- Editorial Board
- President's Message
- Editor's Message
- Current Issue
- Special Issue
- Submit your Manuscript
- Check Manuscript status
- Author Guidelines
- National IMA Committee
- Register As Author
- Register As Reviewer
- Tariff Card & Subscription
- Constitution
- Login Regsiter
- Login Register
Official Publication of the Indian medical Association,
(Mutally affiliated with the British) & Nepal Medical Association,
IMA House, 53, Creek Row, Kolkata 700014
Kolkata,West Bengal,700014
Phone: (033) 2237-8092,2236-0573,2237-0412
The Journal of the Indian Medical Association (JIMA) was founded by doyens of Medical Profession namely Sir Nilratan Sircar, Dr Bidhan Chandra Roy, Dr Kumud Sankar Ray and others in the year 1930 with only 122 Doctors,
Indian Medical Association launched its own journal in the name of “Indian Medical World” . The first issue was published in March 1930, under the able Editorship of Sir Nil Ratan Sircar. Dr. A. N. Ghosh was the Secretary. An All-India Editorial Board of 21 members was also formed. Altogether 18 monthly issues of the “Indian Medical World” in two Volumes of 12 issues and six issues were published. The last issue of the Indian Medical World was dated August 1931.
In the 7th All India Conference of IMA, which was held in Pune, under the Presidentship of Dr. Jivraj N. Mehta, it was resolved to change the name of the journal as “Journal of the Indian Medical Association” . The change was made effective from September, 1931 issue. The change of the name did not connote any change in the policy of the journal.
The main objective of the Journal of the Indian Medical Association (JIMA) was to promote the advancement of medical and allied sciences in the country; the improvement of public health and medical education in India and uphold the honor and dignity of the medical profession.
Journal of the Indian Medical Association (JIMA) publishes Original research articles, Case Reports, Editorials, and Short Communication in all areas of medical science. The journal also considers publication of letters to the editor commenting on research already published in the journal, as well as manuscripts describing new hypotheses or clinical trial protocols. JIMA does not consider research work that has been published, is in press or has been submitted elsewhere (abstracts excepted).

Growth and Development of JIMA
The journal has recorded steady all round growth from year to year. It has recorded its brilliant progress in terms of increasing readership as well as being an “Index Journal” at par with the standard and sophisticated journals listed in Index Medicus (USA) . It is indexed with Copernicus and Scopus now. It is subscribed by most of the Medical Colleges and Libraries in the country.
We accept ethical advertisements of pharmaceutical and non-pharmaceutical products, Instruments, Medical Equipments and Electronic Medical Gadgets, institutions.

Performance Improvement
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Etiam condimentum libero nec ante malesuada, ac ornare massa commodo

Thought Leadership
Quisque at dapibus turpis, in maximus nulla. Curabitur sagittis, leo in rhoncus placerat, dolor enim pretium massa, vitae suscipit purus
JIMA is peerless in its field.
The manuscripts are currently under the double-blinded peer review process and shall be available online as and when they get accepted and ready for publication.
ISSN (Print): 0971-5916 ISSN (Online): Awaited

Privacy Overview
Indian Journal of Medical Research, Supplement
Subject Area and Category
- Biochemistry, Genetics and Molecular Biology (miscellaneous)
- Medicine (miscellaneous)
Publication type
2004-2005, 2012-2021
Information
How to publish in this journal
The set of journals have been ranked according to their SJR and divided into four equal groups, four quartiles. Q1 (green) comprises the quarter of the journals with the highest values, Q2 (yellow) the second highest values, Q3 (orange) the third highest values and Q4 (red) the lowest values.
The SJR is a size-independent prestige indicator that ranks journals by their 'average prestige per article'. It is based on the idea that 'all citations are not created equal'. SJR is a measure of scientific influence of journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals where such citations come from It measures the scientific influence of the average article in a journal, it expresses how central to the global scientific discussion an average article of the journal is.
Evolution of the number of published documents. All types of documents are considered, including citable and non citable documents.
This indicator counts the number of citations received by documents from a journal and divides them by the total number of documents published in that journal. The chart shows the evolution of the average number of times documents published in a journal in the past two, three and four years have been cited in the current year. The two years line is equivalent to journal impact factor ™ (Thomson Reuters) metric.
Evolution of the total number of citations and journal's self-citations received by a journal's published documents during the three previous years. Journal Self-citation is defined as the number of citation from a journal citing article to articles published by the same journal.
Evolution of the number of total citation per document and external citation per document (i.e. journal self-citations removed) received by a journal's published documents during the three previous years. External citations are calculated by subtracting the number of self-citations from the total number of citations received by the journal’s documents.
International Collaboration accounts for the articles that have been produced by researchers from several countries. The chart shows the ratio of a journal's documents signed by researchers from more than one country; that is including more than one country address.
Not every article in a journal is considered primary research and therefore "citable", this chart shows the ratio of a journal's articles including substantial research (research articles, conference papers and reviews) in three year windows vs. those documents other than research articles, reviews and conference papers.
Ratio of a journal's items, grouped in three years windows, that have been cited at least once vs. those not cited during the following year.
Evolution of the percentage of female authors.
Evolution of the number of documents cited by public policy documents according to Overton database.
Evoution of the number of documents related to Sustainable Development Goals defined by United Nations. Available from 2018 onwards.
Leave a comment
Name * Required
Email (will not be published) * Required
* Required Cancel
The users of Scimago Journal & Country Rank have the possibility to dialogue through comments linked to a specific journal. The purpose is to have a forum in which general doubts about the processes of publication in the journal, experiences and other issues derived from the publication of papers are resolved. For topics on particular articles, maintain the dialogue through the usual channels with your editor.
Follow us on @ScimagoJR Scimago Lab , Copyright 2007-2024. Data Source: Scopus®
Cookie settings
Cookie Policy
Legal Notice
Privacy Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(1); 2023 Jan

Prevalence of Depression Among Undergraduate Medical Students in India: A Systemic Review and Meta-Analysis
Gitashree dutta.
1 Community Medicine and Family Medicine, All India Institute of Medical Sciences, Jodhpur, IND
Navin Rajendran
2 Paediatrics, Dr. Sampurnanand (SN) Medical College, Jodhpur, IND
Tarun Kumar
3 Pharmacology, All India Institute of Medical Sciences, Jodhpur, IND
Shoban B Varthya
Vinoth rajendran.
Background: Systematic reviews have proved that there is a high rate of depression among medical students when compared with their age-matched peers. Very few studies have evaluated the pooled prevalence of depression among medical students in India.
Objectives: To determine the pooled prevalence of depression among medical students in India.
Materials and methods: This review was done by searching databases like PubMed, Google Scholar, and Scopus for available original articles published between 2019 and 2022 on depression among Indian medical (MBBS) undergraduate students using PRISMA guidelines.
Results: A total of 19 original research articles were included in this review, involving students at different medical colleges from various regions of India. The pooled prevalence of depression among 5944 medical students was 50.0% (95% CI: (31%-70%)) based on the random effect model. This meta-analysis also found that the pooled prevalence of depression among females (pooled prevalence: 38.0%, 95% CI: 20.0 to 58.0) was slightly higher than among males (pooled prevalence: 34.0%, 95% CI: 15.0 to 55.0).
Conclusion: The high prevalence of depression among medical students demands regular screening for depression along with counselling services. It shows that there is a need to raise awareness among students and other stakeholders, such as parents and medical educators, concerning symptoms and signs of depression among medical students.
Introduction and background
The World Health Organization (WHO) defined health as "a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity", a definition relevant today [ 1 ]. Further, it is stated that "not depressed" is not the end goal as there is a spectrum of well-being, with the disease at one end and optimal well-being at the other. The World Health Organization recognizes mental health disorders as important causes of morbidity and disability, with depression as one of the leading causes of mental health disorders.
In 2016, the age-standardized prevalence of depressive disorders in South Asia was 3.9% (95% UI: 3.6 - 4.2%), 3.7% (95% uncertainty interval (UI): 3.4-4.1%) in Bhutan, 3.9% (95% UI: 3.6-4.2%) in India, 4.4% (95% UI: 4.4-4.8%) in Bangladesh, 3.0% (95% UI: 2.8-3.3%) in Pakistan, and 4.0% (95% UI: 3.7-4.3%) in Nepal [ 2 ]. Systematic reviews have proved that there is a high rate of depression or depressive symptoms (27.2%) among medical students when compared with their age-matched peers before the COVID-19 pandemic [ 3 , 4 ]. All people, including medical students, would benefit from being aware of where they are on the well-being spectrum and what they can do to climb up the spectrum. Students who experience depression also experience additional mental health issues like anxiety, burnout, substance abuse, and suicidal thoughts. Undergraduate students' mental health is a significant public health issue on a global scale [ 5 - 8 ].
The COVID-19 pandemic has taken a toll on the mental health of different individuals worldwide for various containment measures and the disease itself [ 9 ]. During the COVID-19 pandemic, college students are more prone to mental health disorders along with COVID-19 patients and medical personnel. Compared to other training programmes, medical education has the highest academic and emotional requirements. A systematic review and meta-analysis with research works published globally show depression prevalence of 37.9% among medical students [ 10 ].
The pooled prevalence of depression based on standard screening instruments among medical students in India was 40% before the COVID pandemic [ 11 ]. However, no studies have been conducted to date evaluating the effect of this healthcare crisis on medical trainees in India during the pandemic. This meta-analysis includes cross-sectional studies on depression among medical students in India to determine the pooled prevalence of depression among medical students in India.
Materials and methods
This study was completed following the PRISMA checklist [ 12 ], and it was registered in PROSPERO (CRD42022331012) [ 13 ]. Before beginning the literature search, the study's framework was created using PRISMA criteria; after that, no changes were made.
Literature search
A systematic search was undertaken in three databases, namely PubMed, Google Scholar and Scopus, for all the available articles published in the English language during 2019-2021 on the prevalence of depression amongst undergraduate medical students in India by two independent investigators. (Appendices 1) Based on the "PICOS" principle for formulating the search strategy, the search terms include "Depression", "Undergraduate students", "medical students", "undergraduate medical students", and "MBBS students". We have added relevant articles identified by several databases to the search using Rayyan software. It was also attempted to contact the authors of articles whose full texts were unavailable in the databases. Appendices 1 presents a comprehensive search strategy.
Inclusion and exclusion criteria
The inclusion criteria were 1) Cross-sectional study design, 2) The study population was undergraduate medical students from India, 3) Assessing the prevalence of depression using a standardized instrument, and 4) The study period was from January 2019 to April 2022. The articles which did not state the information on the prevalence of depression or outcome data among the undergraduate medical students were excluded.
Study selection and data extraction
The studies were retrieved based on the search strategy discussed a priori. Multiple publications of the same study were identified and collated. Two independent reviewers screened titles and abstracts to identify the studies that meet the inclusion and exclusion criteria. Any disagreements were resolved by discussion or by a third reviewer. Data were extracted using a pre-designed spreadsheet from the studies which included the first author name, year of publication, study period, study setting, sample size, the instrument used for assessing depression, the total number of medical students, number of females, number of males, age (mean) of the student, prevalence of depression overall, and among male students and female students.
Quality assessment/risk of bias (ROB)
Using the Joanna Briggs Institute's (JBI) Critical Appraisal tool for systematic reviews of prevalence studies, we evaluated the study's methodology which was shown in Table Table1 1 [ 14 , 15 ]. The reviewers independently assessed the ROB using the Modified JBI criteria. In case of a mismatch of results, the discrepancies or disputes have been checked, and the reviewers came to a common opinion by discussing it with a third investigator. The evaluated articles were divided into three categories: high ROB (JBI score 49%), moderate ROB (JBI score between 50% and 69%), and low ROB (JBI score >70%) [ 16 ].
NA- Not available, ROB- Risk of bias
Data synthesis and analysis
In this meta-analysis, to determine the prevalence of depression among medical students, the pooled estimates with 95% confidence intervals (95% CI) were calculated using the random-effects model (DerSimonian-Laird method) due to high heterogeneity [ 17 ]. The forest plots have been used to determine the prevalence of pooled estimates. The estimation was calculated using MetaXL version 5.3 and an Excel spreadsheet. A P-value less than 0.05 was considered significant. The Q and I 2 statistics were used as tests for heterogeneity. Q test with P < 0.10 was considered statistically significant heterogeneity and I 2 >75% was labelled as high heterogeneity [ 18 ]. This review used the Doi plot and the LFK index for publication bias. The double arcsine prevalence was taken as the x-axis for the funnel plot. Arcsine transformation was required with data with extreme values like 0 or 1. Otherwise, the confidence interval for the proportion could include values outside the range of 0 and 1, representing 0% and 100%. The y-axis of the graphic was set to the precision obtained from the inverse of Standard Error (SE). Doi plot and the LFK index for publication bias were used to validate the funnel plot's asymmetries. Values describe the publication bias over ±1 of the LFK index [ 19 ]. Sensitivity analysis was done to indicate the major determinant for the pooled prevalence of depression.
Study Characteristics
The initial search from PubMed, Scopus, and Google Scholar yielded 3297 studies. Only 56 pertinent papers were reviewed for eligibility after removing duplicates based on the screening of titles and abstracts. Out of 56 papers, 19 articles were included in the quantitative synthesis after various publications were excluded for multiple reasons (Figure 1 ).

Table 1 shows the study characteristics of the included studies comprising study population, study setting, study tool, study period, sample size and number of depressed undergraduate students along with ROB [ 20 - 38 ].
The Pooled Prevalence of Depression
All the selected studies reported the prevalence of depression among medical students using different instruments for assessing depression. The prevalence of depression in the nineteen studies ranged from 16.0% to 100.0%. The pooled prevalence of nineteen studies, [ 20 - 38 ] 50.0% (95% CI: 31.0 to 70.0), was shown in Figure Figure2 2 .

Minimal depression was seen in only four studies, [ 20 , 24 , 28 , 31 ] with a pooled prevalence of 28.0% (95% CI: 20.0 to 37.0) whereas mild depression was found in six studies, [ 24 , 27 - 30 , 34 ] with pooled prevalence of 14.0% (95% CI: 4.0 to 28.0). The pooled prevalence of thirteen studies that have found moderate depression was found to be 15.0% (95% CI: 11.0 to 19.0) [ 20 , 21 , 24 , 25 , 27 - 31 , 33 - 35 , 37 ]. The pooled prevalence of three studies that have found moderately severe depression was found to be 7.0% (95% CI: 3.0 to 12.0) [ 20 , 24 , 31 ]. Severe depression was seen in eleven studies [ 21 , 24 , 25 , 27 - 29 , 31 , 33 - 35 , 37 ] with a pooled prevalence of 5.0% (95% CI: 3.0 to 7.0), and extremely severe depression was found in five studies [ 21 , 25 , 34 , 35 , 37 ] with a pooled prevalence of 5.0% (95% CI: 2.0 to 11.0). Seven studies have seen the depression of undergraduate medical students among males and females. The pooled estimate of depression among the females (pooled prevalence: 38.0%, 95% CI: 20.0 to 58.0) was slightly higher when compared to males (pooled prevalence: 34.0%, 95% CI: 15.0 to 55.0). Subgroup analysis was calculated for the pooled prevalence of depression based on the instruments used for screening depression. It was found that the pooled prevalence of depression was 27.0% (95% CI: 23.0 to 31.0), 99.0% (95% CI: 96.0 to 100.0), and 37.0% (95% CI: 29.0 to 46.0) in Depression Inventory Scale, Patient Health Questionnaire, and Depression Anxiety Stress Scale respectively.
Heterogeneity and Publication Bias
The nineteen included studies were analyzed for heterogeneity and publication bias [ 20 - 38 ]. High heterogeneity was found in the analysis with the Q test (p <0.001) and I 2 statistics (I 2 = 99.6%). For publication bias, the Doi plot showed no asymmetry confirming the absence of bias (LFK index = 0.15) (Figure (Figure3 3 .)

Sensitivity Analysis
The effect of each study (i.e. nineteen studies) [ 20 - 41 ] on the pooled prevalence of depression has been analysed by excluding each study step by step using sensitivity analysis (Table (Table2). 2 ). It showed that in eight studies, [ 21 , 23 , 26 - 29 , 36 , 38 ] comparatively the prime determinants of the pooled prevalence of depression among undergraduate medical students and the major source of heterogeneity come from five studies [ 25 , 30 , 34 , 35 , 37 ].
Although it is of global public health concern, depression among medical students is still under-recognized and the associated discrimination and stigma deter most of the students from seeking help. Research done among medical students even before the pandemic were showing higher rates of depression and physical distress in comparison to the general population [ 3 - 9 ]. COVID pandemic may have further declined the mental health of all individuals, especially medical students.
This is one of the few systematic reviews and meta-analyses on medical trainees which has ventured into exploring the prevalence of depression amidst the COVID pandemic. It has incorporated 19 original articles published from 2019 to 2022 from medical colleges situated in different regions of India. These articles used various standard screening instruments such as Patient Health Questionnaire (PHQ-9), Depression Anxiety Stress Scale (DASS 21), Beck Depression Inventory (BDI) Scale, Centre for Epidemiologic Studies Depression Scale and Hospital Anxiety and Depression Scale (HADS) for screening depression. The pooled prevalence of depression among medical students (n=5944) was found to be 50.0% [95% CI: (31%-70%] based on a random effect model pertaining to high heterogeneity [Q test (p <0.001) and I2 = 99.6%]; the depression calculated in the various studies ranged from 16.0% to 100.0%. This pooled prevalence is higher than the pooled prevalence value of 40%, which was done before the COVID pandemic, as mentioned in a meta-analysis conducted by Dwivedi N et al. [ 11 ] In Jia Q et al. study, a meta-analysis done in 41 studies among medical students from different countries showed a high pooled prevalence of depression of 37.9% among the students. Comparatively, this meta-analysis has shown a higher prevalence among Indian medical undergraduates, slightly higher in female students [ 10 ]. This variation of the depression may reflect the trend of higher rates of depression in females in the general population [ 42 ]. The severity of depression has also been measured in various studies, though it is not uniform throughout the studies as different screening tools had different cut off for measuring depression. The pooled prevalence of depression in this review varied from 27.0% to 99.0% when stratified based on the study tools. Depression Anxiety Stress Scale was the most commonly used scale among the studies, followed by Patient Health Questionnaire and Beck Depression Inventory.
According to this meta-analysis, one out of two students was found to have some degree of depression which is a concerning number. The prevalence has increased during the COVID pandemic compared to the prevalence before the pandemic since the pandemic itself may have a negative impact on the mental health of the students [ 11 ]. Further, it was also stated that it would increase the burden of depression in South Asian populations and healthcare systems [ 2 ]. There have been multiple explanations behind depression among medical students such as the challenging medical curriculum, lack of sleep and recreational activities due to vast academic tasks given, transition from a familiar to a non-familiar situation, lack of communication skills, etc. Several strategies can be implemented at different levels like changing the grading system, setting clear learning objectives to decrease academic burden, incorporating team-based learning and group activities rather than following traditional didactic lectures, self-directed learning so that students are aware of their shortcomings and promoting professionalism and communication skills for dealing patients properly. This pandemic had led to online teaching of medical students, [ 43 ] further, the effects of social distancing and self-isolation could have made the students more vulnerable to depression and anxiety [ 44 ]. This global health concern can also be taken care of using evidence-based structured programmes for mental upliftment like mindfulness therapy, life skill training, and counselling sessions can be kept for the students [ 45 , 46 ].
Strengths and limitations
The strengths of this study are that it has no asymmetry in the doi plot and is one of the few meta-analyses which has investigated the pooled prevalence of depression among the undergraduate students in India. Despite the strengths, this study has a few limitations like high heterogeneity and there might be a possibility of overestimation of the prevalence of depression because pooled prevalence has been calculated based on screening instruments and in various studies which are self-reporting and does not involve any clinical diagnosis.
Conclusions
The high prevalence of depression among medical students demands regular screening for depression along with counselling services. It shows that there is a need to raise awareness among students and other stakeholders, such as parents and medical educators, concerning symptoms and signs of depression among medical students. Further, effective strategies with health education programs and interventions may be given at individual, family, and community levels for providing mental health services to undergraduate medical students. Research with large sample sizes and multicentric longitudinal research is needed to determine the prevalence and risk factors for depression among medical students in India.
Acknowledgments
The authors are thankful to Dr. Radhika Rajendran, B.tech, PhD., Assistant Professor, Madhav Institute of Science and Technology, Gwalior, Madhya Pradesh, for her valuable inputs.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Eliminating the Pipeline Metaphor in Framing Workforce Equity for American Indian and Alaska Native Communities
- 1 California University of Science and Medicine, Colton, California
- 2 Association of American Indian Physicians, Oklahoma City, Oklahoma
- 3 Mescalero Apache Tribe, Mescalero, New Mexico
- 4 Department of Medicine, University of Illinois College of Medicine, Chicago
- 5 Hispanic Center of Excellence, University of Illinois College of Medicine, Chicago
- 6 JAMA Network Open , Chicago, Illinois
For many years, the term pipeline has been used metaphorically by researchers and policy makers to refer to the progression of students advancing toward a science, technology, engineering, or mathematics (STEM) degree or a career in medicine. 1 Past criticisms of the term pipeline highlight how students, especially those from historically excluded backgrounds, such as American Indian, Black, and Latino/a individuals, “leak” out of the “pipeline” for a variety of personal, social, financial (economic), or cultural reasons. For American Indian and Alaska Native individuals, the term pipeline is especially offensive. More specifically, this term is pejorative for communities where pipeline projects in the US threaten sacred homelands and water supplies. Many people will recall the resistance of the Standing Rock Sioux Tribe and their allies to the Dakota Access Pipeline. Recently, a new pipeline project impacting racially marginalized residents, including Black and low-income residents, living in the Southwest Crossings neighborhood of Houston, Texas, highlighted the continuing practice of divestment and displacement faced by these communities. 2
The American Medical Association (AMA) explored the negative connotations associated with the term pipeline in its “Promising Practices Among Pathway Programs to Increase Diversity in Medicine” report. The report refers to the adverse use of pipeline within “Native American communities that are a prioritized group for recruitment.” 3 In place of pipeline , the term pathways has come into favor by many, including the AMA and the Association of American Medical Colleges. Pipeline implies that there is only 1 entry point and 1 exit, and frames career development as a passive process in which individuals are commodified as a resource to be delivered as a final result. Pipeline leaves out the contexts, complexities, and variations of the myriad pathways students may take in education from elementary and secondary school, through higher education, and on to a STEM or health professions field. Pipeline connotes extraction, transport, and removal from community, rather than investment in and nurturing of people and resources in place. Since many historically marginalized or minoritized racial and ethnic groups of students may take nontraditional or divergent career pathways, it remains critically important to use the more inclusive, accurate term of pathways . Use of pathways for this purpose communicates respect for students’ choices, agency, and career exploration. Pathways connotes many desirable outcomes rather than just 1 and honors the active efforts of both individuals and communities in navigating a career journey. Instead of negatively framing variation in process as “leakage,” transition that values diverse pathways, a variety of outcomes, and the investments in the process can be encouraged. The term pathways communicates value for the unique, powerful attributes and experiences that historically excluded students bring to their education and career journeys.
Equity, diversity, and inclusion efforts have been challenged by performative allyship and the persistent lack of commitment to equitable access from institutional leadership. Proclaiming representative diversity as the end goal establishes dominant cultural norms of tokenism, deficit framing, and devaluation of historically excluded students and their communities. The messaging must evolve to value diversity as a shared value that benefits individuals, communities, institutions, and ultimately, patients. Using pathways terminology can help move beyond representation to inclusive excellence. Medicine as a profession must decommodify the language around workforce development challenges and focus on the power of diversity and inclusion to enhance and improve medicine, primary health care, 4 and health equity.
Leaders and administrators in research, education, and clinical care must be educated about the protected political, sovereign status of tribes and tribal people in the US, and they should incorporate these competencies into medical education for faculty, trainees, and students. Race-based theories and arguments are misapplied and insufficient for American Indian and Alaska Native peoples in many contexts, and lumping American Indian and Alaska Native people together under the term Indigenous or Native may be inaccurate or misleading and should be carefully examined. The federal government has a trust responsibility to uphold congressional treaties based on a Supreme Court decision. 5 Thus, American Indian and Alaska Native individuals have a unique political relationship with the US federal government that allows their status to be considered, regardless of programming or practices that may be race-based or race-conscious. As aptly stated by the Indian Law Resource Center, “Tribes are governments, not racial classifications.” 6 There are countless historic and recent publications using misleading, inaccurate, and harmful terms and classifications. Allies who do not identify as American Indian or Alaska Native, including influential medical educators, researchers, clinicians, authors, and journal editors in the US, should update their language with preference for the terms American Indian or Alaska Native . 7
Despite overwhelming evidence that racial concordance matters in the health outcomes of diverse patient populations, American Indian and Alaska Native tribal members make up less than 1% of all medical students and only 0.3% of all active physicians. 8 , 9 The upcoming relevant US Supreme Court decisions about the consideration of race in college admissions 10 , 11 should have no impact on efforts to recruit American Indian and Alaska Native students into careers in medicine and STEM. Institutions must commit to equitable access, resources, and support to advance representation of American Indian and Alaska Native peoples. The medical profession must rededicate its efforts and resources to investing in the inclusion and thriving of American Indian and Alaska Native students by understanding that talent is universal, while opportunity is not.
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Stern N et al. JAMA Network Open .
Published: July 6, 2023. doi:10.1001/jamanetworkopen.2023.21926
Correction: This article was corrected on May 30, 2024, to correct Dr Stern’s email address.
Corresponding Author: Nicole Stern, MD, Department of Medical Education. California University of Science and Medicine, 1501 Violet St, Colton, CA 92324 ( [email protected] ).
Conflict of Interest Disclosures: None reported.
Disclaimer: Dr Vela is an Associate Editor of JAMA Network Open , but she was not involved in any of the decisions regarding review of the manuscript or its acceptance.

See More About
Stern N , Vela M , Nakae S. Eliminating the Pipeline Metaphor in Framing Workforce Equity for American Indian and Alaska Native Communities. JAMA Netw Open. 2023;6(7):e2321926. doi:10.1001/jamanetworkopen.2023.21926
Manage citations:
© 2024
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

NOVYI MIR Research Journal
Ugc Care Group2 Journal || Issn No:0130-7673 || Submit Your Paper At [email protected]

Welcome To Novyi Mir Journal
Novyi Mir Research Journal is an open access scholastic and peer reviewed monthly international journal for encouraging Researchers, Practitioners, Academicians from Life Sciences, Engineering and Technology Management sectors to contribute to their inventive Research achievements and original work to make superiority information presented for a broader civic of readers and Internet users. Novyi Mir Research Journal targets at promoting the integration of academic theories. Novyi Mir Research Journal is an open access journal, which means that all articles are available on the internet to all users immediately upon publication. Non-commercial use and distribution in any medium is permitted, provided the author and the journal are properly credited. Benefits of open access for authors include: free access for all users worldwide, authors retain copyright to their work, increased visibility and readership, rapid publication, no spatial constraints. Special issues dedicated to international conferences in the topics of the journal are brought out, as well. All submitted manuscripts are initially evaluated by the editor and, if are found suitable, are sent for further consideration, to peer reviewers for an independent and anonymous expert review process.
Submit Your Paper To [email protected] We Will Publish Your Paper Within 24Hrs
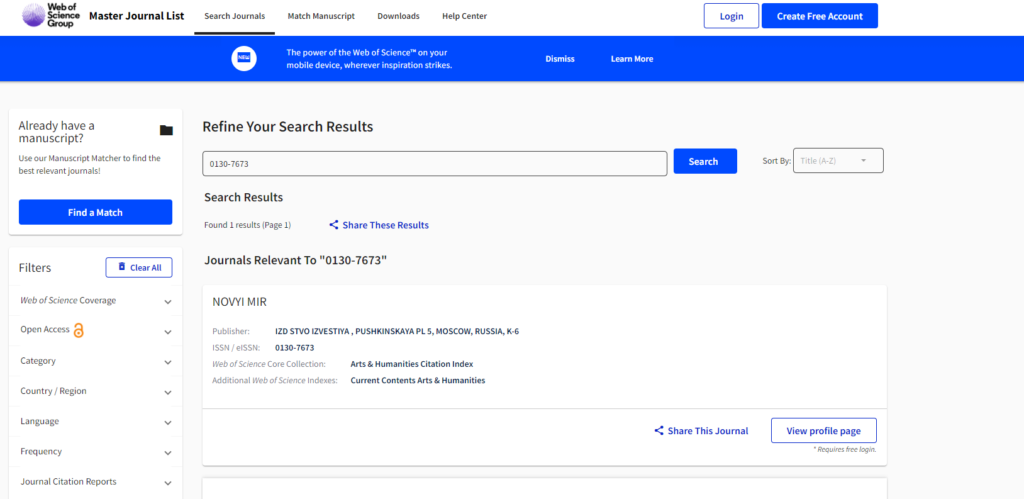
IMPORTANT LINKS UGC-Care Group -II Journals https://ugccare.unipune.ac.in/apps1/home/index https://mjl.clarivate.com/search-results
Submit your paper to: [email protected].

Call For Papers TOPICS Science, Engineering and Technology Arts, Social Sciences and Humanities Physical Sciences and Environment Biological & Medical Sciences Management and Commerce Agriculture and Veterinary Sciences Pharmacy Biomedical Engineering Dental Science Integrative Medicine – viz Healthcare- viz Medical Science Architectural and design research Urban planning research Architectural and design research Architectural and design theory
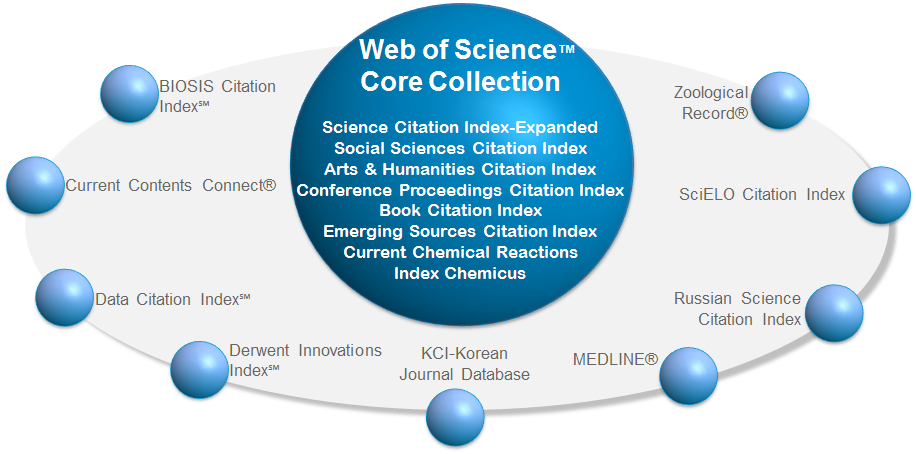
Indexing Of Novyimir Research Journal
Novyimir Research Journal is indexed in more than 15 esteemed online directories followed by DOI, CROSS REF, GOOGLE SCHOLAR, CITEFACTOR, ABEC, DOAJ, LATINDEX, REDIB, CAPESSCILIT and many more. To select the manuscripts we follow stringent guidelines to determine the originality, importance, timeliness, accessibility, grace and astonishing conclusions of the content.


- Conferences
- Current Issue
- Back Issues
Announcements
- Full List of Journals
- Migrate a Journal
- Special Issue Service
- Conference Publishing
- Editorial Board
- Other Journals
Journal of Health, Medicine and Nursing
The journal is a peer-reviewed, international and interdisciplinary research journal. The scope of the journal includes, physical & mental health, diet, exercise, sciences on health issues, public health, self-care, occupational health and safety issues, mechanisms in medicine, technology and manufacturing of medicines, diagosis, surgery, healthcare, nursing practice, nurse training and education, nursing ethics etc.
The journal also covers interdisciplinary research across the topics on policy, technological development, medicine industry.
About the Chief Editor of the journal
Prof. Ignat Ignatov was born on January 1, 1963 in Bulgaria. In 1989 he majored in physics from “Kliment Ohridski” Sofia University and in the same year he began his professional work in the sphere of medical biophysics. In 1996 he founded the Scientific and Research Center of Medical Biophysics (SRCMB). From 2007 Ignat Ignatov is honorable doctor in European Academy of Natural Sciences (Germany). From 2013 he is Doctor of Science and Professor in The Russian Academy for Natural History.
The publication charge of this journal: 160 USD (online publication only) or 165 USD (online publication + 2 hard copies)
IISTE is a member of CrossRef .
The DOI of the journal is: https://doi.org/10.7176/JHMN
Vol 115 (2024)
Table of contents.
Paper submission email: [email protected]
ISSN 2422-8419
Please add our address "[email protected]" into your email contact list.
This journal follows ISO 9001 management standard and licensed under a Creative Commons Attribution 3.0 License.
Copyright © www.iiste.org
Appointments at Mayo Clinic
- Nutrition and healthy eating
Caffeine content for coffee, tea, soda and more
Find out just how much of this stimulant is in coffee, tea, soda and energy drinks.
If you're like most adults, caffeine is a part of your daily routine. But do you know the caffeine content of your favorite drinks?
Up to 400 milligrams of caffeine a day is considered safe for most adults. However, people's sensitivity to caffeine varies. If you're bothered by headaches, restlessness or anxiety, you may want to reevaluate your caffeine intake. Also women who are pregnant, trying to become pregnant or breastfeeding are advised to limit their use of caffeine.
Check the charts for an idea of the caffeine content in popular beverages. Drink sizes are in fluid ounces (oz.) and milliliters (mL). Caffeine is shown in milligrams (mg).
Keep in mind that the actual caffeine content of a cup of coffee or tea can vary quite a bit. Factors such as processing and brewing time affect the caffeine level. So use these numbers as a guide.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Lieberman HR, et al. Daily patterns of caffeine intake and the association of intake with multiple sociodemographic and lifestyle factors in U.S. adults based on the NHANES 2007-2012 surveys. Journal of the American Academy of Nutrition and Dietetics. 2019; doi:10.1016/j.jand.2018.08.152.
- Grosso G, et al. Coffee, caffeine, and health outcomes: An umbrella review. Annual Review of Nutrition. 2019; doi:10.1146/annurev-nutr-071816-064941.
- Is your kid over-caffeinated? Academy of Nutrition and Dietetics. https://www.eatright.org/food/nutrition/healthy-eating/is-your-kid-over-caffeinated. Accessed Feb. 1, 2020.
- Spilling the beans: How much caffeine is too much. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/spilling-beans-how-much-caffeine-too-much. Accessed Sept. 20, 2019.
- 2015-2020 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. http://health.gov/dietaryguidelines/2015/guidelines. Accessed Feb. 1, 2020.
- Duyff RL. Think your drinks. In: Academy of Nutrition and Dietetics Complete Food and Nutrition Guide. 5th ed. Houghton Mifflin Harcourt; 2017.
- Branum AM, et al. Trends in caffeine intake among US children and adolescents. Pediatrics. 2014; doi:10.1542/peds.2013-2877.
- USDA Food Data Central. U.S. Department of Agriculture, Agricultural Research Service. https://fdc.nal.usda.gov/index.html. Accessed April 18, 2022.
- Bordeaux B. Benefits and risks of caffeine and caffeinated beverages. https://www.uptodate.com/contents/search. Accessed March 16, 2022.
- Zeratsky KA (expert opinion). Mayo Clinic. Feb. 5, 2020.
- Wikoff D, et al. Systematic review of the potential adverse effects of caffeine consumption in healthy adults, pregnant women, adolescents, and children. Food and Chemical Toxicology. 2017; doi: 10.1016/j.fct.2017.04.002.
Products and Services
- A Book: Cook Smart, Eat Well
- The Mayo Clinic Diet Online
- A Book: The Mayo Clinic Diet Bundle
- A Book: Mayo Clinic on Digestive Health
- Butter vs. margarine
- Clear liquid diet
- DASH diet: Recommended servings
- Sample DASH menus
- Diverticulitis attack triggers
- Diverticulitis diet
- Eggs and cholesterol
- Enlarged prostate: Does diet play a role?
- Fasting diet: Can it improve my heart health?
- Gluten sensitivity and psoriasis: What's the connection?
- Gluten-free diet
- Gout diet: What's allowed, what's not
- Intermittent fasting
- Low-fiber diet
- Low-glycemic index diet
- Mediterranean diet
- Picnic Problems: High Sodium
- Nutrition and pain
- Vegetarian diet
- Water after meals
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Caffeine content for coffee tea soda and more
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

VIDEO
COMMENTS
The Indian registry on current patient profiles & treatment trends in hypertension (RECORD): One year interim analysis. Rajadhyaksha, Girish Chandrakant; Reddy, Himanshu; Singh, Amresh Kumar; More. Indian Journal of Medical Research. 158 (3):244-255, September 2023. Abstract.
Verbal autopsy to assess causes of mortality among the economically productive age group in the tribal region of Melghat, central India. Satav, Ashish Rambhau; Satav, Kavita Ashish; Kelkar, Abhay Suresh; More. Indian Journal of Medical Research. 158 (3):217-254, September 2023. Abstract. Favorite. PDF. Permissions. Go to Full Text of this Article.
Latest Articles : Indian Journal of Medical Research. Latest Articles. The editors of this journal are pleased to offer electronic publication of accepted papers prior to print publication. These papers can be cited using the date of access and the unique DOI number. Any final changes in manuscripts will be made at the time of print publication ...
The Indian Journal of Medical Research (IJMR) is a biomedical journal with international circulation. It publishes original communications of biomedical research that advance or illuminate medical science or that educate the journal readers. It is issued monthly, in two volumes per year.
The Indian Journal of Medical Research is a peer-reviewed open-access medical journal. [1] [2] It is published by Medknow Publications on behalf of the Indian Council of Medical Research. [1] Since 1977, it has been published monthly with six issues per volume. [3] The journal publishes original "technical and clinical studies related to health ...
Journal List; Indian J Med Res; The Indian Journal of Medical Research Vols. 132 to 159; 2010 to 2024; Vol. 159 2024: v.159(1): 1-116 2024 Jan: v.159(2): 117-258 ... Articles from The Indian Journal of Medical Research are provided here courtesy of Wolters Kluwer -- Medknow Publications. Follow NCBI. Connect with NLM National Library of ...
The Indian Journal of Medical Research (IJMR) is a biomedical journal with international circulation. It publishes original communications of biomedical research that advance or illuminate medical science or that educate the journal readers. It is issued monthly, in two volumes per year. Manuscripts dealing with clinical aspects will be ...
Journal of the Indian Medical Association (JIMA) publishes Original research articles, Case Reports, Editorials, and Short Communication in all areas of medical science. The journal also considers publication of letters to the editor commenting on research already published in the journal, as well as manuscripts describing new hypotheses or ...
Indian Journal of Medical Research Review Latest Developments in the field of Multi Disciplinary. Print ISSN : 0971-5916 | Online ISSN : Awaited Frequency of publication: Monthly | Language of publication: English Starting year: 000 | Format of publication: Print + Online The Indian Journal of Medical Research (IJMR) is an open access peer-reviewed journal […]
The Indian Journal of Medical Research (IJMR) is among the oldest medical Journals in India and in Asia, and is in the 100 th year of publication. It was first published in 1913; the quality and popularity of the journal rose with increasing readership and indexing by various agencies of repute. [ 1] After IJMR, probably the next major ...
The rapid growth of Indian journals, including Perspectives in Clinical Research, is part of this positive trend. Recent rankings released by Thomas Reuters, based on the 2001 to August 31, 2011 time frame, [ 5] support this prediction. India now ranks 11 th in number of papers (293,049) and 16 th in citations (1,727,973), an improvement over ...
Indian Journal of Medical Research - Current Issue. The manuscripts are currently under the double-blinded peer review process and shall be available online as and when they get accepted and ready for publication. Login. Submit Article.
Evaluation of the International Society on Thrombosis & Haemostasis scoring system & its modifications in diagnosis of disseminated intravascular coagulation: A pilot study from southern India. Muddana, Pooja Sai; Kar, Sitanshu Sekhar; Kar, Rakhee. Indian Journal of Medical Research. 155 (2):306-310, February 2022.
Indian Council of Medical Research in Scimago Institutions Rankings. H-Index. 24. Publication type. Journals. ISSN. 03679012. Coverage. 2004-2005, 2012-2021. Information. ... Not every article in a journal is considered primary research and therefore "citable", this chart shows the ratio of a journal's articles including substantial research ...
An official journal of the. Indian Journal of Medical Microbiology (IJMM) provides comprehensive coverage of medical microbiology, as well as infectious diseases. We welcome wide ranging contributions; from basic research at laboratory to clinical trials, including bacteriology, mycobacteriology, virology, mycology and parasitology, infection ...
Indian Journal of Medical Research mainly tackles studies in Coronavirus disease 2019 (COVID-19), Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), 2019-20 coronavirus outbreak, Pandemic and One Health. While Coronavirus disease 2019 (COVID-19) is the focus of the journal, it also provided insights into the studies of Scope (project ...
Indian Journal of Urology, Volume 38, Issue 3, ... Kokilaben Dhirubhai Ambani Hospital and Medical Research . Institute, Mumbai, Maharashtra, 1 Department of Uro‑Oncology,
Diabetes is a global public health challenge, particularly in India, affecting millions. Among diabetic patients, lean type 2 diabetes is a severe subtype with higher microvascular complication risks. While studies on the prevalence, variations and risk factors of diabetes are increasingly available, there has been limited research on the prevalence, variations, and socioeconomic disparities ...
Indian Journal of Medical Research. 155(1):189-196, January 2022. Abstract. Favorite; PDF; Permissions Open. Learning from telepsychiatry during COVID-19 pandemic in India: Boon for public mental health in low- & middle-income countries. Ganesh, Ragul; Verma, Rohit; Deb, Koushik Sinha; More. Indian Journal of Medical Research. 155(1 ...
Research with large sample sizes and multicentric longitudinal research is needed to determine the prevalence and risk factors for depression among medical students in India. Acknowledgments The authors are thankful to Dr. Radhika Rajendran, B.tech, PhD., Assistant Professor, Madhav Institute of Science and Technology, Gwalior, Madhya Pradesh ...
Despite overwhelming evidence that racial concordance matters in the health outcomes of diverse patient populations, American Indian and Alaska Native tribal members make up less than 1% of all medical students and only 0.3% of all active physicians. 8,9 The upcoming relevant US Supreme Court decisions about the consideration of race in college ...
Novyimir Research Journal is indexed in more than 15 esteemed online directories followed by DOI, CROSS REF, GOOGLE SCHOLAR, CITEFACTOR, ABEC, DOAJ, LATINDEX, REDIB, CAPESSCILIT and many more.To select the manuscripts we follow stringent guidelines to determine the originality, importance, timeliness, accessibility, grace and astonishing conclusions of the content.
Indian Journal of Medical Research. 152(1-2):88-94, Jul-Aug 2020. Abstract. Favorite; PDF; Permissions Open. A preliminary study on contact tracing & transmission chain in a cluster of 17 cases of severe acute respiratory syndrome coronavirus 2 infection in Basti, Uttar Pradesh, India ...
About the Chief Editor of the journal. Prof. Ignat Ignatov was born on January 1, 1963 in Bulgaria. In 1989 he majored in physics from "Kliment Ohridski" Sofia University and in the same year he began his professional work in the sphere of medical biophysics. In 1996 he founded the Scientific and Research Center of Medical Biophysics (SRCMB).
Caffeine is shown in milligrams (mg). Keep in mind that the actual caffeine content of a cup of coffee or tea can vary quite a bit. Factors such as processing and brewing time affect the caffeine level. So use these numbers as a guide. Find out just how much caffeine is in coffee, tea, soda and energy drinks.
Dr Harpal Singh, Professor, Centre for Biomedical Engineering, Indian Institute of Technology, New Delhi Dr K.K. Talwar, Former Chairperson, Medical Council of India, New Delhi Dr Radhika Tandon, Professor of Ophthalmology, Dr. Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi Editorial Staff