Cookies on this website
We use cookies to ensure that we give you the best experience on our website. If you click 'Accept all cookies' we'll assume that you are happy to receive all cookies and you won't see this message again. If you click 'Reject all non-essential cookies' only necessary cookies providing core functionality such as security, network management, and accessibility will be enabled. Click 'Find out more' for information on how to change your cookie settings.

- Institutes and units

Oxford Institute of Digital Health
Connected health for better health
This dynamic, interdisciplinary hub for digital health research and teaching address es critical challenges and identif ies solutions harnessing innovations to improve health and health care.
The rapid development of digital technologies is a catalyst for a fundamental shift in both how we live, and how we manage our health. The digital transformation of health systems has the potential to deliver leaner, greener, and more person-centered services. The Oxford Institute of Digital Health is a forward thinking, interdisciplinary, and collaborative hub across academia, industry, health systems, and government agencies to ensure maximum social impact through the shaping of the future of health and health care.
It will harness digital technologies to provide solutions to some of the biggest health challenges for individuals and populations. To create an enduring legacy, the Institute will:
• unite disciplines and sectors to harness digital technology to tackle the health challenges of the twenty-first century;
• provide international leadership in this vital area for the future of health systems;
• develop much needed global capacity through a training pipeline of Master’s and Doctoral students; and
• undertake world-leading research using innovative methods with national and international collaborators.
In the first five years the Institute will focus on transforming primary care and public health in areas where health disparities are most pressing. Based in the Nuffield Department of Primary Care Health Sciences, it will leverage considerable expertise in data science and artificial intelligence, an outstanding track record in the development and evaluation of digital health technology, and leading work investigating the social and ethical aspects of health care to improve patient care and experience across areas such as cardiovascular diseases, mental health, and work with marginalised populations.
Our vision is for digital health to enable those at most risk of illness to be identified and treated earlier and given the tools to manage their health and care better. Richard Hobbs, Head of Department
Supporting the Oxford Institute of Digital Health
HOW YOU CAN HELP – GIVING TO THE OXFORD INSTITUTE OF DIGITAL HEALTH
We are seeking partners who share our vision in shaping the future of global health care and who will support the work of this ground-breaking Institute.
We offer a range of philanthropic opportunities.
Teaching, Capacity Building & Future Leaders

Evidence-Based Health Care

Applied Digital Health

Translational Health Sciences

Global Healthcare Leadership
Our key research themes.
- The Digital Transformation of Care
- Data Science and Artificial Intelligence
- Innovative Methods in Digital Health
- Building a Knowledge Powerhouse

DIGITAL INTERVENTION TO REDUCE SUICIDAL IDEATION FOR SYRIAN REFUGEES
This PhD project explores Syrian refugees’ cultural conceptualisations of mental health and wellbeing, coping strategies and help-seeking behaviour and will co-design the digital intervention to reduce suicidal ideation.

ADOLESCENT MENTAL HEALTH
Using creative arts and digital methods to collect experience data, the ATTUNE collaborative led by will build a digital public health resource and a serious game including elements of narrative exposure therapy.

During the peak of the first wave of COVID-19, Professor Ben Goldacre and colleagues developed the fully open-source, privacy-preserving software platform, OpenSAFELY to allow the open and reproducible analysis of 17 million electronic health records. Following this, the team published the preprint of their first study, examining risk factors for COVID-19 death which has been cited and used globally. This demonstrates the power of novel approaches to data science unlocking evidence from data.

RESEARCH SAVING LIVES THROUGH EARLIER CANCER DETECTION
An innovative new computer algorithm which screens an individual’s medical record to identify their risk of bowel cancer has been trialled successfully in 2.5 million patients.

During the pandemic, we rapidly engineered a secure new Oxford Clinical Informatics Digital Hub (ORCHID) to support clinical research. ORCHID immediately supported two national COVID-19 community treatment trials – PRINCIPLE for repurposed drugs and PANORAMIC for novel antivirals; national flu and COVID-19 surveillance; COVID-19 community diagnostics (RAPTOR); and COVID-19 risk and service recovery. New clinical trials will utilise ORCHID to accelerate recruitment and reduce costs.

DEVELOPING POPULATION BASED SYSTEMS TO DELIVER BETTER VALUE HEALTH CARE
One of our teams is leading work on value-based health care, which aims to get improved outcomes for patients at no greater cost, with the new G20 Hub for value based health care, in Rome and in Sao Paulo for Latin America.
Events and Resources
Events: click here for more information Resources: click here for more information
Digital health news
World hypertension day: How we’re tackling high blood pressure from pregnancy to later life
17 May 2024
Leveraging Digital Health for Better Patient Care and a Greener Healthcare System
23 April 2024
Bennett Institute for Applied Data Science part of project to help evaluate the new NHS Pharmacy First service
13 February 2024
Undergraduate Pathways event – a unique opportunity to explore career opportunities in primary healthcare
2 January 2024
- Insigneo Institute
PhD Programme in Digital Health
We are delighted to announce the launch of The Sheffield Children’s Hospital/Insigneo Institute PhD Programme in Digital Health in collaboration with Great Ormond Street Children’s Hospital.

We are delighted to announce the launch of The Sheffield Children’s Hospital/Insigneo Institute PhD Programme in Digital Health in collaboration with Great Ormond Street Children’s Hospital. There are four competition funded studentships in Paediatric Digital Healthcare Technology.
The PhD students will work together in a pioneering cross-disciplinary programme alongside patients, families, clinicians, engineers, computer scientists and other experts to develop new digital platforms and technologies that can address unmet needs in child health.
The research will focus on paediatric clinical care pathways and span the Insigneo Institute’s research themes of Healthcare Data, Artificial Intelligence and Smart Devices and Sensors. It will develop the concepts of:
- Digital Twins
- Digital Wards
- Digital Healthcare at Home
- Advanced Healthcare Communication
in paediatric real life healthcare settings with Sheffield Children’s Hospital and in collaboration with Great Ormond Street Hospital.
Funding for these PhDs is provided by the NIHR Great Ormond Street Biomedical Research Centre and Sheffield Children’s NHS Foundation Trust as part of their Paediatric Excellence Initiative. The NIHR Great Ormond Street Hospital BRC (GOSH BRC) is a partnership between Great Ormond Street Hospital and the University College London (UCL) Great Ormond Street Institute of Child Health (ICH). Now it’s in its fourth 5-year term, as part of a wider national collaboration - a BRC National Paediatric Excellence Initiative has been set up between GOSH BRC and children’s hospitals in Birmingham, Sheffield and Liverpool. GOSH BRC’s aim is to transform the health of children, and the adults they will become, by combining cutting edge research methods with world-leading clinical trial expertise, to accelerate discovery of new treatments for children with rare and complex conditions.
There are up to four projects available with a closing date of 21 April 2023. Find out more here: https://www.sheffield.ac.uk/insigneo/vacancies
Related information
Insigneo vacancies

Email: [email protected]
Telephone: +44 114 222 0158
Search for PhD opportunities at Sheffield and be part of our world-leading research.
King's College London
Centre for doctoral training in digital twins for healthcare.
Do you want to make a difference in digital advancements of healthcare? Do you want to bridge the gap between healthcare domain-based knowledge, state-of-the art computing, and personalisation techniques? Do you want to test your skills in real-life healthcare applications?
Join our Centre for Doctoral Training (CDT) in Digital Twins for Healthcare (DT4Health) at King’s College London!
DT4Health is an innovative PhD program located at King's, in the heart of London, arising as a joint forces collaboration between the Healthcare Faculties and the Faculty of Natural, Mathematical & Engineering Sciences .
Our mission is to train the next generation of leaders in healthcare technology to improve healthcare systems in the UK in a period of an ageing population and tightening financial constraints using the cutting-edge framework of Digital Twins.
Our Partners
DT4Health is continuously interested in attracting funding. If your organisation wants to be involved in projects on Digital Twins for Healthcare, please email us:
- Visit the Gateway
- Visit the Alliance
- Visit HDR UK Futures
HDR UK-Turing Wellcome PhD Programme in Health Data Science
This truly outstanding and generously funded four-year programme at top UK universities provides you a pathway to join the UK’s leaders in health data research.
What this unique PhD programme offers you
Four-year programme: An initial foundation year allows students to gain real experience and insight into health data research.

Hosted by leading universities: Our host universities are among the very best in health data research.
Nurturing each student: Our programme aims to identify the particular abilities and interests of each student, and gear their PhD experience to effectively develop them.
Leadership Programme: Students benefit from a bespoke expert-led programme to develop the skills they need to understand, collaborate and influence others.
Generous funding: Students have their tuition fees (UK Home rate), college fees (where applicable), research expenses and travel costs paid and receive an enhanced, tax-free stipend with increases every year. (Y1 outside London: £23,955, Y1 in London: £25,954)
Building networks and experience: We actively support students in building networks and contacts in academia, the NHS and industry as well as taking internships and other opportunities to gain real-world experience. This includes a post-PhD bursary to support your next career step.
Team spirit: Strong relationships are built between our entire cohort of students through joint activities that build a genuine team spirit.
Personal support: Each student has their own Director of Studies who is an additional point of contact during their time with us. All students are also further supported by the PhD team.

“The PhD programme has enabled me to gain first-hand experience in modern health data science approaches. It’s a truly unrivalled opportunity.” Steven Wambua
Who is the PhD programme for?
We recruit enthusiastic, talented students who want to use data-driven research to develop and shape the UK’s response to the most complex health challenges of our times.
Applicants must have (or be on track to obtain):
- A first class or 2:1 undergraduate degree in statistics, mathematics, computer / data science, physics or an allied subject or
- Another undergraduate degree subject and outcome but can demonstrate their suitability for this programme through additional qualifications or research experience.
Active or currently registered health care professionals are not eligible and should consider the Wellcome PhD Fellowships for Health Professionals .
Applicants also need to meet the following criteria:
- Successful admission to the specified degree programme at one of our partner universities. Students will be expected to meet the admissions requirements of that department and university but do not need to hold the offer at the point of application.
- Two satisfactory academic or relevant references.
- Proof of a legal right to study in the UK or ability to satisfy the current requirements of UK Visa and Immigration.
Training is in-person, hybrid and virtual throughout the first year.
We are committed to a diverse and inclusive research culture . We welcome those who are returning from the workplace, international candidates and everyone underrepresented in STEM and academia. For further details see our FAQs .
We cannot accept applicants who are looking for a part-time PhD or those who are aiming to study whilst continuing to be employed elsewhere.
We aim to accommodate specific needs and personal circumstances. Please make us aware of individual circumstances when applying or contact us directly at [email protected] . Please note our applicant privacy notice .
If you have questions or require adjustments to the application process, please contact us below via email or telephone (+44 (0)770 847 8846).
There are no nationality restrictions and international students are able to apply. However, applicants are advised the award only covers fees at the UK/Home level. International students will be required to secure an additional scholarship from Queen’s University Belfast (after receiving a offer from us at interview) to cover the difference between Home and Overseas fees. This will limit the university choices available:
(Please be aware that these are usually highly competitive and will need to be applied for separately in your application to Queen’s University Belfast post-offer. A successful application to the PhD programme does not guarantee a fee waiver or scholarship. We do not accept applications from candidates who are self-funding.)
We are currently only recruiting for Queen’s University Belfast.
These are only initial programmes of study for Year 1. Students may transfer to a new university programme from Year 2 after research projects have been confirmed.
Is this the PhD future for you?
Watch our Applicant Open Day hosted by our current students to find out more about the programme and whether it’s for you.
Applications are currently: Closed
The application process.
Details required:
- Contact details
- Details and transcripts of university qualification(s)
- Any relevant job history
- Answers to personal-statement type questions (250-words maximum for each answer)
- Contact details for two referees
- There is no need to apply to the university, submit a research proposal, provide IELTS scores or contact supervisors at this stage
Submitted applications will first be checked for eligibility and then will undergo a first stage review. This will involve triage by the PhD Team in April 2024 . Successful applicants will be invited to an interview in May 2024 .
After receiving an offer, applications will be invited to apply to Queen’s University Belfast.

Selection criteria
Applicants should demonstrate that they meet the following criteria:
* These criteria will be assessed at interview via a pre-interview exercise.
HDR UK reserves the right to reject applicants who do not meet the criteria at any stage. Regretfully, we can only provide feedback for candidates who reach interview.
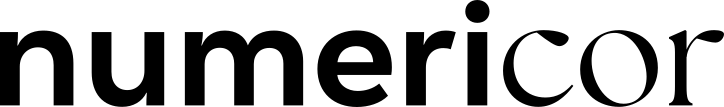
Programme Structure
The four-year programme is divided in two. There is an initial Foundation Year followed by a three-year research project. The first year combines the best in university-based training with HDR UK-led national activities. And we support students to produce game-changing research plans and their projects are backed by substantial research funding.

Foundation year
3-5 day immersion events allow students to gain insight into the work of HDR UK, and our academic, clinical and industry partners. Courses may be residential (expenses provided) with up to a week away from their home university or online. Students undertake an intensive deep dive into an important area of health data science. Immersion topics include risk prediction, oncology, clinical trials, epidemiology and bioinformatics. Past immersion weeks have been hosted by the Universities of Birmingham, Manchester, Oxford and University College London and the European Bioinformatics Institute.
The immersion events encourage students to work together and stimulate new interactions:
- Axes of Prognosis
- The Different Facets of Data
Research areas
PhD research projects can be linked to The Institute’s:
- Research priorities
- Research hubs
- Partnerships
Team working
Students operate as a national cohort and work collaboratively with others, overcoming traditional institutional silos. Students are registered with a partner university but can draw on academic expertise from across the HDR UK network and are supported to formulate research activities that bring together experts from across the UK.
- You can contact us at [email protected] or phone (+44 (0)770 847 8846).
- For details of how we process applicants’ data see PhD Applicant Privacy Notice .
Students have access to graduate-level courses and research project rotation in their university to introduce them to different areas of health data science and enable them to develop a bespoke research project under the guidance of our expert university leads.
Regular workshops and short courses introduce students to the work of HDR UK experts across our hubs, themes and priority areas and to external organisations. Past contributors have included NHSX, IQVIA and AstraZeneca.
Immersion and workshop events allow students to better understand the wider health and social care landscape and accelerate their potential to become sector leaders. They also enable students to develop more ambitious PhD research projects by stimulating collaboration with external academics, industry-based organisations, or by using national data infrastructure.
Training is provided by academic, industry and NHS experts to promote personal and professional development in leadership capability, cross-sector collaborative skills and inter-disciplinary working. In particular, HDR UK is committed to working with public and patients to build increased trust in health data research as well as designing solutions focused on improving patient outcomes and experience. Students will develop communication and collaborative skills to help put them at the forefront of this mission.
At the end of the Foundation Year students design a bespoke three-year research project and a multi-disciplinary supervision team based on their training experiences.
Research proposals will be rigorously reviewed by expert academics and public-patient representatives to ensure they are of the highest standards in terms of ambition, scientific methodology and impact on patient outcomes.
The research will be carried out at their home university and could be linked to HDR UK research priorities , research hubs or partnerships .

This includes short immersions plus longer practical real-world projects with businesses and other organisations at the cutting edge of everything from medical devices, to life sciences, to vaccines. Students also learn about leadership theory and attend specially-convened seminars from senior figures in relevant areas of healthcare.
Networks and experience: Students will be actively supported in building networks and contacts in academia, the NHS and industry as well as taking internships and other opportunities to gain real-world experience.
Team working: Students operate as a national cohort, building strong relationships through joint activities and overcoming traditional institutional silos.
Workshops: Regular workshops and short courses introduce the work of HDR UK experts and to external organisations.
Immersion events: These allow students to better understand the wider health and social care landscape and accelerate students’ potential to become a sector leader. They also enable them to develop an ambitious PhD research project.
Researcher development: Training is provided by academic, industry and NHS experts to promote personal and professional development in cross-sector collaborative skills, communication and inter-disciplinary working.
“Our Leadership Programme will give PhD students the chance to develop the practical skills they need to bring people together to use health data science to deliver much-needed innovations and advances in health and care,” Professor Peter Bannister
Our partners
Programme partners include NHS Digital, AstraZeneca, Moorfields Eye Hospital NHS Foundation Trust, and University Hospitals Birmingham.
More broadly it will work with winners of the NHSX AI Innovation Award , which funds and supports promising artificial intelligence technologies in health and care. There will also be opportunities with businesses on the DTI listed top 100 digital health innovators which are using big data for healthcare innovation.

Master’s Degree Scholarships
We offer 10 annual Master’s degree scholarships worth £10,000 for students with an interest in dementia or diabetes research.

Undergraduate Summer Internship in Health Data Research
Apply for a summer work placement in health data research at a UK research organisation, with an HDR UK-Wellcome Biomedical Vacation Scholarship
Join the HDR UK Alumni Network
HDR UK’s online Alumni Network brings together the amazing people who have been part of our training and education programmes.
Our host universities

- - - - Meet our PhD students
Our PhD students come from a wide range of backgrounds - discover who they are and what their experiences have been as part of the PhD programme
Meet the PhD Programme team

Our wider team consists of leading experts in disciplines including theoretical physics, computer science, mathematics and statistics, applied mathematics and biochemistry.
- Miguel Bernabeu – University of Edinburgh
- Ioanna Manolopoulou – University College London
- Niels Peek – University of Manchester
- Iain Styles – Queen’s University Belfast
- Paul Taylor – University College London
- Catalina Vallejos – University of Edinburgh
- Angela Wood – University of Cambridge
- David Wong – University of Manchester
- Tom Nichols – University of Oxford
- Magnus Rattray – University of Manchester

Alternatively, use our A–Z index

Attend an open day
PhD/MPhil Health Informatics / Course details
Year of entry: 2024
- View full page
Programme description
Our PhD/MPhil Health Informatics programme enables you to undertake a research project that will improve understanding of Health Informatics.
Health informatics and data science is set to revolutionise healthcare by providing a deeper understanding between healthcare delivery, outcomes and patients as well as empowering people to manage their own health.
Manchester has considerable breadth and expertise in this field, being home to the Centre for Health Informatics which encompasses researchers with an international reputation in the field. Our centre is truly multi-disciplinary, blending traditional academia with engineering, infrastructure and project management.
Our main research themes include the following:
- Connected Health (mHealth and wearables)
- Actionable Analytics
- Stratified Medicine
- Data Science Methods (methodological research in statistics, epidemiology and machine learning)
- Predictive Analytics
Please see our website for further details ( Health eResearch Centre ).
Special features
Training and development
All of our postgraduate researchers attend the Doctoral Academy Training Programme delivered by the Researcher Development team . The programme provides key transferable skills and equips our postgraduate researchers with the tools to progress beyond their research degree into influential positions within academia, industry and consultancy. The emphasis is on enhancing skills critical to developing early-stage researchers and professionals, whether they relate to effective communication, disseminating research findings and project management skills.
Teaching and learning
Applicants are specifically matched with a Primary Supervisor and individual project based on their research interests and background.
International applicants interested in this research area can also consider our PhD programme with integrated teaching certificate .
This unique programme will enable you to gain a Postgraduate Certificate in Teaching and Learning, whilst also carrying out independent research on your chosen project.
Scholarships and bursaries
Funded programmes and projects are promoted throughout the year. Funding is available through UK Research Councils, charities and industry. We also have other internal awards and scholarships for the most outstanding applicants from within the UK and overseas.
For more information on available the types of funding we have available, please visit the funded programmes and funding opportunities pages.
What our students say
Disability support.

Digital Health and Social Care research group
Conducting research into digital technologies in health and social care.
The use of digital technologies, such as video consultations, mobile phone apps and ways of monitoring peoples’ symptoms at home are becoming common across health and social care.
The Digital Health and Social Care Research Group (DHSCRG) is based in the Division of Nursing, Midwifery and Social Work at The University of Manchester.
We are a multidisciplinary group that carries out research exploring the use of these technologies in health and social care settings.
We work collaboratively with other research groups in the Division, as well as across the University, UK and internationally.
Our focus is on the use of digital technologies in the nursing, midwifery, allied health professional and social work professions. We hold regular research meetings where we focus on issues related to the development and use of digital technology in health and social care settings.
On this page:
Our research
- Public engagements
- Training opportunties
We work collaboratively with research groups across the Division and the wider University for two key aims.
Developing digital technologies
Aim: To develop digital tools and technologies that can be used to help support health and social care professionals and patients in their care.
Lead: Helen Hawley-Hague
Key researchers
- Emma Stanmore
- Siobhan O’Connor
- Sorrel Burden
- Dawn Dowding
Evaluating digital technologies
Aim: To evaluate how well digital technologies work in health and social care settings and how it impacts on patient care or other outcomes
In this theme we explore:
- How introducing digital technologies affects the way health and social care is delivered.
- How their use can impact on patients, and other care recipients. This includes a focus on potential digital inclusion/exclusion of marginalised groups.
Lead: Dawn Dowding
- Helen Hawley-Hague
- Dharman Jeyasingham
- Paul Clarkson
Amy Vercell
Key projects.
- Assembling the Data Jigsaw: Powering Robust Research on the Causes, Determinants and Outcomes of MSK Disease
- Developing a Social Care Strengths and Vulnerability Index (SC-SVI) for older people
- Development of a decision support tool for older people and their families who pay for social care
- Explore the findings of the evaluation of remote physiotherapy services
- Keep On Keep Up (KOKU app): a digital physical activity programme to prevent falls in older people
- National evaluation of remote physiotherapy services during the COVID-19 Pandemic
- Personalising renal function monitoring and interventions in people living with heart failure: RENAL-HF
- TOGETHER: Using Smartphone Technology in Home Exercise Interventions. Watch the TOGETHER video on YouTube.
< Back to top
Find out more about the people working in the Digital Health and Social Care Research Group.
Professor Dawn Dowding
Dawn is Professor in Clinical Decision Making and Lead for the group.
She has an interest in the development and evaluation of decision support technologies.
View Dawn’s research profile
Dr Helen Hawley-Hague
Helen is a Research Fellow and Deputy Lead for the group.
She has a particular interest in developing and evaluating technologies to support healthy ageing, falls prevention to support rehabilitation, and in the use of healthcare.
View Helen’s research profile
Dr Emma Stanmore
Emma is Reader and Lead of Healthy Ageing Research Group
View Emma’s research profile
Professor Susan Kirk
Susan has long-standing interests in relation to how health technology shapes personal identities and relationships, and its role in supporting self-management for children and adults living with long-term health conditions.
View Susan’s research profile
Dr Alex Hall
Alex is a Research Fellow with interests in implementation of technologies in health and social care settings, and in questions concerning digital inclusion/exclusion of older adults.
View Alex’s research profile
Dr Dharman Jeyasingham
Dharman is a Lecturer in Social Work.
View Dharman’s research profile
Dr Paul Clarkson
Dr Paul Clarkson is a Senior Lecturer in Social Care and undertakes research on service evaluation for adults with serious and longstanding mental health problems; older people and long-term care; psychological and social care services for military veterans; cost-effectiveness analyses (with a particular focus on social care); policy evaluations; preference elicitation studies; dementia home support; preventative assessment in adults and older people.
View Paul’s research profile
Dr Katherine Rogers
Katherine is a Research Fellow, involved in the Social Research for Deaf People (SORD) group, which she co-leads.
View Katherine’s research profile
Dr Ross Atkinson
Dr Ross Atkinson is Programme Manager in the National Institute for Health Research Applied Research Collaboration – Greater Manchester (NIHR ARC-GM) and support the digital health theme within the ARC-GM.
View Ross’s profile here
Dr Janice Christie
Dr Janice Christie is a Senior Lecturer who undertakes research on wound care and community/public health related matters.
View Janice’s profile here
Amy is the Chief Clinical Information Officer for Nursing and Allied Health Professionals and an Acute Oncology Advanced Nurse Practitioner at the Christie NHS Foundation Trust. In 2021, she completed a NIHR ARC GM funded pre-doctoral fellowship supervised by Professor Dawn Dowding and Professor Janelle Yorke. She frequently collaborates with the other digital health researchers, bringing a wealth of clinical expertise, and utilising her research findings within her Christie role to ensure any digital interventions implemented are evidenced based and clinically meaningful.
View Amy’s LinkedIn profile here

Public engagement
Whenever we do anything around technology development we like to get patients and the public involved from the start of the process (conception) through to development.
For example, the Keep On Keep Up (KOKU) app was co-designed with older adults to ensure it was as personalised as possible to meet their needs. Watch a YouTube video by Dr Emma Stanmore who discusses the design and evaluation of this mobile app to encourage physical activity and prevent falls in older people.
The TOGETHER study (NIHR Fellowship) we engaged patients throughout the process and our patient representatives helped demonstrate the technology to new participants interested in taking part in the trial. Watch a YouTube video about the apps designed to support falls rehabilitation and patient and health professionals’ experiences of them.
Training opportunities
We are happy to supervise students who would like to conduct a PhD in the area of digital technologies in the health and social care professions.
A number of our PhD students have funded studentships from the NIHR .
Find PhD projects and information on funding and self-funding at the following links:
- Search for a project
- Find funded programmes
- See all PhD programmes
- Postgraduate research funding
Find out more about the PhD students working in the Digital Health and Social Care Research Group.
Norina Gasteiger
Norina is a PhD student, funded by the NIHR ARC (GM), who is undertaking a realist evaluation of extended reality (augmented and virtual reality) training to upskill care home workers in hand hygiene.
View Norina’s research profile
Claire Ford
Claire Ford is a PhD student who is designing, developing and feasibility testing virtual realtiy (VR) as a method of educating care home and nursing home staff in falls prevention.
View Claire’s LinkedIn profile here
Josh Devlin
Josh is a PhD student, funded by the ESRC / North West Social Science Doctoral Training Partnership, and is exploring the physical, imagined and discursive mobilities and sense-making in child protection social work.
View Josh’s profile here
Jo Fan is a PhD student, funded by the Ministry of Education in Taiwan, and his research is exploring the usability of continuous monitoring and deterioration alerting systems.
View Jo-Fan’s LinkedIn profile here
Sally Hoodless
Sally is a PhD student, funded by the Dunhill Medical Trust, who is examining technology assisted implementation of the FaME falls prevention programme among community-dwelling older adults.
View Sally’s research profile here
If you would like to find out more about our research group or to join, please email the Lead, Professor Dawn Dowding.
Email: [email protected]
+44 (0) 161 306 6000
The University of Manchester Oxford Rd Manchester M13 9PL UK
Connect With Us
The University of Manchester

- Antimicrobial Therapy
- Blood Brain Barrier Disruption
- Cardiovascular Disease
- Mechanobiology
- Orthopaedic Disease
- Targeted Drug Activation
- Publications
- Clinical Themes
- Technical Themes
- Translational Themes
Acute and Critical Care
Complex disease, infectious disease, low and middle-income settings, non-contact vital sign monitoring, remote monitoring in the home, self-management using smartphone apps, translational studies, wearables for digital health.
- Ablative Therapies
- Enhanced Drug Delivery
- Shockwave Therapies
- Therapy Monitoring
- Triggered Drug Release
- Bioelectronic Medicines
- Brain Drug Delivery
- Neural Tissue Engineering
- Neurofeedback Technologies
- Neurovascular Assessment
- Transcranial Magnetic Stimulation
- Transcranial Ultrasound Stimulation
- 3DMed Interreg 2 Seas Consortium
- Early Cancer Detection
- Infectious Disease Home Testing
- Rapid Nucleic Acid Test for Covid-19
- Research Areas
Digital Health covers a wide range of research at the Institute of Biomedical Engineering. It focuses mostly on “AI in healthcare”, sometimes known as Clinical AI, at the interface between machine learning and health informatics, but also on the use of wearables and video cameras to acquire vital-sign data.
The Computational Health Informatics (CHI) Lab shares a common interest in deep learning, Bayesian inference, and related methods. It has access to some of the world’s largest, curated, anonymised healthcare datasets, and includes work with wearables and hospital data, across scales from the massively multivariate (including anonymised genomics) to the high-rate data acquired from medical devices. The systems developed are routinely used in the care of patients within the UK National Health Service, and for improving access to healthcare in low- and middle-income countries (LMICs).
The Biomedical Signal Processing & Machine Learning (BSP-ML) research group aims to deliver patient care agnostic to patient location, through state-of-the art monitoring technology and algorithms, together with alerting systems appropriate to the patient environment, in collaboration with the Critical Care Research Group led by Professor Peter Watkinson. The group’s recent focus has been on adapting the technology, apps and machine learning algorithms developed in the last decade for the fight against COVID-19, through remote patient monitoring, better patient stratification and improved diagnostics.
Clinical collaboration is at the heart of all projects in the Digital Health research area, with biomedical engineers working alongside clinical colleagues, which ensures that each project feeds directly into the care of patients in hospitals or at home.

We use cookies to help our site work, to understand how it is used, and to tailor ads that are more relevant to you and your interests.
By accepting, you agree to cookies being stored on your device. You can view details and manage settings at any time on our cookies policy page.

Digital health research cluster
Our vision is to lead research in collaboration with engineering colleagues, commercial partners and citizens to create health technologies that are accessible for people using health services and their families; and demonstrate evidence of improvements in health, well-being and social care outcomes.
Research interests
Healthcare delivery in 2030 will be vastly different from today. People will be living longer, with multi-morbidity. Integrated care will be central to delivering complex care to this dynamic population and the social context of people’s lives remain the key determinant of how health services are planned and delivered.
Technological innovations will transform the way we diagnose, treat and manage disease. Delivering care closer to people’s homes will be the norm and hospital-based care will be for the seriously ill.
Our research focuses on creating and investigating on technological solutions to improve access and delivery of health care. We are interested in developing personalised models of care that will lead into delivery of patient centred care.
Research areas
- Internet of things and technology integrated health care system
- Remote monitoring and management of conditions
- Digital solutions (apps, wearables, monitors) for patients support
- Predictive risk modelling
- Digital access to primary/community care services (e.g. electronic medical records and e-consultations)
- Digital access and technology use by vulnerable and hard to reach groups.
Methodological expertise
- User-led co-design
- Behaviour change interventions
- Data mining
- eHealth system development
- Evaluation and implementation
- Creating a living laboratory and simulated environments to provide test beds for new technology.
Research projects
- Unlocking data to inform public health policy and practice: Exploring barriers and creating solutions for public health intelligence using integrated datasets across Kent, Sussex and Surrey (KSS). (J Armes)
- Virtual consultations for people with learning disabilities, their families and healthcare providers: Using Experience-Based Co-Design to explore experiences, adapt, develop and implement best-practice guidance and training resources. ARC KSS Towards Changing Practice. (Mold, F., Cooke, D., Armes, J ., Cox, A.)
- The role of Electronic Frailty Index in improving outcomes for newly diagnosed Cancer patients undergoing systemic Chemotherapy treatment - EfFICACY study. (Armes J.)
- AI Health and Care Award Technology Specific Evaluation Team for the evaluation of DERM (Skin Analytics). (Armes J.)
- Methodologies for evaluation of digital health interventions employed to improve management of long term conditions. (N Gityamwi J Armes)
- CLUSTER: Discover, replicate and validate biomarkers for prediction of treatment response to drive stratified medicine approaches in JIA and JIA-uveitis. (Geifman)
- MICA: NURTuRE - changing the landscape of renal medicine to foster a unified approach to stratified medicine (Geifman)
- Identifying biomarkers that improve disease detection in companion animals (Geifman)
- Emergency medical services Streaming-Enabled Evaluation In Trauma: the SEE-IT Trial (Taylor, Lyon, Maben, Magnusson, Munro) www.surrey.ac.uk/SEEITstudy
- Non-inflammatory proteomic signatures of COVID-19 (Geifman)
- Web-based self-management to reduce distress after prostate cancer [ Sara Faithfull and Jane Cockle-Hearn ]
- Developing and trialling a life-long approach to promote diabetes self-management amongst adults with type 1 diabetes-DAFNEplus [ Debbie Cooke ]
- The BEAT diabetes program - an online, supported self-management for adults with type 2 diabetes [ Debbie Cooke ]
- Data driven digital decision-making tool for pharmacists to provide a physical assessment and lifestyle prescription for men with prostate cancer [ Agnieszka Lemanska ]
- TIHM: Technology Integrated Health Management [ Payam Barnaghi (PI, 5G Centre), Emma Ream and Rahim Tafazolli (from 5G Centre) ]
- Randomised controlled trial to evaluate electronic symptom management using the Advanced Symptom Management System (ASyMS) Remote Technology for patients with cancers [ Jo Armes (PI) and Emma Ream ]
Collaborations
The digital health research grouping has a range of multidisciplinary collaborations with patient/public groups, academic organisations and health providers and networks across Kent, Surrey and Sussex, and industry both nationally and internationally. It also contributes to the digital innovation theme of the Applied Research Collaboration (ARC) for Kent, Surrey and Sussex.
Areas of interest for doctoral study
We welcome approaches from people wishing to undertake postgraduate research here with us.
We particularly welcome enquiries in the following areas:
- Remote monitoring and management of symptoms in cancer and other long-term conditions
- Decision support systems for healthcare professionals
- Biosensing to support improved health outcomes for patients
- Online Access in primary care both in terms of patients’ access to medical records or online services, and use by healthcare professionals
- Digital systems/solutions to support student and staff mental health and wellbeing.
Please contact Freda Mold ( [email protected] ) and Jenny Harris ( [email protected] ), our postgraduate research directors, if you are considering postgraduate research.
Publications
- Cooke EA, Lemanska A, Livings J and Thomas SA. The Impact of COVID-19 on Mental Health Services in Scotland, UK. (2022) https://pubmed.ncbi.nlm.nih.gov/35773806/
- Hajira Dambha-Miller, William Hinton, Christopher R Wilcox, Agnieszka Lemanska, Mark Joy, Michael Feher, Beth Stuart, Simon de Lusignan, Julia Hippisley-Cox, Simon Griffin, Mortality from angiotensin-converting enzyme-inhibitors and angiotensin receptor blockers in people infected with COVID-19: a cohort study of 3.7 million people, Family Practice , 2022;, cmac094, https://doi.org/10.1093/fampra/cmac094
- Britt W Jensen, Charlotte Watson, Nophar Geifman, Jennifer L Baker, Ellena Badrick, Andrew G Renehan; Weight changes in type 2 diabetes and cancer risk: a latent class trajectory model study. Obesity Facts (2022)
- Ford, E., Stanley, K., Rees-Roberts, M., Giles, S., & Goddard, K., & Armes, J. (2022). Understanding Public Priorities and Perceptions of the Use of Linked Healthcare Data in South East England. In Challenges of Trustable AI and Added-Value on Health. 0.3233/SHTI220538.
- Oulton K, Williams A, Gibson F. (2022)Acceptability of a novel device to improve child patient experience during venepuncture for blood sampling: Intervention with ‘MyShield’, In: Journal of child health care Sage DOI: 10.1177/13674935221098297
- Britt W Jensen, Charlotte Watson, Nophar Geifman, Jennifer L Baker, Ellena Badrick, Andrew G Renehan; Weight changes in type 2 diabetes and cancer risk: a latent class trajectory model study. Obesity Facts (2022) DOI: 10.1159/000520200
- Sipanoun P, Oulton K, Gibson F, Wray J. (2022)The experiences and perceptions of users of an electronic patient record system in a pediatric hospital setting: a systematc review, In: International journal of medical informatics160104691 Elsevier DOI: 10.1016/j.ijmedinf.2022.104691
- Sipanoun P, Jo Wray J, Kate Oulton K, Gibson F. (2022) What are the ethical and legal considerations of young people and their parents using a hospital patient portal: hospital Ethics Committee members perspectives, In: Clinical ethics Sage
- Callwood A, Gillam L, Christidis A, Doulton J, Harris J, Piano M, Kubacki A, Tiffin P, Roberts K, Tarmey D, Dalton D, Valentin V. (2022) Feasibility of an automated interview grounded in Multiple Mini Interview (MMI) methodology for selection into the health professions: an international multi-methods evaluation, In: BMJ Open
- Smith G, Harcourt S, Hoang U, Lemanska A, Elliot A, Morbey R, Hughes H, Lake I, Edeghere O, Oliver I, Sherlock J, Amlôt R, de Lusignan S. (2022)Observational study of mental health presentations across healthcare setting during the first 9 months of the COVID-19 pandemic in England, In: JMIR Public Health and Surveillance JMIR Publications DOI: 10.2196/32347
- Stephanie JW Shoop-Worrall, Katherine Cresswell, Imogen Bolger, Beth Dillon, Kimme L Hyrich, and Nophar Geifman. Nothing about us without us: involving patient collaborations for machine learning applications in rheumatology. Annals of the Rheumatic Diseases (2021) DOI: 10.1136/annrheumdis-2021-220454
- Mold F, Cooke D, Ip A, Roy, P., Denton, S. & Armes, J. 2021. COVID-19 and beyond: virtual consultations in primary care—reflecting on the evidence base for implementation and ensuring reach: commentary article. BMJ Health & Care Informatics; 28: e100256. doi: 10.1136/bmjhci-2020-100256
- Tucker DA, Hendy J, Chrysanthaki T. (2021) How does policy alienation develop? Exploring street-level bureaucrats' agency in policy context shift in UK telehealthcare, In: Human Relationspp. 1-28 SAGE Publications DOI: 10.1177/00187267211003633
- Jeffreys N, Dambha-Miller H, Fan X, Ferreira F, Liyanage H, Sherlock J, Williams J, Rice R, Stunt A, Faithfull S, Gatenby P, Lemanska A, de Lusignan S. (2021) Using Primary Care Data to Report Real-World Pancreatic Cancer Survival and Symptomatology, In: Studies in health technology and informatics281pp. 168-172 IOS Press DOI: 10.3233/SHTI210142
- Maguire R, McCann L, Kotronoulas G, Kearney N, Ream E, Armes J, Patiraki E, Furlong E, Fox P, Gaiger A, McCrone P, Berg G, Miaskowkski C, Cardone A, Orr D, Flowerday A, Katsaragakis S, Darley A, Lubowitzki S, Harris J, Skene S, Miller M, Moore M, Lewis L, DeSouza N, Donnan PT. Real time remote symptom monitoring during chemotherapy for cancer: European multicentre randomised controlled trial (eSMART). BMJ. 2021 Jul 21;374:n1647. doi: 10.1136/bmj.n1647.
- McMillan B, Davidge G, Brown L, Lyons M, Atherton H, Goulding R, Mold F, Morris RL, Sanders C. (2021) A qualitative exploration of patients' experiences, needs and expectations regarding online access to their primary care record. BMJ Open. 2021 Mar 11;11(3):e044221.
- Taylor C, Harris J, Stenner K, Sevdalis N, Green JSA (2021) A multi-method evaluation of the implementation of a cancer teamwork assessment and feedback improvement programme (MDT-FIT) across a large integrated cancer system. Cancer Medicine : DOI: 10.1002/cam4.3719
- Harris, J., Purssell, E., Cornelius, V., Ream, E., Jones, A. & Armes, J. Development and internal validation of a predictive risk model for anxiety after completion of treatment for early stage breast cancer. (2020), Journal of Patient-Reported Outcomes. 4, 1, 103. https://doi.org/10.1186/s41687-020-00267-w
- Harris, J., Purssell, E., Ream, E., Jones, A., Armes, J. & Cornelius, V. How to Develop Statistical Predictive Risk Models in Oncology Nursing to Enhance Psychosocial and Supportive Care. (2020), Seminars in Oncology Nursing. 36, 6, 151089. https://doi.org/10.1016/j.soncn.2020.151089
- Cheng, K.K-F., Siah, R.C-J., Ream, E., Kanesvaran, R., & Armes J. (2020). Protocol for a scoping review of digital health for older adults with cancer and their families. BMJ Open 10:e038876.doi: http://dx.doi.org/10.1136/bmjopen-2020-038876
- Frohlich DM, Corrigan-Kavanagh E, Campbell S, Chrysanthaki T, Castro P, Zaine I, da Graça Campos Pimentel M. (2020) Assistive media for wellbeing, In: HCI and design in the context of dementia Springer International Publishing DOI: 10.1007/978-3-030-32835-1
- Lemanska A, Faithfull S, Liyanage H, Otter S, Romanchikova M, Sherlock J, Smith N, Thomas S, S de Lusignan S. (2020) Primary Care Prostate Cancer Case Ascertainment, In: Studies in health technology and informatics270pp. 1369-1370 IOS Press DOI: 10.3233/SHTI200446
- Lemanska A, Byford RC, Cruickshank C, Dearnaley DP, Ferreira F, Griffin C, Hall E, Hinton W, de Lusignan S, Sherlock S, Faithfull S. (2020) Linkage of the CHHiP randomised controlled trial with primary care data: a study investigating ways of supplementing cancer trials and improving evidence-based practice, In: BMC Medical Research Methodology20(198) BMC DOI: 10.1186/s12874-020-01078-9
- Davidge G, Sanders C, Hays R, Morris R, Atherton H, Mold F, McMillan B. (2020) What do patients want? A qualitative exploration of patients' needs and expectations regarding online access to their primary care record. Br J Gen Pract. 2020 Jun;70(suppl 1):bjgp20X711245.
- Cheng, K.K-F., Siah, R.C-J., Ream, E., Kanesvaran, R., & Armes J. Protocol for a scoping review of digital health for older adults with cancer and their families. BMJ Open . 2020
- Nwolise C, Carey N , Shawe J. Exploratory study of clinician and patient views regarding the use of a Preconception Care app for women with diabetes, Health Informatics Journal . 2020, 1 (16) DOI: 10.1177/1460458220921707
- Frohlich David M., Corrigan-Kavanagh Emily, Campbell Sarah, Chrysanthaki Theopisti , Castro Paula, Zaine Isabel, Campos Pimentel Maria da Graça (2020) Assistive media for wellbeing, In: HCI and design in the context of dementia Springer International Publishing. DOI: 10.1007/978-3-030-32835-1
- Marcu A, Muller C, Ream E, Whitaker KL. (2019)Online information-seeking about potential breast cancer symptoms Capturing online behaviour with an Internet browsing tracking tool. Journal of Medical Internet Research Journal of Medical Internet Research
- Mold F , Hendy J, Lai YL, de Lusignan S. Electronic Consultation in Primary Care Between Providers and Patients: Systematic Review. JMIR Med Inform. 2019 Dec 3;7(4):e13042. doi: 10.2196/13042
- Frankland Jane, Brodie Hazel, Cooke Debbie , Foster Claire, Foster Rebecca, Gage Heather, Jordan Jake, Mesa-Eguiagaray Ines, Pickering Ruth, Richardson Alison. Follow-up care after treatment for prostate cancer: evaluation of a supported self-management and remote surveillance programme, BMC Cancer . 2019; 19 (1) DOI: 10.1186/s12885-019-5561-0
- Payo RM, Harris J, Armes J . Prescribing fitness apps for people with cancer: a preliminary assessment of content and quality of commercially available apps. Journal of Cancer Survivorship. 2019 Jun 15;13(3):397-405
- Marcu A, Muller C, Ream E , Whitaker KL. Online Information-Seeking About Potential Breast Cancer Symptoms: Capturing Online Behaviour With an Internet Browsing Tracking Tool J Med Internet Res 2019;21(2):e12400 DOI: 10.2196/12400
- Furlong E, Darley A, Fox P, Buick A, Kotronoulas G, Miller M, Flowerday A, Miaskowski C, Patiraki E, Katsaragakis S, Ream E, Armes J , Gaiger A, Berg G, McCrone P, Donnan P, McCann L, Maguire R. Adaptation and Implementation of a Mobile Phone–Based Remote Symptom Monitoring System for People with Cancer in Europe. JMIR cancer . 2019;5(1):e10813
- Papachristou N, Barnaghi P, Cooper B, Kober KM, Maguire R, Paul SM, Hammer M, Wright F, Armes J , Furlong EP, McCann L, Conley YP, Patiraki E, Katsaragakis S, Levine JD, Miaskowski C. Network analysis of the multidimensional symptom experience of oncology. Scientific reports. 2019 Feb 19;9(1):1-1
- Papadatou-Pastou, M., Campbell-Thompson, L., Barley, E . et al. Exploring the feasibility and acceptability of the contents, design, and functionalities of an online intervention promoting mental health, wellbeing, and study skills in Higher Education students. Int J Ment Health Syst 2019; 13 ( 51). https://doi.org/10.1186/s13033-019-0308-5
- Rostill H, Nilforooshan R, Morgan A, Barnaghi P, Ream E, Chrysanthaki T. (2018) Technology integrated health management for dementia, In: British Journal of Community Nursing23(10)pp. 502-508 Mark Allen Healthcare. DOI: 10.12968/bjcn.2018.23.10.502View abstract
- A.R.R. Abrahao, P.F.C. da Silva, D.M. Frohlich, T. Chrysanthaki, A. Gratão, P.C. Castro (2018) Mobile digital storytelling in a Brazilian care home, In: Lecture Notes in Computer Science: HCI International 2018 - Conference Proceedings10926pp. 403-421 Springer DOI: 10.1007/978-3-319-92034-4_31
- Lemanska A, Dearnaley D, Sydes MR, Faithfull F. (2018) Older age, early symptoms and physical function are associated with the severity of late symptom clusters for men undergoing radiotherapy for prostate cancer, In: Clinical Oncology30(6)pp. 334-345 Elsevier DOI: 10.1016/j.clon.2018.01.016
- Mold F, Raleigh M, Alharbi NS, de Lusignan S. (2018) The Impact of Patient Online Access to Computerized Medical Records and Services on Type 2 Diabetes: Systematic Review. Journal of Medical Internet Research. 2018;20(7):e235.
- Liyanage H, Liaw ST, Konstantara E, Mold F, Schreiber R, Kuziemsky C, Terry AL, de Lusignan S. (2018) Benefit-risk of Patients' Online Access to their Medical Records: Consensus Exercise of an International Expert Group. Yearb Med Inform. 2018 Aug;27(1):156-162.
- Mold F , Raleigh M, Alharbi NS, de Lusignan S. The Impact of Patient Online Access to Computerized Medical Records and Services on Type 2 Diabetes: Systematic Review. Journal of Medical Internet Research . 2018;20(7):e235. doi:10.2196/jmir.7858
- Cockle-Hearne J, Barnett D, Hicks J, Simpson M, White I, Faithfull S. A web-based intervention to reduce distress after prostate cancer treatment: development and feasibility of the Getting Down to Coping program in two different clinical settings. JMIR Cancer . 2018; 4(1): e8 . doi: 10.2196/cancer.8918
- Papachristou N, Barneghi P, Cooper BA, Hu X, Maguire R, Apostolidis K, Armes J, Conley YP, Hammer M, Katsaragakis S, Kober KM, Levine JD, McCann L, Patiraki E, Paul SM, Ream E, Wright F, Miaskowski C. Congruence Between Latent Class and K-Modes Analyses in the Identification of Oncology Patients With Distinct Symptom Experiences. Journal of Pain and Symptom Management. 2018; 55(2): 318 - 333. doi : 10.1016/j.jpainsymman.2017.08.020
- Liyanage H, Liaw ST, Konstantara E, Mold F , Schreiber R, Kuziemsky C, Terry AL, de Lusignan S. Benefit-risk of Patients' Online Access to their Medical Records: Consensus Exercise of an International Expert Group. Yearb Med Inform. 2018 Apr 22. doi: 10.1055/s-0038-1641202. [Epub ahead of print] PubMed PMID: 29681044
- Harris J, Cheevers K, Armes J . The emerging role of digital health in monitoring and supporting people living with cancer and the consequences of its treatments. Current opinion in supportive and palliative care . 2018 Sep 1;12(3):268-75
- Chidiebere H, Carey N, Shawe J. Exploring the acceptability and feasibility of a preconception and diabetes information app for women with pregestational diabetes: a mixed methods study protocol. Digital Health . 2017; 3: 1-11. doi: 10.1177/2055207617726418
- Frankland J, Brodie H, Cooke D, Foster C, Foster R, Gage H, Jordan J, Mesa-Eguiagaray I, Pickering R, Richardson A. Follow-up care after treatment for prostate cancer: protocol for an evaluation of a nurse-led supported self-management and remote surveillance programme. BMC Cancer. 2017; 17:656. doi: 10.1186/s12885-017-3643-4
- Maguire R, Fox PA, McCann L, Miaskowski C, Kotronoulas G, Miller M, Furlong E, Ream E, Armes J, Patiraki E, Gaiger A, Berg GV, Flowerday A, Donnan P, McCrone P, Apostolidis K, Harris J, Katsaragakis S, Buick AR, Kearney N. The eSMART study protocol: a randomised controlled trial to evaluate electronic symptom management using the advanced symptom management system (ASyMS) remote technology for patients with cancer. BMJ Open . 2017; 7: e015016. doi: 10.1136/bmjopen-2016-015016
- Miaskowski C, Cooper BA, Aouizerat B, Melisko M, Chen LM, Dunn L, Hu X, Kober KM, Mastick J, Levine JD, Hammer M, Wright F, Harris J, Armes J, Furlong E, Fox P, Ream E, Maguire R, Kearney N. The symptom phenotype of oncology outpatients remains relatively stable from prior to through 1 week following chemotherapy. European Journal of Cancer Care . 2017; 26(3). doi: 10.1111/ecc.12437
- Kidd T, Carey N, Mold F , Westwood S, Miklaucich M, Konstantara E, Sterr A, Cooke D. A systematic review of the effectiveness of self-management interventions in people with multiple sclerosis at improving depression, anxiety and quality of life. PLoS One . 2017 Oct 11;12(10):e0185931. doi: 10.1371/journal.pone.0185931
- Cox A , Lucas G, Marcu A, Piano M, Grosvenor W, Mold F, Maguire R, Ream E. Cancer survivors’ experience with telehealth: a systematic review and thematic synthesis. Journal of Medical Internet Research . 2017;19(1):e11
- Nwolise CH, Carey N, Shawe JA. Preconception care education for women with diabetes: a systematic review of conventional and digital health interventions. JMIR. 2016; 18(11):e291. doi: 10.2196/jmir.5615
- Foster C, Grimmett C, May CM, Ewings S, Myall M, Hulme C, Smith PW, Powers C, Calman L, Armes J , Breckons M. A web-based intervention (RESTORE) to support self-management of cancer-related fatigue following primary cancer treatment: a multi-centre proof of concept randomised controlled trial . Supportive Care in Cancer . 2016 Jun 1;24(6):2445-53
- Cockle Hearne J, Cooke D, Faithfull S. Developing peer support in film for cancer self-management: what do men want other men to know? Supportive Care in Cancer. 24(4): 1625–1631. doi: 10.1007/s00520-015-2938-8
- Foster C, Calman L, Grimmett C, Breckons M, Cotterell P, Yardley L, Joseph J, Hughes S, Jones R, Leonidou C, Armes J, Batehup L, Corner J, Fenlon D, Lennan E, Morris C, Neylon A, Ream E, Turner L, Richardson A. Managing fatigue after cancer treatment: development of RESTORE, a web-based resource to support self-management. Psychooncology . 2015; 24(8): 940 - 949. doi: 10.1002/pon.3747
- Kamps L, Cooke D, Haq SM, Barnes DJ. Does continuous blood glucose monitoring (CGM) improve glycaemic control in patients with Type 1 diabetes who have problematic hypoglycaemia or hyperglycaemia? Diabetic Medicine. 2015; 32: 142-144
- Maguire R, Ream E, Richardson A, Connaghan J, Johnston B, Kotronoulas G, Pedersen V, McPhelim J, Pattison N, Smith A, Webster L, Taylor A, Kearney N. Development of a novel remote patient monitoring system: the advanced symptom management system for radiotherapy to improve the symptom experience of patients with lung cancer receiving radiotherapy (ASyMS-R). Cancer Nursing. 2015; 38(2): E37-E47. doi: 10.1097/NCC.0000000000000150
- Mold F & de Lusignan S. Patients’ Online Access to Their Primary Care Electronic Health Records and Linked Online Services: Implications for Research and Practice. J. Pers. Med. 2015, 5 (4), 452-469
- Mold F , de Lusignan S, Sheikh A, Majeed A, Wyatt JC, Quinn T, Cavill M, Franco C, Chauhan U, Blakey H, Kataria N, Arvanitis TN, Ellis B. Patients' online access to their electronic health records and linked online services: a systematic review in primary care. Br J Gen Pract . 2015 Mar; 65 (632):e141-51
- Breen S, Ritchie D, Schofield P, Hsueh YS, Gough K, Santamaria N, Kamateros R, Maguire R , Kearney N, Aranda S. The Patient Remote Intervention and Symptom Management System (PRISMS)–a Telehealth-mediated intervention enabling real-time monitoring of chemotherapy side-effects in patients with haematological malignancies: study protocol for a randomised controlled trial. Trials . 2015 Dec;16(1):472
- Rutsaert P, Barnett J, Gaspar R, Marcu A , Pieniak Z, Seibt B, Lima ML, Fletcher D, Verbeke W. Beyond information seeking: Consumers’ online deliberation about the risks and benefits of red meat. Food Quality and Preference. 2015 Jan 1;39:191-201
- Tirunagari S, Poh N, Aliabadi K, Windridge D, Cooke D. Patient level analytics using self-organising maps: A case study on Type-1 Diabetes self-care survey responses. 2014 IEEE Symposium on Computational Intelligence and Data Mining (CIDM). doi: 10.1109/CIDM.2014.7008682
- Heller S, Lawton J, Amiel S, Cooke DD, Mansell P, Brennan A, Elliott J, Boote J, Emery C, Baird W, Basarir H, Beveridge S, Bond R, Campbell M, Chater T, Choudhary P, Clark M, de Zoysa N, Dixon S, Gianfrancesco C, Hopkins D, Jacques R, Kruger J, Moore S, Oliver L, Peasgood T, Rankin D, Roberts S, Rogers H, Taylor C, Thokala P, Thompson G, Ward C. Improving management of type 1 diabetes in the UK: the Dose Adjustment For Normal Eating (DAFNE) programme as a research test-bed. A mixed-method analysis of the barriers to and facilitators of successful diabetes self-management, a health economic analysis, a cluster randomised controlled trial of different models of delivery of an educational intervention and the potential of insulin pumps and additional educator input to improve outcomes. Programme Grants for Applied Research. 2014; 2(5). doi: 10.3310/pgfar02050
- Liyanage H, de Lusignan S, Liaw ST, Kuziemsky C, Mold F , Krause P, Fleming D, & Jones S. (2014) Big data usage patterns in the health care domain: A use case driven approach applied to the assessment of vaccination benefits and risks. International Medical Informatics Association (IMIA), Yearb Med Inform. Aug 15; 9 (1):27-35
- de Lusignan S. Mold F et al. (2014) Patients’ online access to their electronic health records and linked online services: an interpretative review. BMJ Open . BMJ Open . 2014 Sep 8; 4 (9):e006021
- Grimmett C, Armes J , Breckons M, Calman L, Corner J, Fenlon D, Hulme C, May CM, May CR, Ream E, Richardson A, Smith, P W F., Yardley, L., Foster, C. RESTORE: an exploratory trial of an online intervention to enhance self-efficacy to manage problems associated with cancer-related fatigue following primary cancer treatment: study protocol for a randomized controlled trial. Trials . 2013 Dec;14(1):184
- Mold F, Ellis B, de Lusignan et al. (2012) The provision and impact of online patient access to their electronic health records and transactional services on the quality and safety of health care: a systematic review protocol, Informatics in Primary Care . 2012; 20 (4):271-82
Researchers
Research theme lead.

Professor Jo Armes
Professor of Cancer Care and Lead for Digital Health
Research theme members

Dr Anand Ahankari
Lecturer in Maternal, Child and Family Health

Postgraduate Research Student


Professor Elizabeth Barley
Professor of Mental Health Sciences and Nursing

Gayasha Batheegama Gamarachchige

Dr Alison Callwood
Senior Lecturer in Integrated Care (Midwifery)

Dr Theopisti Chrysanthaki
Lecturer in Integrated Care/ehealth

Dr Jane Cockle Hearne
Research Fellow

Dr Debbie Cooke

Dr Christos Dadousis
Research Fellow in Health and Biomedical Informatics Research Group

Simon Downs
Paramedic Field Lead & Lecturer (Paramedic Practice)

Professor Sara Faithfull
Visiting Professor of Cancer Nursing Practice, Lead for Clinical Innovation

Hongxin Gao

Professor Nophar Geifman
Professor of Health and Biomedical Informatics

Professor Faith Gibson
Professor of Child Health and Cancer Care

Dr Nyangi Gityamwi

Dr Richard Green
Surrey Future Fellow

Dr Jenny Harris
Senior Lecturer in Cancer Care and Health Statistics

Dr Athena Ip
Dr Haomiao Jin
Lecturer in Health Data Sciences

Dr Agnieszka Lemanska
Senior Lecturer in Health Data Science

Dr Freda Elizabeth Mold
Senior Lecturer in Integrated Care

Professor Caroline Nicholson
Professor of Palliative Care and Ageing

Claire Price

Professor Emma Ream
Professor, Director of Health Sciences Research

Yvonne Smyth
Postgraduate Research Student (PhD)

Professor Cath Taylor
Professor of Healthcare Workforce Organisation and Wellbeing
Latest news

13 MAY 2024
Utilising open research practices to conduct a systematic review and meta-analysis of healthcare data

Modifying a self-efficacy tool for people with learning disabilities using inclusive, open and accessible research

30 APR 2024
Patients diagnosed with cancer in prison more likely to die from the disease
Imperial College London Imperial College London
Latest news.

US health research agency ARPA-H sets out funding vision during Imperial visit

Seven Imperial scientists elected as Fellows of the Royal Society

GSK backs Imperial’s Fleming Initiative with £45m pledge to fight AMR

- Postgraduate taught
Digital Health Leadership
Receive world-class training towards a career as a digital health leader on the flagship programme of the NHS Digital Academy.
Acquire the essential knowledge and skills to work as a leader driving digital health transformation in the NHS
Learn how to identify opportunities for digital transformation and manage large scale projects and organisational change
Benefit from a blended study programme that incorporates online and residential learning
Course key facts
Qualification, september 2024, delivered by, department of surgery and cancer, nhs digital academy, minimum entry standard, 2:2 in a relevant subject, other requirements apply. applicants must also be directly employed by the nhs or non-profit organisation with long-term commission to provide nhs services., course overview.
Receive world-class training towards a career as a digital health leader on the flagship programme of the NHS Digital Academy. Commissioned by Health Education England, this course explores how innovative leadership can help drive digital transformation within a healthcare setting.
You'll apply your learning to your professional practice and build the leadership expertise needed to improve and scale digital workforce capabilities.
You'll also evaluate and implement health information systems and learn how clinical data and insights can be used to drive continuous improvement.
This programme unites a range of experts from Imperial College London's Institute of Global Health Innovation and Imperial College Healthcare NHS Trust.
Teaching is delivered via a blended study programme, with online learning complemented by residential learning opportunities at leadership forums across various sites in London, and the UK.
This page is updated regularly to reflect the latest version of the curriculum. However, this information is subject to change.
Find out more about potential course changes .
Please note: it may not always be possible to take specific combinations of modules due to timetabling conflicts. For confirmation, please check with the relevant department.
Core modules
You’ll study the following core modules.
Essentials of Health Systems
Learn about health systems from a national and international perspective and study current developments in health informatics.
Strategy and Transformational Change
Receive an orientation in the project and programme environment, and analyse how programmes are used to manage a number of related projects and create strategic value for organisations.
Design for Digital Transformation
Provides an insight into the latest developments in human-centred design and consumer health informatics, drawing on in-depth case studies and expert interviews, underpinned by relevant theory and literature.
Principles of Leadership
Understand key concepts in leadership and how these affect your practice, and consider how to lead transformational change in the workplace.
Innovation in Healthcare
Learn about principles of innovation in healthcare, how innovation comes about, the role of different sectors and the health policy implications of future innovation.
Health Information Systems
Critically evaluate an information system selection, implementation and optimisation with relation to technical and business factors.
Data-driven Decision Support
Develop expertise in identifying data sources and review the different types of data available.
Leadership in Practice
Apply concepts, theory and frameworks you have acquired throughout the programme, harnessing the tools and means to lead transformational change.
Teaching and assessment
Teaching and learning methods, balance of assessment.
- Taught modules
- Research project
- 100% Taught modules
- 0% Research project
Assessment methods
Teaching methods.
Students will be provided with access to online content with guidance how to progress through the materials. This will be complemented by live webinars, tutorials, and assessment briefings on each module, delivered by the Module Leads and Teaching Fellows.
The Leadership in Practice module will run throughout the course of the year. The module is centred around developing communities of practice, with experts and practitioners sharing reflection on leadership challenges and experience with operating in health, policy, and innovation settings.
Entry requirements
This course welcomes applications from NHS employees.
Please see a full overview of eligibility criteria . You must be employed by an NHS organisation or commissioned service in England.
- Minimum academic requirement
- English language requirement
- International qualifications
2:2 in a relevant subject
- be a Chief Information Officer, Chief Clinical Information Officer or aspiring digital leader in the NHS or social care
- have five years of relevant experience in informatics or digital health
- have executive level support from your organisation
- be available to attend all residential learning sessions (listed in the overview section of this page)
- provide two references (professional or academic)
If you do not meet the academic requirements above but have substantial relevant industry experience you may be admitted following completion of a ‘Special Qualifying Exam’ (SQE).
All candidates must demonstrate a minimum level of English language proficiency for admission to the university.
For admission to this course, you must achieve the standard university requirement in the appropriate English language qualification. For details of the minimum grades required to achieve this requirement, please see the English language requirements .
We also accept a wide variety of international qualifications.
The academic requirement above is for applicants who hold or who are working towards a UK qualification.
For guidance see our accepted qualifications though please note that the standards listed are the minimum for entry to Imperial , and not specifically this Department .
If you have any questions about admissions and the standard required for the qualification you hold or are currently studying then please contact the relevant admissions team .
How to apply
Interested applicants can get in touch with the programme team.
Eligibility and process
Visit the NHS England website for detailed information about the programme, eligibility, and application process on the Digital Health Leadership web pages.
ATAS certificate
An ATAS certificate is not required for students applying for this course.
Tuition fees
Places on this course are fully funded by a sponsorship arrangement with NHS England.
For more information, learn more about the Digital Health Leadership programme on the NHS England website.
Scholarships
The dean’s master’s scholarships, value per award.
- £10,000
Who it's for
- All students applying to study a Faculty of Medicine Master’s programme beginning in October 2024
How will studying at Imperial help my career?
Learn the skills and knowledge needed to take on senior leadership roles in digital health and care.
Designed for CXOs, CIOs, CNIOs, and CCIOs, this programme provides guidance on advancing transformational digital change across organisations.
Further links
Contact the department.
- Email: [email protected]
Course Director: Professor the Lord Ara Darzi
Visit the Department of Surgery and Cancer website.

Register your interest
Stay up to date on news, events, scholarship opportunities and information related to this course.

Events, tasters and talks
Meet us and find out more about studying at Imperial.
Find an event

Terms and conditions
There are some important pieces of information you should be aware of when applying to Imperial. These include key information about your tuition fees, funding, visas, accommodation and more.
Read our terms and conditions
You can find further information about your course, including degree classifications, regulations, progression and awards in the programme specification for your course.

Research Digital Health & Wellness Research Group (DHaWG)
Developing person-centered accessible digital health and care solutions that make a difference.
We design, develop, implement and evaluate real-world digital health and care solutions.
We are a world-leading digital health and wellness research group.
We are driven by user-centred design and work in close partnership with key stakeholders (citizens, patients, NHS, social care, industry, government) to create smart and connected digital health and care technologies that have a positive impact on individuals, communities, and organisations at scale.
Our key strengths
- we take a ‘whole system’ approach to health and wellbeing (we look at how health, social care, and consumer data and systems work together)
- we are experts in creating and using a variety of co-design and co-production methods (e.g. workshops, ethnography, photo diaries, citizen science panels) to ensure digital solutions and services are usable, accessible and equitable
- we create and use robust and flexible approaches to real-world evaluations of digital health at scale in homes, hospitals and community settings so that our research and innovation have real-world impacts
- our expertise spans the technology readiness pathway from ideation to commercialisation with a focus on making a real-world impact
- we collaborate at a national and international level and have several projects with global reach
- we have funding from Horizon 2020/Europe, CSO, MRC, EPSRC, Innovate UK, ESRC, and AHRC.

Meet the team

Our research areas

Our faculties & departments
Engineering.
- Faculty of Engineering
- Architecture
- Biomedical Engineering
- Chemical & Process Engineering
- Civil & Environmental Engineering
- Design, Manufacturing & Engineering Management
- Electronic & Electrical Engineering
- Mechanical & Aerospace Engineering
- Naval Architecture, Ocean & Marine Engineering
Humanities & Social Sciences
- Faculty of Humanities & Social Sciences
- Centre for Lifelong Learning
- Government & Public Policy
- Psychological Sciences & Health
- Social Work & Social Policy
- Faculty of Science
- Computer & Information Sciences
- Mathematics & Statistics
- Pure & Applied Chemistry
- Strathclyde Institute of Pharmacy & Biomedical Sciences
- Strathclyde Business School
- Accounting & Finance
- Hunter Centre for Entrepreneurship
- Management Science
- MBA & General Management
- Strathclyde Executive Education & Development
- Work, Employment & Organisation

- Data Schools
PhD in Digital Humanities
Requirements.
The PhD in Digital Humanities, run by Cambridge Digital Humanities and based in the Faculty of English, is a research-intensive programme new for 2024 that will enable students to engage at doctoral level with projects demanding the use of digital methods, tools, or adopting critical/theoretical orientations. The programme expands the humanities offering at research postgraduate level at Cambridge by offering a route for cross-disciplinary engagement, responding to the growth of the field of Digital Humanities as a research area.
The programme is designed to enable students from many areas of the arts and humanities to develop practical skills and knowledge and to generate the necessary critical literacy to understand and engage with digital research, and digital cultures, and to respond to questions arise around the ethics of automation, algorithmic analysis, privacy/surveillance, virtual cultures, data sharing, intelligent agency and creativity, archival justice and digital histories, and to explore work in relation to collections and heritage issues. Through supervisions and technical support from a research software engineer, contextualised by a research culture providing research led seminars and lectures, guest seminars, and practice-driven workshops, CDH provides the conditions for original PhD research in Digital Humanities or in other arts and humanities/social science disciplines that make a significant intervention into shaping the field.
Background Digital Humanities is an intrinsically interdisciplinary field: we therefore will consider candidates from almost any academic field. You might have a grounding in History, Archaeology, Literature, Linguistics, Art History, Economics, Computer Science, etc. The degree itself involves working with a range of materials from Cambridge Libraries, Museums and Collections and other disciplines.
Academic qualifications
Applicants for this course should have achieved a UK Masters (Merit) .
If your degree is not from the UK, please check International Qualifications to find the equivalent in your country.
University Minimum Academic Requirements
MPhil students in Digital Humanities from Cambridge who wish to continue to the PhD may apply to do so, subject to meeting certain conditions. The expected standard for continuation to the PhD at Cambridge is normally:
- An overall mark of 70 or more for the MPhil course
- A mark of 70 or more for the dissertation/portfolio submitted as part of the MPhil course
- Other conditions may also be imposed as deemed necessary
General entry requirements for the University of Cambridge: https://www.postgraduate.study.cam.ac.uk/application-process/entry-requirements
2024 Home students: £9,387
2024 Overseas students: £28,401
Anyone who applies to a postgraduate course at Cambridge can also apply to be considered for funding.
Every year the University of Cambridge awards over £100m in scholarships to new postgraduate students. This money comes from many generous University and College endowments, as well as government Research Council (UKRI) funds . A lot of our students also fund their studies from external sources such as charities or government schemes and loans.
Our major internal sources of funding are:
- Cambridge Trust
- Gates Cambridge Trust
- Harding Distinguished Postgraduate Scholars Programme (HDPSP)
- Research Councils (UKRI)
- Colleges and departments
General information found at: https://www.postgraduate.study.cam.ac.uk/funding-overview
European Funding Guide
The European Funding Guide is the largest online-platform in the EU for finding financial aid. The platform contains over 12,000 scholarships, grants and awards across the whole EU worth more than 27 billion Euros per year. Over 4,000 of these are specifically targeted at UK students.
General Enquiries: [email protected]
Postgraduate Administrator (Suzanne Daley): [email protected]
Admissions Enquiries: www.postgraduate.study.cam.ac.uk/contact-form
Twitter: twitter.com/camdighum
Applications for the PhD in Digital Humanities open on 4 September 2023.
The deadline for Gates (US) scholarships is 11 October 2023 ( https://www.gatescambridge.org/apply/timeline/ ).
The deadline for all other applications is in 4 January 2024.
For more information and a link to the application portal, look up Digital Humanities in the Postgraduate Course Directory after applications open.
What kinds of methodologies and projects are most popular at CDH? Moving forward, what areas is CDH most interested in developing?
Our aim is to further an expansive form of Digital Humanities that encompasses work with collections, literature as digital humanities, global digital humanities, critical media theorisation, digital media, methodological advancement, future and emerging technologies including AI and machine learning, and much more. You can find out more about our research activities at cdh.cam.ac.uk/research and a general statement about our research areas at cdh.cam.ac.uk/about . Our supervisors cover a range of research areas. Find a potential CDH supervisor here .
Regarding the application, what do you consider to be an eligible ‘sample of work’? Would essays written for master’s study, for example, or a chapter or two from the master’s thesis be accepted?
Both of these suggestions would work. The sample of work can be one long piece or several shorter essays (max. 5) amounting to around 5,000—7,000 words in total. You will also need to provide an 800-word research proposal. To find the full list of materials required for PhD applications, please visit: postgraduate.study.cam.ac.uk/courses/directory/elelpddgh/apply
Does your PhD programme accept applicants who already hold a PhD?
Yes. Applicants who do not hold a PhD are not at a disadvantage.
If we are currently awaiting results from our MA studies, would it be best to wait for these results to be released before applying, or is it okay to apply beforehand?
You can apply before you have been awarded your marks for your MA, but you will have to have your marks before you are administered to the PhD course. You would simply add a predicted grade to your application form e.g. ‘Merit predicted’.
Are there any specific guidelines or recommendations for creating a research proposal for the PhD programme in Digital Humanities? What should the research proposal look like?
A PhD research proposal should be 800 words long. It needs to give those assessing your application an impression of the strength and originality of your proposed research, and its potential to make a contribution to knowledge. It should be written in clear, jargon-free, and unexceptionable prose. Grammatical mistakes and typographical errors give a very bad impression. You should make sure you cover the following areas (without explicitly dividing the proposal into headings).
- the research topic briefly outline the area and topic of your research.
- the research context relate your proposed research to other work in its field or related fields, and indicate in what ways your research will differ; you might mention monographs on the subject, as well as important theoretical models or methodological exemplars. This is a chance to show your understanding of the background against which your research will be defined.
- the contribution you will make this is your chance to show how you have arrived at your position and recognised the need for your research, and what it is that makes it both new and important; you should indicate what areas and debates it will have an impact on, what methodological example it sets (if appropriate) – in short how it contributes to knowledge and to the practice of our subject. Give examples of the sort of evidence you might consider, and of the questions it might help you to raise. Show that you are already thinking about the area in detail and not only in outline.
- your methods in some cases there will be little to say here, but if there is something striking about your methodology, you should explain it.
- the sources and resources you will use you should delimit your field of enquiry, showing where the project begins and ends; in certain cases, Cambridge will have unique collections and resources of central relevance to your project, and you should mention these.
- how the project will develop you might indicate some of the possible ways in which the project could develop, perhaps by giving a broader or narrower version depending on what materials and issues you uncover
My research looks at a topic that isn’t fully covered by the supervisory team at CDH. Can I still apply to the programme?
Research proposals that move beyond the specialisms of our supervisory team may still work within CDH, however, you may wish to consider applying to a PhD programme in another department. You will be able to engage with our programme and graduate training opportunities as a Cambridge student even if you aren’t based in CDH.
How can I better evaluate whether my research would fit with Cambridge Digital Humanities?
You can find CDH’s team of supervisors here . If you are unsure whether your intended research fits with the specialisms of our supervisors, please contact us at [email protected]
Can we apply for part-time studies at CDH?
Yes, you can apply for part-time study.
Does the October deadline for the Gates scholarship apply to US students already studying in the UK? Is the early round of the Gates scholarship exclusively for US-citizens?
Please see the Cambridge Gates Scholarship website for more details about application deadlines and eligibility.
Can I submit one of my publications as the writing sample for my application?
Absolutely.
How do I find funding? What does three years of funding usually look like?
The main way to find funding is via the University’s Postgraduate Funding Search , which contains:
- University funding opportunities
- Funded studentships and research projects
- Research Council (UKRI) studentships
A lot of our students also fund their studies from external funding sources such as charities or government schemes and loans. Anyone who applies for a postgraduate course at Cambridge can also apply to be considered for funding to help cover their fees and costs . There are also specific funding opportunities available to applicants from underrepresented backgrounds from both UK households and abroad, including application fee waivers. Normally ‘full’ funding covers everything (including fees and living expenses), but there are sometimes opportunities for partial funding though this is less common.
For general information about postgraduate funding visit: postgraduate.study.cam.ac.uk/funding
For contextual data and widening participation funding, visit: postgraduate.study.cam.ac.uk/funding/contextual-data
If you can’t find what you’re looking for, please email us with any questions at [email protected]
Is there a difference between funding opportunities for part-time and full-time PhD applicants?
Tuition fees are essentially the same, just divided up into more years. We don’t control funding directly, so you should check with the specific funder you are targeting.
For more information about postgraduate funding, visit: postgraduate.study.cam.ac.uk/funding
Is it normal to expect to do fieldwork for the PhD project?
It depends on the nature of the project – fieldwork might be appropriate if you are carrying out interviews or observations, but if you are working on archival sources, it wouldn’t be.
Can you provide further information on where applicants can find details relating to the word count and format for the covering letter, the proposal, and writing sample?
To apply for this course, you’ll need to prepare a number of materials. Please see the full list of requirements on the ‘How to Apply’ section of the application portal: postgraduate.study.cam.ac.uk/courses/directory/elelpddgh/apply .
- Two academic references
- Transcript
- Evidence of competence in English If required – you can check using our tool
- Covering letter Applicants need to submit a single page covering letter explaining their rationale for wishing to undertake the course and justifying their case for a place.
- Research proposal (M) Please submit a 800-word research proposal
- Sample of work (max. 5) Please submit a sample of work which can be one long piece or several shorter essays amounting to around 5,000–7,000 words in total.
If you wish to be considered for a Gates Cambridge Scholarship you will also need to provide the following:
- Gates Cambridge Reference
- Research Proposal (PhD applicants only)
See Gates Cambridge for more information.
If we have mitigating, contextual circumstances that have impacted our grades (e.g. health issues, family situations), how can we best share this context with the department on our applications?
There is room on the application form to include contextual circumstances.
When is the deadline to apply?
The general deadline for October 2024 entry is 4 January 2024. US citizens, who are based in the US, and are applying for a Cambridge Gates Scholarship must submit their application by 11 October 2023. For more information, including the application link, visit: postgraduate.study.cam.ac.uk/courses/directory/elelpddgh
Supervisors

Professor Caroline Bassett
Director, Cambridge Digital Humanities; Professor of Digital Humanities

Dr Leonardo Impett
University Assistant Professor in Digital Humanities

Dr Anne Alexander
Senior Research Associate; Learning Director

Dr Hugo Leal
Teaching Associate
Cambridge Digital Humanities
Get in touch.
Cambridge Digital Humanities University of Cambridge 17 Mill Lane Cambridge CB2 1RX
Email: [email protected]
Legal links
- Accessibility
- Freedom of information
- Statement on modern slavery
- Terms and conditions
- Privacy and cookies policy
Stay Connected
Receive our newsletter.
Sign up now
© 2024 Cambridge Digital Humanities. All RIghts Reserved.
Web Design by Chameleon Studios
- Opportunities
- Code of Conduct
- Mailing List
- DH Teaching Forum
- CDH Reactor
- Anti-Computing: Dissent and the Machine’
- CDH Funding
- Research Networks
- Academic Visitors and Fellowships
- Research Funding
- Methods Fellowships 2022/23
- (Anti) Colonial Archives Working Group
- Cambridge Data Schools Terms and Conditions
- Teaching and Assessment
- How to Apply
- How to write your research proposal
Tel: +44 1223 766886 Email [email protected]

- Privacy Overview
- Strictly Necessary Cookies
- 3rd Party Cookies
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
These essential cookies do things like: remembering the notifications you've seen so we do not show them to you again or your progress through a form. They always need to be on.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Digital health: the changing landscape of healthcare
Blog - 13 May 2024

We hear from people all over England about their healthcare experiences. Each month, we look at a snapshot of what they have to say about different areas of healthcare. This gives us a window into how the public feels about how the system is working for them – and it can give an important indication of where it might need improving.
This month, we’ve looked at the stories people have shared about digital healthcare.
Digital innovations, such as technology to monitor medical conditions at home, the NHS App, and virtual appointments, are increasingly impacting healthcare delivery.
In 2022, the Department of Health and Social Care laid out its plan for digital transformation . NHS England aims for most health and social care services to have digital foundations, such as electronic records, in place by March 2025. Right now, only 20% of NHS organisations are digitally mature .
This will transform the way people receive healthcare. It has the potential to lead to better tailored services, more targeted care, and fewer unnecessary interventions.
But for both the NHS and its patients to get the benefits of digital healthcare, it has to work well.
What's needed?
Our work on digital healthcare shows digital tools work best when:
- The people who’ll use the technology have input into designing it, ensuring the tools work for people with different communication needs.
- Tools are tested to ensure they work as intended.
- Patients get information about the reason behind the new way of working, and specific instructions on how to operate new tools.
- Tools are interactive and support two-way communication between patients and professionals.
- Safeguards are in place to ensure patients get alerts if the technology they’re using malfunctions and know who to contact for further support.
Monitoring devices should also be free on the NHS or available to buy at low cost.
“It’s convenient and easy to use. It was inexpensive to buy. [My blood pressure] readings are more reliable as they tend to be higher when taken in GP surgery.” — Story shared by Healthwatch Hampshire
Over the last month, we’ve heard where improvements might be needed.
Technology can be hard, confusing, or time-consuming to use
We heard stories of online submissions taking a long time to process. It could be tedious to find the right information, according to one story, because documents and letters didn’t have titles. And multiple people struggled with uploading test results, such as their blood pressure readings.
“On the NHS app, not all documents have a title – it’s ridiculous, I have to go into each document/letter and read it, which wastes a lot of my time.” — Story shared with Healthwatch Surrey
Online booking caused issues, with someone sharing confusion because the online booking tool they needed was only available for a short window during the day. And Healthwatch Lewisham shared that they’d had multiple complaints about booking systems that didn’t work properly.
“Getting an appointment is becoming more difficult. I called recently and was told because my condition was ongoing and not urgent I needed to go to their website (not the NHS app which would be set up to make appointments). I did fill out the online form which isn't particularly user-friendly. I received a text with a phone appointment for 2 days later. It feels like another barrier has been added to get an appointment and I'm concerned for users who aren’t tech-savvy or have internet access!” — Story shared with Healthwatch Leicestershire
And despite the NHS’s hope that digital innovations could lead to a smoother, more joined-up system, this doesn’t always work.
One person shared a positive experience of using 111 Online – the system directed them to their pharmacist, who was able to diagnose their child with impetigo. But the pharmacist couldn’t prescribe the cream needed to treat the condition. This meant the person had to go back through 111 to be directed to the local injuries unit instead.
While digital healthcare could keep people informed, it’s not always doing that
We heard stories about missing or incomplete information, such as that the NHS App, a cornerstone of the shift towards digitising healthcare, would show a referral to treatment, but didn’t explain what this was for. People also talked about vaccine dates not showing.
The missing information could mean people can’t benefit from the convenience of digital tools – like the person who mentioned that the NHS App didn’t have enough appointments available in the time frame they needed. This meant they had to ring for an appointment anyway.
Another person shared that they could order their prescription digitally, but the tool they used didn’t let them know when it was ready to collect.
Worse still, the information recorded isn’t always accurate
One person was getting notifications that their COVID vaccination is due as they have a compromised immune system – even though they don’t.
“They have me down incorrectly as having a weakened immune system. There is no easy way for me to correct this, no doubt there are thousands of others in a similar position so significant resources are being wasted.” — Story shared with Healthwatch Gloucestershire
Even more seriously, another person found that their NHS App incorrectly showed a ‘Do Not Resuscitate’ flag on their medical records. Their GP surgery was unsure who placed it there, and couldn’t remove it. There were also other reports of people feeling that digital tools didn’t adequately or accurately capture their views and experiences.
And sometimes, digital options don’t suit people’s needs
Even when digital tools are available, people don’t always want to use them. Multiple people shared that they prefer to phone their healthcare providers, rather than using online tools. But in one person’s case, they were repeatedly directed to the online tool anyway – even though the GP surgery knew and agreed that they should be able to keep ordering over the phone.
And while apps could potentially provide helpful minor healthcare interventions, people shared that they weren’t happy with app-based support for areas like their physiotherapy or mental health.
This doesn’t mean it’s all bad news
Just as the NHS hopes is possible, we did hear from people who used digital tools like the NHS App to find the information they needed quickly. Others found it easy to use an online prescription system to order their repeat prescriptions.
And we heard positive comments from people whose GP surgeries used WhatsApp as a means for people to book appointments, allowing them to do so more easily – especially when there was good availability of appointments.
“I put an online medical concern in this morning on e-consult. Received a phone call about an hour later, appointment made to see a GP in the next 30 minutes, referral would be sent and all done and dusted. I have never had any concerns with my surgery, always felt they put the patient at the core and appointments provided in a timely manner. Fabulous service.” — Story shared with Healthwatch Lincolnshire
Digital healthcare that works for everyone
Digital technology has huge implications for the future of healthcare. But people need systems that work well and consistently provide easier access to services and information. If digital healthcare is to work, people also need to feel confident to use the systems available. And the option to speak to a healthcare professional directly, including in person, should still be an option for those who prefer it.
So we’re calling for:
- Traditional models of access and care to remain alongside digital methods.
- Involvement of patients in designing new technological solutions.
- Built-in patient education (tutorials, how-to guides, digital community champions) with any new digital healthcare rollouts.
- Funded, accessible community courses or training for those with low digital literacy.
- A universal right to internet access, with cross-government action to work towards this.
With the right foundations in place, digital technology’s role in healthcare can be one that benefits everyone.
Get the latest news straight to your inbox
Sign up for news alerts if you're interested hearing how people's feedback is improving health and social care.
You might also be interested in

Can I access my GP records online?

Building digital skills and reducing health inequalities for the Nepalese community
Healthwatch network award winners 2021 announced

IMAGES
VIDEO
COMMENTS
Join our Digital Health and Care PhD programme to become part of a new generation of innovators involved in building and developing apps, wearables, smart homes and other digital technologies. Together, these technologies are helping to support health professionals in their decision-making and empowering patients in managing their own health ...
The rapid development of digital technologies is a catalyst for a fundamental shift in both how we live, and how we manage our health. The digital transformation of health systems has the potential to deliver leaner, greener, and more person-centered services. The Oxford Institute of Digital Health is a forward thinking, interdisciplinary, and collaborative hub across academia, industry ...
Our Centre for Doctoral Training in Digital Health and Care offers a four-year PhD course, fully funded by EPSRC, and an MSc in Digital Health and Care which includes scholarships and fee discounts for successful applicants. Both courses welcome applications from UK and overseas students with a background in engineering, computer sciences and ...
The PhD students will work together in a pioneering cross-disciplinary programme alongside patients, families, clinicians, engineers, computer scientists and other experts to develop new digital platforms and technologies that can address unmet needs in child health. The research will focus on paediatric clinical care pathways and span the ...
DT4Health is an innovative PhD program located at King's, in the heart of London, arising as a joint forces collaboration between the Healthcare Faculties and the Faculty of Natural, Mathematical & Engineering Sciences. Our mission is to train the next generation of leaders in healthcare technology to improve healthcare systems in the UK in a ...
Artificial Intelligence (AI) has the potential to transform health and healthcare systems globally, yet few individuals have the required skills and training. To address this challenge, our Centre For Doctoral Training (CDT) in AI-Enabled Healthcare Systems will create a unique interdisciplinary environment to train the brightest and best healthcare artificial intelligence
Transforming Lives PhD Scholarship, Sheffield Hallam University: Predicting and preventing intervention-generated inequalities from new digital health technologies. Applications are invited for a Transforming Lives PhD Scholarship in Health and Social Care commencing 1 October 2024 (negotiable depending on circumstances).
What this unique PhD programme offers you. Four-year programme: An initial foundation year allows students to gain real experience and insight into health data research. Research that makes a difference: The three-year doctoral research projects undertaken by our students are designed to make a genuine contribution to advancing health and care.
This unique multidisciplinary PhD programme brings together students from health and life sciences, computer science, design and engineering. ... The digital health industry is one of the fastest growing, both internationally and in the UK, with current estimates indicating that the sector is increasing at a rate of 15 per cent each year. ...
The Institute of Healthcare Engineering has been awarded a UCL EPSRC DTP-funded PhD studentship via the Faculty of Engineering Sciences. The aim of this studentship is to support interdisciplinary research collaborations on the theme of Digital Health. All studentships are fully funded for 4 years. They provide: 4 years fees (home rate)
PhD Digital Health and Care. This Admissions Statement applies to applications submitted for entry to the programme between 1 October 2022 and 30 September 2023. It should be read in association with the University Admissions Principles and Procedures for Postgraduate programmes, the relevant prospectus entry and general application guidance.
Transforming Lives PhD Scholarship, Sheffield Hallam University: Predicting and preventing intervention-generated inequalities from new digital health technologies. Sheffield Hallam University Health and Social Care Research. Applications are invited for a Transforming Lives PhD Scholarship in Health and Social Care commencing 1 October 2024 ...
Programme description. Our PhD/MPhil Health Informatics programme enables you to undertake a research project that will improve understanding of Health Informatics. Health informatics and data science is set to revolutionise healthcare by providing a deeper understanding between healthcare delivery, outcomes and patients as well as empowering ...
We are happy to supervise students who would like to conduct a PhD in the area of digital technologies in the health and social care professions. A number of our PhD students have funded studentships from the NIHR. Find PhD projects and information on funding and self-funding at the following links: Search for a project; Find funded programmes
In the longer term, the Centre will develop a joint PhD programme to offer opportunities for students to experience time spent with leading digital health experts in the three countries. It will also develop a pipeline to translate digital health technologies between the UK, Canada and Australia.
Digital Health covers a wide range of research at the Institute of Biomedical Engineering. It focuses mostly on "AI in healthcare", sometimes known as Clinical AI, at the interface between machine learning and health informatics, but also on the use of wearables and video cameras to acquire vital-sign data. The Computational Health ...
The digital health research grouping has a range of multidisciplinary collaborations with patient/public groups, academic organisations and health providers and networks across Kent, Surrey and Sussex, and industry both nationally and internationally. It also contributes to the digital innovation theme of the Applied Research Collaboration (ARC ...
Being part of GLIDHE is an opportunity to build a community to generate exciting new ideas in digital health and wellbeing, to improve the health of the world. Please email expressions of interest in a PhD scholarship to: Lesley Payne, GLIDHE Lead [email protected] Useful Links. Bupa Global Institute for Digital Health Excellence
Digital Health Leadership. Digital Health Leadership (PG Dip) Course overview. Receive world-class training towards a career as a digital health leader on the flagship programme of the NHS Digital Academy. Commissioned by NHS England, this course explores how innovative leadership can help drive digital transformation within a healthcare setting.
we create and use robust and flexible approaches to real-world evaluations of digital health at scale in homes, hospitals and community settings so that our research and innovation have real-world impacts. our expertise spans the technology readiness pathway from ideation to commercialisation with a focus on making a real-world impact.
Join a research community making a difference in society with a London Met PhD. Scholarships in Marine Ecosystem Modelling and Sub-surface Characterisation. Apply today to start your PhD in Quantum Technology at The University of Glasgow. Three fully funded PhD Research Studentships in Future Societies.
The digital health industry is expected to grow six times in size over the next five years, at a rate of nearly 30% a year. Driven by the risk of future pandemics and the health needs of ageing populations in countries worldwide, this growth is expected to continue for decades to come. The demand for graduates in this area is therefore ...
The PhD in Digital Humanities, run by Cambridge Digital Humanities and based in the Faculty of English, is a research-intensive programme new for 2024 that will enable students to engage at doctoral level with projects demanding the use of digital methods, tools, or adopting critical/theoretical orientations. The programme expands the ...
This month, we've looked at the stories people have shared about digital healthcare. Digital innovations, such as technology to monitor medical conditions at home, the NHS App, and virtual appointments, are increasingly impacting healthcare delivery. In 2022, the Department of Health and Social Care laid out its plan for digital transformation.