Nutrition in medical education: a systematic review
Affiliations.
- 1 Discipline of Nutrition and Dietetics, Faculty of Medical Health Sciences, The University of Auckland, Auckland, New Zealand. Electronic address: [email protected].
- 2 Menzies Health Institute Queensland, Griffith University, Gold Coast, QLD, Australia.
- 3 Strategic Communication Chair Group, Wageningen University, Wageningen, Netherlands.
- PMID: 31538623
- DOI: 10.1016/S2542-5196(19)30171-8
Background: In many countries, doctors are recommended to provide nutrition care to patients to improve the dietary behaviours of individuals and populations. Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students.
Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel patients, from Nov 1, 2012, to Dec 31, 2018. Search terms related to medical students included "nutrition in medical education", "medical nutrition education", and "undergraduate medical nutrition education". Search terms for topic of interest included "nutrition", "knowledge", "skills", "nutrition counselling", "confidence", "nutrition care", or "nutrition education". Included studies examined any aspect of recently graduated (ie, ≤4 years) or current medical students' nutrition knowledge, attitudes, skills, or confidence (or all three) in nutrition or nutrition counselling; evaluated nutrition curriculum initiatives for medical students; or assessed recently graduated or current medical students' perceptions of nutrition education. Quality assessment appraisal of the studies was done using a Mixed Methods Appraisal Tool. Curriculum initiatives were also appraised.
Findings: 66 studies were identified by the search and 24 were eligible for full-text analysis. 16 quantitative studies, three qualitative studies, and five curriculum initiatives from the USA (n=11), Europe (n=4), the Middle East (n=1), Africa (n=1), and Australasia (n=7) met the inclusion criteria. Our analysis of these studies showed that nutrition is insufficiently incorporated into medical education, regardless of country, setting, or year of medical education. Deficits in nutrition education affect students' knowledge, skills, and confidence to implement nutrition care into patient care. A modest positive effect was reported from curriculum initiatives.
Interpretation: Despite the centrality of nutrition to healthy lifestyle, medical students are not supported to provide high-quality, effective nutrition care. Medical education can be enhanced by institutional commitment to make nutrition education compulsory in medical training, establishment of nutrition competencies to provide a benchmark for nutrition knowledge and skills to be included in curricula, and supported by funding for innovative curriculum initiatives. These initiatives will improve nutrition in medical training to support future doctors for the 21st century.
Funding: Sir John Logan Campbell Medical Fellowship 2017, and an Australian National Health and Medical Research Council Fellowship.
Copyright © 2019 The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY-NC-ND 4.0 license. Published by Elsevier Ltd.. All rights reserved.

Publication types
- Research Support, Non-U.S. Gov't
- Systematic Review
- Curriculum*
- Education, Medical, Undergraduate*
- Nutrition Assessment*
- Nutritional Status*
- Students, Medical*
- Help & FAQ
Nutrition in medical education: a systematic review
- Strategic Communication
Research output : Contribution to journal › Article › Academic › peer-review
Background: In many countries, doctors are recommended to provide nutrition care to patients to improve the dietary behaviours of individuals and populations. Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel patients, from Nov 1, 2012, to Dec 31, 2018. Search terms related to medical students included “nutrition in medical education”, “medical nutrition education”, and “undergraduate medical nutrition education”. Search terms for topic of interest included “nutrition”, “knowledge”, “skills”, “nutrition counselling”, “confidence”, “nutrition care”, or “nutrition education”. Included studies examined any aspect of recently graduated (ie, ≤4 years) or current medical students' nutrition knowledge, attitudes, skills, or confidence (or all three) in nutrition or nutrition counselling; evaluated nutrition curriculum initiatives for medical students; or assessed recently graduated or current medical students' perceptions of nutrition education. Quality assessment appraisal of the studies was done using a Mixed Methods Appraisal Tool. Curriculum initiatives were also appraised. Findings: 66 studies were identified by the search and 24 were eligible for full-text analysis. 16 quantitative studies, three qualitative studies, and five curriculum initiatives from the USA (n=11), Europe (n=4), the Middle East (n=1), Africa (n=1), and Australasia (n=7) met the inclusion criteria. Our analysis of these studies showed that nutrition is insufficiently incorporated into medical education, regardless of country, setting, or year of medical education. Deficits in nutrition education affect students' knowledge, skills, and confidence to implement nutrition care into patient care. A modest positive effect was reported from curriculum initiatives. Interpretation: Despite the centrality of nutrition to healthy lifestyle, medical students are not supported to provide high-quality, effective nutrition care. Medical education can be enhanced by institutional commitment to make nutrition education compulsory in medical training, establishment of nutrition competencies to provide a benchmark for nutrition knowledge and skills to be included in curricula, and supported by funding for innovative curriculum initiatives. These initiatives will improve nutrition in medical training to support future doctors for the 21st century. Funding: Sir John Logan Campbell Medical Fellowship 2017, and an Australian National Health and Medical Research Council Fellowship.
This output contributes to the following UN Sustainable Development Goals (SDGs)
Access to Document
- 10.1016/S2542-5196(19)30171-8 Licence: CC BY-NC-ND
Fingerprint
- Nutrition Social Sciences 100%
- Systematic Review Medicine and Dentistry 100%
- Skill Medicine and Dentistry 71%
- Curriculum Social Sciences 37%
- Skills Social Sciences 31%
- Patient Medicine and Dentistry 28%
- Analysis Medicine and Dentistry 28%
- Counseling Medicine and Dentistry 28%
T1 - Nutrition in medical education: a systematic review
AU - Crowley, Jennifer
AU - Ball, Lauren
AU - Hiddink, Gerrit Jan
PY - 2019/9/1
Y1 - 2019/9/1
N2 - Background: In many countries, doctors are recommended to provide nutrition care to patients to improve the dietary behaviours of individuals and populations. Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel patients, from Nov 1, 2012, to Dec 31, 2018. Search terms related to medical students included “nutrition in medical education”, “medical nutrition education”, and “undergraduate medical nutrition education”. Search terms for topic of interest included “nutrition”, “knowledge”, “skills”, “nutrition counselling”, “confidence”, “nutrition care”, or “nutrition education”. Included studies examined any aspect of recently graduated (ie, ≤4 years) or current medical students' nutrition knowledge, attitudes, skills, or confidence (or all three) in nutrition or nutrition counselling; evaluated nutrition curriculum initiatives for medical students; or assessed recently graduated or current medical students' perceptions of nutrition education. Quality assessment appraisal of the studies was done using a Mixed Methods Appraisal Tool. Curriculum initiatives were also appraised. Findings: 66 studies were identified by the search and 24 were eligible for full-text analysis. 16 quantitative studies, three qualitative studies, and five curriculum initiatives from the USA (n=11), Europe (n=4), the Middle East (n=1), Africa (n=1), and Australasia (n=7) met the inclusion criteria. Our analysis of these studies showed that nutrition is insufficiently incorporated into medical education, regardless of country, setting, or year of medical education. Deficits in nutrition education affect students' knowledge, skills, and confidence to implement nutrition care into patient care. A modest positive effect was reported from curriculum initiatives. Interpretation: Despite the centrality of nutrition to healthy lifestyle, medical students are not supported to provide high-quality, effective nutrition care. Medical education can be enhanced by institutional commitment to make nutrition education compulsory in medical training, establishment of nutrition competencies to provide a benchmark for nutrition knowledge and skills to be included in curricula, and supported by funding for innovative curriculum initiatives. These initiatives will improve nutrition in medical training to support future doctors for the 21st century. Funding: Sir John Logan Campbell Medical Fellowship 2017, and an Australian National Health and Medical Research Council Fellowship.
AB - Background: In many countries, doctors are recommended to provide nutrition care to patients to improve the dietary behaviours of individuals and populations. Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel patients, from Nov 1, 2012, to Dec 31, 2018. Search terms related to medical students included “nutrition in medical education”, “medical nutrition education”, and “undergraduate medical nutrition education”. Search terms for topic of interest included “nutrition”, “knowledge”, “skills”, “nutrition counselling”, “confidence”, “nutrition care”, or “nutrition education”. Included studies examined any aspect of recently graduated (ie, ≤4 years) or current medical students' nutrition knowledge, attitudes, skills, or confidence (or all three) in nutrition or nutrition counselling; evaluated nutrition curriculum initiatives for medical students; or assessed recently graduated or current medical students' perceptions of nutrition education. Quality assessment appraisal of the studies was done using a Mixed Methods Appraisal Tool. Curriculum initiatives were also appraised. Findings: 66 studies were identified by the search and 24 were eligible for full-text analysis. 16 quantitative studies, three qualitative studies, and five curriculum initiatives from the USA (n=11), Europe (n=4), the Middle East (n=1), Africa (n=1), and Australasia (n=7) met the inclusion criteria. Our analysis of these studies showed that nutrition is insufficiently incorporated into medical education, regardless of country, setting, or year of medical education. Deficits in nutrition education affect students' knowledge, skills, and confidence to implement nutrition care into patient care. A modest positive effect was reported from curriculum initiatives. Interpretation: Despite the centrality of nutrition to healthy lifestyle, medical students are not supported to provide high-quality, effective nutrition care. Medical education can be enhanced by institutional commitment to make nutrition education compulsory in medical training, establishment of nutrition competencies to provide a benchmark for nutrition knowledge and skills to be included in curricula, and supported by funding for innovative curriculum initiatives. These initiatives will improve nutrition in medical training to support future doctors for the 21st century. Funding: Sir John Logan Campbell Medical Fellowship 2017, and an Australian National Health and Medical Research Council Fellowship.
U2 - 10.1016/S2542-5196(19)30171-8
DO - 10.1016/S2542-5196(19)30171-8
M3 - Article
C2 - 31538623
AN - SCOPUS:85072169906
SN - 2542-5196
SP - e379-e389
JO - The Lancet Planetary Health
JF - The Lancet Planetary Health
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,882,693 articles, preprints and more)
- Full text links
- Citations & impact
- Similar Articles
Nutrition in medical education: a systematic review.
Author information, affiliations.
- Crowley J 1
- Hiddink GJ 3
ORCIDs linked to this article
- Ball L | 0000-0002-5394-0931
- Crowley J | 0000-0003-1519-4429
The Lancet. Planetary Health , 01 Sep 2019 , 3(9): e379-e389 https://doi.org/10.1016/s2542-5196(19)30171-8 PMID: 31538623
Abstract
Interpretation, full text links .
Read article at publisher's site: https://doi.org/10.1016/s2542-5196(19)30171-8
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Smart citations by scite.ai Smart citations by scite.ai include citation statements extracted from the full text of the citing article. The number of the statements may be higher than the number of citations provided by EuropePMC if one paper cites another multiple times or lower if scite has not yet processed some of the citing articles. Explore citation contexts and check if this article has been supported or disputed. https://scite.ai/reports/10.1016/s2542-5196(19)30171-8
Article citations, general practitioners' experiences of providing lifestyle advice to patients with depression: a qualitative focus group study..
Astaire E , Jennings L , Khundakar M , Silverio SA , Flynn AC
PLoS One , 19(3):e0299934, 11 Mar 2024
Cited by: 0 articles | PMID: 38466705 | PMCID: PMC10927082
The Impact of Education Level on Individual Lifestyle Behaviors among Dietetics Students and Professionals.
Popiolek-Kalisz J , Cakici C , Szczygiel K , Przytula A
Clocks Sleep , 6(1):85-96, 10 Feb 2024
Cited by: 0 articles | PMID: 38390948 | PMCID: PMC10885025
Experiences of Vegans with General Practitioners in the Austrian Health Care System: A Qualitative Study.
Jirovsky-Platter E , Wakolbinger M , Kühn T , Hoffmann K , Rieder A , Haider S
Nutrients , 16(3):392, 29 Jan 2024
Cited by: 0 articles | PMID: 38337677 | PMCID: PMC10856837
Gut microbiota, nutrition, and mental health.
Merlo G , Bachtel G , Sugden SG
Front Nutr , 11:1337889, 09 Feb 2024
Cited by: 0 articles | PMID: 38406183 | PMCID: PMC10884323
FOODWISE (Fostering Optimal Outcomes through Dietary Wisdom, Integration, Spirituality, and Emotionality): A New Model of Integrative Culinary Medicine.
Ring M , Mehta DH , Majd I , Balabanova Shannahan A
J Integr Complement Med , 30(2):95-98, 24 Jan 2024
Cited by: 0 articles | PMID: 38265807 | PMCID: PMC10886423
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Australian and New Zealand Medical Students' Attitudes and Confidence Towards Providing Nutrition Care in Practice.
Lepre B , Crowley J , Mpe D , Bhoopatkar H , Mansfield KJ , Wall C , Beck EJ
Nutrients , 12(3):E598, 25 Feb 2020
Cited by: 6 articles | PMID: 32106539 | PMCID: PMC7146386
Student and educator experiences of maternal-child simulation-based learning: a systematic review of qualitative evidence protocol.
MacKinnon K , Marcellus L , Rivers J , Gordon C , Ryan M , Butcher D
JBI Database System Rev Implement Rep , 13(1):14-26, 01 Jan 2015
Cited by: 18 articles | PMID: 26447004
Impact of an Expansion of a Clinical Nutrition Curriculum on Pre-Clerkship Medical Students' Perception of Their Knowledge and Skills Related to Performing a Nutritional Assessment.
Keel T , Olvet DM , Cavuoto Petrizzo M , John JT , Dougherty R , Sheridan EM
Nutrients , 13(11):4081, 15 Nov 2021
Cited by: 0 articles | PMID: 34836343 | PMCID: PMC8625690
Patient safety education for undergraduate medical students: a systematic review.
Nie Y , Li L , Duan Y , Chen P , Barraclough BH , Zhang M , Li J
BMC Med Educ , 11:33, 14 Jun 2011
Cited by: 56 articles | PMID: 21669007 | PMCID: PMC3128569
The educational effects of portfolios on undergraduate student learning: a Best Evidence Medical Education (BEME) systematic review. BEME Guide No. 11.
Buckley S , Coleman J , Davison I , Khan KS , Zamora J , Malick S , Morley D , Pollard D , Ashcroft T , Popovic C , Sayers J
Med Teach , 31(4):282-298, 01 Apr 2009
Cited by: 172 articles | PMID: 19404891
Europe PMC is part of the ELIXIR infrastructure
Nutrition in medical education: a systematic review
Author: crowley, jennifer, author: ball, lauren, author: hiddink, gerrit jan.
Background: In many countries, doctors are recommended to provide nutrition care to patients to improve the dietary behaviours of individuals and populations. Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel patients, from Nov 1, 2012, to Dec 31, 2018. Search terms related to medical students included “nutrition in medical education”, “medical nutrition education”, and “undergraduate medical nutrition education”. Search terms for topic of interest included “nutrition”, “knowledge”, “skills”, “nutrition counselling”, “confidence”, “nutrition care”, or “nutrition education”. Included studies examined any aspect of recently graduated (ie, ≤4 years) or current medical students' nutrition knowledge, attitudes, skills, or confidence (or all three) in nutrition or nutrition counselling; evaluated nutrition curriculum initiatives for medical students; or assessed recently graduated or current medical students' perceptions of nutrition education. Quality assessment appraisal of the studies was done using a Mixed Methods Appraisal Tool. Curriculum initiatives were also appraised. Findings: 66 studies were identified by the search and 24 were eligible for full-text analysis. 16 quantitative studies, three qualitative studies, and five curriculum initiatives from the USA (n=11), Europe (n=4), the Middle East (n=1), Africa (n=1), and Australasia (n=7) met the inclusion criteria. Our analysis of these studies showed that nutrition is insufficiently incorporated into medical education, regardless of country, setting, or year of medical education. Deficits in nutrition education affect students' knowledge, skills, and confidence to implement nutrition care into patient care. A modest positive effect was reported from curriculum initiatives. Interpretation: Despite the centrality of nutrition to healthy lifestyle, medical students are not supported to provide high-quality, effective nutrition care. Medical education can be enhanced by institutional commitment to make nutrition education compulsory in medical training, establishment of nutrition competencies to provide a benchmark for nutrition knowledge and skills to be included in curricula, and supported by funding for innovative curriculum initiatives. These initiatives will improve nutrition in medical training to support future doctors for the 21st century. Funding: Sir John Logan Campbell Medical Fellowship 2017, and an Australian National Health and Medical Research Council Fellowship.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Med Educ
A review of primary healthcare practitioners’ views about nutrition: implications for medical education
Clare carter.
1 School of Pharmacy, Faculty of Medicine and Health, University of Sydney, New South Wales 2006 Australia
Joanna E. Harnett
Ingrid c. gelissen, associated data.
This study aimed to review literature that reports on the perspectives and opinions of Australian and New Zealand primary healthcare practitioners on their role in nutrition counselling of their patients.
A systematic search of relevant articles reporting on attitudes towards nutrition counselling by Australian and New Zealand doctors/physicians, nurses including midwives, pharmacists and dentists was conducted. The search included literature from the past ten years until March 2021 and identified 21 relevant papers, with most of the studies including medical practitioners and nurses.
Three main themes were identified from qualitative and quantitative data, which included education and training, practitioner experiences and challenges. Consistent with previous literature, health care practitioners acknowledged their important role in the provision of dietary advice to patients. Challenges that influenced the provision of this advice included insufficient education and training, time constraints and limited knowledge and confidence. Time constraints during normal consultations led to a low priority of nutrition counselling. An absence of assessment opportunities to demonstrate nutrition competence and limited coverage of specific nutrition-related advice during training were also reported.
Conclusions
Primary healthcare practitioners acknowledge the importance of playing a role in the provision of nutrition advice but require education and access to evidence-based information that can be utilised effectively within the time constraints of standard consultations. Medical education curricula can be improved to provide more emphasis on nutrition education, including relevant assessment opportunities.
Introduction
The World Health Organisation (WHO) describes nutrition as a ‘fundamental pillar of human life, health and development across the entire life span’. 1 The rise in poor dietary habits, underpinned by the consumption of energy-dense foods high in saturated and trans-fats, refined sugars, and excess salt, has precipitated a worldwide epidemic of non-communicable diseases. 2 Nutrition is a key modifiable determinant of non-communicable diseases, for which evidence illustrates the impact of changing dietary patterns on health outcomes. 2 More specifically, dietary interventions play a crucial role in the prevention and treatment strategy of chronic diseases, including diabetes, cardiovascular disease and hypertension. 2 In 2017, dietary risk factors accounted for 11 million deaths globally. 3
In addition to the valuable role of dieticians, who are instrumental in the education of patients with existing chronic diseases, it has been recognised worldwide that primary healthcare practitioners can also play a fundamental role in the provision of evidence-based nutrition information to patients. 4 For the purpose of this study, the term ‘primary healthcare practitioners’ describes medical doctors/physicians, pharmacists, nurses and/or dentists. Primary healthcare practitioners are regarded as a relatively large, affordable, and accessible community for whom the implementation of strategies to guide the provision of nutrition care could be advantageous. This is apparent in rural settings where access to dieticians may be limited. 5 , 6 An understanding about the knowledge, skills and attitudes of primary healthcare practitioners towards their role in the promotion of healthy nutrition is warranted.
While several studies have reported healthcare practitioners’ perceptions about dietary counselling, a comprehensive review of literature including primary healthcare practitioners of Australia and New Zealand has previously not been conducted. 7 , 8 Therefore, the aim of this review was to identify and summarise the current literature that documents primary healthcare practitioners’ self-perceived knowledge and opinions about the role and readiness to counsel patients on healthy nutrition. The findings of this review will inform the development of education initiatives that aim to equip primary healthcare practitioners with the knowledge and skills required to provide dietary counselling to their patients.
A systematic search and review, as described by Grant and Booth was conducted to identify and summarise peer-reviewed literature that reported perspectives of Australian and New Zealand primary healthcare practitioners about their knowledge and readiness to counsel patients in nutrition. 9 Australia and New Zealand were chosen due to socio-demographic similarities of the populations and similarities in the training of primary health care practitioners.
Search Strategy
Medline, Embase, Web of Science and Scopus were searched for key concepts related to nutrition and primary healthcare practitioners’ provision of dietary counselling. Google Scholar was also searched to capture any articles not identified in the main search. The search was conducted between 19th March and 9th April 2021. The inclusion/exclusion criteria were agreed upon by three authors, and a University of Sydney Faculty of Medicine and Health librarian was consulted regarding the search strategy. The following studies were included: original research studies conducted in Australia and New Zealand adults, written in English, reporting on primary healthcare practitioners’ opinions about dietary counselling, involving doctors/physicians, nurses (including midwives), pharmacists and dentists. Only articles from the past ten years were included to align as much as possible with the most recent curricula provided to health care practitioners. Studies were excluded if they involved allied healthcare professionals, including dieticians, physiotherapists, occupational therapists, chiropractors, naturopaths and complementary medicine practitioners (e.g., herbalists) and complementary medicine products. In addition, any studies involving participants who were students were also excluded. Furthermore, review articles, books, policy documents and conference proceedings were excluded, as were articles in languages other than English or those involving countries other than Australia and New Zealand. Search results were uploaded into EndNote, and duplicates were removed. Titles and abstracts were screened by one author (C.C.) and checked by two additional authors (I.G. and J.H.). Full-text articles included in the study were screened by three authors (C.C., I.G. and J.H.) to confirm eligibility and extraction of relevant data as outlined below. A PRISMA flow diagram of the literature search methodology is included in Appendix 1 .
Data extraction and analysis
Data were extracted, summarised, and tabulated using author, year of publication, aims, study method, sample population and sampling methods, as well as key findings and outcomes ( Table 1 ). As the survey tools utilised in the studies varied substantially, including qualitative data generated from interviews and focus groups, further analysis was performed to assist in the interpretation and organisation of data, utilising the six phases of analysis by Braun and Clarke. 10 This included initial data familiarisation and key concept identification by one author (C.C.), followed by coding and identification of meta themes and sub-themes agreed upon by three authors (C.C., I.G. and J.H.). Discussions throughout the analysis process allowed for consensus between members of the research team regarding the interpretation of data, theme conceptualisation and naming.
*GP = General Practitioner; **Articles also investigated other population samples, including primary healthcare practitioners from other countries, allied health practitioners, students, and the general population. These findings were excluded from our analyses.
A total of 520 articles were identified in the literature search, with an additional article retrieved through Google Scholar. Following the title and abstract screening of 382 articles, 30 articles were assessed for suitability against our inclusion criteria and critically evaluated, with a total of 21 articles included in the systematic review.
An overview of the studies is presented in Table 1 , including the aim, the population studied, the methods utilised, and the major findings reported by the authors. With regards to the primary healthcare practitioners sampled in the articles, the following breakdown of healthcare practitioners was found: general practitioners (n=10), general practitioner registrars (n=3), general practitioner interns (n=1), general nurses (n=10), midwives (n=2) and pharmacists (n=1). Participant numbers averaged 125 (range 9 – 393), with 9 out of 21 studies having >100 participants. Study methods included quantitative methods (questionnaires and surveys; n=16 with a mix of paper and online delivery), qualitative methods (semi-structured interviews n=4; focus groups; n=1) and mixed methods (n=1). The predominant sampling method was convenience sampling. The topics covered included general nutrition (n=7), pregnancy (n=5), nutrition and chronic conditions (including type II diabetes; n=4), nutrition and cancer (n=2), and more specialist branches of nutrition (enteral nutrition, malnutrition and dehydration, and nutrition for patients with brain injuries; n=3).
After coding of articles, three meta themes and fourteen subthemes were identified from the qualitative data as well as the topics and outcomes from the quantitative surveys and questionnaire data. Figure 1 illustrates the meta themes, which were 1) education and training, 2) practitioner experiences and 3) challenges, presented in red, with associated sub-themes in blue. Table 2 provides an overview of selected quotes, supporting the meta themes and sub-themes. The quotes were extracted from individual references and reflected the perspectives of the study participants.

Meta themes (red boxes) and associated subthemes (blue boxes)
This review provides a comprehensive overview of primary healthcare practitioners’ perspectives about the counselling of patients in nutrition in Australia and New Zealand. The results illuminate several key factors that influence the opinions of primary healthcare practitioners regarding the provision of nutrition advice to patients. Firstly, primary healthcare practitioners clearly perceive the provision of nutrition advice as their responsibility, with only one article including general practitioners reporting that the provision of detailed nutrition counselling was not considered part of their role. 7 This is consistent with previous literature, suggesting that healthcare professionals should conduct a nutritional assessment, provide basic evidence-based nutrition advice, and refer patients to a dietician when necessary. 4 , 30 - 32 As healthcare practitioners are accessible to a large proportion of the population, this provides opportunities to discuss nutrition, encourage dietary changes and support the long-term maintenance of these dietary changes. 8 , 22 However, uncertainty regarding an operational definition of basic nutrition care was reported by some primary healthcare practitioners, who found it difficult to differentiate their professional roles. 8 , 13 , 18 Clarification of the scope of practice of healthcare practitioners in relation to nutrition may relieve uncertainty and enhance confidence in the delivery of such information. 21 Professional associations could consider the development of a position statement or guiding principles to achieve this outcome.
Secondly, a recurrent sub-theme across the studies reviewed was the perceived value and impact of primary healthcare practitioners on patient health outcomes. 18 , 22 , 26 Perspectives were positive about the impact of dietary counselling on changing patients’ eating patterns, where healthcare practitioners strongly agreed that nutrition is a key determinant of health outcomes. 18 , 22 , 26 , 27 This concurs with the view of the WHO that the provision of nutrition services is associated with improved maternal, infant, and child health, a lower risk of chronic disease and improved life expectancy. 33 Recognition of the crucial role of dietary interventions in the prevention and treatment of non-communicable diseases can influence the frequency of dietary counselling by primary healthcare practitioners. 8 However, while nurses reported that they believed there is considerable evidence to support the success of dietary interventions, the strength or extent of this evidence was unknown to them .26 The lack of awareness of primary healthcare practitioners, prompted by a deficiency in nutrition knowledge, can precipitate negative beliefs about the effectiveness of nutrition interventions. 13 Health professionals, particularly doctors, are shown to influence patients’ nutrient intake; hence there is a need for healthcare practitioners to lead and promote a collaborative nutrition care approach. 34 This may be achieved by ensuring all healthcare practitioners adopt the view that improving their patients’ nutritional habits will improve patient outcomes. 34 Additionally, the development of objective outcome measures to quantify the benefits of nutrition therapy may modify practitioners’ perspectives and help in this matter. 13
Despite the importance of nutrition and its role in the provision of advice to patients, primary healthcare practitioners were often not able to translate this priority into practice due to a lack of education and training, with a clear gap in knowledge identified across several areas of nutrition. 8 , 13 , 15 , 35 This may lead to the provision by practitioners of nutrition education based on personal experiences and perspectives rather than evidence-based guidelines, which can be of concern. 13 , 35 It was also apparent that primary healthcare practitioners’ knowledge deficits impede their confidence in the delivery of nutrition information to patients. 25 , 28 , 29 Lack of evidence-based nutrition knowledge and associated confidence is underpinned by inadequate nutrition education during and after their formal training. 15 , 17 , 23 , 24 This lack of confidence was also noted in a study from Germany, where less than half of general practitioners surveyed believed that they had successfully changed the dietary habits of their patients. 36 Specifically, studies included in this review emphasised an absence of assessment opportunities to demonstrate nutrition competence and limited coverage of specific nutrition-related advice during training. 12 , 15 Following registration, there is often limited availability and accessibility of nutrition education opportunities and resources. It is therefore unsurprising, that another strong theme identified in this review was primary healthcare practitioners’ interest in receiving additional education and training in nutrition. 8 , 20 , 21 , 29 This concurs with the findings of previous studies that identified insufficient education in nutrition, including a lack of nutrition assessment skills that translate into clinical practice. 30 , 35 , 37 Implementation of a comprehensive nutrition curricula into existing Australian and New Zealand curricula and an increase in available educational opportunities and resources is clearly warranted. In Australia, a Nutrition Competency Framework was developed in 2016 to guide the inclusion of several knowledge and skills-based nutrition competencies in Australian medical curricula. This Framework has, however, to our knowledge, not been formally adopted by the Australian Medical Council, which regulates the Australian and New Zealand medical education. In New Zealand, a nutrition syllabus was introduced in 2012 in general practitioners' training. However, the effectiveness of this syllabus remains to be assessed. 38 , 39 A recent comparative analysis of nutrition incorporated into medical curricula worldwide showed that only 44% of the Australia and New Zealand accreditation documents included in the study had requirements for nutrition education. 40 A systematic review of worldwide literature on the provision of nutrition education to medical students also identified a lack of consensus in education worldwide and concluded that medical students are not provided with adequate nutrition training, calling for institutional commitment to improve nutrition education. 41 Clearly, there is scope to improve nutrition education of medical practitioners worldwide, including assessment opportunities.
The capacity of primary healthcare practitioners to guide and provide evidence-based information to patients is further impacted by additional challenges, including time constraints, funding and prioritisation of nutrition. In Australia and New Zealand, primary health practitioners consistently reported that the time length of patient consultations highly influenced their decision to counsel patients on nutrition. 7 , 8 , 25 - 27 , 35 For example, practitioner nurses and general practitioners indicated that 5-10 minutes and 1-5 minutes respectively were spent on discussions on patients’ diet and the provision of nutrition advice. 22 Literature has stressed that building rapport and getting an understanding of the psycho-social requirements of patients is needed to motivate dietary changes of patients – a process that takes significantly longer than a typical 15-minute healthcare practitioner appointment. 37 Time constraints are clearly a major challenge to the provision of nutrition advice; however, this is not a challenge that can be easily addressed as it would require budgets allocated to the provision of healthcare to include funding time for nutrition assessment and recommendations in consultations with patients. 42 Thus, funding is an additional barrier to the implementation of nutrition advice during counselling as healthcare practitioners are not adequately reimbursed. 8 , 22 , 27 Supplementary solutions for current time constraints include improved education concerning the delivery of brief interventions to promote healthy dietary behaviour change within the context of limited time or the collaboration with other staff that may increase practitioners’ time with patients. 21 The challenge of prioritisation of nutrition is linked to the limited time in standard consultations with patients. 13 , 27 , 28 , 35 Whilst increasing practitioners’ knowledge about the importance of nutrition interventions may encourage the provision of nutrition advice, the matter of time continues to lower the priority of nutrition over acute health-related problems.
Although many studies of the perspectives of nurses and doctors were identified, no articles reported on the opinions of dentists towards nutrition counselling. This is an unexpected finding as poor dietary habits are associated with poor dental outcomes, including cavities and gum disease, and poor dental conditions limit individuals food choices. 43 Dental practitioners recognise the essential role of dietary counselling in the prevention of cavities, but infrequently provide brief and non-specific nutrition advice due to a perceived low level of confidence and competence. 43 The literature also reported various challenges, including financial compensation, insufficient education and training, and time constraints. 44 These findings coincide with the perspectives of other primary healthcare practitioners included in this review. Furthermore, only one study included in this review explored the perspectives of pharmacists toward nutrition and dietarycounselling. 17 The Pharmaceutical Society of Australia’s National Competency Standard Framework indicates that the role of pharmacists encompasses the promotion of dietary recommendations that complements the provision of medications. 45 In previous studies, it has been identified that pharmacists’ lack of knowledge and expertise in nutrition was a major limitation in providing dietary counselling. 46 , 47 Additionally, pharmacists strongly agreed that they are an accessible and credible source of nutrition information for patients but reported low confidence in providing this nutrition-based therapy. 48 Hence the perspectives of pharmacists and dentists align with the perspectives of primary healthcare practitioners explored in this review.
Although this study exclusively analysed the opinions of primary healthcare practitioners, dieticians are clearly specialists in providing detailed dietary advice. According to the Australian Government Department of Health, if an individual is diagnosed with a disease where nutrition plays an important role in disease management (e.g., cardiovascular disease or diabetes), general practitioners can provide a General Practitioner Management Plan (GPMP) and Team Care Arrangement (TCA), which entitles the individual to five visits per year to a registered dietician. 49 However, patient access to dieticians may be limited due to socioeconomic factors, remote location, or patient’s health conditions not qualifying them for this rebate. In addition, the GPMP and TCA do not cover the entire cost of appointments, with out-of-pocket gaps having to be paid by patients. 49 Previous reports highlight a shortage of dieticians in rural and regional areas where populations often demonstrate the greatest need for dietary interventions. 6 Limitations that reduce access of patients to dieticians also include the low rate of referrals by practitioners such as physicians related to patient resistance given the cost of dietician services. 50 Lastly, the role of nutrition in disease prevention is clearly as important as the role of dietary changes after patients are diagnosed with a chronic condition. Therefore, there is an increased obligation of primary healthcare practitioners to provide nutrition advice given their feasibility and accessibility, particularly in remote locations.
Limitations
Although a broad and comprehensive search of key databases was conducted, a perceived limitation of this study may have been the exclusion of the database CINAHL. CINAHL was excluded from the search strategy because it predominantly covers allied health practitioners. In addition, participant numbers were small in some of the articles included, in particular qualitative studies that used interviews and focus groups, which may have been due to data saturation. Lastly, convenience sampling was utilised in the majority of studies, which is common in this line of research.
This review has identified several key challenges that influence the provision of nutrition advice to patients by primary health care providers in Australia and New Zealand, including time constraints, insufficient education and training and associated factors such as low knowledge, confidence and low prioritisation of nutrition. There is clearly scope for improving medical education curricula in the area of nutrition counselling. Primary healthcare education needs to include curricula on evidence-based nutrition that can be implemented effectively within the time constraints of a standard consultation to allow adequate patient counselling in nutrition. This would also require further research to investigate whether brief dietary interventions with patients are indeed effective in improving patients’ dietary habits and nutritional status. Lastly, further research should investigate the perspectives of dentists and pharmacists toward nutrition counselling.
Conflict of Interest
The authors declare that they have no conflict of interest.
Supplementary material
Supplementary file 1.
Appendix 1. PRISMA flow diagram of literature search method
- Search Menu
- Themed Collections
- Editor's Choice
- Ilona Kickbusch Award
- Supplements
- Author Guidelines
- Submission Online
- Open Access Option
- Self-Archiving Policy
- About Health Promotion International
- Editorial Board
- Advertising and Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Strengths and limitations of primary research, strength and limitations of this systematic review, recommendations for future practice, data availability statement.
- < Previous
The effectiveness of physical activity interventions in improving higher education students’ mental health: A systematic review
- Article contents
- Figures & tables
- Supplementary Data
Samantha Donnelly, Kay Penny, Mary Kynn, The effectiveness of physical activity interventions in improving higher education students’ mental health: A systematic review, Health Promotion International , Volume 39, Issue 2, April 2024, daae027, https://doi.org/10.1093/heapro/daae027
- Permissions Icon Permissions
Traditional interventions aiming to improve students’ mental health and quality of life include meditation or canine therapy. The development of physical activity-related interventions has increased over the past decade. We aimed to review all studies using physical activity for improving the mental health and quality of life in higher education students whilst describing the interventions, measurements and effectiveness. A systematic search of six electronic databases including: ProQuest, MEDLINE, Embase, CINAHL, SPORTDiscus and CENTRAL, was conducted following PRISMA guidelines. Randomized or non-randomized controlled trial physical activity-related interventions involving higher education students aiming to improve their mental health and quality of life were included. Searches yielded 58 articles with interventions involving martial arts, sport, mind–body exercises and anaerobic exercises. Psychological measures varied across studies including the State Trait Anxiety Inventory, Beck Depression Inventory and the Perceived Stress Scale. Over half of the studies included in this review ( n = 36) were effective in improving students’ mental health or quality of life. Findings from our review suggest that interventions aiming to be effective in improving students’ mental health quality of life should aim to deliver moderate-vigorous intensity exercises such as dance or Pilates. This systematic review was based on a published protocol in PROSPERO (registration number: CRD42022325975).
We searched academic papers to determine the effectiveness of physical activity for improving the mental health and quality of life of higher education students.
We identified various physical activity-related interventions which are effective in improving students’ mental health and quality of life.
We offer recommendations for the design of future interventions aiming to improve the mental health and quality of life of higher education students through physical activity.
The benefits associated with being physically active are well-recognized. Regular participation in physical activity (PA) has been associated with positive long-term influences on obesity, cardiovascular heart disease and type 2 diabetes mellitus in adults ( Reiner et al ., 2013 ) and is also associated with lower depressive symptoms, anxiety and stress ( UK Government, 2019 ). Interest in the role of PA on mental health and quality of life (QoL) has increased over the past few years due to the Coronavirus Disease-19 (COVID-19) outbreak ( Ozdemir et al ., 2020 ). Nevertheless, the known improvements in outcomes relating to mental health (e.g. depression, anxiety, stress, etc.) and QoL (e.g. personal health (physical, mental and spiritual), relationships, education status, work environment, social status, wealth, etc.) through PA have been observed for decades ( Saxena et al ., 2005 ; Acree et al ., 2006 ; Bize et al ., 2007 ; Farris and Abrantes, 2020 ). To gain the health benefits associated with being physically active, the World Health Organization (WHO) provide PA guidelines for adults aged 18–64 years ( World Health Organization, n.d. ). These outline that adults should participate in at least 150–300 min of moderate-intensity aerobic PA or at least 75–150 min of vigorous-intensity activity weekly. The WHO also recommends that adults should also participate in muscle-strengthening activities and limit sedentary time.
Higher education (HE) students are largely recognized as inactive ( Pengpid et al ., 2015 ), with a decline observed in activity from high school into HE ( Bray and Born, 2004 ). College students indicate that the quality of on-campus facilities, need for social support to encourage exercise and lack of time and motivation are barriers to PA ( LaCaille et al ., 2011 ).
In HE students, meeting PA guidelines has been associated with improved physical health and mental health ( Murphy et al ., 2018 ), and less academic stress compared to students who are inactive ( Gasiūnienė and Miežienė, 2021 ). It is unsurprising that a recent systematic review noted a positive relationship between PA and academic performance in HE students across the USA, France and China ( Wunsch et al ., 2021 ). Alarmingly, findings from a study in 23 low-, middle- and high-income countries found that 41.4% of university students were physically inactive ( Pengpid et al ., 2015 ) ranging from 21.9% in Kyrgyzstan to 80.6% in Pakistan. Whilst the benefits of PA for HE students are clear in relation to health and academic performance, globally these students are inactive.
HE is a time of increased autonomy and self-development for students, however, poor diet and PA behaviours can develop, with research highlighting failings of HE organizations in the promotion of PA for their students ( Keating et al ., 2005 ). Additionally, many HE students face issues with their mental health and QoL ranging from anxiety to alcohol use disorders ( Castillo and Schwartz, 2013 ). HE institutions are promising settings to promote PA opportunities, as the target population can be easily reached, whereby interventions to improve the mental health of HE students can be easily administered ( Martinez et al ., 2016 ). In turn, the improvement of mental health through participation in PA can have positive effects on academic performance ( Al-Drees et al ., 2016 ). To attempt to enhance health-related behaviours in HE students, previous studies have relied on psychological-based therapies to remedy HE student’s mental health problems ( Reiner et al ., 2013 ; Binfet, 2017 ). Findings from a systematic review and meta-analysis exploring the use of cognitive behavioural therapies including mindfulness programmes for the treatment of stress, depression and anxiety in students found a medium effect size for stress and anxiety, but a small effect for depression ( González-Valero et al ., 2019 ). Studies examining the effects of canine therapy on university students’ stress have shown that spending time with therapy canines significantly reduces stress ( Binfet, 2017 ; Binfet et al ., 2018 ). Over the past decade, there has been an increase in interventions employing PA or exercise to improve HE student’s mental health and QoL. Although a review has been conducted examining the effectiveness of interventions targeting PA, nutrition and healthy weight for HE students ( Plotnikoff et al ., 2015 ), this current review is the first to investigate the effectiveness of PA-related interventions in improving the QoL and mental health outcomes in HE students.
The objective of this article is to systematically review the evidence available regarding the impact of PA-related interventions to improve mental health and QoL outcomes in HE students to determine the following research questions:
Are PA or exercise interventions effective in improving the mental health and QoL of HE students?
Does effectiveness of the interventions vary according to the length and type of the intervention?
This systematic review was based on a published protocol in PROSPERO—International prospective register of systematic reviews (registration number: CRD42022325975) following PRISMA guidelines ( Page et al ., 2021 ).
Data sources
An exhaustive search was conducted within six databases: ProQuest, MEDLINE, Embase, CINAHL, SPORTDiscus and CENTRAL, only including peer-reviewed journal articles published up until May 2022. The search strategy was developed through a combination of keywords for each database using the Boolean operators ‘OR’ and ‘AND’: (University students OR College students) AND (Physical activity OR exercise OR movement OR physical fitness) AND (Health-related quality of life OR Stress OR depression OR anxiety) AND (Intervention OR Programme OR randomised controlled trial (RCT) OR non-randomised controlled trial (non-RCT)). Only manuscripts written in English were considered. Two reviewers independently assessed articles for initial study inclusion based on title and abstract. Full texts were then retrieved and assessed based on their eligibility for inclusion.
Study inclusion and exclusion criteria
Type of participants.
Any study including on-campus or remote learning HE students (≥18 years old) full-time or part-time, and undergraduate or postgraduate students were included. Students studying vocational training courses or short courses (i.e. less than 6 months duration) were excluded.
Type of interventions
Interventions deemed eligible for inclusion had to include a PA or movement-based component, aiming to improve student’s mental health and/or QoL. Interventions of all lengths and mode of delivery (e.g. online, on-campus, etc.) were included.
Type of studies
Original quantitative studies including RCTs and non-RCTs were eligible for inclusion. Cross-sectional studies, systematic reviews and meta-analyses were not included.
Type of outcome
This review focuses on the psychological effects of the intervention received relating to the mental health and/or QoL of HE students.
Data extraction
The search results were exported to Zotero® to eliminate duplicates. Titles were screened and eligible studies were downloaded onto excel, reviewed for any remaining duplicates missed by Zotero (S.D.) and the abstracts were manually screened by two researchers independently (S.D. and M.K.). If there was any discrepancy, a third investigator (K.P.) was called to reach a mutual consensus amongst the research team. The full texts of these articles were retrieved. Subsequently, the reference lists of selected studies were reviewed (S.D.) to identify additional relevant studies. From all the eligible full-texts, data were extracted by three researchers (S.D., M.K., K.P.). The following summary data were considered: country, study design, sample size, gender, age (range and mean (standard deviation: SD)), diagnoses, intervention characteristics, analysis, outcomes and effectiveness of intervention.
Data analysis
Across all study designs the purpose of the study, specific population of interest (within HE students); type, duration, and follow-up period of the intervention; and specific mental health measures are described with consideration to key attributes of robustness and generalisability. The reported effectiveness of interventions is described for RCT and non-RCT studies, with the comparators also of interest for the RCTs. The theoretical frameworks underpinning interventions are also described. Due to the heterogeneity of study designs, interventions and outcome measures a meta-analysis was not possible.
Risk of bias (ROB)
ROB was assessed, whereby three reviewers (S.D., M.K., K.P.) reviewed all included studies. Thereafter, the reviewers discussed the assessment of the included studies to come to a final agreement of the assessment of each paper. ROB for RCTs was assessed using the revised version 2 of the Cochrane ROB for randomized trials (RoB 2) ( Sterne et al ., 2019 ). The ROB of all included non-RCTs was assessed using the ROBINS-I tool ( Sterne et al ., 2016 ). This tool provides a systematic way to organize and present the available evidence relating to ROB, and by signalling questions, answers can help identify areas of concern regarding ROB. Similarly, to the RoB 2 tool, outcomes for each individual domain are generated alongside an overall ROB outcome.
Results of literature search
The total search retrieved 1,632 records. Following the removal of duplicates, 1,593 records were screened by title, of which 1,444 titles were excluded, and the remaining 149 abstracts were retrieved and screened. The remaining 101 full-text articles were screened, of which 58 publications from 1991 to 2023 met the inclusion criteria (see Figure 1 ). These publications included 38 RCT studies ( Crocker and Grozelle, 1991 ; Brown et al ., 1993 ; Kim et al ., 2004 ; Mailey et al ., 2010 ; Akandere and Demir, 2011 ; Hemat-Far et al ., 2012 ; Kim et al ., 2013 ; Gallego et al ., 2014 ; Zheng et al ., 2015 ; Li et al ., 2015 ; de Vries et al ., 2016 , 2018 ; Sharp and Caperchione, 2016 ; von Haaren et al ., 2016 ; Huang et al ., 2017 ; López-Rodríguez et al ., 2017 ; Albracht-Schulte and Robert-McComb, 2018 ; Schmalzl et al ., 2018 ; Dinani et al ., 2019 ; Eather et al ., 2019 ; Faro et al ., 2019 ; Herbert et al ., 2020 ; Wan Yunus et al ., 2020 ; Zimmermann and Mangelsdorf, 2020 ; Zheng and Ji, 2021 ; Fukui et al ., 2021 ; Saltan and Ankaralı, 2021 ; Xiao et al ., 2021 ; Ji et al ., 2022 ) and 20 non-RCT studies ( O’Connor et al ., 1995 ; Bass et al ., 2002 ; Wang et al ., 2004 ; Caldwell et al ., 2009 ; Tayama et al ., 2012 ; Koschel et al ., 2017 ; Ezati et al ., 2020 ; Muir et al ., 2020 ; deJonge et al ., 2021 ; Marschin and Herbert, 2021 ; Martínez-Díaz and Carrasco, 2021 ; Salehian et al ., 2021 ; Tong et al ., 2021 ; Forseth et al ., 2022 ; La Count et al ., 2022 ).

PRISMA flow diagram.
Characteristics of included studies
Characteristics of the included studies are summarized in Table 1 . Of the 58 included studies, most ( n = 38, 66%) were RCTs. Furthermore, most studies ( n = 17) were from the USA followed by 11 in China, and 6 in Canada. Four studies were from Iran, and three studies were included from both Germany and Spain. Two studies came from Japan, Turkey and the Netherlands, and the remaining countries were associated with one study each; Australia, Belgium, India, Korea, Malaysia, Norway, Taiwan and the UK (see Table 1 ). Only one RCT study reported the use of behaviour change theory ( Mailey et al ., 2010 ), which was social cognitive theory. No non-RCT studies employed behaviour change theory. Intervention duration ranged from 1 single 10-min session to 20 weeks of intervention. Seven of the RCT ( Kim et al ., 2013 ; Mailey et al ., 2010 ; Philippot et al ., 2022 ; Sun et al ., 2023 ; Wan Yunus et al ., 2020 ; Zhang et al. , 2023a ; Zhu et al ., 2023 ) and 8 of the non-RCT ( Wang et al ., 2004 ; deJonge et al ., 2021 ; Martínez-Díaz and Carrasco, 2021 ; Forseth et al ., 2022 ; Danielsen et al ., 2023 ; Gurung et al ., 2023 ; Sandra et al ., 2023 ; Strehli et al ., 2023 ) studies were designed as pilot trials.
Summary details of included studies
1 Number of participants in the analysis and the median group size as there are slight variations between groups in most studies.
2 Mean age and standard deviations were pooled across groups statistics if overall demographics were not given; NS = not stated; age range (min–max) is stated in lieu of other summary statistics where available.
3 Novice is used to indicate the participants did not need any experience or regular activity; Expert is used to indicate that participants had significant experience in a relevant activity; Medical (phys & psych) indicates that there were medical exclusions for physical and psychological indications, these varied between studies.
4 Intervention dose is given as the minutes per activity session, number of sessions per week and number of weeks of the intervention. This was used to estimate an approximate total length of intervention in minutes. Note these numbers are indicative only as some study designs had variable length sessions and sessions per week; or increased duration/intensity over the length of the study. Abbreviation NSL = no set length.
5 Indicated if the study found a statistically significant difference on one or more psychological outcomes between comparator groups; if there was no comparator group then this indicates effective pre–post comparison as indicated. Psychological measurements with estimated effect sizes for effective RCT studies are listed on a separate table.
6 Description of study indicates it was a randomized controlled trial, however authors describe as quasi-experimental. Due to ambiguity, it is listed with the non-RCT studies.
Incentive to participate
Only 13 (22%) studies outlined small incentives to participate which included the award of additional course credits, money, prize draws (e.g. amazon voucher) and free yoga classes (see Table 1 ).
Diagnoses, psychological outcomes and measurements
Eighteen studies (31%) required participants to have a psychological diagnosis or experience including being referred by the on-campus mental health team, experiencing anxiety, experiencing moderate depression, or having attention deficit hyperactivity disorder (ADHD). Other studies had inclusion criteria based on activity levels or previous exercise experience ( n = 16, 28%) and the remainder ( n = 24, 41%) had no specific inclusion criteria other than being students, although recruitment may have been restricted to sub-groups of students (such as course enrolment or dormitories). Most of the studies ( n = 48, 83%) reported psychological outcomes as their primary outcome, including perceived stress, depression, state anxiety and QoL. In other studies ( n = 10, 17%), non-psychological measures such as cardiorespiratory fitness, heart rate variability and aerobic capacity were reported as their primary outcome, with psychological outcomes being secondary outcomes. Various psychological measurements were used (see Table 2 ) including the Spielberger State-Trait Anxiety Inventory (STAI) and Beck Depression Inventory (BDI).
Summary of psychological instruments used and the language adaptation if known, if no language is stated it is assumed to be in English based on study location
Intervention effectiveness
Interventions were effective in 36 studies (62%) for improving at least one measure of mental health or QOL in HE students ( Akandere and Demir, 2011 ; Bass et al ., 2002 ; Caldwell et al ., 2009 ; Crocker and Grozelle, 1991 ; Danielsen et al ., 2023 ; de Vries et al ., 2016 , 2018 ; deJonge et al ., 2021 ; Dinani et al ., 2019 ; Ezati et al ., 2020 ; Faro et al ., 2019 ; Forseth et al ., 2022 ; Fukui et al ., 2021 ; Gallego et al ., 2014 ; Gurung et al ., 2023 ; Hemat-Far et al ., 2012 ; Herbert et al ., 2020 ; Huang et al ., 2017 ; Ji et al ., 2022 ; Kim et al ., 2013 ; Li et al ., 2022 ; López-Rodríguez et al ., 2017 ; Muir et al ., 2020 ; Philippot et al ., 2022 ; Salehian et al ., 2021 ; Saltan and Ankaralı, 2021 ; Sandra et al ., 2023 ; Strehli et al ., 2023 ; Sun et al ., 2023 ; Tong et al ., 2021 ; von Haaren et al ., 2016 ; Wan Yunus et al ., 2020 ; Wang et al ., 2004 ; Xiao et al ., 2021 ; Zhang and Jiang, 2023b ; Zhao et al ., 2022 ). Five of these studies did not have a comparator so the effectiveness relates only to changes over time (pre-post) and not between groups. Where an intervention was found to be effective the effect sizes were typically medium to large, in either an adjusted repeated measures analysis or a less robust sequence of paired t -tests. No studies which used sequences of t -tests adjusted for multiple comparisons. The effect sizes as reported by the authors or estimated from available information are outlined in ( Supplementary File S1: SF1 ). Nearly half the studies (48%) compared a PA intervention with the ‘usual routine’ (including waitlist control groups). The remaining studies used a variety of comparators including between different PA interventions (e.g. basketball with Taichi) and non-PA interventions such as art, therapy and expressive writing ( Table 1 ). For the purposes of this review, we have categorized these interventions based on the intervention and not the comparator. These are: (a) moderate-vigorous intensity PA (MVIPA) intervention, (b) high-intensity interval training (HIIT), (c) mind–body PA interventions and (d) miscellaneous interventions.
MVIPA interventions.
There were 29 studies which used MVIPA interventions including aerobic strength and resistance exercises, Pilates, running, dance, circuit/gym training and sports games. Of these studies, 25 were found to be effective ( Crocker and Grozelle, 1991 ; Bass et al ., 2002 ; Caldwell et al ., 2009 ; Akandere and Demir, 2011 ; Hemat-Far et al ., 2012 ; Gallego et al ., 2014 ; de Vries et al ., 2016 , 2018 ; von Haaren et al ., 2016 ; Huang et al ., 2017 ; López-Rodríguez et al ., 2017 ; Faro et al ., 2019 ; Ezati et al ., 2020 ; Herbert et al ., 2020 ; Muir et al ., 2020 ; Wan Yunus et al ., 2020 ; deJonge et al ., 2021 ; Fukui et al ., 2021 ; Saltan and Ankaralı, 2021 ; Xiao et al ., 2021 ; Ji et al ., 2022 ; Zhao et al ., 2022 ; Danielsen et al ., 2023 ; Gurung et al ., 2023 ; Sandra et al ., 2023 ). Four studies did not find significant intervention effects. Two of these studies compared an aerobic intervention with a yoga intervention ( Tong et al ., 2021 ; Murray et al ., 2022 ); 1 study compared a home workout with expressive writing ( Marschin and Herbert, 2021 ); and 1 study used cycling/running interventions ( Brown et al ., 1993 ). Notably the cycling/running intervention did not include general student populations, rather it recruited physically challenged students, enrolled in an adaptive physical education class for a single 20-min session.
Nineteen of the 29 studies in this group were RCTs ( Crocker and Grozelle, 1991 ; Brown et al ., 1993 ; Akandere and Demir, 2011 ; Hemat-Far et al ., 2012 ; Gallego et al ., 2014 ; de Vries et al ., 2016 , 2018 ; von Haaren et al ., 2016 ; Huang et al ., 2017 ; López-Rodríguez et al ., 2017 ; Faro et al ., 2019 ; Herbert et al ., 2020 ; Wan Yunus et al ., 2020 ; Fukui et al ., 2021 ; Saltan and Ankaralı, 2021 ; Xiao et al ., 2021 ; Ji et al ., 2022 ; Murray et al ., 2022 , 2022 ; Zhao et al ., 2022 ) and 17 were found to be effective ( Crocker and Grozelle, 1991 ; Akandere and Demir, 2011 ; Hemat-Far et al ., 2012 ; Gallego et al ., 2014 ; de Vries et al ., 2016 , 2018 ; von Haaren et al ., 2016 ; Huang et al ., 2017 ; López-Rodríguez et al ., 2017 ; Faro et al ., 2019 ; Herbert et al ., 2020 ; Wan Yunus et al ., 2020 ; Fukui et al ., 2021 ; Saltan and Ankaralı, 2021 ; Xiao et al ., 2021 ; Ji et al ., 2022 ; Zhao et al ., 2022 ). One was explicitly a pilot study ( Wan Yunus et al ., 2020 ). There were 10 non-RCTs ( Bass et al ., 2002 ; Caldwell et al ., 2009 ; Ezati et al ., 2020 ; Muir et al ., 2020 ; deJonge et al ., 2021 ; Marschin and Herbert, 2021 ; Tong et al ., 2021 ; Danielsen et al ., 2023 ; Gurung et al ., 2023 ; Sandra et al ., 2023 ), 4 of which were pilots ( deJonge et al ., 2021 ; Danielsen et al ., 2023 ; Gurung et al ., 2023 ; Sandra et al ., 2023 ), 8 were found to be effective ( Bass et al ., 2002 ; Caldwell et al ., 2009 ; Ezati et al ., 2020 ; Muir et al ., 2020 ; deJonge et al ., 2021 ; Danielsen et al ., 2023 ; Gurung et al ., 2023 ; Sandra et al ., 2023 ), and 2 did not show statistically significant improvements ( Marschin and Herbert, 2021 ; Tong et al ., 2021 ).

High-intensity interventions.
HIIT interventions ( n = 6) included three RCTs ( Eather et al ., 2019 ; Philippot et al ., 2022 ; Zhu et al ., 2023 ), two of which were pilot ( Philippot et al ., 2022 ; Zhu et al ., 2023 ) and three non-RCTs ( Martínez-Díaz and Carrasco, 2021 ; La Count et al ., 2022 ), one of which was a pilot ( Martínez-Díaz and Carrasco, 2021 ). Only the RCT pilot intervention ( Philippot et al ., 2022 ) showed effectiveness for HIIT interventions. The oldest study in this group describes a procedure of sequential maximal exercises similar to HIIT, although published prior to the popularization of the term ( O’Connor et al ., 1995 ). They found that this training increased anxiety immediately post-training for low-fitness students, although anxiety returned to baseline at follow-up. This study also included maximal treadmill exercises with both highly trained runners and physically fit students who also did not find the sessions effective in reducing anxiety.
Mind–body PA interventions.
There were 19 studies which used mind–body interventions ( Albracht-Schulte and Robert-McComb, 2018 ; Caldwell et al ., 2009 ; Dinani et al ., 2019 ; Forseth et al ., 2022 ; Gao et al ., 2022 ; Kim et al ., 2013 ; Kim et al ., 2004 ; Li et al ., 2015 , , 2022 ; Salehian et al ., 2021 ; Schmalzl et al ., 2018 ; Strehli et al ., 2023 ; Sun et al ., 2023 ; Tong et al ., 2021 ; Wang et al ., 2004 ; Xiao and Zheng, 2022 ; Zhang et al. , 2023a ; Zheng et al ., 2015 ; Zhang and Jiang, 2023 ) including various forms of yoga, Tai-Chi, Qigong (including Baduanjin), Kouk Sun Do, and meridian exercise, where studies ( Caldwell et al ., 2009 ; Tong et al ., 2021 ; Xiao et al ., 2021 ) were also included in the previous section as they were comparisons between mind–body interventions and MVIPA interventions. Overall, these studies provide mixed evidence of effectiveness with only 6 out of 12 RCTs finding at least one significant improvement in a mental health or QOL measure against the comparator (see Supplementary File S1: SF1 ). Eight studies compared with the usual routine, and one each for quiet rest, health education or ujjayi breath. Most of these interventions were lengthy with typically 60-min sessions 2–5 times per week for 8–12 weeks. There were seven non-RCTs, with five claiming the intervention was effective, however, three of these were pilot studies with no comparator. Tong and colleagues (2021) found yoga to be superior to aerobic-style exercises however students self-selected into groups and the effect was primarily considered to be through increased mindfulness rather than a direct measure of mental health or QOL.
Two studies which did not find Tai Chi or Baduanjin to be effective were from the same research group and rigorously designed with similar published protocols ( Zheng et al ., 2013 , 2014 ). They included long interventions (each 12 weeks), the largest sample sizes (approximately 200 participants each) and intention to treat analyses. In both cases, the authors posit that differences with the control group may have been difficult to detect as there were no limits on what activities the control group may have been involved with outside of the trial. The background of the participants may be an important consideration as they were students of traditional Chinese medicine, whereas the three trials which were found to be effective involved nursing ( Kim et al ., 2004 ; Dinani et al ., 2019 ) or general university students ( Xiao et al ., 2021 ). These studies had smaller sample sizes (approximately 30 students per group) and ran for 6, 8 and 12 weeks, respectively. There was also a pilot trial with a small sample size of 18 students which found evidence for the effectiveness of Kouk Sun Do in improving the mental health of students ( Kim et al ., 2013 ). The non-RCT studies which found some evidence for the effectiveness of Tai Chi included a pilot trial with no comparator ( Wang et al ., 2004 ) and, an Iranian study looking specifically at Corona-disease anxiety which did not find Tai Chi effective in comparison with cognitive-spiritual therapy ( Salehian et al ., 2021 ) but was more effective than the control (receiving no intervention). Overall, the evidence is mixed and suggests that mind–body exercises may be effective for improving students’ mental health, however, this may depend on the background of students and which activities they already usually participate in.
Miscellaneous interventions.
There were seven miscellaneous studies including five RCTs ( Mailey et al ., 2010 ; Sharp and Caperchione, 2016 ; Zimmermann and Mangelsdorf, 2020 ; Chawla et al ., 2022 ; Mota et al ., 2023 ) and two non-RCTs ( Tayama et al ., 2012 ; Koschel et al ., 2017 ). None of these studies found the interventions to significantly improve HE students’ mental health and/or QoL. There were three pedometer-based interventions ( Mailey et al ., 2010 ; Tayama et al ., 2012 ; Sharp and Caperchione, 2016 ) which did not specify a number of steps or intervention lengths to participants. It could be argued these are not truly movement-based interventions, but rather tracking-based interventions (with the aim that tracking might increase movement). Similarly, Mota and colleagues (2023) trialled a mobile health app as an intervention which included exercise videos but did not specify the amount of exercise to complete. Another two studies were considered in this category as they involved only a single session or event. One compared a single 20-min creative movement versus art ( Zimmermann and Mangelsdorf, 2020 ) and whilst both groups improved over time there was no difference between the groups. The other allowed students to choose activities within a 3-day on-campus event and whilst it is not called a pilot or feasibility trial, the sample size was 15 students ( Koschel et al ., 2017 ). The final study compared squat exercises with and without whole-body vibration and both groups improved in the domains of depression, anxiety and stress ( Chawla et al ., 2022 ). In this case, the intervention is the addition of the whole-body vibration in conjunction with the exercises, which was not effective.
Assessment of ROB
ROB assessment for included RCT studies is summarized (see Supplementary File S2: SF2 ) and outlined in relation to each RCT study (see Supplementary File S3: SF3 ). Most of the RCT studies included ( n = 22; 58%) scored low in overall ROB, with a further 10 having an unclear ROB, and 6 having high ROB. It is important however to consider that it not possible to blind participants to these types of interventions. Assessment of ROB for included non-RCT studies is summarized (see Supplementary File S4: SF4 ) and outlined in relation to each non-RCT study (see Supplementary File S5: SF5 ). Similarly to the RCT studies, overall, most of the non-RCTs reported low ROB ( n = 12; 60%), whereas five were unclear and the remaining three had a high ROB.
This systematic review suggests that exercise interventions, which are MVIPA, can positively impact the mental health and/or QoL of HE students. Interventions include Pilates, aerobic exercises, basketball, weight, resistance and gym training, dance, exercise games and home workouts and running. Mixed results were observed for mind–body interventions in improving the mental health and/or QoL of HE students. However, there was substantial variability between studies in relation to the context, sample size, intervention duration and outcomes. Interventions involving HIIT were not found to be effective, except for a single pilot study. However, there were only three studies ( Eather et al ., 2019 ; Philippot et al ., 2022 ; Zhu et al ., 2023 ) trialling HIIT in a similar design to other movement-based interventions (in terms of duration) so this area needs further research. Interventions which gave participants access to tracking their physical activity (such as pedometers or mobile app) which did not have a specific session length or duration were not effective ( Mailey et al ., 2010 ; Tayama et al ., 2012 ; Sharp and Caperchione, 2016 ; Mota et al ., 2023 ). Overall, there is substantial variety in the type, duration and measurement of PA interventions, but there is evidence that these can improve aspects of mental health with an appropriate program.
PA trials rely upon the participants volunteering to participate and in turn, conclusions about effectiveness cannot be drawn for students in general as they may not have the internal motivation to initiate or maintain participation in such activities. One study ( Ezati et al ., 2020 ) used a block allocation of students based on dormitories and still found the intervention effective. Further studies of this type could offer insights into general adherence and attrition; however, it may be more challenging in settings where students are not ‘captive’ based on residence. This is discussed further in recommendations. Additionally, most studies fail to detail information surrounding participants’ regular activities and the activities of the control groups after not being assigned to the intervention arm.
Many of the RCT studies included in this review use validated instruments to measure psychological outcomes ( Table 2 ), including the STAI, PSS and BDI. Of the studies included, many included interventions administered over several weeks (≥20 weeks). This is an individual strength within studies only, as such a wide array of instruments are used making any comparisons between studies problematic. Additionally, many studies used multiple measures and sequences of paired t -tests, inflating the type 1 error rate (i.e. false positives). Assessment of multiple psychological outcome measures also raises questions surrounding the accuracy of the results as participants may experience survey fatigue.
A strength of this systematic review is the inclusion of exhaustive searches for relevant peer-reviewed journal articles in six library databases. Although searches were restricted to articles written in the English language only, research findings from a range of different countries where English is not the first language are included. The majority of included studies ( n = 34 studies, 58.6%) had low ROB. Only nine studies (15.5%) were found to have high ROB.
This review has several limitations. First, it was not feasible to conduct meta-analyses due to heterogeneity in study designs, interventions, outcome measures and types of analysis conducted. Second, variations in the length and intensity of interventions limits direct comparison across all included studies. Lastly, this systematic review includes only peer-reviewed journal articles, so publication bias may be a potential limitation of the findings since studies with negative or inconclusive findings may be less likely to have been published ( DeVito and Goldacre, 2019 ).
This review supports the ongoing evaluation of MVIPA interventions for the mental health and wellbeing of HE students. There is evidence that these can be effective for students who are interested in participating. Given the numerous forms of PA, it is valuable to have ongoing research on different interventions. However, it would be helpful to use standardized instruments (e.g. STAI, BDI, PSS and DASS) so that future meta-analysis is possible, and to continue to run trials which continue for several weeks. There is currently only limited evidence of the effectiveness of PA as a general health-promotion activity aimed at all students for mental health. Further research is needed on feasibility, acceptability and adherence within this framework. One study used a block allocation of dormitories ( Ezati et al ., 2020 ) and the intervention group did have slightly higher non-compliance than the control group (i.e. 5 vs 1 students, respectively) but the overall sample size is still relatively low (i.e. 67 students). Additionally, two studies used entire classes as experimental groups ( Marschin and Herbert, 2021 ; Tong et al ., 2021 ), however, these were fitness and psychology classes, respectively, and may not be directly applicable to students in non-health-related fields. From a health-promotion lens, it would be valuable to understand which activities would encourage participation and adherence, and if students who are experiencing symptoms of stress, anxiety and depression can be encouraged to participate.
Most studies found a gender bias in participation (i.e. greater proportion of females than males). This limitation is not unusual. A systematic review on the prevalence of mental health problems in undergraduate students found that more than half had greater than 60% female participation ( Sheldon et al ., 2021 ). The only intervention in this review which skewed to a greater proportion of males (without being exclusively male) included basketball as an intervention ( Xiao et al ., 2021 ). A systematic review of PA interventions for physical health also found that more than half of the studies included predominantly female participants ( Plotnikoff et al ., 2015 ), and that overall interest in the interventions was relatively low. It is possible that a PA intervention explicitly aimed at improving mental health rather than physical health may attract wider and more diverse participation. It would also be of interest to hear student perspectives on the ‘attractiveness’ of programs which are promoted for reducing stress and anxiety, rather than reducing weight. Loneliness was only considered explicitly in one of the studies in this review ( Xiao et al ., 2021 ), however, this is also a growing concern for HE students in wider research ( Bernardon et al ., 2011 ; Diehl et al ., 2018 ).
Pragmatic trials which report initial interest, engagement throughout the semester and the student perspective would complement the existing research on efficacy. It is unlikely that a single PA intervention would be appealing to all students, however, a range of activities which could include a social element, may influence uptake and regular attendance. In this review, only one study offered a range of activities ( Koschel et al ., 2017 ). Although it did not find that the program was effective in reducing stress on quantitative measures before exams, it was only a 3-day intervention with a small sample size and the qualitative feedback found that all students in the intervention group felt it had reduced stress. This approach may provide a framework for a larger and longer program.
This systematic review offers the first detailed synthesis on PA and exercise-specific interventions targeted at improving the mental health and wellbeing of HE students. The evidence suggests that these interventions can positively impact the mental health and QoL of HE students. Evidence shows those interventions which include MVIPA to be the most effective, including aerobics, dance, basketball and running. Mind–body exercises including yoga, Tai Chi and Qigong may also be effective depending on context however this evidence is mixed. HIIT and pedometer/tracking interventions were not effective in improving psychological outcomes in HE students. Implemented long-term and widely across HE institutions, MVIPA interventions may improve mental health in HE students.
This work was not funded.
Data will be made available upon request from the authors.
Acree , L. S. , Longfors , J. , Fjeldstad , A. S. , Fjeldstad , C. , Schank , B. , Nickel , K. J. et al. . ( 2006 ) Physical activity is related to quality of life in older adults . Health and Quality of Life Outcomes , 4 , 37 .
Google Scholar
Akandere , M. and Demir , B. ( 2011 ) The effect of dance over depression . Collegium Antropologicum , 35 , 651 – 656 .
Albracht-Schulte , K. and Robert-McComb , J. ( 2018 ) The effects of yoga and quiet rest on subjective levels of anxiety and physiological correlates: a 2-way crossover randomized trial . BMC Complementary and Alternative Medicine , 18 , 280 .
Al-Drees , A. , Abdulghani , H. , Irshad , M. , Baqays , A. A. , Al-Zhrani , A. A. , Alshammari , S. A. et al. . ( 2016 ) Physical activity and academic achievement among the medical students: a cross-sectional study . Medical Teacher , 38 , S66 – S72 .
Bass , M. A. , Enochs , W. K. and DiBrezzo , R. ( 2002 ) Comparison of two exercise programs on general well-being of college students . Psychological Reports , 91 , 1195 – 1201 .
Bernardon , S. , Babb , K. A. , Hakim-Larson , J. and Gragg , M. ( 2011 ) Loneliness, attachment, and the perception and use of social support in university students . Canadian Journal of Behavioural Science , 43 , 40 – 51 .
Binfet , J. -T. ( 2017 ) The effects of group-administered canine therapy on university students’ wellbeing: a randomized controlled trial . Anthrozoös , 30 , 397 – 414 .
Binfet , J. -T. , Passmore , H. -A. , Cebry , A. , Struik , K. and McKay , C. ( 2018 ) Reducing university students’ stress through a drop-in canine-therapy program . Journal of Mental Health (Abingdon, England) , 27 , 197 – 204 .
Bize , R. , Johnson , J. A. and Plotnikoff , R. C. ( 2007 ) Physical activity level and health-related quality of life in the general adult population: a systematic review . Preventive Medicine , 45 , 401 – 415 .
Bray , S. R. and Born , H. A. ( 2004 ) Transition to University and vigorous physical activity: implications for health and psychological well-being . Journal of American College Health , 52 , 181 – 188 .
Brown , D. R. , Morgan , W. P. and Raglin , J. S. ( 1993 ) Effects of exercise and rest on the state anxiety and blood pressure of physically challenged college students . The Journal of Sports Medicine and Physical Fitness , 33 , 300 – 305 .
Caldwell , K. , Harrison , M. , Adams , M. and Triplett , N. ( 2009 ) Effect of pilates and Taiji Quan training on self-efficacy, sleep quality, mood, and physical performance of college students . Journal of Bodywork and Movement Therapies , 13 , 155 – 163 .
Castillo , L. and Schwartz , S. ( 2013 ) Introduction to the special issue on college student mental health . Journal of Clinical Psychology , 69 , 291 – 297 . https://doi.org/10.1002/jclp.21972
Chawla , G. , Azharuddin , M. , Ahmad , I. and Hussain , M. E. ( 2022 ) Effect of whole-body vibration on depression, anxiety, stress, and quality of life in college students: a randomized controlled trial . Oman Medical Journal , 37 , e408 .
Crocker , P. R. and Grozelle , C. ( 1991 ) Reducing induced state anxiety: effects of acute aerobic exercise and autogenic relaxation . The Journal of Sports Medicine and Physical Fitness , 31 , 277 – 282 .
Danielsen , K. K. , Cabral , D. and Sveaas , S. H. ( 2023 ) ‘Students Moving Together’, tailored exercise for students facing mental health challenges—a pilot feasibility study . International Journal of Environmental Research and Public Health , 20 , 6639 .
de Vries , J. D. , van Hooff , M. L. M. , Geurts , S. A. E. and Kompier , M. A. J. ( 2016 ) Exercise as an intervention to reduce study-related fatigue among university students: a two-arm parallel randomized controlled trial . PLoS One , 11 , e0152137 .
de Vries , J. D. , van Hooff , M. L. M. , Geurts , S. A. E. and Kompier , M. A. J. ( 2018 ) Trajectories of well-being during an exercise randomized controlled trial: the role of exposure and exercise experiences . Stress and Health , 34 , 24 – 35 .
deJonge , M. L. , Jain , S. , Faulkner , G. E. and Sabiston , C. M. ( 2021 ) On campus physical activity programming for post-secondary student mental health: examining effectiveness and acceptability . Mental Health and Physical Activity , 20 , 100391 .
DeVito , N. J. and Goldacre , B. ( 2019 ) Catalogue of bias: publication bias . BMJ Evidence-Based Medicine , 24 , 53 – 54 .
Diehl , K. , Jansen , C. , Ishchanova , K. and Hilger-Kolb , J. ( 2018 ) Loneliness at universities: determinants of emotional and social loneliness among students . International Journal of Environmental Research and Public Health , 15 , 1865 .
Dinani , S. K. , Mehrabi , T. and Sadeghi , R. ( 2019 ) The effect of tai chi exercise on stress, anxiety, depression, and self confidence of nursing students . Jundishapur Journal of Chronic Disease Care , 8 , Article 3 .
Eather , N. , Riley , N. , Miller , A. , Smith , V. , Poole , A. , Vincze , L. et al. . ( 2019 ) Efficacy and feasibility of HIIT training for university students: the uni-HIIT RCT . Journal of Science and Medicine in Sport , 22 , 596 – 601 .
Ezati , M. , Keshavarz , M. , Barandouzi , Z. A. and Montazeri , A. ( 2020 ) The effect of regular aerobic exercise on sleep quality and fatigue among female student dormitory residents . BMC Sports Science, Medicine and Rehabilitation , 12 , 44 .
Faro , J. , Wright , J. A. , Hayman , L. L. , Hastie , M. , Gona , P. N. and Whiteley , J. A. ( 2019 ) Functional resistance training and affective response in female college-age students . Medicine and Science in Sports and Exercise , 51 , 1186 – 1194 .
Farris , S. G. and Abrantes , A. M. ( 2020 ) Mental health benefits from lifestyle physical activity interventions: a systematic review . Bulletin of the Menninger Clinic , 84 , 337 – 372 .
Forseth , B. , Polfuss , M. , Brondino , M. , Hunter , S. D. , Lawlor , M. W. , Beatka , M. J. et al. . ( 2022 ) Adherence to and changes in mental and physiological health during an 8-week yoga intervention: a pilot study . Journal of Bodywork and Movement Therapies , 30 , 203 – 209 .
Fukui , K. , Suzuki , Y. , Kaneda , K. , Kuroda , S. , Komiya , M. , Maeda , N. et al. . ( 2021 ) Do ‘Stay-at-home exercise’ videos induce behavioral changes in college students? A randomized controlled trial . Sustainability , 13 , 11600 .
Gallego , J. , Aguilar-Parra , J. M. , Cangas , A. J. , Langer , I. and Mañas , I. ( 2014 ) Effect of a mindfulness program on stress, anxiety and depression in university students . The Spanish Journal of Psychology , 17 , E109 . https://doi.org/10.1017/sjp.2014.102
Gao , Y. , Wang , J. -Y. , Ke , F. , Tao , R. , Liu , C. and Yang , S. -Y. ( 2022 ) Effectiveness of aromatherapy yoga in stress reduction and sleep quality improvement among Chinese female college students: a quasi-experimental study . Healthcare (Basel, Switzerland) , 10 , 1686 .
Gasiūnienė , L. and Miežienė , B. ( 2021 ) The relationship between students’ physical activity and academic stress . Baltic Journal of Sport and Health Sciences , 4 , 4 – 12 .
González-Valero , G. , Zurita-Ortega , F. , Ubago-Jiménez , J. L. and Puertas-Molero , P. ( 2019 ) Use of meditation and cognitive behavioral therapies for the treatment of stress, depression and anxiety in students. a systematic review and meta-analysis . International Journal of Environmental Research and Public Health , 16 , 4394 .
Gurung , J. , Turner , J. , Freeman , E. , Coleman , C. , Iacovou , S. and Hemingway , S. ( 2023 ) An evaluation of MINDFIT—a student therapeutic running group as a multi-layered intervention in the United Kingdom . Nursing Reports , 13 , 456 – 469 , https://doi.org/10.3390/nursrep13010042
Hemat-Far , A. , Shahsavari , A. and Roholla Mousavi , S. ( 2012 ) Effects of selected aerobic exercises on the depression and concentrations of plasma serotonin in the depressed female students aged 18 to 25 . Journal of Applied Research , 12 ( 1 ).
Herbert , C. , Meixner , F. , Wiebking , C. and Gilg , V. ( 2020 ) Regular physical activity, short-term exercise, mental health, and well-being among university students: the results of an online and a laboratory study . Frontiers in Psychology , 11 , 509 , https://doi.org/10.3389/fpsyg.2020.00509
Huang , H. -C. , Wong , M. -K. , Yang , Y. -H. , Chiu , H. -Y. and Teng , C. -I. ( 2017 ) Impact of playing exergames on mood states: a randomized controlled trial . Cyberpsychology, Behavior, and Social Networking , 20 , 246 – 250 .
Ji , C. , Yang , J. , Lin , L. and Chen , S. ( 2022 ) Physical exercise ameliorates anxiety, depression and sleep quality in college students: experimental evidence from exercise intensity and frequency . Behavioral Sciences , 12 , 61 .
Keating , X. D. , Guan , J. , Piñero , J. C. and Bridges , D. M. ( 2005 ) A meta-analysis of college students’ physical activity behaviors . Journal of American College Health , 54 , 116 – 125 .
Kim , J. -H. , Yang , H. and Schroeppel , S. ( 2013 ) A pilot study examining the effects of Kouk Sun Do on university students with anxiety symptoms . Stress and Health , 29 , 99 – 107 .
Kim , K. B. , Cohen , S. M. , Oh , H. K. and Sok , S. R. ( 2004 ) The effects of meridian exercise on anxiety, depression, and self‐esteem of female college students in Korea . Holistic Nursing Practice , 18 , 230 – 234 .
Koschel , T. L. , Young , J. C. and Navalta , J. W. ( 2017 ) Examining the impact of a university-driven exercise programming event on end-of-semester stress in students . International Journal of Exercise Science , 10 , 754 – 763 .
La Count , P. A. , Hartung , C. M. , Vasko , J. M. , Serrano , J. W. , Wright , H. A. and Smith , D. T. ( 2022 ) Acute effects of physical exercise on cognitive and psychological functioning in college students with attention-deficit/hyperactivity disorder . Mental Health and Physical Activity , 22 , 100443 .
LaCaille , L. J. , Dauner , K. N. , Krambeer , R. J. and Pedersen , J. ( 2011 ) Psychosocial and environmental determinants of eating behaviors, physical activity, and weight change among college students: a qualitative analysis . Journal of American College Health , 59 , 531 – 538 .
Li , K. , Walczak-Kozłowska , T. , Lipowski , M. , Li , J. , Krokosz , D. , Su , Y. et al. . ( 2022 ) The effect of the Baduanjin exercise on COVID-19-related anxiety, psychological well-being and lower back pain of college students during the pandemic . BMC Sports Science, Medicine and Rehabilitation , 14 , 102 .
Li , M. , Fang , Q. , Li , J. , Zheng , X. , Tao , J. , Yan , X. et al. . ( 2015 ) The effect of Chinese traditional exercise-Baduanjin on physical and psychological well-being of college students: a randomized controlled trial . PLoS One , 10 , e0130544 .
Li , X. , Yu , H. and Yang , N. ( 2021 ) The mediating role of resilience in the effects of physical exercise on college students’ negative emotions during the COVID-19 epidemic . Scientific Reports , 11 , Article 1 .
López-Rodríguez , M. M. , Baldrich-Rodríguez , I. , Ruiz-Muelle , A. , Cortés-Rodríguez , A. E. , Lopezosa-Estepa , T. and Roman , P. ( 2017 ) Effects of Biodanza on stress, depression, and sleep quality in university students . Journal of Alternative and Complementary Medicine , 23 , 558 – 565 .
Mailey , E. L. , Wójcicki , T. R. , Motl , R. W. , Hu , L. , Strauser , D. R. , Collins , K. D. et al. . ( 2010 ) Internet-delivered physical activity intervention for college students with mental health disorders: a randomized pilot trial . Psychology, Health & Medicine , 15 , 646 – 659 .
Marschin , V. and Herbert , C. ( 2021 ) A short, multimodal activity break incorporated into the learning context during the covid-19 pandemic: effects of physical activity and positive expressive writing on university students’ mental health—results and recommendations from a pilot study . Frontiers in Psychology , 12 , 645492 , https://doi.org/10.3389/fpsyg.2021.645492 .
Martinez , Y. T. S. , Harmon , B. E. , Nigg , C. R. , Bantum , E. O. and Strayhorn , S. ( 2016 ) Diet and physical activity intervention strategies for college students . Health Behavior and Policy Review , 3 , 336 – 347 .
Martínez-Díaz , I. C. and Carrasco , L. ( 2021 ) Neurophysiological stress response and mood changes induced by high-intensity interval training: a pilot study . International Journal of Environmental Research and Public Health , 18 , 7320 .
Mota , J. F. , Lopes , L. C. C. , Trottier , C. F. , Johnson , S. T. , Lieffers , J. and Prado , C. M. ( 2023 ) A randomized controlled trial of the effects of a web-based intervention on perceived stress and diet quality among first-year university students . Telemedicine Reports , 4 , 327 – 335 .
Muir , M. H. K. , Munroe-Chandler , K. J. , Loughead , T. M. , Sutherland , C. A. and Hawksley , K. G. ( 2020 ) The UWorkItOut UWin program: improving university students’ psychological distress through physical activity . International Journal of Kinesiology and Sports Science , 8 , Article 3 .
Murphy , M. H. , Carlin , A. , Woods , C. , Nevill , A. , MacDonncha , C. , Ferguson , K. et al. . ( 2018 ) Active students are healthier and happier than their inactive peers: the results of a large representative cross-sectional study of university students in Ireland . Journal of Physical Activity and Health , 15 , 737 – 746 .
Murray , A. , Marenus , M. , Cahuas , A. , Friedman , K. , Ottensoser , H. , Kumaravel , V. et al. . ( 2022 ) The impact of web-based physical activity interventions on depression and anxiety among college students: randomized experimental trial . JMIR Formative Research , 6 , e31839 .
O’Connor , P. J. , Petruzzello , S. J. , Kubitz , K. A. and Robinson , T. L. ( 1995 ) Anxiety responses to maximal exercise testing . British Journal of Sports Medicine , 29 , 97 – 102 .
Ozdemir , F. , Cansel , N. , Kizilay , F. , Guldogan , E. , Ucuz , I. , Sinanoglu , B. et al. . ( 2020 ) The role of physical activity on mental health and quality of life during COVID-19 outbreak: a cross-sectional study . European Journal of Integrative Medicine , 40 , 101248 .
Page , M. J. , McKenzie , J. E. , Bossuyt , P. M. , Boutron , I. , Hoffmann , T. C. , Mulrow , C. D. et al. . ( 2021 ) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews . Systematic Reviews , 10 , 89 .
Pengpid , S. , Peltzer , K. , Kassean , H. K. , Tsala Tsala , J. P. , Sychareun , V. and Müller-Riemenschneider , F. ( 2015 ) Physical inactivity and associated factors among university students in 23 low-, middle- and high-income countries . International Journal of Public Health , 60 , 539 – 549 .
Philippot , A. , Moulin , P. , Charon , M. -H. , Balestra , C. , Dubois , V. , de Timary , P. et al. . ( 2022 ) Feasibility of online high-intensity interval training (HIIT) on psychological symptoms in students in lockdown during the COVID-19 pandemic: a randomized controlled trial . Frontiers in Psychiatry , 13 , 904283 .
Plotnikoff , R. C. , Costigan , S. A. , Williams , R. L. , Hutchesson , M. J. , Kennedy , S. G. , Robards , S. L. et al. . ( 2015 ) Effectiveness of interventions targeting physical activity, nutrition and healthy weight for university and college students: a systematic review and meta-analysis . The International Journal of Behavioral Nutrition and Physical Activity , 12 , 45 .
Reiner , M. , Niermann , C. , Jekauc , D. and Woll , A. ( 2013 ) Long-term health benefits of physical activity—a systematic review of longitudinal studies . BMC Public Health , 13 , 813 .
Salehian , M. H. , Yadolazadeh , A. and Ranjbari , S. ( 2021 ) Comparison of the effect of cognitive-spiritual method of hope therapy and tai chi exercises on anxiety caused by corona disease in university students . Pakistan Journal of Medical and Health Sciences , 938 – 947 .
Saltan , A. and Ankaralı , H. ( 2021 ) Does Pilates effect on depression status, pain, functionality, and quality of life in university students? A randomized controlled study . Perspectives in Psychiatric Care , 57 , 198 – 205 .
Sandra , D. A. , Olson , J. A. , Pageaux , B. and Roy , M. ( 2023 ) ‘Ready-to-use’ two-week home exercise program targeting depressive symptoms: Pilot STUDY . Frontiers in Psychiatry , 14 , 1202955 .
Saxena , S. , Van Ommeren , M. , Tang , K. C. and Armstrong , T. P. ( 2005 ) Mental health benefits of physical activity . Journal of Mental Health , 14 , 445 – 451 .
Schmalzl , L. , Powers , C. , Zanesco , A. P. , Yetz , N. , Groessl , E. J. and Saron , C. D. ( 2018 ) The effect of movement-focused and breath-focused yoga practice on stress parameters and sustained attention: a randomized controlled pilot study . Consciousness and Cognition , 65 , 109 – 125 .
Sharp , P. and Caperchione , C. ( 2016 ) The effects of a pedometer-based intervention on first-year university students: a randomized control trial . Journal of American College Health , 64 , 630 – 638 .
Sheldon , E. , Simmonds-Buckley , M. , Bone , C. , Mascarenhas , T. , Chan , N. , Wincott , M. et al. . ( 2021 ) Prevalence and risk factors for mental health problems in university undergraduate students: a systematic review with meta-analysis . Journal of Affective Disorders , 287 , 282 – 292 .
Sterne , J. A. , Hernán , M. A. , Reeves , B. C. , Savović , J. , Berkman , N. D. , Viswanathan , M. et al. . ( 2016 ) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions . BMJ , 355 , i4919 .
Sterne , J. A. C. , Savović , J. , Page , M. J. , Elbers , R. G. , Blencowe , N. S. , Boutron , I. et al. . ( 2019 ) RoB 2: a revised tool for assessing risk of bias in randomised trials . BMJ , 366 , l4898 .
Strehli , I. , Burns , R. D. , Bai , Y. , Ziegenfuss , D. H. , Block , M. E. and Brusseau , T. A. ( 2023 ) Development of an online mind–body physical activity intervention for young adults during COVID-19: a pilot study . International Journal of Environmental Research and Public Health , 20 , 4562 .
Sun , J. , Zhuo , J. , Chu , H. , Wang , J. , Chen , T. , Li , B. et al. . ( 2023 ) Effects of 3-month Qigong exercise on heart rate variability and respiration in anxious college students . Scandinavian Journal of Medicine & Science in Sports , 34 , e14521 , https://doi.org/10.1111/sms.14521
Tayama , J. , Yamasaki , H. , Tamai , M. , Hayashida , M. , Shirabe , S. , Nishiura , K. et al. . ( 2012 ) Effect of baseline self-efficacy on physical activity and psychological stress after a one-week pedometer intervention . Perceptual and Motor Skills , 114 , 407 – 418 .
Tong , J. , Qi , X. , He , Z. , Chen , S. , Pedersen , S. J. , Cooley , P. D. et al. . ( 2021 ) The immediate and durable effects of yoga and physical fitness exercises on stress . Journal of American College Health , 69 , 675 – 683 .
UK Government . ( 2019 ). Physical activity guidelines: Adults and older adults . GOV.UK . Retrieved 17 August 2022 , from https://www.gov.uk/government/publications/physical-activity-guidelines-adults-and-older-adults
von Haaren , B. , Ottenbacher , J. , Muenz , J. , Neumann , R. , Boes , K. and Ebner-Priemer , U. ( 2016 ) Does a 20-week aerobic exercise training programme increase our capabilities to buffer real-life stressors? A randomized, controlled trial using ambulatory assessment . European Journal of Applied Physiology , 116 , 383 – 394 .
Wan Yunus , F. , Tan , X. Z. and Romli , M. H. ( 2020 ) Investigating the feasibility of exergame on sleep and emotion among university students . Games for Health Journal , 9 , 415 – 424 .
Wang , Y. T. , Taylor , L. , Pearl , M. and Chang , L. -S. ( 2004 ) Effects of Tai Chi exercise on physical and mental health of college students . The American Journal of Chinese Medicine , 32 , 453 – 459 .
World Health Organization . ( n.d .). Physical Activity Guidelines World Health Organisation . Retrieved 17 August 2022 , from https://www.who.int/news-room/fact-sheets/detail/physical-activity
Wunsch , K. , Fiedler , J. , Bachert , P. and Woll , A. ( 2021 ) The tridirectional relationship among physical activity, stress, and academic performance in university students: a systematic review and meta-analysis . International Journal of Environmental Research and Public Health , 18 , 739 .
Xiao , T. , Jiao , C. , Yao , J. , Yang , L. , Zhang , Y. , Liu , S. et al. . ( 2021 ) Effects of basketball and Baduanjin exercise interventions on problematic smartphone use and mental health among college students: a randomized controlled trial . Evidence-Based Complementary and Alternative Medicine , 2021 , 8880716 .
Xiao , X. and Zheng , X. ( 2022 ) The effect of parental phubbing on depression in Chinese junior high school students: the mediating roles of basic psychological needs satisfaction and self-esteem . Frontiers in Psychology , 13 , 868354 , https://doi.org/10.3389/fpsyg.2022.868354
Zhang , J. , Gao , T. , Li , Y. , Song , Z. , Cui , M. , Wei , Q. et al. . ( 2023a ) The effect of Bafa Wubu of Tai Chi on college students’ anxiety and depression: a randomized, controlled pilot study . Frontiers in Physiology , 14 , 1036010 .
Zhang , Y. and Jiang , X. ( 2023b ) The effect of Baduanjin exercise on the physical and mental health of college students: a randomized controlled trial . Medicine , 102 , e34897 .
Zhao , Y. , Wang , W. , Wang , M. , Gao , F. , Hu , C. , Cui , B. et al. . ( 2022 ) Personalized individual-based exercise prescriptions are effective in treating depressive symptoms of college students during the COVID-19: a randomized controlled trial in China . Frontiers in Psychiatry , 13 , 1015725 .
Zheng , C. and Ji , H. ( 2021 ) Analysis of the intervention effect and self-satisfaction of sports dance exercise on the psychological stress of college students . Work , 69 , 637 – 649 .
Zheng , G. , Lan , X. , Li , M. , Ling , K. , Lin , H. , Chen , L. et al. . ( 2014 ) The effectiveness of Tai Chi on the physical and psychological well-being of college students: a study protocol for a randomized controlled trial . Trials , 15 , 129 .
Zheng , G. , Lan , X. , Li , M. , Ling , K. , Lin , H. , Chen , L. et al. . ( 2015 ) Effectiveness of Tai Chi on physical and psychological health of college students: results of a randomized controlled trial . PLoS One , 10 , e0132605 .
Zheng , G. , Li , M. , Lan , X. , Yan , X. , Lin , Q. , Chen , L. et al. . ( 2013 ) The effect of Baduanjin exercise for physical and psychological wellbeing of college students: study protocol for a randomized controlled trial . Trials , 14 , 422 .
Zhu , X. , Kostick , M. D. and Haegele , J. A. ( 2023 ) Effects of peer-supported and self-guided exercise on self-reported anxiety and depression among young adults—a pilot study . Journal of Functional Morphology and Kinesiology , 8 , 125 .
Zimmermann , N. and Mangelsdorf , H. ( 2020 ) Emotional benefits of brief creative movement and art interventions . The Arts in Psychotherapy , 70 , 101686 .
Supplementary data
Email alerts, citing articles via.
- Recommend to Your Librarian
- Journals Career Network
Affiliations
- Online ISSN 1460-2245
- Print ISSN 0957-4824
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 17 February 2022
Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review
- Joan Carles Trullàs ORCID: orcid.org/0000-0002-7380-3475 1 , 2 , 3 ,
- Carles Blay ORCID: orcid.org/0000-0003-3962-5887 1 , 4 ,
- Elisabet Sarri ORCID: orcid.org/0000-0002-2435-399X 3 &
- Ramon Pujol ORCID: orcid.org/0000-0003-2527-385X 1
BMC Medical Education volume 22 , Article number: 104 ( 2022 ) Cite this article
31k Accesses
78 Citations
10 Altmetric
Metrics details
Problem-based learning (PBL) is a pedagogical approach that shifts the role of the teacher to the student (student-centered) and is based on self-directed learning. Although PBL has been adopted in undergraduate and postgraduate medical education, the effectiveness of the method is still under discussion. The author’s purpose was to appraise available international evidence concerning to the effectiveness and usefulness of PBL methodology in undergraduate medical teaching programs.
The authors applied the Arksey and O’Malley framework to undertake a scoping review. The search was carried out in February 2021 in PubMed and Web of Science including all publications in English and Spanish with no limits on publication date, study design or country of origin.
The literature search identified one hundred and twenty-four publications eligible for this review. Despite the fact that this review included many studies, their design was heterogeneous and only a few provided a high scientific evidence methodology (randomized design and/or systematic reviews with meta-analysis). Furthermore, most were single-center experiences with small sample size and there were no large multi-center studies. PBL methodology obtained a high level of satisfaction, especially among students. It was more effective than other more traditional (or lecture-based methods) at improving social and communication skills, problem-solving and self-learning skills. Knowledge retention and academic performance weren’t worse (and in many studies were better) than with traditional methods. PBL was not universally widespread, probably because requires greater human resources and continuous training for its implementation.
PBL is an effective and satisfactory methodology for medical education. It is likely that through PBL medical students will not only acquire knowledge but also other competencies that are needed in medical professionalism.
Peer Review reports
There has always been enormous interest in identifying the best learning methods. In the mid-twentieth century, US educator Edgar Dale proposed which actions would lead to deeper learning than others and published the well-known (and at the same time controversial) “Cone of Experience or Cone of Dale”. At the apex of the cone are oral representations (verbal descriptions, written descriptions, etc.) and at the base is direct experience (based on a person carrying out the activity that they aim to learn), which represents the greatest depth of our learning. In other words, each level of the cone corresponds to various learning methods. At the base are the most effective, participative methods (what we do and what we say) and at the apex are the least effective, abstract methods (what we read and what we hear) [ 1 ]. In 1990, psychologist George Miller proposed a framework pyramid to assess clinical competence. At the lowest level of the pyramid is knowledge (knows), followed by the competence (knows how), execution (shows how) and finally the action (does) [ 2 ]. Both Miller’s pyramid and Dale’s cone propose a very efficient way of training and, at the same time, of evaluation. Miller suggested that the learning curve passes through various levels, from the acquisition of theoretical knowledge to knowing how to put this knowledge into practice and demonstrate it. Dale stated that to remember a high percentage of the acquired knowledge, a theatrical representation should be carried out or real experiences should be simulated. It is difficult to situate methodologies such as problem-based learning (PBL), case-based learning (CBL) and team-based learning (TBL) in the context of these learning frameworks.
In the last 50 years, various university education models have emerged and have attempted to reconcile teaching with learning, according to the principle that students should lead their own learning process. Perhaps one of the most successful models is PBL that came out of the English-speaking environment. There are many descriptions of PBL in the literature, but in practice there is great variability in what people understand by this methodology. The original conception of PBL as an educational strategy in medicine was initiated at McMaster University (Canada) in 1969, leaving aside the traditional methodology (which is often based on lectures) and introducing student-centered learning. The new formulation of medical education proposed by McMaster did not separate the basic sciences from the clinical sciences, and partially abandoned theoretical classes, which were taught after the presentation of the problem. In its original version, PBL is a methodology in which the starting point is a problem or a problematic situation. The situation enables students to develop a hypothesis and identify learning needs so that they can better understand the problem and meet the established learning objectives [ 3 , 4 ]. PBL is taught using small groups (usually around 8–10 students) with a tutor. The aim of the group sessions is to identify a problem or scenario, define the key concepts identified, brainstorm ideas and discuss key learning objectives, research these and share this information with each other at subsequent sessions. Tutors are used to guide students, so they stay on track with the learning objectives of the task. Contemporary medical education also employs other small group learning methods including CBL and TBL. Characteristics common to the pedagogy of both CBL and TBL include the use of an authentic clinical case, active small-group learning, activation of existing knowledge and application of newly acquired knowledge. In CBL students are encouraged to engage in peer learning and apply new knowledge to these authentic clinical problems under the guidance of a facilitator. CBL encourages a structured and critical approach to clinical problem-solving, and, in contrast to PBL, is designed to allow the facilitator to correct and redirect students [ 5 ]. On the other hand, TBL offers a student-centered, instructional approach for large classes of students who are divided into small teams of typically five to seven students to solve clinically relevant problems. The overall similarities between PBL and TBL relate to the use of professionally relevant problems and small group learning, while the main difference relates to one teacher facilitating interactions between multiple self-managed teams in TBL, whereas each small group in PBL is facilitated by one teacher. Further differences are related to mandatory pre-reading assignments in TBL, testing of prior knowledge in TBL and activating prior knowledge in PBL, teacher-initiated clarifying of concepts that students struggled with in TBL versus students-generated issues that need further study in PBL, inter-team discussions in TBL and structured feedback and problems with related questions in TBL [ 6 ].
In the present study we have focused on PBL methodology, and, as attractive as the method may seem, we should consider whether it is really useful and effective as a learning method. Although PBL has been adopted in undergraduate and postgraduate medical education, the effectiveness (in terms of academic performance and/or skill improvement) of the method is still under discussion. This is due partly to the methodological difficulty in comparing PBL with traditional curricula based on lectures. To our knowledge, there is no systematic scoping review in the literature that has analyzed these aspects.
The main motivation for carrying out this research and writing this article was scientific but also professional interest. We believe that reviewing the state of the art of this methodology once it was already underway in our young Faculty of Medicine, could allow us to know if we were on the right track and if we should implement changes in the training of future doctors.
The primary goal of this study was to appraise available international evidence concerning to the effectiveness and usefulness of PBL methodology in undergraduate medical teaching programs. As the intention was to synthesize the scattered evidence available, the option was to conduct a scoping review. A scoping study tends to address broader topics where many different study designs might be applicable. Scoping studies may be particularly relevant to disciplines, such as medical education, in which the paucity of randomized controlled trials makes it difficult for researchers to undertake systematic reviews [ 7 , 8 ]. Even though the scoping review methodology is not widely used in medical education, it is well established for synthesizing heterogeneous research evidence [ 9 ].
The specific aims were: 1) to determine the effectiveness of PBL in academic performance (learning and retention of knowledge) in medical education; 2) to determine the effectiveness of PBL in other skills (social and communication skills, problem solving or self-learning) in medical education; 3) to know the level of satisfaction perceived by the medical students (and/or tutors) when they are taught with the PBL methodology (or when they teach in case of tutors).
This review was guided by Arksey and O’Malley’s methodological framework for conducting scoping reviews. The five main stages of the framework are: (1) identifying the research question; (2) ascertaining relevant studies; (3) determining study selection; (4) charting the data; and (5) collating, summarizing and reporting the results [ 7 ]. We reported our process according to the PRISMA Extension for Scoping Reviews [ 10 ].
Stage 1: Identifying the research question
With the goals of the study established, the four members of the research team established the research questions. The primary research question was “What is the effectiveness of PBL methodology for learning in undergraduate medicine?” and the secondary question “What is the perception and satisfaction of medical students and tutors in relation to PBL methodology?”.
Stage 2: Identifying relevant studies
After the research questions and a search strategy were defined, the searches were conducted in PubMed and Web of Science using the MeSH terms “problem-based learning” and “Medicine” (the Boolean operator “AND” was applied to the search terms). No limits were set on language, publication date, study design or country of origin. The search was carried out on 14th February 2021. Citations were uploaded to the reference manager software Mendeley Desktop (version 1.19.8) for title and abstract screening, and data characterization.
Stage 3: Study selection
The searching strategy in our scoping study generated a total of 2399 references. The literature search and screening of title, abstract and full text for suitability was performed independently by one author (JCT) based on predetermined inclusion criteria. The inclusion criteria were: 1) PBL methodology was the major research topic; 2) participants were undergraduate medical students or tutors; 3) the main outcome was academic performance (learning and knowledge retention); 4) the secondary outcomes were one of the following: social and communication skills, problem solving or self-learning and/or student/tutor satisfaction; 5) all types of studies were included including descriptive papers, qualitative, quantitative and mixed studies methods, perspectives, opinion, commentary pieces and editorials. Exclusion criteria were studies including other types of participants such as postgraduate medical students, residents and other health non-medical specialties such as pharmacy, veterinary, dentistry or nursing. Studies published in languages other than Spanish and English were also excluded. Situations in which uncertainty arose, all authors (CB, ES, RP) discussed the publication together to reach a final consensus. The outcomes of the search results and screening are presented in Fig. 1 . One-hundred and twenty-four articles met the inclusion criteria and were included in the final analysis.
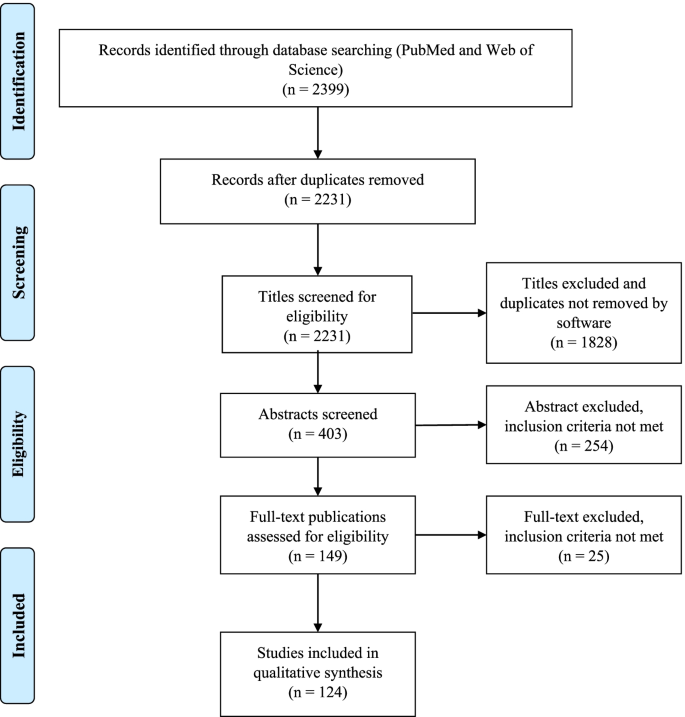
Study flow PRISMA diagram. Details the review process through the different stages of the review; includes the number of records identified, included and excluded
Stage 4: Charting the data
A data extraction table was developed by the research team. Data extracted from each of the 124 publications included general publication details (year, author, and country), sample size, study population, design/methodology, main and secondary outcomes and relevant results and/or conclusions. We compiled all data into a single spreadsheet in Microsoft Excel for coding and analysis. The characteristics and the study subject of the 124 articles included in this review are summarized in Tables 1 and 2 . The detailed results of the Microsoft Excel file is also available in Additional file 1 .
Stage 5: Collating, summarizing and reporting the results
As indicated in the search strategy (Fig. 1 ) this review resulted in the inclusion of 124 publications. Publication years of the final sample ranged from 1990 to 2020, the majority of the publications (51, 41%) were identified for the years 2010–2020 and the years in which there were more publications were 2001, 2009 and 2015. Countries from the six continents were represented in this review. Most of the publications were from Asia (especially China and Saudi Arabia) and North America followed by Europe, and few studies were from Africa, Oceania and South America. The country with more publications was the United States of America ( n = 27). The most frequent designs of the selected studies were surveys or questionnaires ( n = 45) and comparative studies ( n = 48, only 16 were randomized) with traditional or lecture-based learning methodologies (in two studies the comparison was with simulation) and the most frequently measured outcomes were academic performance followed by student satisfaction (48 studies measured more than one outcome). The few studies with the highest level of scientific evidence (systematic review and meta-analysis and randomized studies) were conducted mostly in Asian countries (Tables 1 and 2 ). The study subject was specified in 81 publications finding a high variability but at the same time great representability of almost all disciplines of the medical studies.
The sample size was available in 99 publications and the median [range] of the participants was 132 [14–2061]. According to study population, there were more participants in the students’ focused studies (median 134 and range 16–2061) in comparison with the tutors’ studies (median 53 and range 14–494).
Finally, after reviewing in detail the measured outcomes (main and secondary) according to the study design (Table 2 and Additional file 1 ) we present a narrative overview and a synthesis of the main findings.
Main outcome: academic performance (learning and knowledge retention)
Seventy-one of the 124 publications had learning and/or knowledge retention as a measured outcome, most of them ( n = 45) were comparative studies with traditional or lecture-based learning and 16 were randomized. These studies were varied in their methodology, were performed in different geographic zones, and normally analyzed the experience of just one education center. Most studies ( n = 49) reported superiority of PBL in learning and knowledge acquisition [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 ] but there was no difference between traditional and PBL curriculums in another 19 studies [ 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 ]. Only three studies reported that PBL was less effective [ 79 , 80 , 81 ], two of them were randomized (in one case favoring simulation-based learning [ 80 ] and another favoring lectures [ 81 ]) and the remaining study was based on tutors’ opinion rather than real academic performance [ 79 ]. It is noteworthy that the four systematic reviews and meta-analysis included in this scoping review, all carried out in China, found that PBL was more effective than lecture-based learning in improving knowledge and other skills (clinical, problem-solving, self-learning and collaborative) [ 40 , 51 , 53 , 58 ]. Another relevant example of the superiority of the PBL method over the traditional method is the experience reported by Hoffman et al. from the University of Missouri-Columbia. The authors analyzed the impact of implementing the PBL methodology in its Faculty of Medicine and revealed an improvement in the academic results that lasted for over a decade [ 31 ].
Secondary outcomes
Social and communication skills.
We found five studies in this scoping review that focused on these outcomes and all of them described that a curriculum centered on PBL seems to instill more confidence in social and communication skills among students. Students perceived PBL positively for teamwork, communication skills and interpersonal relations [ 44 , 45 , 67 , 75 , 82 ].
Student satisfaction
Sixty publications analyzed student satisfaction with PBL methodology. The most frequent methodology were surveys or questionnaires (30 studies) followed by comparative studies with traditional or lecture-based methodology (19 studies, 7 of them were randomized). Almost all the studies (51) have shown that PBL is generally well-received [ 11 , 13 , 18 , 19 , 20 , 21 , 22 , 26 , 29 , 34 , 37 , 39 , 41 , 42 , 46 , 50 , 56 , 58 , 63 , 64 , 66 , 78 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 ] but in 9 studies the overall satisfaction scores for the PBL program were neutral [ 76 , 111 , 112 , 113 , 114 , 115 , 116 ] or negative [ 117 , 118 ]. Some factors that have been identified as key components for PBL to be successful include: a small group size, the use of scenarios of realistic cases and good management of group dynamics. Despite a mostly positive assessment of the PBL methodology by the students, there were some negative aspects that could be criticized or improved. These include unclear communication of the learning methodology, objectives and assessment method; bad management and organization of the sessions; tutors having little experience of the method; and a lack of standardization in the implementation of the method by the tutors.
Tutor satisfaction
There are only 15 publications that analyze the satisfaction of tutors, most of them surveys or questionnaires [ 85 , 88 , 92 , 98 , 108 , 110 , 119 ]. In comparison with the satisfaction of the students, here the results are more neutral [ 112 , 113 , 115 , 120 , 121 ] and even unfavorable to the PBL methodology in two publications [ 117 , 122 ]. PBL teaching was favored by tutors when the institutions train them in the subject, when there was administrative support and adequate infrastructure and coordination [ 123 ]. In some experiences, the PBL modules created an unacceptable toll of anxiety, unhappiness and strained relations.
Other skills (problem solving and self-learning)
The effectiveness of the PBL methodology has also been explored in other outcomes such as the ability to solve problems and to self-directed learning. All studies have shown that PBL is more effective than lecture-based learning in problem-solving and self-learning skills [ 18 , 24 , 40 , 48 , 67 , 75 , 93 , 104 , 124 ]. One single study found a poor accuracy of the students’ self-assessment when compared to their own performance [ 125 ]. In addition, there are studies that support PBL methodology for integration between basic and clinical sciences [ 126 ].
Finally, other publications have reported the experience of some faculties in the implementation of the PBL methodology. Different experiences have demonstrated that it is both possible and feasible to shift from a traditional curriculum to a PBL program, recognizing that PBL methodology is complex to plan and structure, needs a large number of human and material resources, requiring an immense teacher effort [ 28 , 31 , 94 , 127 , 128 , 129 , 130 , 131 , 132 , 133 ]. In addition, and despite its cost implication, a PBL curriculum can be successfully implemented in resource-constrained settings [ 134 , 135 ].
We conducted this scoping review to explore the effectiveness and satisfaction of PBL methodology for teaching in undergraduate medicine and, to our knowledge, it is the only study of its kind (systematic scoping review) that has been carried out in the last years. Similarly, Vernon et al. conducted a meta-analysis of articles published between 1970 and 1992 and their results generally supported the superiority of the PBL approach over more traditional methods of medical education [ 136 ]. PBL methodology is implemented in medical studies on the six continents but there is more experience (or at least more publications) from Asian countries and North America. Despite its apparent difficulties on implementation, a PBL curriculum can be successfully implemented in resource-constrained settings [ 134 , 135 ]. Although it is true that the few studies with the highest level of scientific evidence (randomized studies and meta-analysis) were carried out mainly in Asian countries (and some in North America and Europe), there were no significant differences in the main results according to geographical origin.
In this scoping review we have included a large number of publications that, despite their heterogeneity, tend to show favorable results for the usefulness of the PBL methodology in teaching and learning medicine. The results tend to be especially favorable to PBL methodology when it is compared with traditional or lecture-based teaching methods, but when compared with simulation it is not so clear. There are two studies that show neutral [ 71 ] or superior [ 80 ] results to simulation for the acquisition of specific clinical skills. It seems important to highlight that the four meta-analysis included in this review, which included a high number of participants, show results that are clearly favorable to the PBL methodology in terms of knowledge, clinical skills, problem-solving, self-learning and satisfaction [ 40 , 51 , 53 , 58 ].
Regarding the level of satisfaction described in the surveys or questionnaires, the overall satisfaction rate was higher in the PBL students when compared with traditional learning students. Students work in small groups, allowing and promoting teamwork and facilitating social and communication skills. As sessions are more attractive and dynamic than traditional classes, this could lead to a greater degree of motivation for learning.
These satisfaction results are not so favorable when tutors are asked and this may be due to different reasons; first, some studies are from the 90s, when the methodology was not yet fully implemented; second, the number of tutors included in these studies is low; and third, and perhaps most importantly, the complaints are not usually due to the methodology itself, but rather due to lack of administrative support, and/or work overload. PBL methodology implies more human and material resources. The lack of experience in guided self-learning by lecturers requires more training. Some teachers may not feel comfortable with the method and therefore do not apply it correctly.
Despite how effective and/or attractive the PBL methodology may seem, some (not many) authors are clearly detractors and have published opinion articles with fierce criticism to this methodology. Some of the arguments against are as follows: clinical problem solving is the wrong task for preclinical medical students, self-directed learning interpreted as self-teaching is not appropriate in undergraduate medical education, relegation to the role of facilitators is a misuse of the faculty, small-group experience is inherently variable and sometimes dysfunctional, etc. [ 137 ].
In light of the results found in our study, we believe that PBL is an adequate methodology for the training of future doctors and reinforces the idea that the PBL should have an important weight in the curriculum of our medical school. It is likely that training through PBL, the doctors of the future will not only have great knowledge but may also acquire greater capacity for communication, problem solving and self-learning, all of which are characteristics that are required in medical professionalism. For this purpose, Koh et al. analyzed the effect that PBL during medical school had on physician competencies after graduation, finding a positive effect mainly in social and cognitive dimensions [ 138 ].
Despite its defects and limitations, we must not abandon this methodology and, in any case, perhaps PBL should evolve, adapt, and improve to enhance its strengths and improve its weaknesses. It is likely that the new generations, trained in schools using new technologies and methodologies far from lectures, will feel more comfortable (either as students or as tutors) with methodologies more like PBL (small groups and work focused on problems or projects). It would be interesting to examine the implementation of technologies and even social media into PBL sessions, an issue that has been poorly explorer [ 139 ].
Limitations
Scoping reviews are not without limitations. Our review includes 124 articles from the 2399 initially identified and despite our efforts to be as comprehensive as possible, we may have missed some (probably few) articles. Even though this review includes many studies, their design is very heterogeneous, only a few include a large sample size and high scientific evidence methodology. Furthermore, most are single-center experiences and there are no large multi-center studies. Finally, the frequency of the PBL sessions (from once or twice a year to the whole curriculum) was not considered, in part, because most of the revised studies did not specify this information. This factor could affect the efficiency of PBL and the perceptions of students and tutors about PBL. However, the adoption of a scoping review methodology was effective in terms of summarizing the research findings, identifying limitations in studies’ methodologies and findings and provided a more rigorous vision of the international state of the art.
Conclusions
This systematic scoping review provides a broad overview of the efficacy of PBL methodology in undergraduate medicine teaching from different countries and institutions. PBL is not a new teaching method given that it has already been 50 years since it was implemented in medicine courses. It is a method that shifts the leading role from teachers to students and is based on guided self-learning. If it is applied properly, the degree of satisfaction is high, especially for students. PBL is more effective than traditional methods (based mainly on lectures) at improving social and communication skills, problem-solving and self-learning skills, and has no worse results (and in many studies better results) in relation to academic performance. Despite that, its use is not universally widespread, probably because it requires greater human resources and continuous training for its implementation. In any case, more comparative and randomized studies and/or other systematic reviews and meta-analysis are required to determine which educational strategies could be most suitable for the training of future doctors.
Abbreviations
- Problem-based learning
Case-based learning
Team-based learning
References:
Dale E. Methods for analyzing the content of motion pictures. J Educ Sociol. 1932;6:244–50.
Google Scholar
Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9 Suppl):S63–7. https://doi.org/10.1097/00001888-199009000-00045 .
Article Google Scholar
Bodagh N, Bloomfield J, Birch P, Ricketts W. Problem-based learning: a review. Br J Hosp Med (Lond). 2017;78:C167–70. https://doi.org/10.12968/hmed.2017.78.11.C167 .
- Branda LA. El abc del ABP: Lo esencial del aprendizaje basado en problemas. In: Fundación Dr. Esteve, Cuadernos de la fundación Dr. Antonio Esteve nº27: El aprendizaje basado en problemas en sus textos, pp.1–16. 2013. Barcelona.
Burgess A, Matar E, Roberts C, et al. Scaffolding medical student knowledge and skills: team-based learning (TBL) and case-based learning (CBL). BMC Med Educ. 2021;21:238. https://doi.org/10.1186/s12909-021-02638-3 .
Dolmans D, Michaelsen L, van Merriënboer J, van der Vleuten C. Should we choose between problem-based learning and team-based learning? No, combine the best of both worlds! Med Teach. 2015;37:354–9. https://doi.org/10.3109/0142159X.2014.948828 .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. In J Soc Res Methodol. 2005;8:19–32. https://doi.org/10.1080/1364557032000119616 .
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69 .
Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5:371–85. https://doi.org/10.1002/jrsm.1123 .
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73. https://doi.org/10.7326/M18-0850 .
Sokas RK, Diserens D, Johnston MA. Integrating occupational-health into the internal medicine clerkship using problem-based learning. Clin Res. 1990;38:A735.
Richards BF, Ober KP, Cariaga-Lo L, et al. Ratings of students’ performances in a third-year internal medicine clerkship: a comparison between problem-based and lecture-based curricula. Acad Med. 1996;71:187–9. https://doi.org/10.1097/00001888-199602000-00028 .
Gresham CL, Philp JR. Problem-based learning in clinical medicine. Teach Learn Med. 1996;8:111–5. https://doi.org/10.1080/10401339609539776 .
Hill J, Rolfe IE, Pearson SA, Heathcote A. Do junior doctors feel they are prepared for hospital practice? A study of graduates from traditional and non-traditional medical schools. Med Educ. 1998;32:19–24. https://doi.org/10.1046/j.1365-2923.1998.00152.x .
Blake RL, Parkison L. Faculty evaluation of the clinical performances of students in a problem-based learning curriculum. Teach Learn Med. 1998;10:69–73. https://doi.org/10.1207/S15328015TLM1002\_3 .
Hmelo CE. Problem-based learning: effects on the early acquisition of cognitive skill in medicine. J Learn Sc. 1998;7:173–208. https://doi.org/10.1207/s15327809jls0702\_2 .
Finch PN. The effect of problem-based learning on the academic performance of students studying podiatric medicine in Ontario. Med Educ. 1999;33:411–7.
Casassus P, Hivon R, Gagnayre R, d’Ivernois JF. An initial experiment in haematology instruction using the problem-based learning method in third-year medical training in France. Hematol Cell Ther. 1999;41:137–44. https://doi.org/10.1007/s00282-999-0137-0 .
Purdy RA, Benstead TJ, Holmes DB, Kaufman DM. Using problem-based learning in neurosciences education for medical students. Can J Neurol Sci. 1999;26:211–6. https://doi.org/10.1017/S0317167100000287 .
Farrell TA, Albanese MA, Pomrehn PRJ. Problem-based learning in ophthalmology: a pilot program for curricular renewal. Arch Ophthalmol. 1999;117:1223–6. https://doi.org/10.1001/archopht.117.9.1223 .
Curtis JA, Indyk D, Taylor B. Successful use of problem-based learning in a third-year pediatric clerkship. Ambul Pediatr. 2001;1:132–5. https://doi.org/10.1367/1539-4409(2001)001%3c0132:suopbl%3e2.0.co;2 .
Trevena LJ, Clarke RM. Self-directed learning in population health. a clinically relevant approach for medical students. Am J Prev Med. 2002;22:59–65. https://doi.org/10.1016/s0749-3797(01)00395-6 .
Astin J, Jenkins T, Moore L. Medical students’ perspective on the teaching of medical statistics in the undergraduate medical curriculum. Stat Med. 2002;21:1003–7. https://doi.org/10.1002/sim.1132 .
Whitfield CR, Manger EA, Zwicker J, Lehman EB. Differences between students in problem-based and lecture-based curricula measured by clerkship performance ratings at the beginning of the third year. Teach Learn Med. 2002;14:211–7. https://doi.org/10.1207/S15328015TLM1404\_2 .
McParland M, Noble LM, Livingston G. The effectiveness of problem-based learning compared to traditional teaching in undergraduate psychiatry. Med Educ. 2004;38:859–67. https://doi.org/10.1111/j.1365-2929.2004.01818.x .
Casey PM, Magrane D, Lesnick TG. Improved performance and student satisfaction after implementation of a problem-based preclinical obstetrics and gynecology curriculum. Am J Obstet Gynecol. 2005;193:1874–8. https://doi.org/10.1016/j.ajog.2005.07.061 .
Gurpinar E, Musal B, Aksakoglu G, Ucku R. Comparison of knowledge scores of medical students in problem-based learning and traditional curriculum on public health topics. BMC Med Educ. 2005;5:7. https://doi.org/10.1186/1472-6920-5-7 .
Tamblyn R, Abrahamowicz M, Dauphinee D, et al. Effect of a community oriented problem based learning curriculum on quality of primary care delivered by graduates: historical cohort comparison study. BMJ. 2005;331:1002. https://doi.org/10.1136/bmj.38636.582546.7C .
Abu-Hijleh MF, Chakravarty M, Al-Shboul Q, Kassab S, Hamdy H. Integrating applied anatomy in surgical clerkship in a problem-based learning curriculum. Surg Radiol Anat. 2005;27:152–7. https://doi.org/10.1007/s00276-004-0293-4 .
Distlehorst LH, Dawson E, Robbs RS, Barrows HS. Problem-based learning outcomes: the glass half-full. Acad Med. 2005;80:294–9. https://doi.org/10.1097/00001888-200503000-00020 .
Hoffman K, Hosokawa M, Blake R Jr, Headrick L, Johnson G. Problem-based learning outcomes: ten years of experience at the University of Missouri-Columbia school of medicine. Acad Med. 2006;81:617–25. https://doi.org/10.1097/01.ACM.0000232411.97399.c6 .
Kong J, Li X, Wang Y, Sun W, Zhang J. Effect of digital problem-based learning cases on student learning outcomes in ophthalmology courses. Arch Ophthalmol. 2009;127:1211–4. https://doi.org/10.1001/archophthalmol.2009.110 .
Tsou KI, Cho SL, Lin CS, et al. Short-term outcomes of a near-full PBL curriculum in a new Taiwan medical school. Kaohsiung J Med Sci. 2009;25:282–93. https://doi.org/10.1016/S1607-551X(09)70075-0 .
Wang J, Zhang W, Qin L, et al. Problem-based learning in regional anatomy education at Peking University. Anat Sci Educ. 2010;3:121–6. https://doi.org/10.1002/ase.151 .
Abou-Elhamd KA, Rashad UM, Al-Sultan AI. Applying problem-based learning to otolaryngology teaching. J Laryngol Otol. 2011;125:117–20. https://doi.org/10.1017/S0022215110001702 .
Urrutia Aguilar ME, Hamui-Sutton A, Castaneda Figueiras S, van der Goes TI, Guevara-Guzman R. Impact of problem-based learning on the cognitive processes of medical students. Gac Med Mex. 2011;147:385–93.
Tian J-H, Yang K-H, Liu A-P. Problem-based learning in evidence-based medicine courses at Lanzhou University. Med Teach. 2012;34:341. https://doi.org/10.3109/0142159X.2011.531169 .
Hoover CR, Wong CC, Azzam A. From primary care to public health: using problem-based Learning and the ecological model to teach public health to first year medical students. J Community Health. 2012;37:647–52. https://doi.org/10.1007/s10900-011-9495-y .
Li J, Li QL, Li J, et al. Comparison of three problem-based learning conditions (real patients, digital and paper) with lecture-based learning in a dermatology course: a prospective randomized study from China. Med Teach. 2013;35:e963–70. https://doi.org/10.3109/0142159X.2012.719651 .
Ding X, Zhao L, Chu H, et al. Assessing the effectiveness of problem-based learning of preventive medicine education in China. Sci Rep. 2014;4:5126. https://doi.org/10.1038/srep05126 .
Meo SA. Undergraduate medical student’s perceptions on traditional and problem based curricula: pilot study. J Pak Med Assoc. 2014;64:775–9.
Khoshnevisasl P, Sadeghzadeh M, Mazloomzadeh S, Hashemi Feshareki R, Ahmadiafshar A. Comparison of problem-based learning with lecture-based learning. Iran Red Crescent Med J. 2014;16: e5186. https://doi.org/10.5812/ircmj.5186 .
Al-Drees AA, Khalil MS, Irshad M, Abdulghani HM. Students’ perception towards the problem based learning tutorial session in a system-based hybrid curriculum. Saudi Med J. 2015;36:341–8. https://doi.org/10.15537/smj.2015.3.10216 .
Al-Shaikh G, Al Mussaed EM, Altamimi TN, Elmorshedy H, Syed S, Habib F. Perception of medical students regarding problem based learning. Kuwait Med J. 2015;47:133–8.
Hande S, Mohammed CA, Komattil R. Acquisition of knowledge, generic skills and attitudes through problem-based learning: student perspectives in a hybrid curriculum. J Taibah Univ Medical Sci. 2015;10:21–5. https://doi.org/10.1016/j.jtumed.2014.01.008 .
González Mirasol E, Gómez García MT, Lobo Abascal P, Moreno Selva R, Fuentes Rozalén AM, González MG. Analysis of perception of training in graduates of the faculty of medicine at Universidad de Castilla-Mancha. Eval Program Plann. 2015;52:169–75. https://doi.org/10.1016/j.evalprogplan.2015.06.001 .
Yanamadala M, Kaprielian VS, O’Connor Grochowski C, Reed T, Heflin MT. A problem-based learning curriculum in geriatrics for medical students. Gerontol Geriatr Educ. 2018;39:122–31. https://doi.org/10.1080/02701960.2016.1152268 .
Balendran K, John L. Comparison of learning outcomes in problem based learning and lecture based learning in teaching forensic medicine. J Evol Med Dent Sci. 2017;6:89–92. https://doi.org/10.14260/jemds/2017/22 .
Chang H-C, Wang N-Y, Ko W-R, Yu Y-T, Lin L-Y, Tsai H-F. The effectiveness of clinical problem-based learning model of medico-jurisprudence education on general law knowledge for obstetrics/gynecological interns. Taiwan J Obstet Gynecol. 2017;56:325–30. https://doi.org/10.1016/j.tjog.2017.04.011 .
Eltony SA, El-Sayed NH, El-Araby SE-S, Kassab SE. Implementation and evaluation of a patient safety course in a problem-based learning program. Educ Heal. 2017;30:44–9. https://doi.org/10.4103/1357-6283.210512 .
Zhang S, Xu J, Wang H, Zhang D, Zhang Q, Zou L. Effects of problem-based learning in Chinese radiology education: a systematic review and meta-analysis. Medicine (Baltimore). 2018;97: e0069. https://doi.org/10.1097/MD.0000000000010069 .
Hincapie Parra DA, Ramos Monobe A, Chrino-Barcelo V. Problem based learning as an active learning strategy and its impact on academic performance and critical thinking of medical students. Rev Complut Educ. 2018;29:665–81. https://doi.org/10.5209/RCED.53581 .
Ma Y, Lu X. The effectiveness of problem-based learning in pediatric medical education in China: a meta-analysis of randomized controlled trials. Medicine (Baltimore). 2019;98: e14052. https://doi.org/10.1097/MD.0000000000014052 .
Berger C, Brinkrolf P, Ertmer C, et al. Combination of problem-based learning with high-fidelity simulation in CPR training improves short and long-term CPR skills: a randomised single blinded trial. BMC Med Educ. 2019;19:180. https://doi.org/10.1186/s12909-019-1626-7 .
Aboonq M, Alquliti A, Abdulmonem I, Alpuq N, Jalali K, Arabi S. Students’ approaches to learning and perception of learning environment: a comparison between traditional and problem-based learning medical curricula. Indo Am J Pharm Sci. 2019;6:3610–9. https://doi.org/10.5281/zenodo.2562660 .
Li X, Xie F, Li X, et al. Development, application, and evaluation of a problem-based learning method in clinical laboratory education. Clin Chim ACTA. 2020;510:681–4. https://doi.org/10.1016/j.cca.2020.08.037 .
Zhao W, He L, Deng W, Zhu J, Su A, Zhang Y. The effectiveness of the combined problem-based learning (PBL) and case-based learning (CBL) teaching method in the clinical practical teaching of thyroid disease. BMC Med Educ. 2020;20:381. https://doi.org/10.1186/s12909-020-02306 .
Liu C-X, Ouyang W-W, Wang X-W, Chen D, Jiang Z-L. Comparing hybrid problem-based and lecture learning (PBL plus LBL) with LBL pedagogy on clinical curriculum learning for medical students in China: a meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99:e19687. https://doi.org/10.1097/MD.0000000000019687 .
Margolius SW, Papp KK, Altose MD, Wilson-Delfosse AL. Students perceive skills learned in pre-clerkship PBL valuable in core clinical rotations. Med Teach. 2020;42:902–8. https://doi.org/10.1080/0142159X.2020.1762031 .
Schwartz RW, Donnelly MB, Nash PP, Young B. Developing students cognitive skills in a problem-based surgery clerkship. Acad Med. 1992;67:694–6. https://doi.org/10.1097/00001888-199210000-00016 .
Mennin SP, Friedman M, Skipper B, Kalishman S, Snyder J. Performances on the NBME-I, NBME-II, and NBME-III by medical-students in the problem-based learning and conventional tracks at the university-of-new-mexico. Acad Med. 1993;68:616–24. https://doi.org/10.1097/00001888-199308000-00012 .
Kaufman DM, Mann KV. Comparing achievement on the medical council of Canada qualifying examination part I of students in conventional and problem-based learning curricula. Acad Med. 1998;73:1211–3. https://doi.org/10.1097/00001888-199811000-00022 .
Kaufman DM, Mann KV. Achievement of students in a conventional and Problem-Based Learning (PBL) curriculum. Adv Heal Sci Educ. 1999;4:245–60. https://doi.org/10.1023/A:1009829831978 .
Antepohl W, Herzig S. Problem-based learning versus lecture-based learning in a course of basic pharmacology: a controlled, randomized study. Med Educ. 1999;33:106–13. https://doi.org/10.1046/j.1365-2923.1999.00289.x .
Dyke P, Jamrozik K, Plant AJ. A randomized trial of a problem-based learning approach for teaching epidemiology. Acad Med. 2001;76:373–9. https://doi.org/10.1097/00001888-200104000-00016 .
Brewer DW. Endocrine PBL in the year 2000. Adv Physiol Educ. 2001;25:249–55. https://doi.org/10.1152/advances.2001.25.4.249 .
Seneviratne RD, Samarasekera DD, Karunathilake IM, Ponnamperuma GG. Students’ perception of problem-based learning in the medical curriculum of the faculty of medicine, University of Colombo. Ann Acad Med Singapore. 2001;30:379–81.
Alleyne T, Shirley A, Bennett C, et al. Problem-based compared with traditional methods at the faculty of medical sciences, University of the West Indies: a model study. Med Teach. 2002;24:273–9. https://doi.org/10.1080/01421590220125286 .
Norman GR, Wenghofer E, Klass D. Predicting doctor performance outcomes of curriculum interventions: problem-based learning and continuing competence. Med Educ. 2008;42:794–9. https://doi.org/10.1111/j.1365-2923.2008.03131.x .
Cohen-Schotanus J, Muijtjens AMM, Schoenrock-Adema J, Geertsma J, van der Vleuten CPM. Effects of conventional and problem-based learning on clinical and general competencies and career development. Med Educ. 2008;42:256–65. https://doi.org/10.1111/j.1365-2923.2007.02959.x .
Wenk M, Waurick R, Schotes D, et al. Simulation-based medical education is no better than problem-based discussions and induces misjudgment in self-assessment. Adv Health Sci Educ Theory Pract. 2009;14:159–71. https://doi.org/10.1007/s10459-008-9098-2 .
Collard A, Gelaes S, Vanbelle S, et al. Reasoning versus knowledge retention and ascertainment throughout a problem-based learning curriculum. Med Educ. 2009;43:854–65. https://doi.org/10.1111/j.1365-2923.2009.03410.x .
Nouns Z, Schauber S, Witt C, Kingreen H, Schuettpelz-Brauns K. Development of knowledge in basic sciences: a comparison of two medical curricula. Med Educ. 2012;46:1206–14. https://doi.org/10.1111/medu.12047 .
Saloojee S, van Wyk J. The impact of a problem-based learning curriculum on the psychiatric knowledge and skills of final-year students at the Nelson R Mandela school of medicine. South African J Psychiatry. 2012;18:116.
Mughal AM, Shaikh SH. Assessment of collaborative problem solving skills in undergraduate medical students at Ziauddin college of medicine. Karachi Pakistan J Med Sci. 2018;34:185–9. https://doi.org/10.12669/pjms.341.13485 .
Hu X, Zhang H, Song Y, et al. Implementation of flipped classroom combined with problem-based learning: an approach to promote learning about hyperthyroidism in the endocrinology internship. BMC Med Educ. 2019;19:290. https://doi.org/10.1186/s12909-019-1714-8 .
Thompson KL, Gendreau JL, Strickling JE, Young HE. Cadaveric dissection in relation to problem-based learning case sequencing: a report of medical student musculoskeletal examination performances and self-confidence. Anat Sci Educ. 2019;12:619–26. https://doi.org/10.1002/ase.1891 .
Chang G, Cook D, Maguire T, Skakun E, Yakimets WW, Warnock GL. Problem-based learning: its role in undergraduate surgical education. Can J Surg. 1995;38:13–21.
Vernon DTA, Hosokawa MC. Faculty attitudes and opinions about problem-based learning. Acad Med. 1996;71:1233–8. https://doi.org/10.1097/00001888-199611000-00020 .
Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34:151–7. https://doi.org/10.1097/01.CCM.0000190619.42013.94 .
Johnston JM, Schooling CM, Leung GM. A randomised-controlled trial of two educational modes for undergraduate evidence-based medicine learning in Asia. BMC Med Educ. 2009;9:63. https://doi.org/10.1186/1472-6920-9-63 .
Suleman W, Iqbal R, Alsultan A, Baig SM. Perception of 4(th) year medical students about problem based learning. Pakistan J Med Sci. 2010;26:871–4.
Blosser A, Jones B. Problem-based learning in a surgery clerkship. Med Teach. 1991;13:289–93. https://doi.org/10.3109/01421599109089907 .
Usherwood T, Joesbury H, Hannay D. Student-directed problem-based learning in general-practice and public-health medicine. Med Educ. 1991;25:421–9. https://doi.org/10.1111/j.1365-2923.1991.tb00090.x .
Bernstein P, Tipping J, Bercovitz K, Skinner HA. Shifting students and faculty to a PBL curriculum - attitudes changed and lessons learned. Acad Med. 1995;70:245–7. https://doi.org/10.1097/00001888-199503000-00019 .
Kaufman DM, Mann KV. Comparing students’ attitudes in problem-based and conventional curricula. Acad Med. 1996;71:1096–9. https://doi.org/10.1097/00001888-199610000-00018 .
Kalaian HA, Mullan PB. Exploratory factor analysis of students’ ratings of a problem-based learning curriculum. Acad Med. 1996;71:390–2. https://doi.org/10.1097/00001888-199604000-00019 .
Vincelette J, Lalande R, Delorme P, Goudreau J, Lalonde V, Jean P. A pilot course as a model for implementing a PBL curriculum. Acad Med. 1997;72:698–701. https://doi.org/10.1097/00001888-199708000-00015 .
Ghosh S, Dawka V. Combination of didactic lecture with problem-based learning sessions in physiology teaching in a developing medical college in Nepal. Adv Physiol Educ. 2000;24:8–12.
Walters MR. Problem-based learning within endocrine physiology lectures. Adv Physiol Educ. 2001;25:225–7. https://doi.org/10.1152/advances.2001.25.4.225 .
Leung GM, Lam TH, Hedley AJ. Problem-based public health learning - from the classroom to the community. Med Educ. 2001;35:1071–2.
Khoo HE, Chhem RK, Gwee MCE, Balasubramaniam P. Introduction of problem-based learning in a traditional medical curriculum in Singapore - students’ and tutors’ perspectives. Ann Acad Med Singapore. 2001;30:371–4.
Villamor MCA. Problem-based learning (PBL) as an approach in the teaching of biochemistry of the endocrine system at the Angeles University College of Medicine. Ann Acad Med Singapore. 2001;30:382–6.
Chang C-H, Yang C-Y, See L-C, Lui P-W. High satisfaction with problem-based learning for anesthesia. Chang Gung Med J. 2004;27:654–62.
McLean M. A comparison of students who chose a traditional or a problem-based learning curriculum after failing year 2 in the traditional curriculum: a unique case study at the Nelson R. Mandela school of medicine. Teach Learn Med. 2004;16:301–3. https://doi.org/10.1207/s15328015tlm1603\_15 .
Lucas M, García Guasch R, Moret E, Llasera R, Melero A. Canet J [Problem-based learning in an undergraduate medical school course on anesthesiology, recovery care, and pain management]. Rev Esp Anestesiol Reanim. 2006;53:419–25.
Burgun A, Darmoni S, Le Duff F, Weber J. Problem-based learning in medical informatics for undergraduate medical students: an experiment in two medical schools. Int J Med Inform. 2006;75:396–402. https://doi.org/10.1016/j.ijmedinf.2005.07.014 .
Gurpinar E, Senol Y, Aktekin MR. Evaluation of problem based learning by tutors and students in a medical faculty of Turkey. Kuwait Med J. 2009;41:123–7.
Elzubeir MA. Teaching of the renal system in an integrated, problem-based curriculum. Saudi J Kidney Dis Transpl. 2012;23:93–8.
Sulaiman N, Hamdy H. Problem-based learning: where are we now? Guide supplement 36.3–practical application. Med Teach. 2013;35:160–2. https://doi.org/10.3109/0142159X.2012.737965 .
Albarrak AI, Mohammed R, Abalhassan MF, Almutairi NK. Academic satisfaction among traditional and problem based learning medical students a comparative study. Saudi Med J. 2013;34:1179–88.
Nosair E, Mirghani Z, Mostafa RM. Measuring students’ perceptions of educational environment in the PBL program of Sharjah Medical College. J Med Educ Curric Dev. 2015;2:71–9. https://doi.org/10.4137/JMECDECDECD.S29926 .
Tshitenge ST, Ndhlovu CE, Ogundipe R. Evaluation of problem-based learning curriculum implementation in a clerkship rotation of a newly established African medical training institution: lessons from the University of Botswana. Pan Afr Med J. 2017;27:13. https://doi.org/10.11604/pamj.2017.27.13.10623 .
Yadav RL, Piryani RM, Deo GP, Shah DK, Yadav LK, Islam MN. Attitude and perception of undergraduate medical students toward the problem-based learning in Chitwan Medical College. Nepal Adv Med Educ Pract. 2018;9:317–22. https://doi.org/10.2147/AMEP.S160814 .
Asad MR, Tadvi N, Amir KM, Afzal K, Irfan A, Hussain SA. Medical student’s feedback towards problem based learning and interactive lectures as a teaching and learning method in an outcome-based curriculum. Int J Med Res & Heal Sci. 2019;8:78–84. https://doi.org/10.33844/ijol.2019.60392 .
Mpalanyi M, Nalweyiso ID, Mubuuke AG. Perceptions of radiography students toward problem-based learning almost two decades after its introduction at Makerere University. Uganda J Med imaging Radiat Sci. 2020;51:639–44. https://doi.org/10.1016/j.jmir.2020.06.009 .
Korkmaz NS, Ozcelik S. Evaluation of the opinions of the first, second and third term medical students about problem based learning sessions in Bezmialem Vakif University. Bezmialem Sci. 2020;8:144–9. https://doi.org/10.14235/bas.galenos.2019.3471 .
McGrew MC, Skipper B, Palley T, Kaufman A. Student and faculty perceptions of problem-based learning on a family medicine clerkship. Fam Med. 1999;31:171–6.
Kelly AM. A problem-based learning resource in emergency medicine for medical students. J Accid Emerg Med. 2000;17:320–3. https://doi.org/10.1136/emj.17.5.320 .
Bui-Mansfield LT, Chew FS. Radiologists as clinical tutors in a problem-based medical school curriculum. Acad Radiol. 2001;8:657–63. https://doi.org/10.1016/S1076-6332(03)80693-1 .
Macallan DC, Kent A, Holmes SC, Farmer EA, McCrorie P. A model of clinical problem-based learning for clinical attachments in medicine. Med Educ. 2009;43:799–807. https://doi.org/10.1111/j.1365-2923.2009.03406.x .
Grisham JW, Martiniuk ALC, Negin J, Wright EP. Problem-based learning (PBL) and public health: an initial exploration of perceptions of PBL in Vietnam. Asia-Pacific J public Heal. 2015;27:NP2019-27. https://doi.org/10.1177/1010539512436875 .
Khan IA, Al-Swailmi FK. Perceptions of faculty and students regarding Problem Based Learning: a mixed methods study. J Pak Med Assoc. 2015;65:1334–8.
Alduraywish AA, Mohager MO, Alenezi MJ, Nail AM, Aljafari AS. Evaluation of students’ experience with Problem-based Learning (PBL) applied at the College of Medicine, Al-Jouf University. Saudi Arabia J Pak Med Assoc. 2017;67:1870–3.
Yoo DM, Cho AR, Kim S. Satisfaction with and suitability of the problem-based learning program at the Catholic University of Korea College of Medicine. J Educ Eval Health Prof. 2019;16:20. https://doi.org/10.3352/jeehp.2019.16.20 .
Aldayel AA, Alali AO, Altuwaim AA, et al. Problem-based learning: medical students’ perception toward their educational environment at Al-Imam Mohammad Ibn Saud Islamic University. Adv Med Educ Pract. 2019;10:95–104. https://doi.org/10.2147/AMEP.S189062 .
DeLowerntal E. An evaluation of a module in problem-based learning. Int J Educ Dev. 1996;16:303–7. https://doi.org/10.1016/0738-0593(96)00001-6 .
Tufts MA, Higgins-Opitz SB. What makes the learning of physiology in a PBL medical curriculum challenging? Student perceptions. Adv Physiol Educ. 2009;33:187–95. https://doi.org/10.1152/advan.90214.2008 .
Aboonq M. Perception of the faculty regarding problem-based learning as an educational approach in Northwestern Saudi Arabia. Saudi Med J. 2015;36:1329–35. https://doi.org/10.15537/smj.2015.11.12263 .
Subramaniam RM, Scally P, Gibson R. Problem-based learning and medical student radiology teaching. Australas Radiol. 2004;48:335–8. https://doi.org/10.1111/j.0004-8461.2004.01317.x .
Chang BJ. Problem-based learning in medical school: a student’s perspective. Ann Med Surg. 2016;12:88–9. https://doi.org/10.1016/j.amsu.2016.11.011 .
Griffith CD, Blue AV, Mainous AG, DeSimone PA. Housestaff attitudes toward a problem-based clerkship. Med Teach. 1996;18:133–4. https://doi.org/10.3109/01421599609034147 .
Navarro HN, Zamora SJ. The opinion of teachers about tutorial problem based learning. Rev Med Chil. 2014;142:989–97. https://doi.org/10.4067/S0034-98872014000800006 .
Demiroren M, Turan S, Oztuna D. Medical students’ self-efficacy in problem-based learning and its relationship with self-regulated learning. Med Educ Online. 2016;21:30049. https://doi.org/10.3402/meo.v21.30049 .
Tousignant M, DesMarchais JE. Accuracy of student self-assessment ability compared to their own performance in a problem-based learning medical program: a correlation study. Adv Heal Sci Educ. 2002;7:19–27. https://doi.org/10.1023/A:1014516206120 .
Brynhildsen J, Dahle LO, Behrbohm Fallsberg M, Rundquist I, Hammar M. Attitudes among students and teachers on vertical integration between clinical medicine and basic science within a problem-based undergraduate medical curriculum. Med Teach. 2002;24:286–8. https://doi.org/10.1080/01421590220134105 .
Desmarchais JE. A student-centered, problem-based curriculum - 5 years experience. Can Med Assoc J. 1993;148:1567–72.
Doig K, Werner E. The marriage of a traditional lecture-based curriculum and problem-based learning: are the offspring vigorous? Med Teach. 2000;22:173–8.
Kemahli S. Hematology education in a problem-based curriculum. Hematology. 2005;10(Suppl 1):161–3. https://doi.org/10.1080/10245330512331390267 .
Grkovic I. Transition of the medical curriculum from classical to integrated: problem-based approach and Australian way of keeping academia in medicine. Croat Med J. 2005;46:16–20.
Bosch-Barrera J, Briceno Garcia HC, Capella D, et al. Teaching bioethics to students of medicine with Problem-Based Learning (PBL). Cuad Bioet. 2015;26:303–9.
Lin Y-C, Huang Y-S, Lai C-S, Yen J-H, Tsai W-C. Problem-based learning curriculum in medical education at Kaohsiung Medical University. Kaohsiung J Med Sci. 2009;25:264–9. https://doi.org/10.1016/S1607-551X(09)70072-5 .
Salinas Sánchez AS, Hernández Millán I, Virseda Rodríguez JA, et al. Problem-based learning in urology training the faculty of medicine of the Universidad de Castilla-La Mancha model. Actas Urol Esp. 2005;29:8–15. https://doi.org/10.1016/s0210-4806(05)73193-4 .
Amoako-Sakyi D, Amonoo-Kuofi H. Problem-based learning in resource-poor settings: lessons from a medical school in Ghana. BMC Med Educ. 2015;15:221. https://doi.org/10.1186/s12909-015-0501-4 .
Carrera LI, Tellez TE, D’Ottavio AE. Implementing a problem-based learning curriculum in an Argentinean medical school: implications for developing countries. Acad Med. 2003;78:798–801. https://doi.org/10.1097/00001888-200308000-00010 .
Vernon DT, Blake RL. Does problem-based learning work? A meta-analysis of evaluative research. Acad Med. 1993;68:550–63. https://doi.org/10.1097/00001888-199307000-00015 .
Shanley PF. Viewpoint: leaving the “empty glass” of problem-based learning behind: new assumptions and a revised model for case study in preclinical medical education. Acad Med. 2007;82:479–85. https://doi.org/10.1097/ACM.0b013e31803eac4c .
Koh GC, Khoo HE, Wong ML, Koh D. The effects of problem-based learning during medical school on physician competency: a systematic review. CMAJ. 2008;178:34–41. https://doi.org/10.1503/cmaj.070565 .
Awan ZA, Awan AA, Alshawwa L, Tekian A, Park YS. Assisting the integration of social media in problem-based learning sessions in the faculty of medicine at King Abdulaziz University. Med Teach. 2018;40:S37–42. https://doi.org/10.1080/0142159X.2018.1465179 .
Download references
Acknowledgements
Not applicable
No funding was received for conducting this study.
Author information
Authors and affiliations.
Medical Education Cathedra, School of Medicine, University of Vic-Central University of Catalonia, Vic, Barcelona, Spain
Joan Carles Trullàs, Carles Blay & Ramon Pujol
Internal Medicine Service, Hospital de Olot i Comarcal de La Garrotxa, Olot, Girona, Spain
Joan Carles Trullàs
The Tissue Repair and Regeneration Laboratory (TR2Lab), University of Vic-Central University of Catalonia, Vic, Barcelona, Spain
Joan Carles Trullàs & Elisabet Sarri
Catalan Institute of Health (ICS) – Catalunya Central, Barcelona, Spain
Carles Blay
You can also search for this author in PubMed Google Scholar
Contributions
JCT had the idea for the article, performed the literature search and data analysis and drafted the first version of the manuscript. CB, ES and RP contributed to the data analysis and suggested revisions to the manuscript. All authors read and approved the final manuscript.
Ethics declarations
Availability of data and materials.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable for a literature review.
Consent for publication
Competing interests.
All authors declare that they have no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Characteristics ofthe 124 included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Trullàs, J.C., Blay, C., Sarri, E. et al. Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med Educ 22 , 104 (2022). https://doi.org/10.1186/s12909-022-03154-8
Download citation
Received : 03 October 2021
Accepted : 02 February 2022
Published : 17 February 2022
DOI : https://doi.org/10.1186/s12909-022-03154-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Appointments at Mayo Clinic
- Nutrition and healthy eating
- Add antioxidants to your diet
Antioxidants are certain nutrients, such as vitamins C or E, or carotenoids, which may help protect cells against daily damage. As cells do their job, the way they process oxygen results in a molecule called a free radical. These molecules are unstable. As they regain stability, free radicals damage cells and DNA.
Disease and free radical damage
Over time, free radical damage can cause problems for tissues and organs in the body, potentially leading to disease. Research suggests that free radical molecules can add to the risk of health issues linked to aging. Some examples are heart disease, age-related macular degeneration, Alzheimer's disease and cancer.
The body's cells can fix or prevent free radical damage, for example, by making antioxidant enzymes. And some antioxidants, such as vitamin C, come from food and drink.
Eating antioxidants
Plant-based foods are the best source of antioxidants. These include fruits, vegetables, whole grains, nuts, seeds, herbs and spices, and even cocoa. Plants have naturally occurring antioxidants such as carotenoids, flavonoids, isothiocyanates, and phenolic acids.
As a bonus, many foods that have antioxidants also have other benefits. They are often high in fiber, low in saturated fat and cholesterol, and good sources of vitamins and minerals.
Artichokes are a good example.
They naturally have the fiber inulin. But artichokes also have plant chemicals called flavonoids and phenolic acids. Those phytonutrients have the potential to help manage free radicals.

Does cooking affect antioxidants?
Drying, cooking or freezing foods can affect its level of antioxidants. Sometimes cooking allows an antioxidant to be better absorbed. Lycopene in tomatoes is one example.
More lycopene is available in cooked tomatoes than raw ones. And for some foods, such as sweet potatoes, cooked is the only way we could eat them at all.

In addition to cooking, some antioxidants are more available when paired with another nutrient. One example is orange and yellow vegetables with beta carotene and vitamin E. Cooked with a bit of fat, those antioxidants are more available to the body.
Other foods with carotenes also may offer more nutrients cooked. Examples are carrots, red and green peppers, kale, spinach, and broccoli. Some of their phytochemicals may be better absorbed by the body after being cooked.
Other foods have more antioxidants when raw. In jam made of berries, for example, antioxidant levels were lower than in the raw, unprocessed berries.
Fresh or frozen, blueberries, blackberries, raspberries, strawberries and cranberries are among the top fruit sources of antioxidants.

Nuts, seeds and grains
Along with fruits and vegetables, nuts, seeds and grains add antioxidants to the diet. Whole grains, nuts and seeds are a source for selenium, vitamin E and antioxidant phytochemicals.
Unsalted nuts and seeds have protein and fats in addition to other phytochemicals. They are a nutrient dense food.
Nut and seed oils also may help people balance their healthy fat intake. Walnuts and pecans are some of the top nuts for antioxidant content. Not crazy about nuts? Try sunflower seeds.
And don't forget those grains. When made into flour, buckwheat, millet and barley seem to hold on to their phytochemicals best.

Antioxidants add up
Overall, antioxidants from foods taken in over a long period of time seem to support health. Individual antioxidants taken as supplements have less scientific support.
When it comes to adding antioxidants to the diet, no one food or food group can do it all. The best bet is to get a variety of fruits, vegetables, nuts and whole grains into the diet.
Adding foods with different colors can help meet that goal. A food's color hints at its antioxidants. Red, orange, yellow, green, and even blue or black fruits and vegetables provide different antioxidants.
Other things in the diet, such as tea, coffee and some fruit juices also have antioxidants. Some dark chocolate may have antioxidants as well, but it depends on the cocoa contents.
And it can be helpful to make sure to get some antioxidants every day. For example, vitamin C isn't stored in the body. So eating food with that vitamin every day can help make sure the body has enough.
- Antioxidants and health. National Center for Complementary and Integrative Medicine. https://nccih.nih.gov/health/antioxidants/introduction.htm. Accessed March 11, 2024.
- Antioxidants and cancer prevention. National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/risk/diet/antioxidants-fact-sheet. Accessed March 11, 2024.
- Duyff RL. Vitamins and minerals. In: Academy of Nutrition and Dietetics Complete Food and Nutrition Guide. 5th ed. Houghton Mifflin Harcourt; 2017.
- Aune D, et al. Dietary intake and blood concentrations of antioxidants and the risk of cardiovascular disease, total cancer, and all-cause mortality: A systematic review and dose-response meta-analysis of prospective studies. American Journal of Clinical Nutrition. 2018; doi:10.1093/ajcn/nqy097.
- Carlsen MH, et al. The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutrition Journal. 2010; doi:10.1186/1475-2891-9-3.
- Zeratsky KA (expert opinion). Mayo Clinic. March 11, 2024.
- Izquierdo-Vega JA, et al. Evidence of some natural products with antigenotoxic effects. Part 1: Fruits and polysaccharides. Nutrients. 2017; doi:10.3390/nu9020102.
- Lopez-Romero D, et al. Evidence of some natural products with antigenotoxic effects. Part 2: Plants, vegetables, and natural resin. Nutrients. 2018; doi:10.3390/nu10121954.
- Rusu ME, et al. Health benefits of nut consumption in middle-aged and elderly population. Antioxidants (Basel). 2019; doi:10.3390/antiox8080302.
- Artichoke. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed Feb. 14, 2024.
- Neri L. Antioxidant activity in frozen plant foods: Effect of cryoprotectants, freezing process and frozen storage. Foods. 2020; doi:10.3390/foods9121886.
- 2020-2025 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://www.dietaryguidelines.gov. Accessed Feb. 13, 2024.
Products and Services
- The Mayo Clinic Diet Online
- A Book: The Mayo Clinic Diet Bundle
- A Book: Cook Smart, Eat Well
- Cuts of beef
- Grass-fed beef
- Menus for heart-healthy eating
- Organic foods
- Sea salt vs. table salt
- What is BPA?
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Introduction
- Conclusions
- Article Information
Screening pathways incorporating MRI were associated with a reduced number of clinically insignificant disease (A) and biopsies (B); moreover, they also outperformed PSA-only strategies in terms of PPV for clinically significant prostate cancer detection (C). MRI was applied as a sequential screening tool (after PSA-prescreen), with a Prostate Imaging Reporting and Data System score of 3 or higher as a cutoff for biopsy indication. CDR indicates cancer detection rate; OR, odds ratio.
Elevating the PI-RADS cutoff to 4 for the indication of biopsy was associated with lower biopsy rates (B) and less insignificant prostate cancers found (A) compared with prostate-specific antigen (PSA). Moreover, it enhanced the positive predictive value (PPV) for significant disease detection (C). MRI was applied as a sequential screening tool (after PSA prescreening) in this analysis. CDR indicates cancer detection rate; OR, odds ratio.
eAppendix 1. Supplementary methods
eAppendix 2. Reasons for exclusion from full-text selection
eFigure 1. Clinically significant and insignificant prostate cancer detection rate in MRI-based (sequential, PI-RADS 3-5), and PSA-only screening strategies
eFigure 2. Positive predictive value of MRI-based (sequential, PI-RADS 3-5) and PSA-only strategies for the detection of clinically significant and insignificant prostate cancer
eFigure 3. Biopsy indication rates of MRI-based (sequential, PI-RADS 3-5) and PSA-only screening strategies
eFigure 4. MRI rates and adherence to biopsy indication in MRI-based (sequential, PI-RADS 3-5) and PSA-only screening strategies
eFigure 5. Analysis of prostate cancer detection rates with alternative definitions for clinically significant (ISUP≥3) and insignificant (ISUP 1-2) prostate cancers of MRI-based (sequential, PI-RADS 3-5), and PSA-only screening
eFigure 6. Subgroup analysis of MRI-based screening strategies (sequential, PI-RADS 3-5) in terms of prostate cancer detection rates and biopsy indication rates
eFigure 7. Subgroup analysis of MRI-based screening strategies (sequential, PI-RADS 3-5) in terms of positive predictive values
eFigure 8. Clinically significant and insignificant prostate cancer detection rate in MRI-based screening (sequential, PI-RADS 4-5)
eFigure 9. Positive predictive value of MRI-based screening (sequential, PI-RADS 4-5) for the detection of clinically significant and insignificant prostate cancer
eFigure 10. Biopsy indication and adherence rates of MRI-based screening (sequential, PI-RADS 4-5)
eFigure 11. Significant and insignificant prostate cancer detection rates and positive predictive values of screening with MRI, as a first-line screening tool (PI-RADS 4-5)
eFigure 12. Biopsy indication and adherence rates with MRI, as a first-line screening tool (PI-RADS 4-5)
eFigure 13. Risk of bias assessment of randomized controlled trials (RoB 2)
eFigure 14. Risk of bias assessment of prospective cohort studies (ROBINS-I)
eTable 1. PRISMA Checklist
eTable 2. Data extraction
eTable 3. Definitions of Outcomes
eTable 4. Inclusion and exclusion criteria of the studies
eTable 5. Details of MRI imaging and biopsy
Data sharing statement
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Fazekas T , Shim SR , Basile G, et al. Magnetic Resonance Imaging in Prostate Cancer Screening : A Systematic Review and Meta-Analysis . JAMA Oncol. Published online April 05, 2024. doi:10.1001/jamaoncol.2024.0734
Manage citations:
© 2024
- Permissions
Magnetic Resonance Imaging in Prostate Cancer Screening : A Systematic Review and Meta-Analysis
- 1 Comprehensive Cancer Center, Department of Urology, Medical University of Vienna, Vienna, Austria
- 2 Department of Urology, Semmelweis University, Budapest, Hungary
- 3 Centre for Translational Medicine, Semmelweis University, Budapest, Hungary
- 4 Department of Biomedical Informatics, College of Medicine, Konyang University, Daejeon, Republic of Korea
- 5 Unit of Urology, Urological Research Institute, Division of Oncology, IRCCS San Raffaele Scientific Institute, Vita-Salute San Raffaele University, Milan, Italy
- 6 Department of Urology, Assistance Publique des Hôpitaux de Marseille, North Academic Hospital, Marseille, France
- 7 Institute of Mathematics, Department of Stochastics, Budapest University of Technology and Economics, Budapest, Hungary
- 8 Department of Urology, Jagiellonian University Medical College, Krakow, Poland
- 9 Division of Urology, Department of Special Surgery, Jordan University Hospital, The University of Jordan, Amman, Jordan
- 10 The National Center for Diabetes, Endocrinology and Genetics, The University of Jordan, Amman, Jordan
- 11 Department of Urology, La Croix du Sud Hospital, Quint Fonsegrives, France
- 12 Division of Surgery and Interventional Science, University College London, London, England
- 13 Department of Urology, Hospital Universitario La Paz, Madrid, Spain
- 14 Department of Urology, University of Duisburg-Essen and German Cancer Consortium–University Hospital Essen, Essen, Germany
- 15 Department of Radiology and Nuclear Medicine, Erasmus MC Cancer Institute, University Medical Centre, Rotterdam, the Netherlands
- 16 Department of Radiology, Netherlands Cancer Institute, Amsterdam, the Netherlands
- 17 Department of Urology, St Antonius Hospital, Utrecht, the Netherlands
- 18 Department of Urology, Erasmus MC, Rotterdam, the Netherlands
- 19 Department of Urology, Yale School of Medicine, New Haven, Connecticut
- 20 Hourani Center for Applied Scientific Research, Al-Ahliyya Amman University, Amman, Jordan
- 21 Department of Urology, University of Texas Southwestern Medical Center, Dallas
- 22 Department of Urology, Second Faculty of Medicine, Charles University, Prague, Czech Republic
- 23 Department of Urology, Weill Cornell Medical College, New York, New York
- 24 Karl Landsteiner Institute of Urology and Andrology, Vienna, Austria
- 25 Department of Urology, Medical University of Silesia, Zabrze, Poland
Question Do prostate cancer screening pathways that incorporate magnetic resonance imaging (MRI) and targeted biopsies outperform strategies that rely solely on prostate-specific antigen testing and systematic biopsy?
Findings In this systematic review and meta-analysis of 80 114 screened men from 12 studies, MRI-based screening was found to be associated with a reduced number of unnecessary prostate biopsies and detection of clinically insignificant prostate cancer while maintaining the detection of clinically significant prostate cancer compared with prostate-specific antigen–only strategies.
Meaning The findings of this meta-analysis support the integration of prostate MRI in prostate cancer screening to improve the balance of patient harms and benefits.
Importance Prostate magnetic resonance imaging (MRI) is increasingly integrated within the prostate cancer (PCa) early detection pathway.
Objective To systematically evaluate the existing evidence regarding screening pathways incorporating MRI with targeted biopsy and assess their diagnostic value compared with prostate-specific antigen (PSA)–based screening with systematic biopsy strategies.
Data Sources PubMed/MEDLINE, Embase, Cochrane/Central, Scopus, and Web of Science (through May 2023).
Study Selection Randomized clinical trials and prospective cohort studies were eligible if they reported data on the diagnostic utility of prostate MRI in the setting of PCa screening.
Data Extraction Number of screened individuals, biopsy indications, biopsies performed, clinically significant PCa (csPCa) defined as International Society of Urological Pathology (ISUP) grade 2 or higher, and insignificant (ISUP1) PCas detected were extracted.
Main Outcomes and Measures The primary outcome was csPCa detection rate. Secondary outcomes included clinical insignificant PCa detection rate, biopsy indication rates, and the positive predictive value for the detection of csPCa.
Data Synthesis The generalized mixed-effect approach with pooled odds ratios (ORs) and random-effect models was used to compare the MRI-based and PSA-only screening strategies. Separate analyses were performed based on the timing of MRI (primary/sequential after a PSA test) and cutoff (Prostate Imaging Reporting and Data System [PI-RADS] score ≥3 or ≥4) for biopsy indication.
Results Data were synthesized from 80 114 men from 12 studies. Compared with standard PSA-based screening, the MRI pathway (sequential screening, PI-RADS score ≥3 cutoff for biopsy) was associated with higher odds of csPCa when tests results were positive (OR, 4.15; 95% CI, 2.93-5.88; P ≤ .001), decreased odds of biopsies (OR, 0.28; 95% CI, 0.22-0.36; P ≤ .001), and insignificant cancers detected (OR, 0.34; 95% CI, 0.23-0.49; P = .002) without significant differences in the detection of csPCa (OR, 1.02; 95% CI, 0.75-1.37; P = .86). Implementing a PI-RADS score of 4 or greater threshold for biopsy selection was associated with a further reduction in the odds of detecting insignificant PCa (OR, 0.23; 95% CI, 0.05-0.97; P = .048) and biopsies performed (OR, 0.19; 95% CI, 0.09-0.38; P = .01) without differences in csPCa detection (OR, 0.85; 95% CI, 0.49-1.45; P = .22).
Conclusion and relevance The results of this systematic review and meta-analysis suggest that integrating MRI in PCa screening pathways is associated with a reduced number of unnecessary biopsies and overdiagnosis of insignificant PCa while maintaining csPCa detection as compared with PSA-only screening.
Prostate-specific antigen (PSA)–based prostate cancer (PCa) screening has been shown to reduce PCa-specific mortality, but it is also associated with unnecessary biopsies, overdiagnosis, overtreatment, and an unclear effect on overall survival. 1 , 2 To balance these risks and benefits, clinical practice guidelines recommend shared decision-making strategies to identify informed candidates who are most likely to benefit from PCa early detection. 3 , 4 However, this opportunistic approach has been associated with widespread but untargeted testing accompanied by disparities in health care access and literacy. 3 - 5 Moreover, the inherent limitations of PSA-based PCa screening, including excess biopsies and overtreatment of low-grade disease, have not been addressed. 5 , 6
Prebiopsy prostate magnetic resonance imaging (MRI) followed by targeted biopsies has been widely integrated in the diagnostic pathway for PCa, as it is associated with improved detection of clinically significant PCa and reduced numbers of avoidable biopsies and insignificant cancers in the clinical setting. 3 , 7 , 8 As a result, clinical practice guidelines have recommended prebiopsy MRI; however, to our knowledge, there is no consensus about the role of MRI as an integrated PCa screening tool. 3 , 4 Consequently, several ongoing clinical trials are investigating the value of incorporating prebiopsy MRI with targeted biopsy into population-based PCa screening protocols to overcome the limitations of conventional PSA-based screening.
In the setting of a large body of literature addressing the diagnostic role of prostate MRI and its growing global use, there is a need to synthesize evidence to inform clinical practice and help devise a screening strategy that incorporates MRI information. To address this unmet need, in this systematic review and meta-analysis, we summarized the currently available literature on the performance of PCa population-based screening strategies that incorporate MRI and compared them with PSA only–based screening approaches. We hypothesized that PSA-MRI–based PCa screening strategies would outperform PSA only–based screening in terms of clinically relevant end points.
This systematic review and meta-analysis was reported according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses ( PRISMA ) 2020 guideline (eTable 1 in Supplement 1 ) and the Cochrane Handbook. 9 , 10 The study protocol was registered on PROSPERO.
To evaluate the performance of MRI-based screening strategies, we used the population, intervention, control, and outcomes framework. 11 We included studies of men in the general population or those with elevated genetic risk for PCa who were screened for PCa (population) who underwent MRI examination as part of the screening (intervention) and were compared with men screened for PCa using PSA alone (comparison). Studies were selected if they reported data in screening-like populations, while those addressing diagnostic test accuracy or those that enrolled preselected men to undergo biopsy (men with lower urinary tract symptoms, elevated PSA levels, or suspect digital rectal examination results) were excluded. The primary end point was the cancer detection rate (CDR) of clinically significant PCa, defined as an International Society of Urological Pathology (ISUP) grade of 2 or higher (outcome). Secondary end points included the CDR of insignificant PCa (defined as ISUP grade 1), positive predictive values (PPVs) for detecting significant and insignificant PCas, MRI and biopsy indication, biopsy adherence, and complication rates. Moreover, we calculated CDRs using alternative definitions of significant (ISUP ≥3) and insignificant (ISUP 1-2) PCa. This meta-analysis was restricted to prospective observational or randomized studies.
The MEDLINE (via PubMed), Embase, Cochrane/Central, Scopus, and Web of Science databases were queried on May 5, 2023, to identify all available studies containing information on MRI-based screening strategies. After selection by 2 independent review authors (T.F. and G.B.), the following data were extracted from the eligible studies: general information; study population characteristics; details of the intervention and comparator, including screening algorithm (MRI in first-line/sequential screening), sequence (biparametric/multiparametric), and type (1.5T/3T) of MRI; Prostate Imaging Reporting and Data System (PI-RADS) cutoff for the indication of biopsy (PI-RADS ≥3 or ≥4); type of biopsy approach (targeted + systematic/targeted only, cognitive/image-fusion); PSA cutoff; additional novel biomarkers in the screening pathway; and the outcomes of interest described previously. 12 In cases in which studies did not provide information on the specified outcomes, 2 authors (T.F. and G.B.) independently calculated them using the data provided within the studies. Any disagreements on study selection and data extraction were resolved through consensus with a third author (P.R.). Sensitivity, specificity, and negative predictive value could not be evaluated because prostate biopsies were not performed in cases of negative screening test results. To address inconsistencies or overlapping data among studies, we made adjustments to the study samples (eTable 2 in Supplement 1 ). More detailed descriptions of the inclusion criteria, search strategy, selection, and data extraction process are presented in eAppendix 1 and eTables 2 to 3 in Supplement 1 .
Quantitative data synthesis was conducted with the R statistical software (version 4.1; R Core Team) and adhered to the methods recommended by the working group of the Cochrane Collaboration. 10 Based on the likely heterogeneity of the studies included, we used random-effect models for our calculations. 13 , 14 To assess and compare CDR, PPV, MRI, biopsy indication rates, and adherence to biopsy of the different screening pathways, we calculated pooled event rates and odds ratios (ORs) with 95% CIs using the generalized mixed-effect approach. 15 To assess the optimal timing of MRI in the screening pathway, we conducted separate analyses based on different PI-RADS cutoffs for indicating biopsy (≥3, ≥4) and MRI timing (primary/sequential). We used forest plots to visualize event rates and effect measures. To evaluate the moderator effect of different factors, type of MRI sequence, biopsy technique, and study design, we performed subgroup analyses. Heterogeneity was assessed by calculating the I 2 measure and its CI. For all statistical analyses, P ≤ .05 was considered significant. Publication bias could not be assessed due to the low number of articles for 1 outcome. 16 Full details of the statistical analysis are described in eAppendix 1 in Supplement 1 . No ethical approval was required for this systematic review and meta-analysis as already published secondary data were used.
For randomized and nonrandomized studies, the risk of bias (RoB) was evaluated according to the Cochrane Collaboration’s RoB assessment (RoB2) and the Risk of Bias in Nonrandomized Studies of Interventions tools independently by 2 reviewers (T.F. and G.B.). 17 , 18 Disagreements were resolved via consensus with a third author (P.R.).
The search key identified 2037 studies, of which 1464 were screened after removing duplicates. Finally, from the 28 full-text selected studies, 12 and 8 were eligible for qualitative and quantitative evidence synthesis, respectively ( Figure 1 ). A detailed explanation for the exclusion of the studies can be found in eAppendix 2 in Supplement 1 . Table 1 19 - 30 shows the baseline characteristics of the included studies. Overall, we assessed 80 114 screened individuals from 12 studies. We identified 4 population-based randomized clinical trials, 2 prospective cohort studies, and 3 prospective pilot studies. 19 - 25 , 28 - 30 Moreover, we included 2 studies that reported on the efficacy of MRI in a prescreened population. 26 , 27 We identified 4 studies that reported data on the use of novel molecular biomarkers and MRI in PCa screening. 23 , 28 - 30 Most publications included data on the use of MRI as a sequential screening tool (after PSA prescreening); however, 3 studies were identified reporting on up-front MRI. 19 , 24 , 25 Five studies used biparametric MRI (bpMRI), and 8 included multiparametric MRI (mpMRI) ( Table 1 ). As for the method of biopsy, 7 studies used MRI targeted only, while 6 studies used additional systematic sampling ( Table 1 ). For further details on the studies and interventions, please refer to eTables 4 and 5 in Supplement 1 .
We synthesized data from 57 081 men that were derived from 6 articles that applied MRI in a PSA-prescreened population (as part of sequential screening), with a PI-RADS score of 3 or higher as a cutoff as the biopsy indication. 19 - 22 , 26 , 27 A detailed overview of CDRs, PPVs, biopsy indication, and adherence rates can be found in Table 2 and eFigures 1 to 4 in Supplement 1 . The number of men needed to screen to detect 1 significant PCa was 59 and 63 for PSA only and MRI-based strategies, respectively. Although we found no difference between the MRI-only and PSA-only screening methods in terms of clinically significant CDR (OR, 1.02; 95% CI, 0.75-1.37; P = .86) (eFigure 1 in Supplement 1 ), the MRI pathway was associated with lower odds of insignificant PCa detection (OR, 0.34; 95% CI, 0.23-0.49; P = .002) ( Figure 2 ). 19 , 20 , 22 , 26 , 27 These trends in CDR remained similar when alternative definitions were applied for significant (ISUP ≥3: OR, 0.91; 95% CI, 0.54-1.52; P = .40) and insignificant PCas (ISUP 1-2: OR, 0.54; 95% CI, 0.23-1.29; P = .09) (eFigure 5 in Supplement 1 ). Furthermore, screening strategies that incorporated MRI had a higher PPV for detecting significant PCa (OR, 4.15; 95% CI, 2.93-5.88; P = .001) and a lower biopsy rate (OR, 0.28; 95% CI, 0.22-0.36; P < .001) than PSA-only-based ones ( Figure 2 ; eFigures 2 and 3 in Supplement 1 ). 19 , 20 , 22 , 26 , 27 The pooled rate of MRI was 8.5% (95% CI, 2.6%-24.8%; I 2 = 100%) among the screened individuals, and biopsy adherence was higher when MRI was used (OR, 4.61; 95% CI, 2.39-8.89; P = .01) (eFigure 4 in Supplement 1 ). 19 - 22 , 26 , 27 To identify the high rate of heterogeneity among the studies and assess the role of possible confounders, we stratified studies based on the type of MRI sequence, biopsy method, and study design (eFigures 6 and 7 in Supplement 1 ). We observed differences in terms of PPV, but not in CDR and biopsy rates. Compared with mpMRI, the use of bpMRI was associated with a higher PPV for significant PCa (61.1% [95% CI, 26.5%-87.3%] vs 34.8% [95% CI, 25.2%-45.7%]; P < .001) and a lower PPV for insignificant PCa (11.5% [95% CI, 1.3%-55.1%] vs 19.5% [95% CI, 12.3%-29.6%]; P = .01), respectively, without heterogeneity across the subgroups (eFigures 7A and 7E in Supplement 1 ).Targeted + systematic (vs targeted) and image fusion (vs cognitive) biopsies had a lower PPV for insignificant cancers (eFigures 7F and 7G in Supplement 1 ).
Among 19 501 patients who underwent prostate MRI that used a PI-RADS cutoff of 4 or higher as a biopsy indication, we observed even lower odds of insignificant PCa detection (OR, 0.23; 95% CI, 0.05-0.97; P = .048) and biopsy (OR, 0.19; 95% CI, 0.09-0.38; P = .01) with a higher PPV (OR, 7.01; 95% CI, 1.76-27.98; P = .03) and similar CDR (OR, 0.85; 95% CI, 0.49-1.45; P = .23) for significant disease compared with standard PSA-only screening ( Figure 3 ; eFigures 8-10 in Supplement 1 ). 19 , 20 , 27
To evaluate the performance of MRI (PI-RADS ≥4) as a primary screening tool, we synthesized data from 3 articles that involved 983 men. 19 , 24 , 25 Clinically significant and insignificant CDRs were 6% (95% CI, 0.6%-39.4%; I 2 : 92%) and 1.2% (95% CI, 0.2%-7.3%; I 2 : 55%), respectively (eFigures 11A and 11B in Supplement 1 ). The PPV of up-front MRI to detect significant PCa was 41.9% (95% CI, 16.1%-73%; I 2 : 57%) (eFigure 11C in Supplement 1 ). Due to the limited availability of data, comparison of MRI-based screening with PSA-based approaches was only feasible in terms of biopsy selection, which revealed no significant difference between the 2 strategies (OR, 0.81; 95% CI, 0.23-2.87; P = .50) (eFigure 12C in Supplement 1 ). 19 , 24 , 25
We identified 4 articles that reported on the combination of MRI and novel biomarkers; however, given the heterogeneity between populations and interventions within studies, we did not perform a quantitative data synthesis. 23 , 28 - 30 In this subset, the use of novel biomarkers was associated with fewer insignificant PCas while maintaining significant disease detection. 23 , 28 Moreover, MRI has been shown to be an effective screening tool in patients with a genetic predisposition for PCa. 30
The RoB 2 and Risk of Bias in Nonrandomized Studies of Interventions tools identified a low overall RoB in most of the included studies for the CDR, PPV, MRI, and biopsy rates and adherence to biopsy indication outcomes (eFigures 13 and 14 in Supplement 1 ). Among randomized clinical trials, the intervention in the PROBASE trial was found to be biased, as MRI examination was not part of the screening protocol; however, MRI data were available in 79% of participants, and 114 of 120 men (95%) underwent MRI/ultrasonography fusion-targeted and systematic biopsy. 21 Despite some prospective cohort studies that showed a moderate risk in categories that was mainly based on the population of the study, most of these articles displayed a low overall RoB.
To our knowledge, this systematic review and meta-analysis was the first to assess the performance of MRI in the setting of PCa screening. There were several notable and clinically relevant findings from this study. First, these analyses suggested that MRI as part of sequential screening performs similarly to conventional PSA-based strategies in detecting clinically significant PCa while reducing the number of detected insignificant cancers. Second, prebiopsy MRI was associated with a substantially reduced number of unnecessary prostate biopsies performed and enhanced the PPV for significant PCa detection compared with PSA-only screening with standard biopsies. Moreover, modifying the threshold of offering prostate biopsy to a PI-RADS score of 4 or higher and the use of bpMRI may further be associated with a reduced rate of unnecessary biopsies while not meaningfully compromising the detection of significant PCa. Finally, the results of this study suggest that MRI as a first-line screening tool does not seem to exhibit the aforementioned benefits in reducing biopsy rates and the detection of insignificant PCa.
Our findings support and potentially strengthen the cumulative evidence suggesting that the use of MRI following initial PSA prescreen is associated with decreased detection of insignificant PCa compared with PSA-only approaches. Thus, MRI may be a useful tool to mitigate the limitations of PSA-based screening, including overdiagnosis of indolent PCa, which can be associated with overtreatment with avoidable complications associated with any therapy. 31 , 32 However, the 2 screening strategies were similar in terms of CDR for clinically significant disease. Based on our analysis, the number needed to screen to detect 1 significant PCa was 59 and 63 for PSA-only and MRI-based strategies, respectively.
Moreover, use of MRI-based screening strategies was associated with higher PPV for detecting clinically significant PCa and a reduced number of biopsy indications. Based on our findings, the number of biopsies needed to detect 1 significant prostate cancer was 2 and 6 with MRI-based and PSA-only screening, respectively. These findings are notable given the risks of bleeding, infection, discomfort, and expense associated with prostate biopsy, as well as the psychological burden of screening-triggered workup. 33 , 34 Moreover, avoiding biopsy and following up with patients with negative MRI results were shown to be a safe approach in screening. 35 , 36 According to the data presented in this article, patients are more willing to undergo biopsy when the indication is underlined with MRI results, which is an important factor in achieving better outcomes and a more equal distribution of health care resources. 5 , 37 - 39 In modeling studies, MRI-based PCa screening is associated with an improvement in the benefit-harm profile, quality of life, cost-effectiveness, and environmental effect of screening for PCa compared with standard PSA-based screening. 40 - 44 Accordingly, our results synthesizing high-quality prospective data suggested that MRI is effective at identifying individuals who are most likely to require further evaluation and biopsy, potentially reducing the burden on health care resources and sparing patients from having to undergo unnecessary invasive procedures.
This study aggregates performance characteristics of MRI-based screening across PI-RADS cutoffs for biopsy selection, different sequences (multiparametric or biparametric), biopsy methods (targeted only or targeted + systematic), and fusion types (cognitive or image fusion). Our analysis suggests that implementing a PI-RADS score of 4 or higher as a cutoff is further associated with a reduced number of insignificant cancers detected and biopsies performed. Additionally, the choice of MRI sequence, whether biparametric or multiparametric, is an important aspect of screening, as shorter bpMRI protocols are faster, more cost-effective, and are associated with reduced exposure to contrast material, making them valuable in the screening process. 45 , 46 However, bpMRI interpretation may be more challenging, requiring a higher level of expertise. 47 We found that bpMRI is associated with a higher PPV for detecting significant PCa, which may be attributable to preferentially identifying larger, more conspicuous lesions in the absence of contrast. 45 , 48 Lastly, we examined the role of biopsy approach on MRI-based screening outcomes. These results revealed no significant differences in terms of CDR and PPV for significant disease between the targeted-only and targeted + systematic biopsy techniques, as well as between image fusion and cognitive biopsy methods. However, the targeted + systematic and image-fusion biopsies demonstrated a lower PPV for detecting clinically insignificant prostate cancer. These findings suggest that a screening pathway incorporating bpMRI following PSA prescreening coupled with a PI-RADS score of 4 or higher as a cutoff for biopsy indication may be a promising strategy for increasingly accessible and cost-effective screening. However, several questions remain to be addressed in future investigations, including whether to use targeted-only biopsy, the optimal method for fusion biopsy, a comprehensive analysis of screening costs, and an examination of long-term survival outcomes. Furthermore, differences in oncologic risk profiles have been observed between PCa cases diagnosed via MRI-based targeted biopsy and those identified through standard biopsy methods. 49 These findings underscore the need for further research to elucidate the behavior of PCas identified with MRI and targeted biopsy and their implications for treatment strategies.
Our study also highlights the importance of considering the timing and type of MRI and biopsy in the screening process. While MRI following PSA prescreening (sequential pathway) demonstrated numerous advantages compared with PSA-only strategies, up-front MRI as a primary tool did not appear to exhibit the aforementioned benefits in terms of biopsy rates and insignificant PCa detection; however, it was associated with CDR for significant PCa. Although these results are limited by the lack of data for formal statistical comparison, this suggests that while MRI is valuable for refining the selection of patients for biopsy, its use as a primary screening tool needs to be further assessed in the future. Interestingly, among men younger than 55 who harbor breast cancer gene ( BRCA ) germline alterations, up-front MRI has been demonstrated to have the highest clinical benefit, highlighting its diagnostic value for patients with a genetic predisposition for PCa. 30
This study had several limitations. These included a relatively low number of articles that could be included. Subgroup evaluation, heterogeneity, and publication bias assessment were limited. As no biopsy was performed in case of a negative MRI result, sensitivity, specificity, and negative predictive values could not be assessed. Most of the studies assessed a Scandinavian population, limiting the generalizability of our findings. Safety and long-term survival data could not be synthesized, constraining the full-scale interpretation of our results. Finally, the optimal intensity and interval of MRI-based screening rounds have yet to be established, which require consideration of trade-offs regarding frequency of procedures, cancer detection, and associated costs.
The results of this systematic review and meta-analysis suggest that prostate MRI with targeted biopsies is an effective strategy for the early detection of prostate cancer. We found that MRI mitigates pitfalls of standard PSA-based strategies, as it can be associated with fewer unnecessary biopsies and helps to avoid the detection of insignificant cancers while not comprising significant disease detection. Our results highlight the need to reassess our approach to population-based screening; however, the optimal setup of MRI and biopsy scheme in the screening process requires further evaluation.
Accepted for Publication: January 22, 2024.
Published Online: April 5, 2024. doi:10.1001/jamaoncol.2024.0734
Corresponding Author: Shahrokh F. Shariat, MD, DDr(hc), Department of Urology, Comprehensive Cancer Center, Vienna General Hospital, Medical University Vienna, Währinger Gürtel 18-20, A-1090 Vienna, Austria ( [email protected] ).
Author Contributions: Drs Fazekas and Rajwa had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Fazekas, Przydacz, Ploussard, Rivas, Gandaglia, Szarvas, Van Den Bergh, Nyirády, Shariat, Rajwa.
Acquisition, analysis, or interpretation of data: Fazekas, Shim, Basile, Baboudjian, Kói, Abufaraj, Kasivisvanathan, Schoots, Leapman, Shariat, Rajwa.
Drafting of the manuscript: Fazekas, Basile, Kói, Gandaglia, Szarvas, Leapman, Nyirády, Rajwa.
Critical review of the manuscript for important intellectual content: Shim, Basile, Baboudjian, Przydacz, Abufaraj, Ploussard, Kasivisvanathan, Rivas, Schoots, Van Den Bergh, Leapman, Shariat, Rajwa.
Statistical analysis: Fazekas, Shim, Baboudjian, Kói.
Obtained funding: Shariat.
Administrative, technical, or material support: Shim, Przydacz, Abufaraj, Ploussard, Leapman, Shariat, Rajwa.
Supervision: Ploussard, Kasivisvanathan, Rivas, Szarvas, Van Den Bergh, Leapman, Nyirády, Shariat, Rajwa.
Other—validation, software, data curation, methodology: Shim.
Conflict of Interest Disclosures: Dr Fazekas reported grants from the Ministry for Innovation and Technology New National Excellence Program and the European Association of Urology EUSP Scholarship during the conduct of the study. Dr Kasivisvanathan reported personal fees from the European Association of Urology and salary support from Prostate Cancer UK and the John Black Charitable Foundation outside the submitted work. Dr Kói received grant support from the National Research, Development and Innovation Office. No other disclosures were reported.
Funding/Support: This work was supported by the EUSP Scholarship of the European Association of Urology (Dr Fazekas; S-2023-0006) and grants from the New National Excellence Program of the Ministry for Innovation and Technology from the National Research Development, and Innovation Fund (Dr Fazekas; ÚNKP-22-3-1-SE-19) and the Hungarian National Eötvös Grant of the Hungarian state (Dr Fazekas).
Role of the Funder/Sponsor: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Meeting Presentation: This article was presented at the European Association of Urology Congress; April 5, 2024; Paris, France.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

IMAGES
VIDEO
COMMENTS
Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel patients, from Nov 1 ...
This systematic review aims to critically synthesise literature on nutrition education provided to medical students. We will identify new insights into how medical nutrition education can be enhanced to ultimately improve dietary behaviours of individuals and populations across the world. 8.
This systematic review aims to critically synthesise literature on nutrition education provided to medical students. We will identify new insights into how medical nutrition education can be enhanced to ultimately improve dietary behaviours of individuals and populations across the world. 8. Research in contex.
Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel patients, from Nov 1 ...
of Medical Health Sciences, The University of Auckland, Auckland 1142, New Zealand. [email protected]. Nutrition in medical education: a systematic review. Jennifer Crowley, Lauren Ball ...
The review of nutrition education interventions delivered to undergraduate medical students highlights the advantages of utilising interprofessional learning, focusing on student's personal health behaviours and harnessing novel teaching methods such as hands‐on cooking. 10. Highly Influenced. PDF.
Nutrition in medical education: a systematic review Jennifer Crowley, PhD, Lauren Ball, PhD, Gerrit Jan Hiddink, ProfPhD; Affiliations Jennifer Crowley, PhD Discipline of Nutrition and Dietetics, Faculty of Medical Health Sciences, The University of Auckland, Auckland, New Zealand; Correspondence to: Dr Jennifer Crowley, Discipline of Nutrition ...
Abstract. Methods In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel ...
Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for articles on medical students' nutrition knowledge, skills, and confidence to counsel patients, from Nov 1 ...
Search worldwide, life-sciences literature Search. Advanced Search Coronavirus articles and preprints Search examples: "breast cancer" Smith J
Background: In many countries, doctors are recommended to provide nutrition care to patients to improve the dietary behaviours of individuals and populations. Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for...
Several papers have called for a reform in nutrition training in undergraduate medical education and identified barriers such as lack of funding and faculty expertise. 16, 19, 20 Few nutrition education reviews have been completed, but a recent systematic review identified 47 articles from institutions worldwide in multiple health professions ...
The present study aimed to evaluate nutrition education interventions delivered to medical students published between 2015 and 2020 and assess recent efforts in this field subsequent to publication of the prior systematic review on the topic. 15 To the best of the author's knowledge, this is the only review of undergraduate medical nutrition ...
This review highlights the advantages of utilising interprofessional learning, focusing on student's personal health behaviours and harnessing novel teaching methods such as hands-on cooking. ... Increased nutrition training in medical education is needed. A variety of teaching approaches were identified, including novel methods such as ...
nutrition education in medical school curricula,12 which also appears to extend to postgraduate medical train-ing.13 The most recent systematic review on this topic found that, regardless of country, setting or year of medical education, medical students report inadequate knowledge, skills and confidence to support patients in
Nutrition in medical education: a systematic review. Lancet Planet Health. 2019; 3: e379-e389. Abstract; Full Text; Full Text PDF; PubMed; Scopus (235) Google Scholar]. The relationship between dietary habits and non-communicable diseases (NCDs) has been extensively investigated. Numerous long-term prospective observational studies and short ...
These findings show that by implementing appropriate NEIs, it is possible to address the problem of inadequate nutrition education in the medical curriculum. The twenty-three included studies in this review demonstrate the growing recognition of the need to improve medical students' nutrition education experiences.
Background: Whole-food, plant-based (WFPB) dietary patterns can be used as a lifestyle modification to lower blood pressure and lose weight.This study aimed to observe the effects of WFPB dietary patterns and improve nutrition education in medical school. Methods: Forty-six medical students participated in the four-week Plant Plunge challenge, which consisted of a pre- and post-challenge ...
Background: In many countries, doctors are recommended to provide nutrition care to patients to improve the dietary behaviours of individuals and populations. Here, we present a systematic review that aims to critically synthesise literature on nutrition education provided to medical students. Methods: In this systematic review, a literature search was done between May 1 and July 1, 2018, for ...
However, the effectiveness of this syllabus remains to be assessed. 38, 39 A recent comparative analysis of nutrition incorporated into medical curricula worldwide showed that only 44% of the Australia and New Zealand accreditation documents included in the study had requirements for nutrition education. 40 A systematic review of worldwide ...
The findings from a recent systematic review which investigated medical nutrition education throughout the world found that it was insufficiently incorporated into medical education, regardless of country, setting or year of medical education. 1 Innovative and effective ways to increase students' nutrition knowledge, skills and confidence to ...
The effectiveness of physical activity interventions in improving higher education students' mental health: A systematic review ... Medical Sciences and Nutrition, ... Findings from a systematic review and meta-analysis exploring the use of cognitive behavioural therapies including mindfulness programmes for the treatment of stress, ...
Problem-based learning (PBL) is a pedagogical approach that shifts the role of the teacher to the student (student-centered) and is based on self-directed learning. Although PBL has been adopted in undergraduate and postgraduate medical education, the effectiveness of the method is still under discussion. The author's purpose was to appraise available international evidence concerning to the ...
In: Academy of Nutrition and Dietetics Complete Food and Nutrition Guide. 5th ed. Houghton Mifflin Harcourt; 2017. Aune D, et al. Dietary intake and blood concentrations of antioxidants and the risk of cardiovascular disease, total cancer, and all-cause mortality: A systematic review and dose-response meta-analysis of prospective studies.
Findings In this systematic review and meta-analysis of 80 114 screened men from 12 studies, MRI-based screening was found to be associated with a reduced number of unnecessary prostate biopsies and detection of clinically insignificant prostate cancer while maintaining the detection of clinically significant prostate cancer compared with ...