An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can J Public Health
- v.110(3); 2019 Jun
Language: English | French

Why public health matters today and tomorrow: the role of applied public health research
Lindsay mclaren.
1 University of Calgary, Calgary, Canada
Paula Braitstein
2 University of Toronto, Toronto, Canada
David Buckeridge
3 McGill University, Montreal, Canada
Damien Contandriopoulos
4 University of Victoria, Victoria, Canada
Maria I. Creatore
5 CIHR Institute of Population & Public Health and University of Toronto, Toronto, Canada
Guy Faulkner
6 University of British Columbia, Vancouver, Canada
David Hammond
7 University of Waterloo, Waterloo, Canada
Steven J. Hoffman
8 CIHR Institute of Population & Public Health and York University, Toronto, Canada
Yan Kestens
9 Université de Montréal, Montreal, Canada
Scott Leatherdale
Jonathan mcgavock.
10 University of Manitoba and the Children’s Hospital Research Institute of Manitoba, Winnipeg, Canada
Wendy V. Norman
11 University of British Columbia, Vancouver, Canada
Candace Nykiforuk
12 University of Alberta, Edmonton, Canada
Valéry Ridde
13 IRD (French Institute For Research on Sustainable Development), CEPED (IRD-Université Paris Descartes), ERL INSERM SAGESUD, Université Paris Sorbonne Cités, Paris, France
14 University of Montreal Public Health Research Institute (IRSPUM), Montreal, Canada
Janet Smylie
Public health is critical to a healthy, fair, and sustainable society. Realizing this vision requires imagining a public health community that can maintain its foundational core while adapting and responding to contemporary imperatives such as entrenched inequities and ecological degradation. In this commentary, we reflect on what tomorrow’s public health might look like, from the point of view of our collective experiences as researchers in Canada who are part of an Applied Public Health Chairs program designed to support “innovative population health research that improves health equity for citizens in Canada and around the world.” We view applied public health research as sitting at the intersection of core principles for population and public health: namely sustainability, equity, and effectiveness. We further identify three attributes of a robust applied public health research community that we argue are necessary to permit contribution to those principles: researcher autonomy, sustained intersectoral research capacity, and a critical perspective on the research-practice-policy interface. Our intention is to catalyze further discussion and debate about why and how public health matters today and tomorrow, and the role of applied public health research therein.
Résumé
La santé publique est essentielle à une société saine, juste et durable. Pour donner forme à cette vision, il faut imaginer une communauté de la santé publique capable de préserver ses valeurs fondamentales tout en s’adaptant et en réagissant aux impératifs du moment, comme les inégalités persistantes et la dégradation de l’environnement. Dans notre commentaire, nous esquissons un portrait possible de la santé publique de demain en partant de notre expérience collective de chercheurs d’un programme canadien de chaires en santé publique appliquée qui visent à appuyer « la recherche innovatrice sur la santé de la population en vue d’améliorer l’équité en santé au Canada et ailleurs ». Nous considérons la recherche appliquée en santé publique comme se trouvant à la croisée des principes fondamentaux de la santé publique et des populations, à savoir : la durabilité, l’équité et l’efficacité. Nous définissons aussi les trois attributs d’une solide communauté de recherche appliquée en santé publique nécessaires selon nous au respect de ces principes : l’autonomie des chercheurs, une capacité de recherche intersectorielle soutenue et une perspective critique de l’interface entre la recherche, la pratique et les politiques. Nous voulons susciter des discussions et des débats approfondis sur l’importance de la santé publique pour aujourd’hui et pour demain et sur le rôle de la recherche appliquée en santé publique.
Introduction
Public health is critical to a healthy, fair, and sustainable society. Public health’s role in this vision stems from its foundational values of social justice and collectivity (Rutty and Sullivan 2010 ) and—we argue—from its position at the interface of research, practice, and policy.
Realizing this vision requires imagining a public health community that can maintain that foundational core, embrace opportunities of our changing world, and predict and adapt to emerging challenges in a timely manner. Unprecedented ecosystem disruption creates far-reaching health implications for which the public health community is unprepared (CPHA 2015 ; Whitmee et al. 2015 ). Human displacement is at its highest levels on record; those forced from home include “stateless people,” who are denied access to basic rights such as education, health care, employment, and freedom of movement ( http://www.unhcr.org/figures-at-a-glance.html ). Significant growth in urban populations creates an urgent need to improve urban environments, including policies to reduce air pollution and prevent sprawl (CPHA 2015 ; Frumkin et al. 2004 ), to reduce the substantial burden of morbidity and mortality attributable to behaviours such as physical inactivity, which negatively impact quality and quantity of life (Manuel et al. 2016 ). Significant and entrenched forms of economic, social, political, and historical marginalization and exclusion (TRC 2015 ), coupled with inequitable and unsustainable patterns of resource consumption and technological development (CPHA 2015 ; Whitmee et al. 2015 ), cause and perpetuate health inequities. These inequities underlie the now longstanding recognition that the unequal distributions of health-damaging experiences are the main determinants of health (CSDH 2008 ; Ridde 2004 ).
These imperatives demand a broadly characterized public health community. A now classic definition of public health is the science and art of preventing disease, prolonging life, and promoting health through the organized efforts of society (Last 2001 ). Public health, conceptualized in this manner, engages multiple sectors, embraces inclusion and empowerment (Ridde 2007 ), and demands navigating diverse political and economic agendas. Across Canada, a large and growing proportion of provincial spending is devoted to health care, while the proportion devoted to social spending (i.e., the social determinants of health) is small, flat-lining, and in some places declining (Dutton et al. 2018 ). Recent discourse has highlighted a weakening of formal public health infrastructure (Guyon et al. 2017 ) and points of fracture within the field (Lucyk and McLaren 2017 ). Efforts to strengthen public health, in its broadest sense, and to work towards unity of purpose (Talbot 2018 ) are needed now more than ever. What might such efforts look like?
We reflect on this question from our perspectives as researchers who are part of an Applied Public Health Chairs (APHC) program designed to support “innovative population health research that improves health equity for citizens in Canada and around the world.” 1 The applied dimension 2 is facilitated through the program’s focus on “interdisciplinary collaborations and mentorship of researchers and decision makers in health and other sectors” ( http://www.cihr-irsc.gc.ca/e/48898.html ). The APHC program (Box 1) is part of a broader set of efforts to address gaps in public health capacity, including research. Cross-cutting themes for the 2014 cohort (Box 2) include the following: healthy public policy, supportive environments (e.g., cities), diverse methodological approaches, global health, and health equity; many of which 3 align with a Public Health Services and Systems Research perspective in that they “identif[y] the implementation strategies that work, building evidence to support decision-making across the public health sphere” ( http://www.publichealthsystems.org/ ). Applied public health research is broad and could span CIHR Pillars 4 (social, cultural, environmental, and population health research) and 3 (health services research); the 2014 APHC cohort is predominantly aligned with Pillar 4.
The APHC program represents a significant Canadian investment in public health, and thus provides an important vantage point from which to reflect on why public health matters today, and tomorrow.
Box 1 The Applied Public Health Chairs program
Box 2 2014 cohort of Applied Public Health Chairs
More details available at: http://www.cihr-irsc.gc.ca/e/48898.html
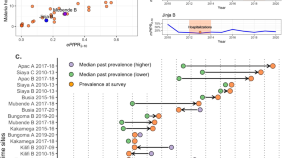
Our proposal
We propose that applied public health research is a critical component of a robust population and public health community. As illustrated in Fig. 1 , we view applied public health research as sitting at the nexus of three core principles: (1) sustainability, (2) equity, and (3) effectiveness, which align with a vision of public health as critical to a healthy, fair, and sustainable society. By sustainability , we mean an approach or way of thinking, about public health in particular (e.g., Schell et al. 2013 ) and population well-being more broadly ( https://sustainabledevelopment.un.org/sdgs ) that emphasizes “meet[ing] the needs of the present generation without compromising the ability of future generations to meet their own needs” (Brundtland et al. 1987 ). Sustainability has social, economic, environmental, and political dimensions. We define equity as a worldview concerned with the embedded or systemic—and often invisible—drivers of unfair distributions of health-damaging experiences. In Canada and elsewhere, inequity is entrenched in legacies of colonial, structural racism designed to sustain inequitable patterns of power and wealth. Equity transcends diverse axes and perspectives, and an equity lens is action-oriented (Ridde 2007 ). Finally, effectiveness refers to impact or benefits for population well-being, as demonstrated by rigorous research. Explicit core values (e.g., equity), while important, are insufficient without translation to demonstrable outcomes (Potvin and Jones 2011 ). These core principles—sustainability, equity, and effectiveness—overlap and are mutually reinforcing; for example, the inequitable concentration of power, wealth, and exploitation of resources precludes sustainability.

Visual depiction of the role and attributes of applied public health research, vis-à-vis core population and public health principles of equity, sustainability, and effectiveness
Although these principles are applicable to the public health community broadly (i.e., including but not limited to researchers), applied public health researchers are uniquely situated to embrace sustainability, equity, and effectiveness when asking questions and generating policy- and practice-relevant knowledge, as illustrated below. Drawing on our collective experiences, we describe three necessary attributes of applied public health research that support our model in Fig. 1 : researcher autonomy, sustained intersectoral research capacity; and a critical perspective on the research-practice-policy interface. We assert that applied public health research is best positioned to contribute meaningfully to the principles of sustainability, effectiveness, and equity if the attributes described below are in place.
Researcher autonomy
Researcher autonomy is a precondition for innovation and independent thinking, and for building and sustaining the conditions for collective efforts. Our working definition of researcher autonomy is the capacity to devote time and energy to activities that, at the researcher’s discretion, facilitate research that embraces principles of sustainability, effectiveness, and equity. Autonomy, beyond the scope of general academic independence, provides the freedom to build and nurture partnerships, and to navigate among universities, health care systems, governments, communities, and across sectors. Effective and respectful partnerships are critical to rigorous intersectoral work and can provide an important platform to discuss systemic forms of inequity (e.g., Olivier et al. 2016 ; Morton Ninomiya et al. 2017 ). Recognizing a potential tension around the role of the researcher in an applied public health context, we deliberately selected the word “autonomy,” which we view as conducive to meaningful collaboration (although that may be experienced differently by different researchers), rather than “independence” which can be seen as contrary to such collaboration. Yet despite their importance, the time and resources to form and sustain those relationships are often not accommodated within funding and academic structures.
Autonomy, when coupled with resources and recognition, permits applied public health researchers to balance foundations of public health with current policy relevance. Although many of us have research programs with particular thematic foci (e.g., physical activity, dental health, HIV), autonomy provides space and credibility to connect those focal issues to enduring and evolving problems in public health (e.g., determinants of population well-being and equity), and to inform the contemporary policy context. Examples include research on health implications of neighbourhood gentrification in urban settings (Steinmetz-Wood et al. 2017 ); using community water fluoridation as a window into public and political understanding and acceptance of public health interventions that are universal in nature (McLaren and Petit 2018 ); and using innovative sampling methods to identify how census methods can perpetuate exclusion (Rotondi et al. 2017 ). That latter work, which estimated that the national census undercounts urban Indigenous populations in Toronto by a factor of approximately 2–4, provides impetus to work towards an inclusive system that respects individual and collective data sovereignty, and that is accountable to the communities from whom data are collected.
These implications of autonomy are consistent with calls for greater reflexivity in public health research (Tremblay and Parent 2014 ).
Insight : To strengthen applied public health research in Canada, researcher autonomy – whereby researchers have the credibility and protected time to set their own agendas in partnerships with the communities they serve – must be privileged.
Sustained intersectoral research capacity
Applied public health research requires funding for resources and infrastructure that are essential to sustain an intersectoral research program, but for which operating funds are otherwise not readily available. Examples include ongoing cohort studies (e.g., Leatherdale et al. 2014 ), research software platforms (e.g., Shaban-Nejad et al. 2017 ), meaningful public sector engagement in developing public health priorities, and knowledge translation activities.
Partnerships, also considered under researcher autonomy above, are one form of intersectoral research capacity. In applied public health research, having strong partnerships in place permits timely response to research opportunities that arise quickly in real-world settings. Examples in our cohort include instances where researchers were able to mobilize for rapid response funding competitions in areas of environment and health, communicable disease in the global South, and Indigenous training networks, because collaborative teams and potential for knowledge co-creation and transfer were already in place.
Insight : A robust applied public health research community requires sustained funding to support foundations of a credible and internationally-competitive research program (e.g., cohort studies, research software platforms, meaningful public sector engagement) that are difficult to resource via usual operating grant channels.
A critical perspective on the research-practice-policy interface
One barrier to evidence-based policy in applied public health is an assumption that evidence is the most important factor in making policy decisions, versus a more holistic view of the policymaking process where evidence is one of many factors, as discussed in recent work (Fafard and Hoffman 2018 ; O’Neill et al. 2019 ; Ridde and Yaméogo 2018 ).
Applied public health research is ideally positioned to embrace a critical perspective on the research-practice-policy interface. Several recent trends are promising in that regard. These include the following: substantive efforts to bridge public health and social science scholarship ( http://www.cihr-irsc.gc.ca/e/50604.html ), growing success by Pillar 4 researchers (including applied public health) in CIHR’s open funding competitions ( http://www.cihr-irsc.gc.ca/e/50488.html ), and the CIHR Health System Impact Fellowship initiative ( http://www.cihr-irsc.gc.ca/e/50612.html ), which could facilitate the placement of doctoral and post-doctoral academic researchers within the public health system and related (e.g., public, NGO) organizations.
Insight : Applied public health researchers are ideally positioned to embrace and model a sophisticated and interdisciplinary perspective on the research-practice-policy interface. To do so, opportunities for researchers (including trainees) to gain skills and experience to navigate the policy context are needed.
Against the backdrop of discourse about a weakening of public health infrastructure and fracture within the field (Guyon et al. 2017 ; Lucyk and McLaren 2017 ), we believe that there is value in working towards a unity of purpose (Talbot 2018 ). This commentary was prompted by a shared belief that through our experience with the Applied Public Health Chair Program, we have seen a glimpse of what is needed to achieve a population and public health community that is positioned to tackle societal imperatives, which includes an important role for applied public health research, spanning CIHR Pillars 3 and 4. Anchored in principles of sustainability, equity, and effectiveness, we assert a strong need for applied research infrastructure that privileges and supports: researcher autonomy, sustained funding to support foundations of a credible and internationally competitive research program, and opportunities for researchers (including trainees) to gain skills and experience to navigate the policy context. We welcome and invite further discussion and debate.
1 Under CIHR-IPPH’s mandate, population health research refers to “research into the complex biological, social, cultural, and environmental interactions that determine the health of individuals, communities, and global populations.”
2 Applied may be defined as follows: “put to practical use,” as opposed to being theoretical ( https://www.merriam-webster.com/dictionary/applied ).
3 For example: https://uwaterloo.ca/compass-system/ (Leatherdale); http://cart-grac.ubc.ca/ (Norman); http://www.healthsystemsglobal.org/ (Ridde).
The original version of this article was revised due to a retrospective Open Access order.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
The article ���Why public health matters today and tomorrow: the role of applied public health research,��� written by Lindsay McLaren et al., was originally published Online First without Open Access.
- Brundtland G, Khalid M, Agnelli S, Al-Athel S, Chidzero B, Fadika L, Hauff V, Lang I, Shijun M, Morino de Botero M, Singh M, Okita S, and et al. (1987). Report of the World Commission on Environment and Development: Our Common Future (‘Brundtland report’). United Nations World Commission on Environment and Development.
- Canadian Public Health Association Discussion Paper . Global change and public health: Addressing the ecological determinants of health. Ottawa: Canadian Public Health Association; 2015. [ Google Scholar ]
- Commission on Social Determinants of Health (CSDH) (2008) . Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization. [ PubMed ]
- Dutton DJ, Forest P-G, Kneebone RD, Zwicker JD. Effect of provincial spending on social services and health care on health outcomes in Canada: an observational longitudinal study. CMAJ. 2018; 190 (3):E66–E71. doi: 10.1503/cmaj.170132. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fafard, P., & Hoffman, S. J. (2018). Rethinking knowledge translation for public health policy. Evidence & Policy . 10.1332/174426418X15212871808802.
- Frumkin H, Frank L, Jackson R. Urban sprawl and public health: designing, planning and building for healthy communities. Washington: Island Press; 2004. [ Google Scholar ]
- Guyon, A., Hancock, T., Kirk, M., MacDonald, J., Neudorf, C., Sutcliffe, P., Talbot, J., Watson-Creed, G. (2017). The weakening of public health: a threat to population health and health care system sustainability. Can J Public Health, 108 (1), 1–6. [ PMC free article ] [ PubMed ]
- Last JM, editor. A dictionary of epidemiology (4th ed) Oxford: Oxford University Press; 2001. [ Google Scholar ]
- Leatherdale ST, Brown KS, Carson V, Childs RA, Dubin JA, Elliott SJ, Faulkner G, Hammond D, Manske S, Sabiston CM, Laxer RE, Bredin C, Thompson-Haile A. The COMPASS study: a longitudinal hierarchical research platform for evaluating natural experiments related to changes in school-level programs, policies and build environment resources. BMC Public Health. 2014; 14 :331. doi: 10.1186/1471-2458-14-331. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lucyk K, McLaren L. Is the future of “population/public health” in Canada united or divided? Reflections from within the field. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice. 2017; 37 (7):223–227. doi: 10.24095/hpcdp.37.7.03. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Manuel DG, Perez R, Sanmartin C, Taljaard M, Hennessy D, Wilson K, Tanuseputro P, Manson H, Benett C, Tuna M, Fisher S, Rosella LC. Measuring burden of unhealthy behaviours using a multivariable predictive approach: life expectancy lost in Canada attributable to smoking, alcohol, physical inactivity, and diet. PLoS Med. 2016; 13 (8):e1002082. doi: 10.1371/journal.pmed.1002082. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McLaren L, Petit R. Universal and targeted policy to achieve health equity: a critical analysis of the example of community water fluoridation cessation in Calgary, Canada in 2011. Crit Public Health. 2018; 28 (2):153–164. doi: 10.1080/09581596.2017.1361015. [ CrossRef ] [ Google Scholar ]
- Morton Ninomiya ME, Atkinson D, Brascoupé S, Firestone M, Robinson N, Reading J, Ziegler CP, Maddox R, Smylie JK. Effective knowledge translation approaches and practices in indigenous health research: a systematic review protocol. Systematic Reviews. 2017; 6 (1):34. doi: 10.1186/s13643-017-0430-x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O’Neill B, Kapoor T, McLaren L. Politics, science and termination: a case study of water fluoridation in Calgary in 2011. Rev Policy Res. 2019; 36 (1):99–120. [ Google Scholar ]
- Olivier C, Hunt MR, Ridde V. NGO-researcher partnerships in global health research: benefits, challenges, and approaches that promote success. Dev Pract. 2016; 26 (4):444–455. doi: 10.1080/09614524.2016.1164122. [ CrossRef ] [ Google Scholar ]
- Potvin L, Jones CM. Twenty-five years after the Ottawa charter: the critical role of health promotion for public health. Canadian Journal of Public Health. 2011; 102 (4):244–248. doi: 10.1007/BF03404041. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ridde V. Une analyse comparative entre le Canada, le Québec et la France: l’importance des rapports sociaux et politiques eu égard aux determinants et aux inégalités de la santé L’antilibéralisme. 2004; 45 (2):343–364. [ Google Scholar ]
- Ridde V. Réduire les inégalités sociales de santé: santé publique, santé communautaire ou promotion de la santé? Promot Educ. 2007; XIV (2):111–114. doi: 10.1177/10253823070140020601. [ CrossRef ] [ Google Scholar ]
- Ridde V, Yaméogo P (2018). How Burkina Faso used evidence in deciding to launch its policy of free healthcare for children under five and women in 2016. Palgrave Communications ;119(4).
- Rotondi MA, O’Campo P, O’Brien K, Firestone M, Wolfe SH, Bourgeois C, Smylie JK. Our Health Counts Toronto: using respondent-driven sampling to unmask census undercounts of an urban indigenous population in Toronto, Canada. BMJ Open. 2017; 7 :e018936. doi: 10.1136/bmjopen-2017-018936. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rutty C, Sullivan SC. This is public health: A Canadian history. Ottawa: Canadian Public Health Association; 2010. [ Google Scholar ]
- Schell SF, Luke DA, Schooley MW, Elliott MB, Herbers SH, Mueller NB, Bunger AC. Public health program capacity for sustainability: A new framework. Implement Sci. 2013; 8 :15. doi: 10.1186/1748-5908-8-15. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shaban-Nejad A, Lavigne M, Okhmatovskaia A, Buckeridge DL. PopHR: a knowledge-based platform to support integration, analysis, and visualization of population health data. Ann N Y Acad Sci. 2017; 1387 (1):44–53. doi: 10.1111/nyas.13271. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Steinmetz-Wood M, Wasfi R, Parker G, Bornstein L, Caron J, Kestens Y. Is gentrification all bad? Positive association between gentrification and individual’s perceived neighbourhood collective efficacy in Montreal, Canada. International Journal of Health Geographics. 2017; 16 (1):24. doi: 10.1186/s12942-017-0096-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Talbot J. (2018). Keynote presentation at Campus Alberta 2018 annual conference, In defense of public health: identifying opportunities to strengthen our field. Calgary, May 9.
- Tremblay MC, Parent AA. Reflexivity in PHIR: let’s have a reflexive talk! Canadian Journal of Public Health. 2014; 105 (3):e221–e223. doi: 10.17269/cjph.105.4438. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Truth and Reconciliation Canada (2015). Honouring the truth, reconciling for the future: Summary of the final report of the Truth and Reconciliation Commission of Canada . Winnipeg: Truth and Reconciliation Commission of Canada.
- Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, Berreira de Souza Dias B, Frumkin H, Gong P, Head P, Horton R, Mace GM, Marten R, Myers SS, Nishtar S, Osofsky SA, Pattanayak SK, Pongsiri MJ, Romanelli C, Soucat A, Vega J, Yach D. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet ommission on planetary health. Lancet. 2015; 386 (10007):1973–2028. doi: 10.1016/S0140-6736(15)60901-1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Public health articles from across Nature Portfolio
Public health is the medical discipline concerned with the prevention and control of disease through population surveillance and the promotion of healthy behaviours. Strategies used to promote public health include patient education, the administration of vaccines, and other components of preventive medicine.
Related Subjects
- Epidemiology
- Population screening
Latest Research and Reviews
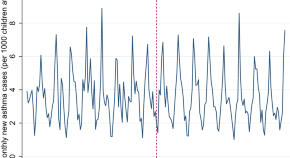
Tobacco control policies and respiratory conditions among children presenting in primary care
- Timor Faber
- Luc E. Coffeng
- Jasper V. Been
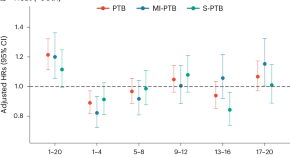
Heat exposure induced risks of preterm birth mediated by maternal hypertension
Findings from a multicenter study of 197,080 singleton live births in China show maternal hypertension as a mediator of the risks imposed by heat exposure between conception and 20 weeks of gestation on preterm birth and its various clinical subtypes.
- Cunrui Huang
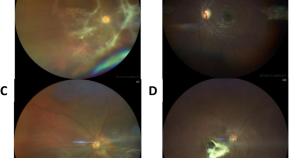
Clinical characteristics and aetiology of uveitis in a viral haemorrhagic fever zone
- Shiama Balendra
- Lloyd Harrison-Williams
- Alasdair Kennedy
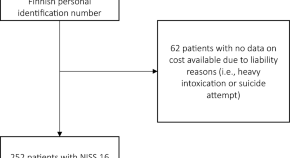
Cumulative costs of severe traffic injuries in Finland: a 2-year retrospective observational study of 252 patients
- Antti Riuttanen
- Erkka Karjalainen
- Ville M. Mattila
Severe outcomes of malaria in children under time-varying exposure
Severe pediatric malaria remains a concern in many countries. Here, the authors use an individual-based modeling approach to evaluate the relationship between malaria prevalence and incidence of malaria pediatric hospitalizations, and show how unsteady transmission patterns affect hospitalization rates.
- Pablo M. De Salazar
- Alice Kamau
- Melissa A. Penny
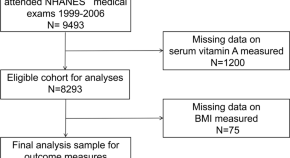
Association between serum vitamin A and body mass index in adolescents from NHANES 1999 to 2006
- Nishant Patel
News and Comment

Neglecting sex and gender in research is a public-health risk
The data are clear: taking sex and gender into account in research and using that knowledge to change health care could benefit billions of people.
- Cheryl Carcel
- Robyn Norton
Interpersonal therapy can be an effective tool against the devastating effects of loneliness
- Myrna M. Weissman
- Jennifer J. Mootz

Is the Internet bad for you? Huge study reveals surprise effect on well-being
A survey of more than 2.4 million people finds that being online can have a positive effect on welfare.
- Carissa Wong

Talking about climate change and health
The climate crisis is also an urgent and ongoing health crisis with diverse human impacts leading to physical, mental and cultural losses. Translating knowledge into action involves broad collaboration, which relies heavily on careful communication of a personal and politicized issue.

Considering health can drive climate action
Last December saw the inaugural Health Day at a Climate Conference of the Parties (COP) and the announcement of the COP28 UAE Declaration on Climate and Health, marking a substantial step in global recognition of the intersecting crises of climate change and health . Nature Climate Change speaks to Maria Neira, director of the Department of Environment, Climate Change and Health at the World Health Organization, about successes and next steps.
- Tegan Armarego-Marriott

How ignorance and gender inequality thwart treatment of a widespread illness
Tens of millions of people have female genital schistosomiasis, a neglected tropical disease that few physicians have even heard of. Efforts are under way to move it out of obscurity and empower women and girls to access sexual and reproductive health care.
- Claire Ainsworth
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
BMC Public Health
Latest collections open to submissions, new: improving the health of incarcerated people.
Guest edited by Jaimie P. Meyer and Heino Johann Stöver
NEW: Exploring barriers to oral health care
Guest Edited by Heather Leggett
NEW: Workplace safety and health
Guest edited by Els Clays, Subas Neupane and Karin Proper
Menstrual health education
Guest edited by HuiJun Chih and Sonia Regina Grover
Editors' picks

- Most accessed
Temporal change in prevalence of BMI categories in India: patterns across States and Union territories of India, 1999–2021
Authors: Meekang Sung, Akhil Kumar, Raman Mishra, Bharati Kulkarni, Rockli Kim and S. V. Subramanian
Unlocking the potential: exploring the impact of dolutegravir treatment on body mass index improvement in underweight adults with HIV in Malawi
Authors: Thulani Maphosa, Shalom Dunga, Lucky Makonokaya, Godfrey Woelk, Alice Maida, Alice Wang, Allan Ahimbisibwe, Rachel K. Chamanga, Suzgo B. Zimba, Dumbani Kayira and Rhoderick Machekano
Sociodemographic determinants of vaccination and willingness to pay for COVID-19 vaccines in Hungary, results of a cross-sectional online questionnaire
Authors: Zsuzsanna Beretzky and Valentin Brodszky
The effects of trade liberalization on inequality in nutrition intake: empirical evidence from Indian districts
Authors: Yali Zhang and Saiya Li
How do labour market conditions explain the development of mental health over the life-course? a conceptual integration of the ecological model with life-course epidemiology in an integrative review of results from the Northern Swedish Cohort
Authors: Anne Hammarström, Hugo Westerlund, Urban Janlert, Pekka Virtanen, Shirin Ziaei and Per-Olof Östergren
Most recent articles RSS
View all articles
Porn video shows, local brew, and transactional sex: HIV risk among youth in Kisumu, Kenya
Authors: Carolyne Njue, Helene ACM Voeten and Pieter Remes
Local government responses for COVID-19 management in the Philippines
Authors: Dylan Antonio S. Talabis, Ariel L. Babierra, Christian Alvin H. Buhat, Destiny S. Lutero, Kemuel M. Quindala III and Jomar F. Rabajante
School grade and sex differences in domain-specific sedentary behaviors among Japanese elementary school children: a cross-sectional study
Authors: Kaori Ishii, Ai Shibata, Minoru Adachi, Yoshiyuki Mano and Koichiro Oka
Oral and anal sex practices among high school youth in Addis Ababa, Ethiopia
Authors: Amsale Cherie and Yemane Berhane
Health literacy and public health: A systematic review and integration of definitions and models
Authors: Kristine Sørensen, Stephan Van den Broucke, James Fullam, Gerardine Doyle, Jürgen Pelikan, Zofia Slonska and Helmut Brand
Most accessed articles RSS
Aims and scope
Editorial board updates.
Join the Editorial Board
We are recruiting new, international Editorial Board Members.
Meet Biplab Kumar Datta
Meet our Editorial Board Members working on the Sustainable Development Goals.
BMC Public Health supports:

The UN Sustainable Development Goals
assisting policy-makers, governments and humanitarian organizations in making research-backed decisions to advance the international well-being agenda.
Equity in academic publishing
for authors based in low- and middle-income countries who might face challenges in publishing their work. Follow us for guidance on submitting your research to us.
BMC Public Health blogs

Highlights of the BMC series – April 2024
15 May 2024

Highlights of the BMC Series – March 2024
10 April 2024

Highlights of the BMC Series – December 2023
30 January 2024
Latest Tweets
Your browser needs to have JavaScript enabled to view this timeline
Important information
Editorial board
For authors
For editorial board members
For reviewers
- Manuscript editing services
Annual Journal Metrics
2022 Citation Impact 4.5 - 2-year Impact Factor 4.7 - 5-year Impact Factor 1.661 - SNIP (Source Normalized Impact per Paper) 1.307 - SJR (SCImago Journal Rank)
2023 Speed 32 days submission to first editorial decision for all manuscripts (Median) 173 days submission to accept (Median)
2023 Usage 24,332,405 downloads 24,308 Altmetric mentions
- More about our metrics
Peer-review Terminology
The following summary describes the peer review process for this journal:
Identity transparency: Single anonymized
Reviewer interacts with: Editor
Review information published: Review reports. Reviewer Identities reviewer opt in. Author/reviewer communication
More information is available here
- Follow us on Twitter
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
Public Health and Epidemiology
Empowering a community publishing articles in all areas of Public Health and Epidemiology, including disease surveillance, infectious disease outbreaks, vaccination, genetic epidemiology, epidemiological transition, sugar taxation, smoking cessation, exercise interventions, behaviour change and much more.
At PLOS, we put researchers and research first.
Our expert editorial boards collaborate with reviewers to provide accurate assessment that readers can trust. Authors have a choice of journals, publishing outputs, and tools to open their science to new audiences and get credit. We collaborate to make science, and the process of publishing science, fair, equitable, and accessible for the whole community.
Your New Open Science Journals
Public health implications of a changing climate.
Feature your research in this collection. We are looking for research that uses climate change to address effects on public health with a particular focus on the spread of infectious diseases. Explore this collection and find out how to submit your research.
Infectious Disease Epidemiology
Feature your research in this collection. We are looking for research that highlights the many interconnected facets of infectious disease epidemiology, including emerging zoonoses, viral genomics, infection dynamics, and more. Explore this collection and find out how to submit your research.
Looking for exciting work in your field?
Discover top cited Public Health & Epidemiology papers from recent years.
PLOS MEDICINE Accelerometer measured physical activity and the incidence of cardiovascular disease: Evidence from the UK Biobank cohort study Read the peer review...
PLOS MEDICINE Cardiovascular health metrics from mid- to late-life and risk of dementia: A population-based cohort study in Finland Read the peer review...
PLOS ONE Comparing the fit of N95, KN95, surgical, and cloth face masks and assessing the accuracy of fit checking Read the preprint...
PLOS ONE is launching a new influenza collection that will focus on every level of influenza prevention. Our panel of expert Guest Editors invite you to submit your research articles by April 9, 2021 to be considered for this collection.
Discover the latest opinion and perspective articles on climate change and infectious diseases in this PLOS Biology Collection. Here we explore one of the most pressing problems facing the world today: understanding how climate change will affect the distribution and dynamics of pathogens and their plant and animal hosts.
Reproducibility is important for the future of science.
PLOS is Open so that everyone can read, share, and reuse the research we publish. Underlying our commitment to Open Science is our data availability policy which ensures every piece of your research is accessible and replicable. We also go beyond that, empowering authors to preregister their research, and publish protocols , negative and null results, and more.

Author Interview: Luca Morgantini on Burnout among Healthcare Professionals in COVID-19

In 2020, PLOS articles were referenced an estimated 107,840 times by media outlets around the world. Read Public Health & Epidemiology articles that made the news.
- The impact of news exposure on collective attention in the United States during the 2016 Zika epidemic
- Residential green space and child intelligence and behavior across urban, suburban, and rural areas in Belgium: A longitudinal birth cohort study of twins
- Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis
Ready to share your study with a wider audience? Help more people read, see, and cite your published research with our Author Media Toolkit
How can we increase adoption of open research practices?

Researchers are satisfied with their ability to share their own research data but may struggle with accessing other researchers’ data. Therefore, to increase data sharing in a findable and accessible way, PLOS will focus on better integrating existing data repositories and promoting their benefits rather than creating new solutions.
Imagining a transformed scientific publication landscape

Open Science is not a finish line, but rather a means to an end. An underlying goal behind the movement towards Open Science is to conduct and publish more reliable and thoroughly reported research.
Infectious disease modeling in a time of COVID-19

As the world grappled with the effects of COVID-19 this year, the importance of accurate infectious disease modeling has become apparent. We invited a few authors to give their perspectives on their research during this global pandemic.
- What do you think is the best way to ensure reproducibility for future generations of researchers?
What is public health?
Health care is vital to all of us some of the time, but public health is vital to all of us all of the time. —C. Everett Koop, former U.S. surgeon general
Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. —World Health Organization
Public health is the science of protecting and improving the health of populations—from neighborhoods to cities to countries to world regions—through education, promotion of healthy lifestyles, research toward prevention of disease and injury, and detecting, preventing, and responding to infectious diseases. Public health experts analyze the effect on health of genetics, personal choice, and the environment to develop interventions and policies that protect the health of families and communities, such as vaccination programs and education on the dangers of tobacco and alcohol. As the American Public Health Association notes, “Public health saves money, improves our quality of life, helps children thrive, and reduces human suffering.”
Public health professionals try to prevent problems from happening or recurring through implementing educational programs, recommending policies, administering services, and conducting research—in contrast to clinical professionals like doctors and nurses, who focus primarily on treating individuals after they become sick or injured. Public health also works to limit health disparities. A large part of public health is promoting health care equity, quality, and accessibility. —CDC Foundation
Academic disciplines involved in public health
The field of public health is highly varied and encompasses many academic disciplines, including the following:
Behavioral science/Health education
Biostatistics
Environmental health
Epidemiology
Health policy
Health services administration/management
Humanitarian and human rights studies
Immunology, molecular biology, genetics, and other basic sciences
International health/global health
Maternal and child health
Public health laboratory practice (e.g., testing of biological and environmental samples)
Public health practice
Public health occupations
Some examples of the many occupations involved in public health include:
Scientists and researchers
Epidemiologists
Public health leaders and policymakers
Public health physicians
Public health nurses
Occupational health and safety professionals
Nutritionists
Social workers
Community planners
Health educators
First responders
Restaurant inspectors
Sanitarians (investigate health and safety within an environment, enforce health and safety regulations, and identify risk factors)
Activities of public health professionals
Some examples of the work undertaken by public health professionals include:
Studying environmental toxins and their health impacts
Monitoring the quality of the air we breathe and the water we drink
Developing plans and strategies to respond to emergencies and disasters
Exploring the causes of injuries and how best to prevent them
Testing biological and environmental samples
Researching risk factors for chronic disease and designing, implementing, and evaluating programs for reducing those risk factors
Implementing childhood and adult vaccination programs
Improving care for pregnant women, mothers, and newborns
Promoting healthy eating and physical activity
Ensuring access to a high-quality fruit and vegetable supply
Investigating infectious-disease outbreaks
Analyzing data for health trends
Undertaking screening programs for certain cancers
Analyzing and implementing public health policy
Principal tools of public health research
Population and numeric disciplines—especially epidemiology, biostatistics, and informatics
Biological sciences disciplines—focusing on infectious and chronic diseases as well as nutritional and environmental links to ill health. Largely laboratory based, and emphasizing the biological, chemical, and genetic basis of health and disease.
Social and policy disciplines—including health policy and management, global health systems, health economics, and the social and behavioral determinants of health and disease
Distinctions between public health and medicine
Because of their shared concern with human health, people often are confused by the difference between public health and medicine. In fact, people’s health is shaped much more by their lifestyle, social networks, environment, and genes than by medical care. Below are some specific distinctions between public health and medicine.
Public health
Primary focus on populations
Emphasis on disease prevention and health promotion for entire communities
Predominant emphasis on promoting healthy behaviors and environments
Specializations organized, for example, by analytical method (epidemiology, toxicology); setting and population (occupational health, global health); substantive health problem (environmental health, nutrition)
Biological sciences central, with a prime focus on major threats to the health of populations, such as epidemics and noncommunicable diseases; research moves between laboratory and field
Social and public policy disciplines an integral part of public health education
Primary focus on individuals
Emphasis on disease diagnosis, treatment, and care of the individual patient
Predominant emphasis on medical care
Specializations organized, for example, by organ system (cardiology, neurology); patient group (obstetrics, pediatrics); etiology and pathophysiology (infectious disease, oncology); technical skill (radiology, surgery)
Biological sciences central, stimulated by needs of patients ; research moves between laboratory and bedside
Social sciences generally an elective part of medical education
Leading causes of death in the United States
Medical view (focuses on the diseases that actually cause deaths).
Heart disease
Chronic lower respiratory diseases
Stroke (cerebrovascular diseases)
Source: Deaths and Mortality, National Center for Health Statistics, Centers for Disease Control and Prevention
Much of this health burden could be prevented or postponed through improved nutrition, increased physical activity, improved vaccination rates, avoidance of tobacco use, adoption of measures to increase motor-vehicle safety, early detection and treatment of risk factors, and health-care quality improvement. — CDC National Health Report: Leading Causes of Morbidity and Mortality and Associated Behavioral Risk and Protective Factors—United States, 2005–2013
Public health view (focuses on the factors that lead to deadly diseases)
Tobacco use
Physical inactivity
Infectious disease
Social determinants of health
“Social determinants of health”—a term often used in the public health field—refers to the conditions in which people are born, grow, work, live, and age and the wider set of forces and systems shaping the conditions of daily life, as defined by the World Health Organization (WHO). These social determinants may describe social inequities that are reflected in the poor health of certain populations, often with devastating consequences. WHO, as noted in its report Health Equity Through Action on the Social Determinants of Health, believes that reducing health inequities is an ethical imperative. “Social injustice,” the report notes, “is killing people on a grand scale.”
Examples of social determinants include:
Availability of resources to meet daily needs (e.g., safe housing and local food markets)
Access to educational, economic, and job opportunities
Access to health care services
Quality of education and job training
Availability of community-based resources in support of community living and opportunities for recreational and leisure-time activities
Transportation options
Public safety
Social support
Social norms and attitudes (e.g., discrimination, racism, and distrust of government)
Exposure to crime, violence, and social disorder (e.g., presence of trash and lack of cooperation in a community)
Socioeconomic conditions (e.g., concentrated poverty and the stressful conditions that accompany it)
Residential segregation
Language/Literacy
Access to mass media and emerging technologies (e.g., cell phones, the Internet, and social media)
Source: Healthy People 2020
People’s health is determined in part by access to social and economic opportunities; the resources and supports available in their homes, neighborhoods, and communities; the quality of their schooling; the safety of their workplaces; the cleanliness of their water, food, and air; and the nature of their social interactions and relationships. Social determinants of health involve economic stability, education, social and community context, health, health care, neighborhood, and the built environment. Each of these five determinant areas reflects a number of key issues that make up the underlying factors in the arena of social determinants of health.
Economic stability
Food insecurity
Housing instability
Early childhood education and development
Enrollment in higher education
High school graduation
Language and literacy
Social and community context
Civic participation
Discrimination
Incarceration
Social cohesion
Health and health care
Access to health care
Access to primary care
Health literacy
Neighborhood and built environment
Access to foods that support healthy eating patterns
Crime and violence
Environmental conditions
“The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition.” —Constitution of the World Health Organization, inscribed in several languages on the FXB Building of the Harvard T.H. Chan School of Public Health
Major global public health challenges
Ending disparities in health between rich and poor and across racial and gender lines
Reducing infant mortality, maternal death rates, and reproductive health problems
Developing solutions and treatments for infectious diseases (e.g., AIDS, tuberculosis, and malaria)
Tackling malnutrition
Preventing the spread of multi-drug-resistant (MDR) diseases, such as MDR tuberculosis
Confronting emerging threats to health from chronic diseases such as diabetes, heart disease, and obesity that are related to lifestyle (e.g., diet, exercise, and tobacco use)
Addressing mental illnesses and social factors in health
Understanding climate change and other environmental health threats
Studying the impacts of war, violence, and terrorism on health
Advancing practices, protocols, and strategies to achieve diverse goals, such as reducing surgical errors, changing social norms around drunk driving
Developing health and communications systems to improve health-related policy and decision-making and increase the speed and effectiveness of responses to emergencies such as disease pandemics, natural disasters, or terrorist attacks
Ten great public health achievements in the United States, 1900–1999
1. vaccination.
Programs of population-wide vaccinations resulted in the eradication of smallpox; elimination of polio in the Americas; and control of measles, rubella, tetanus, diphtheria, Haemophilus influenzae type b, and other infectious diseases in the United States and other parts of the world.
2. Motor-vehicle safety
Improvements in motor-vehicle safety have contributed to large reductions in motor-vehicle-related deaths. These improvements include engineering efforts to make both vehicles and highways safer and successful efforts to change personal behavior (e.g., increased use of safety belts, child safety seats, motorcycle helmets, and decreased drinking and driving).
3. Safer workplaces
Work-related health problems, such as coal workers’ pneumoconiosis (black lung), and silicosis—common at the beginning of the century— have been significantly reduced. Severe injuries and deaths related to mining, manufacturing, construction, and transportation also have decreased; since 1980, safer workplaces have resulted in a reduction of approximately 40% in the rate of fatal occupational injuries.
4. Control of infectious diseases
Control of infectious diseases has resulted from clean water and better sanitation. Infections such as typhoid and cholera, major causes of illness and death early in the 20th century, have been reduced dramatically by improved sanitation. In addition, the discovery of antimicrobial therapy has been critical to successful public health efforts to control infections such as tuberculosis and sexually transmitted diseases (STDs).
5. Decline in deaths from coronary heart disease and stroke
Decline in deaths from coronary heart disease and stroke have resulted from risk-factor modification, such as smoking cessation and blood pressure control coupled with improved access to early detection and better treatment. Since 1972, death rates for coronary heart disease have decreased 51 percent.
6. Safer and healthier foods
Since 1900, safer and healthier foods have resulted from decreases in microbial contamination and increases in nutritional content. Identifying essential micronutrients and establishing food-fortification programs have almost eliminated major nutritional deficiency diseases such as rickets, goiter, and pellagra in the United States. [Healthy Eating Plate sidebar]
7. Healthier mothers and babies
Healthier mothers and babies are a result of better hygiene and nutrition, availability of antibiotics, greater access to health care, and technological advances in maternal and neonatal medicine. Since 1900, infant mortality has decreased 90 percent, and maternal mortality has decreased 99 percent.
8. Family planning
Access to family planning and contraceptive services has altered social and economic roles of women. Family planning has provided health benefits such as smaller family size and longer intervals between the birth of children; increased opportunities for preconceptional counseling and screening; fewer infant, child, and maternal deaths; and the use of barrier contraceptives to prevent pregnancy and transmission of human immunodeficiency virus and other STDs.
9. Fluoridation of drinking water
Fluoridation of drinking water began in 1945 and in 1999 reaches an estimated 144 million persons in the United States. Fluoridation safely and inexpensively benefits both children and adults by effectively preventing tooth decay, regardless of socioeconomic status or access to care. Fluoridation has played an important role in the reductions in tooth decay (40 percent to 70 percent in children) and of tooth loss in adults (40 percent to 60 percent).
10. Recognition of tobacco use as a health hazard
Recognition of tobacco use as a health hazard in 1964 has resulted in changes in the promotion of cessation of use, and reduction of exposure to environmental tobacco smoke. Since the initial Surgeon General’s report on the health risks of smoking, the prevalence of smoking among adults has decreased, and millions of smoking-related deaths have been prevented.
Source: Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report
Ten great public health achievements in the United States, 2001–2010
During the 20th century, life expectancy at birth among U.S. residents increased by 62%, from 47.3 years in 1900 to 76.8 in 2000, and unprecedented improvements in population health status were observed at every stage of life. In 1999, the CDC’s Morbidity and Mortality Weekly Report published a series of reports highlighting 10 public health achievements that contributed to those improvements. This report assesses advances in public health during the first 10 years of the 21st century. Public health scientists at the CDC were asked to nominate noteworthy public health achievements that occurred in the United States during 2001–2010. From those nominations, 10 achievements, not ranked in any order, have been summarized in this report. — Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report
1. Vaccine-preventable diseases
The decade saw substantial declines in cases, hospitalizations, deaths, and health-care costs associated with vaccine-preventable diseases. New vaccines (i.e., rotavirus, quadrivalent meningococcal conjugate, herpes zoster, pneumococcal conjugate, and human papillomavirus vaccines, as well as tetanus, diphtheria, and acellular pertussis vaccine for adults and adolescents) were introduced, bringing to 17 the number of diseases targeted by U.S. immunization policy. A recent economic analysis indicated that vaccination of each U.S. birth cohort with the current childhood immunization schedule prevents approximately 42,000 deaths and 20 million cases of disease, with net savings of nearly $14 billion in direct costs and $69 billion in total societal costs.
The impact of two vaccines has been particularly striking. Following the introduction of pneumococcal conjugate vaccine, an estimated 211,000 serious pneumococcal infections and 13,000 deaths were prevented during 2000–2008. Routine rotavirus vaccination, implemented in 2006, now prevents an estimated 40,000–60,000 rotavirus hospitalizations each year. Advances also were made in the use of older vaccines, with reported cases of hepatitis A, hepatitis B, and varicella at record lows by the end of the decade. Age-specific mortality (i.e., deaths per million population) from varicella for persons age <20 years, declined by 97% from 0.65 in the prevaccine period (1990–1994) to 0.02 during 2005–2007. Average age-adjusted mortality (deaths per million population) from hepatitis A also declined significantly, from 0.38 in the prevaccine period (1990–1995) to 0.26 during 2000–2004.
2. Prevention and control of infectious diseases
Improvements in state and local public health infrastructure along with innovative and targeted prevention efforts yielded significant progress in controlling infectious diseases. Examples include a 30% reduction from 2001 to 2010 in reported U.S. tuberculosis cases and a 58% decline from 2001 to 2009 in central line–associated blood stream infections. Major advances in laboratory techniques and technology and investments in disease surveillance have improved the capacity to identify contaminated foods rapidly and accurately and prevent further spread. Multiple efforts to extend HIV testing, including recommendations for expanded screening of persons aged 13–64 years, increased the number of persons diagnosed with HIV/AIDS and reduced the proportion with late diagnoses, enabling earlier access to life-saving treatment and care and giving infectious persons the information necessary to protect their partners. In 2002, information from CDC predictive models and reports of suspected West Nile virus transmission through blood transfusion spurred a national investigation, leading to the rapid development and implementation of new blood donor screening. To date, such screening has interdicted 3,000 potentially infected U.S. donations, removing them from the blood supply. Finally, in 2004, after more than 60 years of effort, canine rabies was eliminated in the United States, providing a model for controlling emerging zoonoses.
3. Tobacco control
Since publication of the first Surgeon General’s Report on tobacco in 1964, implementation of evidence-based policies and interventions by federal, state, and local public health authorities has reduced tobacco use significantly. By 2009, 20.6% of adults and 19.5% of youths were current smokers, compared with 23.5% of adults and 34.8% of youths 10 years earlier. However, progress in reducing smoking rates among youths and adults appears to have stalled in recent years. After a substantial decline from 1997 (36.4%) to 2003 (21.9%), smoking rates among high school students remained relatively unchanged from 2003 (21.9%) to 2009 (19.5%). Similarly, adult smoking prevalence declined steadily from 1965 (42.4%) through the 1980s, but the rate of decline began to slow in the 1990s, and the prevalence remained relatively unchanged from 2004 (20.9%) to 2009 (20.6%). Despite the progress that has been made, smoking still results in an economic burden, including medical costs and lost productivity, of approximately $193 billion per year.
Although no state had a comprehensive smoke-free law (i.e., prohibit smoking in worksites, restaurants, and bars) in 2000, that number increased to 25 states and the District of Columbia (DC) by 2010, with 16 states enacting comprehensive smoke-free laws following the release of the 2006 Surgeon General’s Report. After 99 individual state cigarette excise tax increases, at an average increase of 55.5 cents per pack, the average state excise tax increased from 41.96 cents per pack in 2000 to $1.44 per pack in 2010. In 2009, the largest federal cigarette excise tax increase went into effect, bringing the combined federal and average state excise tax for cigarettes to $2.21 per pack, an increase from $0.76 in 2000. In 2009, the Food and Drug Administration (FDA) gained the authority to regulate tobacco products. By 2010, FDA had banned flavored cigarettes, established restrictions on youth access, and proposed larger, more effective graphic warning labels that are expected to lead to a significant increase in quit attempts.
4. Maternal and infant health
The past decade has seen significant reductions in the number of infants born with neural tube defects (NTDs) and expansion of screening of newborns for metabolic and other heritable disorders. Mandatory folic acid fortification of cereal grain products labeled as enriched in the United States beginning in 1998 contributed to a 36% reduction in NTDs from 1996 to 2006 and prevented an estimated 10,000 NTD-affected pregnancies in the past decade, resulting in a savings of $4.7 billion in direct costs.
Improvements in technology and endorsement of a uniform newborn-screening panel of diseases have led to earlier life-saving treatment and intervention for at least 3,400 additional newborns each year with selected genetic and endocrine disorders. In 2003, all but four states were screening for only six of these disorders. By April 2011, all states reported screening for at least 26 disorders on an expanded and standardized uniform panel. Newborn screening for hearing loss increased from 46.5% in 1999 to 96.9% in 2008. The percentage of infants not passing their hearing screening who were then diagnosed by an audiologist before age 3 months as either normal or having permanent hearing loss increased from 51.8% in 1999 to 68.1 in 2008.
5. Motor-vehicle safety
Motor vehicle crashes are among the top 10 causes of death for U.S. residents of all ages and the leading cause of death for persons aged 5–34 years. In terms of years of potential life lost before age 65, motor vehicle crashes ranked third in 2007, behind only cancer and heart disease, and account for an estimated $99 billion in medical and lost work costs annually. Crash-related deaths and injuries largely are preventable. From 2000 to 2009, while the number of vehicle miles traveled on the nation’s roads increased by 8.5%, the death rate related to motor vehicle travel declined from 14.9 per 100,000 population to 11.0, and the injury rate declined from 1,130 to 722; among children, the number of pedestrian deaths declined by 49%, from 475 to 244, and the number of bicyclist deaths declined by 58%, from 178 to 74.
These successes largely resulted from safer vehicles, safer roadways, and safer road use. Behavior was improved by protective policies, including effective seat belt and child safety seat legislation; 49 states and the DC have enacted seat belt laws for adults, and all 50 states and DC have enacted legislation that protects children riding in vehicles. Graduated drivers licensing policies for teen drivers have helped reduce the number of teen crash deaths.
6. Cardiovascular-disease prevention
Heart disease and stroke have been the first and third leading causes of death in the United States since 1921 and 1938, respectively. Preliminary data from 2009 indicate that stroke is now the fourth leading cause of death in the United States. During the past decade, the age-adjusted coronary heart disease and stroke death rates declined from 195 to 126 per 100,000 population and from 61.6 to 42.2 per 100,000 population, respectively, continuing a trend that started in the 1900s for stroke and in the 1960s for coronary heart disease. Factors contributing to these reductions include declines in the prevalence of cardiovascular risk factors such as uncontrolled hypertension, elevated cholesterol, and smoking, and improvements in treatments, medications, and quality of care.
7. Occupational safety
Significant progress was made in improving working conditions and reducing the risk for workplace-associated injuries. For example, patient lifting has been a substantial cause of low back injuries among the 1.8 million U.S. health-care workers in nursing care and residential facilities. In the late 1990s, an evaluation of a best practices patient-handling program that included the use of mechanical patient-lifting equipment demonstrated reductions of 66% in the rates of workers’ compensation injury claims and lost workdays and documented that the investment in lifting equipment can be recovered in less than 3 years. Following widespread dissemination and adoption of these best practices by the nursing home industry, Bureau of Labor Statistics data showed a 35% decline in low back injuries in residential and nursing care employees between 2003 and 2009.
The annual cost of farm-associated injuries among youth has been estimated at $1 billion annually. A comprehensive childhood agricultural injury prevention initiative was established to address this problem. Among its interventions was the development by the National Children’s Center for Rural Agricultural Health and Safety of guidelines for parents to match chores with their child’s development and physical capabilities. Follow-up data have demonstrated a 56% decline in youth farm injury rates from 1998 to 2009 (National Institute for Occupational Safety and Health, unpublished data, 2011).
In the mid-1990s, crab fishing in the Bering Sea was associated with a rate of 770 deaths per 100,000 full-time fishers. Most fatalities occurred when vessels overturned because of heavy loads. In 1999, the U.S. Coast Guard implemented Dockside Stability and Safety Checks to correct stability hazards. Since then, one vessel has been lost and the fatality rate among crab fishermen has declined to 260 deaths per 100,000 full-time fishers.
8. Cancer prevention
Evidence-based screening recommendations have been established to reduce mortality from colorectal cancer and female breast and cervical cancer. Several interventions inspired by these recommendations have improved cancer screening rates. Through the collaborative efforts of federal, state, and local health agencies, professional clinician societies, not-for-profit organizations, and patient advocates, standards were developed that have significantly improved cancer screening test quality and use. The National Breast and Cervical Cancer Early Detection Program has reduced disparities by providing breast and cervical cancer screening services for uninsured women. The program’s success has resulted from similar collaborative relationships. From 1998 to 2007, colorectal cancer death rates decreased from 25.6 per 100,000 population to 20.0 (2.8% per year) for men and from 18.0 per 100,000 to 14.2 (2.7% per year) for women. During this same period, smaller declines were noted for breast and cervical cancer death rates (2.2% per year and 2.4%, respectively).
9. Childhood lead-poisoning prevention
In 2000, childhood lead poisoning remained a major environmental public health problem in the United States, affecting children from all geographic areas and social and economic levels. Black children and those living in poverty and in old, poorly maintained housing were disproportionately affected. In 1990, five states had comprehensive lead poisoning prevention laws; by 2010, 23 states had such laws. Enforcement of these statutes as well as federal laws that reduce hazards in the housing with the greatest risks has significantly reduced the prevalence of lead poisoning. Findings of the National Health and Nutrition Examination Surveys from 1976–1980 to 2003–2008 reveal a steep decline, from 88.2% to 0.9%, in the percentage of children aged 1–5 years with blood lead levels ≥10 µg/dL. The risks for elevated blood lead levels based on socioeconomic status and race also were reduced significantly. The economic benefit of lowering lead levels among children by preventing lead exposure is estimated at $213 billion per year.

10. Public health preparedness and response
After the international and domestic terrorist actions of 2001 highlighted gaps in the nation’s public health preparedness, tremendous improvements have been made. In the first half of the decade, efforts were focused primarily on expanding the capacity of the public health system to respond (e.g., purchasing supplies and equipment). In the second half of the decade, the focus shifted to improving the laboratory, epidemiology, surveillance, and response capabilities of the public health system. For example, from 2006 to 2010, the percentage of Laboratory Response Network labs that passed proficiency testing for bioterrorism threat agents increased from 87% to 95%. The percentage of state public health laboratories correctly subtyping Escherichia coli O157:H7 and submitting the results into a national reporting system increased from 46% to 69%, and the percentage of state public health agencies prepared to use Strategic National Stockpile material increased from 70% to 98%. During the 2009 H1N1 influenza pandemic, these improvements in the ability to develop and implement a coordinated public health response in an emergency facilitated the rapid detection and characterization of the outbreak, deployment of laboratory tests, distribution of personal protective equipment from the Strategic National Stockpile, development of a candidate vaccine virus, and widespread administration of the resulting vaccine. These public health interventions prevented an estimated 5–10 million cases, 30,000 hospitalizations, and 1,500 deaths (CDC, unpublished data, 2011).
Existing systems also have been adapted to respond to public health threats. During the 2009 H1N1 influenza pandemic, the Vaccines for Children program was adapted to enable provider ordering and distribution of the pandemic vaccine. Similarly, President’s Emergency Plan for AIDS Relief clinics were used to rapidly deliver treatment following the 2010 cholera outbreak in Haiti.
News from the School

From public servant to public health student

Exploring the intersection of health, mindfulness, and climate change

Conference aims to help experts foster health equity

Building solidarity to face global injustice
- Public Health Research
- Open Access
- First Online: 13 April 2016
Cite this chapter
You have full access to this open access chapter

- Drue H. Barrett PhD 8 ,
- Leonard W. Ortmann PhD 8 ,
- Natalie Brown MPH 9 ,
- Barbara R. DeCausey MPH, MBA 10 ,
- Carla Saenz PhD 11 &
- Angus Dawson PhD 12
Part of the book series: Public Health Ethics Analysis ((PHES,volume 3))
188k Accesses
5 Citations
3 Altmetric
Having a scientific basis for the practice of public health is critical. Research leads to insight and innovations that solve health problems and is therefore central to public health worldwide. For example, in the United States research is one of the ten essential public health services (Public Health Functions Steering Committee 1994). The s of the Ethical Practice of Public , developed by the Public Health Leadership Society (2002), emphasizes the value of having a scientific basis for action. Principle five specifically calls on public health to seek the information needed to carry out effective policies and programs that protect and promote health.
The opinions, findings, and conclusions of the authors do not necessarily reflect the official position, views, or policies of the editors, the editors’ host institutions, or the authors’ host institutions.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others

Research Methods

Evidence-Based Decision-Making 8: Health Policy, a Primer for Researchers
How do we define the policy impact of public health research a systematic review.
- Ethical Challenge
- Public Health Agency
- Public Health Practice
- Informal Payment
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Having a scientific basis for the practice of public health is critical. Research leads to insight and innovations that solve health problems and is therefore central to public health worldwide. For example, in the United States research is one of the ten essential public health services (Public Health Functions Steering Committee 1994). The Principle s of the Ethical Practice of Public Health , developed by the Public Health Leadership Society (2002), emphasizes the value of having a scientific basis for action. Principle five specifically calls on public health to seek the information needed to carry out effective policies and programs that protect and promote health.
This chapter pres ents ethical issues that can arise when conducting public health research. Although the literature about research ethics is complex and rich, it has at least two important limitations when applied to public health research. The first is that much of research ethics has focused on clinical or biomedical research in which the primary interaction is between individuals (i.e., patient-physician or research participant-researcher). Since bioethics tends to focus on the individual, the field of research ethics often neglects broader issues pertaining to communities and population s, including ethical issues raised by some public health research methods (e.g., the use of cluster randomized trials to measure population, not just individual, effects). However, if our discussion of public health research ethics begins by examining public health activities, it becomes apparent that the process of gaining consent involves more than individuals. We must consider that communities bear risks and reap benefits; that not only individuals but also populations may be vulnerable; and that the social, political , and economic context in which research takes place poses ethical challenges. Public health research, with its focus on intervention at community and population levels, has brought these broader ethical considerations to researchers’ attention, demonstrating how ethics guidance based on biomedical research may limit, if not distort, the ethical perspective required to protect human subjects.
The second limitation has to do with how guideline s and regulations are conceived and used. As described in Chaps. 1 and 2 of this casebook, research ethics has mostly evolved out of concern for research abuses. Consequently, the intent of many guidelines and regulations is to strengthen the ethical practice of research with human subjects. These ethical guidance documents include the Nuremberg Code (1947); the Universal Declaration of Human Rights (United Nations 1948); the Declaration of Helsinki (World Medical Association 1964, last revised in 2013); and two documents developed by the Council for International Organizations of Medical Sciences (CIOMS) in collaboration with the World Health Organization (WHO) : International Ethical Guidelines for Biomedical Research Involving Human Subjects (CIOMS 2002) and the International Ethical Guidelines for Epidemiological Studies (CIOMS 2009). In the United States, the primary ethical guidance for protecting human subjects is Title 45, Part 46, of the Code of Federal Regulations (U.S. Department of Health and Human Services 2009). The e thical principles of respect for persons , beneficence , and justice have oft en framed the discussion on ethical conduct of research with human subjects . These principle s were first articulated by the U.S. National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (1979) in the Belmont Report and expanded upon by Beauchamp and Childress (1979) in Principles of Biomedical Ethics .
Such guidelines and regulations often represent a consensus on landmark issues and show ways to consider ethical issues. However, consensus documents can pose obstacles if used uncritically with overgeneralized rules applied blindly. For example, such documents seem to assume that the randomized controlled trial is the gold standard of research methodology, obscuring the fact that all research methods may raise ethical issues. In addition, it is debatable whether these guideline s adequately capture community- and population-oriented values and issues central to public health (Verweij and Dawson 2009). A general concern is that overreliance on guidance documents encourages a legalistic or compliance approach to ethics, rather than encouraging reflection and analysis (Coughlin et al. 2012). Coughlin and colleagues argue that to be successful, research oversight needs to focus on moral judgment and reflection, not on strict rule-like adherence to regulations documented on a checklist. Though formal training in ethics is desirable, moral judgment and discernment are developed by making ethical judgments. This highlights a problem inherent in research oversight. Review of research protocols requires scientific and ethical expertise. However, members of ethics review committees are often unpaid and uncompensated for service time and are frequently asked to perform review duties in addition to their normal work. This lack of regard for their service often results in considerable turnover among committee members and does not allow sufficient time for new members to develop moral discernment. Review of research protocols for human subjects should include consideration of the wider ethical implications of the research and not just focus on compliance with ethics regulations . When inappropriate, guidance should be adapted or even set aside.
Chapter 1 of this casebook provides an account of public health ethics that builds upon the disciplines of both ethics and public health. Following a similar approach, this chapter advances a view of public health research ethics that builds upon concepts of research ethics and public health research. As a result, many ethical issues discussed apply to all health research, including public health research. However, once we examine public health examples, we see that something beyond the traditional resources of current research regulations is needed. We will discuss these ethical issues by reflecting upon traditional research tenets and studying their limitations in a public health context. We will conclude by illustrating via the case studies included in this chapter how ethical challenges arise in public health research. It is impossible to closely analyze all possible ethical issues that may arise either in health research or public health research; thus our intent is to highlight some of the major ethical challenges and considerations.
2 What Is Different About Public Health Research?
The community and population perspective of public health, especially when addressing health issues in resource-poor contexts or in marginalized populations , frequently brings ethical challenges into focus. In public health, research typically occurs outside of the controlled environment that is characteristic of biomedical research . Instead, in public health, research often occurs in real world settings in a particular social, political , and economic context. It may involve interventions with whole communities or populations impacted by catastrophic public health emergencies .
2.1 Can Public Health Research Be Clearly Distinguished from Public Health Practice?
Distinguishing between public health practice and public health research is challenging. Many of the tools and methods are similar. Both involve systematic collection and analysis of data that may lead to generalizable knowledge . Public health research can take forms ranging from descriptive approaches (e.g., correlational studies and cross-sectional surveys) to analytic epidemiologic approaches (e.g., case control studies and cohort studies, including clinical trials ). These same approaches can characterize methods for collecting information as part of public health practice.
A common way to define research is on the basis of its goal to develop generalizable knowledge. For example, the International Ethical Guidelines for Biomedical Research Involving Human Subjects (CIOMS 2002) defines research as “… a class of activity designed to develop or contribute to generalizable knowledge. Generalizable knowledge consists of theories, principle s or relationships, or the accumulation of information on which they are based, that can be corroborated by accepted scientific methods of observation and inference.” Similarly, in the United States, research is defined as “…a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge ” (U.S. Department of Health and Human Services 2009).
In jurisdictions with legal requirements governing research activities, such as the United States, determining what is and is not research becomes critical. Sometimes, however, the line between research and practice-related activities is blurry. One way to identify if an activity is research is to look at intent. The primary intent of public health research is to yield generalizable knowledge. Key characteristics of public health research include (1) benefits beyond the needs of the study participants, (2) collection of data exceeding what is needed to care for study participants, and (3) generation of knowledge with relevance outside the population from which data were collected. In contrast, the primary intent of activities that constitute public health practice are to “… prevent or control disease or injury and improve health, or to improve a public health program or service …” (Centers for Disease Control and Prevention [CDC] 1999, 2010). Key characteristics of public health practice include (1) benefits that focus on activity participants, (2) collection of data needed to improve the activity or the health of the participants, and (3) generation of knowledge that does not go beyond the scope of the activity (CDC 1999, 2010).
Some researchers suggest that the difficulty in distinguishing public health research from public health practice emerges from a deeper conceptual issue relating to the impossibility of satisfactorily defining “research” and related categories (Fairchild and Bayer 2004). For example, public health surveillance might involve identical interventions and risks for public health research as for practice. This has led many public health professional s to call for reorienting ethical review around an activity’s level of risk, which applies to activities in both public health research and practice (Willison et al. 2014). Jurisdictions that do not yet have legal structures or have more flexibility to govern research activities than the United States might have an advantage. Whereas other jurisdictions might need to modify their approach to correlate ethical review with risk instead of on whether something falls under a slippery concept such as research.
3 Ethical Considerations for Protecting the Public during Health Research
This section outlines core aspects of research ethics and not only explains their relevance to public health, but also delves into why research ethics principles might need to be applied differently to public health research than to biomedical research .
3.1 Informed Consent
Informed consent is often treated as the primary means of protecting research participants. Although informed consent can be defined in different ways, it is foremost an active agreement made by someone with the capacity to understand, on the basis of relevant information , and in the absence of pressure or coercion. The common ethical justification for seeking informed consent is an appeal to the notion of autonomy , which holds that individuals have values and preferences and thus should voluntarily decide whether to participate in research. However, gaining consent can result from a more direct appeal to beneficence or to general welfare. Many research ethics guideline s and regulations require an interactive process between the investigator and research participant to best provide information and ensure comprehens ion.
Some potential research participants will always lack capacity to look after their own interests (e.g., children , people with dementia, the unconscious) and thus cannot provide consent. To protect people with diminished autonomy , informed consent is usually obtained from a parent , guardian, or legal representative. While it is clear that research participants with diminished capacity need extra protection, empirical evidence shows that even research participants with full cognitive capacity may not understand information presented as part of the consent process (Dawson 2009). For this reason, informed consent cannot be the only mechanism for protecting research participants. For instance, a research ethics committee can protect participants by assessing risks and benefits. Requiring approval by a research ethics com mittee might be considered a paternalistic judgment, but not an obviously wrong one (Garrard and Dawson 2005; Miller and Wertheimer 2007). Research ethics committees routinely consider waiving informed consent. This is true in public health research where the risk can be less than in biomedical research . Reliance on the judgments of research ethics committees presupposes that members have a high level of profession al trustworthiness and have the skills for ethical deliberation and analysis.
Cultural or social influences can challenge the ideal model of informed consent when conducting public health research. Marshall (2007) provides an excellent overview of challenges with obtaining informed consent, especially in resource-poor settings. These challenges include cultural and social factors that affect comprehension, communication of risks, and decisional authority for consent to do research. Language barriers and low literacy, mistaken beliefs about the benefits of participation , especially when access to health care is limited, and the need to communicate complex scientific information may reduce comprehension of study procedures, benefits, and risks. Marshall (2007) emphasizes the importance of engaging community leaders and soliciting and considering the opinions of community residents when identifying project goals and procedures and establishing consent processes. She notes that in many communities, relying solely on individual consent may not be culturally appropriate. In these situations, adding family or community consent is fitting.
Some research cannot be conducted if the standards of autonomous informed consent are always applied. A good example is emergency research when unconscious victims of head trauma may be randomized to different promising treatments, but the relative effectiveness of each treatment option is unknown. Some countries allow such research via waivers of informed consent if relevant conditions are met (e.g., minimal risk , and the research could not otherwise be carried out) (U.S. Department of Health and Human Services 2009). A public health research method for which it sometimes may be appropriate not to seek informed consent is the cluster randomized trial . By design, a cluster randomized trial compares interventions that target a group (i.e., social entity such as village or town, or a population). Various characteristics of these clusters are matched to ensure a robust comparison of interventions (including no intervention). In some cluster trials, obtaining individual informed consent can seem prohibitively expensive, damaging to a chieving study goals, or even impossible to attain (Sim and Dawson 2012; McRae et al. 2011b). Where consent is impossible to attain, is it right to require it at the expense of not doing the research? Attempts have been made to justify research without first attaining individual consent by appealing to an ethics committee for review, soliciting viewpoints from the community about whether the research is acceptable, or even seeking some form of community consent.
Dickert and Sugarman (2005) make a distinction between community consent and community consultation. Consent means seeking approval , whereas consultation means seeking ideas and opinions . They note, however, that this distinction gets blurred in practice, and that community consultation should not be approached as a box to check off without scrutinizing the input. They identify four ethical goals for any community consultation: enhanced protection, enhanced benefits, legitimacy, and shared responsibility. Adherence to these goals may ensure that risks are identified and protections put into place; that the research benefits not only the researchers, but also the participants and communities being studied; and that the legitimacy of the findings is increased. However, this does not constitute a direct parallel to the individual model of informed consent described previously. Community consent involves meeting with legitimate community representatives empowered to permit researchers to conduct studies involving community members (Weijer and Emanuel 2000; Dickert and Sugarman 2005). The involvement of community representatives in public health research is most clearly seen in community-based participatory research (CBPR) . In CBPR, authorities are involved at all levels of research—from initiation of ideas and projects through data collection, analysis and interpretation, and use of research findings to prompt community change (Flicker et al. 2007).
3.2 Risk/Benefit Analysis
A central concern for research ethics is the weighing of expected benefits against possible harms. The commonly employed criteria for assessing risk to human subjects who participate in health research are that risks are minimized and reasonable in relation to the anticipated benefits. For example, one can argue that procedures used in research are justifiable when already being used for diagnosis or treatment and the risks are proportional to the importance of the knowledge reasonably expected to result from the research. However, one problem in such a determination is the uncertainty of all judgments about risks and benefits. Such determinations have to be made carefully and fairly and on the basis of the best possible evidence.
Research participants may encounter several types of risks. One obvious risk is physical harm, which may include discomfort, pain, or injury from interventions such as drug regimens or medical procedures. Another risk is psychological harm. Research participants may experience stress, anxiety , embarrassment, depression, or other negative emotions. These emotions, which can occur during or after participation in the research, are common in research involving sensitive topics such as sexual preferences or behavior. Social and economic harms are another type of risk. Participants in research that focuses on mental illness, illegal activities, and even certain diseases such as HIV may risk being labeled or stigmatized if precautions are not taken to provide adequate privacy and confidentially. A person’s economic status may be affected if cost s are incurred for participating (e.g., transportation expenses to and from the study site) or by loss of employment (present or future) if a breach of confidentiality occurs (e.g., an employer discovers an employee is being treated for substance abuse ).
One common problem—about which ethics guidelines are typically silent—is how we should conceptualize study participants (McRae et al. 2011a). Consider, for example, that cluster randomized designs and cohort studies commonly compare a group receiving active intervention with a parallel group receiving no intervention. Does the term “participant” apply to those receiving no intervention? This question has far-reaching consequences. If people who do not receive intervention count as participants, researchers may have obligations to them that otherwise would not exist. Another way to think about this is to identify who might be at increased risk, rather than who is a participant. For example, the U.S. National Bioethics Advisory Commission (NBAC) recommends that whenever researchers anticipate that risks will extend beyond study participants, researchers should try to minimize risks to nonpartic ipants (NBAC 2001).
The benefits of health research are any favorable or positive outcome received as a direct result of the research. Put simply, without the research, the outcome would not exist. Sometimes the benefits of health research extend beyond study participants to society; other times, however, research participants do not benefit. And in other instances, only a few participants might benefit. Researchers should thoroughly consider what to do in all these scenarios and how benefits could be provided to those in need. Sometimes research involves reimbursement, incentives, or other tangible goods. Although such items may be provided when someone agrees to participate in research, these items should not be considered benefits arising from the research procedures. In some contexts, such as prisons, offering anything in return for participation in research may be viewed as pressure to participate and therefore should be carefully considered.
The risks of research must be reasonable when compared to the anticipated benefits. This can be difficult to assess because risks will vary depending on the study population . For example, research procedures considered safe for healthy adults may be risky for adults with compromised health or for vulnerable populations such as children , pregnant woman, or seniors. Even if the potential benefits are the same, if the risks differ, the risk/benefit balance is affected. Another consideration for evaluating risks and benefits is the expected result of the research. A higher level of risk may be acceptable if the research can reasonably be expected to benefit the participants. If there is no expectation that the research participants will benefit, the same level of risk may be unacceptable.
Foreseeing the benefits and harms in a study can be challenging. Striking a balance between the two can be difficult and, at times, controversial. A good example of this is the discussion generated by a series of studies conducted in Baltimore that assessed different methods for reducing the exposure of children to lead paint in older rented properties (Mastroianni and Kahn 2002). In this case, the fact was already known that exposure of children to lead is dangerous. However, due to the high cost of removing lead-based paint (the known, best solution), the researchers assessed the effectiveness of cheaper, partial methods of abatement for reducing or even removing the risk of exposure. If found to be effective, these alternative methods would allow treatment of more homes at the same cost, potentially benefiting more children. Monitoring during the study found that some children in the alternative abatement options had elevated blood lead levels. Some health officials believe that the research should not have gone ahead because of this likelihood. Others think that the research was justified because the children were not exposed to any greater level of lead, and in most cases, significantly less than if the research had not been conducted. In other words, no child was put at greater risk through participation , and all children be nefited from blood monitoring. This study demonstrates the complexities of evaluating risks and benefits in public health research.
3.3 Protection of Vulnerable Populations
Altho ugh all segments of society should have the opportunity to participate in research, vulnerable populations may need additional protections to prevent coercion or exploitation. The definition of what it is to be vulnerable is contested (Chap. 7 ). However, NBAC (2001) defines vulnerability in the context of research as a condition, either intrinsic (e.g., mental illness) or situational (e.g., incarceration ), that increases some participants’ risk of being harmed. Regardless of how we define vulnerability, it is often interpreted to require special protections for the safety and well-being of population s such as children, prisoners, pregnant women, mentally disabled people, and economically or educationally disadvantaged people. The CIOMS (2002) international guideline s suggest that special justification is required for inviting vulnerable people to serve as research subjects and, if they are selected, the means of protecting their rights and welfare must be strictly applied. The history of research is replete with examples of unethical treatment of vulnerable populations (Chap. 2 ).
Despite such worries about protecting vulnerable populations, a strong To exclude vulnerable populations violates the spirit of the principle of justice , which requires fair distribution of risks and benefits of research. Inclusion of vulnerable populations may require accommodations to address the specific nature of the vulnerability; however, once these accommodations are in place, vulnerable people with the cognitive capacity to provide informed consent should exercise autonomous choice about their participation . For example, it seems arbitrary to exclude pregnant women from research as a matter of course rather than making a decision based on an assessment of risk levels, the ability to control risks , and the likelihood of direct benefit to the participant .
3.4 Returning Research Results
Public health research tends to focus on population-level research questions. In some cases, for example where data have been anonymized, even when an issue relevant to the clinical care of one or more individuals in the data set is discovered, there is nothing that can be done about it. However, in other cases, public health data sets or surveillance data might hold information that could be crucial to the care of individuals.
When and how should individual-level data, including incidental and secondary findings , be communicated to research participants? The primary argument for an ethical imperative to offer participants research findings, both summary and individual results, rests on the principle of respect for persons ; however, the principles of beneficence and justice are also frequently cited (Presidential Commission for the Study of Bioethical Issues 2013; Miller et al. 2008; Fernandez et al. 2003). The word “offer” is important because giving people the right to decline results is also an expression of respect for persons. The ethical justification for a “duty to disclose research results,” especially individual-level data, has been challenged due to the potential harms of disclosure (Miller et al. 2008). Miller and colleagues argue that the lack of consistent policy guidance for disclosures and the ambiguity about what to disclose undermines any generalized ethical duty to disclose. Clearly, before making a decision to return results, especially individual-level data, the potential benefits and harms from disclosure must be carefully assessed.
The research consent process should describe plans for returning results or provide an option for not receiving results. The consent process should explain the potential harms and benefits associated with receiving research results, the possible strengths and limitations of the results, and the options for follow-up and support if unanticipated consequences occur. If a decision is made to return results, careful considerations must be given to how the results will be returned (e.g., in person, over the telephone, through a letter), whether opt-in or opt-out procedures will be used, and when the results should be returned. Fernandez and colleagues (2003) argue that “research results should, in general, be delayed until the results are published or until they have undergone peer review and been accepted for publication.” This recommendation is based on the need to ensure the integrity of the interpretation of the data and to prevent disclosure of inaccurate information .
To illustrate the diversity of opinion about sharing research data, some researchers have taken the obligation for disclosure further by advocating that research participants be granted access to their raw data via a data repository before these data are analyzed (Lunshof et al. 2014). Lunshof and colleagues suggest that access to raw personal data would increase transparency, personal choice, and reciprocity. Further, such access could equalize the relationship between those who donate data and those who use data for research. However, this rather utopian view raises issues with potential breaches of confidentiality, so more discussion is needed. More discussion is also needed about participants increasingly sharing information about research studies through social media, which can result in breaches of confidentiality and further challenge the integrity of research (Lipset 2014).
3.5 Conflicts of Interest
The potential for conflicts of interest occurs when an individual or group has multiple interests, one of which can compromise the integrity or impartiality of the other. Research involving human subjects often creates this potential when researchers are also involved with participants in the role of health care providers or through engagement with communities in the context of public health research. In resource-poor contexts, the economic impact of the research enterprise can be of such magnitude that it has sociopolitical ramifications o r complexities with potential to spur conflicts of interest. Discussion about conflicts of interest raises issues about integrity in public health and even the very concept of public health as an activity (Coughlin et al. 2012).
Shrinking budgets for public health activities have led many health departments, even those in resource-rich countries, to explore alternative approaches to financing public health research, leading to questions about what constitutes an appropriate partnership and to concerns about real or perceived conflicts of interest. For example, should government s collaborate with vaccine manufacturers to research potential adverse effects of a vaccine? Should researchers collaborate with soda manufactures to study the association between sugar-sweetened beverages and obesity? The U.S. Institute of Medicine (IOM) Committee on Conflicts of Interest in Medical Research, Education, and Practice defines conflict of interest as “a relationship that may place primary interests (e.g., public well-being or research integrity) at risk of being improperly influenced by the secondary, personal interests of the relationship (e.g., financial, professional, or intellectual gains)” (IOM 2009). When Bes-Rastrollo and colleagues (2013) studied systematic reviews of the association between sugar-sweetened beverages and weight gain, they found instances where conflicts of interest influenced scientific findings. The systematic reviews that identified sponsorship or conflicts of interest with food or beverage companies were five times more likely to report “no positive association” between consumption of sugar-sweetened beverages and weight gain or obesity than the reviews that reported having no industry sponsorship or conflicts of interest. These findings point to the need for guidance on how to identify and avoid conflicts of interest with potential to influence outcomes of public health research, especially when the research shapes public policy (IOM 2014).
3.6 Conducting Research during Public Health Emergencies
Sometimes the t raditional elements of research ethics are inappropriate frameworks for decision making. Let’s consider, for example, a decision being contemplated to conduct research during a public health emergency. The research is deemed vitally important to analyze what happened during the emergency, to plan for future scenarios, and to prevent death and illness during disasters. However, such research raises concerns, including the appearance that health officials are more interested in expanding knowledge than in responding to the disaster and that researchers are insensitive to more urgent needs of affected individuals. Still, the case can be made for a strong, ethical imperative that obligates public health officials to conduct research that could yield data useful in preventing future death and illness during disasters (London 2016). The chief ethical task for conducting research during a disaster is to secure future benefits for people without sacrificing the rights or interests of research subjects (Jennings and Arras 2008; WHO 2015). So to justify research during a disaster, public health officials must first demonstrate a real need for the research, which includes its social and scientific value (anticipated results). Generally speaking, research that can be conducted in a nonemergency setting should not be conducted during an emergency response .
If the decision is made to conduct research during a public health emergency, some unique ethical concerns must be considered: the research should not detract resources and personnel from emergency response activities; research activities should be prioritized by highest social and scientific value; and, as people in an emergency are often affected physically and psychologically, and sometimes traumatized, they should be considered a vulnerable population (Jennings and Arras 2008; WHO 2015). At the very least during an emergency, keep in mind that some people may not be able to make reasoned, informed decisions to participate in the research. Consequently, adequate means of protection for participants must be in place. The procedures for an ethics committee review may need to be modified for disaster research projects (Lurie et al. 2013). Possible approaches for ensuring appropriate review include developing just-in-case protocols and establishing centralized or specialized ethics review committees that can approve disaster research protocols quickly (Médecins Sans Frontières 2013).
4 How Ethical Challenges Can Arise in Public Health Research: Lessons Learned from Cases
The cases presented in this chapter illustrate some of the ethical challenges raised by public health research. These challenges range from compliance with research ethics guideline s to the need to address the economic and political implications from the wider societal context in which public health research occurs. Social, economic, and political factors can directly lead to ethical challenges or may affect a researcher’s ability to comply with ethical guidelines.
The case by Boulanger and Hunt illustrates how well-intentioned international efforts to improve access to health care in resource-poor countries can have unintended consequences that present ethical complications. The case raises various interconnected issues that have to do with researchers’ responsibilities and obligations and with conflicts between individual and public goods. Within a collaborative international public health research project, such conflicts can easily arise when local investigators find themselves serving multiple roles that create potential conflicts of interest . Boulanger and Hunt provide an excellent summary of the responsibilitie s and obligations of researchers, including to
Protect participants from harm and ensure they benefit from the research whenever possible;
Support and protect research staff, especially students ;
Support and respect research collaborators, building local capacity when possible; and
Support the research enterprise, which includes building public trust , maximizing the relevance and usefulness of the research, and disseminating findings.
Central to this case is a local researcher’s uncovering of how informal fees for obstetric care are being diverted to senior hospital administrators. The local researcher has a dilemma . If he reveals this ethically dubious informal fee structure, he will not only jeopardize his standing at the hospital, but he could also undermine the availability of obstetric care to women in his community. The director of the research program must ethically weigh the research goal of improving access to health care services with supporting the interests of the research staff while also maintaining good relations with local health agencies. In many contexts, this case would be a clear-cut whistleblower issue demanding revelation. However, where informal fees are standard practice, part of the political culture, or the health infrastructure is already fragile or minimal, the issue becomes complicated, forcing one to prioritize competing values and moral considerations.
The case by Makhoul and colleagues involves research on mental health concerns among youth in a Palestinian refugee camp . The case highlights cultural and social factors that may influence the consent process, especially the power dynamics within communities. Beyond addressing central bioethical and medical principles of trust and respect for persons , the case points to the need for considering broad public health concepts such as respect for community values, empowerment , and advocacy . This case also illustrates how researchers are almost always drawn into a community’s political dynamics by the economic influence of research in resource-poor settings. Efforts by community members to avoid alienating groups that contribute resources to the community may act as a subtle form of pressure to participate in the research.
The case by Kasule and colleagues illustrates the difficult practical choices that resource-poor countries face in processing the increasingly complex volume of research to be ethically reviewed. In these countries, public health officials struggle to complete basic administrative and regulatory aspects of research review and oversight, let alone provide conditions for careful, conscientious ethical analysis. This scenario questions the adequacy of training for members of ethics review committees . Failure to adequately train committee members and fund research oversight will result in lost opportunities and revenues, setting back a resource-poor country’s research or health infrastructure for years. But funding an organization to develop research oversight may divert funds from other more urgent public health needs. Trading short-term public health solutions for long-term research funding presents a classic case of resource allocation and prioritization. Kasule and colleagues consider the pros and cons of reliance upon outside ethics review committees, which might save money at the expense of having less control of oversight.
The case by Kanekar describes the use of an Internet-delivered safe sex health promotion intervention for young black men who have sex w ith men. This case raises a number of practical and ethical considerations and questions that arise in public health research. How does one differentiate research from public health practice? What approaches are required to serve vulnerable populations ? How can one use innovative techniques to target hard-to-reach populations? What are the best ways to protect the privacy of participants and ensure confidentiality of data? How can one reconcile or accommodate conflict among research partners who perceive their primary role or function in radically different ways (e.g., medical provider versus epidemiologist)?
5 Conclusions
Many ethical issues can arise in public health research. The social, economic, and political context within which the research enterprise functions further complicates the ethical landscape. Traditional approaches for considering research ethics issues emerged from biomedical research and initially emphasized ethical considerations at an individual level. However, research in public health demonstrates why this traditional approach to ethics should be expanded. A public health approach to research ethics is apt because it considers community values, the interdependence of citizens, social or population benefit , and social justice . However, as explained in Chap. 1, there is more to ensuring ethical conduct and scientific integrity in public health research than having an ethical review committee apply rule-based guidelines . Researchers need to be familiar with the ethical considerations unique to public health and have sufficient training and experience to exercise moral judgment in all phases of research.
Beauchamp, T.L., and J.F. Childress. 1979. Principles of biomedical ethics . New York: Oxford University Press.
Bes-Rastrollo, M., M.B. Schulze, M. Ruiz-Canela, and M.A. Martinez-Gonzalez. 2013. Financial conflicts of interest and reporting bias regarding the association between sugar-sweetened beverages and weight gain: A systematic review of systematic reviews. PLoS Medicine 10(12): e1001578. doi: 10.1371/journal.pmed.1001578 .
Centers for Disease Control and Prevention (CDC). 1996. Inclusion of women and racial and ethnic minorities in research. http://www.cdc.gov/maso/Policy/Inclusion%20of%20Women%20and%20Racial%20and%20Ethnic%20Minorities%20in%20Research10-18-2007.pdf . Accessed 24 Sept 2014.
Centers for Disease Control and Prevention. 1999. Guidelines for defining public health research and public health non-research . http://www.cdc.gov/od/science/integrity/docs/defining-public-health-research-non-research-1999.pdf . Accessed 24 Sept 2014.
Centers for Disease Control and Prevention. 2010. Distinguishing public health research and public health nonresearch . http://www.cdc.gov/od/science/integrity/docs/cdc-policy-distinguishing-public-health-research-nonresearch.pdf . Accessed 24 Sept 2014.
Coughlin, S.S., A. Barker, and A. Dawson. 2012. Ethics and scientific integrity in public health, epidemiological and clinical research. Public Health Reviews 34(1): 1–13. http://www.publichealthreviews.eu/upload/pdf_files/11/00_Coughlin.pdf . Accessed 24 Sept 2014.
Council for International Organizations of Medical Sciences (CIOMS). 2002. International ethical guidelines for biomedical research involving human subjects . Geneva: CIOMS. http://www.cioms.ch/publications/layout_guide2002.pdf . Accessed 24 Sept 2014.
Council for International Organizations of Medical Sciences. 2009. International ethical guidelines for epidemiological studies . Geneva: CIOMS. http://www.ufrgs.br/bioetica/cioms2008.pdf . Accessed 24 Sept 2014.
Dawson, A. 2009. The normative status of the requirement to gain an informed consent in clinical trials: Comprehension, obligations, and empirical evidence. In The limits of consent: A socio-ethical approach to human subject research in medicine , eds. O. Corrigan, J. McMillan, K. Liddell, M. Richards, and C. Weijer, 99–114. Oxford: Oxford University Press.
Dickert, N., and J. Sugarman. 2005. Ethical goals of community consultation in research. American Journal of Public Health 95(7): 1123–1127.
Fairchild, A.L., and R. Bayer. 2004. Ethics and the conduct of public health surveillance. Science 303(5658): 631–632.
Ferdandez, C.V., E. Kodish, and C. Weijer. 2003. Informing study participants of research results: An ethical imperative. IRB: Ethics & Human Research 25(3): 12–19.
Flicker, S., R. Travers, A. Guta, S. McDonald, and A. Meagher. 2007. Ethical dilemmas in community-based participatory research: Recommendations for institutional review boards. Journal of Urban Health: Bulletin of the New York Academy of Medicine 84(4): 478–493.
Garrard, E., and A. Dawson. 2005. What is the role of the research ethics committee? Paternalism, inducements, and harm in research ethics. Journal of Medical Ethics 31(17): 419–423.
Institute of Medicine (IOM). 2009. Conflicts of interest in medical research, education, and practice . http://www.iom.edu/Reports/2009/Conflict-of-Interest-in-Medical-Research-Education-and-Practice.aspx . Accessed 24 Sept 2014.
Institute of Medicine. 2014. Conflict of interest and medical innovation: Ensuring integrity while facilitating innovation in medical research: Workshop summary . Washington, DC: The National Academies Press.
Jennings, B., and J. Arras. 2008. Ethical guidance for public health emergency preparedness and response: Highlighting ethics and values in a vital public health service . http://www.cdc.gov/od/science/integrity/phethics/docs/White_Paper_Final_for_Website_2012_4_6_12_final_for_web_508_compliant.pdf . Accessed 24 Sept 2014.
Lipset, C.H. 2014. Engage with research participants about social media. Nature Medicine 20(3): 231. doi: 10.1038/nm0314-231 .
London, A.J. 2016. Research in a public health crisis: The integrative approach to managing the moral tensions. In Emergency ethics: Public health preparedness and response, eds. B. Jennings, J.D. Arras, D.H. Barrett, and B.A. Ellis, 220–261. New York: Oxford University Press.
Lunshof, J.E., G.M. Church, and B. Prainsack. 2014. Raw personal data: Providing access. Science 343(6169): 373–374. doi: 10.1126/science.1249382 .
Lurie, N., T. Manolio, A.P. Patterson, F. Collins, and T. Frieden. 2013. Research as a part of public health emergency response. New England Journal of Medicine 368(13): 1251–1255. doi: 10.1056/NEJMsb1209510 .
Marshall, P.A. 2007. Ethical challenges in study design and informed consent for health research in resource-poor settings. In Special topics in social, economic and behavioral (SEB) research, Report number 5 . Geneva: World Health Organization.
Mastroianni, A.C., and J.P. Kahn. 2002. Risk and responsibility: Ethics, Grimes v Kennedy Krieger, and public health research involving children. American Journal of Public Health 92(7): 1073–1076.
McRae, A.D., C. Weijer, A. Binik, J.M. Grimshaw, et al. 2011a. When is informed consent required in cluster randomized trials in health research? Trials 12: 202. doi: 10.1186/1745-6215-12-202 .
McRae, A.D., C. Weijer, A. Binik, A. White, et al. 2011b. Who is the research subject in cluster randomized trials in health research? Trials 12: 183. doi: 10.1186/1745-6215-12-183 .
Médecins Sans Frontières. 2013. Research ethics framework: Guidance document . Brussels: Médecins Sans Frontières. http://fieldresearch.msf.org/msf/bitstream/10144/305288/5/MSF%20Research%20Ethics%20Framework_Guidance%20document%20(Dec2013).pdf . Accessed 24 Sept 2014.
Miller, F.G., and A. Wertheimer. 2007. Facing up to paternalism in research ethics. Hastings Center Report 37(3): 24–34.
Miller, F.A., R. Christensen, M. Giacomini, and J.S. Robert. 2008. Duty to disclose what? Querying the putative obligation to return research results to participants. Journal of Medical Ethics 34(3): 210–213. doi: 10.1136/jme.2006.020289 .
National Bioethics Advisory Commission (NBAC). 2001. Ethical and policy issues in research involving human participants . Bethesda: NBAC. https://bioethicsarchive.georgetown.edu/nbac/human/overvol1.pdf .
Nuremberg Code . 1947. Trials of war criminals before the Nuremberg Military Tribunals under Control Council Law No. 10, Vol. 2, pp. 181–182. Washington, DC: U.S. Government Printing Office, 1949. http://www.hhs.gov/ohrp/archive/nurcode.html . Accessed 24 Sept 2014.
Presidential Commission for the Study of Bioethical Issues. 2013. Anticipate and communicate: Ethical management of incidental and secondary findings in the clinical, research, and direct-to-consumer contexts . Washington, DC: Department of Health and Human Service.
Public Health Functions Steering Committee. 1994. Essential public health services . http://www.health.gov/phfunctions/public.htm . Accessed 24 Sept 2014.
Public Health Leadership Society. 2002. Principles of the ethical practice of public health . http://phls.org/CMSuploads/Principles-of-the-Ethical-Practice-of-PH-Version-2.2-68496.pdf . Accessed 1 Feb 2013.
Sim, J., and A. Dawson. 2012. Informed consent and cluster-randomized trials. American Journal of Public Health 102(3): 480–485. doi: 10.2105/AJPH.2011.300389 .
U.S. Department of Health and Human Services. 2009. Code of Federal Regulations, Title 45, Part 46, Protection of Human Subjects. http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.html . Accessed 24 Sept 2014.
U.S. National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. 1979. The Belmont report: Ethical principles and guidelines for the protection of human subjects of research , Publication No. (OS) 78-0012. Washington, DC: U.S. Government Printing Office.
United Nations. 1948. Universal declaration of human rights . http://www.un.org/en/documents/udhr/ . Accessed 24 Sept 2014.
Verweij, M., and A. Dawson. 2009. Public health research ethics: A research agenda. Public Health Ethics 2(1): 1–6. doi: 10.1093/phe/php008 .
Weijer, C., and E.J. Emanuel. 2000. Protecting communities in biomedical research. Science 289(5482): 1142–1144. doi: 10.1126/science.289.5482.1142 .
Willison, D., N. Ondrusek, A. Dawson, et al. 2014. What makes public health studies ethical? Dissolving the boundary between research and practice. BMC Medical Ethics 15: 61. doi: 10.1186/1472-6939-15-61 .
World Medical Association. 1964/2013. Declaration of Helsinki—Ethical principles for medical research involving human subjects . http://www.wma.net/en/30publications/10policies/b3/ . Accessed 24 Sept 2014.
World Health Organization (WHO). 2015. Ethics in epidemics, emergencies and disasters: Research, surveillance and patient care. Training manual . Geneva: WHO.
6 Case 1: To Reveal or Not to Reveal Potentially Harmful Findings: A Dilemma for Public Health Research
- Renaud F. Boulanger BA &
- Matthew R. Hunt PT, PhD
Biomedical Ethics Unit, McGill University, Montréal, QC, Canada
Renaud F. Boulanger BA
School of Physical and Occupational Therapy, McGill University, Montréal, QC, Canada
Matthew R. Hunt PT, PhD
Centre for Interdisciplinary Research on Rehabilitation, Montréal, QC, Canada
This case is presented for instructional purposes only. The ideas and opinions expressed are the authors ’ own. The case is not meant to reflect the official position , views , or policies of the editors , the editors ’ host institutions , or the authors ’ host institutions .
6.1 Background
In 1987, African health ministers met in Mali to address access to quality primary health care, particularly in rural areas (Anonymous 1988). The resulting Bamako Initiative promoted universal accessibility, though it drew some early criticism for its support of user fees (McPake et al. 1993). For the next decade, user fees were implemented in many African countries to finance health care services. The World Bank supported the measure as part of its Structural Adjustments Programs, which also included austerity measures, trade liberalization, and privatization (McIntyre et al. 2006). However, user fees have since been shown to create access barriers that tend to affect the poor disproportionately (Macha et al. 2012), suggestin g that many vulnerable individuals have been prevented from accessing needed health care services. Against this backdrop, mounting international pressure led to the reform of many user-fees programs, particularly in the last decade. One primary strategy for increasing health care access has been the introduction of selective exemptions of user fees for specific groups (Ben Ameur et al. 2012; Meessen et al. 2011; Ridde et al. 2012). Although this strategy was originally planned in the Bamako Initiative , it was not uniformly implemented. Given the scale of the changes that user fees removal implies for health care systems, there is ongoing research to evaluate their impact (Lagarde and Palmer 2011). Health system investigations such as these may raise ethical questions (Hyder et al. 2014), especially since they involve the study of a public health intervention , often focus on individuals in extreme poverty, and tend to be international and collaborative in nature.
Collaborative international public health research offers the opportunity to build local capacity (Mayhew et al. 2008). However, such research raises a number of issues about researchers’ obligations and responsibilities . First is the responsibility to protect research participants from harm, an obligation recognized by all research ethics guidelines. This duty of protection is heightened when the research participants are from vulnerable populations (Hurst 2008), especially when they are recruited from extremely impoverished populations. Researchers’ responsibilities toward research participants also include ensuring that they benefit from the results of the research whenever possible. For example, the International Ethical Guidelines for Biomedical Research Involving Human Subjects directs that “any intervention or product developed, or knowledge generated, will be made reasonably available for the benefit of that population or community” (Council for International Organizations of Medical Sciences 2002, guideline 10). A second researcher responsibility is to support students and staff hired as part of the research project and to protect them from harm (Wilson 1992). This responsibility can be thought of both as the duty of an employer and the fiduciary duty of an academic supervisor and must extend to situations of whistleblowing. Third, researchers involved in collaborative research have a responsibility to colleagues and collaborators, especially given that research may play a crucial role in capacity building (Garcia and Curioso 2008). Although partnerships with local researchers have been touted as highly valuable (Costello and Zumla 2000), these ties may also result in unexpected ethical dilemmas for local researchers if conflicts arise between their research activities and their established local obligations and responsibilities (Richman et al. 2012). A fourth responsibility of researchers is dedication to the research enterprise. The conduct of public health research can have significant implications for the well-being of large segments of the population, but it requires the trust of the public and of relevant authorities. Endangering the relationship of trust in the context of one specific public health study may jeopardize or ruin other research initiatives (Corbie-Smith et al. 1999). Finally, a fifth responsibility of publicly funded researchers is their duty to the public in whose name they conduct research. Good stewardship requires that researchers strive to maximize the relevance and usefulness of their efforts and that they disseminate their findings (Arzberger et al. 2004). Researchers conducting collaborative international public health research may encounter ethically challenging conflicts among these five lines of responsibilit ies.
6.2 Case Description
Dr. Milena A. is the principal investigator of a large research program that is examining approaches for decreasing inequities in access to health care services in a low-resource setting. She works for an American university, and her research is funded by a U.S. agency. One member of her research team, Dr. Timothy N., is a local physician studying toward a public health degree at Milena’s institution. He is back in his country after finishing his coursework and is ready to conduct fieldwork research. Timothy has taken leave from his position at a local hospital to pursue his studies and, although he wants to continue his clinical work at the hospital, he also wants to expand his focus to include population-level health issues and, eventually, work with his country’s ministry of health. His studies are co-funded by Milena’s research grant and by the ministry of health.
Timothy’s research consists of an examination of the impact of his country’s recent abolishment of health care user fees for children younger than 5 years. User fees had been implemented uniformly in the 1990s without special consideration for poorer families with young children. Initial indicators suggest that health care services continue to be underused in some districts, especially by poor children, despite the recent removal of user fees. Despite the limited uptake, the ministry of health touts the polic y abolishing user fees for children younger than 5 years as an important success. Timothy is conducting his study at several urban health centers, including the hospital from which he is currently on leave. The research project has received ethics approval from Milena’s institution and from the relevant local review boards.
Recently, Timothy r equested a meeting with Milena saying that he needed advice. He reports that he has identified a system of informal fees that undermines the ministry of health’s official policy by making health care once again too expensive for many families with young children. From what Timothy understands, the fees are levied primarily to fund better obstetric care locally, but some indicators point toward senior administrators keeping a small share for themselves. Timothy worries that making his findings public is too risky for him, especially since his involvement in this fieldwork is well-known. He does not think it possible to share his findings without identifying himself as the source of the information . His hospital is one of the sites where he has identified the system of informal payments. He also has good reasons to believe that some members of the ministry of health are already aware of the situation but have not taken action to address it. Disseminating his results will jeopardize his employment at the hospital, his relationships with government officials, and, potentially, the plans to improve obstetric care.
Milena is also conflicted. She recognizes that she has multiple roles, responsibilities, and interests, and that individual and communal goods are at stake. Identifying and seeking to address informal payment structures could improve accessibility of health care services for children, which is the primary goal of her research program. However, the team has responsibilities to Timothy as their student and colleague. Demanding that he upend his career, either for their benefit or for the improvement of health care accessibility , might fail to respect him as an individual. In addition, bringing the situation to light could embarrass the ministry of health. Because the research program depends on the ministry of health’s authorization, tensions in relationships could lead to premature termination of the research. Such an event would have unpredictable outcomes on the careers of everyone on the research team and on the future of health care acces sibility locally.
6.3 Discussion Questions
How should Milena and Timothy prioritize their responsibilities, and what should they ultimately do?
What preemptive actions could the research team have taken to limit the likelihood that the situation described above would happen?
How should the fact that, aside from Timothy, the research team members are not citizens in the country where they are conducting research be considered in the assessment of their obligations?
Is this a case where developing partnerships with local researchers might be counterproductive? Or, could a more robust partnership with local researchers have positioned the team to better address this issue?
How would the ethical analysis differ if, instead of identifying unequal access due to informal fees, Timothy had observed that those exempted from the fees were being offered a lower standard of care than patients whose fees were not waived?
Anonymous. 1988. The Bamako initiative. Lancet 2(8621): 1177–1178.
Arzberger, P., P. Schroeder, A. Beaulieu, et al. 2004. Promoting access to public research data for scientific, economic, and social development. Data Science Journal 3: 135–152.
Ben Ameur, A., V. Ridde, A.R. Bado, M.G. Ingabire, and L. Queuille. 2012. User fee exemptions and excessive household spending for normal delivery in Burkina Faso: The need for careful implementation. BMC Health Services Research 12: 412. doi: 10.1186/1472-6963-12-412 .
Corbie-Smith, G., S.B. Thomas, M.V. Williams, and S. Moody-Ayers. 1999. Attitudes and beliefs of African Americans toward participation in medical research. Journal of General Internal Medicine 14(9): 537–546.
Costello, A., and A. Zumla. 2000. Moving to research partnerships in developing countries. British Medical Journal 321(7264): 827–829.
Council for International Organizations of Medical Sciences. 2002 . International ethical guidelines for biomedical research involving human subjects . http://www.cioms.ch/publications/layout_guide2002.pdf . Accessed 27 Dec 2012.
Garcia, P.J., and W.H. Curioso. 2008. Strategies for aspiring biomedical researchers in resource limited environments. PLoS Neglected Tropical Diseases 2(8): e274. doi: 10.1371/journal.pntd.0000274 .
Hurst, S.A. 2008. Vulnerability in research and health care: Describing the elephant in the room? Bioethics 22(4): 191–202. doi: 10.1111/j.1467-8519.2008.00631.x .
Hyder, A.A., A. Rattani, C. Krubiner, A.M. Bachani, and N.T. Tran. 2014. Ethical review of health systems research in low- and middle-income countries: A conceptual exploration. American Journal of Bioethics 14(2): 28–37. doi: 10.1080/15265161.2013.868950 .
Lagarde, M., and N. Palmer. 2011. The impact of user fees on access to health services in low- and middle-income countries. Cochrane Database of Systematic Reviews 4: CD009094. doi: 10.1002/14651858.CD009094 .
Macha, J., B. Harris, B. Garshong, et al. 2012. Factors influencing the burden of health care financing and the distribution of health care benefits in Ghana, Tanzania and South Africa. Health Policy and Planning 27(suppl 1): i46–i54.
Mayhew, S.H., J. Doherty, and S. Pitayarangsarit. 2008. Developing health systems research capacities through north–south partnership: An evaluation of collaboration with South Africa and Thailand. BMC Health Research Policy and Systems 6: 8. doi: 10.1186/1478-4505-6-8 .
McIntyre, D., M. Thiede, G. Dahlgren, and M. Whitehead. 2006. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Social Science & Medicine 62(4): 858–865.
McPake, B., K. Hanson, and A. Mills. 1993. Community financing of health care in Africa: An evaluation of the Bamako initiative. Social Science & Medicine 36: 1383–1395.
Meessen, B., D. Hercot, M. Noirhomme, et al. 2011. Removing user fees in the health sector: A review of policy processes in six sub-Saharan African countries. Health Policy and Planning 26(suppl 2): ii16–ii29. doi: 10.1093/heapol/czr062 .
Richman, K.A., L.B. Alexander, and G. True. 2012. Proximity, ethical dilemmas, and community research workers. American Journal of Bioethics Primary Research 3(4): 19–29. doi: 10.1080/21507716.2012.714837 .
Ridde, V., E. Robert, and B. Meessen. 2012. A literature review of the disruptive effects of user fee exemption policies on health systems. BMC Public Health 12: 289. doi: 10.1186/1471-2458-12–289 .
Wilson, K. 1992. Thinking about the ethics of fieldwork. In Fieldwork in developing countries , ed. S. Devereux and J. Hoddinott, 179–199. New York: Harvester Wheatsheaf.
7 Case 2: Ethical Challenges in Impoverished Communities: Seeking Informed Consent in a Palestinian Refugee Camp in Lebanon
- Jihad Makhoul DrPH, MPH,
- Rima Afifi PhD, MPH &
- Rima Nakkash DrPH, MPH
Department of Health Promotion and Community Health, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon
Jihad Makhoul DrPH, MPH, Rima Afifi PhD, MPH & Rima Nakkash DrPH, MPH
7.1 Background
Begi nning in 1948, the United Nations Relief and Works Agency (UNRWA) established camps in Lebanon to house refugees from Palestine . As of 2013, 12 camps remained (UNRWA 2013). The typical UNRWA camp houses three generations of refugees, most of whom are unemployed and face economic hardships from state-imposed legal and political restrictions (Chaaban et al. 2010). Camp housing is substandard, usually lacking adequate health care and educational infrastructures. A household survey of camp residents older than 15 years found that the mean length of school attendance is 6–7.5 years, the mean yearly household income is below $3,000, and more than half the respondents consider themselves poor (Makhoul 2003; Khawaja et al. 2006).
Family structures in the camp vary, ranging from matriarchal families, extended families, and traditional patriarchal families to even modern families where parent s jointly make decisions. These family structures also include complex formations where, for example, a remarried father lives with his new wife and stepchildren. In such complex families, children often have several guardians or authority figures. Sociocultural conceptions shared by parents and social workers stress the reliance of children on parental decisions—parents know what is best for children, while children know they must obey parental decisions.
In resource-poor settings like the camps, many nongovernmental organizations (NGOs) supplement UNRWA services, thereby gaining influence. The perceived power that the local Palestinian NGOs hold in the community derives from years of providing supplemental economic and social services to residents. Not surprisingly, if an NGO is politicized, it also will hold political power. In this context, if an NGO agrees to participate in a project, residents may agree to participate without paying close attention to the details or the scope of work. They participate either because they trust the NGO to decide on their behalf or because they want to avoid being perceived as opposing an organization that provides them with needed services. Similarly, international NGOs hold perceived power by providing essential services and distributing needed supplies, especially during emergencies. Universities can acquire such power, even unintentionally, not only from the prestige and status that educational institutions generally enjoy, but also from the potential benefits that research projects bring to the camps. Intentional or not, exercising such power can raise unanticipated problems for the research enterprise.
To p rotect research participants, some national and international commissions have published guidance documents about equitable distribution of benefits and respect for autonomy , beneficence , and social justice . These documents include the Nuremberg Code (1947), the Declaration of Helsinki (World Medical Association 1964), The Belmont Report (National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research 1979), and the International Ethical Guidelines for Biomedical Research Involving Human Subjects (Council for International Organizations of Medical Science 2002). Even though these international guidelines acknowledge the need to consider culture and community, they lack adequate guidance for community-based public health research (Racher 2007; Bledsoe and Hopson 2009). In addition, these guidelines are difficult to apply in nonbiomedical research contexts in community settings. This difficulty could be attributed to applying guideline s without first considering local contexts (Dawson and Kass 2005; Benatar 2002; Chilisa 2009). Many community-oriented practitioners find the principle s too limiting to guide public health research ethics in community settings and recommend incorporating broader conceptions of respect, trust , inclusion , diversity , participation , empowerment , and advocacy (Racher 2007; Bledsoe and Hopson 2009).
Biomedical guidelines often clash with community interactions, especially in the nonindustrialized world (Bledsoe and Hopson 2009; Matsumoto and Jones 2009; Chilisa 2009). One such clash occurs between individual-oriented societies and more collectivist societies that view personhood and individual decision making through the lens of a person’s relation to society (Marshall and Baten 2003). Another clash occurs between the artificially impersonal character of research environments and the centrality of relationships and partnerships in communities. Randomized clinical trials (RCTs), for example, require control of all possible confounders, a nearly impossible standard to achieve in close-knit and dense community settings (Makhoul et al. 2013). Implementing ethical guidelines in the context of power dynamics (Marshall and Baten 2004), like the pronounced power that males wield over females in patriarchal societies , can instigate numerous clashes. In communities like refugee camps that offer few economic or career opportunities, the perceived power that NGO s and, even more so, academic institutions wield is a force that must be taken into account. In such restricted settings, the power dynamics between researchers and research subjects can take on a subtle coercive character.
These same tensions, challenges, and dynamics will emerge in any efforts to obtain informed consent to participate in research. The emergence may stem from failure to appreciate the unique complexity of local familial, cultural, and political structures, or it may represent limitations in the principles being applied.
7.2 Case Description
A community coalition, initiated by researchers from a nearby university, has been meeting for more than a year to prioritize health concerns for youth in a Palestinian refugee camp near Beirut, Lebanon . The camp is a typical UNRWA camp and includes six elementary schools. The coalition comprises camp residents including youth (17–25 years), UNRWA representatives, camp NGO workers, and members of the university research team. The coalition has decided to focus on the mental health of younger ado lescents (11–13 years) in this Palestinian refugee camp and to develop a research intervention on this issue. Cross-sectional studies and evaluation of interventions that link social and life skills to mental health outcomes strongly support the view that these skills enhance the mental health of youth; however, most of the evidence comes from industrialized settings.
The goal of the intervention is to enhance positive mental health by increasing the social and life skills of young adolescents, who will be recruited through the schools. The six elementary schools have comparable resources and student profiles. Each school has been randomly assigned either to the intervention or to the control arm of the study, and only fifth and sixth graders will participate. Participating students in the intervention group will receive 45 extracurricular sessions of 1½ h each over 9 months and gain skills in solving problems, making decisions, building self-esteem, and enhancing relationships with peers, parent s, and teachers. Parents of the students in the intervention group will receive 15 1-h group sessions, and teachers in the intervention schools will be offered six workshops addressing the same topics. Students randomized to the control group will receive 10 sessions over the course of 9 months, but their parents will not participate in the program. However, because teachers often work in more than one camp school, some teachers at the control schools may participate in the intervention workshops. All participants in either the intervention or control condition must complete pre- and post-assessment questionnaires that measure mental health and social and life skills before and after the intervention and at 6 months follow-up.
Recruitment into the research project will unfold in phases. Toward the end of the school year preceding the intervention, parents will be invited to an informational session about the project that will take place in one of the camp schools. After the informational session, meetings will take place with individual families in their homes to recruit students entering grades 5 and 6. Some youth (ages 17–23 years) who live in the camp will receive training to become part of the recruitment team. These youth will visit the homes of all potential intervention and control participants to explain the study and to obtain parental consent . If the parents consent, students will be invited to the school for further discussion (to ensure confidentiality and autonomy of decision making). Once the study has been explained to them, they’ll be asked individually to give their assent .
You are a member of the university research team leading the effort to obtain informed consent. You would like to obtain consent and assent in accordance with standard international procedures, but you realize their application may need to be adjusted to the context of the camp. In particular, you have considered what role principle s such as trust , inclusion , diversity , and broad community participation should play in the research project. That is why you chose to have older youth from the camp obtain both parental consent and student’s assent, but you are concerned about potential problems that this approach may encounter. Also, given the power dynamics and conditions in the camp, you would like the research team to consider how this project can be used to spearhead a discussion with the community coalition about larger issues of empowerment and advocacy . With this in mind, you plan to address the followin g questions with your research team.
7.3 Discussion Questions
How could the history of Palestinian refugee camps potentially impact the informed consent process and the success of this intervention?
Who are the stakeholder s in this case, and what stake, for or against, do they have in the research project? How would you deal with those who believe the project is not in their or the community’s interests?
What are the advantages and potential disadvantages of using older youth to obtain parental consent and student’s assent? What other steps could be taken to enhance the informed consent seeking process in such social contexts?
What incentives, if any, should be given for participation? To whom should these incentives be given? Given the limited opportunities for the inhabitants of the refugee camps and the perceived power of NGOs, at what point would incentives become compulsive to encourage participation?
How do relationships of power influence the application of informed consent procedures specifically, in this context? What steps can be taken to minimize the effects of power?
What bearing, positive or negative, does the background of the researchers have on the researcher-participant interaction, especially for researchers who have never lived in such camp settings and would be considered outsiders to the camp community?
Beyond the informed consent process, are the researchers simply teaching the adolescents how to adjust to an oppressive arrangement instead of exploring, providing and validating strategies to transform the si tuation? If so, what are some alternative intervention strategies that could foster the latter?
By almost any measure, the camp environment is abnormal for a developing adolescent. Given that social determinants severely challenge the health of all members of the camp community, how should the researchers take into account the unusual and extreme circumstances of the adolescents as they implement and evaluate interventions that aim to change individual-level circumstances and attributes?
Benatar, S.R. 2002. Reflections and recommendations on research ethics in developing countries. Social Science & Medicine 54(7): 1131–1141.
Bledsoe, K.L., and R.K. Hopson. 2009. Conducting ethical research and evaluation in underserved communities. In The handbook of social research ethics , ed. D.M. Mertens and P.E. Ginsberg, 391–406. Thousand Oaks: Sage Publications.
Chaaban, J., H., Ghattas, and R.R., Habib, et al. 2010. Socio-economic survey of Palestinian refugees in Lebanon . American University of Beirut (AUB) and the United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA). http://fafsweb.aub.edu.lb/aub-unrwa/files/AUB_UNRWA_report_final_draft.pdf . Accessed 3 Jan 2013.
Chilisa, B. 2009. Indigenous African-centered ethics: Contesting and complementing dominant models. In The handbook of social research ethics , ed. D.M. Mertens and P.E. Ginsberg, 407–425. Thousand Oaks: Sage Publications.
Council for International Organizations of Medical Sciences. 2002 . International ethical guidelines for biomedical research involving human subjects . http://www.cioms.ch/publications/layout_guide2002.pdf . Accessed 18 Feb 2014.
Dawson, L., and N.E. Kass. 2005. Views of US researchers about informed consent in international collaborative research. Social Science & Medicine 61(6): 1211–1222.
Khawaja, M., S. Abdulrahim, R.A. Soweid, and D. Karam. 2006. Distrust, social fragmentation and adolescents’ health in the outer city: Beirut and beyond. Social Science & Medicine 63(5): 1304–1315.
Makhoul, J. 2003. Physical and social contexts of the three urban communities of Nabaa, Borj el Barajneh Palestinian Camp and Hay el Sullum. Unpublished report. CRPH, American University of Beirut, Lebanon.
Makhoul, J., R. Nakkash, T. Harpham, and Y. Qutteina. 2013. Community based participatory research in complex settings: Clean mind–dirty hands. Health Promotion International 29(3): 510–517. doi: 10.1093/heapro/dat049 .
Marshall, A., and S. Batten. 2003. Ethical issues in cross-cultural research. In CONNECTIONS’03 , ed. W.M. Roth, 139–151. http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0CCEQFjAAahUKEwjO7JWKuujIAhXK7CYKHdNyANc&url=http%3A%2F%2Fejournal.narotama.ac.id%2Ffiles%2FEthical%2520Issues%2520in%2520Cross-Cultural%2520Research.pdf&usg=AFQjCNG04xJ3QFK7bIjX_EQUvwrwZRacxg . Accessed 25 Feb 2016.
Marshall, A., and S. Batten. 2004. Researching across cultures: Issues of ethics and power. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research 5(3): Article 39. http://nbnresolving.de/urn:nbn:de:0114-fqs0403396 . Accessed 3 June 2015.
Matsumoto, D., and C.A.L. Jones. 2009. Ethical issues in cross-cultural psychology. In The handbook of social research ethics , ed. D.M. Mertens and P.E. Ginsberg, 323–336. Thousand Oaks: Sage Publications.
National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. 1979. The Belmont report: Ethical principles and guidelines for the protection of human subjects of research . http://www.hhs.gov/ohrp/humansubjects/guidance/belmont.html . Accessed 3 Jan 2013.
Nuremberg Code . 1947. Trials of war criminals before the Nuremberg Military Tribunals under Control Council Law No. 10, Vol. 2, pp. 181–182. Washington, DC: U.S. Government Printing Office, 1949. http://www.hhs.gov/ohrp/archive/nurcode.html . Accessed 23 Feb 2014.
Racher, F.E. 2007. The evolution of ethics for community practice. Journal of Community Health Nursing 24(1): 65–76.
United Nations Relief and Works Agency (UNRWA). 2013. Lebanon . http://www.unrwa.org/etemplate.php?id=65 . Accessed 4 June 2013.
World Medical Association. 1964. Declaration of Helsinki: Ethical principles for medical research involving human subjects. http://www.wma.net/en/30publications/10policies/b3/ . Accessed 23 Feb 2014.
8 Case 3: Improving Review Quality and Efficiency of Resear ch Ethics Committees to Enhance Public Health Practice in Africa
- Mary Kasule PhD,
- Douglas Wassenaar PhD,
- Carel IJsselmuiden MD, MPH &
- Boitumelo Mokgatla
Office of Research and Development, University of Botswana, Gaborone, Botswana
Mary Kasule PhD
South African Research Ethics Training Initiative, School of Applied Human Sciences, University of KwaZulu-Natal, Pietermaritzburg, South Africa
Douglas Wassenaar PhD
Council on Health Research for Development, Geneva, Switzerland
Carel IJsselmuiden MD, MPH
School of Applied Human Sciences, South African Research Ethics Training Initiative, University of KwaZulu-Natal, Pietermaritzburg, South Africa
Africa Office for Council on Health Research for Development, Gaborone, Botswana
Boitumelo Mokgatla
Mapping African Research Ethics Review and Medicines Regulatory Capacity, Gaborone, Botswana
8.1 Background
Many low- to middle-income countries in Africa face a tremendous burden of infectious diseases . Tuberculosis (TB) causes particular concern, with incidence rising and the greatest prevalence in children . Compounding this concern is the lack of an easy-to-use and accurate diagnostic test (World Health Organization 2012). To address these challenges, the World Health Organization’s (WHO) 2011 global plan to stop TB by 2050 urgently calls for more research to develop diagnostics, drugs, and vaccines. WHO’s call reinforces the 2008 Global Ministerial Forum on Research for Health held in Mali, which recommended that each country allocate 2 % of health ministry funds to health care research (Yazdizadeh et al. 2010). All research involving human subjects will require review by institutional review boards (IRBs) or, as they are generally known in Africa, research ethics committees (RECs) . But to expedite the process of high-quality ethical reviews necessary to keep pace with these new research initiatives, a corresponding investment in REC funding and training should be made.
In TB-endemic areas of Africa, the volume and complexity of research have increased without a corresponding strengthening in the capacity of local RECs (WHO 2011). At least 190 RECs operate throughout Africa, but the quality and capacity of each vary widely (IJssemuiden et al. 2012). Although some RECs still lac k adequate research regulatory frameworks, the major challenge to strengthening capacity is lack of funding (Kass et al. 2007). This means, for example, that few, if any, African RECs have tools like electronic information management systems to coordinate submissions efficiently. It also means that few have trained REC administrators, a gap rightly identified as the missing link to improved quality and throughput of ethical review (IJsselmuiden et al. 2012). These factors can delay ethical reviews and create problems with quality and consistency (Milford et al. 2006; Kass et al. 2007). Whenever significant research funds are wasted on managing inefficient RECs, fewer funds are available to study ways to improve public health care services (Tully et al. 2000). This waste of resources on inefficient ethical review affects the timeliness of health services, which, in turn, affects subsequent health care polic y and decision making. Ironically, such wastefulness poses an unethical barrier to potentially beneficial public health research activities. Worse, these inefficiencies can cost research institutions a chance to compete for grants that require prior ethical review of research proposals by the country’s internal REC.
In Africa, external grants are often used to fund health research activities, whereas REC funding typically is either nonexistent or constrained by more pressing health care needs. Attempting to prioritize and allocate resources for activities with outcomes linked to funding puts policy makers in a dilemma . On the one hand, diverting funds from the immediate treatment of life-threatening diseases to a weak, inefficient REC can waste critical resources. On the other hand, not allocating funds to strengthen RECs can lead to the loss of external research funding, the very research that could reduce the burden of disease in the long run. Moreover, external funding, though filling a critical gap, often heightens the tensions at play in prioritizing between immediate needs for health care and long term needs for research and RECs.
8.2 Case Description
A multinational pharmaceutical c ompany put out a call for proposals to research institutions in sub-Saharan Africa to apply for a research grant. The 3-year grant, which provides 500,000 U.S. dollars per year to develop an effective paediatric TB diagnostic tool, would involve conducting clinical trials in five African TB-endemic countries. Successful award of the grant is contingent upon timely review of the proposal by the applicant’s national REC.
In one country eligible for the grant, the ministry of health (MoH) encouraged its National Tuberculosis Research Centre to apply. The grant funding would have boosted the country’s long-term efforts to strengthen the capacity of its public health research by restructuring its TB treatment protocol. The Research Centre promptly submitted a proposal to the national REC, which levies 10 % of the grant as overhead to sustain the REC.
Despite the overhead funding, the country’s national REC l acks an administrator formally trained in research ethics and a robust ethics review structure. Although the REC receives more than 100 applications annually, it only meets every 3 months, often missing deadlines, because it cannot afford essential tools to coordinate submissions efficiently. To have a proposal reviewed; applicants have to submit 20 hard copies of the research application form and 10 copies of all other study materials. The review procedure typically forces the principal investigator of a clinical trial to submit nearly 20 kg of paper copies, a considerable sum in supplies and manpower. Despite its high profile, the TB Research Centre’s grant application does not prove to be an exception to the notoriously slow review process.
Professor Y, a highly capable public health specialist, directs the public health department in the local MoH. She also lectures at a local medical school, serves as Principal Investigator (PI) of an ongoing TB clinical trial in the country, and has extensive experience at all levels of REC activity and oversight. Unfortunately, Professor Y has never had formal training in research ethics, which is critical for anyone involved in managing REC activities. Because of her background, Professor Y became aware of the delays in reviewing the TB Research Centre’s application. Recognizing its importance to the country, Professor Y offered to serve as the primary reviewer for the proposal. Professor Y called an ad hoc REC meeting. At this meeting, the other members, who had only received copies of the grant application form to prepare for their review, unanimously agreed to outsource review of the protocol because they lacked the expertise to evaluate the application. Amid these delays, institutions in other countries competing for the same grant, having already received ethical clearance from their RECs, were awarded the grant. Not only did the delays cost the country a funding opportunity to enhance its public health research capacity, but preparing the application also wasted precious time and scarce resources.
In response to this bungled opportunity, the MoH set up a task force to analyse the situation and offer recommendations. In its report, the task force recommended allocating more resources to RECs to strengthen capacity. Due to budget constraints, the MoH had to divert the money allocated to RECs from the antiretroviral program. Meanwhile, the MoH recommended temporarily outsourcing all REC services to a U.S. based clinical research organization.
8.3 Discussion Questions
What ethical tension or challenges could result from the insufficiencies in REC capacity that forced the MoH’s decision to divert funds from the antiretroviral program to strengthen REC capacity?
How should a country prioritize between the need to foster research, which can have significant long-term impact and immediate health care needs?
Funding for the research grant and temporary outsourcing of ethical reviews will come from multinational or U.S. based partners. What are the advantages and disadvantages for developing countries to accept such funding? What impact does accepting such funding have on a country’s ability to determine its own health priorities?
Professor Y has public health credentials, TB expertise, and extensive experience as an REC administrator. The case suggests that had she followed the procedures for the review process, the grant application might have been successful, even though she apparently lacks formal ethics training.
According to international research ethics regulations, what procedures should Professor Y have followed when distributing the proposal for review, allocating reviewers, and setting up the REC meeting?
How critical is formal ethics training to serving on an REC or to overseeing the development of REC capacity nationwide?
Is it a good use of time for someone like Professor Y to be serving administratively on an REC?
Would you recommend that the MoH create a permanent position for a trained research ethics administrator solely responsible for REC administration issues instead of allowing volunteers like Professor Y, who have multiple roles and respon sibilities, to oversee the activity?
Given the cultural and economic differences between developed Western nations that sponsor research and African host countries, should formal ethics training to prepare for serving on an REC be modelled on Western training or on some other model?
Keeping the interests and values of all stakeholder s in mind, consider the best ways to address the strengthening of REC capacity in African low- to middle-income countries at the local and global levels.
IJssemuiden, C., D. Marias, D. Wassenaar, et al. 2012. Mapping African ethical review committee activity onto capacity needs: The MARC initiative and HRWEB’s interactive database of RECSs in Africa. Developing World Bioethics 12(2): 74–86.
Kass, N.E., A.A. Hyder, A. Ajuwon, et al. 2007. The structure and function of research ethics committees in Africa: A case study. PLoS Medicine 4(1): e3. doi: 10.1371/journal.pmed.0040003 .
Milford, C., D. Wassenaar, and C. Slack. 2006. Resources and needs of research ethics committees in Africa: Preparations for HIV vaccine trials. IRB: Ethics & Human Research 28(2): 1–9.
Tully, J., N. Ninis, R. Booy, and R. Viner. 2000. The new system of review by multi-centre research ethics committees: Prospective study. British Medical Journal 320(7243): 1179–1182.
World Health Organization (WHO). 2011. An international road map for tuberculosis research: Towards a world free of tuberculosis . Geneva: World Health Organization.
World Health Organization (WHO). 2012. Global tuberculosis report 2012 . Geneva:World Health Organization. http://apps.who.int/iris/bitstream/10665/75938/1/9789241564502_eng.pdf . Accessed 3 June 2015.
Yazdizadeh, B., R. Majdzadeh, and H. Salmasian. 2010. Systematic review of methods for evaluating healthcare research economic impact. Health Research Policy and Systems 8: 6. doi: 10.1186/1478-4505-8-6 .
9 Case 4: Internet-Based HIV/AIDS Education and Prevention Programs in Vulnerable Populations: Black Men Who Have Sex with Men
- Amar Kanekar PhD, MPH, MB, MCHES, CPH
Department of Health, Human Performance and Sport Management, University of Arkansas at Little Rock, Little Rock, AR, USA
Amar Kanekar PhD, MPH, MB, MCHES, CPH
This case is presented for instructional purposes only. The ideas and opinions expressed are the author ’ s own. The case is not meant to reflect the official position , views , or policies of the editors , the editors ’ host institutions , or the author ’ s h ost institution .
9.1 Background
Since surfacing more than 30 years ago, the HIV/AIDS pandemic has devastated populations worldwide. Various factors have contributed to this epidemic, such as lack of awareness of HIV status, stigma, homophobia, negative perceptions about HIV testing , socioeconomic factors, behavioral risk factors, and high prevalence of sexually transmitted diseases (Centers for Disease Control and Prevention 2015). In the United States, one goal of the national HIV/AIDS strategy is to re duce HIV-related hea lth disparities. Any reduction in the collective risk of acquiring HIV will require behavior change interventions in communities with the highest HIV prevalence. However, extending the reach of HIV/AIDS preventive interventions in remote areas with limited access to HIV testing and prev ention services has proved difficult (Office of National AIDS Policy 2012).
The challenge of reaching some populations has led many practitioners to consider innovative intervention methods that rely on technologies such as the Internet and mobile telephones. Public health profession als are using these technologies to deliver health education to vulnerable populations in big cities, small towns, and hard-to-reach rural areas. In particular, the past decade has seen more health communication efforts using the Internet to prevent HIV and sexually transmitted diseases (Bull et al. 2007, 2009; Rietmeijer and McFarlane 2009). Studies of interventions that use Internet chat rooms, online modules, and health intervention websites show promising results that bode well for the future of these technolo gies (Chiasson et al. 2009; Moskowitz et al. 2009).
Studies conducted with marginalized and vulnerable populations such as black men who have sex with men (MSM) can pose difficulties. On the technology front, many difficulties reflect the Internet’s relative novelty for conducting studies and the consequent lack of clarity in dealing with the rules, language, and norms of a virtual community culture compared with a traditional community culture (Loue and Pike 2010). On the allocation front, having limited resources usually implies that tailoring interventions to a specific group will mean forgoing benefits to another group. Still, in promoting the health of populations, public health professionals must strive to distribute resources fairly while responding to the specific needs of racial, ethnic, and cultural groups. These concurrent goals require maintaining a delicate balance between targeted and population interventions. On the ethics front, because some projects straddle the line between research and practice, public health profession als can become unsure about whether the ethical guideline s of research or of community work should govern their actions. They must bear in mind that trust , which is essential for conducting community-based participatory research , becomes more crucial when working with vulnerable populations, which tend to show a high degree of mistrust (Loue and Pike 2010). Those who study vulnerable populations need to negotiate community entry either by developing trust or by working closely with local practitioners and building upon established trust.
In the United States , the HIV/AIDS epidemic has hit the African-American population hardest, with black men accounting for 70 % of new HIV infections . Between 2006 and 2009, new HIV infections increased 48 % among black 13- to 24-year-old MSM (Centers for Disease Control and Prevention 2015); by 2009, 37 % of new HIV cases among black men were from black MSM. Given this high prevalence, before the end of 2015, the U.S. national HIV/AIDS strategy calls for a 20 % increase in the proportion of African Americans diagnosed with HIV who have an undetectable viral load (Office of National AIDS Policy 2012). Already, information about HIV issues affecting young MSM (Mustanski et al. 2011) is widely available on the Internet, including messages about how to reduce risk (Hightow-Weidman et al. 2011) and interventions to prevent HIV risk behaviors among MSM (Rhodes et al. 2010) and blacks who inject drugs (Washington and Thomas 2010). Studies show that online delivery of HIV counseling and behavioral interventions for MSM at high risk for HIV are successful, suggesting that the future holds great promise for Internet-delivered interventions for this vulnerable population (Chiasson et al. 2009; Moskowitz et al. 2009).
9.2 Case Description
Dr. Albert, a social scientist, and Dr. Baines, a community worker, are employed by a public health agency in a medium-size U.S. town. The agency has asked them to determine whether a skill-based, Internet-delivered intervention to promote safer sex among young Black MSM will increase HIV knowledge and increase the frequency of using safer-sex practices.
Project participants will be recruited via the Internet in gay chat rooms and be verified electronically by using Internet Protocol and Microsoft Access usernames and passwords (Bull 2011). Participants will be surveyed before they begin the training modules and again at 1- and 6-week intervals after completing the modules. Participants will be randomly assigned to control and experimental arms. Those in the control arm will receive 6 h of online training about health and well-being (e.g., nutrition, physical activity, stress reduction). The experimental arm will receive a 6-h online program including two 1-h modules on each of the following topics: (a) HIV/AIDS-related knowledge; (b) development and improvement of safe sex skills, such as partner communication and monogamous sexual relationships; and (c) self-efficacy in using condoms. The modules will include automated reminders for HIV testing . The study will measure improved knowledge on HIV/AIDS , partner communication about safer sex, and condom usage self-efficacy. Data will be analyzed using statistical software.
Dr. Albert thinks the results could be generalized not only to black MSM in the community but also to black MSM overall. He plans to write an article describing the results for publication in a scientific journal. Although Dr. Baines knows the impact of education on health, especially in underprivileged communities, she wants to educate only a subset of the community they will reach. Besides, since their work is for a public health agency, she believes the intervention ought to reach as many community members possible. She claims the project’s goal is to provide a vulnerable and disadvantaged population with much needed education on health matters and health-promoting behavior and doubts their project constitutes research.
Dr. Albert worries that, because his colleague lacks academic rigor and underappreciates the role of evidence, she fails to appreciate the project’s rationale and design and, as a result, is indifferent to the challenges the Internet poses (e.g., technology-induced bias, protection of confidentiality). Conversely, Dr. Baines believes Dr. Albert has missed the boat and is wasting resources, spuriously introducing statistical analysis of experimental and control arms into what the agency clearly had intended as an education intervention.
9.3 Discussion Questions
Is this a research project? Should approval from an ethics review committee be obtained? Or should the project be considered nonresearch because it will improve the health of the population? How should you decide?
Does the fact that the project is funded by a public health agency play a role in this discussion? Should public health agencies conduct studies to generate evidence about HIV education and prevention interventions? Should agencies focus on the delivery of interventions based on the existing evidence?
How is this black MSM population vulnerable, and how should this vulnerability be addressed in research and nonresearch interventions?
Do Dr. Albert and Dr. Baines have ethical obligations to other community populations? On what basis is the public health agency justified in advancing interventions that target only a subgroup of the community?
How should research studies on Internet-based interventions be conducted to ensure scientific validity, given the difficulties of knowing, for example, whether the participant meets the study’s inclusion criteria? Which measures should be taken to protect the privacy and confidentiality of participants?
How should you decide what level and type of evidence you need to back a public health educational intervention? Should public health professionals always use science to validate educational interventions?
Bull, S. 2011. Technology-based health promotion . Thousand Oaks: Sage Publications.
Bull, S.S., S. Phibbs, S. Watson, and M. McFarlane. 2007. What do young adults expect when they go online? Lessons for development of an STD/HIV and pregnancy prevention website. Journal of Medical Systems 31(2): 149–158.
Bull, S., K. Pratte, N. Whitesell, C. Rietmeijer, and M. McFarlane. 2009. Effects of an Internet based intervention for HIV prevention: The Youthnet trials. AIDS and Behavior 13(3): 474–487. doi: 10.1007/s10461-008-9487-9 .
Centers for Disease Control and Prevention. 2015. HIV Among African Americans. http://www.cdc.gov/HIV/risk/racialethnic/aa/index.html . Accessed 2 June 2015.
Chiasson, M.A., F.S. Shaw, M. Humberstone, S. Hirshfield, and D. Hartel. 2009. Increased HIV disclosure three months after an online video intervention for men who have sex with men (MSM). AIDS Care 21(9): 1081–1089. doi: 10.1080/09540120902730013 .
Hightow-Weidman, L.B., B. Fowler, J. Kibe, et al. 2011. HealthMpowerment.org: Development of a theory-based HIV/STI website for young black MSM. AIDS Education and Prevention 23(1): 1–12. doi: 10.1521/aeap.2011.23.1.1 .
Loue, S., and E.C. Pike. 2010. Case studies in ethics and HIV research . New York: Springer.
Moskowitz, D.A., D. Melton, and J. Owczarzak. 2009. PowerON: The use of instant message counseling and the Internet to facilitate HIV/STD education and prevention. Patient Education and Counseling 77(1): 20–26. doi: 10.1016/j.pec.2009.01.002 .
Mustanski, B., T. Lyons, and S.C. Garcia. 2011. Internet use and sexual health of young men who have sex with men: A mixed-methods study. Archives of Sexual Behavior 40(2): 289–300. doi: 10.1007/s10508-009-9596-1 .
Office of National AIDS Policy. 2012. National HIV/AIDS strategy: Update of 2011–2012 federal efforts to implement the national HIV/AIDS strategy . http://www.aids.gov/federal-resources/national-hiv-aids-strategy/implementation-update-2012.pdf . Accessed 2 June 2015.
Rhodes, S.D., K.C. Hergenrather, J. Duncan, et al. 2010. A pilot intervention utilizing Internet chat rooms to prevent HIV risk behaviors among men who have sex with men. Public Health Reports 125(suppl 1): 29–37.
Rietmeijer, C.A., and M. McFarlane. 2009. Web 2.0 and beyond: Risks for sexually transmitted infections and opportunities for prevention. Current Opinion in Infectious Diseases 22(1): 67–71. doi: 10.1097/QCO.0b013e328320a871 .
Washington, T.A., and C. Thomas. 2010. Exploring the use of Web-based HIV prevention for injection-drug-using black men who have sex with both men and women: A feasibility study. Journal of Gay & Lesbian Social Services 22(4): 432–445. doi: 10.1080/10538720.2010.491747 .
Author information
Authors and affiliations.
Office of Scientific Integrity, Office of the Associate Director for Science, Office of the Director, Centers for Disease Control and Prevention, Atlanta, GA, USA
Drue H. Barrett PhD & Leonard W. Ortmann PhD
Human Research Protections Office, Office of Scientific Integrity, Office of the Associate Director for Science, Office of the Director, Centers for Disease Control and Prevention, Atlanta, GA, USA
Natalie Brown MPH
Clinical Research Branch, Division of Tuberculosis Elimination, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, GA, USA
Barbara R. DeCausey MPH, MBA
Regional Program on Bioethics, Office of Knowledge Management, Bioethics, and Research, Pan American Health Organization, Washington, DC, USA
Carla Saenz PhD
Center for Values, Ethics and the Law in Medicine, Sydney School of Public Health, The University of Sydney, Sydney, Australia
Angus Dawson PhD
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Drue H. Barrett PhD , Matthew R. Hunt PT, PhD , Mary Kasule PhD or Amar Kanekar PhD, MPH, MB, MCHES, CPH .
Editor information
Editors and affiliations.
Centers for Disease Control and Prevention, Atlanta, Georgia, USA
Drue H. Barrett
Centers fo Disease Control and Prevention, Atlanta, Georgia, USA
Leonard W. Ortmann
Angus Dawson
Pan American Health Organization, Washington DC, District of Columbia, USA
Carla Saenz
Global Health Ethics, Department of Information, Evidence and Research, World Health Organization, Geneve, Switzerland
Andreas Reis
Division of STD Prevention National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, USA
Rights and permissions
Open Access This chapter is distributed under the terms of the Creative Commons Attribution-Noncommercial 2.5 License ( http://creativecommons.org/licenses/by-nc/2.5/ ) which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
The images or other third party material in this chapter are included in the work’s Creative Commons license, unless indicated otherwise in the credit line; if such material is not included in the work’s Creative Commons license and the respective action is not permitted by statutory regulation, users will need to obtain permission from the license holder to duplicate, adapt or reproduce the material.
Reprints and permissions
Copyright information
© 2016 The Author(s)
About this chapter
Barrett, D.H., Ortmann, L.W., Brown, N., DeCausey, B.R., Saenz, C., Dawson, A. (2016). Public Health Research. In: H. Barrett, D., W. Ortmann, L., Dawson, A., Saenz, C., Reis, A., Bolan, G. (eds) Public Health Ethics: Cases Spanning the Globe. Public Health Ethics Analysis, vol 3. Springer, Cham. https://doi.org/10.1007/978-3-319-23847-0_9
Download citation
DOI : https://doi.org/10.1007/978-3-319-23847-0_9
Published : 13 April 2016
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-23846-3
Online ISBN : 978-3-319-23847-0
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Public health and research: an overview
Journal of Health Research
ISSN : 2586-940X
Article publication date: 15 October 2020
Issue publication date: 15 June 2021
This paper was to describe the overview of public health research.
Design/methodology/approach
It is a commentary piece of work from own long experience in working with the World Health Organization.
This study has innovative ideas in approaching priority areas in public health research.
Originality/value
This study opens up new thought in public health research.
- Public health
Public health research
Plianbangchang, S. (2021), "Public health and research: an overview", Journal of Health Research , Vol. 35 No. 4, pp. 374-378. https://doi.org/10.1108/JHR-03-2020-0074
Emerald Publishing Limited
Copyright © 2020, Samlee Plianbangchang
Published in Journal of Health Research . Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and non-commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence may be seen at http://creativecommons.org/licences/by/4.0/legalcode
An overview of public health
Public health is the science and art of preventing disease, prolonging life and promoting human health through organized community efforts as well as the informed choice of society, public, private and voluntary organizations and communities at large. Analyzing the health of a population and the threats to that health forms the basis for public health.
Additionally, “health”, as defined in the WHO Constitution in 1948 [ 1 ], considers physical, mental and social well-being and is not merely the absence of disease or infirmity. Furthermore, public health is interdisciplinary, thus, a “public health team” may include several related disciplines in health and other social fields. Access to public health initiatives for comprehensive and integrated health care and services is always a difficult challenge in any population setting.
The objective of this commentary is to provide an overview of public health research and highlight innovative thinking in the field.
Public health systems
Public health systems are commonly defined as “all public, private, and voluntary entities that contribute to the delivery of essential public health services to people within a jurisdiction” [ 2 ]. This concept is to ensure, among other things, that all contributions to the improved health and well-being of the community or state are appropriately recognized and counted in the assessment of the provision of public health services to the community. The public health system includes public health agencies at state and local levels; all healthcare providers; public safety agencies; human services and charity organizations; education and youth development agencies; recreation and art-related organizations; economic and philanthropic agencies and environmental organizations.
The 10 essential public health services/functions
Monitoring community health situations to identify and solve health problems and prevent any health risks in the community;
Investigating and diagnosing specific health threats and health hazards in the community with the view to their early prevention;
Through modern technology in communication, informing, educating and empowering people in the community about health issues and challenges and their interventions;
Identifying/investigating and solving any problems of public health importance;
Through the full participation of people, developing policies and plans that support individual and combined health efforts in the community;
Ensuring effective enforcement of laws and regulations that protect environmental health and assure the safety of the population;
Linking people to needed personal health services and ensuring the provision of quality health care when otherwise unavailable;
Assuring the availability of effective public health workforce and competent healthcare personnel in both public and private facilities;
Objectively evaluating efficiency, effectiveness, accessibility and quality of personal as well as population-based health care facilities and services and
Undertaking study/research for new insights and innovative solutions to effectively counter prevailing and emerging health problems.
Public health rsearch aims to elucidate the influence of factors that determine the health of a population, i.e. genetic, environmental, social-cultural, economic, political, etc. The objective of public health research is to use the knowledge gained to propose policies and interventions, based on scientific evidence, and to help improve the health and well-being of the population and ultimately reduce/eradicate health inequalities.
Public health research is characterized by its multidisciplinary approach. It draws on several disciplines in its development and management, especially epidemiology/human ecology; biostatistics; physical and social sciences as applied to health; biology; genetics and toxicology. It usually entails the analysis of data on population samples on varying scales, depending on the scope and purpose of the research [ 4 ].
In practical terms, public health researchers study the statuses of population health and well-being, disability and loss of independence. They analyze the determining risk factors of these statuses or conditions, whether biological, behavioral, psycho-social or environmental. In addition, the researchers develop and assess the interventions aiming to effectively promote population health, prevent disease and compensate for disabilities and loss of independence. They also develop and assess innovation to improve efficiency and effectiveness of the organization of healthcare facilities and personnel, in public health, medical and other social service areas.
Research in health may be in the fields of health research, medical research, public health research, health services research, health systems research, environmental health research and others. These are interlinked and need to be pursued in a parallel manner in public health development.
Funding agencies
Mission and role of funding agencies
(2)Quality of research proposal
Relevance to current health-related issues and problems; responding to priority public health needs and the challenges of community and country are crucial. Applications should also be in the interest of the international/global health community.
Formulation with rational and logical thinking; Research proposals should be well-conceived and developed according to sound research methodology/protocol on epidemiological principles.
Expected result of the proposal; The result must be of high quality and should imply strong feasibility in its subsequent application/implementation in both technical, managerial and financial terms.
Public health system development research
DEIDS (development and evaluation of integrated health delivery system) (Thailand Lampang Health Development Project), 1973-1978 [ 6 ].
(2)District Health Services Development Project based on the principle of the primary health care approach, Mongar Health Development Project in Bhutan, 1984–1990 [ 7 ].
(3)Comprehensive and Integrated Health Research Development Project on hill- tribe population, 2014–present (still ongoing)
This is a long-term large research and development project with many sub-projects focusing on various specific issues of the target population. It is a multi-agency and interdisciplinary endeavor developed and implemented through the coordination of the Maefah Luang University Center of Excellence on health of the hill-tribe population. It includes the development of integrated and comprehensive social and health care services with an emphasis on equity, social justice and self-reliance in the community. There are multiple sources of funding, however mainly from the National Research Council of Thailand.
Some suggested areas for contemporary public health research
Universal health coverage for all
Financial sustainability in the long term
Equal accessibility by all people, regardless of their social and economic status
The right approach to development, proactive or passive strategy
Affordability in financial and managerial terms of the country concerned.
(2)Social impact of drug abuse /addiction
The social and economic impact of (chaotic situations created by) drug abuse and addiction
The general health of a population that is gradually undermined by drug abuse and drug addiction, leading, among other things to worsened national social and economic growth.
(3)Health and social care of elderly population
Intervention to reduce the degree of morbidity/disability and dependence
Efforts to increase social and economic productivity/independence
Program for self-help and self-reliance in an aged population
Preference between aging and aged programs, the difference between the two.
(4)Emerging infectious disease (EID)
The epidemiological, environmental and ecological approach in an integrated manner
The importance of social and behavioral change
Emerging mutation, assortment and genetic change in infectious agents
Impact of global climate change on EID, etc.
Even though it is mainly conceptual, the article may be able to help open new visions in public health research for better and sustainable health in the entire population in various localities.
1 World Health Organization [WHO] . WHO basic document . 47th ed. Geneva : WHO ; 2009 [cited 2019 Nov 28]. Available from: https://apps.who.int/iris/handle/10665/44192 .
2 World Health Organization [WHO] . What is health policy and systems research (HPSR)? [cited 2019 Nov 28]. Available from: https://www.who.int/alliance-hpsr/about/hpsr/en/ .
3 Centers for Disease Control and Prevention [CDC] , Office for state, tribal, local and territorial support . The 10 Essential Public Health Services: An Overview [cited 2019 Nov 28]. Available from: https://www.cdc.gov/publichealthgateway/publichealthservices/pdf/essential-phs.pdf .
4 Centers for Disease Control and Prevention [CDC] . Public health 101 series [cited 2019 Nov 28]. Available from: https://www.cdc.gov/publichealth101/ .
5 Centers for Disease Control and Prevention [CDC] . 24/7 Saving Lives, Protecting People [cited 2019 Nov 28]. Available from: https://www.cdcfoundation.org/cdc-247-saving-lives-protecting-people# .
6 Memoir on Occasion of the Death Anniversary of Dr. Somboon Vacharothai . Bangkok ; 2014 : 39 - 43 . (On Thailand DEIDS Project) .
7 World Health Organization [WHO] , Regional office for south-east asia [SEARO]. Sasakawa health prize: stories from south-east asia . New Delhi : WHO/SEARO ; 2012 : 125 - 146 [cited 2019 Nov 28]. Available from: https://apps.who.int/iris/bitstream/handle/10665/205878/B4905.pdf?sequence=1&isAllowed=y .
Corresponding author
Related articles, we’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
Public Health Research and Cancer
NCI scientists analyze data to explore how inherited genetic variation contributes to cancer susceptibility and outcomes.
The Importance of Cancer-Related Public Health Research
Cancer has a significant impact on public health in the United States. The years of life lost due to premature deaths, the economic burden to society, the burden to people due to lost wages and the costs associated with treatment, and the long-term effects of cancer and its treatment on the quality of life of survivors take a toll at a population level. Moreover, cancer’s impact on public health will continue to grow as the US population ages and some cancer incidence rates rise.
Researchers are addressing this reality by studying cancer and its burden on a population-wide scale. This research includes:
- maintaining large registries of information about people diagnosed with cancer that can be used to identify important trends in cancer incidence, survival, and mortality; treatment characteristics; and patient outcomes
- investigating behavioral patterns (such as tobacco use, diet, and screening practices); occupational, environmental, medical, and other exposures; and inherited genetic factors that can influence cancer risk
- understanding and addressing factors that contribute to the unequal burden of cancer among certain populations, such as higher cancer death rates, less frequent use of proven screening tests, and higher rates of advanced cancer diagnoses
- analyzing patterns of cancer care and outcomes in different health care settings
- analyzing the economics of cancer and how the health care system affects access to care
- studying ways to improve cancer control programs
- assessing the risks and benefits associated with cancer screening to inform guidance on screening strategies
- working on strategies to communicate and implement evidence-based practices for cancer prevention, detection, diagnosis, treatment, and survivorship into public health, clinical practice, and community settings
Although cancer affects individual patients and their families in different ways, studying its impact on large populations can provide important information that influences practices, policies, and programs that directly affect the health of millions of people in the United States each year.
Selected NCI Activities in Cancer-Related Public Health Research

NCI Fiscal Year 2025 Professional Judgment Budget Proposal
Each year, NCI prepares a professional judgment budget to lead progress against cancer.
NCI supports a diverse array of research that is helping to address issues in cancer-related public health. This research relies on extensive resources, often requires the participation of a large number of people, and can span many years.
NCI plays an important role in public health research by conducting and funding large research studies and assembling large data collections that can be used by researchers worldwide. NCI also engages with other federal agencies and community members to identify, develop, and test culturally appropriate cancer prevention and intervention strategies with communities in mind. Findings from this work inform public health practices to help improve outcomes for all.
Examples of NCI-supported activities in public health research include the following:
Surveillance, Epidemiology, and End Results (SEER) Program
The SEER Program collects data on cancer incidence and survival from cancer registries representing nearly half of the US population. Researchers worldwide use SEER data to identify important cancer-related trends, such as changes in the incidence of or mortality from specific cancers or cancer subtypes, as well as factors associated with prognosis and the risk of second primary cancers . SEER data are a critical source for studies that can spur important new research and inform decisions and policies on cancer control.
Epidemiologic Studies
Epidemiologic studies led or supported by NCI evaluate important factors that affect cancer risk . These factors include diet; tobacco and alcohol use; physical activity; genetics; workplace and environmental exposures, such as medical radiation and diesel exhaust; and infections, such as human papillomavirus (HPV), hepatitis B and C, and HIV.
For example, the Connect for Cancer Prevention Study , is a partnership between NCI and nine health care systems across the Unites States to explore the causes of cancer and to learn how to better prevent it. NCI also conducts and supports research on the long-term effects of cancer and cancer treatment to identify strategies to prevent or lessen adverse effects in cancer survivors.
NCI research findings have had a significant impact on public health by providing key evidence for determining whether specific exposures can cause or prevent cancer and for translating research findings into clinical practice guidelines and individual behavior recommendations. These findings come from studies that take years to conduct and require long-term “detective” work by NCI researchers and NCI grantees .
Health Care Delivery and Cancer Control Research

NCI Health Care Delivery Research and the National Cancer Plan
NCI supports research on cancer care delivery that aligns with the National Cancer Plan’s goal to deliver optimal care. Read about the plan and this goal.
Through NCI’s Healthcare Delivery Research Program and the NCI Community Oncology Research Program (NCORP) , the institute also supports studies assessing patient, clinician, and organizational factors that influence the delivery of cancer care. These studies can provide important information that has the potential to improve cancer care.
Similarly, the Cancer Intervention and Surveillance Modeling Network (CISNET) uses statistical modeling to understand the population-wide impact of cancer control interventions, including prevention, screening, and treatment. CISNET studies, for example, have been used by the US Preventive Services Task Force to inform their recommendations on screening guidelines for lung, breast, colorectal, prostate, and cervical cancers, as well as by the Centers for Medicare and Medicaid Services to inform coverage policies for related screening.
Results from several large clinical trials led by NCI have also contributed to major changes in public health practice. For example, based on findings from the National Lung Screening Trial (NLST) , the US Preventive Services Task Force recommended that people at high risk be offered a low-dose helical CT (LDCT ) scan screening for lung cancer. The Centers for Medicare and Medicaid Services now covers the cost of lung cancer screening with LDCT once a year for Medicare beneficiaries who meet the criteria.
Behavioral Research
Behavioral research is also critical to public health. NCI supports numerous programs that study behavior and cancer from a wide variety of perspectives. For example, NCI funds research to understand the potential impact of e-cigarettes, vapes, and other electronic nicotine delivery systems on individual and population health. Other studies examine the factors that influence how population groups perceive their cancer risk and how it influences their behavior, such as decisions about cancer screening or whether parents have their children vaccinated against HPV.
NCI Cancer Disparities Research and the National Cancer Plan
NCI supports a broad variety of research to understand and address the unequal burden of cancer. This work aligns with the National Cancer Plan’s goal to eliminate inequities. Read about the plan and this goal.
Cancer Disparities Research
Certain populations, including specific racial and ethnic groups, rural populations, sexual and gender minorities, and those in poverty, are affected disproportionately by some cancers . There are many reasons for these disparities, including societal factors and inadequate implementation of cancer prevention and treatment interventions in health care practice.
NCI seeks to address cancer-related disparities by promoting and conducting health equity research that identifies the sources of disparities across the cancer control continuum and throughout the human life span. For example, there are NCI initiatives that support research on cancer control in rural settings and other geographically underserved areas , including research on health disparities in Native American populations .
Cancer Survivorship Research
The number of people who have survived cancer is expected to grow to 26.1 million by 2040, further increasing the importance of understanding and developing interventions that address the unique physical, psychological, and economic issues that cancer survivors often face.
NCI supports a robust research portfolio devoted to helping survivors of adult and pediatric cancers improve both their quality of life and their long-term survival. The institute funds research on adult survivor follow-up care , pediatric and young adult survivorship, survivors with advanced or metastatic disease, and survivorship needs related to primary care . Survivorship-focused studies examine topics such as ways to improve physical activity and diet among survivors, as well as help survivors manage psychological issues such as depression and anxiety. These studies also examine ways to manage physical side effects of cancer and its treatment, such as functional limitations, lymphedema , and sexual dysfunction.
NCI also conducts and funds a number of studies to identify risk factors—related to treatment, behavior, and genetics—for the development of second primary cancers and other outcomes among cancer patients . This research can point to possible interventions for reducing that risk, such as suggesting ways to alter treatments without sacrificing efficacy and guiding the follow-up care of cancer survivors.
One example of NCI-supported survivorship research is the Childhood Cancer Survivor Study (CCSS) . This large cohort study examines the long-term adverse effects of cancer and cancer therapy on survivors of childhood cancer who were diagnosed between 1970 and 1999. The study was created to gain new knowledge about the long-term effects of cancer and its treatment and to educate survivors and the medical community about the potential impacts of a cancer diagnosis and treatment. Results from CCSS are used to help design treatment protocols and interventions that will improve survival, while minimizing harmful late effects .
Recent Findings in Cancer-Related Public Health Research
- Opportunities for Achieving the Cancer Moonshot Goal of a 50% Reduction in Cancer Mortality by 2047
- 3–in–1 Approach Helps Women in Rural Areas Get Cancer Screenings
- Financial Navigation Can Reduce the Financial Toxicity of Cancer Care
- Study Probes Awareness of Alcohol’s Link to Cancer
- Why Have Thyroid Cancer Diagnoses Spiked for US Women?
- Breast Cancer Surgery Choice May Affect Young Survivors’ Quality of Life
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
- 2024 Vaccine Day at Johns Hopkins
- IDARE Working and Steering Groups
- Support Groups
- Strategic Plan
- Why we are named the Department of International Health
- Job Openings
- Student Publications
- Message from the Director
- Ethics, Equity, and Gender
- Global Health Economics
- Global Health Policy
- Global Health Technology and Innovation
- Uttar Pradesh Health Systems Strengthening Project
- Newsletter Archive
- Primary Health Care and Community Health
- Global Disease Epidemiology and Control
- Academic Guides and Competencies
- Frequently Asked Questions
- Program in Applied Vaccine Experiences - PAVE
- Our Work in Action
- Conversations on Sustainable Financing for Development
- Moving from Emergency Response to Post-Recovery: Lessons and Reflections from Ebola
- Polio Eradication: Status, Transition and Legacy
- Supporting Operational AIDS Research (SOAR): Assessing the Geographic Pivot
- The Avahan Experience in India
- Workshop on Strategic Issues in Global Health Program Transitions
- WHERE WE WORK
- Studies by Johns Hopkins Researchers Seek to Improve Mobile Phone Health Surveys in Colombia
- Publications
- Our Publications
- Student Investigators
- Leveraging Primary Health Care Systems for COVID-19
- Mission Afghanistan 2030 In the News
- Mission Afghanistan 2030 Publications
- One Year On: The Pervasive Health Challenges in Afghanistan - Webinar Series
- Sight and Life Global Nutrition Research Institute
- The IDEA Initiative
- The India Primary Health Care Support Initiative (IPSI)
- Faculty Recognition: Excellence in Teaching
- Mathuram Santosham, MD, MPH, ’75
- Primary Faculty Within the Global Disease Epidemiology and Control Program Area
- Primary Faculty Within the Health Systems Program Area
- Primary Faculty Within the Human Nutrition Program Area
- Primary Faculty Within the Social and Behavioral Interventions Program Area
- International Health Endowed Honors and Student Awards
- Student Profile: Abinethaa Paramasivam
- Student Profile: Deja Knight
- Student Profile: Prativa Baral
- Student Profile: Safia Jiwani
- Student Profile: Venessa Chen
- Alumni Profile: Anita Dam
- Alumni Profile: Lani Rice Marquez
- Alumni Profile: Nimi Georgewill
- Allyson Nelson, MSPH ’15
- Alumna Interview | Rebecca Merrill, PhD ’10, MHS ‘07, Senior Epidemiologist, CDC
- Alumni Profile: Brigitta Szeibert, MSPH ’23, RD
- Andrew Nicholson, MSPH '17
- Andrew Thompson, MSPH '12
- Caitlin Quinn, MSPH '17
- Chytanya Kompala, MSPH
- Collrane Frivold, MSPH ’17
- Elizabeth "Libby" Watts, MHS '17
- Katherine Tomaino, MSPH ’14
- Lianne Marie Gonsalves, MSPH '13
- Marie Spiker, MSPH '14, RD program
- Mariya Patwa, MSPH '18
- Mary Qiu, MSPH '16
- Prianca Reddi, MSPH '20
- Tomoka Nakamura, MSPH '15
- Bestselling Author Johnny Saldaña Leads Qualitative Data Workshops
- Faculty Profile | Smisha Agarwal, PHD, MPH, MBA
- Faculty Speaks at UN: Launch of Journal Series on Sexual and Reproductive Health and Rights
- From the Chair
- International Health Faculty Key Contributors to First WHO Guideline on Digital Interventions for Health Systems Strengthening
- International Health Faculty Presents Expert Recommendations On Antimicrobial Resistance to UN Secretary General
- International Health Faculty Receives NIH Fogarty Funding to Establish Research Ethics Training Program in Ethiopia
- International Health Faculty Wins Award for Innovation in Nutrition and Health in Developing Societies
- International Health Student and Faculty Publish New Vaccine Safety Book
- Student Spotlight | Maria Garcia Quesada, MSPH '19
- Student Spotlight | Ryan Thompson, MSPH '19
- Alumna Profile | Collrane Frivold, MSPH ‘17
- Alumna Profile | Katherine Tomaino, MSPH ‘14
- Alumni Reunion | The Program in Applied Vaccine Experiences (PAVE)
- Faculty Profile | Haneefa Saleem, PHD ’14, MPH ’09
- Faculty Profile | Naor Bar-Zeev, PHD, MBBS(HONS), MPH, MBIOSTAT
- Student Practicum Spotlight | Greg Rosen, MSPH Candidate
- Student Spotlight | Nukhba Zia, PHD Candidate
- Make a Gift
- Info for Current Students
Each year the Johns Hopkins Vaccine Initiative (JHVI) hosts Vaccine Day to highlight the advancements in vaccine research by inviting a distinguished scientist to deliver a keynote address on the current status of topics ranging from dengue, rotavirus, COVID-19, measles, and more.
The inaugural Vaccine Day held in 2008 officially launched the JHVI, and 14 Vaccine Day events have been hosted since. Led by Professor Ruth Karron , Vaccine Day works to promote and foster current vaccine research at the Bloomberg School.
This year, Vaccine Day featured two keynote speakers. First Gabriela Paz-Bailey, MD, PhD, MSc, DTM&H, the Chief of the Dengue Branch in the Division of Vector-Borne Diseases from the National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) at the CDC, discussed the basics of dengue transmission and pathogenesis, factors contributing to the increasing global burden of disease from dengue, current outbreak trends, and the current testing and treatments for dengue infections.
Anna Durbin, MD, a professor and the Director of the Center for Immunization Research in the Department of International Health shared the history of dengue vaccine research, an overview of currently available dengue vaccines, her ongoing research developing new vaccines, and the challenges around vaccine implementation and surveillance.
A panel discussion followed with the keynote speakers and two additional vaccine experts, Rupali Limaye, PhD ’12, MPH, MA, an associate professor in the GDEC Program in the Department of International Health and 2nd year MSPH student Morghan Park . During the panel, attendees had the opportunities to ask questions about dengue vaccine research and implementation, issues around vaccine hesitancy, and the importance of improving communication and trust around vaccines within communities.
The event also hosts a poster session that showcases vaccine-related research by students and faculty at the Bloomberg School. Each year this session brings about a rich forum of discussions and knowledge sharing around ongoing research and awards the top 3 student poster presentations. This year over 40 posters were displayed by faculty, staff, and students. The 2024 poster winners are:
1st Place: Binh Nguyen, Zhengrong Li and Samandika Saparamadu – “To Subsidize or Not to Subsidize: The Cost-Effectiveness of RSV Vaccination Among Infants in the U.S.”
2nd Place: Molly Sauer and Prachi Singh – “Characterizing Potential Acceptability of Maternal RSV Vaccination in Kenya: A Latent Class Analysis Approach”
3rd Place: Laura St Clair – “mTOR Activation is associated with greater protective antibody responses following Influenza Vaccination in Young Adult Female compared to Male Mice”
Finally, the new cohort of PAVE Scholars was announced during the event. PAVE, Program in Applied Vaccine Experiences , supports vaccine-focused internships for Johns Hopkins students at international organizations that hold critical roles in global vaccine policy and delivery. Students spend 12 to 16 weeks working full time at one of the partner organizations, gaining valuable experience in vaccine research, policy, and programs of global importance. The outstanding PAVE Scholars 2024 cohort is:
Kedest Mathewos (PhD, Health Systems): Gavi, the Vaccine Alliance
Rithika Rajesh (MSPH, GDEC): Gavi, the Vaccine Alliance
Stella Dlamini (MSPH, GDEC): WHO, Immunization, Vaccines and Biologicals
Georgia Artzberger (MSPH, GDEC): WHO, Immunization, Vaccines and Biologicals
Wally Wennerberg (MSPH, GDEC): UNICEF
Haley Challgren (MSPH, GDEC): PAHO
Watch the recorded keynote addresses and panel session.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
As the FDA evaluates ecstasy treatment for PTSD, questions mount about the evidence

Research on MDMA has shown it can be effective for PTSD, but approval of the treatment isn't yet guaranteed. The Washington Post via Getty Images hide caption
Research on MDMA has shown it can be effective for PTSD, but approval of the treatment isn't yet guaranteed.
In a matter of months, the Food and Drug Administration is expected to decide whether the drug commonly known as ecstasy can be used as a treatment for post-traumatic stress disorder.
An approval by the agency would represent an enormous milestone for the movement to bring psychedelics into the mainstream of mental health care. An FDA rejection of MDMA, the abbreviation of the drug's chemical name, would deal a major setback to the effort.
Clinical trials have inspired optimism in the drug for its potential to help the millions of Americans who experience PTSD. Accounts from some of those who've participated in the trials describe the treatment as transformational.
But new and troubling questions about this research are now threatening to upset the final stretch in the drug's path to market.
The allegations surfaced in a draft report released in March by the Institute for Clinical and Economic Review , a nonprofit that evaluates clinical trials and drug prices, which found "substantial concerns about the validity of the results" of the MDMA clinical trials.
The ICER report was followed in April by a citizen petition to the FDA. In that document, a group of concerned people allege possible misconduct and ethical violations that could compromise the MDMA research. The petition asked the agency to hold a public meeting to address the concerns.
If true, the claims could jeopardize the drug's chances of receiving FDA approval, a decision that is expected to come by early August .
"There's the possibility that the data might not be representative of what's actually happened in clinical trials," says Neşe Devenot , one of the authors of the citizen petition and a senior lecturer in the writing program at Johns Hopkins University who is involved in psychedelic research. "I don't think this has been publicly reckoned with."
That may soon happen. The FDA announced Thursday that it plans to hold a public advisory committee meeting on MDMA-assisted therapy on June 4.
At the heart of the controversy are the organizations that have pioneered research into MDMA: the Multidisciplinary Association for Psychedelic Studies , and the public benefit corporation incubated by MAPS, which was recently rebranded as Lykos Therapeutics .
Lykos sponsored the clinical trials of MDMA. The results are included in the company's application to the FDA seeking approval to market the drug for therapy-assisted PTSD treatment.
Researchers and clinicians involved in the trials have pushed back strongly against the accusations that their clinical data isn't sound.
Jennifer Mitchell , lead author of the published papers from the Phase 3 trials, says she stands behind their findings.
"I didn't feel any pressure from the sponsor to come up with anything different than what the data was providing," says Mitchell, a professor of neurology and psychiatry at the University of California, San Francisco and associate chief of staff for research at the San Francisco VA Medical Center. "I wouldn't have continued to work with them if I had felt that."
Promising MDMA research for PTSD
The Phase 3 trials evaluated MDMA-assisted therapy, a protocol in which the drug is given under the supervision of two therapists.
In the second stage of the trials , 94 people with moderate and severe PTSD received either the drug or a placebo during three sessions, each spaced a month apart. There were also follow up "integration" sessions to help people process their experiences while on MDMA.
By the end of the trial, about 71% of participants in the MDMA arm no longer met the diagnostic criteria for PTSD, compared to about 48% who underwent the same therapy but took a placebo instead. Those findings built on promising results from earlier studies .
The study documented various adverse events in both groups — ranging from nausea and anxiety to heart palpitations — but none of them qualified as serious. The treatment was "generally well tolerated."
"Consistent with PTSD, suicidal ideation was observed in both groups," the authors reported in the journal Nature Medicine , "MDMA did not appear to increase this risk, and no suicidal behavior was observed."
Casey Tylek, a participant in the Phase 3 trials, says he had no experience with the drug prior to the study.
Tylek was in the placebo group, but was later given the opportunity to undergo the therapy with MDMA.
"It was incredibly powerful," says Tylek, a veteran who lives in Massachusetts, "I truly don't know if I would be alive today if I hadn't gone through that trial."
ICER report raises concerns
In its report , ICER acknowledges that the MDMA data suggest it would be an "important addition to treatment options for PTSD," but it questions whether the published findings tell the full story.
Among the concerns, the ICER report details a well-known challenge in psychedelic research around how to make sure study participants don't know if they got the experimental treatment or a placebo. Most of those in the MDMA group were able to identify they had received the drug. It also suggests the method used to assess PTSD — considered the gold-standard — showed improvements in symptoms after the treatment, even though some people were worse overall.
Beyond that, however, the report brings up the possibility that "very strong prior beliefs" among therapists, investigators and patients influenced the results.
"Concerns have been raised by some that therapists encouraged favorable reports by patients and discouraged negative reports by patients including discouraging reports of substantial harms, potentially biasing the recording of benefits and harms," the report states.
ICER does not identify the sources who were interviewed, although it did include two trial participants, a "trial therapist" and those who worked on a podcast called Cover Story , says Dr. David Rind , the chief medical officer for ICER.
"This was a very unusual review," says Rind.
The podcast, produced by New York Magazine and the nonprofit media organization Psymposia , brought to light claims by a participant named Meaghan Buisson, who appeared in a video of two therapists , a married couple, engaged in what Buisson described as inappropriate physical contact while she was under the influence of MDMA at a Phase 2 trial site in Canada.

Enlighten Me with Rachel Martin
This psychedelics researcher approached his death with calm and curiosity.
MAPS determined the therapists "substantially deviated" from the treatment manual. The organization also barred the two therapists from becoming providers of MDMA-assisted therapy in affiliation with MAPS, and health authorities were notified in Canada and the U.S.
The podcast also interviewed two people (their full names were not revealed) who said they received MDMA in the large-scale, or Phase 3, trials and experienced feelings of suicidality and other distress after the studies.
The ICER report is yet to be finalized, but Rind says their analysis showed "there's still a lot of uncertainty" about the treatment.
"You have a group of people who are very upset about how these trials went," he says. "We couldn't tell, even though we talked with people where this happened, whether that represents a tiny fraction of bad events or a number of bad events large enough to have rendered the trial just not believable."
Pushback against the allegations
According to Rind, MAPS and Lykos had "very little" engagement with ICER on the draft report.
But since then, a group of more than 70 clinicians, investigators and others involved in the Phase 3 MDMA trials have published a detailed response , saying that certain aspects of the trials were "misrepresented" and that a number of assertions amount to "hearsay."
Willa Hall , a clinical psychologist in the Phase 3 trials, says she and her colleagues were shocked by how ICER described their work.
"I didn't recognize the study that they were talking about," Hall told NPR. "I think a lot of us felt quite insulted actually by that characterization. I saw nothing like that. I only saw professionalism ."
In their response, Hall and her colleagues write that "[ICER] does not note the many measures taken to train, support, and evaluate therapists on those trials—measures that met, and in some cases exceeded, the accepted standards in the field of psychotherapy research."
They also take issue with ICER relying on "a small number of undisclosed study participants and unnamed 'experts' rather than validated research outcomes." The critiques that participants knew they received the treatment or that the measure of PTSD symptoms might not capture someone's overall condition would also apply to other clinical trials, unrelated to MDMA, they say.
UCSF's Jennifer Mitchell says the clinical trial was designed to safeguard against bias.
Therapists on site were not collecting key data from participants about their PTSD symptoms following the sessions. Instead, that was being done online by "independent assessors" who didn't know who had received the treatment or a placebo.
Hall says therapists "meticulously" captured any adverse events. "We encouraged our participants to be very honest," she says. "We're all invested in knowing how it works and what are the risks for people."
Still, Mitchell acknowledges she doesn't have full insight into what was going on at each trial site on a given day.
"This is my own frustration," she says. "I can't attest to what was happening at one of the sites in Israel on a day to day basis, or on one of the sites in Canada."
But she contends that ICER tried to conduct an investigation without access to the full data.
Luminous: A Series About Psychedelics from 'To The Best Of Our Knowledge'
The FDA granted MDMA "breakthrough therapy" status, she says, which means the agency was involved in the study design and "many aspects" of the trial.
"So there's no keeping things from the FDA," Mitchell says.
The ICER report points out that therapists and participants in the study were "pulled heavily from the existing community of those interested and involved in the use of psychedelics for possible psychological benefits."
For her part though, Mitchell says she's not what some would call a "true believer."
"My personal feeling is that psychedelics are complicated compounds and they do not work for everyone," she says.
Petition adds to controversy ahead of the FDA meeting
On the heels of the ICER report, Neşe Devenot and four others, including Meaghan Buisson, submitted the citizen petition to the FDA calling for a public advisory meeting about the Lykos' application for MDMA.
In it, they ask for extended time for stakeholders who are concerned about the "risks and shortcomings" of the research.
"Evidence from multiple sources indicates that the sponsor has engaged in a pattern of systematic and deliberate omission of adverse events from the public record while minimizing documented harms," the petition states.
It continues: "We cannot rule out the possibility that MAPS/Lykos manipulated clinical trial data to hide adverse events from regulatory agencies."
The petition cites media reports and public statements from figures at Lykos and MAPS — and disclosures from a former employee of the MAPS public benefit corporation "who prefers to maintain anonymity at this juncture."
In addition, the petition alleges that clinical trial investigators would phone MAPS in the event of an incident during the trial to see whether that should be reported as an adverse event and that a suicide attempt during a dosing session was discouraged from being reported.
In an email to NPR, a spokesperson for MAPS rejects the claim.
It's not clear if the FDA's decision to hold a meeting was influenced by Devenot's petition, which has over 80 signatures .
Alaina Jaster , who has a doctorate in pharmacology and toxicology, is another author of the petition.
"We need to listen to people [in the trials] who are having these experiences, instead of telling them that they are liars and that they're going to ruin the psychedelic renaissance," says Jaster who hosts a podcast on psychedelics.
"None of us are against this as a useful tool, or none of us are against treating mental health. We don't have any monetary interests in this not going through," she says.
Neşe Devenot and Brian Pace, another author of the petition, are affiliated with Psymposia , the media organization that produced the podcast, but Devenot says they were not involved in the podcast and are unpaid board members.
In response to the petition's call for a public meeting, a spokesperson for Lykos sent NPR a statement in April saying the company supports holding an advisory meeting. "The voice of the PTSD patient is incredibly important," the email reads.

Shots - Health News
Psychedelic drugs may launch a new era in psychiatric treatment, brain scientists say.
MAPS "remains fully supportive of comprehensive, high-quality research; careful analysis of safety and efficacy; and stringent regulatory oversight of any psychedelic-assisted therapy research or delivery," according to the statement it also sent to NPR in April. "We stand behind Lykos' execution of the clinical program and support the clinical results."
One of those who signed the petition after seeing it posted online is Dr. Boris Heifets , an anesthesiologist at Stanford University whose lab studies psychedelics, including MDMA.
"I don't know if the allegations are true, it just makes me deeply sad if there was actually malfeasance for such an important trial," says Heifets. "The MDMA Phase 3 trials were very important for mental health, important for a lot of people who may benefit from this therapy."
Learning about MAPS several decades ago was, in part, what inspired Heifets to get involved in this type of research.
He says he donates $100 a year to MAPS and that they have supplied his lab with MDMA. He also consults for one company that's developing a derivative of MDMA.
Heifets says the petition contains some "very strong allegations," particularly the claim that certain adverse events were not disclosed.
"I want to hear MAPS respond," he says. " I would really like to understand the risk profile of this drug before it's approved, not after."
- psychedelic drugs
- psychedelics
- clinical trials
- mdma therapy

SPH Researchers Hold Symposium on Energy Systems and Health

Usman Iqbal Selected as 2024 Convocation Alumni Speaker
Sph researchers hold symposium on energy systems and health ..

From left: Jonathan Buonocore, Finlan Mooney, Mary Willis, Breanna Van Loenen, and Brian Sousa at the Power & People Symposium on May 7. Photo: Molly Potter
With support from the School of Public Health and BU’s Institute for Global Sustainability, Jonathan Buonocore and Mary Willis spearheaded the symposium to share with stakeholders their latest research project, a first-of-its-kind database mapping community exposure to energy infrastructure.
Megan jones.
Early analysis of a first-of-its-kind database developed by researchers at the School of Public Health suggests that 91% of census tracts in the United States are close enough to energy infrastructure to warrant consideration of potential adverse health effects.
“There is mounting evidence that living nearby oil and gas infrastructure can be harmful to health, but there is not a single resource showing all the infrastructure, from the well to the compressor to the pipeline, that then also includes the characteristics of the communities living nearby,” says Jonathan Buonocore , an assistant professor of environmental health and a co-principal investigator on the project, The Energy Infrastructure Exposure Intensity and Equity Indices (EI3) Database for Population Health , with Mary Willis , assistant professor of epidemiology. “The information could be used to help usher in a healthy and just energy transition.”
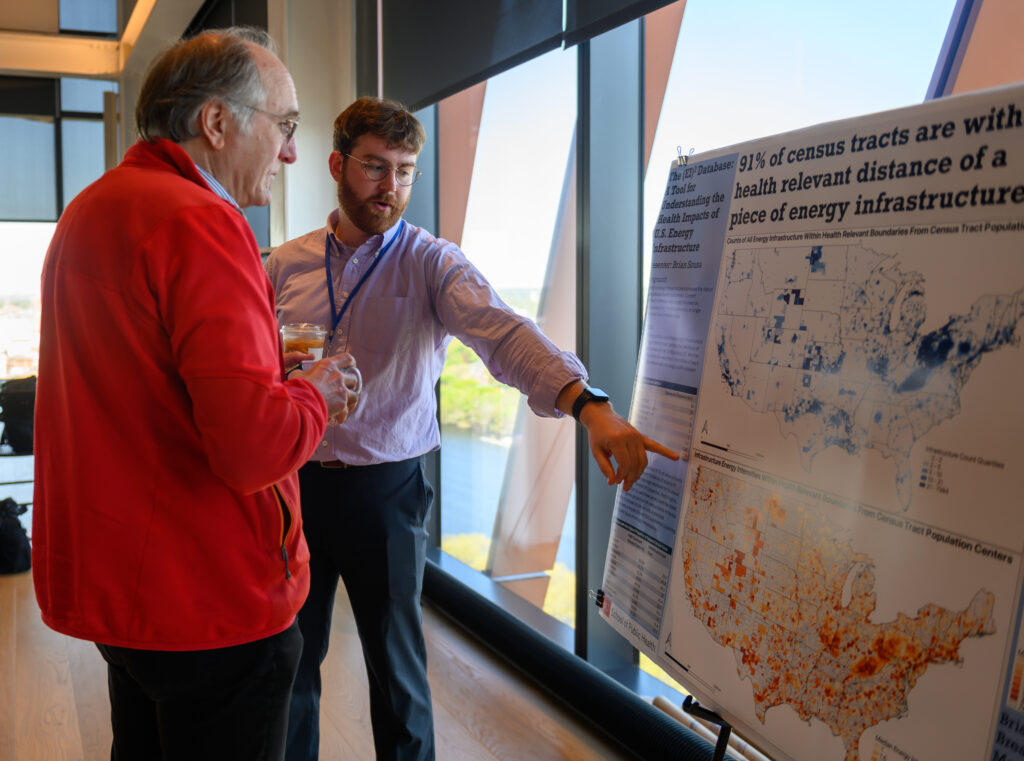
Constructed in a piecemeal fashion as the U.S. rapidly grew and industrialized over the past century, today’s energy infrastructure is a patchwork of millions of components scattered throughout the country. Data on the locations of these components is often available, says Buonocore, but because jurisdiction over energy infrastructure is divided among various government agencies, it can be challenging for communities to access or interpret.
“All the data underlying the [EI3] dataset is public, but this will be the first time it is all in the same place,” he says. Buonocore has previously used geographic data to link oil and gas production to $7.4 billion in annual health damages , including thousands of early deaths and childhood asthma cases largely in surrounding communities, but also in downwind urban centers. “We are hoping that [the dataset] could be used by researchers, policymakers, NGOs, and community groups to really understand what energy infrastructure is near them and the effect that it is having on the community, to then, hopefully, influence the equitable siting of future energy infrastructure.”
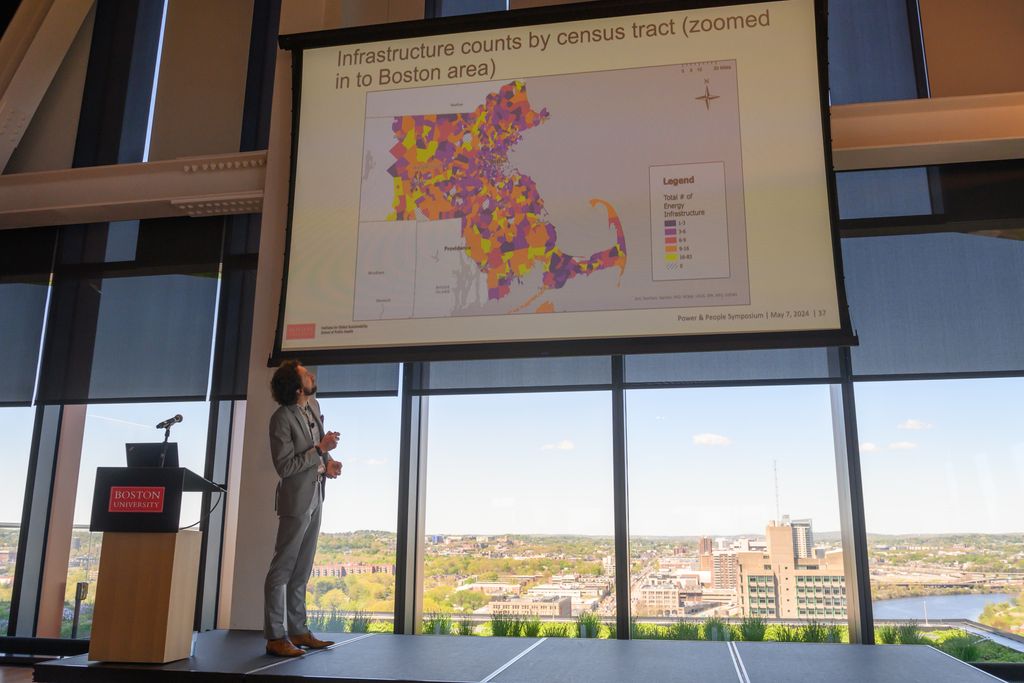
On May 7, Bounocore and Willis spearheaded a symposium, People & Power: Mapping Community Exposure to Energy Infrastructure, to present preliminary insights from and solicit external input on the developing database. The day-long event was hosted in BU’s new Center for Computing and Data Sciences, which, suitably, is the greenest building in BU’s history and one of the most sustainable buildings in the region.
The Boston University Institute for Global Sustainability (IGS), in partnership with SPH, awarded the Buonocore and Willis its first-ever Sustainability Research Grant to fund the establishment of the EI3 database. With the support of Brian Sousa , Breanna Van Loenen , and Fintan Mooney , research data analysts at SPH, as well as faculty and student collaborators in BU’s Earth and Environment Department, the team recently finished entering the locations of active oil, gas, coal, and electrical infrastructure to the database.

“We are still in the information-gathering stage,” noted Willis. Ultimately, the team intends to add a measure of the intensity of exposure and link that to health outcomes using epidemiologic methods, laying the groundwork for future study in areas such as the health impacts of infrastructure hotspots on environmental justice communities and the climate and health co-benefits of clean energy programs.
“But first, we need to show who lives nearby [the infrastructure] because that [relationship] does not currently exist,” says Willis.
During his introductory remarks to the symposium, Dean Sandro Galea highlighted the “enormous potential” of the EI3 database, a sentiment echoed throughout the day by various other speakers and panelists.
“The way we connect is by talking about our families and talking about health—everybody cares about health,” said panelist Andee Krasner of her volunteer work with Mothers Out Front , a national organization that brings together local teams of mothers and other community members to campaign for climate justice at the local and state levels. “Making that connection between energy infrastructure and health will really help us as advocates.”

Altogether, the speakers and attendees represented more than 20 different organizations engaged in the energy sector, ranging from national nonprofits and local grassroots organizations to state and local government agencies, such as the National Resources Defense Council , Environmental Defense Fund , GreenRoots , HEET (Home Energy Efficiency Team), Massachusetts Department of Environmental Protection , and Boston Housing Authority .
The presentation materials from the People & Power symposium, with an introduction to the fledgling EI3 database, are now publicly available on the IGS website . In the future, the research team hopes to make the full database freely available online as well. They are actively seeking additional funding to sustain and advance the promising—and following the symposium, much-anticipated—project.
Explore Related Topics:
- climate and health
- energy systems
- Environmental Health
- environmental justice
- epidemiology
- school news
- Share this story
- 0 Comments Add
Writer/Editor, School News

Megan Jones is the writer and editor focusing on school news at the School of Public Health. Profile
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
Assistant Professor Named Kavli Fellow For Public Health Research On Vulnerable Populations

Benika Dixon , an assistant professor at Texas A&M University School of Public Health , has been named a Kavli Fellow . This prestigious fellowship, awarded annually by the National Academy of Sciences (NAS), recognizes the brightest young scientists who are 45 years old or younger.
More than 6,200 young scientists — including social scientists — have participated since the program’s founding in 1989. Of these Kavli Fellows, 323 have been elected to the NAS and 18 have been awarded the Nobel Prize.
The Fellows, who work in industry, academia and government from a variety of disciplines, have the opportunity to participate in the U.S. and International Kavli Frontiers of Science symposia organized by NAS. Dixon participated recently in the U.S. Kavli Frontiers of Science symposium in California, where she made a presentation titled, “Climate, Disasters and Incarceration: Voices of the Unheard.” She also learned about other fellows’ research and sought out collaborative possibilities.
Giving everyone a voice
Dixon, who grew up in Hartford, Connecticut, began working in health care and nonprofit organizations after earning a bachelor’s degree in chemistry from Spelman College and a master’s degree in public health from Southern Connecticut State University.
She discovered her passion for public health emergency preparedness after moving to the Washington, D.C./Maryland/Virginia area where she assisted elected officials with emergency planning and response.
“I felt oftentimes that the people and the voices at the table weren’t reflective of the communities we served,” Dixon said. “I really wanted to find a way to impact communities that looked like communities I grew up in. I wanted to be a part of helping communities determine what they deemed best for themselves and not have others speaking for them.”
After working for both Baltimore City Health and Austin Public Health as a disaster epidemiologist, Dixon decided to pursue her doctorate, which led her to enroll at the Texas A&M School of Public Health. After graduating, she joined the school’s faculty and focused her research on the mental and physical health implications of environmental exposures, hazards and disasters on vulnerable populations.
“When I say ‘vulnerable populations,’ a lot of my work has been done in environmental justice communities such as the those in the Houston Ship Channel and Houston’s Fifth Ward,” she said.
This focus on vulnerable populations also led Dixon to collaborate with Carlee Purdum from the Texas A&M School of Architecture to start the Prisons, Disasters and Public Health research initiative. Dixon noted that her current work focuses specifically on State of Texas prisons because — unlike federal and county facilities — many of these prisons do not have air conditioning.
“When we’re experiencing 100-plus-degree temperatures, oftentimes we have access to resources such as air conditioning or clean drinking water,” Dixon said. “In comparison, incarcerated individuals may not have access to air conditioning, and they may not have access to resources such as clean water or a place for respite to cool off.”
The researchers’ focus on the effects of extreme temperatures on the mental and physical health of incarcerated individuals led them to develop a partnership with Lioness Justice Impacted Women’s Alliance, an organization led by currently and formerly incarcerated girls and women in Texas with the purpose of ending the incarceration and systematic devaluing experienced within the Texas criminal legal system.
Dixon and Purdum have expanded their work with Lioness to look at the mental health impact of disaster evacuation processes.
“Typically, we think of disasters as hurricanes, wildfires and tornadoes,” Dixon said. “But we’re learning that we have different daily disasters and crises that are happening, so we have to expand the definition of what a disaster looks like.”
These evacuation situations often cause mental stress. “Incarcerated individuals are often silenced or recriminalized in the process of being incarcerated and do not have a voice or any say about what happens to them in the midst of disasters,” Dixon said. “They may not know why or when they are being evacuated or where they are going, so there is an added level of fear and frustration of not knowing in those moments of disaster.”
Expanding her reach
The Kavli fellowship, which honors academics as well as practitioners, already is giving Dixon a wider network and new ideas on how she can extend her research.
“It’s a great opportunity to connect with academics who may look at my work with a different lens,” she said, noting that she met other fellows who were social epidemiologists, virologists and researchers working with climate modeling.
The fellowship also has extended Dixon’s understanding about the potential for her career.
“Being there that week just showed the opportunities that exist to collaborate and grow my work,” Dixon said. “It helped to really validate the work that I’m doing and the science that I’m doing. It really shows that there’s this great trajectory for my career — and there are others out there who are trying to be innovative and create cutting-edge science.”
This article by Dorian Martin originally appeared on Vital Record .
Related Stories

Freestanding Emergency Departments Are Popular, But Do They Function As Intended?
School of Public Health study is the first of its kind to compare characteristics of visits among all emergency department types

Study Finds ‘Digital Humans’ Equally Effective As Real Ones In Ergonomics Training
School of Public Health research shows promising results for virtual training's impact on remote workers' health and behavior.

Monitoring Your Own Blood Pressure Can Save Money — And Possibly Your Life
Study finds self-monitoring of blood pressure has the potential for better health outcomes and cost benefits compared to traditional care.
Recent Stories

Medal Of Honor Recipient, Former Student Dies At 76
Clarence E. Sasser, a Brazoria County native and distinguished veteran of the Vietnam War, earned the nation’s highest military honor in 1969 before studying chemistry at Texas A&M.

Top Barbecue Tips From The ‘Three Brisketeers’
Texas A&M AgriLife experts share four tidbits every barbecue lover should know.

Welch Foundation, Jon Hagler Commit $15 Million To Texas A&M Foundation
The funding aims to bring leading chemistry scholars to Texas A&M University’s Hagler Institute for Advanced Study.

Subscribe to the Texas A&M Today newsletter for the latest news and stories every week.
- Share full article
Advertisement
Supported by
Are We Talking Too Much About Mental Health?
Recent studies cast doubt on whether large-scale mental health interventions are making young people better. Some even suggest they can have a negative effect.

By Ellen Barry
In recent years, mental health has become a central subject in childhood and adolescence. Teenagers narrate their psychiatric diagnosis and treatment on TikTok and Instagram. School systems, alarmed by rising levels of distress and self-harm, are introducing preventive coursework in emotional self-regulation and mindfulness.
Now, some researchers warn that we are in danger of overdoing it. Mental health awareness campaigns, they argue, help some young people identify disorders that badly need treatment — but they have a negative effect on others, leading them to over-interpret their symptoms and see themselves as more troubled than they are.
The researchers point to unexpected results in trials of school-based mental health interventions in the United Kingdom and Australia: Students who underwent training in the basics of mindfulness , cognitive behavioral therapy and dialectical behavior therapy did not emerge healthier than peers who did not participate, and some were worse off, at least for a while.
And new research from the United States shows that among young people, “self-labeling” as having depression or anxiety is associated with poor coping skills, like avoidance or rumination.
In a paper published last year , two research psychologists at the University of Oxford, Lucy Foulkes and Jack Andrews, coined the term “prevalence inflation” — driven by the reporting of mild or transient symptoms as mental health disorders — and suggested that awareness campaigns were contributing to it.
“It’s creating this message that teenagers are vulnerable, they’re likely to have problems, and the solution is to outsource them to a professional,” said Dr. Foulkes, a Prudence Trust Research Fellow in Oxford’s department of experimental psychology, who has written two books on mental health and adolescence.
Until high-quality research has clarified these unexpected negative effects, they argue, school systems should proceed cautiously with large-scale mental health interventions.
“It’s not that we need to go back to square one, but it’s that we need to press pause and reroute potentially,” Dr. Foulkes said. “It’s possible that something very well-intended has overshot a bit and needs to be brought back in.”
This remains a minority view among specialists in adolescent mental health, who mostly agree that the far more urgent problem is lack of access to treatment.
About 60 percent of young Americans with severe depression receive no treatment, according to Mental Health America, a nonprofit research group. In crisis, desperate families fall back on emergency rooms, where teens often remain for days before a psychiatric bed opens up. There is good reason to embrace a preventive approach, teaching schoolchildren basic skills that might forestall crises later, experts say.
Dr. Foulkes said she understood that her argument runs counter to that consensus, and when she began to present it, she braced for a backlash. To her surprise, she said, many educators reached out to express quiet agreement.
“There’s definitely a fear about being the one to say it,” she said.
A deflating result
In the summer of 2022, the results of a landmark study on mindfulness training in British classrooms landed — like a lead balloon.
The trial, My Resilience in Adolescence, or MYRIAD, was ambitious, meticulous and expansive, following about 28,000 teenagers over eight years. It had been launched in a glow of optimism that the practice would pay off, improving the students’ mental health outcomes in later years.
Half of the teenagers were trained by their teachers to direct their attention to the present moment — breathing, physical sensations or everyday activities — in 10 lessons of 30 to 50 minutes apiece.
The results were disappointing . The authors reported “no support for our hypothesis” that mindfulness training would improve students’ mental health. In fact, students at highest risk for mental health problems did somewhat worse after receiving the training, the authors concluded.
But by the end of the eight-year project, “mindfulness is already embedded in a lot of schools, and there are already organizations making money from selling this program to schools,” said Dr. Foulkes, who had assisted on the study as a postdoctoral research associate. “And it’s very difficult to get the scientific message out there.”
Why, one might ask, would a mental health program do harm?
Researchers in the study speculated that the training programs “bring awareness to upsetting thoughts,” encouraging students to sit with darker feelings, but without providing solutions, especially for societal problems like racism or poverty. They also found that the students didn’t enjoy the sessions and didn’t practice at home.
Another explanation is that mindfulness training could encourage “co-rumination,” the kind of long, unresolved group discussion that churns up problems without finding solutions.
As the MYRIAD results were being analyzed, Dr. Andrews led an evaluation of Climate Schools, an Australian intervention based on the principles of cognitive behavioral therapy, in which students observed cartoon characters navigating mental health concerns and then answered questions about practices to improve mental health.
Here, too, he found negative effects. Students who had taken the course reported higher levels of depression and anxiety symptoms six months and 12 months later.
Co-rumination appears to be higher in girls, who tend to come into the program more distressed, as well as more attuned to their friends, he said. “It might be,” he said, “that they kind of get together and make things a little bit worse for each other.”
Dr. Andrews, a Wellcome Trust research fellow, has since joined an effort to improve Climate Schools by addressing negative effects. And he has concluded that schools should slow down until “we know the evidence base a bit more.” Sometimes, he said, “doing nothing is better than doing something.”
The awareness paradox
One problem with mental health awareness, some research suggests, is that it may not help to put a label to your symptoms.
Isaac Ahuvia, a doctoral candidate at Stony Brook University, recently tested this in a study of 1,423 college students . Twenty-two percent “self-labeled” as having depression, telling researchers “I am depressed” or “I have depression,” but 39 percent met the diagnostic criteria for depression.
He found that the students who self-labeled felt that they had less control over depression and were more likely to catastrophize and less likely to respond to distress by putting their difficulties in perspective, compared with peers who had similar depression symptoms.
Jessica L. Schleider, a co-author of the self-labeling study, said this was no surprise. People who self-label “appear to be viewing depression as a biological inevitability,” she said. “People who don’t view emotions as malleable, view them as set and stuck and uncontrollable, tend to cope less well because they don’t see a point to trying.”
But Dr. Schleider, an associate professor of medical social sciences at Northwestern University and the director of the university’s Lab for Scalable Mental Health, pushed back on the prevalence inflation hypothesis. She disagreed with the claim that students are overdiagnosing themselves, noting that Mr. Ahuvia’s findings suggest otherwise.
Awareness campaigns are bound to have multiple effects, helping some students and not others. And ultimately, she argued, the priority for public health should be reaching young people in the most distress.
“The urgency of the mental health crisis is so clear,” she said. “In the partnerships that I have, the emphasis is on the kids truly struggling right now who have nothing — we need to help them — more so than a possible risk for a subset of kids who aren’t really struggling.”
Maybe, she said, we need to look beyond the “universal, school-assembly-style approach,” to targeted, light-touch interventions, which research has shown can be effective at decreasing anxiety and conduct disorders, especially in younger children.
“There is a risk of throwing the baby out with the bathwater,” Dr. Schleider said. “The response can’t be ‘Forget all of it.’ It should be ‘What about this intervention was unhelpful?’”
Other researchers echoed her concern, pointing to studies that show that on average, students benefit from social and emotional learning courses.
One of the largest, a 2023 meta-analysis of 252 classroom programs in 53 countries, found that students who participated performed better academically, displayed better social skills and had lower levels of emotional distress or behavioral problems. In that context, negative effects in a handful of trials appear modest, the researchers said.
“We clearly have not figured out how to do them yet, but I can’t imagine any population-based intervention that the field got right the first time,” said Dr. Andrew J. Gerber, the president and medical director of Silver Hill Hospital and a practicing child and adolescent psychiatrist.
“Really, if you think about almost everything we do in schools, we don’t have great evidence for it working,” he added. “That doesn’t mean we don’t do it. It just means that we’re constantly thinking about ways to improve it.”
‘We want everyone to have it’
These debates are taking place a long way away from classrooms, where mental health curriculums are increasingly commonplace.
Allyson Kangisser, a counselor at Woodsdale Elementary School in Wheeling, W.Va., said the focus in her school is on basic coping skills. In the early grades, students are asked, “What things can you do to take care of yourself when you’re having big feelings?”
Starting in third grade, they take on more complex material, such as watching cartoon characters to distinguish transient stress from chronic conditions like depression. “We’re not trying to have them diagnose themselves,” Ms. Kangisser said. “We are saying, what do you feel — this one? Or this one?”
At the school’s sixth annual mental health fair last month, Woodsdale students walked through a giant inflatable brain, its lobes neatly labeled. They did yoga stretches and talked about regulating their emotions. Ms. Kangisser said the event is valuable precisely because it is universal, so troubled children are not singled out.
“The mental health fair, everybody does it,” she said. “It’s not ‘You need it, and you don’t.’ We want everyone to have it, because you just never know.”
By the time the students reach college, they will have absorbed enormous amounts of information about mental health — from school, but also from social media and from one another.
Dr. Jessica Gold, chief wellness officer for the University of Tennessee system, said the college students she sees are recognizably different — more comfortable speaking about their emotions and more willing to be vulnerable. They also overuse diagnostic terms and have the self-assurance to question a psychiatrist’s judgment.
“It’s sort of a double-edged sword,” she said. “We want people to talk about this more, but we don’t want that to lead to overdiagnosis or incorrect diagnosis or overtreatment. We want it to lead to normalizing of having feelings.”
Lucy Kim, a Yale senior who has lobbied for better mental health support on campus, described the prevalence inflation hypothesis as “disheartening, dismissive and potentially dangerous,” providing another way to discount the experiences of young people.
“As a college student, I see a generation of young people around me impacted by a depth and breadth of loneliness, exhaustion and disillusionment suggestive of a malaise that goes deeper than the general vicissitudes of life,” said Ms. Kim, 23.
Overdiagnosis does happen, she said, and so does glorification of mental health disorders. But stigma and barriers to treatment remain the bigger problem. “I can confidently say I have never heard anyone respond to disclosures of depression with ‘That’s so cool, I wish I had that, too,’” she said.
Ellen Barry is a reporter covering mental health for The Times. More about Ellen Barry
Managing Anxiety and Stress
Stay balanced in the face of stress and anxiety with our collection of tools and advice..
How are you, really? This self-guided check-in will help you take stock of your emotional well-being — and learn how to make changes .
These simple and proven strategies will help you manage stress , support your mental health and find meaning in the new year.
First, bring calm and clarity into your life with these 10 tips . Next, identify what you are dealing with: Is it worry, anxiety or stress ?
Persistent depressive disorder is underdiagnosed, and many who suffer from it have never heard of it. Here is what to know .
New research suggests people tend to be lonelier in young adulthood and late life. But experts say it doesn’t have to be that way .
How much anxiety is too much? Here is how to establish whether you should see a professional about it .
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Cannabis
- Health Effects
- Cannabis FAQs
- Facts and Stats
- Journal Articles
- MMWR Articles
- Related Websites
Cannabis Facts and Stats
At a glance.
A variety of information sources are available to monitor the prevalence and trends of cannabis use in the United States. The resources below cover cannabis-related issues, including data around use, emergency department visits, substance use and misuse, policy measures, and other related tools.
- Cannabis is the most commonly used federally illegal drug in the United States; 52.5 million people, or about 19% of Americans, used it at least once in 2021. 1
- Recent research estimated that approximately 3 in 10 people who use cannabis have cannabis use disorder. 2
- The risk of developing cannabis use disorder is even greater for people who begin to use it before age 18. 3
- Cannabis use directly affects the parts of the brain responsible for memory, learning, attention, decision-making, coordination, emotion, and reaction time. 4 5
- Infants, children, and teens (who still have developing brains) are especially susceptible to the adverse effects of cannabis. 4 5
- Long-term or frequent cannabis use has been linked to increased risk of psychosis or schizophrenia in some users. 6
- Using cannabis during pregnancy may increase the person's risk for pregnancy complications. Pregnant and breastfeeding persons should avoid cannabis. 7
National Surveys That Collect Information About Cannabis Use
Cdc sponsored surveys.
Behavioral Risk Factor Surveillance System (BRFSS)
World's largest, continuously conducted telephone survey that tracks health behaviors, chronic diseases, and preventive health practices among noninstitutionalized adults in the United States.
Youth Risk Behavior Surveillance System (YRBSS)
Monitors six categories of priority health risk behaviors, including cannabis use, among high school youth at national, state, and local levels.
Pregnancy Risk Assessment Monitoring System (PRAMS)
Collects state-specific, population-based data on cannabis use before, during, and shortly after pregnancy.
National Health and Nutrition Examination Survey (NHANES)
Assesses the health and nutritional status of adults and children, aged 12 years and older, in the United States. The survey is unique in that it combines interviews and physical examinations. Voluntary drug use questions ask lifetime cannabis use, age of first use, age when starting to use cannabis regularly, amount used, frequency of use, and time since last use. These data are available from 2005-2007 survey period onward.
Other National Surveys
National Survey on Drug Use and Health (NSDUH)
Ongoing and long-term system, sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA) NSDUH is the primary source of information on the prevalence, patterns, and consequences of alcohol, tobacco, and illegal drug use and abuse in the general U.S. civilian noninstitutionalized population, ages 12 and older.
Monitoring the Future Survey
Ongoing and long-term system, sponsored by the National Institute on Drug Abuse (NIDA) that collects data on the behaviors, attitudes, and values regarding substance use of American teens, college students, and adults. Each year a total of approximately 50,000 students in 8th, 10th, and 12th grades are surveyed about substance use, including cannabis, and a subset are sent follow-up questionnaires through age 45 years.
National Drug Early Warning System (NDEWS)
NDEWS monitors drug use trends in 12 sentinel communities across the United States. Sentinel Site profiles describing drug abuse trends and emerging issues are available on NDEWS website.
National Programs That Collect Information About Cannabis Policies
Alcohol Policy Information System (APIS)
A policy monitoring system sponsored by the National Institute on Alcohol Abuse and Alcoholism (NIAA) that provides detailed information on a wide variety of alcohol-related policies in the United States at both state and federal levels. The system was expanded in 2016 to include policies related to legalizing the cultivation, sale, or use of cannabis for prohibitions and restrictions on such practices.
State Cannabis Policy Enactment Database
A policy monitoring system sponsored by the National Conference of State Legislatures that provides up-to-date information on cannabis legislation that has been enacted in the 50 states, District of Columbia, and its territories. The database is sortable by state, topic, keyword, and primary sponsor.
- Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health (HHS Publication No. PEP22-07-01-005, NSDUH Series H-57). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. 2022. https://www.samhsa.gov/data/report/2021-nsduh-annual-national-report . Accessed on February 9, 2024.
- Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015 Dec;72(12):1235-1242. doi: 10.1001/jamapsychiatry.2015.1858.
- Winters KC, Lee C-YS. Likelihood of developing an alcohol and cannabis use disorder during youth: Association with recent use and age. Drug Alcohol Depend. 2008;92(1-3):239-247. doi: 10.1016/j.drugalcdep.2007.08.005.
- National Academies of Sciences, Engineering, and Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, DC: The National Academies Press; 2017. https://nap.nationalacademies.org/catalog/24625/the-health-effects-of-cannabis-and-cannabinoids-the-current-state. Accessed February 8, 2024.
- Giedd JN. The teen brain: Insights from neuroimaging. J Adolesc Health. 2008;42(4):335–343. doi: 10.1016/j.jadohealth.2008.01.007.
- Volkow ND, Swanson JM, Evins AE, et al. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: A review. JAMA Psychiatry. 2016 Mar;73(3):292-297. doi: 10.1001/jamapsychiatry.2015.3278.
- Ryan SA, Ammerman SD, O’Connor ME, et al. Marijuana use during pregnancy and breastfeeding: Implications for neonatal and childhood outcomes. Pediatrics. 2018;142(3):e20181889. doi: 10.1542/peds.2018-1889.
Cannabis and Public Health
Cannabis—which can also be called marijuana —is the most commonly used federally illegal drug in the United States.
- International edition
- Australia edition
- Europe edition

Public health expert lambasts UK government as fund to tackle inequality launches
Sir Michael Marmot wants cuts reversed as fund backed by L&G and his research institute opens to support local initiatives
One of the UK’s leading public health experts has attacked the Conservative government’s record on health inequality, expressing hope that the next government will “take the right steps” to tackle the problem.
Speaking as he launches a fund to tackle the link between economic deprivation and poor health, Sir Michael Marmot said he had been snubbed by the current government and wanted to see cuts to education and public services reversed.
Marmot authored a seminal 2010 review into the link between health and wealth, which found that people in more deprived areas had shorter life expectancies. Since that report, the UK has got worse on many measures including life expectancy, child poverty and long-term sickness.
The latest study by the Institute of Health Equity at University College London, which Marmot leads, has found that more than 1 million people in England died prematurely in the decade after 2011 owing to a combination of poverty, austerity and Covid.
A Unicef report found that the UK had the biggest increase in child poverty between 2010 and 2020 out of the world’s wealthiest nations, the 39 Organisation for Economic Co-operation and Development countries.
Marmot told the Guardian: “I’d like to see reductions in child poverty … improvement in our public services, reverse the cuts to education. The cuts to education over the decade from 2010 to 2020 were 8% per pupil.
“Why would you do that as a country? The cuts were more extreme in deprived areas than in non-deprived areas. I’d like to see all that change.”
He said he found Labour and the Liberal Democrats more responsive than the current government to the idea of tackling the social conditions that are the main causes of health inequalities.
“I’ve been more than happy to talk to the present government. They haven’t been very happy to talk to me … Let’s hope another government will want to take the right steps.” He noted that Labour’s health mission talked of “making England a Marmot country, tackling the social inequalities that influence health”.
There are nine “Marmot places” – where action is being taken to improve health and reduce health inequalities – across England and Wales including Coventry, Manchester, Leeds, Luton and Gwent. More than 40 local authorities have said they want to reduce health inequalities .

The Institute of Health Equity has set up a £3m health equity fund with the investment group Legal & General (L&G).
after newsletter promotion
The fund, which opens for expressions of interest on 4 June, will support local initiatives to improve housing, education, employment and nutrition. It will finance up to 150 initiatives across the UK, up to £75,000 for each project. Projects could range from funding for schools in deprived areas to community programmes that address the social factors behind pressures on A&E services.
“This fund from Legal & General is a very positive initiative but it’s not going to reverse billions of pounds of cuts,” Marmot said. “We are realistic about that. If you’ve cut funding spending to local government by 34% over the decade, it’s not going to level up by itself but I hope to bring initiatives bubbling up, that scaled up could make a huge difference.”
The first tranche of money, £1m, is going to north-east England where, Marmot said, life expectancy had got shorter and inequalities bigger since 2010. “We’re not going to reverse the mass deindustrialisation of the 1980s … but trying to take initiatives locally, that may reverse some of that damage,” he said.
L&G and the institute have worked together since 2021 and argue that better health will also yield economic benefits such as increased productivity. They are talking to housebuilders and other companies that may want to become involved in the initiative.
Marmot said: “We want to encourage local initiatives, not to let central government off the hook, but to say, what can we do? What can local people do to break the link between poverty, funding cuts and worse health outcomes?”
- Health policy
- Legal and General
- Conservatives
- UCL (University College London)
Most viewed

IMAGES
VIDEO
COMMENTS
Introduction. Public health is critical to a healthy, fair, and sustainable society. Public health's role in this vision stems from its foundational values of social justice and collectivity (Rutty and Sullivan 2010) and—we argue—from its position at the interface of research, practice, and policy.. Realizing this vision requires imagining a public health community that can maintain that ...
Public health is the medical discipline concerned with the prevention and control of disease through population surveillance and the promotion of healthy behaviours. Strategies used to promote ...
The Journal of Public Health Research is an online Open Access, peer-reviewed scholarly journal in the field of public health science. The aim of the journal is to stimulate debate and dissemination of knowledge in the public health field in order to improve efficacy, effectiveness and efficiency of public health interventions to improve health outcomes of populations.
Nichols et al. Tetzlaff et al. Read open access research, editorials, comments, and correspondence from The Lancet Public Health, which contribute to advancing public health practice and policy making worldwide.
Celebrating over 100 years, the American Journal of Public Health ( AJPH) is dedicated to publication of original work in research, research methods, and program evaluation in the field of public health. The Journal also regularly publishes editorials and commentaries and serves as a forum for health policy analysis.
To investigate the potential of embedded research in bridging the gap between research evidence and its implementation in public health practice. Abisope Akintola, Dorothy Newbury-Birch and Stephanie Kilinc. BMC Public Health 2024 24 :1299. Research Published on: 13 May 2024.
Fundamentals of Public Health: Using Policy Tools to Improve Population Health — Combating the U.S. Opioid Crisis. C.L. Barry and B. SalonerN Engl J Med 2021;385:2113-2116. Policy has been ...
BMC Public Health is an open access, peer-reviewed journal that considers articles on the epidemiology of disease and the understanding of all aspects of public health. The journal has a special focus on the social determinants of health, the environmental, behavioral, and occupational correlates of health and disease, and the impact of health policies, practices and interventions on the ...
PLOS Global Public Health is a global journal for public health research of the highest ethical and methodological rigor that reaches across disciplines and regional boundaries to address some of the biggest health challenges and inequities facing our society today. We will work alongside researchers to drive diversity and equity to broaden the ...
Research for Health: our role in the global public health research community. WHO's technical units are just one part of a global web of research for health, encompassing academia, national and regional research bodies, product development partnerships and the private sector. WHO helps to provide global guidance for research priority setting.
Victoria Haldane and colleagues argue that to make covid-19 the last pandemic, public health responses to outbreaks must be strengthened, starting with their most basic functions The covid-19 pandemic has challenged countries to mount and sustain comprehensive public health responses that identify and control an emerging infectious hazard. These challenges have persisted into 2021 and likely ...
Public-private partnerships and other innovative mechanisms for research are concentrating on neglected diseases in order to stimulate the development of vaccines, drugs and diagnostics where market forces alone are insufficient. Research for health spans 5 generic areas of activity: measuring the magnitude and distribution of the health problem;
Published since 1878, Public Health Reports® is the official journal of the Office of the U.S. Surgeon General and the U.S. Public Health Service. It is published bimonthly, plus supplement issues, through an official agreement with the Association of Schools and Programs of Public Health. The journal is peer-reviewed and publishes original ...
Systematic and rigorous inquiry allows us to discover the fundamental mechanisms and causes of disease and disparities. At our Office of Research (research@BSPH), we translate that knowledge to develop, evaluate, and disseminate treatment and prevention strategies and inform public health practice.Research along this entire spectrum represents a fundamental mission of the Johns Hopkins ...
International Journal of Environmental Research and Public Health is a transdisciplinary, peer-reviewed, open access journal published monthly online by MDPI.It covers Global Health, Healthcare Sciences, Behavioral and Mental Health, Infectious Diseases, Chronic Diseases and Disease Prevention, Exercise and Health Related Quality of Life, Environmental Health and Environmental Sciences.
For graduate students who are passionate about putting research and policy recommendations into action, the Johns Hopkins Health Policy Institute (HPI) is an invaluable experience. Among the Spring 2024 HPI Fellows is Glendedora Dolce, now in her second year as a Health and Public Policy doctoral student. Glendora's research aims to prevent ...
Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. Public health is the science of protecting and improving the health of populations—from neighborhoods to cities to countries to world regions—through education, promotion of healthy lifestyles, research toward prevention ...
Abstract. Having a scientific basis for the practice of public health is critical. Research leads to insight and innovations that solve health problems and is therefore central to public health worldwide. For example, in the United States research is one of the ten essential public health services (Public Health Functions Steering Committee 1994).
An overview of public health. Public health is the science and art of preventing disease, prolonging life and promoting human health through organized community efforts as well as the informed choice of society, public, private and voluntary organizations and communities at large. Analyzing the health of a population and the threats to that ...
NCI supports a diverse array of research that is helping to address issues in cancer-related public health. This research relies on extensive resources, often requires the participation of a large number of people, and can span many years. NCI plays an important role in public health research by conducting and funding large research studies and ...
Johns Hopkins Bloomberg School of Public Health. 615 N. Wolfe Street, Baltimore, MD 21205. Each year the Johns Hopkins Vaccine Initiative hosts Vaccine Day to highlight the advancements in vaccine research by inviting a distinguished scientist to deliver a keynote address on the current status of vaccine-related topics.
At the heart of the controversy are the organizations that have pioneered research into MDMA: the Multidisciplinary Association for Psychedelic Studies, and the public benefit corporation ...
With support from the School of Public Health and BU's Institute for Global Sustainability, Jonathan Buonocore and Mary Willis spearheaded the symposium to share with stakeholders their latest research project, a first-of-its-kind database mapping community exposure to energy infrastructure. May 15, 2024. Megan Jones.
News from Texas A&M University. Benika Dixon, an assistant professor at Texas A&M University School of Public Health, has been named a Kavli Fellow.This prestigious fellowship, awarded annually by the National Academy of Sciences (NAS), recognizes the brightest young scientists who are 45 years old or younger.
Lucy Foulkes, a research psychologist at the University of Oxford, wants school systems to proceed cautiously with large-scale mental health interventions. "It's possible that something very ...
Fast facts. Cannabis is the most commonly used federally illegal drug in the United States; 52.5 million people, or about 19% of Americans, used it at least once in 2021. 1. Recent research estimated that approximately 3 in 10 people who use cannabis have cannabis use disorder. 2. The risk of developing cannabis use disorder is even greater for ...
Sir Michael Marmot wants cuts reversed as fund backed by L&G and his research institute opens to support local initiatives One of the UK's leading public health experts has attacked the ...