
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
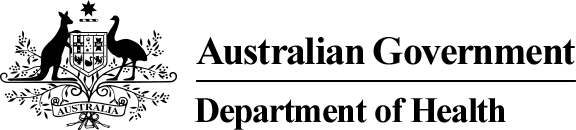
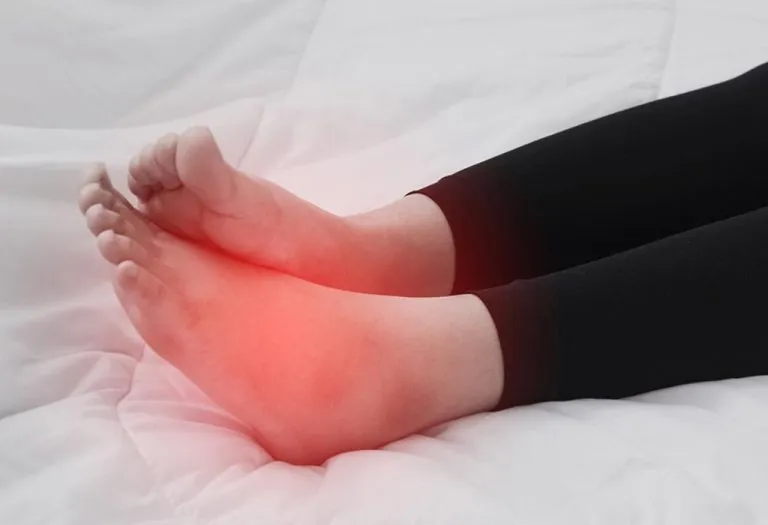
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).
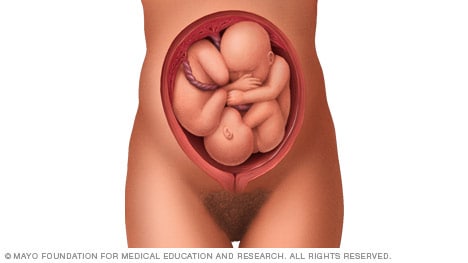
Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Cephalic Position?
The ideal fetal position for labor and delivery
- Why It's Best
Risks of Other Positions
- Determining Position
- Turning a Fetus
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery.
About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy . Your healthcare provider will monitor the fetus's position during the last weeks of gestation to ensure this has happened by week 36.
If the fetus is not in the cephalic position at that point, the provider may try to turn it. If this doesn't work, some—but not all—practitioners will attempt to deliver vaginally, while others will recommend a Cesarean (C-section).
Getty Images
Why Is the Cephalic Position Best?
During labor, contractions dilate the cervix so the fetus has adequate room to come through the birth canal. The cephalic position is the easiest and safest way for the baby to pass through the birth canal.
If the fetus is in a noncephalic position, delivery becomes more challenging. Different fetal positions have a range of difficulties and varying risks.
A small percentage of babies present in noncephalic positions. This can pose risks both to the fetus and the mother, and make labor and delivery more challenging. It can also influence the way in which someone can deliver.
A fetus may actually find itself in any of these positions throughout pregnancy, as the move about the uterus. But as they grow, there will be less room to tumble around and they will settle into a final position.
It is at this point that noncephalic positions can pose significant risks.
Cephalic Posterior
A fetus may also present in an occiput or cephalic posterior position. This means they are positioned head down, but they are facing the abdomen instead of the back.
This position is also nicknamed "sunny-side up."
Presenting this way increases the chance of a painful and prolonged delivery.
There are three different types of breech fetal positioning:
- Frank breech: The legs are up with the feet near the head.
- Footling breech: One or both legs is lowered over the cervix.
- Complete breech: The fetus is bottom-first with knees bent.
A vaginal delivery is most times a safe way to deliver. But with breech positions, a vaginal delivery can be complicated.
When a baby is born in the breech position, the largest part—its head—is delivered last. This can result in them getting stuck in the birth canal (entrapped). This can cause injury or death.
The umbilical cord may also be damaged or slide down into the mouth of the womb, which can reduce or cut off the baby's oxygen supply.
Some providers are still comfortable performing a vaginal birth as long as the fetus is doing well. But breech is always a riskier delivery position compared with the cephalic position, and most cases require a C-section.
Likelihood of a Breech Baby
You are more likely to have a breech baby if you:
- Go into early labor before you're full term
- Have an abnormally shaped uterus, fibroids , or too much amniotic fluid
- Are pregnant with multiples
- Have placenta previa (when the placenta covers the cervix)
Transverse Lie
In transverse lie position, the fetus is presenting sideways across the uterus rather than vertically. They may be:
- Down, with the back facing the birth canal
- With one shoulder pointing toward the birth canal
- Up, with the hands and feet facing the birth canal
If a transverse lie is not corrected before labor, a C-section will be required. This is typically the case.
Determining Fetal Position
Your healthcare provider can determine if your baby is in cephalic presentation by performing a physical exam and ultrasound.
In the final weeks of pregnancy, your healthcare provider will feel your lower abdomen with their hands to assess the positioning of the baby. This includes where the head, back, and buttocks lie
If your healthcare provider senses that the fetus is in a breech position, they can use ultrasound to confirm their suspicion.
Turning a Fetus So They Are in Cephalic Position
External cephalic version (ECV) is a common, noninvasive procedure to turn a breech baby into cephalic position while it's still in the uterus.
This is only considered if a healthcare provider monitors presentation progress in the last trimester and notices that a fetus is maintaining a noncephalic position as your delivery date approaches.
External Cephalic Version (ECV)
ECV involves the healthcare provider applying pressure to your stomach to turn the fetus from the outside. They will attempt to rotate the head forward or backward and lift the buttocks in an upward position. Sometimes, they use ultrasound to help guide the process.
The best time to perform ECV is about 37 weeks of pregnancy. Afterward, the fetal heart rate will be monitored to make sure it’s within normal levels. You should be able to go home after having ECV done.
ECV has a 50% to 60% success rate. However, even if it does work, there is still a chance the fetus will return to the breech position before birth.
Natural Methods For Turning a Fetus
There are also natural methods that can help turn a fetus into cephalic position. There is no medical research that confirms their efficacy, however.
- Changing your position: Sometimes a fetus will move when you get into certain positions. Two specific movements that your provider may recommend include: Getting on your hands and knees and gently rocking back and forth. Another you could try is pushing your hips up in the air while laying on your back with your knees bent and feet flat on the floor (bridge pose).
- Playing stimulating sounds: Fetuses gravitate to sound. You may be successful at luring a fetus out of breech position by playing music or a recording of your voice near your lower abdomen.
- Chiropractic care: A chiropractor can try the Webster technique. This is a specific chiropractic analysis and adjustment which enables chiropractors to establish balance in the pregnant person's pelvis and reduce undue stress to the uterus and supporting ligaments.
- Acupuncture: This is a considerably safe way someone can try to turn a fetus. Some practitioners incorporate moxibustion—the burning of dried mugwort on certain areas of the body—because they believe it will enhance the chances of success.
A Word From Verywell
While most babies are born in cephalic position at delivery, this is not always the case. And while some fetuses can be turned, others may be more stubborn.
This may affect your labor and delivery wishes. Try to remember that having a healthy baby, and staying well yourself, are your ultimate priorities. That may mean diverting from your best laid plans.
Speaking to your healthcare provider about turning options and the safest route of delivery may help you adjust to this twist and feel better about how you will move ahead.
Glezerman M. Planned vaginal breech delivery: current status and the need to reconsider . Expert Rev Obstet Gynecol. 2012;7(2):159-166. doi:10.1586/eog.12.2
Cleveland Clinic. Fetal positions for birth .
MedlinePlus. Breech birth .
UT Southwestern Medical Center. Can you turn a breech baby around?
The American College of Obstetricians and Gynecologists. If your baby is breech .
Roecker CB. Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios . Journal of Chiropractic Medicine . 2013;12(2):74-78. doi:10.1016/j.jcm.2013.06.003
By Cherie Berkley, MS Berkley is a journalist with a certification in global health from Johns Hopkins University and a master's degree in journalism.
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.
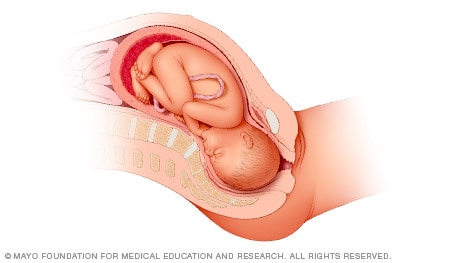
Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.
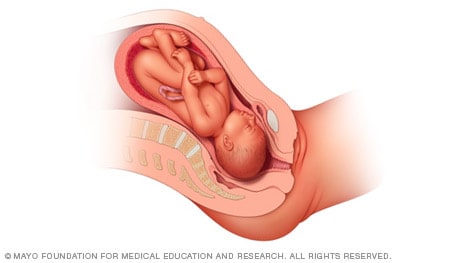
Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

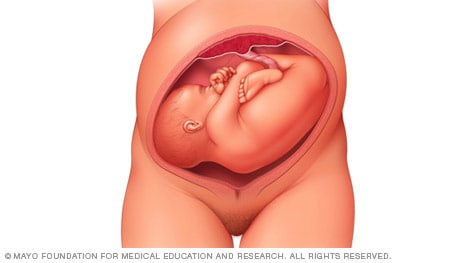
When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.
If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.
- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Your baby in the birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between their head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Alternative Names
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal

Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Review Date 11/10/2022
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Presentation and position of baby through pregnancy and at birth
9-minute read
If you are concerned about your baby’s movements, contact your doctor or midwife for advice immediately.
- If you baby is in a breech presentation, your doctor may recommend trying a technique called an external cephalic version to try and move your baby while they are still in the uterus for an easier birth.
What does presentation and position mean?
Presentation refers to the part of your baby’s body that is facing downwards in the direction of the birth canal.
Position refers to where your baby’s occiput (the bottom part of the back of their head) is in relation to your body.
If your baby is in a breech presentation , then position refers to where your baby’s sacrum (lower back) is in relation to your body.
People — including medical professionals — sometimes use these terms incorrectly. Sometimes when speaking about babies in breech presentation, the word ‘position’ will be used to refer to their presentation. For example, you may read information or hear people say ‘breech position’ instead of ‘breech presentation’.
What are the different types of presentation my baby could be in during pregnancy and birth?
Most babies present headfirst, also known as cephalic presentation. Most babies that are headfirst will be vertex presentation. This means that the crown of their head sits at the opening of your birth canal.
In rare cases, your baby can be headfirst but in face or brow presentation, which may not be suitable for vaginal birth.

If your baby is in a breech presentation, their feet or bottom will be closest to your birth canal. The 3 most common types of breech presentation are:
- frank or extended breech — where your baby’s legs are straight up in front of their body, with their feet up near their face
- complete or flexed breech — where your baby is in a sitting position with their legs crossed in front of their body and their feet near their bottom
- footling breech — where one or both of your baby’s feet are hanging below their bottom, so the foot or feet are coming first
Read more on breech presentation .
What are the different positions my baby could be in during pregnancy and birth?
If your baby is headfirst, the 3 main types of presentation are:
- anterior – when the back of your baby’s head is at the front of your belly
- lateral – when the back of your baby’s head is facing your side
- posterior – when the back of your baby’s head is towards your back

How will I know what presentation and position my baby is in?
Your doctor or midwife can usually work out your baby’s presentation by feeling your abdomen. They may also double check it with a portable ultrasound. Your baby’s presentation is usually checked around 36 weeks .
Your doctor or midwife will also confirm your baby’s head position in labour by examining your belly and using an ultrasound , and they may also do a vaginal examination . During the vaginal examination they are feeling for certain ridges on your baby’s head called sutures and fontanelles that help them work out which way your baby is positioned.
What is the ideal presentation and position for baby to be in for a vaginal birth?
For a vaginal birth, your baby will ideally be headfirst with the back of their head at the front of your belly, also known as being in the anterior position. This position is best for labour and birth since it means that the smallest part of your baby’s head goes down the birth canal first.

When does a baby usually get in the ideal presentation and position for birth?
Your baby will usually be in a headfirst position by 37 weeks of pregnancy. Around 3 in every 100 babies will be in breech presentation after 37 weeks.
Your baby’s position can change with your contractions during labour as they move down the birth canal, so their exact position can change during labour.
What are my options if baby isn't in the ideal presentation or position for a vaginal birth?
If your baby is in a breech presentation, your doctor may recommend a technique called an external cephalic version (ECV) to try and move your baby while they are still in the uterus . An ECV involves your doctor using their hands to apply pressure on your belly and help turn your baby to a headfirst position. It has a 1 in 2 chance of success and is a safe option in most pregnancies.
There is no evidence to show that alternative therapies, such as exercises, acupuncture or chiropractic treatments, help your baby change from a breech presentation to headfirst.
If your baby remains breech, your doctor may discuss having a breech vaginal birth. Not all doctors and hospitals offer this option. They may also suggest you birth your baby with a planned caesarean section .
If your baby’s presentation is headfirst but the position of your baby’s head is not ideal for labour, it can lead to a longer labour, and potential complications . The position of your baby’s head will often change as your labour progresses. If it doesn’t, sometimes you can still give birth without assistance, or you may need your doctor to help turn your baby’s head or help your birth with a vacuum or forceps .
Any procedure or decision for a type of birth will only go ahead with your consent . You will be able to discuss all the options with your doctor, and based on your preferences for yourself and your baby’s safety, make a decision together .
Resources and support
The Royal Australian and New Zealand College of Obstetrics and Gynaecology has a factsheet about the options available to you if your baby is in a breech presentation at the end of your pregnancy .
Mercy Perinatal has information on external cephalic version (ECV) safety and benefits if your baby is in a breech presentation at the end of your pregnancy.
The Women’s Hospital has information about the different presentations and positions your baby could be in, and how it can affect your birthing experience.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: October 2023
Related pages
External cephalic version (ecv), malpresentation, breech pregnancy, search our site for.
- Foetal Version
- Breech Presentation
Need more information?
Top results
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
ECV is a procedure to try to move your baby from a breech position to a head-down position. This is performed by a trained doctor.
Having a baby
The articles in this section relate to having a baby – what to consider before becoming pregnant, pregnancy and birth, and after your baby is born.
Anatomy of pregnancy and birth - pelvis
Your pelvis helps to carry your growing baby and is tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Planned or elective caesarean
There are important things to consider if you are having a planned or elective caesarean such as what happens during and after the procedure.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

- Vishal's account
- Prenatal Care
Fetal Cephalic Presentation During Pregnancy

What Is Cephalic Position?
Types of cephalic position, benefits of cephalic presentation, risks of cephalic position, what are some other positions and their associated risks, when does a foetus get into the cephalic position, how do you know if baby is in cephalic position, how to turn a breech baby into cephalic position, natural ways to turn a baby into cephalic position.
If your baby is moving around in the womb, it’s a good sign as it tells you that your baby is developing just fine. A baby starts moving around in the belly at around 14 weeks. And their first movements are usually called ‘ quickening’ or ‘fluttering’.
A baby can settle into many different positions throughout the pregnancy, and it’s alright. But it is only when you have reached your third and final trimester that the position of your baby in your womb will matter the most. The position that your baby takes at the end of the gestation period will most likely be how your baby will make its appearance in the world. Out of all the different positions that your baby can settle into, the cephalic position at 36 weeks is considered the best position. Read on to learn more about fetal cephalic presentation.
When it comes to cephalic presentation meaning, the following can be considered. A baby is in the cephalic position when he is in a head-down position. This is the best position for them to come out in. In case of a ‘cephalic presentation’, the chances of a smooth delivery are higher. This position is where your baby’s head has positioned itself close to the birth canal, and the feet and bottom are up. This is the best position for your baby to be in for safe and healthy delivery.
Your doctor will begin to keep an eye on the position of your baby at around 34 weeks to 36 weeks . The closer you get to your due date, the more important it is that your baby takes the cephalic position. If your baby is not in this position, your doctor will try gentle nudges to get your baby in the right position.
Though it is pretty straightforward, the cephalic position actually has two types, which are explained below:
1. Cephalic Occiput Anterior
Most babies settle in this position. Out of all the babies who settle in the cephalic position, 95% of them will settle this way. This is when a baby is in the head-down position but is facing the mother’s back. This is the preferred position as the baby is able to slide out more easily than in any other position.
2. Cephalic Occiput Posterior
In this position, the baby is in the head-down position but the baby’s face is turned towards the mother’s belly. This type of cephalic presentation is not the best position for delivery as the baby’s head could get stuck owing to its wide position. Almost 5% of the babies in cephalic presentation settle into this position. Babies who come out in this position are said to come out ‘sunny side up’.
Cephalic presentation, where the baby’s head is positioned down towards the birth canal, is the most common and optimal fetal presentation for childbirth. This positioning facilitates a smoother delivery process for both the mother and the baby. Here are several benefits associated with cephalic presentation:
1. Reduced risk of complications
Cephalic presentation decreases the likelihood of complications during labor and delivery , such as umbilical cord prolapse or shoulder dystocia, which can occur with other presentations.
2. Easier vaginal delivery
With the baby’s head positioned first, vaginal delivery is generally easier and less complicated compared to other presentations, resulting in a smoother labor process for the mother.
3. Lower risk of birth injuries
Cephalic presentation reduces the risk of birth injuries to the baby, such as head trauma or brachial plexus injuries, which may occur with other presentations, particularly breech or transverse positions.
4. Faster progression of labor
Babies in cephalic presentation often help to stimulate labor progression more effectively through their positioning, potentially shortening the duration of labor and reducing the need for medical interventions.
5. Better fetal oxygenation
Cephalic presentation typically allows for optimal positioning of the baby’s head, which facilitates adequate blood flow and oxygenation, contributing to the baby’s well-being during labor and delivery.
Factors such as the cephalic posterior position of the baby and a narrow maternal pelvis can increase the likelihood of complications during childbirth. Occasionally, infants in the cephalic presentation may exhibit a backward tilt of their heads, potentially leading to preterm delivery in rare instances.
In addition to cephalic presentation, there are several other fetal positions that can occur during pregnancy and childbirth, each with its own associated risks. These positions can impact the delivery process and may require different management strategies. Here are two common fetal positions and their associated risks:
1. Breech Presentation
- Babies in breech presentation, where the buttocks or feet are positioned to enter the birth canal first, are at higher risk of birth injuries such as hip dysplasia or brachial plexus injuries.
- Breech presentation can lead to complications during labor and delivery, including umbilical cord prolapse, entrapment of the head, or difficulty delivering the shoulders, necessitating interventions such as cesarean section.
2. Transverse Lie Presentation
- Transverse lie , where the baby is positioned sideways across the uterus, often leads to prolonged labor and increases the likelihood of cesarean section due to difficulties in the baby’s descent through the birth canal.
- The transverse position of the baby may result in compression of the umbilical cord during labor, leading to decreased oxygen supply and potential fetal distress. This situation requires careful monitoring and intervention to ensure the baby’s well-being.
When a foetus is moving into the cephalic position, it is known as ‘head engagement’. The baby stars getting into this position in the third trimester, between the 32nd and the 36th weeks, to be precise. When the head engagement begins, the foetus starts moving down into the pelvic canal. At this stage, very little of the baby is felt in the abdomen, but more is felt moving downward into the pelvic canal in preparation for birth.
You may think that in order to find out if your baby has a cephalic presentation, an ultrasound is your only option. This is not always the case. You can actually find out the position of your baby just by touching and feeling their movements.
By rubbing your hand on your belly, you might be able to feel their position. If your baby is in the cephalic position, you might feel their kicks in the upper stomach. Whereas, if the baby is in the breech position, you might feel their kicks in the lower stomach.
Even in the cephalic position, it may be possible to tell if your baby is in the anterior position or in the posterior position. When your baby is in the anterior position, they may be facing your back. You may be able to feel your baby move underneath your ribs. It is likely that your belly button will also pop out.
When your baby is in the posterior position, you will usually feel your baby start to kick you in your stomach. When your baby has its back pressed up against your back, your stomach may not look rounded out, but flat instead.
Mothers whose placentas have attached in the front, something known as anterior placenta , you may not be able to feel the movements of your baby as well as you might like to.
Breech babies can make things complicated. Both the mother and the baby will face some problems. A breech baby is positioned head-up and bottom down. In order to deliver the baby, the birth canal needs to open a lot wider than it has to in the cephalic position. Besides this, your baby can get an arm or leg entangled while coming out.
If your baby is in the breech position, there are some things that you can do to encourage the baby to get into the cephalic position. There are a few exercises that could help such as pelvic tilts , swimming , spending a bit of time upside down, and belly dancing are a few ways you can try yourself to get your baby into the head-down position .
If this is not working either, your doctor will try an ECV (External Cephalic Version) . Here, your doctor will be hands-on, applying some gentle, but firm pressure to your tummy. In order to reach a cephalic position, the baby will need to be rolled into a bottom’s up position. This technique is successful around 50% of the time. When this happens, you will be able to have a normal vaginal delivery.
Though it sounds simple enough to get the fetal presentation into cephalic, there are some risks involved with ECV. If your doctor notices your baby’s heart rate starts to become problematic, the doctor will stop the procedure right away.
Encouraging a baby to move into the cephalic position, where the head is down towards the birth canal, is often desirable for smoother labor and delivery. While medical interventions may be necessary in some cases, there are natural methods that pregnant individuals can try to help facilitate this positioning. Here are several techniques that may help turn a baby into the cephalic position:
1. Optimal Maternal Positioning
Maintaining positions such as kneeling, hands and knees, or pelvic tilts may encourage the baby to move into the cephalic position by utilizing gravity and reducing pressure on the pelvis.
2. Spinning Babies Techniques
Specific exercises and positions recommended by the Spinning Babies organization, such as Forward-Leaning Inversion or the Sidelying Release, aim to promote optimal fetal positioning and may help encourage the baby to turn cephalic.
3. Chiropractic Care or Acupuncture
Some individuals find that chiropractic adjustments or acupuncture sessions with qualified practitioners can help address pelvic misalignment or relax tight muscles, potentially creating more space for the baby to maneuver into the cephalic position.
4. Prenatal Yoga and Swimming
Engaging in gentle exercises like prenatal yoga or swimming may help promote relaxation, reduce stress on the uterine ligaments, and encourage the baby to move into the cephalic position naturally. These activities also support overall physical and mental well-being during pregnancy.
1. What factors influence whether my baby will be in cephalic presentation?
Several factors can influence your baby’s position during pregnancy, including the shape and size of your uterus, the strength of your abdominal muscles, the amount of amniotic fluid, and the position of the placenta . Additionally, your baby’s own movements and preferences play a role.

2. Is it necessary for my baby to be in cephalic presentation for a vaginal delivery?
While cephalic presentation is considered the optimal position for vaginal delivery, some babies born in non-cephalic presentations can still be safely delivered vaginally with the guidance of a skilled healthcare provider. However, certain non-cephalic presentations may increase the likelihood of needing a cesarean section.
3. What can I do to encourage my baby to stay in the cephalic presentation?
Maintaining good posture, avoiding positions that encourage the baby to settle into a breech or transverse lie, staying active with gentle exercises, and avoiding excessive reclining can all help encourage your baby to remain in the cephalic presentation. Additionally, discussing any concerns with your healthcare provider and following their recommendations can be beneficial.
This was all about fetus with cephalic presentation. Most babies get into the cephalic position on their own. This is the most ideal situation as there will be little to no complications during normal vaginal labour. There are different cephalic positions, but these should not cause a lot of issues. If your baby is in any position other than cephalic in pregnancy, you may need C-Section . Keep yourself updated on the smallest of progress during your pregnancy so that you are aware of everything that is going on. Go for regular check-ups as your doctor will be able to help you if a complication arises during acephalic presentation at 20, 28 and 30 weeks.
References/Resources:
1. Glezerman. M; Planned vaginal breech delivery: current status and the need to reconsider (Expert Review of Obstetrics & Gynecology); Taylor & Francis Online; https://www.tandfonline.com/doi/full/10.1586/eog.12.2 ; January 2014
2. Feeling your baby move during pregnancy; UT Southwestern Medical Center; https://utswmed.org/medblog/fetal-movements/
3. Fetal presentation before birth; Mayo Clinic; https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/fetal-positions/art-20546850
4. Fetal Positions; Cleveland Clinic; https://my.clevelandclinic.org/health/articles/9677-fetal-positions-for-birth
5. FAQs: If Your Baby Is Breech; American College of Obstetricians and Gynecologists; https://www.acog.org/womens-health/faqs/if-your-baby-is-breech
6. Roecker. C; Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios (Journal of Chiropractic Medicine); Science Direct; https://www.sciencedirect.com/science/article/abs/pii/S1556370713000588 ; June 2013
7. Presentation and position of baby through pregnancy and at birth; Pregnancy, Birth & Baby; https://www.pregnancybirthbaby.org.au/presentation-and-position-of-baby-through-pregnancy-and-at-birth
Belly Mapping Pregnancy Belly Growth Chart Baby in Vertex Position during Labour and Delivery
- RELATED ARTICLES
- MORE FROM AUTHOR

Keeping Your Sex Drive Alive in Pregnancy

Is Diarrhoea a Sign of Pregnancy?

Baby Moves or Kicks in the Night During Pregnancy– Is it Safe?
17 Effective Home Remedies for Swollen Feet During Pregnancy

Can You Drink Wine While Pregnant?

Mirror Syndrome During Pregnancy - Causes, Symptoms, and Treatment
Popular on parenting.

245 Rare Boy & Girl Names with Meanings

Top 22 Short Moral Stories For Kids

170 Boy & Girl Names That Mean 'Gift from God'

800+ Unique & Cute Nicknames for Boys & Girls
Latest posts.

Understanding Baby Food Labels - Easy Guide for Parents on How to Read & Use

5 Ways to Maintain Diaper Hygiene in Summer for a Happy Baby!

4 Baby Sleep-Related Questions All New Parents Have Answered by a Paediatrician!

Do Indian Babies Have Different Diaper Needs? Here's an Expert's Opinion!

- Learn /
Why Is Cephalic Presentation Ideal For Childbirth?

5 Dec 2017 | 8 min Read
During labour, contractions stretch your birth canal so that your baby has adequate room to come through during birth. The cephalic presentation is the safest and easiest way for your baby to pass through the birth canal.
If your baby is in a non-cephalic position, delivery can become more challenging. Different fetal positions pose a range of difficulties and varying risks and may not be considered ideal birthing positions.
Two Kinds of Cephalic Positions
There are two kinds of cephalic positions:
- Cephalic occiput anterior , where your baby’s head is down and is facing toward your back.
- Cephalic occiput posterior , where your baby is positioned head down, but they are facing your abdomen instead of your back. This position is also nicknamed ‘sunny-side-up’ and can increase the chances of prolonged and painful delivery.
How to Know if Your Baby is In a Cephalic Position?
You can feel your baby’s position by rubbing your hand on your belly. If you feel your little one’s stomach in the upper stomach, then your baby is in a cephalic position. But if you feel their kicks in the lower stomach, then it could mean that your baby is in a breech position.
You can also determine whether your baby is in the anterior or posterior cephalic position. If your baby is in the anterior position, you may feel their movement underneath your ribs and your belly button could also pop out. If your baby is in the posterior position, then you may feel their kicks in their abdomen, and your stomach may appear rounded up instead of flat.
You can also determine your baby’s position through an ultrasound scan or a physical examination at your healthcare provider’s office.
Benefits of Cephalic Presentation in Pregnancy
Cephalic presentation is one of the most ideal birth positions, and has the following benefits:
- It is the safest way to give birth as your baby’s position is head-down and prevents the risk of any injuries.
- It can help your baby move through the delivery canal as safely and easily as possible.
- It increases the chances of smooth labour and delivery.
Are There Any Risks Involved in Cephalic Position?
Conditions like a cephalic posterior position in addition to a narrow pelvis of the mother can increase the risk of pregnancy complications during delivery. Some babies in the head-first cephalic presentation might have their heads tilted backward. This may, in some rare cases, cause preterm delivery.
What are the Risks Associated with Other Birth Positions?
A small percentage of babies may settle into a non-cephalic position before their birth. This can pose risks to both your and your baby’s health, and also influence the way in which you deliver.
In the next section, we have discussed a few positions that your baby can settle in throughout pregnancy, as they move around the uterus. But as they grow old, there will be less space for them to tumble around, and they will settle into their final position. This is when non-cephalic positions can pose a risk.
Breech Position
There are three types of breech fetal positioning:
- Frank breech : Your baby’s legs stick straight up along with their feet near their head.
- Footling breech: One or both of your baby’s legs are lowered over your cervix.
- Complete breech: Your baby is positioned bottom-first with their knees bent.
If your baby is in a breech position , vaginal delivery is considered complicated. When a baby is born in breech position, the largest part of their body, that is, their head is delivered last. This can lead to injury or even fetal distress. Moreover, the umbilical cord may also get damaged or get wrapped around your baby’s neck, cutting off their oxygen supply.
If your baby is in a breech position, your healthcare provider may recommend a c-section, or they may try ways to flip your baby’s position in a cephalic presentation.
Transverse Lie
In this position, your baby settles in sideways across the uterus rather than being in a vertical position. They may be:
- Head-down, with their back facing the birth canal
- One shoulder pointing toward the birth canal
- Up with their hands and feet facing the birth canal
If your baby settles in this position, then your healthcare provider may suggest a c-section to reduce the risk of distress in your baby and other pregnancy complications.
Turning Your Baby Into A Cephalic Position
External cephalic version (ECV) is a common, and non-invasive procedure that helps turn your baby into a cephalic position while they are in the womb. However, your healthcare provider may only consider this procedure if they consider you have a stable health condition in the last trimester, and if your baby hasn’t changed their position by the 36th week.
You can also try some natural remedies to change your baby’s position, such as:
- Lying in a bridge position: Movements like bridge position can sometimes help move your baby into a more suitable position. Lie on your back with your feet flat on the ground and your legs bent. Raise your pelvis and hips into a bridge position and hold for 5-10 minutes. Repeat several times daily.
- Chiropractic care: A chiropractor can help with the adjustment of your baby’s position and also reduce stress in them.
- Acupuncture: After your doctor’s go-ahead, you can also consider acupuncture to get your baby to settle into an ideal birthing position.
While most babies settle in a cephalic presentation by the 36th week of pregnancy, some may lie in a breech or transverse position before birth. Since the cephalic position is considered the safest, your doctor may recommend certain procedures to flip your baby’s position to make your labour and delivery smooth. You may also try the natural methods that we discussed above to get your baby into a safe birthing position and prevent risks or other pregnancy complications.
When Should A Baby Be In A Cephalic Position?
Your baby would likely naturally drop into a cephalic position between weeks 37 to 40 of your pregnancy .
Is Cephalic Position Safe?
Research shows that 95% of babies take the cephalic position a few weeks or days before their due date. It is considered to be the safest position. It ensures a smooth birthing process.
While most of the babies are in cephalic position at delivery, this is not always the case. If you have a breech baby, you can discuss the available options for delivery with your doctor.
Does cephalic presentation mean labour is near?
Head-down is the ideal position for your baby within your uterus during birth. This is known as the cephalic position. This posture allows your baby to pass through the delivery canal more easily and safely.
Can babies change from cephalic to breech?
The external cephalic version (ECV) is the most frequent procedure used for turning a breech infant.
How can I keep my baby in a cephalic position?
While your baby naturally gets into this position, you can try some exercises to ensure that they settle in cephalic presentation. Exercises such as breech tilt, forward-leaning position (spinning babies program), cat and camel pose can help.
Stitches after a normal delivery : How many stitches do you need after a vaginal delivery? Tap this post to know.
Vaginal birth after caesarean delivery : Learn all about the precautions to consider before having a vaginal delivery after a c-section procedure.
How many c-sections can you have : Tap this post to know the total number of c-sections that you can safely have.
Cover Image Credit: Freepik.com

Related Topics for you
babychakraenglish
cephalicposition
cephalicpresentation
fetaldevelopment
fetalmovement
preganancycare
Suggestions offered by doctors on BabyChakra are of advisory nature i.e., for educational and informational purposes only. Content posted on, created for, or compiled by BabyChakra is not intended or designed to replace your doctor's independent judgment about any symptom, condition, or the appropriateness or risks of a procedure or treatment for a given person.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Womens Health (Lond)
Maternal and fetal characteristics to predict c-section delivery: A scoring system for pregnant women
Rima irwinda.
1 Maternal-Fetal Medicine Division, Department of Obstetrics and Gynaecology, Faculty of Medicine Universitas Indonesia and Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Rabbania Hiksas
2 Faculty of Medicine Universitas Indonesia and Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Angga Wiratama Lokeswara
Noroyono wibowo, introduction:.
Cesarean section is one of the most common obstetrical interventions that has been performed at an increasing rate globally, due to both medical and non-medical reasons. This study aims to develop a prediction tool for pregnant women potentially needing c-section, such that necessary preparations from the mothers, families, and health providers can be made.
A total of 603 pregnant women were recruited in the first phase of c-section prediction tool development. The association between the maternal and fetal factors on the risk of c-section were analyzed, followed by a stepwise multivariate regression analysis. In the next phase, 61 pregnant women were enrolled for external validation. Discrimination was assessed using area under the curve. The calibration plot was then made and assessed using the Hosmer–Lemeshow test.
There were 251 (41.6%) cases of vaginal delivery and 352 (58.4%) of c-section assessed. Multivariate analysis showed that gestational age < 37 wg (OR: 1.66, 95% CI: 1.10–2.51), pre-pregnancy body mass index (underweight) (OR: 0.40, 95% CI: 0.22–0.76), no history of vaginal delivery (OR: 2.66, 95% CI: 1.76–4.02), history of uterine surgery (OR: 8.34, 95% CI: 4.54–15.30), obstetrical complications (OR: 5.61, 95% CI: 3.53–8.90), birthweight ⩾ 3500 g (OR: 4.28, 95% CI: 2.16–8.47), and non-cephalic presentation (OR: 2.74, 95% CI: 1.53–4.89) were independently associated with c-section delivery. Those parameters were included in a 7-item scoring tool, with consecutive predictive scores of 1,–1,2,3,3,2,2,1. The area under the curve result was 0.813 (95% CI: 0.779–0.847), indicating a good predictive ability. The external validation showed AUC: 0.806, 95% CI: 0.694–0.917, Hosmer–Lemeshow test p = 0.666 and calibration plot coefficient of r = 0.939.
Conclusion:
A total of 7 maternal-fetal factors were found to be strongly associated with c-section delivery, including gestational age < 37, maternal underweight body mass index, previous uterine surgery, obstetrical complications, birthweight ⩾ 3500, history of vaginal delivery, and non-cephalic presentation. Using these factors, a prediction tool was developed and validated with good quality.
Introduction
Cesarean section, or more commonly known as c-section, has become the main alternative delivery method in pregnancy with life-threatening complications. 1 The decision to perform c-section should be made under conditions where vaginal delivery is impossible, or poses more risks, and is therefore taken only with certain maternal or fetal indications. 2
Based on the Statement on Cesarean Section Rates by the WHO, 3 a systematic review and ecological analysis have found that a population-based c-section rates above 10% does not correlate with reductions in maternal and neonatal mortality, thus is considered non-optimal, considering the adverse complications in future pregnancies. 4 , 5 Nevertheless, in the last decade, WHO found that the rates of c-section has dramatically increased from 7% in 1990 to more than 1 in 5 childbirths (21%) in 2021, and is projected to reach 29% in 2030, globally. If the trend continues, Eastern Asia and Latin America are projected to reach the highest rates at 63% and 54% respectively. 6
Although c-section can be an imperative, lifesaving surgery in certain cases, one concerning reason behind the trend is the increasing c-section by maternal request, without any medical indications. 7 A systematic review by Begum et al. 8 in 2020 found that c-section by maternal request makes up 0.2%–42% of all childbirths, and 0.9%–60% of all c-sections, with 11-fold increase in c-section by maternal request in upper middle-income countries compared with either high or lower-middle income countries.
In Indonesia, the rate of c-section mimics the global trend, as it increased from 9.8% in 2013 to 17.6% in 2018, with the highest rate found in Jakarta (31.1%). 9 In recent years, the rate of c-section in Cipto Mangunkusumo National Referral Hospital alone reached almost 50%. Despite advanced surgical techniques, c-section poses short-term and long-term complications. Several risks are associated with c-section, including miscarriage and stillbirth, placenta previa, and placenta accreta in the following pregnancy, as well as development of childhood asthma. 10 In Cipto Mangunkusumo hospital, the cases of placenta accreta was found to be at 76 out of 2660 c-section deliveries (2.86%) in 2019. 11 A multi-country survey has also found that c-section performed without medical indications increases risks for severe maternal outcome. 12
Furthermore, in Indonesia, the high maternal morbidity and mortality rates were highly influenced by the poor infrastructure of the healthcare system in remote areas as well as poor awareness of the pregnant mothers, resulting in delayed referrals. 13 In developing countries like Indonesia, poor awareness of the early signs of obstetrical complications also contributes to late consultation to obstetricians. This could eventually delay the c-section, resulting in life-threatening conditions. Therefore, by educating pregnant women with regards to their risks of c-section, maternal and fetal outcomes could potentially be improved.
With varying trends in c-section and its medical and non-medical reasons, the medical risk factors behind today’s trend of c-section becomes unclear. Numbers of scoring system related maternal and fetal characteristics to predict the risk of c-sections have been developed for obstetricians in order to ensure the procedure was done only if indicated. 14 , 15 However, the existing scoring systems were built for obstetrician, hence are too difficult for pregnant women in general population to comprehend, thus many pregnant women remain unaware of their obstetrical condition. Therefore, this study aims to assess the maternal and fetal risk factors of c-section and develop a prediction tool for mothers potentially needing c-section. Hence, necessary preparations from the mothers and families, especially in third trimester, and health providers can be made.
Study setting
The study was carried out at Cipto Mangunkusumo Hospital, Fatmawati Hospital, and Tangerang General hospital, located in Jakarta-Tangerang, Indonesia. All of the hospitals are tertiary referral hospital, which receive and treat referred cases from primary and secondary healthcare facilities. Moreover, Cipto Mangunkusumo Hospital is a national referral hospital in Indonesia, handling patients not only from Jakarta, Indonesia, but also other referred patients from other provinces in Indonesia, mainly the ones with adverse pregnancy complications. These hospitals are also teaching hospitals, where examination and procedures were performed by residents of the Department of Obstetrics and Gynaecology, Faculty of Medicine, University of Indonesia, under close supervision by highly qualified Obstetrics and Gynecology subspecialists and consultants.
Study design and sample recruitment
This was a retrospective cohort study using data from the hospital’s medical records. The first phase of the study was development of a scoring system, which took place in Cipto Mangunkusumo Hospital and Fatmawati Hospital. The minimum sample size calculated was 273; on the basis incidence of c-section rate in Jakarta, 2018 (31.1%), 9 along with 95% confidence interval (CI), and 80% power. 16 The study was restricted to women delivered in those two hospitals from January to April 2019, with gestational age of 22–42 weeks. A total of 753 cases met the criteria. We excluded deliveries with babies weighing 500 g or less (n = 13), cases of intrauterine fetal death at less than 28 weeks (n = 28), and cases with incomplete antenatal data (n = 109). After exclusions, a total of 603 cases complied our eligibility criteria and were put to analysis.
The next phase was a validation of the scoring system, which took place in Tangerang General Hospital. The minimum sample size was also calculated with 95% CI and 80% power. 16 With the effect size 0.26 (low-risk and high-risk difference from the first part of study), the minimum sample requirement for the external validation was 46. Applying similar inclusion and exclusion criteria, the study was restricted to women delivered in the hospital from July to August 2021, with gestational age of 22–42 weeks. Within the period of study, a total 89 cases met the criteria. We excluded deliveries with babies weighing 500 g or less (n = 5), cases of intrauterine fetal death at less than 28 weeks (n = 4), and cases with incomplete antenatal data (n = 19). We continued the external validation using 61 samples. Figure 1 shows the workflow diagram.

The workflow diagram.
This study has been approved by The Ethical Committee for Research in Humans from The Faculty of Medicine, Universitas Indonesia (KET-1491/UN2.F1/ETIK/PPM.00.02/2020). Since this was a retrospective study, we extracted only clinically relevant information from medical records with ensuring patient’s privacy protection. This study also did not affect patients treatment and health, thus written informed consent from all participants was waived by the Ethical Committee.
Outcome measures
All data extracted from medical records were classified into demographic characteristics, pregnancy history, current pregnancy characteristics, and neonatal features. Demographic characteristics; maternal age, gestational age, body height, body weight before pregnancy and during last trimester, body mass index (BMI) before pregnancy and during last trimester which was categorized based on Asia-Pacific BMI criteria including underweight (< 18.5), normal (18.5–22.9), overweight (23–24.9), and obese (⩾ 25). Pregnancy history; gravidity, parity, previous uterine surgery (c-section or myomectomy), history of vaginal delivery. Current pregnancy characteristics; antenatal care (ANC) visit, types of pregnancy (single or twin), pregnancy program, presence of chronic diseases (diabetes, hypertension, heart disease, kidney disease, autoimmune diseases, infections including syphilis, human immunodeficiency virus (HIV), or hepatitis B, and cancer), obstetrical complications [hypertensive disorder in pregnancy, 17 gestational diabetes mellitus (severe hyperglycaemia in pregnancy), 18 intrauterine growth restriction (i.e. estimated fetal weight or abdominal circumference below the 10th percentile, abnormal doppler/amniotic fluid index/biophysical profile), 19 placenta previa, and placental abruption], and the presence of premature rupture of membrane (later than 6 or 12 h). Neonatal features: birth weight, and fetal presentation at the last trimester.
All women were classified into two groups: vaginal delivery and c-section. C-section included both emergency and elective c-section. Vaginal delivery included spontaneous delivery, with or without induction, vacuum extraction, or forceps delivery. The primary outcome of this study was to identify the possible independent factors associated with c-section, which are comprehensible for both non-health care workers and health-care providers.
Statistical analysis
Data analysis was performed using SPSS statistics, version 25 (SPSS Inc, Chicago, Illinois, USA). Mean and standard deviation were used to describe continuous variables with normal distribution, while median and interquartile range for non-normal distribution data. Comparison of proportions was performed by Pearson’s chi-square (χ 2 ) for categorial variables. Variables with p-value < 0.250 in bivariate analysis were put into logistic regression analysis. Each odds ratio (OR) with multivariable log-binomial regression models was estimated with 95% confidence intervals (CIs). A p-value of less than 5% was considered statistically significant.
A predictive scoring tool was developed through stepwise calculations: (1) dividing each prognostic factor’s coefficient B by its standard error (coefficient B/SE); (2) choosing the lowest B/SE value as a reference (3) dividing each B/SE value by the reference value; and (4) picking the rounded number nearest to the result from step 3. In order to evaluate the performance of our scoring system, we analyzed calibration score using the Hosmer–Lemeshow test and discrimination score using receiver operating characteristic (ROC) and area under receiver operating characteristic curve (AUC). These were followed by internal validation using repeated backward logistic regression model for each of predictors with 1000 bootstrap resampling. Finally, the result of external validation of the scoring system were evaluated using repeated discrimination and calibration test using the same method.
Characteristics of study population
There were 603 cases assessed in this study, including 251 (41.6%) cases with vaginal delivery and 352 (58.4%) with c-section delivery. The characteristics of study population is shown in Table 1 . Bivariate and multivariate analysis were performed to evaluate the significances of variables associated with mode of delivery. Among the 18 variables which were analyzed for their association with the risk of c-section, 11 variables found to be significant ( Table 2 ). These 11 variables were then included in the logistic regression analysis, resulting in 7 variables found to be significantly associated with c-section delivery (p < 0.05). The odds ratio of the 11 variables are showed in Table 3 .
Baseline characteristics of study population.
IQR: interquartile range; BMI: body mass index; BP: blood pressure.
Bivariate analysis of factors associated with c-section.
OR: odds ratio; CI: confidence interval; BMI: body mass index; ANC: antenatal care.
Odds ratio for independent variables in multivariate logistic regression analysis.
OR: odds ratio; CI: confidence interval; wg: weeks of gestation; BMI: body mass index.
Development of c-section scoring system
There were seven variables identified in development of scoring system for the final model ( Table 4 ), including gestational age < 37 weeks, underweight pre-pregnancy BMI, previous uterine surgery, obstetrical complications, birth weight ⩾ 3500 g, no history of vaginal delivery, and non-cephalic presentation. Following that, a 7-item scoring system was developed (gestational age < 37 weeks = 1, underweight pre-pregnancy BMI = –1, non-cephalic presentation = 1, no history of vaginal delivery = 2, birthweight ⩾ 3500 g = 2, previous uterine surgery = 3, and obstetrical complications = 3), with a total score 11. The full scoring system is shown in Table 5 .
Derivation of 7-point scoring system to the risk of c-section from stepwise multivariate analysis.
SE: standard error; OR: odds ratio; CI: confidence interval; wg: weeks of gestation; BMI: body mass index.
Sensitivity, specificity, and probability analysis of the scoring system.
Furthermore, the area of AUC was 0.813 (95% CI: 0.779–0.847). ( Figure 2 ). This was considered good as sensitivity of 81% were shown when the score ⩾3 was categorized as high risk for c-section, with a probability score of 53.13% ( Table 5 ). Calibration using Hosmer–Lemeshow showed a good calibration score with p = 0.555 (p > 0.05). An internal validation using 1000× boostraping also showed the same p value (p = 0.555). As the p values of before and after bootstrapping are the same, the scoring system can likely be expected to have similar results in a bigger population.

The ROC curve of the scoring system development the AUC = 0.813, 95% CI: 0.779–0.847.
External validation
We then enrolled 61 subjects for external validation of the scoring tool. Among them, 24 subjects underwent vaginal delivery and 37 subjects underwent c-section delivery. The performance of c-section risk scoring tool was assessed for calibration and discrimination results. As the calibration plot showed a coefficient of r = 0.939 ( Figure 3 ), and the Hosmer–Lemeshow test showed p = 0.624, the scoring system was considered to have a good calibration. In Figure 4 , The AUC was 0.806, with 95% CI (0.694–0.917), showing an excellent discrimination with no big difference from the first part of the study.

The plot calibration diagram of the scoring system in external validation (r = 0.939).

The ROC curve of the scoring system in external validation. The AUC = 0.806, 95% CI: 0.694–0.917.
There were seven variables identified to be independently associated with c-section delivery, including gestational age < 37 weeks, maternal underweight pre-pregnancy, previous uterine surgery, obstetrical complications, no history of vaginal delivery, birth weight ⩾ 3500 g, and non-cephalic presentation. From these variables, a scoring system for the risk of c-section has been developed. Since this scoring system was intended for those without medical background, certain variables which were deemed too technical for general population to understand were not included in the analysis. Therefore, variables such as characteristics of amniotic fluid or umbilical cord were not included in the analysis despite their known associations with the risk of c-section based on previous studies. 14
Among the maternal demographical characteristics, maternal underweight BMI pre-pregnancy was the only variable to independently reduce the risk of c-section by OR: 0.40, 95% CI: 0.22–0.76. This finding was consistent with numbers of study from Asia to Europe, where pre-pregnancy underweight BMI were found to lower the risk of cesarean delivery by almost half, with OR: 0.45–0.66. 20 – 22 In contrast, obese patients who were thought to have increased risks for c-section, showed no significant difference in our study. This was surprising as a previous study had suggested that nulliparous obese pregnant women might have increased risk of c-section. 23 A different cut off value for BMI category between the two criteria, Asian-Pacific and WHO criteria, might have influenced the differing results.
In terms of the obstetrical history, the history of uterine surgery and no history of vaginal delivery were found to be highly associated with c-section. Our study found that the history of uterine surgery was one of two variables with the highest scores in predicting c-section. This finding is in agreement with previous studies which found that a history of c-section in previous births increased the risk of c-section in the following pregnancy, with RR 4.30 (4.24–4.36) and OR: 3.5 (3.4–3.6). 15 , 24 This value may also be increased in deliveries with a history of previous c-section with a gestational distance of less than 19 months. 25 , 26 Although a history of previous c-section is not an absolute indication of c-section in subsequent pregnancies, vaginal birth after cesarean (VBAC) might cause numerous adverse effects including uterine rupture, fetal death, or fetal brain damage due to hypoxia. In addition, other previous uterine surgeries such as myomectomy or resection of adenomyosis were also known as a risk factor for c-section, and are considered indications for c-section in subsequent deliveries. 27 Moreover, history of vaginal delivery also affects the risk of c-section. Mothers in their first pregnancy have a greater risk of having a cesarean delivery compared to those who have already had a vaginal delivery before. This is because the pelvic of multiparous women with previous vaginal delivery was considered to be more flexible and easier to undergo vaginal delivery in the following pregnancies. 15 , 23 , 28
Furthermore, obstetrical complications are also well-established major risk factors of c-section procedure. In this study, we included preeclampsia/eclampsia, gestational diabetes mellitus, IUGR, placenta previa, and placental abruption, since those are the most common pregnancy problems in Indonesia. 9 Previous studies have suggested that those complications of pregnancy had relative risk of around 1.45–1.75 for c-section. 14 , 15 , 24 Our study found that preterm birth (gestational age < 37 wg) increased the risk of c-section. This was consistent with another previous study which showed that birth at < 37 wg increased the risk of c-section with an OR: 1.45, 95% CI: 1.16–1.72. 29 This findings imply that pregnant women who felt the signs of labor such as uterine contractions, bloody mucous discharge or water breaking before 37 weeks of gestation, were predicted to had increased risk of c-section.
The characteristics of the fetus during pregnancy may also affect the risk of c-section delivery, especially during the third trimester. Our study found that birthweight ⩾ 3500 g had OR of 4.28 (95% CI: 2.16–8.47), thus is given a score of “2” in our prediction tool. This is in agreement with a previous study which found that heavier fetal weight was associated with the increased risk of c-section. 14 , 30 Another previous study also supports our finding, suggesting that a total of 60.7% of pregnancies with a fetal weight more than 3500 were delivered by c-section, compared to 39.3% for a fetus weighing < 3500 g. 28 Although our study used the clinical birthweight rather than the estimated fetal weight, previous studies have found that there was no significant difference between estimated fetal weight and actual birth weight in normal weight population. 31 Significant difference of fetal weight usually found in small for gestational age fetus, with differences up to 200 g. 32 Thus, a clinically-determined estimated fetal weight of ⩾ 3500 g, can still be a predictive factor for an increased risk of c-section. In addition, our study also found that non-cephalic presentation is associated with increased risk of c-section. This was not surprising, as numbers of studies have also found its association with increased risk of c-section. A previous study found that the incidence of c-section in non-cephalic presentation was 93.3% (p < 0.001) compared to head presentation, the incidence of which is 37.3%. 28 Nevertheless, studies have suggested that non-cephalic presentation was best diagnosed at 36 weeks of gestational age. 33 Therefore, pregnant women who uses our scoring tool with diagnosed fetal presentation before 36 weeks of gestation, is recommended to repeat the examination in the subsequent weeks of pregnancy. Moreover, interestingly, in our first part of study, we also found 37.18 per 1000 rate of early fetal death. This high number was due to the fact that our study was conducted in tertiary and national referral hospitals, thus the number of cases of adverse pregnancy complications was higher than the national data. 9
To the best of our knowledge, this is the first study to propose a scoring system in the risk of c-section for both non-medical and medical personnel, with variables which were considered simple and easy to evaluate. The internal and external validations have reflected satisfactory calibration and discrimination values of the scoring system. Nevertheless, there were certain limitations of the study. Pregnant women that could confidently use this scoring were the ones with late trimester, as most of variables could only be evaluated during the last trimester. Also, this was a retrospective study, thus the conclusions were limited by the results of this present study. Further studies should explore the application of this predictive scoring tool in a wider range of population with a prospective cohort design.
There were seven independent factors found to be highly associated with c-section delivery, including gestational age < 37, underweight pre-pregnancy BMI, previous uterine surgery, no history of vaginal delivery, obstetrical complications, birthweight ⩾ 3500, and non-cephalic presentation. A predictive scoring tool has been developed and validated with a good quality. Pregnant women were expected to use this scoring tool as a self-administered questionnaire so they are able to self-assess their risks of c-section. High risk of c-section results would encourage mothers, families, and healthcare professionals to arrange for early consultations with obstetricians and make better preparations for the mothers to deliver at the hospitals.
Acknowledgments
We thank Danone Specialized Nutrition Indonesia for supporting this research, as they will further create an online application for the tools.
Author contributions: R.I. and N.W. designed the study. R.H. and A.W.L. conducted the research, performed the analysis, interpretation of data, and wrote the manuscript. R.I. validated the data, revised the paper, and had primary responsibility for the final content. All authors agreed to the published version of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.

Data availability: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
You and your baby at 32 weeks pregnant
Your baby at 32 weeks.
By about 32 weeks, the baby is usually lying with their head pointing downwards, ready for birth. This is known as cephalic presentation.
If your baby is not lying head down at this stage, it's not a cause for concern – there's still time for them to turn.
The amount of amniotic fluid in your uterus is increasing, and your baby is still swallowing fluid and passing it out as urine.
You at 32 weeks
Being active and fit during pregnancy will help you adapt to your changing shape and weight gain. It can also help you cope with labour and get back into shape after the birth.
Find out about exercise in pregnancy .
You may develop pelvic pain in pregnancy. This is not harmful to your baby, but it can cause severe pain and make it difficult for you to get around.
Find out about ways to tackle pelvic pain in pregnancy .
Read about the benefits of breastfeeding for you and your baby. It's never too early to start thinking about how you're going to feed your baby, and you do not have to make up your mind until your baby is born.
Things to think about
- how you might feel after the birth
Start4Life has more about you and your baby at 32 weeks pregnant .
You can sign up for Start4Life's weekly emails for expert advice, videos and tips on pregnancy, birth and beyond.
Page last reviewed: 13 October 2021 Next review due: 13 October 2024
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
How your twins’ fetal positions affect labor and delivery

Twin fetal presentation – also known as the position of your babies in the womb – dictates whether you'll have a vaginal or c-section birth. Toward the end of pregnancy, most twins will move in the head-down position (vertex), but there's a risk that the second twin will change position after the first twin is born. While there are options to change the second twin's position, this can increase the risk of c-section and other health issues. Learn about the six possible twin fetal presentations: vertex-vertex, vertex-breech, breech-breech, vertex-transverse, breech-transverse, and transverse-transverse – and how they'll impact your delivery and risks for complications.
What is fetal presentation and what does it mean for your twins?
As your due date approaches, you might be wondering how your twins are currently positioned in the womb, also known as the fetal presentation, and what that means for your delivery. Throughout your pregnancy, your twin babies will move in the uterus, but sometime during the third trimester – usually between 32 and 36 weeks – their fetal presentation changes as they prepare to go down the birth canal.
The good news is that at most twin births, both babies are head-down (vertex), which means you can have a vaginal delivery. In fact, nearly 40 percent of twins are delivered vaginally.
But if one baby has feet or bottom first (breech) or is sideways (transverse), your doctor might deliver the lower twin vaginally and then try to rotate the other twin so that they face head-down (also called external cephalic version or internal podalic version) and can be delivered vaginally. But if that doesn't work, there's still a chance that your doctor will be able to deliver the second twin feet first vaginally via breech extraction (delivering the breech baby feet or butt first through the vagina).
That said, a breech extraction depends on a variety of factors – including how experienced your doctor is in the procedure and how much the second twin weighs. Studies show that the higher rate of vaginal births among nonvertex second twins is associated with labor induction and more experienced doctors, suggesting that proper delivery planning may increase your chances of a vaginal birth .
That said, you shouldn't totally rule out a Cesarean delivery with twins . If the first twin is breech or neither of the twins are head-down, then you'll most likely have a Cesarean delivery.
Research also shows that twin babies who are born at less than 34 weeks and have moms with multiple children are associated with intrapartum presentation change (when the fetal presentation of the second twin changes from head-down to feet first after the delivery of the first twin) of the second twin. Women who have intrapartum presentation change are more likely to undergo a Cesarean delivery for their second twin.
Here's a breakdown of the different fetal presentations for twin births and how they will affect your delivery.
Head down, head down (vertex, vertex)
This fetal presentation is the most promising for a vaginal delivery because both twins are head-down. Twins can change positions, but if they're head-down at 28 weeks, they're likely to stay that way.
When delivering twins vaginally, there is a risk that the second twin will change position after the delivery of the first. Research shows that second twins change positions in 20 percent of planned vaginal deliveries. If this happens, your doctor may try to rotate the second twin so it faces head-down or consider a breech extraction. But if neither of these work or are an option, then a Cesarean delivery is likely.
In vertex-vertex pairs, the rate of Cesarean delivery for the second twin after a vaginal delivery of the first one is 16.9 percent.
Like all vaginal deliveries, there's also a chance you'll have an assisted birth, where forceps or a vacuum are needed to help deliver your twins.
Head down, bottom down (vertex, breech)
When the first twin's (the lower one) head is down, but the second twin isn't, your doctor may attempt a vaginal delivery by changing the baby's position or doing breech extraction, which isn't possible if the second twin weighs much more than the first twin.
The rates of emergency C-section deliveries for the second twin after a vaginal delivery of the first twin are higher in second twins who have a very low birth weight. Small babies may not tolerate labor as well.
Head down, sideways (vertex, transverse)
If one twin is lying sideways or diagonally (oblique), there's a chance the baby may shift position as your labor progresses, or your doctor may try to turn the baby head-down via external cephalic version or internal podalic version (changing position in the uterus), which means you may be able to deliver both vaginally.
Bottom down, bottom down (breech, breech)
When both twins are breech, a planned C-section is recommended because your doctor isn't able to turn the fetuses. Studies also show that there are fewer negative neonatal outcomes for planned C-sections than planned vaginal births in breech babies.
As with any C-section, the risks for a planned one with twins include infection, loss of blood, blood clots, injury to the bowel or bladder, a weak uterine wall, placenta abnormalities in future pregnancies and fetal injury.
Bottom down, sideways (breech, transverse)
When the twin lowest in your uterus is breech or transverse (which happens in 25 percent of cases), you'll need to have a c-section.
Sideways, sideways (transverse, transverse)
This fetal presentation is rare with less than 1 percent of cases. If both babies are lying horizontally, you'll almost definitely have a C-section.
Learn more:
- Twin fetal development month by month
- Your likelihood of having twins or more
- When and how to find out if you’re carrying twins or more
Was this article helpful?
32 weeks pregnant with twins

36 weeks pregnant with twins

28 weeks pregnant with twins

24 weeks pregnant with twins

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Cleveland Clinic. Fetal Positions for Birth: https://my.clevelandclinic.org/health/articles/9677-fetal-positions-for-birth Opens a new window [Accessed July 2021]
Mayo Clinic. Fetal Presentation Before Birth: https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/multimedia/fetal-positions/sls-20076615?s=7 Opens a new window [Accessed July 2021]
NHS. Giving Birth to Twins or More: https://pubmed.ncbi.nlm.nih.gov/29016498/ Opens a new window [Accessed July 2021]
Science Direct. Breech Extraction: https://www.sciencedirect.com/topics/medicine-and-dentistry/breech-extraction Opens a new window [Accessed July 2021]
Obstetrics & Gynecology. Clinical Factors Associated With Presentation Change of the Second Twin After Vaginal Delivery of the First Twin https://pubmed.ncbi.nlm.nih.gov/29016498/ Opens a new window [Accessed July 2021]
American Journal of Obstetrics and Gynecology. Fetal presentation and successful twin vaginal delivery: https://www.ajog.org/article/S0002-9378(04)00482-X/fulltext [Accessed July 2021]
The Journal of Maternal-Fetal & Neonatal Medicine. Changes in fetal presentation in twin pregnancies https://www.tandfonline.com/doi/abs/10.1080/14767050400028592 Opens a new window [Accessed July 2021]
Reviews in Obstetrics & Gynecology. An Evidence-Based Approach to Determining Route of Delivery for Twin Gestations https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252881/ Opens a new window [Accessed July 2021]
Nature. Neonatal mortality and morbidity in vertex–vertex second twins according to mode of delivery and birth weight: https://www.nature.com/articles/7211408 Opens a new window [Accessed July 2021]
Cochrane. Planned cesarean for a twin pregnancy: https://www.cochrane.org/CD006553/PREG_planned-caesarean-section-twin-pregnancy Opens a new window [Accessed July 2021]
Kids Health. What Is the Apgar Score?: https://www.kidshealth.org/Nemours/en/parents/apgar0.html Opens a new window [Accessed July 2021]
American Journal of Obstetrics & Gynecology. Neonatal mortality in second twin according to cause of death, gestational age, and mode of delivery https://pubmed.ncbi.nlm.nih.gov/15467540/ Opens a new window [Accessed July 2021]
Lancet. Planned cesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group https://pubmed.ncbi.nlm.nih.gov/11052579/ Opens a new window [Accessed July 2021]
Cleveland Clinic. Cesarean Birth (C-Section): https://my.clevelandclinic.org/health/treatments/7246-cesarean-birth-c-section Opens a new window [Accessed July 2021]
St. Jude Medical Staff. Delivery of Twin Gestation: http://www.sjmedstaff.org/documents/Delivery-of-twins.pdf Opens a new window [Accessed July 2021]

Where to go next


- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
- Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Abnormal Fetal lie, Malpresentation and Malposition
Original Author(s): Anna Mcclune Last updated: 1st December 2018 Revisions: 12
- 1 Definitions
- 2 Risk Factors
- 3.2 Presentation
- 3.3 Position
- 4 Investigations
- 5.1 Abnormal Fetal Lie
- 5.2 Malpresentation
- 5.3 Malposition
The lie, presentation and position of a fetus are important during labour and delivery.
In this article, we will look at the risk factors, examination and management of abnormal fetal lie, malpresentation and malposition.
Definitions
- Longitudinal, transverse or oblique
- Cephalic vertex presentation is the most common and is considered the safest
- Other presentations include breech, shoulder, face and brow
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) – this is ideal for birth
- Other positions include occipito-posterior and occipito-transverse.
Note: Breech presentation is the most common malpresentation, and is covered in detail here .
Fig 1 – The two most common fetal presentations: cephalic and breech.
Risk Factors
The risk factors for abnormal fetal lie, malpresentation and malposition include:
- Multiple pregnancy
- Uterine abnormalities (e.g fibroids, partial septate uterus)
- Fetal abnormalities
- Placenta praevia
- Primiparity
Identifying Fetal Lie, Presentation and Position
The fetal lie and presentation can usually be identified via abdominal examination. The fetal position is ascertained by vaginal examination.
For more information on the obstetric examination, see here .
- Face the patient’s head
- Place your hands on either side of the uterus and gently apply pressure; one side will feel fuller and firmer – this is the back, and fetal limbs may feel ‘knobbly’ on the opposite side
Presentation
- Palpate the lower uterus (above the symphysis pubis) with the fingers of both hands; the head feels hard and round (cephalic) and the bottom feels soft and triangular (breech)
- You may be able to gently push the fetal head from side to side
The fetal lie and presentation may not be possible to identify if the mother has a high BMI, if she has not emptied her bladder, if the fetus is small or if there is polyhydramnios .
During labour, vaginal examination is used to assess the position of the fetal head (in a cephalic vertex presentation). The landmarks of the fetal head, including the anterior and posterior fontanelles, indicate the position.
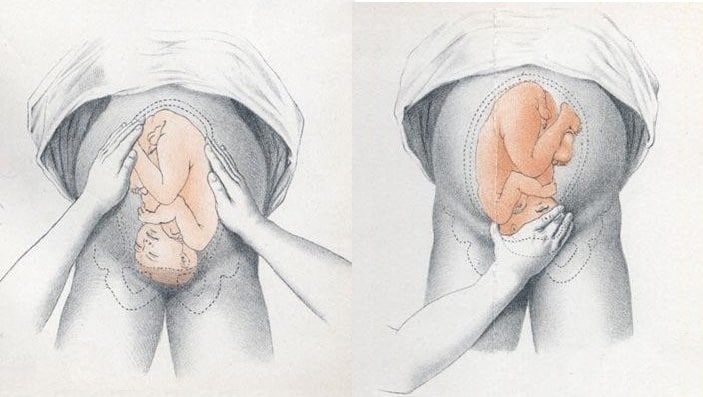
Fig 2 – Assessing fetal lie and presentation.
Investigations
Any suspected abnormal fetal lie or malpresentation should be confirmed by an ultrasound scan . This could also demonstrate predisposing uterine or fetal abnormalities.
Abnormal Fetal Lie
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted – ideally between 36 and 38 weeks gestation.
ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen.
It has an approximate success rate of 50% in primiparous women and 60% in multiparous women. Only 8% of breech presentations will spontaneously revert to cephalic in primiparous women over 36 weeks gestation.
Complications of ECV are rare but include fetal distress , premature rupture of membranes, antepartum haemorrhage (APH) and placental abruption. The risk of an emergency caesarean section (C-section) within 24 hours is around 1 in 200.
ECV is contraindicated in women with a recent APH, ruptured membranes, uterine abnormalities or a previous C-section .
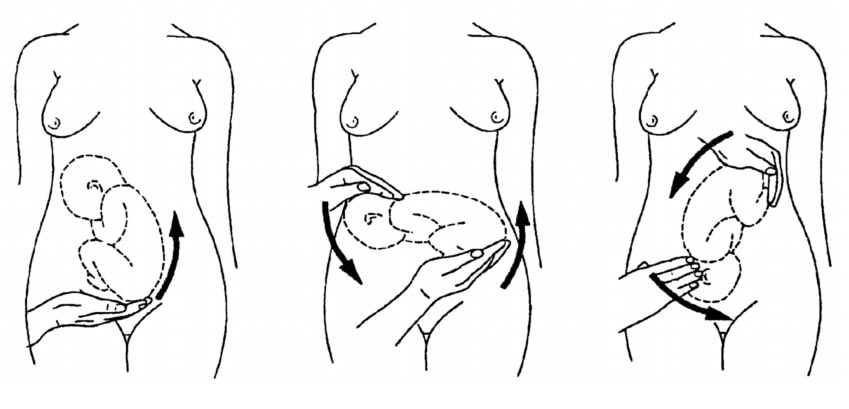
Fig 3 – External cephalic version.
Malpresentation
The management of malpresentation is dependent on the presentation.
- Breech – attempt ECV before labour, vaginal breech delivery or C-section
- Brow – a C-section is necessary
- If the chin is anterior (mento-anterior) a normal labour is possible; however, it is likely to be prolonged and there is an increased risk of a C-section being required
- If the chin is posterior (mento-posterior) then a C-section is necessary
- Shoulder – a C-section is necessary
Malposition
90% of malpositions spontaneously rotate to occipito-anterior as labour progresses. If the fetal head does not rotate, rotation and operative vaginal delivery can be attempted. Alternatively a C-section can be performed.
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) - this is ideal for birth
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation.
- Breech - attempt ECV before labour, vaginal breech delivery or C-section
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
Recommended
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to copy URL
Victoria’s Secret is bringing its controversial fashion show back to the runway
- View Author Archive
- Follow on Twitter
- Get author RSS feed
Thanks for contacting us. We've received your submission.

The Angels are back.
While Victoria’s Secret tried a revamped version of its iconic fashion show in 2023, the brand announced Wednesday that it was bringing the catwalk spectacular back to its original format with a splashy runway show this year.
The new show “will deliver precisely what our customers have been asking for – the glamour, runway, fashion, fun, wings, entertainment – all through a powerful, modern lens reflecting who we are today,” a spokesperson for the brand tells Page Six Style.

Shop 'til you drop with Post Wanted
Save time and money with the latest deals, discounts, trends, reviews and more.
Thanks for signing up!
Please provide a valid email address.
By clicking above you agree to the Terms of Use and Privacy Policy .
Never miss a story with New York Post newsletters.
Victoria’s Secret tested a new format for its fashion show last year after receiving backlash for not including a diverse range of models in its annual TV special.
The show went on a four-year hiatus after facing plummeting ratings in 2018, returning with the “Victoria’s Secret World Tour” in 2023, which was a more fluid pre-taped presentation and streamed on Prime Video.
The brand’s fashion show debuted in 1997 and featured a range of big-name models — dubbed Victoria’s Secret Angels — over the years, with the likes of Heidi Klum, Gisele Bündchen, Naomi Campbell, Kendall Jenner, Claudia Schiffer and Tyra Banks walking the catwalk.

For more Page Six Style …
- See the best celebrity looks of the week in our new series, “Instantly Iconic Style”
- Browse the best fashion and beauty products, according to celebs
- Shop our exclusive merch
Fans eagerly tuned in each year to see the steamy lingerie and performances from artists like Taylor Swift, Rihanna and the Spice Girls, but the special — which swapped between airing on ABC and CBS — dipped in popularity in the wake of the #MeToo movement.
However, it seems like the company is going back to basics after the “World Tour” special featuring Doja Cat shook things up from the typical runway format.
Though there is no date announced, the brand tells us it’s “thrilled to share a women-led articulation of this iconic property later this year.”
Share this article:

Advertisement

COMMENTS
This is called cephalic or occiput anterior presentation. Most fetuses settle into this position by the 36th week of pregnancy. Other fetal positions, like breech presentation, make a vaginal delivery more challenging. ... Your pregnancy care provider may call it fetal presentation or the presentation of the fetus (although this usually refers ...
At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie). Photo credit: Jonathan Dimes for BabyCenter. Fetal presentation and position. During the last trimester of your ...
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder.
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery. About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy.
This positioning is called fetal presentation. Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation.
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation, where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest delivery, as baby's head can easily move down the birth canal and under the pubic bone during childbirth. ... While your baby will likely have been sideways at some point in your pregnancy ...
Cephalic presentation means a fetus is in a head-down position. Vertex refers to the fetus's neck being tucked in. There are other types of cephalic presentations like brow and face. ... It's possible for a fetus to rotate into a cephalic presentation after 36 weeks. Your pregnancy care provider will check the presentation of the fetus ...
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin.
Introduction. Cephalic presentation is the most physiologic and frequent fetal presentation and is associated with the highest rate of successful vaginal delivery as well as with the lowest frequency of complications 1.Studies on the frequency of breech presentation by gestational age (GA) were published more than 20 years ago 2, 3, and it has been known that the prevalence of breech ...
Cephalic presentation, occiput anterior. This is the best position for labor. Your baby is head-down, their face is turned toward your back, and their chin is tucked to their chest. This allows the back of your baby's head to easily enter your pelvis when the time is right. Most babies settle into this position by week 36 of pregnancy.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord. For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor. ... Cephalic presentation occurs in about 97% of deliveries. There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude). ...
Presentation refers to which part of your baby's body is facing towards your birth canal. Position refers to the direction your baby's head or back is facing. Your baby's presentation will be checked at around 36 weeks of pregnancy. Your baby's position is most important during labour and birth.
A baby changes positions frequently throughout pregnancy. At around 36 weeks of pregnancy, most babies will turn so they are in a head-down position. This happens naturally within your uterus as your baby prepares for birth. The head-down position is called cephalic or vertex presentation, and it's the preferred position for a vaginal birth.
External Cephalic Version (ECV): A technique, performed late in pregnancy, in which the doctor attempts to manually move a breech baby into the head-down position. Fetus: The stage of human development beyond 8 completed weeks after fertilization. Fibroids: Growths that form in the muscle of the uterus. Fibroids usually are noncancerous.
Cephalic Occiput Posterior. In this position, the baby is in the head-down position but the baby's face is turned towards the mother's belly. This type of cephalic presentation is not the best position for delivery as the baby's head could get stuck owing to its wide position. Almost 5% of the babies in cephalic presentation settle into ...
Benefits of Cephalic Presentation in Pregnancy. Cephalic presentation is one of the most ideal birth positions, and has the following benefits: It is the safest way to give birth as your baby's position is head-down and prevents the risk of any injuries. It can help your baby move through the delivery canal as safely and easily as possible.
A previous study found that the incidence of c-section in non-cephalic presentation was 93.3% (p < 0.001) compared to head presentation, the incidence of which is 37.3%. 28 Nevertheless, studies have suggested that non-cephalic presentation was best diagnosed at 36 weeks of gestational age. 33 Therefore, pregnant women who uses our scoring tool ...
By about 32 weeks, the baby is usually lying with their head pointing downwards, ready for birth. This is known as cephalic presentation. If your baby is not lying head down at this stage, it's not a cause for concern - there's still time for them to turn. The amount of amniotic fluid in your uterus is increasing, and your baby is still ...
Throughout your pregnancy, your twin babies will move in the uterus, but sometime during the third trimester - usually between 32 and 36 weeks - their fetal presentation changes as they prepare to go down the birth canal. The good news is that at most twin births, both babies are head-down (vertex), which means you can have a vaginal delivery.
Abnormal Fetal Lie. If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation. ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen. It has an approximate success rate of 50% in primiparous women and 60% in multiparous women.
The show went on a four-year hiatus after facing plummeting ratings in 2018, returning with the "Victoria's Secret World Tour" in 2023, which was a more fluid pre-taped presentation and ...