REVIEW article
Environmental and health impacts of air pollution: a review.

- 1 Delphis S.A., Kifisia, Greece
- 2 Laboratory of Hygiene and Environmental Protection, Faculty of Medicine, Democritus University of Thrace, Alexandroupolis, Greece
- 3 Centre Hospitalier Universitaire Vaudois (CHUV), Service de Médicine Interne, Lausanne, Switzerland
- 4 School of Social and Political Sciences, University of Glasgow, Glasgow, United Kingdom
One of our era's greatest scourges is air pollution, on account not only of its impact on climate change but also its impact on public and individual health due to increasing morbidity and mortality. There are many pollutants that are major factors in disease in humans. Among them, Particulate Matter (PM), particles of variable but very small diameter, penetrate the respiratory system via inhalation, causing respiratory and cardiovascular diseases, reproductive and central nervous system dysfunctions, and cancer. Despite the fact that ozone in the stratosphere plays a protective role against ultraviolet irradiation, it is harmful when in high concentration at ground level, also affecting the respiratory and cardiovascular system. Furthermore, nitrogen oxide, sulfur dioxide, Volatile Organic Compounds (VOCs), dioxins, and polycyclic aromatic hydrocarbons (PAHs) are all considered air pollutants that are harmful to humans. Carbon monoxide can even provoke direct poisoning when breathed in at high levels. Heavy metals such as lead, when absorbed into the human body, can lead to direct poisoning or chronic intoxication, depending on exposure. Diseases occurring from the aforementioned substances include principally respiratory problems such as Chronic Obstructive Pulmonary Disease (COPD), asthma, bronchiolitis, and also lung cancer, cardiovascular events, central nervous system dysfunctions, and cutaneous diseases. Last but not least, climate change resulting from environmental pollution affects the geographical distribution of many infectious diseases, as do natural disasters. The only way to tackle this problem is through public awareness coupled with a multidisciplinary approach by scientific experts; national and international organizations must address the emergence of this threat and propose sustainable solutions.

Approach to the Problem
The interactions between humans and their physical surroundings have been extensively studied, as multiple human activities influence the environment. The environment is a coupling of the biotic (living organisms and microorganisms) and the abiotic (hydrosphere, lithosphere, and atmosphere).
Pollution is defined as the introduction into the environment of substances harmful to humans and other living organisms. Pollutants are harmful solids, liquids, or gases produced in higher than usual concentrations that reduce the quality of our environment.
Human activities have an adverse effect on the environment by polluting the water we drink, the air we breathe, and the soil in which plants grow. Although the industrial revolution was a great success in terms of technology, society, and the provision of multiple services, it also introduced the production of huge quantities of pollutants emitted into the air that are harmful to human health. Without any doubt, the global environmental pollution is considered an international public health issue with multiple facets. Social, economic, and legislative concerns and lifestyle habits are related to this major problem. Clearly, urbanization and industrialization are reaching unprecedented and upsetting proportions worldwide in our era. Anthropogenic air pollution is one of the biggest public health hazards worldwide, given that it accounts for about 9 million deaths per year ( 1 ).
Without a doubt, all of the aforementioned are closely associated with climate change, and in the event of danger, the consequences can be severe for mankind ( 2 ). Climate changes and the effects of global planetary warming seriously affect multiple ecosystems, causing problems such as food safety issues, ice and iceberg melting, animal extinction, and damage to plants ( 3 , 4 ).
Air pollution has various health effects. The health of susceptible and sensitive individuals can be impacted even on low air pollution days. Short-term exposure to air pollutants is closely related to COPD (Chronic Obstructive Pulmonary Disease), cough, shortness of breath, wheezing, asthma, respiratory disease, and high rates of hospitalization (a measurement of morbidity).
The long-term effects associated with air pollution are chronic asthma, pulmonary insufficiency, cardiovascular diseases, and cardiovascular mortality. According to a Swedish cohort study, diabetes seems to be induced after long-term air pollution exposure ( 5 ). Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders ( 3 ), leading to infant mortality or chronic disease in adult age ( 6 ).
National reports have mentioned the increased risk of morbidity and mortality ( 1 ). These studies were conducted in many places around the world and show a correlation between daily ranges of particulate matter (PM) concentration and daily mortality. Climate shifts and global planetary warming ( 3 ) could aggravate the situation. Besides, increased hospitalization (an index of morbidity) has been registered among the elderly and susceptible individuals for specific reasons. Fine and ultrafine particulate matter seems to be associated with more serious illnesses ( 6 ), as it can invade the deepest parts of the airways and more easily reach the bloodstream.
Air pollution mainly affects those living in large urban areas, where road emissions contribute the most to the degradation of air quality. There is also a danger of industrial accidents, where the spread of a toxic fog can be fatal to the populations of the surrounding areas. The dispersion of pollutants is determined by many parameters, most notably atmospheric stability and wind ( 6 ).
In developing countries ( 7 ), the problem is more serious due to overpopulation and uncontrolled urbanization along with the development of industrialization. This leads to poor air quality, especially in countries with social disparities and a lack of information on sustainable management of the environment. The use of fuels such as wood fuel or solid fuel for domestic needs due to low incomes exposes people to bad-quality, polluted air at home. It is of note that three billion people around the world are using the above sources of energy for their daily heating and cooking needs ( 8 ). In developing countries, the women of the household seem to carry the highest risk for disease development due to their longer duration exposure to the indoor air pollution ( 8 , 9 ). Due to its fast industrial development and overpopulation, China is one of the Asian countries confronting serious air pollution problems ( 10 , 11 ). The lung cancer mortality observed in China is associated with fine particles ( 12 ). As stated already, long-term exposure is associated with deleterious effects on the cardiovascular system ( 3 , 5 ). However, it is interesting to note that cardiovascular diseases have mostly been observed in developed and high-income countries rather than in the developing low-income countries exposed highly to air pollution ( 13 ). Extreme air pollution is recorded in India, where the air quality reaches hazardous levels. New Delhi is one of the more polluted cities in India. Flights in and out of New Delhi International Airport are often canceled due to the reduced visibility associated with air pollution. Pollution is occurring both in urban and rural areas in India due to the fast industrialization, urbanization, and rise in use of motorcycle transportation. Nevertheless, biomass combustion associated with heating and cooking needs and practices is a major source of household air pollution in India and in Nepal ( 14 , 15 ). There is spatial heterogeneity in India, as areas with diverse climatological conditions and population and education levels generate different indoor air qualities, with higher PM 2.5 observed in North Indian states (557–601 μg/m 3 ) compared to the Southern States (183–214 μg/m 3 ) ( 16 , 17 ). The cold climate of the North Indian areas may be the main reason for this, as longer periods at home and more heating are necessary compared to in the tropical climate of Southern India. Household air pollution in India is associated with major health effects, especially in women and young children, who stay indoors for longer periods. Chronic obstructive respiratory disease (CORD) and lung cancer are mostly observed in women, while acute lower respiratory disease is seen in young children under 5 years of age ( 18 ).
Accumulation of air pollution, especially sulfur dioxide and smoke, reaching 1,500 mg/m3, resulted in an increase in the number of deaths (4,000 deaths) in December 1952 in London and in 1963 in New York City (400 deaths) ( 19 ). An association of pollution with mortality was reported on the basis of monitoring of outdoor pollution in six US metropolitan cities ( 20 ). In every case, it seems that mortality was closely related to the levels of fine, inhalable, and sulfate particles more than with the levels of total particulate pollution, aerosol acidity, sulfur dioxide, or nitrogen dioxide ( 20 ).
Furthermore, extremely high levels of pollution are reported in Mexico City and Rio de Janeiro, followed by Milan, Ankara, Melbourne, Tokyo, and Moscow ( 19 ).
Based on the magnitude of the public health impact, it is certain that different kinds of interventions should be taken into account. Success and effectiveness in controlling air pollution, specifically at the local level, have been reported. Adequate technological means are applied considering the source and the nature of the emission as well as its impact on health and the environment. The importance of point sources and non-point sources of air pollution control is reported by Schwela and Köth-Jahr ( 21 ). Without a doubt, a detailed emission inventory must record all sources in a given area. Beyond considering the above sources and their nature, topography and meteorology should also be considered, as stated previously. Assessment of the control policies and methods is often extrapolated from the local to the regional and then to the global scale. Air pollution may be dispersed and transported from one region to another area located far away. Air pollution management means the reduction to acceptable levels or possible elimination of air pollutants whose presence in the air affects our health or the environmental ecosystem. Private and governmental entities and authorities implement actions to ensure the air quality ( 22 ). Air quality standards and guidelines were adopted for the different pollutants by the WHO and EPA as a tool for the management of air quality ( 1 , 23 ). These standards have to be compared to the emissions inventory standards by causal analysis and dispersion modeling in order to reveal the problematic areas ( 24 ). Inventories are generally based on a combination of direct measurements and emissions modeling ( 24 ).
As an example, we state here the control measures at the source through the use of catalytic converters in cars. These are devices that turn the pollutants and toxic gases produced from combustion engines into less-toxic pollutants by catalysis through redox reactions ( 25 ). In Greece, the use of private cars was restricted by tracking their license plates in order to reduce traffic congestion during rush hour ( 25 ).
Concerning industrial emissions, collectors and closed systems can keep the air pollution to the minimal standards imposed by legislation ( 26 ).
Current strategies to improve air quality require an estimation of the economic value of the benefits gained from proposed programs. These proposed programs by public authorities, and directives are issued with guidelines to be respected.
In Europe, air quality limit values AQLVs (Air Quality Limit Values) are issued for setting off planning claims ( 27 ). In the USA, the NAAQS (National Ambient Air Quality Standards) establish the national air quality limit values ( 27 ). While both standards and directives are based on different mechanisms, significant success has been achieved in the reduction of overall emissions and associated health and environmental effects ( 27 ). The European Directive identifies geographical areas of risk exposure as monitoring/assessment zones to record the emission sources and levels of air pollution ( 27 ), whereas the USA establishes global geographical air quality criteria according to the severity of their air quality problem and records all sources of the pollutants and their precursors ( 27 ).
In this vein, funds have been financing, directly or indirectly, projects related to air quality along with the technical infrastructure to maintain good air quality. These plans focus on an inventory of databases from air quality environmental planning awareness campaigns. Moreover, pollution measures of air emissions may be taken for vehicles, machines, and industries in urban areas.
Technological innovation can only be successful if it is able to meet the needs of society. In this sense, technology must reflect the decision-making practices and procedures of those involved in risk assessment and evaluation and act as a facilitator in providing information and assessments to enable decision makers to make the best decisions possible. Summarizing the aforementioned in order to design an effective air quality control strategy, several aspects must be considered: environmental factors and ambient air quality conditions, engineering factors and air pollutant characteristics, and finally, economic operating costs for technological improvement and administrative and legal costs. Considering the economic factor, competitiveness through neoliberal concepts is offering a solution to environmental problems ( 22 ).
The development of environmental governance, along with technological progress, has initiated the deployment of a dialogue. Environmental politics has created objections and points of opposition between different political parties, scientists, media, and governmental and non-governmental organizations ( 22 ). Radical environmental activism actions and movements have been created ( 22 ). The rise of the new information and communication technologies (ICTs) are many times examined as to whether and in which way they have influenced means of communication and social movements such as activism ( 28 ). Since the 1990s, the term “digital activism” has been used increasingly and in many different disciplines ( 29 ). Nowadays, multiple digital technologies can be used to produce a digital activism outcome on environmental issues. More specifically, devices with online capabilities such as computers or mobile phones are being used as a way to pursue change in political and social affairs ( 30 ).
In the present paper, we focus on the sources of environmental pollution in relation to public health and propose some solutions and interventions that may be of interest to environmental legislators and decision makers.
Sources of Exposure
It is known that the majority of environmental pollutants are emitted through large-scale human activities such as the use of industrial machinery, power-producing stations, combustion engines, and cars. Because these activities are performed at such a large scale, they are by far the major contributors to air pollution, with cars estimated to be responsible for approximately 80% of today's pollution ( 31 ). Some other human activities are also influencing our environment to a lesser extent, such as field cultivation techniques, gas stations, fuel tanks heaters, and cleaning procedures ( 32 ), as well as several natural sources, such as volcanic and soil eruptions and forest fires.
The classification of air pollutants is based mainly on the sources producing pollution. Therefore, it is worth mentioning the four main sources, following the classification system: Major sources, Area sources, Mobile sources, and Natural sources.
Major sources include the emission of pollutants from power stations, refineries, and petrochemicals, the chemical and fertilizer industries, metallurgical and other industrial plants, and, finally, municipal incineration.
Indoor area sources include domestic cleaning activities, dry cleaners, printing shops, and petrol stations.
Mobile sources include automobiles, cars, railways, airways, and other types of vehicles.
Finally, natural sources include, as stated previously, physical disasters ( 33 ) such as forest fire, volcanic erosion, dust storms, and agricultural burning.
However, many classification systems have been proposed. Another type of classification is a grouping according to the recipient of the pollution, as follows:
Air pollution is determined as the presence of pollutants in the air in large quantities for long periods. Air pollutants are dispersed particles, hydrocarbons, CO, CO 2 , NO, NO 2 , SO 3 , etc.
Water pollution is organic and inorganic charge and biological charge ( 10 ) at high levels that affect the water quality ( 34 , 35 ).
Soil pollution occurs through the release of chemicals or the disposal of wastes, such as heavy metals, hydrocarbons, and pesticides.
Air pollution can influence the quality of soil and water bodies by polluting precipitation, falling into water and soil environments ( 34 , 36 ). Notably, the chemistry of the soil can be amended due to acid precipitation by affecting plants, cultures, and water quality ( 37 ). Moreover, movement of heavy metals is favored by soil acidity, and metals are so then moving into the watery environment. It is known that heavy metals such as aluminum are noxious to wildlife and fishes. Soil quality seems to be of importance, as soils with low calcium carbonate levels are at increased jeopardy from acid rain. Over and above rain, snow and particulate matter drip into watery ' bodies ( 36 , 38 ).
Lastly, pollution is classified following type of origin:
Radioactive and nuclear pollution , releasing radioactive and nuclear pollutants into water, air, and soil during nuclear explosions and accidents, from nuclear weapons, and through handling or disposal of radioactive sewage.
Radioactive materials can contaminate surface water bodies and, being noxious to the environment, plants, animals, and humans. It is known that several radioactive substances such as radium and uranium concentrate in the bones and can cause cancers ( 38 , 39 ).
Noise pollution is produced by machines, vehicles, traffic noises, and musical installations that are harmful to our hearing.
The World Health Organization introduced the term DALYs. The DALYs for a disease or health condition is defined as the sum of the Years of Life Lost (YLL) due to premature mortality in the population and the Years Lost due to Disability (YLD) for people living with the health condition or its consequences ( 39 ). In Europe, air pollution is the main cause of disability-adjusted life years lost (DALYs), followed by noise pollution. The potential relationships of noise and air pollution with health have been studied ( 40 ). The study found that DALYs related to noise were more important than those related to air pollution, as the effects of environmental noise on cardiovascular disease were independent of air pollution ( 40 ). Environmental noise should be counted as an independent public health risk ( 40 ).
Environmental pollution occurs when changes in the physical, chemical, or biological constituents of the environment (air masses, temperature, climate, etc.) are produced.
Pollutants harm our environment either by increasing levels above normal or by introducing harmful toxic substances. Primary pollutants are directly produced from the above sources, and secondary pollutants are emitted as by-products of the primary ones. Pollutants can be biodegradable or non-biodegradable and of natural origin or anthropogenic, as stated previously. Moreover, their origin can be a unique source (point-source) or dispersed sources.
Pollutants have differences in physical and chemical properties, explaining the discrepancy in their capacity for producing toxic effects. As an example, we state here that aerosol compounds ( 41 – 43 ) have a greater toxicity than gaseous compounds due to their tiny size (solid or liquid) in the atmosphere; they have a greater penetration capacity. Gaseous compounds are eliminated more easily by our respiratory system ( 41 ). These particles are able to damage lungs and can even enter the bloodstream ( 41 ), leading to the premature deaths of millions of people yearly. Moreover, the aerosol acidity ([H+]) seems to considerably enhance the production of secondary organic aerosols (SOA), but this last aspect is not supported by other scientific teams ( 38 ).
Climate and Pollution
Air pollution and climate change are closely related. Climate is the other side of the same coin that reduces the quality of our Earth ( 44 ). Pollutants such as black carbon, methane, tropospheric ozone, and aerosols affect the amount of incoming sunlight. As a result, the temperature of the Earth is increasing, resulting in the melting of ice, icebergs, and glaciers.
In this vein, climatic changes will affect the incidence and prevalence of both residual and imported infections in Europe. Climate and weather affect the duration, timing, and intensity of outbreaks strongly and change the map of infectious diseases in the globe ( 45 ). Mosquito-transmitted parasitic or viral diseases are extremely climate-sensitive, as warming firstly shortens the pathogen incubation period and secondly shifts the geographic map of the vector. Similarly, water-warming following climate changes leads to a high incidence of waterborne infections. Recently, in Europe, eradicated diseases seem to be emerging due to the migration of population, for example, cholera, poliomyelitis, tick-borne encephalitis, and malaria ( 46 ).
The spread of epidemics is associated with natural climate disasters and storms, which seem to occur more frequently nowadays ( 47 ). Malnutrition and disequilibration of the immune system are also associated with the emerging infections affecting public health ( 48 ).
The Chikungunya virus “took the airplane” from the Indian Ocean to Europe, as outbreaks of the disease were registered in Italy ( 49 ) as well as autochthonous cases in France ( 50 ).
An increase in cryptosporidiosis in the United Kingdom and in the Czech Republic seems to have occurred following flooding ( 36 , 51 ).
As stated previously, aerosols compounds are tiny in size and considerably affect the climate. They are able to dissipate sunlight (the albedo phenomenon) by dispersing a quarter of the sun's rays back to space and have cooled the global temperature over the last 30 years ( 52 ).
Air Pollutants
The World Health Organization (WHO) reports on six major air pollutants, namely particle pollution, ground-level ozone, carbon monoxide, sulfur oxides, nitrogen oxides, and lead. Air pollution can have a disastrous effect on all components of the environment, including groundwater, soil, and air. Additionally, it poses a serious threat to living organisms. In this vein, our interest is mainly to focus on these pollutants, as they are related to more extensive and severe problems in human health and environmental impact. Acid rain, global warming, the greenhouse effect, and climate changes have an important ecological impact on air pollution ( 53 ).
Particulate Matter (PM) and Health
Studies have shown a relationship between particulate matter (PM) and adverse health effects, focusing on either short-term (acute) or long-term (chronic) PM exposure.
Particulate matter (PM) is usually formed in the atmosphere as a result of chemical reactions between the different pollutants. The penetration of particles is closely dependent on their size ( 53 ). Particulate Matter (PM) was defined as a term for particles by the United States Environmental Protection Agency ( 54 ). Particulate matter (PM) pollution includes particles with diameters of 10 micrometers (μm) or smaller, called PM 10 , and extremely fine particles with diameters that are generally 2.5 micrometers (μm) and smaller.
Particulate matter contains tiny liquid or solid droplets that can be inhaled and cause serious health effects ( 55 ). Particles <10 μm in diameter (PM 10 ) after inhalation can invade the lungs and even reach the bloodstream. Fine particles, PM 2.5 , pose a greater risk to health ( 6 , 56 ) ( Table 1 ).
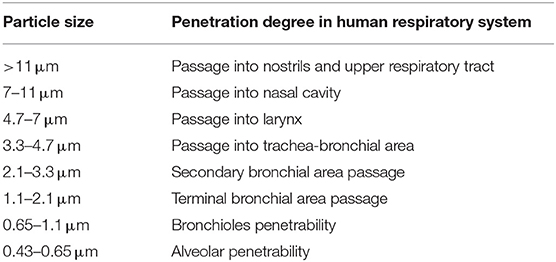
Table 1 . Penetrability according to particle size.
Multiple epidemiological studies have been performed on the health effects of PM. A positive relation was shown between both short-term and long-term exposures of PM 2.5 and acute nasopharyngitis ( 56 ). In addition, long-term exposure to PM for years was found to be related to cardiovascular diseases and infant mortality.
Those studies depend on PM 2.5 monitors and are restricted in terms of study area or city area due to a lack of spatially resolved daily PM 2.5 concentration data and, in this way, are not representative of the entire population. Following a recent epidemiological study by the Department of Environmental Health at Harvard School of Public Health (Boston, MA) ( 57 ), it was reported that, as PM 2.5 concentrations vary spatially, an exposure error (Berkson error) seems to be produced, and the relative magnitudes of the short- and long-term effects are not yet completely elucidated. The team developed a PM 2.5 exposure model based on remote sensing data for assessing short- and long-term human exposures ( 57 ). This model permits spatial resolution in short-term effects plus the assessment of long-term effects in the whole population.
Moreover, respiratory diseases and affection of the immune system are registered as long-term chronic effects ( 58 ). It is worth noting that people with asthma, pneumonia, diabetes, and respiratory and cardiovascular diseases are especially susceptible and vulnerable to the effects of PM. PM 2.5 , followed by PM 10 , are strongly associated with diverse respiratory system diseases ( 59 ), as their size permits them to pierce interior spaces ( 60 ). The particles produce toxic effects according to their chemical and physical properties. The components of PM 10 and PM 2.5 can be organic (polycyclic aromatic hydrocarbons, dioxins, benzene, 1-3 butadiene) or inorganic (carbon, chlorides, nitrates, sulfates, metals) in nature ( 55 ).
Particulate Matter (PM) is divided into four main categories according to type and size ( 61 ) ( Table 2 ).
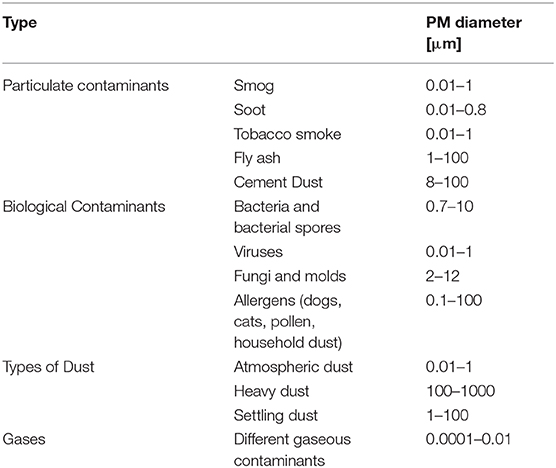
Table 2 . Types and sizes of particulate Matter (PM).
Gas contaminants include PM in aerial masses.
Particulate contaminants include contaminants such as smog, soot, tobacco smoke, oil smoke, fly ash, and cement dust.
Biological Contaminants are microorganisms (bacteria, viruses, fungi, mold, and bacterial spores), cat allergens, house dust and allergens, and pollen.
Types of Dust include suspended atmospheric dust, settling dust, and heavy dust.
Finally, another fact is that the half-lives of PM 10 and PM 2.5 particles in the atmosphere is extended due to their tiny dimensions; this permits their long-lasting suspension in the atmosphere and even their transfer and spread to distant destinations where people and the environment may be exposed to the same magnitude of pollution ( 53 ). They are able to change the nutrient balance in watery ecosystems, damage forests and crops, and acidify water bodies.
As stated, PM 2.5 , due to their tiny size, are causing more serious health effects. These aforementioned fine particles are the main cause of the “haze” formation in different metropolitan areas ( 12 , 13 , 61 ).
Ozone Impact in the Atmosphere
Ozone (O 3 ) is a gas formed from oxygen under high voltage electric discharge ( 62 ). It is a strong oxidant, 52% stronger than chlorine. It arises in the stratosphere, but it could also arise following chain reactions of photochemical smog in the troposphere ( 63 ).
Ozone can travel to distant areas from its initial source, moving with air masses ( 64 ). It is surprising that ozone levels over cities are low in contrast to the increased amounts occuring in urban areas, which could become harmful for cultures, forests, and vegetation ( 65 ) as it is reducing carbon assimilation ( 66 ). Ozone reduces growth and yield ( 47 , 48 ) and affects the plant microflora due to its antimicrobial capacity ( 67 , 68 ). In this regard, ozone acts upon other natural ecosystems, with microflora ( 69 , 70 ) and animal species changing their species composition ( 71 ). Ozone increases DNA damage in epidermal keratinocytes and leads to impaired cellular function ( 72 ).
Ground-level ozone (GLO) is generated through a chemical reaction between oxides of nitrogen and VOCs emitted from natural sources and/or following anthropogenic activities.
Ozone uptake usually occurs by inhalation. Ozone affects the upper layers of the skin and the tear ducts ( 73 ). A study of short-term exposure of mice to high levels of ozone showed malondialdehyde formation in the upper skin (epidermis) but also depletion in vitamins C and E. It is likely that ozone levels are not interfering with the skin barrier function and integrity to predispose to skin disease ( 74 ).
Due to the low water-solubility of ozone, inhaled ozone has the capacity to penetrate deeply into the lungs ( 75 ).
Toxic effects induced by ozone are registered in urban areas all over the world, causing biochemical, morphologic, functional, and immunological disorders ( 76 ).
The European project (APHEA2) focuses on the acute effects of ambient ozone concentrations on mortality ( 77 ). Daily ozone concentrations compared to the daily number of deaths were reported from different European cities for a 3-year period. During the warm period of the year, an observed increase in ozone concentration was associated with an increase in the daily number of deaths (0.33%), in the number of respiratory deaths (1.13%), and in the number of cardiovascular deaths (0.45%). No effect was observed during wintertime.
Carbon Monoxide (CO)
Carbon monoxide is produced by fossil fuel when combustion is incomplete. The symptoms of poisoning due to inhaling carbon monoxide include headache, dizziness, weakness, nausea, vomiting, and, finally, loss of consciousness.
The affinity of carbon monoxide to hemoglobin is much greater than that of oxygen. In this vein, serious poisoning may occur in people exposed to high levels of carbon monoxide for a long period of time. Due to the loss of oxygen as a result of the competitive binding of carbon monoxide, hypoxia, ischemia, and cardiovascular disease are observed.
Carbon monoxide affects the greenhouses gases that are tightly connected to global warming and climate. This should lead to an increase in soil and water temperatures, and extreme weather conditions or storms may occur ( 68 ).
However, in laboratory and field experiments, it has been seen to produce increased plant growth ( 78 ).
Nitrogen Oxide (NO 2 )
Nitrogen oxide is a traffic-related pollutant, as it is emitted from automobile motor engines ( 79 , 80 ). It is an irritant of the respiratory system as it penetrates deep in the lung, inducing respiratory diseases, coughing, wheezing, dyspnea, bronchospasm, and even pulmonary edema when inhaled at high levels. It seems that concentrations over 0.2 ppm produce these adverse effects in humans, while concentrations higher than 2.0 ppm affect T-lymphocytes, particularly the CD8+ cells and NK cells that produce our immune response ( 81 ).It is reported that long-term exposure to high levels of nitrogen dioxide can be responsible for chronic lung disease. Long-term exposure to NO 2 can impair the sense of smell ( 81 ).
However, systems other than respiratory ones can be involved, as symptoms such as eye, throat, and nose irritation have been registered ( 81 ).
High levels of nitrogen dioxide are deleterious to crops and vegetation, as they have been observed to reduce crop yield and plant growth efficiency. Moreover, NO 2 can reduce visibility and discolor fabrics ( 81 ).
Sulfur Dioxide (SO 2 )
Sulfur dioxide is a harmful gas that is emitted mainly from fossil fuel consumption or industrial activities. The annual standard for SO 2 is 0.03 ppm ( 82 ). It affects human, animal, and plant life. Susceptible people as those with lung disease, old people, and children, who present a higher risk of damage. The major health problems associated with sulfur dioxide emissions in industrialized areas are respiratory irritation, bronchitis, mucus production, and bronchospasm, as it is a sensory irritant and penetrates deep into the lung converted into bisulfite and interacting with sensory receptors, causing bronchoconstriction. Moreover, skin redness, damage to the eyes (lacrimation and corneal opacity) and mucous membranes, and worsening of pre-existing cardiovascular disease have been observed ( 81 ).
Environmental adverse effects, such as acidification of soil and acid rain, seem to be associated with sulfur dioxide emissions ( 83 ).
Lead is a heavy metal used in different industrial plants and emitted from some petrol motor engines, batteries, radiators, waste incinerators, and waste waters ( 84 ).
Moreover, major sources of lead pollution in the air are metals, ore, and piston-engine aircraft. Lead poisoning is a threat to public health due to its deleterious effects upon humans, animals, and the environment, especially in the developing countries.
Exposure to lead can occur through inhalation, ingestion, and dermal absorption. Trans- placental transport of lead was also reported, as lead passes through the placenta unencumbered ( 85 ). The younger the fetus is, the more harmful the toxic effects. Lead toxicity affects the fetal nervous system; edema or swelling of the brain is observed ( 86 ). Lead, when inhaled, accumulates in the blood, soft tissue, liver, lung, bones, and cardiovascular, nervous, and reproductive systems. Moreover, loss of concentration and memory, as well as muscle and joint pain, were observed in adults ( 85 , 86 ).
Children and newborns ( 87 ) are extremely susceptible even to minimal doses of lead, as it is a neurotoxicant and causes learning disabilities, impairment of memory, hyperactivity, and even mental retardation.
Elevated amounts of lead in the environment are harmful to plants and crop growth. Neurological effects are observed in vertebrates and animals in association with high lead levels ( 88 ).
Polycyclic Aromatic Hydrocarbons(PAHs)
The distribution of PAHs is ubiquitous in the environment, as the atmosphere is the most important means of their dispersal. They are found in coal and in tar sediments. Moreover, they are generated through incomplete combustion of organic matter as in the cases of forest fires, incineration, and engines ( 89 ). PAH compounds, such as benzopyrene, acenaphthylene, anthracene, and fluoranthene are recognized as toxic, mutagenic, and carcinogenic substances. They are an important risk factor for lung cancer ( 89 ).
Volatile Organic Compounds(VOCs)
Volatile organic compounds (VOCs), such as toluene, benzene, ethylbenzene, and xylene ( 90 ), have been found to be associated with cancer in humans ( 91 ). The use of new products and materials has actually resulted in increased concentrations of VOCs. VOCs pollute indoor air ( 90 ) and may have adverse effects on human health ( 91 ). Short-term and long-term adverse effects on human health are observed. VOCs are responsible for indoor air smells. Short-term exposure is found to cause irritation of eyes, nose, throat, and mucosal membranes, while those of long duration exposure include toxic reactions ( 92 ). Predictable assessment of the toxic effects of complex VOC mixtures is difficult to estimate, as these pollutants can have synergic, antagonistic, or indifferent effects ( 91 , 93 ).
Dioxins originate from industrial processes but also come from natural processes, such as forest fires and volcanic eruptions. They accumulate in foods such as meat and dairy products, fish and shellfish, and especially in the fatty tissue of animals ( 94 ).
Short-period exhibition to high dioxin concentrations may result in dark spots and lesions on the skin ( 94 ). Long-term exposure to dioxins can cause developmental problems, impairment of the immune, endocrine and nervous systems, reproductive infertility, and cancer ( 94 ).
Without any doubt, fossil fuel consumption is responsible for a sizeable part of air contamination. This contamination may be anthropogenic, as in agricultural and industrial processes or transportation, while contamination from natural sources is also possible. Interestingly, it is of note that the air quality standards established through the European Air Quality Directive are somewhat looser than the WHO guidelines, which are stricter ( 95 ).
Effect of Air Pollution on Health
The most common air pollutants are ground-level ozone and Particulates Matter (PM). Air pollution is distinguished into two main types:
Outdoor pollution is the ambient air pollution.
Indoor pollution is the pollution generated by household combustion of fuels.
People exposed to high concentrations of air pollutants experience disease symptoms and states of greater and lesser seriousness. These effects are grouped into short- and long-term effects affecting health.
Susceptible populations that need to be aware of health protection measures include old people, children, and people with diabetes and predisposing heart or lung disease, especially asthma.
As extensively stated previously, according to a recent epidemiological study from Harvard School of Public Health, the relative magnitudes of the short- and long-term effects have not been completely clarified ( 57 ) due to the different epidemiological methodologies and to the exposure errors. New models are proposed for assessing short- and long-term human exposure data more successfully ( 57 ). Thus, in the present section, we report the more common short- and long-term health effects but also general concerns for both types of effects, as these effects are often dependent on environmental conditions, dose, and individual susceptibility.
Short-term effects are temporary and range from simple discomfort, such as irritation of the eyes, nose, skin, throat, wheezing, coughing and chest tightness, and breathing difficulties, to more serious states, such as asthma, pneumonia, bronchitis, and lung and heart problems. Short-term exposure to air pollution can also cause headaches, nausea, and dizziness.
These problems can be aggravated by extended long-term exposure to the pollutants, which is harmful to the neurological, reproductive, and respiratory systems and causes cancer and even, rarely, deaths.
The long-term effects are chronic, lasting for years or the whole life and can even lead to death. Furthermore, the toxicity of several air pollutants may also induce a variety of cancers in the long term ( 96 ).
As stated already, respiratory disorders are closely associated with the inhalation of air pollutants. These pollutants will invade through the airways and will accumulate at the cells. Damage to target cells should be related to the pollutant component involved and its source and dose. Health effects are also closely dependent on country, area, season, and time. An extended exposure duration to the pollutant should incline to long-term health effects in relation also to the above factors.
Particulate Matter (PMs), dust, benzene, and O 3 cause serious damage to the respiratory system ( 97 ). Moreover, there is a supplementary risk in case of existing respiratory disease such as asthma ( 98 ). Long-term effects are more frequent in people with a predisposing disease state. When the trachea is contaminated by pollutants, voice alterations may be remarked after acute exposure. Chronic obstructive pulmonary disease (COPD) may be induced following air pollution, increasing morbidity and mortality ( 99 ). Long-term effects from traffic, industrial air pollution, and combustion of fuels are the major factors for COPD risk ( 99 ).
Multiple cardiovascular effects have been observed after exposure to air pollutants ( 100 ). Changes occurred in blood cells after long-term exposure may affect cardiac functionality. Coronary arteriosclerosis was reported following long-term exposure to traffic emissions ( 101 ), while short-term exposure is related to hypertension, stroke, myocardial infracts, and heart insufficiency. Ventricle hypertrophy is reported to occur in humans after long-time exposure to nitrogen oxide (NO 2 ) ( 102 , 103 ).
Neurological effects have been observed in adults and children after extended-term exposure to air pollutants.
Psychological complications, autism, retinopathy, fetal growth, and low birth weight seem to be related to long-term air pollution ( 83 ). The etiologic agent of the neurodegenerative diseases (Alzheimer's and Parkinson's) is not yet known, although it is believed that extended exposure to air pollution seems to be a factor. Specifically, pesticides and metals are cited as etiological factors, together with diet. The mechanisms in the development of neurodegenerative disease include oxidative stress, protein aggregation, inflammation, and mitochondrial impairment in neurons ( 104 ) ( Figure 1 ).
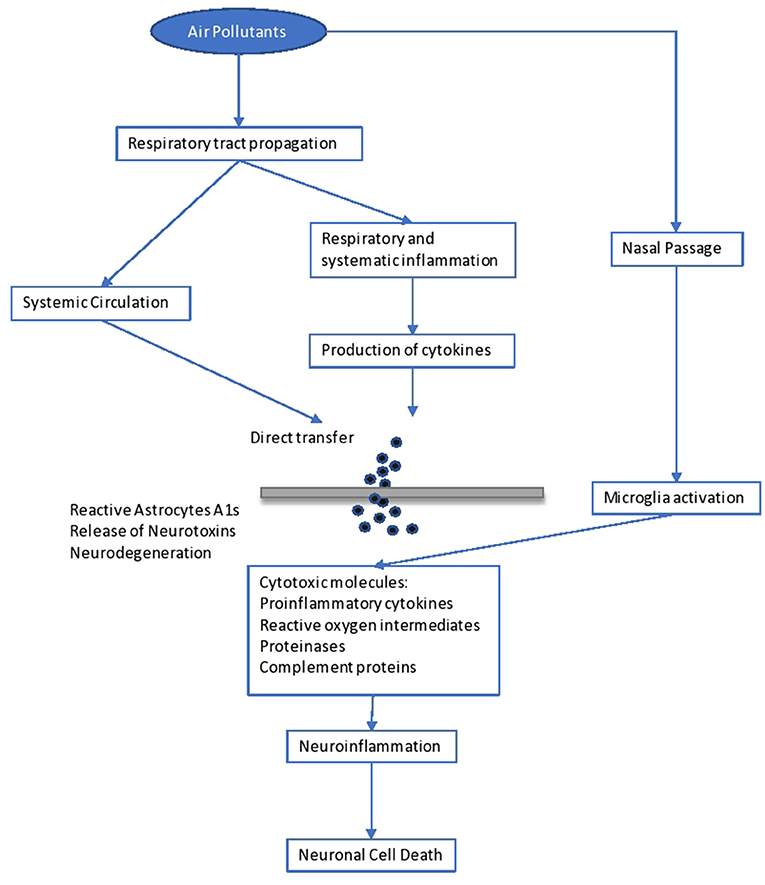
Figure 1 . Impact of air pollutants on the brain.
Brain inflammation was observed in dogs living in a highly polluted area in Mexico for a long period ( 105 ). In human adults, markers of systemic inflammation (IL-6 and fibrinogen) were found to be increased as an immediate response to PNC on the IL-6 level, possibly leading to the production of acute-phase proteins ( 106 ). The progression of atherosclerosis and oxidative stress seem to be the mechanisms involved in the neurological disturbances caused by long-term air pollution. Inflammation comes secondary to the oxidative stress and seems to be involved in the impairment of developmental maturation, affecting multiple organs ( 105 , 107 ). Similarly, other factors seem to be involved in the developmental maturation, which define the vulnerability to long-term air pollution. These include birthweight, maternal smoking, genetic background and socioeconomic environment, as well as education level.
However, diet, starting from breast-feeding, is another determinant factor. Diet is the main source of antioxidants, which play a key role in our protection against air pollutants ( 108 ). Antioxidants are free radical scavengers and limit the interaction of free radicals in the brain ( 108 ). Similarly, genetic background may result in a differential susceptibility toward the oxidative stress pathway ( 60 ). For example, antioxidant supplementation with vitamins C and E appears to modulate the effect of ozone in asthmatic children homozygous for the GSTM1 null allele ( 61 ). Inflammatory cytokines released in the periphery (e.g., respiratory epithelia) upregulate the innate immune Toll-like receptor 2. Such activation and the subsequent events leading to neurodegeneration have recently been observed in lung lavage in mice exposed to ambient Los Angeles (CA, USA) particulate matter ( 61 ). In children, neurodevelopmental morbidities were observed after lead exposure. These children developed aggressive and delinquent behavior, reduced intelligence, learning difficulties, and hyperactivity ( 109 ). No level of lead exposure seems to be “safe,” and the scientific community has asked the Centers for Disease Control and Prevention (CDC) to reduce the current screening guideline of 10 μg/dl ( 109 ).
It is important to state that impact on the immune system, causing dysfunction and neuroinflammation ( 104 ), is related to poor air quality. Yet, increases in serum levels of immunoglobulins (IgA, IgM) and the complement component C3 are observed ( 106 ). Another issue is that antigen presentation is affected by air pollutants, as there is an upregulation of costimulatory molecules such as CD80 and CD86 on macrophages ( 110 ).
As is known, skin is our shield against ultraviolet radiation (UVR) and other pollutants, as it is the most exterior layer of our body. Traffic-related pollutants, such as PAHs, VOCs, oxides, and PM, may cause pigmented spots on our skin ( 111 ). On the one hand, as already stated, when pollutants penetrate through the skin or are inhaled, damage to the organs is observed, as some of these pollutants are mutagenic and carcinogenic, and, specifically, they affect the liver and lung. On the other hand, air pollutants (and those in the troposphere) reduce the adverse effects of ultraviolet radiation UVR in polluted urban areas ( 111 ). Air pollutants absorbed by the human skin may contribute to skin aging, psoriasis, acne, urticaria, eczema, and atopic dermatitis ( 111 ), usually caused by exposure to oxides and photochemical smoke ( 111 ). Exposure to PM and cigarette smoking act as skin-aging agents, causing spots, dyschromia, and wrinkles. Lastly, pollutants have been associated with skin cancer ( 111 ).
Higher morbidity is reported to fetuses and children when exposed to the above dangers. Impairment in fetal growth, low birth weight, and autism have been reported ( 112 ).
Another exterior organ that may be affected is the eye. Contamination usually comes from suspended pollutants and may result in asymptomatic eye outcomes, irritation ( 112 ), retinopathy, or dry eye syndrome ( 113 , 114 ).
Environmental Impact of Air Pollution
Air pollution is harming not only human health but also the environment ( 115 ) in which we live. The most important environmental effects are as follows.
Acid rain is wet (rain, fog, snow) or dry (particulates and gas) precipitation containing toxic amounts of nitric and sulfuric acids. They are able to acidify the water and soil environments, damage trees and plantations, and even damage buildings and outdoor sculptures, constructions, and statues.
Haze is produced when fine particles are dispersed in the air and reduce the transparency of the atmosphere. It is caused by gas emissions in the air coming from industrial facilities, power plants, automobiles, and trucks.
Ozone , as discussed previously, occurs both at ground level and in the upper level (stratosphere) of the Earth's atmosphere. Stratospheric ozone is protecting us from the Sun's harmful ultraviolet (UV) rays. In contrast, ground-level ozone is harmful to human health and is a pollutant. Unfortunately, stratospheric ozone is gradually damaged by ozone-depleting substances (i.e., chemicals, pesticides, and aerosols). If this protecting stratospheric ozone layer is thinned, then UV radiation can reach our Earth, with harmful effects for human life (skin cancer) ( 116 ) and crops ( 117 ). In plants, ozone penetrates through the stomata, inducing them to close, which blocks CO 2 transfer and induces a reduction in photosynthesis ( 118 ).
Global climate change is an important issue that concerns mankind. As is known, the “greenhouse effect” keeps the Earth's temperature stable. Unhappily, anthropogenic activities have destroyed this protecting temperature effect by producing large amounts of greenhouse gases, and global warming is mounting, with harmful effects on human health, animals, forests, wildlife, agriculture, and the water environment. A report states that global warming is adding to the health risks of poor people ( 119 ).
People living in poorly constructed buildings in warm-climate countries are at high risk for heat-related health problems as temperatures mount ( 119 ).
Wildlife is burdened by toxic pollutants coming from the air, soil, or the water ecosystem and, in this way, animals can develop health problems when exposed to high levels of pollutants. Reproductive failure and birth effects have been reported.
Eutrophication is occurring when elevated concentrations of nutrients (especially nitrogen) stimulate the blooming of aquatic algae, which can cause a disequilibration in the diversity of fish and their deaths.
Without a doubt, there is a critical concentration of pollution that an ecosystem can tolerate without being destroyed, which is associated with the ecosystem's capacity to neutralize acidity. The Canada Acid Rain Program established this load at 20 kg/ha/yr ( 120 ).
Hence, air pollution has deleterious effects on both soil and water ( 121 ). Concerning PM as an air pollutant, its impact on crop yield and food productivity has been reported. Its impact on watery bodies is associated with the survival of living organisms and fishes and their productivity potential ( 121 ).
An impairment in photosynthetic rhythm and metabolism is observed in plants exposed to the effects of ozone ( 121 ).
Sulfur and nitrogen oxides are involved in the formation of acid rain and are harmful to plants and marine organisms.
Last but not least, as mentioned above, the toxicity associated with lead and other metals is the main threat to our ecosystems (air, water, and soil) and living creatures ( 121 ).
In 2018, during the first WHO Global Conference on Air Pollution and Health, the WHO's General Director, Dr. Tedros Adhanom Ghebreyesus, called air pollution a “silent public health emergency” and “the new tobacco” ( 122 ).
Undoubtedly, children are particularly vulnerable to air pollution, especially during their development. Air pollution has adverse effects on our lives in many different respects.
Diseases associated with air pollution have not only an important economic impact but also a societal impact due to absences from productive work and school.
Despite the difficulty of eradicating the problem of anthropogenic environmental pollution, a successful solution could be envisaged as a tight collaboration of authorities, bodies, and doctors to regularize the situation. Governments should spread sufficient information and educate people and should involve professionals in these issues so as to control the emergence of the problem successfully.
Technologies to reduce air pollution at the source must be established and should be used in all industries and power plants. The Kyoto Protocol of 1997 set as a major target the reduction of GHG emissions to below 5% by 2012 ( 123 ). This was followed by the Copenhagen summit, 2009 ( 124 ), and then the Durban summit of 2011 ( 125 ), where it was decided to keep to the same line of action. The Kyoto protocol and the subsequent ones were ratified by many countries. Among the pioneers who adopted this important protocol for the world's environmental and climate “health” was China ( 3 ). As is known, China is a fast-developing economy and its GDP (Gross Domestic Product) is expected to be very high by 2050, which is defined as the year of dissolution of the protocol for the decrease in gas emissions.
A more recent international agreement of crucial importance for climate change is the Paris Agreement of 2015, issued by the UNFCCC (United Nations Climate Change Committee). This latest agreement was ratified by a plethora of UN (United Nations) countries as well as the countries of the European Union ( 126 ). In this vein, parties should promote actions and measures to enhance numerous aspects around the subject. Boosting education, training, public awareness, and public participation are some of the relevant actions for maximizing the opportunities to achieve the targets and goals on the crucial matter of climate change and environmental pollution ( 126 ). Without any doubt, technological improvements makes our world easier and it seems difficult to reduce the harmful impact caused by gas emissions, we could limit its use by seeking reliable approaches.
Synopsizing, a global prevention policy should be designed in order to combat anthropogenic air pollution as a complement to the correct handling of the adverse health effects associated with air pollution. Sustainable development practices should be applied, together with information coming from research in order to handle the problem effectively.
At this point, international cooperation in terms of research, development, administration policy, monitoring, and politics is vital for effective pollution control. Legislation concerning air pollution must be aligned and updated, and policy makers should propose the design of a powerful tool of environmental and health protection. As a result, the main proposal of this essay is that we should focus on fostering local structures to promote experience and practice and extrapolate these to the international level through developing effective policies for sustainable management of ecosystems.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
IM is employed by the company Delphis S.A.
The remaining authors declare that the present review paper was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. WHO. Air Pollution . WHO. Available online at: http://www.who.int/airpollution/en/ (accessed October 5, 2019).
Google Scholar
2. Moores FC. Climate change and air pollution: exploring the synergies and potential for mitigation in industrializing countries. Sustainability . (2009) 1:43–54. doi: 10.3390/su1010043
CrossRef Full Text | Google Scholar
3. USGCRP (2009). Global Climate Change Impacts in the United States. In: Karl TR, Melillo JM, Peterson TC, editors. Climate Change Impacts by Sectors: Ecosystems . New York, NY: United States Global Change Research Program. Cambridge University Press.
4. Marlon JR, Bloodhart B, Ballew MT, Rolfe-Redding J, Roser-Renouf C, Leiserowitz A, et al. (2019). How hope and doubt affect climate change mobilization. Front. Commun. 4:20. doi: 10.3389/fcomm.2019.00020
5. Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. Long- term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int . (2014) 70:95–105. doi: 10.1016/j.envint.2014.05.014
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Kelishadi R, Poursafa P. Air pollution and non-respiratory health hazards for children. Arch Med Sci . (2010) 6:483–95. doi: 10.5114/aoms.2010.14458
7. Manucci PM, Franchini M. Health effects of ambient air pollution in developing countries. Int J Environ Res Public Health . (2017) 14:1048. doi: 10.3390/ijerph14091048
8. Burden of Disease from Ambient and Household Air Pollution . Available online: http://who.int/phe/health_topics/outdoorair/databases/en/ (accessed August 15, 2017).
9. Hashim D, Boffetta P. Occupational and environmental exposures and cancers in developing countries. Ann Glob Health . (2014) 80:393–411. doi: 10.1016/j.aogh.2014.10.002
10. Guo Y, Zeng H, Zheng R, Li S, Pereira G, Liu Q, et al. The burden of lung cancer mortality attributable to fine particles in China. Total Environ Sci . (2017) 579:1460–6. doi: 10.1016/j.scitotenv.2016.11.147
11. Hou Q, An XQ, Wang Y, Guo JP. An evaluation of resident exposure to respirable particulate matter and health economic loss in Beijing during Beijing 2008 Olympic Games. Sci Total Environ . (2010) 408:4026–32. doi: 10.1016/j.scitotenv.2009.12.030
12. Kan H, Chen R, Tong S. Ambient air pollution, climate change, and population health in China. Environ Int . (2012) 42:10–9. doi: 10.1016/j.envint.2011.03.003
13. Burroughs Peña MS, Rollins A. Environmental exposures and cardiovascular disease: a challenge for health and development in low- and middle-income countries. Cardiol Clin . (2017) 35:71–86. doi: 10.1016/j.ccl.2016.09.001
14. Kankaria A, Nongkynrih B, Gupta S. Indoor air pollution in india: implications on health and its control. Indian J Comm Med . 39:203–7. doi: 10.4103/0970-0218.143019
15. Parajuli I, Lee H, Shrestha KR. Indoor air quality and ventilation assessment of rural mountainous households of Nepal. Int J Sust Built Env . (2016) 5:301–11. doi: 10.1016/j.ijsbe.2016.08.003
16. Saud T, Gautam R, Mandal TK, Gadi R, Singh DP, Sharma SK. Emission estimates of organic and elemental carbon from household biomass fuel used over the Indo-Gangetic Plain (IGP), India. Atmos Environ . (2012) 61:212–20. doi: 10.1016/j.atmosenv.2012.07.030
17. Singh DP, Gadi R, Mandal TK, Saud T, Saxena M, Sharma SK. Emissions estimates of PAH from biomass fuels used in rural sector of Indo-Gangetic Plains of India. Atmos Environ . (2013) 68:120–6. doi: 10.1016/j.atmosenv.2012.11.042
18. Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M BN. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ . (2008) 86:390–4. doi: 10.2471/BLT.07.044529
19. Kassomenos P, Kelessis A, Petrakakis M, Zoumakis N, Christides T, Paschalidou AK. Air Quality assessment in a heavily-polluted urban Mediterranean environment through Air Quality indices. Ecol Indic . (2012) 18:259–68. doi: 10.1016/j.ecolind.2011.11.021
20. Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med . (1993) 329:1753–9. doi: 10.1056/NEJM199312093292401
21. Schwela DH, Köth-Jahr I. Leitfaden für die Aufstellung von Luftreinhalteplänen [Guidelines for the Implementation of Clean Air Implementation Plans]. Landesumweltamt des Landes Nordrhein Westfalen. State Environmental Service of the State of North Rhine-Westphalia (1994).
22. Newlands M. Environmental Activism, Environmental Politics, and Representation: The Framing of the British Environmental Activist Movement . Ph.D. thesis. University of East London, United Kingdom (2015).
23. NEPIS (National Service Center for Environmental Publications) US EPA (Environmental Protection Agency) (2017). Available online at: https://www.epa.gov/clean-air-act-overview/air-pollution-current-and-future-challenges (accessed August 15, 2017).
24. NRC (National Research Council). Available online at: https://www.nap.edu/read/10728/chapter/1,2014 (accessed September 17, 2019).
25. Bull A. Traffic Congestion: The Problem and How to Deal With It . Santiago: Nationes Unidas, Cepal (2003).
26. Spiegel J, Maystre LY. Environmental Pollution Control, Part VII - The Environment, Chapter 55, Encyclopedia of Occupational Health and Safety . Available online at: http://www.ilocis.org/documents/chpt55e.htm (accessed September 17, 2019).
27. European Community Reports. Assessment of the Effectiveness of European Air Quality Policies and Measures: Case Study 2; Comparison of the EU and US Air Quality Standards and Planning Requirements. (2004). Available online at: https://ec.europa.eu/environment/archives/cafe/activities/pdf/case_study2.pdf (accessed September 22, 2019).
28. Gibson R, Ward S. Parties in the digital age; a review. J Represent Democracy . (2009) 45:87–100. doi: 10.1080/00344890802710888
29. Kaun A, Uldam J. Digital activism: after the hype. New Media Soc. (2017) 20:2099–106. doi: 10.1177/14614448177319
30. Sivitanides M, Shah V. The era of digital activism. In: 2011 Conference for Information Systems Applied Research(CONISAR) Proceedings Wilmington North Carolina, USA . Available online at: https://www.arifyildirim.com/ilt510/marcos.sivitanides.vivek.shah.pdf (accessed September 22, 2019).
31. Möller L, Schuetzle D, Autrup H. Future research needs associated with the assessment of potential human health risks from exposure to toxic ambient air pollutants. Environ Health Perspect . (1994) 102(Suppl. 4):193–210. doi: 10.1289/ehp.94102s4193
32. Jacobson MZ, Jacobson PMZ. Atmospheric Pollution: History, Science, and Regulation. Cambridge University Press (2002). p. 206. doi: 10.1256/wea.243.02
33. Stover RH. Flooding of soil for disease control. In: Mulder D, editor. Chapter 3. Developments in Agricultural and Managed Forest Ecology . Elsevier (1979). p. 19–28. Available online at: http://www.sciencedirect.com/science/article/pii/B9780444416926500094 doi: 10.1016/B978-0-444-41692-6.50009-4 (accessed July 1, 2019).
34. Maipa V, Alamanos Y, Bezirtzoglou E. Seasonal fluctuation of bacterial indicators in coastal waters. Microb Ecol Health Dis . (2001) 13:143–6. doi: 10.1080/089106001750462687
35. Bezirtzoglou E, Dimitriou D, Panagiou A. Occurrence of Clostridium perfringens in river water by using a new procedure. Anaerobe . (1996) 2:169–73. doi: 10.1006/anae.1996.0022
36. Kjellstrom T, Lodh M, McMichael T, Ranmuthugala G, Shrestha R, Kingsland S. Air and Water Pollution: Burden and Strategies for Control. DCP, Chapter 43. 817–32 p. Available online at: https://www.dcp-3.org/sites/default/files/dcp2/DCP43.pdf (accessed September 17, 2017).
37. Pathak RK, Wang T, Ho KF, Lee SC. Characteristics of summertime PM2.5 organic and elemental carbon in four major Chinese cities: implications of high acidity for water- soluble organic carbon (WSOC). Atmos Environ . (2011) 45:318–25. doi: 10.1016/j.atmosenv.2010.10.021
38. Bonavigo L, Zucchetti M, Mankolli H. Water radioactive pollution and related environmental aspects. J Int Env Appl Sci . (2009) 4:357–63
39. World Health Organization (WHO). Preventing Disease Through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease . 1106 p. Available online at: https://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf (accessed September 22, 2019).
40. Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health . (2015) 12:12735–60. doi: 10.3390/ijerph121012735
41. Ethical Unicorn. Everything You Need To Know About Aerosols & Air Pollution. (2019). Available online at: https://ethicalunicorn.com/2019/04/29/everything-you-need-to-know-about-aerosols-air-pollution/ (accessed October 4, 2019).
42. Colbeck I, Lazaridis M. Aerosols and environmental pollution. Sci Nat . (2009) 97:117–31. doi: 10.1007/s00114-009-0594-x
43. Incecik S, Gertler A, Kassomenos P. Aerosols and air quality. Sci Total Env . (2014) 355, 488–9. doi: 10.1016/j.scitotenv.2014.04.012
44. D'Amato G, Pawankar R, Vitale C, Maurizia L. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res . (2016) 8:391–5. doi: 10.4168/aair.2016.8.5.391
45. Bezirtzoglou C, Dekas K, Charvalos E. Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Anaerobe . (2011) 17:337–40. doi: 10.1016/j.anaerobe.2011.05.016
46. Castelli F, Sulis G. Migration and infectious diseases. Clin Microbiol Infect . (2017) 23:283–9. doi: 10.1016/j.cmi.2017.03.012
47. Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters. Emerg Infect Dis . (2007) 13:1–5. doi: 10.3201/eid1301.060779
48. Fenn B. Malnutrition in Humanitarian Emergencies . Available online at: https://www.who.int/diseasecontrol_emergencies/publications/idhe_2009_london_malnutrition_fenn.pdf . (accessed August 15, 2017).
49. Lindh E, Argentini C, Remoli ME, Fortuna C, Faggioni G, Benedetti E, et al. The Italian 2017 outbreak Chikungunya virus belongs to an emerging Aedes albopictus –adapted virus cluster introduced from the Indian subcontinent. Open Forum Infect Dis. (2019) 6:ofy321. doi: 10.1093/ofid/ofy321
50. Calba C, Guerbois-Galla M, Franke F, Jeannin C, Auzet-Caillaud M, Grard G, Pigaglio L, Decoppet A, et al. Preliminary report of an autochthonous chikungunya outbreak in France, July to September 2017. Eur Surveill . (2017) 22:17-00647. doi: 10.2807/1560-7917.ES.2017.22.39.17-00647
51. Menne B, Murray V. Floods in the WHO European Region: Health Effects and Their Prevention . Copenhagen: WHO; Weltgesundheits organisation, Regionalbüro für Europa (2013). Available online at: http://www.euro.who.int/data/assets/pdf_file/0020/189020/e96853.pdf (accessed 15 August 2017).
52. Schneider SH. The greenhouse effect: science and policy. Science . (1989) 243:771–81. doi: 10.1126/science.243.4892.771
53. Wilson WE, Suh HH. Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manag Assoc . (1997) 47:1238–49. doi: 10.1080/10473289.1997.10464074
54. US EPA (US Environmental Protection Agency) (2018). Available online at: https://www.epa.gov/pm-pollution/particulate-matter-pm-basics (accessed September 22, 2018).
55. Cheung K, Daher N, Kam W, Shafer MM, Ning Z, Schauer JJ, et al. Spatial and temporal variation of chemical composition and mass closure of ambient coarse particulate matter (PM10–2.5) in the Los Angeles area. Atmos Environ . (2011) 45:2651–62. doi: 10.1016/j.atmosenv.2011.02.066
56. Zhang L, Yang Y, Li Y, Qian ZM, Xiao W, Wang X, et al. Short-term and long-term effects of PM2.5 on acute nasopharyngitis in 10 communities of Guangdong, China. Sci Total Env. (2019) 688:136–42. doi: 10.1016/j.scitotenv.2019.05.470.
57. Kloog I, Ridgway B, Koutrakis P, Coull BA, Schwartz JD. Long- and short-term exposure to PM2.5 and mortality using novel exposure models, Epidemiology . (2013) 24:555–61. doi: 10.1097/EDE.0b013e318294beaa
58. New Hampshire Department of Environmental Services. Current and Forecasted Air Quality in New Hampshire . Environmental Fact Sheet (2019). Available online at: https://www.des.nh.gov/organization/commissioner/pip/factsheets/ard/documents/ard-16.pdf (accessed September 22, 2019).
59. Kappos AD, Bruckmann P, Eikmann T, Englert N, Heinrich U, Höppe P, et al. Health effects of particles in ambient air. Int J Hyg Environ Health . (2004) 207:399–407. doi: 10.1078/1438-4639-00306
60. Boschi N (Ed.). Defining an educational framework for indoor air sciences education. In: Education and Training in Indoor Air Sciences . Luxembourg: Springer Science & Business Media (2012). 245 p.
61. Heal MR, Kumar P, Harrison RM. Particles, air quality, policy and health. Chem Soc Rev . (2012) 41:6606–30. doi: 10.1039/c2cs35076a
62. Bezirtzoglou E, Alexopoulos A. Ozone history and ecosystems: a goliath from impacts to advance industrial benefits and interests, to environmental and therapeutical strategies. In: Ozone Depletion, Chemistry and Impacts. (2009). p. 135–45.
63. Villányi V, Turk B, Franc B, Csintalan Z. Ozone Pollution and its Bioindication. In: Villányi V, editor. Air Pollution . London: Intech Open (2010). doi: 10.5772/10047
64. Massachusetts Department of Public Health. Massachusetts State Health Assessment . Boston, MA (2017). Available online at: https://www.mass.gov/files/documents/2017/11/03/2017%20MA%20SHA%20final%20compressed.pdf (accessed October 30, 2017).
65. Lorenzini G, Saitanis C. Ozone: A Novel Plant “Pathogen.” In: Sanitá di Toppi L, Pawlik-Skowrońska B, editors. Abiotic Stresses in Plant Springer Link (2003). p. 205–29. doi: 10.1007/978-94-017-0255-3_8
66. Fares S, Vargas R, Detto M, Goldstein AH, Karlik J, Paoletti E, et al. Tropospheric ozone reduces carbon assimilation in trees: estimates from analysis of continuous flux measurements. Glob Change Biol . (2013) 19:2427–43. doi: 10.1111/gcb.12222
67. Harmens H, Mills G, Hayes F, Jones L, Norris D, Fuhrer J. Air Pollution and Vegetation . ICP Vegetation Annual Report 2006/2007. (2012)
68. Emberson LD, Pleijel H, Ainsworth EA, den Berg M, Ren W, Osborne S, et al. Ozone effects on crops and consideration in crop models. Eur J Agron . (2018) 100:19–34. doi: 10.1016/j.eja.2018.06.002
69. Alexopoulos A, Plessas S, Ceciu S, Lazar V, Mantzourani I, Voidarou C, et al. Evaluation of ozone efficacy on the reduction of microbial population of fresh cut lettuce ( Lactuca sativa ) and green bell pepper ( Capsicum annuum ). Food Control . (2013) 30:491–6. doi: 10.1016/j.foodcont.2012.09.018
70. Alexopoulos A, Plessas S, Kourkoutas Y, Stefanis C, Vavias S, Voidarou C, et al. Experimental effect of ozone upon the microbial flora of commercially produced dairy fermented products. Int J Food Microbiol . (2017) 246:5–11. doi: 10.1016/j.ijfoodmicro.2017.01.018
71. Maggio A, Fagnano M. Ozone damages to mediterranean crops: physiological responses. Ital J Agron . (2008) 13–20. doi: 10.4081/ija.2008.13
72. McCarthy JT, Pelle E, Dong K, Brahmbhatt K, Yarosh D, Pernodet N. Effects of ozone in normal human epidermal keratinocytes. Exp Dermatol . (2013) 22:360–1. doi: 10.1111/exd.12125
73. WHO. Health Risks of Ozone From Long-Range Transboundary Air Pollution . Available online at: http://www.euro.who.int/data/assets/pdf_file/0005/78647/E91843.pdf (accessed August 15, 2019).
74. Thiele JJ, Traber MG, Tsang K, Cross CE, Packer L. In vivo exposure to ozone depletes vitamins C and E and induces lipid peroxidation in epidermal layers of murine skin. Free Radic Biol Med. (1997) 23:365–91. doi: 10.1016/S0891-5849(96)00617-X
75. Hatch GE, Slade R, Harris LP, McDonnell WF, Devlin RB, Koren HS, et al. Ozone dose and effect in humans and rats. A comparison using oxygen- 18 labeling and bronchoalveolar lavage. Am J Respir Crit Care Med . (1994) 150:676–83. doi: 10.1164/ajrccm.150.3.8087337
76. Lippmann M. Health effects of ozone. A critical review. JAPCA . (1989) 39:672–95. doi: 10.1080/08940630.1989.10466554
77. Gryparis A, Forsberg B, Katsouyanni K, Analitis A, Touloumi G, Schwartz J, et al. Acute effects of ozone on mortality from the “air pollution and health: a European approach” project. Am J Respir Crit Care Med . (2004) 170:1080–7. doi: 10.1164/rccm.200403-333OC
78. Soon W, Baliunas SL, Robinson AB, Robinson ZW. Environmental effects of increased atmospheric carbon dioxide. Climate Res . (1999) 13:149–64 doi: 10.1260/0958305991499694
79. Richmont-Bryant J, Owen RC, Graham S, Snyder M, McDow S, Oakes M, et al. Estimation of on-road NO2 concentrations, NO2/NOX ratios, and related roadway gradients from near-road monitoring data. Air Qual Atm Health . (2017) 10:611–25. doi: 10.1007/s11869-016-0455-7
80. Hesterberg TW, Bunn WB, McClellan RO, Hamade AK, Long CM, Valberg PA. Critical review of the human data on short-term nitrogen dioxide (NO 2 ) exposures: evidence for NO2 no-effect levels. Crit Rev Toxicol . (2009) 39:743–81. doi: 10.3109/10408440903294945
81. Chen T-M, Gokhale J, Shofer S, Kuschner WG. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci . (2007) 333:249–56. doi: 10.1097/MAJ.0b013e31803b900f
82. US EPA. Table of Historical SO 2 NAAQS, Sulfur US EPA . Available online at: https://www3.epa.gov/ttn/naaqs/standards/so2/s_so2_history.html (accessed October 5, 2019).
83. WHO Regional Office of Europe (2000). Available online at: https://euro.who.int/_data/assets/pdf_file/0020/123086/AQG2ndEd_7_4Sulfuroxide.pdf
84. Pruss-Ustun A, Fewrell L, Landrigan PJ, Ayuso-Mateos JL. Lead exposure. Comparative Quantification of Health Risks . World Health Organization. p. 1495–1542. Available online at: https://www.who.int/publications/cra/chapters/volume2/1495-1542.pdf?ua=1
PubMed Abstract | Google Scholar
85. Goyer RA. Transplacental transport of lead. Environ Health Perspect . (1990) 89:101–5. doi: 10.1289/ehp.9089101
86. National Institute of Environmental Health Sciences (NIH). Lead and Your Health . (2013). 1–4 p. Available online at: https://www.niehs.nih.gov/health/materials/lead_and_your_health_508.pdf (accessed September 17, 2019).
87. Farhat A, Mohammadzadeh A, Balali-Mood M, Aghajanpoor-Pasha M, Ravanshad Y. Correlation of blood lead level in mothers and exclusively breastfed infants: a study on infants aged less than six months. Asia Pac J Med Toxicol . (2013) 2:150–2.
88. Assi MA, Hezmee MNM, Haron AW, Sabri MYM, Rajion MA. The detrimental effects of lead on human and animal health. Vet World . (2016) 9:660–71. doi: 10.14202/vetworld.2016.660-671
89. Abdel-Shafy HI, Mansour MSM. A review on polycyclic aromatic hydrocarbons: source, environmental impact, effect on human health and remediation. Egypt J Pet . (2016) 25:107–23. doi: 10.1016/j.ejpe.2015.03.011
90. Kumar A, Singh BP, Punia M, Singh D, Kumar K, Jain VK. Assessment of indoor air concentrations of VOCs and their associated health risks in the library of Jawaharlal Nehru University, New Delhi. Environ Sci Pollut Res Int . (2014) 21:2240–8. doi: 10.1007/s11356-013-2150-7
91. Molhave L, Clausen G, Berglund B, Ceaurriz J, Kettrup A, Lindvall T, et al. Total Volatile Organic Compounds (TVOC) in Indoor Air Quality Investigations. Indoor Air . 7:225–240. doi: 10.1111/j.1600-0668.1997.00002.x
92. Gibb T. Indoor Air Quality May be Hazardous to Your Health . MSU Extension. Available online at: https://www.canr.msu.edu/news/indoor_air_quality_may_be_hazardous_to_your_health (accessed October 5, 2019).
93. Ebersviller S, Lichtveld K, Sexton KG, Zavala J, Lin Y-H, Jaspers I, et al. Gaseous VOCs rapidly modify particulate matter and its biological effects – Part 1: simple VOCs and model PM. Atmos Chem Phys Discuss . (2012) 12:5065–105. doi: 10.5194/acpd-12-5065-2012
94. WHO (World Health Organization). Dioxins and Their Effects on Human Health. Available online at: https://www.who.int/news-room/fact-sheets/detail/dioxins-and-their-effects-on-human-health (accessed October 5, 2019).
95. EEA (European Environmental Agency). Air Quality Standards to the European Union and WHO . Available online at: https://www.eea.europa.eu/themes/data-and-maps/figures/air-quality-standards-under-the
96. Nakano T, Otsuki T. [Environmental air pollutants and the risk of cancer]. (Japanese). Gan To Kagaku Ryoho . (2013) 40:1441–5.
97. Kurt OK, Zhang J, Pinkerton KE. Pulmonary health effects of air pollution. Curr Opin Pulm Med . (2016) 22:138–43. doi: 10.1097/MCP.0000000000000248
98. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet . (2014) 383:1581–92. doi: 10.1016/S0140-6736(14)60617-6
99. Jiang X-Q, Mei X-D, Feng D. Air pollution and chronic airway diseases: what should people know and do? J Thorac Dis . (2016) 8:E31–40.
100. Bourdrel T, Bind M-A, Béjot Y, Morel O, Argacha J-F. Cardiovascular effects of air pollution. Arch Cardiovasc Dis . (2017) 110:634–42. doi: 10.1016/j.acvd.2017.05.003
101. Hoffmann B, Moebus S, Möhlenkamp S, Stang A, Lehmann N, Dragano N, et al. Residential exposure to traffic is associated with coronary atherosclerosis. Circulation . (2007) 116:489–496. doi: 10.1161/CIRCULATIONAHA.107.693622
102. Katholi RE, Couri DM. Left ventricular hypertrophy: major risk factor in patients with hypertension: update and practical clinical applications. Int J Hypertens . (2011) 2011:495349. doi: 10.4061/2011/495349
103. Leary PJ, Kaufman JD, Barr RG, Bluemke DA, Curl CL, Hough CL, et al. Traffic- related air pollution and the right ventricle. the multi-ethnic study of atherosclerosis. Am J Respir Crit Care Med . (2014) 189:1093–100. doi: 10.1164/rccm.201312-2298OC
104. Genc S, Zadeoglulari Z, Fuss SH, Genc K. The adverse effects of air pollution on the nervous system. J Toxicol . (2012) 2012:782462. doi: 10.1155/2012/782462
105. Calderon-Garciduenas L, Azzarelli B, Acuna H, et al. Air pollution and brain damage. Toxicol Pathol. (2002) 30:373–89. doi: 10.1080/01926230252929954
106. Rückerl R, Greven S, Ljungman P, Aalto P, Antoniades C, Bellander T, et al. Air pollution and inflammation (interleukin-6, C-reactive protein, fibrinogen) in myocardial infarction survivors. Environ Health Perspect . (2007) 115:1072–80. doi: 10.1289/ehp.10021
107. Peters A, Veronesi B, Calderón-Garcidueñas L, Gehr P, Chen LC, Geiser M, et al. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part Fibre Toxicol . (2006) 3:13–8. doi: 10.1186/1743-8977-3-13
108. Kelly FJ. Dietary antioxidants and environmental stress. Proc Nutr Soc . (2004) 63:579–85. doi: 10.1079/PNS2004388
109. Bellinger DC. Very low lead exposures and children's neurodevelopment. Curr Opin Pediatr . (2008) 20:172–7. doi: 10.1097/MOP.0b013e3282f4f97b
110. Balbo P, Silvestri M, Rossi GA, Crimi E, Burastero SE. Differential role of CD80 and CD86 on alveolar macrophages in the presentation of allergen to T lymphocytes in asthma. Clin Exp Allergy J Br Soc Allergy Clin Immunol . (2001) 31:625–36. doi: 10.1046/j.1365-2222.2001.01068.x
111. Drakaki E, Dessinioti C, Antoniou C. Air pollution and the skin. Front Environ Sci Eng China . (2014) 15:2–8. doi: 10.3389/fenvs.2014.00011
112. Weisskopf MG, Kioumourtzoglou M-A, Roberts AL. Air pollution and autism spectrum disorders: causal or confounded? Curr Environ Health Rep . (2015) 2:430–9. doi: 10.1007/s40572-015-0073-9
113. Mo Z, Fu Q, Lyu D, Zhang L, Qin Z, Tang Q, et al. Impacts of air pollution on dry eye disease among residents in Hangzhou, China: a case-crossover study. Environ Pollut . (2019) 246:183–9. doi: 10.1016/j.envpol.2018.11.109
114. Klopfer J. Effects of environmental air pollution on the eye. J Am Optom Assoc . (1989) 60:773–8.
115. Ashfaq A, Sharma P. Environmental effects of air pollution and application of engineered methods to combat the problem. J Indust Pollut Control . (2012) 29.
116. Madronich S, de Gruijl F. Skin cancer and UV radiation. Nature . (1993) 366:23–9. doi: 10.1038/366023a0
117. Teramura A. Effects of UV-B radiation on the growth and yield of crop plants. Physiol Plant . (2006) 58:415–27. doi: 10.1111/j.1399-3054.1983.tb04203.x
118. Singh E, Tiwari S, Agrawal M. Effects of elevated ozone on photosynthesis and stomatal conductance of two soybean varieties: a case study to assess impacts of one component of predicted global climate change. Plant Biol Stuttg Ger . (2009) 11(Suppl. 1):101–8. doi: 10.1111/j.1438-8677.2009.00263.x
119. Manderson L. How global Warming is Adding to the Health Risks of Poor People . The Conversation. University of the Witwatersrand. Available online at: http://theconversation.com/how-global-warming-is-adding-to-the-health-risks-of-poor-people-109520 (accessed October 5, 2019).
120. Ministers of Energy and Environment. Federal/Provincial/Territorial Ministers of Energy and Environment (Canada), editor. The Canada-Wide Acid Rain Strategy for Post-2000 . Halifax: The Ministers (1999). 11 p.
121. Zuhara S, Isaifan R. The impact of criteria air pollutants on soil and water: a review. (2018) 278–84. doi: 10.30799/jespr.133.18040205
122. WHO. First WHO Global Conference on Air Pollution and Health. (2018). Available online at: https://www.who.int/airpollution/events/conference/en/ (accessed October 6, 2019).
123. What is the Kyoto Protocol? UNFCCC . Available online at: https://unfccc.int/kyoto__protocol (accessed October 6, 2019).
124. CopenhagenClimate Change Conference (UNFCCC) . Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
125. Durban Climate Change Conference,. UNFCCC (2011). Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
126. Paris Climate Change Agreement,. (2016). Available online at: https://unfccc.int/process-and-meetings/the-paris-agreement/the-paris-agreement
Keywords: air pollution, environment, health, public health, gas emission, policy
Citation: Manisalidis I, Stavropoulou E, Stavropoulos A and Bezirtzoglou E (2020) Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 8:14. doi: 10.3389/fpubh.2020.00014
Received: 17 October 2019; Accepted: 17 January 2020; Published: 20 February 2020.
Reviewed by:
Copyright © 2020 Manisalidis, Stavropoulou, Stavropoulos and Bezirtzoglou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ioannis Manisalidis, giannismanisal@gmail.com ; Elisavet Stavropoulou, elisabeth.stavropoulou@gmail.com
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Effects of Air Pollution on Health
Air pollution refers to the presence of substances in the air at concentrations that affect human health or the environment. Clean air is important for clean health, and air pollution threatens health in many ways. Every individual has a fundamental right to access free and unlimited clean air. The human lung acts as an interface between the body and the environment. On average, an individual takes in about 10 million breaths annually.
In the process, there is a high possibility of toxic substances reaching the lungs and other organs where they can cause harmful effects. Therefore, there is a need for an appropriate policy response to minimize levels of air pollutants such as particulate matter, nitrogen dioxide, ozone, carbon monoxide, and others (Koenig 165). Reduction in air pollution will bring considerable health benefits to humans. Adequate understanding of these effects is a significant step towards establishing successful policies to minimize these risks. This paper discusses the main effects of air pollution on health, the main air pollutants, and the policies necessary to reduce the levels of air pollution.
Exposure to air pollution causes several health problems, starting from modest changes in the respiratory tract and the affected pulmonary function, moving to restricted performance, emergency rooms visits and hospital admissions, and to deaths (Saldiva 220). Air pollution has adverse effects not only on the respiratory system but affects the cardiovascular system as well. This is true from both acute and chronic exposures to air pollutants.
The most adverse effects of air pollution in terms of the overall health problems include reduction in life expectancy of average populations, related to long-term exposures to high levels of air pollution with particulate matter. It is necessary to understand adequately the nature and magnitude of the effects of air pollutants on health. Air pollutants constitute an important overall component of both outdoor and indoor air and are known to cause health effects, essentially with individuals with pre-existing illnesses.
Air pollution poses a considerable threat to health causing morbidity and reduced life expectancy. The effects of air pollution on human health can be short term or long term. Both short term and long term effects can cause varying degrees of damage to human health. Short term and long term effects may include minor irritations and death respectively (Bauer 1093). Toxic air particles have short term effects such as; immediate irritation to the eyes or throat and in the long term causes death due to respiratory failure or heart attacks (Bauer 1092).
Population subgroups are affected differently by air pollution risks. Variations in terms of sensitivity exposure occur due to nutrition issues, state of general health, and genetic predisposition. Vulnerable groups under high risk include infants and young children, the elderly, pregnant mothers and their unborn fetuses, individuals suffering from other diseases, malnourished, and others (Koenig 165). It is necessary to identify these vulnerable groups because they are the first to be affected as the levels of air pollution increase. Generally, only a minority of the total population is affected by high levels of exposure. Therefore, any excess to mortality due to a pollutant is likely to be restricted to a small group of the population (Bauer 1094).
The Main Air Pollutants
The main constituents of air pollution include a highly variable, complex mixture of different substances, such as smog, that is, photochemical oxidants, carbon monoxide, nitrogen oxides, sulfur oxides, and particulates (Koenig 165). There are many different components in the troposphere that can cause potential effects on human health and the general environment. This paper focuses on pollutants such as particulate matter, ozone, and nitrogen dioxide.
First, long-term exposure to high levels of pollution with particulate matter causes a significant reduction in the life expectancy of the average population (Douglas 6). Important health effects associated with particulate matter in the short term exposure include respiratory problems, increase in mortality, inflammatory reactions in the lungs, increase in hospital admissions, and adverse effects on the cardiovascular system (Dominici et al., 10). The health effects associated with long-term exposure of particulate matter include; reduction in lung function in children and adults, reduced lung function development, reduction in life expectancy due to mainly cardiopulmonary deaths and lung cancer, and others (Koenig 139).
Particulates absorb various chemicals and increase their penetration and longevity in the lungs. They also condense water and vapor and augment the effects of gaseous pollutants like sulphur oxides. The main particulates of concern include; lead, asbestos, mercury, and other major metals. Effects of lead include; anemia, gastrointestinal cramping, and impaired neural functioning (Koenig 128). Asbestos affects pulmonary lesions and mesothelial tissue damages. Asbestos is also associated linked to pulmonary cancer. Lead poisoning on the other hand may affect retardation and possibly hyperactivity in children (Koenig 129).
Second, the ozone is the main toxic element of the oxidants. All photochemical oxidants are manufactured by processes of photosynthesis involving the emissions of hydrocarbon and nitrogen oxides from internal combustion (Evans 107). Health effects associated with short-term exposure to the ozone include; increase in mortality, an increase in hospital admissions, inflammatory reactions to the lungs, an increase in medication usage, adverse effects on pulmonary function, and others. Health effects associated with long term exposure include reduction in lung function (Koenig 139).
Third, the Combustion of fossils is the major source of ambient sulphur oxides. Exposure to ambient sulfur oxides irritates upper respiratory passage in humans, reducing mucus clearance, and reducing pulmonary functioning (Evans 106). Studies on greater exposures cause nasal lesions, bronchitis, pneumonia, and severe pulmonary disorder. Nitrogen oxides are ubiquitous in the air and produced by fossil fuel combustion in motor vehicles and electrical power production. It causes reduced pulmonary functioning, reduced immunity to fight diseases, diminished weight gain, and bronchial inflammation (Evans 107).
The health effects caused by nitrogen dioxide in the short term exposure include; increase in mortality, an increase in hospital admissions, an increase in airwaves allergic inflammation reactions, and effects in pulmonary functions, specifically in asthmatics. Health effects related to long term exposure include increased probability of respiratory symptoms.
Carbon monoxide is caused by incomplete combustion primarily emitted from motor vehicles or cigarette smoking. It causes headaches, nausea, and dizziness associated with deprivation of oxygen. Greater exposure to carbon monoxide can result to result to cortical cellular structure, altered heartbeat, vascular diseases, impaired liver functioning, and fetal growth retardation (Evans 106). Exposure to carbon monoxide is also associated with low birth weight, increased prenatal deaths, increased distress in patients, cardiovascular ailments, and possible infection of cardiovascular disease (Evans 107).
In sum exposure to air pollution specifically, particulate matter, and ozone pose a significant risk to human health. Recent evidence suggests, however, that ozone levels lower than those experienced during episodes of “summer smog” may have considerable effects on human health (Koenig 44).
Policies Necessary to Reduce Air Pollution Levels and Human exposure
The causes and sources of air pollution are more complex and intricate. Therefore the matrix of strategies to reduce air pollution demands broad policy combinations. This necessitates the need to implement appropriate policy strategies to reduce air pollution at all levels and mitigate its adverse effects on human health. These measures include national policy and regulatory framework; local monitoring of air pollution; public information and health warnings; land use planning; transport policy; and energy policy.
First, the national air pollution standards need to be developed to assist local air pollution management. The national government must offer expertise and guidance not available locally. They can also assist local authorities with the fiscal, legal, and institutional mandate for taking action on air pollution locally. Second, local air pollution monitoring must be put in place to identify the changes in pollution concentrations.
The monitoring mechanism must support the overall air pollution management strategy. Three, use public information systems to warn people of severe air pollution consequences, offer control measures, and in the long run increase public awareness of air pollution problems. Fourth, establish education and awareness programs to help people take measures to avoid exposure. Fifth, there is a need to reduce sulfur and organic toxic elements from relevant petroleum products and encouragement of increased use of locally applicable renewable energy to reduce emissions.
In summary, air pollution affects human health. The quality of air affects our health, interpersonal behavior, mood, attitudes, outdoor activities, outdoor activities, and others. Most research on air pollution effects on health tend to concentrate more on physical outcomes such as mortality or diseases. I would suggest the need to look at air quality in terms of policy strategies that may be linked to air quality such as discomfort, irritability, depression, and anxiety.
There is a need to document the adverse effects of different air pollutants on human health, and this should include diseases and the estimated reduction in life expectancy as a result of toxic air. All evidence of increased mortality in highly polluted areas needs to be documented. Relevant authorities must implement regulations by authorities to minimize emissions of toxic air substances. In essence, there is a need for accurate information on the effects of air pollution on health as a basis for establishing effective strategies to minimize these effects.
Works Cited
Brauer, Michael. “Air Pollution from Traffic and Development of Respiratory.” American Journal of Respiratory and Critical Care Medicine, 166 (2002): 1092-1098. Web.
Dominici, Francesca, Peng Roger, Bell Michel, Pham Luu, and Zeger Scot. Particulate Air Pollution and Hospital Admission for Cardiovascular and Respiratory Diseases. The Journal of the American Medical Association , 295 (2006): 10-21.
Douglas, James, and Waller Ryan. Air Pollution and Respiratory Infection in Children. British Medical Association, 20 (1966):1-8.
Evans, Gary. Environmental Stress. Cambridge: Cambridge University Press, 1984.
Koenig, Jane. Health Effects of Ambient Air Pollution. New York: Springer, 2000.
Saldiva, Lichtenfel, and Paiva Barone. Between Air Pollution and Mortality Due to Respiratory Diseases. Environmental Research Journal, 65 (1994): 218-225.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2021, December 9). Effects of Air Pollution on Health. https://studycorgi.com/effects-of-air-pollution-on-health/
"Effects of Air Pollution on Health." StudyCorgi , 9 Dec. 2021, studycorgi.com/effects-of-air-pollution-on-health/.
StudyCorgi . (2021) 'Effects of Air Pollution on Health'. 9 December.
1. StudyCorgi . "Effects of Air Pollution on Health." December 9, 2021. https://studycorgi.com/effects-of-air-pollution-on-health/.
Bibliography
StudyCorgi . "Effects of Air Pollution on Health." December 9, 2021. https://studycorgi.com/effects-of-air-pollution-on-health/.
StudyCorgi . 2021. "Effects of Air Pollution on Health." December 9, 2021. https://studycorgi.com/effects-of-air-pollution-on-health/.
This paper, “Effects of Air Pollution on Health”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: December 9, 2021 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Effects of Air Pollution on Human Health
The World Health Organization (WHO) and other international agencies recognize air pollution as a major threat to human health. Numerous scientific studies have linked air pollution to a variety of health problems (Table 6.2) including: aggravation of respiratory and cardiovascular diseases; decreased lung function; increased frequency and severity of respiratory symptoms such as difficulty breathing and coughing; increased susceptibility to respiratory infections; effects on the nervous system, including the brain, such as IQ loss and impacts on learning, memory, and behavior; cancer; and premature death. Immediate effects of air pollution may show up after a single exposure or repeated exposures. Other health effects may show up either years after exposure has occurred or only after long or repeated periods of exposure.
Immediate effects of air pollution include irritation of the eyes, nose, and throat, headaches, dizziness, and fatigue. Such immediate effects are usually short-term and treatable. Sometimes the treatment is simply eliminating the person’s exposure to the source of the pollution, if it can be identified. Symptoms of some diseases, including asthma, hypersensitivity pneumonitis, and humidifier fever , may also show up soon after exposure to some indoor air pollutants.
Table 6.2: Sources and health effects of criteria pollutants
Source: www.epa.gov
The likelihood of immediate reactions to air pollutants depends on several factors. Age and preexisting medical conditions are two important influences. Some sensitive individuals appear to be at greater risk for air pollution-related health effects, for example, those with pre-existing heart and lung diseases (e.g., heart failure/ischemic heart disease, asthma, emphysema, and chronic bronchitis), diabetics, older adults, and children. In other cases, whether a person reacts to a pollutant depends on individual sensitivity, which varies tremendously from person to person. Some people can become sensitized to biological pollutants after repeated exposures, and it appears that some people can become sensitized to chemical pollutants as well.
Attribution
Zehnder, Caralyn; Manoylov, Kalina; Mutiti, Samuel; Mutiti, Christine; VandeVoort, Allison; and Bennett, Donna, “Introduction to Environmental Science: 2nd Edition” (2018). Biological Sciences Open Textbooks. 4. https://oer.galileo.usg.edu/biology-textbooks/4 This work is licensed under a Creative Commons Attribution-Noncommercial-Share Alike 4.0 License .
Environmental Biology Copyright © by Various Authors is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
Air Pollution and Its Impact on Human Health
Common health problems associated with air pollution.
Indoor and outdoor air pollution causes several common health problems which according to the New Jersey Department of Environmental Protection (2009) are grouped according to the major pollutants. To begin with, carbon monoxide compromises the heart activities hence lethargy and fatigue. It also causes nausea, dizziness, and headaches and in large amounts may even lead to death. Nitrogen dioxide causes nasal and throat irritation and increases the risk of developing respiratory infections. Ozone causes irritation of the respiratory system leading to coughs, chest and throat pains. Particulates cause damage to respiratory tract tissues especially lung tissue leading to lung diseases. Sulfur dioxide is known to make worse existing lung diseases such as bronchitis, asthma, pneumonia and tuberculosis. Lead on the other hand causes damage to the brain and the nervous system with children being most susceptible (New Jersey Department of Environmental Protection, 2009; California Air Resources Board 2007a). From these, it is evident that air pollution has adverse common effects on the respiratory system and to some extent other body parts.
Vulnerability of children to pollutants
The most common health problems in children associated with air pollution occurs in the respiratory system. This is due to the fact that children’s respiratory system is not fully developed therefore immature. This means that the structures are weak and are prone to damage at the slightest exposure to air pollutants. The children’s health study by the California air resources board reported that children are more vulnerable to effects of air pollutants as they are exposed to more air pollution than adults as they have higher respiratory rates and are normally outdoors (California Air Resources Board 2007b). Other factors may include the underdeveloped immune system in children that is not able to effectively and efficiently fight off the effects of air pollution on the body and large surface area to volume ratio that exposes a large surface area to air pollution.
Needs assessment process and the role of Health educator
Community needs assessment is a systematic process in which the health educator, the nurse and other health care professionals together with the members of the community determine the health problems & needs of the community & develop plans of action and implement those plans. In this case the needs assessment process will be in relation to air pollution. The first step is exploration which involves mapping out the community with the purpose of obtaining baseline information that help plan for the rest of the assessment process. The second is step is planning for assessment exercise where by the necessary resources are put into place and objective designed, in this case it will be; to assess health impacts of air pollution and how to combat these effects. The third step is recruitment and training of assistants, fourth step is pretesting and reworking of the tool as it helps to detect faults and shortcomings after which corrections are made. The fifth step is execution of the assessment which basically involves actual going to the community and engaging the community into discussions and giving them the assessment tools so that they can feel it with relevant information. The sixth step is critical analysis of the findings and recommendations. The collected data is analyzed and then findings and recommendations are drawn. One of fundamental recommendation that will be made is to initiate Health Education and Promotion to combat the effects of air pollution. Health education/promotion empowers an individual with the much needed and relevant information that can be of great assistance in management of his/her health and other related issues. The health education and promotion will involve sources of air pollutants, their effects on human health, management and prevention measures. The health educator, the nurse and other stakeholders can carry out this activity with the help of the local health professionals working within the community and even train some community members who will be educating their colleagues; this creates a sense of belonging and ownership among the community members in that they will participate in the health education/promotion activities as their own. This empowers the community and the information stays with them even years after the time of carrying out the assessment. The final step is evaluation and just as in nursing process, evaluations helps in checking if the assessment was a success and whether there has been any positive impact and if interventions put in place had desired results. Evaluation also helps in knowing if the set goals and objectives were met, determining success or failure of the problem and to put corrective measure into place (Zerwekh, 112; Holloway, & Wheeler, 76; Grol 361). The health educator works hand in hand with the community health nurse and other health professionals in the above process where by he/she acts the overall supervisor.
Air pollution has adverse effects on health and majorly affects the respiratory system with children being most vulnerable due to their under developed respiratory system. Health educators are charged with the overall responsibility of overseeing planning, implementation and evaluation of education programs in the community. They also function as consultants to the other health care professionals involved in health education and promotion.
- “Air Pollutants and their health effects”. New Jersey Department of Environmental Protection. 2009. Web.
- “ Health Effects Research .” California Air Resources Board. 2007a. Web.
- The Children’s Health Study . California Air Resources Board. 2007b. Web.
- Grol R. “National standard setting for quality of care in general practice: attitudes of general practitioners and response to a set of standards.” Br J Gen Pract 40 (2000): 361–4.
- Holloway, I., & Wheeler, S. Qualitative Research in Nursing. 2nd Ed. Oxford: Blackwell Publishing, 2002.
- Zerwekh, J. Nursing Today: Transition and Trends. Philadelphia: W. B. Saunders Company, 2003.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, January 16). Air Pollution and Its Impact on Human Health. https://ivypanda.com/essays/air-pollution-and-its-impact-on-human-health/
"Air Pollution and Its Impact on Human Health." IvyPanda , 16 Jan. 2024, ivypanda.com/essays/air-pollution-and-its-impact-on-human-health/.
IvyPanda . (2024) 'Air Pollution and Its Impact on Human Health'. 16 January.
IvyPanda . 2024. "Air Pollution and Its Impact on Human Health." January 16, 2024. https://ivypanda.com/essays/air-pollution-and-its-impact-on-human-health/.
1. IvyPanda . "Air Pollution and Its Impact on Human Health." January 16, 2024. https://ivypanda.com/essays/air-pollution-and-its-impact-on-human-health/.
Bibliography
IvyPanda . "Air Pollution and Its Impact on Human Health." January 16, 2024. https://ivypanda.com/essays/air-pollution-and-its-impact-on-human-health/.
- Throat Cancer With Diagnosis of Human Papillomavirus
- Focused Throat Exam: Differential Diagnosis
- The Best Practices Toward the Treatment of Ear, Nose and Throat Infections
- The Virus That Causes Throat Cancers
- Bacteria Infectious Diseases: Strep Throat
- Environmental Factors and Health Promotion: Indoor and Outdoor Air Pollution
- Sore Throat Differential Diagnosis
- Why Is It Important to Spend Time Outdoors: Essay
- Respiratory Disorder and Nursing Treatment Plan
- SOAP (Subjective, Objective, Assessment and Plan) Note for Throat Exam
- Drugs Affecting the Respiratory System: Bronchodilators
- Asthma Is a Chronic Inflammatory Disorder
- Asthma: Leading Chronic Illness Among Children in the US
- Acute Respiratory Distress Syndrome
- Pharmacotherapy for Respiratory Disorders
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

A Narrative Review on the Human Health Effects of Ambient Air Pollution in Sub-Saharan Africa: An Urgent Need for Health Effects Studies
1 School of Public Health, University of California-Berkeley, Berkeley, CA 94704, USA
Samuel Kizito
2 College of Health Sciences, Makerere University, Kampala, Uganda; moc.oohay@otizikemos
Associated Data
An important aspect of the new sustainable development goals (SDGs) is a greater emphasis on reducing the health impacts from ambient air pollution in developing countries. Meanwhile, the burden of human disease attributable to ambient air pollution in sub-Saharan Africa is growing, yet estimates of its impact on the region are possibly underestimated due to a lack of air quality monitoring, a paucity of air pollution epidemiological studies, and important population vulnerabilities in the region. The lack of ambient air pollution epidemiologic data in sub-Saharan Africa is also an important global health disparity. Thousands of air pollution health effects studies have been conducted in Europe and North America, rather than in urban areas that have some of the highest measured air pollution levels in world, including urban areas in sub-Saharan Africa. In this paper, we provide a systematic and narrative review of the literature on ambient air pollution epidemiological studies that have been conducted in the region to date. Our review of the literature focuses on epidemiologic studies that measure air pollutants and relate air pollution measurements with various health outcomes. We highlight the gaps in ambient air pollution epidemiological studies conducted in different sub-regions of sub-Saharan Africa and provide methodological recommendations for future environmental epidemiology studies addressing ambient air pollution in the region.
1. Introduction
Recent global burden of disease modeling suggests that low-income countries of sub-Saharan Africa (SSA) suffer the highest burden of disease and premature death attributable to environmental pollution [ 1 ]. According to the World Health Organization (WHO), ambient air pollution (AAP) levels exceed recommended limits for as much as 92% of the world’s population [ 2 ], and, compared to all other forms of environmental pollution (e.g., water, soil, and occupational), air pollution causes the largest number of environmental pollution-related deaths [ 1 ]. As a result, the new sustainable development goals places high priority on reducing the impacts of ambient air pollution on non-communicable diseases [ 3 ].
In SSA, there is a paucity of AAP epidemiological studies. In addition, the vast majority of air pollution epidemiological studies in the region are on indoor air pollution (IAP) from household use of cooking fuels. Consequently, the literature regarding the health effects of AAP comes from studies conducted mostly in North America and Western Europe. For instance, the most recent report on the global burden of disease attributable to air pollution derived their AAP burden estimates using integrated exposure–response functions based on data entirely from North American (US and Canada) and European epidemiologic studies [ 4 ]. Several recent systematic reviews and meta-analyses on the health effects of AAP for heart failure [ 5 , 6 ], hypertension [ 7 ], pneumonia [ 8 ], and asthma [ 9 ], included studies from every other continent except SSA. Importantly, there is very good reason to suspect that North American- and European-based exposure–response functions from air pollutants, such as PM 2.5 , may not be readily generalized to such low-income settings in much of SSA, suggesting the possibility that the health burden attributable to AAP may be underestimated in the region.
There are important population-level vulnerabilities and individual-level susceptibilities in SSA which may influence exposure-response relationships of air pollution. Vulnerabilities include multiple overlapping socioeconomic risk factors, access to quality health care, and co-prevalence of chronic and infectious diseases (e.g., tuberculosis (TB) and HIV). Secondly, from the sparse air quality monitoring data that are available for the region, average mean levels of PM 2.5 in some urban areas have been measured at an order of magnitude higher than levels measured in North American and European urban AAP epidemiology studies. Hence, there is greater uncertainty in the magnitude of health effects at high end air pollution exposures since so few studies have been conducted in the most polluted regions [ 4 ]. Thirdly, since air pollution is a complex mixture of gases and particulates that is largely determined by the sources of air pollution, there are likely to be substantive differences in air pollution sources and thus important differences in air pollution components between higher income countries and the lower income countries of SSA. Therefore, the toxicity of air pollutants such as PM 2.5 may be inherently different in ways that place even greater uncertainty in understanding the population health impact of air pollution in the region. It is therefore important to understand the current state of the literature regarding air pollution epidemiologic studies conducted in SSA to date, and to further identify critical gaps in the literature that should help guide future AAP epidemiological research in SSA; a region that lacks adequate air quality monitoring networks and the political will to address air pollution and its impacts [ 3 ], and that also has important population-wide vulnerabilities.
In this review article, we summarize the state of the literature on AAP epidemiologic studies throughout the SSA region. To highlight important gaps in the existing literature, and thus a path forward for future studies in the region, we emphasize the following themes in the review: (1) the regional distribution of AAP epidemiology studies; (2) the types of ambient air pollutants measured; (3) the health outcomes examined; and (4) the observed direction of acute and chronic health effects. This review synthesizes knowledge about a major region of the global population that is severely under-studied in the AAP epidemiology literature and thus addresses an important environmental justice issue in global health [ 1 ].
2.1. Systematic Review
Our systematic review of the published literature focused on original research articles in English language peer-reviewed scientific journals. Search terms were used in a manner that coupled “air pollution” and <country> together or, alternatively, “air quality” and <country> together, with the second search term a designated country ( N = 48) within SSA. In other words, we searched for all studies within SSA with “air pollution” or “air quality” in the text of the article and each search was performed separately for each individual country. We used identical search terms in PubMed, EMBASE, and Google Scholar databases. There was no restriction based on online data base searches in terms of time period of the study or the publication date. From the resultant searches, we reviewed all relevant abstracts and selected out all of those studies that indicated air pollutants were measured as a basis for exposure assessment to air pollution in the study population and where statistical analyses were undertaken to test associations between ambient air pollution measurements and any health outcome of interest and where exposure–response relationships for specific pollutants are reported. We did not restrict the analysis based on any sub-groups (e.g., age, sex, or urban or rural) or by study design. Since IAP and its health effects have been reviewed extensively already, we excluded studies that investigated IAP as the only exposure of interest instead of AAP. In our review of the literature, we decided to only report on those studies with actual air pollutant measurements to highlight the importance of more studies that actually measure air pollutants to derive exposure–response relationships. In addition, since we are strictly interested in epidemiological studies and where pollutant measurements are used to derive an exposure–response relationship, studies were not included in this review if they only related AAP measurements with biomarkers of exposure (e.g., exhaled or urinary markers) nor were they included if factors such as geographic location or occupation were used as air pollution exposure proxies.
In our review, we defined SSA countries as those classified as such by The World Bank [ 10 ]. Hence, in our review, we searched for the SSA countries mapped in Figure 1 .

Map of study area and locations of individual-level AAP epidemiology studies. Countries with individual-level AAP epidemiology studies are indicated with diagonal grey lines and the respective study author and citation number provided for each studied country.
2.2. Descriptive and Narrative Analysis
Our analysis of the reviewed studies is mostly qualitative because we only provide descriptive summaries across all studies and stratified by key aspects of the different studies. Hence, we provide tabular and graphical summaries to help guide the narrative of this review in a focused and consistent manner. We summarized the studies by the following key themes: (1) the regional distribution of AAP epidemiology studies; (2) the types of ambient air pollutants measured; (3) the health outcomes examined; and (4) the observed direction of acute and chronic health effects. We also provide summaries of other subtle, yet important, aspects of the included studies, such as time trends, the study designs, and sub-populations studied. We also review health risk modeling considerations, such as statistical methods used to test exposure–response associations, whether IAP was controlled for in the studies, or whether effect modifiers such as social class, education-level or smoking were considered, or whether a multi-pollutant modeling framework was applied in the analyses.
We did not perform a meta-analysis as part of our systematic review because we felt such an analysis was not warranted given our motivations of the review, the fairly small number of studies, and given that our review is not focused on any single disease or outcome [ 4 ]. While our review was performed systematically but with a narrative and qualitative analysis, we do not argue that the currently available literature precludes other researchers from conducting a meta-analysis, but rather this work represents a jumping-off-point for such future efforts.
A total of twelve studies were identified that satisfied our inclusion criteria of studies that derived exposure-response relationships (for any health outcome) using AAP measurements. A detailed summary of the included studies is presented in the Supplementary Materials (Table S1) . Remarkably, all of the included studies have been published just within the past seven years ( Figure 2 ) and more than half published in the last two years. In the course of our review, we identified a number of other AAP epidemiological studies from SSA [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 ] that did not fit our strict inclusion criteria but are worth noting. While these other studies did not assign air pollution exposure from measurements to derive exposure-response relationships, but instead assigned AAP exposures using proxies such as occupation (e.g., a variety of transportation workers or street vendors), proximity to air pollution sources or intensity of sources, biomarkers (e.g., exhaled CO), perceived air pollutant levels, or comparisons of an air pollution “exposed” region versus a relatively “unexposed” region, each of these AAP exposure-proxy studies show strong and consistent positive associations for health risks such as chronic respiratory, cardiovascular [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 19 ] or adverse birth outcomes [ 18 ]. Since these other exposure-proxy studies are important and may be of interest to readers, a brief summary of these other studies is presented in Table S2 in the Supplementary Materials .

Total number of published ambient air pollution (AAP) epidemiology studies included in the review by year (x-axis).
4. Regional Patterns of Studies
We observed a substantial disparity in terms of the regional patterns of where air pollution epidemiological studies have been carried out in the region. For instance, of the twelve air pollution epidemiology studies included in the review, 10 tested individual-level AAP exposure-response relationships and these were all carried out in just six countries total (Democratic Republic of Congo (DRC), Ghana, Kenya, Niger, Nigeria, and South Africa). Moreover, of the twelve included studies, three-quarters were carried out in South Africa ( N = 9, five of which are multi-country studies), with the city of Durban, South Africa comprising 25% of the twelve studies. Of the two studies that included all of the other SSA countries, each one is a multi-country study with an ecologic country-level or region-level design. All of the study populations in the country-specific studies focused on urban populations.
5. Summary of Study Outcomes
A graphical summary of the study outcomes assessed in the included studies is presented in Figure 3 . More than half of the twelve reviewed studies focus on respiratory outcomes or mortality ( N = 5 and 3, respectively), with the balance focused on stroke, psychosocial (depression), adverse birth outcomes (low birth weight and preterm), and disability. Of the three mortality studies, one is focused on cause-specific mortality (respiratory, cardiovascular, and cerebrovascular) and the other two are focused on population sub-groups (infant, under-five, adult, and maternal mortality). Figure 4 further summarizes the respiratory effects studies by highlighting the types of respiratory outcomes assessed. As indicated in Figure 4 , symptom-based respiratory outcomes predominate, followed by diagnosis- and measurement-based respiratory outcomes. Of the symptom-based outcomes, the most common outcomes studied are cough and wheeze (likely because several studies used the International Study of Asthma and Allergies in Childhood questionnaire). Asthma and bronchitis have been studied only twice and once, respectively. Of the biologic measurement-based outcomes, two studies assessed lung function and one evaluated airway hyperreactivity.

Distribution of types of study by health outcome categories. The smaller pie chart represents the number of mortality outcomes examined within the three different mortality studies identified in our review of the literature.

Distribution of types of respiratory outcomes examined for those classified as respiratory studies.
6. Acute Health Effects Studies
We identified a total of six AAP epidemiologic studies that considered acute health effects. Two respiratory health effect studies considered a range of upper and lower respiratory outcomes (all in children), one study considered stroke, and three other studies considered mortality outcomes. However, we note that only half ( N = 3) of these studies assigned short-term (acute) exposure from AAP measurements to derive exposure–response relationships, while the other three studies assigned exposure using long-term concentrations (e.g., annualized or three-year averages). In addition, two of the three studies that used long-term concentration exposure data may further be classified as “ecological” designs since health outcomes and pollutant exposures were aggregated to large spatial units (e.g., country-level or region-level) rather than studying exposure–response relationships at the individual-level. Two of these studies were prospective designs and both were conducted in Durban, South Africa. Each of these six AAP acute health effects studies are summarized in turn.
6.1. Prospective Studies
A panel study from South Africa recruited school-aged children ( N = 423) from Durban schools [ 20 ]. This study measured PM 10 , SO 2 and CO at the participant’s school and utilized NO 2 and NO ambient air measurements collected from eight government air monitoring sites as well as O 3 ambient air measurements collected at two other government air monitoring sites. Both single-pollutant and bi-pollutant associations were investigated for several acute lower respiratory outcomes. Self-report logs of acute respiratory symptoms were recorded multiple times during the day. Acute symptoms included cough, wheezing, shortness of breath (SOB), chest tightness or heaviness. Significant associations were observed for each air pollutant, with all but one resulting in adverse effects. Cough, SOB and chest symptoms were all higher with increasing PM 10 , SO 2 , NO 2 , and NO concentrations. Wheeze was also higher with increased NO 2 but lower with higher NO. The strength of these associations for each individual pollutant depended on the number of day lags, with cough most consistently stronger for same day or five-day lags and chest tightness consistently strongest on same day exposure. There was no clear pattern for the other outcomes with respect to lag-days. This study did not, apparently, collect important information related to biomass fuel use at participants’ homes.
A prospective cohort study [ 21 ], also carried out in Durban, South Africa, tested the interaction between daily pollutant levels (SO 2 , PM 10 , NO 2 , and NO) and CD14 cell genetic polymorphisms on within-day changes in lung function. The study participants were school-aged children (7–9 years of age) ( N = 71). Forced expiratory volume in 1 s (FEV1) was measured repeatedly every two-hours for three-week periods during different seasons of the year to determine within-day changes in lung function. Continuous air pollutant measurements occurred at the schools, and in some cases, off of school grounds, with exposure assignment based on daily average concentrations from each school or nearest monitor to the school. Generalized estimating equations (GEEs) related exposure–genetic polymorphism interaction terms with daily changes in lung function. Although none of the pollutants were significantly associated with lung function alone, when analyses were stratified by CD14 polymorphism status, only the CD14 CT/TT polymorphism was associated with daily lung function decrements with increasing NO 2 and NO daily exposures. This significant interaction was consistent across one-, two-, and five-day lag exposures for both pollutants. The most important contributions from this study is its prospective design and the consideration of individual-level susceptibility using a biologically plausible polymorphism in a gene related to cellular immunity and asthmatic symptoms.
6.2. Cross-Sectional Studies
A cross–sectional study [ 22 ] utilized household survey data collected between the years 2007 and 2010 in six low- and middle-income countries, which included two SSA countries (South Africa and Ghana). This study tested the association between long–term PM 2.5 and self-report of stroke in the past 12 months in adults ( N = 45,625). PM 2.5 exposure assessment was estimated by deriving three–year average from satellite aerosol optical depth (AOD) measurements (without ground-level measurements). A logistic regression multilevel model resulted in significant positive associations for PM 2.5 and stroke. Statistically significant effect modification was observed for smoking status, physical activity, and fruit and vegetable intake. These interactions were observed to be in the hypothesized direction in some cases (e.g., fruit and vegetable intake mitigated PM 2.5 stroke effects and effects were strongest among those with high physical activity), but interactions were in opposite directions than expected for others (e.g., PM 2.5 effects were strongest in never smokers—possibly due to uncontrolled confounding from environmental tobacco smoke). This study offered several important contributions compared to other studies reviewed; in particular, the authors accounted for IAP sources in the home (such as polluting cooking fuels) and evaluated PM 2.5 effect estimates for effect modification by multiple individual-level biologically plausible risk factors including sex, age, smoking, physical activity, and nutrition (fruit and vegetable intake). Another important contribution of this study, compared to other reviewed studies that used nearest monitor exposure metrics, is the use of satellite derived AOD measures of PM 2.5 exposure. Satellite derived measures provides spatially resolved estimates that may reduce exposure misclassification in epidemiological studies. An important limitation in this study is a reliance on long-term concentrations for acute stroke events; although air pollution and stroke likely have chronic exposure etiology.
The three remaining acute health effects studies are all mortality studies, two of which are ecological designs and one a case-crossover design. The case-crossover study ( N = 149,667), from Cape Town, South Africa, tested the year–round and seasonal associations between daily NO 2 , SO 2 , and PM 10 with respiratory disease (RD) mortality, cardiovascular disease (CVD) mortality, and cerebrovascular disease (CBD) mortality between 2001 and 2006 [ 23 ]. Pollutants were measured hourly at three government air monitoring sites and daily exposures were assigned to the population of Cape Town by averaging across the three monitoring sites to derive daily average values. Daily mortality data, with their corresponding causes of death codes, came from the City of Cape Town mortality records. For NO 2 , statistically significant positive year-round associations were observed for CVD and CBD mortality. PM 10 and SO 2 showed a significant positive year-round association for CBD and CVD mortality, respectively. RD mortality resulted in significant positive associations with NO 2 and PM 10 exposures during warmer times of the year only. No positive associations were seen between study pollutants and any cause-specific mortality outcomes during the colder time of the year [ 23 ]. There are several notable strengths in this Cape Town study. The authors tested for effect modification by sex, age, and distance from monitors (distance from monitor showed significant interaction effects). In addition, this is the only study to have applied a case-crossover design—where individuals serve as their own controls—which is a particularly compelling approach for examining acute health effects from AAP. This was also the only study to explore the potential seasonal trends in pollutant associations.
The two ecological mortality studies are quite different than the Cape Town study primarily because they use either country-level or sub-region-level annual PM estimates and annual mortality estimates. This type of study design has notable weaknesses, such as being susceptible to ecological fallacy and applying long-term exposure estimates to what is essentially an acute health outcome (mortality). Despite these glaring limitations, each of these ecological studies makes unique contributions to the literature on AAP health effects in the region. The study by Aliyu and Ismail [ 24 ] used data from 35 African countries between the years 1995–2001 and explored sex-specific relationships between country-level long-term PM 10 and CO 2 emissions data and rates of adult mortality, infant mortality, and under-five mortality. The authors analyzed the data using an econometric generalized method of moments model (using autoregressive terms on the outcome and exposure) and found that PM 10 and CO 2 emissions were associated with increased male and female adult mortality (though marginally higher in females) and increased under-five and infant mortality. The analysis evaluated effect modification by country-level governmental effectiveness and found that better government effectiveness was associated with lower AAP-mortality risk, suggesting that good governance can play a role in mitigating the health impacts of AAP. The other ecological study, by Owili et al. [ 25 ], took an especially novel PM 2.5 source apportionment approach by using spectral aerosol optical depth satellite data to discriminate PM 2.5 source-specific concentrations as well as source-specific exposure–response relationships with under-five mortality and maternal mortality. The authors used a parametric generalized linear and additive mixed-effect model with natural cubic splines (GLMM + NS) and a Poisson link function as the main analysis for inference (they also supplemented with an alternate non-parametric regression analysis). From the main GLMM + NS analysis, pollutant concentrations for both biomass and anthropogenic PM 2.5 sources were significantly associated with higher under-five and maternal mortality (results were mostly consistent with the non-parametric analysis) (between the years 2000–2015). Conversely, dust PM 2.5 and PM 2.5 from a mixture of sources were both associated with lower under-five and maternal mortality, although there was some conflicting evidence from non-parametric analytic results. While the exposure and outcome data were aggregated at the sub-region level for Africa (Central Africa, Eastern Africa, Northern Africa, Southern Africa, and Western Africa), which is a severe limitation, this study is nonetheless important. The apparent ability to separate out PM 2.5 effects from different sources, by discriminating sources using the spectral nature of light particle scattering, is the most noteworthy contribution of this study [ 25 ]. There are clear regional variations in PM 2.5 sources which may impart spatial variability in the toxicity of airborne PM 2.5 . This appears to be expressed by these findings; with biomass and anthropogenic PM 2.5 sources indicative of higher under-five and maternal mortality risk compared against dust or mixed sources of PM 2.5 with lower risk.
7. Chronic Health Effects Studies
A cross-sectional South Africa study recruited school-aged children ( N = 341) from Durban schools [ 26 ]. This study measured PM 10 and SO 2 at the participant’s school and utilized NO 2 and NO air monitoring data collected from 8 government monitoring sites. Single-pollutant associations were investigated for several chronic lower and upper respiratory outcomes; these included care-giver report on cough, phlegm, bronchitis, wheezing, wheezing with shortness of breath, runny nose, itchy and watery eyes, and asthma. Biologic measurement outcomes included airway hyperreactivity (methacholine challenge tests), pulmonary function measurements, and skin allergy testing. There were no observed associations between air pollutants and study outcomes except only that SO 2 was significantly associated with increased odds of airway hyperreactivity. This was the only reviewed study that examined biologic measures of airway hyperreactivity. While this study did collect information on biomass fuel use (an important risk factor for chronic respiratory illness), this exposure was curiously omitted from the multivariate regression model results, which may partially explain the consistent null findings for most exposure–response relationships.
Another cross-sectional study [ 27 ], conducted in 2004 in the Warri region of Nigeria, recruited schoolchildren (ages 7–14 years; N = 1397)) to examine associations between measurements of traffic-related air pollution and several chronic respiratory symptoms and asthma. Survey questions from the International Study of Asthma and Allergies in Childhood questionnaire were used to determine lower respiratory symptom prevalence and asthma prevalence in the participants. Despite a lack of routine air monitoring in the study area, researchers conducted brief air sampling at the study schools, sampling for carbon monoxide (CO) and PM of varying fraction sizes. Measured CO and PM air concentrations were then combined with indicators of nearby traffic activity in a principal component analysis. The top three principal components were used to assign exposures to participants from study schools which were in turn used as inputs in the logistic regression analyses. Principal component 1 (comprised of traffic pollution) was associated with higher phlegm while principal component 3 (comprised of fine particulates related to truck traffic) was also associated with higher phlegm. No other outcomes showed significant associations. Importantly, this study did control for household IAP sources as determined from study questionnaires. The results from this analysis may be considered a multi-pollutant analysis because it combined concentration data on more than two pollutants, including CO and various PM fraction sizes. Therefore, this study represents the only one in the region to have presented results from a multipollutant analysis, which makes it a particularly important contribution to the literature. By combining information on multiple air pollutants with indicators of traffic-related pollution, the authors were able to demonstrate the importance of traffic-related air pollution on children’s lower respiratory health.
Another cross-sectional study from Nigeria [ 28 ], conducted in 2008 in the city of Ibadan, investigated the relationship between PM 10 concentrations and measures of lung function among selected study participants ( N = 140, ages 15–65). Participants were non-smokers, between the ages of 15–65 years, had no family history of respiratory disease and lived at least for three years in the study area. Air sampling for PM 10 took place over the course of three months in 2008 at time intervals intended to represent air quality during the morning and late afternoon times. Spirometry was performed on study participants to record observed forced expiratory volume in one second (FEV1) and participant body mass index was measured to derive a predicted FEV1 and to calculate percentage predicted FEV1 (% FEV1). Spearman rank test correlation was performed to observe associations between PM 10 concentration and lung function measures. The analysis revealed that only the observed FEV1 measure was significantly associated with lower lung function [ 28 ]. A major limitation of this study was a lack of multivariate analysis leaving the results prone to bias from confounding. Other limitations include a reliance on sampling during certain time-intervals each day, which may not be entirely representative of chronic daily air pollution exposures thus increasing the likelihood of exposure misclassification that would bias findings towards the null. However, this represents the only study to have related AAP measurements with lung function measurements, making it a unique contribution to the literature on AAP health effects studies in SSA.
Two additional cross-sectional studies by Lin et al. [ 29 , 30 ] used household survey of six low and middle income countries, which included data from South Africa and Ghana as well as countries from Asia and Latin America between the years 2007 and 2010, carried out a multilevel regression analysis to determine the association between PM 2.5 and depressive symptoms ( N = 41,785) [ 29 ] and disability score ( N = 45,625) [ 30 ] as chronic outcomes. PM 2.5 exposure assessment was estimated by deriving three-year average from satellite AOD measurements (without ground-level measurements). Estimates of PM 2.5 concentration was positively associated with depressive symptoms [ 29 ] and disability score [ 30 ], controlling for household IAP indicators. Interestingly, smoking was shown to be an effect modifier for depression, with an observed additive interaction between PM 2.5 and smoking on depression. In our review of the current literature, these are the only studies that examined a psychosocial or disability outcome.
The only study to research air pollution associations with adverse birth outcomes in SSA is also a multi-country study, using data on births collected in 2004 and 2005 from study clinics around the world [ 31 ]. Among other countries in Asia and Latin America, several clinic field sites in SSA were included in the study; these were Democratic Republic of Congo (DRC) ( N = 7067), Kenya ( N = 16,694), Niger ( N = 4826) and Nigeria ( N = 6538). This study tested associations between PM 2.5 exposure estimates during pregnancy and preterm birth and term low birth weight. Length of gestation and birth weight were recorded at birth and collected from each study clinic. PM 2.5 exposure during pregnancy was determined with AOD satellite-derived data for 2001–2006 and were combined with vertical column aerosol values from a chemical transport model (these are essentially the same estimates as in Lin et al. [ 22 , 29 ]). Maternal exposure was estimated within a 50-km buffer surrounding each mother’s respective delivery clinic and seasonal adjustments were applied to the long-term pollutant estimates to estimate exposure during the last month of each pregnancy at each mother’s delivery clinic 50-km buffer. Generalized estimating equations (GEE) were implemented in the study to account for clustering of birth outcomes within clinic, with confounder adjustment for maternal and infant factors in one model and country-level factors added in a second model. Only term low birth weight was significantly associated with PM 2.5 exposure levels during pregnancy, at the two highest exposure-level quartiles, although the association was slightly attenuated after controlling for country-level confounders (albeit still statistically significant). Country-level estimates of associations could only be estimated for India and China due to limitations of sample sizes from the other countries, hence no country-level estimates were determined for SSA countries. The primary strength of this multi-country study is the uniform collection of birth and covariate data as well as the exposure estimation procedure across the study sites. However, this study relied heavily on spatial variation in exposure-levels while temporal variability in exposure-levels were extremely limited by way of simple seasonal adjustments. In addition, exposure assignment assumed mothers resided within a 50-km buffer of the health facility, further increasing the risk of exposure misclassification.
8. Discussion
Our review of the AAP epidemiology literature from SSA revealed a very few number of studies relating air pollution measurements with health outcomes as well as extreme geographic disparities in terms of where studies have been conducted. For instance, most of the AAP epidemiology studies were concentrated in a single country (South Africa). While only twelve studies were identified that fit our inclusion criteria, most studies varied in terms of design and the nature of the outcome. On the other hand, each of the studies made a unique and potentially valuable contribution towards not only understanding the relationship between air pollution and health in the region, but also towards guiding future directions for AAP epidemiological studies in the region. From our review of the literature in regards to air monitoring for epidemiology studies in SSA, we identified several important gaps.
8.1. Gaps in Ambient Air Pollution Monitoring and Exposure Estimation
First and foremost, the only region with an adequate air monitoring network that may be leveraged for health effects studies appears to be in South Arica [ 3 ]. This likely played a key role in our determination that South Africa tended to have the highest quality studies, whether it be for testing acute mortality or respiratory outcomes or chronic health outcomes in relation to AAP exposure. Studies from South Africa were able to test associations for several different particulate and gaseous pollutants, whereas studies from Nigeria and Ghana were typically relegated to either a single pollutant or a composite of convenience air pollutant measurements and traffic indicators. Hence, exposure characterization was the most consistent between the South Africa studies and produced the most time-resolved data for acute health effects studies and prospective designs, whereas exposure characterization in the Nigeria studies varied considerably and were not readily comparable.
While air monitoring networks may be emerging in other SSA countries, it is clear that effort should be put towards developing air monitoring networks that can facilitate epidemiology studies throughout the region. We note that low-cost air monitoring instruments have recently been validated and shown to be effective compared against established government air monitoring instruments in the US [ 32 ]. In addition, low-cost passive air samplers for NO 2 have been validated in Durban, South Africa [ 33 ]. Low-cost air samplers may offer a viable alternative compared with costly and complex air monitoring instruments used in higher income countries.
Another glaring gap in the region’s AAP epidemiology literature is a lack of what is now-conventional land use regression (LUR) modeling. Although satellite derived methods have been used in at least four of the reviewed studies, there is still a limited range of pollutants that can be estimated with this method and such exposure metrics are most suitable for chronic exposure and chronic outcome studies. LUR models could be most helpful for exposure assessment in smaller-scale sub-regional AAP epidemiology studies that require spatially- and time-resolved estimates of exposure, especially for acute health effects studies. We identified at least one study on the horizon, in Western Cape, South Africa, that will implement state-of-the-art LUR modelling to derive exposure estimates in a respiratory health effects study [ 34 ].
In the near-term, given the lack of air quality monitoring networks in the region and the high cost of state-of-the-art sampling instrumentation, we recommend the deployment of low-cost and validated air samplers combined with GIS data collection. Such an approach may be leveraged for LUR exposure estimation for chronic or acute health effects studies. Satellite-derived estimates of exposure should also be leveraged in studies where ground-level measurements are not feasible. However, we note there is a general need for ground-level monitoring to validate satellite-derived concentration estimates in the region.
8.2. Health Outcome Gaps
Another important gap that emerged from our review of the literature is a lack of studies that evaluated health care records for cause-specific outcomes (e.g., hospitalizations or hospital visits) or mortality data with the appropriate spatial resolution. Only one of the reviewed studies evaluated cause-specific mortality and none of the studies examined cause-specific hospitalizations or hospital visits. Of the respiratory health studies reviewed, only two studies examined a specific diagnosis (asthma and bronchitis) and these were both self-reported diagnosis instead of documented cases. Moreover, most of the mortality studies we reviewed applied an ecological design with country-level mortality data. Without spatially resolved AAP measurements spatially linked with individual outcomes, findings will continue to be prone to ecological fallacy. Where available, effort should be made to conduct studies that collect hospitalization and mortality data coupled with spatial information that enable data linkage studies for within and between region studies. More studies on cause-specific mortality, hospitalizations, and hospital visits are critically needed to provide insights into the population health impact of AAP in the region. Notably, children comprised the study populations for all of the non-mortality-based and country-specific studies; suggesting a need for more health outcomes studies that include elderly populations in future studies.
In terms of the range of outcomes examined in the included studies, there are some important holes that need to be addressed. Only one study included in our review investigated adverse birth outcomes. Given the epidemiologic evidence for associations between AAP and adverse birth outcomes and the high rates of adverse birth outcomes in SSA, such as low birth weight and preterm birth, there is a need for more such studies. As already mentioned, diagnosis- and measurement-based outcomes are rarely studied in the region. In addition, other respiratory outcomes yet to be explored, in relation to AAP, include pneumonia and TB, which also deserve greater attention given the large burden of these respiratory diseases in the region.
There is also a relatively poor understanding of the AAP sources throughout the region. Like any other part of the world, the sources of AAP in SSA are a mixture of a variety of natural and anthropogenic sources. However, the relative contribution of specific sources of PM pollution is likely to be in stark contrast to the higher income countries of North America and Europe (where most studies have taken place). For instance, of the few source apportionment studies conducted in the region, the predominant sources for PM pollution in Accra, Ghana [ 35 , 36 ] and Kampala, Uganda [ 37 ] included biomass burning, heavily-congested traffic on roadways, loose dirt from road surfaces, fish smoking, and trash burning or incineration. Many of these PM sources are not as typical for urban areas of the higher income countries. In addition, vehicle emissions are poorly regulated and the operating conditions of the ubiquitous use of older emitting vehicles is similarly different compared with higher income countries [ 3 ]. It is therefore important for future studies to take into account the different and unique sources of urban AAP in the region, particularly the impact of biomass and heavy traffic congestion and roadway dust.
8.3. Data Analysis Gaps
Very few studies implemented key analytic elements that should be incorporated into future studies. Only three of the twelve studies controlled for IAP in the home, even though household IAP sources are ubiquitous in the region and the compelling evidence for substantial health effects from IAP in SSA. Since IAP levels are likely to have overlapping health impacts with AAP and likely to be correlated with AAP levels under certain circumstances, there is a clear need to ensure IAP data are collected and incorporated into AAP epidemiologic analyses. On a positive note, at least four of the reviewed studies tested for interaction between AAPs and relevant factors such as smoking, age, sex, season, physical activity, and nutrition. Notably, several of these factors exhibited significant interaction effects, including smoking, warmer seasons, physical activity, and nutrition. These results suggest the need for incorporating effect modification into studies. It is also important to note that none of the reviewed stories explored effect modification by socioeconomic factors like education or poverty, nor was disease co-prevalence (e.g., HIV or TB) explored as an effect modifier. SSA suffers from high poverty and inequality, along with other social stressors and co-prevalence of diseases that can contribute to susceptibility and vulnerability to air pollution impacts on health. There is a critical need to consider these social and comorbidity factors in future AAP epidemiology studies, especially for the rapidly growing urban slum populations of SSA.
For the reviewed studies that measured several pollutants, there was an overall lack of application of a multi-pollutant framework. While this is a well-known and general deficiency in most AAP epidemiology studies, mostly due to the analytic challenges imposed by such a framework, nevertheless future studies should apply a multi-pollutant framework where the data are suited to do so. This may be particularly important for SSA because dust particles and biomass burning comprise a major portion of PM pollution and rapid industrialization and urbanization are co-occurring with these air pollution factors. The study by Owili et al. [ 25 ], which showed variation in mortality effects depending on PM source, highlights the importance of applying a multi-pollutant framework. Additionally, in one of the reviewed studies, air pollution associations with RD mortality were shown to be strongest during the warmer part of the year in South Africa [ 23 ]. This finding may have important implications with respect to the effects of air pollution in the context of warming trends related to climate change. The role of warmer temperatures to act in synergy with air pollution exposure warrants further research in the region [ 38 ].
8.4. Geographic Gaps in AAP Epidemiology Studies
The most obvious gap in our review of the AAP epidemiological literature is the extreme disparities in terms of where studies from SSA have occurred. Not a single individual-level AAP epidemiology study was conducted in Northern SSA and just one in Eastern Africa and one in Central Africa. Even within Western and Southern Africa regions, there are extreme disparities, whereby individual-level studies have occurred in a limited range of areas of South Africa and Nigeria. There is a clear need to conduct studies across a more diverse range of urban areas as well as a need for studies in rural areas where biomass burning could be a contributor to poor air quality.
8.5. Limitations and Strengths
There are some important limitations and strengths regarding our review. There is a possibility that we missed some published articles not represented in PubMed, EMBASE, or Google Scholar. While we recognize this as an important limitation, we are confident that the themes and gaps we identified in our review of the literature is likely to persist. Another limitation is that we did not quantitatively determine effect sizes across studies using a meta-analysis. Even though our motivation here is to simply provide a narrative review to highlight the current state of the literature, there is still a need for a meta-analysis to quantitatively assess effect sizes and compare these with existing literature.
The most important strength of our review is that it synthesizes the range of AAP epidemiology studies carried out in SSA in a consistent manner to highlight important methodological gaps and geographic disparities in the conducting of such studies. We also provide recommendations on future studies in the region to better ascertain the population health impact of AAP.
9. Conclusions
There is a paucity of epidemiological studies regarding ambient air pollution in sub-Saharan Africa, which is worsened by the mal-distribution of the few available studies with most of the studies coming from Southern Africa. More studies are critically needed to provide insights into the population health impact of ambient air pollution in the region; for instance, studies evaluating individual-based and population-based outcomes like cause-specific mortality, hospitalizations, and hospital visits. This review highlights a dire need to improve on the air monitoring networks in sub-Saharan Africa to enable high quality epidemiological studies as a first step in addressing the impacts off ambient air pollution in the region. This can be achieved using the recently validated low-cost air monitoring instruments combined with readily accessible GIS information and methods. This should be coupled with the deployment of data robust analysis techniques, to maximally utilize the few available data. Population susceptibility should also be a focus of future studies, especially regarding the high rates of social deprivation and co-morbidities like HIV and TB. Despite the limited number of studies meeting our strict inclusion, we have been able to demonstrate the profound effect of ambient air pollution on both the acute and chronic health outcomes in the population in sub-Saharan Africa, a region that is hit by a dual burden of infectious and non-infectious risk factors for lung disease.
Acknowledgments
This study was funded by the Global Health Equity Scholars Program, Fogarty TW009338.
Supplementary Materials
The following are available online at http://www.mdpi.com/1660-4601/15/3/427/s1 , Table S1. Tabular summary of studies that met the inclusion criteria. Table S2. Tabular summary of notable studies that did not meet the inclusion criteria.
Author Contributions
E.C. performed summary data analysis of included studies; E.C. reviewed the studies and conducted literature review; E.C. wrote the paper; and S.K. provided substantial guidance, edits and comments to complete this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Advertisement
An overview of atmospheric aerosol and their effects on human health
- Environment and Climate: Role of Humans and Technologies
- Published: 06 September 2023
- Volume 30 , pages 125347–125369, ( 2023 )

Cite this article
- Tanvir Arfin ORCID: orcid.org/0000-0002-5051-614X 1 , 2 ,
- Anupama M Pillai 1 ,
- Nikhila Mathew 1 ,
- Abha Tirpude 1 ,
- Roshani Bang 1 , 2 &
- Pabitra Mondal 1
841 Accesses
7 Citations
1 Altmetric
Explore all metrics
Epidemiologic investigations have previously been published in more than 200 papers, and several studies have examined the impacts of particle air pollution on health. The main conclusions now being made about the epidemiological evidence of particle pollution-induced health impacts are discussed in this article. Although there is no universal agreement, most reviewers conclude that particulate air pollution, particularly excellent combustion-cause contamination prevalent in many municipal and manufacturing environments, is a significant risk for cardiopulmonary sickness and mortality. Most epidemiological research has concentrated on the impacts of acute exposure, although the total public health implications of chronic acquaintance’s outcome may be more extraordinarily significant. According to some reviewers, prolonged, repeated exposure raises the risk of cardiorespiratory death and chronic respiratory illness. A more general (but still universal) agreement is that short-term particle pollution exposure has been shown to aggravate pre-existing pulmonary and cardiovascular diseases and increase the number of community members who become sick, require medical treatment, or die. Several in-depth studies conducted in the global and Indian regions are addressed.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
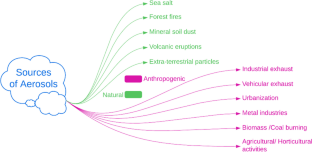
Similar content being viewed by others

Effects on health of air pollution: a narrative review
Pier Mannuccio Mannucci, Sergio Harari, … Massimo Franchini

Respiratory and Cardiovascular Effects of Metals in Ambient Particulate Matter: A Critical Review

Air Pollution and Health Effects
Data availability.
All data generated or analysed during this study are included in this published article.
Adcock IM, Caramori G, Barnes PJ (2011) Chronic obstructive pulmonary disease and lung cancer: new molecular. Respiration 81:265–284. https://doi.org/10.1159/000324601
Article CAS Google Scholar
Ahmad S, Singh R, Arfin T, Neeti K (2022) Fluoride contamination, consequences and removal techniques in water: a review. Environ Sci Adv 1:620–661. https://doi.org/10.1039/D1VA00039J
Albert RE, Lewtas J, Nesnow S, Thorslund TW, Anderson E (1983) Comparative potency method for cancer risk assessment: application to diesel particulate emissions. Risk Anal 3:101–117. https://doi.org/10.1111/j.1539-6924.1983.tb00110.x
Article Google Scholar
Albriet B, Sartelet KN, Lacour S, Carrissimo B, Seigneur C (2010) Modelling aerosol number distributions from a vehicle exhaust with an aerosol CFD model. Atmos Environ 44:1126–1137. https://doi.org/10.1016/j.atmosenv.2009.11.025
Alfaro SC, Gaudichet A, Gomes L, Maille M (1997) Modeling the size distribution of a soil aerosol produced by sandblasting. J Geophys Res Atmos 102:11239–11249. https://doi.org/10.1029/97JD00403
Allen AG, Nemitz E, Shi JP, Harrison RM, Greenwood JC (2001) Size distributions of trace metals in atmospheric aerosols in the United Kingdom. Atmos Environ 35:4581–4591. https://doi.org/10.1016/S1352-2310(01)00190-X
Arey J, Zielinska B, Harger WP, Atkinson R, Winer AM (1988) The contribution of nitrofluoranthenes and nitropyrenes to the mutagenic activity of ambient particulate organic matter collected in southern California. Mutat Res 207:45–51. https://doi.org/10.1016/0165-7992(88)90040-1
Arfin T, Bhaisare DA, Waghmare SS (2021a) Development of a PANI/Fe(NO3)2 nanomaterial for reactive orange 16 (RO16) dye removal. Anal Methods 13:5309–5327. https://doi.org/10.1039/D1AY01402A
Arfin T, Kate P, Singh A, Kumari K (2021b) Alternatives to POPs for a healthy life. In: Kumar K (ed) Persistent organic pollutants: gaps in management and associated challenges, 1st edn. CRC Press, Florida, pp 201–226
Chapter Google Scholar
Atkinson RW, Bremner SA, Anderson HR, Strachan DP, Bland JM, de Leon AP (1999) Short-term associations between emergency hospital admissions for respiratory and cardiovascular disease and outdoor air pollution in London. Arch Environ Health 54(6):398–411. https://doi.org/10.1080/00039899909603371
Balachandran S, Meena BR, Khillare PS (2000) Particle size distribution and its elemental composition in the ambient air of Delhi. Environ Int 26:49–54. https://doi.org/10.1016/s0160-4120(00)00077-5
Berggren D, Bergkvist B, Falkengren-Grerup U, Folkeson L, Tyler G (1990) Metal solubility and pathways in acidified forest ecosystems of south Sweden. Sci Tot Environ 96:103–114. https://doi.org/10.1016/0048-9697(90)90010-R
Brook RD, Brook JR, Rajagopalan S (2003) Air pollution: the heart of the problem. Curr Hypertens Rep 5:32–39. https://doi.org/10.1007/s11906-003-0008-y
Brunekreef B, Holgate ST (2002) Air pollution and health. Lancet 360:1233–1242. https://doi.org/10.1016/S0140-6736(02)11274-8
Brunekreef B, Janssen NA, de Hartog J, Harssema H, Knape M, van Vliet P (1997) Air pollution from truck traffic and lung function in children living near motorways. Epidemiology 8:298–303. https://doi.org/10.1080/08958370600742946
Burgel PR (2011) The role of small airways in obstructive airway diseases. Eur Respir Rev 20:23–33. https://doi.org/10.1183/09059180.00010410
Calderon-Garciduenas L, Solt AC, Henriquez-Roldan C et al (2008) Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid beta-42 and alpha-synuclein in children and young adults. Toxicol Pathol 36:289–310. https://doi.org/10.1177/0192623307313011
Calvo AI, Alves C, Castro A, Pont V, Vicente AM, Fraile R (2013) Research on aerosol sources and chemical composition: past, current and emerging issues. Atmos Res 120-121:1–28. https://doi.org/10.1016/j.atmosres.2012.09.021
Campen MJ, Babu NS, Helms GA, Pett S, Wernly J, Mehran R, McDonald JD (2005) Nonparticulate components of diesel exhaust promote constriction in coronary arteries from ApoE–/– mice. Toxicol Sci 88:95–102. https://doi.org/10.1093/toxsci/kfi283
Canales-Rodriguez M, Quintero-Nunez M, Valdes-Salas B et al (2015) distribution and characterization of PM10 in city and valley of Mexico, Baja California, Mexico. J Environ Prot 6:25–33. https://doi.org/10.4236/jep.2015.61004
Charlson RJ, Lovelock JE, Andreae MO, Warren SG (1987) Oceanic phytoplankton, atmospheric sulphur, cloud albedo and climate. Nature 326:655–661. https://doi.org/10.1038/326655a0
Chubarova N, Ye N, Sviridenkov I, Smirnov A, Slutsker I (2012) Smoke aerosol and its radiative effects during extreme fire event over central Russia in summer 2010. Atmos Meas Tech 5:557–568. https://doi.org/10.5194/amt-5-557-2012
Clark CR, Dutcher JS, Henderson TR, McClellan RO, Marshall WE, Naman TM, Seizinger DE (1984) Mutagenicity of automotive particulate exhaust: influence of fuel extenders, additives and aromatic content. Adv Mod Environ Toxicol 6:109–122
CAS Google Scholar
Contini D, Lin Y-H, Hanninen O, Viana M (2021) Contribution of aerosol sources to health impacts. Atmosphere 12:730. https://doi.org/10.3390/atmos12060730
Cooper CB (2006) The connection between chronic obstructive pulmonary disease symptoms and hyperinflation and its impact on exercise and function. Am J Med 119:21–31. https://doi.org/10.1016/j.amjmed.2006.08.004
Corrigan CJ, Levy ML, Dekhuijzen PR, Crompton GK (2009) The ADMIT series – issues in inhalation therapy. 3 Mild persistent asthma: the case for inhaled corticosteroid therapy. Prim Care Respir J 18:148–158. https://doi.org/10.4104/pcrj.2009.00035
Davies G, Davies JC, Gill DR et al (2011) Safety and expression of a single dose of lipid-mediated cftr gene therapy to the upper and lower airways of patients with cystic fibrosis. Pediatric Pulmonology 281:8755–6863. https://doi.org/10.1136/thoraxjnl-2011-201054a.4
Deepthi Y, Nagendra SMS, Gummadi SN (2019) Characteristics of indoor air pollution and estimation of respiratory dosage under varied fuel-type and kitchen-type in the rural areas of Telangana state in India. Sci Total Environ 650:616–625. https://doi.org/10.10016/j.scitotenv.2018.08.381
DeMarini DM, Brooks LR, Warren SH, Kobayashi T, Gilmour MI, Singh P (2004) Bioassay-directed fractionation and salmonella mutagenicity of automobile and forklift diesel exhaust particles. Environ Health Perspect 112:814–819. https://doi.org/10.1289/ehp.6578
Deng Z, Chen F, Zhang M et al (2016) Association between air pollution and sperm quality: a systematic review and meta-analysis. Environ Pollut 208:663–669. https://doi.org/10.1016/j.envpol.2015.10.044
Dharmage SC, Perret JL, Custovic A (2019a) Epidemiology of asthma in children and adults. Front Pediatr 7:246. https://doi.org/10.3389/fped.2019.00246
Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, Ferris BG Jr, Speizer FE (1993) An association between air pollution and mortality in six US cities. N Engl J Med 329:1753–1759. https://doi.org/10.1056/NEJM199312093292401
Donnelly L, Rogers D (2008) Novel targets and drugs in inflammatory lung disease. Curr Opin Pharmacol 8:219–221. https://doi.org/10.1016/j.coph.2008.04.007
Dung CH, Wu SC, Yen GC (2006) Genotoxicity and oxidative stress of the mutagenic compounds formed in fumes of heated soybean oil, sunflower oil, and lard. Toxicol In Vitro 20:439–447. https://doi.org/10.1016/j.tiv.2005.08.019
Elder A, Couderc JP, Gelein R, Eberly S, Cox C, Xia X, Zareba W, Hopke P, Watts W, Kettelson D, Frampton M, Utell M, Oberdorster G (2007) Effects of on-road highway aerosol exposures on autonomic responses in aged, spontaneously hypertensive rats. Inhal Toxicol 19:1–12. https://doi.org/10.1080/08958370600985735
Feng T, Bei N, Zhao S, Wu J, Li X, Zhang T, Cao J, Zhou W, Li G (2018) Wintertime nitrate formation during haze days in the Guanzhong Basin, China: a case study. Environ Pollut 243:1057–1067. https://doi.org/10.1016/j.envpol.2018.09.069
Finlayson-Pitts BJ (2017) Introductory lecture: atmospheric chemistry in the anthropocene. Faraday Discuss 200:11–58. https://doi.org/10.1039/C7FD00161D
Fitzgerald JW (1991) Marine aerosols: a review. Atmos Environ 25:533–545. https://doi.org/10.1016/0960-1686(91)90050-H
Flower MFJ, Strong DF (1969) The significance of sandstone inclusions in lavas of the comores archipelago. Earth Planet Sci Lett 7:47–50. https://doi.org/10.1016/0012-821X(69)90010-7
Flume PA, O’Sullivan BP, Robinson KA et al (2007) Cystic fibrosis pulmonary guidelines: chronic medications for maintenance of lung health. Am J Respir Crit Care Med 176:957–969. https://doi.org/10.1164/rccm.200705-6640C
Forbes I (2000) Human airway epithelial cell lines for in vitro drug transport and metabolism studies. Pharm Sci Technol Today 3:18–27. https://doi.org/10.1016/s1461-5347(99)00231-x
Gartlehner G, Hansen RA, Carson SS, Lohr KN (2006) Efficacy and safety of inhaled corticosteroids in patients with COPD: a systematic review and meta-analysis of health outcomes. Ann Fam Med 4:253–262. https://doi.org/10.1370/afm.517
Geise M, Kreyling WG (2010) Deposition and biokinetics of inhaled nanoparticles. Part Fibre Toxicol 7:2. https://doi.org/10.1186/1743-8977-7-2
Genc S, Zadeoglulari Z, Fuss SH et al (2012) The adverse effects of air pollution on the nervious system. J Toxicol 2012:782462. https://doi.org/10.1155/2012/782462
Goodman PG, Haw S, Kabir Z Clancy L (2009) Are there health benefits associated with comprehensive smoke-free laws: a review. Int J Public Health 54: 367–378. https://doi.org/10.1007/s00038-009-0089-8
Goudie AS, Middleton NJ (2006) Desert dust in the global system. Springer –Verlag, Berlin Heidelberg
Google Scholar
Groma V, Alfoldy B, Borcsok E et al (2022) Sources and health effects of fine and ultrafine aerosol particles in an urban environment. Atmos Pollut Res 13:101302. https://doi.org/10.1016/j.apr.2021.101302
Gupta SK, Elumalai SP (2017) Size-segregated particulate matter and its association with respiratory deposition doses among outdoor exercises in Dhanbad City, India. J Air Waste Manag Assoc 67:1137–1145. https://doi.org/10.1080/10962247.2017.1344159
Hanania NA, Donohue JF (2007) Pharmacologic interventions in chronic obstructive pulmonary disease: bronchodilators. Proc Am Thorac Soc 4:526–534. https://doi.org/10.1513/pats.200701-016FM
Heisler SL, Frieslander (1977) Gas-to-particle conversion in photochemical smog:aerosol growth laws and mechanisms for organics. Atmos Environ 11:157–168. https://doi.org/10.1016/0004-6981(77)90220-7
Heo JB, Hopke PK, Yi SM (2009) Source apportionment of PM 2.5 in Seoul, Korea. Atmos Chem Phys 9:4957–4971. https://doi.org/10.5194/acp-9-4957-2009
Hinds WC (1999) Aerosol technology: properties, behavior, and measurement of airborne particles. Wiley, New York
Hirtl M, Stuefer M, Arnold D, Grell et al (2019) The effects of simulating volcanic aerosol radiative feedbacks with WRF-Chem during the Eyjafjallajokull eruption, April and May 2010. Atmos Environ 198: 194-206. https://doi.org/10.1016/j.atmosenv.2018.10.058
Ho SSH, Yu JZ, Chu KW, Yeung LL (2006) Carbonyl emissions from commercial cooking sources in Hong Kong. J Air Waste Manage Assoc 56:1091–1098. https://doi.org/10.1080/10473289.2006.10464532
Hoek G, Brunekreef B, Goldbohm S, Fischer P, van den Brandt PA (2002) Association between mortality and indicators of traffic-related air pollution in the Netherlands: a cohort study. Lancet 360:1203–1209. https://doi.org/10.1016/S0140-6736(02)11280-3
Hofmann W (2011) Modelling inhaled particle deposition in the human lung-a review. J Aerosol Sci 42:693–724. https://doi.org/10.1016/j.jaerosci.2011.05.007
Hogg JC (2004) Pathophysiology of airflow limitation in chronic obstructive pulmonary disease. The Lancet 364:21–27. https://doi.org/10.1016/S0140-6736(04)16900-6
Hoppel WA, Fitzgerald JW, Frick GM, Larson RE, Mack EJ (1990) Aerosol size distributions and optical properties found in the marine boundary layer over the Atlantic Ocean. J Geophys Res Atmos 95:3659–3686. https://doi.org/10.1029/JD095iD04p03659
https://ginasthma.org/
Ibald-Mulli A, Stieber J, Wichmann HE et al (2001) Effects of air on blood pressure: a population-based approach. Am J Public Health 91:571–577. https://doi.org/10.2105/ajph.91.4.571
Ikemori F, Uranishi K, Asakawa D et al (2021) Source apportionment in PM2.5 in central Japan using positive matrix factorization focusing on small-scale local biomass burning. Atmos Pollut Res 12:162–172. https://doi.org/10.1016/j.apr.2021.01.006
Jaenicke R (2008) Natural aerosols. Ann N Y Acad Sci 338:317–329. https://doi.org/10.1111/j.1749-6632.1980.tb17129.x
Karar K, Gupta AK (2007) Source apportionment of PM10 at residential and industrial sites of an urban regio of Kolkata, India. Atmos Res 84:30–41. https://doi.org/10.1016/j.atmosres.2006.05.001
Kaufman YJ, Koren I, Remer LA, Tanre D, Ginoux P, Fan S (2005) Dust transport and deposition observed from the Terra-Moderate Resolution Imaging Spectroradiometer (MODIS) spacecraft over the Atlantic Ocean. J Geophys Res Atmos 110. https://doi.org/10.1029/2003JD004436
Khillare PS, Sarkar S (2012) Airborne inhalable metals in residential areas of Delhi, India: distribution, source apportionment and health risks. Atmos Pollut Res 3:46–54. https://doi.org/10.5094/APR.2012.004
Kim JY, Lee EY, Choi I et al (2015) Effects of the particulate matter 2.5 (PM 2.5 ) on lipoprotein metabolism, uptake and degradation, and embryo toxicity. Mol Cells 38:1096–1104. https://doi.org/10.14348/molcells.2015.0194
Klassen CD (2001) Cassarett and Doull’s toxicology: the basic science of poisons. McGraw-Hill, New York
Korhonen A, Relvas H, Miranda AI, Ferreira et al (2021) Analysis of spatial factors, time-activity and infiltration on outdoor generated PM 2.5 exposures of school children in five European cities. Sci Total Environ 785:147111. https://doi.org/10.1016/j.scitotenv.2021.147111
Kothai P, Saradhi IV, Prathibha P et al (2008) Source apportionment of coarse and fine particular matter at Navi Mumbai, India. Aerosol Air Qual Res 8:423–436. https://doi.org/10.4209/aaqr.2008.07.0027
Laden F, Neas LM, Dockery DW, Schwartz J (2000) Association of fine particulate matter from different sources with daily mortality in six US cities. Environ Health Perspect 108:941–947. https://doi.org/10.1289/ehp.00108941
Laeher LP, Brauer M, Lipsett M, Zelikoff JT, Simpson CD, Koenig JQ, Smith KR (2007) Woodsmoke health effects: a review. Inhal Toxicol 19:67–106. https://doi.org/10.1080/08958370600985875
Lai HK, Bayer-Oglesby L, Colvile R, Gotschi T, Jantunen MJ, Kunzli N, Kulinskaya E, Schweizer C, Nieuwenhuijsen MJ (2006) Determinants of indoor air concentrations of PM2.5, black smoke and NO 2 in six European cities (EXPOLIS study). Atmos Environ 40:1299–1313. https://doi.org/10.1016/j.atmosenv.2005.10.03
Lei YC, Hwang JS, Chan CC, Lee CT, Cheng TJ (2005) Enhanced oxidative stress and endothelial dysfunction in streptozotocin-diabetic rats exposed to fine particles. Environ Res 99:335–343. https://doi.org/10.1016/j.envres.2005.03.011
Lelieveld J (2017) Clean air in the Anthropocene. Faraday Discuss 200:693–703. https://doi.org/10.1039/c7fd90032e
Lelieveld J, Evans JS, Fnais M, Giannadaki D, Pozzer A (2015) The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 525:367–371. https://doi.org/10.1038/nature15371
Lewtas J (1988) Genotoxicity of complex mixtures: Strategies for the identification and comparative assessment of airborne mutagens and carcinogens from combustion sources. Fundam Appl Toxicol 10:571–589. https://doi.org/10.1016/0272-0590(88)90184-4
Li N, Sioutas C, Cho A, Schmitz D, Misra C, Sempf J, Wang M, Oberley T, Froines J, Nel A (2003) Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect 111:455–460. https://doi.org/10.1289/ehp.6000
Li Z, Tang Y, Song X et al (2019) Impact of ambient PM2.5 on adverse birth outcome and potential molecular mechanism. Ecotoxicol Environ Saf 169:248–254. https://doi.org/10.1016/j.ecoenv.2018.10.109
Liao BQ, Liu CB, Xie SJ et al (2020) Effects of fine particulate matter (PM2.5) on ovarian function and embryo quality in mice. Environ Int 135:105338. https://doi.org/10.1016/j.envint.2019.105338
Lipfert FW, Baty JD, Miller JP, Wyzga RE (2006) PM 2.5 constituents and related air quality variables as predictors of survival in a cohort of U. S. military veterans. Inhal Toxicol 18:645–657. https://doi.org/10.1080/08958370600742946
Manisalidis I, Stavropoulou E, Starvropoulos A, Bezirtzoglou E (2020) Environmental and health impacts of air pollution: a review. Front Public Health 8:2020. https://doi.org/10.3389/fpubh.2020.00014
Mar TF, Norris GA, Koenig JQ, LarsonTV (2000) Associations between air pollution and mortality in Phoenix, 1995–1997. Environ Health Perspect 108: 347-253. https://doi.org/10.1289/ehp.00108347
Mathew N, Tirpude A, Pillai AM, Mondal P, Arfin T (2023) Emerging contaminants in air pollution and their sources, consequences, and future challenges. In: Kapoor RT, Rafatullah M (eds) Bioremediation technologies: For wastewater and sustainable circular bioeconomy. De Gruyter, Germany, pp 235–274. https://doi.org/10.1515/9783111016825-014
McNeill VF (2017) Atmospheric aerosols: clouds, chemistry, and Climate. Annu Rev Chem Biomol Eng 7:427–444. https://doi.org/10.1146/annurev-chembioeng-060816-101538
Miller RL, Tegen I (1999) Radiative forcing of a tropical direct circulation by soil dust aerosols. J Atmos Sci 56:2403–2433. https://doi.org/10.1175/1520-0469(1999)056
Millman PM (1979) Interplanetary dust. Naturwissenschaften 66:134–139. https://doi.org/10.1007/BF00368706
Mohammad F, Arfin T, Al-Lohedan HA (2019) Biocompatible polylactic acid-reinforced nickel-arsenate composite: studies of electrochemical conductivity, mechanical stability, and cell viability. Mater Sci Eng C 102:142–149. https://doi.org/10.1016/j.msec.2019.04.046
Mohanraj R, Azeez PA (2004) Health effects of airborne particulate matter and the Indian scenario. Curr Sci 87:741–748 https://jstor.org/stable/24109350
Molinelli AR, Santacana GE, Madden MC, Jimenez BD (2006) Toxicity and metal content of organic solvent extracts from airborne particulate matter in Puerto Rico. Environ Res 102:314–325. https://doi.org/10.1016/j.envres.2006.04.010
Möller W, Felten K, Sommerer K, Scheuch G, Meyer G, Meyer P, Haussinger K, Kreyling WG (2008) Deposition, retention, and translocation of ultrafine particles from the central airways and lung periphery. Am J Respir Crit Care Med 177:426–432. https://doi.org/10.1164/rccm.200602-3010C
Moorthy KK, Satheesh SK, Murthy BVK (1997) Investigations of marine aerosols over the tropocal indian ocean. J Geophys Res Atmos 102:18827–18842. https://doi.org/10.1029/97JD01121
Msuderly JL, Chow JC (2008) Health effects of organic aerosols. Inhal Toxicol 20:257–288. https://doi.org/10.1080/08958370701866008
National Collaborating Centre for Chronic Conditions (2004) Chronic obstructive pulmonary disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax 59(Suppl. 1):139–130
Nolan PJ (1972) The photoelectric nucleus counter. The Boyle medal lecture. Scientific Proceedings of the Royal Dublin Society, Series A 4:161–180
O’Donnell DE, Lam M, Webb KA (1999) Spirometric correlates of improvement in exercise performance after anticholinergic therapy in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 160:542–549. https://doi.org/10.1164/ajrccm.160.2.9901038
Obulapuram PK, Arfin T, Mohammad F, Khiste SK, Chavali M, Albalawi AN, Al-Lohedan HA (2021b) Adsorption, equilibrium isotherm, and thermodynamic studies towards the removal of reactive orange 16 dye using Cu(I)-polyaniline composite. Polymers 13:3490. https://doi.org/10.3390/polym13203490
Obulapuram PK, Arfin T, Mohammad F, Kumari K, Khiste SK, Al-Lohedan HA, Chavali M (2021a) surface-enhanced biocompatibility and adsorption capacity of a zirconium phosphate-coated polyaniline composite. ACS Omega 6:33614–33626. https://doi.org/10.1021/acsomega.1c04490
Ogliari KS, Lichtenfels AJF, Marchi MRR et al (2013) intrauterine exposure to diesel exhaust diminishes adult ovarian reserve. Fertil steril 99:1681–1688. https://doi.org/10.1016/j.fertnstert.2013.01.103
Oh H-J, Ma Y, Kim J (2020) Human inhalation exposure to aerosol and health effect: aerosol monitoring and modelling regional deposited doses. Int J Environ Res Public Health 17:1923. https://doi.org/10.3390/ijerph17061923
Ostro B, Broadwin R, Green S, Feng WY, Lipsett M (2006) Fine particulate air pollution and mortality in nine California counties: results from CALFINE. Environ Health Perspect 114:29–33. https://doi.org/10.1289/ehp.8335
Padoan E, Malandrino M, Giacomino A et al (2016) Spatial distribution and potential sources of trace elements in PM10 monitored in urban and rural sites of piedmont region. Chemosphere 145:495–507. https://doi.org/10.1016/j.chemosphere.2015.11.094
Pant P, Baker SJ, Goel R et al (2016) Analysis of size-segregated winter season aerosols data from New Delhi, India. Atmos Pollut Res 7:100–109. https://doi.org/10.1016/j.apr.2015.08.001
Pathak B, Biswas J, Bharali C, Bhuyan PK (2015) Short term introduction of pollutants into the atmosphere at a location in the Brahmaputra Basin: a case study. Atmos Pollut Res 6:220–229. https://doi.org/10.5094/APR.2015.026
Patton JS (1996) Mechanisms of macromolecule absorption by the lungs. Adv Drug Deliv Rev 19:3–36. https://doi.org/10.1016/0169-49X(95)00113-L
Pio C, Legrand M, Alves C, Oliveira T, Afonso J, Caseiro A, Pubaum H, Sanchez-Ochoa A, Gelencser A (2008) Chemical composition of atmospheric aerosols during the 2003 summer intense forest line period. Atmos environ 42:7530–7543. https://doi.org/10.1016/j.atmosenv.2008.05.032
Pope CA, Burnett RT, Thun MJ et al (2002) Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. J Am Med Assoc 287:1132–1141. https://doi.org/10.1001/jama.287.9.1132
Pope CA, Burnett RT, Thurston GD et al (2004) Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation 109:71–77. https://doi.org/10.1161/01.CIR.0000108927.80044.7F
Pope CA, Dockery DW (2006) Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc 56:709–742. https://doi.org/10.1080/10473289.2006.10464485
Prospero JM, Ginoux P, Torres O, Nicholson SE, Gill TE (2002) Environmental characterization of global sources of atmospheric soil dust identified with the nimbus 7 total ozone mapping spectrometer (TOMS) absorbing aerosol product. Rev Geophys 40:2-1–2-31. https://doi.org/10.1029/2000RG000095
Rowe SM, Miller S, Sorscher EJ (2005) Cystic fibrosis. N Engl J Med 352:1992–2001. https://doi.org/10.1056/NEJMra043184
Ruckeri R, Greven S, Ljungman P et al (2007) Air pollution and inflammation (Interleukin-6, C-Reactive Protein, Fibrinogen) in myocardial infarction survivors. Environ Health Perspect 115:1072–1080. https://doi.org/10.11289/ehp.10021
Rudell B, Blomberg A, Helleday R, Ledin MC, Lundback B, Stjernberg N, Horstedt P, Sandstrom T (1999) Bronchoalveolar inflammation after exposure to diesel exhaust: Comparison between unfiltered and particle trap filtered exhaust. Occup Environ Med 56:527–534. https://doi.org/10.1136/oem.56.8.527
Sah D, Verma PK, Kandikonda MK, Lakhani A (2019) Pollution characteristics, human health risk through multiple exposure pathways, and source apportionment of heavy metals in PM 10 at Indo-Gangetic site. Urban Clim 27:149–162. https://doi.org/10.10016/j.uclim.2018.11.010
Samet JM, Dominici F, Curriero FC et al (2000) Fine particulate air pollution and mortality in 20 U.S. Cities, 1987-1994. N Engl J Med 343:1742–1749. https://doi.org/10.1056/NEJM200012143432401
Satir P, Sleigh MA (1990) The physiology of cilia and mucociliary interactions. Annu Rev Physiol 52:137–155. https://doi.org/10.1146/annurev.ph.52.030190.001033
Schaber K (1995) Aerosol formation in absorption processes. Chem Eng Sci 50:1347–1360. https://doi.org/10.1016/0009-2509(95)988846-7
Schuetzle D, Lewtas J (1986) Bioassay-directed chemical analysis in environmental research. Anal Chem 58:1060A–1075A. https://doi.org/10.1021/ac00124a001
Schwarze PE, Ovrevik J, Lag M, Refsnes M, Natstad P, Hetland RB, Dybing E (2006) Particulate matter properties and health effects: consistency of epidemiological and toxicological studies. Hum Exp Toxicol 25:559–579. https://doi.org/10.1177/096032706072520
Seagrave JC, Berger J, Zielinska B, Sagebiel J, Rogers CF, McDonald JD, Mauderly JL (2001) Comparative acute toxicities of particulate matter (PM) and semi-volatile organic compound (SVOC) fractions of traffic tunnel air. Toxicologist 60:192
Seagrave JC, Gigliotti A, McDonald JD, Seilkop SK, Whitney KA, Zielinska B, Mauderly JL (2005) Composition, toxicity, and mutagenicity of particulate and semivolatile emissions from heavy-duty compressed natural gas-powered vehicles. Toxicol Sci 87:232–241. https://doi.org/10.1093/toxsci/kfi230
Sharma SK, Saxena M, Masiwal R, Sharma C (2016) Chemical characterization and source apportionment of aerosol at an urban area of Central Delhi, India. Atmos Pollut Res 7:110–121. https://doi.org/10.1016/j.apr.2015.08.002
Smaldone GC (2006) Advances in aerosols: adult respiratory disease. J Aerosol Med 19:36–46. https://doi.org/10.1089/jam.2006.19.36
Steerenberg PA, van Amelsvoort L, Lovik M, Hetland RB, Alberg T, Halatek T, Bloemen HJT, Rydzynski K, Swaen G, Schwarze P, Dybing E, Cassee FR (2006) Relation between sources of particulate air pollution and biological effect parameters in samples from four European cities: An exploratory study. Inhal Toxicol 18:333–346. https://doi.org/10.1080/08958370500515913
Sturton G, Persson C, Barnes PJ (2008) Small airways: an important but neglected target in the treatment of obstructive airway diseases. Trends Pharmacol Sci 29:340–345. https://doi.org/10.1016/j.tips.2008.04.003
Sun Z, Zhu D (2019) Exposure to putdoor air pollution and its human health outcomes: a scoping review. PLoS One 14:e0216550. https://doi.org/10.1371/journal.pone.0216550
Sunyer J (2008) The neurological effects of air pollution in children. Eur Respir J 32:535–537. https://doi.org/10.1183/09031936.00073708
Suwa T, Hogg JC, Quinlan KB et al (2002) Particulate air pollution induces progression of atherosclerosis. J Am Coll Cardiol 39:935–942. https://doi.org/10.1016/s0735-1097(02)01715-1
Tonne C, Melly S, Mittleman M, Coull B, Goldberg R, Schwartz J (2007) A case-control analysis of exposure to traffic and acute myocardial infarction. Environ Health Perspect 115:53–57. https://doi.org/10.1289/ehp.9587
West JJ, Cohen A, Dentener F, Brunekreef B, Zhu T, Armstrong B, Bell ML, Brauer M, Carmichael G, Costa DL, Dockery DW (2016) What we breathe impacts our health: improving understanding of the link between air pollution and health. Environ Sci Technol 50:4895–4904. https://doi.org/10.1021/acs.est.5b03827
Wichmann HE, Spix C, Tuch T, Wolke G, Peters A, Heinrich J, Kreyling WG, Heyder J (2000) Daily mortality and fine and ultra-fine particles in Erfurt, Germany, Part I. Role of particle number and particle mass. Res Rep Health eff Inst 98:87–94
Wiebert P, Sanchez-Crespo A, Seitz J, Falk R, Philipson K, Kreyling WG, Moller W, Sommerer K, Larrson S, Svartengren M (2006) Negligible clearance of ultrafine particles retained in healthy and affected human lungs. Eur Respir J 28:286–290. https://doi.org/10.1183/09031936.06.00103805
Winter B, Chylek P (1997) Contribution of sea salt aerosol to the planetary clear-sky albedo. Tellus B Chem Phys Meteorol 49:72–79. https://doi.org/10.3402/tellusb.v49i1.15951
World Health Organization (2011) The top 10 causes of death, http://www.who.int/mediacentre/factsheets/fs310/en/index2.html (last accessed 15 August 2013).
Xia W, Wang Y, Chen S, Huang J et al (2021) Double trouble of air pollution by anthropogenic dust. Environ Sci Technol 56:761–769. https://doi.org/10.1021/acs.est.1c04779
Xiao J-Z, Konda S, Yanagisawa N, Miyaji K, Enomoto K, Sakoda T, Iwatsuki K, Enomoto T (2007) Clinical efficacy of probiotic bifidobacterium longum for the treatment of symptoms of Japanese cedar pollen allergy in subjects evaluated in an environmental exposure unit. Allergol Int 56:67–75. https://doi.org/10.2332/allergolint.O-06-455
Xu Q, Wang S, Jiang J, Bhattarai N, Li X, Chang X, Qiu X, Zheng M, Hua Y, Hao J (2019) Nitrate dominates the chemical composition of PM 2.5 during haze event in Beijing, China. Sci Total Environ 689:1293–1303. https://doi.org/10.1016/j.scitotenv.2019.06.294
Yoshizumi K (1986) Regional size distributions of sulfate and nitrate in the Tokyo metropolitan area in summer. Atmos Environ 20:763–766. https://doi.org/10.1016/0004-6981(86)90191-5
Zhang X, Pandis SN, Seinfeld JH (2012) Diffusion-limited versus quasi-equilibrium aerosol growth. and mechanisms for organics. Aerosol Sci Technol 46:874–885. https://doi.org/10.1080/02786826.2012.679344
Zhao X, Zhang X, Xu X et al (2009) Seasonal and diurnal variations of ambient PM2.5 concentration in urban and rural environments in Beijing. Atmos Environ 43:2893–2900. https://doi.org/10.1016/j.atmosenv.2009.03.009
Download references
Acknowledgements
Authors acknowledge the Knowledge Resource Centre, CSIR-NEERI (CSIR-NEERI/KRC/2023/MAR/APC/1) for their support.
Author information
Authors and affiliations.
Air Pollution Control Division, CSIR-National Environmental Engineering Research Institute (CSIR-NEERI), Nehru Marg, Nagpur, 440020, India
Tanvir Arfin, Anupama M Pillai, Nikhila Mathew, Abha Tirpude, Roshani Bang & Pabitra Mondal
Academy of Scientific and Innovative Research (AcSIR), Ghaziabad, 201002, India
Tanvir Arfin & Roshani Bang
You can also search for this author in PubMed Google Scholar
Contributions
Nikhila Mathew: writing—original draft and editing. Abha Tirpude: literature search. Anupama M Pillai: conceptualisation and writing—original draft. Roshani Bang: literature search. Pabitra Mondol: visualisation. Tanvir Arfin: supervision, review, editing, and proofreading. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Tanvir Arfin .
Ethics declarations
Ethics approval.
Not applicable.
Consent to participate
Non applicable.
Consent for publication
Competing interest.
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Arfin, ., Pillai, A.M., Mathew, N. et al. An overview of atmospheric aerosol and their effects on human health. Environ Sci Pollut Res 30 , 125347–125369 (2023). https://doi.org/10.1007/s11356-023-29652-w
Download citation
Received : 14 March 2023
Accepted : 29 August 2023
Published : 06 September 2023
Issue Date : December 2023
DOI : https://doi.org/10.1007/s11356-023-29652-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Air pollution
- Health effects
- Particular matter
- Respiratory
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 13 April 2024
The changing health effects of air pollution exposure for respiratory diseases: a multicity study during 2017–2022
- Siyu Jiang 1 na1 ,
- Longjuan Tang 1 na1 ,
- Zhe Lou 1 na1 ,
- Haowei Wang 2 , 3 ,
- Ling Huang 4 ,
- Wei Zhao 1 ,
- Qingqing Wang 5 ,
- Ruiyun Li 1 , 6 &
- Zhen Ding 5
Environmental Health volume 23 , Article number: 36 ( 2024 ) Cite this article
328 Accesses
7 Altmetric
Metrics details
Multifaceted SARS-CoV-2 interventions have modified exposure to air pollution and dynamics of respiratory diseases. Identifying the most vulnerable individuals requires effort to build a complete picture of the dynamic health effects of air pollution exposure, accounting for disparities across population subgroups.
We use generalized additive model to assess the likely changes in the hospitalisation and mortality rate as a result of exposure to PM2.5 and O 3 over the course of COVID-19 pandemic. We further disaggregate the population into detailed age categories and illustrate a shifting age profile of high-risk population groups. Additionally, we apply multivariable logistic regression to integrate demographic, socioeconomic and climatic characteristics with the pollution-related excess risk.
Overall, a total of 1,051,893 hospital admissions and 34,954 mortality for respiratory disease are recorded. The findings demonstrate a transition in the association between air pollutants and hospitalisation rates over time. For every 10 µg/m 3 increase of PM2.5, the rate of hospital admission increased by 0.2% (95% CI: 0.1–0.7%) and 1.4% (1.0–1.7%) in the pre-pandemic and dynamic zero-COVID stage, respectively. Conversely, O 3 -related hospitalization rate would be increased by 0.7% (0.5–0.9%) in the pre-pandemic stage but lowered to 1.7% (1.5–1.9%) in the dynamic zero-COVID stage. Further assessment indicates a shift of high-risk people from children and young adolescents to the old, primarily the elevated hospitalization rates among the old people in Lianyungang (RR: 1.53, 95%CI: 1.46, 1.60) and Nantong (RR: 1.65, 95%CI: 1.57, 1.72) relative to those for children and young adolescents. Over the course of our study period, people with underlying diseases would have 26.5% (22.8–30.3%) and 12.7% (10.8–14.6%) higher odds of having longer hospitalisation and over 6 times higher odds of deaths after hospitalisation.
Conclusions
Our estimates provide the first comprehensive evidence on the dynamic pollution-health associations throughout the pandemic. The results suggest that age and underlying diseases collectively determines the disparities of pollution-related health effect across population subgroups, underscoring the urgency to identifying the most vulnerable individuals to air pollution.
Peer Review reports
Dynamics and burdens of respiratory diseases are shaped by interacting climatic and societal processes, including exposure to air pollution and human mobility pattern. Mounting evidence suggests that widespread non-pharmacal interventions during early pandemic quickly transformed social mixing and reduced pollution-attributable mortality [ 1 , 2 , 3 , 4 , 5 ]. To make robust assessment of such health benefits, there is a pressing need to critically analyse multifaceted health outcomes such as hospitalisations and mortality over a longer term.
Identifying the most vulnerable individuals to air pollution is a major public health concern. Given the age disparities in social activities and thus air pollution exposure, it is likely that air pollution may have disproportionately affected different age groups [ 6 ]. Recognizing the role of immunity, air pollution threatens to pose a dual burden to individuals with pre-existing diseases [ 7 , 8 ]. This motivates effort to elucidate variations of pollution-related health outcomes across population subgroups. To date, many studies on respiratory diseases have reported findings on the association between ambient air pollution and hospital admissions and mortality [ 9 , 10 , 11 ]. Yet, heterogeneities across age groups and the overlapping burden for those with underlying diseases remain unknown.
The aim of this multicity study is to estimate age-stratified associations between air pollution exposure and health outcomes for respiratory diseases, such that recognizing potential changes between these associations during the COVID-19 pandemic. To this end, we first sought to quantify the health effects of air pollution exposure, both for hospital admissions and mortality. Additionally, we identified vulnerable population subgroups by assessing age differences in pollution-health associations and the excess risk of having underlying diseases.
Study population
Our study is based in 13 cities of Jiangsu province across a broad range of climatic conditions and sociodemographic structures (Supplemental Fig. 1 ). Individual-level records of respiratory diseases related-hospital admissions and mortality from Jan 1, 2017 to Dec 31, 2019 (defined as “pre-pandemic stage”) and from Jan 1, 2020 to Dec 31, 2022 (defined as “dynamic zero-COVID stage”) were retrieved from the surveillance system of Jiangsu Provincial Center for Disease Control and Prevention. The associated characteristics, including age, sex, postcode of residence, date of hospitalisation and mortality, diagnosis, and underlying diseases, were available for each individual. The underlying diseases considered include coronary heart disease, stroke, hypertension, chronic obstructive pulmonary disease, diabetes, chronic kidney disease, cancer, and immune defect.
Health outcomes
Outcomes of interest differ between analyses on population and individual levels. At the population level, outcomes of interest included the daily number of hospital admissions and deaths for respiratory diseases. While a patient’s vulnerability was assessed by using the length of hospitalisations and death after hospitalisation. For simplicity, we categorized the patient’s length of hospital stay as less or longer than the median length among all individuals; and distinguished whether individuals died or recovered after hospitalisation.
Air pollution exposure
We obtained daily air temperature at 2 m (m) and relative humidity from the fifth-generation reanalysis (ERA5) provided by the European Center for Medium-Range Weather Forecasts (ECMWF) [ 12 ]. Additionally, we collected daily 1 km (km) PM2.5 and 10 km O 3 data from the Tracking Air Pollution in China (TAP) platform ( http://tapdata.org.cn ) which provides a near real-time distribution of air pollutants [ 13 , 14 ]. By identifying the nearest grid point to the geographic location of individual’s residence, we further extracted the time-series data of local climate and pollution conditions.
Statistical analyses
We conducted descriptive statistics for the city-stratified rate of hospitalisation and mortality for respiratory diseases. These rates were defined by the number of hospital admissions and deaths per 10,000 people. We quantified the changes of the rates by using the ratio of the rate in pre-pandemic and dynamic zero-COVID stages. All subsequent analyses that investigated potential changes in pollution-related health outcomes were done separately for the pre-pandemic and dynamic zero-COVID stages.
We started with evaluating the overall association between air pollution exposure and different health outcomes in an entire population. To do so, we used generalized additive model (GAM) to collate effects of pollution exposure and weather conditions on the rate of hospitalisations and mortality. Note that we focused on short-term effects of PM2.5 and O 3 and assumed linear associations between pollutant predictors and health outcomes accordingly. We additionally included daily mean temperature and humidity as confounding factors to account for their non-linear effects on both hospitalisations and mortality. Therefore, two-pollutant models were established with the equation as follows:
where \({Y}_{i,j}\) is the number of hospital admissions or mortality on day \(i\) in city \(j\) . The parameter \({\alpha }_{i,j}\) is the overall intercept. \({P}_{i-l1,j}^{1}\) and \({P}_{i-l1,j}^{2}\) is PM2.5 and O 3 on single day, \(l1\) (categorized as 0, 1, 2, or 3 days) prior to hospital admission or deaths, respectively; \({\beta }_{1}\) and \({\beta }_{2}\) are coefficients of two pollutant predictors respectively. \(b\left({T}_{i-l2,j}\right)\) and \(c\left({RH}_{i-l2,j}\right)\) is a smooth function accounting for daily mean temperature and humidity on cumulative days, \(l2\) , (categorized as 0–7, 0–14, 0–21, or 0–28 days) prior to the outcomes of interest, respectively. All models were adjusted for spatial heterogeneity by using a categorical variable to distinguish across cities, \({C}_{j}\) . We fitted models by using records in the dynamic zero-COVID stage and used Generalized Cross-Validation (GCV) to determine the optimal lag effects. Assuming that these optimal lag effects were the same for all subsequent analyses, we further applied models to estimate pollution-health associations at the pre-pandemic stage.
Next, we extended the overall estimates to evaluate the age difference in the association between pollution factors and rate of hospitalisations and mortality. The age groups of the study population was children and young adolescents (aged 0–14 years old), working-age people (aged 15–64 years old), and the old population (over 65 years old). We considered records of hospital admissions among all three age groups; we restricted the analyses of mortality to working-age people and the old as deaths among children and young adolescents were very rare. GAMs were stratified by age groups and applied to each city using the following equation:
where \({Y}_{i,a}\) is the number of hospital admissions or mortality on day \(i\) in age group \(a\) . The parameter \({\alpha }_{i,a}\) is the overall intercept. \({P}_{i-lopt1,j}^{1}\) and \({P}_{i-lopt1,j}^{2}\) are PM2.5 and O 3 on the optimal time lag ( \(opt1\) ); while \(b\left({T}_{i-lopt2,j}\right)\) and \(c\left({RH}_{i-lopt2,j}\right)\) are smooth functions for the multi-day lagged effect ( \(lopt2\) ) of temperature and humidity. Age groups are included as a categorical variable, \(A\) .
Further, we sought to assess the vulnerability of people with underlying diseases. We used multivariable logistic regression to examine the role of having underlying diseases on the odds of longer hospital stay and death after hospitalisation. Models were adjusted for confounding factors, including demographic characteristics (i.e. age and sex), geographic location of residence (rural or urban) and local weather conditions. We additionally accounted for the potential difference in the excess risk among individuals with different number of underlying diseases. We addressed this by evaluating the odds of hospitalisation and mortality for individuals with single disease as compared to those with double or more diseases.
Sensitivity analyses
To validate our findings and insights, we first investigated variations in the pollution-health associations across age groups and cities. Furthermore, we examined potential uncertainty that may arise from the alternative classification of patients with underlying diseases. These individuals were segmented into three categories with single, double and multiple underlying diseases. Recognizing the control measures during the early pandemic and the potential modification of the pollution-related health effects, we make additional assessment of the association between pollutants and health outcomes in the dynamic zero-COVID stage by excluding the records in the first six months of 2020. All analyses were conducted with R version 4.3.0 and ArcGIS 10.8.1.
We retrieved 1,051,893 records of hospital admissions and 34,954 of mortality for respiratory disease during 2017–2022 in Jiangsu Province, China. The rate of hospitalisations and mortality differs significantly between the pre-pandemic and dynamic zero-COVID stages (Supplemental Fig. 2 and Supplemental Fig. 3 ); yet, spatial heterogeneity of such changes is observed (Fig. 1 ).
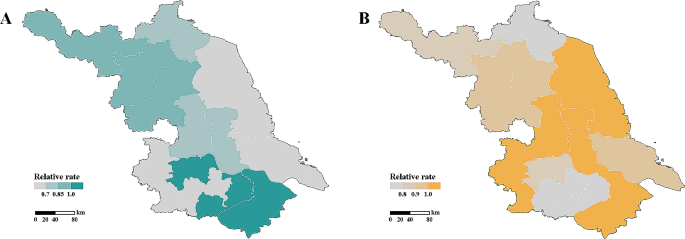
Hospital admissions and mortality for respiratory diseases across 13 cities in Jiangsu province. Cities are coloured by the relative rate of ( A ) hospitalisations and ( B ) mortality, i.e. the number of hospitalisations and death per 10,000, in pre-pandemic and dynamic zero-COVID stages
Overall pollution-health associations
We first identified the overall association between air pollution exposure in the three days before hospital admission and hospitalisation rate for respiratory diseases (Table 1 ). For every 10 µg/m 3 increase of PM2.5 and O 3 , the rate of hospital admission in the pre-pandemic stage increased by 0.2% (95% CI: 0.1–0.7%) and 0.7% (0.5–0.9%), respectively. Mortality of respiratory diseases correlates with pollutants exposure on the previous day (Table 1 ). It is estimated that the rate of mortality would increase by 1.8% (1.3–2.2%) with every 10 µg/m 3 increase of O 3 .
Statistically significant associations between pollutants and health outcomes are also seen in the dynamic zero-COVID stage. We found similar positive association between PM2.5 and hospitalisation rate, with a slightly higher effect (1.4% (1.0–1.7%) increase in hospitalisation rate) compared to pre-pandemic estimates. It is noted that the pattern of association between O 3 and hospitalisations changes, yielding a 1.7% (1.5–1.9%) lower rate of hospitalisation for every 10 µg/m 3 increase of O 3 . Additionally, we observed significant association between O 3 and mortality. It shows that O 3 -related increase in the mortality rate would be lowered to 1.2% (0.6–1.8%) in the dynamic zero-COVID stage. Restricting analyses to subpopulations and geographic areas yield greater variations of the associations among age groups and cities (Supplemental Tables 1 – 2 ).
Age difference in pollution-health associations
Disaggregation of age groups indicates heterogeneity in pollution-health associations within the population (Fig. 2 ). Prior to the COVID-19 pandemic, children and young adolescents were at the highest rate of hospitalisation for respiratory diseases across cities, except for Suqian (Fig. 2 A). However, such age-stratified associations between pollution and hospital admission shifted in the dynamic zero-COVID stage (Fig. 2 B), with substantially elevated rates observed for the old people in Lianyungang (RR: 1.53, 95%CI: 1.46, 1.60) and Nantong (RR: 1.65, 95%CI: 1.57, 1.72) relative to those for children and young adolescents. This increase generates a shift of high-risk people from children and young adolescents to the old. Conversely, we identify that children and the young adolescents turn into the high-risk group with the highest rate of hospitalisation in Suqian (Fig. 2 B). Limiting associations to individuals over 14 years shows that mortality rates are generally greater among the old population, with RR values ranging from 1.12 to 2.96, as compared to those for the working-age people across cities and pandemic stages (Fig. 2 C–D).
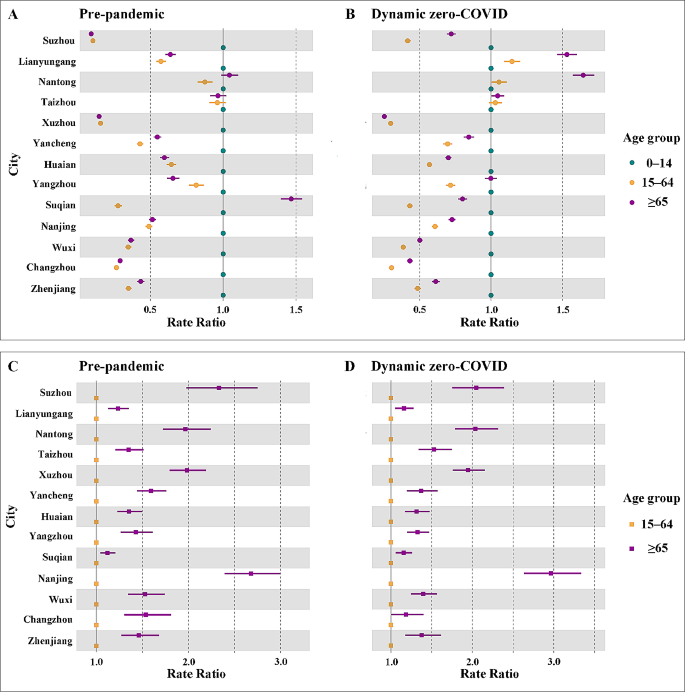
Age disparities in pollution-related rate of hospitalisation and mortality. Estimates of ( A – B ) hospitalisation and ( C – D ) mortality rate across age groups in pre-pandemic and dynamic zero-COVID stage are presented
Excess risk of having underlying diseases
After adjusting for age, sex, and residence, patients having underlying diseases correlate with significantly increased odds of longer hospital stay and death after hospitalisation (Table 2 ). It is estimated that the medium length of hospitalisation over the study period is seven days. Compared with this, our estimates show that people with underlying diseases would have 26.5% (22.8–30.3%) more odds of having longer hospitalisation than those without underlying diseases. Such increase of the odds attributable to underlying diseases are slightly attenuated to 12.7% (10.8–14.6%) in the dynamic zero-COVID stage. Of note, patients with underlying diseases have a strikingly higher odds of deaths after hospitalisation. Over the course of our study period, these patients have odds of deaths that are over 6 times (6.4 (5.6, 7.3) in the pre-pandemic stage and 6.1 (5.7, 6.6) in the dynamic zero-COVID stage) than those in the reference group.
Further assessment indicates disparities in the odds of deaths among patients with single and multiple underlying diseases (Supplemental Table 3 ). Compared to patients without underlying disease, our estimates show that having single underlying disease is associated with around 20% and 540% higher odds of longer hospital stay and death after hospitalisation, respectively. These estimates surge, primarily the odds of deaths in the dynamic zero-COVID stage, among those with double or more underlying diseases. Sensitivity analyses confirm our finding of the increased odds of hospitalisation and death attributable to underlying diseases (Supplemental Table 4 ).
Our multicity study fits well in the current context of the exacerbated health effects of air pollution exposure. In light of emerging evidence that pollution-attributable mortality may have reduced during the pandemic [ 1 , 2 , 3 , 4 , 5 ], we provided the first essential evidence on the dynamic pollution-health associations throughout the pandemic. Unlike previous studies focusing solely on mortality, our multicity study in Jiangsu province extends the analysis to include hospitalizations, thereby offering a more multifaceted understanding how pandemic-related interventions may have modulated the influence of pollutants on health outcomes. We found that air pollution exposure generally associates with multifaceted health outcomes, including hospitalisations and mortality, for respiratory diseases. This finding is broadly consistent with other studies done across a variety of settings [ 15 , 16 , 17 , 18 , 19 , 20 , 21 ]. It is important to note that, over time, there is an opposite shift in the pattern of association between air pollutants and hospitalisation rates. The effect of O 3 on the hospitalisation rate was attenuated which, in turn, may be partially attributed to the lowered level of O 3 during the pandemic. In contrast, risk of PM2.5-related hospitalisation increased in the dynamic zero-COVID stage. Although associations between pollutants and hospital admission evolves, we detected no evidence of deviations from the pre-pandemic association between pollutants exposure and mortality.
When considering the disparities of pollution-related health outcomes among population subgroups, our findings emphasize the importance of two main axes of vulnerability to air pollution exposure: age and underlying diseases. Over the course of the pandemic, the shift in the age profile of high-risk groups may be largely dependent on the relative fraction of hospitalisation across age groups (Supplemental Fig. 3 ). Specifically, the fraction of hospitalisation for respiratory diseases increased among children and young adolescents but reduced among the old in Suqian. Such trade-off generated the shift of the high-risk group from the old to children and young adolescents. Similarly, people over 65 accounted for the greatest fraction of hospitalisation in Lianyungang and Nantong in the dynamic zero-COVID stage, resulting in high-risk population shifts from children and young adolescents to the elderly. Moving beyond the age burden, estimates of an individual’s excess risk would additionally heighten the overlapping burden from air pollution and underlying diseases.
Despite the clear signature of age and underlying diseases on individual’s vulnerability, we provided essential evidence that sex and location of residence are strongly associated with the increased odds of longer hospitalisation and higher risk of death (Table 2 ). We identified that male is more likely to have a higher risk of longer hospital admission (8.6% (95% CI 6.2–11%) in pre-pandemic and 6.6% (95% CI 5.1–8.0%) in dynamic zero-COVID stage) relative to females. Similarly, males tend to have 23.3% (13.9–33.7%) and 16.1% (10.8–21.8%) higher risk of death after hospitalisation in two pandemic stages, respectively. This finding is similar to other environmental health studies, highlighting gender difference in the risk of air pollution exposure [ 22 , 23 , 24 , 25 , 26 ]. Additionally, living in urban areas would associate with a 14.9% (12.3–17.5%) increase in the risk of longer hospitalisation but a 63.8% (60.9–66.4%) lowered mortality risk prior to the pandemic. Although this urban-rural difference is narrowed in the dynamic zero-COVID stage, it is mostly attributed to the health inequalities among areas [ 27 ]. Inadequate health resources yield the limited access to health facilities for people living in rural areas. In such context, people may not seek care in health facilities, leading to a great reduction of hospital admission and the lowered risk of hospitalisation accordingly. With respect to mortality rate, the limited health resources may delay the treatment of respiratory diseases and therefore contribute to higher odds of death after hospitalisation for the rural population.
The key messages of this study are of great public health significance. We provided fundamental estimates of the dynamic pollution-health associations over time, which makes critical contributions to understanding how pandemic-related interventions may have modulated the influence of pollutants on health outcomes. Importantly, by identifying vulnerable population subgroups, particularly the elderly and those with preexisting conditions, we underscore the disproportionate effects of air pollution. These findings support WHO global air quality guidelines where the elderly and those with underlying diseases bear the greatest burden of air pollution [ 28 ]. Additionally, this study based on a multicity approach across 13 cities in Jiangsu province, offers a comprehensive perspective that enhances the generalizability of our findings. In light of these evidence, health authorities will build a complete picture of the heterogeneous health effects of air pollution exposure for respiratory diseases, formulating relevant policies to identify and protect the most vulnerable individuals.
Future studies may build on our findings in several ways. First, we have explicitly estimated air pollution effects on hospitalisation and mortality. Examining across a variety of pollutants and outcomes is essential for differentiating the roles of co-occurring air pollutants on respiratory outcomes. Additionally, assessment of the pollution-related health effects may vary by applying alternative statistical approaches. Evaluating the potential bias of assessment attributable to the statistical approach would be a promising direction for future investigations. Furthermore, our inability to obtain hospitalisation records in 2017–2018 is likely to bias our observed associations which should be validated. Finally, we have reported the excess risk of having underlying diseases. Moving from this finding, prioritizing the most vulnerable subpopulation will require distinguishing contributions across specific underlying diseases.
Data availability
All data were archived within the surveillance system of the Jiangsu Provincial Center for Disease Control and Prevention. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Fifth-generation reanalysis
European Center for Medium-Range Weather Forecasts
Tracking Air Pollution in China
Generalized additive model
Chen K, Wang M, Huang C, Kinney PL, Anastas PT. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020;4(6):e210–2.
Article Google Scholar
Giani P, Castruccio S, Anav A, Howard D, Hu W, Crippa P. Short-term and long-term health impacts of air pollution reductions from COVID-19 lockdowns in China and Europe: a modelling study. Lancet Planet Health. 2020;4(10):e474–82.
Hao X, Li J, Wang H, Liao H, Yin Z, Hu JF, et al. Long-term health impact of PM2.5 under whole-year COVID-19 lockdown in China. Environ Pollut. 2021;290:118118.
Article CAS Google Scholar
Chen G, Tao J, Wang J, Dong M, Li X, Sun X, et al. Reduction of air pollutants and associated mortality during and after the COVID-19 lockdown in China: impacts and implications. Environ Res. 2021;200:111457.
Venter ZS, Aunan K, Chowdhury S, Lelieveld J. Air pollution declines during COVID-19 lockdowns mitigate the global health burden. Environ Res. 2020;192:110403.
Cai W, Zhang C, Zhang S, Bai Y, Callaghan M, Chang N, et al. The 2022 China report of the Lancet countdown on health and climate change: leveraging climate actions for healthy ageing. Lancet Public Health. 2022;7(12):e1073–90.
Hooper LG, Kaufman JD. Ambient air Pollution and clinical implications for susceptible populations. Ann Am Thorac Soc. 2018;15(Suppl 2):S64–8.
Tibuakuu M, Michos ED, Navas-Acien A, Jones MR. Air Pollution and Cardiovascular Disease: a focus on vulnerable populations Worldwide. Curr Epidemiol Rep. 2018;5(4):370–8.
Lin C, Ma Y, Liu R, Shao Y, Ma Z, Zhou L, et al. Associations between short-term ambient ozone exposure and cause-specific mortality in rural and urban areas of Jiangsu, China. Environ Res. 2022;211:113098.
Ma Y, Zhou L, Chen K. Burden of cause-specific mortality attributable to heat and cold: a multicity time-series study in Jiangsu Province, China. Environ Int. 2020;144:105994.
Wang C, Feng L, Chen K. The impact of ambient particulate matter on hospital outpatient visits for respiratory and circulatory system disease in an urban Chinese population. Sci Total Environ. 2019;666:672–9.
Hersbach H, Bell B, Berrisford P, Hirahara S, Horányi A, Muñoz-Sabater J, et al. The ERA5 global reanalysis. Q J Roy Meteor Soc. 2020;146:1999–2049.
Geng XQ, Liu G, Liu S, Meng J, Zhang X Q. Spatiotemporal continuous estimates of daily 1 km PM 2.5 from 2000 to present under the Tracking Air Pollution in China (TAP) framework. Atmos Chem Phys. 2022;22(19):13229–42.
Xue T, Zheng Y, Geng G, Xiao Q, Meng X, Wang M, et al. Estimating Spatiotemporal variation in ambient ozone exposure during 2013–2017 using a Data-Fusion Model. Environ Sci Technol. 2020;54(23):14877–88.
Lu P, Zhang Y, Lin J, Xia G, Zhang W, Knibbs LD, et al. Multi-city study on air pollution and hospital outpatient visits for asthma in China. Environ Pollut. 2020;257:113638.
Zhang Y, Wu Z, Gou K, Wang R, Wang J. The impact of Air Pollution on Outpatient visits of children with asthma in Xi’an, China. Wild Environ Med. 2021;32(1):47–54.
Gu J, Shi Y, Zhu Y, Chen N, Wang H, Zhang Z, et al. Ambient air pollution and cause-specific risk of hospital admission in China: a nationwide time-series study. PLoS Med. 2020;17(8):e1003188.
Wang M, Chen J, Zhang Z, Yu P, Gan W, Tan Z, et al. Associations between air pollution and outpatient visits for arrhythmia in Hangzhou, China. BMC Public Health. 2020;20(1):1524.
Yin P, Chen R, Wang L, Meng X, Liu C, Niu Y, et al. Ambient ozone Pollution and Daily Mortality: a nationwide study in 272 Chinese cities. Environ Health Persp. 2017;125(11):117006.
Perone G. Assessing the impact of long-term exposure to nine outdoor air pollutants on COVID-19 spatial spread and related mortality in 107 Italian provinces. Sci Rep. 2022;12(1):13317.
Orellano P, Reynoso J, Quaranta N, Bardach A, Ciapponi A. Short-term exposure to particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: systematic review and meta-analysis. Environ Int. 2020;142:105876.
Ren M, Li N, Wang Z, Liu Y, Chen X, Chu Y, et al. The short-term effects of air pollutants on respiratory disease mortality in Wuhan, China: comparison of time-series and case-crossover analyses. Sci Rep. 2017;7(1):40482.
Li M, Chen S, Zhao H, Tang C, Lai Y, Oi C, et al. The short-term associations of chronic obstructive pulmonary disease hospitalizations with meteorological factors and air pollutants in Southwest China: a time-series study. Sci Rep. 2021;11(1):12914.
Shin HH, Parajuli RP, Gogna P, Maquiling A, Dehghani P. Pollutant-sex specific differences in respiratory hospitalization and mortality risk attributable to short-term exposure to ambient air pollution. Sci Total Environ. 2020;755:143135.
Niu Y, Zhou Y, Chen R, Yin P, Meng X, Wang W, et al. Long-term exposure to ozone and cardiovascular mortality in China: a nationwide cohort study. Lancet Planet Health. 2022;6(6):e496–503.
Ma Z, Meng X, Chen C, Chao B, Zhang C, Li W. Short-term effects of different PM2.5 ranges on daily all-cause mortality in Jinan, China. Sci Rep. 2022;12(1):5665.
Zhang X, Dupre ME, Qiu L, Zhou W, Zhao Y, Gu D. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC Geriatr. 2017;17(1):151.
WHO global air quality guidelines. Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Geneva: World Health Organization; 2021.
Download references
Acknowledgements
Not applicable.
This work was supported by the Seeds funding of Nanjng Medical University (NMUR20220001), and National Key Research and Development Program of China (2022YFC3700105). The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Author information
Siyu Jiang, Longjuan Tang and Zhe Lou contributed equally to this work.
Authors and Affiliations
School of Public Health, Nanjing Medical University, 101 Longmian AV, Nanjing, 211166, Jiangsu, China
Siyu Jiang, Longjuan Tang, Zhe Lou, Wei Zhao & Ruiyun Li
School of Public Health, Imperial College London, London, UK
Haowei Wang
MRC Centre for Global Infectious Disease Analysis and Abdul Latif Jameel Institute for Disease and Emergency Analytics, Imperial College London, London, UK
College of Urban and Environmental Sciences, Peking University, Beijing, China
Jiangsu Provincial Center for Disease Prevention and Control, 172 Jiangsu Rd, Nanjing, 210009, Jiangsu, China
Qingqing Wang & Zhen Ding
Jiangsu Center for Collaborative Innovation in Geographical Information Resource Development and Application, Nanjing, China
You can also search for this author in PubMed Google Scholar
Contributions
This study was conceptualised by RL and ZD. The research was supervised by ZD. The data analyses were carried out by SJ, LT and ZL. All authors were involved in the data interpretation. SJ, LT and ZL prepared the manuscript. All authors reviewed and approved the final version of the manuscript. RL and ZD had full access to the data and codes used in this study. All authors have final responsibility for the decision to submit the manuscript for publication.
Corresponding authors
Correspondence to Ruiyun Li or Zhen Ding .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for this study was granted through a data sharing agreement from Jiangsu Provincial Center for Disease Prevention and Control.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jiang, S., Tang, L., Lou, Z. et al. The changing health effects of air pollution exposure for respiratory diseases: a multicity study during 2017–2022. Environ Health 23 , 36 (2024). https://doi.org/10.1186/s12940-024-01083-1
Download citation
Received : 27 August 2023
Accepted : 10 April 2024
Published : 13 April 2024
DOI : https://doi.org/10.1186/s12940-024-01083-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Air pollution
- Respiratory disease
- Health risks
- Epidemiology
Environmental Health
ISSN: 1476-069X
- General enquiries: [email protected]
- Biology Article
Effects Of Air Pollution On Human Health
Effects Of Air Pollution On Human Health is very alarming. There are many diseases that can bring about a host of potentially fatal illnesses. From chronic bronchitis to lung cancer, air pollution has the potential to raise the risk of illness.
Air pollution and its link to the respiratory system is quite obvious. However, air pollution is also known to affect the circulatory system and the nervous system. When particular matter enters the nasal cavity, the lining ger irritated and the body may mistake it for an infection, This causes an inflammatory response, which can result in the exacerbation of any pre-existing conditions.
What are the Effects of Air Pollution On Human Health
- Human health is also severely affected by particulates in the atmosphere. The particulates can cause nasal irritation and swelling. It can also cause a running nose.
- Air pollution is also linked to lung damage and limited lung function
- Air pollution can also have an inflammatory effect on the heart – it can elevate blood pressure and aggravate pre-existing conditions of the heart.
- The risk of death significantly increases with long term exposure to polluted air. For instance, people susceptible to heart diseases are at higher risk.
Explore more topics, such as the Causes of Water Pollution , or more only at BYJU’S.
Put your understanding of this concept to test by answering a few MCQs. Click ‘Start Quiz’ to begin!
Select the correct answer and click on the “Finish” button Check your score and answers at the end of the quiz
Visit BYJU’S for all Biology related queries and study materials
Your result is as below
Request OTP on Voice Call
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Post My Comment
- Share Share
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.

This is Air: The "Non-Health" Effects of Air Pollution
A robust body of evidence shows that air pollution exposure is detrimental to health outcomes, often measured as deaths and hospitalizations. This literature has focused less on subclinical channels that nonetheless impact behavior, performance, and skills. This article reviews the economic research investigating the causal effects of pollution on "non-health" endpoints, including labor productivity, cognitive performance, and multiple forms of decision making. Subclinical effects of pollution can be more challenging to observe than formal health care encounters but may be more pervasive if they affect otherwise healthy people. The wide variety of possible impacts of pollution should be informed by plausible mechanisms and require appropriate hypothesis testing to limit false discovery. Finally, any detected effects of pollution, both in the short and long run, may be dampened by costly efforts to avoid exposure ex-ante and remediate its impacts ex-post; these costs must be considered for a full welfare analysis
The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research.
MARC RIS BibTeΧ
Download Citation Data
- March 15, 2022
Published Versions
Mentioned in the news, more from nber.
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .


IMAGES
VIDEO
COMMENTS
The health effects of air pollution are serious - one third of deaths from stroke, lung cancer and heart disease are due to air pollution. This is having an equivalent effect to that of smoking tobacco, and much higher than, say, the effects of eating too much salt. ... These particles are so small that 60 of them make up the width of a human ...
Air pollution has various health effects. The health of susceptible and sensitive individuals can be impacted even on low air pollution days. ... and global warming is mounting, with harmful effects on human health, animals, forests, wildlife, agriculture, and the water environment. ... the main proposal of this essay is that we should focus on ...
Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders ( 3 ), leading to infant mortality or chronic disease in adult age ( 6 ). National reports have mentioned the increased risk of morbidity and mortality ( 1 ).
Abstract. Air pollution is a pressing global environmental challenge with far-reaching consequences for human health and well-being. This research paper presents an extensive examination of air ...
The effects of air pollution on human health can be short term or long term. Both short term and long term effects can cause varying degrees of damage to human health. Short term and long term effects may include minor irritations and death respectively (Bauer 1093). Toxic air particles have short term effects such as; immediate irritation to ...
Immediate effects of air pollution include irritation of the eyes, nose, and throat, headaches, dizziness, and fatigue. Such immediate effects are usually short-term and treatable. Sometimes the treatment is simply eliminating the person's exposure to the source of the pollution, if it can be identified. Symptoms of some diseases, including ...
INTRODUCTION. Air pollution is a major problem of recent decades, which has a serious toxicological impact on human health and the environment. The sources of pollution vary from small unit of cigarettes and natural sources such as volcanic activities to large volume of emission from motor engines of automobiles and industrial activities.[1,2] Long-term effects of air pollution on the onset of ...
The air that we breathe. Air pollution remains one of the biggest and most immediate environmental threats to human health, leading to millions of premature deaths each year and the loss of millions more healthy years of life. It has been linked to a range of adverse health effects, including cardiovascular and respiratory disease, cancer ...
Traffic-Related Air Pollution (TRAP), a mixture of gasses and particles, has most of the elements of human-made air pollution: ground-level ozone, various forms of carbon, nitrogen oxides, sulfur oxides, volatile organic compounds, polycyclic aromatic hydrocarbons, and fine particulate matter. Ozone, an atmospheric gas, is often called smog ...
Effects of air pollution on human health ... Google Scholar, and Web of Science for peer-reviewed research papers published in English only, using search terms "PM", "particulate matter", "mice", "mouse", "rat". ... Ambient air pollution is a health concern in Latin America given its large urban population exposed to levels ...
Indoor and outdoor air pollution causes several common health problems which according to the New Jersey Department of Environmental Protection (2009) are grouped according to the major pollutants. To begin with, carbon monoxide compromises the heart activities hence lethargy and fatigue. It also causes nausea, dizziness, and headaches and in ...
The deleterious effects of pollution manifest in elevated rates of cancer, cardiovascular disease, respiratory ailments, mental disorders, and diarrhea. Each year, approximately 7 million ...
1. Introduction. Air pollution poses a major threat to global health (Cattani-Cavalieri et al., 2020).The World Health Organisation (WHO) air quality data shows 99% of the world's population inhale high levels of pollutants, and as a result of poor air quality an estimated 4.2 million people die each year, with the majority death (91%) from low- and middle-income countries (World Health ...
The lack of ambient air pollution epidemiologic data in sub-Saharan Africa is also an important global health disparity. Thousands of air pollution health effects studies have been conducted in Europe and North America, rather than in urban areas that have some of the highest measured air pollution levels in world, including urban areas in sub ...
Abstract. Air pollution can harm human health, the environment, and cause property damage. Various research have proven the connection of air quality and human health. The epidemiology and laboratory studies demonstrated that ambient air pollutants (for example PM, O3, SO2 and NO2) contributed to various respiratory problems including ...
In this review essay, we pay close attention to how air pollution affects vulnerable groups with respiratory disorders, including children and asthma. This paper will concentrate on the harmful effects of air pollution on people's health in NYC, discuss how the most vulnerable population is affected, and propose a policy solution on the ...
Epidemiologic investigations have previously been published in more than 200 papers, and several studies have examined the impacts of particle air pollution on health. The main conclusions now being made about the epidemiological evidence of particle pollution-induced health impacts are discussed in this article. Although there is no universal agreement, most reviewers conclude that ...
Multifaceted SARS-CoV-2 interventions have modified exposure to air pollution and dynamics of respiratory diseases. Identifying the most vulnerable individuals requires effort to build a complete picture of the dynamic health effects of air pollution exposure, accounting for disparities across population subgroups. We use generalized additive model to assess the likely changes in the ...
Human health is also severely affected by particulates in the atmosphere. The particulates can cause nasal irritation and swelling. It can also cause a running nose. Air pollution is also linked to lung damage and limited lung function. Air pollution can also have an inflammatory effect on the heart - it can elevate blood pressure and ...
This is Air: The "Non-Health" Effects of Air Pollution. A robust body of evidence shows that air pollution exposure is detrimental to health outcomes, often measured as deaths and hospitalizations. This literature has focused less on subclinical channels that nonetheless impact behavior, performance, and skills.
Health effects. Sporadic air pollution events, like the historic London fog in 1952 and a number of short and long term epidemiological studies investigated the effects of air quality changes on human health. A constant finding is that air pollutants contribute to increased mortality and hospital admissions ( Brunekreef and Holgate, 2002 ).
2005. TLDR. Air pollution is associated with a broad spectrum of acute and chronic health effects, the nature of which may vary with the pollutant constituents, and particulate air pollution is consistently and independently related to the most serious effects, including lung cancer and other cardiopulmonary mortality. Expand.
Air pollution is a severe problem in the modern world. Urbanization, industrialization, and traffic emit air pollutants such as carbon monoxide (CO), nitrous oxides (NOx), hydrocarbons (HCs), and particulate matter into the environment. Plants can absorb air pollutants through stomata. They adversely affect the various metabolic and physiological processes of plant species. This review ...
Introduction: Effects of Pollution on Human Health Essay The Earth's population is growing, which leads to the demand for more food, energy, and water. Pollution is also an issue caused by human populations resulting in 54 percent of all deaths occurring because of pollution. Pollution of the Earth can be called one of the most plaguing problems that we have to face.
These human health benefits are strongest when the ocean itself is healthy. Research suggests that countries with more protected ocean areas have lower mortality rates. Conversely, increased ocean pollution has proven negative health effects. For example, a significant amount of toxic microplastic has been found in seafood.