What is kangaroo mother care? Systematic review of the literature
Affiliations.
- 1 Department of Pediatrics, Harvard Medical School, Boston, MA, USA; Department of Global Health and Population, Harvard T.H. Chan School of Public Health, Boston, MA, USA; Saving Newborn Lives, Save the Children, Washington, DC, USA.
- 2 Saving Newborn Lives, Save the Children, Washington, DC, USA.
- 3 Department of Global Health and Population, Harvard T.H. Chan School of Public Health, Boston, MA, USA.
- PMID: 27231546
- PMCID: PMC4871067
- DOI: 10.7189/jogh.06.010701
Background: Kangaroo mother care (KMC), often defined as skin-to-skin contact between a mother and her newborn, frequent or exclusive breastfeeding, and early discharge from the hospital has been effective in reducing the risk of mortality among preterm and low birth weight infants. Research studies and program implementation of KMC have used various definitions.
Objectives: To describe the current definitions of KMC in various settings, analyze the presence or absence of KMC components in each definition, and present a core definition of KMC based on common components that are present in KMC literature.
Methods: We conducted a systematic review and searched PubMed, Embase, Scopus, Web of Science, and the World Health Organization Regional Databases for studies with key words "kangaroo mother care", "kangaroo care" or "skin to skin care" from 1 January 1960 to 24 April 2014. Two independent reviewers screened articles and abstracted data.
Findings: We screened 1035 articles and reports; 299 contained data on KMC and neonatal outcomes or qualitative information on KMC implementation. Eighty-eight of the studies (29%) did not define KMC. Two hundred and eleven studies (71%) included skin-to-skin contact (SSC) in their KMC definition, 49 (16%) included exclusive or nearly exclusive breastfeeding, 22 (7%) included early discharge criteria, and 36 (12%) included follow-up after discharge. One hundred and sixty-seven studies (56%) described the duration of SSC.
Conclusions: There exists significant heterogeneity in the definition of KMC. A large number of studies did not report definitions of KMC. Skin-to-skin contact is the core component of KMC, whereas components such as breastfeeding, early discharge, and follow-up care are context specific. To implement KMC effectively development of a global standardized definition of KMC is needed.

Publication types
- Systematic Review
- Attitude to Health
- Infant, Newborn
- Kangaroo-Mother Care Method / classification*
- Mothers / psychology*
- Physical Stimulation / methods*
- Open access
- Published: 18 November 2022
What influences the implementation of kangaroo mother care? An umbrella review
- Qian Cai 1 , 2 ,
- Dan-Qi Chen 1 , 2 ,
- Hua Wang 2 ,
- Yue Zhang 2 ,
- Rui Yang 1 , 2 ,
- Wen-Li Xu 3 &
- Xin-Fen Xu 2 , 3
BMC Pregnancy and Childbirth volume 22 , Article number: 851 ( 2022 ) Cite this article
4081 Accesses
5 Citations
4 Altmetric
Metrics details
Kangaroo mother care (KMC) is an evidence-based intervention that reduces morbidity and mortality in preterm infants. However, it has not yet been fully integrated into health systems around the world. The aim of this study is to provide a cogent summary of the evidence base of the key barriers and facilitators to implementing KMC.
An umbrella review of existing reviews on KMC was adopted to identify systematic and scoping reviews that analysed data from primary studies. Electronic English databases, including PubMed, Embase, CINAHL and Cochrane Library, and three Chinese databases were searched from inception to 1 July 2022. Studies were included if they performed a review of barriers and facilitators to KMC. Quality assessment of the retrieved reviews was performed by at least two reviewers independently using the Joanna Briggs Institute (JBI) critical appraisal checklist and risk of bias was assessed with the Risk of Bias Assessment Tool for Systematic Reviews (ROBIS) tool. This umbrella review protocol was documented in the PROSPERO registry (CRD42022327994).
We generated 531 studies, and after the removal of duplicates and ineligible studies, six eligible reviews were included in the analysis. The five themes identified were environmental factors, professional factors, parent/family factors, access factors, and cultural factors, and the factors under each theme were divided into barriers or facilitators depending on the specific features of a given scenario.
Conclusions
Support from facility management and leadership and well-trained medical staff are of great significance to the successful integration of KMC into daily medical practice, while the parents of preterm infants and other family members should be educated and encouraged in KMC practice. Further research is needed to propose strategies and develop models for implementing KMC.
Peer Review reports
According to reports from the World Health Organization (WHO), with the development of assisted reproductive technology and the improvement of emergency and critical care technology, the incidence of premature birth is rising, and premature birth has become a global problem [ 1 ]. Nearly fifteen million preterm infants are born each year, and more than one million of them unfortunately die each year [ 2 ]. According to statistics, complications of preterm birth directly account for more than 35% of all neonatal deaths, while the proportion of deaths indirectly caused by preterm birth is even higher because preterm birth increases the risk of infant death from infection [ 3 ]. Many surviving preterm infants encounter plenty of problems due to premature birth, such as sensory impairment and cognitive and language impairment [ 4 , 5 , 6 ]. In addition, the birth of preterm infants may cause a substantial emotional crisis and economic cost to the family, as well as have an impact on public sector services such as education and other social support systems [ 7 , 8 ]. For mothers, preterm birth may also cause a range of perinatal diseases [ 5 , 9 ]. Therefore, effective evidence-based interventions that can be implemented at scale are urgently needed to reduce the incidence of preterm birth complications and neonatal mortality.
Kangaroo mother care (KMC) is one such evidence-based life-saving intervention for preterm infants [ 10 ]. In KMC, the mother (or father) puts her (his) naked preterm infant on her (his) chest in the same way as kangaroo parenting so that the preterm infant is capable of having early, continuous and long-term skin-to-skin contact with his or her mother (father); in addition, measures such as exclusive breastfeeding or breastfeeding, early discharge, and follow-up after discharge are taken for the preterm infants [ 11 , 12 ]. Compared with the conventional nursing mode, KMC is not only able to maintain the body temperature of preterm infants but also significantly reduces the risk of death in low-birth-weight infants by 36% while significantly reducing the risk of sepsis, hypoglycaemia, and hypothermia [ 13 ]. Numerous studies have shown that KMC is a safe, effective, and multifaceted intervention with many short-term and long-term positive effects for preterm infants, such as stabilizing the neonatal physiological state, enhancing immunity, increasing exclusive breastfeeding rates, and promoting mother-infant bonding [ 14 , 15 , 16 , 17 ].
Despite the clear benefits of KMC, this intervention has not yet been fully integrated into health systems around the world [ 18 , 19 ]. There are many barriers impeding the implementation of the KMC, including but not limited to lack of support from family members, lack of parental information, and lack of tools and resources [ 20 , 21 , 22 , 23 ]. Several studies have identified facilitators that may contribute to the implementation of KMC, such as providing KMC training programmes for parents and encouraging physicians to recommend KMC to parents [ 24 , 25 , 26 ]. Undoubtedly, a better understanding of these barriers and facilitators can optimize the implementation of KMC.
Studies on the subject of KMC have developed over many years, with extensive studies from around the world and several systematic reviews on KMC published. These studies spanned different clinical settings, and there are studies that have explored the influencing factors of KMC from different perspectives, such as caregivers (e.g., parents and families) and healthcare workers [ 27 , 28 , 29 ]. A certain number of barriers and facilitators have been identified in these studies. However, the complexity and diversity of conventional studies make KMC difficult to describe and understand and impose challenges for health professionals and administrators who try to apply KMC in health systems [ 22 , 30 ]. Therefore, it is necessary to robustly summarize the evidence base to identify and elucidate key barriers and facilitators to the implementation of KMC.
One available approach is the umbrella review, which involves the synthesis of existing reviews, enabling researchers to collect evidence from multiple healthcare facilities instead of conducting systematic reviews at each facility. Essentially, an umbrella review is a review of existing reviews to provide an overview of the available evidence on a specific topic and allow comparisons of published reviews [ 31 ]. Furthermore, an umbrella review is capable of compiling evidence bases related to specific issues in a relatively short time frame [ 32 ]. We adopted this comprehensive assessment approach to outline factors that may facilitate or inhibit KMC implementation and expansion.
Protocol and registration
A protocol was prospectively developed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) guidelines [ 33 ]. Following current recommendations, the protocol was made openly available through registration with the PROSPERO International Prospective Register of Systematic Reviews platform (registration number CRD42022327994).
Study design
This review was conducted according to the rules for conducting umbrella reviews and published approach [ 32 , 34 ], and was reported following the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA 2020) statement [ 35 ]. The PRISMA checklist is shown in Additional file 1 .
Search strategy
Electronic databases, including PubMed, the Cochrane Database of Systematic Reviews, EMBASE, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the China National Knowledge Infrastructure (CNKI, for Chinese literature), SinoMed (for Chinese literature), and WAN FANG DATA (for Chinese literature), were searched to identify systematic reviews and meta-analyses (published from database inception to 1 July 2022.) of the factors influencing the implementation of KMC in preterm infants. Additionally, we manually searched reference lists from the screened articles to avoid the omission of any related articles. Also, we searched Google Scholar and OpenGrey for grey literature.
The search terms were constructed by combining subject terms and free words, while the language was limited to Chinese or English. The English search terms used were “prematur*/preterm*/premie*/neonat*/infant*/newborn*/low birth weight/LBW/ NICU”, “kangaroo mother care/kangaroo mother method/kangaroo care/kangaroo attachment/kangaroo contact/KMC/KC/skin-to-skin care/skin-to-skin contact/SSC/mother-infant contact”, and “systematic review/meta-analys”, and “早产儿/新生儿/低出生体重儿”“袋鼠护理/袋鼠式护理/皮肤接触”“系统评价/Meta分析/荟萃分析” were adopted as the Chinese search terms. More details of the search strategies are shown in Additional file 2 .
Inclusion criteria
This umbrella review included studies published in peer-reviewed journals and grey literature that addressed the research question. Articles were included if they were published in Chinese, English or in other language with the English version; identified factors impacting KMC implementation, including barriers and facilitators as primary or secondary objectives; and were a systematic review or meta-analysis. Moreover, to retrieve valuable information about the subject under study, we also decided to include scoping reviews, a type of review study that uses a systematic method of searching for information with the aim of accumulating as much evidence as possible and mapping the results. Screening of the searched articles and their subsequent full-text review were carried out based on the following inclusion criteria: (a) studies that used a systematic/scoping review and/or meta-analysis design, (b) studies focused on preterm infants with KMC, and (c) studies that aimed to identify factors associated with KMC implementation. In addition, articles fulfilling the following criteria were excluded: (a) reviews written in any language other than English or Chinese, (b) duplicate publications, and (c) articles or conference abstracts for which the full text was not available.
Study selection
Two researchers independently screened the literature according to the inclusion and exclusion criteria. In case of disagreement, the two researchers first discussed and attempted to resolve the disagreement. If the disagreement could not be resolved, a third researcher was invited to adjudicate. The literature screening process was as follows: (1) Endnote (a literature management software) was used to remove duplicate records; (2) the title and abstract of the articles were read in Endnote, and those that were not related to the subject, population and literature type were removed; (3) the full text of the remaining articles was downloaded, excluding those for which the full text could not be obtained; and (4) the full texts of the articles were read to further exclude literature according to the standard cited in the second step. The study selection process is summarized in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Quality assessment
The quality of the included reviews was assessed using the Joanna Briggs Institute (JBI) critical appraisal checklist for systematic reviews and research syntheses [ 36 ]. This assessment tool comprises 11 items, and the evaluation criteria for each item are “yes”, “no”, “unclear” or “not applicable”. Two members independently assessed the retrieved articles. Any disagreement between them was resolved by a third investigator.
Risk of bias assessment
Risk of bias of the included studies was evaluated by two reviewers using the Risk of Bias Assessment Tool for Systematic Reviews (ROBIS) [ 37 ]. In case of disagreement, a third reviewer was consulted until a final decision was made. ROBIS assesses four domains: 1) study eligibility criteria; 2) identification and selection of studies; 3) data collection and study appraisal; and 4) synthesis and findings. Each domain consists of five to six questions with six possible options: Yes, Probably yes, Probably No, No, Not indicated or Not applicable.
Data extraction
Two researchers independently used a unified Excel form that served as a data extraction sheet used to extract variables that were relevant to the scope of the current review, and another researcher verified the accuracy of the data extraction and quality assessment of all the included reviews. The extracted variables included the type of review, years covered, the total number of studies included in the review, country of origin, settings, aims/objectives and participants. As the aim was to provide a broad overview, all barriers and facilitators in all of the reviews were extracted except for those that were infrequently reported (i.e., those reported by only a few studies).
Data synthesis
After the data were extracted, a qualitative content analysis of the factors impacting KMC implementation was undertaken by the researcher. Each review article was read carefully to identify and extract the reported barriers and facilitators, and the researcher prepared the tables to summarize the data of all articles (see Additional file 3 ). The main key factors extracted from the articles were grouped and classified into themes to enhance the comprehension of the results outcomes. This classification of findings was performed based on the identified factors from the studies included in this review. Any uncertainties regarding the thematic categorizations were resolved through discussion and consensus by the reviewers.
Five hundred and thirty one hits retrieved in the initial search were exported into the reference management software Endnote, and 300 of them was left after duplicate records were excluded. A total of 285 references whose subject and theme were not matched were removed after title and abstract screening. Six eligible reviews were included after further full-text screening of the remaining 15 articles, as shown in Fig. 1 .
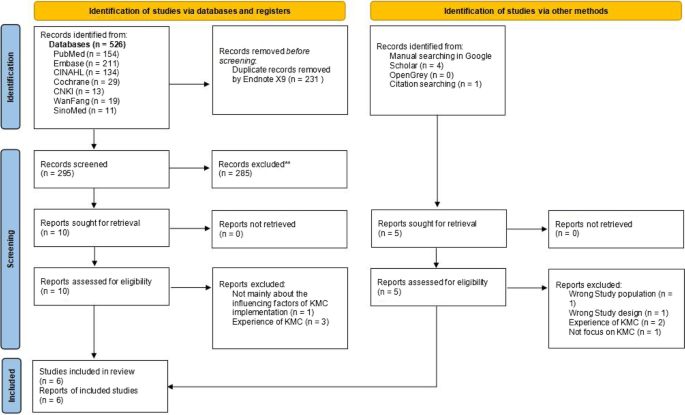
PRISMA flow diagram of barriers and facilitators to implementing KMC
Study characteristics
Table 1 provides an overview of five systematic reviews and one scope review related to KMC implementation as of July 1, 2022, all of which were published in 2015 and later, indicating this topic is relatively fresh. Two of the six articles described barriers and facilitators of KMC implementation from the perspective of caregivers of preterm infants [ 27 , 39 ]; one article explored these influencing factors from the the perspective of healthcare workers [ 28 ]; and the remaining articles discussed the factors affecting KMC implementation from both the perspectives of healthcare workers and parents of preterm infants [ 29 , 38 , 40 ].
The number of studies included in each review varied significantly, which often depended on the inclusion scope of the review [ 27 , 28 , 29 , 38 , 39 , 40 ]. For instance, two most recently published reviews included a smaller number of studies as it defined a specific study area [ 29 , 39 ]. Most of the studies included in the reviews were carried out in low-and middle-income counties and were conducted in health facility.
The methodological quality of the included 6 articles was evaluated by the JBI critical appraisal checklist. The ninth item “Was the likelihood of publication bias assessed” for all the included articles was “No” because publication bias are not assessed in all the included reviews. As the tools for evaluating the quality of the included studies and how to evaluate the quality of the included studies were not described in the two studies conducted by Seidman et al. [ 38 ] and Mathias et al. [ 39 ], so the fifth item “Were the criteria for appraising studies appropriate” and the sixth item “Was critical appraisal conducted by two or more reviewers independently” for these two studied was “No”, and the evaluation results of the remaining items were all “Yes”. The results of the quality appraisal of all the included studies are displayed in Additional file 4 .
After applying the ROBIS tool for risk of bias evaluation, of the six included systematic reviews, four were evaluated to have a high bias risk [ 27 , 28 , 38 , 40 ], and two present an unclear bias risk [ 29 , 39 ] (see Additional file 5 ). Main concerns regarding this aspect were related to (a) limiting searches with language restrictions; (b) lack of risk of bias evaluation; and (c) selection and data extraction not done in duplicate.
Barriers and facilitators of KMC
The five themes identified were environmental factors, professional factors, parent/family factors, access factors, and cultural factors. The subfactors under each theme were divided into barriers or facilitators according to the descriptions provided in the included reviews. A brief summary of the barriers and facilitators identified under each theme is presented in Table 2 . These are described in more detail below.
Environmental factors
This theme comprised facility conditions, resources and materials, and the healthcare system. Facility conditions mainly refer to hardware support in medical institutions, the most common factors being space and privacy. Lack of privacy and insufficient space and supplies directly hinder the implementation of KMC [ 27 , 28 , 29 , 38 , 39 , 40 ], while access to private space/privacy screens and sufficient space and supplies are key facilitators for the implementation of KMC [ 27 , 28 , 29 , 40 ]. In addition, factors such as temperature stability and a quiet and relaxed atmosphere in clinical facilities are conducive to the implementation of KMC [ 27 , 28 , 40 ]. Resources and materials refer to the environmental software support mainly related to resource management and material access. The most common barrier is a lack of KMC guidelines or protocols in the clinical unit [ 27 , 28 , 29 , 38 ], while the implementation of KMC would be enhanced if the clinical unit adopted KMC guidelines or protocols and displayed KMC pictures/posters, etc. [ 28 , 29 , 39 ]. The healthcare system mainly involves educational and policy factors. Inadequate/inconsistent training and unsupportive staffing policies are barriers to KMC implementation [ 28 , 29 , 39 , 40 ], while the integration of KMC into the healthcare curriculum and KMC-related policies are important facilitators for KMC implementation [ 29 , 40 ].
Professional factors
This theme encompassed three subthemes: professional perception, professional characteristics, and professional management. The main barriers under this theme included medical staff’s lack of belief in the efficacy or importance of the KMC [ 38 , 40 ] and their perceptions that KMC is unsafe [ 28 , 39 ] and imposes extra workload on them [ 38 ], the limited level of experience and knowledge of health care workers [ 28 , 29 , 38 ] and lack of communication with each other [ 28 ], high staff and leadership turnover [ 28 , 40 ] and lack of leadership and management support [ 28 , 38 , 40 ]. The main facilitators under this theme included medical staff’s belief in KMC benefits [ 28 , 29 , 40 ] and their sufficient experience, passion, and willingness to implement KMC [ 28 , 29 , 39 ]; leadership and management support [ 29 , 40 ]; and multiple health worker support [ 28 , 39 ].
Parent/family factors
This theme involved parental perception and motivation, parenting capacity, and parental support and empowerment. Experienced and perceived discomfort [ 29 , 39 ], a lack of awareness of the benefits of KMC [ 27 , 29 , 38 , 39 ], and fear/anxiety of hurting the infant [ 38 ] were the most frequently identified barriers to the implementation of KMC. Parenting capacity mainly refers to the health state of the parents of preterm infants. Medical issues such as pain/fatigue [ 27 , 38 , 40 ] and postpartum depression [ 27 , 29 , 38 ] and lack of confidence and knowledge on KMC [ 39 ] were the most common barriers. Support and empowerment refer to the availability of support from family members [ 27 , 29 , 38 , 39 , 40 ], medical staff [ 28 , 29 , 38 , 39 , 40 ], community [ 39 , 40 ], and peers [ 28 , 29 ], which facilitates the implementation of KMC and hinders implementation otherwise.
Access factors
This theme involved time, location, and financing. For medical staff, time was a key barrier; staff perceived that the implementation of KMC would increase their workload [ 28 , 29 , 38 , 40 ] and reduce time with other critical patients [ 28 , 40 ], and they had difficulty finding time for training [ 40 ]. For the parents of preterm infants, commuting from home and the medical unit was another barrier that caregivers were unable to devote sufficient time in KMC practice due to long commutes [ 27 ] or dealing with heavy household chores [ 39 ]. The costs of transportation, accommodation renting, and KMC implementation in the clinical ward were the immediate challenges [ 27 , 38 , 40 ]. Lower hospital costs to family [ 27 , 29 , 40 ], lower cost for health system [ 29 ] and unlimited visitation hours [ 27 , 28 , 40 ] were conducive to the implementation of KMC.
Cultural factors
This theme comprised traditional newborn care, traditional mindset, and gender roles. Traditional newborn care approaches, such as traditional bathing, carrying and breastfeeding practices [ 27 , 28 , 40 ], and the type of wrap [ 39 ] were identified as barriers to the implementation of KMC. However, some aspects of newborn care facilitated the implementation of KMC, i.e., advising mothers to delay bathing [ 28 ]. Some mindsets such as feeling ashamed of having a preterm infant [ 27 , 38 , 40 ], believing that skin-to-skin contact between the preterm infants and their caregivers was inappropriate [ 29 , 38 , 39 ] and considering KMC to be taboo [ 39 ] were identified barriers to the KMC implementation. Additionally, gender inequality existing in the division of labour between fathers and mothers [ 27 , 38 ] was not conducive to the implementation of KMC that KMC was regarded as a role responsibility of the mother, and the father was not allowed to participate in KMC [ 38 , 39 , 40 ] .
Our umbrella review highlighted different factors, each factor comprising barriers and facilitators, that influence the implementation of KMC, provide decision-makers in healthcare with an overview of the field and provide information for the implementation of KMC. All of the included reviews were published in 2015 or later, which confirms the growth and interest in the field of KMC. However, there is considerable heterogeneity in the evidence base on KMC, which makes translation into practice challenging.
Factors related to facility conditions, mainly including lack of privacy and insufficient space and supplies, were mentioned in all six included reviews, which might be related to the operation characteristics of KMC. Skin-to-skin contact is the most important part of the KMC procedure, which requires parents to undress their upper bodies and put their preterm infants on their chests, which is why a suitable physical environment is of great significance [ 11 , 12 ]. Studies have reported that mothers felt uncomfortable and exposed due to the continuous coming and going of medical staff during KMC when insufficient KMC private space was provided, which has proved to be a serious barrier affecting the implementation of KMC in many countries around the world [ 41 , 42 , 43 ]. Therefore, medical units should strive to provide enough quiet, comfortable, and private space for NICUs to implement KMC. Apart from physical facility conditions, resources and materials were another factor. Limited by facility space and human resources, some hospitals in China had to perform intermittent KMC instead of continuous KMC [ 44 ]. A multicountry analysis of health system bottlenecks from 12 African and Asian countries reported that insufficient essential supplies in facilities to support KMC was a barrier to the implementation of KMC [ 21 ].
KMC should be systematically implemented within a facility in accordance with relevant rules and regulations, for example, by adopting standard checklists for mothers and infants to ensure orderly and standardized KMC implementation. In a majority of the hospitals, nurses were required to commit to KMC-related tasks such as KMC recording, assessment, and data monitoring due to the lack of relevant rules and regulations, which meant an extra workload for the nurses [ 45 , 46 ]. Studies have shown that human resource challenges, record keeping, and data collection are barriers to KMC implementation in countries such as Malawi and Indonesia [ 28 , 47 ]. Documentation and annotation of KMC implementation were still not common practices in NICUs, while KMC-related information was imported through electronic medical records in most cases [ 28 , 48 ]. Chan et al. noted that the implementation of KMC was promoted when medical units improved their electronic medical records to allow nurses to record the onset and duration of KMC [ 28 ]. Therefore, the Ministry of Health and government agencies should formulate practical KMC implementation guidelines based on local conditions, and medical units should also formulate and standardize KMC implementation guidelines and programs to promote the implementation of KMC.
Lack of proper leadership, insufficient professionalism of personnel, and insufficient training were also obstacles to KMC implementation. A study on the introduction of KMC in Indonesian hospitals found that government support, hospital management, staff acceptance, and training were identified as key facilitators of KMC implementation [ 47 ]. In some regions, KMC-specific training programs were provisioned for medical staff by the government [ 49 ]. However, the number of staff participating in the training is very limited due to the long distance between the training site and the medical unit and the shortage of personnel in the hospitals, although many medical personnel were willing to participate in the training [ 42 , 50 ]. In other words, although policymakers and decision-makers tried to provide assistance and intervention programs for healthcare workers, they did not anticipate these barriers to attendance. Of course, the support from hospital administrators and leadership could provide more space and human resources to provision KMC, optimize or update the staffing configuration of neonatal care nurses, strengthen the professionalization of neonatal care by healthcare workers, and improve healthcare staff’s attitudes towards and perceptions of KMC [ 43 , 51 ].
The attitudes of the health caregivers towards KMC were also a factor influencing the adoption of KMC for parents. If there were staff in the hospital who were familiar with KMC and willing to educate parents on KMC knowledge, it would help parents of preterm infants to acquire KMC-related knowledge, which would promote KMC preferences and the early initiation of KMC [ 52 , 53 ]. Correspondingly, insufficient awareness of KMC and infant health among parents/family members was a barrier to the practice of KMC [ 22 ]. Despite the generally low awareness of KMC, the reviews reported that it was relatively easier to train mothers on KMC practices and that they were more adherent to KMC practices after understanding and accepting KMC [ 54 ]. Perceived, observed, and experienced effects of KMC could provide comfort and satisfaction to the parents of preterm infants, which promotes KMC use, whereas KMC is inhibited if parents and/or preterm infants experience KMC-related discomfort.
Lack of assistance is a barrier to KMC practice, whereas support from family, friends, and other mothers is a facilitator to the implementation of KMC. There were many different forms of support. For example, family members took turns embracing the preterm infants to free the mother from this practice [ 55 , 56 ]. Evidence from the literature has suggested that emotional support, as well as support and help with household chores, is also a facilitator for mothers [ 57 , 58 ]. Kangaroo nursing can be implemented not only by mothers but also by fathers, grandfathers, grandmothers, and other family members of preterm infants [ 43 , 59 ], and if family members do not understand this point, preterm infants might lose the opportunity to receive kangaroo care [ 60 ]. Therefore, different educational approaches should be adopted to educate families of preterm infants about their roles in KMC, with additional health promotions and activities targeting grandparents and other family members about the benefits of KMC and the significance of supporting mothers, which may increase the number of people receiving KMC.
However, KMC is not suitable for all situations. In some clinical scenarios where mothers of preterm infants have special health conditions, it could be very challenging to train mothers and facilitate KMC implementation. These challenges include the infant being too difficult to embrace, the infant being too heavy, and the mother experiencing chest or back discomfort or pain/fatigue [ 38 ]. The reviews showed that mothers’ medical conditions, including postepisiotomy pain repair [ 61 ], postcesarean recovery [ 62 ], postpartum depression and general maternal illness [ 48 ], were another challenge for KMC practice. Additionally, mothers may mentally struggle with KMC practices, including positioning problems (difficulty sleeping on the chest with infants), breast milk expression, and other breastfeeding-related issues [ 57 , 63 ]. In this case, family support and father involvement make a great difference [ 64 ]. Postpartum depression is a barrier to the implementation of KMC, but interestingly, mothers who practised KMC experienced reduced symptoms of postpartum depression [ 65 , 66 ].
Inviting parents to the NICU to perform KMC could result in extra costs. Studies performed in low-income countries have shown that commuting between home and KMC wards was a barrier to the implementation of KMC, and fees for mothers and babies staying in KMC wards were also considered a barrier [ 39 , 67 ]. Studies have shown that higher economic status is more conducive to the implementation of KMC [ 40 , 43 ]. Therefore, accessing financial resources from hospital administration and/or parental health insurance to facilitate KMC would be a necessary part of KMC expansion. Meanwhile, it is necessary to consider how to reduce hospital charges or provide certain transportation subsidies for families with infants whose hospitalization time exceeds the average length of stay. Limited visiting time in the NICU is another obstacle to the implementation of KMC, especially in the case of closed management such as the NICU in China. Extending the visit time could increase the adoption of KMC to some extent [ 68 , 69 ].
Different cultures, religions, and traditional beliefs in different countries influence perceptions of preterm infants and KMC. In many countries, carrying infants on the chest rather than on the back is considered inappropriate [ 41 ], and some cultures believe that skin-to-skin contact between an infant and his or her caregiver is not appropriate [ 27 ]. Understanding these culturally specific barriers, it is of great importance to adapt KMC promotion programmes to the needs of the population. In some countries, mothers are ridiculed for giving birth to preterm infants, which results in stigma [ 55 , 70 ]. Studies have reported that stigma about preterm infants creates anxiety and guilt in mothers, causing them to abandon their infants, which is a factor hindering the implementation of KMC [ 27 , 38 ]. Muddu et al. [ 71 ] found that fondness was an enabler for parents to accept their preterm infants and utilize KMC to support the improvement of their preterm infants’ health. Cultural barriers also encompass the practice of postpartum confinement and traditional resistance to confinement from grandparents and community members. Most mothers are advised to stay home after delivery in China and India [ 72 , 73 ], which has potential health benefits for mothers and newborns, but it also causes mothers and families to be hesitant to adopt KMC.
Traditional gender role factors were identified as barriers to male participation in neonatal care. KMC was regarded as a breach of social duty or responsibility by mothers in some countries where it is believed that mothers should take care of the family, and when mothers comply with this social duty and gender responsibility, the implementation of KMC becomes a challenge [ 74 ]; meanwhile, fathers are not encouraged to participate in KMC implementation in such cultures. Therefore, it is of great significance to develop interventions on how to encourage fathers to participate in KMC and reduce the stigma surrounding this infant care strategy [ 75 ]. As Dumbaugh et al. [ 76 ] pointed out, the inclusion of males in neonatal care must be done in a way that empowers women. Fathers who are successfully involved in KMC might become peer mentors or examples for others to address the problem of fathers’ reluctance to participate in neonatal care. The name of the intervention, “kangaroo mother care”, could also be modified, e.g., to “kangaroo care”, so that it does not directly imply that the practice is performed only by mothers.
Limitations
The findings in this manuscript are subject to some limitations. First, due to resource constraints, we only searched for English and Chinese reviews, and there was a possibility of missing some relevant studies. Another limitation of the umbrella review approach was that it could only report on what researchers have investigated and published [ 32 ]. For example, some factors might be highly influential, but if they were not adequately investigated in the included studies, they might be reported as less important, or they might not even be included in the review. To mitigate this issue, other key literature not identified in this review was actively referenced. Finally, a potential limitation to the umbrella review approach could be the risk that bias is transmitted upwards from primary studies to the reviews and then to the umbrella review.
Recommendations for future research
KMC implementation issues are likely to differ among different regions, so there remains a need for further research into sustainable development mechanisms in varied settings to promote the adoption of KMC. The generalizability of the findings worldwide and their translation into practice is uncertain. Most of the studies focused at the facility level, such as the NICU, which highlights the lack of community-level studies. Therefore, further research is needed to explore the factors influencing KMC implementation at home and in the community. Male involvement was identified as a facilitator to KMC implementation, but there was no study discussing hindrance factors of father involvement in care specifically. Therefore, further research is also needed to explore the hindrance and/or facilitating factors of male involvement in KMC care from the perspective of fathers. In addition, further research is also needed to test models for addressing barriers and supporting facilitators to promote and implement context-specific health system changes for greater uptake of KMC.
KMC is a complicated intervention that encounters unique barriers and facilitators in different aspects of healthcare systems. Our umbrella review prioritizes the main factors influencing KMC implementation and highlights some key areas that implementers and implementation researchers may need to focus on. KMC should be implemented more systematically and continuously to strengthen and expand its adoption.
The parents of preterm infants and other family members, the medical unit, and the medical staff contribute to a dynamic whole as a triangle, that are closely linked with one another. Support from facility management and leadership and well-trained medical staff are of great significance to the successful integration of KMC into daily medical practice, while the parents of preterm infants and other family members should be educated and encouraged to adopt KMC practice. Effectively integrating KMC into current health systems by addressing barriers and building trust will greatly improve neonatal survival rates.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request. All data were extracted from published systematic reviews and meta-analyses.
World Health Organization. Preterm birth. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/preterm-birth (Accessed 13 May 2022).
Google Scholar
Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7(1):e37–46. https://doi.org/10.1016/S2214-109X(18)30451-0 .
Article PubMed Google Scholar
United Nations Inter-agency Group for Child Mortality Estimation (UN IGME), WHO, World Bank Group and United Nations. Levels & Trends in Child Mortality: Report 2019, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation: United Nations Children’s Fund; 2019. Available online: https://www.unicef.org/reports/levels-and-trends-child-mortality-report-2019 (Accessed 16 May 2022)
Allotey J, Zamora J, Cheong-See F, Kalidindi M, Arroyo-Manzano D, Asztalos E, et al. Cognitive, motor, behavioural and academic performances of children born preterm: a meta-analysis and systematic review involving 64 061 children. BJOG. 2018;125(1):16–25. https://doi.org/10.1111/1471-0528.14832 .
Article CAS PubMed Google Scholar
Ream MA, Lehwald L. Neurologic Consequences of Preterm Birth. Curr Neurol Neurosci Rep. 2018;18(8):48. https://doi.org/10.1007/s11910-018-0862-2 .
Dean B, Ginnell L, Ledsham V, Tsanas A, Telford E, Sparrow S, et al. Eye-tracking for longitudinal assessment of social cognition in children born preterm. J Child Psychol Psychiatry. 2021;62(4):470–80. https://doi.org/10.1111/jcpp.13304 .
Hodek JM, von der Schulenburg JM, Mittendorf T. Measuring economic consequences of preterm birth - Methodological recommendations for the evaluation of personal burden on children and their caregivers. Health Econ Rev. 2011;1(1):6. https://doi.org/10.1186/2191-1991-1-6 .
Article PubMed PubMed Central Google Scholar
Behrman RE, Butler AS, Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes. Preterm Birth: Causes, Consequences, and Prevention. Washington (DC): National Academies Press (US). 2007.
Trumello C, Candelori C, Cofini M, Cimino S, Cerniglia L, Paciello M, et al. Mothers’ Depression, Anxiety, and Mental Representations After Preterm Birth: A Study During the Infant's Hospitalization in a Neonatal Intensive Care Unit. Front Public Health. 2018;6:359. https://doi.org/10.3389/fpubh.2018.00359 .
World Health Organization. WHO Recommendations on Interventions to Improve Preterm Birth Outcomes. Geneva: World Health Organization; 2015. Available online: https://www.who.int/publications/i/item/9789241508988 (Accessed 16 May 2022)
World Health Organization. Kangaroo mother care: a practical guide. Geneva: World Health Organization; 2003. Available online: https://www.who.int/publications/i/item/9241590351 (Accessed 17 May 2022).
Chan GJ, Valsangkar B, Kajeepeta S, Boundy EO, Wall S. What is kangaroo mother care? Systematic review of the literature. J Glob Health. 2016;6(1):010701. https://doi.org/10.7189/jogh.06.010701 .
Boundy EO, Dastjerdi R, Spiegelman D, Fawzi WW, Missmer SA, Lieberman E, et al. Kangaroo Mother Care and Neonatal Outcomes: A Meta-analysis. Pediatrics. 2016;137(1):e20152238. https://doi.org/10.1542/peds.2015-2238 .
Article PubMed Central Google Scholar
Conde-Agudelo A, Díaz-Rossello JL. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst Rev. 2016;2016(8):CD002771. https://doi.org/10.1002/14651858.CD002771 .
Sharma D, Farahbakhsh N, Sharma S, Sharma P, Sharma A. Role of kangaroo mother care in growth and breast feeding rates in very low birth weight (VLBW) neonates: a systematic review. J Matern Fetal Neonatal Med. 2019;32(1):129–42. https://doi.org/10.1080/14767058.2017.1304535 .
Cho ES, Kim SJ, Kwon MS, Cho H, Kim EH, Jun EM, et al. The Effects of Kangaroo Care in the Neonatal Intensive Care Unit on the Physiological Functions of Preterm Infants, Maternal-Infant Attachment, and Maternal Stress. J Pediatr Nurs. 2016;31(4):430–8. https://doi.org/10.1016/j.pedn.2016.02.007 .
Furman L. Kangaroo mother care 20 years later: connecting infants and families. Pediatrics. 2017;139(1):e20163332. https://doi.org/10.1542/peds.2016-3332 .
Stefani G, Skopec M, Battersby C, Matthew H. Why is Kangaroo Mother Care not yet scaled in the UK? A systematic review and realist synthesis of a frugal innovation for newborn care. BMJ Innov. 2022;8:9–20. https://doi.org/10.1136/bmjinnov-2021-000828 .
Article Google Scholar
Salim N, Shabani J, Peven K, Rahman QS, Kc A, Shamba D, et al. Kangaroo mother care: EN-BIRTH multi-country validation study. BMC Pregnancy Childbirth. 2021;21(Suppl 1):231. https://doi.org/10.1186/s12884-020-03423-8 .
Bergh AM, Kerber K, Abwao S, de Graft Johnson J, Aliganyira P, Davy K, et al. Implementing facility-based kangaroo mother care services: lessons from a multi-country study in Africa. BMC Health Serv Res. 2014;14:293. https://doi.org/10.1186/1472-6963-14-293 .
Vesel L, Bergh AM, Kerber KJ, Valsangkar B, Mazia G, Moxon SG, et al. Kangaroo mother care: a multi-country analysis of health system bottlenecks and potential solutions. BMC Pregnancy Childbirth. 2015;15(Suppl 2):S5. https://doi.org/10.1186/1471-2393-15-S2-S5 .
Bilal SM, Tadele H, Abebo TA, Tadesse BT, Muleta M, W/Gebriel F, et al. Barriers for kangaroo mother care (KMC) acceptance, and practices in southern Ethiopia: a model for scaling up uptake and adherence using qualitative study. BMC Pregnancy Childbirth. 2021;21(1):25. https://doi.org/10.1186/s12884-020-03409-6 .
Saltzmann AM, Sigurdson K, Scala M. Barriers to Kangaroo Care in the NICU: A Qualitative Study Analyzing Parent Survey Responses. Adv Neonatal Care. 2022;22(3):261–9. https://doi.org/10.1097/ANC.0000000000000907 .
Mathias CT, Mianda S, Ginindza TG. Facilitating factors and barriers to accessibility and utilization of kangaroo mother care service among parents of low birth weight infants in Mangochi District, Malawi: a qualitative study. BMC Pediatr. 2020;20(1):355. https://doi.org/10.1186/s12887-020-02251-1 .
Maniago JD, Almazan JU, Albougami AS. Nurses’ Kangaroo Mother Care practice implementation and future challenges: an integrative review. Scand J Caring Sci. 2020;34(2):293–304. https://doi.org/10.1111/scs.12755 .
Cattaneo A, Amani A, Charpak N, De Leon-Mendoza S, Moxon S, Nimbalkar S, et al. Report on an international workshop on kangaroo mother care: lessons learned and a vision for the future. BMC Pregnancy Childbirth. 2018;18(1):170. https://doi.org/10.1186/s12884-018-1819-9 .
Smith ER, Bergelson I, Constantian S, Valsangkar B, Chan GJ. Barriers and enablers of health system adoption of kangaroo mother care: a systematic review of caregiver perspectives. BMC Pediatr. 2017;17(1):35. https://doi.org/10.1186/s12887-016-0769-5 .
Chan G, Bergelson I, Smith ER, Skotnes T, Wall S. Barriers and enablers of kangaroo mother care implementation from a health systems perspective: a systematic review. Health Policy Plan. 2017;32(10):1466–75. https://doi.org/10.1093/heapol/czx098 .
Kinshella MW, Hiwa T, Pickerill K, Vidler M, Dube Q, Goldfarb D, et al. Barriers and facilitators of facility-based kangaroo mother care in sub-Saharan Africa: a systematic review. BMC Pregnancy Childbirth. 2021;21(1):176. https://doi.org/10.1186/s12884-021-03646-3 .
Bergh AM, de Graft-Johnson J, Khadka N, Om'Iniabohs A, Udani R, Pratomo H, et al. The three waves in implementation of facility-based kangaroo mother care: a multi-country case study from Asia. BMC Int Health Hum Rights. 2016;16:4. https://doi.org/10.1186/s12914-016-0080-4 .
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39. https://doi.org/10.1186/s13643-018-0695-8 .
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–40. https://doi.org/10.1097/XEB.0000000000000055 .
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1 .
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Mental Health. 2018;21(3):95–100. https://doi.org/10.1136/ebmental-2018-300014 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Joanna Briggs Institute. Joanna Briggs Institute reviewers’ manual: 2017 edition. Australia: The Joanna Briggs Institute; 2017.
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34. https://doi.org/10.1016/j.jclinepi.2015.06.005 .
Seidman G, Unnikrishnan S, Kenny E, Myslinski S, Cairns-Smith S, Mulligan B, et al. Barriers and enablers of kangaroo mother care practice: a systematic review. PLoS One. 2015;10(5):e0125643. https://doi.org/10.1371/journal.pone.0125643 .
Article CAS PubMed PubMed Central Google Scholar
Mathias CT, Mianda S, Ohdihambo JN, Hlongwa M, Singo-Chipofya A, Ginindza TG. Facilitating factors and barriers to kangaroo mother care utilisation in low- and middle-income countries: A scoping review. Afr J Prim Health Care Fam Med. 2021;13(1):e1–e15. https://doi.org/10.4102/phcfm.v13i1.2856 .
Chan GJ, Labar AS, Wall S, Atun R. Kangaroo mother care: a systematic review of barriers and enablers. Bull World Health Organ. 2016;94(2):130–141J. https://doi.org/10.2471/BLT.15.157818 .
Charpak N, Ruiz-Peláez JG. Resistance to implementing kangaroo mother care in developing countries, and proposed solutions. Acta Paediatr. 2006;95(5):529–34. https://doi.org/10.1080/08035250600599735 .
Ferrarello D, Hatfield L. Barriers to skin-to-skin care during the postpartum stay. MCN Am J Matern Child Nurs. 2014;39(1):56–61. https://doi.org/10.1097/01.NMC.0000437464.31628.3d .
Yue J, Liu J, Williams S, Zhang B, Zhao Y, Zhang Q, et al. Barriers and facilitators of kangaroo mother care adoption in five Chinese hospitals: a qualitative study. BMC Public Health. 2020;20(1):1234. https://doi.org/10.1186/s12889-020-09337-6 .
Zhang B, Duan Z, Zhao Y, Williams S, Wall S, Huang L, et al. Intermittent kangaroo mother care and the practice of breastfeeding late preterm infants: results from four hospitals in different provinces of China. Int Breastfeed J. 2020;15(1):64. https://doi.org/10.1186/s13006-020-00309-5 .
Shah RK, Sainju NK, Joshi SK. Knowledge, Attitude and Practice towards Kangaroo Mother Care. J Nepal Health Res Counc. 2018;15(3):275–81. https://doi.org/10.3126/jnhrc.v15i3.18855 .
Adisasmita A, Izati Y, Choirunisa S, Pratomo H, Adriyanti L. Kangaroo mother care knowledge, attitude, and practice among nursing staff in a hospital in Jakarta, Indonesia. PLoS One. 2021;16(6):e0252704. https://doi.org/10.1371/journal.pone.0252704 .
Pratomo H, Uhudiyah U, Sidi IP, Rustina Y, Suradi R, Bergh AM, et al. Supporting factors and barriers in implementing kangaroo mother care in Indonesia. Paediatrica Indonesiana. 2012;52(1):43–50. https://doi.org/10.14238/pi52.1.2012.43-50 .
Lee HC, Martin-Anderson S, Dudley RA. Clinician perspectives on barriers to and opportunities for skin-to-skin contact for premature infants in neonatal intensive care units. Breastfeed Med. 2012;7(2):79–84. https://doi.org/10.1089/bfm.2011.0004 .
Sacks E, Bailey JM, Robles C, Low LK. Neonatal care in the home in northern rural Honduras: a qualitative study of the role of traditional birth attendants. J Perinat Neonatal Nurs. 2013;27(1):62–71. https://doi.org/10.1097/JPN.0b013e31827fb3fd .
Bergh AM, Rogers-Bloch Q, Pratomo H, Uhudiyah U, Sidi IP, Rustina Y, et al. Progress in the implementation of kangaroo mother care in 10 hospitals in Indonesia. J Trop Pediatr. 2012;58(5):402–5. https://doi.org/10.1093/tropej/fmr114 .
Yue J, Liu J, Zhao Y, Williams S, Zhang B, Zhang L, et al. Evaluating factors that influenced the successful implementation of an evidence-based neonatal care intervention in Chinese hospitals using the PARIHS framework. BMC Health Serv Res. 2022;22(1):104. https://doi.org/10.1186/s12913-022-07493-6 .
Deng Q, Zhang Y, Li Q, Wang H, Xu X. Factors that have an impact on knowledge, attitude and practice related to kangaroo care: National survey study among neonatal nurses. J Clin Nurs. 2018;27(21–22):4100–11. https://doi.org/10.1111/jocn.14556 .
Kinshella MW, Salimu S, Chiwaya B, Chikoti F, Chirambo L, Mwaungulu E, et al. “So sometimes, it looks like it's a neglected ward”: Health worker perspectives on implementing kangaroo mother care in southern Malawi. PLoS One. 2020;15(12):e0243770. https://doi.org/10.1371/journal.pone.0243770 .
Gill VR, Liley HG, Erdei C, Sen S, Davidge R, Wright AL, et al. Improving the uptake of Kangaroo Mother Care in neonatal units: A narrative review and conceptual framework. Acta Paediatr. 2021;110(5):1407–16. https://doi.org/10.1111/apa.15705 .
Nguah SB, Wobil PN, Obeng R, Yakubu A, Kerber KJ, Lawn JE, et al. Perception and practice of Kangaroo Mother Care after discharge from hospital in Kumasi, Ghana: a longitudinal study. BMC Pregnancy Childbirth. 2011;11:99. https://doi.org/10.1186/1471-2393-11-99 .
Kymre IG, Bondas T. Skin-to-skin care for dying preterm newborns and their parents--a phenomenological study from the perspective of NICU nurses. Scand J Caring Sci. 2013;27(3):669–76. https://doi.org/10.1111/j.1471-6712.2012.01076.x .
Chugh Sachdeva R, Mondkar J, Shanbhag S, Manuhar M, Khan A, Dasgupta R, et al. A Qualitative Analysis of the Barriers and Facilitators for Breastfeeding and Kangaroo Mother Care Among Service Providers, Mothers and Influencers of Neonates Admitted in Two Urban Hospitals in India. Breastfeed Med. 2019;14(2):108–14. https://doi.org/10.1089/bfm.2018.0177 .
Ariff S, Maznani I, Bhura M, Memon Z, Arshad T, Samejo TA, et al. Understanding Perceptions and Practices for Designing an Appropriate Community-Based Kangaroo Mother Care Implementation Package: Qualitative Exploratory Study. JMIR Form Res. 2022;6(1):e30663. https://doi.org/10.2196/30663 .
Kuo SF, Chen IH, Chen SR, Chen KH, Fernandez RS. The Effect of Paternal Skin-to-Skin Care: A Systematic Review and Meta-analysis of Randomized Control Trials. Adv Neonatal Care. 2022;22(1):E22–32. https://doi.org/10.1097/ANC.0000000000000890 .
Mu PF, Lee MY, Chen YC, Yang HC, Yang SH. Experiences of parents providing kangaroo care to a premature infant: A qualitative systematic review. Nurs Health Sci. 2020;22(2):149–61. https://doi.org/10.1111/nhs.12631 .
Brimdyr K, Widström AM, Cadwell K, Svensson K, Turner-Maffei C. A Realistic Evaluation of Two Training Programs on Implementing Skin-to-Skin as a Standard of Care. J Perinat Educ. 2012;21(3):149–57. https://doi.org/10.1891/1058-1243.21.3.149 .
Kymre IG, Bondas T. Balancing preterm infants’ developmental needs with parents’ readiness for skin-to-skin care: a phenomenological study. Int J Qual Stud Health Well-Being. 2013;8:21370. https://doi.org/10.3402/qhw.v8i0.21370 .
Blomqvist YT, Frölund L, Rubertsson C, Nyqvist KH. Provision of Kangaroo Mother Care: supportive factors and barriers perceived by parents. Scand J Caring Sci. 2013;27(2):345–53. https://doi.org/10.1111/j.1471-6712.2012.01040.x .
Filippa M, Saliba S, Esseily R, Gratier M, Grandjean D, Kuhn P. Systematic review shows the benefits of involving the fathers of preterm infants in early interventions in neonatal intensive care units. Acta Paediatr. 2021;110(9):2509–20. https://doi.org/10.1111/apa.15961 .
Kirca N, Adibelli D. Effects of mother-infant skin-to-skin contact on postpartum depression: A systematic review. Perspect Psychiatr Care. 2021;57(4):2014–23. https://doi.org/10.1111/ppc.12727 .
Scime NV, Gavarkovs AG, Chaput KH. The effect of skin-to-skin care on postpartum depression among mothers of preterm or low birthweight infants: A systematic review and meta-analysis. J Affect Disord. 2019;253:376–84. https://doi.org/10.1016/j.jad.2019.04.101 .
Blencowe H, Kerac M, Molyneux E. Safety, effectiveness and barriers to follow-up using an ‘early discharge’ Kangaroo Care policy in a resource poor setting. J Trop Pediatr. 2009;55(4):244–8. https://doi.org/10.1093/tropej/fmn116 .
Craig JW, Glick C, Phillips R, Hall SL, Smith J, Browne J. Recommendations for involving the family in developmental care of the NICU baby. J Perinatol. 2015;35(Suppl 1):S5–8. https://doi.org/10.1038/jp.2015.142 PMID: 26597804.
Calibo AP, De Leon MS, Silvestre MA, Murray JCS, Li Z, Mannava P, et al. Scaling up kangaroo mother care in the Philippines using policy, regulatory and systems reform to drive changes in birth practices. BMJ Glob Health. 2021;6(8):e006492. https://doi.org/10.1136/bmjgh-2021-006492 .
Hunter EC, Callaghan-Koru JA, Al Mahmud A, Shah R, Farzin A, Cristofalo EA, et al. Newborn care practices in rural Bangladesh: Implications for the adaptation of kangaroo mother care for community-based interventions. Soc Sci Med. 2014;122:21–30. https://doi.org/10.1016/j.socscimed.2014.10.006 .
Muddu GK, Boju SL, Chodavarapu R. Knowledge and awareness about benefits of Kangaroo Mother Care. Indian J Pediatr. 2013;80(10):799–803. https://doi.org/10.1007/s12098-013-1073-0 .
Wong J, Fisher J. The role of traditional confinement practices in determining postpartum depression in women in Chinese cultures: a systematic review of the English language evidence. J Affect Disord. 2009;116(3):161–9. https://doi.org/10.1016/j.jad.2008.11.002 .
Rao CR, Dhanya SM, Ashok K, Niroop SB. Assesment of cultural beliefs and practices during the postnatal period in a costal town of South India - A mixed method research study. Global J Med Public Health. 2014;3(5):1–8.
Opara PI, Okorie EMC. Kangaroo mother care: Mothers experiences post discharge from hospital. J Preg Neonatal Med. 2017;1(1):16–20. https://doi.org/10.35841/neonatal-medicine.1.1.16-20 .
Brotherton H, Daly M, Johm P, Jarju B, Schellenberg J, Penn-Kekana L, et al. “We All Join Hands”: Perceptions of the Kangaroo Method Among Female Relatives of Newborns in The Gambia. Qual Health Res. 2021;31(4):665–76. https://doi.org/10.1177/1049732320976365 .
Dumbaugh M, Tawiah-Agyemang C, Manu A, ten Asbroek GH, Kirkwood B, Hill Z. Perceptions of, attitudes towards and barriers to male involvement in newborn care in rural Ghana, West Africa: a qualitative analysis. BMC Pregnancy Childbirth. 2014;14:269. https://doi.org/10.1186/1471-2393-14-269 .
Download references
Acknowledgments
This research received no external funding.
Author information
Authors and affiliations.
Nursing Department, Zhejiang University School of Medicine, Hangzhou, Zhejiang, China
Qian Cai, Dan-Qi Chen & Rui Yang
Zhejiang University School of Medicine Women’s Hospital, No. 1 Xueshi Road, Shangcheng District, Hangzhou, 310006, Zhejiang Province, China
Qian Cai, Dan-Qi Chen, Hua Wang, Yue Zhang, Rui Yang & Xin-Fen Xu
Women’s Hospital School of Medicine Zhejiang University Haining Branch/Haining Maternity and Child Health Care Hospital, No. 6 Qinjian Road, Haizhou Street, Haining, 314400, Zhejiang Province, China
Wen-Li Xu & Xin-Fen Xu
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, QC, XFX and HW; Methodology, QC, DQC and YZ; Validation, QC, DQC and RY and YZ; Formal Analysis, QC; Resources, QC, YZ and WLX; Writing – Original Draft Preparation, QC; Writing – Review & Editing, QC, DQC, RY and XFX; Supervision, XFX and HW. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Xin-Fen Xu .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
PRISMA 2020 Checklist.
Additional file 2.
Search strategies for English and Chinese databases.
Additional file 3.
1. Articles presenting barriers to implementing KMC. 2. Articles presenting facilitators to implementing KMC.
Additional file 4.
Result of the quality appraisal of included studies.
Additional file 5.
Risk of Bias analysis using ROBIS tool.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Cai, Q., Chen, DQ., Wang, H. et al. What influences the implementation of kangaroo mother care? An umbrella review. BMC Pregnancy Childbirth 22 , 851 (2022). https://doi.org/10.1186/s12884-022-05163-3
Download citation
Received : 07 July 2022
Accepted : 27 October 2022
Published : 18 November 2022
DOI : https://doi.org/10.1186/s12884-022-05163-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Kangaroo mother care
- Preterm birth
- Umbrella review
- Implementation
- Facilitators
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Barriers and Enablers of Kangaroo Mother Care Practice: A Systematic Review
* E-mail: [email protected]
Affiliation Harvard T. H. Chan School of Public Health, Boston, Massachusetts, United States of America
Affiliation Boston Consulting Group, Boston, Massachusetts, United States of America
Affiliation Boston Consulting Group, New York City, New York, United States of America
Affiliation Bill & Melinda Gates Foundation, Seattle, Washington, United States of America
- Gabriel Seidman,
- Shalini Unnikrishnan,
- Emma Kenny,
- Scott Myslinski,
- Sarah Cairns-Smith,
- Brian Mulligan,
- Cyril Engmann

- Published: May 20, 2015
- https://doi.org/10.1371/journal.pone.0125643
- Reader Comments
Kangaroo mother care (KMC) is an evidence-based approach to reducing mortality and morbidity in preterm infants. Although KMC is a key intervention package in newborn health initiatives, there is limited systematic information available on the barriers to KMC practice that mothers and other stakeholders face while practicing KMC. This systematic review sought to identify the most frequently reported barriers to KMC practice for mothers, fathers, and health practitioners, as well as the most frequently reported enablers to practice for mothers. We searched nine electronic databases and relevant reference lists for publications reporting barriers or enablers to KMC practice. We identified 1,264 unique publications, of which 103 were included based on pre-specified criteria. Publications were scanned for all barriers / enablers. Each publication was also categorized based on its approach to identification of barriers / enablers, and more weight was assigned to publications which had systematically sought to understand factors influencing KMC practice. Four of the top five ranked barriers to KMC practice for mothers were resource-related: “Issues with the facility environment / resources,” “negative impressions of staff attitudes or interactions with staff,” “lack of help with KMC practice or other obligations,” and “low awareness of KMC / infant health.” Considering only publications from low- and middle-income countries, “pain / fatigue” was ranked higher than when considering all publications. Top enablers to practice were included “mother-infant attachment” and “support from family, friends, and other mentors.” Our findings suggest that mother can understand and enjoy KMC, and it has benefits for mothers, infants, and families. However, continuous KMC may be physically and emotionally difficult, and often requires support from family members, health practitioners, or other mothers. These findings can serve as a starting point for researchers and program implementers looking to improve KMC programs.
Citation: Seidman G, Unnikrishnan S, Kenny E, Myslinski S, Cairns-Smith S, Mulligan B, et al. (2015) Barriers and Enablers of Kangaroo Mother Care Practice: A Systematic Review. PLoS ONE 10(5): e0125643. https://doi.org/10.1371/journal.pone.0125643
Academic Editor: Zulfiqar A. Bhutta, The Hospital for Sick Children, PAKISTAN
Received: August 22, 2014; Accepted: March 24, 2015; Published: May 20, 2015
Copyright: © 2015 Seidman et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The Bill & Melinda Gates Foundation provided funding for this review. Two authors (BM, CE) were employees of the foundation at the time of writing. They were not involved in collection or analysis of data, but did provide input into revisions / edits of the manuscript.
Competing interests: The authors declare that no competing interests exist.
Introduction
Preterm birth is a major global health issue, with 15 million preterm births occurring each year, and over 1 million of these preterm infants dying each year [ 1 ]. Preterm birth complications directly account for greater than 35% of all neonatal deaths each year, and preterm birth indirectly contributes to an even greater percentage because it increases the risk that an infant will die from infection. Preterm births are on the rise globally, both in high-income and low-income settings [ 1 ]. The 10 countries with highest rates of preterm births include those that are high-income, such as the USA, middle-income such as India, China, the Philippines, Indonesia and Brazil, and low-income such as Nigeria, Pakistan, Bangladesh, Democratic Republic of Congo [ 1 ]. Thus interventions that are feasible and applicable in both high- and low-income settings are highly desired.
Kangaroo mother care (KMC) is an evidence-based approach to reducing mortality and morbidity in preterm infants which was first developed in Bogotá Colombia. According to the World Health Organization's definition, KMC consists of prolonged skin-to-skin (STS) contact between mother and infant, exclusive breastfeeding whenever possible, early discharge with adequate follow-up and support, and initiation of the practice in the facility and continuation at home [ 2 ]. In a meta-analysis, KMC was shown to significantly reduce preterm mortality at 40–41 weeks' corrected gestational age by 40% and to improve other outcomes including severe infection / sepsis, emotional attachment in mothers, and weight gain versus conventional neonatal care in preterm infants [ 3 ]. Another meta-analysis showed a similar mortality benefit, although it included fewer studies in its analysis [ 4 ]. Research from various countries also suggests that KMC is a cost-effective method for treating preterm infants [ 5 , 6 ], that mothers who have practiced KMC may find it acceptable [ 6 – 8 ], and that KMC can have a positive impact on the health of mothers in certain cases [ 9 , 10 ]. Therefore, KMC is a highly relevant intervention that should be considered for scaling across geographies. Although the WHO definition of KMC specifies that the practice should be initiated in a facility setting, several studies and trials have explored whether KMC can be effective in a community-initiated setting, and the effectiveness of KMC in this context has not yet been conclusively determined [ 11 , 12 ].
In spite of these benefits, mothers may face barriers to practice, some of which may prevent them from achieving the continuous STS contact with their infants (a defining feature of KMC). For example, a survey of 46 mothers of preterm infants who were trained on KMC in a facility in Andhra Pradesh, India found that only 6.5% of mothers felt that providing KMC for 12 hours / day or greater was feasible, whereas 52% of mothers felt that only 1 hour / day was practical[ 8 ]. Similarly, in a trial of community-initiated KMC with 1,565 mother-infant pairs, only 23.8% practiced STS for more than 7 hours / day in the first 48 hours of life, and the average number of hours of STS during days 3–7 of life was 2.7 ± 3.4 hours [ 11 ]. Barriers to the other components of KMC, including breastfeeding [ 12 , 13 ], and adequate follow-up after discharge [ 14 , 15 ], have also been noted.
KMC has emerged as a key intervention package for a number of newborn health initiatives, and this is epitomized by the Every Newborn Action Plan (ENAP) [ 16 ]. Additionally a recent convening of ideas from 600 key programmers, policymakers, researchers and stakeholders in newborn health, using the Child Health and Nutrition Research Initiative [CHNRI] method, highlighted KMC as a top preterm intervention agenda [ 17 ]. Many agencies, such as Save the Children's Saving Newborn Lives III (SNL), USAID, WHO and the Bill & Melinda Gates Foundation, and some countries, such as Malawi and South Africa, have also made KMC a priority [ 18 – 22 ].
Therefore, to adequately implement and effectively scale-up this intervention, it is critical to understand the key factors that contribute to a mother's (in)ability to practice KMC. However, there is a dearth of synthesized information on all of the sociocultural, resourcing, and experiential factors that influence a mother's practice of KMC. Accordingly, this review sets out to synthesize existing literature on the factors which influence a mother's ability to practice KMC by answering two questions. First, what are the most frequently cited barriers that could prevent a mother from successfully practicing KMC? These barriers can exist at multiple levels, including barriers to implementation of a KMC program, deficiencies in the program itself, or specific challenges associated with the practice of KMC which the mother has to perform. Second, are there any key positive factors, cited in the relevant literature, that can enable a mother to practice KMC? We believe that it is of utmost importance to consider these different types of barriers together (along with key enablers to practice), even though the solutions for solving each barrier might be different. Even though the specific barriers most relevant for mothers may vary based on context, a comprehensive list of this type will give program implementers, policymakers, and researchers a synthesized set of factors to consider as they attempt to implement new or improve existing KMC programs.
Methodology
Search strategy and selection criteria.
We undertook a systematic review according to PRISMA 2009 guidelines to answer these two questions [ 23 ]. (See S1 Appendix for complete PRISMA checklist). We developed a review protocol with methods and eligibility criteria that were specified in advance. We included any publication in our study that met the following criteria: 1) the aim of the study was to document experiences implementing KMC, STS, or other interventions related to Reproductive, Maternal, Newborn, & Child Health and Nutrition (RMNCH&N) that may have included KMC / STS, or the publication had relevant information on specific barriers to implementation listed in the abstract; 2) the study was published in a peer-reviewed journal; 3) the study included data on the sample population, sample size, and location of implementation; 4) the study was original research; and 5) the study was published in English. Studies testing the efficacy of KMC or STS practice (e.g. randomized controlled trials) were included if issues of acceptability, feasibility, or barriers to practice for parents or practitioners were documented in the abstract. Any publication published before August 13, 2013 (the date of the final database search) was eligible for inclusion. We excluded literature reviews, conference proceedings, letters to the editor, and abstracts in order to prevent double counting of data and to ensure that all barriers were understood in the context of the entire study.
We searched nine electronic databases: PubMed, EMBASE, Scopus, Web of Science, and the WHO Regional Databases (AIM, LILACS, IMEMR, IMSEAR, and WPRIM). We searched all databases using the following search terms: "Kangaroo Mother Care" OR "Kangaroo Care" OR "Skin to skin care". In addition, because at least one relevant article identified from a list of references in a literature review included the terms Kangaroo Mother Care in quotations and the term Skin to skin, we also searched PubMed for "'Kangaroo Mother Care'" and "Skin to skin". We used broad search criteria to ensure that relevant articles were not missed, and we then filtered and excluded many articles based on the eligibility criteria mentioned above. Reference lists from literature reviews identified in the database search were also scanned for relevant titles, and articles were also identified in consultation with the authors on this study. Recommendations for studies to be included in the review were also received from participants at the KMC Acceleration Meeting in Istanbul, October 2013[ 24 ] and in consultation with leaders in the fields of KMC and newborn health.
Data collection
After our initial database search and identification of additional studies through recommendations and scans of reference lists, study titles and abstracts were screened by two reviewers (GS and EK) for inclusion. In situations when a study's eligibility was disputed, a third reviewer (SU) provided an independent assessment until consensus was reached.
96 articles were reviewed to identify a comprehensive list of barriers to KMC practice in advance of the KMC Acceleration Convening [ 24 ]. A data extraction sheet was piloted and tested using these 96 articles. This piloting allowed for preliminary identification of relevant barriers and enablers to be included in the final review as well as final determination of stakeholders to be included in the review: mothers, fathers, community health workers, nurses, physicians, and program managers. The final tool included fields for collecting publication details, relevant study characteristics (sample size, location, and a short description of each study), barriers for each stakeholder group, and enablers to practice for mothers. Results from the preliminary analysis were shared at the KMC Acceleration Convening, ensuring that key stakeholders in the KMC community generally supported the methodology (described in further detail in the next section) and found the preliminary results to be consistent with their experiences [ 24 ]. This convening included researchers and practitioners from many different low- and middle-income countries (LMIC) across Latin America, Sub-Saharan Africa, and Asia, as well as major foundations and civil society organizations involved in RMNCH&N
Once the tool and list of studies was finalized, data was captured from each article into the tool independently by two reviewers (GS and EK) and a third reviewer (SU) provided independent assessment in case of disputes. The main outcome of interest was the frequency with which a barrier / enabler was mentioned across publications. Using frequency of mention allowed for a synthesized view of the barriers / enablers to practice listed in the relevant literature. The data collection process involved identifying barriers and enablers of KMC practice listed in each study (either through qualitative or quantitative findings) and categorizing them into one of the pre-determined categories of barriers / enablers in the tool. There was no limit to the number of barriers / enablers that could be found in a single study, but each study could only count toward a given barrier / enabler once. For example, if a study mentioned several statistics all indicating that mothers' low awareness of KMC was a barrier to practice, this would be coded as a single instance of low awareness among mothers in the tool. In cases where a barrier or enabler was listed for parents in general and did not distinguish between mothers and fathers, this barrier was listed as a barrier for mothers. In cases where a barrier was listed for both nurses and physicians but did not distinguish between the two, this barrier was listed as a barrier for nurses. Barriers / enablers were grouped into three different categories—resourcing, experiential, and sociocultural—based on consensus among all authors. Definitions for these three categories are included in S2 Appendix .
Risk of bias and publication weighting methodology
The goal of this study was to synthesize existing literature on barriers to and enablers of KMC practice. As noted, there is limited systematically organized information on this topic. Therefore, in order to ensure that our review captured as many relevant qualitative and quantitative findings as possible, we chose to include any study identified through our search strategy which had information on barriers and enablers to KMC practice, even if studying this topic was not the primary purpose of the publication.
As one might expect based on this search strategy, our findings included many studies which had observational information on barriers to / enablers of KMC practice. Given the limited amount of synthesized information on barriers to KMC practice, we felt it was important to include these observational findings so that relevant programmatic experience informed this review. At the same time, however, we also sought to ensure that our analysis was weighted toward data from publications which had explicitly studied barriers to KMC practice (rather than giving those data equal weighting to observational findings).
Therefore, we developed a methodology to weight findings from each publication based on the way in which the data was identified and captured. Other public health literature reviews have used similar methods to quantify qualitative data drawn from multiple sources of varying quality and relevance [ 25 – 28 ]. We categorized each publication into one of four types: Indirect study, Exploratory study, Systematic study, and Prioritized study. Indirect studies were defined as those which did not set out to study barriers to / enablers of KMC practice, but which identified and documented these factors (ie, through observational findings). Exploratory studies were defined as those which set out to identify barriers / enablers to KMC practice but which did not pre-specify factors under consideration (ie, were not explicitly testing hypotheses about which barriers / enablers would influence practice). Systematic studies were defined as those which set out to identify barriers / enablers of KMC practice and which did pre-specify the factors under consideration but which did not prioritize among these barriers. Prioritized studies were defined in the same way as systematic studies with the exception that these studies also prioritized the barriers to KMC practice. Our indexed ranking methodology gave the most weight to Prioritized studies, the second-most weight to Systematic studies, the third-most weight to Exploratory studies, and the least weight to Indirect studies. ( S2 Appendix provides more detail on full methodology describing indexed ranking process.) Note that in our findings and discussion, we refer to "top-ranked" barriers to practice for mothers and other groups. Top-ranked barriers are those that received the highest score based on this indexed ranking, which accounts for both frequency of mention across publications and weighting of each piece of evidence based on the publication type.
Each study was placed into one of these categories independently by two reviewers (GS and EK), and in cases of a discrepancy, a third reviewer provided an independent assessment (SU). Of the 103 publications included in this review, there were only 12 discrepancies (11.65%) in categorization between the first two readers, suggesting that this method is reliable for categorizing publications. Our data capture tool included a field to categorize each publication into one of these four categories.
Study selection
From our database search, a total of 1,260 unique publications were identified, and four others were identified through snowballing. Of these 1,264, 168 met preliminary eligibility criteria based on a scan of the title and abstract; all others were excluded because they did not meet at all eligibility criteria discussed in the Methodology section. Of these 168, 51 were eliminated after full-text screening because they did not have relevant data (i.e. barriers to newborn health intervention rollout were listed, but no barriers specific to KMC / STS were listed) or because only an abstract was available, and 14 did not have full text available in English. This resulted in 103 articles deemed relevant for inclusion in the review. Fig 1 represents the study selection for inclusion in the systematic review. A full list of publications included in this review can be found in S3 Appendix .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0125643.g001
Of these 103 articles, 49 were from high-income countries HIC [ 29 ], 22 were from Sub-Saharan Africa, 15 were from South Asia, five were from North Africa / the Middle East, five were from Latin America / Caribbean, three were from Eastern Europe, two were from East Asia / Southeast Asia / Pacific, and two were from LMIC in multiple regions.
Nine of the publications were classified as Prioritized, 48 were classified as Systematic, 31 were classified as Exploratory, and 15 were classified as Indirect. Indirect studies included randomized controlled trials that discussed barriers to implementation and practice, two case studies of individuals' experiences with KMC, and studies on practices throughout the NICU which included information on KMC or STS practice.
A complete dataset used for analyses can be found in S1 Dataset .
Barriers and enablers of KMC practice for mothers
Of the top five barriers to KMC practice identified for mothers, four were resource-related. The top two barriers to practice identified—"Issues with facility environment / resources" and "Negative impressions of staff attitudes or interactions"—were specific to the facility setting. "Fear / anxiety of hurting the infant," an experiential barrier to practice, was ranked third. Resource-related barriers that are relevant both inside and outside the facility—"Lack of help with KMC practice and other obligations" and "Low awareness of KMC / infant health"—were ranked fourth and fifth. When considering publications from LMIC only, four of the five top barriers were the same as when all publications were considered. The only difference is that "Negative impressions of staff attitudes or interactions" dropped significantly (to 11th), and "Pain / fatigue" emerged as the fourth-highest-ranked barrier, just after "Fear / anxiety of hurting the infant." The full rankings of barriers identified for mothers can be found in Fig 2A , and the full ranking of barriers identified for mothers from LMIC only can be found in Fig 2B .
a) Indexed ranking of barriers to adoption of KMC for mothers in all countries, and b) indexed ranking of barriers to adoption of KMC for mothers in LMIC only.
https://doi.org/10.1371/journal.pone.0125643.g002
Experiential factors emerged as the top enablers to KMC practice for mothers. "Mother-infant attachment," "Feelings of confidence / empowerment," and "Ease of practice / preference over traditional care" emerged as three of the top five enablers both when considering all publications and just those from LMIC. "Support from family, friends, and other mothers," a resourcing enabler, was also in the top five enablers when considering all publications, and it was the top-ranked enabler when considering publications only from LMIC. "Support from staff or community health worker (CHW)" was the fourth-highest-ranked enabler when considering all publications, but was ranked seventh when considering LMIC only. "Understanding of efficacy" was also ranked among the top five enablers to practice when considering LMIC only. The full ranking of enablers for mothers across all publications and in LMIC only can be found in Fig 3A and Fig 3B , respectively.
https://doi.org/10.1371/journal.pone.0125643.g003
Barriers of KMC for nurses
Resourcing and sociocultural factors emerged as the top barriers to KMC adoption for nurses. The resourcing barriers "Actual increased workload / staff shortages" and "Lack of clear guidelines / training" were in the top five barriers for nurses when considering publications from all geographies and just those from LMIC. The sociocultural barriers "General lack of buy-in / belief in efficacy" and "Concerns about other medical conditions / care" were also in the top five barriers for nurses when considering publications from all geographies and just those from LMIC. (Note that a data point was counted in the "Concerns about other medical conditions / care" category when the publication indicated that nurses' beliefs countered guidelines for KMC practice or when there was lack of consensus among nurses about whether KMC was safe to practice when an infant had a certain condition). The full ranking of barriers to adoption for nurses across all publications and in LMIC only can be found in Fig 4A and Fig 4B , respectively.
a) Indexed ranking of barriers to adoption of KMC for nurses in all countries, and b) indexed ranking of barriers to adoption of KMC for nurses in LMIC.
https://doi.org/10.1371/journal.pone.0125643.g004
Barriers for fathers, CHW's, physicians, and program managers
Much less data was available for fathers, physicians, and program managers than was for mothers and nurses. Full rankings of barriers for these stakeholders across all publications can be found in Figs 5 – 7 .
https://doi.org/10.1371/journal.pone.0125643.g005
https://doi.org/10.1371/journal.pone.0125643.g006
https://doi.org/10.1371/journal.pone.0125643.g007
The top-ranked barrier for fathers was "Lack of opportunity to practice." The top-ranked barrier for physicians was "General lack of buy-in / belief in efficacy." The top-ranked barrier for program managers was "Need for high-touch support from staff."
The aim of this systematic review was to identify the most frequently cited barriers to KMC adoption, as well as enablers to practice. Given the increasing importance of KMC in addressing the global health challenge of preterm birth and death, synthesizing the experiential, resourcing, and sociocultural barriers that could prevent a mother from effectively practicing KMC is critical to effectively implementing this intervention. Although much has been written on this topic, nearly half (44.6%) of the publications identified for inclusion in this review were categorized as either Exploratory or Indirect, suggesting that there is lots of data relevant to the promotion of KMC that is not organized in a systematic way which can readily guide program implementation.
Based on the list of barriers and enablers found in the publications identified, we have identified five key insights which we believe are relevant for program implementers and researchers. Each of these insights is detailed below.
Mothers are generally able to understand and accept KMC
Low awareness of KMC and infant health more broadly was the fourth-highest-ranked barrier to KMC practice across all publications, and the highest barrier to KMC practice when considering only publications from LMIC. However, this barrier may be over-represented in the literature on KMC because it is easily testable and many publications that implemented KMC in a new setting surveyed pre-existing levels of awareness to establish a baseline. Lack of information about KMC, hypothermia, or newborn health was identified across HIC (Sweden [ 30 , 31 ], Unite[ 32 ]d States[ 33 ]) and LMIC (Bangladesh [ 11 ], Egypt [ 34 , 35 ], Ghana [ 36 , 37 ], India [ 8 , 32 , 38 ], South Africa [ 22 , 39 ], and Zimbabwe [ 40 ]).
In spite of low general awareness of KMC, however, the literature from LMIC suggests that it is easy to train mothers on KMC practices and that they can understand the practice. For example, a training program in India found that 88% of mothers were able to understand KMC with a single training session [ 10 ]. Similarly, during site visits to facilities practicing KMC in Ghana, researchers found that mothers practicing KMC were able name its benefits [ 41 ]. Mothers were also able to understand the KMC messages delivered by community health workers in a community setting in Bangladesh [ 12 ].
Mothers' understanding of the practice also seems to enhance their adherence to practice. In South Africa, for example, mothers' "main motivation for embracing [KMC] was the well-being of their infants" [ 22 ]. Similarly, studies in Ghana found, "all mothers recognised that their babies' small weights put them at risk of illness and death and appreciated that [STS] could improve their health and survival,"[ 37 ] and, "as a motivational factor, mothers and health workers also mentioned various success stories of infants who had survived having been nursed in KMC." [ 41 ] Belief in the efficacy of KMC as an enabling factor for practice was also mentioned in HIC. One case study from the United States describes how the mother used research articles demonstrating KMC's benefits to convince facility staff to let her practice KMC [ 42 ].
Mothers can enjoy practicing KMC, and the practice has benefits for mothers and families
Mothers not only are able to understand and accept KMC, but also they may enjoy the practice. Mother-infant attachment was the top-ranked enabler for KMC practice, and evidence for this enabler came from across HIC and LMIC. In Colombia, for example, sensitivity to infants was significantly higher among mothers practicing KMC compared to control (p<.05), and cognitive fostering was significantly higher among KMC mothers compared to control after 14 days (p<.05) [ 43 ]. Similarly, in India, KMC mothers were more likely to spend time with their baby "beyond the usual care taking" (p<.05), derive pleasure from their baby (p<.05), and only go out for "totally unavoidable" reasons (p<.05) compared to controls [ 44 ]. Qualitative findings from HIC also support these findings [ 13 , 30 , 45 ].
Several studies have shown that KMC has positive impact on the mother. Although postpartum depression can be a barrier to practicing KMC [ 46 ], those mothers who do practice KMC may experience a reduction in postpartum depression symptoms [ 9 , 47 ]. They may also experience an increased sense of competence [ 43 ]. Evidence from HIC also suggests that KMC has a beneficial impact on overall family dynamics. For example, one study from Israel found family cohesiveness was higher among KMC families as compared to controls [ 48 ]. Similarly, qualitative findings from Sweden indicate that KMC "strengthened the mother-father-child unit" [ 49 ]. Although further research may be needed to replicate these findings in low- and middle-income countries, it is clear that KMC can be a beneficial intervention not only for the infant, but also for the mother and the family.
Practicing KMC is often difficult
"Pain / fatigue" emerged as one of the top five barriers to KMC practice when considering all publications and only publications from LMIC. This set of barriers included finding the baby too difficult or heavy to hold [ 12 ], discomfort on the chest or back [ 46 ], and exhaustion [ 50 ], among others. Further, one should note that we identified other barriers that, taken together with the "Pain / fatigue" barrier, indicate that mothers may struggle with the practice. These barriers include "Positioning issues," including difficulty sleeping with the infant on the chest [ 40 ], "Breastmilk expression and other breastfeeding-related issues,"[ 8 ] discomfort related to temperature [ 50 ], and "Issues with clothing / infants' medical devices"[ 30 , 51 ]. Of course, mothers' medical issues also pose a major barrier to practice. These medical issues included pain from episiotomy repair [ 52 ], recovery from caesarean section[ 46 ], postpartum depression[ 46 ], and general maternal illness [ 12 , 53 ].
These barriers suggest that practicing continuous KMC is likely very challenging for mothers, especially those who have low motivation and medical issues.
Support for mothers can make KMC practice easier
In addition to being physically taxing for mothers, KMC also limits the mother's ability to take care of other tasks and obligations. "Lack of help with KMC practice and other obligations" was ranked among the top five barriers to KMC practice across all publications and when looking only at LMIC. Obligations related to mothers' daily routine came up in publications from countries such as Zimbabwe [ 40 ], Uganda [ 54 ], Ghana [ 36 ], and Sweden [ 30 ].
Conversely, "Support from family, friends, and other mothers" emerged as the third-highest-ranked enabler to practice across publications and the top enabler of practice in LMIC. This support took many different forms. Family members would often take turns holding the infant in KMC to give the mother a break from the practice [ 7 , 10 , 55 ]. They would also take care of other tasks that the mother otherwise would have had to deal with, including childcare and housekeeping [ 56 , 57 ]. Qualitative evidence also indicates that emotional support provides an important, and sometimes crucial, enabler to practice. For example, in Malawi, when looking to overcome issues of fear or embarrassment for the mothers, implementers found, "the most effective way to ensure KMC continues at home is to involve the grandma during the admission" [ 58 ]. Similarly critical roles of family members providing emotional support were documented in Ghana [ 36 ] and South Africa [ 39 ].
Several studies also documented the role that other mothers could play in training or supporting mothers in KMC practice. For example, in a study investigating a community-based application of KMC in Bangladesh, one third of mothers who had been trained on community-initiated KMC reported teaching the practice to others [ 11 ]. There is quantitative evidence from Ghana that this phenomenon has an impact on practice; infants in a region where some women had been trained on STS but whose mothers had not been taught STS were more likely to receive STS than infants born in regions where no mothers had been taught STS (RR Any [STS care] : 1.28; 95% CI: 0.92–1.79; RR > 2 h [STS care] : 1.64; 95% CI: 0.80–3.39), thereby suggesting that mothers discussed their STS practice with each other [ 37 ]. Qualitative findings also indicate that KMC mothers support other mothers starting the practice on the ward. In South Africa, for example, KMC mothers supported each other on the ward in various ways: "they reminded each other about the importance of KMC for their babies; discussed how to comfort their babies, and how to kangaroo the infants properly, as demonstrated; and exchanged ideas on how to minimise discomfort" [ 22 ]. Similar experiences were found in Mozambique [ 59 ] and Mexico, Indonesia, and Ethiopia.
Interestingly, "Support from staff or community health workers" was the fourth-highest-ranked enabler for practice across publications but fell to seventh when looking only at publications from LMIC. Although further research is needed, this finding, combined with the finding that support from family, friends, and other mothers is a top enabler to practice, indicates that the community may play a critical role in promoting KMC practice in low-resource settings. Going forward, it will be important for researchers and implementers to understand how the community can complement a facility-based approach to scale-up with community engagement activities, drive demand for the practice, and ensure infants receive quality KMC care.
Physical environment and resourcing factors can be barriers to practice, but these are under-studied in the community setting
"Issues with facility environment / resources" emerged as the top barrier to practice for mothers, and this factor includes an array of different issues. These issues included crowdedness and noisiness [ 22 , 50 , 60 ], lack of privacy [ 61 , 62 ], lack of food and supplies [ 40 , 54 ], and uncomfortable beds [ 13 , 22 ]. It is important to remember that, due to the nature of KMC guidelines, facility-related issues may be over-represented in these findings. Data regarding nurses' barriers to adoption also suggests that resource-related factors, such as workload, play an important role in the implementation of KMC.
It is also important to note that there is a paucity of information available on physical and resourcing barriers to practice for mothers practicing KMC in the community. Of the 103 articles included in this review, only 16 focused on community-initiated KMC or had a substantial focus on community-based practice and perspectives. Thus, although a lack of resources in the community, such as comfortable beds and readily available food, may be an equally common barrier, the data on this topic is currently limited by the focus of existing literature. Of course, institution-initiated KMC is more commonly accepted as an evidence-based practice [ 3 ], which may account for some of the lack of research on practice outside the facility. However, because facility and community practice of KMC actually represent a continuum, with infants moving back and forth between the two, there is still opportunity to study community barriers to practice, even within a facility-initiated KMC program [ 24 ].
Directions for Future Research and Practice
This systematic review prioritizes the main factors that influence KMC practice, and, in doing so, highlights some key areas that implementers and implementation researchers may need to focus on when promoting KMC. Given that local circumstances, including cultural attitudes and support for the mother, have an impact on KMC practice, it is critical to understand the context-specific factors that might impact a KMC program. Qualitative and ethnographic research, including interviews with mothers who have practiced KMC and healthcare providers, as well focus groups with community members, can achieve this goal. Implementers should also study the effectiveness of various user-centric designs for promoting KMC, including different mechanisms to ensure the mother has support for practice.
In addition, this review points out the difficulty that mothers have practicing continuous KMC (at least 20 hours of STS / day). Accordingly, more research and analysis is needed to understand the dose-response effect of KMC. If mothers could practice for shorter periods of time without reducing the mortality impact of the practice, KMC might be more feasible and easier to scale. Researchers should re-examine existing data on the number of hours of STS that infants received and the associated mortality impact, as well as track actual STS hours in forthcoming continuous KMC programs in order to compare infants who received at least 20 hours of STS with those who received fewer (ie, infants whose mothers deviated from the protocol).
Limitations of this Study
This review is limited by definitional challenges related to the practice and implementation of KMC. Since WHO guidelines currently do not recommend community-initiated KMC, there is likely significant bias in the literature toward institution-related barriers to KMC practice [ 2 ]. Therefore, it is likely that more research will focus on issues related to providing KMC in the facility than on issues related to the community, such as cultural perceptions of KMC. However, because mothers and newborns require a continuum of care that extends into both the facility and community, there are likely important barriers to the practice of KMC that relate to community beliefs about newborn care which may be underrepresented in this review.
There also exists some inconsistency in the definition of KMC practice. Even studies included in the Cochrane Review's meta-analysis of KMC , which used rigorous publication inclusion criteria and which helped establish KMC as an evidence-based practice for reducing preterm mortality and morbidity, had widely varying applications of KMC [ 3 ]. For example, Worku et al. did not require infants to be stabilized before beginning KMC, even though most other studies included in the meta-analysis did [ 63 ]. Similarly, the studies included in this meta-analysis had a wide range in the number of hours of STS care actually practiced by mothers and guardians: while some studies reported continuous contact for approximately 20 hours / day [ 64 ], others reported an average of only 1–2 hours of STS care / day [ 65 , 66 ]. Unfortunately, dose-response data for KMC is not available. Given that variations in the application of KMC exist and do not always follow WHO guidelines, our review necessarily includes publications that reflect this variation. By incorporating findings from the broadest range of publications which report barriers to KMC practice, including those publications which only sought to implement STS care (the hallmark component of KMC) and not its other components, we believe we have captured the full range of barriers that one could face when implementing a KMC program.
In addition, the majority of papers identified focuses on mothers and excludes fathers' and other family members' perspectives, and they focus on nurses and exclude physicians' perspectives. Although this likely reflects the reality of the situation that mothers practice KMC more often than fathers and nurses train parents on KMC more often than physicians, future research may need to focus on barriers to practice for fathers and physicians.
There is also a risk that the barriers identified across studies are not the most important barriers to practice, but rather the most easily observable barriers. As mentioned, this review is designed to synthesize the literature on barriers to practice in order to serve as a starting point for future research, rather than to determine which barriers are most critical to overcome in order to ensure the maximum number of hours of STS contact. Because this study included qualitative and observational information from many sources, including publications which did not explicitly set out to address the topic of barriers to KMC practice, it would be impossible to determine which of these barriers are most important (ie, in order to increase the number of hours that a mother can practice STS).
Finally, this review is limited by the fact that only studies published in English were included; in particular, there may be data from non-English-speaking LMIC that have relevant information on barriers / enablers to KMC practice which are not included in this review.
As KMC gains momentum with the rollout of various other Reproductive, Maternal, Newborn, & Child Health and Nutrition programs, including ENAP, it is critical to understand the barriers to practice for the end-users, often the mother, of this life-saving practice, which has many additional benefits for infants and mothers. This systematic review sought to synthesize the most frequently cited barriers to practice for mothers, fathers, CHW's, nurses, physicians, and program managers, as well as the most commonly cited enablers to practice for mothers. The findings from this review can be used to guide future programmatic research efforts aiming to understand how to effectively implement KMC at scale, as well as the design or update of implementation efforts across geographies.
Supporting Information
S1 appendix. prisma checklist..
https://doi.org/10.1371/journal.pone.0125643.s001
S2 Appendix. Detailed methodology for indexed ranking of barriers / enablers.
https://doi.org/10.1371/journal.pone.0125643.s002
S3 Appendix. Full list of publications included in analysis for systematic review.
https://doi.org/10.1371/journal.pone.0125643.s003
S1 Dataset. Complete dataset used for analysis in systematic review.
https://doi.org/10.1371/journal.pone.0125643.s004
Acknowledgments
Funding for this study was provided by the Bill & Melinda Gates Foundation. Funders were not involved in collection, analysis, or interpretation of data. Funders did review drafts of this manuscript. Employees of a for-profit company (Boston Consulting Group) were involved in writing this review, but the outcome of the engagement was not contingent upon the findings or analysis in this paper or any other part of the engagement with the foundation.
Author Contributions
Conceived and designed the experiments: GS SU SCS BM CE. Analyzed the data: GS SU EK SM. Wrote the paper: GS SU CE.
- 1. March of Dimes, PMNCH, Save the Children, WHO (2012) Born Too Soon: The Global Action Report on Preterm Birth. Geneva: World Health Organization. https://doi.org/10.1186/1742-4755-10-S1-S1 pmid:24625113
- 2. Department of Reproductive Health and Research W (2003) Kangaroo mother care: a practical guide. Geneva: World Health Organization.
- 3. Conde-Agudelo A, Díaz-Rossello J (2014) Kangaroo mother care to reduce morbidity and mortality in low birthweight infants (Review).
- View Article
- PubMed/NCBI
- Google Scholar
- 5. Broughton E, Gomez I, N S, Vindell C (2013) The cost-savings of implementing kangaroo mother care in Nicaragua.
- 8. Muddu GK, Boju SL, Chodavarapu R (2013) Knowledge and Awareness about Benefits of Kangaroo Mother Care. Indian J Pediatr.
- 16. PMNCH. "Every Newborn." Available: www.everynewborn.org . Accessed 2013 Dec 1.
- 17. Yoshida S, Rudan I, Lawn JE, Wall S, Souza JP, Bahl R, et al. (2014) Defining newborn health research agenda beyond 2015. Submitted for publication.
- 18. Save the Children (2013) Saving Newborn Lives: Bending the Curve; Accelerating Progress in Newborn Survival and Health. The Bill & Melinda Gates Foundation. [Personal correspondance with Becky Ferguson: August 2013].
- 19. MCHIP (2012). "MCHIP and USAID Host First LAC Conference on Kangaroo Mother Care." Available: http://www.mchip.net/node/699 . Accessed 2014 Jan 16.
- 20. World Health Organization (2014). "Kangaroo mother care to reduce morbidity and mortality and improve growth in low-birth-weight infants." Available: http://www.who.int/elena/titles/kangaroo_care_infants/en/ . Accessed: 2014 Jan 16.
- 21. Bergh A-M, Banda L, Lipato T, Ngwira G, Luhanga R, Ligowe R (2012) Evaluation of kangaroo mother care services in Malawi. MCHIP.
- 29. Central Intelligence Agency (2013) The World Factbook 2013–2014. In: Agency CI, editor. Washington, DC.
- 33. Bramson L, Lee JW, Moore E, Montgomery S, Neish C, Bahjri K, et al. (2010) Effect of early skin-to-skin mother–infant contact during the first 3 hours following birth on exclusive breastfeeding during the maternity hospital stay. Journal of Human Lactation.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Supplements
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 8, Issue 6
- Kangaroo mother care for preterm or low birth weight infants: a systematic review and meta-analysis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-2259-5693 Sindhu Sivanandan 1 ,
- http://orcid.org/0000-0003-1474-1451 Mari Jeeva Sankar 2
- 1 Neonatology , Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER) , Puducherry , India
- 2 Pediatrics , All India Institute of Medical Sciences , New Delhi , India
- Correspondence to Dr Mari Jeeva Sankar; jeevasankar{at}gmail.com
Importance The Cochrane review (2016) on kangaroo mother care (KMC) demonstrated a significant reduction in the risk of mortality in low birth weight infants. New evidence from large multi-centre randomised trials has been available since its publication.
Objective Our systematic review compared the effects of KMC vs conventional care and early (ie, within 24 hours of birth) vs late initiation of KMC on critical outcomes such as neonatal mortality.
Methods Eight electronic databases, including PubMed ® , Embase, and Cochrane CENTRAL, from inception until March 2022, were searched. All randomised trials comparing KMC vs conventional care or early vs late initiation of KMC in low birth weight or preterm infants were included.
Data extraction and synthesis The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered with PROSPERO.
Main outcomes and measures The primary outcome was mortality during birth hospitalization or 28 days of life. Other outcomes included severe infection, hypothermia, exclusive breastfeeding rates, and neurodevelopmental impairment. Results were pooled using fixed-effect and random-effects meta-analyses in RevMan 5.4 and Stata 15.1 (StataCorp, College Station, TX).
Results In total, 31 trials with 15 559 infants were included in the review; 27 studies compared KMC with conventional care, while four compared early vs late initiation of KMC. Compared with conventional care, KMC reduces the risks of mortality (relative risk (RR) 0.68; 95% confidence interval (CI) 0.53 to 0.86; 11 trials, 10 505 infants; high certainty evidence) during birth hospitalisation or 28 days of age and probably reduces severe infection until the latest follow-up (RR 0.85, 95% CI 0.79 to 0.92; nine trials; moderate certainty evidence). On subgroup analysis, the reduction in mortality was noted irrespective of gestational age or weight at enrolment, time of initiation, and place of initiation of KMC (hospital or community); the mortality benefits were greater when the daily duration of KMC was at least 8 hours per day than with shorter-duration KMC. Studies comparing early vs late-initiated KMC demonstrated a reduction in neonatal mortality (RR 0.77, 95% CI 0.66 to 0.91; three trials, 3693 infants; high certainty evidence) and a probable decrease in clinical sepsis until 28-days (RR 0.85, 95% CI 0.76 to 0.96; two trials; low certainty evidence) following early initiation of KMC.
Conclusions and relevance The review provides updated evidence on the effects of KMC on mortality and other critical outcomes in preterm and low birth weight infants. The findings suggest that KMC should preferably be initiated within 24 hours of birth and provided for at least 8 hours daily.
- public health
- systematic review
Data availability statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. Data are available upon reasonable request from the corresponding author.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjgh-2022-010728
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Kangaroo mother care (KMC) is a simple and cost-effective intervention that decreases neonatal mortality and the risk of infection in low birth weight infants.
The WHO recommends the initiation of KMC among low birth weight infants after clinical stabilisation.
WHAT THIS STUDY ADDS
Compared with conventional care, KMC initiated either in the hospital or at home reduces mortality during birth hospitalisation or 28 days of age and probably reduces severe infection until the latest follow-up among preterm and low birth weight infants.
KMC provided for at least 8 hours a day probably results in greater benefits than a shorter duration of KMC.
KMC initiated within 24 hours of birth reduces neonatal mortality and may reduce clinical sepsis until 28 days compared with later initiation.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The results of this updated review will likely influence health providers to initiate KMC in all low birth weight and preterm infants managed in health facilities and at home. Efforts might be undertaken to initiate KMC within 24 hours of birth and to provide it for at least 8 hours a day.
Introduction
Prematurity (gestational age <37 weeks) and low birth weight (defined as <2500 g) are important causes of neonatal and infant mortality and long-term neurodevelopmental disability. 1 Low- and middle-income countries (LMIC) have the highest burden of preterm and low birth weight infants. Kangaroo mother care (KMC) is a simple and cost-effective intervention that has been shown to reduce neonatal mortality and the risk of infection in low birth weight infants. 2 The Cochrane review on KMC, published in 2016, included 21 studies involving 3042 infants and demonstrated a significant reduction in the risks of mortality and severe infection in low birth weight infants. 3
New evidence from large multi-country and community-based randomised trials became available after the publication of the Cochrane review. 4 5 A few of these trials examined the effect of early KMC, that is, KMC initiated within the first 24 hours of delivery. 5 6 The timing of initiation of KMC is critical because KMC is usually commenced after the infant is stabilised. The WHO guidelines also recommend the initiation of KMC after clinical stabilisation. However, stabilisation of preterm/low birth weight neonates may take anything from hours to days, depending on the gestation, birth weight, and general condition at birth. The median age at initiation of KMC in the facility-based studies included in the Cochrane review varied from 3 to 24 days. KMC initiated after 3 days of life would not naturally reduce the risk of deaths occurring in the first 3 days, which account for about 62% of total neonatal deaths. 7 The efficacy and safety of early initiation of KMC – within 24 hours of life – are unknown.
This systematic review aimed to compare the effects of (a) KMC with conventional care and (b) early initiation, that is, KMC within 24 hours of age, with late initiation of KMC on neonatal and infant mortality and severe morbidities among low birth weight and preterm infants. This review would provide critical evidence for policymakers and other stakeholders and may help to formulate clinical practice guidelines.
Inclusion and exclusion criteria
Our review included individually-randomised and cluster-randomised trials that compared KMC with conventional care or early initiation (ie, in the first 24 hours after birth) of KMC with late-initiated KMC among low birth weight and preterm infants, irrespective of the duration of KMC, infant stability at enrolment, study setting, and breastfeeding patterns. Trials reported as only abstracts were included if sufficient information on study methods was available to assess the eligibility and the risk of bias. We excluded quasi-randomised and crossover trials, studies evaluating KMC among term infants or those with birthweight >2500 g, and studies assessing KMC on only physiological parameters, pain scores, maternal mental health, infant colic, or during neonatal transport or as a part of a package of interventions.

Search strategy
We systematically reviewed the relevant publications by searching the electronic databases of MEDLINE (1966 to March 2022) via PubMed ® and OVID, Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1 to March 2022), EMBASE (1988 to March 2022), CINAHL (1981 to March 2022), and the databases PsycINFO, AMED, EMCARE, BNI from inception until March 2022. We used the search terms “kangaroo care,” “kangaroo mother care,” “skin-to-skin care,” and “neonates or infants” in the search strategy. The search was initially conducted until March 2021 (for the presentation of review findings to the WHO Guideline Development Group of the guidelines on the care of low birth weight infants); the search was then updated to March 2022. The search strategy, search results, and the definitions used in the review are provided in online supplemental file 1 . We also searched the databases of clinical trials and reference lists of retrieved articles for eligible studies.
Supplemental material
The primary outcome was mortality during birth hospitalisation or by day 28 of life. Other outcomes were mortality by 6–12 months of age, severe infections, infant growth, neurodevelopment, hypothermia, length of hospital stay, readmission to hospital, and exclusive breastfeeding at discharge and at one and 6 months of age.
Data extraction
The two review authors (SS and MJS) extracted data using a standardised and pre-tested data abstraction form. The data included study characteristics, sample size, details of KMC initiation, duration, breastfeeding, time of hospital discharge, study setting (hospital or community), outcomes including neonatal mortality, hypothermia, sepsis, rates of exclusive breastfeeding, and weight gain. Discrepancies, if any, were resolved by mutual discussion between the reviewers.
Quality assessment and statistical analysis
The review authors independently evaluated the quality of studies using Cochrane’s Risk of Bias-1 tool, extracted data, and synthesised the effect estimates – relative risks (RR) or mean difference (MD) – using RevMan version 5.4 (The Cochrane Collaboration, 2020) or Stata 15.1 (StataCorp, College Station, TX, USA). The RR and 95% confidence intervals (CI) were calculated based on the extracted frequencies and denominators. Results were pooled using fixed-effect meta-analyses using the Mantel-Haenszel method. The heterogeneity of the pooled studies was assessed using the test of homogeneity of study-specific effect sizes and the I 2 statistic, in addition to visual confirmation from forest plots. If substantial heterogeneity was detected, the reasons for heterogeneity were explored. If there was no critical clinical or methodological heterogeneity among the studies, we pooled their results using the random-effects model. We evaluated the likelihood of potential publication bias using funnel plots.
We used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach 8 to assess the quality of evidence for critical outcomes such as mortality at discharge, severe infection/sepsis at the latest follow-up, weight gain, exclusive breastfeeding, and neurodevelopmental outcomes. Evidence from randomised controlled trials was considered high quality; still, it could be downgraded by one or two levels for serious and very serious limitations, respectively, based on the risk of bias, imprecision, inconsistency, indirectness of study results, and publication bias. The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered in PROSPERO (CRD42021240336).
Planned subgroup analyses
For the comparison of KMC vs conventional care, we performed subgroup analyses according to different gestational and birth weight categories and by median duration KMC in hours (<8 hours, 8–16 hours, and >16 hours); time of initiation of KMC – early (≤24 hours of life) vs late initiation; stable vs unstable neonates; health facility vs community settings; and countries (high income vs LMIC settings).
Patient and public involvement
The study is a systematic review of the existing literature on the efficacy of KMC in preterm and low birth weight infants. No subjects were enrolled in the review. Therefore, parents, parent advisors, or the public were not involved in developing the research question and outcome measures.
Role of the funding source
The WHO, Geneva, funded the review. The WHO staff helped finalise the protocol and the manuscript; they had no role in the literature search, data extraction, or data analysis. The corresponding author had the final responsibility for the decision to submit for publication.
Of the 3458 records identified from the database and bibliographic searches, 31 4–6 9–35 studies enrolling 15 559 infants were included in the review ( figure 1 ); 25 studies were conducted in LMIC (two from multiple countries 5 14 while seven were conducted in high-income countries 12 20 24 26 29 30 34 (Appendix). Twenty-seven studies compared KMC with conventional care, while four compared early with late initiation of KMC. 5 6 24 25 KMC was initiated in the health facility in 29 studies and at home (community) in two trials. 4 11 While the sample sizes of earlier hospital-based studies ranged from 28 to 777, the most recent facility-based study – WHO iKMC study 5 – had a sample size of 3211. Of the two community-based studies, one trial had enrolled around 8400 infants. 4 Only six studies included infants with birthweight <1500 g. 12 13 19 28 30 34 Figure 2 depicts the risk of bias in the included studies in specific domains. Many studies had an unclear or high risk of selection bias (due to a lack of information on allocation concealment) and detection bias (because the outcomes assessors were not masked to the intervention group).
- Download figure
- Open in new tab
- Download powerpoint
Flow chart of search results (adapted from PRISMA 2009 flow diagram).
Risk of bias in included studies. Green circle indicates low-risk, red indicates high-risk and yellow, unclear-risk of bias.
KMC versus conventional newborn care
The comparison included 27 studies that enrolled 11 956 infants. The characteristics of included studies are provided in table 1 . All but one study enrolled infants after stabilisation (variably defined in different studies as cardiorespiratory stability, off oxygen or any form of respiratory support, or off intravenous fluids). KMC was started within 24 hours after birth in two studies, between 1 and 7 days in 10 studies, and after 7 days in 12 studies (3 studies did not report the time of initiation). The duration of KMC was <8 hours in 9 studies, 8–16 hours in 9 studies, and >16 hours in 4 studies (5 studies did not report the duration).
- View inline
KMC vs conventional newborn care – characteristics of included studies
Pooled analysis revealed a 32% reduction in mortality during birth hospitalisation or by 28 days after birth or 40 weeks of postmenstrual age (risk ratio (RR) 0.68; 95% CI (CI) 0.53 to 0.86; I 2 =0%; 12 studies; 10 505 infants; fixed-effect model; high certainty evidence; figure 3 ). The funnel plot did not show any evidence of a potential publication bias ( online supplemental efigure 1 ). The benefits of KMC in the primary outcome of mortality during birth hospitalisation or by 28 days of age were observed in all subgroup analyses: gestational age category (≤34 weeks vs. >34 weeks), weight at birth/enrolment (≤2000 g vs. >2000 g), setting (health facility vs. community) and time of initiation of KMC (within 24 hours after birth vs later); the benefits were greater when the daily duration of KMC was at least 8 hours per day than with shorter duration ( online supplemental efigure 2 ). Pooled analysis of 4 studies that had reported mortality by 6 months of age showed a 25% reduction in mortality (RR 0.75; 95% CI 0.62 to 0.92; fixed-effect model; high certainty of evidence).
Kangaroo mother care (KMC) vs. conventional care –Risk ratio of mortality during birth hospitalisation or 28 days of life.
KMC probably results in a 15% reduction in severe infection/sepsis at the latest follow-up (RR 0.85, 95% CI 0.79 to 0.92; 9 trials, 9847 infants; moderate certainty evidence) and 68% reduction in the risk of hypothermia (RR 0.32, 95% CI 0.19 to 0.53; 11 trials, 1169 infants; moderate-certainty evidence). Infants in the KMC arm had a higher gain in anthropometric parameters, namely weight gain per day and length and head circumference gain per week ( table 2 ). The exclusive breastfeeding rates were higher at discharge/28 days of life (RR 1.48, 95% CI 1.44 to 1.52; 9 trials, 9983 infants, very low certainty evidence), but the evidence was uncertain; also, there was no difference in breastfeeding rates at 1–3 months of age. KMC may result in little to no difference in the Griffith Quotients or the risk of cerebral palsy at 12 months of corrected age 36 or IQ scores at 20 years of age.
KMC vs conventional newborn care: key outcomes
Early-initiated versus late-initiated KMC
The evidence was derived from 4 trials that enrolled 3603 infants. One study was done in a high-come country (Sweden), 2 studies were done in low-income countries (Madagascar and The Gambia), and 1 study was multi-country conducted in LMICs (Ghana, India, Malawi, Nigeria, and Tanzania). All trials were conducted in health facilities. Infant stability at enrolment, duration of KMC achieved, and time of initiation of KMC in the included studies are provided in table 3 . In two studies (Mörelius et al 24 and WHO iKMC) 5 KMC was initiated in the delivery room. Brotherton et al 6 enrolled moderately unstable infants in the early KMC arm and stable infants after >24 hour of admission in the control arm. Nagai et al began KMC within 24 hours of birth in the early arm and after 24 hours in the late arm.
Early vs late-initiated KMC – characteristics of included studies
Early-initiated KMC showed a reduction in the risks of mortality by 28 days of age (RR 0.78, 95% CI 0.66 to 0.92; 3 trials, 3533 infants, high certainty evidence; online supplemental efigure 3 ) and hypothermia by discharge or at 28 days (RR 0.74, 95% CI 0.61 to 0.90; high certainty evidence). It probably reduces the risk of clinical sepsis until 28-day follow-up (RR 0.85, 95% CI 0.76 to 0.96; table 4 ; low certainty evidence) and improves exclusive breastfeeding at discharge (RR 1.1.2, 95% CI 1.10 to 1.19; moderate certainty evidence). There was also a decrease in the length of hospital stay ( table 4 ).
Early vs late-initiated KMC – critical outcomes
On subgroup analysis, there was evidence of a reduction in 28-day mortality for infants with GA ≤34 weeks and BW ≤2000, but there was little data for infants >34 weeks and weighing >2000 g at birth. The mortality reduced with a duration of KMC of at least >16 hours per day, with little data for daily KMC duration of <8 hours or 8–16 hours per day.
Quality of the evidence
For the comparison of KMC vs conventional newborn care, the certainty of the evidence was assessed as high for neonatal mortality and moderate for sepsis/severe infection and hypothermia ( table 5 ). For early vs late-initiated KMC, the certainty of the evidence was high for neonatal mortality and hypothermia, moderate for exclusive breastfeeding at discharge, and low for nosocomial clinical sepsis ( table 6 ). A few outcomes, such as weight gain, breastfeeding, and length of hospital stay, showed a high degree of heterogeneity, partly due to clinical and methodological heterogeneity among the studies (varied definitions of hypothermia and time points of assessment; different methods of breastfeeding assessment, etc.).
Summary of findings – KMC vs conventional newborn care
Summary of findings – early initiated KMC vs late-initiated KMC in preterm or low-birth weight infants
The systematic review showed that KMC reduces mortality during birth hospitalisation or by 28 days of age and probably reduces severe infection at the latest follow-up in preterm and low birth weight infants in health facilities and at home. KMC may result in a slight increment in growth parameters (weight and length) and exclusive breastfeeding rates at discharge. KMC may result in little to no difference in neurodevelopmental outcomes at 12 months compared with conventional care. Compared with delayed initiation (>24 hours) of KMC, early-initiated KMC (<24 hours) results in a 33% reduction in mortality by 28 days and a slight reduction in clinical sepsis by 28 days.
Three recent systematic reviews examined the effect of KMC compared with conventional care on infant clinical outcomes. 3 37 38 The Cochrane review in 2016 found 21 studies enrolling 3042 low birth weight infants. 3 Our systematic review used a similar search strategy and inclusion criteria and included studies until 2022. We found 10 newer studies that provided data on 12 517 additional infants with similar gestation and birth weight range. The Cochrane review reported a similar decrease in mortality at discharge or 40 weeks of postmenstrual age (RR 0.60, 95% CI 0.39 to 0.92; 8 trials, 1736 infants) and similar effects on infection, hypothermia, and anthropometry. However, the certainty of the evidence was graded as moderate to very low in the Cochrane review. The addition of information from 12,000-odd infants has improved the precision and certainty of the evidence of the critical outcomes in the current review. In 2020, a systematic review of 416 preterm neonates reported that KMC significantly reduced apneic events in preterm neonates. 38 Another review in 2019 concluded that KMC had a significant positive impact on growth and breastfeeding rates in very low birth weight (VLBW) neonates. 37
We investigated the effect of mean duration KMC in hours and prespecified three categories (<8 hours, 8–16 hours, and >16 hours). The effects on mortality were comparable in the >16 hour and 8–16 hour groups, but there was insufficient data in the <8 hours group. The Cochrane review (2016) explored the effects of the duration of KMC in three different categories; <2 hours and 6–15 hours, and >20 hours per day, and found benefits only when KMC was done for 20 hours or more. We found beneficial effects of KMC in prespecified subgroups of ≤2.0 kg and >2.0 kg and infants with gestational age ≤34 and >34 weeks at birth. T he two community- based studies that enrolled infants at home also showed significant benefits on mortality. We found no additional trials – other than the study by Worku et al included in the Cochrane review – that compared KMC with conventional care in unstable infants.
Only one systematic review – the Cochrane review published in 2016 – has evaluated the effects of early vs late initiation of KMC in low birth weight infants. It also used a cut-off of 24 hours to define early initiation but found only one study of 73 relatively stable low birth weight infants. 25 Our review included three additional studies that recruited 3530 preterm/low birth weight infants and found significant beneficial effects with early initiation of KMC. 5 6 24
The results of our review have substantial implications for policymaking, particularly in LMIC. First, KMC should be provided to all low birth weight and preterm infants irrespective of the settings – both health facilities and at home. Second, given the probable dose-effect response, KMC should preferably be practiced for at least 8 hours a day for optimal benefits. Third, KMC should be initiated within the first 24 hours of life. Indeed, our findings have helped to make recommendations on KMC in the new WHO guidelines on the care of preterm and low birth weight neonates. 39
The strengths of the current review include a comprehensive and systematic search of the literature with updated evidence to March 2022. Compared with the existing Cochrane reviews on KMC, our review identified additional studies that had enrolled almost 13 000 low birth weight infants, which resulted in high precision of estimates and improved the certainty of the evidence. The review also had some limitations. The included studies were not blinded, although outcome assessors were blinded in many studies. However, the risk of bias in the included studies was generally low, and the certainty of the evidence for the primary outcomes was moderate to high. Very low birth weight, extremely preterm neonates, and severely unstable neonates were often excluded from studies. More evidence is needed before extrapolating the study results in these high-risk groups.
To conclude, our findings support the practice of KMC for preterm and low birth weight infants as soon as possible after birth and for at least 8 hours a day. Future research should focus on overcoming barriers and facilitators to large-scale implementation of KMC in facility and community settings. Data on long-term neurodevelopmental outcomes are also needed.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
Acknowledgments.
We acknowledge the support and guidance provided by Dr. Rajiv Bahl, Dr. Karen Edmond, and Dr. Shuchita Gupta from the WHO, Geneva, in finalising the protocol and interpreting the results.
- Milner KM ,
- Roberts G , et al
- Boundy EO ,
- Dastjerdi R ,
- Spiegelman D , et al
- Conde-Agudelo A ,
- Díaz-Rossello JL
- Mazumder S ,
- Dube B , et al
- WHO Immediate KMC Study Group ,
- Naburi H , et al
- Brotherton H ,
- Kebbeh B , et al
- Sankar MJ ,
- Natarajan CK ,
- Das RR , et al
- Balshem H ,
- Helfand M ,
- Schünemann HJ , et al
- Acharya N ,
- Bhatta NK , et al
- Sharma R , et al
- Alisjahbana A ,
- Lrawaty S , et al
- Ferguson AE ,
- Morales Y , et al
- Cattaneo A ,
- Davanzo R ,
- Worku B , et al
- Charpak N ,
- Ruiz-Peláez JG ,
- Figueroa de CZ , et al
- Bhavana DrD ,
- Lakshmi DBV ,
- Sruthi DT , et al
- Pratiwi I ,
- Soetjiningsih S ,
- Gathwala G ,
- Ghavane S ,
- Subramanian S , et al
- Hake-Brooks SJ ,
- Anderson GC
- Kanbur W , et al
- Kumbhojkar S ,
- Md Mahbubul H ,
- Md Maksudur R
- Mörelius E ,
- Örtenstrand A ,
- Theodorsson E , et al
- Andrianarimanana D ,
- Rabesandratana N , et al
- Nimbalkar SM ,
- Patel DV , et al
- Ramanathan K ,
- Deorari AK , et al
- Roberts KL ,
- Paynter C ,
- Quevedo M , et al
- Camacho LW ,
- Rojas EP , et al
- Suman RPN ,
- Zhang Y , et al
- Whitelaw A ,
- Heisterkamp G ,
- Sleath K , et al
- Ruiz-Pelaez JG ,
- Figueroa de C Z , et al
- Farahbakhsh N ,
- Sharma S , et al
- Montealegre-Pomar A ,
- Bohorquez A ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Press release
Handling editor Seema Biswas
Contributors Both authors, MJS and SS, contributed equally to protocol development, literature search, data extraction and analysis and interpretation. SS drafted the manuscript with inputs from MJS. Both authors reviewed and approved the final manuscript. MJS acts as the guarantor of the paper.
Funding The World Health Organization. Grant number- not applicable.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (44,147,016 articles, preprints and more)
- Free full text
- Citations & impact
- Similar Articles
What is kangaroo mother care? Systematic review of the literature.
Author information, affiliations.
- Valsangkar B 2
- Kajeepeta S 3
- Boundy EO 3
Journal of Global Health , 01 Jun 2016 , 6(1): 010701 https://doi.org/10.7189/jogh.06.010701 PMID: 27231546 PMCID: PMC4871067
Abstract
Conclusions, free full text .

What is kangaroo mother care? Systematic review of the literature
Grace j chan.
1 Department of Pediatrics, Harvard Medical School, Boston, MA, USA
2 Department of Global Health and Population, Harvard T.H. Chan School of Public Health, Boston, MA, USA
3 Saving Newborn Lives, Save the Children, Washington, DC, USA
Bina Valsangkar
Sandhya kajeepeta, ellen o boundy, stephen wall.
- Associated Data
Kangaroo mother care (KMC), often defined as skin–to–skin contact between a mother and her newborn, frequent or exclusive breastfeeding, and early discharge from the hospital has been effective in reducing the risk of mortality among preterm and low birth weight infants. Research studies and program implementation of KMC have used various definitions.
To describe the current definitions of KMC in various settings, analyze the presence or absence of KMC components in each definition, and present a core definition of KMC based on common components that are present in KMC literature.
We conducted a systematic review and searched PubMed, Embase, Scopus, Web of Science, and the World Health Organization Regional Databases for studies with key words “kangaroo mother care”, “kangaroo care” or “skin to skin care” from 1 January 1960 to 24 April 2014. Two independent reviewers screened articles and abstracted data.
We screened 1035 articles and reports; 299 contained data on KMC and neonatal outcomes or qualitative information on KMC implementation. Eighty–eight of the studies (29%) did not define KMC. Two hundred and eleven studies (71%) included skin–to–skin contact (SSC) in their KMC definition, 49 (16%) included exclusive or nearly exclusive breastfeeding, 22 (7%) included early discharge criteria, and 36 (12%) included follow–up after discharge. One hundred and sixty–seven studies (56%) described the duration of SSC.
There exists significant heterogeneity in the definition of KMC. A large number of studies did not report definitions of KMC. Skin–to–skin contact is the core component of KMC, whereas components such as breastfeeding, early discharge, and follow–up care are context specific. To implement KMC effectively development of a global standardized definition of KMC is needed.
Globally, 44% of under–five deaths occur during the neonatal period, and the proportion of under–five deaths due to neonatal causes continues to rise [ 1 , 2 ]. Preterm birth (before 37 weeks gestation) accounts for 35% of neonatal deaths. Low birth weight (defined as <2500 g) is commonly used as a surrogate measure of preterm birth [ 3 ]. Preterm and low birth weight infants who survive the neonatal period are more likely to experience neonatal morbidities including acute respiratory, gastrointestinal, immunologic, central nervous system, hearing and vision problems than both term and normal weight infants [ 4 ].
A significant proportion of deaths among preterm and low birth weight infants is preventable. There is evidence that kangaroo mother care (KMC), when compared to conventional neonatal care in resource–limited settings, significantly reduces the risk of mortality in infants born in facilities who are clinically stable and weighing less than 2000 g [ 5 ]. KMC also reduces the risk of hypothermia, severe illness, nosocomial infection, and length of hospital stay, and improves growth, breastfeeding, and maternal–infant attachment [ 5 , 6 ].
Despite strong evidence for mortality and morbidity reduction in low– and middle–income settings and endorsement from the World Health Organization (WHO), country–level adoption and implementation of KMC has been limited. In a systematic assessment of health system bottlenecks among countries with a high burden of neonatal deaths, KMC was identified as an intervention with significant health systems barriers to scale–up including leadership and governance, health financing, health workforce, health service delivery, health information systems, and community ownership and partnership [ 7 ]. Health intervention priority–setting tools, such as the Lives Saved Tool and Child Health and Nutrition Research Initiative methodology, have identified KMC as a high priority intervention based on criteria such as mortality benefit and equity [ 8 , 9 ].
In response to limited global uptake of KMC, in 2013, a group of newborn health stakeholders led by the Bill and Melinda Gates Foundation and Save the Children’s Saving Newborn Lives Program launched a global KMC Acceleration Convening. The goal was to address barriers to implementation, increase uptake of KMC as part of an integrated Reproductive Maternal Newborn and Child Health package, and identify research priorities [ 10 ]. In addition to implementation barriers, a lack of a clear definition of KMC has made effective coverage at scale of KMC challenging. A multi–country study in Africa found variation in KMC implementation across facilities in countries with national commitment to KMC [ 11 ]. Regional, country, and facility differences in health worker capacity, financial resources, leadership, health information systems, and cultural and community structures create challenges to developing and adopting a global definition of KMC.
The WHO has defined KMC as early, continuous, and prolonged skin–to–skin contact (SSC) between the mother and preterm babies; exclusive breastfeeding or breast milk feeding; early discharge after hospital–initiated KMC with continuation at home; and adequate support and follow–up for mothers at home [ 12 ]. While the WHO provides guidance on the components of KMC, guidance on the operationalization and clinical implementation of KMC are needed. There are significant variations in the timing of initiation, duration of SSC, positioning, necessary equipment and supplies, discharge criteria, follow–up frequency, indicators and measurement, and health workforce needs. The variations in these components have differential effects on preterm and low birth weight outcomes. As the global newborn health community begins to accelerate implementation of KMC, a standardized operational definition is needed. We conducted a systematic review of the KMC literature to 1) describe the current definitions of KMC in various settings, 2) analyze the presence or absence of WHO KMC components in each definition, and 3) present a core definition of KMC–common components that are present in at least 70% of all studies and programs–and describe how KMC definitions vary by context. This review provides a basis for development of an operational definition and clinical standards to accelerate the uptake of KMC globally.
We searched PubMed, Embase, Web of Science, Scopus, and WHO regional databases: AIM, LILACS, IMEMR, IMSEAR, and WPRIM using the search terms “kangaroo mother care”, “kangaroo care”, and “skin to skin care” with no language restrictions from 1 January 1960 to 24 April 2014 for original reports including case–control studies, cohort studies, randomized control trials, and case series with 10 or more participants (see Online Supplementary Document (Online Supplementary Document) for the review protocol and full search strategy). Following PRISMA guidelines, studies were included if they contained at least one of the following: the amount of time KMC was practiced, an association between KMC (as an isolated exposure, not part of a larger package) add any outcome, barriers to implementing KMC or factors necessary for successful implementation of KMC. Exclusion criteria were non–human subjects, case series or descriptive studies with fewer than 10 participants, and non–primary data collection or analysis (eg, reviews, meeting abstracts, editorials). Our population of interest included mothers, newborns, or mother–newborn dyads (not restricted to any specific ages) who have practiced KMC as well as health care providers, health facilities, communities, and health systems that have implemented KMC.
We also conducted hand–searches through the reference lists of the articles included in our review and published systematic reviews. Cochrane reviews were searched for relevant articles. To search the “grey literature” for unpublished studies, we explored programmatic reports and requested data from programs implementing KMC to obtain programmatic perspectives in addition to those provided by research studies. Reports were included following the same criteria as above.
Two independent reviewers examined titles, abstracts and full–text articles for inclusion into the review using a screening form based on our inclusion criteria. Using standardized data abstraction forms, two reviewers abstracted data independently from all included articles and reports. At each stage, reviewers compared results to ensure agreement. In the case of disagreement between the two reviewers, a third party acted as a tiebreaker. Native speakers abstracted data from articles in foreign languages. Languages for which a native speaker was not identified (ie, German, Finnish, Korean, Thai and Polish) were translated using an online translation software to assist with data abstraction. If an article or report were missing any information, we contacted the authors to request the data.
Using standardized forms, data were abstracted on study characteristics such as study design, country, sample size, location, and duration of follow–up. We abstracted data on KMC definitions including data on SSC, exclusive breastfeeding, early discharge from the facility, and follow–up and as well as other components [ 12 ]. We generated categorical variables for each component and calculated descriptive frequencies, means, medians and ranges for quantitative data.
Study selection and characteristics

Flow diagram of study selection.
Characteristics of included studies
KMC components
The individual components of KMC varied across studies ( Table 2 ). Kangaroo mother care was not defined in 88 studies (29%). All 211 studies (71%) with KMC definitions included SSC as a component. One–hundred forty–eight studies (50%) included SSC only. For the additional components, 49 studies (16%) included SSC and exclusive or near–exclusive breastfeeding, 36 (12%) included SSC and follow–up after discharge from the health facility, and 22 (7%) included early discharge from the health facility.
Description of kangaroo mother care components in studies
Skin–to–skin contact
Among the studies that defined SSC as part of the KMC package, criteria for SSC initiation, SSC ending, and SSC duration were not well described ( Table 3 and Table 4 ). In 43 studies (14%), SSC was initiated after non–stability criteria were met, 27 studies (9%) promoted immediate initiation of SSC within 60 minutes of birth, 76 studies (25%) encouraged SSC after stability criteria were met, 18 studies (6%) encouraged SSC after a painful procedure, and 135 (45%) did not describe SSC initiation criteria. Forty–three studies observed initiation of SSC of which 4 (9%) observed immediate initiation of SSC. Criteria for stability were non–specific including the terms “clinically stable,” “adapted to extra–uterine life,” “can tolerate handling,” and “without serious illness”. More defined criteria included “satisfactory APGAR score,” “stable weight,” and “stable respiratory and hemodynamic parameters.” Criteria to end SSC were largely non–specific with terms “one day or less,” “until baby no longer accepts,” or “until parent no longer accepts.” More specific terms included “until reaches satisfactory weight [2000 grams or 2500 grams]”. We compared descriptions of SSC with observations of SSC to differentiate promotion vs practice. Most studies (>85%) did not include data on observations of SSC practiced ( Table 3 ).
Promoted skin–to–skin contact characteristics compared to observed skin–to–skin contact characteristics
Promoted skin–to–skin contact duration compared to observed skin–to–skin contact duration
Breastfeeding
Description of breastfeeding characteristics
Discharge criteria from facility
Description of discharge and follow–up characteristics
Other components
Description of clothing and positioning during kangaroo mother care
There is significant heterogeneity in the definition of KMC and a large number of studies did not report a definition of KMC. Of the studies that defined KMC, SSC was present in all studies. Additional KMC components – breastfeeding, early discharge, and follow–up–were missing in the majority of studies. These findings suggest that SSC is accepted in research and programmatic settings as an essential component of KMC, but the other components vary by context, defined as demographic, economic, social, and cultural factors, and newborn characteristics.
The lack of a clear KMC definition and guidance for implementing KMC is a reflection of incomplete evidence. Evidence for KMC is largely based on meta–analyses that combine studies with heterogeneous definitions of KMC and occur in different settings [ 5 , 6 ]. Attempts to stratify the association of KMC on outcomes by KMC components, newborn characteristics (birth weight, gestational age), and high NMR vs low NMR often do not yield statistically significant results because of the limited data available. We do not know the effect of different combinations of KMC components, nor do we understand the feasibility with which each component can be implemented effectively in different contexts. Our study was limited by the lack of data on the duration of SSC. Furthermore, measurement of SSC duration was based on mothers’ report of time with minimal observational data. Studies where SSC duration was measured by an independent observer may be biased by the Hawthorn effect.
To define the optimal duration of SSC, we need additional data on the dose response of SSC duration on mortality and morbidity outcomes. The benefits of SSC are likely dependent on the duration of SSC, however the duration of SSC must also be balanced with the feasibility of practicing SSC for extended periods of time. In most settings promoting SSC 24 hours a day is not feasible. Understanding the minimal duration of SSC that provides the maximal benefits will provide more specific recommendations. Most studies initiated KMC after stabilization of the newborn and the effect of KMC on mortality and morbidity is generalizable to the population of newborns who survive to be stabilized. The effect of KMC immediately after birth before stabilization is unclear due to inconclusive evidence [ 14 – 17 ]. Additional efforts to test the effect of KMC prior to stabilization and to define stability is needed through further studies or by consulting experts at each level of care (primary, secondary, or tertiary care) through a Delphi method.
To operationalize KMC, the simpler the intervention the more likely it is to scale [ 18 ]. A simple and clear operational definition for KMC is needed. Evidence suggests benefits for newborns less than 2000 g, who are stabilized in facilities with SSC as the primary component. More work is needed to improve the measurement of gestational age and improving the recording of birth weights in facilities to better understand the impact of KMC and for whom there are benefits. Our review suggests that skin–to–skin contact is the core minimal component of KMC and variations depend on context and individual clinical needs of the newborn. For example, extremely preterm newborns who are unable to coordinate their suck and swallow will need feeding support such as nasogastric feeding or intravenous fluid. In high resource settings with space and infection precautions, a provider may recommend SSC for a preterm infant but choose not to discharge early from the facility. To operationalize KMC, a simple matrix that lists newborn characteristics in columns and KMC components in rows for different settings, ie, tertiary, secondary, primary or community levels, can take into account the core SSC components with variations based on differences in the newborn and context.
As implementation of KMC begins to accelerate globally, data on the context, individual newborn factors, and KMC components can be collected and harmonized to generate a model that will best define KMC for a set of individual newborn characteristics in specific settings. Research and programmatic agendas to advance KMC should include a standardized set of indicators and measurement tools that document SSC initiation criteria, SSC duration as number of hours per day promoted and ideally observed, feeding protocols, discharge criteria from a facility to community and follow–up standards, and discharge criteria from KMC. To track progress, indicators and standard measurement tools are needed to measure coverage of key newborn interventions including KMC [ 19 ]. The release of the new preterm guidelines by the World Health Organization, where KMC is recommended for all newborns less than 2000 g, will provide an opportunity for programs and researchers to start addressing definition gaps, establish global recommendations of operational definitions and core components of KMC, and accelerate KMC within care of preterm babies.
Developing a standardized operational definition of KMC and employing indicators and measurement tools to measure and evaluate KMC acceleration efforts is needed. More than half of the studies equate KMC with SSC. Moving forward, careful distinction between KMC and SSC is needed. While SSC is beneficial for all newborns, KMC should be clearly defined, at the bare minimum, as a package of interventions including SSC, exclusive breastfeeding, and close monitoring for preterm and/or low birthweight babies. Researchers and program implementers can contribute to building a more solid evidence base for KMC by measuring and reporting how KMC is defined–the components implemented and the feasibility of implementation based on the context–and the outcomes measured. A central and accessible database to share knowledge should contain this data in addition to standardized indicators, such as the proportion of eligible newborns who receive KMC and the barriers and facilitators to implementation of KMC.
- Acknowledgments
We thank Stacie Constantian, Roya Dastjerdi, and Tobi Skotnes for reviewing and abstracting data. Rodrigo Kuromoto and Eduardo Toledo reviewed non–English articles. We acknowledge Kate Lobner for developing and running the search strategy. We would like to thank the mothers and newborns who participated in these studies to better understand how research and programs define KMC.
Funding: Funding for this systematic review was provided by Saving Newborn Lives program of Save the Children Federation, Inc.
Authorship contributions: All authors listed have participated in the concept, design, analysis and interpretation of the data, drafting, or editing of the manuscript. All authors have approved the manuscript as submitted.
Competing interests: The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author). None of the authors has any competing interests to declare. There are no competing interests to disclose.
- Additional Material
Full text links
Read article at publisher's site: https://doi.org/10.7189/jogh.06.010701
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Smart citations by scite.ai Smart citations by scite.ai include citation statements extracted from the full text of the citing article. The number of the statements may be higher than the number of citations provided by EuropePMC if one paper cites another multiple times or lower if scite has not yet processed some of the citing articles. Explore citation contexts and check if this article has been supported or disputed. https://scite.ai/reports/10.7189/jogh.06.010701
Article citations, feasibility and acceptability of a novel biomedical device to prevent neonatal hypothermia and augment kangaroo mother care in kenya: qualitative analysis of focus group discussions and key informant interviews..
Bhuiya NA , Liu S , Muyodi D , Bucher SL
PLOS Glob Public Health , 4(4):e0001708, 16 Apr 2024
Cited by: 0 articles | PMID: 38626201 | PMCID: PMC11020951
Parents' and neonatal healthcare professionals' views on barriers and facilitators to parental presence in the neonatal unit: a qualitative study.
Schmid SV , Arnold C , Jaisli S , Bubl B , Harju E , Kidszun A
BMC Pediatr , 24(1):268, 24 Apr 2024
Cited by: 0 articles | PMID: 38658901 | PMCID: PMC11040849
Microbiome dysbiosis: a modifiable state and target to prevent Staphylococcus aureus infections and other diseases in neonates.
Aneja A , Johnson J , Prochaska EC , Milstone AM
J Perinatol , 44(1):125-130, 30 Oct 2023
Cited by: 0 articles | PMID: 37904005
Determinants of Kangaroo Mother Care among low-birth-weight infants in low resource settings.
Lawal TV , Lawal DI , Adeleye OJ
PLOS Glob Public Health , 3(9):e0002015, 12 Sep 2023
Cited by: 0 articles | PMID: 37699007 | PMCID: PMC10497168
Effects of Kangaroo Care on the development of oral skills and achievement of exclusive oral feeding in preterm infants.
Ciochetto CR , Bolzan GP , Gonçalves DDS , Silveira FPHD , Weinmann ARM
Codas , 35(5):e20220070, 04 Aug 2023
Cited by: 1 article | PMID: 37556686 | PMCID: PMC10449087
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
- http://www.ebi.ac.uk/biostudies/studies/S-EPMC4871067?xr=true
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Kangaroo mother care to reduce morbidity and mortality in low birthweight infants.
Conde-Agudelo A , Díaz-Rossello JL
Cochrane Database Syst Rev , (4):CD002771, 22 Apr 2014
Cited by: 55 articles | PMID: 24752403
Conde-Agudelo A , Diaz-Rossello JL , Belizan JM
Cochrane Database Syst Rev , (2):CD002771, 01 Jan 2003
Cited by: 28 articles | PMID: 12804436
Cochrane Database Syst Rev , (4):CD002771, 01 Jan 2000
Cited by: 31 articles | PMID: 11034759
Conde-Agudelo A , Belizán JM , Diaz-Rossello J
Cochrane Database Syst Rev , (3):CD002771, 16 Mar 2011
Cited by: 80 articles | PMID: 21412879
Barriers and enablers of health system adoption of kangaroo mother care: a systematic review of caregiver perspectives.
Smith ER , Bergelson I , Constantian S , Valsangkar B , Chan GJ
BMC Pediatr , 17(1):35, 25 Jan 2017
Cited by: 52 articles | PMID: 28122592 | PMCID: PMC5267363
Europe PMC is part of the ELIXIR infrastructure
Journal Article
Jun 15, 2016
Kangaroo Mother Care (KMC)
What is kangaroo mother care? Systematic review of the literature

Additional Authors
Grace J Chan, Bina Valsangkar, Sandhya Kajeepeta , Ellen O Boundy, Stephen Wall
Related Topics
Subscribe to our newsletter.
Kangaroo mother care (KMC), often defined as skin– to–skin contact between a mother and her newborn, frequent or exclusive breastfeeding, and early discharge from the hospital has been effective in reducing the risk of mortality among preterm and low birth weight infants. Research studies and program implementation of KMC have used various definitions.
To describe the current definitions of KMC in various settings, analyze the presence or absence of KMC components in each definition, and present a core definition of KMC based on common components that are present in KMC literature.
We conducted a systematic review and searched PubMed, Embase, Scopus, Web of Science, and the World Health Organization Regional Databases for studies with key words “kangaroo mother care”, “kangaroo care” or “skin to skin care” from 1 January 1960 to 24 April 2014. Two independent reviewers screened articles and abstracted data.
We screened 1035 articles and reports; 299 contained data on KMC and neonatal outcomes or qualitative information on KMC implementation. Eighty–eight of the studies (29%) did not define KMC. Two hundred and eleven studies (71%) included skin–to–skin contact (SSC) in their KMC definition, 49 (16%) included exclusive or nearly exclusive breastfeeding, 22 (7%) included early discharge criteria, and 36 (12%) included follow–up after discharge. One hundred and sixty–seven studies (56%) described the hours per day of SSC.
Conclusions
There exists significant heterogeneity in the definition of KMC. A large number of studies did not report definitions of KMC. Skin–to–skin contact is the core component of KMC, whereas components such as breastfeeding, early discharge, and follow–up care are context specific. To implement KMC effectively development of a global standardized definition of KMC is needed.
Related Resources
May 19, 2023
Kangaroo Mother Care (KMC) | Newborn
Follow-up of Kangaroo Mother Care programmes in the last 28 years: results from a cohort of 57 154 low-birth-weight infants in Colombia

May 18, 2023
Infection | Kangaroo Mother Care (KMC)
Effect on neonatal sepsis following immediate kangaroo mother care in a newborn intensive care unit: a post-hoc analysis of a multicentre, open-label, randomised controlled trial

May 16, 2023
Newborn | Kangaroo Mother Care (KMC)
Global Position Paper on Kangaroo Mother Care: A transformative innovation in healthcare

Kangaroo Mother Care: Implementation strategy for scale-up adaptable to different country contexts

We have a new look and feel!
We may look different, but we have not lost the essence of who we are; a learning platform that provides evidence-based knowledge to those working to ensure that newborns survive and thrive. We’d love to hear what you think of the new HNN!
Contact us!
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Kangaroo mother care knowledge, attitude, and practice among nursing staff in a hospital in Jakarta, Indonesia
Asri Adisasmita
1 Department of Epidemiology, and Kangaroo Mother Care Research Project, Faculty of Public Health, Universitas Indonesia, Depok, Indonesia
Yulia Izati
2 Kangaroo Mother Care Research Project, Faculty of Public Health, Universitas Indonesia, Depok, Indonesia
Septyana Choirunisa
Hadi pratomo.
3 Department of Health Education and Behavioural Sciences, and Kangaroo Mother Care Research Project, Faculty of Public Health, Universitas Indonesia, Depok, Indonesia
Luzy Adriyanti
4 Koja District General Hospital, North Jakarta, Jakarta Province, Indonesia
Associated Data
The datasets generated and/or analyzed in this study are not publicly available because they are property of Universitas Indonesia and Koja District General Hospital; however, they may be available from the corresponding author on reasonable request. The authors confirm that there is no special access privileges to the data others would not have. Data can be requested to: 1. Research and Community Engagement Unit, Faculty of Public Health, Universitas Indonesia (Dr. Doni H. Ramadan, email: di.ca.iu@iumkf ) 2. Research and Development Unit, Koja District General Hospital (Ms. Titin Windarti, email: di.og.atrakaj.ajokdusr@ofni )
Kangaroo mother care (KMC) has been proven to decrease rates of morbidity and mortality among premature and low-birth-weight infants. Thus, this study aimed to obtain baseline data regarding KMC knowledge, attitudes, and practices (KAP) among nursing staff caring for mothers and newborns in a hospital in Indonesia.
This cross-sectional study included 65 participants from three hospital wards at Koja District Hospital, North Jakarta. Participants included 29 perinatal ward nurses, 21 postnatal ward nurses and midwives, and 15 labor ward midwives. Data on KAP of KMC were collected using a self-administered questionnaire with closed-ended questions. Each questionnaire can be completed in approximately 1 hour.
Among the included nursing staff, 12.3% (8/65) were determined to have received specific training on KMC, whereas 21.5% (14/65) had received more general training that included KMC content. About 46.2% of the nursing staff had good knowledge concerning KMC, 98.5% had good knowledge of KMC benefits, and 100% had a positive attitude toward KMC. All perinatal ward nurses had some experience assisting and implementing KMC. Some KAP that were observed among the nursing staff included lack of knowledge about the eligible infant weight for KMC and weight gain of infants receiving KMC, lack of education/training about KMC, and concerns regarding necessary equipment in KMC wards.
Conclusions
This study identified several issues that need to be addressed, including knowledge of feeding and weight gain, workload, incubator use, and the need for well-equipped KMC wards. We recommend that hospitals improve their nursing staff’s knowledge of KMC and establish well-equipped KMC wards.
Introduction
Worldwide, nearly 14.8 million babies are born prematurely. In 2014, Indonesia ranked fifth in the world for the number of preterm births (527,672 infants), which comprised 3.5% of preterm births globally for that period [ 1 ]. This is important because preterm infants have considerably higher mortality rates than full-term babies [ 2 ]. Studies have shown that kangaroo mother care (KMC) is safe and effective for managing low-birth-weight (LBW) and preterm babies, and it contributes to decreased mortality rates of preterm infants in both low- and high-income countries [ 2 ]. Lawn et al. reported that KMC was associated with an approximately 50% decrease in deaths among LBW infants weighing less than 2,000 grams at birth [ 3 ]. Moreover, unlike the conventional method of care (incubator), it has been reported that KMC reduces the incidence of severe infection (such as sepsis), nosocomial infection, hypothermia, severe morbidity, lower respiratory tract infection, and prolonged hospital stay. Compared to infants receiving conventional care, those treated with KMC showed more stable body temperature; increased body weight, length, and head circumference; improved breastfeeding; and stronger mother–child bonding [ 3 , 4 ].
Although KMC was introduced in Indonesia in the 1990s, it was not until much later that the Ministry of Health of the Government of Indonesia (GoI) has started to intensively promote KMC in several hospitals throughout the country. With the assistance of the United States Agency for International Development (USAID) and through the Health Service Program (2006–2012), the GoI initiated the KMC program by sending healthcare personnel to attend KMC training in South Africa. Subsequently, the KMC method was implemented across several private and public hospitals [ 5 ]. However, KMC implementation did not progress as expected due to lacking guidelines for KMC implementation and standard operating procedures (SOPS), absence of routine supervision and mentoring, and need for awareness/knowledge in healthcare workers (nursing staff) regarding the importance of KMC for the care of LBW/preterm babies. Those factors may have affected nursing staff knowledge, attitude, and practices (KAP) concerning KMC. Thus, good KAP about KMC are necessary to ensure good implementation of KMC in hospitals. Studies have shown that lack of training, which affected KAP of KMC, substantially hindered KMC adoption among nurses, especially in low- and middle-income countries [ 6 ]. Zhang et al. (2018) identified inadequate formal education among nurses as a substantial barrier to the implementation of KMC in China [ 7 ]. Even informal education about KMC provided improved knowledge of KMC and its benefit among nurses who could support KMC care [ 2 , 7 , 8 ].
To date, information on KAP of KMC among nursing staff in Indonesia remains limited. Therefore, this study aimed to describe the KAP of nursing staff concerning KMC in a hospital setting, serving as a baseline for larger intervention studies as part of efforts to improve the KAP of KMC among nursing staff.
Materials and methods
This descriptive study examining KAP of KMC among nursing staff was conducted as part of a baseline research project on KMC implementation at Koja District Hospital in North Jakarta, Indonesia, and it was funded by the USAID Partnerships for Enhanced Engagement in Research (PEER) program. The study is part of a larger research project that used quantitative and qualitative methods, but this part only focused on the quantitative part of the research. The complete baseline research project included assessment of neonatal morbidity, mortality, and KMC implementation; KAP of KMC among hospital nursing staff; and KAP of KMC among primary health center staff. It also included formative research that explored factors needed to strengthen and enhance KMC implementation in the hospital. Factors included refresher training, facilitative supervision, hospital policies, SOPs for KMC implementation, and the needed supporting facilities to provide input for the development of an intervention package to improve KMC implementation in the hospital. This current study included an analysis of baseline conditions regarding the KAP of KMC among all nurses supporting KMC care before the implementation of the intervention package. This baseline study aimed to provide input for designing a training as part of the intervention to improve KMC care.
The study site, Koja District Hospital, was a secondary-level hospital with a 16-bed neonatal intensive care unit (NICU) and a 40-bed perinatal ward that received perinatal referrals from hospitals near Jakarta. There were no rooms or beds specifically designated for KMC and no written formal KMC SOPs signed by the hospital director. Between June and December 2015, approximately 3,040 neonates were born at or admitted to the hospital. Among those, 412 had LBW (13.5%), with 85% born at the hospital and the remaining admitted after birth. The death rate among LBW infants was recorded to be at 0.9% of the total number of neonatal deaths per total number of those born at or admitted to the hospital during the same period [ 9 ].
All nursing staff at Koja District Hospital who provides in-hospital neonatal care (65 respondents) were included: 29 perinatal ward and NICU nurses, 21 postnatal ward nurses and midwives, and 15 labor ward midwives. The perinatal ward is where neonates are hospitalized, the labor ward is where women deliver their babies, and the postnatal ward is where mothers are transferred after giving birth to a healthy baby. Nursing staff working at an antenatal care (ANC) clinic and those from other hospitals who referred neonates to Koja District Hospital were excluded from the baseline assessment. The hospital nursing staff of each ward was divided into three work shifts. For example, nine nurses provide care for 40 and 16 neonates in the perinatal ward and NICU during each shift, respectively, yielding a ratio of 9 nurses to 56 infants, assuming the usual full occupancy.
Included nursing staff signed a written informed consent form prior to study enrollment. None of them refused to participate in the study. Thereafter, they completed a self-administered questionnaire that included questions related to general knowledge, benefits, attitude, and practices associated with KMC. Data were collected in March 2016. Before data collection, a pre-test of the questionnaire was conducted with nursing staff from another hospital similar to the study site.
The questionnaire consisted of 24 questions on general knowledge, 20 questions on benefits, 12 questions on attitude, and 6 questions on practices associated with KMC. To measure general knowledge, benefits, and practices related to KMC, closed-ended questions (adapted from El-Nagar et al. and KMC Facilitator’s Guide ACCESS) were used [ 10 , 11 ]. For every question on general knowledge and benefits of KMC, a correct response was scored as 1 and incorrect as 0. To measure attitude toward KMC, questions from validated tools were adapted, and a 5-point Likert scale (ranging from “strongly disagree” to “strongly agree”) was used. During analysis, the Likert scale was converted to scores, with 60 being the highest and 12 being the lowest (based on 12 questions and a 5-point Likert scale). A maximum score of 75% or more (i.e., 45 or more) reflected a good attitude toward KMC. Similarly, the same approach was applied to categorize general knowledge and benefits of KMC. Maximum scores for general knowledge and benefits of KMC were 24 and 20, respectively. General knowledge, knowledge on benefits, and attitude score were grouped into four categories (scores 0 to 25 = very low, 25 to below 50 = low, 50 to below 75 = moderate, and 75 to 100 = good/high).
Data collected were entered and analyzed using statistical software. We used descriptive statistics (frequencies, proportions, mean, and median) to summarize knowledge scores and chi-squared or Fisher exact tests if the expected value was less than 5 to measure the associations between two variables. P-values < 0.05 were considered statistically significant. This study was approved by the Ethics Committee of Faculty of Public Health, Universitas Indonesia (Registry number 230/H2.F10/PPM.00.02/2015).
Nursing staff characteristics
Characteristics of the nursing staff in this study are presented in Table 1 . Nursing staff in the perinatal–NICU and postnatal wards were determined to be younger (<30 years of age) than those in the labor ward. Most of the nursing staff (93.2%, 73.3%, and 95.2% in the perinatal, labor, and postnatal wards, respectively) had been working for < 10 years in their current unit. At least 75% of the staff in all three wards had nurse or midwife diplomas (3 years of education).
a Percentages that do not add up to 100% was due to missing data (i.e., one respondent from the postnatal ward did not provide an answer for years of experience working in the current unit).
*p-value < 0.05.
Kangaroo mother care (KMC) training
Most study participants had never attended KMC-specific training (87.7%) or other training that included KMC content (78.5%). Interestingly, a higher proportion of nursing staff in the labor ward than in the perinatal ward attended training that included KMC content (33.3% vs 24.1%, respectively), although the difference was not statistically significant (p = 0.232) ( Table 2 ). Overall, 7.7% of nurses (5/65) had attended both the above-mentioned types of training, 18.5% (12/65) had attended training specific to or including KMC, and 73.8% (48/65) had never attended any KMC-related training.
General knowledge on KMC among nursing staff
General knowledge on KMC was measured through 24 questions, wherein five of those were answered incorrectly by most of the nursing staff in the labor and postnatal wards. The five questions concerned the following: (1) providing nutrition using a small cup, (2) nasogastric tube feeding for LBW infants, (3) early feeding with non-breastmilk, (4) counseling for neonates already at a bodyweight of 2,500 g, and (5) infants gaining adequate weight with the KMC method. Most of the nursing staff (79.3%, 80%, and 100% in the perinatal, labor, and postnatal wards, respectively) incorrectly answered the last question (i.e., weight gain). Nursing staff in the perinatal ward achieved the highest percentage of correct answers (20.7%) for the question on adequate weight gain with the KMC method.
After stratifying participants according to their age, there was no difference observed in the percentage of those with good general knowledge on KMC (63.2% among those aged < 27 years old, compared to 70% among those aged > 27 years old; p = 1.000). The percentage of nursing staff with good general knowledge on KMC was similar between those who had attended training specific to KMC and those who never attended KMC training (50% vs. 68%, respectively; p = 1.000). A higher percentage of perinatal staff who attended training that included KMC content had good general knowledge on KMC compared to those who had never attended such training, although the difference was not statistically significant (71.4% vs. 61.9%, respectively; p = 1.000; Table 3 ). Scores on general knowledge of KMC were good (score > 75) among 65.5% and 60% nursing staff in the perinatal and labor wards, respectively, but only 9.5% nursing staff in the postnatal ward achieved a good score ( Fig 1 ).

General knowledge, knowledge on benefits, and attitude scores were grouped into four categories (scores 0 to 25, 25 to below 50, 50 to below 75, and 75 to 100). The figure represents the percentages of nurses based on those four score categories, with a score of 75–100 representing good knowledge or attitude.
*p-value <0.05.
**p-values cannot be calculated for all participants included in one category.
Nursing staff knowledge on KMC benefits
Most of the nursing staff correctly responded to the 20 questions regarding KMC benefits, which were asked as true or false questions. However, several nursing staff in all three wards incorrectly answered some of these questions. These included questions regarding: (1) using the KMC method for LBW infants kept in an incubator (26.7% and 52.4% of nursing staff in the labor and postnatal ward, respectively, answered incorrectly); (2) disadvantages of KMC implementation with ward hygiene affected because of increased crowdedness (72.4%, 20%, and 23.8% of perinatal–NICU, labor, and postnatal ward nurses, respectively, answered incorrectly), which raised concerns about having a well-equipped KMC ward to support more convenient KMC implementation and prevent cross infection; and (3) whether or not KMC could reduce nursing staff workload (65.5%, 20%, and 4.8% of nursing staff from the perinatal–NICU, labor, and postnatal wards, respectively, stated that KMC increased workload). No difference was observed in the percentage of nursing staff with good knowledge on KMC according to age group. All nursing staff with any training involving KMC content showed good knowledge of KMC benefits, while those with no KMC training had slightly lower knowledge (95.2%) ( Table 3 ). Most nurses in all wards had good/high scores (scores > 75) for knowledge ( Fig 1 ).
Attitude toward KMC
Attitude of the nursing staff toward KMC was assessed through 12 questions. When asked about KMC implementation among infants weighing 1,000–1,800 g, 40% of respondents from the labor ward were not in favor of KMC implementation. No differences were observed after stratifying respondents’ scores according to age group and training experience, and 100% of nurses had a good attitude (score > 75) about KMC ( Table 3 ). These results remained consistent in all wards ( Fig 1 ).
KMC practices by nursing staff were measured based on two parameters: (1) educating mothers/fathers/families on KMC implementation for LBW infants and (2) assisting with KMC implementation. All nursing staff in the perinatal ward stated that they educated and assisted mothers/fathers/families to implement KMC for their infants. For nursing staff working in labor and postnatal wards, 9 of 36 also had the opportunity to educate and assist mothers in KMC.
Several studies have shown that formal and informal KMC education among nursing staff can substantially increase the success of KMC implementation. Unsuccessful KMC implementation is due to, among other factors, uncertainty about including or excluding neonates for KMC, which decreases confidence in implementing KMC. Despite being a single-center study, our results could be generalizable to the status of KAP of KMC among all hospital nursing staff in Indonesia, where such data remain scarce. Our findings showed that only 12.3% of all nurses had attended KMC-specific training and 21.5% attended other training that included KMC content. Zhang et al. (2018) found that KMC-specific training increased the confidence of neonatal nurses in KMC, thus promoting its implementation [ 7 ]. Bergh et al. mentioned that despite enthusiasm about participating in KMC training, the distance to the training site and staff shortages within a hospital could be the reason why a limited number of staff attended KMC training [ 12 ]. Considering that only a few nurses in Koja District Hospital had received KMC-specific training, we recommend that all nurses who provide mother and infant care at Koja District Hospital receive KMC-specific training to increase knowledge and confidence in implementing KMC. This is essential for vulnerable infants, such as those born preterm or LBW. This baseline study was conducted to obtain information to be incorporated into in-house training intervention at Koja District Hospital. Another solution to be considered is to consistently include KMC content in the nurse/midwife training curriculum [ 13 ].
Our findings show that most perinatal–NICU ward nurses had already been implementing KMC and educating parents on KMC, despite their lack of KMC training. Providing actual training to the nursing staff shows promise of substantially improving KMC implementation at Koja District Hospital. Also, the lack of training could result in conflicting knowledge on the timing and duration of KMC [ 14 , 15 ], which could lead to adverse consequences such as mortality [ 16 ] especially among less stable infants.
General knowledge on KMC was surprisingly low among most midwives and nurses working in the postnatal ward. Postnatal ward nursing staff must have adequate knowledge on KMC to ensure its implementation among stable infants born in the hospital, including those rooming-in with the mother and those transferred from the perinatal–NICU ward whose mothers remain hospitalized. The current policy in the study hospital, however, does not support KMC implementation in the postnatal ward. Nonetheless, studies have shown that implementing KMC in the postnatal ward could reduce the length of hospital stay among more stable LBW infants, thereby reducing the cost of care [ 17 – 19 ].
Those who had attended KMC trainings had consistently better general knowledge of KMC and its benefits. However, there was no statistically significant difference in the attitude toward KMC between those who had and had not received KMC training. Our questionnaire was based on previous studies that collected data through interviews [ 10 , 11 ]. However, the self-administered method of collecting data in our study could have hindered our ability to detect differences in attitude toward KMC, as nurses could discuss how to respond to questions while completing the questionnaire.
This present study also showed that certain KAP of KMC, including knowledge and concepts of feeding and weight gain, workload, and incubator use, are in urgent need of improvement to achieve better KMC implementation. One issue that needs to be highlighted in training is knowledge regarding feeding and weight gain, which is central to the success of KMC. An interventional study in India among medical students revealed that education was the most effective method to improve knowledge on infant feeding [ 20 ].
Another noteworthy finding of this study was that KMC did not reduce workload. These results were consistent with those presented in other studies, which found that KMC increased nurses’ workload [ 6 , 21 , 22 ]. A nurse may not have time for training to improve their knowledge and understanding of KMC because of their already high workload, leaving them with partial comprehension regarding KMC. A pre- and post-intervention study in a neonatal unit in Sweden (2008 and 2010) found that before the intervention, several nurses indicated that KMC increased their workload, but others stated that it did not. However, no staff members expressed concern about increased workload with KMC after the intervention. In fact, several staff members stated that KMC decreased nurses’ workload because parents learned to care for their infants [ 23 ]. The Swedish study also concluded that knowledge regarding KMC was especially important, in addition to ensuring the availability of adequate facilities [ 23 ]. That study indicated that an effective intervention could lead to a better atmosphere for implementing KMC. Hence, concerns regarding increased workload with KMC in the current study could be addressed through effective intervention. Furthermore, a parallel study of our KMC PEER project using a qualitative approach revealed that some nurses believed that KMC would decrease workload because the mother of a LBW infant is key in KMC implementation. However, to educate and support the mother/family in KMC, the nursing staff needs formal training to improve their skill and confidence in supporting KMC [ 24 ]. Adequate education on skin-to-skin contact, feeding position, and infant positioning by nursing staff will lead to excellent quality of KMC among mothers/parents/family. Excellent quality of KMC could promote faster weight gain and thermostability, leading to shorter hospitalization and lower morbidity rates among LBW infants [ 19 ]. Proper implementation of KMC could lead to reduced nursing staff workload.
Apart from the lack of understanding of KMC, hospital management often does not prioritize KMC. Provision of facilities and equipment needed to implement KMC, such as KMC beds or couches or a designated ward, could enable the successful and continuous implementation of KMC. The larger study found that the lack of equipment, facilities, and supporting policy were among the reasons why nurses and midwives from wards other than the perinatal ward never implemented KMC. In addition, pediatricians, nursing staff, and management expressed the need of having interventions, such as training, supportive facilitation, and supporting policy, besides facilities and equipment availability to improve KMC implementation [ 9 ].
Responses to our questionnaire indicated that most of the nursing staff were hesitant to implement KMC while infants were in an incubator, which was consistent with the qualitative results [ 24 ], despite studies showing that KMC could improve cardiorespiratory function, promote temperature stability, and prevent infection in addition to its beneficial effect on sleep patterns and breastfeeding [ 2 ]. Therefore, adequate education to address this hesitancy could improve the implementation of KMC with infants in incubators. However, in addition to adequate education, adequate equipment/facilities as well as SOPs and hospital policy supporting KMC implementation are essential for successful KMC in the hospital.
This present study clearly showed that training opportunities should be created to tackle misconceptions and gaps in knowledge of KMC. All nursing staff involved in maternal and infant care (i.e., those in ANC clinics; labor, perinatal, and postnatal wards) should receive adequate training on KMC, even if not directly involved in its implementation. This way, all nursing staff in related wards will be equipped with KMC knowledge that they could use to assist and advise expectant mothers about KMC. An interventional study on KMC knowledge among pregnant women in an ANC clinic in India showed a significant improvement in knowledge regarding the period when KMC should be started, duration of each session, frequency of KMC, and clothing and positioning of the mother and baby [ 25 ]. This illustrates the importance of providing KMC education to pregnant women during ANC visits, given that expectant mothers may be receptive to the concept of KMC. For effective ANC education, nursing staff must have adequate KAP of KMC through effective training.
A study in Norway found that implementing skin-to-skin care among preterm infants in the labor ward may be feasible and safe [ 26 ], indicating that the labor ward staff should also be equipped with KMC knowledge. However, implementing KMC in the labor ward at Koja District Hospital would require a preliminary study to assess its feasibility and safety, especially among preterm infants less than 34 weeks of gestation. Nevertheless, midwives on the labor ward can introduce KMC education for expectant mothers of preterm and LBW infants despite not being directly involved in KMC implementation.
Studies have shown that KMC promotes emotional stability, successful breastfeeding, and reduced neonatal morbidity [ 27 ]. Nurses/midwives should persuade and educate mothers in postnatal wards about KMC, especially those having LBW infants in stable condition. Bergh et al. [ 28 ] suggested that KMC education and training should include all obstetric and neonatal staff members. Indeed, our findings suggest that educational intervention should involve the staff of not only the perinatal ward but also the labor and postnatal wards.
Although all perinatal ward nurses included in this study stated that they had experience in implementing and supporting KMC, the quality of its implementation remained undetermined, with potential for improvement following appropriate intervention. Education has been viewed as an essential tool in improving nurses’ knowledge and skills in facilitating KMC [ 14 , 29 , 30 ]. Nevertheless, even nursing staff who had received training may still need time to become comfortable with the method [ 30 , 31 ]. On-site training could provide additional intervention that would result in the most successful implementation of KMC [ 32 , 33 ]. Moreover, collaboration among healthcare workers with shared goals and team commitments in which inexperienced nurses are partnered with those experienced in KMC can also be helpful [ 31 , 34 , 35 ]. Overall, KMC should be implemented among eligible LBW infants given that it improves weight gain and growth, protects from sepsis and hypothermia, and promotes breastfeeding, thereby playing an integral role in decreasing mortality and morbidity. To effectively implement KMC, the associated KAP among all related hospital nursing staff (including those in the ANC unit) should be improved. This can be attained through interventions involving education, on-site training, and mentoring. The successful implementation of KMC requires relevant education of nurses, education and support of mothers by nursing staff, monitoring of KMC implementation by nurses, identification of institution-specific barriers, and implementation of institution-specific strategies to overcome these barriers.
Our study showed that most nursing staff in the labor and postnatal wards had not received any KMC training. It is worth noting that midwives in the labor ward are in a good position to persuade mothers of LBW infants to implement KMC as a continuation of early breastfeeding initiation (provision of mother’s breast milk to infants within 1 hour of birth) [ 36 ]. Nursing staff in the postnatal ward can also persuade mothers of premature infants to implement KMC through educating them on the benefits of KMC (e.g., preventing hypothermia). Thus, including nurses/midwives in wards other than the perinatal ward in the training intervention is justified considering their opportunity to educate mothers with LBW infants regarding KMC.
One strength of this present study is the inclusion of labor ward nursing staff who are generally not the primary focus of KMC implementation. Therefore, the inclusion of labor ward nursing staff in future intervention would provide additional opportunities to introduce mothers to KMC and support mothers in using KMC.
This current study revealed that nurses and midwives at Koja District Hospital lacked KMC training. Notably, 73.8% of all nurses/midwives have never received relevant training and exhibited inadequate general knowledge on KMC. Moreover, no SOPs existed, and there was the lack of a designated facility for KMC implementation throughout the time of this baseline study. Nonetheless, it should be emphasized that the provision of appropriate KMC facilities does not guarantee successful KMC implementation. Nurses, midwives, and all relevant healthcare providers must also possess the necessary knowledge and attitude to encourage and educate parents to practice and implement KMC.
Recommendation
To improve KMC implementation in hospitals, effective interventions are needed. These should include training that incorporates KMC content into the nurse/midwife curriculum and extracurricular training. Also the provision of facilities that support KMC (such as couches or beds or a designated ward) coupled with on-site training and clear guidelines/SOPs for each relevant ward should also be taken into consideration. Engagement of key stakeholders (e.g., engaging the hospital director and management to obtain their support and commitment) is also a key factor in the success of KMC implementation, given their role in providing the necessary resources and ensuring optimum processes.
Acknowledgments
We acknowledge all the research teams participating in this KMC project under the PEER project; the enumerators who helped execute the study and collect data; Trisari Anggondowati, Ph.D, for her input regarding this manuscript; all the respondents; and the authorities at Koja District Hospital who made this study possible. The authors also would like to thank Enago ( www.enago.com ) for the English language review.
Funding Statement
This study was made possible by the generous support of the American people through the PEER (Partnerships for Enhanced Engagement in Research) Program. The program is supported by USAID and implemented by the U.S. National Academies of Sciences. HP (as the principal investigator of this study) received funding under Sponsor Grant Award Number: AID-OAA-A-11-00012. NAS URL: http://www.nasonline.org/ USAID PEER Program https://www.usaid.gov/what-we-do/GlobalDevLab/international-research-science-programs/peer The contents of this study are the sole responsibility of the authors and do not necessarily reflect the views of the USAID or the United States Government. The publication of this study was made possible by support of Universitas Indonesia (UI research grant 2019: PENG-1/UN2.R3.1/PPM.00/2019) including funding for publication. The funders had no role in the study design; data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
- PLoS One. 2021; 16(6): e0252704.
Decision Letter 0
27 Oct 2020
PONE-D-20-28218
Knowledge, Attitudes, and Practices of Nursing Staff toward Kangaroo Mother Care at Koja Hospital, North Jakarta Municipality, Jakarta, Indonesia: A Cross-sectional Descriptive Study
Dear Dr. Adisasmita,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
Please submit your revised manuscript by Dec 11 2020 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
We look forward to receiving your revised manuscript.
Kind regards,
Elisabete Alves
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please include additional information regarding the survey or questionnaire used in the study and ensure that you have provided sufficient details that others could replicate the analyses. For instance, please include additional details regarding the questionnaire content, development and validation. If the questionnaire is not under a copyright more restrictive than CC-BY, please include a copy, in both the original language and English, as Supporting Information.
3. We note that you have indicated that data from this study are available upon request. PLOS only allows data to be available upon request if there are legal or ethical restrictions on sharing data publicly. For information on unacceptable data access restrictions, please see http://journals.plos.org/plosone/s/data-availability#loc-unacceptable-data-access-restrictions .
In your revised cover letter, please address the following prompts:
a) If there are ethical or legal restrictions on sharing a de-identified data set, please explain them in detail (e.g., data contain potentially identifying or sensitive patient information) and who has imposed them (e.g., an ethics committee). Please also provide contact information for a data access committee, ethics committee, or other institutional body to which data requests may be sent.
b) If there are no restrictions, please upload the minimal anonymized data set necessary to replicate your study findings as either Supporting Information files or to a stable, public repository and provide us with the relevant URLs, DOIs, or accession numbers. Please see http://www.bmj.com/content/340/bmj.c181.long for guidelines on how to de-identify and prepare clinical data for publication. For a list of acceptable repositories, please see http://journals.plos.org/plosone/s/data-availability#loc-recommended-repositories .
We will update your Data Availability statement on your behalf to reflect the information you provide.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #2: No
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: The authors provide a detailed exploration of knowledge attitude and practices of nursing staff in relation to KMC at a single institution.
The study design is appropriate for the objective of the study
The background/introduction is succinct and provides a good synopsis of the topic including a local context.
The methods are well described. However, on line 70, the authors should consider sharing that this is the quantitative portion of a larger study that utilized both qualitative and quantitative methodology. As currently written, it appears unclear. A scale to describe the definition of low/moderate/high knowledge could have been presented in this section. This terminology appeared in the results section and is unclear. Simple descriptive statistics was appropriate for this inquiry.
Results: For all tables, if data is missing, an annotation should be made to signify such. Table 3 has 2 different data points that do not add up to the specified "n". The "n" for "attended training that included KMC" under perinatal ward does not add up to 29 like others and for the same question Postnatal ward does not add up to 21. The authors should maintain consistency in reporting data, presenting as raw number with percentage would be a preferred style. To minimize clutter, the authors should consider presenting Table 3 as a stacked column or bar chart.
Figure 1 Legend should be reviewed for grammar to ensure clarity. Line 197 "dan" vs. "and".
Line 204: they had a negative attitude or they negatively answered a question? Attitude is being described and not a correct or incorrect question? The authors should re-evaluate framing of this section.
Conclusion and Recommendations: accurately describe the findings
I would recommend a review of the manuscript by a language editing service to ensure better structure and grammar.
Reviewer #2: The paper “Knowledge, Attitudes, and Practices of Nursing Staff toward Kangaroo Mother Care at Koja Hospital, North Jakarta Municipality, Jakarta, Indonesia: A Cross-sectional Descriptive Study” is an interest study about the experience of nursing staff on KMC in an Indonesian hospital. The paper needs to be clearer about the innovativeness of its findings because there is a large number of relevant papers in the field tackling these issues.
- Authors should consider choosing a shorter title.
Introduction:
- Authors should consider to update the worldwide and Indonesian preterm birth rates available for 2014 at “Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D, Landoulsi S, Jampathong N, Kongwattanakul K, Laopaiboon M, Lewis C, Rattanakanokchai S, Teng DN, Thinkhamrop J, Watananirun K, Zhang J, Zhou W, Gülmezoglu AM. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019 Jan;7(1):e37-e46. doi: 10.1016/S2214-109X(18)30451-0. Epub 2018 Oct 30. PMID: 30389451; PMCID: PMC6293055.”
- Once the main objective of this study is to inform the design of larger interventions for improving KAP of KMC among nurses, why the authors did not consider to assess the needs of these professionals for implementing this model of care?
- Authors should consider to provide the number and % of PT babies during data collection period.
- Authors should consider explaining the participants’ recruitment process. Is the participation rate 100%? Why?
- This sentence “Study findings are presented in text, tables, and figures” is redundant.
- The chi-squared test is not the most adequate test to use in most of the comparisons because of its assumption that the expected value in each cell is greater than 5.
- Page 6, lines 122-123: This information may be at methods section.
Kangaroo mother care training
- Values from table 2 are very small which compromise the value of the statistical test.
- Is it correct to present a p value for a statistical test with 0 individuals in one of the cells?
- The percentages of the table are not in column neither in line! It is very confusing for the readers. Could the authors explain their option?
Discussion:
- The discussion section is confusing and presents a circular way of thinking. Author should consider structuring it in a better way.
- Page 12, lines 231-234: Authors should discuss the implications of nurses implementing KMC without training. They presume that this is a good thing but there are a lot of negative implications behind that, considering the results on KMC knowledge.
- Page 14, lines 276-284: A reference is needed.
- Pages 14-15, lines 285-295: Authors discussed some findings not reported in the results, namely “the lack of facilities or supporting policy and equipment”. In fact, nurses need this type of facilities to better implement KMC, not only adequate education as the authors suggest at the end of this paragraph.
- Authors should consider do not limit the discussion around the need for training on KMC. There are a bunch of hospital policies that need to be implemented in order to guarantee the basic conditions for a good KMC implementation.
References:
- Some references need to be updated.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: No
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Author response to Decision Letter 0
26 Feb 2021
Dear Reviewers,
Thank you for the useful inputs and review. We have revised our manuscript based on input from reviewers and include responses (blue color text) to reviewers' comments as follows:
Reviewer #1:
1. The authors provide a detailed exploration of knowledge attitude and practices of nursing staff in relation to KMC at a single institution.
The methods are well described. However, on line 70, the authors should consider sharing that this is the quantitative portion of a larger study that utilized both qualitative and quantitative methodology.
We have added in the methods section line 86-88 (of manuscript file without track changes) mentioning that this quantitative study is a portion of a larger study both utilize qualitative and quantitative methodology: “The study is part of a larger research project that used quantitative and qualitative methods, but this part only focused on the quantitative part of the research”.
2. As currently written, it appears unclear. A scale to describe the definition of low/moderate/high knowledge could have been presented in this section. This terminology appeared in the results section and is unclear.
We added description of low/moderate/high knowledge in line 135-138 (of manuscript file without track changes) in methods section: “General knowledge, knowledge on benefit, and attitude score were grouped into four score categories (scores 0 to 25 = very low, 25 to below 50 = low, 50 to below 75 = moderate, and 75 to 100 = good/high).
Simple descriptive statistics was appropriate for this inquiry.
3. Results: For all tables, if data is missing, an annotation should be made to signify such.
We added annotation under table 1: “aPercentages that do not add up to 100% was due to missing data (i.e., one respondent from the postnatal ward did not provide an answer for years of experience working in the current unit)” in line 155-157 of file Manuscript (without track changes).
4. Table 3 has 2 different data points that do not add up to the specified "n". The "n" for "attended training that included KMC" under perinatal ward does not add up to 29 like others and for the same question Postnatal ward does not add up to 21.
We edited table 3 into the current format. The previous table 3 had information on good knowledge (assuming that the rest are not good knowledge). In the current table 3, we provide information including all levels i.e. low, moderate, and good. So the numbers will add up to 29 or 21.
5. The authors should maintain consistency in reporting data, presenting as raw number with percentage would be a preferred style. To minimize clutter, the authors should consider presenting Table 3 as a stacked column or bar chart.
We already edited the reporting data consistently using raw numbers and percentages. We did consider using a graph, but we decide to use table format for table 3 to incorporate much information we want to describe.
6. Figure 1 Legend should be reviewed for grammar to ensure clarity. Line 197 "dan" vs. "and".
We have already edited it in line 214.
7. Line 204: they had a negative attitude or they negatively answered a question?
We mean negatively answered the question. We then edited the sentence into: “When asked about KMC implementation among infants weighing 1,000–1,800 g, 40% of respondents from the labor ward were not in favor of KMC implementation”. in line 219-221 of the file Manuscript (without track changes)
8. Attitude is being described and not a correct or incorrect question? The authors should re-evaluate framing of this section.
We have changed the sentence into: “No differences were observed after stratifying respondents’ scores according to age group and training experience, and 100% of nurses had a good attitude (score > 75) about KMC (Table 3)” in line 221-223 of file Manuscript (without track changes)
9. Conclusion and Recommendations: accurately describe the findings
We have used language editing service to proofread and edit our manuscript.
Reviewer #2:
10. The paper “Knowledge, Attitudes, and Practices of Nursing Staff toward Kangaroo Mother Care at Koja Hospital, North Jakarta Municipality, Jakarta, Indonesia: A Cross-sectional Descriptive Study” is an interest study about the experience of nursing staff on KMC in an Indonesian hospital. The paper needs to be clearer about the innovativeness of its findings because there is a large number of relevant papers in the field tackling these issues.
We have edited our title into: “Kangaroo mother care knowledge, attitude, and practice among nursing staff in a hospital in Jakarta, Indonesia”.
11. Introduction:
We have updated our references in line 46-48 of file Manuscript (without track changes)
12. - Once the main objective of this study is to inform the design of larger interventions for improving KAP of KMC among nurses, why the authors did not consider to assess the needs of these professionals for implementing this model of care?
We did consider assessing the need of this professional for implementing this model of care through our qualitative study (part of the larger study).
From our formative research which is not published yet, the findings were included in our project report (reference no.9), we assessed the needs of the nursing staff, pediatrician, and management, in having intervention (including knowledge, skill, among others) to improve KMC implementation in the hospital.
In addition, we also cited the qualitative findings regarding this issue in the discussion section although not straightforward in line 296-298 “However, to educate and support the mother/family in KMC, the nursing staff needs formal training to improve their skill and confidence in supporting KMC [19]”
13. - Authors should consider explaining the participants’ recruitment process. Is the participation rate 100%? Why?
Yes, the participation rate was 100%. We provide information that all nursing staff willing to participate in line 119 of the file Manuscript (without track changes), although not all of them provide complete data (there is missing data in years of working in current unit).
We have deleted the sentence above to avoid redundancy.
14. - The chi-squared test is not the most adequate test to use in most of the comparisons because of its assumption that the expected value in each cell is greater than 5.
We added Fisher Exact test if the expected value in a cell is less than 5 in line 141
15. Results:
We deleted this sentence in Results section and move it to Methods section in line 118-119.
16. Kangaroo mother care training
The statistical output is presented below:
KMC_training_baseline * Ruang Crosstabulation
Ruang Total
Perinatology Labor Rooming-in
KMC_training_baseline both specific and KMC included training Count 2 2 1 5
% within Ruang 6.9% 13.3% 4.8% 7.7%
specific KMC training Count 2 0 1 3
% within Ruang 6.9% 0.0% 4.8% 4.6%
KMC included training Count 5 3 1 9
% within Ruang 17.2% 20.0% 4.8% 13.8%
not participate in any Count 20 10 18 48
% within Ruang 69.0% 66.7% 85.7% 73.8%
Total Count 29 15 21 65
% within Ruang 100.0% 100.0% 100.0% 100.0%
Chi-Square Tests
Value df Asymptotic Significance (2-sided)
Pearson Chi-Square 4.401a 6 .623
Likelihood Ratio 5.323 6 .503
Linear-by-Linear Association .705 1 .401
N of Valid Cases 65
a. 9 cells (75.0%) have expected count less than 5. The minimum expected count is .69.
17. - The percentages of the table are not in column neither in line! It is very confusing for the readers. Could the authors explain their option?
We have edited table 3
18. Discussion:
We have attempted to revise the discussion section.
19. - Page 12, lines 231-234: Authors should discuss the implications of nurses implementing KMC without training. They presume that this is a good thing but there are a lot of negative implications behind that, considering the results on KMC knowledge.
We added the sentence in the discussion: “Also, the lack of training could result in conflicting knowledge on the timing and duration of KMC [24,35], which could lead to adverse consequences such as mortality [36] especially among less stable infants” in line 256-258.
21. Page 14, lines 276-284: A reference is needed.
We have edited the sentences and provide references that could be seen in line 298-302.
22. - Pages 14-15, lines 285-295: Authors discussed some findings not reported in the results, namely “the lack of facilities or supporting policy and equipment”. In fact, nurses need this type of facilities to better implement KMC, not only adequate education as the authors suggest at the end of this paragraph.
We added the reference regarding lack of facilities or supporting policy and equipment in line 306-308. The information was gathered during formative research (larger study).
23. - Authors should consider do not limit the discussion around the need for training on KMC. There are a bunch of hospital policies that need to be implemented in order to guarantee the basic conditions for a good KMC implementation.
We have added in line 317-319: “However, in addition to adequate education, adequate equipment/facilities as well as SOPs and hospital policy supporting KMC implementation are essential for successful KMC in the hospital”
24. References:
We have updated the references
Submitted filename: Response to Reviewers comment_29 jan 2021.docx
Decision Letter 1
PONE-D-20-28218R1
Please submit your revised manuscript by May 23 2021 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols . Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols .
Please review your reference list to ensure that it is complete and correct. If you have cited papers that have been retracted, please include the rationale for doing so in the manuscript text, or remove these references and replace them with relevant current references. Any changes to the reference list should be mentioned in the rebuttal letter that accompanies your revised manuscript. If you need to cite a retracted article, indicate the article’s retracted status in the References list and also include a citation and full reference for the retraction notice.
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #2: (No Response)
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #2: I would like to thank the authors for their work in answering reviewers' questions.
I think the paper still has some minor issues that should be revised, namely inconsistencies in showing the results in the tables. In table 2 is still missing the row for n(%) as shown in table 1. In table 3 authors reported the p values inconsistently - with and without the 0 before the comma. I think authors should revise all tables again in order to present the results in a consistent way.
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Author response to Decision Letter 1
18 May 2021
Our response:
We would like to thank the reviewer for giving the input for the manuscript. In the revised manuscript:
• We added n (%) in table 2
• We edited p-values in table 3 by adding 0 before the comma
• We revised the tables’ layout to make it consistent and easier to understand
Submitted filename: Response to the reviewer 2.docx
Decision Letter 2
21 May 2021
PONE-D-20-28218R2
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
Acceptance letter
27 May 2021
Dear Dr. Adisasmita:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Elisabete Alves

COMMENTS
We conducted a systematic review and searched PubMed, Embase, Scopus, Web of Science, and the World Health Organization Regional Databases for studies with key words "kangaroo mother care", "kangaroo care" or "skin to skin care" from 1 January 1960 to 24 April 2014. Two independent reviewers screened articles and abstracted data.
Develop and disseminate kangaroo mother care protocols, policies, and guidelines. An absence of protocols, policies, and guidelines was a common barrier discovered in the literature. Without these critical documents, it results in the "default" procedure of separating infants from their mothers, which has been the norm for HCPs.
Kangaroo mother care literature review screening form based on our inclusion criteria. Using stan-dardized data abstraction forms, two reviewers abstracted data independently from all included articles and reports. At each stage, reviewers compared results to ensure agree-ment. In the case of disagreement between the two review-
Kangaroo mother care (KMC) is a cost-effective, natural, safe, and evidence-based intervention that improves maternal-infant bonding, increases breastfeeding rates, and decreases the risk of mortality and morbidity in preterm infants. Although KMC is recommended to be the standard of care for preterm infants, there are significant implementation barriers.
Kangaroo mother care literature review. Skin-to -skin co ntact. Among the studies that de ned SSC as part of the KMC . package, criteria for SSC initiatio n, SSC ending, and SSC .
Among infants with a birth weight between 1.0 and 1.799 kg, those who received immediate kangaroo mother care had lower mortality at 28 days than those who received conventional care with kangaroo ...
Introduction. Kangaroo Mother Care (KMC) is the treatment of preterm infants by their mothers, who make skin-to-skin contact with the infants. 1 KMC improves growth, reduces morbidity, and decreases the duration of hospitalization. 2, 3 It also increases the compatibility between the mothers' and infants' saliva levels 4 and results in a significant improvement in vital physiological ...
Methods: We conducted a systematic review and searched PubMed, Embase, Scopus, Web of Science, and the World Health Organization Regional Databases for studies with key words "kangaroo mother care", "kangaroo care" or "skin to skin care" from 1 January 1960 to 24 April 2014. Two independent reviewers screened articles and abstracted data.
Kangaroo mother care (KMC) is an evidence-based approach to reducing mortality and morbidity in preterm infants which was first developed in Bogotá Colombia. ... In addition, because at least one relevant article identified from a list of references in a literature review included the terms Kangaroo Mother Care in quotations and the term Skin ...
Kangaroo mother care (KMC) is an evidence-based intervention that reduces morbidity and mortality in preterm infants. However, it has not yet been fully integrated into health systems around the world. The aim of this study is to provide a cogent summary of the evidence base of the key barriers and facilitators to implementing KMC. An umbrella review of existing reviews on KMC was adopted to ...
Kangaroo mother care (KMC) is an evidence-based approach to reducing mortality and morbidity in preterm infants. Although KMC is a key intervention package in newborn health initiatives, there is limited systematic information available on the barriers to KMC practice that mothers and other stakeholders face while practicing KMC. This systematic review sought to identify the most frequently ...
In this multicenter trial, the initiation of con-tinuous kangaroo mother care soon after birth in infants with a birth weight between 1.0 and 1.799 kg improved neonatal survival by 25% as compared ...
Importance The Cochrane review (2016) on kangaroo mother care (KMC) demonstrated a significant reduction in the risk of mortality in low birth weight infants. New evidence from large multi-centre randomised trials has been available since its publication. Objective Our systematic review compared the effects of KMC vs conventional care and early (ie, within 24 hours of birth) vs late initiation ...
The review considered studies conducted in sub-Saharan Africa on the perceptions and experiences of mothers who had given birth to preterm babies and had practiced kangaroo mother care wholly or in part at home. Qualitative studies in English and French conducted from January 1979 to March 2019 were considered for inclusion if they exclusively ...
Kangaroo mother care (KMC) is an intervention aimed at improving outcomes among preterm and low birth weight newborns. ... Dr Boundy conceptualized and designed the study, conducted the literature review, collected the data, conducted the analyses, created the tables and figures, and drafted and revised the manuscript; Dr Dastjerdi conducted ...
We conducted a systematic review and searched PubMed, Embase, Scopus, Web of Science, and the World Health Organization Regional Databases for studies with key words "kangaroo mother care", "kangaroo care" or "skin to skin care" from 1 January 1960 to 24 April 2014. Two independent reviewers screened articles and abstracted data.
Methods We conducted a systematic review and searched PubMed, Embase, Scopus, Web of Science, and the World Health Organization Regional Databases for studies with key words "kangaroo mother care", "kangaroo care" or "skin to skin care" from 1 January 1960 to 24 April 2014. Two independent reviewers screened articles and abstracted ...
Immediate kangaroo mother care for preterm and low birthweight babies requires dedicated Mother-Newborn Intensive Care Units GENEVA, 27 May 2021Kangaroo mother care, which involves skin-to-skin contact and exclusive breastfeeding, significantly improves a premature or low birthweight baby's chances of survival Starting kangaroo mother care immediately after birth has the potential to save up ...
We conducted a systematic review and searched PubMed, Embase, Scopus, Web of Science, and the World Health Organization Regional Databases for studies with key words "kangaroo mother care", "kangaroo care" or "skin to skin care" from 1 January 1960 to 24 April 2014. Two independent reviewers screened articles and abstracted data.
Percentages of correct answers on knowledge and attitude toward kangaroo mother care. General knowledge, knowledge on benefits, and attitude scores were grouped into four categories (scores 0 to 25, 25 to below 50, 50 to below 75, and 75 to 100).