The global epidemiology of hypertension
Affiliations.
- 1 Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, USA.
- 2 Tulane University Translational Sciences Institute, New Orleans, LA, USA.
- 3 Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, USA. [email protected].
- 4 Tulane University Translational Sciences Institute, New Orleans, LA, USA. [email protected].
- PMID: 32024986
- PMCID: PMC7998524
- DOI: 10.1038/s41581-019-0244-2
Hypertension is the leading cause of cardiovascular disease and premature death worldwide. Owing to the widespread use of antihypertensive medications, global mean blood pressure (BP) has remained constant or has decreased slightly over the past four decades. By contrast, the prevalence of hypertension has increased, especially in low- and middle-income countries (LMICs). Estimates suggest that 31.1% of adults (1.39 billion) worldwide had hypertension in 2010. The prevalence of hypertension among adults was higher in LMICs (31.5%, 1.04 billion people) than in high-income countries (28.5%, 349 million people). Variations in the levels of risk factors for hypertension, such as high sodium intake, low potassium intake, obesity, alcohol consumption, physical inactivity and unhealthy diet, may explain some of the regional heterogeneity in hypertension prevalence. Despite the increasing prevalence, the proportions of hypertension awareness, treatment and BP control are low, particularly in LMICs, and few comprehensive assessments of the economic impact of hypertension exist. Future studies are warranted to test implementation strategies for hypertension prevention and control, especially in low-income populations, and to accurately assess the prevalence and financial burden of hypertension worldwide.

Publication types
- Research Support, N.I.H., Extramural
- Age Factors
- Antihypertensive Agents / administration & dosage*
- Blood Pressure Determination / methods
- Disease Progression
- Global Health*
- Hypertension / diagnosis*
- Hypertension / drug therapy
- Hypertension / epidemiology*
- Middle Aged
- Risk Assessment
- Sex Factors
- Antihypertensive Agents
Grants and funding
- K12 AR084224/AR/NIAMS NIH HHS/United States
- P20 GM109036/GM/NIGMS NIH HHS/United States
- R01 HL133790/HL/NHLBI NIH HHS/United States
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
High Blood Pressure
- 1 University of California, Davis
- 2 Associate Editor, JAMA Network Open
- Original Investigation Trends in Blood Pressure Control Among US Adults With Hypertension, 1999-2000 to 2017-2018 Paul Muntner, PhD; Shakia T. Hardy, PhD; Lawrence J. Fine, MD; Byron C. Jaeger, PhD; Gregory Wozniak, PhD; Emily B. Levitan, ScD; Lisandro D. Colantonio, MD, PhD JAMA
- Viewpoint A National Commitment to Improve the Care of Patients With Hypertension in the US Jerome M. Adams, MD, MPH; Janet S. Wright, MD JAMA
High blood pressure is a common condition in the US that increases the risk of stroke and heart disease.
Blood pushing against the walls of arteries in the body creates pressure, which generally varies throughout the day. High blood pressure, also known as hypertension , is blood pressure that is consistently higher than what is considered normal. There are 2 types of blood pressure measures: systolic and diastolic . Systolic blood pressure is the pressure in the arteries when the heart beats, while diastolic pressure is the pressure in the arteries when the heart rests. Normal systolic blood pressure is less than 120 millimeters of mercury (mm Hg), and normal diastolic blood pressure is less than 80 mm Hg, together described as 120/80 mm Hg. High blood pressure may be defined slightly differently by clinicians because some guidelines suggest that high blood pressure is that which is consistently higher than 130/80 mm Hg, while other guidelines suggest higher than 140/90 mm Hg.
Symptoms of High Blood Pressure
High blood pressure often has no warning signs or symptoms, which can make it difficult for individuals to know they have it.
Uncontrolled high blood pressure over long periods of time can lead to serious medical conditions such as heart failure or heart attack, stroke, vision problems, and kidney disease.
Preventing High Blood Pressure
There are several known risk factors for developing high blood pressure, including unhealthy diet, physical inactivity, obesity, tobacco use, and excess alcohol use. In the US, older adults, women, and Black individuals also have a higher risk of developing high blood pressure. Some people with a family history of high blood pressure may also have an increased risk.
The most important ways to prevent high blood pressure are to maintain a healthy diet and regular physical activity along with limiting alcohol intake and avoiding tobacco use.
Diagnosis and Treatment
High blood pressure is diagnosed by measuring blood pressure at a doctor’s office, at a pharmacy, or with an at-home monitor. Many people can lower their blood pressure through lifestyle changes such as engaging in 30 minutes of physical activity 5 days a week, eating a healthy diet that includes fresh fruits and vegetables and limits salt and alcohol intake, not smoking, and managing stress. Some people may need to take medication in addition to these lifestyle changes to lower their blood pressure to a healthy range. You may be asked to regularly monitor your blood pressure if you are being treated for high blood pressure, either with a home monitor or at a pharmacy that offers blood pressure monitoring. Talk to your doctor before starting medication to treat high blood pressure.
For More Information
Centers for Disease Control and Prevention www.cdc.gov/bloodpressure/facts.htm
To find this and other JAMA Patient Pages, go to the Patient Information collection at jamanetworkpatientpages.com .
Conflict of Interest Disclosures: None reported.
Sources: Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/facts.htm
American College of Cardiology https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2017/11/09/11/41/2017-guideline-for-high-blood-pressure-in-adults
Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA . Published September 22, 2020. doi: 10.1001/jama.2020.14545
See More About
Desai AN. High Blood Pressure. JAMA. 2020;324(12):1254–1255. doi:10.1001/jama.2020.11289
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics
High Blood Pressure Research
Language switcher.
As part of its broader commitment to research on cardiovascular diseases, the NHLBI leads and supports research and programs on hypertension (high blood pressure). The NHLBI has funded several studies and programs to help develop new treatments for high blood pressure, many of which focus on women’s health, lifestyle interventions, and health disparities. Current studies aim to prevent pregnancy complications and improve blood pressure among people who are at high risk.
NHLBI research that really made a difference
Find funding opportunities and program contacts for high blood pressure research.
- The Dietary Approaches to Stop Hypertension (DASH) Sodium Trial showed that lowering sodium as part of a healthy eating plan significantly lowers blood pressure for people with high blood pressure. Researchers saw the greatest change when lowering sodium was combined with eating a diet rich in fruits and vegetables and low in saturated fat.
- The NHLBI’s Systolic Blood Pressure Intervention Trial (SPRINT) study found that treating to a lower systolic blood pressure target — less than 120 mm Hg — helped lower deaths from heart attack and stroke, particularly among older people who have high blood pressure. These findings informed the latest high blood pressure guidelines in 2017. A follow-up study called SPRINTMIND found that treating to this lower blood pressure target also reduced mild cognitive impairment , a condition that can lead to dementia.
- The NHLBI Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT ) was the largest hypertension clinical trial ever conducted, involving more than 600 clinics and 42,000 participants. The study compared the effectiveness of three commonly used blood pressure-lowering medicines (a calcium channel blocker, amlodipine; an ACE-inhibitor, lisinopril; and an alpha-receptor blocker, doxazosin) with a diuretic, chlorthalidone. The trial concluded that the diuretic worked better than the other medicines to manage high blood pressure and prevent stroke, as well as some types of heart disease, especially heart failure.
Current research funded by the NHLBI
Our Division of Cardiovascular Sciences and its Vascular Biology and Hypertension Branch oversee much of the research we fund on the regulation of blood pressure.
Current research on the treatment of high blood pressure
NHLBI-supported research has led to creating and updating blood pressure treatments that have helped people around the world. High blood pressure affects millions of U.S. adults. We continue to support work on new treatments and also new approaches that tailor the right treatment to the right patient.
- Researchers in the NHLBI-funded Levy Lab are studying the role of genetics in cardiovascular disease using resources from the Framingham Heart Study to develop promising blood pressure medicines and treatments.
- The NHLBI funds research into the connection between inflammation and high blood pressure . Better understanding of the causes of hypertension helps researchers develop treatments to improve blood pressure management and prevent early death from cardiovascular disease.
- The NHLBI supports research to improve adherence to long-term cardiovascular medicines that help regulate blood pressure. Researchers use pharmacy data to identify patients who fail to refill their medicines. They then test whether reminders using text messages or interactive chat bots can improve medicine adherence.
- The NHLBI funds research into the connection between the microbiome and high blood pressure . One study found that bacterial strains in the mouth were linked to high blood pressure in older women. Another study showed that intermittent fasting in an animal model could reduce hypertension by reshaping the gut microbiota.
- Findings from the Offspring Cohort of the Framingham Heart Study (FHS) and the Coronary Artery Risk Development in Young Adults (CARDIA) study showed a close association between hypertension and late-onset epilepsy and other brain changes, respectively, which may increase the risk of cognitive decline later in life.
- A clinical trial called Treating Resistant Hypertension Using Lifestyle Modification to Promote Health (TRIUMPH) showed that lifestyle modification, such as following the DASH eating plan, could significantly reduce blood pressure even in patients with resistant hypertension. Another study found that DASH was effective in adolescents with high blood pressure.
- A clinical trial Chlorthalidone in Chronic Kidney Disease (CLICK) showed that the diuretic chlorthalidone can improve blood pressure control in patients with advanced chronic kidney disease.
- A recent meta-analysis showed that use of anti-hypertension medicines that can cross the blood-brain barrier is linked to more cognitive benefits than those that do not cross the barrier.
Find more NHLBI-funded studies on the high blood pressure treatment at NIH RePORTER.

Find out more about how the DASH diet and exercise help fight resistant high blood pressure.
Current research on women’s health and high blood pressure
NHLBI-supported research has helped reveal how pregnancy complications, including high blood pressure, affect the long-term health of women and their children.
- One study found that women who have a preterm birth have a greater chance of later developing high blood pressure.
- The NHLBI continues to fund the nuMoM2b Heart Health Study , which helps scientists understand how cardiovascular disease starts and develops in women. Researchers, funded by the NHLBI and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, found that women who developed complications during their first pregnancy were more likely to have had higher levels of blood sugar, blood pressure, and inflammation during their first trimester than women who did not develop complications. They are also more likely to develop chronic hypertension within 7 years after delivery. The study is also looking at the links between pregnancy, sleep health, and cardiovascular health .
- The NHLBI’s CHAP Maternal Follow-up Study is examining the impact of treatment for preeclampsia and high blood pressure during pregnancy on a woman’s future chance for developing cardiovascular disease. The results will help identify the best ways to improve the health of women younger than age 40 who have mild, long-term high blood pressure.
Find more NHLBI-funded studies on women’s health and high blood pressure at NIH RePORTER.
Current research on health disparities and high blood pressure
Black adults in the United States have a higher prevalence of high blood pressure than other racial and ethnic groups. The NHLBI supports research to understand and reduce high blood pressure disparities, as part of our broader commitment to addressing health disparities and inequities .
Other studies and research areas we fund to understand and lower the impacts of health disparities are listed below:
- Our RURAL: Risk Underlying Rural Areas Longitudinal Cohort Study reaches 4,000 young and middle-aged men and women from different racial and ethnic groups living in poor rural counties in four southern states. The goal of the study is to understand what causes the high rates of heart and lung disease in these regions and how to lower those rates and improve prevention efforts .
- Co-funded by the NHLBI and the NIH Office of Research on Women’s Health, the Maternal Health Community Implementation Program (MH-CIP) supports community-engaged implementation research, working with affected communities to improve heart, lung, blood, and sleep health before, during, and after pregnancy. MH-CIP focuses on bringing effective maternal health interventions — including projects related to hypertension — into communities severely impacted by maternal health disparities.
- An NHLBI-funded study aims to improve implementation of the SPRINT findings in underserved populations. The study puts into practice a plan for blood pressure treatment at 30 clinics that serve people with little or no income in southeast Louisiana. The study’s findings will help lower barriers to blood pressure treatment faced by people who experience poverty.
Find more NHLBI-funded studies on high blood pressure and health disparities at NIH RePORTER.

High blood pressure research labs at the NHLBI
The NHLBI Division of Intramural Research and its Cardiovascular Branch conduct research on diseases that affect the heart and blood vessels, including high blood pressure. Other Division of Intramural Research groups, such as the Center for Molecular Medicine and Systems Biology Center , perform research on heart and vascular diseases.
Related programs
- In 2023, the NHLBI convened the Transforming Hypertension Diagnosis and Management in the Era of Artificial Intelligence (AI) workshop to discuss gaps and opportunities in leveraging AI technologies for hypertension diagnosis and management.
- Nurse case management, in which a nurse provides behavioral counseling and monitors blood pressure through telehealth, adjusting blood pressure medications as needed
- Community health workers providing health coaching and information about community resources
Read more about the DECIPHeR program .
- In 2019, the NHLBI convened the HIV-associated Comorbidities, Co-infections & Complications Workshop , which led to strategies that support more research into the diseases, infections, and complications related to HIV. People with HIV have a higher risk of developing high blood pressure, even if they actively manage HIV infection with medicine.
Explore more NHLBI research on high blood pressure
The sections above provide you with the highlights of NHLBI-supported research on high blood pressure. You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Risk Factors
- Managing High Blood Pressure
- High Blood Pressure Facts
- Measure Your Blood Pressure
- Hypertension Management Program (HMP) Toolkit
- Publication
- High Blood Pressure Communications Toolkit
- Rapid Evaluations of Telehealth Strategies to Address Hypertension
- Team-Based Care to Improve Blood Pressure Control
- High Blood Pressure Maps and Data Resources
- The Surgeon General's Call to Action to Control Hypertension
- Federal Hypertension Control Leadership Council (The Council)
- About Heart Disease
- About High Blood Pressure
- About Stroke
- About Cholesterol
What to know
- Blood pressure is the pressure of blood pushing against the walls of your arteries.
- Arteries carry blood from your heart to other parts of your body.

Facts about high blood pressure in the United States
In 2017, the American College of Cardiology and the American Heart Association published guidelines for hypertension management. It defined hypertension as a blood pressure at or above 130/80 mmHg. Stage 2 hypertension is defined as a blood pressure at or above 140/90 mmHg. 1
Blood Pressure Category
Systolic Blood Pressure
Diastolic Blood Pressure
<120 mmHg
and <80 mmHg
120-129 mmHg
Stage 1 Hypertension
130-139 mmHg
or 80-89 mmHg
Stage 2 Hypertension
≥140 mmHg
or ≥90 mmHg
- Having high blood pressure puts you at risk for heart disease and stroke , which are leading causes of death in the United States.
- In 2021, high blood pressure was a primary or contributing cause of 691,095 deaths in the United States. 2
- Nearly half of adults have high blood pressure (48.1%, 119.9 million). This is defined as a systolic blood pressure greater than 130 mmHg or a diastolic blood pressure greater than 80 mmHg or are taking medication for high blood pressure. 3
- About 1 in 4 adults with high blood pressure has their blood pressure under control (22.5%, 27.0 million). 3
- About half of adults (45%) with uncontrolled high blood pressure have a blood pressure of 140/90 mmHg or higher. This includes 37 million U.S. adults. 3
- About 34 million adults who should be taking medication according to hypertension guidelines may need a prescription or to fill their prescription and start taking it. Almost two out of three of this group (19 million) have a blood pressure of 140/90 mmHg or higher. 3
- High blood pressure costs the United States about $131 billion each year, averaged over 12 years from 2003 to 2014. 4
Blood pressure control varies by sex and race
Uncontrolled high blood pressure is common, but some groups of people are more likely to have control over their high blood pressure than others.
- A higher percentage of men (50%) have high blood pressure than women (44%). 3
- High blood pressure is more common in non-Hispanic black adults (56%) than in non-Hispanic white adults (48%), non-Hispanic Asian adults (46%), or Hispanic adults (39%). 3
- Among those recommended to take blood pressure medication, blood pressure control is higher among non-Hispanic white adults (32%) than in non-Hispanic black adults (25%), non-Hispanic Asian adults (19%), or Hispanic adults (25%). 3
Rates of high blood pressure vary by geography
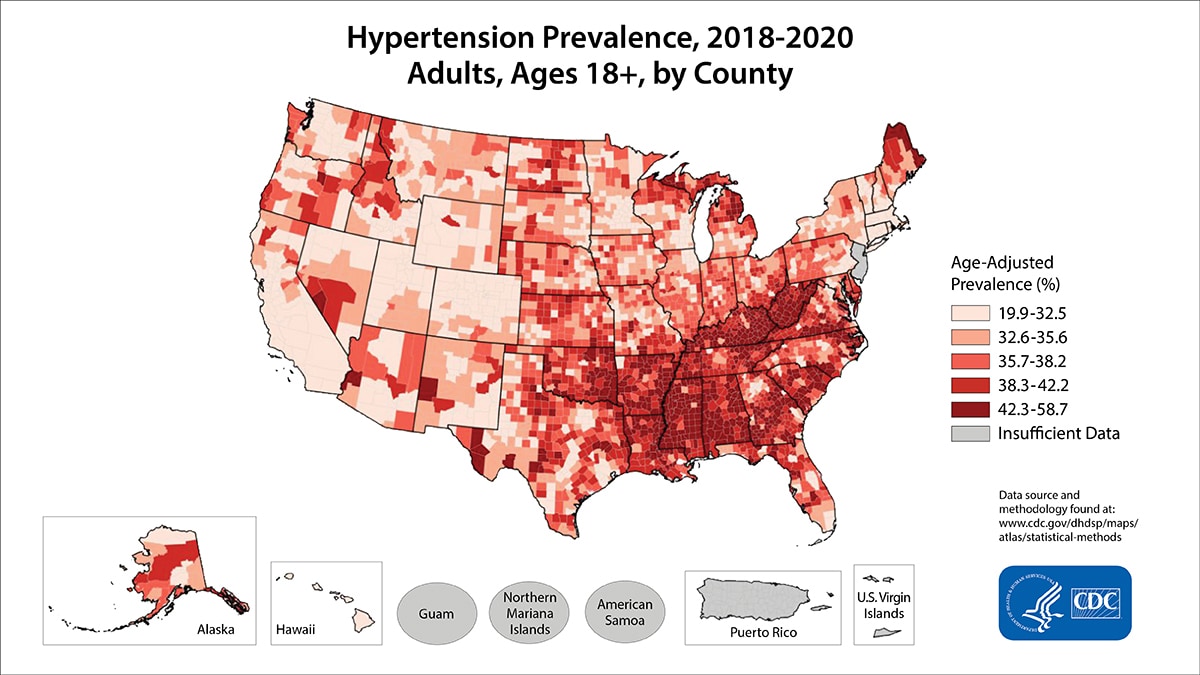
High blood pressure is more common in some areas of the United States. Below is a map showing the self-reported rate of hypertension by county. However, this map likely underreports the true effect of hypertension in each state, because about 1 in 5 adults with high blood pressure is unaware of it and would not report having it. 5
What CDC is doing
- Million Hearts ®
For more information about high blood pressure, visit the following websites:
- Medline Plus
- National Heart, Lung, and Blood Institute
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Hypertension . 2018;71(19):e13–e115.
- National Center for Health Statistics. Multiple Cause of Death 2018–2021 on CDC WONDER Database. Accessed February 2, 2023. https://wonder.cdc.gov/mcd.html
- Centers for Disease Control and Prevention. Hypertension cascade: hypertension prevalence, treatment and control estimates among US adults aged 18 years and older applying the criteria from the American College of Cardiology and American Heart Association's 2017 Hypertension Guideline—NHANES 2017–March 2020. Accessed July 6, 2023. https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html
- Kirkland EB, Heincelman M, Bishu KG, et. al. Trends in healthcare expenditures among US adults with hypertension: national estimates, 2003-2014. J Am Heart Assoc . 2018;7:e008731.
- Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the US by improvements in the use of clinical preventive services. Am J Prev Med . 2010;38(6):600–609.
High Blood Pressure
High blood pressure increases the risk for heart disease and stroke, two leading causes of death for Americans.
For Everyone
Health care providers, public health.
- Open access
- Published: 16 May 2024
Regional and rural-urban patterns in the prevalence of diagnosed hypertension among older U.S. adults with diabetes, 2005–2017
- Jalal Uddin 1 , 2 ,
- Sha Zhu 2 ,
- Gargya Malla 2 ,
- Emily B. Levitan 2 ,
- Deborah B. Rolka 3 ,
- April P. Carson 4 &
- D. Leann Long 5
BMC Public Health volume 24 , Article number: 1326 ( 2024 ) Cite this article
231 Accesses
1 Altmetric
Metrics details
Hypertension prevalence among the overall US adult population has been relatively stable during the last two decades. However, whether this stabilization has occurred across rural-urban communities and across different geographic regions is unknown, particularly among older adults with diabetes who are likely to have concomitant cardiovascular risk factors.
This serial cross-sectional analysis used the 5% national sample of Medicare administrative claims data ( n = 3,516,541) to examine temporal trends (2005–2017) in diagnosed hypertension among older adults with diabetes, across urban-rural communities and US census regions (Northeast, Midwest, South, and West). Joinpoint regression was used to obtain annual percent change (APC) in hypertension prevalence across rural-urban communities and geographic regions, and multivariable adjusted regression was used to assess associations between rural-urban communities and hypertension prevalence.
The APC in the prevalence of hypertension was higher during 2005–2010, and there was a slowdown in the increase during 2011–2017 across all regions, with significant variations across rural-urban communities within each of the regions. In the regression analysis, in the adjusted model, older adults living in non-core (most rural) areas in the Midwest (PR = 0.988, 95% CI: 0.981–0.995) and West (PR = 0.935, 95% CI: 0.923–0.946) had lower hypertension prevalence than their regional counterparts living in large central metro areas.
Conclusions
Although the magnitudes of these associations are small, differences in hypertension prevalence across rural-urban areas and geographic regions may have implications for targeted interventions to improve chronic disease prevention and management.
Peer Review reports
Introduction
Rural-urban disparities in health are well-documented in the US, with persons in rural communities having an excess burden of preventable diseases and mortality [ 1 ]. National data from the US Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) demonstrated that rural-urban disparities in age-adjusted all-cause mortality rates [ 2 ] and mortality from cardiovascular disease [ 3 ] persisted from the late 1990s to early 2010s, although national mortality rates generally declined during this time. Furthermore, over the last two decades, reductions in mortality from ischemic heart disease have been slower for adults aged 65 years living in rural areas than those in urban areas [ 4 ].
The prevalence of hypertension increases with age, such that 77% of US adults aged 65 years have hypertension compared to about 29% of US adults aged 20–44 years [ 5 ]. Moreover, blood pressure control among those with hypertension has declined in recent years [ 6 ], further underscoring the importance of understanding trends in the burden of hypertension.
Existing studies show a mixed pattern in rural-urban differences in cardiovascular risk factors, including hypertension and diabetes. Findings from a contemporaneous cohort study with representation from the contiguous US showed that adults in rural areas were more likely to have hypertension than those in urban areas [ 7 ]. In a separate study using data from primary care practices in the Midwest, adults with diabetes living in rural areas were less likely to have controlled blood pressure than adults with diabetes living in urban areas [ 8 ]. In contrast, in the National Health and Nutrition Examination Survey data (2013–2018), the prevalence of stage II hypertension (BP ≥ 140/90 mm Hg) was higher for adults residing in medium to small metropolitan statistical areas (MSAs) but not for those residing in non-MSAs [ 9 ] Further, CDC’s Diabetes LEAD (Location, Environmental Attributes, and Disparities) Network studies have shown that the new onset type 2 diabetes (T2D) by rural-urban community types varies by region of the US. For instance, the T2D onset was higher in rural areas in the South and in high density urban communities in the Northeast region (the Geisinger sample) [ 10 ]. As hypertension and diabetes are often concomitant [ 11 ], identifying communities that may be differentially impacted by this excess burden is needed.
It is well-documented that diabetes and hypertension, separately, are more prevalent in the southern areas of the US [ 12 , 13 , 14 , 15 ]. While hypertension-related cardiovascular mortality rates increased in both rural and urban areas in the US from 2007 to 2017, this increase was more pronounced in rural areas in the South [ 16 ]. However, evidence is limited on rural-urban disparities in hypertension prevalence over time and across geographic regions among older adults with diabetes, a high-risk group for cardiovascular morbidity and mortality. To address this important gap in the literature, using national level Medicare administrative claims (2005–2017) data, we examined trends in diagnosed hypertension among older adults with diabetes by rural-urban residence and geographic region.
This serial cross-sectional analysis used the 5% national random sample of Medicare data from 2005 to 2017. Medicare is a national program that provides health care insurance to US adults aged ≥ 65 years, and adults with a disability or end-stage renal disease, regardless of age. This analysis included fee-for-service beneficiaries aged ≥ 66 years with at least 12 months of continuous coverage for inpatient (Medicare Part A) and outpatient (Medicare Part B) care, and with a diagnosis for diabetes. As we restricted our analysis to those who were on Medicare for at least 12 months, the lowest age of the participants was 66. Diabetes diagnosis was determined using International Classification of Diseases codes (ICD-9 and ICD-10) from one inpatient claim or two outpatient or carrier claims that were at least seven days apart. Hypertension diagnosis was determined using similar methods. The ICD-9 and ICD-10 codes for diabetes and hypertension, respectively, were obtained from ICD manuals (Supplementary table S1 ) [ 17 , 18 ].
Regions and rural-urban classification
Geographic regions were categorized according to US Census regions (Northeast, Midwest, South, and West). For rural and urban designations, the 2013 CDC National Center for Health Statistics (NCHS) classification scheme [ 19 ] was used to categorize communities at the county-level. The NCHS uses data from the US Census and the Office of Management and Budget to classify counties into the following community types: (1) large central metropolitan; (2) large fringe metropolitan; (3) medium metropolitan; (4) small metropolitan; (5) micropolitan; and (6) and non-core. Large central metropolitan is the most urban classification, and non-core is the most rural classification. The details of the methodology and definitions of these classifications were described previously [ 19 ].
Covariates included age (66–69, 70–74, 75–79, 80–84, and 85 years), sex (male, female), race (White, Black, and Other), and dual eligibility for Medicare and Medicaid; these were obtained from the Medicare Beneficiary Summary File. Additionally, the social vulnerability index (SVI) was also included; this index ranks the relative vulnerability of a geographic area (e.g., county) based on socioeconomic status, household composition and disability, race/ethnicity composition/language, and housing/transportation. We linked publicly available 2010 SVI data to Medicare claims data. The 2010 SVI is based on the 2010 census data and SVI scores ranged from 0 to 1, with a higher score representing higher levels of vulnerability [ 20 , 21 ].
Statistical analysis
We examined sociodemographic characteristics across calendar years. P -value for trend for categorical/ordinal variables was obtained using Mantel-Haenszel Chi-square statistics [ 22 ]. Specifically, non-zero correlation was tested for ordinal covariates (e.g., age group) and linear shift was tested for nominal covariates (e.g., race, sex). Joinpoint regression was used to estimate the annual percent change (APC) in hypertension prevalence [ 23 , 24 , 25 ] by rural-urban community types in each census region. Briefly, joinpoint regression assesses changes in slopes for the outcome of interest between time points across a study period. Estimates were age-standardized to the 2010 US census. Poisson regression with robust standard errors was used to obtain prevalence ratios (PR) to assess the associations of rural-urban categories with hypertension in each census region. Models were unadjusted; adjusted for age, sex, race, and Medicaid-Medicare dual eligibility; and further adjusted for the 2010 social vulnerability index. A two-tailed P < 0.05 was considered statistically significant. Statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc, Cary, NC).
Characteristics of medicare beneficiaries 2005–2017
Table 1 presents sociodemographic characteristics by calendar year. The percentage of study participants aged 66–69 years increased from 2005 to 2017, while the percentages for those aged 75–79 and 80–84 years decreased during this time ( P -value for trend < 0.0001). Women comprised more than half of the study participants across all calendar years, and their percentages decreased from 56.8 in 2005 to 52.8 in 2017 ( P -value for trend < 0.0001). The percentage of study participants in the South and West regions increased from 2005 to 2017, whereas the percentages in the Northeast and Midwest decreased. For community types, there were no significant changes during the study period ( p = 0.86).
Trends in prevalence of hypertension by community types across regions
The age-adjusted hypertension prevalence by rural-urban community types is presented for the Northeast, Midwest, South, and West regions, respectively, in Figs. 1 , 2 , 3 and 4 . The prevalence of diagnosed hypertension among older adults with diabetes increased in all regions, although it differed across rural-urban community types.

Age-adjusted prevalence of diagnosed hypertension among those with diabetes by community types in the Northeast

Age-adjusted prevalence of diagnosed hypertension among those with diabetes by community types in the Midwest

Age-adjusted prevalence of diagnosed hypertension among those with diabetes by community types in the South

Age-adjusted prevalence of diagnosed hypertension among those with diabetes by community types in the West
In the Northeast region (Fig. 1 ), rural communities (non-core) had a lower prevalence of hypertension than more urban communities. From 2005 to 2010, the APC in hypertension prevalence was 1.28% in large fringe metropolitan areas, 1.73% in small metropolitan areas, 1.63% in micropolitan areas, and 1.60% in non-core areas. During 2010–2017, APCs were lower, ranging from 0.02% in non-core to 0.45% in large fringe metropolitan areas.
The prevalence of hypertension was higher in large central and large fringe metropolitan areas than those living in non-core areas in the Midwest region (Fig. 2 ). Between 2005 and 2011, the APC in hypertension was 1.07% in large central metropolitan areas, 1.37% in large fringe metropolitan, and 1.44% in non-core areas. The APC was lower in later years across all community types. Between 2011 and 2017, the APC in hypertension prevalence was 0.23% in large central metropolitan areas, 0.32% in large fringe metropolitan areas, and 0.37% in non-core areas.
Hypertension prevalence was generally higher in the South than in other regions. Additionally, differences in hypertension prevalence across rural-urban communities had smaller magnitudes in the South (Fig. 3 ). Overall, from 2005 to 2017, the APC in hypertension prevalence was higher in earlier years and there was a slowdown in later years across all rural-urban community types. For example, during 2005–2011, the APC was 1.17% in large fringe metropolitan areas, 1.41% in medium metropolitan areas, and 1.47% in non-core areas. During 2011–2017, the APC was 0.42% in large fringe metropolitan areas, 0.38% in medium metropolitan areas, and 0.57% in non-core areas. Interestingly, the rural-urban prevalence gradient in the South region essentially flips through the study period. In general, the prevalences in the beginning were higher in urban counties than in rural counties, but by the end of the study period, prevalences were higher in rural counties compared to urban.
In the West, hypertension prevalence was generally lower than other regions (Fig. 4 ). The prevalence of hypertension was highest in large central metropolitan areas and lowest in non-core areas. During 2005–2011, the APC was 1.25% in large central metropolitan areas and 1.38% in non-core areas. In later years, the APC was lower (APC = 0.00 in non-core areas in 2011–2017 and APC = 0.21 in large fringe metropolitan in 2009–2017).
Association of rural-urban community type with hypertension prevalence
Prevalence ratios (PR) and 95% confidence intervals estimating hypertension prevalence across community types and by geographic region are presented in Table 2 . In the unadjusted model (Model 1), compared to participants residing in large central metropolitan areas, older adults from non-core areas had a lower hypertension prevalence (Northeast PR = 0.958; Midwest PR = 0.934; South PR = 0.993; and West PR = 0.893). However, after adjustment for potential covariates including age, sex, race, Medicare-Medicaid dual-eligibility, and social vulnerability index, associations were weakened to either non-significant or close to 1, indicating very small community type differences in the prevalence of diagnosed hypertension (for example, in non-core areas, Northeast PR = 0.994; Midwest PR = 0.988; South PR = 1.001; and West PR = 0.935), though still statistically significant in the Midwest and West.
This study identified regional and community-level trends in diagnosed hypertension among older adults with diabetes during 2005–2017. Overall, hypertension prevalence increased in each region during the study period, with larger increases occurring from 2005 to around 2010. Additionally, differences in hypertension prevalence by rural-urban community type were observed, although these differences were smaller in the South region than other regions. The prevalence of hypertension was lower in non-core areas than large central metropolitan areas in each region, although these associations were attenuated after multivariable adjustment and the effect estimates were small.
The joinpoint regression analysis revealed interesting changes in the slope of the prevalence trends of hypertension over time for urban/rural categories across all geographic regions. We noticed a larger increase in hypertension prevalence occurring from 2005 to around 2010/2011 and a slowdown in the increase in more recent years (e.g., 2011–2017). One potential reason for this change in the prevalence trend could be healthcare reform in 2011, which has a spillover effect on the health outcomes of Medicare beneficiaries. Since the implementation of the Affordable Care Act (ACA) in 2011, some studies have shown increased utilization of certain clinical preventive services, including blood pressure monitoring among Medicare beneficiaries [ 26 , 27 ]. This is partly because the ACA required most insurance plans and Medicare to cover a range of clinical preventive services without cost-sharing. The inncreased access to preventive services owing to ACA spillover effect may result in better monitoring of high blood pressure and a slowdown in the increase in hypertension prevalence among Medicare beneficiaries in the post-ACA period.
Our analysis found small differences in hypertension prevalence by rural-urban areas. We observed that prevalence estimates were relatively smaller in rural and larger in large metropolitan areas. In contrast, prior studies have reported mixed results, with most studies showing an excess burden of hypertension in rural areas and a few studies showing higher prevalence of hypertension in medium-lower metropolitan areas. For instance, using the similar urban-rural classification that we used, a study using data from the Behavioral Risk Factor Surveillance System (BRFSS) has shown that the age-standardized prevalence of self-reported hypertension was higher in the most rural counties (e.g., non-core and micropolitan) compared to large central metropolitan areas [ 28 ]. In a cohort study of adults 45 years or older, those residing in rural areas had a higher prevalence of hypertension than those residing in large central metropolitan areas [ 7 ]. Further, using a condensed NCHS rural-urban classification scheme, a recent study based on data from the 2013–2018 National Health and Nutrition Examination Survey (NHANES) reports that hypertension (defined as blood pressure (BP) ≥ 140/90) prevalence was higher for adults residing in medium to small metropolitan areas but not for those residing in most rural areas [ 9 ]. In contrast, our study found that among older adults with diabetes, hypertension prevalence was generally lower for those in rural areas than in urban areas within each geographic region, except for the South.
Overall, our analysis stratified by region shows a higher prevalence of age-adjusted hypertension in urban than rural areas in all regions except for the South, where hypertension prevalence is largely similar across community types. Such findings of rural-urban disparities in hypertension by region are consistent with a recent study that examined trends in hypertension-related cardiovascular mortality rates from 2007 to 2017. While hypertension-related mortality rates increased in rural and urban areas during the study period, the hypertension-related mortality rate was higher among those in rural areas in the South [ 16 ]. Our analysis did not specifically examine mortality-related outcomes, but we note that a higher prevalence of hypertension in the South is consistent with previous studies [ 10 , 29 ].
Contrary to some previous studies, our analysis found that rural (i.e., non-core) areas generally had lower hypertension prevalence than urban (i.e., large central metropolitan) areas. To better contextualize our observed higher estimates in urban areas, we note a few methodological and measurement differences in self-report survey data and insurance claims that differ in estimating hypertension. Firstly, validation studies generally report that estimates of hypertension tend to be significantly higher in self-reported surveys than in insurance claims data [ 30 ]. Accuracy of self-reports of chronic conditions may often be limited due to social or personal stigma associated with the conditions and by the presence of other debilitating conditions such as cognitive impairment or severe mental health problems [ 31 ]. Secondly, another potential reason we observed a different association than existing studies is that our study population is Medicare beneficiaries with diabetes. In contrast, most previous studies looked at hypertension among the general population without any disease condition. Future studies can examine whether hypertension prevalence differs between older adults with and without diabetes, especially across urban-rural classification.
Thirdly, unlike most previous studies, we chose to stratify our analysis by region to account for the potential confounding by region [ 10 , 32 ]. Due to confounding by region, we found that urban areas had a higher prevalence in most regions. Finally, administrative claims data is also not without limitations; an insurance claim does not necessarily represent a disease status. At best, an insurance claim represents an episode of care for which a claim was submitted. Most importantly, as access to healthcare facilities is better in urban than rural areas, episodes of care are likely to be higher in urban areas. We note that in light of these methodological and measurement differences, our study findings should be interpreted and compared to existing studies.
Understanding the potential reasons for regional differences in the burden of hypertension is important for the effective prevention and management of chronic conditions. We note that the impact of broader contextual factors, such as community-based economic inequality, lifestyle, healthcare, and environmental factors, may differ across regions and thus differentially affect the burden of chronic disease [ 32 , 33 , 34 ]. Because our findings demonstrate disparities in the prevalence of hypertension in regional and urban-rural settings, future studies might investigate how underlying community characteristics may shape differences in chronic disease conditions within these contexts.
Our study has a few limitations. First, our analysis is limited to Medicare fee-for-service beneficiaries and does not represent those in Medicare Advantage or other commercial insurance plans. The financial incentives and reimbursement structures vary between Medicare fee-for-service and Medicare Advantage. These differences may affect the rate of diagnosis of hypertension. Second, this analysis is based on Medicare administrative claims data that reflect a disease diagnosis and not the prevalence of the condition itself, as those with undiagnosed hypertension or undiagnosed diabetes would not be captured using claims data. Third, the rural-urban classification used was at the county level. Because defining rurality is a complex phenomenon, its classification should represent a nuanced matrix of geographical and population-level characteristics [ 35 ]. Some counties may have urbanized and non-urbanized pockets because of their size, population density, and other area-level characteristics; thus, obtaining and characterizing such a granular rural-urban continuum within a county boundary is challenging. Finally, we could not examine the prevalence of hypertension stratified by race/ethnicity in rural-urban communities due to the smaller sample size in some race/ethnicity categories.
In summary, among older adults with diabetes, the prevalence of diagnosed hypertension in most regions was higher for Medicare beneficiaries residing in urban areas than rural areas. The differential prevalence of diagnosed hypertension in rural-urban communities across geographic regions has implications for targeted interventions to improve chronic disease prevention and management. Although we found smaller yet statistically significant differences, further investigation is needed to examine why older adults living in certain community types have a higher burden of chronic diseases. Understanding underlying contextual and service delivery factors may be immensely useful for designing community-specific preventive interventions to reduce place-based disparities in chronic diseases.
Data availability
The data that support the findings of this study are available from the Data Assistance Center (ResDAC) ( https://resdac.org ), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
Ziller E, Milkowski C. A Century later: rural Public Health’s Enduring challenges and opportunities. Am J Public Health. 2020;110(11):1678–86.
Article PubMed PubMed Central Google Scholar
Cross SH, Califf RM, Warraich HJ. Rural-urban disparity in mortality in the US from 1999 to 2019. JAMA. 2021;325(22):2312–4.
Cross SH, et al. Rural-urban differences in cardiovascular mortality in the US, 1999–2017. JAMA. 2020;323(18):1852–4.
Khan MS, et al. Rural-urban differences in mortality from ischemic heart disease, heart failure, and stroke in the United States. Circulation: Cardiovasc Qual Outcomes. 2021;14(4):e007341.
Google Scholar
Tsao CW, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation. 2023;147(8):e93–621.
Article PubMed Google Scholar
Muntner P, et al. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA. 2020;324(12):1190–200.
Kamin Mukaz D et al. Rural/urban differences in the prevalence of stroke risk factors: a cross-sectional analysis from the REGARDS study. J Rural Health, 2021:1–6.
Kurani SS, et al. Association between Area-Level Socioeconomic Deprivation and Diabetes Care Quality in US Primary Care practices. JAMA Netw open. 2021;4(12):e2138438–2138438.
Ostchega Y, et al. Differences in hypertension prevalence and hypertension control by urbanization among adults in the United States, 2013–2018. Am J Hypertens. 2022;35(1):31–41.
McAlexander TP, et al. Urban and rural differences in new onset type 2 diabetes: comparisons across national and regional samples in the diabetes LEAD network. SSM-Population Health. 2022;19:101161.
Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380(9841):601–10.
Barker LE, et al. Geographic distribution of diagnosed diabetes in the US: a diabetes belt. Am J Prev Med. 2011;40(4):434–9.
Olives C, et al. Prevalence, awareness, treatment, and control of hypertension in United States counties, 2001–2009. PLoS ONE. 2013;8(4):e60308.
Article CAS PubMed PubMed Central Google Scholar
Ward BW, Black LI. State and regional prevalence of diagnosed multiple chronic conditions among adults aged ≥ 18 years—United States, 2014 Morbidity and mortality weekly report, 2016. 65(29): pp. 735–738.
Dwyer-Lindgren L, et al. Diagnosed and undiagnosed diabetes prevalence by county in the US, 1999–2012. Diabetes Care. 2016;39(9):1556–62.
Nambiar L, et al. Decade-long temporal trends in US hypertension-related cardiovascular mortality. J Am Coll Cardiol. 2020;75(20):2644–6.
Optum360º. ICD-9-CM Expert for Physicians, Volumes 1 & 2–2014 (Spiral) 2014 Edition by Optum (2013) 2014.
Optum360º. ICD-10-CM 2021 Expert for Physicians (ICD-10-CM Expert for Physicians 2021.
Ingram DD, Franco SJ. 2013 NCHS Urban-Rural classification Scheme for counties. Vital Health Stat, 2014. 2(166).
Flanagan B et al. A social vulnerability index for disaster management. J Homel Secur Emerg Manag 2011; 8 (1).
Prevention CfDCa. SVI 2010 Documentation https://www.atsdr.cdc.gov/placeandhealth/svi/documentation/pdf/SVI-2010-Documentation-H.pdf 2010.
Stokes ME, Davis CS, Koch GG. Categorical data analysis using SAS. SAS institute; 2012.
Raftery AE. Bayesian model selection in Social Research. Sociol Methodol. 1995;25:111–63.
Article Google Scholar
Kim HJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–51.
Article CAS PubMed Google Scholar
Statistical Methodology and Applications, Branch SRP. National Cancer Institute., Joinpoint Regression Program, Version 4.9.1.0 2022.
Toseef MU, Jensen GA, Tarraf W. Effects of the Affordable Care Act’s enhancement of Medicare benefits on preventive services utilization among older adults in the US. Prev Med. 2020;138:106148.
Mellor JM, et al. The impact of Medicaid expansion on spending and utilization by older low-income Medicare beneficiaries. Health Serv Res. 2023;58(5):1024–34.
Samanic CM, et al. Prevalence of self-reported hypertension and antihypertensive medication use by county and rural-urban classification—United States, 2017. Morb Mortal Wkly Rep. 2020;69(18):533.
Heindl B, et al. Urban-rural differences in hypertension prevalence, blood pressure control, and systolic blood pressure levels. J Hum Hypertens. 2023;37(12):1112–8.
Fortin M, et al. Self-reported versus health administrative data: implications for assessing chronic illness burden in populations. A cross-sectional study. Can Med Association Open Access J. 2017;5(3):E729–33.
Cigolle CT, et al. Inconsistency in the self-report of chronic diseases in panel surveys: developing an adjudication method for the health and retirement study. Journals Gerontology: Ser B. 2018;73(5):901–12.
Uddin J, et al. Trends in diagnosed hypertension prevalence by geographic region for older adults with and without diagnosed diabetes, 2005–2017. J Diabetes Complicat. 2022;36(7):108208.
Article CAS Google Scholar
Myers CA, et al. Diabetes prevalence is associated with different community factors in the diabetes belt versus the rest of the United States. Obesity. 2017;25(2):452–9.
Oates GR, et al. Sociodemographic patterns of chronic disease: how the mid-south region compares to the rest of the country. Am J Prev Med. 2017;52(1):S31–9.
McAlexander TP, et al. Categorizing community type for epidemiologic evaluation of community factors and chronic disease across the United States. Volume 5. Social Sciences & Humanities Open; 2022. p. 100250. 1.
Download references
Acknowledgements
Not Applicable.
This research was conducted by the Diabetes LEAD (Location, Environmental Attributes, and Disparities) Network, funded by C.D.C. cooperative agreements U01DP006302 (University of Alabama at Birmingham) with collaboration with the Drexel University, Geisinger-Johns Hopkins University, New York University School of Medicine, and the US CDC Division of Diabetes Translation. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
Author information
Authors and affiliations.
Department of Community Health and Epidemiology, Dalhousie University, 5790 University Ave, Halifax, Canada
Jalal Uddin
Department of Epidemiology, University of Alabama at Birmingham, Birmingham, USA
Jalal Uddin, Sha Zhu, Gargya Malla & Emily B. Levitan
Division of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Georgia, USA
Deborah B. Rolka
Department of Medicine, University of Mississippi Medical Center, Jackson, USA
April P. Carson
Department of Biostatistics and Data Science, Wake Forest University, Winston-Salem, USA
D. Leann Long
You can also search for this author in PubMed Google Scholar
Contributions
A.P.C., D.L.L., G.M., and J.U. conceptualized the study. J.U. interpreted the data and drafted the manuscript. S.Z. performed statistical analysis. E.B.L., D.L.L., G.M., D.R., and S.Z. interpreted the data and critically reviewed the manuscript. D.L.L. is the guarantor of this work and, as such, had full access to all the data and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Correspondence to Jalal Uddin .

Ethics declarations
Ethics approval and consent to participate.
Ethics approval was granted by the University of Alabama at Birmingham. Informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
A.P.C, E.B.L, and D.L.L. received investigator-initiated research support from Amgen, Inc. No other potential conflicts of interest relevant to this article were reported.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Uddin, J., Zhu, S., Malla, G. et al. Regional and rural-urban patterns in the prevalence of diagnosed hypertension among older U.S. adults with diabetes, 2005–2017. BMC Public Health 24 , 1326 (2024). https://doi.org/10.1186/s12889-024-18802-5
Download citation
Received : 16 November 2023
Accepted : 08 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s12889-024-18802-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Rural-urban classification
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Hypertens
- v.2017; 2017

Prevalence and Associated Risk Factors of Hypertension: A Cross-Sectional Study in Urban Varanasi
Shikha singh.
1 Department of Community Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, India
Ravi Shankar
Gyan prakash singh.
2 Division of Biostatistics, Department of Community Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, India
Hypertension is a major public health problem and important area of research due to its high prevalence and being major risk factor for cardiovascular diseases and other complications. Objectives . (1) To assess the prevalence of hypertension and its associated factors and (2) to estimate awareness, treatment, and adequacy of control of hypertension among study subjects. Methods and Materials . A community based cross-sectional study with multistage sampling design was conducted among urban population of Varanasi. A modified WHO STEPS interview schedule on 640 study subjects aged 25–64 years was used. Results . The prevalence of hypertension was 32.9% (male: 40.9%, female: 26.0%). Mean systolic and diastolic BP were 124.25 ± 15.05 mmHg and 83.45 ± 9.49 mmHg, respectively. Higher odds of being hypertensive were found in male subjects, eldest age group, married subjects, subjects of upper socioeconomic status, illiterate subjects, and retired subjects. Tobacco and alcohol consumption, overweight, obesity, and abdominal obesity were also associated with hypertension. Out of the total hypertensive 211 subjects, only 81 (38.4%) were aware about their hypertension status; out of those, 57 (70.4%) were seeking treatment and 20 (35.08%) had their blood pressure adequately controlled. Conclusion . Around one-third of the subjects were hypertensive and half of the study subjects were prehypertensive in this area. The awareness, treatment, and control of high blood pressure were also very low.
1. Introduction
Hypertension is a major public health problem due to its high prevalence all around the globe [ 1 – 4 ]. Around 7.5 million deaths or 12.8% of the total of all annual deaths worldwide occur due to high blood pressure [ 5 ]. It is predicted to be increased to 1.56 billion adults with hypertension in 2025 [ 6 ].
Raised blood pressure is a major risk factor for chronic heart disease, stroke, and coronary heart disease. Elevated BP is positively correlated to the risk of stroke and coronary heart disease. Other than coronary heart disease and stroke, its complications include heart failure, peripheral vascular disease, renal impairment, retinal hemorrhage, and visual impairment [ 5 ].
Hypertension (or HTN) or high blood pressure is defined as abnormally high arterial blood pressure. According to the Joint National Committee 7 (JNC7), normal blood pressure is a systolic BP < 120 mmHg and diastolic BP < 80 mm Hg. Hypertension is defined as systolic BP level of ≥140 mmHg and/or diastolic BP level ≥ 90 mmHg. The grey area falling between 120–139 mmHg systolic BP and 80–89 mmHg diastolic BP is defined as “prehypertension” [ 7 , 8 ]. Although prehypertension is not a medical condition in itself, prehypertensive subjects are at more risk of developing HTN [ 1 ].
It is a silent killer as very rarely any symptom can be seen in its early stages until a severe medical crisis takes place like heart attack, stroke, or chronic kidney disease [ 8 – 10 ]. Since people are unaware of excessive blood pressure, it is only through measurements that detection can be done. Although majority of patients with hypertension remain asymptomatic, some people with HTN report headaches, lightheadedness, vertigo, altered vision, or fainting episode [ 11 ].
There are several factors predisposing to hypertension. These factors vary from country to country and even there is difference between urban and rural regions of the same place [ 12 ]. Realizing the effect of urbanization on our collective health, World Health Organization has chosen “Urbanization and Health” as the theme for World Health Day 2010 [ 13 ]. Urbanization is considered a determinant of health and one of the key drivers of noncommunicable diseases (NCDs), especially in low- and middle-income countries (LMICs) [ 14 ]. Urban people are more at risk of these diseases as compared to their rural counterparts. As per the findings of National Family Health Survey (NFHS-4), the prevalence of hypertension, obesity, and blood glucose in urban area of Uttar Pradesh was 10.5%, 23.9, and 9.9%, respectively. However, the prevalence of the same phenomenon was 8.3%, 10.8%, and 8.2%, respectively in rural area [ 15 ]. It is clear that all the parameters are having higher prevalence in urban area as compared to rural area. Rapid urbanization, increasing elderly population, mechanization, sedentary life, and dietary changes act together as a web of risk factors which entangles people in it and leads to several chronic diseases. In order to take effective prevention measures, identification of the risk factors is an essential prerequisite. This study intends to generate information on prevalence of hypertension and their associated risk factors in urban area of Varanasi. In addition, it will also look into the awareness and control of hypertension among the study subjects.
2. Materials and Methods
2.1. study area.
Varanasi is an Indian city on the bank of Ganges in Uttar Pradesh. It has total population of 3676841 as per Census 2011. As per Census 2011, out of total population, 52% people live in urban areas, while 48% live in the rural areas. There are 90 Census enumeration wards in Varanasi district. Out of these 90 wards, 5 wards were selected by using simple random sampling.
2.2. Study Design and Sample Size
A community based cross-sectional study was carried out among the people aged 25 to 64 years living in the selected study area. The sample size for the present study was calculated by taking most probable prevalence of hypertension as 50% and permissible error as 5% with 95% confidence interval. Fixing the permissible error as 50%, the minimum sample size was calculated as n = 384. Since sampling procedure was multistage, hence considering the design effect, the sample size was further increased by one and half times. Considering the nonresponse rate of 10% the final sample size in study was fixed as 640. In the present study, a prior written informed consent was also taken from the participants. Prior written informed consent was taken by the participants.
2.3. Sampling Methodology
A multistage sampling was used for this study. There were three stages and for each stage different sampling design was used.
At first, out of these 90 wards, 5 wards were selected by using simple random sampling. At second stage, from each selected ward the households were further selected by using systematic random sampling and probability proportional to size was done. At the third stage, one member of target age group was interviewed from selected household. If the selected family has more than one available eligible person then one was chosen randomly by using lottery method. In case of nonavailability of eligible person in a selected household, at the time of survey, the adjacent household was selected.
2.4. Selection of Study Subjects
2.4.1. inclusion criteria.
Individuals aged 25–64 years in the selected study area who gave consent for participation were considered.
2.4.2. Exclusion Criteria
Individuals who are unable to give response due to serious physical or mental illness and with whom anthropometry measurements cannot be performed were excluded from the study.
2.5. Tools of the Study
Interview schedule [modified and pretested WHO stepwise approach to chronic disease risk factor surveillance (STEPS)], Libra weighing machine, steel anthropometry rod, measuring tape, and Omron BP Machine were used.
2.6. Techniques of the Study
In all study participants, a structured and pretested interview schedule was administered to obtain data on sociodemographic parameters.
2.6.1. Blood Pressure Measurement
Blood pressure was measured two times on the right arm of the selected subject using automatic electronic device (OMRON HEM-7261). The average of two readings was used.
2.6.2. Anthropometric Measurements
All the anthropometric measurements were done by the following standardized technique. Weight was measured by Libra weighing machine having an accuracy of 0.1 kg and height was measured by using a steel anthropometry rod with accuracy of 0.1 cm using standard techniques. Body Mass Index was calculated using the following formula: BMI = weight (kg)/height (mt) 2 . Based on BMI obtained, the subjects were classified into different categories according to the WHO global classification [ 16 ]. Waist circumference (in cm) was measured using a nonstretchable measuring tape. Waist circumference was measured at the smallest horizontal girth between the costal margins and the iliac crest at the end of expiration. Hip circumference (in cm) was measured at the broadest part of the hips by using nonstretchable measuring tape. Waist-to-hip circumference (WHR) was calculated by dividing waist circumference by hip circumference [ 17 ].
2.7. Ethical Consideration
Ethical approval was obtained from the Institute Ethical Committee of the Institute of Medical Sciences, Banaras Hindu University Varanasi. Prior written consent was taken from the subjects who volunteered to participate in the study. Identified hypertensive subjects were referred to the nearby clinic for treatment.
2.8. Definitions Used
- (i) Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) classification was used for hypertension [ 8 ].
- (ii) Hypertension is defined as systolic BP level of ≥140 mmHg and/or diastolic BP level of ≥90 mmHg or being previously diagnosed as hypertensive by any health professional. The area falling between 120–139 mmHg systolic BP and 80–89 mmHg diastolic BP is defined as “prehypertension” [ 8 ].
- (iii) Isolated diastolic hypertension (IDH) having a systolic blood pressure ≤ 140 mmHg and diastolic blood pressure ≥ 90 mmHg and isolated systolic hypertension (ISH) having a systolic blood pressure ≥ 140 mmHg and diastolic blood pressure < 90 mmHg was used to diagnose IDH and ISH, respectively.
- (iv) Awareness was defined as history of hypertension based on diagnosis by a healthcare provider. Treatment was defined as taking any medication or other treatment for hypertension in the last two weeks prior to the survey and control was defined as blood pressure < 140 and <90 mmHg in subjects who were taking medications
- (v) WHO International BMI classification: BMI < 18.5 was classified as “underweight”; <16.00, “severe thinness”; 16.00–16.99, “moderate thinness”; 17.00–18.49, “mild thinness”; 18.50–24.99, “normal range”; BMI ≥ 25.00, “overweight” ; 25.0–29.99, “preobese” ; ≥30.00, “obese” ; 30.00–34.99, “obese class I” ; 35.00–39.99, “obese class II”; and >40.00, “obese class III.”
Revised modified BG Prasad socioeconomic classification scale, January 2014.
- (vii) Current daily smokers are defined as those who were currently smoking cigarettes, bidis, or hookah daily. Current daily smokeless tobacco users are defined as those who were currently using chewable tobacco products, gutka, naswar, khaini, or zarda paan daily. Current alcohol drinkers are defined as those who reported to consuming alcohol within the past one year [ 17 ].
- (viii) Physical activity was measured in three domains that is activity at work, to and from places, and recreational activities as well as time spent sitting. The interview schedule also covered type of activity (vigorous and moderate) at work and for recreational activities. Information was also collected on the number of days in a week spent on different activities and time spent in a day for each activity was also recorded [ 17 ]. Those who were not active in any domain were defined as “inactive,” those who were vigorously active in any category were defined as “vigorously active,” and the rest were “moderately active.”
2.9. Data Processing
The information obtained from the survey was entered into a database developed for the study, using SPSS 16.0 program. Descriptive statistics (mean and standard deviation) were calculated for continuous variables and frequencies and percentages were calculated to summarize qualitative data. Other statistical tests like chi-square test and ANOVA were applied. Logistic regression was applied to identify the risk factors for hypertension. A significance level of 0.05 was used.
A total of 640 study subjects were interviewed for the survey. Out of these, 301 (47%) were male subjects and 339 (53%) were female. The median age (±SD) of the study subjects was 39.0 (±11.9) years and for male and female it was 40.0 (±11.9) years and 38 (±11.8) years, respectively. Regarding religion and caste of the study subjects, around 96% subjects were Hindu and majority of the subjects were in general category, respectively. Majority of the study subjects were married and one-third of the subjects belonged to the upper socioeconomic class. Mean (±SD) BMI of the study subjects was 24.11 ± 3.94 kg/m 2 ; for men it was 23.78 ± 3.95 kg/m 2 and for women it was 24.41 ± 3.92 kg/m 2 . According to Body Mass Index (BMI), more than one-third of the study subjects were either overweight or obese. With regard to abdominal obesity as measured by waist circumference, 40% subjects were at risk ( Table 2 ).
Background characteristics of the study subjects ( N 640).
Table 3 depicts the mean values of systolic and diastolic BP according to age and gender. The mean systolic and diastolic BP of all the study subjects were 124.2 ± 15.0 mmHg and 83.4 ± 9.5 mmHg, respectively. In men, the highest mean systolic BP and mean diastolic BP were among the eldest age group and preceding eldest age group (45–54 years), respectively, while in female the highest mean value of systolic and diastolic BP both were among the 45–54-year age group. With regard to systolic BP, there was significant difference among all the age groups among both male and female study subjects and the same was with diastolic BP as well. The prevalence of isolated systolic BP was found to be 10.6% [95% CI: (8.27–13.37)] and isolated diastolic BP was 19.7% [95% CI: 16.6–23.18]. The proportion was higher in male (14.8%) as compared to female (6.8%). Among both groups (male and female), prevalence was higher among the eldest age group. The prevalence of isolated diastolic BP was higher among male subjects (28.1) against female subjects (12.2%). It was the highest among the second oldest age group among male and oldest age group in female subjects. With regard to systolic BP, age was associated with hypertension status among both genders, whereas diastolic BP was associated with age in male subjects only. There was no association between age and diastolic BP in female subjects.
Mean systolic and diastolic blood pressure (mm hg) and prevalence (%) of isolated systolic hypertensive and isolated diastolic hypertensive by age and gender.
# Excluding known hypertensive.
The overall prevalence of hypertension was 32.96% [95% CI: (29.4–36.7)]. The sex specific prevalence was 40.9% [95% CI: 35.5–46.5] for male and 26.0% [95% CI: 21.6–30.9] for female. Prehypertension was prevalent in 45.9% [95% CI: (40.3–51.5)] of men and 38.05% [95% CI: (33.0–43.2)] of women. In men, hypertension was significantly associated with age but in women, age does not have any effect on their hypertension status. History of hypertension or the prediagnosed cases of hypertension was more among female (6.7%) as compared to male (5.9%) subjects ( Table 4 ).
Prevalence of hypertension and prehypertension by gender and age groups among the study subjects ( N 640).
Table 5 shows the associated factors of prehypertension and hypertension. Gender, age, marital status, occupation, education status, tobacco use, and physical activity were significantly associated with the hypertension status of the study subjects ( p < 0.05). Both the rate of prehypertension and hypertension were higher among male. Hypertension was more prevalent in the 45–54 years, while prehypertension was more in the 35–44-year age group. Being married and government servant were found to be risk factors for both hypertension and prehypertension. Hypertension was found to be more among illiterate subjects, and with regard to prehypertension, primary educated subjects suffered more. Study subjects from lower and upper socioeconomic status were almost equal victims of hypertension. Tobacco use and alcohol use were found to be risk factors for being hypertensive in the study subjects. Although alcohol use was not significantly associated with hypertension status but rate of hypertension was higher among the alcohol users.
Prevalence of prehypertension and hypertension ∗ according to sociodemographic characteristics and behavioral risk factors.
∗ Excluding known hypertensive.
The binary logistic regression analysis showed that odds of being hypertensive were higher among the male subjects (OR: 1.97), eldest age group (OR: 6.49), married subjects (OR: 2.34), uneducated subjects (OR: 1.17), retired subjects (OR: 3.66), and those who were from upper socioeconomic status (1.31). With regard to anthropometric risk factors, being overweight (OR: 1.99), being obese (OR: 3.57), and having abdominal obesity (OR: 1.73) had higher odds of hypertension. Tobacco use (OR: 1.86), alcohol use (OR: 1.55), and nonvegetarian diet (OR: 1.10) also had higher odds of being hypertensive. Gender, age, marital status, occupation, BMI, abdominal obesity, and tobacco use were significantly associated with hypertension. Education, socioeconomic status, and alcohol use were not statistically associated with hypertension. Being female, younger in age, unmarried, highly educated, and staying away from any kind of addiction could serve as protective factors against hypertension ( Table 6 ).
Univariate analysis for the association of hypertension and sociodemographic characteristics, anthropometric measurements, and behavioral risk factors ( N 640).
Out of the total subjects with hypertension, around one-third of the subjects were aware of their condition. Out of those who were aware, 70% were seeking treatment. Only a third of the treated subjects with hypertension had their blood pressure adequately controlled ( Figure 1 ). Females were marginally more aware of their hypertensive status as compared to male counterparts (see Table 4 , history of hypertension). As age, education status, and socioeconomic status were advancing, the awareness of hypertensive status among study subjects was also increasing (not shown in the table).

Flow diagram showing awareness, treatment, and adequacy of control of hypertension among study subjects.
4. Discussion
India is a developing country and like other developing countries, it is going through a rapid demographic and epidemiological transition. In all such transitions, nutrition is the key ingredient and plays prime role. This cross-sectional community based study identified a high prevalence of prehypertension and hypertension in urban areas of Varanasi, which was 41.7% and 32.96%, respectively. Only a quarter of subjects were in the normal category, which highlights the escalating burden of this silent killer.
The prevalence of hypertension in the present study (32.96%) was higher in comparison with the prevalence reported in other studies [ 4 , 6 , 10 , 19 – 22 ]. Few studies reported the results in line with the present study [ 23 , 24 ]. According to World Health Organization (2015), the overall prevalence of hypertension in India was 23.5% and gender specific prevalence was 24.2% and 22.7% among the men and women, respectively [ 25 ].
The prevalence of prehypertension in the present study was 41.7% (male: 45.9% and female: 38.05%). The prevalence estimated in the present study was much higher than that estimated by Nellore (22.3%) [ 10 ] and Bihar (37.95%) [ 20 ]. The difference of prevalence observed between the present study and other studies with respect to hypertension and prehypertension could be due to social and cultural differences, dietary and lifestyle factors, and also the age span as well as the research methodology used.
Men exhibit higher prevalence of hypertension and prehypertension than their female counterparts (M: 40.9% and F: 26.0%) and (M: 45.9% and F: 38.05%), respectively. Similarly, various studies came out with the higher percentage of hypertension in men than women [ 20 , 22 , 23 , 26 – 29 ]. One of the possible explanations for this gender disparity in hypertension prevalence could be partially due to biological sex difference and partially due to behavioral risk factors like smoking, alcohol consumption, or physical activity. We speculate that absentia from alcohol and smoking might be few of those protective factors against hypertension in women. Other than that, women are more interested in health care services utilization and also more frequently report their poor health and therefore they are more likely to have better health [ 6 , 30 ].
Age was found to be an important risk factor for hypertension. As the age was advancing so did the prevalence of hypertension among both the sexes. Similar findings were reported by few other studies also where advancing age was positively related to hypertension [ 1 , 6 , 19 , 21 , 22 , 26 , 31 , 32 ]. With increasing age, the aorta and arteries walls will be stiffened and this contributes to the high prevalence of hypertension in older age groups [ 4 ].
In the present study, marital status, education, occupation, socioeconomic status, BMI, abdominal obesity, tobacco use, alcohol use, and physical activity were significantly associated with the hypertension.
Low literacy level and being too rich were associated with hypertension. The higher education level was negatively correlated to hypertension in the present study. These studies also supported this finding [ 6 , 12 , 33 ]. We speculate that it could be due to the reason that higher education imparts better knowledge and information about hypertension and subsequently those people with higher education had a healthier lifestyle.
Table 5 revealed that education was significantly associated with hypertension ( χ 2 = 17.049, df = 6 and p value = 0.009); however, when adjusted effect of education on hypertension was observed by logistic regression, then no statistical association was observed. Though some studies had shown a significant association of these two variables [ 6 , 12 ], in the study performed in the state of Kerala [ 33 ], insignificant association between education and hypertension was observed. We speculate that this insignificant association could be due to very few subjects in the illiterate and less educated category. There are so many studies which do not refute the finding of the present study that higher socioeconomic status is a risk for hypertension [ 3 , 22 , 24 , 32 , 34 – 36 ]. We assume that better socioeconomic status imparts people with more purchasing power on fast and convenience foods and less physical activity which are already proven to be contributing risk factors for overweight and obesity that subsequently linked to hypertension.
The different anthropometric measurements like BMI, waist circumference, and hip circumference were taken into account to measure overweight, obesity, and central or abdominal obesity. This study showed that overweight and obesity measured by both BMI and waist circumference were major modifiable risk factors to develop hypertension. Overweight subjects had twofold risk of being hypertensive and obese had more than threefold risk for the same in comparison to underweight subjects in this study. There was positive relation observed between increasing BMI and increasing rate of hypertension, which was consistent with other studies [ 1 – 4 , 6 , 12 , 20 , 21 , 23 , 32 , 36 – 39 ]. South Asians have tendency of developing centralized obesity without developing generalized obesity and because of this waist circumference and waist-hip ratio are better measures of body fat [ 40 ]. Abdominal obesity (OR: 1.73) also found to be positively linked to high blood pressure in the present study. Various epidemiological and pathophysiological mechanisms explained the link between obesity and hypertension. One of the probable reasons behind this positive relation between obesity and hypertension could be that increased weight increases cardiac output and increased peripheral resistance of arterioles. Other than that, urbanization is also a cause of changes in dietary habits and reduced physical activity which leads to obesity and subsequently results in hypertension [ 4 ].
Interestingly, we have found inverse association between physical activity and hypertension. Hypertension was more among physically active subjects as compared to inactive subjects (OR: 0.63) but no statistically significant difference was found. Similar result was reported by other study conducted in Turkey [ 1 ]. The exact reason behind this is unknown and yet to be explored. We speculate that they had started physical activity probably under medical advice after being diagnosed for hypertension or other risk factors like overweight or obesity.
As per WHO report, alcohol consumption was the third largest risk factor in the developed countries and tobacco use was being the second major cause of death worldwide [ 17 ]. This study indicated the positive association between alcohol and tobacco use and hypertension. Hypertension was more prevalent in tobacco users (OR: 1.86) and alcohol users (OR: 1.55) as compared to nonusers. This finding is supported by other studies also [ 19 , 23 , 32 , 36 ]. But there are several other studies with contradictory findings [ 1 , 21 , 41 ]. Although not statistically significant, odds of being hypertensive were more among nonvegetarian (OR: 1.10) subjects, while vegetarian diet was proved to be protective against hypertension in this study. Several other studies reported the same result [ 3 , 19 , 33 , 34 ]. A study conducted in Bihar [ 20 ] refutes this finding and reported that vegetarian diet was positively associated with hypertension.
A recent review study revealed that hypertension awareness rate has been doubled from less than 30% in 1980s to around 60% in present among urban populations and less than 10% in 1980s to 35–40% presently among rural population. However, the treatment and control status is still low at around 30% in urban and 20% in rural areas [ 42 ]. Rate of awareness, treatment, and control in the present study was observed as 38.4%, 70.4%, and 35.08%, respectively. Previous study conducted in rural Varanasi reported hypertension awareness, treatment, and control (26.5%, 55.6%, and 40%), respectively [ 7 ].
5. Conclusion & Recommendation
From the results of this study, it can be concluded that the prevalence of both prehypertension and hypertension is very high in urban Varanasi. This makes the people of this area vulnerable to several chronic diseases and other unbearable health consequences. Specifically men are at more risk of being hypertensive than female. Increasing age is proved to be an independent risk factor for hypertension. Programs are needed to improve the surveillance systems and implementation of community based screening programs for early detection of hypertension is also needed. As the awareness of the hypertension status among hypertensive cases was very poor, improving health literacy to increase the awareness of hypertension is also the need of the hour. Interventions like weight management, increased physical activity, increased fruits and vegetables consumption, and reduction in tobacco and alcohol use are required and recommended.
Acknowledgments
The authors would like to thank all the participants for participating in the study.
Additional Points
Limitations of the Study . This study suffers from few of the following limitations. (i) One of the main limitations of this study was the cross-sectional design of the study which restricts examining causal associations. (ii) The study was only conducted in urban areas. (iii) Stress is a major risk factor for hypertension. It could also be considered in the present study for better results.
Conflicts of Interest
There were no conflicts of interest regarding the publication of this article.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 21 May 2024
Another step forward in the introduction of aortic systolic blood pressure assessment into clinical practice?
- Athanase D. Protogerou 1 ,
- Elpida Athanasopoulou 1 &
- Antonios A. Argyris 1 , 2
Hypertension Research ( 2024 ) Cite this article
25 Accesses
1 Altmetric
Metrics details
The Original Article was published on 29 March 2024
In the present issue of the Journal, Cheng C. et al. present evidence from a cohort of more than 2000 patients with non-dialysis chronic kidney disease (CKD), suggesting stronger association between 24-hour aortic systolic blood pressure (aoSBP) and left ventricular hypertrophy (LVH) compared to 24-h brachial SBP (brSBP) [ 1 ]. These results are in absolute accordance with previously published data from the “ Non-invaSive Aortic ambulatory blood pressure monitoring For the detection of tARrget organ damage (SAFAR) study” [ 2 ] in hypertensive individuals, as well as with other studies that followed. Most importantly, the authors provide interesting novel data on a new, previously described diagnostic hypertension phenotype [ 3 ], that derive from cross-classification of brSBP and aoSBP. This approach may open new opportunities for the optimization of hypertension management. After summarizing the current status regarding the clinical value of aoSBP, we will discuss the emerging opportunities - as well as the potential downsides—that seem to evolve ahead.
More than 20 years ago international hypertension guidelines [ 4 ] acknowledged: (i) that the SBP differs substantially between the brachial artery and the aorta (even more than 30 mmHg) and, (ii) that the effect of several classes of antihypertensive drugs, as measured in mmHg of SBP lowering, is not the same at the level of the brachial artery and at the aorta. Based on several meta-analyses thereafter, it has been very well-documented [ 5 ], that aoSBP is significantly associated with mortality and cardiovascular disease (CVD) events. Reference and normal values of aoSBP have been established both for office and 24-hour ambulatory recording [ 6 , 7 ]. Most importantly, aoSBP assessment is nowadays easily feasible simultaneously with brSBP assessment, in a reproducible and quite accurate manner, using automated brachial cuff-based oscillometric devices, even in ambulatory conditions [ 8 ]. Given all the above facts, are we ready to introduce aoSBP assessment in daily clinical practice?
The 2023 European hypertension guidelines [ 9 ] have made a step forward, suggesting that it might be useful to assess aoSBP in the clinical management of isolated systolic hypertension of the youth (ISHy). ISHy is characterized by increased brSBP (in the absence of elevated diastolic blood pressure) often accompanied by very low aoSBP. The underlying hypothesis, i.e., whether the CVD risk of this population is quite inferior, than that “erroneously high” CVD risk as suggested by brSBP, must definitely be further investigated. Apart from that, the recent guidelines [ 9 ] remain quite reluctant to propose wider clinical application of aoSBP, mostly because the: “ …, the incremental prognostic value of central versus conventional office BP measurement is unclear.” Although other clinical applications of aoSBP assessment have been proposed and deserve further investigation (e.g., screening for office masked hypertension [ 10 ]), the available evidence from many observational large studies and their meta-analyses are controversial, largely suggesting a rather limited additional clinical value of aoSBP over brSBP [ 5 , 11 , 12 ]. This fuzzy information is very probably relevant to the fact that for many years the applied methodology to assess aoSBP in most of the above epidemiological studies was not the optimal one. This has now been clearly presented and described in a consensus statement, suggesting that type 2 devices (i.e., those using mean and diastolic pressure [instead of the usually applied systolic/diastolic] to calibrate the recorded peripheral pressure waveform) provide aoSBP values with the best clinical relevance [ 2 , 13 ].
In 2016, we proposed an alternative approach in order to incorporate aoSBP in clinical practice. We defined isolated aortic systolic hypertension (IaoSH; defined as normal office brSBP but high office aoSBP), as a novel diagnostic hypertension phenotype by cross-classification, based on office brSBP and aoSBP [ 3 ]. Individuals with office IaoSH represent up to 10% of that population and have carotid hypertrophy up to 8 times more often in comparison to those with sustained systolic normotension (SSN; both brSBP and aoSBP normal) [ 3 ]. Recently, evidence by IDCARS study [ 13 ], a mortality outcome multicenter study in more than 5000 individuals, suggested that individuals with IaoSH run a 1.28 higher CVD risk when compared to SSN. However, in a previous analysis of the same IDCARS’ population, CVD and mortality were similarly associated with central and peripheral pulsatile blood pressure components [ 11 ]. In other words, it is becoming clear that a clinical approach using the above cross-classification phenotypes, identifies a specific subgroup of the population at higher CVD risk due to elevated aoSBP that cannot be identified by brSBP, even though in the overall population the discriminatory capacity of aoSBP over brSBP is small. Indeed, as just recently shown in a randomized control trial, individuals with IaoSH can safely benefit from more intensive BP lowering drug treatment with spironolactone [ 14 ], suggesting that a potential valid process for more aggressive treatment.
It is therefore very important that in the present issue of the Journal the authors [ 1 ], using 24-hour ambulatory blood pressure monitoring (ABPM) for simultaneous assessment of brSBP and aoSBP, verified in a very high-risk CVD population - due to the presence of CKD - that 24-hour aoSBP with type 2 calibration is superior to 24-hour brSBP for the detection of LVH. It is even more important that they described for the first time in CKD patients, and based on 24-hour ABPM, the novel phenotype of IaoSH, providing evidence that it has more often LVH than SSN; as well as that the isolated brachial systolic hypertension phenotype carries low CVD risk, in accordance with the hypothesis discussed regarding the ISHy phenotype. Needless to say, that this evidence must be further validated. Of note, in this analysis IaoSH was represented by a very small population. Among other issues to be resolved, we might legitimately wonder whether the introduction of even more diagnostic hypertension phenotypes in clinical practice is the right way to improve hypertension management in the future. Certainly, only time will tell.
Cheng C, Lingling L, Sirui L, Ju M, Yu W, Song Q, et al. 24-h central pressure is a valuable predictor for left ventricular hypertrophy in non-dialysis patients with chronic kidney disease. Hyper Res 2024. https://doi.org/10.1038/s41440-024-01654-2
Protogerou AD, Argyris AA, Papaioannou TG, Kollias GE, Konstantonis GD, Nasothimiou E, et al. Left-ventricular hypertrophy is associated better with 24-h aortic pressure than 24-h brachial pressure in hypertensive patients: the SAFAR study. J Hypertens. 2014;32:1805–14.
Article CAS PubMed Google Scholar
Protogerou AD, Aissopou EK, Argyris A, Nasothimiou EG, Konstantonis GD, Karamanou M, et al. Phenotypes of office systolic blood pressure according to both brachial and aortic measurements: frequencies and associations with carotid hypertrophy in 1861 adults. J Hypertens. 2016;34:1325–30.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007;28:1462–536. https://doi.org/10.1093/eurheartj/ehm236 .
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31:1865–71.
Article PubMed Google Scholar
Herbert A, Cruickshank JK, Laurent S, Boutouyrie P, Reference Values for Arterial Measurements C. Reference Values for Arterial Measurements Collaboration. Establishing reference values for central blood pressure and its amplification in a general healthy population and according to cardiovascular risk factors. Eur Heart J. 2014;35:3122–33.
Weber T, Protogerou AD, Agharazii M, Argyris A, Aoun Bahous S, Banegas JR, et al. Twenty-four-hour central (Aortic) systolic blood pressure: reference values and dipping patterns in untreated individuals. Hypertension. 2022;79:251–60.
Protogerou AD, Argyris A, Nasothimiou E, Vrachatis D, Papaioannou TG, Tzamouranis D, et al. Feasibility and reproducibility of noninvasive 24-h ambulatory aortic blood pressure monitoring with a brachial cuff-based oscillometric device. Am J Hypertens. 2012;25:876–82.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41:1874–2071. https://doi.org/10.1097/HJH.0000000000003480 . Epub 2023 Sep 26. Erratum in: J Hypertens. 2024;42:194.
Gkaliagkousi E, Protogerou AD, Argyris AA, Koletsos N, Triantafyllou A, Anyfanti P, et al. Contribution of single office aortic systolic blood pressure measurements to the detection of masked hypertension: data from two separate cohorts. Hypertens Res. 2021;44:215–24.
Huang QF, Aparicio LS, Thijs L, Wei FF, Melgarejo JD, Cheng YB, et al. Cardiovascular end points and mortality are not closer associated with central than peripheral pulsatile blood pressure components. Hypertension. 2020;76:350–8.
Sharman JE, Otahal P, Stowasser M, Stanton T, Reid CM, Nolan M, et al. Blood Pressure Lowering in Patients With Central Hypertension: A randomized Clinical Trial. Hypertension. 2024. https://doi.org/10.1161/HYPERTENSIONAHA.123.21653 . [Epub ahead of print].
Cheng YB, Thijs L, Aparicio LS, Huang QF, Wei FF, Yu YL, et al. Risk stratification by cross-classification of central and brachial systolic blood pressure. Hypertension. 2022;79:1101–11.
Sharman JE, Avolio AP, Baulmann J, Benetos A, Blacher J, Blizzard CL, et al. Validation of non-invasive central blood pressure devices: ARTERY Society task force consensus statement on protocol standardization. Eur Heart J. 2017;38:2805–12.
Article PubMed PubMed Central Google Scholar
Download references
Author information
Authors and affiliations.
Cardiovascular Prevention & Research Unit, Clinic/Laboratory of Pathophysiology, Laiko Hospital, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece
Athanase D. Protogerou, Elpida Athanasopoulou & Antonios A. Argyris
Department of Clinical Therapeutics, Alexandra General Hospital, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece
Antonios A. Argyris
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Athanase D. Protogerou .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Protogerou, A.D., Athanasopoulou, E. & Argyris, A.A. Another step forward in the introduction of aortic systolic blood pressure assessment into clinical practice?. Hypertens Res (2024). https://doi.org/10.1038/s41440-024-01729-0
Download citation
Received : 14 April 2024
Accepted : 23 April 2024
Published : 21 May 2024
DOI : https://doi.org/10.1038/s41440-024-01729-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Aortic blood pressure
- Isolated aortic systolic hypertension
- Hypertension phenotypes
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
COMMENTS
Abstract. Dr Irvine Page proposed the Mosaic Theory of Hypertension in the 1940s advocating that hypertension is the result of many factors that interact to raise blood pressure and cause end-organ damage. Over the years, Dr Page modified his paradigm, and new concepts regarding oxidative stress, inflammation, genetics, sodium homeostasis, and ...
Improvements in the detection, treatment, and control of hypertension have varied substantially across countries, with some middle-income countries now outperforming most high-income nations. The dual approach of reducing hypertension prevalence through primary prevention and enhancing its treatment and control is achievable not only in high-income countries but also in low-income and middle ...
Hypertension Diagnosis. Once a person has been screened and found to have high blood pressure, ambulatory blood pressure monitoring (ABPM) is regarded as the most accurate way to diagnose hypertension and is recommended by guidelines to routinely to confirm elevated blood pressure readings [2, 17, 18].Ambulatory monitors typically involve portable, automated cuffs worn continuously that ...
Hypertension is the leading risk factor for disability and death globally. This is attributed to two major complications of hypertension, cerebrovascular accidents (CVA) and ischemic heart disease. ... All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within ...
Abstract. In 2021, 217 excellent manuscripts were published in Hypertension Research. Editorial teams greatly appreciate the authors' contribution to hypertension research progress. Here, our ...
Hypertension articles from across Nature Portfolio. Hypertension is high blood pressure. It is generally defined in adults as systolic blood pressure greater than or equal to 140mmHg and/or ...
Browse the archive of articles on Hypertension Research. Preoperative blood urea nitrogen-to-serum albumin ratio for prediction of in-hospital mortality in patients who underwent emergency surgery ...
Hypertension is a major cause of cardiovascular disease and deaths worldwide especially in low- and middle-income countries. Despite the availability of safe, well-tolerated, and cost-effective blood pressure (BP)-lowering therapies, <14% of adults with hypertension have BP controlled to a systolic/diastolic BP <140/90 mm Hg.
European Society of Hypertension. J Hypertens 41: 1874-2071 . This ESH Consensus paper contributes to a better standardization of future studies on BPV, and provides clinicians with some indications on how BPV can be managed based on currently available data. J Hypertens 2023; 41: 527-544.
Estimates suggest that 31.1% of adults (1.39 billion) worldwide had hypertension in 2010. The prevalence of hypertension among adults was higher in LMICs (31.5%, 1.04 billion people) than in high-income countries (28.5%, 349 million people). Variations in the levels of risk factors for hypertension, such as high sodium intake, low potassium ...
In Hypertension Research 2021, several important articles on uric acid research were published. Mori et al. reported that a high serum uric acid level is associated with an increase in systolic blood pressure in women but not in men in subjects who underwent annual health checkups [ 188 ].
Kario K, Mogi M, Hoshide S. Latest hypertension research to inform clinical practice in Asia. Hypertens Res. 2022;45:555-72. Article PubMed Google Scholar
High blood pressure is a common condition in the US that increases the risk of stroke and heart disease. Blood pushing against the walls of arteries in the body creates pressure, which generally varies throughout the day. High blood pressure, also known as hypertension, is blood pressure that is consistently higher than what is considered ...
Background. Hypertension is a leading cause of cardiovascular disease (CVD) and affects nearly one in two adults in the United States when defined as a blood pressure of at least 130/80 mm Hg or on antihypertensive medication (Virani et al., 2021, Circulation, 143, e254).Long‐standing disparities in hypertension awareness, treatment, and control among racial and ethnic populations exist in ...
The NHLBI funds research into the connection between the microbiome and high blood pressure. One study found that bacterial strains in the mouth were linked to high blood pressure in older women. Another study showed that intermittent fasting in an animal model could reduce hypertension by reshaping the gut microbiota.
It defined hypertension as a blood pressure at or above 130/80 mmHg. Stage 2 hypertension is defined as a blood pressure at or above 140/90 mmHg. 1. Having high blood pressure puts you at risk for heart disease and stroke, which are leading causes of death in the United States. Nearly half of adults have high blood pressure (48.1%, 119.9 million).
Several rare, monogenic forms of hypertension have been described (for example, the Liddle syndrome, glucocorticoid-remediable aldosteronism (a mineralocorticoid excess state) and mutations in PDE3A (which encodes cGMP-inhibited 3',5'-cyclic phosphodiesterase A)), in which a single gene mutation fully explains the pathogenesis of hypertension and indicates the best treatment modality 7,8,9.
Background Hypertension prevalence among the overall US adult population has been relatively stable during the last two decades. However, whether this stabilization has occurred across rural-urban communities and across different geographic regions is unknown, particularly among older adults with diabetes who are likely to have concomitant cardiovascular risk factors. Methods This serial cross ...
Collections. Hypertension Research, official publication of the Japanese Society of Hypertension, publishes papers reporting original clinical and experimental research in the field of ...
1. Introduction. Hypertension is a major public health problem due to its high prevalence all around the globe [1-4].Around 7.5 million deaths or 12.8% of the total of all annual deaths worldwide occur due to high blood pressure [].It is predicted to be increased to 1.56 billion adults with hypertension in 2025 [].Raised blood pressure is a major risk factor for chronic heart disease, stroke ...
Thomas J. Hoffmann, Carlos Iribarren, Neil Risch, Dongwon Lee and. Aravinda Chakravarti. Hypertension. Learn the benefits of becoming an AHA/ASA Professional Member and join. Current Issue. Immediate Past Issue.
Browse the archive of articles on Hypertension Research. Heterogeneity in longitudinal trajectories of cognitive performance among middle-aged and older individuals with hypertension: Growth ...
New research suggests that hormone replacement therapy (HRT) may improve pulmonary hypertension symptoms in females. Luca Sage/Getty Images. About 1% of the global population has pulmonary ...
hypertension research. research articles. Research articles. Filter By: Article Type. All. All; Article (928) Brief Communication (29) Case Report (18) Guidelines (33) Original Article (1814)
BACKGROUND:Sildenafil, approved for pulmonary arterial hypertension (PAH), ... Free Access Research Article. PDF/EPUB. Randomized, Multicenter Study to Assess the Effects of Different Doses of Sildenafil on Mortality in Adults With Pulmonary Arterial Hypertension. Marius M. Hoeper,
Hypertension Research (Hypertens Res) ISSN 1348-4214 (online) ISSN 0916-9636 (print) nature.com sitemap. About Nature Portfolio. About us; Press releases; Press office; Contact us ...