
Schizophrenia
Apr 14, 2013
780 likes | 1.54k Views
Schizophrenia. Features, Diagnosis, Epidemiology, Etiology, Treatment, Neurochemistry Jack Foust, MD Assistant Professor, Department of Psychiatry and Behavioral Sciences Medical University of South Carolina. Features of Schizophrenia - Positive Symptoms. Hallucinations
Share Presentation
- moghaddam b et al
- hallucinations
- environmental influences
- less likely
- temporal lobe structures
- res brain res rev

Presentation Transcript
Schizophrenia • Features, Diagnosis, Epidemiology, Etiology, Treatment, Neurochemistry • Jack Foust, MD • Assistant Professor, Department of Psychiatry and Behavioral Sciences • Medical University of South Carolina
Features of Schizophrenia - Positive Symptoms • Hallucinations • Disorganized speech/thinking/behavior • Delusions
(from The Hour of the Wolf, directed by Ingmar Bergman)
Features of Schizophrenia - Negative Symptoms • Affective flattening • Alogia • Avolition • Anhedonia • Social Withdrawal
Features of Schizophrenia - Cognitive Deficits • Attention • Memory • Executive functions (organization, planning)
Schizophrenia - DSM Diagnostic Criterion “A” • Characteristic Sxs (2 + for 1 month) • delusions • hallucinations • disorganized speech • grossly disorganized or catatonic behavior • negative Sxs (flat affect, alogia, avolition) • (Only one element required if delusions bizarre, • or hallucinations commentary 2 voices conversing )
Schizophrenia - DSM Diagnostic Criteria B - F • Social/occupational dysfunction (decline) • Duration - 6 months total, 1 month “A” Sxs • Exclusion - SAFD, mood d/o • Exclusion - sub abuse, gen med condition • PDD/Autism - at least 1 month delusions or hallucinations
Schizophrenia - Comorbid Conditions • Depression • Anxiety • Aggression • Substance use disorder
Schizophrenia: Who is at Risk? • Lifetime prevalence • Epidemiologic Catchment Area Study: 1.3% • National Comorbidity Survey: 0.7% • Demographic characteristics • Age - typical onset late teens/early twenties • Gender - earlier age of onset among men • Marital status - less likely to be married
Schizophrenia: Who is at Risk? • Predisposing factors • Season of birth • Pregnancy and birth complications • Genetic background • Precipitating factors • Stress • Substance Abuse
“In addition to interfering with normal brain development, heavy marijuana use in adolescents may also lead to an earlier onset of schizophrenia in individuals who are genetically predisposed” Dr Sanjiv Kumra, Albert Einstein College of Medicine
“Carriers of the COMT valine158 allele were most likely to exhibit psychotic symptoms and to develop schizophreniform disorder if they used cannabis. Cannabis use had no such adverse influence on individuals with two copies of the methionine allele.” Caspi A, et al. Biological Psychiatry.2005; 57:1117-1127.
Genetic Risk Factors
Etiology: Neurodevelopmental Hypothesis • Possible insult during gestation, environmental influences • Disturbance in normal brain maturation • Reduced size medial temporal lobe structures - amygdala, hippocampus • Disturbed cytoarchitecture in hippocampus, entorhinal cortex
Treatment: Psychosocial Interventions • Supportive therapy • Behavioral family therapy • Family education • Social skills training • Community support • Lower relapse; improved functioning, compliance and social adjustment
Treatment: Antipsychotics • Used to treat psychotic disorders, such as schizophrenia, mania, psychotic depression • Include both “typicals” (Haldol) and “atypicals” (Clozaril, Risperdal)
Typical Antipsychotics • Chlopromazine (Thorazine) - prototype • Thioridazine (Mellaril) • Fluphenazine (Prolixin) • Haloperidol (Haldol)
Typical Antipsychotics: Drug/Receptor Effects • Antidopaminergic (D2) • Anticholinergic • Antihistaminic • Anti-alpha 1
Effects of Typical Antipsychotics • Four dopamine pathways • Mesocortical (negative symptoms) • Mesolimbic (positive symptoms) • Nigrostriatal (EPS, TD) • Tuberoinfundibular (hyperprolactinemia)
Guillin O and Laruelle M. Cellscience Reviews. 2005; 2:79-107
DA Receptor Distribution • D1- prefrontal cortex, striatum • D5 - hippocampus and entorhinal cortex • D2 – striatum, low concentration in medial temporal structures (hippocampus, entorhinal cortex, amygdala), thalamus, prefrontal cortex • D3 – striatum and ventral striatum • D4 - prefrontal cortex and hippocampus (have not been detected in the striatum)
Side Effects of Typical Neuroleptics • Extra-pyramidal syndrome (EPS) • Tardive dyskinesia (TD) • Neuroleptic malignant syndrome (NMS) • Prolactin elevation
Extra-Pyramidal Syndrome (EPS) • Acute dystonia • Akathesia • Muscle rigidity • Bradykinesia • Treatment – typically treated with anticholinergic compounds (Cogentin, Benadryl, Artane), Beta-blockers
Tardive Dyskinesia(TD) • 25-year continuous exposure risk: 68% in Yale Incidence Study • Annual incidence: 5% • Risk factors • Increased age • African-American race • Dose and duration of drug exposure • Early and severe EPS
Neuroleptic Malignant Syndrome (NMS) • Potentially fatal complication of neuroleptic Tx • Temperature dysregulation: T >104°F/40°C • Muscle rigidity • Elevated CPK • Elevated WBC • Associated with TaqI A polymorphism in DRD2 • Tx: withdraw neuroleptics, cooling, dantrolene, bromocriptine (DA agonist)
Summary: Limitations of Typical Antipsychotics • Limited efficacy against negative symptoms • A substantial portion of patients (25% to 40%) respond poorly to treatment • EPS occurs at clinically effective doses • Side effects other than EPS (such as NMS) • Liable to cause tardive dyskinesia • Serum prolactin elevation
Advantages of Typical Antipsychotics • No blood monitoring • Efficacious for positive symptoms • Parenteral and depot preparations available • Low-cost
Antipsychotics: Atypical • Clozapine (Clozaril) - prototype • Risperidone (Risperdal) • Olanzepine (Zyprexa) • Quetiapine (Seroquel) • Ziprasidone (Geodon) • Aripiprazole (Abilify)
Atypical Antipsychotics: Clinical and Drug/Receptor Characteristics • Clinically display less EPS, more effective against negative symptoms, some improvement in cognition • Balanced D2/D1 antagonism • Strong 5HT2 antagonists
Serotonin-Dopamine Antagonists and TD: Hypothesized “Site-Specific” Neuromechanisms Psychosis EPS and TD Limbic Cortical Caudate/Putamen A10 A9 Ventral Tegmental Area Substantia Nigra Dopamine/5HT Antagonist Conventional Antipsychotic Agents
Atypical Antipsychotics
Antipsychotic Receptor Affinities • Haloperidol (Haldol)
Antipsychotic Receptor Affinities • Clozapine (Clozaril)
Antipsychotic Receptor Affinities • Risperidone (Risperdal)
Antipsychotic Receptor Affinities • Olanzepine (Zyprexa)
Antipsychotic Receptor Affinities • Quetiapine (Seroquel)
Ziprasidone (Geodon) • High affinity (antagonist) for D2, D3, 5HT2a, 5HT2c, 5HT1d • High affinity (agonist) for 5HT1a • Inhibits re-uptake of 5HT and NE • Moderate affinity for H1, α1 • Low affinity for D1, α2 • Negligible affinity for M1
Ziprasidone (Geodon), cont. • Positive symptoms improved (PANSS) • Negative symptoms improved (PANSS) • Depressive symptoms improved (MADRS) • Low EPS (5HT2a/D2, 5HT1a) • Low weight gain (H1) • Low sexual dysfunction • Minimal CYP450, CBC, LFT or CV effects (some QTc prolongation)
Neurotransmitter Systems Implicated in Schizophrenia Dopamine Acetylcholine Serotonin Norepinephrine GABA Neuropeptides Glutamate
Dopamine Hypothesis • Induction or worsening of psychotic symptoms with dopamine agonists • Amelioration of psychotic symptoms with antipsychotic drugs that are D2-receptor antagonists
Serotonin (5HT) Hypothesis • M-CPP (m-chlorophenylpiperazine) selective 5HT receptor agonist worsens psychotic symptoms • Pretreatment with ritanserin (5HT antagonist) attenuates psychotic symptoms
Glutamate Hypothesis • Psychotomimetic effects of phencyclidine (PCP), a potent N-methyl-D-aspartate (NMDA) type glutamate receptor antagonist - mimics negative, positive and disorganization symptoms • Possible beneficial effects of cycloserine, glutamate receptor agonist
Glutamate, Dopamine, Ketamine • “Subanesthetic doses of ketamine, a noncompetitive NMDA receptor antagonist, impair prefrontal cortex (PFC) function in the rat and produce symptoms in humans similar to those observed in schizophrenia.” • “These findings suggest that ketamine may disrupt dopaminergic neurotransmission in the PFC as well as cognitive functions associated with this region, in part, by increasing the release of glutamate, thereby stimulating postsynaptic non-NMDA glutamate receptors.” Moghaddam B et al. J Neurosci 1997; 17: 2921-2927.
Aghajanian GK, Marek GJ. Brain Res Brain Res Rev 2000; 31:302-312.
Neuronal Circuits in Schizophrenia • Thalamic nuclei relay sensory information to pyramidal neurons in limbic cortex and neocortex through glutaminergic excitatory afferents • Excessive response of pyramidal neurons is putative mechanism of psychosis (overstimulation) Freedman R. Schizophrenia. NEJM. 2003; 349:1738-1749.
- More by User
A group of severe disorders characterized by… disorganized and delusional thinking disturbed perceptions inappropriate emotions and behaviors. Schizophrenia. Often linked to the neurotransmitter dopamine. How Prevalent is Schizophrenia?.
3.29k views • 14 slides
Schizophrenia. Chapter 16. Schizophrenia. Fascinated and confounded healers for centuries One of most severe mental illnesses 1/3 of population 2.5% of direct costs of total budget $46 billion in indirect costs. History of Schizophrenia.
1.52k views • 55 slides
Schizophrenia. Tutorial (6/7/06) O.Arikawe. Definition: Splitting of psychic functions . Incidence : Low incidence but relatively high prevalence Annual incidence using current diagnostic criteria is 0.17 and 0.54 per 1000 population. Types. Acute and chronic
538 views • 16 slides
Schizophrenia. Schizophrenia: The Facts. Affects about .8% of Americans are afflicted Throughout the world over 24 million people suffer from this disease Strikes most commonly in early twenties Affects men and women equally “split mind”. 2. Symptoms of Schizophrenia.
379 views • 11 slides
Schizophrenia. Definition. Schizophrenia is a mental illness that effects the brain that makes the person view reality abnormally. This can consist of delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior. Types.
342 views • 7 slides
Schizophrenia. Chapter 11. Schizophrenia. Positive Symptoms: Type I Delusions Persecutory Delusions of Reference Grandiose Delusions. Schizophrenia. Hallucinations Disorganized Thoughts and Speech Disorganized or Catatonic Behavior http://www.wimp.com/schizophrenicsymptoms/.
372 views • 14 slides
Schizophrenia. By Garren Richardson. What is Schizophrenia?. Schizophrenia is a psychological disorder classified separately from other disorders because it is not easily categorized as an anxiety or mood disorder
379 views • 10 slides
Schizophrenia. The Unwell Brain. Disturbance in the Neurochemistry. The first discovery in the mid 1950s was that chronic usage of large daily doses of Amphetamines could produce a psychosis that was virtually indistinguishable from schizophrenia.
299 views • 12 slides

Schizophrenia. Schizophrenia. Two or more of the following, each present for a significant portion of the time during a 1-month period** Delusions Hallucinations Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms . Schizophrenia.
966 views • 20 slides
Schizophrenia. By Rebecca Stipp. History. Definition. a severe mental disorder characterized by some, but not necessarily all, of the following features: emotional blunting, intellectual deterioration, social isolation, disorganized speech and behavior, delusions, and hallucinations.
268 views • 10 slides
Schizophrenia. What is schizophrenia?. Most disabling and chronic of all mental illnesses Psychosis: type of mental illness- cannot distinguish reality from imagination Psychotic episodes Distorts: Thinking (may believe others are controlling their thoughts) Expression of emotions
296 views • 14 slides
Schizophrenia. Definition Psychotic disorder Thought Disorder Loose associations “Split” from reality NOT split or multiple personality. Symptoms of Schizophrenia. Positive Symptoms Loose associations Word salad Delusions Hallucinations Negative Symptoms Poverty of speech content
546 views • 24 slides
SCHIZOPHRENIA
SCHIZOPHRENIA. Andy Cortez Julian Cruz Period 05. Peter Green. He is the founder of Fleetwood Mac, a famous band He was diagnosed with schizophrenia in the mid 70’s Spent time in psychiatric hospitals and went through electroconvulsive therapy
349 views • 7 slides
Schizophrenia. Unfolding Case Study By Amanda Eymard , DNS, RN and Linda Manfrin-Ledet , DNS, APRN. Assigned Reading to be completed prior to case study. Prior to conducting this unfolding case study, students should read the following:
3.89k views • 82 slides
Schizophrenia. Lecture of 2-14-07. Symptoms. Psychosis Lack of touch with reality Delusions Erroneous beliefs Hallucinations False sensory perceptions Too much dopamine or not enough glutamate. Paranoid Schizophrenia. Delusions of grandeur Believe they are special with special powers
395 views • 22 slides
Schizophrenia. Stacy Zeigler. NIMH. Schizophrenia is a chronic, severe, and disabling brain disorder Affects 1.1% of the U.S. population age 18 and older in a given year.
755 views • 60 slides
Schizophrenia. A group of severe disorders characterized by disorganized and delusional thinking, disturbed perceptions, and inappropriate emotions and behaviours. Those with paranoid tendencies are particularly prone to delusions of persecution.
1.51k views • 7 slides
Schizophrenia. Lyudmyla T. Snovyda. Schizophrenia -.
996 views • 36 slides
Schizophrenia. www.psychlotron.org.uk. Schizophrenia is not a multiple personality A psychotic disorder involving a break with reality Many different manifestations with a few shared features. Schizophrenia diagnosis. Positive Symptoms:
856 views • 24 slides

Schizophrenia. Tiffany Becker Denise Keown Heather Baltz. Overview of Schizophrenia. What is schizophrenia? Schizophrenia behaviors Does schizophrenia affect the brain? What causes schizophrenia? Who gets schizophrenia? Early Onset Schizophrenia Schizophrenia Facts.
1.09k views • 37 slides

Rochelle Blumenstock. Schizophrenia. Etiology. Genetics 10% chance of developing the disorder if you have an immediate relative with it 40-65% chance of both twins being diagnosed with the disorder No single gene associated Many rare genetic mutations . Environment
346 views • 17 slides
schizophrenia
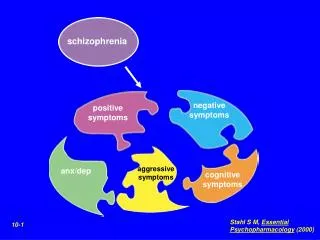
schizophrenia. negative symptoms. positive symptoms. aggressive symptoms. anx/dep. cognitive symptoms. Stahl S M, Essential Psychopharmacology (2000). 10-1. Positive Symptoms of Schizophrenia. Negative Symptoms of Schizophrenia. Stahl S M, Essential Psychopharmacology (2000). 10-20.
648 views • 14 slides
Module 11: Schizophrenia Spectrum and Other Psychotic Disorders
Case studies: schizophrenia spectrum disorders, learning objectives.
- Identify schizophrenia and psychotic disorders in case studies
Case Study: Bryant
Thirty-five-year-old Bryant was admitted to the hospital because of ritualistic behaviors, depression, and distrust. At the time of admission, prominent ritualistic behaviors and depression misled clinicians to diagnose Bryant with obsessive-compulsive disorder (OCD). Shortly after, psychotic symptoms such as disorganized thoughts and delusion of control were noticeable. He told the doctors he has not been receiving any treatment, was not on any substance or medication, and has been experiencing these symptoms for about two weeks. Throughout the course of his treatment, the doctors noticed that he developed a catatonic stupor and a respiratory infection, which was identified by respiratory symptoms, blood tests, and a chest X-ray. To treat the psychotic symptoms, catatonic stupor, and respiratory infection, risperidone, MECT, and ceftriaxone (antibiotic) were administered, and these therapies proved to be dramatically effective. [1]
Case Study: Shanta
Shanta, a 28-year-old female with no prior psychiatric hospitalizations, was sent to the local emergency room after her parents called 911; they were concerned that their daughter had become uncharacteristically irritable and paranoid. The family observed that she had stopped interacting with them and had been spending long periods of time alone in her bedroom. For over a month, she had not attended school at the local community college. Her parents finally made the decision to call the police when she started to threaten them with a knife, and the police took her to the local emergency room for a crisis evaluation.
Following the administration of the medication, she tried to escape from the emergency room, contending that the hospital staff was planning to kill her. She eventually slept and when she awoke, she told the crisis worker that she had been diagnosed with attention-deficit/hyperactive disorder (ADHD) a month ago. At the time of this ADHD diagnosis, she was started on 30 mg of a stimulant to be taken every morning in order to help her focus and become less stressed over the possibility of poor school performance.
After two weeks, the provider increased her dosage to 60 mg every morning and also started her on dextroamphetamine sulfate tablets (10 mg) that she took daily in the afternoon in order to improve her concentration and ability to study. Shanta claimed that she might have taken up to three dextroamphetamine sulfate tablets over the past three days because she was worried about falling asleep and being unable to adequately prepare for an examination.
Prior to the ADHD diagnosis, the patient had no known psychiatric or substance abuse history. The urine toxicology screen taken upon admission to the emergency department was positive only for amphetamines. There was no family history of psychotic or mood disorders, and she didn’t exhibit any depressive, manic, or hypomanic symptoms.
The stimulant medications were discontinued by the hospital upon admission to the emergency department and the patient was treated with an atypical antipsychotic. She tolerated the medications well, started psychotherapy sessions, and was released five days later. On the day of discharge, there were no delusions or hallucinations reported. She was referred to the local mental health center for aftercare follow-up with a psychiatrist. [2]
Another powerful case study example is that of Elyn R. Saks, the associate dean and Orrin B. Evans professor of law, psychology, and psychiatry and the behavioral sciences at the University of Southern California Gould Law School.
Saks began experiencing symptoms of mental illness at eight years old, but she had her first full-blown episode when studying as a Marshall scholar at Oxford University. Another breakdown happened while Saks was a student at Yale Law School, after which she “ended up forcibly restrained and forced to take anti-psychotic medication.” Her scholarly efforts thus include taking a careful look at the destructive impact force and coercion can have on the lives of people with psychiatric illnesses, whether during treatment or perhaps in interactions with police; the Saks Institute, for example, co-hosted a conference examining the urgent problem of how to address excessive use of force in encounters between law enforcement and individuals with mental health challenges.
Saks lives with schizophrenia and has written and spoken about her experiences. She says, “There’s a tremendous need to implode the myths of mental illness, to put a face on it, to show people that a diagnosis does not have to lead to a painful and oblique life.”
In recent years, researchers have begun talking about mental health care in the same way addiction specialists speak of recovery—the lifelong journey of self-treatment and discipline that guides substance abuse programs. The idea remains controversial: managing a severe mental illness is more complicated than simply avoiding certain behaviors. Approaches include “medication (usually), therapy (often), a measure of good luck (always)—and, most of all, the inner strength to manage one’s demons, if not banish them. That strength can come from any number of places…love, forgiveness, faith in God, a lifelong friendship.” Saks says, “We who struggle with these disorders can lead full, happy, productive lives, if we have the right resources.”
You can view the transcript for “A tale of mental illness | Elyn Saks” here (opens in new window) .
- Bai, Y., Yang, X., Zeng, Z., & Yang, H. (2018). A case report of schizoaffective disorder with ritualistic behaviors and catatonic stupor: successful treatment by risperidone and modified electroconvulsive therapy. BMC psychiatry , 18(1), 67. https://doi.org/10.1186/s12888-018-1655-5 ↵
- Henning A, Kurtom M, Espiridion E D (February 23, 2019) A Case Study of Acute Stimulant-induced Psychosis. Cureus 11(2): e4126. doi:10.7759/cureus.4126 ↵
- Modification, adaptation, and original content. Authored by : Wallis Back for Lumen Learning. Provided by : Lumen Learning. License : CC BY: Attribution
- A tale of mental illness . Authored by : Elyn Saks. Provided by : TED. Located at : https://www.youtube.com/watch?v=f6CILJA110Y . License : Other . License Terms : Standard YouTube License
- A Case Study of Acute Stimulant-induced Psychosis. Authored by : Ashley Henning, Muhannad Kurtom, Eduardo D. Espiridion. Provided by : Cureus. Located at : https://www.cureus.com/articles/17024-a-case-study-of-acute-stimulant-induced-psychosis#article-disclosures-acknowledgements . License : CC BY: Attribution
- Elyn Saks. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Elyn_Saks . License : CC BY-SA: Attribution-ShareAlike
- A case report of schizoaffective disorder with ritualistic behaviors and catatonic stupor: successful treatment by risperidone and modified electroconvulsive therapy. Authored by : Yuanhan Bai, Xi Yang, Zhiqiang Zeng, and Haichen Yangcorresponding. Located at : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851085/ . License : CC BY: Attribution

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.7(6); Nov-Dec 2018
Very early-onset psychosis/schizophrenia: Case studies of spectrum of presentation and management issues
Jitender aneja.
1 Department of Psychiatry, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
Kartik Singhai
Karandeep paul.
Schizophrenia occurs very uncommonly in children younger than 13 years. The disease is preceded by premorbid difficulties, familial vulnerability, and a prodromal phase. The occurrence of positive psychotic symptoms such as delusions and hallucinations depends on the level of cognitive development of child. Furthermore, at times it is very difficult to differentiate the psychopathology and sustain a diagnosis of schizophrenia in view of similarities with disorders such as autism, mood disorders, and obsessive compulsive disorders. Here, we present three case studies with varying presentation of childhood-onset psychosis/schizophrenia and associated management issues.
Introduction
Schizophrenia is a chronic severe mental illness with heterogeneous clinical profile and debilitating course. Research shows that clinical features, severity of illness, prognosis, and treatment of schizophrenia vary depending on the age of onset of illness.[ 1 , 2 ] Hence, age-specific research in schizophrenia has been emphasized. Although consistency has been noted in differentiating early-onset psychosis (onset <18 years of age) and adult-onset psychosis (onset >18 years), considerable variation is observed with regard to the age of childhood-onset schizophrenia or very early-onset psychosis/schizophrenia (VEOP/VEOS).[ 2 , 3 ] Most commonly, psychosis occurring at <13 years of age has been considered to be of very early onset and that between 13 and 17 years to be of adolescent onset.[ 4 ] Furthermore, VEOS has been considered to be rare and shown to have differing clinical features (including positive and negative symptoms, cognitive decline, and neuroimaging findings), course, and outcome when compared with that of early-onset or adult-onset schizophrenia.[ 3 ] Progress in acknowledgement of psychotic disorders in children in the recent times has led primary care physicians and paediatricians to increasingly serve as the principal identifiers of psychiatrically ill youth. In recent years, there has been substantial research in early intervention efforts (e.g., with psychotherapy or antipsychotic medicines) focused on the early stages of schizophrenia and on young people with prodromal symptoms.[ 5 ] Here, we report a series of cases with very early onset of psychosis/schizophrenia who had varying clinical features and associated management issues.
Case Reports
A 14-year-old boy, educated up to class 6, belonging to a family of middle socioeconomic status and residing in an urban area was brought with complaints of academic decline since 3 years and hearing voices for the past 2 years. The child was born out of a nonconsanguineous marriage, an unplanned, uneventful, but wanted pregnancy. The child attained developmental milestones as per age. From his early childhood, he was exposed to aggressive behavior of his father, who often attempted to discipline him and in this pursuit at times was abusive and aggressive toward him. Marital problems and domestic violence since marriage lead to divorce of parents when the child attained age of 10 years.
The following year, the child and the mother moved to maternal grandparents’ home and his school was also changed. Within a year of this, a decline in his academic performance with handwriting deterioration, and irritable and sad behaviour was noted. Complaints from school were often received by the mother where the child was found engaged in fist fights and undesirable behavior. He also preferred solitary activities and resented to eat with the rest of the family. In addition, a decline in performance of daily routine activities was seen. No history suggestive of depressive cognitions at that time was forthcoming. A private psychiatrist was consulted who treated him with sodium valproate up to 400 mg/day for nearly 2 months which led to a decline in his irritability and aggression. But the diagnosis was deferred and the medications were gradually tapered and stopped. Over the next 1 year, he also started hearing voices that fulfilled dimensions of commanding type of auditory hallucinations. He suspected that family members including his mother collude with the unknown persons, whose voices he heard and believed it was done to tease him. He eventually dropped out of school and was often found awake till late night, seen muttering to self, shouting at persons who were not around with further deterioration in his socialization and self-care. Another psychiatrist was consulted and he was now diagnosed with schizophrenia and treated inpatient for 2 weeks with risperidone 3 mg, olanzapine 2.5 mg, and oxcarbazepine 300 mg/day with some improvement in his symptoms. Significant weight gain with the medication lead to poor compliance which further led to relapse within 3 months of discharge. Frequent aggressive episodes over the next 1 year resulted in multiple hospital admissions. He was brought to us with acute exacerbation of symptoms and was receiving divalproex sodium 1500 mg/day, aripiprazole 30 mg/day, trifluperazine 15 mg/day, olanzapine 20 mg/day, and lorazepam injection as and when required. He was admitted for diagnostic clarification and rationalization of his medications. He had remarkable physical features of elongated face with large ears. Non-cooperation for mental state examination, and aggressive and violent behavior were noted. He was observed to be muttering and laughing to self. His mood was irritable, speech was laconic, and he lacked insight into his illness. We entertained a diagnosis of very early-onset schizophrenia and explored for the possibilities of organic psychosis, autoimmune encephalitis, and Fragile X syndrome. The physical investigations done are shown in Table 1 . Further special investigations in the form of rubella antibodies (serum IgG = 64.12 U/mL, IgM = 2.44 U/mL) and polymerase chain reaction for Fragile X syndrome (repeat size = 24) were normal. His intelligence quotient measured a year ago was 90, but he did not cooperate for the same during present admission. Initially, we reduced the medication and only kept him on aripiprazole 30 mg/day and added lurasidone 40 mg twice a day and discharged him with residual negative symptoms only. However, his hallucinations and aggression reappeared within 2 weeks of discharge and was readmitted. This time eight sessions of bilateral modified electroconvulsive therapy were administered and he was put on aripiprazole 30 mg/day, chlorpromazine 600 mg/day, sodium divalproex 1000 mg/day, and trihexyphenidyl 4 mg/day. The family was psychoeducated about the illness, and mother's expressed emotions and overinvolvement was addressed by supportive psychotherapy. Moreover, an activity schedule for the child was made, and occupational therapy was instituted. Dietary modifications in view of weight gain were also suggested. In the past 6 months, no episodes of violence came to our notice, though irritability on not meeting his demands is persistent. However, poor socialization, lack of motivation, apathy, weight gain subsequent to psychotropic medications, and aversion to start school are still unresolved. Influence of his multiple medications on bone marrow function is an impending issue of concern.
Details of investigations done in the three children

An 11-year-old boy, educated up to class 3, belonging to a rural family of lower socioeconomic status was brought with complaints of academic decline since 2 years, repetition of acts, irritability since a year, and adoption of abnormal postures since 6 months. He was born out of a nonconsanguineous marriage, uneventful birth, and pregnancy. He was third in birth order and achieved developmental milestones at an appropriate age. Since 2 years, he would not attend to his studies, had poor attention, and difficult memorization. He attributed it to lack of friends at school and asked for school change. There was no history of low mood, depressive cognitions, conduct problems, or bullying and he performed his daily routine like his premorbid self at that time. Since a year, he was observed to repeat certain acts such as pacing in the room from one end to another, continuously for up to 1–2 h, with intermittent stops and often insisted his mother to follow the suit, stand nearby him, or else he would clang on her. He prohibited other family members except his mother near him and would accept his meals only from her. He repeatedly sought assurance of his mother if he had spoken everything right. He also washed his hands repeatedly, up to 10–20 times at one time, and was unable to elaborate reason for the same. His mood during that period was largely irritable with no sadness or fearfulness. He mostly wore the same set of clothes, would be forced to take bath or get nails/hair trimmed, and efforts to these were often met with aggression from the patient. Eventually, he stopped going to school and his family sought faith healing. Within the next 5–6 months, his illness worsened. Fixed gaze, reduced eye blinking, smiling out of context, diminished speech, and refusal to eat food were the reasons for which he was brought to us. His physical examination was unremarkable and his mental state examination using the Kirby's method showed an untidy and ill-kempt child, with infrequent spontaneous acts, and occasional resentment for examination. He had an expressionless face, with occasional smiling to self, negativism, and mutism. No rigidity in any of the limb was observed. He was diagnosed with catatonic schizophrenia and probable obsessive compulsive disorder (vs mannerisms). We performed a battery of physical investigation to rule out organic psychosis [ Table 1 ]. He responded to injection lorazepam with which catatonia melted away. He was also prescribed olanzapine up to 15 mg/day, fluoxetine 20 mg/day, and dietary modification and lactulose for constipation. The family left against medical advice with 50%–60% clinical improvement [rating on Bush Francis Catatonia Rating scale (BFCRS) reduced from 10 to 4]. He relapsed within a month of discharge, initially with predominance of the probable obsessive compulsive symptoms. Fluoxetine was further increased to up to 60 mg/day. But within the next 2 months, the catatonic symptoms reappeared and he was readmitted. He had received olanzapine up to 25 mg/day, which was replaced with risperidone. In view of nonresponse to intravenous lorazepam, we administered him five sessions of modified bilateral Electro-convulsive therapy (ECT) (rating on BFCRS reduced from 8 to 0). The family was psychoeducated about the child's illness and the need for continuous treatment was emphasized. He was discharged with up to 80%–90% improvement. At follow-ups, he started participating at farm work of the family, took care of self, with some repetition of acts such as washing of hands, and denied any associated anxiety symptoms. However, efforts to re-enroll in school had been futile as the child did not agree for it. He has been maintaining at the same level since 6 months of discharge.
A 7-year-old girl, student of second class, belonging to a high socioeconomic status family living in an urban locality was brought with complaints of academic decline, irritability, and abnormal behavior for the past 9 months. The child was born out of a nonconsanguineous marriage, is first in order, and was a wanted child. Maternal health during pregnancy was normal, but the period of labor was prolonged beyond 18 h, so a lower segment caesarean section was performed. There was no history of birth-related complications and the child's birth weight was 2.80 kg. The child attained developmental milestones as per age. The child had a temperament characterized by high activity levels, below average threshold of distractibility, average ability to sustain attention and persist, easy to warm up, adaptation to new situations, and regular bowel and bladder habits. She was enrolled in school at the age of 4 years and progressed well till 9 months back when a decline in her academic interest was observed by her class teacher. Deterioration of her handwriting skills and avoidance of group activities in school were observed. Similarly, at home persistent irritable behavior was seen and her play activities with her siblings reduced. However, her biofunctions were normal during this period.
One month prior to visiting us, she started insisting on wearing the same dress. She wore the same colored or at times the same dress which she would not take off even at bed or bath time. In addition, a change in her mood from largely irritable to cheerful was noted. Her activity levels were increased and it would be difficult to make her sit quietly in class. Her speech output was more than her usual self and she talked incessantly. Her sleep duration also decreased and she started getting up 3–4 h earlier than her usual routine. In view of these symptoms, her family made first contact with us. Her physical examination was normal and mental state examination revealed her to be cheerful, overactive, and difficult to interrupt. She sang and danced during the interview. We diagnosed her with acute mania on the basis of clinical evaluation and assessment on MINI Kid 6.0.[ 6 ] The details of her physical examination are depicted in Table 1 . She was initially treated with olanzapine 5 mg/day which was later on increased to 10 mg/day. However, no response was observed with it in the next 2 weeks, so it was cross tapered with sodium valproate which was built up to 400 mg/day. She improved by nearly 50%, but her mood still remained cheerful/irritable. She did not resume her school and was brought irregularly for the follow-up. Within the next 2 months, she also started muttering to herself and made certain abnormal gestures. She often feared staying alone, or while going to bed insisted the lights to be kept on and ask someone to accompany her in the toilet unlike her previous self. When asked, she reported seeing a lady in white clothes, with no other details. She stopped asking for food on her own and remained lost in her fantasy world. However, her interest in dressing and appreciating herself in mirror persisted. Her mood during this period was mostly labile and often changed from cheerful to sad or irritable. As per the family, the medications were continued as advised. So in view of the emerging picture, the diagnosis was revised to schizo-affective disorder, and in addition to hike in dose of sodium valproate to 500 mg/day, risperidone 2 mg/day was also added. However, even after 8 weeks of treatment with this combination with hike of risperidone to 4 mg/day, there was no relief. The child is still symptomatic, does not go to school, and has significant dysfunction. Psychosocial intervention in the form of psychoeducation, activity scheduling for the child, and occupational therapy has been instituted in addition to the existing treatment regimen, but results are yet to be seen.
The older concept of neurodegenerative etiology of schizophrenia has been superseded by evolving neurodevelopmental nature of this disease. The latter has been attributed to initiation of the underlying pathophysiological processes long before the onset of clinical disease and interaction of the various genetic and environmental factors. The more accommodating theorist propose schizophrenia to be of neurodevelopmental in origin which in turn speeds the process of neurodegeneration.
On clinical front, VEOS is associated with a more insidious onset, prominent negative symptoms, auditory hallucinations, poorly formed delusions which is in part due to less developed cognitive abilities.[ 7 ] The presence of history of speech and language delay as well as motor development deficits have been observed in major studies on childhood-onset schizophrenia, be it the Maudsley early-onset schizophrenia project or the NIMH study.[ 8 , 9 ] Premorbid deficits in social adjustments and presence of autistic symptoms have also been shown. Moreover, the early onset of psychosis is associated with poor prognosis, worse overall functioning, and multiple hospitalizations.[ 7 ] The duration of untreated psychosis in childhood-onset psychosis has been shown to be smaller in hospital-based studies[ 10 ] and larger in community settings.[ 11 ] In addition, the presence of comorbidities and an organic etiology or history of maternal illness during pregnancy is a common finding in VEOS.[ 10 ] In addition, obsessive compulsive symptoms are frequently observed in first-episode drug-naive schizophrenia patients and have a poorer outcome, more severe impairment of social behavior, and lower functioning.[ 12 ] However, in many instances it is very difficult to differentiate the obsessive compulsive symptoms from the motor symptoms of schizophrenia such as stereotypy and mannerisms and varying degree of insight.[ 13 ]
In the present case series, all the children had an insidious onset of illness, with initial symptom of academic decline, and poorly formed psychotic symptoms/psychotic-like experiences. All the children reported here had dropped out of school, showed a shift in their interests, withdrew from social circle, appeared to be distant, had impaired self-care, and often lacked concern for others along with a range of mood disturbances. All these symptoms fit into the classical description of prodromal symptoms of schizophrenia.[ 14 ] In contrast to available evidence, no history of motor, speech, or language delay was noted in any of the child. Furthermore, no history suggestive of autistic features or problems in social adjustments prior to onset of illness was forthcoming.
However, the diagnosis of schizophrenia could be clearly made in the first case, while the second child had predominant catatonic and probably obsessive compulsive symptoms. It is difficult to ascertain the diagnosis of schizophrenia on the basis of presence of only catatonic symptoms and no delusions and hallucinations or negative symptoms as required by Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition or International Classification of Diseases, Tenth Revision. However, it is very difficult to sustain any other diagnosis for the second child. In the third child, the illness has been evolving and the clinical picture changed from predominant mood symptoms to psychotic-like experiences at later stage. Therefore, at present a diagnosis of schizo-affective disorder is entertained. We could not find any possible organic etiology in any of the three cases with the best of our efforts.
With provision of pharmacological and psychosocial treatment in accordance to the available treatment guidelines,[ 15 ] remission was not achieved in two of the three children. Currently, the available evidence also suggests that the prognosis of childhood-onset schizophrenia is mainly poor as it disrupts the social and cognitive development and thus nearly two-third of children do not achieve remission.[ 16 ] On a positive note, we have been able to retain all the children in treatment.
Other issues faced by the families of three children and the treating team are briefly discussed below. In countries like India, where significant expenses are born by patients/family, associated stigma, limited social services, and the anti-psychotic related adverse effects raise the burden of care exponentially. In 2/3 index patients, the family bore the costs of special investigations, which was not possible in the second child and led to financial difficulties for the single mother of the first child. Adding on, the availability of rehabilitation services for children with major mental illnesses is scarce in various parts of our country. Furthermore, we successfully used ECT for management of acute disturbance in two of the three patients prior to the notification of Mental Health Care Act, 2017 that prohibits its use in minors. The case series also put forward a strong case for strengthening and sensitizing primary care physicians and pediatricians in identifying and treating cases of VEOP, since they are more likely to be the first points of contact with patients of the discussed age group. In view of the duration of untreated psychosis being a very eloquent prognostic factor for VEOP and the symptomatology of the same showing significant heterogeneity, armoring primary care physicians and pediatricians with the right skills to identify, treat, or refer patients with VEOP, especially in the prodromal period, might profoundly contribute in decreasing the morbidity and improving prognosis. Citing this lacuna which could be filled and used to our advantage, Stevens et al .[ 17 ] elaborated and discussed various questions which practitioners might find useful.
Childhood-onset schizophrenia is a rare occurrence. The current case series highlights differing clinical presentation of VEOS/VEOP in children and adolescents. Certain other issues pertinent to the management of VEOS/VEOP are also touched upon in this article. With the early recognition of childhood mental health illnesses, we need to build and strengthen ample child and adolescent mental health services in India.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgement
The authors thank Dr. Sonam Arora, MD, DNB (Pathology), for providing assistance in laboratory investigations and article writing.
- 3D Brain Atlas
- Alzheimer’s
- Schizophrenia
- Parkinson’s
Schizophrenia – Neurobiology and Aetiology
This presentation covers aetiology of Schizophrenia.
A working knowledge of the normal structure and function of the nervous system is key to understanding psychiatric disorders like schizophrenia. This slide deck presents an introduction to neuroanatomy, the key components of neurosynaptic transmission, neurotransmitters and the pathophysiology of schizophrenia. Last, it includes a discussion of some underlying causes of schizophrenia, such as genetic and environmental factors.
This slide deck has been developed in collaboration with the former Lundbeck International Neuroscience Foundation.
Index for slide deck
Neurobiology and aetiology, introduction to neuroanatomy, organisation of the nervous system.
To understand psychiatric disorders, it is important to have a working understanding of the normal structure and function of the nervous system. The central nervous system (CNS; brain, spinal cord) and peripheral nervous system (PNS) are made up of neurones and glial cell…
The neurone constitutes the functional unit of the nervous system; there are over 100 billion neurones in the brain. [Purves et al., 2008; Martin, 2003; Kandel et al., 2000] Each neurone has the ability to interact with and influence many other cells, which creates a syste…
Anatomical regions of the brain
The brain is divided into four anatomical regions: the diencephalon, brainstem, cerebrum, and cerebellum, as described on the slide. [Kandel et al., 2000; Tortora & Derrickson, 2009]
References: Kandel ER, Schwartz JH, Jessell TM (eds). Principles of Neural Science. 4th e…
The cerebral cortex is the main functional unit of the cerebrum. [Tortora & Derrickson, 2009] The three main functional areas of the cerebral cortex are: [Tortora & Derrickson, 2009; Prise & Wilson, 2003]
- motor areas that control voluntary movement (primary, secondary, an…
Lobes of the brain
The brain can be thought of as comprising five ‘lobes’ – the four lobes of the cerebral cortex and a fifth lobe, the insula, deep within the brain, as shown on the slide. [Martin, 2003; Tortora & Derrickson, 2009; Price & Wilson, 2003] The lobes of the cerebral cortex are …
Neurosynaptic transmission
Neurotransmission.
Information moves through the nervous system via two integrated forms of communication – electrical neurotransmission and chemical neurotransmission, as shown on the slide. [Kandel et al., 2000] An action potential is generated at the origin of the axon following sufficien…
The synapse
Neurones do not physically touch one another; two neurones are separated by a gap, known as a synaptic cleft. [Kandel et al., 2000] Because neurones do not touch, and an action potential cannot ‘jump’ across a synaptic cleft, the signal must be converted to a chemical sign…
Process of chemical neurotransmission
The idea that neurotransmission occurs at synapses and is mediated by chemicals was, at first, a contentious issue. [Purves et al., 2008] It was in the first half of the 1900s that experiments proved chemical neurotransmission occurred. [Purves et al., 2008] The process is …
Related content

The pathology of ischaemic stroke is complex, but commonly involves the formation of a clot that travels in the blood to or within the brain and becomes lodged in the blood vessels of the brain (a thromboembolism), which can reduce or block blood flow (an occlusion).

Post-stroke fatigue is an under-recognized NPS, which healthcare professionals should anticipate in patients.

Emotional lability describes episodes of involuntary and uncontrollable crying and/or laughing, outside of socially appropriate circumstances and when it is incongruent with the patient’s emotional state.
-300x169.jpg)
Permissions
Permissions for creative use of the resources from neurotorium.
Permission is granted to download images, slides and videos and use them in your own presentations, provided that copyright notices and the Neurotorium logo are not hidden or removed. For use in publications and on websites, proper attribution must be provided together with a link to Neurotorium.org
Your slides will download now. Do you want to get our latest information?
Sign up to our newsletter and receive news in your inbox. We send newsletters every 1-2 months.
You have been subscribed to our newsletter!
Share or print.
Share content with anyone.
Save to workspace
Select language.
We have detected that you are from “France”. You have the option of switching the language to French, if you would prefer that?.

This site uses cookies
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Sign up for our newsletter
Fill in you information below and stay up to date with the latest content on Neurotorium.
We publish newsletters every 2-3 months, keeping you up to date with the latest content on the website. You will receive a welcome e-mail immediately after you sign up for our newsletter. If you do not receive an e-mail, please check your spam folder. Contact support at [email protected] if you require help.
Welcome back
Please enter your details below.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- March 15, 2024 | VOL. 77, NO. 1 CURRENT ISSUE pp.1-42
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Metacognitive Reflection and Insight Therapy for Schizophrenia: Case Study of a Patient With a Co-Occurring Substance Use Disorder
- Alison V. James , Psy.D. ,
- Bethany L. Leonhardt , Psy.D. ,
- Kelly D. Buck , CNS
Search for more papers by this author
Decrements in metacognitive functioning, or the ability to form complex and integrated representations of oneself and others, have been identified as a core feature of schizophrenia. These deficits have been observed to be largely independent of the severity of psychopathology and neurocognitive functioning and are linked to poor outcomes for those with the disorder. This study is a case illustration of the efficacy of metacognitive reflection and insight therapy (MERIT) in increasing the metacognitive capacity of an individual diagnosed as having co-occurring schizophrenia and a substance use disorder during three years of individual therapy. The eight elements of MERIT, which promote metacognitive growth, are presented as they apply to the present case. Case conceptualization, outcomes, and prognosis are also presented. These eight elements enabled the patient to move from a state of gross disorganization—unable to identify his thoughts or present them in a linear fashion—to one in which he was able to develop increasingly complex ideas about himself and others and integrate this understanding into a richer sense of himself, of his psychological challenges, and of the role that substance use played in his life. Results of the study also illustrate the foundational necessity of self-reflectivity in order to facilitate understanding of the mind of others and the relationship between psychological pain and the emergence of disorganization.
Metacognition refers to a spectrum of mental activities that range from discrete acts, such as thinking about one’s own thinking or contemplating the mental activity of others, to an increasingly more complex synthesis of these abilities into an integrated sense of oneself and others ( 1 , 2 ). The absence of these abilities results in difficulties with appropriately responding to psychosocial challenges and, therefore, hinders recovery. Although some researchers consider metacognition to be a component of social cognition ( 3 ), metacognition differs from social cognition in that it is not concerned with the accuracy of one’s emotional or social judgments. Instead, it focuses on how this information is integrated into a more complex understanding of oneself and others. This distinction between social cognition and metacognition as conceptually different factors has been illustrated in previous studies using principal-components analyses ( 4 ).
Deficits in metacognitive capacity among those with schizophrenia have been recognized and observed for more than two decades and are considered to be a stable and key feature that underlies symptoms of the disorder ( 5 ). Intact metacognitive functioning has been found to be associated with psychosocial outcomes, including higher work performance ( 6 ) and intrinsic motivation and learning ( 7 ). Decrements in metacognitive function, in contrast, have been linked to poorer functioning and outcomes ( 8 ). Although metacognition is correlated with severity of psychopathology, previous research suggests that deficits in metacognition cannot solely be explained as reflections of symptoms or features of the disorder ( 9 , 10 ).
Given the identification of metacognitive deficits as a core feature of schizophrenia spectrum disorders, novel interventions that target rebuilding atrophied metacognitive capacities are of paramount importance ( 11 ). One such integrative intervention is metacognitive reflection and insight therapy (MERIT) ( 12 ). MERIT is an integrative treatment that seeks to promote synthetic metacognitive capacity and was developed to target deficits in the four elements of metacognition among individuals with psychotic disorders.
Although MERIT is a manual-based intervention, it does not follow a prescribed treatment protocol. It is instead a flexible and target-driven approach whereby therapists and patients think together, and patients are encouraged to reflect on their ideas of themselves and others. Metacognitive ability is operationalized as a hierarchical capacity within MERIT, with each level of functioning building on the abilities needed for the previous level. As such, interventions within this framework should be tailored to the patient’s current metacognitive capacity and aim to facilitate metacognitive growth toward increasingly complex and integrative metacognitive acts.
MERIT consists of eight interrelated therapeutic elements that should be present in each session. These include attending to the client’s agenda, including the therapist’s thoughts as part of a dialogue, eliciting narrative episodes, defining a psychological problem, discussing interpersonal processes within the session, evaluating progress, stimulating reflective acts about oneself and others, and stimulating the use of knowledge about oneself and others to respond to psychological problems. These elements are each discussed below in the context of the case presented.
Several previous case studies ( 13 – 15 ) have demonstrated the efficacy of MERIT in assisting individuals with schizophrenia with forming more complex ideas about their own mental states and the mental states of others. In addition, MERIT has been shown to help individuals synthesize that information into an integrated sense of themselves and others. These case studies have evaluated patients in both early and later phases of their illness and have included individuals with a range of clinical presentations.
One limitation of the case work to date is a lack of inclusion of clinical cases of individuals presenting with co-occurring substance use disorders. Epidemiological data have shown that approximately 40% to 50% of individuals with schizophrenia also have a substance use disorder ( 16 ). Moreover, substance use disorders among this population are associated with poor outcomes, including poor response to treatment, hospitalization, suicide, and homelessness ( 17 ).
It, therefore, seems especially important to consider this group, given that integrative psychotherapy interventions may reduce the risk of these poor outcomes. People with schizophrenia and co-occurring substance use disorder also appear to possess low levels of metacognition and lower levels of metacognitive mastery, which enables individuals to identify a psychological problem and use their knowledge about themselves to appropriately respond to that problem. Therefore, the current article presents a comprehensive case study of the application of MERIT in the treatment of an individual diagnosed as having co-occurring schizophrenia and substance use disorder.
Case Illustration
Presenting problem and client description.
We refer to the client for this case as Dylan. We have modified details of this case report, such as name and other identifying information, to protect his confidentiality while preserving the illustrative value of the case. Dylan was a Caucasian man in his late 40s who lived in a rural midwestern town with his older brother. He was single and had never married, and he did not have any children.
Dylan’s parents divorced when he was four years old, and he was the youngest of three children. At the time of this therapy, his mother and brother lived in the same state as Dylan, and his father lived in a neighboring state. His eldest brother died approximately 10 years prior from a drug overdose. It was not clear whether there was a history of schizophrenia in Dylan’s family; however, he described instances of his mother’s disorganized behavior, including examples of times when she apparently shouted at someone who was not there and other occasions when she discussed her unusual beliefs with Dylan. He also endorsed a family history significant for alcoholism.
Dylan described a chaotic and conflict-ridden household prior to his parents’ divorce; his father was often drunk and volatile, and his parents frequently fought. After his parents’ divorce, Dylan and his older siblings were raised by his mother. He described a nomadic childhood characterized by poor living conditions. He and his siblings moved to a new home every few years, first moving within the state and then ultimately settling in the southeastern United States.
Largely absent during his childhood and young adulthood were close connections with others, both outside the family (as a result of his frequent moves) as well as within the family in his relationships with his siblings and mother. At the age of 16, frustrated by his mother’s increasingly erratic and disorganized behavior, Dylan decided to hitchhike back home to the Midwest, where he completed high school while living with his uncle. After high school, he worked odd jobs at home before joining the military.
Dylan was diagnosed with schizophrenia in his early 20s, two years into his military career and in the wake of a recent rejection by a woman he was dating. Dylan reported that at this time his drinking and social isolation significantly increased. He was admitted to the hospital by his commander after displaying strange and disorganized behavior and speech, and he remained in the hospital for approximately six months, after which he was discharged from the military.
After his discharge, Dylan moved back to the Midwest to live with his mother in an environment similar to that of his nomadic formative years. During this time, Dylan’s drinking continued to escalate, which he attributed to the stress of living with his mother. His drinking culminated in a citation for driving under the influence of alcohol and a short jail stay, during which his disorganized behavior also briefly intensified.
Ultimately, Dylan chose to move back to his home state to live with his brother, first in a series of trailer homes and later in a home Dylan purchased in a rural town. Over the next several years, his drinking persisted. Coupled with his limited insight and difficulties connecting with others, his alcohol use led Dylan to surround himself with and take in as roommates people who also abused substances. This pattern of behavior ultimately led to a drug-related arrest two years prior to the start of psychotherapy with this provider (AJ).
At the start of psychotherapy, Dylan had been clinically stable with his medication-management regimen for several years. He was serving probation for his drug charge, for which he was required to participate in group psychotherapy and 12-step programming. Prior to psychotherapy with this provider, Dylan had previously participated in individual therapy for a period of one year, but he demonstrated limited engagement in the therapeutic relationship and his treatment.
When Dylan started therapy, he demonstrated significant disorganization of his thoughts and speech and possessed a fragmented account of the narrative events of his psychosocial history. He described hearing voices and seeing strange figures, and he possessed vague delusional beliefs about the government and religion. Dylan also presented with profoundly flat affect, and his sporadic emotional expressions were frequently incongruent with the subject matter being discussed. With regard to his substance use, he demonstrated some awareness that his past drug and alcohol use had caused problems for him, but he lacked an understanding of the factors precipitating his use. Similarly, Dylan’s descriptions of past use contained images of himself as a passive recipient of drugs and alcohol, devoid of any agency or volitional accounts of his use.
Case Formulation
We conceptualized Dylan’s psychosocial difficulties as resulting from low metacognitive capacity, and we therefore used the Metacognition Assessment Scale–Abbreviated (MAS-A) ( 18 ) to illustrate these deficits. The MAS-A is an adaptation of the Metacognition Assessment Scale, which was originally created by Semerari and colleagues ( 2 ) to assess metacognitive function during psychotherapy. The abbreviated version was modified to allow for the assessment of metacognition in personal narratives and was created in conjunction with the original authors.
The MAS-A is subdivided into four scales, each of which measures a separate facet of metacognition. These four subscales include self-reflectivity, or the ability to identify and ultimately integrate information regarding one’s own internal states; understanding the mind of the other, or one’s ability to identify and synthesize information with regard to the mental states of others; decentration, or the capacity to recognize and consider the unique perspective of others; and mastery, or one’s ability to identify a valid psychological problem and use knowledge of oneself to decrease psychological distress. Higher scores on each of the four subscales are reflective of higher metacognitive capacity, whereby individuals are able to form and then synthesize complex representations of themselves and others.
Regarding self-reflectivity, at the onset of psychotherapy Dylan was able to recognize that his thoughts were his own, but he was unable to recognize and differentiate among a variety of cognitive operations aside from his thoughts and memories. Similarly, Dylan was unable identify or distinguish among his emotional states or integrate how his thoughts or feelings might affect his actions, such as his substance use. During these initial stages of treatment, Dylan’s thoughts were often disorganized, resulting in nonlinear and often confusing narratives interjected with delusional thinking and abstractions.
In terms of understanding the mind of the other, Dylan was initially capable of only the most fundamental interpersonal reflections. At a basic level, Dylan was able to recognize the existence of mental functions within the other, but he was unable to distinguish among mental states or identify emotional states within other people. Regarding decentration, Dylan was initially unable to see things from multiple perspectives or differentiate others’ experiences from his own. Thus, he did not possess the capacity to understand that others might possess differing opinions or perceive events differently than he did.
Last, in terms of mastery, at the onset of therapy Dylan was unable to articulate a psychological problem in a nuanced way. Although he was able to acknowledge himself as having a mental illness and recognize a desire to “stay out of trouble” (given that he was on probation at the time), Dylan was unable to articulate more specifically what this meant to him. As a result, his psychological problem appeared to be more a reflection of something he was socialized to report.
Course of Treatment
Element 1: the preeminent role of the client’s agenda..
This first element of MERIT focuses on what the client wants during each therapy session. It is important to note that a client may present with differing agendas in each session, may present with several different agendas simultaneously, or may even be unaware of some or all of the agendas he or she brings to session. Awareness of and attendance to agendas both known and unknown by the client are of paramount importance in the context of the therapeutic relationship.
At first, it was difficult for the therapist to deduce what Dylan wanted out of therapy. In their initial sessions, Dylan described a general desire to “stay out of trouble,” but he was unable to explain in any detail what this meant to him. Given that Dylan was on probation as a result of a recent drug arrest at this time, it was unclear to the therapist whether Dylan attended their sessions for any reason other than meeting his probation requirements for weekly contacts with a mental health provider.
Although seemingly unrelated, it is also of note that during these first several sessions, Dylan presented to therapy with various objects for what he called “show and tell.” These items largely consisted of kitschy household knickknacks, many of which were acquired from garage sales or passed on unceremoniously to Dylan by acquaintances. Although he expressed a desire to share these items with the therapist, the narrative details of the events surrounding his acquisition of the items quickly revealed a lack of emotional attachment to the items. Given this behavior, Dylan’s apparent lack of psychological distress, and his disorganized thought processes during these initial sessions, the therapist had to be willing to endure the uncertainty and discomfort associated with her desire to make sense of his experiences and understand Dylan’s agenda. Thus, she accepted his agenda as unclear and framed it as something they could mutually explore to later establish his psychological problem and clarify the goals of treatment.
With time, the therapist noticed that Dylan’s disorganization often arose at specific times, such as after discussion of difficult interpersonal interactions or losses, or toward the end of sessions spent integrating these interactions throughout his life. For example, in the wake of discussing a narrative about the loss of his brother during one session, Dylan’s thought processes became increasingly more disorganized, and he began to explain his delusional ideas about the role a government conspiracy played in his loss. Dylan also became notably more disorganized for a few sessions at the end of therapy, during which the therapist and Dylan processed the upcoming termination of their work together.
Similarly, with time the therapist also noticed that Dylan’s pattern of substance use primarily occurred within interpersonal contexts. His use was often spurred by attempts at or failed connections with others, or an apparent desire to elicit caring or concern from his therapist. For example, on one occasion after a sustained period of sobriety, Dylan relapsed with a new acquaintance during the therapist’s extended vacation.
The therapist’s observation of Dylan’s disorganization ultimately led her to form the idea that his disorganization served to protect him from the distress caused by his conflicts or lost connection with others. This understanding afforded her a framework for understanding other behaviors, such as Dylan’s “show and tell” and his pattern of substance use, as attempts to connect with others. Thus, the therapist’s understanding of Dylan’s agenda came to be that his objective was to connect with others, but that this effort was impeded by his low abilities to reflect on the minds of others and view others as distinct individuals with lives independent of his own.
Element 2: introduction of the therapist’s thoughts in ongoing dialogue.
This second element involves discussion of the therapist’s thoughts during therapy in a manner that facilitates an open dialogue between client and therapist. Accomplishment of this element requires that the therapist disclose the contents of his or her mind while also encouraging joint reflection about these thoughts. This reflection on the thoughts of the therapist aids in stimulating the client’s metacognitive capacity to understand the mind of the other. It also increases clients’ self-reflectivity as they explore their own reactions to the mental content of the therapist.
During the early stages of therapy, Dylan frequently presented as disorganized and tangential in session and was unable to recognize his own mental activities or those of others. As a result, the therapist was often confused and left therapy sessions frustrated and exhausted from the strain of attempting to follow Dylan’s train of thought. To address this issue, the therapist inserted her own thoughts during sessions to establish her mind as independent from Dylan’s and to reflect her feelings of confusion. She offered comments such as, “I’m confused; help me understand what made you think of that just now,” or, “I’ve noticed that when you have many thoughts in your head, I find myself confused.” These remarks assisted in scaffolding Dylan’s ability to reflect on his own thinking, which ultimately led to more linear and sequential thought processes.
At later stages in therapy, the therapist offered relatively more complex and integrated reflections to increase the salience of the relationship among Dylan’s substance use, emotions, and interpersonal interactions. For example, she offered comments such as, “I notice that you usually drink only when you’re around others. I wonder if that is because it’s harder to get along with others when you’re sober?” or, “When I was away, you chose to use. I’m wondering what I should make of that?” Dylan was invited to reflect on the thoughts of the therapist and whether he agreed with her interpretations. These reflections helped Dylan to differentiate his thoughts from those of the therapist while also laying the groundwork for establishing a shared sense of his psychological problem.
Element 3: the narrative episode.
The third element of MERIT emphasizes eliciting narrative episodes from the client to facilitate construction of a storied sense of the client’s life events. This eliciting of narrative episodes enables a shared sense by therapist and client of the client over time. In addition, it aids the therapist’s conceptualization of the client as a unique and complex being, rather than as merely a compilation of his or her symptoms.
At the start of therapy, Dylan lacked a storied sense of his life, and, as a result, this was a difficult task to engage in. His thought processes vacillated from barren to disorganized, both between as well as within sessions. He was often unable to temporally anchor when events in his life occurred, and he provided vague overviews of interactions and events. For example, Dylan was unable to identify how old he was or where he was living when a given event occurred. This inability to construct a linear narrative was difficult for the therapist as well, because she had to endure barrages of Dylan’s disorganized thoughts. As a result, she also struggled against feelings of confusion and frustration that arose out of her desire to force integration on Dylan’s life and thoughts.
To stimulate narrative episodes, the therapist inquired about whether there were other times in Dylan’s life when a similar event, thought, or feeling occurred or, conversely, whether there had been times when things were different than the event being described. To elicit narrative details when Dylan provided narratives that were barren, the therapist made numerous specific inquiries about the event (e.g., “How old were you when this happened?” or “Where were you living?”) in an effort to model the level of detail necessary for her to formulate a picture in her mind of the event. When Dylan provided disorganized narratives, the therapist intervened without judgment or correction, with questions aimed at eliciting linear thought, such as, “We were just talking about your mom, and now we’re suddenly talking about your car. Did you notice that, too?”
The therapist also maintained a similarly nonjudgmental and nondirective approach while obtaining narrative details about Dylan’s substance use. In gathering these narrative details, the therapist sought to better understand the context in which Dylan used through questions such as, “Who else was there?” “What time of day was it?” or “What were the thoughts in your mind just before using?”
Over time, Dylan began to provide richer and more detailed narrative episodes and started to self-monitor the tangential shifts in his narratives. He also became better able to reflect on the potential internal catalysts to his use of substances (e.g., “Maybe I was bored?”), which afforded a first step in the establishment of Dylan as an active agent in his decisions and life. As Dylan provided more narrative episodes, the therapist was also able to establish a timeline of his life events, which enabled the therapist and Dylan to possess a joint understanding of his life over time as well as the relationship among these events. Themes of isolation, interpersonal conflict, and loneliness arose from narratives describing his frequent and abrupt moves as a child, the end of his only significant romantic relationship, alcohol and drug use throughout his adult life, and his pattern of taking in people in need as roommates. These themes aided in the conceptualization of Dylan’s psychological problem, which is discussed in more detail below.
Element 4: the psychological problem.
The fourth element to be attended to during therapy is the formulation of a psychological problem. To achieve this element, the client and therapist must jointly identify and agree on a valid and plausible psychological problem. Examples of psychological problems that may manifest in treatment include feelings of loneliness stemming from difficulties in connecting with others, interpersonal conflict resulting from a lack of understanding of the mind of others, and feelings of anger and resentment stemming from past events.
During the early stages of therapy, Dylan was unable to clearly articulate a psychological problem. He expressed a desire to “stay out of trouble” but was unable to describe in any nuanced detail what he meant by that statement. It was clear to the therapist that these utterances were largely related to his recent drug-related arrest with a former friend and were likely parroted from his 12-step program or his interactions with his probation officer.
As therapy progressed and Dylan offered more personal narratives, he began to share narratives with themes of his struggles to connect with others and difficulties in understanding the mental states of others and judging their intentions. He described an unstable childhood with frequent moves, which made it difficult for him to form and maintain relationships; a past confusing and abrupt break-up with a former girlfriend; and his more recent behavior of taking in as roommates people who later became problematic and took advantage of Dylan.
At this point, Dylan’s psychological problem became more clearly defined, given that many of his attempts for connection were thwarted by his difficulties in understanding others. This understanding of Dylan’s psychological problem as a difficulty in connecting with others also afforded the therapist a framework for conceptualizing his actions. For example, his substance use with others provided Dylan with a shared experience that he lacked while sober. Similarly, his attendance at 12-step meetings enabled Dylan to establish relationships with individuals who were also stigmatized as part of an “outgroup.”
This development of Dylan’s psychological problem was achieved throughout the processes defined in the first three elements of MERIT. Dylan began to come to his therapy sessions with a purpose, discuss narrative episodes from his life with the therapist, and reflect on her reactions to the events he shared. Through these processes, Dylan was ultimately able to begin to self-reflect about himself and his experiences in a more complex and integrated way.
Elements 5: reflecting on interpersonal processes within the session.
The fifth element of MERIT necessitates that the therapist call attention to the interpersonal dynamics between the client and therapist as they occur within the therapy session. This process was initially a difficult task for Dylan at the start of therapy, given his inability to recognize the therapist as possessing a life largely independent of his own. Moreover, it was compounded by his low levels of self-reflectivity and understanding of the mind of others. To address this in her initial interventions, the therapist focused on helping to cultivate Dylan’s capacity for reflecting on his thinking. The therapist also offered reflections about her own mental activity and offered relevant self-disclosures in an effort to scaffold Dylan’s decentration.
As time passed, the therapist began to note dynamics between herself and Dylan as they arose in sessions. She also encouraged Dylan to reflect on his ideas about the therapist. For example, in several sessions throughout the course of therapy, Dylan disclosed his relapses with drugs and alcohol to the therapist. Early on, the therapist was cognizant that her responses to Dylan’s relapses were often simultaneous feelings of disappointment and concern as well as a desire to control the potential for future relapses. In lieu of engaging Dylan in a skills-based discussion of identifying coping strategies or other safeguards for his substance use, she instead inquired about what Dylan was seeking from her by sharing the information (e.g., comfort and caring, alarm and shock) and disclosed to him how she felt compelled to react.
Discussions such as these laid the groundwork for deeper future explorations of the therapeutic relationship and the ways both Dylan and the therapist were affected by one another. This element was perhaps most salient during the end stages of therapy, during which Dylan and the therapist together reflected on the changes and growth that were facilitated by the therapeutic relationship over the course of therapy.
Element 6: reflecting on the process of therapy within the session.
The sixth element of MERIT requires that the therapist facilitate discussions about the therapy process within sessions as well as the process as a whole. The successful application of this element establishes therapy as an active experience in which reflection is encouraged. Initially, Dylan tended to respond to the therapist’s inquiries about how a given session went with brief positive replies (e.g., “It was good”) but was unable to elaborate more fully regarding the specific elements that made the experience positive for him. As therapy progressed, Dylan began to offer more detailed reflections about the sessions and became better able to differentiate elements that were similar or dissimilar to their other sessions.
As his ability to reflect on his cognitive operations improved, his responses to the therapist’s inquiries began to reflect an increased understanding of himself and their sessions over time. This increased understanding was evidenced by statements such as, “I jumped around more in our discussion today,” or “I think I confused you more today.” Such insights show that Dylan was able to identify periods of increased thought disorganization and how this disorganization affected the processes within the session.
Element 7: stimulating self-reflectivity and awareness of the other’s mind.
The seventh element calls for the therapist’s ongoing assessment of the client’s ability to reflect on the mental states of the self and others. The therapist assesses both self-reflectivity and awareness of the other’s mind using the MAS-A. The therapist then tailors psychosocial interventions during sessions in accordance with the client’s metacognitive capacity in each domain. He or she also provides scaffolding to facilitate metacognitive growth to higher and more complex levels of reflectivity.
At the start of therapy, Dylan presented with low levels of self-reflectivity. He was unable to distinguish different kinds of cognitive operations or recognize and name nuanced emotions in himself. As a result, Dylan was unable to reflect on the link between his mental activity and behaviors, such as substance use. For example, Dylan recalled events from his life during sessions but appeared to be unable to recognize himself as experiencing a memory while recounting the event.
Similarly, he appeared to lack awareness of his own thoughts and how one of his thoughts might create or lead to a new thought. This lack of awareness was especially apparent during times of increased thought disorganization. At times Dylan reported an emotional experience, such as feeling “stressed,” but he was unable to recognize a variety of nuanced emotions.
As a result, the therapist initially did not explicitly address Dylan’s substance use, which necessitated advanced levels of metacognition so that he could identify his thoughts and feelings and reflect on how they might be affected by interpersonal or situational factors. Instead, the therapist’s initial interventions centered on increasing Dylan’s ability to recognize a variety of his own mental operations and reflecting on his mental content as it manifested during sessions. For example, the therapist offered reflections such as, “Your thoughts are confused,” or, “You’re remembering your mother.” The therapist also assisted Dylan through modeling, by offering narrations of her own mental processes such as, “I’m curious…I think…I remember….”
As therapy progressed and Dylan became better able to reflect on his mental activity, the therapist tailored her interventions to target higher levels of self-reflectivity. She encouraged Dylan’s exploration of his emotions by inquiring about the physical sensations in his body and then linking those sensations to an emotional experience: “You said that you felt butterflies in your stomach…I wonder if that was anxiety you were feeling?” The therapist also offered her reflections on how she might feel in similar situations (e.g., “If that happened to me, I would expect that I might feel sad”).
Later interventions focused on identifying and highlighting how Dylan had changed over time and then how reality had unfolded independently from Dylan’s hopes and expectations. To accomplish these goals, the therapist offered reflections aimed at emphasizing these elements as they occurred naturally in Dylan’s narratives (e.g., “You used to think… but now you see things differently”) and offering questions intended to parse Dylan’s expectations and sense of himself over time (e.g., “Were you surprised about how things worked out with your roommate?”).
By the conclusion of therapy, Dylan was at the beginning stages of his ability to integrate how his actions were affected by his thoughts, feelings, and interactions with others within discrete narrative episodes. With this increased capacity for self-reflection, Dylan was able to begin to reflect on the factors that precipitated his substance use. To facilitate this reflection, the therapist began to offer her interpretations to Dylan, such as, “I’m wondering if you drank on Saturday because you were sad and lonely?”
With regard to reflectivity of the mind of the other, Dylan initially possessed low levels of understanding of the minds of others. Although he was able to recognize that others experience thoughts of their own, Dylan could not identify multiple different cognitive operations in the minds of others. The therapist offered similar interventions to those described above for targeting self-reflectivity, including sharing her own mental activity in sessions with Dylan. Toward the middle of their work together, Dylan progressed from identifying a variety of cognitive operations in the minds of others to noticing their emotions (e.g., the anger of a fellow group member, concern and empathy from his therapist).
By the conclusion of their work, Dylan began to demonstrate the next level of understanding of the mind of others on the MAS-A: the ability to make inferences about mental activity of others. This level of metacognitive functioning was evidenced in his ability to recognize the therapist’s facial expression and then use that information to make a hypothesis about her mental activity. For example, at this stage Dylan was able to identify a perplexed expression on the therapist’s face and would then state, “It looks like you have a question.”
Element 8: stimulating mastery.
The eighth and final element of MERIT requires that the therapist help stimulate the client’s utilization of knowledge about him- or herself and others to identify and subsequently respond to a psychological problem. As mentioned above, at the beginning of therapy Dylan was unable to clearly define a psychological problem, reporting a desire to “stay out of trouble” and “not relapse” in the wake of his recent arrest and probation. However, Dylan was unable to further articulate what staying out of trouble might look like or why it was important to him, which left the therapist the impression that this goal was more a reflection of what was expected of Dylan by his probation officer or by those from his 12-step meetings. Additionally, it was unclear to the therapist whether Dylan’s substance use was truly a source of distress to him or whether it was instead a manifestation of more deeply rooted difficulties in forming and maintaining relationships with others that resulted from of his low metacognitive capacity.
During the initial stages of treatment, the therapist’s interventions centered on gathering narrative details of the events surrounding Dylan’s substance use while also eliciting narratives of past moments of distress. As she elicited these narratives, it became clear to the therapist that Dylan’s substance use occurred almost exclusively within the context of social situations in which he was offered drugs or alcohol by his acquaintances. The narratives also revealed Dylan’s past unsuccessful attempts to connect with others and the shared sense of purpose and “otherness” derived from his attendance at meetings or in groups.
Later during treatment, Dylan became increasingly able to articulate his psychological problem of difficulty in understanding and connecting with others. It became clear to the therapist that Dylan’s substance use was largely precipitated by his difficulties in understanding others and his attempts at connection. He progressed from using unhealthy strategies, such as his substance use, to connect with others to more adaptive approaches, such as using the therapist as a support to address other aspects of his presentation (e.g., thought disorganization) that made connecting with others difficult. Overall, the therapist’s interventions assisted Dylan with developing a more nuanced understanding of his psychological problem while also aiding him in considering strategies to address it.
Absent from this element of MERIT was a prescriptive or directive approach whereby the therapist informed Dylan of what his psychological problem was or focused on demanding sobriety of Dylan. Instead, the therapist worked to gain a deeper understanding of the distress Dylan experienced and the underlying function that substance use played in his life. This deeper understanding assisted in providing a context for his experiences and enabled Dylan to better define his psychological problem.
Outcome and Prognosis
When Dylan first began participating in MERIT, he presented with low metacognitive capacities. He was aware that he possessed thoughts, but he was unable to recognize a variety of cognitive operations; identify his emotional experiences; or recognize the interplay among his thoughts, feelings, and actions. Dylan also had difficulty with recognizing these experiences in others and differentiating the experiences of others as separate and unrelated to his own. At the start of treatment, he also a lacked a coherent account of his psychosocial problems, an understanding of the role his substance use played in these problems, and strategies for coping with his psychosocial challenges. Through the application of each of the eight elements of MERIT, Dylan dramatically improved his capacity for metacognition.
By the termination of treatment with his therapist, Dylan was able to form more complex and integrated ideas about himself and others in the context of specific events from his life. He developed the ability to recognize his emotional experiences, fallibility in his thinking, and changes in his thinking over time. Toward the end of treatment, Dylan also was increasingly able to reflect, with scaffolding from the therapist, about how his interactions with others affected his thoughts and emotions and to consider the relationship between these experiences and his substance use.
One could argue that Dylan’s most striking metacognitive gains occurred in his ability to understand the minds of others and view them as independent from himself. At the end of treatment, he was able to recognize a variety of cognitive operations in the minds of others, identify their emotions, and make reasonable conjectures regarding the mental activity of the therapist in response to her facial expressions (e.g., “It looks like you have a question”). Last, Dylan had made steps toward identifying his psychological problem of difficulty with connecting with others.
By the end of therapy, Dylan had less severe positive symptoms, and the frequency and severity of his thought disorganization were greatly diminished. Discussions regarding his delusions about the government and religion in sessions significantly decreased, as did his reports of auditory and visual hallucinations. He was better able to track his own mental activity and self-redirect when he noticed tangential thoughts during sessions.
Dylan was able to maintain sobriety from drugs and alcohol during most of the course of individual therapy. Although Dylan began to occasionally use substances again in the middle stages of treatment, the quantity and frequency of his use were minimal and did not result in significant distress or impairment in functioning. During the final stages of therapy with his provider, Dylan also demonstrated an increased sense of agency in his decisions about his substance use and began to identify and use strategies for managing his use.
Dylan’s increased capacity for self-reflection and awareness of his thought disorganization and his lack of significant exacerbations of his symptoms or hospitalizations are promising factors for his future. Similarly, his significant overall reduction in substance use, greater capacity to reflect on the internal and external precipitants to his use, and increased sense of himself as an active agent in life also bode well for his future. Although gains in all metacognitive domains are possible with continued metacognitive therapy, Dylan has made significant progress in his abilities to understand and identify his own mental activity and has demonstrated increased understanding of the minds of others. He, therefore, appears in a good position for continued recovery and increased interpersonal functioning.
Limitations
This case illustration has a few limitations. This article has described an in-depth study of one person with schizophrenia, who presented with primarily disorganized symptoms. Therefore, these results may not be generalizable to patients with differing demographic characteristics or symptom presentations or those in different phases of their illness. Additionally, this case illustration reflects approximately three years of individual outpatient therapy with Dylan. Therefore, the extent to which these results may be generalizable to those engaged in shorter term treatment or other treatment settings is unclear.
Last, this case study provides an in-depth analysis of only one type of integrative metacognitive therapy. Other metacognitive therapies, such as skills-based metacognitive training ( 19 ), also address metacognitive deficits among those with psychosis. Future researchers may seek to address some of the limitations of the present case illustration, including examination of the effect of long-term integrative metacognitive therapy among clients with differing demographic characteristics and symptom presentations, to assess whether these individuals achieve similar treatment outcomes. More research is also needed that formally assesses metacognitive capacity throughout the course of treatment in both case study and control trial formats.
Summary and Implications for Clinical Practice
In the case presented, the therapist applied the eight elements of MERIT in synergy in the treatment of a middle-aged man with chronic schizophrenia and substance use disorder to attain greater levels of self-reflectivity, understanding of others’ minds, decentration, and mastery. Overall, Dylan’s gains in metacognitive capacity closely mirror results from other case studies ( 15 , 20 , 21 ) using integrative and metacognitively focused psychotherapy. Initial improvements in Dylan’s ability to reflect on his thoughts and feelings gave way to richer narratives, which then led to Dylan’s increased understanding of the problems he faced in his interactions with others. It is also of note that Dylan’s ability to detect, understand, and later intuit the thinking and mental states of others developed only after initial gains in self-reflectivity were achieved. These findings have implications for both conceptualization and intervention, because understanding the course of metacognitive growth may affect the intervention targets used by therapists.
As therapy progressed and Dylan’s narratives became richer and more linear, painful memories emerged of his past experiences with neglect, betrayal, and interpersonal loss. It became clear to the therapist that Dylan’s fragmentation provided him an element of protection from these painful memories. The relationship between his pain and his fragmentation was especially evident during therapy, given that Dylan’s disorganization frequently intensified after he provided narratives about past painful events. Similarly, in the middle stages of treatment he often became increasingly disorganized during the latter half of therapy sessions, which was reflective of the emotional and cognitive fatigue associated with reflecting on his life. These observations are consistent with previous case studies that have noted the relationship of increased insight and reflectivity with feelings of pain and loss ( 22 , 23 ).
The authors report no financial relationships with commercial interests.
1 Lysaker PH, Vohs JL, Ballard R, et al. : Metacognition, self-reflection and recovery in schizophrenia . Future Neurol 2013 ; 8:103–115 Crossref , Google Scholar
2 Semerari A, Carcione A, Dimaggio G, et al. : How to evaluate metacognitive function in psychotherapy? The Metacognition Assessment Scale and its applications . Clin Psychol Psychother 2003 ; 10:238–261 Crossref , Google Scholar
3 Pinkham AE, Penn DL, Green MF, et al. : The Social Cognition Psychometric Evaluation Study: results of the expert survey and RAND panel . Schizophr Bull 2014 ; 40:813–823 Crossref , Medline , Google Scholar
4 Lysaker PH, Gumley A, Luedtke B, et al. : Social cognition and metacognition in schizophrenia: evidence of their independence and linkage with outcomes . Acta Psychiatr Scand 2013 ; 127:239–247 Crossref , Medline , Google Scholar
5 Frith CD : The Cognitive Neuropsychology of Schizophrenia . Hove, UK, Erlbaum, 1992 Google Scholar
6 Lysaker PH, Dimaggio G, Carcione A, et al. : Metacognition and schizophrenia: the capacity for self-reflectivity as a predictor for prospective assessments of work performance over six months . Schizophr Res 2010 ; 122:124–130 Crossref , Medline , Google Scholar
7 Tas C, Brown EC, Esen-Danaci A, et al. : Intrinsic motivation and metacognition as predictors of learning potential in patients with remitted schizophrenia . J Psychiatr Res 2012 ; 46:1086–1092 Crossref , Medline , Google Scholar
8 Hamm JA, Renard SB, Fogley RL, et al. : Metacognition and social cognition in schizophrenia: stability and relationship to concurrent and prospective symptom assessments . J Clin Psychol 2012 ; 68:1303–1312 Crossref , Medline , Google Scholar
9 Abdel-Hamid M, Lehmkämper C, Sonntag C, et al. : Theory of mind in schizophrenia: the role of clinical symptomatology and neurocognition in understanding other people’s thoughts and intentions . Psychiatry Res 2009 ; 165:19–26 Crossref , Medline , Google Scholar
10 Bora E, Yücel M, Pantelis C : Theory of mind impairment in schizophrenia: meta-analysis . Schizophr Res 2009 ; 109:1–9 Crossref , Medline , Google Scholar
11 Lysaker PH, Dimaggio G : Metacognitive capacities for reflection in schizophrenia: implications for developing treatments . Schizophr Bull 2014 ; 40:487–491 Crossref , Medline , Google Scholar
12 Van Donkersgoed RJ, De Jong S, Van der Gaag M, et al. : A manual-based individual therapy to improve metacognition in schizophrenia: protocol of a multi-center RCT . BMC Psychiatry 2014 ; 14:27 Crossref , Medline , Google Scholar
13 Hamm JA, Leonhardt BL : The role of interpersonal connection, personal narrative, and metacognition in integrative psychotherapy for schizophrenia: a case report . J Clin Psychol 2016 ; 72:132–141 Crossref , Medline , Google Scholar
14 Hillis JD, Leonhardt BL, Vohs JL, et al. : Metacognitive reflective and insight therapy for people in early phase of a schizophrenia spectrum disorder . J Clin Psychol 2015 ; 71:125–135. Google Scholar
10.1007/s10879-016-9332-9 Crossref , Google Scholar
16 Blanchard JJ, Brown SA, Horan WP, et al. : Substance use disorders in schizophrenia: review, integration, and a proposed model . Clin Psychol Rev 2000 ; 20:207–234 Crossref , Medline , Google Scholar
17 Dixon L : Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes . Schizophr Res 1999 ; 35(Suppl):S93–S100 Crossref , Medline , Google Scholar
18 Lysaker PH, Carcione A, Dimaggio G, et al. : Metacognition amidst narratives of self and illness in schizophrenia: associations with neurocognition, symptoms, insight and quality of life . Acta Psychiatr Scand 2005 ; 112:64–71 Crossref , Medline , Google Scholar
10.1016/j.cpr.2014.04.004 Crossref , Medline , Google Scholar
20 Lysaker PH, Buck KD, Ringer JM : The recovery of metacognitive capacity in schizophrenia across 32 months of individual psychotherapy: a case study . Psychother Res 2007 ; 17:713–720 Crossref , Google Scholar
21 Hillis JD, Leonhardt BL, Vohs JL, et al. : Metacognitive reflective and insight therapy for people in early phase of a schizophrenia spectrum disorder . J Clin Psychol 2015 ; 71:125–135 Crossref , Medline , Google Scholar
22 Buck KD, Roe D, Yanos P, et al. : Challenges to assisting with the recovery of personal identity and wellness for persons with serious mental illness: considerations for mental health professionals . Psychosis 2012 ; 5:127–133 Google Scholar
23 De Jong S, Van Donkersgoed R, Pijnenborg GHM, et al. : Metacognitive reflection and insight therapy (MERIT) with a patient with severe symptoms of disorganization . J Clin Psychol 2016 ; 72:164–174 Crossref , Medline , Google Scholar
- The Effectiveness of Acceptance and Commitment-Based Therapy on Coping Styles, Distress Tolerance and Metacognitive Beliefs in Substance-Dependent Individuals 1 March 2024 | Research on Addiction, Vol. 17, No. 70
- A Guide for the Implementation of Group-Based Metacognitive Reflection and Insight Therapy (MERITg) 16 September 2022 | Journal of Contemporary Psychotherapy, Vol. 53, No. 1
- Conceptualisation and Measurement of Reflective Process in Psychotherapy: A Systematic Scoping Review 23 September 2022 | Journal of Contemporary Psychotherapy, Vol. 53, No. 1
- Addressing Schizotypy in Metacognitive Reflection and Insight Therapy 10 October 2023
- “I’d Be A Completely Different Person if I Hadn’t Gone to Therapy”: A Qualitative Study of Metacognitive Therapy and Recovery Outcomes in Adults with Schizophrenia 11 November 2021 | Psychiatry, Vol. 85, No. 3
- Introspective accuracy for substance use across a year of treatment for first episode psychosis Schizophrenia Research: Cognition, Vol. 26
- Metacognitive function and fragmentation in schizophrenia: Relationship to cognition, self-experience and developing treatments Schizophrenia Research: Cognition, Vol. 19
- <p>Metacognitive Reflection and Insight Therapy: A Recovery-Oriented Treatment Approach for Psychosis</p> 1 April 2020 | Psychology Research and Behavior Management, Vol. Volume 13
- Disturbances in Self-Experience in Schizophrenia: Metacognition and the Development of an Integrative Recovery-Oriented Individual Psychotherapy 11 December 2018 | Psychopathology, Vol. 52, No. 2
- A Disorder by Any Other Name: Metacognition, Schizophrenia, and Diagnostic Practice 18 July 2018 | Journal of Humanistic Psychology, Vol. 59, No. 1
- Metacognitive deficits and social functioning in schizophrenia across symptom profiles: A latent class analysis 27 March 2019 | Journal of Experimental Psychopathology, Vol. 10, No. 1
- Jay A. Hamm , Psy.D. , and
- Paul H. Lysaker , Ph.D.
- Promoting recovery from severe mental illness: Implications from research on metacognition and metacognitive reflection and insight therapy World Journal of Psychiatry, Vol. 8, No. 1
- Metacognition
- Psychotherapy
- Schizophrenia
- Substance use
Please wait, while we are loading the content...
Similar Documents
Case studies in schizophrenia., chromosome studies in schizophrenia, association of the 3′ region of comt with schizophrenia in taiwan, case studies in schizophrenia, improving social cognition in people with schizophrenia with rc2s: two single-case studies, complete agenesis of the corpus callosum in paranoid schizophrenia—a case report, erratum to: schizophrenia patient or spiritually advanced personality a qualitative case analysis, studies in schizophrenia: a multidisciplinary approach to mind-brain relationships, improving social cognition in people with schizophrenia with rc2s: two single-case studies, about national digital library of india (ndli).
National Digital Library of India (NDLI) is a virtual repository of learning resources which is not just a repository with search/browse facilities but provides a host of services for the learner community. It is sponsored and mentored by Ministry of Education, Government of India, through its National Mission on Education through Information and Communication Technology (NMEICT). Filtered and federated searching is employed to facilitate focused searching so that learners can find the right resource with least effort and in minimum time. NDLI provides user group-specific services such as Examination Preparatory for School and College students and job aspirants. Services for Researchers and general learners are also provided. NDLI is designed to hold content of any language and provides interface support for 10 most widely used Indian languages. It is built to provide support for all academic levels including researchers and life-long learners, all disciplines, all popular forms of access devices and differently-abled learners. It is designed to enable people to learn and prepare from best practices from all over the world and to facilitate researchers to perform inter-linked exploration from multiple sources. It is developed, operated and maintained from Indian Institute of Technology Kharagpur.
Learn more about this project from here .
NDLI is a conglomeration of freely available or institutionally contributed or donated or publisher managed contents. Almost all these contents are hosted and accessed from respective sources. The responsibility for authenticity, relevance, completeness, accuracy, reliability and suitability of these contents rests with the respective organization and NDLI has no responsibility or liability for these. Every effort is made to keep the NDLI portal up and running smoothly unless there are some unavoidable technical issues.
Ministry of Education, through its National Mission on Education through Information and Communication Technology (NMEICT), has sponsored and funded the National Digital Library of India (NDLI) project.
Contact National Digital Library of India
Cite this content.
Sophia Melo Gomes
Write my essay for me frequently asked questions

Reset password
Email not found.
Viola V. Madsen
Finished Papers
Team of Essay Writers
Customer Reviews

Our team of writers is native English speakers from countries such as the US with higher education degrees and go through precise testing and trial period. When working with EssayService you can be sure that our professional writers will adhere to your requirements and overcome your expectations. Pay your hard-earned money only for educational writers.
Paper Writing Service Price Estimation
- Individual approach
- Fraud protection
- Admission/Application Essay
- Annotated Bibliography
- Argumentative Essay
- Book Report Review
- Dissertation
Customer Reviews

IMAGES
VIDEO
COMMENTS
Schizophernia case presentation. 1. Case Presentation on Schizophernia Presenter : Dr Shubham Sadh 3rd Year PG Scholar Guide: Dr Suhas Kumar Shetty Professor. 2. Vital Data • Name : ABC • Age : 33 yrs • Sex : Male • Address : • Religion : Hindu • Education: Post Graduation • Occupation : business • Marital status: Unmarried. 3.
8. PRUNING HYPOTHESIS • Based on the observation that schizophrenia tends to run in families • A group at Harvard Medical School examined the C4 gene, which codes for complement component 4, because it has the strongest ties to schizophrenia. (C4 is part of the immune system pathway that eliminates pathogens and cell debris.) • Found that C4 was expressed at much higher levels in ...
SCHIZOPHRENIA CASE PRESENTATION. Health & Medicine. 1 of 75. Download now. Download to read offline. Schizophrenia case presentation. Schizophrenia case presentation. - Download as a PDF or view online for free.
6. CLINICAL SYMPTOMS OF SCHIZOPHRENIA TYPES SYMPTOMS POSITIVE "Positive" symptoms are referred to as positive because the symptoms are additional behaviors not generally seen in healthy people. For some people, these symptoms come and go. For others, the symptoms become stable over time. Includes: Hallucination, Delusion, Thought & Movement Behavior NEGATIVE "Negative" symptoms refer ...
235045552 case-study-on-schizophrenia - Download as a PDF or view online for free
Case study on schizophrenia. The document provides background information on a case study about a 48-year-old female patient diagnosed with schizophrenia, undifferentiated type. It includes sections on her personal history, symptoms, diagnosis, treatment at a mental health facility over 14 years, and theories about the causes and ...
9. Related disorders • Schizophreniform disorder - symptoms of schizophrenia but for less than 6 months necessary to meet the diagnostic criteria. Social or occupational functioning may or may not be impaired • Delusional disorder - client has one or more delusions, psychosocial functioning is not markedly impaired, and behavior is not obvious odd or bizarre • Brief psychotic ...
Schizophrenia. Unfolding Case Study By Amanda Eymard , DNS, RN and Linda Manfrin-Ledet , DNS, APRN. Assigned Reading to be completed prior to case study. Prior to conducting this unfolding case study, students should read the following: 3.84k views • 82 slides. Schizophrenia. Schizophrenia. Lecture of 2-14-07. Symptoms.
This slide deck covers the course, natural history and prognosis of schizophrenia. Other slides discuss the key components of non-adherence in patients with schizophrenia, highlighting the value of a support system. This slide deck has been developed in collaboration with the former Lundbeck International Neuroscience Foundation.
Case Study: Bryant. Thirty-five-year-old Bryant was admitted to the hospital because of ritualistic behaviors, depression, and distrust. At the time of admission, prominent ritualistic behaviors and depression misled clinicians to diagnose Bryant with obsessive-compulsive disorder (OCD). Shortly after, psychotic symptoms such as disorganized ...
Introduction. Schizophrenia is a chronic severe mental illness with heterogeneous clinical profile and debilitating course. Research shows that clinical features, severity of illness, prognosis, and treatment of schizophrenia vary depending on the age of onset of illness.[1,2] Hence, age-specific research in schizophrenia has been emphasized.Although consistency has been noted in ...
At least one of these must be (1), (2), or (3): Delusions. Hallucinations. Disorganized speech (e.g., frequent derailment or incoherence). Grossly disorganized or catatonic behavior. Negative symptoms (i.e., diminished emotional expression or avolition). Decreased functioning 2.6 months of symptoms with 1 month meeting criterion A. 3.Not ...
This presentation covers aetiology of Schizophrenia. A working knowledge of the normal structure and function of the nervous system is key to understanding psychiatric disorders like schizophrenia. This slide deck presents an introduction to neuroanatomy, the key components of neurosynaptic transmission, neurotransmitters and the ...
Decrements in metacognitive functioning, or the ability to form complex and integrated representations of oneself and others, have been identified as a core feature of schizophrenia. These deficits have been observed to be largely independent of the severity of psychopathology and neurocognitive functioning and are linked to poor outcomes for those with the disorder. This study is a case ...
Schizophrenia is a chronic and severe mental disorder characterized by distortions in thinking, perception, emotions, language, sense of self, and behaviour. This report presents the role of clinical pharmacists in the management of a patient diagnosed with schizophrenia with symptoms of paranoia. A gainfully employed young African male adult reported to be roaming around town moving from one ...
predominance. Schizophrenia is socioeconomic burden with suicidal rate of 10% and expense of .021.65% o- f GDP spent on treatment. -morbid factors associated with Other co Schizophrenia are diabetes, Obesity, HIV infection many metabolic disorders etc. Clinically, schizophrenia is a syndrome of variables symptoms, but profoundly disruptive,
Case study: Schizophrenia Dr.Amra Ahsan* Abstract Ms. S.K. was an unmarried 21 years old, female, single, from middle socio-economic status, came with grandmother along with the complaints of abusive and assaultive behaviour, suspiciousness, bouts of cry, talking to self, laughing without reason from 3 years. On Mental Status Examination,
Case Studies in Schizophrenia; Loading... Please wait, while we are loading the content... 2019 2018 2017 2016 2015 2014 2013 2012 2011 2010 2009 2008 2007 2006 2005 2004 2003 2002 2001 2000 ... Joint Study of Extracranial Arterial Occlusion: V. Progress Report of Prognosis Following Surgery or Nonsurgical Treatment for Transient Cerebral ...
Case Study Scenario Patient with Schizophrenia:- An adult male who was seen at a psychiatric unit complained of hearing voices for the past 10 months and loss of appetite. - He also complained that he roamed around town, and even though he returned home, he was sometimes physically abusive to his mother and sister.
Case Study On Schizophrenia Slideshare. 11 Customer reviews. Toll free 1 (888)499-5521 1 (888)814-4206. ID 28506. View Property. Submit. Nursing Management Business and Economics Psychology +113.
Schizophrenia Case Study Slideshare: 4.8/5. The experts well detail out the effect relationship between the two given subjects and underline the importance of such a relationship in your writing. Our cheap essay writer service is a lot helpful in making such a write-up a brilliant one. View Sample.
Schizophrenia Case Study Slideshare, Arguement Essay, Essay On Coleridges Kubla Khan, Write My Medicine Argumentative Essay, Do I Need A 2nd Cover Letter For A 2nd Interview, What Is The Length Of A Cover Letter, Woody 2000 Case Study Answers Alamat kami ...
Case Study On Schizophrenia Slideshare. As we have previously mentioned, we value our writers' time and hard work and therefore require our clients to put some funds on their account balance. The money will be there until you confirm that you are fully satisfied with our work and are ready to pay your paper writer.