- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical thinking in healthcare and education
- Related content
- Peer review
- Jonathan M Sharples , professor 1 ,
- Andrew D Oxman , research director 2 ,
- Kamal R Mahtani , clinical lecturer 3 ,
- Iain Chalmers , coordinator 4 ,
- Sandy Oliver , professor 1 ,
- Kevan Collins , chief executive 5 ,
- Astrid Austvoll-Dahlgren , senior researcher 2 ,
- Tammy Hoffmann , professor 6
- 1 EPPI-Centre, UCL Department of Social Science, London, UK
- 2 Global Health Unit, Norwegian Institute of Public Health, Oslo, Norway
- 3 Centre for Evidence-Based Medicine, Oxford University, Oxford, UK
- 4 James Lind Initiative, Oxford, UK
- 5 Education Endowment Foundation, London, UK
- 6 Centre for Research in Evidence-Based Practice, Bond University, Gold Coast, Australia
- Correspondence to: J M Sharples Jonathan.Sharples{at}eefoundation.org.uk
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration
Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient’s sex and age, and you begin to think about what questions to ask and what diagnoses and diagnostic tests to consider. You will also need to think about what treatments to consider and how to communicate with the patient and potentially with the patient’s family and other healthcare providers. Some of what you do will be done reflexively, with little explicit thought, but caring for most patients also requires you to think critically about what you are going to do.
Critical thinking, the ability to think clearly and rationally about what to do or what to believe, is essential for the practice of medicine. Few doctors are likely to argue with this. Yet, until recently, the UK regulator the General Medical Council and similar bodies in North America did not mention “critical thinking” anywhere in their standards for licensing and accreditation, 1 and critical thinking is not explicitly taught or assessed in most education programmes for health professionals. 2
Moreover, although more than 2800 articles indexed by PubMed have “critical thinking” in the title or abstract, most are about nursing. We argue that it is important for clinicians and patients to learn to think critically and that the teaching and learning of these skills should be considered explicitly. Given the shared interest in critical thinking with broader education, we also highlight why healthcare and education professionals and researchers need to work together to enable people to think critically about the health choices they make throughout life.
Essential skills for doctors and patients
Critical thinking is not a new concept in education: at the beginning of the last century the US educational reformer John Dewey identified the need to help students “to think well.” 3 Critical thinking encompasses a broad set of skills and dispositions, including cognitive skills (such as analysis, inference, and self regulation); approaches to specific questions or problems (orderliness, diligence, and reasonableness); and approaches to life in general (inquisitiveness, concern with being well informed, and open mindedness). 4
An increasing body of evidence highlights that developing critical thinking skills can benefit academic outcomes as well as wider reasoning and problem solving capabilities. 5 For example, the Thinking, Doing, Talking Science programme trains teachers in a repertoire of strategies that encourage pupils to use critical thinking skills in primary school science lessons. An independently conducted randomised trial of this approach found that it had a positive impact on pupils’ science attainment, with signs that it was particularly beneficial for pupils from poorer families. 6
In medicine, increasing attention has been paid to “critical appraisal” in the past 40 years. Critical appraisal is a subset of critical thinking that focuses on how to use research evidence to inform health decisions. 7 8 9 The need for critical appraisal in medicine was recognised at least 75 years ago, 10 and critical appraisal has been recognised for some decades as an essential competency for healthcare professionals. 11 The General Medical Council’s Good Medical Practice guidance includes the need for doctors to be able to “provide effective treatments based on the best available evidence.” 12
If patients and the public are to make well informed health choices, they must also be able to assess the reliability of health claims and information. This is something that most people struggle to do, and it is becoming increasingly important because patients are taking on a bigger role in managing their health and making healthcare decisions, 13 while needing to cope with more and more health information, much of which is not reliable. 14 15 16 17
Teaching critical thinking
Although critical thinking skills are given limited explicit attention in standards for medical education, they are included as a key competency in most frameworks for national curriculums for primary and secondary schools in many countries. 18 Nonetheless, much health and science education, and education generally, still tends towards rote learning rather than the promotion of critical thinking. 19 20 This matters because the ability to think critically is an essential life skill relevant to decision making in many circumstances. The capacity to think critically is, like a lot of learning, developed in school and the home: parental influence creates advantage for pupils who live in homes where they are encouraged to think and talk about what they are doing. This, importantly, goes beyond simply completing tasks to creating deeper understanding of learning processes. As such, the “critical thinking gap” between children from disadvantaged communities and their more advantaged peers requires attention as early as possible.
Although it is possible to teach critical thinking to adults, it is likely to be more productive if the grounds for this have been laid down in an educational environment early in life, starting in primary school. Erroneous beliefs, attitudes, and behaviours developed during childhood may be difficult to change later. 21 22 This also applies to medical education and to health professionals. It becomes increasingly difficult to teach these skills without a foundation to build on and adequate time to learn them.
Strategies for teaching students to think critically have been evaluated in health and medical education; in science, technology, engineering, and maths; and in other subjects. 23 These studies suggest that critical thinking skills can be taught and that in the absence of explicit teaching of critical thinking, important deficiencies emerge in the abilities of students to make sound judgments. In healthcare studies, many medical students score poorly on tests that measure the ability to think critically , and the ability to think critically is correlated with academic success. 24 25
Evaluations of strategies for teaching critical thinking in medicine have focused primarily on critical appraisal skills as part of evidence based healthcare. An overview of systematic reviews of these studies suggests that improving evidence based healthcare competencies is likely to require multifaceted, clinically integrated approaches that include assessment. 26
Cross sector collaboration
Informed Health Choices, an international project aiming to improve decision making, shows the opportunities and benefits of cross sector collaboration between education and health. 27 This project has brought together people working in education and healthcare to develop a curriculum and learning resources for critical thinking about any action that is claimed to improve health. It aims to develop, identify, and promote the use of effective learning resources, beginning at primary school, to help people to make well informed choices as patients and health professionals, and well informed decisions as citizens and policy makers.
The project has drawn on several approaches used in education, including the development of a “spiral curriculum,” measurement tools, and the design of learning resources. A spiral curriculum begins with determining what people should know and be able to do, and outlines where they should begin and how they should progress to reach these goals. The basic ideas are revisited repeatedly, building on them until the student has grasped a deep understanding of the concepts. 28 29 The project has also drawn on educational research and methods to develop reliable and valid tools for measuring the extent to which those goals have been achieved. 30 31 32 The development of learning resources to teach these skills has been informed by educational research, including educational psychology, motivational psychology, and research and methods for developing learning games. 33 34 35 It has also built on the traditions of clinical epidemiology and evidence based medicine to identify the key concepts required to assess health claims. 29
It is difficult to teach critical thinking abstractly, so focusing on health may have advantages beyond the public health benefits of increasing health literacy. 36 Nearly everyone is interested in health, including children, making it easy to engage learners. It is also immediately relevant to students. As reported by one 10 year old in a school that piloted primary school resources, this is about “things we might actually use instead of things we might use when we are all grown up and by then we’ll forget.” Although the current evaluation of the project is focusing on outcomes relating to appraisal of treatment claims, if the intervention shows promise the next step could be to explore how these skills translate to wider educational contexts and outcomes.
Beyond critical thinking
Exciting opportunities for cross sector collaboration are emerging between healthcare and education. Although critical thinking is a useful example of this, other themes cross the education and healthcare domains, including nutrition, exercise, educational neuroscience, learning disabilities and special education needs, and mental health.
In addition to shared topics, several common methodological and conceptual issues also provide opportunities for sharing ideas and innovations and learning from mistakes and successes. For example, the Education Endowment Foundation is the UK government’s What Works Centre for education, aiming to improve evidence based decision making. Discussions hosted by the foundation are exploring how methods to develop guidelines in healthcare can be adapted and applied in education and other sectors.
Similarly, the foundation’s universal use of independent evaluation for teaching and learning interventions is an approach that should be explored, adapted, and applied in healthcare. Since the development and evaluation of educational interventions are separated, evaluators have no vested interested in the results of the assessment, all results are published, and bias and spin in how results are analysed and presented are reduced. By contrast, industry sponsorship of drug and device studies consistently produces results that favour the manufacturer. 37
Another example of joint working between educators and health is the Best Evidence Medical Education Collaboration, an international collaboration focused on improving education of health professionals. 38 And in the UK, the Centre for Evidence Based Medicine coordinates Evidence in School Teaching (Einstein), a project that supports introducing evidence based medicine as part of wider science activities in schools. 39 It aims to engage students, teachers, and the public in evidence based medicine and develop critical thinking to assess health claims and make better choices.
Collaboration has also been important in the development of the Critical Thinking and Appraisal Resource Library (CARL), 40 a set of resources designed to help people understand fair comparisons of treatments. An important aim of CARL is to promote evaluation of these critical thinking resources and interventions, some of which are currently under way at the Education Endowment Foundation. On 22 May 2017, the foundation is also cohosting an event with the Royal College of Paediatrics and Child Health that will focus on their shared interest in critical thinking and appraisal skills.
Education and healthcare have overlapping interests. Doctors, teachers, researchers, patients, learners, and the public can all benefit from working together to help people to think critically about the choices they make. Events such as the global evidence summit in September 2017 ( https://globalevidencesummit.org ) can help bring people together and build on current international experience.
Contributors and sources: This article reflects conclusions from discussions during 2016 among education and health service researchers exploring opportunities for cross sector collaboration and learning. This group includes people with a longstanding interest in evidence informed policy and practice, with expertise in evaluation design, reviewing methodology, knowledge mobilisation, and critical thinking and appraisal.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare that we have no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Krupat E, Sprague JM, Wolpaw D, Haidet P, Hatem D, O’Brien B. Thinking critically about critical thinking: ability, disposition or both? Med Educ 2011 ; 357 : 625 - 35 . doi:10.1111/j.1365-2923.2010.03910.x pmid:21564200 . OpenUrl
- ↵ Huang GC, Newman LR, Schwartzstein RM. Critical thinking in health professions education: summary and consensus statements of the millennium conference 2011. Teach Learn Med 2014 ; 357 : 95 - 102 . doi:10.1080/10401334.2013.857335 pmid:24405353 . OpenUrl
- ↵ Dewey J. How we think. D C Heath, 1910 . https://archive.org/details/howwethink000838mbp doi:10.1037/10903-000 .
- ↵ Facione PA. Critical thinking: a statement of expert consensus for purposes of educational assessment and instruction. Research findings and recommendations. American Philosophical Association, 1990 , http://files.eric.ed.gov/fulltext/ED315423.pdf .
- ↵ Higgins S, Katsipataki M, Coleman R, et al. The Sutton Trust-Education Endowment Foundation Teaching and Learning Toolkit. Education Endowment Foundation, 2015 .
- ↵ Hanley P, Slavin RE, Elliot L. Thinking, doing, talking science. Evaluation report and executive summary. Education Endowment Foundation, 2015 , https://v1.educationendowmentfoundation.org.uk/uploads/pdf/Oxford_Science.pdf .
- ↵ Sackett DL. How to read clinical journals: I. why to read them and how to start reading them critically . Can Med Assoc J 1981 ; 357 : 555 - 8 . pmid:7471000 . OpenUrl
- ↵ Guyatt G, Cairns J, Churchill D, et al. Evidence-Based Medicine Working Group. Evidence-based medicine. A new approach to teaching the practice of medicine . JAMA 1992 ; 357 : 2420 - 5 . doi:10.1001/jama.1992.03490170092032 pmid:1404801 . OpenUrl
- ↵ Oxman AD, Sackett DL, Guyatt GH. The Evidence-Based Medicine Working Group. Users’ guides to the medical literature. I. How to get started . JAMA 1993 ; 357 : 2093 - 5 . doi:10.1001/jama.1993.03510170083036 pmid:8411577 . OpenUrl
- ↵ Rynearson EH. Endocrinology: a critical appraisal . Cal West Med 1940 ; 357 : 257 - 9 . pmid:18745588 . OpenUrl
- ↵ General Medical Council. Tomorrow's doctors. General Medical Council, 1993. http://www.gmc-uk.org/10a_annex_a.pdf_25398162.pdf
- ↵ General Medical Council. Good medical practice. General Medical Council, 2013. http://www.gmc-uk.org/static/documents/content/GMP_.pdf
- ↵ Edwards A, Elwyn G. Shared decision-making in health care: achieving evidence-based patient choice. 2nd ed . Oxford University Press, 2009 .
- ↵ Sumner P, Vivian-Griffiths S, Boivin J, et al. Exaggerations and caveats in press releases and health-related science news. PLoS One 2016 ; 357 : e0168217 . doi:10.1371/journal.pone.0168217 pmid:27978540 . OpenUrl
- ↵ Schwartz LM, Woloshin S, Andrews A, Stukel TA. Influence of medical journal press releases on the quality of associated newspaper coverage: retrospective cohort study. BMJ 2012 ; 357 : d8164 . doi:10.1136/bmj.d8164 . pmid:22286507 . OpenUrl
- ↵ Glenton C, Paulsen EJ, Oxman AD. Portals to Wonderland: health portals lead to confusing information about the effects of health care. BMC Med Inform Decis Mak 2005 ; 357 : 7 . doi:10.1186/1472-6947-5-7 pmid:15769291 . OpenUrl
- ↵ Moynihan R, Bero L, Ross-Degnan D, et al. Coverage by the news media of the benefits and risks of medications . N Engl J Med 2000 ; 357 : 1645 - 50 . doi:10.1056/NEJM200006013422206 pmid:10833211 . OpenUrl
- ↵ Voogt J, Roblin NP. A comparative analysis of international frameworks for 21st century competences: implications for national curriculum policies. J Curric Stud 2012 ; 357 : 299 - 321 doi:10.1080/00220272.2012.668938 . OpenUrl
- ↵ National Research Council. Taking science to school: learning and teaching science in grades K-8. National Academies Press, 2007 .
- ↵ Nordheim L, Pettersen KS, Flottorp S, Hjälmhult E. Critical appraisal of health claims: science teachers’ perceptions and practices . Health Educ J 2016 ; 357 : 449 - 66 doi:10.1108/HE-04-2015-0016 . OpenUrl
- ↵ Committee on Science Learning. Kindergarten through eighth grade. How children learn science. In: Duschl RA, Schweingruber A, Shouse AW, eds. Taking science to school: learning and teaching science in grades K-8. National Academies Press, 2007 .
- ↵ Vosniadou S. International handbook of research on conceptual change. 2nd ed . Routledge, 2013 .
- ↵ Abrami PC, Bernard RM, Borokhovski E, Waddington DI, Wade CA, Persson T. Strategies for teaching students to think critically a meta-analysis. Rev Educ Res 2015 ; 357 : 275 - 314 . OpenUrl
- ↵ Ross D, Schipper S, Westbury C, et al. Examining critical thinking skills in family medicine residents . Fam Med 2016 ; 357 : 121 - 6 . pmid:26950783 . OpenUrl
- ↵ Ross D, Loeffler K, Schipper S, Vandermeer B, Allan GM. Do scores on three commonly used measures of critical thinking correlate with academic success of health professions trainees? A systematic review and meta-analysis. Acad Med 2013 ; 357 : 724 - 34 . doi:10.1097/ACM.0b013e31828b0823 pmid:23524925 . OpenUrl
- ↵ Young T, Rohwer A, Volmink J, Clarke M. What are the effects of teaching evidence-based health care (EBHC)? Overview of systematic reviews. PLoS One 2014 ; 357 : e86706 . doi:10.1371/journal.pone.0086706 pmid:24489771 . OpenUrl
- ↵ Informed Health Choices Group. Informed health choices. www.informedhealthchoices.org
- ↵ Harden RM, Stamper N. What is a spiral curriculum? Med Teach 1999 ; 357 : 141 - 3 . doi:10.1080/01421599979752 pmid:21275727 . OpenUrl
- ↵ Austvoll-Dahlgren A, Oxman AD, Chalmers I, et al. Key concepts that people need to understand to assess claims about treatment effects. J Evid Based Med 2015 ; 357 : 112 - 25 . doi:10.1111/jebm.12160 pmid:26107552 . OpenUrl
- ↵ Austvoll-Dahlgren A, Nsangi A, Semakula D. Interventions and assessment tools addressing key concepts people need to know to appraise claims about treatment effects: a systematic mapping review. Syst Rev 2016 ; 357 : 215 . doi:10.1186/s13643-016-0389-z pmid:28034307 . OpenUrl
- ↵ Austvoll-Dahlgren A, Semakula D, Nsangi A, et al. The development of the “claim evaluation tools”: assessing critical thinking about effects. BMJ Open forthcoming .
- ↵ Austvoll-Dahlgren A, Guttersrud Ø, Semakula D, Nsangi A, Oxman AD. Measuring ability to assess claims about treatment effects: a latent trait analysis of the claim evaluation tools using Rasch modelling. BMJ Open [ forthcoming ].
- ↵ Sandoval WA, Sodian B, Koerber S, Wong J. Developing children’s early competencies to engage with science . Educ Psychol 2014 ; 357 : 139 - 52 doi:10.1080/00461520.2014.917589 . OpenUrl
- ↵ Pintrich PR. A motivational science perspective on the role of student motivation in learning and teaching contexts . J Educ Psychol 2003 ; 357 : 667 - 86 doi:10.1037/0022-0663.95.4.667 . OpenUrl
- ↵ Clark DB, Tanner-Smith EE, Killingsworth SS. Digital games, design, and learning: a systematic review and meta-analysis . Rev Educ Res 2016 ; 357 : 79 - 122 . doi:10.3102/0034654315582065 pmid:26937054 . OpenUrl
- ↵ Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review . Ann Intern Med 2011 ; 357 : 97 - 107 . doi:10.7326/0003-4819-155-2-201107190-00005 pmid:21768583 . OpenUrl
- ↵ Lundh A, Sismondo S, Lexchin J, Busuioc OA, Bero L. Industry sponsorship and research outcome. Cochrane Database Syst Rev 2012 ; 357 : MR000033 . pmid:23235689 . OpenUrl
- ↵ Thistlethwaite J, Hammick M, The Best Evidence Medical Education (BEME) Collaboration: into the next decade. Med Teach 2010 ; 357 : 880 - 2 . doi:10.3109/0142159X.2010.519068 pmid:21039096 . OpenUrl
- ↵ Centre for Evidence Based Medicine. Einstein—taking EBM to schools. http://www.cebm.net/taking-ebm-schools
- ↵ Castle JC, Chalmers I, Atkinson P, et al. Establishing a library of resources to help people understand key concepts in assessing treatment claims—the Critical Thinking and Appraisal Resource Library (CARL). PLoS One forthcoming .
What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What Is Critical Thinking In Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
You are using an outdated browser
Unfortunately Ausmed.com does not support your browser. Please upgrade your browser to continue.
Cultivating Critical Thinking in Healthcare
Published: 06 January 2019

Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).
Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught , assessed and integrated into the design and development of staff and nurse education and training programs (Papp et al. 2014).
So, what exactly is critical thinking and how can healthcare educators cultivate it amongst their staff?
What is Critical Thinking?
In general terms, ‘ critical thinking ’ is often used, and perhaps confused, with problem-solving and clinical decision-making skills .
In practice, however, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions .
Several formal definitions of critical thinking can be found in literature, but in the view of Kahlke and Eva (2018), most of these definitions have limitations. That said, Papp et al. (2014) offer a useful starting point, suggesting that critical thinking is:
‘The ability to apply higher order cognitive skills and the disposition to be deliberate about thinking that leads to action that is logical and appropriate.’
The Foundation for Critical Thinking (2017) expands on this and suggests that:
‘Critical thinking is that mode of thinking, about any subject, content, or problem, in which the thinker improves the quality of his or her thinking by skillfully analysing, assessing, and reconstructing it.’
They go on to suggest that critical thinking is:
- Self-directed
- Self-disciplined
- Self-monitored
- Self-corrective.

Key Qualities and Characteristics of a Critical Thinker
Given that critical thinking is a process that encompasses conceptualisation , application , analysis , synthesis , evaluation and reflection , what qualities should be expected from a critical thinker?
In answering this question, Fortepiani (2018) suggests that critical thinkers should be able to:
- Formulate clear and precise questions
- Gather, assess and interpret relevant information
- Reach relevant well-reasoned conclusions and solutions
- Think open-mindedly, recognising their own assumptions
- Communicate effectively with others on solutions to complex problems.
All of these qualities are important, however, good communication skills are generally considered to be the bedrock of critical thinking. Why? Because they help to create a dialogue that invites questions, reflections and an open-minded approach, as well as generating a positive learning environment needed to support all forms of communication.
Lippincott Solutions (2018) outlines a broad spectrum of characteristics attributed to strong critical thinkers. They include:
- Inquisitiveness with regard to a wide range of issues
- A concern to become and remain well-informed
- Alertness to opportunities to use critical thinking
- Self-confidence in one’s own abilities to reason
- Open mindedness regarding divergent world views
- Flexibility in considering alternatives and opinions
- Understanding the opinions of other people
- Fair-mindedness in appraising reasoning
- Honesty in facing one’s own biases, prejudices, stereotypes or egocentric tendencies
- A willingness to reconsider and revise views where honest reflection suggests that change is warranted.
Papp et al. (2014) also helpfully suggest that the following five milestones can be used as a guide to help develop competency in critical thinking:
Stage 1: Unreflective Thinker
At this stage, the unreflective thinker can’t examine their own actions and cognitive processes and is unaware of different approaches to thinking.
Stage 2: Beginning Critical Thinker
Here, the learner begins to think critically and starts to recognise cognitive differences in other people. However, external motivation is needed to sustain reflection on the learners’ own thought processes.
Stage 3: Practicing Critical Thinker
By now, the learner is familiar with their own thinking processes and makes a conscious effort to practice critical thinking.
Stage 4: Advanced Critical Thinker
As an advanced critical thinker, the learner is able to identify different cognitive processes and consciously uses critical thinking skills.
Stage 5: Accomplished Critical Thinker
At this stage, the skilled critical thinker can take charge of their thinking and habitually monitors, revises and rethinks approaches for continual improvement of their cognitive strategies.
Facilitating Critical Thinking in Healthcare
A common challenge for many educators and facilitators in healthcare is encouraging students to move away from passive learning towards active learning situations that require critical thinking skills.
Just as there are similarities among the definitions of critical thinking across subject areas and levels, there are also several generally recognised hallmarks of teaching for critical thinking . These include:
- Promoting interaction among students as they learn
- Asking open ended questions that do not assume one right answer
- Allowing sufficient time to reflect on the questions asked or problems posed
- Teaching for transfer - helping learners to see how a newly acquired skill can apply to other situations and experiences.
(Lippincott Solutions 2018)
Snyder and Snyder (2008) also make the point that it’s helpful for educators and facilitators to be aware of any initial resistance that learners may have and try to guide them through the process. They should aim to create a learning environment where learners can feel comfortable thinking through an answer rather than simply having an answer given to them.
Examples include using peer coaching techniques , mentoring or preceptorship to engage students in active learning and critical thinking skills, or integrating project-based learning activities that require students to apply their knowledge in a realistic healthcare environment.
Carvalhoa et al. (2017) also advocate problem-based learning as a widely used and successful way of stimulating critical thinking skills in the learner. This view is echoed by Tsui-Mei (2015), who notes that critical thinking, systematic analysis and curiosity significantly improve after practice-based learning .
Integrating Critical Thinking Skills Into Curriculum Design
Most educators agree that critical thinking can’t easily be developed if the program curriculum is not designed to support it. This means that a deep understanding of the nature and value of critical thinking skills needs to be present from the outset of the curriculum design process , and not just bolted on as an afterthought.
In the view of Fortepiani (2018), critical thinking skills can be summarised by the statement that 'thinking is driven by questions', which means that teaching materials need to be designed in such a way as to encourage students to expand their learning by asking questions that generate further questions and stimulate the thinking process. Ideal questions are those that:
- Embrace complexity
- Challenge assumptions and points of view
- Question the source of information
- Explore variable interpretations and potential implications of information.
To put it another way, asking questions with limiting, thought-stopping answers inhibits the development of critical thinking. This means that educators must ideally be critical thinkers themselves .
Drawing these threads together, The Foundation for Critical Thinking (2017) offers us a simple reminder that even though it’s human nature to be ‘thinking’ most of the time, most thoughts, if not guided and structured, tend to be biased, distorted, partial, uninformed or even prejudiced.
They also note that the quality of work depends precisely on the quality of the practitioners’ thought processes. Given that practitioners are being asked to meet the challenge of ever more complex care, the importance of cultivating critical thinking skills, alongside advanced problem-solving skills , seems to be taking on new importance.
Additional Resources
- The Emotionally Intelligent Nurse | Ausmed Article
- Refining Competency-Based Assessment | Ausmed Article
- Socratic Questioning in Healthcare | Ausmed Article
- Carvalhoa, D P S R P et al. 2017, 'Strategies Used for the Promotion of Critical Thinking in Nursing Undergraduate Education: A Systematic Review', Nurse Education Today , vol. 57, pp. 103-10, viewed 7 December 2018, https://www.sciencedirect.com/science/article/abs/pii/S0260691717301715
- Fortepiani, L A 2017, 'Critical Thinking or Traditional Teaching For Health Professionals', PECOP Blog , 16 January, viewed 7 December 2018, https://blog.lifescitrc.org/pecop/2017/01/16/critical-thinking-or-traditional-teaching-for-health-professions/
- Jacob, E, Duffield, C & Jacob, D 2017, 'A Protocol For the Development of a Critical Thinking Assessment Tool for Nurses Using a Delphi Technique', Journal of Advanced Nursing, vol. 73, no. 8, pp. 1982-1988, viewed 7 December 2018, https://onlinelibrary.wiley.com/doi/10.1111/jan.13306
- Kahlke, R & Eva, K 2018, 'Constructing Critical Thinking in Health Professional Education', Perspectives on Medical Education , vol. 7, no. 3, pp. 156-165, viewed 7 December 2018, https://link.springer.com/article/10.1007/s40037-018-0415-z
- Lippincott Solutions 2018, 'Turning New Nurses Into Critical Thinkers', Lippincott Solutions , viewed 10 December 2018, https://www.wolterskluwer.com/en/expert-insights/turning-new-nurses-into-critical-thinkers
- Papp, K K 2014, 'Milestones of Critical Thinking: A Developmental Model for Medicine and Nursing', Academic Medicine , vol. 89, no. 5, pp. 715-720, https://journals.lww.com/academicmedicine/Fulltext/2014/05000/Milestones_of_Critical_Thinking___A_Developmental.14.aspx
- Snyder, L G & Snyder, M J 2008, 'Teaching Critical Thinking and Problem Solving Skills', The Delta Pi Epsilon Journal , vol. L, no. 2, pp. 90-99, viewed 7 December 2018, https://dme.childrenshospital.org/wp-content/uploads/2019/02/Optional-_Teaching-Critical-Thinking-and-Problem-Solving-Skills.pdf
- The Foundation for Critical Thinking 2017, Defining Critical Thinking , The Foundation for Critical Thinking, viewed 7 December 2018, https://www.criticalthinking.org/pages/our-conception-of-critical-thinking/411
- Tsui-Mei, H, Lee-Chun, H & Chen-Ju MSN, K 2015, 'How Mental Health Nurses Improve Their Critical Thinking Through Problem-Based Learning', Journal for Nurses in Professional Development , vol. 31, no. 3, pp. 170-175, viewed 7 December 2018, https://journals.lww.com/jnsdonline/Abstract/2015/05000/How_Mental_Health_Nurses_Improve_Their_Critical.8.aspx
Anne Watkins View profile
Help and feedback, publications.
Ausmed Education is a Trusted Information Partner of Healthdirect Australia. Verify here .

Critical Thinking in Nursing
- First Online: 02 January 2023
Cite this chapter

- Şefika Dilek Güven 3
Part of the book series: Integrated Science ((IS,volume 12))
1099 Accesses
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered. Nurses should develop their critical thinking skills so that they can analyze the problems of the current century, keep up with new developments and changes, cope with nursing problems they encounter, identify more complex patient care needs, provide more systematic care, give the most appropriate patient care in line with the education they have received, and make clinical decisions. The present chapter briefly examines critical thinking, how it relates to nursing, and which skills nurses need to develop as critical thinkers.
Graphical Abstract/Art Performance

Critical thinking in nursing.
This painting shows a nurse and how she is thinking critically. On the right side are the stages of critical thinking and on the left side, there are challenges that a nurse might face. The entire background is also painted in several colors to represent a kind of intellectual puzzle. It is made using colored pencils and markers.
(Adapted with permission from the Association of Science and Art (ASA), Universal Scientific Education and Research Network (USERN); Painting by Mahshad Naserpour).
Unless the individuals of a nation thinkers, the masses can be drawn in any direction. Mustafa Kemal Atatürk
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bilgiç Ş, Kurtuluş Tosun Z (2016) Birinci ve son sınıf hemşirelik öğrencilerinde eleştirel düşünme ve etkileyen faktörler. Sağlık Bilimleri ve Meslekleri Dergisi 3(1):39–47
Article Google Scholar
Kantek F, Yıldırım N (2019) The effects of nursing education on critical thinking of students: a meta-analysis. Florence Nightingale Hemşirelik Dergisi 27(1):17–25
Ennis R (1996) Critical thinking dispositions: their nature and assessability. Informal Logic 18(2):165–182
Riddell T (2007) Critical assumptions: thinking critically about critical thinking. J Nurs Educ 46(3):121–126
Cüceloğlu D (2001) İyi düşün doğru karar ver. Remzi Kitabevi, pp 242–284
Google Scholar
Kurnaz A (2019) Eleştirel düşünme öğretimi etkinlikleri Planlama-Uygulama ve Değerlendirme. Eğitim yayın evi, p 27
Doğanay A, Ünal F (2006) Eleştirel düşünmenin öğretimi. In: İçerik Türlerine Dayalı Öğretim. Ankara Nobel Yayınevi, pp 209–261
Scheffer B-K, Rubenfeld M-G (2000) A consensus statement on critical thinking in nursing. J Nurs Educ 39(8):352–359
Article CAS Google Scholar
Rubenfeld M-G, Scheffer B (2014) Critical thinking tactics for nurses. Jones & Bartlett Publishers, pp 5–6, 7, 19–20
Gobet F (2005) Chunking models of expertise: implications for education. Appl Cogn Psychol 19:183–204
Ay F-A (2008) Mesleki temel kavramlar. In: Temel hemşirelik: Kavramlar, ilkeler, uygulamalar. İstanbul Medikal Yayıncılık, pp 205–220
Birol L (2010) Hemşirelik bakımında sistematik yaklaşım. In: Hemşirelik süreci. Berke Ofset Matbaacılık, pp 35–45
Twibell R, Ryan M, Hermiz M (2005) Faculty perceptions of critical thinking in student clinical experiences. J Nurs Educ 44(2):71–79
The Importance of Critical Thinking in Nursing. 19 November 2018 by Carson-Newman University Online. https://onlinenursing.cn.edu/news/value-critical-thinking-nursing
Suzanne C, Smeltzer Brenda G, Bare Janice L, Cheever HK (2010) Definition of critical thinking, critical thinking process. Medical surgical nursing. Lippincott, Williams & Wilkins, pp 27–28
Profetto-McGrath J (2003) The relationship of critical thinking skills and critical thinking dispositions of baccalaureate nursing students. J Adv Nurs 43(6):569–577
Elaine S, Mary C (2002) Critical thinking in nursing education: literature review. Int J Nurs Pract 8(2):89–98
Brunt B-A (2005) Critical thinking in nursing: an integrated review. J Continuing Educ Nurs 36(2):60–67
Carter L-M, Rukholm E (2008) A study of critical thinking, teacher–student interaction, and discipline-specific writing in an online educational setting for registered nurses. J Continuing Educ Nurs 39(3):133–138
Daly W-M (2001) The development of an alternative method in the assessment of critical thinking as an outcome of nursing education. J Adv Nurs 36(1):120–130
Edwards S-L (2007) Critical thinking: a two-phase framework. Nurse Educ Pract 7(5):303–314
Rogal S-M, Young J (2008) Exploring critical thinking in critical care nursing education: a pilot study. J Continuing Educ Nurs 39(1):28–33
Worrell J-A, Profetto-McGrath J (2007) Critical thinking as an outcome of context-based learning among post RN students: a literature review. Nurse Educ Today 27(5):420–426
Morrall P, Goodman B (2013) Critical thinking, nurse education and universities: some thoughts on current issues and implications for nursing practice. Nurse Educ Today 33(9):935–937
Raymond-Seniuk C, Profetto-McGrath J (2011) Can one learn to think critically?—a philosophical exploration. Open Nurs J 5:45–51
Download references
Author information
Authors and affiliations.
Nevşehir Hacı Bektaş Veli University, Semra ve Vefa Küçük, Faculty of Health Sciences, Nursing Department, 2000 Evler Mah. Damat İbrahim Paşa Yerleşkesi, Nevşehir, Turkey
Şefika Dilek Güven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Şefika Dilek Güven .
Editor information
Editors and affiliations.
Universal Scientific Education and Research Network (USERN), Stockholm, Sweden
Nima Rezaei
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Güven, Ş.D. (2023). Critical Thinking in Nursing. In: Rezaei, N. (eds) Brain, Decision Making and Mental Health. Integrated Science, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-031-15959-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-15959-6_10
Published : 02 January 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-15958-9
Online ISBN : 978-3-031-15959-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Developing critical thinking skills for delivering optimal care
Scott IA, Hubbard RE, Crock C, et al. Developing critical thinking skills for delivering optimal care. Intern Med J. 2021;51(4):488-493. doi: 10.1111/imj.15272
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care – clinical reasoning, evidence-informed decision-making, and systems thinking – and approaches to develop these skills during clinician training.
Medication use and cognitive impairment among residents of aged care facilities. June 23, 2021
COVID-19 pandemic and the tension between the need to act and the need to know. October 14, 2020
Choosing wisely in clinical practice: embracing critical thinking, striving for safer care. April 6, 2022
Scoping review of studies evaluating frailty and its association with medication harm. June 22, 2022
Countering cognitive biases in minimising low value care. June 7, 2017
'More than words' - interpersonal communication, cognitive bias and diagnostic errors. August 11, 2021
A partially structured postoperative handoff protocol improves communication in 2 mixed surgical intensive care units: findings from the Handoffs and Transitions in Critical Care (HATRICC) prospective cohort study. February 6, 2019
Enabling a learning healthcare system with automated computer protocols that produce replicable and personalized clinician actions. August 4, 2021
Analysis of lawsuits related to diagnostic errors from point-of-care ultrasound in internal medicine, paediatrics, family medicine and critical care in the USA. June 24, 2020
Developing and aligning a safety event taxonomy for inpatient psychiatry. July 13, 2022
Changes in unprofessional behaviour, teamwork, and co-operation among hospital staff during the COVID-19 pandemic. September 28, 2022
Pharmacists reducing medication risk in medical outpatient clinics: a retrospective study of 18 clinics. March 8, 2023
Prevalence and causes of diagnostic errors in hospitalized patients under investigation for COVID-19. April 12, 2023
Barriers to accessing nighttime supervisors: a national survey of internal medicine residents. March 17, 2021
Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016 March 3, 2017
Seroprevalence of SARS-CoV-2 among frontline health care personnel in a multistate hospital network--13 academic medical centers, April-June 2020. September 23, 2020
Transforming the medication regimen review process using telemedicine to prevent adverse events. December 16, 2020
The MedSafer study-electronic decision support for deprescribing in hospitalized older adults: a cluster randomized clinical trial. February 2, 2022
Perceived patient safety culture in a critical care transport program. July 31, 2013
Video-based communication assessment of physician error disclosure skills by crowdsourced laypeople and patient advocates who experienced medical harm: reliability assessment with generalizability theory. May 18, 2022
Implementation of the I-PASS handoff program in diverse clinical environments: a multicenter prospective effectiveness implementation study. November 16, 2022
Patient harm from cardiovascular medications. August 25, 2021
Delays in diagnosis, treatment, and surgery: root causes, actions taken, and recommendations for healthcare improvement. June 1, 2022
Influence of opioid prescription policy on overdoses and related adverse effects in a primary care population. May 19, 2021
Evaluation of a second victim peer support program on perceptions of second victim experiences and supportive resources in pediatric clinical specialties using the second victim experience and support tool (SVEST). November 3, 2021
Diagnostic errors in hospitalized adults who died or were transferred to intensive care. January 17, 2024
Estimation of breast cancer overdiagnosis in a U.S. breast screening cohort. March 16, 2022
Multiple meanings of resilience: health professionals' experiences of a dual element training intervention designed to help them prepare for coping with error. March 31, 2021
Care coordination strategies and barriers during medication safety incidents: a qualitative, cognitive task analysis. March 10, 2021
TRIAD IX: can a patient testimonial safely help ensure prehospital appropriate critical versus end-of-life care? September 15, 2021
Preventing home medication administration errors. March 14, 2022
An act of performance: exploring residents' decision-making processes to seek help. April 14, 2021
A randomized trial of a multifactorial strategy to prevent serious fall injuries. July 29, 2020
Clinical predictors for unsafe direct discharge home patients from intensive care units. October 21, 2020
Association between limiting the number of open records in a tele-critical care setting and retract-reorder errors. July 21, 2021
Standardized assessment of medication reconciliation in post-acute care. April 27, 2022
Estimating the economic cost of nurse sensitive adverse events amongst patients in medical and surgical settings. June 16, 2021
Survey of nurses' experiences applying The Joint Commission's medication management titration standards. November 3, 2021
Effectiveness of acute care remote triage systems: a systematic review. February 5, 2020
Physician task load and the risk of burnout among US physicians in a national survey. December 2, 2020
Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. September 23, 2020
Patient and physician perspectives of deprescribing potentially inappropriate medications in older adults with a history of falls: a qualitative study. May 5, 2021
We asked the experts: the WHO Surgical Safety Checklist and the COVID-19 pandemic: recommendations for content and implementation adaptations. March 17, 2021
Association between surgeon technical skills and patient outcomes. September 9, 2020
Developing the Safer Dx Checklist of Ten Safety Recommendations for Health Care Organizations to address diagnostic errors. October 12, 2022
Influence of psychological safety and organizational support on the impact of humiliation on trainee well-being. June 8, 2022
Comparison of health care worker satisfaction before vs after implementation of a communication and optimal resolution program in acute care hospitals. April 5, 2023
Not overstepping professional boundaries: the challenging role of nurses in simulated error disclosures. September 21, 2011
Temporal associations between EHR-derived workload, burnout, and errors: a prospective cohort study. July 20, 2022
Adherence to national guidelines for timeliness of test results communication to patients in the Veterans Affairs health care system. May 4, 2022
Deferral of care for serious non-COVID-19 conditions: a hidden harm of COVID-19. November 18, 2020
An observational study of postoperative handoff standardization failures. June 23, 2021
Content analysis of patient safety incident reports for older adult patient transfers, handovers, and discharges: do they serve organizations, staff, or patients? January 8, 2020
Exploring the impact of employee engagement and patient safety. September 14, 2022
Deprescribing for community-dwelling older adults: a systematic review and meta-analysis. September 16, 2020
The abrupt expansion of ambulatory telemedicine: implications for patient safety. February 9, 2022
Nurse's Achilles Heel: using big data to determine workload factors that impact near misses. April 14, 2021
A diagnostic time-out to improve differential diagnosis in pediatric abdominal pain. July 14, 2021
What safety events are reported for ambulatory care? Analysis of incident reports from a patient safety organization. October 21, 2020
Expert consensus on currently accepted measures of harm. September 9, 2020
The July Effect in podiatric medicine and surgery residency. July 14, 2021
The calm before the storm: utilizing in situ simulation to evaluate for preparedness of an alternative care hospital during COVID-19 pandemic. June 2, 2021
Missed nursing care in the critical care unit, before and during the COVID-19 pandemic: a comparative cross-sectional study. June 22, 2022
The association between nurse staffing and omissions in nursing care: a systematic review. July 11, 2018
Creating a learning health system for improving diagnostic safety: pragmatic insights from US health care organizations. June 22, 2022
Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. June 8, 2016
Impact of the initial response to COVID-19 on long-term care for people with intellectual disability: an interrupted time series analysis of incident reports. October 14, 2020
Pediatric surgical errors: a systematic scoping review. July 20, 2022
Racial bias in pulse oximetry measurement. December 20, 2020
Accuracy of practitioner estimates of probability of diagnosis before and after testing. May 5, 2021
Recommendations for the safe, effective use of adaptive CDS in the US healthcare system: an AMIA position paper. April 21, 2021
Impact of interoperability of smart infusion pumps and an electronic medical record in critical care. September 23, 2020
Decreased incidence of cesarean surgical site infection rate with hospital-wide perioperative bundle. September 29, 2021
Association of diagnostic stewardship for blood cultures in critically ill children with culture rates, antibiotic use, and patient outcomes: results of the Bright STAR Collaborative. May 18, 2022
Second victim experiences of nurses in obstetrics and gynaecology: a Second Victim Experience and Support Tool Survey December 23, 2020
Understanding the second victim experience among multidisciplinary providers in obstetrics and gynecology. May 19, 2021
eSIMPLER: a dynamic, electronic health record-integrated checklist for clinical decision support during PICU daily rounds. June 16, 2021
Treatment patterns and clinical outcomes after the introduction of the Medicare Sepsis Performance Measure (SEP-1). May 5, 2021
Organizational safety climate and job enjoyment in hospital surgical teams with and without crew resource management training, January 26, 2022
Evaluation of effectiveness and safety of pharmacist independent prescribers in care homes: cluster randomised controlled trial. March 1, 2023
The Critical Care Safety Study: the incidence and nature of adverse events and serious medical errors in intensive care. August 24, 2005
Safety II behavior in a pediatric intensive care unit. August 1, 2018
The working hours of hospital staff nurses and patient safety. January 9, 2005
Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. October 21, 2020
Effects of tall man lettering on the visual behaviour of critical care nurses while identifying syringe drug labels: a randomised in situ simulation. April 20, 2022
Family Input for Quality and Safety (FIQS): using mobile technology for in-hospital reporting from families and patients. March 2, 2022
Bundle interventions including nontechnical skills for surgeons can reduce operative time and improve patient safety. December 9, 2020
COVID-19: an emerging threat to antibiotic stewardship in the emergency department. October 21, 2020
Improving self-reported empathy and communication skills through harm in healthcare response training. January 26, 2022
Association between in-clinic opioid administration and discharge opioid prescription in urgent care: a retrospective cohort study. February 17, 2021
Predicting avoidable hospital events in Maryland. December 1, 2021
Specificity of computerized physician order entry has a significant effect on the efficiency of workflow for critically ill patients. April 21, 2005
Why do hospital prescribers continue antibiotics when it is safe to stop? Results of a choice experiment survey. September 2, 2020
COVID-19: patient safety and quality improvement skills to deploy during the surge. June 24, 2020
Patient safety skills in primary care: a national survey of GP educators. February 4, 2015
Implementing human factors in anaesthesia: guidance for clinicians, departments and hospitals: Guidelines from the Difficult Airway Society and the Association of Anaesthetists. March 1, 2023
Can an electronic prescribing system detect doctors who are more likely to make a serious prescribing error? June 8, 2011
Training in safe opioid prescribing and treatment of opioid use disorder in internal medicine residencies: a national survey of program directors. October 12, 2022
Diagnostic discordance, health information exchange, and inter-hospital transfer outcomes: a population study. June 20, 2018
Systematic review and meta-analysis of interventions for operating room to intensive care unit handoffs. March 10, 2021
All in Her Head. The Truth and Lies Early Medicine Taught Us About Women's Bodies and Why It Matters Today. March 20, 2024
The racial disparities in maternal mortality and impact of structural racism and implicit racial bias on pregnant Black women: a review of the literature. December 6, 2023
A scoping review exploring the confidence of healthcare professionals in assessing all skin tones. October 4, 2023
Patient safety in palliative care at the end of life from the perspective of complex thinking. August 16, 2023
Only 1 in 5 people with opioid addiction get the medications to treat it, study finds. August 16, 2023
Factors influencing in-hospital prescribing errors: a systematic review. July 19, 2023
Introducing second-year medical students to diagnostic reasoning concepts and skills via a virtual curriculum. June 28, 2023
Context matters: toward a multilevel perspective on context in clinical reasoning and error. June 21, 2023
The good, the bad, and the ugly: operative staff perspectives of surgeon coping with intraoperative errors. June 14, 2023
Explicitly addressing implicit bias on inpatient rounds: student and faculty reflections. June 7, 2023
The time is now: addressing implicit bias in obstetrics and gynecology education. May 17, 2023
Listen to the whispers before they become screams: addressing Black maternal morbidity and mortality in the United States. May 3, 2023
Annual Perspective
Formalizing the hidden curriculum of performance enhancing errors. March 22, 2023
Implicit racial bias, health care provider attitudes, and perceptions of health care quality among African American college students in Georgia, USA. January 18, 2023
Structural racism and impact on sickle cell disease: sickle cell lives matter. January 11, 2023
The REPAIR Project: a prospectus for change toward racial justice in medical education and health sciences research: REPAIR project steering committee. January 11, 2023
Using the Assessment of Reasoning Tool to facilitate feedback about diagnostic reasoning. January 11, 2023
Exploring the intersection of structural racism and ageism in healthcare. December 7, 2022
Calibrate Dx: A Resource to Improve Diagnostic Decisions. October 19, 2022
Improved Diagnostic Accuracy Through Probability-Based Diagnosis. September 28, 2022
Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. September 21, 2022
A state-of-the-art review of speaking up in healthcare. August 24, 2022
Skin cancer is a risk no matter the skin tone. But it may be overlooked in people with dark skin. August 17, 2022
Oxford Professional Practice: Handbook of Patient Safety. July 27, 2022
Narrowing the mindware gap in medicine. July 20, 2022
From principles to practice: embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. June 15, 2022
A call to action: next steps to advance diagnosis education in the health professions. June 8, 2022
Does a suggested diagnosis in a general practitioners' referral question impact diagnostic reasoning: an experimental study. April 27, 2022
WebM&M Cases

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
Critical thinking in nursing clinical practice, education and research: From attitudes to virtue
Affiliations.
- 1 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, Consolidated Research Group Quantitative Psychology (2017-SGR-269), University of Barcelona, Barcelona, Spain.
- 2 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, Consolidated Research Group on Gender, Identity and Diversity (2017-SGR-1091), University of Barcelona, Barcelona, Spain.
- 3 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, University of Barcelona, Barcelona, Spain.
- 4 Multidisciplinary Nursing Research Group, Vall d'Hebron Research Institute (VHIR), Vall d'Hebron Hospital, Barcelona, Spain.
- PMID: 33029860
- DOI: 10.1111/nup.12332
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing profession. In this context, the ethics of virtue is a theoretical framework that becomes essential for analyse the critical thinking concept in nursing care and nursing science. Because the ethics of virtue consider how cultivating virtues are necessary to understand and justify the decisions and guide the actions. Based on selective analysis of the descriptive and empirical literature that addresses conceptual review of critical thinking, we conducted an analysis of this topic in the settings of clinical practice, training and research from the virtue ethical framework. Following JBI critical appraisal checklist for text and opinion papers, we argue the need for critical thinking as an essential element for true excellence in care and that it should be encouraged among professionals. The importance of developing critical thinking skills in education is well substantiated; however, greater efforts are required to implement educational strategies directed at developing critical thinking in students and professionals undergoing training, along with measures that demonstrate their success. Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student education and the growth of nursing science.
Keywords: critical thinking; critical thinking attitudes; nurse education; nursing care; nursing research.
© 2020 John Wiley & Sons Ltd.
- Attitude of Health Personnel*
- Education, Nursing / methods
- Nursing Process
- Nursing Research / methods
Grants and funding
- PREI-19-007-B/School of Nursing. Faculty of Medicine and Health Sciences. University of Barcelona

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

1.3: Critical Thinking and Clinical Reasoning
- Last updated
- Save as PDF
- Page ID 63335

- Ernstmeyer & Christman (Eds.)
- Chippewa Valley Technical College via OpenRN
Before learning how to use the nursing process, it is important to understand some basic concepts related to critical thinking and nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” [1] Using critical thinking means that nurses take extra steps to maintain patient safety and don’t just “follow orders.” It also means the accuracy of patient information is validated and plans for caring for patients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” To make sound judgments about patient care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience. [3]
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
Assessment is the first step of the nursing process. The American Nurses Association (ANA) “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” This includes collecting “pertinent data related to the health and quality of life in a systematic, ongoing manner, with compassion and respect for the wholeness, inherent dignity, worth, and unique attributes of every person, including but not limited to, demographics, environmental and occupational exposures, social determinants of health, health disparities, physical, functional, psychosocial, emotional, cognitive, spiritual/transpersonal, sexual, sociocultural, age-related, environmental, and lifestyle/economic assessments.” [1]
A registered nurse uses a systematic method to collect and analyze patient data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized patient in pain includes the patient’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff. Nurses assess patients to gather clues, make generalizations, and diagnose human responses to health conditions and life processes. Patient data is considered either subjective or objective, and it can be collected from multiple sources.
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.” [13] A nursing diagnosis is the nurse’s clinical judgment about the client's response to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses.
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the patient based on their assessment data and nursing diagnoses.
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” [16] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each patient’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the patient’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care. [17]
Nursing Care Plans
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific patient using the nursing process. Registered nurses (RNs) create nursing care plans so that the care provided to the patient across shifts is consistent among health care personnel.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.” Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the patient. Interventions are also documented in the patient’s electronic medical record as they are completed.
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” During evaluation, nurses assess the patient and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, patients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality patient care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a patient’s health care problems
- Improves patient safety
- Improves patient satisfaction
- Identifies a patient’s goals and strategies to attain them
- Increases the likelihood of achieving positive patient outcomes
- Saves time, energy, and frustration by creating a care plan or path to follow
By using these components of the nursing process as a critical thinking model, nurses plan interventions customized to the patient’s needs, plan outcomes and interventions, and determine whether those actions are effective in meeting the patient’s needs. In the remaining sections of this chapter, we will take an in-depth look at each of these components of the nursing process. Using the nursing process and implementing evidence-based practices are referred to as the “science of nursing.” Let’s review concepts related to the “art of nursing” while providing holistic care in a caring manner using the nursing process.
Holistic Nursing Care
The American Nurses Association (ANA) recently updated the definition of nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.”
The ANA further describes nursing is a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.”
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process.
Caring and the Nursing Process
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.” Successful use of the nursing process requires the development of a care relationship with the patient. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the patient and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being. Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, touching, and verbal reassurances while also respecting and being sensitive to the care recipient’s cultural beliefs and meanings associated with caring behaviors.
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41 (4), 215-221. ↵
- Powers, L., Pagel, J., & Herron, E. (2020). Nurse preceptors and new graduate success. American Nurse Journal, 15 (7), 37-39. ↵
- “ The Detective ” by paurian is licensed under CC BY 2.0 ↵
- “ In the Quiet Zone… ” by C.O.D. Library is licensed under CC BY-NC-SA 2.0 ↵
- NCSBN. (n.d.). NCSBN clinical judgment model . https://www.ncsbn.org/14798.htm ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “ The Nursing Process ” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Patient Image in LTC.JPG” by ARISE project is licensed under CC BY 4.0 ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (n.d.). The nursing process . https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- Walivaara, B., Savenstedt, S., & Axelsson, K. (2013). Caring relationships in home-based nursing care - registered nurses’ experiences. The Open Journal of Nursing, 7 , 89-95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3722540/pdf/TONURSJ-7-89.pdf ↵
- “ hospice-1793998_1280.jpg ” by truthseeker08 is licensed under CC0 ↵
- Watson Caring Science Institute. (n.d.). Watson Caring Science Institute. Jean Watson, PHD, RN, AHN-BC, FAAN, (LL-AAN) . https://www.watsoncaringscience.org/jean-bio/ ↵
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Critical thinking: what it is and why it counts. 2020. https://tinyurl.com/ybz73bnx (accessed 27 April 2021)
Faculty of Intensive Care Medicine. Curriculum for training for advanced critical care practitioners: syllabus (part III). version 1.1. 2018. https://www.ficm.ac.uk/accps/curriculum (accessed 27 April 2021)
Guerrero AP. Mechanistic case diagramming: a tool for problem-based learning. Acad Med.. 2001; 76:(4)385-9 https://doi.org/10.1097/00001888-200104000-00020
Harasym PH, Tsai TC, Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci.. 2008; 24:(7)341-55 https://doi.org/10.1016/S1607-551X(08)70131-1
Hayes MM, Chatterjee S, Schwartzstein RM. Critical thinking in critical care: five strategies to improve teaching and learning in the intensive care unit. Ann Am Thorac Soc.. 2017; 14:(4)569-575 https://doi.org/10.1513/AnnalsATS.201612-1009AS
Health Education England. Multi-professional framework for advanced clinical practice in England. 2017. https://www.hee.nhs.uk/sites/default/files/documents/multi-professionalframeworkforadvancedclinicalpracticeinengland.pdf (accessed 27 April 2021)
Health Education England, NHS England/NHS Improvement, Skills for Health. Core capabilities framework for advanced clinical practice (nurses) working in general practice/primary care in England. 2020. https://www.skillsforhealth.org.uk/images/services/cstf/ACP%20Primary%20Care%20Nurse%20Fwk%202020.pdf (accessed 27 April 2021)
Health Education England. Advanced practice mental health curriculum and capabilities framework. 2020. https://www.hee.nhs.uk/sites/default/files/documents/AP-MH%20Curriculum%20and%20Capabilities%20Framework%201.2.pdf (accessed 27 April 2021)
Jacob E, Duffield C, Jacob D. A protocol for the development of a critical thinking assessment tool for nurses using a Delphi technique. J Adv Nurs.. 2017; 73:(8)1982-1988 https://doi.org/10.1111/jan.13306
Kohn MA. Understanding evidence-based diagnosis. Diagnosis (Berl).. 2014; 1:(1)39-42 https://doi.org/10.1515/dx-2013-0003
Clinical reasoning—a guide to improving teaching and practice. 2012. https://www.racgp.org.au/afp/201201/45593
McGee S. Evidence-based physical diagnosis, 4th edn. Philadelphia PA: Elsevier; 2018
Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Acad Med.. 2017; 92:(1)23-30 https://doi.org/10.1097/ACM.0000000000001421
Papp KK, Huang GC, Lauzon Clabo LM Milestones of critical thinking: a developmental model for medicine and nursing. Acad Med.. 2014; 89:(5)715-20 https://doi.org/10.1097/acm.0000000000000220
Rencic J, Lambert WT, Schuwirth L., Durning SJ. Clinical reasoning performance assessment: using situated cognition theory as a conceptual framework. Diagnosis.. 2020; 7:(3)177-179 https://doi.org/10.1515/dx-2019-0051
Examining critical thinking skills in family medicine residents. 2016. https://www.stfm.org/FamilyMedicine/Vol48Issue2/Ross121
Royal College of Emergency Medicine. Emergency care advanced clinical practitioner—curriculum and assessment, adult and paediatric. version 2.0. 2019. https://tinyurl.com/eps3p37r (accessed 27 April 2021)
Young ME, Thomas A, Lubarsky S. Mapping clinical reasoning literature across the health professions: a scoping review. BMC Med Educ.. 2020; 20 https://doi.org/10.1186/s12909-020-02012-9
Advanced practice: critical thinking and clinical reasoning
Sadie Diamond-Fox
Senior Lecturer in Advanced Critical Care Practice, Northumbria University, Advanced Critical Care Practitioner, Newcastle upon Tyne Hospitals NHS Foundation Trust, and Co-Lead, Advanced Critical/Clinical Care Practitioners Academic Network (ACCPAN)
View articles
Advanced Critical Care Practitioner, South Tees Hospitals NHS Foundation Trust

Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. The application of clinical reasoning is central to the advanced non-medical practitioner (ANMP) role, as complex patient caseloads with undifferentiated and undiagnosed diseases are now a regular feature in healthcare practice. This article explores some of the key concepts and terminology that have evolved over the last four decades and have led to our modern day understanding of this topic. It also considers how clinical reasoning is vital for improving evidence-based diagnosis and subsequent effective care planning. A comprehensive guide to applying diagnostic reasoning on a body systems basis will be explored later in this series.
The Multi-professional Framework for Advanced Clinical Practice highlights clinical reasoning as one of the core clinical capabilities for advanced clinical practice in England ( Health Education England (HEE), 2017 ). This is also identified in other specialist core capability frameworks and training syllabuses for advanced clinical practitioner (ACP) roles ( Faculty of Intensive Care Medicine, 2018 ; Royal College of Emergency Medicine, 2019 ; HEE, 2020 ; HEE et al, 2020 ).
Rencic et al (2020) defined clinical reasoning as ‘a complex ability, requiring both declarative and procedural knowledge, such as physical examination and communication skills’. A plethora of literature exists surrounding this topic, with a recent systematic review identifying 625 papers, spanning 47 years, across the health professions ( Young et al, 2020 ). A diverse range of terms are used to refer to clinical reasoning within the healthcare literature ( Table 1 ), which can make defining their influence on their use within the clinical practice and educational arenas somewhat challenging.
The concept of clinical reasoning has changed dramatically over the past four decades. What was once thought to be a process-dependent task is now considered to present a more dynamic state of practice, which is affected by ‘complex, non-linear interactions between the clinician, patient, and the environment’ ( Rencic et al, 2020 ).
Cognitive and meta-cognitive processes
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting. Facione (2020) described critical thinking as ‘purposeful reflective judgement’ that consists of six discrete cognitive skills: analysis, inference, interpretation, explanation, synthesis and self–regulation. Ross et al (2016) identified that critical thinking positively correlates with academic success, professionalism, clinical decision-making, wider reasoning and problem-solving capabilities. Jacob et al (2017) also identified that patient outcomes and safety are directly linked to critical thinking skills.
Harasym et al (2008) listed nine discrete cognitive steps that may be applied to the process of critical thinking, which integrates both cognitive and meta-cognitive processes:
- Gather relevant information
- Formulate clearly defined questions and problems
- Evaluate relevant information
- Utilise and interpret abstract ideas effectively
- Infer well-reasoned conclusions and solutions
- Pilot outcomes against relevant criteria and standards
- Use alternative thought processes if needed
- Consider all assumptions, implications, and practical consequences
- Communicate effectively with others to solve complex problems.
There are a number of widely used strategies to develop critical thinking and evidence-based diagnosis. These include simulated problem-based learning platforms, high-fidelity simulation scenarios, case-based discussion forums, reflective journals as part of continuing professional development (CPD) portfolios and journal clubs.
Dual process theory and cognitive bias in diagnostic reasoning
A lack of understanding of the interrelationship between critical thinking and clinical reasoning can result in cognitive bias, which can in turn lead to diagnostic errors ( Hayes et al, 2017 ). Embedded within our understanding of how diagnostic errors occur is dual process theory—system 1 and system 2 thinking. The characteristics of these are described in Table 2 . Although much of the literature in this area regards dual process theory as a valid representation of clinical reasoning, the exact causes of diagnostic errors remain unclear and require further research ( Norman et al, 2017 ). The most effective way in which to teach critical thinking skills in healthcare education also remains unclear; however, Hayes et al (2017) proposed five strategies, based on well-known educational theory and principles, that they have found to be effective for teaching and learning critical thinking within the ‘high-octane’ and ‘high-stakes’ environment of the intensive care unit ( Table 3 ). This is arguably a setting that does not always present an ideal environment for learning given its fast pace and constant sensory stimulation. However, it may be argued that if a model has proven to be effective in this setting, it could be extrapolated to other busy clinical environments and may even provide a useful aide memoire for self-assessment and reflective practices.
Integrating the clinical reasoning process into the clinical consultation
Linn et al (2012) described the clinical consultation as ‘the practical embodiment of the clinical reasoning process by which data are gathered, considered, challenged and integrated to form a diagnosis that can lead to appropriate management’. The application of the previously mentioned psychological and behavioural science theories is intertwined throughout the clinical consultation via the following discrete processes:
- The clinical history generates an initial hypothesis regarding diagnosis, and said hypothesis is then tested through skilled and specific questioning
- The clinician formulates a primary diagnosis and differential diagnoses in order of likelihood
- Physical examination is carried out, aimed at gathering further data necessary to confirm or refute the hypotheses
- A selection of appropriate investigations, using an evidence-based approach, may be ordered to gather additional data
- The clinician (in partnership with the patient) then implements a targeted and rationalised management plan, based on best-available clinical evidence.
Linn et al (2012) also provided a very useful framework of how the above methods can be applied when teaching consultation with a focus on clinical reasoning (see Table 4 ). This framework may also prove useful to those new to the process of undertaking the clinical consultation process.
Evidence-based diagnosis and diagnostic accuracy
The principles of clinical reasoning are embedded within the practices of formulating an evidence-based diagnosis (EBD). According to Kohn (2014) EBD quantifies the probability of the presence of a disease through the use of diagnostic tests. He described three pertinent questions to consider in this respect:
- ‘How likely is the patient to have a particular disease?’
- ‘How good is this test for the disease in question?’
- ‘Is the test worth performing to guide treatment?’
EBD gives a statistical discriminatory weighting to update the probability of a disease to either support or refute the working and differential diagnoses, which can then determine the appropriate course of further diagnostic testing and treatments.
Diagnostic accuracy refers to how positive or negative findings change the probability of the presence of disease. In order to understand diagnostic accuracy, we must begin to understand the underlying principles and related statistical calculations concerning sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios.
The construction of a two-by-two square (2 x 2) table ( Figure 1 ) allows the calculation of several statistical weightings for pertinent points of the history-taking exercise, a finding/sign on physical examination, or a test result. From this construct we can then determine the aforementioned statistical calculations as follows ( McGee, 2018 ):
- Sensitivity , the proportion of patients with the diagnosis who have the physical sign or a positive test result = A ÷ (A + C)
- Specificity , the proportion of patients without the diagnosis who lack the physical sign or have a negative test result = D ÷ (B + D)
- Positive predictive value , the proportion of patients with disease who have a physical sign divided by the proportion of patients without disease who also have the same sign = A ÷ (A + B)
- Negative predictive value , proportion of patients with disease lacking a physical sign divided by the proportion of patients without disease also lacking the sign = D ÷ (C + D)
- Likelihood ratio , a finding/sign/test results sensitivity divided by the false-positive rate. A test of no value has an LR of 1. Therefore the test would have no impact upon the patient's odds of disease
- Positive likelihood ratio = proportion of patients with disease who have a positive finding/sign/test, divided by proportion of patients without disease who have a positive finding/sign/test OR (A ÷ N1) ÷ (B÷ N2), or sensitivity ÷ (1 – specificity) The more positive an LR (the further above 1), the more the finding/sign/test result raises a patient's probability of disease. Thresholds of ≥ 4 are often considered to be significant when focusing a clinician's interest on the most pertinent positive findings, clinical signs or tests
- Negative likelihood ratio = proportion of patients with disease who have a negative finding/sign/test result, divided by the proportion of patients without disease who have a positive finding/sign/test OR (C ÷ N1) ÷ (D÷N1) or (1 – sensitivity) ÷ specificity The more negative an LR (the closer to 0), the more the finding/sign/test result lowers a patient's probability of disease. Thresholds <0.4 are often considered to be significant when focusing clinician's interest on the most pertinent negative findings, clinical signs or tests.
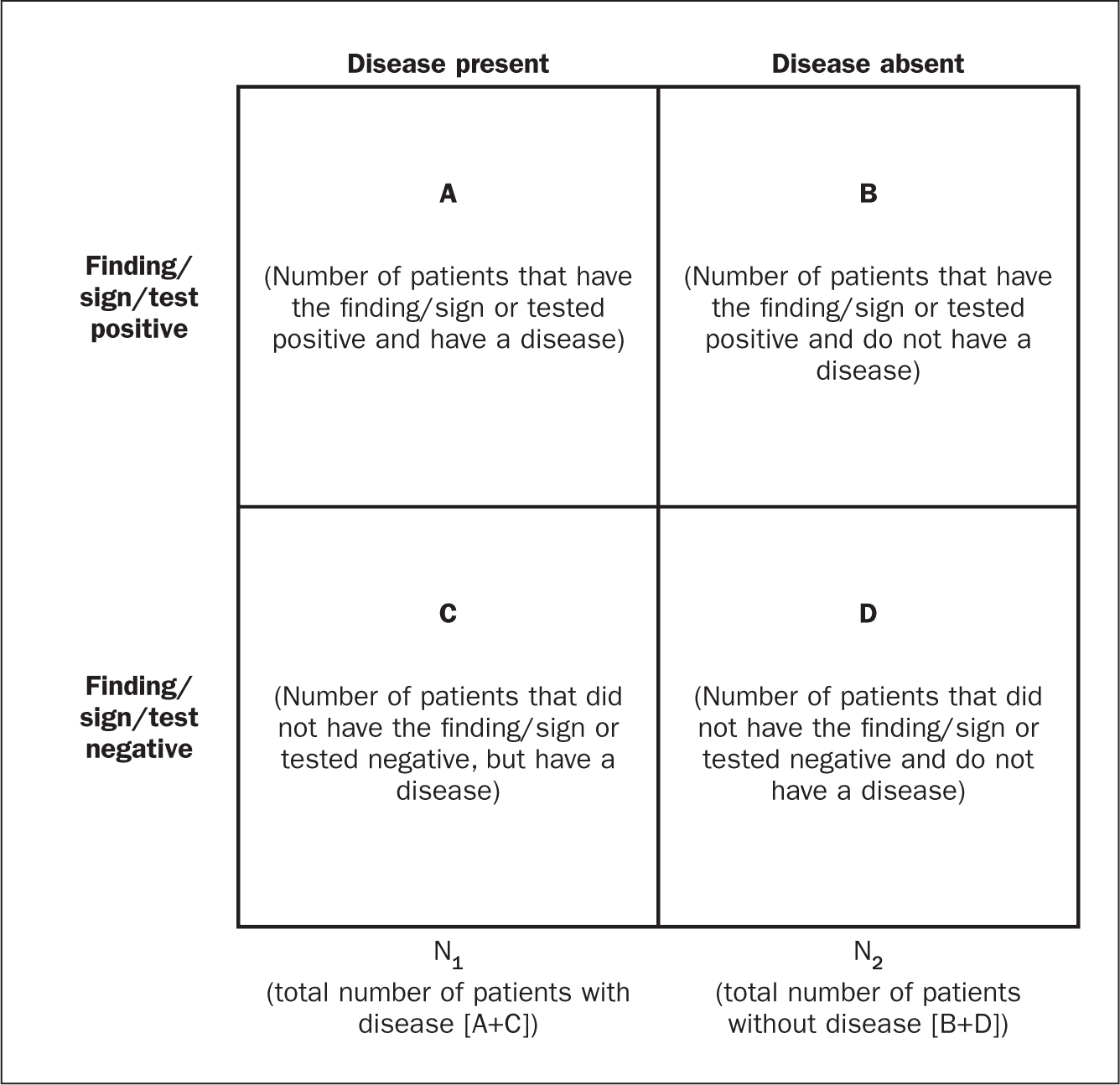
There are various online statistical calculators that can aid in the above calculations, such as the BMJ Best Practice statistical calculators, which may used as a guide (https://bestpractice.bmj.com/info/toolkit/ebm-toolbox/statistics-calculators/).
Clinical scoring systems
Evidence-based literature supports the practice of determining clinical pretest probability of certain diseases prior to proceeding with a diagnostic test. There are numerous validated pretest clinical scoring systems and clinical prediction tools that can be used in this context and accessed via various online platforms such as MDCalc (https://www.mdcalc.com/#all). Such clinical prediction tools include:
- 4Ts score for heparin-induced thrombocytopenia
- ABCD² score for transient ischaemic attack (TIA)
- CHADS₂ score for atrial fibrillation stroke risk
- Aortic Dissection Detection Risk Score (ADD-RS).
Conclusions
Critical thinking and clinical reasoning are fundamental skills of the advanced non-medical practitioner (ANMP) role. They are complex processes and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories. There are multiple constructs to guide these processes, not all of which will be suitable for the vast array of specialist areas in which ANMPs practice. There are multiple opportunities throughout the clinical consultation process in which ANMPs can employ the principles of critical thinking and clinical reasoning in order to improve patient outcomes. There are also multiple online toolkits that may be used to guide the ANMP in this complex process.
- Much like consultation and clinical assessment, the process of the application of clinical reasoning was once seen as solely the duty of a doctor, however the advanced non-medical practitioner (ANMP) role crosses those traditional boundaries
- Critical thinking and clinical reasoning are fundamental skills of the ANMP role
- The processes underlying clinical reasoning are complex and require an array of underpinning knowledge of not only the clinical sciences, but also psychological and behavioural science theories
- Through the use of the principles underlying critical thinking and clinical reasoning, there is potential to make a significant contribution to diagnostic accuracy, treatment options and overall patient outcomes
CPD reflective questions
- What assessment instruments exist for the measurement of cognitive bias?
- Think of an example of when cognitive bias may have impacted on your own clinical reasoning and decision making
- What resources exist to aid you in developing into the ‘advanced critical thinker’?
- What resources exist to aid you in understanding the statistical terminology surrounding evidence-based diagnosis?

COMMENTS
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
The findings suggest that any single definition of critical thinking in the health professions will be inherently contentious and, we argue, should be. Such debates, when made visible to educators and trainees, can be highly productive. ... primary care, geriatrics, paediatrics, mental health, critical care, and various consulting specialties ...
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. ... resulting in the following definition: Critical thinking in nursing is an essential component of professional accountability and quality nursing care. Critical thinkers in nursing exhibit these ...
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood ...
Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).. Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught, assessed and integrated into the design and development of staff and nurse education and training ...
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues ...
Critical thinking in nursing is considered essential for delivering quality care and reflects the professional accountability of registered nurses (Chang et al., 2011 ). It is also a vital part of the clinical assignments and responsibilities nurses are expected to manage. Additionally, nurses' critical thinking has the potential to influence ...
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care - clinical reasoning, evidence-informed decision-making, and systems thinking - and approaches to develop these skills during clinician training.
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
This chapter helps you begin the journey to improving thinking in two steps: (1) First you learn why health care organizations and nursing schools stress the need for critical thinking. (2) Secondly, you examine exactly what critical thinking is and how it relates to clinical reasoning and clinical judgment.
There has been a multidisciplinary plethora of critical thinking definitions stemming from educators in 19121 through and inclusive of today. As nurses' roles change in response to the dynamics of managed care and an increase in use of biotechnology in health care, more is expected of them both in terms of psychomotor and cognitive skills. The American Association for Colleges of Nursing ...
Critical thinking/problem-solving skills should emphasize self-examination. It should teach an individual to accomplish this using a series of steps that progress in a logical fashion, stressing that critical thinking is a progression of logical thought, not an unguided process. Pedagogy.
Critical thinking exposes assumptions, biases, and beliefs that influence clinical reasoning. This scoping review sought to explore instructional approaches for advancing students' critical thinking in healthcare education. Through analysis of 15 articles, no common definition of critical thinking emerged, nor consensus found on measurement ...
The Safe Care Framework ™ is an innovative pedagogy for critical thinking. •. Greater organization and understanding of complex acute care patients. •. Guiding of assessments and priorities. •. Better communication with others. •. Cognitive support for novice nurses to understand complexity.
Critical Thinking and Clinical Reasoning. Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow." [1] Using critical thinking means that nurses take extra steps to maintain patient safety ...
Healthcare systems across the world are challenged with problems of misdiagnosis, non-beneficial care, unwarranted practice variation and inefficient or unsafe practice. In countering these shortcomings, clinicians must be able to think critically, interpret and assimilate new knowledge, deal with uncertainty and change behaviour in response to ...
Critical thinking is the process of gathering information, fully assessing it and then developing an opinion in response. Nurses use critical thinking to make informed decisions about a patient's medical care such as choosing which tests to run and communicating their opinions to doctors. Nurses often are the first to examine a patient in a ...
As detailed in the table, multiple themes surrounding the cognitive and meta-cognitive processes that underpin clinical reasoning have been identified. Central to these processes is the practice of critical thinking. Much like the definition of clinical reasoning, there is also diversity with regard to definitions and conceptualisation of critical thinking in the healthcare setting.
Health care professional curricula need to facilitate the development of critical-thinking skills in students. This systematic review shows that there are mixed results with respect to the acquisition of critical-thinking skills in health care professional students as measured by the CCTST and the WGCTA. There are a limited number of moderate ...
Critical thinking is also called for in medical research and medical writing. Editors of leading medical journals have called for it. Edward Huth [39,40], former editor of Annals of Internal Medicine, has urged that medical articles reflect better and more organized ways of reasoning.Richard Horton [41,42], former editor of The Lancet, has proposed the use in medical writing of a contemporary ...