
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.


Autism Spectrum Disorder: Communication Problems in Children
On this page:
What is autism spectrum disorder?
Who is affected by asd, how does asd affect communication, how are the speech and language problems of asd treated, what research is being conducted to improve communication in children with asd, where can i find additional information about asd.
Autism spectrum disorder (ASD) is a developmental disability that can cause significant social, communication, and behavioral challenges. The term “spectrum” refers to the wide range of symptoms, skills, and levels of impairment that people with ASD can have.
ASD affects people in different ways and can range from mild to severe. People with ASD share some symptoms, such as difficulties with social interaction, but there are differences in when the symptoms start, how severe they are, the number of symptoms, and whether other problems are present. The symptoms and their severity can change over time.
The behavioral signs of ASD often appear early in development. Many children show symptoms by 12 months to 18 months of age or earlier.
ASD affects people of every race, ethnic group, and socioeconomic background. It is four times more common among boys than among girls. The Centers for Disease Control and Prevention (CDC) estimates that about 1 in every 54 children in the U.S. has been identified as having ASD.
The word “autism” has its origin in the Greek word “autos,” which means “self.” Children with ASD are often self-absorbed and seem to exist in a private world in which they have limited ability to successfully communicate and interact with others. Children with ASD may have difficulty developing language skills and understanding what others say to them. They also often have difficulty communicating nonverbally, such as through hand gestures, eye contact, and facial expressions.
The ability of children with ASD to communicate and use language depends on their intellectual and social development. Some children with ASD may not be able to communicate using speech or language, and some may have very limited speaking skills. Others may have rich vocabularies and be able to talk about specific subjects in great detail. Many have problems with the meaning and rhythm of words and sentences. They also may be unable to understand body language and the meanings of different vocal tones. Taken together, these difficulties affect the ability of children with ASD to interact with others, especially people their own age.
Below are some patterns of language use and behaviors that are often found in children with ASD.
- Repetitive or rigid language. Often, children with ASD who can speak will say things that have no meaning or that do not relate to the conversations they are having with others. For example, a child may count from one to five repeatedly amid a conversation that is not related to numbers. Or a child may continuously repeat words he or she has heard—a condition called echolalia. Immediate echolalia occurs when the child repeats words someone has just said. For example, the child may respond to a question by asking the same question. In delayed echolalia, the child repeats words heard at an earlier time. The child may say “Do you want something to drink?” whenever he or she asks for a drink. Some children with ASD speak in a high-pitched or sing-song voice or use robot-like speech. Other children may use stock phrases to start a conversation. For example, a child may say, “My name is Tom,” even when he talks with friends or family. Still others may repeat what they hear on television programs or commercials.
- Narrow interests and exceptional abilities. Some children may be able to deliver an in-depth monologue about a topic that holds their interest, even though they may not be able to carry on a two-way conversation about the same topic. Others may have musical talents or an advanced ability to count and do math calculations. Approximately 10 percent of children with ASD show “savant” skills, or extremely high abilities in specific areas, such as memorization, calendar calculation, music, or math.
- Uneven language development. Many children with ASD develop some speech and language skills, but not to a normal level of ability, and their progress is usually uneven. For example, they may develop a strong vocabulary in a particular area of interest very quickly. Many children have good memories for information just heard or seen. Some may be able to read words before age five, but may not comprehend what they have read. They often do not respond to the speech of others and may not respond to their own names. As a result, these children are sometimes mistakenly thought to have a hearing problem.
- Poor nonverbal conversation skills. Children with ASD are often unable to use gestures—such as pointing to an object—to give meaning to their speech. They often avoid eye contact, which can make them seem rude, uninterested, or inattentive. Without meaningful gestures or other nonverbal skills to enhance their oral language skills, many children with ASD become frustrated in their attempts to make their feelings, thoughts, and needs known. They may act out their frustrations through vocal outbursts or other inappropriate behaviors.
If a doctor suspects a child has ASD or another developmental disability, he or she usually will refer the child to a variety of specialists, including a speech-language pathologist. This is a health professional trained to treat individuals with voice, speech, and language disorders. The speech-language pathologist will perform a comprehensive evaluation of the child’s ability to communicate, and will design an appropriate treatment program. In addition, the speech-language pathologist might make a referral for a hearing test to make sure the child’s hearing is normal.
Teaching children with ASD to improve their communication skills is essential for helping them reach their full potential. There are many different approaches, but the best treatment program begins early, during the preschool years, and is tailored to the child’s age and interests. It should address both the child’s behavior and communication skills and offer regular reinforcement of positive actions. Most children with ASD respond well to highly structured, specialized programs. Parents or primary caregivers, as well as other family members, should be involved in the treatment program so that it becomes part of the child’s daily life.
For some younger children with ASD, improving speech and language skills is a realistic goal of treatment. Parents and caregivers can increase a child’s chance of reaching this goal by paying attention to his or her language development early on. Just as toddlers learn to crawl before they walk, children first develop pre-language skills before they begin to use words. These skills include using eye contact, gestures, body movements, imitation, and babbling and other vocalizations to help them communicate. Children who lack these skills may be evaluated and treated by a speech-language pathologist to prevent further developmental delays.
For slightly older children with ASD, communication training teaches basic speech and language skills, such as single words and phrases. Advanced training emphasizes the way language can serve a purpose, such as learning to hold a conversation with another person, which includes staying on topic and taking turns speaking.
Some children with ASD may never develop oral speech and language skills. For these children, the goal may be learning to communicate using gestures, such as sign language. For others, the goal may be to communicate by means of a symbol system in which pictures are used to convey thoughts. Symbol systems can range from picture boards or cards to sophisticated electronic devices that generate speech through the use of buttons to represent common items or actions.
The federal government’s Autism CARES Act of 2014 brought attention to the need to expand research and improve coordination among all of the components of the National Institutes of Health (NIH) that fund ASD research. These include the National Institute of Mental Health (NIMH), along with the National Institute on Deafness and Other Communication Disorders (NIDCD), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Institute of Environmental Health Sciences (NIEHS), the National Institute of Neurological Disorders and Stroke (NINDS), the National Institute of Nursing Research (NINR), and the National Center for Complementary and Integrative Health (NCCIH).
Together, five institutes within the NIH (NIMH, NIDCD, NICHD, NIEHS, and NINDS) support the Autism Centers of Excellence (ACE), a program of research centers and networks at universities across the country. Here, scientists study a broad range of topics, from basic science investigations that explore the molecular and genetic components of ASD to translational research studies that test new types of behavioral therapies. Some of these studies involve children with ASD who have limited speech and language skills, and could lead to testing new treatments or therapies. You can visit the NIH Clinical Trials website and enter the search term “autism” for information about current trials, their locations, and who may participate.
The NIDCD supports additional research to improve the lives of people with ASD and their families. An NIDCD-led workshop focused on children with ASD who have limited speech and language skills , resulting in two groundbreaking articles. 1 Another NIDCD workshop on measuring language in children with ASD resulted in recommendations calling for a standardized approach for evaluating language skills. The benchmarks will make it easier, and more accurate, to compare the effectiveness of different therapies and treatments.
NIDCD-funded researchers in universities and organizations across the country are also studying:
- Ways to reliably test for developmental delays in speech and language in the first year of life, with the ultimate goal of developing effective treatments to address the communication challenges faced by many with ASD.
- How parents can affect the results of different types of language therapies for children with ASD.
- Enhanced ways to improve communication between children with and without ASD. This could involve a communication board with symbols and pictures, or even a smartphone app.
- Techniques to help researchers better understand how toddlers with ASD perceive words, and the problems they experience with words.
- Cost-effective ways to prevent or reduce the impact of conditions affecting speech, language, and social skills in high-risk children (for example, younger siblings of children with ASD).
- The development of software to help people with ASD who struggle with speech to communicate complex thoughts and interact more effectively in society.
Information from other NIH Institutes and Centers that participate in ASD research is available on the NIH Health Information page by searching on the term “autism.”
In addition, the NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language.
For more information, contact us at:
NIDCD Information Clearinghouse 1 Communication Avenue Bethesda, MD 20892-3456 Toll-free Voice: (800) 241-1044 Toll-free TTY: (800) 241-1055 Email: [email protected]
NIH Pub. No. 97–4315 April 2020
Tager-Flusberg, H., & Kasari, C. (2013). Minimally verbal school-aged children with autism spectrum disorder: the neglected end of the spectrum. Autism Research, 6(6), 468–478. doi: 10.1002/aur.1329. Review.
* Note: PDF files require a viewer such as the free Adobe Reader .
- Patient Care & Health Information
- Diseases & Conditions
- Autism spectrum disorder
Autism spectrum disorder is a condition related to brain development that impacts how a person perceives and socializes with others, causing problems in social interaction and communication. The disorder also includes limited and repetitive patterns of behavior. The term "spectrum" in autism spectrum disorder refers to the wide range of symptoms and severity.
Autism spectrum disorder includes conditions that were previously considered separate — autism, Asperger's syndrome, childhood disintegrative disorder and an unspecified form of pervasive developmental disorder. Some people still use the term "Asperger's syndrome," which is generally thought to be at the mild end of autism spectrum disorder.
Autism spectrum disorder begins in early childhood and eventually causes problems functioning in society — socially, in school and at work, for example. Often children show symptoms of autism within the first year. A small number of children appear to develop normally in the first year, and then go through a period of regression between 18 and 24 months of age when they develop autism symptoms.
While there is no cure for autism spectrum disorder, intensive, early treatment can make a big difference in the lives of many children.
Products & Services
- Children’s Book: My Life Beyond Autism
Some children show signs of autism spectrum disorder in early infancy, such as reduced eye contact, lack of response to their name or indifference to caregivers. Other children may develop normally for the first few months or years of life, but then suddenly become withdrawn or aggressive or lose language skills they've already acquired. Signs usually are seen by age 2 years.
Each child with autism spectrum disorder is likely to have a unique pattern of behavior and level of severity — from low functioning to high functioning.
Some children with autism spectrum disorder have difficulty learning, and some have signs of lower than normal intelligence. Other children with the disorder have normal to high intelligence — they learn quickly, yet have trouble communicating and applying what they know in everyday life and adjusting to social situations.
Because of the unique mixture of symptoms in each child, severity can sometimes be difficult to determine. It's generally based on the level of impairments and how they impact the ability to function.
Below are some common signs shown by people who have autism spectrum disorder.
Social communication and interaction
A child or adult with autism spectrum disorder may have problems with social interaction and communication skills, including any of these signs:
- Fails to respond to his or her name or appears not to hear you at times
- Resists cuddling and holding, and seems to prefer playing alone, retreating into his or her own world
- Has poor eye contact and lacks facial expression
- Doesn't speak or has delayed speech, or loses previous ability to say words or sentences
- Can't start a conversation or keep one going, or only starts one to make requests or label items
- Speaks with an abnormal tone or rhythm and may use a singsong voice or robot-like speech
- Repeats words or phrases verbatim, but doesn't understand how to use them
- Doesn't appear to understand simple questions or directions
- Doesn't express emotions or feelings and appears unaware of others' feelings
- Doesn't point at or bring objects to share interest
- Inappropriately approaches a social interaction by being passive, aggressive or disruptive
- Has difficulty recognizing nonverbal cues, such as interpreting other people's facial expressions, body postures or tone of voice
Patterns of behavior
A child or adult with autism spectrum disorder may have limited, repetitive patterns of behavior, interests or activities, including any of these signs:
- Performs repetitive movements, such as rocking, spinning or hand flapping
- Performs activities that could cause self-harm, such as biting or head-banging
- Develops specific routines or rituals and becomes disturbed at the slightest change
- Has problems with coordination or has odd movement patterns, such as clumsiness or walking on toes, and has odd, stiff or exaggerated body language
- Is fascinated by details of an object, such as the spinning wheels of a toy car, but doesn't understand the overall purpose or function of the object
- Is unusually sensitive to light, sound or touch, yet may be indifferent to pain or temperature
- Doesn't engage in imitative or make-believe play
- Fixates on an object or activity with abnormal intensity or focus
- Has specific food preferences, such as eating only a few foods, or refusing foods with a certain texture
As they mature, some children with autism spectrum disorder become more engaged with others and show fewer disturbances in behavior. Some, usually those with the least severe problems, eventually may lead normal or near-normal lives. Others, however, continue to have difficulty with language or social skills, and the teen years can bring worse behavioral and emotional problems.
When to see a doctor
Babies develop at their own pace, and many don't follow exact timelines found in some parenting books. But children with autism spectrum disorder usually show some signs of delayed development before age 2 years.
If you're concerned about your child's development or you suspect that your child may have autism spectrum disorder, discuss your concerns with your doctor. The symptoms associated with the disorder can also be linked with other developmental disorders.
Signs of autism spectrum disorder often appear early in development when there are obvious delays in language skills and social interactions. Your doctor may recommend developmental tests to identify if your child has delays in cognitive, language and social skills, if your child:
- Doesn't respond with a smile or happy expression by 6 months
- Doesn't mimic sounds or facial expressions by 9 months
- Doesn't babble or coo by 12 months
- Doesn't gesture — such as point or wave — by 14 months
- Doesn't say single words by 16 months
- Doesn't play "make-believe" or pretend by 18 months
- Doesn't say two-word phrases by 24 months
- Loses language skills or social skills at any age
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Autism spectrum disorder has no single known cause. Given the complexity of the disorder, and the fact that symptoms and severity vary, there are probably many causes. Both genetics and environment may play a role.
- Genetics. Several different genes appear to be involved in autism spectrum disorder. For some children, autism spectrum disorder can be associated with a genetic disorder, such as Rett syndrome or fragile X syndrome. For other children, genetic changes (mutations) may increase the risk of autism spectrum disorder. Still other genes may affect brain development or the way that brain cells communicate, or they may determine the severity of symptoms. Some genetic mutations seem to be inherited, while others occur spontaneously.
- Environmental factors. Researchers are currently exploring whether factors such as viral infections, medications or complications during pregnancy, or air pollutants play a role in triggering autism spectrum disorder.
No link between vaccines and autism spectrum disorder
One of the greatest controversies in autism spectrum disorder centers on whether a link exists between the disorder and childhood vaccines. Despite extensive research, no reliable study has shown a link between autism spectrum disorder and any vaccines. In fact, the original study that ignited the debate years ago has been retracted due to poor design and questionable research methods.
Avoiding childhood vaccinations can place your child and others in danger of catching and spreading serious diseases, including whooping cough (pertussis), measles or mumps.
Risk factors
The number of children diagnosed with autism spectrum disorder is rising. It's not clear whether this is due to better detection and reporting or a real increase in the number of cases, or both.
Autism spectrum disorder affects children of all races and nationalities, but certain factors increase a child's risk. These may include:
- Your child's sex. Boys are about four times more likely to develop autism spectrum disorder than girls are.
- Family history. Families who have one child with autism spectrum disorder have an increased risk of having another child with the disorder. It's also not uncommon for parents or relatives of a child with autism spectrum disorder to have minor problems with social or communication skills themselves or to engage in certain behaviors typical of the disorder.
- Other disorders. Children with certain medical conditions have a higher than normal risk of autism spectrum disorder or autism-like symptoms. Examples include fragile X syndrome, an inherited disorder that causes intellectual problems; tuberous sclerosis, a condition in which benign tumors develop in the brain; and Rett syndrome, a genetic condition occurring almost exclusively in girls, which causes slowing of head growth, intellectual disability and loss of purposeful hand use.
- Extremely preterm babies. Babies born before 26 weeks of gestation may have a greater risk of autism spectrum disorder.
- Parents' ages. There may be a connection between children born to older parents and autism spectrum disorder, but more research is necessary to establish this link.
Complications
Problems with social interactions, communication and behavior can lead to:
- Problems in school and with successful learning
- Employment problems
- Inability to live independently
- Social isolation
- Stress within the family
- Victimization and being bullied
More Information
- Autism spectrum disorder and digestive symptoms
There's no way to prevent autism spectrum disorder, but there are treatment options. Early diagnosis and intervention is most helpful and can improve behavior, skills and language development. However, intervention is helpful at any age. Though children usually don't outgrow autism spectrum disorder symptoms, they may learn to function well.
- Autism spectrum disorder (ASD). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/autism/facts.html. Accessed April 4, 2017.
- Uno Y, et al. Early exposure to the combined measles-mumps-rubella vaccine and thimerosal-containing vaccines and risk of autism spectrum disorder. Vaccine. 2015;33:2511.
- Taylor LE, et al. Vaccines are not associated with autism: An evidence-based meta-analysis of case-control and cohort studies. Vaccine. 2014;32:3623.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Overview of management. https://www.uptodate.com/home. Accessed April 4, 2017.
- Autism spectrum disorder. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://dsm.psychiatryonline.org. Accessed April 4, 2017.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Complementary and alternative therapies. https://www.uptodate.com/home. Accessed April 4, 2017.
- Augustyn M. Autism spectrum disorder: Terminology, epidemiology, and pathogenesis. https://www.uptodate.com/home. Accessed April 4, 2017.
- Bridgemohan C. Autism spectrum disorder: Surveillance and screening in primary care. https://www.uptodate.com/home. Accessed April 4, 2017.
- Levy SE, et al. Complementary and alternative medicine treatments for children with autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America. 2015;24:117.
- Brondino N, et al. Complementary and alternative therapies for autism spectrum disorder. Evidence-Based Complementary and Alternative Medicine. http://dx.doi.org/10.1155/2015/258589. Accessed April 4, 2017.
- Volkmar F, et al. Practice parameter for the assessment and treatment of children and adolescents with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53:237.
- Autism spectrum disorder (ASD). Eunice Kennedy Shriver National Institute of Child Health and Human Development. https://www.nichd.nih.gov/health/topics/autism/Pages/default.aspx. Accessed April 4, 2017.
- American Academy of Pediatrics policy statement: Sensory integration therapies for children with developmental and behavioral disorders. Pediatrics. 2012;129:1186.
- James S, et al. Chelation for autism spectrum disorder (ASD). Cochrane Database of Systematic Reviews. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD010766.pub2/abstract;jsessionid=9467860F2028507DFC5B69615F622F78.f04t02. Accessed April 4, 2017.
- Van Schalkwyk GI, et al. Autism spectrum disorders: Challenges and opportunities for transition to adulthood. Child and Adolescent Psychiatric Clinics of North America. 2017;26:329.
- Autism. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed April 4, 2017.
- Autism: Beware of potentially dangerous therapies and products. U.S. Food and Drug Administration. https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm394757.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery. Accessed May 19, 2017.
- Drutz JE. Autism spectrum disorder and chronic disease: No evidence for vaccines or thimerosal as a contributing factor. https://www.uptodate.com/home. Accessed May 19, 2017.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Behavioral and educational interventions. https://www.uptodate.com/home. Accessed May 19, 2017.
- Huebner AR (expert opinion). Mayo Clinic, Rochester, Minn. June 7, 2017.
Associated Procedures
- Cognitive behavioral therapy
News from Mayo Clinic
- 10 significant studies from Mayo Clinic's Center for Individualized Medicine in 2023 Dec. 30, 2023, 12:00 p.m. CDT
- Mayo Clinic 'mini-brain' study reveals possible key link to autism spectrum disorder Aug. 10, 2023, 04:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Speech and Communication in Autism
People diagnosed with an autism spectrum disorder (ASD) can have a wide range of verbal abilities. Some may be entirely nonverbal , some may have limited useful speech, and some may speak fluently and intelligibly. Yet challenges with language and communication are hallmark autism traits.
When a person's verbal abilities are limited, they may sound and behave differently than their neurotypical peers. It can make it hard to communicate—to express ideas appropriately so that others understand them. Depending on their level of support needs , an autistic child can improve their verbal and communication skills with therapies designed to address these challenges.
This article discusses the ways in which it can be hard for autistic kids to express ideas appropriately so that others understand them. It offers information about some of the therapies used to help autistic people to communicate.
Speech and Language in Autism
Common characteristics of speech and language among autistic children include:
- High-pitched or flat intonation: Some autistic children speak in a high-pitched or sing-song voice, or may sound flat and robotic.
- Recitation: It is not uncommon for autistic children to recite lines from a movie word-for-word, or talk endlessly about a favorite topic that is irrelevant to the larger conversation.
- Lack of ability to understand slang: Autistic kids tend to treat language as literal and may not understand slang or the "kidspeak" of their peers.
- Repetition: Often, autistic kids repeat the same phrase over and over. For example, counting from one to five repeatedly or asking questions to which they already know the answer.
- Echolalia: Echolalia occurs when the child echos what someone has just said or asked them. For example, if someone asks "do you want a snack?" They will respond with "do you want a snack?" Or, they may develop "stock phrases" that they use in various situations.
- Uneven verbal and language development: An autistic child with lower support needs (formerly called Asperger's syndrome or high-functioning autism) may develop a strong vocabulary or be a precocious reader, but often only pertaining to a specific interest.
When autistic children are not able to respond when others speak to them, or to their own names, they are sometimes mistakenly thought to have a hearing problem.
Communication Problems
Verbal skills are only one aspect of effective communication. Body language—such as hand gestures, body stance, and making eye contact—conveys to others whether someone is joking or being serious, or angry or happy.
All of the skills involved with social communication presuppose an understanding of complex social expectations, coupled with an ability to self-modulate based on that understanding. Autistic people don't always have those abilities.
Sometimes, autistic people with low support needs find themselves frustrated when their attempts to communicate are met with blank stares or laughter. They may also be mistaken as rude. This is due to:
- A lack of understanding of physical gestures. Autistic children are often unable to give meaning to what they're saying through gestures, such as pointing to an object or using a facial expression.
- An inability to use the right type of speech at the right time. Communicating also requires an understanding of which type of speech is appropriate in a particular situation (known as pragmatic speech). For example, using a loud voice at a funeral can be interpreted as disrespectful, while very formal speech at school can be read as "nerdy." Using the appropriate type of speech involves an understanding of idioms, slang, and an ability to modulate tone, volume, and prosody (ups and downs of the voice).
- Difficulty making eye contact , which can be misinterpreted when autistic people try to communicate
Autistic people often find it challenging to "see" another's perspective. This inability to put yourself in someone else's shoes is often referred to as a lack of "theory of mind."
If your child's healthcare provider suspects autism, they will likely refer you to a speech-language pathologist, who will perform a comprehensive evaluation of your child’s ability to communicate and will then come up with an appropriate treatment program.
Addressing Speech and Communication Skills
Many autistic people are able to improve social communication by learning rules and techniques for better social interaction. Most children (and some adults) participate in treatment programs aimed at improving social communication through a combination of speech-language therapy and social skills therapy .
Speech-language therapy focuses not only on correct pronunciation, but also on intonation, back-and-forth conversation, and other aspects of pragmatic speech. Social skills therapy may involve role-playing exercises and group activities that require practicing collaboration, sharing, and related skills.
Ideally, treatment should begin during the preschool years, when language development occurs. Generally, autistic kids respond well to highly-structured, specialized programs. Parents and those involved in the care of these children should integrate treatment strategies so they become part of the child’s daily life.
Autistic children with intense traits and high support needs may never develop oral speech and language skills. Treatment goals then involve learning to communicate using gestures (such as sign language) or by means of a symbol system in which pictures are used to convey thoughts.
Communication difficulties are a key trait of autism, though they vary depending on the individual and their diagnosis. Some autistic people are nonverbal. Others develop language skills, although often these skills develop or are expressed in a neurodivergent way.
Speech is a factor, with many autistic people finding it hard to modulate speech or understand the patterns of prosody and eye contact. Just as challenging can be the things autistic people talk about, with the repetition of echolalia a common feature.
Speech therapy and other interventions can help autistic kids to develop language and communication skills. Contact your healthcare provider with any concerns about autism, the earlier the better, in order to ensure an accurate diagnosis and treatment.
American Speech-Language-Hearing Association. Autism
National Institute on Deafness and Other Hearing Disorders. Autism Spectrum Disorder: Communication in Children .
Brignell A, Chenausky KV, Song H, Zhu J, Suo C, Morgan AT. Communication interventions for autism spectrum disorder in minimally verbal children . Cochrane Database Syst Rev. 2018 Nov 5;11(11):CD012324. doi: 10.1002/14651858.CD012324.pub2
Adams, C. The Social Communication Intervention Project: a randomized controlled trial of the effectiveness of speech and language therapy for school-age children who have pragmatic and social communication problems with or without autism spectrum disorder . Int J Lang Commun Disord. 2012 May-Jun;47(3):233-44. doi: 10.1111/j.1460-6984.2011.00146.x.
Tierney, CD et al. 'Look at me when I am talking to you': evidence and assessment of social pragmatics interventions for children with autism and social communication disorders . Curr Opin Pediatr. 2014 Apr;26(2):259-64. doi: 10.1097/MOP.0000000000000075.
By Lisa Jo Rudy Rudy is a writer, consultant, author, and advocate who specializes in autism. Her work has appeared in The New York Times and Autism Parenting Magazine.

- Copy/Paste Link Link Copied
Speech-Language Therapy for Autism
Speech-language therapy can help people with autism spectrum disorder (ASD) improve their abilities to communicate and interact with others. 1
Verbal Skills
This type of therapy can help some people improve their spoken or verbal skills, such as:
- Correctly naming people and things
- Better explaining feelings and emotions
- Using words and sentences better
- Improving the rate and rhythm of speech
Nonverbal Communication
Speech-language therapy can also teach nonverbal communication skills, such as:
- Using hand signals or sign language
- Using picture symbols to communicate (Picture Exchange Communication System)
Speech-language therapy activities can also include ways to improve social skills and social behaviors. For example, a child might learn how to make eye contact or to stand at a comfortable distance from another person. These skills make it a little easier to interact with others.
- Paul, R. (2008). Interventions to improve communication in autism. Child and Adolescent Psychiatry Clinics of North America, 17 (4), 835–856.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Autism Spectrum Disorder
What is asd.
Autism spectrum disorder (ASD) is a neurological and developmental disorder that affects how people interact with others, communicate, learn, and behave. Although autism can be diagnosed at any age, it is described as a “developmental disorder” because symptoms generally appear in the first 2 years of life.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) , a guide created by the American Psychiatric Association that health care providers use to diagnose mental disorders, people with ASD often have:
- Difficulty with communication and interaction with other people
- Restricted interests and repetitive behaviors
- Symptoms that affect their ability to function in school, work, and other areas of life
Autism is known as a “spectrum” disorder because there is wide variation in the type and severity of symptoms people experience.
People of all genders, races, ethnicities, and economic backgrounds can be diagnosed with ASD. Although ASD can be a lifelong disorder, treatments and services can improve a person’s symptoms and daily functioning. The American Academy of Pediatrics recommends that all children receive screening for autism. Caregivers should talk to their child’s health care provider about ASD screening or evaluation.
What are the signs and symptoms of ASD?
The list below gives some examples of common types of behaviors in people diagnosed with ASD. Not all people with ASD will have all behaviors, but most will have several of the behaviors listed below.
Social communication / interaction behaviors may include:
- Making little or inconsistent eye contact
- Appearing not to look at or listen to people who are talking
- Infrequently sharing interest, emotion, or enjoyment of objects or activities (including infrequent pointing at or showing things to others)
- Not responding or being slow to respond to one’s name or to other verbal bids for attention
- Having difficulties with the back and forth of conversation
- Often talking at length about a favorite subject without noticing that others are not interested or without giving others a chance to respond
- Displaying facial expressions, movements, and gestures that do not match what is being said
- Having an unusual tone of voice that may sound sing-song or flat and robot-like
- Having trouble understanding another person’s point of view or being unable to predict or understand other people’s actions
- Difficulties adjusting behaviors to social situations
- Difficulties sharing in imaginative play or in making friends
Restrictive / repetitive behaviors may include:
- Repeating certain behaviors or having unusual behaviors, such as repeating words or phrases (a behavior called echolalia)
- Having a lasting intense interest in specific topics, such as numbers, details, or facts
- Showing overly focused interests, such as with moving objects or parts of objects
- Becoming upset by slight changes in a routine and having difficulty with transitions
- Being more sensitive or less sensitive than other people to sensory input, such as light, sound, clothing, or temperature
People with ASD may also experience sleep problems and irritability.
People on the autism spectrum also may have many strengths, including:
- Being able to learn things in detail and remember information for long periods of time
- Being strong visual and auditory learners
- Excelling in math, science, music, or art
What are the causes and risk factors for ASD?
Researchers don’t know the primary causes of ASD, but studies suggest that a person’s genes can act together with aspects of their environment to affect development in ways that lead to ASD. Some factors that are associated with an increased likelihood of developing ASD include:
- Having a sibling with ASD
- Having older parents
- Having certain genetic conditions (such as Down syndrome or Fragile X syndrome)
- Having a very low birth weight
How is ASD diagnosed?
Health care providers diagnose ASD by evaluating a person’s behavior and development. ASD can usually be reliably diagnosed by age 2. It is important to seek an evaluation as soon as possible. The earlier ASD is diagnosed, the sooner treatments and services can begin.
Diagnosis in young children
Diagnosis in young children is often a two-stage process.
Stage 1: General developmental screening during well-child checkups
Every child should receive well-child check-ups with a pediatrician or an early childhood health care provider. The American Academy of Pediatrics recommends that all children receive screening for developmental delays at their 9-, 18-, and 24- or 30-month well-child visits, with specific autism screenings at their 18- and 24-month well-child visits. A child may receive additional screening if they have a higher likelihood of ASD or developmental problems. Children with a higher likelihood of ASD include those who have a family member with ASD, show some behaviors that are typical of ASD, have older parents, have certain genetic conditions, or who had a very low birth weight.
Considering caregivers’ experiences and concerns is an important part of the screening process for young children. The health care provider may ask questions about the child’s behaviors and evaluate those answers in combination with information from ASD screening tools and clinical observations of the child. Read more about screening instruments on the Centers for Disease Control and Prevention (CDC) website.
If a child shows developmental differences in behavior or functioning during this screening process, the health care provider may refer the child for additional evaluation.
Stage 2: Additional diagnostic evaluation
It is important to accurately detect and diagnose children with ASD as early as possible, as this will shed light on their unique strengths and challenges. Early detection also can help caregivers determine which services, educational programs, and behavioral therapies are most likely to be helpful for their child.
A team of health care providers who have experience diagnosing ASD will conduct the diagnostic evaluation. This team may include child neurologists, developmental pediatricians, speech-language pathologists, child psychologists and psychiatrists, educational specialists, and occupational therapists.
The diagnostic evaluation is likely to include:
- Medical and neurological examinations
- Assessment of the child’s cognitive abilities
- Assessment of the child’s language abilities
- Observation of the child’s behavior
- An in-depth conversation with the child’s caregivers about the child’s behavior and development
- Assessment of age-appropriate skills needed to complete daily activities independently, such as eating, dressing, and toileting
Because ASD is a complex disorder that sometimes occurs with other illnesses or learning disorders, the comprehensive evaluation may include:
- Blood tests
- Hearing test
The evaluation may lead to a formal diagnosis and recommendations for treatment.
Diagnosis in older children and adolescents
Caregivers and teachers are often the first to recognize ASD symptoms in older children and adolescents who attend school. The school’s special education team may perform an initial evaluation and then recommend that a child undergo additional evaluation with their primary health care provider or a health care provider who specialize in ASD.
A child’s caregivers may talk with these health care providers about their child’s social difficulties, including problems with subtle communication. For example, some children may have problems understanding tone of voice, facial expressions, or body language. Older children and adolescents may have trouble understanding figures of speech, humor, or sarcasm. They also may have trouble forming friendships with peers.
Diagnosis in adults
Diagnosing ASD in adults is often more difficult than diagnosing ASD in children. In adults, some ASD symptoms can overlap with symptoms of other mental health disorders, such as anxiety disorder or attention-deficit/hyperactivity disorder (ADHD).
Adults who notice signs of ASD should talk with a health care provider and ask for a referral for an ASD evaluation. Although evaluation for ASD in adults is still being refined, adults may be referred to a neuropsychologist, psychologist, or psychiatrist who has experience with ASD. The expert will ask about:
- Social interaction and communication challenges
- Sensory issues
- Repetitive behaviors
- Restricted interests
The evaluation also may include a conversation with caregivers or other family members to learn about the person’s early developmental history, which can help ensure an accurate diagnosis.
Receiving a correct diagnosis of ASD as an adult can help a person understand past challenges, identify personal strengths, and find the right kind of help. Studies are underway to determine the types of services and supports that are most helpful for improving the functioning and community integration of autistic transition-age youth and adults.
What treatment options are available for ASD?
Treatment for ASD should begin as soon as possible after diagnosis. Early treatment for ASD is important as proper care and services can reduce individuals’ difficulties while helping them build on their strengths and learn new skills.
People with ASD may face a wide range of issues, which means that there is no single best treatment for ASD. Working closely with a health care provider is an important part of finding the right combination of treatment and services.
A health care provider may prescribe medication to treat specific symptoms. With medication, a person with ASD may have fewer problems with:
- Irritability
- Repetitive behavior
- Hyperactivity
- Attention problems
- Anxiety and depression
Read more about the latest medication warnings, patient medication guides, and information on newly approved medications at the Food and Drug Administration (FDA) website .
Behavioral, psychological, and educational interventions
People with ASD may be referred to a health care provider who specializes in providing behavioral, psychological, educational, or skill-building interventions. These programs are often highly structured and intensive, and they may involve caregivers, siblings, and other family members. These programs may help people with ASD:
- Learn social, communication, and language skills
- Reduce behaviors that interfere with daily functioning
- Increase or build upon strengths
- Learn life skills for living independently
Other resources
Many services, programs, and other resources are available to help people with ASD. Here are some tips for finding these additional services:
- Contact your health care provider, local health department, school, or autism advocacy group to learn about special programs or local resources.
- Find an autism support group. Sharing information and experiences can help people with ASD and their caregivers learn about treatment options and ASD-related programs.
- Record conversations and meetings with health care providers and teachers. This information may help when it’s time to decide which programs and services are appropriate.
- Keep copies of health care reports and evaluations. This information may help people with ASD qualify for special programs.
How can I find a clinical trial for ASD?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on ASD : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Where can I learn more about ASD?
Free brochures and shareable resources.
- Autism Spectrum Disorder : This brochure provides information about the symptoms, diagnosis, and treatment of ASD. Also available en español .
- Digital Shareables on Autism Spectrum Disorder : Help support ASD awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about ASD.
Federal resources
- Eunice Kennedy Shriver National Institute of Child Health and Human Development
- National Institute of Neurological Disorders and Stroke
- National Institute on Deafness and Other Communication Disorders
- Centers for Disease Control and Prevention (CDC)
- Interagency Autism Coordinating Committee
- MedlinePlus (also available en español )
Research and statistics
- Science News About Autism Spectrum Disorder : This NIMH webpage provides press releases and announcements about ASD.
- Research Program on Autism Spectrum Disorders : This NIMH program supports research focused on the characterization, pathophysiology, treatment, and outcomes of ASD and related disorders.
- Statistics: Autism Spectrum Disorder : This NIMH webpage provides information on the prevalence of ASD in the U.S.
- Data & Statistics on Autism Spectrum Disorder : This CDC webpage provides data, statistics, and tools about prevalence and demographic characteristics of ASD.
- Autism and Developmental Disabilities Monitoring (ADDM) Network : This CDC-funded program collects data to better understand the population of children with ASD.
- Biomarkers Consortium - The Autism Biomarkers Consortium for Clinical Trials (ABC-CT) : This Foundation for the National Institutes of Health project seeks to establish biomarkers to improve treatments for children with ASD.
Last Reviewed: February 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.

- Common misconceptions
- Set Your Location
- Learn the signs
- Symptoms of autism
- What causes autism?
- Asperger syndrome
- Autism statistics and facts
- Learn about screening
- Screening questionnaire
- First Concern to Action
- Autism diagnosis criteria: DSM-5
- Newly diagnosed
- Associated conditions
- Sensory issues
- Interventions
- Access services
- Caregiver Skills Training (CST)
- Information by topic
- Resource Guide
- Autism Response Team
- Our mission
- Our grantmaking
- Research programs
- Autism by the Numbers
- Fundraising & events
- World Autism Month
- Social fundraising
- Ways to give
- Memorial & tributes
- Workplace giving
- Corporate partnership
- Become a partner
- Ways to engage
- Meet our Partners
- Deteccion de autismo
- Deteccion temprana
- My Autism Guide
- Select Your Location
Please enter your location to help us display the correct information for your area.
Speech Therapy
What is speech therapy.
Speech-language therapy addresses challenges with language and communication. It can help people with autism improve their verbal, nonverbal, and social communication. The overall goal is to help the person communicate in more useful and functional ways.
Communication and speech-related challenges vary from person to person. Some individuals on the autism spectrum are not able to speak. Others love to talk, but have difficulty holding a conversation or understanding body language and facial expressions when talking with others.
A speech therapy program begins with an evaluation by a speech-language pathologist (SLP) to assess the person’s communication strengths and challenges. From this evaluation, the SLP creates individual goals for therapy.
Common goals may include improving spoken language, learning nonverbal skills such as signs or gestures, or learning to communicate using an alternative method (such as pictures or technology) .
Examples of the skills that speech therapy may work on include:
- Strengthening the muscles in the mouth, jaw and neck
- Making clearer speech sounds
- Matching emotions with the correct facial expression
- Understanding body language
- Responding to questions
- Matching a picture with its meaning
- Using a speech app on an iPad to produce the correct word
- Modulating tone of voice
Alternative Augmentative Communication (AAC)
Some people with autism find that using pictures or technology to communicate is more effective than speaking. This is known as Alternative Augmentative Communication (AAC) . Examples of AAC methods include:
- Sign language
- Picture exchange communication system (PECS)
- Speech output devices (such as Dynavox)
The speech-language pathologist can help to identify which AAC method (if any) is right for someone with autism and teach him/her how to use the method to communicate.
Learn more about AAC and autism .
You can also visit the American Speech-Language Hearing Association’s AAC webpage for more information.
Social Skills
Speech therapy can also help people work on goals related to social communication. Speech therapists sometimes offer social skills groups in addition to one-on-one therapy.
They may also work on coaching children and adults on communication in different settings. This can include how to communicate with friends, communicating in a relationship, appropriate behavior at work, and more.
Click here for more information on social skills.
Feeding Challenges
Some SLPs are specifically trained to address feeding and swallowing challenges in people with autism. They can evaluate the particular issue a person is dealing with and provide treatment plans for improving feeding-related challenges.
Click here for more information on feeding issues.
Where are services provided?
Speech therapy can take place in a variety of settings:.
- Private clinic setting
- At school, through an Individualized Education Program (IEP)
- At home, as part of an Early Intervention program for children under 3
- In the community, to practice new skills in a natural environment
Services can be provided one-on-one, or in a group setting depending on what skill is being practiced.
Who provides the services?
Speech-Language Pathologists (SLP) provide speech therapy services. They have a master’s degree and are specially licensed to practice through the state.
You may notice that a speech therapist has the credentials “CCC-SLP” after their name. This stands for Certificate of Clinical Competence (CCC) and is a credential through the American Speech-Language Hearing Association (ASHA). It indicates that the speech therapist has achieved excellence in academic and professional standards. You can learn more on the ASHA website.
In some cases, a Speech Therapy Assistant provides direct speech therapy services. This is a person with an associate’s or bachelor’s degree, who is trained and supervised by a certified speech-language pathologist. The assistant works directly with the person with autism to practice skills and work towards goals that are written by the SLP in the clinical treatment plan.
Is it covered by insurance?
Yes, s peech therapy is often covered by health insurance. In some cases, a doctor must state that the therapy is medically necessary for health insurance to provide coverage. [Please see our insurance resources for more information about insurance and coverage for autism services.]
Students can get speech therapy as part of their Individualized Education Program (IEP) at school. Speech therapy is often written into IEPs as a related service. Speech services as part of an IEP are provided at no cost to families.
Some young children receive speech therapy through their Early Intervention program. Early intervention is offered in each state to children under age 3 who are not growing and developing at the same rate as others. These services are free or low-cost based on your family income.
Where do I find a speech therapist?
- Autism Speaks Directory
- American Speech-Language Hearing Association (ASHA)
What questions should I ask?
The following questions can help you learn more about speech therapy before you begin. It can also help you learn whether a particular speech therapist or clinic is a good fit for your family:
- Who will be working directly with my child?
- How many years have you been working with people with autism?
- Where will services be provided?
- What does the initial assessment involve?
- What type of insurance do you accept? Will my insurance cover your services?
- Do you have a waiting list?
- How many hours of therapy per week?
- How long are therapy sessions?
- Can I observe my child’s sessions?
- What is a typical caseload for each therapist?
- How are goals determined? Can clients and parents provide input?
- What does a typical program look like?
- How do you measure progress?
- What are some of the typical milestones for speech and language?
- What can we do to practice at home?
- What progress should we expect?
Your Internet Explorer 11 browser is not supported by this site. Please upgrade to a recent browser for the best experience.
Autism and speech
Published on 13 July 2017
Author: Kathleen Scaler Scott
Kathleen Scaler Scott is Associate Professor at the Department of Speech-Language Pathology, Misericordia University. She explains what fluency disorders are, how they may present in autistic people and what speech and language therapists (SALTs) can do to assist.
Autism and disfluent speech
For decades, researchers have identified patterns of “disfluent speech” in autistic individuals, i.e. speech that exhibits deviations in continuity, fluidity, ease of rate and effort, with hesitations or repetition of sounds, words, or phrases. More recently, the nature and presence of this disfluent speech has become clearer. Three different types of disfluency have been identified:
Stuttering occurs when a person is clear on the words they would like to say, but physically has difficulty getting these words out. People who stutter have difficulty moving forward in producing their words and may:
- repeat sounds(s-s-s-speech)
- repeat syllables (ru-ru-running)
- prolong sounds (sssspeech, whaaat)
- become 'stuck' (blocked) on a sound (s------speech)
During a stuttering block it will take time for the word to come out, and during the block struggled attempts at sound production may be heard, or there may be silence.
Cluttering occurs when a speaker speaks at a rate that is too fast for their system to handle. Those who clutter sound fast to the listener, and listeners have difficulty understanding the person with cluttering due to the presence of at least one of three symptoms:
- excessive repetitions of phrases, revisions of ideas, filler words such as “um” or “uh”
- excessive over-coarticulation. Sounds in words run together and sounds or syllables may be deleted. For example, “It’s like this” may sound like, “slikethi.”
- pauses in places where they would not be expected grammatically.
Atypical disfluency
Atypical disfluencies occur when the speaker has easy repetitions or prolongations of sounds at the ends of words (speech-eech, light-t, misssss) or inserts a sound in the middle of a word (e.g. boy becomes (boy-hoy.). Research is in its infancy regarding these atypical disfluencies. Observations among researchers suggest that these disfluencies differ from stuttering in that the repetitions often occur after the speaker has completed the word. Whereas the individual with stuttering has difficulty starting a word, a speaker with atypical disfluency seems to have difficulty ending the word. Sometimes the end-of-word repetitions occur immediately (speech-eech) and other times after a pause (speech (pause) -eech). The length of the pause varies between individuals, and some have been known to insert another thought in between the pause and the repetition (e.g., “Can you turn out the light (“Oh I like that book”; pause) -ight so I can go to sleep?”).
Life impact
In addition to the outward symptoms of disfluencies, some speakers experience negative feelings and perceptions about their difficulties. Although these negative feelings and perceptions are most common among those who stutter, feelings such as shame, embarrassment, or fear can also occur in response to cluttering, or atypical disfluencies. Additionally, speakers may have cognitive misperceptions about their fluency disorder, such as thoughts that they will always stutter when they say their name, or that they will never be able to be employed in a career that involves speaking. These negative feelings and perceptions can lead to communication avoidance. Individuals with stuttering, in particular, may exhibit tension in their face or other areas of the body when attempting to speak.
Disfluency in autism
Awareness of disfluency is variable in many autistic people, especially among those who clutter and/or exhibit atypical disfluencies. It is important to note that awareness occurs along a continuum. Each person should be assessed as an individual to determine which factors may be contributing to difficulties with efficient and effective communication and therefore may need to be addressed in treatment. Speech and language professionals specifically trained in assessment and treatment of fluency disorders can help with assessing disfluency and any accompanying characteristics. It is important to remember that multiple types of disfluencies can present themselves in the same speaker. Although research continues to emerge, all types of disfluencies have been found in pre-schoolers, school-age children, teens and adults on the autism spectrum. Disfluencies have also been identified across all cognitive abilities. The overall negative impact upon communication should be considered when prioritising goals for speech and language therapy. Communication avoidance and limits to social interaction should be red flags for prioritising fluency assessment and possible therapy.
How speech and language therapy can help autistic individuals
The first thing that a speech and language therapist (SALT) can do is to help identify any disfluencies by type. If there is negative life impact, the SALT can work with the client. If the SALT is not comfortable working with fluency disorders, they can refer the individual to someone experienced in treating fluency disorders.
- If stuttering, treatment strategies will focus on changing the timing and tension of speech.
- If cluttering, treatment will focus upon rate regulation through natural pausing and emphasis of sounds for clarity.
- If atypical disfluency, the proposed function of the disfluency will be determined and the corresponding underlying “root” cause(s) may be addressed. For example, if a client seems to be repeating the end of a word to hold their place due to difficulties with word finding, the SALT may work directly on word finding to eliminate the need to hold their place, as well as natural pausing (instead of repetition) to hold their place when more time is needed.
Further reading
For review of disfluencies in autism spectrum disorders, see:
- Scaler Scott, K., Tetnowski, J. A., Flaitz, J., & Yaruss, J. S. (2014, Jan-Feb). Preliminary study of disfluency in school-age children with autism. International Journal of Language and Communication Disorders, 49(1), 75-89.
For therapy management techniques for cluttering, including cluttering in the ASD population, see:
- Scaler Scott, K., & Ward, D. (2013). Managing Cluttering: A Comprehensive Guidebook of Activities. Austin, TX: Pro-Ed, Inc. 11
For more information regarding assessment, differential diagnosis, and treatment of individuals with fluency disorders and other diagnoses including autism, see the forthcoming guide:
- Scaler Scott, K. (in press). Fluency Plus: Managing Fluency Disorders in Individuals with Multiple Diagnoses. Thorofare, NJ: SLACK, Inc.
Article sources
Related professional practice, sensory differences.

An interview with Peter Vermeulen
Eating disorder or disordered eating?

Differences between avoidant eating and anorexia nervosa
Cookies on this site
Our site uses cookies for key functions and to give you the best experience. Use cookie settings to control which cookies are allowed or click on Allow Optional Cookies to allow all cookies. For more detailed information please see our cookie policy .
Please wait while we check your current settings
Speech and Language Problems in ASD
- Faculty+Staff
- Make an Appointment
- Access Epic CareLink
- Access the Network
- Get Directions
- Request Medical Records
- Find a Specialist
- Find Departments
- Search Jobs
- Donate or Volunteer
- Contact the Institute
- Refer a Patient
- Pay My Bill
Frequently Searched Terms and Topics
- Resources for Patients & Families
Faculty & Staff
Centers & programs.
- , Directions
General Information
Barry Gordon, MD, PhD Professor, Department of Neurology The Johns Hopkins Medical Institutions Department of Neurology Cognitive Neurology/Neuropsychology Baltimore, Maryland, USA
Date Published: April 2, 2007
A Neurologist's Perspective/A Parent's Perspective
Problems with speech and language are one of the defining characteristics of the Autism Spectrum Disorders. However, the difficulties that individuals with autism have with speech and language are very heterogenous and probably have a number of different causes or contributing factors, even in the same individual. My colleagues and I have been trying for some time both to investigate the speech and language problems that can occur in autism and to develop possible treatments for them. In addition, I am the father of a nonverbal 14 year old with autism. What follows is a general overview of my perspective on these problems and how they can be assessed and approached for what treatment is possible. Any actual assessment and treatment plan of any particular individual needs to be far more detailed and follow much more detailed logic than this overview allows. However, I am hopeful that it will still be useful for helping parents and teachers interpret what is wrong, what is right, and what can be done to possibly make things better for such individuals.
Normal Speech and Language
The fullest expression of normal human speech and language requires the desire or intent to communicate something. Also, in its fullest form, it also requires an appreciation of what the other individual understands about a situation and how they are supposed to react to what is being communicated. As the next stage beyond the formulation of an intent or goal in communication, speech and language normally require a mental representation of the message (semantics), next, a representation of the message in terms of words (mentally), and, finally, an articulation of the mental words as physical sounds (articulation of speech). Other ways of expressing mental words are possible, such as gesture (including sign language) or typing. Messages may also have an emotional component that, in English, is signalled by changes in the volume or pitch. Comprehension of speech and language is normally done through sound. This requires paying attention to the sounds, then being able to decipher the sounds in terms of words, then being able to understand the words in terms of intended meanings, and, finally, appreciating the meanings in terms of intentions, actions, or what have you. Vision (perception of gestures and signs or of printed words) and touch (Braille) can also be used as alternative or additional routes into the perception of letters and words.
Impairments in Individuals With Autism
Individuals with autism can have problems with any or all of these aspects involved in producing or understanding speech and language. In particular, for example, because of their deficits in appreciating social situations, they may not feel any need to communicate and may very well not have any understanding of how other people might respond to a communicated message. Individuals with autism frequently appear to have deficits in paying attention to auditory information. They frequently have to be trained to pay attention to sounds. Even when they are paying attention, many individuals with autism seem to have difficulty in decoding what sounds mean and in matching them to words or thoughts. In some individuals with autism, this may be because they actually have difficulties with words and thoughts themselves. In others, it may be more because of a mapping problem. Individuals with autism frequently have difficulties with articulation, often as part of a broader problem of difficulty with oral-motor functions (movements of the lips and tongue and associated breath control). On the plus side, however, individuals with autism are frequently very good with paying attention and appreciating visual materials. Therefore, the visual route is often one way of getting access to their minds and giving them a way of expressing themselves, in turn.
In any given individual, which particular problems they have and which problems are hampering them most in any particular stage of development can only be determined by a careful assessment. Standardized testing can help to some extent, but it requires careful administration and interpretation, in part, because many standardized tests were not developed with a consideration of the kinds of deficits that individuals with autism may have. Therefore, both the administration and the interpretation of such tests may be problematic because of the unusual pattern of performance. To give just one example, because of their markedly restricted interests, individuals with autism may only rarely show any particular verbal ability and may never show the ability when placed in an unusual testing situation with an unfamiliar examiner. In such a case, the reports of parents and teachers who are more familiar with the child’s capabilities can provide an important clue to what is possible for them and what is not.
In our research and educational program, we try to construct for each child an individualized map of their abilities and disabilities. Is the child aware that he or she is being spoken to? Do they ever try to communicate by any means? Are they echolalic (that is, do they repeat sounds or words spoken to them)? Echolalia, for example, is a clue that the child can perceive speech and articulate speech, so any problems that they may be having with speech and language must be beyond those levels.
Individuals with autism may have problems impeding their development of speech and language that are well outside the scope of traditional speech and language therapy (such as social deficits) or, at the very least, in the very frontiers of clinical knowledge as to appropriate treatment (developmental articulation disorders). Parents and teachers are confronted by a bewildering range of options and apparent philosophies of treatment of these individuals. However, what really matters most is the empathy, energy, and flexibility of the particular therapist or therapists. In many cases, for example, therapists with seemingly very different philosophies will have surprisingly similar treatment plans because of the realities of the particular individual they deal with.
Does My Child Have Autism?
Helping your child with autism thrive, autism treatments, interventions, and therapy options, adult autism and relationships.
- Autism at Work: Overcoming Challenges
- Autism in Adults: Recognizing the Signs, Living with a Diagnosis
Autism Behavior Problems
Learning disabilities and disorders.
- Online Therapy: Is it Right for You?
- Mental Health
- Health & Wellness
- Children & Family
- Relationships
Are you or someone you know in crisis?
- Bipolar Disorder
- Eating Disorders
- Grief & Loss
- Personality Disorders
- PTSD & Trauma
- Schizophrenia
- Therapy & Medication
- Exercise & Fitness
- Healthy Eating
- Well-being & Happiness
- Weight Loss
- Work & Career
- Illness & Disability
- Heart Health
- Childhood Issues
- Learning Disabilities
- Family Caregiving
- Teen Issues
- Communication
- Emotional Intelligence
- Love & Friendship
- Domestic Abuse
- Healthy Aging
- Aging Issues
- Alzheimer’s Disease & Dementia
- Senior Housing
- End of Life
- Meet Our Team
Understanding autism spectrum disorders
- What's in a name? Making sense of autism terminology
Autism Spectrum Disorder symptoms
Related signs and symptoms of autism spectrum disorder, how is autism diagnosed, autism spectrum disorders (asd).
This parent’s guide to symptoms and diagnosis can help you better understand your child, decipher all the different autism terms, and make it easier to communicate with doctors, teachers, and therapists.

Ted Hutman, Ph.D. is Assistant Clinical Professor in Psychiatry at the David Geffen School of Medicine at UCLA and a licensed clinical psychologist practicing in Santa Monica, CA.
Autism is not a single disorder, but a spectrum of closely related disorders with a shared core of symptoms. Every individual on the autism spectrum has problems to some degree with social interaction, empathy, communication, and flexible behavior. But the level of disability and the combination of symptoms varies tremendously from person to person. In fact, two kids with the same diagnosis may look very different when it comes to their behaviors and abilities.
If you’re a parent dealing with a child on the autism spectrum, you may hear many different terms including high-functioning autism , atypical autism , autism spectrum disorder , and pervasive developmental disorder . These terms can be confusing, not only because there are so many, but because doctors, therapists, and other parents may use them in dissimilar ways.
But no matter what doctors, teachers, and other specialists call the autism spectrum disorder, it’s your child’s unique needs that are truly important. No diagnostic label can tell you exactly what challenges your child will have. Finding treatment that addresses your child’s needs, rather than focusing on what to call the problem, is the most helpful thing you can do. You don’t need a diagnosis to start getting help for your child’s symptoms.
What’s in a name? Making sense of autism terminology
There is understandably a great deal of confusion about the names of various autism-related disorders. Some professionals speak of “the autisms” to avoid addressing the sometimes subtle differences among the conditions along the autism spectrum. Up to 2013, there were five different “autism spectrum disorders.” The differences among those five were hard to understand for parents trying to figure out which—if any—of these conditions affected their child.
The American Psychiatric Association attempted to simplify matters by combining the pervasive developmental disorders into a single diagnostic classification called “Autism Spectrum Disorder” in the latest edition of the diagnostic bible known as the Diagnostic and Statistical Manual of Mental Disorders . Since many people were diagnosed prior to the change in the classification system and since many professionals still refer to the pre-2013 labels, we summarize them here for your reference. For purposes of clarity, we emphasize that all of the following conditions are now encompassed under the umbrella classification “Autism Spectrum Disorder” (ASD).
The three most common forms of autism in the pre-2013 classification system were Autistic Disorder—or classic autism; Asperger’s Syndrome; and Pervasive Developmental Disorder – Not Otherwise Specified (PDD-NOS). These three disorders share many of the same symptoms, but they differ in their severity and impact. Autistic disorder was the most severe. Asperger’s Syndrome, sometimes called high-functioning autism, and PDD-NOS, or atypical autism, were the less severe variants. Childhood disintegrative disorder and Rett Syndrome were also among the pervasive developmental disorders. Because both are extremely rare genetic diseases, they are usually considered to be separate medical conditions that don’t truly belong on the autism spectrum.
In large part due to inconsistencies in the way that people were classified, all of the above-named variants of autism are now referred to as “Autism Spectrum Disorder.” The single label shifts the focus away from where your child falls on the autism spectrum to whether your child has Autism Spectrum Disorder. If your child is developmentally delayed or exhibits other autism-like behaviors, you will need to visit a medical professional or a clinical psychologist who specializes in diagnostic testing for a thorough evaluation. Your doctor can help you figure out whether your child has Autism Spectrum Disorder and how severely they are affected.
Keep in mind that just because your child has a few autism-like symptoms, it doesn’t mean they have Autism Spectrum Disorder. Autism Spectrum Disorder is diagnosed based on the presence of multiple symptoms that disrupt a person’s ability to communicate, form relationships, explore, play, and learn.
[Read: Does My Child Have Autism?]
( Note: In the DSM-5, the latest version of the diagnostic “Bible” used by mental health professionals and insurers, deficits in social interaction and communication are lumped together in one category. We present problems with social skills separately from problems with speech and language, to make it easier for parents to quickly identify symptoms. )
Social behavior and social understanding
Basic social interaction can be difficult for children with autism spectrum disorders. Symptoms may include:
- Unusual or inappropriate body language, gestures, and facial expressions (e.g. avoiding eye contact or using facial expressions that don’t match what they are saying).
- Lack of interest in other people or in sharing interests or achievements (e.g. showing you a drawing, pointing to a bird).
- Unlikely to approach others or to pursue social interaction; comes across as aloof and detached; prefers to be alone.
- Difficulty understanding other people’s feelings, reactions, and nonverbal cues.
- Resistance to being touched.
- Difficulty or failure to make friends with children the same age.
Speech and language
Many children with Autism Spectrum Disorder struggle with speech and language comprehension. Symptoms may include:
- Delay in learning how to speak (after the age of two) or doesn’t talk at all.
- Speaking in an atypical tone of voice, or with an odd rhythm or pitch.
- Repeating words or phrases over and over without communicative intent.
- Trouble starting a conversation or keeping it going.
- Difficulty communicating needs or desires.
- Doesn’t understand simple statements or questions.
- Taking what is said too literally, missing humor, irony, and sarcasm.
Restricted behavior and play
Children with Autism Spectrum Disorder are often restricted, rigid, and even obsessive in their behaviors, activities, and interests. Symptoms may include:
- Repetitive body movements (hand flapping, rocking, spinning); moving constantly.
- Obsessive attachment to unusual objects (rubber bands, keys, light switches).
- Preoccupation with a narrow topic of interest, sometimes involving numbers or symbols (maps, license plates, sports statistics).
- A strong need for sameness, order, and routines (e.g. lines up toys, follows a rigid schedule). Gets upset by change in their routine or environment.
- Clumsiness, atypical posture, or odd ways of moving.
- Fascinated by spinning objects, moving pieces, or parts of toys (e.g. spinning the wheels on a race car, instead of playing with the whole car).
- Hyper- or hypo-reactive to sensory input (e.g. reacts badly to certain sounds or textures, seeming indifference to temperature or pain).
How children with Autism Spectrum Disorder play
Children with Autism Spectrum Disorder tend to be less spontaneous than other kids. Unlike a typical curious little kid pointing to things that catch their eye, children with ASD often appear disinterested or unaware of what’s going on around them. They also show differences in the way they play. They may have trouble with functional play, or using toys that have a basic intended use, such as toy tools or cooking set. They usually don’t “play make-believe,” engage in group games, imitate others, collaborate, or use their toys in creative ways.
Speak to a Licensed Therapist
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
While not part of autism’s official diagnostic criteria, children with autism spectrum disorders often suffer from one or more of the following problems:
Sensory problems – Many children with autism spectrum disorders either underreact or overreact to sensory stimuli. At times they may ignore people speaking to them, even to the point of appearing deaf. However, at other times they may be disturbed by even the softest sounds. Sudden noises such as a ringing telephone can be upsetting, and they may respond by covering their ears and making repetitive noises to drown out the offending sound. Children on the autism spectrum also tend to be highly sensitive to touch and to texture. They may cringe at a pat on the back or the feel of certain fabric against their skin.
Emotional difficulties – Children with autism spectrum disorders may have difficulty regulating their emotions or expressing them appropriately. For instance, your child may start to yell, cry, or laugh hysterically for no apparent reason. When stressed, they may exhibit disruptive or even aggressive behavior (breaking things, hitting others, or harming themselves). The National Dissemination Center for Children with Disabilities also notes that kids with ASD may be unfazed by real dangers like moving vehicles or heights, yet be terrified of harmless objects such as a stuffed animal.
Uneven cognitive abilities – ASD occurs at all intelligence levels. However, even kids with average to high intelligence often have unevenly developed cognitive skills. Not surprisingly, verbal skills tend to be weaker than nonverbal skills. In addition, children with Autism spectrum disorder typically do well on tasks involving immediate memory or visual skills, while tasks involving symbolic or abstract thinking are more difficult.
Savant skills in autism spectrum disorder
Approximately 10% of people with autism spectrum disorders have special “savant” skills, such as Dustin Hoffman portrayed in the film Rain Man . The most common savant skills involve mathematical calculations, calendars, artistic and musical abilities, and feats of memory. For example, an autistic savant might be able to multiply large numbers in their head, play a piano concerto after hearing it once, or quickly memorize complex maps.
The road to an ASD diagnosis can be difficult and time-consuming. In fact, it is often two to three years after the first symptoms of ASD are noticed before an official diagnosis is made. This is due in large part to concerns about labeling or incorrectly diagnosing the child. However, an ASD diagnosis can also be delayed if the doctor doesn’t take a parent’s concerns seriously or if the family isn’t referred to health care professionals who specialize in developmental disorders.
If you’re worried that your child has ASD , it’s important to seek out a clinical diagnosis. But don’t wait for that diagnosis to get your child into treatment. Early intervention during the preschool years will improve your child’s chances for overcoming their developmental delays. So look into treatment options and try not to worry if you’re still waiting on a definitive diagnosis. Putting a potential label on your kid’s problem is far less important than treating the symptoms.
[Read: Helping Your Child with Autism Thrive]
Diagnosing Autism Spectrum Disorder
In order to determine whether your child has autism spectrum disorder or another developmental condition, clinicians look carefully at the way your child interacts with others, communicates, and behaves. Diagnosis is based on the patterns of behavior that are revealed.
If you are concerned that your child has autism spectrum disorder and developmental screening confirms the risk, ask your family doctor or pediatrician to refer you immediately to an autism specialist or team of specialists for a comprehensive evaluation. Since the diagnosis of autism spectrum disorder is complicated, it is essential that you meet with experts who have training and experience in this highly specialized area.
The team of specialists involved in diagnosing your child may include:
- Child psychologists
- Child psychiatrists
- Speech pathologists
- Developmental pediatricians
- Pediatric neurologists
- Audiologists
- Physical therapists
- Special education teachers
Diagnosing Autism Spectrum Disorder is not a brief process. There is no single medical test that can diagnose it definitively; instead, in order to accurately pinpoint your child’s problem, multiple evaluations and tests may be necessary.
Getting evaluated for Autism Spectrum Disorder
Parent interview – In the first phase of the diagnostic evaluation, you will give your doctor background information about your child’s medical, developmental, and behavioral history. If you have been keeping a journal or taking notes on anything that’s concerned you, share that information. The doctor will also want to know about your family’s medical and mental health history.
Medical exam – The medical evaluation includes a general physical, a neurological exam, lab tests, and genetic testing. Your child will undergo this full screening to determine the cause of their developmental problems and to identify any co-existing conditions.
Hearing test – Since hearing problems can result in social and language delays, they need to be excluded before an Autism Spectrum Disorder can be diagnosed. Your child will undergo a formal audiological assessment where they are tested for any hearing impairments, as well as any other hearing issues or sound sensitivities that sometimes co-occur with autism.
Observation – Developmental specialists will observe your child in a variety of settings to look for unusual behavior associated with the Autism Spectrum Disorder. They may watch your child playing or interacting with other people.
Lead screening – Because lead poisoning can cause autistic-like symptoms, the National Center for Environmental Health recommends that all children with developmental delays be screened for lead poisoning.
Other testing
Depending on your child’s symptoms and their severity, the diagnostic assessment may also include speech, intelligence, social, sensory processing, and motor skills testing. These tests can be helpful not only in diagnosing autism, but also for determining what type of treatment your child needs.
[Read: Autism Treatments, Therapies, and Interventions]
Speech and language evaluation – A speech pathologist will evaluate your child’s speech and communication abilities for signs of autism, as well as looking for any indicators of specific language impairments or disorders.
Cognitive testing – Your child may be given a standardized intelligence test or an informal cognitive assessment.
Adaptive functioning assessment – Your child may be evaluated for their ability to function, problem-solve, and adapt in real-life situations. This may include testing social, nonverbal, and verbal skills, as well as the ability to perform daily tasks such as dressing and feeding themselves.
Sensory-motor evaluation – Since sensory integration dysfunction often co-occurs with autism, and can even be confused with it, a physical therapist or occupational therapist may assess your child’s fine motor, gross motor, and sensory processing skills.
Hotlines and support
Call the Autism Society National Helpline at 1-800-328-8476.
Call the Child Autism UK helpline at 01344 882248 or find help and support at The National Autistic Society .
Call the Early Intervention helpdesk in Perth at 1800 778 581 or Get support for your child from NDIS.
Call the Autism Canada Family Support Representative at 1-800-983-1795.
Find helplines and support in your area at Autism New Zealand .
More Information
- The Autism Revolution - Whole body strategies for making Life all it can be (Harvard Health Books)
- Autism Spectrum Disorders - What should you know? (Centers for Disease Control and Prevention)
- Autism Navigator - Guide to symptoms, causes, diagnosis, and treatment. (Center for Parent Information and Resources)
- Screening and Diagnosis - A guide to the evaluation used to diagnosis autism spectrum disorder. (Centers for Disease Control and Prevention)
- Asperger syndrome and other terms - Including symptoms and diagnosis. (National Autistic Society)
- Pervasive Developmental Disorders Information Page - Jumping off point to resources on Pervasive Developmental Disorder. (NINDS)
- Neurodevelopmental Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders . American Psychiatric Association. Link
More in Autism
Recognizing the early signs and symptoms of Autism

Parenting tips, treatments, and services that can help

Understanding your child’s options

Dealing with challenges and building a partnership together

Autism at Work
Overcoming challenges and finding success in the workplace
Autism in Adults
Recognizing the signs and living with a diagnosis

What’s triggering your child’s outbursts?

The different types of learning disorders and their signs

Professional therapy, done online
BetterHelp makes starting therapy easy. Take the assessment and get matched with a professional, licensed therapist.
Help us help others
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
- Mental Health
Here's What You Need to Know About Autism Spectrum Disorder
ASD affects 1 in 44 children in the US. Here's what you need to know to best support the community and create awareness

- Sleep Science Coach Certification from The Spencer Institute.

Autism spectrum disorder is a broad range of conditions that can affect a person's behavior, social skills and communication. ASD affects people in different ways and continues throughout a person's life.
If you have a loved one or know someone with autism, you are likely well-educated in how it can affect their life and how to best support them. However, the same isn't true for everyone who interacts with a person with ASD -- whether that be friends, teachers, co-workers or even strangers.
Here's what we know about ASD.
What is autism spectrum disorder?
Autism spectrum disorder is a neurological and developmental condition that can affect a person's ability to learn, communicate and interact socially. ASD is considered a spectrum disorder because its symptoms and severity vary from one person to another. Some people with autism can go about life entirely independently, while others may require considerable assistance with daily tasks.
According to 2018 data, the CDC reported that roughly 1 in 44 children in the US is diagnosed with ASD. Here are some statistics you may not know about ASD in the US.
ASD prevalence is pretty similar across all races, ethnicities and socioeconomic groups. Girls are four times less likely to be diagnosed with autism than boys. And 31% of children diagnosed with ASD are classified in the range of intellectual disability, 25% are in the borderline range and 44% are classified in the average to above-average range.
What are the symptoms of autism?
It's important to know that not all people with autism will exhibit the same symptoms. According to a guide created by the American Psychiatric Association to help healthcare providers diagnose mental health disorders, there are three general indications of ASD -- difficulty interacting socially, communication problems and limited repetitive behaviors.
Impact of autism on social interactions
Social interaction is how you act or manage certain situations and interact with other people. This includes interpreting social cues, problem-solving and responding.
People on the autism spectrum often have difficulty socializing and reading other people. They may lack motivation in interacting with those around them or experience social anxiety . However, this is not true for all people with ASD -- others may enjoy social engagement.
Common social skill deficits and indicators include:
Lack of interest in initiating social interactions
Difficulty maintaining eye contact
Inability to read the nonverbal cues of others
Not being able to view another person's perspective
Not understanding sarcasm and metaphors
Impact of autism on communication skills
Communication can be defined as meaningful connections between people in which information is passed and processed -- it can be verbal or nonverbal. People with autism may find communicating with others challenging. Children with ASD often have difficulty developing language skills and fully understanding what others say. People with ASD may also find nonverbal communication like eye contact, facial expressions and body language challenging.
People with ASD may display the following communication patterns :
Rigid or repetitive language
Slow or uneven language development
Limited conversational interests
Poor nonverbal communication skills

Restricted and repetitive behaviors in autism
Repetitive behaviors or "stimming" are amongst the most common symptoms of autism spectrum disorders. People with ASD may present repetitive behaviors in motor skills (fidgeting with hands, turning light switches on and off) or in speech (repeating the same statements or questions).
Many people with autism may experience sensory processing dysfunction . This means that certain senses, like sounds or light, may overstimulate them. Stimming is used as a self-soothing mechanism by distracting them from strong emotions.
Some repetitive behaviors may look like:
Echolalia (repeating words or phrases)
Over or under stimulation by certain sensory outputs
Limited interest in specific topics
Lining up items or toys
Getting upset when changes are made to their routine
Diagnosing ASD
Diagnosing autism spectrum disorders can be challenging because there aren't any biological tests that detect ASD. Healthcare providers analyze a person's behavior and development to make a diagnosis. Most doctors often wait until a child is at least two years old to make a reliable diagnosis. Many pediatricians use the Modified Checklist for Autism in Toddlers (M-CHAT) to help identify if a child is prone to developing ASD.
This screening does not provide a diagnosis but determines if a child is on the right development track for their age or if more in-depth screenings are needed.
Treatments for autism
There is no cure for autism but rather a wide variety of support and intervention plans that can help minimize and manage symptoms. Since autism manifests differently in people, treatment plans will also be unique for every person. Treatments for ASD are designed to reduce symptoms that affect daily activities and overall quality of life. Studies have proven that early diagnosis and intervention are more likely to have long-term effects of minimizing symptoms.
Treatment for people with autism may include one or a combination of the following:
Speech therapy
Training for social skills
Behavioral management therapy
Cognitive behavior therapy
Medication treatment
Nutritional therapy
Occupational therapy
Physical therapy

Common myths and misconceptions about ASD
There are many misconceptions about autism and how it impacts people diagnosed with it. Here are common myths and facts about autism spectrum disorder.
Myth: ASD affects people the same way.
The truth is that people with autism all have different challenges and strengths . It's called a spectrum because people display various symptoms and severity. Some may be highly skilled in certain areas like math, history or speech, while others may present learning difficulty in these topics or may be nonverbal.
Myth: Autism is a mental health disorder.
Autism is not a mental health disorder but a neurological disorder . Neurological disorders affect brain development and the nerves throughout the human body. ASD can affect how a person learns, socializes, communicates and behaves.
Myth: Vaccines cause autism.
There is no single cause of autism; genetics and environment can play a role. Over the years, there have been concerns about vaccines causing ASD. However, studies have shown no link between vaccines and autism.

Why is autism awareness important?
The United Nations declared April 2 as World Autism Awareness Day . The idea behind the decree is to create awareness around ASD to destigmatize the notions associated with autism and promote inclusion. The lack of understanding can significantly affect people with autism and their families.
Whether you, a loved one or someone you know has autism, you can help spread awareness and create a more accepting and safe community for those with ASD.
Other Wellness Guides
- Best Places to Buy Glasses Online
- Best Places to Buy Contacts Online
- Best Prescription Sunglasses
- Best Place to Buy Replacement Prescription Lenses
- Best Blue Light Blocking Glasses
- Best Electric Toothbrush
- Best Invisible Braces
- Best Sunscreen
- Best Mattress
- Best Mattress for Back Pain
- Best Adjustable Mattress
- Purple Mattress
- Saatva Mattress
- Best Headphones for Sleeping
- Best Pillow
- Best Sheets
- Best Elliptical
- Best Treadmill
- Best Rowing Machine
- Best Peloton Alternative
- Best Adjustable Dumbbells
- Best Weightlifting Shoes
- Best Massage Gun
- Theragun Review
- Best Meal Kit Delivery Service
- Best Healthy Meal Delivery Service
- Best Cheap Meal Delivery Service
- Best Plant-Based Meal Delivery Service
- Best Keto Meal Delivery
- Best DNA Test
- Ancestry vs 23 and Me
- Best Continuous Glucose Monitors
- Best Blood Pressure Monitor
- Best Prescription Delivery Services
- Best Portable Humidifiers
- Best Mental Health Apps
- Best Teas for Stress and Anxiety
- Best Fidget Toys for Anxiety
- Best Online Therapy
- Amazon Promo Codes
- Air Up Coupons
Speech Apraxia & Autism: Understanding the Connection
Page Topics
Autism and speech apraxia are comorbid conditions that are closely related. Children with one condition should be screened for the other.
Children with autism may be diagnosed with this developmental condition at a young enough age that they do not have strong capabilities for forming words or sentences. It is important to work with your pediatrician to understand when you can know that your child needs help from a speech therapist.
Speech therapy will typically be given in addition to behavior therapy, which is the primary form of treatment for autism. Adding speech therapy to your child’s treatment regime can help them learn skills to communicate their needs to the rest of the world.
How Does Speech Apraxia Overlap With Autism?
Speech apraxia — also known as apraxia of speech, verbal apraxia, childhood apraxia of speech (CAS), or acquired apraxia of speech — is a disorder of sounds associated with using verbal language. Someone with this condition has difficulty saying what they want to say out loud, clearly, and consistently.
This difficulty is due to a neurological difference affecting brain pathways that are related to planning the mouth muscle movements required to produce spoken words. This is often described as the brain knowing language and sentence structure and creating what it wants to say, but being unable to properly plan out the sequence of words to make speech. Apraxia still involves the person having some level of spoken language rather than being nonverbal.
Apraxia’s severity occurs on a spectrum, so some people may be able to speak with a little stuttering, while others may need extensive support to complete sentences. Symptoms of apraxia include:
- Distorting sounds, especially vowels. The speaker struggles to put the structures for speech, like the tongue, in the right place. Longer and more complex words are more difficult than simple, short words.
- Inconsistent speech errors. This can manifest as saying a difficult word correctly the first time but then saying it incorrectly the second time, or having trouble with one sound one day but having no trouble with it the next day.
- Groping for sounds. The person may attempt to say a word multiple times before they get it right or struggle to find the right pronunciation for a word.
- Errors in rhythm, stress, and tone. This is called prosody. It occurs with inflection and rhythm, as the person is more likely to use equal stress on syllables, omit syllables in words or phrases, segment syllables in a word, or pause inappropriately.
Typically, children with speech apraxia understand language at the normal developmental level, but they are not able to use it at that level. They may also have problems with motor skills and expressive language like gestures.
Apraxia is diagnosed by speech-language pathologists. They look at the cluster of symptoms and rule out other underlying conditions, like muscle weakness, problems producing language (aphasia), or other underlying causes. A speech-language pathologist can also help to treat apraxia.
Formal testing for apraxia may include:
- Repeating a particular word several times.
- Repeating a list of words of increasing length, such as love, loving, and lovingly.
- Examining the ability to read, converse, write, or perform non-speech movements.
Apraxia and autism are both disorders that involve speech and communication, but they are not the same disorder. One recent scientific study suggests that as much as 65% of children with autism have speech apraxia. This suggests that children diagnosed with autism need to be screened for apraxia when they begin speaking.
Autism & Apraxia Are Closely Comorbid Conditions
About 1 in 54 children in the United States has autism , and about 1 in 1,000 children has apraxia.
Children with autism can be especially challenging to diagnose with apraxia, so the assessment with a speech-language pathologist may take a few sessions. Using more than one session with a child on the autism spectrum reduces their stress, so it may be easier to get an accurate diagnosis over multiple sessions.
It may also be a few years before you can get a proper assessment from a speech-language pathologist. Children are diagnosed with autism between 12 months (1 year) and 4 years old, with the average diagnosis age being 2.
However, at this young age, children are still acquiring language capabilities, and they may not speak well enough for a speech therapist to diagnose a speech disorder. The therapist may ask the child to imitate their sounds or repeat words, and this can take a higher level of understanding than a toddler has, especially one with a developmental disorder like autism.
The study finding a high rate of apraxia in children with autism set out to determine if the diagnostic criteria for autism were accidentally overemphasizing speech and language production, leading to several misdiagnoses of apraxia. The 2015 publication reported that data from the study showed 63.6% of children who originally received an autism diagnosis also had apraxia; 36.8% of children with apraxia also had autism; 23.3% of children had neither; and 23.3% of children had both and were diagnosed for both at the same time. Complete diagnostic precision for the autism test is 96.7%.
The study concluded that children with apraxia and children with autism were not misdiagnosed with the other condition. Better pediatric screening for these conditions would improve outcomes for children who experienced these concurrently.
Treating Apraxia in Children With Autism
Treating apraxia in children with autism will likely be separate from behavior therapy, but treatment can occur concurrently. The goals of apraxia treatment include:
- Teaching the child to plan the movements needed to say words.
- Teaching the child to make these movements the correct way.
Speech and occupational therapists will work with your child’s behavior therapist to create a treatment plan, which will include working with and supporting parents like you. Depending on the severity of your child’s apraxia and autism, the speech pathologist or therapist may work on building your child’s communication skills using:
- Visual supports and speech devices. If your child struggles to complete words or sentences to the point that they cannot speak clearly enough to communicate, other devices may be used. Picture cards or a voice-generating computer tablet can help your child or adolescent to communicate when they are not verbally able to do so.
- Gesture cuing. The parent or therapist touches their mouth while saying a sound, which cues the child to form their lips and tongue in certain ways when creating words. This type of visual cue can help children understand where sounds are formed if they cannot transfer what they hear into a shape for their mouth.
- Tools to build vocabulary. Children with autism who are somewhat verbal can learn basic words or phrases that will be important in their daily lives. Parents may work with the therapist to decide which words to use every day, like “mom” and “dad,” or phrases like “I’m hungry.” The specific words and phrases depend on the child’s age and skill level with speaking and remembering.
Speech therapists will use a combination of these approaches in combination with understanding the individual child’s needs. Treatment plans may be frequently adjusted as the child progresses in therapy and builds better verbal skills.
Support Groups for Families of Children With Apraxia & Autism
There are many resources for children with both autism and apraxia and their parents. Here are a few national options to help you get the support you need:
- Apraxia Kids : This organization offers their own support group, along with a resource page of dozens of other support groups.
- PennState Health Children’s Hospital : This hospital offers a page with information on their parent support group as well as links to books on apraxia, autism, and other conditions that are often comorbid with autism.
- Autism Speaks : This national advocacy organization keeps a page of current support groups for people with autism and their loved ones.
The Next Step
If you suspect your child may have co-occurring speech apraxia and autism, the first step is to get an accurate diagnosis. Talk to your child’s pediatrician about your concerns. They may refer you to specialists to get an official diagnosis.
Once you have a diagnosis in hand, you can begin getting your child the treatment they need. This most often includes both behavior therapy and speech therapy.
Apraxia of Speech . (October 2017). National Institute on Deafness and Other Communication Disorders (NIDCD).
Recognizing and Treating Apraxia of Speech in Kids With Autism . Autism Speaks.
Data & Statistics on Autism Spectrum Disorder . (March 2020). Centers for Disease Control and Prevention (CDC).
How Valid is the Checklist for Autism Spectrum Disorder When a Child Has Apraxia of Speech? (October 2015). Journal of Developmental and Behavioral Pediatrics.
Childhood Apraxia of Speech . American Speech-Language-Hearing Association (ASHA).
Questions? We’re here to help
© Copyright 2020-2024 Elemy.
- Privacy Policy
- Terms & Conditions
- Notice of Non-Discrimination
- Notice of Privacy Practices

ADHD vs. Autism: What These Different Disorders Look Like in Children
W henthe Diagnostic and Statistical Manual of Mental Disorders (DSM-5)a.k.a. thediagnostic bible for psychiatrywas updated in 2013, it marked the first time that a person could be diagnosed with both ADHD and autism .
“The conditions themselves look very different on paper, but there’s confusion between the two of them because they can sometimes co-exist,” says Elisa I. Muniz , MD, developmental behavioral pediatrician and assistant professorof pediatrics at the Rose F. Kennedy Childrens Evaluation and Rehabilitation Center at Einstein/Montefiore in New York City.“Though estimates vary widely, it has been reported that up to 50 percent of children with autism have symptoms of ADHD. And approximately 14 percent of children with ADHD have autism. A child can be diagnosed with both conditions because distinguishing between the two can be challenging, especially in younger children.”
According to the Centers for Disease Control and Prevention, 9.4 percent of children in the U.S., or almost 1 in 10, have ADHD, while 1 in 59 has autism . ADHD is a disorder that can affect adults and children and is characterized by trouble with attention (the ability to focus), hyperactivity (the ability to sit still), and impulsivity (the ability to control impulsive actions).
Autism spectrum disorder, on the other hand, is a developmental disability that affects an individual’s ability to communicate, interact socially, and form relationships. It’s a lifelong, complicated condition that can range from mild to severe, and may include an inability to speak or delayed speech, repetitive movements, and repetition of sounds and phrases, among other symptoms.
We asked our experts what these two very different conditions can look like in children.
Social interactions
“A child with ADHD is interested in making friends, seeks out attention from others, and is generally motivated to interact with others,” says Dr. Muniz. That child “is usually persistent in engaging others, utilizing their ability to make good eye contact, and use facial expressions and gestures to engage others in activity. However, someone with ADHDmay have trouble keeping friends. They may face challenges such as having trouble waiting their turn, difficulty participating in an activity that doesn’t capture their attention, and interrupting when others are speaking.”
Children with autism, on the other hand, often“struggle withinitiating social interactionsand in maintaining those relationships over time,” says Dr. Muniz. “They may avoid eye contact when spoken to, and at times, appear to avoid people and social situations. A child with autism may be contently playing alone or even alongside another child, but may struggle to make attempts to engage the other child in their activity.”
Energy levels and focus
The classic high energy level of someone with ADHD differentiates them from someone with autism.“Children with ADHD are more likely to be distractible, having trouble finishing tasks, and can be overly active,” says Geraldine Dawson , PhD, professor of psychiatry and behavioral sciences at Duke University in Durham, North Carolina. “Many children with autism can be unusually focused on a task and have trouble transitioning from one activity to another. Children with autism also tend to have more challenges understanding social cues and interacting with other children.” Girls are often underdiagnosed for ADHD , in fact, because they don’t always have those classic hyperactive qualities .
Sensitivity
A main symptom of autism is an extreme sensitivity to tastes, smells, textures, and soundsespecially loud noises. Many people with the disorder are hypersensitive to bright lights or certain light wavelengths (fluorescent lights, for example). And certain types of touch (light or deep) can feel extremely uncomfortable. Discover other autism symptoms you may not realize .
Organizational skills
Here’s where the two conditions’ differences can be very apparent: Children with autism are very precise and hyper-organizedmaking sure there’s a place for everything and everything in its placewhereas a child with ADHD struggles with organization .“Although both autism and ADHD are associated with some difficulties in organizational skills, children with ADHD are more likely to become distracted and have trouble following through with instructions,” says Dr. Dawson. “Children with autism, on the other hand, have more difficulty flexibly changing their learning strategies to adapt to different tasks.”
Interests and hobbies
Someone with ADHD may have a bunch of varied interests, whereas those with autism will show a restrictive, hyper-focused interest in one particular topic.But that’s not always true. “ADHD describes the pattern of behavior of inattention and/or hyperactivity and impulsivity that is inconsistent with developmental level and causes challenges in functioning,” says Elizabeth Harstad , MD, developmental behavioral pediatrician at Boston Childrens Hospital in Boston, Mass. “Autism describes significant challenges with social communication and restrictive, repetitive patterns of behavior or functioning.” And yet, adds Dr. Harstad, “it’s hard to make a universal statement about how hobbies and interests differ among kids with ADHD versus autism. While some children with autism fixate on certain interests, others have a broad range of interests and hobbies. Additionally, some children with ADHD have a broad range of hobbies and interests, while others prefer only a few things.”
Speech development
While both conditions develop in childhood, it’s evident earlier in children with autism.“Autism generally presents itself in the first few years of life with a child having difficulty communicating, challenges with understanding others’ perspectives, and repetitive or rigid behaviors or movements,” says Dr. Harstad. “ADHD often presents by early- to mid-elementary school age.” (Learn what you should try to avoid saying to a parent of child with autism .)
Early development
Just as with speech, other areas of early development may look different in children with autism versus those with ADHD. “Many of my parents of children with autism say they knew something was different early on,” says Deborah A. Pearson , PhD, professor of psychiatry and behavior sciences at The University of Texas Health Science Center at Houston, in Houston, Texas. “I had one parent, for example, who said, ‘When he was a baby he wouldn’t look me in the eye.’ On the other hand, ADHD doesn’t usually become evident until they’re going to preschool and are compared to other children.”
Nonverbal behavior
“Those with ADHD display pretty typical nonverbal behaviorthey make good eye contact, use gestures, and have a normal range of facial expressions, but in autism, this isn’t the case,” says Dr. Pearson. “With autism, you’ll see inconsistent or nonexistent eye contact, they may not use gestures, and they may have a limited range of expressions or very exaggerated or neutral facial expressions.” (Watch out for these persistent autism myths .)
The post ADHD vs. Autism: What These Different Disorders Look Like in Children appeared first on The Healthy .

What is autism spectrum disorder? How to support the community this Autism Acceptance Month

April marks Autism Acceptance Month with World Autism Day occurring on April 2 every year. The month is meant to be a time for uplifting autistic voices and sharing in the community's joy. But for Samantha Edwards, an autistic content creator and neurodivergent life coach, the month also signifies an influx of harmful myths about autistic people.
"April is a wonderful month to crack down on that and listen to autistic voices and their stories and listen to their struggles," she says. "Acceptance, at the end of the day, is going to promote more inclusivity."
Here’s how you can uplift the neurodivergent community this April and all year long.
What is autism?
Autism is a developmental disability that affects the way people experience the world . This may include differences in processing senses, thinking, physically moving, communicating, socializing and going about daily living.
“We’re born autistic and we’re autistic our whole lives,” says Zoe Gross, the director of advocacy at Autistic Self Advocacy Network . “It affects everything about the way we interact with and perceive the world.”
Autism affects every autistic person differently, and there isn’t one way to be autistic. Gross describes it as an ice cream sundae bar: The traits of autism can be mixed and matched from person to person.
Here’s what autism isn’t, Gross says – something to be scared of or pity.
“In truth, autism is just a neutral fact about us, it’s not necessarily a good or a bad thing,” she says. “It’s just the way our brains are.”
Another misconception is that autistic people don’t have empathy. Gross recalled a time when a teacher asked her if she loved her parents. Of course she loves them, she responded, but the question itself was a symptom of a larger myth about autistic people and emotions.
“Where that comes from is that we may not know what other people are feeling if they don’t tell us because autistic people may not be good at reading body language or other kinds of subtle social cues,” Gross says. “But that doesn’t mean we don’t care what people are feeling.”
World Autism Day: A love letter to parents of a newly-diagnosed child
How common is autism?
About one in 36 children have autism spectrum disorder, the Centers for Disease Control and Prevention states. This number is on the rise, especially as children of color receive more diagnoses after being largely overlooked throughout history.
Edwards started her online autism advocacy journey to combat the misconceptions about autism. As an autistic person and a parent of two autistic children, she says she wants to make the world a more accessible place for future generations.
A large part of her work is advocating for the self-diagnosed community, which she says “are very welcome and included in the autistic community.”
One of the more harmful narratives is that people, especially teenagers, are self-diagnosing after watching a handful of TikTok videos with captions like “Signs you may be autistic” or “10 things that are actually traits of autism.” But that’s “really not the case,” says Edwards. Online platforms like TikTok give the autistic community, like other marginalized communities, more visibility than ever before.
“It is harmful for all of these self-diagnosed autistics that really did put in the research – some have years, even a lifetime of research – to be told, ‘Oh, you watched a couple TikTok videos so you’re not valid,'” Edwards says.
Some medical professionals push back against self-diagnosing, especially when it comes to social media. But there’s also the nuanced issue of access to healthcare services that may lead to a professional diagnosis, which can be limited for some autistic individuals .
What is Autism Acceptance Month?
April is Autism Acceptance Month but many, especially those outside of the autism community, used to refer to the month as " Autism Awareness Month." Autistic advocacy organizations have been using “acceptance” rather than “awareness” for over a decade, and the Autism Society of America shifted the terminology in 2021.
According to ASAN, Autism Acceptance Month was created by and for autistic people to respect the rights and humanity of all autistic people and center “the perspectives and needs of autistic people with intellectual disabilities, nonspeaking autistic people, and autistic people with the highest support needs.”
Using “acceptance” instead of “awareness” is an intentional choice because, as Edwards says, “we’re just moving on.”
“It’s 2023, I do believe most people are aware of what autism is,” she says. “We’ve got the awareness and now we need the resources, we need the advocacy.”
Awareness campaigns have historically focused on how many people have autism or a search for a “cure.” A now-removed 2009 campaign from advocacy organization Autism Speaks opened by saying “I am autism. I’m visible in your children, but if I can help it, I am invisible to you until it’s too late.”
The “awareness” approach, Gross says, further stigmatizes autism as something scary.
“That’s not the way we want to approach giving people information about autism, we want people to view autism as a part of human diversity and autistic people as part of their community,” Gross says.
How to support the autistic community
Don’t speak over autistic voices
“ Nothing about us without us ” is a disability rights slogan that’s top of mind during Autism Acceptance Month.
When it comes to research, policy and advocacy, the most important thing is that autistic people are “in the driver’s seat,” Gross says. It means that decisions about autism need to be made by or with autistic people. It also means centering the stories and experiences of autistic people.
Avoid harmful labels and language
“Low-functioning” and “high-functioning” are labels often ascribed to autistic people. These are harmful , ASAN says, because “we all have things we are good at and things we need help with.”
“People will say, ‘How can I do without the terms low-functioning and high-functioning?’ And what I want to ask is like ‘What are you doing with them now?’” Gross says. “What I encourage people to do is just say what they mean. If they mean this person can’t speak, (say) ‘I’m talking about someone who can’t speak.’ If they mean this person has a job, just say ‘I’m talking about an autistic person who has a job.’”
Neurotypical people may also wonder what’s more appropriate to say – person with autism or autistic person?
Many self-advocates prefer identity first language because it works against the stigma that being autistic is something bad or something that makes you less than. Identity first language (“autistic person”) recognizes and validates that identity.
“Autism is something that you are and not something that you have, you’re not carrying autism around in a bag,” Edwards says. “It’s something that makes your brain different.”
But it’s a personal preference . For example, Gross says people with intellectual disabilities may use person-first language ("person with autism") because “they feel they’ve been so dehumanized and people only see their disability and don’t see them.”
The bottom line: How someone refers to their autism is personal based on what makes them feel the most affirmed and validated.
Support autistic-run organizations and businesses
Edwards recommends supporting organizations that center autistic voices and are run by autistic people, like ASAN and the Autistic Women and Nonbinary Network.
This month, Edwards says she’ll be using her platform to uplift other autistic and disabled creators.
“There’s so many of us that are … trying to make a really big difference in this movement, so I’m really proud of everyone this past year,” she says. “I just want to uplift each other and get the right message out.”
Organizations with primarily neurotypical leadership have led autistic advocates to move away from their symbols (like Autism Speaks’ signature blue color and puzzle piece) in favor of new ones created by autistic self-advocates. The first puzzle piece logo in 1963 featured a crying child in the center and was designed to show autism as a “puzzling condition.” A 2018 study found the general public has a negative implicit bias against the imagery of a puzzle piece, which participants associated with “imperfection, incompletion, uncertainty, difficulty, the state of being unsolved, and, most poignantly, being missing.”
“We recognize discord within the community, including those who dislike the puzzle piece symbol or prefer a different symbol, but there are also many who embrace it and want to continue to see it associated with autism,” Autism Speaks told USA TODAY in a statement.
The organization says it is regularly seeking feedback from those within the autistic community on whether or not to continue its use and encouraged feedback at [email protected] .
Many favor a rainbow or gold infinity symbol and use “ Red Instead ,” which Edwards says symbolizes the passion autistic people have.
Don’t perpetuate myths about autism
Edwards recommends neurotypical people support the neurodiverse community by staying up to date on current research and taking a second glance before sharing something that furthers stereotypes about autistic people.
“We all deserve our human rights, and we all deserve respect,” Gross says. “We all deserve to be able to make choices in our lives, we deserve to live free from neglect and abuse, we deserve to have services that are truly person-centered and individualized for us and that meet our needs. Those aren’t optional, fancy things that you get by being mildly impacted.”
'Surrounded by fighters': Hawthorne school behaviorist plays role in autism book
3-minute read.

HAWTHORNE — A 3-year-old child pointed to a shirt worn by a speech therapist and said “orange.”
Then, the girl looked down at her own shirt, pointed to it and said “yellow.”
Such an exchange may be overlooked by some families, but those with children on the autism spectrum are extra mindful of each little step in the right direction.
A new book by John Fortunato, a professor at Fordham University, traces the lives of real people deeply affected by autism, and the precise instant when the girl assigns colors to the clothing is part of his story.
Disorders as complex as autism do not always lend themselves to happy endings, Fortunato concedes, but “Miracle of Effort” is teeming with mini breakthroughs.
Much of the credit is owed to Lisa Searls, who, in the book’s opening chapter, discovered symptoms of autism in the girl — her second cousin — and set her on a path for proper treatment.
“She was surrounded by fighters,” Searls said. “She was such a fighter. She inspired us to keep working and to keep pushing harder.”
Searls, who now lives in Nazareth, Pennsylvania, about 15 miles northeast of the city of Allentown, works part-time as a behaviorist at Hawthorne’s Washington School on Mohawk Avenue. She also owns a consulting business called Motivating Change , specializing in applied behavior analysis.
Searls’ cousin and the girl depicted throughout the 242-page book is Thalia Morsillo, now 26, who in the end becomes the captain of the high school color guard, graduates with honors from Kean University and takes on a teaching position.
Yes, there are pitfalls along the way.
Her parents move the family to another town when they clash with a child study team in their local district. She struggles in math classes. And by middle school, she starts to resent the help of a teacher’s aide.
But readers will find that the uplifting story comes full circle when Morsillo sees the warning signs of autism in one of her students.
More than anything, the book stresses the importance of early intervention. Had Searls not been there in the beginning, her cousin’s life would not have turned out as it did.
The discovery of Morsillo’s autism was only the first stage — then came the doctor appointments and the official diagnosis. In this case, there were three visits to three different pediatric neurologists.
It can be overwhelming, Searls said, for parents to accept what they hear. Part of the reason for that, she said, is the stigma attached to autism.
Searls said the condition is still misunderstood, but when her cousin was first diagnosed in April 2000, the public perception of it was far worse.
According to the Centers for Disease Control and Prevention , one in 36 children in the U.S. has autism. At the time of Morsillo’s diagnosis, it was more than four times less common to have the disorder.
Fortunato, of Sea Girt, who holds a doctorate in communication from Rutgers, said the book is intended primarily for families dealing with autism and for teachers in special education.
FOOTBALL: Hawthorne High School elevates assistant coach to head job after longtime leader steps down
But its underlying message of hope has wide appeal.
“That’s where the book is relatable,” Fortunato said. “Each child has a unique experience, but there are similarities between the emotions that the family goes through, the challenges overcome and the sacrifices demanded.”
Philip DeVencentis is a local reporter for NorthJersey.com. For unlimited access to the most important news from your local community, please subscribe or activate your digital account today.
Email: [email protected]
Upcoming event
The author will discuss and sign copies of “Miracle of Effort” at the Oakside Bloomfield Cultural Center. The book is also available for purchase on his website at johnafortunato.com.
WHEN: Tuesday, April 9, at 7 p.m.
WHERE: 240 Belleville Ave.
REGISTER: Visit the township website at bloomfieldtwpnj.com.
Advertisement
Autism Spectrum Disorder and auditory sensory alterations: a systematic review on the integrity of cognitive and neuronal functions related to auditory processing
- Neurology and Preclinical Neurological Studies - Review Article
- Open access
- Published: 14 March 2023
- Volume 130 , pages 325–408, ( 2023 )
Cite this article
You have full access to this open access article
- Ana Margarida Gonçalves 1 , 2 &
- Patricia Monteiro ORCID: orcid.org/0000-0003-3288-4560 1 , 2 , 3
6069 Accesses
8 Citations
4 Altmetric
Explore all metrics
Autism Spectrum Disorder (ASD) is a neurodevelopmental condition with a wide spectrum of symptoms, mainly characterized by social, communication, and cognitive impairments. Latest diagnostic criteria according to DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, 2013) now include sensory issues among the four restricted/repetitive behavior features defined as “hyper- or hypo-reactivity to sensory input or unusual interest in sensory aspects of environment”. Here, we review auditory sensory alterations in patients with ASD. Considering the updated diagnostic criteria for ASD, we examined research evidence (2015–2022) of the integrity of the cognitive function in auditory-related tasks, the integrity of the peripheral auditory system, and the integrity of the central nervous system in patients diagnosed with ASD. Taking into account the different approaches and experimental study designs, we reappraise the knowledge on auditory sensory alterations and reflect on how these might be linked with behavior symptomatology in ASD.
Similar content being viewed by others
Elevated levels of atypical handedness in autism: meta-analyses.
Paraskevi Markou, Banu Ahtam & Marietta Papadatou-Pastou
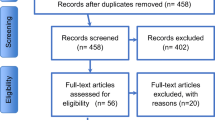
Music Therapy in Autism Spectrum Disorder: a Systematic Review
Amparo V. Marquez-Garcia, Justine Magnuson, … Sylvain Moreno

An Overview of Autism Spectrum Disorder, Heterogeneity and Treatment Options
Anne Masi, Marilena M. DeMayo, … Adam J. Guastella
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder.
Autism spectrum disorder (ASD) is a neurodevelopment condition characterized by deficits in social communication and interaction, and restricted/repetitive behavioral features (Peça et al. 2011 ), showing first symptoms typically around three years old (Robertson and Baron-Cohen 2017 ). In 2018, the Centers for Disease Control and Prevention (CDC) reported approximately one in 44 children diagnosed with ASD, with a four times higher prevalence in boys versus girls. There is a wide variation in the type and severity of symptoms in ASD. Unlike other diagnoses, such as a specific phobia, it is not easy to draw a straight line from symptoms to diagnostic criteria. Each neurodivergent individual with ASD is unique, and the diagnosis is based on behavioral observation.
ASD diagnosis evolution: DSM-5 and ICD-11
The year 2013 was an important landmark for Autism conceptualization, with the release of the latest version of the Diagnostic and Statistical Manual of Mental Disorders (DSM–5) (American Psychiatric Association (APA) 2013 ). Before DSM-5, there were poor diagnostic criteria with limited reliability in assigning subcategory diagnosis (Walker et al. 2004 ). The diagnosis of autism was categorized by subcategories (e.g., autistic disorder, Asperger’s disorder, and pervasive developmental disorder not otherwise specified). With the fifth edition of DSM, there was an important shift in the conceptualization of dimension: Autism became a single diagnosis based on multiple dimensions. The DSM-5 refers to Autism as a Spectrum Disorder, embracing an umbrella of symptoms with wide variety and severity levels. The new diagnosis of ASD includes persistent deficits in social communication and social interaction across multiple contexts, and restricted and repetitive patterns of behavior, interests, or activities (American Psychiatric Association (APA) 2013 ). These symptoms are present in early developmental period, significantly interfering with individuals’ daily functioning (American Psychiatric Association (APA) 2013 ).
In 2018, the World Health Organization updated the classification of autism in the International Classification of Diseases (ICD-11) (Organization 2018 ), to be more in line with DSM-5. The latest version of ICD-11 came into effect on January 2022 (Organization 2018 ). Both authoritative guidebooks used by medical professionals for the diagnosis and treatment of diseases and disorders collapse autism into a single diagnosis of Autism Spectrum Disorder, embracing the same two major aspects: difficulties in initiating and sustaining social communication and social interaction, and restricted interests and repetitive behaviors (Rosen et al. 2021 ).
The evolution of Autism criteria diagnosis reflects the evolving concern of clinicians and, particularly, researchers. If the diagnostic criteria are not easily well defined, people with autistic-like traits might be included, leading to misleading clinical cohorts that might hinder a clear understanding of autism neurobiology. As an example, as DSM-IV (American Psychiatric Association (APA) 1994 ), the previous version of the International Classification of Diseases, ICD-10 (Organization 1993 ), included a third category for language problems. The ICD-10 subdivided communication and social interaction into different clusters. Given that clinicians found it hard to categorize symptoms as either, both DSM-5 and ICD-11 now combine social and language deficits into a single measure. These deficits seem to be interrelated, being understood that a child with limited language or communication problems would have limited social interaction. However, the cause of these communication and language impairments is still unclear.
Sensory processing in ASD
Over the years, the focus of ASD diagnosis was mainly related to cognitive, communication, and social impairments. But more recently, the criteria of diagnosis started to include another feature: the sensory processing domain (Robertson and Baron-Cohen 2017 ). The DSM-5, and more recently the ICD-11, now include sensory hyper- and hypo-sensitivities as part of the restricted and repetitive behavior domain (American Psychiatric Association (APA) 2013 ; Organization 2018 ). Atypical responses to sensory stimuli can also help to differentiate ASD from other developmental disorders (Stewart et al. 2016 ).
Sensory integration is a neurobiological process that refers to the integration and interpretation of sensory stimuli from surrounding context to the brain. Atypical sensory experience seems to occur in 85% of individuals with ASD and can be noticeable early in development (Robertson and Baron-Cohen 2017 ). Symptoms can include hypersensitivity, avoidance, diminished responses, or even sensory seeking behavior (Robertson and Baron-Cohen 2017 ; Sinclair et al. 2017 ). These alterations in sensory processing may interfere with the typical development of higher order functions such as social communication, which requires quick, accurate integration of sensory cues in real time (Robertson and Baron-Cohen 2017 ; Siemann et al. 2020 ). Many studies have looked into multisensory processing, highlighting the role of temporal binding windows as a critical factor in information integration (Robertson and Baron-Cohen 2017 ). The concept of temporal binding window refers to a window of time where specific modalities are perceptually bound (Hillock et al. 2011 ). A recent review from Siemann and colleagues describes numerous findings related to the presence of multisensory and temporal processing deficits in individuals with ASD ( 2020 ) (Siemann et al. 2020 ), suggesting atypical multisensory temporal processing with increased stimulus complexity. Although atypical sensory processing can be present across several sensory domains, atypical behavioral response to environmental sounds is among the most prevalent and disabling sensory feature of autism, with more than 50% of individuals exhibiting impaired sound tolerance (Williams et al. 2021 ).
Auditory sensory processing in ASD
Many individuals diagnosed with ASD have auditory sensitivities, and it is common to observe children with ASD covering their ears, even in the absence of salient background noise. Individuals with ASD can present hyper- or hypo-sensitivity to a variety of sensory stimuli, which can cause a wide range of behavioral manifestations and maladaptations (Sinclair et al. 2017 ). Children underresponsive to sensory input appear to be unaware of auditory stimuli that are salient to others. Studies have shown that pronounced to profound bilateral hearing loss or deafness seems to be present in 3.5% of all cases, and hyperacusis (increased sensitivity or decreased tolerance to sound) affects nearly 18–40% of children with autism (Williams et al. 2021 ; Rosenhall et al. 1999 ; Wilson et al. 2017 ). Individuals with auditory hypersensitivity can notice auditory stimuli at intensity levels that are not salient or would not trouble others, which may cause sensory overload. For a person experiencing sensory overload, everyday sounds can be unpleasant and overwhelming, and that may lead to poor emotional and social regulation (Wilson et al. 2017 ), with impairments at the level of filtering out irrelevant input. The appropriate filtering of sensory information is crucial for healthy brain function, allowing salient awareness and focus on relevant social cues. Deficits in auditory processing can thus affect behavior, with profound effects on a person’s life, especially in the development of higher level skills such as social communication. However, the knowledge about phenomenology or neurocognitive underpinnings that underlie these auditory sensory processing deficits is still scarce. In fact, many studies have been performed before DSM-5 criteria, having a confound effect of potential misdiagnosis or comorbidity with other disorders.
To avoid such potential confounds, we opted for a systematic review of auditory sensory function in patients with ASD, considering studies performed between 2015 and 2022 (2 years after DSM-5 implementation), thus considering the recent adaption of autism diagnosis as a spectrum disorder.
The following questions will be addressed:
What is known about the integrity of Cognitive Function in auditory-related tasks?
What is known about the integrity of Peripheral Auditory System in auditory-related tasks?
What is known about the integrity of Central Auditory Nervous System in auditory-related tasks?
This systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al. 2021 ), and review methods were established before initiating literature screening.
Search strategy and screening criteria
The search strategy started in September 2021 and used MeSH terms from PubMed. Used databases: PubMed, Web of Science (all databases/collections), Scopus, and Scielo. Search terms included “ autis* ” AND “ auditory ”, and were limited to studies published between 2015 and March of 2022. The minimum year of 2015 was considered as the mark of first experimental studies using DSM-5 as a diagnosis of Autism Spectrum Disorders (American Psychiatric Association (APA) 2013 ).
Study design
Studies were eligible if they consisted of original and reported data, with comparison group design, written in English and published in peer-reviewed journals. Conference abstracts, books and documents, editorials, letters, pilot studies, case studies, reviews, and meta-analyses were excluded.
Participants
Only studies with human participants with a clear diagnosis of ASD were considered. To avoid confounding results, studies with ASD participants that were also diagnosed with other symptomatology and/or disorders were excluded: epilepsy, Williams Syndrome, ADHD, Rett Syndrome, Angelman Syndrome, Fragile X Syndrome, etc. Participants diagnosed with ASD in early childhood but without current ASD symptoms, or participants with the diagnosis based on the DSM-IV without other assessments of diagnosis validation (e.g., ICD-11 and ADOS) were also excluded. No restrictions of age, gender, racial, ethnic, and socioeconomic groups were made.
Studies that did not include relevant outcome data were excluded (e.g., ASD parents’ symptomatology; studies focused on visual processing that used auditory cues in the task that are not referred to in the results; studies focused on pilot training or intervention programs).
Results and critical discussion
Most of the tools used to confirm ASD diagnosis in the studies included on this review were: Short-Sensory Profile (SPP) (Dunn 1999 ), Childhood Autism Rating Scale (CARS) (Schopler et al. 2010 ), Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) (Lord et al. 2012 ), and the Peabody test (Dunn and Dunn 1965 ). To estimate global intellectual ability (full-scale IQ), most tests used were the Wechsler Adult Intelligence Scale or the Wechsler Intelligence Scale for Children (Wechsler and Kodama 1949 ), and Raven’s Colored Progressive Matrices Test (Measso et al. 1993 ). Even if there is no official diagnosis for ASD being described as low or high functioning, some papers identified some ASD groups as being high-functioning autism (usually subjects with an IQ mean higher than 85).
Integrity of cognitive function in auditory-related tasks
Cognitive function can be assessed by mental processes such as perception, attention, memory, decision-making, or language comprehension, and in the domain of social cognition (e.g., theory of mind, social and emotional processing). People with ASD have a profile of cognitive strengths and weaknesses, demonstrated by different levels of deficits in social and non-social cognition patterns. To understand how auditory input might influence cognitive function in ASD, it is useful to assess cognitive integrity at several domains, while performing auditory-related tasks.
Attention, detection, and discrimination
Communication in everyday life depends crucially on the ability to detect stimuli and dynamically shift attention between competing auditory streams. We use attention to direct our perceptual systems toward certain stimuli for further processing. Difficulties in attention processes can directly affect social interaction and communication abilities. When compared to neurotypical controls, individuals with ASD seem to have poorer performance in many auditory attention tasks: divided attention (ability to attend to two or more stimuli at the same time), sustained attention (ability to attend stimulus over longer periods), selective attention (ability to ignore details of stimulus not attended), and spatial attention (selecting a stimulus based on its spatial location). Main findings are summarized in Table 1 .
Low-level auditory discrimination ability seems to vary widely within ASD. When different paradigms were compared, no differences were found for adults with ASD regarding selective attention (maintain vs switch tasks) (Emmons et al. 2022 ). However, infants and children with ASD presented poorer performances for sustained and control attention, attentional disengagement, and reorienting (Keehn et al. 2021 ), when compared with typically developing peers (TD). Spatial attention, a key component for social sound orientation, was measured by looking at central or peripheral locations of target sounds location while ignoring nearby sounds (Soskey et al. 2017 ). Adults diagnosed with ASD show diffuse auditory spatial attention independently of stimulus complexity: simple tones, speech sounds (vowels), and complex non-speech sounds (Soskey et al. 2017 ). Interestingly, children with ASD show more diffuse auditory spatial attention, indicated by increased responding to sound at adjacent non-target locations (Soskey et al. 2017 ). Subjects with ASD also seem to be less sensitive to global interference, or mixed cues, when compared with just one cue (local targets processed slower due to the presence of inconsistent global information) (Foster et al. 2016 ).
Responses to sensory stimuli: visual versus auditory—distinctive multisensory integration
Information from different sensory modalities, such as auditory and visual stimuli, can be easily integrated simultaneously by the nervous system. The visual sensory system of ASD individuals seems to be similar to TD peers, as opposed to their auditory system (Little et al. 2018 ). Different sensory modalities combined can create multisensory facilitation. As an example, speech perception is boosted when a listener can see the mouth of a speaker and integrate auditory and visual speech information. However, multisensory integration (MSI) is thought to be distinctive in ASD (Ainsworth et al. 2020 ) (Table 2 ), with temporal processing deficits that are not generalized across multiple sensory domains (Ganesan et al. 2016 ).
Low-level perceptual processes
An experimental design based on Miller’s race model (Miller 1982 ) was tested by assessing the accuracy and reaction times of unisensory and bisensory (visual and auditory) trials and by comparing children with ASD with typically developing peers (TD) as a control group (Stewart et al. 2016 ). Findings did not support impaired bisensory processing for simple non-verbal stimuli in high-functioning children with ASD (Stewart et al. 2016 ). Reduced bisensory facilitation was found for both ASD and TD groups, suggesting intact low-level audiovisual integration. Another study assessed the reaction time of target stimuli detection task (auditory, 3500 Hz tone; visual, white disk ‘flash’; and audiovisual, simultaneous tone and flash) by comparing younger (age 14 or younger) and older participants (age 15 and older) (Ainsworth et al. 2020 ). The authors found greater multisensory reaction time facilitation for neurotypical (NT) adults, increased for older participants, and reduced multisensory facilitation for ASD, both in younger and older participants.
High-level perceptual processes
Audiovisual integration of basic speech and object stimuli was compared in children and adolescents diagnosed with ASD (Smith et al. 2017 ). To measure audiovisual perception, a temporal window of integration was established, where individuals identify which video (temporally aligned or not) matched the auditory stimuli. Results showed similar tolerance of asynchrony for the simple speech and object stimuli for controls, while ASD adolescents showed decreased tolerance of asynchrony for speech stimuli. These results were associated with higher levels of symptom severity (Smith et al. 2017 ). A similar result of instantaneous adaptation to audiovisual asynchrony was found in ASD adults (Turi et al. 2016 ). This means that reduced adaptation effect in ASD individuals, and poorer multisensory temporal acuity, may be hindering speech comprehension and consequently affecting social communication.
Social interaction implies attentional shift, such as joint attention (when a person intentionally focuses attention on another person). A study tested whether impairments in joint attention were influenced by self-relevant processing. Results showed that gaze-triggered attention is influenced by self-relevant processing and symptom severity in ASD individuals, with reduced cueing effect to voice compared to tone targets (Zhao et al. 2019 ).
The stimulus presentation modality can lead to differences in figurative language comprehension, even with high-verbal ASD individuals (matched with TD peers on intelligence and language level) (Chahboun et al. 2016 ). When visual and auditory modalities are compared, individuals with ASD present the poorest performances in the auditory modality, showing difficulties to understand culturally based expressions (Chahboun et al. 2016 ). Greater difficulties in language processing seem to be correlated with higher auditory gap detection thresholds (minimum interval between sequential stimuli needed for individuals to perceive an interruption between the stimuli) (Foss-Feig et al. 2017 ).
The influence of noise on cognitive performance
Multisensory facilitation can be highly valuable, especially in noisy environments. A diminished capacity to integrate sensory information across modalities can potentially contribute to impaired social communication.
Cognitive performance in ASD was assessed with experimental manipulation of noise (quiet and 75 dB gated broadband noise) adding different levels of task difficulty (easier and harder) (Keith et al. 2019 ). Results show that for NT adolescents, it is easier to adapt to the effect of noise. In contrast, the ASD group shows a detrimental effect of noise and increased arousal in the harder condition (Keith et al. 2019 ). Children with ASD who attend more time to the stimulus, such as looking longer to the speaker’s face, show better listening performance (Newman et al. 2021 ). When different levels of signal-to-noise ratio (SNR) are compared, ASD and NT groups exhibited greater benefit at low SNRs relative to high SNRs in phoneme recognition tasks (Stevenson et al. 2017 ). The ASD group shows a reduced performance in both auditory and audiovisual modalities for whole-word recognition tasks with high SNRs (Stevenson et al. 2017 ), when compared with TD peers. High-functioning ASD adults show a speech comprehension rate of nearly 100% in the absence of noise, similar to IQ-matched controls (Piatti et al. 2021 ; Dwyer et al. 2021 ). However, under noise conditions, the ASD group presents worse speech comprehension and neural over-responsiveness (Piatti et al. 2021 ; Dwyer et al. 2021 ). Such results suggest that noise may increase the threshold needed to extract meaningful information from sensory inputs, affecting speech comprehension.
Increased auditory perceptual ability: differences in auditory stimuli detection and discrimination
Regarding auditory perceptual capacity, there is a wide variety of experimental designs, paradigms, and tested parameters, holding different results (Table 3 ). When ASD and TD individuals were compared, significant differences were found in the ASD group regarding several acoustic parameters, such as deficits in the intensity or loudness of stimuli, higher auditory duration discrimination threshold of stimuli, and enhanced memory for vocal melodies (Kargas and Lo 2015 ; Isaksson et al. 2018 ; Weiss et al. 2021 ). Musical and vocal timbre perception seems to be intact for older ASD participants (Schelinski et al. 2016 ), with one study showing decreased music ability, related with deficits at the level of working memory and hyperactivity/inattention of young ASD children (Sota et al. 2018 ).
One of the common parameters used to test auditory perceptual capacity is pitch detection, the degree of highness, or lowness of a tone. Studies have shown a heightened pitch detection in the ASD group, for expected and unexpected sounds (Remington and Fairnie 2017 ). Regarding the developmental trajectory of pitch perception, findings reveal enhanced pitch discrimination in childhood with stability across development in ASD (Mayer et al. 2014 ). Interestingly, this low-level auditory ability seems to vary widely within ASD, being related to IQ level and severity of symptoms (Kargas and Lo 2015 ). Adults diagnosed with ASD show superior pitch perception associated with sensory deficits (Mayer et al. 2014 ). Individual differences in low-level pitch discrimination tasks can predict performance on the higher level global–local tasks (Germain et al. 2018 ). Results seem to vary between detection and discrimination tasks across studies. A discrimination task assesses the ability to detect the presence of a difference between two or more stimuli. Interestingly, no differences were found between low and higher level pitch processing (Chowdhury et al. 2017 ) when ASD children were matched in terms of IQ levels and verbal and non-verbal cognitive abilities, as measured by WASI subtests yield (Wechsler and Kodama 1949 ). For ASD adults without intellectual impairment, when participants were asked to identify modulation-depth differences (e.g., − 3 dB), no differences were found in auditory modulation–depth discrimination tasks (Haigh et al. 2016 ). ASD adults showed difficulties in discriminating, learning, and recognizing unfamiliar voices (particularly pronounced for learning novel voices) (Schelinski et al. 2016 ). These results may allow us to speculate that an increased auditory capacity, such as heightened pitch detection, may lead to better performance at detection or discrimination tasks, but may also entail a sensory overload, greatly enhancing the difficulty of the task for different stimuli parameters.
Auditory processing and language-related impairments
Atypical sound perception and auditory processing deficits may underlie language and learning difficulties in ASD, impairing social communication skills. Studies have found that ASD patients tend to display worst performance in whispered speech compared to normal speech (Venker et al. 2019 ; Georgiou 2020 ) and several differences have been reported in terms of language processing and speech perception (Table 4 ).
The integration of information for successful language processing and speech comprehension relies on precise and accurate temporal integration of auditory and visual cues. Children with ASD seem to possess a wider window of audiovisual temporal integration (Stevenson et al. 2017 ; Noel et al. 2017 ), and higher auditory gap detection thresholds (Foss-Feig et al. 2017 ). Deficits at the level of temporal integration may contribute to impaired speech perception. Studies of auditory processing and language paradigms show that language processing can be facilitated in children with ASD using contextual references such as semantically-constrained verbs compared to neutral verbs (Venker et al. 2019 ).
Language components, such as phonemes, syntax, and context, work together with features to create meaningful communication among individuals. All languages use pitch and contour to carry information about emotions and to communicate non-verbally. The way we say something affects its meaning, just by using different emphasis and intonation. Phonological use of pitch dissimilarities is distinct between tone and non-tone languages at several levels of their phonological hierarchy (prosodic word, phonological phrase, intonational phrase, and utterance tiers) (Beckman and Pierrehumbert 1986 ). Tones are associated with lexical meaning to distinguish words. English, as a non-tone language, uses contrastive pitch specifications at a segmental level, to express syntactic, discourse, grammatical, and attitudinal functions. A tone language, like Mandarin, uses constructive pitch specifications at every level of the phonological hierarchy (Best 2019 ). Pitch processing was assessed in individuals who speak Mandarin, by testing melodic contour and speech intonation (Jiang et al. 2015 ). ASD individuals presented superior melodic contour but comparable contour discrimination, and when compared with controls, ASD performed worse on both identification and discrimination of speech intonation (Jiang et al. 2015 ), suggesting a differential pitch processing in music that does not compensate for speech intonation perception deficits.
Auditory processing and cognitive function assessment: EEG and ERP
Many studies focusing on language processing use electroencephalography (EEG) to measure brain activity in real time. EEG signals reflect electrical activity produced by the brain (brain waves). An approach known as event-related potential (ERP), uses EEG activity that is time-locked with ongoing sensory, motor, or cognitive events, to help identify and classify perceptual, memory, and linguistic operations (Sur and Sinha 2009 ). To avoid confounding effects in the interpretation of ERP results, most studies only include children with normal or corrected-to-normal vision, normal hearing, and absence of genetic or neurological disorders, history of seizures, or past head injury. To check for hearing disabilities, many studies also perform a hearing screening with pure-tone audiometry at 20 dB. However, there is a wide variation regarding the inclusion criteria of participants (Table 5 ).
Event-related potential waveforms have a series of positive and negative voltage deflections, referred by a letter indicating polarity (N, negative; P, positive) and a number indicating their latency in milliseconds (Luck and Kappenman 2012 ). As an example, N100 (also known as N1) indicates a negative polarity between 75 and 130 ms, usually associated with pre-attentive perceptual processing followed by P200 associated with stimulus detection (150–275 ms after stimulus presentation) (Key et al. 2005 ). Other components will be addressed in this review, such as P300 (P3; stimulus categorization and memory updating), N400 (semantics), and P600 (syntactic processing). Mismatch negativity (MMN) is the negative component of a waveform obtained by subtracting event-related potential responses to a frequent stimulus (standard) from those to a rare stimulus (deviant).
Some ASD studies have focused on early ERP components (Table 6 ), mainly showing reduced P1 latencies and amplitude (Patel et al. 2019 ; Arnett et al. 2018 ; Bidet-caulet et al. 2017 ). Looking particularly to patterns of auditory habituation, data suggest reduced habituation for ASD children in the P1 component and a decrease in MMN amplitude (Ruiz-Martínez et al. 2019 ). Pronounced habituation slopes have been observed for neurotypical subjects, with greatest difference at channel Fp1 and in the frontal and fronto-central electrodes (Jamal et al. 2020 ). For neurotypical subjects, P1 is stronger in the initial section of stimuli sequence, showing a gradual reduction in ERP amplitude over time (habituation) (Jamal et al. 2020 ). On the other hand, the ASD group shows absence of reduction between the first and last ERP, or even a positive slope toward the end of the experiment (reduced habituation) (Jamal et al. 2020 ). Regarding temporal processing with gap detection tasks, when compared with TD peers, ASD children with intact cognitive skills present reduced P2 amplitude (Foss-feig et al. 2018 ). The P2 component is associated with attention and stimulus classification, suggesting that the presence of a gap enhances the difficulty of primary level detection, and subsequent perceptual processes may fail to engage. In speech-in-noise tasks, high-functioning ASD adults present higher P2 amplitudes (Borgolte et al. 2021 ). These results suggest that the P2 component can be affected by the audiovisual process and specificities of both stimuli and condition. Early MMN (around 120 ms) show enlarged responses only for pure-tone context, with no other modulations dependent on action sound context (Piatti et al. 2021 ). Individual differences in auditory ERPs with four different loudness intensities (50, 60, 70, 80 dB SPL) (Dwyer et al. 2020 ) were tested using hierarchical clustering analysis based on ERP responses. It was possible to verify a pattern of linear increases in response strength accompanied by a disproportionately strong response to 70 dB stimuli for ASD young children, correlated with auditory distractibility (Dwyer et al. 2020 ). In a similar study, some clusters of ASD individuals presented weak or absent N2 by 60 dB and increased strength with higher intensities (70 or 80 dB) (Dwyer et al. 2021 ). However, there was an overlap between ASD and TD participants in several clusters (Dwyer et al. 2020 , 2021 ), suggesting that sensory impairments in ASD might be largely accounted for the wide interindividual variability that exists within the spectrum.
A large-scale study tested 133 children and young adults in an auditory oddball task, comparing mismatch negativity and P3a results, as well as temporal patterns of habituation (N1 and P3a) (Hudac et al. 2018 ). The P3a component is indexed by different levels of attentional orienting. Results showed heightened sensitivity to change to novel sounds in ASD subjects, increased activation upon repeated auditory stimuli, and dynamic ERP differences driven by early sensitivity and prolonged processing (Ruiz-Martínez et al. 2019 ; Hudac et al. 2018 ). To test the neural indices of early perceptual and later attentional factors underlying tactile and auditory processing, ASD and age- and non-verbal IQ-matched TD peers were compared (Kadlaskar et al. 2021 ). Using an oddball paradigm where children watched a silent video while being presented with tactile and auditory stimuli, results showed reduced amplitudes in early ERP responses for auditory stimuli but not tactile stimuli in ASD children. The differences in neural responsivity were associated with social skills (Kadlaskar et al. 2021 ). Regarding top–down and bottom–up attentional processes, young ASD children with no developmental delay seemed to present more negative MMN voltages and an attenuated response of P3a mean voltages when deviant tones were presented in speech (Piatti et al. 2021 ). When compared with TD peers, bilingual children with ASD seemed to be less sensitive to lexical stress, with reduced MMN amplitude at the right central–parietal, temporal–parietal, and temporal sites (Zhang et al. 2019 ). Children with developmental delay did not differ from the control group in the P3a component (Piatti et al. 2021 ). Compared to adults, there was enhanced bottom–up processing of sensory stimuli in participants with high-functioning autism, with early ERP responses positively correlated to increased sensory sensitivity (Xiaoyue et al. 2017 ). In ASD children, more positive MMR was observed in the processing of speech pitch height (Zhang et al. 2019 ), suggesting hypersensitivity to higher frequency tones.
Another relevant feature for auditory processing is prosody, the rhythmic and intonational aspect of language. Event-related potential (ERP) studies show preserved processing of musical cues in ASD individuals, but with prosodic impairments (Depriest et al. 2017 ). Differences in prosody such as intonation are highly relevant for language-related impairments in ASD with a significant impact on communication. To test prosodic processing, many studies record brain responses to neutral and emotional prosodic deviances reflecting change detection (MMN) and orientation of attention toward change (P3a).
Children with ASD present atypical neural prosody discrimination, with distinct patterns depending on the experimental design. For instance, the P3a component becomes more prominent upon greater difference of stimulus change. Studies using sound-discrimination tasks with lexical tone contrasts based on naturally produced words (e.g., a vowel with neutral or emotional prosody such as sadness) show different P3a depending on the IQ level of ASD children. A study with high-functioning ASD children shows diminished amplitude of P3a (Lindström et al. 2018 ). In a study comparing children and adults, low-functioning children revealed a larger P3a compared to the control, with P3a latencies shorter in ASD adults (Charpentier et al. 2018 ). Regarding change detection, ASD adults presented an earlier MMN (Charpentier et al. 2018 ). Both results suggest atypical neural prosody discrimination and deficits in pre-attentional orientation toward any change in the auditory environment (Lindström et al. 2018 ; Charpentier et al. 2018 ). When vowel and pure tone are compared within tone languages (smaller physical difference between standard and deviants compared to non-tone languages), ASD children still presented diminished response amplitudes and delayed latency of MMN for pure tones, and smaller P3a for vowel (Huang et al. 2018 ). At a pre-attentive perceptual processing level, low-functional ASD children present increased response onset latencies during sustained vowel production, with reduced P1 ERP amplitudes (Patel et al. 2019 ; Bidet-caulet et al. 2017 ; Charpentier et al. 2018 ), lacking neural enhancement in formant-exaggerated speech tasks (Chen et al. 2021 ). When a non-speech sound is followed by a speech sound, TD children present match/mismatch effects at approximately 600 ms, as opposite to ASD (Galilee et al. 2017 ). Interestingly, when speech and non-speech sounds are compared between high-functioning ASD children matched on age, gender, and non-verbal IQ with TD group, ASD children show impaired processing ability regarding speech pitch information, but no differences are observed for non-speech sounds (Zhang et al. 2019 ; Chen et al. 2021 ). Regarding speech differentiation, there seems to be no differences in voice perception. Low-functioning children with ASD seem to present atypical response to non-vocal sounds (Bidet-caulet et al. 2017 ), with atypical consonant differentiation in the 84- to 308-ms period, related to individual differences in non-verbal versus verbal abilities (Key et al. 2016 ).
There is EEG evidence for altered semantic processing in children with ASD, characterized by delayed processing speed and limited integration with mental representations (Piatti et al. 2021 ; Distefano et al. 2019 ). Semantic processing refers to encoding the meaning of a word and relating it to similar words or meanings. During passive and active listening, there is a pre-attentive stage of sound segregation. When individuals attend to auditory stimuli, there are some components that can distinguish the stage of neural processes. The Subject’s own name (SON) is a unique auditory stimulus for triggering an orienting response. Sounds need to stand out from the background to elicit an orienting response. SON is automatically distinguished from other names without reaching awareness, causing involuntary attention take (Tateuchi et al. 2015 ). Children with ASD present the ability to selectively respond to one’s own name with greater negativity over frontal regions, reflecting early automatic pre-attentive detection (Thomas et al. 2019 ), when compared with TD peers. After the pre-attentional level, there is an orienting response to cause a shift of attention, where the auditory system makes use of amplitude and timing cues to differentiate sounds from different spatial locations, giving them context. Although high-functioning adults with ASD do not seem to have general impairment in auditory object formation, they seem to display alterations in attention-dependent aspects of auditory object formation (P400 missing) (Thomas et al. 2019 ), as well as disruption of auditory filtering (Huang et al. 2018 ). These deviations at top–down processing might be linked with deficits in perceptual decision-making.
Some studies highlight the importance of proper ability to anticipate upcoming sensory stimuli. ASD adults seem to be less flexible than controls in the modulation of their local predictions (Goris et al. 2018 ), affecting their function of global top–down expectations. Adults diagnosed with ASD present deficits in predictive coding of sounds and words in action–sound context, with no deficits in predictive coding for neutral, non-action, and sounds (Grisoni et al. 2019 ; Laarhoven et al. 2020 ). When using varied auditory rhythms, both ASD and TD presented decreased MMN, with no difference in error prediction (Knight et al. 2020 ).
There are some interesting data regarding cognitive function lateralization in children with ASD. When comparing ERP responses for speech and non-speech sounds, speech-related events where only detected over temporal electrodes in the left hemisphere (Galilee et al. 2017 ), compared to bilaterally N330 match/mismatch responses in neurotypical children (Galilee et al. 2017 ). Regarding ASD children with impairments specifically at language level, results show hypersensibility to sounds with decreased MMN latency at the left hemisphere (Green et al. 2020 ). Older children with non-verbal IQ impairments presented bilateral attenuation in a word-learning task, as opposed to attenuated P1 amplitude present in the left hemisphere of TD children (Arnett et al. 2018 ). Young children with high-functioning ASD seem to fail to activate right-hemisphere cognitive mechanisms, probably associated with social or emotional features of speech detection.
Increased auditory perceptual capacity: impact on social and emotion perception
Impairments at the level of emotional perception can be related to internal distractions or overload of sensory information that hinder social communication. Studies using sympathetic skin response show that children diagnosed with ASD exhibit delayed habituation to auditory stimuli (Bharath et al. 2021 ). The predominant state of sympathetic nerves can affect the predisposition to filter and perceive cues, and also influence anxiety levels or valence of social cues. Individuals with ASD seem to present higher levels of perceptual capacity, which might be correlated with higher levels of sensory sensitivity (processing more information at any one time) (Brinkert and Remington 2020 ).
Emotional expressiveness is highly important for emotional perception, carrying non-verbal information that helps forming social judgments, and predisposing individuals for further social engagement. A study focusing on emotion recognition in intellectually disabled children with ASD found that these children displayed poorer performance in recognizing surprise and anger in comparison to happiness and sadness (Golan et al. 2018 ). A different study tested emotion performance by comparing ASD children with siblings without ASD diagnosis and TD peers (Waddington et al. 2018 ). Interestingly, the authors found not only poorer emotion performance in terms of speed and accuracy in the ASD group, but also poorer performance in the ASD sibling group compared to TD controls (Waddington et al. 2018 ), suggesting a possible contextual influence in emotional perception.
Children with ASD seem to present lower autonomic reactivity to human voice, with impairments in the vocal emotion recognition tests, albeit normal pro-social functioning (social awareness and social motivation) (Anna et al. 2015 ; Schelinski and Kriegstein 2019 ). This interesting result raises the question whether social impairments in ASD could be a consequence of hyperarousal from sensory overload.
Regarding other assessment paradigms, children with ASD seem to struggle with face-to-face matching, when compared to voice-face and word-face combinations (Golan et al. 2018 ), with worst performance in noisy environments (Newman et al. 2021 ). The ability to integrate facial-voice cues seems to be correlated with socialization skills in children with ASD (Golan et al. 2018 ).
Together, these studies highlight the importance of reappraising cognitive function in light of the sensory systems, such as the auditory system: the Peripheral Auditory System, where auditory pathway starts, as well as the Central Auditory Nervous System, where all auditory information gets integrated and processed.
Assessing the integrity of peripheral auditory system
Sounds are produced by acoustic waves that reach the external auditory canal and travel to the eardrum causing vibration of the tympanic membrane at specific frequencies (the typical hearing frequency range in humans is 20 to 20.000 Hertz, cycles per second) (Peterson et al. 2022 ). The vibration of the tympanic membrane causes vibration of tiny bones in the middle ear that amplify the signal and send it to the cochlea. The signal travels to fluid-filled sections of the cochlea, the scala vestibuli and the scala tympani, and oscillations of these sections transmit energy to the scala media, causing shifts between the tectorial and basilar membrane. The basilar membrane contains receptor hair cells that can be either activated or deactivated by shifts that open or close potassium channels. Cells near the base of the cochlea respond to high frequencies, with increased flexibility to respond to lower frequencies toward the apex of the cochlea (Peterson et al. 2022 ; Zhao and Müller 2015 ; Delacroix and Malgrange 2015 ). Inner hair cells are responsible for the majority of auditory processing. Outer hair cells synapse only on 10% of the spiral ganglion neurons (Delacroix and Malgrange 2015 ). Neurons within the spiral ganglion mostly synapse at the base of hair cells to the auditory nerve (cochlear nerve). The cochlear nerve then sends up information to the brain cortex through a serious of nuclei in the brainstem: the cochlear nuclei (medulla), superior olivary complex (pons), lateral lemniscus (pons), inferior colliculus (midbrain), and medial geniculate nucleus (midbrain) (Felix et al. 2018 ). Although the primary auditory pathway mostly ascends to the cortex through the contralateral side of the brainstem, all levels of the auditory system have crossing fibers, receiving and processing information from both the ipsilateral and contralateral sides (Peterson et al. 2022 ).
The auditory brainstem response (ABR) in ASD
Reported cognitive deficits in ASD regarding speed and accuracy of sound stimuli assessment (Distefano et al. 2019 ; Waddington et al. 2018 ) might potentially be contributed by impairments in impulse initiation at the cochlear nerve, or impairments in the transmission and conduction of signals along the brainstem, as it occurs in demyelinating diseases. One tool used to measure neural functionality of the auditory brainstem is the auditory brainstem response (ABR) (Celesia 2015 ; Jewett and Williston 1971 ). Participants usually perform hearing screenings to exclude hearing disabilities, such as lesions below or within the cochlear nuclei. Of note, since 2015, there are few experimental studies assessing the integrity of the peripheral auditory system in ASD.
The auditory brainstem response (ABR) measures electrical signals associated with the propagation of sound information through the auditory nerve to higher auditory centers, after an acoustic stimulus. Major alterations in neuronal firing along this pathway can be detected as changes in auditory brain response ([ 99 ]). Complementary to the use of a short click as a classical acoustic stimulus, ABR is also often performed with complex sounds, such as syllables, which incorporate an array of complexity more similar to speech. Two major categories of ABR stimulus are detailed below: click-ABR and speech-ABR.
Most ABR studies report differences in auditory brainstem processing for ASD individuals when compared with control groups (Table 7 ). Results are discussed taking into consideration the age of participants and different time-points, their cognitive pattern, type of stimuli, and experimental design.
Click-evoked brainstem responses (click-ABR) in ASD
In the first 10 ms after a click, click-ABR produce five-to-seven waveforms (wave I–VII). These wave peaks reflect the propagation of electrical activity as it travels along the auditory pathway, providing information in terms of latency (speed of transmission), amplitude of the peaks (interpreted as the number of neurons firing), inter-peak latency (time between peaks), and interaural latency (correlation between left and right ear) (Musiek and Lee 1995 ).
Some studies with click-ABR (Table 8 ) show longer latencies for ASD participants in wave V, and longer latency of inter-peak intervals in waves I–V and III–V (Tecoulesco et al. 2020 ; Jones et al. 2020 ). However, these experiments were done with toddlers. Interestingly, a recent study tested older children in a click-ABR paradigm (Claesdotter-Knutsson et al. 2019 ). Results do not show differences in ABR latency, but reveal a higher amplitude of wave III in ASD, suggesting functional alterations at the pons region (Claesdotter-Knutsson et al. 2019 ). This experiment used binaural sound exposure, showing a higher degree of correlation between left and right ear in the ASD group. A different study found absence of asymmetry in the latency of wave V between the right and left sides, both in ASD and control groups (ElMoazen et al. 2020 ). The authors further report a reduced amplitude in the binaural interaction component in younger children with ASD, which might reflect reduced binaural interaction at younger ages not related to artificial latency shift (ElMoazen et al. 2020 ). A recent study looking at newborns later diagnosed with ASD at the age of 3–5 years showed ABR latency delays (Delgado et al. 2021 ), suggesting the emergence of differences in acoustic processing, at the brainstem level, right after birth. A more recent study tested adults with ASD and found no differences in absolute ABR wave latencies (Fujihira et al. 2021 ). The authors showed a shorter summating potential (SP), suggesting normal auditory processing in the brainstem for ASD adults (Fujihira et al. 2021 ).
Speech-evoked brainstem responses (speech-ABR) in ASD
The most common speech-ABR stimulus used is the universal syllable/da/. After the stimulus, a subcortical response emerges as an ABR waveform of seven peaks (V, A, C, D, E, F, O). Peaks can reflect either a change in the stimulus (i.e., onset, offset, or transition) or the periodicity of the stimulus. There are two main components in speech-ABR: the onset response (waves V and A) and the frequency-following response (FFR; waves D, E, and F). The wave C represents the consonant–vowel transition, while the wave O represents the end of the vowel. Analysis of FFR includes measurements of response timing (peaks), magnitude (robustness of encoding of specific frequencies), and fidelity (comparison of FFR consistency across sessions, which gives an index of how stable the FFR is from trial to trial (Krizman and Kraus 2019 )).
Similarly to click-ABR, speech-ABR studies (Table 8 ) also show longer latencies for ASD participants, including high-functioning ASD individuals (Ramezani et al. 2019 ). Recently, a longitudinal study included two assessment time-points (interval of 9.68 months) to look for longitudinal changes in speech-ABR (Chen et al. 2019 ). No differences were found in the TD group, whereas differences were found in the ASD group (shorter latency wave V and increased amplitude wave A and C), suggesting an age effect for ASD (Chen et al. 2019 ). Another study had two assessment time-points to investigate neural response stability, a metric measured by trial-by-trial consistency in the neural encoding of acoustic stimuli (Tecoulesco et al. 2020 ). Results showed that children with a more stable neural encoding of speech sounds, in both groups ASD and TD, demonstrated better language processing at a phonetic discrimination task (Tecoulesco et al. 2020 ). Individuals’ performance was assessed in a different study through listening structured and repetitive listening exercises, with increasing difficulty levels (Ramezani et al. 2021 ). Results showed gradual improvement in ASD individuals’ temporal auditory skills (Ramezani et al. 2021 ).
A relevant association has been found between sensory overload and behavioral measures in ASD, but without relevant auditory processing association (Font-Alaminos et al. 2020 ). For children with ASD, the FFR signal has been described as unstable across trials (Otto-Meyer et al. 2018 ), tending to increase with stimulus repetition (Font-Alaminos et al. 2020 ), which suggests an unstable neural tracking at the level of subcortical auditory system (Table 9 ). The development pattern of auditory information processing was assessed in preschool children with ASD (Chen et al. 2019 ). Results show a positive correlation between wave A and Gesell Developmental Diagnosis Schedules (GDDS) language score (Chen et al. 2019 ). According to authors, the latency between V and A complex could suggest a weakened synchronization of neural response at the beginning of speech stimulus (Chen et al. 2019 ). A different study also revealed longer latencies of the transient FFR components (which include D, E, and F, ABR waves) in the ASD group (Ramezani et al. 2019 ). These results suggest a possible disturbance in brain pathways implicated in FFR generation [the direct pathway to the contra-lateral IC via the lateral lemniscus, and the ipsilateral pathway via superior olivary complex and the lateral lemniscus (Ramezani et al. 2019 )] further raising the question whether this could be a potential compensatory mechanism in ASD.
Otoacoustic emission (OAE) studies in ASD
The integrity of the peripheral auditory system can also be evaluated using otoacoustic emissions (OAEs). Evoked otoacoustic emissions are produced by healthy ears in response to an acoustic stimulus delivered into a sealed ear canal. The acoustic stimulus causes basilar membrane motion which triggers an electromechanical amplification process by the cochlear outer hair cells, producing a sound that echoes back into the middle ear (otoacoustic emissions). These nearly inaudible emissions are measured using a sensitive microphone and help evaluate normal cochlear function. A study tested a group of children and adolescents with ASD (ASD with Full-Scale IQs higher than 85) with normal audiometric thresholds (Bennetto et al. 2016 ). Results showed that children with ASD presented reduced OAEs at 1 kHz frequency range, with no differences outside this critical range (at 0.5 and 4–8 kHz regions) (Bennetto et al. 2016 ), thus suggesting reduced outer hair cell function at 1 kHz. Outer hair cells synapse directly with neurons originating in the nuclei of the superior olivary complex. A morphological post-mortem study of subjects with ASD showed significantly fewer neurons in the Medial Superior Olive (MSO), a specialized nucleus from the superior olivary complex (Mansour and Kulesza 2020 ). Results also showed that the existing fewer neurons in the MSO are smaller, rounder, and with abnormal dendritic orientations (Mansour and Kulesza 2020 ). However, the small sample size, variability of post-mortem tissue origin and quality (7 post-mortem samples from drowning, seizure, or other death causes), may hinder conclusions from this study. Previously, a different study found no evidence regarding asymmetrical or reduced middle ear muscle (MEM) reflexes and binaural efferent suppression of transient evoked otoacoustic emissions responses (Bennetto et al. 2016 ). However, a more recent study showed OAE asymmetry, with the medial olivocochlear system being apparently more effective in the right than the left ear in ASD (Aslan et al. 2022 ).
Assessing the integrity of central auditory nervous system
ASD is a neurodevelopmental disorder with behavior and cognitive traits associated with atypicalities in the central nervous system (CNS). Integrity of the central nervous system can be assessed experimentally by several techniques, such as magnetoencephalography (MEG; Table 10 ), magnetic resonance imaging (MRI; Table 11 ), as well as other multimodal tools (Table 12 ).
Magnetic resonance imaging (MRI) is an imaging technique that is used to assess the anatomy and physiology of brain circuits. Magnetoencephalography (MEG) is a functional neuroimaging technique that detects, records, and analyzes the magnetic fields produced by electrical currents occurring naturally in the brain (Cohen 1972 ). While EEG records brain electrical fields, MEG records magnetic fields. Similar to EEG and ERPs, MEG signals can be also time-locked to particular events, being called event-related magnetic fields (ERFs). As previously described for N100 (EEG signal), M100 (MEG) refers to a peak signal occurring at a latency of about 100 ms after stimulus onset. Both MEG and EEG are non-invasive methods for recording neural activity providing data with high temporal resolution (measured in milliseconds), thus providing unique information in terms of timing, synchrony, and connectivity of neural activity (Port et al. 2015 ). Despite the fact that EEG signals might display superimposed sources of activity, EEG is useful to quickly determine how brain activity can change in response to stimuli and to directly detect abnormal activity, having the advantage of being fully or semi-portable with an accessible cost for researchers. MEG has the advantage that the local variations in conductivity of different brain matter do not attenuate the signal, providing more accurate spatial resolution of neural activity than EEG (Landini et al. 2018 ). Regarding EEG and MEG use in young children, these two techniques offer advantages over some neuroimaging techniques, including fewer physical constraints and the absence of radiation and noise (Port et al. 2015 ). Still, EEG and MEG have limited spatial resolution, making it difficult to determine the precise location of neuronal activity with confidence. In contrast, MRI provides data with good spatial resolution, but lacks a good temporal resolution at the electrophysiological level and cannot provide frequency band discrimination. Functional magnetic resonance imaging (fMRI) uses MRI to measure the oxygenation of blood flowing near active neurons, being a valuable tool for delineating the human neural functional architecture (Cole et al. 2010 ). Combining EEG/MEG with MRI can increase the spatial resolution of electromagnetic source imaging, while tracing the rapid neural processes and information pathways within the brain (Liu et al. 2006 ), making them good candidates for multimodal integration.
Auditory evoked magnetic fields’ studies in ASD
Results from studies with high-functioning ASD individuals show delayed latencies at M50 and M100 auditory evoked responses, suggesting impairments at early auditory processes in the primary and secondary auditory cortex (Claesdotter-Knutsson et al. 2019 ; Matsuzaki et al. 2020 ; Roberts et al. 2019 ; Port et al. 2016 ; Edgar et al. 2013 ). It is thought that the major activity underlying M100 is located in the supratemporal plane, with superior temporal gyrus (STG) as the primer M50 generator (Edgar et al. 2015 ). STG results from the ASD group suggest increased pre-stimulus abnormalities across multiple frequencies with an inability to rapidly return to a resting state before the following stimulus (Edgar et al. 2013 ). Neurotypical individuals present a negative association between age and latency of M50 and M100 (Matsuzaki et al. 2020 ; Roberts et al. 2020 ), which indicates a functional decrease with age. Results show a similar pattern for children with ASD regarding M50, but not with M100 latencies (Matsuzaki et al. 2020 ). A group of ASD children and TD peers were compared at two time-points, from approximately 8 to 11 years old, showing M100 latency and gamma-band maturation rates similar between both groups (Port et al. 2016 ). A study of cascading effects on speech sound processing found lower brain synchronization in the early stage of the M100 component for ASD children (Brennan et al. 2016 ). A group of younger ASD children with approximately 5 years old was assessed in a different study, showing shorter M100 latencies in the left hemisphere (Yoshimura et al. 2021 ). The M200, considered an endogenous response associated with attention and cognition, seems to have a maximum amplitude around 8 years old, decaying with age. This pattern of age-dependent decrease in neurotypical children was less clear in the ASD group (Edgar et al. 2015 ), indicating perhaps a maturational delay.
Looking at data across lifespan from individuals with ASD without intellectual disability, delayed latencies were found above 10 years old versus shorter latencies in younger children, suggesting atypical brain maturation in ASD. Minimally verbal or non-verbal children with ASD (ASD-MVNV) seem to present greater latencies delays in M50 and M100 (components associated with language and communication skills) compared to ASD children without intellectual disabilities (Roberts et al. 2019 ). Similar association for verbal comprehension was found in the left auditory cortex regarding M200 latency response (Matsuzaki et al. 2017 ; Demopoulos et al. 2017 ). In auditory vowel-contrast mismatch field experiments (MMF), an association was found between MMF delay and language impairments in children with ASD (Berman et al. 2016 ). Furthermore, in a study testing pre-attentive discrimination of changes in speech tone, the amplitude of the early MMF component (100–200 ms) seems to be decreased in left temporal auditory areas for ASD children (Yoshimura et al. 2017 ). This group of ASD children, also diagnosed with speech delay, seem to have increased activity in the left frontal cortex compared to other ASD children without speech delay (Yoshimura et al. 2017 ). Deficits in auditory discrimination have also been reported in children with ASD, namely bilaterally delayed MMF latencies (Matsuzaki et al. 2019a ) as well as rightward lateralization of MMF amplitude (Matsuzaki et al. 2019b ) contrasting with the leftward lateralization found in NT children (Matsuzaki et al. 2019a ). ASD children with abnormal auditory sensitivity seem to have longer temporal and frontal residual M100/MMF latencies (Matsuzaki et al. 2017 ). These findings were correlated with the severity of auditory sensitivity in temporal and frontal areas for both hemispheres (Matsuzaki et al. 2017 ). Taking these data together, ASD seems to be characterized by atypical neural activity in the auditory cortex, together with impaired auditory discrimination in brain areas related to attention and inhibitory processing. Such findings seem to be highly associated with language and comprehension deficits.
EEG and MEG frequency bands in auditory tasks
EEG and MEG can be transformed to decompose its raw signal into frequency band components. In adults, the typical frequency bands and their approximate spectral boundaries are delta ( δ , from 1 to 3 Hz), theta ( θ , from 4 to 7 Hz), alpha ( α , from 8 to 12 Hz), beta ( β , from 13 to 30 Hz), and gamma ( γ , from 30 to 100 Hz) (Saby and Marshall 2012 ). Regarding ASD studies, decreased resting alpha power has been observed in children with ASD (Pierce et al. 2021 ). In noise experiment conditions, ASD children seem to have increased recruitment of neural resources, with reduced beta band top–down modulation (required to mitigate the impact of noise on auditory processing) (Mamashli et al. 2017 ). Interestingly, in quiet conditions, no differences were found between ASD and TD peers (Mamashli et al. 2017 ). A different study using sensory distracters (distracters that disrupts the processing of social cue interpretation) found decreased activation in auditory language and frontal regions in high-functioning youth with ASD (Green et al. 2018 ).
In auditory habituation studies measuring galvanic skin response, an aversion effect has been reported in ASD, likely due to sensory information overload. Results show consistent patterns of reduced habituation in ASD individuals, without the predicted steady decline that would be expected for habituation experiments. Instead, ASD adults showed a steady increase in the galvanic skin response over the course of the sessions (Gandhi et al. 2021 ). Regarding phase-lock auditory stimuli, no differences were found in the low gamma frequency range between ASD and TD children around 8 years old. A decrease in low gamma-power was observed in TD subjects around 17 years old but not in the ASD group (Stefano et al. 2019 ). The atypical gamma-band network in ASD seems to be located around the left ventral central sulcus (vCS) in children around 10 years old (Floris et al. 2016 ). Older ASD participants showed more pronounced low gamma deficits (Stefano et al. 2019 ), suggesting an increased background gamma-power that, similar to noise, can affect proper processing of stimuli. Interestingly, a recent study tested ASD children with and without atypical audiovisual behavior and found that only children with atypical audiovisual behavior showed increased theta to low gamma oscillatory power in the bilateral superior temporal sulcus and temporal region (Matsuzaki et al. 2022 ).
Cortical excitatory–inhibitory balance in ASD
Proper development of the central nervous system requires a fine balance between excitatory and inhibitory (E/I) neurotransmission. This E/I balance seems to be very important for cortical gamma-band activity, given that gamma waves are generated through connections between GABAergic inhibitory interneurons and excitatory pyramidal cells (Stefano et al. 2019 ; Port et al. 2017 ). A multimodal imaging study combined MEG, MRI, and GABA magnetic resonance spectroscopy (MRS) to assess physiological mechanisms associated with auditory processing efficiency in high-functioning children/adolescents with ASD. The study found longer M50 latency combined with decreased GABA in the left hemisphere for ASD individuals, suggesting an association between sensory response latency and synaptic activity (Roberts et al. 2020 ). Similar results were shown in a multimodal study that assessed cortical GABA concentrations and gamma-band coherence in the auditory cortex and superior temporal gyrus. Decreased GABA1/Creatine levels were found in children/adolescents with ASD, without the gamma-band coherence association typically seen in neurotypical subjects (Port et al. 2017 ). A different study combining EEG and MRS showed reduced glutamine in the temporal–parietal cortex associated with greater hypersensibility to sensory input detection (Pierce et al. 2021 ). A post-mortem study assessed the cytoarchitecture of the anterior superior temporal area (area of Brodmann), involved in auditory processing and social cognition, by quantifying the number and soma volume of pyramidal neurons in the supragranular and infragranular layers (Kim et al. 2015 ). Results showed no differences between ASD adolescents and adults age-matched with a neurotypical group (Kim et al. 2015 ). A different study looked at cortical neural inhibition for auditory, visual, and motor stimulation (Murray et al. 2020 ). Results showed no increase in the initial transient response in ASD individuals, with widespread changes in stimulus offset responses (Murray et al. 2020 ). Although results show similar patterns of transient response in ASD and TD groups for all cortical regions, larger fMRI amplitudes were found at later response components, approximately 6–8 s after stimulus presentation (stimulus duration of 20 s) (Murray et al. 2020 ). These studies suggest cortical excitatory–inhibitory imbalance in areas related to auditory processing in subjects with ASD.
Auditory sensory sensitivities in ASD
Sensory sensitivities can be assessed at three different stages of sensory processing: initial response to the stimuli, habituation, and generalization of response to novel stimuli. Brain imaging studies in individuals with ASD have found auditory discrimination deficits (Matsuzaki et al. 2019a ; Abrams et al. 2019 ), as well as increased neural responsiveness upon repeated stimuli, with larger fMRI response in the auditory cortex that seems specific to temporal patterns of stimulation (Millin et al. 2018 ). Children with high sensory over-responsivity showed reduced ability to maintain habituation in the amygdala (Green et al. 2019 ), together with increased resting-state functional connectivity between salience network nodes and brain regions implicated in primary sensory processing and attention (Green et al. 2018 ). Children with low sensory over-responsivity showed atypical neural response patterns, with increased prefrontal–amygdala regulation across sensory exposure (Green et al. 2019 ). A different study found intact temporal prediction responses with altered neural entrainment and anticipatory processes in children with ASD (Beker et al. 2021 ). These results might explain atypical behavioral responses observed in ASD during sensory processing, mediated by top–down regulatory mechanisms.
Differences in response to sound familiarity have also been reported in children with ASD, with reduced activity in right-hemisphere planum polare for unfamiliar voices, reduced activity in a broad extent of fusiform gyrus bilaterally, and less activity in the right-hemisphere posterior hippocampus (Abrams et al. 2019 ). In a different fMRI study, the authors compared brain responses to vocal changes with different levels of stimulus saliency (deviancy or novelty) and different emotional content (neutral, angry) (Charpentier et al. 2020 ). Results show no differences between ASD and neurotypical adults regarding vocal stimuli and novelty processing, independently of emotional content. Brain processing appears typical in both groups, with activation in the superior temporal gyrus, and with larger activation for emotional compared to neutral prosody in the right hemisphere (Charpentier et al. 2020 ). These results suggest that the processing of emotional cues may be placed at later processing stages, such as insular activation, or at the hippocampus level. Interestingly, a recent study show altered voice processing in ASD which seems to be present already at the midbrain level of the auditory pathway (Schelinski et al. 2022 ).
Deficits in auditory discrimination have also been found both in MEG and brain imaging studies (Ganesan et al. 2016 ; Claesdotter-Knutsson et al. 2019 ; Abrams et al. 2019 ). Individuals diagnosed with ASD seem to have deficits in predicting the offset of standard tones, engaging less resources for duration tasks compared with pitch discrimination tasks (Lambrechts et al. 2018 ). Spectrally complex sounds can trigger two continuous neural MEG responses in the auditory cortex: the auditory steady-state response (ASSR) at the frequency of stimulation, and the sustained deflection of the magnetic field (sustained field).
The ASSR is an oscillatory response phased-locked to the onset of the stimulus, where the frequency of stimulation is represented by the same frequency in the primary auditory cortex (Stroganova et al. 2020 ). Both ASD and neurotypical children with 5–6 years old seem to show right dominant 40 Hz ASSR (Ono et al. 2020 ). No differences were found regarding neural synchrony at 20 Hz for both ASD and TD children between 5 and 12 years old (Stroganova et al. 2020 ; Ono et al. 2020 ), suggesting a normal maturation of ASSR for low frequencies. Interestingly, the right-side 40 Hz ASSR increased with age in the neurotypical group, as opposed to ASD children (Ono et al. 2020 ). Reduced 40 Hz power was also found in adolescents with ASD at both right and left primary auditory cortex, with no difference in gamma-band responses (Seymour et al. 2021 ). Diminished auditory gamma-band responses were found in ASD children, indicating that peak frequencies likely vary with developmental age (Roberts et al. 2021 ).
The sustained field (SF) is a baseline shift in the electrical and magnetic signals upon exposure to a sound lasting for several seconds. The SF adapts to the probability of a sound pattern, reflecting the integration of pitch information across frequencies within the tonotopic map of the primary auditory cortex (A1) (Stroganova et al. 2020 ). Children diagnosed with ASD seem to have atypical higher order processing in the left hemisphere of the auditory cortex, with cortical sources of SF located in the left and right Heschl’s gyri (primary auditory cortex) (Stroganova et al. 2020 ).
The severity of sensory processing deficits in ASD also seems to be correlated with reduced inter-hemispheric connectivity of auditory cortices (Linke et al. 2018 ; Tanigawa et al. 2018 ) and lower verbal IQ (Linke et al. 2018 ). Interestingly, increased connectivity between the thalamus and the auditory cortex was found in patients with reduced cognitive and behavioral symptomatology (Linke et al. 2018 ; Tanigawa et al. 2018 ), which suggests high thalamocortical connectivity as a potential compensatory mechanism in ASD (Linke et al. 2018 ). Individuals diagnosed with ASD also seem to present abnormal modulation of connectivity between pulvinar and cortex, with greater increases in pulvinar connectivity with the amygdala (Green et al. 2017 ). Regarding processing of social stimuli, reduced connectivity between the left temporal voice area and the superior and medial frontal gyrus was found in ASD patients (Hoffmann et al. 2016 ). Decreased connectivity between the left TVA and the limbic lobe, anterior cingulate and the medial frontal gyrus as well as between the right TVA and the frontal lobe, anterior cingulate, limbic lobe and the caudate seems to be associated with increased symptom severity (Hoffmann et al. 2016 ).
Language and speech processing in ASD
Language acquisition involves the integration of top–down and bottom–up processes. Language deficits present in ASD diagnostic criteria may be related to one of these integration processes or a combination of both. ASD individuals can have sensory deficits in the bottom–up early sensory processing and/or prediction deficits related to higher order assessment.
Phonological processing seems to be disrupted in ASD children, displaying attenuated MEG response in the right auditory cortex to both legal and illegal phonotactic sequences (Brennan et al. 2016 ). Interestingly, ASD children do not seem to have differences in phonological competence but significantly differ in other measures, such as attention, syntax, and pragmatics (Brennan et al. 2016 ; Wagley et al. 2020 ), suggesting impairments at language structure knowledge. An event-related desynchrony of the auditory cortex in the 5–20 Hz range seems to index language ability in both children with ASD and neurotypical controls (Bloy et al. 2019 ). When speech and non-speech were compared, ASD children with poorer language composite scores presented a general auditory processing deficit, with atypical left hemisphere responses in the high order time-window of 200–400 ms (Yau et al. 2016 ), and different neural and behavioral effects of syllable-to-syllable processing in speech segmentation (Wagley et al. 2020 ).
When considering visual-speech recognition tasks, ASD individuals seem to have difficulties in extracting speech information from face movements (Borowiak et al. 2018 ). Decreased Blood Oxygenation Level Dependent (BOLD) responses were detected in the right visual area 5 and left temporal visual-speech area, as well as lower functional connectivity between these two brain regions implicated in visual-speech perception (Borowiak et al. 2018 ). This multimodal fMRI study combined with eye-tracking data showed that the ASD group had reduced responses not only for emotional but also neutral facial movements (Borowiak et al. 2018 ). High-functioning adults with ASD seem to have typical responses for voice-identity tasks, and dysfunctional speech recognition in the right posterior temporal sulcus (Schelinski et al. 2016 ).
Predictive processing was tested in a naturistic environment, by measuring surprisal values, or how much information of word contributes given some linguist context (Brennan et al. 2019 ). Results showed bilateral temporal effect for sentence-context linguistic predictions in an early time-window (from 26 to 254 ms), for both high-functioning ASD children and TD peers with 3–6 years old (Brennan et al. 2019 ). A different study showed that as surprisal values increase, the amplitude of the neural response also increases in the left primary auditory cortex, posterior superior temporal gyrus (pSTG), and inferior frontal gyrus (IFG) in neurotypical children (Wagley et al. 2020 ). However, ASD children with lower IQ levels did not display such learning pattern (Wagley et al. 2020 ).
A longitudinal study tested children in the first months of life (around 4 months old) who later developed ASD, at 3 years old (Lloyd-Fox et al. 2018 ). Using functional near-infrared spectroscopy (fNIRS), infants later diagnosed with ASD showed reduced activation to visual social stimuli across the inferior frontal (IFG) and posterior temporal (pSTS-TPJ) regions of the cortex, reduced activation to vocal sounds, and enhanced activation to non-vocal sounds within left lateralized temporal regions (Lloyd-Fox et al. 2018 ). These results suggest that atypical ASD cortical responses may be detectable at early stages.
A right ASD brain? Lateralization and inter-hemispheric connectivity
The inferior frontal and superior temporal areas in the left hemisphere are crucial for human language processing (Yoshimura et al. 2017 ). Some striking findings report ASD group differences in left and right hemispheres (Edgar et al. 2013 ; Sadeghi Bajestani et al. 2017 ). Results show lower right–left hemispheric synchronization in young children with ASD (Brennan et al. 2016 ), stronger rightward lateralization within the inferior parietal lobule, and reduced leftward lateralization extending the auditory cortex (Floris et al. 2016 ). Neurotypical peers show stronger activation in the left auditory cortex for semantic categorization tasks (Tietze et al. 2019 ), and hemispheric advantage that seems to be absent in ASD children (Edgar et al. 2015 ). Adolescents diagnosed with ASD show weaker cortical activation in the left ventral central sulcus at word comprehension tasks (Tanigawa et al. 2018 ), indicating atypical hemispheric functional asymmetries.
Resting-sate studies of the auditory network in patients with ASD
Resting-state connectivity is a correlated signal between functionally related brain regions in the absence of any stimulus (spontaneous signal fluctuation). Results show dynamic functional brain networks altered in children diagnosed with ASD, including cognitive control, subcortical, auditory, visual, bilateral limbic, and default-mode network (Stickel et al. 2019 ). High-functional ASD adults also present alterations in the anterior sector of the left insula and the middle ventral sub-region of the right insula in the ASD brain (Yamada et al. 2016 ). Atypical spread of activity seems to be present in ASD individuals, indicated by altered dynamic lag patterns in salience, executive, visual, and default-mode networks (Raatikainen et al. 2020 ). Regarding intrinsic neural timescales, both high-functional adults with ASD and TD peers presented longer timescales in frontal and parietal cortices and shorter timescales in sensorimotor, visual, and auditory areas (Watanabe et al. 2019 ). Individuals with ASD also seem to display a volumetric increase in the right insula (Yamada et al. 2016 ). Given that the right insula is primarily specialized for sensory and auditory-related functions, such volumetric expansion might be functionally correlated with previously reported ASD alterations in auditory stimuli processing and auditory sensitivity.
Diffusion MRI studies of the auditory network in patients with ASD
A recent study in children with ASD reports decreased gray matter volume at the fronto-parietal network, associated with the severity of communication score and restricted behaviors. In adults, an increase of gray matter was reported at the regions of auditory and visual networks, with the auditory network being correlated with the severity of the communication core, and visual networks with severity of repetitive and restricted behavior (Yamada et al. 2016 ). Uncoupled structure–function relationships in both auditory and language networks have also been reported in ASD (Berman et al. 2016 ), with changes in the relative weight of white matter contribution to structure–function relationships (Roberts et al. 2020 ).
Final remarks
Experimental design in asd studies.
Despite a large number of studies assessing autism spectrum disorder at the level of auditory processing, it is still not possible to conclude the cause of auditory symptomatology present in ASD. Children and adults diagnosed with ASD have a neurodivergent cognitive profile, and the heterogeneity of both severity and type of symptoms, probably contributes for this lack of causal explanation. Another heterogeneity factor comes from the inclusion criteria for ASD participants, such as the diagnostic assessment confirmation tools or the measurements of IQ levels. Some studies analyze their data considering verbal and non-verbal abilities for ASD children, while other studies refer only to the full performance of IQ levels. To better illustrate this issue, especially for language components assessment, we can look at the study performed by Bloy et al. ( 2019 ) that found no differences in IQ mean values between ASD and TD peers, but highly significant differences in language ability. Future studies should include a wider range of standardized assessment tools to determine discrepancies in autistic traits, and larger sample size to avoid limitations in the assessment of within-group and multiple comparisons.
A consideration should also be made about the accuracy of diagnosis of children with ASD. In a longitudinal study, Port and colleagues referred to the inclusion of a group of children with approximately 8 years old considered to be initially on the spectrum. A later follow-up revealed that these children exhibited optimal outcomes at approximately 12 years old, no longer meeting diagnostic criteria for ASD (Port et al. 2016 ). Interestingly, these children showed results in-between ASD and TD peers. A similar in-between result was found in ASD siblings emotional perceptions (Waddington et al. 2018 ), indicating a possibility of contextual interference in ASD traits, such as parenting. Sometimes, parents’ perception questionnaires are assessed without taking into consideration the social, economic, and affective influence of parenting and/or children’s educators and peers. When designing auditory research studies, it would be important to also consider other relevant daily-life features, such as special talents, levels of anxiety and aggression, and sensory challenges.
One main limitation of brain imaging and EEG auditory studies in ASD is individual discomfort thresholds, such as sensibility to sound levels or immobility requirements during imaging sessions. By analyzing experimental designs, it is possible to see the wide variety of methods and protocols that are applied, even for similar techniques. For instance, some participants are allowed to sleep during ABR recordings (Fujihira et al. 2021 ), while some participants watch videos during the experiment (Jones et al. 2020 ; Chen et al. 2019 ), creating different conditions to assess similar variables across studies. Another important consideration is medication status as an eligibility criterion for ASD studies. Some studies detail the presence or absence of medication, such as risperidone, anxiolytics, or antidepressants (Port et al. 2016 ), or simply exclude ASD-medicated participants, while other do not report any criteria regarding medication.
The underlying conceptualization of autism and associated deficits and impairments through the lens of the DSM might push researchers and clinicians to prioritize the correction of perceived deficits as the major goal of behavioral intervention (American Psychiatric Association (APA) 2013 ; Schuck et al. 2022 ). Given the neurodiversity and individual differences present in ASD subjects, future studies should ensure a comprehensive neuropsychological evaluation, for both ASD and control subjects. As an example, studies often include the term “high or low functioning”, which is not an official medical diagnosis; hence, it is not clear at every study whether this descriptor is based on full-scale IQ and language, verbal and non-verbal, or adaptive behavior and daily functioning measures. To acknowledge cultural differences, future studies could also include social and ecological validity measures (Schuck et al. 2022 ), with assessment of the socio-cultural context at individual, institutional, and family levels, using self-report measures. For a better understanding of the human neurocognitive spectrum, both ASD and control subjects should be assessed at other areas of interest, such as self-determination, self-esteem, social inclusion, well-being, personal development, interpersonal relationships, measures of quality of life, and functional adaptive skills (Schuck et al. 2022 ).
Auditory cortex: a central role in ASD?
Deficits in bottom–up early sensory processing of auditory input.
Low-level auditory stimuli (e.g., pitch discrimination) deficits vary widely within ASD, with some interesting differences when low- and high-functioning children (based on IQ assessment) are compared (Table 13 ). ASD individuals seem better at detecting additional unexpected and expected sounds at several acoustic parameters, showing an increased auditory perceptual capacity, but display deficits in detection and discriminatory tasks, especially in the presence of noise. Difficulties in the processing of sensory stimuli have been confirmed by electrophysiology and brain imaging data at early stages of perceptual processing. ASD patients with verbal disabilities seem to be particularly impaired in terms of cortical processing of acoustic inputs. Larger idiosyncrasy seems to be present in high-level auditory areas, with deficits being associated with severity of social and communication symptoms. One possibility is to look at the core aspects of autism as a cascading effect of unusual auditory and language trajectories (prosody, semantic context). Individuals with ASD seem to have alterations in multisensory integration, displaying poorer performance in multisensory tasks requiring the auditory modality. It is still not clear whether ASD sensory idiosyncrasy affects all types of audiovisual integration and whether these deficits can be compensated by later attentional processes. For non-multimodal studies, further auditory investigation should guarantee that unisensory conditions can be assessed without visual influence (blind conditions) and should control whether auditory processing responses are affected by attention deficits.
Difficulties in understanding others are a core feature of autism spectrum disorders (Baron-Cohen 2001 ). At the emotional level, individuals with ASD seem to have deficits judging auditory valence and vocal emotion recognition, but with normal pro-social functioning, suggesting a normal social awareness and motivation. Future auditory studies should also look into Theory of Mind manifestations, emphasizing social motivation and reward associated with communication. A detrimental effect on communication and increased arousal on ASD children is observed in experiments within a noise context. Interestingly, when the context changes to silent, no differences in speech comprehension are found, suggesting a relevant role of auditory sensory overload in ASD individuals.
Changes in higher-order integration processing of auditory information
Results assessing phonological processing, language components, speech non-speech, and visual-speech recognition, suggest that processing at the auditory cortex is altered in ASD. This atypical sensory processing may interfere with perceptual mechanisms where individuals anticipate what will happen, based on their perceived sensory information. Observed differences in auditory perception in ASD might not be related with attention allocation to acoustic stimuli, but rather to difficulties in recognition and integration of acoustic information, such as the process of understanding speech from other people. Deficits at the level of communicative function would reduce the ability of individuals with ASD to learn several language components, such as phonology, syntax, and semantics. Children use prior information to incrementally narrow down the set of possible interpretations for a sentence, highlight how high-level representations can propagate to low-level processing stages. Deficits in habituation or adaption could potentially lead to an inability to form predictions. Such changes in higher order processing may impact the development of language and interfere with communication.
Integrity of the central nervous system seems to be affected in ASD individuals, with auditory alterations being detectable during early development (Table 14 ). Several studies indicate atypical brain maturation, abnormal neural network synchronization, and functional alterations in the primary auditory cortex, trailed by impaired cognitive function, such as attention, inhibitory processing, and neural discrimination processes. Most individuals diagnosed with ASD have auditory sensory issues, being mainly hypersensitive to sounds. Some reports also indicate that individuals with ASD may have deficits in lateralized cognitive functions as well as functional and brain structural asymmetry, with disproportionate overgrowth of audio and visual sensory networks. In social tasks involving auditory processing of verbal cues, a reduced connectivity between the left temporal voice area and the superior and medial frontal gyrus has been reported. Interestingly, thalamocortical overconnectivity has been reported in several studies albeit with different interpretations: it might reflect lack of thalamocortical inhibition (which could cause difficulties in attentional sensory information), or it might be a compensatory mechanism (that could serve to mitigate reduced synchronization).
Auditory processing in ASD and neurodevelopmental trajectories
Clinical biomarkers can offer the opportunity to improve predictions, diagnosis, stratification by severity and subtypes, and response indices for pharmaceutical development. Such biomarkers should ideally be robust, sensitive, specific to the disorder, and scale with severity (Port et al. 2015 ), but finding biomarkers for ASD requires a deep understanding of its neurobiological underpinnings. A correlation between neuroanatomical, genetic, biochemical, and immune findings with clinical ASD diagnosis is still unclear (Levin and Nelson 2015 ). Furthermore, the heterogeneity of age-related phenotypes in ASD poses a challenge in the pursuit of clinical biomarkers. In that sense, functional signatures derived from electrophysiological and imaging studies might become promising biomarkers given that they offer a temporal layer that could help revealing putative biological trajectories along the development process.
The brain is remarkably malleable, capable of restructuring itself in response to experience. Major sculpting of brain circuits occurs during specific time windows known as critical periods (Leblanc and Fagiolini 2011 ). Distinct critical periods underlie different modalities, ranging from visual processing to language and social development. Critical periods begin in primary sensory areas and occur sequentially in the brain, requiring a precise balance of excitatory/inhibitory (E/I) neurotransmission (Bourgeron 2009 ). These periods close after structural consolidation, diminishing future plasticity as the brain reaches adulthood. Although critical periods provide an exceptional time-window for learning and consolidation, they also represent a period of great vulnerability for the developing brain.
Different neurodevelopmental trajectories and brain maturation processes may explain the heterogeneity of behavioral and cognitive traits observed in ASD. Checking the integrity of the peripheral auditory system as a longitudinal measure of auditory maturation seems to hold some predictive value. ABR studies (both click-ABR and speech-ABR) tend to show longer latencies in children with ASD, and several EEG studies show unstable neural tracking in subcortical auditory processing. However, not all children have the same clinical presentation, suggesting the potential existence of auditory processing-related subtypes of children with ASD. Considering the results from ABR studies, one interesting finding is ABR longitudinal profile across development that seems to indicate shorter latencies in newborns, longer latencies in ASD children compared to newborns, no differences in adolescents, and normal ABR in adults. Infants and toddlers later diagnosed with ASD present delayed auditory brainstem responses, mainly with later wave V latencies (Tecoulesco et al. 2020 ; Ramezani et al. 2019 ; Chen et al. 2019 ), that does not seem to persist through development. These findings highlight a potential difference in terms of auditory brainstem maturation timing, or the existence of compensatory mechanisms such as increasing myelin density. Given that ABR testing is relatively non-invasive and low cost, it could be advantageous to study longitudinal auditory brainstem maturation in children at a higher risk for ASD.
Interestingly, diffusion MRI and MEG studies suggest a deficiency in audiovisual temporal processing, with prolonged cortical response in older children with ASD, mainly mismatch negativity and middle latency delays (M50/M100) (Stevenson et al. 2017 , 2018 ), together with atypical development of white matter and cortical function (Berman et al. 2016 ). Such results could reflect an abnormal maturation of the brainstem that could affect the temporal synchrony of neuronal firing, or/and white matter alterations that could lead to poor signal conduction. Given the range of ASD presentations along development, it could be useful to assess the longitudinal profile of ASD children in a multimodal analysis, comparing the neuropsychological profile, the auditory brainstem maturation, together with an assessment of myelin and cortical response profiles.
The usefulness of longitudinal EEG as a diagnostic tool for uncovering developmental trajectories in ASD has been recently suggested, showing that delta and gamma frequency power trajectories can differentiate autism outcomes, in the first postnatal year (Gabard-Durnam et al. 2019 ). Furthermore, EEG spectral power has been suggested as a marker to differentiate between low- and high-risk ASD infants at 6 months of age (Tierney et al. 2012 ), as well as a marker of disease severity in girls with Rett syndrome (Roche et al. 2019 ). The observation of increased power in the delta band could represent abnormal cortical inhibition due to dysfunctional GABAergic signaling (Roche et al. 2019 ). Given that auditory-related gamma and alpha powers also seem to be altered in ASD subjects along development (Port et al. 2016 ; Pierce et al. 2021 ; Stefano et al. 2019 ), it would be interesting to assess these measures together with social, cognitive, and language abilities, as potential predictors of later outcomes in ASD.
Not many studies have looked into E/I balance related to auditory processing in ASD. The imbalance hypothesis is highly promising, given the suggestion of cortical excitatory–inhibitory imbalance in areas related to auditory processing in subjects with ASD (Murray et al. 2020 ). It is also highly promising, since it provides the basis for a number of ASD biomarkers at various levels, from molecules to the neural networks that ultimately determine behavior (Levin and Nelson 2015 ). For instance, positron emission tomography (PET) is a molecular imaging technique that can be utilized in vivo for dynamic and quantitative measurement of neurotransmitter release in the human brain. Given the clear evidence stemming from animal studies (Castro and Monteiro 2022 ) showing auditory dysfunction and E/I imbalance in different animal models of ASD, it would be interesting to see results from PET studies looking at excitatory and inhibitory neurotransmitter systems, cerebral glucose metabolism, blood flow perfusion, and inflammation in the CNS in ASD patients, while performing specific auditory tasks for assessment of sensory function. In summary, a multivariate combination of biomarkers may be the most promising tool for a better understanding of the significant role of neurodevelopmental change in ASD.
Data availability
All data is provided with this paper.
Abrams DA, Padmanabhan A, Chen T, Odriozola P, Baker AE, Kochalka J et al (2019) Impaired voice processing in reward and salience circuits predicts social communication in children with autism. Elife 8:e39906. https://doi.org/10.7554/eLife.39906
Article PubMed PubMed Central Google Scholar
Aggarwal P and Gupta A (2019) Multivariate graph learning for detecting aberrant connectivity of dynamic brain networks in autism. Med Image Anal 56:11–25. https://doi.org/10.1016/j.media.2019.05.007
Ainsworth K, Ostrolenk A, Irion C, Bertone A (2020) Reduced multisensory facilitation exists at different periods of development in autism. Cortex 134:195–206. https://doi.org/10.1016/j.cortex.2020.09.031
Article PubMed Google Scholar
American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). (American Psychiatric Publishing, Ed.) (4th ed.). Washington, DC
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). (American Psychiatric Publishing, Ed.) (5th ed.). Washington, D.C
Arnett AB et al (2018) Auditory perception is associated with implicit language learning and receptive language ability in autism spectrum disorder. Brain Lang 187:1–8. https://doi.org/10.1016/j.bandl.2018.09.007
Aslan E, Guzel I, Caypinar B, Samanci B, Oysu C (2022) Evaluation of the auditory system in autistic children using evoked otoacoustic emissions and a contralateral suppression test. Ear Nose Throat J. https://doi.org/10.1177/0145561319838934
Baron-Cohen S (2001) Theory of mind in normal development and autism. Prisme 34:74–183
Google Scholar
Beckman ME, Pierrehumbert JB (1986) Intonational structure in Japanese and English. Phonol 3:255–309. https://doi.org/10.1017/S095267570000066X
Article Google Scholar
Beker S, Foxe JJ, Molholm S (2021) Oscillatory entrainment mechanisms and anticipatory predictive processes in Autism Spectrum Disorder. J Neurophysiol 126:1783–1798. https://doi.org/10.1152/jn.00329.2021
Bennetto L, Keith JM, Allen PD, Luebke AE (2016) Children with autism spectrum disorder have reduced otoacoustic emissions at the 1 kHz mid-frequency region. Autism Res 10:337–345. https://doi.org/10.1002/aur.1663
Berman JI, Edgar JC, Blaskey L, Kuschner ES, Levy SE, Ku M et al (2016) Multimodal diffusion-MRI and MEG assessment of auditory and language system development in autism spectrum disorder. Front Neuroanat 10:30. https://doi.org/10.3389/fnana.2016.00030
Best CT (2019) The diversity of tone languages and the roles of pitch variation in non-tone languages: considerations for tone perception research. Front Psychol 10:364. https://doi.org/10.3389/fpsyg.2019.00364
Bharath R, Moodithaya SS, Halahalli H, Undaru SB, Nallilu SK (2021) Evaluation of sympathetic sudomotor responses to auditory stimuli in children with autism spectrum disorders. Indian J Psychiatry 62:494–500. https://doi.org/10.4103/psychiatry.IndianJPsychiatry
Bidet-Caulet A et al (2017) Atypical sound discrimination in children with ASD as indicated by cortical ERPs. J Neurodev Disord. https://doi.org/10.1186/s11689-017-9194-9
Bloy L, Shwayder K, Blaskey L, Roberts TPL, Embick D (2019) A Spectrotemporal correlate of language impairment in autism spectrum disorder. J Autism Dev Disord 49:3181–3190. https://doi.org/10.1007/s10803-019-04040-x
Boets B, Verhoeven J, Wouters J and Steyaert J (2015) Fragile spectral and temporal auditory processing in adolescents with autism spectrum disorder and early language delay. J Autism Dev Disord 56(6):1845–1857. https://doi.org/10.1007/s10803-014-2341-1
Borgolte A et al (2021) Neuropsychologia Enhanced attentional processing during speech perception in adult high-functioning autism spectrum disorder: an ERP-study. Neuropsychologia 161:108022. https://doi.org/10.1016/j.neuropsychologia.2021.108022
Borowiak K, Schelinski S, von Kriegstein K (2018) Recognizing visual speech: reduced responses in visual-movement regions, but not other speech regions in autism. NeuroImage Clin 20:1078–1091. https://doi.org/10.1016/j.nicl.2018.09.019
Bourgeron T (2009) A synaptic trek to autism. Curr Opin Neurobiol 19:231–234. https://doi.org/10.1016/j.conb.2009.06.003
Article CAS PubMed Google Scholar
Brennan JR, Wagley N, Kovelman I, Bowyer SM, Richard AE and Lajiness-O’Neill R et al (2016) Magnetoencephalography shows atypical sensitivity to linguistic sound sequences in autism spectrum disorder. NeuroReport 27:982–986. https://doi.org/10.1097/WNR.0000000000000643
Article CAS PubMed PubMed Central Google Scholar
Brennan JR, Lajiness-O’Neill R, Bowyer S, Kovelman I, Hale JT (2019) Predictive sentence comprehension during story-listening in autism spectrum disorder disorder. Lang Cogn Neurosci 34:428–439. https://doi.org/10.1080/23273798.2018.1560483
Brinkert J, Remington A (2020) Making sense of the perceptual capacities in autistic and non-autistic adults. Autism 24:55–59. https://doi.org/10.1177/1362361320922640
Castro AC, Monteiro P (2022) Auditory dysfunction in animal models of autism spectrum disorder. Front Mol Neurosci 15:1–11. https://doi.org/10.3389/fnmol.2022.845155
Article CAS Google Scholar
Celesia GG (2015) Hearing disorders in brainstem lesions. In: Handbook of Clinical Neurology 509–536
Chahboun S, Vulchanov V, Saldaña D, Eshuis H, Vulchanova M (2016) Can you play with fire and not hurt yourself? A comparative study in figurative language comprehension between individuals with and without autism spectrum disorder. PLoS One 11:e0168571. https://doi.org/10.1371/journal.pone.0168571
Charpentier J, Kovarski K, Malvy J, Saby A, Latinus M (2018) Emotional prosodic change detection in autism Spectrum disorder: an electrophysiological investigation in children and adults. J Neurodev Disord 10:28. https://doi.org/10.1186/s11689-018-9246-9
Charpentier J, Latinus M, Andersson F, Saby A, Cottier JP, Bonnet-Brilhault F et al (2020) Brain correlates of emotional prosodic change detection in autism spectrum disorder. NeuroImage Clin 28:102512. https://doi.org/10.1016/j.nicl.2020.102512
Chen J, Liang C, Wei Z, Cui Z, Kong X, Dong CJ et al (2019) Atypical longitudinal development of speech-evoked auditory brainstem response in preschool children with autism spectrum disorders. Autism Res 12:1022–1031. https://doi.org/10.1002/aur.2110
Chen F, Zhang H, Ding H, Wang S, Peng G and Zhang Y et al (2021) Neural coding of formant-exaggerated speech and nonspeech in children with and without autism spectrum disorders. Autism Res 14:1357–1374. https://doi.org/10.1002/aur.2509
Chowdhury R, Sharda M, Foster N, Germain E, Tryfon A, Doyle-Thomas K et al (2017) Auditory pitch perception in autism spectrum disorder is associated with nonverbal abilities. Perception 46:1298–1320. https://doi.org/10.1177/0301006617718715
Claesdotter-Knutsson E, Åkerlund S, Cervin M, Råstam M, Lindvall M (2019) Abnormal auditory brainstem response in the pons region in youth with autism. Neurol Psychiatry Brain Res 32:122–125. https://doi.org/10.1016/j.npbr.2019.03.009
Cohen D (1972) Magnetoencephalography: detection of the brain’s electrical activity with a superconducting magnetometer. Science (80–) 175:664–666. https://doi.org/10.1126/science.175.4022.664
Cole DM, Smith SM, Beckmann CF (2010) Advances and pitfalls in the analysis and interpretation of resting-state FMRI data. Front Syst Neurosci 4:1–15. https://doi.org/10.3389/fnsys.2010.00008
Crasta JE, Salzinger E, Lin M, Gavin WJ, Davies PL and Lane A (2020) Sensory processing and attention profiles among children with sensory processing disorders and Autism spectrum disorders. Front Integr Neurosci 14(May):1–10. https://doi.org/10.3389/fnint.2020.00022
Delacroix L, Malgrange B (2015) Cochlear afferent innervation development. Hear Res 330:157–169. https://doi.org/10.1016/j.heares.2015.07.015
Delgado CF, Simpson EA, Zeng G, Delgado RE, Miron O (2021) Newborn auditory brainstem responses in children with developmental disabilities. J Autism Dev Disord. https://doi.org/10.1007/s10803-021-05126-1
Demopoulos C, Yu N, Tripp J, Mota N, Brandes-Aitken AN, Desai SS et al (2017) Magnetoencephalographic imaging of auditory and somatosensory cortical responses in children with autism and sensory processing dysfunction. Front Hum Neurosci 11:259. https://doi.org/10.3389/fnhum.2017.00259
Depriest J, Glushko A, Steinhauer K, Koelsch S (2017) Language and music phrase boundary processing in Autism Spectrum Disorder: an ERP study. Sci Rep. https://doi.org/10.1038/s41598-017-14538-y
De Stefano LA, Schmitt LM, White SP, Mosconi MW, Sweeney JA and Ethridge LE (2019) Developmental effects on auditory neural oscillatory synchronization abnormalities in autism spectrum disorder. Front Integr Neurosci 13:34. https://doi.org/10.3389/fnint.2019.00034
Distefano C, Senturk D, Jeste SS (2019) Developmental Cognitive Neuroscience ERP evidence of semantic processing in children with ASD. Dev Cogn Neurosci 36:100640. https://doi.org/10.1016/j.dcn.2019.100640
Dunn W (1999) Sensory profile. Psychological Corporation
Dunn LM and Dunn LM (1965) Peabody picture vocabulary test
Dwyer P, Wang X, Meo-monteil RD, Hsieh F, Saron CD and Rivera SM et al (2020) Defining clusters of young autistic and typically developing children based on loudness-dependent auditory electrophysiological responses. Mol Autism 11:1–17. https://doi.org/10.1186/s13229-020-00352-3
Dwyer P, Wang X, Meo RD, Fushing M, Clifford H and Rivera SM (2021) Using clustering to examine inter-individual variability in topography of auditory event—related potentials in autism and typical development. Brain Topogr 34:681–697. https://doi.org/10.1007/s10548-021-00863-z
Edgar JC et al (2013) Neuromagnetic oscillations predict evoked-response latency delays and core language deficits in autism spectrum disorders. J Autism Dev Disord 45:395–405. https://doi.org/10.1007/s10803-013-1904-x
Edgar JC, Fisk IV CL, Berman JI, Chudnovskaya D, Liu S, Pandey J et al (2015) Auditory encoding abnormalities in children with autism spectrum disorder suggest delayed development of auditory cortex. Mol Autism 6:1–14. https://doi.org/10.1186/s13229-015-0065-5
Eggermont JJ and Schmidt PH (1990) The auditory brainstem response. In: Colon EJ, Viss SL (eds) Evoked potential Man. 41–77
ElMoazen D, Sobhy O, Abdou R, AbdelMotaleb H (2020) Binaural interaction component of the auditory brainstem response in children with autism spectrum disorder. Int J Pediatr Otorhinolaryngol 131:109850. https://doi.org/10.1016/j.ijporl.2019.109850
Emmons KA et al (2022) Auditory attention deployment in young adults with autism spectrum disorder. J Autism Dev Disord. https://doi.org/10.1007/s10803-021-05076-8
Felix R, Gourévitch B, Portfors C (2018) Subcortical pathways: towards a better understanding of auditory disorders. Hear Res 362:48–60. https://doi.org/10.1016/j.heares.2018.01.008
Floris DL, Lai MC, Auer T, Lombardo MV, Ecker C, Chakrabarti B et al (2016) Atypically rightward cerebral asymmetry in male adults with autism stratifies individuals with and without language delay. Hum Brain Mapp 37:230–253. https://doi.org/10.1002/hbm.23023
Font-Alaminos M, Cornella M, Costa-Faidella J, Hervás A, Leung S, Rueda I and Escera C (2020) Increased subcortical neural responses to repeating auditory stimulation in children with autism spectrum disorder. Biol Psychol. https://doi.org/10.1016/j.biopsycho.2019.107807
Foss-Feig JH, Schauder KB, Key AP, Wallace MT, Stone WL (2017) Audition-specific temporal processing deficits associated with language function in children with autism spectrum disorder. Autism Res 10:1845–1856. https://doi.org/10.1002/aur.1820
Foss-feig JH, Stavropoulos KKM, Mcpartland JC, Wallace MT, Stone WL and Key AP (2018) Electrophysiological response during auditory gap detection: biomarker for sensory and communication alterations in autism spectrum disorder? Dev Neuropsychol 43:109–122. https://doi.org/10.1080/87565641.2017.1365869
Foster NEV, Ouimet T, Tryfon A, Doyle-thomas K, Anagnostou E and Hyde KL (2016) Effects of age and attention on auditory global–local processing in children with autism spectrum disorder. J Autism Dev Disord 46:1415–1428. https://doi.org/10.1007/s10803-015-2684-2
Fujihira H, Itoi C, Furukawa S, Kato N, Kashino M (2021) Auditory brainstem responses in adults with autism spectrum disorder. Clin Neurophysiol Pract 6:179–184. https://doi.org/10.1016/j.cnp.2021.04.004
Gabard-Durnam LJ et al (2019) Longitudinal EEG power in the first postnatal year differentiates autism outcomes. Nat Commun. https://doi.org/10.1038/s41467-019-12202-9
Galilee A, Stefanidou C, Mccleery JP (2017) Atypical speech versus non-speech detection and discrimination in 4- to 6- yr old children with autism spectrum disorder: an ERP study. PLoS ONE. https://doi.org/10.1371/journal.pone.0181354
Gandhi TK, Tsourides K, Singhal N, Cardinaux A, Jamal W, Pantazis D et al (2021) Autonomic and electrophysiological evidence for reduced auditory habituation in autism. J Autism Dev Disord 51:2218–2228. https://doi.org/10.1007/s10803-020-04636-8
Ganesan S, Khan S, Garel KA, Hämäläinen MS, Kenet T (2016) Normal evoked response to rapid sequences of tactile pulses in autism spectrum disorders. Front Hum Neurosci 10:433. https://doi.org/10.3389/fnhum.2016.00433
Georgiou GP (2020) Identification of native vowels in normal and whispered speech by individuals with autism spectrum disorder. J Autism Dev Disord. https://doi.org/10.1007/s10803-020-04702-1
Germain E, Foster N, Sharda M, Chowdhury R, Tryfon A, Doyle-Thomas K et al (2018) Pitch direction ability predicts melodic perception in autism. Child Neuropsychol 25:445–465. https://doi.org/10.1080/09297049.2018.1488954
Gonzalez-Gadea ML, Chennu S, Bekinschtein TA, Rattazzi A, Beraudi A, Tripicchio P et al (2015) Predictive coding in autism spectrum disorder and attention deficit hyperactivity disorder. J Neurophysiol 114(5):2625–2636. https://doi.org/10.1152/jn.00543.2015
Golan O, Gordon I, Fichman K, Keinan G (2018) Specific patterns of emotion recognition from faces in children with ASD: results of a cross-modal matching paradigm. J Autism Dev Disord 48:844–852. https://doi.org/10.1007/s10803-017-3389-5
Goris J, Braem S, Nijhof AD, Rigoni D, Deschrijver E, Cruys S et al (2018) Sensory prediction errors are less modulated by global context in autism spectrum disorder. Biol Psychiatry Cogn Neurosci Neuroimaging 3:667–674. https://doi.org/10.1016/j.bpsc.2018.02.003
Green SA, Hernandez L, Bookheimer SY and Dapretto M (2016) Salience network connectivity in autism is related to brain and behavioral markers of sensory over-responsivity. J Am Acad Child Adolescent Psychiatry 55(7):618–626. https://doi.org/10.1016/j.jaac.2016.04.013
Green SA, Hernandez L, Bookheimer SY, Dapretto M (2017) Reduced modulation of thalamocortical connectivity during exposure to sensory stimuli in ASD. Autism Res 10:801–809. https://doi.org/10.1002/aur.1726.Reduced
Green SA, Hernandez LM, Bowman HC, Bookheimer SY, Dapretto M (2018) Sensory over-responsivity and social cognition in ASD: Effects of aversive sensory stimuli and attentional modulation on neural responses to social cues. Dev Cogn Neurosci 29:127–139. https://doi.org/10.1016/j.dcn.2017.02.005
Green SA, Hernandez L, Lawrence KE, Liu J, Tsang T, Yeargin J et al (2019) Distinct patterns of neural habituation and generalization in children and adolescents with autism with low and high sensory overresponsivity. Am J Psychiatry 176:1010–1020. https://doi.org/10.1176/appi.ajp.2019.18121333
Green HL, Shu LC, Levinson L, Shen G, Avery T, Randazzo M et al (2020) Evaluation of mismatch negativity as a marker for language impairment in autism spectrum disorder. J Commun Disord. https://doi.org/10.1016/j.jcomdis.2020.105997
Grisoni L, Moseley R, Motlagh S, Kandia D, Sener N, Pulvermüller F et al (2019) Prediction and mismatch negativity responses reflect impairments in action semantic processing in adults with autism spectrum disorders. Front Hum Neurosci 13:395. https://doi.org/10.3389/fnhum.2019.00395
Haigh SM, Heeger DJ, Heller LM, Gupta A, Dinstein I, Minshew NJ and Behrmann M (2016) No difference in cross-modal attention or sensory discrimination thresholds in autism and matched controls. Vision Res 121:85–94. https://doi.org/10.1016/j.visres.2016.02.001
Hillock AR, Powers AR, Wallace MT (2011) Binding of sights and sounds: age-related changes in multisensory temporal processing. Neuropsychologia 49:461–467. https://doi.org/10.1016/j.neuropsychologia.2010.11.041
Hoffmann E, Brück C, Kreifelts B, Ethofer T, Wildgruber D (2016) Reduced functional connectivity to the frontal cortex during processing of social cues in autism spectrum disorder. J Neural Transm 123:937–947. https://doi.org/10.1007/s00702-016-1544-3
Huang D, Yu L, Wang X, Fan Y, Wang S and Zhang Y (2018) Distinct patterns of discrimination and orienting for temporal processing of speech and nonspeech in Chinese children with autism: an event-related potential study. Eur J Neurosci 47:662–668. https://doi.org/10.1111/ejn.13657
Hudac CM, Deschamps TD, Arnett AB, Cairney BE, Ma R, Jane S and Bernier RA (2018) Early enhanced processing and delayed habituation to deviance sounds in autism spectrum disorder. Brain Cogn 123:110–119. https://doi.org/10.1016/j.bandc.2018.03.004
Isaksson S, Salomäki S, Tuominen J, Arstila V, Falter-wagner CM, and Noreika V (2018) Is there a generalized timing impairment in Autism Spectrum Disorders across time scales and paradigms? 99:111–121. https://doi.org/10.1016/j.jpsychires.2018.01.017
Jamal W, Cardinaux A, Haskins AJ, Kjelgaard M, Sinha P (2020) Reduced sensory habituation in autism and its correlation with behavioral measures. J Autism Dev Disord 51:3153–3164. https://doi.org/10.1007/s10803-020-04780-1
Järvinen A et al (2015) Social functioning and autonomic nervous system sensitivity across vocal and musical emotion in williams syndrome and autism spectrum disorder. Dev Psychobiol 58:17–26. https://doi.org/10.1002/dev.21335
Jewett DL, Williston JS (1971) Auditory-evoked far fields averaged from the scalp of humans. Brain 94:681–696. https://doi.org/10.1093/brain/94.4.681
Jiang J, Liu F, Wan X, Jiang C (2015) Perception of melodic contour and intonation in autism spectrum disorder: evidence from mandarin speakers. J Autism Dev Disord 45:2067–2075. https://doi.org/10.1007/s10803-015-2370-4
Jones MK, Kraus N, Bonacina S, Nicol T, Otto-Meyer S and Roberts MY (2020) Auditory processing differences in toddlers with autism spectrum disorder. J Speech Lang Hear Res 63:1608–1617. https://doi.org/10.1044/2020_JSLHR-19-00061
Kadlaskar G, Bergmann S, Keehn RM, Seidl A, Keehn B (2021) Electrophysiological measures of tactile and auditory processing in children with autism spectrum disorder. Front Hum Neurosci. https://doi.org/10.3389/fnhum.2021.729270
Kargas N, Lo B (2015) The relationship between auditory processing and restricted, repetitive behaviors in adults with autism spectrum disorders. J Autism Dev Disord 45:658–668. https://doi.org/10.1007/s10803-014-2219-2
Keehn B, Kadlaskar G, Bergmann S, McnallyKeehn R, Francis A (2021) Attentional disengagement and the locus coeruleus – norepinephrine system in children with autism spectrum disorder. Front Integr Neurosci. https://doi.org/10.3389/fnint.2021.716447
Keith JM, Jamieson JP, Bennetto L (2019) The influence of noise on autonomic arousal and cognitive performance in adolescents with autism spectrum disorder. J Autism Dev Disord 49:113–126. https://doi.org/10.1007/s10803-018-3685-8
Key APF, Dove GO, Maguire MJ (2005) Linking brainwaves to the brain: an ERP primer. Dev Neuropsychol 27:183–215. https://doi.org/10.1207/s15326942dn2702_1
Key AP, Yoder PJ, Stone WL (2016) Consonant differentiation mediates the discrepancy between non-verbal and verbal abilities in children with ASD. J Intellect Disabil Res 60:478–490. https://doi.org/10.1111/jir.12286
Kim E et al (2015) Preliminary findings suggest the number and volume of supragranular and infragranular pyramidal neurons are similar in the anterior superior temporal area of control subjects and subjects with autism. Neurosci Lett 589:98–103. https://doi.org/10.1016/j.neulet.2015.01.021
Knight EJ, Oakes L, Hyman SL, Freedman EG, Foxe JJ (2020) Individuals with autism have no detectable deficit in neural markers of prediction error when presented with auditory rhythms of varied temporal complexity. Autism Res 13:2058–2072. https://doi.org/10.1002/aur.2362
Krizman J, Kraus N (2019) Analyzing the FFR: a tutorial for decoding the richness of auditory function. Hear Res 382:107779. https://doi.org/10.1016/j.heares.2019.107779
Kurita T, Kikuchi M, Yoshimura Y, Hiraishi H, Hasegawa C, Takahashi T et al (2016) Atypical Bilateral Brain Synchronization in the Early Stage of Human Voice Auditory Processing in Young Children with Autism. PloS One. https://doi.org/10.1371/journal.pone.0153077
Lambrechts A, Falter-Wagner CM, van Wassenhove V (2018) Diminished neural resources allocation to time processing in Autism Spectrum Disorders. NeuroImage Clin 17:124–136. https://doi.org/10.1016/j.nicl.2017.09.023
Landini L, Positano V, Santarelli M (2018) Advanced image processing in magnetic resonance imaging. CRS Press
Book Google Scholar
Leblanc JJ, Fagiolini M (2011) Autism: a critical period disorder? Neural Plast. https://doi.org/10.1155/2011/921680
Levin AR, Nelson CA (2015) Inhibition-based biomarkers for autism spectrum disorder. Neurotherapeutics 12:546–552. https://doi.org/10.1007/s13311-015-0350-1
Lindström R, Lepistö-Paisley T, Makkonen T, Reinvall O, Nieminen-von Wendt T, Alén R and Kujala T (2018) Atypical perceptual and neural processing of emotional prosodic changes in children with autism spectrum disorders. Clin Neurophysiol 129:2411–2420. https://doi.org/10.1016/j.clinph.2018.08.018
Linke AC, JaoKeehn RJ, Pueschel EB, Fishman I, Müller RA (2018) Children with ASD show links between aberrant sound processing, social symptoms, and atypical auditory interhemispheric and thalamocortical functional connectivity. Dev Cogn Neurosci 29:117–126. https://doi.org/10.1016/j.dcn.2017.01.007
Little LM, Dean E, Tomchek S, Dunn W (2018) Sensory processing patterns in autism, attention deficit hyperactivity disorder, and typical development sensory processing patterns in autism, attention deficit hyperactivity disorder, and typical development. Phys Occup Ther Pediatr 38:243–254. https://doi.org/10.1080/01942638.2017.1390809
Liu Z, Ding L, Bin H (2006) Integration of EEG/MEG with MRI and fMRI in functional neuroimaging. IEEE Eng Med Biol Mag 25:46–53. https://doi.org/10.1109/memb.2006.1657787
Lloyd-Fox S, Blasi A, Pasco G, Gliga T, Jones E, Murphy D et al (2018) Cortical responses before six months of life associate with later autism. Eur J Neurosci 47:736–749. https://doi.org/10.1111/ejn.13757
Lodhia V, Hautus MJ, Johnson BW and Brock J (2018) Atypical brain responses to auditory spatial cues in adults with autism spectrum disorder. Eur J Neurosci 47(6):682–689. https://doi.org/10.1111/ejn.13694
Lord C et al (2012) Autism diagnostic observation schedule, 2nd edition (ADOS-2)
Luck S, Kappenman E (2012) The Oxford handbook of event-related potential components. Oxford University Press, p 664
Mamashli F, Khan S, Bharadwaj H, Michmizos K, Ganesan S, Garel K A et al (2017) Auditory processing in noise is associated with complex patterns of disrupted functional connectivity in autism spectrum disorder fahimeh. Autism Res 10:631–647. https://doi.org/10.1002/aur.1714.Auditory
Mansour Y, Kulesza R (2020) Three dimensional reconstructions of the superior olivary complex from children with autism spectrum disorder. Hear Res 393:107974. https://doi.org/10.1016/j.heares.2020.107974
Matsuzaki J, Kagitani-Shimono K, Sugata H, Hanaie R, Nagatani F, Yamamoto T et al (2017) Delayed mismatch field latencies in autism spectrum disorder with abnormal auditory sensitivity: a magnetoencephalographic study. Front Hum Neurosci 11:446. https://doi.org/10.3389/fnhum.2017.00446
Matsuzaki J, Kuschner ES, Blaskey L, Bloy L, Kim M, Ku M et al (2019a) Abnormal auditory mismatch fields are associated with communication impairment in both verbal and minimally verbal/nonverbal children who have autism spectrum disorder. Autism Res 12:1225–1235. https://doi.org/10.1002/aur.2136
Matsuzaki J, Ku M, Berman JI, Blaskey L, Bloy L, Chen Y-H et al (2019b) Abnormal auditory mismatch fields in adults with autism spectrum disorder. Neurosci Lett 698:140–145. https://doi.org/10.1016/j.neulet.2018.12.043
Matsuzaki J, Dipiero M, Saby J, Roberts TPL (2020) Delayed auditory evoked responses in autism spectrum disorder across the life span. Dev Neurosci 41:223–233. https://doi.org/10.1159/000504960
Matsuzaki J et al (2022) Abnormal cortical responses elicited by audiovisual movies in patients with autism spectrum disorder with atypical sensory behavior: a magnetoencephalographic study. Brain Dev 44:81–94. https://doi.org/10.1016/j.braindev.2021.08.007
Mayer JL, Hannent I, Heaton PF (2014) Mapping the developmental trajectory and correlates of enhanced pitch perception on speech processing in adults with ASD. J Autism Dev Disord 46:1562–1573. https://doi.org/10.1007/s10803-014-2207-6
Measso G et al (1993) Raven’s colored progressive matrices: a normative study of a random sample of healthy adults. Acta Neurol Scand 88:70–74. https://doi.org/10.1111/j.1600-0404.1993.tb04190.x
Miller JO (1982) Divided attention: evidence for coactivation withredundant signals. Cogn Psychol 14:247–279. https://doi.org/10.1016/0010-0285(82)90010-x
Mayer JL, Hannent I and Heaton PF (2016) Mapping the Developmental trajectory and correlates of enhanced pitch perception on speech processing in adults with ASD. J Autism Dev Disord 46(5):1562–1573. https://doi.org/10.1007/s10803-014-2207-6
Millin R, Kolodny T, Flevaris AV, Kale AM, Schallmo MP, Gerdts J et al (2018) Reduced auditory cortical adaptation in autism spectrum disorder. Elife 7:e36493. https://doi.org/10.7554/eLife.36493.001
Murray SO, Kolodny T, Schallmo MP, Gerdts J, Bernier RA (2020) Late fMRI response components are altered in autism spectrum disorder. Front Hum Neurosci 14:241. https://doi.org/10.3389/fnhum.2020.00241
Musiek, Frank E, Lee WW (1995) The auditory brain stem response in patients with brain stem or cochlear pathology. Ear Hear 16:631–636. https://doi.org/10.1097/00003446-199512000-00009
Newman RS, Kirby LA, Holzen KV, Redcay E (2021) Read my lips! Perception of speech in noise by preschool children with autism and the impact of watching the speaker’s face. J Dev Disord. https://doi.org/10.1186/s11689-020-09348-9
Noel JP, De Niear MA, Stevenson R, Alais D, Wallace MT (2017) Atypical rapid audio-visual temporal recalibration in autism spectrum disorders. Autism Res 10:121–129. https://doi.org/10.1002/aur.1633
Noel JP, De Niear MA, Lazzara NS and Wallace MT (2018) Uncoupling between multisensory temporal function and non-verbal turn-taking in autism spectrum disorder. IEEE Trans Cogn Dev Syst 10(4):973–982. https://doi.org/10.1109/TCDS.2017.2778141
Ono Y, Kudoh K, Ikeda T, Takahashi T, Yoshimura Y, Minabe Y and Kikuchi M (2020) Auditory steady-state response at 20 Hz and 40 Hz in young typically developing children and children with autism spectrum disorder. Psychiatry Clin Neurosci 74:354–361. https://doi.org/10.1111/pcn.12998
Ostrolenk A, Bao VA, Mottron L, Collignon O and Bertone A (2019) Reduced multisensory facilitation in adolescents and adults on the Autism Spectrum. Sci Reports 9(1):11965. https://doi.org/10.1038/s41598-019-48413-9
Otto-Meyer S, Krizman J, White-Schwoch T, Kraus N (2018) Children with autism spectrum disorder have unstable neural responses to sound. Exp Brain Res 236:733–743. https://doi.org/10.1007/s00221-017-5164-4
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. https://doi.org/10.1136/bmj.n71
Park WJ, Schauder KB, Zhang R, Bennetto L and Tadin D (2017) High internal noise and poor external noise filtering characterize perception in autism spectrum disorder. Sci Reports 7(1):17584. https://doi.org/10.1038/s41598-017-17676-5
Pastor-Cerezuela G, Fernández-Andrés MI, Sanz-Cervera P, and Marín-Suelves D (2020) The impact of sensory processing on executive and cognitive functions in children with autism spectrum disorder in the school context. Res Dev Disabil 96(November 2019):103540. https://doi.org/10.1016/j.ridd.2019.103540
Patel SP, Kim JH, Larson CR, Losh M (2019) Mechanisms of voice control related to prosody in autism spectrum disorder and first-degree relatives. Autism Res 12:1192–1210. https://doi.org/10.1002/aur.2156
Peça J et al (2011) Shank3 mutant mice display autistic-like behaviours and striatal dysfunction. Nature 472:437–442. https://doi.org/10.1038/nature09965
Pegado F, Hendriks M, Amelynck S, Daniels N, Steyaert J, Boets B and Op de Beeck H (2020) Adults with high functioning autism display idiosyncratic behavioral patterns, neural representations and connectivity of the ‘Voice Area’ while judging the appropriateness of emotional vocal reactions. Cortex, 125:90–108. https://doi.org/10.1016/j.cortex.2019.11.008
Peterson D, Reddy V, Hamel R (2022) Neuroanatomy, auditory pathway. StatPearls
Piatti A, Paelt S, Van Der Warreyn P, Roeyers H (2021) Research in autism spectrum disorders atypical attention to voice in toddlers and pre-schoolers with autism spectrum disorder is related to unimpaired cognitive abilities. An ERP study. Res Autism Spectr Disord. https://doi.org/10.1016/j.rasd.2021.101805
Pierce S, Kadlaskar G, Edmondson DA, Keehn RM, Dydak U and Keehn B (2021) Associations between sensory processing and electrophysiological and neurochemical measures in children with ASD: an EEG-MRS study. J Neurodev Disord 13:5. https://doi.org/10.1186/s11689-020-09351-0
Poole D, Miles E, Gowen E and Poliakoff E (2021) Shifting attention between modalities: revisiting the modality-shift effect in autism. Atten Percept Psychophys 83:2498–2509. https://doi.org/10.3758/s13414-021-02302-4
Port RG et al (2015) Prospective MEG biomarkers in ASD: pre-clinical evidence and clinical promise of electrophysiological signatures. Yale J Biol Med 88:25–36
PubMed PubMed Central Google Scholar
Port RG, Edgar JC, Ku M, Bloy L, Murray R, Blaskey L et al (2016) Maturation of auditory neural processes in autism spectrum disorder—a longitudinal MEG study. Clinical 11:566–577. https://doi.org/10.1016/j.nicl.2016.03.021
Port RG et al (2017) Exploring the relationship between cortical GABA concentrations, auditory gamma-band responses and development in ASD: evidence for an altered maturational trajectory in ASD. Autism Res 10:593–607. https://doi.org/10.1002/aur.1686
Raatikainen V, Korhonen V, Borchardt V, Huotari N, Helakari H, Kananen J et al (2020) Dynamic lag analysis reveals atypical brain information flow in autism spectrum disorder. Autism Res. https://doi.org/10.1002/aur.2218
Ramezani M, Lotfi Y, Moossavi A, Bakhshi E (2019) Auditory brainstem response to speech in children with high functional autism spectrum disorder. Neurol Sci 40:121–125. https://doi.org/10.1007/s10072-018-3594-9
Ramezani M, Lotfi Y, Moossavi A, Bakhshi E (2021) Effects of auditory processing training on speech perception and brainstem plastisity in adolescents with autism spectrum disorders. Iran J Child Neurol 15:69–77. https://doi.org/10.22037/ijcn.v15i2.22037
Remington A, Fairnie J (2017) A sound advantage: increased auditory capacity in autism. Cognition 16:459–465. https://doi.org/10.1016/j.cognition.2017.04.002
Roberts TPL, Matsuzaki J, Blaskey L, Bloy L, Edgar JC, Kim M et al (2019) Delayed M50/M100 evoked response component latency in minimally verbal/nonverbal children who have autism spectrum disorder. Mol Autism 10:1–10. https://doi.org/10.1186/s13229-019-0283-3
Roberts TPL, Bloy L, Ku M, Blaskey L, Jackel CR, Edgar JC and Berman JI (2020) A multimodal study of the contributions of conduction velocity to the auditory evoked neuromagnetic response: anomalies in autism spectrum disorder. Autism Res 13:1730–1745. https://doi.org/10.1002/aur.2369
Roberts TPL et al (2021) Magnetoencephalography studies of the envelope following response during amplitude-modulated sweeps: diminished phase synchrony in autism spectrum disorder. Front Hum Neurosci. https://doi.org/10.3389/fnhum.2021.787229
Robertson CE, Baron-Cohen S (2017) Sensory perception in autism. Nat Rev Neurosci 18:671–684. https://doi.org/10.1038/nrn.2017.112
Roche KJ et al (2019) Electroencephalographic spectral power as a marker of cortical function and disease severity in girls with Rett syndrome. J Neurodev Disord 11:1–14. https://doi.org/10.1186/s11689-019-9275-z
Rosen NE, Lord C, Volkmar FR (2021) The diagnosis of autism: from kanner to DSM - III to DSM - 5 and beyond. J Autism Dev Disord 51:4253–4270. https://doi.org/10.1007/s10803-021-04904-1
Rosenhall U, Nordin V, Sandstrom M, Ahlsen G, Gillberg C (1999) Autism and hearing loss. J Autism Dev Disord 29(5):349–357. https://doi.org/10.1023/a:1023022709710
Ruiz-Martínez FJ, Rodríguez-Martínez EI, Wilson CE, Yau S, Saldaña D and Gómez CM et al (2019) Impaired P1 habituation and mismatch negativity in children with autism spectrum disorder. J Autism Dev Disord 50:603–616. https://doi.org/10.1007/s10803-019-04299-0
Saby JN, Marshall PJ (2012) The utility of EEG band power analysis in the study of infancy and early childhood. Dev Neuropsychol 37:253–273. https://doi.org/10.1080/87565641.2011.614663
Sadeghi Bajestani G, Sheikhani A, Hashemi Golpayegani MR, Ashrafzadeh F, Hebrani P (2017) Poincaré Section based Biomarkers of Hemispheric Asymmetry, applied to Autism Spectrum Disorder. Scientia Iranica, 24(6), 3257-3267. https://doi.org/10.24200/sci.2017.4356
Schelinski S, von Kriegstein K (2019) The relation between vocal pitch and vocal emotion recognition abilities in people with autism spectrum disorder and typical development. J Autism Dev Disord 41:68–82. https://doi.org/10.1007/s10803-018-3681-z
Schelinski S, Roswandowitz C, Kriegstein K (2016) Voice identity processing in autism spectrum disorder. Autism Res 10:155–168. https://doi.org/10.1002/aur.1639
Schelinski S, Tabas A, Kriegstein KV (2022) Altered processing of communication signals in the subcortical auditory sensory pathway in autism. Hum Brain Mapp. https://doi.org/10.1002/hbm.25766
Schopler E, Reichler R, Jay R and Barbara R (2010) The childhood autism rating scale (CARS)
Schuck RK et al (2022) Neurodiversity and autism intervention: reconciling perspectives through a naturalistic developmental behavioral intervention framework. J Autism Dev Disord 52:4625–4645. https://doi.org/10.1007/s10803-021-05316-x
Schwartz S, Wang L, Shinn-Cunningham BG and Tager-Flusberg H (2020) Neural evidence for speech processing deficits during a cocktail party scenario in minimally and low verbal adolescents and young adults with autism. Autism Res 13(11):1828–1842. https://doi.org/10.1002/aur.2356
Seymour RA, Rippon G, Gooding-Williams G, Sowman PF, Kessler K (2021) Reduced auditory steady state responses in autism spectrum disorder. Mol Autism 11:56. https://doi.org/10.1186/s13229-020-00357-y
Siemann JK, Veenstra-vanderweele J, Wallace MT (2020) Approaches to understanding multisensory dysfunction in autism spectrum disorder. Autism Res 13:1430–1449. https://doi.org/10.1002/aur.2375
Sinclair D, Oranje B, Razak KA, Siegel SJ, Schmid S (2017) Sensory processing in autism spectrum disorders and Fragile X syndrome—from the clinic to animal models. Neurosci Biobehav Rev 76:235–253. https://doi.org/10.1016/j.neubiorev.2016.05.029
Smith E, Zhang S, Bennetto L (2017) Temporal synchrony and audiovisual integration of speech and object stimuli in autism. Res Autism Spectr Disord 39:11–19. https://doi.org/10.1016/j.rasd.2017.04.001
Soskey LN, Allen PD, Bennetto L (2017) Auditory spatial attention to speech and complex non-speech sounds in children with autism spectrum disorder. Autism Res 10:1405–1416. https://doi.org/10.1002/aur.1790
Sota S, Hatada S, Honjyo K, Takatsuka T (2018) Musical disability in children with autism spectrum disorder Author links open overlay panel. Psychiatry Res 267:354–359. https://doi.org/10.1016/j.psychres.2018.05.078
Stevenson RA et al (2017) Multisensory speech perception in autism spectrum disorder: from phoneme to whole-word perception. Autism Res 10:1280–1290. https://doi.org/10.1002/aur.1776
Stevenson RA, Segers M, Ncube BL, Black KR, Bebko JM, Ferber S and Barense MD (2018) The cascading influence of multisensory processing on speech perception in autism. Autism 22:609–624. https://doi.org/10.1177/1362361317704413
Stewart CR, Sanchez SS, Grenesko EL, Brown CM, Chen CP, Keehn B et al (2016) Sensory symptoms and processing of nonverbal auditory and visual stimuli in children with autism spectrum disorder. J Autism Dev Disord 46:1590–1601. https://doi.org/10.1007/s10803-015-2367-z
Stickel S et al (2019) Audio-visual and olfactory-visual integration in healthy participants and subjects with autism spectrum disorder. Hum Brain Mapp 40:4470–4486. https://doi.org/10.1002/hbm.24715
Stroganova TA, Komarov KS, Sysoeva OV, Goiaeva DE, Obukhova TS, Ovsiannikova TM et al (2020) Left hemispheric deficit in the sustained neuromagnetic response to periodic click trains in children with ASD. Mol Autism 11:100. https://doi.org/10.1186/s13229-020-00408-4
Sur S, Sinha VK (2009) Event-related potential: an overview. Ind Psychiatry J 18:70–73. https://doi.org/10.4103/0972-6748.57865
Tanigawa J, Kagitani-Shimono K, Matsuzaki J, Ogawa R, Hanaie R, Yamamoto T et al (2018) Atypical auditory language processing in adolescents with autism spectrum disorder. Clin Neurophysiol 129:2029–2037. https://doi.org/10.1016/j.clinph.2018.05.014
Tateuchi T, Itoh K, Nakada T (2015) Further characterization of “subject’s own name (SON) negativity”, an ERP component reflecting early preattentive detection of SON. BMC Res Notes. https://doi.org/10.1186/s13104-015-1150-8
Tecoulesco L, Skoe E, Naigles LR (2020) Brain and Language Phonetic discrimination mediates the relationship between auditory brainstem response stability and syntactic performance. Brain Lang 208:104810. https://doi.org/10.1016/j.bandl.2020.104810
Thomas RP, Wang L, Guthrie W, Cola M, McCleery JP, Pandey J et al (2019) What’s in a name? A preliminary event-related potential study of response to name in preschool children with and without autism spectrum disorder. PLoS One 14:1–16. https://doi.org/10.1371/journal.pone.0216051
Tierney AL, Gabard-Durnam L, Vogel-Farley V, Tager-Flusberg H, Nelson CA (2012) Developmental trajectories of resting eeg power: an endophenotype of autism spectrum disorder. PLoS One. https://doi.org/10.1371/journal.pone.0039127
Tietze FA et al (2019) Auditory deficits in audio visual speech perception in adult asperger’s syndrome: fMRI study. Front Psychol 10:2286. https://doi.org/10.3389/fpsyg.2019.02286
Turi M, Karaminis T, Pellicano E, Burr D (2016) No rapid audiovisual recalibration in adults on the autism spectrum. Sci Rep 6:21756. https://doi.org/10.1038/srep21756
van Laarhoven T, Stekelenburg JJ, Eussen MLJM, Vroomen J (2020) Atypical visual-auditory predictive coding in autism spectrum disorder: electrophysiological evidence from stimulus omissions. Autism 24:1849–1859. https://doi.org/10.1177/1362361320926061
Venker CE, Edwards J, Saffran JR, Weismer SE (2019) Thinking ahead: incremental language processing is associated with receptive language abilities in preschoolers with autism spectrum disorder. J Autism Dev Disord 49:1011–1023. https://doi.org/10.1007/s10803-018-3778-4
Waddington F et al (2018) Visual and auditory emotion recognition problems as familial cross-disorder phenomenon in ASD and ADHD. Eur Neuropsychopharmacol 28:994–1005. https://doi.org/10.1016/j.euroneuro.2018.06.009
Wagley N, Lajiness-O’Neill R, Hay J, Ugolini M, Bowyer SM, Kovelman I and Brennan JR (2020) Predictive processing during a naturalistic statistical learning task in ASD. eNeuro. https://doi.org/10.1523/ENEURO.0069-19.2020
Walker DR et al (2004) Specifying PDD-NOS: a comparison of PDD-NOS, Asperger Syndrome, and Autism. J Am Acad Child Adolesc Psychiatry 43:172–180. https://doi.org/10.1097/00004583-200402000-00012
Wang X, Wang S, Fan Y, Huang D and Zhang Y (2017) Speech-specific categorical perception deficit in autism: an event-related potential study of lexical tone processing in Mandarin-speaking children. Sci Reports 7(1):43254. https://doi.org/10.1038/srep43254
Watanabe T and Rees G (2016) Anatomical imbalance between cortical networks in autism. Sci Reports 6:31114. https://doi.org/10.1038/srep31114
Watanabe T, Rees G, Masuda N (2019) Atypical intrinsic neural timescale in autism. Elife 8:1–50. https://doi.org/10.7554/eLife.42256
Wechsler D and Kodama H (1949) Wechsler intelligence scale for children. New York Psychol Corp
Weiss MW, Sharda M, Lense M, Hyde KL, Trehub SE (2021) Enhanced memory for vocal melodies in autism spectrum disorder and Williams syndrome. Autism Res 14:1127–1133. https://doi.org/10.1002/aur.2462
Williams ZJ, He JL, Cascio CJ, Woynaroski TG (2021) Neuroscience and biobehavioral reviews review article a review of decreased sound tolerance in autism: definitions, phenomenology, and potential mechanisms. Neurosci Biobehav Rev 121:1–17. https://doi.org/10.1016/j.neubiorev.2020.11.030
Wilson US, Sadler K, Hancock K, Guinan J Jr, Lichtenhan J (2017) Efferent inhibition strength is a physiological correlate of hyperacusis in children with autism spectrum disorder. J Neurophysiol 118:1164–1172. https://doi.org/10.1152/jn.00142.2017
World Health Organization (1993) The International Classification of Diseases, 10th edition (ICD-10)
World Health Organization (2018) The International Classification of Diseases, 11th edition (ICD-11)
Wang X, Wang S, Fan Y, Huang D, Zhang Y (2017) Speech-specific categorical perception deficit in autism: an Event-Related Potential study of lexical tone processing in Mandarin- speaking children. Sci Rep 7:43254. https://doi.org/10.1038/srep43254
Yamada T, Itahashi T, Nakamura M, Watanabe H, Kuroda M, Ohta H, et al (2016) Altered functional organization within the insular cortex in adult males with high- functioning autism spectrum disorder: evidence from connectivity-based parcellation. Mol Autism. https://doi.org/10.1186/s13229-016-0106-8
Yau SH, Brock J, McArthur G (2016) The relationship between spoken language and speech and nonspeech processing in children with autism: a magnetic event-related field study. Dev Sci 19:834–852. https://doi.org/10.1111/desc.12328
Yoshimura Y, Kikuchi M, Hayashi N, Hiraishi H, Hasegawa C, Takahashi T et al (2017) Altered human voice processing in the frontal cortex and a developmental language delay in 3- to 5-year-old children with autism spectrum disorder. Sci Rep 7:17116. https://doi.org/10.1038/s41598-017-17058-x
Yoshimura Y, Ikeda T, Hasegawa C, An K, Tanaka S, Yaoi K et al (2021) Shorter P1m response in children with autism spectrum disorder without intellectual disabilities. Int J Mol Sci 22:2611. https://doi.org/10.3390/ijms22052611
Zhang J, Meng Y, Tong X, Yuan Z and Wu C (2018) Exploring the neural correlates of lexical stress perception in english among chinese-english bilingual children with autism spectrum disorder: an ERP study. Neurosci Lett 666:158–164. https://doi.org/10.1016/j.neulet.2017.12.031
Zhang J, Meng Y, Wu C, Xiang Y, Yuan Z (2019) Non-speech and speech pitch perception among Cantonese-speaking children with autism spectrum disorder: an ERP study. Neurosci Lett 703:205–212. https://doi.org/10.1016/j.neulet.2019.03.021
Zhao B, Müller U (2015) The elusive mechanotransduction machinery of hair cells. Curr Opin Neurobiol 34:172–179. https://doi.org/10.1016/j.conb.2015.08.006
Zhao S, Uono S, Yoshimura S, Toichi M (2019) A functional but atypical self: influence of self-relevant processing on the gaze cueing effect in autism spectrum disorder. Autism Res 11:1522–1531. https://doi.org/10.1002/aur.2019
Download references
Acknowledgements
We thank all members of the Monteiro Lab and NERD domain for their support and discussions. We thank I. Soares for suggestions that greatly improved the manuscript.
Open access funding provided by FCT|FCCN (b-on).
Author information
Authors and affiliations.
Life and Health Sciences Research Institute, School of Medicine, University of Minho, Campus de Gualtar, 4710-057, Braga, Portugal
Ana Margarida Gonçalves & Patricia Monteiro
ICVS/3B’s—PT Government Associate Laboratory, 4710-057, Braga/Guimarães, Portugal
Experimental Biology Unit, Department of Biomedicine, Faculty of Medicine, University of Porto, Porto, Portugal
Patricia Monteiro
You can also search for this author in PubMed Google Scholar
Contributions
AMG conceptualized and wrote the paper. PM conceptualized and revised the paper. This work has been funded by FEBS (Federation of European Biochemical Societies) Excellence Awards 2021, and Fundação para a Ciência e a Tecnologia (FCT) Grants 2022.05228.PTDC; 2021.01032.CEECIND; PTDC/MED-NEU/28073/2017; POCI-01-0145-FEDER-028073. This work has also been supported by FCT under Project UIDB/50026/2020 and UIDP/50026/2020; and by Norte Portugal Regional Operational Programme (NORTE 2020), under the European Regional Development Fund (ERDF): NORTE-01-0145-FEDER-000013; NORTE- 01-0145-FEDER-000023. A.M.G. was supported by a doctoral fellowship (PD/BD/137759/2018) from FCT, as part of the Inter-University Doctoral Programme in Ageing and Chronic Disease (PhDOC).
Corresponding author
Correspondence to Patricia Monteiro .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Gonçalves, A.M., Monteiro, P. Autism Spectrum Disorder and auditory sensory alterations: a systematic review on the integrity of cognitive and neuronal functions related to auditory processing. J Neural Transm 130 , 325–408 (2023). https://doi.org/10.1007/s00702-023-02595-9
Download citation
Received : 16 August 2022
Accepted : 17 January 2023
Published : 14 March 2023
Issue Date : March 2023
DOI : https://doi.org/10.1007/s00702-023-02595-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Autism spectrum disorder (ASD)
- Neuroscience
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Autism Spectrum Disorder and Childhood Apraxia of Speech: Early Language-Related Hallmarks across Structural MRI Study
Eugenia conti.
1 IRCCS Fondazione Stella Maris, 56128 Pisa, Italy; [email protected] (E.C.); [email protected] (P.B.); [email protected] (L.B.); [email protected] (S.F.); [email protected] (M.T.); [email protected] (P.C.); [email protected] (G.C.); [email protected] (F.M.); [email protected] (A.C.)
Alessandra Retico
2 National Institute for Nuclear Physics (INFN), Pisa Division, 56127 Pisa, Italy; [email protected] (A.R.); [email protected] (L.P.); [email protected] (G.S.)
Letizia Palumbo
Giovanna spera, paolo bosco, laura biagi, simona fiori, michela tosetti, paola cipriani, giovanni cioni.
3 Department of Clinical and Experimental Medicine, University of Pisa, 56126 Pisa, Italy
Filippo Muratori
Anna chilosi, sara calderoni, associated data.
Autism Spectrum Disorder (ASD) and Childhood Apraxia of Speech (CAS) are developmental disorders with distinct diagnostic criteria and different epidemiology. However, a common genetic background as well as overlapping clinical features between ASD and CAS have been recently reported. To date, brain structural language-related abnormalities have been detected in both the conditions, but no study directly compared young children with ASD, CAS and typical development (TD). In the current work, we aim: (i) to test the hypothesis that ASD and CAS display neurostructural differences in comparison with TD through morphometric Magnetic Resonance Imaging (MRI)-based measures (ASD vs. TD and CAS vs. TD); (ii) to investigate early possible disease-specific brain structural patterns in the two clinical groups (ASD vs. CAS); (iii) to evaluate predictive power of machine-learning (ML) techniques in differentiating the three samples (ASD, CAS, TD). We retrospectively analyzed the T1-weighted brain MRI scans of 68 children (age range: 34–74 months) grouped into three cohorts: (1) 26 children with ASD (mean age ± standard deviation: 56 ± 11 months); (2) 24 children with CAS (57 ± 10 months); (3) 18 children with TD (55 ± 13 months). Furthermore, a ML analysis based on a linear-kernel Support Vector Machine (SVM) was performed. All but one brain structures displayed significant higher volumes in both ASD and CAS children than TD peers. Specifically, ASD alterations involved fronto-temporal regions together with basal ganglia and cerebellum, while CAS alterations are more focused and shifted to frontal regions, suggesting a possible speech-related anomalies distribution. Caudate, superior temporal and hippocampus volumes directly distinguished the two conditions in terms of greater values in ASD compared to CAS. The ML analysis identified significant differences in brain features between ASD and TD children, whereas only some trends in the ML classification capability were detected in CAS as compared to TD peers. Similarly, the MRI structural underpinnings of two clinical groups were not significantly different when evaluated with linear-kernel SVM. Our results may represent the first step towards understanding shared and specific neural substrate in ASD and CAS conditions, which subsequently may contribute to early differential diagnosis and tailoring specific early intervention.
1. Introduction
Autism Spectrum Disorder (ASD) and Childhood Apraxia of Speech (CAS) are developmental disorders with distinct definitions and diagnostic criteria. Specifically, ASD includes a set of neurodevelopmental disorders characterized by social communication difficulties as well as restricted interests, repetitive activities and sensory abnormalities [ 1 ]. Recent estimates report an ASD prevalence of about one in 87 children aged 7–9 years [ 2 ] in Italy. ASD is a highly heterogeneous group of disorders, with multiple genetic backgrounds that may reflect multiple neuroanatomical underpinnings, which in turn are expressed with diverse behavioral manifestations [ 3 , 4 ].
CAS is a neurological childhood speech motor disorder in which the precision and consistency of movements underlying speech are impaired in the absence of neuromuscular deficits [ 5 ], and is included among Speech Sound Disorders (SSD) in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [ 1 ]. CAS core-deficit involves the planning and/or programming of the spatiotemporal parameters of movement sequences necessary for speech control [ 5 ] and is very frequently associated with an expressive language disorder [ 6 ].
The prevalence of CAS in the general population is low, 1–2 out of 1000 children [ 7 ], but it rises to 2.4% when considering children with SSD [ 8 ].
Despite the abovementioned differences in epidemiology and symptoms profile, an association between ASD and CAS has been suggested [ 9 , 10 ]. The prevalence of CAS is presumably higher in non-verbal or minimally verbal children with ASD, who represent about 25–30% of the ASD population without useful speech by age 5 [ 11 ].
ASD/CAS association is also supported by a possible shared genetic basis although only few syndromes or genes have been currently identified such as the 16p11.2 deletion syndrome [ 12 ] and the CNTNAP2 gene deletion on 7q35 position. The latter encodes a ‘neurexin’ protein that is associated with several neurodevelopmental disorders, including speech and language disorders [ 13 ] and autism [ 14 , 15 ]. Moreover, studies on the function of FOXP2, which may be mutated in some CAS, underscored molecular intersections between networks involved in spoken language and pathways implicated in Intellectual Disability/ASD [ 16 ]. Furthermore, genes known to be regulated by FOXP2 have been implicated in disorders such as schizophrenia (e.g., DISC1) [ 17 ] and ASD (e.g., MET and MEF2C) [ 18 , 19 ].
From a clinical perspective, both ASD and CAS children experience a delayed expressive language acquisition that might contribute to difficulties in early differential diagnosis between these two conditions. This is of outmost importance as specific and early treatments are now available for these two conditions. A further difficulty relies on the lack of specific neurobiological markers, which would help distinguishing between ASD and CAS at an early age. The use of brain MRI has increased the potential for the application of advanced techniques for detecting brain abnormalities both in ASD and CAS [ 20 , 21 ]. In particular, morphometric and Diffusion-Weighted Imaging (DWI) MRI studies showed an early altered brain trajectory in ASD, involving mainly the fronto-temporal and basal ganglia circuits [ 22 , 23 ]. Morphometric and connectivity brain MRI abnormalities have been also reported in children with CAS and other speech sound disorders, with recurrent abnormalities involving the left supramarginal gyrus, fronto-temporal regions and basal ganglia among other regions [ 21 , 24 , 25 , 26 , 27 , 28 ].
In recent years, there has been a growing interest in the identification of shared brain abnormalities across psychiatric and neurodevelopmental disorders, especially among the disorders that frequently overlap in phenotypic presentation [ 29 ]. In particular, these studies enlarge our understanding of whether symptoms’ overlap between some brain disorders could be at least partly explained by common altered neuroanatomy, or vice-versa, is subtended by disorder-specific brain underpinnings. In this framework, structural imaging studies have directly compared ASD with other neurodevelopmental disorders [ 30 , 31 , 32 ].
To our knowledge, no study has yet compared ASD and CAS through a structural morphometric MRI approach.
The main aim of this work has been to analyze structural MRI differences/similarities between children with ASD and CAS, which might share at least partly a genetic background, as well as of clinical impairment in the language domain, though in different aspects. We decided to exclude comorbid cases (ASD plus CAS) since the presence of comorbidity could be a confounding factor in the identification of disorder-specific brain underpinnings.
In particular, we aimed:
- (1) To test the hypothesis that the two clinical groups (ASD and CAS) display neurostructural differences in comparison with Typically Developing children (TD) through a morphometric MRI approach (ASD vs. TD; CAS vs. TD);
- (2) To investigate possible disease-specific brain structural patterns in the two clinical groups (ASD vs. CAS);
- (3) To evaluate the predictive power of machine-learning analysis in differentiating these three young populations (ASD, CAS, TD).
2. Participants and MRI Data Acquisition
We retrospectively selected MRI brain images of patients diagnosed with ASD and CAS after a comprehensive clinical evaluation at IRCCS Stella Maris Foundation (Pisa, IT), a tertiary care university hospital.
ASD group. Children were rigorously diagnosed with ASD according to the DSM-5 criteria [ 1 ] by a multidisciplinary team including a senior child psychiatrist, an experienced clinical child psychologist and a speech-language pathologist during three–five days of extensive evaluation. The diagnosis was confirmed by the Autism Diagnostic Observation Schedule (ADOS)-2 [ 33 ] administered by clinical psychologists who met standard requirements for research reliability. Inclusion criteria were: (a) age between 34 and 72 months, (b) Non-Verbal Intellectual Quotient (NVIQ) ≥70 and (c) spontaneous no-echolalic language of at least two-word associations, (d) absence of minimal signs potentially indicating comorbid CAS.
CAS group. CAS diagnosis was conducted by a multidisciplinary team on the basis of a comprehensive clinical, instrumental and neurological assessment as well as a video recorded speech–language evaluation. Following the international criteria for CAS diagnosis, speech and language performances were analysed by two independent expert observers according to a checklist including American Speech-Language-Hearing Association (ASHA) criteria [ 5 ] and Strand’s features of CAS [ 6 , 10 , 34 ]. Inclusion criteria were: (a) age between 34 and 71 months, (b) NVIQ ≥ 70, (c) no ASD symptoms documented by neuropsychiatric and psychological observation.
Exclusion criteria for both clinical groups were: (a) structural anomalies detected by MRI; (b) presence of oro-facial structural abnormalities; (c) neurological or genetic diseases; (d) audiological deficits; (e) epilepsy; (f) any identified etiology of the two disorders based on DNA analysis or screening tests for inborn errors of metabolism (plasma and urine amino-acid analysis, urine organic acid measurement, urine muco-polysaccharides quantitation, plasma and urine creatine, and guanidinoacetate analysis).
A group of typically developing children (TD) who had undergone brain MRI for various reasons (including headache, seizures with fever, strabismus, cataract, paroxysmal vertigo, diplopia) was also recruited, as controls.
3. MRI Acquisition and Processing
MRI data were acquired using a GE 1.5 T Signa Neuroptimized System (General Electric Medical Systems) at IRCCS Stella Maris Foundation, fitted with 40 mT/m high-speed gradients. Within the MRI protocol for children, a whole-brain fast spoiled gradient recalled acquisition in the steady-state T1- weighted series (FSPGR) was collected in the axial plane, yielding to contiguous axial slices with voxel size of 1.1 × 1.1 × 1.1 mm. All children were sedated with a general anesthesia with a halogenated agent (Sevoflurane) while spontaneously breathing. For all MRI performed between 2012 and 2018 the same sequence of acquisition was used and the written informed consent from a parent or guardian of children was obtained. This study was approved by the Pediatric Ethic Committee of Tuscany Region (Italy) through the ARIANNA Project (C52I16000020002) and RF 2016-022361560 Project, and was performed according to the Declaration of Helsinki and its later amendments or comparable ethical standards.
We used the ARIANNA platform [ 35 ] for data handling and processing.
4. FreeSurfer Processing and Feature Extraction
Structural MRI data were pre-processed according to the widely used FreeSurfer analysis pipeline (FreeSurfer v.6.0), to finally extract brain descriptive features, such as volume and thickness. FreeSurfer software is well documented and freely available for download at https://surfer.nmr.mgh.harvard.edu/ . FreeSurfer is used as pre-processing workflow for structural MRI data to perform volumetric segmentation and cortical reconstruction through 31 processing steps. The technical details of these procedures are described in the publication by Fischl [ 36 ] and references therein. Briefly, this processing includes motion correction, removal of non-brain tissue using a hybrid watershed/surface deformation procedure, automated Talairach transformation, segmentation of the subcortical white matter and deep grey matter volumetric structures, intensity normalization, tessellation of the grey matter white matter boundary, automated topology correction, and surface deformation following intensity gradients to optimally place the grey/white and grey/cerebrospinal fluid borders at the location where the greatest shift in intensity defines the transition to the other tissue class. FreeSurfer is an extremely time-consuming procedure. It requires in order of a few hours (8 h on average) to segment a 3D volumetric image.
The FreeSurfer analysis pipeline computes for each structure several descriptive features. We considered in our analysis the following regional features: the volumes of subcortical structures and the volumes and thicknesses of the cortical structures, and some volume and thickness global measures. In detail, the cortex was parceled in 34 left and 34 right structures, whose volumes and thicknesses generated 138 cortical features (i.e., 68 volumes, 68 parcel thicknesses plus the mean left and mean right thickness values) contained in the aparc FreeSurfer output file. Thirty additional volume values were considered within those available in the aseg FreeSurfer output file, including the volumes of subcortical structures (thalamus, caudate, putamen, pallidum, hippocampus, amygdala, accumbens nuclei, corpus callosum and brainstem), and those of the ventricles, the subcortical cerebrospinal fluid, the optical chiasm and the cerebellum (white and gray matter). A complete list of the FreeSurfer features considered in this analysis is available in the Supplementary Materials .
5. Statistical Analysis
The entire set of brain features were statistically analysed in order to identify significant differences between patients with ASD, CAS and TD children. The ANOVA test was conducted for normally distributed features, whereas the Kruskal-Wallis test was used in case the features were not normally distributed. The Bonferroni method was used to correct the results for multiple comparisons. The effect sizes were evaluated in terms of Cohen’s d . Furthermore, we performed machine learning (ML)-based multivariate analysis through Support Vector Machine (SVM) binary classifiers [ 37 ]. In particular, linear-kernel SVMs were implemented to evaluate the predictive power of neuroanatomical features in the binary classification of the ASD vs. TD, CAS vs. TD, ASD vs. CAS groups. We implemented a five-fold cross-validation scheme in this analysis to partition the available data in train and test sets and to evaluate the classifier performance. The classification performance was evaluated in terms of the mean and standard deviation of area of the ROC curve (AUC) obtained across 10 repetitions of the five-fold cross-validation.
The statistical analysis and the SVM classification were carried out with Matlab R2018a (The MathWorks, Inc., Natick, Massachusetts, U.S) through in-house developed scripts and functions. In particular, the anova1 , kruskalwallis and multcompare matlab functions were used for statistical analysis and the fitcsvm function for the SVM classification.
6.1. Participants
The initial cohort consisted of 98 patients who underwent brain structural MRI. Eighteen patients were excluded due to detection of minor brain anomalies (i.e., arachnoid cyst; periventricular leukomalacia; cortex anomalies such as heterotopia or dysplasia); seven patients were excluded due to low quality of MRI scans; five patients were excluded due to the presence of clinical comorbidities (other neurodevelopmental disorders).
The final cohort consisted of 68 children aged from 34 to 72 months, belonging to the three groups of ASD, CAS and TD, which were matched for gender and age. The age distributions are showed in Figure 1 .

Age distribution of the subjects in the ASD, CAS and TD groups. The bar plot is shown on the left for the three groups, whereas the box plots with an overlay of the age value of the individual subjects, slightly scattered randomly along the x axis, are shown on the right. Abbreviations: ASD, Autism Spectrum Disorder; CAS, Childhood Apraxia of Speech; TD, Typical Development control.
ASD group: 26 children; mean age ± standard deviation (SD) = 56 ± 11 months; CAS group: 24 children; mean age ± SD = 56 ± 10 months. TD group: 18 children; mean age ± SD = 55 ± 13 months.
Children’s demographic characteristics are shown in Table 1 and Figure 1 .
Demographic characteristics of the cohorts of subjects with ASD, with CAS and TD subjects. The number of subjects in each subgroup is reported ( n ) together with the male/female percentage with respect to the total number of subjects in each cohort.
Abbreviations: ASD, Autism Spectrum Disorder; CAS, Childhood Apraxia of Speech; TD, Typical Development control.
6.2. Statistical Analysis
Statistical analysis of the complete set of FreeSurfer features was carried out. Significant differences in several brain structures across the three cohorts were detected through ANOVA statistical analysis and the Kruskall-Wallis test, as reported in Table 2 for cortical volumes, cortical thicknesses and subcortical volumes. The effect sizes in terms of Cohen’s d are also reported in the table. A visual representation of all altered brain regions, as segmented by FreeSurfer, is shown in Figure 2 , where their overlay on the anatomical image of a representative subject is reported. In particular, brain regions whose features showed statistically significant differences in the comparison among the three groups of children are highlighted. We summarize in the text below the results of the between-group comparisons ASD vs. TD, CAS vs. TD and ASD vs. CAS, reported in Table 2 column (a), Table 2 columns (b) and (c), and Table 2 column (d), respectively.

Visualization of brain regions whose features showed statistically significant differences among the three groups of subjects (see Table 2 for the complete list of features, including also global volumes). The overlay of FreeSurfer segmented regions onto the anatomical image of a representative subject is shown for specific alterations in the ASD vs. TD ( a , b ), CAS vs. TD ( c – e ) and ASD vs. CAS ( f , g ) comparisons. The involved set of features, i.e., the cortical and subcortical volumes, and the cortical thicknesses, are indicated in each figure row.
Cortical volumes showing a statistically significant difference in the comparison among children with ASD, children with CAS and TD children. The test statistics (either ANOVA or Kruskal-Wallis), the p-values, the specification of which group comparisons showed statistically significant differences and the related effect size in terms of Cohen’s d are reported.
Abbreviations. ASD, Autism Spectrum Disorder; CAS, Childhood Apraxia of Speech; TD, Typical Development control. § Features with not-normal distribution undergone Kruskal-Wallis test instead of ANOVA.
6.3. Comparison between ASD and TD
The significant neuroanatomical differences between ASD and TD are reported in Table 2 (a), visualized in Figure 2 a,b and discussed below.
Cortical volumes. Overall, ASD presented increased volumes in comparison with TD. No contra-comparison results were found. The Cohen’s d effect sizes vary from medium effect size to large effect size. ASD presented increased cortical volumes within the fronto-temporal lobe: left paracentral volume ( d = 0.83), left posterior cingulate volume ( d = 0.73), left supramarginal volume ( d = 0.58), right caudal middle frontal volume ( d = 0.77) and right superior temporal volume ( d = 0.95).
Subcortical volumes. Overall, ASD presented increased subcortical volumes in comparison with TD; no contra comparison results were found. ASD presented increased volumes in the following regions: caudate (left d = 1 and right d = 0.89), putamen (left d = 0.89 and right d = 0.88), hippocampus (left d = 1.15 and right d = 1.19) and left nucleus accumbens ( d = 0.92).
Cortical thickness. No statistically significant results were detected.
Global measures and cerebellum. An increase in cortex volumes of the cerebellum (left d = 0.97 and right d = 1) was detected in children with ASD with respect to TD. Children with ASD also presented an increased global subcortical grey matter volume ( d = 0.97) and total grey matter volume ( d = 0.71) with respect to TD.
6.4. Comparison between CAS and TD
The significant neuroanatomical differences between CAS and TD are reported in Table 2 (b) and (c), visualized in Figure 2 c–e, and discussed below.
Cortical volumes. Overall, children with CAS presented higher values of cortical volume within the frontal lobe, in particular in left paracentral ( d = 0.80), right pars triangularis ( d = 0.52) and in left supramarginal ( d = 0.50).
Subcortical volumes. CAS showed an increased volume in left nucleus accumbens ( d = 0.97) with respect to TDs.
Cortical thickness. CAS presented reduced values of cortical thickness in the frontal lobe, in particular in the right frontal pole ( d = 0.97).
Global measures and cerebellum. No statistically significant results were detected.
6.5. Comparison between ASD and CAS
The significant neuroanatomical differences between ASD and CAS are reported in Table 2 (d), visualized in Figure 2 f,g, and discussed below.
Cortical volumes. No statistically significant differences between ASD and CAS were directly detected in cortical volumes.
Subcortical volumes. Statistically significant greater volumes of the left caudate ( d = 0.68) and of the hippocampi (left d = 0.57 and right d = 0.56) have been detected in ASD with respect to CAS.
Cortical thickness. ASD showed statistically significant higher cortical thickness in the right superior temporal ( d = 0.89) in comparison to CAS.
6.6. Machine Learning Analysis
The performances obtained with the binary linear-kernel SVM in the ASD vs. TD, CAS vs. TD, ASD vs. CAS classification are reported in Table 3 . The classification performance achieved by different groups of features (e.g., cortical volumes/thickness, subcortical volumes, and their combinations) are reported in the table in terms of the ROC curve (AUC) values obtained according to a five-fold cross-validation scheme. The error assigned to each AUC value is computed as the standard deviation over 10 repetitions of the five-fold cross-validation.
Classification performance in the binary classification between the ASD vs. TD, CAS vs. TD and ASD vs. CAS groups using structural features. The performances are expressed in terms of the area under the ROC curve (AUC) achieved in the classification of different groups of features (e.g., cortical volumes/thickness, subcortical volumes, global volumes and their combinations). The cross-validation scheme implemented consisted in 10 repetitions of a five-fold cross validation.
Abbreviations: AUC, area under the ROC curve; SD, standard deviation; m, number of features in each selected group of features (each table row); n , number of subjects used in each classification problem (each table column); ASD, Autism Spectrum Disorder; CAS, Childhood Apraxia of Speech; TD, Typical Development control.
It can be noticed from Table 3 that the most informative groups of features driving the discrimination performance between children with ASD and TD are the subcortical volumes, either including or not the global measures. In those cases, AUC values of 0.76 ± 0.14 and of 0.75 ± 0.16 have been obtained. The classification performance remains high when the combination of all features is considered, leading to an AUC of 0.73 ± 0.19.
By contrast, the group of children with CAS does not appear to be distinguishable from the group of TD children by means of a linear-kernel SVM classification. Despite that the classification performance obtained is not above the chance level, the set of cortical thickness features showed an average AUC value of 0.62, and the combination of all features an AUC of 0.61.
It turns out also that the groups of children with ASD and with CAS are indistinguishable from each other by means of a linear-kernel SVM classification, as reported in the rightmost column of Table 3 (all chance-level AUC values). In this case, only the set of cortical thickness features displayed an average AUC value of about 0.64.
7. Discussion
To our knowledge, this is the first structural morphometric MRI study comparing ASD, CAS and TD. This may represent the first step towards understanding the neural substrate that characterizes the two conditions, possibly being of utmost importance for future early tailored intervention strategies. Furthermore, it could be helpful to understand as early as possible whether children with non-verbal or minimally verbal ASD have a CAS on the basis of neuroanatomical brain configuration, given the difficulty of directly testing these children.
7.1. Are ASD and CAS Brain Different from TD Brain?
7.1.1. asd versus td.
ASD children displayed an overall increase of total grey matter volume in comparison with TD, specifically distributed in the fronto-temporal regions.
Grey matter volume increase is one of the most consistent structural findings in ASD, and it is particularly striking in younger children [ 20 ], thus supporting the early brain overgrowth of ASD related to abnormal cortical development and expansion [ 38 , 39 ]. It is of interest that the cortical volumes’ increase found in our ASD children versus TD is mainly distributed in fronto-temporal lobes, known to be crucial for socio-communicative skills development [ 40 ]. The importance of these two brain lobes in the pathophysiology of ASD was further corroborated by two recent studies [ 41 , 42 ], which identified both frontal and temporal lobe volumes as the most discriminative features in the ASD-control classification. Critically, the left supramarginal gyrus, which belongs to the inferior parietal lobule, was also increased in volume in ASD children. This region is massively connected with both Broca’s and Wernicke’s areas, and it is altered during processing of some language aspects, including pragmatics [ 43 ], and sentence comprehension [ 44 ] in children with ASD.
Besides the well-replicated alterations in the fronto-temporal cortical regions, an increased volume in some subcortical structures was detected in the current work. Specifically, both right and left hippocampi were significantly increased in ASD group when compared with TD. The hippocampus is considered relevant for the ASD pathophysiology, since it is connected to the amygdala within the limbic system and implicated in crucial functions of the “social brain” [ 45 ]. Our result of increased hippocampi volumes is consistent with findings from a large study of 98 patients with ASD (age-range: 7.5–18 years) compared to 31 controls [ 46 ], and it is also concordant with a longitudinal investigation in children between the ages of 8 and 12 years [ 47 ]. However, findings on hippocampal volume in autism are quite controversial, as some authors did not identify differences compared with controls [ 48 ], while significantly decreased volumes were found by other authors [ 49 , 50 ].
In addition, we identified a significant enlargement of the striatum (the part of the basal ganglia composed of three subnuclei: caudate, putamen, and nucleus accumbens) in patients with ASD in comparison with TD. Structural alterations of the basal ganglia, and in particular of the caudate nucleus and the putamen, have been frequently detected in ASD, both in children [ 51 ] and adults [ 52 ], and associated with the severity of restricted and repetitive behaviors [ 53 ]. Instead, the nucleus accumbens is generally reported as a critical node within the brain’s reward circuitry, but, more broadly, it is also involved in action selection, integration of cognitive and affective information, and suppression of inappropriate actions [ 54 ].
Interestingly, decreased structural and functional connectivity between the ventral tegmental area of the midbrain and the nucleus accumbens, namely two brain areas crucial for processing social reward, was found in ASD children compared with TD children [ 55 ]. Such brain alterations appear to be related to the level of social interaction impairments in patients with ASD, providing support for the link between abnormalities in reward processing and widespread deficits in social engagement and communication in autism (i.e., the social motivation theory [ 56 ]).
The increased cerebellum volume we found is in agreement with some [ 49 , 57 ], but not all [ 20 , 58 ] literature findings. The cerebellum has been traditionally considered to be primarily involved in motor control and coordination, but its function comprises other domains typically impaired in ASD children, such as language, social cognition, and affective regulation [ 59 ]. In keeping with these data, a consensus paper recently highlighted a crucial role of the neuroanatomical cerebellar alterations in ASD [ 60 ].
We also detected an increased volume in the right superior temporal gyrus (STG), a region implicated in the processing of semantic [ 61 ] and prosodic cues [ 62 ], thus being two language aspects frequently impaired in children with ASD [ 63 ]. In this context, two previous fMRI investigations observed increased brain activation in the right STG of ASD children during processing of prosodic cues, such as anger and irony [ 64 , 65 ], that may reflect a more effortful processing required for the interpretation of prosodic information. The increased grey matter volume in right STG detected in the current study is consistent with three previous sMRI investigations focused respectively on toddlers (mean age: 30 months) [ 66 ], preschoolers (mean age: 53 months) [ 67 ], and children/adolescents (age range: 8.8–18.3 years) [ 68 ] with ASD, supporting the view that volumetric alterations in this region are present across the developmental age.
Cortical thickness analysis reported, in the current sample, no significant differences between ASD patients and TD peers. Some previous studies have shown cortical thickness differences between participants with ASD and controls across the whole brain, and in particular, a greater cortical thickness in fronto-temporal regions implicated in the processing of language and social information [ 69 , 70 , 71 ]. Nevertheless, other investigations have failed to detect between-groups differences in cortical thickness [ 72 ]. Additionally, cortical thinning in the pars opercularis of the inferior frontal gyrus was reported both in preschoolers [ 67 ] and in adults [ 73 ] with ASD. These discrepancies could be partly explained by study differences in sample size, age, patients’ characteristics and clinical symptoms’ severity, MRI acquisition and processing protocols. Longitudinal studies identified that differences in cortical thickness between patients with ASD and TD controls change over time [ 74 , 75 ], suggesting that an altered cortical thickness trajectory may constitute a more reliable neuroanatomical marker in ASD.
7.1.2. CAS Versus TD
Apraxia of speech (AOS) is the main symptom in adults after infarcts to the left hemisphere involving the inferior frontal region, in particular the posterior part of Broca’s area [ 76 ] and the insular cortex [ 77 ] or adjacent white matter [ 78 ]. Instead, Childhood Apraxia of Speech (CAS) is a developmental disorder whose brain correlates remain largely unknown and little evidence is available to date [ 21 , 24 , 28 ].
Our results show structural brain differences in children with CAS in comparison with TD. In particular, altered cortical volumes in areas crucial for speech and language were found, with increased volumes distributed within the parietal lobe (supramarginal gyrus), the frontal lobe (para-central, pars triangularis), and decreased volume in the nucleus accumbens.
The involvement of the left supramarginal gyrus in CAS has been previously described by Kadis [ 24 ], who found an increased thickness of this region in children with CAS aged as in our sample. Anatomo-clinical correlation studies in brain-damaged patients with a selective impairment of the auditory-verbal memory span indicate that the inferior parietal lobule (supramarginal gyrus) of the left hemisphere, at the temporo-parietal junction, represents the main neural correlate of the ‘store’ component of phonological short-term memory [ 79 ]. The left supramarginal gyrus is reported to play an important role in speech production, its damage thus being associated with deficits in phonemic discrimination and speech planning [ 80 ]. Furthermore, the supramarginal gyrus is part of a neural dorsal pathway receiving inputs from the auditory cortex and has reciprocal connections with the opercular part of the inferior frontal gyrus and the ventral premotor area [ 81 , 82 ], both involved in articulatory planning [ 83 ]. Indeed, as recently suggested by Nakamichi et al. [ 84 ] in a functional Near Infrared Spectroscopy (fNIRS) study, the supramarginal gyrus seems to be involved in phonemic processing and articulatory learning through an “articulatory loop” in which phonemic and oral somatosensory information are mapped onto motor representations for articulation. Partially overlapping with our findings, morphological abnormalities of supramarginal gyrus and, bilaterally, of temporal planum and Heschl’s gyrus have been described in children with a subtype of speech sound disorder characterized by persistent speech sound errors [ 27 ].
Another resulting altered region in terms of increased values in CAS vs. TD in the current work was the pars triangularis within the Broca’s area [ 85 , 86 , 87 ]. This region has been associated with linguistic processes, including syntax and semantics [ 86 , 88 , 89 ], but its precise functional role still remains controversial. Recently, Elmer and colleagues [ 90 ] suggested that pars triangularis can be considered as a “hub” region of the language-control network and would have a role in supporting verbal working memory functions during simultaneous language translation.
A further area within the frontal lobe founded as volumetrically increased in CAS vs. TD was the left paracentral region, a sensory-motor area involved in motor control in adults, whose eventual role in the acquisition of speech motor control during development is still unknown.
However it is of note that the paracentral region is contiguous to the precentral region reported as altered in the diffusion study on children with CAS by Fiori et al. [ 21 ].
At subcortical level, the nucleus accumbens, which is part of the ventral striatum and belongs to a broad language learning network [ 91 ], showed a decreased volume in CAS compared to controls.
As far as cortical thickness is concerned, the right frontal pole showed reduced values in CAS compared to TD. It is of note that the frontal pole (Broadmann Area 10) has been described as the most evolved region in humans [ 92 ] and it is essential for attention control, manipulation of stored knowledge and modulation of complex actions, cognition emotion, and behaviour [ 93 ]. However, the interpretation of this finding in children with CAS is still unclear.
7.2. Which Regions Directly Differentiate ASD vs. CAS?
Comparison between ASD and CAS showed that the caudate and the hippocampus volumes, together with the superior temporal thickness, were shown to be increased in ASD vs. CAS.
The basal ganglia (BG), which consist of the striatum, caudate nucleus and putamen, are involved in motor function [ 94 ] as well as in learning and memory processes [ 95 ] and have been widely related to the repetitive and stereotyped behaviors characteristic of autism spectrum [ 96 , 97 ]. Bilaterally reduced grey matter density in the caudate nuclei was described in patients with CAS related to FOXP2 mutations. In particular, MRI studies of the Ke family [ 98 ] and a recent report of an unrelated male child with a FOXP2 intragenic deletion [ 99 ] confirmed reductions of the caudate nucleus bilaterally, as well as of the globus pallidus and hippocampus.
As above mentioned in the ASD vs. TD section, the superior temporal gyrus has been widely described as having a crucial role in the social brain development, and not surprisingly has been found to be increased in our ASD population. Incidentally, the superior temporal gyrus is also involved in language comprehension that is often more severely impaired than language production in children with ASD [ 100 ], whereas an inverse profile characterizes children with CAS.
Data concerning hippocampus increased volumes in ASD are consistent with the findings of other studies, whereas there is only a case report by Liéogeois et al. (2016) [ 99 ] describing bilateral hippocampal and basal ganglia volume reduction (thalamus, globus pallidus, and caudate nucleus) in a 8 years old child with FOXP2 related CAS
Since the abovementioned regions (caudate, superior temporal gyrus and hippocampus) significantly differentiated not only ASD from CAS, but also ASD from TD, it may be hypothesized that these results are more ascribable to ASD higher values than to CAS lower values in the direct comparison.
7.3. Is Machine Learning Informative about Diagnosis Prediction?
Non-invasive brain imaging techniques coupled with advanced image analysis methodologies based on machine learning (ML) have been recently used to provide an automated classification of diseases, including ASD [ 101 ], whereas no application in the CAS field is yet reported. We have included, then, a ML analysis in the current work to estimate the predictive capabilities of neuroanatomical descriptive features in a binary comparison between two out of the three groups of children.
In the cases of CAS vs. TD and of ASD vs. CAS comparisons, the performances achieved did not score above the chance level. This means that the two groups are quite indistinguishable at least with linear-kernel SVM. It has to be noted that the high standard deviation assigned to the AUC values is mainly due to the limited sample size, which did not allow avoidance of the overfitting problem. Increasing the dataset population could sensibly reduce the standard deviation on the AUC values and the classification trends that are barely visible (AUC~0.6) may become apparent. It is also worth mentioning that any subtle relationship between neuroanatomical features that may characterize the two clinical groups of this study could be very hard to catch by a linear classifier. Non-linear approaches could be implemented. However, even in this case, the limited data samples (less than 30 subjects per group) with respect to the large amount of image features (sets from ~30 to more than 150 features have been considered) would not avoid the occurrence of overfitting, which causes a reduction in the generalization ability of the classifier.
In conclusion our ML analysis highlights that the group of children with ASD shows a distinct brain pattern with respect to the control group, focused especially on subcortical brain regions. The comparison between the children with CAS and the control group showed a trend towards the possibility of identifying a relevant pattern focused on cortical thickness, that represents the only relevant trend in the direct comparison between the two clinical groups. Indeed, while ASD present more widespread brain alterations, confirming previous data and opening the possibility to predictive power of ML algorithms based on MRI data, a predictive role of brain patterns in CAS is still not supported by the current sample size.
7.4. Final Considerations
In summary our work reports a general consistency with the previous literature in the brain structural comparison between ASD versus TD and CAS versus TD, with resulting effect size ranging from medium to large. It is of interest that all but one structure showed higher volumes in both ASD and CAS versus TD in this young population, in accordance with previous literature, especially for the ASD group. The only opposite trend regards cortical thickness (CAS < TD in frontal pole cortical thickness), but the significance of this result is not clear, cortical thickness not being univocally interpreted in the literature, and being age-dependent [ 102 ]
The more widespread abnormalities have been observed comparing ASD vs. TD, while more focused alterations have been found by comparing CAS vs. TD. Considering all the structures (cortical and subcortical volumes and cortical thickness), ASD alterations involve fronto-temporal regions together with basal ganglia and cerebellum, while CAS alterations seem to be more focused on and shifted to frontal regions, thus suggesting a possibly more specific speech-language related distribution of anomalies. We can speculate that autistic children’s brain atypicalities are more widespread in the superior temporal gyrus, historically considered the site of sound processing and auditory association cortex, but also linked to social cognition and implicated in visual analysis of social information. Moreover, the superior temporal gyrus has been involved in the perception of the emotional facial stimuli and more generally in social interactions. Conversely, atypicalities in CAS are more shifted in the frontal regions, where sensory motor circuitries are represented. Furthermore, it can be considered that overlapping structural regions between the two conditions can assume a different role at a functional level.
7.5. Strenghts and Weaknesses of the Study
To the best of our knowledge this is the first study comparing young children presenting with ASD, CAS and TD at a neurostructural level. Though our results suggest the possibility of detecting brain correlates potentially able to disentangle the two conditions from typical development from an early age (when clinical specific phenotypization is not easy), ML analysis in our sample has partially reached an optimal predictive power. Indeed, while our ML analyses confirm the possibility of detecting brain patterns with reliable predictive power in the ASD vs. TD comparison, this is not the same for CAS vs. TD and ASD vs. CAS. This can be ascribable to limited sample size, which does not allow a complete representation of the different distribution of possible alterations in the two conditions and also prevents the possibility of implementing more complex non-linear classifier models.
Certainly, the study has strengths and weakness. First, this is a whole brain analysis not driven by an a priori hypothesis, thus minimizing possible interpretation biases. Second, clinical groups, with a short age range, have been evaluated from expert clinicians (multidisciplinary team) in the field of ASD and CAS. Thirdly, the single-site recruitment of study participants limited the noise associated with the collection of data from different MRI scanners and different sequences. Our results should be interpreted in the light of some methodological limitations among which the small sample size is the most crucial. Indeed, our sample size of about 20 children per group is quite small, thus limiting the generalizability of the results and the strength of the conclusions [ 103 ]. Hence, it will be critical in the future to recruit larger samples in order to replicate our findings, and to provide a more robust characterization of the clinical and neuroanatomical profiles of children with ASD and CAS. This study’s limits are mitigated by the fact that patients have been carefully selected so as to be included in a limited age-range, in order to minimize age dependent structural brain alterations. Notably, the sample has been reduced from the initial cohort with the aim of obtaining a well-selected and homogeneous pool of MRI data, coupled with an extensive multidisciplinary clinical characterization of patients.
Furthermore, the retrospective nature of this study has not allowed us to apply appropriate clinical evaluations, such as ADOS-2 to the CAS population and standardized CAS protocols to the ASD population.
Future studies should collect a further group of patients with ASD and comorbid CAS in order to investigate the extent to which these cases differ from the “pure” disorders.
Though remaining cautious about interpretation, our results may represent the first step towards understanding the neural substrate that characterizes ASD and CAS conditions and therefore, in the future, for identifying neurobiological markers that may support early diagnosis of non-verbal or minimally verbal children with ASD.
Furthermore, the identification of a specific motor speech disorder associated to ASD is crucial for tailoring an appropriate early intervention.
Supplementary Materials
The following are available online at https://www.mdpi.com/2075-4426/10/4/275/s1 , Table S1: FreeSurfer features considered in the analysis.
Author Contributions
E.C., A.C., and S.C. conceived the study. E.C. and L.B. collected MRI and clinical data. E.C., A.C., and S.C. were major contributors in writing the manuscript. A.R., S.F., M.T. and P.C. contribute to interpretation of results and to the manuscript finalization. A.R., L.P., G.S., and P.B. performed the analysis. F.M. and G.C. contributed to review and editing the manuscript. All authors have read and agreed to the published version of the manuscript.
This work has been partially funded by the Tuscany Government (Bando FAS Salute by Sviluppo Toscana, ARIANNA Project) and by the Italian Ministry of Health RF 2016 022361560. E.C. and S.C. were partially funded by AIMS-2-Trials European Project.
Conflicts of Interest
The authors have no conflict of interest to declare.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
VIDEO
COMMENTS
Autism Spectrum Disorder (National Institute of Mental Health) Autism is also known as autism spectrum disorder (ASD). People with autism have challenges with communication and social skills. They also have repetitive behaviors or restricted interests. Speech-language pathologists, or SLPs, can help.
Autism spectrum disorder (ASD) is a developmental disability that can cause significant social, communication, and behavioral challenges. ... This is a health professional trained to treat individuals with voice, speech, and language disorders. The speech-language pathologist will perform a comprehensive evaluation of the child's ability to ...
Autism spectrum disorder is a condition related to brain development that impacts how a person perceives and socializes with others, causing problems in social interaction and communication. The disorder also includes limited and repetitive patterns of behavior. The term "spectrum" in autism spectrum disorder refers to the wide range of ...
Speech and Communication in Autism. People diagnosed with an autism spectrum disorder (ASD) can have a wide range of verbal abilities. Some may be entirely nonverbal, some may have limited useful speech, and some may speak fluently and intelligibly. Yet challenges with language and communication are hallmark autism traits.
Speech-language therapy can help people with autism spectrum disorder (ASD) improve their abilities to communicate and interact with others. 1 Verbal Skills This type of therapy can help some people improve their spoken or verbal skills, such as:
Autism spectrum disorder (ASD) is a neurological and developmental disorder that affects how people interact with others, communicate, learn, and behave. Although autism can be diagnosed at any age, it is described as a "developmental disorder" because symptoms generally appear in the first 2 years of life.
What is Speech Therapy? Speech-language therapy addresses challenges with language and communication. It can help people with autism improve their verbal, nonverbal, and social communication. The overall goal is to help the person communicate in more useful and functional ways. Communication and speech-related challenges vary from person to person.
When a child's language abilities (the ability to express oneself , understand spoken language, or both) are significantly lower than a child's intelligence and nonverbal abilities, the child may have a language-based disorder.While all children diagnosed with Autism Spectrum Disorder (ASD) have difficulties associated with communication (for example, pragmatic language difficulties), the ...
Autism spectrum disorder (ASD) is characterized by social communication deficits and restricted and repetitive behaviors (American Psychiatric Association, 2013).Although not required for the diagnosis, many autistic 1 individuals present with concomitant receptive and/or expressive language difficulties that range in severity. Up to 60% of children on the autism spectrum may be diagnosed with ...
Autism and disfluent speech. For decades, researchers have identified patterns of "disfluent speech" in autistic individuals, i.e. speech that exhibits deviations in continuity, fluidity, ease of rate and effort, with hesitations or repetition of sounds, words, or phrases. More recently, the nature and presence of this disfluent speech has ...
Autism, or autism spectrum disorder (ASD), is a developmental disorder that affects a person's ability to learn, behave, communicate, and interact with others.
INTRODUCTION. When it was first observed independently by Leo Kanner 1 and Hans Asperger, 2 autism was viewed as a psychiatric condition with mental retardation as a characteristic feature of the disorder, often accompanied by social awkwardness. The last couple of decades have witnessed an explosion of research in this area, leading to detailed characterization of the behavioral features, and ...
Children with autism are at a higher risk of being affected by speech disorders and often require remedial intervention. Eikeseth and Nesset (Journal of Applied Behavior Analysis, 36(3), 325-337, 2003) used sufficient-response exemplar training of vocal imitation in conjunction with prompting, chaining, and shaping procedures to successfully teach 2 typically developing children to ...
Problems with speech and language are one of the defining characteristics of the Autism Spectrum Disorders. However, the difficulties that individuals with autism have with speech and language are very heterogenous and probably have a number of different causes or contributing factors, even in the same individual.
Many children with Autism Spectrum Disorder struggle with speech and language comprehension. Symptoms may include: Delay in learning how to speak (after the age of two) or doesn't talk at all. Speaking in an atypical tone of voice, or with an odd rhythm or pitch. Repeating words or phrases over and over without communicative intent.
Getty Images Restricted and repetitive behaviors in autism. Repetitive behaviors or "stimming" are amongst the most common symptoms of autism spectrum disorders. People with ASD may present ...
Speech and Autism Spectrum Disorder. Speech is a way of communication which includes articulation, voice and fluency. Speech motor planning is the ability to come up with an idea, plan how to say or express that idea and then finally say it. Muscle tone refers to the muscles and strength needed to move the jaw, tongue and other muscles needed ...
Examining the ability to read, converse, write, or perform non-speech movements. Apraxia and autism are both disorders that involve speech and communication, but they are not the same disorder. One recent scientific study suggests that as much as 65% of children with autism have speech apraxia. This suggests that children diagnosed with autism ...
Autism spectrum disorder, on the other hand, is a developmental disability that affects an individual's ability to communicate, interact socially, and form relationships. ... Just as with speech ...
USA TODAY. 0:04. 0:50. April marks Autism Acceptance Month with World Autism Day occurring on April 2 every year. The month is meant to be a time for uplifting autistic voices and sharing in the ...
It is estimated that 1 in 66 Canadians has an autism spectrum condition (ASC) or Autism Spectrum Disorder (ASD), referred to here as autism (Public Health Agency of Canada, 2018).One defining characteristic of autism is differences or challenges in social communication skills (American Psychological Association [APA], 2013).As specialists in the assessment and treatment of communication ...
NorthJersey.com. 0:07. 1:36. HAWTHORNE — A 3-year-old child pointed to a shirt worn by a speech therapist and said "orange.". Then, the girl looked down at her own shirt, pointed to it and ...
Autism Spectrum Disorder (ASD) is a neurodevelopmental condition with a wide spectrum of symptoms, mainly characterized by social, communication, and cognitive impairments. Latest diagnostic criteria according to DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, 2013) now include sensory issues among the four restricted/repetitive behavior features defined as ...
Autism Spectrum Disorder (ASD) and Childhood Apraxia of Speech (CAS) are developmental disorders with distinct definitions and diagnostic criteria. Specifically, ASD includes a set of neurodevelopmental disorders characterized by social communication difficulties as well as restricted interests, repetitive activities and sensory abnormalities ...