- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Instructional Materials
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning

MyNSTA Community
- My Collections
Good to the Bone
Biological Implications of a Potential Anti-Aging Drug
By Nalini V. Broadbelt, Michelle A. Young
Share Start a Discussion

This case study is designed to introduce students to how the bone’s architecture influences movement and the roles cells play in bone growth and repair. It tells the story of “Maria,” an active 68-year-old woman who works on a farm. Over the last five years, Maria has experienced pain in her wrist and knee joints and has used a nonsteroidal anti-inflammatory drug (ibuprofen) to deal with the pain. In the course of cleaning her home in preparation for a visit from her grandchildren, she falls and breaks a bone in three places. After reading the short case scenario and relevant journal articles, students are asked a series of questions designed to teach facts about bone anatomy, physiology and pathology underlying the patient’s condition. This case study was designed for use in both freshman-level and advanced-level courses in human anatomy and physiology. It could also be used for a biology pathology course. Before starting the case, students should have a basic understanding of the anatomy and physiology of bones.
Download Case
Date Posted
- Compare and contrast the different types of joints and how their structure and shape dictates movement.
- Describe the location and function of bone structures.
- Explain the processes of bone construction and destruction involved in the homeostasis of bone.
- Distinguish the roles of osteochondral progenitor cells, osteoblasts, osteoclasts, and osteocytes.
- Understand the process by which bone is repaired following an injury.
- Describe the process by which bone is repaired following an injury.
- Describe how the drug metformin can influence bone growth and repair and could potentially be used to treat osteoporosis and arthritis.
- Read and analyze graphical data.
Joint; bone; bone repair; fracture; metformin; osteoporosis; arthritis; graph; osteoblasts; osteoclasts; calcium; phosphorus; data analysis; remodeling; osteoporosis
Subject Headings
EDUCATIONAL LEVEL
Undergraduate lower division, Undergraduate upper division
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials, you may also like.
Web Seminar
Join us on Tuesday, June 4, 2024, from 7:00 PM to 8:30 PM ET, to learn about the free lesson plans and storyline units designed for high school studen...
Join us on Thursday, October 24, 2024, from 7:00 PM to 8:00 PM ET, to learn about all NSTA Teacher Awards available and how to apply.Did you come up w...
Join us on Thursday, September 19, 2024, from 7:00 PM to 8:00 PM ET, to learn about NSTA election process for new and interested members of the Board ...

- Eating Disorders
Two Psychiatrists Weigh in on Netflix’s "To the Bone"
A missed opportunity to understand anorexia nervosa..
Posted July 21, 2017 | Reviewed by Ekua Hagan
Co-authored by Jennifer Derenne, MD
As child, adolescent, and adult psychiatrists, we have eagerly been awaiting Netflix’s release of To the Bone . It seems intended to significantly raise awareness, educate viewers, and open conversations about these severe psychiatric disorders.
Eating disorders arise in the context of a “perfect storm” of factors, including biological vulnerability (genetic predisposition, associated mood instability), temperament ( perfectionistic , obsessive, and sensitive to rejection), and a societal preoccupation with the thin ideal. While family dynamics may contribute, it is important to note that eating disorders also, and very often, arise in loving and supportive families.
The film tells the story of Ellen, a 20-year-old Caucasian female with chronic anorexia nervosa, who seeks treatment with the unconventional Dr. Beckham (played by Keanu Reeves). Marti Noxon, the film’s writer and director, has been open about her own struggles with anorexia; Ellen’s story is an autobiographical dramatization of her own journey. Netflix describes the film as revealing Ellen’s “harrowing, funny journey of self-discovery.”
Weeks before its public release, the film has been generating a lot of discussion and controversy. On the heels of the release of 13 Reasons Why , a show that painstakingly describes the events leading to a young woman’s death by suicide through her own lens, Netflix finds itself in the midst of another discussion about responsible film making and distribution.
The major objections noted include concerns about glamorizing and glorifying eating disorders, as well as teaching “tips and tricks” for weight loss and hiding behaviors from treatment providers. In addition, given reports that photos and clips from the film have been used as “thinspiration” on pro-anorexia websites, there is concern that it may be triggering for those who are actively struggling with an eating disorder or are in recovery from their illness. Some worry that perhaps those young people who do not have an eating disorder and would not have otherwise developed one may develop “copycat” behaviors to get the intense attention that is demonstrated in the film. There has also been much debate about perpetuating stereotypes about eating disorders, namely that they are vanity problems affecting affluent white teenage girls. Finally, but perhaps most concerning, Lily Collins, the actress who plays Ellen, was also treated for anorexia nervosa as a teenager , underwent “supervised weight loss” for the role.
The reality is that almost any mention of eating, dieting , weight loss, or exercise can be difficult for someone who is actively dealing with an eating disorder. The film does contain an introductory warning that content may be difficult to watch. As for concerns about Ellen’s story serving as a “how-to” manual or guide to weight loss behaviors, the truth is that much more explicit and detrimental information can be easily found online if someone is actively looking for it. Though many individuals with eating disorders already know the “tricks of the trade” and this film will provide no surprises, it may stimulate copycat behavior in those who have romanticized anorexia nervosa and wish to have an eating disorder.
It seems clear that Ellen is suffering; she is not attaining the normal developmental milestones for someone her age, she lacks fulfilling intimate relationships, and she feels terrible about stressing her family. While she is struggling with the consequences of her illness, she is having trouble making the necessary changes to recover. It is hard to view this depiction of her life as “glamorous." That being said, Ellen is Hollywood beautiful, with meticulously applied eye make-up and cute (although oversized and layered) clothes at her disposal. We would like the film’s message to be more clear: Eating disorders are severe, life-threatening illnesses that have the highest mortality rate of any psychiatric illness.
As mental health clinicians, we struggled with the depiction of eating disorder treatment (including psychiatry) in the film. Recovery from anorexia nervosa is not solely, or even typically, about “hitting bottom” and finding motivation for change; evidence-based treatments exist and are shown to be effective when implemented aggressively and longitudinally. In this sense, the film perpetuates the myth that individuals with psychiatric disorders will, at some point, “see the light” and recover due to a single transformative experience. While dramatic and wishful, emotional and behavioral change rarely occurs in this manner. Recovery from many disorders, and eating disorders, in particular, tend to be marathons and not sprints. Psychiatrists and other mental health professionals can provide excellent, compassionate care for their patients while retaining appropriate boundaries . Earning a patient’s trust takes time, and the film conveys a fairly superficial and glamorized portrayal of the process of developing a therapeutic relationship . No psychiatrist, not even the esteemed Dr. Beckham, has the uncanny ability, the magical talent, to achieve this goal.
As experienced psychiatrists, we argue, that it would be highly unlikely for a treatment program to allow patients to exercise at will and eat (or not eat) whatever they choose. We don’t recommend that families stop talking about food or weight. And, while there are stresses in most families, we see family members as important allies in treatment rather than “problems” that need to be removed. Further, Dr. Beckham’s pronouncement, “I’m not going to treat you if you’re not interested in living,” would be unheard of coming from any sound clinician, no less an expert in anorexia nervosa. In fact, given Ellen’s degree of emaciation and likely medical instability, most clinicians treating a patient as ill as Ellen would have strongly recommended and insisted on a higher level of treatment. In short, Dr. Beckham was fostering substandard care, if not outright malpractice. Should the patient have died (as she almost did) he would be liable for a justified loss of license and civil litigation.
Despite the previous consideration of anorexia nervosa as a “culture-bound” illness of the Caucasian upper class, we now know that eating disorders affect individuals across the lifespan, throughout the gender spectrum, and across all ethnic and socioeconomic backgrounds. In the film, most of the patients, clinicians, and staff are Caucasian, which is not in line with what we see in current clinical practice. Increasing numbers of males seek treatment, as do transgender individuals.

Beyond omitting the diversity of the eating disorder population, the film perpetuated a number of stereotypes. Sadly, the character development in To the Bone was superficial, and there was minimal exploration of family dynamics. And the relationships throughout the film were superficial and sorely lacking any nuance: the African American characters (the patient with apparent binge eating disorder and the caregiver in the residential facility) were both obese. The three mothers were all Caucasian, highly self-preoccupied, and rather superficial in their approach to their children. Ellen’s stepmother is shrill and intrusive, and her mother has moved away. When they reconnect, Ellen’s mother is horrified by her frail condition, stating, "You look like a ghost.” Later, in a frankly bizarre attempt to recapture a lost mother-daughter attachment , she attempts to re-nourish her adult daughter with a baby bottle. There are some lovely moments between Ellen and her sister, but these are few and far between.
The men included a conspicuously (and stereotypically) absent father. Dr. Beckham is portrayed stereotypically as well — he is single, handsome, unconventional (although with little explanation or background as to his experience and motives), difficult to access, and heroic. But perhaps the most complex and interesting character in the film is the male patient — a dancer, a well-read and literate young man, and a sensitive, compassionate friend. Despite any efforts to disparage stereotypes, the film woefully failed and reinforced a significant number of caricatures we often see on the silver screen.
Similarly, the movie fails to capture the loneliness and isolation experienced by individuals with eating disorders. The relative ease with which the characters connect with each other, are open about their struggles, and are willing to be confrontational is unusual for individuals with eating disorders. A budding romance between two patients with anorexia nervosa in the first weeks of treatment is difficult to fathom., as most young women with anorexia nervosa are wary at best about intimate relationships. Though they may fantasize about them, they rarely jump into romances, particularly with individuals they have just met.
At the end of the day, feature movie-making is about entertainment, not advocacy and education . Marti Noxon’s vision and story are based on her own experiences with the illness, and we can appreciate and be respectful of that. However, the film lacked any coherent or complex narrative. It even failed as a vehicle for entertainment. It presents a rather flimsy snapshot of an episode in a young woman’s life.
On the other hand, while we don’t agree with her depiction of mental health treatment for eating disorders, she does convey some very significant messages. As Ellen poignantly points out, individuals with eating disorders are people, not problems. And it is important to remember that full recovery from eating disorders is possible, and there is always reason to be hopeful. The cast filmed this important public service announcement, based on recommendations of the Academy for Eating Disorders :
For parents, it is important to know that the film covers material and uses language that may be too mature for many young people. As is our recommendation with most media consumption, our advice is to have very open conversations with children and teens, before, during, and after viewing the film. We suggest that you watch the movie together. What do they know and think about eating disorders? What was their take on the film? What did they learn? What do they still feel that they need to know?
If your child is in treatment for or in recovery from an eating disorder, have a very frank conversation about whether or not it is a good idea to view the film at this time. We would also encourage schools to lead discussions about the film, using it as an opportunity to focus on eating disorders and body image .
Despite the film’s lack of substance and depth, and what we feel is an incomplete depiction of anorexia nervosa, we want to be clear that we do not support parents censoring or prohibiting teens from viewing it. When supplemented by trustworthy material curated by adults who are experienced with the trajectory of eating disorders, the film may be used as a springboard to discuss the nature, course, and treatment of eating disorders. Watch the movie with teens, and ask them what they think.
- The National Eating Disorders Association and The Academy for Eating Disorders are excellent sources for reputable information.
- Project HEAL , a non-profit that provides scholarships for eating disorder treatment, has developed this Viewing Guide for To the Bone .
A version of this post also appeared and was written by the authors (Beresin and Derenne) on the MGH Clay Center for Young Healthy Minds on July 20, 2017.

Eugene Beresin, M.D. , is a professor of psychiatry at Harvard Medical School.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(4); 2022 Apr

Osteoporosis: A Step-by-Step Case-Based Study
Lokesh goyal.
1 Family Medicine, Christus Spohn, Corpus Christi, USA
Kunal Ajmera
2 Epidemiology and Public Health, Calvert Health Medical Center, Prince Frederick, USA
Osteoporosis is a common disease that affects our elderly population. This disease usually gets undiagnosed for an extended period. Osteoporosis increases the risk of fracture in our elderly population and increases morbidity. The cost associated with osteoporosis does carry a substantial burden in our society. Here, we present a case of osteoporosis with a fracture diagnosed in clinical settings. We discuss different etiology, pathophysiology, and treatment options available to treat this medical condition.
Introduction
Osteoporosis is a disease that causes a decrease in bone mass, increasing bone fragility and fracture [ 1 ]. Osteoporosis is a common disease, and it impacts one in three post-menopausal women and one in five men worldwide. There are roughly 200 million men and women who have osteoporosis in this world. The cost and morbidity associated with osteoporosis carry a substantial burden in our society. According to World Health Organization (WHO), a patient is diagnosed with osteoporosis if the Bone Mineral Density (BMD) T-score = -2.5 [ 1 - 3 ]. The test used to calculate the T score is also called the DXA scan. There are many instruments currently available that calculate the risk of fracture, one of them is called the Fracture risk algorithm (FRAX). FRAX calculates the risk of significant fractures (in ten years) like vertebral and hip fractures due to osteoporosis. FRAX can look at data provided by DXA and use it to predict the risk of fractures more accurately. In this case, we will focus on a patient who has osteoporosis. We will focus on etiology, pathophysiology and treatment options as well.
Case presentation
Patient X is a 62-year-old Caucasian female who presents to the outpatient clinic with right wrist pain and swelling following a fall on an outstretched hand in the garage at home. This patient has a past medical history of hypertension (HTN), chronic heart failure (CHF), pneumonia, chronic obstructive pulmonary disease (COPD), asthma, gastric ulcer, menopause (age 50), stooped posture, and vertebral bone fracture. The patient has a family history of CHF and HTN in her brother (age 55), a pelvic fracture in her mother (age 82), and the mother was also diagnosed with osteoporosis. The patient’s father has HTN. Patient X is married with four children and works in Walmart. She smokes one pack of cigarettes every day and occasionally drinks alcohol. She does no exercise and is fully mobile with no disabilities. The patient does not report symptoms of orthopnea, weakness, chest pain, palpitation, paroxysmal nocturnal dyspnea, or excessive bleeding. The patient is currently taking lisinopril for decreasing afterload; furosemide for reducing edema; atorvastatin for hypercholesterolemia; metoprolol for decreasing heart rate; omeprazole for stomach acidity; fluticasone for her asthma, and epidural steroid injection for lower back pain. Patient X reports to the clinic in acute distress and is oriented to time, person and place. The patient weighs 250 lbs., BP 145/88, pulse 90, and O 2 saturation level of 92%. The patient lungs were clear on auscultation bilaterally. The cardiovascular exam showed a regular rate and rhythm without any murmurs. The right wrist is swollen and hurts to move. There was no edema on the left hand or feet. Radial, femoral, and dorsal pedis pulses were normal bilaterally. The patient was sent to the hospital to get an X-ray of the right hand (Figure (Figure1), 1 ), which revealed Colle’s fracture (distal radius) on the right hand. The hospital then puts a cast on the patient’s hand. The blood test was normal in this patient except for low levels of Vitamin D. The patient was also asked to get a DEXA scan, which revealed a T score of -2.9 (less than -2.5 is osteoporosis). The patient was started on bisphosphonates, raloxifene (selective estrogen receptor modulator [SERM]), and also given Vitamin D (1,000 mg) and calcium tablets. The patient was advised to start exercising daily and eat a healthy diet. She was also asked to be careful while walking.

Pathophysiology
The cause of osteoporosis [ 1 - 3 ] is an imbalance between bone formation and bone reabsorption. A typical bone is constantly being broken down and reformed. Around 10% of our total bone mass is under constant remodeling at any given time [ 4 ]. Due to menopause [ 5 , 6 ], the amount of estrogen secreted in a woman can decline rapidly [ 5 , 7 ]. The lack of estrogen [ 8 ] will increase the risk of bone reabsorption and decrease the deposition of new bone. Due to menopause, we also see an increase in basic multicellular units made of osteoclasts and osteoblasts cells. These osteoclast and osteoblast cells will sequentially resorb old bone and form new bone. This prolongs the osteoclast resorption time and relative shortening of the time for osteoblastic bone formation. The recent studies [ 6 , 9 , 10 ], both done in vitro and in vivo, show that, in the eugonadal state, estrogen will inhibit receptor activators of nuclear factor-κ B ligand (RANKL). RANKL [ 9 , 10 ] is a molecule found on the bone marrow stromal cells/osteoblast precursors and T and B cells. A decrease in the concentration of Vitamin D can also increase the risk of fracture and lower the BMD in the patient’s body. The primary source of Vitamin D comes from sunlight and diet. A severe deficiency of Vitamin D levels can lead to osteomalacia (in adults) or rickets (in children). These diseases cause softening of bones and increase the risk of fracture tremendously. The use of anti-acidity medications [ 2 ] like proton pump inhibitors (PPI) or H2 receptor blockers (Cimetidine) has been shown to increase fracture risk in adults. The increase in the risk of fracture due to anti-acidity medication is that these medications induce hypochlorhydria in the human body. This hypochlorhydria affects the absorption of calcium and therefore leads to a decrease in calcium in the body, increasing the risk of fracture. Any changes in sex hormones [ 8 ] are the most critical factor which affects bone loss due to aging; however, we still need to recognize the non-sex steroid hormonal changes that also occur in the human body. The most important hormone that affects bone physiology is the decrease in growth hormone secretion (as we age) from the pituitary gland. This decrease in growth hormone leads to a decrease in the production of insulin-like growth factors (IGF-1 and IGF-2) [ 4 - 6 ] from the liver. These hormones have a role in osteoblast activity and differentiation. A decrease in IGF is also associated with increased IGF inhibitory binding protein (IGFBP-2). An increase in IGFBP-2 in the human body leads to a decrease in BMD in adults [ 6 - 8 ].
The most pivotal step in the diagnosis of osteoporosis is a DEXA scan (dual-energy x-ray absorptiometry). This test measures BMD. T score of less than -2.5 is considered a diagnosis of osteoporosis. Whereas a score of -1 to -2.5 is considered osteopenia. The NOF guidelines [ 4 - 6 ] state that a patient should undergo osteoporosis treatment not just after a hip/vertebral fracture or with a T- score≤−2.5, but treatment should also be considered in postmenopausal women and men with osteopenia (age > 50). The main goal of osteoporosis treatment is not just to increase BMD but also to prevent fractures in the future. Calcium and Vitamin D deficiency leads to an increase in the risk of bone loss and muscle weakness. This deficiency will, in turn, increase the patient’s risk of falling and fracture. By prescribing calcium and Vitamin D supplements to the patient, we can decrease fracture risk by 10%-15%. Multiple outcomes of the raloxifene evaluation (MORE) [ 6 , 7 ] study has shown that raloxifene, a SERM, reduces the risk of vertebral fracture by 30% if used continuously for three years. National Institute of Health and Care Excellence (NICE) [ 6 , 7 ] recommends using raloxifene in postmenopausal women at increased risk for osteoporosis or women intolerant of Bisphosphonates. Bisphosphonate is the class of drugs used for preventing osteoporosis. It has been the best choice for the treatment of osteoporosis since the 1960s. Bisphosphonates and their analogs bind at sites where bone resorption and new bone formation occur. The osteoclasts will ingest bisphosphonates bound to the mineral and therefore inhibit the function of osteoclasts. This will consequently lead to inhibition of bone resorption.
In addition to her past medical history and family history, these findings put this patient at risk of fracture due to osteoporosis. The past medical history of patient X (menopause, steroid meds, and old age) is consistent with the common risk factors for the development of osteoporosis. Patient X also has a history of vertebral fracture, which is most likely to have been caused due to osteoporosis. The most pertinent physical exam findings for this patient are the presence of stooped posture, history of vertebral fracture, and chronic back pain. The most critical risk factor for fracture in the case of osteoporotic patients is an unstable gait, which increases the risk of falls and, therefore, fractures. To rule out any risk of future fractures, this patient went through a thorough examination (gait abnormalities, orthostatic hypotension, and cognitive impairment). Patient X also went through a thorough neurological examination to rule out any spinal cord or peripheral nerves being compromised. This patient was prescribed bisphosphonates and calcitonin, which will help in inhibiting the osteoclast function. Raloxifene (SERM), this drug, will help decrease the risk of vertebral fractures and breast cancer in women. Vitamin D and Calcium supplements will help in increasing the BMD in the bones and decrease the risk of osteoporosis. The patient was also asked to have a good diet and exercise daily to encourage weight loss. The patient must do some weight-bearing exercise as this helps increase the BMD and helps decrease osteoporosis. Due to an increase in fracture risk from falling, the patient was advised to use a walker while walking.
Conclusions
Through this case presentation, we realize that patients in our society are not appropriately screened for osteoporosis during their lifetime. This is usually due to a lack of medical knowledge among our patient population and sometimes the cost as well. Osteoporosis remains a public health problem and an economic burden to our society. As the incidence of osteoporosis continues to increase, it is clear that preventive interventions must be considered early on and sometimes as early as in utero. Patient education in primary care should focus on the benefits of a healthy lifestyle, a nutritious, and balanced diet (with Vitamin D and calcium supplements) in preventing the risk of osteoporosis. Patients must also avoid smoking, drinking, and illicit drugs as they have been shown to decrease the BMD and increase the risk of osteoporosis.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
To The Bone: Why Netflix’s portrayal of eating disorders has got it all wrong
Reader in TV Studies, University of East Anglia
Disclosure statement
Su Holmes does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
University of East Anglia provides funding as a member of The Conversation UK.
View all partners

Not many films come with a health warning. But the recent Netflix film To The Bone , which tells the story of 20-year-old Ellen – played by Lily Collins – and her journey through treatment for anorexia, has received just that. The UK’s national eating disorder charity Beat said in a statement:
We would strongly urge anyone that might be at risk of an eating disorder to think very carefully before watching this film.
There have also been calls to ban the film because of fears the film might incite eating disorders, or make someone’s problem worse.
Eating disorder sufferers – particularly young girls – have long been presented as especially “vulnerable” to the power of media images and messages. The “anorexic” is often shown as not simply vain, but also unable to separate image from “reality”. And research has shown that people diagnosed with anorexia are routinely presented as being “ suggestively vulnerable ” – that is more likely to be influenced by media images, particularly images of (often unttainable) bodies. But while these cautions most likely come from a place of genuine concern, they can often have the opposite effect and further trivialise anorexia.
Models in magazines
Unwittingly or otherwise, debates such as those over To The Bone perpetuate the idea that girls can be “infected” with anorexia by looking at images of very slim (or starved) bodies – and that this is where the crux of anorexia lies.
But as my own research with people who have experience of an eating disorder shows, not only do such ideas massively simplify the complex reasons why anorexia may develop, they also trivialise it. As one of the people in my research group explained:
So [it is] less like, well there’s a model, a skinny model in a magazine, looking at that, you’ve been looking at that too much and so you just wanna be like them … I don’t agree with that at all. I think that completely trivialises it.
One of the key problems is that there is inadequate understanding of the social and cultural aspects of eating disorders – both in wider society and the media – as well as in the treatment of eating disorders.
Eating disorders are now understood to combine biological, psychological and social factors, and yet the “social” part of the equation is still often marginalised in treatment. So although eating disorders have historically been recognised as primarily affecting girls and women in Western societies, contemporary eating disorder treatment does little to look at the relationship between eating problems and cultural constructs of femininity – notwithstanding the “obvious” fact that most patients are female.
This is despite the wealth of evidence from feminist approaches over the last 40 years which point to the significance of society – and especially gender roles – in the development of eating issues.
These approaches also aim to move beyond the idea of eating disorders as “body image” problems caused by reading too many women’s magazines – and instead look at the complex ways eating disorders might play out inequalities between genders on a broader scale.
Societal expectation
Some of the objections raised about To The Bone claim that it glamorises anorexia, and that it privileges the conventional stereotype of a young, white, fragile “waif”. I for one would like to see more representations that challenge and expand our understanding of what eating disorders “are” in terms of social and cultural identity, and how they might address the stigmatisation and trivialisation of eating disorders, and improve treatment. I don’t see this in To The Bone.
In fact, as the Guardian journalist, Hadley Freeman’s excellent article on the film observes, it perpetuates some of the same gender inequities that are behind eating disorders in the first place. Consider, for example, the fact that Keanu Reeves plays “the brilliant, patriarchal medical professional who can fix women”.

The title To The Bone suggests something about getting to the “truth” of anorexia. Such a possibility is inevitably flawed, as there are many different ways “anorexia” can be viewed and many different experiences of having anorexia.
As someone who lived with the horrifying and debilitating realities of anorexia for over 20 years, I certainly found little sense of my “truth” here. And I’m mad as hell that nobody talked to me about gender during all the time that I was in treatment, or tried to understand what I might have been struggling against. I had to figure this out myself – five years after I was discharged from in-patient treatment. I now know that my anorexia was bound up very clearly with expectations surrounding what it meant to be a “woman”, and all that adult femininity may entail. It wasn’t rocket science.
I still hope for a film that can show such understandings. But in a climate where feminism is as much vilified as welcomed, and with the skinny female body still being spectacularly fetishised in a film that purports to portray the “true” horrors of anorexia, I may well have a long wait ahead of me.
- Eating disorders
- Anorexia nervosa

Program Manager, Scholarly Development (Research)

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

Lecturer/Senior Lecturer, Earth System Science (School of Science)
- Share full article
Advertisement
Supported by
When Is the Best Time to Work Out?
It’s an age-old question. But a few recent studies have brought us closer to an answer.

By Alexander Nazaryan
What is the best time of day to exercise?
It’s a straightforward question with a frustrating number of answers, based on research results that can be downright contradictory.
The latest piece of evidence came last month from a group of Australian researchers, who argued that evening was the healthiest time to break a sweat, at least for those who are overweight. Their study looked at 30,000 middle-aged people with obesity and found that evening exercisers were 28 percent less likely to die of any cause than those who worked out in the morning or afternoon.
“We were surprised by the gap,” said Angelo Sabag, an exercise physiologist at the University of Sydney who led the study. The team expected to see a benefit from evening workouts, but “we didn’t think the risk reduction would be as pronounced as it was.”
So does that mean that evening swimmers and night runners had the right idea all along?
“It’s not settled,” said Juleen Zierath, a physiologist at the Karolinska Institute in Sweden. “It’s an emerging area of research. We haven’t done all the experiments. We’re learning a lot every month.”
No single study can dictate when you should exercise. For many people, the choice comes down to fitness goals, work schedules and plain old preferences. That said, certain times of day may offer slight advantages, depending on what you hope to achieve.
The case for morning exercise
According to a 2022 study , morning exercise may be especially beneficial for heart health. It may also lead to better sleep .
And when it comes to weight loss, there have been good arguments made for morning workouts. Last year, a study published in the journal Obesity found that people who exercised between the hours of 7 a.m. and 9 a.m. had a lower body mass index than counterparts who exercised in the afternoon or at night, though it did not track them over time, unlike the Australian study, which followed participants for an average of eight years.
Of course, the biggest argument for morning exercise may be purely practical. “For a lot of people, the morning is more convenient,” said Shawn Youngstedt, an exercise science professor at Arizona State University. Even if rising early to work out can be challenging at first , morning exercise won’t get in the way of Zoom meetings, play dates or your latest Netflix binge.
The case for afternoon exercise
A few small studies suggest that the best workout time, at least for elite athletes, might be the least convenient for many of us.
Body temperature, which is lower in the morning but peaks in late afternoon, plays a role in athletic performance. Several recent small studies with competitive athletes suggest that lower body temperature reduces performance (though warm-ups exercises help counter that) and afternoon workouts help them play better and sleep longer .
If you have the luxury of ample time, one small New Zealand study found that it can help to nap first. As far as the rest of us are concerned, a Chinese study of 92,000 people found that the best time to exercise for your heart was between 11 a.m. and 5 p.m.
“The main difference is our population,” Dr. Sabag said. While his study was restricted to obese people, the Chinese study was not. “Individuals with obesity may be more sensitive to the time-of-day effects of exercise,” he said.
The case for evening exercise
This latest study may not settle the debate, but it certainly suggests that those struggling with obesity might benefit from a later workout.
Exercise makes insulin more effective at lowering blood sugar levels, which in turn fends off weight gain and Type 2 diabetes, a common and devastating consequence of obesity.
“In the evening, you are most insulin resistant,” Dr. Sabag said. “So if you can compensate for that natural change in insulin sensitivity by doing exercise,” he explained, you can lower your blood glucose levels, and thus help keep diabetes and cardiovascular disease at bay.
One persistent concern about evening exercise is that vigorous activity can disturb sleep. However, some experts have argued that these concerns have been overstated.
The case that it may not matter
While many of these studies are fascinating, none of them is definitive. For one thing, most are simply showing a correlation between exercise times and health benefits, not identifying them as the cause.
“The definitive study would be to actually randomize people to different times,” Dr. Youngstedt said, which would be phenomenally expensive and difficult for academics.
One thing public health experts do agree on is that most Americans are far too sedentary. And that any movement is good movement.
“Whenever you can exercise,” Dr. Sabag urged. “That is the answer.”
In a recent edition of his newsletter that discussed the Australian study, Arnold Schwarzenegger — bodybuilder, actor, former governor — seemed to agree. He cited a 2023 study suggesting that there really isn’t any difference in outcomes based on which time of day you exercise. In which case, it’s all about what works best for you.
“I will continue to train in the morning,” the former Mr. Universe wrote. “It’s automatic for me.”
Alexander Nazaryan is a science and culture writer who prefers to run in the early evening.
Let Us Help You Pick Your Next Workout
Looking for a new way to get moving we have plenty of options..
To get the most out of your strength training, you need to let go of routine and try progressive overload .
What is the best time of day to exercise? A few recent studies have brought us closer to an answer .
Sprinting, at least for short distances, can be a great way to level up your workout routine .
Cycling isn’t just fun. It can also deliver big fitness gains with the right gear and strategy .
Is your workout really working for you? Take our quiz to find out .
Pick the Right Equipment With Wirecutter’s Recommendations
Want to build a home gym? These five things can help you transform your space into a fitness center.
Transform your upper-body workouts with a simple pull-up bar and an adjustable dumbbell set .
Choosing the best running shoes and running gear can be tricky. These tips make the process easier.
A comfortable sports bra can improve your overall workout experience. These are the best on the market .
Few things are more annoying than ill-fitting, hard-to-use headphones. Here are the best ones for the gym and for runners .
Appointments at Mayo Clinic
- Weight loss
Exercise for weight loss: Calories burned in 1 hour
Being active can help you lose weight and keep it off. Find out how much you need.
Being active is vital to losing weight and keeping it off. When active, the body uses more energy in the form of calories. And burning more calories than you take in leads to weight loss.
To lose weight, most people need to cut the number of calories they eat and move more. This is according to the 2020-2025 Dietary Guidelines for Americans. Most often, that means cutting daily calories by 500 to 750 to lose 1 1/2 pounds (0.7 kilograms) a week.
Other factors might be involved in losing weight. Because of changes to the body over time, you might need to cut calories more as you age to keep losing weight or to stay at the same weight.
Diet or exercise: Does one matter more?
Both are important. Diet affects weight loss more than physical activity does. Physical activity, including exercise, has a stronger effect in keeping weight from coming back after weight loss.
Losing weight with diet alone and without physical activity can make people weaker. This is because of age-related losses in bone density and muscle mass. Adding resistance training and aerobic exercise to a weight-loss program helps prevent the loss of bone and muscle.
These are the exercise guidelines for most healthy adults from the U.S. Department of Health and Human Services:
Aerobic activity. Get at least 150 minutes of moderate aerobic activity a week. Or get 75 minutes of vigorous aerobic activity a week. You also can get an equal mix of the two types.
Aim to exercise most days of the week. For even more health benefits, strive for 300 minutes a week or more of moderate aerobic activity or 150 minutes of vigorous activity. Exercising this much may help with weight loss or keeping off lost weight. But even small amounts of physical activity can be helpful. Being active for short periods of time during the day can add up and give you great health benefits.
- Strength training. Do strength training exercises for all major muscle groups at least two times a week. One set of each exercise is enough for health and fitness benefits. Use a weight or resistance level heavy enough to tire your muscles after about 12 to 15 repetitions.
Moderate aerobic exercise includes activities such as brisk walking, biking, swimming and mowing the lawn.
Vigorous aerobic exercise includes activities such as running, swimming hard laps, heavy yardwork and aerobic dancing.
Strength training can include use of weights or weight machines, your own body weight, resistance tubing, or activities such as rock climbing.
How much am I burning?
This list shows about how many calories are burned while doing certain exercises for one hour. This is based on a person who weighs 160 pounds (73 kilograms). The calories you burn depend on the exercise you do, how hard you do it, how much you weigh and other factors.
Based on Ainsworth BE, et al. 2011 compendium of physical activities: A second update of codes and MET values. Medicine & Science in Sports & Exercise. 2011;43:1575.
Remember, to lose weight or to keep weight from creeping up on you as you age, you need to eat less and move more. Moving more means adding more physical activity into your life.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Physical Activity Guidelines for Americans. 2nd ed. U.S. Department of Health and Human Services. https://health.gov/paguidelines/second-edition. Accessed March 13, 2024.
- Physical activity for a healthy weight. Centers for Disease Control and Prevention. https://www.cdc.gov/healthyweight/physical_activity/index.html. Accessed March 13, 2024.
- Ainsworth BE, et al. 2011 compendium of physical activities: A second update of codes and MET values. Medicine & Science in Sports & Exercise. 2011;43:1575.
- 2020-2025 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://www.dietaryguidelines.gov. Accessed March 13, 2024.
- Perreault L, et al. Obesity in adults: Role of physical activity and exercise. https://www.uptodate.com/contents/search. Accessed March 13, 2024.
- AskMayoExpert. Physical activity (adult). Mayo Clinic; 2022.
Products and Services
- A Book: The Mayo Clinic Diet Bundle
- The Mayo Clinic Diet Online
- Aerobic exercise
- Hate to exercise? Try these tips
- Strength training basics
- Walking for weight loss
- Walking for fitness
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities

Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Exercise for weight loss Calories burned in 1 hour
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

What the success of Google Maps on iPhone tells us about Apple and monopolies -- and what the DOJ needs to understand about good products
T here are all manner of navigation apps for the iPhone. Apple Maps is the default choice, and is pretty extensive these days, but it's far from the only option. Just check the App Store. And in the battle to be top map app, Google Maps seems to have nabbed the chequered flag – even on iPhones.
According to this survey by MarketWatch, a whopping 70% of respondents flagged down Google Maps as their go-to navigation copilot. While Waze, Google's other prodigy in the mapping arena, snagged a commendable second place with 27%, Apple Maps trailed with 25%. It's somewhat unexpected that Google Maps is so popular, when Apple Maps comes enabled by default on the best iPhones – the most popular smartphones in the US.
This MarketWatch study wasn't just about counting hands, though; it was a deep dive into the habits of 1,000 US drivers. The study specifically focused on how these mapping applications were used to spot speed traps -- yep, traps on map apps. But it speaks to the popularity of Google's primary navigation app, especially over Apple's default option.
Could it be that good products are more popular?
Despite Apple Maps catching up to Google Maps' feature offerings recently, Google's map app has been a long-time favorite among iPhone owners. Historically, it's offered more features , an integrated experience, and better navigation overall. Plus, you can use it across all Apple devices, most notably CarPlay . In short, it's a good product. Arguably, it's a better product than Apple Maps.
So could it be that Google Maps is more popular because it's a better product? While you'd think that's a simple "yes", the DOJ might disagree with you.
The DOJ filed a landmark lawsuit against Apple last week, alleging the company has a smartphone monopoly. In the suit, the government claimed that one of the world's most successful and valuable companies has a stranglehold on phones, and stated bluntly that Apple uses it to extract more money from consumers. "Apple has gone from revolutionizing the smartphone market to stalling its advancement," said Deputy Attorney General Lisa Monaco. You can read the full lawsuit here .
Google Maps is an interesting case study here, showing that a good product is usually the more popular option. Which is considered by users to be the case with iPhones, even if the tech-averse folks over at the DOJ might disagree.
If anything, this survey showing the popularity of Google Maps goes directly against the DOJ's lawsuit. The DOJ argues that Apple stifles competitors to make it harder for iPhone users to switch away. And I don't know about you, but the popularity of Google Maps on iPhones isn't particularly stifled. And Google is, I don't know, Apple's biggest competitor, perhaps. It's ironic, really.
More from iMore
- Maps App for iPhone and iPad: The ultimate guide
- Apple Maps transit directions: Which cities have them?
- How to share location and directions with Maps for iPhone and iPad
- Open access
- Published: 09 May 2024
Evaluation of integrated community case management of the common childhood illness program in Gondar city, northwest Ethiopia: a case study evaluation design
- Mekides Geta 1 ,
- Geta Asrade Alemayehu 2 ,
- Wubshet Debebe Negash 2 ,
- Tadele Biresaw Belachew 2 ,
- Chalie Tadie Tsehay 2 &
- Getachew Teshale 2
BMC Pediatrics volume 24 , Article number: 310 ( 2024 ) Cite this article
103 Accesses
Metrics details
Integrated Community Case Management (ICCM) of common childhood illness is one of the global initiatives to reduce mortality among under-five children by two-thirds. It is also implemented in Ethiopia to improve community access and coverage of health services. However, as per our best knowledge the implementation status of integrated community case management in the study area is not well evaluated. Therefore, this study aimed to evaluate the implementation status of the integrated community case management program in Gondar City, Northwest Ethiopia.
A single case study design with mixed methods was employed to evaluate the process of integrated community case management for common childhood illness in Gondar town from March 17 to April 17, 2022. The availability, compliance, and acceptability dimensions of the program implementation were evaluated using 49 indicators. In this evaluation, 484 mothers or caregivers participated in exit interviews; 230 records were reviewed, 21 key informants were interviewed; and 42 observations were included. To identify the predictor variables associated with acceptability, we used a multivariable logistic regression analysis. Statistically significant variables were identified based on the adjusted odds ratio (AOR) with a 95% confidence interval (CI) and p-value. The qualitative data was recorded, transcribed, and translated into English, and thematic analysis was carried out.
The overall implementation of integrated community case management was 81.5%, of which availability (84.2%), compliance (83.1%), and acceptability (75.3%) contributed. Some drugs and medical equipment, like Cotrimoxazole, vitamin K, a timer, and a resuscitation bag, were stocked out. Health care providers complained that lack of refreshment training and continuous supportive supervision was the common challenges that led to a skill gap for effective program delivery. Educational status (primary AOR = 0.27, 95% CI:0.11–0.52), secondary AOR = 0.16, 95% CI:0.07–0.39), and college and above AOR = 0.08, 95% CI:0.07–0.39), prescribed drug availability (AOR = 2.17, 95% CI:1.14–4.10), travel time to the to the ICCM site (AOR = 3.8, 95% CI:1.99–7.35), and waiting time (AOR = 2.80, 95% CI:1.16–6.79) were factors associated with the acceptability of the program by caregivers.
Conclusion and recommendation
The overall implementation status of the integrated community case management program was judged as good. However, there were gaps observed in the assessment, classification, and treatment of diseases. Educational status, availability of the prescribed drugs, waiting time and travel time to integrated community case management sites were factors associated with the program acceptability. Continuous supportive supervision for health facilities, refreshment training for HEW’s to maximize compliance, construction clean water sources for HPs, and conducting longitudinal studies for the future are the forwarded recommendation.
Peer Review reports
Integrated Community Case Management (ICCM) is a critical public health strategy for expanding the coverage of quality child care services [ 1 , 2 ]. It mainly concentrated on curative care and also on the diagnosis, treatment, and referral of children who are ill with infectious diseases [ 3 , 4 ].
Based on the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) recommendations, Ethiopia adopted and implemented a national policy supporting community-based treatment of common childhood illnesses like pneumonia, Diarrhea, uncomplicated malnutrition, malaria and other febrile illness and Amhara region was one the piloted regions in late 2010 [ 5 ]. The Ethiopian primary healthcare units, established at district levels include primary hospitals, health centers (HCs), and health posts (HPs). The HPs are run by Health Extension Workers (HEWs), and they have function of monitoring health programs and disease occurrence, providing health education, essential primary care services, and timely referrals to HCs [ 6 , 7 ]. The Health Extension Program (HEP) uses task shifting and community ownership to provide essential health services at the first level using the health development army and a network of woman volunteers. These groups are organized to promote health and prevent diseases through community participation and empowerment by identifying the salient local bottlenecks which hinder vital maternal, neonatal, and child health service utilization [ 8 , 9 ].
One of the key steps to enhance the clinical case of health extension staff is to encourage better growth and development among under-five children by health extension. Healthy family and neighborhood practices are also encouraged [ 10 , 11 ]. The program also combines immunization, community-based feeding, vitamin A and de-worming with multiple preventive measures [ 12 , 13 ]. Now a days rapidly scaling up of ICCM approach to efficiently manage the most common causes of morbidity and mortality of children under the age of five in an integrated manner at the community level is required [ 14 , 15 ].
Over 5.3 million children are died at a global level in 2018 and most causes (75%) are preventable or treatable diseases such as pneumonia, malaria and diarrhea [ 16 ]. About 99% of the global burden of mortality and morbidity of under-five children which exists in developing countries are due to common childhood diseases such as pneumonia, diarrhea, malaria and malnutrition [ 17 ].
In 2013, the mortality rate of under-five children in Sub-Saharan Africa decreased to 86 deaths per 1000 live birth and estimated to be 25 per 1000live births by 2030. However, it is a huge figure and the trends are not sufficient to reach the target [ 18 ]. About half of global under-five deaths occurred in sub-Saharan Africa. And from the top 26 nations burdened with 80% of the world’s under-five deaths, 19 are in sub-Saharan Africa [ 19 ].
To alleviate the burden, the Ethiopian government tries to deliver basic child care services at the community level by trained health extension workers. The program improves the health of the children not only in Ethiopia but also in some African nations. Despite its proven benefits, the program implementation had several challenges, in particular, non-adherence to the national guidelines among health care workers [ 20 ]. Addressing those challenges could further improve the program performance. Present treatment levels in sub-Saharan Africa are unacceptably poor; only 39% of children receive proper diarrhea treatment, 13% of children with suspected pneumonia receive antibiotics, 13% of children with fever receive a finger/heel stick to screen for malaria [ 21 ].
To improve the program performance, program gaps should be identified through scientific evaluations and stakeholder involvement. This evaluation not only identify gaps but also forward recommendations for the observed gaps. Furthermore, the implementation status of ICCM of common childhood illnesses has not been evaluated in the study area yet. Therefore, this work aimed to evaluate the implementation status of integrated community case management program implementation in Gondar town, northwest Ethiopia. The findings may be used by policy makers, healthcare providers, funders and researchers.
Method and material
Evaluation design and settings.
A single-case study design with concurrent mixed-methods evaluation was conducted in Gondar city, northwest Ethiopia, from March 17 to April 17, 2022. The evaluability assessment was done from December 15–30, 2021. Both qualitative and quantitative data were collected concurrently, analyzed separately, and integrated at the result interpretation phase.
The evaluation area, Gondar City, is located in northwest Ethiopia, 740 km from Addis Ababa, the capital city of the country. It has six sub-cities and thirty-six kebeles (25 urban and 11 rural). In 2019, the estimated total population of the town was 338,646, and 58,519 (17.3%) were under-five children. In the town there are eight public health centers and 14 health posts serving the population. All health posts provide ICCM service for more than 70,852 populations.
Evaluation approach and dimensions
Program stakeholders.
The evaluation followed a formative participatory approach by engaging the potential stakeholders in the program. Prior to the development of the proposal, an extensive discussion was held with the Gondar City Health Department to identify other key stakeholders in the program. Service providers at each health facility (HCs and HPs), caretakers of sick children, the Gondar City Health Office (GCHO), the Amhara Regional Health Bureau (ARHB), the Minister of Health (MoH), and NGOs (IFHP and Save the Children) were considered key stakeholders. During the Evaluability Assessment (EA), the stakeholders were involved in the development of evaluation questions, objectives, indicators, and judgment criteria of the evaluation.
Evaluation dimensions
The availability and acceptability dimensions from the access framework [ 22 ] and compliance dimension from the fidelity framework [ 23 ] were used to evaluate the implementation of ICCM.
Population and samplings
All under-five children and their caregivers attended at the HPs; program implementers (health extension workers, healthcare providers, healthcare managers, PHCU focal persons, MCH coordinators, and other stakeholders); and ICCM records and registries in the health posts of Gondar city administration were included in the evaluation. For quantitative data, the required sample size was proportionally allocated for each health post based on the number of cases served in the recent one month. But the qualitative sample size was determined by data saturation, and the samples were selected purposefully.
The data sources and sample size for the compliance dimension were all administrative records/reports and ICCM registration books (230 documents) in all health posts registered from December 1, 2021, to February 30, 2022 (three months retrospectively) included in the evaluation. The registries were assessed starting from the most recent registration number until the required sample size was obtained for each health post.
The sample size to measure the mothers’/caregivers’ acceptability towards ICCM was calculated by taking prevalence of caregivers’ satisfaction on ICCM program p = 74% from previously similar study [ 24 ] and considering standard error 4% at 95% CI and 10% non- responses, which gave 508. Except those who were seriously ill, all caregivers attending the ICCM sites during data collection were selected and interviewed consecutively.
The availability of required supplies, materials and human resources for the program were assessed in all 14HPs. The data collectors observed the health posts and collected required data by using a resources inventory checklist.
A total of 70 non-participatory patient-provider interactions were also observed. The observations were conducted per each health post and for health posts which have more than one health extension workers one of them were selected randomly. The observation findings were used to triangulate the findings obtained through other data collection techniques. Since people may act accordingly to the standards when they know they are observed for their activities, we discarded the first two observations from analysis. It is one of the strategies to minimize the Hawthorne effect of the study. Finally a total of 42 (3 in each HPs) observations were included in the analysis.
Twenty one key informants (14 HEWs, 3 PHCU focal person, 3 health center heads and one MCH coordinator) were interviewed. These key informants were selected since they are assumed to be best teachers in the program. Besides originally developed key informant interview questions, the data collectors probed them to get more detail and clear information.
Variables and measurement
The availability of resources, including trained healthcare workers, was examined using 17 indicators, with weighted score of 35%. Compliance was used to assess HEWs’ adherence to the ICCM treatment guidelines by observing patient-provider interactions and conducting document reviews. We used 18 indicators and a weighted value of 40%.
Mothers’ /caregivers’/ acceptance of ICCM service was examined using 14 indicators and had a weighted score of 25%. The indicators were developed with a five-point Likert scale (1: strongly disagree, 2: disagree, 3: neutral, 4: agree and 5: strongly agree). The cut off point for this categorization was calculated using the demarcation threshold formula: ( \(\frac{\text{t}\text{o}\text{t}\text{a}\text{l}\, \text{h}\text{i}\text{g}\text{h}\text{e}\text{s}\text{t}\, \text{s}\text{c}\text{o}\text{r}\text{e}-\,\text{t}\text{o}\text{t}\text{a}\text{l}\, \text{l}\text{o}\text{w}\text{e}\text{s}\text{t} \,\text{s}\text{c}\text{o}\text{r}\text{e}}{2}) +total lowest score\) ( 25 – 27 ). Those mothers/caregivers/ who scored above cut point (42) were considered as “satisfied”, otherwise “dissatisfied”. The indicators were adapted from the national ICCM and IMNCI implementation guideline and other related evaluations with the participation of stakeholders. Indicator weight was given by the stakeholders during EA. Indicators score was calculated using the formula \(\left(achieved \,in \%=\frac{indicator \,score \,x \,100}{indicator\, weight} \right)\) [ 26 , 28 ].
The independent variables for the acceptability dimension were socio-demographic and economic variables (age, educational status, marital status, occupation of caregiver, family size, income level, and mode of transport), availability of prescribed drugs, waiting time, travel time to ICCM site, home to home visit, consultation time, appointment, and source of information.
The overall implementation of ICCM was measured by using 49 indicators over the three dimensions: availability (17 indicators), compliance (18 indicators) and acceptability (14 indicators).
Program logic model
Based on the constructed program logic model and trained health care providers, mothers/caregivers received health information and counseling on child feeding; children were assessed, classified, and treated for disease, received follow-up; they were checked for vitamin A; and deworming and immunization status were the expected outputs of the program activities. Improved knowledge of HEWs on ICCM, increased health-seeking behavior, improved quality of health services, increased utilization of services, improved data quality and information use, and improved child health conditions are considered outcomes of the program. Reduction of under-five morbidity and mortality and improving quality of life in the society are the distant outcomes or impacts of the program (Fig. 1 ).
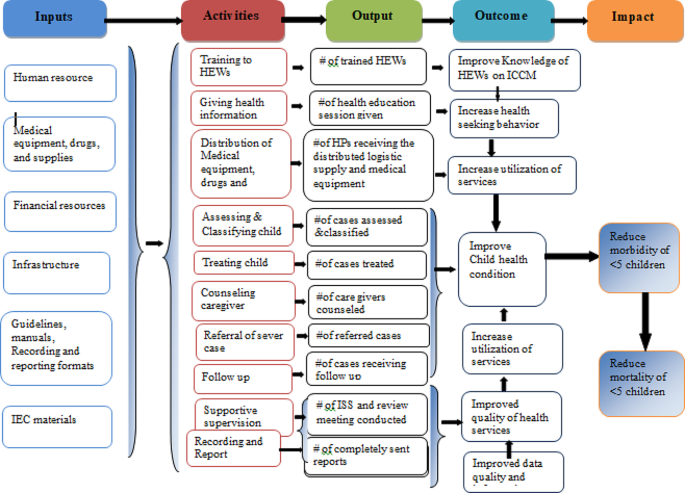
Integrated community case management of childhood illness program logic model in Gondar City in 2022
Data collection tools and procedure
Resource inventory and data extraction checklists were adapted from standard ICCM tool and check lists [ 29 ]. A structured interviewer administered questionnaire was adapted by referring different literatures [ 30 , 31 ] to measure the acceptability of ICCM. The key informant interview (KII) guide was also developed to explore the views of KIs. The interview questionnaire and guide were initially developed in English and translated into the local language (Amharic) and finally back to English to ensure consistency. All the interviews were done in the local language, Amharic.
Five trained clinical nurses and one BSC nurse were recruited from Gondar zuria and Wegera district as data collectors and supervisors, respectively. Two days training on the overall purpose of the evaluation and basic data collection procedures were provided prior to data collection. Then, both quantitative and qualitative data were gathered at the same time. The quantitative data were gathered from program documentation, charts of ICCM program visitors and, exit interview. Interviews with 21 KIIs and non-participatory observations of patient-provider interactions were used to acquire qualitative data. Key informant interviews were conducted to investigate the gaps and best practices in the implementation of the ICCM program.
A pretest was conducted to 26 mothers/caregivers/ at Maksegnit health post and appropriate modifications were made based on the pretest results. The data collectors were supervised and principal evaluator examined the completeness and consistency of the data on a daily basis.
Data management and analysis
For analysis, quantitative data were entered into epi-data version 4.6 and exported to Stata 14 software for analysis. Narration and tabular statistics were used to present descriptive statistics. Based on established judgment criteria, the total program implementation was examined and interpreted as a mix of the availability, compliance, and acceptability dimensions. To investigate the factors associated with ICCM acceptance, a binary logistic regression analysis was performed. During bivariable analysis, variables with p-values less than 0.25 were included in multivariable analysis. Finally, variables having a p-value less than 0.05 and an adjusted odds ratio (AOR) with a 95% confidence interval (CI) were judged statistically significant. Qualitative data were collected recorded, transcribed into Amharic, then translated into English and finally coded and thematically analyzed.
Judgment matrix analysis
The weighted values of availability, compliance, and acceptability dimensions were 35, 40, and 25 based on the stakeholder and investigator agreement on each indicator, respectively. The judgment parameters for each dimension and the overall implementation of the program were categorized as poor (< 60%), fair (60–74.9%), good (75-84.9%), and very good (85–100%).
Availability of resources
A total of 26 HEWs were assigned within the fourteen health posts, and 72.7% of them were trained on ICCM to manage common childhood illnesses in under-five children. However, the training was given before four years, and they didn’t get even refreshment training about ICCM. The KII responses also supported that the shortage of HEWs at the HPs was the problem in implementing the program properly.
I am the only HEW in this health post and I have not been trained on ICCM program. So, this may compromise the quality of service and client satisfaction.(25 years old HEW with two years’ experience)
All observed health posts had ICCM registration books, monthly report and referral formats, functional thermometer, weighting scale and MUAC tape meter. However, timer and resuscitation bag was not available in all HPs. Most of the key informant finding showed that, in all HPs there was no shortage of guideline, registration book and recording tool; however, there was no OTP card in some health posts.
“Guideline, ICCM registration book for 2–59 months of age, and other different recording and reporting formats and booklet charts are available since September/2016. However, OTP card is not available in most HPs.”. (A 30 years male health center director)
Only one-fifth (21%) of HPs had a clean water source for drinking and washing of equipment. Most of Key-informant interview findings showed that the availability of infrastructures like water was not available in most HPs. Poor linkage between HPs, HCs, town health department, and local Kebele administer were the reason for unavailability.
Since there is no water for hand washing, or drinking, we obligated to bring water from our home for daily consumptions. This increases the burden for us in our daily activity. (35 years old HEW)
Most medicines, such as anti-malaria drugs with RDT, Quartem, Albendazole, Amoxicillin, vitamin A capsules, ORS, and gloves, were available in all the health posts. Drugs like zinc, paracetamol, TTC eye ointment, and folic acid were available in some HPs. However, cotrimoxazole and vitamin K capsules were stocked-out in all health posts for the last six months. The key informant also revealed that: “Vitamin K was not available starting from the beginning of this program and Cotrimoxazole was not available for the past one year and they told us they would avail it soon but still not availed. Some essential ICCM drugs like anti malaria drugs, De-worming, Amoxicillin, vitamin A capsules, ORS and medical supplies were also not available in HCs regularly.”(28 years’ Female PHCU focal)
The overall availability of resources for ICCM implementation was 84.2% which was good based on our presetting judgment parameter (Table 1 ).
Health extension worker’s compliance
From the 42 patient-provider interactions, we found that 85.7%, 71.4%, 76.2%, and 95.2% of the children were checked for body temperature, weight, general danger signs, and immunization status respectively. Out of total (42) observation, 33(78.6%) of sick children were classified for their nutritional status. During observation time 29 (69.1%) of caregivers were counseled by HEWs on food, fluid and when to return back and 35 (83.3%) of children were appointed for next follow-up visit. Key informant interviews also affirmed that;
“Most of our health extension workers were trained on ICCM program guidelines but still there are problems on assessment classification and treatment of disease based on guidelines and standards this is mainly due to lack refreshment training on the program and lack of continuous supportive supervision from the respective body.” (27years’ Male health center head)
From 10 clients classified as having severe pneumonia cases, all of them were referred to a health center (with pre-referral treatment), and from those 57 pneumonia cases, 50 (87.7%) were treated at the HP with amoxicillin or cotrimoxazole. All children with severe diarrhea, very severe disease, and severe complicated malnutrition cases were referred to health centers with a pre-referral treatment for severe dehydration, very severe febrile disease, and severe complicated malnutrition, respectively. From those with some dehydration and no dehydration cases, (82.4%) and (86.8%) were treated at the HPs for some dehydration (ORS; plan B) and for no dehydration (ORS; plan A), respectively. Moreover, zinc sulfate was prescribed for 63 (90%) of under-five children with some dehydration or no dehydration. From 26 malaria cases and 32 severe uncomplicated malnutrition and moderate acute malnutrition cases, 20 (76.9%) and 25 (78.1%) were treated at the HPs, respectively. Of the total reviewed documents, 56 (93.3%), 66 (94.3%), 38 (84.4%), and 25 (78.1%) of them were given a follow-up date for pneumonia, diarrhea, malaria, and malnutrition, respectively.
Supportive supervision and performance review meetings were conducted only in 10 (71.4%) HPs, but all (100%) HPs sent timely reports to the next supervisory body.
Most of the key informants’ interview findings showed that supportive supervision was not conducted regularly and for all HPs.
I had mentored and supervised by supportive supervision teams who came to our health post at different times from health center, town health office and zonal health department. I received this integrated supervision from town health office irregularly, but every month from catchment health center and last integrated supportive supervision from HC was on January. The problem is the supervision was conducted for all programs.(32 years’ old and nine years experienced female HEW)
Moreover, the result showed that there was poor compliance of HEWs for the program mainly due to weak supportive supervision system of managerial and technical health workers. It was also supported by key informants as:
We conducted supportive supervision and performance review meeting at different time, but still there was not regular and not addressed all HPs. In addition to this the supervision and review meeting was conducted as integration of ICCM program with other services. The other problem is that most of the time we didn’t used checklist during supportive supervision. (Mid 30 years old male HC director)
Based on our observation and ICCM document review, 83.1% of the HEWs were complied with the ICCM guidelines and judged as fair (Table 2 ).
Acceptability of ICCM program
Sociodemographic and obstetric characteristics of participants.
A total of 484 study participants responded to the interviewer-administered questionnaire with a response rate of 95.3%. The mean age of study participants was 30.7 (SD ± 5.5) years. Of the total caregivers, the majority (38.6%) were categorized under the age group of 26–30 years. Among the total respondents, 89.3% were married, and regarding religion, the majorities (84.5%) were Orthodox Christian followers. Regarding educational status, over half of caregivers (52.1%) were illiterate (unable to read or write). Nearly two-thirds of the caregivers (62.6%) were housewives (Table 3 ).
All the caregivers came to the health post on foot, and most of them 418 (86.4%) arrived within one hour. The majority of 452 (93.4%) caregivers responded that the waiting time to get the service was less than 30 min. Caregivers who got the prescribed drugs at the health post were 409 (84.5%). Most of the respondents, 429 (88.6%) and 438 (90.5%), received counseling services on providing extra fluid and feeding for their sick child and were given a follow-up date.
Most 298 (61.6%) of the caregivers were satisfied with the convenience of the working hours of HPs, and more than three-fourths (80.8%) were satisfied with the counseling services they received. Most of the respondents, 366 (75.6%), were satisfied with the appropriateness of waiting time and 431 (89%) with the appropriateness of consultation time. The majority (448 (92.6%) of caregivers were satisfied with the way of communicating with HEWs, and 269 (55.6%) were satisfied with the knowledge and competence of HEWs. Nearly half of the caregivers (240, or 49.6%) were satisfied with the availability of drugs at health posts.
The overall acceptability of the ICCM program was 75.3%, which was judged as good. A low proportion of acceptability was measured on the cleanliness of the health posts, the appropriateness of the waiting area, and the competence and knowledge of the HEWs. On the other hand, high proportion of acceptability was measured on appropriateness of waiting time, way of communication with HEWs, and the availability of drugs (Table 4 ).
Factors associated with acceptability of ICCM program
In the final multivariable logistic regression analysis, educational status of caregivers, availability of prescribed drugs, time to arrive, and waiting time were factors significantly associated with the satisfaction of caregivers with the ICCM program.
Accordingly, the odds of caregivers with primary education, secondary education, and college and above were 73% (AOR = 0.27, 95% CI: 0.11–0.52), 84% (AOR = 0.16, 95% CI: 0.07–0.39), and 92% (AOR = 0.08, 95% CI: 0.07–0.40) less likely to accept the program as compared to mothers or caregivers who were not able to read and write, respectively. The odds of caregivers or mothers who received prescribed drugs were 2.17 times more likely to accept the program as compared to their counters (AOR = 2.17, 95% CI: 1.14–4.10). The odds of caregivers or mothers who waited for services for less than 30 min were 2.8 times more likely to accept the program as compared to those who waited for more than 30 min (AOR = 2.80, 95% CI: 1.16–6.79). Moreover, the odds of caregivers/mothers who traveled an hour or less for service were 3.8 times more likely to accept the ICCM program as compared to their counters (AOR = 3.82, 95% CI:1.99–7.35) (Table 5 ).
Overall ICCM program implementation and judgment
The implementation of the ICCM program in Gondar city administration was measured in terms of availability (84.2%), compliance (83.1%), and acceptability (75.3%) dimensions. In the availability dimension, amoxicillin, antimalarial drugs, albendazole, Vit. A, and ORS were available in all health posts, but only six HPs had Ready-to-Use Therapeutic Feedings, three HPs had ORT Corners, and none of the HPs had functional timers. In all health posts, the health extension workers asked the chief to complain, correctly assessed for pneumonia, diarrhea, malaria, and malnutrition, and sent reports based on the national schedule. However, only 70% of caretakers counseled about food, fluids, and when to return, 66% and 76% of the sick children were checked for anemia and other danger signs, respectively. The acceptability level of the program by caretakers and caretakers’/mothers’ educational status, waiting time to get the service and travel time ICCM sites were the factors affecting its acceptability. The overall ICCM program in Gondar city administration was 81.5% and judged as good (Fig. 2 ).
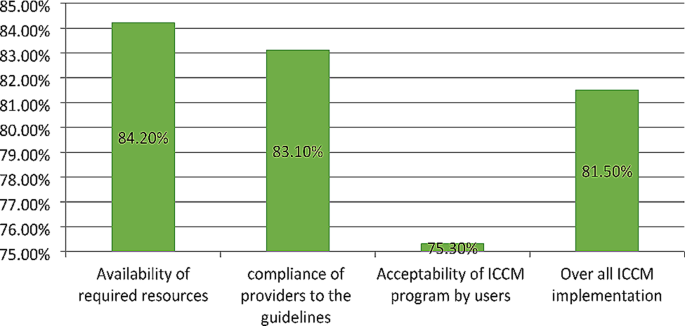
Overall ICCM program implementation and the evaluation dimensions in Gondar city administration, 2022
The implementation status of ICCM was judged by using three dimensions including availability, compliance and acceptability of the program. The judgment cut of points was determined during evaluability assessment (EA) along with the stakeholders. As a result, we found that the overall implementation status of ICCM program was good as per the presetting judgment parameter. Availability of resources for the program implementation, compliance of HEWs to the treatment guideline and acceptability of the program services by users were also judged as good as per the judgment parameter.
This evaluation showed that most medications, equipment and recording and reporting materials available. This finding was comparable with the standard ICCM treatment guide line [ 10 ]. On the other hand trained health care providers, some medications like Zink, Paracetamol and TTC eye ointment, folic acid and syringes were not found in some HPs. However the finding was higher than the study conducted in SNNPR on selected health posts [ 33 ] and a study conducted in Soro district, southern Ethiopia [ 24 ]. The possible reason might be due to low interruption of drugs at town health office or regional health department stores, regular supplies of essential drugs and good supply management and distribution of drug from health centers to health post.
The result of this evaluation showed that only one fourth of health posts had functional ORT Corner which was lower compared to the study conducted in SNNPR [ 34 ]. This might be due poor coverage of functional pipe water in the kebeles and the installation was not set at the beginning of health post construction as reported from one of ICCM program coordinator.
Compliance of HEWs to the treatment guidelines in this evaluation was higher than the study done in southern Ethiopia (65.6%) [ 24 ]. This might be due to availability of essential drugs educational level of HEWs and good utilization of ICCM guideline and chart booklet by HEWs. The observations showed most of the sick children were assessed for danger sign, weight, and temperature respectively. This finding is lower than the study conducted in Rwanda [ 35 ]. This difference might be due to lack of refreshment training and regular supportive supervision for HEWs. This also higher compared to the study done in three regions of Ethiopia indicates that 88%, 92% and 93% of children classified as per standard for Pneumonia, diarrhea and malaria respectively [ 36 ]. The reason for this difference may be due to the presence of medical equipment and supplies including RDT kit for malaria, and good educational level of HEWs.
Moreover most HPs received supportive supervision and performance review meeting was conducted and all of them send reports timely to next level. The finding of this evaluation was lower than the study conducted on implementation evaluation of ICCM program southern Ethiopia [ 24 ] and study done in three regions of Ethiopia (Amhara, Tigray and SNNPR) [ 37 ]. This difference might be due sample size variation.
The overall acceptability of the ICCM program was less than the presetting judgment parameter but slightly higher compared to the study in southern Ethiopia [ 24 ]. This might be due to presence of essential drugs for treating children, reasonable waiting and counseling time provided by HEWs, and smooth communication between HEWs and caregivers. In contrast, this was lower than similar studies conducted in Wakiso district, Uganda [ 38 ]. The reason for this might be due to contextual difference between the two countries, inappropriate waiting area to receive the service and poor cleanness of the HPs in our study area. Low acceptability of caregivers to ICCM service was observed in the appropriateness of waiting area, availability of drugs, cleanness of health post, and competence of HEWs while high level of caregiver’s acceptability was consultation time, counseling service they received, communication with HEWs, treatment given for their sick children and interest to return back for ICCM service.
Caregivers who achieved primary, secondary, and college and above were more likely accept the program services than those who were illiterate. This may more educated mothers know about their child health condition and expect quality service from healthcare providers which is more likely reduce the acceptability of the service. The finding is congruent with a study done on implementation evaluation of ICCM program in southern Ethiopia [ 24 ]. However, inconsistent with a study conducted in wakiso district in Uganda [ 38 ]. The possible reason for this might be due to contextual differences between the two countries. The ICCM program acceptability was high in caregivers who received all prescribed drugs than those did not. Caregivers those waited less than 30 min for service were more accepted ICCM services compared to those more than 30 minutes’ waiting time. This finding is similar compared with the study conducted on implementation evaluation of ICCM program in southern Ethiopia [ 24 ]. In contrary, the result was incongruent with a survey result conducted by Ethiopian public health institute in all regions and two administrative cities of Ethiopia [ 39 ]. This variation might be due to smaller sample size in our study the previous one. Moreover, caregivers who traveled to HPs less than 60 min were more likely accepted the program than who traveled more and the finding was similar with the study finding in Jimma zone [ 40 ].
Strengths and limitations
This evaluation used three evaluation dimensions, mixed method and different data sources that would enhance the reliability and credibility of the findings. However, the study might have limitations like social desirability bias, recall bias and Hawthorne effect.
The implementation of the ICCM program in Gondar city administration was measured in terms of availability (84.2%), compliance (83.1%), and acceptability (75.3%) dimensions. In the availability dimension, amoxicillin, antimalarial drugs, albendazole, Vit. A, and ORS were available in all health posts, but only six HPs had Ready-to-Use Therapeutic Feedings, three HPs had ORT Corners, and none of the HPs had functional timers.
This evaluation assessed the implementation status of the ICCM program, focusing mainly on availability, compliance, and acceptability dimensions. The overall implementation status of the program was judged as good. The availability dimension is compromised due to stock-outs of chloroquine syrup, cotrimoxazole, and vitamin K and the inaccessibility of clean water supply in some health posts. Educational statuses of caregivers, availability of prescribed drugs at the HPs, time to arrive to HPs, and waiting time to receive the service were the factors associated with the acceptability of the ICCM program.
Therefore, continuous supportive supervision for health facilities, and refreshment training for HEW’s to maximize compliance are recommended. Materials and supplies shall be delivered directly to the health centers or health posts to solve the transportation problem. HEWs shall document the assessment findings and the services provided using the registration format to identify their gaps, limitations, and better performances. The health facilities and local administrations should construct clean water sources for health facilities. Furthermore, we recommend for future researchers and program evaluators to conduct longitudinal studies to know the causal relationship of the program interventions and the outcomes.
Data availability
Data will be available upon reasonable request from the corresponding author.
Abbreviations
Ethiopian Demographic and Health Survey
Health Center/Health Facility
Health Extension Program
Health Extension Workers
Health Post
Health Sector Development Plan
Integrated Community Case Management of Common Childhood Illnesses
Information Communication and Education
Integrated Family Health Program
Integrated Management of Neonatal and Childhood Illness
Integrated Supportive Supervision
Maternal and Child Health
Mid Upper Arm Circumference
Non-Government Organization
Oral Rehydration Salts
Outpatient Therapeutic program
Primary health care unit
Rapid Diagnostics Test
Ready to Use Therapeutic Foods
Sever Acute Malnutrition
South Nation Nationalities People Region
United Nations International Child Emergency Fund
World Health Organization
Brenner JL, Barigye C, Maling S, Kabakyenga J, Nettel-Aguirre A, Buchner D, et al. Where there is no doctor: can volunteer community health workers in rural Uganda provide integrated community case management? Afr Health Sci. 2017;17(1):237–46.
Article PubMed PubMed Central Google Scholar
Mubiru D, Byabasheija R, Bwanika JB, Meier JE, Magumba G, Kaggwa FM, et al. Evaluation of integrated community case management in eight districts of Central Uganda. PLoS ONE. 2015;10(8):e0134767.
Samuel S, Arba A. Utilization of integrated community case management service and associated factors among mothers/caregivers who have sick eligible children in southern Ethiopia. Risk Manage Healthc Policy. 2021;14:431.
Article Google Scholar
Kavle JA, Pacqué M, Dalglish S, Mbombeshayi E, Anzolo J, Mirindi J, et al. Strengthening nutrition services within integrated community case management (iCCM) of childhood illnesses in the Democratic Republic of Congo: evidence to guide implementation. Matern Child Nutr. 2019;15:e12725.
Miller NP, Amouzou A, Tafesse M, Hazel E, Legesse H, Degefie T, et al. Integrated community case management of childhood illness in Ethiopia: implementation strength and quality of care. Am J Trop Med Hyg. 2014;91(2):424.
WHO. Annual report 2016: Partnership and policy engagement. World Health Organization, 2017.
Banteyerga H. Ethiopia’s health extension program: improving health through community involvement. MEDICC Rev. 2011;13:46–9.
Article PubMed Google Scholar
Wang H, Tesfaye R, Ramana NV, Chekagn G. CT. Ethiopia health extension program: an institutionalized community approach for universal health coverage. The World Bank; 2016.
Donnelly J. Ethiopia gears up for more major health reforms. Lancet. 2011;377(9781):1907–8.
Legesse H, Degefie T, Hiluf M, Sime K, Tesfaye C, Abebe H, et al. National scale-up of integrated community case management in rural Ethiopia: implementation and early lessons learned. Ethiop Med J. 2014;52(Suppl 3):15–26.
Google Scholar
Miller NP, Amouzou A, Hazel E, Legesse H, Degefie T, Tafesse M et al. Assessment of the impact of quality improvement interventions on the quality of sick child care provided by Health Extension workers in Ethiopia. J Global Health. 2016;6(2).
Oliver K, Young M, Oliphant N, Diaz T, Kim JJNYU. Review of systematic challenges to the scale-up of integrated community case management. Emerging lessons & recommendations from the catalytic initiative (CI/IHSS); 2012.
FMoH E. Health Sector Transformation Plan 2015: https://www.slideshare.net . Accessed 12 Jan 2022.
McGorman L, Marsh DR, Guenther T, Gilroy K, Barat LM, Hammamy D, et al. A health systems approach to integrated community case management of childhood illness: methods and tools. The American Journal of Tropical Medicine and Hygiene. 2012;87(5 Suppl):69.
Young M, Wolfheim C, Marsh DR, Hammamy D. World Health Organization/United Nations Children’s Fund joint statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children. The American journal of tropical medicine and hygiene. 2012;87(5 Suppl):6.
Ezbakhe F, Pérez-Foguet A. Child mortality levels and trends. Demographic Research.2020;43:1263-96.
UNICEF, Ending child deaths from pneumonia and diarrhoea. 2016 report: Available at https://data.unicef.org. accessed 13 Jan 2022.
UNITED NATIONS, The Millinium Development Goals Report 2015: Available at https://www.un.org.Accessed 12 Jan 2022
Bent W, Beyene W, Adamu A. Factors Affecting Implementation of Integrated Community Case Management Of Childhood Illness In South West Shoa Zone, Central Ethiopia 2015.
Abdosh B. The quality of hospital services in eastern Ethiopia: Patient’s perspective.The Ethiopian Journal of Health Development. 2006;20(3).
Young M, Wolfheim C, Marsh DR, Hammamy DJTAjotm, hygiene. World Health Organization/United Nations Children’s Fund joint statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children.2012;87(5_Suppl):6–10.
Obrist B, Iteba N, Lengeler C, Makemba A, Mshana C, Nathan R, et al. Access to health care in contexts of livelihood insecurity: a framework for analysis and action.PLoS medicine. 2007;4(10):e308.
Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implementation science. 2007;2(1):1–9.
Dunalo S, Tadesse B, Abraham G. Implementation Evaluation of Integrated Community Case Management of Common Childhood Illness (ICCM) Program in Soro Woreda, Hadiya Zone Southern Ethiopia 2017 2017.
Asefa G, Atnafu A, Dellie E, Gebremedhin T, Aschalew AY, Tsehay CT. Health System Responsiveness for HIV/AIDS Treatment and Care Services in Shewarobit, North Shewa Zone, Ethiopia. Patient preference and adherence. 2021;15:581.
Gebremedhin T, Daka DW, Alemayehu YK, Yitbarek K, Debie A. Process evaluation of the community-based newborn care program implementation in Geze Gofa district,south Ethiopia: a case study evaluation design. BMC pregnancy and childbirth. 2019;19(1):1–13.
Pitaloka DS, Rizal A. Patient’s satisfaction in antenatal clinic hospital Universiti Kebangsaan Malaysia. Jurnal Kesihatan Masyarakat (Malaysia). 2006;12(1):1–10.
Teshale G, Debie A, Dellie E, Gebremedhin T. Evaluation of the outpatient therapeutic program for severe acute malnourished children aged 6–59 months implementation in Dehana District, Northern Ethiopia: a mixed-methods evaluation. BMC pediatrics. 2022;22(1):1–13.
Mason E. WHO’s strategy on Integrated Management of Childhood Illness. Bulletin of the World Health Organization. 2006;84(8):595.
Shaw B, Amouzou A, Miller NP, Tafesse M, Bryce J, Surkan PJ. Access to integrated community case management of childhood illnesses services in rural Ethiopia: a qualitative study of the perspectives and experiences of caregivers. Health policy and planning.2016;31(5):656 – 66.
Organization WH. Annual report 2016: Partnership and policy engagement. World Health Organization, 2017.
Berhanu D, Avan B. Community Based Newborn Care Baseline Survey Report Ethiopia,October 2014.
Save the children, Enhancing Ethiopia’s Health Extension Package in the Southern Nations and Nationalities People’s Region (SNNPR) Shebedino and Lanfero Woredas report.Hawassa;. 2012: Avalable at https://ethiopia.savethechildren.net
Kolbe AR, Muggah R, Hutson RA, James L, Puccio M, Trzcinski E, et al. Assessing Needs After the Quake: Preliminary Findings from a Randomized Survey of Port-au-Prince Households. University of Michigan/Small Arms Survey: Available at https://deepbluelibumichedu PDF. 2010.
Teferi E, Teno D, Ali I, Alemu H, Bulto T. Quality and use of IMNCI services at health center under-five clinics after introduction of integrated community-based case management (ICCM) in three regions of Ethiopia. Ethiopian Medical Journal. 2014;52(Suppl 3):91 – 8.
Last 10 Km project, Integrated Community Case Management (iCCM) Survey report in Amhara, SNNP, and Tigray Regions, 2017: Avaialable at https://l10k.jsi.com
Tumuhamye N, Rutebemberwa E, Kwesiga D, Bagonza J, Mukose A. Client satisfaction with integrated community case management program in Wakiso District, Uganda, October 2012: A cross sectional survey. Health scrip org. 2013;2013.
EPHI. Ethiopia service provision assessment plus survey 2014 report: available at http://repository.iifphc.org
Gintamo B. EY, Assefa Y. Implementation Evaluation of IMNCI Program at Public Health Centers of Soro District, Hadiya Zone, Southern Ethiopia,. 2017: Available at https://repository.ju.edu.et
Download references
Acknowledgements
We are very grateful to University of Gondar and Gondar town health office for its welcoming approaches. We would also like to thank all of the study participants of this evaluation for their information and commitment. Our appreciation also goes to the data collectors and supervisors for their unreserved contribution.
No funding is secured for this evaluation study.
Author information
Authors and affiliations.
Metema District Health office, Gondar, Ethiopia
Mekides Geta
Department of Health Systems and Policy, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, P.O. Box 196, Gondar, Ethiopia
Geta Asrade Alemayehu, Wubshet Debebe Negash, Tadele Biresaw Belachew, Chalie Tadie Tsehay & Getachew Teshale
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the preparation of the manuscript. M.G. conceived and designed the evaluation and performed the analysis then T.B.B., W.D.N., G.A.A., C.T.T. and G.T. revised the analysis. G.T. prepared the manuscript and all the authors revised and approved the final manuscript.
Corresponding author
Correspondence to Getachew Teshale .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from Institutional Review Board (IRB) of Institute of Public Health, College of Medicine and Health sciences, University of Gondar (Ref No/IPH/1482/2013). Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
Not applicable.
Competing interests
All authors declared that they have no competing interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Geta, M., Alemayehu, G.A., Negash, W.D. et al. Evaluation of integrated community case management of the common childhood illness program in Gondar city, northwest Ethiopia: a case study evaluation design. BMC Pediatr 24 , 310 (2024). https://doi.org/10.1186/s12887-024-04785-0
Download citation
Received : 20 February 2024
Accepted : 22 April 2024
Published : 09 May 2024
DOI : https://doi.org/10.1186/s12887-024-04785-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Integrated community case management
BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Entertainment
- KSAT Insider
- Newsletters
Sweltering heat across Asia was 45 times more likely because of climate change, study finds
Associated Press
Copyright 2024 The Associated Press. All rights reserved
FILE - Parking attendant Andy Tinto uses laundry clips to put a blue towel over his cap to protect himself from the sun in Manila, Philippines on Monday, April 29, 2024. Sizzling heat across Asia and the Middle East in late April that echoed last years destructive swelter was made 45 times more likely in some parts of the continent because of human-caused climate change, a study found. (AP Photo/Aaron Favila)
BENGALURU – Sizzling heat across Asia and the Middle East in late April that echoed last year's destructive swelter was made 45 times more likely in some parts of the continent because of human-caused climate change, a study Tuesday found.
Scorching temperatures were felt across large swaths of Asia, from Gaza in the west — where over 2 million people face clean water shortages, lack of health care and other essentials amid the Israeli bombardment — to the Philippines in the southeast, with many parts of the continent experiencing temperatures well above 40 degrees Celsius (104 degrees Fahrenheit) several days in a row.
Recommended Videos
The study was released by the World Weather Attribution group of scientists, who use established climate models to quickly determine whether human-caused climate change played a part in extreme weather events around the world.
In the Philippines, scientists found the heat was so extreme it would have been impossible without human-caused climate change. In parts of the Middle East, climate change increased the probability of the event by about a factor of five.
“People suffered and died when April temperatures soared in Asia,” said Friederike Otto, study author and climate scientist at Imperial College in London. “If humans continue to burn fossil fuels, the climate will continue to warm, and vulnerable people will continue to die.”
At least 28 heat-related deaths were reported in Bangladesh, as well as five in India and three in Gaza in April. Surges in heat deaths have also been reported in Thailand and the Philippines this year according to the study.
The heat also had a large impact on agriculture, causing crop damage and reduced yields, as well as on education, with school vacations having to be extended and schools closed in several countries , affecting thousands of students.
Myanmar, Laos and Vietnam broke records for their hottest April day, and the Philippines experienced its hottest night ever with a low of 29.8 degrees Celsius (85.6 degrees Fahrenheit). In India, temperatures reached as high as 46 degrees Celsius (115 degrees Fahrenheit). The month was the hottest April on record globally and the eleventh consecutive month in a row that broke the hottest month record .
Climate experts say extreme heat in South Asia during the pre-monsoon season is becoming more frequent and the study found that extreme temperatures are now about 0.85 degrees Celsius (1.5 Fahrenheit) hotter in the region because of climate change.
Internally displaced people, migrants and those in refugee camps were especially vulnerable to the searing temperatures, the study found.
“These findings in scientific terms are alarming," said Aditya Valiathan Pillai, a heat plans expert at New Delhi-based think tank Sustainable Futures Collaborative. "But for people on the ground living in precarious conditions, it could be absolutely deadly.” Pillai was not part of the study.
Pillai said more awareness about heat risks, public and private investments to deal with increasing heat and more research on its impacts are all necessary to deal with future heat waves.
“I think heat is now among the foremost risks in terms of personal health for millions across the world as well as nations’ economic development," he said.
Associated Press writer Seth Borenstein in Washington, D.C. contributed to this report.
Follow Sibi Arasu on Twitter at @sibi123
The Associated Press’ climate and environmental coverage receives financial support from multiple private foundations. AP is solely responsible for all content. Find AP’s standards for working with philanthropies, a list of supporters and funded coverage areas at AP.org .
Copyright 2024 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed without permission.

IMAGES
VIDEO
COMMENTS
This case study is designed to introduce students to how the bone's architecture influences movement and the roles cells play in bone growth and repair. It tells the story of "Maria," an active 68-year-old woman who works on a farm. Over the last five years, Maria has experienced pain in her wrist and knee joints and has used a ...
Case Study - Osteoporosis. Case Study #8 - Muscle Physiology. Notes for Exam Two. Skeletal System Lab Manual Anatomy. professor Dulak case study na tional center for case study teaching in science good to the bone: ee biological implications of potential dru nalini broadbelt.
In vivo studies: Orally administered metformin increases the quality of bone tissue (improving its micro-architecture and mineral density) and facilitates the repair of bone lesions. In addition, metformin may prevent experimental diabetic osteopathy as well as ovariectomy-induced bone loss. Figure 2.
In vitro studies: e results from several in vitro studies show that metformin modulated the phenotypic balance of bone marrow stromal cells towards osteoblastogenesis. In addition, metformin increases in vitro the bone forming capacity of osteoblasts, while decreasing the recruitment and bone-resorbing activity of osteoclasts.
Good to the Bone - professor Dulak case study. Human Anatomy and Physiology I 100% (3) 10. Bio106 Basic A&P Ch. 4 Outline, Skin and Body Membranes. Human Anatomy and Physiology I 100% (3) 3. EXAM 3 Review. Human Anatomy and Physiology I 100% (2) Students also viewed. Homeostasis - Case Study;
The film tells the story of Ellen, a 20-year-old Caucasian female with chronic anorexia nervosa, who seeks treatment with the unconventional Dr. Beckham (played by Keanu Reeves). Marti Noxon, the ...
Osteoporosis is a disease that causes a decrease in bone mass, increasing bone fragility and fracture [ 1 ]. Osteoporosis is a common disease, and it impacts one in three post-menopausal women and one in five men worldwide. There are roughly 200 million men and women who have osteoporosis in this world. The cost and morbidity associated with ...
Good to the Bone: KALEY MOODY CASE STUDY Biological Implications of a Potential Anti-Aging Drug Part 1 - 1. A joint is the connection between two bones. They are classified by the type of tissue that is present. 2. She experiences pain in her wrist and knees. The joints of these are the radiocarpal joint and the ulnocarpal joint for the wrist ...
Good to the bone case study.docx - Part 1- Maria's pain: 1.... Doc Preview. Pages 3. Identified Q&As 21. Solutions available. Total views 58. Georgia Northwestern Technical College. BIOLOGY. BIOLOGY SCIENCE1 1. GeneralBoulder6457. 4/13/2022. View full document. Students also studied. Good to the Bone Case Study .pdf.
TAMIN, Lanzlee M. Reflection Paper MAEd - Biological Science Animal Biology Case Study: Good to the Bone: Biological Implications of a Potential Anti-Aging Drug Speaker: Clarisse Castro Reflection Paper The short case scenario about Maria, has introduced how the bone's architecture influences movement and the roles cells play in bone growth and repair.
X (Twitter) Not many films come with a health warning. But the recent Netflix film To The Bone, which tells the story of 20-year-old Ellen - played by Lily Collins - and her journey through ...
The aim in creating and implementing the cases was to promote active and cooperative learning prior to students taking the bone and muscle physiology exam. The cases also help students to identify gaps in their knowledge prior the exam. Methods: Each case assignment takes about 90 minutes over two class periods.
In this case study, we will be looking at the answers to the Good to the Bone case study. Good to the Bone is a fictional pet food company that launched a new line of dog treats. The company wanted to understand the preferences and buying habits of dog owners to optimize their marketing strategy and increase sales. To gather data, an online ...
Brittle bone disease is a genetic disease that results in abnormal bone formation . Osteoporosis is the loss of bone density and does not mean the bones are abnormally formed . Current treatments for brittle bone disease are medications ( such as bone supplements ) , surgery ( bone surgery ) , and devices including a splint or cast .
Led by Hessam Nowzari, director of the USC Advanced Education in Periodontology program, the researchers have published the first case study of the successful use of a patient's own bone ...
Cracking the Case: The Relationship Between Bones and Hormones. You are starting your second week of a fve-week rotation with a local medical doctor. You have found your experience exciting thus far and you're eager to see what this week will hold. As part of your rotation you get to accompany the physician, Dr. Lee, on rounds and diagnoses.
A group of organized osteoblasts together with the bone made by a unit of cells is usually called the osteon. - Ossification in bone remodeling is the process of laying down new bone material by cells called osteoblasts. Study with Quizlet and memorize flashcards containing terms like Hemmorrhage, fracture, Proximal and more.
3. Callus formation: As minerals (calcium, phosphorus, and magnesium) and new bone matrix are deposited in the osteoid, an unorganized network of bone is formed and woven about the fracture parts. Callus is primarily composed of cartilage, osteoblasts, calcium, and phosphorus.
Good to the Bone Case Study .pdf. Solutions Available. University of West Georgia. BIOLOGY 2021. N4685 Module 1 Introduction and Identification for Capstone project.doc. University of Texas, Arlington. NURS 4685. metformin_bio304.docx. Solutions Available. Roosevelt University. BIOL 315. Good to the Bone.odt.
Define the following terms, used in the case and also in associated questions: a. hemorrhage. b. fracture. c. proximal. d. diaphysis. hemorrhage - bleeding or the abnormal flow of blood. can be external like in this case or internal. fracture- breaks in the continuity of a bone's structure. proximal- point of attachment of a limb clostest to ...
Their study looked at 30,000 middle-aged people with obesity and found that evening exercisers were 28 percent less likely to die of any cause than those who worked out in the morning or afternoon ...
To lose weight, most people need to cut the number of calories they eat and move more. This is according to the 2020-2025 Dietary Guidelines for Americans. Most often, that means cutting daily calories by 500 to 750 to lose 1 1/2 pounds (0.7 kilograms) a week. Other factors might be involved in losing weight. Because of changes to the body over ...
10. Bio106 Basic A&P Ch. 4 Outline, Skin and Body Membranes. Human Anatomy and Physiology I100% (3) 3. Case Study - Osteoporosis. Human Anatomy and Physiology I100% (2) More from: Human Anatomy and Physiology IHSCI.1010. University of Massachusetts Lowell.
The Japanese duo is collaborating on new EVs, but partnerships like these can be good for their respective brands. As per a report by Automotive News, the duo is expected to team up on three ...
Google Maps is an interesting case study here, showing that a good product is usually the more popular option. Which is considered by users to be the case with iPhones, even if the tech-averse ...
Background Integrated Community Case Management (ICCM) of common childhood illness is one of the global initiatives to reduce mortality among under-five children by two-thirds. It is also implemented in Ethiopia to improve community access and coverage of health services. However, as per our best knowledge the implementation status of integrated community case management in the study area is ...
Reconstruction of craniomaxillofacial bone defects using 3D-printed hydroxyapatite (HA) bioceramic patient-specific implants (PSIs) is a new technique with great potential. This study aimed to investigate the advantages, disadvantages, and clinical outcomes of these implants in craniomaxillofacial surgeries. The PubMed and Embase databases were searched for patients with craniomaxillofacial ...
The study was released by the World Weather Attribution group of scientists, who use established climate models to quickly determine whether human-caused climate change played a part in extreme ...
case study practice national center for case study teaching in science good to the bone: biological implications of potential drug nalini broadbelt and. Skip to document. University; High School. Books; Discovery. ... Bone case study. case study practice. Course. Anatomy and Physiology 2 (BIO 2112) 9 Documents. Students shared 9 documents in ...
Week 6 Case Study: Bone. 1. Describe the bone cells that are involved in generation of bone tissue. Some of the bone cells that are involved in the generation of bone tissues are the osteoblasts, osteoclasts, and osteocytes. The balance between these three types of cells contribute to bone homeostasis.