

15 Organ Donation Pros and Cons
We never know when tragedy might strike. We never known when an illness may develop. Some people may even be born with a genetic disorder or disease and require help. That is why the current system of organ donations is such an integral part of our healthcare system.
Thanks to modernizing technologies, it is possible for more people to become living donors than ever before. It is also very easy to list yourself as an organ donor should something happen to you, allowing you to save multiple lives with one final act of caring and grace.
There are some organ donation pros and cons that should be thought about if you’re wondering if becoming an organ donor is the right decision for you.
Here Are the Pros of Organ Donation
1. It is possible for one organ donor to save up to 8 lives. More than 100,000 people just in the United States are waiting for an organ transplant right now. This includes critical organs, such as the heart, the liver, and the kidneys. When a person registers as an organ donor, it becomes possible to help save lives in ways that you may have never thought possible before.
2. It offers people a second chance at life. People who are waiting for an organ transplant are often dependent on costly treatments to survive. A person waiting for a kidney transplant, for example, may need to visit a dialysis clinic multiple times per week to have their blood cleaned. By being able to donate an organ, it becomes possible for that individual to return to a somewhat normal lifestyle that doesn’t have the same costly procedures that need to happen on a regular basis.
3. It can offer a sense of closure. For organ donations which occur out of tragedy, the process of organ donation can help families to find a sense of closure that wouldn’t happen otherwise. Knowing that the heart of a son, daughter, father, or mother continues to beat on in the chest of someone else can be a comforting experience. It won’t eliminate the grief that comes from losing a loved one, but it does communicate the idea that their loss is not in vain. Letting someone continue with their life is a gift that really does keep on giving.
4. It is possible to help someone right now. If someone is a direct match for an individual on the organ transplant list, then it is possible to help a person in need right now. You can donate certain organs while you are still alive. Living donations right now include a kidney, portions of the liver, portions of the lung or pancreas, and some intestinal tissues as well. If you are not comfortable with this type of living donation, then consider donating blood.
5. There are no age restrictions on being an organ donor. Anyone can be an organ donor, including children. The only restrictions in place are related to the age of certain organs for some individuals and that children under the age of 18 must have the consent of a parent or guardian to provide a donation.
6. It allows for the potential of medical research advances. Organ donation may not always be possible to help someone else live a normal life, but that doesn’t completely exclude the ability to donate to help others. People can make donation to benefit science and medical research. This may include donating a specific organ, such as a heart or their brain. It can even include donating their entire body. For those who may have a rare disease or genetic condition, a donation such as this offers the potential of saving more lives through the knowledge gained.
7. Living donations are free. If you are approved as a match and make a living donation for someone in need, then the medical procedure and recovery needs you have are free of charge. The costs related to you are usually not passed on to the organ recipient either, as many physicians will provide their services free of charge. Even if there are recovery complications, your medical costs are covered.
8. More organ transplants are happening today than ever before. In 2016, there were more than 33,500 organ transplants that occurred in the United States. That set a new record for completed transplants. Thanks to improvements in medical procedures and technology innovations, there has been a 20% increase in successful transplants from 2012-2016. With more than 8,000 transplants completed in the first quarter of 2017, that is a trend which looks to be continuing.
Here Are the Cons of Organ Donation
1. It can prolong the grieving period of a family. For an organ donation to be successful, it may be necessary to keep a loved one on life support for an extended period. This helps to keep the tissues which will be donated in a healthy state. Organ donations do not occur unless a person is declared to be brain dead, but the process of life support can make it feel like a loved one is still alive. When there is the presence of life, there is often hope, and having that hope can make the grief even stronger.
2. There is not always a choice for the donation. Many families do not have a choice in who gets the organs that are being donated by a loved one through tragedy. They are simply given to the person who is on the organ donation list who is a match and in the direst of need. This means someone of a different faith, a different political position, or different culture may receive the organ and that can be difficult for some families to accept. Living donations are often matched to other family members, while direct matches for humanitarian purposes are also possible, so this key point doesn’t always apply.
3. Not everyone can become an organ donor. Although many people can become an organ donor through a simple authorization process, not everyone is eligible. There are age-related restrictions on certain organs. You cannot be over 80 years old to make a cornea donation and must be younger than 60 to donate heart valves or tendons. People with certain existing medical conditions, such as being HIV-positive, having metastasized cancer in the last 12 months, or being diagnosed with Creuzfeldt-Jacob Disease will also prevent a donation.
4. Organ donations can lead to other health problems. To become a living donor, a surgery or medical procedure is required. Any surgery offers a risk to the person that may include death. Other health problems can develop after a surgery that requires a lifestyle change. People who donate bone marrow, for example, may be restricted in the future activities for a lifetime. Those who donate a kidney may be prohibited from consuming alcohol. For those who receive an organ, there is a 10% risk of diabetes development.
5. Not every organ which is donated will be accepted. Organ rejection is a very real possibility for those who receive a transplant. Even when there is a direct match, there is always the chance that the transplant will be rejected. Those who receive a transplant will often be required to take immunosuppressant medications for the rest of their lives to reduce the chances of this issue from occurring.
6. Employers do not always have leave policies for living donations. Only 12 states in the US currently have organ or bone marrow donor leave policies that impact private sector employees. Federal government employees receive 30 days of paid leave for an organ donation and 7 days of paid leave for a bone marrow donation that is over and above the employee’s sick and annual leave. Most states have similar donor leave laws for state employees, but some offer the 30 days of leave unpaid.
7. Organ transplants are incredibly expensive. In the United States, the cost of a liver transplant is $71,000, plus an additional $25,000 for every 30 days of care pre-transplant. For those who need a heart-lung transplant, the cost is $130,000, with an additional $56,000 for every 30 days of care pre-transplant. For many organ recipients, their total care cost exceeds $1 million, with heart-lung transplant recipients facing a cost of $2.3 million. Part of this cost is due to the wait time to receive an organ transplant. For some organs, the average wait time can be 3-5 years in some regions of the United States.
The pros and cons of organ donation show that you can get involved in some way right now. You can register to become an organ donor. You can register your children. You can also be tested to see if you could become a living donor for someone who is in need right now. Someone is added to the national organ transplant waiting list every 10 minutes, on average, in the United States. Since one organ donor can save up to 8 lives, the time to act is now.
- Organ Donation
5 Pros and Cons of Being an Organ Donor Explained
Updated 06/13/2022
Published 11/13/2020

Sherrie Johnson, BA in Liberal Studies
Contributing writer

Cake values integrity and transparency. We follow a strict editorial process to provide you with the best content possible. We also may earn commission from purchases made through affiliate links. As an Amazon Associate, we earn from qualifying purchases. Learn more in our affiliate disclosure .
If you’re thinking about becoming an organ donor, it’s important to weigh all the pros and cons before making the choice. Becoming a living donor or a donor after you die is a decision that you shouldn’t take lightly. Not only does your being a donor potentially impact you, but it can also impact your immediate family and even your closest friends. Learn how to become a donor, what it involves, and familiarize yourself with the pros and cons of organ donation.
Jump ahead to these sections:
Pros of becoming an organ donor, cons of becoming an organ donor.
There are numerous benefits to becoming an organ donor, whether you decide to become a living donor or a donor after your death. Here are some of the things you can look forward to if you choose to sign up for the national organ donor registry.
1. Anyone can donate at any age
Many people assume that they can’t be an organ donor because they’re not the right age, in good enough health, or even have the right ethnic background to donate. However, that isn’t the case at all!
You can choose to become an organ donor at any age. If you’re under 18, you can sign up to become a living donor or a donor after death with the consent of a parent. For all other ages, you can choose to become a donor at any time.
People of all ages need organs, making your donation critical — no matter your age. Donors range from newborns all the way up to those in their 90s.
Worried about a health condition? There are very few reasons why your organs wouldn’t be accepted for donation.
Outside of active cancer or a systemic infection, your organs would likely be healthy enough to be used. Common health issues like high blood pressure and diabetes — reasons why some might think they’d become ineligible — are not reasons for rejection at all.
If religious beliefs cause you to question whether you should sign up, many religions do believe in the validity of being a donor. Religions that specifically support organ donation include most branches of Christianity, Judaism, and Islam.
Living or deceased
Not only can you decide to become a donor at the point of your death, but you can also decide to become a living donor. While the majority of organs needed by patients can only be taken after someone dies, several organs can be donated by those still living including:
- Part of a liver
- Part of a lung
- Part of a pancreas
- Part of an intestine
- Some tissues
Since we have two kidneys and only need one to function, the whole organ can be removed from a living donor. Pieces of the liver, lung, pancreas, or intestine can be taken and the body will compensate for the missing piece.
2. You can save one life — or more
When you choose to be an organ donor, you’re not just impacting one person’s life. As a donor, you have the opportunity to save up to eight lives with your:
- Pair of lungs
Once each of these organs is removed, they can go to eight different people in desperate need. And that’s just the major organs. If you choose to donate tissue, eyes, and other parts, your donation can go even further.
3. Your death can be more meaningful
For many families, the tragic and untimely death of a loved one lacks meaning and feels senseless. Some would even say their death is “wasteful” as such a young life was wasted when they had so much life left to live.
By donating your organs, even tragic and untimely deaths don’t have to be meaningless. Though death is still tragic and loss deeply painful, many families of organ donors say that they were given hope when their loved one’s organs were given to someone in need. A seemingly meaningless death becomes something meaningful and allows a loved one’s legacy to live on through the life of the organ recipient.
4. You can further medical research
If you don’t want to be buried and you’re looking for alternatives to cremation , consider donating your body to science . When you do, your body might be used to help medical students train and become doctors.
Your body could also be used to provide study and research on diseases. Who knows? Your donation could be the reason for a major medical breakthrough that transforms the medical world.
5. You can help someone right now
As a living donor, you don’t have to wait until your death to donate. You can help someone in need right now.
You could be a match for a kidney for a close friend or family member, or give part of your liver, pancreas, lungs, or intestines to a complete stranger. By becoming a living donor, you can do something to change the world right now.
You can find numerous benefits to becoming an organ donor but there are some cons to think through as well. Here are several to consider before deciding what to choose.
1. It can lengthen the grieving process
When an organ donor passes away, the hospital keeps the deceased person on life support until recipient matches can be found for their organs. This is done to keep blood flowing through the body and the organs alive even though the person is legally and clinically deceased.
This can be difficult for family members who must wait until the organs have been taken for the body to be transported and prepared for burial. It lengthens the waiting process and can prolong grieving while the family waits for closure.
In some cases, keeping the person on life support can also provide a false sense of hope that a loved one will somehow get better. Once the organs are removed and the person is taken off of life support, it can feel like the family has to deal with death a second time.
2. You may not get to choose the recipient
If you’re a living donor, you might choose who to give your kidney to. If a family member or friend, for example, needs a kidney and you’re a match, you can volunteer to have your kidney go to that person.
When you pass away, your organs will go to the most eligible recipient on the waiting list. You won’t get to choose who receives your heart or liver. Some potential donors and their family members might find this aspect difficult to deal with.
Family members also may not get to meet the recipient or their families. If organ donation is chosen to provide a legacy, the family may be disappointed. Not all donors and recipients are able to meet each other.
3. Living donors can encounter health complications
As a living donor, you will undergo surgery to remove the organ or pieces of organs you plan to donate. As with any surgery, health complications can occur, from excessive bleeding during surgery to infection and scarring.
Though there is little long-term information with regard to health complications for living donors, some studies have shown that kidney donors may deal with long-term issues including high blood pressure. A small percentage end up needing dialysis or a transplant themselves.
Living liver donors are at a slightly greater risk for long-term health complications, including abdominal bleeding, intestinal problems such as blockages or tears, organ impairment or failure, and the need for a transplant.
4. Organ rejection could happen for recipients
Organ donation and the medications that help a recipient’s body accept the organ have gotten better and better over the years. Unfortunately, the reality still exists that a recipient’s body may reject the organ, despite anti-rejection medications. If this is the case, it can be hard on the donor’s family.
In the case where a donor’s family gets to know the recipient, it can be especially painful if, after several months, the transplanted organ fails or is rejected. For the families of donors, it can feel like they’re losing their loved one all over again, this time because the recipient hasn’t been helped permanently by the donated organ.
5. Families may not agree with the decision
Not all families accept the practice of organ donation and you may find that your family disagrees with your choice. Disagreements arise due to religious and personal preferences. The decision can cause some family members to become upset.
Should you wish to sign up for the national registry of organ donors and your family does not agree with your choice, it’s essential that you express your wishes in writing. In addition to placing the donor sticker on your driver’s license, file an advanced directive.
Once notarized, the advanced directive is a legally binding document that communicates to doctors and caregivers what you want to happen medically should you become uncommunicative or die. Have a copy placed in your permanent medical files and give copies to your immediate family members as well.
To avoid confusion and arguments at the time of your death, be sure that your funeral wishes are known by all close relatives and even close friends.
Giving Hope and Life
Organ donation is a powerful tool used to offer thousands of people the gift of hope and new life each year. If you don’t have any objections to signing up, you can become an organ donor and give people across America a second chance at life.
- “Benefits and Risks of Becoming a Living Donor.” Living Donation, American Transplant Foundation, 2020. americantransplantfoundation.org/about-transplant/living-donation/about-living-donation/#:~:text=Risks%20to%20the%20Donor,other%20organs%2C%20and%20even%20death
- “Organ Donation Statistics.” Organ Donor, U.S. Government Information on Organ Donation and Transplantation, 2020. organdonor.gov/statistics-stories/statistics.html
- “Making Your Last Wishes Known.” A to Z Guides, WebMD, 7 July 2000. webmd.com/a-to-z-guides/features/making-your-last-wishes-known#1
Categories:
- How To Share Your Wishes
You may also like

What’s the Organ Donation Process After Death? 10 Steps

How to Become an Organ Donor in the US (2021 Update)

Donor Stewardship Plans: Definition+ FREE Template

How to Organize & Share Your Final Wishes for Free

Benefits and risks of becoming a living organ donor

Please check out our Living Donation Guide for more information and resources.
Living Donation Benefits
For the recipient:.
- Quality of life: Transplants can greatly improve a recipient’s health and quality of life, allowing them to return to normal activities. They can spend more time with family and friends, be more physically active, and pursue their interests more fully.
- Increased life span: A kidney transplant dramatically increases the life span of a patient by about 10 years and improves their quality of life. Dialysis, while clearly a life-saving treatment, it is a less-than-perfect replacement for an actual human kidney. In addition, people who undergo a transplant will no longer require weekly dialysis treatments or have the side effects of dialysis such as nausea, vomiting, low blood pressure, muscle cramping, and itchy skin.
- Shorter waiting time : Due to the lack of organs available for transplant, patients on the national transplant list often face long wait times (sometimes several years) before they are able to receive a transplant from a deceased donor. Patients who find a suitable living donor do not have to wait on the list.
- Better results : Transplant candidates generally have better results when they receive organs from living donors as compared to organs from deceased donors. Often, transplanted organs from living donors have greater longevity than those from deceased donors. Genetic matches between living donors and candidates may lessen the risk of rejection.
- Kidneys and Livers Function Almost Immediately : A kidney or liver from a living donor usually functions immediately in the recipient. In uncommon cases, some kidneys from deceased donors do not work immediately, and as a result, the patient may require dialysis until the kidney starts to function.
For the Living Donor:
- Positive emotional experiences: The gift of an organ can save the life of a transplant candidate. The experience of providing this special gift to a person in need can serve be a positive aspect of donation.
- More time with your loved one: Donating an organ can increase the time you have to spend with your loved one as well as the quality of that time.
For Both the Recipient and the Living Donor:
- Flexible time frame : Surgery can be scheduled at a time that is convenient for both the donor and recipient.
- Removes a candidate from the list: A living donor removes a candidate from the national transplant waiting list, which is currently above 114,000 people. This allows the people on the waiting list who cannot find a living donor a better chance of receiving the gift of life from a deceased donor.
- Immediate impact: The impact of a transplant is so striking that recipients often look noticeably healthier as soon as they emerge from surgery.
Living Donation Impacts/Risks
Living donation does not change life expectancy, and after recovery from the surgery, most donors go on to live happy, healthy, and active lives.
For kidney donors, the usual recovery time after the surgery is short, and donors can generally resume their normal home and working lives within two to six weeks. Liver donors typically need a minimum of two months to resume their normal home and working lives.
Although transplantation is highly successful, complications for the donor and recipient can arise. Make sure to check out common myths and concerns about living donation. Be sure to talk to your doctor about what to expect.
Effects on the Body
For living kidney donors, the remaining kidney will enlarge slightly to do the work that two healthy kidneys share. The liver has the ability to regenerate and regain full function. Lungs and pancreas do not regenerate, but donors usually do not experience problems with reduced function.
Risks to the Donor
As with any other surgery, there are both short and long term risks involved in living donation. Surgical complications can include pain, infection, blood loss, blood clots, allergic reactions to anesthesia, pneumonia, injury to surrounding tissue or other organs, and even death. As transplant surgeries are becoming more common and surgical techniques are advancing, risks involved with living donation continue to decrease.
There has been no national systematic long-term data collection on the risks associated with living organ donation. However, there are studies that are currently gathering such information. Based upon limited information that is currently available, overall risks are considered to be low. Risks can differ among donors and the type of organ.
For kidney donors, there is only a 1% lifetime increase in the donor’s own risk of kidney failure. To put this into perspective, the general population has a 3% risk for kidney failure. Overall, there is only a three in 10,000 risk of dying during surgery and in general donation neither reduces life expectancy nor prevents donors from living normal, healthy lives. Some possible long-term risks of donating a kidney may include high blood pressure (hypertension); large amount of protein in the urine; hernia; organ impairment or failure that leads to the need for dialysis or transplantation.
Liver transplantation carries greater risk for both the donor and the recipient than kidney transplantation. Some possible long-term risks associated with donating a lobe of the liver may include wound infections; hernia; abdominal bleeding; bile leakage; narrowing of the bile duct; intestinal problems including blockages and tears; organ impairment or failure that leads to the need for transplantation.
Limited Long-Term Data about Living Donors
The Organ Procurement and Transplantation Network (OPTN) has limited long-term data available on how living donors do over time. Based on OPTN data from 1998 through 2007, of the 3,086 individuals who were living liver donors, at least four* have been listed for a liver transplant due to complications related to the donation surgery. Of the 59,075 individuals who were living kidney donors from 1998 to 2007, at least 11* have been listed for a kidney transplant. However, the medical problems that caused these kidney donors to be listed for transplant may or may not be connected to the donation.
*This total only captures data on transplant candidates who are known to the OPTN/UNOS to be previous donors.
Real Life Living Donor Heroes!

Chelsey donated a kidney to her college roommate, Ellen. Chelsey is now a 1+1=LIFE Mentorship mentor and member of our Young Professionals Group (TLC).

Steve donated a kidney to his daughter, Kelsey. He is now a Team Transplant cyclist and 1+1=LIFE Mentorship mentor .

Keith (right) received the GIFT OF LIFE when he was given a kidney from his step-son Jonny (left). Keith is now a mentor in our 1+1=LIFE Mentorship Program .
Other Considerations
Studies have shown that donating a kidney or part of the liver does not affect a woman’s ability to have children. However, it is important that you tell your doctors of your plans to have children. Each case is different, and your doctor may have additional recommendations given your medical history. A recent study from Toronto says that women who have donated a kidney are at higher risk of developing gestational hypertension or pre-eclampsia during pregnancies that follow the donation. The study suggests the increase in risk is not enormous (about a 6% increase), and in fact most women who have donated a kidney can safely carry a pregnancy to term. More information about the study can be found here.
Police, Fire, and Military Service
Some police and fire departments or branches of the military will not accept individuals with only one kidney. Be sure to talk to your superior if you are considering becoming a living donor.
Please note: As detailed in our Privacy Policy , the information contained on this site does NOT substitute medical advice. Please discuss any medical questions, considerations, and decisions with your doctor
Living organ donations are categorized in the following ways:
- Non-Directed Living Organ Donation
- Directed Living Organ donation
Living organ donors are usually between the ages of 18 and 60 year old . However, acceptable ages may vary by transplant center and the health of the donor candidate.
The prospective donor must have several points of compatibility including a compatible blood type , tissue type, and other markers.
The donor candidate is carefully evaluated by lab tests, physical examination, and psychological evaluation to ensure that the candidate is healthy enough to donate and that he or she is making an informed decision. The decision about whether to accept the donor is then made by the health care team at the transplant center.
Please note: It is illegal to sell human organs for the purpose of transplantation. Federal law stipulates that no person may be paid and/or receive valuable consideration for donating an organ.
See Living Donor Laws – Federal and State by State
Need support? Connect with a Mentor .
See our Living Donor Guide for more information.
Other Living Donation Resources
The American Transplant Foundation (ATF) is the only 501 (c)(3) nonprofit in the country that provides three tiers of support for living donors, transplant recipients, and their families. We go beyond awareness by providing real help to patients who need it the most. Join us and be part of the community fighting for the lives of those on the transplant wait list.
Join our online community where you can share, reflect, connect.
Quick links.
Donate Today! Honor a Loved One Potential Living Donor Database Download our Media Kit Legislation 1+1=LIFE Mentorship Program Join Save a Life Giving Club Fundraise Online Shop
Sign up now to receive alerts, updates, and invitations to events
Email Address *
Why Don't More People Want to Donate Their Organs?
Around 21 Americans die each day waiting for transplants. What's behind the reluctance to posthumously save a life?
In 1998, Adam Vasser, a 13-year-old teenager who loved playing baseball, was vacationing in Montana with his family when he suddenly came down with what felt like the flu. When he had trouble breathing and his ankles became swollen, his parents took him to a nearby clinic where the doctor on duty checked his vitals and sent him directly to the hospital across the street. By the time the family arrived at the hospital a few minutes later, Adam was in complete heart failure.
For months, Adam waited in a hospital for a heart transplant, during which time his heart was only able to pump with the assistance of a left-ventricular assist device (LVAD). “It was the size of a washing machine and it had two tubes that went through my chest into my left ventricle to help it pump blood,” Adam, now a 30-year-old teacher in the San Francisco Bay Area, recalls. “My official diagnosis was idiopathic viral cardiomyopathy. Meaning, basically, a virus of unknown origin had attacked my heart.” Four and a half months after getting sick, Adam underwent a heart transplant that saved his life.
But thousands of people aren’t as lucky. In the United States alone, 21 people die everyday waiting for an organ transplant. Though about 45 percent of American adults are registered organ donors, it varies widely by state. More than 80 percent of adults in Alaska were registered donors in 2012, compared to only 12.7 percent in New York, for example . In New York alone, there are more than 10,000 people currently waiting for organ transplants. According to data compiled by the Organ Procurement and Transplantation Network , more than 500 people died in New York last year, waiting for an organ to become available.
Given this shortage of organs, why don’t more people donate?
It’s a touchy question, something non-donors aren’t necessarily keen to answer. But experts say there is a large disparity between the number of people who say that they support organ donation in theory and the number of people who actually register. In the U.K., for example, more than 90 percent of people say they support organ donation in opinion polls, but less than one-third are registered donors. What keeps well-intentioned people from ultimately donating is something that academics, doctors, and organ-donation activists are trying to figure out.
In a recent literature review , researchers at the University of Geneva examined several social and psychological reasons why people choose not to donate, either by not registering as an organ donor during their lives, or electing not to donate the organs of their next of kin.
The study cites mistrust in the medical field and lack of understanding about brain death as major barriers to donation. A 2002 study in Australia, for example, illustrates the controversy surrounding brain death . Some participants indicated that they wouldn’t donate the organs of their next of kin if his or her heart were still beating, even if they were proclaimed brain-dead.
Studies have also shown that the less people trust medical professionals, the less likely they are to donate. The mistrust can come from personal experience—one study in New York showed , for example, that next of kin who perceived a lower quality of care during a loved one’s final days were less likely to consent to donation—or from misconceptions about how the medical community treats registered organ donors.
“There are a lot of people who subscribe to the belief that if a doctor knows you are a registered donor, they won’t do everything they can to save your life,” says Brian Quick , an associate professor of communication at the University of Illinois.
More than half of people, one study shows, have gotten information regarding organ donation from TV, so it makes sense that researchers are concerned with how fictional medical dramas can influence our attitudes toward medical professionals (a topic The Atlantic covered in August ).
Recommended Reading
When are you really an adult.

A Kidnapping Gone Very Wrong

Dear Therapist: I Don’t Approve of My Daughter-in-Law’s Parenting
Quick and his colleagues have studied how watching Grey’s Anatomy can influence people’s attitudes toward the medical community. “We found that heavy viewers of the show saw Grey’s Anatomy as realistic, meaning that they felt the images and the stories were realistic. And the more realistic they saw these stories, the more likely they were to buy into medical mistrust.”
Religion is another factor that repeatedly comes up in research. While many religions consider organ donation an act of love, some research has shown that Catholics are less likely to donate than other religious groups, despite the Vatican’s official position in favor of it. It seems that this is due to a belief in the afterlife and the concern for maintaining body integrity .
It could be that people are simply uncomfortable or unwilling to talk about death at all. In a survey of more than 4,000 students and their families from six universities throughout the United States, some people indicated concern that making plans for death would bring it about prematurely (which might also account for the fact that only 25 percent of Americans have advance directives). Others can’t shake the “ick” factor. Defined by researchers as “a basic disgust response to the idea of organ procurement or transplantation,” a 2011 study in Scotland found that non-donors reported higher levels of the ick factor and concern with body integrity than donors.
In a study of British women who had not signed up to be donors, researchers found that they were uncomfortable talking about death, with one participant saying, “The underlying taboo is that you have to be dead, potentially, well, you have to be dead […] Nobody really wants to think about that.” The research suggests that the more matter-of-fact attitude people have when talking about death and normalizing the issue of organ donation, the more likely they are to sign up as donors.
And this is where a lot of people think the solution comes in. “What we’re trying to do in New York is move the cultural needle on the issue,” says Aisha Tator, executive director of the New York Alliance for Donation . “Organized tissue donation should be a cultural norm like we did with bike helmet and seatbelt interventions.” Her organization isn’t the only one. Throughout the United States there have been a smattering of recent educational campaigns and studies on their efficacy. Campaigns have targeted the young , the old , nurses , DMV employees , and ethnic minorities who tend to donate less than white Americans or white Brits.
Another, more ambitious, strategy people point to is to change from the United States’ current opt-in system to an opt-out system, which would mean that everyone would be a donor by default, unless they actively opted out.
In a recent study conducted in the U.K., researchers studied the organ-donation systems of 48 countries over 13 years and concluded that Spain, with an opt-out style of consent, had the highest rate of organ donation of the countries studied and represents a successful model to emulate.
But beyond being a political and bureaucratic nightmare to actually make happen, changing the American system to an opt-out system might not fix the problem.
“The Spanish model is held up as the ideal, and in many ways it is,” says Eamonn Ferguson, a professor of health psychology at the University of Nottingham and one of the researchers on the study. “They have an opt-out system, but they also have a very coordinated, hierarchical, interlinked system of well-trained organ-transplant professionals.” Adding to the complexity of the issue is the fact that the rate of live organ donations is lower in countries with opt-out systems.
Some groups of people have tried to take the issue into their own hands. Lifesharers and other organ sharing networks, in which members promise to donate organs upon their death and give priority to fellow member donors, highlight that notions of reciprocity and fairness are incentives for at least some people.
The transplant system in Israel is a case study for how these ideas can be systematized. A change of law in 2010 that prioritizes patients with a history of donation—if a family member donated his or her organs or the patient himself made a living donation or if the patient has been on the donor list for at least three years—has incentivized a significant portion of the population to register as donors.
Preliminary results, published last year, show that the annual deceased organ-donation rate increased from 7.8 organs per million people in 2010 to 11.4 organs per million people in 2011. The number of new registrations per month more than doubled and the total number of candidates waiting for a transplant fell for the first time ever.
The new law, which was coupled with a multimedia campaign called ‘Sign and Be Prioritized’ and a streamlined registration process, has also changed who receives organs.
“More than 35 percent of those who actually got organs after the law was passed got them because of the prioritizing system,” says Dr. Jacob Levee, director of the Heart Transplantation Unit at Sheba Medical Center who spearheaded the change and authored the results. “It’s not just a dead-letter law. We’ve seen an actual change in how organs are being allocated.”
Though the Israeli case is compelling, for some, the decision to donate might not be rational at all. If the idea of someone cutting them open makes people feel sick, they are probably unlikely to sign up.
“Unfortunately unless you’re personally touched by the issue, unless you have a child that gets a virus and suddenly needs a new heart, you don’t really think about it,” Tator says. But it’s not only recipients like Vasser who can be touched by a transplant. The parents of at least one donor have become vocal advocates of organ donation after the loss of their son.

In 2003, Matthew Messina, a 25-year-old student at Chico State, was struck by a drunk driver while riding his bike home from a barbecue. Soon after his family arrived from New York, Matthew was in a coma. After running a series of tests, the neurosurgeon determined that he was brain-dead and recommended taking him off life support.
Matthew’s father Sam Messina says that when the organ-procurement team approached him and his wife, they knew it was something that Matthew, who was a reservist in the Marines and volunteered with handicapped children in his spare time, would have wanted to do.
“We stay in touch with two women in California who received organs from him. Both are married with families,” Sam Messina, who now gives talks about organ donation and is on the board of directors at the Center for Donation and Transplant , told me. “When I look into their eyes, I see a little bit of Matthew moving on.”
Appointments at Mayo Clinic
- Consumer health
Organ donation: Don't let these myths confuse you
Unsure about donating organs for transplant? Don't let wrong ideas keep you from saving lives.
Connect with others
News, connections and conversations for your health
- Transplant Page - Connect with others Transplant Page
- Transplant Group - Connect with others Transplant Group
Answers to common organ donation questions and concerns.
More than 100,000 people in the U.S. are waiting for an organ transplant.
Sadly, many may never get the call saying that a donor organ has been found. Many may not get that second chance at life. Every day in the U.S., about 17 people die because there aren't enough donor organs for all who wait for a transplant.
It can be hard to think about dying. It can be even harder to think about donating organs and tissue. But organ donors save lives.
Here are answers to some common organ donation myths and concerns.
Myth: If I agree to donate my organs, the hospital staff won't work as hard to save my life.
Fact: When you go to the hospital for treatment, the health care team tries to save your life, not someone else's. You get the best care you can get.
Myth: Maybe I won't really be dead when they sign my death certificate.
Fact: This is a popular topic in tabloids. But in reality, people don't start to wiggle their toes after a health care provider says they're dead. In fact, people who have agreed to organ donation are given more tests to make sure they're dead than are those who aren't donating organs. These tests are done at no charge to their families.
Myth: Organ donation is against my faith.
Fact: Most major faiths accept organ donation. These include Catholicism, Islam, Buddhism, most branches of Judaism and most Protestant faiths. Some religions believe organ donation to be an act of charity. If you don't know where your faith stands on organ donation, ask a member of your clergy.
Myth: I'm younger than 18. I'm too young to make this decision.
Fact: Many states let people younger than 18 register as organ donors. But if you die before your 18th birthday, your parents or legal guardian will make the decision. If you want to be an organ donor, make sure your family is OK with your wishes. Remember, children, too, need organ transplants. They often need organs smaller than adult size.
Myth: People who donate organs or tissues can't have an open-casket funeral.
Fact: Donors' bodies are treated with care and respect. And they're dressed for burial. No one can see that they donated organs or tissues.
Myth: I'm too old to donate. Nobody wants my organs.
Fact: There's no standard cutoff age for donating organs. The decision to use your organs is based on the health of your organs, not age. Let the health care team decide at the time of your death whether your organs and tissues can be transplanted.
Myth: I'm not in the best health. Nobody wants my organs or tissues.
Fact: Very few medical conditions keep you from donating organs. Maybe you can't donate some organs, but other organs and tissues are fine. Again, let the health care team decide at the time of your death whether your organs and tissues can be transplanted.
Myth: I'd like to donate one of my kidneys now. Can I do that if it's not going to a family member?
Fact: Yes. Most living donations are between family members and friends. But you can choose to donate a kidney to a stranger, so long as you're a match. You also can donate other organs and tissues, such as a lung or part of a lung or liver.
If you decide to become a living donor, the health care team at the transplant center asks a lot of questions. They want to make sure you know the risks.
You'll have tests to make sure you're healthy and that the organ you want to donate is in good shape. The health care team also will want to be as sure as possible that the donation won't damage your health.
Myth: Rich and famous people go to the top of the list when they need a donor organ.
Fact: The rich and famous are treated the same as everyone else when it comes to organ donation. True, famous people might get a lot of press after a transplant. But who they are and how much money they have don't help them get an organ. A computer system and strict standards ensure fairness.
Myth: My family will be charged if I donate my organs.
Fact: The organ donor's family never pays for donation. The donor family pays for all the medical care given to save your life before your organs are donated. Sometimes families think those costs are for the organ donation. But the person who gets the organs for transplant pays the costs for removing the organs.
Why you should think about donating organs
Now that you have the facts, you can see that being an organ donor can have a big impact. And your donation helps not just the person getting the organ. By donating your organs and tissue after you die, you can save up to eight lives and improve 75 more. Many families say that knowing their loved one helped others helped them cope with their loss.
Think about being an organ donor if you belong to an ethnic minority group. These include Black Americans, Asian Americans and Pacific Islanders, Native Americans, and Hispanics. People in these groups are more likely than white people to have certain illnesses that affect the kidneys, heart, lung, pancreas and liver.
Some blood types are more common among minority groups. The blood type of the donor usually needs to match the blood type of the person getting an organ. So the need for minority donor organs is high.
How to donate
Becoming an organ donor is easy. Just do the following:
- Sign up with your state's donor registry. Most states have ways to sign up. Check the list at organdonor.gov.
- Mark your choice on your driver's license. Do this when you get or renew your license.
- Tell your family. Make sure your family knows you want to be an organ donor.
Being on your state's organ donation registry and marking your choice on your driver's license or state ID are the best ways to make sure you become a donor. But telling your family also is important because hospitals ask next of kin before taking organs.
However, hospitals don't need to ask for consent if you are 18 or older and are on your state's donor registry or have marked your driver's license or state ID card for organ donation.
If you have named someone to decide about your health care for you if you are not able to do so, make sure that person knows that you want to be an organ donor. You also can include your wishes in a living will if you have one. But the will might not be read right at the time of your death.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Organ donation statistics. Organdonor.gov. https://www.organdonor.gov/learn/organ-donation-statistics. Accessed Dec. 29, 2022.
- Franklin GF, et al. Evaluation of the potential deceased organ donor (adult). https://www.uptodate.com/contents/search. Accessed Dec. 29, 2022.
- Theological perspective on organ and tissue donation. United Network for Organ Sharing. https://unos.org/transplant/facts/theological-perspective-on-organ-and-tissue-donation/. Accessed Dec. 29, 2022.
- Equity access to transplant. United Network for Organ Sharing. https://insights.unos.org/equity-in-access/. Accessed Dec. 29, 2022.
- Frequently asked questions about organ donation for older adults. National Institute on Aging. https://www.nia.nih.gov/health/frequently-asked-questions-about-organ-donation-older-adults. Accessed Dec. 29, 2022.
- Facts about organ donation. United Network for Organ Sharing. https://unos.org/transplant/facts/. Accessed Dec. 29, 2022.
- Donate organs while alive. Organdonor.gov. https://www.organdonor.gov/learn/process/living-donation. Accessed Dec. 29, 2022.
Products and Services
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Assortment of Health Products from Mayo Clinic Store
- The Mayo Clinic Diet Online
- A Book: The Mayo Clinic Diet Bundle
- A Book: Live Younger Longer
- A Book: Mayo Clinic on Digestive Health
- Myths about cancer causes
- Emergency essentials: Putting together a survival kit
- Emergency health information
- Kidney donation: Are there long-term risks?
- Living wills
- Osteopathic medicine
- Personal health records
- Telehealth: Technology meets health care
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Organ donation Dont let these myths confuse you
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Disadvantages of Organ Donation: What to Know
Mary Beth holds a Bachelor's Degree in Communications and Journalism and has held several roles in the media industry.
Learn about our Editorial Policy .
Terri is a critical care nurse with over 35 years of experience. She is also a freelance writer and author.
Religious beliefs and fear of the unknown are only two of the several cons of organ donation. Some feel that ethics - both the patient's and the doctor's - also play a large role.
Organ Donation at a Glance
According to Donate Life America , there were a total of 138 million registered organ and tissue donors in the United States. While it is reported that 95% of adults in the U.S. support organ donation, only 54% are registered organ and tissue donors. However, the amount of people who actually need transplants is on the rise, topping out at more than 114,000 individuals on the national waiting list .
Why is it then that roughly 46% percent (nearly half) of the U.S. population who are eligible to be organ donors aren't even registered? Could it be that the benefits of organ donation do not outweigh the disadvantages?
Understanding the Cons of Organ Donation
While some may shun the thought of having their body buried without all of its organs, others don't have a problem with it. Besides not being a suitable donor, there are many reasons why individuals are against organ donation.
Religious and Ethnic Beliefs
Organ and tissue donation is a very personal decision, and most organized religions don't oppose it. Many encourage it and consider it an act of charity. However, some religious and ethnic groups do have stipulations:
- Amish : Approves in organ donation if a person's life will definitely be improved or saved, but is reluctant to participate if the outcome of the transplant is questionable.
- Gypsies (Romany) : Because this group of people share common folk beliefs, they oppose any and all organ and tissue donation. They also believe that a body should be buried with all of its organs intact because the soul maintains its physical self for one year after the individual dies.
- Jehovah's Witnesses : While organ donation is a personal decision, if one decides to go through with the procedure, all organs and tissues must be completely drained of blood first.
- Shinto : The religion concurs with folk belief that a dead body is "impure and dangerous" and injuring a person after he or she dies is a "serious crime." Therefore, they do not support organ or tissue donation.
Fear of Unethical Selling and Buying of Organs
It's true, there is a black market out there for some types of donated organs, especially kidneys and most often, not in the United States. Countries including Bosnia, China, Ukraine, Iran, and Pakistan, where populations are poor, are frequently in the news because residents there illegally - and in some cases legally - sell certain human organs for cash. In the United States, selling your organs is illegal, although some argue that if individuals were paid for the viable organs upon their demise, those on the transplant waiting list may be helped a little sooner. But is buying human organs ethical if it is a matter of life or death? In some countries, citizens don't have much of a choice. Organs from living donors are transplanted from those living in Third World countries into prominent individuals living elsewhere. All because the money is needed for the donors to live. However, in others, organs are stolen. For instance:
- Because of the Japanese cultural beliefs regarding the body after death, there are not many viable donors living there. For many years, affluent citizens went to countries such as Singapore and Taiwan to purchase organs from executed prisoners even though the inmates did not authorize the donation. This was outlawed in 1994 by the World Medical Association.
- However, in China, it is still legal to remove and sell organs from executed prisoners without their consent, sometimes even on the eve of the execution when the individual is still alive.
- In 2004, the director of Willed Body Program at the University of California, Los Angeles was arrested for illegally selling body parts and organs donated to the program by individuals who have died. The deceased individuals donated their bodies to science for research, but instead, the former head of the program received more than $1 million for the organs and body parts when sold on the black market.
Uneducated About the Process
Still, many Americans are unwilling to become donors simply because they don't understand everything that goes along with the procedure. To help with this, health care providers are working adamantly with organizations such as Donate Life America to ensure that both the patient and patient's family have a clear understanding as to what occurs when organs are donated and transplanted. Some myths , that help explain the cons of organ donating, include:
- Donor would be unable to have an open-casket funeral
- Under 18 is too young to donate
- Patient is too old to donate
- Family members will be billed if an organ donation occurs
Prolongs the Family's Grieving Process
Another issue with organ donation is can potentially arise with the donor's family. It may be necessary to keep a loved one on life support for an extended period in order to keep the tissues healthy that are to be donated. Unfortunately, this may give the family a sense of false hope since they are still seeing 'life' and this may intensify the grief as well.
Family May Have a Problem With the Recipient
The family may have a problem with the fact that they do not have a choice on who receives their loved one's organs. It simply goes to the next organ recipient on the list that is a match. This means someone of a different culture, ethnicity, political belief or religion could receive their loved one's organs and this may be difficult for some families to accept.
Cons of Living Organ Donors
The most common organs supplied by living donors are kidneys and liver. While being a living organ donor can be very rewarding, unforeseen circumstances can arise and there is no way to know in advance if there will be problems. Some cons of being a living donor include:
Medical Cons
There are short-term and long-term medical cons for being a living donor.
Possible short-term cons may include:
- Blood clots
- Allergic reaction to anesthesia
- Bulging of stitches
- Feeling sick, vomiting, diarrhea
Possible long-term cons include:
- Pain (chronic)
- Adhesions from scars
If you're a living kidney donor, you may experience high blood pressure, diabetes, loss of kidney function (25-35%), chronic kidney disease and bowel blockage. A small percentage of donors end up needing a kidney transplant themselves but you will get priority since you're a living donor.
Emotional Cons
Emotional short-term cons include worry or anxiety about the surgery itself and stress during the recovery process.
Long-term emotional cons could include anger if the patient's body rejects the organ. You may feel sadness or regret as well.
Financial Cons
Short-term financial cons include the cost of travel and lodging. Also, lost wages for time off work due to testing, surgery, and recovery.
Long-term financial cons include having difficulty getting health or life insurance or having to pay a higher premium after the surgery. There is also a chance you would have trouble being accepted into the military or having a career in law enforcement or with the fire department.
Cons of Mandatory Organ Donation
There is a definite need for more organ donors and mandatory organ donation has been considered as an option. The cons of mandatory organ donation include:
- Organ donation, in general, may contradict personal, family or religious beliefs.
- People would lose their rights and freedom to decide what happens to their body after death.
- This change may not correlate with the deceased's wishes which could be very distressing for the family
- This change could allow certain doctors to spend less time saving lives in order to secure an organ that is needed by a patient.
An opt-out system or a program to recruit more donors may be a better option than making organ donation mandatory.
Benefits of Organ Donation
Many people have considered the pros and cons of being an organ donor. They understand the benefits of organ donation and believe it is not only a privilege but a social responsibility. Organs donated from one individual can save eight lives and enhance the quality of about 50 lives. Other benefits of organ donation are:
- It helps grieving families make some sense out of their loved one's death.
- It allows some individuals to improve or have a better quality of life.
- It is more cost-effective in the long run over the cost of lifelong medical care.
Weigh All Organ Donation Pros and Cons
When it really comes down to it, becoming an organ or tissue donor is really a personal decision that should be discussed with your next of kin, personal physician and spiritual leader. Before you sign up to be a donor, make sure you are completely educated about the process.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Iran J Nurs Midwifery Res
- v.27(2); Mar-Apr 2022
Concerns and Challenges of Living Donors When Making Decisions on Organ Donation: A Qualitative Study
Raziyeh sadat bahador.
Nursing Research Center, Kerman University of Medical Sciences, Kerman, Iran
Jamileh Farokhzadian
Parvin mangolian, esmat nouhi, background:.
Mental concerns of living donors can be a solid barrier to logical and informed decision-making for organ donation. The present study explores living donors' mental concerns and problems during the process of decision-making for organ donation.
Materials and Methods:
present study was performed using qualitative content analysis. Twenty-one participants were selected by purposive sampling. The data were collected and recorded through semistructured interviews and analyzed by MAX Qualitative Data Analysis software 12, based on Graneheim and Lundman's contractual content analysis method.
Data analysis extracted 425 codes, 13 subcategories, 3 main categories, and 1 core theme (conflict between doubt and certainty). The three main categories were individual barriers and concerns (faced by the donor), interpersonal concerns and barriers (experienced by the family), and socio-organizational concerns and barriers (at the community).
Conclusions:
Based on the results, donors have significant concerns and face major problems when deciding on organ donation. Therefore, health-care professionals should take into account organ donors' concerns, raise awareness of donor associations, and formulate policies to increase living donors' satisfaction.
Introduction
Studies have shown that deceased donors cannot meet the growing demand for organs such as the kidneys, liver, etc. Sometimes cultural, religious, and legal considerations may even be reluctant to donate organs after death.[ 1 ] Thus, because of the high demand for organ transplantation and the increased wait time for transplantation, receiving organs from living donors is a primary strategy to meet patients' needs and overcome their problems.[ 2 ] Popoola et al .[ 3 ] reported that the low number of living donors had been identified as a significant challenge worldwide. Furthermore, donors go through a tough decision-making process for organ donation. They may encounter problems, worries, and concerns. Recent studies have shown that the decision to donate an organ is influenced by issues related to personal life, family status, and the relationship with the recipient, leading to a wide range of problems during the decision-making process.[ 4 ] The decision-making process has been significantly influenced by various concerns such as medical uncertainty, post-donation recovery, family responsibilities, recipient health-related concerns, and donors' health in the future.[ 5 ] According to Kim et al .,[ 6 ] barriers to the proliferation of live donors are multifactorial and need to be addressed using extensive nationwide studies. They stated that common concerns of living kidney donors include the impact of donation on future health, increased risk of chronic medical conditions with future weight gain or return to unhealthy lifestyles, and the inability to return to previous activities. Other studies have shown that obesity[ 7 , 8 , 9 ] and social factors may also prevent many potential donors from becoming donor candidates.[ 6 , 10 ]
Other studies have shown that despite unique liver transplant needs, many transplant programs and transplant-related activities have been suspended or severely restricted due to the rapid growth of the COVID-19 pandemic.[ 11 ] Another study showed that the prevalence of COVID-19 was one of the concerns that led to a significant reduction in the number of living and deceased liver transplant donors and the inactivation of the waiting list.[ 12 ]
In addition to the issues mentioned above, the acceptance of organ donation depends on cultural, ethnic, and religious factors in the community. For instance, Farid and Mou[ 1 ] stated that although organ donation and transplantation can be hopeful for dying patients, attitudes toward organ donation and transplantation can be different depending on religious, cultural, and legal issues in the community. Thus, community-related issues are some challenges beyond the individual decision to transplant an organ. Living donors' concerns always hinder making logical decisions. Thus, some strategies need to be adopted to educate donors and empower them to make informed decisions about donation. It is believed that as national policies require centers to inform potential donors of the specific risks associated with organ donation, comprehensive donor training is needed to address living donors' other concerns and possible misconceptions.[ 13 ]
Many studies have addressed barriers, challenges, and concerns of organ donation in brain-dead patients. However, problems faced by living donors have been less qualitatively examined. The present study used a qualitative approach and provided an in-depth analysis of barriers and problems faced by living donors. It tried to explore their mental concerns about the decision to donate organs to direct policies governing the community toward accurate assessment of possible risks and problems encountered by potential donors when making informed decisions and managing these mental concerns. It is not reasonable to encourage living people to give their organs to others for any reason, for example, in exchange for money. Thus, given the high demand for organ donation and the low number of donors, more investigations are needed to identify factors affecting donors' decisions for organ donation. To this end, the study explores the mental living donors' concerns and problems faced by them during the process of decision-making for organ donation.
Materials and Methods
This study was part of a larger research project that aimed to provide solutions to advance the decision-making on organ donation and was conducted from August 2019 to December 2020. A qualitative approach following contractual content analysis was adopted to explain the impact of organ donation on living donors. The participants were selected using purposive sampling from living organ donors, their family members, organ recipients, and medical staff in the Organ Donation Center, Kidney, and Bone Marrow Donation Commission in Afzalipour Hospital, and Kidney Donation Association in southeastern Iran. The interviews with the participants were conducted in places preferred by participants (hospital, private home, park, nursing school, etc.) so that they felt relaxed and unstressed during the interview since this study was conducted during the COVID-19 outbreak and given its possible risks for the participants, the research procedures were conducted with strict adherence to health and social protocols.
The data were collected through the interviews with 21 participants, including 16 organ donors, 1 member from the family of the donor, 1 organ recipient, 1 surgeon from the organ donation commission, 1 person who had given up to donate an organ, and 1 psychologist. Nine of the donors participating in the study were kidney donors, five were nonrelated (for sale), and four were related (not for sale). Four of them had bone-marrow donations, one nonrelated (for sale) and three related (not for sale), and the remaining three donors, who were related (not for sale), donated a portion of the liver.
Data analysis was performed simultaneously with data collection. Sampling continued without any restrictions until the data were saturated. Proper links were established between the identified categories. The first author conducted interviews. However, all the researchers reviewed the interviews like outside observers. After each interview, the researchers studied the interviews, identified the interview's strengths and weaknesses, and reviewed the items to be considered in the subsequent interview. According to the written reminders, the proposed questions required researchers to conduct additional interviews with two participants during the analysis of the data. Two interviews were conducted with participants 2 and 1. The researchers conducted a total of 22 interviews with 20 participants. The interview questions focused on the implications of organ donation in living donors. First, each interview started with warm-up questions followed by open-ended questions like “Would you mind sharing your experience of the organ donation you did?”, and probing questions for further clarification of the interviewee's statements. Each interview took 45–90 min. At the end of the interview, the participants were given the interviewer's mobile phone number and asked to discuss any issues with the interviewer if they remembered any of the implications of organ donation and the possibility of further interviews. Finally, the participants were appreciated with a small gift.
Data collection and analysis were performed simultaneously. The MAX Qualitative Data Analysis 12 was used to facilitate the organization and comparison of the data. The transcript of each interview was reviewed several times. The qualitative data content analysis process was performed according to the method proposed by Graneheim and Lundman, including transcribing the interview, reading the transcripts several times to come up with a general understanding of their content and get immersed in the data, determining semantic units, and summarizing them, extracting the primary codes, classifying the similar primary codes under the same subcategories, classifying similar codes under more comprehensive categories, extracting latent and manifest concepts from the data, and formulating the final themes.[ 14 ] To this end, after preparing the transcripts, each text was reviewed several times. Later, the semantic units were identified based on the research questions, and appropriate codes were assigned to each semantic unit. As shown in Table 1 , the preliminary codes were placed into subcategories and labeled based on their conceptual similarity. The subcategories were compared and placed under the more abstract categories (main categories). The main categories were further categorized under a more abstract concept (theme). All extracted codes and categories were reviewed and approved by the second and fifth authors of this study. The initially extracted codes were reduced by continuous data analysis and comparisons. Finally, the categories and subcategories were abstracted. The criteria proposed by Lincoln and Guba (credibility, dependability, confirmability, and transferability) were used to ensure the trustworthiness of the data.[ 15 ] To ensure the credibility of the results, the participants were asked to review and confirm the codes extracted from the interview and revise the contents on demand (member check). Collecting the data from interviews with family caregivers with great diversity in terms of the relationship with the patient, ethnicity, and religion established credibility. To enhance the confirmability of the findings, all texts of the interviews, codes, and categories were reviewed and confirmed by the second, third, and fifth authors of this study (peer check) as well as a faculty member that was not a member of the research team (faculty check). To ensure the dependability of the results, all stages of the study were recorded. The participants were selected by maximum variation in terms of ethnicity, education, religion, economic status, relation to the patient, and social class, which enhanced the transferability of the findings of the study.
The participants’ demographic characteristics
Ethical considerations
To observe ethical considerations, the researcher asked the participants to complete the informed consent form. Moreover, before starting the interview, the participants' permission was obtained for recording the interviews and taking notes. They were also assured their demographic information would remain confidential. After the final report, the audio files would be removed, and, if desired, they could receive the audio file of the interview and be informed of the overall results. The participants were reassured that they were free to leave the study at any stage of the study. The Ethics Committee of Kerman University of Medical Sciences approved this study with the code of IR.KMU.REC.1398.222.
The participants were 21 persons including 16 organ donors, 1 donor family member, 1 organ recipient, a surgeon member of the donation commission, 1 person who has given up to donate an organ, and a psychologist. The participants were in the 26–58 age range. Table 1 displays participants' characteristics including gender, marital status, education level, age, etc., Following the analysis of the participants' statements about organ donation implications, 425 codes, 13 subcategories, 3 main categories, and 1 theme were extracted [ Table 2 ].
Themes, categories, and subcategories extracted from the data
The theme emerging from all categories was the conflict between doubt and certainty, which covered three main categories: “individual concerns and barriers (perceived by the donor),” “interpersonal concerns and barriers (experienced by the family),” and “socio-organizational barriers and concerns (apparent in the community).”
Individual concerns and barriers
This main category accounts for the mental concerns of the donor that disrupt the process of decision-making for organ donation and is the most critical category. It consists of five subcategories: “Fear of negative implications in the future,” “Fear of having Covid-19,” “Doubtfulness due to lack of knowledge,” “Lack of independence,” and “Fear of surgery and anesthesia.”
Fear of negative implications in the future
Sometimes, thinking about possible problems causes anxiety. Each decision may have positive and negative consequences that the donor must consider logically before making a decision. The donors expressed concerns such as fear of disability and the possibility of regret in the future, the possibility of rejection by others, fear of the unknown, etc., when making decisions on organ donation. Accordingly, one of the participants said: ”One of the fears that preoccupied my mind is what should I do in case of my kidney dysfunctions? What happens if I cannot find a kidney on time? If so, I may blame myself, but as soon as I leave everything to God, I will calm down” (P3).
Fear of getting COVID-19
Fear and anxiety about having COVID-19 raised some concerns for organ donors. Fear and anxiety weaken the immune system and raised shared concerns in donors in the current state of society. The participants pointed out to the possibility of developing COVID-19 during hospitalization, the impact of COVID-19 on the recovery process, and the possibility of deterioration due to having one kidney as the leading causes of concerns. One of the participants said: ”My only concern was the risk of getting Covid-19 during hospitalization. I was terrified of it; otherwise, I had made this decision, and I would rest assured If they made me ascertained” (P4).
Lack of knowledge and awareness
Having sufficient and up-to-date information leads to making rational and prudent decisions. A critical issue to consider in decision-making is collecting reliable information. Sharing information increases trust. The participants believed that the lack of knowledge and awareness could be due to the donor's unwillingness to obtain information, the time limit to get information, unavailability of a reliable source of information, obsession with acquiring more information, etc. One of the participants said: ”Although I inquired a lot, I was worried that I had not got enough information or my information was wrong, as if I was obsessed. I also feared that I did not have access to reliable information (physicians)” (P15).
Lack of independence
Some people constantly ask others for advice when faced with challenging life situations instead of making decisions based on their inner and personal needs. Fearing from the consequences of their choices, these people either constantly delay decisions or completely submit to the opinions of others. Making decisions to donate an organ depends on individual will and independence. The decision-maker must have an intention to decide and accept the responsibility. However, some participants pointed to some issues such as dependence on others in decision-making, fear of individual decision-making, and inability to take responsibility for decision-making. A participant said: ”I left it to my family to decide so that if something went wrong, they wouldn't blame me for making the wrong decision alone. Because I was afraid the transplant would be rejected, then my family would blame me for the uselessness of my transplanted organ” (P12).
Fear of surgery and anesthesia
Anesthesia, where general or local, is an integral part of the surgery. Anesthesia-related death news has left many people fearful of anesthesia during surgery. Fear and anxiety resulting from anesthesia are normal, but unfortunately, they may appear in the form of phobia. An influx of negative thoughts, not waking up after anesthesia, following similar bad news, and inability to overcome fear were some of the issues extracted from the participants' statements. One participant said: ”I am terrified of being anesthetized and not awakening then. I also feel horrible imagining myself in the waiting and operating room as I am intensively stressful” (P11).
Interpersonal concerns and barriers
This main category accounted for the concerns of family members for the donor. It had the subcategories such as “diversity of opinions,” “family opposition,” “history of chronic family diseases,” and “family beliefs and misconceptions.”
Variety of opinions
It is advisable to consult knowledgeable and educated people who are aware of the ups and downs of the path, but sometimes asking for views of ordinary people may confuse the donor. Diversity of opinions raises doubts in decision-making. One of the participants, who had a large family, said: ”It was confusing. Everyone had an idea. I was baffled about what the right decision was. But I think one should first think deeply to decide what to do and get advice from his family or friends” (P14).

Opposition from family members
Strong opposition from family members was another problem especially for unrelated donors. Some participants found it a reason to conceal the decision from the family. Related donors faced objections due to their age and education. In some cases, the recipient firmly refuses to accept organs for fear of harming the donor and feeling indebted to the donor. ”I really could not accept any organ of my family members because I was afraid something bad would happen to them or the organ would be rejected. Then, I could not forgive myself” said one recipient.
Another donor said: “My sister, who had dialysis every week, disagreed. She said she never got an organ from me. ” She did not want to get me into the same trouble she had. My mother disagreed initially” (P1).
A member of the donor family said: ”As a woman, it is tough to hear that your husband sold his kidney because he couldn't make a living. I told him right before the donation that I would leave you forever if he did this” (P13).
History of chronic diseases in the family
Currently, diseases such as diabetes and hypertension have affected many people. Although the history of these diseases in the family's medical records is not an absolute contraindication of organ donation, some donors have difficulty making decisions because of congenital diseases of donors and recipients. Having a history of kidney and liver disorders in the family, improper family lifestyles such as inactivity, an unhealthy diet, etc., are factors that make donors doubtful in decisions. ”I had made up my mind and even had a kidney test, but my doctor said my blood creatine was high, and it may be congenital in my family, so I gave up donating. The association introduced another donor” (P21), said one participant who gave up donating and was a recipient family member.
Another participant stated: ”My mother had a history of high blood pressure and diabetes. I was afraid that it would be congenital and I have the same problem later. These thoughts preoccupied my mind a lot” (P2).
Family beliefs and misconceptions
Misconceptions in the family were mentioned by the donors as issues that cast doubt on donation. The participants pointed to consequences such as the shortening of life span, the weakening of the body, and not returning to everyday life after donation until the end of life. ”One of the main concerns of donors and their families is their concern if they can have a normal life after donation. I have always told their families that donating a kidney will never cause disorders in their health and well-being, and the life expectancy of kidney donors is not shorter than non-donors. The kidney failure is not also associated with previous donations” (P17), said a surgeon who participated in our study.
Socio-organizational concerns and barriers
Socio-organizational concerns were the issues in the community that caused concern for the donor. These concerns were subcategorized into “distrust in the medical system,” “lack of welfare facilities in the community for the donor,” “fear of losing reputation,” and “inappropriate working conditions.”
Distrust in the medical system
Organ donation candidates need to trust the health-care system. Some donors misconceive that the medical team may not be skilled at performing the transplant. Donors' concerns include mistakes made during the operation, refusing a transplant and returning the patient to dialysis, the disclosure of private information by treatment staff, and the possibility of transmitting the disease from the donor to the recipient. ”I did not want anyone to find out that I donated, but I was unsure whether this information would remain confidential. I had never been in such a stressful situation during hospitalization. Because if someone spotted me in the hospital, he would find that I was a donor. There was no privacy in the hospital at all” (P7).
Another participant stated: ”I was always afraid that something bad would happen to me during the surgery. Honestly, I was not sure, but I had no other choice” (P10).
Lack of community welfare facilities for donors
The organ donors complained about the nonsupportive government. Lack of medical insurance coverage including life insurance, non-prioritization in government-supporting schemes, lack of post-donation support due to the prolonged recovery process, and unavailability of caregivers during the recovery process were among the points mentioned by the donors. One of the donors said: ”I underwent liver surgery willingly, but I had no other choice. They did the operation and tests for me at a lower price. But as my recovery process took a long time, there was no financial, professional, or educational support. I lost my job during this time” (P8).
Fear of losing reputation and being stigmatized
Undoubtedly, there is a negative social attitude toward specific groups of people in society. Some people label donors and their families as dealers. This issue is more commonly found in unrelated donors who receive money from the recipient's family. A member of the donors' family said: ”We were more afraid of losing our reputation, so we were against it. They did not know we did it to pay for our child's operation, but unfortunately, we were misjudged” (P15).
Unfavorable working conditions
Organ donors need good working conditions and a lively social life after organ donation. Some people are doubtful about deciding to donate due to their working conditions. Occupations involving hard and tedious work, especially in hot weather, heavy sports, constant exposure to radiation and pathogens, etc., were among the concerns of the donors. One participant said: ”I was just worried after the transplant. I was wondering if I could do a lot of work with this medical condition or not. I am a worker. I work hard. I was worried about the future because I had hard days before the donation” (P9).
The present study explored the concerns and problems of living donors when deciding to donate an organ. The core theme identified in this study was “Conflict between doubt and certainty,” which included three main categories: “individual concerns and barriers,” “interpersonal concerns and barriers,” and “socio-organizational concerns and barriers.” Liver donors reported the most server concerns and problems. In contrast, people with bone marrow transplantation reported fewer challenges and problems. The severity of these problems was the same in related and nonrelated donors but was more severe for donors who decided urgently or coercively.
The donors reported some personal concerns and challenges. They typically believed that organ donation would have severe health-related complications. Half of the people who were to decide to donate organs to their loved ones did not do so due to health and safety concerns.[ 16 ] Studies have shown that fear is a significant barrier to living organ donation. Interestingly, this fear may be strongly associated with a lack of knowledge about living organ donation processes and outcomes.[ 17 ] This fear is caused by side effects such as kidney failure,[ 13 ] risk of hypertension, proteinuria, and cardiovascular events,[ 18 ] and fear of surgery and death.[ 13 , 19 ] Fear of rejection[ 20 ] was another concern for the health and well-being of the recipient.[ 13 ] In the present study, most of these fears were associated with the possibility of getting COVID-19 during the organ donation process or during the recovery period, which could significantly reduce organ donation in the community.[ 11 , 12 ]
Lack of knowledge about living organ donation was another challenge found in many previous studies. Alvaro et al .[ 17 ] stated that the lack of knowledge about organ donation is due to the difficulty in obtaining such knowledge. Many participants reported that learning more about donation helped them overcome fears or worries about organ donation.[ 13 ] The results of the present study, as in recent studies, suggested that potential living donors support more effective and more explicit educational content as well as more explicit discussions with health-care professionals.[ 17 , 20 ] In the present study, the donors reported more concern about reliable information about the organ donation process and were more likely to seek information obsessively.
On the contrary, the recipients played a passive role in this regard. Donors have other options to choose from, while recipients have to wait for their decision. Other data, however, indicate that potential recipients requested information about the living donor.[ 20 ]
Regarding barriers and interpersonal concerns, Ruck et al .[ 13 ] believe that donors have personal concerns about donation and hear concerns about organ donation from family and friends. The decision-making process is dramatically influenced by post-donation recovery concerns, family responsibilities, recipient health-related concerns, and the donor's health in the future.[ 5 ] Irving et al .[ 21 ] stated that the opinions of participants' families often shape viewpoints about organ donation. Such influences can positively or often negatively affect individuals' decisions, with some feeling that they have to ask permission from family members. There is a general consensus on respect for autonomy in decision-making by potential donors about transplants.[ 22 ] However, another study found that a series of intra- and interpersonal negotiations were involved in the decisions on the transplant to be made by both the donor and recipient.[ 23 ]
Some evidence from the recipient's refusal to receive an organ from a family member indicated that patients are unlikely to ask their family members to be evaluated for a living organ donation.[ 24 ] They were not happy with this request.[ 17 , 20 ] Potential recipients raised concerns about the impact of kidney donation on the donor's health. They were concerned about the negative implications of surgery, including fear of rejection by the recipient and uncertainty about possible donor reactions,[ 17 ] loss of the donor's kidney, and the possibility that he or she may need his or her donated kidney in the future.[ 17 , 25 , 26 , 27 ] In addition to concerns about physical harm to donors, recipients expressed model concerns. The patients stated that they may feel indebted to their donors.[ 19 ] Some are concerned that younger family members may later need all of their potential donors.[ 28 ] The present study showed that the recipients who received an organ from a related donor felt obliged and owed, and the severity of this feeling depended on the intimacy between the donor and the recipient. It is more prominent in Iran due to the expansion of families and closeness between family members. Accordingly, Asian studies have shown that living donation can impose an unsatisfactory commitment.[ 20 ] Another study found that feeling owed varies significantly across cultures, with more substantial interpersonal commitments seen in collectivist cultures.[ 17 ]
In the present study, the families of unrelated donors disagree strongly with the donation. Related donor families were less likely to oppose the donor due to the patient's presence in the family. The reasons for the objections were the fear of endangering the donor, devaluating the effort in case of transplant rejection, the possibility of blaming the patient for doubling family problems, and feeling indebtedness to the donor till the end of life. However, the opposition in nonrelated families was primarily due to the misconceptions of the family.
Gan Kim Soon et al .[ 16 ] believed that participants' occupational discomfort results from a nonsupportive system and workplace restrictions. For instance, employers did not approve medical certificates, so donors were forced to take unpaid sick leave during surgery. Other studies indicated that the decision-making process was significantly influenced by other concerns, including uncertainty about the medical system.[ 19 , 21 ] The participants attributed this concern to the distrust in the health system and organ donation process, previous negative experiences with the health system, and lack of proper care.[ 21 ] However, in the present study, these fears and worries were mainly related to the surgical process and the fear of the disclosure of organ transplantation. The present study showed that the most common social concern in relative donors was the distrust in the medical system. Unrelated donors complained about the fear of being stigmatized, not receiving government support, and unacceptable working conditions. This study also showed that people who belonged to minority groups were more likely to have social concerns in society. They often expressed fears of a lack of support from the government and insurance organizations. Therefore, health officials are recommended to provide medical, care-support, educational, and insurance facilities for these people in the community. In their recent study, Fernández-Alonso et al .[ 29 ] stated that the organ donation process requires specialized training to avoid organizational problems. Accordingly, Allahverdi et al .[ 30 ] suggested the necessity to start nurses university education in this regard. Attitudes toward organ donation and transplantation can differ according to religious, cultural, and legal issues at the community. Since this issue has been accepted in Iran, the participants did not express any concerns. However, in other cultures, this can be a deterrent beyond the individual decision to transplant.[ 1 ]
Since this study was conducted in southeastern Iran, so cultural beliefs, economic, and even educational problems in this region may restrict the generalizability of the results to the other areas. However, it was attempted to include participants with maximum diversity in terms of socio-cultural background, work experience, and educations to make the results more applicable to similar populations. In addition, this study was retrospective in nature, so its findings may be subjected to misreporting and memory biases.
Following the results of the present study, the worries and concerns of living donors act as barriers to logical and informed decision-making for organ donation. After deciding to donate an organ, the donor may struggle with its implications for the rest of his life. Given the growing number of living donors, it is essential to understand the concerns of living donors in the organ donation decision-making process. It is recommended to manage these concerns and prohibit donors who experience more significant challenges from donating organs. Health-care professionals also need to use these experiences to raise awareness of donation associations, develop health policies at higher levels, and most importantly, increase the satisfaction of living donors.
Financial support and sponsorship
Kerman University of Medical Sciences
Conflicts of interest
Nothing to declare.
Acknowledgments
The present study is the result of a student doctoral dissertation. We appreciate the officials at Kerman University of Medical Sciences for supporting this study and the participants. Kerman University of Medical Sciences approved this study with the code 98000437.
Organ Donations: Cause and Effect Essay
Introduction.
Over the years, organ transplantation has developed into a successful treatment for organ failure. More than a million lives have been successfully extended and improved because of advancements in organ transplantation. These achievements are evidence of the medical community’s innovation and commitment, as well as the shifting attitudes and character of people worldwide. However, despite these advancements, there is still a global scarcity of organs. There are numerous legal, socio-cultural, and other restrictions on the implementation of organ donation from deceased person programs in both developing and developed countries. The rising demand for organs has not yet been addressed, even in those nations where the rate of dead organ donation is still more significant than that of other countries. While the number of donors is steady, the number of people needing organ transplants is continuously increasing.
One of the most remarkable developments in medicine is organ transplantation. Since the initial successful transplantations, organ transplantation has helped many patients live longer and healthier lives. A rising number of patients who require substitute organs are selecting transplantation due to recent improvements in human organ transplants (Sarabu & Hricik, 2019). There is a supply-demand dilemma due to recent technological developments, with more people needing new organs than there are attainable. International commerce in human organs is increasing, and organ donations have grown due to the comparatively high demand for organs. When organs are in tall order, they are frequently taken from the impoverished and given to the wealthy. Most transplant organizations and the world’s leading faiths have condemned the complex phenomenon, which has horrified the medical world, the media, and several governments.
Every day, on average, 22 individuals may be away while awaiting an organ transplant that cannot be performed due to a lack of organ donors. Since most nations forbid the sale of organs, a solution must be found to accommodate the rising demand for donors. The issue seems to be that the United States has to do a better job of persuading the living and the departed to remark on organ donations while they are still alive. It is stated that 85% of Americans would give their organs (Abbassi & Toso, 2022). By educating people on how they may prolong life by giving their loved one’s organs to those who are waiting for organ donors. It must be done in a way that appeals to Americans’ hearts and inspires them to sign up as organ donors. The times to do this are not when patients are taken into critical units when they may be brain-dead or in cardiac arrest and are likely to be lifeless with little chance of recovery. The moment has come for the US to improve its organ donation education efforts.
The general population is unaware of the specifics of being an organ donor and the critical need for live rather than deceased organ donations. The US has a donor shortage, thus finding ways to increase donor attraction has been discussed but to little avail. The opt-in method, which is used in the United States, allows a person to choose whether or not they want to be a donor before death. The person does this by adding their name to a national organ donor register, or they might have their driver’s license flagged as an organ donor. Only 28% of those in the opt-in system agree to revisit the program to address the fatal organ shortage and figure out how to increase organ donations (Abbassi & Toso, 2022). This has been hotly discussed by many, and some solutions being examined include encouraging incentives, implementing an opt-out mechanism, and requiring first-person permission approval.
There has never been a lower rate of organ donation, and some people think there should be rewards for both live and deceased donors. Although it is currently illegal in the United States and other nations, this is a topic that is being considered. Although kidney donation is not practiced in the United States, it has been found to be effective in other nations. For example, Iran pays its residents up to $1,200 for kidney donations, but the recipients must be Iranian nationals and get long-term medical attention (Monday & Ogugua, 2020). There should be discussions regarding possible legislative incentives that may be used to fulfill the demand for organ donations given the high number of people who are waiting for kidney transplants who pass away every day and the high number of kidney transplant waiting list fatalities. Government officials consider incentives for organ donors to be a kind of selling body parts in exchange for money. Not as a reward, as was previously said, which is now affecting the Iranian economy.
The Open Philanthropy Project is conducting a study into the likelihood of establishing incentives and has incorporated many ways incentives might be used as a part of their research to increase the likelihood of organ donors. Although nothing has been decided yet, this project is looking into how to interpret what may be called an incentive. Setting up a donor to get a payment that goes to a family member or estate has been thought about. It has been criticized to hope that the incentive will be compelling enough to convince people to give the organs of loved ones, but an incentive need not involve a monetary payout. There have been discussions of compensating for funeral costs or donor insurance for potential organ donors, whereby each donor voluntarily agrees to give in advance, with the benefiting estates receiving compensation following the transplant. To make these kinds of incentives lawful in the United States, legislation will need to be altered. Concerns include the possibility that the body will thereafter be seen as a good to be bought and sold, with brokers in charge of the transaction and the poor being excluded (Okumura et al., 2022).
The altruistic model notion was employed by American politicians, and they do not like this approach. Additionally, the opt-out model program, in which a person is a donor by default unless they expressly state otherwise before death, is not taken into account. Despite the fact that the opt-out system is not used in the United States, it has been demonstrated to be effective in 25 European nations, where organ donation rates “typically exceed 90% for those who participate in opt-out programs and fail to reach 15% in opt-in countries like the United States” (Samuel, 2017). The adoption of this procurement scheme by the United States has not been prompted, and it is unknown if this method will improve conditions there or make them worse. Only a small percentage of Americans who have registered with the Department of Health and Human Services have useable organs after they pass away, despite the fact that the majority of Americans favor organ donation. This is due to the fact that, according to Anne Pasche, “When a donor dies, the oxygenated blood must be flowing through the organs,” but only 2% do so (Samuel, 2017). Senator Ted Kenney Jr., a cancer survivor and healthcare attorney, submitted a measure to implement the opt-out scheme while he was representing Connecticut in 2011 and 2014, however, it was rejected by Republicans and voters. Senator Kennedy sought to initiate discussions and raise awareness of the 1,500 Connecticut residents who are waiting list members. It was opposed because the bill’s text implies that the corpse would automatically become state property after death unless a prior opt-out was indicated in written documentation.
The opt-out program is fantastic in nations that have universal health care, but in the United States health care is for profit and has to solve that issue first before taking the opt-out system into account, said Mark Stales, according to a quote (Roh, 2018). Another option to boost organ donations is through the first-person permission organ donation clause, which the government may formally enforce by bringing legal action against family members who opted to ignore the dead donor’s desire to become a donor after their death. A person’s next of kin is not allowed to override a person’s recorded choice to donate their organs under the rule known as brain death first-person consent. Individual family members who have not been informed of the deceased’s per-determine consent to donate organs may find this to be very unsettling.
However, once it has been established that the patient has reached that legal fiction, the Organ Procurement Organization intervenes and instructs the surgical team to remove the organs. In order to combat the reduction in organ donations, the law was created. There have been cases where family members have litigated to overturn someone’s decision to donate their organs, but their efforts ultimately proved futile, thus the family chose to discontinue the case.
How difficult or simple a decision would it be for any person to make if individuals had to decide whether to give the organs of somebody they love? What is known is that something needs to be done to help patients who are waiting for organ donors enjoy longer lives. If people can come up with intriguing ways to catch the attention of potential donors, the number of individuals who die every day is disturbing. A genuine talk about anything of interest to them that could give them the idea to become a donor needs to be had, and efforts need to be taken to make it happen. The United States must simultaneously investigate alternatives to the current technique since it is not able to fulfill demand. There have been some legal actions, but overall not enough has been done, thus this is long overdue. It is truly a question of life and death, thus the laws that are being proposed ought to be reintroduced under pressure from all quarters.
In conclusion, it is critical to acknowledge the dramatically rising need for organ transplantation caused by various health issues everywhere. However, studies on the international organ trade need to be more comprehensive, which perfectly illustrates the lack of prior attempts to compile and synthesize essential data. As a result, it is critical to control the organ trade while pursuing further medical and social science studies. The creation of platforms on which government agencies, professional associations, and decision-makers pool their resources to acquire and disseminate vital information is a significant step toward the result of a health policy that is both more comprehensive and long-lasting.
Abbassi, F., & Toso, C. (2022). Organ donation, distribution, and allocation in the United States, Europe, and Asia . Textbook of Liver Transplantation , 157–173. Web.
Monday, O. I., & Ogugua, P. (2020). Review paper – A critique of living altruistic organ donation . Global Bioethics Enquiry Journal , 8 (2), 61–65. Web.
Okumura, K., Dhand, A., & Ohira, S. (2022). Letter regarding “Cardiac outcomes in isolated heart and simultaneous kidney and heart transplants in the United States.” Kidney International Reports , 7 (1), 125. Web.
Roh, Y.-N. (2018). Organ donation . Organ donation and transplantation – Current status and future challenges , 3 (35), 5–35. Web.
Samuel, Leah, (2017). To solve organ shortage states consider opt-out organ donation laws . Web.
Sarabu, N., & Hricik1, D. E. (2019). They are pushing the age envelope: Kidney transplantation for elderly patients with prior nonkidney solid organ transplants . Transplantation , 103 (11), 2221–2222. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, April 13). Organ Donations: Cause and Effect. https://ivypanda.com/essays/organ-donations-cause-and-effect/
"Organ Donations: Cause and Effect." IvyPanda , 13 Apr. 2024, ivypanda.com/essays/organ-donations-cause-and-effect/.
IvyPanda . (2024) 'Organ Donations: Cause and Effect'. 13 April.
IvyPanda . 2024. "Organ Donations: Cause and Effect." April 13, 2024. https://ivypanda.com/essays/organ-donations-cause-and-effect/.
1. IvyPanda . "Organ Donations: Cause and Effect." April 13, 2024. https://ivypanda.com/essays/organ-donations-cause-and-effect/.
Bibliography
IvyPanda . "Organ Donations: Cause and Effect." April 13, 2024. https://ivypanda.com/essays/organ-donations-cause-and-effect/.
- Advantages and Disadvantages of Organ Transplantation
- Organ and Blood Donation
- Organ Donation and Transplantation Medicine
- Workplace Incidences Prevention
- Discussion: Legalizing Drugs of Abuse
- Increase in Mental Health and Depression Rates: An Overview
- Smoking Cessation Treatment: The System-Level Intervention
- A "Step Too Far" or "Perfect Sense?" by Stead et al
- Research article
- Open access
- Published: 06 November 2019
‘If I donate my organs it’s a gift, if you take them it’s theft’ : a qualitative study of planned donor decisions under opt-out legislation
- Jordan Miller ORCID: orcid.org/0000-0003-2068-5951 1 ,
- Sinéad Currie 1 &
- Ronan E. O’Carroll 1
BMC Public Health volume 19 , Article number: 1463 ( 2019 ) Cite this article
28k Accesses
22 Citations
7 Altmetric
Metrics details
There is a worldwide shortage of donor organs for transplantation. To overcome this, several countries have introduced an opt-out donor consent system. This system, soon planned for Scotland and England means individuals are automatically deemed to consent for organ donation unless they register an opt-out decision. This study was designed to explore the reasons underpinning donor choices for people who plan to actively opt-in to the register, take no action and be on the register via deemed consent, opt-out, and those who are unsure of their decision.
This study reports the analysis of free-text responses obtained from a large survey of intentions towards opt-out legislation in Scotland, England and Northern Ireland ( n = 1202). Of the n = 1202 participants who completed the questionnaire, n = 923 provided a free text response explaining their views. Thematic analysis was used to explore the reasons why participants plan to: opt-in ( n = 646), follow deemed consent ( n = 205), opt-out ( n = 32) and those who were not sure ( n = 40).
A key theme for people planning to opt-in is that it ensures one’s donor choice is explicitly clear and unequivocal . Some regarded deemed consent as unclear and open to ambiguity, thus actively opting-in was viewed as a way of protecting against family uncertainty and interference. For the deemed consent group, a key theme is that it represents a simple effortless choice. This is important from both a pragmatic time-saving point of view and because it protects ambivalent participants from making a challenging emotive choice about organ donation. Key themes for those planning to opt-out relate to fears around medical mistrust and bodily integrity . Notably, both participants who plan to opt-out and opt-in perceived presumed consent as “authoritarian” and a method of increasing Government control of organs. In response, registering an active decision protected their freedom of choice.
Conclusions
The findings highlight the importance of registering deliberate active consent for people who choose opt-in, due to concerns over possible family refusal under deemed consent. These findings could inform the development of communication campaigns that encourage family communication before the implementation of opt-out legislation.
Peer Review reports
Despite widespread public support for the principle of organ donation around the world, there is a critical shortage of available organs for transplantation. Although transplant activity has increased globally by 7.2% since 2015, there remains an insufficient supply of organs to satisfy demand [ 1 ]. To overcome the shortage of organ donors, several countries have changed organ donation laws and introduced an opt-out system of consent. This legislative change removes the requirement for individuals to actively sign-up and join the organ donor register (ODR). Rather, an opt-out system follows deemed consent; meaning that if no active donor decision (opt-in or opt-out) has been registered, individuals are automatically deemed to consent for organ donation. If an individual does not want to be an organ donor, they are required to actively opt-out and remove themselves from the ODR. As such, an opt-out system will enable consent for donation to be deemed without the need for people to action an intention to donate [ 2 ]. The rationale behind this system is that it should bridge the gap between the publics’ largely favourable intentions towards organ donation and inaction, thus increasing the pool of potential donors. This is important, as although around 90% of the UK public are found to support organ donation, in practice, just 40% have registered as donors [ 3 ]. The shortage of UK organ donors is further compounded by poor rates of family consent. Despite continued efforts from the UK Organ Donation Taskforce to increase rates of family consent for donation, they remain low, with 35% of families in Scotland and England refusing consent for donation between 2018/2019 [ 4 ]. This is notably heightened for individuals from Black, Asian and minority ethnic backgrounds (BAME), where family refusal rates for donation increase to 58%.
In 2017, the Scottish and English Parliaments announced plans to introduce an opt-out system (also referred to as a deemed consent system). This system has now been in operation in Wales for over 3 years. The latest figures from 2018/19 indicate that the number of donors and subsequent rates of transplantation have now increased, from 181 recorded transplants in 2017/18 to a total of 216 transplants between 2018/19 [ 5 ]. Many other countries across the world have implemented an opt-out system of donor consent. The most recent evidence suggests that donation rates (per million population), in countries with opt-out consent systems are, on average higher in comparison to countries with opt-in legislation [ 6 , 7 ]. However, there is considerable variance found in donation rates, with some opt-in countries having much higher donation rates than opt-out. Moreover, both reviews emphasised that it may be difficult to disentangle the role of other causative factors, including transplantation infrastructure, health care provision, public awareness and underlying public attitudes.
Indeed, a recent review designed to inform the development of the planned opt-out system in Scotland echoed these concerns, reporting limited evidence that in isolation, an opt-out system would increase transplantation rates [ 8 ]. The review however, did report strong evidence advocating the importance of public awareness and attitudes towards opt-out consent. This is critical, as extensive research has shown emotional beliefs and attitudes, for example, discomfort at thinking about one’s death, to be key determinants of donor behaviour in countries with opt-in legislation [ 9 , 10 , 11 ]. Recent work has also confirmed negative emotional beliefs to be heightened for participants who plan to opt-out of the donor register if deemed consent laws are introduced in Scotland and England [ 12 ].
Attitudes towards opt-out consent
Within the last 40 years, there has been a shift in attitudes towards opt-out consent laws in the UK. Evidence from a systematic review of survey data from 1976 and 2007 reported levels of support for opt-out legislation in the UK to vary between 34 and 64% [ 7 ]. Notably, the highest levels of support were recorded in surveys conducted after the year 2000. However, the authors note, the review’s conclusions are limited due to methodological inconsistencies in the reporting of the included surveys. As such, the findings may not be fully representative of current viewpoints and attitudes towards organ donation and opt-out consent laws.
While the aforementioned review suggests public support for opt-out laws to have increased, the proposals for opt-out legislation in Scotland and England were met with some controversy. In fact, an independent report from the UK Organ Donation Taskforce advocated against opt-out laws in 2008 over concerns that the system may incur a loss of public faith in the health service and the Government [ 13 ]. The belief that opt-out consent increases government control was also echoed within a qualitative report from the Welsh Government prior to the introduction of opt-out consent [ 14 ]. Notably, it was these factors that contributed to opt-out legislation being reversed in Brazil [ 15 ].
In addition, the introduction of deemed consent may unintentionally result in confusion and ambiguity regarding the role of the family/next-of-kin during the donation decision-making process. Under opt-out laws, it is now the families’ role to confirm whether their loved one had objected to donation, otherwise consent is deemed. Although next of kin will continue to be consulted, in practice, the opt-out system does not provide next-of-kin the legal rights to override or “veto” consent for donation unless explicit evidence of the deceased’s objection is provided [ 16 ]. However, international evidence suggests that next-of-kin continue to have a substantial influence during the decision-making process in countries with opt-out consent [ 17 ]. For example, after an opt-out system was implemented in Chile, a considerable increase in family refusal rates, and a decrease in donations were reported [ 18 ]. The legislation was subsequently revised. Increased rates of family refusal were also reported following the introduction of opt-out laws in Wales [ 19 ]. These findings suggested possible confusion among the public regarding the role of the family under the opt-out system [ 20 ].
Despite these concerns, little is known about the factors influencing planned donor decisions under opt-out consent laws in Scotland and England. As the Bill for opt-out legislation has now been passed in Scotland and England and is planned for implementation in 2020, a timely investigation of these factors is warranted. Given the emotive nature of the topic of organ donation, the application of qualitative methods may offer a richer understanding of the motivations behind participant’s donor decisions. This study explores the reasons why people plan to make a particular donor choice (opt-in, deemed consent, opt-out and not sure) under an opt-out organ donation system. This data was obtained from free-text responses from a large survey of intentions towards opt-out consent legislation in Scotland, England and Northern Ireland [ 12 ].
The aims of this study were: [ 1 ] to explore the differences between participants donor choices (opt-in, deemed consent, opt-out and not sure) following the planned introduction of opt-out consent laws, [ 2 ] to investigate the key differences between participants who plan to actively opt-in and opt-out of the donor register, and [ 3 ] to examine the key differences and similarities between people who provide consent for donation by actively opting-in to the register and those who plan to follow deemed consent.
Study procedure
The qualitative data reported in this study was acquired from free-text responses obtained from a questionnaire survey that assessed; previous experience of organ donation, knowledge of organ donation, attitudes towards organ donation and also, examined the donor intentions of participants in Scotland, England and Northern Ireland in a opt-out consent organ donor system. The detailed methodology and results for the quantitative aspects of the questionnaire study are reported elsewhere [ 12 ].
The qualitative data in this study describes the reasons underpinning participants donor choice (opt-in, deemed consent, opt-out or not sure) following the introduction of opt-out laws. This was acquired in two stages. To initially obtain a measure of anticipated donor status following the introduction of opt-out consent laws, participants were presented with information describing the proposed opt-out legislative changes (see Fig. 1 ). Participants were then asked, ‘ If the organ donation laws in your country change to an opt-out system, what would your choice be ?’ The potential responses were as follows; I would opt-in (I want to be an organ donor), I have no objection to donating my organs (deemed consent to be an organ donor), I would opt-out (I do not want to be an organ donor) and not sure. After selecting one of these responses, participants were presented with a free-text entry box and asked to ‘ Please briefly provide the reason behind your choice’. The qualitative responses obtained from this open-ended response option are the focus of the current study.
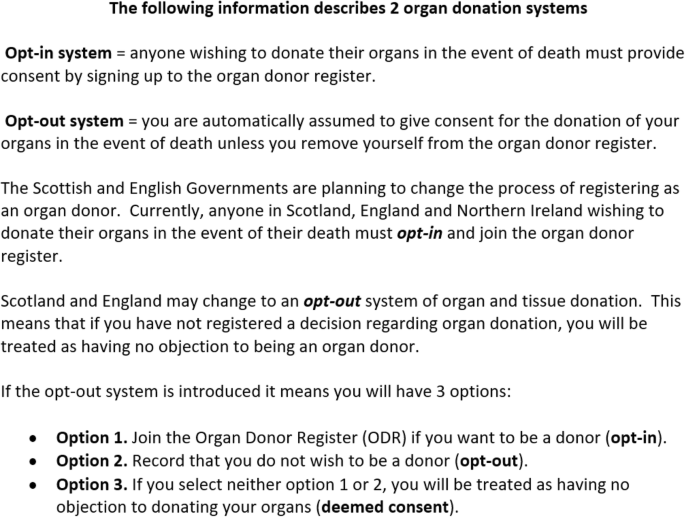
Information presented to participants regarding the planned changes to organ donor laws
Study recruitment and inclusion
Ethical approval for this study was granted by the General University Ethics Panel at the University of Stirling. Members of the general public over 18 years of age who were currently resident in Scotland, England or Northern Ireland, were opportunistically recruited for this online study. To recruit participants, online advertisements were posted to a university portal page and the social media websites Facebook, Twitter and Reddit. The advertisements presented brief details about the study and contained a URL link to the study, hosted via a Qualtrics questionnaire. Potential participants were initially presented with information about the study before informed consent was requested via an electronic selection box. Aside from three questions addressing consent and eligibility, participants were informed that they could omit a response to any question they felt unable to answer. Recruitment for the study began on the 24th of January and continued until the 12th of March 2018.
Questionnaire participants
In total, 1202 members of the UK public completed the full online questionnaire. In response to the question: If the organ donation laws in your country change to an opt-out system, what would your choice be? 66.1% ( n = 794) of participants selected to ‘opt-in’ to the donor register, 24.3% ( n = 292) of participants selected ‘deemed consent to be an organ donor’, 4.2%, ( n = 50) of participants selected to ‘opt-out’ and 5.2% ( n = 63) of participants selected ‘not sure’.
Qualitative free-text responses
Of the total sample of questionnaire respondents, 76.79% ( n = 923) provided a free-text written response explaining their reasons for this choice. This qualitative data is the focus of the current study. Of these responses, n = 646 were obtained from participants who plan to opt-in, n = 205 from participants who would follow deemed consent, n = 32 from opt-out respondents, and n = 40 from participants who selected not sure.
Data preparation and analysis
The data was analysed using thematic analysis [ 21 ]. Thematic analysis was selected due to its flexibility and suitability for identifying patterns within large datasets. The analysis was conducted based on the four respective response groups (opt-in, deemed consent, opt-out and not sure). To enable data familiarisation, each response was read multiple times and preliminary ideas noted. Following this, potential features of interest within each response were systematically highlighted and assigned an appropriate code in MS Word. The responses and respective codes were then organised, reviewed and collated into themes and respective subthemes. To reduce researcher bias, the resulting themes and subthemes were independently reviewed by two members of the research team (JM and SC). Discrepancies in the resulting themes were resolved through discussion with the research team (JM, SC & ROC).
Participant characteristics
The age of respondents who provided free-text comments ( n = 923) ranged from 18 to 82 ( M = 40.34, SD = 12.68). The majority of respondents 80.5% (743) identified as female, 18.3% (169) as male, four participants identified as transgender and seven as “other”. The majority of respondents, 87.3% (806) reported to be living in Scotland, 11.6% (107) in England and 1.1% [ 10 ] in Northern Ireland. The demographic information for each response group is presented below in Table 1 .
Overview of key themes
The overall dataset revealed 13 main themes; organised into each of the four donor response categories (opt-in, deemed consent, not sure and opt-out) see Fig. 2 . The four main themes identified for participants who plan to actively opt-in were: (1) my choice is explicitly clear and unequivocal; (2) my organs could save lives, (3) reciprocity - If willing to receive I should be willing to give, and (4) personal experience of donation (please see Table 2 for themes and respective sub-themes). For participants who plan to follow deemed consent, the themes are displayed in Table 3 . For participants who are unsure of their decision, the themes are shown in Table 4 . Lastly, themes and respective sub-themes for respondents who plan to opt-out of the donor register are available in Table 5 .
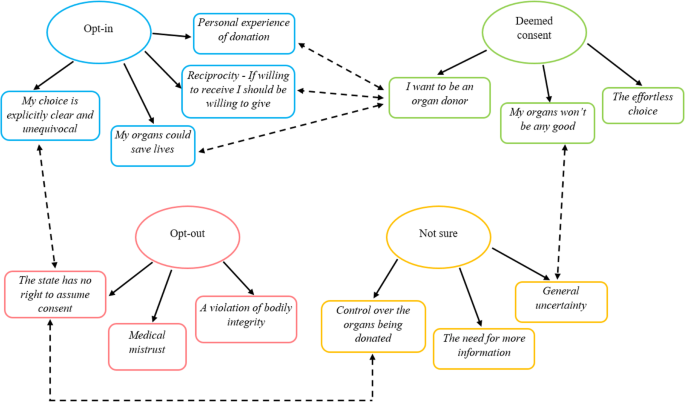
Key themes for the opt-in, deemed consent, opt-out and not sure response groups. Single directional arrows represent the key themes from each donor choice; bi-directional dotted arrows demonstrate a relationship between themes
The illustrative quotes are identified by the corresponding participants’ sex and age, e.g. Female 24 years. Some participants expressed multiple reasons for their choice, therefore some quotes can be assigned to more than one thematic category.
Themes from opt-in respondents
Theme 1: my choice is explicitly clear and unequivocal.
This theme represents the view that actively opting-in to the donor register, provides a stronger indication of participants’ wishes to be an organ donor. This theme encompasses three sub-themes, (1) my wishes are set in stone, (2) reduces family distress and, (3) protection against family interference. Throughout, the act of opting-in was reported to signify clear recorded evidence of participants’ donor intentions, in contrast to passively taking no action and following deemed consent. Participants in this group described deemed consent as ambiguous and open to uncertainty. Actively opting-in to the donor register was perceived as a way of ensuring their wishes to donate were explicitly clear and unambiguous (sub-theme 1).
I wouldn't want any confusion about my intentions to donate my organs after I die so I would opt-in so it was conclusive proof. (Female 28 years)
Providing no objection is not actually consenting to donating especially if people are unaware of the system, I think it’s safer to opt-in so it is definitely my choice. (Female 20 years)
A few participants who plan to actively opt-in perceived opt-out legislation as a threat to their individual responsibility and choice. In the following excerpt, automatically presuming consent for organ donation was thought to indicate the state’s ownership of the body after death. Therefore, the process of actively registering an opt-in decision was viewed as a way of protecting their autonomy and right to decide.
I do not believe that my body belongs to the state and as such I want to decide what happens after death. (Male 39 years)
Before organ donation can proceed, the eligible donors’ next of kin are approached and consulted during the donation decision-making process. Participants expressed that by actively opting-in to the donor register and thereby clearly indicating a preference to donate, potential uncertainty and confusion regarding their wishes would be minimised. It was hoped that a recorded informed decision would ameliorate distress when newly bereaved families are confronted with the emotive decision to donate their loved one’s organs (sub-theme 2).
I would prefer this to be a conscience [conscious] decision on my part and not something left to the state. Making arrangements myself would also grant some comfort to my family to know that the harvesting of my organs was something I wanted and not something which was decided for me. (Male 30 years)
I would still like to be perceived as an active organ donor, indicating it was my own choice so that my family does not have to make any difficult decision in such difficult time. (Female 32 years)
Some participants expressed concerns that members of their family, who “don ’ t like the idea ” of organ donation, may potentially disregard their wishes and overturn their decision. Therefore, for these participants, actively opting-in to the register was a method of safeguarding their choice and preventing potential family interference after their death (sub-theme 3).
I want there to be no confusion on my death, and I do not want my family (some who do not hold my views) to be upset by, or interfere in my decision after death. (Female 53 years)
I want to donate and think the option of “deemed to give consent” is wishy washy and family members could argue against it, saying you didn’t know. I want my choice to be clear. (Female 41 years)
Theme 2: my organs could save lives
Throughout, participants in the opt-in group described a strong desire to save someone’s life as an important reason for opting-in to the donor register. This theme encompasses two distinct subthemes (1) dead people don’t need organs, and (2) it’s just the “right thing to do”. Many participants described simple pragmatic reasons for donating their organs after death and questioned why others did not share the same view. To these participants, their organs were described as personally useless for them, but potentially lifesaving for others (sub-theme 1). As such, the act of discarding functional organs was labelled as “wasteful ” and “selfish ” . Often, participants in this response group displayed limited psychological attachment to their organs and likened the act of organ donation to everyday activities such as recycling or donating unwanted items to charity.
What is the point in letting perfectly good organs rot away inside a dead body when they could be used to save lives? I see it as the same principle as taking things you don't need to the charity shop. Why keep it if you don’t need it but it could really benefit someone else? (Female 33 years)
Personally, I just think that it makes sense to donate healthy organs when you can no longer use them yourself. We make a conscious effort to recycle paper etc. so why should it not make sense to recycle valuable organs? (Female 20 years)
Some participants also expressed the view that ethically, donating their organs after death is simply “the right thing to do” (sub-theme 2). For some, donating organs after death represented their last act of kindness that was somewhat expected as part of their civic and societal duty.
I believe it would be the most ethical choice, as I would be maximizing my utility to my society through allowing my organs to be given to those who need them most. (Male 24 years)
I would like to be able to help someone after my death if I can. Organs are obviously not needed after death it seems like the obvious socially responsible action to take. (Female 52 years )
While, others viewed the act of organ donation as a method of balancing out any negative actions that may have occurred during their lifetime.
You’re doing a good thing when you're dead. It balances the bad things you've done when alive. A bit. (Male 44 years)
Theme 3: reciprocity - if willing to receive I should be willing to give
Participants who plan to actively opt-in to the register described the notion of reciprocity as an important factor in their decision to donate. Participants explained that if they ever required an organ transplant, a donor organ would be gratefully accepted; therefore, many felt it would be hypocritical not to offer the same opportunity to other people. For some participants, the donor system was likened to a banking system; as such, it was believed that one should only receive what they put in. In this instance, if a person is unwilling to donate their organs, they should not be eligible to receive an organ if they ever needed one.
I think it should work like a bank if you don't put anything in then you shouldn't be allowed to take anything out. I believe every person who is ABLE to opt in should and those who simply don't fancy it should not be allowed an organ if they find themselves in need of one. If a person cannot donate on genuine medical grounds then they should be allowed to receive an organ if needed. (Female 39 years)
If I or one of my children needed an organ I would hope there would be a donor for us, therefore, I expect any of us to be a donor for any other human being in need or an organ. It’s an equalities issue as well as a humanity and compassionate issue. (Female 47 years)
Theme 4: personal experience of donation
Some respondents shared personal experiences of organ donation as the influential factor in their decision to become an organ donor. In the following extracts, participants described how the lives of family and friends had been completely transformed through organ donation. Others described the experience of losing a loved one during the wait for a lifesaving transplant as their motivation for becoming an organ donor. Whilst for some participants, knowing that their loved ones had saved multiple lives by donating their organs upon their death, cemented the importance of organ donation.
My mum, uncles and papa have all had or having a kidney transplant! My mum had hers 8 years ago and seeing how it's not only changed my life and my dads, but also hers and it’s amazing to see her healthy again! (Female 23 years)
My dad needed a liver transplant and I was going to be a “live donor” We had to wait till he was strong enough for the operation but unfortunately he died before we could complete it. Organ donation is giving someone a second chance. (Male 36 years)
When my Grandfather passed away, he helped 5 different people from donating organs. This has made me aware of the importance of donating organs and the great difference that it can make for others. (Female 21 years)
Themes from deemed consent respondents
Theme 1: the effortless choice.
This theme encompasses the view that a deemed consent system (taking no action and thereby becoming an organ donor by default) serves as the easiest way of indicating a donor choice. This theme consists of two sub-themes, (1) I’m lazy, and this means less hassle, and (2) it saves me a difficult choice. Participants explained that a system of deemed consent was favourable as becoming an organ donor will now require no conscious effort or unwarranted paperwork to be completed on their part. Many participants expressed a wish to donate their organs yet, had not actively registered as a result of “laziness”. For these participants, deemed consent was viewed as a pragmatic and effortless system that would automatically indicate their wishes (sub-theme 1).
I'm happy to be opted in without having to fill out any paper work. I hate paperwork so the less I have to do, the better! (Female 43 years)
I'm rather lazy and so wouldn't want to have to ‘do’ anything! Besides which I'm happy to donate my organs or whatever's left of them. (Female 28 years)
Deemed consent was also regarded by some participants as a way of indicating a desire to be an organ donor without the need to make a challenging or emotive decision (sub-theme 2). At times, participants described general support for organ donation yet, reported the thought of organ donation to evoke unease and stated fears of “being cut open after death”. For these participants, deemed consent is considered a way of indicating their underlying preference to donate whilst, avoiding barriers that may have previously prevented these participants from registering an active opt-in decision.
I’m not against them using my organs after I die but I don’t really want to volunteer for it or anything. (Female 20 years)
Opting in means confronting your own mortality, general support for the principal of organ donation and not wishing to confront your own mortality means option 3 [deemed consent] satisfies both. (Male 55 years)
Whilst I don’t want to think about my organs being used or being cut open after death I also think if my organs could be used to save someone that’s acceptable. (Female 50 years)
Theme 2: my organs won’t be any good
Some participants that plan to follow deemed consent, expressed both a desire to donate their organs, however, were unsure if they were medically suitable to be an organ donor due to physical illnesses and poor lifestyle choices. For these participants, taking no action and following deemed consent will enable them to maintain a positive stance regarding organ donation, whilst allowing medical professionals to assess their suitability for donation in the event of their death.
I would happily opt in but due to a medical condition, I understand they cannot be accepted. I won't actively opt out & leave it to the doctors to decide whether they can use anything. (Male 57 years)
Due to being a smoker and overweight I have thought that most of my organs would be of no use. I have no objection to my organs being used if required. (Female 35 years)
Theme 3: I want to be an organ donor
While the aforementioned themes describe the reasons why participants made a choice of deemed consent, the following theme describes participant’s motivations for becoming an organ donor. This is because these participants, satisfied that deemed consent indicated consent to donate, described general reasons why they would donate their organs after death. This theme is comprised of three sub-themes: [ 1 ] no need for organs when you’re dead, [ 2 ] reciprocity, and [ 3 ] personal experience of donation. For many, motivations to become an organ donor centred on helping others and giving life after death. Participants frequently stated that after death they would have no requirement for their organs and expressed frustration at the thought of their valuable organs “rotting in a coffin or being incinerated”. Organ donation was subsequently seen as a way of utilising otherwise useless organs to give life to people in desperate need (sub-theme 1).
I choose it as I have no longer any need for these organs when I'm dead so someone else should benefit from my life - goodness knows I've done bugger all else with it, this is my tiny contribution to humanity. (Female 42 years)
Why should we take valuable organs with us when we die, when there are still people who are fighting to live, needing an organ? Organ donation is an amazing thing. (Female 25 years)
For some, the decision to become an organ donor was driven by the concept of reciprocity. These participants, similar to those in the opt-in group, described feeling duty bound to agree to be an organ donor as they would accept an organ if they or someone close to them ever required a transplant. Therefore, participants felt it would otherwise be “selfish” not to agree to donate (sub-theme 2).
I'd want an organ if I needed it, so would have to agree with donation. (Female 39 years)
I would hope an organ would be available if myself or any friend or family needed. I therefore feel I should be prepared to donate my own organs. (Female 36 years)
In a similar way to the opt-in group, some participants reflected on their own personal experience of family members whose lives had been transformed through organ donation as their motivation for becoming an organ donor (sub-theme 3).
My dad waited 3 years for a kidney transplant it transformed his life when he received it. Another friend’s husband had a heart transplant over 20 years ago and he’s still living a full life- it is an honor to help others live full lives once mine ends. (Female 43 years)
My father had a heart transplant and would not have survived without the selflessness of organ donors. (Female 33 years)
Themes from not sure responses
Theme 1: general uncertainty.
This theme encapsulates feelings of uncertainty around the decision to become an organ donor and encompasses two sub-themes, (1) I’m still not sure I want to be a donor and, (2) medical uncertainty. Throughout, participants in this group described the enormity of the decision to become an organ donor. Although several participants explained that they had been contemplating organ donation for a long period of time, they remain undecided and uncertain (sub-theme 1).
I have been thinking about this for many years and am yet to decide what route I'd like to take. (Female 29 years)
It’s a big decision and not one that I have ever been confident about making … (Female 51 years)
Still really unsure as to whether or not I'm 100% committed to donating organs. (Male 40 years)
For some participants, pre-existing medical conditions or episodes of physical illness contributed towards uncertainty around the suitability of their organs for use in transplantation. This led to some individuals reporting concerns about transmitting illness’ or poor quality organs to the recipient (sub-theme 2).
I do not think I am able to donate as I previously had skin cancer. If it would be permitted I would be happy to select opt-out system. (Female 53 years)
I have experienced a 2-year period of illness diagnosed as Chronic fatigue syndrome, as I do not know the cause I would not wish others to experience this due to any donation of my organs or blood. Until such times as I can be assured that such would not be the case I would not be happy to donate. (Male 57 years)
Theme 2: the need for more information
Participants felt that they lacked the appropriate information about organ donation in general, and in relation to the proposals for opt-out consent laws. As this legislation has not yet been enacted in Scotland, England and Northern Ireland, many were uninformed of the proposals. For some, more information was required in order to make an informed choice.
Don’t know enough about organ donation. (Male 49 years)
Really don't have enough information, but would like to have more information about this. (Female 42 years)
Theme 3: control over the organs being donated
Participants who were unsure of their decision also described a desire to choose which of their organs would be donated. Some expressed unease at the thought of donating particular organs and tissue, for these participants, a perceived lack of control over the donation process was an important factor in their decision.
I think not sure covers it. I think there are certain organs I wouldn't want to donate. (Male 43 years)
I would like control of which organs are used. (Female 42 years)
Opt-out themes
Theme 1: medical mistrust.
Participants expressed feelings of distrust in the medical profession in the event of life-threatening injuries as a key reason in their decision to opt-out. This theme comprised of two sub-themes, (1) what if I’m not dead?, and (2) reduced lifesaving care. In particular, some participants expressed concerns regarding the validity of a brainstem death diagnosis, and described fears that doctors would hastily harvest their organs before they were really dead. As a result, participants expressed fears that they would be alive and aware of their organs being removed (sub-theme 1).
I am scared that there would not be enough checks that I was really brain dead before my organs were removed. (Female 61 years)
I have no wish to be “kept alive” on a ventilator until my organs are taken out for transplantation on the basis that some doctor has declared me to be “brain dead”. (Female 65 years)
Participants also voiced concerns regarding the degree of life-saving treatment they would receive if doctors were aware they were organ donors. Throughout participants’ accounts, there appeared to be a dichotomy between donor care and non-donor care. As such, there were concerns that registered donors would receive a reduced lifesaving effort in lieu of saving a potential recipient’s life with viable donor organs (sub-theme 2).
I have a cynical approach to the care an organ donor would receive in the event of life threatening injuries as oppose to a non-donor in the same position. (Female 44 years)
Theme 2: a violation of bodily integrity
This theme broadly represents concerns expressed by participants that organ donation would violate the physical integrity of their body after death. This theme encompassed three sub-themes, [ 1 ] a desire to remain whole after death, [ 2 ] organ donation damages the body, and [ 3 ] a barrier to a peaceful passing. Participants recurrently expressed concerns that removing organs after death would jeopardise the completeness of their body. It was important for these participants to remain bodily intact after death (sub-theme 1).
I was born with them I would like to die with them. (Male 29 years)
I just want to go out of the world the way I came in. (Female 47 years)
Participants also reported fears that organ donation would cause unnecessary, additional physical damage to their body after death (sub-theme 2). This was frequently epitomised through powerful word choice that represents harm, e.g. “cut open” when describing the process of organ donation.
Just do not like the idea of being cut open after death. (Female 24 years)
Simply do not wish to be used for any reason after death, put to rest with no damage to body. (Male 57 years)
Individuals who plan to opt-out viewed organ donation as incongruous to a peaceful passing (sub-theme 3). Throughout, participants expressed distress at the thought of unnecessary medical interventions, such as the use of mechanical ventilation during their death. Participants wanted their death to be a peaceful and natural process; organ donation, however, was believed to delay and interfere with deaths natural course.
I find it totally gruesome and weird. Let nature take its course and leave things as they are. (Female 21 years)
Theme 3: the state has no right to assume consent
Participants held strong views concerning the ownership of their own body. Therefore, this theme encompasses the belief that opt-out consent laws give the government unwarranted control over your body after death. Participants expressed concerns that following the enactment of deemed consent laws, the absence of a clear objection will now be regarded as consent for organ donation. The importance of individual responsibility and informed consent was marked within participants’ responses; this was believed to be threatened under the opt-out system.
I am a firm believer in individual responsibility and object to the Government making assumptions on my behalf. (Female 82 years)
The creation of an opt-out system is inherently wrong in my opinion. The rational conclusion of such a policy is that the state has authority and ownership over your body and organs without ever getting consent. (Male 22 years)
For some participants, this was considered to criminalise the act of organ donation. In the following excerpt, organ donation under the current opt-in system is viewed as an altruistic gift, yet, under a system which presumes or deems consent, it is theft.
If I donate my organs it’s a gift. If you take them it’s theft. My body belongs to me. It does not belong to the state to do with as it sees fit. I am a registered organ donor. I will not be if it goes to opt out. (Female 60 years)
Following the introduction of opt-out consent legislation, if an individual has not registered an active donor choice, consent for organ donation is automatically presumed through deemed consent. This qualitative study prospectively explored the reasons underpinning the planned choice to either, opt-in, follow deemed consent, or opt-out of the donor register following the introduction of opt-out legislation in Scotland, England and Northern Ireland.
Key similarities between opt-in and deemed consent responses
For participants who want to be an organ donor, either by following deemed consent or by actively opting-in to the register, personal experiences of organ donation were important factors that cemented their decision. Throughout, participants shared emotive anecdotal stories of; loved ones whose lives had been “transformed” after receiving an organ transplant. Others shared experiences of losing a loved one during the wait for a transplant. For many, this personal insight increased their awareness of the importance of organ donation and motivated them to register. These findings are consistent with previous literature, which found personal organ donation experience to be a powerful factor that increases one’s willingness to become an organ donor [ 22 , 23 ].
Participants in the opt-in and deemed consent group shared a largely pragmatic view of their body after death. These respondents expressed limited psychological attachment to their organs and viewed donation as akin to recycling. Therefore, the prospect of reusing potentially lifesaving organs was an influential factor for both groups.
Another important factor shared by both people who plan to opt-in and follow deemed consent, centred on the concept of reciprocity. Participants in both groups reflected on the impact a donated organ would have if they themselves, or someone they loved required one. This in turn, elicited a sense of obligation to offer the same opportunity to another person. For some, willingly accepting an organ without being willing to register as a donor was considered “ hypocritical”. The findings from this study support existing research into the use of reciprocity primes and organ donation. For example, priming individuals to think about accepting a donated organ has been found to increase intentions to register as an organ donor [ 24 , 25 ]. Moreover, research from the Behavioural Insights Team found campaigns that focus on reciprocity to increase active registrations on the ODR. In the aforementioned research, approximately one million participants were exposed to one of eight organ donation campaigns during the process of renewing vehicle tax or registering for a driving licence on the GOV.UK webpage. The campaign that focused on reciprocity by asking, “If you needed an organ transplant, would you have one? If so please help others” was most successful at increasing active donor registrations [ 26 ].
Although people who plan to opt-in and follow deemed consent are both indicating a choice to be an organ donor, their reasoning for selecting either an active opt-in or a passive deemed consent decision revealed important distinctions; these are discussed below.
Key differences between opt-in and deemed consent responses
A predominant reason participants plan to actively opt-in to the ODR when legislation changes, is that it signifies a clear and unambiguous intention to donate organs after death. Conversely, the notion of deemed consent, although largely supported by this group was perceived as being unclear (“ wishy washy ”) and susceptible to ambiguity. Therefore, participants felt that actively opting-in would safeguard their wishes after death. This was important for a number of reasons; for some, this was viewed as a way of preventing family interference, while for others it was hoped that explicitly giving consent would relieve a grieving family of an incredibly difficult choice.
Throughout, participants expressed the belief that the decision to become an organ donor should be a conscious, autonomous choice, and expressed unease at the thought of family members interfering with their decision. To reduce the chance of family interference, participants in this group felt strongly about taking every action possible to ensure their wishes were upheld upon their death. This finding is supported by data from the NHS Blood and Transplant (NHSBT) 2017–18 potential donor audit. This indicated that if an individual had actively registered an opt-in decision, 92% of families consented for organ donation upon their loved one’s death. However, if the individual had not registered a decision to be an organ donor, family consent substantially decreases to 52% [ 4 ]. Therefore, in instances where an active donor choice is recorded, consent for donation is markedly higher.
Participants in the opt-in group recognised the enormity and emotive nature of the donation decision-making process faced by grieving families. As a result, many expressed concerns that taking no action and following deemed consent was not sufficiently clear to indicate their wishes to their family. Participants in this group felt that simply providing no objection is not actually consenting, which raised concerns that a grieving family may be left feeling confused. Our findings suggest that opting-in was regarded as an unambiguous way of clarifying donor wishes to families which, would in turn, reduce uncertainty and relieve them of the decision. This is supported by evidence from existing literature, which found confusion and uncertainty regarding the deceased wishes to be a key factor behind family refusal for organ donation [ 27 ]. This is important, as data from 2016/17, the year after the introduction of deemed consent laws in Wales, reported 21 instances of family refusal for organ donation. This compared to only eight instances in 2015/16 [ 19 ]. The heightened rates of family refusal were attributed to uncertainty regarding the role of the family under the opt-out system [ 20 ]. As a result, an extensive communication campaign that focused on encouraging people to share their donor wishes with family and friends was introduced. Family consent rates in Wales are now 70% and highest in the UK [ 4 ]. Therefore, before the introduction of deemed consent laws in Scotland and England, the development of campaigns that encourage families to discuss their wishes should be a priority.
The enormity and emotive nature of a donor decision was also a recurrent theme expressed by participants who plan to follow deemed consent. However, for some participants in this group, taking no action and thereby becoming an organ donor by default was viewed as a way of avoiding this difficult choice. The findings of this study suggest participants experienced ambivalence when considering organ donation; simultaneously describing both support for organ donation whilst citing fears and emotional barriers as a major deterrent to a donor choice. The concept of ambivalence and affect is recognised as an important factor for donor relevant decisions [ 28 ]. The participants in the present study described fears of being “ cut open after death ” or general discomfort about “ confronting your own mortality ” when contemplating a donor relevant decision. These factors are recognised deterrents to donor registrations [ 9 , 10 , 11 ]. However, this was also accompanied by affirmations of support for the principle of organ donation. Therefore, deemed consent emerged as a preferred option by some, as it signifies the underlying wish to be an organ donor without the need to confront aversive emotional barriers during the active registration process. Ultimately, this system may increase the pool of potential donors by including ambivalent individuals who previously felt unable to register an active opt-in decision yet want to donate their organs.
The effortless nature of deemed consent may also increase the pool of donors; by including people with favorable viewpoints towards organ donation who have not registered an active opt-in decision as a result of “ laziness ”. Throughout, participants in this group favored the simplistic nature of a deemed consent system as, unlike the current opt-in system, consent can be recorded without any required action. Consistently, research has shown that one’s positive intentions do not exclusively predict behavior [ 29 ]. Organ donation is a particularly powerful example of this tendency; as although the majority of the UK public support organ donation, just 40% of people are registered as donors [ 3 ]. Therefore, a default system that removes the requirement for active registration may reduce this discrepancy by capturing those who have not yet actioned their intentions.
Key differences between opt-in and opt-out responses
For the participants who plan to actively opt-out of the donor register, fears surrounding the medical profession were salient among participants’ reasons for opting-out. Notably, this concerned the validity of using brainstem death criteria as a method of defining irreversible total-body death. The complex and misunderstood nature of brainstem death has been recognised in previous qualitative research in organ donation [ 30 ]. Participants who plan to opt-out often did not equate brainstem death as a “real” death; this manifested as fears of premature withdrawal of care and donation occurring while patients were still alive. To ensure potential donor organs are in optimal condition, they require an adequate supply of oxygen. As the patient’s breathing is maintained using mechanical support, it can be challenging for families to comprehend that the person is no longer alive. These views may also be compounded by misleading depictions of brainstem death and organ donation portrayed within the media [ 31 ]. As the main source of information and knowledge regarding organ donation, damaging media misrepresentations rapidly propagate and influence the development of harmful beliefs [ 32 ].
Concerns that organ donation would violate the physical integrity of the body were also prominent within participants’ reasons for planning to actively opt-out. Expressions of bodily integrity concerns were expressed through fears over a loss of completeness without organs, disfigurement and concerns over unnecessary intervention to prevent a peaceful death. Participants expressed worries that organ donation would involve “ cutting-up” the body for organs to be “ harvested”. Such concerns have consistently emerged as key factors that deter potential registrants [ 9 , 10 , 11 ]. The concept of bodily integrity is rooted in mortality and personal autonomy [ 33 ]. As these beliefs centre around transgressions of the body after death and have consequences for the afterlife, they are intrinsically challenging to falsify and overcome. These may be exacerbated by conflicting viewpoints of organ donation and religion. Although major religions in the UK support organ donation, a recent UK survey found that over 50% of respondents believed organ donation was against most religious beliefs [ 12 ].
Another reason for choosing to opt-out focused on perceptions of heightened government control of organs after death. The importance of free choice and autonomy were central reasons for opting-out; signifying that participants’ choice was perceived to be threatened under proposals for opt-out. This may reflect the wider psychological concept of reactance, an unpleasant emotional response experienced following a perceived threat to one’s freedom [ 34 ]. Consequently, perceptions of presumed consent as an impingement of rights may result in the public taking action to protect their free choice ( opting-out ). Indeed, some critics of opt-out legislation have reported that accepting the absence of objection as permission for donation, to undermine the ethical principles of informed consent [ 35 ]. Moreover, the absence of active informed consent was perceived as reducing the altruistic nature of organ donation to an act synonymous with theft. Although concerns over government control were reported in Wales prior to the introduction of opt-out consent laws, limited research has investigated these issues. Given such concerns have contributed to the reversal of opt-out consent in other countries [ 15 ] a timely exploration of these factors is necessary.
The concept of reactance was not exclusively reported by individuals who plan to opt-out but was also evident among individuals who plan to opt-in. Interestingly, although this group plan to actively register as organ donors, some perceived the plans to introduce deemed consent as a coercive action from the government. Our findings suggest that a sense of ownership over one’s body is important for both those who plan to opt-in and opt-out. Therefore, registering an active donor choice was viewed as a way of safeguarding particpants’ freedom of choice and eliciting control over their donor decision.
Implications for future research
This study has important implications that may inform future research and practice. In particular, our findings demonstrate the importance of encouraging clear unambiguous consent for people who would opt-in, and illustrate concerns of confusion and the potential for family refusal under deemed consent. This finding could inform the development of communication campaigns in Scotland and England that focus on explaining the role of the family before the implementation of opt-out laws. This is important, as after the enactment of opt-out legislation in Wales, instances of family refusal doubled [ 19 ]. Now, following extensive campaigns designed to encourage family communication and to prevent families from overturning their loved one’s wishes, Wales has the highest rate of family consent for organ donation in the UK [ 4 ]. This is particularly important for individuals within BAME communicates, where family refusal rates are markedly higher. Given that 21% of individuals who died while waiting for a transplant last year were from BAME communities, there is an urgent need to increase family consent and rates of donation among minority ethnic groups [ 36 ]. Secondly, our findings also highlighted fears of medical mistrust and perceptions of government control under opt-out laws. To reduce the number of people planning to opt-out of the organ donor register, the evaluation and development of targeted campaigns to challenge concerns of medical mistrust and heightened government control under opt-out laws are urgently required.
Strengths and limitations
It is important to first acknowledge some limitations of our study. As is common in this field, there was a recruitment bias, in that the majority of free-text responses were obtained from female participants and individuals living in Scotland. We also recognise that there were a limited number of participants from BAME communities. Secondly, as survey methods do not permit exploration or probing of salient response topics, the use of a questionnaire will have to some degree limited the depth of participants’ responses. However, the use of an open-ended free-text response option, enabled participants to explain in their own words, the reasons important to them. As such, the data was suitably rich and detailed to provide a breadth of information and insights into donor decisions under opt-out consent. Although interview-based methods are preferred in qualitative research, the number of studies collecting data using questionnaire-based methods are increasing, particularly when exploring potentially sensitive topics [ 37 , 38 ]. This method also has a number of strengths. Importantly, the use of an online survey was effective at obtaining a large sample of over 900 respondents across different donor choices (opt-in, opt-out and deemed consent). This is, to the authors’ knowledge, the largest qualitative study to examine donor decisions under the new opt-out organ donation system. A particular strength of this method is that it may reduce socially desirable responding often experienced when using quantitative methods to investigate potentially emotive topics, such as in this study [ 39 ]. Moreover, these methods offer participants anonymity to express potentially complex and contentious viewpoints. This is particularly important for people who plan to opt-out of the donor register who may be hesitant to express their decision not to donate within a face to face or group setting. Before the introduction of opt-out laws in Scotland and England, future research using qualitative interview methodology is warranted to obtain a comprehensive understanding of the factors influencing donor decisions under opt-out consent.
This research provides deeper insights into donor relevant decisions following the enactment of opt-out consent legislation in Scotland and England. The findings highlight the importance of an active indisputable choice for individuals in the opt-in group, to ensure their wishes are safeguarded and not overridden by distressed families at the time of death. The introduction of deemed consent is advantageous primarily for those who have not actioned intentions to be an organ donor due to “laziness”, and for those with psychological ambivalence towards organ donation as it protects them from making a difficult choice. Our findings from participants who plan to opt-out, reinforce the existing opt-in organ donation literature around concerns of medical mistrust and violations of bodily integrity, and highlight a novel deterrent for the opt-out system, namely concerns of heightened government control. Although implementing a system of deemed consent may increase the pool of eligible organ donors, the potential for confusion should not be overlooked. Two primary concerns with deemed consent, family interference and reactance due to perceptions of unwarranted government control have emerged from this study. Before the introduction of deemed consent laws, the development of campaigns to target these factors is imperative.
Availability of data and materials
The datasets used during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Black, Asian and Minority Ethnic
NHS Blood and Transplant
Organ Donation Register
United Kingdom
Global Observatory on Donation and Transplantation. Organ Donation and Transplantation Activities: 2016 Activity Report. Global Observatory on Donation and Transplantation WHO-ONT collaboration; 2016. Available from: http://www.transplant-observatory.org/download/2016-activity-data-report/
Google Scholar
Johnson EJ, Goldstein D. Do defaults save lives? Science. 2003;302:1338–9.
Article CAS Google Scholar
NHSBT. Organ Donation and Transplantation Activity Data: UNITED KINGDOM; 2019. Available from: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/15236/nhsbt-united-kingdom-summary-report-jan-19.pdf
NHSBT. Organ Donation and Transplantation: Activity Report 2018/19; 2019. Available from: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/16469/organ-donation-and-transplantation-activity-report-2018-2019.pdf
NHSBT. Organ Donation and Transplantation Activity Data: WALES; 2019. Available from: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/15914/nhsbt-wales-summary-report-mar-19.pdf
Shepherd L, O’Carroll RE, Ferguson E. An international comparison of deceased and living organ donation/transplant rates in opt-in and opt-out systems: a panel study. BMC Med. 2014;12(1):131.
Article Google Scholar
Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A. A systematic review of presumed consent systems for deceased organ donation. Health Technol Assess (Winchester, England). 2009;13(26):iii, ix-xi):1–95.
Opt out organ donation: a rapid evidence review. Scotland: Scottish Government; 2018. Available from: https://www.gov.scot/publications/opt-out-organ-donation-rapid-evidence-review/pages/11/
Morgan SE, Stephenson MT, Harrison TR, Afifi WA, Long SD. Facts versusFeelings’ how rational is the decision to become an organ donor? J Health Psychol. 2008;13(5):644–58.
Shepherd L, O’Carroll RE. Do affective attitudes predict organ donor registration? A prospective study. J Health Psychol. 2014;19(10):1329–33.
O’Carroll RE, Foster C, McGeechan G, Sandford K, Ferguson E. The “ick” factor, anticipated regret, and willingness to become an organ donor. Health Psychol. 2011;30(2):236.
Miller J, Currie S, O'Carroll RE. ‘What if I'm not dead?’–myth-busting and organ donation. Br J Health Psychol. 2019;24(1):141–58.
Organ Donation Taskforce. The potential impact of an opt out system for organ donation in the UK. London: Organ donation Taskforce; 2008. Available from: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/4250/thepotentialimpactofanoptoutsystemfororgandonationintheuk.pdf
Welsh Government. Research to support Wales’ organ donation opt-out proposal consultation: qualitative research report 2012. Available from: https://gweddill.gov.wales/docs/caecd/research/120418organdonationen.pdf
Csillag C. Brazil abolishes “presumed consent” in organ donation. Lancet. 1998;352(9137):1367.
Welsh Government. Human transplantation (Wales) bill: explanatory memorandum. 2012.
Rosenblum AM, Horvat LD, Siminoff LA, Prakash V, Beitel J, Garg AX. The authority of next-of-kin in explicit and presumed consent systems for deceased organ donation: an analysis of 54 nations. Nephrol Dial Transplant. 2011;27(6):2533–46.
Dominguez J, Rojas JL. Presumed consent legislation failed to improve organ donation in Chile. Transplant Proc. 2013;45(4):1316–7.
Welsh Government. Organ donation annual report 2017. 2017. Available from: https://gov.wales/sites/default/files/publications/2018-07/organ-donation-annual-report-2017.pdf
Welsh Government. Organ donation Wales: communications activity 2017. 2017. Available from: https://gov.wales/sites/default/files/publications/2018-07/171204-organ-donation-wales-communications-activity-2017.pdf
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Irving MJ, Jan S, Tong A, Wong G, Craig JC, Chadban S, et al. What factors influence people's decisions to register for organ donation? The results of a nominal group study. Transpl Int. 2014;27(6):617–24.
Feeley TH, Reynolds-Tylus T, Anker AE, Evans M. Reasons for (not) signing the state registry: surveying Department of Motor Vehicles customers in New York state. Prog Transplant. 2014;24(1):97–105.
O’Carroll RE, Haddow L, Foley L, Quigley J. If you needed an organ transplant would you have one? The effect of reciprocity priming and mode of delivery on organ donor registration intentions and behaviour. Br J Health Psychol. 2017;22(3):577–88.
O’Carroll RE, Quigley J, Miller CB. The effect of reciprocity priming on organ donor registration intentions and behavior. Ann Behav Med. 2019;53(6):592–5.
Behavioural Insights Team. Applying behavioural insights to organ donation: Preliminary results from a randomised controlled trial. Depertment of Health, London: Cabinet Office; 2013.
Anker AE, Feeley TH. Why families decline donation: the perspective of organ procurement coordinators. Prog Transplant. 2010;20(3):239–46.
van den Berg H, Manstead AS, van der Pligt J, Wigboldus DH. The role of affect in attitudes toward organ donation and donor-relevant decisions. Psychol Health. 2005;20(6):789–802.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Morgan SE, Harrison TR, Afifi WA, Long SD, Stephenson MT. In their own words: the reasons why people will (not) sign an organ donor card. Health Commun. 2008;23(1):23–33.
Lewis A, Weaver J, Caplan A. Portrayal of brain death in film and television. Am J Transplant. 2017;17(3):761–9.
Aykas A, Uslu A, Şimşek C. Editors. Mass media, online social network, and organ donation: old mistakes and new perspectives. Transplant Proc. 2015;47(4):1070–2.
Viens A. Bodily integrity as a barrier to organ donation. In: Jox RJ, Assadi G, Marckmann G. (eds.) Organ Transplantation in Times of Donor Shortage. Challenges and Solutions. Heidelberg: Springer. 2015;19–26.
Steindl C, Jonas E, Sittenthaler S, Traut-Mattausch E, Greenberg J. Understanding psychological reactance. Z Psychol. 2015;223(4):205–14.
PubMed PubMed Central Google Scholar
Truog RD. Consent for organ donation—balancing conflicting ethical obligations. N Engl J Med. 2008;358(12):1209–11.
NHSBT. Government campaign will focus on urgent shortage of black, Asian and minority ethnic organ donors. 2019. Available from: https://www.organdonation.nhs.uk/get-involved/news/government-campaign-will-focus-on-urgent-shortage-of-black-asian-and-minority-ethnic-organ-donors/
Halley MC, Rustagi AS, Torres JS, Linos E, Plaut V, Mangurian C, Choo E, Linos E. Physician mothers’ experience of workplace discrimination: a qualitative analysis. bmj. 2018;363:k4926.
Opperman E, Braun V, Clarke V, Rogers C. “It feels so good it almost hurts”: young adults’ experiences of orgasm and sexual pleasure. J Sex Res. 2014;51(5):503–15.
Van de Mortel TF. Faking it: social desirability response bias in self-report research. Australian J Adv Nurs. 2008;25(4):40.
Download references
Acknowledgements
Not applicable.
This study was funded by a PhD studentship from the University of Stirling awarded to JM.
Author information
Authors and affiliations.
Faculty of Natural Sciences, Division of Psychology, University of Stirling, Stirling, FK9 4LA, Scotland
Jordan Miller, Sinéad Currie & Ronan E. O’Carroll
You can also search for this author in PubMed Google Scholar
Contributions
JM SC and ROC designed the study. JM monitored recruitment. JM conducted a thematic analysis of the data. JM and SC independently reviewed the codes and resulting themes. JM drafted the manuscript with a significant contribution from both SC and ROC. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jordan Miller .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was obtained from the General University Ethics Panel at the University of Stirling. All participants gave informed consent prior to participation via an electronic selection box on the online questionnaire. The paper contains no potentially identifiable information.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Miller, J., Currie, S. & O’Carroll, R.E. ‘If I donate my organs it’s a gift, if you take them it’s theft’ : a qualitative study of planned donor decisions under opt-out legislation. BMC Public Health 19 , 1463 (2019). https://doi.org/10.1186/s12889-019-7774-1
Download citation
Received : 07 March 2019
Accepted : 14 October 2019
Published : 06 November 2019
DOI : https://doi.org/10.1186/s12889-019-7774-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Organ donation
- Opt-out consent
- Medical mistrust
- Bodily integrity
- Family refusal
- Qualitative study
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
After assessing the lungs of a deceased patient, the thoracic surgeon Thomas Charrier (second from right) gives the green light for transplantation to his colleagues on the phone at the Foch hospital in Suresnes, Paris. This and all photos below taken on 9 December 2022 by Christophe Archambault/AFP. Courtesy Getty Images
Last hours of an organ donor
In the liminal time when the brain is dead but organs are kept alive, there is an urgent tenderness to medical care.
by Ronald W Dworkin + BIO
My patient was dead before I even saw her. She had been in a car accident. Now she was scheduled for organ donation.
She was called an ‘ASA 6’. To estimate operative risk, the American Society of Anesthesiologists (ASA) has a classification system built around how sick a patient is, ranging from a healthy ASA 1 to a moribund ASA 5, the latter meaning someone is not expected to live 24 hours. When the system was created in the mid-20th century, a sixth class for dead people seemed pointless. Death was known to the dead only, and life to the living only, and between the two there had been no bridge. When the definition of death changed in the late 1960s, making it possible for a person to be ‘brain dead’ but with organs still very much alive and available for donation, a bridge appeared and a sixth class was created in the early 1980s. Since 1988, when officials started collecting organ transplant data, almost a million organ transplants have been performed in the United States. Most of the organs have come from brain-dead donors. In 2021 alone, the US had almost 10,000 such donors.
When told of my upcoming case, I had mixed feelings. On the one hand, being in perfect health, unaccustomed to suffering and therefore easily disconcerted by the thought of death, I was horrified. My attitude toward death was like that of a young person standing blindfolded and tied to a post, awaiting a volley from a firing squad. The whole concept made my blood run cold. Yet the case also aroused in me a feeling of relief. Simply put, there was no risk of malpractice, as my patient was already dead. Many anaesthesiologists have such self-centred thoughts when taking care of ASA 6 patients.
I n her early 30s, she had a youthful face, without the traces of severe illness that ICU patients typically have. With her hair wrapped inside a bright, polka-dotted kerchief, she gave off an expression of almost pleasant, good-humoured cheeriness.
Who was this young person whose life had been tragically snuffed out? I jabbed into every crack of her medical record to find out. But little had been written down. Both her life and death seemed simple enough to be chronicled in a few lines. Something had happened inside her brain with the car accident, and the end came.
We wheeled her toward the operating room. Before departing, I pulled the sheet over her exposed feet. Why? I had an objection to her being dead, but I had an even more serious objection to her being undignified. With my patient still partly in the world of the living, I wanted to keep a place for her in the part that pretends to be genteel.
Six hours she had been officially dead. Now she had re-entered the world of the living
When we arrived in the operating room, something turned over inside me, sank, and went cold. After all, she was dead. The day before, she was as whole as me – and now look. She would never rise again.
After we moved her from the gurney to the operating table, the doctors and nurses, so used to taking care of living patients, stared at one another stupidly, as if not knowing why they had come together or why they stood around the table. For a brief moment, each one of us likely had the same supernatural vision, how for the past six hours, after being declared brain dead, this woman had lain under the measureless power of death. Six hours she had been officially dead. Six times had the hour hand on the clock moved – and she had lain dead. Now she had re-entered the world of the living. I would support her blood pressure and pulse. I would make her blood bright red with oxygen. Indeed, she might even wake up and look at us, I fantasised. She might be raised from the dead.

Ghoulish thinking, yet I do not write about this case to be ghoulish. Nor am I trying to stake out a new position in the bioethics debate. My purpose is more practical. Today, artificial intelligence (AI) looms over medical practice. Although unlikely to replace doctors completely, AI makes some medical activities especially ripe targets for takeover, including the harvesting of organs from brain-dead donors. And why not? Bedside manner and the common touch cease to be concerns. Using AI machines rather than doctors to harvest organs also promises to save money.
Yet this impersonal, nonhuman method of organ retrieval may discourage people from becoming organ donors , or from letting dead relatives become so, thereby exacerbating the current organ shortage. People will see pictures of organ retrieval being carried on all around by inanimate machinery in a room completely abandoned by human beings. Bodies will be brought in and sent out, while the invisible, sleepless work of the machines goes on. ‘Please, tell me this is not my end,’ people will fret privately. And they will resist consenting to organ donation.
O rgan retrieval can take place at odd hours because the time between retrieval and transplantation must be minimised. A donor heart or lungs can last only four to six hours outside the body. A kidney, liver or pancreas can last a bit longer. Because donation and transplantation must be synched perfectly, surgical teams must be allowed to work at any hour of the day.
Although donors are dead, managing their anaesthesia can be tricky. To keep their organs healthy, their physiology must be carefully attended to, yet brain death affects each organ system differently. High intracranial pressure can lead to an enormous outpouring of adrenaline, which can injure the heart and other organs as circulation fails. Brain death can cause pulmonary oedema (fluid in the lungs), making it hard to oxygenate the blood, thereby damaging the organs by a second route. Brain death also wreaks havoc on the body’s endocrine system, causing vital hormone levels to fall and damaging organs by a third route.
My patient lay stretched out on the table. The room was silent, as I had not yet placed any vital sign monitors on her body. It was a sinister silence. The monitors typically emit sounds that resemble the unconcerned twitter of birds. In an operating room, they symbolise life. Their absence suggests that a patient is not alive. In fact, mine wasn’t.
Nature will never permit anyone to know the exact point where brain death becomes real death
Ready to cut, the surgeon spoke through his headphones to surgeons in other cities waiting for the organs. The rest of us said nothing as he gave them an estimated time of arrival. The team had a real need for a stout word in these last few moments before the operation began. Sensing the mood, the surgeon said some dignified things about how our patient was giving other people a chance to live. Everyone nodded in agreement. He seemed thankful and sincere, yet he had to be that way for, at such a moment, anyone with even a modicum of intelligence would have felt anything else as an affront.

The surgeon cut into the patient’s chest. Almost immediately the patient’s heart rate and blood pressure jumped. It resembled the powerful surge of life that comes during a period when a person’s very existence and survival are at stake. The jump originated in a spinal reflex that stimulated the woman’s sympathetic nervous system below the level of the brain. Still, it seemed a manifestation of her will to live. Even more so when her hand moved – a sure sign of life! But that, too, was mediated through a spinal reflex.
I gave the patient some anaesthetic gas. I also gave her some opioids. Why the latter? After all, a dead patient doesn’t feel pain. In part because opioids help to lower heart rate and blood pressure directly, but also, I must admit, because I thought my patient might still be a ‘little alive’, whatever that means, and therefore in pain. Irrational on my part, yes, but the secret of life, including the definition of life, still remains the deepest and most mysterious one. Here Nature permits no eavesdroppers; never will she permit anyone to know the exact point where brain death becomes real death. At this, she draws a veil. I wanted to hedge my bets.
The woman’s blood pressure soon dropped too low. I poured fluid into her intravenous line. In the meantime, the surgeon moved hurriedly to extract her heart, clamping the large blood vessels leading both to and from it. Our fast pace betrayed another incongruence. Speed is thought to be a bit unrefined in an operating room. True, it is needed to save money, but ideally the operating room is an ordered world with calm transitions, a world without haste, except during an emergency to save a patient’s life. The visibly hasty fashion in which I and the surgeon worked made it seem like one of those urgent situations. In fact, I was trying to keep her circulation going long enough for the surgeon to tear her heart out.
I transfused a unit of blood, as excessive blood clotting, common after brain death, had made her dangerously anaemic. I turned on the warming mattress lying underneath her to keep her body temperature from dropping below 36 degrees Celsius. Brain death interferes with the body’s ability to regulate temperature, and the resulting hypothermia poses a risk to the organs. Finally, I gave her insulin to control her blood sugar level, as brain death often causes blood sugar to rise. All of these are routine lifesaving measures. In the past, I had used them to fight off death in my sickest patients, but here I had to remind myself that my patient was already dead.
T he surgeon removed her heart. The irrevocable instant had come. It was as when a train starts with a violent jerk, as if to overcome a disinclination to change its state of inertia. For many in the operating room, this was the moment when the woman’s life really ended.
A minute before, I had heard the melodies of the electrocardiogram (EKG) and pulse oximeter without really thinking about them. An anaesthesiologist’s ear is so capable of adapting itself that a continuous din, like the noise of a street or the rushing sound of a river, adjusts itself completely to their consciousness. But the unexpected halt in the sounds startled me into listening – and looking. I stared over the ether screen into the woman’s now-vacant chest cavity. It was shameful and terrible to gaze upon. Part of me felt as if I had abetted a murder around the corner.
I tried to make this last sigh worthy of the moment, a sigh that only another human being could replicate
The surgeon injected the heart with cold preservative and put it in a box. His next target was the lungs. He asked me to manually give the woman one last deep breath so that he could confirm that all parts of her lungs had been expanded before their removal. The breath I gave her was slow and gentle, like a sigh. Indeed, medically speaking, it was a sigh. On ventilators, there is a function labelled ‘sigh’ which, when pressed, gives a patient a single sustained deep breath to open up the lung’s small air sacs. Almost proudly, I imagined the sigh I gave this woman to be more human than what a machine could give. Compressing the anaesthesia bag with my hand, I imagined how she might have sighed in the past, on her own, in the face of some bitter reality, some trick or force of fate, crushing her heart but also uplifting her. I tried to make this last sigh worthy of the moment, a sigh that only another human being could replicate, a deep breath that begins with disappointment, passes into resignation, and ends in acceptance. I crafted that last sigh as if it were the epilogue to a tragedy.
When the woman exhaled her last bit of sigh, I removed her breathing tube. The surgeon took out her lungs and stapled her windpipe shut. At this point, there was little for me to do, and my inactivity plunged me into a sense of nothingness. I felt I was going to gag on my thoughts if I didn’t do something. I walked away from my patient to look inside a cupboard. I opened a few drawers. Then I felt badly for doing so. Although one of us was dead, still there seemed to be two of us here. It’s as if the woman and I were friends and I didn’t want to leave my friend. I went back and stood by her head.
The surgical team removed the rest of her organs and the case finished. Here the woman and I reached a parting of the ways. I stared at her face seriously and fixedly as though I wanted to look my fill and imprint forever on my memory her image. I cannot recall for how long I looked. Great moments are always outside of time.
Our relationship proved significant. Nothing is more characteristic of the total lack of spiritual connection between myself and other patients than the fact that I have forgotten most of their names and faces. But this woman’s name and face I remember. And when I speak of memory, I do not mean something akin to a register kept in a well-ordered office, a place in which documents are laid away in store. I mean something submerged in the rushing stream of my blood, memory as a living organ in which every feeling experienced that day retains its natural essence, its original intensity, its primary historical form.

M y patient lived longer than what her death certificate says. She lived in my mind during the organ retrieval and continues to live in my memory because I do not want to forget her, and because I cannot forget her. Although I know only her general outlines, our connection satisfies some deep law of harmony underlying all life, in which every person must enter into communion with another person in order fully to live. By that standard, my patient lived past her official time of death.
When AI replaces the anaesthesiologist during organ retrievals, you, the organ donor, will not live any longer than what’s listed on your death certificate. The air inside the operating room is already cold, dry and unpleasant. Various monitors will sit on the top shelf of the anaesthesia machine, regulated by AI. Their special melodic rings will no longer be necessary, as their data will be sent along to AI in silence. Care will be delivered without the mediation of human minds, senses or hands.
Before your lungs are removed, the machine’s ventilator bellows will go up, down, up, down. Capable only of whooshing and not ringing, the bellows will seem to call sadly through the cold air to the monitors sitting above, waiting fruitlessly for a response. What a simple, insignificant movement: up, down, up, down, never getting away from the same place. It will be the only activity surrounding your head amid the metal machines, with their cold, menacing gleam. Nobody will be sitting next to you to wonder about what you were like, or about the things that distinguished your personality and made it special. A vision of the future arises: similarly deserted operating rooms with AI machines all moving automatically, while the people who used to work in them have gone off somewhere to sit dreamily on the grass beneath the sky.
Medicine has tapped a new source of organs in the form of donation after circulatory death
It seems a decidedly unpleasant environment in which to meet one’s end, and enough to discourage those on the fence from becoming potential organ donors. Rather than live a bit longer in the mind of another person, rather than have that person think about you and wonder about you, entertain irrational imaginary concerns about you, slip a little extra narcotic into your intravenous line ‘just in case’, engage in metaphysical speculations about your breathing pattern, and imagine you a friend, you will be alone on the table, and your surgery will more closely resemble a bandit raid. The machines will be determined to take everything, every organ. Reduced to financial terms, it will be as if you were left penniless.
Worse, a new danger will come to overlie the chilling sense of emptiness, scaring even more people away from becoming organ donors. Because there are already too few brain-dead donors – each year, more than 8,000 people in the US die while on the waiting list for organs – medicine has tapped a new source of organs in the form of donation after circulatory death (DCD). These organ donors are not brain dead, although many of them are unconscious. Instead, they lack circulatory or respiratory activity after being disconnected from artificial life-support systems. Without such activity after a few minutes of so-called ‘no touch’, they are declared dead, and their organs become available for donation. Their numbers have been growing over the past two decades. Today, they account for about 10 per cent of transplanted organs in the US.
The problem is that certain medicines necessarily given to these donors before death, but in expectation of death, may hasten their death. The medicines are given for the sole purpose of making their organs more viable for transplantation. Heparin, for example, prevents blood clotting, while phentolamine dilates blood vessels and improves blood flow to the organs. Yet heparin also increases the chances of bleeding into the brain, while phentolamine may lower blood pressure to the degree that a person goes into shock. Although these patients are near death for other reasons, the medicines may become their actual cause of death. This makes doctors uneasy; hence the rule not to give these medicines to donors prone to bleeding or with low blood pressure.
Y et the rule risks driving away potential donors, who will naturally think: ‘Doctors won’t give you these medicines to kill you; on the other hand, they won’t give you these medicines to help you. At some point, doctors aren’t really on your side. But when?’ As the number of brain-dead donors drops, medicine will increasingly rely on DCD donors to compensate. Already sensitised by the image of surrendering their organs to machines in a metallic desert, potential donors will fear being herded into the ‘imminent death’ category to meet some organ quota, a fear only heightened when word gets out that doctors are not always their advocates.
Currently, doctors in the US must get consent before declaring people DCD donors, but another model, called the ‘presumed consent model’, already operates in other countries and allows the recovery of organs without prior authorisation. A cascade of events threatens to turn organ retrieval into a kind of science-fiction nightmare, where organ shortages lead to medicines being given to people to preserve their organs while possibly hastening their death, all without telling them the plan or asking for their permission.
My experience in the operating room serves as a warning to those eager to cut corners and replace doctors with AI machines
Whenever people start to think about becoming an organ donor, they immediately make a leap to their own precious person. Who am I, what am I, what am I without my organs, and so forth. It is part and parcel of being a human being. That some people are willing to surrender their organs after death suggests that, to feel oneself human, they need more than merely having a whole body; they also need an atmosphere of simple humanity. To feel human, people need to feel that they occupy space in the thoughts and feelings of others. It is why they consider becoming organ donors in the first place. They imagine helping others by giving up a part of themselves in the future. In exchange, they imagine the recipients thinking from time to time about what they, their donors, were like. In that way, the donors feel a connection with whomever those recipients might be, and feel somehow fulfilled.

I’d like to think that caring for my brain-dead patient satisfied some small part of this need to feel human, whether on the part of my patient before she died and who perhaps lived in expectation of becoming a donor one day, or on the part of her relatives who gave their consent to the procedure after she was declared brain dead. Either way, I connected with her or with her family.
My experience in the operating room serves as a warning to those eager to cut corners and replace doctors with AI machines willy-nilly. You don’t satisfy people’s urge to feel human by making the bridge to the next world a totally inhuman one.
The lesson extends far beyond organ donation. AI promises to make healthcare quicker, more precise, and error-free. To the degree that it replaces doctors and nurses, it portends a massive shift in medicine that seems to come every 30 years, when people are so overwhelmed by the burden of their own technological creations, they need every iota of their strength to adjust. Once again, with the advent of AI, advancements promise to put healthcare on an entirely new footing and, once again, the inevitable backlash will be there. So it was in the 1960s, when new medical technologies and procedures, such as home dialysis machines and coronary artery bypass surgery, improved life, and yet, during this same period, the medical profession’s reputation plummeted, as patients complained that doctors had grown cold and impersonal. So it was in the 1990s, when the rise of managed care promised greater efficiency at less cost, and a ‘win-win’ strategy anchored in preventive medicine, led to a patient rebellion against being treated like cattle, including their inability to choose their own doctor, and rushed visits to practitioners ‘on the plan’.
Now, in the 2020s, the stage is set for outrage, yet again. AI promises to elevate healthcare; but, to the degree that it replaces doctors and nurses, it also threatens to depersonalise patients and to wash off their distinctive colours until everyone has the same drab tint. In the crucible that looms, patients are going to rebel. And it is in the arena of organ donation, where they face death by machine, that they are likely to baulk loudest, and first.

Building embryos
For 3,000 years, humans have struggled to understand the embryo. Now there is a revolution underway
John Wallingford

Design and fashion
Sitting on the art
Given its intimacy with the body and deep play on form and function, furniture is a ripely ambiguous artform of its own
Emma Crichton Miller

Learning to be happier
In order to help improve my students’ mental health, I offered a course on the science of happiness. It worked – but why?

The environment
We need to find a way for human societies to prosper while the planet heals. So far we can’t even think clearly about it
Ville Lähde

Stories and literature
Do liberal arts liberate?
In Jack London’s novel, Martin Eden personifies debates still raging over the role and purpose of education in American life

Alien life is no joke
Not long ago the search for extraterrestrials was considered laughable nonsense. Today, it’s serious and scientific
The arguments for and against ‘opt out’ organ donation
Mother of seriously ill patient says system still not working despite change in law
- Newsletter sign up Newsletter

The mother of a seriously ill patient has described an organ donation scheme that came into effect last year as “flawed”.
Blood donation rules: who can donate? Bereaved families blocked hundreds of organ transplants from registered donors Record 5.45m people on NHS England waiting lists
The change in law, which came into effect on 20 May 2020, meant it could be assumed that all adults in England would automatically become organ donors when they die, unless they opted out or were members of an “excluded group”.
The change - known as Max and Kiera’s Law - was intended to make it easier for people to donate their organs. A total of 296 donations took place in the 12 months after it came into effect, the BBC reports.
Subscribe to The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.
Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
But Cathy Meredith, the mother of 28-year-old Sarah Meredith, who is seriously ill with cystic fibrosis, says that family are still able to prevent their relative’s organs from being donated, even with this change in the law.
Speaking to South Hams Gazette , Meredith said it is wrong that “people now believe that if they do wish to donate their organs they need do nothing”.
She told the paper that people should sign up to the NHS Organ Donor Register (ODR), so that “clinicians can approach the family knowing that person wanted to be a donor”. In cases where families are unaware their relative’s intentions, 69% “will decline consent”, she said.
MP for Totnes Anthony Mangnall has agreed to raise the issue in parliament. “I am proud not only to carry my organ donation card with me but also to have actively joined the organ donor register,” he said.
What is automatic organ opt-out?
Under the scheme, patients aged 18 or over have to opt out if they do not want to be an organ donor. Families of those donating their organs are still able to withdraw consent on behalf of their loved ones.
Before the change, organs and tissues could only be taken from patients in England if the deceased joined the Organ Donor Register (ODR) or informed their relatives before their death that they wished to donate.
More than 5,800 people are on the organ waiting list in England, and an average of three people in need of an organ transplant die each day. In 2018, more than 400 people died in the UK waiting for a transplant, the BBC reports.
In the financial year to March 2021, the number of lives potentially saved or improved by receiving an organ donation fell by 30%, NHS figures show. However, the number of people opting into the ODR rose from 26 million to 26.7 million by the end of March 2021.
What is family refusal?
Family refusal is currently the “biggest obstacle to donation”, says the NHS. Around 91% of families agree to organ donation if their relative is on the organ donation register (ODR), according to figures from the NHS Blood and Transplant potential donor audit.
However, when patients are not on the ODR then 55% of families say no to a donation.
The number of people from black, Asian and minority ethnic communities who received a life-saving transplant hit a record high in 2020, at 1,187. People from these communities usually have to wait longer for an organ transplant, due to a lower number of donors from these ethnic backgrounds being registered as donors.
It was hoped that the introduction of the new law would reduce this discrepancy, and initial figures indicate this may be starting to happen. Millie Banerjee, chair of NHS Blood and Transplant, has said: “It’s really encouraging to see the number of people from ethnic minority groups receiving the lifesaving transplants they need.”
“However, there is still a long way to go to close the gap between the number of people donating organs and those waiting for a transplant”, she continued.
The pros and cons of automatic organ donation
Arguments for automatic organ donation:
- More than 5,500 people in the UK need a transplant, but a shortage of donors means that around 3,500 transplants are carried out annually
- Advances in medical science mean that the number of people whose lives could be saved by a transplant is rising more rapidly than the number of willing donors.
- The law as it was previously condemned many, some of them children, to an unnecessary death, simply because of the shortage of willing donors while, as the British Medical Association puts it, “bodies are buried or cremated complete with organs that could have been used to save lives”.
- Doctors and surgeons can be trusted not to abuse the licence which a change of the law would grant them.
- Objections to a change in the law are sheer sentimentality. A dead body is an inanimate object, incapable of feeling.
Arguments against automatic organ donation:
- Few question the value of transplant operations or the need for more donors. But a programme designed to recruit more donors is preferable to a change in the law.
- The law change implies that our bodies belong to the state as soon as we are dead. The assumption is offensive.
- Organ removal without the expressed wish of the deceased could be distressing for his or her family.
- The change in the law is open to abuse, with the possibility of death being hastened to secure an organ needed by some other patient.
- The safeguard - that is, the right to refuse permission for your organs to be removed - is inadequate. A terminally ill patient or his/her relatives would be made to feel selfish if permission was withheld.
- Families may feel the wishes of their loved ones are more ambiguous compared to opt-in systems, leading to higher risk of family refusal.
Sign up for Today's Best Articles in your inbox
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com

In Depth Sorting through the noise and controversies of modern survey research
By David Faris Published 16 May 24

Speed Read New CDC data shows drug overdose deaths dropped for the first time in five years
By Peter Weber, The Week US Published 16 May 24
Cartoons Thursday's cartoons - reminiscing, political pollen, and more
By The Week US Published 16 May 24

The Explainer Research shows that the treatment could provide significant relief from symptoms for many hay fever sufferers
By Richard Windsor, The Week UK Published 26 April 24

Pros and Cons A medical system that serves everyone comes with its own costs, and they're not only financial
By Rebecca Messina, The Week UK Published 24 April 24

The Explainer Hospitals in England will launch new scheme that will allow access to a rapid treatment review
By Richard Windsor, The Week UK Published 21 February 24

The Explainer Widely regarded as the worst treatment disaster in the history of the NHS, the public inquiry is due to publish its report in May
By The Week UK Published 10 February 24

The Explainer New proposals include more money for dentists working in under-served areas
By Richard Windsor, The Week UK Published 7 February 24

The Explainer Demise of UK tech start-up is a cautionary tale for politicians seeking quick fixes to complicated problems
By The Week UK Last updated 26 November 23

Two-thirds of women surgeons claim to have been sexually harassed and a third alleged assaults
By Chas Newkey-Burden Published 12 September 23

Today's Big Question Procedure could be offered more widely including to transgender people
By Chas Newkey-Burden Published 23 August 23
- Contact Future's experts
- Terms and Conditions
- Privacy Policy
- Cookie Policy
- Advertise With Us
The Week is part of Future plc, an international media group and leading digital publisher. Visit our corporate site . © Future US, Inc. Full 7th Floor, 130 West 42nd Street, New York, NY 10036.
Home — Essay Samples — Nursing & Health — Organ Donation — Shortcomings and Benefits of Organ Donation
Shortcomings and Benefits of Organ Donation
- Categories: Organ Donation Surgery
About this sample

Words: 1088 |
Published: Jan 29, 2019
Words: 1088 | Pages: 2 | 6 min read
Table of contents
Advantages of organ donation, disadvantages of organ donation, works cited, social responsibility, helps the families of the deceased to overcome grief, imparts a new hope to live a fruitful life, provides material for medical research, complications during and after surgery.
- Anderson, L. (2015). Organ Donation: Opportunities for Action. John Wiley & Sons.
- Callender, C. O., & Sade, R. M. (Eds.). (2011). The Global Organ Shortage: Economic Causes, Human Consequences, Policy Responses. University of South Carolina Press.
- Caplan, A. L., McCartney, J. J., & Sisti, D. A. (2018). Health, Disease, and Illness: Concepts in Medicine. Georgetown University Press.
- Delmonico, F. L. (2011). Organ Transplantation: Ethical, Legal, and Psychosocial Aspects. John Wiley & Sons.
- Gordon, E. J., & Wolf, S. M. (2013). Donation in a Changing World: The Ethical Challenges. MIT Press.
- Gruessner, A. C., & Benedetti, E. (Eds.). (2019). Transplantation at a Glance. Wiley Blackwell.
- Hippen, B. (2012). Is Altruistic Organ Donation an Unjustified Gift? In S. J. Youngner, R. M. Arnold, & R. Shapiro (Eds.), The Definition of Death: Contemporary Controversies (pp. 95-107). Johns Hopkins University Press.
- Price, D. (2019). Organ Transplantation: A Clinical Guide. Cambridge University Press.
- Radcliffe-Richards, J., Daar, A. S., Guttmann, R. D., & Hoffenberg, R. (Eds.). (2014). The Case for the Living Donor. Routledge.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1215 words
1 pages / 673 words
6 pages / 2570 words
2 pages / 891 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
The case of Baby Theresa, a newborn born with anencephaly in 1992, ignited a profound ethical debate regarding organ donation, the definition of death, and the boundaries of medical intervention. This essay delves into the [...]
Organ donation is a medical marvel that saves countless lives each year, offering a ray of hope to those in dire need of organ transplants. However, beneath the altruistic act of organ donation lie complex ethical issues that [...]
Organ donation is a pure act of kindness. However, it is often debated about whether it should be mandatory or not. Donating your organ is a social cause which is all together a decision of the person who is willing to donate [...]
The act of organ donation stands as a powerful testament to human solidarity and compassion, offering the gift of life to those in dire need. Organ donation has the potential to transform the lives of individuals grappling with [...]
Despite many possible life-concerning consequences following an allogeneic organ transplantation such as graft rejection, side effects from long-term immunosuppression and unquantifiable risk of disease transmissions, many [...]
Ionising radiation is a method of treatment that commonly used to treat cancer. Radiation therapy uses high-energy particles or waves, such as x-rays, gamma rays, electron beams, or protons, to destroy or damage cancer cells. [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Essay on Organ Donation for Students and Children
500+ words essay on organ donation.
Essay on Organ Donation – Organ donation is a process in which a person willingly donates an organ of his body to another person. Furthermore, it is the process of allowing the removal of one’s organ for its transplanting in another person. Moreover, organ donation can legally take place by the consent of the donor when he is alive. Also, organ donation can also take place by the assent of the next of kin of a dead person. There has been a significant increase in organ donations due to the advancement of medical science.

Organ Donation in Different Countries
First of all, India follows the opt-in system regarding organ donation. Furthermore, any person wishing to donate an organ must fill a compulsory form. Most noteworthy, this form is available on the website of the Ministry of Health and Family Welfare Government of India. Also, The Transplantation of Human Organs Act 1994, controls organ donation in India.
The need for organ donation in the United States is growing at a considerable rate. Furthermore, there has also been a significant rise in the number of organ donors in the United States. Most noteworthy, organ donation in the United States takes place only by the consent of the donor or their family. Nevertheless, plenty of organizations are pushing for opt-out organ donation
Within the European Union, the regulation of organ donation takes place by the member states. Furthermore, many European countries have some form of an opt-out system. Moreover, the most prominent opt-out systems are in Austria, Spain, and Belgium. In England, no consent is presumed and organ donation is a voluntary process.
Argentina is a country that has plenty of awareness regarding organ donation. Most noteworthy, the congress of Argentina introduced an opt-out organ donation policy. Moreover, this means that every person over 18 years of age will be a donor unless they or their family state their negative. However, in 2018, another law was passed by congress. Under the new law, the family requirement was removed. Consequently, this means that the organ donor is the only person who can state their negative.
Get the huge list of more than 500 Essay Topics and Ideas
Benefits of Organ Donation
First of all, organ donation is very helpful for the grieving process. Furthermore, many donor families take relief and consolation due to organ donation. This is because they understand that their loved one has helped save the life of other people. Most noteworthy, a single donor can save up to eight lives.
Organ donation can also improve the quality of life of many people. An eye transplant could mean the ability to see again for a blind person. Similarly, donating organs could mean removing the depression and pain of others. Most noteworthy, organ donation could also remove the dependency on costly routine treatments.
Organ donation is significantly beneficial for medical science research. Donated organs offer an excellent tool for conducting scientific researches and experiments. Furthermore, many medical students can greatly benefit from these organs. Most noteworthy, beneficial medical discoveries could result due to organ donation. Organ donation would also contribute to the field of Biotechnology.
To sum it up, organ donation is a noble deed. Furthermore, it shows the contribution of an individual even after death. Most noteworthy, organ donation can save plenty of lives. Extensive awareness regarding organ donation must certainly be spread among the people.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

What are the risks involved with donating a kidney? A transplant expert explains why pig organs may be the only option for some
- Search Search
Northeastern Global News spoke with Dami Ko, an assistant professor of nursing at Northeastern and a transplant expert, to learn more about kidney transplantation and what could be done to address the donation shortage.
- Copy Link Link Copied!

The first man to receive a pig kidney died over the weekend , nearly two months after undergoing the transplant.
Doctors at Massachusetts General Hospital, where 62-year-old Richard Slayman underwent the procedure, said there is “no indication” that his death was the result of the pig kidney failing. The man had previously received a transplanted kidney from a human, but it had to be taken out due to complications.
The surgery, known as a xenotransplantation, was seen as a medical breakthrough in helping address the major global organ donation shortage.
And the shortage is pretty significant, according to the data.
Every day, 17 people in the United States die waiting for an organ transplant, according to the U.S. Health Resources and Services Administration. Kidneys in particular are in high demand. An estimated 786,000 patients were living with kidney failure in 2021, but only about 25,000 received a transplant, the National Kidney Foundation reported.
Transplantation numbers have gone up since then, but organ donor proponents continue to argue that if more people donated one of their kidneys, operations requiring organs from genetically modified pigs would be less necessary.
But what kind of risks are involved in donating a kidney?
Northeastern Global News spoke with Dami Ko , an assistant professor of nursing at Northeastern and a transplant expert, to learn more about kidney transplantation and what could be done to address the donation shortage.
This interview has been edited and condensed for clarity.
What factors must be considered in a kidney transplant?
First of all, there are two types of donations. One is you donate a kidney as a living donor, meaning that you give one of your kidneys to another person in need. In a deceased donation, you get a kidney from someone who has had brain death. So before we confirm someone’s death, when they are on life support, we start talking about organ donation and get consent [from family members].
When we decide on a donation, there are so many factors that need to be matched between recipients and donors. There are so many things that need to match like blood types, and also their DNA-like HLA, which is called human leukocyte antigens. Those are the key things that need to be matched.
There are some risk scores in the registry, but those who are in relatively good condition but really in need of those organs will get first place to those donated organs if they are a match.
What are the risks for a living person to donate one of their kidneys?
A lot of people would say the risk would be very low because it’s simply taking out their organ and giving it to someone else, but it’s a major surgery. It’s not a simple surgery.
You will need some time for recovery afterwards. During the process, you may also experience some kind of physical and psychological complications. It could be depression or pain. Some people may say, ‘Hey, I donated my organ but all the attention is being given to the recipient and not to me, and there is no one who is really supporting myself.’
Most people will recover pretty well, but some may have some long-term complications, and that may affect your ability to go back to work or go back to a normal life.
All those things may interfere with the living donor’s decision about whether they would want to give their organ to someone else.
Featured Stories

A historic homecoming for congresswoman and the actress who plays her in the Netflix biopic ‘Shirley’

Northeastern’s Barnett Institute of Chemical and Biological Analysis celebrates 50th anniversary by looking to the future

Election 2024: New, easy-to-read poll tracker plots changes within pollsters

CPI report shows inflation eased in April, but consumer prices still rose 3.4% from a year ago
Do kidney donations often come from family members do cultural and religious beliefs become considerations.
If it’s within the family, the kidney disease might be genetic. For example, if your parent has the end stages of kidney disease, the child who is thinking about giving the kidney to the parent may also have a higher risk of getting that disease.
If they give one of their kidneys to their parent, that donor will be living with just one kidney themeslves. What if something happens to their kidney? They will need to get a kidney transplantation in the future.
Also, based on my perspective, another thing that really needs to be considered is cultural and religious beliefs.
I’m from South Korea, and at the time I was practicing there, probably 80% of donations were from living donors. It’s because of filial piety like the need to respect your parents and you should be willing to give your organs to your parents when they are in need.
And also, they think that donating your organs after life is not really good. You don’t want to harm your body. You want to keep an intact body for your afterlife or next life.
If the demand for kidney donations is not met, can xenotransplantation fill the gap?
It’s really hard to make someone donate their organs. It’s a really hard decision and many people don’t know much about organ donation. I think xenotransplantation can help reduce the mismatch between the demand and the shortage.
But not everyone can have the privilege of having a xenotransplantation, so I think increasing organ donation is really important, but we don’t know much about what would be the best strategy to increase the donor shortage.
Also, if we were to increase organ donations, some people still might not be able to find a good match to get a transplant. They may need to go with xenotransplantation when it becomes more popular and a more common practice in the future.
Northeastern Global News, in your inbox.
Sign up for NGN’s daily newsletter for news, discovery and analysis from around the world.
What kind of strategies can bridge the gap between those who need organ transplants and potential donors?
A lot of researchers have tried to bridge the gaps, but I don’t think they are up to date with the most effective strategies yet.
A lot of interventions have been conducted on the population level. You might have seen campaigns asking ‘Have you considered a donation?’ from the United Network for Organ Sharing, it’s a national department. Also, on the community level, if you go to the RMV or DMV, they ask questions about whether you’d like to be a donor.
At the education level, some people provide education programs at schools, like universities and high schools.
Hospital wise, they try to implement interventions and think about ways they can identify potential donors via brain death and actually use their organ to be transplanted from someone.
Although there are many different strategy levels, there is not one single effective way to improve donation sizes or attitudes. Research is still ongoing and I can’t give an answer on what would be the best way to do it, but I think a multilevel approach is a good way to do it because it will be effective to many people in the community from multiple levels.
The cultural perspective should also be considered. Every culture has different ideas about donations, especially those who are immigrants or those who are from a low socioeconomic status. They may not really trust the health care system, so they may not be willing to become a donor or willing to sign for their deceased family member.
All these things need to be considered, but I can tell a lot of researchers are working on it, and I really hope to see some progress in the future.

Recent Stories

- Share full article
Advertisement
Supported by
Patient Dies Weeks After Kidney Transplant From Genetically Modified Pig
Richard Slayman received the historic procedure in March. The hospital said it had “no indication” his death was related to the transplant.

By Virginia Hughes
Richard “Rick” Slayman, who made history at age 62 as the first person to receive a kidney from a genetically modified pig, has died about two months after the procedure.
Massachusetts General Hospital, where Mr. Slayman had the operation, said in a statement on Saturday that its transplant team was “deeply saddened” at his death. The hospital said it had “no indication that it was the result of his recent transplant.”
Mr. Slayman, who was Black, had end-stage kidney disease, a condition that affects more than 800,000 people in the United States, according to the federal government, with disproportionately higher rates among Black people.
There are far too few kidneys available for donation. Nearly 90,000 people are on the national waiting list for a kidney.
Mr. Slayman, a supervisor for the state transportation department from Weymouth, Mass., had received a human kidney in 2018. When it began to fail in 2023 and he developed congestive heart failure, his doctors suggested he try one from a modified pig.
“I saw it not only as a way to help me, but a way to provide hope for the thousands of people who need a transplant to survive,” he said in a hospital news release in March.
His surgery, which lasted four hours, was a medical milestone. For decades, proponents of so-called xenotransplantation have proposed replacing ailing human organs with those from animals. The main problem with the approach is the human immune system, which rejects animal tissue as foreign, often leading to serious complications.
Recent advances in genetic engineering have allowed researchers to tweak the genes of the animal organs to make them more compatible with their recipients.
The pig kidney that was transplanted into Mr. Slayman was engineered by eGenesis, a biotech company based in Cambridge, Mass. Scientists there removed three genes and added seven others to improve compatibility. The company also inactivated retroviruses that pigs carry and could be harmful to humans.
“Mr. Slayman was a true pioneer,” eGenesis said in a statement on social media on Saturday. “His courage has helped to forge a path forward for current and future patients suffering from kidney failure.”
Mr. Slayman was discharged from the hospital two weeks after his surgery, with “one of the cleanest bills of health I’ve had in a long time,” he said at the time.
In a statement published by the hospital, Mr. Slayman’s family said he was kind, quick-witted and “fiercely dedicated to his family, friends and co-workers.” They said they had taken great comfort in knowing that his case had inspired so many people.
“Millions of people worldwide have come to know Rick’s story,” they said in the statement. “We felt — and still feel — comforted by the optimism he provided patients desperately waiting for a transplant.”
Virginia Hughes is an editor on the Health and Science desk. More about Virginia Hughes

IMAGES
VIDEO
COMMENTS
Here Are the Pros of Organ Donation. 1. It is possible for one organ donor to save up to 8 lives. More than 100,000 people just in the United States are waiting for an organ transplant right now. This includes critical organs, such as the heart, the liver, and the kidneys.
1. Introduction. Alone in the USA over an estimated 120.000 people are waiting for a donor organ with 21 patients dying per day due to the deficit [].In Germany around 1.000 persons die per year while awaiting organ transplantation [], with similar numbers for other developed nations, although most of them implement significant national campaigns and other incentives toward an increase in ...
1. It can lengthen the grieving process. When an organ donor passes away, the hospital keeps the deceased person on life support until recipient matches can be found for their organs. This is done to keep blood flowing through the body and the organs alive even though the person is legally and clinically deceased.
The other advantage of organ transplantation is that it improves the quality of life of a patient. Organ transplantation improves the quality of patients' lives since it reduces or eliminates dependency and hospitalization costs (Thomas, 2011). Organ damage leads to frequent hospitalization of individuals.
Based upon limited information that is currently available, overall risks are considered to be low. Risks can differ among donors and the type of organ. For kidney donors, there is only a 1% lifetime increase in the donor's own risk of kidney failure. To put this into perspective, the general population has a 3% risk for kidney failure.
Preliminary results, published last year, show that the annual deceased organ-donation rate increased from 7.8 organs per million people in 2010 to 11.4 organs per million people in 2011. The ...
Organ donation "is a civic gesture that should be taught at school," said Noel. In a conversation after the symposium, Wikler, a former chief ethicist at WHO, made another suggestion for increasing the number of donated organs. Years ago, while serving on a committee to advise then Secretary of Health and Human Services Donna Shalala, he ...
Here are answers to some common organ donation myths and concerns. Myth: If I agree to donate my organs, the hospital staff won't work as hard to save my life. Fact: When you go to the hospital for treatment, the health care team tries to save your life, not someone else's. You get the best care you can get.
This guideline will help improve organ transplant outcomes, leading to more individuals being able to live healthier and longer lives. The science and evidence are clear and will improve the safety of organs, balanced with a clear and conscious regard for donors and recipients. It is the human aspect of donation and transplantation—helping ...
This can lead to saving many lives that would otherwise have been lost. In Michigan, a positive attitude towards organ donation would assist the many people in need, and would be a heroic move. I want to call upon people to save life today by signing for organ donation. This is not enough.
Benefits of Organ Donation . Many people have considered the pros and cons of being an organ donor. They understand the benefits of organ donation and believe it is not only a privilege but a social responsibility. Organs donated from one individual can save eight lives and enhance the quality of about 50 lives. Other benefits of organ donation ...
Organ donation is a remarkable act of compassion and generosity that saves lives and improves the quality of life for countless individuals. It is a practice that embodies the values of altruism, solidarity, and empathy. As we conclude this article, it is crucial to recognize the importance of individual decisions regarding organ donation.
organ donation, the act of giving one or more organs (or parts thereof), without compensation, for transplantation into someone else. Organ donation is a very personal yet complex decision, intertwined with medical, legal, religious, cultural, and ethical issues. Today organ donation, strictly defined, encompasses the donation and transplantation of the heart, intestines, kidneys, liver, lungs ...
Introduction. Studies have shown that deceased donors cannot meet the growing demand for organs such as the kidneys, liver, etc. Sometimes cultural, religious, and legal considerations may even be reluctant to donate organs after death.[] Thus, because of the high demand for organ transplantation and the increased wait time for transplantation, receiving organs from living donors is a primary ...
Although kidney donation is not practiced in the United States, it has been found to be effective in other nations. For example, Iran pays its residents up to $1,200 for kidney donations, but the recipients must be Iranian nationals and get long-term medical attention (Monday & Ogugua, 2020). There should be discussions regarding possible ...
A disadvantage to living organ donation is that all surgery carries the risk of medical error, infection and even death 2. There is also a risk of future health problems. For instance, if you donate a kidney, there is no guarantee your remaining kidney will remain healthy throughout your life. An additional disadvantage is the donation may be ...
Living donation serves as a viable option, especially in cases of kidney and liver transplantation, and saves the life of both the recipient and the next person on the waiting list. "A large number of transplant patients do extremely well, improving the quality and timespan of their life," Andreoni said. "It also drastically increases the ...
However, despite its critical importance, there persists a significant gap in awareness and understanding surrounding organ donation. This essay embarks on a journey to shed light on the multifaceted dimensions of organ donation, encompassing its types, benefits, and the misconceptions that often shroud this life-saving practice.
Ultimately, leaving the decision up to family members during the crucial time of grief tends to work against organ donation as the family feels it is best to keep the body intact. This ends up leaving several viable organs going to waste. According to Clara a respondent (as cited in Nizza, Britton and Smith 2014), who was interviewed feels it ...
Background There is a worldwide shortage of donor organs for transplantation. To overcome this, several countries have introduced an opt-out donor consent system. This system, soon planned for Scotland and England means individuals are automatically deemed to consent for organ donation unless they register an opt-out decision. This study was designed to explore the reasons underpinning donor ...
A donor heart or lungs can last only four to six hours outside the body. A kidney, liver or pancreas can last a bit longer. Because donation and transplantation must be synched perfectly, surgical teams must be allowed to work at any hour of the day. Although donors are dead, managing their anaesthesia can be tricky.
The pros and cons of automatic organ donation. Arguments for automatic organ donation: More than 5,500 people in the UK need a transplant, but a shortage of donors means that around 3,500 ...
Imparts a New Hope to Live a Fruitful Life. Organ donation gives a new ray of hope to the recipients. The recipients are patients suffering from dysfunctional or failed organs/tissues. A sheer gesture of donating one's healthy organs to such patients would give them a chance to live a healthy life for the second time.
500+ Words Essay on Organ Donation. Essay on Organ Donation - Organ donation is a process in which a person willingly donates an organ of his body to another person. Furthermore, it is the process of allowing the removal of one's organ for its transplanting in another person. Moreover, organ donation can legally take place by the consent of ...
The surgery, known as a xenotransplantation, was seen as a medical breakthrough in helping address the major global organ donation shortage. And the shortage is pretty significant, according to the data. Every day, 17 people in the United States die waiting for an organ transplant, according to the U.S. Health Resources and Services ...
Richard "Rick" Slayman, who made history at age 62 as the first person to receive a kidney from a genetically modified pig, has died about two months after the procedure. Massachusetts General ...