Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 01 August 1997

Researching alternative medicine
- Wayne B. Jonas 1
Nature Medicine volume 3 , pages 824–827 ( 1997 ) Cite this article
132 Accesses
28 Citations
3 Altmetric
Metrics details
In 1992 the US Congress created the Office of Alternative Medicine (OAM), placing it within the NIH, one of the foremost bio-medical research establishments world-wide. The OAM is currently funded to the tune of $40 million per year. Although alternative and unconventional medicine attracts considerable attention (and finances) from the public in Western societies, many within the established medical and research communities are outwardly cynical and dismissive of alternative medical practices. We have asked Wayne B. Jonas. Director of the OAM, to discuss what the OAM hopes to achieve and how it is going about it.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Eisenberg, D.M., Kessler, R.C., Foster, C., Norlock, F.E., Calkins, D.R., Delbanco, T.L. Unconventional medicine in the United States - prevalence, costs, and patterns of use. N. Engl. J. Med. , 328 , 246–252 (1993).
Article CAS Google Scholar
Fisher, P. & Ward, A. Complementary medicine in Europe. British Medical Journal. 309 , 107–111 (1994).
MacLennan, A.H., Wilson, D.H. & Taylor, A.W. Prevalence and cost of alternative medicine in Australia. Lancet. 347 , 569–573 (1996).
Cassileth, B.R., Lussk, E.J., Strouss, T.B. & Bodenheimer, B.J. Contemporary unorthodox treatments in cancer medicine: a study of patients, treatments, and practitioners. Annals Int. Med. 101 , 105–112 (1984).
Anderson, W.H. et al . Patient use and assessment of conventional and alternative therapies for HIV infection and AIDS. AIDS. 74 , 561–564 (1993).
Article Google Scholar
Blumberg, D.L., Grant, W.D., Hendricks, S.R., Kamps, C.A. & Dewan, M.J. The physician and unconventional medicine. Alternative Therapies in Health & Medicine. 1 , 31–35 (1995).
CAS Google Scholar
Ernst,, E. Complementary medicine: what physicians think of it: a meta-analysis. Arch Intern Med 155 , 2405–2408 (1995).
Halliday, J., Taylor, M., Jenkins, A. & Reilly, D. Medical students and complementary medicine. Complementary Therapies in Medicine 1 (suppl), 32–33 (1993).
Google Scholar
Carlston, M., Stuart, M. & Jonas, W. Alternative Medicine Instruction in American Medical Schools and Family Medicine Residency Programs. Fam. Med. (in the press) (1997).
Description PoDa. Defining and describing complementary and alternative medicine. Alternative Therapies in Health and Medicine. 3 , 49–57 (1997).
Furnham, A. & Forey, J. The attitudes, behaviors and beliefs of patients of conventional vs. complementary (alternative) medicine. Journal of Clinical Psychology. 50 , 458–469 (1994).
Kleijnen, J. & Knipschild, P. Gingko biloba for cerebral insufficiency. Br. J. Clin. Pharm. 34 , 352–358 (1992).
Di Silverio, F. et al . Plant extracts in BPH. Minerva Urologica e Nefrologica 45 , 143–49 (1993).
CAS PubMed Google Scholar
Neil, A. & Silagy, C. Garlic: Its cardio-protective properties. Curr. Opin. Lipid. 5 , 6–10 (1994).
Linde, K., Ramirez, G., Mulrow, C.D., Pauls, A., Weidenhammer, W. & Melchart, D. St John's wort for depression — an overview and meta-analysis of randomised clinical trials [see comments]. Br. Med. J. 313 , 253–258 (1996).
Gibson, R.G., Gibson, S., MacNeill, A.D. & Watson, B.W. Homeopathic therapy in rheumatoid arthritis: Evaluation by double-blind clinical therapeutical trial. Br. J. Clin. Pharm. 9 , 453–459 (1980).
Berman, B.M. et al . Efficacy of traditional Chinese acupuncture in the treatment of symptomatic knee osteoarthritis: A pilot study. Osteoarthritis Cartilage 3 , 139–142 (1995).
Jonas, W.B., Rapoza, C.P. & Blair, W.F. The effect of niacinamide on osteoarthritis: A pilot study. Inflammation Research. 45 , 330–334 (1996).
Tao, X.L., Dong, Y. & Zhang, N.Z. A double-blind study of T2 (tablets of polygly-cosides of Tripterygium wilfodii hook) in the treatment of rheumatoid arthritis. [Chinese]. Chung-Hua Nei Ko Tsa Chih Chinese Journal of Internal Medicine. 26 , 399–402, 444–445 (1987).
Altman, R.D. et al . Capsaicin cream 0.025% as monotherapy for osteoarthritis: A double-blind study. Seminars in Arthritis & Rheumatism. 23 (suppl) 25–33 (1994).
Kjeldsen-Kragh, J. et al . Changes in laboratory variables in rheumatoid arthritis patients during a trial of fasting and one-year vegetarian diet. Scand J Rheumatol. 24 , 85–93 (1995).
Lavigne, J.V., Ross, C.K., Berry, S.L., Hayford, J.R. & Pachman, L.M. Evaluation of a psychological treatment package for treating pain in juvenile rheumatoid arthritis. Arthritis Care Res. 5 , 101–110 (1992).
Assendelft, W.J., Koes, B.W., Knipschild, P.G. & Bouter, L.M. The relationship between methodological quality and conclusions in reviews of spinal manipulation. JAMA 274 , 1942–1948 (1995).
Ader, R. Conditioned Immunopharmacological effects in animals: Implications for a conditioning model of pharmacotherapy. In: White, L., Tursky, B., Schwartz, G.E., editors. Placebo Theory, Research and Mechanisms (The Guilford Press) 306–323 (New York, 1985).
Vickers, A.J. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. J. R. Soc. Med. 89 , 303–311 (1996).
Dowie, J. Evidence based medicine. Needs to be within framework of decision making based on decision analysis. Br. Med. J. 313 , 170–171 (1996).
Methods PoRGa. How should we research unconventional therapies? Int. J. Tech. Assess. Health Care 13 , 111–121 (1997).
Davenas, E. et al . Human basophil degranulation triggered by very dilute anti-serum against IgE. Nature 333 , 816–818 (1988).
Kleijnen, J., Knipschild, P. & Rietter, G. Clinical trials of homoeopathy. Br. Med. J. 302 , 316–323 (1991).
Linde, K. et al . Critical review and meta-analysis of serial agitated dilutions in experimental toxicology. Human and Experimental Toxicology 13 , 481–492 (1994).
Boissel, J.P., Cucherat, M., Haugh, M. & Gauthier, E. Critical literature review on the effectiveness of homoeopathy: overview of data from homoeopathic medicine trials. Brussels: Homoeopathic Medicine Research Group. Report to the European Commission, 1996.
Radin, D.I. & Nelson, R.D. Evidence for Consciousness-Related Anomalies in Random Physical Systems. Found. Physics 19 , 1499–1514 (1989).
Braud, W.G. & Schlitz, M.J. Consciousness interactions with remote biological systems: Anomalous intentionality effects. Subtle Energies 2 , 1–46 (1992).
Bern, D.J. & Honorton, C. Does psi exist? Replicable evidence for anomalous information transfer. Psychological Bulletin 115 , 4–18 (1994).
Download references
Author information
Authors and affiliations.
Director, Office of Alternative Medicine, National Institutes of Health, 9000 Rockville Pike, Building 31, Room 5B35 MSC 2182, Bethesda, Maryland, 20892, USA
Wayne B. Jonas
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Jonas, W. Researching alternative medicine. Nat Med 3 , 824–827 (1997). https://doi.org/10.1038/nm0897-824
Download citation
Issue Date : 01 August 1997
DOI : https://doi.org/10.1038/nm0897-824
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Herbal biomedicines: a new opportunity for aquaculture industry.
- Thavasimuthu Citarasu
Aquaculture International (2010)
What is the state of the evidence on the mind–cancer survival question, and where do we go from here? A point of view
- Joanne E. Stephen
- Michelle Rahn
Supportive Care in Cancer (2007)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Alternative Medicine and Healthcare Delivery: A Narrative Review
- First Online: 07 January 2023
Cite this chapter

- Ibrahim Adekunle Oreagba 3 &
- Kazeem Adeola Oshikoya 4
456 Accesses
1 Altmetric
The global trend toward increased acceptability and use of complementary and alternative medicines (CAMs), across all age groups, is well documented in the literature. Consequently, further systematic evaluation and meta-analysis are necessary to evaluate the quality, efficacy, safety, and regulation of these range of therapies by combining all the available evidence in the literature. Furthermore, the role of CAM in healthcare delivery and its utilization in a digital age cannot be overemphasized. Evidence-based results would guide both patients willing to use CAMs and their providers in making an informed decision. This narrative review addressed the above points. There is subtle evidence supporting the quality, efficacy, and safety of CAM therapies and products; however, much of the evidence is inconsistent due to the varied CAM types and regulatory policies from country to country. More research is required in this field to further harness the gains of CAM therapies and products globally. CAM users and providers should exercise caution with the available therapies and products. Care should also be taken when consulting CAM therapies online.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Adib-Hajbaghery, M., & Hoseinian, M. (2014). Knowledge, attitude and practice toward complementary and traditional medicine among Kashan health care staff. Complementary Therapies in Medicine, 22 , 126–132.
Google Scholar
Allen, D., Bilz, M., Leaman, D. J., Miller, R. M., Timoshyna, A., & Window, J. (2014). European red list of medicinal . Publications Office of the European Union.
Aronson, J. K. (2016). Meyler’s side effects of drugs (16th ed. pp. 488–424). Elsevier Publishing House.
Ayoubi, R. A., Nassour, N. S., Saidy, E. G., Aouad, D. K., Maalouly, J. S., & Daou, E. B. (2020). Physical manipulation-induced femoral neck fracture: A case report. Case Reports in Orthopaedic Research, 3 , 118–122. https://doi.org/10.1159/000509704
Article Google Scholar
Barnes, J. (2003). Quality, efficacy and safety of complementary medicines: Fashions, facts and the future. Part I. Regulation and quality. British Journal of Clinical Pharmacology, 55 , 226–233.
Bent, S., Tiedt, T. N., Odden, M. C., & Shlipak, M. G. (2003). The relative safety of ephedra compared with other herbal products. Annals of Internal Medicine, 138 , 468–471.
Bordes, C., Leguelinel-Blache, G., Lavigne, J. P., Mauboussin, J. M., Laureillard, D., Faure, H., Rouanet, I., Sotto, A., & Loubet, P. (2020). Interactions between antiretroviral therapy and complementary and alternative medicine: A narrative review. Clinical Microbiology and Infection., 26 (9), 1161–1170. https://doi.org/10.1016/j.cmi.2020.04.019.p420-421
Bouziri, A., Hamdi, A., Menif, K., & Ben Jaballah, N. (2010). Hepatorenal injury induced by cutaneous application of Atractylis gummifera L. Clin Toxicol (Phila), 48 (7), 752–754. https://doi.org/10.3109/15563650.2010.498379 . PMID: 20615152.
Bowden, D., Goddard, L., & Gruzelier, J. (2011). A randomized controlled single-blind trial of the efficacy of reiki at benefitting mood and well-being. Evid Based Complement Alternat Med, 2011 , 381862. https://doi.org/10.1155/2011/381862
Campbell-Hall, V., Petersen, I., Bhana, A. et al. (2010). Collaboration between traditional practitioners and primary health care staff in South Africa: Developing a workable partnership for community mental health services. Transcultural Psychiatry, 47 , 610–628.
Charnock, D., Shepperd, S., Needham, G., & Gann, R. (1999). DISCERN: An instrument for judging the quality of written consumer health information on treatment choices. Journal of Epidemiology and Community Health, 53 (2), 105–111.
Chitindingu, E., George, G., & Gow, J. (2014). A review of the integration of traditional, complementary and alternative medicine into the curriculum of South African medical schools. BMC Medical Education, 14 , 40.
Colombo, F., Di Lorenzo, C., Biella, S., Vecchio, S., Frigerio, G., & Restani, P. (2020). Adverse effects to food supplements containing botanical ingredients. Journal of Functional Foods, 72 ,. https://doi.org/10.1016/j.jff.2020.103990
De Maat, M. M. R., Hoetelmans, R. M. W., Mathôt, R. A. A., van Gorp, E. C. M., Meenhorst, P. L., Mulder, J. W., & Beijnen, J. H. (2001). Drug interaction between St John’s wort and nevirapine. AIDS, 15 (3).
Dwyer, J. T., Coates, P. M., & Smith, M. J. (2018). Dietary supplements: Regulatory challenges and research resources. Nutrients, 10 (1), 41. Published 2018 Jan 4. https://doi.org/10.3390/nu10010041
Eisenberg, D. M., Davis, R., Ettner, S. L., Appel, S., Wilkey, S., Van Rompay, M., et al. (1998). Trends in alternative medicine use in the United States 1990–1997. Journal of the American Medical Association, 280 , 1569–1575.
Ekor, M. (2014). The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Frontiers in Pharmacology, 4 , 177.
Ernst, E., & Thompson-Coon, J. (2002). Heavy metals in traditional Chinese medicines: A systematic review. Clinical Pharmacology & Therapeutics, 70 (6), 497–504. https://doi.org/10.1067/mcp.2001.120249
European Medicines Agency. Compilation of Union Procedures on Inspections and Exchange of Information. 21 September 2021, EMA/INS/428126/2021, Rev 18, Inspections Office, Quality and Safety of Medicines Department. Available at: https://www.ema.europa.eu/en/documents/regulatory-procedural-guideline/compilation-union-procedures-inspections-exchange-information_en.pdf (Accessed 30 March 2022).
Frass, M., Strassl, R. P., Friehs, H., Müllner, M., Kundi, M., & Kaye, A. D. (2012). Use and acceptance of complementary and alternative medicine among the general population and medical personnel: A systematic review. The Ochsner Journal, 12 , 45–56. Google Scholar | Medline
Fjær, E. L., Landet, E. R., McNamara, C. L. (2020). The use of complementary and alternative medicine (CAM) in Europe. BMC Complement Med Ther, 20 , 108. https://doi.org/10.1186/s12906-020-02903-w
Food Drug and Administration. (2016). Dietary supplements: New dietary ingredient notifications and related issues: Guidance for Industry April 1.
Food Drugs and Administration. Alerts, Advisories and Safety Information: Food, Beverages, Dietary Supplements, and Infant Formula . Available at https://www.fda.gov/food/recalls-outbreaks-emergencies/alerts-advisories-safety-information (Accessed 29 March 2022).
Forsyth, A., Blamey, G., Lobet, S., & McLaughlin, P. (2020). Practical guidance for nonspecialist physical therapists managing people with hemophilia and musculoskeletal complications. Health, 12 (2), 158–179.
Goksu, E., Kilic, T., & Yilmaz, D. (2012). Hepatitis: A herbal remedy Germander. Clinical Toxicology, 50 (2), 158. https://doi.org/10.3109/15563650.2011.647993
Guido, P. C., Ribas, A., Gaioli, M., Quattrone, F., & Macchi, A. (2015). The state of the integrative medicine in Latin America: The long road to include complementary, natural, and traditional practices in formal health systems. European Journal of Integrative Medicine, 7 , 5–12.
Health Canada. (2016). About natural health product regulation in Canada . Available at: https://www.canada.ca/en/health-canada/services/drugs-health-products/natural-nonprescription/regulation.html (Accessed 31 March 2022).
Hofgard, M. W., & Zipin, M. L. (1999) Complementary and alternative medicine--a business opportunity? Medical Group Management Journal, 46 (3), 16–24, 26–7. PMID: 10539335.
Horrigan, B., Lewis, S., Abrams, D. I., & Pechura, C. (2012). Integrative medicine in America—How integrative medicine is being practiced in clinical centers across the United States. Global Advances in Health and Medicine 1 (3), 18–94. https://doi.org/10.7453/gahmj.2012.1.3.006
Hudson, A., Lopez, E., Almalki, A. J., Roe, A. L., & Calderón, A. I. (2018). A review of the toxicity of compounds found in herbal dietary supplements. Planta Medica, 84 (9–10), 613–626. https://doi.org/10.1055/a-0605-3786 . Epub 2018 Apr 19.
James, P. B., Wardle, J., Steel, A., & Adams, J. (2018). Traditional, complementary and alternative medicine use in Sub-Saharan Africa: A systematic review. BMJ Global Health, 3 , e000895. https://doi.org/10.1136/bmjgh-2018-000895
Kasilo, O. M., Trapsida, J.-M., & Mwikisa Ngenda, C. (2010) An overview of the traditional medicine situation in the African region. African Health Monitor , 7–15.
Kalumbi, M. H., Likongwe, M. C., Mponda, J., Zimba, B. L., Phiri, O., Lipenga, T., Mguntha, T., & Kumphanda, J. (2020). Bacterial and heavy metal contamination in selected commonly sold herbal medicine in Blantyre, Malawi. Malawi Medical Journall, 32 (3), 153–159.
Keshari P. (2021). Controversy, adulteration and substitution: Burning problems in ayurveda practices. In H. El-Shemy (Ed.), Medicinal plants from nature [Working Title] [Internet]. IntechOpen; [cited 2022 Mar 29]. Available from: https://www.intechopen.com/online-first/77108 . https://doi.org/10.5772/intechopen.98220
Komlaga, G., Agyare, C., Dickson, R. A., Mensah, M. L. K., Annan, K., &, Loiseau, P. M. (2015). Medicinal plants and finished marketed herbal products used in the treatment of malaria in the Ashanti region, Ghana. Journal of Ethnopharmacology, 4 , 172:333–346.
LiverTox. (2017). Clinical and research information on drug-Induced liver injury [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Chaparral. [Updated 2017 Jan 23]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548355/
LiverTox. (2018). Clinical and research information on drug-Induced liver injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Jin Bu Huan. [Updated 2018 Apr 26]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548147/
LiverTox. (2020). Clinical and research information on drug-Induced liver injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Pennyroyal Oil. [Updated 2020 Mar 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548673/
Luo, L., Wang, B., Jiang, J., Fitzgerald, M., Huang, Q., Yu, Z., Li, H., Zhang, J., Wei, J., Yang, C., Zhang, H., Dong, L., & Chen, S. (2020). Heavy metal contaminations in herbal medicines: Determination, comprehensive risk assessments, and solutions. Frontiers in Pharmacology, 14 (11), 595335. https://doi.org/10.3389/fphar.595335.PMID:33597875;PMCID:PMC7883644
Ministry for Primary Industries. (2016). Food standard: New Zealand food (supplemented food) standard, 2016 (2016) https://www.mpi.govt.nz/dmsdocument/11365-new-zealand-food-supplemented-food-standard-2016 (Accessed 31 March 2022).
Mingzhe, X., Baobin, H., Fang, G., Chenchen, Z., Yueying, Y., Lulu, L., Wenya, W., & Luwen. (2019). Assessment of adulterated traditional Chinese medicines in China: 2003–2017. Front Pharmacol (10). https://doi.org/10.3389/fphar.2019.01446
National Center on Complementary and Integrative Health (NCCIH). (2005). Energy medicine: An overview . Backgrounders; NCCIH: Rockville Pike, MD, USA.
National Center for Complementary and Integrative Health (NCCIH). Alerts and advisories . Available at https://www.nccih.nih.gov/news/alerts (Accessed 29 March 2022).
National Institute of Health. (2005a). Institute of Medicine (US) Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington (DC): National Academies Press (US), 7, Integration of CAM and Conventional Medicine. Available from: https://www.ncbi.nlm.nih.gov/books/NBK83807/
National Institute of Health. (2005b). Institute of Medicine (US) Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington (DC): National Academies Press (US), 5, State of Emerging Evidence on CAM. Available from: https://www.ncbi.nlm.nih.gov/books/NBK83790/
National Center for Complementary and Integrative Health. (2020). Natural Does not Necessarily Mean Safer, or Better [Internet]. U.S. Department of Health and Human Services [cited 2020 May 24]. https://www.nccih.nih.gov/health/know-science/natural-doesnt-mean-better .
Neuman, M. G., Cohen, L., Opris, M., Nanau, R. M., & Hyunjin, J. (2015). Hepatotoxicity of pyrrolizidine alkaloids. Journal of Pharmacy & Pharmaceutical Sciences, 18 (4), 825–843. https://doi.org/10.18433/j3bg7j PMID: 26626258.
Newmaster, S. G., Grguric, M., Shanmughanandhan, D., et al. (2013). DNA barcoding detects contamination and substitution in North American herbal products. BMC Medicine, 11 , 11–222.
Ng, J. Y., Munford, V., & Thakar, H. (2020). Web-based online resources about adverse interactions or side effects associated with complementary and alternative medicine: A systematic review, summarization and quality assessment. BMC Medical Informatics and Decision Making, 20 , 290. https://doi.org/10.1186/s12911-020-01298-5
Ng, J. Y. (2020). The regulation of complementary and alternative medicine professions in Ontario. Canada. Integrative Medicine Research, 9 (1), 12–16.
Nielsen, A., Tick, H., Mao, J. J., & Hecht, F. (2019). Consortium pain task force. Academic consortium for integrative medicine & health commentary to CMS; RE: National Coverage Analysis (NCA) Tracking Sheet for Acupuncture for Chronic Low Back Pain (CAG-00452N). Global Advance Health and Medicine,8 , 2164956119857648. Published 2019 Jul 11. https://doi.org/10.1177/2164956119857648 .
Oshikoya, K. A., Oreagba, I. A., Ogunleye, O. O., et al. (2014). Use of complementary medicines among HIV-infected children in Lagos. Nigeria. Complement Ther Clin Pract, 20 , 118–124.
Oshikoya, K. A., Oreagba, I. A., Ogunleye, O. O., Oluwa, R., Senbanjo, I. O., & Olayemi, S. O. (2013). Herbal medicines supplied by community pharmacies in Lagos, Nigeria: Pharmacists’ knowledge. Pharmacy Practice, 11 (4), 219–227.
Oreagba, I. A., Kazeem Adeola Oshikoya and Mercy Amachree. (2011). Herbal medicine use among urban residents in Lagos, Nigeria BMC Complementary and Alternative Medicine 11, 117. http://www.biomedcentral.com/1472-6882/11/117 .
Paoloni, M., Agostini, F., Bernasconi, S., Bona, G., Cisari, C., Fioranelli, M., Invernizzi, M., Madeo, A., Matucci-Cerinic, M., Migliore, A., Quirino, N., Ventura, C., Viganò, R., & Bernetti, A. (2022). Information survey on the use of complementary and alternative medicine. Medicina (Kaunas), 14 , 58(1), 125.
Robinson, M. M., & Zhang, X. (2011a). Traditional medicines: Global situation, issues and challenges. In Proceedings of the world medicines situation. World Health Organization, pp. 1–14. https://digicollection.org/hss/documents/s18063en/s18063en.pdf .
Robinson, M. M., & Zhang, X. (2011b) Traditional medicines: Global situation, issues and challenges. In: Proceedings of the world medicines situation. World Health Organization, pp. 1–14. https://digicollection.org/hss/documents/s18063en/s18063en.pdf .
Pantano, F., Mannocchi, G., Marinelli, E., Gentili, S., Graziano, S., Busardò, F. P., & di Luca, N. M. (2017). Hepatotoxicity induced by greater celandine (Chelidonium majus L.): A review of the literature. European Review Medical and Pharmacol ogical Sciences, 21 (1 Suppl), 46–52. PMID: 28379595.
Paoloni, M., Agostini, F., Bernasconi, S., Bona, G., Cisari, C., Fioranelli, M., Invernizzi, M., Madeo, A., Matucci-Cerinic, M., Migliore, A., Quirino, N., Ventura, C., Viganò, R., & Bernetti, A. (2022). Information survey on the use of complementary and alternative medicine. Medicina (kaunas, Lithuania), 58 (1), 125.
Perez-Garcia, M., & Figueras, A. (2011). The lack of knowledge about the voluntary reporting system of adverse drug reactions as a major cause of underreporting: Direct survey among health professionals. Pharmacoepidemiol Drug Safety, 20 (12), 1295–1302.
Raman, A., & Lau, C. (1996). Anti-diabetic properties and phytochemistry of Momordica charantia L. (Cucurbitaceae). Phytomedicine, 2 (4), 349–362.
Robinson, N. (2006). Integrated traditional Chinese medicine. Complementary Therapies in Clinical Practice, 12 (2), 132–140.
Romm, A. (2009, May 22). Botanical medicine for women’s health E-Book . Elsevier Health Sciences .
Sambo, L. (2011). Health systems and primary health care in the African region. African Health Monitor 14, 2–3.
Sbaffi, L., & Rowley, J. (2017). Trust and credibility in web-based health information: A review and agenda for future research. Journal of Medical Internet Research, 19 (6), e218.
Schulz, V., Hänsel, R., & Tyler, V. E. (2000). Rational Phytotherapy. A Physicians’ Guide to Herbal Medicine (4th ed.). Springer.
Sharad, S., Manish, P., Mayank, B., Mitul, C., & Sanjay, S. (2011). Regulatory status of traditional medicines in Africa Region. International Journal of Research in Ayurveda and Pharmacy 2 (1), 103–110.
Sharma, O. P., Sharma, S., Pattabhi, V., Mahato, S. B., & Sharma, P. D. A. (2007). Review of the hepatotoxic plant Lantana camara. Critical Reviews in Toxicology., 37 , 313–352.
Sharples, F. M., van Haselen, R., & Fisher, P. (2003). NHS patients’ perspective on complementary medicine: A survey. Complementary Therapies in Medicine, 11 , 243–248.
Snyman, T., Stewart, M. J., Grove, A., & Steenkamp, V. (2005). Adulteration of South African Traditional Herbal Remedies. Therapeutic Drug Monitoring, 27 (1), 86–89. https://doi.org/10.1097/00007691-200502000-00015
Summaries for Patients. (2003). Ephedra is associated with more adverse effects than other herbs. Ann Intern Med 138, I.56
Tabish, S. A. (2008). Complementary and alternative healthcare: Is it evidence-based? International Journal Health Science (Qassim) 2(1), V–IX.
Teschke, R. (2010). Kava hepatotoxicity: Pathogenetic aspects and prospective considerations. Liver International, 30 (9), 1270–1279. https://doi.org/10.1111/j.1478-3231.2010.02308.x PMID: 20630022.
Upton, R., Romm, A. (2010). Chapter 4—Guidelines for herbal medicine use. In A. Romm, Mary L. Hardy, & S. Mills (Eds.), Botanical Medicine for Women’s Health , Churchill Livingstone, pp. 75–96, ISBN 9780443072772, https://doi.org/10.1016/B978-0-443-07277-2.00004-0 . https://www.sciencedirect.com/science/article/pii/B9780443072772000040
Van Andel, T., Myren, B., & Van Onselen, S. (2012). Ghana’s herbal market. Journal of Ethno- Pharmacology., 140 (2), 368–378.
Valli, G., & Giardina, E. G. (2002). Benefits adverse effects and drug interactions of herbal therapies with cardiovascular effects. Journal of the American College of Cardiology, 39 (7), 1083–1095.
Vega, L. C., Montague, E., & DeHart, T. (2011). Trust between patients and health websites: A review of the literature and derived outcomes from empirical studies. Health Technology, 1 (2–4), 71–80.
Ventola, C. L. (2010). Current issues regarding complementary and alternative medicine (CAM) in the United States: Part 1: The widespread Use of CAM and the need for better-Informed health care professionals to provide patient counselling. Pharmacy and Therapeutics., 35 (8), 461–468.
Wang, J., & Xiong, X. (2012). Current situation and perspectives of clinical study in integrative medicine in China. Evidence-Based Complementary and Alternative Medicine, 2012, Article ID 268542, p. 11. https://doi.org/10.1155/2012/268542
World Health Organization. (2000). WHO General guidelines for methodologies on research and evaluation of traditional medicine . Available at: https://apps.who.int/iris/bitstream/10665/66783/1/WHO_EDM_TRM_2000.1.pdf (Accessed 30 March 2022).
World Health Organization. (2019). WHO global report on traditional and complementary medicine 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Available at: http://apps.who.int/iris/rest/bitstreams/1217520/retrieve (Accessed 30 March 2022).
Zhang, C. S., Tan, H. Y., Zhang, G. S., Zhang, A. L., Xue, C. C., & Xie, Y. M. (2015, November 4). Placebo Devices as Effective Control Methods in Acupuncture Clinical Trials: A Systematic Review. PLoS ONE, 10 (11), e0140825. https://doi.org/10.1371/journal.pone.0140825
Download references
Author information
Authors and affiliations.
Department of Pharmacology, Therapeutics and Toxicology, College of Medicine, University of Lagos, Idi-Araba, Lagos, Nigeria
Ibrahim Adekunle Oreagba
Department of Pharmacology, Therapeutics and Toxicology, College of Medicine, Lagos State University, Ikeja, Lagos, Nigeria
Kazeem Adeola Oshikoya
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ibrahim Adekunle Oreagba .
Editor information
Editors and affiliations.
Business (Entrepreneurship), Universiti Brunei Darussalam, Bandar Seri Begawan, Brunei Darussalam
Lukman Raimi
College of Medicine, University of Lagos, Lagos, Nigeria
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Oreagba, I.A., Oshikoya, K.A. (2023). Alternative Medicine and Healthcare Delivery: A Narrative Review. In: Raimi, L., Oreagba, I.A. (eds) Medical Entrepreneurship. Springer, Singapore. https://doi.org/10.1007/978-981-19-6696-5_21
Download citation
DOI : https://doi.org/10.1007/978-981-19-6696-5_21
Published : 07 January 2023
Publisher Name : Springer, Singapore
Print ISBN : 978-981-19-6695-8
Online ISBN : 978-981-19-6696-5
eBook Packages : Business and Management Business and Management (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Research article
- Open access
- Published: 23 November 2020
Potential factors that influence usage of complementary and alternative medicine worldwide: a systematic review
- Mayuree Tangkiatkumjai ORCID: orcid.org/0000-0002-9442-970X 1 ,
- Helen Boardman 2 &
- Dawn-Marie Walker 3
BMC Complementary Medicine and Therapies volume 20 , Article number: 363 ( 2020 ) Cite this article
32k Accesses
77 Citations
40 Altmetric
Metrics details
To determine similarities and differences in the reasons for using or not using complementary and alternative medicine (CAM) amongst general and condition-specific populations, and amongst populations in each region of the globe.
A literature search was performed on Pubmed, ScienceDirect and EMBASE. Keywords: ‘herbal medicine’ OR ‘herbal and dietary supplement’ OR ‘complementary and alternative medicine’ AND ‘reason’ OR ‘attitude’. Quantitative or qualitative original articles in English, published between 2003 and 2018 were reviewed. Conference proceedings, pilot studies, protocols, letters, and reviews were excluded. Papers were appraised using valid tools and a ‘risk of bias’ assessment was also performed. Thematic analysis was conducted. Reasons were coded in each paper, then codes were grouped into categories. If several categories reported similar reasons, these were combined into a theme. Themes were then analysed using χ 2 tests to identify the main factors related to reasons for CAM usage.
231 publications were included. Reasons for CAM use amongst general and condition-specific populations were similar. The top three reasons for CAM use were: (1) having an expectation of benefits of CAM (84% of publications), (2) dissatisfaction with conventional medicine (37%) and (3) the perceived safety of CAM (37%). Internal health locus of control as an influencing factor was more likely to be reported in Western populations, whereas the social networks was a common factor amongst Asian populations ( p < 0.05). Affordability, easy access to CAM and tradition were significant factors amongst African populations ( p < 0.05). Negative attitudes towards CAM and satisfaction with conventional medicine (CM) were the main reasons for non-use ( p < 0.05).
Conclusions
Dissatisfaction with CM and positive attitudes toward CAM, motivate people to use CAM. In contrast, satisfaction with CM and negative attitudes towards CAM are the main reasons for non-use.
Peer Review reports
Use of complementary and alternative medicine (CAM) has become widespread in the last two decades. The prevalence of CAM use in general populations worldwide ranges from 9.8% to 76% [ 1 ]. Twelve systematic reviews report reasons for CAM use mainly in cancer populations compared to other condition-specific populations [ 2 , 3 , 4 , 5 ].
Five of the systematic reviews aimed to determine reasons for CAM use in either general or condition-specific populations [ 2 , 5 , 6 , 7 , 8 ]. The reviews reported that the main reasons for CAM use were: (a) expected benefits and perceived safety of CAM, (b) control and participation in their therapy, and (c) alignment of socioculture, beliefs and needs. The other six reviews also reported reasons for CAM use, but this issue was not their main aim [ 3 , 4 , 9 , 10 , 11 , 12 ]. Their findings showed various reasons for CAM use, such as: (1) the benefits and safety of CAM, (2) availability and accessibility of CAM, (3) influence from friends, family, and the mass media, and (4) dissatisfaction with conventional medicine (CM). One systematic review from sub-Saharan Africa also reported barriers to CAM use that included: (a) the absence of conclusive scientific evidence for CAM, (b) a lack of belief in safety and efficacy of CAM, and (c) unhygienic practice in product preparation [ 9 ].
A narrative review (Jones et al., 2019) aimed to determine factors influencing CAM use in Australia and reported that cancer and other condition-specific populations shared some reasons for CAM use: (a) self-perceived ill health, (b) sense of well-being and (c) integrative treatment [ 13 ].
However these reviews do not directly compare similarities and differences in the reasons for CAM use between populations. There are also limited systematic reviews reporting reasons for not using CAM. The present review aimed to provide comprehensive understanding of factors influencing different populations to use/not use CAM.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement was employed in the present systematic review [ 14 ]. Research questions of this review were 1) What were the similarities and differences in reasons for using/not using CAM amongst general and condition specific populations? and 2) What were the similarities and differences in reasons for using/not using CAM amongst populations in each region?
Search strategy
The databases – PubMed: National Library of Medicine, ScienceDirect and EMBASE were searched. It is recommended that two or more databases are searched. EMBASE alone has the highest percentage recall of papers and, as a result, gains in searching resources beyond EMBASE are modest [ 15 , 16 , 17 ]. Keywords used were ‘herbal medicine’ OR, ‘herbal and dietary supplement’ OR, ‘complementary and alternative medicine’, AND ‘reason’ OR ‘attitude’. Free-text terms combined with Boolean operators and filters were used for searching relevant studies [ 18 ]. For example, ‘complementary and alternative medicine’ AND ‘reason’; ‘complementary and alternative medicine’ AND ‘attitude’. All permutations of these key words were performed. Herbal medicine and dietary supplements were used as keywords due to these products being extensively used worldwide, compared to other types of CAM [ 19 , 20 , 21 , 22 , 23 , 24 , 25 ]. Pubmed and EMBASE were chose because they are the main sources suggested by the Cochrane centre and provide relevant studies in this field [ 26 ]. Meanwhile, the ScienceDirect database has published information relating to the social sciences A date range of January 2003 to December 2018 was set as the World Health Organization’s (WHO) 2002 definition of CAM was used to underpin this research: “CAM are used to refer to a broad set of health care practices that are not part of a country’s own tradition, or not integrated into its dominant health care system” [ 27 ]. This current review began in 2019 and has reviewed relevant sources published ovevr a 15 year period from 2003 to 2018.
Selection criteria
Original articles published in English from 2003 to 2018 were reviewed. Quantitative, and qualitative studies, and mixed-methods research were included as each type of publication provided a different informational perspective and complemented each other. No limits were set regarding country of origin or type of population. This process was conducted by two independent reviewers.
Exclusion criteria
Conference proceedings, pilot studies, study protocols, letters, literature reviews or systematic reviews were excluded. The studies which did not report on factors or reasons for using, or not using, CAM were excluded. Furthermore, papers which studied some specific groups were also excluded, i.e. students, medical professionals, pregnant women, people aged less than 15 years, care givers, or specific sexual identities or ethnic groups. This exclusion was due to the premise that each group has a specific characteristic which may underpin their reasons for CAM usage, which may deviate from other populations. As the present review focused on the reasons and attitudes influencing people to use/not use CAM, efficacy trials of CAM were also excluded.
Data extraction and risk of bias assessment
The process of extracting data from publications was conducted by two independent reviewers. Any disagreements were resolved by discussion with a third reviewer. The included quantitative studies were appraised using a standard tool adapted from Gan’s study, which contained 10 items and assessed a study’s internal and external validity [ 22 ]. Meanwhile, the qualitative studies were assessed by a standard tool from Jakes’ study, which evaluated agreement between research questions, methods, representation, interpretation of results, influence of researchers, evidence of ethical approve and a flow from the analysis to conclusion [ 12 ]. These tools have been used for evaluating studies in the CAM field and seem to be appropriate to assessing the methodologies of the observational and qualitative studies included in this present systematic review.
Data synthesis and statistical analysis
Data in the present systematic review was analysed by both qualitative and quantitative methods conducted by two independent reviewers [ 28 ]. An inductive thematic approach was performed to identify themes of reasons for use and non-use of CAM [ 28 ]. All use or non-use reasons in each publication were coded by hand, and then grouped into a category according to the reason(s). If several categories reported similar reasons, such categories were combined into one theme. The themes, therefore, emerged from this process. This process was forward and backward analysed until the themes were consistent. Then, similarities and differences of the themes between general and condition-specific populations, and between Western and Asia populations were analysed by χ 2 -tests. Tests were two-tailed and a p -value < 0.05 was considered statistically significant.
Searching via the three databases provided 10,887 publications. After excluding irrelevant publications based on their title and abstract, 2,007 publications remained, from which 861 duplicates were removed. 799 publications met the exclusion criteria and were therefore not included. From the 347 full-text articles reviewed, 116 publications were excluded due to an absence of reporting factors or reasons for CAM use, resulting in 231 publications from 51 countries being included in the analysis (Fig. 1 ).
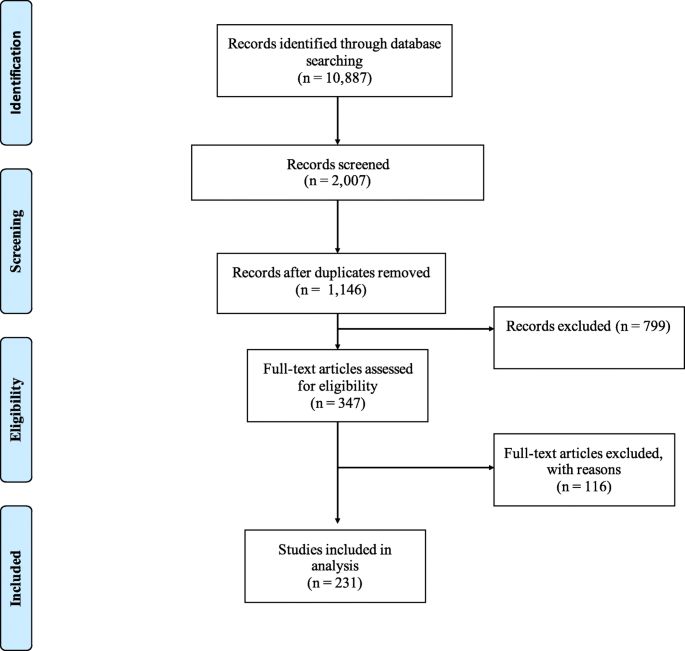
Flowchart of study identification process
Thirty-seven out of the 231 included publications were qualitative studies (16%) mainly from the United Kingdom (UK) [ 29 , 30 , 31 , 32 , 33 , 34 ], the United States (US) [ 35 , 36 , 37 , 38 ], Australia [ 39 , 40 , 41 ] or Canada [ 42 , 43 , 44 ]; a survey or cross-sectional study were the most commonly employed quantitative methods in the included publications (80.5%). Only eight mixed method papers (3.5%) reported the reasons for CAM use [ 32 , 45 , 46 , 47 , 48 , 49 , 50 , 51 ]. Eleven papers (4.8%) were conducted in elderly populations [ 35 , 39 , 42 , 43 , 52 , 53 , 54 , 55 , 56 , 57 , 58 ], and six (2.6%) in women only populations [ 29 , 38 , 39 , 59 , 60 , 61 ].
The highest number of all included publications originated in Asia (25.5%), followed by Europe (20.9%), North America (20.0%) and the Middle East (14.7%). A small number of publications from Australia were also included in the present systematic review (7.8%).
To gather information the majority of the quantitative papers utilised questionnaires which provided a list of factors or reasons for using CAM based on previous studies. The majority of the included qualitative studies utilised interviews or focus groups with open-ended questions and employed thematic or inductive analyses. Sixty-four percent of the included publications defined CAM based on the National Center for Complementary and Alternative Medicine (NCCAM), the World Health Organization (WHO, 7%), and the others, e.g. the Food and Drug Administration, the Dietary Supplement and Health Education Act (DSHEA), Ernst’s definition, Eisenberg’s definition, etc.
Figure 2 shows an increase in the number of publications related to reasons for CAM use amongst condition-specific populations since 2013, compared with publications involving general populations. The total number of publications dealing with CAM use amongst general and condition-specific populations in this review was 48 (21%) and 179 (77%), respectively. The number of the papers in condition-specific populations is higher than in general populations (Fig. 2 ), i.e. cancer (29.0% of publications), diabetes (5.6% of publications), cardiovascular disease and hypertension (5.2% of publications), human immunodeficiency virus (HIV) (3.5% of publications), inflammatory bowel disease (3% of publications), pain (3% of publications), chronic kidney disease (2.6% of publications), and depression (0.9% of publications). The majority of studies in the present review reported various types of CAM use (69%), followed by herbal medicine (18%) and traditional medicine, including traditional Chinese medicine (1%).
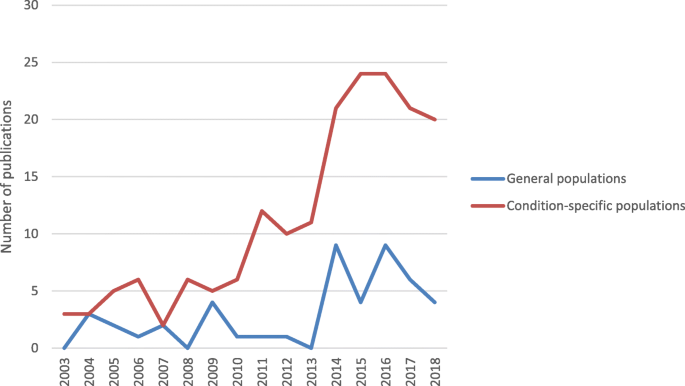
Trend in numbers of the publications of reasons for CAM use
The risk of bias assessment resulted in one quantitative publication being excluded due to poor internal and external validity. The included studies addressing general populations had a low bias risk (mode of a total score = 10, range 7-10), and for condition-specific populations there was a moderate risk of bias (mode of a total score = 7, range 5 – 10). The weaknesses of studies involving condition-specific populations was mainly due to a lack of reporting of their randomisation procedure (73% of the publications), how representative the sample was (64%), and non-response bias (48%). Details of the risk of bias assessment provided in a supplementary material no. 1 .
Lack of reporting the researcher’s background (69% of the publications) and the influence of reseachers on the research (60%) were the main weaknesses of the included qualitative studies in both general and condition-specific populations.
Themes of reasons for use and non-use of CAM
Both quantitative and qualitative studies reported similar reasons for CAM use. Thirty-three (14.3%) publications provided reasons for use as well as non-use of CAM. The present systematic review found three main factors related to reasons for CAM use: positive attitudes toward CAM, negative attitudes toward CM, and other factors, i.e. influence of their social network, their doctor’s recommendation, having an internal health locus of control and tradition (Fig. 3 ). Reasons for non-use of CAM were having negative attitudes toward CAM and positive attitudes toward CM.
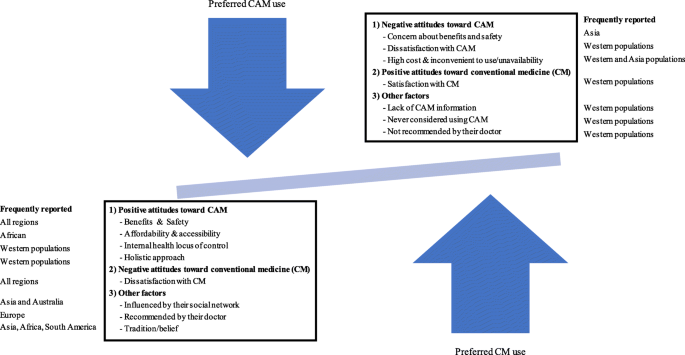
Factors related to reasons for CAM use and non-use
Reasons for CAM use amongst general and condition-specific populations
There was no difference in reasons for CAM use between general and condition-specific populations. The top three reported reasons for CAM use in all populations were perceived benefits (84% of publications), and safety of CAM (37%), and dissatisfaction with CM (37%). The most reported expected benefits of CAM were treatment of illnesses, alleviation of symptoms, reducing side effects of CM, maintenance of well-being, or prevention of disease. People also reported that using CAM was a last resort [ 29 , 44 , 52 , 62 , 63 , 64 ]. Improving physical and emotional well-being, and quality of life were further reasons for using CAM in patients with cancer [ 50 , 63 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 ]. The cancer patients also reported using CAM to reduce side effects of CM [ 33 , 45 , 65 , 66 , 69 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 ]. Western populations in both the general and condition-specific populations were more likely to report combining CAM and CM helped them [ 33 , 54 , 74 , 81 , 82 , 83 , 84 ]. Likewise, condition-specific populations in some Asian and Middle East countries perceived that CAM complemented CM [ 63 , 85 , 86 , 87 , 88 , 89 ]. Even though CAM is more likely to be a mainstream therapy in Asian countries, the Asian condition-specific populations tend not use CAM as a substitute for CM. However, CM is substituted with CAM amongst general populations in Japan [ 90 ].
Regarding dissatisfaction with CM, being ineffective and/or causing side effects were the most frequently reported reasons in both general and condition-specific populations for their lack of satisfaction [ 29 , 36 , 40 , 54 , 81 , 87 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 ]. Some patients wanted to use CAM in order to either avoid side effects resulting from CM or to decrease the number of conventional medicines taken [ 49 , 92 , 103 , 108 , 109 , 110 , 111 , 112 ]. A lack of trust in CM as the reason for using CAM was reported in three publications from Asia, two from the Middle East and one from Europe [ 61 , 94 , 113 , 114 , 115 , 116 ]. Additionally, condition-specific populations decided to use CAM to avoid invasive care or aggressive treatment [ 80 , 111 ]; or they were disappointed with or had negative experience of conventional care and/or the staff providing it [ 41 , 80 , 86 , 97 , 103 , 105 , 117 , 118 , 119 ]. CAM users in both Asian and Western populations preferred to visit CAM practitioners because they provided fuller explanations and more time when compared with conventional health professionals [ 34 , 66 , 86 ]. Condition-specific populations in Asia and Africa often found it difficult to access CM; a circumstance which drove them to use CAM [ 97 , 120 ].
Only 8.7% of publications found that condition-specific populations viewed CAM as natural, and thus safe [ 21 , 29 , 49 , 65 , 67 , 76 , 92 , 100 , 106 , 107 , 112 , 114 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 ]. Six studies from Europe, Asia and Africa also reported ‘being curious’ as the reason for using CAM [ 92 , 97 , 130 , 131 , 132 , 133 ].
Other factors were influenced by CAM users’ social networks (27% of publications), having an internal health locus of control defined as preferring to control or decide choices of health treatments themselves (28%), affordability of CAM (24%), willingness to try or use CAM (including hope) (21%), conventional health professionals’ recommendation (18%), easy access to CAM (14%), belief in a holistic approach (12%), and tradition/belief (12%). Internal health locus of control and a holistic approach were more likely to reported by Western populations, as such reasons may be developed from or informed by a Western perspective [ 30 , 31 , 34 , 37 , 42 , 45 , 46 , 48 , 50 , 55 , 56 , 67 , 68 , 71 , 73 , 80 , 91 , 93 , 95 , 106 , 107 , 125 , 126 , 127 , 128 , 130 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 ].
Similarities and differences in reasons for CAM use amongst patients with cancer and other chronic illnesses
The literature shows that patients with various illnesses share the main reasons for CAM use, such as perceived benefits of CAM use or dissatisfaction with CM rather than having different reasons in specific diseases [ 36 , 40 , 41 , 48 , 57 , 62 , 84 , 86 , 87 , 92 , 96 , 99 , 104 , 108 , 125 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 ]. However, being influenced by social media, having an internal health locus of control, or willingness to try CAM were reported more frequently by cancer patients than other members of condition-specific populations (Fig. 4 ). Meanwhile dissatisfaction with CM, affordability of CAM and easy access to CAM were more frequently reported by patients with other chronic illnesses ( p < 0.05). Patients with cancer, whilst accepting the efficacy and safety of CM, may use CAM in order to complement the efficacy of chemotherapy and/or reduce its unpleasant side effects (36% of publications in cancer populations) [ 33 , 34 , 45 , 63 , 64 , 65 , 66 , 67 , 69 , 71 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 88 , 122 , 123 , 124 , 139 , 152 ].
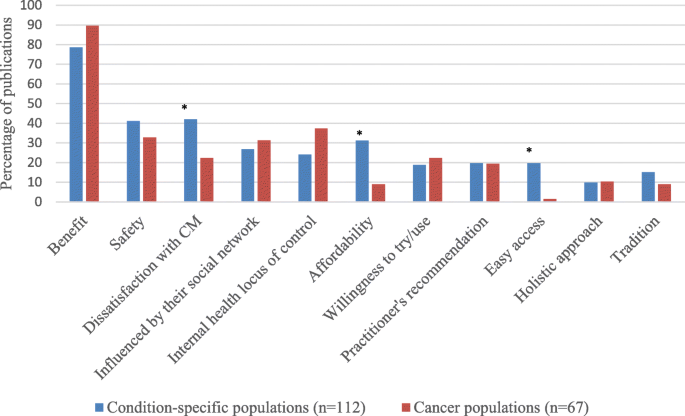
Comparing the reasons for CAM use amongst cancer patients and patients with other chronic illnesses. * Statistical significant at p < 0.05
Reasons for CAM use in each region
There was no global difference in the reported reasons for using CAM, namely the benefits of CAM, dissatisfaction with CM, and safety of CAM, see Fig. 5 . However, the number of publications in Europe (35% of publication), North America (48%) and South America (75%) that reported dissatisfaction with CM as the reason for using CAM was higher than in other populations. The benefits (89% of publications) and safety of CAM (50%) were reported as of the main reasons for CAM use in Australian populations.
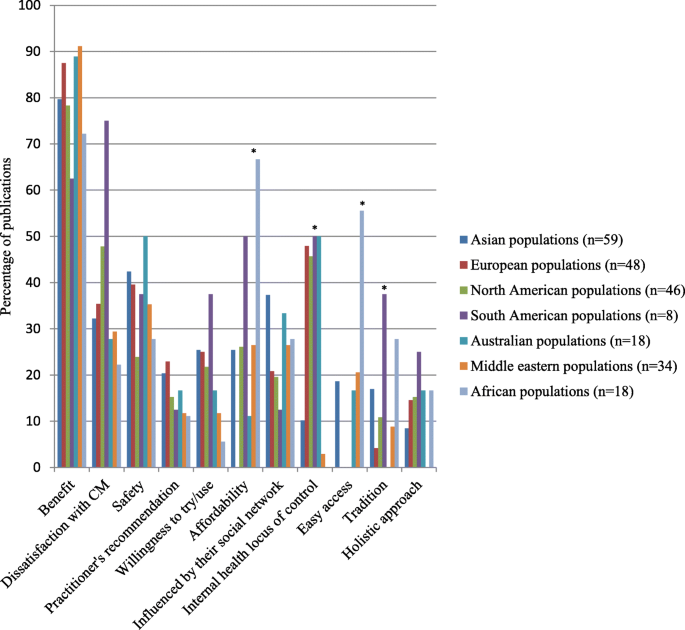
Comparison of the reasons for CAM use worldwide. * Statistical significant at p < 0.05
An internal health locus control, affordability and easy access of CAM, as well as tradition/belief were significantly different in each region ( p < 0.05). Internal health locus control influenced people in Australia (50% of publications), South America (50%), and Europe (48%). Additionally, tradition significantly influenced CAM use in South America (38% of publications), Africa (28%) and Asia (17%), compared with other regions. A high proportion of publications in Asian (37%) and Australian populations (33%) reported that social networks influenced them to use CAM, compared with other regions. African populations had the highest proportion of reported affordability of CAM (67%) and easy access (56%) as reasons for CAM use, whilst no report of these reasons was found in European populations. European populations (23% of publications) are more likely to report conventional health professionals’ recommendations for CAM use as their reason, compared with other regions.
Regarding reasons for CAM use amongst Western and Asian populations, Asian populations more frequently reported using CAM due to being influenced by members of their social network, low costs of CAM, easier access to CAM and tradition than Western populations ( p < 0.05), Fig. 6 . Meanwhile, having an internal health locus of control is the main reason for CAM use in Western populations ( p < 0.05).
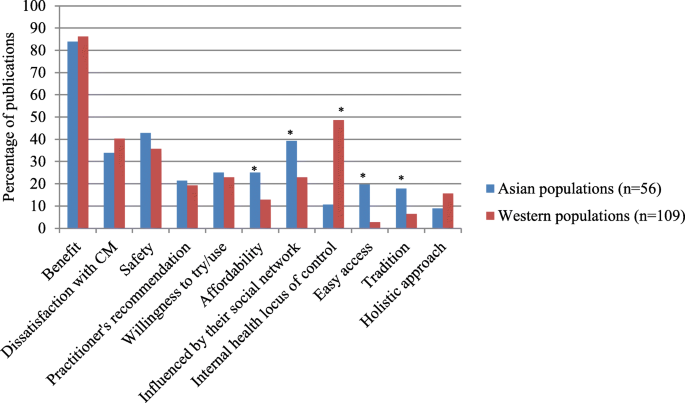
Comparison of the reasons for CAM use between Asian and Western populations. * Statistical significant at p < 0.05
Reasons for non-use amongst Western and Asian populations
The studies of reasons for non-use are limited compared to the reasons for using CAM, so comparison of the reasons for non-use in each region cannot be made. No publications from the Middle East or South America were included in the present systematic review. Two publications from Africa and Australia were included. The majority of studies in the included publications were conducted in Asia, Europe or North America. Therefore, we compared Asian and Western populations.
Thirty papers in condition-specific populations [ 45 , 47 , 65 , 75 , 79 , 80 , 95 , 107 , 115 , 120 , 123 , 124 , 130 , 150 , 152 , 157 , 162 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 ], six in general populations [ 180 , 181 , 182 , 183 , 184 , 185 ], one publication involving elderly people [ 53 ] and one publication involving females [ 61 ] reported the reasons for not using CAM. Asian populations more frequently reported doubt about the efficacy of CAM or lower effectiveness of CAM compared to CM, concerns about side effects of CAM, and inconvenience or unavailability of CAM than did members of Western populations ( p < 0.05), Fig. 7 [ 47 , 75 , 79 , 120 , 170 , 172 , 174 , 175 , 176 , 177 , 179 , 180 , 181 ]. Some publications in Asian populations also reported concern about CAM reducing the efficacy of CM as a reason for non-use [ 169 , 170 ].
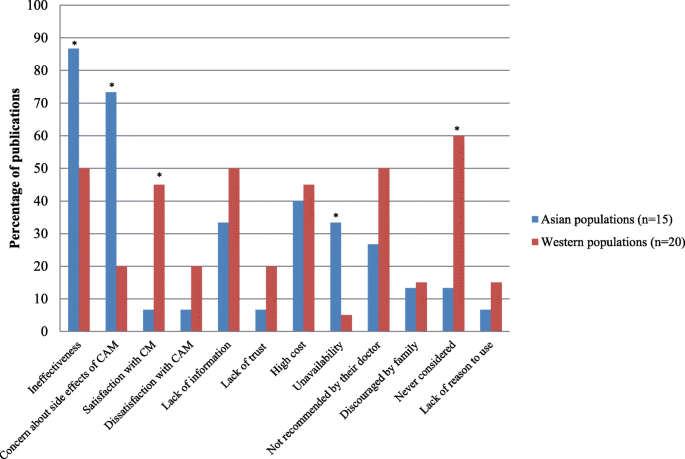
Reasons for non-use between Asian and Western populations. * Statistical significant at p < 0.05
Meanwhile, Western populations mainly reported satisfaction with CM (45% of publications, p < 0.05) or had never considered using CAM (60%, p < 0.05) [ 45 , 65 , 95 , 123 , 124 , 130 , 150 , 152 , 157 , 162 , 171 , 182 , 184 , 186 ]. Other reasons for the non-use of CAM were lack of reliable information about the efficacy of CAM, the high cost of CAM, and it not being recommended by conventional health professionals or the ‘patient’s’ family.
The included studies in the present systematic review can be seen to represent CAM use worldwide as they were mainly from Asia, Europe, North America, Middle East, and Australia. Recently, researchers in Asia have become interested in this field as several CAMs are embedded in their culture and society. Publications from this region has been rising since 2008; however, readers should be aware that the present systematic review included a small number of eligible publications from Australia and South America. Although a high number of publications originated in Australia, they tended to study specific populations, e.g. middle-aged women, and other topics, rather than reasons for CAM use. Researchers may less likely to investigate reasons for CAM use in South America, compared to other regions. Therefore, the findings in the present systematic review may be less likely to be generalisable in Australian and South American populations.
The present systematic review included a high number of publications amongst cancer, diabetic, cardiovascular disease, and HIV populations. It would therefore seem that illnesses, such as these which cannot be satisfactorily treated by CM, or when CM has significant unpleasant side-effects, drive some patients to seek CAM. Cancer populations have been studied regarding reasons for CAM use more than other condition-specific populations. There are six systematic reviews of the reasons for CAM use in patients with cancer [ 2 , 3 , 5 , 8 , 187 , 188 ].
As expected, three main factors related to reasons for CAM use in the present systematic review were positive attitudes toward CAM, negative attitudes toward CM and other factors, i.e. the influence of their social network, their doctor’s recommendation, having an internal health locus of control and tradition. The top three reported reasons for CAM use were perceived benefits and safety of CAM, and dissatisfaction with CM. These findings are consistent with previous systematic reviews [ 3 , 9 , 10 , 11 , 12 ]. These reasons are similar in both general and condition-specific populations, and in populations from different global regions, as cited frequently above. Although the present systematic review included a limited number of publications from Australia, benefits and safety of CAM were reported as the main reasons for CAM use in Australian populations. These findings agree with a previous systematic review in Australia [ 6 ].
Despite limited scientific evidence for the benefits of CAM [ 189 ], the ‘expected benefits’ of CAM was the most frequently reported reason for CAM use. This finding is not surprising as people tend to seek CAM as a way of meeting their needs or filling a gap left by conventional medicine. The included publications amongst the cancer population are more likely to report CAM use for reducing the negative and often unpleasant side effects of CM. This finding is consistent with systematic reviews of CAM users with prostate or advanced cancer [ 3 , 4 ]. Additionally, the cancer population seems to accept the efficacy and side effects of CM, and therefore uses CAM to complement CM.
Previously, people believed that CAM is natural and safe [ 190 ]. This idea may have led many patients with chronic illnesses on using CAM instead of CM. However, the present systematic review indicates that a small number of the included publications amongst condition-specific populations reported that CAM is safe as a reason for CAM use. Therefore, CAM as natural therapy is not the main reason for CAM use; a point which may be linked to the high number of reported adverse events from using CAM [ 191 , 192 , 193 ]. Patients therefore should use CAM with caution or under supervision from conventional or CAM practitioners.
Regarding other factors related to CAM use in each region, nearly half of the included publications reported that internal health locus control influenced people in Australia, South America, and Europe. However, this reason may have been reported less by Asian, Middle Eastern and African people, as they may not explain their reasons in such terms. Tradition also significantly influenced CAM use in South America, Africa and Asia, compared with other global regions. This orientation may be because CAM, for example, herbal medicine, is embedded in such regions and therefore aligns with their populations’ socio-culture values. Social networks influenced Asian and Australian populations to use CAM, compared with other regions, as they may have a close-knot family or community structure.
Affordability of CAM, together with easy access, are likely to be the main reasons for CAM use amongst African populations. The high cost of, and poor accessibility to, CM appears to influence people to use CAM in Africa [ 57 , 58 , 97 , 164 , 183 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 ]. Meanwhile, no report of these reasons was found in European populations. CAM may not be cheap and easy to access in Europe, compared with CM as users have to personally pay for CAM and it can be difficult to access [ 19 ]. Moreover, European populations are more likely to report conventional health professionals’ recommendations for CAM use as their reason for choosing that option, compared with other global regions. This option may be because health care is readily available in most European countries; so when they have a health problem, they visit their general practitioner.
There are limited publications reporting reasons for non-use of CAM in each region. Further studies relating to this issue are required, particularly in populations from Africa, the Middle East and South America. The present systematic review found that Asian populations are more likely to question the efficacy and safety of CAM, and to be concerned about potentially harmful interactions between herbal medicines and CM. These findings imply that Asian populations seem to understand the limitations of CAM, the efficacy and safety of CAM, and are aware of herb-drug interactions.
The findings confirm that Western populations do not use CAM if they are satisfied with the efficacy and safety of CM. This outcome may be because they can easily access CM, and CAM is less likely to be considered as an option for chronic illnesses in Western countries. However, if they were to become disappointed with the CM/staff, they may decide to use CAM. This possibility is consistent with the systematic review of patients with cancer, which reported that the patients who were satisfied with CM did not use CAM [ 3 ]. Lack of reliable information about the efficacy of CAM, as a barrier to CAM use reported in the present systematic review, is consistent with the findings from a previous systematic review [ 9 ].

Limitations of this review
Although this review only selected a small number of key words, and only three search engines in order to search the literature the findings returned 43% duplicate publications. Further reviews should search using a wide range of CAM types as keywords, e.g. yoga, acupuncture, relaxation, etc., in order to confirm the findings from the present review. There was a small number of publications addressing the reasons for CAM use in South America (n = 8); thus the findings from that continent should be interpreted with caution. This review included only publications in English; as a result the findings did not represent publications in other languages. Regarding the results from the search strategy used in this review, only 5% of the papers were excluded due to being non-English. This outcome is unlikely to have any significant impact on the findings of the present review, as most of the studies were conducted in Europe, from where a high number of publications in English were identified for inclusion in this review.
Results of publications in condition-specific populations representing a national population should also be interpreted with caution due to only 36% of these studies being designed to represent the patient population. The present systematic review found poor external validity of the included studies amongst condition-specific populations, therefore future studies should be aware of this issue.
Impact of the findings for conventional health professionals
Expected benefits of CAM are the main reason for CAM use despite a lack of clinical trials. To promote the rational use of CAM, health care providers should be ready to provide such information to their patients and conventional medicine guidelines should report reliable information about CAM, and be easily available to, health care providers. The findings in the present review have confirmed that being disappointed with CM or associated professional providers, particularly in Western populations, is more likely to influence condition-specific populations to use CAM. To prevent patients from using CAM inappropriately, health care providers should spend more time clearly explaining treatment options, the likely treatment outcomes and potential negative effects of CAM, including herb-drug interactions.
Having an internal health locus of control seems to be a main reason for CAM use in Western populations. This finding implies that patients prefer deciding a therapy by and for themselves. To decrease inappropriate use of CAM, conventional health care providers should offer sufficient health information to their patients, as well as holding a discussion with a patient, before deciding upon a health therapy.
A person’s social network is more likely to influence their decision making regarding CAM in Asian populations. Therefore, health care providers should educate not only patients about how to properly use CAM, but also their friends and family members.
It is clear that the main reasons for CAM use in all populations are a positive attitude toward CAM, that is the perceived benefit and safety of CAM, and a negative attitude toward CM, a dissatisfaction with CM. Having an internal health locus of control is a more frequently reported reason for CAM use in Western populations, whilst being influenced by social networks is a common reason for its adoption amongst Asian populations. Affordability, easy access to CAM and tradition are the most common reasons amongst African populations. Negative attitudes towards CAM and satisfaction with CM are more likely to be the reason for non-use. Conventional health professionals should acknowledge that people may turn to CAM in order to serve their needs. Therefore, health care providers should regularly ask their patients about their use of CAM before that providers prescribes any conventional medicines, in order to prevent undesirable adverse effects or CAM-drug interactions. Further studies are required to investigate reasons for CAM use in South America and reasons for non-use in all global regions, in order to provide more conclusive evidence in this field.
Availability of data and materials
The included publications in this systematic review were assessed their risk of bias in order to evaluate the quality of publications. This information provided in its supplementary information file. The other datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Complementary and Alternative Medicine
Conventional Medicine
Human Immunodeficiency Virus
The Preferred Reporting Items for Systematic Revews and Meta-Analyses
The United Kingdom
The United States
Harris PE, Cooper KL, Relton C, Thomas KJ. Prevalence of complementary and alternative medicine (CAM) use by the general population: a systematic review and update. Int J Clin Pract. 2012;66(10):924–39.
Article CAS PubMed Google Scholar
Weeks L, Balneaves LG, Paterson C, Verhoef M. Decision-making about complementary and alternative medicine by cancer patients: integrative literature review. Open Med. 2014;8(2):e54–66.
PubMed PubMed Central Google Scholar
Truant TL, Porcino AJ, Ross BC, Wong ME, Hilario CT. Complementary and alternative medicine (CAM) use in advanced cancer: a systematic review. J Support Oncol. 2013;11(3):105–13.
Article PubMed Google Scholar
Bishop FL, Rea A, Lewith H, Chan YK, Saville J, Prescott P. Elm Ev, Lewith GT: complementary medicine use by men with prostate cancer: a systematic review of prevalence studies. Prostate Cancer Prostatic Dis. 2011;14(1):1–13.
Verhoef MJ, Balneaves LG, Boon HS, Vroegindewey A. Reasons for and characteristics associated with complementary and alternative medicine use among adult cancer patients: a systematic review. Integr Cancer Ther. 2005;4(4):274–86.
Reid R, Steel A, Wardle J, Trubody A, Adams J. Complementary medicine use by the Australian population: a critical mixed studies systematic review of utilisation, perceptions and factors associated with use. BMC Complement Altern Med. 2016;16(1):176.
Article PubMed PubMed Central Google Scholar
Franzel B, Schwiegershausen M, Heusser P, Berger B. Individualised medicine from the perspectives of patients using complementary therapies: a meta-ethnography approach. BMC Complement Altern Med. 2013;13:124.
Bishop FL, Yardley L, Lewith GT. A systematic review of beliefs involved in the use of complementary and alternative medicine. J Health Psychol. 2007;12(6):851–67.
James PB, Wardle J, Steel A, Adams J. Traditional, complementary and alternative medicine use in sub-Saharan Africa: a systematic review. BMJ Glob Health. 2018;3(5):e000895.
Qureshi NA, Khalil AA, Alsanad SM. Spiritual and religious healing practices: some reflections from Saudi National Center for Complementary and Alternative Medicine, Riyadh. J Relig Health. 2018.
Yang L, Sibbritt D, Adams J. A critical review of complementary and alternative medicine use among people with arthritis: a focus upon prevalence, cost, user profiles, motivation, decision-making, perceived benefits and communication. Rheumatol Int. 2017;37(3):337–51.
Jakes D, Kirk R, Muir L. A qualitative systematic review of patients’ experiences of acupuncture. J Altern Complement Med. 2014;20(9):663–71.
Jones E, Nissen L, McCarthy A, Steadman K, Windsor C. Exploring the use of complementary and alternative medicine in cancer patients. Integr Cancer Ther. 2019;18:1534735419854134.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017;6(1):245.
Halladay CW, Trikalinos TA, Schmid IT, Schmid CH, Dahabreh IJ. Using data sources beyond PubMed has a modest impact on the results of systematic reviews of therapeutic interventions. J Clin Epidemiol. 2015;68(9):1076–84.
Suarez-Almazor ME, Belseck E, Homik J, Dorgan M, Ramos-Remus C. Identifying clinical trials in the medical literature with electronic databases: MEDLINE alone is not enough. Control Clin Trials. 2000;21(5):476–87.
Keene MR, Heslop IM, Sabesan SS, Glass BD. Complementary and alternative medicine use in cancer: a systematic review. Complement Ther Clin Pract. 2019;35:33–47.
CAMbrella – A pan-European research network for Complementary and Alternative Medicine (CAM) [ https://cordis.europa.eu/project/rcn/92501/reporting/en ].
Ock SM, Choi JY, Cha YS, Lee J, Chun MS, Huh CH, et al. The use of complementary and alternative medicine in a general population in South Korea: results from a national survey in 2006. J Korean Med Sci. 2009;24(1):1–6.
Singh V, Raidoo DM, Harries CS. The prevalence, patterns of usage and people's attitude towards complementary and alternative medicine (CAM) among the Indian community in Chatsworth, South Africa. BMC Complement Altern Med. 2004;4:3.
Gan WC, Smith L, Luca EJ, Harnett JE. The prevalence and characteristics of complementary medicine use by Australian and American adults living with gastrointestinal disorders: a systematic review. Complement Ther Med. 2018;41:52–60.
Jatau AI, Aung MM, Kamauzaman TH, Chedi BA, Sha'aban A, Rahman AF. Use and toxicity of complementary and alternative medicines among patients visiting emergency department: systematic review. J Intercult Ethnopharmacol. 2016;5(2):191–7.
The Use of Complementary and Alternative Medicine in the United States [ https://nccih.nih.gov/research/statistics/2007/camsurvey_fs1.htm ].
Posadzki P, Watson LK, Alotaibi A, Ernst E. Prevalence of use of complementary and alternative medicine (CAM) by patients/consumers in the UK: systematic review of surveys. Clin Med (Lond). 2013;13(2):126–31.
Article Google Scholar
Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Searching for and selecting studies. Cochrane Handbook Syst Rev Interv. 2019:67–107.
World Health Organization. WHO traditional medicine strategy 2002-2005. Geneva: World Health Organization; 2002.
Google Scholar
Gough D, Oliver S, Thomas J. An introduction to systematic reviews. 2nd ed. London: SAGE Publications Inc.; 2017.
Vickers KA, Jolly KB, Greenfield SM. Herbal medicine: women's views, knowledge and interaction with doctors: a qualitative study. BMC Complement Altern Med. 2006;6:40.
Soundy A, Lee RT, Kingstone T, Singh S, Shah PR, Edwards S, et al. Experiences of healing therapy in patients with irritable bowel syndrome and inflammatory bowel disease. BMC Complement Altern Med. 2015;15:106.
Little CV. Simply because it works better: exploring motives for the use of medical herbalism in contemporary U. K, health care. Complement Ther Med. 2009;17(5-6):300–8.
Holmes MM, Bishop FL, Calman L. “I just googled and read everything”: exploring breast cancer survivors’ use of the internet to find information on complementary medicine. Complement Ther Med. 2017;33:78–84.
MacArtney JI. Balancing exercises: Subjectivised narratives of balance in cancer self-health. Health (London). 2016;20(4):329–45.
de Valois B, Asprey A, Young T. “The monkey on your shoulder”: a qualitative study of lymphoedema patients’ attitudes to and experiences of acupuncture and moxibustion. Evid Based Complement Alternat Med. 2016;2016:4298420.
Oberg EB, Thomas MS, McCarty M, Berg J, Burlingham B, Bradley R. Older adults’ perspectives on naturopathic medicine’s impact on healthy aging. Explore (NY). 2014;10(1):34–43.
Hwang JP, Roundtree AK, Suarez-Almazor ME. Attitudes toward hepatitis B virus among Vietnamese, Chinese and Korean Americans in the Houston area, Texa. J Community Health. 2012;37(5):1091–100.
Eaves ER, Sherman KJ, Ritenbaugh C, Hsu C, Nichter M, Turner JA, et al. A qualitative study of changes in expectations over time among patients with chronic low back pain seeking four CAM therapies. BMC Complement Altern Med. 2015;15:12.
Kabel A. Fighting for wellness: strategies of mid-to-older women living with cancer. J Cross Cult Gerontol. 2015;30(1):107–17.
McLaughlin D, Lui CW, Adams J. Complementary and alternative medicine use among older Australian women - a qualitative analysis. BMC Complement Altern Med. 2012;12:34.
McIntyre E, Saliba AJ, Moran CC. Herbal medicine use in adults who experience anxiety: a qualitative exploration. Int J Qual Stud Health Well-being. 2015;10:29275.
Brijnath B, Antoniades J, Adams J. Investigating patient perspectives on medical returns and buying medicines online in two communities in Melbourne, Australia: results from a qualitative study. Patient. 2015;8(2):229–38.
Fries CJ. Older adults’ use of complementary and alternative medical therapies to resist biomedicalization of aging. J Aging Stud. 2014;28:1–10.
Williamson AT, Fletcher PC, Dawson KA. Complementary and alternative medicine: use in an older population. J Gerontol Nurs. 2003;29(5):20–8.
Read SC, Carrier ME, Whitley R, Gold I, Tulandi T, Zelkowitz P. Complementary and alternative medicine use in infertility: cultural and religious influences in a multicultural Canadian setting. J Altern Complement Med. 2014;20(9):686–92.
Fox P, Butler M, Coughlan B, Murray M, Boland N, Hanan T, et al. Using a mixed methods research design to investigate complementary alternative medicine (CAM) use among women with breast cancer in Ireland. Eur J Oncol Nurs. 2013;17(4):490–7.
Niemi M, Stahle G. The use of ayurvedic medicine in the context of health promotion--a mixed methods case study of an ayurvedic Centre in Sweden. BMC Complement Altern Med. 2016;16:62.
Tangkiatkumjai M, Boardman H, Praditpornsilpa K, Walker DM. Reasons why Thai patients with chronic kidney disease use or do not use herbal and dietary supplements. BMC Complement Altern Med. 2014;14:473.
Skovgaard L. Use and users of complementary and alternative medicine among people with multiple sclerosis in Denmark. Dan Med J. 2016;63(1):B5159.
PubMed Google Scholar
Hendershot KA, Dixon M, Kono SA, Shin DM, Pentz RD. Patients’ perceptions of complementary and alternative medicine in head and neck cancer: a qualitative, pilot study with clinical implications. Complement Therapies Clin Pract. 2014;20(4):213–8.
Scarton LA, Del Fiol G, Oakley-Girvan I, Gibson B, Logan R, Workman TE. Understanding cancer survivors’ information needs and information-seeking behaviors for complementary and alternative medicine from short- to long-term survival: a mixed-methods study. J Med Libr Assoc. 2018;106(1):87–97.
Mulkins AL, McKenzie E, Balneaves LG, Salamonsen A, Verhoef MJ. From the conventional to the alternative: exploring patients’ pathways of cancer treatment and care. J Complement Integr Med. 2016;13(1):51–64.
Levine MAH, Xu S, Gaebel K, Brazier N, Bedard M, Brazil K, et al. Self-reported use of natural health products: a cross-sectional telephone survey in older Ontarians. J Geriatr Pharmacother. 2009;7(6):383–92.
Cheung CK, Wyman JF, Halcon LL. Use of complementary and alternative therapies in community-dwelling older adults. J Altern Complement Med. 2007;13(9):997–1006.
Bruno JJ, Ellis JJ. Herbal use among US elderly: 2002 National Health Interview Survey. Ann Pharmacother. 2005;39(4):643–8.
Johnson PJ, Jou J, Rhee TG, Rockwood TH, Upchurch DM. Complementary health approaches for health and wellness in midlife and older US adults. Maturitas. 2016;89:36–42.
Murthy V, Sibbritt D, Broom A, Kirby E, Frawley J, Refshauge KM, et al. Back pain sufferers’ attitudes toward consultations with CAM practitioners and self- prescribed CAM products: a study of a nationally representative sample of 1310 Australian women aged 60-65 years. Complement Ther Med. 2015;23(6):782–8.
Ayele AA, Tegegn HG, Haile KT, Belachew SA, Mersha AG, Erku DA. Complementary and alternative medicine use among elderly patients living with chronic diseases in a teaching hospital in Ethiopia. Complement Ther Med. 2017;35:115–9.
Bayuo J. Experiences with out-patient hospital service utilisation among older persons in the Asante Akyem North District- Ghana. BMC Health Serv Res. 2017;17(1):652.
Faqueti A, Tesser CD. Use of complementary and alternative medicine in primary healthcare in Florianopolis, Santa Catarina, Brazil: user perception. Cien Saude Colet. 2018;23(8):2621–30.
Johnson PJ, Kozhimannil KB, Jou J, Ghildayal N, Rockwood TH. Complementary and alternative medicine use among women of reproductive age in the United States. Womens Health Issues. 2016;26(1):40–7.
Mahmoudi GA, Almasi V, Lorzadeh N, Khansari A. The reasons for using and not using alternative medicine in Khorramabad women, west of Iran. J Pak Med Assoc. 2015;65(6):623–5.
Lambert TD, Morrison KE, Edwards J, Clarke CE. The use of complementary and alternative medicine by patients attending a UK headache clinic. Complement Ther Med. 2010;18(3-4):128–34.
Puataweepong P, Sutheechet N, Ratanamongkol P. A survey of complementary and alternative medicine use in cancer patients treated with radiotherapy in Thailand. Evid Based Complement Alternat Med. 2012;2012:670408.
Ustundag S, Demir Zencirci A. Complementary and alternative medicine use among cancer patients and determination of affecting factors: a questionnaire study. Holist Nurs Pract. 2015;29(6):357–69.
Molassiotis A, Fernadez-Ortega P, Pud D, Ozden G, Scott JA, Panteli V, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16(4):655–63.
Roberts D, Wilson C, Todd C, Long AF, Mackereth P, Stringer J, et al. Complementary therapies in cancer: patients’ views on their purposes and value pre and post receipt of complementary therapy - a multi-Centre case study. Eur J Integr Med. 2013;5(5):443–9.
Hok J, Falkenberg T, Tishelman C. Lay perspectives on the use of biologically based therapies in the context of cancer: a qualitative study from Sweden. J Clin Pharm Ther. 2011;36(3):367–75.
Lengacher CA, Bennett MP, Kip KE, Gonzalez L, Jacobsen P, Cox C. Relief of symptoms, side effects, and psychological distress through use of complementary and alternative medicine in women with breast cancer. Oncol Nurs Forum. 2006;33(1):97–104.
Kremser T, Evans A, Moore A, Luxford K, Begbie S, Bensoussan A, et al. Use of complementary therapies by Australian women with breast cancer. Breast. 2008;17(4):387–94.
Al-Naggar RA, Bobryshev YV, Abdulghani M, Rammohan S, Osman MT, Kadir SYA. Complementay/alternative medicine use among cancer patients in Malaysia. World J Med Sci. 2013;8(2):157–64.
Helpman L, Ferguson SE, Mackean M, Rana A, Le L, Atkinson MA, et al. Complementary and alternative medicine use among women receiving chemotherapy for ovarian cancer in 2 patients populations. Int J Gynecol Cancer. 2011;21(3):587–93.
Sewitch MJ, Yaffe M, Maisonneuve J, Prchal J, Ciampi A. Use of complementary and alternative medicine by cancer patients at a Montreal hospital. Integr Cancer Ther. 2011;10(4):305–11.
Gillett J, Lentile C, Hiscock J, Plank A, Martin JM. Complementary and alternative medicine use in radiotherapy: what are patients using? J Altern Complement Med. 2012;18(11):1014–20.
Lövgren M, Wilde-Larsson B, Hök J, Leveälahti H, Tishelman C. Push or pull? Relationships between lung cancer patients’ perceptions of quality of care and use of complementary and alternative medicine. Eur J Oncol Nurs. 2011;15(4):311–7.
Farooqui M, Hassali MA, Shatar AKA, Shafie AA, Seang TB, Farooqui MA. Complementary and alternative medicine (CAM) use by Malaysian oncology patients. Complement Ther Clin Pract. 2012;18(2):114–20.
Xu W, Towers AD, Li P, Collet JP. Traditional Chinese medicine in cancer: perspectives and experiences of patients and professionals in China. Eur J Cancer Care. 2006;15(4):397–403.
Article CAS Google Scholar
Akyol AD, Oz B. The use of complementary and alternative medicine by patients with cancer: in Turkey. Complement Ther Clin Pract. 2011;17(4):230–4.
Wong LYE, Leung PC, Tang JL, Mercer SW. Use of dietary supplements by breast cancer patients undergoing conventional cancer treatment. Patient Prefer Adherence. 2010;4:407–14.
Jaradat NA, Shawahna R, Eid AM, Al-Ramahi R, Asma MK, Zaid AN. Herbal remedies use by breast cancer patients in the West Bank of Palestine. J Ethnopharmacol. 2016;178:1–8.
Boon H, Brown JB, Gavin A, Westlake K. Men with prostate cancer: making decisions about complementary/alternative medicine. Med Decis Mak. 2003;23(6):471–9.
Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;343:1–19.
Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. Am J Cardiol. 2006;98(5):673–80.
Kanodia AK, Legedza ATR, Davis RB, Eisenberg DM, Phillips RS. Perceived benefit of complementary and alternative medicine (CAM) for back pain: a national survey. J Am Board Fam Med. 2010;23(3):354–62.
Jong MC, van de Vijver L, Busch M, Fritsma J, Seldenrijk R. Integration of complementary and alternative medicine in primary care: what do patients want? Patient Educ Couns. 2012;89(3):417–22.
Moolasarn S, Sripa S, Kuessirikiet V, Sutawee K, Huasary J, Chaisila C, et al. Usage of and cost of complementary/alternative medicine in diabetic patients. J Med Assoc Thail. 2005;88(11):1630–7.
Peleg R, Liberman O, Press Y, Shvartzman P. Patients visiting the complementary medicine clinic for pain: a cross-sectional study. BMC Complement Altern Med. 2011;11:36.
See A, Teo B, Kwan R, Lim R, Lee J, Tang MBY, et al. Use of complementary and alternative medicine among dermatology outpatients in Singapore. Australas J Dermatol. 2011;52(1):7–13.
Kang E, Yang EJ, Kim SM, Chung IY, Ah HS, Ku DH, et al. Complementary and alternative medicine use and assessment of qulity of life in Korean breast cancer patiens: a descriptive study. Support Care Cancer. 2012;20(3):461–73.
Kamel FO, Magadmi RM, Hagras MM, Magadmi B, AlAhmad RA. Knowledge, attitude, and beliefs toward traditional herbal medicine use among diabetics in Jeddah Saudi Arabia. Complement Ther Clin Pract. 2017;29:207–12.
Chiba T, Sato Y, Nakanishi T, Yokotani K, Suzuki S, Umegaki K. Inappropriate usage of dietary supplements in patients by miscommunication with physicians in Japan. Nutrients. 2014;6(12):5392–404.
Weizman AV, Ahn E, Thanabalan R, Leung W, Croitoru K, Silverberg MS, et al. Characterisation of complementary and alternative medicine use and its impact on medication adherence in inflammatory bowel disease. Aliment Pharmacol Ther. 2012;35(3):342–9.
D'Inca R, Garribba AT, Vettorato MG, Martin A, Martines D, Di Leo V, et al. Use of alternative and complementary therapies by inflammatory bowel disease patients in an Italian tertiary referral Centre. Dig Liver Dis. 2007;39(6):524–9.
Brunelli B, Gorson KC. The use of complementary and alternative medicines by patients with peripheral neuropathy. J Neurol Sci. 2004;218(1-2):59–66.
Hasan SS, Ahmed SI, Bukhari NI, Loon WCW. Use of complementary and alternative medicine among patients with chronic diseases at outpatient clinics. Complement Ther Clin Pract. 2009;15(3):152–7.
Nayak S, Matheis RJ, Schoenberger NE, Shiflett SC. Use of unconventional therapies by individuals with multiple sclerosis. Clin Rehabil. 2003;17(2):181–91.
Zaman T, Agarwal S, Handa R. Complementary and alternative medicine use in rheumatoid arthritis: an audit of patients visiting a tertiary care Centre. Natl Med J India. 2007;20(5):236–9.
Olisa NS, Oyelola FT. Evaluation of use of herbal medicines among ambulatory hypertensive patients attending a secondary health care facility in Nigeria. Int J Pharm Pract. 2009;17(2):101–5.
Huri HZ, Lian GTP, Hussain S, Pendek R, Widodo RT. A survey amongst complementary alternative medicine (CAM) users with types 2 diabetes. Int J Diab Metab. 2009;17:9–15.
Purohit MP, Wells RE, Zafonte RD, Davis RB, Phillips RS. Neuropsychiatric symptoms and the use of complementary and alternative medicine. PM R. 2013;5(1):24–31.
Khalil SHA, Zaki A, Ibrahim AM, El-Moughazi AM, Khater AM, Youssef AM, et al. Pattern of use of complementary and alternative medicine among type 2 diabetes mellitus patients in Alexandria, Egypt. J Egypt Public Health Assoc. 2013;88(3):137–42.
Delgoda R, Younger N, Barrett C, Braithwaite J, Davis D. The prevalence of herbs use in conjunction with conventional medicines in Jamaica. Complement Ther Med. 2010;18(1):13–20.
Welz AN, Emberger-Klein A, Menrad K. Why people use herbal medicine: insights from a focus-group study in Germany. BMC Complement Altern Med. 2018;18(1):92.
Behnood-Rod A. Afzali poor Khoshkbejari M, Pourzargar P, Hassanzadeh M, Moharamzad Y, Foroughi F: complementary and alternative medicine use among Iranian patients attending urban outpatient general practices. Complement Ther Clin Pract. 2018;30:58–63.
Bahall M, Edwards M. Perceptions of complementary and alternative medicine among cardiac patients in South Trinidad: a qualitative study. BMC Complement Altern Med. 2015;15:99.
Bahall M. Complementary and alternative medicine usage among cardiac patients: a descriptive study. BMC Complement Altern Med. 2015;15:100.
Bozza C, Gerratana L, Basile D, Vitale MG, Bartoletti M, Agostinetto E, et al. Use and perception of complementary and alternative medicine among cancer patients: the CAMEO-PRO study : complementary and alternative medicine in oncology. J Cancer Res Clin Oncol. 2018;144(10):2029–47.
Singh H, Maskarinec G, Shumay DM. Understanding the motivation for conventional and complementary/alternative medicine use among men with prostate cancer. Integr Cancer Ther. 2005;4(2):187–94.
Alshagga MA, Al-Dubai SA, Faiq SSM, Yusuf AA. Use of complementary and alternative medicine among asthmatic patients in primary care clinics in Malaysia. Ann Thorac Med. 2011;6(3):115–9.
Spanner ED, Duncan AM. Prevalence of dietary supplement use in adults with chronic renal insufficiency. J Ren Nutr. 2005;15(2):204–10.
Trangmar P, Diaz VA. Investigating complementary and alternative medicine use in a Spanish-speaking Hispanic community in South Carolina. Ann Fam Med. 2008;6(Suppl 1):s12–5.
Shmueli A, Shuval J. Use of complementary and alternative medicine in Israel: 2000 vs. Isr Med Assoc. 1993;6(1):3–8.
AlGhamdi KM, Khurrum H, Al-Natour SH, Alghamdi W, Mubki T, Alzolibani A, et al. Use of complementary and alternative medicine among dermatology outpatients: results from a national survey. J Cutan Med Surg. 2015;19(6):570–9.
Lim MK, Sadarangani P, Chan HL, Heng JY. Complementary and alternative medicine use in multiracial Singapore. Complement Ther Med. 2005;13(1):16–24.
Sawalha AF. Complementary and alternative medicine (CAM) in Palestine: use and safety implcations. J Altern Complement Med. 2007;13(2):263–9.
Portela F, Dias CC, Caldeira P, Cravo M, Deus J, Goncalves R, et al. The who-when-why triangle of CAM use among Portuguese IBD patients. Dig Liver Dis. 2017;49(4):388–96.
Al Akeel MM, Al Ghamdi WM, Al Habib S, Koshm M, Al Otaibi F. Herbal medicines: Saudi population knowledge, attitude, and practice at a glance. J Family Med Prim Care. 2018;7(5):865–75.
Bahall M. Prevalence, patterns, and perceived value of complementary and alternative medicine among HIV patients: a descriptive study. BMC Complement Altern Med. 2017;17(1):422.
Anbari K, Gholami M. Evaluation of trends in the use of complementary and alternative medicine in health centers in Khorramabad (west of Iran). Global J Health Sci. 2016;8(2):72–6.
Yonekura S, Okamoto Y, Sakurai D, Sakurai T, Iinuma T, Yamamoto H, et al. Complementary and alternative medicine for allergic rhinitis in Japan. Allergol Int. 2017;66(3):425–31.
Broom A, Wijewardena K, Sibbritt D, Adams J, Nayar KR. The use of traditional, complementary and alternative medicine in Sri Lankan cancer care: results from a survey of 500 cancer patients. Public Health. 2010;124(4):232–7.
Caliskaner Z, Kartal O, Gulec M, Ozturk S, Erel F, Sener O, et al. Awareness of allergy patients about herbal remedies: a cross-sectional study of residents of Ankara, Turkey. Allergol Immunopathol (Madr). 2010;38(2):78–82.
Molassiotis A, Margulies A, Fernandez-Ortega P, Pud D, Panteli V, Bruyns I, et al. Complementary and alternative medicine use in patients with haematological malignancies in Europe. Complement Ther Clin Pract. 2005;11(2):105–10.
Molassiotis A, Ozden G, Platin N, Scott JA, Fernandez-Ortega P, Milovics L, et al. Complementary and alternative medicine use in patients with head and neck cancers in Europe. Eur J Cancer Care. 2006;15(1):19–24.
Molassiotis A, Panteli V, Patiraki E, Ozden G, Platin N, Madsen E, et al. Complementary and alternative medicine use in lung cancer patients in eight European countries. Complement Ther Clin Pract. 2006;12(1):34–9.
Hung A, Kang N, Bollom A, Wolf JL, Lembo A. Complementary and alternative medicine use is prevalent among patients with gastrointestinal diseases. Dig Dis Sci. 2015;60(7):1883–8.
Dossett ML, Davis RB, Lembo AJ, Yeh GY. Complementary and alternative medicine use by US adults with gastrointestinal conditions: results from the 2012 National Health Interview Survey. Am J Gastroenterol. 2014;109(11):1705–11.
Arentz S, Smith CA, Abbott JA, Bensoussan A. A survey of the use of complementary medicine by a self-selected community group of Australian women with polycystic ovary syndrome. BMC Complement Altern Med. 2014;14:472.
Lert F, Grimaldi-Bensouda L, Rouillon F, Massol J, Guillemot D, Avouac B, et al. Characteristics of patients consulting their regular primary care physician according to their prescribing preferences for homeopathy and complementary medicine. Homeopathy. 2014;103(1):51–7.
Arslan C, Guler M. Alternative medicine usage among solid tumour patients receiving chemotherapy. Eur J Cancer Care (Engl). 2017;26(5):e12530.
Rossi P, Torelli P, Lorenzo CD, Sances G, Manzoni GC, Tassorelli C, et al. Use of complementary and alternative medicine by patients with cluster headache: results of a multi-Centre headache clinic survey. Complement Ther Med. 2008;16(4):220–7.
Zhou F, Wu HJ, Zhai JP, Zhang GY, Shao Y, Tian X, et al. Who are the users of a traditional Chinese sanfu acupoint herbal patching therapy in China?: a cross-sectional survey. Medicine (Baltimore). 2016;95(49):e5414.
Koç Z, Çınarlı T. The determination of complementary and alternative medicine use in patients presenting at the emergency room. Complement Ther Clin Pract. 2018;31:164–9.
Loraschi A, Bellantonio P, Bortolon F, Capra R, Cavalla P, Costantino G, et al. Use of herbal remedies by multiple sclerosis patients: a nation-wide survey in Italy. Neurol Sci. 2016;37(4):613–22.
Kristoffersen AE, Stub T, Musial F, Fonnebo V, Lillenes O, Norheim AJ. Prevalence and reasons for intentional use of complementary and alternative medicine as an adjunct to future visits to a medical doctor for chronic disease. BMC Complement Altern Med. 2018;18(1):109.
Burke A, Lam CN, Stussman B, Yang H. Prevalence and patterns of use of mantra, mindfulness and spiritual meditation among adults in the United States. BMC Complement Altern Med. 2017;17(1):316.
Thomson P, Jones J, Browne M, Leslie SJ. Why people seek complementary and alternative medicine before conventional medical treatment: a population based study. Complement Ther Clin Pract. 2014;20(4):339–46.
Huebner J, Muenstedt K, Prott FJ, Stoll C, Micke O, Buentzel J, et al. Online survey of patients with breast cancer on complementary and alternative medicine. Breast Care (Basel). 2014;9(1):60–3.
McCall M, Thorne S, Ward A, Heneghan C. Yoga in adult cancer: an exploratory, qualitative analysis of the patient experience. BMC Complement Altern Med. 2015;15:245.
Huebner J, Prott FJ, Micke O, Muecke R, Senf B, Dennert G, et al. Online survey of cancer patients on complementary and alternative medicine. Oncol Res Treat. 2014;37(6):304–8.
Upchurch DM, Rainisch BW. The importance of wellness among users of complementary and alternative medicine: findings from the 2007 National Health Interview Survey. BMC Complement Altern Med. 2015;15:362.
McIntyre E, Saliba AJ, Wiener KKK, Bishop FL. Predicting the intention to use herbal medicines for anxiety symptoms: a model of health behaviour. J Ment Health. 2017:1–8.
Rhee TG, Westberg SM, Harris IM. Complementary and alternative medicine in US adults with diabetes: reasons for use and perceived benefits. J Diabetes. 2018;10(4):310–9.
Nguyen GC, Croitoru K, Silverberg MS, Steinhart AH, Weizman AV. Use of complementary and alternative medicine for inflammatory bowel disease is associated with worse adherence to conventional therapy: the COMPLIANT study. Inflamm Bowel Dis. 2016;22(6):1412–7.
Oxelmark L, Lindberg A, Lofberg R, Sternby B, Eriksson A, Almer S, et al. Use of complementary and alternative medicine in Swedish patients with inflammatory bowel disease: a controlled study. Eur J Gastroenterol Hepatol. 2016;28(11):1320–8.
Schmacke N, Muller V, Stamer M. What is it about homeopathy that patients value? And what can family medicine learn from this? Qual Prim Care. 2014;22(1):17–24.
Leach MJ, Lauche R, Zhang AL, Cramer H, Adams J, Langhorst J, et al. Characteristics of herbal medicine users among internal medicine patients: a cross-sectional analysis. J Herb Med. 2017;10:59–63.
Shorofi SA. Complementary and alternative medicine (CAM) among hospitalised patients: reported use of CAM and reasons for use, CAM preferred during hospitalisation, and the socio-demographic determinants of CAM users. Complement Ther Clin Pract. 2011;17(4):199–205.
Kuo GM, Hawley ST, Todd WL, Balkrishnan R, Volk RJ. Factors associated with herbal use among urban multiethnic primary care patients: a cross-sectional survey. BMC Complement Altern Med. 2004;4:18.
Hierl M, Pfirstinger J, Andreesen R, Holler E, Mayer S, Wolff D, et al. Complementary and alternative medicine: a clinical study in 1,016 hematology/oncology patients. Oncology. 2017;93(3):157–63.
Lettner S, Kessel KA, Combs SE. Complementary and alternative medicine in radiation oncology : survey of patients’ attitudes. Strahlenther Onkol. 2017;193(5):419–25.
Loquai C, Dechent D, Garzarolli M, Kaatz M, Kaehler KC, Kurschat P, et al. Use of complementary and alternative medicine: a multicenter cross-sectional study in 1089 melanoma patients. Eur J Cancer. 2017;71:70–9.
Kessel KA, Lettner S, Kessel C, Bier H, Biedermann T, Friess H, et al. Use of complementary and alternative medicine (CAM) as part of the oncological treatment: survey about patients’ attitude towards CAM in a university-based oncology Center in Germany. PLoS One. 2016;11(11):e0165801.
Article PubMed PubMed Central CAS Google Scholar
Salamonsen A. Use of complementary and alternative medicine in patients with cancer or multiple sclerosis: possible public health implications. Eur J Pub Health. 2016;26(2):225–9.
Wortmann JK, Bremer A, Eich HT, Wortmann HP, Schuster A, Fuhner J, et al. Use of complementary and alternative medicine by patients with cancer: a cross-sectional study at different points of cancer care. Med Oncol. 2016;33(7):78.
King N, Balneaves LG, Levin GT, Nguyen T, Nation JG, Card C, et al. Surveys of cancer patients and cancer health care providers regarding complementary therapy use, communication, and information needs. Integr Cancer Ther. 2015;14(6):515–24.
Salamonsen A. Mind the gap! Lay and medical perceptions of risks associated with the use of alternative treatment and conventional medicine. Forsch Komplementmed. 2015;22(1):24–9.
Sullivan A, Gilbar P, Curtain C. Complementary and alternative medicine use in cancer patients in rural Australia. Integr Cancer Ther. 2015;14(4):350–8.
Huebner J, Micke O, Muecke R, Buentzel J, Prott FJ, Kleeberg U, et al. User rate of complementary and alternative medicine (CAM) of patients visiting a counseling facility for CAM of a German comprehensive cancer center. Anticancer Res. 2014;34(2):943–8.
Egger S, Hughes S, Smith DP, Chambers S, Kahn C, Moxey A, et al. Factors associated with the use of complementary and alternative medicines for prostate cancer by long-term survivors. PLoS One. 2018;13(3):e0193686.
Osman NA, Hassanein SM, Leil MM, NasrAllah MM. Complementary and alternative medicine use among patients with chronic kidney disease and kidney transplant recipients. J Ren Nutr. 2015;25(6):466–71.
Tangkiatkumjai M, Boardman H, Praditpornsilpa K, Walker DM. Prevalence of herbal and dietary supplement usage in Thai outpatients with chronic kidney disease: a cross-sectional survey. BMC Complement Altern Med. 2013;13:153.
Wood MJ, Stewart RL, Merry H, Johnstone DE, Cox JL. Use of complementary and alternative medical therapies in patients with cardiovascular disease. Am Heart J. 2003;145(5):806–12.
Atwine F, Hultsjo S, Albin B, Hjelm K. Health-care seeking behaviour and the use of traditional medicine among persons with type 2 diabetes in South-Western Uganda: a study of focus group interviews. Pan Afr Med J. 2015;20:76.
Haile KT, Ayele AA, Mekuria AB, Demeke CA, Gebresillassie BM, Erku DA. Traditional herbal medicine use among people living with HIV/AIDS in Gondar, Ethiopia: do their health care providers know? Complement Ther Med. 2017;35:14–9.
Fernandez A, Simian D, Quera R, Flores L, Ibanez P, Lubascher J, et al. Complementary and alternative medicine in patients with inflammatory bowel disease: a survey performed in a tertiary center in Chile. Complement Ther Med. 2018;40:77–82.
Basedow M, Runciman WB, March L, Esterman A. Australians with osteoarthritis; the use of and beliefs about complementary and alternative medicines. Complement Ther Clin Pract. 2014;20(4):237–42.
Siu JY. Coping with future epidemics: tai chi practice as an overcoming strategy used by survivors of severe acute respiratory syndrome (SARS) in post-SARS Hong Kong. Health Expect. 2016;19(3):762–72.
Jones D, Cohen L, Rieber AG, Urbauer D, Fellman B, Fisch MJ, et al. Complementary and alternative medicine use in minority and medically underserved oncology patients: assessment and implications. Integr Cancer Ther. 2018;17(2):371–9.
Sun L, Mao JJ, Vertosick E, Seluzicki C, Yang Y. Evaluating cancer patients’ expectations and barriers toward traditional Chinese medicine utilization in China: a patient-support group-based cross-sectional survey. Integr Cancer Ther. 2018;17(3):885–93.
Chen G, Qiao TT, Ding H, Li CX, Zheng HL, Chen XL, et al. Use of Chinese herbal medicine therapies in comprehensive hospitals in Central China: a parallel survey in cancer patients and clinicians. J Huazhong Univ Sci Tech Med Sci. 2015;35(6):808–14.
Mani J, Juengel E, Arslan I, Bartsch G, Filmann N, Ackermann H, et al. Use of complementary and alternative medicine before and after organ removal due to urologic cancer. Patient Prefer Adherence. 2015;9:1407–12.
Nagashekhara M, Murthy V, Mruthyunjaya AT, Li Ann L. An empirical study on traditional, complementary and alternative medicine usage among Malaysian cancer patients. Asian Pac J Cancer Prev. 2015;16(15):6237–41.
Naja F, Fadel RA, Alameddine M, Aridi Y, Zarif A, Hariri D, et al. Complementary and alternative medicine use and its association with quality of life among Lebanese breast cancer patients: a cross-sectional study. BMC Complement Altern Med. 2015;15:444.
Lail G, Luck N, Tasneem AA, Rai A, Laeeq SM, Majid Z. The usage of complementary and alternative medicine in gastrointestinal patients visiting the outpatients’ department of a large tertiary care Centre-views from Pakistan. Pan Afr Med J. 2016;24:247.
Lee K, Mokhtar HH, Krauss SE, Ong BK. Hypertensive patients’ preferences for complementary and alternative medicine and the influence of these preferences on the adherence to prescribed medication. Complement Ther Clin Pract. 2014;20(2):99–105.
Chu FY, Yan X, Zhang Z, Xiong XJ, Wang J, Liu HX. Features of complementary and alternative medicine use by patients with coronary artery disease in Beijing: a cross-sectional study. BMC Complement Altern Med. 2013;12:287.
Leung GKK, Wong SWH, GKB N, Hung KN. Concomitant use of Western and Chinese medicine treatments in neurosurgical patients in Hong Kong. Chin J Integr Med. 2011; Epub ahead of print.
Richmond JA, Bailey DE, Patel K, Jezsik JA, Muir A, Lin JR, et al. The use of complementary and alternative medicine by patients with chronic hepatitis C. Complement Ther Clin Pract. 2010;16(3):124–31.
Saw JT, Bahari MB, Ang HH, Lim YH. Herbal use amongst multiethnic medical patients in Penang hospital: pattern and perceptions. Med J Malaysia. 2006;61(4):422–32.
CAS PubMed Google Scholar
Jang S, Kim KH, Sun SH, Go HY, Lee EK, Jang BH, et al. Characteristics of herbal medicine users and adverse events experienced in South Korea: a survey study. Evid Based Complement Alternat Med. 2017;2017:4089019.
Yeong SW, Choong YC. Knowledge and characteristics of herbal supplement usage among community pharmacy customers in a Malaysian population. Complement Ther Med. 2017;35:92–108.
Burke A, Nahin RL, Stussman BJ. Limited health knowledge as a reason for non-use of four common complementary health practices. PLoS One. 2015;10(6):e0129336.
Lawrence D, Smith H, Magala E, Cooper M. Young people’s opinions about herbal medicines in a suburban district of Central Uganda. Int Health. 2014;6(4):337–8.
Upchurch DM, Rainisch BW. A sociobehavioral wellness model of acupuncture use in the United States, 2007. J Altern Complement Med. 2014;20(1):32–9.
Aziato L, Antwi HO. Facilitators and barriers of herbal medicine use in Accra, Ghana: an inductive exploratory study. BMC Complement Altern Med. 2016;16:142.
Leong EM, Semple SJ, Angley M, Siebert W, Petkov J, McKinnon RA. Complementary and alternative medicines and dietary interventions in multiple sclerosis: what is being used in South Australia and why? Complement Ther Med. 2009;17(4):216–23.
Gratus C, Damery S, Wilson S, Warmington S, Routledge P, Grieve R, et al. The use of herbal medicines by people with cancer in the UK: a systematic review of the literature. Q J Med. 2009;102(12):831–42.
Eardley S, Bishop FL, Prescott P, Cardini F, Brinkhaus B, Santos-Rey K, et al. A systematic literature review of complementary and alternative medicine prevalence in EU. Forsch Komplementmed. 2012;19(Suppl 2):18–28.
Ernst E. How much of CAM is based on research evidence? Evid Based Complement Alternat Med. 2011;2011:676490.
Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328(4):246–52.
Haller CA, Kearney T, Bent S, Ko R, Benowitz NL, Olson K. Dietary supplement adverse events: reports of a one-year poison center surveillance project. J Med Toxicol. 2008;4(2):84–92.
Lee WJ, Kim HW, Lee HY, Son CG. Systematic review on herb-induced liver injury in Korea. Food Chem Toxicol. 2015;84:47–54.
Luyckx VA. Nephrotoxicity of alternative medicine practice. Adv Chronic Kidney Dis. 2012;19(3):129–41.
Belachew N, Tadesse T, Gube AA. Knowledge, attitude, and practice of complementary and alternative medicine among residents of Wayu town, Western Ethiopia. J Evid Based Complement Altern Med. 2017;22(4):929–35.
Bamidele JO, Adebimpe WO, Oladele EA. Knowledge, attitude and use of alternative medical therapy amongst urban residents of Osun state, southwestern Nigeria. Afr J Tradit Complement Altern Med. 2009;6(3):281–8.
Amaeze OU, Aderemi-Williams RI, Ayo-Vaughan MA, Ogundemuren DA, Ogunmola DS, Anyika EN. Herbal medicine use among type 2 diabetes mellitus patients in Nigeria: understanding the magnitude and predictors of use. Int J Clin Pharm. 2018;40(3):580–8.
Lulebo AM, Mapatano MA, Mutombo PB, Mafuta EM, Samba G, Coppieters Y. Prevalence and determinants of use of complementary and alternative medicine by hypertensive patients attending primary health care facilities in Kinshasa, Democratic Republic of the Congo: a cross-sectional study. BMC Complement Altern Med. 2017;17(1):205.
Kretchy IA, Owusu-Daaku F, Danquah S. Patterns and determinants of the use of complementary and alternative medicine: a cross-sectional study of hypertensive patients in Ghana. BMC Complement Altern Med. 2014;14:44.
O'Neill S, Gryseels C, Dierickx S, Mwesigwa J, Okebe J, d'Alessandro U, et al. Foul wind, spirits and witchcraft: illness conceptions and health-seeking behaviour for malaria in the Gambia. Malar J. 2015;14:167.
Aboyade OM, Beauclair R, Mbamalu ON, Puoane TR, Hughes GD. Health-seeking behaviours of older black women living with non-communicable diseases in an urban township in South Africa. BMC Complement Altern Med. 2016;16(1):410.
Article CAS PubMed PubMed Central Google Scholar
Agyei-Baffour P, Kudolo A, Quansah DY, Boateng D. Integrating herbal medicine into mainstream healthcare in Ghana: clients’ acceptability, perceptions and disclosure of use. BMC Complement Altern Med. 2017;17(1):513.
Download references
Acknowledgements
Not applicable.
This research did not receive support from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Clinical Pharmacy, Faculty of Pharmacy, Srinakharinwirot University, Nakhonnayok, 26120, Thailand
Mayuree Tangkiatkumjai
Division of Pharmacy Practice and Policy, School of Pharmacy, University of Nottingham, Nottingham, UK
Helen Boardman
School of Health Sciences, University of Southampton, Southampton, UK
Dawn-Marie Walker
You can also search for this author in PubMed Google Scholar
Contributions
All the authors designed the study. MT and DW searched and extracted the publications. All the authors analysed, reviewed and approved the contents of the manuscript. MT drafted the manuscript. HB designed the study and analysed reviewed and approved the contents of the manuscript.
Corresponding author
Correspondence to Mayuree Tangkiatkumjai .
Ethics declarations
Ethics approval and consent to participate.
Not applicable
Consent for publication
Competing interests.
The authors declare that they have no competing interests
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Risk of bias.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tangkiatkumjai, M., Boardman, H. & Walker, DM. Potential factors that influence usage of complementary and alternative medicine worldwide: a systematic review. BMC Complement Med Ther 20 , 363 (2020). https://doi.org/10.1186/s12906-020-03157-2
Download citation
Received : 29 June 2020
Accepted : 12 November 2020
Published : 23 November 2020
DOI : https://doi.org/10.1186/s12906-020-03157-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Conventional medicine
- Complementary and alternative medicine
BMC Complementary Medicine and Therapies
ISSN: 2662-7671
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.322(7279); 2001 Jan 20
Research into complementary and alternative medicine: problems and potential
Richard l nahin.
a Division of Extramural Research, Training and Review, National Center for Complementary and Alternative Medicine, National Institutes of Health, 9000 Rockville Pike, Bethesda MD 20892-2182, USA, b National Center for Complementary and Alternative Medicine
Stephen E Straus
The growing use of unsubstantiated complementary and alternative medicine therapies by people in the United States 1 along with its increasing coverage by third party payers 2 encouraged Congress to create the National Center for Complementary and Alternative Medicine (NCCAM) at the National Institutes of Health. The centre's mission is “to explore complementary and alternative healing practices in the context of rigorous science; to educate and training CAM researchers; and to disseminate authoritative information to the public and professionals.” 3 To complete this mission, NCCAM supports publicly relevant and scientifically rigorous research to identify those complementary and alternative medicine practices that are safe and effective.
The centre's resources, although generous ($68.3m (£46m) for fiscal year 2000), are not sufficient to study all complementary and alternative medicine practices. NCCAM therefore developed criteria to help prioritise the many possible research opportunities (box). As part of the evaluation process, NCCAM seeks advice from its national advisory council, complementary and alternative medicine and conventional clinicians, members of the scientific research community, the public, sister federal agencies, and other stakeholders.
Summary points
- Many early clinical trials investigating complementary and alternative medicine have had serious flaws
- Clinical investigations of complementary and alternative medicine are made difficult by factors such as use of complex, individualised treatments and lack of standardisation of herbal medicines
- Other problems include difficulties in accruing, randomising, and retaining patients and in identifying appropriate placebo interventions
- Despite these complexities, rigorously designed clinical trials are possible, including pragmatic studies of complete complementary and alternative medicine systems
- Strong commitment is required from the research community to provide information about complementary and alternative medicines to the public and health professionals
Allocation of resources
Staff at the centre are often asked why limited resources are being spent on research that is perceived as replicating previously published work, especially when other western countries have already integrated some of these practices into standard care. Unfortunately, many of the studies have been small, their results variable or inconsistent, and their research designs inadequate. Systematic reviews have found that many clinical trials testing complementary or alternative medicine have major flaws, such as insufficient statistical power, poor controls, inconsistency of treatment or product, and lack of comparisons with other treatments, with placebo, or with both. These reviews typically conclude that larger, well designed studies are necessary before making authoritative recommendations. Specific examples of such reviews include the use of Hypericum perforatum (St John's wort) to treat depression 4 ; Ginkgo biloba to delay cognitive decline in patients with Alzheimer's disease 5 ; Serenoa repens (saw palmetto) to relieve symptoms associated with benign prostatic hyperplasia 6 ; and glucosamine and chondroitin sulphate to treat osteoarthritis. 7 NCCAM is currently supporting randomised controlled trials for these four dietary supplements that have been designed with the scientific rigour demanded by experienced scientists and the American public.
One reason for investing so much in research into dietary supplements is that their use is growing rapidly in the United States. Although consultations with complementary and alternative medicine practitioners (acupuncturists, chiropractors, naturopathic physicians, etc) remained stable on a percentage basis from 1993 8 to 1998, 1 use of dietary supplements greatly increased. Billions of dollars are spent on dietary supplements in the United States every year. The Dietary Supplement Health and Education Act, which was passed in 1994, made it easier to obtain these natural products. The act also loosened the federal control over dietary supplements, with the result that most commercially available products are not well characterised or standardised. Another issue is that the optimal dose, schedule, and route of administration of most dietary supplements have not been determined systematically; nor are the frequency and extent of drug reactions and interactions known. NCCAM therefore believes that most dietary supplements are not yet ready for large, expensive trials despite their wide use by patients. At a minimum, preclinical studies, pharmacokinetics testing, and developmental phase I and II trials are necessary before these products can be launched into definitive clinical trials. NCCAM is vigorously encouraging research in these areas through a series of focused initiatives. 9
Criteria for prioritising research opportunities
- Quantity and quality of available preliminary data to help determine the most appropriate type of research (basic versus clinical research; phase I or II clinical trial versus phase III trial)
- Extent of use by the US public (greatest weight given to interventions in wide use)
- Public health importance of disease being treated (greatest weight to diseases associated with highest mortality or morbidity or for which conventional medicine has not proved optimal)
- Feasibility of conducting the research
- Cost of research

Problems with research design
Although many people in the United States self medicate with dietary supplements, many others seek care from practitioners of traditional systems of medicine, including Ayurveda (from India), Kampo (from Japan), traditional Chinese medicine, Native American medicine, and more recently developed systems such as naturopathy and chiropractic. 1 , 10 – 12 Despite the diverse cultures, geographical locations, and beliefs from which these systems developed, they share several common characteristics such as the use of complex interventions often including botanical medications; individualised diagnosis and treatment of patients; an emphasis on maximising the body's inherent healing ability; and treatment of the “whole” patient by addressing their physical, mental, and spiritual attributes rather than focusing on a specific pathogenic process as emphasised in western biomedicine.
Despite this emphasis on multimodality treatment regimens, most research investigating traditional systems of medicine have examined only one, or perhaps two, interventions taken from a whole treatment system. For instance, there are hundreds of small studies examining the efficacy of acupuncture needling alone for treating asthma, pain, hypertension, or nausea. Yet in real practice, acupuncture needling would be just one of an arsenal of interventions used by a licensed acupuncturist including botanical potions, cupping, dietary changes, exercise therapy (such as Tai Chi or Qi Gong), moxibustion, and Chinese massage. Similarly interventions such as yoga, a single botanical medication, or meditation are just single components of complex systems of medicine. So investigators are faced with either designing a trial of a single intervention that does not accurately reflect true clinical practice or undertaking a multifaceted intervention trial that is complicated to design and implement.
Research design is further confounded by the wide variation in how many forms of complementary and alternative medicine are practised. For instance, there are multiple approaches of chiropractic medicine and acupuncture practised in the United States. Within these approaches the treatment may vary for individual patients presenting with the same conventional diagnosis because practitioners often focus on the symptoms of the disease rather than a primary pathology. Furthermore, the number and length of treatments and the specific treatment used may vary both between individuals and for an individual during the course of treatment. For example, when designing a randomised controlled trial for acupuncture, the investigator is faced with choices concerning the selection of points, the depth of needle insertion, and the frequency and scheduling of treatment. Unless these choices are made in an evidence based fashion, the trial will be compromised.
Difficulties in accruing, randomising, and retaining patients are other potential areas of concern. Some issues common to all clinical trials, such as the use of broad exclusion criteria and inadequate outreach to underserved populations, can limit patient participation and reduce generalisability. We also know that patients with a strong preference for a particular treatment will refuse randomisation. 13 – 15 Moreover, should patients accept randomisation, the easy access of dietary supplements and other complementary interventions in the open market greatly increases the likelihood of “cheating” by the control group. This problem has also been found in trials of dietary and behavioural interventions used in conventional medicine. 16
Finding appropriate placebos or shams for treatments such as acupuncture, chiropractic, massage therapy, or complex herbal mixtures is challenging. Complementary and alternative treatments typically involve extended and intensive interactions between the patient and the practitioner, which greatly increase the possibility of a placebo effect. 17 , 18 Double blinding of the interventions may not be possible because the experienced practitioner will know which treatment is sham and which the intervention. The practitioner, in turn, may consciously or unconsciously convey this information to the patient. The variability of practice also affects the choice of a placebo. 19 For instance, superficial insertion of acupuncture needles at valid acupuncture points has been used as a control in many acupuncture trials. 20 , 21 Yet, the Japanese school of acupuncture advocates that such superficial needling is effective, and some research supports this view. 22
Approaches to good design
Given the complex nature of diagnosis and treatment in traditional systems of medicine, how should we design clinical trials? Approaches vary from that of the typical pharmaceutical drug trial, in which strict, standardised diagnostic criteria are used with a defined and standardised treatment, to the other extreme, in which investigations of a whole system are undertaken in its proper context so that both the diagnosis and treatment may be highly individualised.
In studies of a system of traditional medicine to treat a specific disease the investigators consider the system as a whole, instead of a single core modality. These full spectrum studies can be done without identifying the underlying mechanism of action for each intervention, provided there is a clear, clinically relevant end point. For example, NCCAM is currently supporting a phase II randomised trial comparing three approaches to treating women with temporomandibular disorder: naturopathic medicine, traditional Chinese medicine, and usual conventional care. Patients randomised to receive either naturopathic or Chinese medicine are diagnosed and treated in the traditional manner. The end points for the study include validated measures of temporomandibular disease as well as reassessment of the naturopathic or Chinese medicine diagnosis, with all variables being analysed on an intention to treat basis.
A second approach is to study a specific modality adapted from a traditional system of medicine for treating a specific disease. NCCAM currently supports several such trials, including a double blind randomised controlled trial of acupuncture using traditional Chinese medicine needling points specific for depression. The treatment is compared with acupuncture at points that are used to treat other conditions and a waiting list control. The acupuncture treatments are individualised and based on the Chinese medicine diagnosis. Blinding is maintained by having different practitioners diagnose, treat, and evaluate the patients. Monthly assessment by the diagnosing acupuncturist allows for modifications of the treatment plan as needed. The outcome measures include both standard measures of depression (such as the Hamilton rating scale for depression) and reassessment of the Chinese medicine diagnosis, with all analysis done on an intention to treat basis.
A third approach is a trial of a single intervention, such as a herbal medicine to treat a conventionally diagnosed disease. This is the most common approach currently used to investigate complementary and alternative medicine, and ongoing trials are studying hypericum for depression; acupuncture for symptomatic relief of osteoarthritis; G biloba for preventing dementia; shark cartilage as an adjunctive therapy for non-small cell lung cancer; and glucosamine and chondroitin for osteoarthritis.
All of the above examples are randomised controlled trials. They show that despite increases in complexity and possibly cost, it is possible to design high quality trials investigating complementary and alternative medicine. However, the trials require much more preparation than trials of conventional medicine and individual trial components (blinding, placebo, consistency of intervention even if individualised, etc) often need extensive piloting before the trial.
Although randomised controlled trials are the accepted standard of clinical research, NCCAM values other types of high quality research, including careful observational studies. For many complementary and alternative therapies, there is no reliable information concerning the types of practices used for particular diseases or conditions; the numbers and types of patients who use them; how the practices are delivered (including dose used); how well patients respond to treatment; and relevant side effects. These issues can be investigated in observational studies. In addition, observational studies afford pragmatic ways of answering some types of questions, such as the evaluation of rare adverse events, as well as being a viable research option when randomisation of patients might be considered unethical or unacceptable.
The conduct of high quality research on complementary and alternative medicine requires a commitment by the research community, as well as sustained financial support from governments and industry. This commitment is essential if the public and healthcare providers are to have sufficient information on safety and efficacy to make informed decisions concerning use of complementary and alternative medicine. We envision that compelling data will facilitate meaningful interactions between conventional and complementary practitioners and ultimately lead to the development of interdisciplinary partnerships that incorporate validated complementary practices into patient care.

National Institutes of Health data show steep growth in expenditure on dietary supplements
Competing interests: None declared.
Phone Numbers
Routine and emergency care.
Companion Animal Hospital in Ithaca, NY for cats, dogs, exotics, and wildlife
Equine and Nemo Farm Animal Hospitals in Ithaca, NY for horses and farm animals
Cornell Ruffian Equine Specialists, on Long Island for every horse
Ambulatory and Production Medicine for service on farms within 30 miles of Ithaca, NY
Animal Health Diagnostic Center New York State Veterinary Diagnostic Laboratory
General Information
Cornell University College of Veterinary Medicine Ithaca, New York 14853-6401

Study demonstrates the advantages of S/U grades for D.V.M. students

While S/U grading has been used at other institutions, it has not been widely applied at CVM, and the research team took advantage of the opportunity to explore the effects of an alternative system. Photo: Chris Montgomery/Unsplash
Researchers from the Cornell University College of Veterinary Medicine (CVM) found that a satisfactory/unsatisfactory (S/U) grading system used during the early months of COVID-19 increased veterinary students’ well-being and time for self-care without sacrificing academic performance. According to their paper, published in the Journal of Veterinary Medical Education , D.V.M. students performed similarly on letter-graded and S/U coursework, offering the opportunity to consider alternative grading systems that support both students’ health and learning.
Research has shown that workplace burnout is prevalent among veterinarians, highlighting the importance of promoting well-being during training and beyond. “In our profession we have a responsibility to investigate ways to improve the lives of our D.V.M. students as they transition into their professional careers,” said study co-author and assistant clinical professor in the Department of Population Medicine and Diagnostic Sciences Ashleigh Newman ‘06.
Pandemic grading alternative offers research opportunity
After stay-at-home orders were issued in New York, Cornell temporarily offered an S/U grading system for the spring 2020 semester before returning to standard-letter grading in the fall. First author Kelly Lyboldt, D.V.M. ‘05, an associate professor of practice in the Department of Biomedical Sciences, said that professors were concerned about the impacts the rapid conversion to online courses might have on students’ stress levels and learning. The college ultimately decided to institute S/U grading for DVM students.
While pass/fail grading isn’t common in academia, human medicine programs have experimented with S/U grading since the 1960s to allay students’ anxiety. Studies showed that S/U grading positively affected students’ well-being without altering academic outcomes. Opponents have argued that alternatives to letter grades could undermine the rigor of medical training. Still, human medical students have received S/U grades on United States Medical Licensing Examinations since 2022, shifting the emphasis from numerical scores to clinical excellence and interpersonal skills.
While S/U grading has been used at other institutions, it has not been widely applied at CVM,, and thus the team took advantage of the opportunity to explore the effects of an alternative system. A cohort of veterinary students took a core course that spanned the spring and fall 2020 semesters, and faculty were able to compare the results of S/U and letter-graded classes. According to Lyboldt, the research team hypothesized that the S/U system would alleviate students’ stress over their GPAs without sacrificing motivation or academic success.
The team used academic performance data from the 2020 Foundation Course III — a two-part course on animal organ systems covering physiology, pharmacology, clinical pathology, and anatomic pathology — along with a questionnaire about students’ educational experiences and well-being during the course. While students received S/U grades for the spring 2020 course, administrative support kept track of their numerical and letter grades for both semesters, since a “Satisfactory” grade requires a final score above C –. Out of 118 students in the cohort, 68% responded to the questionnaire.

Gaining time for self-care while maintaining motivation to learn
In terms of academic performance, the grading system made little difference in students’ final numerical grades: 83.7% and 84.3% for the spring and fall 2020 semesters, respectively. Data also supported the team’s prediction that, without the pressure of achieving a particular letter grade, 95% of students reported redirecting some of their energy to achieving a healthier balance between academics and caring for their physical and mental wellbeing.
A majority of students saw S/U grading and the open-book exams that accompanied it positively.
One critique around S/U grading in educational literature involves motivation: will students still work hard if they’re not striving for a high GPA? Fortunately, students said their motivation to study was unchanged by the grading system. Around half of those who agreed that S/U grading contributed to their well-being on the survey reported improved learning and enjoyment of the material.
“A lot of us noticed our conversations with students in the spring S/U semester were drastically different than those in the fall,” said Lyboldt. “They seemed more curious about the material, and asked about content instead of points on a quiz.”
Not everyone enjoyed the temporary grading system. Almost 50% of questionnaire responders would have preferred a final letter grade in the spring 2020 class. The authors suspect that’s because grades are important for internships, and their spring 2020 grades would have enhanced their overall GPAs.

The future of S/U grading at CVM
While CVM isn’t throwing in the towel on letter grades, the college did move to S/U grading for fourth-year D.V.M. students performing clinical rotations. Foundation Course III is now hybrid, with weekly S/U quizzes and built-in reflection opportunities for graded assignments, along with a letter-graded final exam and letter for the final grade.
Eleni Casseri, M.P.H. ’19, D.V.M. ’24, took a hybrid version of Foundation Course III. “The pass/fail grading on the quizzes took a lot of pressure off me,” she said. “It wasn’t about whether I got 80% or 85%; it was about learning material because I’m going to be a doctor someday. I felt like I wasn’t just trying to pass another class.”
The research team also believes that S/U grading allows students the space for low-stakes failures and learning resilience. “Our veterinary students are very intelligent and motivated individuals,” said Kathryn D. Bach ‘04, M.S. ‘09, Ph.D. ‘19, paper co-author and lecturer in the Department of Population Medicine and Diagnostic Sciences. “We want them to focus on growing after their mistakes instead of stressing about impacts to their GPAs.”
Antonia Jameson Jordan, D.V.M. ‘99, Ph.D. ’08, is a senior lecturer in the Department of Biomedical Sciences and paper co-author who sees S/U grades within a larger context. “Our students have been pushing for years for the college to support their wellness,” she explained. “It’s great to find systems that support students’ learning, health, and ability to be great veterinarians.”
As CVM continues to examine and refine its curriculum, these findings will help in establishing approaches that optimize long-term learning and healthy habits for sustaining a lifetime of career satisfaction in veterinary medicine.
Written by Jennifer DeMoss
Recent News

Cornell University College of Veterinary Medicine recognizes newest graduates

CVM faculty, staff, awarded SUNY Chancellor’s Awards for Excellence

Wing skeleton evolution may be less restricted in small birds
Cornell immunology symposium -- june 3-5, 2024, why children die and what we can do about it, social behavior change in food safety: levers to drive food system transformation, educating generalists for adaptive expertise.

IMAGES
VIDEO
COMMENTS
Abstract. Alternative medicine has renewed its growing public interest in recent times due to inequality of patients and healthcare professionals' ratios with increased work-load for the latter ...
PDF | On Mar 16, 2020, Charles Wagner published Complementary and Alternative Medicine | Find, read and cite all the research you need on ResearchGate
For some authors, traditional medicine dif-fers from conventional medicine by relying on theories not based on scientific data upon which modern medicine is based, thus bypass-ing the scientific evidence-based paradigm.15 The attributes "additional" or "alternative" translate an epistemological discomfort on the identity of
Evidence-based medicine is described by Stacks as "the thoughtful, explicit, and prudent application of the best available evidence in making decisions concerning the care of specific patients" [ 33 ]. It emphasizes the use of data from carefully planned and executed studies to facilitate decision-making [ 34 ].
Complementary medicine The terms "complementary medicine" and "alternative medicine" refer to a broad set of health care practices that are not part of that country's own traditional or conventional medicine and are not fully integrated into the dominant health care system. They are used interchangeably with traditional medicine in some
In 1992 the US Congress created the Office of Alternative Medicine (OAM), placing it within the NIH, one of the foremost bio medical research establishments world-wide. The OAM is currently funded ...
PDF | On Jan 1, 2021, M. TRINADH RAO and others published Alternative Medicine: New Ways to Treat Diseases and Therapies | Find, read and cite all the research you need on ResearchGate
rural populations.8 Research on plant and use of traditional medicinal information has again received considerable interest. Indeed, herbal medicine is an integral part of any traditional ... 68 Journal of Evidence-Based Complementary & Alternative Medicine 18(1) use of medicinal plants has gained a respectable position today,
Abstract. The global trend toward increased acceptability and use of complementary and alternative medicines (CAMs), across all age groups, is well documented in the literature. Consequently, further systematic evaluation and meta-analysis are necessary to evaluate the quality, efficacy, safety, and regulation of these range of therapies by ...
Use of complementary and alternative medicine (CAM) has become widespread in the last two decades. The prevalence of CAM use in general populations worldwide ranges from 9.8% to 76% [].Twelve systematic reviews report reasons for CAM use mainly in cancer populations compared to other condition-specific populations [2,3,4,5].Five of the systematic reviews aimed to determine reasons for CAM use ...
AbsTrACT. background The WHO estimates that a considerable number of people in Sub-Saharan Africa (SSA) rely on traditional, complementary and alternative medicine (TCAM) to meet their primary healthcare needs, yet there remains a dearth of research evidence on the overall picture of TCAM utilisation in the region.
Integrative Medicine Research (IMR) is the official journal of Korea Institute of Oriental Medicine (KIOM). The journal is a quarterly, single-blind peer-reviewed, open access journal focused on evidence-based scientific research in integrative medicine, traditional medicine, and complementary and …. View full aims & scope.
mentary and Alternative Medicine, "a group of diverse medical and health care systems, practices, ... internal validityinternal validity of a research study—the certainty with which conclusions can be drawn from the study because of its rigor and design. But, the more complex, controlled, and rigorous the study, ...
It is difficult to draw strong conclusions about trends in prevalence or impact of the four types of alternative medicine research (Figs. 4, ,5, 5, ,6 6 and and7) 7) because there are few papers published per year, particularly within broad fields. Moreover, these papers are often concentrated in specialist journals and the inclusion or ...
Introduction. Complementary and alternative medicine (CAM) encompasses several millennia of therapeutic systems such as Ayurvedic medicine and traditional Chinese medicine (TCM), as well as contemporary systems like anthroposophical medicine, naturopathic medicine, chiropractic medicine and homeopathy. CAM is usually associated with specific ...
This paper is based on a presentation at the NIH Conference on Complementary and Alternative Medicine Research Methodology; April 26-28, 1995; Bethesda, Maryland. It represents the final report of the NIH Working Group on Quantitative Methods in Alternative Medicine (Jeffrey S. Levin, PhD, MPH, Chairman). The work of the first author was ...
Alternative medicine; the tendency of using complimentary alternative medicine in patients of different hospitals of Lahore, Pakistan. Professional Med J 2014; 21(6):1178-1184. INTRODUCTION Complimentary alternative medicine denotes to medical interventions and techniques that have neither included in residency training nor usually
Alternative medicine is a term that describes medical treatments that are used instead of traditional therapies. Some people also refer to it as "integrative or "complementary" medicine. Whereas complementary ... Research into alternative therapies often fails to follow proper research protocols, providing invalid results. ...
Herbal Medicine Today: Clinical and Research Issues. Fabio Firenzuoli and Luigi Gori. Center of Natural Medicine, S.Giuseppe Hospital, Empoli, Italy. Herbal medicine is the use of medicinal plants ...
traditional medicine. Keywords: Alternative medicine, Students, Hearing-impaired, Cultural belief, Nigeria 1. Introduction Traditional medicine has remained the most affordable and easily accessible source of treatment in primary health care system of poor communities where alternative therapy is the major means of medical treatment in
Problems with research design. Although many people in the United States self medicate with dietary supplements, many others seek care from practitioners of traditional systems of medicine, including Ayurveda (from India), Kampo (from Japan), traditional Chinese medicine, Native American medicine, and more recently developed systems such as naturopathy and chiropractic. 1,10 - 12 Despite the ...
cost of malaria treatment at a health clinic ranged from ¢1,900 to ¢3,000 (US$1.30 to US$2.00 in 1997), treatment at home using drugs bought from pharmacies or health care workers ranged between ¢200 and ¢1,000 (US$0.10 to US$0.70), and treatment by an herbalist was virtually free (Ahorlu and others 1997).
We randomly assigned patients with type 2 diabetes and chronic kidney disease (defined by an estimated glomerular filtration rate [eGFR] of 50 to 75 ml per minute per 1.73 m 2 of body-surface area ...
The research team also believes that S/U grading allows students the space for low-stakes failures and learning resilience. "Our veterinary students are very intelligent and motivated individuals," said Kathryn D. Bach '04, M.S. '09, Ph.D. '19, paper co-author and lecturer in the Department of Population Medicine and Diagnostic Sciences.