A Brief Review of Cardiovascular Diseases, Associated Risk Factors and Current Treatment Regimes
Affiliation.
- 1 Department of Internal Medicine, University of Iowa, Iowa City, IA 52242, United States.
- PMID: 31553287
- DOI: 10.2174/1381612825666190925163827
Cardiovascular diseases (CVDs) are the leading cause of premature death and disability in humans and their incidence is on the rise globally. Given their substantial contribution towards the escalating costs of health care, CVDs also generate a high socio-economic burden in the general population. The underlying pathogenesis and progression associated with nearly all CVDs are predominantly of atherosclerotic origin that leads to the development of coronary artery disease, cerebrovascular disease, venous thromboembolism and, peripheral vascular disease, subsequently causing myocardial infarction, cardiac arrhythmias or stroke. The aetiological risk factors leading to the onset of CVDs are well recognized and include hyperlipidaemia, hypertension, diabetes, obesity, smoking and, lack of physical activity. They collectively represent more than 90% of the CVD risks in all epidemiological studies. Despite high fatality rate of CVDs, the identification and careful prevention of the underlying risk factors can significantly reduce the global epidemic of CVDs. Beside making favorable lifestyle modifications, primary regimes for the prevention and treatment of CVDs include lipid-lowering drugs, antihypertensives, antiplatelet and anticoagulation therapies. Despite their effectiveness, significant gaps in the treatment of CVDs remain. In this review, we discuss the epidemiology and pathology of the major CVDs that are prevalent globally. We also determine the contribution of well-recognized risk factors towards the development of CVDs and the prevention strategies. In the end, therapies for the control and treatment of CVDs are discussed.
Keywords: Atherosclerosis; epidemiological studies; hypertension; platelets; stroke; thrombosis..
Copyright© Bentham Science Publishers; For any queries, please email at [email protected].

Publication types
- Research Support, Non-U.S. Gov't
- Cardiovascular Diseases / complications*
- Cardiovascular Diseases / prevention & control*
- Cardiovascular Diseases / therapy*
- Diabetes Mellitus
- Hyperlipidemias / complications
- Hypertension / complications
- Risk Factors
- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
Spotlight Issues
- Image Gallery
- ESC Journals App
- ESC Content Collections
- Author Guidelines
- Submission Site
- Open Access Options
- Read & Publish
- Author Resources
- Self-Archiving Policy
- About Cardiovascular Research
- About the European Society of Cardiology
- ESC Publications
- Journal Career Network
- Editorial Board
- ESC membership
- Advertising and Corporate Services
- Developing Countries Initiative
- Dispatch Dates
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Latest articles

Editor's Choice

NEW: Spotlight Issue
Discover Cardiovascular Research 's latest Spotlight Issue on Obesity, Metabolism, and Diabetes. This issue contains a number of invited expert reviews alongside original research papers.
Start Reading
IMPACT FACTOR
CARDIAC & CARDIOVASCULAR SYSTEMS
12 out of 143
JOURNAL CITATION INDICATOR
11 out of 215

Follow @CVR_TomaszGuzik on X
Connect with Editor-in-Chief, Tomasz J. Guzik, and stay up to date with the latest news and content from CVR .
Join the conversation with #CardiovascularResearch
Obesity, Metabolism, and Diabetes
Read the Spotlight Issue

Heart Failure

Cardiovascular Immunology

Browse all the Cardiovascular Research Spotlight Issues
Start reading

CVR Discoveries
Enjoy the new webinar series delivered by Cardiovascular Research and the ESC Council on Basic Cardiovascular Science.
Watch the webinars

CVR On life
Cardiovascular Research On life is the online platform linking the journal with the wider scientific community.
Find out more
Connect on social media
Stay up to date with all the latest news from Cardiovascular Research by connecting with us on X.
Follow here

War in Ukraine
ESC Journal Family editors-in-chief fully support the official ESC statement .
From the ESC

Discover Cardiovascular Research ’s top 20 most read articles published within the past 12 months.
Explore the collection

Discover the ESC Content Collections hub, now home to the latest content and collections from the ESC publications.
Read the latest collections

Visit the ESC Publications website to browse journals, books, guidelines, and online resources from the ESC. Stay up to date with the latest journal news.
Explore ESC Publications
Related titles
- Recommend to Your Librarian
- Journals Career Network
Affiliations
- Online ISSN 1755-3245
- Print ISSN 0008-6363
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
This paper is in the following e-collection/theme issue:
Published on 22.4.2024 in Vol 26 (2024)
Evaluation of Prompts to Simplify Cardiovascular Disease Information Generated Using a Large Language Model: Cross-Sectional Study
Authors of this article:

Research Letter
- Vishala Mishra 1 * , MBBS, MMCi ;
- Ashish Sarraju 2 , MD ;
- Neil M Kalwani 3, 4 , MD, MPP ;
- Joseph P Dexter 5, 6, 7 * , PhD
1 Department of Biostatistics and Bioinformatics, Duke University School of Medicine, Durham, NC, United States
2 Department of Cardiovascular Medicine, Cleveland Clinic, Cleveland, OH, United States
3 Veterans Affairs Palo Alto Health Care System, Palo Alto, CA, United States
4 Division of Cardiovascular Medicine and the Cardiovascular Institute, Department of Medicine, Stanford University School of Medicine, Stanford, CA, United States
5 Data Science Initiative, Harvard University, Allston, MA, United States
6 Department of Human Evolutionary Biology, Harvard University, Cambridge, MA, United States
7 Institute of Collaborative Innovation, University of Macau, Taipa, Macao
*these authors contributed equally
Corresponding Author:
Joseph P Dexter, PhD
Data Science Initiative
Harvard University
Science and Engineering Complex 1.312-10
150 Western Avenue
Allston, MA, 02134
United States
Phone: 1 8023381330
Email: [email protected]
In this cross-sectional study, we evaluated the completeness, readability, and syntactic complexity of cardiovascular disease prevention information produced by GPT-4 in response to 4 kinds of prompts.
Introduction
Many web-based patient educational materials about cardiovascular disease (CVD) are inaccessible for the general public [ 1 ]. Artificial intelligence (AI) chatbots powered by large language models (LLMs) are a potential source of public-facing CVD information [ 2 - 4 ]. Generative language models present risks related to information quality but also opportunities for producing accessible information about CVD at scale, which could advance the American Heart Association’s 2020 impact goals related to health literacy [ 5 ]. Recent studies have used LLMs to simplify medical information in different contexts [ 3 , 6 - 8 ], but quantitative comparison of prompt engineering strategies is needed to assess and optimize performance and to ensure that the rapid deployment of clinical AI tools proceeds in an equitable manner [ 9 ]. In this cross-sectional study, we evaluated the completeness, readability, and syntactic complexity of CVD prevention information produced by GPT-4 in response to 4 kinds of prompts.
A set of 25 questions about fundamental CVD prevention topics was drawn from a previous study, which found that the GPT 3.5 version of ChatGPT provided generally appropriate responses [ 2 ]. We devised 3 prompt strategies for generating simplified ChatGPT responses to these questions, including a zero-shot prompt to use plain and easy-to-understand language, a one-shot prompt with a sample simplified passage on an unrelated subject, and a combined prompt to use simplified language and cover specific key points (which we termed “rubric prompting”; Multimedia Appendix 1 ). Responses to these three prompts were compared to baseline responses for which the prompt contained only the question about CVD. The full set of responses is provided in Multimedia Appendix 2 .
For each question and prompt type, 3 independent responses were generated between April and June 2023, using the GPT-4 version of ChatGPT with default parameters, which was available from OpenAI through a ChatGPT Plus subscription. Two authors, who are preventive cardiologists (AS and NWK), scored the responses as “complete,” “incomplete,” or “inconsistent” according to a custom rubric ( Multimedia Appendix 3 ); disagreements were resolved by consensus. For all generated responses, we calculated 5 readability scores, using Readability Studio Professional (version 2019.3; Oleander Software), and 2 measures of syntactic complexity, using the L2 Syntactic Complexity Analyzer (version 3.3.3), as described previously [ 10 ].
Differences from baseline completeness were assessed using the Fisher exact test, and 2-sample readability and syntactic complexity comparisons were done using the Wilcoxon rank-sum test. Statistical significance was set as P <.05.
Baseline responses to 80% (20/25) of the questions were scored as “complete” ( Table 1 ). Completeness was significantly lower for both the zero-shot (8/25, 32%; P =.001) and one-shot (8/25, 32%; P =.001) simplification prompts but significantly higher for the rubric prompts (25/25, 100%; P =.001). All 3 prompts significantly improved readability according to every metric and lowered 1 measure of syntactic complexity ( Table 2 ).
a For every prompt strategy, we generated 3 responses to each of the 25 questions about cardiovascular disease prevention. “Complete” indicates that all 3 responses received a full score according to our coverage rubric, “Incomplete” indicates that all 3 responses received less than a full score, and “Inconsistent” indicates that some responses were “Complete” and others were “Incomplete.” Grades shown were determined by consensus between 2 reviewers.
b LDL: low-density lipoprotein.
a For every prompt strategy, we generated 3 responses to each of the 25 questions about cardiovascular disease prevention. Lower scores indicate higher readability.
b Difference between responses to the baseline prompts and prompts for plain language. P values are from a 1-tailed Wilcoxon signed rank test.
c Difference between responses to the baseline prompts and prompts for plain language with an example. P values are from a 1-tailed Wilcoxon signed rank test.
d Difference between responses to the baseline prompts and prompts for plain language with coverage. P values are from a 1-tailed Wilcoxon signed rank test.
e FKGL: Flesch-Kincaid Grade Level.
f SMOG: Simple Measure of Gobbledygook.
g GFI: Gunning Fog Index.
h FORCAST: Ford, Caylor, Sticht formula.
i CLI: Coleman-Liau Index.
j MLC is a measure of elaboration at the clause level (ie, number of words per clause), and DC/T is a measure of subordination.
k MLC: mean length of clause.
l DC/T: dependent clauses/T-unit.
We found that zero- and one-shot prompting of GPT-4 to produce simplified information about CVD generated more readable but less comprehensive responses. This loss of information, however, could be averted by combining a zero-shot simplification prompt with a short reminder to include critical information (rubric prompting). Our findings highlight the importance of optimizing prompts and incorporating expert clinical judgment when considering the use of LLMs to produce patient education materials, including AI-drafted replies to patient messages [ 3 , 6 , 7 ]. Accordingly, prospective guidelines for the use of AI in medicine should address best practices for prompt engineering, standardized evaluation of model outputs, and outreach to clinicians and the public to cultivate relevant skills [ 11 ]. Such guidelines will provide important parameters for clinician-in-the-loop information simplification systems [ 6 , 12 , 13 ], which have already been deployed to improve the accessibility of surgical consent forms [ 14 ].
The limitations of this study include the evaluation of a single model at a specific point in time and the absence of reading comprehension data from patients. Since the prompt strategies developed herein are not model specific, it should be straightforward to extend these strategies to other LLMs. Future research should further evaluate trade-offs between prompt engineering and fine-tuning of LLMs for medical applications using multiple models. It would also be useful to integrate ongoing user testing with structured health literacy assessment of generated responses to identify types of simplification that are especially important for improving patient understanding.
Acknowledgments
We thank Stephen Blackwelder, PhD (Duke University Health System), for helpful discussions and comments on the manuscript and Vasudha Mishra, MBBS (AIIMS Patna), for assistance with data collection. JPD was supported by a Harvard Data Science Fellowship and the Institute of Collaborative Innovation at the University of Macau. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Authors' Contributions
VM, AS, and JPD designed the study. VM and JPD generated the ChatGPT responses and performed the computational and statistical analyses. AS and NWK performed the completeness scoring. VM and JPD wrote the manuscript. All authors edited and reviewed the manuscript.
Conflicts of Interest
None declared.
Example prompt types.
Full ChatGPT responses.
Custom scoring rubric.
- Pearson K, Ngo S, Ekpo E, Sarraju A, Baird G, Knowles J, et al. Online patient education materials related to lipoprotein(a): readability assessment. J Med Internet Res. Jan 11, 2022;24(1):e31284. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sarraju A, Bruemmer D, Van Iterson E, Cho L, Rodriguez F, Laffin L. Appropriateness of cardiovascular disease prevention recommendations obtained from a popular online chat-based artificial intelligence model. JAMA. Mar 14, 2023;329(10):842-844. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee P, Bubeck S, Petro J. Benefits, limits, and risks of GPT-4 as an AI chatbot for medicine. N Engl J Med. Mar 30, 2023;388(13):1233-1239. [ CrossRef ] [ Medline ]
- Sarraju A, Ouyang D, Itchhaporia D. The opportunities and challenges of large language models in cardiology. JACC Adv. Sep 2023;2(7):100438. [ FREE Full text ] [ CrossRef ]
- Magnani JW, Mujahid MS, Aronow HD, Cené CW, Dickson VV, Havranek E, et al. American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Peripheral Vascular Disease; Council on Quality of Care and Outcomes Research; and Stroke Council. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation. Jul 10, 2018;138(2):e48-e74. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lyu Q, Tan J, Zapadka ME, Ponnatapura J, Niu C, Myers KJ, et al. Translating radiology reports into plain language using ChatGPT and GPT-4 with prompt learning: results, limitations, and potential. Vis Comput Ind Biomed Art. May 18, 2023;6(1):9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Haver HL, Lin CT, Sirajuddin A, Yi PH, Jeudy J. Use of ChatGPT, GPT-4, and Bard to improve readability of ChatGPT's answers to common questions about lung cancer and lung cancer screening. AJR Am J Roentgenol. Nov 2023;221(5):701-704. [ CrossRef ] [ Medline ]
- Shah NH, Entwistle D, Pfeffer MA. Creation and adoption of large language models in medicine. JAMA. Sep 05, 2023;330(9):866-869. [ CrossRef ] [ Medline ]
- Singh N, Lawrence K, Richardson S, Mann DM. Centering health equity in large language model deployment. PLOS Digit Health. Oct 24, 2023;2(10):e0000367. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mishra V, Dexter JP. Comparison of readability of official public health information about COVID-19 on websites of international agencies and the governments of 15 countries. JAMA Netw Open. Aug 03, 2020;3(8):e2018033. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Meskó B. Prompt engineering as an important emerging skill for medical professionals: tutorial. J Med Internet Res. Oct 04, 2023;25:e50638. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Liu X, Wu J, Shao A, Shen W, Ye P, Wang Y, et al. Uncovering language disparity of ChatGPT on retinal vascular disease classification: cross-sectional study. J Med Internet Res. Jan 22, 2024;26:e51926. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chen S, Li Y, Lu S, Van H, Aerts HJWL, Savova GK, et al. Evaluating the ChatGPT family of models for biomedical reasoning and classification. J Am Med Inform Assoc. Apr 03, 2024;31(4):940-948. [ CrossRef ] [ Medline ]
- Mirza FN, Tang OY, Connolly ID, Abdulrazeq HA, Lim RK, Roye GD, et al. Using ChatGPT to facilitate truly informed medical consent. NEJM AI. Jan 10, 2024;1(2):AIcs2300145. [ CrossRef ]
Abbreviations
Edited by T de Azevedo Cardoso; submitted 11.12.23; peer-reviewed by R Mpofu; comments to author 12.01.24; revised version received 25.01.24; accepted 31.01.24; published 22.04.24.
©Vishala Mishra, Ashish Sarraju, Neil M Kalwani, Joseph P Dexter. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 22.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Advance in the treatment of acute heart failure identified
A multicenter study led by Vanderbilt University Medical Center (VUMC) and Lipscomb University College of Pharmacy in Nashville has identified a potential new treatment for acute heart failure, a leading cause of hospitalization and death.
The drug, dapagliflozin, was initially approved for the treatment of Type 2 diabetes, but it since has been shown to reduce the risk of hospitalization for heart failure and death in patients with serious health problems that include heart and chronic kidney disease and heightened cardiovascular risk.
Reporting this month in the Journal of the American College of Cardiology , the researchers found that dapagliflozin also benefits patients after admission to the hospital for acute heart failure. The drug improves diuresis, the elimination of excess fluid from the lungs, thereby relieving congestion, and it can reduce hospital stays.
"We demonstrated safety and efficacy of initiating dapagliflozin within the first day of hospitalization for acute heart failure," said the paper's first author, Zachary Cox, PharmD, professor of Pharmacy Practice at Lipscomb University. This "will have international impact on the treatment of acute heart failure."
Each year 800,000 patients with acute heart failure are admitted to U.S. hospitals from emergency rooms. These patients are at high risk for prolonged hospital stays and death. The annual cost of treating acute heart failure in the United States is estimated to exceed $34 billion.
Diuretics are administered to most patients with acute heart failure to improve symptoms and lung congestion caused by fluid buildup. However, the optimal approach to diuretic therapy in patients hospitalized for acute heart failure remains poorly defined and contributes to prolonged inpatient stays and high death and readmission rates.
Furthermore, many patients do not respond to diuretics, and about half of patients are discharged with persistent congestion. This can result in patients returning to the hospital soon after discharge and being readmitted for further heart failure therapy.
Dapagliflozin is a sodium-glucose cotransporter 2 (SGLT2) inhibitor that acts on the kidneys to increase the removal of sodium and glucose from the body. In April 2020, VUMC began a randomized, clinical trial of the drug in patients hospitalized with acute heart failure.
The study was designed by VUMC's JoAnn Lindenfeld, MD, and Sean Collins, MD, MSc, and by Cox, a member of VUMC's heart failure research team.
Lindenfeld, professor of Medicine in the Division of Cardiology, is nationally known for her innovative contributions to the field of heart failure.
Collins, professor of Emergency Medicine, directs the Center for Emergency Care Research and Innovation (CERI), a national leader in emergency care research, co-directs the Vanderbilt Coordinating Center, which supports VUMC-led clinical research, and is associate director for clinical trials research in the Vanderbilt Institute for Medicine and Public Health.
Cox is a fellow of the Heart Failure Society of America who has published extensively in the field.
Despite the COVID-19 pandemic, which reached its crescendo in the middle of the study, the researchers were able to enroll 240 patients and complete the trial, "thanks to the diligent effort and collaboration between the CERI research team, and … the departments of emergency medicine and cardiology," Cox said.
"This unique partnership allows VUMC to conduct trials in acute heart failure that are only possible in a small number of medical centers across the world," he said.
The trial "really highlights the novelty of our Emergency Medicine infrastructure, and why we are a leader in designing and conducting highly impactful clinical trials such as this one," Collins added.
Patients were enrolled at five sites in addition to VUMC: TriStar Centennial Medical Center and Ascension St. Thomas Hospital West in Nashville, the University of North Carolina at Chapel Hill, the University of Mississippi Medical Center in Jackson, and INTEGRIS Health Baptist Medical Center in Oklahoma City.
Within 24 hours of admission for acute heart failure, patients were randomized to receive either dapagliflozin or conventional diuretic treatment.
While early administration of dapagliflozin did not improve weight-based diuretic efficiency compared to conventional treatment, patients who received the drug experienced no increase in adverse events, required shorter periods of IV diuresis, and were discharged faster during the five-day study period.
The trial demonstrated the safety and efficacy of starting a drug during early hospitalization that will continue to be prescribed upon discharge to help achieve optimal outpatient therapy and reduce the likelihood of readmission.
"It is a way to both improve diuresis AND get a head start on implementing Guideline Directed Medical Therapy in patients with acute heart failure," Lindenfeld said.
Other VUMC co-authors are Cathy Jenkins, MS, and Frank Harrell Jr., PhD, Department of Biostatistics, and Christina Kampe, MAcc, Karen Miller, RN, MPA, and William Stubblefield, MD, MPH, Department of Emergency Medicine.
The study was an investigator-initiated trial funded by AstraZeneca but independently conducted by VUMC investigators. Dapagliflozin is marketed under the brand name FARXIGA. Acute heart failure research at VUMC is supported in part by the National Heart, Lung and Blood Institute of the National Institutes of Health.
- Heart Disease
- Stroke Prevention
- Diseases and Conditions
- Today's Healthcare
- Kidney Disease
- Cholesterol
- Heart failure
- Ischaemic heart disease
- Ovarian cancer
- Cardiac arrest
- Programmed cell death
Story Source:
Materials provided by Vanderbilt University Medical Center . Original written by Bill Snyder. Note: Content may be edited for style and length.
Journal Reference :
- Zachary L. Cox, Sean P. Collins, Gabriel A. Hernandez, A. Thomas McRae, Beth T. Davidson, Kirkwood Adams, Mark Aaron, Luke Cunningham, Cathy A. Jenkins, Christopher J. Lindsell, Frank E. Harrell, Christina Kampe, Karen F. Miller, William B. Stubblefield, JoAnn Lindenfeld. Efficacy and Safety of Dapagliflozin in Patients With Acute Heart Failure . Journal of the American College of Cardiology , 2024; 83 (14): 1295 DOI: 10.1016/j.jacc.2024.02.009
Cite This Page :
Explore More
- Loneliness Runs Deep Among Parents
- Food in Sight? The Liver Is Ready!
- Acid Reflux Drugs and Risk of Migraine
- Do Cells Have a Hidden Communication System?
- Mice Given Mouse-Rat Brains Can Smell Again
- How Do Birds Flock? New Aerodynamics
- Cancer: Epigenetic Origin Without DNA Mutation
- Climate Change Driving Biodiversity Loss
- Why Can't Robots Outrun Animals?
- Evolution of Gliding in Marsupials
Trending Topics
Strange & offbeat.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Cardiovascular disease.
Edgardo Olvera Lopez ; Brian D. Ballard ; Arif Jan .
Affiliations
Last Update: August 22, 2023 .
- Continuing Education Activity
The cardiovascular system consists of the heart and its blood vessels. A wide array of problems can arise within the cardiovascular system, a few of which include endocarditis, rheumatic heart disease, and conduction system abnormalities. Cardiovascular disease, also known as heart disease, refers to the following 4 entities: coronary artery disease (CAD) which is also referred to as coronary heart disease (CHD), cerebrovascular disease, peripheral artery disease (PAD), and aortic atherosclerosis. CAD results from decreased myocardial perfusion that causes angina due to ischemia and can result in myocardial infarction (MI), and/or heart failure. It accounts for one-third to one-half of all cases of cardiovascular disease. Cerebrovascular disease is the entity associated with strokes, also termed cerebrovascular accidents, and transient ischemic attacks (TIAs). Peripheral arterial disease (PAD) is arterial disease predominantly involving the limbs that may result in claudication. Aortic atherosclerosis is the entity associated with thoracic and abdominal aneurysms. This activity reviews the evaluation and treatment of cardiovascular disease and the role of the medical team in evaluating and treating these conditions.
- Review the cause of coronary artery disease.
- Describe the pathophysiology of atherosclerosis.
- Summarize the treatment options for heart disease.
- Outline the evaluation and treatment of cardiovascular disease and the role of the medical team in evaluating and treating this condition.
- Introduction
The cardiovascular system consists of the heart and blood vessels. [1] There is a wide array of problems that may arise within the cardiovascular system, for example, endocarditis, rheumatic heart disease, abnormalities in the conduction system, among others, cardiovascular disease (CVD) or heart disease refer to the following 4 entities that are the focus of this article [2] :
- Coronary artery disease (CAD): Sometimes referred to as Coronary Heart Disease (CHD), results from decreased myocardial perfusion that causes angina, myocardial infarction (MI), and/or heart failure. It accounts for one-third to one-half of the cases of CVD.
- Cerebrovascular disease (CVD): Including stroke and transient ischemic attack (TIA)
- Peripheral artery disease (PAD): Particularly arterial disease involving the limbs that may result in claudication
- Aortic atherosclerosis: Including thoracic and abdominal aneurysms
Although CVD may directly arise from different etiologies such as emboli in a patient with atrial fibrillation resulting in ischemic stroke, rheumatic fever causing valvular heart disease, among others, addressing risks factors associated to the development of atherosclerosis is most important because it is a common denominator in the pathophysiology of CVD.
The industrialization of the economy with a resultant shift from physically demanding to sedentary jobs, along with the current consumerism and technology-driven culture that is related to longer work hours, longer commutes, and less leisure time for recreational activities, may explain the significant and steady increase in the rates of CVD during the last few decades. Specifically, physical inactivity, intake of a high-calorie diet, saturated fats, and sugars are associated with the development of atherosclerosis and other metabolic disturbances like metabolic syndrome, diabetes mellitus, and hypertension that are highly prevalent in people with CVD. [3] [2] [4] [5]
According to the INTERHEART study that included subjects from 52 countries, including high, middle, and low-income countries, 9 modifiable risks factors accounted for 90% of the risk of having a first MI: smoking, dyslipidemia, hypertension, diabetes, abdominal obesity, psychosocial factors, consumption of fruits and vegetables, regular alcohol consumption, and physical inactivity. It is important to mention that in this study 36% of the population-attributable risk of MI was accounted to smoking. [6]
Other large cohort studies like the Framingham Heart Study [7] and the Third National Health and Nutrition Examination Survey (NHANES III) [5] have also found a strong association and predictive value of dyslipidemia, high blood pressure, smoking, and glucose intolerance. Sixty percent to 90% of CHD events occurred in subjects with at least one risk factor.
These findings have been translated into health promotion programs by the American Heart Association with emphasis on seven recommendations to decrease the risk of CVD: avoiding smoking, being physically active, eating healthy, and keeping normal blood pressure, body weight, glucose, and cholesterol levels. [8] [9]
On the other hand, non-modifiable factors as family history, age, and gender have different implications. [4] [7] Family history, particularly premature atherosclerotic disease defined as CVD or death from CVD in a first-degree relative before 55 years (in males) or 65 years (in females) is considered an independent risk factor. [10] There is also suggestive evidence that the presence of CVD risk factors may differently influence gender. [4] [7] For instance, diabetes and smoking more than 20 cigarettes per day had increased CVD risk in women compared to men. [11] Prevalence of CVD increases significantly with each decade of life. [12]
The presence of HIV (human immunodeficiency virus), [13] history of mediastinal or chest wall radiation, [14] microalbuminuria, [15] , increased inflammatory markers [16] [17] have also been associated with an increased rate and incidence of CVD.
Pointing out specific diet factors like meat consumption, fiber, and coffee and their relation to CVD remains controversial due to significant bias and residual confounding encountered in epidemiological studies. [18] [19]
- Epidemiology
Cardiovascular diseases (CVD) remain among the 2 leading causes of death in the United States since 1975 with 633,842 deaths or 1 in every 4 deaths, heart disease occupied the leading cause of death in 2015 followed by 595,930 deaths related to cancer. [2] CVD is also the number 1 cause of death globally with an estimated 17.7 million deaths in 2015, according to the World Health Organization (WHO). The burden of CVD further extends as it is considered the most costly disease even ahead of Alzheimer disease and diabetes with calculated indirect costs of $237 billion dollars per year and a projected increased to $368 billion by 2035. [20]
Although the age-adjusted rate and acute mortality from MI have been declining over time, reflecting the progress in diagnosis and treatment during the last couple of decades, the risk of heart disease remains high with a calculated 50% risk by age 45 in the general population. [7] [21] The incidence significantly increases with age with some variations between genders as the incidence is higher in men at younger ages. [2] The difference in incidence narrows progressively in the post-menopausal state. [2]
- Pathophysiology
Atherosclerosis is the pathogenic process in the arteries and the aorta that can potentially cause disease as a consequence of decreased or absent blood flow from stenosis of the blood vessels. [22]
It involves multiple factors dyslipidemia, immunologic phenomena, inflammation, and endothelial dysfunction. These factors are believed to trigger the formation of fatty streak, which is the hallmark in the development of the atherosclerotic plaque [23] ; a progressive process that may occur as early as in the childhood. [24] This process comprises intimal thickening with subsequent accumulation of lipid-laden macrophages (foam cells) and extracellular matrix, followed by aggregation and proliferation of smooth muscle cells constituting the formation of the atheroma plaque. [25] As this lesions continue to expand, apoptosis of the deep layers can occur, precipitating further macrophage recruitment that can become calcified and transition to atherosclerotic plaques. [26]
Other mechanisms like arterial remodeling and intra-plaque hemorrhage play an important role in the delay and accelerated the progression of atherosclerotic CVD but are beyond the purpose of this article. [27]
- History and Physical
The clinical presentation of cardiovascular diseases can range from asymptomatic (e.g., silent ischemia, angiographic evidence of coronary artery disease without symptoms, among others) to classic presentations as when patients present with typical anginal chest pain consistent of myocardial infarction and/or those suffering from acute CVA presenting with focal neurological deficits of sudden onset. [28] [29] [28]
Historically, coronary artery disease typically presents with angina that is a pain of substernal location, described as a crushing or pressure in nature, that may radiate to the medial aspect of the left upper extremity, to the neck or the jaw and that can be associated with nausea, vomiting, palpitations, diaphoresis, syncope or even sudden death. [30] Physicians and other health care providers should be aware of possible variations in symptom presentation for these patients and maintain a high index of suspicion despite an atypical presentation, for example, dizziness and nausea as the only presenting symptoms in patients having an acute MI [31] ), particularly in people with a known history of CAD/MI and for those with the presence of CVD risk factors. [32] [33] [34] [33] [32] Additional chest pain features suggestive of ischemic etiology are the exacerbation with exercise and or activity and resolution with rest or nitroglycerin. [35]
Neurologic deficits are the hallmark of cerebrovascular disease including TIA and stroke where the key differentiating factor is the resolution of symptoms within 24 hours for patients with TIA. [36] Although the specific symptoms depend on the affected area of the brain, the sudden onset of extremity weakness, dysarthria, and facial droop are among the most commonly reported symptoms that raise concern for a diagnosis of a stroke. [37] [38] Ataxia, nystagmus and other subtle symptoms as dizziness, headache, syncope, nausea or vomiting are among the most reported symptoms with people with posterior circulation strokes challenging to correlate and that require highly suspicion in patients with risks factors. [39]
Patients with PAD may present with claudication of the limbs, described as a cramp-like muscle pain precipitated by increased blood flow demand during exercise that typically subsides with rest. [40] Severe PAD might present with color changes of the skin and changes in temperature. [41]
Most patients with thoracic aortic aneurysm will be asymptomatic, but symptoms can develop as it progresses from subtle symptoms from compression to surrounding tissues causing cough, shortness of breath or dysphonia, to the acute presentation of sudden crushing chest or back pain due to acute rupture. [42] The same is true for abdominal aortic aneurysms (AAA) that cause no symptoms in early stages to the acute presentation of sudden onset of abdominal pain or syncope from acute rupture. [43]
A thorough physical examination is paramount for the diagnosis of CVD. Starting with a general inspection to look for signs of distress as in patients with angina or with decompensated heart failure, or chronic skin changes from PAD. Carotid examination with the patient on supine position and the back at 30 degrees for the palpation and auscultation of carotid pulses, bruits and to evaluate for jugular venous pulsations on the neck is essential. Precordial examination starting with inspection, followed by palpation looking for chest wall tenderness, thrills, and identification of the point of maximal impulse should then be performed before auscultating the precordium. Heart sounds auscultation starts in the aortic area with the identification of the S1 and S2 sounds followed by characterization of murmurs if present. Paying attention to changes with inspirations and maneuvers to correctly characterize heart murmurs is encouraged. Palpating peripheral pulses with bilateral examination and comparison when applicable is an integral part of the CVD examination. [44]
Thorough clinical history and physical exam directed but not limited to the cardiovascular system are the hallmarks for the diagnosis of CVD. Specifically, a history compatible with obesity, angina, decreased exercise tolerance, orthopnea, paroxysmal nocturnal dyspnea, syncope or presyncope, and claudication should prompt the clinician to obtain a more detailed history and physical exam and, if pertinent, obtain ancillary diagnostic test according to the clinical scenario (e.g., electrocardiogram and cardiac enzymes for patients presenting with chest pain).
Besides a diagnosis prompted by clinical suspicion, most of the efforts should be oriented for primary prevention by targeting people with the presence of risk factors and treat modifiable risk factors by all available means. All patient starting at age 20 should be engaged in the discussion of CVD risk factors and lipid measurement. [9] Several calculators that use LDL-cholesterol and HDL-cholesterol levels and the presence of other risk factors calculate a 10-year or 30-year CVD score to determine if additional therapies like the use of statins and aspirin are indicated for primary prevention, generally indicated if such risk is more than ten percent. [10] Like other risk assessment tools, the use of this calculators have some limitations, and it is recommended to exert precaution when assessing patients with diabetes and familial hypercholesterolemia as their risk can be underestimated. Another limitation to their use is that people older than 79 were usually excluded from the cohorts where these calculators were formulated, and individualized approach for these populations is recommended by discussing risk and benefits of adjunctive therapies and particular consideration of life expectancy. Some experts recommend a reassessment of CVD risk every 4 to 6 years. [9]
Preventative measures like following healthy food habits, avoiding overweight and following an active lifestyle are pertinent in all patients, particularly for people with non-modifiable risk factors such as family history of premature CHD or post-menopause. [9] [8]
The use of inflammatory markers and other risk assessment methods as coronary artery calcification score (CAC) are under research and have limited applications that their use should not replace the identification of people with known risk factors, nonetheless these resources remain as promising tools in the future of primary prevention by detecting people with subclinical atherosclerosis at risk for CVD. [45]
- Treatment / Management
Management of CVD is very extensive depending on the clinical situation (catheter-directed thrombolysis for acute ischemic stroke, angioplasty for peripheral vascular disease, coronary stenting for CHD); however, patients with known CVD should be strongly educated on the need for secondary prevention by risk factor and lifestyle modification. [9] [46]
- Differential Diagnosis
- Acute pericarditis
- Angina pectoris
- Artherosclerosis
- Coronary artery vasospasm
- Dilated cardiomyopathy
- Giant cell arteritis
- Hypertension
- Hypertensive heart disease
- Kawasaki disease
- Myocarditis
The prognosis and burden of CVD have been discussed in other sections.
- Complications
The most feared complication from CVD is death and, as explained above, despite multiple discoveries in the last decades CVD remains in the top leading causes of death all over the world owing to the alarming prevalence of CVD in the population. [2] Other complications as the need for longer hospitalizations, physical disability and increased costs of care are significant and are the focus for health-care policymakers as it is believed they will continue to increase in the coming decades. [20]
For people with heart failure with reduced ejection fraction (HFreEF) of less than 35%, as the risk of life-threatening arrhythmias is exceedingly high in these patients, current guidelines recommend the implantation of an implantable-cardioverter defibrillator (ICD) for those with symptoms equivalent to a New York Heart Association (NYHA) Class II-IV despite maximal tolerated medical therapy. [47]
Strokes can leave people with severe disabling sequelae like dysarthria or aphasia, dysphagia, focal or generalized muscle weakness or paresis that can be temporal or cause permanent physical disability that may lead to a complete bedbound state due to hemiplegia with added complications secondary to immobility as is the higher risk of developing urinary tract infections and/or risk for thromboembolic events. [48] [49]
There is an increased risk of all-cause death for people with PAD compared to those without evidence of peripheral disease. [50] Chronic wounds, physical limitation, and limb ischemia are among other complications from PAD. [51]
- Consultations
An interprofessional approach that involves primary care doctors, nurses, dietitians, cardiologists, neurologists, and other specialists is likely to improve outcomes. This has been shown to be beneficial in patients with heart failure, [52] coronary disease, [53] and current investigations to assess the impact on other forms of CVD are under planning and promise encouraging results.
- Deterrence and Patient Education
Efforts should be directed toward primary prevention by leading a healthy lifestyle, and an appropriate diet starting as early as possible with the goal of delay or avoid the initiation of atherosclerosis as it relates to the future risk of CVD. The AHA developed the concept of "ideal cardiovascular health" defined by the presence of [8] :
- Ideal health behaviors: Nonsmoking, body mass index less than 25 kg/m2, physical activity at goal levels, and the pursuit of a diet consistent with current guideline recommendations
- Ideal health factors: Untreated total cholesterol less than 200 mg/dL, untreated blood pressure less than 120/80 mm Hg, and fasting blood glucose less than 100 mg/dL) with the goal to improve the health of all Americans with an expected decrease in deaths from CVD by 20%
Specific attention should be made to people at higher risk for CVD as are people with diabetes, hypertension, hyperlipidemia, smokers, and obese patients. Risk factors modification by controlling their medical conditions, avoiding smoking, taking appropriate measures to lose weight and maintaining an active lifestyle is of extreme importance. [8] [9] [10] The recommendations on the use of statins and low-dose aspirin for primary and secondary prevention has been discussed in other sections.
- Pearls and Other Issues
Cardiovascular disease generally refers to 4 general entities: CAD, CVD, PVD, and aortic atherosclerosis.
CVD is the main cause of death globally.
Measures aimed to prevent the progression of atherosclerosis are the hallmark for primary prevention of CVD.
Risk factor and lifestyle modification are paramount in the prevention of CVD.
- Enhancing Healthcare Team Outcomes
An interprofessional and patient-oriented approach can help to improve outcomes for people with cardiovascular disease as shown in patients with heart failure (HF) who had better outcomes when the interprofessional involvement of nurses, dietitians, pharmacists, and other health professionals was used (Class 1A). [52]
Similarly, positive results were obtained in people in an intervention group who were followed by an interprofessional team comprised of pharmacists, nurses and a team of different physicians. This group had a reduction in all-cause mortality associated with CAD by 76% compared to the control group. [53] Healthcare workers should educate the public on lifestyle changes and reduce the modifiable risk factors for heart disease to a minimum.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Atherosclerosis as a result of coronary heart disease. Contributed by National Heart, Lung and Blood Institute (NIH)
Coronary artery disease Image courtesy S Bhimji MD
Disclosure: Edgardo Olvera Lopez declares no relevant financial relationships with ineligible companies.
Disclosure: Brian Ballard declares no relevant financial relationships with ineligible companies.
Disclosure: Arif Jan declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Olvera Lopez E, Ballard BD, Jan A. Cardiovascular Disease. [Updated 2023 Aug 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP

Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review De-risking primary prevention: role of imaging. [Ther Adv Cardiovasc Dis. 2021] Review De-risking primary prevention: role of imaging. Shafter AM, Shaikh K, Johanis A, Budoff MJ. Ther Adv Cardiovasc Dis. 2021 Jan-Dec; 15:17539447211051248.
- Shared and non-shared familial susceptibility of coronary heart disease, ischemic stroke, peripheral artery disease and aortic disease. [Int J Cardiol. 2013] Shared and non-shared familial susceptibility of coronary heart disease, ischemic stroke, peripheral artery disease and aortic disease. Calling S, Ji J, Sundquist J, Sundquist K, Zöller B. Int J Cardiol. 2013 Oct 3; 168(3):2844-50. Epub 2013 Apr 30.
- Stenting for peripheral artery disease of the lower extremities: an evidence-based analysis. [Ont Health Technol Assess Ser....] Stenting for peripheral artery disease of the lower extremities: an evidence-based analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2010; 10(18):1-88. Epub 2010 Sep 1.
- Polyvascular disease and long-term cardiovascular outcomes in older patients with non-ST-segment-elevation myocardial infarction. [Circ Cardiovasc Qual Outcomes....] Polyvascular disease and long-term cardiovascular outcomes in older patients with non-ST-segment-elevation myocardial infarction. Subherwal S, Bhatt DL, Li S, Wang TY, Thomas L, Alexander KP, Patel MR, Ohman EM, Gibler WB, Peterson ED, et al. Circ Cardiovasc Qual Outcomes. 2012 Jul 1; 5(4):541-9. Epub 2012 Jun 19.
- Review Prevention of ventricular fibrillation, acute myocardial infarction (myocardial necrosis), heart failure, and mortality by bretylium: is ischemic heart disease primarily adrenergic cardiovascular disease? [Am J Ther. 2004] Review Prevention of ventricular fibrillation, acute myocardial infarction (myocardial necrosis), heart failure, and mortality by bretylium: is ischemic heart disease primarily adrenergic cardiovascular disease? Bacaner M, Brietenbucher J, LaBree J. Am J Ther. 2004 Sep-Oct; 11(5):366-411.
Recent Activity
- Cardiovascular Disease - StatPearls Cardiovascular Disease - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- For Journalists
- News Releases
- Latest Releases
- News Release
Studying the role of inflammation in heart disease
Northwestern Medicine will lead a national research center with support from the American Heart Association
- Link to: Northwestern Now Story
Media Information
- Release Date: April 22, 2024
Media Contacts
Kristin Samuelson
- (847) 491-4888
- Email Kristin
- Northwestern will focus on inflammation’s role in heart failure with preserved ejection fraction (HFpEF)
- HFpEF accounts for more than half of all heart failure cases in the U.S.
- Goal is to understand why some people experience unresolving inflammation while others do not
CHICAGO --- Northwestern Medicine scientists have been selected to lead one of only three research centers nationally as part of a $15 million American Heart Association (AHA) research initiative studying the role of inflammation in heart disease.
While inflammation is critical for mounting immune responses against pathogens or injuries, inflammatory dysregulation can fuel numerous diseases, including those in the heart.
“Fundamentally, we know that inflammation is an immune response to something, we understand the ‘something’ to a reasonable degree and we’re starting to understand the immune response better,” said Dr. Matthew Feinstein , associate professor of cardiology at Northwestern University Feinberg School of Medicine, who will direct one research center in the collaboration. “But there’s so much more work we need to do to understand the diversity of human immune responses that can lead some people to have inflammation go off the rails and some people to actually be able to resolve that inflammation and do it in a way that doesn’t lead to disease development.”
The four-year awards, funded by the AHA’s Strategically Focused Research Network (SFRN) on Inflammation in Cardiac and Neurovascular Disease, started April 1.
Partnering with Chicago State University, Northwestern’s research center will undertake three different projects focused on understanding inflammatory responses and how to treat heart disease caused by inflammation, specifically in patients with heart failure with preserved ejection fraction (HfpEF).
HfpEF is marked by excessive inflammation and accounts for more than half of all heart failure cases in the U.S. The condition also carries a significant public health burden: 50% of people diagnosed with HfpEF die within five years, according to the AHA.
Northwestern’s research initiatives will focus on immune cells, which regulate inflammation in the body, and how the cells are affected by stressors. Investigators will also analyze existing and novel approaches to modulating metabolism and immune cell responses in HfpEF with the ultimate goal of targeting inflammation to address the disease.
“We’ll do this by bringing together patient-centered approaches and experimental model systems, all coalescing around the question of ‘What is turning inflammation on and off in the setting of cardiometabolic risk factors and HfpEF?’” Feinstein said. “The goal is that this knowledge will inform approaches that modulate harmful, unresolving inflammation to curb cardiometabolic disease and HfpEF.”
The AHA funds SFRNs as part of its mission to advance cardiovascular health for all. Research teams apply for the program’s four-year grants with novel and innovative ideas to better understand cardiovascular diseases impacted by each research network’s focus, the latest of which is inflammation.
Other research teams selected as part of the network include investigators at the University of Pittsburgh, which will focus onidentifying and treating interrelated conditions of brain and vascular pathology; and University of Michigan, which will study the driving forces behind inflammatory processes linked to aging and obesity and how to prevent inflammation that could lead to heart failure, dementia and other diseases.
“Often times, the way we investigate inflammation in the heart and vascular disease can be really siloed,” Feinstein said. “We’re thrilled to start to break down some of these walls to understand fundamental features and mechanisms of cardiometabolic inflammation, and to do so in a patient-relevant way.”
Additional Feinberg faculty serving as principal investigators on projects in the Feinberg-based center include Dr. Sanjiv Shah , the Neil J. Stone, MD, professor of cardiology; Edward Thorp , the Frederick Robert Zeit Professor of Pathology; and Kiarri Kershaw , associate professor of preventive medicine (epidemiology).
Christopher Botanga, professor of biology and principal investigator at Chicago State University (CSU), will serve as director of training phase synergy. This collaboration will increase the pipeline of opportunities — which includes the NUCATS -supported Science Immersion Program — for CSU students to collaborate on specific projects as well as have near-peer mentoring from SFRN postdoctoral fellows. Obayed Raihan, assistant professor of pharmaceutical sciences at CSU, will help lead the project’s bioinformatics consortium, which will engage in shared methods development work on using bioinformatic approaches to understand immune-inflammatory contributors to cardiovascular disease.
“We are grateful to the AHA and excited for the opportunity to answer essential questions about how inflammation is regulated in cardiometabolic disease and HFpEF,” Feinstein said. “Ultimately, we hope that this knowledge will inform viable inflammation-modulating approaches to prevent and treat human disease.”
- Share full article
Advertisement
Supported by
Why Are Younger Adults Developing This Common Heart Condition?
New research suggests that A-fib may be more prevalent, and more dangerous, in people under 65 than previously thought.

By Dani Blum
Atrial fibrillation, a common cardiac condition that raises the risk of stroke, is increasingly affecting the health of people under the age of 65.
For years, experts thought that A-fib, a type of irregular heartbeat, primarily occurred in people age 65 and older, and that younger people with the condition most likely wouldn’t develop other cardiac issues, said Dr. Aditya Bhonsale, a cardiac electrophysiologist at the University of Pittsburgh Medical Center. But in new research published Monday, Dr. Bhonsale and his colleagues examined data on more than 67,000 patients with A-fib who were treated at the center, nearly one-quarter of whom were under the age of 65. Those patients had an increased risk of death, compared to people without the condition. They also often had risk factors for A-fib like high blood pressure, obesity and sleep apnea, which could make cardiovascular health issues worse.
What is A-fib?
In A-fib, the upper and lower chambers of the heart are not coordinated as they should be, which makes the heart beat chaotically — sometimes too slow, sometimes too fast, often just irregularly. People with the condition can experience a fluttering heartbeat and palpitations.
Dr. Geoffrey Barnes, a cardiologist and vascular medicine specialist at University of Michigan Health, said that he frequently saw patients who say “I felt like my heart was racing away” or “I felt like it was skipping beats.” People with A-fib can also experience shortness of breath and chest discomfort. Some people have occasional episodes; others will continuously experience an irregular heartbeat. People often have no symptoms and don’t even realize they have the condition, Dr. Barnes said.
Increasingly, doctors said, patients are seeking care because their smart watches have detected an irregular heartbeat. That might help explain why more younger people are being diagnosed, said Dr. Hugh Calkins, a professor of cardiology at Johns Hopkins Medicine. “The more you screen, the more you’re going to find,” he said.
Doctors typically diagnose atrial fibrillation with an electrocardiogram while factoring in your medical and family history. They will sometimes give patients a portable monitor to wear for up to a month to look for an irregular heartbeat.
A-fib can cause clots to form in the heart that can travel to the brain and lead to strokes, even in younger patients, Dr. Bhonsale said. The condition may also raise the risk of cognitive decline and dementia , as well as heart failure. In the study, researchers found that people with A-fib under the age of 65 were at a significantly higher risk of hospitalization for heart failure, stroke and heart attack, compared to people without A-fib.
What’s driving the increase in younger adults?
Atrial fibrillation may also be increasing among younger adults because many of the risk factors for the condition — including pre-existing heart disease and diabetes — are on the rise in that age group, too, Dr. Bhonsale said.
Nearly one in five people in the study who had A-fib also had obstructive sleep apnea , which is a significant risk factor for the condition. People with sleep apnea stop and restart breathing in the night; they struggle to get sufficient rest. The condition, which often goes undiagnosed , is tied to a range of cardiovascular issues .
There is also a correlation between how much alcohol people consume and the likelihood they will develop A-fib, said Dr. Bradley Knight, the medical director of electrophysiology at the Northwestern Medicine Bluhm Cardiovascular Institute. Smoking cigarettes and vaping are also linked with a greater risk of A-fib, Dr. Barnes said.
While exercise in general is associated with a lower risk of cardiac conditions, extreme endurance exercise, like marathons and triathlons, are linked with a higher risk of A-fib, Dr. Calkins said.
How is A-fib treated?
Doctors work with patients to address factors that make A-fib more likely to occur, such as by making sure someone with sleep apnea is using a CPAP machine or by helping patients quit smoking. Sometimes, particularly for younger patients, physicians will recommend a procedure called catheter ablation , which doctors use to get rid of tissue in the heart that may be causing an irregular heartbeat.
Doctors may also prescribe blood thinners, to reduce stroke risk, as well as other medications to manage symptoms. These include drugs that can help regulate heart rate and rhythm , Dr. Knight said. While medications can help reduce the frequency and duration of A-fib episodes, “they rarely eliminate the A-fib,” he added. He tells patients that the disease is like high blood pressure: It must be continuously managed.
“If you are diagnosed with A-fib at any age, but in particular at a younger age, you have been given a great opportunity to now say, OK, what things can I do to help better manage my health and reduce the chance of having a problem later in life?” Dr. Barnes said. “I almost think of it like a wake-up call.”
Dani Blum is a health reporter for The Times. More about Dani Blum
Tips for Better Sleep
Tired of tossing and turning there are some strategies you could try to maximize your hours in bed..
Four out of five people say that they suffer from sleep problems at least once a week and wake up feeling exhausted. Use our guide for a better night’s sleep .
Poor sleep can make anxiety, depression and other mental health issues worse. Here’s what to do about it .
Sleep deprivation doesn’t just feel terrible — it can also hamper your ability to form and recall memories .
The “sleepy girl mocktail” has gone viral on TikTok, where wellness influencers are touting it as a must-have to help you sleep. But is it effective ?
Do sleeping pills work? We asked experts about the different types of medications for treating insomnia .
Sharing a bed with a restless partner doesn’t have to be torture. Try these tips .
Turn Your Bedroom Into a Sleep Sanctuary With Wirecutter’s Recommendations
Good rest starts with a great mattress. These tips can help you pick the right one for you out of the countless options available .
Next, you’ll need a good pillow. These customizable models offer the comfort you need — whether you sleep on your stomach, side or back.
Looking for a more luxe experience? The right sheets can make a big difference. Here is a selection to choose from .
White noise machines have the power to mask yapping dogs, clanky radiators and late-night parties. Consider buying one .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Cardiovascular diseases articles from across Nature Portfolio
Cardiovascular diseases are pathological conditions affecting the heart and/or blood vessels that is, the cardiovascular system.
Related Subjects
- Acute coronary syndromes
- Arrhythmias
- Cardiomyopathies
- Congenital heart defects
- Dyslipidaemias
- Heart failure
- Hypertension
- Valvular disease
- Vascular diseases
Latest Research and Reviews
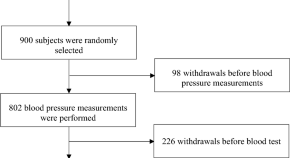
Sex-specific associations between the environmental exposures and low-grade inflammation and increased blood pressure in young, healthy subjects
- Wojciech M. Marchewka
- Krzysztof L. Bryniarski
- Tomasz J. Guzik

LINC317.5 as a novel biomarker for hypertriglyceridemia in normal glucose metabolism

P2X7 receptor knockout does not alter renal function or prevent angiotensin II-induced kidney injury in F344 rats
- Josselin Nespoux
- Marie-Louise T. Monaghan
- Matthew A. Bailey

Targeting immune cell recruitment in atherosclerosis
In this Review, the authors discuss the receptors, ligands and interactors that regulate immune cell recruitment in atherosclerosis, describe mechanisms that promote the resolution of inflammation in atherosclerotic lesions, and highlight potential strategies to target these pathways for the treatment of atherosclerotic cardiovascular disease.
- Yvonne Döring
- Emiel P. C. van der Vorst
- Christian Weber
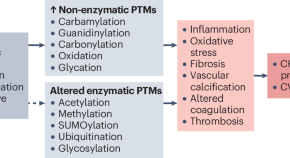
Post-translational modifications in kidney diseases and associated cardiovascular risk
Chronic kidney disease (CKD) is associated with several alterations in protein post-translational modifications. Here, the authors examine the evidence of these alterations, their links with CKD progression and cardiovascular risk in patients with CKD, and their potential clinical applications.
- Heidi Noels
- Vera Jankowski
- Joachim Jankowski
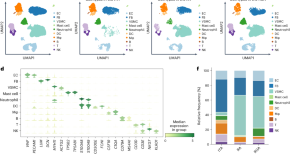
Strategies for arterial graft optimization at the single-cell level
Based on comparative single-cell transcriptomics of arterial grafts deriving from internal thoracic, radial and right gastroepiploic arteries, Hu, Dai, Chang, et al. identify factors that might prevent extracellular matrix deposition and fibrosis and improve the outcomes of coronary artery bypass grafting.
- Jiangping Song
News and Comment
Periodontal treatment reduces af recurrence.
Treatment for periodontal disease might reduce the recurrence of atrial fibrillation (AF) in patients undergoing ablation, suggesting that periodontitis is a modifiable risk factor for AF.
- Gregory B. Lim
The coronary sinus reducer improves angina symptoms in patients with stable CAD
Findings from the ORBITA-COSMIC trial show that treatment of patients with stable coronary artery disease using a coronary sinus reducer improves angina symptoms but does not increase transmural myocardial perfusion.
- Karina Huynh

Benefits of ninerafaxstat in non-obstructive hypertrophic cardiomyopathy
According to data from the IMPROVE-HCM trial, ninerafaxstat is well tolerated by patients with symptomatic non-obstructive hypertrophic cardiomyopathy and improves exercise performance among those who are most symptomatically limited.

Heart pump increases survival in STEMI-related cardiogenic shock
Data from the DanGer Shock trial demonstrate that implantation of a microaxial flow pump in patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock increases the survival rate compared with standard care alone.
- Jennifer Harman
RNA-based therapies targeting APOC3 lower triglyceride levels in patients with hypertriglyceridaemia
Three randomized clinical trials presented at ACC.24 demonstrate that olezarsen and plozasiran, RNA-based therapies that target APOC3 , can robustly reduce plasma triglyceride levels in patients with moderate to severe hypertriglyceridaemia.
No benefit of β-blockers after myocardial infarction with preserved ejection fraction
In the REDUCE-AMI trial, the use of β-blockers in patients with acute myocardial infarction (MI) who have undergone early coronary angiography and have a preserved left ventricular ejection fraction did not reduce the risk of death or new MI compared with no β-blocker use.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
The independent source for health policy research, polling, and news.
A New Use for Wegovy Opens the Door to Medicare Coverage for Millions of People with Obesity
Juliette Cubanski , Tricia Neuman , Nolan Sroczynski , and Anthony Damico Published: Apr 24, 2024
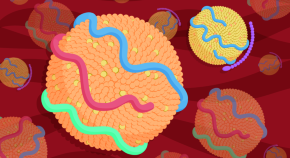
The FDA recently approved a new use for Wegovy (semaglutide), the blockbuster anti-obesity drug, to reduce the risk of heart attacks and stroke in people with cardiovascular disease who are overweight or obese. Wegovy belongs to a class of medications called GLP-1 (glucagon-like peptide-1) agonists that were initially approved to treat type 2 diabetes but are also highly effective anti-obesity drugs. The new FDA-approved indication for Wegovy paves the way for Medicare coverage of this drug and broader coverage by other insurers. Medicare is currently prohibited by law from covering Wegovy and other medications when used specifically for obesity. However, semaglutide is covered by Medicare as a treatment for diabetes, branded as Ozempic.
What does the FDA’s decision mean for Medicare coverage of Wegovy?
The FDA’s decision opens the door to Medicare coverage of Wegovy, which was first approved by the FDA as an anti-obesity medication. Soon after the FDA’s approval of the new use for Wegovy, the Centers for Medicare & Medicaid Services (CMS) issued a memo indicating that Medicare Part D plans can add Wegovy to their formularies now that it has a medically-accepted indication that is not specifically excluded from Medicare coverage . Because Wegovy is a self-administered injectable drug, coverage will be provided under Part D , Medicare’s outpatient drug benefit offered by private stand-alone drug plans and Medicare Advantage plans, not Part B, which covers physician-administered drugs.
How many Medicare beneficiaries could be eligible for coverage of Wegovy for its new use?
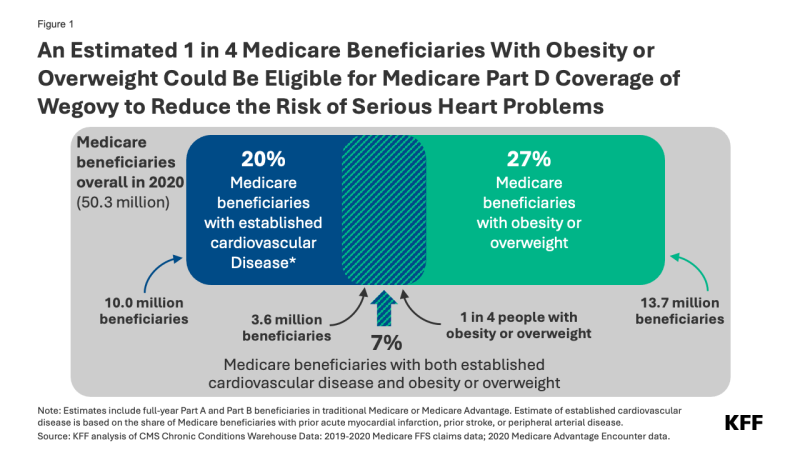
Of these 3.6 million beneficiaries, 1.9 million also had diabetes (other than Type 1) and may already have been eligible for Medicare coverage of GLP-1s as diabetes treatments prior to the FDA’s approval of the new use of Wegovy.
Not all people who are eligible based on the new indication are likely to take Wegovy, however. Some might be dissuaded by the potential side effects and adverse reactions . Out-of-pocket costs could also be a barrier. Based on the list price of $1,300 per month (not including rebates or other discounts negotiated by pharmacy benefit managers), Wegovy could be covered as a specialty tier drug, where Part D plans are allowed to charge coinsurance of 25% to 33%. Because coinsurance amounts are pegged to the list price, Medicare beneficiaries required to pay coinsurance could face monthly costs of $325 to $430 before they reach the new cap on annual out-of-pocket drug spending established by the Inflation Reduction Act – around $3,300 in 2024, based on brand drugs only, and $2,000 in 2025. But even paying $2,000 out of pocket would still be beyond the reach of many people with Medicare who live on modest incomes . Ultimately, how much beneficiaries pay out of pocket will depend on Part D plan coverage and formulary tier placement of Wegovy.
Further, some people may have difficulty accessing Wegovy if Part D plans apply prior authorization and step therapy tools to manage costs and ensure appropriate use. These factors could have a dampening effect on use by Medicare beneficiaries, even among the target population.
When will Medicare Part D plans begin covering Wegovy?
Some Part D plans have already announced that they will begin covering Wegovy this year, although it is not yet clear how widespread coverage will be in 2024. While Medicare drug plans can add new drugs to their formularies during the year to reflect new approvals and expanded indications, plans are not required to cover every new drug that comes to market. Part D plans are required to cover at least two drugs in each category or class and all or substantially all drugs in six protected classes . However, facing a relatively high price and potentially large patient population for Wegovy, many Part D plans might be reluctant to expand coverage now, since they can’t adjust their premiums mid-year to account for higher costs associated with use of this drug. So, broader coverage in 2025 could be more likely.
How might expanded coverage of Wegovy affect Medicare spending?
The impact on Medicare spending associated with expanded coverage of Wegovy will depend in part on how many Part D plans add coverage for it and the extent to which plans apply restrictions on use like prior authorization; how many people who qualify to take the drug use it; and negotiated prices paid by plans. For example, if plans receive a 50% rebate on the list price of $1,300 per month (or $15,600 per year), that could mean annual net costs per person around $7,800. If 10% of the target population (an estimated 360,000 people) uses Wegovy for a full year, that would amount to additional net Medicare Part D spending of $2.8 billion for one year for this one drug alone.
It’s possible that Medicare could select semaglutide for drug price negotiation as early as 2025, based on the earliest FDA approval of Ozempic in late 2017 . For small-molecule drugs like semaglutide, at least seven years must have passed from its FDA approval date to be eligible for selection, and for drugs with multiple FDA approvals, CMS will use the earliest approval date to make this determination. If semaglutide is selected for negotiation next year, a negotiated price would be available beginning in 2027. This could help to lower Medicare and out-of-pocket spending on semaglutide products, including Wegovy as well as Ozempic and Rybelsus, the oral formulation approved for type 2 diabetes. As of 2022, gross Medicare spending on Ozempic alone placed it sixth among the 10 top-selling drugs in Medicare Part D, with annual gross spending of $4.6 billion, based on KFF analysis . This estimate does not include rebates, which Medicare’s actuaries estimated to be 31.5% overall in 2022 but could be as high as 69% for Ozempic, according to one estimate.
What does this mean for Medicare coverage of anti-obesity drugs?
For now, use of GLP-1s specifically for obesity continues to be excluded from Medicare coverage by law. But the FDA’s decision signals a turning point for broader Medicare coverage of GLP-1s since Wegovy can now be used to reduce the risk of heart attack and stroke by people with cardiovascular disease and obesity or overweight, and not only as an anti-obesity drug. And more pathways to Medicare coverage could open up if these drugs gain FDA approval for other uses . For example, Eli Lilly has just reported clinical trial results showing the benefits of its GLP-1, Zepbound (tirzepatide), in reducing the occurrence of sleep apnea events among people with obesity or overweight. Lilly reportedly plans to seek FDA approval for this use and if approved, the drug would be the first pharmaceutical treatment on the market for sleep apnea.
If more Medicare beneficiaries with obesity or overweight gain access to GLP-1s based on other approved uses for these medications, that could reduce the cost of proposed legislation to lift the statutory prohibition on Medicare coverage of anti-obesity drugs. This is because the Congressional Budget Office (CBO), Congress’s official scorekeeper for proposed legislation, would incorporate the cost of coverage for these other uses into its baseline estimates for Medicare spending, which means that the incremental cost of changing the law to allow Medicare coverage for anti-obesity drugs would be lower than it would be without FDA’s approval of these drugs for other uses. Ultimately how widely Medicare Part D coverage of GLP-1s expands could have far-reaching effects on people with obesity and on Medicare spending.
- Medicare Part D
- Chronic Diseases
- Heart Disease
- Medicare Advantage
news release
- An Estimated 1 in 4 Medicare Beneficiaries With Obesity or Overweight Could Be Eligible for Medicare Coverage of Wegovy, an Anti-Obesity Drug, to Reduce Heart Risk
Also of Interest
- An Overview of the Medicare Part D Prescription Drug Benefit
- FAQs about the Inflation Reduction Act’s Medicare Drug Price Negotiation Program
- What Could New Anti-Obesity Drugs Mean for Medicare?
- Medicare Spending on Ozempic and Other GLP-1s Is Skyrocketing

IMAGES
VIDEO
COMMENTS
Abstract. Cardiovascular disease has become a growing global and public health concern among non-communicable diseases (NCDs). The purpose of the study was to focus on the increasing prevalence of the risk factors of cardiovascular diseases (CVD), irrespective of age and gender, and its effect on public health worldwide.
Background: The American Heart Association, in conjunction with the National Institutes of Health, annually reports the most up-to-date statistics related to heart disease, stroke, and cardiovascular risk factors, including core health behaviors (smoking, physical activity, diet, and weight) and health factors (cholesterol, blood pressure, and glucose control) that contribute to cardiovascular ...
F. Böhm and OthersN Engl J Med 2024;390:1481-1492. In a registry-based trial, FFR-guided PCI of nonculprit lesions did not result in a lower risk of a composite of death from any cause ...
This study shows that the release of neutrophil extracellular traps (NETs) after stroke and myocardial infarction triggers B cell apoptosis and reduces the number of IgA-producing plasma cells ...
Patients with cardiovascular disease (CVD) have an increased risk of cancer, and patients with cancer have an increased risk of CVD. In this Review, the authors discuss the shared modifiable risk ...
Heart disease is a fatal human disease, rapidly increases globally in both developed and undeveloped countries and consequently, causes death. Normally, in this disease, the heart fails to supply ...
Cardiovascular diseases (CVDs), principally ischemic heart disease (IHD) and stroke, are the leading cause of global mortality and a major contributor to disability. This paper reviews the magnitude of total CVD burden, including 13 underlying causes of cardiovascular death and 9 related risk factors, using estimates from the Global Burden of ...
Cardiovascular diseases (CVDs), principally ischemic heart disease (IHD) and stroke, are the leading cause of. global mortality and a major contributor to disability. This paper reviews the ...
Abstract. Cardiovascular diseases (CVDs) are the leading cause of premature death and disability in humans and their incidence is on the rise globally. Given their substantial contribution towards the escalating costs of health care, CVDs also generate a high socio-economic burden in the general population.
Discover Cardiovascular Research's latest Spotlight Issue on Obesity, Metabolism, and Diabetes. This issue contains a number of invited expert reviews alongside original research papers. Start Reading. IMPACT FACTOR. 10.9 . CARDIAC & CARDIOVASCULAR SYSTEMS. 12 out of 143 ... Atherosclerotic cardiovascular disease (ASCVD) is characterized by a ...
1. Introduction. Cardiovascular (CV) disease (CVD) is still a major cause of morbidity and mortality in many countries in Europe although considerable efforts have been made in recent decades to address this disease in an even more "comprehensive" approach [].The so-called "traditional" CV risk factors are arterial hypertension, dyslipidemia, diabetes, cigarette smoking, family history ...
Cholenahalli Nanjappa Manjunath. December 2013 View PDF. More opportunities to publish your research: Browse open Calls for Papers. Read the latest articles of Journal of Cardiovascular Disease Research at ScienceDirect.com, Elsevier's leading platform of peer-reviewed scholarly literature.
The following are highlights from the new series, Circulation: Cardiovascular Quality and Outcomes Topic Review. This series will summarize the most important manuscripts, as selected by the Editor, that have published in the Circulation portfolio. The objective of this new series is to provide our readership with a timely, comprehensive selection of important papers that are relevant to the ...
Background: The American Heart Association, in conjunction with the National Institutes of Health, annually reports on the most up-to-date statistics related to heart disease, stroke, and cardiovascular risk factors, including core health behaviors (smoking, physical activity, diet, and weight) and health factors (cholesterol, blood pressure, and glucose control) that contribute to ...
Study characteristics. Table 2 shows the basic characteristics of the included studies. In total, our meta-analysis of ML and cardiovascular diseases included 103 cohorts (55 studies) with a total ...
Journal of cardiovascular Disease Research (JCDR) (J Cardiovasc. Dis. Res.) [www.jcdronline.org] J Cardiovasc. Dis. Res. [ISSN: Print -0975-3583, Online - 0976-2833] is a double-blind peer-reviewed, open access international circulating professional journal led by a group of research scientists, JCDR publishes a wide range of topics covering ...
Research Letter (26) mHealth for Data Collection and Research (832) Chatbots and Conversational Agents (402) Artificial Intelligence (1097) Natural Language Processing (605) Machine Learning (1323) Cardiology (104) Cardiovascular Disease Prevention (117) Generative Language Models Including ChatGPT (146)
The drug, dapagliflozin, was initially approved for the treatment of Type 2 diabetes, but it since has been shown to reduce the risk of hospitalization for heart failure and death in patients with ...
The cardiovascular system consists of the heart and blood vessels.[1] There is a wide array of problems that may arise within the cardiovascular system, for example, endocarditis, rheumatic heart disease, abnormalities in the conduction system, among others, cardiovascular disease (CVD) or heart disease refer to the following 4 entities that are the focus of this article[2]:
The AHA funds SFRNs as part of its mission to advance cardiovascular health for all. Research teams apply for the program's four-year grants with novel and innovative ideas to better understand cardiovascular diseases impacted by each research network's focus, the latest of which is inflammation.
New research suggests that A-fib may be more prevalent, and more dangerous, in people under 65 than previously thought. By Dani Blum Atrial fibrillation, a common cardiac condition that raises the ...
Cardiovascular disease (CVD) remains a leading cause of morbidity and mortality in type 1 diabetes mellitus and type 2 diabetes mellitus (T2D). 1-3 Beyond the inherent increase in mortality in diabetic subjects, when diabetes mellitus is combined with manifestations of CVD, such as myocardial infarction or stroke, the mortality rate is nearly doubled, leading to an estimated reduction in ...
Cardiovascular disease, also known as heart disease, affects the heart or blood vessels, or both. It is the leading cause of death in women and about 30% of women die from some form of it. Poor sleep quality and insomnia are prevalent among women, especially during midlife, often defined as age 40 to 65 years, with up to 50% of women reporting ...
Cardiovascular diseases are pathological conditions affecting the heart and/or blood vessels that is, the cardiovascular system. ... Research Highlights 23 Apr 2024 Nature Reviews Cardiology. P: 1.
Heart failure is a chronic, progressive condition in which the heart's ability to squeeze and then pump blood throughout the body weakens. Two main types are defined by a measure called ejection ...
The FDA recently approved a new use for Wegovy, the blockbuster anti-obesity drug, to reduce the risk of heart attacks and stroke in people with cardiovascular disease who are overweight or obese ...