

The Ultimate Guide to Nursing Assignments: 7 Tips and Strategies
Nursing assignments are a critical component of every nursing student’s academic journey. They serve as opportunities to test your knowledge, apply theoretical concepts to real-world scenarios, and develop essential skills necessary for your future nursing career. However, tackling nursing assignments can often be overwhelming, particularly when you’re juggling multiple responsibilities. In this comprehensive guide, we provide valuable tips, strategies, and expert assignment help services to help you excel in your nursing assignments. Whether you’re struggling with research, structuring your assignment, or proofreading, we’re here to support you every step of the way.
Understanding the Nursing Assignments
To excel in nursing assignments , it’s crucial to start by thoroughly understanding the requirements. Take the time to carefully read the assignment prompt, paying close attention to the topic, word count, formatting guidelines, and any specific instructions provided by your instructor. Understanding these key components will ensure that you meet all the necessary criteria.
Conducting Thorough Research
Once you have a clear understanding of the assignment, it’s time to conduct thorough research. Solid research forms the foundation of any successful nursing assignment. Begin by gathering relevant and credible sources, such as nursing textbooks, scholarly articles, reputable websites , and academic databases specific to nursing. These resources will provide you with evidence-based information to support your arguments and demonstrate your understanding of the topic.
Creating a Well-Structured Outline
A well-structured outline is essential for organizing your thoughts and ensuring a logical flow in your nursing assignment. An effective outline acts as a roadmap, guiding you through the writing process and ensuring that you cover all the necessary points.
At [Your Service Name], our expert writers can assist you in creating a comprehensive outline tailored to your specific assignment. By collaborating with us, you can receive personalized guidance in organizing your ideas effectively and structuring your assignment in a logical manner. Our writers understand the nuances of nursing assignments and can help you identify the most important concepts and supporting evidence to include.
Using a Professional Tone
Maintaining a professional tone throughout your nursing assignment is crucial. As aspiring healthcare professionals, it’s essential to communicate your ideas with clarity, conciseness, and professionalism. Use clear and concise language, avoiding jargon or slang that may hinder the reader’s understanding. Present your arguments and supporting evidence in a logical and coherent manner, demonstrating your ability to think critically and apply nursing principles.
Our expert writers have extensive experience in academic writing within the field of nursing. They possess a deep understanding of the professional tone required for nursing assignments and can ensure that your assignment is written to the highest standards. By collaborating with us, you can receive guidance in maintaining a professional tone and effectively conveying your ideas.
Incorporating Practical Examples
In addition to a professional tone, incorporating practical examples into your nursing assignment can greatly enhance its quality. Practical examples bring theoretical concepts to life, illustrating their application in real-life scenarios. They demonstrate your understanding of nursing principles and showcase your ability to bridge the gap between theory and practice.
Our team consists of experienced nursing professionals who can assist you in incorporating relevant practical examples into your assignment. Drawing from their extensive knowledge and expertise, they can provide you with real-life scenarios or case studies that strengthen the impact and credibility of your work. By collaborating with us, you can elevate the quality of your assignment by demonstrating your ability to apply nursing concepts in practical settings.
Proofreading and Editing
Proofreading and editing are essential steps in the assignment writing process. They ensure that your nursing assignment is polished, error-free, and effectively communicates your ideas. After completing the initial draft, it’s crucial to take a break and return to your work with fresh eyes. During the proofreading stage, carefully review your assignment for grammar, spelling, punctuation, and sentence structure. Correct any errors and inconsistencies that may affect the clarity and professionalism of your writing.
At nursingresearchhelp.com , we have a dedicated team of proofreaders and editors who specialize in nursing assignments. They meticulously review your work, ensuring that it adheres to formatting guidelines and meets the highest standards of academic writing. Our proofreaders and editors will help you refine your assignment, ensuring that it is polished and error-free. By collaborating with us, you can rest assured that your assignment will be thoroughly reviewed and refined before submission.
Seeking Help When Needed
In addition to proofreading and editing, it’s important to seek help when needed. Nursing assignments can be challenging, and it’s perfectly normal to require assistance. Whether you’re facing difficulties in understanding the assignment prompt, need guidance in specific areas, or simply want a fresh perspective on your work, don’t hesitate to reach out for support.
Our friendly and knowledgeable support team is always available to address any questions or concerns you may have. We understand the unique challenges faced by nursing students and can provide you with the guidance and clarification you need. By seeking help when needed, you can overcome obstacles and ensure the successful completion of your nursing assignments.
Mastering nursing assignments is within your reach with the right tips, strategies, and expert assignment help services. At nursingresearchhelp.com we are committed to supporting nursing students in excelling in their academic pursuits. Our experienced writers, proofreaders, and editors can provide personalized assistance throughout the assignment writing process, ensuring that your assignments meet the highest standards of quality and professionalism.
With our help, you can confidently tackle your nursing assignments and overcome any challenges you may face. Visit our website nursingresearchhelp.com to learn more about our services and how we can support you in achieving academic excellence. Whether you need guidance in understanding the assignment, conducting thorough research, creating a well-structured outline, using a professional tone, incorporating practical examples, or ensuring a polished final product, we are here to assist you. Trust us for reliable and professional assignment help tailored to your needs.
Don’t let the challenges of nursing assignments hold you back—reach out to us for reliable and professional assignment help tailored to your needs.
You might also like
Nursingresearchhelp.com is the fastest, easiest and most reliable way to have content written for your website. You’ll be able to post a project and 1000s of freelance writers from across the globe will have instant access to write your content quickly, professionally, and affordably.
QUICK LINKS
- HOW IT WORKS
- OUR SERVICES
- TERMS OF USE

Call/Text: +1 608 912 3884

How To Refuse an Unsafe Patient Assignment as a Nurse
What is a safe nursing assignment, when should you refuse an assignment, how to refuse a patient assignment.

You walk into work, ready to spend the next 12 hours taking care of your patients and providing them with the best nursing care possible. You look at your patient assignment and see you have one extra patient than usual, as well as only one CNA for your entire nursing unit. Your charge nurse has a full patient assignment too, making her less available to offer help and support. You hear machines beeping, bed alarms sounding, and patients yelling, and you stop and think to yourself “is this safe?”
Does this scenario sound familiar to you as a nurse?
Being given an inappropriate assignment can be very overwhelming and stressful. Your patients need you to show up and take care of them, and your nursing team needs you, and you want to help.
But where do you draw the line, and say “NO”, to a patient assignment? What is an unsafe assignment, and can a nurse refuse an assignment?
An appropriate nursing assignment is any patient assignment where the nurse can safely and effectively provide all the necessary care for their patients, and have the necessary tools, training, medications, knowledge, resources, and equipment to perform their nursing duties for those patients.
The definition of a safe and appropriate nursing assignment is variable, has to do with much more than patient ratios alone, and will vary by state and facility.
Per the American Nurses Association (ANA), nurses have not only a right but also an obligation to assess and determine if they can safely and appropriately provide care on any given patient assignment. They provide this list of questions that every nurse should be asking themselves before accepting any patient assignment.
What does an inappropriate or unsafe patient assignment look like, and what are some reasons you might stop and consider refusing the assignment or asking your leader for changes to the assignment?
Too Many Patients
There are only 2 states in the US that have laws mandating nurse-to-patient ratios , California and Massachusetts. Some states, but not all of them, have mandatory reporting requirements for staffing. Others have staffing committees with some nurse members to assist in making staffing decisions, but still no mandated ratios.
You will learn as you gain more nursing experience how many patients are too much for you as one nurse. This will depend on your unit’s acuity level, patient population, and the individual staffing policies at your facility.
- Inappropriate distribution of patient acuity
5 “walkie-talkie” patients are vastly different from 5 patients on high-level oxygen. The ability to understand what constitutes high acuity will also come with more nursing experience. You may not know or understand, what the acuity level is of a COVID patient on continuous BIPAP, until you have cared for that type of patient.
Also take into consideration how many discharges or empty rooms you have, if you have any patients on continuous drips or pain pumps, your patient’s mobility level, and if your patient is scheduled for any procedure that will warrant intense post-procedure monitoring when they return.
A particular patient’s acuity can change with each shift, which means nursing management must be in close communication with the team and get accurate patient acuity updates before making each assignment.
Inadequate knowledge or training
Are you being asked to care for a post-surgical patient on gynecology, when you normally take care of patients recovering from a stroke? Are you being asked to care for pediatric patients when you have only ever cared for adults? Maybe you are being asked to do something you think may be out of your scope of practice as a nurse. This would be a reason to voice concern and ultimately refuse a particular assignment.
No Supplies or Help
Do you have all of the equipment you need to do your job? Do you know where your code cart is, and can you safely and effectively help your patient in an emergency? Are your medications stocked, machines in good working order, and can you get extra help if you need it?
If you don’t have all of the above, keeping your patients safe could be a challenge, and this alone would deem your assignment unsafe.
If you find yourself in any of the above situations, or others in which you feel your license and patient safety are in jeopardy, can you refuse to take the assignment ?
The ANA upholds that “ registered nurses – based on their professional and ethical responsibilities – have the professional right to accept, reject or object in writing to any patient assignment that puts patients or themselves at serious risk for harm. Registered nurses have the professional obligation to raise concerns regarding any patient assignment that puts patients or themselves at risk for harm.” Read the full ANA position statement here.
It is not only your right as a nurse, but also your duty, to raise concern and ultimately refuse an unsafe, inappropriate assignment. Here are some tips on how you can bring up these concerns and refuse your assignment as a nurse.
Know your rights, and be prepared to state them
It is solely your responsibility as a nurse to know your rights, as well as your responsibilities, in the state in which you practice as a nurse. Each state has its own Nurse Practice Act, which defines by law what you can, and cannot do, as a nurse. It also contains your nursing scope of practice. Visit the NCSBN website to quickly navigate to each state's Nurse Practice Act .
The NCSBN also provides a great decision-making tool to help explain the proper process of determining whether or not a certain activity is within the nurse’s scope.
Be prepared to refer to the Nursing Code of Ethics , and verbalize any statement of your nursing rights when communicating about your patient assignment with your leader. By knowing your rights as a nurse, and being ready to state them, you can clearly and effectively communicate with your manager why you want to refuse an assignment when placed in an unsafe situation.
Don’t Create a Nurse-Patient Relationship
Before you decide to accept any patient assignment, you need to avoid any activity that could be considered creating a nurse-patient relationship. There is a fine line between refusing a patient assignment, and nurse abandonment, which also varies state by state.
For example in Arizona, the board of nursing defines patient abandonment as a nurse severing or ending the nurse-patient relationship, after creating the relationship, without giving handoff or reporting to another capable nurse to take over that patient's care.
Here are some things that may be considered for establishing a nurse-patient relationship:
Viewing the patient’s electronic medical record
Saying hi to the patient, or going into their room at all
Taking orders from a doctor regarding that patient
Administering any type of patient care such as assisting them to the bathroom, taking them a food tray, or administering them any medications.
It is critical to read up on your state’s Nurse Practice Act and get a very clear definition of what patient abandonment is in your state. Your state’s board of nursing will have the resources needed to give you directions on the correct process of refusing an assignment in your state of licensure.
Do Your Research and Be Prepared
Nurses are always thinking ahead, preparing for what can go wrong with our patients, and ready to act in case of any emergency. We know exactly what equipment we will need for our patients, and would never allow our patients to be without adequate IV access.
Apply this same principle to the safety of your nursing license, your patients, and your team, by doing your research on the process of refusing a patient assignment correctly. Study your facilities policies, your nursing rights, and your state’s Nurse Practice Act.
It is your responsibility to know these things, and you don’t want to be scrambling at the very last second trying to do this research when you are being pressured at the moment to take a dangerous assignment.
Keep Everything in Writing
If you do end up voicing any sort of staffing or patient safety concerns, or ultimately refusing an assignment, always make sure you are communicating it to all of the appropriate leaders and follow your chain of command.
Send an email to all members of your leadership team to summarize the situation, and provide thorough documentation of why you are refusing an assignment, with adequate details.
Keep any paper records for yourself, just in case.
Help Find Solutions
Refusing a patient assignment will have an impact on all of the patients in the unit, the entire hospital, as well as the rest of the members of the healthcare team. It is your right, and duty, to refuse an inappropriate assignment. But try to be as professional and flexible as possible, keeping the ultimate goal of patient safety in mind.
Can you and your team brainstorm with your nursing leader on other ways to make everyone’s assignments safe and appropriate, such as:
Calling in a resource RN to help with patient care tasks
Re-arranging the patient assignment to re-distribute patient acuity better among all nurses
Obtaining a 1:1 sitter for all confused patients, ensuring their safety and also freeing up your extra time for your other patients?
Better assigning the patients to nurses based on their appropriate certifications, and expertise?
Ultimately you are a team, and you are there for your patients and each other. The goal is patient safety, and if you don’t speak up and refuse to take an inappropriate assignment, your patient’s well-being and your nursing license are on the line.
Be prepared to have these conversations, and be well-versed in your rights as a nurse. By refusing inappropriate assignments, you are advocating for yourself, and your patients, and being a voice for positive change in healthcare.

Amy was surgical PCU/Telemetry unit as a new grad for over 10 years; the last year and a half of that time being Telemetry COVID nursing. She stepped away from the bedside and is currently working PRN as a concierge nurse. Amy has a passion for budgeting. Follow her on Instagram, Facebook, and on her website Real Desert Mama , where she talks about budgeting, saving money, and tips and motivation on how to live a great life and achieve your financial goals through budgeting

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
3.3 Assignment
Nursing team members working in inpatient or long-term care settings receive patient assignments at the start of their shift. Assignment refers to routine care, activities, and procedures that are within the legal scope of practice of registered nurses (RN), licensed practical/vocational nurses (LPN/VN), or assistive personnel (AP). [1] Scope of practice for RNs and LPNs is described in each state’s Nurse Practice Act. Care tasks for AP vary by state; regulations are typically listed on sites for the state’s Board of Nursing, Department of Health, Department of Aging, Department of Health Professions, Department of Commerce, or Office of Long-Term Care. [2]
See Table 3.3a for common tasks performed by members of the nursing team based on their scope of practice. These tasks are within the traditional role and training the team member has acquired through a basic educational program. They are also within the expectations of the health care agency during a shift of work. Agency policy can be more restrictive than federal or state regulations, but it cannot be less restrictive.
Patient assignments are typically made by the charge nurse (or nurse supervisor) from the previous shift. A charge nurse is an RN who provides leadership on a patient-care unit within a health care facility during their shift. Charge nurses perform many of the tasks that general nurses do, but also have some supervisory duties such as making assignments, delegating tasks, preparing schedules, monitoring admissions and discharges, and serving as a staff member resource. [3]
Table 3.3a Nursing Team Members’ Scope of Practice and Common Tasks [4]
|
| ||
|---|---|---|
| RN |
| |
| LPN/VN | Tasks That Potentially Can Be Delegated According to the Five Rights of Delegation: | |
| AP |
|
An example of a patient assignment is when an RN assigns an LPN/VN to care for a client with stable heart failure. The LPN/VN collects assessment data, monitors intake/output throughout the shift, and administers routine oral medication. The LPN/VN documents this information and reports information back to the RN. This is considered the LPN/VN’s “assignment” because the skills are taught within an LPN educational program and are consistent with the state’s Nurse Practice Act for LPN/VN scope of practice. They are also included in the unit’s job description for an LPN/VN. The RN may also assign some care for this client to AP. These tasks may include assistance with personal hygiene, toileting, and ambulation. The AP documents these tasks as they are completed and reports information back to the RN or LPN/VN. These tasks are considered the AP’s assignment because they are taught within a nursing aide’s educational program, are consistent with the AP’s scope of practice for that state, and are included in the job description for the nursing aide’s role in this unit. The RN continues to be accountable for the care provided to this client despite the assignments made to other nursing team members.
Special consideration is required for AP with additional training. With increased staffing needs, skills such as administering medications, inserting Foley catheters, or performing injections are included in specialized training programs for AP. Due to the impact these skills can have on the outcome and safety of the client, the National Council of State Board of Nursing (NCSBN) recommends these activities be considered delegated tasks by the RN or nurse leader. By delegating these advanced skills when appropriate, the nurse validates competency, provides supervision, and maintains accountability for client outcomes. Read more about delegation in the “ Delegation ” section of this chapter.
When making assignments to other nursing team members, it is essential for the RN to keep in mind specific tasks that cannot be delegated to other nursing team members based on federal and/or state regulations. These tasks include, but are not limited to, those tasks described in Table 3.3b.
Table 3.3b Examples of Tasks Outside the Scope of Practice of Nursing Assistive Personnel
|
| |
|---|---|
| LPN/VN | refers to adjusting the dosage of medication until the desired effects are achieved.) |
| Assistive Personnel (AP) |
As always, refer to each state’s Nurse Practice Act and other state regulations for specific details about nursing team members’ scope of practice when providing care in that state.
Find and review Nurse Practice Acts by state at www.ncsbn.org/npa.
Read more about the Wisconsin’s Nurse Practice Act and the standards and scope of practice for RNs and LPNs Wisconsin’s Legislative Code Chapter N6.
Read more about scope of practice, skills, and practices of nurse aides in Wisconsin at DHS 129.07 Standards for Nurse Aide Training Programs.
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation . https://www.ncsbn.org/NGND-PosPaper_06.pdf ↵
- McMullen, T. L., Resnick, B., Chin-Hansen, J., Geiger-Brown, J. M., Miller, N., & Rubenstein, R. (2015). Certified nurse aide scope of practice: State-by-state differences in allowable delegated activities. Journal of the American Medical Directors Association, 16 (1), 20–24. https://doi.org/10.1016/j.jamda.2014.07.003 ↵
- RegisteredNursing.org. (2021, April 13). What is a charge nurse? https://www.registerednursing.org/specialty/charge-nurse/ ↵
- RegisteredNursing.org. (2021, January 27). Assignment, delegation and supervision: NCLEX-RN. https://www.registerednursing.org/nclex/assignment-delegation-supervision/ ↵
- State of Wisconsin Department of Health Services. (2018). Medication administration by unlicensed assistive personnel (UAP): Guidelines for registered nurses delegating medication administration to unlicensed assistive personnel. https://www.dhs.wisconsin.gov/publications/p01908.pdf ↵
Routine care, activities, and procedures that are within the authorized scope of practice of the RN, LPN/VN, or routine functions of the assistive personnel.
Making adjustments to medication dosage per an established protocol to obtain a desired therapeutic outcome.
Nursing Management and Professional Concepts Copyright © by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Development of a Nursing Assignment Tool Using Workload Acuity Scores
To determine a just and consistent practice for creating nursing assignments.
BACKGROUND:
Traditional methods of assigning patients to nurses may lead to unbalanced nursing workload. This article describes the ongoing, hospital-wide effort to evaluate and implement a nursing assignment tool based on electronic health record (EHR) functionality and auto-calculated nursing workload scores.
EHR records of individual patient workload scores from all hospital units were collected from August 2017 to June 2018. A nurse-specific total workload score was summed for each staff. Then, each hospital unit’s mean nurse workload score and standard deviation, along with the unit’s nurse-to-patient ratio, were used to calculate levels of high, medium, and low nursing workload measurement (NWM).
Mean patient-specific workload scores varied greatly across hospital units. Unit-specific nurse-to-patient ratios were factored into NWM scores to create ranges for assignments that were relatively consistent across the institution.
CONCLUSION:
The use of objective, electronically generated nursing workload scores, combined with traditional nurse-to-patient ratios, provides accurate real-time nurse staffing needs that can inform best practice in staffing. The confirmation of individual patient workload scores and an appreciation for the complexity of EHR vendor rules are necessary for successful implementation. Automation ensures patient safety, staff satisfaction, and optimal resource allocation.
The focus in healthcare has been to increase quality while maintaining costs. Donabedian’s model for improving quality is based on the triad of structure, process, and outcomes and is often used in current patient outcomes and value-based payment models. 1 Newer methodologies include the Quality Health Outcome Model, which uses pathways for associating nursing care and quality. Others focus on the National Database of Nursing Quality Indicators (NDNQI) to review nurse staffing and outcomes. 2 Research has shown that when administrators decrease staff in an effort to lower costs, quality decreases and adverse events increase. 3 , 4 Given that nurse staffing comprises 40% of hospital budgets, it is imperative that optimal nurse assignments continue to meet standards of quality care and improve patient outcomes. 3 , 4 The process of how nursing assignments are distributed in healthcare settings has evolved from uninformed to scientific. 5 Multiple factors, from budgeting and operations to staff satisfaction and patient safety, have driven this evolution. Nursing assignments are often based on room proximity, mandated nurse-to-patient ratio, patient’s medical diagnosis, and continuity of care from shift to shift. In reality, nursing activity will vary throughout a patient’s length of stay based on a combination of prescribed tasks including education, nursing interventions, and psychosocial needs, in addition to medical diagnosis. The NDNQI method for staff assignments uses the hours per patient day (HPPD) as a standard when evaluating staffing. 4 – 6 Managers take into account the average number of staff they have on a given unit and compute the assignment from that information. However, using the traditional methods of creating assignments without objective data may lead to unbalanced nurse workload; in other words, intensity of nursing care varies based on patient-specific needs and abilities. Ideally, assignments should take into account changes in any patient-related tasks, inclusive of psychosocial status, medical status, care transitions, and nursing plans of care. NDNQI has proven to be more accurate than HPPD in determining patient needs as it includes admission, discharge, transfer, and other activities that take up a nurse’s time. 7 Through appropriate documentation of patient-specific activity and utilization of a standard and reliable workload measurement system, nursing assignments become more equitable. 2 To create a process that takes the complexity of nursing care into consideration when making shift assignments, it is 1st necessary to assess the amount of nursing activity required by a single patient and translate into a workload score. 8 – 10
The 2nd step, and focus of the current article, is to sum the patient workload score attributed to each nurse on duty to plan nursing assignments and distribute the total work of the unit safely and equitably. Workload-based staffing technology satisfies an essential function that meets diverse patient needs when determining nursing assignments.
Calculating a workload score takes into account dynamic patient care demands that often change from shift to shift or even hour to hour. Historically, resource allocation and staff assignment did not take the ever-changing patient care requirements into consideration. 5 According to the American Nurses Association (ANA), “Greater benefit can be derived from staffing models that consider the number of nurses and/or the nurse-to-patient ratios and can be adjusted to account for unit and shift level factors.” 11 Using a workload score in combination with an electronic health record (EHR)–based assignment tool offers an opportunity for real-time patient-centered resource allocation. By leveraging existing documentation, the nursing workload measurement (NWM) allows for agility and accuracy in nurse staffing assignments.
It has been well documented that HPPD-based or diagnostic related group–based assignments do not accurately equate to perceived nursing workload. 7 The term workload is interpreted differently among healthcare professionals. Given that, according to Merriam-Webster, 12 the medical definition of workload is keenness of sense perception , it is vital to clarify this in relation to patient care. For this project, the operational definition of workload included the amount of nursing care needed, patient reliance on nursing, staff allocation, and workload measurement. 5 , 13 The term workload-based reflects an aggregate of medical- and nursing-related tasks, as well as other aspects, such as risk factors, admission, transfer, and discharge activities. 14 The intention of a patient-specific workload score generated by EHR documentation is to estimate the intensity of nursing work the patient will require in the upcoming shift. Unless a standard is applied to account for the intensity of nursing activity required for a patient during a shift, the process of distributing nursing assignments becomes biased.
Significance
Aiken et al 15 have led the battle regarding patient safety and the level of staffing needed to maintain this goal. There are currently no federal regulations to establish appropriate guidelines for safe patient care related to nurse staffing. The Safe Staffing for Nurse and Patient Safety Act of 2018 (S. 2446, H.R. 5052) proposes clear directives related to nurse staffing levels for hospitals that receive reimbursement from Medicare. 15 One such requirement is that minimum ratios are identified and adaptable based on “the level and variability of intensity of care required by patient under existing conditions.” 16 In this Act, Congress acknowledged the abundance of evidence supporting the correlation between safe nurse staffing and improved patient outcomes. The fact that this federal legislation has not passed should not negate its importance when addressing safe staffing. States are also actively addressing safe staffing legislation. Regulations are beginning to affect payments based on staffing models, and union contracts are demanding that healthcare organizations adopt workload-driven systems. 11 The proposed federal legislation acknowledged that Connecticut, Illinois, Nevada, Ohio, Oregon, Texas, and Washington have enacted this as recommended. 11 As stated in the Lippincott Blog: “14 states currently addressed nurse staffing in hospitals in law/regulations: CA, CT, IL, MA, MN, NV, NJ, NY, OH, OR, RI, TX, VT, and WA.” 17 California is the only state with unit-specific mandated minimum nurse ratios, whereas other states have developed committees and public disclosure of ratios. Massachusetts has written into law specific nurse-to-patient ratios for the ICU of 1:1 or 1:2. Man-dating a minimum nurse-to-patient ratio by no means restricts the ability of organizations to increase ratios according to need. 16
In this study, we are motivated by the current national discussion to provide insight on how to harness emerging EHR technologies to provide hospital-wide nurse staffing assignments based on real-time patient need. Our aim is to incorporate the ANA position on staffing, namely, that staffing should focus not only on ratio, and there is variation between nurse experience, hospitals, units, and shifts. 11 The current study integrates regularly captured patient workload scores with traditional nurse-to-patient ratios into an automated data nursing assignment tool (NAT).
Materials and Methods
In the fall of 2017, our organization, an approximately 400-bed tertiary care, rural academic medical center, located in New England, implemented an EHR-based workload tool that measures patient-specific nursing workload. The institutional review board granted exempt status to conduct this quality improvement work.
Prior to implementation, decisions were made by the organization to adapt EHR rules to a point value associated with each nursing task. There are 9 components that make up an individual patient score: assessments, medications, lines/drains/airways, risks, wounds, orders, activities of daily living, admission and transfer/discharge. The tool automates an individual patient workload score based on 300 available rules that look retrospectively and prospectively for certain elements within existing documentation as well as orders. The proprietary nature of the tool does not allow the authors to disclose the details of the rules that drive the workload score. The score is updated at the following times: 3:00 AM, 9:00 AM, 3:00 PM, and 9:00 PM. The times are set to allow for “filed status” of scores. It is important to note that the times were not set to allow for late documentation, but for the batch job to run. The next phase, and the focus of this article, was to use this individual patient-level EHR data as the driver to implement a patient-centered objective and automated NAT.
To create an impartial assignment, the average workload scores on each unit were addressed. The authors felt this was important to compare unit scores so we would know if it was appropriate to use a universal assignment score, or whether this should be department specific. Having implemented the nursing workload tool, data were collected from August 2017 to June 2018. EHR-generated data were obtained using a web-based report of all patients and their workload numbers. We compiled the summary score of all patients assigned to one nurse, which is equivalent to the total workload score for that nurse. We examined the mean, SD, and median values to understand the distribution of the data. Nurse workload scores were aggregated at the department level and transformed into 3 categories indicating low, medium, and high workload, based on 1 SD from the mean department score. To set the ranges for these categories, the department level mean ± 1 SD was multiplied by each department-specific nurse-to-patient ratio. In some instances, fractional numbers were used to accommodate for units that have different nurse-to-patient ratios on the night shift. For example, a nurse-to-patient ratio of 3.5:1 was used for a unit with a 3:1 nurse-to-patient ratio on days and 4:1 nurse-to-patient ratio on nights. The result was department-specific NWM categories for nurse assignments that were represented with a color to indicate when the combined patient assignments for each nurse fell within a low, medium, or high range. The upper limit of the high range was determined by adding 200 to the lower limit of the high category. This value is only needed to program the ranges in the EHR, so it is somewhat arbitrary. However, after examining maximum values since August 2017, it is unlikely that this number will be exceeded.
The mean patient workload score varied greatly across departments, ranging from a mean score in pediatrics of 64 to a mean in ICU medical of 196 ( Table 1 ). Aggregated patient scores at the nurse level were summed across all units and compared. This aggregated number represents the NWM for a single nurse assignment having taken into account the unit’s nurse-to-patient ratio. The NWM score falls within the predefined ranges of low, medium, or high. For medium, the optimal NWM range in pediatrics with a nurse-to-patient ratio multiplier of 4 is 144 to 432, whereas in ICU medical, a nurse-to-patient ratio multiplier of 2 defines an optimal range of 272 to 512. As a visual indicator of the ranges, the NAT will be implemented with stoplight colors, with green representing the medium-level, or ideal, range. Yellow will indicate that the assignment is in the low range, indicating that a nurse still has capacity to care for additional patients, and red is in the high range relative to nursing workload. These categories will provide decision support to charge nurses and managers to determine nurse-to-patient ratios and assignments in real time, according to patient-centered needs.
Patient-Level and Nurse Assignment–Level Work Acuity Scores Across Departments in an Academic Hospital
| Individual Patient Scoring Data | Aggregate Patient Scores for Nurse Assignment | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Department | No. of Observations | Mean | SD | Median | Low Threshold (Mean − 1 SD) | High Threshold (Mean + 1 SD) | Unit Standard Nurse-to-Patient Ratio | Nurse-to-Patient Ratio Multiplier | Product of Low Threshold × Nurse-to-Patient Ratio Multiplier | Product of High Threshold × Nurse-to-Patient Ratio Multiplier | Range for Low Assignment (Yellow) | Range for Optimal Assignment (Green) | Range for High Assignment (Red) |
| Oncology | 2798 | 9.1 | 29 | 91 | 64 | 122 | 1:4 day; 1:5 night | 4.5 | 288 | 554 | 0–287 | 288–554 | 555–754 |
| Surgical unit 1 | 1780 | 81 | 30 | 76 | 51 | 110 | 1:4 | 4.0 | 204 | 444 | 0–203 | 204–444 | 445–644 |
| Medical unit | 1179 | 106 | 34 | 98 | 72 | 139 | 1:4 | 4.0 | 288 | 560 | 0–287 | 288–560 | 561–760 |
| ICU medical | 1322 | 196 | 59 | 196 | 136 | 255 | 1:2 | 2.0 | 272 | 512 | 0–271 | 272–512 | 513–712 |
| Surgical unit 2 | 882 | 94 | 32 | 90 | 63 | 126 | 1:4 | 4.0 | 248 | 508 | 0–247 | 248–508 | 509–708 |
| ICU surgical | 372 | 151 | 59 | 138 | 92 | 209 | 1:2 | 2.0 | 184 | 420 | 0–183 | 184–420 | 421–620 |
| Pediatrics | 421 | 64 | 32 | 57 | 33 | 96 | 1:4 day; 1:5 night | 4.5 | 144 | 432 | 0–143 | 144–432 | 433–632 |
All scores from Web Intelligence over 11.5 months (7/17 to 6/18 four times per day).
Nurse-to-patient ratio multiplier is an average in cases when a unit has different ratio standards for day and night shifts.
Strengths and Limitations
Because of the proprietary limitations of the EHR vendor, the direct application of ranges reported in our study cannot be generalized to other institutions. Nonetheless, the process of evaluating department-specific measures to derive appropriate ranges and staffing assignments can be universally adopted. Data were collected from a single academic center, which reduces the generalizability of our study. However, the sample size included 26,985 records and covered a 12-month period across all departments.
The major finding of this article demonstrates that patient workload scores, combined with minimum department-specific nurse-to-patient ratios, provide accurate patient needs to generate fair, hospital-wide staff assignments. As expected, patient workload scores varied by department. What was not expected were the higher scores observed in departments that were traditionally viewed as having lower patient care needs; that is, in the hospice unit, when we looked closer, scores were comparable to the ICU.
Our work demonstrates that a NAT allows the person responsible for making nursing assignments, usually the charge nurse, to quickly assess and adjust a nurse’s workload. The cumulative NWM score is translated into a visual indicator using color and a slide bar. The colors change based on a range of scores customized to each unit. When developing our approach, research into other organizations’ strategy to develop the ranges for the NAT yielded sparse results. It was determined that a descriptive statistical approach would be utilized to define and maintain each unit’s optimal range. Nurse managers were presented with the proposed ranges and educated on the logic behind the process and development of the tool. Work is ongoing to fully implement this assignment tool into everyday practice at the institution to ensure staff assignments are fair and unbiased. Most managers responded positively and are eager to use this tool when available. However, there was some reluctance to using patient workload scores as a basis for a staff assignment tool. The inpatient psychiatric unit staff initially did not feel this tool would be applicable to their care model. The range of scores for this unit was 30 to 90, with an outlier of 205. Data revealed that outliers in the psychiatric unit were dramatically visible and could be directly attributed to increased patient care needs, which we believe reinforced the reliability of the workload scores.
The next phase of developing an improved practice of assigning staff will require that staff schedules are batch uploaded to the EHR and into the NAT. The availability of the daily nurse schedule is a vital component for successful implementation; however, it was outside the scope of the current project. Once implemented, the staff responsible for assigning patients will drag and drop a patient’s name to the assigned nurse. A bar under the staff nurse’s name will fill with the color to indicate the current status of his/her assigned workload. The patient’s workload score will be automatically updated 4 times per day to adjust to real-time documentation and upcoming orders. As the score is dependent on nursing documentation, complete and real-time documentation of patient care will produce the most reliable score ( Figure 1 ).

Nursing assignment tool workflow.
There will be ongoing monitoring of this tool to ensure usability following implementation. Some nurse managers expressed concern with the stoplight color scheme and have suggested that a gradation of a single color may be more useful. The middle range is the optimal assignment. An assignment classified as red may be construed as precarious or undesirable. Color scheme changes will be considered pending feedback after implementation. Continued review of the ranges will also be necessary as documentation standards change or updates to the EHR are made that may lead to breakage of rules used to calculate scores.
Patient safety issues are rightly at the center of concern regarding ineffective staffing models. Studies have drawn a direct line between nursing workload and staffing ratios and avoidable deaths. 6 , 10 , 16 Patient safety is only one of the concerns that can be addressed by utilizing a NAT for staffing decisions. Other areas of concern that may be addressed include staff retention, burnout, and work satisfaction. 8 Identifying and remediating workload disparities will allow managers to allocate staffing resources appropriately, including using flexible staff when needed. 13 “Fixed staffing numbers or ratios only identify minimum staffing levels and do not adjust for the ever-changing nature of patient care needs.” 3
The national conversation continues to reflect positively on agile nursing assignment processes that flex with patient needs. 9 , 18 , 19 However, there are logistic and cultural barriers to implementation. Another challenge to the adoption of this technology may be the geography related to specific patient locations in the hospital unit. Adjusting nursing assignments based strictly on nursing workload may fail to take location of patients into consideration. Some departments currently base assignment on room location, as there are physical barriers in the unit design. Changing the status quo of the process to assign patients to nurses may be challenging in some units. One unit manager reported that they assign nurses up to 24 hours in advance, making the every 6-hour update to the nurse workload score less valuable and less sensitive to acuity and condition changes, as well as nurse competence. Clearly, each institution will require adjustments that can be easily managed from the back end of this flexible product. Engagement with operational leaders is a vital component of implementation. Such systems that leverage EHR technology have the potential to impact excellence in nursing practice.
Future versions of this tool will allow a charge nurse to quickly match patients to nurses based on continuity of care, expertise, and location. Coordinating care at this level of granularity will help ensure the patient is paired with the right nurse for the current phase of care to achieve patient safety, staff satisfaction, and optimal resource allocation. The use of objective, data-driven, electronically generated NWM scores based on actual patient workload, combined with nurse-to-patient ratios, provides accurate real-time nurse staffing needs that can lead to best practice in staffing. The validation of workload scores and an appreciation for the complexity of vendor rules are necessary for successful implementation.
Acknowledgments
The authors acknowledge Geoffrey Tarbox, MBA, RN, for his work on the Excel spreadsheets; and Petrice DiDominic, MSN, RNC-OB, for her help with the Workload Acuity Tool.
R.T.E. was supported by award number UL1TR001086 from the National Center for Advancing Translational Sciences of the National Institutes of Health.
The authors declare no conflicts of interest.

- Walden University
- Faculty Portal
Common Assignments: Writing in Nursing
Although there may be some differences in writing expectations between disciplines, all writers of scholarly work are required to follow basic writing standards such as writing clear, concise, and grammatically correct sentences; using proper punctuation; demonstrating critical thought; and, in all Walden programs, using APA style. When writing in nursing, however, students must also be familiar with the goals of the discipline and discipline-specific writing expectations.
Nurses are primarily concerned about providing quality care to patients and their families, and this demands both technical knowledge and the appropriate expression of ideas (“Writing in nursing,” n.d). As a result, nursing students are expected to learn how to present information succinctly, and even though they may often use technical medical terminology (“Writing in nursing,” n.d.), their work should be accessible to anyone who may read it. Among many goals, writers within this discipline are required to:
- Document knowledge/research
- Demonstrate critical thinking
- Express creative ideas
- Explore nursing literature
- Demonstrate understanding of learning activities. (Wagner, n.d., para. 2)
Given this broad set of objectives, nursing students would benefit from learning how to write diverse literature, including scholarly reports, reviews, articles, and so on. They should aim to write work that can be used in both the research and clinical aspects of the discipline. Walden instructors often ask nursing students to write position and reflective papers, critique articles, gather and analyze data, respond to case studies, and work collaboratively on a project. Although there may be differences between the writing expectations within the classroom and those in the workplace, the standards noted below, though more common in scholarly writing, require skills that are transferrable to the work setting.
Because one cannot say everything there is to say about a particular subject, writers present their work from a particular perspective. For instance, one might choose to examine the shortage of nurses from a public policy perspective. One’s particular contribution, position, argument, or viewpoint is commonly referred to as the thesis and, according to Gerring et al. (2004), a good thesis is one that is “new, true, and significant” (p. 2). To strengthen a thesis, one might consider presenting an argument that goes against what is currently accepted within the field while carefully addressing counterarguments and adequately explaining why the issue under consideration matters (Gerring et al., 2004). The thesis is particularly important because readers want to know whether the writer has something new or worthwhile to say about the topic. Thus, as you review the literature, before writing, it is important to find gaps and creative linkages between viewpoints with the goal of contributing innovative ideas to an ongoing discussion. For a contribution to be worthwhile you must read the literature carefully and without bias; doing this will enable you to identify some of the subtle differences in the viewpoints presented by different authors and help you to better identify the gaps in the literature. Because the thesis is essentially the heart of your discussion, it is important that it is argued objectively and persuasively.
With the goal of providing high quality care, the healthcare industry places a premium on rigorous research as the foundation for evidence-based practices. Thus, students are expected to keep up with the most current research in their field and support the assertions they make in their work with evidence from the literature. Nursing students also must learn how to evaluate evidence in nursing literature and identify the studies that answer specific clinical questions (Oermann & Hays, 2011). Writers are also expected to critically analyze and evaluate studies and assess whether findings can be used in clinical practice (Beyea & Slattery, 2006). (Some useful and credible sources include journal articles, other peer-reviewed sources, and authoritative sources that might be found on the web. If you need help finding credible sources contact a librarian.)
Like other APA style papers, research papers in nursing should follow the following format: title, abstract, introduction, literature review, method, results, discussion, references, and appendices (see APA 7, Sections 2.16-2.25). Note that the presentation follows a certain logic: In the introduction one presents the issue under consideration; in the literature review, one presents what is already known about the topic (thus providing a context for the discussion), identifies gaps, and presents one’s approach; in the methods section, one would then identify the method used to gather data; and in the results and discussion sections, one then presents and explains the results in an objective manner, noting the limitations of the study (Dartmouth Writing Program, 2005). Note that not all papers need to be written in this manner; for guidance on the formatting of a basic course paper, see the appropriate template on our website.
In their research, nursing researchers use quantitative, qualitative, or mixed methods. In quantitative studies, researchers rely primarily on quantifiable data; in qualitative studies, they use data from interviews or other types of narrative analyses; and in mixed methods studies, they use both qualitative and quantitative approaches. A researcher should be able to pose a researchable question and identify an appropriate research method. Whatever method the researcher chooses, the research must be carried out in an objective and scientific manner, free from bias. Keep in mind that your method will have an impact on the credibility of your work, so it is important that your methods are rigorous. Walden offers a series of research methods courses to help students become familiar with the various research methods.
Instructors expect students to master the content of the discipline and use discipline- appropriate language in their writing. In practice, nurses may be required to become familiar with standardized nursing language as it has been found to lead to the following:
- better communication among nurses and other health care providers,
- increased visibility of nursing interventions,
- improved patient care,
- enhanced data collection to evaluate nursing care outcomes,
- greater adherence to standards of care, and
- facilitated assessment of nursing competency. (Rutherford, 2008)
Like successful writers in other disciplines and in preparation for diverse roles within their fields, in their writing nursing students should demonstrate that they (a) have cultivated the thinking skills that are useful in their discipline, (b) are able to communicate professionally, and (c) can incorporate the language of the field in their work appropriately (Colorado State University, 2011).
If you have content-specific questions, be sure to ask your instructor. The Writing Center is available to help you present your ideas as effectively as possible.
Beyea, S. C., & Slattery, M. J. (2006). Evidence-based practice in nursing: A guide to successful implementation . http://www.hcmarketplace.com/supplemental/3737_browse.pdf
Colorado State University. (2011). Why assign WID tasks? http://wac.colostate.edu/intro/com6a1.cfm
Dartmouth Writing Program. (2005). Writing in the social sciences . http://www.dartmouth.edu/~writing/materials/student/soc_sciences/write.shtml
Rutherford, M. (2008). Standardized nursing language: What does it mean for nursing practice? [Abstract]. Online Journal of Issues in Nursing , 13 (1). http://ojin.nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/Health-IT/StandardizedNursingLanguage.html
Wagner, D. (n.d.). Why writing matters in nursing . https://www.svsu.edu/nursing/programs/bsn/programrequirements/whywritingmatters/
Writing in nursing: Examples. (n.d.). http://www.technorhetoric.net/7.2/sectionone/inman/examples.html
Didn't find what you need? Email us at [email protected] .
- Previous Page: Collaborative Writing in Business & Management
- Next Page: Learning Agreements (LAs)
- Office of Student Disability Services
Walden Resources
Departments.
- Academic Residencies
- Academic Skills
- Career Planning and Development
- Customer Care Team
- Field Experience
- Military Services
- Student Success Advising
- Writing Skills
Centers and Offices
- Center for Social Change
- Office of Academic Support and Instructional Services
- Office of Degree Acceleration
- Office of Research and Doctoral Services
- Office of Student Affairs
Student Resources
- Doctoral Writing Assessment
- Form & Style Review
- Quick Answers
- ScholarWorks
- SKIL Courses and Workshops
- Walden Bookstore
- Walden Catalog & Student Handbook
- Student Safety/Title IX
- Legal & Consumer Information
- Website Terms and Conditions
- Cookie Policy
- Accessibility
- Accreditation
- State Authorization
- Net Price Calculator
- Contact Walden
Walden University is a member of Adtalem Global Education, Inc. www.adtalem.com Walden University is certified to operate by SCHEV © 2024 Walden University LLC. All rights reserved.

Nursing School Assignments and Tips to Ace All of Them

If you are about to start nursing school or considering enrolling in a nursing program, you would want to know what to expect. You will write many papers in nursing school and do many other assignments. This is true whether you pursue ADN, BSN, MSN, DNP, or PhD in Nursing.
Before we delve into the types of assignments and papers to expect in nursing school, let us begin by dispelling the myth that nursing school is hell; it is NOT. Instead, it is a beautiful and exciting journey into a noble profession. It entails a commitment to life-long continuous learning for you to grow.
Nursing school writing assignments are an excellent way for students to understand concepts taught in the classroom. You might wonder what kinds of assignments nursing students do. These assignments come in various forms and help students build critical thinking, creativity, research, clinical reasoning, and problem-solving skills that are critical in clinical settings.
This blog post looks at the diverse assignments you should expect or will cover in nursing school, including some tips to help you ace them and get better grades.
Common Nursing School Writing Assignments
Classwork forms the core of most nursing programs. You must have high-quality assignment submissions to attain better grades in nursing school. As soon as you decide to become a nursing student, you sign up for a marathon of writing different types of papers.
Whether you love or hate it, you will write papers before graduating from nursing school; that is the norm. Although not so many, you will encounter a few homework and assignments where you must submit a well-researched, formatted, and organized nursing paper.
The typical nursing school assignments include essays, research papers, term papers, and case studies. Others are article critiques/reviews, critical appraisal, evidence synthesis tables (synthesis matrix), PowerPoint Presentations, posters, discussion posts/ responses, and policy analysis papers. Other advanced papers include nursing care plans, SBAR template papers, evidence-based papers, capstone projects, theses, dissertations, proposals, etc.
These assignments are submitted either individually or as a group. Let us expound on this so you have a clear picture.
Essays for nursing classes come in various forms, including admission essays , scholarship essays, descriptive essays, persuasive essays, speech essays, expository essays, and narrative essays.
Notably, nursing essays focus on a single perspective, argument, or idea, which constantly forms the thesis of the paper.
Nursing essays focus on various topics relating to nursing practice and the broader healthcare field. You can write an essay examining a nursing theory or non-nursing theory or discuss a nursing issue .
Some essays, such as reflective nursing essays, use reflective models to reflect, analyze, and understand personal and professional encounters during clinical practice.
Each nursing essay should demonstrate your understanding of the topic, critical analysis, and organization skills. Besides, you should use evidence from peer-reviewed scholarly sources to support your arguments and ideas.
Discussion Board Posts
If you pursue a hybrid or exclusively online nursing program, you will be assigned to write weekly discussion forum posts and responses. Discussion board posts are short essay-like assignments posted in a threaded format so students can discuss nursing and healthcare topics.
You will write an original discussion post, between 200 and 300 words long, and post it on the forum. You are also expected to write a peer-response post in response to or to comment on an original post done by your peers.
Discussion boards help nursing students advance theoretical concepts, learn from one another, share ideas, and get feedback that can help them advance their knowledge in clinical reasoning and practice.
Research Papers
Nursing practice is evidence-driven, translating evidence into practice to ensure quality, accessible, and affordable healthcare. As such, nursing research takes precedence during studies and when practicing.
Nursing professors assign nursing students to write research papers on various evidence-based practice topics. The students must prove their worth by researching, analyzing, and organizing facts.
Related Writing Guides:
- How to write a nursing school research paper.
- Systematic Reviews vs Literature Review
Research papers help student nurses to review literature, conduct research, implement solutions, and draw evidence-based conclusions.
Research papers are critical in developing research and writing skills, maintaining good communication, and fostering creativity and clinical reasoning.
Potential nursing research paper topics can be quality improvement, healthcare/nursing informatics , healthcare policies, practice privileges, nursing ethics, ethical dilemmas , pathophysiology, and epidemiology .
Term Papers
In nursing school, a term paper is a type of assignment completed and submitted toward the end of the semester.
Usually, a professor can assign you a specific term paper topic, or they can let you choose a topic and consult with them for approval.
Term papers can be done individually or as a group project. A term paper has an impact on your final grade.
You should use credible scholarly sources published within the last five years for recent information.
Besides, also ensure that you plan your time well, do everything as per the instructions, and submit the nursing term paper before the deadline.
A term paper can also be a nursing process change report that is expected to address an area that needs change.
Case Studies
Nursing school case study assignments are an essential learning tool.
Most professors assign hypothetical clinical case studies or case scenarios (snippets) to test your clinical reasoning skills.
As a nursing educational tool, nursing case studies help you to develop practical, theoretical knowledge by simulating real-world experiences.
When analyzing a case study, you must use concepts and knowledge from class and class text to assess a patient, plan and implement care, and evaluate the outcomes.
Sometimes, you encounter simulated or digital clinical experience case studies such as iHuman and Shadow Health .
You should be very keen when analyzing a case study and when writing the analysis report.
Case studies help you get beyond books and use your creativity, clinical reasoning, problem-solving, and analytical skills to apply theoretical knowledge to real-world problems.
Your professor can give you a case study of a patient presenting with a given condition and expect you to take them through the care planning process, including admission and discharge, as you would in a real healthcare setting.
Other times, you can be asked to develop a hypothetical case study of a patient presenting with a chronic disease or a disorder and then use the case study guidelines, including head-to-toe assessment , diagnosis , nursing care planning , and discharge planning.
Related Guides:
- How to write a great nursing case study.
- How to complete a case conceptualization report (for psychiatric nursing students)
Nursing Care Plans and SOAP Notes
A nursing care plan can be part of a case study or a stand-alone assignment. Nursing care plans are essential in nursing education as they help students develop effective nursing care planning. Formulating a nursing care plan for a patient scenario or case helps treat them as you define the guidelines and roles of nurses in caring for the patient.
You also develop solid action plans for focused and patient-centred care by documenting the patient's needs. When they are part of an assignment, you can tabulate the nursing care plan using columns so that you explore every aspect independently.
Remember to use evidence from peer-reviewed scholarly sources when giving rationale.
The SOAP notes are a clinical tool healthcare professionals use to organize patient information to minimize confusion and assess, diagnose, and treat patients. Check our comprehensive guide on developing good SOAP Notes in nursing school .
Concept Maps
Another common nursing school assignment is concept maps. Concept mapping helps you visually organize, compartmentalize, and categorize information about nursing care planning, medical diagnosis, pathophysiology, SBAR, nursing responsibilities, etc.
A nursing concept map assignment equips you with strong critical thinking, analytical, and problem-solving skills. You also hone your clinical reasoning skills in the process.
Whether it is part of an assignment or a stand-alone, learn how to write great concept maps to score the best grades.
Concept Analysis Papers
If you are taking BSN, MSN, or DNP, you will likely be assigned to write a concept analysis paper. Make sure to distinguish this from a concept paper that is a proposal. A concept analysis paper examines the structure and function of a nursing concept.
The process entails a review of the literature and creativity in coming up with borderline, related, contrast, inverted, and illegitimate cases.
You also explore the antecedents and consequences of the concept before finalizing with empirical referents.
If you need to learn about the structure of a good concept analysis paper, check out our nursing concept analysis guide . We have listed concepts you can analyze depending on your speciality, instructions, and passion.
Capstone Projects
At an advanced stage in nursing school, students are expected to submit longer research papers; capstone project papers. A nursing capstone project is a final project that allows students to demonstrate the skills, knowledge, and concepts gained throughout the nursing program.
In nursing education, the capstone project typically covers an evidence-based practice issue or problem. You can write a nursing change paper, look into a clinical process, problem, or issue, and then develop recommendations based on a study.
Most of the MSN and DNP capstone projects focus on clinical change or quality improvement. You will be expected to develop a PICOT question and formulate a research study to examine the issue, implement a change process using evidence-based models, and make recommendations.
Nursing capstone projects are individual research projects based on nursing topics either of your professional or personal interest. You have to demonstrate competency and commitment to improve health outcomes.
Apart from capstone projects, you will also write a nursing thesis and dissertation papers, which depend on the program requirements and your professor's preferences.
Check out these specific writing guides for advanced papers:
- How to write a nursing dissertation or thesis
- Tips for choosing the best nursing dissertation topic
- How to write an excellent capstone project paper
- List of capstone project topics for nursing school
- How to formulate a PICOT question
- PICOT question examples to inspire nursing students
Group Assignments
In nursing school and practice, collaboration and teamwork are highly recommended. You will encounter collaborative group assignments such as presentations (PowerPoint slides, Prezi, or other platforms), simulation assignments, writing nursing reports, and group research projects.
Group projects allow you to research, learn, and organize ideas together so that you can understand concepts better. It is essential to avoid social loafing in a group to gain more. Besides, plan your time well and avoid excuses.
You can also be assigned to work on simulation exercises as a group of nursing students. The aim of such exercises is to build a collaborative, teamwork, and decision-making spirit among the team.
When in such groups, expect to work with your peers to assess the hypothetical patient, communicate with your peers, formulate a care plan, and manage any arising issues as you would in clinical settings. Do not take such activities for granted; they contribute significantly to your grade.
Presentations
Your professor can assign you to design a PowerPoint Slide accompanied by speaker notes and send it for grading or present it online or in class. Under presentations, you will also be requested to design flyers, posters, and other visual documents to disseminate information.
It could be about a disease, health promotion, or nursing research. You must also make PowerPoint slides when presenting a thesis, dissertation, or capstone for assessments. Remember, this is the chance to bring out your creativity.
Expect other assignments such as dosage calculations, HESI test exams, skills checkoffs, electronic medical record documentation, nursing student portfolio, online quizzes, drug write-ups, process recordings, group drug presentations, etc.
In most cases, you will be given a template to use wisely and make it as appealing as possible.
Tips to Help You Ace Nursing Assignments
A lot goes into getting the best grades in nursing school. One of the main determinants of your nursing school grades is the assignments, which you are required to do and complete within set deadlines.
Even though many nursing students perform better on clinical, that needs to reflect in written assignments. Most students fear research and writing or do not take writing assignments seriously. Regardless of the assignment, here are some practical and effective tips to help you ace your nursing school writing assignments and surprise everyone, including yourself.
1. Plan your Time
The number one challenge for nursing students that inhibits them from completing assignments is the need for more time management.
Most students are juggling studies and work to make ends meet. It worsens when you have a massive workload from more than one class and a family to look after.
The simple trick to beat this is to manage your time well. You can schedule your assignments for periods when you are free and when you can concentrate and cover more. Assignments have deadlines ranging from hours to days or a few weeks.
To succeed, keep track of your assignments and other academic activities, such as mid-term and final examinations, so that you can plan your study periods. You can use online time management tools and apps to allocate your nursing school homework time.
With proper planning, you should be reassured about the last-minute rush to complete your assignment, which is responsible for the colossal failure we are experiencing in nursing schools.
2. Follow the Course Guidelines to the T
Guidelines, prompts, and reading materials accompany each writing assignment and homework. Sometimes a professor can be generous enough also to give you access to the Rubric, which breaks down how they will assess assignments. Ensure you read everything and note what is required before working on any paper.
Pay attention to these, read, and familiarize yourself with the course guidelines. Understand the formatting requirements preferred by your school, such as Vancouver, APA, or Harvard. Most nursing schools will specify this in the course documents. Also, check the databases and journal articles you can use when writing your nursing assignments.
Preparing in advance by reading the course materials to identify the recommended study materials. You will have a deeper understanding, knowledge, and skills to handle every nursing assignment correctly.
3. Have an Active Study Buddy
A nursing study buddy can be one of your classmates whom you study with. Study buddies offer mutual support, which comes in handy when completing assignments.
Select a bright and committed person with something to offer so you are not only giving. Set the study hours and have accountability follow-ups to ensure you cover much of the syllabus and concepts in time.
A study buddy can help you understand nursing concepts, theories, models, and frameworks. They can also help you review your written papers and give valuable feedback when editing and proofreading your nursing papers.
A knowledgeable, accountable, committed study partner can help you revamp your grades by submitting high-quality assignments.
4. Join a Study Group
A study group is a tried and tested means of completing nursing assignments. Apart from building your teamwork and collaborative skills, you can brainstorm ideas, critique one another, and learn more about the class assignments. With diversity in thoughts, you can get valuable insights and inputs for personal-level work.
Besides, you are also guaranteed to ace the nursing group assignments with ease. When doing group work, try to rotate into new groups so that you can appreciate the diversity of thoughts and reasoning. You can also identify individuals from your groups, those that are active, as your study buddies.
When you have accountability partners within the group, you commit to given tasks and make necessary follow-ups. If you are a part-time student, consider having students whose free time is similar to yours to benefit everyone.
5. Get Writing Assignment Help
As with other subjects in college and university, nursing students face challenges such as time management, complexity of assignments, too many assignments, and writer's block. When you feel overwhelmed with completing your nursing class assignments, you can always pay someone to handle the class for you or at least do your coursework or assignments.
One sure way to get assistance without drawing too much attention is by trusting assignment help websites like NurseMyGrade.com with your papers. Many students do not have time to complete assignments or find them challenging. Consequently, many hire nursing assignment helpers from nursing paper writing platforms.
If you feel like hiring the right professionals, use NurseMyGrade. We offer customized writing solutions to nursing students at different academic levels. Our nursing experts can complete short and lengthy assignments. You will have a well-researched and formatted paper written in Vancouver, APA, MLA, ASA, AMA, Harvard, or any citation style you choose.
You can use the tips and insights above to master nursing school assignments. We wish you all the best as you strive towards excellence. Don't worry about the many assignments. Instead, be grateful that they will equip you with knowledge, skills, and experience to make you the best nurse.
How Many Papers to Write in Nursing School
We have so far covered the general aspects of the types of assignments to expect in nursing school. Under the assignments, you may ask yourself if you must write many papers in nursing school.
While the answer depends on your professor, institutional curriculum requirements, and nursing level, you will undoubtedly write a couple of academic papers before graduating from nursing school. You will write research papers, essays, proposals, white papers, policy analysis papers, capstone project papers, case studies, scholarship essays, personal statements, quality improvement reports, etc.
Suppose you are pursuing a Licensed Practical Nurse (LPN) program. In that case, you will likely write between 13 and 15 papers during the LPN program, including short and long essays, reflective journals, essays, patient-based case studies, and others as your professor pleases.
If you are in a 2-year ADN program, expect to complete about 20 to 30 papers, including care plans, SBAR reports, essays, case studies analyses, research papers, reports, and other assignments.
For a 4-year Bachelor of Science in Nursing (BSN) program, you will write between 35 and 50 papers. If you are taking the online class program options, like the WGU BSN program, you might write more papers because they form the basis for your assessment.
BSN-level papers are demanding because you must strictly adhere to the formatting styles and be critical and organized in your presentation.
If you are taking a Master of Science in Nursing (MSN) program, an advanced-level study for registered nurses (RNs), you will do about 20-50 papers, given that it offers the foundation for nursing research. Again, at an advanced level, the MSN writing assignments are complex.
You need to plan well, research widely, and analyze facts thoroughly before drawing conclusions. During this level, expect to write papers such as MSN essays, discussion posts and responses, specialized case studies, research papers, clinical reports, advanced SOAP notes, nursing care plans, policy papers, position papers (white papers), dissertations, theses, capstone papers, project papers, and change project papers.
You are expected to show exquisite research skills for the Doctor of Nursing Practice (DNP) program, considered the highest level or terminal degree in nursing practice. At this level, you have specialized, advanced your knowledge, and have adequate experience.
Mostly, DNP papers are a little longer. You will write between 20-30 papers; depending on your nursing school curriculum and supervisor's preference, it could be less or more.
If you opt for the research route, you will write many research papers, technical papers, policy analysis papers, white papers, reflection papers, nursing dissertations, PICOT-based change project papers (DNP change project papers), and other assignments.
Finally, for the Doctor of Philosophy (PhD) in nursing programs, you should expect to write between 10 and 15 papers covering research-oriented topics.
Attaining this degree makes you the epitome of success in the field. You can advance into a nursing researcher, educator, leader, or manager.
We have writers that can help you handle all these types of papers regardless of the academic level. Our Online Nursing Writing pros are available for hire anytime and any day.
Having worked successfully with many nursing clients/students, we are confident to help you achieve your dreams.
Before you go …
There are many assignments and papers to complete in nursing school, including written assignments, quizzes, exams (oral and written), reflective journals, journal entries, e-Portfolio, integrative reviews, teaching plans, presentations, etc. Whether taking an LPN program or advancing your career by pursuing a Ph.D. in Nursing, you will do many nursing school assignments.
Do not take assignments as a punishment. Instead, consider them as tools to equip and shape you into a desirable nurse practitioner.
If you feel overwhelmed, stressed, and anxious about completing the assignments, you can hire our nursing writers to help you. We can help you ace nursing assignments online and ensure that you get 100% well-researched, organized, and proofread papers.
Our papers are 100% original and non-plagiarized. The writers understand how to structure nursing papers, formulate great paragraphs using the MEAN, PEEL, or TEEL formats, and write desirable papers consistently, scoring the best grades. You can call us your nursing assignment slayers or acers because, in a few hours, we will help you get it all behind you. We can help you ace online nursing classes and tests/quizzes .
Click on the Order button and fill out the form to get our writers started in making you a nursing paper that gives the best grade. No topic is challenging for us, and we allow you direct communication with the writer in the process of getting help.
Struggling with
Related Articles

How to Write a Policy Analysis Paper : A Nursing/Med Student Guide

Drug Calculations: Using Math Skills for Patient Care

Writing a Nursing Research Paper that Meets Professor's Requirements
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Delegating vs. assigning: What you need to know
Registered nurses (RNs) often delegate to other RNs, licensed practical nurses/vocational nurses (LPN/LVNs), and assistive personnel (AP). (In some states or jurisdictions, LPN/LVNs may be allowed to delegate, so “licensed nurses” will be used in this article.) Delegating appropriately protects patients and reduces the risk of legal liability, yet the parameters of delegation often are not fully understood.
One common area of misunderstanding is delegation vs. assignment. Knowing the differences between the two is essential to ensure you delegate appropriately. The primary difference relates to scope of practice and where the clinician learned the activities to be carried out.
According to national guidelines for nursing delegation from the National Council of State Boards of Nursing (NCSBN) and American Nurses Association (ANA), an assignment refers to the “routine care, activities, and procedures that are within the authorized scope of practice of the RN or LPN/VN or part of the routine functions of the AP.” This definition covers fundamental skills that the assignee would have learned in a basic education program. A licensed nurse is still responsible for ensuring the assignment is carried out correctly.
According to the NCSBN/ANA guideline, delegation applies when the delegatee is performing a “specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed.” As opposed to work that is part of an assignment, the work associated with delegation was not learned in a basic education program. Therefore, the delegatee must have obtained additional education and have verified competence in the delegated area for which they will be responsible. The licensed nurse maintains overall accountability for the patient, but the delegatee is responsible for the delegated activity, skill, or procedure.
Licensed nurses can’t delegate activities that involve clinical reasoning, nursing judgment, or critical decision making, and the delegated responsibility has to be within the delegator’s scope of practice under the state’s or jurisdiction’s nurse practice act (NPA).
Responsibilities
Organizational administrators, the delegator, and the delegatee each have responsibilities when an activity, skill, or procedure is delegated.
Professionals who work at the administrative or managerial level of the organization set the cultural tone for the nursing work environment and are responsible for managing the delegation processes. Those at the administrative level within an organization define what nursing responsibilities may be delegated, to whom, and under what set(s) of circumstances. They are also responsible for developing and maintaining policies and procedures associated with delegation, periodically evaluating the efficacy and safety of delegation processes, and training and educating staff.
The delegator is responsible for determining the needs of the patient, when delegation is appropriate, and if the delegatee is competent to complete the delegated task. Delegators must follow delegation guidelines in the NPA and relevant organizational policies and procedures. Clear communication is key, and the delegator must be available as a resource to the delegatee. Delegators also need to evaluate outcomes as they maintain overall accountability for the patient. Delegators must be prepared to step in at any point if it appears the delegatee is not handling the assignment appropriately. Any problems should be reported to nursing leadership.
The delegatee is responsible for only accepting activities that fall within their competence and that they feel comfortable completing safely. Delegatees must communicate with the delegator, particularly if the patient’s condition changes, and complete the activity correctly, including fulfilling any documentation requirements. Delegatees maintain accountability for the delegated activity and need to notify the delegator immediately if they have difficulty completing the task.
One special case
NCSBN notes that in some cases, APs are taught how to perform skills that were previously thought to be exclusively RN and LPN/LVN responsibilities, such as certified medical assistants administering injections. In these cases, it’s best to consider such tasks as being delegated and, therefore, validate competency.
Keeping patients safe
Knowing the differences between assigning and delegating helps protect patients and avoid legal action should an error occur. Assignments involve routine tasks learned in basic education and that fall under designated scope of practice, while delegation involves tasks that were learned through additional education and for which competency has been determined.
Good communication and an understanding of the responsibilities of delegators and delegatees is essential to avoid misunderstanding. Remember, the licensed nurse remains accountable for the patient, but the delegatee is responsible for the delegated task.
Five rights of delegation
The ncsbn outlines five rights of delegation. in the case of a lawsuit, a key component would be whether you adhered to these rights:.
- Right task . The task needs to fall within the delegatee’s job description or is part of organizational policies and procedures.
- Right circumstance . The patient must be stable.
- Right person . The delegatee must have the appropriate skills and knowledge to perform the task.
- Right directions and communication . Clear directions need to be given, with the delegator verifying understanding by the delegatee. Communication must be two-way, with the delegatee asking questions as needed.
- Right supervision and evaluation . The delegator needs to monitor the delegated activity, including evaluating patient outcomes.
Article by: Cynthia Saver, MS, RN, President of CLS Development, Inc., in Columbia, Md and Georgia Reiner, MS, CPHRM, Risk Analyst, NSO
National Council of State Boards of Nursing. National guidelines for nursing delegation. J Nurs Reg. 2016;7(1):5-12.
NCSBN, ANA. National guidelines for nursing delegation. 2019.
#Delegating #RN
Share this article:
Frequently Asked Questions
You have questions. We have answers. (It's why we're here.)
What kinds of activities might trigger a disciplinary action by a licensing board or regulatory agency?
The fact is anyone can file a complaint against you with the state board for any reason—even your own employer—and it doesn’t have to be solely connected to your professional duties. All complaints need to be taken seriously, no matter how trivial or unfounded they may appear.
How does a shared limit policy work?
The business, and all eligible employees and sub-contractors you regularly employ, will be considered when determining your practice’s premium calculation and share the same coverage limits you select for the business.
We have a shared limit policy. Are employees covered if they practice outside our office?
If your employees are moonlighting, either for pay or as a volunteer, they should carry an individual professional liability insurance policy to cover those services. Otherwise, they might not be covered for claims that arise out of these activities.
There are plenty more where those came from.
See more FAQs
More learning right here
Check out these related articles.
Nurse Case Study: Failure to monitor and inadequate documentation in home health setting
RN working in home health setting fails to monitor and properly document ulcer wounds in post-surgical Alzheimer’s patient.
Nurse Case Study: Failure to monitor high fall risk ICU patient; failure to educate family on fall prevention
This medical malpractice case study, presented by NSO and CNA, involves a registered nurse working in a critical care setting.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
A practical guide to making patient assignments in acute care
Affiliation.
- 1 Definitive Observation Unit, Kaiser Permanente San Diego Medical Center, CA, USA. [email protected]
- PMID: 23232175
- DOI: 10.1097/NNA.0b013e3182785fff
Charge nurses have integral roles in healthcare organizations. Making patient assignments is an important charge nurse role that lacks theoretical support and practical guidelines. Based on a concept analysis of the charge nurse role, the author looks at a theory-gap analysis regarding how patient assignments are made and proposes a framework to guide the process of patient assignments.
PubMed Disclaimer
Similar articles
- The Nurse-Patient Assignment: Purposes and Decision Factors. Allen SB. Allen SB. J Nurs Adm. 2015 Dec;45(12):628-35. doi: 10.1097/NNA.0000000000000276. J Nurs Adm. 2015. PMID: 26565641
- Comparison of nurse workload approaches. Beswick S, Hill PD, Anderson MA. Beswick S, et al. J Nurs Manag. 2010 Jul;18(5):592-8. doi: 10.1111/j.1365-2834.2010.01124.x. J Nurs Manag. 2010. PMID: 20636508
- Building a nursing productivity measure based on the synergy model: first steps. Kohr LM, Hickey PA, Curley MA. Kohr LM, et al. Am J Crit Care. 2012 Nov;21(6):420-30; quiz 431. doi: 10.4037/ajcc2012859. Am J Crit Care. 2012. PMID: 23117905
- Nurse staffing and patient, nurse, and financial outcomes. Unruh L. Unruh L. Am J Nurs. 2008 Jan;108(1):62-71; quiz 72. doi: 10.1097/01.NAJ.0000305132.33841.92. Am J Nurs. 2008. PMID: 18156863 Review.
- Nurse staffing. [No authors listed] [No authors listed] Prairie Rose. 2005 Nov-2006 Jan;74(4):18-9. Prairie Rose. 2005. PMID: 16594185 Review. No abstract available.
- Clinical decision support system for clinical nurses' decision-making on nurse-to-patient assignment: a scoping review protocol. Kwon H, Lee D. Kwon H, et al. BMJ Open. 2024 Jan 31;14(1):e080208. doi: 10.1136/bmjopen-2023-080208. BMJ Open. 2024. PMID: 38296282 Free PMC article.
- Search in MeSH
Related information
- Cited in Books

LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Wolters Kluwer
Other Literature Sources
- scite Smart Citations
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Nursing Care Plans (NCP) Ultimate Guide and List
Writing the best nursing care plan requires a step-by-step approach to complete the parts needed for a care plan correctly. This tutorial will walk you through developing a care plan. This guide has the ultimate database and list of nursing care plans (NCP) and nursing diagnosis samples for our student nurses and professional nurses to use—all for free! Care plan components, examples, objectives, and purposes are included with a detailed guide on writing an excellent nursing care plan or a template for your unit.
Table of Contents
Standardized care plans, individualized care plans, purposes of a nursing care plan, three-column format, four-column format, student care plans, step 1: data collection or assessment, step 2: data analysis and organization, step 3: formulating your nursing diagnoses, step 4: setting priorities, short-term and long-term goals, components of goals and desired outcomes, types of nursing interventions, step 7: providing rationale, step 8: evaluation, step 9: putting it on paper, basic nursing and general care plans, surgery and perioperative care plans, cardiac care plans, endocrine and metabolic care plans, gastrointestinal, hematologic and lymphatic, infectious diseases, integumentary, maternal and newborn care plans, mental health and psychiatric, musculoskeletal, neurological, pediatric nursing care plans, reproductive, respiratory, recommended resources, references and sources, what is a nursing care plan.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes a client’s potential needs or risks. Care plans provide a way of communication among nurses, their patients, and other healthcare providers to achieve healthcare outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
Nursing care planning begins when the client is admitted to the agency and is continuously updated throughout in response to the client’s changes in condition and evaluation of goal achievement. Planning and delivering individualized or patient-centered care is the basis for excellence in nursing practice .
Types of Nursing Care Plans
Care plans can be informal or formal: An informal nursing care plan is a strategy of action that exists in the nurse ‘s mind. A formal nursing care plan is a written or computerized guide that organizes the client’s care information.
Formal care plans are further subdivided into standardized care plans and individualized care plans: Standardized care plans specify the nursing care for groups of clients with everyday needs. Individualized care plans are tailored to meet a specific client’s unique needs or needs that are not addressed by the standardized care plan.
Standardized care plans are pre-developed guides by the nursing staff and health care agencies to ensure that patients with a particular condition receive consistent care. These care plans are used to ensure that minimally acceptable criteria are met and to promote the efficient use of the nurse’s time by removing the need to develop common activities that are done repeatedly for many of the clients on a nursing unit.
Standardized care plans are not tailored to a patient’s specific needs and goals and can provide a starting point for developing an individualized care plan .
Care plans listed in this guide are standard care plans which can serve as a framework or direction to develop an individualized care plan.
An individualized care plan care plan involves tailoring a standardized care plan to meet the specific needs and goals of the individual client and use approaches shown to be effective for a particular client. This approach allows more personalized and holistic care better suited to the client’s unique needs, strengths, and goals.
Additionally, individualized care plans can improve patient satisfaction . When patients feel that their care is tailored to their specific needs, they are more likely to feel heard and valued, leading to increased satisfaction with their care. This is particularly important in today’s healthcare environment , where patient satisfaction is increasingly used as a quality measure.
Tips on how to individualize a nursing care plan:
- Perform a comprehensive assessment of the patient’s health, history, health status, and desired goals.
- Involve the patient in the care planning process by asking them about their health goals and preferences. By involving the client, nurses can ensure that the care plan is aligned with the patient’s goals and preferences which can improve patient engagement and compliance with the care plan.
- Perform an ongoing assessment and evaluation as the patient’s health and goals can change. Adjust the care plan accordingly.
The following are the goals and objectives of writing a nursing care plan:
- Promote evidence-based nursing care and render pleasant and familiar conditions in hospitals or health centers.
- Support holistic care , which involves the whole person, including physical, psychological, social, and spiritual, with the management and prevention of the disease.
- Establish programs such as care pathways and care bundles. Care pathways involve a team effort to reach a consensus regarding standards of care and expected outcomes. In contrast, care bundles are related to best practices concerning care for a specific disease.
- Identify and distinguish goals and expected outcomes.
- Review communication and documentation of the care plan.
- Measure nursing care.
The following are the purposes and importance of writing a nursing care plan:
- Defines nurse’s role. Care plans help identify nurses’ unique and independent role in attending to clients’ overall health and well-being without relying entirely on a physician’s orders or interventions.
- Provides direction for individualized care of the client. It serves as a roadmap for the care that will be provided to the patient and allows the nurse to think critically in developing interventions directly tailored to the individual.
- Continuity of care. Nurses from different shifts or departments can use the data to render the same quality and type of interventions to care for clients, therefore allowing clients to receive the most benefit from treatment.
- Coordinate care. Ensures that all members of the healthcare team are aware of the patient’s care needs and the actions that need to be taken to meet those needs preventing gaps in care.
- Documentation . It should accurately outline which observations to make, what nursing actions to carry out, and what instructions the client or family members require. If nursing care is not documented correctly in the care plan, there is no evidence the care was provided.
- Serves as a guide for assigning a specific staff to a specific client. There are instances when a client’s care needs to be assigned to staff with particular and precise skills.
- Monitor progress. To help track the patient’s progress and make necessary adjustments to the care plan as the patient’s health status and goals change.
- Serves as a guide for reimbursement. The insurance companies use the medical record to determine what they will pay concerning the hospital care received by the client.
- Defines client’s goals. It benefits nurses and clients by involving them in their treatment and care.
A nursing care plan (NCP) usually includes nursing diagnoses , client problems, expected outcomes, nursing interventions , and rationales . These components are elaborated on below:
- Client health assessment , medical results, and diagnostic reports are the first steps to developing a care plan. In particular, client assessment relates to the following areas and abilities: physical, emotional, sexual, psychosocial, cultural, spiritual/transpersonal, cognitive, functional, age-related, economic, and environmental. Information in this area can be subjective and objective.
- Nursing diagnosis . A nursing diagnosis is a statement that describes the patient’s health issue or concern. It is based on the information gathered about the patient’s health status during the assessment.
- Expected client outcomes. These are specific goals that will be achieved through nursing interventions . These may be long and short-term.
- Nursing interventions . These are specific actions that will be taken to address the nursing diagnosis and achieve expected outcomes . They should be based on best practices and evidence-based guidelines.
- Rationales. These are evidence-based explanations for the nursing interventions specified.
- Evaluation . These includes plans for monitoring and evaluating a patient’s progress and making necessary adjustments to the care plan as the patient’s health status and goals change.
Care Plan Formats
Nursing care plan formats are usually categorized or organized into four columns: (1) nursing diagnoses, (2) desired outcomes and goals, (3) nursing interventions, and (4) evaluation. Some agencies use a three-column plan where goals and evaluation are in the same column. Other agencies have a five-column plan that includes a column for assessment cues.
The three-column plan has a column for nursing diagnosis, outcomes and evaluation, and interventions.
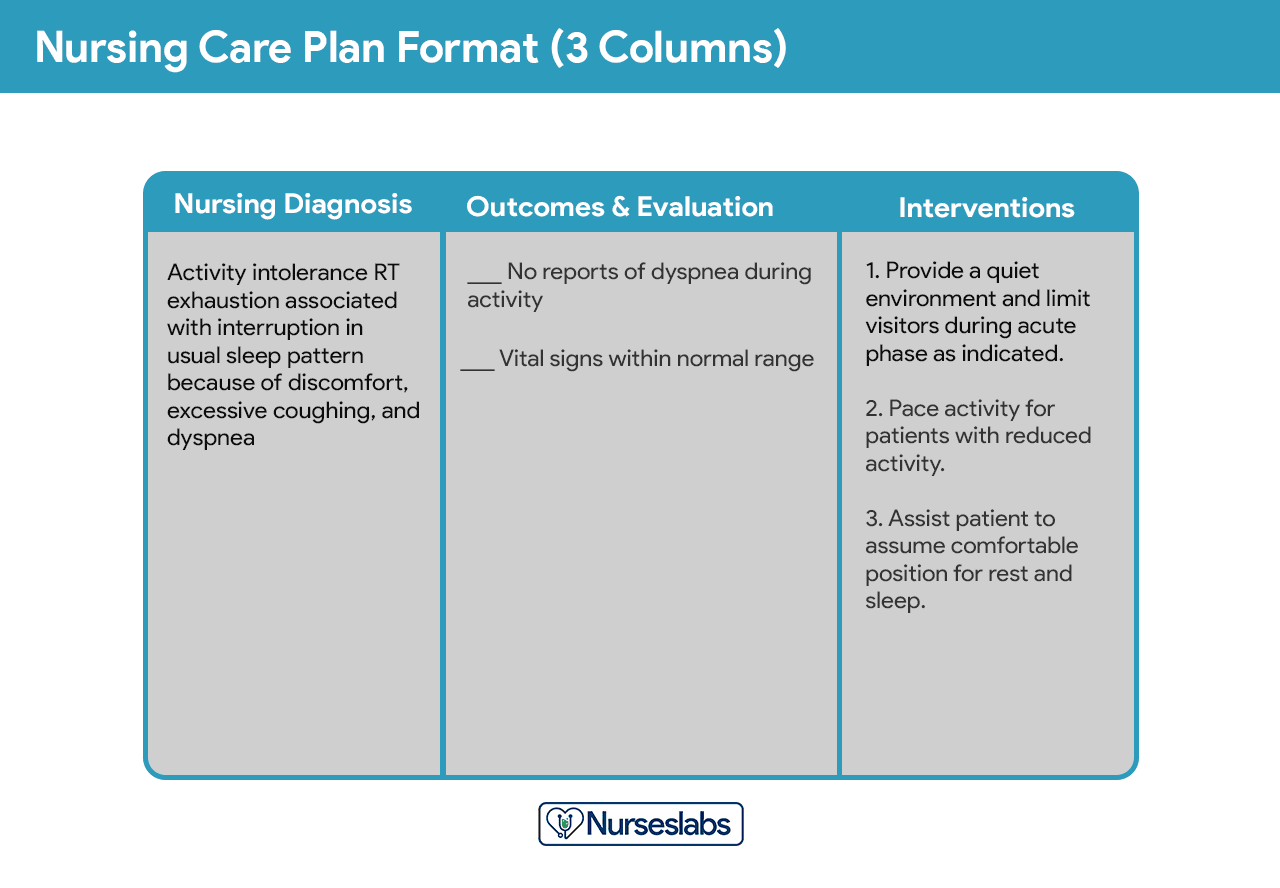
This format includes columns for nursing diagnosis, goals and outcomes, interventions, and evaluation.
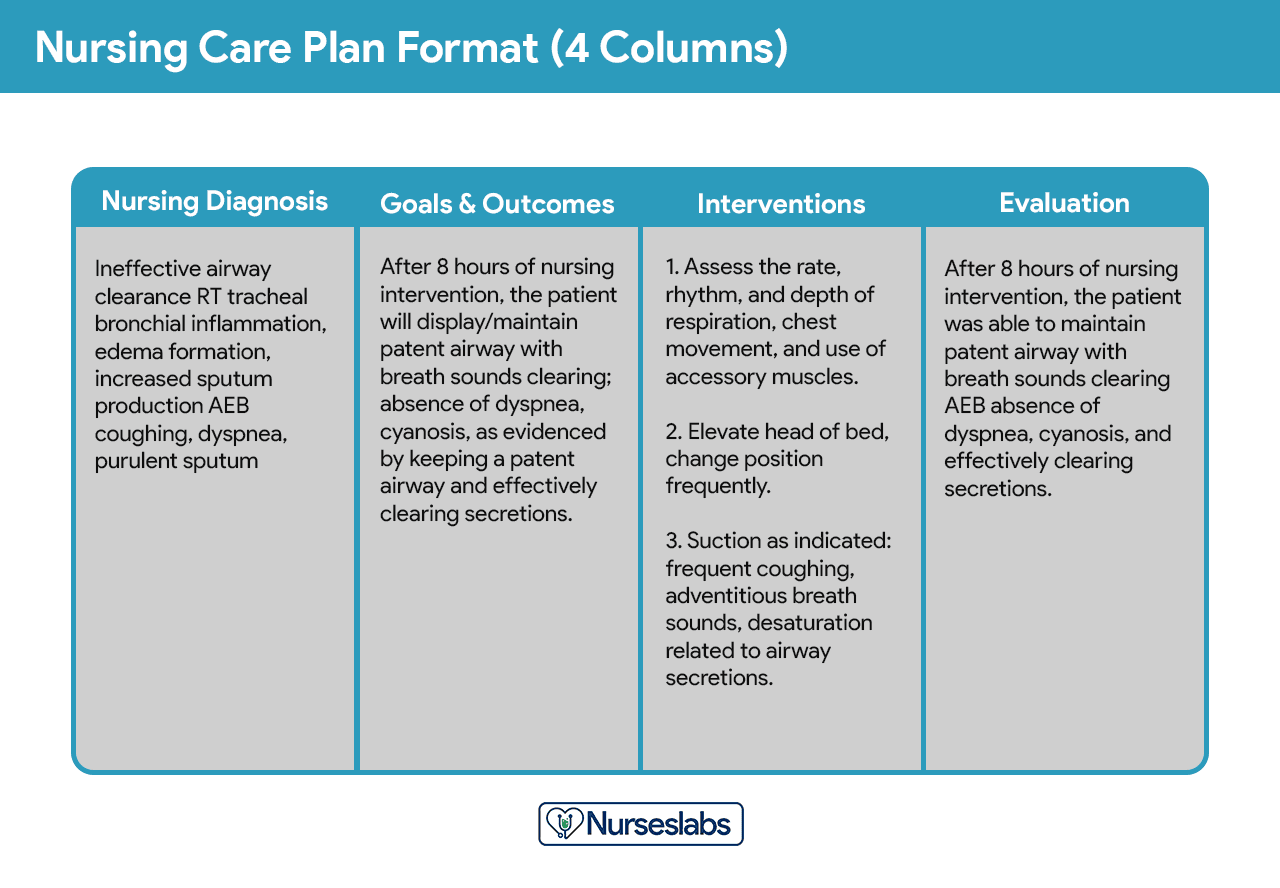
Below is a document containing sample templates for the different nursing care plan formats. Please feel free to edit, modify, and share the template.
Download: Printable Nursing Care Plan Templates and Formats
Student care plans are more lengthy and detailed than care plans used by working nurses because they serve as a learning activity for the student nurse.
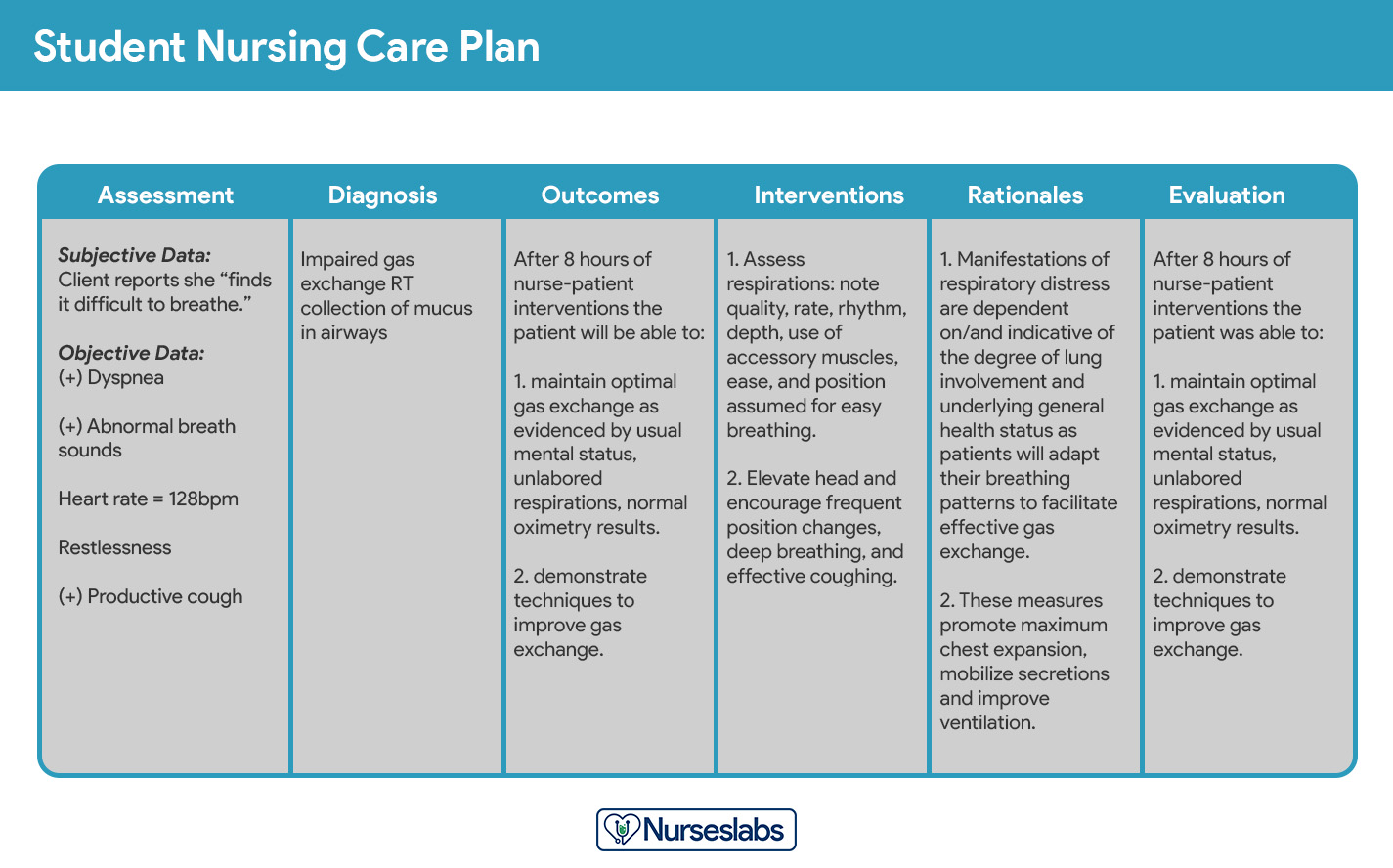
Care plans by student nurses are usually required to be handwritten and have an additional column for “Rationale” or “Scientific Explanation” after the nursing interventions column. Rationales are scientific principles that explain the reasons for selecting a particular nursing intervention.
Writing a Nursing Care Plan
How do you write a nursing care plan (NCP)? Just follow the steps below to develop a care plan for your client.
The first step in writing a nursing care plan is to create a client database using assessment techniques and data collection methods ( physical assessment , health history , interview, medical records review, and diagnostic studies). A client database includes all the health information gathered . In this step, the nurse can identify the related or risk factors and defining characteristics that can be used to formulate a nursing diagnosis. Some agencies or nursing schools have specific assessment formats you can use.
Critical thinking is key in patient assessment, integrating knowledge across sciences and professional guidelines to inform evaluations. This process, crucial for complex clinical decision-making , aims to identify patients’ healthcare needs effectively, leveraging a supportive environment and reliable information
Now that you have information about the client’s health, analyze, cluster, and organize the data to formulate your nursing diagnosis, priorities, and desired outcomes.
Nursing diagnoses are a uniform way of identifying, focusing on and dealing with specific client needs and responses to actual and high-risk problems. Actual or potential health problems that can be prevented or resolved by independent nursing intervention are termed nursing diagnoses.
We’ve detailed the steps on how to formulate your nursing diagnoses in this guide: Nursing Diagnosis (NDx): Complete Guide and List .
Setting priorities involves establishing a preferential sequence for addressing nursing diagnoses and interventions. In this step, the nurse and the client begin planning which of the identified problems requires attention first. Diagnoses can be ranked and grouped as having a high, medium, or low priority. Life-threatening problems should be given high priority.
A nursing diagnosis encompasses Maslow’s Hierarchy of Needs and helps to prioritize and plan care based on patient-centered outcomes. In 1943, Abraham Maslow developed a hierarchy based on basic fundamental needs innate to all individuals. Basic physiological needs/goals must be met before higher needs/goals can be achieved, such as self-esteem and self-actualization. Physiological and safety needs are the basis for implementing nursing care and interventions. Thus, they are at the base of Maslow’s pyramid, laying the foundation for physical and emotional health.
Maslow’s Hierarchy of Needs
- Basic Physiological Needs: Nutrition (water and food), elimination (Toileting), airway (suction)-breathing (oxygen)-circulation (pulse, cardiac monitor, blood pressure ) (ABCs), sleep , sex, shelter, and exercise.
- Safety and Security: Injury prevention ( side rails , call lights, hand hygiene , isolation , suicide precautions, fall precautions, car seats, helmets, seat belts), fostering a climate of trust and safety ( therapeutic relationship ), patient education (modifiable risk factors for stroke , heart disease).
- Love and Belonging: Foster supportive relationships, methods to avoid social isolation ( bullying ), employ active listening techniques, therapeutic communication , and sexual intimacy.
- Self-Esteem: Acceptance in the community, workforce, personal achievement, sense of control or empowerment, accepting one’s physical appearance or body habitus.
- Self-Actualization: Empowering environment, spiritual growth, ability to recognize the point of view of others, reaching one’s maximum potential.
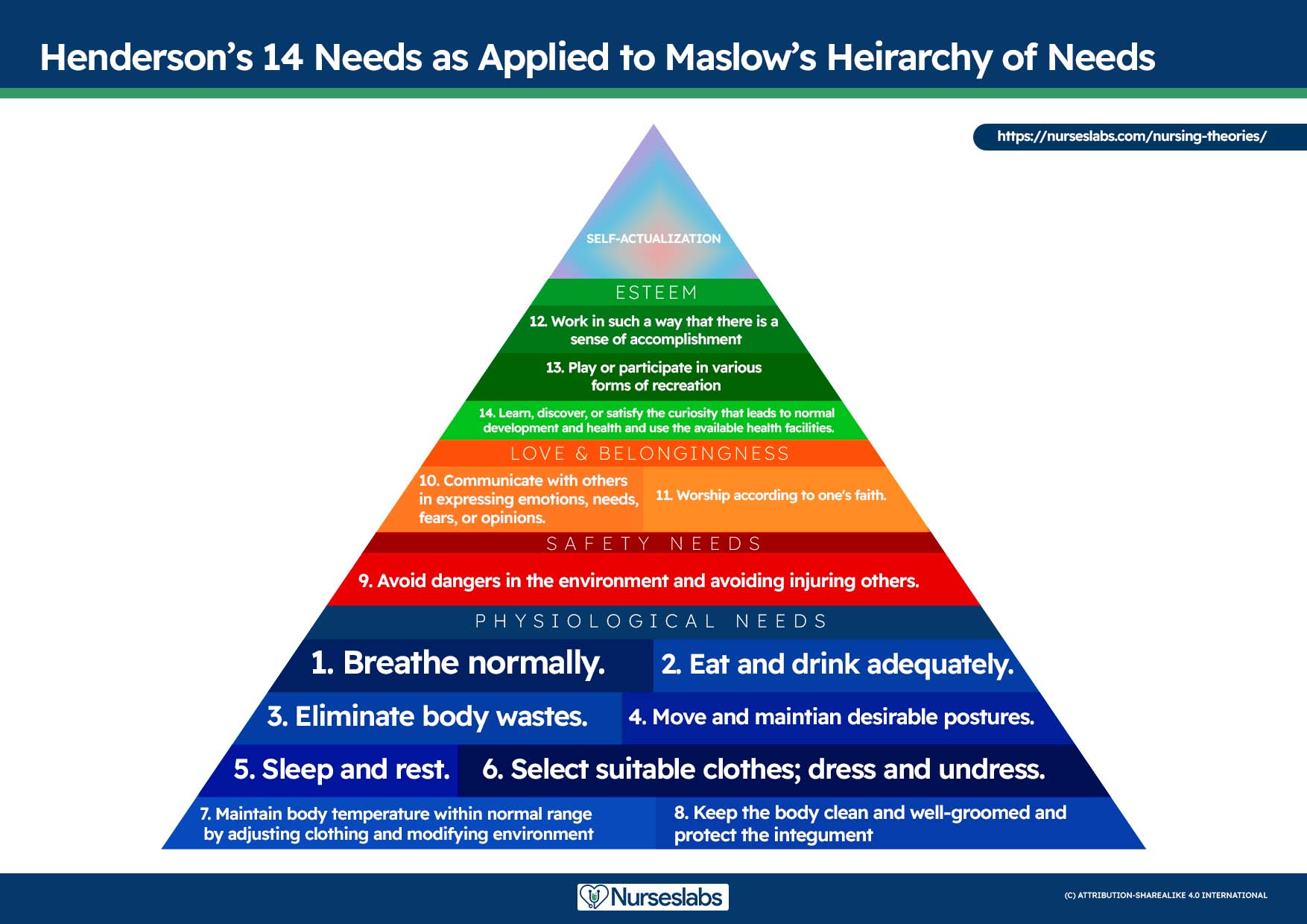
The client’s health values and beliefs, priorities, resources available, and urgency are factors the nurse must consider when assigning priorities. Involve the client in the process to enhance cooperation.
Step 5: Establishing Client Goals and Desired Outcomes
After assigning priorities for your nursing diagnosis, the nurse and the client set goals for each determined priority. Goals or desired outcomes describe what the nurse hopes to achieve by implementing the nursing interventions derived from the client’s nursing diagnoses. Goals provide direction for planning interventions, serve as criteria for evaluating client progress, enable the client and nurse to determine which problems have been resolved, and help motivate the client and nurse by providing a sense of achievement.
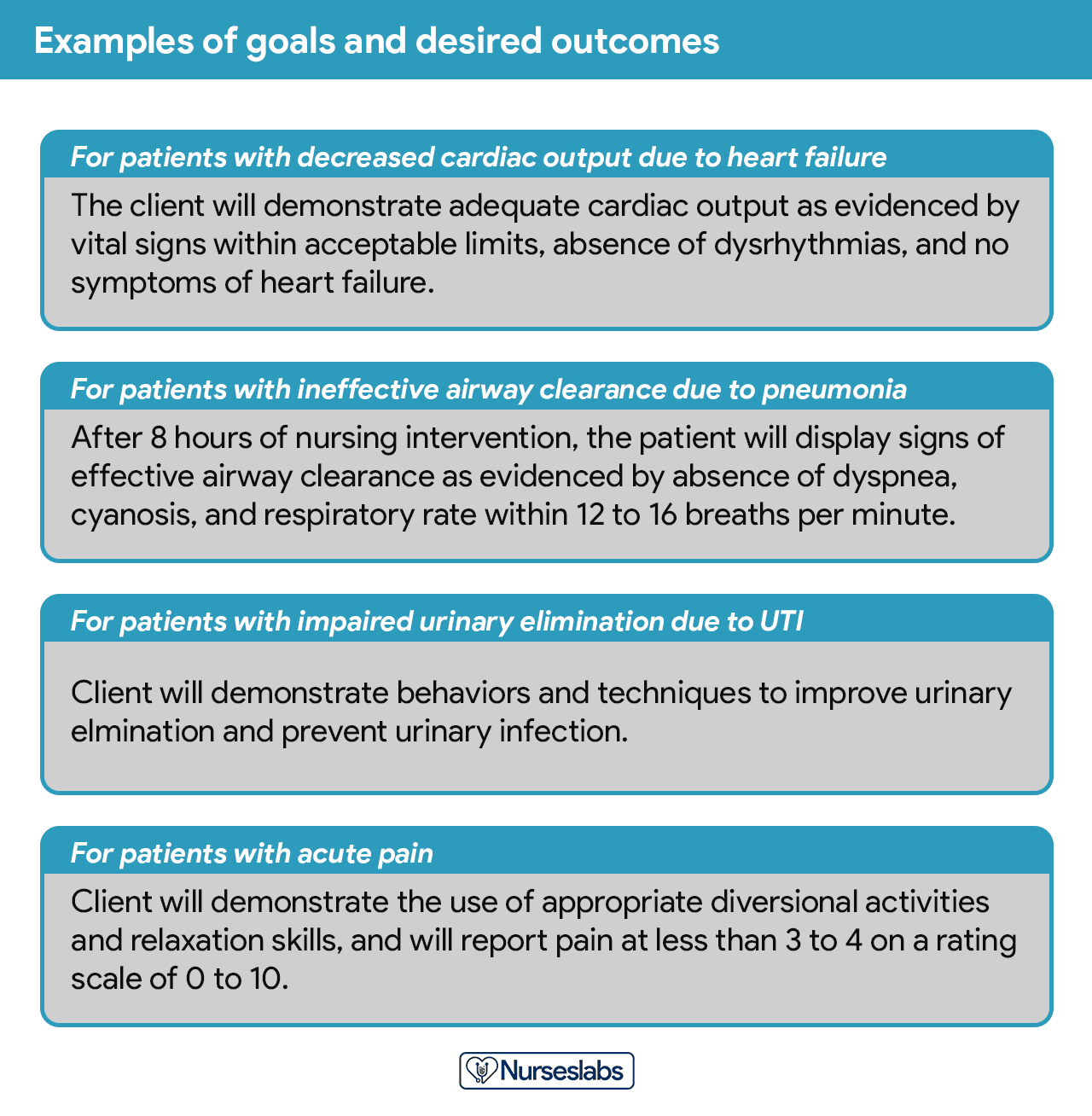
One overall goal is determined for each nursing diagnosis. The terms “ goal outcomes “ and “expected outcome s” are often used interchangeably.
According to Hamilton and Price (2013), goals should be SMART . SMART stands for specific, measurable, attainable, realistic, and time-oriented goals.
- Specific. It should be clear, significant, and sensible for a goal to be effective.
- Measurable or Meaningful. Making sure a goal is measurable makes it easier to monitor progress and know when it reaches the desired result.
- Attainable or Action-Oriented. Goals should be flexible but remain possible.
- Realistic or Results-Oriented. This is important to look forward to effective and successful outcomes by keeping in mind the available resources at hand.
- Timely or Time-Oriented. Every goal needs a designated time parameter, a deadline to focus on, and something to work toward.
Hogston (2011) suggests using the REEPIG standards to ensure that care is of the highest standards. By this means, nursing care plans should be:
- Realistic. Given available resources.
- Explicitly stated. Be clear about precisely what must be done, so there is no room for misinterpretation of instructions.
- Evidence-based. That there is research that supports what is being proposed.
- Prioritized. The most urgent problems are being dealt with first.
- Involve. Involve both the patient and other members of the multidisciplinary team who are going to be involved in implementing the care.
- Goal-centered. That the care planned will meet and achieve the goal set.
Goals and expected outcomes must be measurable and client-centered. Goals are constructed by focusing on problem prevention, resolution, and rehabilitation. Goals can be short-term or long-term . Most goals are short-term in an acute care setting since much of the nurse’s time is spent on the client’s immediate needs. Long-term goals are often used for clients who have chronic health problems or live at home, in nursing homes, or in extended-care facilities.
- Short-term goal . A statement distinguishing a shift in behavior that can be completed immediately, usually within a few hours or days.
- Long-term goal . Indicates an objective to be completed over a longer period, usually weeks or months.
- Discharge planning . Involves naming long-term goals, therefore promoting continued restorative care and problem resolution through home health, physical therapy, or various other referral sources.
Goals or desired outcome statements usually have four components: a subject, a verb, conditions or modifiers, and a criterion of desired performance.
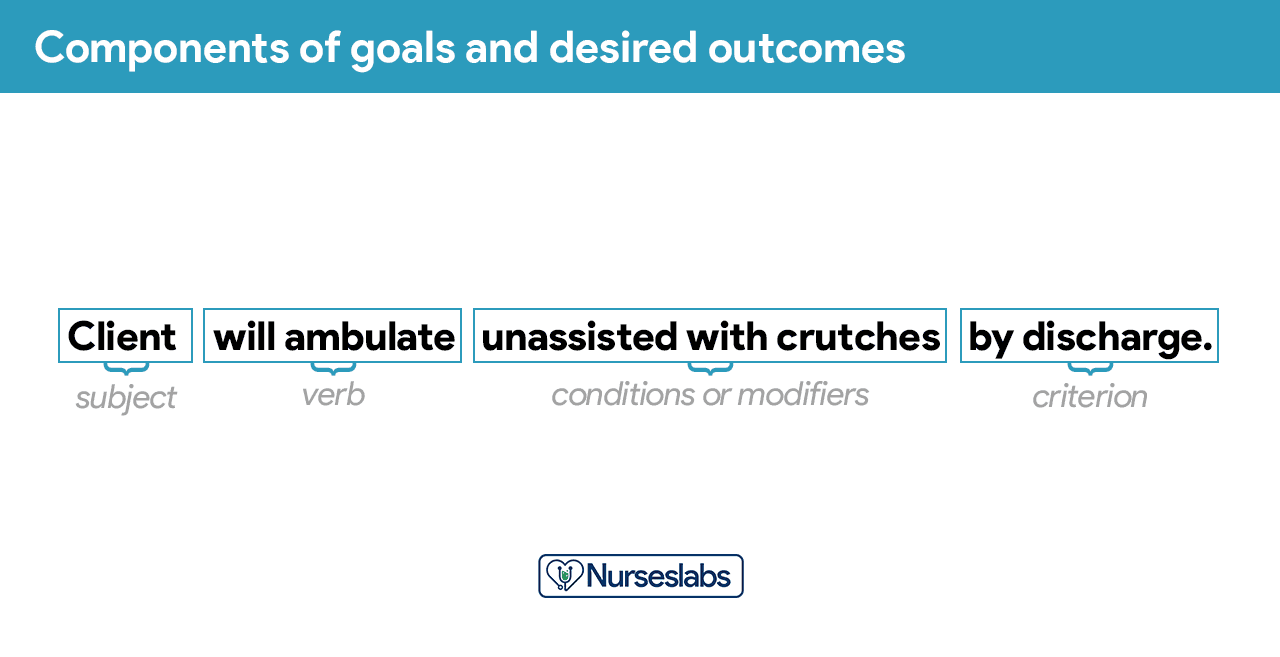
- Subject. The subject is the client, any part of the client, or some attribute of the client (i.e., pulse, temperature, urinary output). That subject is often omitted in writing goals because it is assumed that the subject is the client unless indicated otherwise (family, significant other ).
- Verb. The verb specifies an action the client is to perform, for example, what the client is to do, learn, or experience.
- Conditions or modifiers. These are the “what, when, where, or how” that are added to the verb to explain the circumstances under which the behavior is to be performed.
- Criterion of desired performance. The criterion indicates the standard by which a performance is evaluated or the level at which the client will perform the specified behavior. These are optional.
When writing goals and desired outcomes, the nurse should follow these tips:
- Write goals and outcomes in terms of client responses and not as activities of the nurse. Begin each goal with “Client will […]” help focus the goal on client behavior and responses.
- Avoid writing goals on what the nurse hopes to accomplish, and focus on what the client will do.
- Use observable, measurable terms for outcomes. Avoid using vague words that require interpretation or judgment of the observer.
- Desired outcomes should be realistic for the client’s resources, capabilities, limitations, and on the designated time span of care.
- Ensure that goals are compatible with the therapies of other professionals.
- Ensure that each goal is derived from only one nursing diagnosis. Keeping it this way facilitates evaluation of care by ensuring that planned nursing interventions are clearly related to the diagnosis set.
- Lastly, make sure that the client considers the goals important and values them to ensure cooperation.
Step 6: Selecting Nursing Interventions
Nursing interventions are activities or actions that a nurse performs to achieve client goals. Interventions chosen should focus on eliminating or reducing the etiology of the priority nursing problem or diagnosis. As for risk nursing problems, interventions should focus on reducing the client’s risk factors. In this step, nursing interventions are identified and written during the planning step of the nursing process ; however, they are actually performed during the implementation step.
Nursing interventions can be independent, dependent, or collaborative:
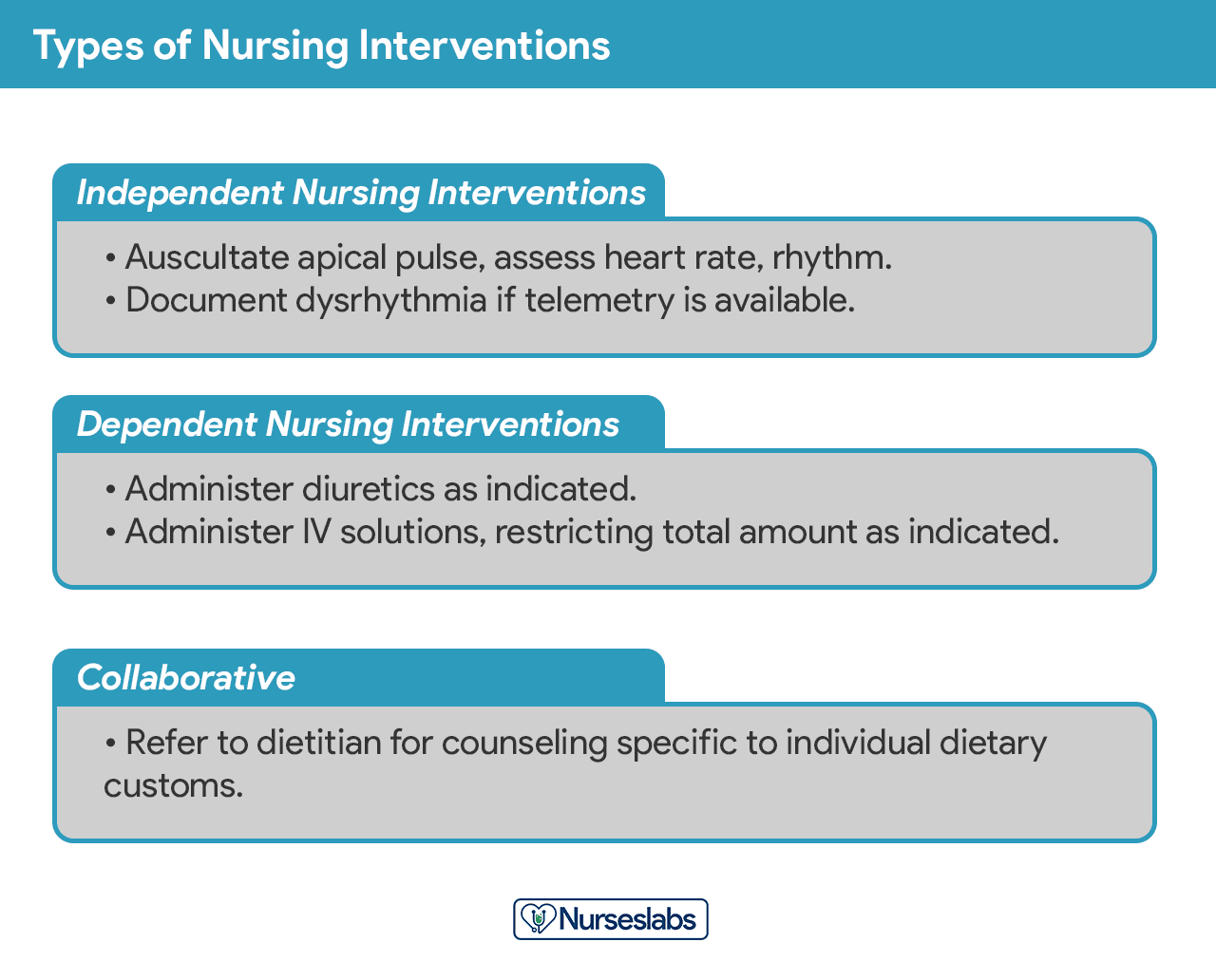
- Independent nursing interventions are activities that nurses are licensed to initiate based on their sound judgement and skills. Includes: ongoing assessment, emotional support, providing comfort , teaching, physical care, and making referrals to other health care professionals.
- Dependent nursing interventions are activities carried out under the physician’s orders or supervision. Includes orders to direct the nurse to provide medications, intravenous therapy , diagnostic tests, treatments, diet, and activity or rest. Assessment and providing explanation while administering medical orders are also part of the dependent nursing interventions.
- Collaborative interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, dietitians, and therapists. These actions are developed in consultation with other health care professionals to gain their professional viewpoint.
Nursing interventions should be:
- Safe and appropriate for the client’s age, health, and condition.
- Achievable with the resources and time available.
- Inline with the client’s values, culture, and beliefs.
- Inline with other therapies.
- Based on nursing knowledge and experience or knowledge from relevant sciences.
When writing nursing interventions, follow these tips:
- Write the date and sign the plan. The date the plan is written is essential for evaluation, review, and future planning. The nurse’s signature demonstrates accountability.
- Nursing interventions should be specific and clearly stated, beginning with an action verb indicating what the nurse is expected to do. Action verb starts the intervention and must be precise. Qualifiers of how, when, where, time, frequency, and amount provide the content of the planned activity. For example: “ Educate parents on how to take temperature and notify of any changes,” or “ Assess urine for color, amount, odor, and turbidity.”
- Use only abbreviations accepted by the institution.
Rationales, also known as scientific explanations, explain why the nursing intervention was chosen for the NCP.
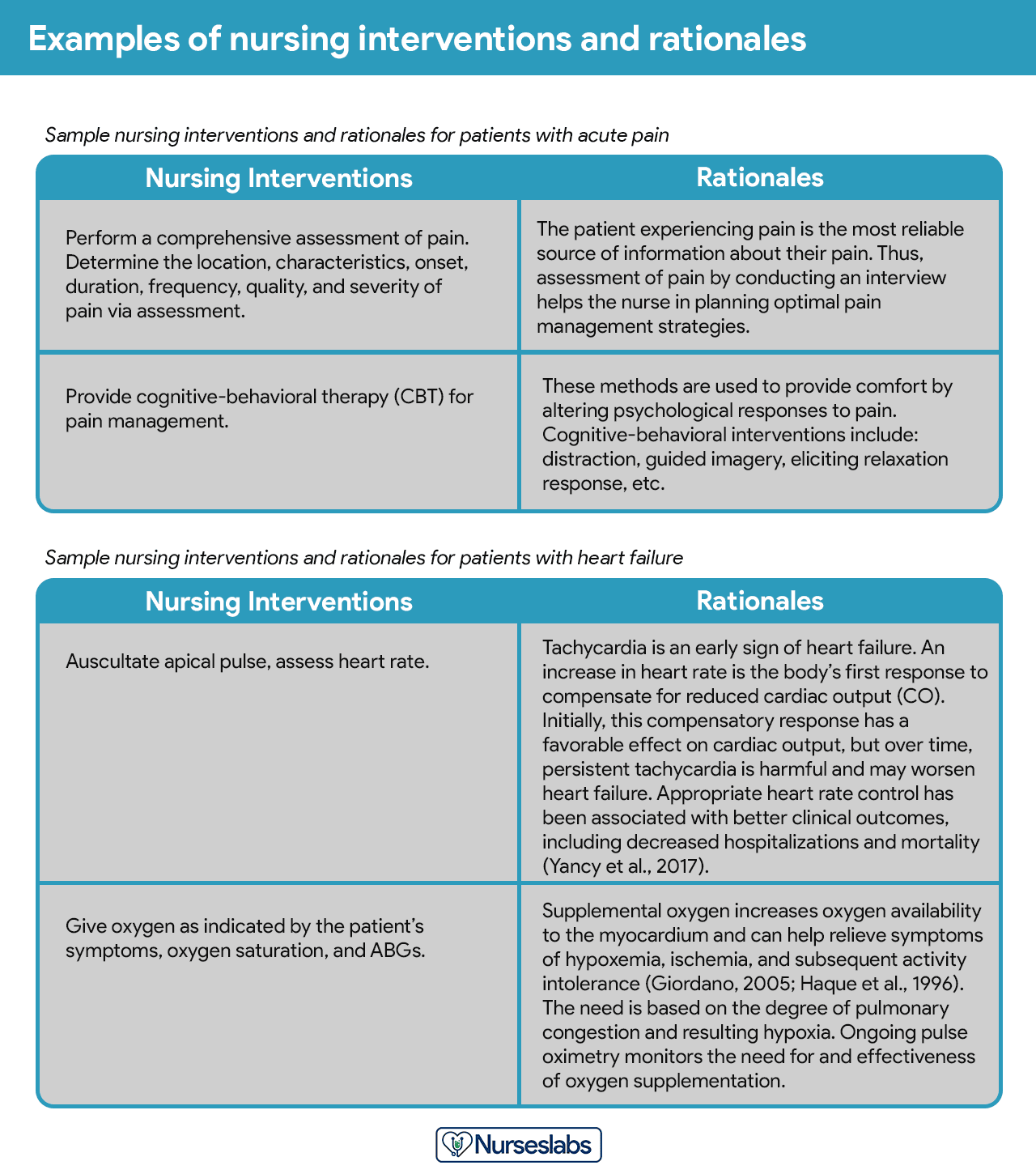
Rationales do not appear in regular care plans. They are included to assist nursing students in associating the pathophysiological and psychological principles with the selected nursing intervention.
Evaluation is a planned, ongoing, purposeful activity in which the client’s progress towards achieving goals or desired outcomes is assessed, and the effectiveness of the nursing care plan (NCP). Evaluation is an essential aspect of the nursing process because the conclusions drawn from this step determine whether the nursing intervention should be terminated, continued, or changed.
The client’s care plan is documented according to hospital policy and becomes part of the client’s permanent medical record, which may be reviewed by the oncoming nurse. Different nursing programs have different care plan formats. Most are designed so that the student systematically proceeds through the interrelated steps of the nursing process , and many use a five-column format.
Nursing Care Plan List
This section lists the sample nursing care plans (NCP) and nursing diagnoses for various diseases and health conditions. They are segmented into categories:
Miscellaneous nursing care plans examples that don’t fit other categories:
Care plans that involve surgical intervention .
| Surgery and Perioperative Care Plans |
|---|
Nursing care plans about the different diseases of the cardiovascular system :
| Cardiac Care Plans |
|---|
Nursing care plans (NCP) related to the endocrine system and metabolism:
| Endocrine and Metabolic Care Plans |
|---|
| Acid-Base Imbalances |
|---|
| Electrolyte Imbalances |
|---|
Care plans (NCP) covering the disorders of the gastrointestinal and digestive system :
| Gastrointestinal Care Plans |
|---|
Care plans related to the hematologic and lymphatic system:
| Hematologic & Lymphatic Care Plans |
|---|
NCPs for communicable and infectious diseases:
| Infectious Diseases Care Plans |
|---|
All about disorders and conditions affecting the integumentary system:
| Integumentary Care Plans |
|---|
Nursing care plans about the care of the pregnant mother and her infant. See care plans for maternity and obstetric nursing:
| Maternal and Plans |
|---|
Care plans for mental health and psychiatric nursing:
| Mental Health and Psychiatric Care Plans |
|---|
Care plans related to the musculoskeletal system:
| Musculoskeletal Care Plans |
|---|
Nursing care plans (NCP) for related to nervous system disorders:
| Neurological Care Plans |
|---|
Care plans relating to eye disorders:
| Care Plans |
|---|
Nursing care plans (NCP) for pediatric conditions and diseases:
| Pediatric Nursing Care Plans |
|---|
Care plans related to the reproductive and sexual function disorders:
| Reproductive Care Plans |
|---|
Care plans for respiratory system disorders:
| Respiratory Care Plans |
|---|
Care plans related to the kidney and urinary system disorders:
| Urinary Care Plans |
|---|
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition) Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

Recommended reading materials and sources for this NCP guide:
- Björvell, C., Thorell-Ekstrand, I., & Wredling, R. (2000). Development of an audit instrument for nursing care plans in the patient record. BMJ Quality & Safety , 9 (1), 6-13. [ Link ]
- DeLaune, S. C., & Ladner, P. K. (2011). Fundamentals of nursing: Standards and practice . Cengage learning .
- Freitas, F. A., & Leonard, L. J. (2011). Maslow’s hierarchy of needs and student academic success . Teaching and learning in Nursing , 6 (1), 9-13.
- Hamilton, P., & Price, T. (2007). The nursing process, holistic. Foundations of Nursing Practice E-Book: Fundamentals of Holistic Care , 349.
- Lee, T. T. (2004). Evaluation of computerized nursing care plan: instrument development . Journal of Professional Nursing , 20 (4), 230-238.
- Lee, T. T. (2006). Nurses’ perceptions of their documentation experiences in a computerized nursing care planning system . Journal of Clinical Nursing , 15 (11), 1376-1382.
- Rn , B. O. C., Rn, H. M., Rn, D. T., & Rn, F. E. (2000). Documenting and communicating patient care : Are nursing care plans redundant?. International Journal of Nursing Practice , 6 (5), 276-280.
- Stonehouse, D. (2017). Understanding the nursing process . British Journal of Healthcare Assistants , 11 (8), 388-391.
- Yildirim, B., & Ozkahraman, S. (2011). Critical thinking in nursing process and education . International journal of humanities and social science , 1 (13), 257-262.
66 thoughts on “Nursing Care Plans (NCP) Ultimate Guide and List”
This page is helpful!
Thank you! Hope we’ve helped you write better nursing care plans!
Will definitely use this site to help write care plans. How should I cite this link when using APA format. Thank You
HI Can some one help me to do assignment on Impaired renal perfusion. 1.Goal 2.Related Action 3.Rational 4.Evaluate outcome
Wow God bless plenty Nurseslabs really relieve my burdens 😊😊
Thank you for all this useful info! I have been looking for something like this online.
You’re welcome! :)
Quite educative thank you
The notes were indeed useful
I hope to learn more and improve my skills towards nursing
Thank you so so much! This website is of great assistance to me. God bless you.
It’s so great for nursing student
Very beautiful ,Good work keep it up
Nice work. Well done
Very helpful
Great job,thank you
Thanks so much , it’s of much support for students .
Risk for ineffective thermoregulation would be a good one for you to do next for newborn.
Hi, i have learnt a lot THANK YOU. i would kindly like to learn more on paper 1 since am yet to sit for my nursing council exams and feel challenged on the paper.please do assist me thank you.
This site is a total lifesaver!
What is a nursing care plan a mother in second stage of labour?
Please see: 36 Labor Stages, Induced and Augmented Labor Nursing Care Plans
What is the nursing care plan for pulmonary oedema?
I m interest in receiving a blank nursing care plan template for my students to type on. I was wondering if it was available and if so can you please direct me on where to find it?
Hi! You can download it here: Nursing Care Plan Template
I love this website!!! Is there a textbook version of the Nurseslabs that I can purchase??
Thank you Nurseslabs. This is a wonderful note you’ve prepared for all nurses. I would like a pdf of this. Thanks.
I wish I had had this resource when i was in nursing school 2008!!
Yeah! It’s nice
Thanks for this information!
God bless you sis…Thank you for all this useful info!
This is the kind of step-by-step guidance that I needed. Thank you!
Thank you. I have learned a lot!
Wow! This is a hidden treasure!
Thanks a lot for this, it is really helpful!
Hi Matt! I would like to purchase a textbook of your nursing care plan. Where I can purchase pls help!
Hi Criselda,
Sorry, we don’t have a textbook. All of our resources are here on the website and free to use.
Good day, I would like to know how can I use your website to help students with care plans.
Sincerely, Oscar A. Acosta DNP, RN
Oh I love your works. Your explanations
I’m glad I’ve met your website. It helps me a lot. Thank you
I love this, so helpful.
These care plans are great for using as a template. I don’t have to reinvent the wheel, and the information you provided will ensure that I include the important data without leaving things out. Thanks a million!
Hi, I have learnt a lot, this is a wonderful note you’ve prepared for all nurses thank you.
Matt, this page is very informative and I especially appreciate seeing care plans for patients with neurological disorders. I notice, though, that traumatic brain injury is not on your list. Might you add a care plan page for this?
Thanks alot I had gained much since these are detailed notes 🙏🙏
OMG, this is amazing!
Wow very helpful.thank you very much🙏🙏
Hi, is there a downloadable version of this, pdf or other files maybe this is awesome!
Hi Paul, on your browser go to File > Print > Save as PDF. Hope that helps and thanks for visiting Nurseslabs!
Matt, I’m a nursing instructor looking for tools to teach this. I am interested in where we can find “rules” for establishing “related to” sections…for example –not able to utilize medical diagnosis as a “related to” etc. Also, resources for nursing rationale.
Hello, please check out our guide on how to write nursing diagnoses here: https://nurseslabs.com/nursing-diagnosis/
Nursing care plan is very amazing
Thanks for your time. Nursing Care Plan looks great and helpful!
complete knowledge i get from here
great resource. puts it all together. Thank for making it free for all
Hello Ujunwa, Thanks a lot for the positive vibes! 🌟 It’s super important to us that everyone has access to quality resources. Just wondering, is there any specific topic or area you’d love to see more about? We’re always looking to improve and add value!
Great work.
Hi Abbas, Thank you so much! Really glad to hear you found the nursing care plans guide useful. If there’s a specific area or topic you’re keen on exploring more, or if you have any suggestions for improvement, feel free to share. Always aiming to make our resources as helpful as possible!
It has been good time me to use these nursing guides.
What is ncp for acute pain
For everything you need to know about managing acute pain, including a detailed nursing care plan (NCP), definitely check out our acute pain nursing care plan guide . It’s packed with insights on assessment, interventions, and patient education to effectively manage and alleviate acute pain.
Good morning. I love this website
what is working knowledge on nursing standard, and Basic Life Support documentation?
Leave a Comment Cancel reply
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Brooker D. Person-centred dementia care.London: Jessica Kingsley; 2007
What is a nursing intervention: a beginner's guide. 2019. https://tinyurl.com/mh2mwhb6 (accessed 1 November 2021)
Butterworth C. How to achieve a person-centred writing style in care plans. Nurs Older People. 2012; 24:(8)21-26 https://doi.org/10.7748/nop2012.10.24.8.21.c9310
Centre for Policy on Ageing. The effectiveness of care pathways in health and social care. 2014. https://tinyurl.com/3t835kfd (accessed 1 November 2021)
Clinical and service integration. The route to improved outcomes. 2010. https://tinyurl.com/whb87xd6 (accessed 1 November 2021)
Department of Health. Refocusing the Care Programme Approach. Policy and positive practice guidance. 2008. https://tinyurl.com/anyrzhy6 (accessed 3 November 2021)
Department of Health. Personalised care planning: improving care for people with Long term conditions. 2011. https://tinyurl.com/uc3u3tkh (accessed 1 November 2021)
Department of Health. Care planning in the treatment of long term conditions: final report of the CAPITOL Project. 2013a. https://tinyurl.com/7399vphc
Department of Health. Mental health payment by results guidance 2013-2014. 2013b. https://tinyurl.com/9zyfmy87 (accessed 1 November 2021)
Dimond B. Exploring the legal status of healthcare documentation in the UK. Br J Nurs. 2005; 14:(9)517-518 https://doi.org/10.12968/bjon.2005.14.9.18078
Foundations of nursing practice: making the difference, 2nd edn. In: Hogston R, Simpson PM (eds). London: Palgrave Macmillan; 2002
Kozier B, Erb G, Berman A, Snyder S, Lake R, Harvey S. Fundamentals of nursing: concepts, process and practice, 8th edn. Harlow: Pearson Education; 2008
Leach M. Clinical decision making in complementary & alternative medicine.Chatswood (NSW, Australia): Elsevier; 2010
Lloyd M. A practical guide to care planning in health and social care.Maidenhead: Open University Press; 2010
Matthews E. Nursing care planning made incredibly easy!.Philadelphia (PA): Lippincott Williams and Wilkins; 2010
Monitor. Delivering better integrated care: A summary of what delivering better integrated care means and how Monitor is supporting the sector. 2015. https://tinyurl.com/825k8kd6 (accessed 1 November 2021)
NHS website. NHS launches accredited suppliers for electronic patient records. 2019. https://tinyurl.com/4fzs4up5 (accessed 1 November 2021)
National Institute for Clinical Excellence. What to expect during assessment and care planning. 2021. https://tinyurl.com/63hm5vvp (accessed 1 November 2021)
NHS England. Personalised care and support planning handbook: the journey to person-centred care: Core information. 2016a. https://tinyurl.com/9fyrtw45 (accessed 1 November 2021)
NHS England. Mental health clustering booklet v5.0 (2016/17). 2016b. https://tinyurl.com/7p6dfnry (accessed 1 November 2021)
NurseChoice. Nursing smart goals: how to set smart goals for Nursing. 2018. https://tinyurl.com/s292baez (accessed 1 November 2021)
Nursing and Midwifery Council. Future nurse: standards of proficiency for registered nurses. 2018a. http://tinyurl.com/yddpadva (accessed 1 November 2021)
Nursing and Midwifery Council. The code: professional standards of practice and behaviour for nurses, midwives and nursing associates. 2018b. https://tinyurl.com/gozgmtm (accessed 1 November 2021)
Nursing and Midwifery Council. Keep records of all evidence and decisions. 2021. https://tinyurl.com/4pcabhms (accessed 1 November 2021)
Revello K, Fields W. An educational intervention to increase nurse adherence in eliciting patient daily goals. Rehabil Nurs. 2015; 40:(5)320-326 https://doi.org/10.1002/rnj.201
Royal College of Nursing. RCN factsheet on nurse prescribing in the UK. 2014. https://tinyurl.com/hkndnbhv (accessed 3 November 2021)
Nursing process. 2021. https://www.ncbi.nlm.nih.gov/books/NBK499937 (accessed 1 November 2021)
Wing JK, Beevor AS, Curtis RH, Park SGB, Hadden J, Burns A. Health of the Nation Outcome Scales (HoNOS). Br J Psychiatry. 1998; 172:(1)11-18 https://doi.org/10.1192/bjp.172.1.11
World Health Organization. Integrated care models: an overview. 2016. https://tinyurl.com/6encn9a5 (accessed 1 November 2021)
Yeomans D. Clustering in mental health payment by results: a critical summary for the clinician. Adv Psychiatr Treat. 2014; 20:(4)227-234 https://doi.org/10.1192/apt.bp.113.011320
Assessing the patient's needs and planning effective care
Benjamin Ajibade
Senior Lecturer, Mental Health Nursing, Northumbria University
View articles · Email Benjamin

Nurses have an essential role to play in the assessment and planning of patient care. This is emphasised in the Nursing and Midwifery Council's 2018Future Nurse proficiency standards. In this article, the author discusses the importance of person-centred care in assessing needs and highlights the need for all nursing interventions to be evidence based. The topics covered include assessing people's needs, care planning, stages of care planning, benefits of care planning, models of care, care pathways, and care clustering in mental health care. The article also highlights the significance of record-keeping.
The central role of nurses in assessing patient needs and planning care is one of the core areas emphasised in Future Nurse, the Nursing and Midwifery Council's (NMC) (2018a) nursing proficiency standards. The document categorises ‘assessing needs and planning care’ as the third of seven areas of proficiency, which are grouped into ‘platforms’. Future Nurse emphasises that the delivery of person-centred care and evidence-based nursing interventions are vital components for effective patient assessment and care planning. The standards further highlight that the nurse should understand the need to assess each patient's capacity to make their own decisions and to allow them the opportunity to give and withdraw consent.
An assessment is a form of a dialogue between client and practitioner, in which they discuss the needs of the former to promote their wellbeing and what they expect to happen in their daily life ( National Institute for Health and Care Excellence (NICE), 2021 ). Nursing assessment involves collecting data from the patient and analysing the information to identify the patient's needs, which are sometimes described as problems.
The process of planning care employs different strategies to resolve the needs identified as part of an assessment. Ideally, this will include the selection of appropriate evidence-based nursing interventions. When planning care, the patient's needs and wishes should be prioritised, and the individual must be involved in the decision-making process to ensure a person-centred approach. The planned care must take into account the patient's conditions, personal attributes and choices. It is worth noting that the principles of care planning are transferable between hospital, home and care home settings.
Section 2 of the NMC Code highlights the importance of partnership working with patients to ensure the delivery of effective high-quality care and of involving them in their care, which includes empowering patients by enabling them to make their own decisions ( NMC, 2018b ). The patient should be viewed holistically, with importance placed on the physical, psychological, social and spiritual aspects of the person's life, which are inextricable.
The intrinsic factors of a patient's condition will often affect their concordance with the advice and treatment offered. Consequently, it is important to understand the reasons for non-concordance and to tailor treatments/recommendations to each individual, which will improve the quality of care delivered.
Brooker (2007) developed the acronym VIPS to address some of the confusion surrounding what should or should not be perceived as person-centred care. VIPS stresses the following:
- V is a value base that affirms the value of each human being, irrespective of age and cognitive ability. This is the foundation for individualised care
- I is individualised care that considers the individual's distinctiveness and holistic needs
- P is about seeing the world from the patient's perspective, to ensure that the health professional takes the patient's point of view into account when providing care
- S is about maintaining a social environment that supports the patient's psychological needs, including their mental, emotional and spiritual needs.
Health professionals should endeavour to involve the patient in decision-making and enable them to make choices as much as possible, using a range of approaches to achieve this ( Lloyd, 2010 ). Unless proven otherwise, a nurse must assume that a patient has the capacity to make their own decisions, in line with the Mental Capacity Act 2005.
The following draws on the author's experience in mental health nursing but can be applied to other areas of nursing care.
Care planning
Planning care is essential in the delivery of appropriate nursing care. Following assessment of a patient's needs, the next stage is to ‘plan care’ to address the actual and potential problems that have been identified. This helps to prioritise the client's needs and assists in setting person-centred goals. Planned care will change as a patient's needs change and as the nurse and/or other health professionals identify new needs. Care planning assists professionals to communicate information about the patient's care to others ( Department of Health (DH), 2013a ; NICE, 2021 ), to facilitate continuity of care. Communication may be predominantly verbal, but it will also always involve documentation in a variety of formats, including computer-based, handwritten or preprinted care plans.
It is essential for nurses to consider their consultation style when developing a care plan in order to reduce the risk of paternalism when communicating with the patient and discussing their needs. Collaborative consultation encourages patients to participate in their care and improves rapport, while a paternalistic approach will generally minimise an individual's part in, and responsibility for, their own care needs and may compromise care outcomes and concordance ( Leach, 2010 ). A collaborative/partnership consultation style facilitates a person-centred approach by the practitioners and involves the patient in their care. Such an approach can include asking questions such as: ‘We have different types of treatment approaches that could be considered, what are your preferences?’ This is in contrast to a paternalistic consultation style with the health professional announcing any decisions with a statement such as: ‘I am going to prescribe a certain treatment for you.’
When drawing up a care plan with a patient the nurse should take into account a number of considerations ( Box 1 ).
Box 1.Nursing considerations
- The patient should know the reason for the assessment
- The assessment should be flexible and adaptable to the needs of the individual
- The patient must be fully involved and their dignity, independence, and interests should be paramount
- The patient can have someone with them, if preferred
- Appropriate language and terminologies should be used throughout the consultation
- The diversity of the individual client, their beliefs, values, culture and their circumstances must be considered
- It is essential to consider the patient's gender, sexuality, ethnicity, disability and religion as part of the assessment
- Be open to listening to the patient's personal history and life story
- The entire family's needs should be considered, inclusive of the patient and their carers: remember the importance of providing holistic care
- Cost-effectiveness should also be taken into account
Sources: Department of Health, 2011; National Institute for Health and Care Excellence, 2021
Stages of care planning
Care planning has been described as the third stage of the nursing process ( NMC, 2018a ; Toney-Butler and Thayer, 2021 ). It includes assessing the patient's needs, identifying the problem(s), setting goals, developing evidence-based interventions and evaluating outcomes ( Matthews, 2010 ). This will require the health professional to apply high-level critical thinking, decision-making and problem-solving skills. It is important to note that a care plan can be prescriptive: it is devised after a patient has been assessed through the prescription of nursing actions ( Hogston and Simpson, 2002 ) or through collaborative working involving the multidisciplinary team.
In some situations there will be differences between what the nurse sees as a priority in terms of the patient's needs and what the patient wants. An example of this would be a patient with mental health problems who may be at high risk of self-harm, who may need to be put on intermittent 15-minute observation. In such cases, a patient would be deemed as not having capacity to make decisions and the nurse will need to use their clinical judgement to prescribe the best treatment option. The care plan can still be agreed in conjunction with the patient once the nurse has explained the reasons for the interventions and acknowledged in the care plan that this is not the patient's preferred choice.
In situations where the patient has capacity to make decisions, the care plan should be agreed in collaboration with the service user ( NHS England, 2016a ).
Identifying needs
As part of the care planning process, the nurse will identify a patient's needs/problems and propose a set of interventions to address them in order of priority, ensuring that everything is in agreement with the patient. To ensure that appropriate goals are set, a patient's needs will be classified as high, intermediate and low.
Each goal provides an indication as to the expected outcome, along with the proposed interventions required to meet the patient's problems/needs, all of which must be patient centred. It is important, in collaboration with the patient, to set both short-term, achievable goals and longer-term goals that may take days, weeks or months to accomplish. One way nurses can ensure this is to apply the SMART goal-setting approach to ensure that the goals are ( Revello and Fields, 2015 ; NurseChoice, 2018 ):
- M easurable
- A chievable
- T imely (within a defined time frame).
Interventions
Interventions are nursing actions/procedures or treatments built on clinical judgement and knowledge, performed to meet the needs of patients. The actions should be evidence based and indicate who will carry them out, when and how often ( Hogston and Simpson, 2002 ). The scheduled interventions will have been agreed with the patient with the aim of improving their health condition, and each subsequent action should strive to meet the goals set at the previous stage. Brooks (2019) outlined three types of intervention:
- Those independently initiated by nurses
- Those that are dependent on a physician or other health professionals
- Those that are interdependent, that is, those rely on the experience, skills and knowledge of multiple professionals.
Independent nursing interventions are planned and actioned by nurses autonomously ( NMC, 2018a ), and these actions do not require the nurse to have direction from another health professional. When actioning interventions dependent on other health professionals, the nurses must determine the appropriateness of any directions from other health professionals before carrying them out because the nurse remains accountable for the actions, for example, the administration of prescribed medication ( NMC, 2018a ). Due to developments in the nursing profession, some advanced nurse practitioners can now prescribe interventions, eg prescription of medication can be done by nurse independent prescribers or nurse supplementary prescribers ( Royal College of Nursing, 2014 ). Interdependent interventions are usually recorded in collaborative care plans reviewed in multidisciplinary (MDT) meetings and must be agreed by all parties involved. Both the goals and interventions must be communicated in a timely manner to all those involved in the patient's care.
This is the stage when a planned intervention is evaluated to assess whether or not it has been achieved. This can be an ongoing process, and the care plan should document the frequency and time frame for evaluating the intervention. If the initial goal becomes unachievable, the nurse will be required to reassess the patient's needs, and review and revise the interventions.
Benefits of care planning
The DH (2011) highlighted that the aim of care planning is to improve the quality of care and outcomes by respecting individual wishes and enabling patients to acknowledge the ownership of their condition and ensuring they have the ability to influence the outcomes. Health professionals should engage individuals in decision-making and facilitate them to take control of their health by agreeing common goals to improve outcomes. This will have additional benefits for both the patient and health services as it should reduce the number of GP appointments and emergency admissions the patient may require. Promoting self-management of long-term conditions can also help slow progression of illness.
Care planning empowers patients to care for themselves when they are self-managing their health and when they may have difficulty accessing a health professional. This became evident during the pandemic, with patients often having to go for extended periods between appointments with their health professionals. Care planning has really come into its own in community care in the past few years, which became evident during the pandemic—particularly in the field of mental health—because it leads to better patient concordance with treatment and other care needs without the need for constant input by health professionals. This benefits both health professionals and the NHS: it increases job satisfaction, brings efficiency savings and improves the quality of patient care ( DH, 2011 ).
Model of care
Models of care are used to deliver best practice in health care. An integrated services care model is multifaceted and enables the co-ordination of care by different health and social care professionals to meet individual patient needs. It encompasses patient-centred care and enables care staff across different providers to reduce duplication, confusion, delay and gaps in services ( Monitor, 2015 ). In the modern NHS, this is the preferred model of care.
The care plan is an integral part of this model because it enables the creation of shared care plans that map different care processes. It becomes a point of reference for various providers involved in the care of the patients, ensuring the co-ordination of care across services ( Curry and Ham, 2010 ; World Health Organization, 2016 ).
Care pathways
Care pathways, which are also known as critical pathways, clinical pathways, integrated care pathways, care paths and care maps, are used to describe a specific patient journey that dictates the care to be provided or process to be followed for a patient's particular condition or needs. An evidence-based care process is established for specific conditions by considering expert opinion that takes into account the evidence to recommend interventions that have been shown to achieve better health outcomes cost-effectively ( Centre for Policy on Ageing, 2014 ).
Care pathways are often developed at local level and have been shown to be efficacious at meeting local needs. They are also known to improve cross-setting collaborations. Clinical pathways are aimed at providing effective health care appropriate for the patient group of conditions, thereby reducing hospital stays, leading to cost-effective health care ( Kozier et al, 2008 ).
Care clusters
Care clustering is a needs assessment tool that is used to rate a patient's care need against specific scales:
‘A cluster is a global description of a group of people with similar characteristics as identified from a holistic assessment and then rated using the Mental Health Clustering Tool (MHCT).’
NHS England, 2016b
This framework is used to plan and organise mental health services, including the care and support provided to individuals based on their illness and individual needs. One of the care clustering tools used in the NHS is the Health of the Nations Outcome Scales (HoNOS) ( Wing et al, 1998 ; Yeomans, 2014 ; NHS England, 2016b ).
Mental health services were brought under the scope of Payment by Results (PbR) in the NHS in 2012-2013.
‘Payment by Results (PbR) is the transparent rules-based payment system in England under which commissioners pay healthcare providers for each patient seen or treated, taking into account the complexity of the patient's healthcare needs.’
Consequently, as part of the care planning process, nurses need to take into account the cost-effectiveness of any interventions in order to consider how much funding is likely to be available for an initial completion of assessments, during scheduled reassessment and at any subsequent reassessment after a significant change in the patient's needs.
Box 2.Importance of complying with guidelines when undertaking assessment and planning care
- You must be compliant with the Nursing and Midwifery Council (2018b ; 2021 ) guidelines for record and record-keeping
- Adhere to the employing local organisation's policy on record-keeping, eg local trust policy
- Follow the NHS trust Care Programme Approach (CPA) policy ( Department of Health, 2008 )
- Collaborate with all those involved in a patient's care planning process
Importance of record-keeping
Accurate record-keeping is essential in the assessment of needs and planning care. This complies with the NMC (2018b) which states that record-keeping is fundamental to nursing practice, emphasising that records must be accurate and precise.
Health professionals should be aware of the need for legal accountability when documenting care in a written record because such records could be used in any legal proceedings ( Dimond, 2005 ). A record refers to not only a patient's record, but encompasses all records related to an individual nurse's range of practice. It is important to include the person being cared for in the record-keeping process, who should be asked to sign the plan of care, if they have capacity to do so ( NMC, 2021 ).
It is good practice to make an entry in the care documentation if a service user is unable to sign or agree to their planned care and state the reason for this ( Butterworth, 2012 ). In addition to paper-based records, care plans can be entered into the electronic health/patient record system used in the practitioner's service ( NHS website, 2019 ).
Best practice in writing care plans
There are some critical factors to consider when writing a focused person-centred care plan. One of these is to clearly document in detail the needs of the patient and to use the patient's language whenever possible, for example: ‘Mr D likes to dress smart every morning, but has been finding it difficult to make the choice of clothing to wear.’ An example of a poor way to record the same issue might be: ‘Mr D is unable to dress by himself’ and the aim is ‘Mr D will appear to dress smartly’.
The documented goal/aim of the care plan should be determined by applying the SMART acronym. It is therefore vital to ensure that the aim is specific by focusing on issues that can be measured, with goals that are achievable and realistic. It is also important to suggest and record a time frame within which a patient's short-term and long-term goals could be achieved. In relations to Mr D's clothing, a daily time frame might be appropriate. To come to an agreement over this issue, Mr D might be asked: ‘Mr D, would you like to be able to make your own choice of clothes to wear every day with the support of staff?’ The projected daily goal would then be recorded as part of the care plan documentation.
An intervention must specify how a goal/aim will be achieved, including who will be responsible for implementing each task. This could be the staff nurse on duty, team nurse, team leader, the nurse in charge and/or the patient (please put the patient's name). Evaluation should be carried out regularly and documented, and should conform with the proposed time frame outlined as part of the suggested intervention. Evaluations should be undertaken whenever actions are performed in accordance with each proposed intervention, and details of the progress of the patient's problem/needs documented.
In conclusion, the article has discussed the importance of assessing patients' needs, emphasising person-centred care using the VIPS acronym devised by Brooker (2007) . It has stressed the notion for all nursing interventions to be evidence based. The stages of care planning were discussed, and the application of the SMART goal-setting approach was highlighted. Record-keeping is an integral part of care planning in the communication of patient's care and progress. The benefits of care planning in improving quality of care and outcomes, respecting individual wishes, thereby empowering the patient was recognised.
LEARNING OUTCOMES
- Nurses must ensure that assessment of patient needs and care planning are always focused on the person
- All nursing interventions must be evidence based
- The goals set out in a patient's care plan must be achievable and measurable, and should include time frames within which both short- and long-term goals can be achieved
- Record-keeping is a vital component of care planning and is part of communicating aspects of a patient's care, and their progress towards their goals, with other health professionals involved in their care
CPD reflective questions
- In the context of a patient's health, what should you aim to do when care planning?
- Who should you involve in the care planning and why? Should the patient have a copy of the care plan?
- Is it acceptable to destroy care plans or other records?
- When should care plans be reviewed?
- Visit Nurse.com on Facebook
- Visit Nurse.com on YouTube
- Visit Nurse.com on Instagram
- Visit Nurse.com on LinkedIn
Nurse.com by Relias . © Relias LLC 2024. All Rights Reserved.

Patient acuity tool on a medical-surgical unit
Use a tool for consistent, objective, and quantifiable patient assignments..
- Patient assignments can lead to dissatisfaction among nursing staff, especially when they’re not consistent, objective, and quantifiable.
- Dissatisfaction can create barriers to the adaptability and teamwork that are critical to good patient care.
- The patient acuity tool addresses the important issue of unbalanced nurse-patient assignments and helps nurses influence decision-making in their organizations.
Patient assignments can lead to dissatisfaction among nursing staff, especially when they’re not consistent, objective, and quantifiable. This dissatisfaction can create barriers to the adaptability and teamwork that are so critical to good patient care.
In 2016, three RNs on a complex 23-bed medical-surgical unit at Durham VA Health Care System identified a recurring complaint by nursing staff that patient assignments were inconsistent and unequal. An average of five RNs and one charge nurse were assigned five patients per nurse per shift. The nursing assignment system included placing patients in one of two categories: “standard patient” or “involved care” patient. The problem was the subjectivity of these terms; they had no supporting evidence. The result was frustrated nurses, which prompted the unit to develop a process improvement project.
Standardizing handoff communication
The Bedside Mobility Assessment Tool 2.0
Hours per patient day: Understanding this key measure of productivity
Purpose and goals
We used evidence-based information to create an objective acuity tool to establish patient assignments. The tool uses both clinical patient characteristics and workload indicators to score patients from 1 to 4 based on acuity level. This approach gives nurses the power to score their patient, then report to the charge nurse so that RN assignments for the oncoming shift are quantifiable and equitable. It also gives them the opportunity to assess the level of patient safety risk.
The goals of the tool are to:
- increase nurse satisfaction with their patient assignment
- increase nurse perception of patient safety by assigning patients with high acuity scores equitably.
The patient acuity tool
Each patient is scored on a 1-to-4 scale (1, stable patient; 2, moderate-risk patient; 3, complex patient; 4, high-risk patient) based on the clinical patient characteristics and the care involved (workload.) Each nurse scores his or her patients, based on acuity, for the upcoming shift and relays this information to the charge nurse, who then assigns patients before the shift change. The handoff report between RNs allows each to validate patients’ current acuity and care needs. (See Patient acuity tool .)

Methodology
Anecdotal reports by the RN staff and our observations prompted the collection of data from staff. Some of the staff comments about the current system included:
- “Why are my patient assignments so unfair?”
- “How will I care for all of my patients effectively?”
- “Involved care is a subjective term.”
We conducted a literature review and eventually combined two existing tools and restructured them to create our acuity tool. Before implementing the process improvement project, we used the newly created tool to assess the current average distribution of total acuity among nurse assignments, and we asked RNs to complete a 10-question survey to measure their satisfaction with patient assignments and perceptions of patient safety. We then taught the RNs how to use the tool and placed color-coded, laminated copies at every nursing computer.
The tool was pilot tested for 28 days. After the first 14 days, we conducted an audit to assess compliance, which revealed that average compliance among all four shifts was 35%. We then collected data on the average distribution of total acuity among nurse assignments. Progress e-mails were sent to staff, and individual follow-ups were held to promote compliance. At the end of the 28 days, we conducted another compliance audit, which revealed an average compliance among all four shifts of 77%, an increase of 220%.
At the end of the pilot study, we reviewed patient assignments before and after implementing the acuity tool to assess their equality, and we surveyed RNs about the two goals we set for the project: improve nurse satisfaction and increase nurse perception of patient safety.
Equality of patient assignments
To determine the equality of nurses’ assignments within a shift, the difference in total acuity between the highest and lowest scoring assignments was obtained. (See RN assignments using acuity tool .)

Before implementing the acuity tool, the average distribution of total acuity between highest and lowest nurse assignments for each shift was 4.83 (using a scale of 1 = lowest acuity and 4 = highest acuity). After implementation, the average distribution of total acuity between highest and lowest nurse assignments was 3.06, a 36.6% improvement in equality and accuracy.
Goal 1: Improve nurse satisfaction
Three of the 10 questions in the nurse survey were aimed at nurse satisfaction, including RN perception of patient assignment equality, having input into making assignments, and frequency of feeling overwhelmed with patient assignments. The most significant change occurred with the question “Please rate how frequently you feel overwhelmed with your patient assignment.” Response options were never (1), rarely (2), sometimes (3), frequently (4), and every shift (5). According to the survey, the weighted average of nurse satisfaction was 3.19 before implementing the acuity tool and 2.84 (11% improvement) after.
Goal 2: Increase nurse perception of patient safety
When asked to respond to the statement “I feel like patient safety is a concern when I accept my patient assignment,” RN staff chose from the following options: never (1), rarely (2), sometimes (3), frequently (4), and every shift (5). The weighted average was 3.38 pre-implementation and 3.21 post-implementation, a 5% improvement in RNs’ perception of patient safety. After reviewing the annual performance improvement data, we found no direct correlation between using the acuity tool and patient safety measurements (rate of falls, medication errors, and restraint use). However, by distributing high-acuity patients among nurses, this tool, used in conjunction with other current actions, can reduce the need for patient safety measures such as using sitters and frequent rounding.
We attributed many of the challenges faced during the implementation of this project to staff assignment changes during some 24-hour periods. Sometimes patient assignments changed every 4 hours because of differences in nurse shift length, which left the staff with no consistent communication between shifts. The charge nurse would also occasionally take a patient assignment when patient acuity was high and RN census was low, resulting in outliers in data.
Another challenge included RN staff changes during the pilot study, leading to gaps in education about proper use of the tool, decreased feedback, and less data in post-implementation than pre-implementation. As part of our sustainment plan, we’ll incorporate education on the tool in new staff orientation, adapt it to other medical-surgical units in the hospital, and continue quarterly audits to assess compliance.
Given the original concern by staff that assignments were unequal, one of the strengths of this acuity tool is that it allows nurses to become stakeholders in making patient assignments. In addition, it also gives the charge nurse an objective way to justify assignment rationale. The tool costs no money to implement and requires no special technology. In addition, it’s noninvasive to the unit’s workflow, easy to implement, and easily adapted to different units and their specific needs. We’ve also found that the tool enhances the shift-to-shift handoff report and that it can be used to assign patients based on nurse competence (novice nurses, expert nurses, etc.).
Striking a balance
The patient acuity tool addresses the important issue of unbalanced nurse-patient assignments and helps nurses influence decision-making in their organizations. Our research found that an objective patient acuity tool on a medical-surgical floor could increase assignment equality, improve nurse satisfaction, and improve nurse perception of patient safety. The tool is now being piloted on other units at this facility, and we’ve received consults from other facilities in the Veterans Affairs Health Care System.
| Use these strategies to create sustainable happiness. Spending time with family and friends is the most important thing you can do to be happy, so create a good work/life balance. Appreciate the present moment and find time for daily meditation. Health and happiness are strongly connected, so exercise regularly and eat healthy. Whether religion-based or not, spirituality offers a foundation for happiness. Rather than spending money on material things, spend it on experiences—family vacations, activities with friends, a mindfulness retreat. Learn the art of bouncing back from adversity. Gratitude is linked to happiness. Take time once a day to think of one thing you’re grateful for. Some experts say you can “fake it till you make it”; smiling and engaging in positive behavior can help you become more positive even if that’s not how you initially felt. Connect with goals that have meaning to you and find joy in the journey. |
Andrea Ingram is a medical-surgical certified nurse at the VA Health Care System in Durham, North Carolina. Jennifer Powell is a neonatal intensive care unit nurse at Novant Health Hemby Children’s Hospital in Charlotte, North Carolina.
Selected references
Chiulli KA, Thompson J, Reguin-Hartman KL. Development and implementation of a patient acuity tool for a medical-surgical unit . Academy of Medical-Surgical Nurses. 2014;23(2):1, 9-12.
Kidd M, Grove K, Kaiser M, Swoboda B, Taylor A. A new patient-acuity tool promotes equitable nurse-patient assignments . American Nurse Today. 2014;9(3):1-4.
Comments are closed.

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Increasing diversity in nursing with support from Nurses on Boards Coalition

Adventures in lifelong learning

The power of language

Making peace with imperfection

When laws and nursing ethics collide

Taking on health disparities

Medication safety and pediatric health

Confidence is in

Tailored falls prevention plans

Men in nursing

Chylothorax: A stepwise approach to care

Aortic dissection

FAQs: AI and prompt engineering

Caring for adults with autism spectrum disorder

Known fallers

ANA Nursing Resources Hub
Search Resources Hub

RN to BSN: Advancing Your Nursing Career
4 min read • February, 09 2024
If you’re a registered nurse (RN) with an Associate Degree in Nursing (ADN) looking for more job security, earning potential, and job satisfaction, an RN to BSN program may be the ideal next step in your career. Obtaining a Bachelor of Science in Nursing (BSN) can open new financial, leadership, and learning opportunities in your nursing career while providing a solid foundation for future growth.
What Is an RN to BSN Program?
An RN to BSN program provides ADN nurses with a straightforward path to completing their BSNs. It typically takes four years to complete an undergraduate BSN degree. However, if you’ve already earned an ADN, you can complete an RN to BSN program in two years or less.
Having a BSN can open the door to more advanced nursing leadership roles, increasing your career options and salary while positioning you to pursue more advanced degrees.
RN to BSN Requirements
Many public and private colleges and universities offer RN to BSN programs. Each institution sets its own admission policies, but specific requirements generally apply. All programs require you to have an ADN, and your license to practice as an RN must be active and unrestricted. Other RN to BSN requirements may include:
- A minimum GPA. Your previous college and high school academic performance may impact admission decisions.
- Standardized test scores. Most schools require the SAT or ACT.
- Prerequisite classes. ADN coursework generally satisfies this requirement. (Note that some older STEM (science, technology, engineering, and mathematics) credits may need to be retaken depending on admission requirements.)
RN to BSN Curriculum
The RN to BSN program curriculum picks up where your ADN ends. RN to BSN classes delve into nursing theory, public health and policy, specialized health sciences, and management and administration. The total credit hours required vary by program, and there’s usually flexibility in the number of hours taken each semester for full-time and part-time students. RN to BSN programs typically occur on-site, but many schools also offer accredited RN to BSN online programs, including some without clinicals . An online program is a convenient and manageable option for nurses working while in school.

How Much Does an RN to BSN Program Cost?
The cost of an RN to BSN program varies depending on the institution you choose. The average tuition for an in-state resident at a public university is typically about $9,600 per year. Private universities are significantly more expensive, with average annual tuition and fees closer to $34,000 . Financial aid for nursing students is available through various sources, such as scholarships, grants, fellowships, loans, and work-study programs.
The Benefits of an RN to BSN Program
Obtaining a BSN gives RNs more opportunities for career advancement. Many health care facilities and employers actively seek nurses with a BSN. Studies indicate patients have better outcomes , shorter stays, and incur fewer costs in hospitals that have more BSN nurses on staff. Some states, including New York, have even enacted laws that require RNs to complete a BSN within ten years of licensure.
Beyond the industry’s structural change toward hiring BSN nurses, consider an RN to BSN program’s financial, professional, and personal advantages.
Financial Benefits
Compensation for BSN nurses is significantly higher than for ADN RNs. Depending on where you live, you could earn upwards of $90K as a BSN nurse, according to ZipRecruiter , compared to an average salary of $75K for an ADN nurse . With the career opportunities available to BSN nurses, the differential expands as you assume more advanced roles and responsibilities.
Professional Benefits
A BSN allows greater professional flexibility and more access to leadership opportunities. Whether you want to specialize in cardiology or oncology, join the staff at a Magnet-designated hospital, or become a nurse administrator or educator, a BSN is essential. This status is also required for admission to graduate nursing programs.
Personal Benefits
Many nurses find the intellectual challenge and pride of accomplishment in earning a BSN inspiring and fulfilling. Besides the new skills and training you’ll receive, obtaining a BSN gives you more freedom and control over your career.
If you’re an RN who wants to make significant contributions to health care, an RN to BSN program is a rewarding investment that gives you a competitive edge.
Images sourced from Getty Images
Related Resources

Item(s) added to cart

IMAGES
VIDEO
COMMENTS
Proofreading and Editing. Proofreading and editing are essential steps in the assignment writing process. They ensure that your nursing assignment is polished, error-free, and effectively communicates your ideas. After completing the initial draft, it's crucial to take a break and return to your work with fresh eyes.
It has clues to the information you need. It provides the framework for the assignment-making process, including staff constraints, additional duties that must be covered, and patient factors most impor-tant on your unit. Use the electronic health record (EHR) to generate various useful pieces of patient in-formation.
What is a Safe Nursing Assignment? An appropriate nursing assignment is any patient assignment where the nurse can safely and effectively provide all the necessary care for their patients, and have the necessary tools, training, medications, knowledge, resources, and equipment to perform their nursing duties for those patients.
3.3 Assignment. Nursing team members working in inpatient or long-term care settings receive patient assignments at the start of their shift. Assignment refers to routine care, activities, and procedures that are within the legal scope of practice of registered nurses (RN), licensed practical/vocational nurses (LPN/VN), or assistive personnel ...
Introduction. Nursing assignments are the backbone of patient care. They encompass a wide range of tasks that nurses perform daily, contributing significantly to the recovery and well-being of ...
Nursing assignments are often based on room proximity, mandated nurse-to-patient ratio, patient's medical diagnosis, and continuity of care from shift to shift. In reality, nursing activity will vary throughout a patient's length of stay based on a combination of prescribed tasks including education, nursing interventions, and psychosocial ...
Improved workload management may reduce stress and its negative impact on nurses, leading them to work with a higher level of integrity and loyalty to their organization. Research indicates that using a workload tool can help promote equitable nurse-patient assignments, which may improve nurse job satisfaction.
Nurse-patient assignments help coordinate daily unit activities, matching nurses with patients to meet unit and patient needs for a specific length of time. If you are new to this challenge, try these eight tips as a guide for making nurse-patient assignments. 1. Find a mentor . Most nurses learn to make nurse-patient assignments from a colleague.
Walden instructors often ask nursing students to write position and reflective papers, critique articles, gather and analyze data, respond to case studies, and work collaboratively on a project. Although there may be differences between the writing expectations within the classroom and those in the workplace, the standards noted below, though ...
Nurse-patient assignments are created based on knowledge and understanding of nursing unit environment, nurse qualities, and patient characteristics. Clinical nurses are vital resources for critical changes in patient status. Nurse-patient assignments should be frequently reassessed and changed as needed to ensure continuous, safe, quality ...
Similarly, the ability for nurses to predict change, employ improvement strategies, and exercise fiscal prudence are critical skills. System awareness, innovation, and design also are needed to address such issues as structural racism and systemic inequity. Entry-Level Professional Nursing Education.
Summary. The American Nurses Association (ANA) upholds that registered nurses - based on their professional and ethical responsibilities - have the professional right to accept, reject or object in writing to any patient assignment that puts patients or themselves at serious risk for harm. Registered nurses have the professional obligation ...
Pediatric Nursing: Scope and Standards of Practice is a collaborative effort of the ANA, the Society for Pediatric Nurses (SPN), and NAPNAP. The American Psychiatric Nurses Association (APNA) Web site provides information about the role of the advanced practice psychiatric nurse organized by topic, workplace setting, and/or specialty.
A nursing care plan can be part of a case study or a stand-alone assignment. Nursing care plans are essential in nursing education as they help students develop effective nursing care planning. Formulating a nursing care plan for a patient scenario or case helps treat them as you define the guidelines and roles of nurses in caring for the patient.
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of ...
A licensed nurse is still responsible for ensuring the assignment is carried out correctly. Delegation. According to the NCSBN/ANA guideline, delegation applies when the delegatee is performing a "specific nursing activity, skill, or procedure that is beyond the delegatee's traditional role and not routinely performed." As opposed to work ...
Abstract. Charge nurses have integral roles in healthcare organizations. Making patient assignments is an important charge nurse role that lacks theoretical support and practical guidelines. Based on a concept analysis of the charge nurse role, the author looks at a theory-gap analysis regarding how patient assignments are made and proposes a ...
Nursing workloads directly influence a nurse's ability to assess thoroughly and promote excellent patient outcomes. When patient assignments aren't equitable, nurses. may feel inadequate and frustrated. Problems also can arise when all nurses are assigned the same number of patients without regard for acuity levels.
A nursing care plan (NCP) usually includes nursing diagnoses, client problems, expected outcomes, nursing interventions, and rationales. These components are elaborated on below: Client health assessment, medical results, and diagnostic reports are the first steps to developing a care plan.
Planning care is essential in the delivery of appropriate nursing care. Following assessment of a patient's needs, the next stage is to 'plan care' to address the actual and potential problems that have been identified. This helps to prioritise the client's needs and assists in setting person-centred goals. Planned care will change as a patient's needs change and as the nurse and/or other ...
A licensed nurse is still responsible for ensuring the assignment is carried out correctly. Delegation According to the NCSBN/ANA guideline, delegation applies when the delegatee is performing a "specific nursing activity, skill, or procedure that is beyond the delegatee's traditional role and not routinely performed."
Nurse definition: At its core, the definition of a nurse is a healthcare professional who uses their clinical skills to care for patients, as well as their families. Nurses also work in communities where they promote good health and well-being practices. Nurses work in myriad settings such as healthcare systems, outpatient care centers ...
Questions to Ask in Making the Decision to Accept a Staffing Assignment for Nurses. Registered nurses need to know their rights and responsibilities when considering a patient assignment. If you feel that you lack expertise on a unit and patient population , you don't just have the right to refuse an assignment there, you have an obligation ...
What is Nursing? Case study: Jack. This assignment will largely focus between the biological, psychological and social factors regarding the case study Jack and the link between what the nurse's role is. It will give attention to his injury, a fractured Distal Tibia and Fibula, which is effectively the shin bone. (Waugh, A and Grant, A. 2018).
The patient acuity tool. Each patient is scored on a 1-to-4 scale (1, stable patient; 2, moderate-risk patient; 3, complex patient; 4, high-risk patient) based on the clinical patient characteristics and the care involved (workload.) Each nurse scores his or her patients, based on acuity, for the upcoming shift and relays this information to ...
10 examples of professional development goals. Here are ten examples of professional development goals to inspire your own: 1. Develop a new skill set. Growing professionally often means expanding the arsenal of things you're able to do. What skill you choose to develop can depend on your industry, job, and personal preferences.
Welcome! You can use this tool to find and compare different types of Medicare providers (like physicians, hospitals, nursing homes, and others). Use our maps and filters to help you identify providers that are right for you. Find Medicare-approved providers near you & compare care quality for nursing homes, doctors, hospitals, hospice centers ...
Compensation for BSN nurses is significantly higher than for ADN RNs. Depending on where you live, you could earn upwards of $90K as a BSN nurse, according to ZipRecruiter, compared to an average salary of $75K for an ADN nurse. With the career opportunities available to BSN nurses, the differential expands as you assume more advanced roles and ...