- Case report
- Open access
- Published: 03 March 2021

Severe primary hypothyroidism in an apparently asymptomatic 19-year-old woman: a case report
- Rania Dannan ORCID: orcid.org/0000-0003-2456-572X 1 ,
- Sulaiman Hajji 2 &
- Khaled Aljenaee 2
Journal of Medical Case Reports volume 15 , Article number: 108 ( 2021 ) Cite this article
9157 Accesses
1 Altmetric
Metrics details
Hypothyroidism is diagnosed on the basis of laboratory tests because of the lack of specificity of the typical clinical manifestations. There is conflicting evidence on screening for hypothyroidism.
Case presentation
We report a case of an apparently healthy 19-year-old Kuwaiti woman referred to our clinic with an incidental finding of extremely high thyroid-stimulating hormone (TSH), tested at the patient’s insistence as she had a strong family history of hypothyroidism. Despite no stated complaints, the patient presented typical symptoms and signs of hypothyroidism on evaluation. Thyroid function testing was repeated by using different assays, with similar results; ultrasound imaging of the thyroid showed a typical picture of thyroiditis. Treatment with levothyroxine alleviated symptoms and the patient later became biochemically euthyroid on treatment.
There is controversy regarding screening asymptomatic individuals for hypothyroidism; therefore, it is important to maintain a high index of suspicion when presented with mild signs and symptoms of hypothyroidism especially with certain ethnic groups, as they may be free of the classical symptoms of disease.
Peer Review reports
We report a case of an apparently healthy 19-year-old Kuwaiti woman referred to our clinic with an incidental finding of extremely high thyroid-stimulating hormone (TSH), tested at the patient’s insistence as she had a strong family history of hypothyroidism. Despite no stated complaints, the patient presented typical symptoms and signs of hypothyroidism on evaluation. This raised the question of who should be screened for hypothyroidism. Screening for hypothyroidism refers to the measurement of thyroid function in asymptomatic populations who are at high risk of having thyroid disease, or patients who have mild, nonspecific symptoms, such as tiredness. Here, we summarize the conflicting evidence regarding screening for hypothyroidism, and emphasize the importance of maintaining a high index of suspicion for hypothyroidism even when presented with mild signs and symptoms.
A previously healthy, seemingly asymptomatic 19-year-old woman was referred to us by her general practitioner because of an extremely high TSH level of 1099 mlU/L, detected on random testing at the patient’s request because of her family’s history of autoimmune thyroid disease. The patient reported fatigue with excessive sleepiness lasting more than 14 hours per day, depressed mood, inexplicable weight gain, decreased appetite, hair loss, constipation, and menorrhagia, all indicative of a hypothyroid state. There was no history of chronic medical conditions or regular medication use, although the patient reported the use of over-the-counter paracetamol for headaches and dysmenorrhea. Physical examination showed normal vital parameters (weight 72 kg; height 160 cm; blood pressure 124/80 mmHg; pulse 56 bpm) and classical signs of hypothyroidism: periorbital puffiness and loss of outer third of her eyebrows and dry skin that was not coarse. Neck examination showed no scars and upward thyroid movement with deglutition, a smooth palpable goiter without nodules, and no palpable lymph nodes. Lower limb tone and power were intact despite slow relaxation of ankle reflexes.
Laboratory findings from before and after treatment initiation are presented in Table 1 . At the baseline in April 2019, the patient’s TSH was 1099 mlU/L (Roche assay) and free thyroxin (T4) was 0.7 pmol/L; the TSH level was retested in a Siemens assay, with a similar result (TSH 991 mlU/L). A subsequent anti-thyroid peroxidase (anti-TPO) antibodies test showed high levels (42 lU/mL). Complete blood count, renal function, liver enzymes, and lipid profile were tested; the hemoglobin level was 10 g/dL, with a microcytic hypochromic picture, most likely due to iron-deficiency anemia because the ferritin level was 6 ng/mL. The lipid profile showed dyslipidemia (total cholesterol 6.50 mmol/L, low-density lipoprotein 4.09 mmol/L, triglycerides 1.56 mmol/L). Renal function was normal. Ultrasound imaging of the thyroid showed diffuse cystic changes replacing much of the normal thyroid tissue with a “Swiss cheese” appearance (Fig. 1 ). The patient was started on levothyroxine in April 2019, and subsequent TSH and free T4 tested in December 2019 were 2.320 mIU/L and 17.5 pmol/L, respectively; symptom resolution was noted after a few weeks on levothyroxine (100 µg) supplementation, and the patient became biochemically euthyroid after 6 months.
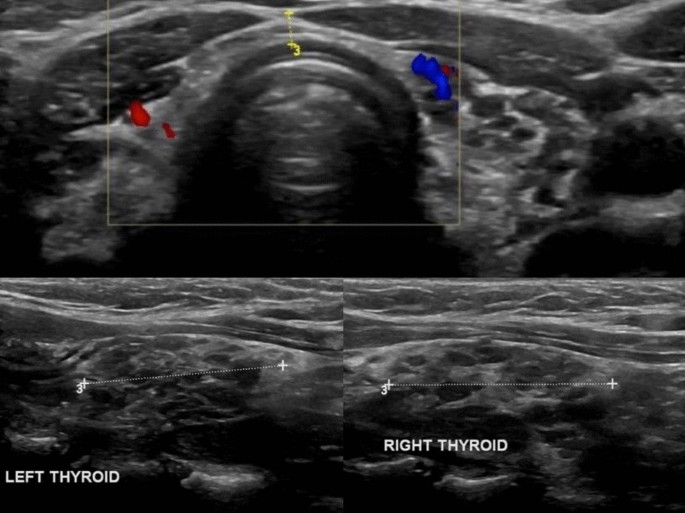
Ultrasound of the thyroid showing diffuse cystic changes replacing much of the normal thyroid tissue with a “Swiss cheese” appearance
Hypothyroidism is a disorder of thyroid hormone deficiency that affects 0.2–5.3% of Europeans and 0.3–3.7% of Americans [ 1 ]. Clinical manifestations vary by patient age as well as the duration and severity of thyroid hormone deficiency. Therefore, a definite diagnosis is primarily made on the basis of biochemical testing [ 2 ]. There is an ongoing debate about the optimal normal ranges of TSH and T4. A TSH level higher than 4.2–4.5 mlU/L and a free T4 less than 10 pmol/L confirms hypothyroidism [ 3 ]. Therapy aims to supplement thyroxine to alleviate signs and symptoms of hypothyroidism, and to normalize serum thyrotropin without overtreatment [ 2 ].
In younger populations, typical symptoms of hypothyroidism are usually present and can facilitate diagnosis, whereas a diagnosis in the elderly is difficult because of seemingly asymptomatic presentation and thus necessitates a high index of suspicion in clinicians to predict hypothyroidism [ 2 ]. Moreover, symptoms and signs of hypothyroidism vary from person to person depending on age, gender, and origin [ 4 , 5 , 6 ]. Table 2 presents the commonest symptoms and signs of patients with hypothyroidism in Saudi Arabia, Oman, and Australia; in all three countries, tiredness, which was documented in 56%, 25%, and 84% of patients, respectively, was the most common presenting symptom [ 4 , 5 , 6 ]. Our patient presented with symptom unawareness despite an extremely high TSH level incidentally detected on biochemical testing, but had typical symptoms of hypothyroidism on clinical evaluation. This raises the question of hypothyroidism screening: who should be screened? And when should they be screened?
Screening for hypothyroidism refers to the measurement of thyroid function in asymptomatic populations who are at high risk of having thyroid disease, or patients who have mild, nonspecific symptoms, such as tiredness. Screening is carried out by measuring serum TSH levels [ 6 ], but there are conflicting recommendations on screening. The American Thyroid Association (ATA) recommends screening for hypothyroidism in all adults 35 years and older every 5 years and in certain high-risk individuals [ 6 ]. However, the US Preventative Task Force (USPTF) found insufficient evidence for screening of thyroid dysfunction and emphasizes the uncertainties surrounding potential clinical benefits [ 7 ]. Similarly, the Royal College of Physicians in London found no justification for screening for hypothyroidism even in the elderly and individuals with a strong family history of thyroid disease [ 8 ]. Exceptions include screening of newborn babies for congenital hypothyroidism and patients with previous thyroid surgery or radioactive iodine treatment as well as patients receiving long-term lithium or amiodarone therapy [ 8 ]. There are no strong recommendations for screening of the non-pregnant asymptomatic population for hypothyroidism. Therefore, many asymptomatic patients with overt hypothyroidism could remain undiagnosed and untreated.
Our 19-year-old patient presented to the clinic with no complaints, but further assessment revealed typical signs and symptoms of hypothyroidism and a TSH level higher than 1000 mlU/L. All symptomatic patients should be evaluated for hypothyroidism, but screening of asymptomatic individuals is controversial and not recommended by certain organizations. This report is presented to recommend a lowering of the screening threshold for hypothyroidism and to motivate physicians to boost their index of suspicion to diagnose the disease, especially with certain ethnic groups, as they may be free of the classical symptoms so severe hypothyroidism can be missed.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
Anti-thyroid peroxidase
American Thyroid Association
High-density lipoprotein
Low-density lipoprotein
Mean corpuscular volume
Thyroid-stimulating hormone
The United States Preventive Services Task Force
Taylor PN, Albrecht D, Scholz A, et al . Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. 2018;14(5):301–16.
Article Google Scholar
Carle A, Pedersen IB, Knudsen N, et al. Hypothyroid symptoms fail to predict thyroid insufficiency in old people: a population-based case–control study. Am J Med. 2016;129(10):1082–92. https://doi.org/10.1016/j.amjmed.2016.06.013 .
Article PubMed Google Scholar
Lewandowski K. Reference ranges for TSH and thyroid hormones. Thyroid Res. 2015;8(Suppl 1):A17.
El-Shafie KT. Clinical presentation of hypothyroidism. J Fam Community Med. 2003;10(1):55–8.
Google Scholar
Al-Sultan AI, Larbi EB, Magbool G, Karima T, Bagshi M. Clinical presentation of spontaneous primary hypothyroidism in adults. Ann Saudi Med. 1995;15(2):143–7.
Article CAS Google Scholar
Oddie TH, Boyd CM, Fisher DA, Hales IB. Incidence of signs and symptoms in thyroid disease. Med J Aust. 1972;2(18):981–6.
Garber JR, Cobin RH, Gharib H, et al . Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012;22(12):1200–35.
LeFevre ML, Siu AL, Bibbins-Domingo K, et al . Screening for thyroid dysfunction: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;162(9):641–50.
Vanderpump MPJ, Ahlquist JAO, Franklyn JA, Clayton RN. Consensus statement for good practice and audit measures in the management of hypothyroidism and hyperthyroidism. Br Med J. 1996;313(7056):539–44.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Kuwaiti Board of Internal Medicine, Ahmadi, Kuwait
Rania Dannan
Al-Adan Hospital, Kuwait City, Kuwait
Sulaiman Hajji & Khaled Aljenaee
You can also search for this author in PubMed Google Scholar
Contributions
RD was responsible for the literature review and writing of the article and is the corresponding author; SH edited the manuscript and gained consent from the patient; KJ supplied most of the patient information and images. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Rania Dannan .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dannan, R., Hajji, S. & Aljenaee, K. Severe primary hypothyroidism in an apparently asymptomatic 19-year-old woman: a case report. J Med Case Reports 15 , 108 (2021). https://doi.org/10.1186/s13256-021-02677-w
Download citation
Received : 21 November 2020
Accepted : 11 January 2021
Published : 03 March 2021
DOI : https://doi.org/10.1186/s13256-021-02677-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypothyroidism
- Asymptomatic
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
MINI REVIEW article
Crash landing of thyroid storm: a case report and review of the role of extra-corporeal systems.

- 1 Department of Cardiology, National University Heart Center, Singapore, Singapore
- 2 Division of Endocrinology, Department of Medicine, National University Hospital, Singapore, Singapore
- 3 Department of Hematology-Oncology, National University Cancer Institute, Singapore, Singapore
- 4 Cardiothoracic Intensive Care Unit, National University Heart Center, Singapore, Singapore
- 5 Department of Surgery, Yong Loo Lin School of Medicine, Singapore, Singapore
- 6 Department of Medicine, Yong Loo Lin School of Medicine, Singapore, Singapore
Thyroid storm is a rare but life-threatening endocrinological emergency with significant mortality ranging from 10-30% with multi-organ involvement and failure. In view of the rarity of this condition and efficacy of established first line medical treatment, use of extra-corporeal treatments are uncommon, not well-studied, and its available evidence exists only from case reports and case series. We describe a 28-year-old man who presented with an out-of-hospital cardiac arrest secondary to thyroid storm. Despite conventional first-line pharmacotherapy, he developed cardiogenic shock and circulatory collapse with intravenous esmolol infusion, as well as multi-organ failure. He required therapeutic plasma exchange, concurrent renal replacement therapy, and veno-arterial extra-corporeal membrane oxygenation, one of the few reported cases in the literature. While there was clinical stabilization and improvement in tri-iodothyronine levels on three extra-corporeal systems, he suffered irreversible hypoxic-ischemic brain injury. We reviewed the use of early therapeutic plasma exchange and extra-corporeal membrane oxygenation, as well as the development of other novel extra-corporeal modalities when conventional pharmacotherapy is unsuccessful or contraindicated. This case also highlights the complexities in the management of thyroid storm, calling for caution with beta-blockade use in thyrocardiac disease, with close monitoring and prompt organ support.
Introduction
Thyroid storm (TS) is a life-threatening exacerbation of the hyperthyroid state characterized by multi-organ dysfunction of the cardiovascular, thermoregulatory, gastrointestinal-hepatic and central nervous systems. While the incidence among hospitalized patients is estimated to be low at 1-2% ( 1 ), the overall mortality is 10-30% ( 2 ), with a 12-fold increase in mortality compared to individuals with thyrotoxicosis ( 3 ). The diagnosis of TS is additionally challenging due to the absence of specific clinical or laboratory findings. Early recognition of this condition is key, as it allows for prompt and specific treatment, as well as early identification of organ dysfunction with initiation of supportive measures in the intensive care setting if required.
We present a case of TS in a young patient with undiagnosed Graves’ disease, presenting with an out-of-hospital cardiac arrest. Initially hemodynamically stable following return of spontaneous circulation, he developed circulatory collapse after intravenous esmolol infusion, initiated for control of tachycardia. There was consequent multi-organ failure which contraindicated the use of standard anti-thyroid drug therapy. He required three extra-corporeal systems of continuous renal replacement therapy (CRRT), veno-arterial extra-corporeal membrane oxygenation (VA-ECMO) and therapeutic plasma exchange (TPE) for stabilization, one of the few reported cases in the literature.
Case Description
A 28-year-old male presented with an out-of-hospital ventricular fibrillation (VF) arrest, preceded by an acute respiratory illness. There was return of spontaneous circulation after 60 minutes of resuscitation with bystander cardiopulmonary resuscitation and external defibrillation by paramedics. In the Emergency Department, he was febrile at 40.5 degrees Celsius, hypertensive with a blood pressure of 146/83mmHg and tachycardic with a heart rate of 155 beats per minute. Physical examination was unremarkable, except for a Glasgow Coma Scale of 3. No goiter was seen on examination. Corroborative history from his family confirmed symptoms of heat intolerance, loss of weight, hand tremors and palpitations in the preceding two months, as well as a maternal history of Graves’ thyrotoxicosis.
Initial investigations showed elevated inflammatory markers, mixed respiratory and metabolic acidosis, raised troponin I, but with normal electrolyte levels. Electrocardiogram confirmed sinus tachycardia. Chest radiograph showed prominent pulmonary vasculature without evidence of pneumonia. Point-of-care echocardiogram showed impaired left ventricular systolic function without other obvious abnormalities; the marked sinus tachycardia precluded accurate estimation of the left ventricular ejection fraction (LVEF). Computed tomographic (CT) scan of the brain was normal, and urine drug screen was negative. A coronary angiogram performed was normal, and a provisional diagnosis of acute myocarditis was made. Thyroid function test, sent as part of investigations for myocarditis, showed thyrotoxicosis with an elevated serum free thyroxine (FT4) level of 42.1pmol/L (reference range: 8.0-16.0pmol/L) and a suppressed serum thyroid stimulating hormone (TSH) at <0.01mIU/L (reference range: 0.45-4.50mIU/L) ( Figure 1 ) – our patient had thyroid storm complicated by thyrocardiac disease, with a Burch-Wartofsky score of 105. His thyroid-stimulating hormone receptor antibody eventually returned elevated at >40IU/L (normal ≤2.0IU/L), confirming underlying Graves’ disease.
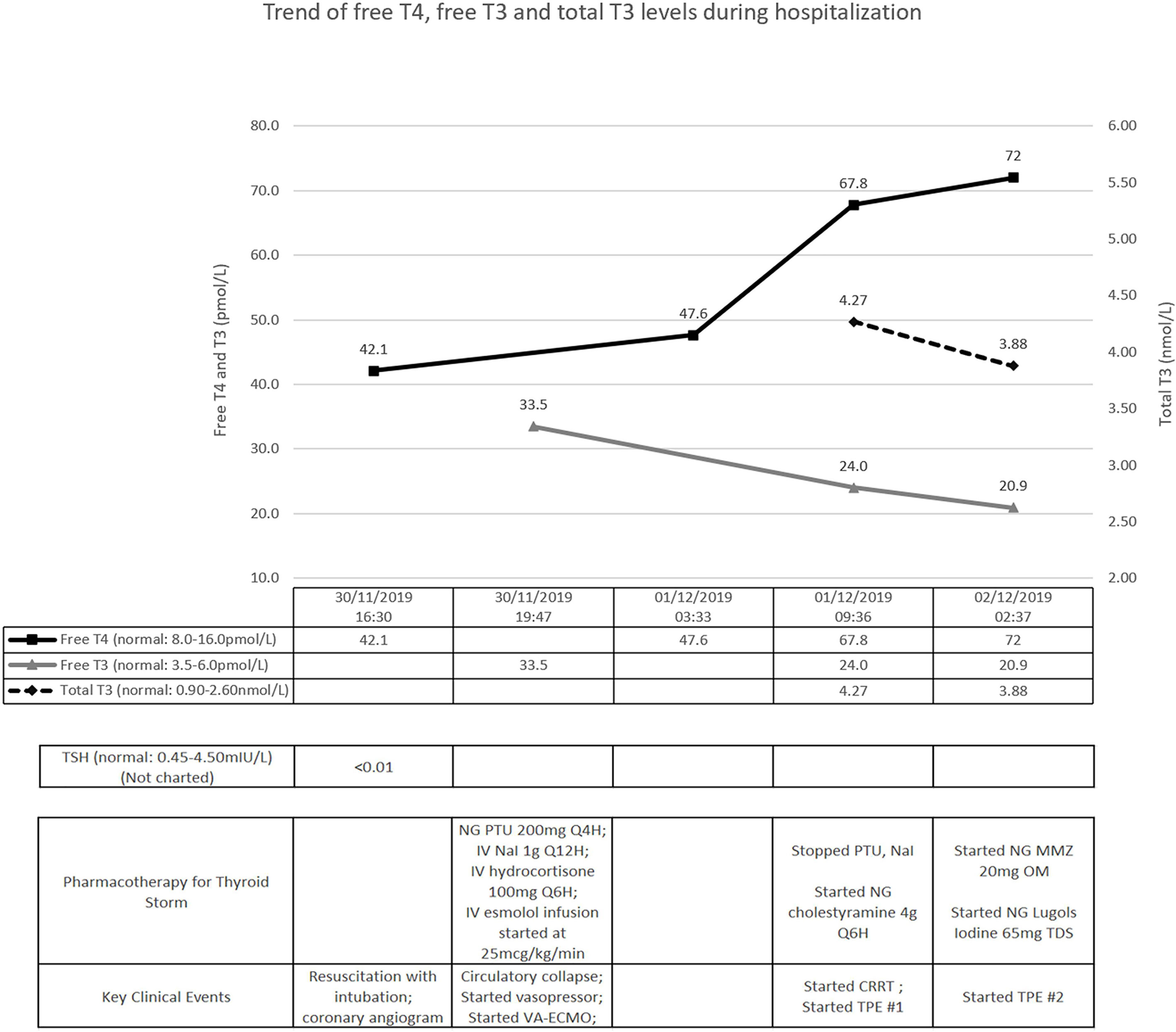
Figure 1 Timeline of key clinical events. T4, thyroxine; T3, tri-iodothyronine; TSH, thyroid-stimulating hormone; NG, nasogastric; IV, intravenous; PTU, propylthiouracil; NaI, sodium iodide; VA-ECMO, veno-arterial extra-corporeal membrane oxygenation; CRRT, continuous renal replacement therapy; TPE, therapeutic plasma exchange; MMZ, methimazole.
Treatment was promptly initiated with nasogastric propylthiouracil, intravenous sodium iodide and hydrocortisone ( Figure 1 ). Temperature was controlled with a cooling blanket. Judicious low dose esmolol infusion was commenced at 25mcg/kg/min to manage the tachycardia. This was followed shortly by a pulseless electrical activity arrest. Despite a short downtime of three minutes and prompt cessation of beta-blockade, he required high doses of noradrenaline and vasopressin thereafter. He remained persistently hypotensive with maximal dual vasopressor support, and was initiated on VA-ECMO support ( Figure 2 ).
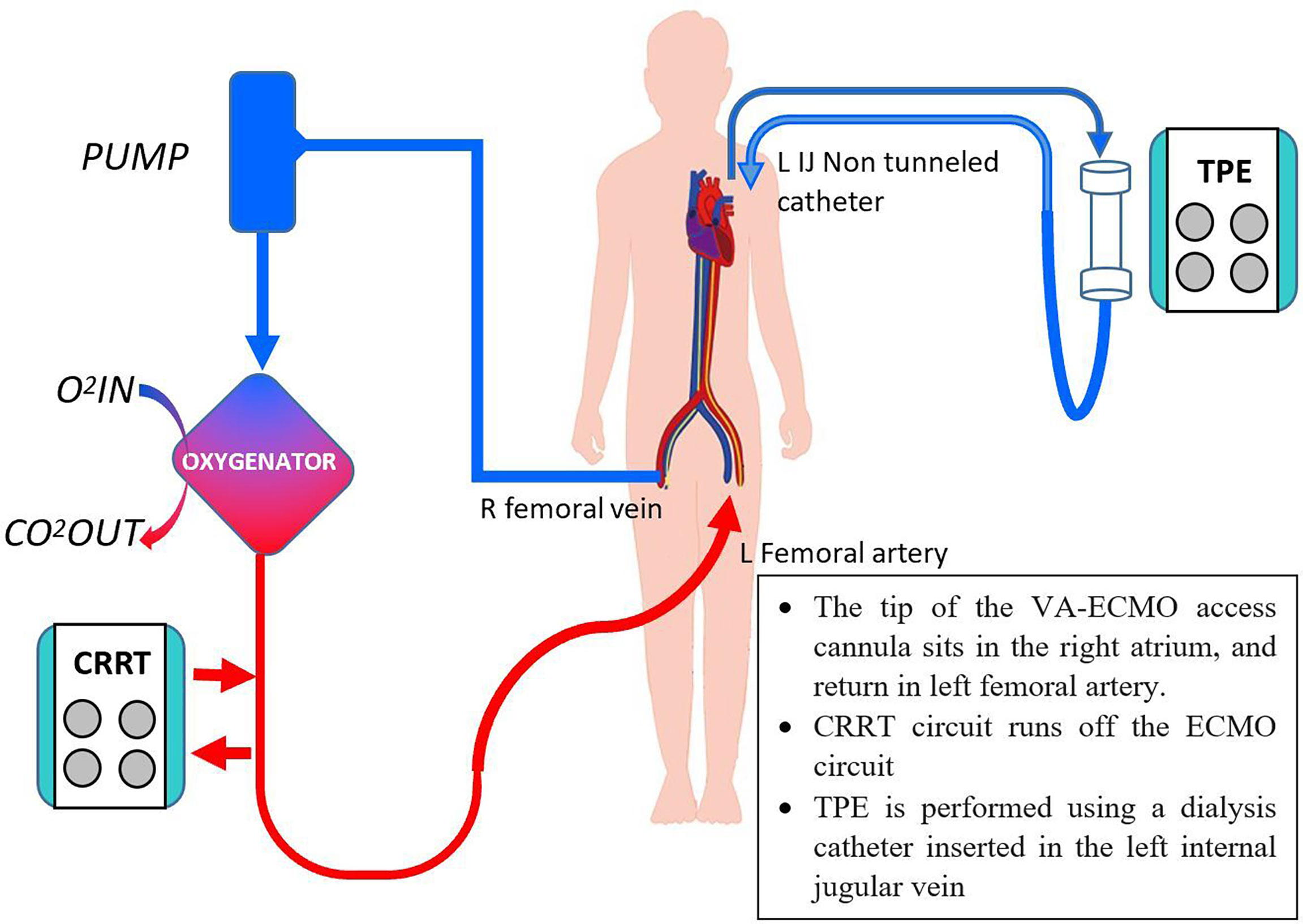
Figure 2 Concurrent CRRT, VA-ECMO and TPE. O 2 , oxygen, CO 2 , carbon dioxide, others as per Figure 1 .
Further investigations revealed worsening transaminitis and anuric acute kidney injury, requiring CRRT. Transthoracic echocardiogram showed severe left ventricular systolic dysfunction with estimated LVEF of 10%. Pharmacological options were now limited to cholestyramine and hydrocortisone. We decided to institute TPE; with the first cycle performed on day 2 of admission, with 2.5L of albumin and 0.5L of saline ( Figure 1 ). After the first cycle, his vasopressor support reduced significantly (only requiring low dose noradrenaline infusion) and his tri-iodothyronine (T3) levels improved ( Figure 1 ). As his FT4 continued to worsen, nasogastric methimazole and Lugol’s iodine were cautiously started, along with second TPE cycle, on the third day.
His pupils were noted to be fixed and dilated with the second cycle of TPE ongoing. Urgent CT scan of the brain revealed diffuse cerebral edema with severe mass effect and tonsillar herniation. A decision was made in conjunction with his family for withdrawal of care, given the grave prognosis.
Evidence of Use of Extra-Corporeal Systems in TS
Our patient is one of the few reported cases where multiple extra-corporeal systems were used (TPE, CRRT, and VA-ECMO) in TS management. On review of the medical literature of articles in English, there has only been four case reports describing the concurrent use of TPE and ECMO in patients with thyrotoxicosis with circulatory collapse ( 4 – 7 ), with one of them reporting the use of three extra-corporeal systems ( 4 ).
Characterized by extreme multi-systemic manifestations of thyrotoxicosis, TS is uncommon but potentially fatal, with a mortality rate of 10-30% ( 2 ). Standard first-line pharmacotherapy in TS aims to block production and release of thyroid hormones with propylthiouracil or methimazole, inhibit release of pre-formed thyroid hormones with iodine, decrease peripheral conversion of T4 to T3 with propylthiouracil and steroids, and treat adrenergic symptoms with beta-blockade, prior to definitive treatment in the form of surgery or radioactive iodine (RAI) ablation. These methods are efficacious and rapid acting. However, certain patients are not able to tolerate, or fail pharmacotherapy, as seen in our patient with multi-organ failure precluding the use of conventional treatment. In such cases, alternative treatment including use of extra-corporeal systems must be considered, of which TPE is the most well established.
TPE is an extra-corporeal blood purification technique used for eliminating large molecular substances. Currently, TPE has a Class II indication for TS in the 2019 American Society for Apheresis (ASFA) guidelines, either as a standalone or adjunct therapy, although the grade 2C level of recommendation suggests the evidence arises mostly from case reports and case series, with an absence of prospective randomized controlled trials ( 8 ). TPE is postulated to work by several mechanisms including: 1) reducing protein-bound thyroid hormones of which 99.97% of total serum T4 and 99.7% of total serum T3 are bound to plasma proteins thyroxine binding globulin (TBG), transthyretin and albumin ( 9 ), 2) additionally reducing autoantibodies and cytokines of a predominantly Th1 pattern including interleukin-2, interferon-γ and tumor necrosis factor-α ( 10 – 12 ), and 3) removing 5’-monodeiodinase which converts T4 to T3 ( 12 ). TPE is shown to reduce all of free and total T4 and T3 ( 13 ), by an estimated 10-80% ( 12 ), and at a greater rate than standard medical therapy for patients with hyperthyroidism ( 14 ). However, these effects are transient and usually last for only 24-48 hours, with a potential risk for rebound thyrotoxicosis ( 12 ). This appears related to the fact that only thyroid hormones from the intravascular compartment is removed, with rapid re-equilibrium from the extravascular spaces. A study in 13 healthy individuals showed the intravascular component of thyroxine accounts for only 26% of the distribution ( 15 ), with the other sites of distribution found to be 14% in the liver, 34% in extrahepatic tissue and 26% in extracellular fluid pools. These transient effects suggest that multiple cycles of TPE may be required, and should be used only as a temporizing measure for definitive treatment ( 12 ). TPE can be performed with either plasma or albumin replacement, and the ASFA guideline does not preferentially recommend the use of plasma or albumin. It has been proposed that plasma has the theoretical advantage of containing binding proteins TBG and transthyretin, which has higher affinity to bind free T4 and T3, as well as avoid depleting coagulation factors thus avoiding complications of bleeding ( 13 ). However, there is similarly a theoretical risk of the presence of thyroid hormones from donor plasma, as well as higher risks of transfusions reactions and infections with use of plasma. Till date, there are no direct head-to-head trials between the use of plasma and albumin in TPE in patients with TS. TPE is generally well tolerated, with risks of minor side effects ranging from about 5% ( 9 ) to 36% ( 16 ), including nausea and vomiting, vagal or hypotensive response and transfusion reactions. The risk of death with TPE for any indication is exceedingly rare at 0.05% ( 17 ), and this is usually attributed to the severity of the underlying condition.
ECMO is an established life-saving treatment option for patients who develop acute cardiopulmonary failure ( 18 ), although its use in endocrinological emergencies is still under research ( 19 ). Use of ECMO in patients with thyrotoxicosis have largely been reported in the form of case reports or case series within the literature. In 2011, Hsu et al. ( 20 ) first reported a series with the use of supportive ECMO ranging from 19-114 hours in four cases of thyrotoxicosis-induced cardiovascular collapse. Three patients survived, with normalization of thyroid function and improved cardiovascular function. A subsequent review by White et al. ( 21 ) published in 2018 reported the successful use of ECMO with survival in 11 out of 14 patients ( 22 – 24 ) between 1970 to 2017 with thyrotoxicosis-induced cardiomyopathy, with near complete recovery of left ventricular function. A review of the cases with the use of ECMO and other extra-corporeal systems in patients with severe thyrotoxicosis or thyroid storm has been summarized in Table 1 , including additional new cases reported from 2018 to 2021 ( 25 – 28 ) and conference poster reports ( 29 – 32 ). These 27 cases (inclusive of our case) showed survival in 85.2% (23 of the 27 cases), with survival in all four of the reported cases requiring additional extra-corporeal support of TPE or CRRT ( 4 – 7 ). ECMO was initiated for either cardiovascular collapse or circulatory shock, and lasted between 19 hours to 18 days. Within the reports of successful outcomes, all cases reported clinical and biochemical improvement in thyrotoxicosis, as well as improvement in cardiac function, although numerical data were not available in some of the reports. The details of these cases are reported in Table 1 . The use of ECMO however, must be weighed against the contraindications and complications of ECMO use, including bleeding, thromboembolism, strokes and access injuries such as hemorrhage, arterial dissection, and distal limb ischemia ( 18 ).
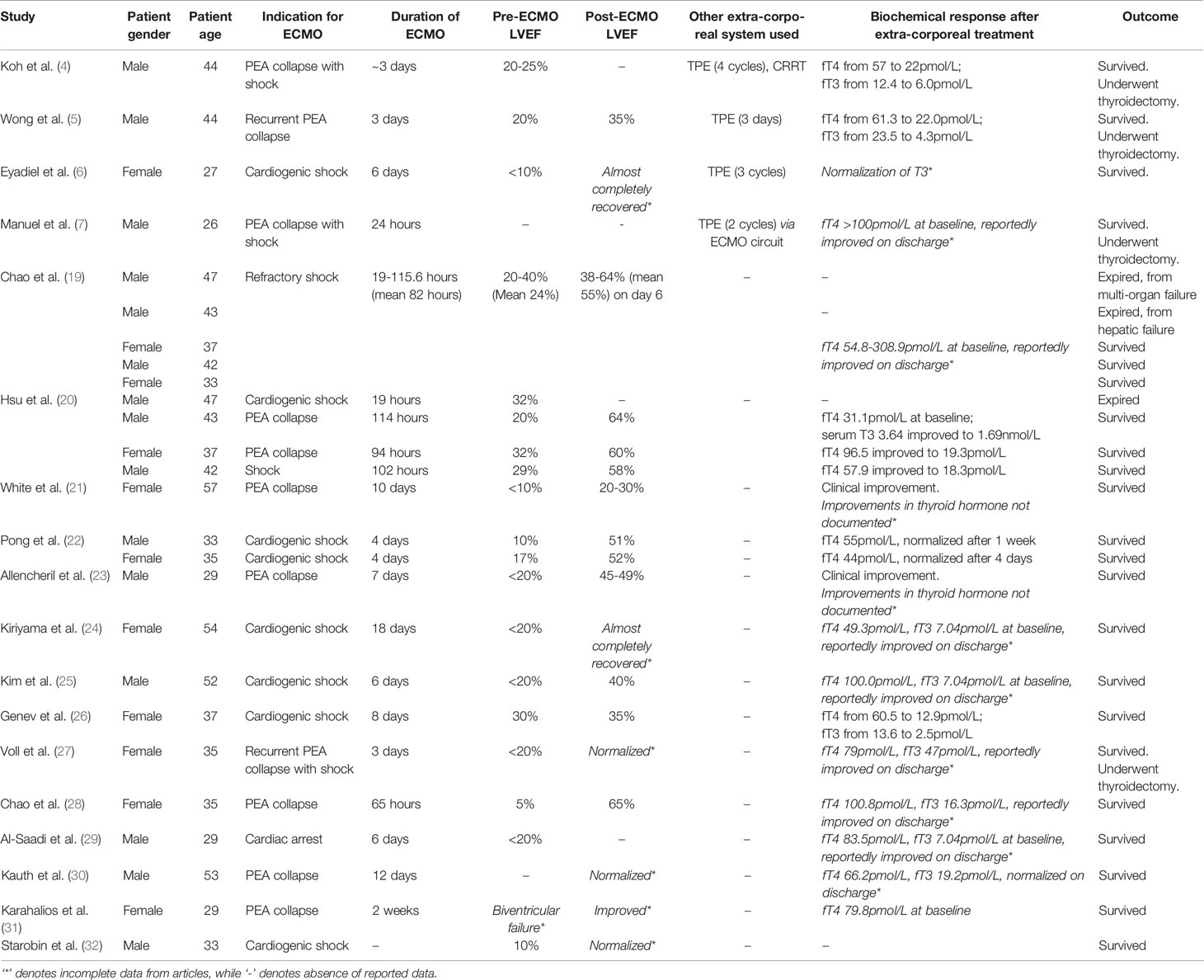
Table 1 Summary of cases with use of ECMO and other extra-corporeal systems in patients with severe thyrotoxicosis or thyroid storm.
Novel therapies are also increasingly considered for TS, using principles similar to TPE by removing protein bound thyroid hormones. Case reports with the use of dialysis has been proposed in management of thyroid storm, most notably with CRRT, which is preferred due to its better tolerability in hemodynamically unstable patients due to its slower rate of exchange of fluids and solutes. Parikh et al. ( 33 ) and Koball et al. ( 34 ) illustrated the sequential use of single pass continuous veno-venous albumin dialysis after limited response to TPE, demonstrating a more sustained improvement in thyroid hormones with less rebound thyrotoxicosis, as well as greater removal of thyroid hormones overall. Other studies have shown the additive effects of TPE and CRRT in removal of thyroid hormones ( 35 ), while another study reported a correlation of improvement of total T3 and free T4 levels of up to 80% with concomitant CRRT and standard medical therapy (without TPE), although the exact mechanisms are unclear ( 36 ). The Molecular Adsorption Recirculation Systems (MARS) has also been used, with one case report with TS and severe liver dysfunction showing rapid resolution of thyroid hormones and improvement of bilirubin ( 37 ). A retrospective case series also demonstrated significant improvement in thyroid hormone levels in patients with hyperthyroidism with severe liver dysfunction (although this study was primarily powered to show improvement and safety of use of RAI with combined with MARS in patients with severe hyperthyroidism and liver disease) ( 38 ). These reports provide early evidence of the utility of novel extra-corporeal systems in correcting thyroid hormone levels especially in patients with either kidney or liver dysfunction, although more research into the underlying mechanism and validation of results are required before recommendations can be made for its supportive use.
These cases provide some evidence of the use and benefits of extra-corporeal systems in the management of TS, after conventional pharmacotherapy is unsuccessful or contraindicated. Owing to the efficacy of pharmacotherapy and risks of extra-corporeal systems, conventional pharmacotherapy should be always be instituted as initial therapy. Comparison trials between pharmacotherapy and extra-corporeal systems or randomized controlled trials are unavailable due to the rarity of TS, and are unlikely to be performed now given the established efficacy of first line pharmacological agents. Retrospective analysis from the National Inpatient Database in Japan has shown that use of extra-corporeal systems is associated with higher mortality. It reported increased mortality in patients requiring hemodialysis and TPE with adjusted odds ratio for mortality at 4.81. The mortality was 61.9% in 13 out of 21 patients, compared to a mortality of 43.3% requiring either hemodialysis or TPE, and 7.8% requiring neither support. The use of ECMO had a trend towards increased mortality (2.86, CI 0.69-11.92), with a mortality of 72.2% among 13 of 18 patients, as compared to 9.3% in patients not requiring ECMO ( 39 ). These numbers, albeit small, suggest a significantly higher mortality in patients requiring use of extra-corporeal systems, and this differs from the established mortality rate of 10-30%, and vary significantly from the numbers in our review and White et al.’s review in patients requiring ECMO ( 21 ). Similarly Muller et al. ( 12 ) showed the use of TPE showed significant clinical and biochemical improvement. As patients requiring extra-corporeal systems are typically patients who are more critically ill and have multi-organ failure, as well as the possibility of publication bias, it is likely that the true survival rate of these patients in thyroid storm treated with extra-corporeal systems is likely lower than the published literature. Further research, possibly in the form of prospective multinational studies, may be required in view of the small numbers and limited data currently.
Beta-Blockade – A Double-Edged Sword in TS
While our patient received guideline-directed TS pharmacological therapy in a timely fashion, the development of circulatory collapse with consequent multi-organ failure following intravenous esmolol infusion, an ultra-short acting beta-blocker, deserves further discussion.
The cardiovascular effects in TS are driven largely by T3, leading to increased chronotropy and inotropy, improved diastolic relaxation and decreased peripheral resistance, eventually resulting in high cardiac output (CO) heart failure (HF), estimated to be seen in 6% of patients with thyrotoxicosis. This is thought to be reversible with treatment with thyrotoxicosis, with a small study showing improving in LVEF from 28% to 55% ( 40 ). Cardiomyopathy and LV dysfunction, on the other hand, are only seen in 1% ( 20 , 41 ). HF with low CO has been reported with prolonged severe hyperthyroidism, consequent to persistent tachycardia, and pathologic increase in cardiac workload with demand-supply mismatch ( 42 ). Aside from cardiomyopathy, there is an increased risk of arrhythmias with thyrotoxicosis, typically supraventricular, with rare reported cases of thyrotoxicosis-related VF related to congenital coronary anomalies, hypokalemia, coronary vasospasm and early repolarization ( 43 ), none of which were present in our patient. It is plausible that our patient had low CO thyrocardiac disease with an additional component of myocardial stunning post-cardiac arrest, but his stormy course precluded detailed cardiac imaging.
Tachycardia is almost always present in TS, and patients with tachycardia exceeding 150 beats per minute are associated with a higher mortality rate in a retrospective Japanese cohort ( 44 ). Accordingly, the Japanese Thyroid Association and Japanese Endocrine Society 2016 guidelines ( 45 ) recommend aggressive control of tachycardia including the use of ultra-short acting beta-blockers including esmolol or landiolol. New data are emerging which support the use of esmolol over propranolol, due to its shorter half-life elimination (nine minutes, versus 2.3 hours respectively) and duration of action, as well as its relatively higher beta 1-selectivity ( 46 ). The comparative use of esmolol and propranolol has been studied in other populations such as patients with supraventricular tachycardia, which showed similar response rate but more adverse effect of hypotension seen in the esmolol group (45%, as compared to 18%), although these were mostly asymptomatic and resolved quickly with no complications ( 47 ). Regardless of choice of beta-blockers, its use must be considered with caution in patients with decompensated HF or other features of low CO, where the thyroid-induced hyperadrenergic state plays an important compensatory role in maintaining CO. This is related to either direct catecholamine action or an interaction between the adrenergic system and excessive circulating thyroid hormone ( 48 ). The abolishment of that sympathetic drive through the use of beta-blockers is postulated to lead to the circulatory collapse, as seen in our case. Though initially hypertensive, the temporal association of esmolol infusion and PEA arrest led us to conclude it caused or at least triggered the hemodynamic decompensation in our patient. Abubaker et al. ( 49 ) reviewed a total of 11 cases of circulatory collapse with the use of beta-blockade, mostly with long acting agents including bisoprolol, metoprolol, propranolol, with all but one patient showing evidence of underlying heart failure or cardiomyopathy. The author also highlighted the challenges in managing uncontrolled tachycardia in these patients, with two cases eventually requiring esmolol and landiolol use. To date, there has been no head-to-head trials between the longer acting propranolol as compared to the ultra-short acting esmolol or landiolol. There has no reports of circulatory collapse with use of intravenous esmolol, and only one case report with landiolol ( 50 ). Despite the use of ultra-short acting esmolol, circulatory collapse in our case underscores its class effect, and is strongly associated with fatal outcomes in TS. Close cardiac monitoring and prompt institution of VA ECMO support, as what was done in this case, are recommended. Other forms of supportive therapy including CRRT may be considered until effective and definitive therapies can be instituted to treat TS.
We highlight a case of TS presenting with out-of-hospital cardiac arrest, with further hemodynamic decompensation following beta-blockade and multi-organ failure which limited therapeutic options. Despite prompt initiation of CRRT, VA-ECMO and TPE, he sustained hypoxic-ischemic brain injury. Underscoring the complexities in TS, this case calls for caution with beta-blockade in thyrocardiac disease, close monitoring and prompt organ support, and consideration of early TPE when conventional options fail. A review of the use of TPE and other extra-corporeal systems shows that TPE may be an underutilized rescue treatment for severe thyroid storm not amenable to conventional pharmacotherapy or contraindicated due to side effects or multi-organ involvement. Further study of novel extra-corporeal therapies for TS is needed to uncover its therapeutic potential, especially in the Intensive Care setting.
Author Contributions
All authors were involved in the management of the patient. SL, KW, and SY wrote the first draft of the manuscript. PL and KR reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Klubo-Gwiezdzinska J, Wartofsky L. Thyroid Emergencies. Med Clin North Am (2012) 96(2):385–403. doi: 10.1016/j.mcna.2012.01.015
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Chiha M, Samarasinghe S, Kabaker AS. Thyroid Storm: An Updated Review. J Intensive Care Med (2015) 30(3):131–40. doi: 10.1177/0885066613498053
3. Galindo RJ, Hurtado CR, Pasquel FJ, Tome RG, Peng L, Umpierrez GE. National Trends in Incidence, Mortality, and Clinical Outcomes of Patients Hospitalized for Thyrotoxicosis With and Without Thyroid Storm in the United States, 2004-2013. Thyroid (2019) 29(1):36–43. doi: 10.1089/thy.2018.0275
4. Koh H, Kaushik M, Loh JK, Chng CL. Plasma Exchange and Early Thyroidectomy in Thyroid Storm Requiring Extracorporeal Membrane Oxygenation. Endocrinol Diabetes Metab Case Rep (2019) 1):1–6. doi: 10.1530/EDM-19-0051
CrossRef Full Text | Google Scholar
5. Wong IMJ, Lim JY, Goh JTK, Tan QL, Tay CK. Thyroid Storm Rescued by Extracorporeal Membrane Oxygenation Support, Plasmapheresis and Thyroidectomy: A Case Report. J Emerg Crit Care Med (2021) 5:19. doi: 10.21037/jeccm-20-147
6. Eyadiel L, Amjad A, Pisani B, Miller P, Jain R. Use of Therapeutic Plasma Exchange and ECMO Support With Impella for LV Vent as Treatment for Cardiogenic Shock in Acute Thyrotoxicosis/Thyroid Storm. J Card Fail (2018) 24:S84–5. doi: 10.1016/j.cardfail.2018.07.337
7. Manuel L, Fong LS, Lahanas A, Grant P. How to do it: Plasmapheresis via Venoarterial Extracorporeal Membrane Oxygenation Circuit for Thyroid Storm. Ann Med Surg (Lond) (2021) 67:102485. doi: 10.1016/j.amsu.2021.102485
8. Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E, et al. Guidelines on the Use of Therapeutic Apheresis in Clinical Practice – Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Eighth Special Issue. J Clin Apher (2019) 34(3):171–354. doi: 10.1002/jca.21705
9. Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ. Williams Textbook of Endocrinology . 14th Edition. Philadelphia, PA: Elsevier (2020).
Google Scholar
10. Ganesh BB, Bhattacharya P, Gopisetty A, Prabhakar BS. Role of Cytokines in the Pathogenesis and Suppression of Thyroid Autoimmunity. J Interferon Cytokine Res (2011) 31(10):721–31. doi: 10.1089/jir.2011.0049
11. Tan AWK, Lim BSP, Hoe JKM, Hoi WH, Leow MKS. Therapeutic Plasma Exchange for Control of Thyroid Storm. J Clin Apher (2021) 36:189–95. doi: 10.1002/jca.21832
12. Muller C, Perrin P, Faller B, Richter S, Chantrel F. Role of Plasma Exchange in the Thyroid Storm. Ther Apher Dial (2011) 15(6):522–31. doi: 10.1111/j.1744-9987.2011.01003.x
13. Garla V, Kovvuru K, Ahuja S, Palabindala V, Malhotra B, Salim SA. Severe Hyperthyroidism Complicated by Agranulocytosis Treated With Therapeutic Plasma Exchange: A Case Report and Review of the Literature. Case Rep Endocrinol (2008) 4135940. doi: 10.1155/2018/4135940
14. Binimelis J, Bassas L, Marruecos L, Rodriguez J, Domingo ML, Madoz P, et al. Massive Thyroxine Intoxication: Evaluation of Plasma Extraction. Intensive Care Med (1987) 13(1):33–8. doi: 10.1007/BF00263555
15. Nicoloff JT, Dowling JT. Estimation of Thyroxine Distribution in Man. J Clin Invest (1986) 47(1):26–37. doi: 10.1172/JCI105712
16. Shemin D, Briggs D, Greenan M. Complications of Therapeutic Plasma Exchange: A Prospective Study of 1,727 Procedures. J Clin Apher (2007) 22(5):270–6. doi: 10.1002/jca.20143
17. McLeod BC, Sniecinski I, Ciavarella D, Owen H, Price TH, Randels MJ, et al. Frequency of Immediate Adverse Effects Associated With Therapeutic Apheresis. Transfusion (1999) 39(3):282–8. doi: 10.1046/j.1537-2995.1999.39399219285.x
18. Ventetuolo CE, Muratore CS. Extracorporeal Life Support in Critically Ill Adults. Am J Respir Crit Care Med (2014) 190(5):497–508. doi: 10.1164/rccm.201404-0736CI
19. Chao A, Wang CH, You HC, Chou NK, Yu HY, Chi NH, et al. Highlighting Indication of Extracorporeal Membrane Oxygenation in Endocrine Emergencies. Sci Rep (2015) 5:13361. doi: 10.1038/srep13361
20. Hsu LM, Ko WJ, Wang CH. Extracorporeal Membrane Oxygenation Rescues Thyrotoxicosis-Related Circulatory Collapse. Thyroid (2011) 21(4):439–41. doi: 10.1089/thy.2010.0230
21. White A, Bozso SJ, Moon MC. Thyrotoxicosis Induced Cardiomyopathy Requiring Support With Extracorporeal Membrane Oxygenation. J Crit Care (2018) 45:140–3. doi: 10.1016/j.jcrc.2018.01.026
22. Pong V, Yeung C, Ko RL, Tse H, Siu C. Extracorporeal Membrane Oxygenation in Hyperthyroidism-Related Cardiomyopathy: Two Case Reports. J Endocrinol Metab (2013) 3(1-2):24–8. doi: 10.4021/jem144w
23. Allencherril J, Birnbaum I. Heart Failure in Thyrotoxic Cardiomopathy: Extracorporeal Membrane Oxygenation Treatment for Graves’ Disease. J Extra Corpor Technol (2015) 47(4):231–2.
PubMed Abstract | Google Scholar
24. Kiriyama H, Amiya E, Hatano M, Hosoya Y, Maki H, Nitta D, et al. Rapid Improvement of Thyroid Storm-Related Hemodynamic Collapse by Aggressive Anti-T Hyroid Therapy Including Steroid Pulse: A Case Report. Med (Baltimore) (2017) 96(22):e7053. doi: 10.1097/MD.0000000000007053
25. Kim S, Seol SH, Kim YS, Kim DK, Kim KH, Kim DI. Thyrotoxicosis Induced Cardiogenic Shock Rescued by Extracorporeal Membrane Oxygenation. J Geriatr Cardiol (2018) 15:203–4. doi: 10.11909/j.issn.1671-5411.2018.02.003
26. Genev I, Lundholm MD, Emanuele MA, McGee E, Mathew V. Thyrotoxicosis-Induced Cardiomyopathy Treated With Venoarterial Extracorporeal Membrane Oxygenation. Heart Lung (2020) 49:165–6. doi: 10.1016/j.hrtlng.2019.06.006
27. Voll M, Øystese KA, Høiskar E, Johansen O, Nyvold C, Norheim I, et al. Case Report: A Patient With Thyroid Storm, Refractory Cardiogenic Shock, and Cardiac Arrest Treated With Lugol's Iodine Solution and Veno-Arterial Extra Corporal Membrane Oxygenation Support. Eur Heart J - Case Rep (2021) 5(2):ytab017. doi: 10.1093/ehjcr/ytab017
28. Chao J, Cook R, Dhingra V. Escaping a Storm Alive: A Case Report of a Young Woman’s Acute Presentation of Thyroid Storm Leading to Cardiac Arrest Salvaged by VA-ECMO. J Clin Anesth Intensive Care (2021) 2(1):26–30.
29. Al-Saadi M, Sista R, Lan C. Veno-Arterial Extracorporeal Membrane Oxygenation Saved A Young Patient In Refractory Cardiogenic Shock Precipitated By Thyroid Storm. Am J Respir Crit Care Med (2016) 193:A6918.
30. Kauth M, Sheikh A, Hinkle L. In the "I" of the Storm: Thyroid Storm Induced by Iodine Contrast in Thyrotoxicosis. Am J Respir Crit Care Med (2019) 199:A1713. doi: 10.1164/ajrccm-conference.2019.199.1_MeetingAbstracts.A1713
31. Karahalios BA, Singh R, Boyd K, Ogbonna M. A Perfect Storm: A Case Of Managing Cardiogenic Shock Due To Thyrotoxic Cardiomyopathy With Extracorporeal Membrane Oxygenation. J Hosp Med (2020).
32. Starobin B, Afari M. Through The Storm: Veno-Arterial Extracorporeal Membranous Oxygenation Therapy For Treatment Of Thyroid Storm Induced Cardiogenic Shock. J Am Coll Cardiol (2021) 77(18_Supplement_1):215.
33. Parikh T, Sharma M, Hegde A. SUN-559 Refractory Thyroid Storm: Role of Single Pass Albumin Dialysis (SPAD). J Endocr Soc (2019) 3(Suppl 1):SUN–559. doi: 10.1210/js.2019-SUN-559
34. Koball S, Hickstein H, Gloger M, Hinz M, Henschel J, Stange J, et al. Treatment of Thyrotoxic Crisis With Plasmapheresis and Single Pass Albumin Dialysis: A Case Report. Artif Organs (2010) 34(2):E55–58. doi: 10.1111/j.1525-1594.2009.00924.x
35. Haley PA, Zabaneh I, Bandak DN, Iskapalli MD. The Resolution of Thyroid Storm Using Plasma Exchange and Continuous Renal Replacement Therapy. J Adv Biol Biotechnol (2019) 20(1):1–4. doi: 10.9734/JABB/2018/45719
36. Park HS, Kwon SK, Kim YN. Successful Treatment of Thyroid Storm Presenting as Recurrent Cardiac Arrest and Subsequent Multiorgan Failure by Continuous Renal Replacement Therapy. Endocrinol Diabetes Metab Case Rep (2017) 1:16–0115. doi: 10.1530/EDM-16-0115
37. Tan YW, Sun L, Zhang K, Zhu L. Therapeutic Plasma Exchange and a Double Plasma Molecular Absorption System in the Treatment of Thyroid Storm With Severe Liver Injury: A Case Report. World J Clin Cases (2019) 7(10):1184–90. doi: 10.12998/wjcc.v7.i10.1184
38. Zhang Q, Guan Y, Xiang T, Liu S, Chen Q, Zhang Q. Combination of Molecular Adsorbent Recirculating System and Radioiodine for the Treatment of Concurrent Hyperthyroiditism and Severe Liver Dysfunction: A Retrospective Cohort Study. Endocr Pract (2017) 23(2):141–8. doi: 10.4158/EP161417.OR
39. Ono Y, Ono S, Yasunaga H, Matsui H, Fushimi K, Tanaka Y. Factors Associated With Mortality of Thyroid Storm: Analysis Using a National Inpatient Database in Japan. Med (Baltimore) (2016) 95(7):e2848. doi: 10.1097/MD.0000000000002848
40. Umpierrez GE, Challapalli S, Patterson C. Congestive Heart Failure Due to Reversible Cardiomyopathy in Patients With Hyperthyroidism. J Med Sci (1995) 310(3):99–102. doi: 10.1097/00000441-199531030-00003
41. Dahl P, Danzi S, Klein I. Thyrotoxic Cardiac Disease. Curr Heart Fail Rep (2008) 5(3):170–6. doi: 10.1007/s11897-008-0026-9
42. Klein I, Danzi S. Thyroid Disease and the Heart. Circulation (2007) 116(15):1725–35. doi: 10.1161/CIRCULATIONAHA.106.678326
43. Nakashima Y, Kenzaka T, Okayama M, Kajii E. A Case of Thyroid Storm With Cardiac Arrest. Int Med Case Rep J (2014) 7:89–92. doi: 10.2147/IMCRJ.S63475
44. Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, et al. Diagnostic Criteria, Clinical Features, and Incidence of Thyroid Storm Based on Nationwide Surveys. Thyroid (2012) 22:661–79. doi: 10.1089/thy.2011.0334
45. Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, Tsuboi K, et al. 2016 Guidelines for the Management of Thyroid Storm From The Japan Thyroid Association and Japan Endocrine Society (First Edition). Endocr J (2016) 63(12):1025–64. doi: 10.1507/endocrj.EJ16-0336
46. Brunette DD, Rothong C. Emergency Department Management of Thyrotoxic Crisis With Esmolol. Am J Emerg Med (1991) 9:232–4. doi: 10.1016/0735-6757(91)90083-V
47. Morganroth J, Horowitz LN, Anderson J, Turlapaty P. Comparative Efficacy and Tolerance of Esmolol to Propranolol for Control of Supraventricular Tachyarrhythmia. Am J Cardiol (1985) 56(11):33F–9F. doi: 10.1016/0002-9149(85)90914-2
48. Landsberg L. Catecholamines and Hyperthyroidism. Clin Endocrinol Metab (1977) 6:697–718. doi: 10.1016/S0300-595X(77)80076-5
49. Abubakar H, Singh V, Arora A, Alsunaid S. Propranolol-Induced Circulatory Collapse in a Patient With Thyroid Crisis and Underlying Thyrocardiac Disease: A Word of Caution. J Investig Med High Impact Case Rep (2017) 5(4):2324709617747903. doi: 10.1177/2324709617747903
50. Misumi K, Kodera S, Nagura F, Kushida S, Shiojiri T, Kanda J. Cardiac Arrest Caused by Landiolol in a Patient in Thyroid Crisis. J Cardiol Cases (2016) 14(2):62–4. doi: 10.1016/j.jccase.2016.04.002
Keywords: thyroid storm, multi-organ failure, extra-corporeal membrane oxygenation, therapeutic plasma exchange, continuous renal replacement therapy, out-of-hospital cardiac arrest
Citation: Lim SL, Wang K, Lui PL, Ramanathan K and Yang SP (2021) Crash Landing of Thyroid Storm: A Case Report and Review of the Role of Extra-Corporeal Systems. Front. Endocrinol. 12:725559. doi: 10.3389/fendo.2021.725559
Received: 15 June 2021; Accepted: 06 August 2021; Published: 20 August 2021.
Reviewed by:
Copyright © 2021 Lim, Wang, Lui, Ramanathan and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shir Lynn Lim, [email protected]
† These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Search Menu
- Sign in through your institution
- Volume 2024, Issue 6, June 2024 (In Progress)
- Volume 2024, Issue 5, May 2024
- Bariatric Surgery
- Breast Surgery
- Cardiothoracic Surgery
- Colorectal Surgery
- Colorectal Surgery, Upper GI Surgery
- Gynaecology
- Hepatobiliary Surgery
- Interventional Radiology
- Neurosurgery
- Ophthalmology
- Oral and Maxillofacial Surgery
- Otorhinolaryngology - Head & Neck Surgery
- Paediatric Surgery
- Plastic Surgery
- Transplant Surgery
- Trauma & Orthopaedic Surgery
- Upper GI Surgery
- Vascular Surgery
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Submit
- About Journal of Surgical Case Reports
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- Introduction
- Materials and methods
- Conclusions
- Conflict of interest statement
- Ethics approval and consent to participate
- Data availability
- < Previous
Diffuse large B-cell lymphoma associated with papillary thyroid carcinoma: a case report and systematic review on management and outcomes
- Article contents
- Figures & tables
- Supplementary Data
Eddy P Lincango, Luis F Serrano, Sebastian Vallejo, Paola Solis-Pazmino, Andrea Garcia-Bautista, William Acosta, Oscar J Ponce, Jorge Salazar-Vega, Cristhian Garcia, Diffuse large B-cell lymphoma associated with papillary thyroid carcinoma: a case report and systematic review on management and outcomes, Journal of Surgical Case Reports , Volume 2024, Issue 5, May 2024, rjad658, https://doi.org/10.1093/jscr/rjad658
- Permissions Icon Permissions
Primary thyroid lymphoma is a rare thyroid cancer, comprising ˂5% of thyroid neoplasms. Most cases are diffuse large B-cell lymphoma (DLBCL). Coexistence with papillary thyroid cancer (PTC) is extremely rare. This study presents a case of a 55-year-old woman with DLBCL and micropapillary thyroid cancer who underwent lobectomy, chemotherapy, and radiotherapy. Additionally, we performed a systematic review of 10 cases, including the reported case. The risk of bias in case reports varied. DLBCL diagnoses were mainly made after surgery, with total thyroidectomy being the most common surgical procedure. Chemotherapy was administered in most cases, and radiotherapy was used in some cases. Long-term outcomes indicated a low recurrence rate. While some debate the role of surgery in thyroid lymphoma, this study suggests that surgery should be considered in selected cases. Further research is needed to determine optimal treatment strategies for DLBCL with PTC.
- radiation therapy
- chemotherapy regimen
- diffuse large b-cell lymphoma
- surgical procedures, operative
- thyroid neoplasms
- thyroidectomy
- thyroid cancer
- thyroid lymphoma
- thyroid carcinoma, papillary
Email alerts
Citing articles via, affiliations.
- Online ISSN 2042-8812
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Clinical Features of Nivolumab-Induced Thyroiditis: A Case Series Study
Affiliations.
- 1 1 Department of Diabetes, Endocrinology and Nutrition, Kyoto University Graduate School of Medicine , Kyoto, Japan .
- 2 2 Preemptive Medicine and Lifestyle Disease Research Center, Kyoto University Hospital , Kyoto, Japan .
- PMID: 28537531
- DOI: 10.1089/thy.2016.0562
Background: The programmed cell death-1 (PD-1) pathway is a novel therapeutic target in immune checkpoint therapy for cancer. It consists of the PD-1 receptor and its two ligands, programmed death-ligand 1 (PD-L1) and programmed death-ligand 2 (PD-L2). Nivolumab is an anti-PD-1 monoclonal antibody approved for malignant melanoma, advanced non-small cell lung cancer, and advanced renal cell carcinoma in Japan. Thyrotoxicosis and hypothyroidism have both been reported in international Phase 3 studies and national post-marketing surveillance of nivolumab in Japan.
Methods: This study analyzed five consecutive cases with thyroid dysfunction associated with nivolumab therapy. Second, it examined the mRNA and protein expressions of PD-L1 and PD-L2 by reverse transcription polymerase chain reaction and Western blotting.
Results: All patients were diagnosed with painless thyroiditis. Thyrotoxicosis developed within four weeks from the first administration of nivolumab and normalized within four weeks of onset in three of the five patients. Hypothyroidism after transient thyrotoxicosis developed in two patients, and preexisting hypothyroidism persisted in one patient. The other two patients were treated with glucocorticoids and discontinued nivolumab therapy for comorbid adverse events. One did not develop hypothyroidism, and the other developed mild, transient hypothyroidism. In addition, it was verified that normal thyroid tissue expresses PD-L1 and PD-L2 mRNA and those proteins.
Conclusions: In the present cases, nivolumab-induced thyrotoxicosis seemed to be associated with painless thyroiditis, while no patient with Graves' disease was observed. A transient and rapid course with subsequent hypothyroidism was observed in nivolumab-induced thyroiditis. In addition, it was verified that PD-L1 and PD-L2 are expressed in normal thyroid tissue. This suggests that nivolumab therapy reduces immune tolerance, even in normal thyroid tissue, and leads to the development of thyroiditis. Treating thyrotoxicosis with only supportive care and considering levothyroxine replacement therapy once subsequent hypothyroidism occurs is proposed. Further investigations are required to confirm whether glucocorticoid therapy and discontinuation of nivolumab therapy prevent subsequent hypothyroidism.
Keywords: PD-1; immune checkpoint inhibitor; nivolumab; painless thyroiditis; thyrotoxicosis.
Publication types
- Case Reports
- Antibodies, Monoclonal / adverse effects*
- Antineoplastic Agents / adverse effects*
- Breast Neoplasms / drug therapy
- Lung Neoplasms / drug therapy
- Melanoma / drug therapy
- Middle Aged
- Skin Neoplasms / drug therapy
- Symptom Assessment
- Thyroiditis / blood
- Thyroiditis / chemically induced*
- Thyroiditis / diagnosis*
- Thyrotoxicosis / blood
- Thyrotoxicosis / chemically induced*
- Thyrotoxicosis / diagnosis*
- Thyrotropin / blood
- Thyroxine / blood
- Triiodothyronine / blood
- Antibodies, Monoclonal
- Antineoplastic Agents
- Triiodothyronine
- Thyrotropin
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (44,166,401 articles, preprints and more)
- Available from publisher site using DOI. A subscription may be required. Full text

The Relationship Between Thyroid Dysfunction and Sleep Quality Among Population of Saudi Arabia.
Author information, affiliations.
- Alreshidi NF 1
- Alrashidi R 1
- Aljaloud LZ 1
- Alshammari AB 1
ORCIDs linked to this article
- Alreshidi NF | 0000-0001-6501-7223
International Journal of General Medicine , 29 May 2024 , 17: 2497-2505 https://doi.org/10.2147/ijgm.s462512 PMID: 38831928
Abstract
Patients and methods, full text links .
Read article at publisher's site: https://doi.org/10.2147/ijgm.s462512
Europe PMC is part of the ELIXIR infrastructure
Medullary Thyroid Carcinoma Surveillance Study: A Case-Series Registry
Add to collection, downloadable content.
- Other Affiliation: Novo Nordisk Inc
- Other Affiliation: Eli Lilly and Company, Indianapolis, IN, United States
- Affiliation: School of Medicine
- Other Affiliation: BioPharmaceuticals Medical, AstraZeneca,Wilmington, DE, United States
- Other Affiliation: Massachusetts General Hospital, Boston, MA, United States
- Other Affiliation: GlaxoSmithKline Research and Development Limited, Collegeville, PA, United States
- Other Affiliation: Memorial Sloan Kettering Cancer Center, New York, NY, United States
- Other Affiliation: United BioSource LLC, Blue Bell, PA, United States
- The Medullary Thyroid Carcinoma (MTC) Surveillance Study [the MTC registry (1)] is a case-series registry established in 2010 as a Food and Drug Administration (FDA) postmarketing commitment for liraglutide, the first long-acting glucagon-like peptide-1 receptor agonist (GLP-1 RA) approved in the United States. Subsequently, other GLP-1 RAs have been developed and brought to market, including exenatide (AstraZeneca, PLC), albiglutide (GlaxoSmithKline, PLC), dulaglutide (Eli Lilly and Company), and semaglutide (Novo Nordisk A/S), and are included in the MTC registry. Additional pharmaceutical companies (sponsors) who receive FDA approval for new GLP-1 RA products may also be asked to participate in this registry.
- thyroid tumor
- Thyroid Neoplasms
- cancer risk
- priority journal
- drug industry
- diabetes mellitus
- cancer registry
- glucagon like peptide 1 receptor
- cancer epidemiology
- telephone interview
- health care personnel
- thyroid medullary carcinoma
- semaglutide
- United States
- Glucagon-Like Peptide-1 Receptor
- dulaglutide
- cancer patient
- medical history
- Product Surveillance, Postmarketing
- albiglutide
- postmarketing surveillance
- drug approval
- Carcinoma, Neuroendocrine
- risk factor
- liraglutide
- Drug Approval
- institutional review
- Food and Drug Administration
- https://doi.org/10.17615/5bzv-n840
- https://doi.org/10.1089/thy.2019.0591
- In Copyright
- Attribution-NonCommercial 4.0 International
- Whole Biome
- Eli Lilly and Company
- American Diabetes Association, ADA
- Johnson and Johnson, J&J
- GlaxoSmithKline, GSK
- National Cancer Institute, NCI, (P30 CA008748)
- Novo Nordisk
- vTv Therapeutics
- Elcelyx Therapeutics
- CSL Behring
- National Institutes of Health, NIH, (U01DK098246, U54DK118612, UC4DK108612, UL1TR002489)
- Intarcia Therapeutics
- Cirius Therapeutics
- Mary Ann Liebert Inc.
This work has no parents.
Select type of work
Master's papers.
Deposit your masters paper, project or other capstone work. Theses will be sent to the CDR automatically via ProQuest and do not need to be deposited.
Scholarly Articles and Book Chapters
Deposit a peer-reviewed article or book chapter. If you would like to deposit a poster, presentation, conference paper or white paper, use the “Scholarly Works” deposit form.
Undergraduate Honors Theses
Deposit your senior honors thesis.
Scholarly Journal, Newsletter or Book
Deposit a complete issue of a scholarly journal, newsletter or book. If you would like to deposit an article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Deposit your dataset. Datasets may be associated with an article or deposited separately.
Deposit your 3D objects, audio, images or video.
Poster, Presentation, Protocol or Paper
Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.

Case Studies in Thyroid and Parathyroid Tumors
- © 2023
- Amit Agarwal 0 ,
- Ranil Fernando 1 ,
- Rajeev Parameswaran 2 ,
- Anand Mishra 3 ,
- Roma Pradhan 4
Department of Endocrine and Breast Surgery, Medanta Hospital, Lucknow, India
You can also search for this author in PubMed Google Scholar
Faculty of Medicine, University of Moratuwa, Moratuwa, Sri Lanka
Department of surgery, yong loo lin school of medicine, national university of singapore, singapore, singapore, department of endocrine surgery, king george’s medical university, lucknow, india.
- Comprises interesting common and uncommon cases of the thyroid and parathyroid surgery
- Covers questions that may arise on surgical rounds or in operation theatres
- Includes figures and tables to reinforce the critical elements of the disease process virtually
18k Accesses
This is a preview of subscription content, log in via an institution to check access.
Access this book
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions
Table of contents (90 chapters)
Front matter, primary hyperparathyroidism (phpt): unusual clinical presentation, phpt presenting as osteitis fibrosa cystica.
- Amit Agarwal, Ranil Fernando, Rajeev Parameswaran, Anand Mishra, Roma Pradhan
Truncal Calciphylaxis in Primary Hyperparathyroidism Without Renal Failure
Hypercalcemic crisis resulting in acute kidney failure, familial isolated hyperparathyroidism (fihp), phpt presenting as pulmonary thromboembolism, juvenile phpt, loss of height in phpt, maternal phpt, phpt presenting with psychiatric symptoms, phpt presenting with severe proximal muscle weakness, phpt with ckd, phpt presenting with poor mentation, phpt presenting as a jaw tumor, lithium-induced primary hyperparathyroidism, hyperparathyroidism with femur fracture, hypercalcemic crisis, phpt presenting as pancreatitis, phpt: diagnostic dilemma.
- Benign thyroid tumors
- Malignant thyroid tumors
- Thyroid emergencies
- Benign parathyroid tumors
- Malignant parathyroid tumors
- Endocrine surgery
About this book
Authors and affiliations.
Amit Agarwal, Roma Pradhan
Ranil Fernando
Rajeev Parameswaran
Anand Mishra
About the authors
Bibliographic information.
Book Title : Case Studies in Thyroid and Parathyroid Tumors
Authors : Amit Agarwal, Ranil Fernando, Rajeev Parameswaran, Anand Mishra, Roma Pradhan
DOI : https://doi.org/10.1007/978-981-99-0938-4
Publisher : Springer Singapore
eBook Packages : Medicine , Medicine (R0)
Copyright Information : The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd. 2023
Hardcover ISBN : 978-981-99-0937-7 Published: 09 June 2023
Softcover ISBN : 978-981-99-0940-7 Due: 10 July 2023
eBook ISBN : 978-981-99-0938-4 Published: 08 June 2023
Edition Number : 1
Number of Pages : XVI, 408
Number of Illustrations : 11 b/w illustrations, 192 illustrations in colour
Topics : General Surgery , Endocrinology , Oncology , Internal Medicine
- Publish with us
Policies and ethics
- Find a journal
- Track your research

- Events & Education
- ATA Publications
- ATA Guidelines & Statements
- Research Grants
- Thyroid Cancer Patient Information
- Trainees Corner
- Corporate Leadership Council
- ATA Career Center
- Laboratory Services Library
- Scientific & Professional Interest
- Thyroid Cancer Staging Calculator
- (CEA) Doubling Time Calculator
- Change In Thyroid Nodule Volume Calculator
- Thyroid Patient Information
- Find an Endocrinology – Thyroid Specialist
- Patient Support Links
- Clinical Thyroidology for the Public
- Friends of the ATA Newsletter
- ATA Practice Guidelines
- Clinical Trials
- ATA Research Accomplishments
- Member Benefits
- Become an ATA Member
- Renew Your Membership
- Member Guidelines & Categories
- Society Committees
- Member Directory
- Trainee Membership
- Meet our Members
- Women in Thyroidology
- Thyroid Online Access
- Clinical Thyroidology Online
- Video Endocrinology
- Leadership & Staff
- Committees & Workgroups
- Diversity, Equity, Inclusion
- Awards & Recognition
- Our History
- Give Online
- Valerie Anne Galton Fund
- Samuel Refetoff Fund
- Ridgway Legacy Fund
- Memorial or Tribute Gift Donation
- Workplace Giving
- Estate and Planned Giving
- Donate by Mail/Fax/Phone
- Research Accomplishments
Case Studies
Publications
About the ata.
© 2024 American Thyroid Association.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Gen Fam Med
- v.19(5); 2018 Sep
Thyroid follicular carcinoma in a teenager: A case report
1 Department of General Medicine, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan
Tadahiko Shien
2 Department of Breast and Endocrine Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan
Fumio Otsuka
A 19‐year‐old girl complained of an enlarged cervical mass. Based on clinical and cytological assessments, it was diagnosed as thyroid follicular carcinoma and left thyroidectomy was performed. Although thyroid neoplasms are rare in young people, differentiation is needed when the rapid growth of a goiter is detected.
1. INTRODUCTION
Thyroid carcinomas, especially thyroid follicular carcinoma, are rare in young people. Papillary carcinoma in the thyroid accounts for about 90% of thyroid carcinomas, and follicular carcinoma accounts for about 6% of thyroid carcinomas; the incidence of thyroid cancer in people in their twenties or younger is approximately 1 in 100 000 in Japan. 1 Herein, we introduce a case of juvenile thyroid follicular carcinoma showing the rapid growth of a goiter.
2. CASE PRESENTATION
A 19‐year‐old girl who had a complaint of a swollen and enlarged feeling of her cervical mass for a few months visited our hospital (Figure 1 ). The patient had no particular past or family history including thyroidal disorders or other neoplasms. Cervical examination by ultrasonography revealed a diffusely enlarged left thyroid tumor showing a heterogenous pattern without clear capsule formation (Figure 2 A), in which internal blood flow was augmented by a Doppler scan (Figure 2 B). Endocrine examination showed that the patient was euthyroid and there were no thyroid autoantibodies (Table 1 ). A chest X‐ray showed a tracheal shift to the right and a dense shadow of the neck (Figure 3 A). Computed tomography showed enlargement of the left thyroidal lesion and airway constriction (Figure 3 B, coronal view; Figure 3 C, horizontal view). Based on the results of cytology of a fine‐needle aspiration specimen, a follicular neoplasm was suspected. Left thyroidectomy was then performed, and a pathological diagnosis of follicular carcinoma (pT3N0M0 pStage I) was made on the basis of examination of the resected thyroid lesion (Figure 4 ). Cancer recurrence was not observed for a period of 1 year after surgery.

Swollen cervical mass

Ultrasonography revealed a diffusely enlarged left thyroid tumor (A). A Doppler scan showed augmented blood flow in the thyroid tumor (B)
Thyroid‐related laboratory data

A chest X‐ray showed a tracheal shift to the right and a high‐density area in her neck (A, arrow). Computed tomography showed an enlarged thyroid tumor shifting the trachea to the right (B) and constricting the airway (C)

Pathology of the resected thyroid tumor stained with hematoxylin and eosin showed proliferation of heteromorphic follicular carcinoma cells with capsular invasion
3. DISCUSSION
Thyroid follicular carcinoma is very rare in teenagers. In general, a simple goiter is seen in young females, and thyroid carcinomas tend to be found in middle‐aged to elderly women. In adults, nodule prevalence has been estimated to be 2%‐6% by palpation and 19%‐35% by ultrasound. 2 Some studies using sonography showed that the prevalence of thyroid nodules in pediatrics is 0.2%‐5.1%. 3 However, it has been estimated that 25% of thyroid nodules are malignant in children, while only 5% of them are malignant in adults. 3 There has been no well‐documented report regarding the occurrence of follicular carcinoma in teenagers; however, in a 20‐year study on thyroid cancer in children and adolescents in China, 7 (8.4%) of 83 patients were reported to have follicular carcinoma. 4
Childhood‐onset thyroid carcinoma is a more metastatic and aggressive local disease than thyroid carcinoma in adults. 5 Therefore, management of thyroid nodules in children needs more attention than that in adults, and early detection is important. Nevertheless, children with thyroid carcinoma, especially those with follicular carcinoma, have a relatively good prognosis even if they have neck or distant metastasis. 6 In addition, the general development and thyroid function of children born from mothers with childhood‐onset thyroid carcinoma do not seem to be affected by their former diseases. 7
Not only thyroidectomy but also radioiodine ablation can be chosen as treatment for childhood‐onset thyroid carcinoma. Although radioiodine therapy is effective even for inoperable cases and adjuvant radioiodine therapy has been reported to reduce the risk of locoregional and distant recurrence, 8 other cancer risk is increased by radioiodine therapy, particularly in the salivary gland, rectum, and colon; the risk of cancer in soft tissue and bone, leukemia, and pulmonary fibrosis might also be increased. 9 Therefore, the balance of benefits and risks should be carefully considered. Pediatric follicular carcinoma has a lower frequency of metastasis and a lower grade of malignancy than those of papillary carcinoma. 10
Considering this rare case, cervical lesions in children should be carefully followed up, and when growing potential is detected in young cases, thyroidal neoplasms should be readily differentiated by clinical and cytological assessments.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Oka K, Shien T, Otsuka F. Thyroid follicular carcinoma in a teenager: A case report . J Gen Fam Med . 2018; 19 :170–172. 10.1002/jgf2.185 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

COMMENTS
Hypothyroidism is diagnosed on the basis of laboratory tests because of the lack of specificity of the typical clinical manifestations. There is conflicting evidence on screening for hypothyroidism. We report a case of an apparently healthy 19-year-old Kuwaiti woman referred to our clinic with an incidental finding of extremely high thyroid-stimulating hormone (TSH), tested at the patient's ...
Introduction. Hypothyroidism is a chronic disease associated with deficiency in the thyroid hormones, thyroxine (T4) and triiodothyronine (T3) [1, 2].The consequences of untreated or inadequately treated hypothyroidism include infertility, cardiovascular disease, and neurological and musculoskeletal symptoms [3-5].Environmental iodine deficiency is the most common cause of thyroid disorders ...
On examination, the blood pressure was 128/74 mm Hg, the pulse 66 beats per minute, the weight 66.7 kg, and the height 165.1 cm. A nodule was palpable in the thyroid on the right side; there was ...
Abstract. Papillary thyroid carcinoma (PTC) is the most common malignant thyroid neoplasm with the median age at presentation for papillary carcinoma being around 50 years. This case report describes the author's experience of being diagnosed with PTC at the age of 25, as well as the course of treatment, and eventual outcome.
1. Introduction. Thyroid nodules are overgrown masses of normal thyroid cells in the gland [], which are classified into several types: single, multiple, solid, or cystic [].A previous study reported that the global prevalence of thyroid nodules has reached 4-7%, of which 8-16% turn into thyroid cancer [].In recent years, the prevalence of thyroid nodules in China has shown a concerning ...
Case presentation. A 62-year-old Caucasian woman was referred by her general practitioner in February 2016 in view of hypothyroid symptoms but with biochemical thyrotoxic picture. She did have a right-sided subtotal thyroidectomy in March 1989 (histology: colloid goitre with marked fibrosis; thyroglobulin antibodies—1:640; thyroid microsomes ...
The majority of patients with thyroid cancer are at low risk for recurrence (<5%), 1-3 and their risk of cancer-related death is even lower. 4 After thyroidectomy, radioiodine (iodine-131) is ...
A retrospective case series also demonstrated significant improvement in thyroid hormone levels in patients with hyperthyroidism with severe liver dysfunction (although this study was primarily powered to show improvement and safety of use of RAI with combined with MARS in patients with severe hyperthyroidism and liver disease) . These reports ...
International Journal of Endocrinology. Volume 2014, Issue 1 ... (FT4) and provide a more eligible and economic strategy to assess thyroid function. A total of 2,673 participants (500 patients with hyperthyroidism, 500 patients with hypothyroidism, and 1,673 healthy people) were involved in our study. Serums TT3, TT4, FT3, and FT4 and ...
Associations of Combined Exposure to Metabolic and Inflammatory Indicators with Thyroid Nodules in Adults: A Nested Case-Control Study, International Journal of Endocrinology, 2024, (1-11), (2024 ...
Introduction. Papillary thyroid cancer (PTC) is the most frequent thyroid neoplasm (90%). It tends to be slow growing and associated with a favorable prognosis [].On the other hand, primary thyroid lymphoma (PTL) is an unusual endocrine malignancy comprising ˂5% of thyroid neoplasms [].PTL usually presents with a rapidly enlarging painless thyroid mass that can cause obstructive symptoms like ...
Acute suppurative thyroiditis (AST) is a rare but potentially life-threatening condition. Well-protected from infection, the thyroid gland has a fibrous capsule and fascial planes separating it from other neck structures and shielding it from local spread of pathogens. 1,2 The thyroid gland has an extensive vascular supply and lymphatic drainage, which further protects it from infection.
Thyroid®. The definitive peer-reviewed journal package in thyroid disease, care, and research, providing multidisciplinary original research and patient-focused reports, reviews and commentary, and an innovative videojournal companion covering new surgical and diagnostic imaging techniques and technologies. This subscription also includes:
Methods: This study analyzed five consecutive cases with thyroid dysfunction associated with nivolumab therapy. Second, it examined the mRNA and protein expressions of PD-L1 and PD-L2 by reverse transcription polymerase chain reaction and Western blotting. Results: All patients were diagnosed with painless thyroiditis.
Thyroid nodules (TN) are prevalent in the general population and represent a common complaint in clinical practice. Most are asymptomatic and are associated with a 7%-15% risk of malignancy ( [1][1] ). Methods: PubMed and Medline were searched for articles with a focus on the epidemiology, diagnosis, and management of TN over the past 5 y. Results: The increase in frequency of imaging has ...
Malignancy in struma ovarii is rare and observed in only 5%-10% of patients. Here, we present a patient with malignant struma ovarii and coexisting intrathyroidal papillary thyroid carcinoma, with recurrence (large pouch-of-Douglas mass) and metastases (bilateral pulmonary and iliac nodal metastases) presenting 12 y after surgery. The notable features in this case were a concurrent ...
The study employed an observational cross-sectional design and included a representative Saudi Arabian cohort. The Pittsburgh Sleep Quality Index (PSQI) was included in a digital self-administered survey that participants were asked to complete. Results There were 1044 responders in the study, most of whom (54%) were between the ages of 21 and 30.
The Medullary Thyroid Carcinoma (MTC) Surveillance Study [the MTC registry (1)] is a case-series registry established in 2010 as a Food and Drug Administration (FDA) postmarketing commitment for liraglutide, the first long-acting glucagon-like peptide-1 receptor agonist (GLP-1 RA) approved in the United States.
Case Studies in Thyroid and Parathyroid Tumors ... She is onthe editorial board of the World Journal of Endocrine Surgery, the official journal of the Asian Association of Endocrine Surgeons. Dr. Pradhan was the first to use continuous neuromonitoring in entire north India in thyroid surgery. Her clinical interests include thyroid, minimally ...
1. Introduction. Impaired sensitivity to thyroid hormone (ISTH) syndromes are a group of disorders characterized by an apparent discrepancy between serum levels of thyroid-stimulating hormone (TSH) and thyroid hormones (TH) and/or hormone action at the tissue and cell levels [].This group includes all defects that could interfere with the biological activity of properly synthesized THs.
A rare case of papillary thyroid cancer associated with hyperthyroidism is described here. Case: A 49-year-old male presented to the authors' outpatient clinic with complaints of a painless left-sided anterior neck swelling that had persisted for the past 8 months. He also reported weight loss for the same duration.
Conclusions In a highly selected group of patients with relapsed GD and predominantly small thyroid glands, single-session RFA may achieve disease remission. Smaller total thyroid volume may be a favorable factor associated with disease remission after RFA. The results of this study need to be confirmed with a long-term clinical trial.
Thyroid hormones are major regulators of a number of vital organ systems. Therefore, it is obvious that in a state of depressed hormone production, all the body's major organs are affected. ... Patient consent form has been procured prior to the case report study. Statement of Authorship. All authors have given approval to the final version ...
A thyroid panel revealed a TSH of <.01 uIU/mL, triiodothyronine of 282.8 ng/dL, and a free thyroxine of 5.77 ng/dL, confirming a diagnosis of thyrotoxicosis. ... Bakhsh ZK, Gad HA, Bashir MT, Elmoheen A. An unusual case of thyroid storm masquerading as an intestinal obstruction in a patient with malrotation of the gut. Cureus. 2021;13(3):e13948 ...
2013 Case Studies - Thyroid Nodules. 1. View Larger More Details. 2013 Case Studies - Thyroid Cancer. 0. MEETINGS 2024 ATA Annual Meeting Annual Scientific Abstracts ... ATA Member Thyroid Journal Bundle Access ATA Guidelines & Statements Guideline Pocketcards Clinical Thyroidology for the Public (CTFP) AWARDS Recognition
s. The thyroid gland regulates the body's metabolism and growth. In Ayurveda, this is attributed to a function of Agni. Clinical symptoms of this disease closely resemble Agnimandya and symptoms precipitated consequentially. A 24-year-old female patient visited the hospital with complaints of irregular menstruation, heaviness all over the body, gradual weight gain, and constipation. After ...
Journal of Medical Virology is a clinical virology journal focused on the diagnosis, ... In this case-control study, 14 patients diagnosed with AMN-SARS-CoV-2 between 2022/12 and 2023/3 were enrolled and compared with 14 SARS-CoV-2-infected individuals without AMN, who served as controls (SARS-CoV-2-no AMN). Metabolomic profiling using ...
Thyroid follicular carcinoma is very rare in teenagers. In general, a simple goiter is seen in young females, and thyroid carcinomas tend to be found in middle‐aged to elderly women. In adults, nodule prevalence has been estimated to be 2%‐6% by palpation and 19%‐35% by ultrasound. 2 Some studies using sonography showed that the ...