The Healthcare System in the U.S. Essay
The book, “Essentials of the U.S. Health Care System” provides information and insights regarding the health care system in the U.S. The first point that stood out to me is that today the main concern of the health care system is public health rather than patient-centered care. Chapter 3 addresses a historical overview of the healthcare system in the U.S. It points out that there is a shift from patient-oriented healthcare to a focus on the need for chronic disease managers (Shi, 2017). I think that this is a crucial change in the system as the modern world is experiencing an increase in chronic diseases and the spread of new viruses like COVID-19. The world was in lockdown and the issue of public health was critical. I am now wondering if the shift in the health care system would influence the quality of services as now the majority is a priority over individual cases.
The second point that stood out to me is that the healthcare system is very pricy and that there are many racial and socioeconomic disparities regarding access to care, its quality, and delivery. Everyone knows that U.S. health care is expensive, but I do not think about the issue in detail. African American people and other non-white people were not able to obtain good health care throughout many years of the struggle against racial discrimination (Shi, 2017). Even in the modern world, some medical professionals still have prejudices regarding race and ethnicity that hinder health care delivery. As such, it is crucial to address such racial and socio-economic issues to prevent them from happening in the future.
Shi, L. (2017). Essentials of the U.S. Health Care System . Burlington, Massachusetts: Jones & Bartlett Learning.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, June 9). The Healthcare System in the U.S. https://ivypanda.com/essays/the-healthcare-system-in-the-us/
"The Healthcare System in the U.S." IvyPanda , 9 June 2023, ivypanda.com/essays/the-healthcare-system-in-the-us/.
IvyPanda . (2023) 'The Healthcare System in the U.S'. 9 June.
IvyPanda . 2023. "The Healthcare System in the U.S." June 9, 2023. https://ivypanda.com/essays/the-healthcare-system-in-the-us/.
1. IvyPanda . "The Healthcare System in the U.S." June 9, 2023. https://ivypanda.com/essays/the-healthcare-system-in-the-us/.
Bibliography
IvyPanda . "The Healthcare System in the U.S." June 9, 2023. https://ivypanda.com/essays/the-healthcare-system-in-the-us/.
- The Convenience of the Emergency Care System
- Explaining the Importance of Introducing U.S. Health Care Reforms
- Non-White Experience: Stereotyping and Discrimination
- Hear Her Healthcare Campaign Evaluation
- The Socioeconomic and Political Impact of COVID-19
- Addressing the Social Determinants of Health
- The Relevance of Bedsores: Background to the Study
- Quitting Smoking and Related Health Benefits
Suggestions or feedback?

MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
What has the pandemic revealed about the US health care system — and what needs to change?
Press contact :.

Previous image Next image
With vaccinations for Covid-19 now underway across the nation, MIT SHASS Communications asked seven MIT scholars engaged in health and health care research to share their views on what the pandemic has revealed about the U.S. health care system — and what needs to change. Representing the fields of medicine, anthropology, political science, health economics, science writing, and medical humanities, these researchers articulate a range of opportunities for U.S. health care to become more equitable, more effective and coherent, and more prepared for the next pandemic.
Dwaipayan Banerjee , associate professor of science, technology, and society
On the heels of Ebola, Covid-19 put to rest a persistent, false binary between diseases of the rich and diseases of the poor. For several decades, health care policymakers have labored under the impression of a great epidemiological transition. This theory holds that the developed world has reached a stage in its history that it no longer needs to worry about communicable diseases. These "diseases of the poor" are only supposed to exist in distant places with weak governments and struggling economies. Not here in the United States.
On the surface, Covid-19 made clear that diseases do not respect national boundaries. More subtly, it tested the hypothesis that the global north no longer need concern itself with communicable disease. And in so doing, it undermined our assumptions about global north health-care infrastructures as paradigmatically more evolved. Over the last decades, the United States has been focused on developing increasingly sophisticated drugs. While this effort has ushered in several technological breakthroughs, a preoccupation with magic-bullet cures has distracted from public health fundamentals. The spread of the virus revealed shortages in basic equipment and hospitals beds, the disproportionate effects of disease on the marginalized, the challenge of prevention rather than cure, the limits of insurance-based models to provide equitable care, and our unacknowledged dependence on the labor of underpaid health care workers.
To put it plainly, the pandemic did not create a crisis in U.S. health care. For many in the United States, crisis was already a precondition of care, delivered in emergency rooms and negotiated through denied insurance claims. As we begin to imagine a "new normal," we must ask questions about the old. The pandemic made clear that the "normal" had been a privilege only for a few well-insured citizens. In its wake, can we imagine a health-care system that properly compensates labor and recognizes health care as a right, rather than a privilege only available to the marginalized when an endemic crisis is magnified by a pandemic emergency?
Andrea Campbell , professor of political science
No doubt, the pandemic reveals the dire need to invest in public-health infrastructure to better monitor and address public-health threats in the future, and to expand insurance coverage and health care access. To my mind, however, the pandemic’s greatest significance is in revealing the racism woven into American social and economic policy.
Public policies helped create geographic and occupational segregation to begin with; inadequate racist and classist public policies do a poor job of mitigating their effects. Structural racism manifests at the individual level, with people of color suffering worse housing and exposure to toxins, less access to education and jobs, greater financial instability, poorer physical and mental health, and higher infant mortality and shorter lifespans than their white counterparts. Residential segregation means many white Americans do not see these harms.
Structural racism also materializes at the societal level, a colossal waste of human capital that undercuts the nation’s economic growth, as social and economic policy expert Heather McGhee shows in her illuminating book, "The Sum of Us." These society-wide costs are hidden as well; it is difficult to comprehend the counterfactual of what growth would look like if all Americans could prosper. My hope is that the pandemic renders this structural inequality visible. There is little point in improving medical or public-health systems if we fail to address the structural drivers of poor health. We must seize the opportunity to improve housing, nutrition, and schools; to enforce regulations on workplace safety, redlining, and environmental hazards; and to implement paid sick leave and paid family leave, among other changes. It has been too easy for healthy, financially stable, often white Americans to think the vulnerable are residual. The pandemic has revealed that they are in fact central. It’s time to invest for a more equitable future.
Jonathan Gruber , Ford Professor of Economics
The Covid-19 pandemic is the single most important health event of the past 100 years, and as such has enormous implications for our health care system. Most significantly, it highlights the importance of universal, non-discriminatory health insurance coverage in the United States. The primary source of health insurance for Americans is their job, and with unemployment reaching its highest level since the Great Depression, tens of millions of workers lost, at least temporarily, their insurance coverage.
Moreover, even once the economy recovers, millions of Americans will have a new preexisting condition, Covid-19. That’s why it is critical to build on the initial successes of the Affordable Care Act to continue to move toward a safety net that provides insurance options for all without discrimination.
The pandemic has also illustrated the power of remote health care. The vast majority of patients in the United States have had their first experience with telehealth during the pandemic and found it surprisingly satisfactory. More use of telehealth can lead to increased efficiency of health care delivery as well as allowing our system to reach underserved areas more effectively.
The pandemic also showed us the value of government sponsorship of innovation in the health sciences. The speed with which the vaccines were developed is breathtaking. But it would not have been possible without decades of National Institute of Health investments such as the Human Genome Project, nor without the large incentives put in place by Operation Warp Speed. Even in peacetime, the government has a critical role to play in promoting health care innovation
The single most important change that we need to make to be prepared for the next pandemic is to recognize that proper preparation is, by definition, overpreparation. Unless we are prepared for the next pandemic that doesn’t happen, we won’t possibly be ready for the next pandemic that does.
This means working now, while the memory is fresh, to set up permanent, mandatorily funded institutions to do global disease surveillance, extensive testing of any at-risk populations when new diseases are detected, and a permanent government effort to finance underdeveloped vaccines and therapeutics.
Jeffrey Harris , professor emeritus of economics and a practicing physician The pandemic has revealed the American health care system to be a non-system. In a genuine system, health care providers would coordinate their services. Yet when Elmhurst Hospital in Queens was overrun with patients, some 3,500 beds remained available in other New York hospitals. In a genuine system, everyone would have a stable source of care at a health maintenance organization (HMO). While our country has struggled to distribute the Covid-19 vaccine efficiently and equitably, Israel, which has just such an HMO-based system, has broken world records for vaccination.
Germany, which has all along had a robust public health care system, was accepting sick patients from Italy, Spain, and France. Meanwhile, U.S. hospitals were in financial shock and fee-for-service-based physician practices were devastated. We need to move toward a genuine health care system that can withstand shocks like the Covid-19 pandemic. There are already models out there to imitate. We need to strengthen our worldwide pandemic and global health crisis alert systems. Despite concerns about China’s early attempts to suppress the bad news about Covid-19, the world was lucky that Chinese investigators posted the full genome of SARS-CoV-2 in January 2020 — the singular event that triggered the search for a vaccine. With the recurrent threat of yet another pandemic — after H1N1, SARS, MERS, Ebola, and now SARS-Cov-2 — along with the anticipated health consequences of global climate change, we can’t simply cross our fingers and hope to get lucky again.
Erica Caple James , associate professor of medical anthropology and urban studies The coronavirus pandemic has revealed some of the limits of the American medical and health care system and demonstrated many of the social determinants of health. Neither the risks of infection nor the probability of suffering severe illness are equal across populations. Each depends on socioeconomic factors such as type of employment, mode of transportation, housing status, environmental vulnerability, and capacity to prevent spatial exposure, as well as “preexisting” health conditions like diabetes, obesity, and chronic respiratory illness.
Such conditions are often determined by race, ethnicity, gender, and “biology,” but also poverty, cultural and linguistic facility, health literacy, and legal status. In terms of mapping the prevalence of infection, it can be difficult to trace contacts among persons who are regular users of medical infrastructure. However, it can be extraordinarily difficult to do so among persons who lack or fear such visibility, especially when a lack of trust can color patient-clinician relationships.
One’s treatment within medical and health care systems may also reflect other health disparities — such as when clinicians discount patient symptom reports because of sociocultural, racial, or gender stereotypes, or when technologies are calibrated to the norm of one segment of the population and fail to account for the severity of disease in others.
The pandemic has also revealed the biopolitics and even the “necropolitics” of care — when policymakers who are aware that disease and death fall disproportionately in marginal populations make public-health decisions that deepen the risks of exposure of these more vulnerable groups. The question becomes, “Whose lives are deemed disposable?” Similarly, which populations — and which regions of the world — are prioritized for treatment and protective technologies like vaccines and to what degree are such decisions politicized or even racialized?
Although no single change will address all of these disparities in health status and access to treatment, municipal, state, and federal policies aimed at improving the American health infrastructure — and especially those that expand the availability and distribution of medical resources to underserved populations — could greatly improve health for all.
Seth Mnookin , professor of science writing
The Covid-19 pandemic adds yet another depressing data point to how the legacy and reality of racism and white supremacy in America is lethal to historically marginalized groups. A number of recent studies have shown that Black, Hispanic, Asian, and Native Americans have a significantly higher risk of infection, hospitalization, and death compared to white Americans.
The reasons are not hard to identify: Minority populations are less likely to have access to healthy food options, clean air and water, high-quality housing, and consistent health care. As a result, they’re more likely to have conditions that have been linked to worse outcomes in Covid patients, including diabetes, hypertension, and obesity.
Marginalized groups are also more likely to be socioeconomically disadvantaged — which means they’re more likely to work in service and manufacturing industries that put them in close contact with others, use public transportation, rely on overcrowded schools and day cares, and live in closer proximity to other households. Even now, more vaccines are going to wealthier people who have the time and technology required to navigate the time-consuming vaccine signup process and fewer to communities with the highest infection rates.
This illustrates why addressing inequalities in Americans’ health requires addressing inequalities that infect every part of society. Moving forward, our health care systems should take a much more active role in advocating for racial and socioeconomic justice — not only because it is the right thing to do, but because it is one of the most effective ways to improve health outcomes for the country as a whole.
On a global level, the pandemic has illustrated that preparedness and economic resources are no match for lies and misinformation. The United States, Brazil, and Mexico have, by almost any metric, handled the pandemic worse than virtually every other country in the world. The main commonality is that all three were led by presidents who actively downplayed the virus and fought against lifesaving public health measures. Without a global commitment to supporting accurate, scientifically based information, there is no amount of planning and preparation that can outflank the spread of lies.
Parag Pathak , Class of 1922 Professor of Economics The pandemic has revealed the strengths and weaknesses of America’s health care systems in an extreme way. The development and approval of three vaccines in roughly one year after the start of the pandemic is a phenomenal achievement. At the same time, there are many innovations for which there have been clear fumbles, including the deployment of rapid tests and contact tracing. The other aspect the pandemic has made apparent is the extreme inequality in America’s health systems. Disadvantaged communities have borne the brunt of Covid-19 both in terms of health outcomes and also economically. I’m hopeful that the pandemic will spur renewed focus on protecting the most vulnerable members of society. A pandemic is a textbook situation in economics of externalities, where an individual’s decision has external effects on others. In such situations, there can be major gains to coordination. In the United States, the initial response was poorly coordinated across states. I think the same criticism applies globally. We have not paid enough attention to population health on a global scale. One lesson I take from the relative success of the response of East Asian countries is that centralized and coordinated health systems are more equipped to manage population health, especially during a pandemic. We’re already seeing the need for international cooperation with vaccine supply and monitoring of new variants. It will be imperative that we continue to invest in developing the global infrastructure to facilitate greater cooperation for the next pandemic.
Prepared by MIT SHASS Communications Editor and designer: Emily Hiestand Consulting editor: Kathryn O'Neill
Share this news article on:
Related links.
- Program in Science, Technology and Society
- Graduate Program in Science Writing
- MIT Anthropology
- Department of Economics
- Department of Political Science
- Department of Urban Studies and Planning
Related Topics
- Anthropology
- Political science
- Program in STS
- Science writing
- Public health
- Health care
- Diversity and inclusion
- Science, Technology, and Society
- School of Humanities Arts and Social Sciences
Related Articles

Reflecting on a year of loss, grit, and pulling together
Building equity into vaccine distribution.

In online vigil, MIT community shares grief, anger, and hope
Previous item Next item
More MIT News

Elaine Liu: Charging ahead
Read full story →
Scientists use generative AI to answer complex questions in physics
New tool empowers users to fight online misinformation

2024 MIT Supply Chain Excellence Awards given to 35 undergraduates

Faces of MIT: Reimi Hicks

John Joannopoulos receives 2024-2025 Killian Award
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Care Financ Rev
- v.14(1); Fall 1992

A layman's guide to the U.S. health care system
This article provides an overview of the U.S. health care system and recent proposals for health system reform. Prepared for a 15-nation comparative study for the Organization for Economic Cooperation and Development (OECD), the article summarizes descriptive data on the financing, utilization, access, and supply of U.S. health services; analyzes health system cost growth and trends; reviews health reforms adopted in the 1980s; and discusses proposals in the current health system reform debate.
Introduction
This article was prepared for a 15-country comparative analysis of health system reforms in the 1980s in Organization for Economic Cooperation and Development (OECD) countries. 1 This OECD project follows up on an earlier 7—country comparative study ( Schneider, 1991 ). This article pulls together basic structural information, reviews trends in the growth of health system costs and indicators, discusses the major health system reforms of the 1980s, and summarizes the proposed changes currently being debated. As a part of this OECD project, a comparative study of all 15 countries is currently being written and will be published by OECD, along with the individual country papers early next year.
The United States spends more on health care services than does any other nation—on average, more than twice as much per person as the other OECD countries ( Schieber, Poullier, and Greenwald, 1991 ). These expenditures are financed by a complex mixture of public payers (Federal, State, and local government), as well as private insurance and individual payments: There is no single nationwide system of health insurance. The United States primarily relies on employers to voluntarily provide health insurance coverage to their employees and dependents; government programs are confined to the elderly, the disabled, and some of the poor. These private and public health insurance programs all differ with respect to benefits covered, sources of financing, and payments to medical care providers. There is little coordination between private and public programs: Some people have both public and private insurance while others have neither. Nevertheless, persons without health insurance are not entirely without health care. Although they receive fewer and less coordinated services than those with insurance, many of these “uninsured” individuals receive health care services through public clinics and hospitals, State and local health programs, or private providers who finance the care through charity and by shifting costs to other payers.
Organization
Health services are provided by a loosely structured delivery system organized at the local level. Hospitals can open or close according to community resources, preferences, and the dictates of an open market for hospital services. Also, physicians are free to establish their practice where they choose. There is no health planning at the Federal level, and State planning efforts vary from none to stringent review of hospital and nursing home construction projects. In areas without sufficient private providers (e.g., inner cities and remote rural areas), Federal-and State-funded programs provide some primary care to populations not otherwise served by the fee-for-service (FFS) system. Municipal and county public health departments provide limited primary care services through public health clinics and regulate sanitation, water supply, and environmental hazards.
Most hospitals are owned by private non-profit institutions; the remainder are owned by governments or private for-profit corporations. Physicians, the vast majority of whom are in private practice and paid on an FFS basis, see their patients in their offices, and admit them to hospitals where they can continue to serve them. About two-fifths of physicians are in solo practice. Although there is a long-term trend toward the formation of more and larger group practices, the proportion of solo practices is shrinking only at a very slow rate ( Marder et al., 1988 ). A relatively small number of physicians is not in the FFS sector but is employed by the government, corporations, managed care networks, or hospitals.
Health reform in the 1980s and 1990s
In recent years, health reform in the United States has focused on controlling rapidly rising health costs and increasing financial access to health care. A variety of cost-control strategies have been attempted at the Federal, State, and local levels of government and by private payers. Despite these efforts, health care costs continue to escalate. The resulting pressure on public, private, and individual budgets keeps the issue of control of health care costs high on the public agenda.
Sources of health insurance
The vast majority of the population, about 74 percent, is covered by private health insurance ( Figure 1 ). Those under 65 years of age and their dependents obtain private health insurance either through their employers (61 percent of the population) or by direct purchase of non-group health insurance (13 percent of the population). A small proportion of the population, 13 percent, has multiple health insurance coverage 2 (e.g., both private and public health insurance), and 14 percent have no insurance ( U.S. Bureau of the Census, 1991b ). Not all firms offer health insurance. In fact the majority of the uninsured (75 percent) are employees or their dependents ( Short, Monheit, and Beauregard, 1989 ).

There are more than 1,000 private health insurance companies providing health insurance policies with different benefit structures, premiums, and rules for paying the insured or medical care providers. These companies are regulated by State insurance commissioners; the Federal Government does not generally regulate insurance companies. States sometimes specify that certain, often narrowly defined, benefits or providers (e.g., chiropractic services) be covered by all health insurance policies sold in the State. States may also regulate insurance premium increases and other aspects of the insurance industry. In recent years, most large employers have opted to “self-insure,” or cover health expenses as they occur, rather than purchase insurance from a company, because this exempts them from State insurance regulation as detailed later.
Although employer-provided health insurance is voluntary, it is encouraged by tax policy. Employer-paid contributions to employee health costs are basically a substitute for cash wages. This substitution has increased in recent years. Health benefits rose from 2.4 percent of total compensation in 1970 to 5.8 percent in 1989, and from 23 percent of total benefits in 1970 to 36 percent in 1989 ( Employee Benefit Research Institute, 1991 ). When employers pay wages in the form of health benefits, they are subject neither to the personal income tax nor to the Social Security tax. If such wages were taxed as income, then Federal revenues would have increased by an estimated $56 billion in 1990 ( U.S. Department of the Treasury, 1990 ). Individuals with relatively high medical expenses, more than 7.5 percent of their taxable income, may be able to deduct out-of-pocket health care expenditures from their Federal income taxes, for a 1990 cost of about $2.9 billion ( U.S. Department of the Treasury, 1990 ). Employer contributions to group health insurance were estimated to be $139 billion in 1990 ( Levit and Cowan, 1991 ).
The majority of those with private health insurance are covered for inpatient hospital services and physician services; the breadth and depth of coverage of other services vary. Industries with strong unions (e.g., steel, automobile) have the broadest benefit packages. On the other hand, service industries (e.g., restaurants) may provide little or no coverage ( Friedman, 1991 ). The amount of patient cost sharing also varies. For example, as many as 55 million Americans with private health insurance are underinsured, that is, they do not have a limit on their out-of-pocket health expenses and are at risk of being impoverished should they experience a costly, major illness ( Farley, 1985 ). Home care is covered in most insurance plans after a hospitalization for an acute episode of illness in order to allow recovery in a less costly setting. Home care and long-term care for chronic conditions and frailty related to aging are not generally covered by public or private insurance. Most long-term care and home care are purchased out-of-pocket or provided informally by family and friends. In the last few years, some private health insurers have been marketing long-term care policies, primarily to upper income individuals who can afford the premiums. However, Medicaid (described later) does pay for long-term care and home care services for the poor, and finances nearly one-half of the annual nursing home expenditure of $53.1 billion ( Levit et al., 1991b ).
Medicare is a uniform national health insurance program for the aged and disabled. Administered by the Federal Government, it is the single largest health insurer in the country, covering about 13 percent of the population, including virtually all the elderly 65 years of age or over (31 million people), and certain persons with disabilities or kidney failure (3 million people) ( Board of Trustees of the Federal Hospital Insurance Trust Fund, 1992 ). The program is financed by a combination of payroll taxes, general Federal revenues, and premiums. It is comprised of two parts: Coverage under Part A is earned through payment of a payroll tax during one's working years; coverage under Part B is voluntarily obtained through payment of a premium once eligibility for Medicare is established (through receipt of retirement or disability benefits under the Social Security income assistance program).
Medicare is an inter-generational transfer program primarily funded by taxes from working people to provide services to aged beneficiaries. However, this financing approach is not actuarially sound: Expenses are increasing faster than revenues, leading to a projected trust fund bankruptcy early in the next century ( Boards of Trustees of the Federal Hospital Insurance Trust Fund, 1992 ). As the population ages, there will be fewer workers supporting each beneficiary. There were 5 workers for each beneficiary in 1960, there will be 3 workers per beneficiary in 2000, and 1.9 by the year 2040 ( U.S. House of Representatives, 1991 ).
Coverage under Part A includes inpatient hospital care, very limited nursing home services, and some home health services. The Part A payroll tax is paid by virtually all employed individuals. The payroll tax is 1.45 percent of payroll for both the employer and the employee (for a total of 2.9 percent) up to a maximum of $125,000 of income. This maximum was raised in 1990 from $51,300. Employer contributions to Medicare Part A were nearly $30 billion in 1990 ( Levit and Cowan, 1991 ). Coverage under Part B includes physician and other ambulatory services, durable medical equipment (e.g., wheelchairs), and certain other services. It is funded through premiums (about 25 percent of the program cost), by enrollees ($31.80 per month in 1992), and by general Federal revenues (about 75 percent of the program cost).
Medicare is oriented towards acute care, and such services as long-term nursing home care, routine eye care, and outpatient prescription drugs are not covered. Moreover, Medicare patients must also pay coinsurance and deductibles: These account for an average of 17 percent of the services covered by Medicare, and consume an average of 6 percent of their per capita income ( U.S. House of Representatives, 1991 ). Medicare covers less than one-half of the total medical care expenses of the elderly ( Waldo et al., 1989 ). To pay for Medicare coinsurance and deductibles and, in some cases, uncovered benefits, about 68 percent of Medicare beneficiaries have private supplemental health plans, provided by former employers or self-purchased, and an additional 9 percent have Medicaid ( U.S. Bureau of the Census, 1991a ). Despite all of these sources of health insurance, the elderly spend an increasing share of their after-tax income on health expenses, up from 7.8 percent in 1972 to 12.5 percent in 1988 ( U.S. House of Representatives, 1991 ).
Medicaid is a health insurance program for certain groups of the poor. It covers preventive, acute, and long-term care services for 25 million people, or 10 percent of the population. Medicaid is jointly financed by Federal and State governments. The Federal Government matches State Medicaid outlays at rates which vary by State personal-income levels: The Federal share of total expenditures ranges from 50 to 83 percent, with the poorer States receiving a higher match from the Federal Government. Medicaid is administered by the States under broad Federal guidelines governing the scope of services, the level of payments to providers, and population groups eligible for coverage.
In order to be eligible for Medicaid, a person must be poor as well as aged, blind, disabled, pregnant, or the parent of a dependent child. Mothers and dependent children comprise about 68 percent of Medicaid recipients, the elderly 13 percent, the blind and disabled 15 percent, and others 4 percent. States further define eligibility levels (e.g., maximum income and asset levels) within certain broad parameters. Consequently, about 60 percent of the poor below the Federal poverty line are excluded from Medicaid ( Swartz and Lipson, 1989 ). Childless, non-disabled adults under 65 years of age, no matter how poor or how high their medical expenses, are not eligible, nor are individuals with assets above State-defined levels. On the other hand, because Medicaid is the only public program that finances long-term nursing home care, a significant number of middle-class elderly have become eligible for Medicaid-covered nursing home care by intentionally transferring assets to their children and exhausting their income on nursing home expenses ( Burwell, 1991 ). About 43 percent of Medicaid expenditures are spent on skilled nursing facilities and intermediate care facilities ( Ruther et al., 1991 ).
The uninsured receive fewer health services than insured individuals with comparable health status ( Freeman et al., 1987 ). Services for the uninsured are provided through a variety of sources, the amount and scope of which vary by community. Federal, State, and local governments support public health clinics and hospitals with a primary mission of providing care to the indigent. In some cases they pay private providers to care for the indigent as well. Public health expenditures support preventive health measures such as vaccinations, cancer screening programs, and well-child care. The services are often available to all, although a fee which varies according to income may be charged.
Providers sometimes subsidize the costs of services to uninsured individuals from operating margins. Charity care and bad debt represented 5 percent of hospital expenses in 1988 ( Prospective Payment Assessment Commission, 1991 ). Estimates of physician charity care are difficult to make because, unlike hospitals, physicians do not submit detailed cost reports to the Federal Government. A recent study estimated that physicians provide $3 billion worth of free services and nearly $4 billion of reduced-fee services annually ( American Medical Association, 1991 ). However, as insurers and employers try to control their own costs, the ability of hospitals and other providers to cross-subsidize care for the uninsured, by cost-shifting to insurers and employers, may decrease.
Health spending
National income and health.
In 1990, about 12.2 percent of GNP was devoted to health expenditures. This amounted to $666.2 billion ($2,566 per capita), an increase of 10.3 percent over 1989 levels ( Levit et al., 1991a ). The United States spent a higher percentage of its wealth on health than any other OECD country ( Schieber, Poullier, and Greenwald, 1991 ). Health expenditures have been growing rapidly both as a share of GNP and in absolute terms. For example, health expenditures in 1980 accounted for 9.1 percent of GNP and are projected to rise to more than 16 percent of GNP by the year 2000 ( Sonnefeld et al., 1991 ). One reason for this rapid growth is the sluggish U.S. economy and slow GNP growth. However, inflation in medical prices has long been significantly higher than general inflation ( Levit et al., 1991b ).
Source of funds
Public budgets accounted for 42 percent of health spending in 1990, and private sector spending accounted for 58 percent ( Figure 2 ) ( Levit et al., 1991a ). The proportion of total health care expenditures covered by public sources is lower in the United States than in all but one of the OECD member countries ( Schieber, Poullier, and Greenwald, 1991 ). The Federal budget paid for 29 percent of all health spending, primarily through the Medicare and Medicaid programs, but also through health spending by the Departments of Defense and Veterans Affairs for current and retired military personnel and their dependents. Of the 13 percent State and local share of health spending, approximately 5 percent was for Medicaid, and 8 percent was for other State and local health programs ( Levit et al., 1991a ).

Health expenditures comprise a growing share of public budgets. In 1990, health represented 15 percent of the Federal budget and 11 percent of State and local budgets. By contrast, health expenditures in 1980 comprised 12 percent of the Federal budget and 9 percent of State budgets. Medicare alone is now 9 percent of the Federal budget ( Levit et al., 1991a ). Of the 58 percent of all health spending that was not financed by public budgets, 33 percent was paid for by private insurance payments, 20 percent by individuals out-of-pocket, and 5 percent by other private payments, including philanthropy ( Levit et al., 1991a ). In 1990, approximately 39 percent of total health spending was for hospital care, 19 percent for physician services, 8 percent for nursing home care, 22 percent for other personal health care spending, and 12 percent for other non-personal health care items such as research and construction ( Levit et al., 1991a ).
Trends in spending
The annual growth rate of health spending in the 1980s was about 10.4 percent as a whole, but varied by type of service. Hospital spending grew by about 15 percent per year in the early 1980s, slowed to about 7 percent in the mid-1980s, and increased to about 10 percent by the end of the decade. Physician spending growth through the decade averaged about 15 percent per year, but moderated somewhat toward the end of the decade ( Levit et al., 1991a ).
The share of all health spending accounted for by private health insurance and government programs rose slightly over the 1980s, while out-of-pocket spending marginally declined ( Levit et al., 1991a ). The increased use of cost sharing as a cost-containment measure, described later, has not kept pace with rapidly rising health care costs.
Insurance coverage by service
Insurance coverage varies by service. Hospital care is the best insured, and nursing home care and dental care are the least well insured. Out-of-pocket payments for hospital care cover only 6 percent of total hospital spending, public programs (Medicare and Medicaid) 40 percent, other State and local programs 14 percent, private insurance 36 percent, and private charity care the remaining 4 percent. On the other hand, out-of-pocket payments for nursing home expenditures finance 44 percent of total nursing home spending, Medicaid covers 43 percent, Medicare and other non-Medicaid State and local funds cover 7 percent, private charity covers 2 percent, and private insurance covers only 1 percent ( Levit et al., 1991a ). Most employer-sponsored group health plans cover outpatient prescription drugs as does Medicaid, while Medicare does not.
Patient cost sharing
As employers and insurers try to contain costs, patient cost sharing is becoming a more common feature of almost all U.S. health plans ( Employee Benefit Research Institute, 1991 ). Typical deductibles are $100 to $500 per person per year, and typical coinsurance rates are 20 percent per service ( Employee Benefit Research Institute, 1990 ). The RAND Corporation national health insurance experiment found that the use of cost sharing as a cost-containment tool reduced utilization without adversely affecting health status, except for low-income individuals with hypertension, vision, or dental problems ( Newhouse et al., 1981 ). The impact on the health status of the low-income and the exclusion of the elderly and chronically ill from the experiment suggest some caution about the general use of cost sharing as a cost-containment tool. The proportion of private health plans with limits on out-of-pocket spending increased steadily during the last decade. Nevertheless, as previously noted, many policies still do not offer full protection against catastrophic expenses ( U.S. Bureau of Labor Statistics, 1989 , 1982 ).
Health services delivery system
There are about 6,700 hospitals in the United States, including 5,480 community, acute care hospitals, 880 specialty hospitals (e.g., psychiatric, rehabilitation, long-term care), and 340 Federal hospitals open only to military personnel, veterans, or native Americans. Of the 5,480 community hospitals, non-profit hospitals represent 59 percent, local government hospitals 27 percent, and for-profit hospitals 14 percent. There are 3.9 community hospital beds for each 1,000 residents, although this varies around the country. There were 33 million hospital admissions in 1990 with an average length of stay per admission of 9.2 days. Hospital stays are shorter and admission rates are lower in the United States compared with other OECD countries. The average hospital occupancy rate, 66 percent, is lower in the United States than in other OECD countries, however this rate varies and may be 40 percent or lower in rural areas ( American Hospital Association, 1990 ; National Center for Health Statistics, 1991 ).
Hospitals finance capital purchases through a variety of means including savings, tax-exempt bond issues, and philanthropy. Although Federal and State mortgage loan guarantee programs assist some hospitals to secure financing for construction and renovation projects, it is more common for hospitals to secure private mortgage insurance when floating a construction bond. Some States require prior approval before certain capital projects can be undertaken, while other States have no prior approval procedures.
Because physicians in the community admit their patients to hospitals, hospitals must be attractive to physicians in order to obtain patients. This makes it difficult for hospitals to deny physician requests to purchase expensive equipment, because purchasing such equipment is a way that hospitals attempt to attract physicians. As a result, hospitals engage in what has been called a medical arms race, in which each competes to own state-of-the-art technology. The United States has 8 times more magnetic resonance imaging machines (MRIs) per capita, 6 times more lithotripsy centers, and 3 times more cardiac catheterization and open heart surgery units than Canada ( Rublee, 1989 ).
There were more than 574,000 physicians in active practice in 1988, or 2.3 active physicians per 1,000 population ( National Center for Health Statistics, 1991 ). In the early 1980s, a national physician surplus was forecasted for the 1990s ( U.S. Department of Health and Human Services, 1981 ). Now this forecast is being debated. A physician surplus causes concern because some argue that physicians can create demand and thereby add to rising health costs ( Rice and LaBelle, 1989 ).
Nonetheless, problems exist in the geographic and specialty distribution of physicians. For instance, the physician-to-population ratio averages 0.9 active physicians per 1,000 population in rural areas ( U.S. Office of Technology Assessment, 1990 ). Of those in active practice, about 33 percent are primary care physicians (family practice, general pediatrics, and internal medicine) and the remainder are specialists (Politzer et al., 1989). There is concern that the proportion of primary care physicians will continue to fall in the coming decade. The United States has a much higher percentage of specialists than do other OECD countries ( Rosenblatt, 1992 ).
Individuals can access specialists directly except in some coordinated care settings (described later). Some specialists (e.g., radiologists, anesthesiologists, and pathologists) practice in hospitals under contract. Compensation arrangements with hospital-based physicians vary but often include a salary as well as FFS billings of which the physician retains a percentage.
In the past, most high-technology equipment was purchased by hospitals. Recently, however, physicians, either alone or in joint ventures, have been purchasing high-technology equipment outside the traditional confines of the hospital. Joint ventures are arrangements where investors pool capital to purchase expensive equipment and build facilities such as ambulatory surgery centers. Some argue that these practices rapidly diffuse high technologies, create competition with hospitals for ambulatory procedures, increase utilization, and fuel health inflation ( Florida Health Care Cost Containment Board, 1991 ).
Medical education is financed by a combination of student tuition payments, Federal and State education programs, and private funds. Public funds support medical education through State-supported medical schools (about 60 percent of all medical schools), Federal and State student loan programs, Federal health education programs, and Medicare payments for graduate medical education in teaching hospitals. In 1990, about 80 percent of medical students had an average debt of $46,224 upon graduation from medical school (Jolin et al., 1991). High-paid specialties are more attractive to medical students than the lower paid family and general practice for a variety of reasons ( Colwill, 1992 ). Reform of medical education financing, in order to influence new physicians' choice of specialty and geographic location, is an important public policy goal. Proposals include reducing Medicare payments to new physicians who locate in overserved areas, and increasing funds for the current Federal program (the National Health Service Corps) which forgives student debt in return for practicing in underserved areas.
Coordinated care
In recent years, coordinated care arrangements have become increasingly popular as a way to control costs in both the private and public sectors. The term coordinated care refers to a diverse and rapidly changing set of alternative health care delivery models. These models differ from traditional FFS medicine by integrating the financing and delivery of health services with the goal of controlling costs by managing utilization and provider payment levels.
The oldest model of coordinated care is the health maintenance organization (HMO); several have existed for decades, although most have been formed in recent years. Individuals who enroll in an HMO receive a comprehensive benefit package available only from a defined network of providers for a fixed payment, usually a monthly or yearly premium. To compensate for the restricted choice of providers, enrollees often face lower cost sharing and have little billing paperwork compared with FFS medicine. HMOs themselves range from long-established organizations that employ physicians, build their own hospitals and clinics, and only serve HMO enrollees, to recent affiliations of solo practice physicians and hospitals who may also practice traditional FFS medicine. Nearly 37 million Americans, 15 percent of the population, are enrolled in HMOs ( Porter, Ball, and Kraus, 1992 ).
A more recent model is the preferred provider organization (PPO) which selectively contracts with or arranges for a network of doctors, hospitals, and others to provide services at a discounted price schedule. Individuals pay lower coinsurance rates if they visit physicians who have agreed to accept a lower price. Similar to HMOs, the PPO model includes utilization review, and formal standards are used to select and maintain network providers and physicians. PPO enrollment grew from only 1 percent of participants in medium and large employer health plans in 1986 to 10 percent in 1989 ( U.S. Department of Labor, 1990 ).
A recent development is the point-of-service (POS) network. POS networks start with an HMO and add a PPO component in an attempt to achieve both cost containment and freedom of choice of providers. Enrollees are encouraged to use HMO doctors by paying a higher coinsurance charge if they use doctors not affiliated with the HMO. By contrast, in a PPO, the doctor simply accepts a lower price for certain patients with no equivalent HMO structure with its emphasis on coordinated care. It is expected that the features of POS networks will continue to evolve.
Studies suggest that HMOs can save about 20-30 percent compared with FFS insurance, primarily by reducing inpatient hospital days ( Manning et al., 1984 ). However, in some instances these savings are the result of favorable selection of enrollees rather than more cost effective use of health services. The cost advantages of HMOs compared with FFS medicine may be reduced as utilization controls are increasingly introduced into the FFS sector. Quality assurance at HMOs is an important issue. There is concern that HMOs, and especially for-profit HMOs, have economic incentives to underserve their enrollees in order to live within the capitated payment. On the other hand, HMOs may need to offer care of at least reasonable quality in order to be attractive to enrollees.
Coordinated care, as used broadly, includes not only HMOs and PPOs but also a variety of other cost-control techniques, influencing patient care decisions before services are provided. These techniques, increasingly imposed by third-party payers, include prior approval of hospital admissions, management of high-cost patient care, control of referrals to specialists through primary care physicians, selective contracting with hospitals and other providers, required second opinions for surgical procedures, profile analysis of provider utilization and practice patterns, and screening of claims prior to payment to avoid duplicate and inappropriate payments. Although the evidence on utilization review is not complete, some of these techniques, such as preadmission certification and review during an inpatient hospital stay, are cost effective ( Scheffler, Sullivan, and Ko, 1991 ).
Health outcomes
Despite the highest health expenditures in the world, the United States does not perform particularly well in terms of gross health outcome measures. For instance, in 1988 the United States had a life expectancy at birth of 71.5 years for males and 78.3 years for females, and an infant mortality rate of 10.0 per 100,000 births. Compared with the other OECD countries, it ranked 17th in male life expectancy, 16th in female life expectancy, and 20th in infant mortality ( Schieber, Poullier, and Greenwald, 1991 ).
However, direct comparisons of U.S. health costs and outcomes with OECD nations can be misleading because of exacerbated social problems in the United States which have significant health costs and adversely affect U.S. health outcomes. The 20,000 annual U.S. homicides result in per capita homicide rates 10 times those of Great Britain and 4 times those of Canada. There are 100 assaults reported by U.S. emergency rooms for every homicide. About 25 percent of spinal cord injuries result from assaults; lifetime care for a quadriplegic averages $600,000. The United States has about 375,000 drug-exposed babies, and estimated 5-year costs of treatment are $63,000 per child. U.S. child poverty rates are double those of former West Germany and Canada, and triple those of Switzerland and Sweden ( Schwartz, 1991 ; Rich, 1991 ; Smeeding et al., 1988 ).
The United States has had a total of 206,000 acquired immunodeficiency syndrome (AIDS) cases, and there were 39,000 AIDS deaths in 1990 alone. The U.S. AIDS infection rate is more than four times that of Canada ( Pan American Health Organization, 1992 ). The average lifetime health costs of an AIDS patient are now $85,000. These costs may increase as new drugs are developed to prolong the life of AIDS patients. AIDS is putting budget pressures on inner-city hospitals and emergency rooms because many AIDS patients do not have adequate insurance. Recent studies estimate that the United States will spend $5.8 billion caring for AIDS patients in 1991, and that these costs will rise rapidly to $10.4 billion by 1994 ( Hellinger, 1991 ).
Health outcomes for some minority groups are significantly worse than the U.S. average. The infant mortality rate for Native Americans is 1.5 times the rate for white people and the rate for black people is 2.1 times the rate for white people ( National Center for Health Statistics, 1991 ). Life expectancy has been significantly higher for white people than for black people for the last 20 years. Homicide is the leading cause of death for black people between 15 and 44 years of age, with the rate for black males more than 8 times the rate for white males of the same age ( National Center for Health Statistics, 1991 ).
Data and evaluation systems
When evaluating health services, the United States is both data rich and poor. Compared with health systems where there is a single payer, U.S. data are divided among many insurers, making it virtually impossible to produce comprehensive provider or beneficiary profiles. However, the United States also requires detailed diagnostic and procedural information on each bill paid in an FFS system. Moreover, hospital admissions and major surgery often require preadmission review. Consequently, a great deal of information that is unavailable in systems which do not require detailed bills is produced at the patient level.
Various systems to improve data and to coordinate data systems are under development. The Institute of Medicine of the National Academy of Sciences has issued several reports calling for more health outcomes research and improved data systems, including computerized patient records ( Institute of Medicine, 1991 ). The Federal Government publishes uniform mortality statistics for hospitals based on Medicare billing records and quality information on nursing homes based on periodic inspections. The Medicare program is also developing a uniform clinical data set to evaluate the quality of care and outcomes of Medicare patients. The Federal research effort on medical outcomes, including the development of medical practice guidelines, is coordinated by the Agency for Health Care Policy and Research.
Data are also used by commercial firms in order to evaluate providers for inclusion in managed care networks. Such firms analyze companies' claims experience, health utilization, and outcomes. These data help to identify efficient providers with whom the purchasers should contract, and inefficient providers who should be excluded. Other firms analyze drug prescription data to identify over-prescribers, as well as potential adverse drug interactions which may produce avoidable hospitalizations.
Background for reform in the 1980s
Enactment of medicare and medicaid.
The first nationwide hospital insurance bill was introduced in Congress in 1942, but failed to pass. Discussions of various forms of national health insurance over the next two decades culminated in the enactment of Medicare and Medicaid in 1965. Medicare and Medicaid were a compromise between those who wanted national health insurance for everyone, and those who wanted the private sector to continue to be the source of insurance coverage. The elderly and the poor were at high risk for health expenses beyond their means and were less likely than other population groups to have health insurance. The elderly were generally considered to be uninsurable or bad risks by the private insurance market. In 1963, 75 percent of adults under age 65 had hospital insurance compared with 56 percent of people 65 years of age or over. In 1966, following passage of Medicare, about 19 million elderly people, or 10 percent of the population, received health insurance coverage. This nearly doubled the number of insured 65 years of age or over. Medicare coverage was extended to the under age 65 population with disabilities or end stage renal disease, about 2 million new enrollees, in 1972 ( Cohen, 1986 ; Gornick et al., 1986; Mills, 1986 ).
Medicaid initially covered about 10 million people, adding an unknown number of recipients to those covered under other State and local welfare programs. By 1973, there were 19.6 million Medicaid enrollees. Most Medicaid enrollees are children and mothers under the income assistance program called Aid to Families with Dependent Children (AFDC) ( Cohen, 1986 ; Gornick et al., 1986; Mills, 1986 ).
This large expansion of third-party coverage combined with generous payment methods (both Medicare and Medicaid originally paid hospitals their costs and Medicare largely paid physicians their charges) was one of the principal engines of health care cost growth in the 1970s and 1980s. In addition, the passage of Medicare and Medicaid gave the Federal Government an institutional interest in health care cost containment as it suddenly became the single largest health insurer.
Health care in the 1970s
The 1970s were characterized by rapid expansions in health care costs, and the development of strategies for their containment. Cost-control strategies emphasized regulation and planning. The National Health Planning Act of 1974 created a system of State and local health planning agencies largely supported by Federal funds. States passed certificate-of-need laws designed to limit investment in expensive hospital and nursing home facilities. The Carter Administration (1977-81) advocated direct Federal controls on hospital spending, however, Congress failed to enact them. With the installation of the Reagan Administration in 1980, a pro-competitive approach to cost containment was advanced and the health planning legislation was repealed in 1986 by Public Law 99-660.
Significant expansion of government support for medical education was designed to address a perceived shortage of physicians. Medical school enrollment doubled over the course of the decade. Government funds also supported a growing biomedical research and development community, with its hub at the National Institutes of Health.
Although not generally recognized at the time as a bill affecting health care, the 1974 Employee Retirement Income and Security Act (ERISA) has had a profound impact on health policy ( Fox et al., 1989 ). The legislation was passed to regulate corporate use of pension funds, but it also pre-empted State regulation of self-insuring employee benefit plans generally. Growing numbers of larger employers were already moving to self-insured health benefits as a cost-control mechanism prior to ERISA's passage. The ERISA pre-emption provided further incentives to employers to convert their employee health benefit plans to self-insurance. Employers now have a large stake in the ERISA Federal pre-emption because many have structured their health benefit plans to take advantage of its provisions and exemptions.
U.S. health system in the 1980s
As frequently noted, the U.S. health care system suffers from rapid escalation of health costs, lack of universal access to insurance coverage, geographic maldistribution of providers, underutilization of primary care and preventive services, gaps in the continuity of care, and a high rate of inappropriate utilization of health services. These problems coexist with widely acknowledged strengths such as providing the vast majority of the population with state-of-the-art care, offering consumers freedom of choice among a variety of highly skilled providers using the latest technology, and promoting a vigorous biomedical research and development sector. There are sophisticated quality assurance and data systems, and virtually no queues for elective surgery for those with insurance.
Health care cost growth
Growth in U.S. health care costs results in part from such unique features as the predominant FFS payment system, extensive third-party insurance coverage, a fragmented multipayer system, and a vigorous biomedical research establishment combined with rapid diffusion of new technologies. The fragmented U.S. structure gives providers incentives to provide additional services and to bill for higher levels of service to increase revenues. Although coordinated care arrangements encourage provision of services within fixed budgets, they have only recently become more widespread. Moreover, coordinated care itself may have difficulty in controlling utilization in a system whose basic structure continues to reward increased FFS billings. In contrast to the United States, other OECD countries control health costs through central control of budgets and all-payer ratesetting.
Health care costs are perceived as reducing the international competitiveness of American business, however, there is debate on this issue. For example, Chrysler states that health care costs add $700 to the price of every American manufactured car. By comparison, health care costs add $350 to the cost of a car in Germany and France, or $225 in Japan ( Graig, 1991 ). (This, of course, reflects health benefits provided in lieu of past and present wages to retirees and current workers, and the aging labor force of the industrial sector.) Others argue that the issue is the total labor compensation package, not fringe benefits alone ( Reinhardt, 1989 ).
Because health insurance in the United States is primarily employer-based, cost containment must be a high priority for employers if cost-control goals are to be attained. However, employers provide health benefits as a means of attracting a trained and stable labor force. Employers may become ambivalent about aggressive cost-containment strategies if the result is potential labor unrest (there have been several recent strikes 3 over employer health benefit reductions). Moreover, the business community has been split between industries that provide comprehensive benefits to older, unionized workers, and newer service industries that provide much more limited fringe benefits of all types to younger and healthier workers. The former, such as the automobile industry, is increasingly concerned about high health costs resulting from an aging labor force, and the shifting of costs to them for the health care provided to uninsured workers in the service sectors. This creates a new political situation in which the business community is no longer united against fundamental reform of the health care system.
Administrative costs
U.S. administrative costs are high and a source of unnecessary expenditures. Efforts are under way to standardize electronic billing across all payers in order to reduce administrative costs ( Sullivan, 1992 ). Despite consensus that administrative efficiencies are possible, there is disagreement about the extent to which adopting a single payer system or alternative health insurance arrangements would reduce administrative or total systems costs.
Advocates of national health insurance argue that Canada has been able to provide universal health insurance coverage while spending substantially less than the United States. In particular, they compare administrative costs in the United States and Canada, and suggest that the difference in these alone (an estimated $60 to $70 billion, or about 10 percent of total 1991 U.S. health costs) could finance health coverage for the uninsured ( Woolhandler and Himmelstein, 1991 ; U.S. General Accounting Office, 1991 ; Newhouse, Anderson, and Roos, 1988 ). Others argue that these comparisons are unsound. They fail to properly value the positive effect of those administrative costs designed to coordinate care, assure quality, and control utilization, misapprehend that cost differences result from factors other than the single payer mechanism, and ignore or do not capture other costs of the Canadian system, for example, increased patient waiting time ( Danzon, 1991 ).
Medical malpractice
Another alleged source of excessive health spending is the high cost of medical malpractice premiums and defensive medicine. (The fear of a malpractice suit is said to induce doctors to order unnecessary tests and services. However, this behavior also maximizes FFS physicians' practice income.) Professional liability costs for physician services are estimated to be about $20 billion, only $5 billion of which are malpractice premiums, or less than 1 percent of all health spending. The remainder, or $15 billion (another 3 percent of health spending), is the estimated cost of defensive medicine ( American Medical Association, 1990 ).
Malpractice insurance premiums average 6 percent of physician practice costs. The average premium masks considerable variation in premiums by specialty and State: Obstetricians and neurologists can pay up to $100,000 or more a year in malpractice insurance premiums in Florida and New York. Patients who win malpractice cases can receive awards in the millions of dollars.
A recent study found that adverse events occurred in slightly less than 4 percent of hospital admissions. Medical negligence caused the adverse event in 25 percent of these cases, or 1 percent of all admissions. The incidence of injured patients seeking redress in the courts (8 times as many patients were injured than filed a claim) or receiving compensation from the courts was smaller still (16 times as many patients were injured than received compensation). The study also found that many malpractice cases in the courts did not involve adverse events or negligence, and that physicians' perceived probability of suit was significantly higher than actual experience warranted ( Harvard Medical Study, 1990 ).
Inappropriate utilization
Studies have documented high variation across geographic areas in the performance of certain surgical procedures ( Wennberg, 1973 ; Chassin et al., 1986 ). They raise questions about why this variation, even within small geographic areas, exists: Are patients sicker in some towns than others? Are physicians trained to practice medicine differently? In order to measure the extent of this variation, panels of physician experts have developed and applied medical appropriateness criterion retrospectively to medical records. They have found that the incidence of inappropriate use of such expensive and potentially dangerous procedures as coronary artery bypass surgery accounts for between 20 and 35 percent of care ( Chassin et al., 1987 ). Additional RAND Corporation studies of a small number of medical procedures ( Brook et al., 1989 ; Merrick et al., 1986 ) found that about 15-30 percent of those medical procedures were inappropriate, unnecessary, or both, meaning the medical evidence did not justify the medical intervention. If the estimate for clearly inappropriate procedures alone were applied to all medical spending, this would amount to unnecessary expenditures of between $99 billion and $198 billion in 1990. Inappropriate utilization may result from several factors including incentives inherent in FFS medicine, inadequate communication or knowledge among medical professionals, defensive medicine, and patient demand on physicians to render more services. As a consequence, the Federal Government is investing more than $100 million a year in research to study outcomes and inappropriate utilization, and to develop practice guidelines for physicians.
Of course, an unestimated number of people who need appropriate procedures do not receive them. Groups at risk of underservice include minorities, the poor, and uninsured ( Freeman et al., 1987 ; Hadley, Steinberg, and Feder, 1991 ; Goldberg et al., 1992 ). It is unknown whether providing appropriate procedures to all would result in net savings or costs.
Delivery system under stress
In many areas of the country, the distribution of providers does not adequately reflect the population's need for services. Some inner-city areas have insufficient physician, clinic, and hospital capacity to provide needed services, resulting in backlogs of patients in emergency rooms which too often serve, inappropriately, as providers of last resort. Some rural areas of the country have excess hospital capacity combined with a paucity of physicians. In 1988, about 34 million people (collectively 29 percent of the rural population and 9 percent of the urban population) lived in underserved areas ( U.S. Office of Technology Assessment, 1990 ). Other parts of the country have a surfeit of hospital beds and physicians.
Utilization review
Utilization review techniques are designed to prevent unnecessary services and control costs. They require physicians to fill out forms, write special justifications of the appropriateness of the services they order, and subject providers to utilization review of their services. Medicare peer review activities assess the medical necessity, appropriateness, and quality of care in the hospital setting. Efforts are under way to extend Medicare peer review to other settings (e.g., coordinated care). Some argue that health systems that budget physician expenditures as a cost-control mechanism grant them more clinical freedom than U.S. physicians enjoy. In the United States, physicians guard the right to set their own fees, but as a result find themselves increasingly subject to utilization controls which may constrain their clinical freedom ( Reinhardt, 1987 ).
Long-term care
In common with other OECD countries, long-term care services in the United States are not integrated with acute care health services in terms of delivery, providers, or financing. Because long-term care and acute care are not routinely covered by the same private or social insurance systems (with the exception of Medicaid), there are few incentives to overcome the separation of services. Social and health services have been effectively integrated in only a few federally funded demonstration projects in selected cities. Municipal, State, and local governments pay for long-term care or home care only in rare and limited cases.
Reforms in the 1980s
When President Reagan took office in 1981, tax reform was a priority. The combination of the tax reforms passed in the early 1980s, and increased military spending during the Reagan Presidency, together with Congress dominated by the opposition party which defended domestic program spending, led to a growing Federal deficit ( Sawhill, 1982 ). In this context, the 1980s was a decade of constant pressure to find budget savings from Medicare and Medicaid because these programs are not subject to annual budget limits (i.e., spending increases as enrollees utilize services) and they represent a large and rapidly growing share of the Federal domestic budget.
At the Federal level, the intellectual paradigm to control health costs shifted from regulation and planning to managed competition. Some economists theorize that health care competition is capable of systematically bringing market-oriented economic incentives to bear on medical care in order to control costs and enhance efficiency. These theories suggest that in the face of appropriate incentive forces, health care insurance plans will themselves seek to control both the price and volume of services as they competitively seek to increase market share and attract enrollees ( Enthoven, 1978 ).
Federal-level reforms
Federal Government reforms have been an opportunistic mix of competitive and regulatory strategies. The Reagan Administration developed an agenda based on competitive principles in the early 1980s, but in large measure these proposals were not enacted by Congress. The result was a mixture of pragmatic reforms such as Medicare hospital prospective payment, which combined aspects of regulation (uniform, Government-set prices) with aspects of competition (per admission payments give hospitals incentives both to attract more patients and to cut costs).
Competition as a strategy
The competitive strategy builds from its critique of the current financing and delivery system in which the provider has little incentive to contain costs as long as a third-party insurer-payer will honor any bill submitted. The third-party insurer-payer has little incentive to pressure providers to control costs if the insured (or his representative, typically an employer) is willing to pay an ever-increasing health insurance premium. The patient has little incentive to control utilization because with insurance coverage, typically paid by his employer as a tax-advantaged alternative to taxable wages, the employee-patient is indifferent to costs. Advocates of competition seek to create incentives to overcome such indifference to costs.
There are various techniques for fostering competition. First, advocates of competition encourage HMOs and similar entities to compete for members on the basis of quality and premiums as an effective way to control health care inflation. Because HMOs and similar entities receive a fixed payment in advance for each enrollee, regardless of actual utilization, they have strong incentives to control costs by limiting utilization, whereas the risk of underutilization is moderated by the entity's need to maintain membership.
Another approach builds on vouchers and tax credits ( Pauly et al., 1991 , Butler et al., 1989 ). These proposals would replace the current open-ended tax subsidy to businesses with income-related tax credits for the purchase of health insurance. Low-income families would be given purchasing power in the form of insurance vouchers, allowing them to select among plans ( Butler et al., 1989 ). This would shift the current subsidy away from high-income toward low-income groups, including low-income workers without employer-sponsored insurance. The Butler variation would alter the role of employer groups, making families directly responsible for the purchase of insurance, using available tax credits. This variation has been criticized because it would end the administrative efficiencies provided by large-employer groups. The Pauly variation assumes, but does not require, that employers will continue to act as purchasing agents on behalf of their employees. It has raised concerns that employers might have fewer incentives to negotiate lower group insurance rates on behalf of employees if the ultimate purchasing power is shifted to the employee, and that the purchasing power of the tax credit or voucher might be inadequate for an individual or family without the negotiating power of the employer ( Pauly et al., 1991 ).
Competition proposals
Proposals for a tax cap, advanced in the early 1980s by the Reagan Administration, called for limiting the amount of health insurance an employer could provide tax-free to a fixed amount per employee per month. The rationale for these proposals is that the current tax treatment of employer-provided health insurance fuels cost-inflation because it encourages first dollar coverage, excessive utilization, and high provider payment levels by shielding everyone from the true cost of health care choices. Because unlimited health benefits would no longer be tax-free, both employees and employers would become more cost-conscious, and consequently would pressure providers and insurers to contain costs. They also would be encouraged to seek cost-efficient plans, such as HMOs, that are more likely to provide broad benefits within the capped tax-free monthly amount. Congress did not agree with the Reagan tax cap proposals, and the proposed legislation was never enacted.
Another proposal would have encouraged employers who provide retiree health benefits supplementing Medicare to go at-risk much like an HMO, and manage the basic Medicare benefit as well as their supplemental benefits as a single integrated plan. This was proposed by the Administration in the mid-1980s as the Medicare voucher bill. Congress subsequently permitted limited demonstrations of this concept, called Medicare Insured Groups, which are currently under way.
Medicare managed care reform
In 1982, Congress changed the structure of Medicare payments from a retrospectively adjusted cost-reimbursement system to a prospective, risk-based one. The goal was to build incentives for HMOs to accept Medicare enrollees, while bringing an element of competition into the Medicare program. Prior to 1982, Medicare interim payments were adjusted at the end of the year based on the actual costs incurred by Medicare enrollees. HMO's preferred the post-1982 method where they received a monthly capitated at-risk payment for each Medicare enrollee because that is how they insured non-Medicare enrollees. Medicare pays HMOs 95 percent of what it otherwise pays on a geographically adjusted basis for the average Medicare enrollee in the FFS sector controlling for age, sex, and disability. Regardless of whether the Medicare payment is more or less than an HMO's costs at the end of the year, there is no further adjustment. This payment method, because it places them at financial risk, provides HMOs with a strong incentive to contain costs.
With these changes in place, Medicare enrollment in HMOs increased rapidly to a level of about 1.5 million enrollees in risk-based HMOs, or 3 percent of total Medicare enrollees. However, for two key reasons, growth then leveled off. First, HMOs did not offer sufficient enrollment incentives to entice Medicare beneficiaries to give up their free choice of providers. Second, HMOs are reluctant to enroll Medicare beneficiaries in some areas where Medicare payments are considered to be too low to make Medicare beneficiaries good risks. On the other hand, some studies have shown that Medicare enrollees in HMOs tend to be healthier than Medicare enrollees in FFS medicine ( Mathematica Policy Research, 1989 ). This phenomenon is called favorable selection for the HMO and adverse selection for the Medicare program.
Medicare hospital payment reform
In 1983, the Federal Government adopted a regulatory approach to Medicare hospital payment that changed hospital reimbursement from a cost-based retrospective system, in which a hospital was paid its costs, to a fixed-price prospective payment system (PPS) in order to create incentives for hospitals to be efficient in the delivery of services. Under PPS, hospitals receive an average payment for each patient based upon the patient's diagnosis. If the hospital spends less than the Medicare PPS payment, it keeps the difference as profit, and if it spends more, it takes a loss. The payment system change was made after a period in which hospital costs had grown about 16 percent annually. Although PPS is essentially a Government administered price system, it was not regarded as incompatible with a pro-competitive reform strategy because hospitals, to survive, still had to attract patients. This significant change in hospital payment resulted primarily from Federal budget pressures and only secondarily from a consensus within the health policy community about how to reform hospital payments.
PPS was successful in reducing Medicare's rate of increase in inpatient hospital spending, and in increasing hospital productivity although the effect on overall cost growth is not clear ( Coulam and Gaumer, 1992 ). A number of State Medicaid programs adopted variations of the PPS in order to reduce their hospital spending. Total hospital spending—inpatient and outpatient—still continued to increase because of increased volume of more expensive diagnoses (so-called “upcoding”), and technological change which permitted surgical procedures to move to the outpatient setting. One-half of all surgeries are now performed in the outpatient setting where spending controls are less vigorous ( American Hospital Association, 1992 ). Because PPS makes a payment for each admission, hospitals have incentives to increase admissions. However, hospital inpatient admissions declined substantially during the 1980s for all patients. This decline occurred because of:
- Increased review of hospital admissions by both private and public payers.
- Increased use of hospital deductibles and coinsurance by private payers.
- Technological advances permitting more surgery to be performed in the outpatient setting.
The decline in admissions and days leveled off by the end of the decade.
Medicare physician payment reform
After the growth rate in Federal hospital expenditures declined, attention turned to the 15-percent average annual increase in Medicare physician spending. In 1989, the Medicare system of paying physician charges was changed to a resource-based relative value scale (RBRVS) to be phased-in starting in 1992. The prior system of charge-based reimbursement was considered inflationary because physicians had incentives to raise their charges in order to increase their Medicare payments.
RBRVS, like hospital PPS, is regulatory in that it sets a price based on the input resources required to produce each physician service. On the other hand, because physician prices for each procedure will be published, consumers will have more information about physician costs, fostering competition when compared with the old payment system in which it was difficult for physicians or patients to know in advance what Medicare would pay. There are more than 7,000 physician procedure codes which must be priced, compared with less than 500 hospital payment groups.
At the same time that the Medicare physician fee schedule was enacted, a process for setting spending goals for Medicare physician services was developed. If physicians exceed the goal, they can be penalized in a future year by receiving a lower payment update than they otherwise would have received. Conversely, if they meet the goal, they can be rewarded with a larger payment update. In addition, physicians must now submit bills directly to Medicare on behalf of patients (formerly the physician had the right to refuse to submit the bill to Medicare for the patient) and they are restricted in the amount they can charge patients above and beyond what Medicare will pay (balance billing).
It is too early to tell whether the RBRVS will be successful in limiting Medicare physician spending. Similarly, it is not yet clear whether private payers will voluntarily adopt the Medicare fee schedule structure, thereby enhancing the prospects for system-wide savings. If RBRVS is broadly adopted by private payers, the ability of physicians to recoup revenue by increasing charges to other payers (cost shifting—a dynamic that also applies to hospitals under PPS) would be significantly reduced.
Medicare catastrophic coverage act
The Medicare Catastrophic Coverage Act (MCCA), Public Law 100-360, enacted in 1988, was the most significant expansion of Medicare benefits since the beginning of the program. Prior to MCCA, Medicare patients without supplemental coverage (i.e., private insurance or Medicaid) were vulnerable to significant out-of-pocket expenses if they exhausted Medicare hospital coverage or had high outpatient drug or physician expenses. Under MCCA, Medicare coverage was extended to cover a portion of the costs of outpatient prescription drugs, increasing post-hospital nursing home extended care benefits, increasing home health benefits, limiting beneficiary cost-sharing liability for covered Medicare services, and expanding inpatient hospital benefits.
MCCA also significantly expanded the Medicaid program by reducing cost sharing for spouses of Medicaid-covered nursing home residents, increasing the number of eligible pregnant women and children, and requiring State Medicaid programs to pay Medicare premiums and cost sharing for Medicare beneficiaries near the poverty line who were not otherwise eligible for Medicaid.
The new Medicare benefits were beneficiary-financed, first through an increase in Medicare Part B premiums affecting all enrollees, and also through a surcharge on the income taxes of high-income elderly. As a result of a tax revolt initiated by high-income beneficiaries, Medicare provisions were repealed 1 year after enactment. This experience makes it unlikely that Congress will attempt to pay for expanded benefits (e.g., long-term care) for the poor elderly by taxing the high-income elderly or reducing their benefits. It can also be argued that Congress and the President are less likely to propose expanded health benefits for those without insurance coverage paid for by taxing or reducing the benefits and tax advantages of those currently with insurance coverage.
Medicaid reform
In 1981, the Administration proposed and Congress enacted reductions in Medicaid eligibility coupled with additional State flexibility in setting payment levels for providers. States used this new flexibility to constrain provider payments by engaging in selective contracting with hospitals, developing PPSs similar to Medicare for hospitals, increasing enrollment in managed care networks, and restricting rates of increase in payments to all providers. By the end of the decade, hospitals were challenging the adequacy of Medicaid payment levels in the courts arguing that States had violated the statutory requirement to set payment rates high enough to cover the costs of an efficiently run hospital. In some cases, the courts have ruled that States have presented insufficient evidence to justify their payment levels ( U.S. Congressional Budget Office, 1992 ). As a result, some States have begun to increase their Medicaid payments to hospitals.
Although budget cutting goals continued to be the norm for the fast-growing Medicare program throughout the 1980s, during the second half of the 1980s, Congress began to expand the number of people eligible for Medicaid resulting in dramatically increased spending. The expanded Federal mandates meant that States were required to devote new resources to Medicaid. By the end of the decade, Medicaid was the fastest-growing component of State budgets. Given the recent recession and consequent declines in State revenues, States are now highly resistant to additional Medicaid expansions absent their full financing by the Federal Government.
State-level reforms
All-payer systems.
In the 1970s and 1980s, several States, including Maryland, New Jersey, New York, and Massachusetts, started all-payer ratesetting systems for hospital services. Ratesetting is a regulatory method of budgeting hospitals designed to provide adequate revenue for all patients, including those without insurance, prevent cost shifting between payers, and provide incentives for cost containment. These systems budget hospitals either by establishing payment rates for the treatment of each patient as in PPS, no matter who pays (hence the term all-payer), or by directly establishing annual budgets. Evaluations indicate that all-payer ratesetting has been a successful cost-control strategy ( Anderson, 1992 ). The rate of hospital cost growth has been reduced on a per capita basis compared with the national average. Most of the ratesetting States started with comparatively higher hospital costs, making it unclear whether or not these savings would have resulted if the system were adopted in States with lower costs. Despite their success in cost control, all-payer ratesetting programs have not been adopted by additional States. All-payer systems require consensus among health insurers, employers, hospitals, and State government as well as a sophisticated State regulatory bureaucracy. Some States reject as inappropriate such significant State intervention in the health marketplace.
Employer health insurance mandates
Prior to the 1980s, Hawaii adopted an employer health insurance mandate and has virtually universal coverage. However, the passage of ERISA (previously discussed) prevents additional States from requiring employers to provide insurance. Employer mandates have not resulted in significant problems in Hawaii for a variety of reasons, including a history of employer paternalism (employer-provided health benefits were widespread prior to the State mandate), and the State's geographic isolation that prevents employers and health care providers from easily moving to a different State. In addition, the State has a fast-growing economy which increases employer competition for relatively scarce labor ( Friedman, 1990 ; Van Ellet, 1981 ).
The State of Massachusetts adopted a variant of an employer mandate called play or pay. Under play or pay, an employer must provide health insurance to employees or pay a tax which is used by the State to provide public insurance for the firm's employees and other uninsured individuals. However, the Massachusetts play or pay plan was not implemented because of the State's recent fiscal crises, and election of a new governor who campaigned, in part, on a platform opposing the program ( Kronick, 1991 ).
Risk pools for the uninsurable
Twenty-five States have legislatively approved risk-pool legislation to provide insurance to those who, because of an expensive pre-existing health condition, cannot purchase insurance in the private market. Generally, risk pools are financed by a mixture of State general revenues, health insurance premium taxes, and individual premiums. Several States have actually implemented such pools. However, because risk-pool premiums are high (even though insufficient on an actuarial basis)—typically 125 to 150 percent of equivalent policies—many of the uninsurable cannot afford to participate. Consequently, these pools have limited enrollments, but require substantial subsidies, nonetheless. Enrollment in State risk pools ranges from 94 people in Wyoming to 25,000 in Minnesota ( Trippler, 1991 ).
Oregon health priorities demonstration
In order to increase the number of people with health insurance, the State of Oregon has proposed a three-part program ( Eddy, 1991 ). First, it proposes to expand Medicaid eligibility to all persons below the poverty line, whether or not they are categorically eligible, and to partly finance these expansions in health insurance coverage by not paying for medical services that are determined annually by the legislature to be of low priority. Oregon constructed a partial enumeration of health services. Based on available medical information and on the values expressed by Oregonians toward those outcomes, as assessed through public forums and surveys, 709 pairs of conditions and treatments were ranked from most- to least-expected positive outcomes.
The annual Medicaid budget will determine how far down the list services can be funded in any given year. Only mothers and children would be covered under the demonstration's first year, and the elderly and disabled populations would be phased in at a later date. This policy has been described as rationing, and criticized as funding expansions for one group of the poor at the expense of another. However, it has been defended as achieving greater equity among the poor by giving a smaller but higher priority benefit package to a larger group of people, and allowing explicit public participation in publicly funded health insurance choices. Because of the nature of the changes to the Medicaid program, Federal approval of the demonstration is required before it can be implemented. To date, approval has not been given.
In addition to the Medicaid changes, the Oregon proposal includes two other components. It would require employers, on a play or pay basis, to extend insurance coverage to employees not currently insured; and, it would allow low-income people not covered by the employer mandate or Medicaid to purchase publicly-subsidized State-sponsored insurance.
Private sector reforms
In recent years, employers and private insurers have used a number of strategies to control health-care costs. These include the development of coordinated care networks, such as HMOs and PPOs, previously noted, increases in employee cost sharing, and the employment of a variety of utilization review techniques. All of these approaches are designed to decrease utilization of health care services thought to have marginal value to the individual case.
Another cost-control strategy that many large employers use is to self-insure, paying for employee health expenses rather than purchasing a health insurance policy from an insurance company. Under ERISA, employers who self-insure escape State regulations, including mandated benefits and taxes on premiums. Some self-insured companies have placed limits (for example, $5,000) on payments for specific conditions such as AIDS. This has been challenged in the courts ( McGann v. H and H Music Co., 1991 ). Self-insuring employers also avoid the profit, marketing, and sales components of private health insurance policies, and reserve for themselves the financial benefits which other insurers secure through investment of premiums and reserves. Such employers may contract with a health insurer for claims processing services only. More than one-half of all group insurance company coverage is now provided by self-insurance ( Health Insurance Association of America, 1991 ). 4
Despite all of these efforts, employers may find that offering a coordinated care product (PPO or HMO) as a choice to the employee group may not reduce overall costs. Although healthy employees opt for the coordinated care network (which they do not expect to use) to obtain lower premiums, the premium for the employer's traditional indemnity plan is driven up by the sicker risk pool that remains in the FFS sector. One recent study of a PPO found that enrollees used it for preventive care and minor illnesses, but went outside the network about one-half the time for specialty care and hospitalization without surgery ( Wouters and Hester, 1988 ). This suggests a dilemma for public policy in relation to encouraging PPOs: If the price for going outside the network is not punitive, enrollees will go outside for much of their care. However, if the price is punitive, the plan may no longer be attractive to enrollees.
Health-system reform
By the early 1990s, continued large premium increases in the small group health insurance market led to increasing recognition that reforms were needed at the State or National level. The heavy use of medical underwriting by small group insurers combined with such practices as increasing premium rates when illnesses occurred meant that many companies faced the choice of dropping coverage, excluding employees with medical conditions from their policies, or shopping for a new insurer in an ever-tightening and expensive market.
Despite pressure for fundamental reform in recent years, major changes in the U.S. health care system have not occurred for several reasons: 1) no consensus has yet emerged on the direction fundamental reform should take; 2) there is divided political control of the Administration and Congress; 3) budget pressures at both the Federal and State levels make it unlikely that there will be substantial new money to finance reforms; 4) the public is unhappy with the health system as a whole but satisfied with their own doctor; and 5) the public is unwilling to pay more than a small amount in new taxes to finance changes ( Blendon and Edwards, 1991 ; Blendon and Donelan, 1990 ).
Health has emerged as an important issue in the 1992 election. Candidates and all the major interest groups have advanced proposals, and bills have been introduced in Congress. The Republican Party tends to support voluntary market-based proposals and the Democratic Party tends to support mandatory government-directed proposals, but there are still significant differences within each party. Proposals tend to differ on one or more of several dimensions: the extent to which they rely on the private sector or government to provide health insurance coverage; whether they call for cost control through market forces, government ratesetting, or government-determined budgets; and whether they are universal and mandatory, or voluntary and incentive-based.
It is an open question whether the country will unite behind any of the broad-scale proposals outlined later, or support incremental changes to components of the current system.
President Bush's proposal
President Bush has advanced a broad, market-based reform approach that builds on the present health care delivery system ( Executive Office of the President, 1992 ). The plan minimizes the role of Government in providing health insurance in favor of providing individuals with tax credits for the purchase of private insurance but also contains regulatory aspects. The plan has numerous elements. It would:
- Provide health insurance tax credits to the poor for the purchase of private insurance.
- Increase tax subsidies to the middle class for the purchase of insurance.
- Regulate the ability of private insurers to select whom to insure and how much to charge.
- Encourage the growth of coordinated care in public and private programs.
- Reduce administrative costs in public and private programs.
- Reform the medical liability system.
- Expand access to services in underserved areas by increasing funding for public health clinics and health personnel.
Advantages of the proposal include that it builds on the current system, which minimizes disruption for those who are satisfied with their current arrangements, and allows those newly enfranchised with a tax credit or otherwise assisted in purchasing health care coverage to choose their health insurance plan. However, critics argue that the proposal does not guarantee universal coverage, and hence the problems surrounding the uninsured will not be fully remediated. They also assert that market incentives and managed care approaches will not adequately control costs.
Employer-based proposals
Some members of the Democratic Party have endorsed play or pay. This type of proposal requires employers to provide a minimum health insurance package or pay a tax to support public provision of coverage to their employees. Variations, such as the proposal of the National Leadership Coalition, include an overall health budget target, set by a quasi-governmental board, which would constrain real growth in health spending, over time, to the growth in the gross national product ( National Leadership Coalition for Health Care Reform, 1991 ).
Play or pay proposals address the problem of self-selection by allowing employers to choose between provision of insurance or payment of the tax. Employers facing high health insurance expenses may save money by paying the tax, while those with low health expenses may save money by purchasing insurance. The public plan could become very expensive if private insurance covers low-cost employer groups, leaving high-cost groups to the public plan. The play or pay approach differs from an employer mandate primarily by having a back-up public plan that would shift significant dollars from the private to the public sector. However, this back-up public plan could potentially include all of the uninsured, while an employer mandate, by itself, would leave uncovered the 25 percent of the uninsured who are not connected to the labor force.
Advantages of employer-based approaches (either a mandate or play or pay) include expanding, rather than replacing, the current employer-based insurance system to uncovered workers thereby reducing the current problem of cost shifting. When compared with government-sponsored national health insurance, employer-based proposals limit the costs shifted to public budgets. However, critics argue that employer-based approaches will increase unemployment as employers, particularly small businesses, are forced to lay off workers because they cannot or choose not to incur the tax or the cost of health insurance. They also characterize mandated coverage as a tax on employers and employees. Critics of play or pay argue that the public plan would be unstable, grow rapidly, and likely would evolve into national health insurance ( Butler, 1991 ).
Government-sponsored national health insurance
Advocates of publicly financed or budgeted approaches, which include some members of the Democratic Party, are split between two possible versions: the Canadian or State-budgeted model, and the Medicare or federally budgeted model. Arguments for the Federal model are that a global budget and a single payer would be the most efficient in reducing duplicative administrative costs, negotiating payment levels with health providers, and assuring universal coverage ( Himmelstein and Woolhandler, 1989 ). Proponents for the State model argue that State budgets are constrained by the inability to run deficits or print money, so States may have a greater stake in restraining cost growth than the Federal Government. In addition, consolidating health programs at the State level would build on existing State functions such as licensing providers and inspecting health facilities. Opponents argue that national health insurance would lead to burdensome regulation, rationing, and objectionable new taxes.
Recent blue ribbon commission proposals
Several recent Commissions have examined the question of universal health insurance coverage and cost control. These include the Pepper Commission (a bipartisan group representing Congress, the Administration, and the public), the Quadrennial Social Security Advisory Commission, the National Governors' Association (NGA), and the National Leadership Coalition for Health Care Reform (1991) , a group of big business, unions, consumers, and health care professionals. The Quadrennial Commission recommended a series of demonstrations in the States prior to fundamental reform at the Federal level ( Advisory Council on Social Security, 1991 ). NGA recommended federalizing the long-term care portion of Medicaid and allowing States to engage in demonstrations, such as Hawaii's employer mandate and Maryland's all-payer system. The Pepper Commission ( U.S. Bipartisan Commission, 1990 ) and the National Leadership Coalition (1991) recommended variations on an employer-based play or pay approach.
Summary and conclusion
As of this writing, December 1992, it appears that the new Administration's approach to national health reform will build upon the existing employer- sponsored health insurance system. It is unclear, however, how universal coverage will be achieved or costs controlled. Health reform will remain high on the political agenda because of the continuing growth in health care expenditures in the United States and the resulting pressure on Federal, State, corporate, and individual budgets.
Acknowledgments
We wish to thank Chris Bladen and other staff of the Office of the Assistant Secretary for Planning and Evaluation, George Schieber, Health Care Financing Administration (HCFA), Richard Saltman, OECD project consultant, Emory University, HCFA reviewers, and the OECD staff for comments on earlier versions of this article.
1 This article is a slightly shorter version of the official U.S. Government paper submitted to the OECD.
Reprint requests: George Greenberg, Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, 200 Independence Avenue, SW., Room 442E, Washington, DC. 20201.
2 The numbers presented in this document reflect this duplicative coverage and consequently do not sum to 100 percent.
3 Recent strikes—Pittson Coal strike in West Virginia in 1989, and Communication Workers of America in 1989 struck in 15 States against three regional telephone companies: Bell Atlantic, NYNEX, and Pacific Telesis ( Gorman, 1989 ).
4 Self-insured plans here include administrative services only plans, in which the corporation or organization self-insures but contracts out for the processing of claims, and minimum premium plans in which the corporation or organization self-insures but also purchases health insurance for very large claims.
- Advisory Council on Social Security. Commitment to Change: Foundations for Reform. Washington: 1991. [ Google Scholar ]
- American Hospital Association. Annual Survey of Hospitals, 1980-92. In Lane, L., A decade of growth in outpatient surgery. Hospitals. 1992 May 5; 66 (9):34–35. [ Google Scholar ]
- American Hospital Association. Hospital Statistics. Chicago: 1990-91. [ Google Scholar ]
- American Medical Association. Physician Provision of Charity Care. Chicago: 1991. [ Google Scholar ]
- American Medical Association. The Cost of Medical Professional Liability in the 1980s. Chicago: 1990. [ Google Scholar ]
- Anderson GF. Health Care Financing Review. 1991 Annual Supplement. Washington: U.S. Government Printing Office; Mar. 1992. All-payer ratesetting: Down but not out; pp. 42–44. HCFA Pub. No. 03322. Office of Research and Demonstrations, Health Care Financing Administration. [ PubMed ] [ Google Scholar ]
- Blendon R, Donelon K. The Public and the Emerging Debate Over National Health Insurance. New England Journal of Medicine. 1990 Jul 19; 323 (3):208–212. [ PubMed ] [ Google Scholar ]
- Blendon R, Edwards J. Caring for the uninsured: Choices for reform. Journal of the American Medical Association. 1991 May 15; 265 (19):2563–2565. [ PubMed ] [ Google Scholar ]
- Boards of Trustees of the Federal Hospital Insurance Trust Fund. 1992 Annual Report of the Board of Trustees of the Federal Hospital Insurance Trust Fund. Washington, DC.: Apr. 1992. [ Google Scholar ]
- Brook R, Kamberg C, Mayer-Oakes A, et al. Appropriateness of Acute Medical Care for the Elderly: An Analysis of the Literature. Santa Monica, CA.: RAND Corporation; 1989. [ PubMed ] [ Google Scholar ]
- Brown ER. Medicare and Medicaid: The process, value, and limits of health care reforms. Journal of Public Health Policy. 1983 Sept. 4 (3):335–366. [ PubMed ] [ Google Scholar ]
- Burwell B. Middle-Class Welfare: Medicaid Estate Planning for Long-Term Care Coverage. Lexington, MA.: SysteMetrics/McGraw Hill Inc.; Sept. 1991. [ Google Scholar ]
- Butler S. Why ‘play or pay’ national health is doomed to fail. The Heritage Lectures. 1991; 329 :1–9. [ Google Scholar ]
- Butler S, Haislmaier EF, editors. A National Health System for America. Washington: The Heritage Foundation; 1989. [ Google Scholar ]
- Chassin MR, Brook RH, Park RE, et al. Variations in the Use of Medical and Surgical Services by the Medicare Population. New England Journal of Medicine. 1986 Jan. 314 (5):285–290. [ PubMed ] [ Google Scholar ]
- Chassin MR, Kosecoff J, Park RE. Does Inappropriate Use Explain Geographic Variation in the Use of Health Care Services. Journal of the American Medical Association. 1987 Nov. 258 (18):2533–2537. [ PubMed ] [ Google Scholar ]
- Cohen W. Health Care Financing Review. 1985 Annual Supplement. Washington: U.S. Government Printing Office; 1986. Reflections on the enactment of Medicare and Medicaid; pp. 3–11. HCFA Pub. No. 03217. Office of Research and Demonstration, Health Care Financing Administration. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Colwill J. Where Have All the Primary Care Applicants Gone? New England Journal of Medicine. 1992 Feb. 326 (6):387–393. [ PubMed ] [ Google Scholar ]
- Coulam R, Gaumer GL. Health Care Financing Review. 1991 Annual Supplement. Washington: U.S. Government Printing Office; Mar. 1992. Medicare's prospective payment system: A critical appraisal; pp. 45–78. HCFA Pub. No. 03322. Office of Research and Demonstration, Health Care Financing Administration. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Danzon P. The Hidden Costs of Budget-Constrained Health Insurance Systems. Paper presented at the American Enterprise Institute Conference; Washington, DC.. Oct. 3, 1991. [ Google Scholar ]
- Eddy D. Oregon's plan: Should it be approved? Journal of the American Medical Association. 1991 Nov. 266 (17):2439–2445. [ PubMed ] [ Google Scholar ]
- Employee Benefit Research Institute. Fundamentals of Employee Benefit Programs. Washington: 1990. [ Google Scholar ]
- Employee Benefit Research Institute. Issue Brief, No 118. Washington: Sept. 1991. [ Google Scholar ]
- Enthoven AC. Consumer-Choice Health Plan: A National Health Insurance Proposal Based on Regulated Competition in the Private Sector. New England Journal of Medicine. 1978 Mar. 298 (13):709–720. [ PubMed ] [ Google Scholar ]
- Executive Office of the President. The President's Comprehensive Health Reform Program. Washington: U.S. Government Printing Office; 1992. [ Google Scholar ]
- Farley P. Who are the uninsured? The Milbank Memorial Fund Quarterly, Health and Society. 1985; 63 :476–503. [ PubMed ] [ Google Scholar ]
- Florida Health Care Cost Containment Board. Joint Ventures Among Health Care Providers in Florida. Sept. Tallahassee, FL.: 1991. [ Google Scholar ]
- Fox DM, Schaffer DC. Health Policy and ERISA: Interest Groups and Semipreemption. Journal of Health Politics, Policy and Law. 1989 Summer; 14 (2):239–260. [ PubMed ] [ Google Scholar ]
- Freeman HE, Blendon RJ, Aiken LH, et al. Americans Report on Their Access to Health Care. Health Affairs. 1987 Spring; 6 (1):6–18. [ PubMed ] [ Google Scholar ]
- Friedman E. The Uninsured: From Dilemma to Crisis. Journal of the American Medical Association. 1991 May 15; 265 (19):2491–2495. [ PubMed ] [ Google Scholar ]
- Friedman E. Health insurance in Hawaii: Paradise Lost or Found? Business and Health. 1990 Jun; 8 :52–59. [ PubMed ] [ Google Scholar ]
- Glaser WA. Health Insurance in Practice. San Francisco: Jossey-Bass; 1991. [ Google Scholar ]
- Goldberg K, Hartz A, Jacobsen S, et al. Racial and Community Factors Influencing Coronary Artery Bypass Graft Surgery Rates for all 1986 Medicare Patients. Journal of the American Medical Association. 1992 Mar. 267 (11):1473–1477. [ PubMed ] [ Google Scholar ]
- Gorman C. Can't afford to get sick. Time. 1989 Aug. 134 :43. [ Google Scholar ]
- Gornick M, Greenberg JN, Eggers PW, et al. Health Care Financing Review. 1985 Annual Supplement. Washington: U.S. Government Printing Office; 1968. Twenty years of Medicare and Medicaid: Covered populations, use of benefits, and program expenditures; pp. 13–59. HCFA Pub. No. 03217. Office of Research and Demonstration, Health Care Financing Administration. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Graig L. Health of Nations, An International Perspective on US Health Care Reform. Washington, DC.: The Wyatt Company; 1991. [ Google Scholar ]
- Hadley J, Steinberg E, Feder J. Comparisons of Uninsured and Privately Insured Hospital Patients: Condition on Admission, Resource Use, and Outcome. Journal of the American Medical Association. 1991 Jan. 265 (3):374–379. [ PubMed ] [ Google Scholar ]
- Harvard Medical Practice Study. Patients, Doctors, and Lawyers: Medical Injury, Malpractice Litigation, and Patient Compensation in New York. Cambridge, MA.: President and Fellows of Harvard College; 1990. [ Google Scholar ]
- Health Insurance Association of America. Source Book of Health Insurance Data. Washington: 1991. [ Google Scholar ]
- Hellinger F. Forecasting the Medical Care Costs of the HIV Epidemic: 1991-1994. Inquiry. 1991 Fall; 28 (3):213–225. [ PubMed ] [ Google Scholar ]
- Himmelstein DU, Woolhandler S. A National Program for the U.S.—A Physicians' Proposal. New England Journal of Medicine. 1989 Jan. 320 (2):102–108. [ PubMed ] [ Google Scholar ]
- Iglehart JK. The American Health Care System: Introduction. New England Journal of Medicine. 1992 Apr. 326 (14):962–967. [ PubMed ] [ Google Scholar ]
- Institute of Medicine. Computer-Based Patient Records: An Essential Technology for Health Care. Washington, DC.: National Academy Press; Apr. 1991. [ Google Scholar ]
- John LD, Jolly P, Krakower JY, et al. U.S. Medical School Finances. Journal of the American Medical Association. 1991 Aug. 266 (7):985–990. [ PubMed ] [ Google Scholar ]
- Jonas HS, Etzel SI, Barzansky B. Educational Programs in U.S. Medical Schools. Journal of the American Medical Association. 1991 Aug. 266 (7):913–920. [ PubMed ] [ Google Scholar ]
- Kronick R. Can Massachusetts Pay for Health Care for All? Health Affairs. 1991 Spring; 10 (1):26–44. [ PubMed ] [ Google Scholar ]
- Langenbrunner JC. Improving the Cost-Effectiveness of Health Care Under the Medicare and Medicaid Programs in the United States: Experience and Future Directions. Paper presented at the International Social Security Association Meeting; Ottawa, Canada. Oct. 1991. [ Google Scholar ]
- Levit KR, Lazenby HC, Cowan CA, et al. Health Care Financing Review. 1. Vol. 13. Washington: U.S. Government Printing Office; Fall. 1991a. National health expenditures, 1990; pp. 29–54. HCFA Pub. No. 03341. Office of Research and Demonstration, Health Care Financing Administration. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Levit KR, Lazenby HC, Letsch SW, et al. National Health Care Spending, 1989. Health Affairs. 1991b Spring; 10 (1):117–130. [ PubMed ] [ Google Scholar ]
- Levit KR, Cowan CA. Health Care Financing Review. 2. Vol. 13. Washington: U.S. Government Printing Office; Winter. 1991. Business, households, and governments: Health care costs, 1990; pp. 83–93. HCFA Pub. No. 03326. Office of Research and Demonstrations, Health Care Financing Administration. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Manning WG, Leibowitz A, Goldberg GA, et al. A Controlled Trial of the Effect of a Prepaid Group Practice on Use of Services. New England Journal of Medicine. 1984 Jun 7; 310 (23):1505–1510. [ PubMed ] [ Google Scholar ]
- Marder W, Emmons D, Kletke P, et al. Physician Payment Patterns: Challenging Conventional Wisdom. Health Affairs. 1988 Winter; 7 (5):137–145. [ PubMed ] [ Google Scholar ]
- Mathematica Policy Research. National Evaluation of the Medicare Competition Demonstrations Summary Report. Washington, DC.: Jan. 1989. Contract Number 500-83-0047. Prepared for the Health Care Financing Administration. [ Google Scholar ]
- McGann v. H and H Music Company: U.S. Court of Appeals, Fifth Circuit, Number 90-2672. Nov. 4, 1991.
- Merrick NJ, Brook RH, Fink A, et al. Use of Carotid Endarterectomy in Five California Veterans Administration Medical Centers. Journal of the American Medical Association. 1986 Nov. 256 (18):2531–2535. [ PubMed ] [ Google Scholar ]
- Mills WD. Health Care Financing Review. 1985 Annual Supplement. Washington: U.S. Government Printing Office; 1986. Building a better safety net; pp. 1–2. HCFA Pub. No. 03217. Office of Research and Demonstrations, Health Care Financing Administration. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- National Center for Health Statistics. Health, United States, 1990. Washington: U.S. Government Printing Office; 1991. DHHS Pub. No. (PHS) Public Health Service. [ Google Scholar ]
- National Leadership Coalition for Health Reform. Excellent Health Care for All Americans at a Reasonable Cost. Washington, DC.: 1991. [ Google Scholar ]
- Newhouse JP, Anderson G, Roos L. Hospital Spending in the United States and Canada: A Comparison. Health Affairs. 1988 Winter; 7 (5):6–16. [ PubMed ] [ Google Scholar ]
- Newhouse JP, Manning WG, Morris CN, et al. Some Interim Results From a Controlled Trial of Cost-Sharing in Health Insurance. New England Journal of Medicine. 1981 Dec. 305 (25):1501–1507. [ PubMed ] [ Google Scholar ]
- Pan American Health Organization. AIDS surveillance in the Americas. Washington, DC.: Mar. 1992. [ Google Scholar ]
- Pauly MV, Danzon P, Feldstein P, et al. A plan for ‘Responsible National Health Insurance’ Health Affairs. 1991 Spring; 10 (1):5–25. [ PubMed ] [ Google Scholar ]
- Pauly MV. Taxation, Health Insurance, and Market Failure in the Medical Economy. Journal of Economic Literature. 1986 Jun; 24 (2):629–675. [ PubMed ] [ Google Scholar ]
- Politzer RM, Harris DL, Gaston MH, et al. Primary Care Physician Supply and the Medically Underserved. Journal of the American Medical Association. 1991 Jul 3; 266 (1):104–109. [ PubMed ] [ Google Scholar ]
- Porter M, Ball P, Kraus N. The Interstudy Competitive Edge. 2. Vol. 1. Excelsior, MN.: Jan. 1992. [ Google Scholar ]
- Prospective Payment Assessment Commission. The trend and distribution of hospital uncompensated care costs 1980-1989. Washington: U.S. Government Printing Office; Oct. 1991. Technical report I-91-04. [ Google Scholar ]
- Reinhardt U. Health Care Spending and American Competitiveness. Health Affairs. 1989 Winter; 8 (4):5–21. [ PubMed ] [ Google Scholar ]
- Reinhardt U. Resource Allocation in Health Care: The Allocation of Lifestyles to Providers. The Milbank Quarterly. 1987; 65 (2):153–176. [ PubMed ] [ Google Scholar ]
- Rice TH, Labelle RJ. Do Physicians Induce Demand for Medical Services? Journal of Health Politics, Policy and Law. 1989 Fall; 14 (3):587–600. [ PubMed ] [ Google Scholar ]
- Rich S. Tracing Medical Costs to Social Problems. The Washington Post. 1991 Aug. [ Google Scholar ]
- Roper W, Winkenwerder W, Hackbarth G, et al. Effectiveness in Health Care: An Initiative to Evaluate and Improve Medical Practice. New England Journal of Medicine. 1988 Nov. 319 (18):1197–1202. [ PubMed ] [ Google Scholar ]
- Rosenblatt R. Specialists or Generalists: On Whom Should We Base the American Health Care System? Journal of the American Medical Association. 1992 Mar. 267 (12):1665–1667. [ PubMed ] [ Google Scholar ]
- Rublee D. Medical Technology in Canada, Germany, and the United States. Health Affairs. 1989 Fall; 8 (3):178–181. [ PubMed ] [ Google Scholar ]
- Ruther M, Reilly TW, Silverman HA, et al. Medicare and Medicaid Data Book, 1990. Washington: U.S. Government Printing Office; Mar. 1991. Health Care Financing Program Statistics. HCFA Pub. No. 03314. Office of Research and Demonstrations, Health Care Financing Administration. [ Google Scholar ]
- Sawhill I. Economic Policy. In: Palmer JL, Sawhill IV, editors. The Reagan Experiment. Washington, DC.: The Urban Institute Press; 1982. [ Google Scholar ]
- Scheffler R, Sullivan S, Ko T. The Impact of Blue Cross and Blue Shield Plan Utilization Management Programs, 1980-1988. Inquiry. 1991 Fall; 28 (3):263–275. [ PubMed ] [ Google Scholar ]
- Schieber G, Poullier J, Greenwald LM. Health Care Systems in Twenty-Four Countries. Health Affairs. 1991 Fall; 10 (3):22–38. [ PubMed ] [ Google Scholar ]
- Schneider M. Health Care Financing Review. 3. Vol. 12. Washington: U.S. Government Printing Office; Jun, 1991. Health care cost containment in the Federal Republic of Germany; pp. 87–101. HCFA Pub. No. 03317. Office of Research and Demonstrations, Health Care Financing Administration. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schwartz L. The Medical Costs of America's Social Ills. Wall Street Journal. 1991 Jun 24; [ Google Scholar ]
- Short P, Monheit A, Beauregard K. National Medical Expenditure Survey: A profile of uninsured Americans. National Center for Health Services Research and Health Care Technology Assessment; Rockville, MD.: 1989. Research findings. [ Google Scholar ]
- Smeeding T, Torrey BB, Rein M. Patterns of Income and Poverty: The Economic Status of Children and the Elderly in Eight Countries. In: Palmer J, Smeeding T, Torrey BB, editors. The Vulnerable. Washington, DC.: The Urban Institute Press; 1988. [ Google Scholar ]
- Sonnefeld S, Waldo D, Lemieux J, et al. Health Care Financing Review. 1. Vol. 13. Office of Research and Demonstrations, Health Care Financing Administration; Fall. 1991. Projections of national health expenditures through the year 2000; pp. 1–27. HCFA Pub. No. 03321. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sullivan L. President Bush's Comprehensive Health Reform Package. Journal of American Health Policy. 1992 Mar-Apr; 2 (2):15–18. [ PubMed ] [ Google Scholar ]
- Swartz K, Lipson D. Strategies for Assisting the Medically Uninsured. Washington, DC.: The Urban Institute and the Intergovernmental Health Policy Project; 1989. [ Google Scholar ]
- Trippler A. Comprehensive Health Insurance for High Risk Individuals. Bloomington, MN.: Communicating for Agriculture, Inc.; Aug. 1991. [ Google Scholar ]
- U.S. Bipartisan Commission on Comprehensive Health Care. Access to Health Care and Long-Term Care for all Americans. Recommendations to Congress. Washington, DC.: 1990. [ Google Scholar ]
- U.S. Bureau of the Census. Current Population Reports. No. 175. Washington: U.S. Government Printing Office; 1991a. Poverty in the United States: 1990. (P-60). [ Google Scholar ]
- U.S. Bureau of the Census. Current Population Survey File. Washington, DC.: Mar, 1991b. Tabulations by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. [ Google Scholar ]
- U.S. Bureau of Labor Statistics. Employee benefits in medium and large firms, 1988. Bulletin 2336:39. Washington: Government Printing Office; Aug. 1989. U.S. Department of Labor. [ Google Scholar ]
- U.S. Bureau of Labor Statistics. Employee benefits in medium and large firms, 1981. Bulletin 2140:5. Washington: Government Printing Office; Aug. 1982. U.S. Department of Labor. [ Google Scholar ]
- U.S. Congressional Budget Office. Factors Contributing to the Growth of the Medicaid Program. Washington: May, 1992. [ Google Scholar ]
- U.S. Congressional Research Service. Health Insurance and the Uninsured: Background Data and Analysis. Washington: U.S. Government Printing Office; May, 1988. [ Google Scholar ]
- U.S. Department of Health and Human Services. Summary Report of the Graduate Medical Education Advisory Committee to the Secretary. Washington: U.S. Government Printing Office; 1981. DHHS publication (HRA) 81-651. [ Google Scholar ]
- U.S. Department of Labor. Employee Benefits in Medium and Large Firms, 1989. Bulletin Number 2363. Washington: U.S. Government Printing Office; Jun, 1990. Bureau of Labor Statistics. [ Google Scholar ]
- U.S. Department of the Treasury. Financing Health and Long-Term Care Report to the President and to Congress. Washington: U.S. Government Printing Office; Mar. 1990. [ Google Scholar ]
- U.S. General Accounting Office. Canadian Health Insurance: Lessons for the United States. Washington: Jun, 1991. Pub. No. HRD-91-90. [ Google Scholar ]
- U.S. House of Representatives, Committee on Ways and Means. Overview of Entitlement Programs, 1991 Green Book. Washington: U.S. Government Printing Office; May 7, 1991. [ Google Scholar ]
- U.S. Office of Technology Assessment. Health Care in Rural America. Washington: U.S. Government Printing Office; Sep, 1990. Pub. No. OTA-H-434. [ Google Scholar ]
- Van Ellet T. State Comprehensive and Catastrophic Health Insurance Programs: An overview. Washington: Intergovernmental Health Policy Project. George Washington University; 1981. [ Google Scholar ]
- Waldo DR, Sonnefeld ST, McKusick DR, et al. Health Care Financing Review. 4. Vol. 10. Washington: U.S. Government Printing Office; Summer. 1989. Health expenditures by age group, 1977 and 1987; pp. 111–120. HCFA Pub. No. 03284. Office of Research and Demonstrations, Health Care Financing Administration. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wennberg J, Gittelsohn A. Small area variations in health care delivery. Science. 1973; 182 :1102–1108. [ PubMed ] [ Google Scholar ]
- Woolhandler S, Himmelstein D. The Deteriorating Administrative Efficiency of the U.S. Health Care System. New England Journal of Medicine. 1991 May 2; 324 (18):1253–1258. [ PubMed ] [ Google Scholar ]
- Wouters AZ, Hester J. Patient Choice of Providers in a Preferred Provider Organization. Medical Care. 1988 Mar. 26 (3):240–255. [ PubMed ] [ Google Scholar ]
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
5 Critical Priorities for the U.S. Health Care System
- Marc Harrison

A guide to making health care more accessible, affordable, and effective.
The pandemic has starkly revealed the many shortcomings of the U.S. health care system — as well as the changes that must be implemented to make care more affordable, improve access, and do a better job of keeping people healthy. In this article, the CEO of Intermountain Healthcare describes five priorities to fix the system. They include: focus on prevention, not just treating sickness; tackle racial disparities; expand telehealth and in-home services; build integrated systems; and adopt value-based care.
Since early 2020, the dominating presence of the Covid-19 pandemic has redefined the future of health care in America. It has revealed five crucial priorities that together can make U.S. health care accessible, more affordable, and focused on keeping people healthy rather than simply treating them when they are sick.
- Marc Harrison , MD, is president and CEO of Salt Lake City-based Intermountain Healthcare.
Partner Center
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Confronting Challenges in the US Health Care System : Potential Opportunity in a Time of Crisis
- 1 Deputy Editor, JAMA Health Forum
- 2 Department of Health Policy, Vanderbilt University School of Medicine, Nashville, Tennessee
- Editorial The Near-Term Future of Health Care Reform Ezekiel J. Emanuel, MD, PhD JAMA
- Editorial Crucial Questions for US Health Policy in the Next Decade John Z. Ayanian, MD, MPP JAMA
The sheer number of challenges facing the Biden Administration and the 117th Congress in the health policy sphere is staggering, as is the range of potential solutions offered by the authors of the Viewpoints in the JAMA Health Policy series. 1 The most pressing challenges involve addressing the global COVID-19 pandemic. Yet policy makers would be remiss if they did not leverage this opportunity to also address the fundamental problems with the US health system laid bare by the nation’s response to the pandemic. These include major challenges related to health insurance coverage, the solvency of publicly funded programs, the stability of the health care safety net, market power and consolidation, inequities in health care access and outcomes, public health infrastructure, and the failure to effectively use technology to help counteract these problems.
Personal health crises, such as experiencing a myocardial infarction, can spur patients and their care teams to work to improve underlying health habits and conditions that contributed to the health event. Similarly, the havoc wrought by the COVID-19 pandemic is a clarion call to improve US health care coverage, financing, and organization. The status quo practices of the health system in the US—like poor health habits of a patient with heart disease—have left it susceptible to poor outcomes.
The high cost of the US health care system is its biggest weakness. In the US, national expenditures on health care goods and services were approximately $4 trillion in 2020, accounting for an estimated 18% of gross domestic product. 2 High prices for care explain a large part of the difference in spending between the US and other developed countries. Surprise billing is just one aspect of the pricing problem, but one that, as Colla 3 describes, illustrates many troubling trends in medicine. Consolidation of hospitals, insurers, and large and small practices has accelerated during the pandemic and as Dafny 4 explains, can be expected to lead to higher prices in the commercial market in the future. Chernew 5 elegantly discusses how market power and consolidation in the health care industry, exacerbated by the pandemic, could lead to still higher prices and a cycle of harms for individuals, governments, and society as a whole.
Those harms include incomplete insurance coverage, both in terms of numbers of people covered and the generosity of that coverage, due to high prices that lead to high insurance premiums. Higher premiums have meant that many people who are not eligible for subsidies on the health insurance exchanges find insurance unaffordable. The Biden campaign proposals to extend subsidies to higher income groups are designed to help solve this problem but will not address its root causes. High premiums have also contributed to wage stagnation for US workers with employment-based health insurance and to higher cost-sharing, which has been shown to reduce access to necessary care.
In addition, higher health care costs put pressure on state and federal budgets. As Gee et 6 al discuss, 12 states have not chosen to expand Medicaid to date, and a concern that even being responsible for 10% of the increased costs could be burdensome is one of the reasons cited for this choice. Frank and Neuman 7 emphasize that the looming deficits in the Medicare Part A Trust Fund will also put pressure on federal policy makers to find sources of new revenues or to cut benefits or payment rates. Perhaps even more important, as described by Venkataramani and colleagues, 8 high health care prices contribute to limited budgets for other social goods like education and housing that could improve health outcomes, possibly even more than direct spending on health care.
Similarly, it is now clear that the US has spent an increasing amount of resources on health care, but spending on public health has been inadequate. Investments in surveillance officers and systems and in stockpiles of equipment and medications are less appealing ways to spend public resources than covering new drugs or services. The pandemic has revealed the shortcomings of the US public health infrastructure and illustrates that neglecting to reinvest in public health after a pandemic will more severely compromise the ability to respond effectively to the next public health crisis. 9 Although none of the Viewpoints in this series focused on specific public health proposals, they should be part of every discussion of improving health and health care going forward. Public health policy must be central not only to health policy, but to economic policy and national security policy as well.
High health care prices might be less of a problem if the US health care system was uniformly delivering high-quality care and yielding high value. The US does prioritize health as a society and voters are reluctant to endorse solutions that limit access to the latest innovations in health care. However, a fundamental shortcoming in the US health care system is the tendency to create and perpetuate incentives to deliver higher-margin treatments and specialty care instead of primary care, preventive care, and public health. The central need to refine the focus on value was highlighted in many articles in the series.
Several Viewpoints in the Health Policy series provided worthy suggestions and policy recommendations the could help the US health care system recover from the current crises stronger. Berwick and Gilfillan 10 call for speeding the cycle time of demonstrations under the Center for Medicare and Medicaid Innovation, Dafny 4 suggests examining mergers and acquisitions more closely, and Chernew 5 proposes implementing “backstop” prices in commercial markets.
Another important step will be using data and technology strategically. During the pandemic, the health care system rapidly adopted telemedicine in clinical care. Millions of people accessed readily available data dashboards that illustrated the course of the pandemic and the extent of infections in specific areas, and many used the information to demand better and more equal care. As described by Adler-Milstein, 11 a digital transformation in the US health care system could make it possible to continuously monitor and use real-time data to inform preparedness and population-level care planning. Such data systems also could be used to help address and reduce disparities and inequities in care and to improve health system transparency, including around prices. Moreover, these systems could save money and reduce the reporting and patient tracking burdens on health care centers, physicians, and other clinicians participating in value-based care; administrative costs are estimated by Kocher et al 12 at $2500 per person per year.
Can commitments to improving health care coverage, financing, and organization be made in the midst of a pandemic and an affordability crisis? There are reasons to hope the answer is yes. The pandemic has substantially changed care patterns, shown the risks of fee-for-service payment and a reliance on highly reimbursed surgical procedures, and revealed the need for a stronger public health infrastructure and greater preparedness. Health systems will be increasingly held accountable for ensuring delivery of high-value care and for addressing health equity issues in ways that do not rely on outdated models of care. No one could have imagined or would wish the current economic, societal, or health care challenges of the COVID-19 pandemic on a new administration or Congress. But all have hope that leaders can confront these crises as potential opportunities for developing solutions to address the ongoing major challenges in the US health care system.
Correction: This article was updated on June 7, 2021, to correct the spelling of Dr Venkataramani’s name in the fifth paragraph.
Corresponding Author: Melinda B. Buntin, PhD, Department of Health Policy, Vanderbilt University School of Medicine, 2525 West End Ave, Ste 1200, Nashville, TN 37203 ( [email protected] ).
Conflict of Interest Disclosures: Dr Buntin reported being an unpaid board member of the Harvard Medical Faculty Practice in Boston, Massachusetts.

See More About
Buntin MB. Confronting Challenges in the US Health Care System : Potential Opportunity in a Time of Crisis . JAMA. 2021;325(14):1399–1400. doi:10.1001/jama.2021.1471
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
Health Care in the United States, Essay Example
Pages: 4
Words: 1013
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
In the United States, there has long been discussion about the quality and nature of the delivery of healthcare. The debates have included who may receive such services, whether or not healthcare is a privilege or an entitlement, whether and how to make patient care affordable to all segments of the population, and the ways in which the government should, or should not, be involved in the provision of such services. Indeed, many people feel that the healthcare in this country is the best in the world; others believe tha (The Free Dictionary)t our health delivery system is broken. This paper shall examine different aspects of the healthcare system in our country, discussing whether it has been successful in providing essential services to American citizens.
The delivery of healthcare services is considered to be a system; according to the Free Diction- ary (Farlex, 2010), a system is defined as “a group of interacting, interrelated, or interdependent elements forming a complex whole.” This is an apt description of our healthcare structure, as it is compiled of patients, medical and mental health providers, hospitals, clinics, laboratories, insurance companies, and many other parties that are reliant on each other and that, when combined, make up the entity known as our healthcare system.
Those who believe that our healthcare system is the best in the world often point to the fact that leaders as well as private citizens from countries throughout the world frequently come to the United States to have surgeries and other treatments that they require for survival. A more cynical view of this phenomenon is that if people have the money, they are able to purchase quality care in the U.S., a “survival of the fittest” situation. Those who lack the resources to travel to the U.S. for medical treatment are simply out of luck, and often will die without the needed care.
In fact, reports by the World Health Organization and other groups consistently indicate that while the United States spends more than any other country on healthcare costs, Americans receive lower quality, less efficient and less fairness from the system. These conclusions come as a result of studying quality of care, access to care, equity and the ability to lead long, productive lives. (World Health Organization,2001.) What cannot be disputed is that the cost of healthcare is constantly rising, a fact which was the precipitant to the large movement to reform healthcare in our country in 2010. More than 10 years ago, the goal of managed care was to drive down the costs of healthcare, but those promises did not materialize (Garsten, 2010.) A large segment of the population is either uninsured or underinsured, and it is speculated that over the next decade, these problems will only increase while other difficulties will arise (Garson, 2010.)
When examining the healthcare system, there are three aspects of care that call for evaluation: the impact of delivering care on the patient, the benefits and harms of that treatment, and the functioning of the healthcare system, as described in an article by Adrian Levy. Levy argues that each of these outcomes should be assessed and should include both the successes and the limitations of each aspect. The idea is that there should be operational measurements of patients’ interactions with the healthcare system that would include patients’ experiences in hospitals, using measurements of their functional abilities and their qualities of life following discharge. The results of patients’ interactions with the healthcare system should be utilized to develop and improve the delivery of healthcare treatment, as well as to develop policy changes that would affect the entire field of healthcare in the United States.
One view of the state of American healthcare is that the system is fragmented; there have been many failed attempts by several presidents to introduce the idea of universal healthcare. Instead, American citizens are saddled with a system in which government pays either directly or indirectly for over 50% of the healthcare in our country, but the actual delivery of insurance and of care is undertaken by an assortment of private insurers, for-profit hospitals, and other parties who raise costs without increasing quality of service (Wells, Krugman, 2006.) If the United States were to switch to a single-payer system such as that provided in Canada, the government would directly provide insurance which would most likely be less expensive and provide better results than our current system.
It is clear that throwing money at a problem does not necessarily resolve it; the fact that the United States spends more than twice as much on healthcare provision as any other country in the world only makes it more ironic that when it comes to evaluating the service, Americans fall appallingly flat. In my opinion, if the new healthcare reform bill had included a public option which would have taken the profit margin out of the equation, the nation and its citizens would have been in a much better position to receive quality healthcare. The fact that people die every day from preventable illnesses and conditions simply because they do not have affordable insurance is a national disgrace. In addition, many of the people who have been the most adamantly against government “intrusion” into their healthcare are actually on Medicaid or Medicare, federally-funded programs. Their lack of understanding of what the debate actually involves is striking, and they are rallying against what is in their own best interests. These are people that equate Federal involvement in healthcare as socialism. Unless and until our healthcare system is able to provide what is needed to all of its citizens, all claims that we have the best healthcare system in the world are, sadly, utterly hollow.
Adrian R Levy (2005, December). Categorizing outcomes of Health Care delivery. Clinical and investigative medicine, pp. 347-351.
Arthur Garson (2000). The U.S. Healthcare System 2010: Problems Principles and Potential Solutions. Retrieved July 3, 2010, from Circulation: The Journal of the American Heart Association: http://circ.ahajournals.org/cgi/reprint/101/16/2015
The Free Dictionary. (n.d.). Farlex. Retrieved July 3, 2010. http://www.thefreedictionary.com/system
World Health Organization. (2003, July). WHO World Health Report 2000. Retrieved July 3, 2010, from State of World Health: http://faculty.washington.edu/ely/Report2000.htm
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Using Learning Journals in Continuing and Higher Education, Article Critique Example
Prolonged Exposure Therapy, Research Paper Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Why the US healthcare...
Why the US healthcare system is failing, and what might rescue it
- Related content
- Peer review
- Arnold Relman , professor emeritus of medicine and social medicine, Harvard Medical School, Boston, Massachusetts, USA
- arnoldrelman{at}gmail.com
The US healthcare system is by far the most expensive in the world, but it now leaves about 50 million of its citizens totally without coverage and fails to provide adequate protection for millions more. And the quality of care is on average inferior to that of countries that spend much less. Can the rise of multispecialty groups make US medical care much more affordable and efficient?
The US healthcare system seems headed for bankruptcy because of its ever increasing and unsustainable costs. These costs will be effectively controlled only by legislative reforms in the insurance and payment for medical care, but the prospects of such legislation will depend on a more favourable political climate and stronger public support. However, legislation will accomplish little unless the organisation of medical services also changes. The recent movement of US physicians into large multispecialty groups suggests that this reorganisation of medical care may already be under way. If this trend continues, it could not only facilitate the enactment of legislation, but also help to make our medical care much more affordable and efficient.
At present, most US physicians are in solo practice or belong to small, single specialty partnerships, but new social and economic forces are beginning to make employment in large multispecialty groups a more attractive option. About a quarter of all US practitioners are now employed in such groups, which are being formed by independent physician organisations and by hospitals. If their number continues to increase and if they eventually represent the great majority of practising physicians, a wave of legislative reforms could be initiated that transforms our currently dysfunctional healthcare system. But before I say more about this move towards group practice and how it might improve prospects for reform, readers need to understand how and why our health system has been failing. I should also describe the extensive health legislation enacted by the Democrats in 2010, and explain how it falls short of providing the kind of major reforms that would be required to rescue our healthcare system.
The US system is a confusing hodgepodge that makes no sense to informed observers. Although it is by far the most expensive in the world, it now leaves about 50 million of its citizens totally without coverage and fails to provide adequate protection for millions more. Most people also have no support for the cost of long term or rehabilitative care. And, despite huge expenditures, the quality of care is highly variable—but on average inferior to many advanced countries that spend much less. The best physicians and hospitals and the best care available in the US are among the finest to be found anywhere, but access to that care is grossly uneven. Many receive substandard care and far too many receive virtually no care except when illness is far advanced or there is an emergency. 1 2
Why the huge cost and the inefficiency?
What explains this paradox? Why do we spend so much on medical care without anything like a commensurate return, and how does our system differ from those in other countries that spend barely half as much but do so much better? In my view, by far the most important explanation—the primary cause of our unique problems—is that the US, alone among all advanced Western countries, has allowed its healthcare system to become a market and its physicians to behave as if they were in business. 3 In the US medical care has become a huge, competitive industry with many private investors, but with relatively little government regulation. Involving more than $2.7 trillion (£1.7 trillion; €2 trillion), the US healthcare industry now constitutes nearly 18% of our entire economy and it continues to expand. Its growth has slowed during the past two years, largely reflecting the effect of the recession in reducing employment based insurance and the ability of most people to afford care that is not mostly paid by insurance. Expenditures will probably resume their rise when the economy improves and new federal commitments to pay for care are implemented in the years ahead.
The US is a clear example of what happens when medical care becomes a commodity in trade rather than a social service. Because the market for medical care differs so much from other markets, classical market forces do not exert their usual control over buyers and sellers and hence do not regulate supply and demand. 4 In the US medical market, those who largely control the supply of services (physicians) also largely determine the demand. Of course, the patients’ complaints, illnesses, and injuries also play an important role, but it is the physician who interprets them and knows what services are needed for diagnosis, treatment, and prevention. It is also the physician on whom the consumer (that is, the patient) relies for advice. The fee for service payment system through which most physicians are paid gives them a strong economic incentive to be overly generous in their recommendations and provision of services, especially since they are well aware of their reimbursement for the services they provide, but are usually unfamiliar with the charges made to insurers by laboratories, hospitals, and other facilities for the services they recommend.
These facilities, whether paid for each individual item of service or for an episode of care (for example, a day in the hospital or a visit to a clinic), also have strong economic incentives to maximise the volume of their profitable services and increase the referral of paying patients. So, in addition to direct marketing to consumers, they encourage doctors to use their facilities and to refer patients by offering many kinds of favours and financial arrangements. Medical products (prescription drugs, devices, and equipment), which account for more than 15% of costs, are also promoted by manufacturers like commodities in trade rather than being used only according to medical need. Marcia Angell’s much discussed 2011 article documents this behaviour by manufacturers of psychoactive drugs. 5 To increase their sales, manufacturers depend on direct marketing to patients, and give financial and other inducements to the physicians who prescribe them. While not unique to the US, these practices are more pervasive in the US than elsewhere. The conflicts of interest that stem from attempts by manufacturers to influence the behaviour of physicians add to the unnecessary costs of the system.
Not only is there little or no government regulation of the volume of services and products in the US healthcare market, but there is also very little regulation of prices—far less than in most other advanced countries. The commercial competition encouraged by this lax regulation affects the behaviour of all players in the market. No more than half of the US health economy involves investor owned organisations and institutions, but most of the others (so called not-for-profits) also see themselves as businesses competing for market share, so they act very much like their for-profit, investor owned competitors. Virtually all organisations and many physicians seek to maximise their income. The net result is the virtually unrestrained growth of health costs, driven not simply by medical need but by economic incentives.
In addition to the cost of a medical care system driven by these economic incentives, there is the huge cost exacted by the dependence of the US system on private for-profit insurance plans. Numbering in the hundreds, but increasingly being consolidated within a relatively few giant corporations, these private plans insure or provide billing and collecting services for more than half of the total population. This includes most of those covered through their place of employment and those who are self insured. In addition, about a quarter of those over 65 have opted to have Medicare pay for their care through private plans, apparently in response to vigorous marketing by private insurers who offer a few services not available in Medicare. Altogether, private insurance plans comprise a huge and growing industry, with a gross income of more than $800bn. Their profits and business overheads vary considerably but average between 15% and 25% of their premiums. The US government estimates private insurance plans added over $150bn to the cost of healthcare in 2011. 6 (The overhead expenses of Medicare are less than 5% of total expenditures.) Despite their claims to the contrary, these plans add little or nothing to the value of the insurance they sell or service that is even close to their added cost. 7 No other country is as dependent on relatively unregulated private for-profit insurance plans as is the US. Other advanced countries, such as France and Switzerland, include private insurance plans as a central part of their health system, but these plans are not-for-profit and are much more tightly regulated by government than in the US.
The costs of both halves of the US healthcare system—the publicly insured and the privately insured—have been rising at an unsustainable rate, but over the years the privately insured half has risen slightly more rapidly. Despite its much lower overheads and its not-for-profit organisation, the rising cost of public insurance has continued to follow the inflationary trajectory of the private sector. This rise is explained in part by the ageing of the population and the increasing number of citizens reaching the Medicare eligible age of 65. But the chief reasons are that the payment methods and the economic incentives of doctors and hospitals are largely the same throughout the system.
Furthermore, since both public and private insurance plans function largely through billing by fee for service, they are both open to fraudulent billing and inflated charges that enable unscrupulous providers to game the system and extract larger than justified payments. Estimates often made in the media by experts place the cost of fraud and abuse at about 5% to 10% of the total cost of personal care. Another factor driving costs in both publicly and privately insured sectors of the US system is the fear of malpractice litigation and the so called defensive behaviour of physicians who order many tests and procedures to protect themselves against possible lawsuits if anything should go wrong. There are no reliable estimates of how much unnecessary medical service results from defensive practice, but most experts agree it may be a significant but not major contribution to health costs.
The Affordable Care Act of 2010
Although the crisis in the US system is primarily caused by its costs, most of the healthcare legislation enacted in the past few years has been concerned with extending and protecting insurance benefits. A landmark bill, the Affordable Care Act (ACA) was passed by the Democratic controlled Congress in March of 2010. An excellent, readable summary of this huge and complicated legislation can be found in a recent book by McDonough. 8 Democrats have acclaimed the ACA as a major step forward in solving the US system’s problems, but many liberals, like me, have reservations. 9 The act does promise to cover more of the cost of drugs, to offer subsidised private coverage to about 16 million uninsured citizens, to help states extend Medicaid coverage to another 16 million and prevent private insurers from denying coverage to those with pre-existing illnesses or dropping coverage of those who develop expensive illnesses while being insured. Most of these benefits are not scheduled to start until 2014—although a few have already begun. The law does contain major advances but, despite its name, it has no provisions that will reliably control rising costs. To persuade the politically powerful private insurance industry to support (or, at least, not oppose) the passage of this legislation, President Obama had to agree to include in the law a requirement that all uninsured individuals buy private insurance or be fined—the so called insurance mandate. He also agreed to eliminate from the law a provision that would have allowed those with private insurance to choose a “public option,” that is, to choose a public plan similar to Medicare.
Republicans are strongly opposed to the ACA, and particularly to its insurance mandate. They believe it gives more power to the executive branch of government than the US Constitution allows, and they have brought the issue to the Supreme Court, which heard the case in March and will probably announce a decision in June. The ACA will be a central issue in the upcoming presidential campaign, with all potential Republican nominees pledged to seek immediate legislative annulment of the law if they are elected—assuming it is still standing after the Supreme Court hands down its opinion. The future shape of our healthcare system will therefore depend greatly on legal and electoral decisions made this year.
Some provisions in the ACA that have not yet been fully implemented, and a few initiatives already started by private insurers experiment with replacing the fee for service payment system with new arrangements. They pay providers for episodes of care, or encourage groups of physicians to share in any savings from assuming the comprehensive care of a designated panel of patients. These physician groups, affiliated with one or more hospitals, are called “accountable care organisations” and 32 such organisations in various parts of the country have recently signed contracts to try this model. It is much too early to know whether these initiatives will save money and be acceptable to doctors and their patients—or even whether they can function as expected—but they are being hailed by the Obama administration and by those who believe that modest changes in the present insurance and payments systems can control costs and improve the quality of care. I believe this is unrealistic, because they may never be fully completed and because they do not address the basic problems with the current system. 9
Major reform is needed
I am convinced that the impending national cost crisis and the bankruptcy of our healthcare system will not be averted unless there is much more drastic and systematic reform. 7 We will have to replace all our insurance systems, public and private, with a single public plan that guarantees universal access to prepaid, comprehensive care, and this plan should be funded by a progressive healthcare tax that all citizens (including government officials) must pay according to their means. Prepaid comprehensive care funded in this way would give government firm control over its total health expenditures while leaving decisions on the specific use of available resources where it should be—in the hands of physicians and their patients. By setting the rate of the healthcare tax, government would in effect be capping its costs. Any medical services provided outside the system would be at the patients’ expense.
To provide this kind of prepaid comprehensive care, we will need a reorganised medical care system based on private, non-profit, multispecialty group practices, in which physicians are paid largely or entirely by salary. If fee for service payment is to be largely or entirely replaced by prepaid, capitated payment, we will need medical organisations that can accept such payment and distribute an agreed, total percentage to physicians through salaries. The kind of multispecialty group practice that I have described in more detail elsewhere would be the ideal organisation to serve this function. 10
There are ample reasons and considerable empirical evidence to suggest that group practices can deliver care more efficiently than unorganised physicians in solo or small, single specialty partnership practices who compete for income and depend on fee for service payment. 11 Multispecialty groups usually include adequate numbers of primary care physicians who integrate and moderate the procedure based behaviour of the specialists. Most experts agree that substantial savings, as well as improved care, can be anticipated when primary care physicians collaborate with specialists in well organised groups. Without the fee for service incentive, prepaid salaried groups of this kind are less driven to unnecessary or duplicative services. And if the system is funded entirely by government without involving bills, the costs of insurance overheads and fraudulent billing are avoided. The potential savings would be enormous—a reduction of 30% to 40% in total expenditures would be a conservative estimate.
Multispecialty practices—the future
Multispecialty, physician managed group practices already exist in many parts of the US, mostly in the west, and least in the southeastern states. Some are well known, long established, and highly reputed. Only a few groups pay full salaries and most are still dependent on fee for service payment from multiple public and private insurers. However, the number of group practices in the country of all kinds and the number of physicians employed in these practices are increasing rapidly. There are at present over 400 such groups, employing nearly 200 000 physicians (about 25% of all practising physicians). These numbers are increasing at about 10% per year, according to information recently given to me by the American Medical Group Association, the organisation that represents most multispecialty groups.
There are many reasons why so many US physicians seem to be abandoning private practice in favour of seeking employment in large groups. Many starting physicians have acquired large personal debts during the course of their education and cannot afford the investment and financial risk of setting up their own practice. The supporting staff and facilities available in group practices and the assistance they offer with the business and administrative expenses of practice are very attractive; so are the retirement and fringe benefits. Furthermore, young US physicians nowadays are much more interested than formerly in practice settings that allow them to share responsibilities with colleagues and to work specified hours rather than assuming the heavy time demands of solo or small partnership practice. This is particularly true of women physicians, who shortly will constitute half of the physician workforce. But physicians of both genders are increasingly interested in a professional career that allows them more time for family and personal affairs. Employment (full or part time) in large groups provides that opportunity.
For their part, hospitals and physician organisations are eager to establish group practices because of the growing interest of public and private insurance plans in controlling costs by contractual arrangements with groups of physicians rather than individual practitioners. If this trend continues, soon the great majority of US physicians will be employed in large multispecialty groups and the prospects for major reform of the healthcare system will have greatly improved.
With so many physicians employed in multispecialty practices it would be much easier to institute new payment methods that replace insurance based reimbursement for itemised services with tax supported prepaid access to comprehensive care. If group practice proves popular with patients and physicians, and is increasingly perceived as an effective way to control costs and improve quality of care, it would also be much easier to persuade physicians in the groups to accept payment by salaries instead of fee for service. Popular pressure on Congress to enact reforms that are now politically impossible is more likely to be successful when most physicians are happily employed in multispecialty groups, and these groups are delivering good, affordable care.
Fierce resistance to reform can be expected from the private insurance industry, from Republicans in Congress, and from all those with vested financial interests in the status quo, so it is quite possible that the necessary legislation would be stalled until our health system faces bankruptcy, or even for an indefinite time after that. The misguided view that healthcare is primarily a business and that it requires the intervention of private insurance plans is so deeply embedded in US culture that legislation changing it to a universal right supported by government may be a long time in coming, and will certainly depend on how the political climate changes. But sooner or later reality will prevail, because a health system largely shaped by free market forces and heavily dependent on private insurance will never provide the whole US population with good medical care at an affordable cost.
The inevitable change in the health system, when it finally comes, won’t be achieved by a single legislative act of Congress. There will probably be stepwise increments—perhaps starting with reforms in various states. But I am convinced that tax supported, not-for-profit multispecialty group practice is necessary for the rescue of the US healthcare system. So the prospects for major health reform in the US depend on whether its physicians continue to choose employment in groups, and whether insurance plans are ultimately replaced by a single public payer that provides universal access to comprehensive care rather than itemised reimbursement for services.
Arnold Relman biography
Arnold Relman was editor of the New England Journal of Medicine from 1977 to 1991. He is the author of A Second Opinion: Rescuing America’s Health Care . He qualified in medicine at Columbia University, New York, in 1946, and then began research in nephrology and electrolyte balance while at Yale. In 1966 and 1974 he coedited two volumes of Controversy in Internal Medicine.
Cite this as: BMJ 2012;344:e3052
Competing interests: The author has completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review: Commissioned, externally peer reviewed.
- ↵ Davis K, Schoen C, Stremikis K. Mirror, mirror on the wall: How the performance of the U.S. health care system compares internationally: 2010 update. The Commonwealth Fund, June 2010.
- ↵ Squires DA. The U.S. health system in perspective: A comparison of twelve industrialized nations. The Commonwealth Fund, July 2011.
- ↵ Relman AS. A second opinion. Rescuing America’s health care. Public Affairs, 2010.
- ↵ Arrow KJ. Uncertainty and the welfare economics of medical care. American Economic Review 1963 ; 53 : 941 -73. OpenUrl CrossRef Web of Science
- ↵ Angell ME. The epidemic of mental illness: Why? The New York Review , June 23, 2011 :20-2.
- ↵ Keehan SP, Sisko AM, Truffer CJ, et al. National health spending projections through 2020: Economic recovery and reform drive faster spending growth. Health Aff 2011 ; 30 : 1594 -1605. OpenUrl Abstract / FREE Full Text
- ↵ Relman AS. In dire health. The American Prospect 2012 ; 23 : 34 -7. OpenUrl
- ↵ McDonough JE. Inside national health reform. University of California Press, 2011.
- ↵ Relman AS. Health care: The disquieting truth. The New York Review 30 September 2010 :45-8.
- ↵ Relman AS. How doctors could rescue health care. The New York Review 27 October 2011 :14-18.
- ↵ Enthoven AC, Tollen LA, eds. Toward a 21st century health system. The contributions and promise of prepaid group practice. Jossey-Bass, 2004.
How to build a better health system: 8 expert essays

We need to focus on keeping people healthy, not just treating them when they're sick Image: REUTERS/Rupak De Chowdhuri
.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Global Future Council on Health and Healthcare
Introduction
By Francesca Colombo , Head, Health Division, Organisation for Economic Co-operation and Development (OECD) and Helen E. Clark , Prime Minister of New Zealand (1999-2008), The Helen Clark Foundation
Our healthy future cannot be achieved without putting the health and wellbeing of populations at the centre of public policy.
Ill health worsens an individual’s economic prospects throughout the lifecycle. For young infants and children, ill health affects their capacity to acumulate human capital; for adults, ill health lowers quality of life and labour market outcomes, and disadvantage compounds over the course of a lifetime.
And, yet, with all the robust evidence available that good health is beneficial to economies and societies, it is striking to see how health systems across the globe struggled to maximise the health of populations even before the COVID-19 pandemic – a crisis that has further exposed the stresses and weaknesses of our health systems. These must be addressed to make populations healthier and more resilient to future shocks.
Each one of us, at least once in our lives, is likely to have been frustrated with care that was inflexible, impersonal and bureaucratic. At the system level, these individual experiences add up to poor safety, poor care coordination and inefficiencies – costing millions of lives and enormous expense to societies.
This state of affairs contributes to slowing down the progress towards achieving the sustainable development goals to which all societies, regardless of their level of economic development, have committed.
Many of the conditions that can make change possible are in place. For example, ample evidence exists that investing in public health and primary prevention delivers significant health and economic dividends. Likewise, digital technology has made many services and products across different sectors safe, fast and seamless. There is no reason why, with the right policies, this should not happen in health systems as well. Think, for example, of the opportunities to bring high quality and specialised care to previously underserved populations. COVID-19 has accelerated the development and use of digital health technologies. There are opportunities to further nurture their use to improve public health and disease surveillance, clinical care, research and innovation.
To encourage reform towards health systems that are more resilient, better centred around what people need and sustainable over time, the Global Future Council on Health and Health Care has developed a series of stories illustrating why change must happen, and why this is eminently possible today. While the COVID-19 crisis is severally challenging health systems today, our healthy future is – with the right investments – within reach.
1. Five changes for sustainable health systems that put people first
The COVID-19 crisis has affected more than 188 countries and regions worldwide, causing large-scale loss of life and severe human suffering. The crisis poses a major threat to the global economy, with drops in activity, employment, and consumption worse than those seen during the 2008 financial crisis . COVID-19 has also exposed weaknesses in our health systems that must be addressed. How?
For a start, greater investment in population health would make people, particularly vulnerable population groups, more resilient to health risks. The health and socio-economic consequences of the virus are felt more acutely among disadvantaged populations, stretching a social fabric already challenged by high levels of inequalities. The crisis demonstrates the consequences of poor investment in addressing wider social determinants of health, including poverty, low education and unhealthy lifestyles. Despite much talk of the importance of health promotion, even across the richer OECD countries barely 3% of total health spending is devoted to prevention . Building resilience for populations also requires a greater focus on solidarity and redistribution in social protection systems to address underlying structural inequalities and poverty.
Beyond creating greater resilience in populations, health systems must be strengthened.
High-quality universal health coverage (UHC) is paramount. High levels of household out-of-pocket payments for health goods and services deter people from seeking early diagnosis and treatment at the very moment they need it most. Facing the COVID-19 crisis, many countries have strengthened access to health care, including coverage for diagnostic testing. Yet others do not have strong UHC arrangements. The pandemic reinforced the importance of commitments made in international fora, such as the 2019 High-Level Meeting on Universal Health Coverage , that well-functioning health systems require a deliberate focus on high-quality UHC. Such systems protect people from health threats, impoverishing health spending, and unexpected surges in demand for care.
Second, primary and elder care must be reinforced. COVID-19 presents a double threat for people with chronic conditions. Not only are they at greater risk of severe complications and death due to COVID-19; but also the crisis creates unintended health harm if they forgo usual care, whether because of disruption in services, fear of infections, or worries about burdening the health system. Strong primary health care maintains care continuity for these groups. With some 94% of deaths caused by COVID-19 among people aged over 60 in high-income countries, the elder care sector is also particularly vulnerable, calling for efforts to enhance control of infections, support and protect care workers and better coordinate medical and social care for frail elderly.
Third, the crisis demonstrates the importance of equipping health systems with both reserve capacity and agility. There is an historic underinvestment in the health workforce, with estimated global shortages of 18 million health professionals worldwide , mostly in low- and middle-income countries. Beyond sheer numbers, rigid health labour markets make it difficult to respond rapidly to demand and supply shocks. One way to address this is by creating a “reserve army” of health professionals that can be quickly mobilised. Some countries have allowed medical students in their last year of training to start working immediately, fast-tracked licenses and provided exceptional training. Others have mobilised pharmacists and care assistants. Storing a reserve capacity of supplies such as personal protection equipment, and maintaining care beds that can be quickly transformed into critical care beds, is similarly important.
Fourth, stronger health data systems are needed. The crisis has accelerated innovative digital solutions and uses of digital data, smartphone applications to monitor quarantine, robotic devices, and artificial intelligence to track the virus and predict where it may appear next. Access to telemedicine has been made easier. Yet more can be done to leverage standardised national electronic health records to extract routine data for real-time disease surveillance, clinical trials, and health system management. Barriers to full deployment of telemedicine, the lack of real-time data, of interoperable clinical record data, of data linkage capability and sharing within health and with other sectors remain to be addressed.
Fifth, an effective vaccine and successful vaccination of populations around the globe will provide the only real exit strategy. Success is not guaranteed and there are many policy issues yet to be resolved. International cooperation is vital. Multilateral commitments to pay for successful candidates would give manufacturers certainty so that they can scale production and have vaccine doses ready as quickly as possible following marketing authorisation, but could also help ensure that vaccines go first to where they are most effective in ending the pandemic. Whilst leaders face political pressure to put the health of their citizens first, it is more effective to allocate vaccines based on need. More support is needed for multilateral access mechanisms that contain licensing commitments and ensure that intellectual property is no barrier to access, commitments to technology transfer for local production, and allocation of scarce doses based on need.
The pandemic offers huge opportunities to learn lessons for health system preparedness and resilience. Greater focus on anticipating responses, solidarity within and across countries, agility in managing responses, and renewed efforts for collaborative actions will be a better normal for the future.
OECD Economic Outlook 2020 , Volume 2020 Issue 1, No. 107, OECD Publishing, Paris
OECD Employment Outlook 2020 : Worker Security and the COVID-19 Crisis, OECD Publishing, Paris
OECD Health at a Glance 2019, OECD Publishing, Paris
https://www.un.org/pga/73/wp-content/uploads/sites/53/2019/07/FINAL-draft-UHC-Political-Declaration.pdf
OECD (2020), Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Health Policy Studies, OECD Publishing, Paris
Working for Health and Growth: investing in the health workforce . Report of the High-Level Commission on Health Employment and Economic Growth, Geneva.
Colombo F., Oderkirk J., Slawomirski L. (2020) Health Information Systems, Electronic Medical Records, and Big Data in Global Healthcare: Progress and Challenges in OECD Countries . In: Haring R., Kickbusch I., Ganten D., Moeti M. (eds) Handbook of Global Health. Springer, Cham.
2. Improving population health and building healthy societies in times of COVID-19
By Helena Legido-Quigley , Associate Professor, London School of Hygiene and Tropical Medicine
The COVID-19 pandemic has been a stark reminder of the fragility of population health worldwide; at time of writing, more than 1 million people have died from the disease. The pandemic has already made evident that those suffering most from COVID-19 belong to disadvantaged populations and marginalised communities. Deep-rooted inequalities have contributed adversely to the health status of different populations within and between countries. Besides the direct and indirect health impacts of COVID-19 and the decimation of health systems, restrictions on population movement and lockdowns introduced to combat the pandemic are expected to have economic and social consequences on an unprecedented scale .
Population health – and addressing the consequences of COVID-19 – is about improving the physical and mental health outcomes and wellbeing of populations locally, regionally and nationally, while reducing health inequalities.¹ Moreover, there is an increasing recognition that societal and environmental factors, such as climate change and food insecurity, can also influence population health outcomes.
The experiences of Maria, David, and Ruben – as told by Spanish public broadcaster RTVE – exemplify the real challenges that people living in densely populated urban areas have faced when being exposed to COVID-19.¹
Maria is a Mexican migrant who has just returned from Connecticut to the Bronx. Her partner Jorge died in Connecticut from COVID-19. She now has no income and is looking for an apartment for herself and her three children. When Jorge became ill, she took him to the hospital, but they would not admit him and he was sent away to be cared for by Maria at home with their children. When an ambulance eventually took him to hospital, it was too late. He died that same night, alone in hospital. She thinks he had diabetes, but he was never diagnosed. They only had enough income to pay the basic bills. Maria is depressed, she is alone, but she knows she must carry on for her children. Her 10-year old child says that if he could help her, he would work. After three months, she finds an apartment.
David works as a hairdresser and takes an overcrowded train every day from Leganés to Chamberi in the centre of Madrid. He lives in a small flat in San Nicasio, one of the poorest working-class areas of Madrid with one of the largest ageing populations in Spain. The apartments are very small, making it difficult to be in confinement, and all of David’s neighbours know somebody who has been a victim of COVID-19. His father was also a hairdresser. David's father was not feeling well; he was taken to hospital by ambulance, and he died three days later. David was not able to say goodbye to his father. Unemployment has increased in that area; small local shops are losing their customers, and many more people are expecting to lose their jobs.
Ruben lives in Iztapalapa in Mexico City with three children, a daughter-in-law and five grandchildren. Their small apartment has few amenities, and no running water during the evening. At three o’clock every morning, he walks 45 minutes with his mobile stall to sell fruit juices near the hospital. His daily earnings keep the family. He goes to the central market to buy fruit, taking a packed dirty bus. He thinks the city's central market was contaminated at the beginning of the pandemic, but it could not be closed as it is the main source of food in the country. He has no health insurance, and he knows that as a diabetic he is at risk, but medication for his condition is too expensive. He has no alternative but to go to work every day: "We die of hunger or we die of COVID."
These real stories highlight the issues that must be addressed to reduce persistent health inequalities and achieve health outcomes focusing on population health. The examples of Maria, David and Ruben show the terrible outcomes COVID-19 has had for people living in poverty and social deprivation, older people, and those with co-morbidities and/or pre-existing health conditions. All three live in densely populated urban areas with poor housing, and have to travel long distances in overcrowded transport. Maria’s loss of income has had consequences for her housing security and access to healthcare and health insurance, which will most likely lead to worse health conditions for her and her children. Furthermore, all three experienced high levels of stress, which is magnified in the cases of Maria and David who were unable to be present when their loved ones died.
The COVID-19 pandemic has made it evident that to improve the health of the population and build healthy societies, there is a need to shift the focus from illness to health and wellness in order to address the social, political and commercial determinants of health; to promote healthy behaviours and lifestyles; and to foster universal health coverage.² Citizens all over the world are demanding that health systems be strengthened and for governments to protect the most vulnerable. A better future could be possible with leadership that is able to carefully consider the long-term health, economic and social policies that are needed.
In order to design and implement population health-friendly policies, there are three prerequisites. First, there is a need to improve understanding of the factors that influence health inequalities and the interconnections between the economic, social and health impacts. Second, broader policies should be considered not only within the health sector, but also in other sectors such as education, employment, transport and infrastructure, agriculture, water and sanitation. Third, the proposed policies need to be designed through involving the community, addressing the health of vulnerable groups, and fostering inter-sectoral action and partnerships.
Finally, within the UN's Agenda 2030 , Sustainable Development Goal (SDG) 3 sets out a forward-looking strategy for health whose main goal is to attain healthier lives and wellbeing. The 17 interdependent SDGs offer an opportunity to contribute to healthier, fairer and more equitable societies from which both communities and the environment can benefit.
The stories of Maria, David and Ruben are real stories featured in the Documentary: The impact of COVID19 in urban outskirts, Directed by Jose A Guardiola. Available here. Permission has been granted to narrate these stories.
Buck, D., Baylis, A., Dougall, D. and Robertson, R. (2018). A vision for population health: Towards a healthier future . [online] London: The King's Fund. [Accessed 20 Sept. 2020]
Wilton Park. (2020). Healthy societies, healthy populations (WP1734). Wiston House, Steyning. Retrieved from https://www.wiltonpark.org.uk/event/wp1734/ Cohen B. E. (2006). Population health as a framework for public health practice: a Canadian perspective. American journal of public health , 96 (9), 1574–1576.
3. Imagine a 'well-care' system that invests in keeping people healthy
By Maliha Hashmi , Executive Director, Health and Well-Being and Biotech, NEOM, and Jan Kimpen , Global Chief Medical Officer, Philips
Imagine a patient named Emily. Emily is aged 32 and I’m her doctor.
Emily was 65lb (29kg) above her ideal body weight, pre-diabetic and had high cholesterol. My initial visit with Emily was taken up with counselling on lifestyle changes, mainly diet and exercise; typical advice from one’s doctor in a time-pressured 15-minute visit. I had no other additional resources, incentives or systems to support me or Emily to help her turn her lifestyle around.
I saw Emily eight months later, not in my office, but in the hospital emergency room. Her husband accompanied her – she was vomiting, very weak and confused. She was admitted to the intensive care unit, connected to an insulin drip to lower her blood sugar, and diagnosed with type 2 diabetes. I talked to Emily then, emphasizing that the new medications for diabetes would only control the sugars, but she still had time to reverse things if she changed her lifestyle. She received further counselling from a nutritionist.
Over the years, Emily continued to gain weight, necessitating higher doses of her diabetes medication. More emergency room visits for high blood sugars ensued, she developed infections of her skin and feet, and ultimately, she developed kidney disease because of the uncontrolled diabetes. Ten years after I met Emily, she is 78lb (35kg) above her ideal body weight; she is blind and cannot feel her feet due to nerve damage from the high blood sugars; and she will soon need dialysis for her failing kidneys. Emily’s deteriorating health has carried a high financial cost both for herself and the healthcare system. We have prevented her from dying and extended her life with our interventions, but each interaction with the medical system has come at significant cost – and those costs will only rise. But we have also failed Emily by allowing her diabetes to progress. We know how to prevent this, but neither the right investments nor incentives are in place.
Emily could have been a real patient of mine. Her sad story will be familiar to all doctors caring for chronically ill patients. Unfortunately, patients like Emily are neglected by health systems across the world today. The burden of chronic disease is increasing at alarming rates. Across the OECD nearly 33% of those over 15 years live with one or more chronic condition, rising to 60% for over-65s. Approximately 50% of chronic disease deaths are attributed to cardiovascular disease (CVD). In the coming decades, obesity, will claim 92 million lives in the OECD while obesity-related diseases will cut life expectancy by three years by 2050.
These diseases can be largely prevented by primary prevention, an approach that emphasizes vaccinations, lifestyle behaviour modification and the regulation of unhealthy substances. Preventative interventions have been efficacious. For obesity, countries have effectively employed public awareness campaigns, health professionals training, and encouragement of dietary change (for example, limits on unhealthy foods, taxes and nutrition labelling).⁴,⁵ Other interventions, such as workplace health-promotion programmes, while showing some promise, still need to demonstrate their efficacy.

The COVID-19 crisis provides the ultimate incentive to double down on the prevention of chronic disease. Most people dying from COVID-19 have one or more chronic disease, including obesity, CVD, diabetes or respiratory problems – diseases that are preventable with a healthy lifestyle. COVID-19 has highlighted structural weaknesses in our health systems such as the neglect of prevention and primary care.
While the utility of primary prevention is understood and supported by a growing evidence base, its implementation has been thwarted by chronic underinvestment, indicating a lack of societal and governmental prioritization. On average, OECD countries only invest 2.8% of health spending on public health and prevention. The underlying drivers include decreased allocation to prevention research, lack of awareness in populations, the belief that long-run prevention may be more costly than treatment, and a lack of commitment by and incentives for healthcare professionals. Furthermore, public health is often viewed in a silo separate from the overall health system rather than a foundational component.
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
Fee-for-service models that remunerate physicians based on the number of sick patients they see, regardless the quality and outcome, dominate healthcare systems worldwide. Primary prevention mandates a payment system that reimburses healthcare professionals and patients for preventive actions. Ministries of health and governmental leaders need to challenge skepticism around preventive interventions, realign incentives towards preventive actions and those that promote healthy choices by people. Primary prevention will eventually reduce the burden of chronic diseases on the healthcare system.
As I reflect back on Emily and her life, I wonder what our healthcare system could have done differently. What if our healthcare system was a well-care system instead of a sick-care system? Imagine a different scenario: Emily, a 32 year old pre-diabetic, had access to a nutritionist, an exercise coach or health coach and nurse who followed her closely at the time of her first visit with me. Imagine if Emily joined group exercise classes, learned where to find healthy foods and how to cook them, and had access to spaces in which to exercise and be active. Imagine Emily being better educated about her diabetes and empowered in her healthcare and staying healthy. In reality, it is much more complicated than this, but if our healthcare systems began to incentivize and invest in prevention and even rewarded Emily for weight loss and healthy behavioural changes, the outcome might have been different. Imagine Emily losing weight and continuing to be an active and contributing member of society. Imagine if we invested in keeping people healthy rather than waiting for people to get sick, and then treating them. Imagine a well-care system.
Anderson, G. (2011). Responding to the growing cost and prevalence of people with multiple chronic conditions . Retrieved from OECD.
Institute for Health Metrics and Evaluation. GBD Data Visualizations. Retrieved here.
OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris.
OECD. (2017). Obesity Update . Retrieved here.
Malik, V. S., Willett, W. C., & Hu, F. B. (2013). Global obesity: trends, risk factors and policy implications. Nature Reviews Endocrinology , 9 (1), 13-27.
Lang, J., Cluff, L., Payne, J., Matson-Koffman, D., & Hampton, J. (2017). The centers for disease control and prevention: findings from the national healthy worksite program. Journal of occupational and environmental medicine , 59 (7), 631.
Gmeinder, M., Morgan, D., & Mueller, M. (2017). How much do OECD countries spend on prevention? Retrieved from OECD.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198.
Richardson, A. K. (2012). Investing in public health: barriers and possible solutions. Journal of Public Health , 34 (3), 322-327.
Yong, P. L., Saunders, R. S., & Olsen, L. (2010). Missed Prevention Opportunities The healthcare imperative: lowering costs and improving outcomes: workshop series summary (Vol. 852): National Academies Press Washington, DC.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved here .
McDaid, D., F. Sassi and S. Merkur (Eds.) (2015a), “Promoting Health, Preventing Disease: The Economic Case ”, Open University Press, New York.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved from OECD.
4. Why e arly detection and diagnosis is critical
By Paul Murray , Head of Life and Health Products, Swiss Re, and André Goy , Chairman and Executive Director & Chief of Lymphoma, John Theurer Cancer Center, Hackensack University Medical Center
Although healthcare systems around the world follow a common and simple principle and goal – that is, access to affordable high-quality healthcare – they vary significantly, and it is becoming increasingly costly to provide this access, due to ageing populations, the increasing burden of chronic diseases and the price of new innovations.
Governments are challenged by how best to provide care to their populations and make their systems sustainable. Neither universal health, single payer systems, hybrid systems, nor the variety of systems used throughout the US have yet provided a solution. However, systems that are ranked higher in numerous studies, such as a 2017 report by the Commonwealth Fund , typically include strong prevention care and early-detection programmes. This alone does not guarantee a good outcome as measured by either high or healthy life expectancy. But there should be no doubt that prevention and early detection can contribute to a more sustainable system by reducing the risk of serious diseases or disorders, and that investing in and operationalizing earlier detection and diagnosis of key conditions can lead to better patient outcomes and lower long-term costs.
To discuss early detection in a constructive manner it makes sense to describe its activities and scope. Early detection includes pre-symptomatic screening and treatment immediately or shortly after first symptoms are diagnosed. Programmes may include searching for a specific disease (for example, HIV/AIDS or breast cancer), or be more ubiquitous. Prevention, which is not the focus of this blog, can be interpreted as any activities undertaken to avoid diseases, such as information programmes, education, immunization or health monitoring.
Expenditures for prevention and early detection vary by country and typically range between 1-5% of total health expenditures.¹ During the 2008 global financial crisis, many countries reduced preventive spending. In the past few years, however, a number of countries have introduced reforms to strengthen and promote prevention and early detection. Possibly the most prominent example in recent years was the introduction of the Affordable Care Act in the US, which placed a special focus on providing a wide range of preventive and screening services. It lists 63 distinct services that must be covered without any copayment, co-insurance or having to pay a deductible.

Whilst logic dictates that investment in early detection should be encouraged, there are a few hurdles and challenges that need to be overcome and considered. We set out a few key criteria and requirements for an efficient early detection program:
1. Accessibility The healthcare system needs to provide access to a balanced distribution of physicians, both geographically (such as accessibility in rural areas), and by specialty. Patients should be able to access the system promptly without excessive waiting times for diagnoses or elective treatments. This helps mitigate conditions or diseases that are already quite advanced or have been incubating for months or even years before a clinical diagnosis. Access to physicians varies significantly across the globe from below one to more than 60 physicians per 10,000 people.² One important innovation for mitigating access deficiencies is telehealth. This should give individuals easier access to health-related services, not only in cases of sickness but also to supplement primary care.
2. Early symptoms and initial diagnosis Inaccurate or delayed initial diagnoses present a risk to the health of patients, can lead to inappropriate or unnecessary testing and treatment, and represents a significant share of total health expenditures. A medical second opinion service, especially for serious medical diagnoses, which can occur remotely, can help improve healthcare outcomes. Moreover, studies show that early and correct diagnosis opens up a greater range of curative treatment options and can reduce costs (e.g. for colon cancer, stage-four treatment costs are a multiple of stage-one treatment costs).³
3. New technology New early detection technologies can improve the ability to identify symptoms and diseases early: i. Advances in medical monitoring devices and wearable health technology, such as ECG and blood pressure monitors and biosensors, enable patients to take control of their own health and physical condition. This is an important trend that is expected to positively contribute to early detection, for example in atrial fibrillation and Alzheimers’ disease. ii. Diagnostic tools, using new biomarkers such as liquid biopsies or volatile organic compounds, together with the implementation of machine learning, can play an increasing role in areas such as oncology or infectious diseases.⁴
4. Regulation and Intervention Government regulation and intervention will be necessary to set ranges of normality, to prohibit or discourage overdiagnosis and to reduce incentives for providers to overtreat patients or to follow patients' inappropriate requests. In some countries, such as the US, there has been some success through capitation models and value-based care. Governments might also need to intervene to de-risk the innovation paradigm, such that private providers of capital feel able to invest more in the development of new detection technologies, in addition to proven business models in novel therapeutics.
OECD Health Working Papers No. 101 "How much do OECD countries spend on prevention" , 2017
World Health Organization; Global Health Observatory (GHO) data; https://www.who.int/gho/health_workforce/physicians_density/en/
Saving lives, averting costs; A report for Cancer Research UK, by Incisive Health, September 2014
Liquid Biopsy: Market Drivers And Obstacles; by Divyaa Ravishankar, Frost & Sullivan, January 21, 2019
Liquid Biopsies Become Cheap and Easy with New Microfluidic Device; February 26, 2019
How America’s 5 Top Hospitals are Using Machine Learning Today; by Kumba Sennaar, February 19, 2019
5. The business case for private investment in healthcare for all
Pascal Fröhlicher, Primary Care Innovation Scholar, Harvard Medical School, and Ian Wijaya, Managing Director in Lazard’s Global Healthcare Group
Faith, a mother of two, has just lost another customer. Some households where she is employed to clean, in a small town in South Africa, have little understanding of her medical needs. As a type 2 diabetes patient, this Zimbabwean woman visits the public clinic regularly, sometimes on short notice. At her last visit, after spending hours in a queue, she was finally told that the doctor could not see her. To avoid losing another day of work, she went to the local general practitioner to get her script, paying more than three daily wages for consultation and medication. Sadly, this fictional person reflects a reality for many people in middle-income countries.
Achieving universal health coverage by 2030, a key UN Sustainable Development Goal (SDG), is at risk. The World Bank has identified a $176 billion funding gap , increasing every year due to the growing needs of an ageing population, with the health burden shifting towards non-communicable diseases (NCDs), now the major cause of death in emerging markets . Traditional sources of healthcare funding struggle to increase budgets sufficiently to cover this gap and only about 4% of private health care investments focus on diseases that primarily affect low- and middle-income countries.
In middle-income countries, private investors often focus on extending established businesses, including developing private hospital capacity, targeting consumers already benefiting from quality healthcare. As a result, an insufficient amount of private capital is invested in strengthening healthcare systems for everyone.

Why is this the case? We discussed with senior health executives investing in Lower and Middle Income Countries (LMIC) and the following reasons emerged:
- Small market size . Scaling innovations in healthcare requires dealing with country-specific regulatory frameworks and competing interest groups, resulting in high market entry cost.
- Talent . Several LMICs are losing nurses and doctors but also business and finance professionals to European and North American markets due to the lack of local opportunities and a significant difference in salaries.
- Untested business models with relatively low gross margins. Providing healthcare requires innovative business models where consumers’ willingness to pay often needs to be demonstrated over a significant period of time. Additionally, relatively low gross margins drive the need for scale to leverage administrative costs, which increases risk.
- Government Relations. The main buyer of health-related products and services is government; yet the relationship between public and private sectors often lacks trust, creating barriers to successful collaboration. Add to that significant political risk, as contracts can be cancelled by incoming administrations after elections. Many countries also lack comprehensive technology strategies to successfully manage technological innovation.
- Complexity of donor funding. A significant portion of healthcare is funded by private donors, whose priorities might not always be congruent with the health priorities of the government.
Notwithstanding these barriers, healthcare, specifically in middle-income settings, could present an attractive value proposition for private investors:
- Economic growth rates . A growing middle class is expanding the potential market for healthcare products and services.
- Alignment of incentives . A high ratio of out-of-pocket payments for healthcare services is often associated with low quality. However, innovative business models can turn out of pocket payments into the basis for a customer-centric value proposition, as the provider is required to compete for a share of disposable income.
- Emergence of National Health Insurance Schemes . South Africa, Ghana, Nigeria and others are building national health insurance schemes, increasing a population’s ability to fund healthcare services and products .
- Increased prevalence of NCDs. Given the increasing incidence of chronic diseases and the potential of using technology to address these diseases, new business opportunities for private investment exist.
Based on the context above, several areas in healthcare delivery can present compelling opportunities for private companies.
- Aggregation of existing players.
- Leveraging primary care infrastructure. Retail companies can leverage their real estate, infrastructure and supply chains to deploy primary care services at greater scale than is currently the case.
- Telemedicine . Telecommunications providers can leverage their existing infrastructure and customer base to provide payment mechanisms and telehealth services at scale. As seen during the COVID-19 pandemic, investment in telemedicine can ensure that patients receive timely and continuous care in spite of restrictions and lockdowns.
- Cost effective diagnostics . Diagnostic tools operated by frontline workers and combined with the expertise of specialists can provide timely and efficient care.
To fully realize these opportunities, government must incentivise innovation, provide clear regulatory frameworks and, most importantly, ensure that health priorities are adequately addressed.
Venture capital and private equity firms as well as large international corporations can identify the most commercially viable solutions and scale them into new markets. The ubiquity of NCDs and the requirement to reduce costs globally provides innovators with the opportunity to scale their tested solutions from LMICs to higher income environments.
Successful investment exits in LMICs and other private sector success stories will attract more private capital. Governments that enable and support private investment in their healthcare systems would, with appropriate governance and guidance, generate benefits to their populations and economies. The economic value of healthy populations has been proven repeatedly , and in the face of COVID-19, private sector investment can promote innovation and the development of responsible, sustainable solutions.
Faith – the diabetic mother we introduced at the beginning of this article - could keep her client. As a stable patient, she could measure her glucose level at home and enter the results in an app on her phone, part of her monthly diabetes programme with the company that runs the health centre. She visits the nurse-led facility at the local taxi stand on her way to work when her app suggests it. The nurse in charge of the centre treats Faith efficiently, and, if necessary, communicates with a primary care physician or even a specialist through the telemedicine functionality of her electronic health system.
Improving LMIC health systems is not only a business opportunity, but a moral imperative for public and private leaders. With the appropriate technology and political will, this can become a reality.
6. How could COVID-19 change the way we pay for health services?
John E. Ataguba, Associate Professor and Director, University of Cape Town and Matthew Guilford, Co-Founder and Chief Executive Officer, Common Health
The emergence of the new severe acute respiratory syndrome coronavirus (SARS-Cov-2), causing the coronavirus disease 2019 (COVID-19), has challenged both developing and developed countries.
Countries have approached the management of infections differently. Many people are curious to understand their health system’s performance on COVID-19, both at the national level and compared to international peers. Alongside limited resources for health, many developing countries may have weak health systems that can make it challenging to respond adequately to the pandemic.
Even before COVID-19, high rates of out-of-pocket spending on health meant that every year, 800 million people faced catastrophic healthcare costs ,100 million families were pushed into poverty, and millions more simply avoided care for critical conditions because they could not afford to pay for it.
The pandemic and its economic fallout have caused household incomes to decline at the same time as healthcare risks are rising. In some countries with insurance schemes, and especially for private health insurance, the following questions have arisen: How large is the co-payment for a COVID-19 test? If my doctor’s office is closed, will the telemedicine consultation be covered by my insurance? Will my coronavirus care be paid for regardless of how I contracted the virus? These and other doubts can prevent people from seeking medical care in some countries.
In Nigeria, like many other countries in Africa, the government bears the costs associated with testing and treating COVID-19 irrespective of the individual’s insurance status. In the public health sector, where COVID-19 cases are treated, health workers are paid monthly salaries while budgets are allocated to health facilities for other services. Hospitals continue to receive budget allocations to finance all health services including the management and treatment of COVID-19. That implies that funds allocated to address other health needs are reduced and that in turn could affect the availability and quality of health services.
Although health workers providing care for COVID-19 patients in isolation and treatment centres in Nigeria are paid salaries that are augmented with a special incentive package, the degree of impact on the quality improvement of services remains unclear. The traditional and historical allocation of budgets does not always address the needs of the whole population and could result in poor health services and under-provision of health services for COVID-19 patients.
In some countries, the reliance on out-of-pocket funding is hardly better for private providers, who encounter brand risks, operational difficulties, and – in extreme cases – the risk of creating “debtor prisons” as they seek to collect payment from patients. Ironically, despite the huge demand for medical services to diagnose and treat COVID-19, large healthcare institutions and individual healthcare practitioners alike are facing financial distress.
Dependence on a steady stream of fee-for-service payments for outpatient consultations and elective procedures is leading to pay cuts for doctors in India , forfeited Eid bonuses for nurses in Indonesia , and hospital bankruptcies in the United States . In a recent McKinsey & Company survey, 77% of physicians reported that their business would suffer in 2020 , and 46% were concerned about their practice surviving the coronavirus pandemic.
COVID-19 is exposing how fee-for-service, historical budget allocation and out-of-pocket financing methods can hinder the performance of the health system. Some providers and health systems that deployed “value-based” models prior to the pandemic have reported that these approaches have improved financial resilience during COVID-19 and may support better results for patients. Nevertheless, these types of innovations do not represent the dominant payment model in any country.
How health service providers are paid has implications for whether service users can get needed health services in a timely fashion, and at an appropriate quality and an affordable cost. By shifting from fee-for-service reimbursements to fixed "capitation" and performance-based payments, these models incentivize providers to improve quality and coordination while also guaranteeing a baseline income level, even during times of disruption.
Health service providers could be paid either in the form of salaries, a fee for services they provide, by capitation (whether adjusted or straightforward), through global budgets, or by using a case-based payment system (for example, the diagnostics-related groups), among others. Because there are different incentives to consider when adopting any of the methods, they could be combined to achieve a specific goal. For example, in some countries, health workers are paid salaries , and some specific services are paid on a fee-for-service basis.
Ideally, health services could be purchased strategically , incorporating aspects of provider performance in transferring funds to providers and accounting for the health needs of the population they serve.
In this regard, strategic purchasing for health has been advocated and should be highlighted as crucial with the emergence of the COVID-19 pandemic. There is a need to ensure value in the way health providers are paid, inter alia to increase efficiency, ensure equity, and improve access to needed health services. Value-based payment methods, although not new in many countries, provide an avenue to encourage long-term value for money, better quality, and strategic purchasing for health, helping to build a healthier, more resilient world.
7. L essons in integrated care from the COVID-19 pandemic
Sarah Ziegler, Postdoctoral Researcher, Department of Epidemiology and Biostatistics, University of Zurich, and Ninie Wang, Founder & CEO, Pinetree Care Group.
Since the start of the COVID-19 pandemic, people suffering non-communicable diseases (NCDs) have been at higher risk of becoming severely ill or dying. In Italy, 96.2% of people who died of COVID-19 lived with two or more chronic conditions.
Beyond the pandemic, cardiovascular disease, cancer, respiratory disease and diabetes are the leading burden of disease, with 41 million annual deaths. People with multimorbidity - a number of different conditions - often experience difficulties in accessing timely and coordinated healthcare, made worse when health systems are busy fighting against the pandemic.
Here is what happened in China with Lee, aged 62, who has been living with Chronic Obstructive Pulmonary Disease (COPD) for the past five years.
Before the pandemic, Lee’s care manager coordinated a multi-disciplinary team of physicians, nurses, pulmonary rehabilitation therapists, psychologists and social workers to put together a personalized care plan for her. Following the care plan, Lee stopped smoking and paid special attention to her diet, sleep and physical exercises, as well as sticking to her medication and follow-up visits. She participated in a weekly community-based physical activity program to meet other COPD patients, including short walks and exchange experiences. A mobile care team supported her with weekly cleaning and grocery shopping.
Together with her family, Lee had follow-up visits to ensure her care plan reflected her recovery and to modify the plan if needed. These integrated care services brought pieces of care together, centered around Lee’s needs, and provided a continuum of care that helped keep Lee in the community with a good quality of life for as long as possible.
Since the COVID-19 outbreak, such NCD services have been disrupted by lockdowns, the cancellation of elective care and the fear of visiting care service . These factors particularly affected people living with NCDs like Lee. As such, Lee was not able to follow her care plan anymore. The mobile care team was unable to visit her weekly as they were deployed to provide COVID-19 relief. Lee couldn’t participate in her community-based program, follow up on her daily activities, or see her family or psychologists. This negatively affected Lee’s COPD management and led to poor management of her physical activity and healthy diet.
The pandemic highlights the need for a flexible and reliable integrated care system to enable healthcare delivery to all people no matter where they live, uzilizing approaches such as telemedicine and effective triaging to overcome care disruptions.
Lee’s care manager created short videos to assist her family through each step of her care and called daily to check in on the implementation of the plan and answer questions. Lee received tele-consultations, and was invited to the weekly webcast series that supported COPD patient communities. When her uncle passed away because of pneumonia complications from COVID-19 in early April, Lee’s care manager arranged a palliative care provider to support the family through the difficult time of bereavement and provided food and supplies during quarantine. Lee could even continue with her physical activity program with an online training coach. There were a total of 38 exercise videos for strengthening and stretching arms, legs and trunk, which she could complete at different levels of difficulty and with different numbers of repetitions.
Lee’s case demonstrates that early detection, prevention, and management of NCDs play a crucial role in a global pandemic response. It shows how we need to shift away from health systems designed around single diseases towards health systems designed for the multidimensional needs of individuals. As part of the pandemic responses, addressing and managing risks related to NCDs and prevention of their complications are critical to improve outcomes for vulnerable people like Lee.
How to design and deliver successful integrated care
The challenge for the successful transformation of healthcare is to tailor care system-wide to population needs. A 2016 WHO Framework on integrated people-centered health services developed a set of five general strategies for countries to progress towards people-centered and sustainable health systems, calling for a fundamental transformation not only in the way health services are delivered, but also in the way they are financed and managed . These strategies call for countries to:
- Engage and empower people / communities: an integrated care system must mobilize everyone to work together using all available resources, especially when continuity of essential health and community services for NCDs are at risk of being undermined.
- Strengthen governance and accountability, so that integration emphasizes rather than weakens leadership in every part of the system, and ensure that NCDs are included in national COVID-19 plans and future essential health services.
- Reorient the model of care to put the needs and perspectives of each person / family at the center of care planning and outcome measurement, rather than institutions.
- Coordinate services within and across sectors, for example, integrate inter-disciplinary medical care with social care, addressing wider socio-economic, environmental and behavioral determinants of health.
- Create an enabling environment, with clear objectives, supportive financing, regulations and insurance coverage for integrated care, including the development and use of systemic digital health care solutions.
Whether due to an unexpected pandemic or a gradual increase in the burden of NCDs, each person could face many health threats across the life-course.
Only systems that dynamically assess each person’s complex health needs and address them through a timely, well-coordinated and tailored mix of health and social care services will be able to deliver desired health outcomes over the longer term, ensuring an uninterrupted good quality of life for Lee and many others like her.
- Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 2020;12: 6049–57.
- WHO. Noncommunicable diseases in emergencies. Geneva: World Health Organization, 2016.
- WHO. COVID-19 significantly impacts health services for noncommunicable diseases. June 2020.
- Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicalbe diseases in the COVID-19 response. The Lancet. 2020. 395:1678-1680
- WHO. Framework on integrated people-centred health services. Geneva: World Health Organization, 2016.
8 . Why access to healthcare alone will not save lives
Donald Berwick, President Emeritus and Senior Fellow, Institute for Healthcare Improvement; Nicola Bedlington, Special Adviser, European Patient Forum; and David Duong, Director, Program in Global Primary Care and Social Change, Harvard Medical School.
Joyce lies next to 10 other women in bare single beds in the post-partum recovery room at a rural hospital in Uganda. Just an hour ago, Joyce gave birth to a healthy baby boy. She is now struggling with abdominal pain. A nurse walks by, and Joyce tries to call out, but the nurse was too busy to attend to her; she was the only nurse looking after 20 patients.
Another hour passes, and Joyce is shaking and sweating profusely. Joyce’s husband runs into the corridor to find a nurse to come and evaluate her. The nurse notices Joyce’s critical condition - a high fever and a low blood pressure - and she quickly calls the doctor. The medical team rushes Joyce to the intensive care unit. Joyce has a very severe blood stream infection. It takes another hour before antibiotics are started - too late. Joyce dies, leaving behind a newborn son and a husband. Joyce, like many before her, falls victim to a pervasive global threat: poor quality of care.
Adopted by United Nations (UN) in 2015, the Sustainable Development Goals (SDG) are a universal call to action to end poverty, protect the planet and ensure that all enjoy peace and prosperity by 2030. SDG 3 aims to ensure healthy lives and promote wellbeing for all. The 2019 UN General Assembly High Level Meeting on Universal Health Coverage (UHC) reaffirmed the need for the highest level of political commitment to health care for all.
However, progress towards UHC, often measured in terms of access, not outcomes, does not guarantee better health, as we can see from Joyce’s tragedy. This is also evident with the COVID-19 response. The rapidly evolving nature of the COVID-19 pandemic has highlighted long-term structural inefficiencies and inequities in health systems and societies trying to mitigate the contagion and loss of life.
Systems are straining under significant pressure to ensure standards of care for both COVID-19 patients and other patients that run the risk of not receiving timely and appropriate care. Although poor quality of care has been a long-standing issue, it is imperative now more than ever that systems implement high-quality services as part of their efforts toward UHC.
Poor quality healthcare remains a challenge for countries at all levels of economic development: 10% of hospitalized patients acquire an infection during their hospitalization in low-and-middle income countries (LMIC), whereas 7% do in high-income countries. Poor quality healthcare disproportionally affects the poor and those in LMICs. Of the approximately 8.6 million deaths per year in 137 LMICs, 3.6 million are people who did not access the health system, whereas 5 million are people who sought and had access to services but received poor-quality care.
Joyce’s story is all too familiar; poor quality of care results in deaths from treatable diseases and conditions. Although the causes of death are often multifactorial, deaths and increased morbidity from treatable conditions are often a reflection of defects in the quality of care.
The large number of deaths and avoidable complications are also accompanied by substantial economic costs. In 2015 alone, 130 LMICs faced US $6 trillion in economic losses. Although there is concern that implementing quality measures may be a costly endeavor, it is clear that the economic toll associated with a lack of quality of care is far more troublesome and further stunts the socio-economic development of LMICs, made apparent with the COVID-19 pandemic.
Poor-quality care not only leads to adverse outcomes in terms of high morbidity and mortality, but it also impacts patient experience and patient confidence in health systems. Less than one-quarter of people in LMICs and approximately half of people in high-income countries believe that their health systems work well.
A lack of application and availability of evidenced-based guidelines is one key driver of poor-quality care. The rapidly changing landscape of medical knowledge and guidelines requires healthcare workers to have immediate access to current clinical resources. Despite our "information age", health providers are not accessing clinical guidelines or do not have access to the latest practical, lifesaving information.
Getting information to health workers in the places where it is most needed is a delivery challenge. Indeed, adherence to clinical practice guidelines in eight LMICs was below 50%, and in OECD countries, despite being a part of national guidelines, 19-53% of women aged 50-69 years did not receive mammography screening.4 The evidence in LMICs and HICs suggest that application of evidence-based guidelines lead to reduction in mortality and improved health outcomes.
Equally, the failure to change and continually improve the processes in health systems that support the workforce takes a high toll on quality of care. During the initial wave of the COVID-19 pandemic, countries such as Taiwan, Hong Kong, Singapore and Vietnam, which adapted and improved their health systems after the SARS and H1N1 outbreaks, were able to rapidly mobilize a large-scale quarantine and contact tracing strategy, supported with effective and coordinated mass communication.
These countries not only mitigated the economic and mortality damage, but also prevented their health systems and workforce from enduring extreme burden and inability to maintain critical medical supplies. In all nations, investing in healthcare organizations to enable them to become true “learning health care systems,” aiming at continual quality improvement, would yield major population health and health system gains.
The COVID-19 pandemic underscores the importance for health systems to be learning systems. Once the dust settles, we need to focus, collectively, on learning from this experience and adapting our health systems to be more resilient for the next one. This implies a need for commitment to and investment in global health cooperation, improvement in health care leadership, and change management.
With strong political and financial commitment to UHC, and its demonstrable effect in addressing crises such as COVID-19, for the first time, the world has a viable chance of UHC becoming a reality. However, without an equally strong political, managerial, and financial commitment to continually improving, high-quality health services, UHC will remain an empty promise.
1. United Nations General Assembly. Political declaration of the high-level meeting on universal health coverage. New York, NY2019.
2. Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Health equity in England: the Marmot review 10 years on. Institute of Health Equity;2020.
3. National Academies of Sciences, Engineering, and Medicine: Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: Improving health care worldwide. Washington, DC: National Academies Press;2018.
4. World Health Organization, Organization for Economic Co-operation and Development, World Bank Group. Delivering quality health services: a global imperative for universal health coverage. World Health Organization; 2018.
5. Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health. 2018;6(11):e1196-e1252.
6. Ricci-Cabello I, Violán C, Foguet-Boreu Q, Mounce LT, Valderas JM. Impact of multi-morbidity on quality of healthcare and its implications for health policy, research and clinical practice. A scoping review. European Journal of General Practice. 2015;21(3):192-202.
7. Valtis YK, Rosenberg J, Bhandari S, et al. Evidence-based medicine for all: what we can learn from a programme providing free access to an online clinical resource to health workers in resource-limited settings. BMJ global health. 2016;1(1).
8. Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America . Washington, DC: National Academies Press 2012.
- Impact & Innovation

Reimagining the U.S. healthcare system
Subscribe to Impact & Innovation in Apple Podcasts , Spotify , Google Podcasts , SoundCloud , or your favorite podcast player .
Peter Hagan is the Digital Health Director at Commonwealth Care Alliance, and former team member at Iora Health. Iora was a start up that created a new model for value-based care, to improve health outcomes and lower costs. Ten years after launching, it was acquired by One Medical, a primary care provider, which was later acquired by Amazon. Peter initially started out as a patient at one of Iora's first pilot sites, and later became a health coach, playing a critical role in Iora's team-based care model. His third role before leaving Iora to pursue his MPH was to work on the backend of Iora's digital health products, which included a patient-friendly electronic health record system that allowed each patient and their care team to seamlessly coordinate care. In this episode, Pete and I discuss the challenge of shifting from the dominant fee-for-service care model in the U.S., to the value-based care model which focuses on improving people's health rather than profiting from their care needs. Rather than waiting and hoping for existing players to make these changes, could it be the new entrants into the field that disrupt and transform it?
The gathering storm in US healthcare: How leaders can respond and thrive
Addie Fleron is an associate partner in McKinsey’s Chicago office and Shubham Singhal is a senior partner in the Detroit office.
The authors wish to thank Katherine Baicker, Gretchen Berlin, Daniel Brown, Brandon Carrus, Christopher Chen, Sam Hazen, David Knott, Bob Kocher, Pooja Kumar, Sarah London, Steve Markovich, Peter McCanna, Emad Rizk, Jim Skogsbergh, Sven Smit, Mandy Tilton, Drew Ungerman, and Nithya Vinjamoori for their contributions to this article.
Explore a career with us
Related articles.

The next frontier of care delivery in healthcare
The future of US healthcare: What’s next for the industry post-COVID-19
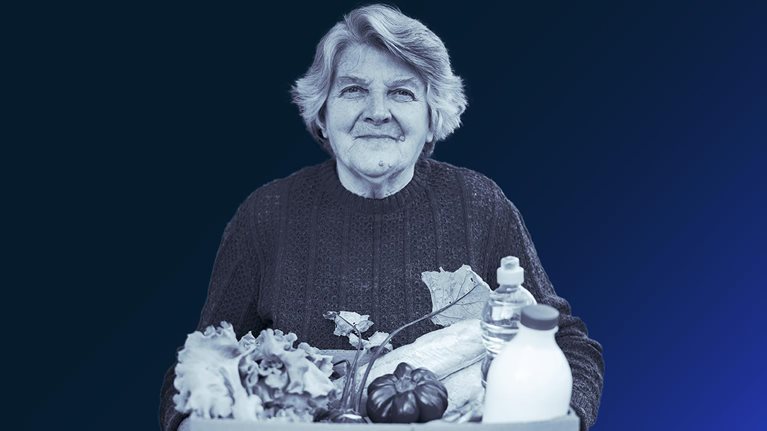
How providers are meeting patients’ basic needs—and where they could do more

- < Previous
Home > Andrew Young School of Policy Studies > Dissertations > 83
AYSPS Dissertations
The intersection of aging, health, & correctional systems: an exploration of experiences, approaches, & policies using a person-centered framework.
Victoria Helmly , Georgia State University
Author ORCID Identifier
0000-0002-9474-2739
Date of Award
Spring 5-6-2024
Degree Type
Dissertation
Degree Name
Doctor of Philosophy (PhD)
Criminal Justice
First Advisor
William J Sabol
Second Advisor
Elizabeth Beck
Third Advisor
Thaddeus Johnson
Fourth Advisor
Dean Dabney
This dissertation consists of three interconnected papers that study the intersection of correctional systems and aging in the United States, specifically in prisons and community supervision. The papers examine existing policies and the experiences of older adults using a person-centered framework. The first two papers explore data collected through semi-structured interviews with community supervision officers and people with experience under community supervision. The first paper investigates a person-centered community supervision model and highlights how it applies specifically to older adults, defined as those aged 50 or older. There is evidence of the implementation of this model, but there is an opportunity for further development. The data presented underscores the need for a more precise definition of a person-centered approach in community supervision and more attention to the age-related needs of people under supervision. The second paper explores the unique challenges of people aged 50 or older who are under community supervision, such as adapting to technology, securing stable housing, and managing chronic health conditions. It further reveals the gaps in knowledge of officers concerning aging-specific resources and the universal experiences pertinent to all age groups. The third paper is a content analysis of end-of-life decision-making policies in U.S. departments of corrections. It underscores the variability in accessibility and specificity of such policies, advocating for a more person-centered model that aligns with community standard quality of care. The research signifies that current prison systems have opportunities for enhancing policy and potentially affecting the quality of end-of-life care in prisons. Collectively, these papers emphasize potential improvement and growth in person-centered approaches for correctional systems and the opportunities to address the challenges of a growing older adult population. These findings highlight the need for additional research and collaboration between the fields of criminal justice and gerontology. The relevance extends beyond research to practitioners and policymakers in criminal justice and aging services whose work directly impacts this population.
Recommended Citation
Helmly, Victoria, "The Intersection of Aging, Health, & Correctional Systems: An Exploration of Experiences, Approaches, & Policies Using a Person-centered Framework." Dissertation, Georgia State University, 2024. https://scholarworks.gsu.edu/aysps_dissertations/83
Since May 15, 2024
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
- Submit ETD (Thesis/Dissertation)
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
The Essential Roles of the Muscular System in Human Health and Movement
This essay about the muscular system elucidates its critical roles beyond mere movement. It highlights how muscles are integral to various bodily functions, from movement and posture stabilization to circulation and temperature regulation. The primary function of muscles is to facilitate movement through contraction and relaxation, controlled by the nervous system. Muscles also stabilize our posture, assist in blood circulation by helping the heart pump blood, and generate heat through contractions to maintain body temperature. Additionally, muscular activity aids digestion through the rhythmic contractions of smooth muscles in the gastrointestinal tract and supports respiratory functions via the diaphragm and intercostal muscles. This essay underlines the muscular system’s versatility, adaptability, and essential contribution to overall health and bodily functions, emphasizing its significance far beyond physical strength and endurance.
How it works
When we think about our muscles, images of lifting weights at the gym or sprinting to catch a bus might spring to mind. But the muscular system, a complex network of more than 600 muscles, does far more than help us execute physical tasks like these; it’s central to nearly every function in the body, from the obvious to the obscure.
Starting with the basics, the primary role of the muscular system is movement. Muscles, by contracting and relaxing, facilitate not just our ability to walk and jump but also the fine motor skills required to write with a pen or type on a keyboard.
This dance of contraction and relaxation happens under the command of the nervous system, which sends signals to different muscles to initiate action. Muscles work in pairs—while one contracts, the other relaxes, creating a push-pull dynamic that moves limbs and other body parts.
But the impact of muscles goes beyond moving from point A to point B. They are also crucial for posture and stability. Whether you’re sitting in a chair, standing in line, or performing a yoga pose, muscles are at work. Postural muscles in the core and lower back constantly adjust and counterbalance to keep us upright and aligned. Without this muscle activity, maintaining a stable posture would be an impossible task.
Beyond helping us move and stay upright, muscles play an essential role in the circulatory system. Take the heart, for instance. This vital organ, essentially a muscular pump, contracts to push blood through a vast network of vessels, delivering oxygen and nutrients to every part of the body. Peripheral muscles support this function by helping pump blood back to the heart. When you exercise, your muscle contractions help drive this process, improving circulation and enhancing overall cardiovascular health.
Muscles also keep us warm. They generate heat as a byproduct of their contractions—a process that’s vital for maintaining body temperature. When you’re cold, your muscles begin to shiver, producing rapid, involuntary contractions to generate additional warmth. This ability to regulate temperature is a perfect example of how the muscular system quietly supports our survival in ways we might not immediately recognize.
Let’s not forget digestion. The muscles in the stomach and intestines play a critical role here. Smooth muscles in the walls of these organs rhythmically contract in a process called peristalsis, which pushes food through the digestive tract. These movements are crucial for the mechanical breakdown of food, allowing nutrients to be absorbed and waste to be expelled.
The respiratory system is yet another area where muscles prove indispensable. The diaphragm, a large muscle located below the lungs, is the prime mover of the respiratory system. It contracts and flattens out, expanding the chest cavity and pulling air into the lungs. The intercostal muscles between the ribs also play a part, helping expand and contract the chest cavity, increasing or decreasing the lungs’ volume as required for breathing.
Even with such diverse and vital roles, the muscular system’s capacity for adaptation and healing is perhaps its most remarkable feature. Muscles can grow stronger with use and shrink in times of inactivity. They have a remarkable ability to recover from injury, regenerating and adapting to new challenges.
In essence, the muscular system is a testament to the complexity and marvel of the human body. Every heartbeat, every breath, and every movement are possible because of this intricate system. It’s not just about strength or fitness—it’s about foundational activities that enable us to live, breathe, and function. The muscular system doesn’t just help us move through the world; it’s integral to almost every aspect of what keeps us alive and healthy. Understanding this system’s broad scope highlights the interconnectedness of body functions and the sheer elegance of our biological architecture. Whether it’s digesting a meal, taking a deep breath, or simply standing still, the muscular system is involved, working tirelessly behind the scenes to keep our bodies in motion and in balance.
Cite this page
The Essential Roles of the Muscular System in Human Health and Movement. (2024, May 12). Retrieved from https://papersowl.com/examples/the-essential-roles-of-the-muscular-system-in-human-health-and-movement/
"The Essential Roles of the Muscular System in Human Health and Movement." PapersOwl.com , 12 May 2024, https://papersowl.com/examples/the-essential-roles-of-the-muscular-system-in-human-health-and-movement/
PapersOwl.com. (2024). The Essential Roles of the Muscular System in Human Health and Movement . [Online]. Available at: https://papersowl.com/examples/the-essential-roles-of-the-muscular-system-in-human-health-and-movement/ [Accessed: 16 May. 2024]
"The Essential Roles of the Muscular System in Human Health and Movement." PapersOwl.com, May 12, 2024. Accessed May 16, 2024. https://papersowl.com/examples/the-essential-roles-of-the-muscular-system-in-human-health-and-movement/
"The Essential Roles of the Muscular System in Human Health and Movement," PapersOwl.com , 12-May-2024. [Online]. Available: https://papersowl.com/examples/the-essential-roles-of-the-muscular-system-in-human-health-and-movement/. [Accessed: 16-May-2024]
PapersOwl.com. (2024). The Essential Roles of the Muscular System in Human Health and Movement . [Online]. Available at: https://papersowl.com/examples/the-essential-roles-of-the-muscular-system-in-human-health-and-movement/ [Accessed: 16-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Divisions and Offices
- Our Organization
- Our Success Stories
- Partnerships
- Where We Work
- Global Health Observances
- Regional Offices
- Our Newsletter
- Global Immunization
- Global Health Equity
Strengthening Cameroon's Health Systems
U.S. CDC helped Cameroon respond to COVID-19 by strengthening the country's health systems. CDC supported the establishment and upgrade of the National Public Health Laboratory to distribute, process, and report the results of COVID-19 test kits to country leaders and the World Health Organization. CDC and Cameroon's partnership contributed to a regional COVID-19 preparedness plan with an impact extending beyond Cameroon's borders.

Photo essay

Global Health
CDC's Global Health Center works 24/7 to reduce illness and respond to health threats worldwide.

Cost of living help and a future made in Australia
Strengthening medicare and the care economy.
Building a better health system than improves outcomes
Print or save page
On this page
High‑quality health services through Medicare
Boosting access to essential health services
Building a better healthcare system
The Government is investing $2.8 billion to continue its commitment to strengthen Medicare. This includes the $1.2 billion package to address pressures facing the health system, which provides:
- $882.2 million to support older Australians avoid hospital admission, be discharged from hospital earlier and improve their transition out of hospital to other appropriate care.
- $227 million to deliver a further 29 Medicare Urgent Care Clinics and boost support for regional and remote clinics. This will increase the total number of clinics across Australia to 87. Since commencing last year, existing clinics have already provided almost 400,000 bulk‑billed visits.
- $90 million to address health workforce shortages by making it simpler and quicker for international health practitioners to work in Australia.

Rohan’s daughter Zoya has been off school with a runny nose and a cough. By 6pm, she is lethargic and has a fever.
Rohan is concerned because his regular GP is now closed. Instead of waiting for hours at the emergency department, he takes Zoya to a Medicare Urgent Care Clinic, without having to make an appointment.
During the bulk billed visit, Zoya is diagnosed with an infection by the doctor and prescribed appropriate medication. Rohan and Zoya leave within an hour of arrival. Zoya makes a full recovery.
Improving health outcomes
Almost half of Australians live with a chronic condition. This Budget will provide $141.1 million for research and services for people living with chronic conditions, including bowel and skin cancer, diabetes and dementia.
To improve health outcomes, the Government is providing:
- Support for Australians to enjoy healthier, more active lives by investing $132.7 million in sport participation and performance programs.
- $825.7 million to ensure Australians can continue to access testing for and vaccinations against COVID‑19. The Government is also ensuring continued access to oral antiviral medicines on the Pharmaceutical Benefits Scheme.
- $41.6 million over two years to continue funding for alcohol and other drug treatment and support services, including the Good Sports alcohol management program for community sporting clubs.
The Government is allocating an additional $411.6 million (for a total $1.6 billion over 13 years) through the Medical Research Future Fund to continue existing research and introduce two new research missions for low‑survival cancers and reducing health inequities.
Improving access to medicines
The Government is investing $3.4 billion for new and amended listings to the Pharmaceutical Benefits Scheme, which means eligible patients can save on treatment costs.
By expanding the Closing the Gap Pharmaceutical Benefits Scheme Co‑payment Program, eligible First Nations patients will have free or cheaper access to all Pharmaceutical Benefits Scheme medicines.
Australians will benefit from $141.1 million to support and expand the National Immunisation Program.
Mental health support
The Government’s $888.1 million mental health package over eight years will help people get the care they need, while relieving pressure on the Better Access initiative and making it easier to access services.
A free, low‑intensity digital service will be established to address the gap for people with mild mental health concerns. From 1 January 2026, Australians will be able to access the service without a referral and receive timely, high‑quality mental health support. Once fully established, 150,000 people are expected to make use of this service each year.
The Government is improving access to free mental health services through a network of walk‑in Medicare Mental Health Centres, built on the established Head to Health network. The upgraded national network of 61 Medicare Mental Health Centres will open by 30 June 2026. They will provide clinical services for adults with moderate‑to‑severe mental health needs.
For Australians with complex mental health needs, funding will be provided for Primary Health Networks to partner with GPs to deliver multidisciplinary, wraparound support services and care coordination.
Improving the aged care system
Providing quality care
The Budget provides $2.2 billion to deliver aged care reforms and continue implementing recommendations from the Royal Commission into Aged Care Quality and Safety.
The new Aged Care Act will put the rights and needs of older people at the centre of the aged care system. The new Act will provide the framework for fundamental change within the aged care sector.
More Home Care Packages
The Government is investing $531.4 million to release an additional 24,100 Home Care Packages in 2024–25. This will help reduce average wait times and enable people to age at home if they prefer to do so.
Improving aged care regulation
Funding of $110.9 million over four years will support an increase in the Aged Care Quality and Safety Commission’s regulatory capabilities.
The Government is investing $1.2 billion in critical digital systems to support the introduction of the new Aged Care Act and contemporary IT systems.
The My Aged Care Contact Centre will receive $37 million to reduce call‑waiting times for people seeking information and access to aged care.
Higher wages for aged care workers
The Government has committed to fund the Fair Work Commission decision to increase the award wage for direct and indirect aged care workers once the final determination is made. This will build on the $11.3 billion already allocated to support the interim 15 per cent wage increase for aged care workers.
The Government is providing $87.2 million for workforce initiatives to attract nurses and other workers into aged care.
Reforming the disability sector
Better and more sustainable services
Getting the National Disability Insurance Scheme (NDIS) back on track
A further $468.7 million is being provided to support people with disability and get the NDIS back on track. This includes:
- $214 million over two years to fight fraud and to co‑design NDIS reforms with people with disability, announced earlier this year
- $160.7 million to upgrade the NDIS Quality and Safeguards Commission’s information technology
- $45.5 million to establish a NDIS Evidence Advisory Committee
- $20 million to start consultation and design on reforms to help NDIS participants and people with disability navigate services.
This builds on $732.9 million provided in the 2023–24 Budget.
In December 2023, National Cabinet agreed to work together to improve the experience of participants and restore the original intent of the Scheme to support people with permanent and significant disability, within a broader ecosystem of supports. This builds on an earlier decision by National Cabinet to ensure Scheme sustainability and achieve an 8 per cent growth target by 1 July 2026, with further moderation as the NDIS matures.
Improving employment for people with disability
A $227.6 million investment will support a new specialised disability employment program to replace the existing Disability Employment Services program by 1 July 2025. This includes a modern digital platform for providers and participants. These reforms will support more people with disability into sustainable work, through a program with greater flexibility, increased individual supports, and better service quality. Eligibility will be expanded to include volunteers outside the income support system and those with less than eight hours per week work capacity.
Delivering essential services
Investing in reliability and security
Strengthening resourcing for Services Australia
The Government is delivering safer and more efficient government services for all Australians.
A $1.8 billion provision will support delivery of customer and payment services. This includes funding for frontline and service delivery staff to manage claims, respond to natural disasters and improve the cyber security environment. The Government is providing $314.1 million over two years to strengthen safety and security at Services Australia centres.
The Government is investing $580.3 million over four years and $139.6 million per year ongoing to sustain the myGov platform and identify potential enhancements. A further $50 million will improve usability, safety and security of the myGov platform and ensure Services Australia can support people to protect their information and privacy.
Strengthening the Australian Taxation Office (ATO) against fraud
There will be $187.4 million to better protect taxpayer data and Commonwealth revenue against fraudulent attacks on the tax and superannuation systems. Funding will upgrade the ATO’s information and communications technologies and increase fraud prevention capabilities to manage increasing risk, prevent revenue loss, and support victims of fraud and cyber crime.
Looking after our veterans
Veterans’ claims processing is prioritised with an additional $186 million for staffing resources and $8.4 million to improve case management and protect against cyber risk. The Government will provide $222 million to harmonise veterans’ compensation and rehabilitation legislation.
A further $48.4 million will be available for Veterans’ Home Care and Community Nursing programs and $10.2 million to provide access to funded medical treatment for ill and injured veterans while their claims for liability are processed.
Back to top

IMAGES
VIDEO
COMMENTS
The book, "Essentials of the U.S. Health Care System" provides information and insights regarding the health care system in the U.S. The first point that stood out to me is that today the main concern of the health care system is public health rather than patient-centered care. Chapter 3 addresses a historical overview of the healthcare ...
The National Academy of Medicine defines healthcare quality as "the degree to which health care services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge." Many factors contribute to the quality of care in the United States, including access to timely care, affordability of care, and use of evidence ...
The U.S. health system is a mix of public and private, for-profit and nonprofit insurers and health care providers. The federal government provides funding for the national Medicare program for adults 65 and ... United States HEALTH SYSTEM OVERVIEW Data: 2019 OECD Health Data except: diabetes prevalence from Health at a Glance 2019 (IDF Atlas ...
3. Argument for Universal Healthcare. Universal healthcare in the U.S., which may or may not include private market-based options, offer several noteworthy advantages compared to exclusive systems with inequitable access to quality care including: (i) addressing the growing chronic disease crisis; (ii) mitigating the economic costs associated with said crisis; (iii) reducing the vast health ...
healthcare systems consistently earn better ratings than the United States' current healthcare system. The contents of Chapter Two targets some of the more outstanding problems in the American healthcare system including escalated pharmaceutical prices, disparities in hethcare al by race or ethnicity, and the repeated failure of healthcare ...
Germany, which has all along had a robust public health care system, was accepting sick patients from Italy, Spain, and France. Meanwhile, U.S. hospitals were in financial shock and fee-for-service-based physician practices were devastated. We need to move toward a genuine health care system that can withstand shocks like the Covid-19 pandemic.
The United States spends far more money on healthcare per head than any other country. Compared to other high-income countries, however, life expectancy in the United States is lower and mortality is higher. Moreover, international comparison shows a varied picture with respect to quality and outcomes - with very good indicators for some ...
A Crisis in Public Health. The United States has 4% of the world's population but, as of July 16, approximately 26% of its Covid-19 cases and 24% of its Covid-19 deaths. 17 These startling ...
There are 100 assaults reported by U.S. emergency rooms for every homicide. About 25 percent of spinal cord injuries result from assaults; lifetime care for a quadriplegic averages $600,000. The United States has about 375,000 drug-exposed babies, and estimated 5-year costs of treatment are $63,000 per child.
The US Healthcare System Essay. Sort By: Page 1 of 50 - About 500 essays. Better Essays. Healthcare System in Us. 1290 Words; 6 Pages ... On the other hand, a large mindset is that the United States' health care system is inefficient because. 2534 Words; 10 Pages; Better Essays. Preview. Decent Essays. Us Vs Us Healthcare System. 731 Words; 3 ...
They include: focus on prevention, not just treating sickness; tackle racial disparities; expand telehealth and in-home services; build integrated systems; and adopt value-based care. Since early ...
The high cost of the US health care system is its biggest weakness. In the US, national expenditures on health care goods and services were approximately $4 trillion in 2020, accounting for an estimated 18% of gross domestic product. 2 High prices for care explain a large part of the difference in spending between the US and other developed ...
The delivery of healthcare services is considered to be a system; according to the Free Diction- ary (Farlex, 2010), a system is defined as "a group of interacting, interrelated, or interdependent elements forming a complex whole.". This is an apt description of our healthcare structure, as it is compiled of patients, medical and mental ...
During the COVID-19 pandemic, while some countries succeeded in reducing their rate of death after SARS-CoV-2 infection via vaccination by the end of 2021, some of them also faced hospital capacity strain, leading to social anxiety about delays in the diagnosis and treatment of patients with other diseases. This essay presents an allegory to explain the situation during the COVID-19 pandemic ...
The US healthcare system seems headed for bankruptcy because of its ever increasing and unsustainable costs. These costs will be effectively controlled only by legislative reforms in the insurance and payment for medical care, but the prospects of such legislation will depend on a more favourable political climate and stronger public support.
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
The technology accounts for 38 to 65 percent of healthcare spending in America (Johnson, 2011). The annual spending of health care increased from 75 billion in 1970 to 2.0 trillion in 2005 and is estimated to reach 4.0 trillion in 2015 (Kaiser Foundation, 2013). U.S. citizens spent 5,267 per capita for health care in 2002- 53 percent more than ...
U. Health Care System Essay. Macie Smith HCA 255 Professor Kevin Hayes March 20th, 2022. Assuring public health care get entry to insurance has been established to be a challenge in many nations - one which is still a hot topic in monetary, political, or even non-public debates.
United States Healthcare System Essay. Healthcare within the United States has captured different people within the field such as business leaders, policy makers, and health experts to give the system a reformation. Within the year of 1993 and 1994 the United States government has changed over the course of the year and made sure that the ...
Iora was a start up that created a new model for value-based care, to improve health outcomes and lower costs. Ten years after launching, it was acquired by One Medical, a primary care provider, which was later acquired by Amazon. Peter initially started out as a patient at one of Iora's first pilot sites, and later became a health coach ...
It threatens affordability and access to care for consumers, and it poses material risks to profitability for providers, payers, and other healthcare stakeholders. McKinsey research reveals the combined effects of these forces could accelerate the increase in NHE by approximately $600 billion through 2027. Downloads.
Whether it's childbirth, caring for a family member, or dealing with one's own injury or illness, a bill inevitably comes in the mail leaving most people asking, "Why does everything cost so ...
This dissertation consists of three interconnected papers that study the intersection of correctional systems and aging in the United States, specifically in prisons and community supervision. The papers examine existing policies and the experiences of older adults using a person-centered framework. The first two papers explore data collected through semi-structured interviews with community ...
Essay Example: When we think about our muscles, images of lifting weights at the gym or sprinting to catch a bus might spring to mind. But the muscular system, a complex network of more than 600 muscles, does far more than help us execute physical tasks like these; it's central to nearly
U.S. CDC helped Cameroon respond to COVID-19 by strengthening the country's health systems. CDC supported the establishment and upgrade of the National Public Health Laboratory to distribute, process, and report the results of COVID-19 test kits to country leaders and the World Health Organization. CDC and Cameroon's partnership contributed to ...
The Government is investing $2.8 billion to continue its commitment to strengthen Medicare. This includes the $1.2 billion package to address pressures facing the health system, which provides: $882.2 million to support older Australians avoid hospital admission, be discharged from hospital earlier and improve their transition out of hospital ...