
Transforming the understanding and treatment of mental illnesses.
Información en español

Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Anxiety Disorders
What is anxiety.
Occasional anxiety is a normal part of life. Many people worry about things such as health, money, or family problems. But anxiety disorders involve more than temporary worry or fear. For people with an anxiety disorder, the anxiety does not go away and can get worse over time. The symptoms can interfere with daily activities such as job performance, schoolwork, and relationships.
There are several types of anxiety disorders, including generalized anxiety disorder, panic disorder, social anxiety disorder, and various phobia-related disorders.
What are the signs and symptoms of anxiety?
Generalized anxiety disorder.
Generalized anxiety disorder (GAD) usually involves a persistent feeling of anxiety or dread, which can interfere with daily life. It is not the same as occasionally worrying about things or experiencing anxiety due to stressful life events. People living with GAD experience frequent anxiety for months, if not years.
Symptoms of GAD include:
- Feeling restless, wound-up, or on-edge
- Being easily fatigued
- Having difficulty concentrating
- Being irritable
- Having headaches, muscle aches, stomachaches, or unexplained pains
- Difficulty controlling feelings of worry
- Having sleep problems, such as difficulty falling or staying asleep
Panic disorder
People with panic disorder have frequent and unexpected panic attacks. Panic attacks are sudden periods of intense fear, discomfort, or sense of losing control even when there is no clear danger or trigger. Not everyone who experiences a panic attack will develop panic disorder.
During a panic attack, a person may experience:
- Pounding or racing heart
- Trembling or tingling
- Feelings of impending doom
- Feelings of being out of control
People with panic disorder often worry about when the next attack will happen and actively try to prevent future attacks by avoiding places, situations, or behaviors they associate with panic attacks. Panic attacks can occur as frequently as several times a day or as rarely as a few times a year.
Social anxiety disorder
Social anxiety disorder is an intense, persistent fear of being watched and judged by others. For people with social anxiety disorder, the fear of social situations may feel so intense that it seems beyond their control. For some people, this fear may get in the way of going to work, attending school, or doing everyday things.
People with social anxiety disorder may experience:
- Blushing, sweating, or trembling
- Stomachaches
- Rigid body posture or speaking with an overly soft voice
- Difficulty making eye contact or being around people they don’t know
- Feelings of self-consciousness or fear that people will judge them negatively
Phobia-related disorders
A phobia is an intense fear of—or aversion to—specific objects or situations. Although it can be realistic to be anxious in some circumstances, the fear people with phobias feel is out of proportion to the actual danger caused by the situation or object.
People with a phobia:
- May have an irrational or excessive worry about encountering the feared object or situation
- Take active steps to avoid the feared object or situation
- Experience immediate intense anxiety upon encountering the feared object or situation
- Endure unavoidable objects and situations with intense anxiety
There are several types of phobias and phobia-related disorders:
Specific phobias (sometimes called simple phobias) : As the name suggests, people who have a specific phobia have an intense fear of, or feel intense anxiety about, specific types of objects or situations. Some examples of specific phobias include the fear of:
- Specific animals, such as spiders, dogs, or snakes
- Receiving injections
Social anxiety disorder (previously called social phobia) : People with social anxiety disorder have a general intense fear of, or anxiety toward, social or performance situations. They worry that actions or behaviors associated with their anxiety will be negatively evaluated by others, leading them to feel embarrassed. This worry often causes people with social anxiety to avoid social situations. Social anxiety disorder can manifest in a range of situations, such as within the workplace or the school environment.
Agoraphobia: People with agoraphobia have an intense fear of two or more of the following situations:
- Using public transportation
- Being in open spaces
- Being in enclosed spaces
- Standing in line or being in a crowd
- Being outside of the home alone
People with agoraphobia often avoid these situations, in part, because they think being able to leave might be difficult or impossible in the event they have panic-like reactions or other embarrassing symptoms. In the most severe form of agoraphobia, an individual can become housebound.
Separation anxiety disorder: Separation anxiety is often thought of as something that only children deal with. However, adults can also be diagnosed with separation anxiety disorder. People with separation anxiety disorder fear being away from the people they are close to. They often worry that something bad might happen to their loved ones while they are not together. This fear makes them avoid being alone or away from their loved ones. They may have bad dreams about being separated or feel unwell when separation is about to happen.
Selective mutism: A somewhat rare disorder associated with anxiety is selective mutism. Selective mutism occurs when people fail to speak in specific social situations despite having normal language skills. Selective mutism usually occurs before the age of 5 and is often associated with extreme shyness, fear of social embarrassment, compulsive traits, withdrawal, clinging behavior, and temper tantrums. People diagnosed with selective mutism are often also diagnosed with other anxiety disorders.
What are the risk factors for anxiety?
Researchers are finding that both genetic and environmental factors contribute to the risk of developing an anxiety disorder.
The risk factors for each type of anxiety disorder vary. However, some general risk factors include:
- Shyness or feeling distressed or nervous in new situations in childhood
- Exposure to stressful and negative life or environmental events
- A history of anxiety or other mental disorders in biological relatives
Anxiety symptoms can be produced or aggravated by:
- Some physical health conditions, such as thyroid problems or heart arrhythmia
- Caffeine or other substances/medications
If you think you may have an anxiety disorder, getting a physical examination from a health care provider may help them diagnose your symptoms and find the right treatment.
How is anxiety treated?
Anxiety disorders are generally treated with psychotherapy, medication, or both. There are many ways to treat anxiety, and you should work with a health care provider to choose the best treatment for you.
Psychotherapy
Psychotherapy or “talk therapy” can help people with anxiety disorders. To be effective, psychotherapy must be directed at your specific anxieties and tailored to your needs.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is an example of one type of psychotherapy that can help people with anxiety disorders. It teaches people different ways of thinking, behaving, and reacting to situations to help you feel less anxious and fearful. CBT has been well studied and is the gold standard for psychotherapy.
Exposure therapy is a CBT method that is used to treat anxiety disorders. Exposure therapy focuses on confronting the fears underlying an anxiety disorder to help people engage in activities they have been avoiding. Exposure therapy is sometimes used along with relaxation exercises.
Acceptance and commitment therapy
Another treatment option for some anxiety disorders is acceptance and commitment therapy (ACT). ACT takes a different approach than CBT to negative thoughts. It uses strategies such as mindfulness and goal setting to reduce discomfort and anxiety. Compared to CBT, ACT is a newer form of psychotherapy treatment, so less data are available on its effectiveness.
Medication does not cure anxiety disorders but can help relieve symptoms. Health care providers, such as a psychiatrist or primary care provider, can prescribe medication for anxiety. Some states also allow psychologists who have received specialized training to prescribe psychiatric medications. The most common classes of medications used to combat anxiety disorders are antidepressants, anti-anxiety medications (such as benzodiazepines), and beta-blockers.
Antidepressants
Antidepressants are used to treat depression, but they can also be helpful for treating anxiety disorders. They may help improve the way your brain uses certain chemicals that control mood or stress. You may need to try several different antidepressant medicines before finding the one that improves your symptoms and has manageable side effects.
Antidepressants can take several weeks to start working so it’s important to give the medication a chance before reaching a conclusion about its effectiveness. If you begin taking antidepressants, do not stop taking them without the help of a health care provider. Your provider can help you slowly and safely decrease your dose. Stopping them abruptly can cause withdrawal symptoms.
In some cases, children, teenagers, and adults younger than 25 may experience increased suicidal thoughts or behavior when taking antidepressant medications, especially in the first few weeks after starting or when the dose is changed. Because of this, people of all ages taking antidepressants should be watched closely, especially during the first few weeks of treatment.
Anti-anxiety medications
Anti-anxiety medications can help reduce the symptoms of anxiety, panic attacks, or extreme fear and worry. The most common anti-anxiety medications are called benzodiazepines. Although benzodiazepines are sometimes used as first-line treatments for generalized anxiety disorder, they have both benefits and drawbacks.
Benzodiazepines are effective in relieving anxiety and take effect more quickly than antidepressant medications. However, some people build up a tolerance to these medications and need higher and higher doses to get the same effect. Some people even become dependent on them.
To avoid these problems, health care providers usually prescribe benzodiazepines for short periods of time.
If people suddenly stop taking benzodiazepines, they may have withdrawal symptoms, or their anxiety may return. Therefore, benzodiazepines should be tapered off slowly. Your provider can help you slowly and safely decrease your dose.
Beta-blockers
Although beta-blockers are most often used to treat high blood pressure, they can help relieve the physical symptoms of anxiety, such as rapid heartbeat, shaking, trembling, and blushing. These medications can help people keep physical symptoms under control when taken for short periods. They can also be used “as needed” to reduce acute anxiety, including to prevent some predictable forms of performance anxieties.
Choosing the right medication
Some types of drugs may work better for specific types of anxiety disorders, so people should work closely with a health care provider to identify which medication is best for them. Certain substances such as caffeine, some over-the-counter cold medicines, illicit drugs, and herbal supplements may aggravate the symptoms of anxiety disorders or interact with prescribed medication. People should talk with a health care provider, so they can learn which substances are safe and which to avoid.
Choosing the right medication, medication dose, and treatment plan should be done under an expert’s care and should be based on a person’s needs and their medical situation. Your and your provider may try several medicines before finding the right one.
Support groups
Some people with anxiety disorders might benefit from joining a self-help or support group and sharing their problems and achievements with others. Support groups are available both in person and online. However, any advice you receive from a support group member should be used cautiously and does not replace treatment recommendations from a health care provider.
Stress management techniques
Stress management techniques, such as exercise, mindfulness, and meditation, also can reduce anxiety symptoms and enhance the effects of psychotherapy. You can learn more about how these techniques benefit your treatment by talking with a health care provider.
How can I find a clinical trial for anxiety?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Anxiety Disorders : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Adults - Anxiety Disorders : List of studies being conducted on the NIH Campus in Bethesda, MD
- Join a Study: Children - Anxiety Disorders : List of studies being conducted on the NIH Campus in Bethesda, MD
Where can I learn more about anxiety?
Free brochures and shareable resources.
- Generalized Anxiety Disorder (GAD): When Worry Gets Out of Control : This brochure describes the signs, symptoms, and treatment of generalized anxiety disorder.
- I’m So Stressed Out! : This fact sheet intended for teens and young adults presents information about stress, anxiety, and ways to cope when feeling overwhelmed.
- Obsessive-Compulsive Disorder: When Unwanted Thoughts Take Over : This brochure describes the signs, symptoms, and treatment of OCD.
- Panic Disorder: When Fear Overwhelms : This brochure describes the signs, symptoms, and treatments of panic disorder.
- Social Anxiety Disorder: More Than Just Shyness : This brochure describes the signs, symptoms, and treatment of social anxiety disorder.
- Shareable Resources on Anxiety Disorders : Help support anxiety awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about anxiety disorders.
- Mental Health Minute: Anxiety Disorders in Adults :Take a mental health minute to watch this video about anxiety disorders in adults.
- Mental Health Minute: Stress and Anxiety in Adolescents : Take a mental health minute to watch this video about stress and anxiety in adolescents.
- NIMH Expert Discusses Managing Stress and Anxiety : Learn about coping with stressful situations and when to seek help.
- GREAT : Learn helpful practices to manage stress and anxiety. GREAT was developed by Dr. Krystal Lewis, a licensed clinical psychologist at NIMH.
- Getting to Know Your Brain: Dealing with Stress : Test your knowledge about stress and the brain. Also learn how to create and use a “ stress catcher ” to practice strategies to deal with stress.
- Guided Visualization: Dealing with Stress : Learn how the brain handles stress and practice a guided visualization activity.
- Panic Disorder: The Symptoms : Learn about the signs and symptoms of panic disorder.
Federal resources
- Anxiety Disorders (MedlinePlus – also en español )
Research and statistics
- Journal Articles : References and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Anxiety Disorder : This webpage provides information on the statistics currently available on the prevalence and treatment of anxiety among people in the U.S.
Last Reviewed: April 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
Signs of Anxiety
Reviewed by Psychology Today Staff
Everybody gets anxious sometimes, whether in response to something reality-based—such as the possibility of getting seriously ill with COVID-19—or something wholly imagined, such as the possibility of financial ruin when well off. But the reactions tend to be short-lived. Anxiety is meant to keep you safe, and the system is rigged to err on the side of survival. Anxiety is regarded as a disorder when the worry is more intense than a situation warrants, it persists for weeks or months, the thoughts of worry are difficult to control, and they interfere with everyday functioning. In generalized anxiety disorder, worry can focus on any of the major domains of life circumstances—health, work, or family—or minor matters.
Anxiety has two basic components: There is a cognitive load of worry, or the apprehensive expectation of some bad outcome. And there are physical symptoms, notably restlessness and edginess, muscle tension, sleep disturbance, and difficulty concentrating. Like depression, anxiety can make its presence felt in many systems of the body—disrupting digestion, speeding heart rate, setting off ringing in the ears. More women than men experience anxiety, by a factor of two to one. Over the course of a lifetime, Americans have a 10 percent chance of developing anxiety. But rates of the disorder have been rising rapidly over the past decade. The median age of onset is 31. Studies show that in Europe and in China, the chance of developing generalized anxiety is less than 6 percent.
On This Page
- Is anxiety in the mind or the body?
- At what age are people most likely to get anxiety?
- What are the major signs of anxiety?
- What does it mean to have clinical anxiety?
- Why do I feel like I might be having a heart attack?
- Why do I feel like something terrible is about to happen?
- Why does my body shake?
- Why can’t I concentrate on anything?
- Why do I sometimes feel like I can't breathe?
- Is anxiety the same thing as fear?
- What is the course of clinical anxiety?
- Why am I not interested in sex?
- Do children get anxiety?
Anxiety shows itself both in the mind and the body . As a threat is perceived—whether it is a reality-based one such as the possibility of being fired for an offense or an imagined one—the brain’s amygdala signals the hypothalamus, a central command center, which broadcasts the signal through the autonomic nervous system and sets off a cascade of hormones, including adrenaline. It in turn stimulates the multiple physical symptoms of anxiety. Your heart beats faster and your pulse rate increases. So does your blood pressure. Breathing accelerates; you may feel short of breath. Other symptoms include:
• dizziness
• muscle tension
• trembling or shaking
• dry mouth
• sweating
• stomachache
• headache.
Studies show that the bodily symptoms often lead to misdiagnosis in which the symptoms are ascribed to physical causes, and the true source of the problem continues undiscovered.
Although children can develop anxiety, the average age of onset of any anxiety disorder is 21.3 years. Nevertheless, the age of onset is decreasing, and the National Institutes of Health reports that 32 percent of adolescents had one form or another of an anxiety disorder: generalized anxiety, phobia, panic disorder, or social anxiety disorder. Observers cite new cultural pressures linking youth and anxiety . Some anxiety disorders show up sooner than others: Separation anxiety, specific phobias, and social anxiety disorder most often begin before age 15. General anxiety disorder and other anxiety disorders begin, on average, between 21.1 and 34.9 years.
Generalized anxiety disorder declares itself in both the mind and the body. People with anxiety experience excessive worry more often than not for at least six months and are unable to control the worry. They also experience a number of physical symptoms. The presence of at least three physical signs along with excessive worry is the criterion for clinical diagnosis.
• Restlessness, or feeling on edge
• Being easily fatigued
• Difficulty concentrating
• Irritability
• Muscle tension
• Sleep disturbance
Phobia is a common anxiety disorder in which fear is focused on a very specific object or situation and anxiety is experienced only in that situation or in anticipation of exposure to it.
Occasional bouts of anxiety are a normal part of life. And a moderate amount of anxiety in some situations—say, before taking a test, giving a talk, engaging in a new activity, or doing something risky—is good. It heightens alertness and can boost performance. But when anxiety is intense or overwhelming, persistent, beyond unpleasant, interferes with everyday functioning or important activities, and is out of proportion to the actual dangers faced then it is considered a disorder, or clinical condition.
In anxiety, and especially during a panic attack, the heart, prompted by hormones that are part of the stress response, speeds up and intensifies its work in an effort to quickly supply the muscles with oxygen, in the possibility that fight or flight might be called for. You feel palpitations , a sense that your heart is pounding or racing or even beating irregularly. Breathing quickens, too, and can create the feeling of not getting enough oxygen. These automatic reactions create the sense of having a heart attack. In physically healthy people, the symptoms are harmless, although the fear of having a heart attack tends to trigger even more anxiety. However, after a quick crescendo, the physical sensations generally subside.
A sense of impending doom is a common accompaniment to bouts of anxiety and especially panic attacks. Not only may it seemingly strike out of the blue, it also tends to exacerbate the anxiety. The feeling that something bad is about to happen is triggered by the body’s response when the mind senses a threat. Hormones released as part of the body’s stress response put the brain on high alert, scanning relentlessly for danger, and a strong stress response can lead to the feeling that catastrophe awaits. Measures to tamp down the stress response, such as deep-breathing for a few minutes, can dampen the sense of impending doom.
Anxiety plays out in the body as well as the mind. It puts much of the nervous system on high alert for danger and ready to fight or flee. The aroused nervous system is poised to expend energy, and shaking is a manifestation of that tension. The nervous tension may reveal itself in trembling hands or even a whole-body tremor. Shaky hands and body tremors can come and go in waves or they can be relatively constant. Unpleasant as they are, they carry no danger and eventually pass. Taking steps to reduce anxiety—deep-breathing, going for a walk or run—can reduce the level of anxiety and quell the shakiness.,
The worry of anxiety disrupts other cognitive functions, and concentration and memory are both casualties. Anxiety undermines working memory, so that it’s hard to hold onto incoming information for long; you feel like you can’t focus long enough to get anything done and tasks seem especially difficult. Brain fog . In addition, the normal bias of the brain to register negative events is exaggerated in anxiety, and the brain is preoccupied with scanning for danger. Compounding the problem, anxiety disrupts sleep, and lack of sleep erodes working memory and the ability to focus even further,
Breathlessness is a common symptom of anxiety, and especially in its most extreme expression, panic. The feeling of being short of breath is caused directly by hormones released by the body any time the mind senses or chews over a threat—whatever it is that fills you with worry. Linked to the deep-seated stress response that automatically prepares the body for fight or flight, breathlessness is the sensation you get as the body speeds up heart rate and breathing in an attempt to speed extra oxygen to muscles.
The experience of breathlessness, especially in combination with awareness of a pounding heart, can set off a vicious cycle, itself exacerbating anxiety, leading to even more breathlessness. Breathlessness may last 10 minutes or more, but it eventually dissipates. Directly countering breathlessness with a minute or two of deep-breathing exercises is one of the most effective anti-anxiety measures —it not only sends oxygen to your overworking brain, it stimulates the parasympathetic nerve, the calming branch of the autonomic nervous system..
Fear is a response to immediate danger. it is usually highly focused , triggered by a very specific object or circumstance, and meant to mobilize fast action. There may not be any external trigger for anxiety; it is a response to real or imagined future threat, and it is typically more diffuse, setting in motion the need for constant vigilance in anticipation of some possible undesirable outcome. It usually stimulates avoidance behavior.
What makes a person anxious is highly subjective and idiosyncratic. Fear, on the other hand, has a social side. Fear stimulates a set of distinctive and universally understood changes in facial expression—widened pupils, pale skin —that are thought to silently warn others that a danger is present. Anxiety shares some of the physiological signs of fear—heightened alertness and fast heart rate, similarly, set off by the hormones related to the stress response—but it singularly places a heavy load of worry on the brain in the form of repeated thoughts about what might possibly go wrong in the future.
Generalized anxiety disorder tends to be a chronic condition. The symptoms of anxiety occur when the brain’s amygdala identifies a threat and sends out a signal for the body and brain to prepare for danger. The brain goes into overdrive, searching for bad things. The body alerts organ systems to prepare to fight or flee.
Studies show that some people are born with a low threshold of reactivity of the amygdala, so that it’s constantly turning on the alarm system. In others, adverse experiences during childhood permanently reset the response level of the amygdala in an effort to ward off the possibility of being harmed in the future. Both situations set up chronic vulnerability to anxiety. The sources of anxiety may change over the course of a lifetimes, but the tendency to react to difficult situations with anxiety endures.
Anxiety is guaranteed buzzkill. Anxiety is a response originally designed to promote survival in a world of danger. The brain center that regulates such basic behaviors as eating and sex (the hypothalamus) shuts down activity in any system not related to immediate survival. One result is lack of libido, or low sex drive . In addition, the on-edge feeling that anxiety stirs prevents the relaxation needed to sense as pleasurable the physical stimulation that leads to orgasm. Particularly for women, orgasm requires the ability to let go; anxiety does exactly the opposite. The sex drive typically returns when the brain senses that the environment is safe.
Studies show that just over 7 percent of children aged 3 to 17 have a current anxiety problem. That’s approximately 4.4 million children in the U.S.. More and more children are being diagnosed with anxiety—incidence rose from 5.5 percent to 6.4 percent between 2007and 2012 alone.
Experts point to several factors; prominent among them is the way that parents often try to shield their kids from feeling bad over the normal lumps and bumps of life. Noah is disappointed because he didn’t get chosen for the soccer team. Instead of helping the child understand which athletic skills might need more work, and helping him process the dejection, a parent protests to the school or coach. The net effect is that the child fails to develop coping skills for minor disappointments, and the lack of coping skills turns even minor challenges into significant sources of anxiety. In that way, the anxieties of the adults create anxious children .

Setting boundaries is hard. Here are 5 tips to help you be better at setting them.

Musicians can experience performance as either a challenge or a threat. When a performance task is perceived as threatening, symptoms of performance anxiety are likely.

The evidence strongly points to the perils of long-term use of benzos. This warning is more credible after recent studies have revealed the mechanisms of cognitive impairments.

Going away to college is a big decision, and being far from home might not be right for everyone. Here are four questions to ask yourself and your child.

Learning to integrate the feelings of grief and cope with the loss of the mother is painful. It is a hero’s journey that changes you and helps you understand more about your self.

Cultivating mindful awareness can be immensely helpful with anxiety. Here's how.
A simple exercise can shift your attention from fearful and negative to positive. This can dramatically shift your emotional state.

Embedded within our culture of competition is a hidden cycle of danger, disconnection, and distrust pitted against our biological quest for safety, trust, and connection.

Sharing struggles not just with family and friends but with strangers can help those in a time of grief.

Here are some keys to coping with chronic stress for psychologists, with a focus on symptom management and the influence of societal factors.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Suma P. Chand ; Raman Marwaha .
Affiliations
Last Update: April 24, 2023 .
- Continuing Education Activity
Fear is an automatic neurophysiological state of alarm characterized by a fight or flight response to a cognitive appraisal of present or imminent danger (real or perceived). Anxiety is linked to fear and manifests as a future-oriented mood state that consists of a complex cognitive, affective, physiological, and behavioral response system associated with preparation for the anticipated events or circumstances perceived as threatening. This activity reviews the pathophysiology of anxiety, its presentation, diagnosis and highlights the role of the interprofessional team in its management.
- Identify the DSM V criteria for anxiety disorders.
- Describe the presentation of a patient with anxiety.
- Outline the treatment and management options available for anxiety.
- Discuss interprofessional team strategies for improving care coordination and outcomes for patients with anxiety.
- Introduction
Fear is an automatic neurophysiological state of alarm characterized by a fight or flight response to a cognitive appraisal of present or imminent danger (real or perceived). Anxiety is linked to fear and manifests as a future-oriented mood state that consists of a complex cognitive, affective, physiological, and behavioral response system associated with preparation for the anticipated events or circumstances perceived as threatening. Pathological anxiety is triggered when there is an overestimation of perceived threat or an erroneous danger appraisal of a situation which leads to excessive and inappropriate responses. [1] [2] [3]
Anxiety is one of the most common psychiatric disorders but the true prevalence is not known as many people do not seek help or clinicians fail to make the diagnosis.
Anxiety disorders appear to be caused by an interaction of biopsychosocial factors. Genetic vulnerability interacts with situations that are stressful or traumatic to produce clinically significant syndromes.
Anxiety can be caused by the following conditions:
- Medications
- Herbal medications
- Substance abuse
- Childhood experiences
- Panic disorders
- Epidemiology
Anxiety is one of the most common psychiatric disorders in the general population. Specific phobia is the most common with a 12-month prevalence rate of 12.1%. Social anxiety disorder is the next most common, with a 12-month prevalence rate of 7.4%. The least common anxiety disorder is agoraphobia with a 12-month prevalence rate of 2.5%. Anxiety disorders occur more frequently in females than in males with an approximate 2:1 ratio. [4]
- Pathophysiology
The significant mediators of anxiety in the central nervous system are thought to be norepinephrine, serotonin, dopamine, and gamma-aminobutyric acid (GABA). The autonomic nervous system, especially the sympathetic nervous system, mediates most of the symptoms.
The amygdala plays an important role in tempering fear and anxiety. Patients with anxiety disorders have been found to show heightened amygdala response to anxiety cues. The amygdala and limbic system structures are connected to prefrontal cortex regions, and prefrontal-limbic activation abnormalities may be reversed with psychological or pharmacologic interventions.
- History and Physical
Characteristic Symptoms Pathological Anxiety
Cognitive symptoms: fear of losing control; fear of physical injury or death; fear of "going crazy"; fear of negative evaluation by others; frightening thoughts, mental images, or memories; perception of unreality or detachment; poor concentration, confusion, distractible; narrowing of attention, hypervigilance for threat; poor memory; and difficulty speaking.
Physiological symptoms: increased heart rate, palpitations; shortness of breath, rapid breathing; chest pain or pressure; choking sensation; dizzy, light-headed; sweaty, hot flashes, chills; nausea, upset stomach, diarrhea; trembling, shaking; tingling or numbness in arms and legs; weakness, unsteadiness, faintness; tense muscles, rigidity; and dry mouth.
Behavioral symptoms: avoidance of threat cues or situations; escape, flight; pursuit of safety, reassurance; restlessness, agitation, pacing; hyperventilation; freezing, motionless; and difficulty speaking.
Affective symptoms: nervous, tense, wound up; frightened, fearful, terrified; edgy, jumpy, jittery; and impatient, frustrated.
Anxiety Disorders as defined in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM–5; American Psychiatric Association, 2013):
- Separation Anxiety Disorder: An individual with separation anxiety disorder displays anxiety and fear atypical for his/her age and development level of separation from attachment figures. There is persistent and excessive fear or anxiety about harm to, loss of, or separation from attachment figures. The symptoms include nightmares and physical symptoms. Although the symptoms develop in childhood, they can be expressed throughout adulthood as well.
- Selective Mutism: This disorder is characterized by a consistent failure to speak in social situations where there is an expectation to speak even though the individual speaks in other circumstances, can speak, and comprehends the spoken language. The disorder is more likely to be seen in young children than in adolescents and adults.
- Specific Phobia: Individuals with specific phobias are fearful or anxious about specific objects or situations which they avoid or endure with intense fear or anxiety. The fear, anxiety, and avoidance are almost always immediate and tend to be persistently out of proportion to the actual danger posed by the specific object or situation. There are different types of phobias: animal, blood-injection-injury, and situational.
- Social Anxiety Disorder: This disorder is characterized by marked or intense fear or anxiety of social situations in which one could be the subject of scrutiny. The individual fears that he/she will be negatively evaluated in such circumstances. He/she also fears being embarrassed, rejected, humiliated or offending others. These situations always provoke fear or anxiety and are avoided or endured with intense fear and anxiety.
- Panic Disorder: Individuals with this disorder experience recurrent, unexpected panic attacks and experience persistent concern and worry about having another panic attack. They also have changes in their behavior linked to panic attacks which are maladaptive, such as avoidance of activities and situations to prevent the occurrence of panic attacks. Panic attacks are abrupt surges of intense fear or extreme discomfort that reach a peak within minutes, accompanied by physical and cognitive symptoms such as palpitations, sweating, shortness of breath, fear of going crazy, or fear of dying. Panic attacks can occur unexpectedly with no obvious trigger, or they may be expected, such as in response to a feared object or situation.
- Agoraphobia: Individuals with this disorder are fearful and anxious in two or more of the following circumstances: using public transportation, being in open spaces, being in enclosed spaces like shops and theaters, standing in line or being in a crowd, or being outside of the home alone. The individual fears and avoids these situations because he/she is concerned that escape may be difficult or help may not be available in the event of panic-like symptoms, or other incapacitating or embarrassing symptoms (e.g., falling or incontinence).
- Generalized Anxiety Disorder: The key feature of this disorder is persistent and excessive worry about various domains, including work and school performance, that the individual finds hard to control. The person also may experience feeling restless, keyed up, or on edge; being easily fatigued; difficulty concentrating or mind going blank; irritability, muscle tension, and sleep disturbance.
- Substance/Medication-Induced Anxiety Disorder: This disorder involves anxiety symptoms due to substance intoxication or withdrawal or to medical treatment.
- Anxiety Disorder Due to Other Medical Conditions: Anxiety symptoms are the physiological consequence of another medical condition. Examples include endocrine disease: hypothyroidism, hypoglycemia, and hypercortisolism; cardiovascular disorders: congestive heart failure, arrhythmia, and pulmonary embolism; respiratory illness: asthma and pneumonia; metabolic disturbances: B12 or porphyria; neurological illnesses: neoplasms, encephalitis, and seizure disorder.
When the history and examination do not suggest the symptoms as arising from any other medical disorder, the initial laboratory studies may be limited to the following: complete blood cell count (CBC) chemistry profile, thyroid function tests, urinalysis, and urine drug screen. [5] [6] [7]
If the anxiety symptoms are atypical or there are some abnormalities noted in the physical examination more detailed evaluations may be indicated to identify or exclude underlying medical conditions. This would include the following: electroencephalography, brain computed tomography (CT) scan, electrocardiography, tests for infection, arterial blood gas analysis, chest radiography, and thyroid function tests.
- Treatment / Management
Acute anxiety may require treatment with a benzodiazepine. Chronic anxiety treatment consists of psychotherapy, pharmacotherapy, or a combination of both.
Pharmacotherapy: selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), benzodiazepines, tricyclic antidepressants, mild tranquilizers, and beta-blockers treat anxiety disorders. [3] [8] [9]
- SSRIs (fluoxetine, sertraline, paroxetine, escitalopram, and citalopram) are an effective treatment for all anxiety disorders and considered first-line treatment.
- SNRIs (venlafaxine and duloxetine) are considered as effective as SSRIs and also are considered first-line treatment, particularly for generalized anxiety disorder (GAD).
- Tricyclic antidepressants (amitriptyline, imipramine, and nortriptyline) are useful in the treatment of anxiety disorders but cause significant adverse effects.
- Benzodiazepines (alprazolam, clonazepam, diazepam, and lorazepam) are used for short-term management of anxiety. They are fast-acting and bring relief within 30 minutes to an hour. They are effective in promoting relaxation and reducing muscular tension and other symptoms of anxiety. Because they work quickly, they are effective when taken for panic attacks or overwhelming episodes. Long-term use may require increased doses to achieve the same effect, which may result in problems related to tolerance and dependence.
- Buspirone is a mild tranquilizer that is slow acting as compared to benzodiazepines and takes about 2 weeks to start working. It has the advantage of being less sedating and also not being addicting with minimal withdrawal effects. It works for GAD.
- Beta-blockers (propranolol and atenolol) control the physical symptoms of anxiety such as rapid heart rate, a trembling voice, sweating, dizziness, and shaky hands. They are most helpful for phobias, particularly social phobia.
Psychotherapy: One of the most effective forms of psychotherapy is cognitive-behavioral therapy. It is a structured, goal-oriented, and didactic form of therapy that focuses on helping individuals identify and modify characteristic maladaptive thinking patterns and beliefs that trigger and maintain symptoms. This form of therapy focuses on building behavioral skills so that patients can behave and react more adaptively to anxiety-producing situations. Exposure therapy is utilized to move individuals towards facing the anxiety-provoking situations and stimuli which they typically avoid. This exposure results in a reduction in anxiety symptoms as they learn that their anxiety is causing them to experience false alarms and they do not need to fear the situation or stimuli and can cope effectively with such a situation.
- Differential Diagnosis
- Pheochromocytoma
- Atrial fibrillation
- Hyperthyroidism
- Diabetic ketoacidosis
Anxiety disorders have very high morbidity including substance abuse, alcoholism, and major depression. In addition, constant anxiety also increases the risk of adverse cardiac events. In others, anxiety impairs the ability to develop social relationships and worsens the quality of life. Severe anxiety has also been linked to high rates of suicide.
- Pearls and Other Issues
Characteristic Features Noted in Individuals with Clinical Anxiety
- False alarms: The presence of intense fear in the absence of threat cues or very minimal threat provocation.
- Persistence: There is a future-oriented perspective that involves the anticipation of threat or danger which causes the patient to experience a heightened level of apprehension and thoughts about impending potential threat, regardless of whether it materializes.
- Impaired Functioning: Anxiety interferes with effective and adaptive coping in the face of a perceived threat and the person’s daily social or occupational life.
- Stimulus hypersensitivity: In clinical states, fear is elicited by a wider range of stimuli or situations of relatively mild intensity that would be innocuous to a person who does not have clinical anxiety.
- Dysfunctional cognition and cognitive symptoms: Thinking characterized by overestimation of threat or danger appraisal of a situation that is not confirmed in any way.
- Enhancing Healthcare Team Outcomes
Anxiety disorders are very common and can present in diverse ways. Because the condition is underdiagnosed and associated with high morbidity, it is best managed by an interprofessional team consisting of a mental health nurse, psychiatrist, psychotherapist, social worker, and a primary care provider. Family members need to be educated about the disorder and help monitor the symptoms and provide support. A mental health nurse should closely follow these patients as suicidal ideations are not rare. The pharmacist should educate the patient on different medications, their benefits, and potential adverse effects. Collaboration between the team members is vital to ensure that no patient is neglected and that all patients are receiving an acceptable standard of care.
The outlook for patients with anxiety is guarded. Data indicate that the high rates of mortality are associated with adverse cardiac events. In those with social phobia, the condition leads to significant functional impairment and a very poor quality of life. The risk of suicides is also high in this population. Patients with anxiety need lifelong follow-up because, despite drug therapy, relapse rates are high. [2] [10] [11] (Level V)
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Suma Chand declares no relevant financial relationships with ineligible companies.
Disclosure: Raman Marwaha declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Chand SP, Marwaha R. Anxiety. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Anxiety (Nursing). [StatPearls. 2024] Anxiety (Nursing). Chand SP, Marwaha R, Bender RM. StatPearls. 2024 Jan
- Separation Anxiety Disorder. [StatPearls. 2024] Separation Anxiety Disorder. Feriante J, Torrico TJ, Bernstein B. StatPearls. 2024 Jan
- Review Models and mechanisms of anxiety: evidence from startle studies. [Psychopharmacology (Berl). 2008] Review Models and mechanisms of anxiety: evidence from startle studies. Grillon C. Psychopharmacology (Berl). 2008 Aug; 199(3):421-37. Epub 2007 Dec 6.
- Implicit evaluations and physiological threat responses in people with persistent low back pain and fear of bending. [Scand J Pain. 2017] Implicit evaluations and physiological threat responses in people with persistent low back pain and fear of bending. Caneiro JP, O'Sullivan P, Smith A, Moseley GL, Lipp OV. Scand J Pain. 2017 Oct; 17:355-366. Epub 2017 Oct 12.
- Review Making a mountain out of a molehill: on the role of the rostral dorsal anterior cingulate and dorsomedial prefrontal cortex in conscious threat appraisal, catastrophizing, and worrying. [Neurosci Biobehav Rev. 2014] Review Making a mountain out of a molehill: on the role of the rostral dorsal anterior cingulate and dorsomedial prefrontal cortex in conscious threat appraisal, catastrophizing, and worrying. Kalisch R, Gerlicher AM. Neurosci Biobehav Rev. 2014 May; 42:1-8. Epub 2014 Feb 10.
Recent Activity
- Anxiety - StatPearls Anxiety - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
How to Manage Public Speaking Anxiety
Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.
:max_bytes(150000):strip_icc():format(webp)/ArlinCuncic_1000-21af8749d2144aa0b0491c29319591c4.jpg)
Amy Morin, LCSW, is a psychotherapist and international bestselling author. Her books, including "13 Things Mentally Strong People Don't Do," have been translated into more than 40 languages. Her TEDx talk, "The Secret of Becoming Mentally Strong," is one of the most viewed talks of all time.
:max_bytes(150000):strip_icc():format(webp)/VW-MIND-Amy-2b338105f1ee493f94d7e333e410fa76.jpg)
Luis Alvarez / Getty Images
Speech Anxiety and SAD
How to prepare for a speech.
Public speaking anxiety, also known as glossophobia , is one of the most commonly reported social fears.
While some people may feel nervous about giving a speech or presentation if you have social anxiety disorder (SAD) , public speaking anxiety may take over your life.
Public speaking anxiety may also be called speech anxiety or performance anxiety and is a type of social anxiety disorder (SAD). Social anxiety disorder, also sometimes referred to as social phobia, is one of the most common types of mental health conditions.
Public Speaking Anxiety Symptoms
Symptoms of public speaking anxiety are the same as those that occur for social anxiety disorder, but they only happen in the context of speaking in public.
If you live with public speaking anxiety, you may worry weeks or months in advance of a speech or presentation, and you probably have severe physical symptoms of anxiety during a speech, such as:
- Pounding heart
- Quivering voice
- Shortness of breath
- Upset stomach
Causes of Public Speaking Anxiety
These symptoms are a result of the fight or flight response —a rush of adrenaline that prepares you for danger. When there is no real physical threat, it can feel as though you have lost control of your body. This makes it very hard to do well during public speaking and may cause you to avoid situations in which you may have to speak in public.
How Is Public Speaking Anxiety Is Diagnosed
Public speaking anxiety may be diagnosed as SAD if it significantly interferes with your life. This fear of public speaking anxiety can cause problems such as:
- Changing courses at college to avoid a required oral presentation
- Changing jobs or careers
- Turning down promotions because of public speaking obligations
- Failing to give a speech when it would be appropriate (e.g., best man at a wedding)
If you have intense anxiety symptoms while speaking in public and your ability to live your life the way that you would like is affected by it, you may have SAD.
Public Speaking Anxiety Treatment
Fortunately, effective treatments for public speaking anxiety are avaible. Such treatment may involve medication, therapy, or a combination of the two.
Short-term therapy such as systematic desensitization and cognitive-behavioral therapy (CBT) can be helpful to learn how to manage anxiety symptoms and anxious thoughts that trigger them.
Ask your doctor for a referral to a therapist who can offer this type of therapy; in particular, it will be helpful if the therapist has experience in treating social anxiety and/or public speaking anxiety.
Research has also found that virtual reality (VR) therapy can also be an effective way to treat public speaking anxiety. One analysis found that students treated with VR therapy were able to experience positive benefits in as little as a week with between one and 12 sessions of VR therapy. The research also found that VR sessions were effective while being less invasive than in-person treatment sessions.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
If you live with public speaking anxiety that is causing you significant distress, ask your doctor about medication that can help. Short-term medications known as beta-blockers (e.g., propranolol) can be taken prior to a speech or presentation to block the symptoms of anxiety.
Other medications may also be prescribed for longer-term treatment of SAD, including selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). When used in conjunction with therapy, you may find the medication helps to reduce your phobia of public speaking.
In addition to traditional treatment, there are several strategies that you can use to cope with speech anxiety and become better at public speaking in general . Public speaking is like any activity—better preparation equals better performance. Being better prepared will boost your confidence and make it easier to concentrate on delivering your message.
Even if you have SAD, with proper treatment and time invested in preparation, you can deliver a successful speech or presentation.
Pre-Performance Planning
Taking some steps to plan before you give a speech can help you better control feelings of anxiety. Before you give a speech or public performance:
- Choose a topic that interests you . If you are able, choose a topic that you are excited about. If you are not able to choose the topic, try using an approach to the topic that you find interesting. For example, you could tell a personal story that relates to the topic as a way to introduce your speech. This will ensure that you are engaged in your topic and motivated to research and prepare. When you present, others will feel your enthusiasm and be interested in what you have to say.
- Become familiar with the venue . Ideally, visit the conference room, classroom, auditorium, or banquet hall where you will be presenting before you give your speech. If possible, try practicing at least once in the environment that you will be speaking in. Being familiar with the venue and knowing where needed audio-visual components are ahead of time will mean one less thing to worry about at the time of your speech.
- Ask for accommodations . Accommodations are changes to your work environment that help you to manage your anxiety. This might mean asking for a podium, having a pitcher of ice water handy, bringing in audiovisual equipment, or even choosing to stay seated if appropriate. If you have been diagnosed with an anxiety disorder such as social anxiety disorder (SAD), you may be eligible for these through the Americans with Disabilities Act (ADA).
- Don’t script it . Have you ever sat through a speech where someone read from a prepared script word for word? You probably don’t recall much of what was said. Instead, prepare a list of key points on paper or notecards that you can refer to.
- Develop a routine . Put together a routine for managing anxiety on the day of a speech or presentation. This routine should help to put you in the proper frame of mind and allow you to maintain a relaxed state. An example might be exercising or practicing meditation on the morning of a speech.
Practice and Visualization
Even people who are comfortable speaking in public rehearse their speeches many times to get them right. Practicing your speech 10, 20, or even 30 times will give you confidence in your ability to deliver.
If your talk has a time limit, time yourself during practice runs and adjust your content as needed to fit within the time that you have. Lots of practice will help boost your self-confidence .
- Prepare for difficult questions . Before your presentation, try to anticipate hard questions and critical comments that might arise, and prepare responses ahead of time. Deal with a difficult audience member by paying them a compliment or finding something that you can agree on. Say something like, “Thanks for that important question” or “I really appreciate your comment.” Convey that you are open-minded and relaxed. If you don’t know how to answer the question, say you will look into it.
- Get some perspective . During a practice run, speak in front of a mirror or record yourself on a smartphone. Make note of how you appear and identify any nervous habits to avoid. This step is best done after you have received therapy or medication to manage your anxiety.
- Imagine yourself succeeding . Did you know your brain can’t tell the difference between an imagined activity and a real one? That is why elite athletes use visualization to improve athletic performance. As you practice your speech (remember 10, 20, or even 30 times!), imagine yourself wowing the audience with your amazing oratorical skills. Over time, what you imagine will be translated into what you are capable of.
- Learn to accept some anxiety . Even professional performers experience a bit of nervous excitement before a performance—in fact, most believe that a little anxiety actually makes you a better speaker. Learn to accept that you will always be a little anxious about giving a speech, but that it is normal and common to feel this way.
Setting Goals
Instead of trying to just scrape by, make it a personal goal to become an excellent public speaker. With proper treatment and lots of practice, you can become good at speaking in public. You might even end up enjoying it!
Put things into perspective. If you find that public speaking isn’t one of your strengths, remember that it is only one aspect of your life. We all have strengths in different areas. Instead, make it a goal simply to be more comfortable in front of an audience, so that public speaking anxiety doesn’t prevent you from achieving other goals in life.
A Word From Verywell
In the end, preparing well for a speech or presentation gives you confidence that you have done everything possible to succeed. Give yourself the tools and the ability to succeed, and be sure to include strategies for managing anxiety. These public-speaking tips should be used to complement traditional treatment methods for SAD, such as therapy and medication.
Crome E, Baillie A. Mild to severe social fears: Ranking types of feared social situations using item response theory . J Anxiety Disord . 2014;28(5):471-479. doi:10.1016/j.janxdis.2014.05.002
Pull CB. Current status of knowledge on public-speaking anxiety . Curr Opin Psychiatry. 2012;25(1):32-8. doi:10.1097/YCO.0b013e32834e06dc
Goldstein DS. Adrenal responses to stress . Cell Mol Neurobiol. 2010;30(8):1433-40. doi:10.1007/s10571-010-9606-9
Anderson PL, Zimand E, Hodges LF, Rothbaum BO. Cognitive behavioral therapy for public-speaking anxiety using virtual reality for exposure . Depress Anxiety. 2005;22(3):156-8. doi:10.1002/da.20090
Hinojo-Lucena FJ, Aznar-Díaz I, Cáceres-Reche MP, Trujillo-Torres JM, Romero-Rodríguez JM. Virtual reality treatment for public speaking anxiety in students. advancements and results in personalized medicine . J Pers Med . 2020;10(1):14. doi:10.3390/jpm10010014
Steenen SA, van Wijk AJ, van der Heijden GJ, van Westrhenen R, de Lange J, de Jongh A. Propranolol for the treatment of anxiety disorders: Systematic review and meta-analysis . J Psychopharmacol (Oxford). 2016;30(2):128-39. doi:10.1177/0269881115612236
By Arlin Cuncic, MA Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
- Signs and Symptoms
Understanding the Different Types of Anxiety Disorders
- Generalized Anxiety Disorder
Panic Disorder
- Social Anxiety Disorder
Separation Anxiety Disorder
- OCD and PTSD Classification
Living With Anxiety Disorders
- Next in Anxiety Disorder Guide Causes and Risk Factors of Anxiety
An anxiety disorder is a mental health condition that involves intense feelings of fear or worry. Different types of anxiety disorders affect millions of Americans. For example, 15 million U.S. adults experience social anxiety disorder, and 6 million experience panic disorder.
Anxiety disorders can be challenging and may greatly impact daily life. Learn about the different types of anxiety disorders, their causes, treatment, coping, and more.
Kseniya Ovchinnikova / Getty Images
Generalized Anxiety Disorder (GAD)
People with GAD experience intense feelings of worry or fear that occur most days for six months or longer. This anxiety is related to a variety of different areas of life, such as relationships, careers, health, and safety. GAD affects nearly 6% of adults at some point in their lives.
In addition to worry and fear that is difficult to control, symptoms of GAD may include:
- Changes in sleep or difficulty sleeping
- Difficulty concentrating
- Digestive issues
- Feeling restless
- Irritability
- Tense muscles , often in the neck and shoulders
While some people may be genetically prone to GAD, this condition may run in families partially because of life circumstances and the home environment. The specific causes are not fully understood.
Diagnosis involves an evaluation with a healthcare provider or mental health professional (such as a psychiatrist, psychologist, or social worker) who will ask questions and assesses the condition.
Treatment can include the following, which may be combined:
- Psychotherapy : Cognitive behavioral therapy (CBT) teaches how to modify your thinking, behavior, and reaction to situations. Acceptance and commitment therapy teach strategies to address negative thoughts and reduce anxiety.
- Medication : Antidepressants or antianxiety medications may be prescribed.
Panic disorder is a condition in which a person experiences many panic attacks over a long period of time. The panic attacks come on suddenly, without any known danger, and involve intense feelings of fear or feelings of losing control. This condition is more than twice as common among females than males.
Symptoms of a panic attack include:
- Difficulty breathing
- Feeling weak
- Increased heart rate
- Light-headedness
- Pain in the chest
- Shaking or chills
- Sweating with our without feeling hot
- Upset stomach
A person with panic disorder is intensely fearful of experiencing another panic attack, and they often fear or avoid places where they have had a panic attack.
Like GAD, it is not entirely clear what causes panic disorder. People who experience traumatic events or loss are at an increased risk. A mental health professional such as a psychiatrist can diagnose this condition with an evaluation that involves asking questions.
Panic disorder can be treated with talk therapy (psychotherapy) techniques such as cognitive behavioral therapy (CBT), coping techniques, relaxation exercises , support groups, lifestyle changes, and medications (antidepressants, antianxiety drugs, beta-blockers ).
Social Anxiety Disorder (SAD)
SAD involves fear or worry related to social interactions. Women are more likely to experience SAD than men, especially among teens and young women. Additionally, their symptoms tend to be more severe.
Social anxiety disorder symptoms include:
- Avoiding social situations or interactions
- Extreme shyness or fear of talking to new people
- Feelings of nervousness , embarrassment, or being judged
- Overthinking conversations
- Ruminating about interactions with others
The specific causes of social anxiety disorder are unclear. It may run in families, and stress and environmental factors also may play a role.
Similar to other types of anxiety disorders, SAD can be diagnosed by talking with a mental health professional. Some providers offer virtual appointments, which tend to be easier for people experiencing symptoms of SAD. Treatment may involve talk therapy, medications, or both.
Separation anxiety disorder involves intense fear or reaction related to being apart from those to whom the individual is attached. These fears and reactions are normal for babies and young children but can become a concern if they do not grow out of it around school age. This condition may also affect teens and adults.
Symptoms of separation anxiety disorder include:
- Difficulty sleeping, leaving the house, or taking part in activities that involve being away from a primary caregiver
- Extreme reaction when separated from a primary caregiver
- Fear or worry related to danger for a primary caregiver or self
- Feeling physically ill when separated from a primary caregiver
- Intense desire to constantly be with a specific person
The causes of separation anxiety disorder are not fully known. Traumatic experiences, instability at home, and stressful situations can increase the risk of this condition. It can be diagnosed with an evaluation from a mental health professional.
This condition can be treated with talk therapy or play therapy for children and talk therapy or medications for adults.
A phobia is a continuous, irrational, and intense fear of something that poses little or no actual danger. Most people who have a specific phobia have more than one. For example, a person may have a phobia of both spiders and heights.
Phobia symptoms include:
- Avoiding something specific due to fear, such as needles or dogs
Phobias can be caused by a traumatic event involving the thing that is feared or someone repeatedly or intensely expressing the dangers of what is feared. However, sometimes the cause is unrelated to the specific phobia, or the cause is unknown.
Phobias can be evaluated and diagnosed by a mental health professional. Treatment options include talk therapy and exposure therapy.
New Classifications for OCD and PTSD
Obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD) used to be considered anxiety disorders, but are now classified independently.
Obsessive-Compulsive Disorder
OCD involves repeated, unwanted thoughts or urges (obsessions) and feeling the need to do something repeatedly (compulsions). It affects up to 3 million American adults.
Symptoms of OCD include:
- Feeling fear of losing control of their behavior
- Feeling the need to clean excessively or an intense fear of germs
- Fear of forgetting or losing things
- Placing items in a specific order
- Repeatedly checking that things have been completed
OCD may be caused by genetics or traumatic experiences, especially in childhood, but the causes are not fully understood. This condition can be diagnosed with an evaluation from a mental health professional such as a psychiatrist. It is treated with talk therapy , medications, or both.
Post-Traumatic Stress Disorder
PTSD can result from experiencing a traumatic event. It involves a nervous system response after the event has ended and the person is no longer in danger.
PTSD affects about 6% of Americans at some point in their life. It affects about 8% of women compared to 4% of men due to trauma such as sexual assault being more commonly experienced by women.
PTSD symptoms include:
- Intrusive thoughts, which may include flashbacks
- Avoiding situations, places, and people that remind them of the traumatic event.
- Negative thoughts, guilt, shame, fear, distorted beliefs about themself or others
- Constant vigilance for potential danger
- Difficulty sleeping
- Jumpiness or being scared easily
PTSD is caused by a past experience of a traumatic event or events. Risk factors include abuse, accidents, and war. After an evaluation, this condition can be diagnosed by a mental health professional. It is treated with talk therapy such as cognitive behavioral therapy CBT, eye movement desensitization and reprocessing (EMDR) , and medications.
Anxiety disorders are challenging, and often severe enough to impact daily life. They are also treatable. Up to 85% of people who receive treatment for anxiety disorders find it to be effective. Additionally, there are many ways to cope with anxiety disorders long term.
Coping methods include:
- Relaxation exercises
- Breathing techniques
- Mindfulness and meditation
- Connecting with a trusted friend or family member
- Lifestyle behaviors such as prioritizing sleep, eating nutritious foods, and exercising regularly
Anxiety disorders involve intense feelings of fear or worry that recur for six months or longer. There are different types of anxiety disorders, such as social anxiety disorder, which is an intense fear of social interactions that may be severe enough to interfere with daily life.
Panic disorder involves sudden episodes of intense fear called panic attacks. Separation anxiety disorder is when an older child, teen, or adult experiences an extreme reaction to being away from a primary caregiver or another loved one.
Generalized anxiety disorder is when anxiety is related to a variety of different areas of life rather than a specific object or situation.
Obsessive-compulsive disorder and post-traumatic stress disorder were once considered anxiety disorders, but they are now considered separate conditions.
Anxiety disorders are treatable. It is important to seek help for these conditions to get relief and prevent further complications. If you or someone you know is experiencing symptoms of an anxiety disorder, reach out to a primary care provider or mental health professional for support.
A Note on Gender and Sex Terminology
Verywell Health acknowledges that sex and gender are related concepts, but they are not the same. To reflect our sources accurately, this article uses terms like “female,” “male,” “woman,” and “man” as the sources use them.
Anxiety and Depression Association of America. Anxiety disorders - facts and statistics .
National Institute of Mental Health. Generalized anxiety disorder .
National Institute of Mental Health. Anxiety disorders .
National Institute of Mental Health. Generalized anxiety disorder: when worry gets out of control .
National Institute of Mental Health. Panic disorder .
National Institute of Mental Health. Panic disorder: when fear overwhelms .
Asher M, Asnaani A, Aderka IM. Gender differences in social anxiety disorder: a review . Clinical Psychology Review . 2017;56:1-12. doi:10.1016/j.cpr.2017.05.004
National Institute of Mental Health. Social anxiety disorder: more than just shyness .
Laicher H, Int-Veen I, Torka F, et al. Trait rumination and social anxiety separately influence stress-induced rumination and hemodynamic responses . Sci Rep . 2022;12(1):5512. doi:10.1038/s41598-022-08579-1
Nemours KidsHealth. Separation anxiety .
Boston Children's Hospital. Separation anxiety disorder .
Wardenaar KJ, Lim CCW, Al-Hamzawi AO, et al. The cross-national epidemiology of specific phobia in the World Mental Health Surveys . Psychol Med . 2017;47(10):1744-1760. doi:10.1017/S0033291717000174
MedlinePlus. Phobia—simple/specific .
International OCD Foundation. Who gets OCD ?
National Institute of Mental Health. Obsessive-compulsive disorder.
Department of Veteran Affairs. How common is PTSD in adults?
American Psychiatric Association. What is post-traumatic stress disorder?
Garakani A, Murrough JW, Freire RC, et al. Pharmacotherapy of anxiety disorders: current and emerging treatment options . Front Psychiatry . 2020;11:595584. doi:10.3389/fpsyt.2020.595584
By Ashley Olivine, Ph.D., MPH Dr. Olivine is a Texas-based psychologist with over a decade of experience serving clients in the clinical setting and private practice.
Appointments at Mayo Clinic
Fear of public speaking: how can i overcome it, how can i overcome my fear of public speaking.
Fear of public speaking is a common form of anxiety. It can range from slight nervousness to paralyzing fear and panic. Many people with this fear avoid public speaking situations altogether, or they suffer through them with shaking hands and a quavering voice. But with preparation and persistence, you can overcome your fear.
These steps may help:
- Know your topic. The better you understand what you're talking about — and the more you care about the topic — the less likely you'll make a mistake or get off track. And if you do get lost, you'll be able to recover quickly. Take some time to consider what questions the audience may ask and have your responses ready.
- Get organized. Ahead of time, carefully plan out the information you want to present, including any props, audio or visual aids. The more organized you are, the less nervous you'll be. Use an outline on a small card to stay on track. If possible, visit the place where you'll be speaking and review available equipment before your presentation.
- Practice, and then practice some more. Practice your complete presentation several times. Do it for some people you're comfortable with and ask for feedback. It may also be helpful to practice with a few people with whom you're less familiar. Consider making a video of your presentation so you can watch it and see opportunities for improvement.
- Challenge specific worries. When you're afraid of something, you may overestimate the likelihood of bad things happening. List your specific worries. Then directly challenge them by identifying probable and alternative outcomes and any objective evidence that supports each worry or the likelihood that your feared outcomes will happen.
- Visualize your success. Imagine that your presentation will go well. Positive thoughts can help decrease some of your negativity about your social performance and relieve some anxiety.
- Do some deep breathing. This can be very calming. Take two or more deep, slow breaths before you get up to the podium and during your speech.
- Focus on your material, not on your audience. People mainly pay attention to new information — not how it's presented. They may not notice your nervousness. If audience members do notice that you're nervous, they may root for you and want your presentation to be a success.
- Don't fear a moment of silence. If you lose track of what you're saying or start to feel nervous and your mind goes blank, it may seem like you've been silent for an eternity. In reality, it's probably only a few seconds. Even if it's longer, it's likely your audience won't mind a pause to consider what you've been saying. Just take a few slow, deep breaths.
- Recognize your success. After your speech or presentation, give yourself a pat on the back. It may not have been perfect, but chances are you're far more critical of yourself than your audience is. See if any of your specific worries actually occurred. Everyone makes mistakes. Look at any mistakes you made as an opportunity to improve your skills.
- Get support. Join a group that offers support for people who have difficulty with public speaking. One effective resource is Toastmasters, a nonprofit organization with local chapters that focuses on training people in speaking and leadership skills.
If you can't overcome your fear with practice alone, consider seeking professional help. Cognitive behavioral therapy is a skills-based approach that can be a successful treatment for reducing fear of public speaking.
As another option, your doctor may prescribe a calming medication that you take before public speaking. If your doctor prescribes a medication, try it before your speaking engagement to see how it affects you.
Nervousness or anxiety in certain situations is normal, and public speaking is no exception. Known as performance anxiety, other examples include stage fright, test anxiety and writer's block. But people with severe performance anxiety that includes significant anxiety in other social situations may have social anxiety disorder (also called social phobia). Social anxiety disorder may require cognitive behavioral therapy, medications or a combination of the two.
Craig N. Sawchuk, Ph.D., L.P.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Social anxiety disorder (social phobia). In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association, 2013. http://dsm.psychiatryonline.org. Accessed April 18, 2017.
- 90 tips from Toastmasters. Toastmasters International. https://www.toastmasters.org/About/90th-Anniversary/90-Tips. Accessed April 18, 2017.
- Stein MB, et al. Approach to treating social anxiety disorder in adults. http://www.uptodate.com/home. Accessed April 18, 2017.
- How to keep fear of public speaking at bay. American Psychological Association. http://www.apa.org/monitor/2017/02/tips-sidebar.aspx. Accessed April 18, 2017.
- Jackson B, et al. Re-thinking anxiety: Using inoculation messages to reduce and reinterpret public speaking fears. PLOS One. 2017;12:e0169972.
- Sawchuk CN (expert opinion). Mayo Clinic, Rochester, Minn. April 24, 2017.
Products and Services
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Anxiety disorders
- Cognitive behavioral therapy
- Specific phobias
- Sweating and body odor
- Tachycardia
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Fear of public speaking How can I overcome it
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Anxiety Guide
- Help & Advice
Complete List of Anxiety Symptoms (241 Total)
Fact checked.
Micah Abraham, BSc
Last updated November 26, 2022
Anxiety is a mental, emotional, and physical condition. Anyone who has anxiety or knows someone who has struggled with it can identify it by some of its most common symptoms: nervousness, sweating, exaggerated or irrational fear, and rapid heartbeat among others.
But these are not the only symptoms of anxiety. Anxiety is occasionally called “the Great Imitator” due to its ability to mimic other health conditions.
For those who live with chronic anxiety, its range of symptoms, from the usual to the rare, is extensive.
Anxiety changes the way you think.
Anxiety alters your hormone levels.
Anxiety changes your perception and awareness so that you notice physical sensations that someone without anxiety would never notice .
Anxiety can even amplify physical sensations. For example, someone without anxiety may have a knee pain so mild that they don’t even notice it, but a person with anxiety feels that knee pain severely because their mind has been altered, making it hypersensitive to the way the body feels.
Anxiety can also create symptoms that are not there at all.
Anxiety Symptoms List: Learn More About Anxiety
The best way to stop anxiety is to understand it. The more you understand what causes your symptoms, what they mean, why you struggle with them, and what you can do to stop them, the more you’ll be able to start making real progress on your own anxiety symptoms.
We have broken each symptom down into categories for easy navigation. You can click on any of the links below to be taken to the section of your choice immediately, or you can scroll down to start reading more about the symptoms as a whole.
Note: Some people experience anxiety symptoms that are 100% mental with no physical symptoms. Others experience anxiety symptoms that are 100% physical: they are anxious physically even though they have no worries and their minds are clear. Most people experience some combination of the two. There is no right or wrong way to experience anxiety.
Keep in mind that categorizing some anxiety symptoms is difficult . For example, you may feel that what we consider to be a whole-body symptom is more of a chest symptom, and vice versa. So if you don’t find a symptom you struggle with in the section you expect, it may be in another section.
- Most Common Symptoms of Anxiety
- Mental Symptoms of Anxiety – Thoughts and More
Emotional Symptoms of Anxiety
Symptoms of anxiety that affect the whole body, symptoms of anxiety that affect the organs.
- Symptoms of Anxiety Affecting that Affect the Head
- Symptoms of Anxiety that Affect the Upper Body
- Symptoms of Anxiety that Affect the Lower Body
Other Symptoms of Anxiety
Within each of these categories are sub-categories that will allow you to learn more about specific groupings of symptoms. If you find that a symptom you struggle with not on this list, and you’d like to discuss it in the future, please feel free to contact us at any time, and we’ll do our best to address it.
Note: Every Type of Anxiety Has Different Symptoms
Anxiety is not a single disorder.
Anxiety has hundreds of symptoms, but these symptoms may change depending on the type of anxiety you have. “Anxiety disorders” is an umbrella term for a group of anxiety conditions, each of which has unique signs and symptoms. These anxiety disorders include the following:
- Acute Stress Disorder
- Agoraphobia Without a History of Panic Disorder
- Anxiety Disorder Due to a General Medical Condition
- Anxiety Disorder not Otherwise Specified
- Generalized Anxiety Disorder
- Obsessive-Compulsive Disorder
- Panic Disorder with Agoraphobia
- Panic Disorder Without Agoraphobia
- Post-Traumatic Stress Disorder
- Social Phobia
- Specific Phobia
- Substance-Induced Anxiety Disorder
Keep in mind how different these anxiety disorders may be as you learn about the symptoms of anxiety. It’s also important to note that not everyone’s anxiety fits into a neat little bubble. Many people with one type of anxiety struggle with symptoms that are similar to those of another type.
Finally, as you explore the symptoms below, you should recognize that you are not alone. We asked those on our Facebook page if they had weird anxiety symptoms. They had hundreds of responses, ranging from “forgetting how to swallow” to a “loud pop, like a firecracker, in their ear.” An individual suffering from an anxiety disorder perceives a wide range of feelings and sensations, which are unique, complex, and often difficult to explain.
The Most Common Symptoms of Anxiety
Although there are many strange and unusual anxiety symptoms, there are also those that are common. The most common anxiety symptoms are those directly caused by the fight-or-flight system — the system in your brain that is responsible for keeping you safe from harm. When it works improperly, it causes anxiety.
Typically, if you have anxiety, you will experience some combination of these symptoms. Much depends on the anxiety disorder, how long you’ve had it, what you’re paying attention to, and more. For example, some symptoms, like chest pains, are more common in panic attacks than in generalized anxiety disorder or OCD.
Don’t take this list to mean that you do or do not have anxiety. Anxiety is more complex than that. But if you do have an anxiety disorder, you will likely experience at least 50% of the following common anxiety symptoms (click on each symptom to learn more):
- Breathing Difficulties
- Chest Pressure / Chest Tightness
- Concentration Problems
- Depersonalization / Derealization
- Difficulty Speaking
- Digestion Issues
- Feeling Ill
- Feeling Overwhelmed
- Feeling Shaky
- “Heart Attack Symptoms”
- Heart Pounding / Heart Palpitations
- Hyperventilation
- Insomnia / Drowsiness
- Lack of Air
- Lightheadedness
- Muscle Tension / Sore Muscles
- Nervousness
- Shallow Breathing
These are some of the most common anxiety symptoms. If your symptoms do not appear on this list, that does not make them rare. There are still thousands of anxiety symptoms that millions of people all over the world experience.
For those who are interested in learning more about their anxiety symptoms, the following are all of the slightly less common, but no less important, symptoms of anxiety that they may experience, broken down by category.
Mental Symptoms of Anxiety: Thoughts and Cognitive Habits
Anxiety is a mental health condition, so the best way to start talking about anxiety symptoms is to look at the mental ones.
Anxiety alters your brain. It changes how you think, how you perceive, and how you process information. For example, someone without anxiety may see a random person looking at them and think nothing of it. Someone with anxiety may see the same person looking at them and worry that they’re being judged or that the person is dangerous.
The exact same situation is processed differently.
Similarly, anxiety can cause strange mental symptoms. It can cause anhedonia — which is a total loss of the ability to feel pleasure. It can cause obtrusive thoughts, like imagining yourself being violent to a child even though you have no violent tendencies. It can even cause you to forget who you are.
Anxiety changes the neurochemicals in your brain that tell you how to think and act.
But rest assured, curing anxiety can also change your brain back to its prior state. Like a disease, anxiety changes your brain, but none of those changes have to be permanent.
Thought Symptoms of Anxiety
The following are some of the most common symptoms of anxiety related to thoughts. Thought symptoms are especially common among those struggling with Obsessive-Compulsive Disorder but play some role in nearly all forms of anxiety.
Anxiety thought symptoms include:
- Bad Thoughts
- Crazy Thoughts
- Disturbing Thoughts
- Intrusive Thoughts
- Irrational Thoughts
- Obsessive Thoughts
- Racing Thoughts
- Scary Thoughts
- Violent Thoughts
- Weird Thoughts
If you struggle with one of these types of thoughts, it’s important to remind yourself time and time again that they are caused by anxiety and that anxiety changes how you think, making these types of thoughts more frequent.
Cognitive Functioning Symptoms of Anxiety
In this case, cognitive functioning refers to how your brain acts, not necessarily how you think. An example might be memory loss. Memory loss, especially regarding smaller details, is common in those with anxiety.
The following are some anxiety symptoms that affect how your mind functions:
- Disorientation
- Distorted Reality
- Forgetfulness
- Hallucinations
- Memory Loss
- Memory Problems
It could be argued that emotional issues, like we discuss in the next section of the guide, are related to cognitive functioning as are some types of thoughts (such as racing thoughts), but this list of anxiety symptoms should give you a bit more of an idea of the different types of mental anxiety symptoms.
Anxiety has a strong effect on your emotions. In some ways, anxiety itself is an emotion.
As a result, it’s not uncommon for anxiety to affect your emotions. You can have almost any emotion as a result of anxiety. Some people actually experience anxiety euphoria. This means anxiety triggers extreme happiness in them (although usually this occurs only when they have some relief from anxiety).
Because anxiety alters the neurochemicals associated with mood, many emotional anxiety symptoms are common. We have broken them down into two sections, mood-based emotion anxiety symptoms and fear-based emotional symptoms.
Mood-Based Anxiety Symptoms
If you have anxiety, the changes it makes to your brain chemicals will affect your mood. But its impact will vary from one person to the next because the human mind translates neurotransmitters differently. You can experience some, all, or only one of the many mood anxiety symptoms, including:
- Aggression and Violence
- The Development of Apathy
- Hyperactivity
- Impaired Communication
- Impulsivity
- Irritability
- Isolation and Loneliness
- Mood Swings
- Numb Feelings
- “Psychotic” Behaviors
- Severe Sadness
- A Suicidal Mindset
- The Emotional Brain
- Toying with Emotions
Many of them make perfect sense for the condition. For example, if you are struggling with stress because of anxiety, it makes sense that you may also be irritable. The different levels of neurotransmitters in the brain may directly cause other symptoms, like mood swings.
Fear-Based Anxiety Symptoms
Anxiety itself is a form of fear. Indeed, fears often constitute a type of anxiety disorder. Phobias are significant fears of a specific stimulus and cause anxiety symptoms. The following, however, are a few types of fears that are also symptoms of anxiety:
- Being Easily Scared
- Fear of Death and Dying
- Fear of Going Crazy
- Hypochondriasis
In some ways, fear of flying may be an anxiety symptom as well as a fear of going outside. Fears may also cause anxiety. This shows how linked the causes and symptoms of anxiety can be.
We will now start to list physical anxiety symptoms. These sections are broken up to correspond to individual parts of the body — the head, the chest, and more. But there are also some symptoms that affect the entire body. These are symptoms of that kind.
Muscle-Related Anxiety Symptoms
Anxiety affects the muscles in many ways. The following are several of the symptoms of anxiety that may affect nearly any muscle in the body. Click on each link to explore what causes those specific symptoms to occur when you have anxiety.
- Muscle Aches
- Muscle Cramps
- Muscle Pain
- Muscle Spasms / Behavioral Spasms
- Muscle Stiffness
- Muscle Twitching
- Muscle Weakness
This list excludes muscle tension because we listed it in the “Common Anxiety Symptom” section.
In addition, several types of pain and discomfort in specific areas of the body may be caused by muscles, but because they are specific to a body part, you will find them in a different list.
Blood and Circulatory System-Related Anxiety Symptoms
Anxiety can also affect how your heart pumps blood, how your body communicates, and so much more. The following are some anxiety symptoms of the blood and circulatory system:
- Circulation Problems
- Hormonal Changes
- Hypertension
- Low Blood Pressure
Anxiety can also make some issues that you already struggle with worse. Luckily, most of the time, these issues are only temporary, and do not cause any long-term damage or lead to any long-term risks.
Temperature Perception-Based Anxiety Symptoms
Anxiety also affects the way you perceive ambient temperature, which in turn can make you feel hot, cold, or both. The following are some associated anxiety symptoms:
- Body Temperature Changes
- Feeling Cold
- Hot and Cold Flashes
- Hyperhidrosis
In most cases, they are largely harmless.
Other Whole-Body (Somatic) Anxiety Symptoms
The following are some symptoms of anxiety that affect the entire body but do not necessarily fit into any one category. Be sure to explore the links below to learn more about each symptom as well as what may cause it and what you can do about it.
- Aches and Pains
- Pins and Needles
- Restlessness
- Trouble Moving
- A Weakened Immune System
Anxiety symptoms can also migrate, making them feel like they affect your entire body.
Although slightly less common, anxiety can also affect the organs, especially the largest organ of your body — your skin. We discussed chest pains and a rapid heartbeat earlier as the adrenaline from anxiety frequently affects your heart. But you may also find that anxiety affects your organs or leads to similar organ symptoms. See the following:
- Atrial Fibrillation
- Burning Skin
- Heart Palpitations
- Irregular Heartbeat
- Kidney Problems
- Red Blotches
- Skin Color Changes
- Slow Heart Rate
- Spleen Issues
- Tachycardia
If you struggle with any of these issues, it makes sense to see a doctor for safety. But anxiety really does cause all of these conditions, and if you struggle with them, curing your anxiety may be the only way to eliminate them.
Symptoms of Anxiety that Affect the Eyes, Nose, Mouth
Since anxiety is a mental health condition, it does seem to make some sense that it would cause a wide range of physical symptoms involving the eyes, mouth, etc.

Eye-Related Anxiety Symptoms
Anxiety may affect the eyes and perception. This is partially a result of the fight-or-flight response. At the same time, since the eyes are dependent on a fully functioning brain, it’s not a surprise that anxiety causes a lot of eye symptoms, including:
- Blurred Vision
- Double Vision
- Eye Problems
- Pupil Changes
- Seeing Spots
- Vision Problems
Often, if these issues are caused by anxiety, the symptoms seem to come and go at different times. This means glasses alone may not fix them.
Head Anxiety Symptoms
It’s not always clear why stress and anxiety seem to affect the head so much. Muscle tension is likely one of the most common culprits. But there are many symptoms that specifically affect the head, including:
- Hair Problems
- Head Pressure
- Itchy Scalp
These don’t even include the symptoms that often affect the face, which are listed below.
Nose-Related Symptoms
Anxiety and stress can cause many different nose-related anxiety symptoms. They can also make allergies worse. The symptoms include:
- Changes in Smell
This is another way in which oversensitivity may be a problem. Anxiety can make you more sensitive in your perception of these symptoms. So if you would normally be able to ignore a slightly runny nose, anxiety will make you more aware of it.
Mouth-Related Symptoms
That same oversensitivity is often specifically linked to issues of the mouth. Indeed, while anxiety can literally cause a bad taste in your mouth, it can also make you hyper-aware of how your mouth “tastes” when you’d normally be able to enjoy it. Common mouth-related anxiety symptoms include:
- A Bad Taste in the Mouth
- A Constrained Voice
- A Dry Mouth
- A Metallic Taste
- Taste Changes
- Teeth Problems
Trouble swallowing and related issues are also common, but those are a bit more linked to the throat.
Hearing- and Ear-Related Symptoms
Some people describe strange hearing sensations with anxiety, like a loud “pop” noise that seems to come out of nowhere. You may experience any number of hearing- and ear-related anxiety symptoms, including:
- Hearing Problems
- Ringing Ears
- Sensitivity to Sound
These don’t include auditory hallucinations, which we listed above under the cognitive functioning section.
Speech-Related Symptoms
Because anxiety affects both your thoughts and your mouth, speech problems may be common. If you struggle to speak as a symptom of your anxiety, see if you have one of the anxiety-related speech symptoms below:
- Slurred Speech
- Speech — Concentration and Swallowing
- Speech Patterns
Of course, anxiety can also cause fear of speaking in public, and those with anxiety — especially social anxiety — may have symptoms that include overthinking before speaking or speaking too fast.
Other Head Symptoms (Including Those Related to the Face and Throat)
There are also some head symptoms that simply do not seem to fit into any of the above sections. The following are such symptoms of anxiety:
- Choking Sensations
- Face Issues
- Lump in the Throat
- Sore Throat
Some issues, like sore throat, may have very complex causes – such as anxiety triggering acid reflux, which in turn causes a sore throat. Don’t forget to explore the links to see if you can learn more about your own anxiety symptoms.
Symptoms of Anxiety that Affect the Upper Body — Including the Arms, Neck, Back, Chest
As we move down the body, we get to symptoms that relate to the upper body — including the arms, neck, back, and chest.
We’ve done our best to break down each of these symptoms into their appropriate categories, but some may be hard to categorize. So explore the text below to find symptoms you may be experiencing.
Arm- and Hand-Related Anxiety Symptoms
Anxiety doesn’t have a “strong” effect on the arms and the hands, but it does affect them. The main culprits are the nerves — which can misfire when you have anxiety — and blood flow. Some common arm- and hand-related anxiety symptoms include
- Armpit Problems and Sweating
- Finger Symptoms
- Hand Symptoms
- Nail Biting
- A Tingling Sensation in the Hands and Arms
Be careful about oversensitivity as well. Anxiety makes you so sensitive to normal sensations that they feel worse. This occasionally happens with tingling hands, for example, although anxiety can also cause the hands to tingle all on its own.
Chest, Digestive, and Breathing Anxiety Symptoms
Your chest is more than muscles. Inside your chest are your lungs, which affect breathing, and several parts of your digestive tract. These can lead to a variety of chest anxiety symptoms, including:
- Angina-like symptoms
- Esophagus Problems
- Heartburn and Acid Reflux
- Indigestion
- Respiratory Problems
Some of the most common anxiety symptoms include chest pains, rapid heartbeat, and trouble breathing, so be sure to review that section as well for other anxiety symptoms of the chest.
Abdomen-Related Anxiety Symptoms
Right below the chest is your abdomen, which houses your stomach and has some of the most sensitive muscles in your entire body. Those who struggle with stress regularly have abdominal pain and other conditions. See some of them below:
- Abdominal Pain
- Stomach Cramps
- Stomach Pain
- Stomach Problems
- Upset Stomach
Stress has a strong effect on stomach acids and digestion.
Other Upper Body-Related Anxiety Symptoms
Of course, symptoms are not limited to those parts of the upper body. You may find that you have a variety of additional symptoms, including:
- Armpit Pain and Sweating
You may also find yourself concerned about flank pain, lower back pain, upper back pain, and other, related symptoms. These may also be anxiety-related symptoms.
Symptoms of Anxiety that Affect the Lower Body – Including the Legs, Feet, Genitals
Anxiety may elicit a variety of symptoms in your genitals, buttocks, legs, feet, and more.
Sometimes, the symptoms aren’t easy to pin down. People who struggle with panic attacks, for example, often find that automatic movements become less automatic. Something as simple as walking suddenly becomes difficult because they are so aware of their bodies that they essentially override their muscle memory and have to figure out how to walk again.
Still, we have attempted to categorize the lower body symptoms into the following groups:
Pelvis-Related Anxiety Symptoms
Problems with sex can be both causes and symptoms of anxiety, and — due to stress, changes in blood flow, and how the brain works — anxiety can also create a lot of unique issues that affect urination, sexual desire, and more. The following are several pelvis-related symptoms of anxiety:
- Bowel Problems
- Constipation
- Fertility Problems
- Genital Symptoms
- Incontinence/Loss of Bladder Control
- Infertility
- Irritable Bowel Syndrome
- Decreased Libido
- Urination Issues
- Vaginal Discomfort
- Yellow Stool
Leg and Feet Anxiety Symptoms
Your legs and feet can be surprisingly sensitive to anxiety. The relationship between adrenaline/blood flow and your legs and feet is well known, which is why anxiety can cause many leg and foot symptoms, including
- Foot Discomfort
- Tingling Feet
- Toe Problems
Walking can often help with anxiety leg symptoms, but only if anxiety hasn’t affected your ability to walk.
Even in the most comprehensive list of anxiety symptoms, it can be difficult to find a category for each symptom. The following are some miscellaneous anxiety symptoms that did not fit into any of the groups listed above.
Sleep-Related Anxiety Symptoms
Anxiety has a profound effect on sleep, which is why “insomnia” is up there with the most common anxiety symptoms. But many other sleep-related issues exist, including:
- Night Sweats
- Sleep Problems
- Sleep Apnea
Some people sleep more, others less. Some people sleep like a rock, others toss and turn. Stress is so complex that it can have a different impact on how each person sleeps, how often they sleep, and how they dream.
Behavior-Related Anxiety Symptoms
The simple act of avoiding a social situation because you have social fears or that of having your partner drive because you hate freeways — these are arguably behavioral anxiety symptoms. The following are a few of the many that currently exist:
- Behavioral Changes
- Collapsing/Fainting
- Social Withdrawal
- Weight Gain
Those with Obsessive-Compulsive Disorder are especially prone to behavioral symptoms.
Illness-Related and Miscellaneous Anxiety Symptoms
Finally, some common issues do not fit into any of the above categories. For example, there are illness-related anxiety symptoms that seem to mimic real disorders, as well as strange and unusual symptoms, like itchiness, that are different for different people. The following are some of the anxiety symptoms that do not quite fit in the previous groups:
- Fibromyalgia
- Increased Risk of Infection
- Peripheral Neuropathy
- Swollen Glands/Swollen Lymph Nodes
Anxiety: It Does it All
Anxiety really can seem to cause almost every symptom imaginable because it does. It mimics health conditions. It can make you so sensitive to how you feel that normal perceptions feel abnormal. It can create its own issues — such as acid reflux, which then causes hoarseness or chronic cough.
In nearly any mental health book, the list of anxiety symptoms is extremely short, and this leads to people developing even more anxiety as they worry that they may have something else, that something else may be wrong with them.
But if you talk to people who have anxiety, do research, and learn more about the condition, you will quickly find that there are hundreds of anxiety symptoms out there: all the more reason to find ways to cure it.
Questions? Comments?
Do you have a specific question that this article didn’t answered? Send us a message and we’ll answer it for you!
Where can I go to learn more about Jacobson’s relaxation technique and other similar methods? – Anonymous patient
You can ask your doctor for a referral to a psychologist or other mental health professional who uses relaxation techniques to help patients. Not all psychologists or other mental health professionals are knowledgeable about these techniques, though. Therapists often add their own “twist” to the technqiues. Training varies by the type of technique that they use. Some people also buy CDs and DVDs on progressive muscle relaxation and allow the audio to guide them through the process. – Timothy J. Legg, PhD, CRNP
Read This Next

What Happens During an Anxiety Attack?
Fact Checked by Denise Griswold, MSc, LCAS Updated on December 8, 2020.
Panic disorder is one of the least understood types of anxiety by those that have never experienced an anxiety attack....

7 Tips How to Fight Anxiety
Written by Micah Abraham, BSc Updated on October 10, 2020.
Anxiety is a constant struggle. You need to get it under control in order to live an enjoyable life., This...
What Anxiety Treatments Are There?
Fact Checked by Faiq Shaikh, M.D. Updated on October 10, 2020.
Anxiety disorders are life-altering issues. Anxiety is a condition that creates real, measurable changes to your brain, and alters the...
Anxiety vs. Depression: What is the Relationship?
Fact Checked by Sally-Anne Soameson, Psychiatrist Updated on October 10, 2020.
While psychologists look at mental health in terms of specific disorders, the truth is that mental health isn't always quite...
Anxiety and the Brain: An Introduction
Fact Checked by Denise Griswold, MSc, LCAS Updated on October 10, 2020.
It should come as little surprise that your brain is the source of your anxiety. Not only does anxiety manifest...

The 6 Main Types of Anxiety - Which Do You Have?
Everyone experiences anxiety differently. Some people have general anxiety that is manageable but never seems to go away. Others suffer...

5 Strategies for Instant Anxiety Relief
Millions and millions of people suffer from anxiety, and yet according to statistics less than 50% of those with anxiety...
Get advice that’s rooted in medical expertise:
Sign up for our newsletter and get science-backed tips to better manage anxiety and boost your mental health. Nurture yourself with mental health advice that’s rooted in medical expertise.
Your privacy is important to us. Any information you provide to us via this website may be placed by us on servers located in countries outside of the EU. If you do not agree to such placement, do not provide the information.
🍪 Pssst, we have Cookies!
We use Cookies to give you the best online experience. More information can be found here . By continuing you accept the use of Cookies in accordance with our Cookie Policy.
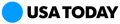
Anxiety symptoms: What to understand about the condition and how to calm anxiety.
A nxiety is a feeling that just about everyone can relate to. We feel anxious when we're unsure what will happen next, are worried about what to say or do in a given situation or don't know how to react to a pending change. Understanding anxiety is mental health 101.
While mild feelings of anxiety are common, anxiety can also be debilitating for many people. Some such individuals have learned coping mechanisms and techniques that experts say anyone can use to improve symptoms of anxiety − even when they don't recognize that anxiety is what they're experiencing.
"Some may have anxiety and not know, while others may be aware they have anxiety but don't want others to know," says Jimmy Noorlander, LCSW, a clinical social worker at Deseret Counseling in Utah. "We are all put in different situations and how each of us responds can be different."
Start the day smarter. Get all the news you need in your inbox each morning.
Anxiety symptoms: What are they?
Anxiety is a persistent worry that can manifest in any everyday situation but is often rooted in concerns about something unknown or yet to come. A fast heart rate , a sense of impending danger, perspiration , trembling and rapid breathing sometimes accompany anxiety. While the degree of one's symptoms can vary, some measure of anxiousness is both natural and common. "Fear and anxiety are wired into our DNA as part of our fight or flight mechanism of survival," explains Siggie Cohen, PhD, a child development specialist and popular parenting coach . "Anxiety is a universal human trait," she adds.
Anxiety is often triggered by a real or perceived threat, especially in situations where one is unsure of potential consequences or possible outcomes. "It's the overthinking about such outcomes...that precipitates the anxiety," explains Juanita Guerra, PhD, a clinical psychologist in New Rochelle, New York.
What causes anxiety?
Many things contribute to anxiety. A lack of sleep , core personality traits, physical changes such as puberty or aging, and many social experiences and interactions commonly trigger feelings of anxiety. Persons who have ever experienced neglect, emotional or physical abuse, bullying or the loss of a loved one are especially prone. "Anxiety can also spike due to unexpected circumstances such as crisis or trauma," explains Cohen.
Anxiety is frequently present in many children and teens, and "continues to increase but generally peaks somewhere between 25-45 years of age," says Guerra. At that point, anxiety may ebb for some people, but retirement , children moving out and the uncertainties of old age commonly cause anxious feelings to return for many elderly adults. "Anxiety generally affects all age groups," says Noorlander, "though each person can present it in different ways."
How to calm anxiety
Regardless of when or how one experiences anxiety, knowing ways to prevent or calm it can be helpful. Exercise has been shown to reduce anxiety and stress; a healthy diet has, too. Calming techniques such as deep breathing , placing one's hands under warm water or meditation can also be effective practices. Cutting down on alcohol, caffeine and tobacco is important as well as such substances often exacerbate symptoms of anxiety. "Some different techniques I like to use are going for a walk , journaling or thinking of a relaxing place," suggests Noorlander. Distracting oneself from worry with an activity such as watching a movie, listening to music or talking with a friend can also be helpful.
Above all, being willing to recognize and deal with feelings of anxiety is critical. "Avoidance, denial and working hard to get rid of the anxiety all have the unintended effect of keeping anxiety alive," explains Cohen. She says that awareness and mindfulness are the first steps toward managing and coping with anxiety. "One wants to develop an understanding of what their personal triggers are, be transparent about emotions in general, seek and accept support and keep an open mind," she advises.
'I wish I could live a normal life': What your friend with an anxiety disorder wishes you knew
This article originally appeared on USA TODAY: Anxiety symptoms: What to understand about the condition and how to calm anxiety.

83% of Adults With Generalized Anxiety Disorder Symptoms Are Undiagnosed
— researchers urge for better screening and intervention.
by Kristen Monaco , Senior Staff Writer, MedPage Today May 8, 2024
NEW YORK CITY -- Almost a quarter of surveyed U.S. adults met criteria for generalized anxiety disorder (GAD), though the vast majority of them were undiagnosed, a retrospective cross-sectional study suggested here.
Out of 75,261 respondents to the online 2022 National Health and Wellness Survey, 23.3% screened positive for anxiety using the 7-Item GAD Questionnaire , Daniel Karlin, MD, chief medical officer of MindMed in New York City, reported here at the American Psychiatric Association annual meeting.
Of those who screened positive, 83.1% had never received a GAD diagnosis. Most (55.1%) of the individuals screening positive had moderate symptoms while 44.9% had severe symptoms.
Last year, the U.S. Preventive Services Task Force recommended that all adults up to age 64 be screened for anxiety in the primary care setting, including for GAD, in order to avoid delays in diagnosis and treatment. But Karlin explained that estimates of undiagnosed GAD had been outdated or based on small samples.
If the proportions identified by Karlin and his team were broadened to the entire U.S. population, it would represent around 59 million adults with GAD, 49 million of whom are undiagnosed.
"There are a lot of people walking around with symptoms that are severe enough for them to have moderate to severe GAD who've never been diagnosed," he told MedPage Today . "The burden of illness of undiagnosed GAD is remarkably high."
"These findings reflect something that we're missing as a healthcare system, that there are people who have this severe anxiety, they aren't sure what to do [or] what there is to be done about it," he said. "We need to be doing a better job of screening for anxiety disorders, and then intervening when we detect them."
Karlin said that for a long time there has been a greater focus placed on diagnosing and treating major depressive disorder (MDD), but GAD and MDD are "overlapping diseases," he noted.
"We need to continue to recognize that distress comes in different flavors, and that no single flavor is more important than any other," Karlin added. "Let's make sure we're paying attention to anxiety as well as depression."
A few characteristics stood out among adults with GAD who were undiagnosed. They were more likely to be younger, male, smokers, alcohol drinkers, employed, and have a higher income when compared with controls without GAD symptoms or those already diagnosed with GAD:
- Age: 37.5 vs 51.8 vs 42.1 years, respectively
- Male: 54% vs 49% vs 26%
- Current smoker: 36% vs 15% vs 23%
- Alcohol drinker: 72% vs 64% vs 65%
- Employed: 75% vs 55% vs 50%
- Income of $75,000 or higher: 59% vs 46% vs 26%
The group with undiagnosed GAD were also less likely to be white (51% vs 65% vs 69%, respectively) and less likely to have overweight or obesity (45% vs 62% vs 68%).
Karinn Glover, MD, MPH, a psychiatrist at Albert Einstein College of Medicine in New York City, wasn't surprised to see people with GAD report higher rates of alcohol use, pointing out how untreated anxiety is linked with substance use.
"I certainly wonder how many of those who screened positive for anxiety also have relied heavily on alcohol or cannabis to manage anxiety and to what extent that use might meet criteria for misuse or a disorder," Glover, who wasn't involved with the research, told MedPage Today .
In another poster presented here led by Karlin and colleagues, adults with undiagnosed GAD also tended to have a poorer quality of life. Compared with diagnosed adults, undiagnosed adults had significantly fewer healthcare provider visits in the past 6 months (3.0 vs 8.7) but had a significantly higher number of hospitalizations (1.2 vs 0.3) and emergency room (ER) visits (1.3 vs 0.5; P <0.001 for all).
The Work Productivity and Activity Impairment Questionnaire also showed that undiagnosed adults had scores for absenteeism, presenteeism, overall work productivity impairment, and activity impairment that were 3.1, 1.9, 1.9, and 1.6 times higher, respectively, than diagnosed adults ( P <0.001 for all).
As for RAND-36 Physical, Mental, and Global Health Composite scores, undiagnosed adults trended toward lower but not significantly different physical (36.1 vs 39.6) and global health composite scores (32.3 vs 33.5), but higher mental health composite scores (32.8 vs 32.1).
Interestingly, adults with undiagnosed GAD were less likely to report certain comorbidities like depression (15% vs 79%) and pain (10% vs 44%) than diagnosed adults.
In order to catch more cases of undiagnosed anxiety, Karlin recommended healthcare providers screen patients using the 7-Item GAD Questionnaire. Agreeing, Glover said these findings support the use of the collaborative care model -- a brief anxiety screening at every primary care visit followed by a warm handoff to a clinician providing evidence-based treatment in the primary care setting for each patient who screens positive and is interested.
"Collaborative care decreases barriers like waitlists and avoids some of the stigma often associated with obtaining care in more specialized psychiatric settings," Glover said. "Additionally, screening in primary care has been shown to decrease healthcare costs like ER visits in the long run."
![presentation of anxiety symptoms author['full_name']](https://clf1.medpagetoday.com/media/images/author/kristenMonaco_188.jpg)
Kristen Monaco is a senior staff writer, focusing on endocrinology, psychiatry, and nephrology news. Based out of the New York City office, she’s worked at the company since 2015.
Disclosures
Both studies were funded by MindMed.
Karlin and several co-investigators reported employment with MindMed. No other disclosures were reported.
Glover had no disclosures.
Primary Source
American Psychiatric Association
Source Reference: Karlin D, et al "Screening adults in the U.S. general population to detect cases of undiagnosed generalized anxiety disorder" APA 2024; Poster P03-020.
Secondary Source
Source Reference: Karlin D, et al "Quantifying the burden of undiagnosed generalized anxiety disorder in the U.S. general adult population" APA 2024; Poster P03-019.
EZH2-dependent epigenetic reprogramming in the central nucleus of amygdala regulates adult anxiety in both sexes after adolescent alcohol exposure
Affiliations.
- 1 Center for Alcohol Research in Epigenetics, Department of Psychiatry, University of Illinois Chicago, Chicago, IL, 60612, USA.
- 2 Jesse Brown Veterans Affairs Medical Center, Chicago, IL, 60612, USA.
- 3 Center for Alcohol Research in Epigenetics, Department of Psychiatry, University of Illinois Chicago, Chicago, IL, 60612, USA. [email protected].
- 4 Jesse Brown Veterans Affairs Medical Center, Chicago, IL, 60612, USA. [email protected].
- 5 Department of Anatomy and Cell Biology, University of Illinois Chicago, Chicago, IL, 60612, USA. [email protected].
- PMID: 38670959
- PMCID: PMC11053082
- DOI: 10.1038/s41398-024-02906-y
Alcohol use and anxiety disorders occur in both males and females, but despite sharing similar presentation and classical symptoms, the prevalence of alcohol use disorder (AUD) is lower in females. While anxiety is a symptom and comorbidity shared by both sexes, the common underlying mechanism that leads to AUD and the subsequent development of anxiety is still understudied. Using a rodent model of adolescent intermittent ethanol (AIE) exposure in both sexes, we investigated the epigenetic mechanism mediated by enhancer of zeste 2 (EZH2), a histone methyltransferase, in regulating both the expression of activity-regulated cytoskeleton-associated protein (Arc) and an anxiety-like phenotype in adulthood. Here, we report that EZH2 protein levels were significantly higher in PKC-δ positive GABAergic neurons in the central nucleus of amygdala (CeA) of adult male and female rats after AIE. Reducing protein and mRNA levels of EZH2 using siRNA infusion in the CeA prevented AIE-induced anxiety-like behavior, increased H3K27me3, decreased H3K27ac at the Arc synaptic activity response element (SARE) site, and restored deficits in Arc mRNA and protein expression in both male and female adult rats. Our data indicate that an EZH2-mediated epigenetic mechanism in the CeA plays an important role in regulating anxiety-like behavior and Arc expression after AIE in both male and female rats in adulthood. This study suggests that EZH2 may serve as a tractable drug target for the treatment of adult psychopathology after adolescent alcohol exposure.
© 2024. This is a U.S. Government work and not under copyright protection in the US; foreign copyright protection may apply.
Publication types
- Research Support, N.I.H., Extramural
- Research Support, Non-U.S. Gov't
- Alcoholism / genetics
- Alcoholism / metabolism
- Anxiety* / genetics
- Anxiety* / metabolism
- Central Amygdaloid Nucleus* / drug effects
- Central Amygdaloid Nucleus* / metabolism
- Cytoskeletal Proteins / genetics
- Cytoskeletal Proteins / metabolism
- Disease Models, Animal
- Enhancer of Zeste Homolog 2 Protein* / genetics
- Enhancer of Zeste Homolog 2 Protein* / metabolism
- Epigenesis, Genetic*
- Ethanol* / pharmacology
- GABAergic Neurons / drug effects
- GABAergic Neurons / metabolism
- Nerve Tissue Proteins / genetics
- Nerve Tissue Proteins / metabolism
- Rats, Sprague-Dawley
- Enhancer of Zeste Homolog 2 Protein
- EZH2 protein, rat
- activity regulated cytoskeletal-associated protein
- Cytoskeletal Proteins
- Nerve Tissue Proteins
Grants and funding
- UO1AA019971/U.S. Department of Health & Human Services | NIH | National Institute on Alcohol Abuse and Alcoholism (NIAAA)
- U24AA024605/U.S. Department of Health & Human Services | NIH | National Institute on Alcohol Abuse and Alcoholism (NIAAA)
- P50AA022538/U.S. Department of Health & Human Services | NIH | National Institute on Alcohol Abuse and Alcoholism (NIAAA)
- RO1AA010005/U.S. Department of Health & Human Services | NIH | National Institute on Alcohol Abuse and Alcoholism (NIAAA)
- F32AA027410/U.S. Department of Health & Human Services | NIH | National Institute on Alcohol Abuse and Alcoholism (NIAAA)
- Open access
- Published: 02 May 2024
Assessing the impact of migraine on benign paroxysmal positional vertigo symptoms and recovery
- Seda Çakır 1 ,
- Aysenur Sahin 1 ,
- Ozlem Gedik-Soyuyuce 2 ,
- Zeynep Gence Gumus 2 ,
- İbrahim Sertdemir 3 ,
- Nazım Korkut 4 &
- Pınar Yalınay Dikmen ORCID: orcid.org/0000-0001-7112-2142 1
BMC Neurology volume 24 , Article number: 148 ( 2024 ) Cite this article
211 Accesses
1 Altmetric
Metrics details
During episodes of benign paroxysmal positional vertigo (BPPV), individuals with migraine, compared with individuals without migraine, may experience more severe vestibular symptoms because of their hyperexcitable brain structures, more adverse effects on quality of life, and worse recovery processes from BPPV.
All patients with BPPV were assigned to the migraine group (MG, n = 64) and without migraine group (BPPV w/o MG, n = 64) and completed the Vertigo Symptom Scale (VSS), Vertigo Dizziness Imbalance Symptom Scale (VDI-SS), VDI Health-Related Quality of Life Scale (VDI-HRQoLS), Beck Anxiety Inventory (BAI), and Beck Depression Inventory (BDI) at the time of BPPV diagnosis (baseline) and on the one-month follow-up. Headache Impact Test-6 and Migraine Disability Assessment Scale were used for an assessment of headache. Motion sickness was evaluated based on the statement of each patient as present or absent.
Compared with the BPPV w/o MG, the MG had higher VSS scores at baseline [19.5 (10.7) vs. 11.3 (8.5); p < 0.001] and on one-month follow-up [10.9 (9.3) vs. 2.2 (2.7), p < 0.001]; experienced more severe dizziness and imbalance symptoms based on the VDI-SS at baseline (61.9% vs. 77.3%; p < 0.001) and after one month (78.9% vs. 93.7%, p < 0.001); and more significantly impaired quality of life according to the VDI-HRQoLS at baseline (77.4% vs. 91.8%, p < 0.001) and after one month (86.3% vs. 97.6%, p < 0.001).
On the one-month follow-up, the subgroups of patients with moderate and severe scores of the BAI were higher in the MG (39.2%, n = 24) than in the BPPV w/o MG (21.8%, n = 14) and the number of patients who had normal scores of the BDI was lower in the MG than in the BPPV w/o MG (67.1% vs. 87.5%, p = 0.038).
Clinicians are advised to inquire about migraine when evaluating patients with BPPV because it may lead to more intricate and severe clinical presentation. Further studies will be elaborated the genuine nature of the causal relationship between migraine and BPPV.
Peer Review reports
Migraine is a vastly prevalent and disabling neurological disorder worldwide [ 1 ]. It is not defined as merely headache, which is only one of the phases of a migraine attack. In addition to pain, the several symptoms during migraine attacks reflect a complex pathophysiology and the diffuse involvement of multiple neural networks and anatomical regions, such as the autonomic, affective, cognitive, and sensory systems, as well as the brainstem [ 2 ]. Compared with individuals without migraine, those who have migraine have brains that are hyperexcitable from the influence of genetic and epigenetic factors and exhibit distinct characteristics in their ability to cope with internal and external stimuli that disrupt homeostasis [ 3 ]. Functional imaging and neurophysiological studies have provided concrete proof that the brains of individuals with migraine exhibited increased responsiveness to sensory stimuli, even during the interictal phase [ 3 , 4 ]. Moreover, compared with individuals without migraine, those with migraine were reported to exhibit increased activation in the primary visual cortex and the other visual processing regions, such as the lateral geniculate nucleus and the motion-responsive middle temporal cortex, when exposed to visual stimuli [ 5 , 6 ]. The clinical implication of the results of functional imaging and electrophysiological studies was that individuals experienced migraine attacks when exposed to internal (e.g., menstruation, sleep disturbances, skipping meals, and stress) or external (e.g., changes in air pressure, crowded environments, entering poorly ventilated spaces, and tying up hair) triggers that surpass their allostatic loads [ 7 ]. In this context, the ability of individuals with migraine to cope with stressors was assumed to differ from that of individuals without migraine [ 2 , 8 , 9 , 10 ]. The exact mechanisms of the increased cortical responsiveness in migraine (i.e., increased excitability or decreased inhibition in the brain and central or peripheral origin) have not been fully elucidated and remain a topic of debate [ 11 ].
Benign paroxysmal positional vertigo (BPPV) is the most common cause of vertigo [ 12 ]. Individuals with migraine were reported to be more likely to experience BPPV [ 13 , 14 , 15 , 16 ]. Owing to the maladaptive or hypersensitive brains in individuals with migraine, symptoms that may arise from stimulation or dysfunction of the peripheral vestibular system can be severe and bothersome [ 8 , 9 , 10 ]. In this context, BPPV could be an acute trigger for the disruption of the peripheral vestibular system balance in individuals with migraine. Compared with individuals without migraine, those with migraine may experience more severe vestibular symptoms during a BPPV attack because of their hyperexcitable brain structures, experience a greater impact on their quality of life (QoL), and have a longer recovery process.
In this study, we hypothesized a heightened severity of vestibular symptoms, such as vertigo and dizziness, during episodes of BPPV among individuals with migraine and vestibular migraine (VM), which had been increasingly recognized in recent years as the most common cause of spontaneous episodic vertigo and is the second most common vestibular disorder following BPPV. Furthermore, we anticipated a more negative impact on overall QoL and a less effective recovery from BPPV in this group than in individuals without a history of migraine. To test our hypothesis, we aimed to compare the vertigo, dizziness, and QoL scales at the time of BPPV diagnosis and on one-month follow-up between individuals with migraine and those without migraine. In addition, we aimed to test the validity of our hypothesis in the subgroup of patients with VM.
Study population and study design
In this study, 128 consecutive patients who had BPPV that presented as dizziness or vertigo and were clinically evaluated at the ear nose throat (ENT) and neurology outpatient clinics of Acıbadem Maslak Hospital between April 2022 and November 2022 were prospectively recruited for six months. The diagnosis of BPPV was confirmed based on the results of videonistagmography (VNG), which was done at the audiology laboratory. Clinical assessment included complete medical history and neurootological, neurological, and physical examinations. The study was conducted in accordance with the ethical principles stated in the Declaration of Helsinki. Institutional review board approval was granted by Acibadem University School of Medicine (2022–02/17). Written informed consent was obtained from all the participants prior to enrolment.
The inclusion criteria were age ≥ 18 years and < 65 years, literate, provision of consent, and at least one year of headache in patients who had migraine. The diagnosis of migraine was made by a neurology specialist according to the International Classification of Headache Disorders, third edition [ 17 ]. The exclusion criteria were the presence of conditions that can affect cognitive performance; severe physical illness or clinical laboratory findings that indicated a serious illness, such as malignancy; history of severe neurological disease, such as cerebrovascular disease; being under the influence of psychoactive substances; history of debilitating central or peripheral vestibular diseases, such as vestibular neuritis, persistent postural perceptual dizziness (PPPD) and having Meniere’s disease. During the one-month follow-up period, the participants did not receive any new treatment to suppress vestibular symptoms or migraine. Based on the aforementioned criteria, patients were excluded because of unwillingness to participate ( n = 15), age < 18 years ( n = 57), age > 65 years ( n = 191), history of malignancy ( n = 9), the presence of Meniere’s disease and PPPD ( n = 22) and vestibular neuritis ( n = 28), being lost to follow-up within one month ( n = 14). Therefore, a total of 128 eligible patients who met the criteria were included in the study (Fig. 1 ). Among the patients with BPPV who were included in the study, those with migraine were classified as the migraine group (MG) and those without migraine were classified as the BPPV without migraine group (BBPV w/o MG).
Flow diagram
Assessments
After being diagnosed by the participating experts in the study, all patients filled out the standardized questionnaires and measurement tools during the interview with the same neurology research assistant (SC). The patients were interviewed twice; the first was during the diagnosis of BPPV (baseline) and lasted for approximately 60 min, and the second was during the follow-up visit after one month and lasted for about 30 min. During the first interview, the demographic characteristics of all patients were recorded. The patients completed the data form on the clinical features of BPPV and migraine, as well as the other clinical scales that were used in the study (Additional file 1 ). Individuals experiencing 4–14 headache days per month were categorized as having frequent episodic migraine (EM), while those with 0–3 headache days per month or fewer were classified as having infrequent episodic migraine (EM). Patients experiencing ≥ 15 headache days per month were classified as chronic migraine (CM).
Risk factors of BPPV were also questioned in the data form. Recent trauma was defined to injuries to the head and neck regions within the previous month. The presence of viral or bacterial infections affecting the upper or lower respiratory system within the past month was investigated as a potential risk factor. The term "prolonged rest" was employed to characterize bed rest following surgery within the preceding month. Heavy alcohol consumption was defined to the excessive intake of alcohol within the 3-day period before the appearance of BPPV-related complaints, typically exceeding recommended daily limits or surpassing moderate drinking guidelines. Vitamin deficiency was characterized by a blood level of 25-hydroxy vitamin D below 25 ng/mL. Stress positivity was evaluated as the patient expressing his or her stress level as normal or increased following the negative life events experienced in the last month. Acute insomnia was characterized by disruptions in sleep continuity, involving difficulty in initiating and/or maintaining sleep, and occurring for a duration of at least three days per week, lasting anywhere between one week and three months.
For the evaluation of the clinical features of vertigo, the Vertigo Symptom Scale (VSS), Vertigo Dizziness Imbalance Symptom Scale (VDI-SS), and Health-Related Quality of Life Scale (VDI-HRQoLS) were used. For the evaluation of headache, the Headache Impact Test (HIT-6) was applied. For the assessment of migraine-related disability, the Migraine Disability Assessment Scale (MIDAS) was used. The Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI) were used to assess anxiety and depression symptoms. In the absence of a clinically validated and reliable Turkish scale for evaluating motion sickness, participants were classified as either having a history of motion sickness (present) or not having it (absent), relying on their past or current experiences.
Motion sickness was evaluated based on the statement of each patient as present or absent. The MG were given a headache diary during the baseline interview. All patients were invited for a follow-up appointment after one month for repeat completion of the clinical scales and collection of the headache diaries from the MG.
Vertigo symptom scale
The VSS was developed for the assessment of vertigo symptoms [ 18 , 19 ]. The VSS short form comprised 15 items, which were evaluated on a 0–4 Likert-type scale, based on the frequency during the past month (0: never, 1: very rarely, 2: most of the time, 3: often- every week, or 4: very often- most days). The patients were asked to choose the most appropriate response that reflected their condition. The total score ranged from 0 to 60; a score of ≥ 24 was classified as severe vertigo, and a score of < 24 was classified as mild vertigo.
The VDI comprised two subscales, as follows: the VDI-SS, which contained 14 items, and the VDI-HRQoLS, which contained 22 items. Each item was classified into five subcategories using a 0–5 Likert-type scale (0: always, 1: most of the time, 2: often, 3: sometimes, 4: very rarely, and 5: never). The patients were asked to select the most appropriate response that reflected their condition. The total score ranged from 0 to 100%; a score of 100% indicated no symptoms or no impact on the QoL, whereas a score approaching 0% indicated worsening of symptoms and QoL.
Headache impact test
The HIT-6 evaluates the impact of headaches on an individual’s life. It comprises six subdomains, including pain, social functioning, role functioning, vitality, cognitive functioning, and psychological distress caused by pain [ 20 , 21 ]. The total score ranged from 36 to 78, with higher scores indicating a greater impact. The HIT-6 score was categorized into four groups, such as ≤ 49 (little to no impact), 50–55 (partial impact), 56–59 (significant impact), and ≥ 60 (severe impact).
Migraine disability assessment scale
The MIDAS had been used to evaluate the impact of migraine on the performance of daily activities in the past three months, based on the answers to five questions in three areas, such as work or school, household chores, and activities that are related to family, social life, and leisure [ 22 , 23 ]. In this study, the scores were categorized based on the severity of the disability caused by migraine attacks, as follows: 0–5 points for no or very mild disability, 6–10 points for mild disability, 11–20 points for moderate disability, and > 21 points for severe disability.
Beck anxiety inventory
The BAI is a self-reported inventory that assesses the frequency and severity of anxiety symptoms [ 24 , 25 ]. It comprises 21 symptom categories, each with four response options. Each item is scored from 0 to 3. The maximum possible score on the scale is 63. The total score was categorized as follows: 0–7 points for no anxiety, 8–15 points for mild anxiety, 16–25 points for moderate anxiety, and 26–63 points for severe anxiety.
Beck depression inventory
The BDI is one of the commonly used self-reported instruments in research and daily practice [ 26 , 27 ] and comprises 21 questions. The patients were asked to choose the most appropriate response that reflected their current state. The total score ranged from 0 to 63. The results were categorized as follows: 0–9 indicated no or minimal depression, 10–18 indicated mild depression, 19–29 indicated moderate depression, and 30–63 indicated severe depression.
Statistical analysis
The primary outcome variables were the changes in the VSS, VDI, and VDI-HRQoLS from baseline to follow-up at one month. In our study, two types of comparative statistics were conducted to investigate the severity of the BPPV symptoms in the MG and the impact of having migraine on BPPV recovery. First, the severity of vestibular symptoms and QoL were compared between the MG and the BPPV w/o MG. In addition, the BPPV recovery process was evaluated by comparing the three scales between baseline and one-month follow-up in each group.
Statistical analysis was carried out using RStudio software V2022.12.0 (RStudio Team, 2022) and the R programming language V4.2.2 (R Core Team, 2022) with the aid of R-based packages. All the analyses were performed on the available data. A priori statistical power calculation was conducted. The sample size was based on the available data. The normality of data was assessed by the Shapiro–Wilk test. Hypothesis testing was two-tailed. For comparisons between groups, T-test, or Mann–Whitney U-test was used for numerical variables, whereas chi-square test and two-sample proportion test were used for categorical data. Posthoc pairwise comparisons were performed using Bonferroni-corrected Mann–Whitney U-test. The relationship between numerical variables was explored using Spearman’s rank correlation coefficient. The data were expressed as number and percentage for categorical variables. Numerical variables was expressed as mean, standard deviation, range, median, and interquartile range according to parametric or nonparametric distribution properties. A value of p < 0.05 was considered statistically significant.
Demographic features
Table 1 presents the demographic data of all participants. The mean age was significantly lower in the MG than in the BPPV w/o MG [39.1 years (10.2 years) vs. 44.6 years (9.5 years), p = 0.002]. The MG had a preponderance of women ( n = 55, 85.9%), whereas the proportion of women in the BPPV w/o MG was lower ( n = 36, 56.2%) ( p < 0.001). The participants in the MG ( n = 64) were divided into the VM ( n = 26) and nonVM ( n = 38) groups; there were no differences in the demographic data between the two groups.
Migraine features
Migraine group
In this study, 15.6% ( n = 10) had migraine with aura (MWA) and 84.4% ( n = 54) had migraine without aura (MWoA). In 81.3% ( n = 52) of patients, a diagnosis of migraine was previously known and 65.6% ( n = 42) had a family history of migraine. The mean duration of migraine was 13.5 years (10.7 years). Migraine patients were categorized into three groups based on the frequency of their headaches: infrequent EM (81.2%, n = 52), frequent EM (7.8%, n = 5) and CM (11.0%, n = 7). In our study, 89% of the participants reported experiencing headache frequency within the range of EM. The mean and median MIDAS scores in the MG were 14.4 (19.6) and 9 (3; 21), respectively. In the MG, the mean HIT-6 score was 57,7 ± 9,0 at baseline and 54,7 [ 2 , 9 ] on the first month. At baseline, 21.8% ( n = 14) of the MG was under a prophylactic medication for migraine. In preceding month, the mean and median of monthly headache days (MHDs) and number of days of acute attack medication intake were [5.0 (6.4) - 3 (1; 5.25)] and [4.7 (7.1) - 3 (1; 5.0)], respectively. On the first month of follow-up based on the headache diaries of the patients, the mean and median MHDs and number of days of acute attack medication intake were [5.2 (6.1) - 4 (1.75;7.25)] and [4.3 (6.3) – 3 (0.75;4.25)], respectively.
Comparison of the vestibular migraine and nonvestibular migraine groups
In the VM group, 19.2% ( n = 5) had MWA and 80.8% ( n = 21) had MWoA. In the nonVM group, 13.2% ( n = 5) had MWA and 86.8% ( n = 33) had MWoA. A pre-existing diagnosis of migraine was identified in 92.3% ( n = 24) of individuals in the VM group, and a family history of migraine was reported by 80.7% ( n = 21). In contrast, in the nonVM group, 73.6% ( n = 28) had a previously known migraine diagnosis, and 55.2% (n = 21) reported a family history of migraine. Family history of migraine was statistically different between two groups ( p = 0.04).
The average durations of migraine in the VM and nonVM groups were 9.0 years (8.3 years) and 15.7 years (11.5 years), respectively ( p = 0.04). EM in the VM and nonVM groups was infrequent in 73.0% ( n = 19) and 86.7% ( n = 33), respectively, and was frequent in 11.5% ( n = 3) and 5.2% ( n = 2), respectively. CM was diagnosed in 15.3% ( n = 4) and 7.8% ( n = 3) of the VM and nonVM groups, respectively. There were no significant differences in the occurrences of EM and CM between the two groups ( p = 0.59).
At baseline, the mean MHDs for the preceding month did not differ between the two groups ( p = 0.312). On one-month follow-up, the median MHD was significantly higher in the VM group than in the nonVM group [5 (3; 8) vs. 3 (1; 4), p = 0.02]. The median MIDAS score was significantly higher in the VM group than in the nonVM group [15 (6; 24) vs. 6 (3; 15), p = 0.04]. There were no significant differences in the HIT-6 scores at baseline [59.3 ± 8,3 vs. 56.8 ± 9,5; p = 0.270] and on one-month follow-up [56.1 ± 8.3 vs. 53.8 ± 9.9; p = 0.32] between the VM and nonVM groups.
Benign paroxysmal positional vertigo features
Table 2 summarizes the BPPV-related data for the MG and BPPV w/o MG. Among the patients with BPPV, the affected ear was classified as the right, left, or bilateral. There was no significant difference in the affected ear between the two groups ( p = 0.278). BPPV was classified as affecting the posterior, horizontal, anterior, or mixed canals. In both groups, the posterior canal (PC) was most frequently affected. The proportion of patients in whom the PC was affected was not significantly different between the groups [MG ( n = 52, 81.2%) vs. BPPV w/o MG ( n = 43, 67.1%); p = 0.085].
In our cohort, most participants had a previous history of BPPV [MG ( n = 47, 73.4%) vs. BPPV w/o MG ( n = 45, 70.3%); p = 0.844]. The median number of repositioning maneuvers was similar between the two groups [MG 2 (1; 3) vs. BPPV w/o MG 2 (1; 2), p = 0.25]. Regarding the BPPV risk factors, recent history of trauma (15.6% vs. 1.5%, p = 0.01) and past or current history of motion sickness (84.3% vs. 53.1%, p < 0.001) were significantly more prevalent in the MG than in the BPPV w/o MG.
Description of vertigo or dizziness
Table 3 shows the answers of the participants, according to the Barany Society classification of vestibular symptoms in the International Classification of Vestibular Diseases [ 28 ]. Visual stimulus-triggered vertigo (48.4% vs. 26.5%, p = 0.02) and dizziness triggered by head movement (82.8% vs. 65.6%, p = 0.04) were significantly different between the MG and BPPV w/o MG. The terms that were usually used by the patients to describe their vestibular symptoms during BPPV were evaluated under 13 headings [ 29 ]. As shown in Table 4 , compared with the BPPV w/o MG, the MG reported significantly more frequent sensations of rocking back and forth (37.5% vs. 17.1%, p = 0.017); unsteadiness (71.8% vs. 39.0%, p < 0.001); feeling of fogginess in the head (40.6% vs. 20.3%, p = 0.021); and feeling like being drunk (50% vs. 29.6%, p = 0.030).
Motion sickness
The prevalence of motion sickness was significantly higher in the MG than in the BPPV w/o MG (82.9% vs. 54.7%, p < 0.001) .
Comparison of clinical scales
Comparison of the mg with the bppv w/o mg.
Table 5 displays the baseline and 1–month follow-up VSS, VDI-SS, VDI-HRQoLS, BAI, and BDI scores for both groups. The median VSS score was significantly higher in the MG than in the BPPV w/o MG at baseline [16.5 (12; 27) vs. 9 (5.75; 15), p < 0.001] and on one-month follow-up [8 (5; 14.25) vs. 2 (0; 3), p < 0.001]. However, the change in VSS the scores from baseline to one-month follow-up was not significantly different between the groups [7.5 (4; 13) vs. 7 (4; 11.25), p = 0.939].
Impairment was classified as mild or severe based on the median VSS scores. Severe impairment (i.e., higher VSS scores) was more prevalent in the MG than in the BPPV w/o MG both at baseline ( p < 0.001 ) and on one- month follow-up ( p = 0.010 ) . At baseline, the percentage of patients with mild scores was significantly higher in the BPPV w/o MG than in the MG [68.7% ( n = 44) vs. 93.7% ( n = 60)], whereas that of patients with severe scores was significantly higher in the MG than in the BPPV w/o MG [31.2% ( n = 20) vs. 6.2% (n = 4), p < 0.001]. Notably, one-third of the MG had severe VSS scores at baseline. By the first month of follow-up, severe VSS scores were not observed in the BPPV w/o MG but were persistent in 12.5% ( n = 8) of the MG ( p = 0.010).
The median VDI-SS score was significantly lower in the MG than in the BPPV w/o MG at baseline [61.5 (54.25; 73) vs. 80.5 (69; 87.25), p < 0.001] and on one-month follow-up [83 (72.75; 89) vs. 95 (91.5; 98), p < 0.001]. However, the change in VDI-SS scores from baseline to one-month follow-up did not show a significant difference between the groups [-17 (-25.5; -7.75) vs. -13.5 (-24; -7), p = 0.507].
The median VDI-HRQoLS scores were significantly lower in the MG than in the BPPV w/o MG at baseline [81 (69; 92) vs. 95 (87.5; 99), p < 0.001] and on one-month follow-up [92 (79.5; 97.25) vs. 99.5 (97; 100), p < 0.001]. However, there was no significant difference between the groups in terms of the change in the VDI-HRQoLS scores from baseline to the first month of follow-up [-5 (-14; -1.75) vs. -3 (-7.5; 0), p = 0.122].
The median BAI scores were significantly higher in the MG than in the BPPV w/o MG at baseline [12 (6.5; 19.25) vs. 4.5 (1.75; 14), p < 0.001] and on one-month follow-up [8 (3; 16) vs. 2 (0; 6), p < 0.001]. However, there was no significant difference between the groups in terms of the change in the BAI scores from baseline to the first month of follow-up [3 (1; 6) vs. 2.5 (1; 5), p = 0.755].
Using a categorical distribution (i.e., normal, mild, moderate, or severe), the BAI scores were significantly different between two groups at baseline ( p < 0.001) and on one-month follow-up ( p < 0.001). At baseline, the BAI score was normal in 62.5% ( n = 40) of the BPPV w/o MG and in 31.2% ( n = 20) of the MG showed. On follow-up after one month, the distributions of patients with normal and mild BAI scores were similar to those at baseline, but the subgroups of patients with moderate and severe BAI scores were higher in the MG (39.2%, n = 24) than in the BPPV w/o MG (21.8%, n = 14) (Table 5 ).
The median BDI scores were significantly higher in the MG than in the BPPV w/o MG at baseline [8 (5; 14) vs. 2 (0; 8.25), p < 0.001] and on the one-month follow-up [7 (2; 11.25) vs. 1 (0; 5), p < 0.001]. However, the change in the BDI scores from baseline to the first month of follow-up was not significantly different between the two groups [0.5 (0; 3) vs. 0 (0; 2), p = 0.122]. Using a categorical distribution, the BDI scores did not differ between the two groups at baseline ( p = 0.084); however, on the first month, the number of patients who had normal scores was lower in the MG than in the BPPV w/o MG (67.1% vs. 87.5%, p = 0.038) (Table 5 ).
Table 6 demonstrates the comparison of the clinical scales between the VM and nonVM groups. The median VSS was not significantly different between the two groups at baseline [19.5 (12; 27.75) vs. 15 (11.25; 24.25), p = 0.385]. However, on the first month, the median VSS score was significantly higher in the VM group than in the nonVM group [12 (6.5; 17) vs. 6 (4.25; 10.75), p = 0.043]. The change in the VSS scores between the two time points was not significantly different between the two groups ( p = 0.411). Furthermore, the subgroupings to mild and severe impairment were not different between the two groups in the two time points.
The VDI-SS scores were not significantly different between the VM and nonVM groups at baseline [61.3 (15.0) vs. 62.3 (16.0), p = 0.793] and on one-month follow-up [79 (64.25; 86.5) vs. 85.5 (77.5; 89.75), p = 0.074]. However, the median VDI-HRQoLS indicated a significantly higher impairment in the VM group than in the nonVM group both at baseline [73 (61; 85.75) vs. 89 (71.5; 94.75), p = 0.003] and on one-month follow-up [85 (73; 92.75) vs. 94 (87; 98), p = 0.005].
The mean/median scores and categorical distributions of the BAI did not show any significant differences at baseline and on one-month follow-up between the two groups. Moreover, the median BDI scores were not significantly different between the VM and nonVM groups at baseline [9.5 (7; 13.5) vs. 7 (3.25; 13.75), respectively, p = 0.233]. In one-month follow-up, the BDI score did not show any statistical difference between the VM group than in the nonVM group [8.5 (7; 11.75) vs. 4.5 (1; 9.75), p = 0.089]. In addition to that, the categorical distribution of the BDI in the groups was not significantly different between the two groups.
Correlation analysis for vestibular migraine
In the VM group, the HIT-6 score had a moderate positive correlation with the VSS ( p = 0.018, rho = 0.457) and a moderate negative correlation with the VDI-SS ( p = 0.010, rho = − 0.491). Moreover, MIDAS was strongly correlated with the VSS ( p = 0.001, rho = 0.60) and moderately correlated with the VDI-SS ( p = 0.002, rho = − 0.56).
In the nonVM group, the HIT-6 score had a weak relationship with the BAI ( p = 0.024, rho = 0.36) and a moderate relationship with the BDI ( p = 0.006, rho = 0.431).
In this study, during at both the diagnosis and on the one-month follow-up for BPPV, patients with migraine experienced more severe vestibular symptoms and a greater adverse impact on their quality of life compared to those without migraine. At all assessment points, the MG who exceeded the VSS cut-off score associated with severe vestibular symptoms was statistically more prevalent to those without migraine. The similar rate of improvement in both groups indicated that suffering from migraine did not negatively affect the recovery from BPPV within a one-month period. Patients diagnosed with VM exhibited a frequent family history with migraine and longer migraine duration, along with higher baseline MIDAS scores and increased MHDs at the one-month follow-up, when compared to patients without VM. Individuals with VM exhibited higher VVS scores during the follow-up period and experienced significantly more impaired health-related quality of life at all assessment points compared to those without VM. Finally, in patients with VM, the MIDAS demonstrated a strong correlation with the VSS, and a significant negative correlation with the VDI-SS.
Studies have shown that BPPV was more common in individuals with migraine than in healthy controls [ 14 , 30 , 31 ] and that having migraine increased the risk of BPPV [ 13 ]. Migraine was relatively frequent in women and young patients with a history of BPPV [ 32 ]. Ishiyama et al. [ 31 ] demonstrated that in patients with BPPV without migraine, the age of onset age was older, reaching a peak in the eighth decade. Nearly half (47%) of the patients who experienced BPPV before the age of 50 years had a history of migraine. Faralli et al. [ 33 ] showed that the mean age of BPPV onset was 39 ± 9.2 years in patients with migraine and 53 ± 7.3 years in individuals without migraine. In alignment with prior research, we observed that the MG was significantly younger, compared with the BPPV w/o MG.
In a comprehensive retrospective study in the United States, the factors that affected the coexistence of migraine and BPPV were investigated using a substantial participant pool ( n = 1481) [ 32 ]. The results showed that the self-reported prevalence of migraine among patients with BPPV was 25.8% ( n = 382). The authors identified female sex, young age, history of previous BPPV, and absence of diabetes mellitus (DM) as the common comorbidities of migraine and BPPV. That study revealed a greater prevalence of coexistent BPPV and migraine in individuals who had a prior history of BPPV than in those who had no BPPV (OR 1.6, 95% CI 1.2–2.1, p < 0.002). Similarly, in our cohort, the patients were younger and were predominantly women in the MG than in the BPPV w/o MG. In other previous studies, vascular comorbidities, such as hypertension, DM, and hyperlipidemia, may have negative effects on the occurrence [ 34 ] or recurrence [ 35 ] of BPPV. In our study, hypertension was significantly more prevalent in the BPPV w/o MG than in the MG ( p = 0.038); this may have been associated with relatively old age of the patients in the BPPV w/o MG. However, considering the limited number of participants, this finding should be interpreted with caution. Consistent with the literature [ 36 ], our study reported a significantly higher prevalence of a recent history of head trauma in the MG than in the BPPV w/o MG.
Most cases of BPPV develop in the posterior and horizontal canals. In our cohort, involvement of the PC was observed in 81.2% of the MG and 67.1% of the BPPV w/o MG, consistent with the literature [ 37 ]. The rate of BPPV recurrence has been reported to range from 7 to 56% [ 34 , 38 , 39 ]. In a study on general population, Luryi et al. [ 40 ] found a BPPV recurrence rate of 37%, an increased risk of recurrence in females and individuals who had a history of BPPV, and a previous history of BPPV as the most significant factor associated with BPPV recurrence [ 40 ]. In our study, most participants had a history of BPPV, although we did not find an increased rate of BPPV recurrence in the MG. The high rates of BPPV recurrence in this study might be related to the setting of a tertiary referral center. Similarly, Ishiyama et al. [ 31 ] reported high BPPV recurrence rates in both migraineurs (77%, n = 62) and nonmigraineurs (66%, n = 154).
In this present study, the prevalence of motion sickness was significantly higher in the MG than in the BPPV w/o MG and only tended to be higher in the VM group than in the nonVM group. In our previous study, more frequent headaches and more intense vestibular symptoms during caloric testing were observed in patients with migraine, particularly those who had motion sickness alone and those who had both migraine and motion sickness, than in patients without migraine and motion sickness [ 41 ].
In this study, the incidence of visually-induced vertigo and dizziness triggered by head movement was higher in the patients with migraine than in those without migraine. After a BPPV episode, patients may experience vertigo or dizziness in different forms and rates. In patients with VM, vestibular findings were also experienced in different ways [ 42 ]. Activation of the noradrenergic locus coeruleus and serotonergic dorsal raphe nucleus has been demonstrated in migraineurs [ 43 ]. These regions are important anatomical areas for modulating the intensity of sensory stimuli, such as light and sound [ 44 ]. We believed that the significantly higher incidence of visually-induced vertigo in migraineurs may be related to the modulation of the vestibuloocular reflex and spatial processing in the high cortical centers, which are thought to be affected in the pathophysiology of VM with BPPV.
In our study, the sensations of forward and backward swaying, unsteadiness, head heaviness, and a feeling of being drunk were significantly more frequent in migraineurs than in nonmigraineurs. These differences in the perception of vestibular symptoms highlighted the importance of taking the time to dig deep into the history to differentiate and diagnose vertigo [ 29 ].
Consistent with our hypothesis, we observed that the assessment scales for the severity of the vertigo symptoms and the feeling of dizziness were higher in migraineurs than in nonmigraineurs both at baseline and on the first month. In addition, we concluded that having migraine with BPPV had a greater impact on QoL at the time of BPPV diagnosis and on the first month of follow-up. In a cross-sectional study on patients with MWA, MWoA, CM, and healthy control subjects ( n = 60 for each), the dizziness handicap inventory scores were significantly higher in the patients with migraine than in the healthy controls ( p < 0.001) [ 45 ], and the disability was more pronounced in the patients with MWA and CM than in the patients with MWoA. However, we were unable to make a direct comparison between the results of that previous study and our study, because majority of our cohort comprised patients with EM, most of our patients had MWoA, and the number of patients with CM was limited.
In a recent study on 58 patients diagnosed as BPPV, the duration of dizziness following BPPV episodes was reported to be longer in patients with migraine than in patients without migraine [ 46 ]. In our study, the assessment scales for the severity of the vertigo symptoms and the feeling of dizziness were higher in migraineurs than in nonmigraineurs at baseline and after one month, but the MG and BPPV w/o MG showed similar improvements in the VSS, VDI-SS, and VDI-HRQoLS scores after one month. If both BPPV and migraine are thought to be risk factors for the development of PPPD, one of the shortcomings of this study is that the vertigo and dizziness that persist in migraine patients in the first month after BPPV were not re-evaluated at the end of the third month.
Both the BAI and BDI scores were higher in the MG than in the BPPV w/o MG at the baseline and on one-month follow-up. Psychiatric comorbidities reduce the QoL of patients with migraine and may complicate migraine management [ 47 ]. The findings of our study highlighted the importance of considering psychiatric comorbidities in migraineurs who are being diagnosed as BPPV and during the recovery process following BPPV.
In a recent prospective study that compared patients with VM ( n = 50) and patients with migraine only ( n = 35), the MIDAS, Visual Analogue Score, and BDI score were significantly higher in the latter ( p < 0.05), whereas the Balance Confidence scores were significantly lower in the former ( p < 0.001) [ 48 ]. These findings indicated that headache was more prominent in patients with migraine only, but vestibular complaints were more prominent in patients with VM. In our study, although many patients reported the frequency of EM, the MIDAS scores indicated a mild level of disability in all patients with migraine. Moreover, the MIDAS was significantly higher in the VM group than in the nonVM group. Notably, there was no increase in the number of MHDs in the MG after one month. This finding suggested that VM might influence migraine-related disability independently of headache frequency. Based on our correlation analysis in the VM group, the severity of vertigo and dizziness seemed to be related with the impact of headache and migraine-related disability. However, in the nonVM group, the impact of headache correlated with psychiatric comorbidities. Our findings highlighted the need to ask about headache and psychiatric comorbid conditions when managing patients with BPPV.
Our study had strengths and weaknesses. Although all interviews were conducted by the same neurology resident, some patients refused to participate and some were lost to follow-up, probably because the total duration of the baseline and follow-up interviews was 1.5 h. One of the strengths of our study was its prospective design that evaluated the severity of vestibular symptoms, QoL, and psychiatric comorbidities in patients with and without migraine using a comprehensive methodology. Additionally, the study assessed the course of BPPV and its effects on migraine frequency through one-month follow-up. Another strength was the subgroup analysis of patients with VM. However, it should be noted that VM can be confused with BPPV, both clinically and in terms of the VNG findings. During acute VM attacks, spontaneous and positional nystagmus alone or in combination can be observed [ 49 ]. In the study by Beh et al. [ 50 ], the incidence of positional vertigo was as high as 25.2% during VM attacks but was only13% outside of the attacks. In our study, the patients were evaluated for VM by both neurology and ENT specialists. VM was diagnosed based on clinical interview, whereas BPPV diagnosis was confirmed by VNG. PPPD patients were not included in the study. All patients were evaluated and VNG was performed by the same experts, and the clinical interviews were conducted by only one neurology resident; these supported the reliability of our findings.
Some limitations of our study need to be addressed. There were more women and younger participants in the MG than in the BPPV w/o MG. We did not have sex–age matched patients with BBPV without migraine. These inequalities might have affected our results. However, previous studies showed that compared with patients with BPPV alone, patients with BPPV with migraine were younger and had a preponderance of women. Our cohort reflected a real life setting in that way. Because our study was conducted at a tertiary referral center, it should be emphasized that our results may not reflect the findings in the general population, and caution should be exercised when generalizing our findings. Another weakness was the limited number of participants. Although the minimum recommended number of participants was achieved after a power analysis during the planning phase, the results may vary if the number of subjects is increased. Furthermore, majority of the participants had EM. The relationship between migraine and BPPV could have been more effectively evaluated if the participants were evenly divided into the EM and CM groups. In this study, 21.8% of our patients with migraine were under prophylactic treatment, which might have influenced the severity and course of BPPV symptoms in these patients. In our study, during the BPPV diagnosis, the number of MHDs in the preceding month was based on memory recall of the patients in the MG. Because these data did not involve objective tracking, the actual situation might not have been fully reflected. Moreover, our patients were not evaluated as two subgroups (i.e., canalolithiasis and cupulolithiasis). This omission may have affected the assessment of the severity of symptoms during BPPV and the disease course and prognosis, thereby, possibly affecting our results. In addition, a substantial proportion of patients in the MG exhibited VM (40.6%). Hence, it is plausible that the heightened vestibular morbidity observed in the BPPV group with migraine might be attributed to the supplementary vestibular symptoms present in the VM subgroup. Finally, PPPD is one of the most common reasons of chronic dizziness. For a diagnosis of PPPD, persistent symptoms need to be lasted for 3 months or longer. The cross-sectional nature of our study does not allow us to assess whether our patients developed PPPD. This underlines the need to be careful in interpreting our results and to keep PPPD in mind.
Conclusions
Our findings highlighted the importance of asking patients with BPPV about migraine and psychiatric comorbidities. Prospective studies with a larger participant pool and a focused examination of how being migraine affects the onset, progression, and recovery of BPPV will offer valuable insights for physicians managing these prevalent conditions in the future.
Availability of data and materials
The datasets of the current study are available from the corresponding author upon reasonable request.
Abbreviations
- Benign paroxysmal positional vertigo
BPPV without migraine group
Vertigo Symptom Scale
Vertigo Dizziness Imbalance Symptom Scale
VDI Health-Related Quality of Life Scale
Beck Anxiety Inventory
Beck Depression Inventory
Quality of life
Vestibular migraine
Ear nose throat
Videonistagmography
Headache Impact Test
Migraine Disability Assessment Scale,
Migraine with aura
Migraine without aura
Episodic migraine
Chronic migraine
Monthly headache days
Diabetes mellitus
Persistent postural perceptual dizziness
Group GBDNDC. Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Neurol. 2017;16(11):877–897.
Sprenger T, Borsook D. Migraine changes the brain: neuroimaging makes its mark. Curr Opin Neurol. 2012;25(3):252–62.
Article PubMed PubMed Central Google Scholar
Coppola G, Chen W-T. Neurophysiology of the Migraine Brain: Springer; 2021.
Schwedt TJ, Chiang CC, Chong CD, Dodick DW. Functional MRI of migraine. Lancet Neurol. 2015;14(1):81–91.
Article PubMed Google Scholar
Denuelle M, Boulloche N, Payoux P, Fabre N, Trotter Y, Geraud G. A PET study of photophobia during spontaneous migraine attacks. Neurology. 2011;76(3):213–8.
Article CAS PubMed Google Scholar
Boulloche N, Denuelle M, Payoux P, Fabre N, Trotter Y, Geraud G. Photophobia in migraine: an interictal PET study of cortical hyperexcitability and its modulation by pain. J Neurol Neurosurg Psychiatry. 2010;81(9):978–84.
Borsook D, Burstein R. The enigma of the dorsolateral pons as a migraine generator. Cephalalgia. 2012;32(11):803–12.
Article CAS PubMed PubMed Central Google Scholar
Cozma S, Ghiciuc CM, Damian L, Pasquali V, Saponaro A, Lupusoru EC, et al. Distinct activation of the sympathetic adreno-medullar system and hypothalamus pituitary adrenal axis following the caloric vestibular test in healthy subjects. PLoS ONE. 2018;13(3):e0193963.
Burstein R, Noseda R, Borsook D. Migraine: multiple processes, complex pathophysiology. J Neurosci. 2015;35(17):6619–29.
Saman Y, Bamiou DE, Gleeson M, Dutia MB. Interactions between stress and vestibular compensation - a review. Front Neurol. 2012;3:116.
Do TP, Hougaard A, Dussor G, Brennan KC, Amin FM. Migraine attacks are of peripheral origin: the debate goes on. J Headache Pain. 2023;24(1):3.
von Brevern M, Bertholon P, Brandt T, Fife T, Imai T, Nuti D, et al. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res. 2015;25(3–4):105–17.
Article Google Scholar
Chu CH, Liu CJ, Lin LY, Chen TJ, Wang SJ. Migraine is associated with an increased risk for benign paroxysmal positional vertigo: a nationwide population-based study. J Headache Pain. 2015;16:62.
Lempert T, Leopold M, von Brevern M, Neuhauser H. Migraine and benign positional vertigo. Ann Otol Rhinol Laryngol. 2000;109(12 Pt 1):1176.
CAS PubMed Google Scholar
Uneri A. Migraine and benign paroxysmal positional vertigo: an outcome study of 476 patients. Ear Nose Throat J. 2004;83(12):814–5.
Kayan A, Hood JD. Neuro-otological manifestations of migraine. Brain. 1984;107(Pt 4):1123–42.
Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
Yanik B, Kulcu DG, Kurtais Y, Boynukalin S, Kurtarah H, Gokmen D. The reliability and validity of the vertigo symptom scale and the vertigo dizziness imbalance questionnaires in a turkish patient population with benign paroxysmal positional vertigo. J Vestib Res. 2008;18(2–3):159–70.
Yardley L, Masson E, Verschuur C, Haacke N, Luxon L. Symptoms, anxiety and handicap in dizzy patients: development of the vertigo symptom scale. J Psychosom Res. 1992;36(8):731–41.
Dikmen PY, Bozdag M, Gunes M, Kosak S, Tasdelen B, Uluduz D, et al. Reliability and validity of Turkish Version of Headache Impact Test (HIT-6) in patients with migraine. Noro Psikiyatr Ars. 2021;58(4):300–7.
PubMed Google Scholar
Bayliss MS, Dewey JE, Dunlap I, Batenhorst AS, Cady R, Diamond ML, et al. A study of the feasibility of Internet administration of a computerized health survey: the headache impact test (HIT). Qual Life Res. 2003;12(8):953–61.
Ertas M, Siva A, Dalkara T, Uzuner N, Dora B, Inan L, et al. Validity and reliability of the Turkish Migraine Disability Assessment (MIDAS) questionnaire. Headache. 2004;44(8):786–93.
Stewart WF, Lipton RB, Kolodner KB, Sawyer J, Lee C, Liberman JN. Validity of the Migraine Disability Assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain. 2000;88(1):41–52.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7.
Ulusoy M, Sahin NH, Erkmen H. Turkish version of the beck anxiety inventory: psychometric properties. J Cogn Psychother. 1998;12(2):163.
Google Scholar
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71.
Kapci EG, Uslu R, Turkcapar H, Karaoglan A. Beck Depression Inventory II: evaluation of the psychometric properties and cut-off points in a Turkish adult population. Depress Anxiety. 2008;25(10):E104–10.
Bisdorff AR, Staab JP, Newman-Toker DE. Overview of the International classification of vestibular disorders. Neurol Clin. 2015;33(3):541–50 ( vii ).
Huang TC, Wang SJ, Kheradmand A. Vestibular migraine: an update on current understanding and future directions. Cephalalgia. 2020;40(1):107–21.
Neuhauser H, Leopold M, von Brevern M, Arnold G, Lempert T. The interrelations of migraine, vertigo, and migrainous vertigo. Neurology. 2001;56(4):436–41.
Ishiyama A, Jacobson KM, Baloh RW. Migraine and benign positional vertigo. Ann Otol Rhinol Laryngol. 2000;109(4):377–80.
Hilton DB, Luryi AL, Bojrab DI, Babu SC, Hong RS, Bojrab DI 2nd, et al. Comparison of associated comorbid conditions in patients with benign paroxysmal positional vertigo with or without migraine history: a large single institution study. Am J Otolaryngol. 2020;41(6):102650.
Faralli M, Cipriani L, Del Zompo MR, Panichi R, Calzolaro L, Ricci G. Benign paroxysmal positional vertigo and migraine: analysis of 186 cases. B-ENT. 2014;10(2):133–9.
von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78(7):710–5.
Zhu CT, Zhao XQ, Ju Y, Wang Y, Chen MM, Cui Y. Clinical characteristics and risk factors for the recurrence of benign paroxysmal positional vertigo. Front Neurol. 2019;10:1190.
Andersson H, Jablonski GE, Nordahl SHG, Nordfalk K, Helseth E, Martens C, et al. The risk of benign paroxysmal positional vertigo after head trauma. Laryngoscope. 2022;132(2):443–8.
Lee SH, Kim JS. Benign paroxysmal positional vertigo. J Clin Neurol. 2010;6(2):51–63.
Perez P, Franco V, Cuesta P, Aldama P, Alvarez MJ, Mendez JC. Recurrence of benign paroxysmal positional vertigo. Otol Neurotol. 2012;33(3):437–43.
Lopez-Escamez JA, Gamiz MJ, Fernandez-Perez A, Gomez-Finana M. Long-term outcome and health-related quality of life in benign paroxysmal positional vertigo. Eur Arch Otorhinolaryngol. 2005;262(6):507–11.
Luryi AL, Lawrence J, Bojrab DI, LaRouere M, Babu S, Zappia J, et al. Recurrence in benign paroxysmal positional vertigo: a large single-institution study. Otol Neurotol. 2018;39(5):622–7.
Gedik-Soyuyuce O, Yalinay-Dikmen P, Korkut N. The effect of migraine and motion sickness on symptoms evoked by the caloric vestibular test. J Vestib Res. 2022;32(2):135–44.
Teggi R, Colombo B, Albera R, Asprella Libonati G, Balzanelli C, Batuecas Caletrio A, et al. Clinical features, familial history, and migraine precursors in patients with definite vestibular migraine: the VM-phenotypes projects. Headache. 2018;58(4):534–44.
Maniyar FH, Sprenger T, Monteith T, Schankin C, Goadsby PJ. Brain activations in the premonitory phase of nitroglycerin-triggered migraine attacks. Brain. 2014;137(Pt 1):232–41.
Dodick DW. Migraine Lancet. 2018;391(10127):1315–30.
Carvalho GF, Vianna-Bell FH, Florencio LL, Pinheiro CF, Dach F, Bigal ME, et al. Presence of vestibular symptoms and related disability in migraine with and without aura and chronic migraine. Cephalalgia. 2019;39(1):29–37.
Bruss D, Abouzari M, Sarna B, Goshtasbi K, Lee A, Birkenbeuel J, et al. Migraine features in patients with recurrent benign paroxysmal positional vertigo. Otol Neurotol. 2021;42(3):461–5.
Minen MT, Begasse De Dhaem O, Kroon Van diest A, Powers S, Schwedt TJ, Lipton R, et al. Migraine and its psychiatric comorbidities. J Neurol Neurosurg Psychiatry. 2016;87(7):741–9.
Ozcelik P, Kocoglu K, Ozturk V, Keskinoglu P, Akdal G. Characteristic differences between vestibular migraine and migraine only patients. J Neurol. 2022;269(1):336–41.
von Brevern M, Zeise D, Neuhauser H, Clarke AH, Lempert T. Acute migrainous vertigo: clinical and oculographic findings. Brain. 2005;128(Pt 2):365–74.
Beh SC, Masrour S, Smith SV, Friedman DI. The Spectrum of vestibular migraine: clinical features, triggers, and examination findings. Headache. 2019;59(5):727–40.
Download references
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and affiliations.
Department of Neurology, Acıbadem University School of Medicine, İçerenköy. Kayışdağı Cad. No: 32. Ataşehir, İstanbul, 34752, Turkey
Seda Çakır, Aysenur Sahin & Pınar Yalınay Dikmen
Department of Audiology, Acıbadem Maslak Hospital, İstanbul, Turkey
Ozlem Gedik-Soyuyuce & Zeynep Gence Gumus
Department of Biostatistics and Bioinformatics, Acıbadem University, İstanbul, Turkey
İbrahim Sertdemir
Department of Otorhinolaryngology, Acıbadem Maslak Hospital, İstanbul, Turkey
Nazım Korkut
You can also search for this author in PubMed Google Scholar
Contributions
PYD conceptualized and designed the study. SC, OGS, ZGG, AS, NK, PYD contributed to the data acquisition. IS performed the data analyses. PYD and SC made interpretation of data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Pınar Yalınay Dikmen .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the ethical principles stated in the Declaration of Helsinki. The present study has been approved by the ethics committee of the Acıbadem University School of Medicine (leading ethics committee, (2022–02/17). Informed consent was obtained from every subject before participation.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Çakır, S., Sahin, A., Gedik-Soyuyuce, O. et al. Assessing the impact of migraine on benign paroxysmal positional vertigo symptoms and recovery. BMC Neurol 24 , 148 (2024). https://doi.org/10.1186/s12883-024-03606-2
Download citation
Received : 08 October 2023
Accepted : 18 March 2024
Published : 02 May 2024
DOI : https://doi.org/10.1186/s12883-024-03606-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Neurology
ISSN: 1471-2377
- General enquiries: [email protected]

COMMENTS
For some people, anxiety may be linked to an underlying health issue. In some cases, anxiety signs and symptoms are the first indicators of a medical illness. If your doctor suspects your anxiety may have a medical cause, he or she may order tests to look for signs of a problem. Examples of medical problems that can be linked to anxiety include:
Gastrointestinal symptoms: Running to the bathroom just before giving an important speech is a classic presentation of anxiety. People who feel anxiety in their gut may have diarrhea and vomiting. ... Symptoms of Generalized Anxiety Disorder Among Adults: United States, 2019. Published September 2020. Accessed May 2022.
Anti-anxiety medications. Anti-anxiety medications can help reduce the symptoms of anxiety, panic attacks, or extreme fear and worry. The most common anti-anxiety medications are called benzodiazepines. Although benzodiazepines are sometimes used as first-line treatments for generalized anxiety disorder, they have both benefits and drawbacks.
Anxiety has two basic components: There is a cognitive load of worry, or the apprehensive expectation of some bad outcome. And there are physical symptoms, notably restlessness and edginess ...
In any of these situations, you may notice several signs of anxiety. You can have a physical response, like: A racing heart. Sudden perspiration. A knot in your stomach. Nausea and vomiting ...
Anxiety disorders are a type of mental health condition. Anxiety makes it difficult to get through your day. Symptoms include feelings of nervousness, panic and fear as well as sweating and a rapid heartbeat. Treatments include medications and cognitive behavioral therapy. Your healthcare can design a treatment plan that's best for you.
Anxiety Disorder Symptoms. The main symptom of anxiety disorders is excessive fear or worry. Anxiety disorders can also make it hard to breathe, sleep, stay still, and concentrate. Your specific ...
Takeaway. Anxiety is a natural emotion. However, it can also cause physical symptoms, such as shaking and sweating. Anxiety disorders can affect daily life and can improve with treatment. Anxiety ...
Anxiety disorders are very common and can have a diverse presentation of signs and symptoms. The condition has very high morbidity and mortality and is best managed by an interprofessional team that includes a mental health nurse, pharmacist, psychologist, psychiatrist, and primary care provider.
Effects of anxiety on your mind. These can include: feeling tense, nervous or unable to relax. having a sense of dread, or fearing the worst. feeling like the world is speeding up or slowing down. feeling like other people can see you're anxious and are looking at you. feeling like you can't stop worrying, or that bad things will happen if you ...
experiencing depersonalization or derealization. Physical symptoms of anxiety may include: racing heart or chest pain. shortness of breath. sweating, hot flashes, or cold flashes. dizziness or ...
This activity reviews the pathophysiology of anxiety, its presentation, diagnosis and highlights the role of the interprofessional team in its management. ... If the anxiety symptoms are atypical or there are some abnormalities noted in the physical examination more detailed evaluations may be indicated to identify or exclude underlying medical ...
Explore the symptoms and causes of presentation anxiety and how to overcome a fear of public speaking. Plus, 7 mindful techniques to prepare for a presentation. Presentation anxiety, a form of performance anxiety, can be paralyzing. For someone with this condition, the thought of having to speak in front of an audience triggers a range of ...
Some psychological symptoms you might have include: feelings of intense worry and nervousness. fear, stress, and panic in public speaking situations. feelings of dread and fear before speaking in ...
Public speaking anxiety may be diagnosed as SAD if it significantly interferes with your life. This fear of public speaking anxiety can cause problems such as: Changing courses at college to avoid a required oral presentation. Changing jobs or careers. Turning down promotions because of public speaking obligations.
A panic attack is an abrupt period of intense fear or discomfort accompanied by four or more of the following 13 systemic symptoms: Palpitations, pounding heart, or accelerated heart rate. Sweating. Trembling or shaking. Shortness of breath or feeling of smothering. Feelings of choking. Chest pain or discomfort.
An anxiety disorder is a mental health condition that involves intense feelings of fear or worry. Different types of anxiety disorders affect millions of Americans. For example, 15 million U.S. adults experience social anxiety disorder, and 6 million experience panic disorder. Anxiety disorders can ...
Cognitive behavioral therapy is a skills-based approach that can be a successful treatment for reducing fear of public speaking. As another option, your doctor may prescribe a calming medication that you take before public speaking. If your doctor prescribes a medication, try it before your speaking engagement to see how it affects you.
Anxiety, or the anticipation of a future threat, isn't always a negative. While occasional feelings of anxiety may be intense, they're a sign the mind and body are working together to maintain ...
Anxiety is a mental, emotional, and physical condition. Anyone who has anxiety or knows someone who has struggled with it can identify it by some of its most common symptoms: nervousness, sweating, exaggerated or irrational fear, and rapid heartbeat among others. But these are not the only symptoms of anxiety.
How to calm anxiety. Regardless of when or how one experiences anxiety, knowing ways to prevent or calm it can be helpful. Exercise has been shown to reduce anxiety and stress; a healthy diet has ...
The group with undiagnosed GAD were also less likely to be white (51% vs 65% vs 69%, respectively) and less likely to have overweight or obesity (45% vs 62% vs 68%).
Alcohol use and anxiety disorders occur in both males and females, but despite sharing similar presentation and classical symptoms, the prevalence of alcohol use disorder (AUD) is lower in females. While anxiety is a symptom and comorbidity shared by both sexes, the common underlying mechanism that …
The Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI) were used to assess anxiety and depression symptoms. In the absence of a clinically validated and reliable Turkish scale for evaluating motion sickness, participants were classified as either having a history of motion sickness (present) or not having it (absent), relying on ...