- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic


Executive Editor
Michael Eriksen, USA
New Special Issue: Read Now
Health Education Research proudly presents a new Special Issue: Refugee, Immigrant, and Migrant Health. This issue explores the hidden global public health crisis.

Health Education Research deals with all the vital issues involved in health education and promotion worldwide - providing a valuable link between the health education research and practice communities.

Editor's Choice Articles
Executive Editor, Michael Eriksen, has hand-picked a collection of outstanding research articles from the journal, freely available to read.
Explore now

Why should you publish with HER ?
Health Education Research publishes original, peer-reviewed studies that deal with all the vital issues involved in health education and promotion worldwide—providing a valuable link between the health education research and practice communities. Explore the reasons why HER is the perfect home for your research.

Public Health at OUP
Latest articles.

Recommend to your library
Fill out our simple online form to recommend Health Education Research to your library.
Recommend now

Promote Your Article
Have you published an article? What should you do now? Read our top tips on promoting your work to reach a wider audience and ensure your work makes an impact.

Discover a more complete picture of how readers engage with research in Health Education Research through Altmetric data. Now available on article pages.

Email alerts
Register to receive table of contents email alerts as soon as new issues of Health Education Research are published online.
Related Titles
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Health Education
School-based health education helps adolescents acquire functional health knowledge, strengthen attitudes and beliefs, and practice skills needed to adopt and maintain healthy behaviors throughout their lives.

Schools can play a critical role in reducing adolescent health risks through the delivery of effective health education. 1-3
The specific content and skills addressed in health education, including sexual health and other related topic areas (e.g., violence prevention, mental and emotional health, food and nutrition), are commonly organized into a course of study or program and often summarized in a curriculum framework.
Health education curriculum should include:
A set of intended learning outcomes or objectives that directly relate to students’ acquisition of health-related knowledge, attitudes, and skills.
A planned progression of developmentally appropriate lessons or learning experiences that lead to achieving health objectives.
Continuity between lessons or learning experiences that clearly reinforce the adoption and maintenance of specific health-enhancing behaviors.
Content or materials that correspond with the sequence of learning events and help teachers and students meet the learning objectives.
Assessment strategies to determine if students have achieved the desired learning.
Health education is effective at addressing adolescent behaviors
Youth behaviors and experiences set the stage for adult health. 1-3 In particular, health behaviors and experiences related to early sexual initiation, violence, and substance use are consistently linked to poor grades and test scores and lower educational attainment. 4-7 In turn, providing health education as early as possible can help youth to develop positive well-being, academic success, and healthy outcomes into adulthood.
Health education tends to be more effective when it is taught by qualified teachers, connects students to health services, engages parents and community partners, and fosters positive relationships between adolescents and adults who are important to them.
Research suggests that well-designed and well-implemented school health programs can influence multiple health outcomes, including reducing sexual risk behaviors related to HIV, sexually transmitted diseases (STDs) and unintended pregnancy, decreasing substance and tobacco use, and improving academic performance. 8-10
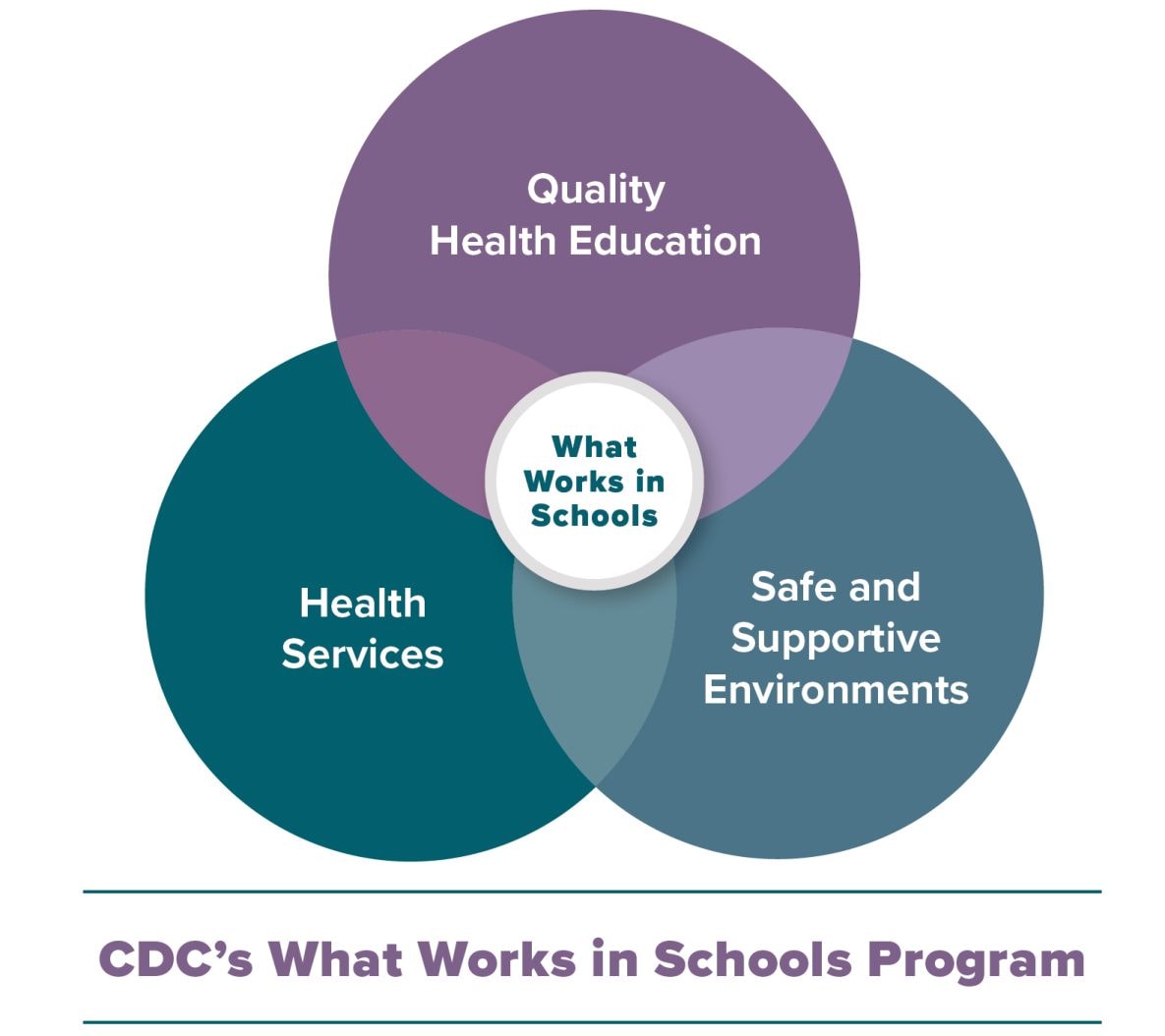
Schools can promote safe and supportive environments by improving students’ connections to schools and increasing the support they receive from parents.
See CDC’s Characteristics of an Effective Health Education Curriculum to learn more about research on effective curricula in school health education.
Standards for Health Education
Health education standards are designed to establish, promote, and support health-enhancing behaviors for students in all grade levels. 11 These learning standards have been updated or are currently being revised by multiple professional organizations in school health. Versions of these standards are available here and here .
Sexual health is a critical component of health education
School-based sexual health education provides youth with the knowledge and skills they need to protect their health and become successful learners. Increasing the number of schools that provide health education on key health risks facing youth, including HIV, STDs and unintended pregnancy, is a critical health objective for improving our nation’s health. 12
National Sex Education Standards

The National Sex Education Standards outline foundational knowledge and skills students need to navigate sexual development and grow into sexually healthy adults. The standards are designed to help schools focus on what is most essential for students to learn by the end of a grade level or grade span and can be used to create lessons and curricula with aligned learning objectives. 13
Learn more about CDC's program guidance for school-based HIV/STD prevention.
Access CDC resources to support health education teaching and learning.
Develop, revise, and evaluate health education curriclua using CDC's Health Education Curriculum Analysis Tool (HECAT).
- Eisen M, Pallitto C, Bradner C, Bolshun N. Teen Risk-Taking: Promising Prevention Programs and Approaches . Washington, DC: Urban Institute; 2000.
- Lohrmann DK, Wooley SF. Comprehensive School Health Education. In: Marx E, Wooley S, Northrop D, editors. Health Is Academic: A Guide to Coordinated School Health Programs. New York: Teachers College Press; 1998:43–45.
- Nation M, Crusto C, Wandersman A, Kumpfer KL, Seybolt D, Morrissey-Kane, E, Davino K. What works: principles of effective prevention programs . American Psychologist 2003;58(6/7):449–456.
- Centers for Disease Control and Prevention. School Health Profiles 2018: Characteristics of Health Programs Among Secondary Schools . Atlanta: Centers for Disease Control and Prevention; 2019.
- Rasberry CN, Tiu GF, Kann L, et al. Health-Related Behaviors and Academic Achievement Among High School Students— United States, 2015 . MMWR Morb Mortal Wkly Rep 2017 ;66:921–927
- Basch CE. Healthier students are better learners: high-quality, strategically planned, and effectively coordinated school health programs must be a fundamental mission of schools to help close the achievement gap . J Sch Health . 2011 Oct;81(10):650-62.
- Murray NG, Low BJ, Hollis C, Cross AW, Davis SM. Coordinated school health programs and academic achievement: A systematic review of the literature . J Sch Health 2007;77:589-600.
- Kirby D, Coyle K, Alton F, Rolleri L, Robin L. Reducing Adolescent Sexual Risk: A Theoretical Guide for Developing and Adapting Curriculum-Based Programs . Scotts Valley, CA: ETR Associates; 2011.
- U.S. Department of Health and Human Services. Preventing Tobacco Use Among Young People–An Update: A Report of the Surgeon General . Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2011: 6-22–6-45.
- Centers for Disease Control and Prevention. Youth Risk Behavior Survey: Data Summary & Trends Report: 2009-2019 . Atlanta: Centers for Disease Control and Prevention; 2020.
- Centers for Disease Control and Prevention. Health Education Curriculum Analysis Tool , 2021, Atlanta, GA: CDC; 2021.
- United States Department of Health and Human Services. HP 2020 Topics and Objectives: Early and Middle Childhood . Healthy People website. Accessed February 2021.
- Future of Sex Education Initiative. (2020). National Sexuality Education Standards: Core Content and Skills, K-12 .
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Open access
- Published: 06 April 2020
The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015
- Viju Raghupathi 1 &
- Wullianallur Raghupathi 2
Archives of Public Health volume 78 , Article number: 20 ( 2020 ) Cite this article
216k Accesses
267 Citations
172 Altmetric
Metrics details
A clear understanding of the macro-level contexts in which education impacts health is integral to improving national health administration and policy. In this research, we use a visual analytic approach to explore the association between education and health over a 20-year period for countries around the world.
Using empirical data from the OECD and the World Bank for 26 OECD countries for the years 1995–2015, we identify patterns/associations between education and health indicators. By incorporating pre- and post-educational attainment indicators, we highlight the dual role of education as both a driver of opportunity as well as of inequality.
Adults with higher educational attainment have better health and lifespans compared to their less-educated peers. We highlight that tertiary education, particularly, is critical in influencing infant mortality, life expectancy, child vaccination, and enrollment rates. In addition, an economy needs to consider potential years of life lost (premature mortality) as a measure of health quality.
Conclusions
We bring to light the health disparities across countries and suggest implications for governments to target educational interventions that can reduce inequalities and improve health. Our country-level findings on NEET (Not in Employment, Education or Training) rates offer implications for economies to address a broad array of vulnerabilities ranging from unemployment, school life expectancy, and labor market discouragement. The health effects of education are at the grass roots-creating better overall self-awareness on personal health and making healthcare more accessible.
Peer Review reports
Introduction
Is education generally associated with good health? There is a growing body of research that has been exploring the influence of education on health. Even in highly developed countries like the United States, it has been observed that adults with lower educational attainment suffer from poor health when compared to other populations [ 36 ]. This pattern is attributed to the large health inequalities brought about by education. A clear understanding of the health benefits of education can therefore serve as the key to reducing health disparities and improving the well-being of future populations. Despite the growing attention, research in the education–health area does not offer definitive answers to some critical questions. Part of the reason is the fact that the two phenomena are interlinked through life spans within and across generations of populations [ 36 ], thereby involving a larger social context within which the association is embedded. To some extent, research has also not considered the variances in the education–health relationship through the course of life or across birth cohorts [ 20 ], or if there is causality in the same. There is therefore a growing need for new directions in education–health research.
The avenues through which education affects health are complex and interwoven. For one, at the very outset, the distribution and content of education changes over time [ 20 ]. Second, the relationship between the mediators and health may change over time, as healthcare becomes more expensive and/or industries become either more, or less hazardous. Third, some research has documented that even relative changes in socioeconomic status (SES) can affect health, and thus changes in the distribution of education implies potential changes in the relationship between education and health. The relative index of inequality summarizes the magnitude of SES as a source of inequalities in health [ 11 , 21 , 27 , 29 ]. Fourth, changes in the distribution of health and mortality imply that the paths to poor health may have changed, thereby affecting the association with education.
Research has proposed that the relationship between education and health is attributable to three general classes of mediators: economic; social, psychological, and interpersonal; and behavioral health [ 31 ]. Economic variables such as income and occupation mediate the relationship between education and health by controlling and determining access to acute and preventive medical care [ 1 , 2 , 19 ]. Social, psychological, and interpersonal resources allow people with different levels of education to access coping resources and strategies [ 10 , 34 ], social support [ 5 , 22 ], and problem-solving and cognitive abilities to handle ill-health consequences such as stress [ 16 ]. Healthy behaviors enable educated individuals to recognize symptoms of ill health in a timely manner and seek appropriate medical help [ 14 , 35 ].
While the positive association between education and health has been established, the explanations for this association are not [ 31 ]. People who are well educated experience better health as reflected in the high levels of self-reported health and low levels of morbidity, mortality, and disability. By extension, low educational attainment is associated with self-reported poor health, shorter life expectancy, and shorter survival when sick. Prior research has suggested that the association between education and health is a complicated one, with a range of potential indicators that include (but are not limited to) interrelationships between demographic and family background indicators [ 8 ] - effects of poor health in childhood, greater resources associated with higher levels of education, appreciation of good health behaviors, and access to social networks. Some evidence suggests that education is strongly linked to health determinants such as preventative care [ 9 ]. Education helps promote and sustain healthy lifestyles and positive choices, nurture relationships, and enhance personal, family, and community well-being. However, there are some adverse effects of education too [ 9 ]. Education may result in increased attention to preventive care, which, though beneficial in the long term, raises healthcare costs in the short term. Some studies have found a positive association between education and some forms of illicit drug and alcohol use. Finally, although education is said to be effective for depression, it has been found to have much less substantial impact in general happiness or well-being [ 9 ].
On a universal scale, it has been accepted that several social factors outside the realm of healthcare influence the health outcomes [ 37 ]. The differences in morbidity, mortality and risk factors in research, conducted within and between countries, are impacted by the characteristics of the physical and social environment, and the structural policies that shape them [ 37 ]. Among the developed countries, the United States reflects huge disparities in educational status over the last few decades [ 15 , 24 ]. Life expectancy, while increasing for all others, has decreased among white Americans without a high school diploma - particularly women [ 25 , 26 , 32 ]. The sources of inequality in educational opportunities for American youth include the neighborhood they live in, the color of their skin, the schools they attend, and the financial resources of their families. In addition, the adverse trends in mortality and morbidity brought on by opioids resulting in suicides and overdoses (referred to as deaths of despair) exacerbated the disparities [ 21 ]. Collectively, these trends have brought about large economic and social inequalities in society such that the people with more education are likely to have more health literacy, live longer, experience better health outcomes, practice health promoting behaviors, and obtain timely health checkups [ 21 , 17 ].
Education enables people to develop a broad range of skills and traits (including cognitive and problem-solving abilities, learned effectiveness, and personal control) that predispose them towards improved health outcomes [ 23 ], ultimately contributing to human capital. Over the years, education has paved the way for a country’s financial security, stable employment, and social success [ 3 ]. Countries that adopt policies for the improvement of education also reap the benefits of healthy behavior such as reducing the population rates of smoking and obesity. Reducing health disparities and improving citizen health can be accomplished only through a thorough understanding of the health benefits conferred by education.
There is an iterative relationship between education and health. While poor education is associated with poor health due to income, resources, healthy behaviors, healthy neighborhood, and other socioeconomic factors, poor health, in turn, is associated with educational setbacks and interference with schooling through difficulties with learning disabilities, absenteeism, or cognitive disorders [ 30 ]. Education is therefore considered an important social determinant of health. The influence of national education on health works through a variety of mechanisms. Generally, education shows a relationship with self-rated health, and thus those with the highest education may have the best health [ 30 ]. Also, health-risk behaviors seem to be reduced by higher expenditure into the publicly funded education system [ 18 ], and those with good education are likely to have better knowledge of diseases [ 33 ]. In general, the education–health gradients for individuals have been growing over time [ 38 ].
To inform future education and health policies effectively, one needs to observe and analyze the opportunities that education generates during the early life span of individuals. This necessitates the adoption of some fundamental premises in research. Research must go beyond pure educational attainment and consider the associated effects preceding and succeeding such attainment. Research should consider the variations brought about by the education–health association across place and time, including the drivers that influence such variations [ 36 ].
In the current research, we analyze the association between education and health indicators for various countries using empirical data from reliable sources such as the Organization for Economic Cooperation and Development (OECD) and World Bank. While many studies explore the relationship between education and health at a conceptual level, we deploy an empirical approach in investigating the patterns and relationships between the two sets of indicators. In addition, for the educational indicators, we not only incorporate the level of educational attainment, but also look at the potential socioeconomic benefits, such as enrollment rates (in each sector of educational level) and school life expectancy (at each educational level). We investigate the influences of educational indicators on national health indicators of infant mortality, child vaccinations, life expectancy at birth, premature mortality arising from lack of educational attainment, employment and training, and the level of national health expenditure. Our research question is:
What are some key influencers/drivers in the education-health relationship at a country level?
The current study is important because policy makers have an increasing concern on national health issues and on policies that support it. The effect of education is at the root level—creating better overall self-awareness on personal health and making healthcare more accessible. The paper is organized as follows: Section 2 discusses the background for the research. Section 3 discusses the research method; Section 4 offers the analysis and results; Section 5 provides a synthesis of the results and offers an integrated discussion; Section 6 contains the scope and limitations of the research; Section 7 offers conclusions with implications and directions for future research.
Research has traditionally drawn from three broad theoretical perspectives in conceptualizing the relationship between education and health. The majority of research over the past two decades has been grounded in the Fundamental Cause Theory (FCT) [ 28 ], which posits that factors such as education are fundamental social causes of health inequalities because they determine access to resources (such as income, safe neighborhoods, or healthier lifestyles) that can assist in protecting or enhancing health [ 36 ]. Some of the key social resources that contribute to socioeconomic status include education (knowledge), money, power, prestige, and social connections. As some of these undergo change, they will be associated with differentials in the health status of the population [ 12 ].
Education has also been conceptualized using the Human Capital Theory (HCT) that views it as a return on investment in the form of increased productivity [ 4 ]. Education improves knowledge, skills, reasoning, effectiveness, and a broad range of other abilities that can be applied to improving health. The third approach - the signaling or credentialing perspective [ 6 ] - is adopted to address the large discontinuities in health at 12 and 16 years of schooling, which are typically associated with the receipt of a high school diploma and a college degree, respectively. This perspective considers the earned credentials of a person as a potential source that warrants social and economic returns. All these theoretical perspectives postulate a strong association between education and health and identify mechanisms through which education influences health. While the HCT proposes the mechanisms as embodied skills and abilities, FCT emphasizes the dynamism and flexibility of mechanisms, and the credentialing perspective proposes educational attainment through social responses. It needs to be stated, however, that all these approaches focus on education solely in terms of attainment, without emphasizing other institutional factors such as quality or type of education that may independently influence health. Additionally, while these approaches highlight the individual factors (individual attainment, attainment effects, and mechanisms), they do not give much emphasis to the social context in which education and health processes are embedded.
In the current research while we acknowledge the tenets of these theoretical perspectives, we incorporate the social mechanisms in education such as level of education, skills and abilities brought about by enrollment, school life expectancy, and the potential loss brought about by premature mortality. In this manner, we highlight the relevance of the social context in which the education and health domains are situated. We also study the dynamism of the mechanisms over countries and over time and incorporate the influences that precede and succeed educational attainment.
We analyze country level education and health data from the OECD and World Bank for a period of 21 years (1995–2015). Our variables include the education indicators of adult education level; enrollment rates at various educational levels; NEET (Not in Employment, Education or Training) rates; school life expectancy; and the health indicators of infant mortality, child vaccination rates, deaths from cancer, life expectancy at birth, potential years of life lost and smoking rates (Table 1 ). The data was processed using the tools of Tableau for visualization, and SAS for correlation and descriptive statistics. Approaches for analysis include ranking, association, and data visualization of the health and education data.
Analyses and results
In this section we identify and analyze patterns and associations between education and health indicators and discuss the results. Since countries vary in population sizes and other criteria, we use the estimated averages in all our analyses.
Comparison of health outcomes for countries by GDP per capita
We first analyzed to see if our data reflected the expectation that countries with higher GDP per capita have better health status (Fig. 1 ). We compared the average life expectancy at birth, average infant mortality, average deaths from cancer and average potential year of life lost, for different levels of GDP per capita (Fig. 1 ).
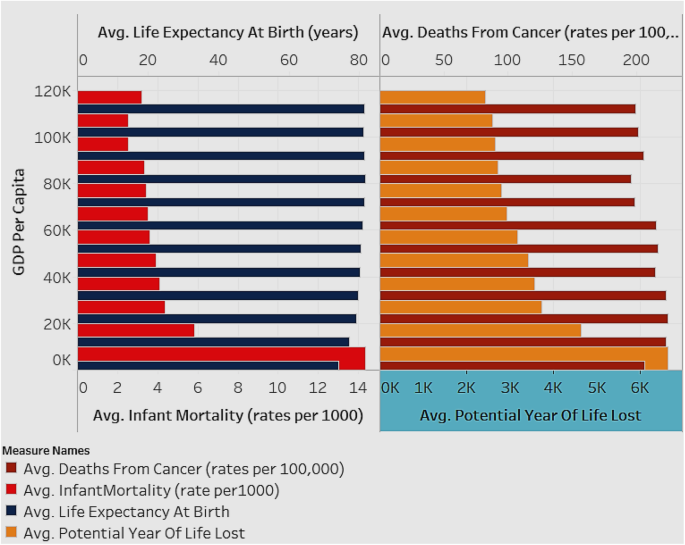
Associations between Average Life Expectancy (years) and Average Infant Mortality rate (per 1000), and between Deaths from Cancer (rates per 100,000) and Average Potential Years of Life Lost (years), by GDP per capita (for all countries for years 1995–2015)
Figure 1 depicts two charts with the estimated averages of variables for all countries in the sample. The X-axis of the first chart depicts average infant mortality rate (per 1000), while that of the second chart depicts average potential years of life lost (years). The Y-axis for both charts depicts the GDP per capita shown in intervals of 10 K ranging from 0 K–110 K (US Dollars). The analysis is shown as an average for all the countries in the sample and for all the years (1995–2015). As seen in Fig. 1 , countries with lower GDP per capita have higher infant mortality rate and increased potential year of life lost (which represents the average years a person would have lived if he or she had not died prematurely - a measure of premature mortality). Life expectancy and deaths from cancer are not affected by GDP level. When studying infant mortality and potential year lost, in order to avoid the influence of a control variable, it was necessary to group the samples by their GDP per capita level.
Association of Infant Mortality Rates with enrollment rates and education levels
We explored the association of infant mortality rates with the enrollment rates and adult educational levels for all countries (Fig. 2 ). The expectation is that with higher education and employment the infant mortality rate decreases.
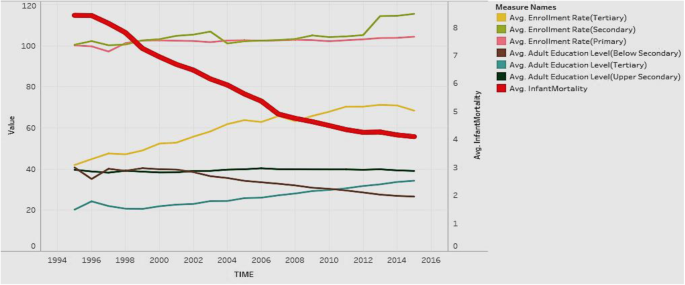
Association of Adult Education Levels (ratio) and Enrollment Rates (ratio) with Infant Mortality Rate (per 1000)
Figure 2 depicts the analysis for all countries in the sample. The figure shows the years from 1995 to 2015 on the X axis. It shows two Y-axes with one axis denoting average infant mortality rate (per 1000 live births), and the other showing the rates from 0 to 120 to depict enrollment rates (primary/secondary/tertiary) and education levels (below secondary/upper secondary/tertiary). Regarding the Y axis showing rates over 100, it is worth noting that the enrollment rates denote a ratio of the total enrollment (regardless of age) at a level of education to the official population of the age group in that education level. Therefore, it is possible for the number of children enrolled at a level to exceed the official population of students in the age group for that level (due to repetition or late entry). This can lead to ratios over 100%. The figure shows that in general, all education indicators tend to rise over time, except for adult education level below secondary, which decreases over time. Infant mortality shows a steep decreasing trend over time, which is favorable. In general, countries have increasing health status and education over time, along with decreasing infant mortality rates. This suggests a negative association of education and enrollment rates with mortality rates.
Association of Education Outcomes with life expectancy at birth
We explored if the education outcomes of adult education level (tertiary), school life expectancy (tertiary), and NEET (not in employment, education, or training) rates, affected life expectancy at birth (Fig. 3 ). Our expectation is that adult education and school life expectancy, particularly tertiary, have a positive influence, while NEET has an adverse influence, on life expectancy at birth.
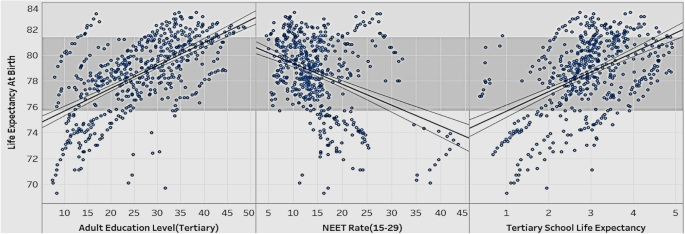
Association of Adult Education Level (Tertiary), NEET rate, School Life Expectancy (Tertiary), with Life Expectancy at Birth
Figure 3 show the relationships between various education indicators (adult education level-tertiary, NEET rate, school life expectancy-tertiary) and life expectancy at birth for all countries in the sample. The figure suggests that life expectancy at birth rises as adult education level (tertiary) and tertiary school life expectancy go up. Life expectancy at birth drops as the NEET rate goes up. In order to extend people’s life expectancy, governments should try to improve tertiary education, and control the number of youths dropping out of school and ending up unemployed (the NEET rate).
Association of Tertiary Enrollment and Education with potential years of life lost
We wanted to explore if the potential years of life lost rates are affected by tertiary enrollment rates and tertiary adult education levels (Fig. 4 ).
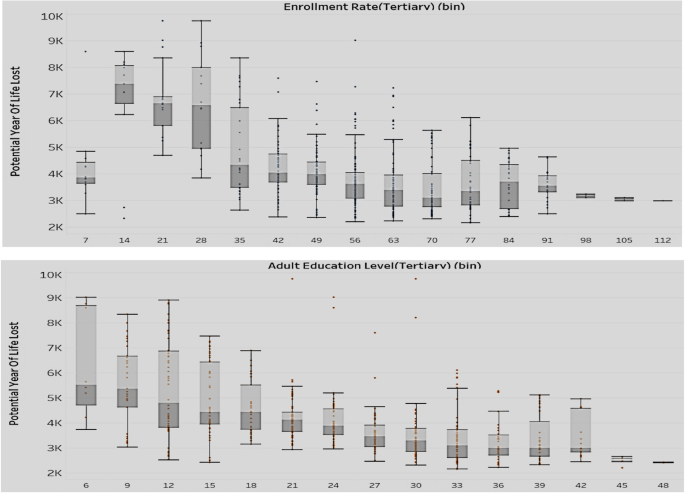
Association of Enrollment rate-tertiary (top) and Adult Education Level-Tertiary (bottom) with Potential Years of Life Lost (Y axis)
The two sets of box plots in Fig. 4 compare the enrollment rates with potential years of life lost (above set) and the education level with potential years of life lost (below set). The analysis is for all countries in the sample. As mentioned earlier, the enrollment rates are expressed as ratios and can exceed 100% if the number of children enrolled at a level (regardless of age) exceed the official population of students in the age group for that level. Potential years of life lost represents the average years a person would have lived, had he/she not died prematurely. The results show that with the rise of tertiary adult education level and tertiary enrollment rate, there is a decrease in both value and variation of the potential years of life lost. We can conclude that lower levels in tertiary education adversely affect a country’s health situation in terms of premature mortality.
Association of Tertiary Enrollment and Education with child vaccination rates
We compared the performance of tertiary education level and enrollment rates with the child vaccination rates (Fig. 5 ) to assess if there was a positive impact of education on preventive healthcare.
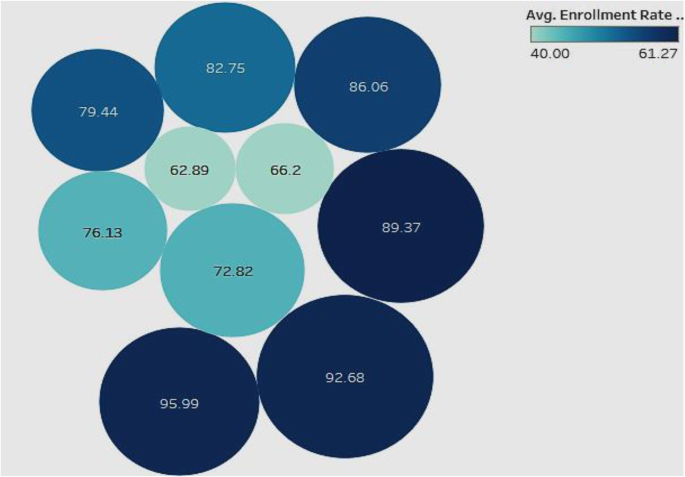
Association of Adult Education Level-Tertiary and Enrollment Rate-Tertiary with Child Vaccination Rates
In this analysis (Fig. 5 ), we looked for associations of child vaccination rates with tertiary enrollment and tertiary education. The analysis is for all countries in the sample. The color of the bubble represents the tertiary enrollment rate such that the darker the color, the higher the enrollment rate, and the size of the bubble represents the level of tertiary education. The labels inside the bubbles denote the child vaccination rates. The figure shows a general positive association of high child vaccination rate with tertiary enrollment and tertiary education levels. This indicates that countries that have high child vaccination rates tend to be better at tertiary enrollment and have more adults educated in tertiary institutions. Therefore, countries that focus more on tertiary education and enrollment may confer more health awareness in the population, which can be reflected in improved child vaccination rates.
Association of NEET rates (15–19; 20–24) with infant mortality rates and deaths from Cancer
In the realm of child health, we also looked at the infant mortality rates. We explored if infant mortality rates are associated with the NEET rates in different age groups (Fig. 6 ).
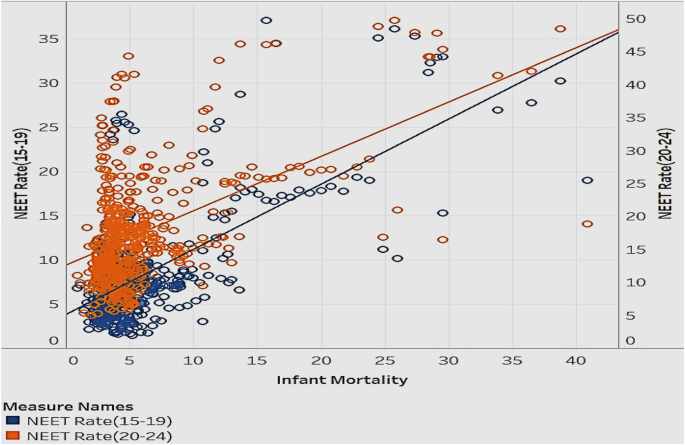
Association of Infant Mortality rates with NEET Rates (15–19) and NEET Rates (20–24)
Figure 6 is a scatterplot that explores the correlation between infant mortality and NEET rates in the age groups 15–19 and 20–24. The data is for all countries in the sample. Most data points are clustered in the lower infant mortality and lower NEET rate range. Infant mortality and NEET rates move in the same direction—as infant mortality increases/decrease, the NEET rate goes up/down. The NEET rate for the age group 20–24 has a slightly higher infant mortality rate than the NEET rate for the age group 15–19. This implies that when people in the age group 20–24 are uneducated or unemployed, the implications on infant mortality are higher than in other age groups. This is a reasonable association, since there is the potential to have more people with children in this age group than in the teenage group. To reduce the risk of infant mortality, governments should decrease NEET rates through promotional programs that disseminate the benefits of being educated, employed, and trained [ 7 ]. Additionally, they can offer financial aid to public schools and companies to offer more resources to raise general health awareness in people.
We looked to see if the distribution of population without employment, education, or training (NEET) in various categories of high, medium, and low impacted the rate of deaths from cancer (Fig. 7 ). Our expectation is that high rates of NEET will positively influence deaths from cancer.
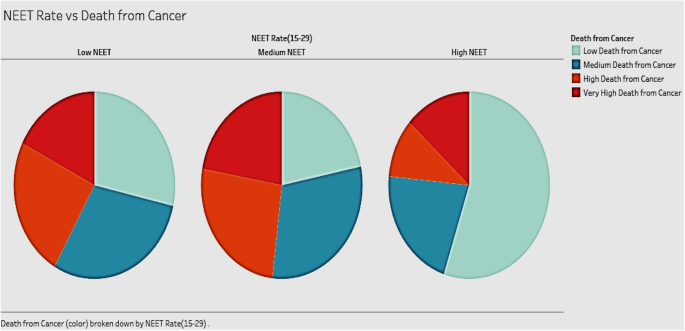
Association of Deaths from Cancer and different NEET Rates
The three pie charts in Fig. 7 show the distribution of deaths from cancer in groups of countries with different NEET rates (high, medium, and low). The analysis includes all countries in the sample. The expectation was that high rates of NEET would be associated with high rates of cancer deaths. Our results, however, show that countries with medium NEET rates tend to have the highest deaths from cancer. Countries with high NEET rates have the lowest deaths from cancer among the three groups. Contrary to expectations, countries with low NEET rates do not show the lowest death rates from cancer. A possible explanation for this can be attributed to the fact that in this group, the people in the labor force may be suffering from work-related hazards including stress, that endanger their health.
Association between adult education levels and health expenditure
It is interesting to note the relationship between health expenditure and adult education levels (Fig. 8 ). We expect them to be positively associated.
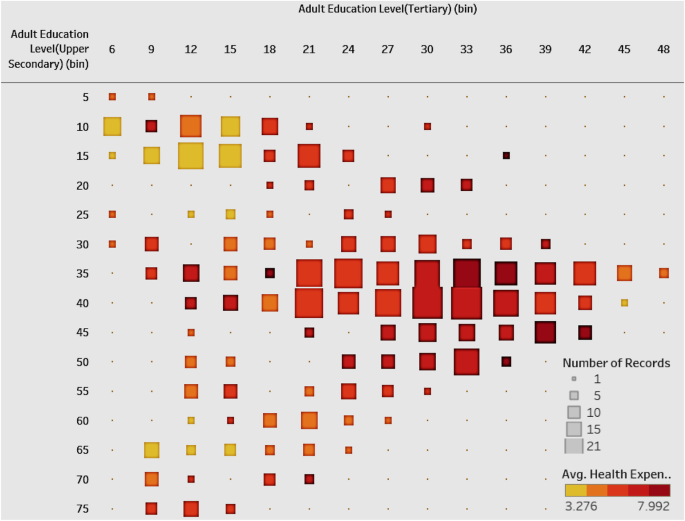
Association of Health Expenditure and Adult Education Level-Tertiary & Upper Secondary
Figure 8 shows a heat map with the number of countries in different combinations of groups between tertiary and upper-secondary adult education level. We emphasize the higher levels of adult education. The color of the square shows the average of health expenditure. The plot shows that most of the countries are divided into two clusters. One cluster has a high tertiary education level as well as a high upper-secondary education level and it has high average health expenditure. The other cluster has relatively low tertiary and upper secondary education level with low average health expenditure. Overall, the figure shows a positive correlation between adult education level and compulsory health expenditure. Governments of countries with low levels of education should allocate more health expenditure, which will have an influence on the educational levels. Alternatively, to improve public health, governments can frame educational policies to improve the overall national education level, which then produces more health awareness, contributing to national healthcare.
Association of Compulsory Health Expenditure with NEET rates by country and region
Having explored the relationship between health expenditure and adult education, we then explored the relationship between health expenditure and NEET rates of different countries (Fig. 9 ). We expect compulsory health expenditure to be negatively associated with NEET rates.
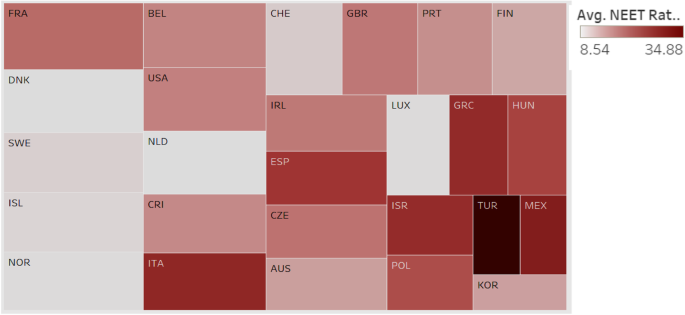
Association between Compulsory Health Expenditure and NEET Rate by Country and Region
In Fig. 9 , each box represents a country or region; the size of the box indicates the extent of compulsory health expenditure such that a larger box implies that the country has greater compulsory health expenditure. The intensity of the color of the box represents the NEET rate such that the darker color implies a higher NEET rate. Turkey has the highest NEET rate with low health expenditure. Most European countries such as France, Belgium, Sweden, and Norway have low NEET rates and high health expenditure. The chart shows a general association between low compulsory health expenditure and high NEET rates. The relationship, however, is not consistent, as there are countries with high NEET and high health expenditures. Our suggestion is for most countries to improve the social education for the youth through free training programs and other means to effectively improve the public health while they attempt to raise the compulsory expenditure.
Distribution of life expectancy at birth and tertiary enrollment rate
The distribution of enrollment rate (tertiary) and life expectancy of all the countries in the sample can give an idea of the current status of both education and health (Fig. 10 ). We expect these to be positively associated.
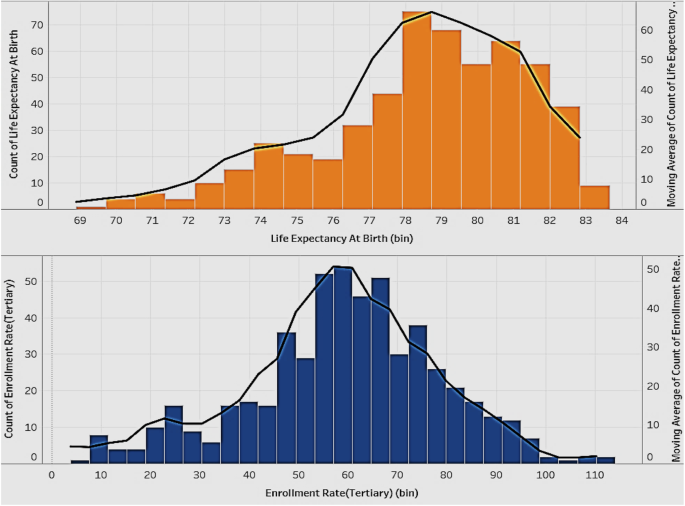
Distribution of Life Expectancy at Birth (years) and Tertiary Enrollment Rate
Figure 10 shows two histograms with the lines representing the distribution of life expectancy at birth and the tertiary enrollment rate of all the countries. The distribution of life expectancy at birth is skewed right, which means most of the countries have quite a high life expectancy and there are few countries with a very low life expectancy. The tertiary enrollment rate has a good distribution, which is closer to a normal distribution. Governments of countries with an extremely low life expectancy should try to identify the cause of this problem and take actions in time to improve the overall national health.
Comparison of adult education levels and deaths from Cancer at various levels of GDP per capita
We wanted to see if various levels of GDP per capita influence the levels of adult education and deaths from cancer in countries (Fig. 11 ).
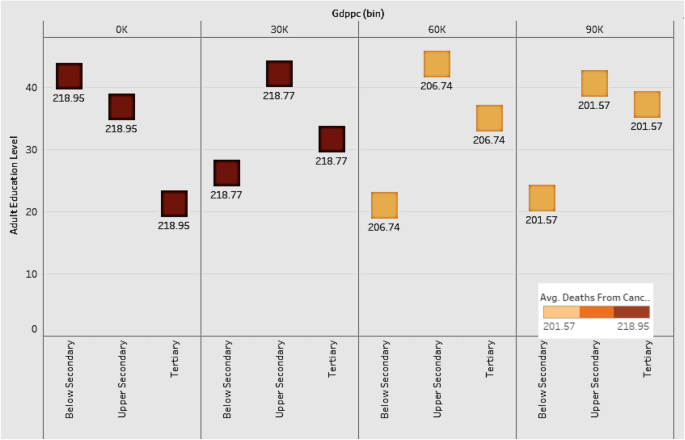
Comparison of Adult Education Levels and Deaths from Cancer at various levels of GDP per capita
Figure 11 shows the distribution of various adult education levels for countries by groups of GDP per capita. The plot shows that as GDP grows, the level of below-secondary adult education becomes lower, and the level of tertiary education gets higher. The upper-secondary education level is constant among all the groups. The implication is that tertiary education is the most important factor among all the education levels for a country to improve its economic power and health level. Countries should therefore focus on tertiary education as a driver of economic development. As for deaths from cancer, countries with lower GDP have higher death rates, indicating the negative association between economic development and deaths from cancer.
Distribution of infant mortality rates by continent
Infant mortality is an important indicator of a country’s health status. Figure 12 shows the distribution of infant mortality for the continents of Asia, Europe, Oceania, North and South America. We grouped the countries in each continent into high, medium, and low, based on infant mortality rates.
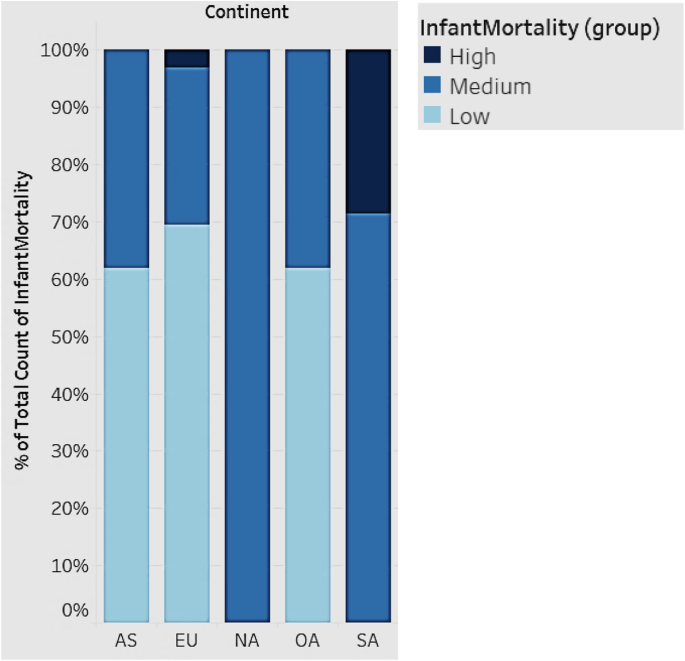
Distribution of Infant Mortality rates by Continent
In Fig. 12 , each bar represents a continent. All countries fall into three groups (high, medium, and low) based on infant mortality rates. South America has the highest infant mortality, followed by Asia, Europe, and Oceania. North America falls in the medium range of infant mortality. South American countries, in general, should strive to improve infant mortality. While Europe, in general, has the lowest infant mortality rates, there are some countries that have high rates as depicted.
Association between child vaccination rates and NEET rates
We looked at the association between child vaccination rates and NEET rates in various countries (Fig. 13 ). We expect countries that have high NEET rates to have low child vaccination rates.
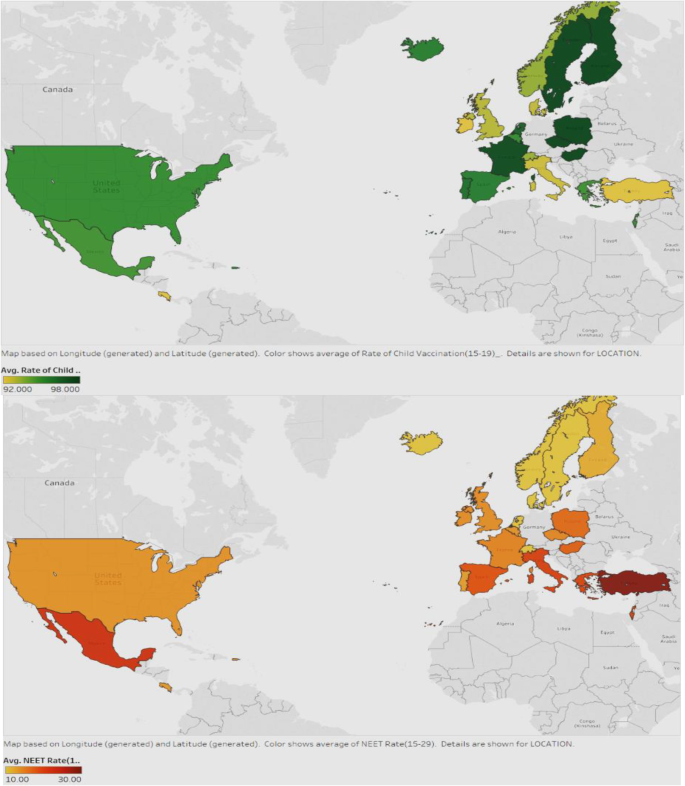
Association between Child Vaccination Rates and NEET rates
Figure 13 displays the child vaccination rates in the first map and the NEET rates in the second map, for all countries. The darker green color shows countries with higher rates of vaccination and the darker red represents those with higher NEET rates. It can be seen that in general, the countries with lower NEET also have better vaccination rates. Examples are USA, UK, Iceland, France, and North European countries. Countries should therefore strive to reduce NEET rates by enrolling a good proportion of the youth into initiatives or programs that will help them be more productive in the future, and be able to afford preventive healthcare for the families, particularly, the children.
Average smoking rate in different continents over time
We compared the trend of average smoking rate for the years 1995–201 for the continents in the sample (Fig. 14 ).
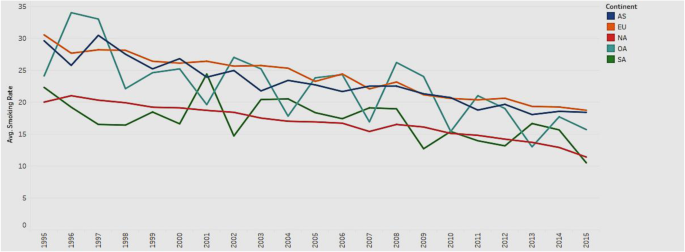
Trend of average smoking rate in different continents from 1995 to 2015
Figure 14 depicts the line charts of average smoking rates for the continents of Asia, Europe, Oceania, North and South America. All the lines show an overall downward trend, which indicates that the average smoking rate decreases with time. The trend illustrates that people have become more health conscious and realize the harmful effects of smoking over time. However, the smoking rate in Europe (EU) is consistently higher than that in other continents, while the smoking rate in North America (NA) is consistently lower over the years. Governments in Europe should pay attention to the usage of tobacco and increase health consciousness among the public.
Association between adult education levels and deaths from Cancer
We explored if adult education levels (below-secondary, upper-secondary, and tertiary) are associated with deaths from cancer (Fig. 15 ) such that higher levels of education will mitigate the rates of deaths from cancer, due to increased awareness and proactive health behavior.
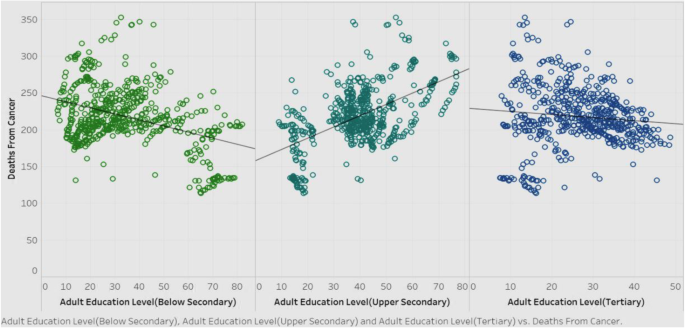
Association of deaths from cancer with adult education levels
Figure 15 shows the correlations of deaths from cancer among the three adult education levels, for all countries in the sample. It is obvious that below-secondary and tertiary adult education levels have a negative correlation with deaths from cancer, while the upper-secondary adult education level shows a positive correlation. Barring upper-secondary results, we can surmise that in general, as education level goes higher, the deaths from cancer will decrease. The rationale for this could be that education fosters more health awareness and encourages people to adopt healthy behavioral practices. Governments should therefore pay attention to frame policies that promote education. However, the counterintuitive result of the positive correlation between upper-secondary levels of adult education with the deaths from cancer warrants more investigation.
We drilled down further into the correlation between the upper-secondary education level and deaths from cancer. Figure 16 shows this correlation, along with a breakdown of the total number of records for each continent, to see if there is an explanation for the unique result.
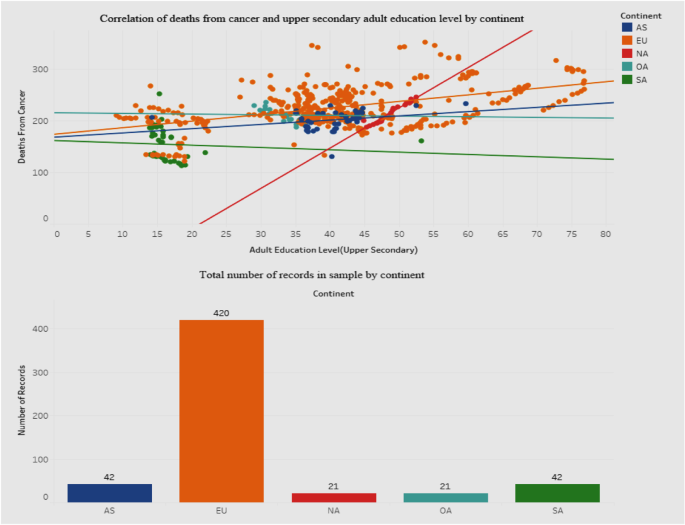
Association between deaths from cancer and adult education level-upper secondary
Figure 16 shows a dashboard containing two graphs - a scatterplot of the correlation between deaths from cancer and education level, and a bar graph showing the breakdown of the total sample by continent. We included a breakdown by continent in order to explore variances that may clarify or explain the positive association for deaths from cancer with the upper-secondary education level. The scatterplot shows that for the European Union (EU) the points are much more scattered than for the other continents. Also, the correlation between deaths and education level for the EU is positive. The bottom bar graph depicts how the sample contains a disproportionately high number of records for the EU than for other continents. It is possible that this may have influenced the results of the correlation. The governments in the EU should investigate the reasons behind this phenomenon. Also, we defer to future research to explore this in greater detail by incorporating other socioeconomic parameters that may have to be factored into the relationship.
Association between average tertiary school life expectancy and health expenditure
We moved our focus to the trends of tertiary school life expectancy and health expenditure from 1995 to 2015 (Fig. 17 ) to check for positive associations.
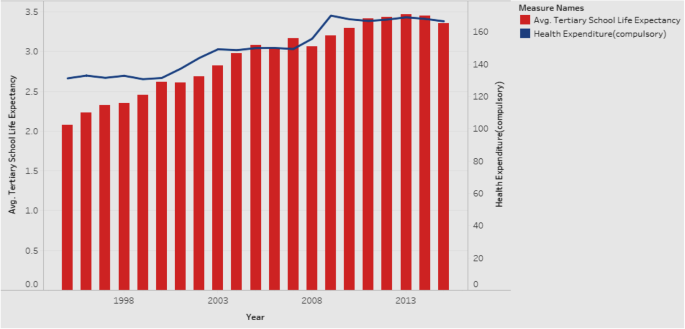
Association between Average Tertiary School Life Expectancy and Health Expenditure
Figure 17 is a combination chart explaining the trends of tertiary school life expectancy and health expenditure, for all countries in the sample. The rationale is that if there is a positive association between the two, it would be worthwhile for the government to allocate more resources towards health expenditure. Both tertiary school life expectancy and health expenditure show an increase over the years from 1995 to 2015. Our additional analysis shows that they continue to increase even after 2015. Hence, governments are encouraged to increase the health expenditure in order to see gains in tertiary school life expectancy, which will have positive implications for national health. Given that the measured effects of education are large, investments in education might prove to be a cost-effective means of achieving better health.
Our results reveal how interlinked education and health can be. We show how a country can improve its health scenario by focusing on appropriate indicators of education. Countries with higher education levels are more likely to have better national health conditions. Among the adult education levels, tertiary education is the most critical indicator influencing healthcare in terms of infant mortality, life expectancy, child vaccination rates, and enrollment rates. Our results emphasize the role that education plays in the potential years of life lost, which is a measure that represents the average years a person would have lived had he/she not died prematurely. In addition to mortality rate, an economy needs to consider this indicator as a measure of health quality.
Other educational indicators that are major drivers of health include school life expectancy, particularly at the tertiary level. In order to improve the school life expectancy of the population, governments should control the number of youths ending up unemployed, dropping out of school, and without skills or training (the NEET rate). Education allows people to gain skills/abilities and knowledge on general health, enhancing their awareness of healthy behaviors and preventive care. By targeting promotions and campaigns that emphasize the importance of skills and employment, governments can reduce the NEET rates. And, by reducing the NEET rates, governments have the potential to address a broad array of vulnerabilities among youth, ranging from unemployment, early school dropouts, and labor market discouragement, which are all social issues that warrant attention in a growing economy.
We also bring to light the health disparities across countries and suggest implications for governments to target educational interventions that can reduce inequalities and improve health, at a macro level. The health effects of education are at the grass roots level - creating better overall self-awareness on personal health and making healthcare more accessible.
Scope and limitations
Our research suffers from a few limitations. For one, the number of countries is limited, and being that the data are primarily drawn from OECD, they pertain to the continent of Europe. We also considered a limited set of variables. A more extensive study can encompass a larger range of variables drawn from heterogeneous sources. With the objective of acquiring a macro perspective on the education–health association, we incorporated some dependent variables that may not traditionally be viewed as pure health parameters. For example, the variable potential years of life lost is affected by premature deaths that may be caused by non-health related factors too. Also there may be some intervening variables in the education–health relationship that need to be considered. Lastly, while our study explores associations and relationships between variables, it does not investigate causality.
Conclusions and future research
Both education and health are at the center of individual and population health and well-being. Conceptualizations of both phenomena should go beyond the individual focus to incorporate and consider the social context and structure within which the education–health relationship is embedded. Such an approach calls for a combination of interdisciplinary research, novel conceptual models, and rich data sources. As health differences are widening across the world, there is need for new directions in research and policy on health returns on education and vice versa. In developing interventions and policies, governments would do well to keep in mind the dual role played by education—as a driver of opportunity as well as a reproducer of inequality [ 36 ]. Reducing these macro-level inequalities requires interventions directed at a macro level. Researchers and policy makers have mutual responsibilities in this endeavor, with researchers investigating and communicating the insights and recommendations to policy makers, and policy makers conveying the challenges and needs of health and educational practices to researchers. Researchers can leverage national differences in the political system to study the impact of various welfare systems on the education–health association. In terms of investment in education, we make a call for governments to focus on education in the early stages of life course so as to prevent the reproduction of social inequalities and change upcoming educational trajectories; we also urge governments to make efforts to mitigate the rising dropout rate in postsecondary enrollment that often leads to detrimental health (e.g., due to stress or rising student debt). There is a need to look into the circumstances that can modify the postsecondary experience of youth so as to improve their health.
Our study offers several prospects for future research. Future research can incorporate geographic and environmental variables—such as the quality of air level or latitude—for additional analysis. Also, we can incorporate data from other sources to include more countries and more variables, especially non-European ones, so as to increase the breadth of analysis. In terms of methodology, future studies can deploy meta-regression analysis to compare the relationships between health and some macro-level socioeconomic indicators [ 13 ]. Future research should also expand beyond the individual to the social context in which education and health are situated. Such an approach will help generate findings that will inform effective educational and health policies and interventions to reduce disparities.
Availability of data and materials
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
Fundamental Cause Theory
Human Capital Theory
Not in Employment, Education, or Training
Organization for Economic Cooperation and Development
Socio-economic status
Andersen RM, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95–124.
Article CAS Google Scholar
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Social Behav. 1995;36(1):1–10.
Baker DP. The Schooled Society: The Educational Transformation of Global Culture. Stanford, CA: Stanford Univ. Press: 2014; 360.
Becker GS. Human capital: a theoretical and empirical analysis, with special reference to education. Chicago: Univ. Chicago Press; 1964.
Google Scholar
Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Oxford Acad J. 1979;109(2):186–204.
CAS Google Scholar
Crimmins EM, Kim JK, Vasunilashorn S. Biodemography: new approaches to understanding trends and differences in population health and mortality. Demography. 2010;47:S41–64.
Article Google Scholar
Spence M. Job market signalling. The Quarterly J Econ. 1973;87:355–79.
Cutler DM, Lleras-Muney A. Education and Health: Evaluating Theories and Evidence: NBER Working Papers; 2006. p. 12352.
Feinstein L. What are the effects of education on health? OECD Proceedings of the Copenhagen Symposium; 2006 . .
Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980;21(3):219–39.
Freedman VA, Martin LG. The role of education in explaining and forecasting trends in functional limitations among older Americans. Demography. 1999;36(4):461–73.
Freese J, Lutfey K. Fundamental causality: challenges of an animating concept for medical sociology. In: Pescosolido BA, Martin JK, McLeod JD, Rogers A, editors. Handbook of the Sociology of Health, Illness, and Healing: a blueprint for the 21st century. New York: Springer; 2011. p. 67–81.
Chapter Google Scholar
Fouweather T, Gillies C, Wohland P, Van Oyen H, Nusselde W, Robine J, Cambois E, Jagger C. Comparison of socio-economic indicators explaining inequalities in healthy life years at age 50 in Europe: 2005 and 2010. Eur J Pub Health. 2015;25:978–83.
George LK, Gwyther LP. Caregiver Weil-being: a multidimensional examination of family caregivers of demented adults. Gerontologist. 1986;26(3):253–9.
Goldman D, Smith JP. The increasing value of education to health. Soc Sc Med. 2011;72(10):1728–37.
Harper AC, Lambert LJ. The health of populations: an introduction. New York: Springer Publishing Company; 1994.
Health 2020: Education and health through the life-course. WHO Europe Sector Brief on Education Health; 2015. http://www.euro.who.int/__data/assets/pdf_file/0007/324619/Health-2020-Education-and-health-through-the-life-course-en.pdf?ua=1 .
Kino S, Bernabé E, Sabbah W. The role of healthcare and education systems in co-occurrence of health risk behaviours in 27 European countries. Eur J Public Health. 2018;28(1):186–92.
Landerman LR, Burns BJ, Swartz MS, Wagner HR, George LK. The relationship between insurance coverage and psychiatric disorder in predicting use of mental health services. Am J Psychol. 1994;151(12):1785.
Lynch SM. Cohort and life-course patterns in the relationship between education and health: a hierarchical approach. Demography. 2003;40(2):309–31.
Mackenbach J, Kunst A. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44(6):757–71. https://doi.org/10.1016/S0277-9536(96)00073-1 .
Article CAS PubMed Google Scholar
Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982-1994. Natl Acad Sci. 1997;94(6):2593–8.
Mirowski J, Ross CE. Education, learned effectiveness and health. London Rev Edu. 2005;3(3):205–20.
Montez JK, Berkman LF. Trends in the educational gradient of mortality among US adults aged 45 to 84 years: bringing regional context into the explanation. Am J Pub Health. 2014;104(1):e82–90.
Montez JK, Zajacova A. Trends in mortality risk by education level and cause of death among US white women from 1986 to 2006. Am J Pub Health. 2013;103:473–9.
Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, Carnes BA, Carstensen LL, Fried LP, Goldman DP, Jackson J, Kohli M, Rother J, Zheng Y, Rowe J. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff. 2012;31(8):1803–13.
Pamuk ER. Social-class inequality in infant mortality in England and Wales from 1921 to 1980. Eur J Popul 1988; 4 , 1–21, https://doi.org/10.1007/BF01797104.
Phelan JC , Link BG , Tehranifar P . Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications . J Health Soc Behav 2010 ; 51 : S28 S40 . doi : 10.1177/0022146510383498.
Renard F, Devleesschauwer B, Speybroeck N, Deboosere P. Monitoring health inequalities when the socio-economic composition changes: are the slope and relative indices of inequality appropriate? Results of a simulation study. BMC Public Health 2019; 19: 662. https://doi.org/10.1186/s12889-019-6980-1.
Ro A, Geronimus A, Bound J, Griffith D, Gee G. Educational gradients in five Asian immigrant populations: do country of origin, duration and generational status moderate the education-health relationship? Prev Med Rep. 2016;4:338–43.
Ross CE, Wu CL. The links between education and health. Am Soc Rev. 1995;60(5):719–45.
Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA. Diverging trends in premature mortality in the U.S. by sex, race, and ethnicity in the 21st century. Lancet. 2017;389:1043–54.
Tsou MT. Association of Education, health behaviors, concerns, and knowledge with metabolic syndrome among urban elderly in one medical Center in Taiwan. Int J Gerontology. 2017;11(3:138–43.
Wheaton B. Stress, personal coping resources, and psychiatric symptoms: an investigation of interactive models. J Health Soc Behav. 1983;24(3):208–29.
Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Ann Rev Soc. 1995;21:349–86.
Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Ann Rev Pub Health. 2018;39:273–89.
Zimmerman EB, Woolf SH. Understanding the relationship between education and health. Discussion Paper, Inst Med. Washington DC; 2014. https://nam.edu/wp-content/uploads/2015/06/BPH-UnderstandingTheRelationship1.pdf .
Zhong H. An over time analysis on the mechanisms behind the education–health gradients in China. China Econ Rev. 2015;34(C):135–49.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Koppelman School of Business, Brooklyn College of the City University of New York, 2900 Bedford Ave, Brooklyn, NY, 11210, USA
Viju Raghupathi
Gabelli School of Business, Fordham University, 140 W. 62nd Street, New York, NY, 10023, USA
Wullianallur Raghupathi
You can also search for this author in PubMed Google Scholar
Contributions
Both authors contributed equally to all parts of the manuscript.
Corresponding author
Correspondence to Viju Raghupathi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Raghupathi, V., Raghupathi, W. The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. Arch Public Health 78 , 20 (2020). https://doi.org/10.1186/s13690-020-00402-5
Download citation
Received : 16 October 2019
Accepted : 26 February 2020
Published : 06 April 2020
DOI : https://doi.org/10.1186/s13690-020-00402-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Education level
- Enrollment rate
- Life expectancy
- Potential years of life lost
- Infant mortality
- Deaths from cancer
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
- Subject List
- Take a Tour
- For Authors
- Subscriber Services
- Publications
- African American Studies
- African Studies
- American Literature
- Anthropology
- Architecture Planning and Preservation
- Art History
- Atlantic History
- Biblical Studies
- British and Irish Literature
- Childhood Studies
- Chinese Studies
- Cinema and Media Studies
- Communication
- Criminology
- Environmental Science
- Evolutionary Biology
- International Law
- International Relations
- Islamic Studies
- Jewish Studies
- Latin American Studies
- Latino Studies
- Linguistics
- Literary and Critical Theory
- Medieval Studies
- Military History
- Political Science
Public Health
- Renaissance and Reformation
- Social Work
- Urban Studies
- Victorian Literature
- Browse All Subjects
How to Subscribe
- Free Trials
In This Article Expand or collapse the "in this article" section Health Education
Introduction, definition and scope of practice.
- Historical and Philosophical Foundations
- Theories and Models
- Community Assessment
- Implementation and Best Practices
- Relationship to Health Professions, Health-Enhancing Systems, and Sectors
- Health Communication, Social Marketing, and Policy Advocacy
- Professionalism and Ethics
Related Articles Expand or collapse the "related articles" section about
About related articles close popup.
Lorem Ipsum Sit Dolor Amet
Vestibulum ante ipsum primis in faucibus orci luctus et ultrices posuere cubilia Curae; Aliquam ligula odio, euismod ut aliquam et, vestibulum nec risus. Nulla viverra, arcu et iaculis consequat, justo diam ornare tellus, semper ultrices tellus nunc eu tellus.
- Air Quality: Health Effects
- Air Quality: Indoor Health Effects
- Attachment as a Health Determinant
- Behavior Change Theory in Health Education and Promotion
- Cancer Screening
- Climate Change and Human Health
- Community Development
- Community Health Interventions
- Critical Health Literacy
- Cultural Safety
- Dietary Guidelines
- Evidence-Based Pediatric Dentistry
- Food Security and Food Banks
- Functional Literacy
- Global Health Promotion
- Health Administration
- Health Communication
- Health Literacy
- Health Literacy and Noncommunicable Diseases
- Health Planning
- Health Promotion
- Knowledge Translation and Exchange
- Media Advocacy
- Mental Health
- Mental Health Promotion
- Ottawa Charter
- Parenting Skills and Capacity
- Prenatal Health
- Sex Education in HIV/AIDS Prevention
- Skin Cancer Prevention
Other Subject Areas
Forthcoming articles expand or collapse the "forthcoming articles" section.
- Housing as a Determinant of Health
- Quackery as a Public Health Problem
- Social Vulnerability in Public Health
- Find more forthcoming articles...
- Export Citations
- Share This Facebook LinkedIn Twitter
Health Education by Elaine Auld , Stephen F. Gambescia LAST REVIEWED: 23 February 2011 LAST MODIFIED: 23 February 2011 DOI: 10.1093/obo/9780199756797-0044
Health education is defined as “any combination of learning experiences designed to facilitate voluntary actions conducive to health” ( Green and Kreuter 2005 ). Although the history of health education dates back to the 19th century, it was not until the 1940s that the field began evolving as a distinct discipline. Over time, health education’s theory and practice base have broadened from focusing on one-to-one and mass media behavioral interventions to encompass responsibility for policies, systems, and environments that affect population health. In the early 21st century, the terms health education and health promotion (i.e., the latter including an ecological approach) are often used interchangeably in the United States, while internationally health promotion is used as an overarching concept that includes health education. Health education is considered a mature profession given that it has developed a discrete body of knowledge, defined competencies, a certification system for individuals, a code of ethics, a federal occupational classification, and recognized accreditation processes in higher education. Health education is generally aligned with the behavioral and social sciences as one of the core dimensions of public health study and practice. Additionally, the field draws from theories and models from education, health studies, communications, and other diverse areas. The unique combination of these knowledge areas forms the basis for health education competencies. Health educators employ a core set of competencies, regardless of the diverse practice settings in which they work (i.e., schools, universities, health departments, community-based organizations, health-care settings, worksites, and international organizations). This bibliography is organized around major areas of health education practice, such as assessing, planning, implementing, managing, and evaluating health education or health promotion programs, services, and interventions. It includes historical and philosophical foundations, and development of its professionalism and ethics. The discipline embraces both qualitative and quantitative methods, community-based participatory research, health communication and social marketing principles, and policy and media advocacy to accomplish program objectives. Health educators are stalwarts in the fight for social justice and believe that the health of a population should be a priority in any society.
The definition and scope of health education have evolved since the 1950s, particularly in relation to improved understanding of behavioral and socio-ecological influences on health. The early definition of health education in Griffiths 1972 primarily emphasized the provision of learning experiences to promote voluntary changes to individual health. Subsequent work in Robertson and Minkler 1994 , Schwartz, et al. 1995 , and Downie, et al. 1996 provides a broader context of health education in relation to policy, systems, and environmental changes inherent in the practice of health promotion and related philosophies. Taub, et al. 2009 provides a concise overview of how the terms health education and health promotion are used differently in the early 21st century in the United States versus internationally, due to historical, cultural, and political considerations. Gold and Miner 2002 and Modeste, et al. 2004 provide good sources of contemporary definitions for many other terms, which is especially important due to the eclectic base from which health education draws.
Downie, Robert, Carol Tannahill, and Andrew Tannahill. 1996. Health promotion: Models and values . 2d ed. Oxford: Oxford Univ. Press.
A comprehensive and systematic review of how to define health promotion and the range of underlying values held by those in practice. One of the few works that addresses the influence of values held by the profession, government entities, and communities on health promotion.
Gold, Robert S., and Kathleen R. Miner. 2002. 2000 Joint Committee on Health Education and Promotion Terminology. Journal of School Health 7.2: 3–7.
DOI: 10.1111/j.1746-1561.2002.tb06501.x
The Joint Committee convenes every decade to evaluate the current terminology in health education, which changes with the advancement of scholarship, technological developments, and professional practice. This citation is the seventh major health education terminology report issued during the past seventy years.
Griffiths, William. 1972. Health education definitions, problems, and philosophies. Health Education Monographs 31:12–14.
This health education pioneer defines health education as an “attempt to close the gap between what is known about optimum health practice and that which is actually practiced.” Later, as part of the views offered to President Richard M. Nixon’s First White House Conference on Health Education, Griffiths also asserted the health educator’s role in changing societal conditions that influence health.
Modeste, Naomi, Teri Tamayose, and Helen H. Marshak. 2004. Dictionary of public health promotion and education: Terms and concepts . 2d ed. San Francisco: Jossey-Bass.
Brief dictionary of the most common and more esoteric terms used in health promotion and education. Expands on concepts beyond a rote definition, which is useful to both students and practitioners.
Robertson, A., and Meredith Minkler. 1994. New health promotion movement: A critical examination. Health Education Quarterly 21:295–312.
Explores the various meanings of health education to date and identifies the characteristics of a new health promotion movement and implications for practice and research.
Schwartz, Randy, Robert Goodman, and Alan Steckler. 1995. Policy advocacy interventions for health promotion and education: Advancing the state of practice. Health Education Quarterly 22.4: 421–426.
This theme issue outlines the role of policy advocacy in achieving health education and health promotion objectives. Includes seminal articles on environmental and policy change for tobacco, cardiovascular disease, physical activity, and nutrition.
Taub, Alyson, John P. Allegrante, Margaret P. Barry, and Keiko Sakagami. 2009. Perspectives on terminology and conceptual and professional issues in health education and health promotion credentialing. Health Education & Behavior 36.3: 439–450.
DOI: 10.1177/1090198109333826
Explains how the terms health education and health promotion have been defined and used differently in the United States and other countries, and includes a succinct and useful table. Also addresses key international perspectives on professional competencies, standards, and accreditation.
back to top
Users without a subscription are not able to see the full content on this page. Please subscribe or login .
Oxford Bibliographies Online is available by subscription and perpetual access to institutions. For more information or to contact an Oxford Sales Representative click here .
- About Public Health »
- Meet the Editorial Board »
- Access to Health Care
- Action Research
- Active Aging
- Active Living
- Adolescent Health, Socioeconomic Inequalities in
- Adolescent Risk-Taking Behavior in the United States
- Advocacy, Public Health
- Agricultural Safety and Public Health
- Alcohol Availability and Violence
- Alternative Research Designs
- Ambient Air Quality Standards and Guidelines
- American Perspectives on Chronic Disease and Control
- Antimicrobial Resistance (AMR)
- Arts in Health
- Asthma in Children
- Asthma, Work-Related
- Behavioral Risk Factor Surveillance
- Bicycling and Cycling Safety
- Birth and Death Registration
- Birth Cohort Studies
- Board of Health
- Breastfeeding
- Built Environment and Health, The
- Business and Corporate Practices
- Cancer Communication Strategies in North America
- Cancer Prevention
- Capacity Building
- Capacity Building for NCDs in LMICs
- Capacity-Building for Applied Public Health in LMIC: A US ...
- Cardiovascular Health and Disease
- Child Labor
- Child Maltreatment
- Children, Air Pollution and
- Children, Injury Risk-Taking Behaviors in
- Children, Obesity in
- Citizen Advisory Boards
- Climate Change: Institutional Response
- Clinical Preventive Medicine
- Community Air Pollution
- Community Gardens
- Community Health Assessment
- Community Partnerships and Coalitions
- Community-Based Participatory Research
- Complexity and Systems Theory
- Cultural Capital and Health
- Culture and Public Health
- Definition of Health
- Dental Public Health
- Design and Health
- Directions in Global Public Health Graduate Education
- Driving and Public Health
- Ecological Approaches
- Enabling Factors
- Environmental Health, Pediatric
- Environmental Laws
- Environmental Protection Agency
- Ethics of Public Health
- Evidence-Based Public Health Practice
- Family Planning Services and Birth Control
- Food Safety
- Food Systems
- Frail Elderly
- Genomics, Public Health
- Geographic Information Systems
- Geography and Health
- Global Health
- Global Health Diplomacy
- Global Health Security
- Guide to Community Preventive Services, The
- Health Disparities
- Health Education
- Health Impact Assessment
- Health in All Policies
- Health in All Policies in European Countries
- Health Measurement Scales
- Health Promoting Hospitals
- Health Promotion Foundations
- Health Promotion Workforce Capacity
- Health Systems of Low and Middle-Income Countries, The
- Healthy People Initiative
- Healthy Public Policy
- Hepatitis C
- High Risk Prevention Strategies
- Homelessness
- Human Rights, Health and
- Human Sexuality and Sexual Health: A Western Perspective
- IANPHI and National Public Health Institutes
- Immigrant Populations
- Immunization and Pneumococcal Infection
- Immunization in Pregnancy
- Indigenous Peoples, Public Health and
- Indigenous Populations of North America, Australasia, and ...
- Indoor Air Quality Guidelines
- Infant Mortality
- Internet Applications in Promoting Health Behavior
- Intersectoral Action
- Intersectoral Strategies in Low - Middle Income Countries ...
- Justice, Social
- Knowledge Utilization and Exchange
- Law of Public Health in the United States
- Migrant Health
- Migrant Worker Health
- Motor Vehicle Injury Prevention
- Multi-Drug-Resistant Tuberculosis
- Nanotechnology
- National Association of Local Boards of Health
- National Public Health Institutions
- Needs Assessment
- Needs Assessments in International Disasters and Emergenci...
- Obesity Prevention
- Occupational Cancers
- Occupational Exposure to Benzene
- Occupational Exposure to Erionite
- Occupational Safety and Health
- Occupational Safety and Health Administration (OSHA)
- Oral Health Equity for Minority Populations in the United ...
- Parenting and Work
- Participatory Action Research
- Patient Decision Making
- Pesticide Exposure and Pesticide Health Effects
- Physical Activity and Exercise
- Physical Activity Promotion
- Pneumoconiosis
- Polio Eradication in Pakistan
- Population Aging
- Population Determinants of Unhealthy Foods and Beverages
- Population Health Objectives and Targets
- Precautionary Principle
- Preparedness
- Program Evaluation in American Health Education
- Program Planning and Evaluation
- Public Health, History of
- Public Health Surveillance
- Public-Private Partnerships in Public Health Research and ...
- Public-Private Partnerships to Prevent and Manage Obesity ...
- Quantitative Microbial Risk Assessment
- Racism as a Structural Determinant of Health
- Radiation Emergencies and Public Health: Impacts, Prepared...
- Randomized Controlled Trials
- Real World Evaluation Strategies
- Reducing Obesity-Related Health Disparities in Hispanic an...
- Research Integrity in Public Health
- Resilient Health Systems
- Rural Health in the United States
- Safety, Patient
- School Health Programs in the Pacific Region
- Smoking Cessation
- Social Determinants of Health
- Social Epidemiology
- Social Marketing
- Statistics in Public Health
- STI Networks, Patterns, and Control Strategies
- Stillbirths
- Sustainable Development Goals
- Systems in the United States, Public Health
- Systems Modeling and Big Data for Non-Communicable Disease...
- Systems Theory in Public Health
- Traditional, Complementary, Alternative, and Integrative M...
- Translation of Science to Practice and Policy
- Traumatic Stress and Post-Traumatic Stress Disorder
- Tuberculosis among Adults and the Determinants of Health
- UK Public Health Systems
- Unintentional Injury Prevention
- Urban Health
- Vaccination, Mandatory
- Vaccine Hesitancy
- Vermiculite
- Violence Prevention
- Vulnerability, Intersectionality and Health in Migration
- Water Quality
- Water Quality and Water-Related Disease
- Weight Management in US Occupational Settings
- Welfare States, Public Health and Health Inequalities
- Worksite Health Promotion
- World Health Organization (WHO)
- Privacy Policy
- Cookie Policy
- Legal Notice
- Accessibility
Powered by:
- [66.249.64.20|185.66.15.189]
- 185.66.15.189

Health and education
Education has the power to transform the lives of children and young people, and the world around them. At UNESCO, inclusive and transformative education starts with healthy, happy and safe learners. Because children and young people who receive a good quality education are more likely to be healthy, and likewise those who are healthy are better able to learn and complete their education.
Guided by the UNESCO Strategy on education for health and well-being , UNESCO works to improve the physical and mental health, well-being and education outcomes of all learners. By reducing health-related barriers to learning, such as gender-based violence, gender inequality, HIV and sexually transmitted infections (STIs), early and unintended pregnancy, bullying and discrimination, and malnutrition, UNESCO, governments and school systems empower learners to understand their rights, learn better and lead fulfilling lives.
What you need to know about education for health and well-being
Helping children learn about health and well-being
For healthy, informed and empowered learners
Supporting comprehensive sexuality education for adolescents and young people in Sub-Saharan Africa
Preventing and addressing violence in and around school
Key figures
is bullied at school every month globally
occur each year among adolescent girls aged 15–19
and almost half do not have handwashing facilities with water and soap
in 161 countries – nearly half of all children in primary school – receive school meals

A foundation for life and love campaign
What does comprehensive sexuality education mean to you?
A foundation for life and love
First technical brief in a series of four.

More publications

- Open access
- Published: 21 May 2024
Effectively teaching cultural competence in a pre-professional healthcare curriculum
- Karen R. Bottenfield 1 ,
- Maura A. Kelley 2 ,
- Shelby Ferebee 3 ,
- Andrew N. Best 1 ,
- David Flynn 2 &
- Theresa A. Davies 1 , 2
BMC Medical Education volume 24 , Article number: 553 ( 2024 ) Cite this article
208 Accesses
Metrics details
There has been research documenting the rising numbers of racial and ethnic minority groups in the United States. With this rise, there is increasing concern over the health disparities that often affect these populations. Attention has turned to how clinicians can improve health outcomes and how the need exists to educate healthcare professionals on the practice of cultural competence. Here we present one successful approach for teaching cultural competence in the healthcare curriculum with the development of an educational session on cultural competence consisting of case-based, role-play exercises, class group discussions, online discussion boards, and a lecture PowerPoint presentation.
Cultural competence sessions were delivered in a pre-dental master’s program to 178 students between 2017 and 2020. From 2017 to 2019, the sessions were implemented as in-person, case-based, role-play exercises. In 2020, due to in-person limitations caused by the COVID-19 pandemic, students were asked to read the role-play cases and provide a reflection response using the online Blackboard Learn discussion board platform. Evaluation of each session was performed using post-session survey data.
Self-reported results from 2017 to 2020 revealed that the role-play exercises improved participant’s understanding of components of cultural competence such as communication in patient encounters (95%), building rapport with patients (94%), improving patient interview skills (95%), and recognition of students own cultural biases when working with patients (93%).
Conclusions
Students were able to expand their cultural awareness and humility after completion of both iterations of the course session from 2017 to 2019 and 2020. This session can be an effective method for training healthcare professionals on cultural competence.
Peer Review reports
It is projected that by the year 2050, racial and ethnic minority groups will make up over 50% of the United States population [ 1 ]. With a more multicultural society, growing concern has emerged over how to address the health disparities that effect these populations and the ways in which healthcare professionals can increase positive health outcomes. Continuing evidence suggests that many patients from racial and ethnic minority groups are not satisfied with the current state of healthcare which has been attributed to implicit bias on the part of physicians and current challenges faced by practitioners who feel underprepared to address these issues due to differences in language, financial status, and healthcare practice [ 2 , 3 , 4 ].
To contend with health disparities and the challenges faced by practitioners working with a more diverse population, healthcare educators have begun to emphasize the importance of educating healthcare workforce on the practice of cultural competence and developing a skilled-based set of behaviors, attitudes and policies that effectively provides care in the wake of cross-cultural situations and differences [ 4 , 5 , 6 ]. There are several curricular mandates from both medical and dental accreditation bodies to address this issue [ 7 , 8 , 9 ], and large amounts of resources, ideas, and frameworks that exist for implementing and training future and current healthcare providers on the inadequacies of the healthcare system and cultural competence [ 10 , 11 , 12 ]. These current institutional guidelines for accreditation and the numerous amounts of resources for training cultural competence, continue to evolve with work documenting the need for blended curriculum that is continuous throughout student education, starting early as we have done here with pre-dental students, including in-person didactic or online sessions, a service learning component, community engagement and a reflective component [ 4 , 5 , 13 , 14 ].
This study investigates teaching cultural competence in a healthcare curriculum. We hypothesized that early educational exposure to cultural competence through role playing case studies, can serve as an effective mechanism for training early pre-doctoral students the practice of cultural competence. Utilizing student self-reported survey data conducted in a predental master’s curriculum, in which two iterations of role-playing case studies were used to teach components of cultural competence, this study aims to evaluate and support research that suggests role-playing case studies as effective means for educating future clinical professionals on the practice of cultural competence.
This study was determined to be exempt by the Institutional Review Board of Boston University Medical Campus, Protocol # H-37,232. Informed consent was received from all subjects.
Data collection
The role-playing, case-based simulated patient encounter exercises were developed and administered at Boston University Chobanian & Avedisian School of Medicine to predental students in the Master of Science in Oral Health Sciences Program (see Table 1 ). From 2017 to 2020, we administered patient encounter cases [see Additional File 1 ] to students ( n = 178) in the program as a portion of a case-based, role-playing exercise to teach the importance of cultural competence and cultural awareness during patient encounters. During years 2017–2019, real actors portrayed the patient and physician. In 2020, the session was conducted online via a discussion board through a Blackboard Course Site. The original case was published as part of a master’s students thesis work in 2021 [ 15 ].
Description of patient encounter cases 1 and 2
Patient Encounter Case 1 [see Additional file 1 ] is composed of two subsections, scenario 1 A and scenario 1B, and is centered around a patient/physician interaction in which a patient who is pregnant presents with pain upon urination. The physician in 1 A is short and terse with the patient, immediately looking at a urine sample, prescribing medication for a urinary tract infection, and telling the patient to return for a follow-up in 2 weeks. In scenario 1B, a similar situation ensues; however, in this scenario the physician takes more time with the patient providing similar care as the physician in 1 A, but asking for more information about the patients personal and medical history. At the conclusion of the scenario, the patient is offered resources for an obstetrician and a dentist based on the information that is provided about the patient’s background. The patient is then sent on their way and asked to follow-up in 2 weeks. The patient does not return.
Patient Encounter Case 2 [see Additional file 1 ] follows a similar format to the Patient Encounter Case 1. In scenario 2 A, the same patient from Case 1 returns with tooth pain after giving birth. The physician in 2 A, like 1 A, is short with the patient and quickly refers the patient to a dentist. In 2B, the physician again takes more time with the patient to receive background information on the patient, make a connection, and provides an antibiotic and dental referral.
Each Patient Encounter Case explored topics such as the importance of building a trusting physician/patient relationship, the importance of asking a patient for patient history, making a connection, and the importance of a physician taking all facets of a patient’s circumstances into consideration [ 15 ].
Session outline
The sessions conducted between 2017 and 2019 were composed of three parts: (1) enactment of an abridged patient encounter facilitated by session administrators, (2) group discussion and reflection during which time students were asked to critically reflect and discuss the theme and key take-aways from the role play exercise, and (3) a PowerPoint presentation emphasizing take-away points from the role-play exercise. At the conclusion of the cultural competence training sessions, students participated in a post-session Qualtrics generated survey administered electronically to assess each student’s feelings about the session [see Additional file 3 ].
Role-play enactment
Facilitators dressed-up in clothing to mimic both the physician and patient for all case scenarios in Patient Encounter Case 1 and Case 2. At the conclusion of the role play portion of each of the cases, the facilitators paused to lead students in a real-time class group discussion. After Case 1, students were asked questions such as: What did you think ? Were the patient’s needs met? Did you expect the patient to return? Following Case 2, similar questions were asked by the facilitators, including: What did you think ? Were the patient’s needs met? Did you expect the patient to accept help?
At the conclusion of this portion of the session, the facilitators led a larger general discussion about both cases and how they related to one another. Finally, the course session concluded with a PowerPoint presentation that reinforced the take-home points from the session [see Additional file 2 ] [ 15 ].
Change in session modality due to COVID-19 pandemic
In Fall 2020, due to the COVID-19 pandemic, the course modality moved to an online platform and consisted of three parts on a Blackboard Discussion Board (Blackboard, Inc.). Students were required to: (1) read each of the Patient Encounter Cases and add a brief reflection comparing the scenarios, (2) then comment on at least two peer’s posts in the discussion forum and (3) attend class to hear a PowerPoint presentation by a course session facilitator on the key take-aways from each scenario [ 15 ].
Student surveys
At the conclusion of the cultural competence training sessions, students participated in a post-session Qualtrics ( https://www.qualtrics.com ) generated survey administered electronically to assess each student’s feelings about the sessions [see Additional file 3 ]. The format of the survey included 5 questions with the following Likert scale response options: strongly agree, agree, disagree, strongly disagree. These post-session surveys were not required but rather optional [ 15 ].
A total of 178 students completed the cultural competence sessions between 2017 and 2020. Of these participants, 112 voluntarily completed a post-session survey on the effectiveness of the course in teaching cultural competence and cultural awareness during patient encounters. Between 2017 and 2019, 99 students completed post-session surveys following sessions with role play exercises. In 2020, 13 students completed post-session surveys following discussion board sessions.
Role-play exercises enhanced cultural competence
In responding to post-session survey questions following cultural competence sessions that included role-play exercises (2017–2019), 71% of students surveyed strongly agreed and 24% agreed that the role-play exercises helped them to identify the importance of communication in patient encounters. In asking participants if the role-play exercises made them more aware of different strategies to improve their patient interview skills, 72% strongly agreed and 23% agreed. Also, 68% of the students strongly agreed and 26% agreed that the exercises helped them to better identify the importance of building rapport and trust during patient encounters. When asked if the exercises helped the students to better understand their own bias and/or cultural awareness when working with patients, the results of the survey showed that 62% of students strongly agreed and 31% agreed with this statement. In addition, most students found the role-play exercises to be enjoyable (72% strongly agreed and 22% agreed). See results shown in Fig. 1 .
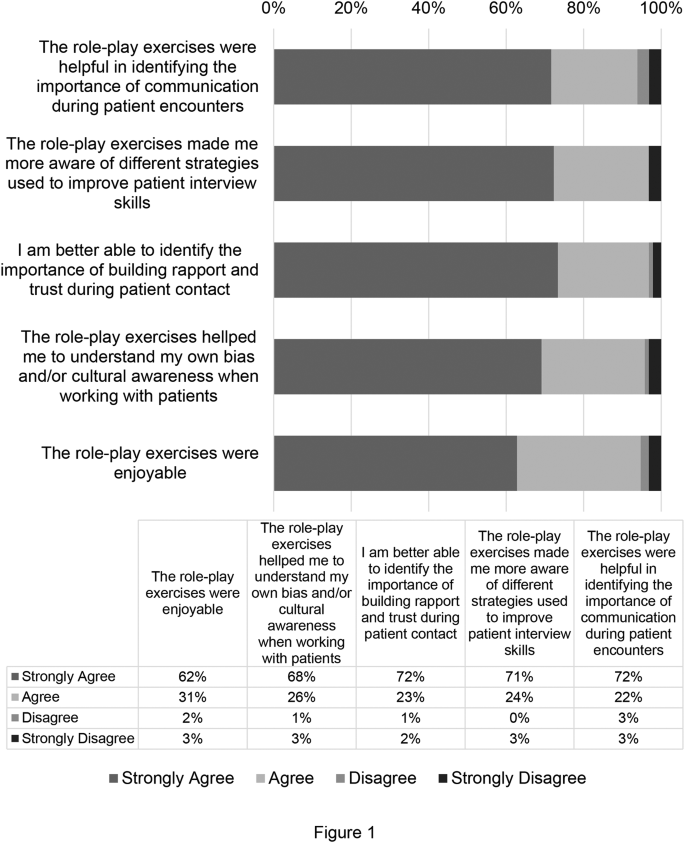
Cultural Competence Session Survey Data from the Year 2017–2019. Survey data from students at Boston University’s Oral Health Sciences Program for the years 2017–2019. Data is presented as percent of respondents ( n = 99)
Discussion boards and reflections enhanced cultural competence
Cultural competence sessions held during 2020 did not include role-play exercises due to the Covid-19 pandemic. Instead, students participated in discussion boards and reflections on Blackboard. In response to the post-session survey question asking if the discussion board exercises were helpful in identifying the importance of communication during patient encounters, 67% of students strongly agreed and 25% agreed with this statement. Also, 75% of students strongly agreed and 17% agreed that the discussion board exercises helped them identify the importance of building rapport and trust during patient contact. When asked if the exercises helped the students to better understand their own bias and/or cultural awareness when working with patients, the results of the survey showed that 67% of students strongly agreed and 25% agreed with this statement. In addition, most students found the discussion board exercises to be enjoyable (67% strongly agreed and 22% agreed). See results shown in Fig. 2 .
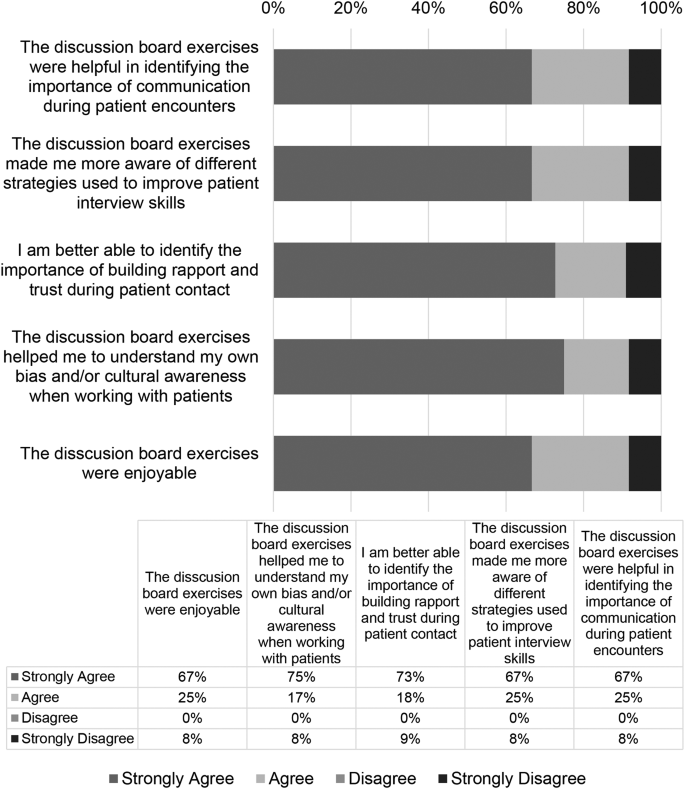
Cultural competence session survey data from the Year 2020. Survey data from students at Boston University’s Oral Health Sciences Program for the year 2020. Data is presented as percent of respondents ( n = 13)
Student responses to the reflection portion of the online cultural competency sessions were recorded and categorized. Five themes were selected and 441 reflection responses were coded using NVivo (Version 12). The results showed that 29% of reflections demonstrated student’s ability to understand a holistic approach to clinical care, 24.3% understood the importance of collecting a patient history, 6.8% recognized the socioeconomic factors during a patient encounter, 27.9% reflected on the importance of the patient clinical relationship, and 12% on the effects on improving health outcomes (Table 1 ). Representative student responses to these themes are shown in Table 1 .
There exists a need to develop novel and effective means for teaching and training the next generation of healthcare professionals the practice of cultural competence. Thus, two iterations of a course session using case-based patient centered encounters were developed to teach these skills to pre-professional dentals students. Overall, the results of this study demonstrated that participation in the course, subsequent group discussion sessions, and take-away PowerPoint sessions significantly improved the participant’s understanding of the importance of communication skills and understanding of socioeconomic, environmental, and cultural disparities that can affect a patient’s health outcome.
According to results from the course session implemented in-person from 2017 to 2019, the role-playing exercise significantly improved participants understanding of important components that can be used to improve health outcomes that may be affected due to health disparities. Students were strongly able to identify the importance of communication in patient encounters, to understand strategies such as communication and compassionate care in patient encounters, identify the importance of building a patient-physician relationship with patients, and were able to recognize their own cultural biases. Similarly, in 2020, even with a change in course modality to on-line learning due to COVID-19, students were able to understand the same key take-aways from the course session as demonstrated by reflections using the discussion board regarding the need for a holistic approach to care, importance of the patient clinician relationship, and importance of taking a patient history. Despite promising implications of both iterations of the session, students completing the session online did not find the same success in “understanding my own bias/and or cultural awareness when working with patients.” This decrease may be attributed to change in course modality and the strengths of the role-play enactment of the patient encounter. It is important to recognize that additional learning components, including video recordings of the role-play enactment, may be necessary if the discussion board is used as the primary learning method in the future.
In contrast to previous studies that attempted to determine the effectiveness of cultural competence training methods, this session had many unique characteristics. The simulated role-playing exercise enabled student participants to see first-hand an interactive patient scenario that could be used as an example for when students begin working with patients or communicating with patients who are culturally diverse. Additionally, the nature of the cases created for the course session which were divided into a part A in which the patient physician was more straightforward when diagnosing and treating the patient and a part B with a more comprehensive and nurturing approach to care, allowed the students to compare the scenarios and make their own assumptions and comments on the effectiveness of each portion of the case. Another strength of this training, was the faculty with cultural competence training were uniquely involved in case creation and facilitation of the course session. According to previous studies with similar aims, it was noted that direct observation and feedback from a faculty member who had cultural competence training and direct contact with patients can provide students with a more memorable and useful experience when educating students [ 12 ]. The facilitators of this session were able to emphasize from their own personal experiences how to work with culturally diverse populations.
An important aspect of the 2020 iteration of the course session in which a discussion board format was used, was that it allowed students who may feel uncomfortable with sharing their thoughts on a case and their own biases, the opportunity to share in a space that may feel safer than in person [ 4 ]. Previous studies have mentioned challenges with online discussion boards [ 4 ] but here we had robust participation, albeit required. Students often contributed more than the required number of comments and they were often lengthy and engaging when responding to peers. Finally, in contrast to previous studies, this course session took place in a pre-professional master’s program, the M.S. in Oral Health Sciences Program at Boston University Chobanian & Avedisian School of Medicine. This program, in which students are given the opportunity to enhance their credentials for professional school, provided students with early exposure to cultural competence training. Students that completed this session in their early pre-professional curriculum should be better prepared than peers who did not receive any cultural competence training until they entered their designated professional school. This session is part of an Evidence Based Dentistry course, which incorporates a larger component of personal reflection that serves to engage students in critical thinking as they begin to develop the skills to be future clinicians. Students that understand different cultures, society and themselves through self-assessments will grow and be best suited in time to treat future patients [ 4 , 16 , 17 ].
One limitation of the present study was the number of survey participants that competed the post-session surveys, as survey completion was not required. Thus, the number of student participants declined over the years, reaching its lowest number of participants in 2020 when the discussion board course session was implemented, and students may have been over surveyed due to the pandemic. Another limitation to this study, was the lack of both a pre and post survey that could be used to determine how student’s understanding of cultural competence had evolved from their entry into the course to the conclusion of the course as well as individual bias and self-reporting measures.
In the future, the course should implement both a role-playing format and subsequent discussion board reflections within the same course session. Studies have shown that alternatives ways of drawing students to reflect whether role play, personal narratives, etc. can be extremely advantageous in developing personal reflection and awareness building competency [ 4 , 16 , 17 , 18 ]. It is noted that role-playing exercises that allow students to provide feedback with student colleagues can provide students with more insight into their own behaviors. It has also been shown in previous studies that student writing and reflection activities can also facilitate student’s reflections on their own beliefs and biases [ 4 , 11 ]. Reflective writing skills are an important and effective means for students to continue to gauge their cultural competence throughout the remainder of their academic training and as future clinicians [ 4 , 17 , 19 ]. Further, students may experience emotional responses through the process of reflective writing as they recognize personal bias or stereotypes, creating a profound and impactful response resulting in enhanced understanding of cultural differences and beliefs [ 4 ]. By combining both learning techniques, students would be able to understand their own bias and their classmates and create a dialogue that could be more beneficial than just one learning method alone. Furthermore, by implementing the discussion board into the role-playing session, as stated previously, students that are more cautious about sharing their point of view or about their own implicit bias in a traditional classroom setting would be able to express their opinions and facilitate a more comprehensive discussion more thoroughly.
Here we show an effective means to utilize role-play of a multi-scenario case-based patient encounter to teach pre-professional healthcare student’s components of cultural competence, emphasizing the importance of provider-patient interactions, holistic patient care, and patient history and socioeconomic factors in provider care. This study contributes to the larger body of work that seeks to address this important aspect of education as it relates to enhancing patient health care outcomes.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Albino JEN, Inglehart MR, Tedesco LA. Dental education and changing oral health care needs: disparities and demands. J Dent Educ. 2012;76(1):75–88.
Article Google Scholar
Constantinou CS, Papageorgiou A, Samoutis G, McCrorie P. Acquire, apply, and activate knowledge: a pyramid model for teaching and integrating cultural competence in medical curricula. Patient Educ Couns. 2018;101(6):1147–51.
DallaPiazza M, Padilla-Register M, Dwarakanath M, Obamedo E, Hill J, Soto-Greene ML. Exploring racism and health: an intensive interactive session for medical students. MedEdPORTAL. 2018;14:10783.
Forsyth CJ, Irving MJ, Tennant M, Short SD, Gilroy JA. Teaching Cultural competence in Dental Education: a systematic review and exploration of implications for indigenous populations in Australia. J Dent Educ. 2017;81(8):956–68.
Betancourt JR. Cultural competence and medical education: many names, many perspectives, one goal. Acad Med. 2006;81(6):499–501.
Jernigan VBB, Hearod JB, Tran K, Norris KC, Buchwald D. An examination of cultural competence training in US medical education guided by the tool for assessing cultural competence training. J Health Disparities Res Pract. 2016;9(3):150–67.
Google Scholar
Behar-Horenstein LS, Warren RC, Dodd VJ, Catalanotto FA. Addressing oral Health disparities Via Educational Foci on Cultural competence. Am J Public Health. 2017;107(S1):S18–23.
Lie D, Boker J, Cleveland E. Using the tool for assessing cultural competence training (TACCT) to measure faculty and medical student perceptions of cultural competence instruction in the first three years of the curriculum. Acad Med. 2006;81(6):557–64.
Holyfield LJ, Miller BH. A tool for assessing cultural competence training in dental education. J Dent Educ. 2013;77(8):990–7.
Vasquez Guzman CE, Sussman AL, Kano M, Getrich CM, Williams RL. A comparative case study analysis of cultural competence training at 15 U.S. medical schools. Acad Med. 2021;96(6):894–9.
Jernigan VB, Hearod JB, Tran K, Norris KC, Buchwald D. An examination of cultural competence training in US medical education guided by the tool for assessing cultural competence training. J Health Dispar Res Pract. 2016;9(3):150–67.
Kripalani S, Bussey-Jones J, Katz MG, Genao I. A prescription for cultural competence in medical education. J Gen Intern Med. 2006;21(10):1116–20.
Mariño R, Satur J, Tuncer E, Tran M, Milford E, Tran VMTH, Tran PQ, Tsai RP. Cultural competence of Australian dental students. BMC Med Educ. 2021;21(1):155.
Beagan BL. Teaching social and cultural awareness to medical students: it’s all very nice to talk about it in theory, but ultimately it makes no difference. Acad Med. 2003;78(6):605–14.
Ferrebee S, Boston University School of Medicine Master’s Thesis. (2021). Effectively Teaching Cultural Competence in Healthcare Education. Available at Boston University Libraries: Open BU: https://open.bu.edu/handle/2144/43838 .
Crosson JC, Deng W, Brazeau C, Boyd L, Soto-Greene M. Evaluating the effect of cultural competency training on medical student attitudes. Fam Med. 2004;36(3):199–203.
Cathryn F, Michelle I, Short S, Tennant M, Gilroy J. Strengthening indigenous cultural competence in dentistry and oral health education: academic perspectives. Eur J Dent Educ. 2019;23(1). https://doi.org/10.1111/eje.12398
DasGupta S, Meyer D, Calero-Breckheimer A, Costley AW, Guillen S. Teaching cultural competency through narrative medicine: intersections of classroom and community. Teach Learn Med. 2006;18(1):14–7.
Woldt JL, Nenad MW. Reflective writing in dental education to improve critical thinking and learning: A systematic review. J Dent Educ. 2021;85(6):778–785. https://doi.org/10.1002/jdd.12561 . Epub 2021 Feb 11. PMID: 33576055.
Download references
Acknowledgements
We would like to acknowledge Boston University’s Chobanian & Avedisian School of Medicine’s Graduate Medical Science students and study participants.
No funding was used for the completion of this study.
Author information
Authors and affiliations.
Graduate Medical Sciences, Boston University Chobanian & Avedisian School of Medicine, 72 East Concord Street, L317, R-1017, Boston, MA, 02118, USA
Karen R. Bottenfield, Andrew N. Best & Theresa A. Davies
Department of Medical Sciences & Education, Boston University Chobanian & Avedisian School of Medicine, 72 East Concord Street, Boston, MA, 02118, USA
Maura A. Kelley, David Flynn & Theresa A. Davies
University of Maryland School of Dentistry, 650 W Baltimore Street, Baltimore, MD, 21201, USA
Shelby Ferebee
You can also search for this author in PubMed Google Scholar
Contributions
TAD designed the original study concept, taught the classes (roleplay), conducted the surveys, and collected data; MAK designed the original case and PowerPoint, and performed roleplay; DBF and SF evaluated data and drafted original figures; ANB assisted in drafting the manuscript; KRB finalized figures and the manuscript.
Corresponding author
Correspondence to Theresa A. Davies .
Ethics declarations
Ethics approval and consent to participate.
This study was determined to be EXEMPT by the Institutional Review Board of Boston University Medical Campus, Protocol # H-37232.
Consent for publication
Not applicable.
Informed consent
Informed consent was received from all subjects.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bottenfield, K.R., Kelley, M.A., Ferebee, S. et al. Effectively teaching cultural competence in a pre-professional healthcare curriculum. BMC Med Educ 24 , 553 (2024). https://doi.org/10.1186/s12909-024-05507-x
Download citation
Received : 27 October 2023
Accepted : 02 May 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s12909-024-05507-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Communication
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Share full article
Advertisement
Supported by
She Just Earned Her Doctorate at 17. Now, She’ll Go to the Prom.
Dorothy Jean Tillman II of Chicago made history as the youngest person to earn a doctoral degree in integrated behavioral health at Arizona State University.

By Alexandra E. Petri
When Dorothy Jean Tillman II successfully defended her dissertation in November 2023 to earn her doctoral degree from Arizona State University, she couldn’t wait to share the news with her best friend.
“It was a surreal moment,” Dr. Tillman said, “because it was crazy I was doing it in the first place.”
Dr. Tillman, at only 17, became the youngest person to earn a doctoral degree in integrated behavioral health from Arizona State’s College of Health Solutions, all before she was eligible to vote. Earlier this month, Dr. Tillman, now 18, took part in Arizona State’s commencement ceremony and delivered remarks as the outstanding 2024 graduate at the College of Health Solution’s convocation.
Lesley Manson, program director for the doctorate of behavioral health at Arizona State and Dr. Tillman’s doctoral chair, said Dr. Tillman displayed extraordinary perseverance, hard work and dedication for her young age, tackling every challenge head-on.
“She can serve as a real role model,” Ms. Manson said.
Dr. Tillman, called D.J. by her family and friends, was an early bloomer. She grew up in Chicago and was home-schooled from a young age, first in a group setting through online classes, and then by her mother, Jimalita Tillman, a single parent with a background in community theater.
Dr. Tillman was part of a gifted program before transitioning to home-schooling. Jimalita Tillman continued her daughter on an accelerated track: By the time she was 8, she was taking high school classes. While most 9-year-olds were learning math and reading, Dr. Tillman was starting college online.
At the time, they lived with Jimalita Tillman’s mother, Dorothy Wright Tillman, a civil rights activist who worked alongside the Rev. Dr. Martin Luther King Jr. and was a Chicago alderman. Dr. Tillman is her grandmother’s namesake (hence the II at the end of Dr. Tillman’s name).
During her early college days, Dr. Tillman’s classroom was often a Starbucks in Chicago, and her days began as soon it opened, she said. Her go-to order was an iced peach green tea with lemonade.
“Around the time when kids went to lunch, we’d be closing the computer,” said Dr. Tillman, who said her discipline and focus come from her grandmother.
Because of her age, Dr. Tillman lived at home while pursuing her higher education, and most of her coursework was online — a challenge for a self-described social butterfly. “I do love meeting new people and talking to people and understanding them and how their brains work,” she said. She found other ways to stay connected with friends through after-school activities.
At 10, she earned her associate degree in psychology at the College of Lake County in Illinois. At 12, she received her Bachelor of Science in humanities at Excelsior College in New York, and at 14, she earned a Master of Science from Unity College in Maine. She chose those fields because they can help scientists “understand why people treat the environment the way they do,” she told Time for Kids in a July 2020 interview.
Ellen Winner, a professor of psychology at Boston College and the author of “Gifted Children: Myths and Realities,” said that children like Dr. Tillman have a motivational intensity she calls a “rage to master.”
“One of the reasons they push themselves is they have a high, innate ability of some kind, and so learning, in whatever they are gifted in, comes easily to them and it’s very pleasurable,” she said. Schools are often not equipped for such gifted children, she added, which may lead parents to home-school their children. The trade-off, she and some experts say, is missing out on socialization and learning with children their age.
“There’s no perfect solution to kids like this,” Ms. Winner said.
Jimalita Tillman said she was sure her daughter was finished with higher education after earning her master’s degree. Dr. Tillman had just launched an organization to support Black youth in Chicago interested in STEM and the arts called the Dorothy Jeanius STEAM Leadership Institute. It was 2020, just after the beginning of the pandemic.
She was surprised when her daughter said she wanted to pursue her doctorate, and even tried to dissuade Dr. Tillman. But Dr. Tillman wanted to help young people with their mental health. She told her mother to trust her.
“I had to follow her lead,” Jimalita Tillman, 42, said.
Dr. Tillman was accepted into the management concentration at Arizona State’s College of Health Solutions, an online doctorate program. Her thesis on developing programs to reduce the stigma for college students seeking mental health services was based on a study she conducted for an in-person internship at the Illinois Institute of Technology in Chicago. Dr. Tillman hopes her story resonates with girls who are talkative, outgoing “out-there kind of girls who are trying to figure themselves out but are very smart.”
“I want them to see someone who has taken that energy, sparkle and excitement and packaged it in a way that is classy and beautiful,” she said.
Dr. Tillman may now have her doctorate, but she’s also excited about teenage things — like attending a prom. On Saturday, she going as her best friend’s date to his senior dance. They’re taking an Escalade outfitted with stars on the ceiling, she said, a feature she requested and that her mother made happen.
Dr. Tillman has been focused on school and her professional pursuits, and she plans to host her institute’s summer camp again. Then, she said, she plans to take a beat and have a “fun teenage summer,” doing things she loves, discovering new hobbies and figuring herself out in the process.
“I want to focus on who I am,” she said.
CVS Seeks Private Equity Funding for Oak Street Health, Bloomberg News Reports

FILE PHOTO: A general view shows the CVS Health Finance Center at CVS headquarters of CVS Health Corp in Woonsocket, Rhode Island, U.S. October 30, 2023. REUTERS/Faith Ninivaggi/File Photo
(Reuters) -CVS Health Corp has been seeking a private equity partner to fund growth at Oak Street Health, a primary care provider it bought a year ago, Bloomberg News reported on Thursday.
The company has been working with financial advisers to help find capital to back new clinics that will be opened by Oak Street, the report said, citing people familiar with the matter.
The deliberations are in a preliminary stage and the structure could change, while there is no guarantee a deal will be reached, according to the report.
CVS declined a request for comment from Reuters.
A potential CVS-private equity partnership would help lessen the capital investment burden associated with the build out of the Oak Street Health clinic base, Leerink Partners analyst Michael Cherny said in a note.
"Overall, we see this move as prudent on the surface, but need more details on the potential joint venture," he added.
The U.S. healthcare conglomerate bought Oak Street Health for about $9.5 billion in February last year.
CVS had said in February it planned to nearly double the business to 300 clinics by 2026 and aimed to grow the number of Oak Street patients over time.
(Reporting by Sneha S K in Bengaluru; Editing by Shailesh Kuber)
Copyright 2024 Thomson Reuters .
Tags: funds , United States
The Best Financial Tools for You
Credit Cards

Personal Loans

Comparative assessments and other editorial opinions are those of U.S. News and have not been previously reviewed, approved or endorsed by any other entities, such as banks, credit card issuers or travel companies. The content on this page is accurate as of the posting date; however, some of our partner offers may have expired.

Subscribe to our daily newsletter to get investing advice, rankings and stock market news.
See a newsletter example .
You May Also Like
7 best long-term stocks to buy.
Glenn Fydenkevez May 24, 2024

What Is Par Value for Stocks and Bonds?
Coryanne Hicks May 24, 2024

11 Top Sector ETFs to Buy
Jeff Reeves May 24, 2024

Stock Market Holidays in 2024
Daniel J. Lee May 24, 2024

George Soros' 6 Top Stock Picks
Brian O'Connell May 23, 2024

5 Best Undervalued Blue-Chip Stocks
Glenn Fydenkevez May 23, 2024

15 Best Dividend Stocks to Buy for 2024
Ian Bezek May 23, 2024

7 Best Semiconductor ETFs to Buy in 2024
Tony Dong May 23, 2024
Best Investments for 2024
Kate Stalter May 23, 2024

7 Best Cryptocurrency Exchanges
Jeff Reeves May 22, 2024

6 Best Biotech Stocks to Buy for 2024
Wayne Duggan May 22, 2024

Bill Gates Portfolio: 7 Best Stocks
Brian O'Connell May 22, 2024

Top Fidelity Funds for Retirement
Tony Dong May 22, 2024

7 Stocks That Outperform in a Recession

8 Best High-Yield REITs to Buy
Tony Dong May 21, 2024

Elon Musk's Record of Overpromising
Wayne Duggan May 21, 2024

What Are Magnificent 7 Stocks?

9 Biggest Financial Fraud Cases
Brian O'Connell May 21, 2024

6 Best Vanguard Funds for Retirement
Coryanne Hicks May 21, 2024

Sell in May and Go Away in 2024?
Dmytro Spilka May 20, 2024

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- FASEB Bioadv
- v.2(12); 2020 Dec

The future of health professions education: Emerging trends in the United States
George e. thibault.
1 Daniel D. Federman Professor of Medicine and Medical Education, Emeritus, Harvard Medical School, Boston Massachusetts, USA
1. INTRODUCTION
In February 2020 when I was asked to submit some thoughts on trends in the future of health professions education, I had no idea that we were about to experience a once in a century pandemic that would profoundly change health care and the lives and education of health professionals in this country. As I write these personal reflections, we are still in the midst of the COVID‐19 pandemic and cannot yet define what the “new normal” will be for health care, health professional education or society as a whole on the other side of the pandemic. Acknowledging this uncertainty, I believe that the trends I have identified will be more relevant than ever in the post‐COVID world with some specific caveats.
The six trends that I have identified for the future of health professions education are:
- Interprofessional education in order to better prepare health professionals for future collaborative practice.
- Longitudinal integrated clinical education that is more patient, community, and chronic disease oriented.
- Education in the social determinants of health and the social and humanistic missions of the health professions.
- More emphasis on the continuum of health professions education for the life‐long learning and long‐term well‐being of health professionals.
- A shift to competency‐based, time variable health professions education to better fulfill our social contract and to produce the most competent practitioners most efficiently.
- The integration of artificial intelligence and new educational and information technologies into the continuum of health professions education and practice.
It is impossible, of course, to touch on all of the educational issues relevant to every health profession, but I believe I have identified high level trends that will impact all health professions education.
The observations that follow are based on my personal experiences of four decades as a faculty member at Harvard Medical School and several of its affiliated hospitals (Massachusetts General, Brigham and Women's, and West Roxbury Veterans Administration), two decades as a board member and chair of a graduate school of health professions education (the MGH Institute of Health Professions) and a decade leading the only national foundation devoted to improving the nation's health through innovations in health professions education (the Josiah Macy Jr. Foundation).
As I reflect on my five decades in health professions education my observation is that for the first four decades the pace of health‐care delivery reform far exceeded the pace of health professions education reform. The passage of Medicare and Medicaid in the 1960s, advances in science and technology to improve both diagnosis and treatment stimulated by rising NIH budgets in the 1960s and 1970s, increases in the costs of care leading to managed care and mergers and acquisitions in the 1980s and 1990s, the quality improvement and patient safety movements of the 1990s and beyond, and the rise in consumerism with more open access to medical information have all contributed to dramatic changes in the organization and delivery of health care in this country without a parallel transformation in the education of health professionals. Happily, I have witnessed in the past decade a significant openness and willingness to change in health professions education with notable experimentation in both prelicensure (undergraduate) and postlicensure (graduate) education. These changes are heartening, but much more needs to be done to keep pace with this rapidly changing health‐care world and changing societal demographics and expectations.
When I assumed the Presidency of the Macy Foundation in January 2008, I outlined a vision for educational reform that would better align health professional education with societal needs and with an evolving health‐care delivery system. I felt that the health professions education enterprise must not view itself as a closed system in the ivory tower, but as one closely interconnected with the delivery system in which its graduates would work and with the society that they would serve. Health professions education needed to derive its curricular goals from outside rather than inside, and it in turn must be accountable to society in measuring and fulfilling those goals. This framework was very similar to that developed by the Lancet Commission 1 2 years later in their work assessing health professions education worldwide. It is a framework that has been adopted by Canada and some western European countries.
The themes to create this alignment became the funding priorities for the Foundation for a decade. The trends that I have identified grew out of this work to align health professions education with societal needs. The trends have been refined and modified based on experience and continuous monitoring of the external environment. In elucidating these trends, I am drawing on very personal experiences as a medical educator and Foundation President.
For each of these six trends I will explain why it is important, provide some examples (drawn heavily from my Macy Foundation experience), identify some challenges, and speculate about the future. I will then conclude with some additional comments about the potential lasting impact of COVID‐19 on health professions education and how the lessons derived from COVID‐19 relate to these trends.
1.1. Trend number one: Interprofessional education in order to better prepare health professions for true collaborative practice
The practice of medicine is more and more dependent on teams of professionals caring for complex patients and patients with multiple chronic conditions. Access to reliable, high‐quality primary care is also enhanced by a team approach. 2 , 3 There is an increasing body of evidence that care delivered by highly functioning, collaborative teams leads to better patient outcomes. Yet, until recently, health professional education has been designed to keep the professions apart until the completion of the training process. This is in spite of the fact that interprofessional education (IPE) has been written about in the United States since the 1960s, and a 1972 Institute of Medicine Report (“Education for the Health Team”) 4 strongly recommended IPE.
There are many reasons why IPE did not gain traction in the United States; among these are the logistical obstacles, the strong cultures of each of the professions, the political dominance of physicians who as a group did not embrace IPE, and the lack of a sense of urgency about changing the design of the health‐care delivery system. The tide began to turn in the last decade as several institutions demonstrated that logistical barriers could be overcome, educational leaders in many professions (including MDs) saw the advantages of IPE, and there developed greater urgency about the need for health‐care reform that met the “triple aim” of better health outcomes, better patient experiences, and lower costs. The time was right to assert that the ability to work in a team is a core competency that should be possessed by all health professionals. 5
I am proud that the Macy Foundation was a leader in this change. In the decade 2008 to 2018 the Macy Foundation supported 44 large grants and 41 small grants with IPE as the primary or secondary theme. In addition, 24 educational innovation projects of Macy Faculty Scholars were interprofessional. IPE was the largest investment that the Macy Foundation made in any of its priority areas. The reasons for the decision to make the investment were that this seemed to be a propitious time to take advantage of the alignment of forces favoring IPE, the belief that IPE could have a large positive impact on improving the health of the public, and the hope that by creating a critical mass of affirmative work we could make this the norm in health professions education. By design, all of the large IPE grants included medical schools and nursing schools. Many included other health professional schools, such as pharmacy, dentistry, public health, and social work. We reasoned that since nurses and doctors were the most numerous and visible of the health professionals caring for patients, changing the culture in those two professions would be models for others.
In reviewing this body of work, 6 we derived five important lessons that informed our subsequent grant giving. 1) Leadership from the top is essential. Deans, Provosts, Chancellors, and Presidents must embrace IPE and make it a high priority as expressed by budget and organizational structure (such as an office of IPE). Only in this way can the inevitable logistical and political barriers be overcome. 2) Intensive planning with clear educational goals and metrics must lay the groundwork for all IPE initiatives. IPE experiences must be as rigorous as all other parts of the formal curriculum. 3) Interprofessional learners must be engaged through real, meaningful work that advances patient care and their own professional development. These experiences must be reinforced in a developmentally appropriate way throughout the entire educational trajectory. 4) Innovative use of educational technology such as simulation and on‐line, asynchronous learning can help overcome logistical barriers and complement face to face encounters and real patient experiences. 5) Much attention must be paid to faculty development since most faculty have had little or no experience working with faculty or learners from other health professions.
One of the other lessons learned is that IPE is at its best when each profession has the strongest possible educational program—strong uni ‐professional education leads to strong inter ‐professional education. This is consistent with the experiences of those who have studied successful teams—it is the diversity of points of view and experiences that are brought to bear on the problem that leads to the most successful outcomes. Health science campuses or universities with multiple health science schools that have made IPE a high priority have found that it has helped bring about a cultural change towards greater openness and inclusion that has benefited all faculty and students.
The Health Professions Accreditation Collaborative, which started with Medicine, Nursing, and Pharmacy and now includes 25 entry level health professions education accrediting boards, reports that 22 of its 25 members have or are developing an IPE standard.
So now that IPE is being required by nearly all the health professional prelicensure accrediting bodies (who are also working on a common set of definitions of IPE), can we declare victory and move on? Hardly. There is still great unevenness in the quality, robustness, and penetrance of IPE across all our health professional schools nationally. Free‐standing health professional schools without nursing or medical partners are particularly challenged. We still have more to learn about which are the most meaningful IPE experiences and what are the ideal timing and duration. We also need to solve the challenge of incorporating more IPE in the core clinical experiences of both prelicensure and postlicensure of health professionals.
Almost all of the formal IPE programs to date involve prelicensure health professionals. Though there have been many logistical barriers to overcome to reach our current level of success in prelicensure education, the challenges are even greater in the heterogenous and complex postlicensure world where education takes place virtually entirely in the health‐care delivery system and not in health professional schools. But if IPE is to truly demonstrate a positive impact on the practice of health professionals and the health outcomes of patients, it must become more a part of these later stages of professional development (including what we have called “continuing medical education”). There are some encouraging movements in this direction including a VA primary care program that has medical residents and nurse practitioners sharing practices, a Macy funded pilot study of Ob/Gyn residents and midwifery students training together, and work by the Accreditation Council for Continuing Medical Education (ACCME) to jointly certify interprofessional continuing education programs in nursing, pharmacy and medicine. But much more needs to be done in this arena if our patients are to get the maximum benefit of IPE. This should be an important source of pilot projects and innovations in the future.
Finally, we need to consider the potential contributions of non‐health professionals in a broader definition of IPE. Biomedical Sciences, Engineering, Architecture, Law, Public Policy—to name just a few professions—have important intersections with health and health‐care delivery. There are only a handful of instances that I am aware of in which learners from these professions interact with learners from the health professions, and in each case, it has proven to be beneficial. One can imagine a future real or virtual university where such IPE experiences are more routine.
IPE is here to stay. I regard the last decade as proof of concept. Now that concept needs to be refined, broadened, and linked more closely to improved patient outcomes,
1.2. Trend number two: Longitudinal integrated clinical education that is more patient, community and chronic disease oriented.
Since the Flexner Report in 1910 medical school education in the United States has been predominately hospital based and scheduled as a series of rotations on hospital services. As formal graduate medical education (GME) programs for physicians evolved in the decades following the Flexner Report these followed the hospital‐based models. Subsequently, Medicare became the predominant funder of GME in the United States with the payment through the hospital, which reinforced the hospital‐based rotational model. To varying degrees, other health professions have followed this model of hospital‐based rotational clinical education and training.
There are many good reasons why the hospital became the principal site of education in the health professions. The hospital contains the highest concentration of sick patients and this afforded ready access to “teaching material.” It also brought together faculty and learners in one place for increased efficiency of combining teaching and care delivery. As technology and specialization increased, the hospital became even more important as the sole place to have access to all technologies and all specialties. While many of these positive attributes of hospitals continue today, it has been increasingly apparent over the last two decades that there are significant limitations of the hospital and the rotational system as the sole or even principal pedagogical site and method for clinical education in the health professions.
First, the patient population in the hospital of academic medical centers today is less and less representative of the patients that our graduates will care for. Because of both economic and technologic factors hospitals care for only the sickest and most complex patients and for a shorter and shorter period of time. Second, the intensity of care and changes in the schedules of both learners and staff have made it more difficult to accomplish optimal learning environments and achieve educational goals. Third, the rotational model of clinical education lessens the opportunity for learners to appreciate the full impact of illness on patients or to form meaningful relations with patients, faculty, and staff. This is particularly true as logistical and regulatory issues have led to shorter and shorter rotations with more frequent turnover of staff. There is less opportunity for meaningful supervision, assessment, and feedback.
For these reasons, a number of medical schools have piloted and then established a new model for clinical education based on the principles of continuity: continuity of care, continuity of curriculum, and continuity of supervision. 7
In the full expression of this model, the specialty‐specific rotational clerkships are entirely replaced by a year‐long longitudinal experience that integrates the specialties and emphasizes the care of patients over time with mentoring and supervision by a constant group of faculty. Many of these experiences employ small group problem‐based learning which has been more common in the preclinical than clinical curriculum. A high percentage of the teaching is in the ambulatory setting, but learners also spend time in the hospital when their patients are hospitalized and for certain planned specialty experiences. Some schools have developed hybrid models that retain the traditional specialty clerkships at least in part, and overlay more longitudinal ambulatory and didactic experiences to achieve some of the continuity goals.
The continuity principles are consistent with what we know about successful experiential learning. 8 The longitudinal integrated clerkship (LIC) permit both horizontal (across disciplines) and vertical (basic science to clinical science) integration and allow for a more planned developmentally appropriate curriculum. Studies comparing LIC students with traditional clerkship students show comparable knowledge and clinical skills in the two groups, but LIC students show greater satisfaction, higher confidence, and a strong sense of patient centeredness. 9 Perhaps because of markers of more successful professional development, they are more likely to retain the idealism expressed on entry to medical school, which many studies have shown to erode in the clerkship year.
This model has not been as fully tested for other health professions, but one can readily see applicability in other frontline clinical health professions such as nursing, pharmacy, or physician assistant.
In addition to the evidence of improved learner performance and attitudes, there are a number of other potential benefits to a more widespread adoption of this model for at least a portion of health professions clinical education. Many of these relate to the other educational trends discussed in this paper. First, this model creates opportunities for interprofessional learning and the development of team‐based skills, which are much harder to accomplish in short rotations in the intense hospital environment. Second, the appreciation of the impact of an illness on patients over time and the location of the education in ambulatory settings afford more opportunities to understand the social determinants of health and to develop true partnerships with patients and their families. Third, the continuity of the relationship between learner and faculty affords the opportunity to do much more meaningful assessment and give feedback more continuously in the developmental process. This is a prerequisite to achieving competency‐based education. Fourth, the evidence of higher learner satisfaction with the meaningful work they are able to engage in may be at least a partial antidote to the alarming rates of burnout reported among learners in the health professions. 10 It is also likely that these experiences better prepare them to be life‐long learners. Fifth, there is much concern about the added burden learners place on stressed health‐care delivery sites. Learners in longitudinal experiences can be much more successfully integrated into the workflow of care organizations. Trust can only be developed with time, and with trust comes greater opportunity to make meaningful contributions to the work of the organization in which the learner is embedded.
There are many obstacles to the widespread implementation of the longitudinal integrated clerkship and these include less infrastructure to support teaching in many ambulatory settings, economic pressures for productivity, departmentally based culture and deficiencies in faculty development and incentives for teaching. Pilot programs in a number of institutions have shown that these obstacles can be overcome on a site‐specific basis. In fact, when successful, the LIC model is more popular with both faculty and the host sites. Several new medical schools have been able to institute the LIC model for the entire class, as they have had the advantage of small class size and no prior history of traditional clerkships.
The principles of continuity also should be applied to graduate education, but they will look different than the LIC on the undergraduate or prelicensure level. They may take the form of differentiation into tracks that are tailored to the career goals of the graduate learner. The graduate learner would spend larger blocks of time in specific settings (hospital or ambulatory) that are designed to prepare her for independent practice. This means she would spend less time repeating rotations for which she has already demonstrated competence. In this model the final stages of training look more and more like the beginning of practice, emphasizing the concept of the continuum. The well‐established primary care tracks in many US Internal Medicine programs are an example of this model, but I believe these can be made even more robust and differentiated. In these longer experiences the trainee (about to become practitioner) has the advantage of continuity with patients, site, staff, and mentors.
There will always be a role for shorter, intensive experiences in the hospital or some other technology‐rich site for early learners, graduate learners, and life‐long learners. The ideal educational model will be a blend of experiences designed specifically for the needs of the learners in a developmentally appropriate way. I believe there is growing evidence that some part of the core clinical educational experiences of all prelicensure health professional students should be in a longitudinal experience that is based on the principles of educational continuity.
1.3. Trend number three: Education in the social determinants of health and the social and humanistic missions of the health professions
Much of health professions education appropriately focuses on understanding normal human anatomy and physiology, the pathogenesis of disease, diagnostic and therapeutic decision making, and communication skills. It is absolutely essential that every health professional has a keen understanding of the basic and clinical sciences as they pertain to their practice and keep current in them. All of these together contribute to what we call health care. But we realize that health is more than health care. In fact, it has been estimated that all we do in health care contributes about 20% to the health of the public. Larger contributions to health are what have been called the “social determinants of health.” The WHO defines social determinants of health as “the conditions in which people are born, grow, work, live and age, including the health system. These circumstances are shaped by the distribution of money, power and resources….” 11 Social determinants of health are important not only because they are major contributors to health, but because they also are the principle cause of health disparities (or inequities) that we find in our society. WHO defines health inequities as “the unfair and avoidable differences in health status.” These health inequities have been documented to be prevalent in the US health‐care system.
If the ultimate goal of health professions education is to improve the health of the public (which I believe it is), then one would be incomplete as a health professional without an understanding of the social determinants of health. Therefore, teaching about the social determinants of health should be a part of the education of all health professions.
A recent consensus study of the National Academy of Medicine has provided “A Framework for Education Health Professionals to Address the Social Determinants of Health.” 12 There are several aspects of this framework which are synchronous with the trends we are discussing in this paper. First, this requires an interprofessional approach to education in order to gain insights from both the direct care health professions (nursing, social work, medicine, etc.) as well as public health and many other professions whose work affects health (architecture, urban planning, law, public policy, clergy to name but a few). Understanding and influencing the social determinants of health requires a collaborative approach. Second, a true understanding of the social determinants of health requires longitudinal and community‐based educational experiences. This reinforces the need for the kind of experiential learning exemplified by the longitudinal integrated clerkships. Third, addressing the social determinants of health requires a commitment to life‐long learning across the whole continuum of the career from the prelicensure learner to fully independent practice.
There are several consequences that will follow from making this commitment to teaching and addressing the social determinants of health. It reminds us that the health professions are at their core humanistic professions, which mean that they place human interests, values, and dignity at the center of their focus. 13 The health professions are unique among the professions in combining a humanistic heritage and a scientific heritage. In recent decades the scientific heritage has received much more attention, and the challenges of today call for a restoration of the balance. Humanism is elevated not at the expense of science, but to be allied with science so that they together can improve the health of the public.
Addressing the social determinants of health also forces us to confront the issue of diversity and inclusion within our professions and institutions. We cannot dismantle racism, which is one of the most powerful social determinants of health in our society, if we do not exemplify inclusiveness and equity in our own work and organizations.
Addressing the social determinants of health also reminds us that as health professionals we have a social contract. Society has given us special privileges, and in return we are expected to put their interests above our own and use our special knowledge and standing to improve society. We, therefore, have a responsibility not only to understand the social determinants of health, but to help address health inequities. Sometimes we will do this working individually, sometimes through professional organizations, and sometimes through our institutional policies and practices. 14 Health professionals should learn to be advocates for constructive social change; it is part of our professional responsibility to fulfill our social contract. 15
Addressing the social determinants of health will better position us to truly partner with patients, families, and communities in linking better interprofessional education and collaborative practice with better health for the public. We cannot achieve better health for the public without these partnerships. 16
Addressing these goals will not be easy and will require some fundamental changes in our educational processes and the cultures of our institutions. It will require breaking down the silos between the professions and breaking down the walls that have separated the professions from the public we serve. It also will mean introducing new content (social science, humanities, economics) across the continuum of health professions education, and it will require new models for clinical education and community engagement. There have been encouraging movements in these directions in the changes of the last decade. But the pace must accelerate if we are to prepare health professionals who can understand and address the social determinants of health in order to lessen the widening health disparities and improve health for all.
1.4. Trend number four: More emphasis on the continuum of health professions education for the life‐long learning and long‐term well‐being of health professionals
Historically each phase of health professional education has been treated separately with different administrative structures, different regulatory structures, and even sometimes different nomenclature. There has been a sense that each phase has the equivalent of a “final exam” and produces a “finished product.” The education of physicians in the United States is an example. There is a clear separation between medical school (undergraduate education) and residency and fellowship (graduate medical education). Undergraduate education occurs within one of 150+ (the number is growing) medical schools in the United States, each with its own administrative structure for education, and nationally it is regulated by the Liaison Committee on Medical Education (LCME) a partnership of the American Medical Association and the Association of American Medical Colleges. The medical school graduate (the “finished product”) then enters into the world of graduate medical education, overseen by over 1,500 hospitals and academic systems as program sponsors, each with their own unique educational administrative structures. Regulation is by the independent Accreditation Council of Graduate Medical Education (ACGME). The “finished products” of this GME system enter practice where they must comply with state licensure laws and hospital/health systems standards. All are required to have some degree of continuing medical education which is administered by a large array of academic institutions, professional associations, delivery systems, and private entities. This enterprise is regulated by the Accreditation Council of Continuing Education (ACCME). Other health professions have similar, if not as complicated, fragmentation of the educational continuum.
The reality is that there is no “final exam,” and there are no “finished” products. Ideally, the health professional is always learning, always in the state of becoming (perhaps that is why we call it “practice”). It is necessary and appropriate that there be milestones and checkpoints along the way to assure the progress of the learner/practitioner and to fulfill our social contract to assure competency. External regulations notwithstanding, it is essential that the attitudes and skills required for life‐long, self‐motivated learning be instilled in all of our learners from the beginning of the educational trajectory. That is what will ultimately assure competency across the continuum.
An important aspect of this is a much greater attention to the quality of the learning environments in which learning and work take place across the life span of the health professional. 17 , 18 Without improved environments for learning (and working) other initiatives for educational enhancement and improvement will be for naught. There are many elements to these environments: the personal perspective of the learner, the community in which teaching and learning occur, the organizational culture and practices that surround that learning, and the physical and virtual spaces in which it occurs. 19 That environment is often shared by learners and practitioners across the whole spectrum of health professions education, which is why the continuum should be the conceptual model.
Another important aspect of the continuum conceptual model and the emphasis on life‐long learning is that it also facilitates the focus on learner and clinician well‐being. There has been an alarming rise in the reported rate of burnout among health professional learners and clinicians, and a recent report of the National Academy of Medicine (“Taking Actions Against Clinician Burnout”) (reference 10) made many concrete recommendations on how system changes can help lessen burnout and promote well‐being. Many of those recommendations deal directly with the learning and working environment. Suboptimal learning environments (across the continuum) contribute to burnout.
Another consequence of this renewed and enhanced emphasis on the continuum, life‐long learning and the learning environment is that this conceptual model is more likely to lead to empowered learners who feel they are doing meaningful work. 20 Understanding that the ultimate goal of all health professions education is improved health of the patient, the progressive increase in responsibility across the educational continuum enables learners to find purpose in their work and feel like they are making contributions. This is likely another antidote to burnout.
While there are some encouraging movements toward this conceptual model of the continuum of education, this will not be any easy change. Administrative and regulatory structures are well embedded in our system, and there is a lot of territoriality. Academic institutions and health‐care delivery systems need to work more closely together to improve both education and care across the continuum. 21 And regulatory bodies must work to eliminate the barriers to common language and standards for assessment across the continuum and facilitate smoother and more flexible transitions.
1.5. Trend number five: A shift to competency‐based time‐variable health professions education to better fulfill our social contract and produce the most competent practitioners most efficiently
Health professions education has the responsibility to society to produce practitioners who are competent across broad domains of knowledge, attitudes, and skills. Each profession is responsible for establishing its competencies and the educational program to achieve them. All agree that assessment of these competencies is critical in fulfilling our social contract, but historically that assessment has not been rigorous. “Time in place” has often been accepted as a proxy for competency assessment. The required number of months in a given site or discipline and the required number of years in a given program are taken as assurance of competency. This has led to a fragmented and rigid time‐based system of education that does not meet the needs of learners or of the public.
While elements of a competency‐based, time‐variable approach exist within our current educational system, few programs or institutions have fully embraced this model. Two major concepts drive this model: (1) There is a comprehensive curricular, instructional, and assessment strategy based on a framework of observable and assessable competencies derived from patient and societal needs (2) Time is used as an educational resource rather than a limitation or a rule with the consequence that learners and teachers will use time as necessary to achieve the desired competencies.
The connection between the competencies and the needs of society is absolutely central to the success of this model; “competency‐based education begins with an uncompromising focus on translating the needs of contemporary society for improved health care into competencies that must be mastered by health professionals across all disciplines.” 22 This is an ongoing process across the education/practice continuum and it must be accompanied by robust assessment.
The concept of time as a resource has a liberating effect on both learner and teacher. Learners are allowed adequate time to achieve educational goals but are not required to spend time that is not needed to achieve these goals. Teachers are afforded adequate time for observation, assessment, and coaching to feel comfortable with their judgments. This could result in some learners achieving competencies and moving on in the continuum in less time (and some may take more time). In many instances the total time may be the same, but how that time is used will be different from one learner to another. Thus, the instructional program becomes more individualized, even more so as the learner is farther along the educational trajectory.
This model creates an entirely different dynamic between learners and teachers, and the role of feedback is entirely different than in the traditional model. The learner becomes much more self‐motivated to achieve the competency in order to move to the next level and actively seeks feedback. The teacher becomes the helper and enabler.
There are many challenges in making this paradigm shift, and it will require changes across many domains. 23 Some of those changes are directly within the control of each educational enterprise, such as curriculum and faculty development reforms. Other changes will involve external bodies for regulatory changes to permit greater flexibility in accrediting programs and certifying individuals. There will need to be more research done to develop more rigorous assessment systems and to evaluate outcomes. Some of the other trends we are discussing in this paper should facilitate this transformation. This work must be interprofessional, emphasize continuity and the continuum of education, and will be facilitated by educational technologies.
Though these changes will be difficult, several programs have demonstrated their feasibility. (reference 23 ). The Education in Pediatrics Across the Continuum (EPAC) program has successfully integrated undergraduate and graduate medical education for pediatrics in a competency‐based, time‐variable fashion in a pilot program at four US institutions (University of California, San Francisco; University of Colorado; University of Minnesota; and University of Utah). Oregon Health and Science University School of Medicine has implemented a competency‐based, time‐variable curriculum for its entire medical school class. The University of Wisconsin, Milwaukee has a Flex‐Option Program for RN to BSN completion that is competency based and time variable. Queens University in Canada has instituted a competency‐based, time‐variable system for all of its graduate medical education programs. Canada has now made a commitment that all of the GME programs nationally will be competency based and time variable. There are many examples of such programs in Europe and many more pilots underway in the United States.
All of these examples represent “proof of concept” and gives encouragement that both the internal and external changes that are necessary are possible. As in other areas of innovation, the early adopters will pave the way for those that follow.
1.6. Trend number six: The integration of artificial intelligence and new educational and information technologies into the continuum of health professions education and practice
Technology is changing in every aspect of our lives, and the pace of that change is accelerating. Health professions education has been slow in adopting new technology, but that pace, too, has now accelerated. 24 There are now many technologies embedded in our educational system that have improved efficiency and pedagogy and have helped to accomplish other educational goals. Simulation has provided safe and controllable settings for skill development, learning clinical reasoning and developing communication and teamwork skills. It also has been a powerful tool for promoting interprofessional education. Online learning has provided efficient means for knowledge acquisition so that student/faculty time can be more productively spent in higher level functions of interpretation, reasoning, and team skills (the “flipped classroom”). Computerized models have largely replaced cadavers for learning anatomy, and computerized images have largely replaced microscopes in the classroom. Asynchronous, interactive learning has helped to resolve some of the logistic problems with IPE and with distributed models of education and training at multiple sites. Large databases (sometimes obtained from computerized medical records) are being successfully used to direct curricular content and to evaluate educational and clinical performance. All of these changes have helped to improve the education process and also to create closer links between education and our health‐care deliver system, but these changes are small compared with those that are likely to follow.
I will consider three separate aspects of this trend: (1) the increased use of technology as an alternative to traditional education, (2) increased education about technology and artificial intelligence to produce practitioners who are able to successfully use and integrate these tools, and (3) an increased focus on how to capture and utilize time freed by technology to devote to other important functions that cannot be accomplished by technology.
In the realm of technology as an alternate to traditional education, there are now a multitude of online degree and certificate programs in the health professions. This trend will only accelerate as pressures increase to produce more health professionals at a lower cost. There will be an ongoing challenge for quality control and a continued need for faculty development and technological support to adjust to this new educational model. For the clinical disciplines there will always be a need for some real, nonvirtual experiences. More research will be needed to understand the optimal dose and timing of face to face encounters in these “hybrid” models.
Much more time needs to be spent in the future educating and preparing health professionals for a career in which they will be constantly using information technologies and artificial intelligence. By artificial intelligence I mean all of the ways that machines use large data sets to replicate or approximate human cognition. This concept has been around since the 1950s, and for a long time the focus was on the projections that this would someday replace the doctor or other professionals. A more likely scenario is that successful clinicians will harness artificial intelligence to assist them in clinical practice—the two together will be better than either alone. To do that the health professional of tomorrow must have a better understanding of probabilities, confidence intervals, and the use and limitations of large data bases. There is much concern that the algorithms used in AI could actually exacerbate health disparities because of built‐in biases. The health professional of the future must understand the strengths and limitations of these algorithms.
The health professional of tomorrow also will need to be trained in the uses and limitations of telemedicine for both patient and student encounters. All health professional will need training in using the computerized medical record and other technological aids in ways that enhance the patient experience and the patient–clinician relationship rather than detract from them. Our current disappointing experiences with electronic medical records that were developed for business rather than clinical transactions should be a warning to us. Health professionals must be actively involved in developing the systems of the future.
And that brings us to the last aspect of this trend—educators, learners, and clinicians must work together to see that technology enables them at each step along the continuum to devote more time to the higher level functions of reasoning, communication, compassion, and empathy. It will be easy to continue to lament the intrusion of technology or to be nostalgic about the past, but it will take effort and creativity to seize this opportunity to actually elevate the status and role of health professions education and clinical practice. The greatest dividend of the technological revolution will come when all health professionals are freed up to truly “work up to license.” Machine learning can never provide the human touch that all patients want and need in a healing relationship with their clinicians. We must harness technology to enable us to make clinical practice more humanistic.
This sixth trend may in many ways be the most exciting, but it also can be the scariest and most threatening. That is why engagement with the issues should not be delayed, and these concepts must be built into the earliest phases of health professions education and reinforced across the continuum.
1.7. Significance of COVID‐19 on these trends
It is, of course, impossible to predict today the long‐term effects of the disruption we are now experiencing from the COVID‐19 pandemic. That disruption has profoundly affected the health of the public with corollary challenges to the health‐care delivery system and health professions education. Beyond that, the economic, social, and psychological effects on society are likely to be felt for years, if not decades. But with those caveats, I will posit that it is likely that the COVID‐19 experience will actually reinforce and accelerate these trends I have identified. I will also note some other issues it has raised about the preparation of health professionals for the future.
First, as to COVID‐19 and the trends. It is quite clear that the enormous stress placed on our health‐care delivery and public health systems could not have been dealt with without a collaborative and interprofessional approach. The daily heroic stories of frontline health workers have stressed the interdependence of the team. If we ever had any doubt that we are preparing health‐care workers of the future to work in teams, the COVID‐19 story has put that doubt to rest.
Regarding the second trend, the disruption in hospital‐based education during the pandemic has been profound. For all practical purposes clinical education in the hospital stopped. This was done to protect the learners and to conserve scarce personal protective equipment, but also because of the realization that the COVID‐19 hospital was not an environment conducive to education. On the other hand, ambulatory education did continue in many settings, and students who have acquired both the trust and skills that are part of a successful longitudinal integrated experience were actually able to be helpful to their patients and the care sites in these stressful times. I received a personal communication from one of the leaders of these experiences with the following observation. 25 “LICs are proving particularly resilient and beneficial in the time of Covid. Indeed, I keep learning of stories in the United States, and in other countries, of how LIC students are able to continue to benefit their patients, preceptors, offices/institutions, and communities precisely because of the model—with the LIC model, students are known and trusted and the students know their patients and clinical microsystem so well. All this is to say that on top of all the proven educational benefits over these many years, we now see that the power of time affords the trust, connectivity, systems training, patient–preceptor–system relationships need to address current COVID needs and the likely care delivery that is coming. LICs create time and relationships AND flexibility and these offer enormous benefits for education and service.”
The pandemic has also highlighted the importance of the social determinants of health because of the striking differences in outcome based on race, ethnicity, economic status, and zip code. The relationship between social factors (racism, housing, job, transportation, air quality, access to care) and health outcomes has never been clearer or starker. COVID‐19 has called for us to not only better understand these relationships but to do something about them. And health‐care professionals must be central to that discussion and action.
The importance of the environments in which we work and learn and the importance of focusing on the long‐term well‐being and resilience of our health professionals have also been drawn in sharp relief by the pandemic. The other side of the coin of the heroism of health‐care workers has been the effect of this continually stressful environment on increasing the likelihood of burnout, depression, and suicide. We will not know for some time the long‐term psychological and morale consequences of the pandemic on health‐care workers, but we will need to pay more even more attention to these environmental factors at each point in the education and clinical continuum going forward. The extraordinary humanism shown by our health professionals must be returned in kind by developing and maintaining humanistic systems of care and learning.
The stress on the whole health‐care system showed the importance of assuring competence at all levels of the health professions and also of assuring that we have enough health professionals with the right skills in the right places. That is, after all, our social contract.
Finally, the pandemic has shown very clearly the increasing role that technology will play in education and care. Most health professional schools went to entirely online learning, and that is likely to continue in some fashion into the next academic year. In the clinics, a high percentage of visits become telemedicine visits. This enforced rapid transition in both these domains is likely to lead to rapid improvement in and acceptance of these technologies, and I expect some of these changes will be permanent.
So, each of the trends has been reinforced and I suspect accelerated by the pandemic. As traumatic as has been this disruption, we may look back at it as an accelerant of change albeit at a very high price.
There are some other changes that also are likely to stay that were not part of the trends I have identified. There must be a greater emphasis going forward in health professional education on emergency preparedness, with the likelihood that other epidemics and pandemics will occur in the professional lives of all of our trainees. Also, the pandemic has reminded us of the enormous importance of public health and epidemiology in our health‐care system. This has profound implications at a policy level because we have so woefully underinvested in public health and public health planning. But it also has implications at the education and practice level in that we must much more actively integrate these disciplines with the other health professions—consistent with the interprofessional education trend.
2. CONCLUSION
This is an exciting time in health professions education. Building on a decade of innovations that provided proofs of concept and some guiding principles, we are poised for a decade of explosive innovation along the six trends outlined. It is good that we are ready for this, because the public we serve desperately needs these changes to enable it to achieve the health that is our goal.
It should also be apparent that these trends are not totally independent from one another; they are, indeed, interconnected. Interprofessional education helps to create the culture for addressing the social determinants of health and life‐long sustaining learning environments. Longitudinal integrated clinical experiences facilitate insights into the social determinants of health and create the continuity environment for competency‐based assessment and professional development. Educational technologies and big data, properly harnessed, can help promote all of these changes. These are but a few examples of the interconnectedness of the trends, and illustrate why these changes need to be done together.
All of these changes together will in fact be needed if we want to produce the health professionals we need for an optimal health‐care system and a healthy public. This will require leadership and culture change. We must break down the barriers that separate the professions and the barriers that separate education from health‐care delivery and that separate both from the patients, families, and communities we serve. We must remember that health professions education and health‐care delivery both have the same goal—the improved health of the public. That will only happen if we produce health‐care professionals who are truly collaborative, community oriented, cognizant of the social determinants of health, resilient, competent life‐long learners who are adept at harnessing technology to serve their patients, and who possess empathy and compassion. In other words, they model the ideal blend of humanism and science. It is a tall order, but we can do it.
Thibault GE. The future of health professions education: Emerging trends in the United States. . FASEB BioAdvances . 2020; 2 :685–694. 10.1096/fba.2020-00061 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
This article is part of the Biomedical Education Special Collection.
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
For the children of Gaza, war means no school — and no indication when formal learning might return
Since the war between Israel and Hamas erupted on October 7, all of Gaza’s schools have closed. That has left hundreds of thousands of students without formal schooling or safe places to spend their days. (AP video shot by Abdel Kareem Hana and Mahmoud Essa)
Children attend an activity at a makeshift class in Deir al Balah, on Sunday, April 21, 2024. Since the war erupted Oct 7, all schools in Gaza have closed, and nearly 90% of school buildings are damaged or destroyed, according to aid groups. (AP Photo/Abdel Kareen Hana)
- Copy Link copied
Manal Al Buhaisi works with children at a makeshift class in Deir al Balah, on Sunday, April 21, 2024. Since the war erupted Oct 7, all schools in Gaza have closed, and nearly 90% of school buildings are damaged or destroyed, according to aid groups. (AP Photo/Abdel Kareen Hana)
Children play near their family’s tent in Deir al Balah, on Saturday, April 20, 2024. Since the war erupted Oct 7, all of Gaza’s schools have closed, and aid groups are scrambling to keep children off the streets and their minds focused on something other than the war. (AP Photo/Abdel Kareen Hana)
DEIR AL-BALAH, Gaza (AP) — Atef Al-Buhaisi, 6, once dreamed of a career building houses. Now, all he craves is to return to school.
In Israel’s war with Hamas, Atef’s home has been bombed, his teacher killed and his school in Nuseirat turned into a refuge for displaced people. He lives in a cramped tent with his family in Deir al-Balah in central Gaza, where he sleeps clinging to his grandmother and fears walking alone even during the day.
Since the war erupted Oct. 7 , all of Gaza’s schools have closed — leaving hundreds of thousands of students like Atef without formal schooling or a safe place to spend their days. Aid groups are scrambling to keep children off the streets and their minds focused on something other than the war, as heavy fighting continues across the enclave and has expanded into the southern city of Rafah and intensified in the north.
“What we’ve lost most is the future of our children and their education,” said Irada Ismael, Atef’s grandmother. “Houses and walls are rebuilt, money can be earned again ... but how do I compensate for (his) education?”
Gaza faces a humanitarian crisis, with the head of the U.N.'s World Food Program determining a “full-blown famine” is already underway in the north. More than 35,000 Palestinians have been killed in the war, according to the Gaza Health Ministry, which does not distinguish between civilians and combatants in its figures. About 80% of Gaza’s population has been driven from homes. Much of Gaza is damaged or destroyed, including nearly 90% of school buildings, according to aid group estimates.
Children are among the most severely affected , with the U.N. estimating some 19,000 children have been orphaned and nearly a third under the age of 2 face acute malnutrition. In emergencies, education takes a back seat to safety, health and sanitation, say education experts, but the consequences are lasting.
“The immediate focus during conflict isn’t on education, but the disruption has an incredibly long-term effect,” said Sonia Ben Jaafar, of the Abdulla Al Ghurair Foundation, a philanthropic organization focused on education in the Arab world. “The cost at this point is immeasurable.”
Before the war, Gaza was home to more than 625,000 students and some 20,000 teachers in its highly literate population, according to the U.N. In other conflicts, aid groups can create safe spaces for children in neighboring countries — for example, Poland for shelter and schooling during the war in Ukraine.
That’s not possible in Gaza, a densely populated enclave locked between the sea, Israel and Egypt. Since Oct 7, Palestinians from Gaza haven’t been allowed to cross into Israel. Egypt has let a small number of Palestinians leave.
“They’re unable to flee, and they remain in an area that continues to be battered,” said Tess Ingram, of UNICEF. “It’s very hard to provide them with certain services, such as mental health and psychosocial support or consistent education and learning.”
Aid groups hope classes will resume by September. But even if a cease-fire is brokered, much of Gaza must be cleared of mines, and rebuilding schools could take years .
In the interim, aid groups are providing recreational activities — games, drawing, drama, art — not for a curriculum-based education but to keep children engaged and in a routine, in an effort for normalcy. Even then, advocates say, attention often turns to the war — Atef’s grandmother sees him draw pictures only of tents, planes and missiles.
Finding free space is among the biggest challenges . Some volunteers use the outdoors, make do inside tents where people live, or find a room in homes still standing.
It took volunteer teachers more than two months to clear one room in a school in Deir al-Balah to give ad hoc classes to children. Getting simple supplies such as soccer balls and stationery into Gaza can also take months, groups report.
“Having safe spaces for children to gather to play and learn is an important step,” Ingram said, but “ultimately the children of Gaza must be able to return to learning curriculum from teachers in classrooms, with education materials and all the other support schooling provides.”
This month, UNICEF had planned to erect at least 50 tents for some 6,000 children from preschool to grade 12 for play-based numbers and literacy learning in Rafah. But UNICEF says those plans could be disrupted by Israel’s operation there.
Lack of schooling can take a psychological toll — it disrupts daily life and, compounded with conflict, makes children more prone to anxiety and nervousness, said Jesus Miguel Perez Cazorla, a mental health expert with the International Committee of the Red Cross.
Children in conflicts are also at increased risk of forced labor, sexual violence, trafficking and recruitment by gangs and armed groups, experts warn.
“Not only are children vulnerable to recruitment by Hamas and other militant groups, but living amid ongoing violence and constantly losing family members makes children psychologically primed to want to take action against the groups they consider responsible,” said Samantha Nutt of War Child USA, which supports children and families in war zones.
Palestinians say they’ve seen more children take to Gaza’s streets since the war, trying to earn money for their families.
“The streets are full of children selling very simple things, such as chocolate, canned goods,” said Lama Nidal Alzaanin, 18, who was in her last year of high school and looking forward to university when the war broke out. “There is nothing for them to do.”
Some parents try to find small ways to teach their children, scrounging for notebooks and pens and insisting they learn something as small as a new word each day. But many find the kids are too distracted, with the world around them at war.
Sabreen al-Khatib, a mother whose family was displaced to Deir al-Balah from Gaza City, said it’s particularly hard for the many who’ve seen relatives die.
“When you speak in front of children,” al-Khatib said, “what do you think he is thinking? Will he think about education? Or about himself, how will he die?”
On Oct. 7, 14-year-old Layan Nidal Alzaanin — Lama’s younger sister — was on her way to her middle school in Beit Hanoun when missiles flew overhead, she said. She fled with her family to Rafah, where they lived crowded in a tent. Since Israel ordered evacuations there, she fled to Deir al-Balah.
“It is a disaster,” she said. “My dreams have been shattered. There is no future for me without school.”
Mednick reported from Tel Aviv, Israel.


COMMENTS
The education of health professionals substantially changed before, during, and after the COVID-19 pandemic. A 2010 Lancet Commission examined the 100-year history of health-professional education, beginning with the 1910 Flexner report. Since the publication of the Lancet Commission, several transformative developments have happened, including in competency-based education, interprofessional ...
Health Education Journal is a peer reviewed journal publishing high quality papers on health education as it relates to individuals, populations, groups and communities vulnerable to and/or at risk of health issues and problems. A strongly educational perspective is adopted with a focus on activities, interventions and programmes that work well in the contexts in which they are applied.
The third article, "Quality Assurance in Teaching K-12 Health Education: Paving a new Path Forward," outlines the current context of health education pedagogy in K-12 schools in which health education is often relegated to teachers who are not professionally prepared in the discipline (Birch et al., 2019). The authors present four ...
Health Education Research publishes original, peer-reviewed studies that deal with all the vital issues involved in health education and promotion worldwide—providing a valuable link between the health education research and practice communities. Explore the reasons why HER is the perfect home for your research.
Abstract. Health education is a crucial consideration in the healthcare system and has the potential to improve global health. Recently, researchers have expressed interest in streamlining health education, utilizing digital tools and flexible curriculums to make it more accessible, and expanding beyond disease and substance abuse prevention.
Introduction. This NAM Perspectives paper provides an overview of health education in schools and challenges encountered in enacting evidence-based health education; timely policy-related opportunities for strengthening school health education curricula, including incorporation of essential health literacy concepts and skills; and case studies ...
Health Education & Behavior (HEB) is a peer-reviewed bi-monthly journal that provides empirical research, case studies, program evaluations, literature reviews, and discussions of theories of health behavior and health status, as well as strategies to improve social and behavioral health.HEB also examines the processes of planning, implementing, managing, and assessing health education and ...
Health education is effective at addressing adolescent behaviors. Youth behaviors and experiences set the stage for adult health. 1-3 In particular, health behaviors and experiences related to early sexual initiation, violence, and substance use are consistently linked to poor grades and test scores and lower educational attainment. 4-7 In turn, providing health education as early as possible ...
The link between education to health and well-being is clear. Education develops the skills, values and attitudes that enable learners to lead healthy and fulfilled lives, make informed decisions, and engage in positive relationships with everyone around them. Poor health can have a detrimental effect on school attendance and academic performance.
A clear understanding of the macro-level contexts in which education impacts health is integral to improving national health administration and policy. In this research, we use a visual analytic approach to explore the association between education and health over a 20-year period for countries around the world. Using empirical data from the OECD and the World Bank for 26 OECD countries for ...
URGENT NEED FOR NEW DIRECTIONS IN EDUCATION-HEALTH RESEARCH. Americans have worse health than people in other high-income countries, and have been falling further behind in recent decades ().This is partially due to the large health inequalities and poor health of adults with low education ().Understanding the health benefits of education is thus integral to reducing health disparities and ...
reviews health education theories and definitions, identifies the components of evidence-based health education and outlines the abilities necessary to engage in effective practice. Much has been written over the years about the relationship and overlap between health education, health promotion and other concepts, such as health literacy.
Health education is defined as "any combination of learning experiences designed to facilitate voluntary actions conducive to health" ( Green and Kreuter 2005 ). Although the history of health education dates back to the 19th century, it was not until the 1940s that the field began evolving as a distinct discipline.
At UNESCO, inclusive and transformative education starts with healthy, happy and safe learners. Because children and young people who receive a good quality education are more likely to be healthy, and likewise those who are healthy are better able to learn and complete their education. Guided by the UNESCO Strategy on education for health and ...
Abstract. The aim of this study was to explore the school principal's role in promoting physical activity for inactive children in school settings. Exploratory qualitative interview study. The study was conducted in seven elementary schools ... Open AccessResearch articleFirst published March 14, 2024pp. 282-292.
Health Education. Health education is defined as a continuous, dynamic, complex and planned teaching-learning process throughout the lifespan and in different settings that is implemented through an equitable and negotiated client and health professional 'partnership' to facilitate and empower the person to promote/initiate lifestyle-related behavioural changes that promote positive health ...
We provide programs, resources and advocacy to support health and physical educators at every level, from preschool to university graduate programs. For more information, visit www.shapeamerica.org. Publication office: Taylor & Francis, Inc., 530 Walnut Street, Suite 850, Philadelphia, PA 19106. Authors can choose to publish gold open access in ...
Dental education and changing oral health care needs: disparities and demands. J Dent Educ. 2012;76(1):75-88. Article Google Scholar Constantinou CS, Papageorgiou A, Samoutis G, McCrorie P. Acquire, apply, and activate knowledge: a pyramid model for teaching and integrating cultural competence in medical curricula. Patient Educ Couns. 2018 ...
Equality in Education and Health Care. For Amy Li, a sophomore majoring in public health studies, her fascinations with equality and policy were apparent as soon as she arrived on campus in August 2022. She promptly became involved in student government, currently serving as secretary of the Student Government Association, and successfully ...
Education is a critical component of health and, we argue, education is a major, long-term, multifaceted cause of health. In particular, education is a powerful means of breaking the cycle of poverty (which greatly affects ethnic and racial minority populations) and promoting health equity.
Ms. Tillman earned her doctoral degree in integrated behavioral health from the school at age 17. Tillman Family, via Associated Press. When Dorothy Jean Tillman II successfully defended her ...
The Senate Committee on Health, Education, Labor and Pensions May 23 passed legislation that included proposals on mental health and emergency pediatric services during a markup session.The AHA submitted a statement for the hearing, expressing support for the passage of the Dr. Lorna Breen Health Care Provider Protection Reauthorization Act (S. 3679), which would reauthorize grants for health ...
Health Education Journal: Create email alert. Also from Sage. CQ Library Elevating debate opens in new tab; Sage Data Uncovering insight opens in new tab; Sage Business Cases Shaping futures opens in new tab; Sage Campus Unleashing potential opens in new tab; Sage Knowledge Multimedia learning resources opens in new tab;
State lawmakers have targeted restricting sex education since the Dobbs ruling, especially in states banning abortion. Link Copied! Less than halfway through the year, 2024 has already broken the ...
The U.S. healthcare conglomerate bought Oak Street Health for about $9.5 billion in February last year. CVS had said in February it planned to nearly double the business to 300 clinics by 2026 and ...
RCSI Medical University of Bahrain hosted a ceremony to celebrate the winners of the Health Awareness Art Competition 2023-2024, in the presence of His Excellency Dr Mohamed bin Mubarak Juma, Minister of Education Chairman of the Board of Trustees of the Higher Education Council, Professor Sameer Otoom, President of RCSI Medical University of Bahrain, and invitees from both institutions.
The six trends that I have identified for the future of health professions education are: Interprofessional education in order to better prepare health professionals for future collaborative practice. Longitudinal integrated clinical education that is more patient, community, and chronic disease oriented.
Nutbeam D (2000) Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International 15 (3): 259-267. Nutbeam D (2008a) The evolving concept of health literacy. Social Science & Medicine 67 (12): 2072-2078.
In emergencies, education takes a back seat to safety, health and sanitation, say education experts, but the consequences are lasting. "The immediate focus during conflict isn't on education, but the disruption has an incredibly long-term effect," said Sonia Ben Jaafar, of the Abdulla Al Ghurair Foundation, a philanthropic organization ...