An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Apgar score.
Leslie V. Simon ; Manan Shah ; Bradley N. Bragg .
Affiliations
Last Update: March 19, 2024 .
- Continuing Education Activity
The Apgar score is a standardized assessment of a neonate's status immediately after birth and the response to resuscitation efforts and remains the gold standard for evaluating neonates. Although the Apgar score was initially designed to assess the need for intervention to establish breathing at 1 minute, the Neonatal Resuscitation Program guidelines state that Apgar scores should not be used to determine the initial need for intervention, what interventions are indicated, or when to initiate them, as resuscitation must be commenced before the 1-minute Apgar score is assigned. The Apgar score should not be interpreted in isolation but as part of a complete assessment, with resuscitation always taking precedence over scoring.
This course delves into the clinical significance and intricacies of Apgar scoring, which involves evaluating 5 vital signs of newborns: color, heart rate, reflexes, muscle tone, and respiration. While a score of 7 to 10 at 1 and 5 minutes is considered reassuring, factors such as gestational age, birth weight, maternal medications, and congenital anomalies can influence scores. Healthcare professionals will better understand Apgar scores in predicting outcomes, emphasizing the need for ongoing monitoring and care beyond the initial scoring period when evaluating and managing newborns.
- Identify the physiological criteria used for calculating the Apgar score.
- Interpret the clinical relevance of the Apgar score.
- Determine the limitations of the Apgar score.
- Apply interprofessional team strategies to improve care coordination and patient outcomes when evaluating newborns using the Apgar score.
- Introduction
The Apgar score is a rapid method for assessing a neonate immediately after birth and in response to resuscitation. Apgar scoring remains the accepted assessment method endorsed by the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics. While originally designed in 1952 by Dr. Virginia Apgar, an anesthesiologist at Columbia University, to assess the need for intervention to establish breathing at 1 minute, the guidelines for the Neonatal Resuscitation Program state that Apgar scores should not be used to determine the initial need for intervention, what interventions are indicated, or when to initiate them, as resuscitation must be commenced before the 1-minute Apgar score is assigned. [1] [2] [3]
Elements of the Apgar score include color, heart rate, reflexes, muscle tone, and respiration. Apgar scoring is designed to assess for signs of hemodynamic compromise, including cyanosis, hypoperfusion, bradycardia, hypotonia, respiratory depression, or apnea. Each element is scored 0, 1, or 2. The score is recorded at 1 minute and 5 minutes after delivery in all infants, with expanded recording at 5-minute intervals for infants who score ≤7 at 5 minutes and in those requiring resuscitation as a method for monitoring response; scores of 7 to 10 are considered reassuring.
Apgar scores may vary with gestational age, birth weight, maternal medications, drug use or anesthesia, and congenital anomalies. Several components of the score are also subjective and prone to inter-rater variability. Thus, the Apgar score is limited because it provides somewhat subjective information about an infant’s physiology at a point in time. Apgar score alone should not be interpreted as evidence of asphyxia, and its significance in outcome studies, while widely reported, is often inappropriate. Resuscitation should always take precedence over calculating a clinical score.
- Indications
Apgar scoring is indicated in all newborn infants at 1 and 5 minutes and should be documented in the clinical record. In infants scoring <7, expanded Apgar score recording is encouraged by the American College of Obstetrics and Gynecology and the American Academy of Pediatrics as a method of monitoring response to resuscitation. [4] [5] [6]
- Contraindications
Apgar scoring has no known contraindications in the evaluation of newborns. However, in certain situations (eg, an infant who needs to be paralyzed or undergo surgery at birth), the score may not reflect the underlying physiology.
While most auscultation is performed with a stethoscope rather than by palpation, the most accurate method remains an electrocardiogram. [7] No other equipment is required. A pulse oximeter may also be used. Ideally, a radiant warmer and an electrocardiogram should be readily available in the delivery suite to provide the necessary warmth for neonates with hypothermia and to provide a more accurate heart rate if resuscitation is required. Alternatively, warm blankets and a stethoscope could be used.
Any trained healthcare professional may calculate the Apgar score depending on the situation, including:
- Neonatologist
- Pediatrician
- Nurse practitioner
- Family physician
- Respiratory Therapist
- Technique or Treatment
There are 5 parts to an Apgar score. Each category is weighted evenly and assigned a 0, 1, or 2 value. The components are then added to give a score recorded 1 and 5 minutes after birth. A score of 7 to 10 is considered reassuring, a score of 4 to 6 is moderately abnormal, and a score of 0 to 3 is deemed low in full-term and late preterm infants, at 5 minutes, when an infant has a score of <7, Neonatal Resuscitation Program guidelines recommend continued recording at 5-minute intervals up to 20 minutes. Scoring during resuscitation is not equivalent to an infant not undergoing resuscitation because resuscitative efforts alter several score elements. [8] [9]
The score is calculated using the following assessment:
- If the neonate is not breathing, the respiratory score is 0.
- If respirations are slow and irregular, weak, or gasping, the respiratory score is 1.
- If the neonate is crying vigorously, the respiratory score is 2.
- The heart rate is evaluated with a stethoscope or an electrocardiogram and is the most critical part of the score in determining the need for resuscitation.
- If there is no heartbeat, the heart rate score is 0.
- If the heart rate is <100 bpm, the heart rate score is 1.
- If the heart rate is >100 bpm, the heart rate score is 2.
- In inactive neonates with loose and floppy muscle tone, the score for muscle tone is 0.
- In neonates demonstrating some tone and flexion, the score for muscle tone is 1.
- In neonates in active motion with a flexed muscle tone that resists extension, the muscle tone score is 2.
- In a neonate with no response to stimulation, the reflex irritability response score is 0.
- A neonate grimacing in response to stimulation has a reflex irritability response score of 1.
- In a neonate who cries, coughs, or sneezes on stimulation, the reflex irritability response is 2.
- Most infants will score 1 for color even at the 5-minute, as peripheral cyanosis is common among normal infants. Color can also be misleading in non-white infants. [10]
- If the neonate is pale or blue, the score for color is 0.
- If the infant is pink, but the extremities are blue, the score for color is 1.
- If the neonate is entirely pink, the score for color is 2.
- Clinical Significance
Apgar scores were designed to help identify infants that require respiratory support or other resuscitative measures, not as an outcome measure. The Apgar score alone should not be considered evidence of asphyxia or proof of an intrapartum hypoxic event. While there is some evidence of poor long-term outcomes with a low Apgar score at 1 minute, the change in scores from 1 to 5 minutes and the individual scores at 5 and 10 minutes are more predictive. [11] [12] [11] [13] [14] [15]
Low Apgar scores at 5 minutes correlate with mortality and may confer an increased risk of cerebral palsy in population studies but not necessarily with an individual neurologic disability. [16] Most infants with low Apgar scores do not go on to develop cerebral palsy, but lower scores over time increase the population's risk of poor neurologic outcomes. Scores <5 at 5 and 10 minutes correlate with an increased relative risk of cerebral palsy. Neonates with scores <5 at 5 minutes after delivery should have cord blood gas sampling performed. Apgar scores that remain at 0 after 10 minutes are predictive of a poor outcome, though a significant portion of those babies survive, and many have no neurodevelopmental disabilities. [16] [17] Experts no longer recommended that resuscitative efforts be terminated at 10 minutes with an Apgar score of 0. [17]
- Enhancing Healthcare Team Outcomes
Physicians, advanced practitioners, midwives, respiratory therapists, and nurses play pivotal roles in Apgar scoring, with consistency in scoring crucial to mitigate inter-rater variability. Interprofessional team members are each instrumental in assessing neonates and promptly communicating any changes in Apgar scores to the attending clinician. Health professionals each play a crucial role in documenting scores at 1 and 5 minutes and working with other clinicians in initial resuscitative measures for low-scored neonates. Interprofessional communication ensures findings are shared with the mother and family, facilitating collaborative care planning. Physicians, advanced practitioners, midwives, and nurses should address family concerns, provide education leaflets, and emphasize patient education for managing neonates with low Apgar scores. This collaborative approach fosters optimal patient-centered care, enhancing outcomes and safety through effective team performance.
- Nursing, Allied Health, and Interprofessional Team Interventions
Nurses looking after newborns should know the Apgar score and its significance. Nurses should understand that a score between 7-10 is average; a score between 4-6 needs proper reevaluation. A score of less than 3 is never good, and immediate attention is mandatory. In this situation, the nurse should immediately call a code and inform the clinician.
- Nursing, Allied Health, and Interprofessional Team Monitoring
- Apgar scoring at 1 and 5 minutes
- The general condition of the neonate
- Vital signs of the newborn
- Umbilical cord pH
- Arterial blood gases of the newborn
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Leslie Simon declares no relevant financial relationships with ineligible companies.
Disclosure: Manan Shah declares no relevant financial relationships with ineligible companies.
Disclosure: Bradley Bragg declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Simon LV, Shah M, Bragg BN. APGAR Score. [Updated 2024 Mar 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Effect of a statewide neonatal resuscitation training program on Apgar scores among high-risk neonates in Illinois. [Pediatrics. 2001] Effect of a statewide neonatal resuscitation training program on Apgar scores among high-risk neonates in Illinois. Patel D, Piotrowski ZH, Nelson MR, Sabich R. Pediatrics. 2001 Apr; 107(4):648-55.
- The Apgar Score. [Pediatrics. 2015] The Apgar Score. AMERICAN ACADEMY OF PEDIATRICS COMMITTEE ON FETUS AND NEWBORN, AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS COMMITTEE ON OBSTETRIC PRACTICE. Pediatrics. 2015 Oct; 136(4):819-22.
- Committee Opinion No. 644: The Apgar Score. [Obstet Gynecol. 2015] Committee Opinion No. 644: The Apgar Score. . Obstet Gynecol. 2015 Oct; 126(4):e52-e55.
- Review The Apgar cycle: a new view of a familiar scoring system. [Arch Dis Child Fetal Neonatal ...] Review The Apgar cycle: a new view of a familiar scoring system. Pinheiro JM. Arch Dis Child Fetal Neonatal Ed. 2009 Jan; 94(1):F70-2. Epub 2008 Aug 14.
- Review The value of autopsy in determining the cause of failure to respond to resuscitation at birth. [Semin Neonatol. 2004] Review The value of autopsy in determining the cause of failure to respond to resuscitation at birth. Squier W, Cowan FM. Semin Neonatol. 2004 Aug; 9(4):331-45.
Recent Activity
- APGAR Score - StatPearls APGAR Score - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Introduction
Limitations of the apgar score, apgar score and resuscitation, prediction of outcome, other applications, conclusions, recommendations, aap committee on fetus and newborn, 2014–2015, acog committee on obstetric practice, 2014–2015, the apgar score.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
AMERICAN ACADEMY OF PEDIATRICS COMMITTEE ON FETUS AND NEWBORN , AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS COMMITTEE ON OBSTETRIC PRACTICE , Kristi L. Watterberg , Susan Aucott , William E. Benitz , James J. Cummings , Eric C. Eichenwald , Jay Goldsmith , Brenda B. Poindexter , Karen Puopolo , Dan L. Stewart , Kasper S. Wang , Jeffrey L. Ecker , Joseph R. Wax , Ann Elizabeth Bryant Borders , Yasser Yehia El-Sayed , R. Phillips Heine , Denise J. Jamieson , Maria Anne Mascola , Howard L. Minkoff , Alison M. Stuebe , James E. Sumners , Methodius G. Tuuli , Kurt R. Wharton; The Apgar Score. Pediatrics October 2015; 136 (4): 819–822. 10.1542/peds.2015-2651
Download citation file:
- Ris (Zotero)
- Reference Manager
The Apgar score provides an accepted and convenient method for reporting the status of the newborn infant immediately after birth and the response to resuscitation if needed. The Apgar score alone cannot be considered as evidence of, or a consequence of, asphyxia; does not predict individual neonatal mortality or neurologic outcome; and should not be used for that purpose. An Apgar score assigned during resuscitation is not equivalent to a score assigned to a spontaneously breathing infant. The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists encourage use of an expanded Apgar score reporting form that accounts for concurrent resuscitative interventions.
In 1952, Dr Virginia Apgar devised a scoring system that was a rapid method of assessing the clinical status of the newborn infant at 1 minute of age and the need for prompt intervention to establish breathing. 1 Dr Apgar subsequently published a second report that included a larger number of patients. 2 This scoring system provided a standardized assessment for infants after delivery. The Apgar score comprises 5 components: (1) color; (2) heart rate; (3) reflexes; (4) muscle tone; and (5) respiration. Each of these components is given a score of 0, 1, or 2. Thus, the Apgar score quantitates clinical signs of neonatal depression, such as cyanosis or pallor, bradycardia, depressed reflex response to stimulation, hypotonia, and apnea or gasping respirations. The score is reported at 1 minute and 5 minutes after birth for all infants, and at 5-minute intervals thereafter until 20 minutes for infants with a score less than 7. 3 The Apgar score provides an accepted and convenient method for reporting the status of the newborn infant immediately after birth and the response to resuscitation if it is needed; however, it has been inappropriately used to predict individual adverse neurologic outcome.
The purpose of the present statement was to place the Apgar score in its proper perspective. This statement revises the 2006 College Committee Opinion/American Academy of Pediatrics policy statement to include updated guidance from the 2014 report Neonatal Encephalopathy and Neurologic Outcome (second edition) 4 published by the American College of Obstetricians and Gynecologists in collaboration with the American Academy of Pediatrics, along with new guidance on neonatal resuscitation. The guidelines of the Neonatal Resuscitation Program state that the Apgar score is useful for conveying information about the newborn infant’s overall status and response to resuscitation. However, resuscitation must be initiated before the 1-minute score is assigned. Therefore, the Apgar score is not used to determine the need for initial resuscitation, what resuscitation steps are necessary, or when to use them. 3
An Apgar score that remains 0 beyond 10 minutes of age may, however, be useful in determining whether continued resuscitative efforts are indicated because very few infants with an Apgar score of 0 at 10 minutes have been reported to survive with a normal neurologic outcome. 3 , 5 , 6 In line with this outcome, the 2011 Neonatal Resuscitation Program guidelines state that “if you can confirm that no heart rate has been detectable for at least 10 minutes, discontinuation of resuscitative efforts may be appropriate.” 3
The Neonatal Encephalopathy and Neurologic Outcome report defines a 5-minute Apgar score of 7 to 10 as reassuring, a score of 4 to 6 as moderately abnormal, and a score of 0 to 3 as low in the term infant and late-preterm infant. 4 In that report, an Apgar score of 0 to 3 at 5 minutes or more was considered a nonspecific sign of illness, which “may be one of the first indications of encephalopathy.” However, a persistently low Apgar score alone is not a specific indicator for intrapartum compromise. Furthermore, although the score is widely used in outcome studies, its inappropriate use has led to an erroneous definition of asphyxia. Asphyxia is defined as the marked impairment of gas exchange, which, if prolonged, leads to progressive hypoxemia, hypercapnia, and significant metabolic acidosis. The term asphyxia, which describes a process of varying severity and duration rather than an end point, should not be applied to birth events unless specific evidence of markedly impaired intrapartum or immediate postnatal gas exchange can be documented on the basis of laboratory test results.
It is important to recognize the limitations of the Apgar score. It is an expression of the infant’s physiologic condition at 1 point in time, which includes subjective components. There are numerous factors that can influence the Apgar score, including maternal sedation or anesthesia, congenital malformations, gestational age, trauma, and interobserver variability. 4 In addition, the biochemical disturbance must be significant before the score is affected. Elements of the score, such as tone, color, and reflex irritability, can be subjective and partially depend on the physiologic maturity of the infant. The score may also be affected by variations in normal transition. For example, lower initial oxygen saturations in the first few minutes need not prompt immediate supplemental oxygen administration; the Neonatal Resuscitation Program targets for oxygen saturation are 60% to 65% at 1 minute and 80% to 85% at 5 minutes. 3 The healthy preterm infant with no evidence of asphyxia may receive a low score only because of immaturity. 7 , 8 The incidence of low Apgar scores is inversely related to birth weight, and a low score cannot predict morbidity or mortality for any individual infant. 8 , 9 As previously stated, it is also inappropriate to use an Apgar score alone to diagnose asphyxia.
The 5-minute Apgar score, and particularly a change in the score between 1 minute and 5 minutes, is a useful index of the response to resuscitation. If the Apgar score is less than 7 at 5 minutes, the Neonatal Resuscitation Program guidelines state that the assessment should be repeated every 5 minutes for up to 20 minutes. 3 However, an Apgar score assigned during resuscitation is not equivalent to a score assigned to a spontaneously breathing infant. 10 There is no accepted standard for reporting an Apgar score in infants undergoing resuscitation after birth because many of the elements contributing to the score are altered by resuscitation. The concept of an assisted score that accounts for resuscitative interventions has been suggested, but the predictive reliability has not been studied. To correctly describe such infants and provide accurate documentation and data collection, an expanded Apgar score reporting form is encouraged ( Fig 1 ). This expanded Apgar score may also prove useful in the setting of delayed cord clamping, in which the time of birth (ie, complete delivery of the infant), the time of cord clamping, and the time of initiation of resuscitation can all be recorded in the comments box.

Expanded Apgar score reporting form. Scores should be recorded in the appropriate place at specific time intervals. The additional resuscitative measures (if appropriate) are recorded at the same time that the score is reported by using a checkmark in the appropriate box. The comment box is used to list other factors, including maternal medications and/or the response to resuscitation between the recorded times of scoring. ETT, endotracheal tube; PPV/NCPAP, positive pressure ventilation/nasal continuous positive airway pressure.
The Apgar score alone cannot be considered to be evidence of or a consequence of asphyxia. Many other factors, including nonreassuring fetal heart rate–monitoring patterns and abnormalities in umbilical arterial blood gas results, clinical cerebral function, neuroimaging studies, neonatal electroencephalography, placental pathology, hematologic studies, and multisystem organ dysfunction, need to be considered in diagnosing an intrapartum hypoxic–ischemic event. 6 When a category I (normal) or category II (indeterminate) fetal heart rate tracing is associated with Apgar scores of 7 or higher at 5 minutes, a normal umbilical cord arterial blood pH (±1 SD), or both, it is not consistent with an acute hypoxic–ischemic event. 4
A 1-minute Apgar score of 0 to 3 does not predict any individual infant’s outcome. A 5-minute Apgar score of 0 to 3 correlates with neonatal mortality in large populations 11 , 12 but does not predict individual future neurologic dysfunction. Population studies have uniformly reassured us that most infants with low Apgar scores will not develop cerebral palsy. However, a low 5-minute Apgar score clearly confers an increased relative risk of cerebral palsy, reported to be as high as 20- to 100-fold over that of infants with a 5-minute Apgar score of 7 to 10. 9 , 13 , – 15 Although individual risk varies, the population risk of poor neurologic outcomes also increases when the Apgar score is 3 or less at 10 minutes, 15 minutes, and 20 minutes. 16 When a newborn infant has an Apgar score of 5 or less at 5 minutes, umbilical arterial blood gas samples from a clamped section of the umbilical cord should be obtained, if possible. 17 Submitting the placenta for pathologic examination may be valuable.
Monitoring of low Apgar scores from a delivery service may be useful. Individual case reviews can identify needs for focused educational programs and improvement in systems of perinatal care. Analyzing trends allows for the assessment of the effect of quality improvement interventions.
The Apgar score describes the condition of the newborn infant immediately after birth and, when properly applied, is a tool for standardized assessment. 18 It also provides a mechanism to record fetal-to-neonatal transition. Apgar scores do not predict individual mortality or adverse neurologic outcome. However, based on population studies, Apgar scores of less than 5 at 5 and 10 minutes clearly confer an increased relative risk of cerebral palsy, and the degree of abnormality correlates with the risk of cerebral palsy. Most infants with low Apgar scores, however, will not develop cerebral palsy. The Apgar score is affected by many factors, including gestational age, maternal medications, resuscitation, and cardiorespiratory and neurologic conditions. If the Apgar score at 5 minutes is 7 or greater, it is unlikely that peripartum hypoxia–ischemia caused neonatal encephalopathy.
The Apgar score does not predict individual neonatal mortality or neurologic outcome and should not be used for that purpose.
It is inappropriate to use the Apgar score alone to establish the diagnosis of asphyxia. The term asphyxia, which describes a process of varying severity and duration rather than an end point, should not be applied to birth events unless specific evidence of markedly impaired intrapartum or immediate postnatal gas exchange can be documented.
When a newborn infant has an Apgar score of 5 or less at 5 minutes, umbilical arterial blood gas samples from a clamped section of the umbilical cord should be obtained. Submitting the placenta for pathologic examination may be valuable.
Perinatal health care professionals should be consistent in assigning an Apgar score during resuscitation; therefore, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists encourage use of an expanded Apgar score reporting form that accounts for concurrent resuscitative interventions.
Kristi L. Watterberg, MD, FAAP, Chairperson
Susan Aucott, MD, FAAP
William E. Benitz, MD, FAAP
James J. Cummings, MD, FAAP
Eric C. Eichenwald, MD, FAAP
Jay Goldsmith, MD, FAAP
Brenda B. Poindexter, MD, FAAP
Karen Puopolo, MD, FAAP
Dan L. Stewart, MD, FAAP
Kasper S. Wang, MD, FAAP
Captain Wanda D. Barfield, MD, MPH, FAAP – Centers for Disease Control and Prevention
James Goldberg, MD – American College of Obstetricians and Gynecologists
Thierry Lacaze, MD – Canadian Pediatric Society
Erin L. Keels, APRN, MS, NNP-BC – National Association of Neonatal Nurses
Tonse N.K. Raju, MD, DCH, FAAP – National Institutes of Health
Jim Couto, MA
Jeffrey L. Ecker, MD, Chairperson
Joseph R. Wax, MD, Vice Chairperson
Ann Elizabeth Bryant Borders, MD
Yasser Yehia El-Sayed, MD
R. Phillips Heine, MD
Denise J. Jamieson, MD
Maria Anne Mascola, MD
Howard L. Minkoff, MD
Alison M. Stuebe, MD
James E. Sumners, MD
Methodius G. Tuuli, MD
Kurt R. Wharton, MD
Debra Bingham, DrPh, RN – Association of Women’s Health Obstetric Neonatal Nurses
Sean C. Blackwell, MD – Society for Maternal–Fetal Medicine
William M. Callaghan, MD – Centers for Disease Control and Prevention
Julia Carey-Corrado, MD – US Food and Drug Administration
Beth Choby, MD – American Academy of Family Physicians
Joshua A. Copel, MD – American Institute of Ultrasound in Medicine
Nathaniel DeNicola, MD, MS – American Academy of Pediatrics Council on Environmental Health (ACOG liaison)
Tina Clark-Samazan Foster, MD – Committee on Patient Safety and Quality Improvement – Ex-Officio
William Adam Grobman, MD – Committee on Practice Bulletins-Obstetrics – Ex-Officio
Rhonda Hearns-Stokes, MD – US Food and Drug Administration
Tekoa King, CNM, FACNM – American College of Nurse-Midwives
Uma Reddy, MD, MPH – National Institute of Child Health and Human Development
Kristi L. Watterberg, MD – American Academy of Pediatrics
Cathy H. Whittlesey – Executive Board – Ex-Officio
Edward A. Yaghmour, MD – American Society of Anesthesiologists
Gerald F. Joseph, Jr, MD
Mindy Saraco, MHA
Debra Hawks, MPH
Margaret Villalonga
Amanda Guiliano
This document is copyrighted and is the property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
Policy statements from the American Academy of Pediatrics benefit from expertise and resources of liaisons and internal (AAP) and external reviewers. However, policy statements from the American Academy of Pediatrics may not reflect the views of the liaisons or the organizations or government agencies that they represent.
The guidance in this statement does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All policy statements from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
Also published in Obstetrics & Gynecology . Copyright October 2015 by the American College of Obstetricians and Gynecologists, 409 12th Street, SW, PO Box 96920, Washington, DC 20090-6920 and the American Academy of Pediatrics, 141 Northwest Point Blvd, PO Box 927, Elk Grove Village, IL 60009-0927. All rights reserved. ISSN 1074-861×
The American College of Obstetricians and Gynecologists Committee Opinion no. 644: The Apgar score. Obstet Gynecol . 2015;126:e52–e55. Accepted for publication Jul 22, 2015
Re:Time for the Combined Apgar
We thank the authors for their recently published study of the ability of alternative versions of the Apgar score to predict perinatal mortality. Your study is consistent with the main points of our statement regarding the limitations of the Apgar score: (1) the Apgar score does not predict individual outcomes and should not be used for that purpose; (2) the Apgar score alone does not establish a diagnosis of asphyxia; and (3) the use of an expanded Apgar score can provide additional information detailing resuscitative efforts. The suggestion that adding a second number to the existing Apgar score to summarize the interventions described in the expanded Apgar score table is certainly intriguing, and could potentially improve communication. We look forward to confirmation of your findings in subsequent cohorts.
Conflict of Interest:
None declared
Time for the Combined Apgar
on behalf of the TEST-APGAR study group
In regard to The AAP and the ACOG report on the usage of the Apgar-Score in the current issue of Pediatrics.
We agree with the authors that it is necessary "to place the Apgar score in its proper perspective", especially in the light of recent advances in delivery room management (1). Furthermore, we strongly support their conclusion that "perinatal health care professionals should be consistent in assigning an Apgar score during resuscitation." However, to our disappointment the authors missed the opportunity to give - based on current scientific evidence (2,3) - a suggestion on how to make the assignment more consistent. The authors encourage the use of the Expanded-Apgar as already suggested in 2006 without giving a practical approach on how to report its results in daily work and discharge letters (4). In addition to these practical issues, the Expanded-Apgar will be less predictive and uncertainties remain without a specification of the conventional Apgar score (2). The combination of both, a Specified-Apgar (which scores infant`s condition irrespective of treatment or gestational age) plus the Expanded- Apgar (scoring the interventions the infant has received), will solve both problems (2). In contrast to author's statement, this combination of two scores - named Combined-Apgar - was prospectively tested in about 2000 infants. A large international multicenter study in VLBW infants proved the Combined-Apgar at 5 and 10 minutes to have a high predictive value on perinatal mortality: A Combined-Apgar of 0 to 5 (many interventions with poor response) at 5 and/or 10 minutes was associated with a 30-fold increase in mortality in 1855 VLBW infants (2). A similar good predictive value of the Combined-Apgar was shown in term infants (2). Thus, as previously stated, "... changes to perinatal care necessitate a reformation of the conventional Apgar and the Combined-Apgar Score represents a chance to do so" (5).
1) Statement P. The Apgar Score. Pediatrics. 2015;136(4):819-822. doi:10.1542/peds.2015-2651. 2) Rudiger M, Braun N, Aranda J, et al. Neonatal assessment in the delivery room - Trial to Evaluate a Specified Type of Apgar (TEST-Apgar). BMC Pediatr. 2015;15:18. doi:10.1186/s12887-015-0334-7. 3) Dalili H, Nili F, Sheikh M, Hardani AK, Shariat M, Nayeri F. Comparison of the four proposed apgar scoring systems in the assessment of birth asphyxia and adverse early neurologic outcomes. PLoS One. 2015;10(3):e0122116. doi:10.1371/journal.pone.0122116. 4) Statement P. The Apgar score. Pediatrics. 2006;117(4):1444-1447. doi:10.1542/peds.2006-0325. 5) Rudiger M, Konstantelos D. Apgar score and risk of cause-specific infant mortality. Lancet. 2015;385(9967):505-6. doi:10.1016/S0140- 6736(15)60196-9.
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 20 May 2024
Neuromuscular components of Apgar score in predicting delivery room respiratory support
- Manoj Biniwale ORCID: orcid.org/0000-0002-6616-7132 1
Pediatric Research ( 2024 ) Cite this article
27 Accesses
Metrics details
Newborn wellbeing is documented by use of Apgar scores after every delivery of the infant all over the world. Scores developed by Dr Virginia Apgar in 1952 are still considered as the gold standard for the assessment of newborns at 1 and 5 min of age by both the American College of Obstetricians and Gynecologists, and the American Academy of Pediatrics. 1 Five elements of Apgar scores namely heart rate, respiration, color, activity (muscle tone) and grimace (reflexes) constitute equal points ranging from 0 to 2 leading to maximum score of 10 points. Neonatal resuscitation program typically focuses on heart rate, breathing and color (oxygen saturations) for steps in performing resuscitation. There is less emphasis given for grimace and activity during decision making at the time of resuscitation. Even though activity and grimace essentially reflect neuromuscular response of the infant with tone and reflexes respectively its utility has been limited especially in preterm infants. While assessment of heart rate, breathing and color are easy to interpret with placement of cardiac monitor and pulse oximeter in preterm infants there is significant variability between delivery room personnel to interpret scoring of activity and grimace as compared to term infants. 2
Majority of very preterm infants require some form of resuscitation ranging from oxygen through mask or nasal cannula, continuous positive airway pressure (CPAP), positive pressure ventilation (PPV) to intubation with advanced cardiopulmonary resuscitation. It is of utmost importance to provide the optimum respiratory support in these preterm infants to avoid further morbidities which may lead to long term consequences. Current delivery room decisions while caring for preterm infants are based on the response to initial steps of resuscitation as well as individual experience of personnel leading resuscitation and local practice standards. Predicting stability in these infants is the highest priority in order to avoid unnecessary escalation of support. Even if the decisions to provide or escalate respiratory support are made based on heart rate and oxygen saturations in reality getting accurate heart rate and oxygen saturations in the first minutes of life in very preterm infants may not be always feasible with pulse oximetry. 3 The study by Tuttle et al in this edition of Pediatric Research have addressed the concerns in predicting interpersonal variability and assessing need for respiratory support while focusing on two of the least relied upon components of Apgar score namely grimace and activity. 4
The authors hypothesize that initial grimace and activity reported in Apgar scores can predict reliably what respiratory support is required for these very preterm infants to successfully achieve stabilization. The study uses videos of prerecorded resuscitation conducted from previous study and quality improvement measures to calculate grimace and activity scores at early stages of resuscitation in very preterm infants. It is interesting to note that seven neonatal consultants were blinded to report the grimace and activity scores on the video clips prior to receiving the respiratory support. The videos were condensed to get immediate reflection of scores from the blinded personnel. Additionally, the authors deleted audios from all clips to avoid any bias. Assessors scored the video clips only once and median scores were considered for analyses. Further, the scores for grimace and activity were combined, and infants were separated in two groups. The infants were labeled non-vigorous if combined score was <2 and vigorous if score was ≥2. Outcome of respiratory support was divided into three categories of no respiratory support/CPAP, PPV for longer than 15 seconds and attempts for intubations. Additionally, the team assessed interobserver variability for scoring these two components of Apgar score.
Authors did not find any significant difference in the requirement of respiratory support when they analyzed activity and grimace as individual factors. On the other hand, when the scores were combined together, the infants labeled as non-vigorous were at significantly higher risk for requiring greater level of respiratory support. Further, these infants were less likely to be stabilized by CPAP alone. Another interesting finding was that initially there was some correlation between lower heart rate in non-vigorous infants. Over time authors noted a poor correlation between non-vigorous infants when compared to heart rate and oxygen saturations. Decision making for the respiratory support in the delivery room is more complex than simply following the algorithm especially in extremely preterm infants. One must weigh in the facts that even if heart rate and oxygen saturations are relatively within the range whether it is sustainable for the non-vigorous infants to achieve a longer term stabilization without needing additional respiratory support. Additionally, immaturity of lungs plays a significant role due to variability in surfactant production.
Heart rate, respiration and color typically assess cardiorespiratory wellbeing of the newborn infants whereas grimace and activity of Apgar scores typically assess neuromuscular response. Thus combining these two neuromuscular components may give better perception of overall infant wellbeing. It makes sense that the neuromuscular factors would predict the need for initial respiratory support independent of heart rate and oxygen saturations as shown in the present study. There are several causes of having abnormal tone and reflexes at birth. Predominant prenatal causes include compromised blood flow through placenta due to maternal hypertension or abruption. Maternal medications such as magnesium sulfate or administration of general anesthesia can compromise the tone in preterm infants. Additionally, infant causes typically include sepsis, metabolic derangements and neurological insult among other. 1 , 5 The present study only includes few of these factors to differentiate the etiology of having low grimace and activity scores, and their effects on the outcomes.
Video recordings of neonatal resuscitation is practiced at several institutions all over the world mainly to review local practices and improve the performance of resuscitation. 6 The video recordings have been also used in clinical research studies to get accurate time points for the resuscitation and used as a tool in the training to assess adherence with algorithms and guidelines as well as technical, cognitive and behavioral skills. 7 The present study used small clips of videos recorded during the resuscitation of preterm infants. The clips shown to the blinded consultants were only 5–20 s in length. It is interesting to note that even the brief clips were assessed accurately by these blinded consultants to predict the decision making for the need of respiratory support during the resuscitation. Further, it is impressive to see a very little variability among the consultants with most of them showing agreement to similar scores of grimace and activity. One may argue that the scoring consultants were from only two large institutions compared to previous studies showing more variability among neonatologists from several centers with different backgrounds. 2 , 8
Overall this study brings very unique aspects of Apgar scoring components. Activity and grimace are typically assigned in retrospect for the majority of very preterm resuscitations. These two components are generally not considered as priority and ignored for initialing resuscitation measures or assessing response. The present study may lead to more clinical research questions on how to interpret grimace and activity, and whether these two factors play more role than we think especially in very preterm infants. Previous studies have shown a low predictability of Apgar scores in assessing long term neurodevelopmental outcomes in preterm infants which was partly due to variability in scoring. 9 Recently using machine learning algorithms researchers have assessed various factors including all components of Apgar scores that play roles in robust prediction of survival in extremely preterm infants. 10 One may use the resuscitation videos along with pertinent clinical information into the artificial intelligence models which may improve accuracy and limit variability in predicting the need for respiratory support in preterm infants. Additionally, whether neuromuscular responses at birth have any impact of future general movement assessment is remained to be studied. Researchers may also assess correlation between the response to resuscitation using brain oxygen levels with near infrared spectroscopy and initial neurological responses recorded through grimace and activity. Further studies may focus on assessing long term consequences of having low scores in activity and grimace to independently predict neurodevelopmental outcomes.
Simon L. V., Hashmi M. F. & Bragg B. N. APGAR Score. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470569/ (2024).
Bashambu, M. T., Whitehead, H., Hibbs, A. M., Martin, R. J. & Bhola, M. Evaluation of interobserver agreement of apgar scoring in preterm infants. Pediatrics 130 , e982–e987 (2012).
Katheria, A., Rich, W. & Finer, N. Electrocardiogram provides a continuous heart rate faster than oximetry during neonatal resuscitation. Pediatrics 130 , e1177–e1181 (2012).
Tuttle Z. et al. Combining activity and grimace scores reflects perinatal stability in infants <32 weeks gestational age. Pediatr Res. https://doi.org/10.1038/s41390-024-03130-6 (2024).
Yozawitz, E., Delfiner, L. & Moshé, S. L. Neonatal hypotonia. Neoreviews 19 , e445–e455 (2018).
Olson, L. et al. Neonatal resuscitation monitoring: A low-cost video recording setup for quality improvement in the delivery room at the resuscitation table. Front Pediatr. 10 , 952489 (2022).
Article PubMed PubMed Central Google Scholar
Simma B. et al. Video recording in the delivery room: Current status, implications and implementation. Pediatr Res. https://doi.org/10.1038/s41390-021-01865-0 (2021).
Rüdiger, M. et al. Variations of Apgar score of very low birth weight infants in different neonatal intensive care units. Acta Paediatr . 98 , 1433–1436 (2009).
Ehrhardt, H. et al. Apgar score and neurodevelopmental outcomes at age 5 years in infants born extremely preterm. JAMA Netw. Open 6 , e2332413 (2023).
Li, A., Mullin, S. & Elkin, P. L. Improving prediction of survival for extremely premature infants born at 23 to 29 weeks gestational age in the neonatal intensive care unit: development and evaluation of machine learning models. JMIR Med. Inf. 12 , e42271 (2024).
Article Google Scholar
Download references
Open access funding provided by SCELC, Statewide California Electronic Library Consortium.
Author information
Authors and affiliations.
Department of Pediatrics, Keck Medical School of USC, 1200 N State Street, Los Angeles, CA, 90033, USA
Manoj Biniwale
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Manoj Biniwale .
Ethics declarations
Competing interests.
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions

About this article
Cite this article.
Biniwale, M. Neuromuscular components of Apgar score in predicting delivery room respiratory support. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03281-6
Download citation
Received : 23 April 2024
Accepted : 29 April 2024
Published : 20 May 2024
DOI : https://doi.org/10.1038/s41390-024-03281-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Factors associated with 5-min APGAR score, death and survival in neonatal intensive care: a case-control study
Affiliations.
- 1 Federal University of Pará (UFPA), Belém, PA, Brazil.
- 2 State University of Pará (UEPA), Belém, PA, Brazil.
- 3 Ceres Faculty of Medicine (FACERES), São José do Rio Preto, SP, Brazil.
- 4 Federal University of Pará (UFPA), Belém, PA, Brazil. [email protected].
- 5 Clinical and Experimental Research Unit of the Urogenital System (UPCEURG), Institute of Health Sciences of the Federal University of Pará. João de Barros Barreto Hospital, Mundurucus street, 4487; Guamá, Belém, PA, CEP: 66073-000, Brazil. [email protected].
- PMID: 36151512
- PMCID: PMC9502588
- DOI: 10.1186/s12887-022-03592-9
Background: The 5-minute APGAR score is clinically used as a screening tool to assess how the newborn has reacted to previous care, remaining relevant for predicting neonatal survival. This study aimed to analyze the determinants of the 5th minute APGAR score, and the factors associated with the death and survival of newborns with low APGAR scores hospitalized in the neonatal intensive care unit (NICU) at a referral public hospital in North Brazil.
Methods: This was a hospital-based retrospective case-control study with 277 medical records. Newborns who presented with a 1-minute APGAR score < 7 followed by a 5-minute APGAR score < 7 were considered cases, while a score ≥ 7 was categorized as controls. Univariate and multivariable logistic regression analyses were used to establish the determinant factors of the low APGAR score and death outcome in this group. Survival curves were obtained using the Kaplan-Meier estimator, and then univariate and multivariate Cox regression was performed.
Results: After adjusted analysis, the factor associated with low APGAR scores was vaginal delivery (OR = 3.25, 95%CI = 1.60-6.62, p = 0.001). Birth injury (OR = 0.39, 95%CI = 0.19-0.83, p = 0.014) was associated with upper APGAR scores. No significant independent associations were observed between the variables analyzed and death in the low APGAR score group. The Kaplan-Meier curve showed that individuals who presented Cesarean delivery had a shorter survival time in the ICU.
Conclusion: In this setting, a 5-minute Apgar score < 7 was associated with the occurrence of vaginal delivery and birth injury with a 5-minute Apgar score ≥ 7. Survival in ICU was lower in newborns that were delivered via cesarean section.
Keywords: Apgar score; Child health services; Intensive care units, neonatal.
© 2022. The Author(s).
Publication types
- Research Support, Non-U.S. Gov't
- Apgar Score
- Birth Injuries*
- Case-Control Studies
- Cesarean Section
- Infant, Newborn
- Infant, Newborn, Diseases*
- Intensive Care, Neonatal
- Retrospective Studies
Assessment of Deafness in Term Infants with Birth Asphyxia with Otoacoustic Emission and Brain Stem Evoked Response Audiometry: A Prospective Observational Study
- Original Article
- Published: 22 May 2024
Cite this article

- Reshma P. Chavan ORCID: orcid.org/0000-0002-4267-7285 1 ,
- Sujit M. Shivsharan 1 &
- Akshay B. Nalte 1
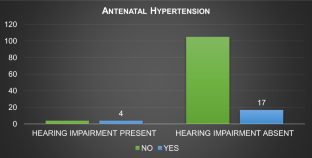
To assess deafness in term infant with birth asphyxia by otoacoustic emission and brain stem evoked response audiometry. A Prospective observational study was done at Tertiary care government hospital from 15/02/2021 to 15/10/2022.Total 130 patients were included in the study by consecutive sampling method. All the patients fulfilling the inclusion criteria during the study period were included. After explaining the aims, objectives and methods of study, written informed consent was obtained from the parents to undergo Otoacoustic Emission (OAE) and Brain Stem Evoked Response Audiometry Test (BERA). Data was entered in case record form. Collected data was analysed by appropriate statistical methods. Hearing impairment was present in eight (6.15%) asphyxiated term infants. A mild degree of hearing loss was seen in three (37.5%), a moderate degree of hearing loss was seen in four (50%), severe degree of hearing loss was seen in one (12.5%) asphyxiated term infant. In asphyxiated term infants, no significant difference in hearing loss was seen with respect to gender, Obstetrics history, and type of delivery. Significant difference in hearing loss was seen in antenatal Diabetes mellitus, hypertension, family history of SNHL and APGAR Score less than 6. Severe degree of hearing loss was seen in prolonged labour and HTN mother. Significant difference in hearing loss was seen in antenatal Diabetes mellitus, hypertension, family history of SNHL and APGAR Score less than 4 and 6 in one and five minutes respectively. Severe degree of hearing loss was seen in prolonged labour and HTN mother.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Mishra G, Sharma Y, Mehta K, Patel G (2013) Efficacy of distortion product oto-acoustic emission (OAE)/auditory brainstem evoked response (ABR) protocols in universal neonatal hearing screening and detecting hearing loss in children <2 years of age. Indian J Otolaryngol Head Neck Surg 65(2):105–110
Article PubMed Google Scholar
Sachdeva K, Sao T (2017) Outcomes of newborn hearing screening program: a hospital based study. Indian J Otolaryngol Head Neck Surg 69(2):194–198
Article PubMed PubMed Central Google Scholar
Wroblewska-Seniuk KE, Dabrowski P, Szyfter W, Mazela J (2016) Universal newborn hearing screening: methods and results, obstacles, and benefits. Pediatr Res 81(3):415–422. https://doi.org/10.1038/pr.2016.250
Parving A (1993) Congenital hearing disability: epidemiology and identification: a comparison between two health authority districts. Int J Pediatr Otorhinolaryngol 27:29–46
Article CAS PubMed Google Scholar
Kim SY, Bothwell NE, Backous DD (2002) The expanding role of the otolaryngologist in managing infants and children with hearing loss. Otolaryngol Clin N Am 35(4):699–710
Article Google Scholar
White KR, Maxon AB (1995) Universal screening for infant hearing impairment: simple, beneficial, and presently justified. Int J Pediatric Otorhinolaryngol 32(3):201–211. https://doi.org/10.1016/0165-5876(95)01165-8
Article CAS Google Scholar
Aradhana A, Sarangi G, Saboth P, Tripathy R (2020) Assessment of hearing impairment in NICU graduates by otoacoustic emission and brainstem evoked response audiometry tests. J Neonatol 34(3):109–117
Wilson DF, Hodgson RS, Gustafson MF, Hogue S, Mills L (1992) The sensitivity of auditory brainstem response testing in small acoustic neuromas. Laryngoscope 102(9):961–964
Sharma P, Chhangani NP, Meena KR et al (2006) Brainstem evoked response audiometry (BAER) in infants with hyperbilirubinemia. Indian J Pediatr 73(5):413–416
Yousefi J, Ajalloueyan M, Amirsalari S, Hassanali Fard M (2013) The specificity and sensitivity of transient otoacustic emission in neonatal hearing screening compared with diagnostic test of auditory brain stem response in tehran hospitals. Iran J Pediatr 23(2):199–204
PubMed PubMed Central Google Scholar
Amini E, Kasheh Farahani Z, Rafiee Samani M et al (2014) Assessment of hearing loss by OAE in asphyxiated newborns. Iran Red Crescent Med J 16(1):e6812. https://doi.org/10.5812/ircmj.6812
Singh R, Vates E. Brainstem Auditory Evoked Response Test. [Updated 2023 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK597358
Eiserman WD, Hartel DM, Shisler L, Buhrmann J, White KR, Foust T (2008) Using otoacoustic emissions to screen for hearing loss in early childhood care settings. Int J pediatr otorhinolaryngol 72(4):475–482
Davis A, Wood S (1992) The epidemiology of childhood hearing impairment: factors relevant to planning of services. Br J Audiol 26(2):77–90
Pourarian S, Khademi B, Pishva N, Jamali A (2012) Prevalence of hearing loss in newborns admitted to neonatal intensive care unit. Iran J otorhinolaryngol 24(68):129
Kilickan L, Gürkan Y, Aydin Ö, Etiler N (2003) The effect of combined spinal-epidural (CSE) anaesthesia and size of spinal needle on postoperative hearing loss after elective caesarean section. Clin Otolaryngol Allied Sci 28(3):267–272
Ohl C, Dornier L, Czajka C, Chobaut JC, Tavernier L (2009) Newborn hearing screening on infants at risk. Int J Pediatr Otorhinolaryngol 73(12):1691–1695
Thornberg E, Thiringer K, Odeback A, Milsom I (1995) Birth asphyxia: incidence, clinical course and outcome in a Swedish population. Acta Paediatr 84(8):927–932
Alfirevic Z, Devane D, Gyte GM, Cuthbert A (2017) Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labor. Cochrane Database Syst Rev, 2: CD006066.
Bahl R (2010) Newborn and infant hearing screening. In: Kocur I (ed) Current issues and guiding principles for action. WHO Press, Geneva
Google Scholar
World Health Organization (WHO). Situation review and update on deafness, hearing loss and intervention programs proposed plans of action for prevention and alleviation of hearing impairment in countries of the South East Asia Region. New Delhi WHO Regional Office for South East Asia; 2007.
Yoshinaga Itano C, Sedey AL, Coulter DK, Mehl AL (1998) Language of early and later identified children with hearing loss. Pediatrics 102(5):1161–1171
Yoshinaga-Itano C (1995) Efficacy of early identification and intervention. Semin Hear 16:115–120
Martines F, Porrello M, Ferrara M, Martines M, Martines E (2007) Newborn hearing screening project using transient evoked otoacoustic emissions: western sicily experience. Int J Pediatr Otorhinolaryngol 71(1):107–112
Martines F, Bentivegna D, Ciprì S, Costantino C, Marchese D, Martines E (2012) On the threshold of effective well infant nursery hearing screening in Western Sicily. Int J Pediatr Otorhinolaryngol 76(3):423–427
Salvago P, Martines E, Martines F (2013) Prevalence and risk factors for sensorineural hearing loss: western sicily overview. Eur Arch Otorhinolaryngol 270(12):3049–3056
Pawar R, Illalu S, Fattepur SR (2019) A study on prevalence of hearing impairment in newborns with birth asphyxia admitted to neonatal intensive care unit. Int J Pediatr Res 6(1):42–49
Meqbel AL, AS, Al BAGHLI HA, (2015) The prevalence of hearing impairment in high-risk infants in Kuwait. Aud Vest Res 24(1):11–16
Bakhshaee M, Boskabadi H, Hassanzadeh M, Nourizadeh N, Ghassemi MM, Khazaeni K, Moghiman T, Tale MR (2008) Hearing impairment in the neonate of preeclamptic women. Otolaryngol Head Neck Surg 139(6):846–849
Amini E, Kasheh Farahani Z, Rafiee Samani M, Hamedi H, Zamani A, Karimi Yazdi A, Nayeri F, Nili F, Rezaeizadeh G (2014) Assessment of hearing loss by OAE in asphyxiated newborns. Iran Red Crescent Med J 16(1):e6812
Stanton SG, Ryerson E, Moore SL, Sullivan-Mahoney M, Couch SC (2005) Hearing screening outcomes in infants of pregestational diabetic mothers. Am J Audiol 14(1):86–93
Zhou JH, Yu K, Ding H, Zhu ZH, Han LH, Zhang T (2021) A clinical study on gestational diabetes mellitus and the hearing of newborns. Diabet Metab Syndr Obes Targets Ther 14:2879
Kountakis SE, Skoulas I, Phillips D, Chang CJ (2002) Risk factors for hearing loss in neonates: a prospective study. Am J Otolaryngol 23(3):133–137
Ewart-Toland A, Yankowitz J, Winder A, Imagire R, Cox VA, Aylsworth AS et al (2000) Oculoauriculovertebral abnormalities in children of diabetic mothers. Am J Med Genet 90(4):303–309
Alan C, Alan MA (2021) Maternal hypertension, pre-eclampsia, eclampsia and newborn hearing: a retrospective analysis of 454 newborns. Int J Pediatr Otorhinolaryngol 146:110748
Kattah AG, Garovic VD (2013) The management of hypertension in pregnancy. Adv Chronic Kidney Dis 20(3):229–239. https://doi.org/10.1053/j.ackd.2013.01.014
Berg CJ, Callaghan WM, Syverson C, Henderson Z (2010) Pregnancy-related mortality in the United States, 1998 to 2005. Obstet Gynecol 9(3):1302–1309
Tabrizi AG, Asadi M, Naini AS (2016) Preeclamsia: A New Risk Factor for Hearing Loss. Biomed Pharmacol J 9(3):1135–1138
Bakhshaee M, Hassanzadeh M, Nourizadeh N, Karimi E, Moghiman T, Shakeri M (2008) Hearing impairment in pregnancy toxemia. Otolaryngol Head Neck Surg 139(2):298–300. https://doi.org/10.1016/j.otohns.2008.04.016
Kunnath AZ, Aboobakker ASC, Kunjimon BN, Sreedhar S (2021) Hearing impairment among high risk neonates born in a tertiary care hospital in north Kerala–a cross sectional study. Int J Otorhinolaryngol Head Neck Surg 7:452–458
Gouri ZU, Sharma D, Berwal PK, Pandita A, Pawar S (2015) Hearing impairment and its risk factors by newborn screening in north-western India. Matern health, neonatol perinatol 1(1):1–7
Binay C, Kavuncuoglu S, Fidan V, Binay O, Altuncu E, Taskin U (2016) Screening for abnormal hearing in newborns and assessment of high-risk group. Austin J Otolaryngol. 3(2):1073
Regina M, Moideen SP, Mohan M, Mohammed MT, Afroze KH (2017) Audiological screening of high risk infants and prevalence of risk factors. Int J Contemp Pediatr. 4(2):507–511
Sun P, Liang Y, Tan M, Yuan Y, Yang C, Liu Y et al (2015) Correlation between risk factors of hearing lose and results of initial hearing screening in 1021 neonates. J Clinical Otorhinolaryngology Head Neck Surg 29(10):893–898
American Academy of Paediatrics (2007) Years 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Paediatrics 120(4):898
Beswick R, Driscoll C, Kei J (2012) Monitoring for postnatal hearing loss using risk factors: a systematic literature review. Ear Hearing 33(6):745–756
Güven SG (2019) The effect of mode of delivery on newborn hearing screening results. Turk Arch Otolaryngol 57(1):19–23
Shahid R, Vigilante M, Deyro H, Reyes I, Gonzalez B, Kliethermes S (2016) Risk factors for failed newborn otoacoustic emissions hearing screen. Clin Pediatr 55(12):1138–1142
Olusanya BO (2009) Newborns at risk of sensorineural hearing loss in low-income countries. Arch Dis Child 94(3):227–230
Xiao T, Li Y, Xiao L, Jiang L, Hu Q (2015) Association between mode of delivery and failure of neonatal acoustic emission test: a retro-spective analysis. Int J Pediatr Otorhinolaryngol 79(4):516–519
Roth DA, Hildesheimer M, Maayan-Metzger A, Muchnik C, Hamburger A, Mazkeret R, Kuint J (2006) Low prevalence of hearing impairment among very low birthweight infants as detected by universal neonatal hearing screening. Arch Dis Child Fetal Neonatal Ed 91(4):F257–F262
Article PubMed Central Google Scholar
Poonual W, Navacharoen N, Kangsanarak J, Namwongprom S (2016) Risk factors for hearing loss in infants under universal hearing screening program in Northern Thailand. J Multidiscip Healthc 9:1–5
PubMed Google Scholar
Joint Committee on Infant Hearing, American Academy of Audiology, American Academy of Pediatrics et al (2000) position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics 106(4):798–817
Baradaranfar M, Mehrparvar A, Mostagahci M, Mollasadeghi A, Naghshineh E, Davari M (2014) Hearing abnormality in neonate intensive care unit (NICU). Yazd-Iran Int J Pediatr 2(2):113–117
Nagapoornima P, Ramesh A, Rao S et al (2007) Universal hearing screening. Indian J Pediatr 74(6):545–549
John M, Balraj A, Kurien M (2009) Neonatal screening for hearing loss: pilot study from a tertiary care centre. Indian J Otolaryngol Head Neck Surg 61(1):23–26
Article CAS PubMed PubMed Central Google Scholar
Rance G (2005) Auditory neuropathy/dys-synchrony and its perceptual consequences. Trends in Amplif 9(1):1–43
Vare R et al (2022) Neonatal hearing screening programme-efficacy of otoacoustic emissions in detecting hearing loss. Int J Recent Sci Res 13(04):984–988
Heikkinen T (2001) The role of respiratory viruses in otitis media. Vaccine 19:S51–S55
Sano S, Kamide Y, Schachern PA, Paparella MM (1994) Micropathologic changes of pars tensa in children with otitis media with effusion. Arch Otolaryngol Head Neck Surg 120:815–819
Heikkinen T, Thint M, Chonmaitree T (1999) Prevalence of various respiratory viruses in the middle ear during acute otitis media. N Engl J Med 340:260–264
Olusanya BO, Davis AC, Hoffman HJ (2019) Hearing loss grades and the International classification of functioning, disability and health. Bull World Health Organ 97(10):725–728. https://doi.org/10.2471/BLT.19.230367
Ramanjaneyulu J, Kumar SR, Chaitanya VK, Kusumanjali A (2021) Oto acoustic emissions in early detection of sensorineural hearing loss in high-risk neonates. Int J Otorhinolaryngol Head Neck Surg 7:1794–1798
Labaeka AA, Tongo OO, Ogunbosi BO, Fasunla JA (2018) Prevalence of hearing impairment among high-risk newborns in Ibadan. Nigeria Frontiers in pediatrics 6:194
Hess M, Finckh-Krumer U, Bartsch M, Kewitz G, Versmold H, Gross M (1998) Hearing screening in at-risk neonate cohort. Int J Pediatr Otorhinolaryngol 46(1–2):81–89
Download references
Author information
Authors and affiliations.
Department of ENT, GMC Miraj, Miraj, Maharashtra, India
Reshma P. Chavan, Sujit M. Shivsharan & Akshay B. Nalte
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Reshma P. Chavan .
Ethics declarations
Conflict of interest.
Ethical Approval
Ethical Approval was taken by Institutional Ethical Board as per ICMR guidelines by letter no. GMCM/IEC-C/7/2021.
Human and Animal Rights
This article is a retrospective analysis of data and does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed Consent was obtained from parents of all Infants included in the study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (XLSX 32 KB)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Chavan, R.P., Shivsharan, S.M. & Nalte, A.B. Assessment of Deafness in Term Infants with Birth Asphyxia with Otoacoustic Emission and Brain Stem Evoked Response Audiometry: A Prospective Observational Study. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-04736-2
Download citation
Received : 01 January 2024
Accepted : 29 April 2024
Published : 22 May 2024
DOI : https://doi.org/10.1007/s12070-024-04736-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Otoacoustic emission
- Brain stem evoked response audiometry
- Hearing loss
- Hearing assessment
- Find a journal
- Publish with us
- Track your research
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Adverse Childhood Experiences
- Risk and Protective Factors
- Program: Essentials for Childhood: Preventing Adverse Childhood Experiences through Data to Action
- Adverse childhood experiences can have long-term impacts on health, opportunity and well-being.
- Adverse childhood experiences are common and some groups experience them more than others.

What are adverse childhood experiences?
Adverse childhood experiences, or ACEs, are potentially traumatic events that occur in childhood (0-17 years). Examples include: 1
- Experiencing violence, abuse, or neglect.
- Witnessing violence in the home or community.
- Having a family member attempt or die by suicide.
Also included are aspects of the child’s environment that can undermine their sense of safety, stability, and bonding. Examples can include growing up in a household with: 1
- Substance use problems.
- Mental health problems.
- Instability due to parental separation.
- Instability due to household members being in jail or prison.
The examples above are not a complete list of adverse experiences. Many other traumatic experiences could impact health and well-being. This can include not having enough food to eat, experiencing homelessness or unstable housing, or experiencing discrimination. 2 3 4 5 6
Quick facts and stats
ACEs are common. About 64% of adults in the United States reported they had experienced at least one type of ACE before age 18. Nearly one in six (17.3%) adults reported they had experienced four or more types of ACEs. 7
Preventing ACEs could potentially reduce many health conditions. Estimates show up to 1.9 million heart disease cases and 21 million depression cases potentially could have been avoided by preventing ACEs. 1
Some people are at greater risk of experiencing one or more ACEs than others. While all children are at risk of ACEs, numerous studies show inequities in such experiences. These inequalities are linked to the historical, social, and economic environments in which some families live. 5 6 ACEs were highest among females, non-Hispanic American Indian or Alaska Native adults, and adults who are unemployed or unable to work. 7
ACEs are costly. ACEs-related health consequences cost an estimated economic burden of $748 billion annually in Bermuda, Canada, and the United States. 8
ACEs can have lasting effects on health and well-being in childhood and life opportunities well into adulthood. 9 Life opportunities include things like education and job potential. These experiences can increase the risks of injury, sexually transmitted infections, and involvement in sex trafficking. They can also increase risks for maternal and child health problems including teen pregnancy, pregnancy complications, and fetal death. Also included are a range of chronic diseases and leading causes of death, such as cancer, diabetes, heart disease, and suicide. 1 10 11 12 13 14 15 16 17
ACEs and associated social determinants of health, such as living in under-resourced or racially segregated neighborhoods, can cause toxic stress. Toxic stress, or extended or prolonged stress, from ACEs can negatively affect children’s brain development, immune systems, and stress-response systems. These changes can affect children’s attention, decision-making, and learning. 18
Children growing up with toxic stress may have difficulty forming healthy and stable relationships. They may also have unstable work histories as adults and struggle with finances, jobs, and depression throughout life. 18 These effects can also be passed on to their own children. 19 20 21 Some children may face further exposure to toxic stress from historical and ongoing traumas. These historical and ongoing traumas refer to experiences of racial discrimination or the impacts of poverty resulting from limited educational and economic opportunities. 1 6
Adverse childhood experiences can be prevented. Certain factors may increase or decrease the risk of experiencing adverse childhood experiences.
Preventing adverse childhood experiences requires understanding and addressing the factors that put people at risk for or protect them from violence.
Creating safe, stable, nurturing relationships and environments for all children can prevent ACEs and help all children reach their full potential. We all have a role to play.
- Merrick MT, Ford DC, Ports KA, et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep 2019;68:999-1005. DOI: http://dx.doi.org/10.15585/mmwr.mm6844e1 .
- Cain KS, Meyer SC, Cummer E, Patel KK, Casacchia NJ, Montez K, Palakshappa D, Brown CL. Association of Food Insecurity with Mental Health Outcomes in Parents and Children. Science Direct. 2022; 22:7; 1105-1114. DOI: https://doi.org/10.1016/j.acap.2022.04.010 .
- Smith-Grant J, Kilmer G, Brener N, Robin L, Underwood M. Risk Behaviors and Experiences Among Youth Experiencing Homelessness—Youth Risk Behavior Survey, 23 U.S. States and 11 Local School Districts. Journal of Community Health. 2022; 47: 324-333.
- Experiencing discrimination: Early Childhood Adversity, Toxic Stress, and the Impacts of Racism on the Foundations of Health | Annual Review of Public Health https://doi.org/10.1146/annurev-publhealth-090419-101940 .
- Sedlak A, Mettenburg J, Basena M, et al. Fourth national incidence study of child abuse and neglect (NIS-4): Report to Congress. Executive Summary. Washington, DC: U.S. Department of Health an Human Services, Administration for Children and Families.; 2010.
- Font S, Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse Negl. 2016;51:390-399.
- Swedo EA, Aslam MV, Dahlberg LL, et al. Prevalence of Adverse Childhood Experiences Among U.S. Adults — Behavioral Risk Factor Surveillance System, 2011–2020. MMWR Morb Mortal Wkly Rep 2023;72:707–715. DOI: http://dx.doi.org/10.15585/mmwr.mm7226a2 .
- Bellis, MA, et al. Life Course Health Consequences and Associated Annual Costs of Adverse Childhood Experiences Across Europe and North America: A Systematic Review and Meta-Analysis. Lancet Public Health 2019.
- Adverse Childhood Experiences During the COVID-19 Pandemic and Associations with Poor Mental Health and Suicidal Behaviors Among High School Students — Adolescent Behaviors and Experiences Survey, United States, January–June 2021 | MMWR
- Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004 Feb;113(2):320-7.
- Miller ES, Fleming O, Ekpe EE, Grobman WA, Heard-Garris N. Association Between Adverse Childhood Experiences and Adverse Pregnancy Outcomes. Obstetrics & Gynecology . 2021;138(5):770-776. https://doi.org/10.1097/AOG.0000000000004570 .
- Sulaiman S, Premji SS, Tavangar F, et al. Total Adverse Childhood Experiences and Preterm Birth: A Systematic Review. Matern Child Health J . 2021;25(10):1581-1594. https://doi.org/10.1007/s10995-021-03176-6 .
- Ciciolla L, Shreffler KM, Tiemeyer S. Maternal Childhood Adversity as a Risk for Perinatal Complications and NICU Hospitalization. Journal of Pediatric Psychology . 2021;46(7):801-813. https://doi.org/10.1093/jpepsy/jsab027 .
- Mersky JP, Lee CP. Adverse childhood experiences and poor birth outcomes in a diverse, low-income sample. BMC pregnancy and childbirth. 2019;19(1). https://doi.org/10.1186/s12884-019-2560-8 .
- Reid JA, Baglivio MT, Piquero AR, Greenwald MA, Epps N. No youth left behind to human trafficking: Exploring profiles of risk. American journal of orthopsychiatry. 2019;89(6):704.
- Diamond-Welch B, Kosloski AE. Adverse childhood experiences and propensity to participate in the commercialized sex market. Child Abuse & Neglect. 2020 Jun 1;104:104468.
- Shonkoff, J. P., Garner, A. S., Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. https://doi.org/10.1542/peds.2011-2663
- Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsych. 2017;87(1):3. https://doi.org/10.1037/ort0000133 .
- Schofield TJ, Donnellan MB, Merrick MT, Ports KA, Klevens J, Leeb R. Intergenerational continuity in adverse childhood experiences and rural community environments. Am J Public Health. 2018;108(9):1148-1152. https://doi.org/10.2105/AJPH.2018.304598 .
- Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. J Adolesc Health. 2013;53(4 Suppl):S32-38. https://doi.org/10.1016/j.jadohealth.2013.05.004 .
Adverse Childhood Experiences (ACEs)
ACEs can have a tremendous impact on lifelong health and opportunity. CDC works to understand ACEs and prevent them.

VIDEO
COMMENTS
Study with Quizlet and memorize flashcards containing terms like A nurse is discussing Apgar scoring with a newly licensed nurse. The nurse should identify that which of the following factors can affect the Apgar score?, A nurse is discussing Apgar scoring with a newly licensed nurse. Which of the following information should the nurse include in the teaching?, A nurse is conducting an app car ...
Study with Quizlet and memorize flashcards containing terms like A nurse is discussing Apgar scoring with a newly licensed nurse. The nurse should identify that which of the following factors can affect the Apgar score?, A nurse is collecting data from a newborn who is 5 minutes old. The newborn has a slow and weak cry, flaccid tone, pale color, grimace, and a heart rate of 120/min.
Students read about the importance of the Apgar score in assessing the newborn after delivery. Each sign of the Apgar score is identified with illustrations...
The Apgar score is a rapid method for assessing a neonate immediately after birth and in response to resuscitation. Apgar scoring remains the accepted assessment method endorsed by the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics. While originally designed in 1952 by Dr. Virginia Apgar, an anesthesiologist at Columbia University, to assess the need ...
STEP 2: PLAY A VIDEO CASE STUDY TO WATCH AS A GROUP. Using your video-conferencing platform, open the Video Case Study and play it for the group. At the end, a Video Challenge Question will be offered. At this point, you can ask students to key in their answer using the chat function.
What is an Apgar Score? This video covers the basics of performing an Apgar Score assessment on a newborn infant.💥Neonatal and Pediatric Assessment [Full Gu...
An easy way to learn APGAR, a scoring system designed to assess newborns. Includes APGAR mnemonic! For more medicine videos consider subscribing (if you foun...
Video Case Studies RN Cases & Concepts Adult Medical-Surgical Heart Failure Perfusion Informatics & Nursing Informatics Acid-Base Acid-Base Imbalances Oxygenation ... Apgar Scoring Breastfeeding Health Promotion Complications of Pregnacy Reproduction & Sexuality Fundal Assessment Reproduction & Sexuality Maternal Newborn 4
The Apgar score is a quick assessment of a newborn baby 1 minute and 5 minutes after birth. ... with infants with an Apgar score of 7-10. Similarly, a 2018 study found that the risk of epilepsy ...
Quizlet has study tools to help you learn anything. Improve your grades and reach your goals with flashcards, practice tests and expert-written solutions today. ... practice tests and expert-written solutions today. Flashcards. 1 / 5 ATI Video Case Studies: Apgar Scoring. Log in. Sign up. Get a hint. A nurse is discussing Apgar scoring with a ...
Pediatric Education Online. Home; Podcasts; Videos; Notes; Cases; Links; Get Involved; About. About Pedscases; Our Team
The Apgar Score. Pediatrics (2015) 136 (4): 819-822. The Apgar score provides an accepted and convenient method for reporting the status of the newborn infant immediately after birth and the response to resuscitation if needed. The Apgar score alone cannot be considered as evidence of, or a consequence of, asphyxia; does not predict ...
The Apgar score has stood the test of time and has become an internationally accepted method of scoring judgments about the physiological status of newborns infant in case notes. 2-4 Apgar scores are also widely used in clinical audit and research, but there has been surprisingly little research into how accurately they are assigned. Table 1:
Make lesson planning and integration a little easier by exploring ATI's Video Case Studies Educator Implementation Guide (EIG). Get even more from our nurse-educator-written clinical replacement lesson plans, specially designed for each case. Access lesson plans and the EIG in your ATI faculty portal under Resources > Products & Integration.
Describe the physical presentation of a newborn who has an Apgar score of 2. The newborn with this means that the baby is not responsive. SCENARIO: You are caring for a mother who just delivered, and you are responsible for assessing the newborn's Apgar score based on the information below. Determine the 1-minute and 5-minute Apgar scores.
View Video Case Study.docx from MED SURG 324 at Chamberlain College of Nursing. Apgar Scoring What Apgar score would you give the newborn in the video if the heart rate is 120 BPM? Activity: 2 Pulse: ... ATI Video Case Study_ Apgar Scoring clinical 204.docx. Solutions Available. Sinclair Community College. BIO 1211.
ATI APGAR Scoring Case study Test. Get a hint. A nurse is assisting with the care of a newborn immediately following birth which of the following action should the nurse take first? Click the card to flip 👆. Place the newborn skin to skin on the mothers chest. Click the card to flip 👆. 1 / 5.
An APGAR score under 4 indicates the need for resuscitation, an APGAR score between 4 and 7 indicates the need for stimulation and a score of 7 to 10 indicates a newborn in good condition and requires only nasopharyngeal suctioning. (Davidson, London, Ladewig, 2020) 7. What emotional support should the nurse provide to the parents for a newborn ...
Biology document from West Coast University, 3 pages, Module Report Tutorial: Video Case Studies RN 3.0 Module: Reproduction: Apgar Scoring Individual Name: Sabrina Bajwa Institution: West Coast U Ontario BSN Program Type: BSN Overview Of Most Recent Use Case Date 2/23/2023 Reproduction: Apgar Scoring 2/23/2
Scores developed by Dr Virginia Apgar in 1952 are still considered as the gold standard for the assessment of newborns at 1 and 5 min of age by both the American College of Obstetricians and ...
Background: The 5-minute APGAR score is clinically used as a screening tool to assess how the newborn has reacted to previous care, remaining relevant for predicting neonatal survival. This study aimed to analyze the determinants of the 5th minute APGAR score, and the factors associated with the death and survival of newborns with low APGAR scores hospitalized in the neonatal intensive care ...
Study with Quizlet and memorize flashcards containing terms like A nurse is discussing Apgar scoring with a newly licensed nurse. The nurse should identify that which of the following factors can affect the Apgar score?, A nurse is collecting data from a newborn who is 5 minutes old. The newborn has a slow and weak cry, flaccid tone, pale color, grimace, and a heart rate of 120/min.
Similar study conducted by Joint committee on infant hearing suggests that babies with APGAR score of 0-4 at 1 min and 0-6 at 5 min were at risk of having hearing impairment . Study conducted by Baradaranfar et al. [ 54 ] found that 2.9% of babies with birth asphyxia and APGAR Scores of < 5 at 5 min was with hearing impairment.
ATI Video Case Study Apgar Scoring.docx. Solutions Available. Cincinnati State Technical and Community College. NUR 204. EDUC 750 Quiz 5 Mixed Methods and Evaluation.docx. Solutions Available. Thomas Edison State College. EDUCATION 750. COLANGELO - 7.3 - Problems- Graphical Method of Aggregate Planning.xlsx.
Rationale: Apgar scoring is a rapid assessment of the newborn's transition to extrauterine life & is based on 5 components: heart rate, respiratory effort, muscle tone, reflex irritability, & color. BP is NOT included in Apgar scoring. A nurse is assessing a newborn who is 5 min old. The newborn has a slow & weak cry, flaccid tone, pale color ...
Toxic stress, or extended or prolonged stress, from ACEs can negatively affect children's brain development, immune systems, and stress-response systems. These changes can affect children's attention, decision-making, and learning. 18. Children growing up with toxic stress may have difficulty forming healthy and stable relationships.