Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

How your twins’ fetal positions affect labor and delivery

What happens to your baby right after birth

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

- Tuesday, April 23, 2024
- Nursing Article
4 Key Steps of the Leopold Maneuver for Accurate Fetal Positioning
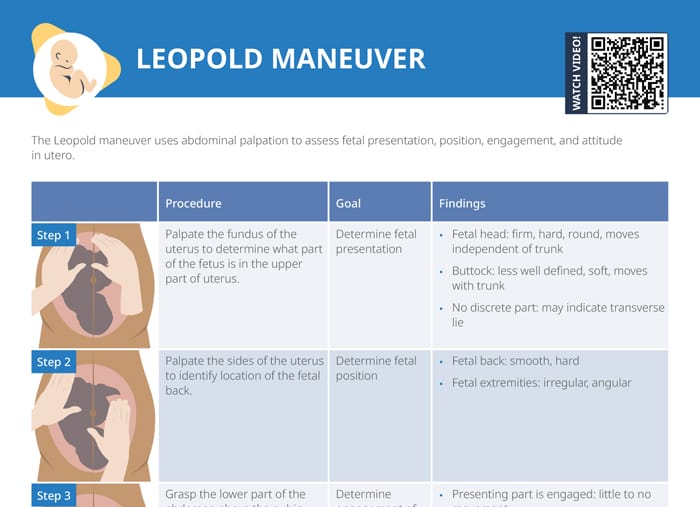
The Leopold Maneuver is a fundamental examination technique used to assess fetal presentation, position, and size during pregnancy . It has been widely employed as a routine prenatal assessment tool by obstetricians and midwives for over a century. The technique involves a series of four maneuvers that allow the examiner to palpate the maternal abdomen and identify the fetal presentation and position.
In this article, we will explore the history, purpose, benefits, and limitations of the Leopold Maneuver , as well as provide a step-by-step guide on how to perform the examination. We will also discuss the importance of the Leopold Maneuver in prenatal care, common issues that may arise during the examination , and the role of the procedure in diagnosing fetal position.
Table of Contents
Definition of the Leopold Maneuver
The Leopold maneuver is a four-step procedure used by healthcare professionals to assess the fetal presentation, fetal lie, and fetal position . This technique involves feeling the abdomen, identifying the location of the fetal back, and palpating the fetal head, buttocks, and limbs to determine their position within the uterus .
History of the Leopold Maneuver
The Leopold maneuver was first described in 1899 by Christian Gerhard Leopold , a German obstetrician. Since then, it has become a standard procedure in obstetrics worldwide. Over the years, the technique has undergone several modifications to make it more accurate and reliable.
Importance of Leopold Maneuver in Obstetrics
The Leopold maneuver is a vital tool in assessing fetal presentation, lie, and position. The information obtained from this technique helps healthcare professionals determine the best mode of delivery and anticipate potential complications during labor and delivery. It also assists in identifying multiple gestations and abnormal fetal presentations , ensuring the safe delivery of the baby.
Purpose and Benefits of the Leopold Maneuver
Assessment of fetal presentation.
The Leopold maneuver is used to determine fetal presentation, which refers to the part of the fetus that enters the maternal pelvis first. The most common fetal presentation is the cephalic presentation, where the baby is head-down. However, other presentations, such as breech or transverse, require special attention during labor and delivery. The Leopold maneuver helps healthcare professionals determine the fetal presentation to prepare for the most optimal delivery for both the mother and baby.
Estimating Fetal Weight
During the Leopold maneuver, healthcare professionals can estimate fetal weight by palpating the mother’s abdomen. This information is crucial in assessing fetal growth and development and determining the need for intervention or delivery in cases where the fetus is too large or too small.
Identifying Fetal Lie and Attitude
The Leopold maneuver also helps healthcare professionals identify fetal lie and attitudes. Fetal lie refers to the orientation of the fetus in the uterus , while fetal attitude refers to the position of the fetus’s head and limbs in relation to its body . Accurate identification of fetal lie and attitudes is essential in preparing for safe and successful delivery.
Step-by-Step Guide on Performing the Leopold Maneuver
Preparing the Patient for the Examination
Before beginning the Leopold maneuver, the mother should empty her bladder, lie down, and relax her abdominal muscles. The healthcare professional should wash their hands and warm them before beginning the examination.
Step 1: Identification of the Fundus

Palpation of the fundus: The first maneuver is also called Fundal Grip . The healthcare professional palpates the uppermost part of the uterus (fundus) to determine the fetal lie, presentation, and engagement . The healthcare professional should identify the position of the fundus, which is the top of the uterus, by palpating the abdomen with both hands. The fundus is usually located near the navel.
Your Findings Should Be Recorded as, Head : round, more mobile Breach : Large, nodular mass
Step 2: Identification of the Fetal Back

Palpation of the sides of the uterus : The second maneuver is also called Umbilical Grip . The healthcare professional palpates the sides of the uterus to determine the fetal presentation and position . The healthcare professional should identify the location of the fetal back by feeling a smooth, firm, and long surface on one side of the uterus.
Your Findings Should Be Recorded as,
Back : Hard, resistant structure, directed anteriorly, posteriorly, or transversely Fetal Extremities : Numerous small irregular mobile parts
Step 3: Identification of the Fetal Part occupying the Pelvic Inlet

Palpation of the fetal parts : This maneuver is also known as the first Pawlik Grip . The healthcare professional palpates the fetal parts to determine the fetal position and engagement . The healthcare professional should identify the fetal part occupying the pelvic inlet by palpating the lower abdomen . Depending on the fetal presentation, this could be the fetal head or buttocks.
When the head has descended, can feel the anterior shoulder or the space created by the neck from the head.
- Palpate the lower abdomen to identify the presenting part of the fetus (e.g., “The fetal buttocks are presenting at the inlet.”)
- Note the position of the presenting part in relation to the mother’s pelvis (e.g., “The presenting part is in a transverse lie.”)
Step 4: Identification of the Fetal Part in the Pelvic Cavity

Palpation of the pelvic inlet : This maneuver is also known as the second Pawlik Grip . The healthcare professional palpates the pelvic inlet to determine fetal engagement . Finally, the healthcare professional should identify the fetal part in the pelvic cavity . This could be the fetal head, buttocks, or limbs.
Not engaged: Movable mass is felt
Engaged : Fixed mass is felt
Importance of the Leopold Maneuver in Prenatal Care
Identification of abnormal fetal presentation.
The Leopold maneuver is crucial in identifying abnormal fetal presentations , such as breech or transverse, which require special attention during labor and delivery to ensure the safety of both the mother and baby.
Assessment of Fetal Growth and Development
The Leopold maneuver provides healthcare professionals with vital information about fetal growth and development and helps them anticipate potential complications during labor and delivery.
Identification of Multiple Gestations
The Leopold maneuver is an essential tool in identifying multiple gestations to ensure appropriate prenatal care and delivery planning for mothers carrying more than one baby.
Common Issues and Solutions During the Leopold Maneuver
The Leopold maneuver is an obstetric examination technique used to assess fetal presentation, position, and engagement. However, performing this maneuver can be challenging due to various factors. Here are some common issues and solutions during the Leopold maneuver.
Difficulty in Assessing the Fetal Presentation
One common issue during the Leopold maneuver is difficulty in identifying fetal presentation . This can happen when the fetal presentation is not well defined or when there are multiple fetuses. To solve this issue, the examiner should carefully palpate the abdomen and try to differentiate between the fetal parts.
Difficulties in Identifying the Fetal Parts
Another common issue during the Leopold maneuver is difficulty in identifying fetal parts . This can happen when the fetus is in an atypical position or when there are fetal anomalies. To solve this issue, the examiner should use various techniques such as ultrasound or auscultation to guide them in identifying the fetal parts.
Confounding Factors that May Affect the Examination
There are confounding factors that may affect the accuracy of the Leopold maneuver, including obesity, polyhydramnios, fetal anomalies, and fetal movements . These factors can make it more challenging to perform the Leopold maneuver accurately. To solve this issue, examiners should try to minimize these factors or use additional examination techniques to confirm fetal presentation and position.
The Role of the Leopold Maneuver in Diagnosing Fetal Position
The Leopold maneuver is a crucial examination technique for diagnosing fetal position, and it plays a significant role in obstetric care. Here are some important factors to consider when using the Leopold maneuver to diagnose fetal position.
Importance of Diagnosing Fetal Position
Diagnosing fetal position is essential for obstetricians and midwives to ensure safe delivery. By knowing the fetal position, they can anticipate any potential complications during delivery and prepare accordingly. This can help minimize the risk of fetal distress, maternal injury, and other delivery-related complications .
Accuracy of Leopold Maneuver in Diagnosing Fetal Position
The Leopold maneuver is an accurate technique for diagnosing fetal position, with a sensitivity of up to 84%. It is a non-invasive and cost-effective method that can be performed by most healthcare providers. Therefore, it is widely used in obstetric care to diagnose fetal position.
Limitations of the Leopold Maneuver in Diagnosing Fetal Position
However, the Leopold maneuver has some limitations in diagnosing fetal position. It may not be accurate in identifying fetal presentation in cases of multiple pregnancies, fetal anomalies, or when the fetus is in an atypical position . Additionally, the examiner’s experience and skill level can also affect the accuracy of the Leopold maneuver.
Complications
The Leopold maneuver is generally considered a safe and non-invasive examination, but as with any medical procedure, there are potential complications that can occur. Some possible complications of the Leopold maneuver include:
- Discomfort: The Leopold maneuver can cause some discomfort or mild pain for the patient, especially if the examiner is pressing too hard or manipulating the fetus in a way that causes discomfort.
- False results: In some cases, the Leopold maneuver can produce false results, which can lead to incorrect decisions about delivery options or interventions. This can occur if the fetus is in an unusual position or if the examiner is inexperienced or unable to accurately interpret the results of the exam.
- Fetal distress: In rare cases, the Leopold maneuver can cause fetal distress or other complications, such as premature labor or rupture of the amniotic sac. This can occur if the examiner is too forceful or aggressive during the exam or if the fetus is in a vulnerable position.
- Infection: While the Leopold maneuver is a non-invasive exam, there is still a small risk of infection if the examiner does not follow proper hygiene protocols, such as washing their hands before and after the exam.
Nurse’s Responsibilities
The Leopold maneuver is a technique used by healthcare professionals, including nurses, to assess the position of a fetus in the mother’s uterus. As a nurse, your responsibilities during Leopold maneuvers include:
- Explaining the procedure to the patient: Before performing the Leopold maneuver, it is important to explain the procedure to the patient and ensure that they understand what will happen during the exam. This can help reduce anxiety and improve the patient’s overall experience.
- Preparing the patient: Before performing the exam, you will need to ensure that the patient is positioned correctly and that their clothing is adjusted to allow access to their abdomen. You may also need to provide a drape or cover for modesty.
- Assisting the healthcare provider: During the Leopold maneuver, you may be asked to assist the healthcare provider by holding the patient’s abdomen or providing support as needed. You may also need to help position the patient to allow for optimal access to the uterus.
- Monitoring the patient: As the Leopold maneuver can cause some discomfort or pain for the patient, it is important to monitor their vital signs and overall comfort level throughout the exam. If the patient experiences any discomfort or pain, you may need to provide comfort measures, such as adjusting their position or providing pain relief medication.
- Documenting the exam: After the Leopold maneuver, it is important to document the results of the exam in the patient’s medical record. This includes noting the fetal presentation, position, and engagement, as well as any other relevant information.
- Providing patient education: Following the exam, you may need to provide the patient with education about the results of the exam, as well as any next steps that may be needed. This can include discussing delivery options, potential complications, and follow-up appointments.
What is the Leopold Maneuver?
The Leopold Maneuver is a manual examination technique used by obstetricians and midwives to assess the fetal presentation, position, and size during pregnancy. The technique involves a series of four maneuvers that allow the examiner to palpate the maternal abdomen and identify the fetal presentation and position.
How is the Leopold Maneuver performed?
The Leopold Maneuver involves four maneuvers, which are performed in sequence. The first maneuver involves palpating the fundus to determine the location of the fetal head or buttocks. The second maneuver involves identifying the location of the fetal back. The third maneuver involves palpating the lower abdomen to identify the presenting part of the fetus. The fourth maneuver involves determining fetal descent and engagement.
What is the purpose of the Leopold Maneuver?
The purpose of the Leopold Maneuver is to assess the fetal presentation, position, and size during pregnancy. The examination can provide valuable information to obstetricians and midwives to ensure the health and safety of both the mother and the baby. The Leopold Maneuver can help identify abnormal fetal presentation, and multiple gestations, and estimate fetal weight.
Can the Leopold Maneuver be performed at home?
No, the Leopold Maneuver is a medical examination technique that should only be performed by trained healthcare professionals, such as obstetricians or midwives. It requires specialized knowledge, training, and experience to perform the examination accurately.
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
Fetal Positions for Labor and Birth
Knowing your baby's position can you help ease pain and speed up labor
In the last weeks of pregnancy , determining your baby's position can help you manage pain and discomfort. Knowing your baby's position during early labor can help you adjust your own position during labor and possibly even speed up the process.
Right or Left Occiput Anterior
Illustration by JR Bee, Verywell
Looking at where the baby's head is in the birth canal helps determine the fetal position.The front of a baby's head is referred to as the anterior portion and the back is the posterior portion. There are two different positions called occiput anterior (OA) positions that may occur.
The left occiput anterior (LOA) position is the most common in labor. In this position, the baby's head is slightly off-center in the pelvis with the back of the head toward the mother's left thigh.
The right occiput anterior (ROA) presentation is also common in labor. In this position, the back of the baby is slightly off-center in the pelvis with the back of the head toward the mother's right thigh.
In general, OA positions do not lead to problems or additional pain during labor or birth.
Right or Left Occiput Transverse
Illustration by JR Bee, Verywell
When facing out toward the mother's right thigh, the baby is said to be left occiput transverse (LOT). This position is halfway between a posterior and anterior position. If the baby was previously in a posterior position (in either direction), the LOT position indicates positive movement toward an anterior position.
When the baby is facing outward toward the mother's left thigh, the baby is said to be right occiput transverse (ROT). Like the previous presentation, ROT is halfway between a posterior and anterior position. If the baby was previously in a posterior position, ROT is a sign the baby is making a positive move toward an anterior position.
When a baby is in the left occiput transverse position (LOT) or right occiput transverse (ROT) position during labor, it may lead to more pain and a slower progression.
Tips to Reduce Discomfort
There are several labor positions a mother can try to alleviate pain and encourage the baby to continue rotating toward an anterior position, including:
- Pelvic tilts
- Standing and swaying
A doula , labor nurse, midwife , or doctor may have other suggestions for positions.
Right or Left Occiput Posterior
When facing forward, the baby is in the occiput posterior position. If the baby is facing forward and slightly to the left (looking toward the mother's right thigh) it is in the left occiput posterior (LOP) position. This presentation can lead to more back pain (sometimes referred to as " back labor ") and slow progression of labor.
In the right occiput posterior position (ROP), the baby is facing forward and slightly to the right (looking toward the mother's left thigh). This presentation may slow labor and cause more pain.
To help prevent or decrease pain during labor and encourage the baby to move into a better position for delivery, mothers can try a variety of positions, including:
- Hands and knees
- Pelvic rocking
Mothers may try other comfort measures, including:
- Bathtub or shower (water)
- Counter pressure
- Movement (swaying, dancing, sitting on a birth ball )
- Rice socks (heat packs)
How a Doctor Determines Baby's Position
Leopold's maneuvers are a series of hands-on examinations your doctor or midwife will use to help determine your baby's position. During the third trimester , the assessment will be done at most of your prenatal visits. Knowing the baby's position before labor begins can help you prepare for labor and delivery.
Once labor begins, a nurse, doctor, or midwife will be able to get a more accurate sense of your baby's position by performing a vaginal exam. When your cervix is dilated enough, the practitioner will insert their fingers into the vagina and feel for the suture lines of the baby's skull as it moves down in the birth canal. It's important to ensure the baby is head down and moving in the right direction.
Labor and delivery may be more complicated if the baby is not in a head-down position, such as in the case of a breech presentation.
How You Can Determine Baby's Position
While exams by health practitioners are an important part of your care, from the prenatal period through labor and delivery, often the best person to assess a baby's position in the pelvis is you. Mothers should pay close attention to how the baby moves and where different movements are felt.
A technique called belly mapping can help mothers ask questions of themselves to assess their baby's movement and get a sense of the position they are in as labor approaches.
For example, the position of your baby's legs can be determined by asking questions about the location and strength of the kicking you feel. The spots where you feel the strongest kicks are most likely where your baby's feet are.
Other landmarks you can feel for include a large, flat plane, which is most likely your baby's back. Sometimes you can feel the baby arching his or her back.
At the top or bottom of the flat plane, you may feel either a hard, round shape (most likely your baby's head) or a soft curve (most likely to be your baby's bottom).
Guittier M, Othenin-Girard V, de Gasquet B, Irion O, Boulvain M. Maternal positioning to correct occiput posterior fetal position during the first stage of labour: a randomised controlled trial . BJOG: An International Journal of Obstetrics & Gynaecology . 2016;123(13):2199-2207. doi:10.1111/1471-0528.13855
Gizzo S, Di Gangi S, Noventa M, Bacile V, Zambon A, Nardelli G. Women’s Choice of Positions during Labour: Return to the Past or a Modern Way to Give Birth? A Cohort Study in Italy . Biomed Res Int . 2014;2014:1-7. doi:10.1155/2014/638093
Ahmad A, Webb S, Early B, Sitch A, Khan K, MacArthur C. Association between fetal position at onset of labor and mode of delivery: a prospective cohort study . Ultrasound in Obstetrics & Gynecology . 2014;43(2):176-182. doi:10.1002/uog.13189
Nishikawa M, Sakakibara H. Effect of nursing intervention program using abdominal palpation of Leopold’s maneuvers on maternal-fetal attachment . Reprod Health . 2013;10(1). doi:10.1186/1742-4755-10-12
Choi S, Park Y, Lee D, Ko H, Park I, Shin J. Sonographic assessment of fetal occiput position during labor for the prediction of labor dystocia and perinatal outcomes . The Journal of Maternal-Fetal & Neonatal Medicine . 2016;29(24):3988-3992. doi:10.3109/14767058.2016.1152250
Bamberg C, Deprest J, Sindhwani N et al. Evaluating fetal head dimension changes during labor using open magnetic resonance imaging . J Perinat Med . 2017;45(3). doi:10.1515/jpm-2016-0005
Gabbe S, Niebyl J, Simpson J et al. Obstetrics . Philadelphia, Pa.: Elsevier; 2012.
By Robin Elise Weiss, PhD, MPH Robin Elise Weiss, PhD, MPH is a professor, author, childbirth and postpartum educator, certified doula, and lactation counselor.
Lecturio Nursing
Cheat Sheets
Nursing Knowledge
Leopold Maneuvers
Table of contents, what is the leopold maneuver .
The Leopold maneuvers are a common, non-invasive assessment for pregnant clients. It involves palpating the abdomen using specific hand movements in four steps to gather valuable information about the fetal position, which is essential for safe and effective labor and delivery management.
What is the purpose of the Leopold maneuvers?
The purpose of the Leopold maneuvers is to assess the position, presentation, attitude, and engagement of the fetus inside the uterus:
- Position: whether the fetus is positioned longitudinally, transversely, or obliquely
- Presentation: which part of the fetus is presenting first, such as head or breech
- Engagement: how far the presenting part has descended into the pelvis
- Attitude: relationship of fetal head to body (ideal: fetus curled with back rounded and chin tucked to chest, arms crossed over chest and legs folded at knees)
This information is important for planning the delivery and can guide decisions during labor. Usually, the Leopold maneuvers are done to determine if the fetus is in an optimal position for labor. They are also used to identify the location of the fetal back, which is where fetal heart tones are best auscultated.
Related videos
Leopold maneuvers steps , maneuver 1: fundus palpation to determine fetal presentation.
Palpate the fundus of the uterus to determine what part of the fetus is in the upper part of the uterus. Findings:
- Fetal head: firm, hard, round, moves independent of trunk
- Buttock: less well defined, soft, moves with trunk
- No discrete part: may indicate transverse lie
Maneuver 2: Palpation of sides to determine fetal position
Palpate the sides of the uterus to identify the location of the fetal back. Findings:
- Fetal back: smooth, hard
- Fetal extremities: irregular, angular
Maneuver 3: Palpation of lower abdomen to determine engagement of presenting part
Grasp the lower part of the abdomen above the pubic symphysis to engage the fetal presenting part. Gently move from side to side. Findings:
- Presenting part is engaged: little to no movement
- Presenting part is not engaged: part is easily moved, ballotable
Maneuver 4: Palpation to determine fetal attitude
Facing the foot of the client, use both hands to assess the position of the fetal head. Findings:
- Fetal head is well flexed: resistance from the brow is palpated opposite the fetal back.
- Fetal head is extended: occiput is palpated on the same side as the fetal back.
Factors that may affect findings
Factors that may affect findings include:
- Maternal body habitus
- Polyhydramnios
- Full maternal bladder
RELATED TOPIC:
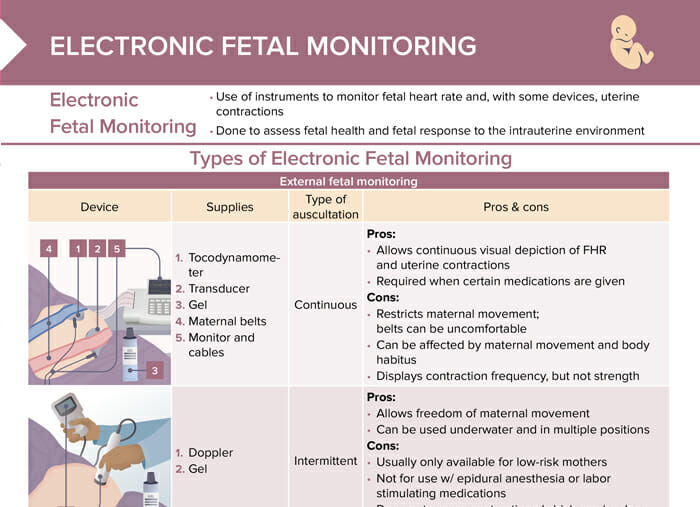
Electronic Fetal Monitoring: Types & Strip Assessment
FREE CHEAT SHEET
Free Download
Nursing Cheat Sheet
Master the topic with a unique study combination of a concise summary paired with video lectures.
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
User Reviews
Get premium to test your knowledge.
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.

Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Determining fetal position (Leopold’s maneuvers)
Determining fetal position (Leopold’s maneuvers) You can determine fetal position, presentation, and attitude by performing Leopold’s maneuvers. Ask the patient to empty her bladder; then assist her to a supine position and expose her abdomen. Perform these four maneuvers in order. First maneuver Face the patient and warm your hands. Place your hands on the patient’s abdomen to determine fetal position in the uterine fundus. Curl your fingers around the fundus. When the fetus is in the vertex position (head first), the buttocks should feel irregularly shaped and firm. When the fetus is in the breech position, the head should feel hard, round, and movable.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Cultural childbearing practices
- Multiple gestations
- Coombs’ test, direct
- Phototherapy
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

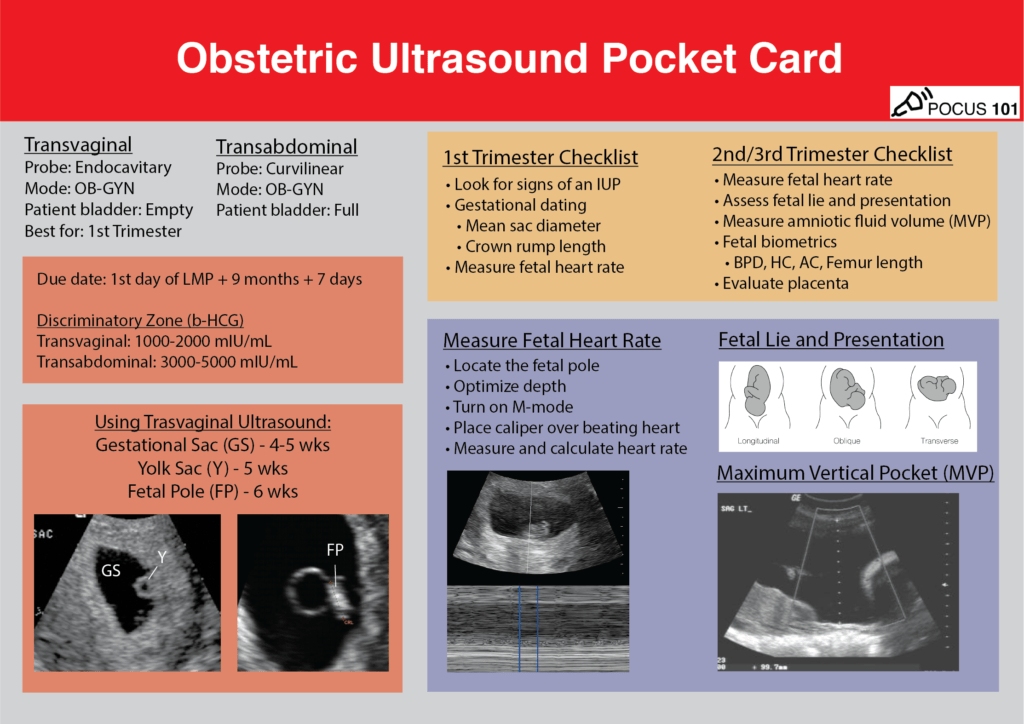
Obstetric/OB Ultrasound Made Easy: Step-By-Step Guide
- OB/Gyn , Ultrasound Basics , Ultrasound Protocols , Ultrasound Tutorials
Primary Authors: Satchel Genobaga , Vi Dinh ; Co-authors: Jessica Ahn , Jade Deschamps, Annalise Lang , Victor Lee, Reed Krause , Devin Tooma, Seth White. Oversight, Review, and Final Edits by Vi Dinh (POCUS 101 Editor) .
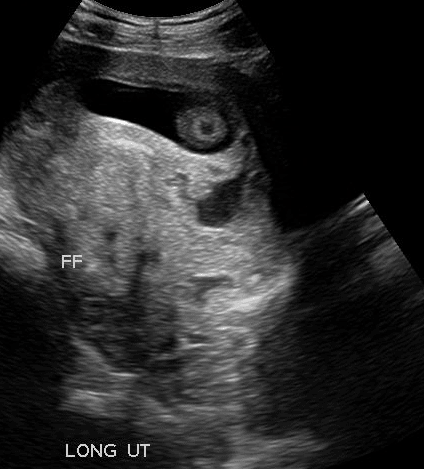
Obstetric (OB) Point of Care Ultrasound (POCUS) can be used in all stages of pregnancy for a wide range of applications: from diagnosing the patient presenting with vaginal bleeding, gestational dating, to measuring fetal cardiac activity.
After reading this post, you will learn how to use basic obstetrical ultrasound to do the following:
- Recognize an intrauterine pregnancy and 1st-trimester findings (gestational sac, yolk sac, fetal pole)
- Estimate gestational age
- Measure fetal cardiac activity
- Recognize the ultrasonographic findings of pregnancy pathologies
- Assess fetal lie, viability, biometrics, and placental location in the 2nd & 3rd trimester
Table of Contents
Obstetric (OB) Ultrasound POCKET CARD PDF
Download ob ultrasound protocol card pdf here.
Like this Post? Sign Up For POCUS 101 Updates!

Obstetric/OB Ultrasound Indications
- Vaginal bleeding in pregnancy
- Abdominal/Pelvic pain in pregnancy
- Gestational dating
- Positive pregnancy test with increased B-hCG
- Assessing for fetal viability
- Maternal trauma
Pre-Exam Preparation
Determining estimated due date based on lmp.
It is important to estimate the gestational age prior to Obstetric/OB ultrasound assessment to determine if the findings are normal. Naegele’s Rule is a simple way to calculate the due date based on the last menstrual period (LMP) and estimate gestational age prior to the Obstetric/OB ultrasound assessment.
Due Date = Date of first day of last menstrual period (LMP) + 9 Calendar months + 7 days For example, if the LMP was 7/16/20, add 9 months (4/16/21), then add 7 days = 4/23/21
Gestational age is estimated in weeks from the first day of the LMP. The gestational age as well as the estimated due date can be refined using ultrasound findings which we’ll discuss below.
B-hCG Discriminatory Zone
It is generally accepted that an intrauterine pregnancy should be seen on transvaginal ultrasound with a B-hCG level of 1000-2000 mIU/mL , and on transabdominal ultrasound with a level of 3000-5000 mIU/mL ; this is called the discriminatory zone (Bree et al). If an intrauterine pregnancy (IUP) isn’t seen at this time, you should be suspicious of an ectopic pregnancy or non-viable intrauterine pregnancy.
However, there has been some debate on the utility of the discriminatory zone, with evidence showing the chance of a viable IUP developing later on despite no IUP detected below the discriminatory zones ( Doubilet et al, Wang 2011 ).
OB Ultrasound Transabdominal Approach
For full details on how to perform transabdominal pelvic ultrasound read our Complete Pelvic Ultrasound Post HERE .
Patient Preparation
- Full urinary bladder is preferred if in the 1st-trimester
Ultrasound Machine Preparation
- Tra nsducer: Curvilinear Ultrasound Probe (Ideal Choice) or Phased Array Probe.
- Preset : Pelvic or Abdomen
- Machine Placement : Position the ultrasound machine on the right side of the patient with the screen facing you. With this configuration you can face both the patient and the ultrasound screen, scanning with your right hand and manipulating buttons on the machine with the left hand.

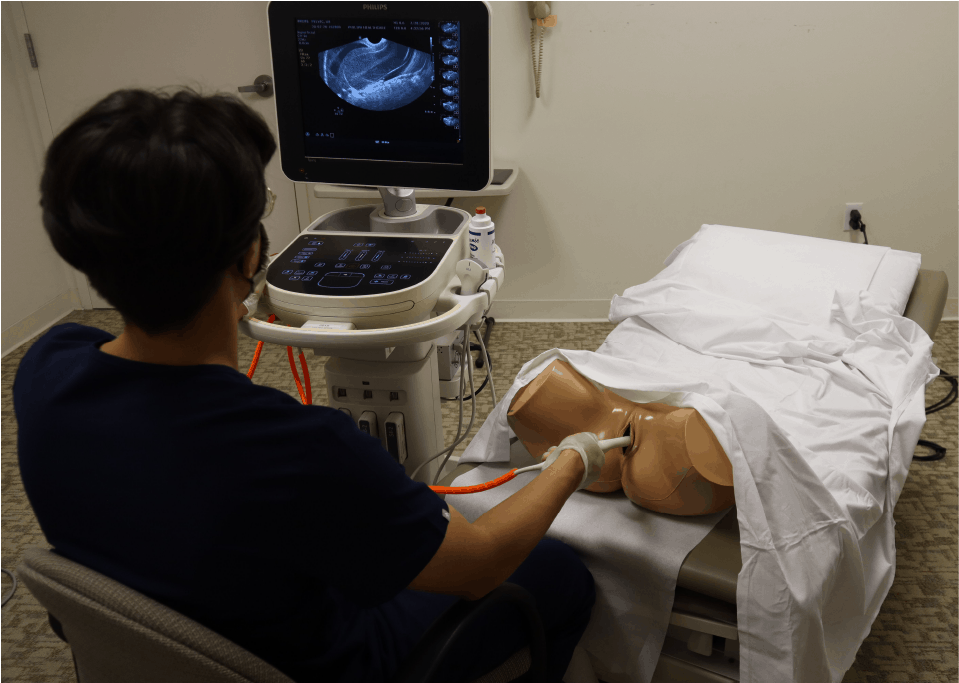
OB Ultrasound Transvaginal Approach
Transvaginal ultrasound is primarily used in the 1st trimester since signs of pregnancy can be seen earlier than transabdominal ultrasound. For complete details on how to perform transvaginal ultrasound read our Complete Pelvic Ultrasound Post HERE .
- Dorsal Lithotomy position. Make sure to have a drape/sheet and cover the patient properly. Position them similarly to how you would perform a normal pelvic exam.
- Empty bladder (if possible)
- Have a chaperone present in the room with you.
- Transducer : Transvaginal/Endocavitary probe.
- Preset : Gyn/Pelvic
- Will also need a sterile condom (or sterile glove) and sterile gel.
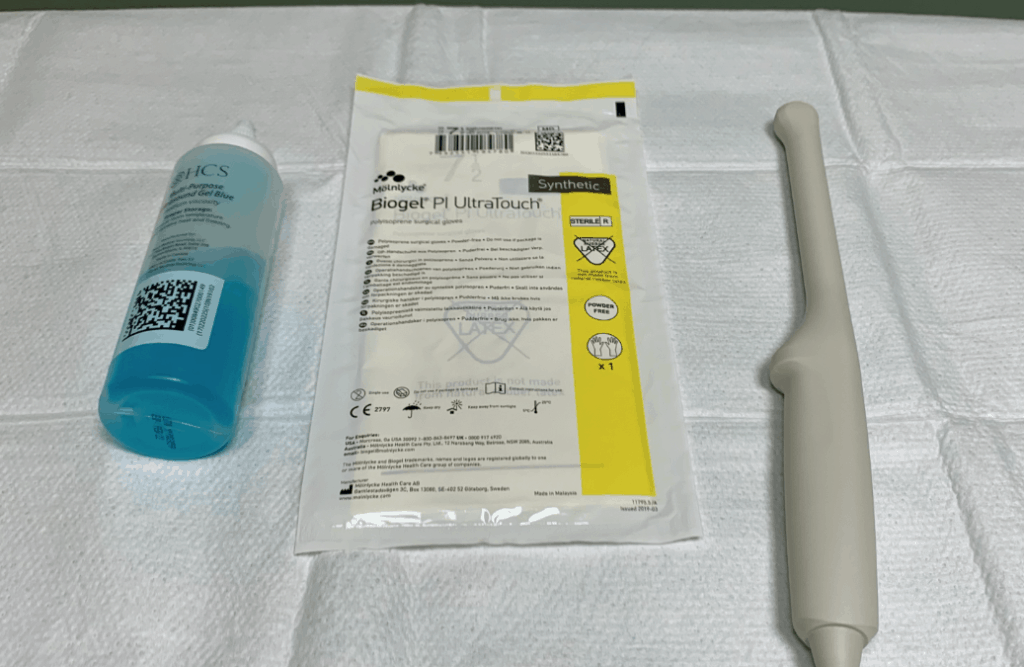
- The indicator is located at the 12 o’clock position of the probe.
- Place gel at the tip of the endocavitary probe.
- Apply sterile glove or sterile condom over the endocavitary probe
- Apply sterile gel to the tip of the covered endocavitary probe.
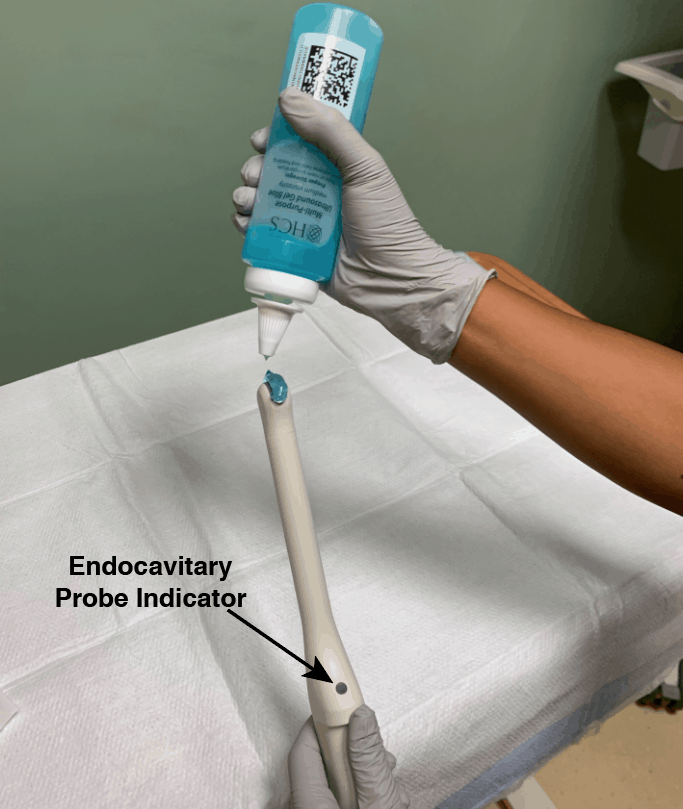
- Machine Positioning : Position the ultrasound machine on the right side of the patient with the screen facing you. With this configuration you can face both the patient and the ultrasound screen, scanning with your right hand and manipulating buttons on the machine with the other hand. Also position a chair at the foot of the bed to sit in while performing the scan.
1st Trimester Obstetric/OB Ultrasound Protocol
Identifying an intrauterine pregnancy.
To definitively diagnose an intrauterine pregnancy, either a yolk sac or a fetal pole must be seen within a gestational sac inside of the uterus.
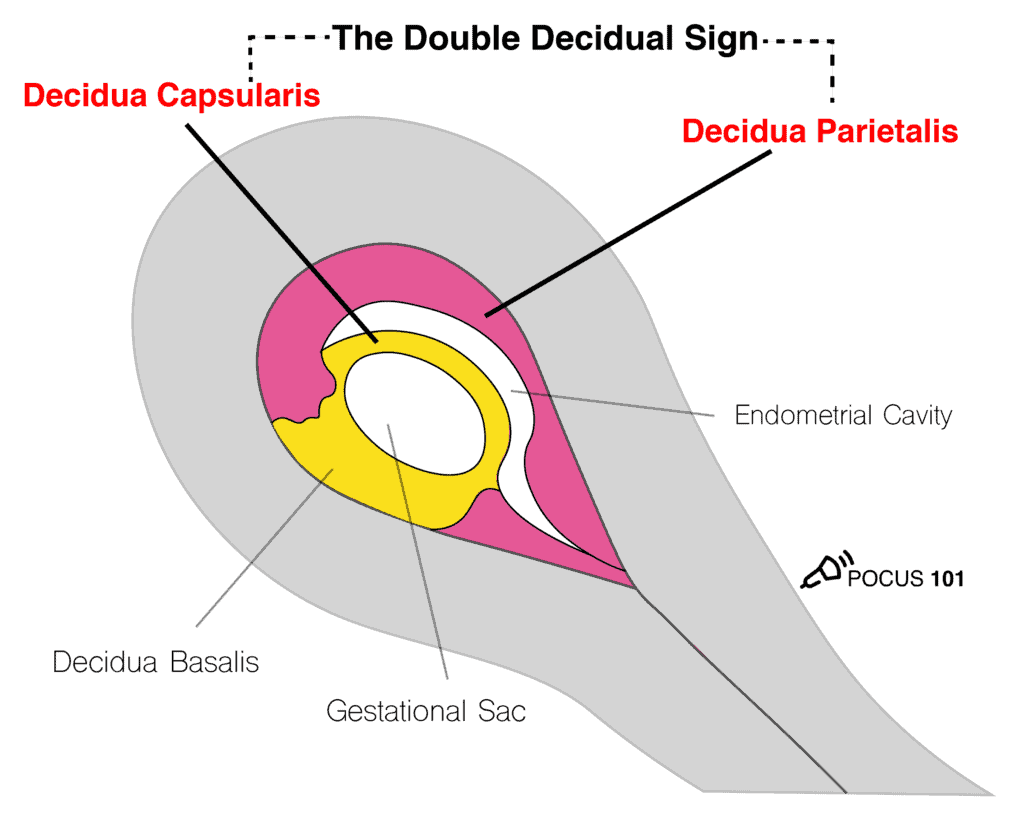
Gestational Sac (4-5 weeks)
The gestational sac is a collection of fluid surrounding the embryo and yolk sac. It is the first structure to be seen in the development of an IUP. It will have these features:
- Anechoic (dark), round structure with an echogenic (bright) border.
- Typically, it is in the upper 1/3 of the uterine fundus.
- You should expect to see the gestational sac at 4.5-5 weeks gestational age with transvaginal ultrasound.
- Make sure the sac is actually in the uterus by tracking the vaginal stripe to the uterus.
Shortly after the appearance of the gestational sac, the decidual layers are commonly seen. This is called the Double Decidual Sign . They will appear as 2 echogenic rings surrounding the gestational sac. The outer ring is the decidua parietalis (lining the uterine cavity) and the inner ring the decidua capsularis (lining the gestational sac). The presence of a Double Decidual Sign is highly indicative of an early intrauterine pregnancy. However, a definitive diagnosis of IUP will require the presence of a yolk sac or fetal pole.
POCUS101 Tip: Don’t diagnose a IUP until you see a yolk sac or fetal pole within a uterine gestational sac.
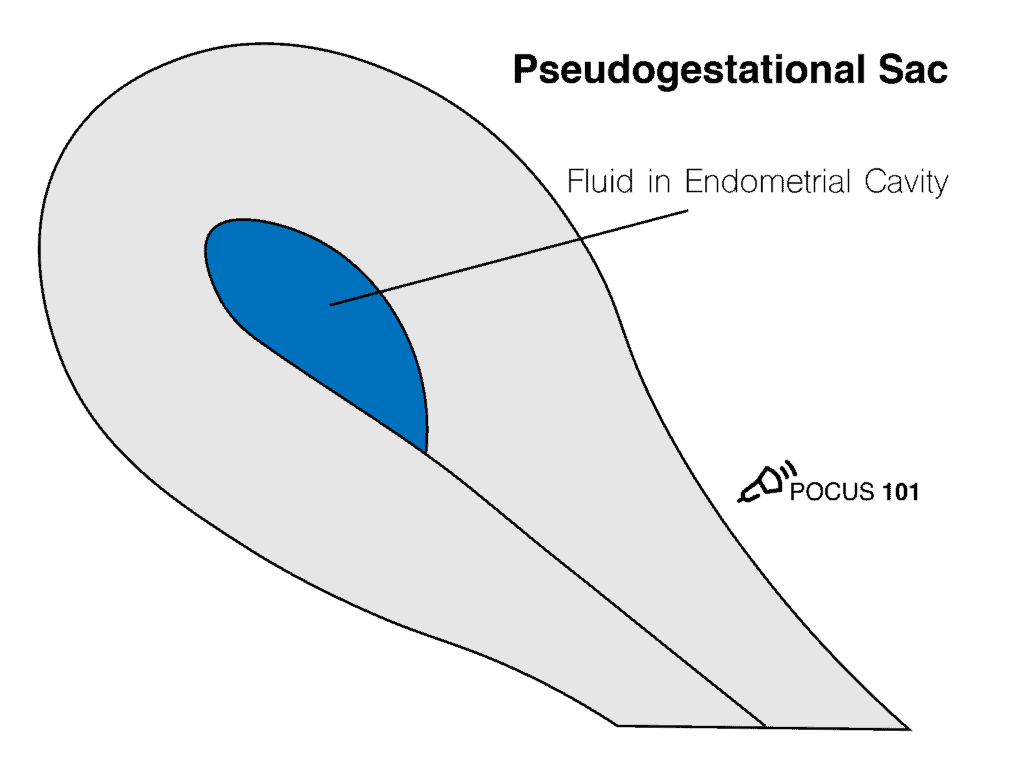
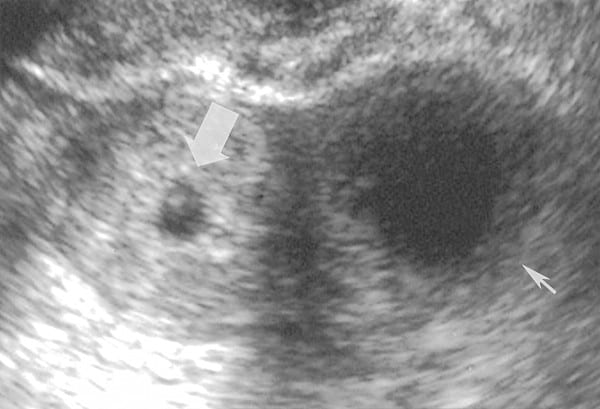
Pseudogestational Sac
A common pitfall is to falsely identify a gestational sac. Small collections of fluid can look very similar to gestational sacs and are appropriately called Pseudogestational sacs . How can we tell them apart? Pseudogestational sacs will usually have one or more of the following characteristics ( Benson et al, 2013 ):
- A pseudogestational sac is more irregularly shaped or pointy-edged than a round gestational sac.
- The border surrounding the sac is not as echogenic as that of a true gestational sac.
- The fluid within a pseudo-gestational sac is not completely anechoic, there are some echoes seen in the fluid.
- The fluid of a pseudo-gestational sac will not be found in the decidua like a true gestational sac, but in the uterine cavity .
- A pseudo-gestational sac will not have the contents of a maturing gestational sac such as the yolk sac and embryo .
Correctly distinguishing between a true and pseudo-gestational sac is important because intrauterine fluid collections reportedly occur in 9-20% of ectopic pregnancies ( Benson et al, 2013 ). Additionally, misdiagnosing a pseudo-gestational sac for an early IUP can lead to improper treatment.
Note the irregular shape, lack of double decidual sign, presence of echoes in the fluid, and lack of embryonic contents in Pseudogestational Sac.
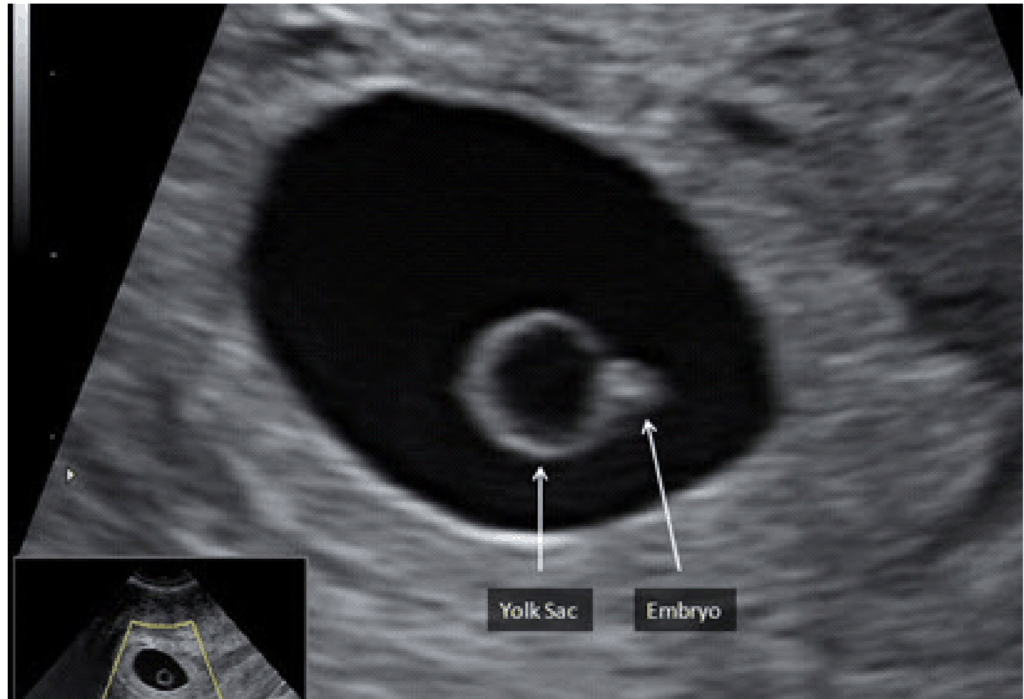
Yolk Sac – (5 weeks)
Typically seen at around 5 weeks gestational age by transvaginal OB ultrasound, the yolk sac is an early source of nutrition for the developing embryo which usually isn’t yet visible. The yolk sac is a circular, echogenic ring with an anechoic center seen eccentrically (not in the center) in the gestational sac.
Fetal Pole – (5.5-6 weeks)
The fetal pole, or developing embryo, should be seen at 5.5-6 weeks gestational age by transvaginal ultrasound. It grows directly adjacent to the yolk sac. With transvaginal ultrasound, the fetal pole should be seen when it is 2-4mm in length.
Pregnancy Dating in the 1st Trimester
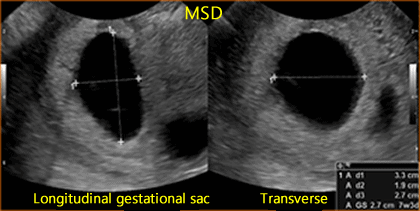
Mean sac diameter (msd).
Prior to the appearance of a fetal pole, the mean sac diameter can be used to estimate the gestational age.
- Step 1 – Optimize depth to see gestational sac
- Step 2 – Obtain a sagittal view of the gestational sac
- Step 3 – Measure the height and length of the sac using the mean sac diameter calculation package.
- Step 4 – Rotate the probe 90º to obtain a transverse view of the gestational sac.
- Step 5 – Measure the width of the gestational sac.
Generally, the formula for calculating gestational age from mean sac diameter is:
MSD (in mm) + 30 = Gestational age (in days)
Crown-Rump Length (CRL)
Once a fetal pole is present, the crown-rump length should be used to estimate the gestational age as it is the most accurate method of dating the pregnancy. The crown-rump length is defined as the measurement between the top of the head and the bottom of the torso.
- Step 1 – Optimize depth to clearly see the entire fetal pole or embryo.
- Step 2 – Acquire a proper view of the fetus ( Wanyonyi et al, Ioannou et al )
- Step 3 – Measure the crown-rump length using your machine’s calculation package.

If your ultrasound does not have an OB package use this formula: CRL (in mm) + 42 = Gestational age (in days)
POCUS 101 Tip: Make sure that the view of the fetus is in the mid-sagittal plane . Having an oblique section or an off-center longitudinal section of the fetus will lead to underestimation of the crown-rump length.
Cardiac Activity (Fetal Heart Rate Measurement)
Assessing cardiac activity is a crucial task in obstetric ultrasound. Fetal cardiac activity should be seen at a crown rump length (CRL) of 5-7mm.
M-mode is the preferred way to measure fetal cardiac activity over pulsed wave doppler because it subjects the fetus to lower ultrasound energy.
- Step 1 – Locate the fetal heart and optimize the depth
- Step 2 – Properly place the M-Mode cursor over the beating heart and activate M-Mode
- Step 3 – Open the OB calculation package and place the vertical cursors at one heartbeat cycle (some machines measure at 2 heartbeat cycles)
- Step 4 – The machine should automatically calculate the fetal heart rate from your measurement.
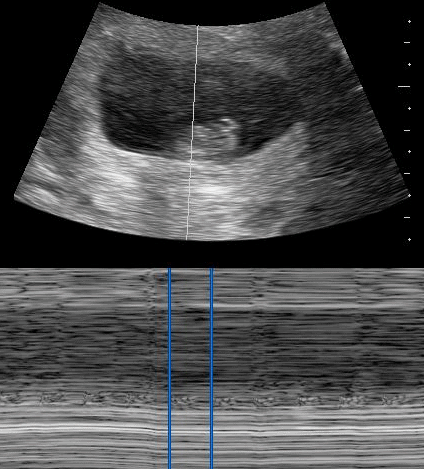
Normal fetal heart rate ranges:
Here is a quick video summarizing how to measure fetal heart rate using M-Mode:
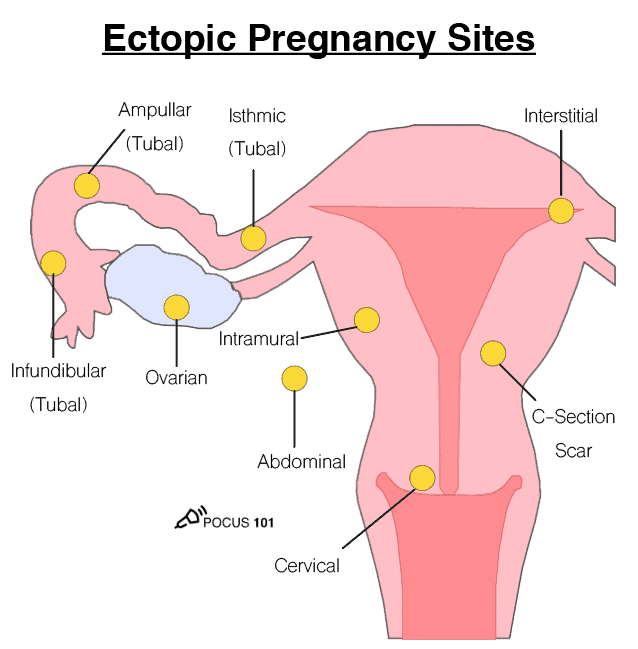
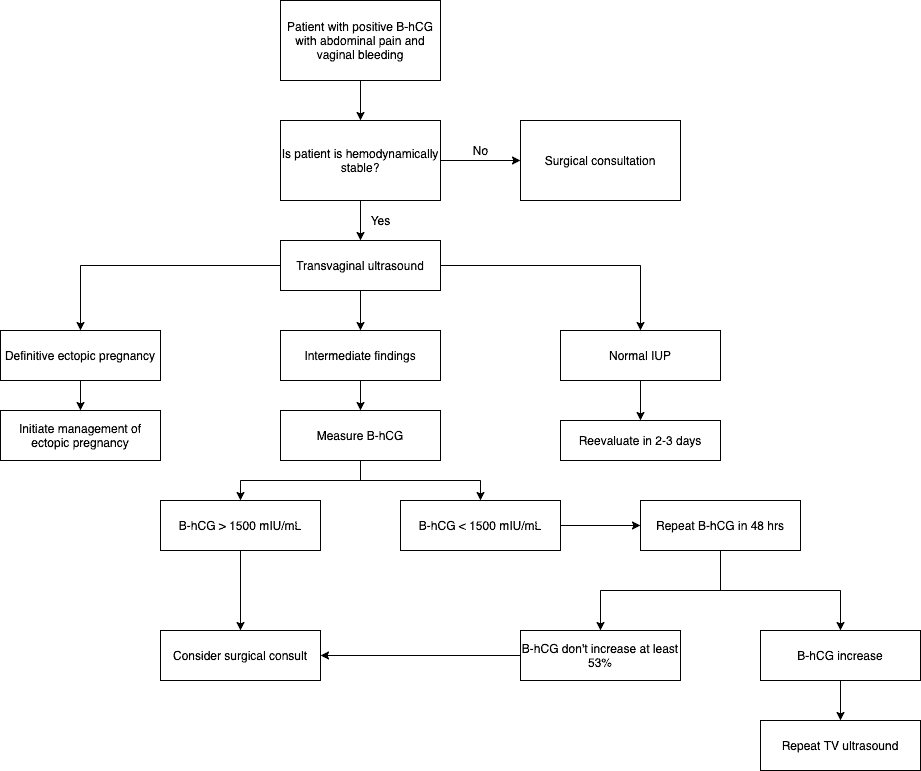
Ectopic Pregnancies
An ectopic pregnancy refers to any pregnancy occurring outside of the uterus. They pose a substantial risk to the mother and thus must be diagnosed accurately. Ectopic pregnancies cannot be missed.
- These patients commonly present with abdominal pain , pelvic pain , or vaginal bleeding .
- Peritoneal irritation
- Cervical motion tenderness
- Lack of fetal heart tones
- Previous tubal surgery
- Prior ectopic pregnancy
The vast majority of ectopic pregnancies are found in the fallopian tubes, particularly in the ampullary region of the tube. They can be seen in many different locations, however. Because there are many places in which an ectopic pregnancy can be, the primary goal of ultrasound should be not to definitively rule in an ectopic pregnancy, but rather to rule in an intrauterine pregnancy; therefore making an ectopic pregnancy highly unlikely.
Follow these steps to look for an ectopic pregnancy:
Step 1 – Scan the uterus for a gestational sac with a yolk sac, fetal pole, or cardiac activity within the uterus. If detected then the patient has IUP and unlikely a concurrent ectopic (unless IVF therapy)
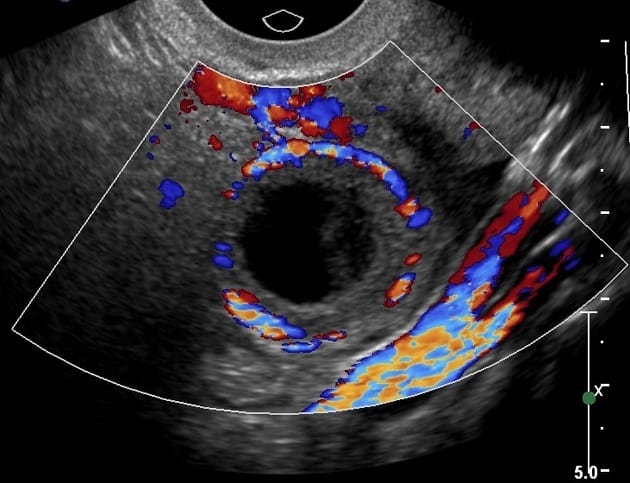
- The tubal ring sign ( Stein et al ) is a common ultrasound finding with an ectopic pregnancy . This is a thick hyperechoic ring around a tubal mass.
- The ring of fire sign ( Pellerito et al ) can be seen in ectopic pregnancy but can also be seen in corpus luteum cysts. The ring of fire sign describes the high-velocity flow seen on color Doppler imaging due to the high vascularization of the area surrounding the ectopic pregnancy.
- Finding a gestational sac and fetal pole with cardiac activity outside of the uterus is diagnostic of an ectopic pregnancy .
Step 3 – Assess the Pouch of Douglas for free fluid.
Step 4 – Integrate ultrasound findings with B-hCG levels
- Fetus visible in the uterus
- B-hCG level of 1000-2000 mIU/mL
- Ectopic mass
- Fluid in the cul de sac
- Abnormal serum B-hCG pattern*
*Normally, B-hCG levels rise at least 50% in a 48 hour period. In ectopic pregnancies, B-hCG levels commonly rise 50% or less in the same timeframe. Additionally, B-hCG levels plateau sooner than IUPs (IUPs usually plateau at around 10-12 weeks) ( Lin et al ).
Corpus Luteal Cyst
A corpus luteal cyst develops due to the growth, instead of the normal regression, of the corpus luteum. These cysts will appear very similar to a tubal ectopic pregnancy.
How can you tell the difference between the two?
Miscarriage
It is important to use proper terminology when describing miscarriages:
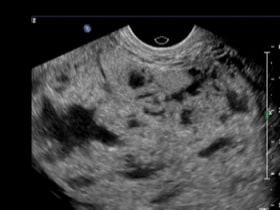
Molar Pregnancy
A molar pregnancy is a tumor due to the uncontrolled proliferation of trophoblasts, which are cells that surround the blastocyst and later become the placenta. These “moles” are categorized into complete and partial.
Presentation:
- Vaginal bleeding
- Exaggerated uterine size for gestational age
- Hyperemesis
- Pregnancy-induced hypertension
A molar pregnancy will appear on ultrasound as a “snowstorm” inside the uterus. The contents of the uterus are complex and heterogeneous and often contain many small cystic structures . In addition, there may be theca-lutein cysts in the ovaries which are thin-walled cystic structures (these are more common in 2nd-trimester complete moles) ( Benson et al, 2000 ).

2nd-3rd Trimester Obstetric/OB Ultrasound Protocol
Like in the 1st trimester, identifying fetal cardiac activity is essential to determining the viability of a pregnancy. Now that the fetus has grown to the point where we can identify its anatomy, we can directly visualize the 4 chambers of the heart. We can still use M-mode to measure fetal heart rate. Use the steps described above to calculate the fetal heart rate.
- Acquire a 4-chamber view of the fetal heart. This view can be found by scanning through the fetus in a transverse plane.
- Optimize the magnification and gain so that the fetal heart takes up the majority of the screen.
- The left atrium will be closest to the spine.
- The axis of the heart will be pointing to the left of the fetus.
- Use the calipers to measure the length of 1 (or 2 depending on the machine) cardiac cycle(s). The fetal heart rate should be calculated by the machine.
A refresher on how to use M-mode to measure fetal heart rate:
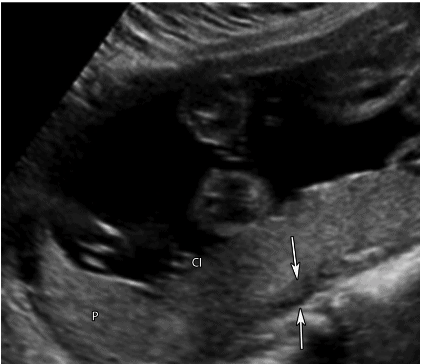
Fetal Presentation
The presentation of the fetus refers to which part of the fetus is closest to the birth canal.
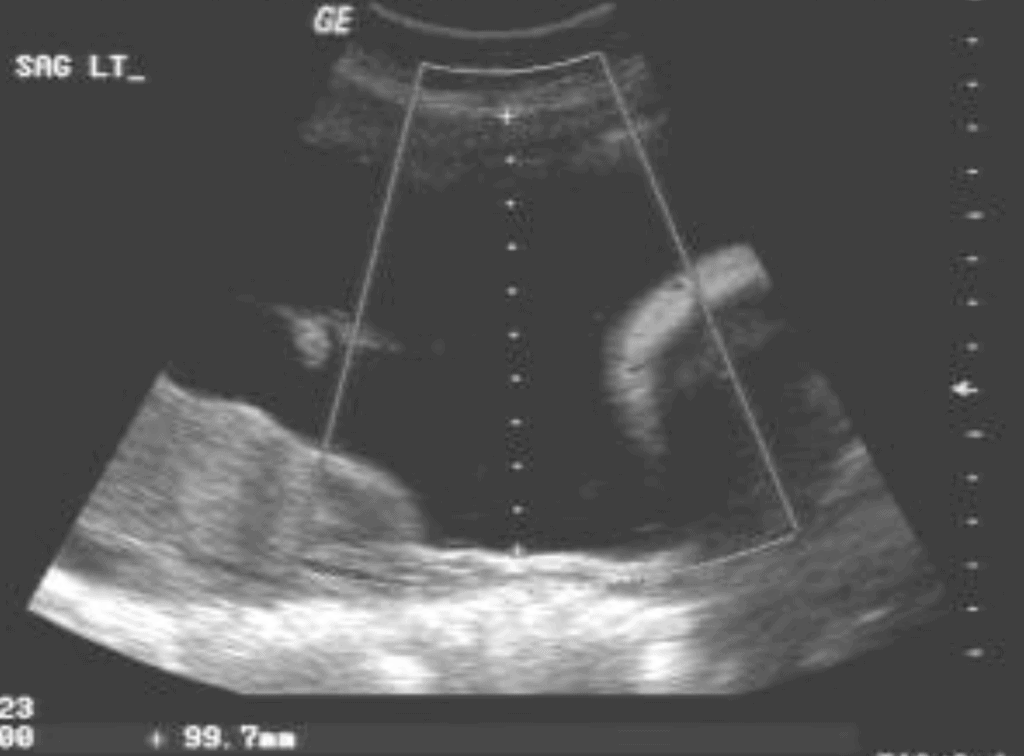
- Obtain a midline sagittal view of the lower uterus.
- Determine which part of the fetus is closed to the maternal pelvic inlet.
Cephalic Presentation — Head first
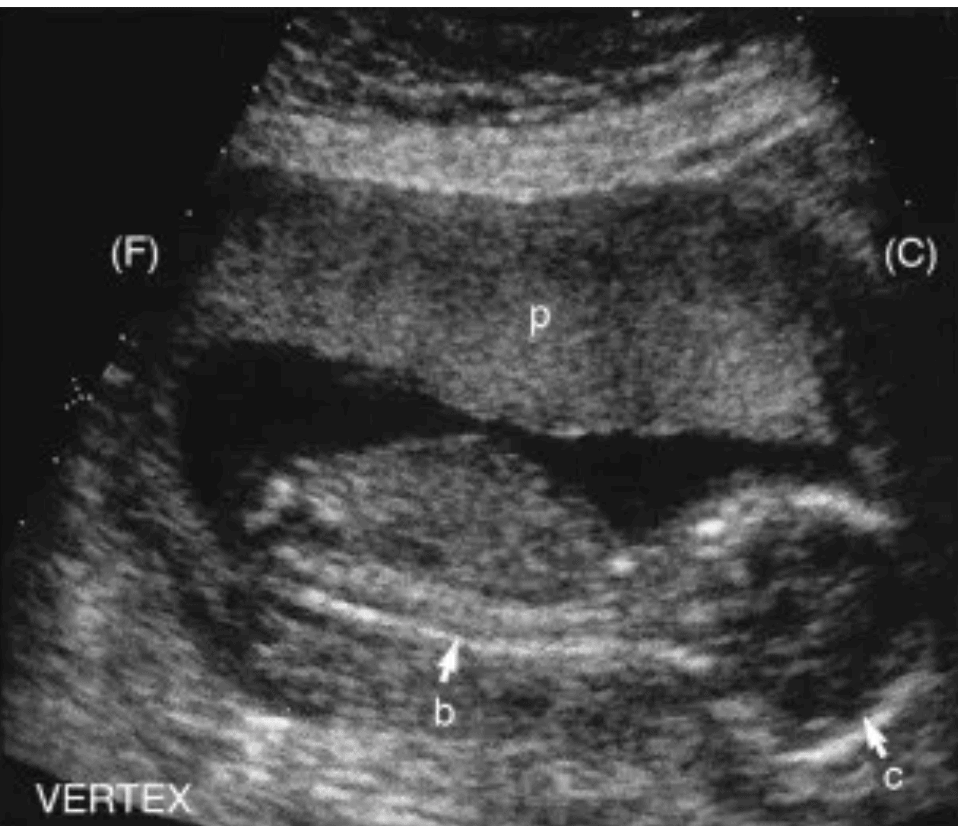
Breech Presentation — Buttocks/Feet first
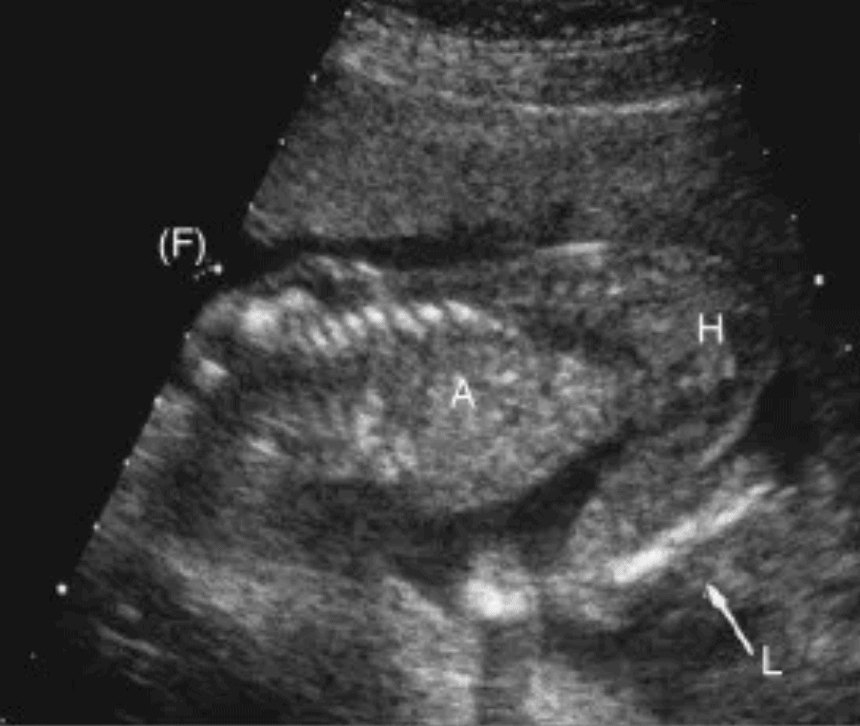
Shoulder Presentation — Shoulder/Arm first
- This presentation will show a transverse (short axis) or oblique cross-section of the fetus in a mid-sagittal view of the uterus.
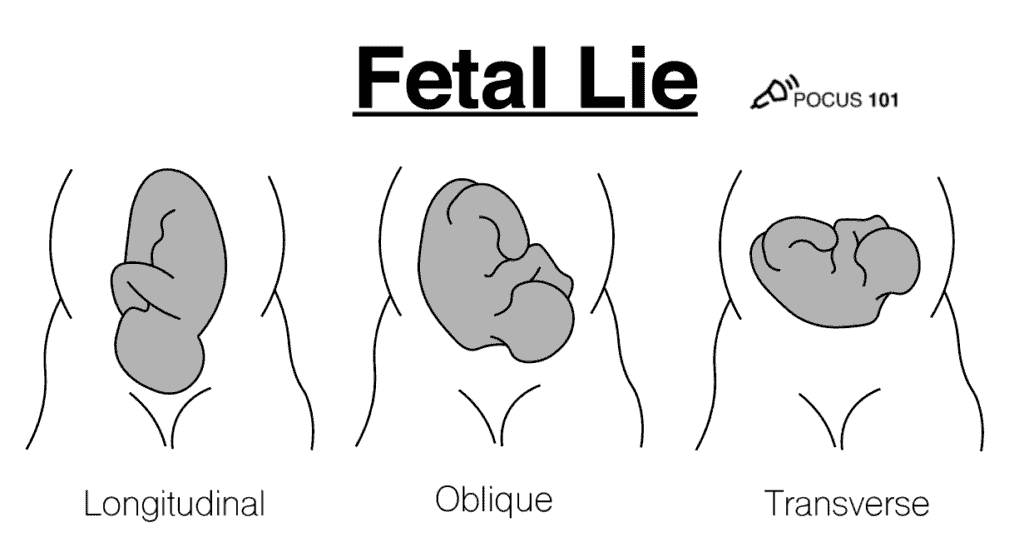
Fetal lie refers to the relative orientation of the fetal and maternal spines and can either be longitudinal, oblique, or transverse .
To determine the fetal lie, acquire a mid-sagittal view of the fetal spine and compare it to the maternal spine.
Longitudinal Lie – The maternal and fetal spines are parallel (can be breech or cephalic presentations)
Oblique Lie – The fetal spine is at an oblique angle to the maternal spine
Transverse Lie – The maternal and fetal spines are perpendicular
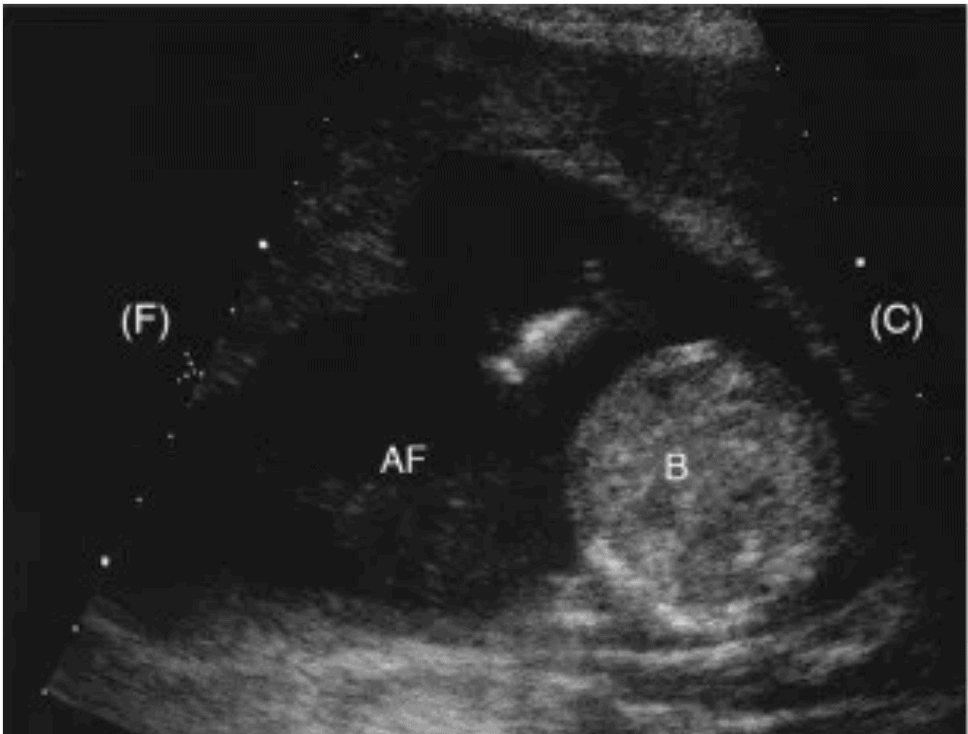
Amniotic Fluid Volume (Maximum Vertical Pocket)
Amniotic fluid accompanies the fetus in the amniotic sac. It functions as a cushion for the fetus, helps protect it from infection, and promotes muscle, lung, and digestive system development. Polyhydramnios refers to having too much amniotic fluid while oligohydramnios refers to having too little. Polyhydramnios is associated with fetal malformations, developmental delay, and neurologic disorders ( Yefet & Daniel-Spiegel ). Oligohydramnios is associated with increased perinatal morbidity and mortality ( Casey et al ).
Amniotic fluid volume can be assessed with ultrasound by measuring the maximum vertical pocket of amniotic fluid.
- Oligohydramnios: <2 cm
- Normal: 2-8 cm
- Polyhydramnios: >8 cm
Here’s how to measure the maximum vertical pocket:
- Scan the amniotic sac from left to right in a sagittal view.
- Estimate a location that has the deepest vertical pocket and measure it with the calipers.
- The caliper line must be in a vertical orientation.
- The caliper line must be free of any fetal parts or the umbilical cord.
Fetal Biometrics
In the 2nd and 3rd trimester, various measurements of the fetus, known as fetal biometrics, can be used to estimate the weight and gestational age. These aren’t as accurate as the 1st-trimester crown-rump length measurement, but they can be helpful nonetheless.
The ultrasound OB calculation package will automatically calculate the weight and gestational age for you. However, if you don’t have an OB calculation package, a great resource for normal ranges of these measurements by gestational age can be found HERE .
Biparietal Diameter
- The midline falx
- Septum cavi pellucidi (labelled in the image below)
- You should not see the cerebral hemispheres.
- The structures on each side of the midline falx should be symmetrical.
- Activate the BPD measurement package on the OB/GYN preset.
- The caliper line should be perpendicular to the midline falx.
- Place the near caliper (top of the screen) on the outside of the parietal bone wall.
- Place the far caliper (bottom of the screen) on the inside of the parietal bone wall.
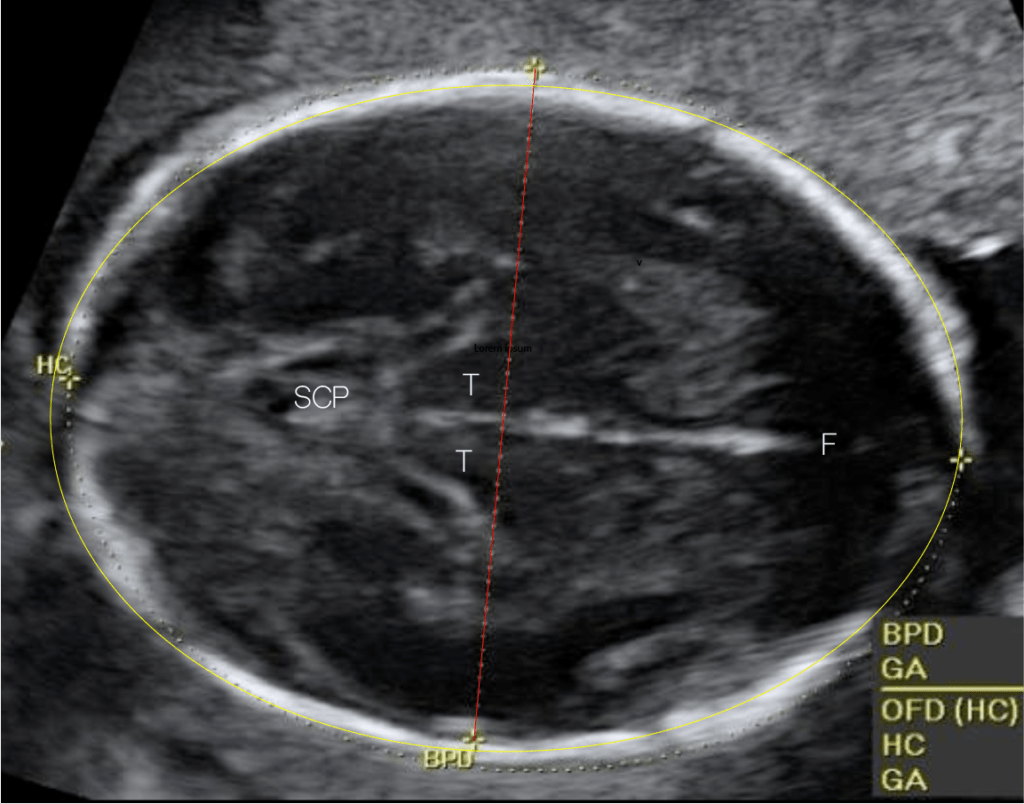
Head Circumference
- Use the same view that you acquired for the biparietal diameter measurement.
- Activate the head circumference (HC) measurement package on the OB/GYN preset.
- Trace the head circumference.
- If an ellipse tool is not available on your machine, measure the long axis diameter (OFD) of the head. The machine should calculate the head circumference from the BPD and OFD.
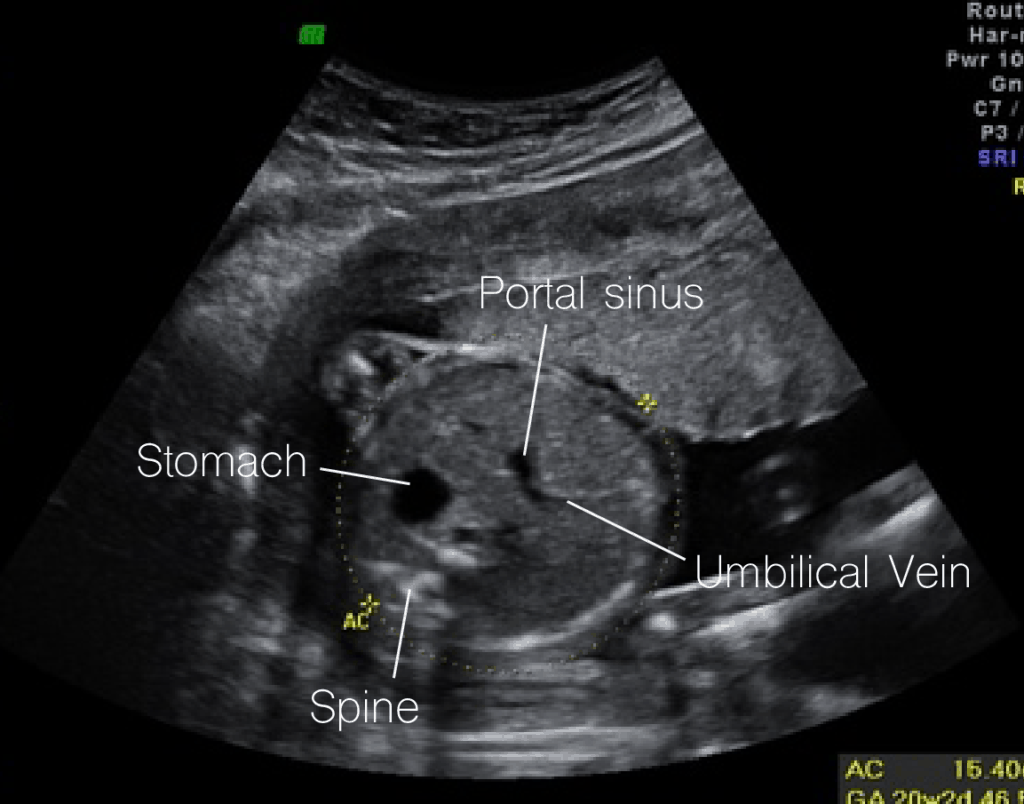
Abdominal Circumference
- Along the same transverse plane, scan down towards the fetus’ upper abdomen.
- Portal sinus
- Umbilical vein
- You should not see the kidneys.
- Activate the abdominal circumference (AC) measurement package on the OB/GYN preset.
- Trace the abdominal circumference.
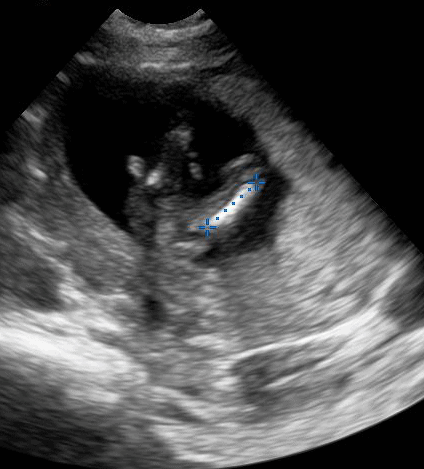
Femur Length
- Acquire a long axis view of one of the femurs.
- Activate the femur length (FL) measurement package on the OB/GYN preset.
- Place the calipers on each end of the bone.
Placental Evaluation
Normal placenta.
The placenta should be clearly visible by the beginning of 2nd trimester. Here are the characteristics of a normal placenta:
- Uniform echogenicity (shade of gray) and rounded margins
- Slight hypoechoic area behind the placenta
- Usually, the cord will be centrally inserted
- Average thickness of 2-4 cm ( Fadl et al )
To locate the placenta follow these steps:
- Starting at the superior end of the uterus, sweep from left to right in a sagittal plane.
- Follow the same pattern for more inferior sections of the uterus
- Identify the margins of the placenta.
- If the fetus is creating artifact and obscuring a posterior placenta, scan laterally.
Placenta Previa
Placenta previa refers to when the placenta is covering the internal os. This will commonly present as painless vaginal bleeding.
The earlier that placenta previa is detected, the less likely it is to be present at delivery since the placenta appears to migrate during pregnancy. However, if the placenta is covering the internal os at the onset of labor, a C-section is indicated.
Transvaginal ultrasound is preferred over transabdominal ultrasound for detecting low lying placenta and placenta previa.
Marginal placenta previa is when the placenta is extending to the edge of the internal os.
A low lying placenta is when the placenta is within 2 cm of the internal os.
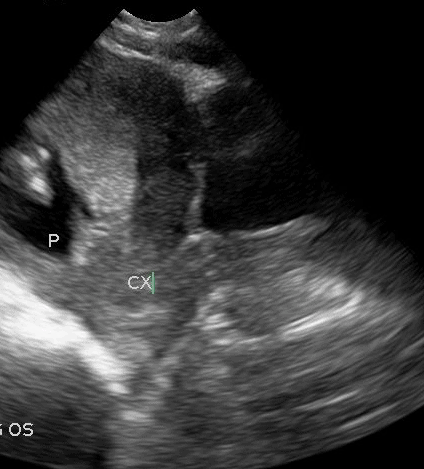
Placenta Accreta Spectrum
Placenta accreta spectrum, also known as morbidly adherent placenta or just placenta accreta, is the excessive proliferation of the placenta into the myometrium. It is defined along a spectrum based on how deep into the myometrium the placenta invades (see figure below).
- Risk factors: Prior uterine surgery, placenta previa , assisted reproduction
- Placenta Accreta: Placenta is in contact with the myometrium
- Placenta Increta: Placenta invades the myometrium
- Placenta Percreta: Placenta invades past the myometrium into adjacent structures
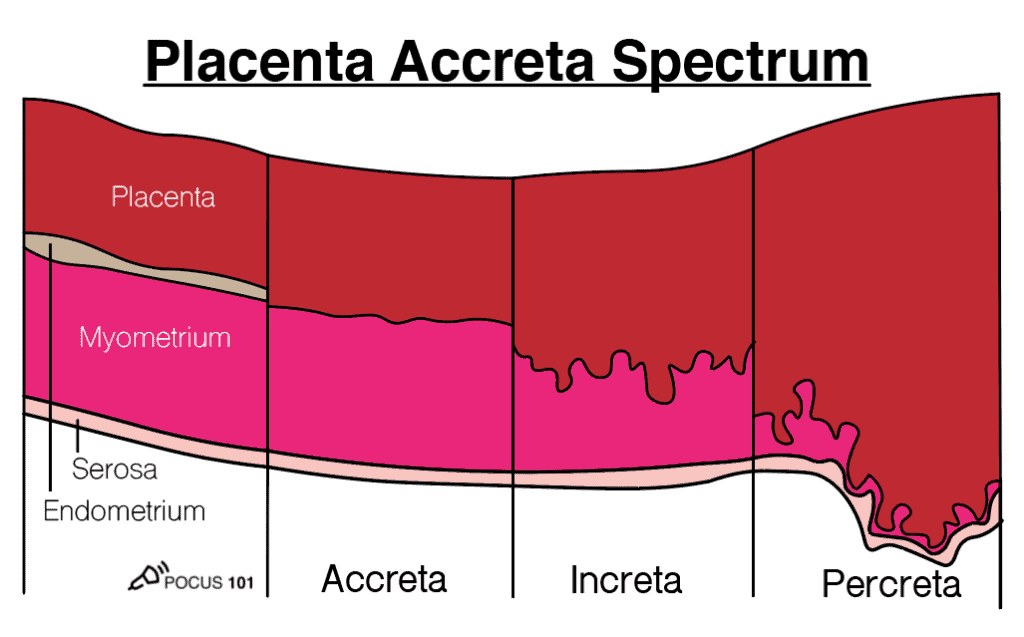
Placenta accreta spectrum has these features on ultrasound:
- Discontinuous myometrium or thin (<1 mm) myometrium
- Absent retroplacental hypoechoic space that is seen in a normal placenta
- Increased retroplacental vascularity
- This is said to look like Swiss cheese
- These will have turbulent blood flow on color doppler
- In placenta percreta: Abnormal or loss of interface between uterus and adjacent structures (e.g. bladder) with chaotic vascularity
Placental Abruption
Placental abruption occurs when the placenta prematurely separates from the uterine wall. For the fetus, this can lead to preterm birth or stillbirth. For the mother, abruption can lead to large blood loss, DIC, or even death.
Diagnosing placental abruption with ultrasound can be difficult due to the varying presentation and severity. The clinical and ultrasound appearance of abruption depends on several factors:
- The location of the placenta
- The location of the separation and bleeding (pre-placental, retroplacental, placental margin)
- How old the bleeding is
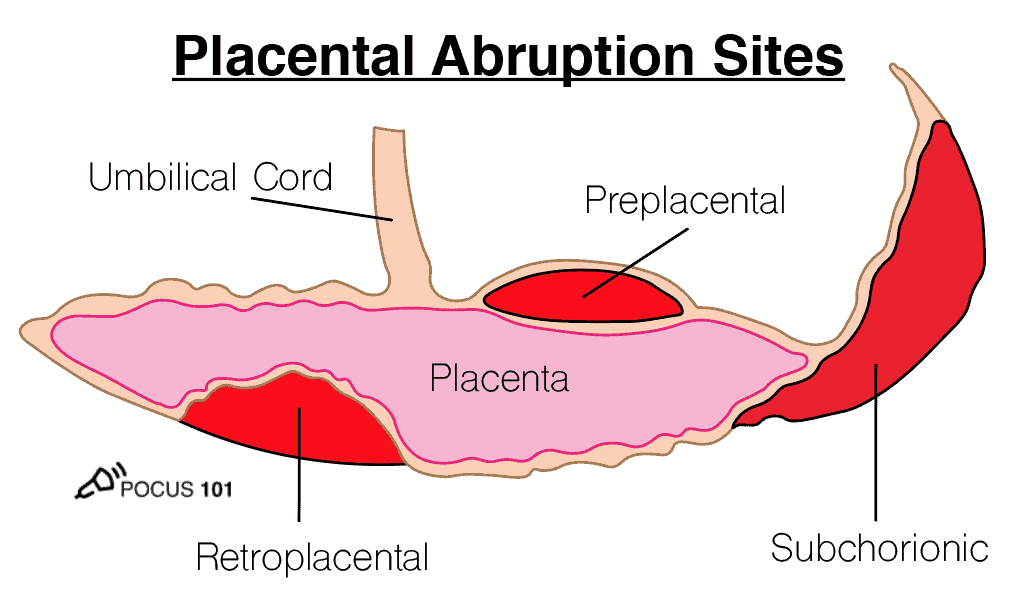
How do these factors influence ultrasound findings? Acute bleeding will appear as hypoechoic or isoechoic to the placenta. The blood will appear hyperechoic after 1-2 weeks. Therefore, a blood clot over the internal os can look similar to a placenta previa. Additionally, a retroplacental abruption can mimic the appearance of the hypoechoic space behind a normal placenta ( Oyelese & Anath ).
With those factors in mind, here are some ultrasound findings that may suggest the presence of an abruption ( Fadl et al ):
- The placenta “jiggles” with quick transducer pressure. This is known as the jello sign .
- Retroplacental, preplacental, or placental margin collection of fluid — will have a lack of flow.
- Placental heterogeneity
- Varying placental thickness
- Bree, R., Edwards, M., Bohm-Velez, M., Beyler, S., Roberts, J., Mendelson, E. (1989). Transvaginal sonography in the evaluation of normal early pregnancy: correlation with HCG level American Journal of Roentgenology 153(1), 75-79. https://dx.doi.org/10.2214/ajr.153.1.75
- Doubilet, P., Benson, C., Bourne, T., Blaivas, M., Pregnancy, S., Barnhart, K., Benacerraf, B., Brown, D., Filly, R., Fox, J., Goldstein, S., Kendall, J., Lyons, E., Porter, M., Pretorius, D., Timor-Tritsch, I. (2013). Diagnostic Criteria for Nonviable Pregnancy Early in the First Trimester New England Journal of Medicine 369(15), 1443-1451.
- Chiang, G., Levine, D., Swire, M., McNamara, A., Mehta, T. (2004). The Intradecidual Sign: Is It Reliable for Diagnosis of Early Intrauterine Pregnancy? American Journal of Roentgenology 183(3), 725-731.
- Benson, C., Doubilet, P., Peters, H., Frates, M. (2013). Intrauterine Fluid With Ectopic Pregnancy Journal of Ultrasound in Medicine 32(3), 389-393 .
- Wanyonyi, S., Napolitano, R., Ohuma, E., Salomon, L., Papageorghiou, A. (2014). Image-scoring system for crown-rump length measurement Ultrasound in Obstetrics & Gynecology 44(6), 649-654. https://dx.doi.org/10.1002/uog.13376
- Ioannou, C., Sarris, I., Hoch, L., Salomon, L., Papageorghiou, A., Century, I. (2013). Standardisation of crown-rump length measurement BJOG: An International Journal of Obstetrics & Gynaecology 120(s2), 38-41. https://dx.doi.org/10.1111/1471-0528.12056
- Stein, M., Ricci, Z., Novak, L., Roberts, J., Koenigsberg, M. (2004). Sonographic Comparison of the Tubal Ring of Ectopic Pregnancy With the Corpus Luteum Journal of Ultrasound in Medicine 23(1), 57-62 .
- Pellerito, J., Taylor, K., Quedens-Case, C., Hammers, L., Scoutt, L., Ramos, I., Meyer, W. (1992). Ectopic pregnancy: evaluation with endovaginal color flow imaging. Radiology 183(2), 407-411.
- Lin, E., Bhatt, S., Dogra, V. (2008). Diagnostic Clues to Ectopic Pregnancy RadioGraphics 28(6), 1661-1671. https://dx.doi.org/10.1148/rg.286085506
- Lozeau, A., Potter, B. (2005). Diagnosis and management of ectopic pregnancy. American family physician 72(9), 1707-14.
- Benson, C., Genest, D., Bernstein, M., Soto-Wright, V., Goldstein, D., Berkowitz, R. (2000). Sonographic appearance of first trimester complete hydatidiform moles: First trimester moles Ultrasound in Obstetrics and Gynecology 16(2), 188-191. https://dx.doi.org/10.1046/j.1469-0705.2000.00201.x
- Yefet, E., Daniel-Spiegel, E. (2016). Outcomes From Polyhydramnios With Normal Ultrasound PEDIATRICS 137(2), e20151948-e20151948. https://dx.doi.org/10.1542/peds.2015-1948
- Casey, B., McIntire, D., Bloom, S., Lucas, M., Santos, R., Twickler, D., Ramus, R., Leveno, K. (2000). Pregnancy outcomes after antepartum diagnosis of oligohydramnios at or beyond 34 weeks’ gestation American Journal of Obstetrics and Gynecology 182(4), 909-912. https://dx.doi.org/10.1016/s0002-9378(00)70345-0
- Fadl, S., Moshiri, M., Fligner, C., Katz, D., Dighe, M. (2017). Placental Imaging: Normal Appearance with Review of Pathologic Findings RadioGraphics 37(3), 979-998.
- Oyelese, Y., Ananth, C. (2006). Placental Abruption Obstetrics & Gynecology 108(4), 1005-1016.
- Abuhamad, A., Chaoui, R., Jeanty, P., Paladini, D. Ultrasound in Obstetrics & Gynecology: A Practical Approach
- Jones, R., Goldstein, J., Boulger, C., Dschaak, T., Gibson, K., Gramer, D., Kehrl, T., Kennedy, M., Lappen, J., Minardi, J., Smalley, C., Tabbut, M. (2016). Point-of-Care OB Ultrasound
- Print Friendly
- StumbleUpon
Thanks for Reading! Sign Up for POCUS 101 Updates!
[…] Obstetric/OB Ultrasound Tutorial […]
The earlier that placenta previa is detected, the less likely it is to be present at delivery since the placenta appears to migrate during pregnancy. However, if the placenta is covering the internal os at the onset of labor, a C-section is indicated.Santhathi is one of the best ivf center and gives a good treatment on fertility
It appears that you have mislabeled your BPD fetal head image. The Cavum Septum Pellucidum is in the anterior brain, and you placed it in the posterior brain. I do see it in the image you used. FYI!
Get Started Now !
Sign Up for POCUS 101 Updates!
Start scanning today .

Let's Connect!
Contact: [email protected]
© 2023 - POCUS 101
Pin it on pinterest.
Get notified about new Posts!
- Normal Normal and Abnormal First Trimester Exam Normal Fetal Ultrasound Biometry Fetal Heart Ultrasound Determining Fetal Situs Fetal Urinary System Umbilical Cord CNS Critical Anatomy CNS Embryology and Early Development CNS Later Development CNS Ultrasound Brain Anatomy
- Fetal Anomalies Fetal Heart Fetal Chest Fetal Colon Fetal Central Nervous System Facial Clefts Skeletal Dysplasia Genetic Markers
- Doppler Editorial Board Fetal Doppler Middle Cerebral Artery Doppler
- Fetal/Maternal Conditions Transvaginal Ultrasound Fetal Anemia Interventions Preterm Labor Placenta and Umbilical Cord
- Twins Key Views Twins: Videos Diamniotic Dichorionic and Diamniotic Monochorionic Twins Monochorionic Monoamniotic Twins Twin to Twin Transfusion Syndrome Fetal Growth Restriction Twin Reversed Arterial Perfusion Conjoined Twins
- Video Topics
- Access CMEs
- Other Links Topics A-Z Links CME Videos Upload Your Case Editorial Board
- Take A Free Tour
- Free Videos
- Editorial Board

Determining Normal Fetal Situs (Situs Solitus)
One of the first steps in obtaining cardiac views is to determine how the fetus is oriented within the uterus and to determine the right and left side of the abdominal contents versus the right and left side of the heart and thoracic contents. This is not as easy as it might seem since the fetal left side can be on the maternal right and the opposite can be true.
In summary, situs refers to the right and left orientation of fetal organs. For example situs solitus is the normal left to right axis arrangement in the fetus with the stomach and spleen on the left side of the body, and the liver and gallbladder on the right side.

Visual Summary of Normal Fetal Situs
Below are steps required to determine situs related to cephalic or breech presentation, and whether the spine or back is up (anterior) or down (posterior).
1. Determine the lie of the fetus:
A. Is the fetus head first with the head in front of the ultrasound screen? This could also be termed cephalic or vertex presentation. B. Is the fetal feet or bottom first with the head behind the screen? This could also be termed footling or breech presentation. C. Determine whether the spine or back is anterior (back up) or posterior (back down).
2. Obtain a transverse cut of the thorax to demonstrate a 4-chamber view. The left atrium is nearest the spine and the cardiac axis points to the left.
Detailed Method to Determine Fetal Situs
1. Define within the uterus the presentation of the fetus (generally vertex or breech; less often the presentation is oblique or transverse.).
2. Determine whether the fetal spine is parallel or transverse to the maternal spine. In sagittal view, if the fetal and maternal spine are parallel, the fetus is in longitudinal lie. When the fetal spine is perpendicular to the maternal spine, the fetus is in a transverse lie.
3. Determine the position of the fetal left side. The fetal left side will be as follows: A. With respect to the maternal abdomen, the fetal left side is anterior and near to the ultrasound transducer. B. With respect to the posterior uterine wall, the fetal left side is posterior and farthest from the transducer. C. With respect to the right uterine wall, the fetal left side will be on the maternal right. D. With respect to the left uterine wall, the fetal left side will be on the maternal left.
4. Obtain a transverse view of the abdomen and define the fetal stomach which is positioned in the left side of the fetal abdomen.
5. Obtain a 4-chamber view of the heart by obtaining a transverse view of the thorax. The left atrium and descending aorta are nearest to the spine and the cardiac axis points to the left.
6. Finally, ascertain if the stomach and heart are in their correct respective locations, i.e., the stomach is on the left side and the cardiac axis points to the left.
7. Place a transverse image of the fetal abdomen and heart side by side and validate that the left side of the fetal abdomen (stomach near to the spine) is concordant with the left side of the fetal heart (left atrium and descending aorta near to the spine). This is done by displaying a side by side comparison of a transverse view through the fetal stomach and a 4-chamber cardiac view.

Above. Normal ultrasound orientation for situs solitus.
Right Hand Rule of Thumb: Introduction
In their article “Sonographic definition of the fetal situs,” Bronshtein, Gover, and Zimmer [ 1 ] describe a “right hand rule of thumb” to define fetal situs during transabdominal scanning, and a “left hand rule of thumb” for transvaginal scanning.

Right Hand Rule of Thumb: Cephalic, supine, back down

Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The palm of the hand is anterior, or represents the ventral or face surface of the fetus. The fetus is therefore face up, back down, and the thumb points to the fetal left.
Right. Again, the imaginary fetus is back down with the stomach and cardiac axis pointing to the left. (Ignore color scheme of fetal heart and vessels.)

Right Hand Rule of Thumb: Cephalic, prone, back up
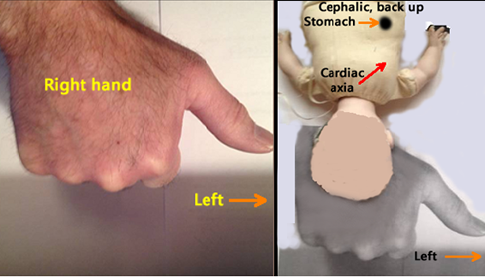
Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The top of the hand (dorsal surface or prone position) represents back up.
Right. The imaginary fetus is back up with the stomach and cardiac axis pointing to the fetal left.

Right Hand Rule of Thumb: Breech, supine, back down
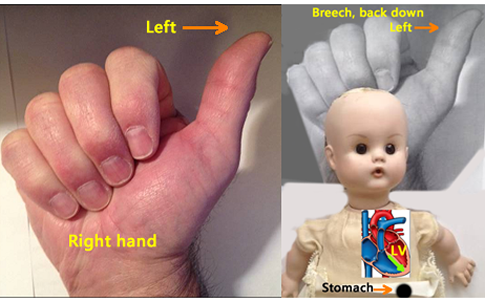
Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The palm of the sonographer’s hand is anterior, or represents the ventral surface of the fetus. The fetus is therefore face up, back down, and the thumb points to the fetal left.
Right . The imaginary fetus is back down with the stomach and cardiac axis pointing to the left. (Ignore color scheme of fetal heart and vessels).

Right Hand Rule of Thumb: Breech, prone, back up

Right . The imaginary fetus is back up with the stomach and cardiac axis pointing to the fetal left side.

- Normal CNS Anatomy
- Fetal Situs
- Normal Fetal Ultrasound Biometry
All are web-based courses. Subscribe Today!
- Literature Reviews
- Terms of Use
Fastest Obstetric, Gynecology and Pediatric Insight Engine
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Fetal Situs
● INTRODUCTION The first step in the ultrasonographic evaluation of the fetus is the assessment of fetal visceral situs as some organs are arranged symmetrically and others, such as the abdominal and thoracic organs, are arranged asymmetrically ( 1 ). A clear definition of left and right sidedness in the body is noted since early embryogenesis. A good understanding of fetal situs is important during ultrasound examinations, as some fetal anomalies are associated with abnormal laterality of abdominal and/or thoracic organs. Evaluating the orientation and position of the fetal heart in the thorax and the anatomic relationship of the abdominal organs is part of the targeted fetal cardiac examination. Knowledge of the anatomic landmarks in the chest and abdomen can facilitate the routine cardiac screening examination and provide clues to the presence of cardiac abnormality ( 1 , 2 ). This chapter will focus on the fetal situs, including the anatomic orientation of the organs in the chest and upper abdomen. ● SEQUENTIAL SEGMENTAL ANALYSIS In evaluating fetal cardiac anatomy, a sequential segmental approach helps in the description of cardiac abnormalities in a clear and simple approach. For many years, pathologists and pediatric cardiologists have been using this approach to describe normal and abnormal hearts ( 1 , 3 , 4 ). In the sequential segmental approach, the cardiovascular system is divided into segments, and for each segment, the anatomy, the position, and the connection with the next segment are described. This sequential segmental analysis involves three anatomic regions: the atria, the ventricles, and the arterial trunks. Each anatomic region is also partitioned into a right- and left-sided component. Atrioventricular valves separate the atria from the ventricles, and the semilunar valves separate the ventricles from the arterial trunks. A fourth anatomic segment, systemic and pulmonary venous connections, should also be evaluated. The cardiac chambers are therefore recognized by their morphologic structures rather than their anatomic locations. The direction of blood flow also helps assess the atrioventricular and ventriculoarterial connections. Assessment of visceral situs and cardiac position, which is described in detail in this chapter, should be part of this sequential segmental approach ( 1 , 3 , 4 ). Table 6.1 presents the steps for the sequential segmental analysis in fetal cardiac evaluation. Detailed anatomic evaluation of cardiac chambers, valvular structures, arterial trunks, and venous systems will be presented in the following chapters. TABLE 6.1 Steps for Sequential Segmental Analysis in the Fetus 1. Identify visceral situs 2. Identify atrial arrangement (morphologic right and left atrium) 3. Identify atrioventricular (AV) connections (AV valves) 4. Identify ventricular arrangement (morphologic right and left ventricle) 5. Identify ventriculoarterial connections (semilunar valves) 6. Identify arterial trunk arrangement (aorta and pulmonary artery) 7. Identify systemic and pulmonary venous connections ● FETAL VISCERAL SITUS Assessment of the fetal thoracic and visceral situs is the initial approach to the sequential segmental analysis of the fetal heart by ultrasound ( 5 ). Heterotaxy syndrome commonly involves cardiac and abdominal anomalies, and thus focusing on the fetal heart without an evaluation of the upper abdomen often results in an incomplete diagnosis. Although the current method for the determination of fetal situs relies on the position of the stomach and heart in the abdomen and chest, respectively, careful attention should also be paid to the position of the aorta and inferior vena cava below the diaphragm ( 4 , 5 ) ( Fig. 6.1 ), the orientation of the umbilical vein with the portal sinus, the presence and position of the gallbladder, and when feasible the presence and location of the spleen. It is generally agreed that the positions of the aorta and inferior vena cava below the diaphragm are more reliable criteria for the determination of right or left isomerism than the location of the stomach in the abdomen. Technique 1. Locate the fetal head within the uterus and determine the presenting part (e.g., cephalic, breech) ( Fig. 6.2 ). 2. Determine the fetal lie within the uterus by obtaining a sagittal view of the fetal spine. (Longitudinal lie: when the fetal spine is parallel to the maternal spine; transverse lie: when the fetal spine is perpendicular to the maternal spine; oblique lie: when the fetal spine is oblique to the maternal spine.) 3. After establishing the exact position of the fetus with steps 1 and 2, determine the location of the fetal left side with regard to the maternal abdomen (fetal left side is anterior [closer to the transducer], posterior [closer to the posterior uterine wall], right lateral [closer to the maternal right uterine wall], left lateral [closer to the maternal left uterine wall]) ( Fig. 6.2 ). 4. Obtain a transverse view of the fetal abdomen by rotating the transducer 90 degrees from the sagittal view of the lower thoracic spine. The fetal stomach is imaged in the left side of the abdomen, the descending aorta is posterior to the left, and the inferior vena cava is anterior to the right ( Figs. 6.1 and 6.3 ). In addition, the intrahepatic part of the umbilical vein is seen connecting with the left portal vein and portal sinus with an L-shape to the right ( Figs. 6.1 and 6.3 ). By sliding the transducer toward the fetal chest, a four-chamber view of the heart is imaged. Note that the apex of the heart is pointing toward the left side of the fetal chest ( Figs. 6.2 and 6.4 ). Determining that the stomach, descending aorta, and cardiac apex are located on the fetal left side and the inferior vena cava is located on the right side establishes normal visceral situs ( Figs. 6.1 and 6.3 ). Figure 6.1: Schematic drawing of a cross section of the upper abdomen for the assessment of the abdominal situs. The vertical line divides this plane into right and left. The right-sided structures include the gallbladder, the portal sinus, a large part of the liver, and inferior vena cava (IVC). The left-sided structures include the descending aorta, the stomach, and the spleen. Figure 6.3 is the corresponding ultrasound plane. Figure 6.2: Determining fetal situs in longitudinal lie: In A , the fetus is in a cephalic presentation with the fetal spine close to the left uterine wall, resulting in the right side being anterior and left side posterior. In B , the fetus is in a cephalic presentation with the fetal spine close to the right uterine wall, resulting in the left side being anterior and right side posterior. In C , the fetus is in a breech presentation with the fetal spine close to the left uterine wall, resulting in the left side being anterior and right side posterior. In D , the fetus is in a breech presentation with the fetal spine close to the right uterine wall, resulting in the right side being anterior and left side posterior. Note the corresponding transverse ultrasound planes of the chest and abdomen. Blue arrows point to fetal stomach, red arrows to the apex of the heart, and yellow arrows to the descending aorta. See text for details. Several methods for determining fetal situs during the ultrasound examination have been described. Cordes et al. ( 6 ) described a technique that involves orienting the transducer in a standardized way so that the fetal head is on the right side of the screen in a fetal sagittal plane as a starting point and then rotating the transducer 90 degrees in clockwise to obtain the caudocranial transverse views. Another method reported by Bronshtein et al. ( 7 ) is referred to as the right-hand rule for abdominal scanning and the left-hand rule for transvaginal scanning ( Fig. 6.5 ). The palm of the hand corresponds to the face of the fetus, and the examiner holds the hand according to the side of the fetal face; the fetal heart and stomach are shown by the examiner’s thumb. Figure 6.3: Axial view of the fetal abdomen in a fetus with situs solitus. Note the location of the liver, portal sinus (PS), and inferior vena cava (IVC) in right side (R); and the stomach (St) and descending aorta (Ao) in left side (L). The umbilical vein (UV) is located in the midline. Compare with Figure 6.1 . Figure 6.4: Schematic drawing of a cross section of the thorax at the level of the four-chamber view in a fetus with situs solitus. Note the position of the heart in the left chest with a normal cardiac axis of 45 degrees. See text for details. LA, left atrium; RA, right atrium; LV, left ventricle; RV, right ventricle; Ao, Aorta; L, left; R, right. Situs Solitus, Situs Inversus, and Situs Ambiguous Three types of visceral situs exist: situs solitus, situs inversus, and situs ambiguous ( Table 6.2 ). a.) Situs solitus refers to the normal arrangement of vessels and organs within the body ( Fig. 6.1 ). b.) Situs inversus, with an incidence of about 0.01% of the population, refers to a mirror-image arrangement of organs and vessels to situs solitus. Situs inversus is associated with a slight increase in the incidence of complex congenital heart disease (CHD), in the order of 0.3% to 5% ( 8 ), and with the presence of Kartagener syndrome in about 20% of the cases ( 9 ). Kartagener syndrome, with an autosomal recessive transmission, primarily involves ciliary dysfunction with recurrent respiratory infection and reduced fertility. c.) Situs ambiguous (heterotaxy), which refers to visceral malpositions and malformations different from situs solitus or inversus, is commonly associated with complex CHD, abnormalities in venous drainage, bowel malrotations and obstruction, and splenic, biliary, and bronchial tree abnormalities. The incidence of situs ambiguous has been estimated around 1 per 10,000 infants ( 10 ). Two types of heterotaxy exist: right isomerism and left isomerism. In right isomerism, also referred to as asplenia, both sides of the body show the right morphology; in left isomerism, also referred to as polysplenia, both sides of the body show the left morphology. Chapter 30 presents a detailed overview of heterotaxy and isomerism in the fetus. Figure 6.5: Determining fetal situs: A diagram of the fetus is presented in back posterior ( 1 and 3 ) and back anterior ( 2 and 4 ) positions. In transabdominal scanning, the ultrasound beam (S) is directed from top to bottom. The palm of the right hand represents the face of the fetus, and the fetal heart and stomach are on the same side of the examiner’s thumb. (Modified from Bronshtein M, Gover A, Zimmer EZ. Sonographic definition of the fetal situs. Obstet Gynecol. 2002;99( 6 ):1129–1130, with permission.)
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Fetal Cardiac Measurements and Reference Ranges
- Color Doppler in Fetal Echocardiography
- The Three-Vessel-Trachea View and Upper Mediastinum
- Three- and Four-Dimensional Ultrasound of the Fetal Heart
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree


- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Original Author(s): Minesh Mistry Last updated: 12th November 2018 Revisions: 7
- 1 Introduction
- 2 Preparation
- 3 General Inspection
- 4 Abdominal Inspection
- 5.1 Fundal Height
- 5.3 Presentation
- 5.4 Liquor Volume
- 5.5 Engagement
- 6 Fetal Auscultation
- 7 Completing the Examination
The obstetric examination is a type of abdominal examination performed in pregnancy.
It is unique in the fact that the clinician is simultaneously trying to assess the health of two individuals – the mother and the fetus.
In this article, we shall look at how to perform an obstetric examination in an OSCE-style setting.
Introduction
- Introduce yourself to the patient
- Wash your hands
- Explain to the patient what the examination involves and why it is necessary
- Obtain verbal consent
Preparation
- In the UK, this is performed at the booking appointment, and is not routinely recommended at subsequent visits
- Patient should have an empty bladder
- Cover above and below where appropriate
- Ask the patient to lie in the supine position with the head of the bed raised to 15 degrees
- Prepare your equipment: measuring tape, pinnard stethoscope or doppler transducer, ultrasound gel
General Inspection
- General wellbeing – at ease or distressed by physical pain.
- Hands – palpate the radial pulse.
- Head and neck – melasma, conjunctival pallor, jaundice, oedema.
- Legs and feet – calf swelling, oedema and varicose veins.
Abdominal Inspection
In the obstetric examination, inspect the abdomen for:
- Distension compatible with pregnancy
- Fetal movement (>24 weeks)
- Surgical scars – previous Caesarean section, laproscopic port scars
- Skin changes indicative of pregnancy – linea nigra (dark vertical line from umbilicus to the pubis), striae gravidarum (‘stretch marks’), striae albicans (old, silvery-white striae)
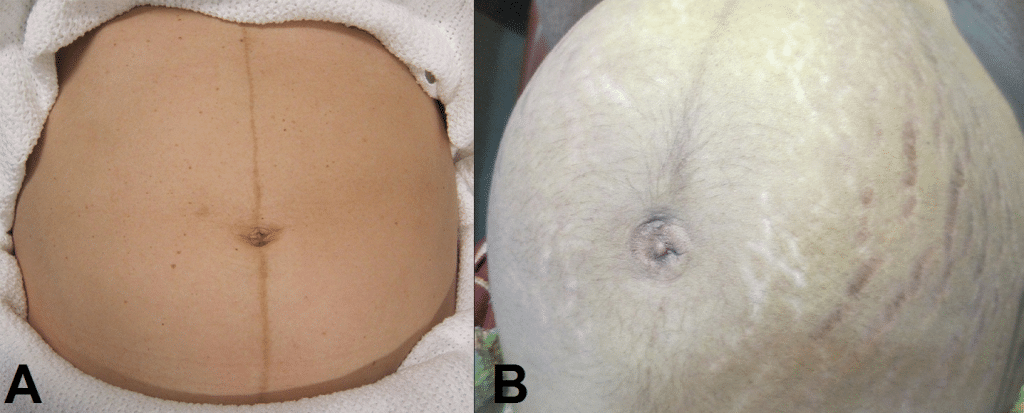
Fig 1 – Skin changes in pregnancy. A) Linea nigra. B) Striae gravidarum and albicans.
Ask the patient to comment on any tenderness and observe her facial and verbal responses throughout. Note any guarding.
Fundal Height
- Use the medial edge of the left hand to press down at the xiphisternum, working downwards to locate the fundus.
- Measure from here to the pubic symphysis in both cm and inches. Turn the measuring tape so that the numbers face the abdomen (to avoid bias in your measurements).
- Uterus should be palpable after 12 weeks, near the umbilicus at 20 weeks and near the xiphisternum at 36 weeks (these measurements are often slightly different if the woman is tall or short).
- The distance should be similar to gestational age in weeks (+/- 2 cm).
- Facing the patient’s head, place hands on either side of the top of the uterus and gently apply pressure
- Move the hands and palpate down the abdomen
- One side will feel fuller and firmer – this is the back. Fetal limbs may be palpable on the opposing side
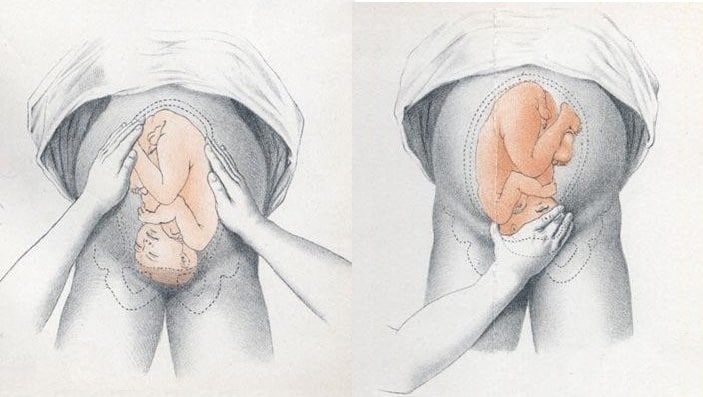
Fig 2 – Assessing fetal lie and presentation.
Presentation
- Palpate the lower uterus (below the umbilicus) to find the presenting part.
- Firm and round signifies cephalic, soft and/or non-round suggests breech. If breech presentation is suspected, the fetal head can be often be palpated in the upper uterus.
- Ballot head by pushing it gently from one side to the other.
Liquor Volume
- Palpate and ballot fluid to approximate volume to determine if there is oligohydraminos/polyhydramnios
- When assessing the lie, only feeling fetal parts on deep palpation suggests large amounts of fluid
- Fetal engagement refers to whether the presenting part has entered the bony pelvis
- Note how much of the head is palpable – if the entire head is palpable, the fetus is unengaged.
- Engagement is measured in 1/5s
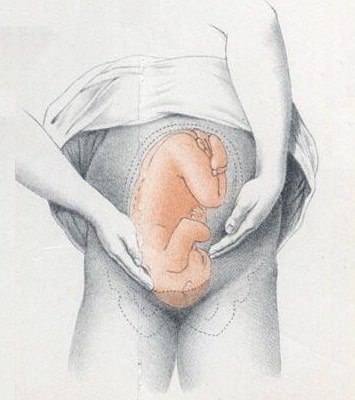
Fig 3 – Assessing fetal engagement.
Fetal Auscultation
- Hand-held Doppler machine >16 weeks (trying before this gestation often leads to anxiety if the heart cannot be auscultated).
- Pinard stethoscope over the anterior shoulder >28 weeks
- Feel the mother’s pulse at the same time
- Should be 110-160bpm (>24 weeks)
Completing the Examination
- Palpate the ankles for oedema and test for hyperreflexia (pre-eclampsia)
- Thank the patient and allow them to dress in private
- Summarise findings
- Blood pressure
- Urine dipstick
- Hands - palpate the radial pulse.
- Skin changes indicative of pregnancy - linea nigra (dark vertical line from umbilicus to the pubis), striae gravidarum ('stretch marks'), striae albicans (old, silvery-white striae)
- One side will feel fuller and firmer - this is the back. Fetal limbs may be palpable on the opposing side
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Turk Ger Gynecol Assoc
- v.21(3); 2020 Sep

A novel technique for determining the axis of the fetal heart: Clock position method
Sezgin dursun.
1 Private Clinic, Ağrı, Turkey
Fatih Aktoz
2 Clinic of Obstetrics and Gynecology, Ağrı State Hospital, Ağrı, Turkey
To the Editor,
Determination of the fetal heart axis via ultrasonography is crucial as some cardiovascular diseases can only be diagnosed according to the accuracy of fetal heart position. There are reliable methods for ultrasonographic assessment of the left/right axis by using fetal stomach or gallbladder as a landmark. However, if there is a malposition of an indicator organ, it may be difficult to distinguish the left side from the right side. For this reason, these methods sometimes require more experienced physicians to obtain reliable results. For inexperienced clinicians this can be more difficult because both understanding the position of fetus and ultrasound probe orientation can be confusing. There is a need for a practical technique that can be used easily and reliably by perinatologists or obstetricians.
We suggest an easy method for assessment of the fetal heart axis. In our method, the physician should be seated on the right side of the patient, hold the probe with the right hand and perform a transabdominal examination. The left side of the probe should be on the left side of the ultrasound screen. The fetus should be scanned in a transverse plane. The thoracic cavity is imagined as a watch dial and the fetal spine refers the 12 o’clock position. If the fetus is in breech presentation, the axis of the heart should be approximately at the 7 o’clock position ( Figure 1a ) and similarly, if the fetus is in cephalic presentation, the axis of the heart should be approximately at the 5 o’clock position ( Figure 1b ). If the fetus is in a transverse lie, indicator of the probe should point to patient’s head for sagittal imaging and the fetal structure nearest to clinician (in other words closest part of the fetus to maternal right side) is accepted as the presenting part.

Clock position method to determine fetal heart axis. The spine always refers to the 12 o’clock position (a) Breech presentation; the axis of the heart at the 7 o’clock position. (b) Cephalic presentation; the axis of the heart at the 5 o’clock position
Other methods have been described to assess of the fetal heart position. Cordes et al. ( 1 ) described a technique in 1994. The left and right side of the fetus was distinguished depending on parameters such as position of fetus and mother, ultrasound probe orientation and video screen. Although being accurate and reliable, it is not easy to learn and perform for all practitioners. Bronshtein et al. ( 2 ) suggested a simple technique to determine fetal situs. They used forearm, hand and thumb for orientation. In this method, right hand for transabdominal examination and left hand for transvaginal examination was used. The dorsal side of the forearm referred to the fetal back and thumb showed the fetal left side. It is more user-friendly than Cordes et al.’s ( 1 ) technique but clinicians can be confused when they choose the appropriate hand to use for evaluation. The method that we described can be used by any clinician. It does not require calculation. Thus, it requires less time compared to others. In addition, our method is not affected by fetal movements. In conclusion, we believe that this technique may be a good option for clinicians at every level of experience.

IMAGES
VIDEO
COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
It is used to determine the position, presentation, and engagement of the fetus in utero. This activity describes the four Leopold maneuvers and explains the method of systematic abdominal palpation used to assess fetal presentation and position in the third trimester of pregnancy. Objectives: Describe the normal fetal presentation and position.
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.. In brow presentation, the neck is moderately arched so that the brow presents first.. Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech ...
Fetal position reflects the orientation of the fetal head or butt within the birth canal. Anterior Fontanel. The bones of the fetal scalp are soft and meet at "suture lines." Over the forehead, where the bones meet, is a gap, called the "anterior fontanel," or "soft spot." This will close as the baby grows during the 1st year of life, but at ...
The Leopold maneuver is used to determine fetal presentation, which refers to the part of the fetus that enters the maternal pelvis first. The most common fetal presentation is the cephalic presentation, where the baby is head-down. However, other presentations, such as breech or transverse, require special attention during labor and delivery. ...
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
The fetus undergoes a series of changes in position, attitude, and presentation during labor. This process is essential for the accomplishment of a vaginal delivery. The presence of a fetal malpresentation or an abnormality of the maternal pelvis can significantly impede the likelihood of a vaginal delivery. The contractile aspect of the uterus ...
Looking at where the baby's head is in the birth canal helps determine the fetal position.The front of a baby's head is referred to as the anterior portion and the back is the posterior portion. There are two different positions called occiput anterior (OA) positions that may occur. ... The right occiput anterior (ROA) presentation is also ...
Determining fetal lie, position, presentation and attitude Follow the 4 steps of the Leopold Maneuver for abdominal palpation to determine fetal lie and presentation. Diagnose Count for 60 seconds to have the fetal heart rate bpm (beats per minute) or count for 15 seconds and multiply by 4. A normal heart rate is between 120 and 160 bpm.
Fetal presentation. Fetal presentation refers to which anatomical part of the fetus is closest to the pelvic inlet. Assess the gravid uterus to determine fetal presentation: 1. Ensure you are facing the patient to observe for signs of discomfort and warn the patient this may feel a little uncomfortable. 2.
Maneuver 1: Fundus palpation to determine fetal presentation. Palpate the fundus of the uterus to determine what part of the fetus is in the upper part of the uterus. Findings: Fetal head: firm, hard, round, moves independent of trunk. Buttock: less well defined, soft, moves with trunk. No discrete part: may indicate transverse lie.
Place your hands on the patient's abdomen to determine fetal position in the uterine fundus. Curl your fingers around the fundus. When the fetus is in the vertex position (head first), the buttocks should feel irregularly shaped and firm. When the fetus is in the breech position, the head should feel hard, round, and movable.
Compound presentation means that a fetal hand is coming out with the fetal head. This is a problem because: The amount of baby that must come through the birth canal at one time is increased. There is increased risk of mechanical injury to the arm and shoulder, including fractures, nerve injuries and soft tissue injury.
Use the steps described above to calculate the fetal heart rate. Acquire a 4-chamber view of the fetal heart. This view can be found by scanning through the fetus in a transverse plane. ... Fetal Presentation. The presentation of the fetus refers to which part of the fetus is closest to the birth canal. Obtain a midline sagittal view of the ...
Detailed Method to Determine Fetal Situs. 1. Define within the uterus the presentation of the fetus (generally vertex or breech; less often the presentation is oblique or transverse.). 2. Determine whether the fetal spine is parallel or transverse to the maternal spine. In sagittal view, if the fetal and maternal spine are parallel, the fetus ...
Figure 6.2: Determining fetal situs in longitudinal lie: In A, the fetus is in a cephalic presentation with the fetal spine close to the left uterine wall, resulting in the right side being anterior and left side posterior.In B, the fetus is in a cephalic presentation with the fetal spine close to the right uterine wall, resulting in the left side being anterior and right side posterior.
Lie. Facing the patient's head, place hands on either side of the top of the uterus and gently apply pressure. Move the hands and palpate down the abdomen. One side will feel fuller and firmer - this is the back. Fetal limbs may be palpable on the opposing side. Fig 2 - Assessing fetal lie and presentation.
Figure 1. Clock position method to determine fetal heart axis. The spine always refers to the 12 o'clock position (a) Breech presentation; the axis of the heart at the 7 o'clock position. (b) Cephalic presentation; the axis of the heart at the 5 o'clock position. Other methods have been described to assess of the fetal heart position.
About Press Copyright Contact us Creators Advertise Developers Terms Privacy Policy & Safety How YouTube works Test new features NFL Sunday Ticket Press Copyright ...