Summary of Symptoms, Causes, and Treatment of Hypertension Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment

Hypertension
Target audience and health literacy.
Improvements in the quality of life and access to healthcare worldwide are associated with greater longevity – for instance, in some countries, life expectancy may amount up to 80 years and more. While a longer life is a positive tendency, it gives rise to an increase in age-related health disorders which contributes to the global and national burden of disease. One of the most prevalent health conditions associated with age is hypertension. According to a report by World Health Organization, almost half of the people over the age of 25 suffered from hypertension at least once in their lives (Kishore, Gupta, Kohli, & Kumar, 2016). This essay will provide an informative summary of symptoms, causes, and treatment of hypertension.
Hypertension is a health condition that is characterized by high blood pressure (HBP). For blood pressure to be considered abnormally high, the readings should consistently display 140 over 90 or higher. It is essential to understand that a single occasion of HBP due to some factors be it stress or environmental conditions does not mean that a patient suffers from hypertension. For a proper diagnosis, a patient showing typical symptoms and making complaints should make regular appointments at his or her GP’s and measure blood pressure at home as well.
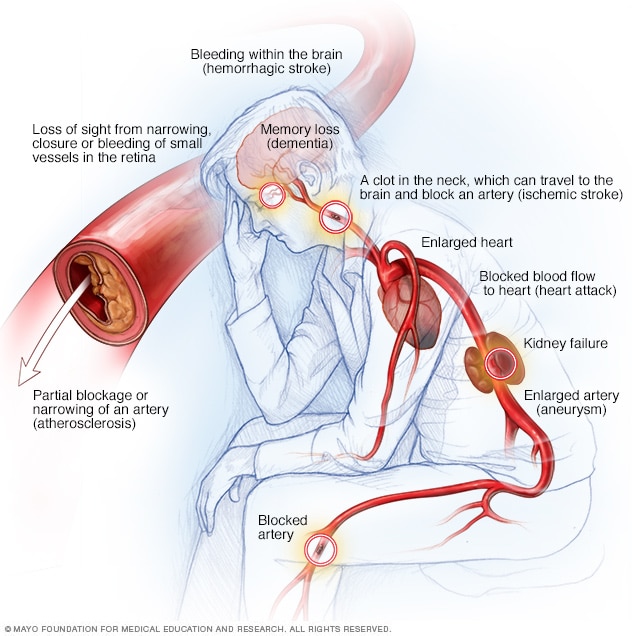
The symptoms of hypertension can be very mild, and the condition may go unnoticed for years on end. The signs may vary from patient to patient, but typically, if symptoms are present, they include severe headaches, chest ache, difficulty breathing, the feeling of weakness, and fatigue. The main reason why it is imperative to pay attention to symptoms and make an early diagnosis is the extensive list of possible complications. When neglected and untreated, HBP can lead to heart attack or a stroke, aneurysm, heart failure, and even dementia; in some cases, HBP can be lethal.
The primary risk factor for HBP is old age since blood vessels lose their elasticity over time (Buford, 2016). Among other factors is the presence of the condition in a patient’s close relatives. Other underlying causes are associated with a patient’s lifestyle: drinking alcohol in excess, smoking tobacco, and not being physically active (Leung et al., 2017). If diagnosed with HBP, a patient is usually prescribed beta-blockers, diuretics, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin II receptor blockers (ARBs) (Weber et al., 2014). However, taking medication alone does not solve the problem, and a patient should revise his or her daily habits and make improvements.
A study by McNaughton et al. (2014) showed that the lack of medical knowledge was associated with elevated blood pressure especially in those patients who had not been officially diagnosed with HBP. Hence, it is critical that a patient takes charge of his or her health and takes measures to prevent or control the condition and improve their overall health literacy. The target audience of the health brochure on hypertension would consist of patients over 45 years – a typical age of onset.
It is also reasonable to spread the brochure among patients belonging to risk groups – for instance, among those suffering from obesity or diabetes. Even though hypertension is associated with mature or old age, as per the report by the World Health Organization, young people might also be susceptible to developing HBP. Thus, a health practitioner could promote better dietary habits and a fitness routine to help to eliminate risks.
Over the last few decades, heightened blood pressure has become a significant public health challenge as it was found to be one of the risks of cardiovascular mortality. Hypertension, or high blood pressure, is alarmingly prevalent among individuals over the age of 45. While health practitioners are trained to address the issue, the patients should gain control of their lifestyle as well. An informative health brochure with links to credible sources can help patients make well-informed health decisions.
Buford, T. W. (2016). Hypertension and aging . Ageing Research Reviews , 26 , 96-111. Web.
Kishore, J., Gupta, N., Kohli, C., & Kumar, N. (2016). Prevalence of hypertension and determination of its risk factors in rural Delhi. International Journal of Hypertension , 2016, 7962595.
Leung, A. A., Daskalopoulou, S. S., Dasgupta, K., McBrien, K., Butalia, S., Zarnke, K. B.,… & Gelfer, M. (2017). Hypertension Canada’s 2017 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults . Canadian Journal of Cardiology , 33 (5), 557-576. Web.
McNaughton, C. D., Kripalani, S., Cawthon, C., Mion, L. C., Wallston, K. A., & Roumie, C. L. (2014). Association of health literacy with elevated blood pressure: A cohort study of hospitalized patients . Medical Care , 52 (4), 346-353. Web.
Weber, M. A., Schiffrin, E. L., White, W. B., Mann, S., Lindholm, L. H., Kenerson, J. G.,… & Cohen, D. L. (2014). Clinical practice guidelines for the management of hypertension in the community: A statement by the American Society of Hypertension and the International Society of Hypertension . The Journal of Clinical Hypertension , 16 (1), 14-26. Web.
- What is Hypertension?
- The Hypertension Condition Analysis
- Creating Awareness Through Education: Hypertension
- Lifestyle Habits and Cardiac Changes
- Disorders of the Veins and Arteries
- Heart Attack: Health Information Patient Handout
- Cardiovascular Disorders: Pharmacotherapy
- Core Measures of Acute Myocardial Infarction
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, July 8). Summary of Symptoms, Causes, and Treatment of Hypertension. https://ivypanda.com/essays/summary-of-symptoms-causes-and-treatment-of-hypertension/
"Summary of Symptoms, Causes, and Treatment of Hypertension." IvyPanda , 8 July 2021, ivypanda.com/essays/summary-of-symptoms-causes-and-treatment-of-hypertension/.
IvyPanda . (2021) 'Summary of Symptoms, Causes, and Treatment of Hypertension'. 8 July.
IvyPanda . 2021. "Summary of Symptoms, Causes, and Treatment of Hypertension." July 8, 2021. https://ivypanda.com/essays/summary-of-symptoms-causes-and-treatment-of-hypertension/.
1. IvyPanda . "Summary of Symptoms, Causes, and Treatment of Hypertension." July 8, 2021. https://ivypanda.com/essays/summary-of-symptoms-causes-and-treatment-of-hypertension/.
Bibliography
IvyPanda . "Summary of Symptoms, Causes, and Treatment of Hypertension." July 8, 2021. https://ivypanda.com/essays/summary-of-symptoms-causes-and-treatment-of-hypertension/.
Hypertension: Introduction, Types, Causes, and Complications
Cite this chapter.
- Yoshihiro Kokubo MD, PhD, FAHA, FACC, FESC, FESO 4 ,
- Yoshio Iwashima MD, PhD, FAHA 5 &
- Kei Kamide MD, PhD, FAHA 6
8739 Accesses
4 Citations
Hypertension remains one of the most significant causes of mortality worldwide. It is preventable by medication and lifestyle modification. Office blood pressure (BP), out-of-office BP measurement with ambulatory BP monitoring, and self-BP measurement at home are reliable and important data for assessing hypertension. Primary hypertension can be defined as an elevated BP of unknown cause due to cardiovascular risk factors resulting from changes in environmental and lifestyle factors. Another type, secondary hypertension, is caused by various toxicities, iatrogenic disease, and congenital diseases. Complications of hypertension are the clinical outcomes of persistently high BP that result in cardiovascular disease (CVD), atherosclerosis, kidney disease, diabetes mellitus, metabolic syndrome, preeclampsia, erectile dysfunction, and eye disease. Treatment strategies for hypertension consist of lifestyle modifications (which include a diet rich in fruits, vegetables, and low-fat food or fish with a reduced content of saturated and total fat, salt restriction, appropriate body weight, regular exercise, moderate alcohol consumption, and smoking cessation) and drug therapies, although these vary somewhat according to different published hypertension treatment guidelines.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Article PubMed Google Scholar
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Article CAS PubMed Google Scholar
National Clinical Guideline Centre (UK). Hypertension: The Clinical Management of Primary Hypertension in Adults: Update of Clinical Guidelines 18 and 34 [Internet]. London: Royal College of Physicians (UK); 2011 Aug. Available from http://www.ncbi.nlm.nih.gov/books/NBK83274 . PubMed PMID: 22855971.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32:3–15.
Go AS, Bauman MA, Coleman King SM, Fonarow GC, Lawrence W, Williams KA, et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014;63:878–85.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–387.
Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham heart study: a cohort study. Lancet. 2001;358:1682–6.
Kokubo Y, Nakamura S, Watanabe M, Kamide K, Kawano Y, Kawanishi K, et al. Cardiovascular risk factors associated with incident hypertension according to blood pressure categories in non-hypertensive population in the Suita study: an Urban cohort study. Hypertension. 2011;58:E132.
Google Scholar
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10.
Kokubo Y. Traditional risk factor management for stroke: a never-ending challenge for health behaviors of diet and physical activity. Curr Opin Neurol. 2012;25:11–7.
Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(12):3754–832.
European Stroke Organisation (ESO) Executive Committee, ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25:457–507.
Article Google Scholar
Guild SJ, McBryde FD, Malpas SC, Barrett CJ. High dietary salt and angiotensin II chronically increase renal sympathetic nerve activity: a direct telemetric study. Hypertension. 2012;59:614–20.
Mu S, Shimosawa T, Ogura S, Wang H, Uetake Y, Kawakami-Mori F, et al. Epigenetic modulation of the renal beta-adrenergic-WNK4 pathway in salt-sensitive hypertension. Nat Med. 2011;17:573–80.
WHO. Guideline: Sodium intake for adults and children. Geneva, World Health Organization (WHO), 2012. http://www.ncbi.nlm.nih.gov/books/NBK133309/pdf/TOC.pdf .
Kokubo Y. Prevention of hypertension and cardiovascular diseases: a comparison of lifestyle factors in westerners and east Asians. Hypertension. 2014;63:655–60.
Ascherio A, Rimm EB, Giovannucci EL, Colditz GA, Rosner B, Willett WC, et al. A prospective study of nutritional factors and hypertension among US men. Circulation. 1992;86:1475–84.
Ascherio A, Hennekens C, Willett WC, Sacks F, Rosner B, Manson J, et al. Prospective study of nutritional factors, blood pressure, and hypertension among US women. Hypertension. 1996;27:1065–72.
Stamler J, Liu K, Ruth KJ, Pryer J, Greenland P. Eight-year blood pressure change in middle-aged men: relationship to multiple nutrients. Hypertension. 2002;39:1000–6.
Miura K, Greenland P, Stamler J, Liu K, Daviglus ML, Nakagawa H. Relation of vegetable, fruit, and meat intake to 7-year blood pressure change in middle-aged men: the Chicago Western Electric study. Am J Epidemiol. 2004;159:572–80.
Tsubota-Utsugi M, Ohkubo T, Kikuya M, Metoki H, Kurimoto A, Suzuki K, et al. High fruit intake is associated with a lower risk of future hypertension determined by home blood pressure measurement: the OHASAMA study. J Hum Hypertens. 2011;25:164–71.
Ueshima H, Stamler J, Elliott P, Chan Q, Brown IJ, Carnethon MR, et al. Food omega-3 fatty acid intake of individuals (total, linolenic acid, long-chain) and their blood pressure: INTERMAP study. Hypertension. 2007;50:313–9.
Geleijnse JM, Giltay EJ, Grobbee DE, Donders AR, Kok FJ. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. J Hypertens. 2002;20:1493–9.
Kromhout D, Bosschieter EB, de Lezenne CC. The inverse relation between fish consumption and 20-year mortality from coronary heart disease. N Engl J Med. 1985;312:1205–9.
Yamori Y. Food factors for atherosclerosis prevention: Asian perspective derived from analyses of worldwide dietary biomarkers. Exp Clin Cardiol. 2006;11:94–8.
PubMed Central CAS PubMed Google Scholar
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84.
Hamer M, Chida Y. Active commuting and cardiovascular risk: a meta-analytic review. Prev Med. 2008;46:9–13.
Hayashi T, Tsumura K, Suematsu C, Okada K, Fujii S, Endo G. Walking to work and the risk for hypertension in men: the Osaka Health Survey. Ann Intern Med. 1999;131:21–6.
Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298:2296–304.
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33.
Groppelli A, Giorgi DM, Omboni S, Parati G, Mancia G. Persistent blood pressure increase induced by heavy smoking. J Hypertens. 1992;10:495–9.
Makris TK, Thomopoulos C, Papadopoulos DP, Bratsas A, Papazachou O, Massias S, et al. Association of passive smoking with masked hypertension in clinically normotensive nonsmokers. Am J Hypertens. 2009;22:853–9.
Zanchetti A. Intermediate endpoints for atherosclerosis in hypertension. Blood Press Suppl. 1997;2:97–102.
CAS PubMed Google Scholar
Iwashima Y, Kokubo Y, Ono T, Yoshimuta Y, Kida M, Kosaka T, et al. Additive interaction of oral health disorders on risk of hypertension in a Japanese urban population: the Suita study. Am J Hypertens. 2014;27:710–9.
Zelkha SA, Freilich RW, Amar S. Periodontal innate immune mechanisms relevant to atherosclerosis and obesity. Periodontol 2000. 2010;54:207–21.
Article PubMed Central PubMed Google Scholar
Tsioufis C, Kasiakogias A, Thomopoulos C, Stefanadis C. Periodontitis and blood pressure: the concept of dental hypertension. Atherosclerosis. 2011;219:1–9.
Kubo M, Hata J, Doi Y, Tanizaki Y, Iida M, Kiyohara Y. Secular trends in the incidence of and risk factors for ischemic stroke and its subtypes in Japanese population. Circulation. 2008;118:2672–8.
Sjol A, Thomsen KK, Schroll M. Secular trends in blood pressure levels in Denmark 1964–1991. Int J Epidemiol. 1998;27:614–22.
Kokubo Y, Kamide K, Okamura T, Watanabe M, Higashiyama A, Kawanishi K, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease in a Japanese urban cohort: the Suita study. Hypertension. 2008;52:652–9.
Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke. 2004;35:776–85.
Briasoulis A, Agarwal V, Tousoulis D, Stefanadis C. Effects of antihypertensive treatment in patients over 65 years of age: a meta-analysis of randomised controlled studies. Heart. 2014;100:317–23.
Asayama K, Thijs L, Brguljan-Hitij J, Niiranen TJ, Hozawa A, Boggia J, et al. Risk stratification by self-measured home blood pressure across categories of conventional blood pressure: a participant-level meta-analysis. PLoS Med. 2014;11:e1001591.
Bussemaker E, Hillebrand U, Hausberg M, Pavenstadt H, Oberleithner H. Pathogenesis of hypertension: interactions among sodium, potassium, and aldosterone. Am J Kidney Dis. 2010;55:1111–20.
Kokubo Y, Nakamura S, Okamura T, Yoshimasa Y, Makino H, Watanabe M, et al. Relationship between blood pressure category and incidence of stroke and myocardial infarction in an urban Japanese population with and without chronic kidney disease: the Suita study. Stroke. 2009;40:2674–9.
Kokubo Y. The mutual exacerbation of decreased kidney function and hypertension. J Hypertens. 2012;30:468–9.
Kokubo Y, Okamura T, Watanabe M, Higashiyama A, Ono Y, Miyamoto Y, et al. The combined impact of blood pressure category and glucose abnormality on the incidence of cardiovascular diseases in a Japanese urban cohort: the Suita study. Hypertens Res. 2010;33:1238–43.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–32.
Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348:g2301.
Aranda P, Ruilope LM, Calvo C, Luque M, Coca A, Gil de Miguel A. Erectile dysfunction in essential arterial hypertension and effects of sildenafil: results of a Spanish national study. Am J Hypertens. 2004;17:139–45.
Sharp SI, Aarsland D, Day S, Sonnesyn H, Alzheimer’s Society Vascular Dementia Systematic Review Group, Ballard C. Hypertension is a potential risk factor for vascular dementia: systematic review. Int J Geriatr Psychiatry. 2011;26:661–9.
Ninomiya T, Ohara T, Hirakawa Y, Yoshida D, Doi Y, Hata J, et al. Midlife and late-life blood pressure and dementia in Japanese elderly: the Hisayama study. Hypertension. 2011;58:22–8.
Thukkani AK, Bhatt DL. Renal denervation therapy for hypertension. Circulation. 2013;128:2251–4.
Myat A, Redwood SR, Qureshi AC, Thackray S, Cleland JG, Bhatt DL, et al. Renal sympathetic denervation therapy for resistant hypertension: a contemporary synopsis and future implications. Circ Cardiovasc Interv. 2013;6:184–97.
Bhatt DL, Kandzari DE, O’Neill WW, D’Agostino R, Flack JM, Katzen BT, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393–401.
Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755–62.
Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703–13.
Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW, et al. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group. N Engl J Med. 1994;330:877–84.
Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and Bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123:2799–810, 2799 p following 2810.
Steg PG, Bhatt DL, Wilson PW, D’Agostino Sr R, Ohman EM, Rother J, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–206.
Perry Jr HM, Davis BR, Price TR, Applegate WB, Fields WS, Guralnik JM, et al. Effect of treating isolated systolic hypertension on the risk of developing various types and subtypes of stroke: the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 2000;284:465–71.
Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350:757–64.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
American DA. Standards of medical care in diabetes–2014. Diabetes Care. 2014;37 Suppl 1:S14–80.
Hollenberg NK, Price DA, Fisher ND, Lansang MC, Perkins B, Gordon MS, et al. Glomerular hemodynamics and the renin-angiotensin system in patients with type 1 diabetes mellitus. Kidney Int. 2003;63:172–8.
Mezzano S, Droguett A, Burgos ME, Ardiles LG, Flores CA, Aros CA, et al. Renin-angiotensin system activation and interstitial inflammation in human diabetic nephropathy. Kidney Int Suppl. 2003:(86);S64–70.
Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366:1545–53.
Jamerson K, Weber MA, Bakris GL, Dahlof B, Pitt B, Shi V, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359:2417–28.
Bakris GL, Toto RD, McCullough PA, Rocha R, Purkayastha D, Davis P, et al. Effects of different ACE inhibitor combinations on albuminuria: results of the GUARD study. Kidney Int. 2008;73:1303–9.
ONTARGET Investigators, Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547–59.
Download references
Sources of Funding
This study was supported by grants-in-aid from the Ministry of Education, Science, and Culture of Japan (Nos. 25293147 and 26670320), the Ministry of Health, Labor, and Welfare of Japan (H26-Junkankitou [Seisaku]-Ippan-001), the Rice Health Database Maintenance industry, Tojuro Iijima Memorial Food Science, the Intramural Research Fund of the National Cerebral and Cardiovascular Center (22-4-5).
Author information
Authors and affiliations.
Department of Preventive Cardiology, National Cerebral and Cardiovascular Center, 5-7-1, Fujishiro-dai, Suita, Osaka, 565-8565, Japan
Yoshihiro Kokubo MD, PhD, FAHA, FACC, FESC, FESO
Divisions of Hypertension and Nephrology, National Cerebral and Cardiovascular Center, 5-7-1, Fujishiro-dai, Suita, Osaka, 565-8565, Japan
Yoshio Iwashima MD, PhD, FAHA
Division of Health Science, Osaka University Graduate School of Medicine, Suita, Osaka, Japan
Kei Kamide MD, PhD, FAHA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yoshihiro Kokubo MD, PhD, FAHA, FACC, FESC, FESO .
Editor information
Editors and affiliations.
Center for Drug Evaluation and Research Division of Cardiovascular and Renal Products, US Food and Drug Administration, Silver Spring, Maryland, USA
Gowraganahalli Jagadeesh
Pharmacology Unit, AIMST University, Bedong, Malaysia
Pitchai Balakumar
Khin Maung-U
Rights and permissions
Reprints and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Kokubo, Y., Iwashima, Y., Kamide, K. (2015). Hypertension: Introduction, Types, Causes, and Complications. In: Jagadeesh, G., Balakumar, P., Maung-U, K. (eds) Pathophysiology and Pharmacotherapy of Cardiovascular Disease. Adis, Cham. https://doi.org/10.1007/978-3-319-15961-4_30
Download citation
DOI : https://doi.org/10.1007/978-3-319-15961-4_30
Publisher Name : Adis, Cham
Print ISBN : 978-3-319-15960-7
Online ISBN : 978-3-319-15961-4
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Taking a summer road trip? Enter for a chance to win $4,000 cash with AARP Rewards.
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
AARP MEMBERSHIP
AARP Membership — $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products, hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

Get Happier
Creating Social Connections

Brain Health Resources
Tools and Explainers on Brain Health

Your Health
8 Major Health Risks for People 50+
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

How to Protect What You Collect
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Outdoor Vacation Ideas
Camping Vacations

Plan Ahead for Summer Travel

AARP National Park Guide
Discover Canyonlands National Park

History & Culture
8 Amazing American Pilgrimages
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

Movies for Grownups
Summer Movie Preview

Jon Bon Jovi’s Long Journey Back

Looking Back
50 World Changers Turning 50

Sex & Dating
Spice Up Your Love Life

Friends & Family
How to Host a Fabulous Dessert Party

Home Technology
Caregiver’s Guide to Smart Home Tech

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul
AARP Solves 25 of Your Problems
Driver Safety
Maintenance & Safety
Trends & Technology

AARP Smart Guide
How to Clean Your Car

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page
High Blood Pressure (Hypertension): A Guide to Symptoms, Causes and Tests
Explore risk factors for high blood pressure, testing options and why it is known as the silent killer.
Kimberly Hayes,
Merle Myerson, M.D.

High Blood Pressure Guide
- Symptoms, causes and tests
- High blood pressure myths
- Alcohol and blood pressure
- Hypertension headache myths
Smoking and high blood pressure
- Anxiety, stress and hypertension
- Is hypertension genetic?
- Medications that raise blood pressure
- Home blood pressure monitoring
- Surprising causes of hypertension
A staggering three-quarters of Americans over age 60 have high blood pressure, otherwise known as hypertension, putting them at increased risk for stroke, heart attack and heart failure. Men tend to have higher blood pressure rates in their younger years, but women catch up around the time of menopause.
Hypertension increases with age: Only 22.4 percent of people ages 18–39 have the condition. But those numbers rise to 54.5 percent for people age 40–59 and 74.5 percent for people 60 and over. These alarming rates are even higher for people of color, especially for African Americans. Hypertension prevalence across all ages is higher among non-Hispanic Black adults (57.1 percent) than non-Hispanic white (43.6 percent) or Hispanic (43.7 percent) adults.
What causes high blood pressure?
“The main cause of high blood pressure is aging blood vessels,” said Jordana Cohen, MD, MSCE, Associate Professor of Medicine, Renal-Electrolyte and Hypertension at the Hospital of the University of Pennsylvania. She is also chair of the Hypertension Science Committee for the American Heart Association.
Blood vessels tend to stiffen with age and becomes less flexible, which can drive up the pressure inside them. However, studies have found that there are populations of older people who don’t have high blood pressure, for example the remote South American Yanomami tribe, whose members live in near-total isolation in the rainforests in southern Venezuela and northern Brazil. They eat very little salt and fat and have a diet high in plantains, fruit and meat, and their blood pressures stay the same as when they were younger.

Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
Research suggests that this could be related to their lower consumption of salt , and the fact that they eat a lot of potassium, Cohen said. They also have less exposure to modern-day risk factors such as pollution, stress and other diseases that are prevalent in our society, such as diabetes, heart disease and kidney disease, which all contribute to high blood pressure, Cohen added.
Understanding a blood pressure reading
Blood pressure is measured in stages, with a normal range being less than 120/80. The top number — the systolic— measures the pressure in your arteries when your heart beats. The bottom number — the diastolic — measures the pressure in your arteries when the blood is flowing back to the heart through the veins. Your blood pressure numbers are measured in millimeters of mercury (mm Hg). Stages at or above 120/80 include: elevated, stage 1 hypertension and stage 2 hypertension. A severely elevated blood pressure of 180/120 or greater can be a hypertensive crisis and could require guidance from your doctor, or in some cases, emergency care.
“The top number is what’s mostly considered our biggest indicator of risk,” Cohen said. It also tends to be the most responsive to treatment. The bottom number tends to be higher in younger people and then gets lower with age. Older patients can see a very wide split between their top and the bottom number, which can be concerning, Cohen said, especially if the bottom number gets too low as it can increase the risk of falls and kidney problems. “This is something that I see in my much older patients in their 80s, 90s and 100s.”
What are symptoms of high blood pressure?
Most people with hypertension shouldn’t expect to experience symptoms from high blood pressure.
“If your expectation is that you’re going to feel it, then you’re going to be somebody who’s missing it 90 percent of the time,” Cohen said.
Generally, people will not feel any symptoms of high blood pressure unless they are having the severely elevated blood pressure, which occurs when a patient’s underlying high blood pressure has accelerated to 180/120 or above and is damaging their vital organs, including the brain, heart, kidneys or eyes. In this scenario the person could face additional symptoms including sudden headache, blurred vision or vomiting, and should seek emergency medical assistance. It’s important to note that people with poorly controlled blood pressure could have readings in this higher range, but as long as they are not having other symptoms it may not be an emergency. However, they still should follow up with their doctor within a couple of days.
Measuring your blood pressure
While patients may assume a blood pressure measurement at a doctor’s office is the most accurate, that’s not always the case. To get a good blood pressure reading, it’s recommended the person sit in a quiet environment with their feet flat on the floor and their arms on a table or desk in front of them, which may not always be how you are positioned at the doctor’s office. Couple that with the stress of a doctor’s visit, and it’s easy to see how readings may not be 100 percent accurate.
White coat hypertension and masked hypertension
According to the Cleveland Clinic, between 15 to 30 percent of people have so-called white coat hypertension, which means their blood pressure is higher at a health care provider’s office, but normal at home. Estimates vary, however, with some research saying up to 50 percent or more people have white coat hypertension.

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
But it’s important not to discount these higher doctor’s office readings totally. “I think white coat can be used to deny high blood pressure,” said Beverly Green, M.D., senior investigator for Kaiser Permanente Washington Health Research Institute. “There’s literature showing that people with white coat hypertension are higher risk of eventually getting high blood pressure.”
At the opposite end of white coat hypertension is masked hypertension. Approximately 10 to 40 percent of people have this condition, which occurs when blood pressure is normal in the doctor’s office but high in everyday life. This can happen among people who typically smoke but avoid doing so right before a doctor’s visit. People who have sleep apnea could also be at risk, Cohen said.
The importance of home blood pressure monitoring
With home monitoring, patients can hopefully control their environment and take their readings at ideal times. (Look for guidelines on checking your blood pressure at home at the end of this article.)
It’s important to make sure you are using an accurate device, and more than two-thirds of devices on the market right now are not, Cohen said. The website validatebp.org from the American Medical Association provides a list of devices that have been validated for accuracy and includes price ranges.
It is of course important to still get your blood pressure checked at your doctor’s office and to discuss the readings you take at home with them. Some providers use an automated office blood pressure machine, which provides multiple readings over a series of intervals. This can be used in a quiet room without a medical professional present, hopefully reducing white coat hypertension.
Ambulatory blood pressure monitoring
Some patients are referred for ambulatory blood pressure monitoring, where your blood pressure is measured on a continuous basis for 24 hours as you live your daily life, even as you sleep. Your doctor will calculate the average blood pressure and also look at the range, how often readings are high or low, and if there is a “dip,” meaning a lowering of blood pressure during nighttime hours, which is normal. Ambulatory monitoring can be used for patients who have had high blood pressure readings but haven’t yet started treatment, need changes to their medications, or whose blood pressure is not responding to medications, or who have felt dizziness or have had fainting episodes.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
Green has used ambulatory monitoring herself and, to her surprise, found that she had high blood pressure during the workday. “I wouldn’t have known that I had high blood pressure while at work, and there are a lot of people walking around just like that whose hypertension wouldn’t have been caught otherwise,” Green added.
It’s been shown both home monitors and the ambulatory monitors do a better job predicting heart attacks , strokes and death because they catch the variability in the average blood pressure much better than you can get from occasional blood pressure readings in the doctor’s office, Green said.
Unfortunately, ambulatory monitoring can be difficult for some patients to access as it’s a subspecialty in medicine and not available in every doctor’s office, Cohen says. But studies have shown that home blood pressure monitoring with a store-bought monitor is a good surrogate for ambulatory. “It’s not expensive and everyone can do it.”
Read more about home blood pressure monitoring .
This high blood pressure guide shows you the science behind high blood pressure and the various factors that can play a role in high blood pressure causes and symptoms:
High blood pressure myths
Blood pressure myths about types of salt, wine intake and medications persist in popular culture. Here’s a look at six blood pressure myths, plus tips you can use to maintain a healthy blood pressure.
Read more about high blood pressure myths .

LEARN MORE ABOUT AARP MEMBERSHIP.
Alcohol and high blood pressure
Research has traditionally shown that heavy drinking raises your risk for high blood pressure, but now experts believe even light to moderate drinking can carry risks.
Read more about alcohol and high blood pressure .
While smoking is not a primary risk factor for high blood pressure, the habit can damage blood vessels, contributing to plaque buildup and hardening arteries. Nicotine, the addictive chemical compound in cigarettes, can also increase blood pressure.
Read more about smoking and high blood pressure .
Anxiety, stress and high blood pressure
Stress can trigger blood pressure to rise in the short-term, and if that happens frequently enough, it could damage the blood vessels, heart and kidneys, similar to what happens in people with long-term hypertension. But that’s different from saying stress or anxiety themselves produce high blood pressure.
Read more about the links between anxiety, stress and high blood pressure .
Is high blood pressure genetic?
A May 2024 study in Nature Genetic s analyzed the genes of more than 1 million people of European heritage and uncovered some 113 gene variants associated with high blood pressure. While you can’t change your genes, there are lifestyle changes you can make that will likely have a much bigger impact on your risk for high blood pressure.
Read more about high blood pressure and genetics .
Medications that cause high blood pressure
Pain and migraine medicines, decongestants, corticosteroids and some herbal supplements are all examples of pills that could raise your blood pressure. Yet a 2021 study revealed that 18.5 percent of adults with hypertension were taking one or more of these medications.
Read more about medications that can raise blood pressure .
Surprising causes of high blood pressure
While salt is one of the most associated risk factors for high blood pressure, there are a handful of unsuspected foods, habits and health issues that can play a role, too.
Read more surprising things that can raise your blood pressure .
Hypertension headache
A common myth persists among some patients that they can sense their blood pressure is creeping up because they’ve started getting headaches. Yet research shows the link between high blood pressure and headaches is shaky, particularly for mild and moderate high blood pressure.
Read more about high blood pressure headaches .

How to properly measure your blood pressure at home
- Make sure your blood pressure monitor has been validated at validatebp.org. Confirm that the cuff fits by measuring around your upper arm and choosing a monitor with the correct cuff size. Wrist and finger monitors are not recommended due to less reliable readings.
- Be in a quiet room , avoid conversation and relax for three to five minutes before taking your blood pressure.
- Make sure that you’re positioned correctly : Sit at a kitchen table or a desk where your feet are flat on the floor, your back is supported and your arms are resting on the table at the level of your heart.
- Put the cuff on your bare arm. If you must push your sleeve up, make sure it is loose fitting. A tight sleeve could create a tourniquet effect and raise your blood pressure.
- Empty your bladder prior to a reading. Having a full bladder can raise your blood pressure, according to the AMA.
- Take your blood pressure twice . People often get a surge of adrenaline when they first take the reading.
- Record your blood pressure measurements , along with the time of day you took them, and discuss these results with your doctor. The AHA offers a printable blood pressure log .
- Smoke, eat or drink coffee or other caffeinated beverages at least 30 minutes before taking your blood pressure.
“We usually recommend checking two back-to-back readings about 30 seconds to a minute apart in the morning, before taking medications … and two back-to-back readings in the evening before going to bed, at least an hour after dinner, for a minimum of three days per month,” said Jordana Cohen, MD, MSCE, Associate Professor of Medicine, Renal-Electrolyte and Hypertension at the Hospital of the University of Pennsylvania. “That’s the minimum needed to get a really accurate reading.”
Doing this series of checks once a month is recommended for people currently being treated with blood pressure medication. If your blood pressure is borderline, three days of monitoring every two to three months is recommended, Cohen said.
While these are general guidelines, you should discuss how frequently to take your blood pressure with your doctor, based on your individual medical needs.
The website Targetbp.org offers additional tools and guides for measuring your blood pressure accurately at home as does the AHA .
Kimberly Hayes is an editor-writer for AARP and has written on health and social justice issues for numerous organizations, including the National Organization for Women, the Robert Wood Johnson Foundation and the Lawyers’ Committee for Civil Rights. She previously served as editor of Native American Report . Dr. Merle Myerson is a board-certified cardiologist with specialties in sports medicine, lipids, women’s health and prevention of cardiovascular disease.
A Guide to High Blood Pressure
Discover the risk factors, diagnostic process and potential symptoms of hypertension
Discover AARP Members Only Access
Already a Member? Login

More From AARP

6 Ways to Lower Your Blood Pressure Without Medication
Try these tactics to help fight hypertension and bring your numbers down

9 Best (and 8 Worst) Foods for High Blood Pressure

8 Major Health Risks for People 50 and Older
A look at the top killers — and how to dodge them
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
Appointments at Mayo Clinic
High blood pressure dangers: hypertension's effects on your body.
High blood pressure is a risk factor for more than heart disease. Learn what other health conditions high blood pressure can cause.
High blood pressure complications
High blood pressure can cause many complications.
High blood pressure, also called hypertension, can quietly damage the body for years before symptoms appear. Without treatment, high blood pressure can lead to disability, a poor quality of life, or even a deadly heart attack or stroke.
Blood pressure is measured in millimeters of mercury (mm Hg). In general, hypertension is a blood pressure reading of 130/80 mm Hg or higher.
Treatment and lifestyle changes can help control high blood pressure to lower the risk of life-threatening health conditions.
Damage to the arteries
Healthy arteries are flexible, strong and elastic. Their inner lining is smooth so that blood flows freely, supplying vital organs and tissues with nutrients and oxygen.
Over time, high blood pressure increases the pressure of blood flowing through the arteries. This may cause:
- Damaged and narrowed arteries. High blood pressure can damage the cells of the arteries' inner lining. When fats from food enter the bloodstream, they can collect in the damaged arteries. In time, the artery walls become less elastic. This limits blood flow throughout the body.
- Aneurysm. Over time, the constant pressure of blood moving through a weakened artery can cause part of the artery wall to bulge. This is called an aneurysm. An aneurysm can burst open and cause life-threatening bleeding inside the body. Aneurysms can form in any artery. But they're most common in the body's largest artery, called the aorta.
Damage to the heart
High blood pressure can cause many heart conditions, including:
- Coronary artery disease. High blood pressure can narrow and damage the arteries that supply blood to the heart. This damage is known as coronary artery disease. Too little blood flow to the heart can lead to chest pain, called angina. It can lead to irregular heart rhythms, called arrhythmias. Or it can lead to a heart attack.
- Heart failure. High blood pressure strains the heart. Over time, this can cause the heart muscle to weaken or become stiff and not work as well as it should. The overwhelmed heart slowly starts to fail.
- Enlarged left heart. High blood pressure forces the heart to work harder to pump blood to the rest of the body. This causes the lower left heart chamber, called the left ventricle, to thicken and to enlarge. A thickened and enlarged left ventricle raises the risk of heart attack and heart failure. It also increases the risk of death when the heart suddenly stops beating, called sudden cardiac death.
- Metabolic syndrome. High blood pressure raises the risk of metabolic syndrome. This syndrome is a cluster of health conditions that can lead to can lead to heart disease, stroke and diabetes. The health conditions that make up metabolic syndrome are high blood pressure, high blood sugar, high levels of blood fats called triglycerides, low levels of HDL cholesterol, which is the "good" cholesterol, and too much body fat around the waist.
Damage to the brain
The brain depends on a nourishing blood supply to work right. High blood pressure may affect the brain in the following ways:
- Transient ischemic attack (TIA). Sometimes this is called a ministroke. A TIA happens when the blood supply to part of the brain is blocked for a short time. Hardened arteries or blood clots caused by high blood pressure can cause TIAs. A TIA is often a warning sign of a full-blown stroke.
- Stroke. A stroke happens when part of the brain doesn't get enough oxygen and nutrients. Or it can happen when there is bleeding inside or around the brain. These problems cause brain cells to die. Blood vessels damaged by high blood pressure can narrow, break or leak. High blood pressure also can cause blood clots to form in the arteries leading to the brain. The clots can block blood flow, raising the risk of a stroke.
- Dementia. Narrowed or blocked arteries can limit blood flow to the brain. This could lead to a certain type of dementia, called vascular dementia. A single stroke or multiple tiny strokes that interrupt blood flow to the brain also can cause vascular dementia.
- Mild cognitive impairment. This condition involves having slightly more troubles with memory, language or thinking than other adults your age have. But the changes aren't major enough to impact your daily life, as with dementia. High blood pressure may lead to mild cognitive impairment.
Damage to the kidneys
Kidneys filter extra fluid and waste from the blood — a process that requires healthy blood vessels. High blood pressure can damage the blood vessels in and leading to the kidneys. Having diabetes along with high blood pressure can worsen the damage.
Damaged blood vessels prevent the kidneys from being effective at filtering waste from the blood. This allows dangerous levels of fluid and waste to collect. When the kidneys don't work well enough on their own, it's a serious condition called kidney failure. Treatment may include dialysis or a kidney transplant. High blood pressure is one of the most common causes of kidney failure.
Damage to the eyes
High blood pressure can damage the tiny, delicate blood vessels that supply blood to the eyes, causing:
- Damage to the blood vessels in the retina, also called retinopathy. The retina is a layer of light-sensing cells at the back of the eye. Damage to the blood vessels in the retina can lead to bleeding in the eye, blurred vision and complete loss of vision. Having diabetes along with high blood pressure raises the risk of retinopathy.
- Fluid buildup under the retina, also called choroidopathy. This condition can result in distorted vision or sometimes scarring that makes vision worse.
- Nerve damage, also called optic neuropathy. Blocked blood flow can damage the nerve that sends light signals to the brain, called the optic nerve. The damage can lead to bleeding within the eye or vision loss.
Sexual conditions
Trouble getting and keeping an erection is called erectile dysfunction. It becomes more and more common after age 50. But people with high blood pressure are even more likely to have erectile dysfunction. That's because limited blood flow caused by high blood pressure can block blood from flowing to the penis.
High blood pressure can reduce blood flow to the vagina. Reduced blood flow to the vagina can lead to less sexual desire or arousal, vaginal dryness, or trouble having orgasms.
High blood pressure emergencies
High blood pressure usually is an ongoing condition that slowly causes damage over years. But sometimes blood pressure rises so quickly and seriously that it becomes a medical emergency. When this happens, treatment is needed right away, often with hospital care.
In these situations, high blood pressure can cause:
- Chest pain.
- Complications in pregnancy, such as the blood pressure-related conditions preeclampsia or eclampsia.
- Heart attack.
- Memory loss, personality changes, trouble concentrating, irritable mood or gradual loss of consciousness.
- Serious damage to the body's main artery, also called aortic dissection.
- Sudden impaired pumping of the heart, leading to fluid backup in the lungs that results in shortness of breath, also called pulmonary edema.
- Sudden loss of kidney function.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Basile J, et al. Overview of hypertension in adults. https://www.uptodate.contents/search. Accessed Aug. 11, 2023.
- Health threats from high blood pressure. American Heart Association. https://www.heart.org/en/health-topics/high-blood-pressure/health-threats-from-high-blood-pressure. Accessed Aug. 11, 2023.
- High blood pressure. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/high-blood-pressure. Accessed Aug. 11, 2023.
- Hypertensive crisis: When you should call 9-1-1 for high blood pressure. American Heart Association. https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings/hypertensive-crisis-when-you-should-call-911-for-high-blood-pressure. Accessed Aug. 11, 2023.
- How high blood pressure can lead to vision loss. American Heart Association. https://www.heart.org/en/health-topics/high-blood-pressure/health-threats-from-high-blood-pressure/how-high-blood-pressure-can-lead-to-vision-loss. Accessed Aug. 11, 2023.
- Transient ischemic attack (TIA). American Stroke Association. https://www.stroke.org/en/about-stroke/types-of-stroke/tia-transient-ischemic-attack. Accessed Aug. 11, 2023.
- Petersen R. Mild cognitive impairment: Epidemiology, pathology, and clinical assessment. https://www.uptodate.contents/search. Accessed Aug. 11, 2023.
- Whelton PK, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; doi:10.1161/HYP.0000000000000065.
- Arnett DK, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019; doi:10.1161/CIR.0000000000000678.
- Unger T, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Journal of Hypertension. 2020; doi:10.1097/HJH.0000000000002453.
- U.S. Preventive Services Task Force. Screening for hypertension in adults: US Preventive Services Task Force reaffirmation recommendation statement. JAMA. 2021; doi:10.1001/jama.2021.4987.
- Coles S, et al. Blood pressure targets in adults with hypertension: A clinical practice guideline from the AAFP. American Family Physician. 2022; https://www.aafp.org/pubs/afp/issues/2022/1200/practice-guidelines-hypertension.html. Accessed Aug. 11, 2023.
- The anatomy of blood pressure. American Heart Association. https://watchlearnlive.heart.org/index.php?moduleSelect=bpanat. Accessed Aug. 11, 2023.
- What is aortic aneurysm? National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/aortic-aneurysm. Accessed Aug. 11, 2023.
- What is metabolic syndrome? American Heart Association. https://www.heart.org/en/health-topics/metabolic-syndrome/about-metabolic-syndrome. Accessed Aug. 11, 2023.
- How high blood pressure can lead to kidney damage or failure. American Heart Association. https://www.heart.org/en/health-topics/high-blood-pressure/health-threats-from-high-blood-pressure/how-high-blood-pressure-can-lead-to-kidney-damage-or-failure. Accessed Sept. 19, 2023.
Products and Services
- A Book: Mayo Clinic on High Blood Pressure
- Blood Pressure Monitors at Mayo Clinic Store
- The Mayo Clinic Diet Online
- Medication-free hypertension control
- Alcohol: Does it affect blood pressure?
- Alpha blockers
- Amputation and diabetes
- Angiotensin-converting enzyme (ACE) inhibitors
- Angiotensin II receptor blockers
- Anxiety: A cause of high blood pressure?
- Arteriosclerosis / atherosclerosis
- Artificial sweeteners: Any effect on blood sugar?
- AskMayoMom Pediatric Urology
- Beta blockers
- Beta blockers: Do they cause weight gain?
- Beta blockers: How do they affect exercise?
- Birth control pill FAQ
- Blood glucose meters
- Blood glucose monitors
- Blood pressure: Can it be higher in one arm?
- Blood pressure chart
- Blood pressure cuff: Does size matter?
- Blood pressure: Does it have a daily pattern?
- Blood pressure: Is it affected by cold weather?
- Blood pressure medication: Still necessary if I lose weight?
- Blood pressure medications: Can they raise my triglycerides?
- Blood pressure readings: Why higher at home?
- Blood pressure test
- Blood pressure tip: Get more potassium
- Blood sugar levels can fluctuate for many reasons
- Blood sugar testing: Why, when and how
- Bone and joint problems associated with diabetes
- How kidneys work
- Bump on the head: When is it a serious head injury?
- Caffeine and hypertension
- Calcium channel blockers
- Calcium supplements: Do they interfere with blood pressure drugs?
- Can whole-grain foods lower blood pressure?
- Central-acting agents
- Choosing blood pressure medicines
- Chronic daily headaches
- Chronic kidney disease
- Chronic kidney disease: Is a clinical trial right for me?
- Coarctation of the aorta
- COVID-19: Who's at higher risk of serious symptoms?
- Cushing syndrome
- DASH diet: Recommended servings
- Sample DASH menus
- Diabetes and depression: Coping with the two conditions
- Diabetes and exercise: When to monitor your blood sugar
- Diabetes and heat
- 10 ways to avoid diabetes complications
- Diabetes diet: Should I avoid sweet fruits?
- Diabetes diet: Create your healthy-eating plan
- Diabetes foods: Can I substitute honey for sugar?
- Diabetes and liver
- Diabetes management: How lifestyle, daily routine affect blood sugar
- Diabetes symptoms
- Diabetes treatment: Can cinnamon lower blood sugar?
- Using insulin
- Diuretics: A cause of low potassium?
- Diuretics: Cause of gout?
- Do infrared saunas have any health benefits?
- Drug addiction (substance use disorder)
- Eating right for chronic kidney disease
- High blood pressure and exercise
- Fibromuscular dysplasia
- Free blood pressure machines: Are they accurate?
- Home blood pressure monitoring
- Glomerulonephritis
- Glycemic index: A helpful tool for diabetes?
- Guillain-Barre syndrome
- Headaches and hormones
- Headaches: Treatment depends on your diagnosis and symptoms
- Heart and Blood Health
- Herbal supplements and heart drugs
- High blood pressure (hypertension)
- High blood pressure and cold remedies: Which are safe?
- High blood pressure and sex
- How does IgA nephropathy (Berger's disease) cause kidney damage?
- How opioid use disorder occurs
- How to tell if a loved one is abusing opioids
- What is hypertension? A Mayo Clinic expert explains.
- Hypertension FAQs
- Hypertensive crisis: What are the symptoms?
- Hypothermia
- I have IgA nephrology. Will I need a kidney transplant?
- IgA nephropathy (Berger disease)
- Insulin and weight gain
- Intracranial hematoma
- Isolated systolic hypertension: A health concern?
- What is kidney disease? An expert explains
- Kidney disease FAQs
- Kratom: Unsafe and ineffective
- Kratom for opioid withdrawal
- L-arginine: Does it lower blood pressure?
- Late-night eating: OK if you have diabetes?
- Lead poisoning
- Living with IgA nephropathy (Berger's disease) and C3G
- Low-phosphorus diet: Helpful for kidney disease?
- Medications and supplements that can raise your blood pressure
- Menopause and high blood pressure: What's the connection?
- Molar pregnancy
- MRI: Is gadolinium safe for people with kidney problems?
- New Test for Preeclampsia
- Nighttime headaches: Relief
- Obstructive sleep apnea
- Obstructive Sleep Apnea
- Opioid stewardship: What is it?
- Pain Management
- Pheochromocytoma
- Picnic Problems: High Sodium
- Pituitary tumors
- Polycystic kidney disease
- Polypill: Does it treat heart disease?
- Poppy seed tea: Beneficial or dangerous?
- Postpartum preeclampsia
- Preeclampsia
- Prescription drug abuse
- Primary aldosteronism
- Pulse pressure: An indicator of heart health?
- Mayo Clinic Minute: Rattlesnakes, scorpions and other desert dangers
- Reactive hypoglycemia: What can I do?
- Renal diet for vegetarians
- Resperate: Can it help reduce blood pressure?
- Scorpion sting
- Secondary hypertension
- Serotonin syndrome
- Sleep deprivation: A cause of high blood pressure?
- Spider bites
- Stress and high blood pressure
- Symptom Checker
- Takayasu's arteritis
- Tapering off opioids: When and how
- Tetanus shots: Is it risky to receive 'extra' boosters?
- The dawn phenomenon: What can you do?
- Understanding complement 3 glomerulopathy (C3G)
- Understanding IgA nephropathy (Berger's disease)
- Vasodilators
- Vegetarian diet: Can it help me control my diabetes?
- Vesicoureteral reflux
- Video: Heart and circulatory system
- How to measure blood pressure using a manual monitor
- How to measure blood pressure using an automatic monitor
- Obstructive sleep apnea: What happens?
- What is blood pressure?
- Can a lack of vitamin D cause high blood pressure?
- What are opioids and why are they dangerous?
- White coat hypertension
- Wrist blood pressure monitors: Are they accurate?
- Effectively managing chronic kidney disease
- Mayo Clinic Minute: Do not share pain medication
- Mayo Clinic Minute: Avoid opioids for chronic pain
- Mayo Clinic Minute: Be careful not to pop pain pills
- Mayo Clinic Minute: Out of shape kids and diabetes
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- High blood pressure dangers - Hypertensions effects on your body
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 05 June 2024
Consider hypertension risk factors once again
- Masaki Mogi 1 ,
- Satoshi Hoshide 2 &
- Kazuomi Kario 2
Hypertension Research volume 47 , pages 1443–1444 ( 2024 ) Cite this article
2 Altmetric
Metrics details
Takase et al. examined risk factors for hypertension using data from the Tohoku Medical Megabank cohort study, and found that body mass index, salt intake, urinary Na/K ratio, γ-GTP level, and alcohol intake were associated with risk factors for elevated systolic blood pressure [ 1 ]. Aida et al. examined the relationship between income and blood pressure using data from the National Database of Health Insurance Claims and Specific Health Checkups of Japan, and found that the lowest income group had 15.3% more hypertension than the highest income group in men and 18.7% in women, and the effects of lifestyle habits such as smoking, alcohol consumption, and obesity were considered [ 2 ]. In a similar report, Gupta et al. looked at the incidence of hypertension in India by region and attributed the increase in hypertension among the younger generation in the less developed rural areas to a lack of knowledge and adequate treatment for hypertension via inequalities [ 3 ]. Using data on 920,000 individuals from the Japan Health Insurance Association, Mori et al. examined the association between excessive antihypertensive treatment and cardiovascular events in patients at low risk for cardiovascular disease and reported that the incidence of events increases when diastolic blood pressure falls below 60 mmHg, sounding the alarm against excessive diastolic blood pressure reduction [ 4 ]. Sleep apnea in obese individuals is a known risk factor for hypertension. However, Inoue et al. found that the 3% oxygen desaturation index (3% ODI) obtained by polysomnography correlated with the presence of hypertension even in non-obese individuals, and the possibility of sleep disorders should be considered in hypertensive patients, even in non-obese individuals [ 5 ]. In addition, because women who experience gestational hypertension are at higher risk for future cardiovascular disease and metabolic syndrome, postpartum care is needed. Ushida et al. include a review article on the importance and methods of such care [ 6 ]. Detailed risk management in women who experience hypertension during pregnancy is desirable. Moreover, Yan et al. reported that a follow-up study of 330 very elderly hypertensive patients aged 80 years or older with a mean follow-up of 3.8 years showed a U-shaped relationship between baseline systolic blood pressure and pulse pressure values and the development of future frailty, with nadir values of systolic blood pressure 140 mmHg, pulse pressure was 77 mmHg [ 7 ]. Furthermore, as biomarkers of risk factors for cardiovascular disease, An et al. reported high uric acid levels as a risk factor for elevated arterial stiffness [ 8 ], and Ding et al. reported the importance of serum total homocysteine levels in relation to renal function [ 9 ].
In addition, two studies on atrial fibrillation are reported in this month’s issue. The first examined the presence of atrial fibrillation in 4161 hypertensive patients aged 65 years or older in Shanghai and found that the incidence was 2.21 times higher in newly hypertensive patients than in those who were already hypertensive, suggesting the need to be aware of the development of atrial fibrillation in newly hypertensive patients [ 10 ]. The second, from Chichareon et al. in Thailand, showed that in 3172 patients with atrial fibrillation, the higher the blood pressure variability, the higher the risk of stroke, cerebral hemorrhage, and death [ 11 ].
In short, this month’s Special Issue - Asian Studies is a reminder of the dangers of hypertension and the need for meticulous hypertension care.
Takase M, Nakaya N, Tanno K, Kogure M, Hatanaka R, Nakaya K, et al. Relationship between traditional risk factors for hypertension and systolic blood pressure in the Tohoku Medical Megabank Community-based Cohort. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01582-1 .
Aida J, Inoue Y, Tabuchi T, Kondo N. Modifiable risk factors of inequalities in hypertension: Analysis of 100 million health checkups recipients. Hypertens Res. 2024. https://doi.org/10.1038/s41440-024-01615-9 .
Rajeev Gupta R, Gaur K, Ahuja S, Anjana RM. Recent Studies on Hypertension Prevalence and Control in India 2023. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01585-y .
Mori Y, Mizuno A, Fukuma S. Low on-treatment blood pressure and cardiovascular events in patients without elevated risk: A nationwide cohort study. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01593-y .
Inoue M, Sakata S, Arima H, Yamato I, Oishi E, Ibaraki A, et al. Sleep-related breathing disorder in a Japanese occupational population and its association with hypertension - Stratified analysis by obesity status. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01612-y .
Ushida T, Tano S, Imai K, Matsuo S, Kajiyama H, Kotani T. Postpartum and interpregnancy care of women with a history of hypertensive disorders of pregnancy. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01641-7 .
Yan J, Wu B, Lu B, Zhu Z, Di N, Yang C, et al. Association between baseline office blood pressure level and the incidence and development of long-term frailty in the community-dwelling very elderly with hypertension. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01613-x .
An L, Wang Y, Liu L, Miao C, Zu L, Wang G, et al. High serum uric acid is a risk factor for arterial stiffness in a Chinese hypertensive population: A cohort study. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01591-0 .
Ding C, Li J, Wei Y, Fan W, Cao T, Chen Z, et al. Associations of total homocysteine and kidney function with all-cause and cause-specific mortality in hypertensive patients: a mediation and joint analysis. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01614-w .
Zhang W, Chen Y, Hu LX, Xia JH, Ye XF, Cheng YB, et al. New-onset hypertension as a contributing factor to the incidence of atrial fibrillation in the elderly. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01617-7 .
Chichareon P, Methavigul K, Lip GYH, Krittayaphong R. Systolic blood pressure visit-to-visit variability and outcomes in Asians patients with atrial fibrillation. Hypertens Res. 2024 https://doi.org/10.1038/s41440-024-01592-z .
Download references
Author information
Authors and affiliations.
Department of Pharmacology, Ehime University Graduate School of Medicine, Toon, Japan
Masaki Mogi
Division of Cardiovascular Medicine, Jichi Medical University School of Medicine, Shimotsuke, Japan
Satoshi Hoshide & Kazuomi Kario
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Masaki Mogi .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mogi, M., Hoshide, S. & Kario, K. Consider hypertension risk factors once again. Hypertens Res 47 , 1443–1444 (2024). https://doi.org/10.1038/s41440-024-01680-0
Download citation
Received : 21 March 2024
Accepted : 26 March 2024
Published : 05 June 2024
Issue Date : June 2024
DOI : https://doi.org/10.1038/s41440-024-01680-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Risk factors
- Atrial fibrillation
- Hypertensive disorders of pregnancy
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies


Essay on Hypertension
Students are often asked to write an essay on Hypertension in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Hypertension
What is hypertension.
Hypertension is when blood pushes too hard against the walls of your blood vessels. Imagine a garden hose with too much water pressure; it’s similar for your blood vessels. It’s often called high blood pressure and is a common health issue.
Causes of High Blood Pressure
High blood pressure can come from eating too much salt, not exercising, stress, or family history. Sometimes, it happens for no clear reason. It’s important to eat healthy and stay active to prevent it.
Why It’s Serious
If not treated, hypertension can hurt important organs like the heart and kidneys. It can lead to heart attacks, strokes, and other health problems. That’s why checking your blood pressure regularly is crucial.
Treatment and Control
Doctors usually suggest changes in diet and exercise to manage high blood pressure. In some cases, medicine is also needed. Eating less salt, more fruits and vegetables, and regular physical activity can help control it.
250 Words Essay on Hypertension
Hypertension is another name for high blood pressure. It’s a health problem where the force of your blood against your artery walls is too high. Imagine a garden hose with too much water pressure; it’s similar with blood in your body’s pipes.
Causes of Hypertension
Many things can make your blood pressure go up. Eating too much salt, not exercising, being overweight, and stress are common causes. Sometimes, it runs in families, so your parents might have it too.
Why Hypertension is Bad
High blood pressure is sneaky because you can’t feel it, but it can hurt your body. It can make your heart work too hard and weaken your blood vessels. Over time, this can lead to heart problems and strokes, which are very serious.
How to Know If You Have It
Doctors can check your blood pressure with a cuff that squeezes your arm. It’s quick and doesn’t hurt. Numbers tell if your pressure is normal, a bit high, or too high. Regular checks are important.
Keeping Blood Pressure Normal
To keep your blood pressure in check, eat healthy foods like fruits and veggies, stay active, and keep a healthy weight. If your doctor says so, you might need medicine too. Remember, taking care of your blood pressure is taking care of your heart.
500 Words Essay on Hypertension
What is hypertension.
Hypertension is the medical term for high blood pressure. Imagine the water pipes in your house. When the water pressure is too high, pipes can get damaged. Similarly, when blood moves through your body with too much force, it can harm your blood vessels and organs.
There are often no clear causes of hypertension, but many things can play a role. Eating a lot of salty foods, not exercising enough, being overweight, and smoking can increase your risk. Also, if your family members have high blood pressure, you might be more likely to have it too.
Why Is High Blood Pressure Bad?
If your blood pressure is high for too long, it can cause problems. It can make your heart work too hard and become weak. It can also damage your blood vessels, making it hard for blood to reach important parts of your body. This can lead to heart attacks, strokes, or kidney problems.
How Do You Know You Have It?
High blood pressure doesn’t usually make you feel sick, so many people don’t know they have it. That’s why it’s called a “silent killer.” The only way to know for sure is to get your blood pressure checked by a doctor or nurse.
How to Control Hypertension
If you have high blood pressure, your doctor might give you medicine to help control it. But there are also things you can do on your own. Eating healthy foods, staying at a good weight, exercising, and not smoking can all help lower your blood pressure. Cutting back on salt is especially important because salt makes your body hold on to water, which raises blood pressure.
Living with High Blood Pressure
People with high blood pressure can live normal, healthy lives if they take care of themselves. It’s important to follow your doctor’s advice, take your medicine, and make good choices like eating right and staying active. Checking your blood pressure at home and writing down the numbers can help you and your doctor know how well your treatment is working.
Hypertension, or high blood pressure, is a health issue that can lead to serious problems if not managed. It’s often caused by things we can change, like our diet or how much we exercise. By getting regular check-ups, eating well, staying active, and following your doctor’s advice, you can control your blood pressure and live a healthy life. Remember, even though high blood pressure can be dangerous, taking the right steps can help you keep it in check.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Non Communicable Diseases
- Essay on Gambling Addiction
- Essay on No Smoking
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.


ESSAY SAUCE
FOR STUDENTS : ALL THE INGREDIENTS OF A GOOD ESSAY
Essay: Hypertension
Essay details and download:.
- Subject area(s): Health essays
- Reading time: 15 minutes
- Price: Free download
- Published: 5 November 2016*
- File format: Text
- Words: 4,397 (approx)
- Number of pages: 18 (approx)
Text preview of this essay:
This page of the essay has 4,397 words. Download the full version above.
Introduction Hypertension is a multifactor disease characterized by chronic elevation in blood pressure to levels equal to or above 140 mmHg systolic blood pressure (SBP) and above 90 mmHg of diastolic blood pressure (DBP). Considered a worldwide epidemic disease, hypertension is the main risk factor for cardiovascular disease, being epidemiologically closely associated with metabolic diseases such as obesity and diabetes. Hypertension is the main risk factor for cardiovascular diseases, which include stroke, coronary artery disease (CAD), and heart failure (HF) leading to ∼1.8 million deaths worldwide every year, cardiovascular disease leads to ∼17 millions of death per year, and, from this total, it is reported that high blood pressure is estimated to cause more than half of these deaths (over 9 million deaths every year), making it also the main risk factor in the global disease burden. Aging is a major risk factor for developing hypertension. The prevalence of the disease increases with age, with a higher rate in men than women. People who don’t have hypertension at age 55 have 90% chance of developing it later in life. The goal of hypertension treatment is to prevent death and complication by achieving and maintaining the blood pressure at 140/90 mm Hg or lower. Life style modification is the first line of intervention for all patients with hypertension, but pharmacological is the cornerstone for the disease treatment to reduce the high blood pressure and prevent complications such as cardiovascular and renal morbidity and mortality. For many years the right ventricle was grossly undervalued and considered to function mainly as a conduit, while its contractile performance was considered haemodynamically unimportant. Since the early 1950s, however, the relevance of the chamber in the maintenance of normal cardiac physiology was recognized in several cardiovascular disorders. Tricuspid annular plane systolic excursion (TAPSE) has been proposed as a simple and reproducible parameter for quantitative assessment of RV ejection fraction. It provides a simple method for global RV functional assessment and is a strong predictor of prognosis in heart failure. Although the right ventricle can now be imaged and studied in several ways, two-dimensional (2D) guided M-mode echocardiography is an attractive tool due to its simplicity. Studies on RV function among patients with hypertensive heart disease (HHD) are rather few and have focused mainly on the diastolic function of the chamber. Aim of Work This study is aiming to assess the systolic function of the right ventricle in patients with systemic hypertension using tricuspid annular plane systolic excursion (TAPSE). Chapter (1) Systemic Hypertension • Definition of Hypertension The cut-off mark for the definition of hypertension has evolved over time. Hypertension is defined as a systolic blood pressure (SBP) of 140 mm Hg or more, or a diastolic blood pressure (DBP) of 90 mm Hg or more, or taking antihypertensive medication. • Classification of hypertension Hypertension has been classified according to 2013 ESH/ESC guidelines, as shown in Table 1. • Prevalence of Hypertension Hypertension is one of the most significant risk factors for cardiovascular diseases and cerebro-vascular, which ranks as the first and third most frequent causes of death in elderly population all over the world. Blood pressure is a complex genetic trait with heritability estimates of 30–50%, but the intrinsic origin of essential hypertension remains obscure although many environmental factors are known. Available data on the prevalence of hypertension and the temporal trends of BP values are limited comparable data. Overall the prevalence of hypertension appears to be around 30–45% of the general population, with a steep increase with ageing, also a noticeable difference appear to be in the average BP levels across countries, with no systematic trends towards BP changes in the past decade. Stroke mortality is a good candidate, because hypertension is by far the most important cause of this event. A close relationship between prevalence of hypertension and mortality for stroke has been reported. • Path-physiology of hypertension The path-physiology of hypertension is an area of active research, attempting to explain causes of hypertension, which is a chronic disease characterized by elevation of blood pressure. Hypertension can be classified as either essential or secondary. Essential hypertension indicates that no specific medical cause can be found to explain a patient’s condition. About 90-95% of hypertension is essential hypertension. Secondary hypertension indicates that high blood pressure is a result of another underlying condition, such as kidney disease or tumors (adrenal-adenoma or pheochromocytoma). Persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure and arterial aneurysm, and is a leading cause of chronic renal failure. Most mechanisms leading to secondary hypertension are well understood. The path-physiology of essential hypertension remains an area of active research, with many theories and different links to many factors. Cardiac and peripheral resistance are the two determinants of arterial pressure. Hence, for understanding the pathogenesis and treatment of hypertensive disorders, it is useful to understand factors involved in the regulation of normal and elevated arterial blood pressure. Cardiac output (CO) and peripheral vascular resistance (PVR) are the two determinants of arterial blood pressure (ABP), ABP = CO X PVR. Cardiac output is the volume of the blood pumped by the heart in a specific period of time (usually 1 minute), while peripheral vascular resistance is the force in the blood vessels that the left ventricle must overcome to eject blood from the heart. Resistance of blood flow is determined primarily by the diameter of blood vessels and blood viscosity. Increased peripheral vascular resistance results from a narrowing of the arteries and arterioles or and increased in fluid volume in the blood vessels that results from sodium and water retention. Increased peripheral vascular resistance is the most prominent characteristic of hypertension. The aging process is associated with multiple structural and functional alterations in cardiovascular system that can influence blood pressure regulation. Arterial stiffness, especially in the large arteries, is the pathological characteristic that best exemplifies geriatric hypertension. Histological, the changes are apparent in the vascular sub endothelial and media layers, which thickness of the arteries due to the accumulation of collagenous fibers, calcium deposition, and loss of elastic fibers, resulting in narrowing and increased stiffness of blood vessels. It is directly leads to increase in peripheral vascular resistance, a path gnomic characteristic of hypertension in the elderly population. Moreover, with increasing the age, blood vessels also become less responsive to B- adrenergic stimulation, which is necessary for vasodilatation. On the other hand, alpha- adrenergic responsiveness remains unchanged. These changes also contribute to increase peripheral vascular resistance and lead to hypertension. Beyond this structural change in the arteries, the regulation of vascular resistance is also affected by age related changes in the autonomic nervous system. There is an age associated decline in the sensitivity of the arterial baroreceptor. This effects the regulation of vascular resistance in two important ways. First, a larger change in blood pressure is required to stimulate the baroreceptor to invoke the appropriate compensatory response in heart rate. This also contributes to the age related increase in blood pressure variability. Second, the decrease in baroreceptor sensitivity leads to relatively greater activation of sympathetic nervous system outflow for a given level of blood pressure. An age associated increase in sympathetic nervous system activity has been demonstrated by higher plasma epinephrine and nor epinephrine levels. These hormones called catecholamine are vasoconstrictors which they cause the blood pressure to constrict making the diameter smaller. By constricting blood vessels, nor-epinephrine increases peripheral vascular resistance and raises blood pressure. Epinephrine constricts blood vessels and increases the force of cardiac contraction, causing blood pressure to rise. Regulation of peripheral vascular resistance by the vascular endothelium is also changed in relation to age. the cell of which become smaller and less uniformly aligned, this change may result in decrease production of endogenous vasodilating substances (e.g., Nitric Oxide ) and decline in local control of vascular tone. Impaired nitric oxide – mediated vasodilatation is a potential contributor to the age related increase in peripheral vascular resistance. Age related changes in renal function, particularly in renal regulation of sodium balance may also contribute to an increase in blood pressure. Decreased renal blood flow and glomelular filtration rate impair the aging kidney’s ability to excrete a sodium load. These renal changes in the regulation of sodium balance create a tendency for sodium retention. This likely plays a part in the finding that a high proportion of older hypertensive individuals, perhaps as high as two thirds, are characterized as having salt sensitivity. Slat sensitivity is operationally defined as an increase in mean arterial blood pressure, commonly 5 mmHg or more, during a high compared to a low dietary sodium intake. Additionally, aging also alter the Rennin – Angiotensin – Aldosterone – System (RAAS). This affects blood pressure through control of angiotensin II, which has been found to be responsible for sodium and volume retention, vasoconstriction, sympathetic activation, cell growth and proliferation, and possibility atherogenesis. With age, plasma rennin levels decline, and rennin response to sodium depletion, diuretic administration, and upright posture declines as well. • Risk factors for hypertension In most cases, the underlying causes of hypertension remain unknown. These risk factors can be classified as modifiable and non modifiable. Modifiable determinants include factors that can be altered, such as individual and community influences, living and working condition, and socio – cultural factors. On the other hand, non modifiable determinants include those factors that are beyond the control of the individual. A- Non modifiable risk factors: Non modifiable risk factors are inherited characteristics in a particular individual that cannot be changed such as age, sex, race or ethnicity, and heredity. i. Age Age is the most powerful risk factor for developing hypertension. The worldwide increase in the elderly population (age ≤65 years) is associated with concurrent increases in the prevalence of systemic hypertension and morbidity and mortality from vascular complications of hypertensive disease. Cardiovascular disease becomes increasingly common with advancing age. As a person gets older, the heart undergoes subtle physiologic changes, even in the absence of disease. The heart muscle of the aged heart may relax less completely between beats, and as a result, the pumping chambers become stiffer and may work less efficiently. The combination of changes probably reflects stiffening of the blood vessels (reduced arterial compliance) and leads to a large increase in pulse pressure with aging. Age related hypertension appears to be predominantly systolic rather than diastolic. Both systolic blood pressure and diastolic blood pressure increase with age. Systolic blood pressure rises progressively until the age of 70 or 80 years, whereas diastolic blood pressure increases until the age 50 or 60 years and tends to level off or even decline slightly. ii. Sex The overall incidence of hypertension is higher in men than in women until the age 55 years. After that, women’s risk for hypertension increases sharply. The National Health and Nutrition Examination Survey (NHANES) in USA (2003) showed that, the prevalence of hypertension was higher in women than in men aged 70 years old and above. iii. Heredity Family history of hypertension among first degree relatives (e.g. parents, siblings, and off-spring) is considered a risk factor for developing hypertension. First degree relatives of patients with hypertension have two fold greater risk of hypertension , and the risk increases to four fold when more family member are hypertensive. A family history of hypertension at an early age increases the risk. iv. Race or Ethnicity Prevalence of hypertension is twice as high in African American as in whites. The reason for the increased prevalence of hypertension among blacks is unclear, but the increase has been attributed to lower rennin levels, greater sensitivity to vasopressin, higher salt intake, and greater environmental stress. B. Modifiable risk factors: Modifiable risk factors could be controlled through life style modification or by medical intervention. These risk factors include diabetes mellitus, elevated serum lipids, sleep apnea, and unhealthy lifestyle as physical inactivity, consumption of unhealthy diet, obesity, smoking, excessive alcohol or caffeine intake, and poor stress management. i. Diabetes mellitus Patients with diabetes have 1.5 to 2 time increased risk of having hypertension. WHO reported that, about 60 to 65% of people with diabetes have high blood pressure. Diabetes mellitus accelerates atherosclerosis via numerous metabolic events: chronic hyperglycemia, insulin resistance, and dyslipidemia, which alter the function of multiple cell types, including endothelium, smooth muscle cells, and platelets leading to build up of atheroma in the arterial wall. Insulin resistance is a cardinal defect in type II diabetes in elderly. Insulin resistance and hyper-insulinemia are associated with hypertension. The mechanism of developing hypertension in elderly with insulin resistance may be due to increase the activity of sympathetic nervous system leading to increases in cardiac output and peripheral vascular resistance. Recent evidence suggests that glycemic control may decrease the hypertension risk. Keeping sugar well controlled minimize potential damage to blood vessels, offering strong protection against the development of high blood pressure. ii. Elevated serum lipids Raised blood cholesterol increases the risk of heart disease and stroke. Elevated levels of serum lipids (cholesterol and triglycerides are extremely common and are one of the most important risk factors that can be changed. Lowering raised blood cholesterol reduces the risk of heart disease. The prevalence of raised total cholesterol noticeably increases according to the income level of the country. In low-income countries, around 25 percent of adults have raised total cholesterol, while in high-income countries; over 50 per cent of adults have raised total cholesterol. The major lipid particles, cholesterol and triglycerides, both have important functions in the body. Cholesterol is an essential component of the cell membranes functioning to provide stability while permitting membrane transport. It is a precursor to adrenal steroids, sex hormones, bile and bile acids. Triglycerides are the major source of energy for the body. Both cholesterol and triglycerides are in soluble molecules and are transported in the circulation as lipoproteins. Normal serum cholesterol level is below 200mg/dl. When there is too much cholesterol in the body because of diet and the rate at which the cholesterol is processed, it is slowly build up in the inner lining of the arteries. This can lead to narrowing of the arteries and build up atherosclerosis. Most cholesterol in the blood is carried in two kinds of a protein called (lipoproteins): low-density lipoprotein (LDL), and high density lipoprotein (HDL). Low-density lipoprotein cholesterol, which is “bad” cholesterol causing the build-up of plaque. The optimal level of LDL cholesterol is less than 100 mg/dl. High-density lipoprotein cholesterol is the “good” cholesterol because it tends to carry excess cholesterol back to the liver where it is removed from the body. The HDL level of 60 mg/dl and above is considered protective against cardiovascular disease (CVD). People with a low level of HDL cholesterol (less than 40 mg/dl) have a higher risk of cardiovascular disease. Triglycerides are the most common type of fat in the body. The normal triglycerides level is less than 150 mg/dl. Many people who have CVD or DM have high triglycerides level combined with low HDL cholesterol or high LDL cholesterol seems to speed up atherosclerosis. Epidemiological study conducted in Japan (2004) has shown that, the level of total cholesterol in the blood is a strong predictor of elevated blood pressure. Other studies confirmed that the relation between the incidence of hypertension and high plasma cholesterol levels is gradually attenuated after the age of 65 years. Decreasing fat content in the diet is the first step in reducing cholesterol levels. Several clinical trials have shown the efficiency of lipid lowering agent as statins for reducing cardiovascular risk in patients with elevated serum lipid. iii. Sleep apnea Obstructive sleep apnea (OSA) is the most common category of sleep-disordered breathing. The term “sleep-disordered breathing” is commonly used in the U.S. to describe the full range of breathing problems during sleep in which not enough air reaches the lungs (hypopnea and apnea). Hypertension occurs in more than 50% of individuals with obstructive sleep apnea. Approximately 70% of patients with obstructive sleep apnea are obese. Hypertension related to (OSA) should also be considered in patients with drug–resistant hypertension and in patients with a history of snoring. Despite extensive research, the underlying mechanisms of obstructive sleep apnea induced hypertension are not entirely understood. Evidence indicates that sympathetic activation plays a central role on OSA–induced hypertension. iv. Lifestyle factors Lifestyle changes are important for preventing and treating high blood pressure. Healthy changes include maintaining a normal weight, exercising regularly, quitting smoking, limiting alcohol consumption to no more than one or two drinks a day, reducing sodium (salt) intake, and increasing potassium intake. • Lifestyle factors include: A) Physical inactivity: Lack of physical activity increases the risk of blood vessel disease, heart disease, and stroke. It also makes it easier to put on unwanted pounds. In addition, when you are out of shape, it takes more effort for your heart to pump blood. This increases the force exerted on arteries, which can lead to high blood pressure. Regular exercise and increasing amount of physical activity have been shown to favorably affect positively on blood pressure in people with hypertension, independent of changes in body weight and also prevent hypertension in normo-tensive individuals. An epidemiological study in USA illustrates that regular exercise and physical activity can attenuate systolic and diastolic blood pressure by 11 and 8 mmHg respectively. B) Unhealthy diet: A diet that’s high in calories, fats and sugars and low in essential nutrients contributes directly to poor health as well as to obesity. In addition, there are some problems that can happen from eating too much salt. Some people are “salt sensitive,” meaning a high-salt (sodium) diet raises their high blood pressure. Salt keeps excess fluid in the body that can add to the burden on the heart. While too much salt can be dangerous, healthy food choices can actually lower blood pressure. High dietary sodium intake is associated with an increased incidence of hypertension. At least 40% of elders who eventually develop hypertension are salt sensitive and the excess salt may be the precipitating cause of hypertension in these individuals. Decrease intake of fresh fruits and vegetables has been proposed to be a vascular risk factor. Most of this food are antioxidants and protect the arterial intima from oxidative damage. Diet low in potassium is associated with an increased risk of hypertension. Some clinical trials suggest that increasing dietary potassium by approximately (54 mmol) per day can reduce systolic blood pressure by 2-3 mmHg in hypertensive patients. C) Obesity: The prevalence of obesity is increasing drastically in the recent decade and it has become particularly high in the elderly population. The prevalence of overweight and obesity is commonly assessed by using body mass index (BMI), defined as the weight in kilograms divided by the square of the height in meters (kg/m2). A BMI ≤ 25 kg/m2 is defined as overweight and a BMI ≤ 30 kg/m2 as obese. In the elderly, obesity has been associated not only with increased mortality, but also with elevated risks of hypertension and other CVD. Anyone who is overweight has a risk for developing hypertension 50% more than people with normal weight. D) Smoking: Cigarette smoking is a major risk factor for high blood pressure. Cigarette smokers have twice the chance of developing hypertension and four times the chance of sudden death compared with non smokers. Smoking is one of the leading causes of preventable death in the United States, and it increases the risk of having a heart attack or stroke. With each cigarette you smoke, blood pressure also shoots up by as much as 10 points and stays higher for up to an hour. If you constantly have a cigarette in your hand, that could keep your blood pressure elevated for much of the day. High amounts of secondhand smoke, environmental smoke, and passive smoking can also contribute to high blood pressure; it is best to avoid cigarette smoke as much as possible. The mechanism of hypertension risk associated with smoking is complex. The main mechanism appears to be through the development and progression of atherosclerosis. Cigarette tobacco contains high concentration of oxidants and free radicals (like Nitric oxide), as well as nicotine, a major constituent of cigarettes. These constituents are considered to be absorbed into the systemic circulation, to injure the arterial endothelium and thus promote atherogenesis. Nicotine has been suggested to contribute to atherosclerosis via its effect on changes in the lipid metabolism, endothelial damage and production of growth factors. Smoking also increases insulin resistance enhances sympathetic activity which increases heart rate and blood pressure. E) Alcohol consumption: Heavy and regular use of alcohol can increase blood pressure dramatically. It can also cause heart failure, lead to stroke and produce irregular heartbeats. Too much alcohol can contribute to high triglycerides, cancer and other diseases, obesity, alcoholism, suicide and accidents. The effect of alcohol appears to be depending on the amount consumed. Reducing alcohol gradually in hypertensive patients can lower blood pressure by average of 13 mmHg systole and 15 mmHg diastole. However, the abrupt cessation of alcohol intake in individuals consuming great amounts resulted in a rapid increase in their blood pressure. F) Caffeine consumption: Caffeine can cause a short-lived but dramatic rise in blood pressure. The amount of caffeine in two to three cups of coffee can raise systolic pressure 3 to 14 millimeters of mercury (mm Hg). Diastolic pressure can be increased 4 to 13 mm Hg. However, this transient rise in blood pressure due to caffeine has not been shown to increase risk of hypertension. Caffeine actually increases blood pressure, but the association between habitual consumption of caffeinated beverages and incidence of hypertension is uncertain. However, a recent longitudinal study found a positive association between caffeine consumption and blood pressure. G) Poor stress management: Severe stress can lead to a temporary but dramatic spike in blood pressure. Over time, this might contribute to high blood pressure, although that has never been conclusively proved. In addition, some people cope with stress by overeating, drinking too much, or smoking. A study carried out in Brazil shows that people exposed to high levels of repeated psychological stress develop hypertension to a greater extent than those who do not experience as much stress. Left Ventricular hypertrophy in Hypertension Left ventricular hypertrophy (LVH) is defined as an increase in the mass of the left ventricle, which can be secondary to an increase in wall thickness, an increase in cavity size, or both. LVH as a consequence of hypertension usually presents with an increase in wall thickness, with or without an increase in cavity size. This increase in mass predominantly results from a chronic increase in afterload of the LV caused by the hypertension, although there is also a genetic component. A significant increase in the number and /or size of sarcomeres within each myocardial cell is the pathologic mechanism. Left ventricular wall thickness and/or mass is the best studied marker of hypertensive heart disease. Increased left ventricular wall thickness and mass have continuously been found to be associated with the level of blood pressure and age. However, without increased systolic blood pressure, clinically significant increases in left ventricular mass do not occur with advancing age. Chronic systolic hypertension therefore seems to be the principal cause of left ventricular hypertrophy . LVH serves as an integrated surrogate for cumulated blood pressure load and is best described as being proportional to the area under the lifetime BP curve. This is also supported by the fact that there is a strong association of left ventricular mass and mean 24-hour ambulatory blood pressure. The increase of LV mass with age might reflect the influence that other risk factors exert with time on the development of LVH. The relationship between echocardiographic LV mass and clinical blood pressure is usually weak. Twenty-four-hour blood pressure recordings have shown a much closer correlation between LV mass and average daily blood pressure. Non-haemodynamic factors, such as age, sex, race, body mass index, diabetes, and dietary salt intake, may contribute to determine who among hypertensive patients develop LVH and to what degree LVM is increased. In fact, the coexistence of hypertension with diabetes increases the prevalence of LVH. Moreover, insulin resistance and high insulin levels are associated with the development of LVH in hypertensive patients. Other major cardio-metabolic risk factors, notably hyper-cholesterolaemia and hyper-glycaemia, may also modify the extent of LVM and the prevalence of LVH in the hypertensive population. Genetic factors might also exert a powerful modulation of LV mass; in fact monozygotic twins have more similar LV mass values then di-zygotic twins. • Pathogenesis of Left Ventricular Hypertrophy: Two major triggers for LVH are biomechanical stress and neuro –hormonal factors. LVH is mainly due to pressure or volume overload on the heart. Common causes of pressure overload are systemic hypertension, aortic stenosis, coarctation of the aorta and hypertrophic cardiomyopathy. It is thought that a mechanical signal initiates a cascade of biological events which lead to coordinated cardiac growth. There is then an increased myosin heavy chain synthesis (by about 35%) within hours of pressure overload. This increase is initially predicted by an increase in translational efficiency. Neurohormonal factors that have been implicated in left ventricular hypertrophy include: Angiotensin II, endothelin, calcineurin, metallo proteinases and heterometrimeric G. Angiotensin II – It has been postulated that angiotensin II, via the AT1 receptor, plays a key role in the induction of hypertrophy because it can directly induce the molecular events of early cardiac growth. Cardiac rennin-angiotensin system has been proposed as an important determinant of hypertrophic response. The importance of angiotensin II in the development of LVH in hypertensive subjects is also suggested indirectly by the observation that an ACE inhibitor causes regression of left ventricular hypertrophy, more than other antihypertensive drugs. Endothelin – Some animal studies suggest that endothelin plays a role in the development of left ventricular wall hypertrophy in response to elevated blood pressure. Calcineurin – Calcineurin is a calcium calmodulin–dependent phosphatase. It serves as a master switch for clinical hypertrophy. In animal studies, that transgenic mice that over-express components of the calcineurin signaling pathway, develop a hypertrophic phenotype that can be expressed by pharmacological inhibitors of calcineurin. Metalloproteinase (MMPs) – Matrix metalloproteinase is a family of zinc dependant interstitial enzymes. Their tissue inhibitors (TIMPs) control the breakdown of collagen. The role of MMPs in concentric hypertrophy is not fully understood, but preliminary observations show that they are activated in experimental pressure overload hypertrophy. Studies have also shown that imbalance between MMPs and TIMPs could lead to LVH and diastolic dysfunction. Heterometrimeric G Proteins – Many hormones and neurotransmitters implicated in the initiation and exacerbation of myocardial hypertrophy including angiotensin II and endothelin, bind to cell membrane receptors which couple to a subset of intracellular hetero-metrimeric G proteins – the G (q) class.
...(download the rest of the essay above)
About this essay:
If you use part of this page in your own work, you need to provide a citation, as follows:
Essay Sauce, Hypertension . Available from:<https://www.essaysauce.com/health-essays/hypertension/> [Accessed 05-06-24].
These Health essays have been submitted to us by students in order to help you with your studies.
* This essay may have been previously published on Essay.uk.com at an earlier date.
Essay Categories:
- Accounting essays
- Architecture essays
- Business essays
- Computer science essays
- Criminology essays
- Economics essays
- Education essays
- Engineering essays
- English language essays
- Environmental studies essays
- Essay examples
- Finance essays
- Geography essays
- Health essays
- History essays
- Hospitality and tourism essays
- Human rights essays
- Information technology essays
- International relations
- Leadership essays
- Linguistics essays
- Literature essays
- Management essays
- Marketing essays
- Mathematics essays
- Media essays
- Medicine essays
- Military essays
- Miscellaneous essays
- Music Essays
- Nursing essays
- Philosophy essays
- Photography and arts essays
- Politics essays
- Project management essays
- Psychology essays
- Religious studies and theology essays
- Sample essays
- Science essays
- Social work essays
- Sociology essays
- Sports essays
- Types of essay
- Zoology essays
- Open access
- Published: 01 June 2024
Blood pressure and heart failure: focused on treatment
- Kyeong-Hyeon Chun 1 &
- Seok-Min Kang ORCID: orcid.org/0000-0001-9856-9227 2
Clinical Hypertension volume 30 , Article number: 15 ( 2024 ) Cite this article
146 Accesses
Metrics details
Heart failure (HF) remains a significant global health burden, and hypertension is known to be the primary contributor to its development. Although aggressive hypertension treatment can prevent heart changes in at-risk patients, determining the optimal blood pressure (BP) targets in cases diagnosed with HF is challenging owing to insufficient evidence. Notably, hypertension is more strongly associated with HF with preserved ejection fraction than with HF with reduced ejection fraction. Patients with acute hypertensive HF exhibit sudden symptoms of acute HF, especially those manifested with severely high BP; however, no specific vasodilator therapy has proven beneficial for this type of acute HF. Since the majority of medications used to treat HF contribute to lowering BP, and BP remains one of the most important hemodynamic markers, targeted BP management is very concerned in treatment strategies. However, no concrete guidelines exist, prompting a trend towards optimizing therapies to within tolerable ranges, rather than setting explicit BP goals. This review discusses the connection between BP and HF, explores its pathophysiology through clinical studies, and addresses its clinical significance and treatment targets.
Heart failure (HF) remains a major public health burden, with a rapidly increasing global prevalence. In the United States, more than 5 million people aged ≥20 years are affected by HF [ 1 ], and this number is expected to increase by 46%, resulting in an estimated 8 million Americans with HF in 2030 [ 2 ]. Hypertension is one of the most frequent comorbidities [ 3 ], playing a pivotal role in the development of HF [ 4 ]. In the Framingham Heart Study, hypertension progressed to HF in 91% of patients > 20 years of age, with a doubling and tripling of the risk of HF in male and female hypertensive patients, respectively [ 5 , 6 ]. Chronic hypertension causes functional and structural changes in the heart, culminating in HF and further increasing the rate of mortality and morbidity [ 7 ]. Intensive treatment of hypertension can prevent and reverse myocardial changes in patients at risk of HF; however, defining optimal blood pressure (BP) targets for patients who have already developed HF is challenging owing to a lack of evidence.
Currently, HF is classified depending on the left ventricular ejection fraction (LVEF), with LVEF ≤40% defined as HF with reduced ejection fraction (HFrEF) and LVEF ≥50% as HF with preserved ejection fraction (HFpEF) [ 8 ]. In addition, if the LVEF is between 41 and 49%, the definition of HF with mildly reduced ejection fraction (HFmrEF) is commonly used in a dynamic trajectory to denote improvement from or deterioration to HFrEF [ 9 ]. HFmrEF occupies a spectrum between HFrEF and HFpEF, exhibiting the characteristics of both. However, this classification system is often ambiguous [ 10 ]. In the present review, rather than focusing on this detailed classification of LVEF, we focus on the classical phenotypes of HFrEF and HFpEF (implicitly including the concept of HFmrEF) and their association with BP from a more comprehensive perspective.
Development of hypertensive heart disease and HF
Traditionally, the development and progression of HF in hypertensive patients has been classified into four stages: (1) isolated left ventricular (LV) diastolic dysfunction without LV hypertrophy; (2) LV diastolic dysfunction with concentric LV hypertrophy; (3) clinical HFpEF accompanied by pulmonary edema; and (4) dilated cardiac chambers with HFrEF [ 6 ]. These stages suggest that diastolic dysfunction is an early phenomenon, and hypertension-induced LV hypertrophy leads to remodeling of the left atrium and ventricle, ultimately resulting in advanced diastolic and systolic dysfunction.
As reviewed in the article by Messerli et al. [ 6 ], hypertensive heart disease plays a pivotal role in the pathophysiology of HF through a sequential and intricate process. Initially, the LV responds to elevated BP by adapting to the hemodynamic wall stress, which results in pressure overload. This adaptation involves the thickening of the LV wall and an increase in LV mass, resulting in concentric LV hypertrophy. During this phase, the initial manifestation of cardiac dysfunction is LV diastolic dysfunction. With a persistent pressure overload, diastolic dysfunction progresses, ultimately leading to the onset of HFpEF. In the advanced stages of hypertensive heart disease, typically due to prolonged exposure to pressure overload with or without concurrent myocardial ischemia, the condition evolves into a dilated LV dimension. The final stage is characterized by reduced LVEF and development of HFrEF.
However, HFrEF and HFpEF should be considered from a slightly different perspective than that presented by Messerli et al. [ 6 ]. If HFrEF and HFpEF are considered part of a unified disease spectrum, they may be expected to respond similarly to HF treatment. However, numerous medications that have demonstrated clear improvements in HFrEF have not shown comparable beneficial effects on HFpEF [ 11 ]. Angiotensin receptor blockers (ARBs) [ 12 ], angiotensin-converting enzyme inhibitors (ACEis) [ 13 ], β-blockers [ 14 , 15 ], and mineralocorticoid receptor antagonists (MRAs) [ 16 ], all of which are also used as antihypertensive drugs, have failed to show clinically significant prognostic improvements in HFpEF, unlike in HFrEF. These differences were also evident in epidemiological studies. For example, a Japanese chronic HF registry-based study showed that most patients with HFpEF and nearly half of those with HFrEF remained in their respective categories throughout a 3-year follow-up period [ 10 ]. A study consisting of 3480 consecutive Japanese patients with HF showed that HFpEF transitioned to HFrEF in only 4% of them after 3 years, whereas HFrEF at registration transitioned to HFpEF and HFmrEF in 26 and 21% of patients, respectively, at 3 years, suggesting reverse remodeling after treatment [ 10 ]. These findings further support the idea that HFpEF and HFrEF are distinct syndromes with fundamental pathophysiological differences and etiologies. Similarly, in another long-term longitudinal study of ambulatory HFpEF patients, LVEF remained ≥50% in most patients with HFpEF for 11 years, and only 1.6% of patients evolved to LVEF < 50% [ 17 ]. Therefore, approaching HFrEF and HFpEF differently when examining their associations with hypertension is imperative.
Association between hypertension and HF
Hypertension is widely recognized as one of the most important risk factors of HFpEF [ 18 ]. Increased LV filling pressure and chronic myocardial remodeling due to hypertension are considered the primary mechanisms leading to the development of HFpEF [ 19 ]. Elevated systolic BP (SBP) is notably observed in patients with HFpEF, with a 3% rise in the likelihood of prevalent HFpEF for every 1 mmHg increase in SBP > 120 mmHg in an acute HF setting [ 20 ].
In terms of HFrEF, the association manifests distinctively. According to the European Society of Cardiology Heart Failure Long-Term Registry, the largest pan-European cohort of patients with real-world chronic HF in the full spectrum of LVEF, HFrEF accounts for approximately 60% of all patients in the registry [ 21 ]. This registry data showed that mean SBP tends to be lower in HFrEF than in other categories, with 121.6 ± 20.8 mmHg in HFrEF, 126.5 ± 21.1 mmHg in HFmrEF, and 130.9 ± 21.4 mmHg in HFpEF. The use of antihypertensive therapy differed notably between the HFrEF and HFpEF groups, with 56% for HFrEF and 67% for HFpEF. Regarding the underlying etiology of HF, nearly half of HFrEF cases (49%) occur due to ischemic heart disease, approximately one-third (35%) is caused by idiopathic dilated cardiomyopathy, and only 4.5% is due to hypertension itself. In contrast, HFpEF has a different etiology, with 18% of cases occurring due to hypertension, approximately a quarter due to ischemic heart disease, and 12% due to idiopathic dilated cardiomyopathy.
An analysis of the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry based on the United States population mirrors these distinctions [ 14 ]. The etiology of HF was ischemic in a higher percentage of patients with HFrEF than in those with HFpEF (54% vs. 38%, P < 0.0001), whereas the hypertensive etiology was more common in patients with HFpEF than in those with HFrEF (28% vs. 17%, P < 0.0001). Interestingly, when further stratified by LVEF, a hypertensive etiology was significantly predominant in HFpEF (LVEF, > 50%) than in HFmrEF (LVEF, 41–49%) at a rate of 31% versus 22% ( P < 0.0001). In the Korean Acute Heart Failure (KorAHF) registry, which is a prospective multicenter cohort registry including more than 5600 patients with acute heart failure from 10 tertiary hospitals in the Republic of Korea, the prevalence of hypertension was 62.2%; ischemic etiology accounted for 37.6%, and idiopathic dilated cardiomyopathy comprised 15.3% of the cases [ 22 ], which is in line with the European HF registry. When divided based on LVEF, the prevalence of hypertension was higher in patients with HFpEF (64%) than in those with HFrEF (56%).
These observations suggest that while some variability may be influenced by factors such as race, region, and specific registry characteristics, a stronger association exists between high BP and HFpEF than between high BP and HFrEF in the overall population with HF.
Hypertensive AHF
Acute HF (AHF) is caused by the acute or subacute deterioration of heart function, leading to pulmonary edema and subsequent symptoms such as dyspnea or edema. Given that these symptoms are primarily caused by volume overload, treatment strategies are based on this assumption [ 23 ]. However, a closer look reveals that the aggravating factors of HF are diverse, resulting in distinct phenotypes of AHF that necessitate more specialized treatments. These phenotypes can occur as acute exacerbation of preexisting chronic HF, or as a new onset (de novo) HF. Concerning the relationship between BP and AHF, lowering the ventricular filling pressure plays a crucial role in AHF management, especially when hypertension is concurrently present [ 24 ].
AHF is a complex and multifaceted condition characterized by diverse etiologies, distinct pathophysiological mechanisms, varying risk profiles, and treatment responses [ 25 , 26 ]. This heterogeneity poses significant challenges when conducting randomized controlled trials aimed at comprehensively investigating AHF. In this context, we often encounter a specific form of AHF where “high BP” is clearly the cause or is strongly suspected of contributing to the pathogenesis, which is commonly referred to as “hypertensive acute heart failure (H-AHF)”. This clinical phenomenon is characterized by a dramatic improvement in clinical signs and symptoms by BP-lowering treatment, which is also the goal of treatment. In previous studies, the H-AHF has often been defined by the following two features [ 23 , 24 , 27 , 28 ]: (1) SBP ≥ 140 mmHg and (2) acute cardiogenic pulmonary edema, often with rapid onset.
Within the spectrum of AHF, approximately half of the patients may exhibit an SBP > 140 mmHg [ 29 , 30 , 31 ], although not all cases are categorized as H-AHF. H-AHF is particularly characterized by the sudden onset of symptoms, notably pulmonary edema, which distinguishes it from other forms of AHF [ 23 , 28 ]. A more obvious characteristic of H-AHF is the presence of severely elevated BP (≥160–180 mmHg), with pulmonary edema developing in a matter of hours, and no other cause of AHF except hypertension [ 24 , 31 ]. However, because of this vague definition and characterization, there is a large variation in prevalence between the registries; this phenotype is reported as 4% in the KorAHF registry [ 22 ] and approximately 11% in the European or US HF registries [ 21 , 30 , 31 ]. In particular, for HFrEF, hypertensive etiology is reported as 4.5% in the European registry [ 21 ] and 2.9% in the KorAHF registry [ 22 ]. This difference is thought to be due to demographic variations and ambiguity in the definition of diagnosis.
Several studies have investigated the association between symptom duration and the clinical features of patients with H-AHF. One study examined whether dyspnea occurred in ≤7 or > 7 days, and found that the latter was associated with higher in-hospital worsening of HF and 1-year cardiovascular mortality and less improvement in symptoms within 48 hours [ 32 ] . In the group with onset ≤7 days, SBP was significantly higher (138 mmHg vs. 121 mmHg) and moderate-to-severe pulmonary edema was more frequent (33% vs. 8%) compared to cases with onset > 7 days. Although these findings do not precisely delineate the threshold for a “rapid” onset indicative of H-AHF pathophysiology, they do provide knowledge regarding the phenotype. In other words, H-AHF may manifest as the most severe form of AHF with high BP; however, it also exhibits a relatively favorable prognosis [ 24 , 32 , 33 , 34 , 35 , 36 ]. This is supported by studies showing that among patients with AHF presenting to the emergency department, high BP is often a predictor of low risk [ 27 , 34 , 35 , 36 ].
A recent post hoc analysis demonstrated that treatment effectiveness varied with BP [ 37 ]. It has been recommended that SBP should be lowered by ≤25% in H-AHF [ 24 , 27 , 38 ]. Patients treated with vasodilators who achieved an SBP reduction ≤25% within 6 hours of emergency room arrival had a better diuretic response and lower 1-year mortality than those with SBP reduction > 25% [ 39 ]. In this regard, vasodilators are hypothesized to improve outcomes by mitigating end-organ damage in patients with H-AHF, potentially by influencing both preload and/or afterload [ 24 ], and they can generally be used safely in H-AHF and may provide benefits when applied to appropriate patients. Unfortunately, despite numerous randomized clinical trials in this population over the past two decades, no vasodilator has shown any mortality benefit [ 40 ]. This is due to the fact that AHF is a heterogeneous condition with diverse etiologies and pathophysiology, and stratifying and enrolling specific subgroups with predictable treatment responses is challenging. Although there is a lack of evidence from randomized clinical trials, intravenous nitroglycerin, which is still the most familiar vasodilative agent among clinicians, can be administered safely and effectively to improve outcomes in patients with AHF and severely high BP [ 41 ].
Prognostic value of BP in HF
We recognize that there is no alternative to BP measurement as a source of clinical information regarding the hemodynamic status of patients with HF. Indeed, owing to its simplicity in measurement and widespread availability, BP is of paramount clinical importance in guiding the treatment of patients with HF. Furthermore, arterial hypertension is considered one of the most common comorbidities [ 3 ] and a precursor of HF [ 4 ]. Table 1 [ 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 ] shows the previous clinical trials and observational studies on the prognosis of BP in patients with and without HF.
In general, associating a higher BP with a greater incidence of HF is reasonable. In a population-based longitudinal observational study including 5888 adults aged ≥65 years, isolated systolic hypertension (SBP ≥140 mmHg) was associated with an increased risk of incident HF compared to subjects without isolated systolic hypertension during a follow-up duration of 8.7 years [ 54 ]. Regarding the clinical prognosis of low versus high BP, the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) trial, which enrolled a high-risk population of 15,244 hypertensive patients, showed no evidence for an increased risk of adverse outcome in patients with low BP [ 56 ]. This observation holds true for hypertensive patients in general and for those at high risk of cardiovascular disease without a history of HF. However, in patients who have already been diagnosed with HF, the clinical significance of BP appears to differ from that in the general population or in those with other cardiovascular diseases.
A retrospective longitudinal study showed that a low SBP (< 90 mmHg) was associated with poor survival in patients with chronic HF [ 21 ]. Notably, when the subjects were categorized based on SBP levels (< 90, 90–109, 110–129, and > 129 mmHg), as BP increased, the prognosis tended to improve in the group with SBP > 129 mmHg. Interestingly, this study also showed that pronounced long-term changes in SBP were associated with poor prognosis in this population. This result is in line with a previous study, which suggested the concept of “reverse epidemiology” that implies an improved survival rate in patients with HF with an elevated BP [ 58 ]. Several studies have reported a similar association, and this correlation is reminiscent of the “obesity paradox,” the relationship between HF and obesity. A post hoc analysis of OPTIMIZE-HF registry showed that, compared to SBP ≥ 130 mmHg at discharge, SBP < 130 mmHg was not associated with outcomes, but SBP < 120 mmHg at discharge was associated with a higher risk of death among hospitalized elderly HFpEF patients with hypertension [ 52 ]. Recent observational studies have also indicated that low SBP is associated with poor prognosis in patients with HFpEF [ 59 , 60 ].
It is not surprising that low BP might be considered harmful, as it can serve as a marker of worse health conditions. Even among patients on maximal guideline-directed medication therapy (GDMT), those with SBP < 110 mmHg have been shown to be at increased risk of readmission for HF [ 44 ], and this association remained significant despite no evidence of more severe disease or a greater burden of comorbidities in those with low BP [ 46 ].
While most of these data analyzed prognosis based on baseline BP, the analysis from the KorAHF registry focused on on-treatment BP during follow-up [ 50 ]. Among the 4487 patients hospitalized for acute HF, SBP and diastolic BP (DBP) above and below the reference BP were associated with increased mortality. A nadir of 132.4/74.2 mmHg was associated with the lowest mortality rate in this cohort, especially for those with HFpEF. However, in patients with HFrEF, the mortality risk increased significantly only in the lower BP range and not in the higher BP range. In detail, the lowest risk of mortality was observed at an SBP/DBP of 136.0/76.6 mmHg for HFrEF, and at 127.9/72.7 mmHg for HFpEF. This pattern of association with BP profile was also described in a previous study [ 61 ], although the classification of HF was comparatively different; patients with mild-to-moderate LV systolic dysfunction (LVEF, 30–50%) had a U-shaped association with mortality, but patients with severe LV systolic dysfunction (LVEF, < 30%) had a linear relationship with lower SBP, which was associated with increased mortality. Thus, it can be inferred that the association among HFrEF, HFpEF, and BP had a relatively different pattern. Taken together, these results suggest that there may be a safer BP range in HF, although it is not clear-cut; lower BP is associated with a higher risk in HFrEF and HFpEF, and while HFrEF has a wider margin of safety for higher BP, HFpEF has a narrower margin of safety because higher BP is also associated with increased risk in HFpEF compared to that in HFrEF (Fig. 1 ).
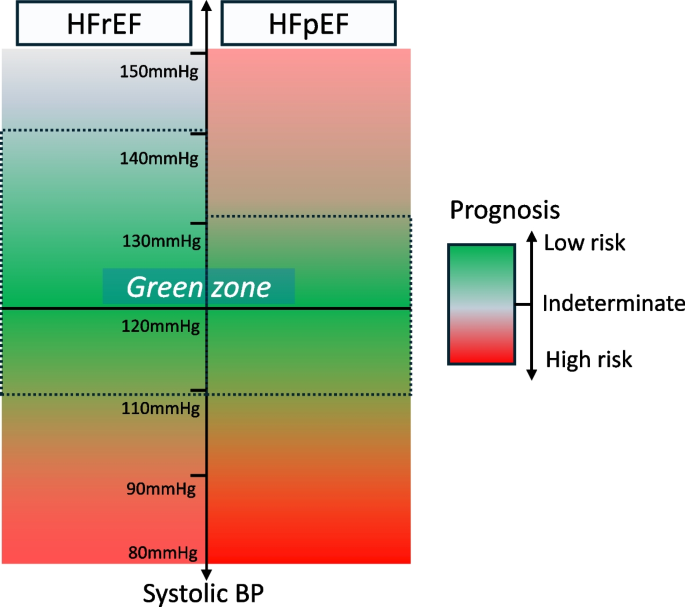
A conceptual safety margin (“green zone”) for blood pressure (BP) in each heart failure group. Heart failure with reduced ejection fraction (HFrEF) has a wide safety margin for BP, with a lower BP being at higher risk. Heart failure with preserved ejection fraction (HFpEF) has a relatively narrow safety margin for BP, with both higher and lower BP being at higher risk
Medication affecting BP in HF
Most agents proven to have a survival benefit in HF have the potential to lower BP (such as ACEis, ARBs, β-blockers, angiotensin receptor-neprilysin inhibitors [ARNIs], MRAs, and sodium glucose cotransporter 2 [SGLT2] inhibitors) to a greater or lesser extent; however, not all BP-lowering treatments have the same beneficial effects, as summarized in Table 2 [ 12 , 13 , 16 , 42 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 ]. It is challenging to establish a direct relationship between the probability of clinical benefit and BP-lowering alone, particularly in more recent studies where the number of medications used in the study population was higher than that in previous studies. Additionally, in some cases, lowering the BP was neither beneficial nor detrimental, thereby complicating the assessment of contribution of BP to the benefits of GDMT in HF. These conflicting results have raised the question of whether reduction in BP is due to the positive effects of drugs with BP-lowering effects or, conversely, whether these drugs have deleterious effects that are offset by the benefits of neurohumoral regulation [ 79 ]. Nevertheless, the importance of treating BP in HF is consensually recognized in the HF and hypertension guidelines [ 38 , 80 , 81 ] both of which recommend drugs that have been reliably demonstrated in randomized clinical trials to improve outcomes as first-line therapy, especially for HFrEF [ 82 ].
Given that certain agents (such as metoprolol, carvedilol, and MRAs) without clear evidence of BP-lowering effect, significantly improved outcomes in HFrEF [ 70 , 83 ] and that some agents (such as calcium channel blockers [CCBs], moxonidine, and α-blockers) with significant BP-lowering effects in the general hypertensive population had no/harmful effects on HFrEF [ 84 , 85 ], it is now established that lowering BP per se is not associated with improved outcomes in HF. Instead, the focus has shifted to the class of drugs and how early they are initiated, forming the foundation of the current HF pharmacotherapy with individualized combination therapy in addition to existing agents. In this regard, patients with HF who have low BP are often undertreated, and as the Change the Management of Patients with Heart Failure (CHAMP-HF) registry data show, low BP is an independent predictor of the underuse or underdosing of neurohormonal antagonists [ 86 ]. Emphasizing that in certain cases, optimizing GDMT can be advantageous when patient tolerance permits, rather than refraining from medication solely due to BP concerns remains crucial.
Treatment for BP in patients with HF
Management of bp for incident hf.
Recognizing the explicit risk of cardiovascular disease progression in patients with uncontrolled BP, considering hypertension as a precursor to HF remains crucial. The Staging Classification of Heart Failure (A, B, C, D), introduced by the American College of Cardiology/American Heart Association in 2003, highlights the preventive aspect of HF and underscores the significance of risk factor management [ 87 , 88 ]. Accumulating evidence shows that that antihypertensive treatment is beneficial for incident HF. In a meta-analysis that demonstrated substantial reductions in cardiovascular death, stroke, and HF compared to placebo, the most significant benefit derived from antihypertensive therapy was the prevention of HF [ 89 ]. This analysis included 42 clinical trials with a total of 192,478 randomized patients and showed that low-dose diuretics significantly reduced the risk of stroke, cardiovascular mortality, and total mortality compared to placebo, with relative risks of 0.71, 0.81, and 0.90, respectively. The greatest reduction was observed in the risk of HF (relative risk, 0.51; 95% confidence interval, 0.42–0.62). More specifically, another meta-analysis by Ettehad et al. [ 90 ] showed that for each 10-mmHg reduction in SBP, the risk of HF significantly decreased by 28%.
In Hypertension in the Very Elderly Trial (HYVET) study, active antihypertensive treatment with indapamide, with or without perindopril, reduced the risk of incident HF by 64% in patients aged ≥80 years [ 91 ]. When comparing BP after 2 years of treatment, BP reduction was more modest in the perindopril group than that in the placebo group, with an additional reduction in SBP/DBP of 15.0/6.1 mmHg. In addition to placebo-controlled trials, several studies comparing active treatment with standard treatment for hypertension have reported data on the incidence of HF. The Systolic Blood Pressure Intervention Trial (SPRINT), which assessed the role of intensive antihypertensive treatment with a target SBP < 120 mmHg, showed a 38% reduction of relative risk in the development of HF in the intensive treatment group [ 57 ].
Despite increasing evidence highlighting the significant burden of HF associated with hypertensive heart disease, current hypertension treatment guidelines lack specific pharmacological strategies for managing patients beyond BP reduction [ 80 , 81 ]. However, a position paper by the Heart Failure Association, in collaboration with the European Association of Preventive Cardiology, suggests utilizing diuretics, ACEis, and ARBs to prevent HF in hypertensive patients [ 92 ]. This recommendation is based on a network meta-analysis encompassing 26 trials, which showed that these three classes of antihypertensive drugs were most effective in lowering the incidence of HF compared to placebo. Furthermore, the 2023 European Society of Hypertension guidelines recommended lowering BP with five major antihypertensive drugs including CCBs and β-blockers, in addition to the above three classes of drugs, to prevent HF development [ 93 ]. In addition, if the target blood pressure is not achieved with these medications alone, additional medications (e.g., α-blockers) are recommended as needed.
Management of BP in established HF
For patients with established HF, the prognostic meaning of BP is relatively different. Given that many HF drugs have BP-lowering effects, and that BP is one of the most important hemodynamic markers in cardiovascular disease and one of the few that can be measured directly in the clinic, BP targeting in HF is always of interest. However, there is no compelling evidence or guidelines on this aspect. Interestingly, standard HF therapy (with ACEi/ARBs, ARNIs, and β-blockers) may induce hypotension, occasionally leading to drug discontinuation. However, current HF guidelines recommend uptitrating medications to the tolerance of patients and emphasize that repeated attempts at uptitration can result in optimization, even if the initial attempts may fail [ 9 , 94 ]. This is a substantial challenge and a gap between the ideal and the reality frequently encountered in clinical practice. The following questions arise: Should we aggressively pursue different classes of HF medications, even in those who have low BP, high frailty, and especially, intolerance to BP-lowering medications? Alternatively, should we maintain a certain target BP, for example, an SBP between 110 and 130 mmHg, even if it means discontinuing certain medications? The answers to these questions can be estimated through previous literature, and we should at least attempt to learn from existing evidence.
Recommendations on BP in the treatment of HF from several guidelines for HF and hypertension are summarized in Table 3 [ 9 , 38 , 81 , 93 , 95 , 97 , 98 ]. The 2021 European Society of Cardiology HF guideline emphasizes striving to achieve target dose of each HF medication, and the 2023 European Society of Hypertension guideline recommends combining the medications (ACEis [ARBs if not tolerated], ARNIs, BBs, MRAs, and SGLT2 inhibitors) that have been shown to have outcome benefits, particularly in HFrEF. It was common across guidelines that nondihydropyridine CCB agents were not recommended in HFrEF.
Target BP in established HF
The 2017 American College of Cardiology Foundation/American Heart Association guidelines for the management of HF recommend that optimal BP in those with hypertension and an increased risk of HF (stage A) should be < 130/80 mmHg [ 81 ]. In addition, patients with HFrEF and hypertension should be treated by GDMT titration to attain a target SBP < 130 mmHg. The target BP was also updated based on several clinical trials, primarily the SPRINT trial [ 99 ]. The 2022 focused update of Korean Hypertension Society guideline for the management of hypertension also mentioned that in patients with hypertension who are at high risk for HF or with HF, it is reasonable to control BP below 130/80 mmHg [ 98 ]. However, thus far, there are no compelling data to identify a simple BP target in patients with established HF.
In 2022, the American Heart Association/American College of Cardiology/Heart Failure Society of America updated guidelines for the management of HF, which stated that the optimal BP or antihypertensive regimens are not known for HFpEF and did not mention any BP goals for HFrEF at all [ 100 ]. As more pharmacological options become available in the modern era, the recent trend is toward maximizing GDMT within a tolerable range rather than providing a target BP. Here, the tolerability of an individual to treatment is assessed using safety indicators such as hypotension or renal insufficiency. If there are no adverse events, maximizing GDMT is deemed more important, suggesting that clinicians should not passively treat by solely providing a target BP.
Differences in BP management between those with HFrEF and HFpEF
In general, guideline-recommended BP management for HFpEF was not significantly different from that for HFrEF. The difference is that hypertension is not as prevalent in HFrEF as in HFpEF, and patients with HFrEF rarely have uncontrolled BP [ 95 ]. In hypertensive patients, CCB is an option for BP control, although as mentioned above, the role of CCBs in HFrEF is limited (Table 2 ). However, the role of CCBs in HFpEF in the current era is not necessarily associated with worse HF outcomes. Although the Prospective Randomized Amlodipine Survival Evaluation-2 (PRAISE-2) study, which did not show the efficacy of amlodipine in HFrEF, had limited baseline medical treatment to ACEi (99%) and β-blocker use (19%) [ 78 ], a recent observational study on CCBs in HFpEF showed the noninferiority of CCBs, both dihydropyridines and nondihydropyridines, in addition to multiple drug usage, with β-blocker being used in more than two-thirds and MRA in one-quarter of the cases [ 101 ]. Although randomized clinical studies are required, evidence from studies on HFpEF suggests that CCB may still be effective in lowering BP and improving outcomes. In other words, it suggests that more aggressive BP management is feasible and effective by utilizing conventional antihypertensive agents to improve outcomes in patients with HFpEF compared to those with HFrEF. The 2023 European Society of Hypertension guideline also mentioned that the use of all major antihypertensive drugs including CCBs are recommended in HFpEF, and the use of ARNIs or MRAs can be considered in HFpEF with lower LVEF spectrum (Table 3 ).
Time in BP target range in HF
A practical limitation of what we learn from clinical research is that BP measurements are taken only at a certain point in time. BP is a continuous metric that changes over time, so continuous BP monitoring and “time in target range” is also important for BP management, and some recent studies reinforce this point of view. Huang et al. [ 102 ] reported a post hoc analysis of the Treatment of Preserved Cardiac Function HF with an Aldosterone Antagonist (TOPCAT) trial, which compared the efficacy of spironolactone in patients with HFpEF and showed that the duration in the target range of SBP between 110 and 130 mmHg was associated with better clinical outcomes, including mortality and hospitalizations for HF. Moreover, subgroup analyses showed that it was more significant in younger patients than in older patients.
In addition, Chen et al. [ 103 ] reported another post hoc analysis of data from the TOPCAT trial and the Beta-Blocker Evaluation of Survival Trial (BEST), which showed that a longer duration of BP in the target range of SBP between 120 and 130 mmHg was associated with a lower risk of major adverse cardiovascular events in hypertensive patients with HF. Since the BEST trial enrolled patients with HFrEF and the TOPCAT trial enrolled patients with HFpEF, this post hoc study concluded that a longer duration in the target range was highly associated with better cardiovascular outcomes regardless of LVEF. However, these studies were still limited by the fact that they did not analyze different combinations of various HF drug classes. Therefore, additional studies with similar designs are anticipated to provide additional insights into BP management in the HFrEF population.
Conclusions
Most of the HF medications have a mechanism and effect of lowering BP. Addressing patients with marginal BP poses significant therapeutic challenges, particularly considering that several other medications or clinical situations can also lower BP. Given the association of low BP with adverse prognosis, establishing a target BP and determining the ideal treatment strategy are critical, yet complex.
Many of these questions remain unanswered. How do we set a target BP? Can we unify all patients with HF using a single target BP? How do we individualize treatment and divide that subgroup? What evidence should we base our treatment on, and how do we categorize these patients for clinical research? How do we identify those who can benefit from further BP reduction and those who cannot? Which of the various HF medications should be titrated first for BP, when, and how much? Determining the optimal timing, dosage adjustments, and titration strategies for HF medication in the context of BP management requires further investigation.
Furthermore, the target BP varies depending on factors such as the patient’s condition, underlying comorbidities, etiology of HF, and the response of BP to medications. Some individuals have preserved tissue perfusion and no symptoms or signs of exercise intolerance or organ hypoperfusion even at lower BP, whereas others develop these dysfunctions even at normal or high BP. This highlights the difficulty of adopting a one-size-fits-all approach for treating HF, and it is hoped that more targeted treatments will become available depending on the underlying pathogenesis of HF.
Availability of data and materials
Not applicable.
Abbreviations
Angiotensin-converting enzyme inhibitor
American Heart Association
Acute heart failure
Angiotensin receptor blocker
Angiotensin receptor-neprilysin inhibitor
Beta-blocker Evaluation of Survival Trial
- Blood pressure
Calcium channel blocker
Change the Management of Patients with Heart Failure
Candesartan in Heart failure Assessment of Reduction in Mortality and Morbidity
Confidence interval
Carvedilol Prospective Randomized Cumulative Survival
Cardiovascular
Dapagliflozin and Prevention of Adverse outcomes in Heart Failure
Diastolic blood pressure
Dapagliflozin Evaluation to Improve the Lives of patients with Preserved Ejection Fraction Feart Failure
Digitalis Investigation Group
Empagliflozin Outcome Trial in patients with Chronic Heart Failure
Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure
European Society of Cardiology
European Society of Hypertension
Guideline-Directed Medication Therapy
Hypertensive acute heart failure
- Heart failure
Heart failure with mildly reduced ejection fraction
Heart failure with preserved ejection fraction
Heart failure with reduced ejection fraction
Hospitalization for heart failure
Hazard ratio
Hypertension in the Very Elderly Trial
Irbesartan in heart failure with Preserved ejection fraction
Korean Acute Heart Failure
Korean Society of Hypertension
Left ventricular
Left ventricular ejection fraction
Left ventricular hypertrophy
Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure
Myocardial infarction
Mineralocorticoid receptor antagonist
Not applicable
New York Heart Association
Organized Program to Initiate Lifesaving Treatment In Hospitalized patients with Heart Failure
Prospective Comparison of ARNI with ACEi to determine Impact on Global Mortality and Morbidity in Heart Failure
Prospective Comparison of ARNI with ARB Global Outcomes in Heart Failure with preserved ejection fraction
Perindopril in Elderly People with Chronic Heart Failure
Prospective Randomized Amlodipine Survival Evaluation-2
Prospective Randomized Trial of the Optimal Evaluation of Cardiac Symptoms and Revascularization
Renin-angiotensin system
Randomized controlled trial
Systolic blood pressure
Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors with Heart Failure
Sodium glucose cotransporter 2
Studies Of Left Ventricular Dysfunction
Systolic Blood Pressure Intervention Trial
Treating to new targets
Treatment Of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist
Valsartan-Heart Failure Trial
Valsartan Antihypertensive Long-term Use Evaluation
Vericiguat Global study in subjects with Heart Failure with Reduced Ejection Fraction
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics: 2014 update: a report from the American Heart Association. Circulation. 2014;129:e28-292.
PubMed Google Scholar
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–19.
Article CAS PubMed PubMed Central Google Scholar
Meta-analysis global Group in Chronic Heart Failure (MAGGIC). The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur Heart J. 2012;33:1750–7.
Article Google Scholar
Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41.
Article PubMed Google Scholar
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62.
Article CAS PubMed Google Scholar
Messerli FH, Rimoldi SF, Bangalore S. The transition from hypertension to heart failure: contemporary update. JACC Heart Fail. 2017;5:543–51.
Oh GC, Cho HJ. Blood pressure and heart failure. Clin Hypertens. 2020;26:1.
Article PubMed PubMed Central Google Scholar
Cho JY, Cho DH, Youn JC, Kim D, Park SM, Jung MH, et al. Korean Society of Heart Failure Guidelines for the management of heart failure: definition and diagnosis. Int J Heart Fail. 2023;5:51–65.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022;145:e895-1032.
Tsuji K, Sakata Y, Nochioka K, Miura M, Yamauchi T, Onose T, et al. Characterization of heart failure patients with mid-range left ventricular ejection fraction-a report from the CHART-2 study. Eur J Heart Fail. 2017;19:1258–69.
Borlaug BA, Redfield MM. Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation. 2011;123:2006–14.
Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet. 2003;362:777–81.
Cleland JG, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J, et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338–45.
Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF registry. J Am Coll Cardiol. 2007;50:768–77.
Arnold SV, Silverman DN, Gosch K, Nassif ME, Infeld M, Litwin S, et al. Beta-blocker use and heart failure outcomes in mildly reduced and preserved ejection fraction. JACC Heart Fail. 2023;11(8 Pt 1):893–900.
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370:1383–92.
Lupón J, Gavidia-Bovadilla G, Ferrer E, de Antonio M, Perera-Lluna A, López-Ayerbe J, et al. Heart failure with preserved ejection fraction infrequently evolves toward a reduced phenotype in long-term survivors. Circ Heart Fail. 2019;12:e005652.
Lee CJ, Park S. Hypertension and heart failure with preserved ejection fraction. Heart Fail Clin. 2021;17:337–43.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–60.
Styron JF, Jois-Bilowich P, Starling R, Hobbs RE, Kontos MC, Pang PS, et al. Initial emergency department systolic blood pressure predicts left ventricular systolic function in acute decompensated heart failure. Congest Heart Fail. 2009;15:9–13.
Chioncel O, Lainscak M, Seferovic PM, Anker SD, Crespo-Leiro MG, Harjola VP, et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: an analysis of the ESC heart failure long-term registry. Eur J Heart Fail. 2017;19:1574–85.
Cho JH, Choe WS, Cho HJ, Lee HY, Jang J, Lee SE, et al. Comparison of characteristics and 3-year outcomes in patients with acute heart failure with preserved, mid-range, and reduced ejection fraction. Circ J. 2019;83:347–56.
Viau DM, Sala-Mercado JA, Spranger MD, O’Leary DS, Levy PD. The pathophysiology of hypertensive acute heart failure. Heart. 2015;101:1861–7.
Collins SP, Levy PD, Martindale JL, Dunlap ME, Storrow AB, Pang PS, et al. Clinical and research considerations for patients with hypertensive acute heart failure: a consensus statement from the Society of Academic Emergency Medicine and the Heart Failure Society of America acute heart failure working group. J Card Fail. 2016;22:618–27.
Collins SP, Levy PD, Fermann GJ, Givertz MM, Martindale JM, Pang PS, et al. What’s next for acute heart failure research? Acad Emerg Med. 2018;25:85–93.
Girbes ARJ, de Grooth HJ. Time to stop randomized and large pragmatic trials for intensive care medicine syndromes: the case of sepsis and acute respiratory distress syndrome. J Thorac Dis. 2020;12(Suppl 1):S101–9.
Collins S, Martindale J. Optimizing hypertensive acute heart failure management with afterload reduction. Curr Hypertens Rep. 2018;20:9.
Liu JX, Uppal S, Patel V. Management of acute hypertensive heart failure. Heart Fail Clin. 2019;15:565–74.
Adams KF Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the acute decompensated heart failure National Registry (ADHERE). Am Heart J. 2005;149:209–16.
Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, et al. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: findings from OPTIMIZE-HF. Arch Intern Med. 2008;168:847–54.
Arrigo M, Gayat E, Parenica J, Ishihara S, Zhang J, Choi DJ, et al. Precipitating factors and 90-day outcome of acute heart failure: a report from the intercontinental GREAT registry. Eur J Heart Fail. 2017;19:201–8.
Sokolska JM, Sokolski M, Zymliński R, Biegus J, Siwołowski P, Nawrocka-Millward S, et al. Patterns of dyspnoea onset in patients with acute heart failure: clinical and prognostic implications. ESC Heart Fail. 2019;6:16–26.
Lee DS, Lee JS, Schull MJ, Borgundvaag B, Edmonds ML, Ivankovic M, et al. Prospective validation of the emergency heart failure mortality risk grade for acute heart failure. Circulation. 2019;139:1146–56.
Rosman Y, Kopel E, Shlomai G, Goldenberg I, Grossman E. The association between admission systolic blood pressure of heart failure patients with preserved systolic function and mortality outcomes. Eur J Intern Med. 2015;26:807–12.
Collins SP, Jenkins CA, Harrell FE Jr, Liu D, Miller KF, Lindsell CJ, et al. Identification of emergency department patients with acute heart failure at low risk for 30-day adverse events: the STRATIFY decision tool. JACC Heart Fail. 2015;3:737–47.
Chioncel O, Mebazaa A, Harjola VP, Coats AJ, Piepoli MF, Crespo-Leiro MG, et al. Clinical phenotypes and outcome of patients hospitalized for acute heart failure: the ESC heart failure long-term registry. Eur J Heart Fail. 2017;19:1242–54.
Cotter G, Davison BA, Butler J, Collins SP, Ezekowitz JA, Felker GM, et al. Relationship between baseline systolic blood pressure and long-term outcomes in acute heart failure patients treated with TRV027: an exploratory subgroup analysis of BLAST-AHF. Clin Res Cardiol. 2018;107:170–81.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200.
Kitai T, Tang WH, Xanthopoulos A, Murai R, Yamane T, Kim K, et al. Impact of early treatment with intravenous vasodilators and blood pressure reduction in acute heart failure. Open Heart. 2018;5:e000845.
Harrison N, Pang P, Collins S, Levy P. Blood pressure reduction in hypertensive acute heart failure. Curr Hypertens Rep. 2021;23:11.
Levy P, Compton S, Welch R, Delgado G, Jennett A, Penugonda N, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med. 2007;50:144–52.
Rouleau JL, Roecker EB, Tendera M, Mohacsi P, Krum H, Katus HA, et al. Influence of pretreatment systolic blood pressure on the effect of carvedilol in patients with severe chronic heart failure: the carvedilol prospective randomized cumulative survival (COPERNICUS) study. J Am Coll Cardiol. 2004;43:1423–9.
Lee TT, Chen J, Cohen DJ, Tsao L. The association between blood pressure and mortality in patients with heart failure. Am Heart J. 2006;151:76–83.
Desai RV, Banach M, Ahmed MI, Mujib M, Aban I, Love TE, et al. Impact of baseline systolic blood pressure on long-term outcomes in patients with advanced chronic systolic heart failure (insights from the BEST trial). Am J Cardiol. 2010;106:221–7.
Banach M, Bhatia V, Feller MA, Mujib M, Desai RV, Ahmed MI, et al. Relation of baseline systolic blood pressure and long-term outcomes in ambulatory patients with chronic mild to moderate heart failure. Am J Cardiol. 2011;107:1208–14.
Böhm M, Young R, Jhund PS, Solomon SD, Gong J, Lefkowitz MP, et al. Systolic blood pressure, cardiovascular outcomes and efficacy and safety of sacubitril/valsartan (LCZ696) in patients with chronic heart failure and reduced ejection fraction: results from PARADIGM-HF. Eur Heart J. 2017;38:1132–43.
Selvaraj S, Claggett BL, Böhm M, Anker SD, Vaduganathan M, Zannad F, et al. Systolic blood pressure in heart failure with preserved ejection fraction treated with sacubitril/valsartan. J Am Coll Cardiol. 2020;75:1644–56.
Lam CS, Mulder H, Lopatin Y, Vazquez-Tanus JB, Siu D, Ezekowitz J, et al. Blood pressure and safety events with vericiguat in the VICTORIA trial. J Am Heart Assoc. 2021;10:e021094.
Vidán MT, Bueno H, Wang Y, Schreiner G, Ross JS, Chen J, et al. The relationship between systolic blood pressure on admission and mortality in older patients with heart failure. Eur J Heart Fail. 2010;12:148–55.
Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, Choi JO, et al. Reverse J-curve relationship between on-treatment blood pressure and mortality in patients with heart failure. JACC Heart Fail. 2017;5:810–9.
Arundel C, Lam PH, Gill GS, Patel S, Panjrath G, Faselis C, et al. Systolic blood pressure and outcomes in patients with heart failure with reduced ejection fraction. J Am Coll Cardiol. 2019;73:3054–63.
Faselis C, Lam PH, Zile MR, Bhyan P, Tsimploulis A, Arundel C, et al. Systolic blood pressure and outcomes in older patients with HFpEF and hypertension. Am J Med. 2021;134:e252–63.
D’Agostino RB, Belanger AJ, Kannel WB, Cruickshank JM. Relation of low diastolic blood pressure to coronary heart disease death in presence of myocardial infarction: the Framingham study. BMJ. 1991;303:385–9.
Ekundayo OJ, Allman RM, Sanders PW, Aban I, Love TE, Arnett D, et al. Isolated systolic hypertension and incident heart failure in older adults: a propensity-matched study. Hypertension. 2009;53:458–65.
Bangalore S, Messerli FH, Wun CC, Zuckerman AL, DeMicco D, Kostis JB, et al. J-curve revisited: an analysis of blood pressure and cardiovascular events in the treating to new targets (TNT) trial. Eur Heart J. 2010;31:2897–908.
Kjeldsen SE, Berge E, Bangalore S, Messerli FH, Mancia G, Holzhauer B, et al. No evidence for a J-shaped curve in treated hypertensive patients with increased cardiovascular risk: the VALUE trial. Blood Press. 2016;25:83–92.
Upadhya B, Rocco M, Lewis CE, Oparil S, Lovato LC, Cushman WC, et al. Effect of intensive blood pressure treatment on heart failure events in the systolic blood pressure reduction intervention trial. Circ Heart Fail. 2017;10:e003613.
Güder G, Frantz S, Bauersachs J, Allolio B, Wanner C, Koller MT, et al. Reverse epidemiology in systolic and nonsystolic heart failure: cumulative prognostic benefit of classical cardiovascular risk factors. Circ Heart Fail. 2009;2:563–71.
Tsujimoto T, Kajio H. Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol. 2018;263:69–74.
Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic blood pressure and outcomes in patients with heart failure with preserved ejection fraction. JAMA Cardiol. 2018;3:288–97.
Ather S, Chan W, Chillar A, Aguilar D, Pritchett AM, Ramasubbu K, et al. Association of systolic blood pressure with mortality in patients with heart failure with reduced ejection fraction: a complex relationship. Am Heart J. 2011;161:567–73.
Investigators SOLVD, Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293–302.
Cohn JN, Tognoni G. Valsartan heart failure trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–75.
McMurray JJ, Ostergren J, Swedberg K, Granger CB, Held P, Michelson EL, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-added trial. Lancet. 2003;362:767–71.
Massie BM, Carson PE, McMurray JJ, Komajda M, McKelvie R, Zile MR, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456–67.
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004.
Solomon SD, McMurray JJ, Anand IS, Ge J, Lam CS, Maggioni AP, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381:1609–20.
Packer M, Fowler MB, Roecker EB, Coats AJ, Katus HA, Krum H, et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation. 2002;106:2194–9.
Packer M, Colucci WS, Sackner-Bernstein JD, Liang CS, Goldscher DA, Freeman I, et al. Double-blind, placebo-controlled study of the effects of carvedilol in patients with moderate to severe heart failure. The PRECISE trial. Prospective randomized evaluation of carvedilol on symptoms and exercise. Circulation. 1996;94:2793–9.
Effect of metoprolol CR/XL in chronic heart failure. Metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet. 1999;353:2001–7.
Flather MD, Shibata MC, Coats AJ, Van Veldhuisen DJ, Parkhomenko A, Borbola J, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005;26:215–25.
Zannad F, McMurray JJ, Krum H, van Veldhuisen DJ, Swedberg K, Shi H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11–21.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–24.
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61.
McMurray JJ, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Solomon SD, Vaduganathan M, Claggett BL, de Boer RA, DeMets D, Hernandez AF, et al. Baseline characteristics of patients with HF with mildly reduced and preserved ejection fraction: DELIVER trial. JACC Heart Fail. 2022;10:184–97.
Armstrong PW, Pieske B, Anstrom KJ, Ezekowitz J, Hernandez AF, Butler J, et al. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382:1883–93.
Packer M, Carson P, Elkayam U, Konstam MA, Moe G, O’Connor C, et al. Effect of amlodipine on the survival of patients with severe chronic heart failure due to a nonischemic cardiomyopathy: results of the PRAISE-2 study (prospective randomized amlodipine survival evaluation 2). JACC Heart Fail. 2013;1:308–14.
Hartupee J, Mann DL. Neurohormonal activation in heart failure with reduced ejection fraction. Nat Rev Cardiol. 2017;14:30–8.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127–248.
Pinho-Gomes AC, Rahimi K. Management of blood pressure in heart failure. Heart. 2019;105:589–95.
Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. carvedilol heart failure study group. N Engl J Med. 1996;334:1349–55.
Udelson JE, DeAbate CA, Berk M, Neuberg G, Packer M, Vijay NK, et al. Effects of amlodipine on exercise tolerance, quality of life, and left ventricular function in patients with heart failure from left ventricular systolic dysfunction. Am Heart J. 2000;139:503–10.
Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, Tristani FE, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure: results of a veterans administration cooperative study. N Engl J Med. 1986;314:1547–52.
Greene SJ, Butler J, Albert NM, DeVore AD, Sharma PP, Duffy CI, et al. Medical therapy for heart failure with reduced ejection fraction: the CHAMP-HF registry. J Am Coll Cardiol. 2018;72:351–66.
Pfeffer MA. Heart failure and hypertension: importance of prevention. Med Clin North Am. 2017;101(1):19–28.
Jessup M, Brozena S. Heart failure. N Engl J Med. 2003;348:2007–18.
Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003;289:2534–44.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
Piepoli MF, Adamo M, Barison A, Bestetti RB, Biegus J, Böhm M, et al. Preventing heart failure: a position paper of the heart failure association in collaboration with the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2022;29:275–300.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European renal association (ERA). J Hypertens. 2023;41:1874–2071.
Greene SJ, Butler J, Fonarow GC. Simultaneous or rapid sequence initiation of quadruple medical therapy for heart failure-optimizing therapy with the need for speed. JAMA Cardiol. 2021;6:743–4.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726.
Khan SS, Ning H, Shah SJ, Yancy CW, Carnethon M, Berry JD, et al. 10-year risk equations for incident heart failure in the general population. J Am Coll Cardiol. 2019;73:2388–97.
Park SM, Lee SY, Jung MH, Youn JC, Kim D, Cho JY, et al. Korean Society of Heart Failure Guidelines for the management of heart failure: management of the underlying etiologies and comorbidities of heart failure. Int J Heart Fail. 2023;5:127–45.
Kim HL, Lee EM, Ahn SY, Kim KI, Kim HC, Kim JH, et al. The 2022 focused update of the 2018 Korean hypertension society guidelines for the management of hypertension. Clin Hypertens. 2023;29:11.
SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol. 2022;79:e263–421.
Matsumoto S, Kondo T, Yang M, Campbell RT, Docherty KF, de Boer RA, et al. Calcium channel blocker use and outcomes in patients with heart failure and mildly reduced and preserved ejection fraction. Eur J Heart Fail. 2023;25:2202–14.
Huang R, Lin Y, Liu M, Xiong Z, Zhang S, Zhong X, et al. Time in target range for systolic blood pressure and cardiovascular outcomes in patients with heart failure with preserved ejection fraction. J Am Heart Assoc. 2022;11:e022765.
Chen K, Li C, Cornelius V, Yu D, Wang Q, Shi R, et al. Prognostic value of time in blood pressure target range among patients with heart failure. JACC Heart Fail. 2022;10:369–79.
Download references
Acknowledgements
Author information, authors and affiliations.
Division of Cardiology, National Health Insurance Service Ilsan Hospital, Goyang, Republic of Korea
Kyeong-Hyeon Chun
Division of Cardiology, Severance Hospital, Cardiovascular Research Institute, Yonsei University College of Medicine, Seoul, Republic of Korea
Seok-Min Kang
You can also search for this author in PubMed Google Scholar
Contributions
KHC wrote the draft and SMK edited and supervised the whole article. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Seok-Min Kang .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chun, KH., Kang, SM. Blood pressure and heart failure: focused on treatment. Clin Hypertens 30 , 15 (2024). https://doi.org/10.1186/s40885-024-00271-y
Download citation
Received : 19 January 2024
Accepted : 17 April 2024
Published : 01 June 2024
DOI : https://doi.org/10.1186/s40885-024-00271-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
Clinical Hypertension
ISSN: 2056-5909
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Home — Essay Samples — Nursing & Health — Other Diseases & Conditions — Hypertension
Essays on Hypertension
Brief description of hypertension.
Hypertension, or high blood pressure, is a common but serious medical condition that can lead to heart disease, stroke, and other health problems. It affects millions of people worldwide and is often referred to as a "silent killer" due to its lack of noticeable symptoms. Managing hypertension is crucial for overall health and well-being.
Importance of Writing Essays on This Topic
Essays on hypertension are important for both academic and personal exploration. They provide an opportunity to delve into the causes, effects, and management of this prevalent health issue. Through researching and writing about hypertension, individuals can gain a deeper understanding of the condition and its impact on society.
Tips on Choosing a Good Topic
- Select a specific aspect of hypertension to focus on, such as its relationship to lifestyle choices or its impact on certain demographics.
- Consider the relevance and significance of the topic in current medical research and public health discussions.
- Choose a topic that allows for critical analysis and exploration of potential solutions or interventions for hypertension.
Essay Topics
- The Role of Genetics in Hypertension
- The Impact of Diet and Nutrition on Hypertension
- Gender Disparities in Hypertension Diagnosis and Treatment
- The Relationship Between Stress and Hypertension
- The Effectiveness of Exercise in Managing Hypertension
- Public Health Interventions for Hypertension Prevention
- Hypertension in Aging Populations
- The Link Between Hypertension and Cardiovascular Disease
- Social Determinants of Hypertension in Underserved Communities
- The Psychological Impact of Hypertension Diagnosis
Concluding Thought
Writing essays on hypertension offers a valuable opportunity to explore the complexities of this prevalent health issue and contribute to the ongoing dialogue surrounding its prevention and management. By engaging with this topic through academic writing, individuals can deepen their understanding and potentially make a positive impact on public health.
Essay on High Blood Pressure
Hypertension - the "silent killer", made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
The Heart Disease of Hypertension
High blood pressure and the measures to prevent cardiovascular disease of hypertension, preventing and controlling hypertension for improved population health, hypertension in children: overview of healthcare policy concern and solution, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Important Public Health Challenges of Hypertension and Obesity
The concept of preeclampsia, investigation of the link between poverty and hypertension, understanding hypertension: causes, effects, management, functions of minerals and water in the human body, relevant topics.
- Myocardial Infarction
- Hearing Loss
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Br J Gen Pract
- v.66(652); November 2016

Hypertension from the patient’s perspective
Treating hypertension.
Every day, countless prescriptions are signed for antihypertensive medications, many of which are never taken. When managing hypertension we demand a lot from our patients: lifestyle changes that can be difficult and disruptive; and, if necessary, regular use of antihypertensive medication. These come with risks and many patients struggle to remember to take their tablets as prescribed. Hypertension is a largely silent condition and treatment aims to reduce the risks of future diseases, in particular strokes, ischaemic heart disease, and renal failure, rather than to reduce current suffering. It is perhaps not surprising, then, that studies tend to find very poor levels of patient compliance with antihypertensive medication regimes. 1 , 2 This is because patients do not have debilitating symptoms as a motivator to comply, nor the reward of relief of suffering to encourage continued adherence.
In order to motivate patients to comply, and to ensure that they use the medications appropriately and with informed consent, we must ensure they understand the potential benefits (and risks) of treating hypertension.
PATIENT VIEWS
In order to better understand patients’ perceptions of hypertension and its treatment, in early 2015 I undertook semi-structured interviews (including the Morisky MMAS8 medication compliance questionnaire) 3 with patients at a GP practice in central Manchester who were attending their annual hypertension reviews. Excluded from the survey were patients not taking antihypertensive medication at the time of the interview, those who would not comply with the survey, and those unable to speak English sufficiently to complete it, leaving 27 patients.
All patients felt that treating hypertension was either ‘very’ or ‘quite’ important. This may not be representative of the practice’s patients with hypertension as a whole because the patients included in the study had all agreed to attend an annual hypertension review; others were invited but did not attend.
The mean MMAS8 compliance score for those answering that treating hypertension is ‘very’ important was 0.8 (high adherence); the mean for those answering ‘quite’ was 2 (medium adherence). Patients were asked why they thought treating hypertension is important. Answers ranged from the specific (reduced vision, painful legs) to the vague (‘ something would happen’ , ‘it isn’t healthy’ ), with an occasional ‘because the doctor tells you to!’ Most patients volunteered one or both of heart attacks and strokes as being reasons to treat hypertension; just 8/27 were unaware of either of these potential consequences. Interestingly, the group that thought hypertension control ‘very important’ and the group considering it ‘quite important’ had the same rates of recognition of heart attacks and strokes as complications.
A total of 17/27 patients said they had experienced symptoms as a result of their hypertension. The most commonly reported symptoms were headaches, dizziness, hot flushes, and mood disorders (low mood, frustration, irritability). Other answers included chest tightness, palpitations, backache, constipation, and reduced vision. These symptoms would not normally be expected with the non-accelerated hypertension documented for these 27 patients. We certainly cannot assume that the existence of these symptoms was a direct result of the hypertension.
The patients’ belief that their symptoms were hypertension related was resulting in potential harm. Symptoms that might normally prompt the patient to seek medical advice (for example, palpitations, dizziness, low mood) were being ignored, presumed treated by the antihypertensive medications. One patient was treating her severe headaches with extra doses of her drugs. Many patients expected that they would feel better if their blood pressure was lower, giving the potential for poor compliance as a result of perceived ineffectiveness.
HOME BLOOD PRESSURE MONITORING
A common theme among patients who believed their symptoms were a result of their hypertension was the use of home blood pressure monitoring. Patients described how a painful or worrying symptom would arise and so, in something of a panic, they would measure their blood pressure and find it to be high, thereby strengthening their belief that the symptom was a result of high blood pressure.
MORE PATIENT EDUCATION NEEDED
In conclusion, many patients in this group did not understand why they were being treated for hypertension, and most attributed symptoms to this condition. More patient education into what to expect from hypertension and antihypertensive medications, and into the risk reduction aims of treatment, is required in order to promote patient autonomy for managing hypertension and to improve safe compliance with treatment regimes. The gaps and inaccuracies in patients’ understanding identified by this study are being addressed with a leaflet for practitioners to give to newly diagnosed patients and to patients at annual hypertension reviews. A similar approach may benefit patients elsewhere.

IMAGES
VIDEO
COMMENTS
The lack of physical activity is one of the leading causes of hypertension (Centers for Disease Control and Prevention, 2021). Moreover, poor dietary habits with the prevalence of unhealthy foods can promote problems with blood vessels and cause increased blood pressure. For this reason, in some cases, individuals can avoid the condition ...
The symptoms of hypertension can be very mild, and the condition may go unnoticed for years on end. The signs may vary from patient to patient, but typically, if symptoms are present, they include severe headaches, chest ache, difficulty breathing, the feeling of weakness, and fatigue.
Introduction: The state of clinical hypertension in 2021: According to the 2017 guidelines of the American Heart Association, almost one half of the adult population in the United States has hypertension, 1 and the Global Burden of Disease study ranks elevated systolic pressure as the leading cause of lost years of quality life. 2 Despite advances in medical therapy, hypertension remains a ...
1 Introduction. Hypertension is defined as a persistence increase in blood pressure above the normal range of 120/80 mmHg. The prevalence of hypertension increases with advancing age. The persistent and chronic elevated arterial pressure causes marked pathological changes in the vasculature and heart.
Understanding a blood pressure reading. Blood pressure is measured in stages, with a normal range being less than 120/80. The top number — the systolic — measures the pressure in your arteries when your heart beats. The bottom number — the diastolic - measures the pressure in your arteries when the blood is flowing back to the heart ...
Several rare, monogenic forms of hypertension have been described (for example, the Liddle syndrome, glucocorticoid-remediable aldosteronism (a mineralocorticoid excess state) and mutations in PDE3A (which encodes cGMP-inhibited 3',5'-cyclic phosphodiesterase A)), in which a single gene mutation fully explains the pathogenesis of hypertension and indicates the best treatment modality 7,8,9.
INTRODUCTION. Hypertension is the leading preventable risk factor for cardiovascular disease (CVD) and all-cause mortality worldwide. 1,2 In 2010, 31.1% of the global adult population (1.39 billion people) had hypertension, defined as systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg. 3 The prevalence of hypertension is rising globally owing to ageing of the population and increases in ...
When you have high blood pressure, the heart has to work harder to pump blood. The strain causes the walls of the heart's pumping chamber to thicken. This condition is called left ventricular hypertrophy. Eventually, the heart can't pump enough blood to meet the body's needs, causing heart failure. Kidney problems.
High blood pressure may affect the brain in the following ways: Transient ischemic attack (TIA). Sometimes this is called a ministroke. A TIA happens when the blood supply to part of the brain is blocked for a short time. Hardened arteries or blood clots caused by high blood pressure can cause TIAs. A TIA is often a warning sign of a full-blown ...
Hypertension and Healthy People 2020. Hypertension remains one of the most prevalent and treatable risk factors for cardiovascular disease and is associated with an enormous public health burden in terms of morbidity, mortality, and healthcare spending. 1 Both clinical and policy interventions have important roles to play in primary prevention ...
Hypertension, often referred to as high blood pressure, is a prevalent health condition that affects a significant portion of the population. It is characterized by elevated blood pressure levels, which can have detrimental effects on the cardiovascular system, kidneys, vision, and overall quality of life.This essay will explore the causes, effects, and management of hypertension in order to ...
Introduction. According to data from the National Health and Nutrition Examination Survey (NHANES) 2017 to 2018, 56.3% of US adults with hypertension have uncontrolled blood pressure (BP), defined by systolic BP (SBP) ≥140 mm Hg or diastolic BP (DBP) ≥90 mm Hg. 1 In October 2020, the US Surgeon General published a Call to Action to Control Hypertension that emphasized improving the ...
Hypertension or high blood pressure (HTN) means the pressure in arteries is consistently above normal 140/90 mmHg, or high than it should be resulting in excessive pressure on the walls of the arteries. Hypotension is an abnormally low blood pressure, which may be caused by emotional or traumatic shock; hemorrhage and chronic wasting disease.
High blood pressure is defined as having a systolic pressure above 140 mmHg and/or a diastolic pressure above 90 mmHg. There are two types of high blood pressure: primary (essential) and secondary. Primary hypertension is the most common form and typically develops gradually over time without any identifiable cause.
Takase et al. examined risk factors for hypertension using data from the Tohoku Medical Megabank cohort study, and found that body mass index, salt intake, urinary Na/K ratio, γ-GTP level, and ...
Causes of High Blood Pressure. High blood pressure can come from eating too much salt, not exercising, stress, or family history. Sometimes, it happens for no clear reason. It's important to eat healthy and stay active to prevent it. Why It's Serious. If not treated, hypertension can hurt important organs like the heart and kidneys.
Essay Writing Service. Blood pressure (BP) is defined as the amount of pressure exerted, when heart contract against the resistance on the arterial walls of the blood vessels. In a clinical term high BP is known as hypertension. Hypertension is defined as sustained diastolic BP greater than 90 mmHg or sustained systolic BP greater than 140 mmHg.
Background: Hypertension, or high blood pressure, is a major cause of disability and the leading risk factor for death around the world. Ongoing surveillance is necessary to monitor and assess the ...
1. Introduction. Hypertension is a major public health problem due to its high prevalence all around the globe [1-4].Around 7.5 million deaths or 12.8% of the total of all annual deaths worldwide occur due to high blood pressure [].It is predicted to be increased to 1.56 billion adults with hypertension in 2025 [].Raised blood pressure is a major risk factor for chronic heart disease, stroke ...
High blood pressure increases your risk for heart disease and stroke, two leading causes of death for both Florida and the United States (Centers for disease control, 2017). High blood pressure, also called hypertension, is known as the "silent killer" because it often has no warning signs or symptoms, and many people do not know they have it.
Secondary hypertension indicates that high blood pressure is a result of another underlying condition, such as kidney disease or tumors (adrenal-adenoma or pheochromocytoma). Persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure and arterial aneurysm, and is a leading cause of chronic renal failure.
Heart failure (HF) remains a significant global health burden, and hypertension is known to be the primary contributor to its development. Although aggressive hypertension treatment can prevent heart changes in at-risk patients, determining the optimal blood pressure (BP) targets in cases diagnosed with HF is challenging owing to insufficient evidence. Notably, hypertension is more strongly ...
Hypertension (high blood pressure) is one of the most preventable causes of premature morbidity and mortality world-wide. Made-to-order essay as fast as you need it Each essay is customized to cater to your unique preferences + experts online Get my essay Hypertension is known as...
If your readings are still very high, contact your health care professional immediately. You could be having a hypertensive crisis . Written by American Heart Association editorial staff and reviewed by science and medicine advisors. See our editorial policies and staff. For most people, high blood pressure has no signs or symptoms.
A total of 17/27 patients said they had experienced symptoms as a result of their hypertension. The most commonly reported symptoms were headaches, dizziness, hot flushes, and mood disorders (low mood, frustration, irritability). Other answers included chest tightness, palpitations, backache, constipation, and reduced vision.
The Causes Of Hypertension. This essay sample was donated by a student to help the academic community. Papers provided by EduBirdie writers usually outdo students' samples. Hypertension can be described as, the level of blood pressure reached when treatment is advantageous to an individual. Ideal blood pressure is seen to be between 90/60mmHg ...
This type of hypertension is known as essential or primary hypertension. High blood pressure caused by an underlying condition. This type of blood pressure is known as secondary hypertension, which tends to appear suddenly and cause high blood pressure, the condition such as obstructive sleep apnea, kidney disease, and medications.