Psychological Theories of Depression
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
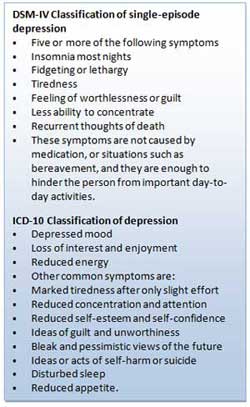
Depression is a mood disorder that prevents individuals from leading a normal life at work, socially, or within their family. Seligman (1973) referred to depression as the ‘common cold’ of psychiatry because of its frequency of diagnosis.
Depending on how data are gathered and how diagnoses are made, as many as 27% of some population groups may be suffering from depression at any one time (NIMH, 2001; data for older adults).

Behaviorist Theory
Behaviorism emphasizes the importance of the environment in shaping behavior. The focus is on observable behavior and the conditions through which individuals” learn behavior, namely classical conditioning, operant conditioning, and social learning theory.
Therefore, depression is the result of a person’s interaction with their environment.
For example, classical conditioning proposes depression is learned through associating certain stimuli with negative emotional states. Social learning theory states behavior is learned through observation, imitation, and reinforcement.
Operant Conditioning
Operant conditioning states that depression is caused by the removal of positive reinforcement from the environment (Lewinsohn, 1974). Certain events, such as losing your job, induce depression because they reduce positive reinforcement from others (e.g., being around people who like you).
Depressed people usually become much less socially active. In addition, depression can also be caused by inadvertent reinforcement of depressed behavior by others.
For example, when a loved one is lost, an important source of positive reinforcement has lost as well. This leads to inactivity. The main source of reinforcement is now the sympathy and attention of friends and relatives.
However, this tends to reinforce maladaptive behavior, i.e., weeping, complaining, and talking of suicide. This eventually alienates even close friends leading to even less reinforcement and increasing social isolation and unhappiness. In other words, depression is a vicious cycle in which the person is driven further and further down.
Also, if the person lacks social skills or has a very rigid personality structure, they may find it difficult to make the adjustments needed to look for new and alternative sources of reinforcement (Lewinsohn, 1974). So they get locked into a negative downward spiral.
Critical Evaluation
Behavioral/learning theories make sense in terms of reactive depression, where there is a clearly identifiable cause of depression. However, one of the biggest problems for the theory is that of endogenous depression. This is depression that has no apparent cause (i.e., nothing bad has happened to the person).
An additional problem of the behaviorist approach is that it fails to consider cognitions (thoughts) influence on mood.
Psychodynamic Theory
During the 1960s, psychodynamic theories dominated psychology and psychiatry. Depression was understood in terms of the following:
- inwardly directed anger (Freud, 1917),
- introjection of love object loss,
- severe super-ego demands (Freud, 1917),
- excessive narcissistic , oral, and/or anal personality needs (Chodoff, 1972),
- loss of self-esteem (Bibring, 1953; Fenichel, 1968), and
- deprivation in the mother-child relationship during the first year (Kleine, 1934).
Freud’s psychoanalytic theory is an example of the psychodynamic approach . Freud (1917) proposed that many cases of depression were due to biological factors.
However, Freud also argued that some cases of depression could be linked to loss or rejection by a parent. Depression is like grief in that it often occurs as a reaction to the loss of an important relationship.
However, there is an important difference because depressed people regard themselves as worthless. What happens is that the individual identifies with the lost person so that repressed anger towards the lost person is directed inwards towards the self. The inner-directed anger reduces the individual’s self-esteem and makes him/her vulnerable to experiencing depression in the future.
Freud distinguished between actual losses (e.g., the death of a loved one) and symbolic losses (e.g., the loss of a job). Both kinds of losses can produce depression by causing the individual to re-experience childhood episodes when they experience loss of affection from some significant person (e.g., a parent).
Later, Freud modified his theory stating that the tendency to internalize lost objects is normal and that depression is simply due to an excessively severe super-ego. Thus, the depressive phase occurs when the individual’s super-ego or conscience is dominant. In contrast, the manic phase occurs when the individual’s ego or rational mind asserts itself, and s/he feels control.
In order to avoid loss turning into depression, the individual needs to engage in a period of mourning work, during which s/he recalls memories of the lost one.
This allows the individual to separate himself/herself from the lost person and reduce inner-directed anger. However, individuals very dependent on others for their sense of self-esteem may be unable to do this and so remain extremely depressed.
Psychoanalytic theories of depression have had a profound impact on contemporary theories of depression.
For example, Beck’s (1983) model of depression was influenced by psychoanalytic ideas such as the loss of self-esteem (re: Beck’s negative view of self), object loss (re: the importance of loss events), external narcissistic deprivation (re: hypersensitivity to loss of social resources) and oral personality (re: sociotropic personality).
However, although highly influential, psychoanalytic theories are difficult to test scientifically. For example, its central features cannot be operationally defined with sufficient precision to allow empirical investigation. Mendelson (1990) concluded his review of psychoanalytic theories of depression by stating:
“A striking feature of the impressionistic pictures of depression painted by many writers is that they have the flavor of art rather than of science and may well represent profound personal intuitions as much as they depict they raw clinical data” (p. 31).
Another criticism concerns the psychanalytic emphasis on the unconscious, intrapsychic processes, and early childhood experience as being limiting in that they cause clinicians to overlook additional aspects of depression. For example, conscious negative self-verbalization (Beck, 1967) or ongoing distressing life events (Brown & Harris, 1978).
Cognitive Explanation of Depression
This approach focuses on people’s beliefs rather than their behavior. Depression results from systematic negative bias in thinking processes.
Emotional, behavioral (and possibly physical) symptoms result from cognitive abnormality. This means that depressed patients think differently from clinically normal people. The cognitive approach also assumes changes in thinking precede (i.e., come before) the onset of a depressed mood.
Beck’s (1967) Theory
One major cognitive theorist is Aaron Beck. He studied people suffering from depression and found that they appraised events in a negative way.
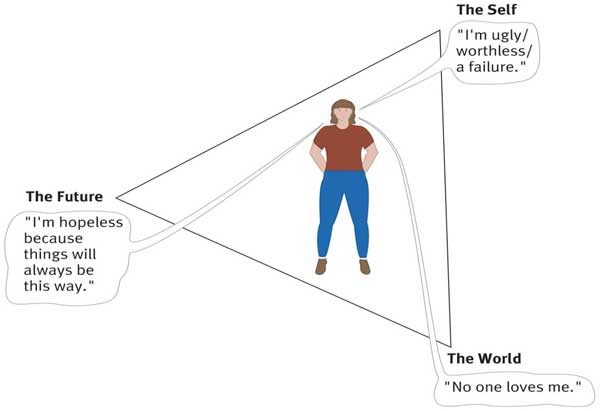
Beck (1967) identified three mechanisms that he thought were responsible for depression:
The cognitive triad (of negative automatic thinking) Negative self schemas Errors in Logic (i.e. faulty information processing)
The cognitive triad is three forms of negative (i.e., helpless and critical) thinking that are typical of individuals with depression: namely, negative thoughts about the self, the world, and the future. These thoughts tended to be automatic in depressed people as they occurred spontaneously.
For example, depressed individuals tend to view themselves as helpless, worthless, and inadequate. They interpret events in the world in an unrealistically negative and defeatist way, and they see the world as posing obstacles that can’t be handled.
Finally, they see the future as totally hopeless because their worthlessness will prevent their situation from improving.
As these three components interact, they interfere with normal cognitive processing, leading to impairments in perception, memory, and problem-solving, with the person becoming obsessed with negative thoughts.
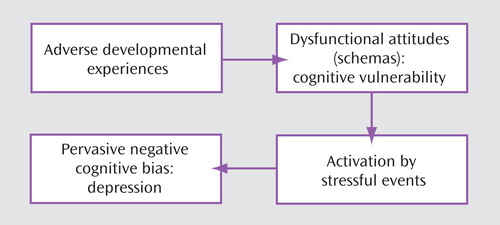
Beck believed that depression-prone individuals develop a negative self-schema . They possess a set of beliefs and expectations about themselves that are essentially negative and pessimistic. Beck claimed that negative schemas might be acquired in childhood as a result of a traumatic event. Experiences that might contribute to negative schemas include:
- Death of a parent or sibling.
- Parental rejection, criticism, overprotection, neglect, or abuse.
- Bullying at school or exclusion from a peer group.
However, a negative self-schema predisposes the individual to depression, and therefore someone who has acquired a cognitive triad will not necessarily develop depression.
Some kind of stressful life event is required to activate this negative schema later in life. Once the negative schema is activated, a number of illogical thoughts or cognitive biases seem to dominate thinking .
People with negative self-schemas become prone to making logical errors in their thinking, and they tend to focus selectively on certain aspects of a situation while ignoring equally relevant information.
Beck (1967) identified a number of systematic negative biases in information processing known as logical errors or faulty thinking. These illogical thought patterns are self-defeating and can cause great anxiety or depression for the individual. For example:
- Arbitrary Inference: Drawing a negative conclusion in the absence of supporting data.
- Selective Abstraction: Focusing on the worst aspects of any situation.
- Magnification and Minimisation: If they have a problem, they make it appear bigger than it is. If they have a solution they make it smaller.
- Personalization: Negative events are interpreted as their fault.
- Dichotomous Thinking: Everything is seen as black and white. There is no in between.
Such thoughts exacerbate and are exacerbated by the cognitive triad. Beck believed these thoughts or this way of thinking become automatic.
When a person’s stream of automatic thoughts is very negative, you would expect a person to become depressed. Quite often these negative thoughts will persist even in the face of contrary evidence.
Alloy et al. (1999) followed the thinking styles of young Americans in their early 20s for six years. Their thinking style was tested, and they were placed in either the ‘positive thinking group’ or ‘negative thinking group’.
After six years, the researchers found that only 1% of the positive group developed depression compared to 17% of the ‘negative’ group. These results indicate there may be a link between cognitive style and the development of depression.
However, such a study may suffer from demand characteristics. The results are also correlational. It is important to remember that the precise role of cognitive processes is yet to be determined. The maladaptive cognitions seen in depressed people may be a consequence rather than a cause of depression.
Learned Helplessness
Martin Seligman (1974) proposed a cognitive explanation of depression called learned helplessness .
According to Seligman’s learned helplessness theory, depression occurs when a person learns that their attempts to escape negative situations make no difference.
Consequently, they become passive and will endure aversive stimuli or environments even when escape is possible.
Seligman based his theory on research using dogs.
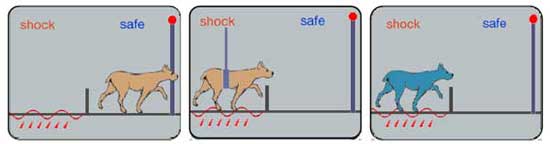
A dog put into a partitioned cage learns to escape when the floor is electrified. If the dog is restrained whilst being shocked, it eventually stops trying to escape.
Dogs subjected to inescapable electric shocks later failed to escape from shocks even when it was possible to do so. Moreover, they exhibited some of the symptoms of depression found in humans (lethargy, sluggishness, passive in the face of stress, and appetite loss).
This led Seligman (1974) to explain depression in humans in terms of learned helplessness , whereby the individual gives up trying to influence their environment because they have learned that they are helpless as a consequence of having no control over what happens to them.
Although Seligman’s account may explain depression to a certain extent, it fails to take into account cognitions (thoughts). Abramson, Seligman, and Teasdale (1978) consequently introduced a cognitive version of the theory by reformulating learned helplessness in terms of attributional processes (i.e., how people explain the cause of an event).
The depression attributional style is based on three dimensions, namely locus (whether the cause is internal – to do with a person themselves, or external – to do with some aspect of the situation), stability (whether the cause is stable and permanent or unstable and transient) and global or specific (whether the cause relates to the “whole” person or just some particular feature characteristic).
In this new version of the theory, the mere presence of a negative event was not considered sufficient to produce a helpless or depressive state. Instead, Abramson et al. argued that people who attribute failure to internal, stable, and global causes are more likely to become depressed than those who attribute failure to external, unstable, and specific causes.
This is because the former attributional style leads people to the conclusion that they are unable to change things for the better.
Gotlib and Colby (1987) found that people who were formerly depressed are actually no different from people who have never been depressed in terms of their tendencies to view negative events with an attitude of helpless resignation.
This suggests that helplessness could be a symptom rather than a cause of depression. Moreover, it may be that negative thinking generally is also an effect rather than a cause of depression.
Humanist Approach
Humanists believe that there are needs that are unique to the human species. According to Maslow (1962), the most important of these is the need for self-actualization (achieving our potential). The self-actualizing human being has a meaningful life. Anything that blocks our striving to fulfill this need can be a cause of depression. What could cause this?
- Parents impose conditions of worth on their children. I.e., rather than accepting the child for who s/he is and giving unconditional love , parents make love conditional on good behavior. E.g., a child may be blamed for not doing well at school, develop a negative self-image and feel depressed because of a failure to live up to parentally imposed standards.
- Some children may seek to avoid this by denying their true selves and projecting an image of the kind of person they want to be. This façade or false self is an effort to please others. However, the splitting off of the real self from the person you are pretending to cause hatred of the self. The person then comes to despise themselves for living a lie.
- As adults, self-actualization can be undermined by unhappy relationships and unfulfilling jobs. An empty shell marriage means the person is unable to give and receive love from their partner. An alienating job means the person is denied the opportunity to be creative at work.
Abramson, L. Y., Seligman, M. E., & Teasdale, J. D. (1978). Learned helplessness in humans: critique and reformulation . Journal of abnormal psychology, 87(1) , 49.
Alloy, L. B., Abramson, L. Y., Whitehouse, W. G., Hogan, M. E., Tashman, N. A., Steinberg, D. L., … & Donovan, P. (1999). Depressogenic cognitive styles : Predictive validity, information processing and personality characteristics, and developmental origins. behavior research and therapy, 37(6) , 503-531.
Beck, A. T. (1967). Depression: Causes and treatment . Philadelphia: University of Pennsylvania Press.
Beck, A. T., Epstein, N., & Harrison, R. (1983). Cognitions, attitudes and personality dimensions in depression. British Journal of Cognitive Psychotherapy .
Bibring, E. (1953). The mechanism of depression .
Brown, G. W., & Harris, T. (1978). Social origins of depression: a reply. Psychological Medicine, 8(04) , 577-588.
Chodoff, P. (1972). The depressive personality: A critical review. Archives of General Psychiatry, 27(5) , 666-673.
Fenichel, O. (1968). Depression and mania. The Meaning of Despair . New York: Science House.
Freud, S. (1917). Mourning and melancholia. Standard edition, 14(19) , 17.
Gotlib, I. H., & Colby, C. A. (1987). Treatment of depression: An interpersonal systems approach. Pergamon Press.
Klein, M. (1934). Psychogenesis of manic-depressive states: contributions to psychoanalysis . London: Hogarth.
Lewinsohn, P. M. (1974). A behavioral approach to depression .
Maslow, A. H. (1962). Towards a psychology of being . Princeton: D. Van Nostrand Company.
National Institute of Mental Health. (2001). Depression research at the National Institute of Mental Health http://www.nimh.nih.gov/health/publications/depression/complete-index.shtml.
Seligman, M. E. (1973). Fall into helplessness. Psychology today, 7(1) , 43-48.
Seligman, M. E. (1974). Depression and learned helplessness . John Wiley & Sons.
Further Information
- List of Support Groups
- Campaign against Living Miserably
- Men do cry: one man’s experience of depression
- NHS Self Help Guides
Depression: A cognitive perspective
Affiliations.
- 1 University of British Columbia, Canada. Electronic address: [email protected].
- 2 Stanford University, United States.
- PMID: 29961601
- DOI: 10.1016/j.cpr.2018.06.008
Cognitive science has been instrumental in advancing our understanding of the onset, maintenance, and treatment of depression. Research conducted over the last 50 years supports the proposition that depression and risk for depression are characterized by the operation of negative biases, and often by a lack of positive biases, in self-referential processing, interpretation, attention, and memory, as well as the use of maladaptive cognitive emotion regulation strategies. There is also evidence to suggest that deficits in cognitive control over mood-congruent material underlie these cognitive processes. Specifically, research indicates that difficulty inhibiting and disengaging from negative material in working memory: (1) increases the use of maladaptive emotion regulation strategies (e.g., rumination), decreases the use of adaptive emotion regulation strategies (e.g., reappraisal), and potentially impedes flexible selection and implementation of emotion regulation strategies; (2) is associated with negative biases in attention; and (3) contributes to negative biases in long-term memory. Moreover, studies suggest that these cognitive processes exacerbate and sustain the negative mood that typifies depressive episodes. In this review, we present evidence in support of this conceptualization of depression and discuss implications of research findings for theory and practice. Finally, we advance directions for future research.
Keywords: Cognition; Cognitive control; Depression; Emotion regulation strategies; Information-processing biases.
Copyright © 2018 Elsevier Ltd. All rights reserved.
Publication types
- Research Support, N.I.H., Extramural
- Research Support, Non-U.S. Gov't
- Adaptation, Psychological / physiology*
- Cognitive Dysfunction / physiopathology*
- Depressive Disorder / physiopathology*
- Emotional Regulation / physiology*
- Executive Function / physiology*
Grants and funding
- R37 MH101495/MH/NIMH NIH HHS/United States
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Evolution of the Cognitive Model of Depression and Its Neurobiological Correlates
- Aaron T. Beck M.D.
Search for more papers by this author
Although the cognitive model of depression has evolved appreciably since its first formulation over 40 years ago, the potential interaction of genetic, neurochemical, and cognitive factors has only recently been demonstrated. Combining findings from behavioral genetics and cognitive neuroscience with the accumulated research on the cognitive model opens new opportunities for integrated research. Drawing on advances in cognitive, personality, and social psychology as well as clinical observations, expansions of the original cognitive model have incorporated in successive stages automatic thoughts, cognitive distortions, dysfunctional beliefs, and information-processing biases. The developmental model identified early traumatic experiences and the formation of dysfunctional beliefs as predisposing events and congruent stressors in later life as precipitating factors. It is now possible to sketch out possible genetic and neurochemical pathways that interact with or are parallel to cognitive variables. A hypersensitive amygdala is associated with both a genetic polymorphism and a pattern of negative cognitive biases and dysfunctional beliefs, all of which constitute risk factors for depression. Further, the combination of a hyperactive amygdala and hypoactive prefrontal regions is associated with diminished cognitive appraisal and the occurrence of depression. Genetic polymorphisms also are involved in the overreaction to the stress and the hypercortisolemia in the development of depression—probably mediated by cognitive distortions. I suggest that comprehensive study of the psychological as well as biological correlates of depression can provide a new understanding of this debilitating disorder.
I was privileged to start my research on depression at a time when the modern era of systematic clinical and biological research was just getting underway. Consequently, the field for new investigations was wide open. The climate at the time was friendly for such research. The National Institute of Mental Health had only recently been funding research and providing salary support for full-time clinical investigators. The Group for Advancement of Psychiatry, under the leadership of pioneers like David Hamburg, was providing guidelines as well as the impetus for clinical research.
Caught up with the contagion of the times, I was prompted to start something on my own. I was particularly intrigued by the paradox of depression. This disorder appeared to violate the time-honored canons of human nature: the self-preservation instinct, the maternal instinct, the sexual instinct, and the pleasure principle. All of these normal human yearnings were dulled or reversed. Even vital biological functions like eating or sleeping were attenuated. The leading causal theory of depression at the time was the notion of inverted hostility. This seemed a reasonable, logical explanation if translated into a need to suffer. The need to punish one’s self could account for the loss of pleasure, loss of libido, self-criticism, and suicidal wishes and would be triggered by guilt. I was drawn to conducting clinical research in depression because the field was wide open—and besides, I had a testable hypothesis.
Cross-Sectional Model of Depression
I decided at first to make a foray into the “deepest” level: the dreams of depressed patients. I expected to find signs of more hostility in the dream content of depressed patients than nondepressed patients, but they actually showed less hostility. I did observe, however, that the dreams of depressed patients contained the themes of loss, defeat, rejection, and abandonment, and the dreamer was represented as defective or diseased. At first I assumed the idea that the negative themes in the dream content expressed the need to punish one’s self (or “masochism”), but I was soon disabused of this notion. When encouraged to express hostility, my patients became more, not less, depressed. Further, in experiments, they reacted positively to success experiences and positive reinforcement when the “masochism” hypothesis predicted the opposite (summarized in Beck [1] ).
Some revealing observations helped to provide the basis for the subsequent cognitive model of depression. I noted that the dream content contained the same themes as the patients’ conscious cognitions—their negative self-evaluations, expectancies, and memories—but in an exaggerated, more dramatic form. The depressive cognitions contained errors or distortions in the interpretations (or misinterpretations) of experience. What finally clinched the new model (for me) was our research finding that when the patients reappraised and corrected their misinterpretations, their depression started to lift and—in 10 or 12 sessions—would remit (2) .
Thus, I undertook the challenge of attempting to integrate the different psychological pieces of the puzzle of depression. The end product was a comprehensive cognitive model of depression. At the surface, readily accessible level was the negativity in the patients’ self-reports, including their dreams and their negative interpretations of their experiences. These variables seemed to account for the manifestations of depression, such as hopelessness, loss of motivation, self-criticism, and suicidal wishes. The next level appeared to be a systematic cognitive bias in information processing leading to selective attention to negative aspects of experiences, negative interpretations, and blocking of positive events and memories. These findings raised the question: “What is producing the negative bias?” On the basis of clinical observations supported by research, I concluded that when depressed, patients had highly charged dysfunctional attitudes or beliefs about themselves that hijacked the information processing and produced the negative cognitive bias, which led to the symptoms of depression (1 , 3 , 4) .
A large number of studies have demonstrated that depressed patients have dysfunctional attitudes, show a systematic negative attentional and recall bias in laboratory experiments, and report cognitive distortions (selective abstraction, overgeneralizing, personalization, and interpretational biases [4] ). Dysfunctional attitudes, measured by the Dysfunctional Attitudes Scale (5) , are represented by beliefs such as “If I fail at something, it means I’m a total failure.” During a full-blown episode of depression, the hypersalient dysfunctional attitudes lead into absolute negative beliefs about the self, their personal world, and the future (“I am a failure”). I suggested that these dysfunctional attitudes are embedded within cognitive structures, or schemas, in the meaning assignment system and thus have structural qualities, such as stability and density as well as thresholds and levels of activation. The degree of salience (or “energy”) of the schemas depends on the intensity of a negative experience and the threshold for activation at a given time (successive stressful experiences, for example, can lower the threshold [1] ).
When the schemas are activated by an event or series of events, they skew the information processing system, which then directs attentional resources to negative stimuli and translates a specific experience into a distorted negative interpretation. The hypersalience of these negative schemas leads not only to a global negative perception of reality but also to the other symptoms of depression, such as sadness, hopelessness, loss of motivation, and regressive behaviors such as social withdrawal and inactivity. These symptoms are also subjected to negative evaluation (“My poor functioning is a burden on my family” and “My loss of motivation shows how lazy I am”). Thus, the depressive constellation consists of a continuous feedback loop with negative interpretations and attentional biases with the subjective and behavioral symptoms reinforcing each other.
Developmental Model of Depression
Cognitive vulnerability.
What developmental event or events might lead to the formation of dysfunctional attitudes and how these events might relate to later stressful events leading to the precipitation of depression was another piece of the puzzle. In our earlier studies, we found that severely depressed patients were more likely than moderately or mildly depressed patients to have experienced parental loss in childhood (6) . We speculated that such a loss would sensitize an individual to a significant loss at a later time in adolescence or adulthood, thus precipitating depression. Brij Sethi, a member of our group, showed that the combination of a loss in childhood with an analogous loss in adulthood led to depression in a significant number of depressed patients (7) . The meaning of the early events (such as “If I lose an important person, I am helpless”) is transformed into a durable attitude, which may be activated by a similar experience at a later time. A recent prospective study observed that early life stress sensitizes individuals to later negative events through impact on cognitive vulnerability leading to depression (8) .

Is the Serotonin Theory of Depression Dead?
The complicated history of the serotonin hypothesis.
Posted August 11, 2022 | Reviewed by Hara Estroff Marano
- What Is Depression?
- Find a therapist to overcome depression
- Research has shown that depression is not simply caused by low monoamines such as serotonin, dopamine, and norepinephrine in the brain.
- Scientific understanding of depression has grown to include genetic factors, stress responses, and other brain changes.
- While depression treatment should include psychotherapy and lifestyle changes, antidepressants may still have an important role in recovery.
Recently, Moncrieff and colleagues published a review of the evidence for the serotonin theory of depression , concluding that there was “no consistent evidence of there being an association between serotonin and depression,” which was shocking news to the general public .
Many news organizations commented on this “long-held theory” being debunked. Some critics touted the paper as evidence that psychiatric treatments are a sham . One politician even cited the paper to suggest, in a baseless and confusing argument, that somehow antidepressants were responsible for mass shootings . Here, we hope to clarify what we know about serotonin and depression.
The serotonin hypothesis is a version of the “monoamine hypothesis of depression.” Monoamines are a group of chemicals that act as neurotransmitters in the brain and include serotonin, dopamine , and norepinephrine. As early as the 1950s, psychiatrists thought these chemicals might be important for mood regulation based on the serendipitous discovery that some drugs were effective for treating depression and all of them seemed to work by increasing the levels of monoamines in the brain. There were other clues, such as certain drugs that lowered monoamine levels seemed to make some people depressed.
For a time, it seemed there was a biological explanation for depression. However, it did not take long for people to see cracks in this theory. Most antidepressants take weeks to work even though they increase brain monoamine levels only a few hours after ingestion. Furthermore, even though there was an occasional positive finding, studies looking at how levels of monoamines in the brain correlate with symptoms of depression were inconclusive (before modern neuroimaging, these studies were notoriously difficult to do).
The results suggested a much more complex process . As early as 1965, Harvard psychiatrist Joseph Schildkraut summarized the theory and supporting data. He concluded, much like Professor Moncrieff half a century later, that “it is not possible…to confirm…or to reject” the hypothesis .
So why did it persist, even if experts knew it was, if not wholly wrong, at least inadequate? Like many imperfect explanations, it survived because it had utility for modeling the role of monoamine chemicals in the brain, especially for drug development. After all, the first antidepressants all worked by increasing the level of monoamines in the brain. Although effective, they were not targeted and had many side effects.
Researchers then began concentrating on a specific monoamine, serotonin, as a target for drugs. What followed was a revolution in antidepressant treatment. Fluoxetine (Prozac) was the first SSRI, or serotonin reuptake inhibitor introduced in the US. Approved in 1987, it was an almost immediate success, and a flurry of other serotonergic drugs followed. Even today, nearly all drug treatments for depression target one or more monoamines, and serotonin is usually one of those.
Even if most mental health experts understood that the monoamine hypothesis was inadequate, it became one way to explain to patients what might be causing depression. It was not uncommon for doctors to tell patients that they had a “chemical imbalance.” This biological explanation was perceived less stigmatizing for most patients, who tended to blame themselves for something outside their control.
As Dr. Montcrieff fairly points out in a blog discussing her study, “even if leading psychiatrists were beginning to doubt the [serotonin hypothesis]…no one told the public.” Many of us thought, “what is the harm.” Even if not exactly true, the point of the explanation is well intended: that depression is a biological disease, not a moral failing or, in some other way, the patient’s fault .
Although the monoamine theory spurred drug discovery and integrated a biological element into our understanding of mood disorders, it may have also limited it. Most antidepressants for the last several decades were “me too” drugs that differed little from their predecessors. The success of the monoamine approach, along with the expense of drug development, may have made pharmaceutical companies reluctant to explore new approaches to depression. It may also have dissuaded patients and their doctors from pursuing other proven approaches to depression, such as psychotherapy , exercise, and a healthy diet .
Professor Moncrieff and her coauthors are doing a service in getting the news out. However, we caution against misrepresentations of the report as a way to conclude that medications have no role in mental health treatment.
Since the monoamine theory emerged in the 1950s, thousands of scientists have added to knowledge about depression and its treatment. The whole puzzle isn't solved yet, but we know a lot. Most modern theories take an integrative approach, meaning that many things cause depression, all working (or not working) together. The “perfect storm” of depression includes genetic vulnerabilities that put people at risk, epigenetic responses to stress , and changes in certain vulnerable parts of the brain that, yes, include the serotonin system.

Is there still a role for antidepressants? Depending on the person, antidepressants are not always needed. However, for many patients, they can be lifesaving, especially those with severe depression. Our understanding of how they work continues to evolve. For example, one mechanism thought to underly the efficacy of antidepressants is their ability to either directly or indirectly lead to an increase in brain-derived neurotrophic factor (BDNF), which is involved in the growth, maturation, and survival of neurons . New research also suggests that some antidepressants may work better for individuals of specific age, sex , medical history, and symptoms .
As our scientific knowledge grows, so should our communication to those directly affected. We believe that the serotonin theory isn’t dead; it just has grown up a lot.
About the Authors
Robert J Boland, MD is the Chief of Staff and a Senior Vice President at The Menninger Clinic. He is also vice chair of the Menninger Department of Psychiatry and Behavioral Science at Baylor College of Medicine and the Brown Foundation Endowed Chair in Psychiatry at Baylor. He is also the co-host of the Menninger Clinic’s Mind Dive Podcast , which examines dilemmas faced by mental health professionals.
Kelly Truong MD is a staff psychiatrist at The Menninger Clinic and an assistant professor at Baylor College of Medicine. She specializes in addiction psychiatry, psychodynamic psychotherapy, and addiction psychopharmacology . She is a member of the American Academy of Addiction Psychiatry, American Psychoanalytic Association and the Houston Psychoanalytic Society.
Alemi, F., Min, H., Yousefi, M., Becker, L. K., Hane, C. A., Nori, V. S., & Wojtusiak, J. (2021). Effectiveness of common antidepressants: A post market release study. EClinicalMedicine, 41. https://doi.org/10.1016/j.eclinm.2021.101171
Boku, S., Nakagawa, S., Toda, H., & Hishimoto, A. (2018). Neural basis of major depressive disorder: Beyond monoamine hypothesis. Psychiatry and Clinical Neurosciences, 72(1), 3–12. https://doi.org/10.1111/pcn.12604
Casarotto, P. C., Girych, M., Fred, S. M., Kovaleva, V., Moliner, R., Enkavi, G., Biojone, C., Cannarozzo, C., Sahu, M. P., Kaurinkoski, K., Brunello, C. A., Steinzeig, A., Winkel, F., Patil, S., Vestring, S., Serchov, T., Diniz, C. R. A. F., Laukkanen, L., Cardon, I., … Castrén, E. (2021). Antidepressant drugs act by directly binding to TRKB neurotrophin receptors. Cell, 184(5), 1299-1313.e19. https://doi.org/10.1016/j.cell.2021.01.034
How to take the news that depression has not been shown to be caused by a chemical imbalance. (2022, July 24). Joanna Moncrieff. https://joannamoncrieff.com/2022/07/24/how-to-take-the-news-that-depres…
Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2022). The serotonin theory of depression: A systematic umbrella review of the evidence. Molecular Psychiatry, 1–14. https://doi.org/10.1038/s41380-022-01661-0
Schildkraut, J. J. (1965). The catecholamine hypothesis of affective disorders: a review of supporting evidence. The American Journal of Psychiatry, 122(5), 509–522. https://doi.org/10.1176/ajp.122.5.509

Mind Matters is a collaborative blog written by Menninger staff and an occasional invited guest to increase awareness about mental health. Launched in 2019, Mind Matters is curated and edited by an expert clinical team, which is led by Robyn Dotson Martin, LPC-S. Martin serves as an Outpatient Assessment team leader and staff therapist.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
April 23, 2024
Research in Context: Treating depression
Finding better approaches.
While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.

Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness, anxiety, hopelessness, frustration, or guilt. You may not enjoy the activities you usually do. These feelings tend to be only temporary. Once circumstances change, and the source of stress goes away, your mood usually improves. But sometimes, these feelings don’t go away. When these feelings stick around for at least two weeks and interfere with your daily activities, it’s called major depression, or clinical depression.
In 2021, 8.3% of U.S. adults experienced major depression. That’s about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain. People with major depression may become unable to meet their responsibilities at work or home. Depression can also lead people to use alcohol or drugs or engage in high-risk activities. In the most extreme cases, depression can drive people to self-harm or even suicide.
The good news is that effective treatments are available. But current treatments have limitations. That’s why NIH-funded researchers have been working to develop more effective ways to treat depression. These include finding ways to predict whether certain treatments will help a given patient. They're also trying to develop more effective drugs or, in some cases, find new uses for existing drugs.
Finding the right treatments
The most common treatments for depression include psychotherapy, medications, or a combination. Mild depression may be treated with psychotherapy. Moderate to severe depression often requires the addition of medication.
Several types of psychotherapy have been shown to help relieve depression symptoms. For example, cognitive behavioral therapy helps people to recognize harmful ways of thinking and teaches them how to change these. Some researchers are working to develop new therapies to enhance people’s positive emotions. But good psychotherapy can be hard to access due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some cases.
There are many antidepressant drugs on the market. Different drugs will work best on different patients. But it can be challenging to predict which drugs will work for a given patient. And it can take anywhere from 6 to 12 weeks to know whether a drug is working. Finding an effective drug can involve a long period of trial and error, with no guarantee of results.
If depression doesn’t improve with psychotherapy or medications, brain stimulation therapies could be used. Electroconvulsive therapy, or ECT, uses electrodes to send electric current into the brain. A newer technique, transcranial magnetic stimulation (TMS), stimulates the brain using magnetic fields. These treatments must be administered by specially trained health professionals.
“A lot of patients, they kind of muddle along, treatment after treatment, with little idea whether something’s going to work,” says psychiatric researcher Dr. Amit Etkin.
One reason it’s difficult to know which antidepressant medications will work is that there are likely different biological mechanisms that can cause depression. Two people with similar symptoms may both be diagnosed with depression, but the causes of their symptoms could be different. As NIH depression researcher Dr. Carlos Zarate explains, “we believe that there’s not one depression, but hundreds of depressions.”
Depression may be due to many factors. Genetics can put certain people at risk for depression. Stressful situations, physical health conditions, and medications may contribute. And depression can also be part of a more complicated mental disorder, such as bipolar disorder. All of these can affect which treatment would be best to use.
Etkin has been developing methods to distinguish patients with different types of depression based on measurable biological features, or biomarkers. The idea is that different types of patients would respond differently to various treatments. Etkin calls this approach “precision psychiatry.”
One such type of biomarker is electrical activity in the brain. A technique called electroencephalography, or EEG, measures electrical activity using electrodes placed on the scalp. When Etkin was at Stanford University, he led a research team that developed a machine-learning algorithm to predict treatment response based on EEG signals. The team applied the algorithm to data from a clinical trial of the antidepressant sertraline (Zoloft) involving more than 300 people.

EEG data for the participants were collected at the outset. Participants were then randomly assigned to take either sertraline or an inactive placebo for eight weeks. The team found a specific set of signals that predicted the participants’ responses to sertraline. The same neural “signature” also predicted which patients with depression responded to medication in a separate group.
Etkin’s team also examined this neural signature in a set of patients who were treated with TMS and psychotherapy. People who were predicted to respond less to sertraline had a greater response to the TMS/psychotherapy combination.
Etkin continues to develop methods for personalized depression treatment through his company, Alto Neuroscience. He notes that EEG has the advantage of being low-cost and accessible; data can even be collected in a patient’s home. That’s important for being able to get personalized treatments to the large number of people they could help. He’s also working on developing antidepressant drugs targeted to specific EEG profiles. Candidate drugs are in clinical trials now.
“It’s not like a pie-in-the-sky future thing, 20-30 years from now,” Etkin explains. “This is something that could be in people's hands within the next five years.”
New tricks for old drugs
While some researchers focus on matching patients with their optimal treatments, others aim to find treatments that can work for many different patients. It turns out that some drugs we’ve known about for decades might be very effective antidepressants, but we didn’t recognize their antidepressant properties until recently.
One such drug is ketamine. Ketamine has been used as an anesthetic for more than 50 years. Around the turn of this century, researchers started to discover its potential as an antidepressant. Zarate and others have found that, unlike traditional antidepressants that can take weeks to take effect, ketamine can improve depression in as little as one day. And a single dose can have an effect for a week or more. In 2019, the FDA approved a form of ketamine for treating depression that is resistant to other treatments.
But ketamine has drawbacks of its own. It’s a dissociative drug, meaning that it can make people feel disconnected from their body and environment. It also has the potential for addiction and misuse. For these reasons, it’s a controlled substance and can only be administered in a doctor’s office or clinic.
Another class of drugs being studied as possible antidepressants are psychedelics. These include lysergic acid diethylamide (LSD) and psilocybin, the active ingredient in magic mushrooms. These drugs can temporarily alter a person’s mood, thoughts, and perceptions of reality. Some have historically been used for religious rituals, but they are also used recreationally.
In clinical studies, psychedelics are typically administered in combination with psychotherapy. This includes several preparatory sessions with a therapist in the weeks before getting the drug, and several sessions in the weeks following to help people process their experiences. The drugs are administered in a controlled setting.
Dr. Stephen Ross, co-director of the New York University Langone Health Center for Psychedelic Medicine, describes a typical session: “It takes place in a living room-like setting. The person is prepared, and they state their intention. They take the drug, they lie supine, they put on eye shades and preselected music, and two therapists monitor them.” Sessions last for as long as the acute effects of the drug last, which is typically several hours. This is a healthcare-intensive intervention given the time and personnel needed.
In 2016, Ross led a clinical trial examining whether psilocybin-assisted therapy could reduce depression and anxiety in people with cancer. According to Ross, as many as 40% of people with cancer have clinically significant anxiety and depression. The study showed that a single psilocybin session led to substantial reductions in anxiety and depression compared with a placebo. These reductions were evident as soon as one day after psilocybin administration. Six months later, 60-80% of participants still had reduced depression and anxiety.
Psychedelic drugs frequently trigger mystical experiences in the people who take them. “People can feel a sense…that their consciousness is part of a greater consciousness or that all energy is one,” Ross explains. “People can have an experience that for them feels more ‘real’ than regular reality. They can feel transported to a different dimension of reality.”
About three out of four participants in Ross’s study said it was among the most meaningful experiences of their lives. And the degree of mystical experience correlated with the drug’s therapeutic effect. A long-term follow-up study found that the effects of the treatment continued more than four years later.
If these results seem too good to be true, Ross is quick to point out that it was a small study, with only 29 participants, although similar studies from other groups have yielded similar results. Psychedelics haven’t yet been shown to be effective in a large, controlled clinical trial. Ross is now conducting a trial with 200 people to see if the results of his earlier study pan out in this larger group. For now, though, psychedelics remain experimental drugs—approved for testing, but not for routine medical use.
Unlike ketamine, psychedelics aren’t considered addictive. But they, too, carry risks, which certain conditions may increase. Psychedelics can cause cardiovascular complications. They can cause psychosis in people who are predisposed to it. In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called “bad trip”—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may prevent many people from having access to it.
Better, safer drugs
Despite the promise of ketamine or psychedelics, their drawbacks have led some researchers to look for drugs that work like them but with fewer side effects.
Depression is thought to be caused by the loss of connections between nerve cells, or neurons, in certain regions of the brain. Ketamine and psychedelics both promote the brain’s ability to repair these connections, a quality called plasticity. If we could understand how these drugs encourage plasticity, we might be able to design drugs that can do so without the side effects.

Dr. David Olson at the University of California, Davis studies how psychedelics work at the cellular and molecular levels. The drugs appear to promote plasticity by binding to a receptor in cells called the 5-hydroxytryptamine 2A receptor (5-HT2AR). But many other compounds also bind 5-HT2AR without promoting plasticity. In a recent NIH-funded study, Olson showed that 5-HT2AR can be found both inside and on the surface of the cell. Only compounds that bound to the receptor inside the cells promoted plasticity. This suggests that a drug has to be able to get into the cell to promote plasticity.
Moreover, not all drugs that bind 5-HT2AR have psychedelic effects. Olson’s team has developed a molecular sensor, called psychLight, that can identify which compounds that bind 5-HT2AR have psychedelic effects. Using psychLight, they identified compounds that are not psychedelic but still have rapid and long-lasting antidepressant effects in animal models. He’s founded a company, Delix Therapeutics, to further develop drugs that promote plasticity.
Meanwhile, Zarate and his colleagues have been investigating a compound related to ketamine called hydroxynorketamine (HNK). Ketamine is converted to HNK in the body, and this process appears to be required for ketamine’s antidepressant effects. Administering HNK directly produced antidepressant-like effects in mice. At the same time, it did not cause the dissociative side effects and addiction caused by ketamine. Zarate’s team has already completed phase I trials of HNK in people showing that it’s safe. Phase II trials to find out whether it’s effective are scheduled to begin soon.
“What [ketamine and psychedelics] are doing for the field is they’re helping us realize that it is possible to move toward a repair model versus a symptom mitigation model,” Olson says. Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That’s likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
—by Brian Doctrow, Ph.D.
Related Links
- How Psychedelic Drugs May Help with Depression
- Biosensor Advances Drug Discovery
- Neural Signature Predicts Antidepressant Response
- How Ketamine Relieves Symptoms of Depression
- Protein Structure Reveals How LSD Affects the Brain
- Predicting The Usefulness of Antidepressants
- Depression Screening and Treatment in Adults
- Serotonin Transporter Structure Revealed
- Placebo Effect in Depression Treatment
- When Sadness Lingers: Understanding and Treating Depression
- Psychedelic and Dissociative Drugs
References: An electroencephalographic signature predicts antidepressant response in major depression. Wu W, Zhang Y, Jiang J, Lucas MV, Fonzo GA, Rolle CE, Cooper C, Chin-Fatt C, Krepel N, Cornelssen CA, Wright R, Toll RT, Trivedi HM, Monuszko K, Caudle TL, Sarhadi K, Jha MK, Trombello JM, Deckersbach T, Adams P, McGrath PJ, Weissman MM, Fava M, Pizzagalli DA, Arns M, Trivedi MH, Etkin A. Nat Biotechnol. 2020 Feb 10. doi: 10.1038/s41587-019-0397-3. Epub 2020 Feb 10. PMID: 32042166. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. J Psychopharmacol . 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512. PMID: 27909164. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, Bossis AP, Grigsby J, Fischer S, Ross S. J Psychopharmacol . 2020 Feb;34(2):155-166. doi: 10.1177/0269881119897615. Epub 2020 Jan 9. PMID: 31916890. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE. Science . 2023 Feb 17;379(6633):700-706. doi: 10.1126/science.adf0435. Epub 2023 Feb 16. PMID: 36795823. Psychedelic-inspired drug discovery using an engineered biosensor. Dong C, Ly C, Dunlap LE, Vargas MV, Sun J, Hwang IW, Azinfar A, Oh WC, Wetsel WC, Olson DE, Tian L. Cell . 2021 Apr 8: S0092-8674(21)00374-3. doi: 10.1016/j.cell.2021.03.043. Epub 2021 Apr 28. PMID: 33915107. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. Nature . 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355.
Connect with Us
- More Social Media from NIH
- Warning Signs and Symptoms
- Mental Health Conditions
- Common with Mental Illness
- Mental Health By the Numbers
- Individuals with Mental Illness
- Family Members and Caregivers
- Kids, Teens and Young Adults
- Veterans & Active Duty
- Identity and Cultural Dimensions
- Frontline Professionals
- Mental Health Education
- Support Groups
- NAMI HelpLine
- Publications & Reports
- Podcasts and Webinars
- Video Resource Library
- Justice Library
- Find Your Local NAMI
- Find a NAMIWalks
- Attend the NAMI National Convention
- Fundraise Your Way
- Create a Memorial Fundraiser
- Pledge to Be StigmaFree
- Awareness Events
- Share Your Story
- Partner with Us
- Advocate for Change
- Policy Priorities
- NAMI Advocacy Actions
- Policy Platform
- Crisis Intervention
- State Fact Sheets
- Public Policy Reports
Recognizing the Lesser-Known Symptoms of Depression
February 09, 2022
By Ginger Robertson

Thanks to sensationalized media depictions of mental illness and stigma surrounding mental health conditions, people tend to have a limited view of what depression actually looks like. When you think of a “depressed person,” perhaps you envision an image from a movie or medication commercial: Someone lying alone in a dark room, crying into a box of tissues, overcome with feelings of hopelessness.
This picture is not necessarily inaccurate; it is simply incomplete. There are many more manifestations of depression — symptoms that aren’t necessarily visible or immediately obvious.
Knowing the seldom discussed symptoms of depression is a valuable skill; being able to recognize the less obvious signs may help you or a loved one identify and seek treatment for depression, if needed. Additionally, knowing and fully understanding these symptoms allows us to be more compassionate and helpful to those who are living with mental health conditions.
Here are a few lesser-known symptoms to look out for:
Studies have shown that depression can reduce cognitive functions , including working memory, long-term memory, decision making and ability to focus. Research also suggests that people with depression often have “widespread grey matter structural abnormalities” in the brain — observable structural differences that contribute to such cognitive deficits.
This often presents in what we refer to as a “brain fog,” in which people may experience an inability to focus on tasks, slower reaction times, forgetfulness and feelings of being mentally “blocked.” Naturally, this can lead to a number of professional, personal and emotional challenges; combating cognitive symptoms can be a frustrating and demoralizing experience.
If this is a symptom you have observed in yourself or someone else, remember to have patience; you and those around you are deserving of grace while navigating a health issue.
Substance Use
While substance use disorders are complex conditions, they are often linked to depression . People experiencing substance use challenges often face the consequences of misinformation and stigma; many are blamed for “poor choices” and irresponsibility.
However, this misguided discourse fails to recognize many of the facets of addiction, including the fact that many people misuse drugs and alcohol to self-medicate their depression. They may not be aware that they are depressed, may not have the resources to treat their depression or may grapple with the stigma surrounding seeking help.
We all have a role to play in dismantling stigma surrounding treatment for mental health conditions; if we can acknowledge that mental health is health, seek help ourselves and encourage others to follow suit, we may, in result, see a decline in substance use.
Weight Changes
While weight changes can be indicative of a shift in physical health, they can also be connected to mental health. Depression is known to affect appetite; some people with depression experience increased appetite and report eating more, while others experience a decrease in appetite and undereat. Accordingly, large weight fluctuations may be a symptom of unmanaged depression.
The challenge of coping with depression is often compounded by stigma surrounding weight and body size; one person may be “fat shamed” for their weight gain while another is praised for their weight loss, despite both weight changes being a result of mental illness. Overeating and undereating — and grappling with public opinion about bodies — only adds to the physical and emotional challenges of depression. A holistic approach to treating depression requires a degree of body positivity: An acceptance of all sizes with the goal of mind and body health.
Irritability
Irritability , anger and impatience often accompany depression. Perhaps you have experienced the surprise of these negative emotions that seemingly “come out of nowhere” — either when you experience them or are on the receiving end of an outburst from someone else.
Often, these outbursts are referred to as anger attacks , sudden intense spells of anger could be considered uncharacteristic and inappropriate in the moment. In turn, this can lead to feelings of shame and confusion surrounding an inability to control these intense emotions. A 2009 study found that angry reactions in depressed individuals may stem from rejection, guilt, fear and “ineffective management of the experience and expression of anger.”
While this experience can be distressing, sharing your concerns with a trusted health care professional could prevent further attacks.
Extreme Fatigue
Often, the chemical imbalances that accompany depression can strip people of their energy. Individuals with depression often have low levels of norepinephrine, serotonin and dopamine. Without appropriate levels of these chemicals, we can experience fatigue, sleep issues, low motivation, decreased interest in once-enjoyed activities and a general lack of joy.
For these reasons, many antidepressants work to increase these chemicals in the body.
From the outside, these symptoms may be judged as a personal failing. Perhaps someone appears lazy, disorganized or unclean — but in reality, they are doing their very best to cope when they are struggling to simply get out of bed. In these moments, chores may go undone, hygiene may falter and basic tasks may get overlooked.
Rather than passing judgment or demanding change, we need to remember that, often, compassion and medical intervention are the appropriate response.
Physical Pain
Other possible physical manifestations of depression are vague aches and pains. The chemicals serotonin and norepinephrine don’t simply affect mood — they also influence how we feel pain. Accordingly, the chemical imbalance linked to depression is also linked to many types of physical pain.
Additionally, research shows that there are biological factors that increase inflammation and decrease immunity during depressive episodes. Those with depression may experience headaches, body aches and stomach aches, among other ailments.
Ultimately, it’s important to remember that depression is complex. It is a mental health condition that doesn’t always look like the tired trope we see played out in the media and stigma-laden conversations.
Depression manifests in a wide variety of symptoms — both mental and physical — that most people may not be aware of. Of course, it is certainly possible to experience brain fog, misuse substances, battle fatigue and feel pain without having depression. But if you are noticing these behaviors and feelings in yourself or someone else, remain vigilant and consider seeking help. Prioritizing your health is not only wise; it is brave.
Ginger Robertson is a registered nurse and mental health blogger. She hopes her work can end the stigma surrounding mental illness and seeking mental health care.
Submit To The NAMI Blog
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness. Most importantly: We feature your voices. Check out our Submission Guidelines for more information.

Recent Posts
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264 , text “helpline” to 62640 , or chat online. In a crisis, call or text 988 (24/7).
- What is a recession?
Recessions and the business cycle
- What is a depression?
Recession vs. depression
- How recessions affect you
- Recession FAQs
What is a recession?
Paid non-client promotion: Affiliate links for the products on this page are from partners that compensate us (see our advertiser disclosure with our list of partners for more details). However, our opinions are our own. See how we rate investing products to write unbiased product reviews.
- A recession and a depression describe periods during which the economy shrinks, but they differ in severity, duration, and scale.
- A recession is a decline in economic activity spread across the economy that lasts more than a few months.
- A depression is a more extreme economic downturn, and there has only been one in US history: The Great Depression, which lasted from 1929 to 1939.
Economic downturns are a lousy time for everyone. You may be worried about losing your job and being able to pay your bills — or you may be alarmed at just how abruptly that little red line that represents your investment portfolio has dropped. It's even worse if that red line represents your 401(k) savings. As a result, it can be helpful to know the signs of a recession, as well as the different ways this term is defined.
While you've probably heard the terms "recession" and "depression" before, you may not know what they actually mean and what the difference is between the two. Chiefly, a depression is a more severe, long-lasting recession that extends beyond the confines of a single country's border and into the economies of other nations.
To help you better understand the business cycle and prepare for the twists and turns of an economic crisis, here's what you need to know about recessions, depressions, and how they're different.
What is a recession?
Defining a recession , technical definition .
The technical definition of a recession is "a significant decline in economic activity that is spread across the economy and that lasts more than a few months," according to the National Bureau of Economic Research (NBER), a nonprofit organization that officially declares U.S. recessions and expansions.
An economic recession is often defined as a decline of real (meaning inflation-adjusted) gross domestic product (GDP) for two consecutive quarters — but it's not that simple. Over the course of a business cycle, you might see GDP contract for a period of time, but that doesn't necessarily mean that there's a recession.
The NBER takes a broader view. The group defines recessions as "a significant decline in economic activity spread across the economy, lasting more than a few months," with indicators including:
- Decline in real GDP
- Decline in real income
- Rise in unemployment
- Slowed industrial production and retail sales
- Lack of consumer spending
The NBER's view of recessions takes a more holistic outlook of the economy, meaning recessions are not necessarily defined by one single factor. But many of these factors are intertwined, meaning a significant drop in something like GDP could rattle consumer spending or unemployment.
In simpler terms
A recession can be defined as a time during which the economy shrinks, businesses make less money and the unemployment rate goes up. The business cycle is not characterized by neverending increases in GDP. As a result, there are times when this economic yardstick is decreasing, and if it declines for a long enough time, the economy has entered recession.
These periods of economic decline frequently last about a year, according to figures provided by the International Monetary Fund (IMF).
During these times, many economic indicators experience notable declines. Investment and production both decline, according to an IMF paper. Consumption also declines, which reduces the overall demand for goods and services created by corporations.
This, in turn, can reduce profitability and motivate companies to lay off employees in an effort to ensure their bottom line remains healthy.
It is worth noting that while recessions frequently last about a year, expansions generally last longer , as the economy is usually growing in size, according to the IMF.
More specifically, the global organization examined 21 advanced economies between 1960 and 2007, revealing that they were in recession roughly 10% of the time, at least according to this sample.
Causes of recession
Generally speaking, expansion and growth in an economy cannot last forever. A significant decline in economic activity is usually triggered by a complex, interconnected combination of factors, including:
Economic shocks
An economic shock is an unpredictable event that causes widespread economic disruption, such as a natural disaster or a terrorist attack. The most recent example of such a shock was the COVID-19 outbreak, which triggered a brief recession.
Another example of an event that served as a shock to the economy was Hurricane Katrina. One estimate was that this natural disaster caused $200 billion worth of damage, according to figures from the U.S. Bureau of Labor Statistics.
High interest rates
High interest rates make it more expensive for consumers to borrow money. This means that they are less likely to spend, especially on major purchases like houses or cars. Companies will probably reduce their spending and growth plans as well because the cost of financing is too high.
Asset bubbles
During an asset bubble, for example a housing bubble , the prices of investments like tech stocks in the dot-com era or real estate before the Great Recession rise rapidly, far beyond their fundamentals. These high prices are supported only by artificially inflated demand, which is caused by overly optimistic expectations of future asset values. This artificially inflated demand eventually dissipates, and the bubble bursts. At this point, people lose money and confidence collapses. Both consumers and businesses cut down on spending and the economy goes into recession.
Loss of confidence
The sentiment of consumers has a substantial impact on the economy. Consumer spending accounts for close to 70% of U.S. GDP, so when these individuals tighten up their purse strings, it can tip the economy into recession. Even if this change in mindset is not enough to trigger a recession, a drop in consumer demand gives companies less incentive to produce goods and services, which can in turn motivate them to lay off employees in order to maintain profitability.
It is worth noting that the confidence of business executives, as well as other key decision makers in corporations, has a substantial impact on the health of the economy. If these decision makers become less confident, then they could cut budgets, laying off workers and potentially reducing expenditure on capital equipment in an effort to bolster profitability.
To understand the macroeconomic variables that constitute recessions, Giacomo Santalego , PhD, a senior lecturer of economics at Fordham University, says it's important to acknowledge the relationship between recessions and the business cycle.
A business cycle tracks the up-and-down fluctuations natural to any capitalistic economies. Because the cycle traces the wide-ranging upward and downward comovements of economic indicators, it is often a focal point for monetary and fiscal policy as governments attempt to curtail the effects of these peaks and valleys.
Business cycles are understood as having four distinct phases:
- Expansion: This phase represents a period of economic growth, also considered the "normal" phase of the business cycle. It is often characterized by an increase in employment and a swelling of consumer spending and demand, which leads to an increase in the production and cost of goods and services.
- Peak: The highest point of a business cycle that signifies when an economy has reached its crest of output. Here, there's nowhere to go but down, sending the economy into a contraction phase. This can happen for any number of reasons, either investors get too speculative and create an asset bubble or industrial production starts outpacing demand. This is commonly seen as the turning point into the contraction phase.
- Contraction: A period that is marked by a decline in economic activity often identified by a rise in unemployment as well as a bear market . Additionally, GDP growth falls under 2%. As growth contracts, the economy enters a recession.
- Trough: A peak is to an expansion what a trough is to a contraction. A trough marks the bottom of a business cycle's economic activity and marks the start of a new wave of expansion and a new business cycle. This is a turning point that's followed by a new wave of expansion.
It's important to note that business cycles do not occur at predictable intervals. Instead, they are irregular in length, and their severity is reflected by the economic variables of the time. That said, the average post-World War II business cycle lasted 65 months, according to the Congressional Research Service .
What is a depression?
An economic depression is typically understood as an extreme downturn in economic activity lasting several years, but the exact definition and specifications of a depression are less clear.
"The way people think about it is a depression is a more widespread and severe recession," says Laura Ullrich, senior regional economist with the Federal Reserve Bank of Richmond, says, "but there is no clear-cut moment where we can say 'we hit X unemployment rate or Y GDP growth — we're now officially in a depression.'"
The NBER notes that economists differ on the period of time that designates a depression. Some experts believe a depression lasts only when economic activity is declining, while the more common understanding is that a depression extends until economic activity has returned to close to normal levels.
A depression is a more severe recession. However, it's a little tricky to concretely, quantifiably describe the difference between a recession and a depression, mainly because there's only been one.
Because economists do not have a set definition for what constitutes a depression, the general public sometimes uses it interchangeably with the term recession. However, the difference makes itself evident when you compare the Great Recession to the Great Depression.
Generally speaking, a depression spans years, rather than months, and typically sees higher rates of unemployment and a sharper decline in GDP. And while a recession is often limited to a single country, a depression is usually severe enough to have global impacts.
How recessions affect you
Job losses .
One major consequence of economic downturns is job losses. When the economy starts to contract, revenues decline, which gives companies substantial incentive to lay off employees in order to turn a profit. A perfect example of how a downturn can cause employers to eliminate jobs is the recession that coincided with the COVID-19 pandemic. The global pandemic began in early 2020, and during March, April and May of that year, the nation's employers shed 1.5 million jobs, according to figures from the Bureau of Labor Statistics. Further, economic downturns result in reduced tax revenue, which can prompt governments to lay off workers. Many state governments, in particular, need to balance their budgets each year, which can cause them to slash jobs.
Reduced income
Economic downturns can lower the income of residents by eliminating jobs and lowering wages. In addition, companies reduce investment in capital equipment during recessions, which lowers productivity. This can, in turn, adversely impact wages. Lowered incomes can have significant impacts on the economy in the long-term, for example undermining nutrition and making it more difficult for people to pursue college education. Both of these adverse effects can impact productivity in the long-run.
Difficulty finding work
One very noticeable impact of an economic downturn is a tighter labor market. When the economy goes into recession, many jobs will get eliminated, both in the public and private sectors. This can increase the number of applicants for every available position, resulting in a highly competitive labor market. This increased competition for jobs can undermine the power that employees have to demand adequate compensation, which can in turn place downward pressure on salaries and wages.
Declining investments
One common challenge that investors encounter during economic downturns is the impact that falling asset values can have on their net worth. When the economy goes into recession, the value of assets held by everyday investors, for example stocks and real estate, can decline substantially. This can undermine the value of their retirement accounts and also wealth they hold outside of these accounts, for example in brokerage accounts. When investors feel less wealthy, it can make them less likely to spend, something referred to as the wealth effect . This can in turn contribute to further economic contraction.
Recession FAQs
The length of a recession varies, from a matter of months to multiple years. According to IMF research cited in this piece, recessions typically last a year.
Economists at the National Bureau of Economic Research (NBER) officially declare US recessions.
Yes, you can prepare for a recession by paying off debt, building up savings and also creating a diversified investment portfolio.
Governments may respond to recessions by cutting taxes or spearheading other forms of economic stimulus in order to fuel expansion.
Yes, there are different types of recessions, which can vary in terms of length and intensity. A depression, for example, is a severe recession.
- Main content
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Stress, coping, and depression: testing new hypotheses in a prospectively studied general population sample of U.S. born Whites and Blacks
1 Department of Epidemiology, Columbia University, New York, NY
The scarcity of empirically supported explanations for the Black/White prevalence difference in depression in the U.S. is a conspicuous gap in the literature. Recent evidence suggests that the paradoxical observation of decreased risk of depression but elevated rates of physical illness among Blacks in the U.S. compared with Whites may be accounted for by the use of coping behaviors (e.g., alcohol and nicotine consumption, overeating) among Blacks exposed to high stress levels. Such coping behaviors may mitigate deleterious effects of stressful exposures on mental health while increasing the risk of physical ailments. The racial patterning in mental and physical health outcomes could therefore be explained by this mechanism if a) these behaviors were more prevalent among Blacks than Whites and/or b) the effect of these behavioral responses to stress was differential by race. The present study challenges this hypothesis using longitudinal, nationally-representative data with comprehensive DSM-IV diagnoses. Data are drawn from 34,653 individuals sampled in Waves 1 (2001-2002) and 2 (2004-2005) as part of the US National Epidemiologic Survey on Alcohol and Related Conditions. Results showed that a) Blacks were less likely to engage in alcohol or nicotine consumption at low, moderate, and high levels of stress compared to Whites, and b) there was a significant three-way interaction between race, stress, and coping behavior for BMI only (F=2.11, df=12, p=0.03), but, contrary to the hypothesis, elevated BMI was protective against depression in Blacks at low, not high, levels of stress. Further, engagement in unhealthy behaviors, especially at pathological levels, did not protect against depression in Blacks or in Whites. In sum, the impact of stress and coping processes on depression do not appear to operate differently in Blacks versus Whites. Further research testing innovative hypotheses that would explain the difference in Black/White depression prevalence is warranted.
Introduction
Epidemiologic studies have consistently documented that Blacks living in the United States have higher rates of physical illness such as hypertension and diabetes, and higher rates of mortality, compared with non-Hispanic Whites controlling for indicators of socio-economic position (SEP) ( Heckler 1985 ; McCord and Freeman 1990 ; Williams and Jackson 2005 ). Conversely, major psychiatric epidemiologic household surveys have reported that Blacks have equal or lower rates of most psychiatric disorders, including major depression ( Kessler, McGonagle et al. 1994 ; Hasin, Goodwin et al. 2005 ; Breslau, Aguilar-Gaxiola et al. 2006 ; Williams, Gonzalez et al. 2007 ). These divergent patterns for mental and physical health outcomes have been termed a ‘paradox’ ( Williams 2001 ). Blacks in the U.S. face historic and contemporary institutionalized discrimination which exposes them to disadvantaged SEP, worse living conditions, and greater stress and adversity due to marginalized social status ( Kessler, Mickelson et al. 1999 ; Kreiger 2000 ; Williams and Williams-Morris 2000 ), all of which seemingly place Blacks at greater risk for depression compared with Whites ( Dohrenwend 2000 ). Indeed, among Blacks in the U.S., perception of discrimination and adversity due to race is associated with greater psychological distress and depressive symptoms ( Kessler, Mickelson et al. 1999 ; Williams and Williams-Morris 2000 ). However, absolute rates of depression remain lower among Blacks compared with Whites.
Many pathways have been posited to explain the elevated rates of physical health problems among Blacks in the U.S. compared with Whites. One well-studied mechanism is stress associated with disadvantaged social status. The physiologic responses to stress via allostatic load have been hypothesized to influence health by a process of ‘wear and tear’ whereby the body can no longer effectively regulate itself ( McEwen 2000 ; McEwen 2004 ). “Weathering” ( Geronimus 1994 ; Geronimus 1996 ), which describes a process of accelerated aging as an effect of the cumulative experience of stress and adversity, has been hypothesized to explain why Blacks have lower birthweights as well as higher mortality at younger ages than Whites after controlling for SEP. Further, interpersonal discrimination appraised by the individual as negative can result in fear, anger, and denial, thereby inducing injurious physiologic responses in cardiovascular, endocrine, neurologic and immune systems ( Krieger 1990 ; Krieger and Sidney 1996 ; Kreiger 2000 ). Adverse neighborhood conditions, to which Blacks have greater exposure than Whites, can influence health through inadequate access to social and health services, exposures to health hazards, and reduction in social cohesion and connectedness ( Massey 1985 ; Massey 2004 ). Greater stress, worse bodily wear and tear, reduced access to medical services, and greater exposure to deleterious neighborhood conditions are all risk factors for depression ( Leonard 2000 ; McEwen 2003 ; Stansfeld 2005 ), and yet Blacks consistently generate estimates of depression below those of Whites; this poses a perplexing, unresolved issue for social and psychiatric epidemiology.
Two methodological hypotheses advanced to explain this mental/physical health paradox posit that rates of depression among Blacks are underestimated in major psychiatric epidemiologic studies due to selection bias and measurement error. The selection bias hypothesis reflects the fact that all major psychiatric epidemiologic surveys conducted in the U.S. exclude institutionalized populations. Young Black men in the U.S. are overrepresented in prison and jail populations ( Petit and Western 2004 ), where depression is more prevalent compared with household populations ( Teplin 1990 ; Teplin, Abram et al. 1996 ). Thus, the underestimation of depression prevalence in household samples could affect Blacks to a greater extent compared with Whites, though the effect of this bias would primarily be age- and gender-specific. The measurement error hypothesis suggests potential diagnostic bias in the major survey instruments used to capture depression. Given the same symptom presentation, Blacks interviewed by clinicians in unstructured or semi-structured formats are more likely to be diagnosed as having a disorder in the psychotic spectrum and Whites as having a disorder in the mood spectrum ( Neighbors, Trierweiler et al. 1999 ; Neighbors, Trierweiler et al. 2003 ; Strakowski, Keck et al. 2003 ). Additionally, some argue that depression may manifest differently in Blacks compared with Whites, and current diagnostic nosology more appropriately captures depression in Whites compared with Blacks ( Rogler 1999 ; Baker 2001 ; Brown 2003 ; Kleinman 2004 ). Available data suggest that while these hypotheses may explain some of the Black/White difference in depression, methodological issues cannot account for the all of the difference ( Williams, Gonzalez et al. 2007 ; Breslau, Javaras et al. 2008 ). Thus, hypotheses exploring alternative mechanisms through which Blacks may have a lower prevalence of depression compared with Whites remain necessary.
In contrast to methodological hypotheses explaining the mental/physical health ‘paradox’, a recently advanced alternative hypothesis is that the patterning in physical and mental health outcomes in Blacks versus Whites arises from mechanisms for coping with stressors that on average operate differently for Black and White Americans ( Jackson and Knight 2006 ; Jackson, Knight et al. 2009 ). Jackson and colleagues have argued that Blacks in the U.S. face greater, and unique, stressors compared with Whites, and that strategies deployed to cope emotionally with this increased stress may protect mental health while having deleterious consequences for physical health. Recently, Jackson and colleagues reported that at high levels of stress, Blacks with elevated body mass index (BMI) and/or who smoke cigarettes and/or drink alcohol (collectively termed ‘unhealthy behaviors’ or ‘UHBs’ ( Jackson, Knight et al. 2009 )) were less likely than Blacks not engaging in these behaviors to develop depression, whereas the pattern trended in the opposite direction for Whites ( Jackson, Knight et al. 2009 ). Further empirical support for this hypothesis was recently reported using data from the Baltimore Epidemiologic Catchment Area Study ( Mezuk, Rafferty et al. 2010 ). Evidence indicates that UHBs can ameliorate immediate anxiety and depressive symptoms in response to stressful experiences by regulating corticotropin-releasing factor in the hypothalamic-pituitary-adrenalcortical (HPA) axis ( Benowitz 1988 ; Koob, Roberts et al. 1998 ; Dallman, Pecoraro et al. 2003 ). However, long-term heavy alcohol consumption, smoking, and high BMI can lead to a cascade of physical health consequences. This hypothesis suggests that, in the context of chronic stress, Blacks’ engagement in UHBs may serve to buffer the deleterious consequences of stress on depression through the HPA pathway, leading to a lower prevalence of depression but a greater prevalence of physical health problems than would have otherwise occurred. This hypothesis also suggests that the same processes operate differently or with different consequences in Whites. In the interest of brevity, we refer to these potentially differential patterns in the relationships between stress, coping, and depression between Blacks and Whites as “group-specific,” meaning that they arise from the unequal distribution of exposures and coping resources engendered by a racialized environment, rather than differences embedded in the individual.
Differences in stress and coping processes between Blacks and Whites could account for the mental/physical health ‘paradox’ under two scenarios. (1) UHBs are indeed protective against depression, among both Blacks and Whites, but Blacks are much more likely to engage in them compared with Whites at a given level of stress. This is unlikely in light of previous epidemiologic evidence suggesting that a) substance disorders and obesity are comorbid with depression ( Reiger, Farmer et al. 1990 ; Kessler, Crum et al. 1997 ; Hasin, Goodwin et al. 2005 ) and b) Blacks are less likely than Whites to engage in alcohol and nicotine consumption ( Grant, Hasin et al. 2004 ; Hasin, Stinson et al. 2007 ). However, patterns of comorbidity and Black/White differences in depression at all levels of stress have not been investigated systematically. (2) UHBs operate differentially by race, whereby they protect against depression to a greater extent among Blacks compared with Whites (either overall or variably by level of stress). This hypothesis is supported by data from the Americans’ Changing Lives Survey ( Jackson, Knight et al. 2009 ) and the Baltimore Epidemiologic Catchment Area Study ( Mezuk, Rafferty et al. 2010 ), as described above.
We propose to comprehensively investigate each of the above scenarios in a large nationally representative prospective study of U.S. adults. The present study is intended to both replicate and extend the analyses presented in Jackson et al. (2009) to provide a comprehensive test of the underlying theory. Using the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) we accomplish five main aims. First, we construct as exact a replication as possible of Jackson et al. (2009) in order to provide a baseline for comparison and from which to broaden the analyses. The remaining four aims systematically test the theory underlying the two scenarios outlined above. We examine whether alcohol consumption, nicotine consumption, and body mass index (as a proxy for overeating, consistent with Jackson et al., (2009) ) are prospectively protective against depression; we examine whether Blacks engage in more of these behaviors than Whites at low, moderate, and/or high levels of stress; and we test the hypothesis that Blacks exposed to high levels of stress are protected against depression if engaged in UHBs at the time of the stressors and, simultaneously, that Whites are not similarly conferred such protection from these behaviors. Finally, the hypothesis outlined by Jackson et al. (2009) suggests that the stress exposure of Blacks is qualitatively different compared to that of Whites. The NESARC data allows us to examine a measure of perceived racial discrimination in order to test whether Blacks who report high levels of discrimination and engage in UHBs have less depression than Blacks who report high levels of discrimination and do not engage in UHBs.
The data used in the present study have distinct advantages over those in ( Jackson, Knight et al. 2009 ): namely a larger sample size, DSM-IV diagnoses of major depression at two time points, DSM-IV diagnoses of nicotine dependence and alcohol use disorders, and comprehensive measures of nicotine, alcohol consumption, and stressful life events. Extending the analyses of Jackson et al, (2009) to include pathological alcohol and nicotine consumption is important in testing the hypothesis, as high and chronic levels of nicotine and alcohol use are behaviors most associated with poor physical health outcomes; if the Black/White “paradox” can be attributed to discrepant mental and physical health consequences of unhealthy behaviors, the nature and degree of engagement in those behaviors most implicated in poor somatic health should be considered.
Data are drawn from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a two-wave longitudinal survey of adults in the United States residing in households and group quarters. Wave 1 was conducted in 2001-2002 (N=43,093); young adults, Hispanics and Blacks were oversampled, with an overall response rate of 81%. Respondents were re-interviewed for Wave 2 approximately three years after Wave 1, with 34,653 (80.4%) successfully re-interviewed. More information on the study methods is found elsewhere ( Grant, Goldstein et al. 2009 ). The research protocol, including written informed consent procedures, received full ethical review and approval from the U.S. Census Bureau and the U.S. Office of Management and Budget.
All measures were assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV). We used measures of race/ethnicity, UHBs, and stressful life events ascertained at Wave 1 and measures of the outcomes, major depression and physical illness, from Wave 2. This design established the temporality of the exposures as occurring prior to the outcome; we controlled for major depression at Wave 1 in all analyses for which depression at Wave 2 was an outcome to further establish temporal sequence.
Race/ethnicity
We included self-identified non-Hispanic Whites (N=19,216) and non-Hispanic Blacks (N=6,065) who reported being born in the U.S. Foreign-born Blacks (N=664) and Whites (N=1,264) were excluded from the present analysis because patterns of substance use, depression and stressful life events differ between foreign- and non-foreign born individuals.
‘Unhealthy behaviors’ (UHBs)
We considered three types of ‘UHBs’: alcohol consumption, nicotine consumption, and body mass index (BMI). While a compelling argument can be made regarding the validity of terming alcohol consumption, nicotine consumption, and BMI collectively as ‘UHBs’ (e.g., moderate consumption of alcohol may be cardioprotective ( Klatsky 2009 )), we have used this terminology to remain consistent with the prior empirical support for the hypothesis we are testing ( Jackson, Knight et al. 2009 ). For our replication analysis, we use definitions exactly consistent with Jackson, Knight et al. (2009) , namely a UHB count measure (0-3) indicating if the individual ever consumed at least one alcoholic beverage in their lifetime, ever smoked at least 100+ cigarettes in their lifetime, and whether they currently have a BMI≥30. For our extended test of the overall theory, we used the following definitions:
- Alcohol consumption in the past 12 -months at Wave 1 was operationalized as a three-level variable: no consumption (N=2,293); non-pathological consumption (i.e., any level of consumption but no alcohol abuse/dependence diagnosis) at levels less than weekly binge (>4 drinks for men or >3 drinks per women on at least one occasion in the past year) (N=13,765); and DSM-IV alcohol abuse/dependence or at least weekly binge drinking (N=8,593). Measurement of alcohol consumption and diagnoses is a particular strength of the AUDADIS-IV instrument; diagnoses are made based on assessment of over 40 symptom items, and the excellent reliability and validity of alcohol diagnosis in the AUDADIS-IV have been extensively documented both the United States and internationally (see Hasin et al., 2007 ). Limited differential item functioning by race/ethnicity has been noted for alcohol disorder criteria in Item Response Theory analysis ( Saha, Chou et al. 2006 ).
- Nicotine consumption in the past 12 -months at Wave 1 was operationalized as a three-level variable: no nicotine use (N=18,601); non-pathological use (any level of use but no DSM-IV-defined nicotine dependence diagnosis) (N=3,358); and DSM-IV nicotine dependence (N=3,313). The good reliability and validity of nicotine dependence in the AUDADIS-IV have been well-documented ( Grant, Hasin et al. 2004 ). Limited differential item functioning by race/ethnicity has been noted for nicotine dependence criteria in Item Response Theory analysis ( Saha, Compton et al. 2010 ).
- Unhealthy eating in the past 12 -months at Wave 1 was operationalized using current BMI based on respondent’s self-reported height and weight. BMI an imperfect proxy for unhealthy eating; BMI is known to be determined by more than simply caloric intake, including exercise patterns and genetic vulnerability ( Hetherington and Cecil 2010 ). However, empirical studies have documented a robust correlation between unhealthy eating and BMI (e.g., ( Haimoto, Iwata et al. 2008 ; Kent and Worsley 2009 )). Three categories were created: BMI<25 (N=10,252), BMI greater than or equal to 25 but less than 35 (N=12,615), and BMI≥35 (N=2,414). While conventional cut-points define overweight as BMI between 25 and <30 and obese as ≥30 ( Centers for Disease Control and Prevention 2010 ), we chose more conservative cut points due to known error in the measurement BMI ( Rothman 2008 ), often overestimating an individual’s true body size.
- UHB count . The three measures described above were combined to create an overall measure of UHBs, comparable to that in Jackson et al. (2009) . Respondents were given a score of 0 for the least severe level of each behavior (i.e., no alcohol consumption, no nicotine consumption, or BMI<25), one point for the moderate level, and two points for the most severe level (i.e., DSM-IV alcohol abuse/dependence or at-least weekly binge drinking, DSM-IV nicotine dependence, or BMI≥35) within each unhealthy behavior category. Based on this summary score, we created a three level variable indicating no unhealthy behaviors (count was equal to zero) (N=2,539), low levels of unhealthy behavior (count was 1, 2, or 3) (N=20,077), and high levels of unhealthy behaviors (count of 4 or more) (N=2,656).
Stressful life events in the past 12-months
Twelve stressful life events were assessed at Wave 1 using a checklist with dichotomous response options: family member or close friend had a serious illness (38.4%), family member or close friend died (32.1%), respondent changed jobs/job responsibilities/work hours (23.8%), moved or someone new came to live with respondent (15.8%), major financial crisis/unable to pay bills/bankruptcy (10.6%), trouble with a boss or co-worker (8.7%), unemployed and looking for work >1 month (7.7%), respondent or family member was the victim of a crime (6.7%), fired or laid off (5.9%), problems with neighbor/friend/relative (5.8%), separated/divorced/broke up (5.4%), and respondent or a family member had trouble with police/got arrested/sent to jail (5.1%).
Figure 1 shows the relationship between number of past year stressful life events, race, and depression. As shown, the number of stressful life events at Wave 1 was not linearly related to depression at Wave 2 among Blacks, though the difference in prevalence between Blacks and Whites was not statistically significantly different at any level of stressful life events save for among those with one stressful life event (p=0.04). Also shown in Figure 1 , the confidence intervals for the proportions substantially overlap, indicative of the small sample sizes among those with high levels of stress. Therefore, we created a categorical measure of the number of stressful life events reported by the respondent. We extensively evaluated the appropriate threshold for ‘high stress’, and found that the direction and magnitude of the results were not dependent on the upper cutpoint used. We also evaluated whether the data would fit a quadratic term for past year stressful life events; the results did not change when a quadratic term was used. Therefore, to maximize statistical power and to provide the best fit to these data, we used the following cut points: no stressful life events in the past-year (N=7,274), one or two stressful life events (N=11,832), and three or more (N=6,175). Finer categorizations could not be utilized due to the minimum cell sizes required to conduct large-sample statistics.

Prevalence of depression at Wave 2 by number of past year stressor among non-Hispanic U.S.-born Whites (N=19,216) and non-Hispanic U.S.-born Blacks (N=6,065) in the general population
Perceived discrimination
Respondents self-reporting Black race were asked at the Wave 2 interview, “How often have you experienced discrimination, been prevented from doing something, or been hassled or made to feel inferior in any of the following situations because of your race?” The frequencies of seven discrimination experiences in the past 12 months were assessed (e.g., obtaining health care or health insurance coverage, obtaining a job or while on the job, or being called a racist name) ( Krieger, Smith et al. 2005 ). The scale showed good internal consistency reliability (α=0.76) ( Ruan, Goldstein et al. 2008 ). Responses were summed and a three-level variable was created indicating: no discriminatory experiences reported (N=3,708), a low level of discriminatory experiences (more than zero but less than the 75 th percentile on the scale, N=1,753), and a high level of discriminatory experiences (75 th percentile or greater, N=604).
Major Depressive Episode (MDE)
The good reliability and validity of DSM-IV major depression diagnosis in the AUDADIS-IV have been well-documented ( Hasin, Goodwin et al. 2005 ). At Wave 1, major depression in the past 12-months or prior to the past 12-months was assessed; we combined these timeframes to create a W1 lifetime depression diagnosis, and used this variable as a control in all analyses predicting major depression at Wave 2. At Wave 2, major depression was assessed in the past 12-months, and since the last interview but prior to the past 12-months. We combined these times frames to create a W2 depression diagnosis.
Physical illness
We examined Black/White differences in fourteen physical illnesses (e.g., arteriosclerosis, hypertension, diabetes, heart attack, high cholesterol, ulcer) assessed at Wave 2. Physical illness status was based on respondent self-report of a physician diagnosis.
Control variables
In all analyses we also controlled for age, sex, past-year personal income, education, and region of residence as assessed at Wave 1. We also controlled for major depression at prior to the past-year or the past-year Wave 1; Blacks had a lower prevalence of past year (OR=0.80, 95% C.I. 0.66-0.96) and lifetime depression (OR=0.56, 95% C.I. 0.49-0.64) at Wave 1.
Statistical analysis
Prevalence estimates by race, stressful life events, and UHBs were generated using cross-tabulations. Odds ratios and 95% confidence intervals were generated using logistic regression. All interaction tests are on the multiplicative scale. All analyses were conducted using SUDAAN software to adjust standard errors for the non-random probability of selection into the sample. All prevalence estimates and odds ratios are sample weighted to be representative of the U.S. population based on the year 2000 census.
Overall Black/White differences in the NESARC data
Consistent with prior literature, Blacks were less likely to have Wave 2 major depression (OR=0.80, 95% C.I. 0.70-0.91) and more likely to have a Wave 2 physical illness (OR=1.20, 95% C.I. 1.08-1.35) compared with Whites (data not shown).
Results of the Jackson et al. (2009) replication attempt
Our findings did not replicate those of Jackson et al. (2009) . Figures 2a and 2b show the predicted probability of depression based on the results of a logistic regression model categorizing UHB consumption (any lifetime smoking, any lifetime drinking, and/or current obesity) and past-year stressful life events, and controlling for age, sex, past-year personal income, education, region of residence, and major depression at Wave 1. Among Whites, the figures indicate a higher predicted probability of depression with each increasing level of UHB consumption and each increasing level of stressful life events. Among Blacks, the pattern is less consistent, but no evidence emerges suggesting that those who engage in more UHB consumption have less depression. There were no significant interactions between stressful life events and UHBs predicting depression among Blacks (F=1.20, df=6, p=0.32) or Whites (F=0.43, df=6, p=0.86), and no significant three-way interaction between stressful life events, UHBs, and race (F=1.05, df=17, p=0.42).

Predicted probability of depression at Wave 2 based on unhealthy behaviors as defined by Jackson et al. (2009) * and past-year stressful life events at Wave 1, by race, among non-Hispanic U.S.-born Whites (Figure 2a, N=19,216) and non-Hispanic U.S.-born Blacks Figure 2b, N=6,065) in the general population
* UHBs defined to be consistent with Jackson et al. (2009) : any consumption of at least one alcoholic beverage in lifetime, any consumption of 100+ cigarettes in lifetime, and/or current BMI≥30.
As part of our replication attempt, we also conducted an analysis with a mean centered, continuous stress variable in order to more closely approximate Jackson et al. (2009) and Mezuk et al. (2010) , despite the evident violation of the linearity assumption among Blacks (shown in Figure 1 ). Among Blacks at high levels of mean-centered stress, those with 0 UHBs have a higher predicted probability of depression compared to those with 1 UHB, and those with 1 UHB have a higher predicted probability of depression compared to those with 2 or 3 UHBs (consistent with Jackson et al. (2009) and Mezuk et al. (2010) ). The same pattern is not evident among Whites (results not shown). However, this result arises entirely from the misspecification of the regression model by entering stress as a continuous variable among Blacks. Further, none of the interactions were significant when using the mean centered, continuous stress variable (interaction of stress and UHBs among Blacks: F=0.89, df=3, p=0.45; interaction of stress and UHBs among Whites: F=1.46, df=3, p=0.23; three way interaction of stress, UHBs, and race: F=1.37, df=7, p=0.23).
Results of the extended test of the Jackson et al hypothesis
Are uhbs protective against depression and is stress associated with more depression.
We found that Wave 1 UHBs, at any level, are not protective against Wave 2 depression. Stress, however, is prospectively predictive of Wave 2 depression. Table 1 shows the odds of Wave 2 depression given Wave 1 UHBs among the whole sample, and for Blacks and Whites separately. Among Whites, greater Wave 1 alcohol, nicotine, BMI severity, and overall UHB score predicted higher odds of depression at Wave 2. Among Blacks, no significant odds ratios were observed for the relation between Wave 1 UHBs and Wave 2 depression. However, all four odds ratios for the highest UHB category were in the direction consistent with high levels of UHB predicting greater odds of depression. Among both Whites and Blacks, more stressful life events at Wave 1 predicted greater odds of depression at Wave 2 (see Table 1 ).
Alcohol consumption, nicotine consumption, BMI, and stressful life events prospectively predicting major depression three years later among non-Hispanic U.S.-Born Whites (N=19,216) and non-Hispanic U.S-born Blacks (N=6,065)
Bold text indicates statistical significance at p<0.05
AOR = odds ratio adjusted for age, sex, past-year personal income, education, region of residence, and major depression at Wave 1
Do Blacks report higher levels of UHBs?
Blacks had lower odds of Wave 1 alcohol consumption, nicotine consumption, and any UHBs compared with Whites, but a higher proportion of Blacks were in high Wave 1 BMI categories compared with Whites. This finding held in every level of Wave 1 stressful life events (see Table 2 ) save the lowest level. Among those with no stressful life events, there was no significant relationship between UHBs and race. The magnitude and strength of the relationship between UHB and race increased with each level of stressful life event category.
Odds of alcohol consumption, nicotine consumption, high BMI, and ‘unhealthy behaviors’ in non-Hispanic U.S.-born Blacks (N=6, 065) compared to non-Hispanic U.S.-born Whites (N=19,216) at low, moderate, and high levels of stress
AOR = odds ratio adjusted for age, sex, past-year personal income, education, and region of residence
Do UHBs have a differential effect on depression among Blacks and Whites at certain stress levels?
Little support was found for the hypothesis that UHBs have a differential effect on Blacks and Whites at high levels of stress. We examined whether the effect of Wave 1 UHBs on Wave 2 depression differed by race and Wave 1 stressful life event status ( Table 3 ). Results indicated that a low level of unhealthy behaviors is protective against depression in Blacks (OR=0.06, 95% C.I. 0.01-0.24) but not Whites (OR=2.14, 95% C.I. 0.71-6.48) among those at low levels of stress. However, the three-way interaction test was not significant, limiting the conclusions that can be drawn from this association. We did find a significant three-way interaction between race, Wave 1 stress, and Wave 1 BMI (F=2.11, df=12, p=0.03). Based on the patterns of odds ratios shown in Table 3 , we conclude that there is evidence to suggest a protective effect of Wave 1 BMI 25-34 on Wave 2 depression in Blacks but not Whites, but only at very low levels of stress.
Odds of depression at Wave 2 based on unhealthy behaviors and past-year stressful life events at Wave 1, by race and sex, among non-Hispanic U.S.-born Blacks (N=6,065) and non-Hispanic U.S.-born Whites (N=19,216) in the general population
We also examined these patterns by sex (results not shown). UHBs significantly interacted with race among men only (F=6.07, df=2, p=0.004), whereby Black men reporting a low level of unhealthy behaviors had significantly lower odds of depression compared to White men (OR=0.06, 95% C.I. 0.01-0.24). Similar to the aggregated analysis, a three way interaction between Wave 1 BMI, race, and Wave 1 stress was statistically significant in men (F=2.28, df=12, p=0.02). This interaction was significant at the trend level among women (F=1.7, df=12, p=0.09).
Are UHBs protective against depression among Blacks reporting more race-specific stress?
Wave 1 UHBs did not moderate the effect of perceived discrimination reported at Wave 2 among Blacks. The observed prevalence of Wave 2 depression by UHB consumption and discrimination experiences are shown in Figure 3 . In unadjusted analyses, Wave 1 non-pathological nicotine use was associated with a lower odds of depression at Wave 2 compared to no nicotine use (OR=0.48, 95% C.I. 0.24-0.96) (data not shown). However, the effect was no longer significant when lifetime depression at Wave 1 was controlled (OR=0.52, 95% C.I. 0.26, 1.05) (data not shown). No other odds ratios were significant in unadjusted or adjusted analyses. We also replicated these analyses using UHBs defined at Wave 2 (concurrent to measurement of discrimination): results were unchanged.

Prevalence of depression at Wave 2 based on unhealthy behaviors and lifetime perceived discrimination exposure among non-Hispanic U.S.-born Blacks (N=6,065) in the general population
The present study did not find support for the hypothesis that engaging in unhealthy behaviors ameliorates major depression among Blacks in the U.S. exposed to high levels of stress, or that a differential effect of UHBs on depression among Blacks compared with Whites accounts for the mental/physical health paradox. First, we showed that the results presented in Jackson et al. (2009) and Mezuk et al (2010) do not replicate in a nationally-representative sample using model specification to account for the non-linear association between stress and depression among Blacks that we observed in these data. Next, as part of a more in-depth investigation of the hypothesis, we demonstrated that the relationship between depression and alcohol consumption, nicotine consumption, and BMI among Blacks is not statistically significant and, in fact, the direction of association between UHBs and depression is positive, not negative. Third, we documented that Blacks are less likely to engage in alcohol and nicotine consumption but have higher BMI than Whites at all levels of stress. We note, however, that an overall count of UHBs was not associated with race among those with no stressful life events. This suggests a complex patterning of unhealthy behaviors and race across stress levels that should be more comprehensively examined in these and other data in future analyses.
Finally, we showed that while race, stress, and BMI did interact significantly to predict depression in this sample, being overweight was protective against depression among Blacks only at very low levels of stress . Similarly, among those with no stressful life events, we found that low levels of UHBs were associated with less depression in Blacks but not Whites, though this result was significant among men only and a three-way interaction test was not significant. Furthermore, examination of perceived discrimination as a measure of stress in Blacks revealed no significant effects of unhealthy behaviors on depression at any exposure level. Taken together, these results indicate that engagement in unhealthy behaviors, especially at pathological levels, does not protect against depression, and that stress pathways do not operate differently in Blacks compared with Whites in the U.S. Thus, our confidence in the group-specific stress and coping hypothesis proposed by Jackson and colleagues ( Jackson and Knight 2006 ; Jackson, Knight et al. 2009 ; Mezuk et al. 2010 ) is diminished. Although UHBs may have immediate positive psychological effects via the HPA axis, the evidence presented here suggests these effects are not robust enough to prevent the clinical manifestation of major depression.
We did find evidence that some measures of unhealthy behaviors were significant predictors of depression in Whites but not Blacks. For example, at high levels of stress, Whites with high BMI, nicotine dependence, and a high unhealthy behavior count were more likely to evidence depression compared with Whites without these unhealthy behaviors, but the same predictors were not significant among Blacks. However, we caution against over-interpretation of these findings; as noted by Gelman and Stern: “The Difference Between ‘Significant’ and ‘Not Significant’ is not Itself Statistically Significant” ( Gelman and Stern 2006 ). There were no significant interactions between race and unhealthy behaviors at high levels of stress, indicating that the odds ratios across race categories were not statistically distinguishable. Further, ignoring significance levels, thirty-two of forty-eight odds ratios calculated (67%) in the total sample were in the same direction for Whites and Blacks. Thus, the most appropriate conclusion from these data is the pathway through which unhealthy behaviors and stress impact depression does not differ in Blacks compared with Whites in the U.S., and that in general, UHBs increase the risk for depression at all levels of stress.
In the present analysis we predicted major depression during a three-year follow-up based on stressful events and UHBs assessed at baseline. While this strategy is most appropriate to establish temporality, it may overlook a key component of the hypothesis, namely, that UHBs in response to stress are active coping strategies for the suppression of immediate depressive symptoms ( Benowitz 1988 ; Koob, Roberts et al. 1998 ; Dallman, Pecoraro et al. 2003 ; Jackson and Knight 2006 ; Jackson, Knight et al. 2009 ). Thus, we may have failed to capture protective effects because we did not examine major depressive episodes concurrent with stressors and unhealthy behaviors. To explore this possibility, we re-analyzed our data using stress, UHBs and depression diagnoses all measured concurrently, at both baseline and follow-up. Neither analysis suggested different conclusions; results were generally consistent with those presented in our main analyses. Thus, we conclude that these data, analyzed multiple ways at multiple time points, do not provide sufficient evidence for either a protective effect of UHBs on depression, or a differential pathway through which unhealthy behaviors affect depression in Blacks compared with Whites, regardless of the exposure to stress.
These results decrease confidence in the validity of the hypothesis that group-specific stress processes explain the depression difference in Blacks and Whites, leaving open other theories to be tested. Measurement and selection bias hypotheses are unlikely to fully explain the “paradox” ( Breslau, Javaras et al. 2008 ), suggesting the need for both new theories and more direct tests of existing theories based on the premise that the lower prevalence of depression in Blacks is not artefactual. Studies suggest that Blacks develop different coping strategies when faced with life stress compared with Whites ( Smith 1985 ; Wilson 1989 ; Maton, Teti et al. 1996 ), which, given the extraordinary nature and degree of stress to which Blacks are exposed starting at a young age, are hypothesized to develop over the life course. Compared with Whites, Blacks are more likely to find emotional strength and support in religious communities ( Taylor, Chatters et al. 1996 ; Gibson and Hendricks 2006 ; Giger, Appel et al. 2008 ), and develop racial self-esteem and strong ethnic identity ( Nagel 1994 ). Further, extensive research has documented the ‘John Henryism’ effect among Blacks in the U.S., the personality trait characterized by active coping with stressful and negative experiences and associated with worse health outcomes for Blacks at high levels of socio-economic position ( James, Strogatz et al. 1987 ; James 1994 ). Alternatively, the present DSM nosology may not accurately tap Black psychological responses to their unique stress exposures, and therefore DSM-IV depression as currently defined may not be the appropriate outcome to fully understand racial differences in depressive mood states ( Brown 2003 ; Kendrick, Anderson et al. 2007 ). Support for this theory can be drawn from the multiple studies showing that Blacks report lower levels of well-being, higher levels of distress, and higher depressive scores when measured on non-DSM instruments ( Brown 2003 ; Mabry and Kiecolt 2005 ). Taken together, the results from the present study should serve as a catalyst to promote the advancement of innovative and alternative theories to explain the Black/White paradox in mental and physical health. Few studies are conducted with the primary aim of untangling this paradox, a situation that should be redressed. Such research should include rich measurement of the social and political context, and conduct in-depth examination of the role of ethnic identity, religion, and responses to group-specific stressor, such as racial discrimination.
Several limitations should be noted. First, our measure of stressful life events is a checklist of experiences susceptible to respondent subjectivity and appraisal processes, and without regard to salience, severity, or context of experience. Substantial evidence indicates that objective measures of stressful experiences as well as information on the context of the experience is necessary to fully analyze and interpret stress in mental health research ( Dohrenwend 1998 ; Dohrenwend 2006 ). Additionally, the stressful events experienced by Blacks in the U.S. may be more chronic and race-specific than what is captured in the scale of past-year stressors ( Jones 2000 ; Kreiger 2000 ). We attempted to mitigate this limitation by also using a measure of perceived racial/ethnic discrimination. Further, we evaluated whether results changed if higher cut-offs of past-year stressful experiences were used to define the ‘high stress’ exposure group; higher cut-offs did not change the results. Thus, the conclusions from these data are limited by the available stress measure.
In conclusion, the persistent differences in health outcomes between White and Black adults remain one of the most challenging public health issues in the U.S. As theories regarding the etiology of these differences continue to develop, the mental health ‘paradox’ will be increasingly important to explain as part of a robust etiologic pathway. Substantive etiologic hypotheses that simultaneously explain why Blacks in the U.S. have higher rates of physical illness and lower rates of mood disorders need to be tested directly in order to resolve the ‘paradox’ and progress toward intervention and prevention efforts.
Hypothesis that Black-White depression paradox is due to protective effects of unhealthy behaviors at high stress unsupported.
Blacks less likely to engage in alcohol consumption or cigarette smoking compared with Whites, but have higher average BMI.
Engaging in unhealthy behaviors is not protective against depression at any stress level in either Blacks or Whites.
Acknowledgments
This research was supported in part by a fellowship from the National Institute of Mental Health (T32MH013043-36, Barnes) and a fellowship from the National Institute of Drug Abuse (F31-DA026689, K. Keyes).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
- Baker FM. Diagnosing depression in African Americans. Community Mental Health Journal. 2001; 37 (1):31–38. [ PubMed ] [ Google Scholar ]
- Benowitz NL. Drug therapy. Pharmacologic aspects of cigarette smoking and nicotine addition. N Engl J Med. 1988; 319 (20):1318–30. [ PubMed ] [ Google Scholar ]
- Breslau J, Aguilar-Gaxiola S, et al. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006; 36 (1):57–68. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Breslau J, Javaras KN, et al. Differential item functioning between ethnic groups in the epidemiological assessment of depression. J Nerv Ment Dis. 2008; 196 (4):297–306. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown T. Critical race theory speaks to the sociology of mental health: mental health problems produced by racial stratification. Journal of Health and Social Behavior. 2003; 44 (3):292–301. [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention. 2010. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html .
- Dallman MF, Pecoraro N, et al. Chronic stress and obesity: a new view of “comfort food” Proc Natl Acad Sci U S A. 2003; 100 (20):11696–701. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dohrenwend BP. Adversity, stress, and Psychopathology. New York: Oxford University Press, USA; 1998. [ Google Scholar ]
- Dohrenwend BP. The role of adversity and stress in psychopathology: some evidence and its implications for theory and research. J Health Soc Behav. 2000; 41 (1):1–19. [ PubMed ] [ Google Scholar ]
- Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychol Bull. 2006; 132 (3):477–95. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gelman A, Stern H. The Difference Between “Significant” and “Not Significant” is not Itself Statistically Significant. American Statistician. 2006; 60 (4):328–331. [ Google Scholar ]
- Geronimus AT. Power and Decision: The Social Control of Reproduction. Cambridge, MA: Harvard University Press; 1994. The weathering hypothesis and the health of African American women and infants: Implicatins for reproductive strategies and policy analysis. [ Google Scholar ]
- Geronimus AT. Black/White differences in the relationship of maternal age to brithweight: A population basd test of the weathering hypothesis. Soc Sci Med. 1996; 42 (4):589–597. [ PubMed ] [ Google Scholar ]
- Gibson LM, Hendricks CS. Integrative review of spirituality in African American breast cancer survivors. ABNF J. 2006; 17 (2):67–72. [ PubMed ] [ Google Scholar ]
- Giger JN, Appel SJ, et al. Church and spirituality in the lives of the African American community. J Transcult Nurs. 2008; 19 (4):375–83. [ PubMed ] [ Google Scholar ]
- Grant BF, Goldstein RB, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009; 14 (11):1051–66. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Grant BF, Hasin DS, et al. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004; 61 (11):1107–15. [ PubMed ] [ Google Scholar ]
- Haimoto H, Iwata M, et al. Long-term effects of a diet loosely restricting carbohydrates on HbA1c levels, BMI and tapering of sulfonylureas in type 2 diabetes: a 2-year follow-up study. Diabetes Res Clin Pract. 2008; 79 (2):350–6. [ PubMed ] [ Google Scholar ]
- Hasin DS, Goodwin RD, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005; 62 (10):1097–106. [ PubMed ] [ Google Scholar ]
- Hasin DS, Stinson FS, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007; 64 (7):830–42. [ PubMed ] [ Google Scholar ]
- Heckler MM. Report of the Secretary’s Task Force on Black and Minority Health. Wasington, DC: Natl. Academy Press; 1985. Task Force on Black and Minority Health. [ Google Scholar ]
- Hetherington MM, Cecil JE. Gene-environment interactions in obesity. Forum Nutr. 2010; 63 :195–203. [ PubMed ] [ Google Scholar ]
- Jackson JS, Knight KM. Race and self-regulatory behaviors: the role of the stress response and HPA axis in physical and mental health disparities. In: Carstensen LL, Schaie KW, editors. Social structure, Aging, and Self-Regulation in the Elderly. New York, NY: Springer; 2006. [ Google Scholar ]
- Jackson JS, Knight KM, et al. Race and Unhealthy Behaviors: Chronic Stress, the HPA Axis, and Physical and Mental Health Disparities Over the Life Course. Am J Public Health 2009 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- James SA. John Henryism and the health of African Americans. Culture of Medicine and Psychiatry. 1994; 18 :163–182. [ PubMed ] [ Google Scholar ]
- James SA, Strogatz DS, et al. Socioeconomic status, John Henryism, and hypertension in blacks and whites. Am J Epidemiol. 1987; 126 (4):664–73. [ PubMed ] [ Google Scholar ]
- Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000; 90 (8):1212–5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kendrick L, Anderson NLR, et al. Perceptions of depression among young African American men. Family and Community Health. 2007; 30 (1):63–73. [ PubMed ] [ Google Scholar ]
- Kent LM, Worsley A. Trends in BMI, diet and lifestyle between 1976 and 2005 in North Sydney. Asia Pac J Clin Nutr. 2009; 18 (3):453–61. [ PubMed ] [ Google Scholar ]
- Kessler RC, Crum RM, et al. Lifetime co-occurrence of DSM-III-R Alcohol Abuse and Dependence WIth Other Psychiatric Disorders in the National COmorbidity Survey. Arch Gen Psychiatry. 1997; 54 :313–321. [ PubMed ] [ Google Scholar ]
- Kessler RC, McGonagle KA, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994; 51 (1):8–19. [ PubMed ] [ Google Scholar ]
- Kessler RC, Mickelson KD, et al. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999; 40 (3):208–30. [ PubMed ] [ Google Scholar ]
- Klatsky AL. Alcohol and cardiovascular diseases. Expert Rev Cardiovasc Ther. 2009; 7 (5):499–506. [ PubMed ] [ Google Scholar ]
- Kleinman A. Culture and depression. N Engl J Med. 2004; 351 (10):951–3. [ PubMed ] [ Google Scholar ]
- Koob GF, Roberts AJ, et al. Neurocircuitry targets in ethanol reward and dependence. Alcohol Clin Exp Res. 1998; 22 (1):3–9. [ PubMed ] [ Google Scholar ]
- Kreiger N. Social Epidemiology. New York: Oxford University Press; 2000. Discrimination and health; pp. 36–75. [ Google Scholar ]
- Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990; 30 (12):1273–81. [ PubMed ] [ Google Scholar ]
- Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. Am J Public Health. 1996; 86 (10):1370–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Krieger N, Smith K, et al. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005; 61 (7):1576–96. [ PubMed ] [ Google Scholar ]
- Leonard B. Stress, Depression, and the Activation of the Immune System. World Journal of Biological Psychiatry. 2000; 1 (1):17–25. [ PubMed ] [ Google Scholar ]
- Mabry JB, Kiecolt KJ. Anger in black and white: race, alienation, and anger. J Health Soc Behav. 2005; 46 (1):85–101. [ PubMed ] [ Google Scholar ]
- Massey DS. Residential segregation and neighborhood conditions in U.S. metropolitan areas. In: Smesler N, Wilson WJ, Mitchell F, editors. America Becoming Racial: Trends and Their Consequences. Wasington, D.C.: Natl Acad Press; 1985. pp. 391–434. [ Google Scholar ]
- Massey DS. Segregation and stratification: a biosocial perspective. DuBois Reviews of Social Science. 2004; 1 :7–25. [ Google Scholar ]
- Maton KI, Teti DM, et al. Cultural specificity of support sources, correlates and contexts: three studies of African-American and caucasian youth. Am J Community Psychol. 1996; 24 (4):551–87. [ PubMed ] [ Google Scholar ]
- McCord C, Freeman HP. Excess mortality in Harlem. N Engl J Med. 1990; 322 (3):173–7. [ PubMed ] [ Google Scholar ]
- McEwen BS. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000; 22 (2):108–24. [ PubMed ] [ Google Scholar ]
- McEwen BS. Mood disordesr and allostatic load. Biological Psychiatry. 2003; 54 (3):200–207. [ PubMed ] [ Google Scholar ]
- McEwen BS. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann N Y Acad Sci. 2004; 1032 :1–7. [ PubMed ] [ Google Scholar ]
- Mezuk B, Rafferty JA, et al. Reconsidering the Role of Social Disadvantage in Physical and Mental Health: Stressful Life Events, Health Behaviors, Race, and Depression. Am J Epidemiology. 2010; 172 (11):1238–1249. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nagel J. Constructing Ethnicity: Creating and Recreating Ethnic Identity and Culture. Social Problems. 1994; 41 (1) [ Google Scholar ]
- Neighbors HW, Trierweiler SJ, et al. Racial differences in DSM diagnosis using a semi-structured instrument: the importance of clinical judgment in the diagnosis of African Americans. J Health Soc Behav. 2003; 44 (3):237–56. [ PubMed ] [ Google Scholar ]
- Neighbors HW, Trierweiler SJ, et al. Psychiatric diagnosis of African Americans: diagnostic divergence in clinician-structured and semistructured interviewing conditions. J Natl Med Assoc. 1999; 91 (11):601–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Petit B, Western B. Mass imprisonment and the life course: race and class inequality in U.S. incarceration. American Sociological Review. 2004; 69 :601–612. [ Google Scholar ]
- Reiger DA, Farmer ME, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA. 1990; 264 (19):2511–2518. [ PubMed ] [ Google Scholar ]
- Rogler LH. Methodological sources of cultural insensitivity in mental health research. Am Psychol. 1999; 54 (6):424–33. [ PubMed ] [ Google Scholar ]
- Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes (Lond) 2008; 32 (Suppl 3):S56–9. [ PubMed ] [ Google Scholar ]
- Ruan WJ, Goldstein RB, et al. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008; 92 (1-3):27–36. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Saha TD, Chou SP, et al. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006; 36 (7):931–41. [ PubMed ] [ Google Scholar ]
- Saha TD, Compton WM, et al. Dimensionality of DSM-IV nicotine dependence in a national sample: an item response theory application. Drug Alcohol Depend. 2010; 108 (1-2):21–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith E. Ethnic minorities: life stress, social support, and mental health issues. The Counseling Psychologist. 1985; 13 :537–579. [ Google Scholar ]
- Stansfeld SA. Social support and social cohesion. In: Marmot MG, Wilkinson RG, editors. Social determinants of health. New York: Oxford University Press; 2005. [ Google Scholar ]
- Strakowski SM, Keck PE, Jr, et al. Ethnicity and diagnosis in patients with affective disorders. J Clin Psychiatry. 2003; 64 (7):747–54. [ PubMed ] [ Google Scholar ]
- Taylor RJ, Chatters LM, et al. Black and white differences in religious participation: A multi-sample comparison. Journal for the Scientific Study of Religion. 1996; 35 :403–410. [ Google Scholar ]
- Teplin LA. The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area Program. Am J Public Health. 1990; 80 (6):663–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Teplin LA, Abram KM, et al. Prevalence of psychiatric disorders among incarcerated women. I. Pretrial jail detainees. Arch Gen Psychiatry. 1996; 53 (6):505–12. [ PubMed ] [ Google Scholar ]
- Williams DR. Racial variations in adult health status: patterns, paradoxes, and prospects. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America Becoming: Racial Trends and Their Consequences. Washington, D.C.: National Academy Press; 2001. [ Google Scholar ]
- Williams DR, Gonzalez HM, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007; 64 (3):305–15. [ PubMed ] [ Google Scholar ]
- Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood) 2005; 24 (2):325–34. [ PubMed ] [ Google Scholar ]
- Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethn Health. 2000; 5 (3-4):243–68. [ PubMed ] [ Google Scholar ]
- Wilson MN. Child development in the context of the Black extended family. American Psychologist. 1989; 44 :380–383. [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
The serotonin hypothesis of depression is still influential. We aimed to synthesise and evaluate evidence on whether depression is associated with lowered serotonin concentration or activity in a ...
Psychodynamic Theory. Cognitive Explanation of Depression. Learned Helplessness. Humanist Approach. Depression is a mood disorder that prevents individuals from leading a normal life at work, socially, or within their family. Seligman (1973) referred to depression as the 'common cold' of psychiatry because of its frequency of diagnosis.
Although "the serotonin hypothesis of depression is still influential," Moncrieff and coauthors noted, citing widely adopted textbooks published as recently as 2020 and surveys indicating that ...
Depression can start early in the lifecourse and, if it remains unmanaged, may increase the risk for substance abuse, chronic conditions, such as cardiovascular disease, and premature mortality [4,5,6,7,8]. Treatment for depression exists, such as pharmacotherapy, cognitive behavioural therapy, and other modalities.
1. Introduction. Depression as described by the World Health Organization (WHO) is a mood disorder characterized by specific symptoms including sadness, loss of interest, anhedonia (loss of pleasure), lack of appetite, feelings of guilt, low self-esteem or self-worth, sleep disturbance, feelings of tiredness, and poor concentration [1].Individuals suffering from depression describe varying ...
Depression is a common and debilitating mental health condition whose underlying aetiology and pathophysiology is still relatively poorly understood. In this article, we first turn to the past and briefly review what neuroscientific investigations have taught us so far about depression.
The serotonin (5-HT) hypothesis of depression dates from the 1960s. It originally postulated that a deficit in brain serotonin, corrected by antidepressant drugs, was the origin of the illness. Nowadays, it is generally accepted that recurring mood disorders are brain diseases resulting from the combination, to various degrees, of genetic and ...
The serotonin hypothesis of depression is still influential. We aimed to synthesise and evaluate evidence on whether depression is associated with lowered serotonin concentration or activity in a systematic umbrella review of the principal relevant areas of research. PubMed, EMBASE and PsycINFO were searched using terms appropriate to each area ...
The main areas of research do not provide support for the most well-known neurochemical hypothesis, the serotonin theory of depression—the idea that depression is caused by low levels or low ...
This hypothesis is relevant because most antidepressant drugs either prevent or reverse the damage caused by increased cortisol release, over-excitation, and inflammation [70,71]. Additionally, ECT is one possible adjunctive therapy for depression that canprevent or reverse the effects of cortisol and overexcitation . The factor linking ...
Cognitive science has been instrumental in advancing our understanding of the onset, maintenance, and treatment of depression. Research conducted over the last 50 years supports the proposition that depression and risk for depression are characterized by the operation of negative biases, and often by a lack of positive biases, in self-referential processing, interpretation, attention, and ...
The monoamine hypothesis of depression postulates a deficiency in serotonin or norepinephrine neurotransmission in the brain. Monoaminergic neurotransmission is mediated by serotonin (5 ...
According to Freud's psychodynamic theory, depression results from exaggerated self-blame and guilt that arises from early life experiences and interactions. Psychodynamic theories form the ...
The leading causal theory of depression at the time was the notion of inverted hostility. This seemed a reasonable, logical explanation if translated into a need to suffer. The need to punish one's self could account for the loss of pleasure, loss of libido, self-criticism, and suicidal wishes and would be triggered by guilt. ...
The serotonin hypothesis is a version of the "monoamine hypothesis of depression." Monoamines are a group of chemicals that act as neurotransmitters in the brain and include serotonin ...
A second theory for this time-lag effect has now become more widely accepted, which is consistent with the monoamine hypothesis that depression is due to underactivity of 5-HT neurons. However, this theory still relies on the concepts of neural compensation and subsensitivity. The crucial difference is that according to what we'll call the ...
This theory assumes that depression is due to deficits in the self-control process, which consists of three phases: self-monitoring, self-evaluation, and self-administration of consequences (Rehm, 1977; Rehm et al., 1979). In the self-monitoring phase, individuals attend only to negative events and tend to recognize only immediate, short-term ...
The neurotrophic hypothesis of depression [1] proposes that major depressive disorder (MDD) is caused, at least partly, by impaired neurotrophic support. Neurotrophic factors (also known as neurotrophins) are a family of closely related proteins which regulate the survival, development, and function of neurons in both the central and peripheral ...
This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs. Choat / Adobe Stock. Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness ...
The serotonin hypothesis of depression. The monoamine neurotransmitter serotonin (5-hydroxytryptamine, 5-HT) is synthesized by neurons in the dorsal raphe (DR) nucleus. These neurons integrate inputs from multiple brain regions, including the nucleus accumbens (NAc), amygdala, lateral habenula (LHb), and PFC, and send projections throughout the ...
Those with depression may experience headaches, body aches and stomach aches, among other ailments. Ultimately, it's important to remember that depression is complex. It is a mental health condition that doesn't always look like the tired trope we see played out in the media and stigma-laden conversations.
This hypothesis proposes that depression results from decreased neurotrophic support, leading to neuronal atrophy, decreased hippocampal neurogenesis and loss of glia, and that antidepressant treatment blocks or reverses this neurotrophic factor deficit, and thereby reverses the atrophy and cell loss [6,13].
Recession. Depression. The Great Recession lasted two years, from 2007 to 2009. The only documented depression lasted a decade, from 1929 to 1939. In the Great Recession, unemployment rose to 10.6%
This hypothesis suggests that, in the context of chronic stress, Blacks' engagement in UHBs may serve to buffer the deleterious consequences of stress on depression through the HPA pathway, leading to a lower prevalence of depression but a greater prevalence of physical health problems than would have otherwise occurred.