- Open access
- Published: 30 July 2021

Impact of tobacco and/or nicotine products on health and functioning: a scoping review and findings from the preparatory phase of the development of a new self-report measure
- Esther F. Afolalu ORCID: orcid.org/0000-0001-8866-4765 1 ,
- Erica Spies 1 ,
- Agnes Bacso 1 ,
- Emilie Clerc 1 ,
- Linda Abetz-Webb 2 ,
- Sophie Gallot 1 &
- Christelle Chrea 1
Harm Reduction Journal volume 18 , Article number: 79 ( 2021 ) Cite this article
16k Accesses
4 Citations
10 Altmetric
Metrics details
Measuring self-reported experience of health and functioning is important for understanding the changes in the health status of individuals switching from cigarettes to less harmful tobacco and/or nicotine products (TNP) or reduced-risk products (RRP) and for supporting tobacco harm reduction strategies.
This paper presents insights from three research activities from the preparatory phase of the development of a new self-report health and functioning measure. A scoping literature review was conducted to identify the positive and negative impact of TNP use on health and functioning. Focus groups ( n = 29) on risk perception and individual interviews ( n = 40) on perceived dependence in people who use TNPs were reanalyzed in the context of health and functioning, and expert opinion was gathered from five key opinion leaders and five technical consultants.
Triangulating the findings of the review of 97 articles, qualitative input from people who use TNPs, and expert feedback helped generate a preliminary conceptual framework including health and functioning and conceptually-related domains impacted by TNP use. Domains related to the future health and functioning measurement model include physical health signs and symptoms, general physical appearance, functioning (physical, sexual, cognitive, emotional, and social), and general health perceptions.
Conclusions
This preliminary conceptual framework can inform future research on development and validation of new measures for assessment of overall health and functioning impact of TNPs from the consumers’ perspective.
As a leading cause of preventable morbidity and mortality worldwide, smoking remains a major public health problem. Compared with those who do not smoke, people who smoke are significantly more likely to develop heart diseases, lung cancer, chronic obstructive pulmonary disease (COPD), and other diseases [ 1 , 2 ]. It is well established that the best way to avoid the health risks associated with smoking is for people to never start and for those who smoke to quit [ 1 , 3 ]. Tobacco harm reduction is one way to alleviate the health risk for individuals who choose not to quit smoking [ 4 ], by providing less harmful tobacco and/or nicotine products (TNP), such as reduced-risk products (RRP) (used here to refer to products that present, are likely to present, or have the potential to present, less risk of harm to people who smoke and switch to these products versus continued smoking) or modified risk tobacco products (MRTP).
Several smokeless tobacco products and a heated tobacco product were recently authorized for marketing with modified risk claims through the United States (US) Food and Drug Administration (FDA) MRTP pathway [ 5 ]. The guidance on MRTP applications [ 6 ] specifies that health outcomes should be assessed during premarket evaluation and postmarket surveillance of modified risk TNPs such as these. These health outcomes comprise not only objective clinical and biological measures but also self-reported outcomes [ 6 , 7 ]. Studies and reports have recently started providing evidence on the health impact of new TNPs [ 8 ]. For instance, recent papers have investigated the effects of e-cigarettes and heated tobacco products on cardiopulmonary outcomes [ 9 , 10 , 11 , 12 , 13 , 14 ]. However, the papers have mainly focused on clinical measurements, such as spirometry and other lung function tests; consumer perception is rarely explored or the focus of the research. Measuring self-reported experience is important for understanding the changes in the health status of individuals switching from cigarettes to RRPs and is a key component of tobacco harm reduction strategies [ 7 ]. Self-reported ratings of RRP effectiveness or adverse events might differ from clinical measures and provide another perspective as useful as the clinicians. In addition, consumer perception of positive changes in health status, functioning and other behavioral outcomes will also subsequently influence use behaviors and switching to RRPs rather than continuing smoking.
Self-perceived health status is a complex concept to define and measure, particularly within the context of TNP use [ 15 ]. While generic health status measures, such as the Medical Outcomes Study 36-item Short-Form Health Survey (SF-36), have been used to evaluate the health status of people who smoke [ 16 , 17 ], comparisons have mainly been made between those who currently smoke, those who used to smoke, and those who never smoked [ 18 , 19 ]. Results from these studies strongly suggest that, in healthy populations, existing generic measures are not sensitive enough to detect change over time when stopping or switching from cigarettes to other TNPs, owing to high ceiling effects [ 20 ]. While a few smoking-specific quality of life measures have been developed, these measures have not been widely implemented or standardized [ 15 , 17 , 21 , 22 ], and the application of these smoking-specific measures to different TNP use across the risk continuum is scarce [ 20 ].
As part of the A ssessment of B ehavioral OU tcomes related to T obacco and Nicotine Products (ABOUT™) Toolbox initiative [ 23 ], the present project aims at developing a new self-report measure (ABOUT™— Health and Functioning ) to address the current gap and assess the impact of TNPs on health and functioning (including health status, functional status and other health-related quality of life constructs). This paper presents insights from three research activities [ 24 , 25 ] from the preparatory phase of development of the measure—that is, a scoping literature review, reanalysis of consumer focus groups/interviews, and expert opinion. These three activities serve as background research to support the development of a preliminary conceptual framework of health and functioning associated with the use of TNPs.
Scoping literature review
The purpose of the review was to address two main questions among individuals who use TNPs:
What are the positive and negative health and functioning impacts of TNP use?
What concepts are evaluated by measures used to assess the positive and negative impacts of TNP use?
Given the nature and breadth of the research questions and the number of potentially relevant publications, a scoping literature review was used as it provides a means of identifying the literature and mapping the concepts and evidence on a topic by using an informative and iterative research process [ 26 ]. The scoping review involved a PubMed search (August 2018) and application of Sciome’s rapid Evidence Mapping (rEM) [ 27 ], followed by additional manual screening and review. rEM is a proprietary methodology developed by Sciome ( https://www.sciome.com/ ) to rapidly summarize and produce a quantitative representation of the available body of scientific evidence in a particular area. The study by Lam et al. demonstrated a proof-of-concept application of the rEM methodology [ 27 ]. The PubMed search terms targeted qualitative and quantitative research among people who use TNPs (Table 1 ). This was supplemented by a second, parallel step of manually identifying relevant literature through other known sources. Table 2 describes the general inclusion and exclusion criteria that were applied to the scoping literature review.
After the initial rEM exercise, two reviewers (EC, SG) further manually screened the titles and abstracts of the articles identified through the automated rEM exercise against the inclusion and exclusion criteria. Finally, the selected publications underwent a full screening by two reviewers (VL and DF) for determining their relevance to the research questions for data extraction and one of the co-authors (LA-W) cross-checked the screening and resolved differences in opinion among the reviewers.
The World Health Organization (WHO) International Classification of Functioning, Disability and Health (ICF) [ 28 ] framework and the revised Wilson and Cleary [ 29 , 30 ] model were used as a guide to broadly inform categories for data extraction from the literature on TNP use and health and functioning. These established models enable the conceptualization and description of health status and functioning (the combination of which is often referred to as health-related quality of life) [ 31 , 32 ], and related outcomes and determinants. To complement and refine this and to ensure relevance to those who use TNPs, the data extracted from the literature was also grouped and labeled based on the contents of the literature reviewed.
The elements extracted from the selected papers were as follows:
Author, citation details, and publication type
Objectives and/or research questions
Sample type, size, and principle demographics
Type(s) of TNP and definitions of levels of consumption
Methodology, questionnaires, and statistical methods used
Main results
Results grouped in broad categories: Health Signs and Symptoms; General Health Perceptions; Quality of Life, Health-Related Quality of Life, and Functional Status; Individual Characteristics; Environmental and Social Characteristics; Biomarkers and Biological Endpoints.
Reanalysis of focus groups/in-depth interviews
The objective of the secondary analyses of existing qualitative data in people who use TNPs was to inform the drafting of the initial conceptual framework, as well as interview guides for planned concept elicitation qualitative studies to identify concepts and develop items to detect what is relevant to measure in this context. Two sets of qualitative data containing information related to health and functioning were reanalyzed and participants had consented for their data to be used in future studies. The first was from 29 focus groups (total number of participants n = 229) that were originally designed to discuss perceived risk, appeal, and intent to use TNPs [ 33 , 34 ]. The focus groups—stratified by smoking status—were conducted in the United States (US; n = 12), Japan ( n = 4), Italy ( n = 4), and the United Kingdom (UK; n = 9) between December 2012 and August 2013. The second dataset included 40 in-depth interviews conducted in North Carolina, USA, with people who use TNPs, to discuss issues centered on perceived dependence on TNPs [ 35 ]. While 21 interviewees were people who were poly-TNPs users, 19 were people who were exclusive users of one of the following types of TNPs: cigarettes ( n = 5), smokeless tobacco ( n = 5), e-cigarettes ( n = 5), or another type of TNP (pipes, waterpipes, or nicotine replacement therapy [NRT] products; n = 4). These interviews were conducted in August 2017. The demographics of both data sets are presented in Table 3 . For reanalyzing the data, an initial codebook guided by the literature review data extraction categories was developed; however, new codes were created to complement these categories based on the thematic content analysis of the transcripts. The qualitative analysis software Quirkos [ 36 ] was used for the reanalysis.
Expert panel review
An expert panel consisting of five key opinion leaders (KOL) and five technical consultants was convened in August 28, 2018, in Neuchâtel, Switzerland. The KOLs were subject matter experts in the fields of nicotine and smoking cessation ( n = 1), Patients Reported Outcomes (PRO) evaluation and scale development ( n = 3), and health economics ( n = 1). The consultants were experts on nicotine dependence ( n = 1), psychometric validation ( n = 2), market research ( n = 1), and PRO development and validation ( n = 1). The meeting followed an agenda and semi-structured discussion guide to facilitate conversations. First, the panel was presented with the principles underlying the tobacco harm reduction assessment strategy [ 4 ]. This session was followed by an open elicitation phase, during which two experienced moderators asked the panel to identify and discuss concepts related to health and functioning in people who use TNPs that different stakeholders might find important. Then, the panel was asked to review and respond to the concepts identified in the literature review and in the qualitative research reanalysis. These findings were discussed in depth to arrive at a consolidated preliminary conceptual framework. Each concept was presented, and the experts were asked to rank and agree on concepts to be included and how the concepts should be grouped by domains in the framework. In generating the framework, the project team and expert panel considered the themes and concepts identified under each of the categories from the scoping literature review, specific concepts from the secondary analyses of the qualitative data, and the expert panel meeting. The authors then synthesized and re-organized concepts emerging from the different preparatory phase activities under main health and functioning and conceptually-related domains. The participants also provided their input on the best strategies for planned qualitative studies to inform and support the development and validity of the proposed health and functioning measure.
The literature search identified 4761 articles. Figure 1 (flow diagram) depicts the results of the search and screening process. Titles and abstracts were screened by the rEM exercise until the machine learning algorithms predicted 97.7% relevant references; thus, 707 abstracts were not screened. After applying the inclusion/exclusion criteria to the remaining 4,054 abstracts, 281 were identified as part of the rEM exercise. After additional manual screening and review of the abstracts and articles against the inclusion/exclusion criteria, 90 full-text articles were included for data extraction [ 20 , 37 – 125 ]. Seven additional full-text articles were also included on the basis of a manual search [ 126 , 127 , 128 , 129 , 130 , 131 , 132 ]. Findings are summarized in Table 4 and a detailed description and data extracted from all the articles from the literature review is presented in Additional File 1 .
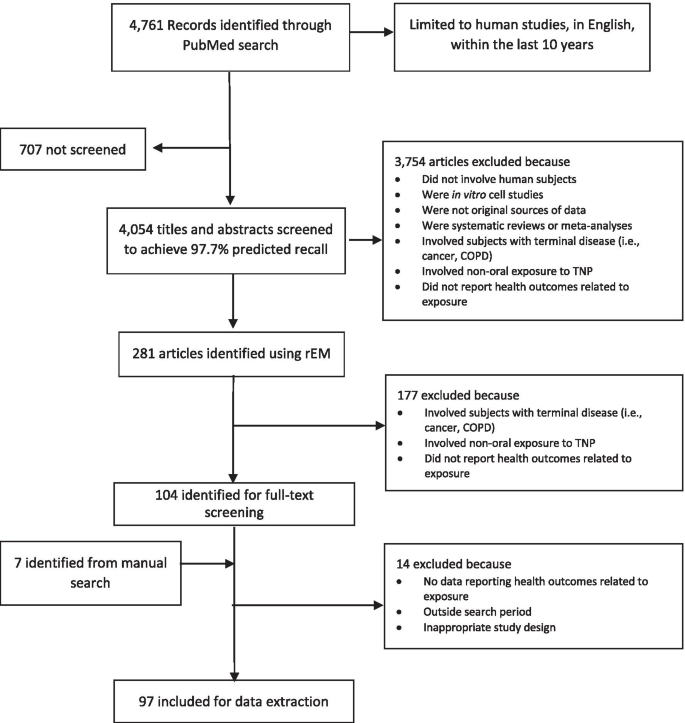
Flow diagram Sciome’s rapid Evidence Mapping (rEM) and manual screening processes of the scoping literature review
Fifty-six publications (56/97; 58%) presented data related to health signs and symptoms . These are grouped under five core areas: mental health and cognitive functioning (28/97; 29%); pain and physical trauma (6/97; 6%); respiratory, cardiovascular and inflammatory conditions (5/97; 5%); “other” health conditions , which included insomnia, liver disease, eye health, and hearing loss (5/97; 5%); and oral health (4/97; 4%). There were also eight publications related to the effects of smoking cessation on health signs and symptoms, mostly benefits of cessation but also including perceived dependence, addiction, and withdrawal symptoms (8/97; 8%). Overall, the burden and impact of cigarette smoking on both physical and mental health symptoms was negative and generally worse among people who smoke relative to those who do not smoke. On the other hand, quitting smoking was accompanied by improvements in general physical health and psychological wellbeing. However, in spite of the positive impact of quitting smoking, loss of moments of pleasure, struggle to manage stress, the social aspects of smoking, and withdrawal symptoms were seen as barriers to quitting.
The general health perceptions of various adults who use TNPs were reported in 18 of the 97 articles (18%), with 9 of them detailing the general health perceptions related to cigarettes and 9 being related to e-cigarettes and other TNPs. Perceptions were determined by questionnaires and focus groups for evaluating the health impacts, fear of diseases, harm to others and self, social impacts (both positive [e.g., inclusion and looking “cool”] and negative [e.g., stigma and exclusion]), and other reasons for taking up or considering/attempting smoking cessation.
Quality of life, health-related quality of life, and functional status was studied in 9 of the 97 included articles (9%). These studies mostly demonstrated with generic and specific QoL, HRQoL, or functional status questionnaires that cigarette smoking was associated with a worse quality of life and that smoking cessation often resulted in an improved quality of life. However, in some cases, the use of TNPs also reportedly enabled individuals to manage their levels of anxiety and improve some aspects of social engagement and functional status.
Individual, environmental and social characteristics were found to influence the decision to smoke and/or consider or attempt to quit smoking or switching to other TNPs, as reported in 8 (8%) and 11 (11%) of 97 publications, respectively. Some key characteristics and determinants of smoking behavior included low socioeconomic status, male sex, living alone, family, and close social environment, societal stigma, and local regulations.
Finally, 12 of the 97 publications (12%) were related to studies on biomarkers and biological endpoints in people who use TNPs and showed that smoking cigarettes negatively influenced cardiovascular, respiratory, oral, renal, stress, metabolic, and inflammatory-related biomarkers and physiological assessments.
The themes from this reanalysis are summarized below and organized on the basis of the narrative of the participants of their experiences.
Perceived negative impact of smoking
Other than health, the biggest and most salient reported negative impact of smoking was the perceived lack of control related to addiction and emotional health and wellbeing. Participants reported feeling that cigarette smoking was running their lives or “holding them hostage.” They reported that this perceived lack of a sense of control or willpower often led to feelings of weakness or a feeling that they were a “slave” to cigarettes. Many respondents reported smoking even when they did not necessarily want to and experiencing feelings of obsession and craving.
Perceived lack of control and addiction were also related to the activities of the participants throughout the day. People who smoke often reported altering their activities to smoke because of patterns of behavior or routine and the experienced need for a smoke. They reported that the “need for a smoke” sensation would cause them to leave work or social events early, not attend events if smoking was not allowed, interrupt what they were doing to smoke, and get up in the middle of the night.
Fear of withdrawal symptoms, with a strong emphasis on mental/emotional health, was also prominent among reported negative impacts of smoking. This fear was often reported as limiting the willingness of individuals to try to quit smoking or facilitating a return to prior smoking behavior. Individuals reported fearing the following symptoms they associated with withdrawal: mood swings and irritability, violent or aggressive behavior, inability to concentrate, anxiety, anger, and weight gain.
Perceived benefits of smoking
Several perceived benefits were identified that keep individuals smoking or using cigarettes. These included perceptions of enhanced cognitive functioning, relaxation, a way to take a break, use as a coping strategy, a social function, a weight management tool, the perception that it feels good, and being part of one’s identity. It is also important to note that the perceived benefits of smoking often outweighed the risks and the feeling of lack of control in the participant discussions. Even people who used to smoke noted they missed the relaxation and breaks they associated with smoking.
Recognition of symptoms/diseases related to smoking
Table 5 summarizes the negative symptoms and diseases related to smoking recognized by participants in both the focus groups and interviews. These were mostly related to six main body systems (cardiovascular, digestive, oral, neurological, reproductive, and respiratory).
Impacts on physical functioning
The participants noted how smoking impacts their physical functioning. In particular, they noted how their exercise capacity during running, playing sports, walking upstairs, and general physical activity was diminished. They also reported reduced stamina and endurance, decreased physical strength, and feeling tired more easily.
Effects on emotional health
The participants also described how smoking impacts their emotional health and wellbeing. People who smoke reported feelings of shame, guilt, weakness, and a lack of control or powerlessness. They also reported feelings of depression and anxiety associated with worry about health risks. Furthermore, the participants indicated that they experienced a fear of going to places where they could not smoke, being a bad role model for their children, and (in case of people who used to smoke) going back to smoking.
Positive and negative social impacts
Smoking was perceived to have both negative and positive impacts on the social lives of participants. Smoking impacted life negatively when it was not allowed in certain environments, such as in homes, at work, and in cars and airplanes. Stigma was also associated with smoking in an environment where peers and family members do not smoke, but it was also seen as a source of group identity within social networks that had a higher prevalence of smoking behaviors. Participants reported that smoking had some positive impacts on their social interaction, because it facilitated work breaks and increased communication with peers.
Reasons people decided to try to quit
Throughout the focus groups and interviews, individuals identified several reasons why they tried to quit smoking. These included: health, diagnosis of cancer (self, family, or friend), gum disease, pregnancy, hospital stay, worry that it will “kill me,” dislike of taste or odor, social reasons, change in surroundings (fewer smoking spaces), and price.
Reasons people do not like alternatives to cigarettes
The participants’ reasons for not liking alternatives to cigarettes (i.e., less harmful TNPs/RRPs) included perceptions that the alternatives did not work (i.e., the participants still had cravings and experienced withdrawal symptoms), made them feel or get ill (nausea and vomiting), were not “the same” as cigarettes in terms of the ritual, taste, or “feeling,” or were inconvenient/too big to carry.
The conclusions of the expert panel widely supported the findings of the literature review and the input from the reanalyzed focus groups and interviews. Some of the experts working in field of tobacco and nicotine provided additional insights based on their extensive experience with people who use TNPs; they highlighted the importance of the enjoyment of smoking for people who find it difficult to quit, the positive immediate benefits of quitting, and the smoking-related biomarkers that might be on a causal pathway between switching and changes in health and functioning status.
The following main areas were discussed and agreed during the meeting: (1) utility of use, referring to the perceived satisfaction and enjoyment of smoking (e.g., craving relief, weight control, and social affiliation); (2) signs and symptoms of withdrawal (e.g., anxiety, depression, and anger) and the positive immediate physical health effects of quitting smoking (e.g., better general and oral hygiene, less coughing, and improved exercise capacity); (3) functioning, including cognitive, physical, sexual, social, emotional, and role functioning; (4) worry associated with smoking and smoking-related diseases; (5) general health perceptions and quality of life; (6) association with smoking-related biomarkers that could be on the causal pathway between switching and changes in health and functioning; and (7) TNP use patterns and maintenance of switching to RRPs.
Generation of the preliminary conceptual framework
Triangulation of the findings from the literature review, qualitative input from people who use TNPs, and expert panel feedback helped generate a preliminary descriptive conceptual framework that includes the health and functioning and conceptually-related domains impacted by TNP use (Fig. 2 ).
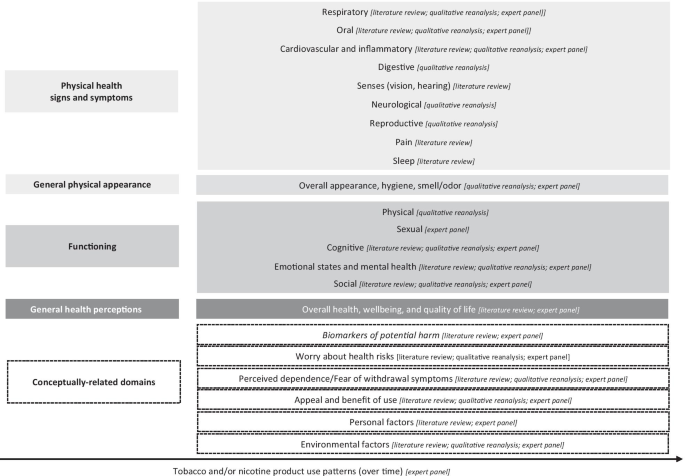
Health and functioning conceptual framework related to tobacco and/or nicotine product use from the preparatory phase research findings
Four domains related to the future health and functioning measurement model for TNP use are indicated in grey rectangular boxes and include (moving down from proximal to distal parameters) physical health symptoms (e.g., oral and respiratory symptoms), general physical condition (e.g., appearance and hygiene), functioning (physical, sexual, cognitive, emotional, and social functioning), and general health perceptions, which will be the most distal measure of health and functioning. The preparatory phase research also identified six conceptually-related domains (in dashed rectangular boxes), which are not direct indicators of health status but might influence the impact of TNP use on health and functioning. These include attitudinal variables (worry about the health risks of using TNPs and perceived dependence/fear of withdrawal symptoms associated with quitting smoking), and utilitarian ones (perceived appeal, satisfaction, and benefits of TNP use). In addition, personal factors (e.g., sociodemographic) and environmental factors (e.g., peer/family influence, policies and regulations and sociocultural context) are also reflected in the conceptual framework as indirect indicators of health and functioning.
The framework further indicates that specific behavioral indicators (i.e., TNP use patterns over time) might influence any impact of TNP use on health and functioning. Whilst other causal and reciprocal relationships and hierarchies might exist within the domains, these are not explicitly characterized in this initial draft of the framework and will have to be tested with further empirical data. Finally, identified biomarkers of potential harm (in italics and dashed box) are also integrated in this conceptual framework as part of the conceptually-related domains, because they are on a causal pathway between TNP use and changes in health and functioning [ 133 , 134 ]. Biomarkers are not part of the measurement model that will be considered for a new self-report measure; however, because they are the most proximal parameters to health and functioning, they will be assessed independently as appropriate endpoints by objective clinical or biological analyses.
Triangulation of published literature, reanalysis of qualitative data, and expert opinion helped develop the presented preliminary conceptual framework as the foundation for a new measure to assess the impact of TNPs on self-reported health and functioning. This is essential for identifying relevant concepts and understanding what is important to measure in people who use TNPs. The findings reveal the importance of not only the perceived impacts of TNP use on physical health and physical functioning, but also on aspects of mental health and social interactions and functioning, and general perceptions of health and health-related quality of life.
For the literature review, the WHO ICF [ 28 ] and Wilson and Cleary model [ 29 , 30 ] served as useful guides to develop categories for data abstraction. The scoping literature review yielded 97 articles on TNP use and the relationship to health, perceptions of health, social and individual functioning, and quality of life. Overall, most studies had focused on the known negative effects of cigarette smoking (e.g., mental, respiratory, and oral health) and the rationale and motivation to quit smoking. The WHO ICF and Wilson and Clearly models were not always sufficient for identifying the breadth of relevant concepts, especially from the perspective of TNP use. Development of new codes for the reanalysis of existing qualitative data allowed for the development, extension, and exploration of the topic and provided valuable insights reported in the qualitative data reanalysis, such as the perceived benefits/satisfaction from cigarette smoking, and the rationale for quitting smoking or switching to an RRP. The findings show how this manner of secondary analysis can be valuable in health-related fields where the topic is broad and an existing body of knowledge can contribute by offering a different perspective [ 135 ].
The presentation of the preliminary conceptual framework from this preparatory phase is specific to TNP use and marks a slight departure from the established norms and characterization of the variables typically observed in existing generic health and functioning and health-related quality of life models, such as the WHO ICF and Wilson and Clearly models. Notably, specific hypothesized relationships and the hierarchy between domains are not explicitly characterized in the current draft of the framework. The framework provided an exploratory representation of the current findings to reflect a measurement instrument in people who use TNPs that would ideally be able to assess and demonstrate improvements in self-reported health and functioning status, stability of perceived positive aspects of using TNPs, and no worsening in key areas of physical and emotional health and functioning upon switching to RRPs. Nevertheless, the framework could still undergo further refinement to support the development and validation of a new measure and to further characterize and test the relationships and hierarchies between domains.
This work is not without limitations. For the scoping literature review, among the reviewed articles, not many reported on the use of e-cigarettes and other alternative tobacco or nicotine-delivery devices, because most studies had focused exclusively on cigarettes. It is possible that concepts associated with health and functioning that are relevant to other TNPs were not identified. This is most likely the consequence of the large number of publications related to cigarette use. Some concepts might also have been missed, given the large evidence base on health and functioning-related themes and concepts. However, this was also not a systematic literature search; a scoping review is generally broader than a systematic review in terms of the former having a less-defined research question, broader inclusion and exclusion criteria, and no systematic appraisal of study quality [ 26 ]. Nevertheless, the present scoping review methodology provides a lens on the overall evidence base, and regular updates on the search—specifically related to RRPs and novel TNPs and their health and functioning impacts—could be considered for fully understanding the evolving state of the art in this context. The reanalysis of existing qualitative data also has limitations related to data fit and completeness of preexisting data [ 136 ]. The insights collected from these reanalyzed studies were originally for a different purpose several years prior to the present research, and this might not completely and accurately reflect the objectives of the new project.
Considering the findings of the current research, the development of a health and functioning measure can continue to follow the FDA’s Guidance on PRO measures. As specified within the guideline, gaining input directly from the intended use populations through concept elicitation is a critical activity for ensuring content validity during the development of any new self-reported measure [ 137 ]. Continuous engagement with an expert panel can also support the refinement of the conceptual framework as well as the development of the draft and final measure.
The goal of this research was to identify from varied research activities key concepts and aspects of health and functioning and related changes associated with the use of TNPs. The resulting preliminary conceptual framework provides the basis for informing future research to further understand health and functioning concepts important to measure in individual who switch to RRPs and to develop a new self-report measure to assess this from the consumers’ perspective.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
Assessment of Behavioral OUtcomes related to Tobacco and Nicotine Products Toolbox
Chronic obstructive pulmonary disease
Food and Drug Administration
Health-related quality of life
International Classification of Functioning, Disability and Health
- Modified risk tobacco products
Nicotine replacement therapy
Patient-Reported Outcomes
Quality of life
Reduced-risk products
Rapid Evidence Mapping
- Tobacco and/or nicotine products
United Kingdom
United States
36-Item Short-Form Health Survey
World Health Organization
U.S. Department of Health and Human Services. The health consequences of smoking: 50 years of progress. A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
Google Scholar
Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJL, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6(4):e1000058.
Article PubMed PubMed Central Google Scholar
Bilano V, Gilmour S, Moffiet T, d’Espaignet ET, Stevens GA, Commar A, et al. Global trends and projections for tobacco use, 1990–2025: an analysis of smoking indicators from the WHO Comprehensive Information Systems for Tobacco Control. Lancet. 2015;385(9972):966–76.
Article PubMed Google Scholar
Zeller M, Hatsukami D. The strategic dialogue on tobacco harm reduction: a vision and blueprint for action in the US. Tob Control. 2009;18(4):324–32.
Food and Drug Administration. Modified risk orders 2020. https://www.fda.gov/tobacco-products/advertising-and-promotion/modified-risk-orders .
Food and Drug Administration. Modified risk tobacco product applications: draft guidance for industry 2012. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/modified-risk-tobacco-product-applications .
Institute of Medicine. Scientific standards for studies on modified risk tobacco products. Washington, DC: The National Academies Press; 2012. p. 370.
Stratton K, Kwan LY, Eaton DL, editors. National Academies of Sciences Engineering and Medicine. Public health consequences of e-cigarettes. Washington, DC: The National Academies Press; 2018. p. 774.
Lappas AS, Tzortzi AS, Konstantinidi EM, Teloniatis SI, Tzavara CK, Gennimata SA, et al. Short-term respiratory effects of e-cigarettes in healthy individuals and smokers with asthma. Respirology. 2018;23(3):291–7.
Meo SA, Ansary MA, Barayan FR, Almusallam AS, Almehaid AM, Alarifi NS, et al. Electronic cigarettes: impact on lung function and fractional exhaled nitric oxide among healthy adults. Am J Men’s Health. 2019;13(1):1557988318806073.
Article Google Scholar
Polosa R, Cibella F, Caponnetto P, Maglia M, Prosperini U, Russo C, et al. Health impact of E-cigarettes: a prospective 3.5-year study of regular daily users who have never smoked. Sci Rep. 2017;7(1):13825.
Article PubMed PubMed Central CAS Google Scholar
Sharman A, Zhussupov B, Sharman D, Kim I, Yerenchina E. Lung function in users of a smoke-free electronic device with HeatSticks (iQOS) versus smokers of conventional cigarettes: protocol for a longitudinal cohort observational study. JMIR Res Protoc. 2018;7(11):e10006.
Skotsimara G, Antonopoulos AS, Oikonomou E, Siasos G, Ioakeimidis N, Tsalamandris S, et al. Cardiovascular effects of electronic cigarettes: a systematic review and meta-analysis. Eur J Prev Cardiol. 2019;26(11):1219–28.
Wang JB, Olgin JE, Nah G, Vittinghoff E, Cataldo JK, Pletcher MJ, et al. Cigarette and e-cigarette dual use and risk of cardiopulmonary symptoms in the Health eHeart Study. PLoS ONE. 2018;13(7):e0198681.
Ware JE Jr, Gandek B, Kulasekaran A, Guyer R. Evaluation of smoking-specific and generic quality of life measures in current and former smokers in Germany and the United States. Health Qual Life Outcomes. 2015;13:128.
Frendl DM, Ware JE Jr. Patient-reported functional health and well-being outcomes with drug therapy: a systematic review of randomized trials using the SF-36 health survey. Med Care. 2014;52(5):439–45.
Goldenberg M, Danovitch I, IsHak WW. Quality of life and smoking. Am J Addict. 2014;23(6):540–62.
Olufade AO, Shaw JW, Foster SA, Leischow SJ, Hays RD, Coons SJ. Development of the smoking cessation quality of life questionnaire. Clin Ther. 1999;21(12):2113–30.
Article CAS PubMed Google Scholar
Sarna L, Bialous SA, Cooley ME, Jun HJ, Feskanich D. Impact of smoking and smoking cessation on health-related quality of life in women in the Nurses’ Health Study. Qual Life Res. 2008;17(10):1217–27.
Kulasekaran A, Proctor C, Papadopoulou E, Shepperd CJ, Guyer R, Gandek B, et al. Preliminary evaluation of a new german translated tobacco quality of life impact tool to discriminate between healthy current and former smokers and to explore the effect of switching smokers to a reduced toxicant prototype cigarette. Nicotine Tob Res. 2015;17(12):1456–64.
Edelen MO. The PROMIS smoking assessment toolkit–background and introduction to supplement. Nicotine Tob Res. 2014;16(Suppl 3):S170–4.
Shaw JW, Coons SJ, Foster SA, Leischow SJ, Hays RD. Responsiveness of the Smoking Cessation Quality of Life (SCQoL) questionnaire. Clin Ther. 2001;23(6):957–69.
Chrea C, Acquadro C, Afolalu EF, Spies E, Salzberger T, Abetz-Webb L, et al. Developing fit-for-purpose self-report instruments for assessing consumer responses to tobacco and nicotine products: the ABOUT Toolbox initiative. F1000Res. 2018;7:1878.
Food and Drug Administration. Patient-reported outcome measures: use in medical product development to support labeling claims 2009. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-reported-outcome-measures-use-medical-product-development-support-labeling-claims .
Food and Drug Administration. Patient-focused drug development: methods to identify what is important to patients guidance for industry, Food and Drug Administration Staff, and Other Stakeholders 2019. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-methods-identify-what-important-patients-guidance-industry-food-and .
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143.
Lam J, Howard BE, Thayer K, Shah RR. Low-calorie sweeteners and health outcomes: a demonstration of rapid evidence mapping (rEM). Environ Int. 2019;123:451–8.
World Health Organisation. International classification of functioning, disability and health (ICF) 2001. https://www.who.int/classifications/icf/en/ .
Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. Conceptual model of health-related quality of life. J Nurs Scholarsh. 2005;37(4):336–42.
Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273(1):59–65.
Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645–9.
Moons P. Why call it health-related quality of life when you mean perceived health status? Eur J Cardiovasc Nurs. 2004;3(4):275–7.
Cano S, Chrea C, Salzberger T, Alfieri T, Emilien G, Mainy N, et al. Development and validation of a new instrument to measure perceived risks associated with the use of tobacco and nicotine-containing products. Health Qual Life Outcomes. 2018;16(1):192.
Salzberger T, Chrea C, Cano SJ, Martin M, Atkison M, Emilien G, et al. Perceived risks associated with the use of tobacco and nicotine-containing products: findings from qualitative research. Tobacco Sci Technol. 2017;50:32–42.
Chrea C, Salzberger T, Abetz-Webb L, Afolalu EF, Cano S, Rose J, et al. PRM183—development of a fit-for-purpose tobacco and nicotine products dependence instrument. Barcelona: ISPOR Europe; 2018.
Book Google Scholar
Quirkos 2.3.1 [Computer Software] 2020. https://www.quirkos.com .
Abu-Helalah MA, Alshraideh HA, Al-Serhan AA, Nesheiwat AI, Da’na M, Al-Nawafleh A. Epidemiology, attitudes and perceptions toward cigarettes and hookah smoking amongst adults in Jordan. Environ Health Prev Med. 2015;20(6):422–33.
Akturk E, Yağmur J, Açıkgöz N, Ermi N, Cansel M, Karaku Y, et al. Assessment of atrial conduction time by tissue Doppler echocardiography and P-wave dispersion in smokers. J Interv Card Electrophysiol. 2012;34(2):247–53.
Aubin HJ, Peiffer G, Stoebner-Delbarre A, Vicaut E, Jeanpetit Y, Solesse A, et al. The French Observational Cohort of Usual Smokers (FOCUS) cohort: French smokers perceptions and attitudes towards smoking cessation. BMC Public Health. 2010;10(100):1–8.
Becoña E, Vázquez MI, Míguez MC, Fernández del Río E, López-Durán A, Martínez Ú, et al. Smoking habit profile and health-related quality of life. Psicothema. 2013;25(4):421–6.
PubMed Google Scholar
Bennasar Veny M, Pericas Beltrán J, González Torrente S, Segui González P, Aguiló Pons A, Tauler RP. Self-perceived factors associated with smoking cessation among primary health care nurses: a qualitative study. Rev Latino-Am Enfermagem. 2011;19(6):1437–44.
Bommelé J, Schoenmakers TM, Kleinjan M, van Straaten B, Wits E, Snelleman M, et al. Perceived pros and cons of smoking and quitting in hard-core smokers: a focus group study. BMC Public Health. 2014;14:175–85.
Borland R, Yong HH, O’Connor RJ, Hyland A, Thompson ME. The reliability and predictive validity of the Heaviness of Smoking Index and its two components: findings from the International Tobacco Control Four Country study. Nicotine Tob Res. 2010;12(Suppl 1):S45-50.
Bot M, Vink J, Milaneschi Y, Smit JH, Kluft C, Neuteboom J, et al. Plasma cotinine levels in cigarette smokers: impact of mental health and other correlates. Eur Addict Res. 2014;20(4):183–91.
Brody AL, Olmstead RE, Abrams AL, Costello MR, Khan A, Kozman D, et al. Effect of a history of major depressive disorder on smoking-induced dopamine release. Biol Psychiatry. 2009;66(9):898–901.
Article CAS PubMed PubMed Central Google Scholar
Brook DW, Rubenstone E, Zhang C, Brook JS. Trajectories of cigarette smoking in adulthood predict insomnia among women in late mid-life. Sleep Med. 2012;13(9):1130–7.
Brotman RM, He X, Gajer P, Fadrosh D, Sharma E, Mongodin EF, et al. Association between cigarette smoking and the vaginal microbiota: a pilot study. BMC Infect Dis. 2014;14:471–82.
Brown-Johnson CG, Cataldo JK, Orozco N, Lisha NE, Hickman NJ 3rd, Prochaska JJ. Validity and reliability of the Internalized Stigma of Smoking Inventory: an exploration of shame, isolation, and discrimination in smokers with mental health diagnoses. Am J Addict. 2015;24(5):410–8.
Bush T, Hsu C, Levine MD, Magnusson B, Miles L. Weight gain and smoking: perceptions and experiences of obese quitline participants. BMC Public Health. 2014;14:1229.
Caldirola D, Cavedini P, Riva A, Di Chiaro NV, Perna G. Cigarette smoking has no pro-cognitive effect in subjects with obsessive-compulsive disorder: a preliminary study. Psychiatr Danub. 2016;28(1):86–90.
Caldirola D, Daccò S, Grassi M, Citterio A, Menotti R, Cavedini P, et al. Effects of cigarette smoking on neuropsychological performance in mood disorders: a comparison between smoking and nonsmoking inpatients. J Clin Psychiatry. 2013;74(2):e130–6.
Carpenter MJ, Gray KM. A pilot randomized study of smokeless tobacco use among smokers not interested in quitting: changes in smoking behavior and readiness to quit. Nicotine Tob Res. 2010;12(2):136–43.
Croucher R, Haque MF, Kassim S. Oral pain before and after smokeless tobacco cessation in U.K.-resident Bangladeshi women: cross-sectional analyses. Nicotine Tobacco Res. 2013;15(5):896–903.
Article CAS Google Scholar
Depp CA, Bowie CR, Mausbach BT, Wolyniec P, Thornquist MH, Luke JR, et al. Current smoking is associated with worse cognitive and adaptive functioning in serious mental illness. Acta Psychiatr Scand. 2015;131(5):333–41.
Ditre JW, Zale EL, Heckman BW, Hendricks PS. A measure of perceived pain and tobacco smoking interrelations: pilot validation of the pain and smoking inventory. Cogn Behav Ther. 2017;46(6):339–51.
Doiron M, Dupré N, Langlois M, Provencher P, Simard M. Smoking history is associated to cognitive impairment in Parkinson’s disease. Aging Ment Health. 2017;21(3):322–6.
Gonzalez A, Zvolensky MJ, Vujanovic AA, Leyro TM, Marshall EC. An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: relation to smoking motives and barriers to quitting. J Psychiatr Res. 2008;43(2):138–47.
Grogan S, Fry G, Gough B, Conner M. Smoking to stay thin or giving up to save face? Young men and women talk about appearance concerns and smoking. Br J Health Psychol. 2009;14(1):175–86.
Hawari FI, Obeidat NA, Ghonimat IM, Ayub HS, Dawahreh SS. The effect of habitual waterpipe tobacco smoking on pulmonary function and exercise capacity in young healthy males: A pilot study. Respir Med. 2017;122:71–5.
Heffernan TM, O’Neill TS, Moss M. Smoking-related prospective memory deficits in a real-world task. Drug Alcohol Depend. 2012;120(1–3):1–6.
Highland KB, McChargue DE. Stress-induced cardiovascular reactivity among African American smokers. Am J Health Behav. 2011;35(1):51–9.
Holley AL, Law EF, Tham SW, Myaing M, Noonan C, Strachan E, et al. Current smoking as a predictor of chronic musculoskeletal pain in young adult twins. J Pain. 2013;14(10):1131–9.
Ichikawa Y, Kitagawa K, Kato S, Dohi K, Hirano T, Ito M, et al. Altered coronary endothelial function in young smokers detected by magnetic resonance assessment of myocardial blood flow during the cold pressor test. Int J Cardiovasc Imaging. 2014;30:73–80.
Javed F, Abduljabbar T, Vohra F, Malmstrom H, Rahman I, Romanos GE. Comparison of periodontal parameters and self-perceived oral symptoms among cigarette smokers, individuals vaping electronic cigarettes, and never-smokers. J Periodontol. 2017;88(10):1059–65.
Johnson AL, McLeish AC. Differences in panic psychopathology between smokers with and without asthma. Psychol Health Med. 2017;22(1):110–20.
Kahler CW, Daughters SB, Leventhal AM, Rogers ML, Clark MA, Colby SM, et al. Personality, psychiatric disorders, and smoking in middle-aged adults. Nicotine Tob Res. 2009;11(7):833–41.
Karadoğan D, Önal Ö, Şahin D, Yazıcı S, Kanbay Y. Evaluation of school teachers’ sociodemographic characteristics and quality of life according to their cigarette smoking status: a cross-sectional study from eastern Black Sea region of Turkey. Tuberkuloz ve toraks. 2017;65(1):18–24.
Kim J, Gall SL, Dewey HM, Macdonell RA, Sturm JW, Thrift AG. Baseline smoking status and the long-term risk of death or nonfatal vascular event in people with stroke: a 10-year survival analysis. Stroke. 2012;43(12):3173–8.
Kim J, Lee S. Using focus group interviews to analyze the behavior of users of new types of tobacco products. J Prev Med Public Health. 2017;50(5):336–46.
Kralikova E, Novak J, West O, Kmetova A, Hajek P. Do e-cigarettes have the potential to compete with conventional cigarettes?: a survey of conventional cigarette smokers’ experiences with e-cigarettes. Chest. 2013;144(5):1609–14.
Lao XQ, Jiang CQ, Zhang WS, Adab P, Lam TH, Cheng KK, et al. Smoking, smoking cessation and inflammatory markers in older Chinese men: The Guangzhou Biobank Cohort Study. Atherosclerosis. 2009;203(1):304–10.
Lappan S, Thorne CB, Long D, Hendricks PS. Longitudinal and reciprocal relationships between psychological well-being and smoking. Nicotine Tob Res. 2018;22(1):18–23.
Article PubMed Central Google Scholar
Lynch ME, Johnson KC, Kable JA, Carroll J, Coles CD. Smoking in pregnancy and parenting stress: maternal psychological symptoms and socioeconomic status as potential mediating variables. Nicotine Tob Res. 2011;13(7):532–9.
Lyvers M, Carlopio C, Honours VB, Edwards MS. Mood, mood regulation, and frontal systems functioning in current smokers, long-term abstinent ex-smokers, and never-smokers. J Psychoactive Drugs. 2014;46(2):133–9.
Martin LM, Sayette MA. A review of the effects of nicotine on social functioning. Exp Clin Psychopharmacol. 2018;26(5):425–39.
Martinasek MP, McDermott RJ, Bryant CA. Antecedents of university students’ hookah smoking intention. Am J Health Behav. 2013;37(5):599–609.
Mattey DL, Dawson SR, Healey EL, Packham JC. Relationship between smoking and patient-reported measures of disease outcome in ankylosing spondylitis. J Rheumatol. 2011;38(12):2608–15.
McCann SJ. Subjective well-being, personality, demographic variables, and American state differences in smoking prevalence. Nicotine Tob Res. 2010;12(9):895–904.
McDonald EA, Ling PM. One of several “toys” for smoking: young adult experiences with electronic cigarettes in New York City. Tob Control. 2015;24(6):588–93.
McLeish AC, Zvolensky MJ, Del Ben KS, Burke RS. Anxiety sensitivity as a moderator of the association between smoking rate and panic-relevant symptoms among a community sample of middle-aged adult daily smokers. Am J Addict. 2009;18(1):93–9.
Melis M, Lobo SL, Ceneviz C, Ruparelia UN, Zawawi KH, Chandwani BP, et al. Effect of cigarette smoking on pain intensity of TMD patients: a pilot study. Cranio. 2010;28(3):187–92.
Memon A, Barber J, Rumsby E, Parker S, Mohebati L, de Visser RO, et al. What factors are important in smoking cessation and relapse in women from deprived communities? A qualitative study in Southeast England. Public Health. 2016;134:39–45.
Mendiondo MS, Alexander LA, Crawford T. Health profile differences for menthol and non-menthol smokers: findings from the National Health Interview Survey. Addiction. 2010;105(Suppl 1):124–40.
Miyatake N, Numata T, Nishii K, Sakano N, Suzue T, Hirao T, et al. Influence of cigarette smoking on estimated glomerular filtration rate (eGFR) in Japanese male workers. Acta Med Okayama. 2010;64:385–90.
CAS PubMed Google Scholar
Mohammadi S, Mazhari MM, Mehrparvar AH, Attarchi MS. Cigarette smoking and occupational noise-induced hearing loss. Eur J Public Health. 2009;20(4):452–5.
Mohammadnezhad M, Tsourtos G, Wilson C, Ratcliffe J, Ward P. “I have never experienced any problem with my health. So far, it hasn’t been harmful”: older Greek-Australian smokers’ views on smoking: a qualitative study. BMC Public Health. 2015;15:304–15.
Morris MC, Mielock AS, Rao U. Salivary stress biomarkers of recent nicotine use and dependence. Am J Drug Alcohol Abuse. 2016;42(6):640–8.
Muir S, Marshall B. Changes in health perceptions of male prisoners following a smoking cessation program. J Correct Health Care. 2016;22(3):247–56.
Nelson JP, Pederson LL, Lewis J. Tobacco use in the Army: illuminating patterns, practices, and options for treatment. Mil Med. 2009;174(2):162–9.
Nemeth JM, Liu ST, Klein EG, Ferketich AK, Kwan MP, Wewers ME. Factors influencing smokeless tobacco use in rural Ohio Appalachia. J Community Health. 2012;37(6):1208–17.
Nikcevic AV, Spada MM. Metacognitions about smoking: a preliminary investigation. Clin Psychol Psychother. 2010;17(6):536–42.
Nunes SO, Vargas HO, Brum J, Prado E, Vargas MM, de Castro MR, et al. A comparison of inflammatory markers in depressed and nondepressed smokers. Nord J Psychiatry. 2012;14:540–6.
CAS Google Scholar
Oh DL, Heck JE, Dresler C, Allwright S, Haglund M, Del Mazo SS, et al. Determinants of smoking initiation among women in five European countries: a cross-sectional survey. BMC Public Health. 2010;10(74):1–11.
Pasco JA, Williams LJ, Jacka FN, Ng F, Henry MJ, Nicholson GC, et al. Tobacco smoking as a risk factor for major depressive disorder: population-based study. Br J Psychiatry. 2008;193(4):322–6.
Pina JA, Namba MD, Leyrer-Jackson JM, Cabrera-Brown G, Gipson CD. Social influences on nicotine-related behaviors. Int Rev Neurobiol. 2018;140:1–32.
Poole-Di Salvo E, Liu YH, Brenner S, Weitzman M. Adult household smoking is associated with increased child emotional and behavioral problems. J Dev Behav Pediatr. 2010;31(2):107–15.
Rahman MA, Mahmood MA, Spurrier N, Rahman M, Choudhury SR, Leeder S. Why do Bangladeshi people use smokeless tobacco products? Asia-Pacific J Public Health. 2015;27(2):NP2197–209.
Rollini F, Franchi F, Cho JR, Degroat C, Bhatti M, Ferrante E, et al. Cigarette smoking and antiplatelet effects of aspirin monotherapy versus clopidogrel monotherapy in patients with atherosclerotic disease: results of a prospective pharmacodynamic study. J Cardiovasc Transl Res. 2014;7(1):53–63.
Romijnders K, van Osch L, de Vries H, Talhout R. Perceptions and reasons regarding e-cigarette use among users and non-users: a narrative literature review. Int J Environ Res Public Health. 2018;15(6):1190.
Rooke C, Cunningham-Burley S, Amos A. Smokers’ and ex-smokers’ understanding of electronic cigarettes: a qualitative study. Tob Control. 2016;25:e60–6.
Roth B, Bengtsson M, Ohlsson B. Diarrhoea is not the only symptom that needs to be treated in patients with microscopic colitis. Eur J Intern Med. 2013;24(6):573–8.
Sales MP, Oliveira MI, Mattos IM, Viana CM, Pereira ED. The impact of smoking cessation on patient quality of life. J Bras Pneumol. 2009;35(5):436–41.
Schane RE, Prochaska JJ, Glantz SA. Counseling nondaily smokers about secondhand smoke as a cessation message: a pilot randomized trial. Nicotine Tob Res. 2013;15(2):334–42.
Schnoll RA, Goren A, Annunziata K, Suaya JA. The prevalence, predictors and associated health outcomes of high nicotine dependence using three measures among US smokers. Addiction. 2013;108(11):1989–2000.
Segarra R, Zabala A, Eguíluz JI, Ojeda N, Elizagarate E, Sánchez P, et al. Cognitive performance and smoking in first-episode psychosis: the self-medication hypothesis. Eur Arch Psychiatry Clin Neurosci. 2011;261(4):241–50.
Sherratt FC, Newson L, Marcus MW, Field JK, Robinson J. Perceptions towards electronic cigarettes for smoking cessation among Stop Smoking Service users. Br J Health Psychol. 2015;21(2):421–33.
Soneji SS, Sung HY, Primack BA, Pierce JP, Sargent JD. Quantifying population-level health benefits and harms of e-cigarette use in the United States. PLoS ONE. 2018;13(3):e0193328.
Talati A, Wickramaratne PJ, Keyes KM, Hasin DS, Levin FR, Weissman MM. Smoking and psychopathology increasingly associated in recent birth cohorts. Drug Alcohol Depend. 2013;133(2):724–32.
Tan QH. Smoking spaces as enabling spaces of wellbeing. Health Place. 2013;24:173–82.
Tatullo M, Gentile S, Paduano F, Santacroce L, Marrelli M. Crosstalk between oral and general health status in e-smokers. Medicine. 2016;95(49):e5589.
Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ. 2014;348:g1151-g.
Thompson TP, Greaves CJ, Ayres R, Aveyard P, Warren FC, Byng R, et al. An exploratory analysis of the smoking and physical activity outcomes from a pilot randomized controlled trial of an exercise assisted reduction to stop smoking intervention in disadvantaged groups. Nicotine Tob Res. 2016;18(3):289–97.
Torigian DA, Green-McKenzie J, Liu X, Shofer FS, Werner T, Smith CE, et al. A study of the feasibility of FDG-PET/CT to systematically detect and quantify differential metabolic effects of chronic tobacco use in organs of the whole body—a prospective pilot study. Acad Radiol. 2017;24:930–40.
Ulvik A, Ebbing M, Hustad S, Midttun Ø, Nygård O, Vollset SE, et al. Long- and short-term effects of tobacco smoking on circulating concentrations of B vitamins. Clin Chem. 2010;56(5):755–63.
Vidrine JI, Businelle MS, Cinciripini P, Li Y, Marcus MT, Waters AJ, et al. Associations of mindfulness with nicotine dependence, withdrawal, and agency. Subst Abus. 2009;30(4):318–27.
Volkman JE, DeRycke EC, Driscoll MA, Becker WC, Brandt CA, Mattocks KM, et al. Smoking status and pain intensity among OEF/OIF/OND veterans. Pain Med. 2015;16(9):1690–6.
Vujanovic AA, Marshall-Berenz EC, Beckham JC, Bernstein A, Zvolensky MJ. Posttraumatic stress symptoms and cigarette deprivation in the prediction of anxious responding among trauma-exposed smokers: a laboratory test. Nicotine Tob Res. 2010;12(11):1080–8.
Wadsworth E, Neale J, McNeill A, Hitchman SC. How and why do smokers start using e-cigarettes? Qualitative study of Vapers in London, UK. Int J Environ Res Public Health. 2016;13(7):661–74.
Article PubMed Central CAS Google Scholar
Xie X, Dijkstra AE, Vonk JM, Oudkerk M, Vliegenthart R, Groen HJ. Chronic respiratory symptoms associated with airway wall thickening measured by thin-slice low-dose CT. Am J Roentgenol. 2014;203(4):W383–90.
Yang T, Shiffman S, Rockett IR, Cui X, Cao R. Nicotine dependence among Chinese city dwellers: a population-based cross-sectional study. Nicotine Tob Res. 2011;13(7):556–64.
Yu A, Cai X, Zhang Z, Shi H, Liu D, Zhang P, et al. Effect of nicotine dependence on opioid requirements of patients after thoracic surgery. Acta Anaesthesiol Scand. 2015;59(1):115–22.
Zhang X, Kahende J, Fan AZ, Barker L, Thompson TJ, Mokdad AH, et al. Smoking and visual impairment among older adults with age-related eye diseases. Prev Chronic Dis. 2011;8(4):A84.
PubMed PubMed Central Google Scholar
Zhao L, Xu L, Lai Y, Che C, Zhou Y. Temporal changes of smoking status and motivation in Chinese patients with hepatitis B: relationship with anxiety and depression. J Clin Nurs. 2012;21(15–16):2193–201.
Zorlu N, Cropley VL, Zorlu PK, Delibas DH, Adibelli ZH, Baskin EP, et al. Effects of cigarette smoking on cortical thickness in major depressive disorder. J Psychiatr Res. 2017;84:1–8.
Miyatake N, Numata T, Nishii K, Sakano N, Suzue T, Hirao T, et al. Relation between cigarette smoking and ventilatory threshold in the Japanese. Environ Health Prev Med. 2011;16(3):185–90.
Bjørngaard JH, Gunnell D, Elvestad MB, Davey Smith G, Skorpen F, Krokan H, et al. The causal role of smoking in anxiety and depression: a Mendelian randomization analysis of the HUNT study. Psychol Med. 2012;43(4):711–9.
Chen SC, Chen HF, Peng HL, Lee LY, Chiang TY, Chiu HC. Psychometric testing of the Chinese-Version Glover-Nilsson Smoking Behavioral Questionnaire (GN-SBQ-C) for the identification of nicotine dependence in adult smokers in Taiwan. Int J Behav Med. 2017;24(2):272–9.
Doran N, Spring B, McChargue D, Pergadia M, Richmond M. Impulsivity and smoking relapse. Nicotine Tob Res. 2004;6:641–7.
Haller CS, Etter JF, Courvoisier DS. Trajectories in cigarette dependence as a function of anxiety: a multilevel analysis. Drug Alcohol Depend. 2014;139:115–20.
Jamal M, Van der Does AJW, Cuijpers P, Penninx BW. Association of smoking and nicotine dependence with severity and course of symptoms in patients with depressive or anxiety disorder. Drug Alcohol Depend. 2012;126(1–2):138–46.
Krishnan-Sarin S, Reynolds B, Duhig A, Smith A, Liss T, McFetridge A, et al. Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug Alcohol Depend. 2007;88:79–82.
Tidey JW, Pacek LR, Koopmeiners JS, Vandrey R, Nardone N, Drobes DJ, et al. Effects of 6-week use of reduced-nicotine content cigarettes in smokers with and without elevated depressive symptoms. Nicotine Tob Res. 2017;19(Suppl 1):59–67.
Chang CM, Cheng YC, Cho TM, Mishina EV, Del Valle-Pinero AY, van Bemmel DM, et al. Biomarkers of potential harm: summary of an FDA-sponsored public workshop. Nicotine Tob Res. 2019;21(1):3–13.
Haziza C, de La Bourdonnaye G, Donelli A, Skiada D, Poux V, Weitkunat R, et al. Favorable changes in biomarkers of potential harm to reduce the adverse health effects of smoking in smokers switching to the menthol tobacco heating system 2.2 for three months (part 2). Nicotine Tob Res. 2019;22(4):549–59.
Bishop L, Kuula-Luumi A. Revisiting qualitative data reuse: a decade on. SAGE Open. 2017;7(1):1–15.
Sherif V. Evaluating preexisting qualitative research data for secondary analysis. In: Forum: qualitative social research, vol. 19, no. 2. 2018.
Patrick D, Burke L, Gwaltney C, Leidy N, Martin M, Molsen E, et al. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: part 1—eliciting concepts for a new PRO instrument. Value Health. 2011;14(8):967–77.
Download references
Acknowledgements
We thank the team at Sciome LLC for their assistance and contribution to the literature review. We thank Vivienne Law and David Floyd for their contributions to the literature review, reanalysis of qualitative data, and assistance with review of the draft manuscript. We thank Catherine Acquadro for her review of the draft manuscript. We also thank John Ware, Jed Rose, Ashley Slagle, Donald Patrick, Karl Fagerström, Stefan Cano, and Thomas Salzberger for their input and review.
Philip Morris International is the sole source of funding and sponsor of this research.
Author information
Authors and affiliations.
PMI R&D, Philip Morris Product S.A., Quai Jeanrenaud 5, 2000, Neuchâtel, Switzerland
Esther F. Afolalu, Erica Spies, Agnes Bacso, Emilie Clerc, Sophie Gallot & Christelle Chrea
Patient-Centered Outcomes Assessments Ltd., 1 Springbank, Bollington, Macclesfield, Cheshire, SK10 5LQ, UK
Linda Abetz-Webb
You can also search for this author in PubMed Google Scholar
Contributions
EA, ES and CC performed conceptualization. EA, ES and LA-W performed methodology. EA, ES, SG, EC and LA-W were involved in the investigation. EA and ES were involved in writing—original draft. EA, EC, LA-W and CC were involved in writing—review & editing. EA performed visualization. ES and CC performed supervision. AB, EC and SG were involved in data curation. AB and EC were involved in project administration. LA-W performed formal analysis. CC was involved in funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Esther F. Afolalu .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
Esther F. Afolalu, Emilie Clerc, and Christelle Chrea are employees of Philip Morris International. Agnes Bacso, Erica Spies, and Sophie Gallot completed the work during prior employment with Philip Morris International. Linda Abetz-Webb is a consultant for Philip Morris International.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Work completed during prior affiliation with PMI R&D: Erica Spies, Agnes Bacso, Sophie Gallot.
Supplementary Information
Additional file 1..
Summary tables of results of scoping literature review
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Afolalu, E.F., Spies, E., Bacso, A. et al. Impact of tobacco and/or nicotine products on health and functioning: a scoping review and findings from the preparatory phase of the development of a new self-report measure. Harm Reduct J 18 , 79 (2021). https://doi.org/10.1186/s12954-021-00526-z
Download citation
Received : 14 October 2020
Accepted : 21 July 2021
Published : 30 July 2021
DOI : https://doi.org/10.1186/s12954-021-00526-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health and functioning
- Scoping review
- Qualitative research
- Conceptual framework
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 24 March 2022
Tobacco and nicotine use
- Bernard Le Foll 1 , 2 ,
- Megan E. Piper 3 , 4 ,
- Christie D. Fowler 5 ,
- Serena Tonstad 6 ,
- Laura Bierut 7 ,
- Lin Lu ORCID: orcid.org/0000-0003-0742-9072 8 , 9 ,
- Prabhat Jha 10 &
- Wayne D. Hall 11 , 12
Nature Reviews Disease Primers volume 8 , Article number: 19 ( 2022 ) Cite this article
35k Accesses
70 Citations
96 Altmetric
Metrics details
- Disease genetics
- Experimental models of disease
- Preventive medicine
Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will die prematurely from tobacco-related complications. In addition, people who smoke have a significant reduction in their quality of life. Neurobiological findings have identified the mechanisms by which nicotine in tobacco affects the brain reward system and causes addiction. These brain changes contribute to the maintenance of nicotine or tobacco use despite knowledge of its negative consequences, a hallmark of addiction. Effective approaches to screen, prevent and treat tobacco use can be widely implemented to limit tobacco’s effect on individuals and society. The effectiveness of psychosocial and pharmacological interventions in helping people quit smoking has been demonstrated. As the majority of people who smoke ultimately relapse, it is important to enhance the reach of available interventions and to continue to develop novel interventions. These efforts associated with innovative policy regulations (aimed at reducing nicotine content or eliminating tobacco products) have the potential to reduce the prevalence of tobacco and nicotine use and their enormous adverse impact on population health.
Similar content being viewed by others

Associations between classic psychedelics and nicotine dependence in a nationally representative sample
Use of electronic cigarettes and heated tobacco products during the covid-19 pandemic.
Smoking cessation behaviors and reasons for use of electronic cigarettes and heated tobacco products among Romanian adults
Introduction.
Tobacco is the second most commonly used psychoactive substance worldwide, with more than one billion smokers globally 1 . Although smoking prevalence has reduced in many high-income countries (HICs), tobacco use is still very prevalent in low-income and middle-income countries (LMICs). The majority of smokers are addicted to nicotine delivered by cigarettes (defined as tobacco dependence in the International Classification of Diseases, Tenth Revision (ICD-10) or tobacco use disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)). As a result of the neuro-adaptations and psychological mechanisms caused by repeated exposure to nicotine delivered rapidly by cigarettes, cessation can also lead to a well-characterized withdrawal syndrome, typically manifesting as irritability, anxiety, low mood, difficulty concentrating, increased appetite, insomnia and restlessness, that contributes to the difficulty in quitting tobacco use 2 , 3 , 4 .
Historically, tobacco was used in some cultures as part of traditional ceremonies, but its use was infrequent and not widely disseminated in the population. However, since the early twentieth century, the use of commercial cigarettes has increased dramatically 5 because of automated manufacturing practices that enable large-scale production of inexpensive products that are heavily promoted by media and advertising. Tobacco use became highly prevalent in the past century and was followed by substantial increases in the prevalence of tobacco-induced diseases decades later 5 . It took decades to establish the relationship between tobacco use and associated health effects 6 , 7 and to discover the addictive role of nicotine in maintaining tobacco smoking 8 , 9 , and also to educate people about these effects. It should be noted that the tobacco industry disputed this evidence to allow continuing tobacco sales 10 . The expansion of public health campaigns to reduce smoking has gradually decreased the use of tobacco in HICs, with marked increases in adult cessation, but less progress has been achieved in LMICs 1 .
Nicotine is the addictive compound in tobacco and is responsible for continued use of tobacco despite harms and a desire to quit, but nicotine is not directly responsible for the harmful effects of using tobacco products (Box 1 ). Other components in tobacco may modulate the addictive potential of tobacco (for example, flavours and non-nicotine compounds) 11 . The major harms related to tobacco use, which are well covered elsewhere 5 , are linked to a multitude of compounds present in tobacco smoke (such as carcinogens, toxicants, particulate matter and carbon monoxide). In adults, adverse health outcomes of tobacco use include cancer in virtually all peripheral organs exposed to tobacco smoke and chronic diseases such as eye disease, periodontal disease, cardiovascular diseases, chronic obstructive pulmonary disease, stroke, diabetes mellitus, rheumatoid arthritis and disorders affecting immune function 5 . Moreover, smoking during pregnancy can increase the risk of adverse reproductive effects, such as ectopic pregnancy, low birthweight and preterm birth 5 . Exposure to secondhand cigarette smoke in children has been linked to sudden infant death syndrome, impaired lung function and respiratory illnesses, in addition to cognitive and behavioural impairments 5 . The long-term developmental effects of nicotine are probably due to structural and functional changes in the brain during this early developmental period 12 , 13 .
Nicotine administered alone in various nicotine replacement formulations (such as patches, gum and lozenges) is safe and effective as an evidence-based smoking cessation aid. Novel forms of nicotine delivery systems have also emerged (called electronic nicotine delivery systems (ENDS) or e-cigarettes), which can potentially reduce the harmful effects of tobacco smoking for those who switch completely from combustible to e-cigarettes 14 , 15 .
This Primer focuses on the determinants of nicotine and tobacco use, and reviews the neurobiology of nicotine effects on the brain reward circuitry and the functioning of brain networks in ways that contribute to the difficulty in stopping smoking. This Primer also discusses how to prevent tobacco use, screen for smoking, and offer people who smoke tobacco psychosocial and pharmacological interventions to assist in quitting. Moreover, this Primer presents emerging pharmacological and novel brain interventions that could improve rates of successful smoking cessation, in addition to public health approaches that could be beneficial.
Box 1 Tobacco products
Conventional tobacco products include combustible products that produce inhaled smoke (most commonly cigarettes, bidis (small domestically manufactured cigarettes used in South Asia) or cigars) and those that deliver nicotine without using combustion (chewing or dipping tobacco and snuff). Newer alternative products that do not involve combustion include nicotine-containing e-cigarettes and heat-not-burn tobacco devices. Although non-combustion and alternative products may constitute a lesser risk than burned ones 14 , 15 , 194 , no form of tobacco is entirely risk-free.
Epidemiology
Prevalence and burden of disease.
The Global Burden of Disease Project (GBDP) estimated that around 1.14 billion people smoked in 2019, worldwide, increasing from just under a billion in 1990 (ref. 1 ). Of note, the prevalence of smoking decreased significantly between 1990 and 2019, but increases in the adult population meant that the total number of global smokers increased. One smoking-associated death occurs for approximately every 0.8–1.1 million cigarettes smoked 16 , suggesting that the estimated worldwide consumption of about 7.4 trillion cigarettes in 2019 has led to around 7 million deaths 1 .
In most populations, smoking prevalence is much higher among groups with lower levels of education or income 17 and among those with mental health disorders and other co-addictions 18 , 19 . Smoking is also more frequent among men than women (Figs 1 – 3 ). Sexual and/or gender minority individuals have disproportionately high rates of smoking and other addictions 17 , 20 . In addition, the prevalence of smoking varies substantially between regions and ethnicities; smoking rates are high in some regions of Asia, such as China and India, but are lower in North America and Australia. Of note, the prevalence of mental health disorders and other co-addictions is higher in individuals who smoke compared with non-smokers 18 , 19 , 21 . For example, the odds of smoking in people with any substance use disorder is more than five times higher than the odds in people without a substance use disorder 19 . Similarly, the odds of smoking in people with any psychiatric disorder is more than three times higher than the odds of smoking in those without a psychiatric diagnosis 22 . In a study in the USA, compared with a population of smokers with no psychiatric diagnosis, subjects with anxiety, depression and phobia showed an approximately twofold higher prevalence of smoking, and subjects with agoraphobia, mania or hypomania, psychosis and antisocial personality or conduct disorders showed at least a threefold higher prevalence of smoking 22 . Comorbid disorders are also associated with higher rates of smoking 22 , 23 .
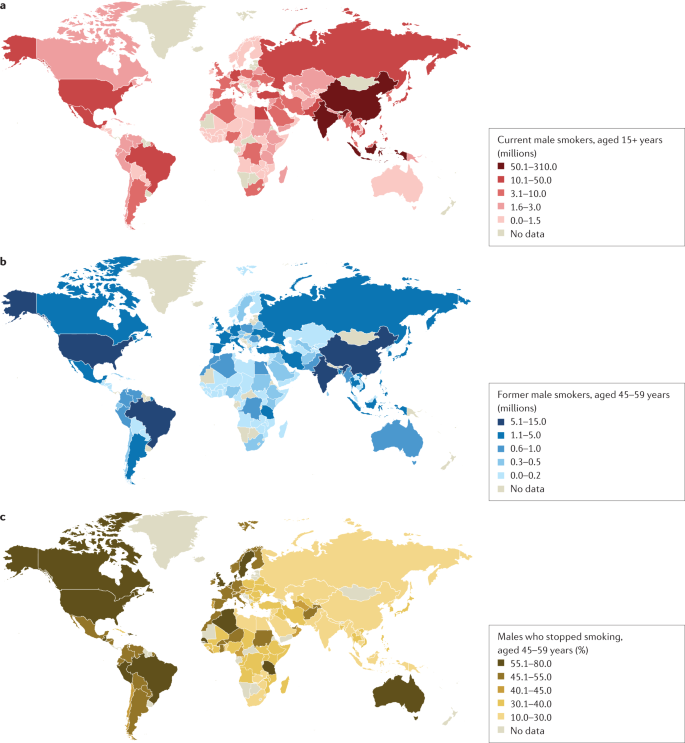
a | Number of current male smokers aged 15 years or older per country expressed in millions. b | Former male smokers aged 45–59 years per country expressed in millions. c | Former male smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for male smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among males is less variable than among females. Data from ref. 1 .
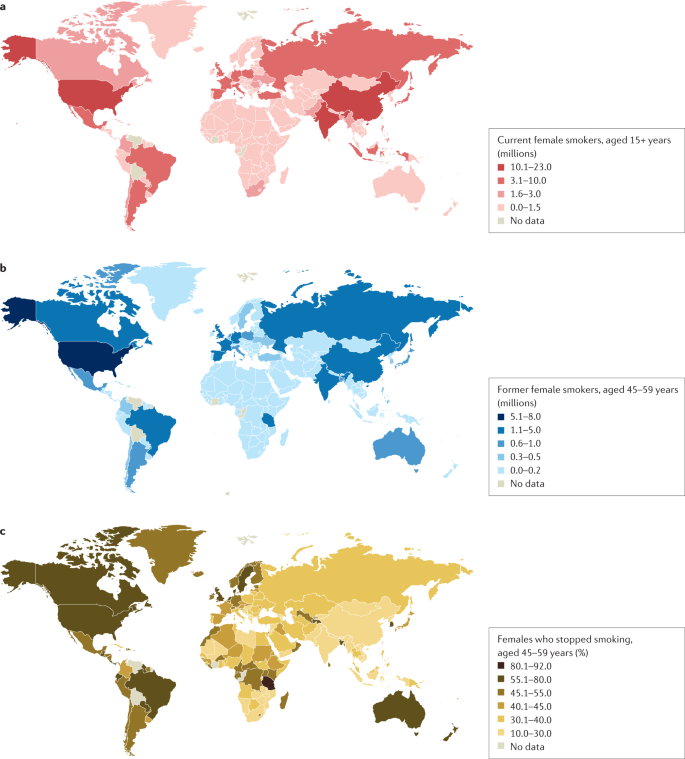
a | Number of current female smokers aged 15 years or older per country expressed in millions. b | Former female smokers aged 45–59 years per country expressed in millions. c | Former female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for female smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among females is much lower in East and South Asia than in Latin America or Eastern Europe. Data from ref. 1 .
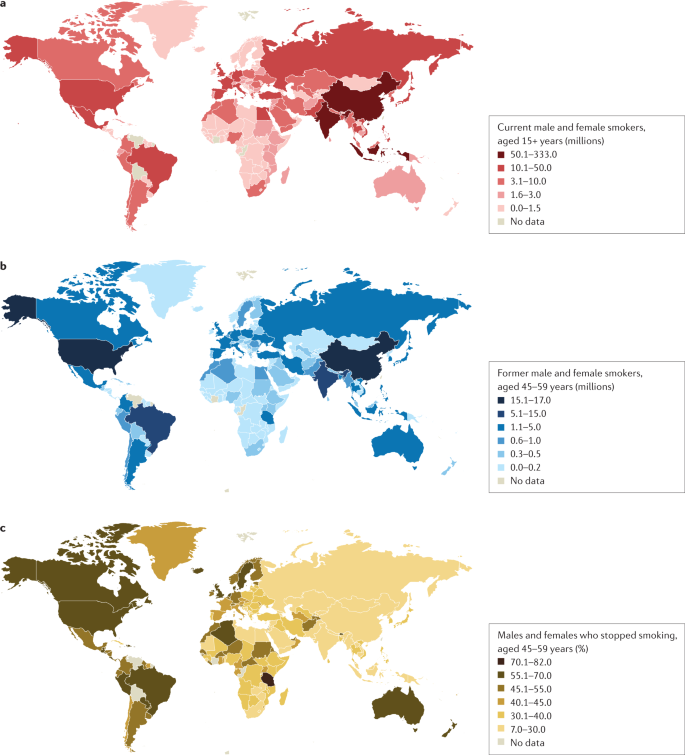
a | Number of current male and female smokers aged 15 years or older per country expressed in millions. b | Former male and female smokers aged 45–59 years per country expressed in millions. c | Former male and female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for the period 2015–2019 from countries with direct smoking surveys. Cessation rates are higher in high-income countries, but also notably high in Brazil. Cessation is far less common in South and East Asia and Russia and other Eastern European countries, and also low in South Africa. Data from ref. 1 .
Age at onset
Most smokers start smoking during adolescence, with almost 90% of smokers beginning between 15 and 25 years of age 24 . The prevalence of tobacco smoking among youths substantially declined in multiple HICs between 1990 and 2019 (ref. 25 ). More recently, the widespread uptake of ENDS in some regions such as Canada and the USA has raised concerns about the long-term effects of prolonged nicotine use among adolescents, including the possible notion that ENDS will increase the use of combustible smoking products 25 , 26 (although some studies have not found much aggregate effect at the population level) 27 .
Smoking that commences in early adolescence or young adulthood and persists throughout life has a more severe effect on health than smoking that starts later in life and/or that is not persistent 16 , 28 , 29 . Over 640 million adults under 30 years of age smoke in 22 jurisdictions alone (including 27 countries in the European Union where central efforts to reduce tobacco dependence might be possible) 30 . In those younger than 30 years of age, at least 320 million smoking-related deaths will occur unless they quit smoking 31 . The actual number of smoking-related deaths might be greater than one in two, and perhaps as high as two in three, long-term smokers 5 , 16 , 29 , 32 , 33 . At least half of these deaths are likely to occur in middle age (30–69 years) 16 , 29 , leading to a loss of two or more decades of life. People who smoke can expect to lose an average of at least a decade of life versus otherwise similar non-smokers 16 , 28 , 29 .
Direct epidemiological studies in several countries paired with model-based estimates have estimated that smoking tobacco accounted for 7.7 million deaths globally in 2020, of which 80% were in men and 87% were current smokers 1 . In HICs, the major causes of tobacco deaths are lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas and bladder cancer 28 , 29 . In some lower income countries, tuberculosis is an additional important cause of tobacco-related death 29 , 34 , which could be related to, for example, increased prevalence of infection, more severe tuberculosis/mortality and higher prevalence of treatment-resistant tuberculosis in smokers than in non-smokers in low-income countries 35 , 36 .
Despite substantial reductions in the prevalence of smoking, there were 34 million smokers in the USA, 7 million in the UK and 5 million in Canada in 2017 (ref. 16 ), and cigarette smoking remains the largest cause of premature death before 70 years of age in much of Europe and North America 1 , 16 , 28 , 29 . Smoking-associated diseases accounted for around 41 million deaths in the USA, UK and Canada from 1960 to 2020 (ref. 16 ). Moreover, as smoking-associated diseases are more prevalent among groups with lower levels of education and income, smoking accounts for at least half of the difference in overall mortality between these social groups 37 . Any reduction in smoking prevalence reduces the absolute mortality gap between these groups 38 .
Smoking cessation has become common in HICs with good tobacco control interventions. For example, in France, the number of ex-smokers is four times the number of current smokers among those aged 50 years or more 30 . By contrast, smoking cessation in LMICs remains uncommon before smokers develop tobacco-related diseases 39 . Smoking cessation greatly reduces the risks of smoking-related diseases. Indeed, smokers who quit smoking before 40 years of age avoid nearly all the increased mortality risks 31 , 33 . Moreover, individuals who quit smoking by 50 years of age reduce the risk of death from lung cancer by about two-thirds 40 . More modest hazards persist for deaths from lung cancer and emphysema 16 , 28 ; however, the risks among former smokers are an order of magnitude lower than among those who continue to smoke 33 .
Mechanisms/pathophysiology
Nicotine is the main psychoactive agent in tobacco and e-cigarettes. Nicotine acts as an agonist at nicotinic acetylcholine receptors (nAChRs), which are localized throughout the brain and peripheral nervous system 41 . nAChRs are pentameric ion channels that consist of varying combinations of α 2 –α 7 and β 2 –β 4 subunits, and for which acetylcholine (ACh) is the endogenous ligand 42 , 43 , 44 . When activated by nicotine binding, nAChR undergoes a conformational change that opens the internal pore, allowing an influx of sodium and calcium ions 45 . At postsynaptic membranes, nAChR activation can lead to action potential firing and downstream modulation of gene expression through calcium-mediated second messenger systems 46 . nAChRs are also localized to presynaptic membranes, where they modulate neurotransmitter release 47 . nAChRs become desensitized after activation, during which ligand binding will not open the channel 45 .
nAChRs with varying combinations of α-subunits and β-subunits have differences in nicotine binding affinity, efficacy and desensitization rate, and have differential expression depending on the brain region and cell type 48 , 49 , 50 . For instance, at nicotine concentrations found in human smokers, β 2 -containing nAChRs desensitize relatively quickly after activation, whereas α 7 -containing nAChRs have a slower desensitization profile 48 . Chronic nicotine exposure in experimental animal models or in humans induces an increase in cortical expression of α 4 β 2 -containing nAChRs 51 , 52 , 53 , 54 , 55 , but also increases the expression of β 3 and β 4 nAChR subunits in the medial habenula (MHb)–interpeduncular nucleus (IPN) pathway 56 , 57 . It is clear that both the brain localization and the type of nAChR are critical elements in mediating the various effects of nicotine, but other factors such as rate of nicotine delivery may also modulate addictive effects of nicotine 58 .
Neurocircuitry of nicotine addiction
Nicotine has both rewarding effects (such as a ‘buzz’ or ‘high’) and aversive effects (such as nausea and dizziness), with the net outcome dependent on dose and others factors such as interindividual sensitivity and presence of tolerance 59 . Thus, the addictive properties of nicotine involve integration of contrasting signals from multiple brain regions that process reward and aversion (Fig. 4 ).
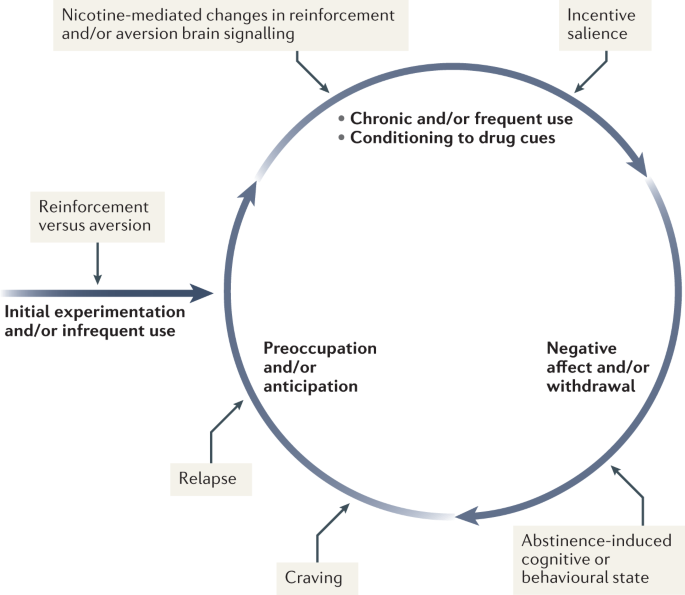
During initial use, nicotine exerts both reinforcing and aversive effects, which together determine the likelihood of continued use. As the individual transitions to more frequent patterns of chronic use, nicotine induces pharmacodynamic changes in brain circuits, which is thought to lead to a reduction in sensitivity to the aversive properties of the drug. Nicotine is also a powerful reinforcer that leads to the conditioning of secondary cues associated with the drug-taking experience (such as cigarette pack, sensory properties of cigarette smoke and feel of the cigarette in the hand or mouth), which serves to enhance the incentive salience of these environmental factors and drive further drug intake. When the individual enters into states of abstinence (such as daily during sleep at night or during quit attempts), withdrawal symptomology is experienced, which may include irritability, restlessness, learning or memory deficits, difficulty concentrating, anxiety and hunger. These negative affective and cognitive symptoms lead to an intensification of the individual’s preoccupation to obtain and use the tobacco/nicotine product, and subsequently such intense craving can lead to relapse.
The rewarding actions of nicotine have largely been attributed to the mesolimbic pathway, which consists of dopaminergic neurons in the ventral tegmental area (VTA) that project to the nucleus accumbens and prefrontal cortex 60 , 61 , 62 (Fig. 5 ). VTA integrating circuits and projection regions express several nAChR subtypes on dopaminergic, GABAergic, and glutamatergic neurons 63 , 64 . Ultimately, administration of nicotine increases dopamine levels through increased dopaminergic neuron firing in striatal and extrastriatal areas (such as the ventral pallidum) 65 (Fig. 6 ). This effect is involved in reward and is believed to be primarily mediated by the action of nicotine on α 4 -containing and β 2 -containing nAChRs in the VTA 66 , 67 .
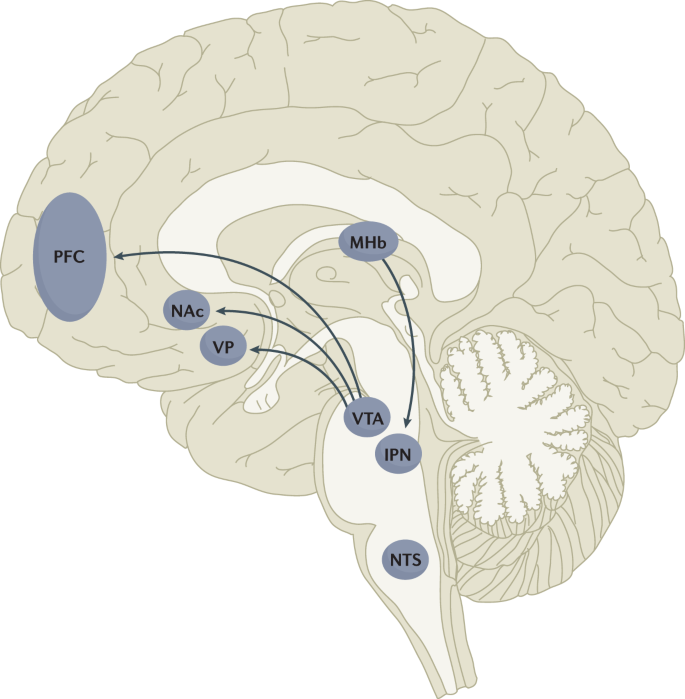
Multiple lines of research have demonstrated that nicotine reinforcement is mainly controlled by two brain pathways, which relay predominantly reward-related or aversion-related signals. The rewarding properties of nicotine that promote drug intake involve the mesolimbic dopamine projection from the ventral tegmental area (VTA) to the nucleus accumbens (NAc). By contrast, the aversive properties of nicotine that limit drug intake and mitigate withdrawal symptoms involve the fasciculus retroflexus projection from the medial habenula (MHb) to the interpeduncular nucleus (IPN). Additional brain regions have also been implicated in various aspects of nicotine dependence, such as the prefrontal cortex (PFC), ventral pallidum (VP), nucleus tractus solitarius (NTS) and insula (not shown here for clarity). All of these brain regions are directly or indirectly interconnected as integrative circuits to drive drug-seeking and drug-taking behaviours.
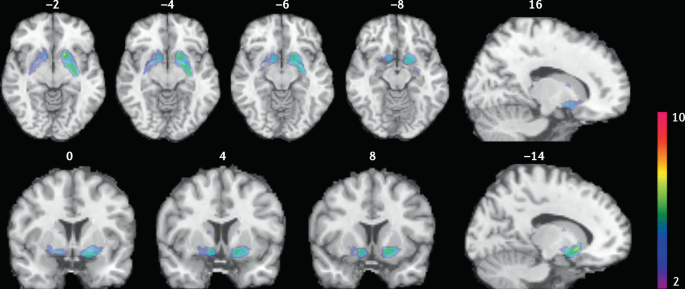
Smokers received brain PET scans with [ 11 C]PHNO, a dopamine D 2/3 PET tracer that has high sensitivity in detecting fluctuations of dopamine. PET scans were performed during abstinence or after smoking a cigarette. Reduced binding potential (BP ND ) was observed after smoking, indicating increased dopamine levels in the ventral striatum and in the area that corresponds to the ventral pallidum. The images show clusters with statistically significant decreases of [ 11 C]PHNO BP ND after smoking a cigarette versus abstinence condition. Those clusters have been superimposed on structural T1 MRI images of the brain. Reprinted from ref. 65 , Springer Nature Limited.
The aversive properties of nicotine are mediated by neurons in the MHb, which project to the IPN. Studies in rodents using genetic knockdown and knockout strategies demonstrated that the α 5 -containing, α 3 -containing and β 4 -containing nAChRs in the MHb–IPN pathway mediate the aversive properties of nicotine that limit drug intake, especially when animals are given the opportunity to consume higher nicotine doses 68 , 69 , 70 , 71 , 72 . In addition to nAChRs, other signalling factors acting on the MHb terminals in the IPN also regulate the actions of nicotine. For instance, under conditions of chronic nicotine exposure or with optogenetic activation of IPN neurons, a subtype of IPN neurons co-expressing Chrna5 (encoding the α 5 nAChR subunit) and Amigo1 (encoding adhesion molecule with immunoglobulin-like domain 1) release nitric oxide from the cell body that retrogradely inhibits MHb axon terminals 70 . In addition, nicotine activates α 5 -containing nAChR-expressing neurons that project from the nucleus tractus solitarius to the IPN, leading to release of glucagon-like peptide-1 that binds to GLP receptors on habenular axon terminals, which subsequently increases IPN neuron activation and decreases nicotine self-administration 73 . Taken together, these findings suggest a dynamic signalling process at MHb axonal terminals in the IPN, which regulates the addictive properties of nicotine and determines the amount of nicotine that is self-administered.
Nicotine withdrawal in animal models can be assessed by examining somatic signs (such as shaking, scratching, head nods and chewing) and affective signs (such as increased anxiety-related behaviours and conditioned place aversion). Interestingly, few nicotine withdrawal somatic signs are found in mice with genetic knockout of the α 2 , α 5 or β 4 nAChR subunits 74 , 75 . By contrast, β 2 nAChR-knockout mice have fewer anxiety-related behaviours during nicotine withdrawal, with no differences in somatic symptoms compared with wild-type mice 74 , 76 .
In addition to the VTA (mediating reward) and the MHb–IPN pathway (mediating aversion), other brain areas are involved in nicotine addiction (Fig. 5 ). In animals, the insular cortex controls nicotine taking and nicotine seeking 77 . Moreover, humans with lesions of the insular cortex can quit smoking easily without relapse 78 . This finding led to the development of a novel therapeutic intervention modulating insula function (see Management, below) 79 , 80 . Various brain areas (shell of nucleus accumbens, basolateral amygdala and prelimbic cortex) expressing cannabinoid CB 1 receptors are also critical in controlling rewarding effects and relapse 81 , 82 . The α 1 -adrenergic receptor expressed in the cortex also control these effects, probably through glutamatergic afferents to the nucleus accumbens 83 .
Individual differences in nicotine addiction risk
Vulnerability to nicotine dependence varies between individuals, and the reasons for these differences are multidimensional. Many social factors (such as education level and income) play a role 84 . Broad psychological and social factors also modulate this risk. For example, peer smoking status, knowledge on effect of tobacco, expectation on social acceptance, exposure to passive smoking modulate the risk of initiating tobacco use 85 , 86 .
Genetic factors have a role in smoking initiation, the development of nicotine addiction and the likelihood of smoking cessation. Indeed, heritability has been estimated to contribute to approximatively half of the variability in nicotine dependence 87 , 88 , 89 , 90 . Important advances in our understanding of such genetic contributions have evolved with large-scale genome-wide association studies of smokers and non-smokers. One of the most striking findings has been that allelic variation in the CHRNA5 – CHRNA3 – CHRNB4 gene cluster, which encodes α 5 , α 3 and β 4 nAChR subunits, correlates with an increased vulnerability for nicotine addiction, indicated by a higher likelihood of becoming dependent on nicotine and smoking a greater number of cigarettes per day 91 , 92 , 93 , 94 , 95 . The most significant effect has been found for a single-nucleotide polymorphism in CHRNA5 (rs16969968), which results in an amino acid change and reduced function of α 5 -containing nAChRs 92 .
Allelic variation in CYP2A6 (encoding the CYP2A6 enzyme, which metabolizes nicotine) has also been associated with differential vulnerability to nicotine dependence 96 , 97 , 98 . CYP2A6 is highly polymorphic, resulting in variable enzymatic activity 96 , 99 , 100 . Individuals with allelic variation that results in slow nicotine metabolism consume less nicotine per day, experience less-severe withdrawal symptoms and are more successful at quitting smoking than individuals with normal or fast metabolism 101 , 102 , 103 , 104 . Moreover, individuals with slow nicotine metabolism have lower dopaminergic receptor expression in the dopamine D2 regions of the associative striatum and sensorimotor striatum in PET studies 105 and take fewer puffs of nicotine-containing cigarettes (compared with de-nicotinized cigarettes) in a forced choice task 106 . Slower nicotine metabolism is thought to increase the duration of action of nicotine, allowing nicotine levels to accumulate over time, therefore enabling lower levels of intake to sustain activation of nAChRs 107 .
Large-scale genetic studies have identified hundreds of other genetic loci that influence smoking initiation, age of smoking initiation, cigarettes smoked per day and successful smoking cessation 108 . The strongest genetic contributions to smoking through the nicotinic receptors and nicotine metabolism are among the strongest genetic contributors to lung cancer 109 . Other genetic variations (such as those related to cannabinoid, dopamine receptors or other neurotransmitters) may affect certain phenotypes related to smoking (such as nicotine preference and cue-reactivity) 110 , 111 , 112 , 113 , 114 , 115 .
Diagnosis, screening and prevention
Screening for cigarette smoking.
Screening for cigarette smoking should happen at every doctor’s visit 116 . In this regard, a simple and direct question about a person’s tobacco use can provide an opportunity to offer information about its potential risks and treatments to assist in quitting. All smokers should be offered assistance in quitting because even low levels of smoking present a significant health risk 33 , 117 , 118 . Smoking status can be assessed by self-categorization or self-reported assessment of smoking behaviour (Table 1 ). In people who smoke, smoking frequency can be assessed 119 and a combined quantity frequency measure such as pack-year history (that is, average number of cigarettes smoked per day multiplied by the number of years, divided by 20), can be used to estimate cumulative risk of adverse health outcomes. The Association for the Treatment of Tobacco Use and Dependence recommends that all electronic health records should document smoking status using the self-report categories listed in Table 1 .
Owing to the advent of e-cigarettes and heat-not-burn products, and the popularity of little cigars in the US that mimic combustible cigarettes, people who use tobacco may use multiple products concurrently 120 , 121 . Thus, screening for other nicotine and tobacco product use is important in clinical practice. The self-categorization approach can also be used to describe the use of these other products.
Traditionally tobacco use has been classified according to whether the smoker meets criteria for nicotine dependence in one of the two main diagnostic classifications: the DSM 122 (tobacco use disorder) and the ICD (tobacco dependence) 123 . The diagnosis of tobacco use disorder according to DSM-5 criteria requires the presence of at least 2 of 11 symptoms that have produced marked clinical impairment or distress within a 12-month period (Box 2 ). Of note, these symptoms are similar for all substance use disorder diagnoses and may not all be relevant to tobacco use disorder (such as failure to complete life roles). In the ICD-10, codes allow the identification of specific tobacco products used (cigarettes, chewing tobacco and other tobacco products).
Dependence can also be assessed as a continuous construct associated with higher levels of use, greater withdrawal and reduced likelihood of quitting. The level of dependence can be assessed with the Fagerström Test for Nicotine Dependence, a short questionnaire comprising six questions 124 (Box 2 ). A score of ≥4 indicates moderate to high dependence. As very limited time may be available in clinical consultations, the Heaviness of Smoking Index (HSI) was developed, which comprises two questions on the number of cigarettes smoked per day and how soon after waking the first cigarette is smoked 125 . The HSI can guide dosing for nicotine replacement therapy (NRT).
Other measures of cigarette dependence have been developed but are not used in the clinical setting, such as the Cigarette Dependence Scale 126 , Hooked on Nicotine Checklist 127 , Nicotine Dependence Syndrome Scale 128 , the Wisconsin Inventory of Smoking Dependence Motives (Brief) 129 and the Penn State Cigarette Dependence Index 130 . However, in practice, these are not often used, as the most important aspect is to screen for smoking and encourage all smokers to quit smoking regardless of their dependence status.
Box 2 DSM-5 criteria for tobacco use disorder and items of the Fagerström Test for nicotine dependence
DSM-5 (ref. 122 )
Taxonomic and diagnostic tool for tobacco use disorder published by the American Psychiatric Association.
A problematic pattern of tobacco use leading to clinically significant impairment or distress as manifested by at least two of the following, occurring within a 12-month period.
Tobacco often used in larger amounts or over a longer period of time than intended
A persistent desire or unsuccessful efforts to reduce or control tobacco use
A great deal of time spent in activities necessary to obtain or use tobacco
Craving, or a strong desire or urge to use tobacco
Recurrent tobacco use resulting in a failure to fulfil major role obligations at work, school or home
Continued tobacco use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of tobacco (for example, arguments with others about tobacco use)
Important social, occupational or recreational activities given up or reduced because of tobacco use
Recurrent tobacco use in hazardous situations (such as smoking in bed)
Tobacco use continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco use
Tolerance, defined by either of the following.
A need for markedly increased amounts of tobacco to achieve the desired effect
A markedly diminished effect with continued use of the same amount of tobacco
Withdrawal, manifesting as either of the following.
Withdrawal syndrome for tobacco
Tobacco (or a closely related substance, such as nicotine) taken to relieve or avoid withdrawal symptoms
Fagerström Test for Nicotine Dependence 124
A standard instrument for assessing the intensity of physical addiction to nicotine.
How soon after you wake up do you smoke your first cigarette?
Within 5 min (scores 3 points)
5 to 30 min (scores 2 points)
31 to 60 min (scores 1 point)
After 60 min (scores 0 points)
Do you find it difficult not to smoke in places where you should not, such as in church or school, in a movie, at the library, on a bus, in court or in a hospital?
Yes (scores 1 point)
No (scores 0 points)
Which cigarette would you most hate to give up; which cigarette do you treasure the most?
The first one in the morning (scores 1 point)
Any other one (scores 0 points)
How many cigarettes do you smoke each day?
10 or fewer (scores 0 points)
11 to 20 (scores 1 point)
21 to 30 (scores 2 points)
31 or more (scores 3 points)
Do you smoke more during the first few hours after waking up than during the rest of the day?
Do you still smoke if you are so sick that you are in bed most of the day or if you have a cold or the flu and have trouble breathing?
A score of 7–10 points is classified as highly dependent; 4–6 points is classified as moderately dependent; <4 points is classified as minimally dependent.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Young people who do not start smoking cigarettes between 15 and 25 years of age have a very low risk of ever smoking 24 , 131 , 132 . This age group provides a critical opportunity to prevent cigarette smoking using effective, evidence-based strategies to prevent smoking initiation and reduce escalation from experimentation to regular use 131 , 132 , 133 , 134 , 135 .
Effective prevention of cigarette uptake requires a comprehensive package of cost-effective policies 134 , 136 , 137 to synergistically reduce the population prevalence of cigarette smoking 131 , 135 . These policies include high rates of tobacco taxation 30 , 134 , 137 , 138 , widespread and rigorously enforced smoke-free policies 139 , bans on tobacco advertising and promotions 140 , use of plain packaging and graphic warnings about the health risks of smoking 135 , 141 , mass media and peer-based education programmes to discourage smoking, and enforcement of laws against the sale of cigarettes to young people below the minimum legal purchase age 131 , 135 . These policies make cigarettes less available and affordable to young people. Moreover, these policies make it more difficult for young people to purchase cigarettes and make smoking a much less socially acceptable practice. Of note, these policies are typically mostly enacted in HICs, which may be related to the declining prevalence of smoking in these countries, compared with the prevalence in LMICs.
Pharmacotherapy
Three evidence-based classes of pharmacotherapy are available for smoking cessation: NRT (using nicotine-based patches, gum, lozenges, mini-lozenges, nasal sprays and inhalers), varenicline (a nAChR partial agonist), and bupropion (a noradrenaline/dopamine reuptake inhibitor that also inhibits nAChR function and is also used as an antidepressant). These FDA-approved and EMA-approved pharmacotherapies are cost-effective smoking cessation treatments that double or triple successful abstinence rates compared with no treatment or placebo controls 116 , 142 .
Combinations of pharmacotherapies are also effective for smoking cessation 116 , 142 . For example, combining NRTs (such as the steady-state nicotine patch and as-needed NRT such as gum or mini-lozenge) is more effective than a single form of NRT 116 , 142 , 143 . Combining NRT and varenicline is the most effective smoking cessation pharmacotherapy 116 , 142 , 143 . Combining FDA-approved pharmacotherapy with behavioural counselling further increases the likelihood of successful cessation 142 . Second-line pharmacotherapies (for example, nortriptyline) have some potential for smoking cessation, but their use is limited due to their tolerability profile.
All smokers should receive pharmacotherapy to help them quit smoking, except those in whom pharmacotherapy has insufficient evidence of effectiveness (among adolescents, smokeless tobacco users, pregnant women or light smokers) or those in whom pharmacotherapy is medically contraindicated 144 . Table 2 provides specific information regarding dosing and duration for each FDA-approved pharmacotherapy. Extended use of pharmacotherapy beyond the standard 12-week regimen after cessation is effective and should be considered 116 . Moreover, preloading pharmacotherapy (that is, initiating cessation medication in advance of a quit attempt), especially with the nicotine patch, is a promising treatment, although further studies are required to confirm efficacy.
Cytisine has been used for smoking cessation in Eastern Europe for a long time and is available in some countries (such as Canada) without prescription 145 . Cytisine is a partial agonist of nAChRs and its structure was the precursor for the development of varenicline 145 . Cytisine is at least as effective as some approved pharmacotherapies for smoking cessation, such as NRT 146 , 147 , 148 , and the role of cytisine in smoking cessation is likely to expand in the future, notably owing to its much lower cost than traditional pharmacotherapies. E-cigarettes also have the potential to be useful as smoking cessation devices 149 , 150 . The 2020 US Surgeon General’s Report concluded that there was insufficient evidence to promote cytisine or e-cigarettes as effective smoking cessation treatments, but in the UK its use is recommended for smoking cessation (see ref. 15 for regularly updated review).
Counselling and behavioural treatments
Psychosocial counselling significantly increases the likelihood of successful cessation, especially when combined with pharmacotherapy. Even a counselling session lasting only 3 minutes can help smokers quit 116 , although the 2008 US Public Health Service guidelines and the Preventive Services Task Force 151 each concluded that more intensive counselling (≥20 min per session) is more effective than less intensive counselling (<20 min per session). Higher smoking cessation rates are obtained by using behavioural change techniques that target associative and self-regulatory processes 152 . In addition, behavioural change techniques that will favour commitment, social reward and identity associated with changed behaviour seems associated with higher success rates 152 . Evidence-based counselling focuses on providing social support during treatment, building skills to cope with withdrawal and cessation, and problem-solving in challenging situations 116 , 153 . Effective counselling can be delivered by diverse providers (such as physicians, nurses, pharmacists, social workers, psychologists and certified tobacco treatment specialists) 116 .
Counselling can be delivered in a variety of modalities. In-person individual and group counselling are effective, as is telephone counselling (quit lines) 142 . Internet and text-based intervention seem to be effective in smoking cessation, especially when they are interactive and tailored to a smoker’s specific circumstances 142 . Over the past several years, the number of smoking cessation smartphone apps has increased, but there the evidence that the use of these apps significantly increases smoking cessation rates is not sufficient.
Contingency management (providing financial incentives for abstinence or engagement in treatment) has shown promising results 154 , 155 but its effects are not sustained once the contingencies are removed 155 , 156 . Other treatments such as hypnosis, acupuncture and laser treatment have not been shown to improve smoking cessation rates compared with placebo treatments 116 . Moreover, no solid evidence supports the use of conventional transcranial magnetic stimulation (TMS) for long-term smoking cessation 157 , 158 .
Although a variety of empirically supported smoking cessation interventions are available, more than two-thirds of adult smokers who made quit attempts in the USA during the past year did not use an evidence-based treatment and the rate is likely to be lower in many other countries 142 . This speaks to the need to increase awareness of, and access to, effective cessation aids among all smokers.
Brain stimulation
The insula (part of the frontal cortex) is a critical brain structure involved in cigarette craving and relapse 78 , 79 . The activity of the insula can be modulated using an innovative approach called deep insula/prefrontal cortex TMS (deep TMS), which is effective in helping people quit smoking 80 , 159 . This approach has now been approved by the FDA as an effective smoking cessation intervention 80 . However, although this intervention was developed and is effective for smoking cessation, the number of people with access to it is limited owing to the limited number of sites equipped and with trained personnel, and the cost of this intervention.
Quality of life
Generic instruments (such as the Short-Form (SF-36) Health Survey) can be used to evaluate quality of life (QOL) in smokers. People who smoke rate their QOL lower than people who do not smoke both before and after they become smokers 160 , 161 . QOL improves when smokers quit 162 . Mental health may also improve on quitting smoking 163 . Moreover, QOL is much poorer in smokers with tobacco-related diseases, such as chronic respiratory diseases and cancers, than in individuals without tobacco-related diseases 161 , 164 . The dimensions of QOL that show the largest decrements in people who smoke are those related to physical health, day-to-day activities and mental health such as depression 160 . Smoking also increases the risk of diabetes mellitus 165 , 166 , which is a major determinant of poor QOL for a wide range of conditions.
The high toll of premature death from cigarette smoking can obscure the fact that many of the diseases that cause these deaths also produce substantial disability in the years before death 1 . Indeed, death in smokers is typically preceded by several years of living with the serious disability and impairment of everyday activities caused by chronic respiratory disease, heart disease and cancer 2 . Smokers’ QOL in these years may also be adversely affected by the adverse effects of the medical treatments that they receive for these smoking-related diseases (such as major surgery and radiotherapy).
Expanding cessation worldwide
The major global challenge is to consider individual and population-based strategies that could increase the substantially low rates of adult cessation in most LMICs and indeed strategies to ensure that even in HICs, cessation continues to increase. In general, the most effective tools recommended by WHO to expand cessation are the same tools that can prevent smoking initiation, notably higher tobacco taxes, bans on advertising and promotion, prominent warning labels or plain packaging, bans on public smoking, and mass media and educational efforts 29 , 167 . The effective use of these policies, particularly taxation, lags behind in most LMICs compared with most HICs, with important exceptions such as Brazil 167 . Access to effective pharmacotherapies and counselling as well as support for co-existing mental health conditions would also be required to accelerate cessation in LMICs. This is particularly important as smokers living in LMICs often have no access to the full range of effective treatment options.
Regulating access to e-cigarettes
How e-cigarettes should be used is debated within the tobacco control field. In some countries (for example, the UK), the use of e-cigarettes as a cigarette smoking cessation aid and as a harm reduction strategy is supported, based on the idea that e-cigarette use will lead to much less exposure to toxic compounds than tobacco use, therefore reducing global harm. In other countries (for example, the USA), there is more concern with preventing the increased use of e-cigarettes by youths that may subsequently lead to smoking 25 , 26 . Regulating e-cigarettes in nuanced ways that enable smokers to access those products whilst preventing their uptake among youths is critical.
Regulating nicotine content in tobacco products
Reducing the nicotine content of cigarettes could potentially produce less addictive products that would allow a gradual reduction in the population prevalence of smoking. Some clinical studies have found no compensatory increase in smoking whilst providing access to low nicotine tobacco 168 . Future regulation may be implemented to gradually decrease the nicotine content of combustible tobacco and other nicotine products 169 , 170 , 171 .
Tobacco end games
Some individuals have proposed getting rid of commercial tobacco products this century or using the major economic disruption arising from the COVID-19 pandemic to accelerate the demise of the tobacco industry 172 , 173 . Some tobacco producers have even proposed this strategy as an internal goal, with the idea of switching to nicotine delivery systems that are less harmful ( Philip Morris International ). Some countries are moving towards such an objective; for example, in New Zealand, the goal that fewer than 5% of New Zealanders will be smokers in 2025 has been set (ref. 174 ). The tobacco end-game approach would overall be the best approach to reduce the burden of tobacco use on society, but it would require coordination of multiple countries and strong public and private consensus on the strategy to avoid a major expansion of the existing illicit market in tobacco products in some countries.
Innovative interventions
The COVID-19 pandemic has shown that large-scale investment in research can lead to rapid development of successful therapeutic interventions. By contrast, smoking cessation has been underfunded compared with the contribution that it makes to the global burden of disease. In addition, there is limited coordination between research teams and most studies are small-scale and often underpowered 79 . It is time to fund an ambitious, coordinated programme of research to test the most promising therapies based on an increased understanding of the neurobiological basis of smoking and nicotine addiction (Table 3 ). Many of those ideas have not yet been tested properly and this could be carried out by a coordinated programme of research at the international level.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 397 , 2337–2360 (2021). This study summarizes the burden of disease induced by tobacco worldwide .
Google Scholar
West, R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol. Health 32 , 1018–1036 (2017).
PubMed PubMed Central Google Scholar
West, R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD 6 , 277–283 (2009).
PubMed Google Scholar
Fagerström, K. Determinants of tobacco use and renaming the FTND to the Fagerström test for cigarette dependence. Nicotine Tob. Res. 14 , 75–78 (2012).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Doll, R. & Hill, A. B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 2 , 739–748 (1950).
CAS PubMed PubMed Central Google Scholar
Royal College of Physicians. Smoking and health. Summary of a report of the Royal College of Physicians of London on smoking in relation to cancer of the lung and other diseases (Pitman Medical Publishing, 1962).
Henningfield, J. E., Smith, T. T., Kleykamp, B. A., Fant, R. V. & Donny, E. C. Nicotine self-administration research: the legacy of Steven R. Goldberg and implications for regulation, health policy, and research. Psychopharmacology 233 , 3829–3848 (2016).
Le Foll, B. & Goldberg, S. R. Effects of nicotine in experimental animals and humans: an update on addictive properties. Hand. Exp. Pharmacol. https://doi.org/10.1007/978-3-540-69248-5_12 (2009).
Article Google Scholar
Proctor, R. N. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll. Tob. Control. 21 , 87–91 (2012).
Hall, B. J. et al. Differential effects of non-nicotine tobacco constituent compounds on nicotine self-administration in rats. Pharmacol. Biochem. Behav. 120 , 103–108 (2014).
Musso, F. et al. Smoking impacts on prefrontal attentional network function in young adult brains. Psychopharmacology 191 , 159–169 (2007).
CAS PubMed Google Scholar
Goriounova, N. A. & Mansvelder, H. D. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb. Perspect. Med. 2 , a012120 (2012).
Fagerström, K. O. & Bridgman, K. Tobacco harm reduction: the need for new products that can compete with cigarettes. Addictive Behav. 39 , 507–511 (2014).
Hartmann-Boyce, J. et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 9 , CD010216 (2021).
Jha, P. The hazards of smoking and the benefits of cessation: a critical summation of the epidemiological evidence in high-income countries. eLife https://doi.org/10.7554/eLife.49979 (2020).
Article PubMed PubMed Central Google Scholar
Palipudi, K. M. et al. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS ONE 7 , e33466 (2012).
Goodwin, R. D., Pagura, J., Spiwak, R., Lemeshow, A. R. & Sareen, J. Predictors of persistent nicotine dependence among adults in the United States. Drug Alcohol. Depend. 118 , 127–133 (2011).
Weinberger, A. H. et al. Cigarette use is increasing among people with illicit substance use disorders in the United States, 2002-14: emerging disparities in vulnerable populations. Addiction 113 , 719–728 (2018).
Evans-Polce, R. J., Kcomt, L., Veliz, P. T., Boyd, C. J. & McCabe, S. E. Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. Am. J. Psychiatry 177 , 1073–1081 (2020).
Hassan, A. N. & Le Foll, B. Survival probabilities and predictors of major depressive episode incidence among individuals with various types of substance use disorders. J. Clin. Psychiatry https://doi.org/10.4088/JCP.20m13637 (2021).
Article PubMed Google Scholar
Smith, P. H., Mazure, C. M. & McKee, S. A. Smoking and mental illness in the U.S. population. Tob. Control. 23 , e147–e153 (2014).
Bourgault, Z., Rubin-Kahana, D. S., Hassan, A. N., Sanches, M. & Le Foll, B. Multiple substance use disorders and self-reported cognitive function in U.S. adults: associations and sex-differences in a nationally representative sample. Front. Psychiatry https://doi.org/10.3389/fpsyt.2021.797578 (2022).
Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990-2019. Lancet Public Health 6 , e472–e481 (2021).
Warner, K. E. How to think–not feel–about tobacco harm reduction. Nicotine Tob. Res. 21 , 1299–1309 (2019).
Soneji, S. et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 171 , 788–797 (2017).
Levy, D. T. et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob. Control. 28 , 629–635 (2019).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking — 50 years of progress: a report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Jha, P. & Peto, R. Global effects of smoking, of quitting, and of taxing tobacco. N. Engl. J. Med. 370 , 60–68 (2014). This review covers the impact of tobacco, of quitting smoking and the importance of taxation to impact prevalence of smoking .
Jha, P. & Peto., R. in Tobacco Tax Reform: At the Crossroads of Health and Development . (eds Marquez, P. V. & Moreno-Dodson, B.) 55–72 (World Bank Group, 2017).
Jha, P. et al. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 368 , 341–350 (2013).
Banks, E. et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 13 , 38 (2015).
Pirie, K. et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381 , 133–141 (2013).
Jha, P. et al. A nationally representative case-control study of smoking and death in India. N. Engl. J. Med. 358 , 1137–1147 (2008).
Chan, E. D. et al. Tobacco exposure and susceptibility to tuberculosis: is there a smoking gun? Tuberculosis 94 , 544–550 (2014).
Wang, M. G. et al. Association between tobacco smoking and drug-resistant tuberculosis. Infect. Drug Resist. 11 , 873–887 (2018).
Jha, P. et al. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 368 , 367–370 (2006).
Jha, P., Gelband, H, Irving, H. & Mishra, S. in Reducing Social Inequalities in Cancer: Evidence and Priorities for Research (eds Vaccarella, S et al.) 161–166 (IARC, 2018).
Jha, P. Expanding smoking cessation world-wide. Addiction 113 , 1392–1393 (2018).
Jha, P. Avoidable global cancer deaths and total deaths from smoking. Nat. Rev. Cancer 9 , 655–664 (2009).
Wittenberg, R. E., Wolfman, S. L., De Biasi, M. & Dani, J. A. Nicotinic acetylcholine receptors and nicotine addiction: a brief introduction. Neuropharmacology 177 , 108256 (2020).
Boulter, J. et al. Functional expression of two neuronal nicotinic acetylcholine receptors from cDNA clones identifies a gene family. Proc. Natl Acad. Sci. USA 84 , 7763–7767 (1987).
Couturier, S. et al. A neuronal nicotinic acetylcholine receptor subunit (α7) is developmentally regulated and forms a homo-oligomeric channel blocked by α-BTX. Neuron 5 , 847–856 (1990).
Picciotto, M. R., Addy, N. A., Mineur, Y. S. & Brunzell, D. H. It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog. Neurobiol. 84 , 329–342 (2008).
Changeux, J. P. Structural identification of the nicotinic receptor ion channel. Trends Neurosci. 41 , 67–70 (2018).
McKay, B. E., Placzek, A. N. & Dani, J. A. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem. Pharmacol. 74 , 1120–1133 (2007).
Wonnacott, S. Presynaptic nicotinic ACh receptors. Trends Neurosci. 20 , 92–98 (1997).
Wooltorton, J. R., Pidoplichko, V. I., Broide, R. S. & Dani, J. A. Differential desensitization and distribution of nicotinic acetylcholine receptor subtypes in midbrain dopamine areas. J. Neurosci. 23 , 3176–3185 (2003).
Gipson, C. D. & Fowler, C. D. Nicotinic receptors underlying nicotine dependence: evidence from transgenic mouse models. Curr. Top. Behav. Neurosci. 45 , 101–121 (2020).
Hamouda, A. K. et al. Potentiation of (α4)2(β2)3, but not (α4)3(β2)2, nicotinic acetylcholine receptors reduces nicotine self-administration and withdrawal symptoms. Neuropharmacology 190 , 108568 (2021).
Lallai, V. et al. Nicotine acts on cholinergic signaling mechanisms to directly modulate choroid plexus function. eNeuro https://doi.org/10.1523/ENEURO.0051-19.2019 (2019).
Benwell, M. E., Balfour, D. J. & Anderson, J. M. Evidence that tobacco smoking increases the density of (-)-[3H]nicotine binding sites in human brain. J. Neurochem. 50 , 1243–1247 (1988).
Perry, D. C., Davila-Garcia, M. I., Stockmeier, C. A. & Kellar, K. J. Increased nicotinic receptors in brains from smokers: membrane binding and autoradiography studies. J. Pharmacol. Exp. Ther. 289 , 1545–1552 (1999).
Marks, M. J. et al. Nicotine binding and nicotinic receptor subunit RNA after chronic nicotine treatment. J. Neurosci. 12 , 2765–2784 (1992).
Le Foll, B. et al. Impact of short access nicotine self-administration on expression of α4β2* nicotinic acetylcholine receptors in non-human primates. Psychopharmacology 233 , 1829–1835 (2016).
Meyers, E. E., Loetz, E. C. & Marks, M. J. Differential expression of the beta4 neuronal nicotinic receptor subunit affects tolerance development and nicotinic binding sites following chronic nicotine treatment. Pharmacol. Biochem. Behav. 130 , 1–8 (2015).
Zhao-Shea, R., Liu, L., Pang, X., Gardner, P. D. & Tapper, A. R. Activation of GABAergic neurons in the interpeduncular nucleus triggers physical nicotine withdrawal symptoms. Curr. Biol. 23 , 2327–2335 (2013).
Jensen, K. P., Valentine, G., Gueorguieva, R. & Sofuoglu, M. Differential effects of nicotine delivery rate on subjective drug effects, urges to smoke, heart rate and blood pressure in tobacco smokers. Psychopharmacology 237 , 1359–1369 (2020).
Villanueva, H. F., James, J. R. & Rosecrans, J. A. Evidence of pharmacological tolerance to nicotine. NIDA Res. Monogr. 95 , 349–350 (1989).
Corrigall, W. A., Coen, K. M. & Adamson, K. L. Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res. 653 , 278–284 (1994).
Nisell, M., Nomikos, G. G., Hertel, P., Panagis, G. & Svensson, T. H. Condition-independent sensitization of locomotor stimulation and mesocortical dopamine release following chronic nicotine treatment in the rat. Synapse 22 , 369–381 (1996).
Rice, M. E. & Cragg, S. J. Nicotine amplifies reward-related dopamine signals in striatum. Nat. Neurosci. 7 , 583–584 (2004).
Mameli-Engvall, M. et al. Hierarchical control of dopamine neuron-firing patterns by nicotinic receptors. Neuron 50 , 911–921 (2006).
Picciotto, M. R., Higley, M. J. & Mineur, Y. S. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 76 , 116–129 (2012).
Le Foll, B. et al. Elevation of dopamine induced by cigarette smoking: novel insights from a [11C]-+-PHNO PET study in humans. Neuropsychopharmacology 39 , 415–424 (2014). This brain imaging study identified the brain areas in which smoking elevates dopamine levels .
Maskos, U. et al. Nicotine reinforcement and cognition restored by targeted expression of nicotinic receptors. Nature 436 , 103–107 (2005). This article discusses the implication of the β 2 - containing nAChRs in the VTA in mammalian cognitive function .
Picciotto, M. R. et al. Acetylcholine receptors containing the beta2 subunit are involved in the reinforcing properties of nicotine. Nature 391 , 173–177 (1998). This article discusses the implication of the β 2 - containing nAChRs in addictive effects of nicotine .
Fowler, C. D., Lu, Q., Johnson, P. M., Marks, M. J. & Kenny, P. J. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature 471 , 597–601 (2011). This article discusses the implication of the α5 nicotinic receptor located in the MHb in a mechanism mediating the aversive effects of nicotine .
Elayouby, K. S. et al. α3* Nicotinic acetylcholine receptors in the habenula-interpeduncular nucleus circuit regulate nicotine intake. J. Neurosci. https://doi.org/10.1523/JNEUROSCI.0127-19.2020 (2020).
Ables, J. L. et al. Retrograde inhibition by a specific subset of interpeduncular α5 nicotinic neurons regulates nicotine preference. Proc. Natl Acad. Sci. USA 114 , 13012–13017 (2017).
Frahm, S. et al. Aversion to nicotine is regulated by the balanced activity of β4 and α5 nicotinic receptor subunits in the medial habenula. Neuron 70 , 522–535 (2011).
Jackson, K. J. et al. Role of α5 nicotinic acetylcholine receptors in pharmacological and behavioral effects of nicotine in mice. J. Pharmacol. Exp. Ther. 334 , 137–146 (2010).
Tuesta, L. M. et al. GLP-1 acts on habenular avoidance circuits to control nicotine intake. Nat. Neurosci. 20 , 708–716 (2017).
Salas, R., Pieri, F. & De Biasi, M. Decreased signs of nicotine withdrawal in mice null for the β4 nicotinic acetylcholine receptor subunit. J. Neurosci. 24 , 10035–10039 (2004).
Salas, R., Sturm, R., Boulter, J. & De Biasi, M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J. Neurosci. 29 , 3014–3018 (2009).
Jackson, K. J., Martin, B. R., Changeux, J. P. & Damaj, M. I. Differential role of nicotinic acetylcholine receptor subunits in physical and affective nicotine withdrawal signs. J. Pharmacol. Exp. Ther. 325 , 302–312 (2008).
Le Foll, B. et al. Translational strategies for therapeutic development in nicotine addiction: rethinking the conventional bench to bedside approach. Prog. Neuropsychopharmacol. Biol. Psychiatry 52 , 86–93 (2014).
Naqvi, N. H., Rudrauf, D., Damasio, H. & Bechara, A. Damage to the insula disrupts addiction to cigarette smoking. Science 315 , 531–534 (2007). This article discusses the implication of the insular cortex in tobacco addiction .
Ibrahim, C. et al. The insula: a brain stimulation target for the treatment of addiction. Front. Pharmacol. 10 , 720 (2019).
Zangen, A. et al. Repetitive transcranial magnetic stimulation for smoking cessation: a pivotal multicenter double-blind randomized controlled trial. World Psychiatry 20 , 397–404 (2021). This study validated the utility of deep insula/prefrontal cortex rTMS for smoking cessation .
Le Foll, B., Forget, B., Aubin, H. J. & Goldberg, S. R. Blocking cannabinoid CB1 receptors for the treatment of nicotine dependence: insights from pre-clinical and clinical studies. Addict. Biol. 13 , 239–252 (2008).
Kodas, E., Cohen, C., Louis, C. & Griebel, G. Cortico-limbic circuitry for conditioned nicotine-seeking behavior in rats involves endocannabinoid signaling. Psychopharmacology 194 , 161–171 (2007).
Forget, B. et al. Noradrenergic α1 receptors as a novel target for the treatment of nicotine addiction. Neuropsychopharmacology 35 , 1751–1760 (2010).
Garrett, B. E., Dube, S. R., Babb, S. & McAfee, T. Addressing the social determinants of health to reduce tobacco-related disparities. Nicotine Tob. Res. 17 , 892–897 (2015).
Polanska, K., Znyk, M. & Kaleta, D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health 22 , 72 (2022).
Volkow, N. D. Personalizing the treatment of substance use disorders. Am. J. Psychiatry 177 , 113–116 (2020).
Li, M. D., Cheng, R., Ma, J. Z. & Swan, G. E. A meta-analysis of estimated genetic and environmental effects on smoking behavior in male and female adult twins. Addiction 98 , 23–31 (2003).
Carmelli, D., Swan, G. E., Robinette, D. & Fabsitz, R. Genetic influence on smoking–a study of male twins. N. Engl. J. Med. 327 , 829–833 (1992).
Broms, U., Silventoinen, K., Madden, P. A. F., Heath, A. C. & Kaprio, J. Genetic architecture of smoking behavior: a study of Finnish adult twins. Twin Res. Hum. Genet. 9 , 64–72 (2006).
Kendler, K. S., Thornton, L. M. & Pedersen, N. L. Tobacco consumption in Swedish twins reared apart and reared together. Arch. Gen. Psychiat 57 , 886–892 (2000).
Saccone, N. L. et al. The CHRNA5-CHRNA3-CHRNB4 nicotinic receptor subunit gene cluster affects risk for nicotine dependence in African-Americans and in European-Americans. Cancer Res. 69 , 6848–6856 (2009).
Bierut, L. J. et al. Variants in nicotinic receptors and risk for nicotine dependence. Am. J. Psychiatry 165 , 1163–1171 (2008). This study demonstrates that nAChR gene variants are important in nicotine addiction .
Bierut, L. J. et al. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum. Mol. Genet. 16 , 24–35 (2007).
Berrettini, W. et al. α-5/α-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol. Psychiatry 13 , 368–373 (2008).
Sherva, R. et al. Association of a single nucleotide polymorphism in neuronal acetylcholine receptor subunit alpha 5 (CHRNA5) with smoking status and with ‘pleasurable buzz’ during early experimentation with smoking. Addiction 103 , 1544–1552 (2008).
Thorgeirsson, T. E. et al. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat. Genet. 42 , 448–453 (2010).
Ray, R., Tyndale, R. F. & Lerman, C. Nicotine dependence pharmacogenetics: role of genetic variation in nicotine-metabolizing enzymes. J. Neurogenet. 23 , 252–261 (2009).
Bergen, A. W. et al. Drug metabolizing enzyme and transporter gene variation, nicotine metabolism, prospective abstinence, and cigarette consumption. PLoS ONE 10 , e0126113 (2015).
Mwenifumbo, J. C. et al. Identification of novel CYP2A6*1B variants: the CYP2A6*1B allele is associated with faster in vivo nicotine metabolism. Clin. Pharmacol. Ther. 83 , 115–121 (2008).
Raunio, H. & Rahnasto-Rilla, M. CYP2A6: genetics, structure, regulation, and function. Drug Metab. Drug Interact. 27 , 73–88 (2012).
CAS Google Scholar
Patterson, F. et al. Toward personalized therapy for smoking cessation: a randomized placebo-controlled trial of bupropion. Clin. Pharmacol. Ther. 84 , 320–325 (2008).
Rodriguez, S. et al. Combined analysis of CHRNA5, CHRNA3 and CYP2A6 in relation to adolescent smoking behaviour. J. Psychopharmacol. 25 , 915–923 (2011).
Strasser, A. A., Malaiyandi, V., Hoffmann, E., Tyndale, R. F. & Lerman, C. An association of CYP2A6 genotype and smoking topography. Nicotine Tob. Res. 9 , 511–518 (2007).
Liakoni, E. et al. Effects of nicotine metabolic rate on withdrawal symptoms and response to cigarette smoking after abstinence. Clin. Pharmacol. Ther. 105 , 641–651 (2019).
Di Ciano, P. et al. Influence of nicotine metabolism ratio on [11C]-(+)-PHNO PET binding in tobacco smokers. Int. J. Neuropsychopharmacol. 21 , 503–512 (2018).
Butler, K. et al. Impact of Cyp2a6 activity on nicotine reinforcement and cue-reactivity in daily smokers. Nicotine Tob. Res. https://doi.org/10.1093/ntr/ntab064 (2021).
Benowitz, N. L., Swan, G. E., Jacob, P. 3rd, Lessov-Schlaggar, C. N. & Tyndale, R. F. CYP2A6 genotype and the metabolism and disposition kinetics of nicotine. Clin. Pharmacol. Ther. 80 , 457–467 (2006).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51 , 237–244 (2019).
McKay, J. D. et al. Large-scale association analysis identifies new lung cancer susceptibility loci and heterogeneity in genetic susceptibility across histological subtypes. Nat. Genet. 49 , 1126–1132 (2017).
Chukwueke, C. C. et al. The CB1R rs2023239 receptor gene variant significantly affects the reinforcing effects of nicotine, but not cue reactivity, in human smokers. Brain Behav. 11 , e01982 (2021).
Ahrens, S. et al. Modulation of nicotine effects on selective attention by DRD2 and CHRNA4 gene polymorphisms. Psychopharmacology 232 , 2323–2331 (2015).
Harrell, P. T. et al. Dopaminergic genetic variation moderates the effect of nicotine on cigarette reward. Psychopharmacology 233 , 351–360 (2016).
Lerman, C. et al. Role of functional genetic variation in the dopamine D2 receptor (DRD2) in response to bupropion and nicotine replacement therapy for tobacco dependence: results of two randomized clinical trials. Neuropsychopharmacology 31 , 231–242 (2006).
Le Foll, B., Gallo, A., Le Strat, Y., Lu, L. & Gorwood, P. Genetics of dopamine receptors and drug addiction: a comprehensive review. Behav. Pharmacol. 20 , 1–17 (2009).
Chukwueke, C. C. et al. Exploring the role of the Ser9Gly (rs6280) dopamine D3 receptor polymorphism in nicotine reinforcement and cue-elicited craving. Sci. Rep. 10 , 4085 (2020).
The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. Public Health Service report. Am. J. Prev. Med. 35 , 158–176 (2008).
Hackshaw, A., Morris, J. K., Boniface, S., Tang, J. L. & Milenković, D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 360 , j5855 (2018).
Qin, W. et al. Light cigarette smoking increases risk of all-cause and cause-specific mortality: findings from the NHIS cohort study. Int. J. Env. Res. Public Health https://doi.org/10.3390/ijerph17145122 (2020).
Rodu, B. & Plurphanswat, N. Mortality among male smokers and smokeless tobacco users in the USA. Harm Reduct. J. 16 , 50 (2019).
Kasza, K. A. et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 376 , 342–353 (2017).
Richardson, A., Xiao, H. & Vallone, D. M. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob. Res. 14 , 927–932 (2012).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental disorders 5th edn (American Psychiatric Association, 2013).
World Health Organization. Tobacco fact sheet. WHO https://www.who.int/news-room/fact-sheets/detail/tobacco (2021).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C. & Fagerström, K. O. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br. J. Addict. 86 , 1119–1127 (1991).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W. & Robinson, J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 84 , 791–799 (1989).
Etter, J. F., Le Houezec, J. & Perneger, T. V. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology 28 , 359–370 (2003).
DiFranza, J. R. et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Arch. Pediatr. Adolesc. Med. 156 , 397–403 (2002).
Shiffman, S., Waters, A. & Hickcox, M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 6 , 327–348 (2004).
Smith, S. S. et al. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob. Res. 12 , 489–499 (2010).
Foulds, J. et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob. Res. 17 , 186–192 (2015).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing tobacco use among youth and young adults: a report of the Surgeon General (Centers for Disease Control and Prevention, 2012).
World Health Organization. Tobacco control to improve child health and development. Thematic brief (WHO, 2021).
Lantz, P. M. et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob. Control. 9 , 47–63 (2000).
Leão, T., Kunst, A. E. & Perelman, J. Cost-effectiveness of tobacco control policies and programmes targeting adolescents: a systematic review. Eur. J. Public Health 28 , 39–43 (2018).
Royal College of Physicians. Smoking and health 2021: a coming of age for tobacco control? (RCP, 2021).
Higashi, H. et al. Cost effectiveness of tobacco control policies in Vietnam: the case of population-level interventions. Appl. Health Econ. Health Policy 9 , 183–196 (2011).
Ranson, M. K., Jha, P., Chaloupka, F. J. & Nguyen, S. N. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tob. Res. 4 , 311–319 (2002).
International Agency for Research on Cancer. I ARC Handbooks of Cancer Prevention: Tobacco control Vol. 14 (IARC, 2011).
Frazer, K. et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2 , CD005992 (2016).
Hoffman, S. J. & Tan, C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health 15 , 744 (2015).
McNeill, A. et al. Tobacco packaging design for reducing tobacco use. Cochrane Database Syst. Rev. 4 , CD011244 (2017).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General (Department of Health and Human Services, 2020).
Lindson, N. et al. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 4 , CD013308 (2019).
Krist, A. H. et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA 325 , 265–279 (2021).
Tutka, P. & Zatonski, W. Cytisine for the treatment of nicotine addiction: from a molecule to therapeutic efficacy. Pharmacol. Rep. 58 , 777–798 (2006).
Courtney, R. J. et al. Effect of cytisine vs varenicline on smoking cessation: a randomized clinical trial. JAMA 326 , 56–64 (2021).
Walker, N. et al. Cytisine versus nicotine for smoking cessation. N. Engl. J. Med. 371 , 2353–2362 (2014). This study validated the utility of cytisine for smoking cessation .
West, R. et al. Placebo-controlled trial of cytisine for smoking cessation. N. Engl. J. Med. 365 , 1193–1200 (2011).
Hajek, P. et al. E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technol. Assess. 23 , 1–82 (2019).
Walker, N. et al. Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. Lancet Respir. Med. 8 , 54–64 (2020).
Siu, A. L., U.S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 163 , 622–634 (2015).
Black, N. et al. Behaviour change techniques associated with smoking cessation in intervention and comparator groups of randomized controlled trials: a systematic review and meta-regression. Addiction 115 , 2008–2020 (2020).
Center for Substance Abuse and Treatment. Detoxification and Substance Abuse Treatment (Center for Substance Abuse and Treatment, 2006).
Cahill, K., Hartmann-Boyce, J. & Perera, R. Incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub5 (2015).
Secades-Villa, R., Aonso-Diego, G., García-Pérez, Á. & González-Roz, A. Effectiveness of contingency management for smoking cessation in substance users: a systematic review and meta-analysis. J. Consult. Clin. Psychol. 88 , 951–964 (2020).
Cahill, K. & Perera, R. Competitions and incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub4 (2011).
Trojak, B. et al. Transcranial magnetic stimulation combined with nicotine replacement therapy for smoking cessation: a randomized controlled trial. Brain Stimul. 8 , 1168–1174 (2015).
Wing, V. C. et al. Brain stimulation methods to treat tobacco addiction. Brain Stimul. 6 , 221–230 (2013).
Dinur-Klein, L. et al. Smoking cessation induced by deep repetitive transcranial magnetic stimulation of the prefrontal and insular cortices: a prospective, randomized controlled trial. Biol. Psychiatry 76 , 742–749 (2014).
Goldenberg, M., Danovitch, I. & IsHak, W. W. Quality of life and smoking. Am. J. Addict. 23 , 540–562 (2014).
Heikkinen, H., Jallinoja, P., Saarni, S. I. & Patja, K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicotine Tob. Res. 10 , 1199–1207 (2008).
Moayeri, F., Hsueh, Y. A., Dunt, D. & Clarke, P. Smoking cessation and quality of life: insights from analysis of longitudinal Australian data, an application for economic evaluations. Value Health 24 , 724–732 (2021).
Taylor, G. M. et al. Smoking cessation for improving mental health. Cochrane Database Syst. Rev. 3 , CD013522 (2021).
López-Nicolás, Á., Trapero-Bertran, M. & Muñoz, C. Smoking, health-related quality of life and economic evaluation. Eur. J. Health Econ. 19 , 747–756 (2018).
Morris, A. Linking nicotine addiction and T2DM. Nat. Rev. Endocrinol. 16 , 6 (2020).
Willi, C., Bodenmann, P., Ghali, W. A., Faris, P. D. & Cornuz, J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama 298 , 2654–2664 (2007).
World Health Organization. WHO report on the global tobacco epidemic (WHO, 2019).
Donny, E. C. et al. Randomized trial of reduced-nicotine standards for cigarettes. N. Engl. J. Med. 373 , 1340–1349 (2015). This study tested the impact of reducing the quantity of nicotine present in cigarettes on smoking .
Benowitz, N. L. & Henningfield, J. E. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N. Engl. J. Med. 331 , 123–125 (1994).
Benowitz, N. L. & Henningfield, J. E. Reducing the nicotine content to make cigarettes less addictive. Tob. Control. 22 , i14–i17 (2013).
Gottlieb, S. & Zeller, M. A nicotine-focused framework for public health. N. Engl. J. Med. 377 , 1111–1114 (2017).
Hall, W. & West, R. Thinking about the unthinkable: a de facto prohibition on smoked tobacco products. Addiction 103 , 873–874 (2008).
Ioannidis, J. P. A. & Jha, P. Does the COVID-19 pandemic provide an opportunity to eliminate the tobacco industry? Lancet Glob. Health 9 , e12–e13 (2021).
Smokefree. Smokefree 2025. Smokefree https://www.smokefree.org.nz/smokefree-in-action/smokefree-aotearoa-2025 (2021).
Morgan, C. J., Das, R. K., Joye, A., Curran, H. V. & Kamboj, S. K. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict. Behav. 38 , 2433–2436 (2013).
Elsaid, S., Kloiber, S. & Le Foll, B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog. Mol. Biol. Transl. Sci. 167 , 25–75 (2019).
Butler, K. & Le Foll, B. Novel therapeutic and drug development strategies for tobacco use disorder: endocannabinoid modulation. Expert Opin. Drug Discov. 15 , 1065–1080 (2020).
D’Souza, D. C. et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2a single-site randomised controlled trial. Lancet Psychiatry 6 , 35–45 (2019).
Robinson, J. D. et al. Pooled analysis of three randomized, double-blind, placebo controlled trials with rimonabant for smoking cessation. Addict. Biol. 23 , 291–303 (2018).
Gueye, A. B. et al. The CB1 neutral antagonist AM4113 retains the therapeutic efficacy of the inverse agonist rimonabant for nicotine dependence and weight loss with better psychiatric tolerability. Int. J. Neuropsychopharmacol. https://doi.org/10.1093/ijnp/pyw068 (2016).
Yammine, L. et al. Exenatide adjunct to nicotine patch facilitates smoking cessation and may reduce post-cessation weight gain: a pilot randomized controlled trial. Nicotine Tob. Res. 23 , 1682–1690 (2021).
Eren-Yazicioglu, C. Y., Yigit, A., Dogruoz, R. E. & Yapici-Eser, H. Can GLP-1 be a target for reward system related disorders? A qualitative synthesis and systematic review analysis of studies on palatable food, drugs of abuse, and alcohol. Front. Behav. Neurosci. 14 , 614884 (2020).
Vanderkam, P. et al. Effectiveness of drugs acting on adrenergic receptors in the treatment for tobacco or alcohol use disorders: systematic review and meta-analysis. Addiction 116 , 1011–1020 (2021).
Sokoloff, P. & Le Foll, B. The dopamine D3 receptor, a quarter century later. Eur. J. Neurosci. 45 , 2–19 (2017).
David, S. P., Lancaster, T., Stead, L. F., Evins, A. E. & Prochaska, J. J. Opioid antagonists for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003086.pub3 (2013).
Ray, L. A. et al. Efficacy of combining varenicline and naltrexone for smoking cessation and drinking reduction: a randomized clinical trial. Am. J. Psychiatry 178 , 818–828 (2021).
Mooney, M. E. et al. Bupropion and naltrexone for smoking cessation: a double-blind randomized placebo-controlled clinical trial. Clin. Pharmacol. Ther. 100 , 344–352 (2016).
Justinova, Z., Le Foll, B., Redhi, G. H., Markou, A. & Goldberg, S. R. Differential effects of the metabotropic glutamate 2/3 receptor agonist LY379268 on nicotine versus cocaine self-administration and relapse in squirrel monkeys. Psychopharmacology 233 , 1791–1800 (2016).
Le Foll, B., Wertheim, C. E. & Goldberg, S. R. Effects of baclofen on conditioned rewarding and discriminative stimulus effects of nicotine in rats. Neurosci. Lett. 443 , 236–240 (2008).
Franklin, T. R. et al. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol. Depend. 103 , 30–36 (2009).
Lotfy, N., Elsawah, H. & Hassan, M. Topiramate for smoking cessation: systematic review and meta-analysis. Tob. Prev. Cessat. 6 , 14 (2020).
Shanahan, W. R., Rose, J. E., Glicklich, A., Stubbe, S. & Sanchez-Kam, M. Lorcaserin for smoking cessation and associated weight gain: a randomized 12-week clinical trial. Nicotine Tob. Res. 19 , 944–951 (2017).
Higgins, G. A., Fletcher, P. J. & Shanahan, W. R. Lorcaserin: a review of its preclinical and clinical pharmacology and therapeutic potential. Pharmacol. Ther. 205 , 107417 (2020).
Stead, L. F. & Lancaster, T. Interventions to reduce harm from continued tobacco use. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD005231.pub2 (2007).
Download references
Acknowledgements
B.Le F. is supported by a clinician-scientist award from the Department of Family and Community Medicine at the University of Toronto and the Addiction Psychiatry Chair from the University of Toronto. The funding bodies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The authors thank H. Fu (University of Toronto) for assistance with Figs 1–3.
Author information
Authors and affiliations.
Translational Addiction Research Laboratory, Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada
Bernard Le Foll
Departments of Family and Community Medicine, Psychiatry, Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada
Department of Medicine, University of Wisconsin, Madison, WI, USA
Megan E. Piper
University of Wisconsin Center for Tobacco Research and Intervention, Madison, WI, USA
Department of Neurobiology and Behaviour, University of California Irvine, Irvine, CA, USA
Christie D. Fowler
Section for Preventive Cardiology, Department of Endocrinology, Morbid Obesity and Preventive Medicine, Oslo University Hospital, Oslo, Norway
Serena Tonstad
Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, USA
Laura Bierut
Institute of Mental Health, Peking University Sixth Hospital, Peking University, Beijing, China
National Institute on Drug Dependence, Peking University Health Science Center, Beijing, China
Centre for Global Health Research, Unity Health Toronto, University of Toronto, Toronto, Ontario, Canada
- Prabhat Jha
National Centre for Youth Substance Use Research, The University of Queensland, St Lucia, Queensland, Australia
Wayne D. Hall
Queensland Alliance for Environmental Health Sciences, The University of Queensland, Woolloongabba, Queensland, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (B.Le F.); Epidemiology (P.J. and W.D.H.); Mechanisms/pathophysiology (C.D.F., L.B., L.L. and B.Le F.); Diagnosis, screening and prevention (P.J., M.E.P., S.T. and B.Le F.); Management (M.E.P., S.T., W.D.H., L.L. and B.Le F.); Quality of life (P.J. and W.D.H.); Outlook (all); Conclusions (all). All authors contributed substantially to the review and editing of the manuscript.
Corresponding author
Correspondence to Bernard Le Foll .
Ethics declarations
Competing interests.
B.Le F. has obtained funding from Pfizer (GRAND Awards, including salary support) for investigator-initiated projects. B.Le F. has received some in-kind donations of cannabis product from Aurora and medication donation from Pfizer and Bioprojet and was provided a coil for TMS study from Brainsway. B.Le F. has obtained industry funding from Canopy (through research grants handled by CAMH or the University of Toronto), Bioprojet, ACS, Indivior and Alkermes. B.Le F. has received in-kind donations of nabiximols from GW Pharma for past studies funded by CIHR and NIH. B.Le F. has been an advisor to Shinoghi. S.T. has received honoraria from Pfizer the manufacturer of varenicline for lectures and advice. All other authors declare no competing interests.
Peer review
Peer reviewer information.
Nature Reviews Disease Primers thanks Jamie Brown, Elisardo Iglesias and Ming Li for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
CTRI website: https://d3futrf33lk36a.cloudfront.net/wp-content/uploads/sites/240/2019/04/Meds-Chart.pdf
Philip Morris International: https://www.pmi.com/
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Le Foll, B., Piper, M.E., Fowler, C.D. et al. Tobacco and nicotine use. Nat Rev Dis Primers 8 , 19 (2022). https://doi.org/10.1038/s41572-022-00346-w
Download citation
Accepted : 07 February 2022
Published : 24 March 2022
DOI : https://doi.org/10.1038/s41572-022-00346-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrated mrna- and mirna-sequencing analyses unveil the underlying mechanism of tobacco pollutant-induced developmental toxicity in zebrafish embryos.
- Jiasheng Chen
- Xiaoping Zhong
Journal of Translational Medicine (2024)
Influence of substance use on male reproductive health and offspring outcomes
- Jamie O. Lo
- Jason C. Hedges
- Charles A. Easley
Nature Reviews Urology (2024)
Reductions in smoking due to ratification of the Framework Convention for Tobacco Control in 171 countries
- Guillermo Paraje
- Mauricio Flores Muñoz
Nature Medicine (2024)
Impact of benzoic acid and 2,2’-methylenebis (6-tert-butyl-4-methylphenol) on the metabolome of flue-cured tobacco and rhizosphere microbial communities: implications for continuous cropping obstacles
- Qiulian Peng
- Jiayan Zhang
Plant and Soil (2024)
Nicotinic regulation of microglia: potential contributions to addiction
- Alexa R. Soares
- Marina R. Picciotto
Journal of Neural Transmission (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Perceptions of health risks of cigarette smoking: A new measure reveals widespread misunderstanding
Affiliation Department of Communication, Stanford University, Stanford, California, United States of America
Affiliation Graduate School of Business, Stanford University, Stanford, California, United States of America
* E-mail: [email protected]
Affiliations Department of Political Science, Vanderbilt University, Nashville, Tennessee, United States of America, Hoover Institution, Stanford University, Stanford, California, United States of America
Affiliation U.S. Department of Treasury, Washington, D.C., United States of America
Affiliation LinChiat Chang Consulting, LLC, San Francisco, California, United States of America
Affiliation Department of Communication Studies, University of Michigan, Ann Arbor, Michigan, United States of America
Affiliation GfK Custom Research North America, New York City, New York, United States of America
- Jon A. Krosnick,
- Neil Malhotra,
- Cecilia Hyunjung Mo,
- Eduardo F. Bruera,
- LinChiat Chang,
- Josh Pasek,
- Randall K. Thomas

- Published: August 14, 2017
- https://doi.org/10.1371/journal.pone.0182063
- Reader Comments
15 Feb 2019: Krosnick JA, Malhotra N, Mo CH, Bruera EF, Chang L, et al. (2019) Correction: Perceptions of health risks of cigarette smoking: A new measure reveals widespread misunderstanding. PLOS ONE 14(2): e0212705. https://doi.org/10.1371/journal.pone.0212705 View correction
Most Americans recognize that smoking causes serious diseases, yet many Americans continue to smoke. One possible explanation for this paradox is that perhaps Americans do not accurately perceive the extent to which smoking increases the probability of adverse health outcomes. This paper examines the accuracy of Americans’ perceptions of the absolute risk, attributable risk, and relative risk of lung cancer, and assesses which of these beliefs drive Americans’ smoking behavior. Using data from three national surveys, statistical analyses were performed by comparing means, medians, and distributions, and by employing Generalized Additive Models. Perceptions of relative risk were associated as expected with smoking onset and smoking cessation, whereas perceptions of absolute risk and attributable risk were not. Additionally, the relation of relative risk with smoking status was stronger among people who held their risk perceptions with more certainty. Most current smokers, former smokers, and never-smokers considerably underestimated the relative risk of smoking. If, as this paper suggests, people naturally think about the health consequences of smoking in terms of relative risk, smoking rates might be reduced if public understanding of the relative risks of smoking were more accurate and people held those beliefs with more confidence.
Citation: Krosnick JA, Malhotra N, Mo CH, Bruera EF, Chang L, Pasek J, et al. (2017) Perceptions of health risks of cigarette smoking: A new measure reveals widespread misunderstanding. PLoS ONE 12(8): e0182063. https://doi.org/10.1371/journal.pone.0182063
Editor: Raymond Niaura, Legacy, Schroeder Institute for Tobacco Research and Policy Studies, UNITED STATES
Received: May 7, 2016; Accepted: June 20, 2017; Published: August 14, 2017
This is an open access article, free of all copyright, and may be freely reproduced, distributed, transmitted, modified, built upon, or otherwise used by anyone for any lawful purpose. The work is made available under the Creative Commons CC0 public domain dedication.
Data Availability: Data are available at: https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/JP2JHH , doi: 10.7910/DVN/JP2JHH .
Funding: LC and RKT have commercial affiliations with LinChiat Chang Consulting and GfK Custom Research North America, respectively. These companies provided support in the form of salaries for authors LC and RKT, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
Competing interests: LC and RKT have commercial affiliations with LinChiat Chang Consulting and GfK Custom Research North America, respectively. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
Introduction
Despite a constant flow of messages reminding Americans of the health risks of cigarette smoking, and despite a steady decline in the proportion of Americans who smoke during the last 50 years, more than 20% of Americans continue to smoke regularly today [ 1 ]. This paper explores whether the continued prevalence of smoking may, in part, stem from a failure to acknowledge these risks. At first blush, this assertion may seem patently implausible; much research indicates that increasingly large proportions of Americans recognize the various dangers of smoking, and some studies even suggest that most Americans overestimate the proportion of smokers who suffer from certain smoking-related ailments [ 2 ]. Nonetheless, it is possible that people underestimate the magnitude of some of the health risks caused by smoking. Because individuals seem to base their decisions about whether to smoke on how they believe the act of smoking changes the risk of contracting specific diseases, correcting any underestimation of risk may yield future reductions in smoking onset and increases in cessation [ 3 ]. To explore these possibilities, we conducted three studies of national samples of American adults documenting risk perceptions and their relations to smoking behavior.
Challenges in the study of risk perception
One way to gauge the accuracy of people’s perceptions of the health dangers of smoking is to focus simply on the list of maladies that become more likely as a result of smoking. This list includes various cancers, heart diseases, respiratory diseases, premature death, and more [ 4 , 5 ]. By asking representative national samples of American adults to identify which diseases and medical conditions on a provided list are linked with smoking, researchers have illuminated three interesting patterns. First, since the 1950s, the proportion of Americans who failed to identify any health risks of smoking dropped consistently [ 6 ]. Second, according to Gallup [ 7 ], a sizable proportion of Americans still fails to recognize a link between smoking and some related ailments (see S1 Fig ). Other contemporary surveys support these same conclusions [ 8 – 10 ]. The proportion of American adults who associate smoking with a particular ailment varies considerably across ailments, from a high of 81% who report a link between smoking and cancer to single-digit proportions who identify links with asthma, hypertension, bronchitis, and stroke [ 11 ]. Thus, even today, Americans apparently underestimate the breadth of the danger.
A more refined way to gauge the accuracy of perceptions is to focus on the amount of increased risk of each malady that results from smoking. According to epidemiological studies, each of these increases is a function of many attributes, including age of smoking onset, number of years of regular smoking, number of cigarettes consumed per day, and more [ 4 , 5 ]. Therefore, actual risks must be expressed as variables that are functions of such factors, and perceptions of these risks must be ascertained specifying such factors.
Furthermore, even holding constant age of onset, length of smoking, and dosage, a smoking-related risk can be perceived in three different ways: (1) absolute risk (i.e., “what is the chance that a person will get lung cancer if he/she smokes?”), (2) attributable risk (i.e., “how much does smoking raise the chances that a person will get lung cancer compared to not smoking?”), and (3) relative risk (i.e., “how much more likely is a person to get lung cancer if he/she smokes?”) [ 12 , 13 ]. Mausner and Bahn [ 14 ] provide a thorough review of how epidemiologists calculate and use each of these different measures of risk. Assessing Americans’ perceptions of all three seems most sensible in order to determine whether people tend to perceive all types of risk accurately, overestimate all types of risk, underestimate all types of risk, or overestimate some while underestimating others. Attributable fraction is another measure of risk perceptions, but we do not investigate this measure in this study [ 15 ].
One way to think about the goal of such an investigation is to identify any ways in which people underestimate risk, so that public health education campaigns can correct this misunderstanding. But it could turn out that people underestimate one particular type of risk (e.g., absolute risk) and yet do not use that particular perception of risk in their decision-making about whether to start or stop smoking. Therefore, efforts to correct the public’s misunderstanding would not translate into changes in smoking behavior. So to draw out implications of measurements of perceived risk, we need evidence indicating which perceptions may be behaviorally consequential.
The research described in this paper set out to do so by gauging perceptions of absolute risk, attributable risk, and relative risk with a focus specifically on lung cancer. And we explored which of these risk perceptions might drive smoking onset and cessation. We focus on lung cancer specifically rather than all health risks associated with smoking following Viscusi’s seminal work on smoking-related risks [ 2 ]. While the share of American adults who associate smoking with a particular health malady varies across maladies [ 11 ], an assessment of which type of risk perception—absolute risk, attributable risk, and relative risk—impacts Americans’ smoking behavior the most should not be sensitive to the health malady of interest. In other words, if perceptions of relative risk of lung cancer affects smoking behavior more than perceptions of absolute and attributable risk of lung cancer, then perceptions of relative risk of another disease should similarly be most effective at driving smoking behavior.
Prior studies of perceptions of the magnitude of risk
A number of past studies have attempted to measure perceptions of the magnitude of the risk of smoking in representative samples of American adults, but their methodologies entailed a series of limitations, as we outline next. It is worth noting that this paper focuses on the U.S. and therefore does not discuss the many interesting studies of smoking-related risk perceptions that have been done in countries other than the U.S [ 16 – 18 ].
We also do not discuss studies that examined people’s perceptions of their own personal smoking-related risks (e.g., Boney-McCoy et al. [ 19 ]; Strecher et al. [ 20 ]) because our focus is on Americans’ perceptions of the risk of smoking to people in general. Many studies have produced interesting results involving people’s perceptions of their own personal risks of smoking-related health problems (e.g., [ 19 , 21 – 27 ]). However, according to Gigerenzer [ 28 ], people naturally think about the population rather than personal chance, and perceptions of personal risk likely mediate the relationship between general risk and behavior.
Because this paper is focused on the beliefs of adults, we also do not discuss the findings of many interesting studies of youth. For example, Romer and Jamieson [ 29 ] asked questions similar to Viscusi’s [ 2 ] of a national sample of 14- and 15-year-olds: “Out of every 100 cigarette smokers, how many do you think will: (a) get lung cancer because they smoke? (b) have heart problems, like a heart attack, because they smoke? (c) die from a smoking-related illness?” Their results mirror Viscusi’s [ 2 ]: on average; respondents said 61.4% of smokers would develop lung cancer, much higher than the true rate. Likewise, a representative sample of 20–22 year olds said 52.6% on average. Many other studies have explored the beliefs of children and adolescents as well [ 21 , 30 – 37 ].
Some past studies have asked people to describe their perceptions of the magnitude of a smoking-related risk of some malady by asking people to select a point on a rating scale with a small number of verbally labeled response options. For example, Weinstein et al. [ 27 ] asked “How likely do you think it is that (the average male cigarette smoker/the average female cigarette smoker/you) will develop lung cancer in the future?” and offered a 5-point scale ranging from “very low” to “very high.” Similarly, Romer and Jamieson [ 29 ] asked respondents “In your opinion, is smoking very risky for a person’s health, somewhat risky, only a little risky, or not risky at all?” It is not clear whether “somewhat risky” or “very risky” is an overestimate or underestimate of risk. In other words, measures that assess perceptions of smoking’s dangers on these non-numeric subjective probability scales do not permit assessing the degree to which magnitudes of perceived risk reflect true numeric risk levels.
Other studies have measured perceptions of risks quantitatively but did not specify the population of people being described or the dosage of smoking being addressed. For example, in a survey conducted by Audits & Surveys Worldwide, respondents were asked, “Among 100 cigarette smokers, how many of them do you think will get lung cancer because they smoke?” [ 2 ]. The characteristics of a smoker are important contextual considerations with regards to actual health risks a given smoker faces. The probabilities of various smoking-related ailments differ for occasional and daily smokers and depend on the age of a smoker as well as the duration of smoking. Because this type of question does not specify what population is to be described or how much smoking was done for how long, it is impossible to gauge the accuracy of responses by comparing them with the results of epidemiological studies, which show risk to vary across populations and age, smoking duration, and dosage. Some scholarly work has begun to remedy this issue, specifying the exact quantity of cigarettes smoked per day [ 38 ].
Another potential limitation of the Audits & Surveys question is the phrase “because they smoke.” This phrase was presumably meant to lead respondents to estimate the number of lung cancer cases completely attributable to smoking. As Slovic [ 36 ] observed, this phrase can be interpreted in various different ways. Specifically, people may believe that smoking, along with other factors, enhances the chances of contracting lung cancer, leading them to respond that smoking is partially responsible for some lung cancer cases. This, too, makes it difficult to identify the appropriate true rate of smoking-induced lung cancer cases to which to compare risk perceptions.
Finally, the notions of “subadditivity” and “the focus of judgment effect” point to another potential problem with the Audits & Surveys question [ 39 – 41 ]. The question, “Among 100 cigarette smokers, how many of them do you think will get lung cancer because they smoke?” focuses respondents’ attention on just one possible outcome of smoking: getting lung cancer. This approach typically leads to overestimation of the probability of the event in question. Asking respondents instead to report the number of smokers who will not get lung cancer would focus attention on that outcome instead, probably leading to overstatement of that probability. So the sum of the average answers to these two forms of the question would most likely total more than 100. A more desirable measurement approach would overcome the bias induced by arbitrarily asking about only one outcome (e.g., either getting lung cancer or not getting lung cancer).
The present research
To overcome the limitations of past studies, we conducted three surveys measuring Americans’ beliefs about smoking-related health risks in different ways. To gauge perceived risk, we asked two questions: one about the risk to nonsmokers, and the other about the risk to smokers. This approach is advantageous if a researcher wants to measure perceptions of attributable risk or relative risk, because (1) subadditivity is likely to bias both reports upward, so subtracting or dividing one judgment from or by the other will minimize the impact of overestimation, (2) answers to these questions can be used to generate assessments of perceived absolute risk, attributable risk, and relative risk, and (3) this approach employs the principle of decomposition, which enhances the accuracy of measures of people’s beliefs [ 15 ]. It is worth noting one limitation of our research is the fact that we only ask about lung cancer, and do not consider other health risks linked with smoking. However, most likely people’s perceptions of risk across multiple disease categories would be positively correlated. Consequently, our general conclusions about lung cancer would likely be similar if respondents were forced to consider multiple disease categories.
In decomposition, a single, global judgment is broken down into a series of sub-judgments, each of which a respondent must make in the process of generating the global judgment. Here, in order to gauge people’s perceptions of relative risk, we could ask, “how many more times likely is a smoker to get lung cancer than a nonsmoker?” To answer the global question, a respondent must estimate both the likelihood a nonsmoker will get lung cancer and estimate the likelihood that a smoker will get lung cancer, and then mentally compute the ratio of the probabilities. Because respondents can accidentally make a computational error when executing that last step, surveyors can more accurately measure people’s beliefs by asking directly about the sub-judgments, leaving the researcher to compute the ratio. The same logic applies to the measurement of perceived attributable risk (see S1 Appendix for a discussion of measuring probabilities and numeracy).
When measuring perceptions of the lung cancer risks of nonsmokers and smokers, we expressed specifically a volume of smoking and at what age it began, so we could more accurately gauge the extent to which people overestimated or under-estimated the health risks of smoking. And rather than asking survey respondents to report probabilities, we asked them to report frequencies, since a variety of studies suggest that people think more naturally in terms of frequencies [ 42 , 43 ].
We compared the three risk perception measures (absolute, attributable, and relative risk) in terms of their associations with cessation among a sample of current and former smokers. We also compared the risk perception measures in terms of their associations with the desire to quit among current smokers. Although previous studies have found positive and significant correlations between risk perceptions and the desire to quit, none of these studies compared different risk perception measures to one another or analyzed numerical risk estimates [ 27 , 44 , 45 ].
Such associations can occur for at least two reasons. First, beliefs about the health risks of smoking may be instigators of smoking cessation (for a review of this literature, see S2 Appendix ). Second, people may adjust their beliefs about smoking’s health risks in order to rationalize their status as a smoker or a non-smoker [ 46 – 48 ]. If perceptions of health risks are motivators of smoking cessation and/or if quitting smoking induces people to inflate their risk perceptions, then perceived risk should be lower among people who currently smoke than among people who have quit. That is, the higher a person’s perceived risk, the more likely he or she is to have quit. Likewise, the higher a current smoker’s perception of risk, the more motivated he or she should be to quit smoking. Therefore, the more strongly a risk perception measure is associated with whether a person has quit smoking and a smoker’s desire to quit, the more likely that risk perception is to capture the way people naturally think about risk in this arena.
Many possible patterns of risk perception types could be found in a population. The most heterogeneous pattern would be one in which one-third of people think in terms of absolute risk, while another one-third of people think in terms of attributable risk, and the remaining people think in terms of relative risk. The most homogeneous case would be one in which everyone thinks in terms of just one of these risk perceptions to make behavioral choices regarding smoking. Our analyses explored the extent of use of each of the three risk perception measures.
We also explored whether people who felt more certain about risk perceptions manifested stronger relations of those perceptions with cessation and desire to quit. Psychological research on attitude strength suggests that people hold beliefs and attitudes with varying degrees of certainty, and beliefs held with more certainty are more likely to shape thinking and action [ 49 ]. Therefore, we explored whether any of the risk perceptions were more strongly related to cessation among people who held their risk perceptions with more certainty.
Three studies
Our three studies explored five main questions: (1) How many people overestimate and underestimate absolute risk, attributable risk, and relative risk of lung cancer due to smoking? (2) How strongly are perceived absolute risk, attributable risk, and relative risk related to quitting? (3) How strongly are perceived absolute risk, attributable risk, and relative risk related to desire to quit among current smokers? (4) Are the relations between risk perceptions and quitting strongest among respondents who are most certain about their risk perceptions? (5) How strongly are perceived absolute risk, attributable risk, and relative risk related to having initiated smoking?
Study 1 was a random digit dial telephone survey of a nationally representative sample of American adults who were current or former smokers, conducted in 2000 by Schulman, Ronca, and Bucuvalas, Inc. (hereafter SRBI). Study 2 was a 2006 survey of a national non-representative sample of current and former smokers who volunteered to complete Internet surveys for Harris Interactive in exchange for points that could be redeemed for gifts. Study 3 was a 2009 survey of a nationally representative sample of all Americans, including people who had never smoked, via the Face-to-Face Recruited Internet Survey Platform (the FFRISP; see S3 Appendix for descriptions of the methodologies of the three studies, and see S4 Appendix for the demographic characteristics of the three samples).
The telephone survey respondents who were current or former smokers were asked:
(1) “Next, I'd like to turn to a different topic: what you personally think about the effect of cigarette smoking on people's health. I'm going to read these next two questions very slowly to let you think about each part of them, and I can repeat each question as many times as you like before you answer, so you can be sure they are clear to you. First, if we were to randomly choose one thousand American adults who never smoked cigarettes at all during their lives, how many of those one thousand people do you think would get lung cancer sometime during their lives?” (2) “And if we were to randomly choose one thousand American adults who each smoked one pack of cigarettes a day every day for 20 years starting when they were 20 years old, how many of those one thousand people do you think would get lung cancer sometime during their lives?” (3) “You said that smokers are [more likely/as likely/less likely] to get lung cancer than nonsmokers. How certain are you about this? Extremely certain, very certain, moderately certain, slightly certain, or not certain at all?”
We ask respondents to assess the prospect of lung cancer incidence generally like Viscusi [ 2 ]. We emphasized “personally” so that people would feel comfortable providing their own best guess of a fact, specifically general population risk of contracting lung cancer. This wording is designed to avoid the question seeming like a “quiz” (or their guess of what a public health authority might say), but rather their personal assessment of risk. For the two Internet surveys, the wording was adapted for self-administration. In all three studies, the response choices for the last question were presented in descending order for a randomly chosen half of the respondents and in ascending order for the other half. By implementing the same internally valid research design three separate times, it is possible to assess whether our findings are replicable.
Each of the three studies discussed above were deemed as suitable for exempt IRB review status by Stanford University’s review board, as no identifying information on the respondents was retained, and disclosure of answers to the survey questions would not place the respondents at risk. Informed consent for Study 1 was provided verbally given that Study 1 was a telephone survey. Written informed consent was provided for both Study 2 and Study 3, and Stanford’s IRB approved use of oral consent in Study 1 and written consent in Study 2 and 3.
Actual risk
We used data reported by Peto et al. [ 50 ] to compute the actual absolute risk, attributable risk, and relative risk of contracting lung cancer for one-pack-a-day smokers who started smoking at age 20 and smoked for 20 years. To do so, we divided the absolute risk of mortality due to lung cancer among these smokers (about 3%) by the absolute risk of mortality due to lung cancer among non-smokers (about 0.4%, yielding a relative risk of about 7). Although Peto et al. [ 50 ] examined mortality instead of incidence, the probability of dying from lung cancer conditional on developing lung cancer is 74.4% within a thirteen-year period according to Marcus et al. [ 51 ], and even higher among smokers [ 52 ]. If relative risk is higher, then our results understate the proportion of Americans who underestimate this relative risk. According to these figures, the attributable risk of lung cancer due to smoking is then about 3% (3% minus 0.4%, rounds to 3%). It is worth noting that although one might imagine that it is difficult to estimate risk rates because of complex functional forms, interactions of smoking with other risk factors, cohort effects, and other complications, research suggests that in fact, risk rates are largely robust to some potential complexities [ 53 – 55 ].
Perceived risk
In Study 1, the mean of current and former smokers’ perceptions of absolute risk of lung cancer among smokers was 48% (i.e., 480.1 smokers out of 1,000 smokers would get lung cancer); the median was 50% (see columns 1 and 2 of Table 1 ). 10.3% of respondents perceived absolute risks between 0% and 5.0%, and the remaining respondents gave answers above 5.0%. 99.5% of respondents overestimated absolute risk, only about 0.3% estimated it correctly (by giving an answer of 30), and 0.2% underestimated it (by giving an answer less than 30).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0182063.t001
As expected, the mean and median perceived absolute risk of nonsmokers getting lung cancer were less: 22% and 10%, respectively. Thirty-six percent of respondents gave answers between 0% and 5.0%. Thus, most people vastly overestimated this absolute risk.
Only 5.2% of respondents thought smokers were less likely to get lung cancer than nonsmokers (a belief revealed by attributable risks less than 0; see columns 1 and 2 of Table 2 ). Attributable risk was calculated by subtracting each respondent’s answer to the question about nonsmokers from his or her answer to the question about smokers. 9.6% of respondents thought smokers and nonsmokers were equally likely to contract lung cancer, reporting an attributable risk of 0. A large majority, 85.2% of respondents, reported that smokers were more likely than nonsmokers to contract lung cancer. 76.1% overestimated attributable risk by reporting figures greater than 4%. The mean perceived attributable risk was about 27%, and the median was 20%.
https://doi.org/10.1371/journal.pone.0182063.t002
In contrast, a large majority of respondents (74.6%) underestimated relative risk, because they reported perceptions that implied a relative risk less than 7 (see columns 1 and 2 of Table 3 ). Relative risk was computed by dividing each respondent's answer to the question about 1,000 smokers by his or her answer to the question about 1,000 nonsmokers. Because this quantity is undefined for respondents who said none of the 1,000 nonsmokers would get lung cancer (because the denominator would be zero), 1 was added to these respondents’ answers to the questions about smokers and nonsmokers to allow the relative risk quantity to be defined for all respondents. Note that re-computing all analyses reported below treating these people as having missing data on the relative risk measure had negligible impact on the reported results. 54.6% of the respondents could be said to have vastly underestimated relative risk, because their reports implied a value less than 3. Only about 1.5% of respondents perceived relative risk approximately correctly (e.g., 7), and only 23.9% of respondents overestimated relative risk. 5.2% of respondents perceived a relative risk of less than 1, meaning they thought smokers developed lung cancer less often than nonsmokers, and 9.6% of the sample perceived a relative risk of 1.0, meaning they thought smokers and nonsmokers were equally likely to develop lung cancer. Mean perceived relative risk was 26.7, much higher than the true value, and the median was 2.5, lower than the true value. Thus, relative risk tells a very different story about the prevalent errors in risk perceptions than does attributable risk: most people overestimated the latter, whereas most people underestimated the former.
https://doi.org/10.1371/journal.pone.0182063.t003
Compared to the representative sample of current and formers smokers interviewed in Study 1, Study 2’s non-probability sample of current and former smokers reported: (1) lower perceived absolute risk of lung cancer among nonsmokers and smokers (e.g., 49.5% and 25.7%, respectively, gave answers between 0 and 50 out of 1,000 who would get lung cancer, compared to 36.0% and 10.3% in Study 1; see seventh and eighth columns in Table 1 ); (2) lower perceived attributable risk (e.g., 50.9% had a value of 99 or less, compared to 30.7% of the Study 1 respondents; see the eighth column of Table 2 ); and (3) lower perceived relative risk (e.g., 59.5% had values of 2.99 or less, as compared with 54.6% of the Study 1 respondents; see the eighth column of Table 3 ).
Using all three risk measures, Study 3’s representative sample of current and former smokers perceived less risk than the Study 1’s respondents did 9 years earlier. Study 3’s current and former smokers reported lower absolute risk among nonsmokers (mean = 11.9%, median = 5%) than did the Study 1 respondents (mean = 21.5%, median = 10%; see columns nine and one, respectively, of Table 1 ). Study 3’s current and former smokers perceived lower absolute risk for smokers than did the Study 1 respondents (means = 33.1% vs. 48.0%; medians = 30.0% vs. 50.0%; see columns ten and two, respectively, of Table 1 ). And Study 3’s current and former smokers perceived lower attributable risk of smoking than did the Study 1 respondents (means = 21.1% vs. 26.7%; medians = 11.5% vs. 20.0%; see columns nine and one, respectively, of Table 2 ) and lower relative risk than did the Study 1 respondents (means = 12.9 vs. 26.7; medians = 2.5 vs. 2.5; see columns 9 and 1, respectively, of Table 3 ).
Study 3 suggests that the perceived risk of lung cancer may have declined among current and former smokers between 2000 and 2009. That is, the two representative sample surveys indicated that respondents’ assessments of the absolute risk of lung cancer for both smokers and non-smokers became notably more accurate during this period.
Comparing risk measures
Which of these measures is an appropriate focus for claims about public risk perceptions and their accuracy? One way to answer this question is to determine which of these risk perceptions drives people’s decisions about whether or not to smoke. Many possible patterns of risk perception use are possible in any population. The most heterogeneous pattern would be one in which some people decide whether to smoke or quit based upon their perceptions of the attributable risk, while others make this decision with reference to perceptions of relative risk, and still others make their decisions based on perceptions of absolute risk, with the three groups being of roughly equal size. The most homogeneous case is that in which everyone uses just one of these risk perceptions to make their behavioral choices regarding smoking. By gauging which risk perceptions have how much impact for how many people, we can begin to understand whether smoking behavior overall in a population is driven mostly by perceptions that overestimate risk, mostly by perceptions that underestimate risk, or by a mixture of perceptions that sometimes overestimate and other times underestimate.
The data of all three studies allowed us to explore whether perceptions of attributable risk, relative risk, and absolute risk inspire people to quit smoking by comparing current and former smokers. If perceptions of health risks are indeed a principal motivator of smoking cessation, then perceived risk should be lower among people who currently smoke than among people who used to smoke but have quit. In other words, the higher a person’s perceived risk, the more likely he or she should be to have quit smoking. Based upon this assumption, the better a risk perception measure predicts whether a person has quit smoking, the more likely that risk perception is to have driven quitting decisions.
To adjudicate whether absolute risk, attributable risk, or relative risk drove people’s decisions to quit, we estimated the parameters of generalized additive models (GAMs) comparing current smokers to former smokers by using a Gaussian link function predicting a binary variable representing whether a respondent was a current or former smoker using the various measures of perceived risk and the weights for unequal probability of selection and demographic post-stratification (see S5 Appendix for more details on GAMs). GAMs are especially useful for estimating models containing two highly correlated predictors (as we have here) because relaxing the assumption of linearity prevents model misspecification, allowing for better isolation of the unique relations of different risk perceptions with other variables.
Using this flexible approach, we first estimated a model in which relative and attributable risk predicted quitting (more precisely, having quit). It might seem appealing to estimate GAMs predicting quitting using all three measures, but non-independence among the three measures of perceived risk makes that impossible. When examining Study 1’s data, we see that perceptions of relative risk were sensibly correlated with diminished chances of remaining a smoker (see the top-left panel of S2 Fig ). The dark line in the figure represents the estimated relation, and the two light lines demark the bounds of the 95% confidence interval around the estimates. The small vertical lines at the bottom of the figure (called “rugmarks”) indicate whether one or more respondents provided a data point at each point along the x-axis. Increasing perceived relative risk was associated with decreased log-odds of remaining a smoker. Movement from the 25 th percentile to the 75 th percentile (weighted) of relative risk increased the probability of quitting by 13.8 percentage points (see the first row of the first column of Table 4 ).
https://doi.org/10.1371/journal.pone.0182063.t004
In contrast, over the range of the bulk of the data (where the majority of the rugmarks on the x-axis are located), the relation between attributable risk and quitting was fairly flat (see bottom-left panel of S2 Fig ). Movement across the interquartile range of attributable risk increased the probability of quitting negligibly, by only 0.3% (see second row of the first column of Table 4 ).
To more formally gauge and compare these relations, we estimated a set of nested GAMs. First, we estimated a model predicting quitting using only attributable risk and then observed the improvement in goodness of fit of the model when we added relative risk as a predictor. A likelihood ratio (hereafter LR) test comparing the log likelihood of the two-variable model to the nested one-variable model indicated that the addition of the extra variable resulted in a significantly better fit (p=.03), meaning that relative risk was a reliable unique predictor of quitting (see third row of the first column of Table 4 ). Next, we estimated a model predicting quitting using only relative risk and then estimated the improvement in goodness of fit when attributable risk was added as a predictor. This addition did not improve the model’s fit significantly (p=.64; see fourth row of the first column of Table 4 ). Thus, relative risk perceptions appear to have been related to decisions to quit smoking, whereas perceptions of attributable risk were not.
To explore whether absolute risk outperforms relative risk, we estimated a GAM in which quitting was predicted by both measures. As shown in the right panels of S2 Fig , relative risk was again sensibly related to quitting (with probability of remaining a smoker declining smoothly as perceived risk increased), whereas absolute risk was not. Again, adding relative risk to a model fitted with only absolute risk improved the fit significantly (p=.002), whereas adding absolute risk to a model with relative risk did not yield a significant improvement in fit (p=.15; see rows seven and eight of the first column of Table 4 ). Movement across the interquartile range of absolute risk was associated with a 10.5% decrease in the chances of quitting, whereas movement across the interquartile range of relative risk was associated with a sizable and more reasonable 15.2% increase in the likelihood of quitting (see rows five and six of the first column of Table 4 ). As shown in columns two and three of Table 4 (as well as S3 and S4 Figs), these same results were replicated in Studies 2 and 3.
There may be an illusion hidden in these results. When people are asked to report a probability but do not know the answer, they sometimes answer “50,” meaning “fifty-fifty” or “I don’t know,” rather than meaning a 50% chance [ 56 ]. To explore the impact of this potential source of measurement error on our conclusions, we re-estimated the logistic GAM by: (1) dropping the respondents who answered “500” to the question about nonsmokers or to the question about smokers; (2) replacing the 500s with values generated by multiple imputation; and (3) replacing the 500s with answers obtained by a follow-up probe. The results supported the above conclusions even more strongly (for details of these approaches and results, see S6 Appendix ).
Next, we explored whether certainty moderated the associations of risk perceptions with quitting behavior. In Study 1, as expected, the correlation of relative risk with quitting was significantly stronger among high certainty respondents (people who were extremely certain, 27% of the sample) than among lower certainty respondents. Among the high certainty respondents, the probability of quitting increased over the interquartile range of relative risk by 23.7 percentage points (p=.008), a much larger increase than among the low certainty respondents, whose positive change was just 10.5 percentage points (p=.054). Accounting for certainty significantly improved the goodness of fit of the model (p=.03).
Likewise, in Study 2, the positive relation between perceived relative risk and quitting was significantly stronger among high certainty respondents than among low certainty respondents (p=.009). Among the high certainty respondents (18% of the sample), movement across the interquartile range of relative risk increased the probability of quitting by 44.1% (p<.001), whereas movement across this interquartile range in the low certainty group was associated with an increase in quitting probability of only 13.6% (p<.001). Accounting for certainty significantly improved the goodness of fit of the model (p=.009).
In Study 3, among high certainty individuals (30.5% of the sample), movement across the interquartile range of relative risk was associated with an increased probability of quitting smoking of 15.8% (p=.06), whereas movement across this interquartile range in the low certainty group was associated with an increase in quitting probability of 11.1% (p=.03). Accounting for certainty again significantly improved the goodness of fit of the model (p=.03).
Desire to quit.
Next, we examined whether current smokers’ risk perceptions were associated with their desire to quit. While a desire to quit does not automatically translate to smoking cessation, a strong desire to quit is predictive of subsequent quitting behavior, and is a necessary condition for quitting [ 57 ]. In Study 1, adding relative risk to a GAM model predicting desire to quit among current smokers with attributable risk caused a marginally non-significant improvement in fit (p=.09; see the third row of column four in Table 4 ). Movement from the 25 th to the 75 th percentile of relative risk raised the probability of wanting to quit by 17.0% (see the first row of column four in Table 4 ). But adding attributable risk to a model predicting desire to quit with relative risk did not improve fit significantly (p=.27; see row four of column four in Table 4 ). Movement across the interquartile range of attributable risk slightly lowered desire to quit by 1.1% (see row two of column four in Table 4 ). Likewise, adding relative risk to a model including absolute risk yielded a significant improvement in fit (p=.046; see row seven of column four in Table 4 ). Movement across the interquartile range of relative risk increased desire to quit by 13.9% (see row five in Table 4 ). But adding absolute risk to a model including relative risk marginally significantly decreased desire to quit (interquartile range movement = 15.6%, p=.06; see rows six and eight of column four in Table 4 ). The data from Studies 2 and 3 yielded similar results (see columns five and six of Table 4 ). This further supports the contention that people think in terms of relative risk perceptions.
Smoking onset.
We observed the expected results when we used the three measures in Study 3 to explore whether perceived risk was greater among people who ever smoked than among people who never smoked. Comparing the distributions in the ninth and tenth columns in Table 1 with the distributions in the last two columns of the table, we see that: (1) both groups had similar expectations for the proportion of nonsmokers who would get lung cancer (mean = 11% for people who never smoked vs. 12% for people who ever smoked), but (2) the expected proportion of smokers who would get lung cancer was higher among people who had never smoked (mean = 43.3%) than among people who ever smoked (mean = 33.1%).
Also as expected, people who never smoked perceived higher attributable risk of smoking than did people who ever smoked (see the last two columns in Table 2 ): (1) 3.9% thought that smokers were less likely to contract lung cancer than nonsmokers (attributable risk of less than 0); (2) 6.3% thought that smokers and nonsmokers were equally likely to get lung cancer (attributable risk of 0); and (3) 89.7% thought that smokers were more likely to contract lung cancer than nonsmokers. Respondents who never smoked thought smokers were 32 percentage points more likely than nonsmokers to get lung cancer, on average (see columns 11 and 12 of Table 2 ). Thus, these individuals perceived a higher attributable risk than did current and former smokers (21.1 percentage points; see column nine of Table 2 ). Likewise, respondents who never smoked also perceived higher relative risk than did current and former smokers (compare the last two columns of Table 3 with the ninth and tenth columns of that table).
As expected, perceptions of relative risk were strongly associated with status as a never smoker vs. a current smoker in GAMs (see the left panels of S5 Fig ). Adding relative risk to a model predicting current smoking with attributable risk considerably improved fit (p<.001), whereas adding attributable risk to a model with relative risk did not significantly improve fit (p=.57). Movement across the interquartile range of relative risk yielded a 22.7 percentage point decrease in the likelihood that respondents were smokers. Movement across the interquartile range of attributable risk yielded a decrease in the probability of being a smoker of only 0.7 percentage points.
Likewise, adding relative risk to a model with only absolute risk improved fit significantly (p<.001), whereas adding absolute risk to a model including relative risk was associated with only a marginally significant improvement in fit (p=.07). Movement across the interquartile range of relative risk (when controlling for absolute risk) was associated with a 22.3 percentage point decrease in the probability of ever having smoked (see the right panels of S5 Fig ). In contrast, movement across the interquartile range of absolute risk (when controlling for relative risk) produced only an 8.5 percentage point decrease in the likelihood of ever having smoked.
Summary and implications
Taken together, this evidence suggests that while Americans have overestimated the absolute risk and risk difference of lung cancer associated with cigarette smoking, Americans have generally underestimated the relative risk. Furthermore, this evidence suggests that people may think more about smoking health risks in terms of relative risk than in terms of absolute risk or risk difference. The relations we saw here may result from the influence of health risk beliefs on decisions to quit smoking, decisions to start smoking, and regret about smoking, or these relations may occur because people rationalize their smoking status by adjusting their risk perceptions, or from some other process. Having seen here that these are possibilities, we look forward to future research exploring them to characterize the basis for the relations we observed.
Communication of risk has been a difficult task for medical professionals, and our findings encourage consideration of a different approach to communicating health risks than has been typical on American cigarette packages and in other prominent health communications [ 58 , 59 ]. There are a large number of studies that show that the design of and warnings on cigarette packs can influence perceptions of the risks of smoking [ 60 – 68 ]. However, much constructive work can perhaps still be done by informing individuals about how much smoking increases their health risks. If the findings reported here are correct in suggesting that people use perceptions of relative risk when deciding whether to quit smoking, and if relative risk is indeed underestimated by most current and former smokers, corrective steps in this regard might be consequential. More specifically, if public health efforts are initiated in the future to encourage Americans to more accurately recognize the magnitudes of relative risks for various undesirable health outcomes of cigarette consumption, this may well lead to a reduction in the nation’s smoking rate and a consequent reduction in smoking-related morbidity and mortality. This may be why quantitative information about relative risk on cigarette packages in Australia (e.g., “Tobacco smoking causes more than four times the number of deaths caused by car accidents.”) appears to have been effective in encouraging smoking cessation [ 69 ].
Future research could explore these possibilities with experiments gauging the effects of different ways of describing risks on cigarette packages and other health communication mediums like television advertisements, poster campaigns, and doctor-patient communication [ 70 ]. Our findings suggest that when conducting such experiments, it may be desirable to attempt to alter people’s perceptions of relative risk in order to most directly address people’s natural approach to thinking about health risks in this arena. Perceptions of relative risk might be changed best by making such direct statements. But it may also be that such perceptions can be changed even more effectively by inducing affective reactions or in other non-quantitative ways, while simultaneously maximizing trust in the source of the information [ 71 , 72 ]. It is important to bear in mind that even successful efforts to change risk perceptions may not produce changes in behavior, so it will be important for future investigations to assess whether risk perception changes are translated into action [ 73 ].
In addition to their applied value, the findings reported here are interesting in basic psychological terms. By distinguishing between absolute, attributable, and relative risk, the present findings encourage future study with such measures to understand how people make many types of risky decisions and, more generally, how people trade off probabilities when making choices. And many important questions remain regarding risk perceptions involving smoking, such as how people arrive at their perceptions of relative, attributable, and absolute risk, and when and why some people use one measure rather than another to make behavioral decisions. Future studies of these sorts of issues seem merited, both in the smoking and other domains.
Resonance with other findings
Various findings reported here resonate with findings of some past studies. For example, Viscusi [ 2 ] and Borland [ 69 ] found that people overestimated the absolute risk of smoking. Khwaja et al. [ 74 ] found that both smokers and non-smokers overestimated their risks of dying from all sorts of causes [ 69 ]. When Weinstein et al. [ 27 ] asked respondents to assess the relative risk of smoking (“Would you say the average smoker has about the same lung cancer risk as a nonsmoker, a little higher lung cancer risk than a nonsmoker, twice the nonsmoker’s risk, five times the nonsmoker’s risk, or ten times the nonsmoker’s risk?”), smokers offered underestimates.
Boney-McCoy et al. [ 19 ] found that current smokers perceived the absolute risk of smoking to be significantly lower than that perceived by former smokers. This is consistent with the evidence reported here that when considered alone, absolute risk perceptions are related to quitting in the same way. However, when controlling for relative risk, the relation of quitting to absolute risk perceptions was close to zero in the present data.
Antoñanzas et al. [ 75 ] found distributions of Spaniards’ perceptions of attributable and relative risk (regarding the impact of cigarette smoking on lung cancer and heart disease) very similar to those reported here. Viscusi et al. [ 76 ] found that each of these risk perceptions predicted Spaniards’ status as a smoker or nonsmoker when considered alone, and relative risk was a considerably stronger predictor than attributable risk, though Viscusi et al. [ 76 ] did not assess the predictive abilities of perceived attributable risk and relative risk in a single regression equation.
The present evidence that people seem to think in terms of relative risk rather than attributable or absolute risk resonates with research on effective ways to communicate risks to patients [ 77 , 78 ]. For example, Malenka et al. [ 13 ] asked respondents to imagine they had a disease and could choose to take one of two medications—one described in terms of its impact on relative risk (“reduces risk of dying by 80%”) and the other (statistically equivalent) described in terms of impact on attributable risk (“can prevent 8 deaths per 100 people”). Most respondents preferred the medication described in terms of relative risk, perhaps because this portrayal resonated with people’s natural way of thinking about medication benefits found that relative risk information had more impact than did attributable risk information [ 79 – 83 ]. These findings contrast with Saitz’s [ 84 ] and Gigerenzer et al.’s [ 85 ] speculations that people will respond as well or better to attributable risk information (presented as two absolute risks) than to relative risk information, a finding challenged by our data as well.
A preference for thinking about health risks in terms of relative risk is also apparent in news media stories. In one study, 83% of such stories reported benefits of medications in terms of relative risk only, 2% reported benefits in terms of attributable risk only, and 15% reported benefits in terms of both indicators [ 86 ]. Similarly, medical journal articles tend to focus on reports of relative risk rather than attributable risk [ 87 ].
Other directions for further research
Future research might gain more insight into people’s natural ways of thinking about health risks by asking people to describe the health risks of smoking with whatever language they wish. With enough probing, open-ended data gathering might reveal whether people naturally use language evoking absolute risk, attributable risks, or relative risk levels, or a non-numeric representation, and such evidence is worthwhile to collect in future research [ 37 , 88 ]. Future work should also incorporate how much life is lost when calculating risk (see Viscusi [ 38 ] for a discussion of how this might affect an understanding of these results).
Generalizing beyond lung cancer
The focus of the analyses reported here has been people’s perceptions of the risk of getting lung cancer due to smoking. Because lung cancer is one of the best-known health risks of smoking [ 11 ], Americans may be less likely to underestimate the relative risk of lung cancer than of other diseases that are known to be caused by smoking. If we had asked survey questions about heart disease, oral cancers, or stroke instead of lung cancer, the prevalence of underestimation of relative risk may have been even greater than was observed for lung cancer. Correcting these misunderstandings may decrease the expected smoking rate even more. Future studies can explore these possibilities.
Implications regarding other domains of risk perception.
Differentiating perceived relative risk from perceived attributable risk may be useful in other health domains as well. For example, Meltzer and Egleston [ 89 ] reported that patients with diabetes vastly overestimated their own absolute risk of experiencing various complications. But perhaps their perceptions of relative risk are more accurate.
Implications for health education.
Psychological research on health counseling communication has revealed errors in people’s understanding of risk information [ 90 – 92 ]. However, educational efforts can present risk rates in various different ways, and some presentation approaches can cause misunderstandings [ 93 , 92 ]. The present evidence bolsters the conclusions of some past studies suggesting that future research may be most successful when presenting relative risk information to yield better quality decisions [ 94 – 99 ].
Supporting information
S1 fig. proportions of americans who failed to assert that smoking is dangerous to human health: gallup organization surveys..
https://doi.org/10.1371/journal.pone.0182063.s001

S2 Fig. Generalized Additive Models predicting the probability of being a current smoker: SRBI Survey (n = 456).
https://doi.org/10.1371/journal.pone.0182063.s002
S3 Fig. Generalized Additive Models predicting the probability of being a current smoker: Harris Interactive Survey (n = 795).
https://doi.org/10.1371/journal.pone.0182063.s003
S4 Fig. Generalized Additive Models predicting the probability of being a current smoker vs. former smoker: FFRISP (n = 471).
https://doi.org/10.1371/journal.pone.0182063.s004
S5 Fig. Generalized Additive Models predicting the probability of being a current smoker vs. never smoker: FFRISP (n = 714).
https://doi.org/10.1371/journal.pone.0182063.s005
S1 Appendix. Measuring risk.
https://doi.org/10.1371/journal.pone.0182063.s006
S2 Appendix. Literature on the relation of health risk perceptions with quitting smoking.
https://doi.org/10.1371/journal.pone.0182063.s007
S3 Appendix. Survey methodology.
https://doi.org/10.1371/journal.pone.0182063.s008
S4 Appendix. Demographics of current and former smokers in the SRBI Survey, current and former smokers in the Harris Interactive Survey, all individuals in the FFRISP Survey, and the nation’s population.
https://doi.org/10.1371/journal.pone.0182063.s009
S5 Appendix. GAMs.
https://doi.org/10.1371/journal.pone.0182063.s010
S6 Appendix. Exploring responses of 500.
https://doi.org/10.1371/journal.pone.0182063.s011
S7 Appendix. References for supporting information.
https://doi.org/10.1371/journal.pone.0182063.s012
Acknowledgments
The first survey described in this paper was funded by Empire Blue Cross/Blue Shield of New York. The third data set described was collected via the Face-to-Face Recruited Internet Survey Platform (FFRISP), funded by NSF Grant 0619956, Jon A. Krosnick, Principal Investigator. The authors thank Geoffrey Fong and Paul Slovic for very helpful suggestions. The authors acknowledge the excellent research assistance of Virginia Lovison. Jon Krosnick is University Fellow at Resources for the Future.
Author Contributions
- Conceptualization: JAK LC.
- Data curation: JAK NM CHM LC JP RKT.
- Formal analysis: NM CHM LC JP.
- Funding acquisition: JAK RKT.
- Investigation: JAK LC RKT.
- Methodology: NM LC JP.
- Project administration: JAK NM CHM.
- Resources: JAK RKT.
- Software: NM CHM LC JP RKT.
- Supervision: JAK.
- Validation: NM CHM JP.
- Visualization: NM CHM LC JP.
- Writing – original draft: JAK NM CHM EFB JP.
- Writing – review & editing: JAK NM CHM EFB JP.
- 1. Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2007.
- 2. Viscusi WK. Smoking: Making the risky decision. New York: Oxford University Press; 1992.
- View Article
- Google Scholar
- PubMed/NCBI
- 6. Newport F, Moore DW, Saad L (Gallup O. Long term Gallup Poll trends: A portrait of American public opinion through the century [Internet]. http://www.gallup.com/poll/3400/longterm-gallup-poll-trends-portrait-american-public-opinion.aspx
- 7. Gallup Organization. National survey. Retrieved from iPOLL Databank, The Roper Center for Public Opinion Research, University of Connecticut. http://www.ropercenter.uconn.edu/ipoll.html . Accessed August 1, 2014.
- 8. Department of Health and Human Services, Public Health Service, Office of the Assistant Secretary for Health, Office on Smoking and Health. Use of Tobacco Survey (ARC Identifier 607143),1986.
- 9. American Lung Association and Gallup Organization. National survey, June 1987. Retrieved from iPOLL Databank, The Roper Center for Public Opinion Research, University of Connecticut. http://www.ropercenter.uconn.edu/ipoll.html . Accessed.
- 12. Manski CF. Identification problems in the social sciences. Cambridge, MA: Harvard University Press; 1995.
- 14. Mausner JS, Bahn JK. Epidemiology: An introductory text. Philadelphia, PA: Saunders; 1974.
- 47. Festinger L. A theory of cognitive dissonance. Stanford, CA: Stanford University Press; 1957.
- 49. Petty RE, Krosnick JA. Attitude strength: Antecedents and consequences. Hillsdale, NJ: Erlbaum; 1995.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Anniversary
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 12, Issue suppl 1
- Smoking on the rise among young adults: implications for research and policy
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Correspondence to: Paula M Lantz, PhD, Department of Health Management & Policy, University of Michigan School of Public Health, 109 Observatory Rd. Room M3116, Ann Arbor, MI 48109-2029, USA; plantz{at}umich.edu
This paper investigates hypotheses regarding the cause of the recent apparent increase in young adult smoking, compares trends in smoking among young adults with trends in the use of other substances, and considers the implications for youth tobacco control research and policy. Time series analyses of national data suggest that the recent observed increase in smoking among young adults is primarily an artefact of the almost simultaneous increase in smoking among high school students. In addition, however, it also appears that there have been real changes in smoking patterns among young adults. While many questions remain regarding recent trends in tobacco and other drug use among adolescents and young adults, what is known leads to a clarion call for increased intervention and policy action for the prevention and control of tobacco use among young adults in the USA.
- adolescence
- young adults, high school students
- college students
- smoking patterns
- CAS, College Alcohol Study
- CPS, Current Population Survey
- NHIS, National Health Interview Survey
https://doi.org/10.1136/tc.12.suppl_1.i60
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
In the late 1990s, evidence from a number of different sources pointed to a disquieting trend: cigarette smoking among college students in the USA was on the rise. Wechsler et al sounded one of the first alarms, reporting that longitudinal data from 130 college campuses showed that the prevalence of self reported smoking in the past 30 days increased from 22.3% in 1993 to 28.5% in 1997, an increase of approximately 28%. 1 A 1999 follow up survey (also conducted on a nationally representative sample of four year colleges) confirmed an increase in the prevalence of cigarette smoking among college students. 2
Data from the Monitoring the Future project also demonstrate that there was an increase in the prevalence of cigarette smoking among college students in the late 1990s. This upsurge, however, was observed among young adults in general—both those enrolled and not enrolled in college. 3 Between 1993 and 1999, the 30 day prevalence of cigarette smoking rose by 25% among college students 1–4 years beyond high school, and by about 21% for young adults 19–24 who were not in college. Although year 2000–01 data suggest a decrease in smoking among both college students and young adults not in school, these trends remain quite disturbing. At the present time, it is estimated that there are approximately 11 million smokers between the ages of 19 and 25 in the USA. 4
Several questions emerging from these general trends should resonate with those interested in youth tobacco prevention and control. A primary issue is the extent to which trends among young adults are reflections of previous trends in smoking behaviour among teenagers—that is, the apparent increase among young adults may be a cohort effect reflecting increased use among adolescents a few years earlier. In addition, however, these trends raise the spectre that there has been a true increase in the number of young adults initiating cigarette smoking after high school. From this, a cascade of concerns and additional questions flows. What might explain the apparent increase in the initiation of tobacco use among young adults? Is it possible that some tobacco control strategies aimed at adolescents are merely delaying or deferring initiation rather than preventing it? Have tobacco control advocates and policymakers been remiss in not focusing more resources on young adults?
The purpose of this paper is to explore the issue of recent trends in cigarette smoking among young adults in significant depth. This paper has the following objectives: (1) to review the published literature regarding trends in smoking behaviour among young adults in the USA over the past two decades, comparing college students and non-college young adults; (2) to investigate hypotheses regarding the causes of the apparent increase in smoking in the late 1990s; (3) to explore key issues that arise from a deeper understanding of these concurrent trends and various explanations regarding the causes and driving forces behind them; and (4) to make recommendations for tobacco control research and policy.
Review of published literature and trend data
Much of the information presented and reviewed in this paper was obtained from published manuscripts and abstracts. In addition, information on trends in adolescent and young adult smoking was obtained from a number of published reports and public websites. A major source of information for this paper came from the Monitoring the Future project, including a recent report on substance use among college students and adults aged 19–40 years. 3
Trend analysis of Monitoring the Future data
Annual data from the Monitoring the Future project were analysed using time series analytic techniques to detect whether or not the trend toward increasing smoking among high school students in the mid 1990s is related to the subsequent increase in smoking among college students. The goal here was to explore the hypothesis that the recent increase in young adult smoking is an artefact (or cohort effect) of the observed increase in smoking among teenagers. Using time series modelling (with lag functions), an analysis was conducted to see if there is statistical evidence of such a cohort effect. The dependent variable used for this analysis was 30 day prevalence of cigarette smoking (that is, whether or not someone had smoked a cigarette in the past 30 days).
Secondary analysis of 2000 NHIS data
Data from the 2000 National Health Interview Survey (NHIS) were analysed to assess recent trends in smoking behaviour among young adults. Following the methods of Pierce et al , 5 adult survey respondents were classified into birth cohorts (in this case, single year birth cohorts). Analyses were performed on 18 birth cohorts from 1960 through 1977. People in these birth cohorts turned 18 from 1978 to 1995, and turned 21 from 1981 to 1998. Restricting the sample to these birth cohorts means that all subjects for these analyses were 23–40 years old at the time of the NHIS 2000 survey. Including more recent birth cohorts was possible, but given that the people in these cohorts were 18–22 years old at the time of the survey and thus had not yet completed their early adult years, results regarding tobacco use patterns during this time period would be biased (and almost certainly in the direction of underestimation).
During the NHIS interview process, respondents who report smoking 100 or more cigarettes during their lifetime are categorised as “ever smokers” and asked a series of additional questions. The main variable of interest for this analysis was the age at which “ever smokers” reported becoming regular smokers (worded as “at what age did you become a fairly regular smoker?”). Subjects responded with an age, that they never were a regular smoker, that they didn’t know, or that they refused to answer the question. Age at initiation of regular smoking was recoded to create a number of new variables including the establishing of regular smoking before age 15, before age 18, at age 18, or at ages 19–21. Other NHIS variables under analysis included ones related to current cigarette smoking status, the use of other tobacco products, and smoking cessation behaviour.
Variables of interest were analysed by birth cohort to detect any trends or changes over time. Most analyses were conducted for the entire sample and by sex. All analyses used weighted data to correct for the complex sampling design of the NHIS. The strengths of the NHIS data—which present a cross-sectional picture across a number of age groups and thus birth cohorts—are that the experiences of several cohorts can be analysed using only one year of data. A limitation, however, is that everyone is answering questions in the year 2000, when they were asked to recall specific aspects of their smoking initiation and early smoking behaviour. The further people are away from these experiences, the more likely recall bias might influence their responses. Thus, any changes observed across cohorts may reflect, in part, the fact that older cohorts are further away from the actual experiences in question.
Recent trends in smoking among young adults
Monitoring the future results.
A very useful and informative source of information on trends in tobacco and other drug use among American youth is the Monitoring the Future project, an ongoing research programme conducted since 1975 out of the Institute for Social Research at the University of Michigan. 3, 6 Since 1976, a representative sample of the high school seniors participating in the Monitoring the Future surveys has received periodic follow up surveys. Thus, the Monitoring the Future project provides information on the drug related behaviour of high school students and adults through the age of 40 at the present time.
Data available from the Monitoring the Future Project demonstrate that there has been a significant increase in cigarette use among young adults during the past decade, for both those in and not in college. Figure 1 shows trends in the 30 day prevalence of cigarette smoking (panel A) and the 30 day prevalence of daily smoking (panel B) over the past two decades, for full time college students, for others 1–4 years past high school, and high school seniors. 3 For all three groups, the trends are similar. There was a decrease in cigarette smoking behaviour during the 1980s. In the early 1990s, however, smoking prevalence began to increase among all three groups, with an especially strong increase among high school seniors. The 30 day prevalence of smoking continued to increase through the 1990s for high school seniors, peaking in 1997 and decreasing thereafter. The trend lines for full time college students and other young adults peaked in 1999, and showed a decrease for the first time in many years in 2000.
- Download figure
- Open in new tab
- Download powerpoint
Monitoring the Future trend data regarding smoking. Reproduced from Johnston et al , 3 with permission. (A) Trends in 30 day prevalence of cigarette use. (B) Trends in 30 day prevalence of daily cigarette use.
Regarding college students, Johnston et al report: “Between 1990 and 1999, the 30-day prevalence of cigarette smoking by college students rose from 23% to 31%, or by about one-third, and daily smoking rose from 14% to 19%—or by about 40%.” 3 Between 1980 and 1994, female college students had higher rates of smoking than males. However, a crossover occurred in 1995, and since this time rates of smoking among college males have been slightly higher than those for females. It is believed that this crossover reflects a similar sex crossover in smoking behaviour that occurred among high school seniors a few years earlier. 3
Young adults 1–4 years beyond high school but not in college have a higher prevalence of smoking than those in college, with 30 day prevalence rates in the mid to late 1990s ranging from 35–42%. Rates of heavy smoking are also significantly greater among young adults not in college. For example, in the year 2000, 23.7% of young adults not in college reported smoking a half pack or more a day, compared with 10.1% of full time college students. Despite the greater prevalence of smoking among non-college young adults, the relative increases in smoking were much greater among college students. For example, between 1990 and 1999, the 30 day prevalence of daily smoking increased by approximately 25% for non-college young adults, yet by almost 60% for full time college students. 3
In summary, Monitoring the Future data provide clear and credible evidence that there were significant and alarming increases in cigarette smoking among both male and female high school students and young adults during the 1990s. 3, 6 Trends in self reported smoking behaviour are paralleled by trends in the percentage of high school seniors and young adults reporting that most or all of their friends smoke. 3 While the most recent data are suggestive of a decline or at least a plateau in the trend line, the results for the 1990s are unmistakable: high school students, college students, and young adults not in college all experienced a significant upsurge in cigarette smoking during the 1990s.
Harvard School of Public Health College Alcohol Studies
Another very useful source of information regarding trends in cigarette smoking among college students in the USA is the Harvard School of Public Health College Alcohol Study (CAS). The CAS involves a random sample of undergraduates at a nationally representative sample of four year colleges. While the primary focus of the survey is alcohol behaviour, information about cigarette smoking is included as well.
Results from the 1993 CAS included that 22.3% of full time college students had smoked in the past 30 days, with an additional 25% reporting that they were former smokers. 7 Wechsler et al looked at changes in smoking prevalence between the 1993 and 1997 surveys, and discovered the alarming finding reported above. 1 Over this five year period, there had been a 27.8% increase in cigarette smoking prevalence (defined as smoking during the past 30 days). In addition, it was reported that there was a decrease in smoking rates at the “extremes” of smoking behaviour: there were fewer very light smokers (< 1 cigarette per day) and fewer heavy smokers (> 20 per day).
More recently, Rigotti et al analyzed data from a third CAS, conducted in 1999. 2 Their findings included that more than 60% of college students had tried some sort of tobacco product in their life, that almost half (45.7%) had used some sort of tobacco product in the past year, and that a third (32.9%) were current users in terms of 30 day prevalence of any tobacco use. 2 The 30 day prevalence rate of cigarette use in 1999 was similar to the rate in 1997, suggesting a plateau in the upsurge among college students. While cigarettes accounted for the majority of tobacco ingested by college students in 1999, cigars also were a significant source of tobacco for males. Even though cigarette smoking rates were similar for males and females (28.4% v 28.5%, respectively), males had a higher overall rate of tobacco use in the past 30 days because of their higher use of cigars (15.7% v 3.9%) and smokeless tobacco (8.7% v 0.4%). 2
Other studies
Selected major findings from a number of data sources are summarised in table 1. The 1995 National College Health Risk Behaviour Survey included students at both two and four year institutions. 8 Nearly three quarters of the respondents (74.8%) reported that they had ever tried a cigarette, and 29% had smoked at least one cigarette in the past 30 days. Whites and those at two year institutions were more likely to report ever and recent smoking. This study was not longitudinal. Thus it cannot offer insights regarding trends.
- View inline
Prevalence of smoking in past 30 days among young adults in major national studies
Results from the NHIS suggest that the rate of current smoking among 18–24 year olds was 23.5% in 1991. 9 This rate had risen to 28.6% in 1997, a 22% increase. 10 Although the definition of current smoking in the NHIS changed slightly in 1992 (from having ever smoked 100 or more cigarettes and currently smoking to having ever smoked 100 or more cigarettes and now smoking every day or some days), this change is not responsible for the increase in smoking observed among 18–24 year olds during the 1990s. In fact, no other adult age group experienced an increase in smoking rates over this time; the only increase in current smoking occurred in the youngest adult age group.
Data from the NHIS also signal that, starting around 1997, the prevalence of smoking among those 18–24 years old was as high as those 25–44 years (for example, 28.7% v 28.6% in 1997, and 26.8% v 27.0% in 2000) (Gary Giovino, personal communication on unpublished NHIS results, May 2002). In prior years, NHIS results consistently showed the highest prevalence of smoking in the 25–44 age group, and significantly lower rates in the youngest adult years. This changed, however, in 1997 when two important trend lines met: while smoking rates for adults 25–44 years old were declining in the early to mid 1990s, they were simultaneously increasing among younger adults. NHIS data also suggest that, between 1997 and 2000, the prevalence of smoking among young adults 18–24 years old and those 25–44 was similar and was decreasing slightly.
NHIS results from the year 2000 (data not shown) also demonstrate that young adult males are significantly more likely to use other types of tobacco products than females, and that this pattern holds across birth cohorts. The use of cigars and bidis among males appears to have increased somewhat across birth cohorts reaching age 21 between the years of 1991 and 1998, and a significant proportion of males (over 25%) report having used smokeless tobacco products. This is alarming given the finding that smokeless tobacco use is a significant predictor of cigarette smoking initiation among young adult males. 11, 12 Also alarming are data suggesting that the consumption of cigars increased dramatically between 1993 and 1998, with a slight decrease after that year. 13
Major explanations for trends in young adult smoking
The compositional change hypothesis.
There are many possible explanations for the trends in young adult cigarette smoking described above. One explanation for the increase in smoking among college students is that it is an artefact of a compositional change in the US college student population. Historically, young adults not in college have had higher rates of smoking than those of a similar age but enrolled in college. 3 If more young adults are attending college, it is possible that increases in student smoking represent a change in the types of young adults attending school rather than a true increase in the prevalence of cigarette smoking. According to data from the Current Population Survey (CPS), 14 there has been a slight increase in the proportion of high school graduating seniors who attend college. In 1995, 62.0% of graduating high school seniors were enrolled in a college or university in the fall. This proportion climbed to 67.0% in the fall of 1997, which was a record high. In 1998, the proportion dropped to 65.6%, and fell to 62.9% in 1999 and 63.0% in 2000.
The CPS statistics suggest that the increase in the proportion of high school seniors attending college occurred at the same time that college smoking rates were increasing. Thus, it is possible that part of the increase in smoking observed among college students is due to a compositional change in the types of students who are attending college. The amount of the increase explained by such a change, however, is likely to be quite small. First, the increase in college enrolment, while certainly noteworthy, is not of such a magnitude that it would have a significant compositional effect. Second, there have been increases in smoking among young adults both in and not enrolled in college. Thus, the compositional change explanation, while worth considering, is not credible as a major explanation for the increase in young adult smoking.
The cohort effect hypothesis
A second hypothesis to consider is that the recent observed increase in smoking among young adults in the USA is an artefact of the almost simultaneous increase in smoking among high school students. Between 1991 and 1997, cigarette smoking among youth increased significantly according to several different data sources. 3, 15 Monitoring the Future data suggest a 32% increase in 30 day prevalence of any smoking among high school seniors during this time period. 10 Longitudinal analysis of Monitoring the Future data have established the existence of cohort effects: “if a class (or birth) cohort establishes an unusually high rate of smoking at an early age relative to other cohorts, the rate is likely to remain high throughout the life cycle relative to that of other birth cohorts at equivalent ages.” 3
Given the significant increase in smoking among high school students in the 1990s, the observed increase in smoking among young adults is often presumed to reflect the aging of adolescent cohorts with higher smoking rates. 2, 3 There are indeed data to support the cohort hypothesis. First, Monitoring the Future results do suggest that the increase in smoking among high school seniors predates the observed increase among young adults ages 19–24. An increase in 30 day prevalence of smoking was first observed in 1993 for high school seniors, and increases were subsequently observed for 19–20 year olds in 1994, for 21–22 year olds in 1995, and for 23–24 year olds in 1996. These results are quite suggestive of an aging cohort effect.
Second, time series modelling results suggest that the two trend lines—that is, trends in the 30 day smoking prevalence rates for high school seniors and young adults 1–4 years out of high school between 1980 and 2000—are significantly related to one another. Specifically, the results showed that rates of current smoking among high school seniors explained three quarters of the variance in the rates of smoking among all 19–20 year olds over the 21 year time period under study, using a one year lag function (R 2 = 0.756, p < 0.001). In addition, smoking rates among high school seniors explained two thirds of the variance in current smoking rates among all 21–22 year olds, using a three year lag function (R 2 = 0.67, p < 0.001). Similarly, smoking rates among high school seniors explained three quarters of the variance in smoking among college students 1–4 years out of high school, using a two year lag function (R 2 = 0.765, p < 0.001). Thus, rates of smoking among high school seniors are highly correlated with and explain the majority of the variance in subsequent smoking rates among young adults.
Nonetheless, there are also some disturbing aspects of observed trends that argue against a pure cohort effect. First, when the trend lines for college students and young adults not in school are separated (fig 1), one can see that increases in 30 day prevalence of any smoking and the 30 day prevalence of daily smoking among college students really started before 1990. 3 As such, it appears that the increase in smoking among college students actually was apparent before the upsurge in smoking among high school seniors (which appears to have started in 1992–93).
Second, similar to trends in cigarette consumption, the use of illicit drugs increased dramatically among high school students and young adults in the USA during the 1990s. 16, 17 Between 1980 and 1992, most illicit drugs showed a strong decrease in use among high school students, college students and young adults not in college. 3 After 1992, however, a number of drugs—including marijuana—showed a clear increase in use among adolescents (both males and females), with smaller increases for a number of substances among young adults. Rates of any illicit drug use increased in a startlingly way between 1992 and 2000 as follows: from 27.1% to 40.9% for high school seniors, from 29.7% to 39.3% for young adults ages 19–20, and from 30.0% to 36.9% for young adults ages 21–22. 3, 18 These rates began to stabilise slightly in the late 1990s.
Monitoring the Future investigators believe that much of the increase in illicit drug use among young adults is a cohort phenomenon, the result of adolescent cohorts with significant increases in use aging into young adulthood. 3 However, increases in the use of some drugs occurred simultaneously among high school students and young adults (both those in and not in college), including increases in the use of marijuana, hallucinogens, and amphetamines. Interestingly, Gledhill-Hoyt et al report that nearly a third of college marijuana users initiated use while in college. 16
Compared with other substances, trends in alcohol use are somewhat different. During the time period that smoking was significantly increasing among high school students and young adults in general, alcohol consumption was experiencing a slight increase in terms of 30 day prevalence and binge drinking. 19, 20 These increases are especially noteworthy as they started in the mid 1990s after a nearly decade long decline. 20, 21 Thus, while the observed increases are not as dramatic as those for smoking or for illicit drug use, these small increases represent a clear and definite shift in a trend line.
In summary, while the cohort hypothesis likely has some degree of explanatory power, it is probably not the full explanation for the observed increase in smoking among young adults. The story becomes more complex when we look at some of the details in the trend lines, and we also consider the fact that a broader phenomenon regarding other substance use among adolescents and young adults was occurring at the same time. In general it appears that increases in smoking have occurred at the same time as increases in the use of other tobacco products, binge drinking, and the use of many types of illicit drugs, including marijuana. Given the strong evidence that risk taking behaviour regarding substances in general was on the rise among youth and young adults during the 1990s, it is clear that the case of cigarette smoking should not be viewed as an isolated phenomenon.
The change in age at initiation or habitual smoking hypothesis
In attempting to explain the increase in cigarette smoking among young adults in the USA, it is also important to consider whether there have been any changes in the age of smoking initiation or habitual smoking. Becoming a regular or habitual smoker is described as a process or a series of transitions through several stages, starting with the first “initiating” puff on a cigarette. 22, 23
The epidemiology of cigarette smoking initiation in the USA includes one clear and consistent finding: the majority of people who end up being habitual smokers initiate experimentation with smoking as children or adolescents. 15 Data from a variety of sources consistently have shown that the vast majority of people who try a cigarette for the first time are under 18, and that the majority who become daily smokers do so by or at age 18.
There is no doubt that, even in the face of increased smoking rates among young adults, cigarette smoking initiation remains primarily an activity of minors. Even so, there may have been changes in some aspects of the process of being a regular or habitual smoker. In particular, it may be that there have been changes in age distribution of habitual or regular smoking. Below, results from an analysis of data from the 2000 NHIS regarding smoking behaviour in early adulthood across birth cohorts (from 1960 to 1977) are presented in an attempt to shed a bit more light on the hypothesis that there have been changes in age specific smoking patterns concomitant with the observed increase in cigarette use among young adults.
Trends in ever smoking 100 cigarettes
NHIS data from 2000 show that, across the 18 age cohorts, between a third and a half of adults ages 23–40 reported that they have smoked 100 or more cigarettes in their lifetime (table 2). There does appear to have been a slight increase in the proportion of adults reporting ever smoking 100 cigarettes for more recent birth cohorts (those turning 21 between 1996 and 1998), although this change is not statistically significant. There also appears to have been a slight increase in the rate of current smokers over time, with people from younger age cohorts (those born in 1975–77) having a higher rate of current smoking than those in older cohorts. This is consistent with the findings regarding an increase in smoking prevalence among young adults described above. However, given that the NHIS findings presented here involve cross-sectional analysis only, it is possible that this pattern is explained in part by older respondents having had more time to engage in smoking cessation.
2000 National Health Interview Survey results: smoking prevalence by birth cohort
Trends in age at initiation of regular smoking
The 2000 NHIS survey data suggest that the mean and median age at which regular smoking was established did not change much over these 18 birth cohorts. On average, over time, the mean age for regular smoking has been 20.8 years (with a median of 17 years). While there was a decrease in the mean age of establishment of regular smoking for the 1973 and 1974 birth cohorts (17.5 and 18.7 years, respectively), more recent birth cohorts have average ages of initiation of regular smoking that are quite similar to the general pattern over time.
As shown in table 3, the proportion of ever smokers establishing habitual smoking habits by the age of adulthood has fluctuated some over time, but does appear to have risen somewhat for cohorts born after 1970 (that is, for those turning 18 during the early 1990s). For example, 66.8% of ever smokers in the 1970 birth cohort became regular smokers by age 18, compared with 74.5% in the 1976 birth cohort. When coupled with trends regarding the mean age at initiation, these results support a well accepted tenet in tobacco prevention circles: that most smokers initiate smoking behaviour as adolescents, and that—for the vast majority of smokers—smoking became a regular activity or habit at age 18 or younger. Data from the 2000 NHIS do not suggest any sort of significant deviation from well established and well understood patterns of regarding youth smoking in the USA.
2000 National Health Interview Survey results: patterns in the age of initiation of regular smoking by birth cohort
However, the NHIS results do suggest that the rate at which ever smokers establish regular smoking between the ages of 19–21 has experienced an increase in recent years (table 3). In particular, the proportion of ever smokers who report the establishment of habitual smoking at the ages of 19, 20, or 21 appears to have increased for more recent birth cohorts, specifically the 1975–77 birth cohorts. People in these birth cohorts turned 21 between 1996 and 1998, years in which smoking among young adults was increasing. For example, 13.5% of ever smokers in the 1974 birth cohort reported becoming regular smokers in early adulthood (as opposed to age 18 or younger), compared with 17.8% in the 1975 birth cohort and 21.7% in the 1977 birth cohort (table 3). For the most recent cohorts, approximately one out of four smokers became a regular smoker between the ages of 19 and 21. Time series analysis shows that the change in the slope of this trend line is close to being significant at the 0.05 level (p = 0.058). While more data points are needed to reach any solid conclusions, the current data do suggest that a significant proportion of smokers are making the transition to habitual smoking as young adults and that this appears to have increased in frequency among more recent birth cohorts.
It is also interesting to note that the proportion of ever smokers (100 or more cigarettes) who report that they never became a “habitual smoker” was similarly low (less than 6%) across the birth cohorts under study (table 3). Thus, it appears that most people who have ever had 100 cigarettes become what they consider to be a regular smoker at some point, and that the rate of experimenters who do not become regular smokers has not changed much over the past two decades. Even so, some people who smoke regularly can do so without smoking daily. These people are referred to as “intermittent smokers”. 24 NHIS data show that the prevalence of intermittent or non-daily smokers has increased over the birth cohorts under study, from a rate of 12.1% of ever smokers in the 1960 cohort to 20.8% in the 1977 cohort (table 3). Time series analysis revealed that there has been a significant change in the slope of this trend line (p = 0.001), suggesting that the rate of intermittent smoking among adults is indeed higher among more recent birth cohorts, or those who reached young adulthood during the years where smoking prevalence among young adults was increasing.
Sex difference
Some interesting sex differences in smoking patterns are apparent in the 2000 NHIS data (table 4). First, the proportion reporting ever smoking 100 cigarettes is higher among males than females in all birth cohorts. Second, changes in the age at regular smoking are stronger for males than females. Using the last four years of available NHIS data (representing those who turned 23 between 1997 and 2000), the proportion of males establishing regular smoking by age 18 decreased from 80.3% for the 1974 birth cohort to 67.4% for the 1977 birth cohort, compared with 77.8% and 73.6% for the 1974 and 1977 birth cohorts, respectively, for females. Similarly, the proportion of males who reported becoming a regular smoker at ages 19–21 increased by 75% comparing the 1970 birth cohort with the 1977 birth cohort (14.0% v 24.5%). The proportion for females across this same time period increased by 5.5% (with some fluctuations—see table 4). These trend data suggest that the phenomenon of an increase in the rate of habitual smoking initiation is much stronger for males.
2000 National Health Interview Survey results: age at which respondent became a regular smoker by birth cohort and sex
In summary, the epidemiology of cigarette smoking indicates that smoking initiation primarily occurs during adolescence. Evidence from a number of sources suggests that this pattern has intensified during the past two decades. The majority of smokers are still trying their first cigarette in early adolescence, and making the transition to habitual smoking by age 19. However, it is also the case that a significant proportion of smokers establish regular or habitual smoking as young adults. Analyses of NHIS survey data suggest that this proportion has been sizeable for some time, and that it increased, particularly among males, during the late 1990s. In addition, the proportion of current smokers who do not smoke daily has significantly increased among younger birth cohorts.
These findings are paralleled by data from a number of other recent surveys, including results from the 1999 National Youth Tobacco Survey, which show that the proportion of 18 and 19 year olds classified as “non-daily smokers” or “experimenters” was greater than the proportion of current smokers. 25 In addition, trend data from the National Household Survey on Drug Abuse show that the rate of initiation of daily cigarette use among both 12–17 year olds and 18–25 year olds increased during the 1990s. 26 For young adults (18–25 years), the rate of initiation for daily smoking (per 1000 person years of exposure) jumped from 28.9 in 1990 to 34.7 in 1997. 26
Along with a “cohort effect” (whereby cohorts with increased rates of adolescent smoking carried their smoking rates into their young adult years), the increase in smoking prevalence among young adults also appears to be occurring because there has been an increase in the rate at which young adults who have experimented with cigarettes become regular smokers. For those who turned 21 in 1998, approximately 1 out of 5 female smokers and 1 out of 4 male smokers established regular smoking after the age of 18. It appears that there have been some changes in smoking behaviour patterns among young adults above and beyond an increase in prevalence caused by a cohort effect.
INDIVIDUAL RISK FACTORS AND SOCIAL ENVIRONMENT CONSIDERATIONS
Recent results from the 1998–99 Tobacco-Use Supplement to the CPS suggest that, among young adults ages 18–24, current smokers (26% of the sample overall) were more likely to be male (29%), white (31%) or American Indian (35%), unemployed (36%), or blue collar (34%) or services workers (32%). 27 There is very little in the published literature regarding risk factors for smoking among young adults not in college. In contrast, the Harvard College CAS have provided valuable insights regarding individual risk factors for smoking among college students.
Multivariable analysis of the 1993 CAS data led Emmons et al to conclude that other lifestyle choices are significantly associated with cigarette smoking in the past 30 days among college students. 7 This includes using marijuana, heavy drinking, and having multiple sex partners. The attitudes that parties are a very important or important part of college life and that collegiate athletics and religion are not very important also were significantly related to smoking. In addition, Emmons et al found that white students, those belonging to a fraternity or sorority, and women living in a co-ed dorm had a higher risk of smoking. Similar to findings from the 1993 CAS data, 1999 college students who used tobacco were more likely to be white and to experiment with other risky behaviours (for example, binge drinking, marijuana use, and multiple sexual partners) than non-smokers. 2
Analysing predictors of “late onset smoking” (defined as establishment of smoking after high school), Ellickson et al found that lower parental education, worse grades in high school, and younger age relative to others in a grade cohort were significant risk factors. 28 In a longitudinal study of college bound high school students who reported never experimenting with tobacco, Choi et al found that—four years later—14% had initiated smoking. 29 Risk factors for this late initiation included being white, having more depressive symptoms, attending church less often, believing that peers approve of smoking, and believing that experimenting with cigarettes is safe.
Wee et al found that adults younger than 30—both male and female—are more likely to smoke if they are trying to lose weight. 30 Weschler et al reported that a prominent perception among health centre directors on college campuses is that students smoke for a variety of reasons—including as a response to stress and as tool for weight control—and that many students do not believe they are addicted and that they will quit upon graduation. 31
In addition, it is believed that smoking reduces and, for some people, fully relieves anxiety in a variety of social situations. Sonntag et al reported that social anxiety has been significantly associated with nicotine dependence in both cross-sectional and longitudinal studies. 32 In addition Anda et al claimed that their results from the Adverse Childhood Experiences Study contribute to a growing literature suggesting that “nicotine use is associated with self-medicating efforts to cope with negative emotional and social experiences”. 33 A significant, graded relation was found between smoking and the number of adverse childhood experiences, including emotional, physical, and sexual abuse; a battered mother; parental separation/divorce; and growing up with a substance abusing, mentally ill, or incarcerated household member.
Are adolescents and young adults smoking cigarettes more because of increased feelings of social anxiety and pressure? Are they trying to “self medicate” to relieve stress or emotional pain in some way? The myriad reasons that adolescents and young adults are smoking cigarettes and using other substances are complex and not well understood. A full review of the literature on this topic is outside of the scope of this paper. However, a prominent social environment hypothesis regarding the increase in smoking among young adults is that the tobacco industry has intensified its activity in this market segment—that is, more aggressive industry marketing activities may be partly responsible for the increase in smoking observed among college students and young adults in general.
Using tobacco industry documents that have become public in the wake of litigation, Katz and Lavack, 34 Sepe et al , 35 and Sepe and Glantz 36 have argued that changes in industry promotional tactics correspond with the increase in smoking observed among young adults. These marketing tactics have taken many forms since the late 1980s: (1) promotions in bars, nightclubs, comedy clubs, and other venues that use person-to-person interactions, free samples, free promotional accessories, contests, and games; (2) efforts to cultivate “brand presence” in bars, including company branded items (such as napkins, coasters, clothing for employees, etc), and financial incentives for owners and employees; and (3) increased use of the alternative press (especially weekly alternative newspapers in urban areas) for several purposes, including product advertisement, event promotion, and bar promotion.
Adult only facilities—such as bars and nightclubs—are exempt from the 1998 Master Settlement Agreement in terms of marketing activities. Sepe et al argue that tobacco industry bar and nightclub promotions “protect the industry from advertising regulations, clean indoor air laws, and accusations of marketing to adolescents. Bar promotions help the industry engineer peer influence to encourage tobacco use among young adults.” 35
Sepe and Glantz wrote that young adults “are not immune to ‘late’ initiation of smoking . . .. Directed marketing toward young adults in social settings such as bars and nightclubs may raise the age at initiation toward what it was in the past. Current increases in young adult smoking, in terms of both overall prevalence and first use, suggest that this directed marketing is having an impact.” 36 Thus, the argument is being made that observed increases in smoking among young adults are in part explained by tobacco industry promotional tactics.
There is a growing body of research literature reporting associations between exposure to tobacco industry marketing/promotions and smoking behaviours, particularly among youth. 37– 40 Thus, is not unreasonable to consider the hypothesis that increased efforts targeting young adults have reaped benefits for the industry. Although spending on tobacco advertising remained relatively constant between 1988 and 1998, promotional allowances tripled in size during this time period. 41, 42 As has been argued in the past, the industry’s continued investment in specific types of promotion and marketing suggests that those within in the industry itself must have some evidence or reason to believe that these tactics are effective. 43
Ling and Glantz have attempted to shed light on why the tobacco industry has intensified its marketing efforts among young adults. They explain:
“First, the industry views the transition from smoking the first cigarette to becoming a confirmed pack-a-day smoker as a series of stages that may extend to age 25, and it has developed marketing strategies not only to encourage initial experimentation (often as teens), but also to carry new smokers through each stage of this process. Second, industry marketers encourage solidification of smoking habits and increases in cigarette consumption by focusing on key transition moments when young adults adopt new behaviors, such as entering new workplaces, school, military, and especially leisure and social activities. Third, tobacco companies study young adults’ attitudes, social groups, values, aspirations, role models, and activities, and infiltrate both their physical and social environments.” 44
Evidence from industry documents confirms that the tobacco industry has invested significant time and resources into studying youth and young adult development, motivations, and social environments, and that this research has helped them to divide potential and actual smokers into different markets or segments. 22, 40, 45 As described above, a number of recent articles provide provocative new evidence and ideas regarding tobacco industry strategies and trends in smoking among young adults. A note of caution, however, needs to be raised. The evidence to date is of a simple ecological nature: smoking rates among young adults rose several years after the industry first introduced promotional activities in bars, nightclubs, and other venues targeting young adults (in the late 1980s), and shortly after these types of efforts were intensified (in the early to mid 1990s). Rigotti et al recently found that, controlling for a number of potential confounders, those college students who report exposure to bar and campus tobacco promotional events do have higher rates of smoking, and that this association is only observed among those who became smokers as adults. 46 However, showing temporal associations and establishing causation are, of course, two different things. Thus, although certainly provocative and compelling, the evidence to date does not conclusively show a causal link between industry tactics and the increase in smoking among young adults.
RESEARCH AND POLICY IMPLICATIONS
As described above, much has been written about the apparent increase in smoking among college students. Increases in smoking, however, have not been observed exclusively in the college population. Significant increases also have been witnessed among young adults in general, and importantly among high school students. There is credible evidence that some of the observed increase among young adults is an artifactual result of the aging of cohorts with increased smoking among youth. In addition, there is information indicating that other factors may be at play as well. Recent NHIS data suggest that there was an increase in the rate at which young adults became “regular” or habitual smokers at the same time as the observed increase in smoking prevalence, especially among males. In addition, the increase in cigarette smoking has occurred concomitantly with an increase in other risk taking behaviours regarding substance use, including binge drinking and the use of marijuana and other illicit drugs.
The reasons for the increase in smoking among young adults are not clear, and there are many questions that remain unanswered at this point in time. Additional research is needed in multiple areas, including research that will help to answer the following questions:
What sociodemographic and behavioural characteristics are associated with changes in the smoking behaviour of young adults? What subgroups are at higher risk for becoming habitual smokers as young adults? Are the characteristics or risk factors for habitual smoking initiation the same among college students and those not in school? Is the recent increase really largely a male phenomenon?
How is the increase in cigarette smoking among young adults related to the increase in the use of other substances? Are some of the same causal factors involved across substances?
Are there any tobacco control policies and interventions aimed at adolescents that may be delaying or deferring initiation of habitual smoking rather than preventing it?
How do we best intervene with adults who have just “come of age”? Are young adults more like adults or adolescents in terms of their knowledge and understanding of risk, their motivations, their self perceptions, their attitudes, the social influences that affect them, etc? What needs to be understood about young adults to better inform the design of smoking prevention and control interventions?
Even in the face of these and a number of other unanswered questions, we do have sufficient information and knowledge in hand to consider a number of programmatic and policy responses. The following is a list of potential policy responses and intervention strategies that need to be investigated, debated, and discussed as the tobacco control community further develops an agenda for addressing tobacco use among young adults.
Invest in smoking cessation interventions aimed at young adults
Although rates of smoking cessation have increased among adults over the past two decades, this has primarily been observed among adults ages 45 and older. Among young adults (ages 18–24), the percentage of ever smokers who have quit smoking has remained relatively stable, especially over the past 10 years (Gary Giovino, personal communication on unpublished NHIS results, May 2002). This does not mean, however, that young adult smokers are not interested in quitting. Results from the 1995 National College Health Risk Behaviour Survey included that 59% of current smokers had made at least one quit attempt, and that this rate was 82% among daily smokers. 47 Furthermore, recent results from the 2000 NHIS suggest that among those ages 18–24, over three quarters of current smokers who attempted to quit in the past still would like to quit, and that almost half (44.2%) of those who have zero quit attempts also would like to quit (Gary Giovino, personal communication on unpublished NHIS results, May 2002).
Given the prevalence of smoking and of the desire to quit among young adults, it is important that interventions and resources regarding smoking cessation be made available. According to the 2000 CPS, over 60% of young adults who graduated from high school are enrolled in a college or university; and 80% of young adults who are not full time students are in the labour force. Thus, a significant proportion of young adults can be reached with messages and resources offered through educational institutions and work sites.
Unfortunately, there is very little evaluation literature on smoking cessation interventions aimed at young adults. Thus, it is not possible at this time to make specific recommendations regarding cessation intervention approaches that have proven effective among young adults. We also should recognise that smoking cessation interventions that have been developed for adults in general may not be the best approach to take with younger adults. Those between the ages of 18–25 may be more like adolescents than older adults in their perceptions of risk, their perceptions of themselves as “smokers” or as having an addiction, their attitudes towards different types of cessation messages, and thus their responses to behavioural interventions. Thus, simply increasing the exposure of young adults to the existing arsenal of cessation tools/interventions is likely not the best way to proceed. A significant amount of formative research needs to be conducted in this area (for a start see O’Neill et al , 48 and Martinelli 49 ).
Even so, at this point in time it does seem reasonable to recommend that smoking cessation interventions that have been shown to be effective with adults in general be offered through student health services on college campuses, and that they be part of employee health benefit packages and resources, including typical employment venues of young adults not enrolled in college. Interventions should be tailored to address the attitudes and tobacco use patterns of young adults, recognising that a significant proportion have only recently become regular smokers or still may be intermittent smokers, and that a non-trivial proportion of males also use tobacco products other than cigarettes. Analysis of the impact of standard smoking cessation interventions in the young adult population need to be conducted so we can have some notion of their degree of effectiveness relative to older adults.
Unfortunately, many young adults are without health insurance, and people in this age group (especially males) do not have frequent contact with health care providers. Thus, it will admittedly be a challenge to expose young adult habitual smokers to proven cessation strategies involving clinical interventions combined with nicotine replacement therapy. In addition, data suggest that adolescents and young adults are infrequently asked about their smoking status and counselled regarding cessation during encounters with primary care providers. 50, 51 As such, interventions that do not rely on “teachable moments” with health care providers also must be designed and evaluated.
Wechsler et al conducted a survey of 393 college health centre directors to assess their attitudes about and efforts regarding student smoking. 52 The findings included that while 85% of directors considered smoking to be a serious problem, only 27% prohibit smoking in all indoor areas (which includes private offices and dormitories). In addition, almost half reported that there were no smoking cessation programmes available on their campus, and—among those who do provide cessation resources—the prominent perception was that demand was quite low. Similarly, a study conducted at 11 public colleges in Massachusetts found that “tobacco use among college students was not regarded as a high-priority problem by students or administrators”. 53 Thus, an obvious first step is to engage in efforts that will assist in making tobacco control a priority issue among college and university administrators and health care providers. It is likely that similar educational and “problem definition” efforts will have to be directed at employers and work site health managers.
Invest in smoking prevention interventions aimed at young adults
Given the epidemiology of smoking initiation, focusing prevention and control activities on youth has made great sense. 22, 37 However, the view that this focus on youth may be myopic and even dangerous in some ways has been expressed. Glantz has argued that a primary focus on youth in tobacco control efforts may be counterproductive, as it reinforces tobacco industry depictions of smoking as an “adult” behaviour, and shifts attention away from more comprehensive efforts. 54 Hill has made a similar argument, with a primary concern being that messages that youth should not smoke are likely to reinforce adolescents’ natural rebellious attitudes toward adults. 55 Even if one believes that it is essential to target serious tobacco prevention efforts toward youth, an important admission is that efforts to date, involving a wide variety of interventions, programmes and policies, have been met with limited success. 22, 37
Given current trends and the recognition that an increasing proportion of adult smokers initiate regular smoking after age 18, the time has come to increase prevention and control activities in the young adult population. It is still the case that the majority of smokers are fully engrained in this activity by the time they are 19. However, it appears that currently over 20% of smokers make the transition from occasional to habitual smoker as young adults. As Ling and Glantz have argued: “During the critical years of young adulthood, public health efforts dwindle while tobacco industry efforts intensify . . . Public health efforts should match tobacco industry interest in young adults. Each place where young adults adopt new behaviours also provides opportunities for public health interventions.” 44
Just what these prevention interventions and policies should look like is unclear at the moment. Again, there is very little literature regarding efforts to prevent tobacco use among young adults. Ling and Glantz suggest: “public health campaigns that resonate with the psychological needs and values of both smokers and nonsmokers may improve smoking prevention and cessation efforts. Interventions that affect cigarette prices, acceptance of the tobacco industry, the social acceptability of smoking, and secondhand tobacco smoke particularly threaten the industry.” 45 Jacobson et al suggested that public health practitioners and policymakers can learn a great deal from how the tobacco industry has skilfully marketed its products: “Just as tobacco marketing can influence smoking behaviour, social marketing is a promising approach to smoking prevention, although it does require significant resources and skillful execution.” The literature on social marketing suggests that mass media campaigns increase their chance for effectiveness if: (1) the campaign strategies are based on sound social marketing principles; (2) the effort is large and intense; (3) target groups are carefully differentiated; (4) messages for specific target groups are based on empirical findings regarding the attitudes, beliefs, needs and interests of the groups; and (5) the campaign is of sufficient duration. 22 Ling and Glantz recommend that media messages should not simply attempt to convince individuals not to smoke. 44 They also should support clean indoor air policies, social environments that challenge the social acceptability of smoking, and tobacco excise taxes.
Focusing prevention and control activities among young adults begs the question of the relative degree of focus on the college versus non-college populations. Given that smoking rates have increased more among college students than those not in school, and given the attention that the tobacco industry is giving to this market, one could argue that college students should be the number one priority. However, it is also the case that smoking rates are significantly higher among those not in school. It is likely that the most effective interventions will need to be tailored differently for these different groups of young adults. Tough discussions regarding the best use of limited prevention resources need to occur.
Consider potential counterproductive effects of interventions targeting adolescents
Even if one believes that a strong focus on youth is essential, it is possible that specific types of interventions and strategies are having the counterproductive effect of delaying rather than totally preventing tobacco use. Thus, it is important to consider whether any current youth focused strategies are delaying, deferring, or even encouraging smoking initiation among young adults rather than preventing it. To answer this issue, we would need to review a wide range of evaluations in which the long term effects of interventions were actually tracked into the early adult years. Unfortunately, follow up periods for youth tobacco interventions rarely extend beyond adolescence. An exception to this is the work of Rigotti et al , who analysed 1999 data regarding tobacco use among students at public colleges in Massachusetts and found that those students from this state (and thus ostensibly exposed to the Massachusetts’s youth focused tobacco control programme) had significantly lower rates of current use than those who attended high school in another state (31.5% v 42.6%). 56 These results suggest that exposure to a multiple component, comprehensive tobacco control programme as an adolescent has positive effects that last into young adulthood.
Additional information on the long term effects of youth tobacco prevention and control activities is greatly needed. In addition, it is critical that the tobacco control community invest some time and energy into considering whether or not specific types of youth focused strategies do indeed have the potential for counterproductive delaying effects. For example, it has become increasingly common for youth in possession of cigarettes to receive sanctions through the legal system (including such penalties as a ticket/fine or loss of driving privileges). 22, 54, 57 Such sanctions, of course, do not apply to adults. These negative consequences likely do not prevent experimentation with smoking, yet they may actually reduce youth access and/or persuade some minors to avoid smoking in public places. If such sanctions actually do decrease some minors’ ability and/or willingness to smoke, the transition to habitual smoking may be delayed. However, the desire to be “rebellious” and to engage in what is sanctioned as adult behaviour may have been reinforced (perhaps even intensified) and may remain strong as the adolescent reaches the “legal age” for the behaviour. As such, this may lead to increased smoking among young adults. While one might consider the proposed scenario rather far-fetched, it does seem worthwhile to contemplate potential negative side effects of various types of youth focused interventions. We need to entertain the uncomfortable possibility that strategies and tactics focusing on youth tobacco control are in part contributing to the recent changes in smoking behaviour observed among young adults.
Promote smoke-free environments
The promotion of smoke-free environments should be considered a potentially effective mechanism for decreasing smoking among young adults. These environments include work sites, campuses, restaurants, bars and nightclubs, and even homes. There is a growing amount of evidence that clean indoor air policies can have a positive effect on smokers as well as those at risk for exposure to environmental tobacco smoke. 22, 58 Such policies create social environments that reinforce messages about the negative aspects of tobacco smoke. Such environments may also encourage current smokers to quit or reduce their consumption, and in doing so may prevent some smokers from transitioning into regular, habitual smoking.
Ling and Glantz recommend the promotion of smoke-free homes among young adults: “ . . .educating young adults about the dangers of secondhand smoke may be particularly effective because they are starting new households and new families. Educating young adult parents (and parents to be) about the dangers of secondhand smoke will provide benefits not only for the new child (who will avoid the morbidity associated with involuntary smoking) but may also prompt cessation among the adults.” 44
Several people have argued for the creation of campus wide smoke-free environments (including dormitories and other residences, eating and recreation facilities, classrooms, and private offices). 5, 52 The results of their survey of college health centre directors suggest that some schools are attempting to counter trends in student smoking by implementing no-smoking policies. Such policies, however, must be promoted and enforced if they are to have any effect. Regarding smoke-free bars, Sepe et al stated that the “[c]reation of smoke-free bars—with appropriate ground-work and public education—may be a key to undermining the tobacco industry’s efforts to use bars to reestablish the social acceptability of smoking and secondhand smoke”. 35
Consider smoking in a broader context of risk taking behaviour
Adolescents and young adults will be done a great disservice if researchers and policy advocates do not consider tobacco use in the larger context of social environments and risk taking behaviour, in particular risky sexual behaviour and the use of alcohol and illicit drugs. A tobacco focused approach to policy and intervention is not likely to be the most effective strategy, since it is clear that a number of risky behaviours are linked with each other and with some identifiable attitudes and perspectives. The root causes of youth and young adult smoking are likely not tobacco specific, but rather things that motivate or drive people to engage in other forms of risky or rebellious behaviour. Malcolm Gladwell, in his book The tipping point , makes the important observation that what leads to smoking is not positive perceptions or attitudes about the act of smoking itself: “Over the past decade, the anti-smoking movement has railed against the tobacco companies for making smoking cool and has spent untold millions of dollars of public money trying to convince teenagers that smoking isn’t cool But that’s not the point. Smoking was never cool. Smokers are cool..” 59 Thus, it is possible that risk taking behaviours cluster together because adolescents (or young adults) are trying to project an overall image or persona of themselves that they view positively (a person who is rebellious, takes risk, is independent, etc). As such, the phenomenon may be more about a process of attempting to become a specific type of person than an isolated decision to engage in a specific type of behaviour (that is, cigarette smoking). Furthermore, while it is certainly reasonable to point fingers at the tobacco industry, insinuating sole blame on industry marketing tactics for the broad phenomenon of increased smoking among young adults is too simplistic. Efforts to reduce tobacco use among young adults need to include, but also have a broader vision and scope than, counteracting industry marketing/promotional activities
The recent increase in smoking among young adults should be of grave concern to those engaged in tobacco prevention and control among youth. The increase is partly a residual effect of increases in cigarette smoking that have occurred among adolescents. In addition, however, the upsurge in smoking among young adults appears to be part of a broader phenomenon involving changes in substance use and risk taking behaviours among youth making the transition to adulthood. While there are many unanswered questions about recent trends in cigarette smoking and other drug use among both adolescents and young adults, what is known to date leads to a clarion call for increased intervention and policy action regarding the prevention and control of substance abuse among young adults—both on and off campus—in the USA.
Acknowledgments
Nicole Kuiper provided valuable research assistance and support on this project. David Mendez and Harold Pollack provided guidance regarding analysis, and Gary Giovino offered useful data and comments. Nancy Rigotti, Pam Ling, Ken Warner, Peter Jacobson, and Ernest Dopp provided excellent substantive comments on earlier drafts of the paper. In addition, numerous colleagues attending the Innovations in Youth Tobacco Control Conference (July 2002) shared useful and provocative feedback.
- ↵ Wechsler H , Rigotti N, Gledhill-Hoyt J, et al. Increased levels of cigarette use among college students. JAMA 1998 ; 280 1673 –78. OpenUrl CrossRef PubMed Web of Science
- ↵ Rigotti NA , Lee JE, Wechsler H. U.S. College students’ use of tobacco products: results of a national survey. JAMA 2000 ; 248 : 699 –705.
- ↵ Johnston LD , O’Malley PM, Bachman JG. Monitoring the Future national survey results on drug use, 1975–2000 . Volume II: College students and adults ages 19–40. Bethesda, Maryland: National Institute on Drug Abuse, 2001. (NIH Publication No. 01–4925.)
- ↵ Substance Abuse and Mental Health Services Administration . Summary of findings from the 2000 National Household Survey on Drug Abuse. Rockville, Maryland: Office of Applied Studies, Report No: (SMA) 01–3549, September 2001 .
- ↵ Pierce JP , Naquin M, Gilpin E, et al. Smoking initiation in the United States: a role for worksite and college smoking bans. J Natl Cancer Inst 1991 ; 83 : 1009 –13. OpenUrl Abstract / FREE Full Text
- ↵ Monitoring the Future . University of Michigan News and Information Services: Ann Arbor, Michigan, Access date: 30 August 2002. URL: http://monitoringthefuture.org
- ↵ Emmons KM , Wechsler H, Dowdall G, et al. Predictors of smoking among U.S. college students. Am J Public Health 1998 ; 88 : 104 –7. OpenUrl CrossRef PubMed Web of Science
- ↵ Centers for Disease Control and Prevention . Tobacco use among high school students – United States, 1997. MMWR Morb Mortal Wkly Rep 1998 ; 47 : 229 –33. OpenUrl PubMed
- ↵ National Center for Health Statistics . Health, United States, 1993. Hyattsville, Maryland: Public Health Service, 1994 . (DHHS Publication Number (PHS) 94–1232.)
- ↵ Centers for Disease Control and Prevention . Tobacco use – United States, 1900–1999. MMWR Morb Mortal Wkly Rep 1999 ; 48 : 986 –93. OpenUrl PubMed
- ↵ Haddock CK , Web MV, DeBon M, et al. Evidence that smokeless tobacco use is a gateway for smoking initiation in young adult males. Prev Med 2001 ; 32 : 262 –7. OpenUrl CrossRef PubMed Web of Science
- ↵ Glover E , Laflin M, Edwards S. Age of initiation and switching patterns between smokeless tobacco and cigarettes among college students in the United States. Am J Public Health 1989 ; 79 : 207 –8. OpenUrl PubMed Web of Science
- ↵ Nyman AL , Taylor TM, Biener L. Trends in cigar smoking and perceptions of health risks among Massachusetts adults. Tobacco Control 2002 ; 11 (suppl II): ii25 –8. OpenUrl Abstract / FREE Full Text
- ↵ National Center for Education Statistics . The Condition of Education 2000. Access date: 5 February 2003. URL: http://nces.ed.gov/pubs2000/2000062.pdf
- ↵ Giovino GA . Epidemiology of tobacco use among US adolescents. Nicotine Tob Res 1999 ; 1 (supp 1): 31 –40.
- ↵ Gledhill-Hoyt J , Lee H, Strote J, et al. Increased use of marijuana and other illicit drugs at U.S. colleges in the 1990s: results of three national surveys. Addiction 2000 ; 95 : 1655 –67. OpenUrl CrossRef PubMed Web of Science
- ↵ Johnson RA , Gerstein DR. Initiating of use of alcohol, cigarettes, marijuana, cocaine and other substances in US birth cohorts since 1919. Am J Public Health 1998 ; 88 : 27 –33. OpenUrl PubMed Web of Science
- ↵ Bachman JG , Johnston LD, O’Malley PM. Explaining recent increases in students’ marijuana use: impacts of perceived risks and disapproval, 1976 through 1996. Am J Public Health 1998 ; 88 : 887 –92. OpenUrl PubMed Web of Science
- ↵ O’Malley PM , Johnston DL, Bachman JG. Alcohol use among adolescents. Alcohol Health & Research World 1998 ; 2 : 85 –93.
- ↵ Schulenberg J , Bachman JG, O’Malley PM, et al. High school educational success and subsequent substance use: a panel analysis following adolescents into young adulthood. J Health Soc Behav 1994 ; 35 : 45 –62. OpenUrl CrossRef PubMed Web of Science
- ↵ Schulenberg J , O’Malley PM, Bachman JG, et al. Getting drunk and growing up: trajectories of frequent binge drinking during the transition to young adulthood. J Stud Alcohol 1996 ; 57 : 289 –304. OpenUrl PubMed Web of Science
- ↵ Jacobson PD , Lantz PM, Warner KE, et al. Combating teen smoking: research and policy strategies . Ann Arbor, Michigan: University of Michigan Press, 2001 .
- ↵ Flay BR , Hu FB, Richardson J. Psychosocial predictors of different stages of cigarette smoking among high school students. Prev Med 1998 ; 27 : A9 –18. OpenUrl CrossRef PubMed Web of Science
- ↵ Husten CG , McCarty MC, Giovino GA, et al. Intermittent smokers: a descriptive analysis of persons who have never smoked daily. Am J Public Health 1998 ; 88 : 86 –9. OpenUrl PubMed Web of Science
- ↵ American Legacy Foundation . Legacy First Look Report 3: pathways to established smoking: results from the 1999 National Youth Tobacco Survey. Washington DC: American Legacy Foundation, October 2000 .
- ↵ SAMHSA , Office of Applied Statistics. Tobacco use in America: findings from the 1999 National Household Survey on Drug Abuse. Access date: 30 August 2002. URL: http://www.samhsa.gov/OAS/NHSDA/tobacco/appendixd.htm
- ↵ Lawrence D , Fagan P, Backinger C, et al. Smoking patterns among young adults ages 18–24 in the US: data from the Current Population Survey, 1998–1999. Abstract from the Society for Research on Nicotine and Tobacco Annual Meeting, Savannah, Georgia, February 2002 .
- ↵ Ellickson PL , McGuigan KA, Klein DJ. Predictors of late-onset smoking and cessation over 10 years. J Adolesc Health 2001 ; 29 : 101 –8. OpenUrl
- ↵ Choi WS , Harris KJ, Okuyemi K et al. Predictors of smoking initiation among college-bound high school students. Abstract from the Society for Research on Nicotine and Tobacco Annual Meeting, Savannah, Georgia, February 2002 .
- ↵ Wee CC , Rigotti NA, Davis RB, et al. Relationship between smoking and weight control efforts among adults in the United States. Arch Intern Med 2001 ; 161 : 546 –50. OpenUrl CrossRef PubMed Web of Science
- ↵ Wechsler H , Lee JE, Nelson TF, et al. Drinking levels, alcohol problems and secondhand effects in substance-free college residences: results of a national study. J Stud Alcohol 2001 ; 61 : 23 –32. OpenUrl
- ↵ Sonntag H , Wittchen HU, Hofler M, et al . Are social fears and DSM-IV social anxiety disorder associated with smoking and nicotine dependence in adolescents and young adults? Eur Psychiatry 2000 ; 15 : 67 –74. OpenUrl CrossRef PubMed Web of Science
- ↵ Anda RF , Croft JB, Felitti, VJ, et al . Adverse childhood experiences and smoking during adolescence and adulthood. JAMA 1999 ; 282 : 1652 –8. OpenUrl CrossRef PubMed Web of Science
- ↵ Katz SK , Lavack AM. Tobacco related bar promotions: insights from tobacco industry documents. Tobacco Control 2002 ; 11 (suppl I): i92 –101. OpenUrl Abstract / FREE Full Text
- ↵ Sepe E , Ling PM, Glantz SA. Smooth moves: tobacco bar and nightclub promotions target young adults. Am J Public Health 2002 : 92 : 414 –9. OpenUrl CrossRef PubMed Web of Science
- ↵ Sepe E , Glantz SA. Bar and club tobacco promotions in the alternative press: targeting young adults. Am J Public Health 2002 : 92 : 75 –8. OpenUrl PubMed Web of Science
- ↵ Lantz P , Jacobson PD, Warner KE, et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tobacco Control 2000 ; 9 : 47 –63. OpenUrl Abstract / FREE Full Text
- Gilpin EA , Pierce JP, Rosbrook B. Are adolescents receptive to current sales promotion practices of the tobacco industry? Prev Med 1997 ; 26 : 14 –21. OpenUrl CrossRef PubMed Web of Science
- Pierce JP , Gilpin EA, Choi WS. Sharing the blame: smoking experimentation and future smoking-attributable mortality due to Joe Camel and Marlboro advertising and promotions. Tobacco Control 1999 ; 8 : 37 –44. OpenUrl Abstract / FREE Full Text
- ↵ Perry CL . The tobacco industry and underage youth smoking: tobacco industry documents from the Minnesota litigation. Pediatr Adolesc Med 1999 ; 153 : 935 –41. OpenUrl
- ↵ King C , Siegel M. The Master Settlement Agreement with the tobacco industry and cigarette advertising in magazines. N Engl J Med 2001 ; 345 : 504 –11. OpenUrl CrossRef PubMed Web of Science
- ↵ Rosenberg NJ , Siegel M. Use of corporate sponsorship as a tobacco marketing tool: A review of tobacco industry sponsorship in the USA, 1995–99. Tobacco Control 2001 ; 10 : 239 –46. OpenUrl Abstract / FREE Full Text
- ↵ Tye JB , Warner KE, Glantz SA. Tobacco advertising and consumption: evidence of a causal relationship. J Public Health Policy 1987 ; 8 : 492 –508. OpenUrl CrossRef PubMed
- ↵ Ling PM , Glantz SA. Why and how the tobacco industry sells cigarettes to young adults: evidence from industry documents. Am J Public Health 2002 ; 92 : 908 –16. OpenUrl CrossRef PubMed Web of Science
- ↵ Ling PM , Glantz SA. Using tobacco industry marketing research to design more effective tobacco control campaigns. JAMA 2002 ; 287 : 2983 –9. OpenUrl CrossRef PubMed Web of Science
- ↵ Rigotti NA , Moran SE, Wechsler H. College students’ exposure to tobacco promotions at bars, clubs and campus social events: prevalence and relationship to tobacco use. Abstract from the Society for Research on Nicotine and Tobacco Annual Meeting, New Orleans, February 2003 .
- ↵ Everett SA , Husten CG, Kann LK, et al. Smoking initiation and smoking patterns among U.S. college students. J Am Coll Health 1999 ; 48 : 55 –60. OpenUrl PubMed Web of Science
- ↵ O’Neill HK , Gillispie MA, Slobin K. Stages of change and smoking cessation: a computer-administered intervention program for young adults. Am J Health Promotion 2000 ; 15 : 93 –96. OpenUrl PubMed Web of Science
- ↵ Martinelli AM . An explanatory model of variables influencing health promotion behaviors in smoking and nonsmoking college students. Public Health Nurs 1999 ; 16 : 263 –9. OpenUrl CrossRef PubMed Web of Science
- ↵ Foote J , Harris R, Giles M, et al. Physician advice and tobacco use: a survey of 1st-year college students. J Am Coll Health 1996 ; 45 : 129 –32. OpenUrl PubMed Web of Science
- ↵ Thorndike A , Ferris T, Stafford R, et al. Rates of U.S. physicians counseling adolescents about smoking. J Natl Cancer Inst 1999 ; 91 : 1857 –62. OpenUrl Abstract / FREE Full Text
- ↵ Wechsler H , Kelley K, Seibring M, et al. College smoking policies and smoking cessation programs: results of a survey of college health center directors. J Am Coll Health 2001 : 49 : 205 –12. OpenUrl PubMed Web of Science
- ↵ Majchrzak N , Park E, Rigotti N. Tobacco use by Massachusetts public college students: discussing issues with students and administrators. Abstract from the Society for Research on Nicotine and Tobacco Annual Meeting, Savannah, Georgia, February 2002 .
- ↵ Glantz SA . Preventing tobacco use—the youth access trap. Am J Public Health 1996 ; 86 : 1156 –8. OpenUrl
- ↵ Hill D . Why we should tackle adult smoking first. Tobacco Control 1999 ; 8 : 333 –5. OpenUrl FREE Full Text
- ↵ Rigotti NA , Regan S, Majchrzak NE, et al. Tobacco use by Massachusetts public college students in 1999. Tobacco Control 2002 ; 11 (suppl II): ii20 –4. OpenUrl Abstract / FREE Full Text
- ↵ Wakefield M , Giovino G. Teen penalties for tobacco possession, use, and purchase: evidence and issues. Tobacco Control 2003 ; 12 (suppl I): 6 –13. OpenUrl FREE Full Text
- ↵ Brownson RC , Eriksen MP, Davis RM, et al. Environmental tobacco smoke: health effects and policies to reduce exposure. Ann Rev Public Health 1997 ; 18 : 163 –85. OpenUrl CrossRef PubMed Web of Science
- ↵ Gladwell M . The tipping point: how little things can make a big difference. New York: Little, Brown & Co, 2000 .
Read the full text or download the PDF:
Tobacco, Nicotine, and E-Cigarettes Research Report What research is being done on tobacco use?
New scientific developments can improve our understanding of nicotine addiction and spur the development of better prevention and treatment strategies.
Genetics and Epigenetics
An estimated 50-75 percent of the risk for nicotine addiction is attributable to genetic factors. 221 A cluster of genes (CHRNA5-CHRNA3-CHRNB4) on chromosome 15 that encode the α5, α3, and β4 protein subunits that make up the brain receptor for nicotine 221–223 are particularly implicated in nicotine dependence and smoking among people of European descent. Variation in the CHRNA5 gene influences the effectiveness of combination NRT, but not varenicline. 224 Other research has identified genes that influence nicotine metabolism and therefore, the number of cigarettes smoked, 225 responsiveness to medication, 204,205 and chances of successfully quitting. 226 For example, the therapeutic response to varenicline is associated with variants for the CHRNB2, CHRNA5, and CHRNA4 genes, while bupropion-related cessation is linked with variation in genes that affect nicotine metabolism. 227
Smoking can also lead to persistent changes in gene expression (epigenetic changes), which may contribute to associated medical consequences over the long term, even following cessation. 228 Epigenetic changes may serve as a potential biomarker for prenatal tobacco smoke exposure. Researchers found tobacco-specific changes at 26 sites on the epigenome, and this pattern predicted prenatal exposure with 81 percent accuracy. 229 A large scale meta-analysis of data on epigenetic changes associated with prenatal exposure to cigarette smoke also identified many epigenetic changes that persisted into later childhood. 230 More research is needed to understand the long-term health impacts of these changes.
Neuroimaging
Cutting-edge neuroimaging technologies have identified brain changes associated with nicotine dependence and smoking. Using functional magnetic resonance imaging (fMRI), scientists can visualize smokers’ brains as they respond to cigarette-associated cues that can trigger craving and relapse. 231 Such research may lead to a biomarker for relapse risk and for monitoring treatment progress, as well as point to regions of the brain involved in the development of nicotine addiction. 29
A neuroimaging technology called default-mode or resting-state fMRI (rs-fMRI) reveals intrinsic brain activity when people are alert but not performing a particular task. Using this technique, researchers are examining the neurobiological profile associated with withdrawal and how nicotine impacts cognition. 232 Comparisons between smokers and nonsmokers suggest that chronic nicotine may weaken connectivity within brain circuits involved in planning, paying attention, and behavioral control—possibly contributing to difficulty with quitting. 233 fMRI studies also reveal the impact of smoking cessation medications on the brain—particularly how they modulate the activity of different brain regions to alleviate withdrawal symptoms and reduce smoking. A review of these studies suggested that NRT enhances cognition during withdrawal by modulating activity in default-network regions, but may not affect neural circuits associated with nicotine addiction. 234
Some imaging techniques allow researchers to visualize neurotransmitters and their receptors, further informing our understanding of nicotine addiction and its treatment. 27 Using these techniques, researchers have established that smoking increases the number of brain receptors for nicotine. Individuals who show greater receptor upregulation are less likely to stop smoking. 28 Combining neuroimaging and genetics may yield particularly useful information for improving and tailoring treatment. For example, nonsmoking adolescents with a particular variant in the CHRNA5-CHRNA3-CHRNB4 gene cluster (which is associated with nicotine dependence and smoking) showed reduced brain activity in response to reward in the striatum as well as the orbitofrontal and anterior cingulate cortex. This finding suggests that genetics can influence how the brain processes rewards which may influence vulnerability to nicotine dependence. 235 Neuroimaging genetics also shows that other genes, including ones that influence dopamine neurotransmission, influence reward sensitivity and risk for addiction to nicotine. 236
235 Smoking Essay Topics & Examples
Looking for smoking essay topics? Being one of the most serious psychological and social issues, smoking is definitely worth writing about.
🏆 Best Smoking Essay Examples & Topic Ideas
🥇 good titles for smoking essay, 👍 best titles for research paper about smoking, ⭐ simple & easy health essay titles, 💡 interesting topics to write about health, ❓ essay questions about smoking.
In your essay about smoking, you might want to focus on its causes and effects or discuss why smoking is a dangerous habit. Other options are to talk about smoking prevention or to concentrate on the reasons why it is so difficult to stop smoking. Here we’ve gathered a range of catchy titles for research papers about smoking together with smoking essay examples. Get inspired with us!
Smoking is a well-known source of harm yet popular regardless, and so smoking essays should cover various aspects of the topic to identify the reasons behind the trend.
You will want to discuss the causes and effects of smoking and how they contributed to the persistent refusal of large parts of the population to abandon the habit, even if they are aware of the dangers of cigarettes. You should provide examples of how one may become addicted to tobacco and give the rationales for smokers.
You should also discuss the various consequences of cigarette use, such as lung cancer, and identify their relationship with the habit. By discussing both sides of the issue, you will be able to write an excellent essay.
Reasons why one may begin smoking, are among the most prominent smoking essay topics. It is not easy to begin to enjoy the habit, as the act of smoke inhalation can be difficult to control due to a lack of experience and unfamiliarity with the concept.
As such, people have to be convinced that the habit deserves consideration by various ideas or influences. The notion that “smoking is cool” among teenagers can contribute to the adoption of the trait, as can peer pressure.
If you can find polls and statistics on the primary factors that lead people to tweet, they will be helpful to your point. Factual data will identify the importance of each cause clearly, although you should be careful about bias.
The harmful effects of tobacco have been researched considerably more, with a large body of medical studies investigating the issue available to anyone.
Lung cancer is the foremost issue in the public mind because of the general worry associated with the condition and its often incurable nature, but smoking can lead to other severe illnesses.
Heart conditions remain a prominent consideration due to their lethal effects, and strokes or asthma deserve significant consideration, as well. Overall, smoking has few to no beneficial health effects but puts the user at risk of a variety of concerns.
As such, people should eventually quit once their health declines, but their refusal to do so deserves a separate investigation and can provide many interesting smoking essay titles.
One of the most prominent reasons why a person would continue smoking despite all the evidence of its dangers and the informational campaigns carried out to inform consumers is nicotine addiction.
The substance is capable of causing dependency, a trait that has led to numerous discussions of the lawfulness of the current state of cigarettes.
It is also among the most dangerous aspects of smoking, a fact you should mention.
Lastly, you can discuss the topics of alternatives to smoking in your smoking essay bodies, such as e-cigarettes, hookahs, and vapes, all of which still contain nicotine and can, therefore, lead to considerable harm. You may also want to discuss safe cigarette avoidance options and their issues.
Here are some additional tips for your essay:
- Dependency is not the sole factor in cigarette consumption, and many make the choice that you should respect consciously.
- Cite the latest medical research titles, as some past claims have been debunked and are no longer valid.
- Mortality is not the sole indicator of the issues associated with smoking, and you should take chronic conditions into consideration.
Find smoking essay samples and other useful paper samples on IvyPanda, where we have a collection of professionally written materials!
- Conclusion of Smoking Should Be Banned on College Campuses Essay However, it is hard to impose such a ban in some colleges because of the mixed reactions that are held by different stakeholders about the issue of smoking, and the existing campus policies which give […]
- Smoking: Problems and Solutions To solve the problem, I would impose laws that restrict adults from smoking in the presence of children. In recognition of the problems that tobacco causes in the country, The Canadian government has taken steps […]
- How Smoking Is Harmful to Your Health The primary purpose of the present speech is to inform the audience about the detrimental effects of smoking. The first system of the human body that suffers from cigarettes is the cardiovascular system.
- Should Smoking Be Banned in Public Places? Besides, smoking is an environmental hazard as much of the content in the cigarette contains chemicals and hydrocarbons that are considered to be dangerous to both life and environment.
- Causes and Effects of Smoking Some people continue smoking as a result of the psychological addiction that is associated with nicotine that is present in cigarettes.
- Smoking Cigarette Should Be Banned Ban on tobacco smoking has resulted to a decline in the number of smokers as the world is sensitized on the consequences incurred on 31st May.
- Smoking: Effects, Reasons and Solutions This presentation provides harmful health effects of smoking, reasons for smoking, and solutions to smoking. Combination therapy that engages the drug Zyban, the concurrent using of NRT and counseling of smokers under smoking cessation program […]
- On Why One Should Stop Smoking Thesis and preview: today I am privileged to have your audience and I intend to talk to you about the effects of smoking, and also I propose to give a talk on how to solve […]
- Smoking and Its Negative Effects on Human Beings Therefore, people need to be made aware of dental and other health problems they are likely to experience as a result of smoking.
- Smoking Among Teenagers as Highlighted in Articles The use of tobacco through smoking is a trend among adolescents and teenagers with the number of young people who involve themselves in smoking is growing each day.
- Advertisements on the Effect of Smoking Do not Smoke” the campaign was meant to discourage the act of smoking among the youngsters, and to encourage them to think beyond and see the repercussions of smoking.
- Hookah Smoking and Its Risks The third component of a hookah is the hose. This is located at the bottom of the hookah and acts as a base.
- Should Smoking Tobacco Be Classified As an Illegal Drug? Although this is the case, the tobacco industry is one of the most profitable industries, a fact that has made it very hard for the government to illegalize the use of tobacco products.
- Health Promotion Plan: Smokers in Mississippi The main strategies of the training session are to reduce the number of smokers in Mississippi, conduct a training program on the dangers of smoking and work with tobacco producers.
- Public Health Education: Anti-smoking Project The workshop initiative aimed to achieve the following objectives: To assess the issues related to smoking and tobacco use. To enhance the health advantages of clean air spaces.
- Smoking and Its Effects on Human Body The investigators explain the effects of smoking on the breath as follows: the rapid pulse rate of smokers decreases the stroke volume during rest since the venous return is not affected and the ventricles lose […]
- Causes and Effects of Smoking in Public The research has further indicated that the carcinogens are in higher concentrations in the second hand smoke rather than in the mainstream smoke which makes it more harmful for people to smoke publicly.
- Smoking and Youth Culture in Germany The report also assailed the Federal Government for siding the interest of the cigarette industry instead of the health of the citizens.
- Summary of “Smokers Get a Raw Deal” by Stanley Scott Lafayette explains that people who make laws and influence other people to exercise these laws are obviously at the top of the ladder and should be able to understand the difference between the harm sugar […]
- Aspects of Anti-Smoking Advertising Thus, it is safe to say that the authors’ main and intended audience is the creators of anti-smoking public health advertisements.
- Introducing Smoking Cessation Program: 5 A’s Intervention Plan The second problem arises in an attempt to solve the issue of the lack of counseling in the unit by referring patients to the outpatient counseling center post-hospital discharge to continue the cessation program.
- Teenage Smoking and Solution to This Problem Overall, the attempts made by anti-smoking campaigners hardly yield any results, because they mostly focus on harmfulness of tobacco smoking and the publics’ awareness of the problem, itself, but they do not eradicate the underlying […]
- Smoking Qualitative Research: Critical Analysis Qualitative research allows researchers to explore a wide array of dimensions of the social world, including the texture and weave of everyday life, the understandings, experiences and imaginings of our research participants, the way that […]
- Tobacco Debates in “Thank You for Smoking” The advantage of Nick’s strategy is that it offers the consumer a role model to follow: if smoking is considered to be ‘cool’, more people, especially young ones, will try to become ‘cool’ using cigarettes.
- Smoking Habit, Its Causes and Effects Smoking is one of the factors that are considered the leading causes of several health problems in the current society. Smoking is a habit that may be easy to start, but getting out of this […]
- The Change of my Smoking Behavior With the above understanding of my social class and peer friends, I was able to create a plan to avoid them in the instances that they were smoking.
- “Thank You For Smoking” by Jason Reitman Film Analysis Despite the fact that by the end of the film the character changes his job, his nature remains the same: he believes himself to be born to talk and convince people.
- Health Promotion for Smokers The purpose of this paper is to show the negative health complications that stem from tobacco use, more specifically coronary heart disease, and how the health belief model can help healthcare professionals emphasize the importance […]
- Gender-Based Assessment of Cigarette Smoking Harm Thus, the following hypothesis is tested: Women are more likely than men to believe that smoking is more harmful to health.
- Hazards of Smoking and Benefits of Cessation Prabhat Jha is the author of the article “The Hazards of Smoking and the Benefits of Cessation,” published in a not-for-profit scientific journal, eLife, in 2020.
- The Impact of Warning Labels on Cigarette Smoking The regulations requiring tobacco companies to include warning labels are founded on the need to reduce nicotine intake, limit cigarette dependence, and mitigate the adverse effects associated with addiction to smoking.
- Psilocybin as a Smoking Addiction Remedy Additionally, the biotech company hopes to seek approval from FDA for psilocybin-based therapy treatment as a cigarette smoking addiction long-term remedy.
- Investing Savings from Quitting Smoking: A Financial Analysis The progression of interest is approximately $50 per year, and if we assume n equal to 45 using the formula of the first n-terms of the arithmetic progression, then it comes out to about 105 […]
- Smoking as a Community Issue: The Influence of Smoking A review of the literature shows the use of tobacco declined between 1980 and 2012, but the number of people using tobacco in the world is increasing because of the rise in the global population.
- Smoking Public Education Campaign Assessment The major influence of the real cost campaign was to prevent the initiation of smoking among the youth and prevent the prevalence of lifelong smokers.
- Smoking Cessation Therapy: Effectiveness of Electronic Cigarettes Based on the practical experiments, the changes in the patients’ vascular health using nicotine and electronic cigarettes are improved within one-month time period. The usage only of electronic cigarettes is efficient compared to when people […]
- Quitting Smoking and Related Health Benefits The regeneration of the lungs will begin: the process will touch the cells called acini, from which the mucous membrane is built. Therefore, quitting the habit of smoking a person can radically change his life […]
- Smoking and Stress Among Veterans The topic is significant to explore because of the misconception that smoking can alleviate the emotional burden of stress and anxiety when in reality, it has an exacerbating effect on emotional stress.
- Smoking as a Predictor of Underachievement By comparing two groups smoking and non-smoking adolescents through a parametric t-test, it is possible to examine this assumption and draw conclusions based on the resulting p-value.
- Smoking and the Pandemic in West Virginia In this case, the use of the income variable is an additional facet of the hypothesis described, allowing us to evaluate whether there is any divergence in trends between the rich and the poor.
- Anti-Smoking Policy in Australia and the US The anti-smoking policy is to discourage people from smoking through various means and promotion of a healthy lifestyle, as well as to prevent the spread of the desire to smoke.
- Smoking Prevalence in Bankstown, Australia The secondary objective of the project was to gather and analyze a sufficient amount of auxiliary scholarly sources on smoking cessation initiatives and smoking prevalence in Australia.
- Drug Addiction in Teenagers: Smoking and Other Lifestyles In the first part of this assignment, the health problem of drug addiction was considered among teens and the most vulnerable group was established.
- Anti-Smoking Communication Campaign’s Analysis Defining the target audience for an anti-smoking campaign is complicated by the different layers of adherence to the issue of the general audience of young adults.
- Smoking Cessation Project Implementation In addition, the review will include the strengths and weaknesses of the evidence presented in the literature while identifying gaps and limitations.
- Smoking Cessation and Health Promotion Plan Patients addicted to tobacco are one of the major concerns of up-to-date medicine as constant nicotine intake leads to various disorders and worsens the health state and life quality of the users.
- Maternal and Infant Health: Smoking Prevention Strategies It is known that many women know the dangers of smoking when pregnant and they always try to quit smoking to protect the lives of themselves and the child.
- A Peer Intervention Program to Reduce Smoking Rates Among LGBTQ Therefore, the presumed results of the project are its introduction into the health care system, which will promote a healthy lifestyle and diminish the level of smoking among LGBTQ people in the SESLHD.
- Tackling Teenage Smoking in Community The study of the problem should be comprehensive and should not be limited by the medical aspect of the issue. The study of the psychological factor is aimed at identifying the behavioral characteristics of smoking […]
- Peer Pressure and Smoking Influence on Teenagers The study results indicate that teenagers understand the health and social implications of smoking, but peer pressure contributes to the activity’s uptake.
- Smoking Cessation Programs Through the Wheel of Community Organizing The first step of the wheel is to listen to the community’s members and trying to understand their needs. After the organizer and the person receiving treatment make the connection, they need to understand how […]
- Smoking: Benefits or Harms? Hundreds of smokers every day are looking for a way to get rid of the noose, which is a yoke around the neck, a cigarette.
- The Culture of Smoking Changed in Poland In the 1980-90s, Poland faced the challenge of being a country with the highest rates of smoking, associated lung cancer, and premature mortality in the world.
- The Stop Smoking Movement Analysis The paper discusses the ideology, objective, characteristics, context, special techniques, organization culture, target audience, media strategies, audience reaction, counter-propaganda and the effectiveness of the “Stop Smoking” Movement.”The Stop Smoking” campaign is a prevalent example of […]
- Smoking Health Problem Assessment The effects of smoking correlate starkly with the symptoms and diseases in the nursing practice, working as evidence of the smoking’s impact on human health.
- Integration of Smoking Cessation Into Daily Nursing Practice Generally, smoking cessation refers to a process structured to help a person to discontinue inhaling smoked substances. It can also be referred to as quitting smoking.
- E-Cigarettes and Smoking Cessation Many people argue that e-cigarettes do not produce secondhand smoke. They believe that the e-fluids contained in such cigarettes produce vapor and not smoke.
- Outdoor Smoking Ban in Public Areas of the Community These statistics have contributed to the widespread efforts to educate the public regarding the need to quit smoking. However, most of the chronic smokers ignore the ramifications of the habit despite the deterioration of their […]
- Nicotine Replacement Therapy for Adult Smokers With a Psychiatric Disorder The qualitative research methodology underlines the issue of the lack of relevant findings in the field of nicotine replacement therapy in people and the necessity of treatment, especially in the early stages of implementation.
- Smoking and Drinking: Age Factor in the US As smoking and drinking behavior were both strongly related to age, it could be the case that the observed relationship is due to the fact that older pupils were more likely to smoke and drink […]
- Poland’s Smoking Culture From Nursing Perspective Per Kinder, the nation’s status as one of Europe’s largest tobacco producers and the overall increase in smoking across the developing nations of Central and Eastern Europe caused its massive tobacco consumption issues.
- Smoking Cessation Clinic Analysis The main aim of this project is to establish a smoking cessation clinic that will guide smoker through the process of quitting smoking.
- Cigarette Smoking Among Teenagers in the Baltimore Community, Maryland The paper uses the Baltimore community in Maryland as the area to focus the event of creating awareness of cigarette smoking among the teens of this community.
- Advocating for Smoking Cessation: Health Professional Role Health professionals can contribute significantly to tobacco control in Australia and the health of the community by providing opportunities for smoking patients to quit smoking.
- Lifestyle Management While Quitting Smoking Realistically, not all of the set goals can be achieved; this is due to laxity in implementing them and the associated difficulty in letting go of the past lifestyle.
- Smoking in the Actuality The current use of aggressive marketing and advertising strategies has continued to support the smoking of e-cigarettes. The study has also indicated that “the use of such e-cigarettes may contribute to the normalization of smoking”.
- Analysis of the Family Smoking Prevention and Tobacco Control Act The law ensures that the FDA has the power to tackle issues of interest to the public such as the use of tobacco by minors.
- “50-Year Trends in Smoking-Related Mortality in the United States” by Thun et al. Thun is affiliated with the American Cancer Society, but his research interests cover several areas. Carter is affiliated with the American Cancer Society, Epidemiology Research Program.
- Pulmonology: Emphysema Caused by Smoking The further development of emphysema in CH can lead to such complications caused by described pathological processes as pneumothorax that is associated with the air surrounding the lungs.
- Smoking and Lung Cancer Among African Americans Primarily, the research paper provides insight on the significance of the issue to the African Americans and the community health nurses.
- Health Promotion and Smoking Cessation I will also complete a wide range of activities in an attempt to support the agency’s goals. As well, new studies will be conducted in order to support the proposed programs.
- Maternal Mental Health and Prenatal Smoking It was important to determine the variables that may lead to postpartum relapse or a relapse during the period of pregnancy. It is important to note that the findings are also consistent with the popular […]
- Nursing Interventions for Smoking Cessation For instance, the authors are able to recognize the need to classify the level of intensity in respect to the intervention that is employed by nurses towards smoking cessation.
- Smoking and Cancer in the United States In this research study, data on tobacco smoking and cancer prevalence in the United States was used to determine whether cancer in the United States is related to tobacco smoking tobacco.
- Marketing Plan: Creating a Smoking Cessation Program for Newton Healthcare Center The fourth objective is to integrate a smoking cessation program that covers the diagnosis of smoking, counseling of smokers, and patient care system to help the smokers quit their smoking habits. The comprehensive healthcare needs […]
- Smoking Among the Youth Population Between 12-25 Years I will use the theory to strengthen the group’s beliefs and ideas about smoking. I will inform the group about the relationship between smoking and human health.
- Risks of Smoking Cigarettes Among Preteens Despite the good news that the number of preteen smokers has been significantly reducing since the 1990s, there is still much to be done as the effects of smoking are increasingly building an unhealthy population […]
- Healthy People Program: Smoking Issue in Wisconsin That is why to respond to the program’s effective realization, it is important to discuss the particular features of the target population in the definite community of Wisconsin; to focus on the community-based response to […]
- Health Campaign: Smoking in the USA and How to Reduce It That is why, the government is oriented to complete such objectives associated with the tobacco use within the nation as the reduction of tobacco use by adults and adolescents, reduction of initiation of tobacco use […]
- Smoking Differentials Across Social Classes The author inferred her affirmations from the participant’s words and therefore came to the right conclusion; that low income workers had the least justification for smoking and therefore took on a passive approach to their […]
- Cigarette Smoking Side Effects Nicotine is a highly venomous and addictive substance absorbed through the mucous membrane in the mouth as well as alveoli in the lungs.
- Long-Term Effects of Smoking The difference between passive smoking and active smoking lies in the fact that, the former involves the exposure of people to environmental tobacco smoke while the latter involves people who smoke directly.
- Smoking Cessation Program Evaluation in Dubai The most important program of this campaign is the Quit and Win campaign, which is a unique idea, launched by the DHCC and is in the form of an open contest.
- Preterm Birth and Maternal Smoking in Pregnancy The major finding of the discussed research is that both preterm birth and maternal smoking during pregnancy contribute, although independently, to the aortic narrowing of adolescents.
- Enforcement of Michigan’s Non-Smoking Law This paper is aimed at identifying a plan and strategy for the enforcement of the Michigan non-smoking law that has recently been signed by the governor of this state.
- Smoking Cessation for Patients With Cardio Disorders It highlights the key role of nurses in the success of such programs and the importance of their awareness and initiative in determining prognosis.
- Legalizing Electronic Vaping as the Means of Curbing the Rates of Smoking However, due to significantly less harmful effects that vaping produces on health and physical development, I can be considered a legitimate solution to reducing the levels of smoking, which is why it needs to be […]
- Inequality and Discrimination: Impact on LGBTQ+ High School Students Consequently, the inequality and discrimination against LGBTQ + students in high school harm their mental, emotional, and physical health due to the high level of stress and abuse of various substances that it causes.
- Self-Efficacy and Smoking Urges in Homeless Individuals Pinsker et al.point out that the levels of self-efficacy and the severity of smoking urges change significantly during the smoking cessation treatment.
- “Cigarette Smoking: An Overview” by Ellen Bailey and Nancy Sprague The authors of the article mentioned above have presented a fair argument about the effects of cigarette smoking and debate on banning the production and use of tobacco in America.
- “The Smoking Plant” Project: Artist Statement It is the case when the art is used to pass the important message to the observer. The live cigarette may symbolize the smokers while the plant is used to denote those who do not […]
- Dangers of Smoking While Pregnant In this respect, T-test results show that mean birthweight of baby of the non-smoking mother is 3647 grams, while the birthweight of smoking mother is 3373 grams. Results show that gestation value and smoking habit […]
- The Cultural Differences of the Tobacco Smoking The Middle East culture is connected to the hookah, the Native American cultures use pipes, and the Canadian culture is linked to cigarettes.
- Ban on Smoking in Enclosed Public Places in Scotland The theory of externality explains the benefit or cost incurred by a third party who was not a party to the reasoning behind the benefit or cost. This will also lead to offer of a […]
- How Smoking Cigarettes Effects Your Health Cigarette smoking largely aggravates the condition of the heart and the lung. In addition, the presence of nicotine makes the blood to be sticky and thick leading to damage to the lining of the blood […]
- Alcohol and Smoking Abuse: Negative Physical and Mental Effects The following is a range of effects of heavy alcohol intake as shown by Lacoste, they include: Neuropsychiatric or neurological impairment, cardiovascular, disease, liver disease, and neoplasm that is malevolent.
- Smoking Prohibition: Local Issues, Personal Views This is due to the weakening of blood vessels in the penis. For example, death rate due to smoking is higher in Kentucky than in other parts of the country.
- Smoking During Pregnancy Issues Three things to be learned from the research are the impact of smoking on a woman, possible dangers and complications and the importance of smoking cessation interventions.
- The Smoking Problem: Mortality, Control, and Prevention The article presents smoking as one of the central problems for many countries throughout the world; the most shocking are the figures related to smoking rate among students. Summary: The article is dedicated to the […]
- Tobacco Smoking: Bootleggers and Baptists Legislation or Regulation The issue is based on the fact that tobacco smoking also reduces the quality of life and ruins the body in numerous ways.
- Ban Smoking in Cars Out of this need, several regulations have been put in place to ensure children’s safety in vehicles is guaranteed; thus, protection from second-hand smoke is an obvious measure that is directed towards the overall safety […]
- Smoking: Causes and Effects Considering the peculiarities of a habit and of a disease, smoking can be considered as a habit rather than a disease.
- Smoking Behavior Under Clinical Observation The physiological aspect that influences smokers and is perceived as the immediate effect of smoking can be summarized as follows: Within ten seconds of the first inhalation, nicotine, a potent alkaloid, passes into the bloodstream, […]
- Smoking and Its Effect on the Brain Since the output of the brain is behavior and thoughts, dysfunction of the brain may result in highly complex behavioral symptoms. The work of neurons is to transmit information and coordinate messengers in the brain […]
- Smoking Causes and Plausible Arguments In writing on the cause and effect of smoking we will examine the issue from the point of view of temporal precedence, covariation of the cause and effect and the explanations in regard to no […]
- Post Smoking Cessation Weight Gain The aim of this paper is to present, in brief, the correlation between smoking cessation and weigh gain from biological and psychological viewpoints.
- Marketing a Smoking Cessation Program In the case of the smoking cessation program, the target group is made up of smokers who can be further subdivided into segments such as heavy, medium, and light smokers.
- Smoking Cessation for Ages 15-30 The Encyclopedia of Surgery defines the term “Smoking Cessation” as an effort to “quit smoking” or “withdrawal from smoking”. I aim to discuss the importance of the issue by highlighting the most recent statistics as […]
- Motivational Interviewing as a Smoking Cessation Intervention for Patients With Cancer The dependent variable is the cessation of smoking in 3 months of the interventions. The study is based on the author’s belief that cessation of smoking influences cancer-treated patients by improving the efficacy of treatment.
- Factors Affecting the Success in Quitting Smoking of Smokers in West Perth, WA Australia Causing a wide array of diseases, health smoking is the second cause of death in the world. In Australia, the problem of smoking is extremely burning due to the high rates of diseases and deaths […]
- Media Effects on Teen Smoking But that is not how an adult human brain works, let alone the young and impressionable minds of teenagers, usually the ads targeted at the youth always play upon elements that are familiar and appealing […]
- “Passive Smoking Greater Health Hazard: Nimhans” by Stephen David The article focuses on analyzing the findings of the study and compares them to the reactions to the ban on public smoking.
- Partnership in Working About Smoking and Tobacco Use The study related to smoking and tobacco use, which is one of the problematic areas in terms of the health of the population.
- Cigar Smoking and Relation to Disease The article “Effect of cigar smoking on the risk of cardiovascular disease, chronic obstructive pulmonary disease and cancer in Men” by Iribarren et al.is a longitudinal study of cigar smokers and the impact of cigar […]
- Quitting Smoking: Motivation and Brain As these are some of the observed motivations for smoking, quitting smoking is actually very easy in the sense that you just have to set your mind on quitting smoking.
- Health Effects of Tobacco Smoking in Hispanic Men The Health Effects of Tobacco Smoking can be attributed to active tobacco smoking rather than inhalation of tobacco smoke from environment and passive smoking.
- Smoking in Adolescents: A New Threat to the Society Of the newer concerns about the risks of smoking and the increase in its prevalence, the most disturbing is the increase in the incidences of smoking among the adolescents around the world.
- The Importance of Nurses in Smoking-Cessation Programs When a patient is admitted to the hospital, the nursing staff has the best opportunity to assist them in quitting in part because of the inability to smoke in the hospital combined with the educational […]
- New Jersey Legislation on Smoking The advantages and disadvantages of the legislation were discussed in this case because of the complexity of the topic at hand as well as the potential effects of the solution on the sphere of public […]
- Environmental Health: Tabaco Smoking and an Increased Concentration of Carbon Monoxide The small size of the town, which is around 225000 people, is one of the reasons for high statistics in diseases of heart rate.
- Advanced Pharmacology: Birth Control for Smokers The rationale for IUD is the possibility to control birth without the partner’s participation and the necessity to visit a doctor just once for the device to be implanted.
- Legislation Reform of Public Smoking Therefore, the benefit of the bill is that the health hazard will be decreased using banning smoking in public parks and beaches.
- Female Smokers Study: Inferential Statistics Article The article “Differential Effects of a Body Image Exposure Session on Smoking Urge between Physically Active and Sedentary Female Smokers” deepens the behavioral mechanisms that correlate urge to smoke, body image, and physical activity among […]
- Smoking Bans: Protecting the Public and the Children of Smokers The purpose of the article is to show why smoking bans aim at protecting the public and the children of smokers.
- Clinical Effects of Cigarette Smoking Smoking is a practice that should be avoided or controlled rigorously since it is a risk factor for diseases such as cancer, affects the health outcomes of direct and passive cigarette users, children, and pregnant […]
- Public Health and Smoking Prevention Smoking among adults over 18 years old is a public health issue that requires intervention due to statistical evidence of its effects over the past decades.
- Smoking in the US: Statistics and Healthcare Costs According to the Centers for Disease Control and Prevention, tobacco smoking is the greatest preventable cause of death in the US.
- Smoking Should Be Banned Internationally The questions refer to the knowledge concerning the consequences of smoking and the opinions on smoking bans. 80 % of respondents agree that smoking is among the leading causes of death and 63, 3 % […]
- Microeconomics: Cigarette Taxes and Public Smoking Ban The problem of passive smoking will be minimized when the number of smokers decreases. It is agreeable that the meager incomes of such families will be used to purchase cigarettes.
- Alcohol and Smoking Impact on Cancer Risk The research question is to determine the quantity of the impact that different levels of alcohol ingestion combined with smoking behavioral patterns make on men and women in terms of the risks of cancer.
- Teenagers Motivated to Smoking While the rest of the factors also matter much in the process of shaping the habit of smoking, it is the necessity to mimic the company members, the leader, or any other authority that defines […]
- Indoor Smoking Restriction Effects at the Workplace Regrettably, they have neglected research on the effect of the legislation on the employees and employers. In this research, the target population will be the employees and employers of various companies.
- Hypnotherapy Session for Smoking Cessation When I reached the age of sixty, I realized that I no longer wanted to be a smoker who was unable to take control of one’s lifestyle.
- Stopping Tobacco Smoking: Lifestyle Management Plan In addition, to set objective goals, I have learned that undertaking my plan with reference to the modifying behaviour is essential for the achievement of the intended goals. The main intention of the plan is […]
- Smoking Epidemiology Among High School Students In this way, with the help of a cross-sectional study, professionals can minimalize the risk of students being afraid to reveal the fact that they smoke. In this way, the number of students who smoke […]
- Social Marketing: The Truth Anti-Smoking Campaign The agreement of November 1998 between 46 states, five territories of the United States, the District of Columbia, and representatives of the tobacco industry gave start to the introduction of the Truth campaign.
- Vancouver Coastal Health Smoking Cessation Program The present paper provides an evaluation of the Vancouver Coastal Health smoking cessation program from the viewpoint of the social cognitive theory and the theory of planned behavior.
- Smoking Experience and Hidden Dangers When my best college friend Jane started smoking, my eyes opened on the complex nature of the problem and on the multiple negative effects of smoking both on the smoker and on the surrounding society.
- South Illinois University’s Smoking Ban Benefits The purpose of this letter is to assess the possible benefits of the plan and provide an analysis of the costs and consequences of the smoking ban introduction.
- Smoking Cessation in Patients With COPD The strategy of assessing these papers to determine their usefulness in EBP should include these characteristics, the overall quality of the findings, and their applicability in a particular situation. The following article is a study […]
- Smoking Bans: Preventive Measures There have been several public smoking bans that have proved to be promising since the issue of smoking prohibits smoking in all public places. This means it is a way of reducing the exposure to […]
- Ban Smoking Near the Child: Issues of Morality The decision to ban smoking near the child on father’s request is one of the demonstrative examples. The father’s appeal to the Supreme Court of California with the requirement to prohibit his ex-wife from smoking […]
- The Smoking Ban: Arguments Comparison The first argument against banning smoking employs the idea that smoking in specially designated areas cannot do harm to the health of non-smokers as the latter are supposed to avoid these areas.
- Smoking Cessation and Patient Education in Nursing Pack-years are the concept that is used to determine the health risks of a smoking patient. The most important step in the management plan is to determine a date when the man should quit smoking.
- Philip Morris Company’s Smoking Prevention Activity Philip Morris admits the existence of scientific proof that smoking leads to lung cancer in addition to other severe illnesses even after years of disputing such findings from health professionals.
- Tobacco Smoking and Its Dangers Sufficient evidence also indicates that smoking is correlated with alcohol use and that it is capable of affecting one’s mental state to the point of heightening the risks of development of disorders.
- Virginia Slims’ Impact on Female Smokers’ Number Considering this, through the investigation of Philip Morris’ mission which it pursued during the launch of the Virginia Slims campaign in 1968-1970 and the main regulatory actions undertaken by the Congress during this period, the […]
- Cigarette Smoking and Parkinson’s Disease Risk Therefore, given the knowledge that cigarette smoking protects against the disease, it is necessary to determine the validity of these observations by finding the precise relationship between nicotine and PD.
- Tuberculosis Statistics Among Cigarette Smokers The proposal outlines the statistical applications of one-way ANOVA, the study participants, the variables, study methods, expected results and biases, and the practical significance of the expected results.
- Smoking Ban and UK’s Beer Industry However, there is an intricate type of relationship between the UK beer sector, the smoking ban, and the authorities that one can only understand by going through the study in detail The history of smoking […]
- Status of Smoking around the World Economic factors and level of education have contributed a lot to the shift of balance in the status of smoking in the world.
- Redwood Associates Company’s Smoking Ethical Issues Although employees are expected to know what morally they are supposed to undertake at their work place, it is the responsibility of the management and generally the Redwood’s hiring authority to give direction to its […]
- Smokers’ Campaign: Finding a Home for Ciggy Butts When carrying out the campaign, it is important to know what the situation on the ground is to be able to address the root cause of the problem facing the population.
- Mobile Applications to Quit Smoking A critical insight that can be gleaned from the said report is that one of the major factors linked to failure is the fact that smokers were unable to quit the habit on their own […]
- Behavior Modification Technique: Smoking Cessation Some of its advantages include: its mode of application is in a way similar to the act of smoking and it has very few side effects.
- Quitting Smoking: Strategies and Consequences Thus, for the world to realize a common positive improvement in population health, people must know the consequences of smoking not only for the smoker but also the society. The first step towards quitting smoking […]
- Effects of Thought Suppression on Smoking Behavior In the article under analysis called I suppress, Therefore I smoke: Effects of Thought Suppression on Smoking Behavior, the authors dedicate their study to the evaluation of human behavior as well as the influence of […]
- Suppressing Smoking Behavior and Its Effects The researchers observed that during the first and the second weeks of the suppressed behavior, the participants successfully managed to reduce their intake of cigarettes.
- Smoking Cessation Methods These methods are a part of NRT or nicotine replacement therapy, they work according to the principle of providing the smoker with small portions of nicotine to minimize the addiction gradually and at the same […]
- Understanding Advertising: Second-Hand Smoking The image of the boy caught by the smoke is in the center of the picture, and it is in contrast with the deep black background.
- People Should Quit Smoking
- Importance of Quitting Smoking
- Cigarette Smoking in Public Places
- Ban of Tobacco Smoking in Jamaica
- Anti-Smoking Campaign in Canada
- Electronic Cigarettes: Could They Help University Students Give Smoking Up?
- Psychosocial Smoking Rehabilitation
- The Program on Smoking Cessation for Employees
- Tips From Former Smokers (Campaign)
- Combating Smoking: Taxation Policies vs. Education Policies
- The Program to Quit Smoking
- Smoking Culture in Society
- Possible Smoking Policies in Florida
- Smoking Ban in the State of Florida
- Core Functions of Public Health in the Context of Smoking and Heart Disease
- Smoking: Pathophysiological Effects
- Putting Out the Fires: Will Higher Taxes Reduce the Onset of Youth Smoking?
- Smoking Bans in US
- Smoking as Activity Enhancer: Schizophrenia and Gender
- Health Care Costs for Smokers
- Medical Coverage for Smoking Related Diseases
- Exposure to mass media proliferate smoking
- The Realm of reality: Smoking
- Ethical Problem of Smoking
- The Rate of Smoking Among HIV Positive Cases.
- Studying the Government’s Anti-Smoking Measures
- Smoking Should Be Banned In the United States
- Effectiveness of Cognitive Behavioral Theory on Smoking Cessation
- Effectiveness of the Cognitive Behavioral Therapy for Smoking Cessation
- Wayco Company’s Non-smoking Policy
- Adverse Aspects of Smoking
- Negative Impacts of Smoking on Individuals and Society
- Dealing With the Increase in the Number of Smokers Between Ages 17 and 45
- Cannabis Smoking in Canada
- Smoking Ban in the United States of America
- Dangers of Smoking Campaign
- Should Cigarettes Be Banned? Essay
- Smoking Ban in New York
- Smoking and Adolescents
- Trends in Smoking Prevalence by Race/Ethnicity
- Business Ethics: Smoking Issue
- Where Does the Path to Smoking Addiction Start?
- Public Health Communication: Quit Smoking
- Are Estimated Peer Effects on Smoking Robust?
- Are There Safe Smoking and Tobacco Options?
- What Are the Health Risks of Smoking?
- Does Cigarette Smoking Affect Body Weight?
- Does Cigarette Smuggling Prop Up Smoking Rates?
- What Foods Help You Quit Smoking?
- How Can People Relax Without Smoking?
- Does Education Affect Smoking Behaviors?
- Is Vaping Worse Than Smoking?
- Do Movies Affect Teen Smoking?
- What Is Worse: Drinking or Smoking?
- Does Smoking Affect Breathing Capacity?
- Does Smoking Cause Lung Cancer?
- Does Having More Children Increase the Likelihood of Parental Smoking?
- Does Smoking Cigarettes Relieve Stress?
- Does Time Preference Affect Smoking Behavior?
- How Does Smoking Affect Cardiovascular Endurance?
- How Hypnosis Can Help You Quit Smoking?
- How Does Smoking Affect Brain?
- How Nicotine Affects Your Quit Smoking Victory?
- How Does Secondhand Smoking Affect Us?
- Why Is Smoking Addictive?
- How Smoking Bans Are Bad for Business?
- Why Smoking Should Not Be Permitted in Restaurants?
- Why Public Smoking Should Be Banned?
- Why Has Cigarette Smoking Become So Prominent Within the American Culture?
- What Makes Smoking and Computers Similar?
- Does Smoking Affect Schooling?
- What Effects Can Cigarette Smoking Have on the Respiratory System?
- What Are the Most Prevalent Dangers of Smoking and Drinking?
- Social Security Paper Topics
- Drugs Titles
- Cannabis Essay Titles
- Global Issues Essay Topics
- Cardiovascular Diseases Titles
- Marijuana Ideas
- NHS Research Ideas
- Hypertension Topics
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 29). 235 Smoking Essay Topics & Examples. https://ivypanda.com/essays/topic/smoking-essay-examples/
"235 Smoking Essay Topics & Examples." IvyPanda , 29 Feb. 2024, ivypanda.com/essays/topic/smoking-essay-examples/.
IvyPanda . (2024) '235 Smoking Essay Topics & Examples'. 29 February.
IvyPanda . 2024. "235 Smoking Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/smoking-essay-examples/.
1. IvyPanda . "235 Smoking Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/smoking-essay-examples/.
Bibliography
IvyPanda . "235 Smoking Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/smoking-essay-examples/.
Home — Essay Samples — Nursing & Health — Addictions — Smoking
Essays About Smoking
Smoking essay, types of essay about smoking.
- Cause and Effect Essay: This type of essay focuses on the causes and effects of smoking. It discusses why people start smoking and the consequences of smoking on both the smoker and those around them.
- Argumentative Essay: This essay type aims to persuade the reader about the negative effects of smoking. It presents an argument and provides supporting evidence to convince the reader that smoking is harmful and should be avoided.
- Persuasive Essay: Similar to an argumentative essay, this type of essay aims to persuade the reader to quit smoking. It presents facts, statistics, and other relevant information to convince the reader to stop smoking.
Smoking Essay Example: Cause and Effect
- Identify the causes of smoking: Start by examining why people start smoking in the first place. Is it peer pressure, addiction, stress, or curiosity? Understanding the reasons why people smoke is crucial in creating an effective cause and effect essay.
- Discuss the effects of smoking: Highlight the impact smoking has on an individual's health and the environment. Discuss the risks associated with smoking, such as lung cancer, heart disease, and respiratory problems, and explain how smoking affects non-smokers through secondhand smoke.
- Use reliable sources: To make your essay more convincing, ensure that you use credible sources to back up your claims. Use scientific studies, government reports, and medical journals to support your arguments.
- Provide statistical evidence: Incorporate statistical data to make your essay more impactful. Use figures to show the number of people who smoke, the effects of smoking on the environment, and the costs associated with smoking.
- Offer solutions: Conclude your essay by suggesting solutions to the problem of smoking. Encourage smokers to quit by outlining the benefits of quitting smoking and offering resources for those who want to quit.
Smoking: Argumentative Essay
- Choose a clear position: The writer should choose a side on the issue of smoking, either for or against it, and be clear in presenting their stance.
- Gather evidence: Research and collect facts and statistics to support the writer's argument. They can find data from reliable sources like scientific journals, government reports, and reputable news organizations.
- Address counterarguments: A good argumentative essay will acknowledge opposing viewpoints and then provide a counterargument to refute them.
- Use persuasive language: The writer should use persuasive language to convince the reader of their position. This includes using rhetorical devices, such as ethos, pathos, and logos, to appeal to the reader's emotions and logic.
- Provide a clear conclusion: The writer should summarize the key points of their argument and reiterate their stance in the conclusion.
Persuasive Essay on Smoking
- Identify your audience and their beliefs about smoking.
- Present compelling evidence to support your argument, such as statistics, research studies, and personal anecdotes.
- Use emotional appeals, such as stories or images that show the negative impact of smoking.
- Address potential counterarguments and refute them effectively.
- Use strong and clear language to persuade the reader to take action.
- When choosing a topic for a smoking persuasive essay, consider a specific aspect of smoking that you would like to persuade the audience to act upon.
Hook Examples for Smoking Essays
Anecdotal hook.
Imagine a teenager taking their first puff of a cigarette, unaware of the lifelong addiction they're about to face. This scenario illustrates the pervasive issue of smoking among young people.
Question Hook
Is the pleasure derived from smoking worth the serious health risks it poses? Dive into the contentious debate over tobacco use and its consequences.
Quotation Hook
"Smoking is a habit that drains your money and kills you slowly, one puff after another." — Unknown. Explore the financial and health impacts of smoking in today's society.
Statistical or Factual Hook
Did you know that smoking is responsible for nearly 8 million deaths worldwide each year? Examine the alarming statistics and data associated with tobacco-related illnesses.
Definition Hook
What exactly is smoking, and what are the various forms it takes? Delve into the definitions of smoking, including cigarettes, cigars, pipes, and emerging alternatives like e-cigarettes.
Rhetorical Question Hook
Can we truly call ourselves a smoke-free generation when new nicotine delivery devices are enticing young people? Investigate the impact of vaping and e-cigarettes on the youth.
Historical Hook
Trace the history of smoking, from its ancient roots to its prevalence in different cultures and societies. Explore how perceptions of smoking have evolved over time.
Contrast Hook
Contrast the images of the suave, cigarette-smoking characters from classic films with the grim reality of tobacco-related diseases and addiction in the modern world.
Narrative Hook
Walk in the shoes of a lifelong smoker as they recount their journey from that first cigarette to a battle with addiction and the quest to quit. Their story reflects the struggles of many.
Shocking Statement Hook
Prepare to uncover the disturbing truth about smoking—how it not only harms the smoker but also affects non-smokers through secondhand smoke exposure. It's an issue that goes beyond personal choice.
Smoking Informative Speech
Can smoking be prevented by making tobacco illegal, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Rhetorical Analysis of Anti-smoking Campaigns
The effects of smoking on your body, the effects of smoking on health, the importance of quitting smoking, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
The History of Tobacco Use and Its Dangers
The dangers of smoke from cigarettes, a research paper on smoking cigarettes: should society ban it, effect of tobacco: why cigarette smoking should be banned, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
How Smoking Can Ruin Your Health
Fight addiction with the help willpower, should smoking be made illegal: argumentative, look of maturity: why smoking is "good" for you, nevada's smoking freedom at stake as joelle babula argues that local government should enforce strict laws, the effects of smoking ban, the challenges of quitting smoking, discussion on whether cigarette smoking should be banned in public places, the motif of smoking in all the pretty horses, the issue of smoking and alcohol drinking among adolescents, my personal experience of the effects of vaping, why vaping is bad for you: effects and dangers, feminist theory and communication, the toxic truth of smoking and vaping, the different harmful effects of smoking marijuana, pieces of advice that will help you to select the best vape shop in las vegas, facts of herbal cigarettes versus tobacco cigarettes, vaping: all you need to know about this trend, from cure to poison: the negative effects of tobacco, global efforts to diminish tobacco usage, relevant topics.
- Post Traumatic Stress Disorder
- Healthy Food
- Sleep Deprivation
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Smoking Research Paper

View sample smoking research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Cigarette smoking has great societal and clinical significance. It is a major cause of several diseases, including a variety of cancers. The practice of cigarette smoking is pervasive; about a quarter of all adult Americans smoke cigarettes, and smoking rates are even higher in many other countries. Despite the high personal cost associated with cigarette smoking, it is a prototypical addictive disorder manifesting such features as tolerance, withdrawal, and chronic use. The peak age for smoking prevalence is between eighteen and twenty-five years. Retrospective data from the National Household Survey on Drug Abuse suggests that the average age of first use of tobacco products in 1999 among all persons who ever used in their lifetime was 15.4 for cigarettes, 20.5 for cigars, and 16.7 for smokeless tobacco across all age groups (Kopstein 2001). Data from the National Comorbidity Survey suggests that the onset of nicotine dependence is delayed for at least one year after the onset of daily smoking. Smoking rates decline among people who have reached their mid-twenties, but these declines are modest in comparison to other forms of substance use. This may be due to the fact that cigarette smoking is highly addictive, legal, and not immediately performance-impairing.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code, biological aspects of nicotine addiction.
Nicotine, independently, yields the trademark effects of an addictive drug. It produces tolerance and physical dependence, and heightened doses produce euphoria and satisfaction (Corrigall 1999; USDHHS 1998). Smokers will not self-administer tobacco on a chronic basis if it does not contain nicotine. Nicotine is essential for the development and maintenance of a smoking habit. However, once nicotine dependence is established, cues related to nicotine release become greatly influential in controlling self-administration behaviors. When a cigarette is smoked, about 80 percent of the inhaled nicotine is absorbed in the lungs (Armitage et al. 1975). Absorption is both efficient and extremely rapid. Despite the overall recognition that the rapid onset of drug action promotes addictive drug use, it remains unclear why this is so. Researchers do not fully understand which characteristics of drug pharmacokinetics are most determinant of addictiveness.
Behavioral Aspects And Environmental Influence
Data published in 2002 suggest that smoking among American adolescents is fairly common, with 27 percent of twelfth graders, 18 percent of tenth graders, and 11 percent of eighth graders reporting that they had smoked in the past month (Johnston et al. 2002). This level of smoking prevalence represents a decline from peaks in the mid-1990s. Much less is known about the epidemiology of tobacco dependence in adolescents. Dependence is a term often correlated with addiction, and adolescent smokers are less likely to be diagnosed with tobacco dependence than are adult smokers (Colby et al. 2000), although many adolescent smokers consider themselves addicted. Adolescents who are dependent report the same symptoms as do dependent adults, including cravings, withdrawal, tolerance, and a desire to reduce smoking (Colby et al. 2000). Compared to adults at the same level of self-reported intake, adolescents who smoke are more likely to be diagnosed as dependent, which suggests that adolescents may be especially vulnerable to dependence or sensitive to the effects of nicotine (Kandel and Chen 2000).
Before they experiment with cigarettes, adolescents form beliefs and attitudes about the effects of smoking. These attitudes and beliefs prospectively predict both the onset and escalation of smoking. Many adolescents believe that there are no health risks related to smoking in the first few years, and they believe that they will stop smoking before any damage is done. Existing evidence suggests that adolescents and adults exhibit unrealistic optimism about the personalized risks of smoking (Arnett 2000; Weinstein 1999). Whether adolescents are any more likely than adults to underestimate the personalized risks of smoking is unclear.
Evidence indicates that as smokers become more dependent, there is a shift in the motivational basis for their tobacco use. Social motives and contextual factors are rated as influential to beginner smokers, while heavy smokers emphasize the importance of control over negative moods and urges, and the fact that smoking has become involuntary (Piper et al. 2004). When smoking becomes less linked to external cues and more linked to internal stimuli, smokers are classified as dependent. There is also evidence suggesting that smoking cigarettes may lead to the use of illicit drugs. Cigarette smoking is endemic among substance abusers, with rates as high as 74 percent to 88 percent (Kalman 1998), compared to 23 percent of the general population (CDC 2002).
Greater parental education is associated with less likelihood of smoking in offspring. Additionally, girls appear to be more influenced by peer smoking than boys (Mermelstein 1999). In the United States, the highest smoking rates are among American Indian and Alaska Native adolescents, followed by whites and then Hispanics, with lowers rates among Asian Americans and African Americans. While studies that sample multiethnic groups are sparse, research has suggested that African American and Asian American adolescents report stronger antismok-ing socialization messages from parents and that African American parents report feeling particularly empowered to influence their children’s smoking (for reviews, see Mermelstein 1999; USDHHS 1998). Peer smoking is a relatively weak predictor of smoking for African American adolescents compared to white adolescents.
Adolescents sometimes start smoking as a result of self-image. The social image of an adolescent smoker is an ambivalent one, with negative aspects but also images of toughness, sociability, and precocity that may be particularly valued by “deviance-prone” adolescents who are at risk to smoke (Barton et al. 1982). Additionally, adolescents may start smoking and continue smoking because of their perception of the effect that smoking has on weight control and dieting. The belief that smoking can control body weight has been shown to predict smoking initiation among adolescent girls, but not boys (Austin and Gortmaker 2001). In addition, this belief is held more widely by white girls than by African American girls (Klesges et al. 1997). Despite the above-mentioned indicators, peer smoking is the most consistently identified predictor of adolescent smoking (Derzon and Lipsey 1999). In addition to cigarette smoking by peers, affiliation with peers who engage in high levels of other problem behaviors also prospectively predicts smoking initiation, as does self-identification with a high-risk social group (Sussman et al. 1994).
Smoking Cessation And Prevention
The tobacco industry spends millions of dollars per day on advertising and promotional materials to keep their products in the public eye. Beyond such reminders of the availability of tobacco products, smoking is not an easy habit to break. Smokers must not only break the physical addiction to nicotine, but also the habit of lighting up at certain times of the day. Successful quitters confess that quitting is often a lengthy process that involves several unsuccessful attempts. Although one-third of smokers attempt to quit each year, 90 percent or more of those who attempt to quit will fail.
Nicotine replacement therapies (NRTs) have been used to help some people quit smoking. The two most common forms of NRTs are chewing gum and the nicotine patch, both of which are available over the counter. Nicorette, a prescription chewing gum containing nicotine, is often used to help reduce the consumption of nicotine over time. Users have reported experiencing fewer cravings for nicotine as the dosage is reduced, until they are completely weaned. The nicotine patch was first marketed in 1991 for smokers with a desire to quit. Generally, the nicotine patch is used in conjunction with a comprehensive smoking-behavior cessation program. Additionally, a nicotine nasal spray, nicotine inhaler, and nicotine pill have been approved by the FDA to help cigarette smokers quit smoking. In order to prevent the initiation and maintenance of smoking, there has been an increase since the mid-1980s in the development and implementation of smoking cessation and prevention programs, especially for young people and adolescents.
Global Economics Of Smoking
Approximately 80 percent of the world’s 1.1 billion smokers live in low- and middle-income countries. In 1998 about four million people died of tobacco-related disease worldwide (WHO 1999). This number is projected to increase to ten million annually by 2030, with 70 percent of these deaths occurring in low-income countries. Death counts of this magnitude could be prevented if current smokers quit, but it is rare for smokers living in low- to middle-income countries to attempt to quit smoking (Jha and Chaloupka 2000). Although few dispute that smoking is damaging to human health on a global scale (Peto and Lopez 2000), governments have avoided taking action to control smoking. This is mainly due to concerns that such interventions might have harmful economic consequences, such as permanent job losses. Despite these concerns, several common measures aimed at the control of smoking, such as higher tobacco taxes, consumer information, bans on advertising and promotion, and regulatory policies, have had a significant impact. Each will be discussed below.
An increase in tobacco taxes is the single most effective intervention to reduce the demand for tobacco. A review by Prabhat Jha and Frank Chaloupka (2000) suggests that a price increase of 10 percent would reduce smoking by 4 percent in high-income countries and by about 8 percent in low- and middle-income countries. This evidence also implies that young people, individuals on low incomes, and those with less education are more responsive to price changes (Chaloupka et al. 2000). Policies to improve the quality and extent of tobacco information can also reduce smoking, particularly in low-and middle-income countries. For example, in the 1960s and 1970s, the promulgation in the United States and Britain of new evidence on the health risks of smoking helped reduce consumption between 4 and 9 percent. In addition, warning labels on cigarette packages were also found to reduce consumption during that era (Kenkel and Chen 2000). In a review of 102 countries and econometric analyses of income, Henry Saffer and Chaloupka (2000) revealed that bans on advertising and promotion led to considerable reductions in tobacco consumption.
Enforcing regulatory policies designed to prevent smoking in public places, worksites, and other facilities can also significantly reduce cigarette consumption worldwide (Yurekli and Zhang 2000). Attempts to impose restrictions on the sale of cigarettes to young people in high-income countries have mostly been unsuccessful (Siegel et al. 1999). Furthermore, it may be difficult to implement and enforce such restrictions in low-income countries. Evidence indicates that freer trade in tobacco products has led to an increase in smoking and other types of tobacco use. One solution is for countries to adopt measures that effectively reduce demand and apply those measures to both imported and domestically produced cigarettes (Taylor et al. 2000).
Bibliography:
- Armitage, A. K., C. T. Dollery, C. F. George, et al. 1975. Absorption and Metabolism of Nicotine from Cigarettes. British Medical Journal 4: 313–316.
- Arnett, Jeffrey Jensen. 2000. Optimistic Bias in Adolescent and Adult Smokers and Nonsmokers. Addictive Behavior 25: 625–632.
- Austin, S. Bryn, and Steven L. Gortmaker. 2001. Dieting and Smoking Initiation in Early Adolescent Girls and Boys: A Prospective Study. American Journal of Public Health 91: 446–450.
- Barton, John, Laurie Chassin, Clark Presson, and Steven J. Sherman. 1982. Social Image Factors as Motivators of Smoking Initiation in Early and Middle Adolescence. Child Development 53 (6): 1499–1511. Centers for Disease Control and Prevention (CDC). 2002.
- Cigarette Smoking among Adults—United States, 2000. Morbidity and Mortality Weekly Report 51: 642–645.
- Chaloupka, Frank J., Teh-Wei Hu, Kenneth E. Warner, et al. 2000. The Taxation of Tobacco Products. In Tobacco Controlin Developing Countries, eds. Prabhat Jha and Frank Chaloupka, 237–272. Oxford: Oxford University Press.
- Colby, Suzanne, Stephen T. Tiffany, Saul Shiffman, and Raymond S. Niaura. 2000. Are Adolescent Smokers Dependent on Nicotine? A Review of the Evidence. Drug Alcohol Dependence 59 (suppl.): 83–95.
- Corrigall, William A. 1999. Nicotine Self-Administration in Animals as a Dependence Model. Nicotine Tobacco Resistance 1: 11–20.
- Derzon, James H., and Mark W. Lipsey. 1999. Predicting Tobacco Use to Age 18: A Synthesis of Longitudinal Research. Addiction 94: 995–1006.
- Jha, Prabhat, and Frank J. Chaloupka. 2000. The Economics of Global Tobacco Control. British Medical Journal 321: 358–361.
- Johnston, Lloyd D., Patrick M. O’Malley, Jerold Bachman, and John E. Schulenberg. 2002. National Survey Results on Drug Use from the Monitoring the Future Study, 1975–2002. Vol. 1: Secondary School Students. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, and National Institutes of Health.
- Kalman, David. 1998. Smoking Cessation Treatment for Substance Misusers in Early Recovery: A Review of the Literature and Recommendations for Practice. Substance Use and Misuse 33: 2021–2047.
- Kandel, Denise B., and Kevin Chen. 2000. Extent of Smoking and Nicotine Dependence in the United States, 1991–1993. Nicotine and Tobacco Research 2: 263–275.
- Kenkel, Donald, and Lisa Chen. 2000. Consumer Information and Tobacco Use. In Tobacco Control in Developing Countries, eds. Prabhat Jha and Frank Chaloupka, 177–214. Oxford: Oxford University Press.
- Klesges, Robert C., Vanessa E. Elliot, and Leslie A. Robinson. 1997. Chronic Dieting and the Belief that Smoking Controls Body Weight in a Biracial Population-based Adolescent Sample. Tobacco Control 6: 89–94.
- Kopstein, Andrea. 2001. Tobacco Use in America: Findings from the 1999 National Household Survey on Drug Abuse.
- Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration.
- Mermelstein, Robin. 1999. Ethnicity, Gender, and Risk Factors for Smoking Initiation: An Overview. Nicotine and Tobacco Research 1 (suppl.): 45–51.
- Peto, Richard, and Alan D. Lopez. 2000. The Future Worldwide Health Effects of Current Smoking Patterns. In Critical Issues in Global Health, eds. C. Everett Koop, Clarence E. Pearson, and M. Roy Schwartz, 154–161. San Francisco: Jossey-Bass.
- Piper, Megan E., Thomas M. Piasecki, E. Belle Federman, et al. 2004. A Multiple Motives Approach to Tobacco Dependence: The Wisconsin Inventory of Smoking Dependence Motives (WISDM). Journal of Consulting in Clinical Psychology 72 (2): 139–154.
- Saffer, Henry, and Frank J. Chaloupka. 2000. Tobacco Advertising: Economic Theory and International Evidence. Journal of Health Economics 19: 1117–1137.
- Siegel, Michael, Lois Biener, and Nancy A. Rigotti. 1999. The Effect of Local Tobacco Sales Laws on Adolescent Smoking Initiation. Prevention Medicine 29: 334–342.
- Sussman, Steve, Clyde W. Dent, Lou Anne McAdams, et al. 1994. Group Self-identification and Adolescent Cigarette Smoking: A 1-year Prospective Study. Journal of Abnormal Psychology 103: 576–580.
- Taylor, Allyn L., Frank J. Chaloupka, Emmanuel Guindon, and Michaelyn Corbett. 2000. The Impact of Trade Liberation on Tobacco Consumption. In Tobacco Control in Developing Countries, eds. Prabhat Jha and Frank Chaloupka, 343–364. Oxford: Oxford University Press.
- U.S. Department of Health and Human Services (USDHHS). 1998. Tobacco Use among US Racial/Ethnic Minority Groups: African Americans, American Indians, and Alaska Natives, Asian Americans and Pacific Islanders, Hispanics, Report of the Surgeon General. Atlanta, GA: USDHHS, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
- Weinstein, Neil D. 1999. Accuracy of Smokers’ Risk Perceptions. Nicotine and Tobacco Research 1 (suppl.): 123–130.
- World Health Organization (WHO). 1999. Making a Difference, World Health Report 1999. Geneva, Switzerland: Author.
- Yurekli, Ayda A., and Ping Zhang. 2000. The Impact of Clean Indoor-Air Laws and Cigarette Smuggling on Demand for Cigarettes: An Empirical Model. Health Economics 9: 159–170.
ORDER HIGH QUALITY CUSTOM PAPER


Review of Related Literature (RRL) in Research Paper
Ai generator.
1. Introduction: This review examines how technology affects education, focusing on student engagement, learning outcomes, and teacher practices over the past decade.
2. Theoretical Framework: Based on Constructivist Learning Theory and TPACK, this review explores how technology integration enhances education.
3. Review of Empirical Studies
Student Engagement
- Interactive Whiteboards : Smith & Jones (2015) found increased student participation in 20 elementary classrooms using interactive whiteboards.
- Gamification : Lee & Hammer (2011) reported improved motivation and engagement with educational games in 300 middle school students.
Learning Outcomes
- Online Learning Platforms : Johnson & Brown (2017) observed better standardized test performance among 500 high school students using online platforms.
- Blended Learning : Clark & Mayer (2016) found higher academic achievement in 200 college students in blended learning environments.
Teacher Practices
- Professional Development : Williams & Davis (2018) highlighted improved instructional practices from ongoing tech training in 150 teachers.
- Digital Assessment Tools : Thompson & Peterson (2019) showed enhanced instructional strategies using digital tools in 30 high school classrooms.
4. Methodological Review: Studies used surveys, experiments, and longitudinal designs. Surveys provided broad data but had self-report biases. Experiments showed causation but lacked ecological validity. Longitudinal studies provided long-term data but were resource-intensive.
5. Synthesis and Critique: Technology positively impacts engagement, outcomes, and practices. Challenges include digital divide and training. More longitudinal and experimental research is needed.
6. Conclusion: Research shows technology’s potential to enhance education but highlights the need for further study on sustainable implementation and overcoming barriers.
7. References :
- Clark, R. C., & Mayer, R. E. (2016). E-learning and the Science of Instruction . Wiley.
- Johnson, L., & Brown, A. (2017). Impact of Online Learning on Student Performance . Journal of Educational Technology, 12(3), 45-56.
- Lee, J. J., & Hammer, J. (2011). Gamification in Education . Academic Exchange Quarterly, 15(2), 1-5.
- Smith, K., & Jones, L. (2015). Interactive Whiteboards in Elementary Education . Educational Technology Research, 63(4), 123-135.
- Thompson, M., & Peterson, D. (2019). Digital Assessment Tools in High Schools . Journal of Education, 14(1), 78-89.
- Williams, P., & Davis, R. (2018). Professional Development for Technology Integration . Journal of Teacher Education, 20(4), 100-110.
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.10(3); 2021 Mar
A qualitative study on attitude towards smoking, quitting and tobacco control policies among current smokers of different socio-economic status
Lalitha rani chellappa.
1 Department of Public Health Dentistry, Saveetha Dental College, Saveetha Institute of Management and Technical Sciences, Saveetha University, No. 162, Poonamallee High Road, Chennai, Tamil Nadu, India
Arthi Balasubramaniam
Meignana arumugham indiran, pradeep kumar rathinavelu, introduction:.
Tobacco consumed as smoke and smokeless forms is an important preventable public health issue projected to be the single largest cause of mortality worldwide. The aim of the study was to qualitatively assess the attitudes towards smoking, quitting and tobacco control policies among current smokers of different socio-economic status.
Materials and Methods:
An in-depth interview for 10 current smokers and a focus group discussion comprising of 10 current smokers was conducted with a guide and moderator which was audio recorded. About 6, 8 and 6 subjects from white collar, blue collar, and black collar employee status participated in the study. Their tobacco consumption and dependence using the Fagerstrom Test for Nicotine Dependence scale (FTNDS) was assessed.
About 50% of the participants had low; 30% had moderate and 20% had high nicotine dependency. Most of the participants started smoking by peer influence and continued as it made them to socialize. Relapses during their quit attempt was mainly due to work stress. Participants heard about the control of tobacco act but were unsure of the features in it. They perceived that no changes will happen if government bans production and selling of tobacco products. Also anti-tobacco commercials in social media will have no use. Nicotine replacement therapy may help in quitting the habit.
Conclusion:
The study concluded that people in low socio-economic status had high nicotine dependency with inadequate knowledge on tobacco control policies. They strongly believe that an individual's self-restrain only can succeed him in quitting the habit.
Introduction
Tobacco remains as a single largest cause for heart diseases and stroke in India, with more than one million deaths/year.[ 1 ] India faces an enormous economic burden for treating tobacco-related diseases amounted to $907 and $285 million for smoke and smokeless tobacco respectively.[ 2 ] Control and prevention of tobacco use becomes a major public health issue in limiting morbidity and mortality.[ 3 ] The prevalence of adult current smokers and smokeless tobacco users is 24.3% and 25.9%, respectively. With increasing tobacco control measures (surveillance and monitoring, tobacco control policy, legislation, capacity building) by the Government of India, still prevention of smoking remains a major challenge.[ 4 ] Although the prevalence of tobacco users has been decreasing over last two decades, about 19% of adult males and 2% of adult females continue using tobacco currently. Evidence says that 55.4% and 49.6% of smoke and smokeless tobacco users planned to or were thinking about quitting.[ 5 ] However only <2% tobacco users have made an attempt to quit using mCessation program – Quit Tobacco For Life.[ 6 ] Though use of tobacco among the adults dropped from 35% in 2009–10 to 29% in 2016–17 still a high economic burden is posed on India.[ 7 ]
Studies have demonstrated that a brief physician-delivered intervention (as brief as three minutes) using cognitive behavioural therapy (CBT) for smoking cessation in primary care setting significantly increases patients' smoking cessation rates.[ 8 ] Smoking cessation produces immediate and substantial health benefits.[ 9 ] The nicotine replacement medications and psychotic drugs have produced reasonable results in smoking cessation among high tobacco dependence individuals.[ 10 ] Thus there is a need for population-based interventions to complement individual-based behavioural or pharmacological interventions, capacity building for smoking cessation and treatment of tobacco dependence.[ 11 ] Social support for quitting, training of health professionals and integration of smoking cessation in other health programmes are essential for successful implementation of tobacco cessation programmes.[ 12 ] Recognizing the importance of tobacco cessation, there are 19 tobacco cessation clinics (TCCs) in India with the support of the World Health Organization.[ 13 ]
The Quit Tobacco International (QTI) has embarked on a project of incorporating tobacco cessation intervention in the undergraduate medical curriculum in two countries: India and Indonesia. As part of this project in India, 15 course modules were developed, piloted, implemented and evaluated in various departments of five medical colleges in Kerala and Karnataka States.[ 14 ]
Recent study suggested that even after being diagnosed with Head and Neck Cancer, one third of the study population continued to use tobacco.[ 15 ] Thus, it becomes an integral part of health professionals to provide a structured approach to initiate smoking cessation, manage withdrawal symptoms, and provide long-term support.[ 16 ] However, these cessation programs are usually customised according to individuals. This necessitates an in-depth understanding of the perception towards smoking and quitting in bringing out a targeted behavioural change.
The aim of the study was to qualitatively assess the attitudes towards smoking, quitting and tobacco control policies among current smokers of different socio-economic status attending a private dental college in Chennai.
Materials and Methods
Qualitative in-depth interviews and focus group discussions were conducted among current smokers visiting a private dental college in Chennai, Tamil Nadu. Ethical clearance was obtained from Institutional ethics committee, Saveetha University with the number SRB/SDC/PHD-1802/19/03. Approval obtained on 19/4/2019. The study population included white collar, blue collar, and black collar employees according to Friedrich in 2013.[ 17 ] A white-collar worker is a salaried professional, typically referring to general office workers and management. Blue-collar worker is a member of the working class who performs manual labour and either earns an hourly wage or is paid piece rate for the amount of work done. Black collar worker is a manual labourer in industries.
The study included current tobacco users, using tobacco for more than a year and aged 18 years and above. Former smokers and those who were not willing to participate in the study were excluded. The snowballing sampling method was used to recruit the study participants. Written informed consent was obtained from the study participants and the anonymity of the participants was maintained. The study was conducted during December 2019 in the department of Public Health Dentistry in a private room. The participants had varying levels of motivation to quit in the future. Interview was carried out until new responses or new ideas were generated. A baseline data on tobacco consumption, dependence was assessed using the Fagerstrom Test for Nicotine Dependence scale (FTNDS).
In depth interview
The study included an initial in-depth interview for 10 participants with 3 from black and white collar group and 4 participants from blue collar group. In-depth interview was conducted by a moderator along with an assistant. An interview guide was formulated so that we could probe into various aspects of smoking behaviour. The information's given by the participants were audio-recorded. The interview lasted 30 – 45 minutes for each participant.
The areas of discussion included reasons to start smoking and to continue, their perception as smokers, attitude towards non-smokers and their knowledge regarding health effects of smoking. Further probing was done to obtain details regarding their quit attempts and anti- health warnings on multimedia such as television, newspaper, or the cigarettes packets. The last part of the discussion included their knowledge and attitude towards nicotine replacement therapy (NRT) and tobacco control policies in the country.
Focus group discussion
A focus group discussion was conducted comprising 10 current smokers. The participants involved in the in-depth interview were not included for the focus group discussion. About 3 participants from black collar, 4 from blue collar and 3 from white collar group participated. Like in-depth interview, there was one moderator and one assistant. The discussion lasted for one hour and was audio-recorded. The moderator prompted the topics and the discussion continued. The areas of discussion included knowledge and attitude about cigarettes and other tobacco products act (COTPA), attitude about the situation what will happen if India closes the production of tobacco products. The discussion was healthy and each individual participated in briefing their perception.
Data analysis was done in accordance with thematic framework analysis to allow themes to be generated from the data collected. The audio recordings were transcribed to their verbatim format. The recordings were read and familiarised multiple times to generate themes. The focus group guide helped to sort the emerging keys points and the new themes to be segregated according to the responses. Initial analysis was undertaken manually, and the responses from each participant were identified and charted under the respective key points. Finally, interpretative analysis was done to group together similar points and to identify recurrent themes which enabled the various aspects of smoking behaviour among the participants of the three groups.
Among the 20 participants, 6 were white collar, 8 were in blue collar and 6 were black collar employees. About 50% had low nicotine dependency; 30% had medium nicotine dependency and 20% had high nicotine dependency. Low dependency was seen among 40% and 20% of white and black collar employees respectively. Medium dependency was seen among 60% and 33.33% of white and blue collar employees. However, high nicotine dependency was observed among 80% of black collar and 66.67% of blue collar employees. The responses generated after the focus group discussion were segregated and the following themes were produced.
Reasons for start of smoking
Most of them started smoking at the age of 18 years. The main reason to start smoking was due to the influence of peers and friends. The reason was found similar in black and blue- collar employees while white collar employees had a different perception
- One of the black collar employees said “I saw my friends smoking, was curious to know what it is about and how it would feel”
- One of the blue-collar employee said “all my friends in my gang were using it and they asked me to use. I wanted to be included too”
- White collar employee said “in college, only when a guy smokes, he was considered matured, macho and can impress girl classmates”
Reasons to continue smoking
All the participants considered smoking as a stress buster and a major way to socialise. They could divert their mind from what was troubling them.
- “Whenever I have tension I want to smoke and relax. It gives relaxation and I would forget all the tension in association with drinking” - Black collar employee
- “It's a good pass time and to socialize with friends in tea shop” - Blue collar employee
- We received another dimension for the reason to continue from a white - collar employee.
- “I have smoking zone in my office and major decisions were made here. Also I get chances to interact with the higher officials” - white collar employee.
Knowledge regarding health effects and COTPA
When asked about the harmful effects of tobacco on health, all the three groups said they are aware of the ill effects of tobacco and it affects lungs. White and blue-collar employees learned from books and movies, black collar employees learned from movies and advertisements. And some of the participants have had relatives who had suffered of health problems due to constant tobacco use. They were not aware of the COTPA act and its regulations, however watched anti-tobacco advertisements and heard from people that smoking in public is prohibited. They all never smoke in front of women and children but do smoke in public. Their usual place is the local tea shop where women and children won't be there.
Aspects related to quitting attempts
- Everyone has attempted to quit tobacco. “whenever I feel financially low, I try to quit but relapsed because of tension”–blue collar employee
- One of the blue-collar employees said “I want to quit when I get married and start a family”.
- Stress was the main reason for relapse. One of the white-collar employees said that “I tried to quit for a month but I relapsed due to work pressure though had sufficient knowledge on ill-effects”
What will happen if tobacco is stopped manufacturing
We explained about Indian Tobacco Company (ITC) and its share in producing tobacco in the country. And we questioned what will happen if the country stops production and selling tobacco products
- The black collar employees were so lethargic about the question and said its hypothetical “We can only talk about but the government will never stop manufacturing cigarettes”
- “When government bans the cigarettes, people will go for other addictions of cheaper tobacco forms” – Blue collar employee
- The white-collar employees said that “high dependent people may go for other addiction but people in officer ranks may try to quit”
Anti - tobacco commercials
We asked about the anti-tobacco commercials which are shown on television, theatres and on the tobacco packets.
- The black collar employees were aware of the commercials and uncertain of the purpose of those commercials as they are run by the same government and companies which are selling them.
- One of the blue-collar employee said “It doesn't affect me”
- The white-collar employees said they feel guilty inside but -they couldn't quit it. One of the white-collar employee said “I convince myself that I know the limits of tobacco that will cause ill effects and I will stay in my limits”
Nicotine replacement therapy
We shared some knowledge about nicotine and its effects and how nicotine replacement therapy helps in quitting tobacco.
- “We are not aware and can't afford for such things” -Black collar employee said
- One of the blue-collar employees had an experience with NRT and he said that “I have tried one of NRT gums once but I don't like the taste of it and it doesn't satisfy me as cigarettes do”
- White-collar employees were more aware of NRT and none of them had tried and they were ready to try with proper professional advice.
Summary of the responses given by the participants for different categories
People who are highly addicted inhale it deeply into the brain and get high instantly and exhale via nose. People who medium dependent will exhale via mouth. That’s a way u can identify how addicted they are
Qualitative research pivots in apprehending a research query as a humanistic or idealistic approach. Though quantitative approach is viewed as a reliable method which can be made objectively and propagated by other researchers, qualitative method helps to understand people's beliefs, experiences, behaviour, attitudes, and interactions.[ 18 ] Although once viewed as philosophically incongruent with experimental research, qualitative research is now being recognized for its ability to add a new dimension into interventional studies that cannot be obtained through measurement of variables alone.[ 19 ] Qualitative research gives voice to the participants in the study permitting them to share their experiences of effects of the drug of interest in a clinical trial. This can open our eyes to new aspects and help modify the design of the clinical trial.[ 20 ]
In the present study, peer pressure was the main reason the participants started smoking. A study by Sharma et al . in 2016, it was found that main reason to start smoking was due to the influence of peer groups and friends, while a few felt it created a high esteem among the others.[ 21 ] The reason to continue smoking and relapse in quit attempts in the present study was stress which was similar to statement in the previous studies.[ 22 , 23 , 24 , 25 ]
High nicotine dependency was seen among black and blue-collar employees. This proves the role of socioeconomic status and education in nicotine dependency. Previous research suggests that people in socioeconomically deprived neighbourhoods smoke more than those in affluent neighbourhoods, independently of individual-level socioeconomic status.[ 26 , 27 ]
Tobacco cessation in primary care
Qualitative study is all about connecting to the psychological aspect of the participants that can play a role in the intervention. Early detection, diagnosis and treatment are important to increase the awareness of the population. Primary health centre physicians and dentists are the first contact of medicine. Easy accessibility of the oral cavity to examine renders it an ideal target for improved screening practices. Due to the modest investments of time and cost required by screening exams, primary care physicians assume a frontline role in the battle against tobacco and oral cancer.[ 28 ]
Regarding the health sector, more investment in training of health professionals from primary care to psychology, biopsies, in addition to intersectoral and multidisciplinary actions are necessary.[ 29 ] Further training is required at both undergraduate and postgraduate levels to increase awareness of tobacco usage, its associated risk factors to strengthen primary care practitioners' abilities.[ 30 ]
Findings of the study show that people in low socio-economic status had high nicotine dependency with inadequate knowledge on tobacco control policies. There is a need for interdisciplinary approach to prevent tobacco use that involves various disciples of medicine, with the support of government and the broader community. Dentists are one of the professionals who can detect the smoking habit by examining the oral cavity. A public health dentist, often are the primary contact of health worker for many of the low socio - economic groups. It is important for us to understand the various interventions and aspects of the nicotine intoxication and assist in cessation of the habit.
In the present study, among the 20 people participated in-depth interview and focus group discussions, 30% were white collar, 40% were blue collar and 30% included black collar employees. The results showed that 50% of the participants had low nicotine dependency; 30% had medium nicotine dependency and 20% had high nicotine dependency. During the focus group discussion and in depth interviews, most of the participants stated that they started the habit due to peer pressure and they were aware about the ill effects of tobacco use. Most of the participants relapsed from their quitting due to family or work tension. During focus group discussion, one of the participants from white collar employees who have had previous unsuccessful attempt in quitting said that “people who are highly addicted inhales it deeply into the brain, gets high instantly and exhale via nose”. People with medium dependency will exhale through mouth. All the participants were unaware of tobacco control policies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.

IMAGES
VIDEO
COMMENTS
Background and objectives: Despite reductions in prevalence in recent years, tobacco smoking remains one of the main preventable causes of ill-health and premature death worldwide.This paper reviews the extent and nature of harms caused by smoking, the benefits of stopping, patterns of smoking, psychological, pharmacological and social factors that contribute to uptake and maintenance of ...
We identified three outcomes with a 4-star association with smoking: COPD (72% increase in risk based on the BPRF, 0.54 ROS), lower respiratory tract infection (54%, 0.43) and pancreatic cancer ...
Almost 35 years ago, the Office of the Surgeon General of the United States Health Service reviewed over 7000 research papers on the topic of smoking and health, and publicly recognized the role of smoking in various diseases, including lung cancer. Since then, numerous studies have been published that substantiate the strong association of ...
Background Cigarettes and their by-products (i.e., smoke; ash) are a complex, dynamic, and reactive mixture of around 5,000 chemicals. Cigarette smoking potentially harms nearly every organ of the human body, causes innumerable diseases, and impacts the health of smokers and those interacting with the smokers. Smoking brings greater health problems in the long-term like increased risk of ...
Measuring self-reported experience of health and functioning is important for understanding the changes in the health status of individuals switching from cigarettes to less harmful tobacco and/or nicotine products (TNP) or reduced-risk products (RRP) and for supporting tobacco harm reduction strategies. This paper presents insights from three research activities from the preparatory phase of ...
Tobacco smoking: Health impact, prevalence, correlates and interventions. Background and objectives: Despite reductions in prevalence in recent years, tobacco smoking remains one of the main preventable causes of ill-health and premature death worldwide. This paper reviews the extent and nature of harms caused by smoking, the benefits of ...
In their Article in The Lancet Public Health, Marissa Reitsma and colleagues1 report their comprehensive analysis of smoking tobacco use in young people from more than 3000 tobacco surveys from 204 countries and territories around the world. The result is an invaluable overview of an epidemic that causes millions of deaths every year. Their detailed mapping of the prevalence of smoking tobacco ...
Abstract. Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will ...
Most Americans recognize that smoking causes serious diseases, yet many Americans continue to smoke. One possible explanation for this paradox is that perhaps Americans do not accurately perceive the extent to which smoking increases the probability of adverse health outcomes. This paper examines the accuracy of Americans' perceptions of the absolute risk, attributable risk, and relative ...
This paper aims to identify the causal effects of smoking on mental health using data from the Lung Health Study, a randomized trial of smoking cessation treatment with five years of follow-up interviews. In the short-run, distress increases, likely reflecting the effects of nicotine withdrawal.
estimated that smoking increases the risk of. coronary heart disease about 2-4 times, stroke 2-4 times, lung cancer 25 times in. men, and 25.7 times in women. Be sides, smoking can lead to an ...
This paper investigates hypotheses regarding the cause of the recent apparent increase in young adult smoking, compares trends in smoking among young adults with trends in the use of other substances, and considers the implications for youth tobacco control research and policy. Time series analyses of national data suggest that the recent observed increase in smoking among young adults is ...
There is also emerging data suggesting that e-cigarettes may facilitate smoking cessation but further research is needed to compare the effectiveness and safety of e-cigarettes compared to other nicotine replacement therapies [13,14]. Consistent with the U.S. FDA regulatory oversight and the U.S. Surgeon General report, it may be prudent to ...
Many studies have been done on the health risks of smoking and driving. In a survey of 'the effects of smoking on society: a case study', Gupta and Kumar (2018) observe that smoking is very ...
The number of daily smokers aged > 10 years in Aceh Province was 25%, occasional smokers were 4.3%, former smokers 2.5% and non-smokers were as much as 68.2%. Based on gender, men smoke and 11.7% of women smoke. The amongst reported smokers, 18% report first trying cigarettes between ages 10 and 14 years and 55.4% between ages 15 and 19. 5.
Cutting-edge neuroimaging technologies have identified brain changes associated with nicotine dependence and smoking. Using functional magnetic resonance imaging (fMRI), scientists can visualize smokers' brains as they respond to cigarette-associated cues that can trigger craving and relapse. 231 Such research may lead to a biomarker for ...
Here we've gathered a range of catchy titles for research papers about smoking together with smoking essay examples. Get inspired with us! Smoking is a well-known source of harm yet popular regardless, and so smoking essays should cover various aspects of the topic to identify the reasons behind the trend. You will want to discuss the causes ...
In conclusion, a smoking persuasive essay is a powerful tool to persuade readers to take action against smoking. With the right research, evidence, and persuasive language, it is possible to change attitudes and behaviors related to smoking. Conclusion Writing an essay on smoking can be a difficult endeavor. However, with the help of expertly ...
For example, in the 1960s and 1970s, the promulgation in the United States and Britain of new evidence on the health risks of smoking helped reduce consumption between 4 and 9 percent. In addition, warning labels on cigarette packages were also found to reduce consumption during that era (Kenkel and Chen 2000).
Prevalence and burden of tobacco smoking. In 2012, approximately 45,500 deaths (18% of all deaths in Canada) were attributed to tobacco smoking [].Smoking continues to be a leading cause of preventable death and disability [2, 3].Among smoking-related deaths, most were attributable to cancers, cardiovascular disease, and respiratory diseases [1, 4].
1)The paper identifies an impactful vulnerability in Ap-ple's Wi-Fi positioning system and demonstrates ways of exploiting it to track users, including in the context of military and natural disaster situations. 2)The paper collects a longitudinal dataset that could benefit future research. 3)The paper provides recommendations for remediation.
Significance of the Study on the Impact of Remote Work on Employee Productivity in the Tech Industry. 1. Introduction: The shift to remote work due to the COVID-19 pandemic has significantly altered workplace dynamics, particularly in the tech industry.This research paper explores the impact of remote work on employee productivity, offering comprehensive insights through both qualitative and ...
Introduction. Tobacco is a well established cause of at least 13 cancers; 1 however, until recently there have been no large evidence-based assessments of the effects of smoking on cancer treatment outcomes. The 2014 Surgeon General's Report 1 is the "first large evidence review to report a causal association between tobacco use and adverse clinical outcomes for patients with cancer".
1. Introduction: This review examines how technology affects education, focusing on student engagement, learning outcomes, and teacher practices over the past decade. 2. Theoretical Framework: Based on Constructivist Learning Theory and TPACK, this review explores how technology integration enhances education. 3.
Introduction. Tobacco remains as a single largest cause for heart diseases and stroke in India, with more than one million deaths/year.[] India faces an enormous economic burden for treating tobacco-related diseases amounted to $907 and $285 million for smoke and smokeless tobacco respectively.[] Control and prevention of tobacco use becomes a major public health issue in limiting morbidity ...