- Signs of Addiction

Addiction Research
Discover the latest in addiction research, from the neuroscience of substance use disorders to evidence-based treatment practices. reports, updates, case studies and white papers are available to you at hazelden betty ford’s butler center for research..

Why do people become addicted to alcohol and other drugs? How effective is addiction treatment? What makes certain substances so addictive? The Butler Center for Research at the Hazelden Betty Ford Foundation investigates these and other questions and publishes its scientific findings in a variety of alcohol and drug addiction research papers and reports. Research topics include:
- Evidence-based treatment practices
- Addiction treatment outcomes
- Addiction, psychiatry and the brain
- Addictive substances such as prescription opioids and heroin
- Substance abuse in youth/teens, older adults and other demographic groups such as health care or legal professionals
These research queries and findings are presented in the form of updates, white papers and case studies. In addition, the Butler Center for Research collaborates with the Recovery Advocacy team to study special-focus addiction research topics, summarized in monthly Emerging Drug Trends reports. Altogether, these studies provide the latest in addiction research for anyone interested in learning more about the neuroscience of addiction and how addiction affects individuals, families and society in general. The research also helps clinicians and health care professionals further understand, diagnose and treat drug and alcohol addiction. Learn more about each of the Butler Center's addiction research studies below.
Research Updates
Written by Butler Center for Research staff, our one-page, topic-specific summaries discuss current research on topics of interest within the drug abuse and addiction treatment field.
View our most recent updates, or view the archive at the bottom of the page.
Patient Outcomes Study Results at Hazelden Betty Ford
Trends and Patterns in Cannabis Use across Different Age Groups
Alcohol and Tobacco Harm Reduction Interventions
Harm Reduction: History and Context
Racial and Ethnic Health Disparities and Addiction
Psychedelics as Therapeutic Treatment
Sexual and Gender Minority Youth and SUDs
Health Care Professionals and Mental Health
Grief and Addiction
Helping Families Cope with Addiction
Emerging Drug Trends Report and National Surveys
Shedding New Light on America’s No. 1 Health Problem
In collaboration with the University of Maryland School of Public Health and with support from the Butler Center for Research, the Recovery Advocacy team routinely issues research reports on emerging drug trends in America. Recovery Advocacy also commissions national surveys on attitudes, behaviors and perspectives related to substance use. From binge drinking and excessive alcohol use on college campuses, to marijuana potency concerns in an age of legalized marijuana, deeper analysis and understanding of emerging drug trends allows for greater opportunities to educate, inform and prevent misuse and deaths.
Each drug trends report explores the topic at hand, documenting the prevalence of the problem, relevant demographics, prevention and treatment options available, as well as providing insight and perspectives from thought leaders throughout the Hazelden Betty Ford Foundation.
View the latest Emerging Drug Trends Report:
Pediatricians First Responders for Preventing Substance Use
- Clearing Away the Confusion: Marijuana Is Not a Public Health Solution to the Opioid Crisis
- Does Socioeconomic Advantage Lessen the Risk of Adolescent Substance Use?
- The Collegiate Recovery Movement Is Gaining Strength
- Considerations for Policymakers Regarding Involuntary Commitment for Substance Use Disorders
- Widening the Lens on the Opioid Crisis
- Concerns Rising Over High-Potency Marijuana Use
- Beyond Binging: “High-Intensity Drinking”
View the latest National Surveys :
- College Administrators See Problems As More Students View Marijuana As Safe
College Parents See Serious Problems From Campus Alcohol Use
- Youth Opioid Study: Attitudes and Usage
About Recovery Advocacy
Our mission is to provide a trusted national voice on all issues related to addiction prevention, treatment and recovery, and to facilitate conversation among those in recovery, those still suffering and society at large. We are committed to smashing stigma, shaping public policy and educating people everywhere about the problems of addiction and the promise of recovery. Learn more about recovery advocacy and how you can make a difference.
Evidence-Based Treatment Series
To help get consumers and clinicians on the same page, the Butler Center for Research has created a series of informational summaries describing:
- Evidence-based addiction treatment modalities
- Distinctive levels of substance use disorder treatment
- Specialized drug and alcohol treatment programs
Each evidence-based treatment series summary includes:
- A definition of the therapeutic approach, level of care or specialized program
- A discussion of applicability, usage and practice
- A description of outcomes and efficacy
- Research citations and related resources for more information
View the latest in this series:
Motivational Interviewing
Cognitive Behavioral Therapy
Case Studies and White Papers
Written by Hazelden Betty Ford Foundation researchers and clinicians, case studies and white papers presented by the Butler Center for Research provide invaluable insight into clinical processes and complex issues related to addiction prevention, treatment and recovery. These in-depth reports examine and chronicle clinical activities, initiatives and developments as a means of informing practitioners and continually improving the quality and delivery of substance use disorder services and related resources and initiatives.
- What does it really mean to be providing medication-assisted treatment for opioid addiction?
Adolescent Motivational Interviewing
Peer Recovery Support: Walking the Path Together
Addiction and Violence During COVID-19
The Brain Disease Model of Addiction
Healthcare Professionals and Compassion Fatigue
Moving to Trauma-Responsive Care
Virtual Intensive Outpatient Outcomes: Preliminary Findings
Driving Under the Influence of Cannabis
Vaping and E-Cigarettes
Using Telehealth for Addiction Treatment
Grandparents Raising Grandchildren
Substance Use Disorders Among Military Populations
Co-Occurring Mental Health and Substance Use Disorders
Women and Alcohol
Prescription Rates of Opioid Analgesics in Medical Treatment Settings
Applications of Positive Psychology to Substance Use Disorder
Substance Use Disorders Among Legal Professionals
Factors Impacting Early Alcohol and Drug Use Among Youths
Animal-Assisted Therapy for Substance Use Disorders
Prevalence of Adolescent Substance Misuse
Problem Drinking Behaviors Among College Students
The Importance of Recovery Management
Substance Use Factors Among LGBTQ individuals
Prescription Opioids and Dependence
Alcohol Abuse Among Law Enforcement Officers
Helping Families Cope with Substance Dependence
The Social Norms Approach to Student Substance Abuse Prevention
Drug Abuse, Dopamine and the Brain's Reward System
Women and Substance Abuse
Substance Use in the Workplace
Health Care Professionals: Addiction and Treatment
Cognitive Improvement and Alcohol Recovery
Drug Use, Misuse and Dependence Among Older Adults
Emerging Drug Trends
Does Socioeconomic Advantage Lessen the Risk of Adolescent Substance Use
The Collegiate Recovery Movement is Gaining Strength
Involuntary Commitment for Substance Use Disorders
Widening the Lens of the Opioid Crisis
Beyond Binge Drinking: High Intensity Drinking
High Potency Marijuana
National Surveys
College Administrators See Problems as More Students View Marijuana as Safe
Risky Opioid Use Among College-Age Youth
Case Studies/ White Papers
What does it really mean to be providing medication-assisted treatment for opioid addiction
Are you or a loved one struggling with alcohol or other drugs? Call today to speak confidentially with a recovery expert. Most insurance accepted.
Harnessing science, love and the wisdom of lived experience, we are a force of healing and hope for individuals, families and communities affected by substance use and mental health conditions..
We use cookies to give you the best experience possible. By continuing we’ll assume you’re on board with our cookie policy

- A Research Guide
- Research Paper Topics
- 40 Drug Abuse & Addiction Research Paper Topics
40 Drug Abuse & Addiction Research Paper Topics
Drug Abuse and Sociology
Drug abuse and medicine, drug abuse and psychology.
- Drug abuse and the degradation of neuron cells
- The social aspects of the drug abuse. The most vulnerable categories of people
- Drugs and religion. Drug abuse as the part of the sacred rituals
- Chronic Lymphocytic Leukemia
- Drug abuse as the part of human trafficking and as psychological defence of victims
- Reversible and irreversible consequences of drug abuse
- Drug abuse and minors
- Ethnic and cultural traditions that may lead to drug abuse
- Medical marijuana. Can legalizing it lead to drug abuse?
- The ethical questions of abusing painkiller drugs or other drugs that ease the state of a person
- The “club culture”. May it enhance the danger of drug abuse?
- Preventing drug abuse. Mandatory examination or voluntary learning: what will help most?
- The abstinence after the drug abuse. Rehabilitation and resocialization of the victims of it
- The harm done by drug abuse to the family and social relations
- The types of drugs and the impact of their abuse to the human body
- The positive effects of drugs. May they be reached without drawbacks of drug abuse?
- Alcoholics Anonymous, similar organisations and their role in overcoming the dependency
- Is constant smoking a drug abuse? Quitting smoking: government and social decisions
- Exotic addictions: game addiction, porn addiction etc. Do they have the effects similar to drug abuse?
- Substance abuse during pregnancy and before conceiving. What additional harm it causes?
- The correlation between drugs and spreading of HIV/AIDS
- Drug abuse and crime rates
- History of drug abuse. Opium houses, heroin cough syrup and others
- Drunk driving and drunk violence. The indirect victims of alcohol abuse
- The social rejection of the former drug abusers and the way to overcome it
- The main causes of drug abuse in the different social groups
- Drug abuse and mental health
- LGBTQ+ and drug abuse
- The development of drug testing. The governmental implementation of it
- Geniuses and drug abuse. Did drugs really helped them to create their masterpieces?
- Shall the laws about drug abuse be changed?
- Health Care Information Technology
- Drug abuse and global health throughout the 20-21 centuries
- Personal freedom or the safety of society: can drugs be allowed for personal use?
- Legal drinking age in different countries and its connection to the cultural diversity
- The different attitude to drugs and drug abuse in the different countries. Why it differs so much?
- Teenage and college culture. Why substance abuse is considered to be cool?
- Drugs, rape and robbery. Drugging people intentionally as the way to prevent them defending themselves
- 12-Step Programs and their impact on healing the drug addiction
- Alcohol, tobacco and sleeping pills advertising. Can it lead to more drug abuse?
By clicking "Log In", you agree to our terms of service and privacy policy . We'll occasionally send you account related and promo emails.
Sign Up for your FREE account
Addiction Science

About Addiction Science
Many people don't understand why or how other people become addicted to drugs. They may mistakenly think that those who use drugs lack moral principles or willpower and that they could stop their drug use simply by choosing to. In reality, drug addiction is a complex disease, and quitting usually takes more than good intentions or a strong will. Drugs change the brain in ways that make quitting hard, even for those who want to. Fortunately, researchers have found treatments that can help people recover from drug addiction and lead productive lives. Read the DrugFacts
Looking for Treatment?
Use the SAMHSA Treatment Locator or call 1-800-662-HELP (4357) .
Drugs, Brains, and Behavior: The Science of Addiction
Provides scientific information about the disease of drug addiction, including the many harmful consequences of drug...
Can AI learn the language of addiction?
Dr. Curtis uses AI, social media, and smartphone sensors to gain a better understanding of substance use and misuse

Can science keep up with designer drugs?
What’s really in bath salts, N-bombs, and synthetic opioids? What are the health risks of taking these drugs?
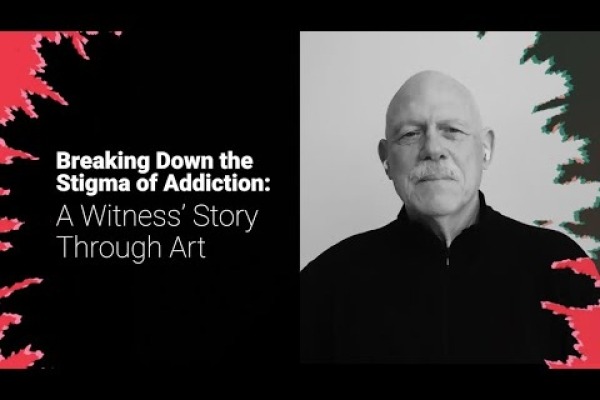
Breaking Down the Stigma of Addiction: A Witness’ Story Through Art
Watch artist and advocate William Stoehr’s intimate testimony, as he shares his story of loss to an opioid overdose and...

Investigating Drug Use: Brain Imaging
Thomas Ross, staff scientist in the Neuroimaging Research Branch at the NIDA, uses brain imaging techniques such as...
Teen Brain Development
NIDA explores in this video the intriguing similarities between the processes of brain development and computer...

Why are Drugs so Hard to Quit?
New NIDA animation tackles a common question and explains the science behind drug use and addiction to help light the...

Investigating Drug Use: Building Molecular Tools
The primary objective of the Optogenetics and Transgenic Technology Core at the NIDA IRP was to build molecular tools...
Innovative projects answer nida’s challenge to implement substance use prevention in primary care, is it too soon to start talking about a cure for addiction, five areas where “more research” isn’t needed to curb the overdose crisis, time to start talking about pre-addiction, related resources.
- NIH Director’s Blog on Addiction Science
- Words Matter: Preferred Language for Talking About Addiction

- MJC Library & Learning Center
- Research Guides
Drug Abuse, Addiction, Substance Use Disorder
- Research Drug Abuse
Start Learning About Your Topic
Create research questions to focus your topic, find books in the library catalog, find articles in library databases, find web resources, cite your sources, key search words.
Use the words below to search for useful information in books and articles .
- substance use disorder
- substance abuse
- drug addiction
- substance addiction
- chemical dependency
- war on drugs
- names of specific drugs such as methamphetamine, cocaine, heroin
- opioid crisis
Background Reading:
It's important to begin your research learning something about your subject; in fact, you won't be able to create a focused, manageable thesis unless you already know something about your topic.
This step is important so that you will:
- Begin building your core knowledge about your topic
- Be able to put your topic in context
- Create research questions that drive your search for information
- Create a list of search terms that will help you find relevant information
- Know if the information you’re finding is relevant and useful
If you're working from off campus , you'll be prompted to log in just like you do for your MJC email or Canvas courses.
All of these resources are free for MJC students, faculty, & staff.
- Gale eBooks This link opens in a new window Use this database for preliminary reading as you start your research. Try searching these terms: addiction, substance abuse
Other eBooks from the MJC Library collection:
Use some of the questions below to help you narrow this broad topic. See "substance abuse" in our Developing Research Questions guide for an example of research questions on a focused study of drug abuse.
- In what ways is drug abuse a serious problem?
- What drugs are abused?
- Who abuses drugs?
- What causes people to abuse drugs?
- How do drug abusers' actions affect themselves, their families, and their communities?
- What resources and treatment are available to drug abusers?
- What are the laws pertaining to drug use?
- What are the arguments for legalizing drugs?
- What are the arguments against legalizing drugs?
- Is drug abuse best handled on a personal, local, state or federal level?
- Based on what I have learned from my research what do I think about the issue of drug abuse?
Why Use Books:
Use books to read broad overviews and detailed discussions of your topic. You can also use books to find primary sources , which are often published together in collections.
Where Do I Find Books?
You'll use the library catalog to search for books, ebooks, articles, and more.
What if MJC Doesn't Have What I Need?
If you need materials (books, articles, recordings, videos, etc.) that you cannot find in the library catalog , use our interlibrary loan service .
All of these resources are free for MJC students, faculty, & staff.
- EBSCOhost Databases This link opens in a new window Search 22 databases simultaneously that cover almost any topic you need to research at MJC. EBSCO databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Gale Databases This link opens in a new window Search over 35 databases simultaneously that cover almost any topic you need to research at MJC. Gale databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Psychology and Behavioral Sciences Collection This link opens in a new window Contains articles from nearly 560 scholarly journals, some dating as far back as 1965
- Access World News This link opens in a new window Search the full-text of editions of record for local, regional, and national U.S. newspapers as well as full-text content of key international sources. This is your source for The Modesto Bee from January 1989 to the present. Also includes in-depth special reports and hot topics from around the country. To access The Modesto Bee , limit your search to that publication. more... less... Watch this short video to learn how to find The Modesto Bee .
Use Google Scholar to find scholarly literature on the Web:

Browse Featured Web Sites:
- National Institute on Drug Abuse NIDA's mission is to lead the nation in bringing the power of science to bear on drug abuse and addiction. This charge has two critical components. The first is the strategic support and conduct of research across a broad range of disciplines. The second is ensuring the rapid and effective dissemination and use of the results of that research to significantly improve prevention and treatment and to inform policy as it relates to drug abuse and addiction.
- Drug Free America Foundation Drug Free America Foundation, Inc. is a drug prevention and policy organization committed to developing, promoting and sustaining national and international policies and laws that will reduce illegal drug use and drug addiction.
- Office of National Drug Control Policy A component of the Executive Office of the President, ONDCP was created by the Anti-Drug Abuse Act of 1988. ONDCP advises the President on drug-control issues, coordinates drug-control activities and related funding across the Federal government, and produces the annual National Drug Control Strategy, which outlines Administration efforts to reduce illicit drug use, manufacturing and trafficking, drug-related crime and violence, and drug-related health consequences.
- Drug Policy Alliance The Drug Policy Alliance (DPA) is the nation's leading organization promoting alternatives to current drug policy that are grounded in science, compassion, health and human rights.
Your instructor should tell you which citation style they want you to use. Click on the appropriate link below to learn how to format your paper and cite your sources according to a particular style.
- Chicago Style
- ASA & Other Citation Styles
- Last Updated: Apr 25, 2024 1:28 PM
- URL: https://libguides.mjc.edu/drugabuse
Except where otherwise noted, this work is licensed under CC BY-SA 4.0 and CC BY-NC 4.0 Licenses .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 February 2021
Addiction as a brain disease revised: why it still matters, and the need for consilience
- Markus Heilig 1 ,
- James MacKillop ORCID: orcid.org/0000-0003-4118-9500 2 , 3 ,
- Diana Martinez 4 ,
- Jürgen Rehm ORCID: orcid.org/0000-0001-5665-0385 5 , 6 , 7 , 8 ,
- Lorenzo Leggio ORCID: orcid.org/0000-0001-7284-8754 9 &
- Louk J. M. J. Vanderschuren ORCID: orcid.org/0000-0002-5379-0363 10
Neuropsychopharmacology volume 46 , pages 1715–1723 ( 2021 ) Cite this article
90k Accesses
105 Citations
326 Altmetric
Metrics details
A Correspondence to this article was published on 03 May 2021
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Similar content being viewed by others
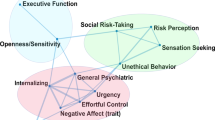
Subtypes in addiction and their neurobehavioral profiles across three functional domains

Drug addiction: from bench to bedside

The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex
Introduction.
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 , 5 , 6 , 7 , 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .
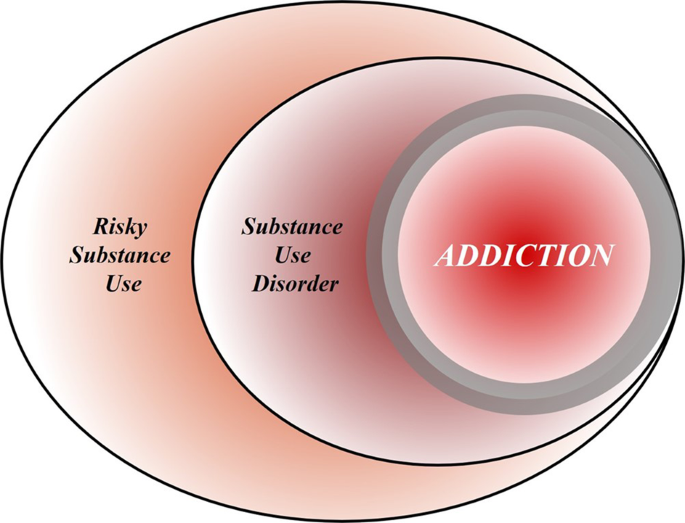
Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 , 118 , 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].
Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 , 64 , 65 , 66 , 67 , 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].
Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 , 88 , 89 , 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 , 92 , 93 , 94 , 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 , 6 , 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–7.
Article CAS PubMed Google Scholar
McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95.
Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12.
Heyman GM. Addiction and choice: theory and new data. Front Psychiatry. 2013;4:31.
Article PubMed PubMed Central Google Scholar
Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res Theory. 2018;26:249–55.
Article Google Scholar
Pickard H, Ahmed SH, Foddy B. Alternative models of addiction. Front Psychiatr.y 2015;6:20.
Google Scholar
Hall W, Carter A, Forlini C. The brain disease model of addiction: is it supported by the evidence and has it delivered on its promises? Lancet Psychiatr. 2015;2:105–10.
Hart CL. Viewing addiction as a brain disease promotes social injustice. Nat Hum Behav. 2017;1:0055.
Heilig M, Epstein DH, Nader MA, Shaham Y. Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosc.i 2016;17:592–9.
Article CAS Google Scholar
Jellinek EM. The disease concept of alcoholism. Hillhouse Press on behalf of the Christopher J. Smithers Foundation: New Haven, CT; 1960.
Stevenson A. Oxford dictionary of English. 3 ed. New York, NY: Oxford University Press; 2010.
Fan J, May SJ, Zhou Y, Barrett-Connor E. Bimodality of 2-h plasma glucose distributions in whites: the Rancho Bernardo study. Diabetes Care 2005;28:1451–6.
King AC, Vena A, Hasin D, De Wit D, O’Connor CJ, Cao D. Subjective responses to alcohol in the development and maintenance of alcohol use disorder (AUD). Am J Psychiatry. 2021. https://doi.org/10.1176/appi.ajp.2020.20030247 .
GBD. 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1:1058–61.
Article CAS PubMed PubMed Central Google Scholar
Epstein DH, Heilig M, Shaham Y. Science-based actions can help address the opioid crisis. Trends Pharm Sci. 2018;39:911–16.
Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abus Treat. 2005;28:321–9.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Datab System Rev. 2013;5:CD009329.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings a systematic review and meta-analysis. JAMA. 2014;311:1889–900.
Article PubMed CAS Google Scholar
Mark TL, Kranzler HR, Song X. Understanding US addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend. 2003;71:219–28.
Article PubMed Google Scholar
Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–65.
Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–83.
Laing RD. The divided self; a study of sanity and madness. London: Tavistock Publications; 1960.
Foucault M, Khalfa J. History of madness. New York: Routledge; 2006.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. et al.Comorbidity of mental disorders with alcohol and other drug abuse. Results Epidemiologic Catchment Area (ECA) study.JAMA. 1990;264:2511–8.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16.
Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–69.
Humphreys K. Addiction treatment professionals are not the gatekeepers of recovery. Subst Use Misuse. 2015;50:1024–7.
Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–21.
Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72.
Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI Jr, Porjesz B, et al. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: an evaluation after 5 years. Arch Gen Psychiatry. 2005;62:753–60.
Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharm Toxicol. 2018;58:143–59.
Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harv Rev Psychiatry. 2015;23:76–89.
Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:102–23.
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–66.
Article PubMed PubMed Central CAS Google Scholar
Lee MR, Sher KJ. “Maturing Out” of binge and problem drinking. Alcohol Res: Curr Rev. 2018;39:31–42.
Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92.
Berridge V. The rise, fall, and revival of recovery in drug policy. Lancet. 2012;379:22–23.
Parvaz MA, Moeller SJ, d’Oleire Uquillas F, Pflumm A, Maloney T, Alia-Klein N, et al. Prefrontal gray matter volume recovery in treatment-seeking cocaine-addicted individuals: a longitudinal study. Addict Biol. 2017;22:1391–401.
Korponay C, Kosson DS, Decety J, Kiehl KA, Koenigs M. Brain volume correlates with duration of abstinence from substance abuse in a region-specific and substance-specific manner. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:626–35.
PubMed PubMed Central Google Scholar
Janes AC, Datko M, Roy A, Barton B, Druker S, Neal C, et al. Quitting starts in the brain: a randomized controlled trial of app-based mindfulness shows decreases in neural responses to smoking cues that predict reductions in smoking. Neuropsychopharmacology. 2019;44:1631–38.
Humphreys K, Bickel WK. Toward a neuroscience of long-term recovery from addiction. JAMA Psychiatry. 2018;75:875–76.
Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med. 2015;45:1061–72.
Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005;6:521–32.
Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. AJ Psychiatry. 2003;160:687–95.
Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50:668–81.
Wray NR, Lin T, Austin J, McGrath JJ, Hickie IB, Murray GK, et al. From basic science to clinical application of polygenic risk scores: a primer. JAMA Psychiatry. 2021;78:101–9.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Visscher PM, Wray NR. Concepts and misconceptions about the polygenic additive model applied to disease. Hum Hered. 2015;80:165–70.
Heilig M, Leggio L. What the alcohol doctor ordered from the neuroscientist: theragnostic biomarkers for personalized treatments. Prog Brain Res. 2016;224:401–18.
Rasmussen K, White DA, Acri JB. NIDA’s medication development priorities in response to the Opioid Crisis: ten most wanted. Neuropsychopharmacology. 2019;44:657–59.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. AJ Psychiatry. 2010;167:748–51.
Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, et al. Neurofunctional domains derived from deep behavioral phenotyping in alcohol use disorder. AJ Psychiatry. 2019;176:744–53.
Kwako LE, Bickel WK, Goldman D. Addiction biomarkers: dimensional approaches to understanding addiction. Trends Mol Med. 2018;24:121–28.
Xiao P, Dai Z, Zhong J, Zhu Y, Shi H, Pan P. Regional gray matter deficits in alcohol dependence: a meta-analysis of voxel-based morphometry studies. Drug Alcohol Depend. 2015;153:22–8.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24.
Klugah-Brown B, Di X, Zweerings J, Mathiak K, Becker B, Biswal B. Common and separable neural alterations in substance use disorders: a coordinate-based meta-analyses of functional neuroimaging studies in humans. Hum Brain Mapp. 2020;41:4459–77.
Volkow ND, Fowler JS, Wang GJ. The addicted human brain: insights from imaging studies. J Clin Investig. 2003;111:1444–51.
Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci. 2011;12:652–69.
Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72:305–15.
Scofield MD, Heinsbroek JA, Gipson CD, Kupchik YM, Spencer S, Smith AC, et al. The nucleus accumbens: mechanisms of addiction across drug classes reflect the importance of glutamate homeostasis. Pharm Rev. 2016;68:816–71.
Korpi ER, den Hollander B, Farooq U, Vashchinkina E, Rajkumar R, Nutt DJ, et al. Mechanisms of action and persistent neuroplasticity by drugs of abuse. Pharm Rev. 2015;67:872–1004.
Luscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron. 2011;69:650–63.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories–indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82.
Lesscher HM, Vanderschuren LJ. Compulsive drug use and its neural substrates. Rev Neurosci. 2012;23:731–45.
Cruz FC, Koya E, Guez-Barber DH, Bossert JM, Lupica CR, Shaham Y, et al. New technologies for examining the role of neuronal ensembles in drug addiction and fear. Nat Rev Neurosci. 2013;14:743–54.
Crick F. The astonishing hypothesis: the scientific search for the soul. Scribner; Maxwell Macmillan International: New York, NY; 1994.
Vanderschuren LJ, Achterberg EJ, Trezza V. The neurobiology of social play and its rewarding value in rats. Neurosci Biobehav Rev. 2016;70:86–105.
Venniro M, Zhang M, Caprioli D, Hoots JK, Golden SA, Heins C, et al. Volitional social interaction prevents drug addiction in rat models. Nat Neurosci. 2018;21:1520–29.
Martinez D, Orlowska D, Narendran R, Slifstein M, Liu F, Kumar D, et al. Dopamine type 2/3 receptor availability in the striatum and social status in human volunteers. Biol Psychiatry. 2010;67:275–8.
Wiers CE, Shokri-Kojori E, Cabrera E, Cunningham S, Wong C, Tomasi D, et al. Socioeconomic status is associated with striatal dopamine D2/D3 receptors in healthy volunteers but not in cocaine abusers. Neurosci Lett. 2016;617:27–31.
Morgan D, Grant KA, Gage HD, Mach RH, Kaplan JR, Prioleau O, et al. Social dominance in monkeys: dopamine D2 receptors and cocaine self-administration. Nat Neurosci. 2002;5:169–74.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e66.
Gilbert PA, Zemore SE. Discrimination and drinking: a systematic review of the evidence. Soc Sci Med 2016;161:178–94.
Oshri A, Gray JC, Owens MM, Liu S, Duprey EB, Sweet LH, et al. Adverse childhood experiences and amygdalar reduction: high-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreat. 2019;24:400–10.
Holmes CJ, Barton AW, MacKillop J, Galván A, Owens MM, McCormick MJ, et al. Parenting and salience network connectivity among African Americans: a protective pathway for health-risk behaviors. Biol Psychiatry. 2018;84:365–71.
Brody GH, Gray JC, Yu T, Barton AW, Beach SR, Galván A, et al. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;171:46–52.
Hanson JL, Gillmore AD, Yu T, Holmes CJ, Hallowell ES, Barton AW, et al. A family focused intervention influences hippocampal-prefrontal connectivity through gains in self-regulation. Child Dev. 2019;90:1389–401.
Borsboom D, Cramer A, Kalis A. Brain disorders? Not really… why network structures block reductionism in psychopathology research. Behav Brain Sci. 2018;42:1–54.
Field M, Heather N, Wiers RW. Indeed, not really a brain disorder: Implications for reductionist accounts of addiction. Behav Brain Sci. 2019;42:e9.
Pascoli V, Hiver A, Van Zessen R, Loureiro M, Achargui R, Harada M, et al. Stochastic synaptic plasticity underlying compulsion in a model of addiction. Nature. 2018;564:366–71.
James W. The dilemma of determinism. Whitefish, MT: Kessinger Publishing; 2005.
Gessell B. Indeterminism in the brain. Biol Philos. 2017;32:1205–23.
Jedlicka P. Revisiting the quantum brain hypothesis: toward quantum (neuro)biology? Front Mol Neurosci. 2017;10:366.
Heyman GM. Addiction: a disorder of choice. Cambridge, MA: Harvard University Press; 2010.
Heather NQ. Is addiction a brain disease or a moral failing? A: Neither. Neuroethics. 2017;10:115–24.
Ahmed SH, Lenoir M, Guillem K. Neurobiology of addiction versus drug use driven by lack of choice. Curr Opin Neurobiol. 2013;23:581–7.
Hogarth L, Lam-Cassettari C, Pacitti H, Currah T, Mahlberg J, Hartley L, et al. Intact goal-directed control in treatment-seeking drug users indexed by outcome-devaluation and Pavlovian to instrumental transfer: critique of habit theory. Eur J Neurosci. 2019;50:2513–25.
Mathis V, Kenny PJ. From controlled to compulsive drug-taking: the role of the habenula in addiction. Neurosci Biobehav Rev. 2019;106:102–11.
Luscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21:247–63.
Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–89.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–68.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–91.
Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat Neurosci. 2005;8:1442–4.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Prim. 2019;5:52.
Vanderschuren LJ, Everitt BJ. Drug seeking becomes compulsive after prolonged cocaine self-administration. Science 2004;305:1017–9.
American_Psychiatric_Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc; 2013.
Book Google Scholar
Spragg SDS. Morphine addiction in chimpanzees. Comp Psychol Monogr. 1940;15:132–32.
Lenoir M, Cantin L, Vanhille N, Serre F, Ahmed SH. Extended heroin access increases heroin choices over a potent nondrug alternative. Neuropsychopharmacology. 2013;38:1209–20.
Caprioli D, Venniro M, Zeric T, Li X, Adhikary S, Madangopal R, et al. Effect of the novel positive allosteric modulator of metabotropic glutamate receptor 2 AZD8529 on incubation of methamphetamine craving after prolonged voluntary abstinence in a rat model. Biol Psychiatry. 2015;78:463–73.
Augier E, Barbier E, Dulman RS, Licheri V, Augier G, Domi E, et al. A molecular mechanism for choosing alcohol over an alternative reward. Science. 2018;360:1321–26.
Bigelow GE. An operant behavioral perspective on alcohol abuse and dependence. In: Heather N, Peters TJ, Stockwell T, editors. International handbook of alcohol dependence and problems. John Wiley & Sons Ltd; 2001. p. 299–315.
Higgins ST, Heil SH, Lussier JP. Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol. 2004;55:431–61.
Satel S, Lilienfeld SO. Brainwashed: the seductive appeal of mindless neuroscience. New York, NY: Basic Books; 2015.
Wilson EO. Consilience: the unity of knowledge. New York, NY: Vintage Books; 1999.
Saunders JB, Degenhardt L, Reed GM, Poznyak V. Alcohol use disorders in ICD-11: past, present, and future. Alcohol Clin Exp Res 2019;43:1617–31.
Organization. WH. ICD-11 for mortality and morbidity statistics. 2018. https://icd.who.int/browse11/l-m/en . Accessed 21 Oct 2020.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7–30.
Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res 2017;41:179–86.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. AJ Psychiatry. 2013;170:834–51.
Rosenthal RJ, Faris SB. The etymology and early history of ‘addiction’. Addict Res Theory. 2019;27:437–49.
Martin CS, Steinley DL, Verges A, Sher KJ. The proposed 2/11 symptom algorithm for DSM-5 substance-use disorders is too lenient. Psychol Med. 2011;41:2008–10.
Degenhardt L, Bharat C, Bruno R, Glantz MD, Sampson NA, Lago L, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction. 2019;114:534–52.
PubMed Google Scholar
Lago L, Bruno R, Degenhardt L. Concordance of ICD-11 and DSM-5 definitions of alcohol and cannabis use disorders: a population survey. Lancet Psychiatry. 2016;3:673–84.
Lundin A, Hallgren M, Forsman M, Forsell Y. Comparison of DSM-5 classifications of alcohol use disorders with those of DSM-IV, DSM-III-R, and ICD-10 in a general population sample in Sweden. J Stud Alcohol Drugs. 2015;76:773–80.
Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry. 2016;80:179–89.
Rehm J, Heilig M, Gual A. ICD-11 for alcohol use disorders: not a convincing answer to the challenges. Alcohol Clin Exp Res. 2019;43:2296–300.
Download references
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author information
Authors and affiliations.
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Markus Heilig
Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
- James MacKillop
Homewood Research Institute, Guelph, ON, Canada
New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY, USA
Diana Martinez
Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada
Jürgen Rehm
Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON, Canada
Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD, USA
Lorenzo Leggio
Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
Louk J. M. J. Vanderschuren
You can also search for this author in PubMed Google Scholar
Contributions
All authors jointly drafted the paper.
Corresponding author
Correspondence to Markus Heilig .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Heilig, M., MacKillop, J., Martinez, D. et al. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacol. 46 , 1715–1723 (2021). https://doi.org/10.1038/s41386-020-00950-y
Download citation
Received : 10 November 2020
Revised : 11 December 2020
Accepted : 14 December 2020
Published : 22 February 2021
Issue Date : September 2021
DOI : https://doi.org/10.1038/s41386-020-00950-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The importance of choice and agency in animal models of addiction.
- Serge H. Ahmed
Journal of Neural Transmission (2024)
Neuromarkers in addiction: definitions, development strategies, and recent advances
- Nicholas R. Harp
- Tor D. Wager
What Do We Know About Informal Caregiving in the Field of Addiction?: A Scoping Review
- Mélissa Côté
- Eve-Emmanuelle Morency
- Nadine Blanchette-Martin
International Journal of Mental Health and Addiction (2024)
Persistent impacts of smoking on resting-state EEG in male chronic smokers and past-smokers with 20 years of abstinence
- Yoonji Jeon
- Dongil Chung
Scientific Reports (2023)
A contextualized reinforcer pathology approach to addiction
- Samuel F. Acuff
- James G. Murphy
Nature Reviews Psychology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Loading metrics
Open Access
Peer-reviewed
Research Article
Functional connectivity changes in the brain of adolescents with internet addiction: A systematic literature review of imaging studies
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Child and Adolescent Mental Health, Department of Brain Sciences, Great Ormond Street Institute of Child Health, University College London, London, United Kingdom
Roles Conceptualization, Supervision, Validation, Writing – review & editing
* E-mail: [email protected]
Affiliation Behavioural Brain Sciences Unit, Population Policy Practice Programme, Great Ormond Street Institute of Child Health, University College London, London, United Kingdom
- Max L. Y. Chang,
- Irene O. Lee

- Published: June 4, 2024
- https://doi.org/10.1371/journal.pmen.0000022
- Peer Review
- Reader Comments
Internet usage has seen a stark global rise over the last few decades, particularly among adolescents and young people, who have also been diagnosed increasingly with internet addiction (IA). IA impacts several neural networks that influence an adolescent’s behaviour and development. This article issued a literature review on the resting-state and task-based functional magnetic resonance imaging (fMRI) studies to inspect the consequences of IA on the functional connectivity (FC) in the adolescent brain and its subsequent effects on their behaviour and development. A systematic search was conducted from two databases, PubMed and PsycINFO, to select eligible articles according to the inclusion and exclusion criteria. Eligibility criteria was especially stringent regarding the adolescent age range (10–19) and formal diagnosis of IA. Bias and quality of individual studies were evaluated. The fMRI results from 12 articles demonstrated that the effects of IA were seen throughout multiple neural networks: a mix of increases/decreases in FC in the default mode network; an overall decrease in FC in the executive control network; and no clear increase or decrease in FC within the salience network and reward pathway. The FC changes led to addictive behaviour and tendencies in adolescents. The subsequent behavioural changes are associated with the mechanisms relating to the areas of cognitive control, reward valuation, motor coordination, and the developing adolescent brain. Our results presented the FC alterations in numerous brain regions of adolescents with IA leading to the behavioural and developmental changes. Research on this topic had a low frequency with adolescent samples and were primarily produced in Asian countries. Future research studies of comparing results from Western adolescent samples provide more insight on therapeutic intervention.
Citation: Chang MLY, Lee IO (2024) Functional connectivity changes in the brain of adolescents with internet addiction: A systematic literature review of imaging studies. PLOS Ment Health 1(1): e0000022. https://doi.org/10.1371/journal.pmen.0000022
Editor: Kizito Omona, Uganda Martyrs University, UGANDA
Received: December 29, 2023; Accepted: March 18, 2024; Published: June 4, 2024
Copyright: © 2024 Chang, Lee. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The behavioural addiction brought on by excessive internet use has become a rising source of concern [ 1 ] since the last decade. According to clinical studies, individuals with Internet Addiction (IA) or Internet Gaming Disorder (IGD) may have a range of biopsychosocial effects and is classified as an impulse-control disorder owing to its resemblance to pathological gambling and substance addiction [ 2 , 3 ]. IA has been defined by researchers as a person’s inability to resist the urge to use the internet, which has negative effects on their psychological well-being as well as their social, academic, and professional lives [ 4 ]. The symptoms can have serious physical and interpersonal repercussions and are linked to mood modification, salience, tolerance, impulsivity, and conflict [ 5 ]. In severe circumstances, people may experience severe pain in their bodies or health issues like carpal tunnel syndrome, dry eyes, irregular eating and disrupted sleep [ 6 ]. Additionally, IA is significantly linked to comorbidities with other psychiatric disorders [ 7 ].
Stevens et al (2021) reviewed 53 studies including 17 countries and reported the global prevalence of IA was 3.05% [ 8 ]. Asian countries had a higher prevalence (5.1%) than European countries (2.7%) [ 8 ]. Strikingly, adolescents and young adults had a global IGD prevalence rate of 9.9% which matches previous literature that reported historically higher prevalence among adolescent populations compared to adults [ 8 , 9 ]. Over 80% of adolescent population in the UK, the USA, and Asia have direct access to the internet [ 10 ]. Children and adolescents frequently spend more time on media (possibly 7 hours and 22 minutes per day) than at school or sleeping [ 11 ]. Developing nations have also shown a sharp rise in teenage internet usage despite having lower internet penetration rates [ 10 ]. Concerns regarding the possible harms that overt internet use could do to adolescents and their development have arisen because of this surge, especially the significant impacts by the COVID-19 pandemic [ 12 ]. The growing prevalence and neurocognitive consequences of IA among adolescents makes this population a vital area of study [ 13 ].
Adolescence is a crucial developmental stage during which people go through significant changes in their biology, cognition, and personalities [ 14 ]. Adolescents’ emotional-behavioural functioning is hyperactivated, which creates risk of psychopathological vulnerability [ 15 ]. In accordance with clinical study results [ 16 ], this emotional hyperactivity is supported by a high level of neuronal plasticity. This plasticity enables teenagers to adapt to the numerous physical and emotional changes that occur during puberty as well as develop communication techniques and gain independence [ 16 ]. However, the strong neuronal plasticity is also associated with risk-taking and sensation seeking [ 17 ] which may lead to IA.
Despite the fact that the precise neuronal mechanisms underlying IA are still largely unclear, functional magnetic resonance imaging (fMRI) method has been used by scientists as an important framework to examine the neuropathological changes occurring in IA, particularly in the form of functional connectivity (FC) [ 18 ]. fMRI research study has shown that IA alters both the functional and structural makeup of the brain [ 3 ].
We hypothesise that IA has widespread neurological alteration effects rather than being limited to a few specific brain regions. Further hypothesis holds that according to these alterations of FC between the brain regions or certain neural networks, adolescents with IA would experience behavioural changes. An investigation of these domains could be useful for creating better procedures and standards as well as minimising the negative effects of overt internet use. This literature review aims to summarise and analyse the evidence of various imaging studies that have investigated the effects of IA on the FC in adolescents. This will be addressed through two research questions:
- How does internet addiction affect the functional connectivity in the adolescent brain?
- How is adolescent behaviour and development impacted by functional connectivity changes due to internet addiction?
The review protocol was conducted in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (see S1 Checklist ).
Search strategy and selection process
A systematic search was conducted up until April 2023 from two sources of database, PubMed and PsycINFO, using a range of terms relevant to the title and research questions (see full list of search terms in S1 Appendix ). All the searched articles can be accessed in the S1 Data . The eligible articles were selected according to the inclusion and exclusion criteria. Inclusion criteria used for the present review were: (i) participants in the studies with clinical diagnosis of IA; (ii) participants between the ages of 10 and 19; (iii) imaging research investigations; (iv) works published between January 2013 and April 2023; (v) written in English language; (vi) peer-reviewed papers and (vii) full text. The numbers of articles excluded due to not meeting the inclusion criteria are shown in Fig 1 . Each study’s title and abstract were screened for eligibility.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmen.0000022.g001
Quality appraisal
Full texts of all potentially relevant studies were then retrieved and further appraised for eligibility. Furthermore, articles were critically appraised based on the GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) framework to evaluate the individual study for both quality and bias. The subsequent quality levels were then appraised to each article and listed as either low, moderate, or high.
Data collection process
Data that satisfied the inclusion requirements was entered into an excel sheet for data extraction and further selection. An article’s author, publication year, country, age range, participant sample size, sex, area of interest, measures, outcome and article quality were all included in the data extraction spreadsheet. Studies looking at FC, for instance, were grouped, while studies looking at FC in specific area were further divided into sub-groups.
Data synthesis and analysis
Articles were classified according to their location in the brain as well as the network or pathway they were a part of to create a coherent narrative between the selected studies. Conclusions concerning various research trends relevant to particular groupings were drawn from these groupings and subgroupings. To maintain the offered information in a prominent manner, these assertions were entered into the data extraction excel spreadsheet.
With the search performed on the selected databases, 238 articles in total were identified (see Fig 1 ). 15 duplicated articles were eliminated, and another 6 items were removed for various other reasons. Title and abstract screening eliminated 184 articles because they were not in English (number of article, n, = 7), did not include imaging components (n = 47), had adult participants (n = 53), did not have a clinical diagnosis of IA (n = 19), did not address FC in the brain (n = 20), and were published outside the desired timeframe (n = 38). A further 21 papers were eliminated for failing to meet inclusion requirements after the remaining 33 articles underwent full-text eligibility screening. A total of 12 papers were deemed eligible for this review analysis.
Characteristics of the included studies, as depicted in the data extraction sheet in Table 1 provide information of the author(s), publication year, sample size, study location, age range, gender, area of interest, outcome, measures used and quality appraisal. Most of the studies in this review utilised resting state functional magnetic resonance imaging techniques (n = 7), with several studies demonstrating task-based fMRI procedures (n = 3), and the remaining studies utilising whole-brain imaging measures (n = 2). The studies were all conducted in Asiatic countries, specifically coming from China (8), Korea (3), and Indonesia (1). Sample sizes ranged from 12 to 31 participants with most of the imaging studies having comparable sample sizes. Majority of the studies included a mix of male and female participants (n = 8) with several studies having a male only participant pool (n = 3). All except one of the mixed gender studies had a majority male participant pool. One study did not disclose their data on the gender demographics of their experiment. Study years ranged from 2013–2022, with 2 studies in 2013, 3 studies in 2014, 3 studies in 2015, 1 study in 2017, 1 study in 2020, 1 study in 2021, and 1 study in 2022.
https://doi.org/10.1371/journal.pmen.0000022.t001
(1) How does internet addiction affect the functional connectivity in the adolescent brain?
The included studies were organised according to the brain region or network that they were observing. The specific networks affected by IA were the default mode network, executive control system, salience network and reward pathway. These networks are vital components of adolescent behaviour and development [ 31 ]. The studies in each section were then grouped into subsections according to their specific brain regions within their network.
Default mode network (DMN)/reward network.
Out of the 12 studies, 3 have specifically studied the default mode network (DMN), and 3 observed whole-brain FC that partially included components of the DMN. The effect of IA on the various centres of the DMN was not unilaterally the same. The findings illustrate a complex mix of increases and decreases in FC depending on the specific region in the DMN (see Table 2 and Fig 2 ). The alteration of FC in posterior cingulate cortex (PCC) in the DMN was the most frequently reported area in adolescents with IA, which involved in attentional processes [ 32 ], but Lee et al. (2020) additionally found alterations of FC in other brain regions, such as anterior insula cortex, a node in the DMN that controls the integration of motivational and cognitive processes [ 20 ].
https://doi.org/10.1371/journal.pmen.0000022.g002
The overall changes of functional connectivity in the brain network including default mode network (DMN), executive control network (ECN), salience network (SN) and reward network. IA = Internet Addiction, FC = Functional Connectivity.
https://doi.org/10.1371/journal.pmen.0000022.t002
Ding et al. (2013) revealed altered FC in the cerebellum, the middle temporal gyrus, and the medial prefrontal cortex (mPFC) [ 22 ]. They found that the bilateral inferior parietal lobule, left superior parietal lobule, and right inferior temporal gyrus had decreased FC, while the bilateral posterior lobe of the cerebellum and the medial temporal gyrus had increased FC [ 22 ]. The right middle temporal gyrus was found to have 111 cluster voxels (t = 3.52, p<0.05) and the right inferior parietal lobule was found to have 324 cluster voxels (t = -4.07, p<0.05) with an extent threshold of 54 voxels (figures above this threshold are deemed significant) [ 22 ]. Additionally, there was a negative correlation, with 95 cluster voxels (p<0.05) between the FC of the left superior parietal lobule and the PCC with the Chen Internet Addiction Scores (CIAS) which are used to determine the severity of IA [ 22 ]. On the other hand, in regions of the reward system, connection with the PCC was positively connected with CIAS scores [ 22 ]. The most significant was the right praecuneus with 219 cluster voxels (p<0.05) [ 22 ]. Wang et al. (2017) also discovered that adolescents with IA had 33% less FC in the left inferior parietal lobule and 20% less FC in the dorsal mPFC [ 24 ]. A potential connection between the effects of substance use and overt internet use is revealed by the generally decreased FC in these areas of the DMN of teenagers with drug addiction and IA [ 35 ].
The putamen was one of the main regions of reduced FC in adolescents with IA [ 19 ]. The putamen and the insula-operculum demonstrated significant group differences regarding functional connectivity with a cluster size of 251 and an extent threshold of 250 (Z = 3.40, p<0.05) [ 19 ]. The molecular mechanisms behind addiction disorders have been intimately connected to decreased striatal dopaminergic function [ 19 ], making this function crucial.
Executive Control Network (ECN).
5 studies out of 12 have specifically viewed parts of the executive control network (ECN) and 3 studies observed whole-brain FC. The effects of IA on the ECN’s constituent parts were consistent across all the studies examined for this analysis (see Table 2 and Fig 3 ). The results showed a notable decline in all the ECN’s major centres. Li et al. (2014) used fMRI imaging and a behavioural task to study response inhibition in adolescents with IA [ 25 ] and found decreased activation at the striatum and frontal gyrus, particularly a reduction in FC at inferior frontal gyrus, in the IA group compared to controls [ 25 ]. The inferior frontal gyrus showed a reduction in FC in comparison to the controls with a cluster size of 71 (t = 4.18, p<0.05) [ 25 ]. In addition, the frontal-basal ganglia pathways in the adolescents with IA showed little effective connection between areas and increased degrees of response inhibition [ 25 ].
https://doi.org/10.1371/journal.pmen.0000022.g003
Lin et al. (2015) found that adolescents with IA demonstrated disrupted corticostriatal FC compared to controls [ 33 ]. The corticostriatal circuitry experienced decreased connectivity with the caudate, bilateral anterior cingulate cortex (ACC), as well as the striatum and frontal gyrus [ 33 ]. The inferior ventral striatum showed significantly reduced FC with the subcallosal ACC and caudate head with cluster size of 101 (t = -4.64, p<0.05) [ 33 ]. Decreased FC in the caudate implies dysfunction of the corticostriatal-limbic circuitry involved in cognitive and emotional control [ 36 ]. The decrease in FC in both the striatum and frontal gyrus is related to inhibitory control, a common deficit seen with disruptions with the ECN [ 33 ].
The dorsolateral prefrontal cortex (DLPFC), ACC, and right supplementary motor area (SMA) of the prefrontal cortex were all found to have significantly decreased grey matter volume [ 29 ]. In addition, the DLPFC, insula, temporal cortices, as well as significant subcortical regions like the striatum and thalamus, showed decreased FC [ 29 ]. According to Tremblay (2009), the striatum plays a significant role in the processing of rewards, decision-making, and motivation [ 37 ]. Chen et al. (2020) reported that the IA group demonstrated increased impulsivity as well as decreased reaction inhibition using a Stroop colour-word task [ 26 ]. Furthermore, Chen et al. (2020) observed that the left DLPFC and dorsal striatum experienced a negative connection efficiency value, specifically demonstrating that the dorsal striatum activity suppressed the left DLPFC [ 27 ].
Salience network (SN).
Out of the 12 chosen studies, 3 studies specifically looked at the salience network (SN) and 3 studies have observed whole-brain FC. Relative to the DMN and ECN, the findings on the SN were slightly sparser. Despite this, adolescents with IA demonstrated a moderate decrease in FC, as well as other measures like fibre connectivity and cognitive control, when compared to healthy control (see Table 2 and Fig 4 ).
https://doi.org/10.1371/journal.pmen.0000022.g004
Xing et al. (2014) used both dorsal anterior cingulate cortex (dACC) and insula to test FC changes in the SN of adolescents with IA and found decreased structural connectivity in the SN as well as decreased fractional anisotropy (FA) that correlated to behaviour performance in the Stroop colour word-task [ 21 ]. They examined the dACC and insula to determine whether the SN’s disrupted connectivity may be linked to the SN’s disruption of regulation, which would explain the impaired cognitive control seen in adolescents with IA. However, researchers did not find significant FC differences in the SN when compared to the controls [ 21 ]. These results provided evidence for the structural changes in the interconnectivity within SN in adolescents with IA.
Wang et al. (2017) investigated network interactions between the DMN, ECN, SN and reward pathway in IA subjects [ 24 ] (see Fig 5 ), and found 40% reduction of FC between the DMN and specific regions of the SN, such as the insula, in comparison to the controls (p = 0.008) [ 24 ]. The anterior insula and dACC are two areas that are impacted by this altered FC [ 24 ]. This finding supports the idea that IA has similar neurobiological abnormalities with other addictive illnesses, which is in line with a study that discovered disruptive changes in the SN and DMN’s interaction in cocaine addiction [ 38 ]. The insula has also been linked to the intensity of symptoms and has been implicated in the development of IA [ 39 ].
“+” indicates an increase in behaivour; “-”indicates a decrease in behaviour; solid arrows indicate a direct network interaction; and the dotted arrows indicates a reduction in network interaction. This diagram depicts network interactions juxtaposed with engaging in internet related behaviours. Through the neural interactions, the diagram illustrates how the networks inhibit or amplify internet usage and vice versa. Furthermore, it demonstrates how the SN mediates both the DMN and ECN.
https://doi.org/10.1371/journal.pmen.0000022.g005
(2) How is adolescent behaviour and development impacted by functional connectivity changes due to internet addiction?
The findings that IA individuals demonstrate an overall decrease in FC in the DMN is supported by numerous research [ 24 ]. Drug addict populations also exhibited similar decline in FC in the DMN [ 40 ]. The disruption of attentional orientation and self-referential processing for both substance and behavioural addiction was then hypothesised to be caused by DMN anomalies in FC [ 41 ].
In adolescents with IA, decline of FC in the parietal lobule affects visuospatial task-related behaviour [ 22 ], short-term memory [ 42 ], and the ability of controlling attention or restraining motor responses during response inhibition tests [ 42 ]. Cue-induced gaming cravings are influenced by the DMN [ 43 ]. A visual processing area called the praecuneus links gaming cues to internal information [ 22 ]. A meta-analysis found that the posterior cingulate cortex activity of individuals with IA during cue-reactivity tasks was connected with their gaming time [ 44 ], suggesting that excessive gaming may impair DMN function and that individuals with IA exert more cognitive effort to control it. Findings for the behavioural consequences of FC changes in the DMN illustrate its underlying role in regulating impulsivity, self-monitoring, and cognitive control.
Furthermore, Ding et al. (2013) reported an activation of components of the reward pathway, including areas like the nucleus accumbens, praecuneus, SMA, caudate, and thalamus, in connection to the DMN [ 22 ]. The increased FC of the limbic and reward networks have been confirmed to be a major biomarker for IA [ 45 , 46 ]. The increased reinforcement in these networks increases the strength of reward stimuli and makes it more difficult for other networks, namely the ECN, to down-regulate the increased attention [ 29 ] (See Fig 5 ).
Executive control network (ECN).
The numerous IA-affected components in the ECN have a role in a variety of behaviours that are connected to both response inhibition and emotional regulation [ 47 ]. For instance, brain regions like the striatum, which are linked to impulsivity and the reward system, are heavily involved in the act of playing online games [ 47 ]. Online game play activates the striatum, which suppresses the left DLPFC in ECN [ 48 ]. As a result, people with IA may find it difficult to control their want to play online games [ 48 ]. This system thus causes impulsive and protracted gaming conduct, lack of inhibitory control leading to the continued use of internet in an overt manner despite a variety of negative effects, personal distress, and signs of psychological dependence [ 33 ] (See Fig 5 ).
Wang et al. (2017) report that disruptions in cognitive control networks within the ECN are frequently linked to characteristics of substance addiction [ 24 ]. With samples that were addicted to heroin and cocaine, previous studies discovered abnormal FC in the ECN and the PFC [ 49 ]. Electronic gaming is known to promote striatal dopamine release, similar to drug addiction [ 50 ]. According to Drgonova and Walther (2016), it is hypothesised that dopamine could stimulate the reward system of the striatum in the brain, leading to a loss of impulse control and a failure of prefrontal lobe executive inhibitory control [ 51 ]. In the end, IA’s resemblance to drug use disorders may point to vital biomarkers or underlying mechanisms that explain how cognitive control and impulsive behaviour are related.
A task-related fMRI study found that the decrease in FC between the left DLPFC and dorsal striatum was congruent with an increase in impulsivity in adolescents with IA [ 26 ]. The lack of response inhibition from the ECN results in a loss of control over internet usage and a reduced capacity to display goal-directed behaviour [ 33 ]. Previous studies have linked the alteration of the ECN in IA with higher cue reactivity and impaired ability to self-regulate internet specific stimuli [ 52 ].
Salience network (SN)/ other networks.
Xing et al. (2014) investigated the significance of the SN regarding cognitive control in teenagers with IA [ 21 ]. The SN, which is composed of the ACC and insula, has been demonstrated to control dynamic changes in other networks to modify cognitive performance [ 21 ]. The ACC is engaged in conflict monitoring and cognitive control, according to previous neuroimaging research [ 53 ]. The insula is a region that integrates interoceptive states into conscious feelings [ 54 ]. The results from Xing et al. (2014) showed declines in the SN regarding its structural connectivity and fractional anisotropy, even though they did not observe any appreciable change in FC in the IA participants [ 21 ]. Due to the small sample size, the results may have indicated that FC methods are not sensitive enough to detect the significant functional changes [ 21 ]. However, task performance behaviours associated with impaired cognitive control in adolescents with IA were correlated with these findings [ 21 ]. Our comprehension of the SN’s broader function in IA can be enhanced by this relationship.
Research study supports the idea that different psychological issues are caused by the functional reorganisation of expansive brain networks, such that strong association between SN and DMN may provide neurological underpinnings at the system level for the uncontrollable character of internet-using behaviours [ 24 ]. In the study by Wang et al. (2017), the decreased interconnectivity between the SN and DMN, comprising regions such the DLPFC and the insula, suggests that adolescents with IA may struggle to effectively inhibit DMN activity during internally focused processing, leading to poorly managed desires or preoccupations to use the internet [ 24 ] (See Fig 5 ). Subsequently, this may cause a failure to inhibit DMN activity as well as a restriction of ECN functionality [ 55 ]. As a result, the adolescent experiences an increased salience and sensitivity towards internet addicting cues making it difficult to avoid these triggers [ 56 ].
The primary aim of this review was to present a summary of how internet addiction impacts on the functional connectivity of adolescent brain. Subsequently, the influence of IA on the adolescent brain was compartmentalised into three sections: alterations of FC at various brain regions, specific FC relationships, and behavioural/developmental changes. Overall, the specific effects of IA on the adolescent brain were not completely clear, given the variety of FC changes. However, there were overarching behavioural, network and developmental trends that were supported that provided insight on adolescent development.
The first hypothesis that was held about this question was that IA was widespread and would be regionally similar to substance-use and gambling addiction. After conducting a review of the information in the chosen articles, the hypothesis was predictably supported. The regions of the brain affected by IA are widespread and influence multiple networks, mainly DMN, ECN, SN and reward pathway. In the DMN, there was a complex mix of increases and decreases within the network. However, in the ECN, the alterations of FC were more unilaterally decreased, but the findings of SN and reward pathway were not quite clear. Overall, the FC changes within adolescents with IA are very much network specific and lay a solid foundation from which to understand the subsequent behaviour changes that arise from the disorder.
The second hypothesis placed emphasis on the importance of between network interactions and within network interactions in the continuation of IA and the development of its behavioural symptoms. The results from the findings involving the networks, DMN, SN, ECN and reward system, support this hypothesis (see Fig 5 ). Studies confirm the influence of all these neural networks on reward valuation, impulsivity, salience to stimuli, cue reactivity and other changes that alter behaviour towards the internet use. Many of these changes are connected to the inherent nature of the adolescent brain.
There are multiple explanations that underlie the vulnerability of the adolescent brain towards IA related urges. Several of them have to do with the inherent nature and underlying mechanisms of the adolescent brain. Children’s emotional, social, and cognitive capacities grow exponentially during childhood and adolescence [ 57 ]. Early teenagers go through a process called “social reorientation” that is characterised by heightened sensitivity to social cues and peer connections [ 58 ]. Adolescents’ improvements in their social skills coincide with changes in their brains’ anatomical and functional organisation [ 59 ]. Functional hubs exhibit growing connectivity strength [ 60 ], suggesting increased functional integration during development. During this time, the brain’s functional networks change from an anatomically dominant structure to a scattered architecture [ 60 ].
The adolescent brain is very responsive to synaptic reorganisation and experience cues [ 61 ]. As a result, one of the distinguishing traits of the maturation of adolescent brains is the variation in neural network trajectory [ 62 ]. Important weaknesses of the adolescent brain that may explain the neurobiological change brought on by external stimuli are illustrated by features like the functional gaps between networks and the inadequate segregation of networks [ 62 ].
The implications of these findings towards adolescent behaviour are significant. Although the exact changes and mechanisms are not fully clear, the observed changes in functional connectivity have the capacity of influencing several aspects of adolescent development. For example, functional connectivity has been utilised to investigate attachment styles in adolescents [ 63 ]. It was observed that adolescent attachment styles were negatively associated with caudate-prefrontal connectivity, but positively with the putamen-visual area connectivity [ 63 ]. Both named areas were also influenced by the onset of internet addiction, possibly providing a connection between the two. Another study associated neighbourhood/socioeconomic disadvantage with functional connectivity alterations in the DMN and dorsal attention network [ 64 ]. The study also found multivariate brain behaviour relationships between the altered/disadvantaged functional connectivity and mental health and cognition [ 64 ]. This conclusion supports the notion that the functional connectivity alterations observed in IA are associated with specific adolescent behaviours as well as the fact that functional connectivity can be utilised as a platform onto which to compare various neurologic conditions.
Limitations/strengths
There were several limitations that were related to the conduction of the review as well as the data extracted from the articles. Firstly, the study followed a systematic literature review design when analysing the fMRI studies. The data pulled from these imaging studies were namely qualitative and were subject to bias contrasting the quantitative nature of statistical analysis. Components of the study, such as sample sizes, effect sizes, and demographics were not weighted or controlled. The second limitation brought up by a similar review was the lack of a universal consensus of terminology given IA [ 47 ]. Globally, authors writing about this topic use an array of terminology including online gaming addiction, internet addiction, internet gaming disorder, and problematic internet use. Often, authors use multiple terms interchangeably which makes it difficult to depict the subtle similarities and differences between the terms.
Reviewing the explicit limitations in each of the included studies, two major limitations were brought up in many of the articles. One was relating to the cross-sectional nature of the included studies. Due to the inherent qualities of a cross-sectional study, the studies did not provide clear evidence that IA played a causal role towards the development of the adolescent brain. While several biopsychosocial factors mediate these interactions, task-based measures that combine executive functions with imaging results reinforce the assumed connection between the two that is utilised by the papers studying IA. Another limitation regarded the small sample size of the included studies, which averaged to around 20 participants. The small sample size can influence the generalisation of the results as well as the effectiveness of statistical analyses. Ultimately, both included study specific limitations illustrate the need for future studies to clarify the causal relationship between the alterations of FC and the development of IA.
Another vital limitation was the limited number of studies applying imaging techniques for investigations on IA in adolescents were a uniformly Far East collection of studies. The reason for this was because the studies included in this review were the only fMRI studies that were found that adhered to the strict adolescent age restriction. The adolescent age range given by the WHO (10–19 years old) [ 65 ] was strictly followed. It is important to note that a multitude of studies found in the initial search utilised an older adolescent demographic that was slightly higher than the WHO age range and had a mean age that was outside of the limitations. As a result, the results of this review are biased and based on the 12 studies that met the inclusion and exclusion criteria.
Regarding the global nature of the research, although the journals that the studies were published in were all established western journals, the collection of studies were found to all originate from Asian countries, namely China and Korea. Subsequently, it pulls into question if the results and measures from these studies are generalisable towards a western population. As stated previously, Asian countries have a higher prevalence of IA, which may be the reasoning to why the majority of studies are from there [ 8 ]. However, in an additional search including other age groups, it was found that a high majority of all FC studies on IA were done in Asian countries. Interestingly, western papers studying fMRI FC were primarily focused on gambling and substance-use addiction disorders. The western papers on IA were less focused on fMRI FC but more on other components of IA such as sleep, game-genre, and other non-imaging related factors. This demonstrated an overall lack of western fMRI studies on IA. It is important to note that both western and eastern fMRI studies on IA presented an overall lack on children and adolescents in general.
Despite the several limitations, this review provided a clear reflection on the state of the data. The strengths of the review include the strict inclusion/exclusion criteria that filtered through studies and only included ones that contained a purely adolescent sample. As a result, the information presented in this review was specific to the review’s aims. Given the sparse nature of adolescent specific fMRI studies on the FC changes in IA, this review successfully provided a much-needed niche representation of adolescent specific results. Furthermore, the review provided a thorough functional explanation of the DMN, ECN, SN and reward pathway making it accessible to readers new to the topic.
Future directions and implications
Through the search process of the review, there were more imaging studies focused on older adolescence and adulthood. Furthermore, finding a review that covered a strictly adolescent population, focused on FC changes, and was specifically depicting IA, was proven difficult. Many related reviews, such as Tereshchenko and Kasparov (2019), looked at risk factors related to the biopsychosocial model, but did not tackle specific alterations in specific structural or functional changes in the brain [ 66 ]. Weinstein (2017) found similar structural and functional results as well as the role IA has in altering response inhibition and reward valuation in adolescents with IA [ 47 ]. Overall, the accumulated findings only paint an emerging pattern which aligns with similar substance-use and gambling disorders. Future studies require more specificity in depicting the interactions between neural networks, as well as more literature on adolescent and comorbid populations. One future field of interest is the incorporation of more task-based fMRI data. Advances in resting-state fMRI methods have yet to be reflected or confirmed in task-based fMRI methods [ 62 ]. Due to the fact that network connectivity is shaped by different tasks, it is critical to confirm that the findings of the resting state fMRI studies also apply to the task based ones [ 62 ]. Subsequently, work in this area will confirm if intrinsic connectivity networks function in resting state will function similarly during goal directed behaviour [ 62 ]. An elevated focus on adolescent populations as well as task-based fMRI methodology will help uncover to what extent adolescent network connectivity maturation facilitates behavioural and cognitive development [ 62 ].
A treatment implication is the potential usage of bupropion for the treatment of IA. Bupropion has been previously used to treat patients with gambling disorder and has been effective in decreasing overall gambling behaviour as well as money spent while gambling [ 67 ]. Bae et al. (2018) found a decrease in clinical symptoms of IA in line with a 12-week bupropion treatment [ 31 ]. The study found that bupropion altered the FC of both the DMN and ECN which in turn decreased impulsivity and attentional deficits for the individuals with IA [ 31 ]. Interventions like bupropion illustrate the importance of understanding the fundamental mechanisms that underlie disorders like IA.
The goal for this review was to summarise the current literature on functional connectivity changes in adolescents with internet addiction. The findings answered the primary research questions that were directed at FC alterations within several networks of the adolescent brain and how that influenced their behaviour and development. Overall, the research demonstrated several wide-ranging effects that influenced the DMN, SN, ECN, and reward centres. Additionally, the findings gave ground to important details such as the maturation of the adolescent brain, the high prevalence of Asian originated studies, and the importance of task-based studies in this field. The process of making this review allowed for a thorough understanding IA and adolescent brain interactions.
Given the influx of technology and media in the lives and education of children and adolescents, an increase in prevalence and focus on internet related behavioural changes is imperative towards future children/adolescent mental health. Events such as COVID-19 act to expose the consequences of extended internet usage on the development and lifestyle of specifically young people. While it is important for parents and older generations to be wary of these changes, it is important for them to develop a base understanding of the issue and not dismiss it as an all-bad or all-good scenario. Future research on IA will aim to better understand the causal relationship between IA and psychological symptoms that coincide with it. The current literature regarding functional connectivity changes in adolescents is limited and requires future studies to test with larger sample sizes, comorbid populations, and populations outside Far East Asia.
This review aimed to demonstrate the inner workings of how IA alters the connection between the primary behavioural networks in the adolescent brain. Predictably, the present answers merely paint an unfinished picture that does not necessarily depict internet usage as overwhelmingly positive or negative. Alternatively, the research points towards emerging patterns that can direct individuals on the consequences of certain variables or risk factors. A clearer depiction of the mechanisms of IA would allow physicians to screen and treat the onset of IA more effectively. Clinically, this could be in the form of more streamlined and accurate sessions of CBT or family therapy, targeting key symptoms of IA. Alternatively clinicians could potentially prescribe treatment such as bupropion to target FC in certain regions of the brain. Furthermore, parental education on IA is another possible avenue of prevention from a public health standpoint. Parents who are aware of the early signs and onset of IA will more effectively handle screen time, impulsivity, and minimize the risk factors surrounding IA.
Additionally, an increased attention towards internet related fMRI research is needed in the West, as mentioned previously. Despite cultural differences, Western countries may hold similarities to the eastern countries with a high prevalence of IA, like China and Korea, regarding the implications of the internet and IA. The increasing influence of the internet on the world may contribute to an overall increase in the global prevalence of IA. Nonetheless, the high saturation of eastern studies in this field should be replicated with a Western sample to determine if the same FC alterations occur. A growing interest in internet related research and education within the West will hopefully lead to the knowledge of healthier internet habits and coping strategies among parents with children and adolescents. Furthermore, IA research has the potential to become a crucial proxy for which to study adolescent brain maturation and development.
Supporting information
S1 checklist. prisma checklist..
https://doi.org/10.1371/journal.pmen.0000022.s001

S1 Appendix. Search strategies with all the terms.
https://doi.org/10.1371/journal.pmen.0000022.s002
S1 Data. Article screening records with details of categorized content.
https://doi.org/10.1371/journal.pmen.0000022.s003
Acknowledgments
The authors thank https://www.stockio.com/free-clipart/brain-01 (with attribution to Stockio.com); and https://www.rawpixel.com/image/6442258/png-sticker-vintage for the free images used to create Figs 2 – 4 .
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. 5 ed. Washington, D.C.: American Psychiatric Publishing; 2013.
- 10. Stats IW. World Internet Users Statistics and World Population Stats 2013 [ http://www.internetworldstats.com/stats.htm .
- 11. Rideout VJR M. B. The common sense census: media use by tweens and teens. San Francisco, CA: Common Sense Media; 2019.
- 37. Tremblay L. The Ventral Striatum. Handbook of Reward and Decision Making: Academic Press; 2009.
- 57. Bhana A. Middle childhood and pre-adolescence. Promoting mental health in scarce-resource contexts: emerging evidence and practice. Cape Town: HSRC Press; 2010. p. 124–42.
- 65. Organization WH. Adolescent Health 2023 [ https://www.who.int/health-topics/adolescent-health#tab=tab_1 .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Bentham Open Access

Internet Addiction: A Brief Summary of Research and Practice
Hilarie cash.
a reSTART Internet Addiction Recovery Program, Fall City, WA 98024
Cosette D Rae
Ann h steel, alexander winkler.
b University of Marburg, Department for Clinical Psychology and Psychotherapy, Gutenbergstraße 18, 35032 Marburg, Germany
Problematic computer use is a growing social issue which is being debated worldwide. Internet Addiction Disorder (IAD) ruins lives by causing neurological complications, psychological disturbances, and social problems. Surveys in the United States and Europe have indicated alarming prevalence rates between 1.5 and 8.2% [1]. There are several reviews addressing the definition, classification, assessment, epidemiology, and co-morbidity of IAD [2-5], and some reviews [6-8] addressing the treatment of IAD. The aim of this paper is to give a preferably brief overview of research on IAD and theoretical considerations from a practical perspective based on years of daily work with clients suffering from Internet addiction. Furthermore, with this paper we intend to bring in practical experience in the debate about the eventual inclusion of IAD in the next version of the Diagnostic and Statistical Manual of Mental Disorders (DSM).
INTRODUCTION
The idea that problematic computer use meets criteria for an addiction, and therefore should be included in the next iteration of the Diagnostic and Statistical Manual of Mental Disorders (DSM) , 4 th ed. Text Revision [ 9 ] was first proposed by Kimberly Young, PhD in her seminal 1996 paper [ 10 ]. Since that time IAD has been extensively studied and is indeed, currently under consideration for inclusion in the DSM-V [ 11 ]. Meanwhile, both China and South Korea have identified Internet addiction as a significant public health threat and both countries support education, research and treatment [ 12 ]. In the United States, despite a growing body of research, and treatment for the disorder available in out-patient and in-patient settings, there has been no formal governmental response to the issue of Internet addiction. While the debate goes on about whether or not the DSM-V should designate Internet addiction a mental disorder [ 12 - 14 ] people currently suffering from Internet addiction are seeking treatment. Because of our experience we support the development of uniform diagnostic criteria and the inclusion of IAD in the DSM-V [ 11 ] in order to advance public education, diagnosis and treatment of this important disorder.
CLASSIFICATION
There is ongoing debate about how best to classify the behavior which is characterized by many hours spent in non-work technology-related computer/Internet/video game activities [ 15 ]. It is accompanied by changes in mood, preoccupation with the Internet and digital media, the inability to control the amount of time spent interfacing with digital technology, the need for more time or a new game to achieve a desired mood, withdrawal symptoms when not engaged, and a continuation of the behavior despite family conflict, a diminishing social life and adverse work or academic consequences [ 2 , 16 , 17 ]. Some researchers and mental health practitioners see excessive Internet use as a symptom of another disorder such as anxiety or depression rather than a separate entity [e.g. 18]. Internet addiction could be considered an Impulse control disorder (not otherwise specified). Yet there is a growing consensus that this constellation of symptoms is an addiction [e.g. 19]. The American Society of Addiction Medicine (ASAM) recently released a new definition of addiction as a chronic brain disorder, officially proposing for the first time that addiction is not limited to substance use [ 20 ]. All addictions, whether chemical or behavioral, share certain characteristics including salience, compulsive use (loss of control), mood modification and the alleviation of distress, tolerance and withdrawal, and the continuation despite negative consequences.
DIAGNOSTIC CRITERIA FOR IAD
The first serious proposal for diagnostic criteria was advanced in 1996 by Dr. Young, modifying the DSM-IV criteria for pathological gambling [ 10 ]. Since then variations in both name and criteria have been put forward to capture the problem, which is now most popularly known as Internet Addiction Disorder. Problematic Internet Use (PIU) [ 21 ], computer addiction, Internet dependence [ 22 ], compulsive Internet use, pathological Internet use [ 23 ], and many other labels can be found in the literature. Likewise a variety of often overlapping criteria have been proposed and studied, some of which have been validated. However, empirical studies provide an inconsistent set of criteria to define Internet addiction [ 24 ]. For an overview see Byun et al . [ 25 ].
Beard [ 2 ] recommends that the following five diagnostic criteria are required for a diagnosis of Internet addiction: (1) Is preoccupied with the Internet (thinks about previous online activity or anticipate next online session); (2) Needs to use the Internet with increased amounts of time in order to achieve satisfaction; (3) Has made unsuccessful efforts to control, cut back, or stop Internet use; (4) Is restless, moody, depressed, or irritable when attempting to cut down or stop Internet use; (5) Has stayed online longer than originally intended. Additionally, at least one of the following must be present: (6) Has jeopardized or risked the loss of a significant relationship, job, educational or career opportunity because of the Internet; (7) Has lied to family members, therapist, or others to conceal the extent of involvement with the Internet; (8) Uses the Internet as a way of escaping from problems or of relieving a dysphoric mood (e.g., feelings of helplessness, guilt, anxiety, depression) [ 2 ].
There has been also been a variety of assessment tools used in evaluation. Young’s Internet Addiction Test [ 16 ], the Problematic Internet Use Questionnaire (PIUQ) developed by Demetrovics, Szeredi, and Pozsa [ 26 ] and the Compulsive Internet Use Scale (CIUS) [ 27 ] are all examples of instruments to assess for this disorder.
The considerable variance of the prevalence rates reported for IAD (between 0.3% and 38%) [ 28 ] may be attributable to the fact that diagnostic criteria and assessment questionnaires used for diagnosis vary between countries and studies often use highly selective samples of online surveys [ 7 ]. In their review Weinstein and Lejoyeux [ 1 ] report that surveys in the United States and Europe have indicated prevalence rates varying between 1.5% and 8.2%. Other reports place the rates between 6% and 18.5% [ 29 ].
“Some obvious differences with respect to the methodologies, cultural factors, outcomes and assessment tools forming the basis for these prevalence rates notwithstanding, the rates we encountered were generally high and sometimes alarming.” [ 24 ]
There are different models available for the development and maintenance of IAD like the cognitive-behavioral model of problematic Internet use [ 21 ], the anonymity, convenience and escape (ACE) model [ 30 ], the access, affordability, anonymity (Triple-A) engine [ 31 ], a phases model of pathological Internet use by Grohol [ 32 ], and a comprehensive model of the development and maintenance of Internet addiction by Winkler & Dörsing [ 24 ], which takes into account socio-cultural factors ( e.g. , demographic factors, access to and acceptance of the Internet), biological vulnerabilities ( e.g. , genetic factors, abnormalities in neurochemical processes), psychological predispositions ( e.g. , personality characteristics, negative affects), and specific attributes of the Internet to explain “excessive engagement in Internet activities” [ 24 ].
NEUROBIOLOGICAL VULNERABILITIES
It is known that addictions activate a combination of sites in the brain associated with pleasure, known together as the “reward center” or “pleasure pathway” of the brain [ 33 , 34 ]. When activated, dopamine release is increased, along with opiates and other neurochemicals. Over time, the associated receptors may be affected, producing tolerance or the need for increasing stimulation of the reward center to produce a “high” and the subsequent characteristic behavior patterns needed to avoid withdrawal. Internet use may also lead specifically to dopamine release in the nucleus accumbens [ 35 , 36 ], one of the reward structures of the brain specifically involved in other addictions [ 20 ]. An example of the rewarding nature of digital technology use may be captured in the following statement by a 21 year-old male in treatment for IAD:
“I feel technology has brought so much joy into my life. No other activity relaxes me or stimulates me like technology. However, when depression hits, I tend to use technology as a way of retreating and isolating.”
REINFORCEMENT/REWARD
What is so rewarding about Internet and video game use that it could become an addiction? The theory is that digital technology users experience multiple layers of reward when they use various computer applications. The Internet functions on a variable ratio reinforcement schedule (VRRS), as does gambling [ 29 ]. Whatever the application (general surfing, pornography, chat rooms, message boards, social networking sites, video games, email, texting, cloud applications and games, etc.), these activities support unpredictable and variable reward structures. The reward experienced is intensified when combined with mood enhancing/stimulating content. Examples of this would be pornography (sexual stimulation), video games (e.g. various social rewards, identification with a hero, immersive graphics), dating sites (romantic fantasy), online poker (financial) and special interest chat rooms or message boards (sense of belonging) [ 29 , 37 ].
BIOLOGICAL PREDISPOSITION
There is increasing evidence that there can be a genetic predisposition to addictive behaviors [ 38 , 39 ]. The theory is that individuals with this predisposition do not have an adequate number of dopamine receptors or have an insufficient amount of serotonin/dopamine [ 2 ], thereby having difficulty experiencing normal levels of pleasure in activities that most people would find rewarding. To increase pleasure, these individuals are more likely to seek greater than average engagement in behaviors that stimulate an increase in dopamine, effectively giving them more reward but placing them at higher risk for addiction.
MENTAL HEALTH VULNERABILITIES
Many researchers and clinicians have noted that a variety of mental disorders co-occur with IAD. There is debate about which came first, the addiction or the co-occurring disorder [ 18 , 40 ]. The study by Dong et al . [ 40 ] had at least the potential to clarify this question, reporting that higher scores for depression, anxiety, hostility, interpersonal sensitivity, and psychoticism were consequences of IAD. But due to the limitations of the study further research is necessary.
THE TREATMENT OF INTERNET ADDICTION
There is a general consensus that total abstinence from the Internet should not be the goal of the interventions and that instead, an abstinence from problematic applications and a controlled and balanced Internet usage should be achieved [ 6 ]. The following paragraphs illustrate the various treatment options for IAD that exist today. Unless studies examining the efficacy of the illustrated treatments are not available, findings on the efficacy of the presented treatments are also provided. Unfortunately, most of the treatment studies were of low methodological quality and used an intra-group design.
The general lack of treatment studies notwithstanding, there are treatment guidelines reported by clinicians working in the field of IAD. In her book “Internet Addiction: Symptoms, Evaluation, and Treatment”, Young [ 41 ] offers some treatment strategies which are already known from the cognitive-behavioral approach: (a) practice opposite time of Internet use (discover patient’s patterns of Internet use and disrupt these patterns by suggesting new schedules), (b) use external stoppers (real events or activities prompting the patient to log off), (c) set goals (with regard to the amount of time), (d) abstain from a particular application (that the client is unable to control), (e) use reminder cards (cues that remind the patient of the costs of IAD and benefits of breaking it), (f) develop a personal inventory (shows all the activities that the patient used to engage in or can’t find the time due to IAD), (g) enter a support group (compensates for a lack of social support), and (h) engage in family therapy (addresses relational problems in the family) [ 41 ]. Unfortunately, clinical evidence for the efficacy of these strategies is not mentioned.
Non-psychological Approaches
Some authors examine pharmacological interventions for IAD, perhaps due to the fact that clinicians use psychopharmacology to treat IAD despite the lack of treatment studies addressing the efficacy of pharmacological treatments. In particular, selective serotonin-reuptake inhibitors (SSRIs) have been used because of the co-morbid psychiatric symptoms of IAD (e.g. depression and anxiety) for which SSRIs have been found to be effective [ 42 - 46 ]. Escitalopram (a SSRI) was used by Dell’Osso et al . [ 47 ] to treat 14 subjects with impulsive-compulsive Internet usage disorder. Internet usage decreased significantly from a mean of 36.8 hours/week to a baseline of 16.5 hours/week. In another study Han, Hwang, and Renshaw [ 48 ] used bupropion (a non-tricyclic antidepressant) and found a decrease of craving for Internet video game play, total game play time, and cue-induced brain activity in dorsolateral prefrontal cortex after a six week period of bupropion sustained release treatment. Methylphenidate (a psycho stimulant drug) was used by Han et al . [ 49 ] to treat 62 Internet video game-playing children diagnosed with attention-deficit hyperactivity disorder. After eight weeks of treatment, the YIAS-K scores and Internet usage times were significantly reduced and the authors cautiously suggest that methylphenidate might be evaluated as a potential treatment of IAD. According to a study by Shapira et al . [ 50 ], mood stabilizers might also improve the symptoms of IAD. In addition to these studies, there are some case reports of patients treated with escitalopram [ 45 ], citalopram (SSRI)- quetiapine (antipsychotic) combination [ 43 ] and naltrexone (an opioid receptor antagonist) [ 51 ].
A few authors mentioned that physical exercise could compensate the decrease of the dopamine level due to decreased online usage [ 52 ]. In addition, sports exercise prescriptions used in the course of cognitive behavioral group therapy may enhance the effect of the intervention for IAD [ 53 ].
Psychological Approaches
Motivational interviewing (MI) is a client-centered yet directive method for enhancing intrinsic motivation to change by exploring and resolving client ambivalence [ 54 ]. It was developed to help individuals give up addictive behaviors and learn new behavioral skills, using techniques such as open-ended questions, reflective listening, affirmation, and summarization to help individuals express their concerns about change [ 55 ]. Unfortunately, there are currently no studies addressing the efficacy of MI in treating IAD, but MI seems to be moderately effective in the areas of alcohol, drug addiction, and diet/exercise problems [ 56 ].
Peukert et al . [ 7 ] suggest that interventions with family members or other relatives like “Community Reinforcement and Family Training” [ 57 ] could be useful in enhancing the motivation of an addict to cut back on Internet use, although the reviewers remark that control studies with relatives do not exist to date.
Reality therapy (RT) is supposed to encourage individuals to choose to improve their lives by committing to change their behavior. It includes sessions to show clients that addiction is a choice and to give them training in time management; it also introduces alternative activities to the problematic behavior [ 58 ]. According to Kim [ 58 ], RT is a core addiction recovery tool that offers a wide variety of uses as a treatment for addictive disorders such as drugs, sex, food, and works as well for the Internet. In his RT group counseling program treatment study, Kim [ 59 ] found that the treatment program effectively reduced addiction level and improved self-esteem of 25 Internet-addicted university students in Korea.
Twohig and Crosby [ 60 ] used an Acceptance & Commitment Therapy (ACT) protocol including several exercises adjusted to better fit the issues with which the sample struggles to treat six adult males suffering from problematic Internet pornography viewing. The treatment resulted in an 85% reduction in viewing at post-treatment with results being maintained at the three month follow-up (83% reduction in viewing pornography).
Widyanto and Griffith [ 8 ] report that most of the treatments employed so far had utilized a cognitive-behavioral approach. The case for using cognitive-behavioral therapy (CBT) is justified due to the good results in the treatment of other behavioral addictions/impulse-control disorders, such as pathological gambling, compulsive shopping, bulimia nervosa, and binge eating-disorders [ 61 ]. Wölfling [ 5 ] described a predominantly behavioral group treatment including identification of sustaining conditions, establishing of intrinsic motivation to reduce the amount of time being online, learning alternative behaviors, engagement in new social real-life contacts, psycho-education and exposure therapy, but unfortunately clinical evidence for the efficacy of these strategies is not mentioned. In her study, Young [ 62 ] used CBT to treat 114 clients suffering from IAD and found that participants were better able to manage their presenting problems post-treatment, showing improved motivation to stop abusing the Internet, improved ability to control their computer use, improved ability to function in offline relationships, improved ability to abstain from sexually explicit online material, improved ability to engage in offline activities, and improved ability to achieve sobriety from problematic applications. Cao, Su and Gao [ 63 ] investigated the effect of group CBT on 29 middle school students with IAD and found that IAD scores of the experimental group were lower than of the control group after treatment. The authors also reported improvement in psychological function. Thirty-eight adolescents with IAD were treated with CBT designed particularly for addicted adolescents by Li and Dai [ 64 ]. They found that CBT has good effects on the adolescents with IAD (CIAS scores in the therapy group were significant lower than that in the control group). In the experimental group the scores of depression, anxiety, compulsiveness, self-blame, illusion, and retreat were significantly decreased after treatment. Zhu, Jin, and Zhong [ 65 ] compared CBT and electro acupuncture (EA) plus CBT assigning forty-seven patients with IAD to one of the two groups respectively. The authors found that CBT alone or combined with EA can significantly reduce the score of IAD and anxiety on a self-rating scale and improve self-conscious health status in patients with IAD, but the effect obtained by the combined therapy was better.
Multimodal Treatments
A multimodal treatment approach is characterized by the implementation of several different types of treatment in some cases even from different disciplines such as pharmacology, psychotherapy and family counseling simultaneously or sequentially. Orzack and Orzack [ 66 ] mentioned that treatments for IAD need to be multidisciplinary including CBT, psychotropic medication, family therapy, and case managers, because of the complexity of these patients’ problems.
In their treatment study, Du, Jiang, and Vance [ 67 ] found that multimodal school-based group CBT (including parent training, teacher education, and group CBT) was effective for adolescents with IAD (n = 23), particularly in improving emotional state and regulation ability, behavioral and self-management style. The effect of another multimodal intervention consisting of solution-focused brief therapy (SFBT), family therapy, and CT was investigated among 52 adolescents with IAD in China. After three months of treatment, the scores on an IAD scale (IAD-DQ), the scores on the SCL-90, and the amount of time spent online decreased significantly [ 68 ]. Orzack et al . [ 69 ] used a psychoeducational program, which combines psychodynamic and cognitive-behavioral theoretical perspectives, using a combination of Readiness to Change (RtC), CBT and MI interventions to treat a group of 35 men involved in problematic Internet-enabled sexual behavior (IESB). In this group treatment, the quality of life increased and the level of depressive symptoms decreased after 16 (weekly) treatment sessions, but the level of problematic Internet use failed to decrease significantly [ 69 ]. Internet addiction related symptom scores significantly decreased after a group of 23 middle school students with IAD were treated with Behavioral Therapy (BT) or CT, detoxification treatment, psychosocial rehabilitation, personality modeling and parent training [ 70 ]. Therefore, the authors concluded that psychotherapy, in particular CT and BT were effective in treating middle school students with IAD. Shek, Tang, and Lo [ 71 ] described a multi-level counseling program designed for young people with IAD based on the responses of 59 clients. Findings of this study suggest this multi-level counseling program (including counseling, MI, family perspective, case work and group work) is promising to help young people with IAD. Internet addiction symptom scores significantly decreased, but the program failed to increase psychological well-being significantly. A six-week group counseling program (including CBT, social competence training, training of self-control strategies and training of communication skills) was shown to be effective on 24 Internet-addicted college students in China [ 72 ]. The authors reported that the adapted CIAS-R scores of the experimental group were significantly lower than those of the control group post-treatment.
The reSTART Program
The authors of this article are currently, or have been, affiliated with the reSTART: Internet Addiction Recovery Program [ 73 ] in Fall City, Washington. The reSTART program is an inpatient Internet addiction recovery program which integrates technology detoxification (no technology for 45 to 90 days), drug and alcohol treatment, 12 step work, cognitive behavioral therapy (CBT), experiential adventure based therapy, Acceptance and Commitment therapy (ACT), brain enhancing interventions, animal assisted therapy, motivational interviewing (MI), mindfulness based relapse prevention (MBRP), Mindfulness based stress reduction (MBSR), interpersonal group psychotherapy, individual psychotherapy, individualized treatments for co-occurring disorders, psycho- educational groups (life visioning, addiction education, communication and assertiveness training, social skills, life skills, Life balance plan), aftercare treatments (monitoring of technology use, ongoing psychotherapy and group work), and continuing care (outpatient treatment) in an individualized, holistic approach.
The first results from an ongoing OQ45.2 [ 74 ] study (a self-reported measurement of subjective discomfort, interpersonal relationships and social role performance assessed on a weekly basis) of the short-term impact on 19 adults who complete the 45+ days program showed an improved score after treatment. Seventy-four percent of participants showed significant clinical improvement, 21% of participants showed no reliable change, and 5% deteriorated. The results have to be regarded as preliminary due to the small study sample, the self-report measurement and the lack of a control group. Despite these limitations, there is evidence that the program is responsible for most of the improvements demonstrated.
As can be seen from this brief review, the field of Internet addiction is advancing rapidly even without its official recognition as a separate and distinct behavioral addiction and with continuing disagreement over diagnostic criteria. The ongoing debate whether IAD should be classified as an (behavioral) addiction, an impulse-control disorder or even an obsessive compulsive disorder cannot be satisfactorily resolved in this paper. But the symptoms we observed in clinical practice show a great deal of overlap with the symptoms commonly associated with (behavioral) addictions. Also it remains unclear to this day whether the underlying mechanisms responsible for the addictive behavior are the same in different types of IAD (e.g., online sexual addiction, online gaming, and excessive surfing). From our practical perspective the different shapes of IAD fit in one category, due to various Internet specific commonalities (e.g., anonymity, riskless interaction), commonalities in the underlying behavior (e.g., avoidance, fear, pleasure, entertainment) and overlapping symptoms (e.g., the increased amount of time spent online, preoccupation and other signs of addiction). Nevertheless more research has to be done to substantiate our clinical impression.
Despite several methodological limitations, the strength of this work in comparison to other reviews in the international body of literature addressing the definition, classification, assessment, epidemiology, and co-morbidity of IAD [ 2 - 5 ], and to reviews [ 6 - 8 ] addressing the treatment of IAD, is that it connects theoretical considerations with the clinical practice of interdisciplinary mental health experts working for years in the field of Internet addiction. Furthermore, the current work gives a good overview of the current state of research in the field of internet addiction treatment. Despite the limitations stated above this work gives a brief overview of the current state of research on IAD from a practical perspective and can therefore be seen as an important and helpful paper for further research as well as for clinical practice in particular.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Nearly One-Third of U.S. Adults Know Someone Who’s Died of Drug Overdose
Survey also finds ‘overdose loss’ bolsters recognition of addiction as an important policy issue that spans party lines
Losing a loved one to drug overdose has been a common experience for many Americans in recent years, crossing political and socioeconomic divides and boosting the perceived importance of the overdose crisis as a policy issue, according to a new survey led by researchers at the Johns Hopkins Bloomberg School of Public Health.
A nationally representative survey of more than 2,300 Americans, fielded in spring 2023, suggests that 32 percent of the U.S. adult population, or an estimated 82.7 million individuals, has lost someone they know to a fatal drug overdose. For nearly one-fifth of survey respondents—18.9 percent, representing an estimated 48.9 million adults—the person they knew who died of overdose was a family member or close friend.
The rates of reported loss due to overdose did not differ significantly by political party affiliation, but those who experienced overdose loss were more likely to view addiction as an extremely or very important policy issue.
The study was published online May 31 in JAMA Health Forum .
“The drug overdose crisis is a national tragedy,” says Alene Kennedy-Hendricks, PhD, assistant professor in the Department of Health Policy and Management at the Bloomberg School, who led the analysis. “Although large numbers of U.S. adults are bereaved due to overdose, they may not be as visible as other groups who have lost loved ones to less stigmatized health issues. Movements to build support for policy change to overcome the devastating toll of the overdose crisis should consider the role of this community.”
Over one million Americans have died from drug overdoses since the late 1990s, including more than 100,000 per year in the last few years, according to the Centers for Disease Control and Prevention. Last year, overdose deaths declined slightly for the first time in five years, decreasing three percent from 2022, according to preliminary data from the CDC’s National Center for Health Statistics. At about 108,000 estimated deaths, the CDC 2023 preliminary numbers remain near historic highs.
The overdose crisis has evolved over several phases, beginning with prescription opioids such as oxycodone playing a key role, followed by heroin and, more recently, powerful synthetic opioids like illicitly manufactured fentanyl and polysubstance use. Opioids can suppress breathing as a side effect, and the unpredictability of the illicit drug supply and the potency of fentanyl have dramatically increased the risk of overdose.
While the survey questions did not specifically identify opioids, the majority of overdose deaths over the last two decades have been opioid-related.
The overdose crisis has not only impacted its direct victims but also their relatives, friends, and acquaintances. Kennedy-Hendricks and her colleagues at the Bloomberg School’s Center for Mental Health and Addiction Policy set up the study to help illuminate this wider impact, which otherwise has been little studied.
The paper was co-written with colleagues from Boston University School of Public Health, the University of Minnesota, and the de Beaumont Foundation. The study’s senior author is Sandro Galea, MD, DrPH, MPH, dean of Boston University School of Public Health.
The survey is part of the CLIMB (COVID-19 and Life Stressors Impact on Mental Health and Well-being) study. Led by Catherine Ettman, PhD, an assistant professor in the Bloomberg School’s Department of Health Policy and Management, the CLIMB study has surveyed a nationally representative sample of adult Americans annually since 2020. For this overdose loss study, questions to participants from March 28 to April 17, 2023—CLIMB Wave 4—included “Do you personally know anyone who has died from a drug overdose?” A total of 2,326 participants responded to the question. Participants answering “yes” were then asked “Who do you know that has died from a drug overdose?”
Overdose losses were reported across all income groups. Forty percent of lower-income respondents (defined as annual household incomes less than $30,000) reported overdose loss. Over one-quarter—26 percent—of respondents in the $100,000 and higher annual household income category reported an overdose loss.
The rate of reported overdose loss was not significantly different across self-described Republicans, Democrats, and Independents, adding to the picture of a far-reaching phenomenon.
The data suggested a high level of endorsement across all groups—greater than 60 percent, even among those reporting no overdose loss—that addiction is an extremely or very important policy issue. Respondents who reported overdose loss had 37 percent greater odds of viewing addiction as a very or extremely important policy priority.
“This study contributes new evidence that the addiction crisis and the losses that come with it are common across Americans, but the burden is greater among those who are more economically precarious,” says Ettman. “Addressing addiction can be a unifying theme in increasingly divided times.”
The researchers plan to follow up with further studies in future CLIMB survey waves, looking at associations between overdose loss and other social variables such as trust in institutions.
“ Experience of Personal Loss Due to Drug Overdose Among U.S. Adults ” was co-authored by Alene Kennedy-Hendricks, Catherine Ettman, Sarah Gollust, Sachini Bandara, Salma Abdalla, Brian Castrucci, and Sandro Galea.
CLIMB Study Wave 4 was funded by a grant from the de Beaumont Foundation.
Media contacts: Kate Sam [email protected] or Kris Henry [email protected]
Related Content

Health in All Policies

A Brief History of Traffic Deaths in the U.S.

The Hunger Gap

Rewriting the Story of Life’s Later Years

Amsterdam’s Struggle to Improve Sex Worker Health
- Skip to main content
- Keyboard shortcuts for audio player
Weekend Edition Sunday
- Latest Show
Sunday Puzzle
- Corrections
Listen to the lead story from this episode.
Politics chat: How voters are responding to Trump's felony conviction
by Ayesha Rascoe , Mara Liasson
The Americas
Mexico votes for a new president after a campaigning season plagued by violence.
by Eyder Peralta , Ayesha Rascoe
Middle East
Aid workers in gaza say nowhere is safe after israeli attacks on 'humanitarian zones'.
by Hadeel Al-Shalchi
Girls in the U.S. are getting their period earlier. Here's what parents should know
by Ayesha Rascoe , Maria Godoy
Bookstores have come under attack in Ukraine. But interest in reading is only growing
by Joanna Kakissis
25 years ago, Napster changed how we listen to music forever
by Ayesha Rascoe
What locals think of the proposal to build U.S.'s tallest building in Oklahoma City
by Graycen Wheeler

Sunday Puzzle NPR hide caption
Sunday Puzzle: Second in Line
by Will Shortz
Movie Interviews
A new animated film follows a lonely dog and his robot friend in new york city.
by Ayesha Rascoe , Matthew Schuerman , Andrew Craig
Conservative media sows doubt about the verdict in Trump's felony convictions
by Ayesha Rascoe , David Folkenflik
Supreme Court judge accused of bias towards Trump declines to recuse himself from case
by Ayesha Rascoe , Matthew Schuerman , Hiba Ahmad
Some states are adopting a new form of reading instruction to combat falling scores
by Juma Sei
A new movie tells the story of Kemba Smith Pradia, race and incarceration
Strange news, meet abby lampe, two-time champion of the cheese-wheel-chasing race, meet abby lampe, two-time champion of the chees-wheel-chasing race, 100 years ago, indigenous people were granted u.s. citizenship by law.
by Sandhya Dirks
The first professional women's hockey league in the U.S. has a winner
Music interviews, jon lampley, a veteran of stephen colbert's talk show, releases his debut album.
by D. Parvaz , Ayesha Rascoe , Ryan Benk
Searching for a song you heard between stories? We've retired music buttons on these pages. Learn more here.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
June 5, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
written by researcher(s)
Whose health matters? The diversity deficit in clinical trials
by Sonia Anand, The Conversation

Most people are aware that the process of bringing new medical products to market is rigorous, complex and tightly regulated. Diagnostic tests, therapies and treatments all go through lengthy, expensive trials to make sure they're safe and effective before being approved for public use. The gold standard for clinical trials— randomized controlled studies —often require thousands of research subjects.
Society generally agrees such effort is necessary. Our medical system is built on evidence and trust, and reliable research is essential to both.
As a professor of medicine and a researcher with an interest in ethnic variation and health, I have reflected on who is included and who is left out of clinical trials. Unfortunately, clinical trials all too often fail to reflect the communities that stand to be most affected by the outcomes of that research.
Under-representation in clinical trials
The underrepresented of racialized , or non-white, people in clinical trials is a serious and largely unrecognized problem that needs more scrutiny as part of the growing movement to foster health equity.
Like other broad efforts to build a fairer, more inclusive society, there is an ongoing movement toward health equity —the effort to assure every person in society has equal access to health care.
There are multiple reports that show the majority of studies of genetic variants linked to type 2 diabetes focused on higher-income white people of European background , whereas diabetes is more frequent in non-white ethnic groups. That led my colleagues and me to wonder if the same might be true of clinical trials for type 2 diabetes treatments.
It turns out it was. That's a significant concern, given that about 422 million people worldwide —roughly one in 20—have diabetes, which disproportionately affects non-white ethnic populations such as South Asian, East Asian, Indigenous and Black people. The number of cases and the prevalence of diabetes have been steadily increasing for decades.
My research colleagues and I looked at 20 years' worth of data for our January paper in the journal Diabetologia , and found that in diabetes-related clinical trials , there is a clear difference between the pool of research subjects and the populations statistically more likely to develop type 2 diabetes.
While racialized, or non-white, populations carry a heavier burden of diabetes, the body of research subjects enrolled in type 2 diabetes trials is disproportionately white.
We analyzed 83 studies that took place between 2000 and 2020, involving 283,000 research subjects. We found racialized people were somewhat under-represented in government-funded research and significantly under-represented in industry-funded research relative to the distribution of diabetes by ethnicity or race in the regions being studied.
The differences between government- and industry-funded study subjects may be attributable to government guidelines that call for proportional representation by gender, ethnicity and racial groups. In industry-funded research, there's not much regulation at all in terms of ethnic diversity.
It isn't necessarily racism—at least not direct, overt racism—that drives this dynamic. The answer is likely more banal: habit and convenience. Physicians who recruit research subjects for studies, as they often do , are likely to lean on the same patients they've recruited before, and their research coordinators are more likely to seek patients in local hospitals and clinics.
My study discusses how this reliance on traditional recruitment tools, such as posters in English in hospitals and clinics inviting people to volunteer, without considering the distribution of the disease of interest by ethnicity, leads to over-represention of white European participants, as there is no specific plan to engage high-risk communities.
Being motivated to collect data as quickly and efficiently as possible, pharmaceutical companies also usually go to clinical or academic research organizations they've worked with before. They generally recruit in ways they've used previously, which typically nets them higher-income, white European subjects.
Researchers may also avoid traditionally underrepresented groups, believing they don't want to participate in research, when research in North America and England shows people from such groups would like to participate in research but are rarely asked .
Does underrepresentation affect results?
One may wonder whether the failure to balance the pool of diabetes research participants twists the results. The short answer is that in general, it likely does not.
While there is a genetic component to diabetes , we know from other research that physiologically speaking, people are more often similar in terms of responding to disease and to treatments , so the drugs we prescribe are legitimately effective.
However, detecting ethnic differences in serious adverse reactions to experimental drugs is more difficult because they are less frequent. Some may occur more frequently in ethnically diverse groups due to differences in the frequency of genetic variants or physiologic responses, leaving some vulnerable to hidden problems that a more diversified clinical trial participant pool could have exposed.
A broader problem is trust. We know racialized people are less likely to trust the medical system, all too often with good reason. Participating in trials would allow racialized people to develop a greater sense of inclusion and control—and feel they are players in the medical system, not outsiders to structures that have historically excluded or even abused them. Improving trust encourages more people to seek medical help when they need it.
The person who hesitates to seek care because of mistrust is more likely to develop more severe symptoms . A cancer discovered sooner rather than later is typically easier to treat. A diabetic who receives care earlier is far less likely to need a toe or limb amputation later .
Even a small improvement in the percentage of racialized people who seek care and receive effective therapies can make a significant difference in the overall health of the population and the total cost of health care. The Institute of Medicine in the United States found that closing the health equity gap by just one percent would reduce health-care costs by billions of dollars .
Recruiting representative study participants
The way to fix this problem is to require and fund researchers to recruit ethnically diverse participants that more closely resemble the demographic makeup of Canada, or distribution of disease by ethnic group. Government-funded research grants can be tagged to requirements for disease proportional recruitment, and corporate-funded research should be required by government regulators to show evidence of the same.
Specifically targeting underrepresented populations to build an appropriately representative pool of participants takes more effort, time and money, so it rarely happens, especially when funding is already tight.
Without a better understanding of the consequences of unbalanced recruiting, and stricter regulations to enforce it, many sponsors and researchers will continue to take the path of least resistance to get their study numbers.
Explore further
Feedback to editors

Evidence-based design or Feng Shui in hospital rooms might benefit patients, online study finds
39 minutes ago

Researchers unveil pioneering approach to combat age-related vision loss

Brain imaging study shows how THC in cannabis disrupts brain activity and may cause cognitive impairment

Researchers suggest that amyloid contributes to calcific aortic valve disease development

Prostate cancer study reveals molecular switch linked to lineage plasticity, therapy resistance

New AI technique can identify seizure types, including rare forms of epilepsy

Researchers find a poor quality diet may lead to brain changes associated with depression and anxiety

Psychologist discovers goosebumps happen far more often than we think

Study reveals how 'forever chemicals' may impact heart health in older women

Mass incarceration may worsen gun violence in Black communities, study finds
Related stories.

Newer diabetes treatments are understudied in Black populations and may be less beneficial
Sep 21, 2023

Diversity among research staff found to increase participation of underrepresented patients in clinical studies
Oct 19, 2023

Ethnicity and early menopause increase risk of type 2 diabetes, finds study
Sep 26, 2023

OB-GYN research lacks racial, ethnic inclusivity
Dec 21, 2022

Participants in health research not representative of the UK's diverse population, finds study
Nov 30, 2023
Q&A: How medicine can achieve more diversity in clinical trials—an expert's perspective
Sep 15, 2023
Recommended for you

Lung cancer treatment produces progression-free survival results in Phase III trial
4 hours ago

Research team finds almost a million potential sources of next-gen antibiotics in the natural world
3 hours ago

New molecular tool shows how telomeres relate to heart health
23 hours ago

Phase III trial shows lorlatinib highly effective against ALK-positive non–small cell lung cancer
Jun 4, 2024

Study suggests textbooks are wrong about how the tongue tastes things

Allergy or infection? Scientists discover what distinguishes these two immune system responses
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
Research Topics. En español. The National Institute on Drug Abuse (NIDA) is the largest supporter of the world's research on substance use and addiction. Part of the National Institutes of Health, NIDA conducts and supports biomedical research to advance the science on substance use and addiction and improve individual and public health.
JAM Impact Factor Reaches 5.5. The Journal of Addiction Medicine's (JAM) Impact Factor (IF), released in June 2023 by Clarivate's Journal Citation Reports, jumped by nearly a full point to 5.5 in 2022 from 4.6 in 2021. JAM's 2020 IF was 3.9 and has been steadily increasing since 2014. The IF metric is a ratio of the number of citations ...
Introduction. Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that "addiction is a brain disease", articulated a set of implications of this position, and outlined an agenda for realizing its promise [].The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the ...
Inhibitory control, a core deficit in drug addiction, may be amenable to targeted prefrontal cortex interventions. ... Research Highlights 22 Sept 2023 Neuropsychopharmacology. Volume: 49, P: 357-358.
For much of the past century, scientists studying drugs and drug use labored in the shadows of powerful myths and misconceptions about the nature of addiction. When scientists began to study addictive behavior in the 1930s, people with an addiction were thought to be morally flawed and lacking in willpower. Those views shaped society's ...
The Canadian Journal of Psychiatry. Exposure to state violence and substance use by Alexandra Domike Blackman, Sarah Kammourh, and Elizabeth R Nugent. Research & Politics. COVID-19: Changing the Landscape of Substance Use by Laura G. Leahy [email protected] and Susan E. Caverly.
How does science provide solutions for drug abuse and addiction? Scientists study the effects that drugs have on the brain and on people's behavior. They use this information to develop programs for preventing drug abuse and for helping people recover from addiction. Further research helps transfer these ideas into practice in our communities. 3
Drug addiction including smoking, alcohol and illicit drug use is indirectly or directly responsible for 11.8 million deaths each year in the world [].According to the Global Burden of Disease ...
Addiction is the official journal of the Society for the Study of Addiction, and has been in publication since 1884. The journal publishes peer-reviewed research reports on pharmalogical and behavioural addictions, bringing together research conducted within many different disciplines.
Addiction is psychological and/or physical dependence on the use of drugs or other substances, or on activities or behaviors. Substance abuse is a pattern of continued substance use despite substance-related problems, distress, and/or impairment. ... Topics in Psychology. Explore how scientific research by psychologists can inform our ...
Journal scope statement. Psychology of Addictive Behaviors® publishes peer-reviewed original articles related to the psychological aspects of addictive behaviors. The journal includes articles on the following topics: alcohol use and alcohol use disorders. drug use and drug use disorders. smoking and nicotine use and disorders.
Abstract. Alcohol is a major contributor to global disease and a leading cause of preventable death, causing approximately 88,000 deaths annually in the United States alone. Alcohol use disorder is one of the most common psychiatric disorders, with nearly one-third of U.S. adults experiencing alcohol use disorder at some point during their lives.
Journal overview. Since being founded in 1993, Addiction Research and Theory has been the leading outlet for research and theoretical contributions that view addictive behaviour as arising from psychological processes within the individual and the social context in which the behaviour takes place as much as from the biological effects of the ...
It includes 14 empirical research articles and one intervention paper from Bosnia, Croatia, Hong Kong, Italy, mainland China, Norway, Poland, Singapore, South Korea, Spain, Slovenia, Sweden and the United States, and covers the topics of substance misuse and addiction amongst various social groups, different types and forms of illicit and ...
These research queries and findings are presented in the form of updates, white papers and case studies. In addition, the Butler Center for Research collaborates with the Recovery Advocacy team to study special-focus addiction research topics, summarized in monthly Emerging Drug Trends reports. Altogether, these studies provide the latest in ...
The global issue of substance abuse demands ongoing initiatives aligned with the United Nations Sustainable Development Goals. With drug use remaining prevalent worldwide, interventions are critical to addressing the associated health challenges and societal implications. Exercise and physical activities have emerged as integral components of substance use disorder (SUD) treatment, offering ...
Over the past years, popular and scholarly discourse around the topic of "smartphone addiction" (more generally referred to as "tech addiction") has boomed. Over 10,000 scientific papers using the phrase "smartphone addiction" have been published since 2017. 3 This growing interest has so far not been translated into any medically ...
Drug abuse and Medicine. The obvious topic for a medical research paper. The impact of drugs on the human body, the changes in its physiology and the nature of addiction are well studied also, but, unfortunately, the drugs evolve along with the science, so the new synthetic drugs that are sometimes considered harmless "energy club pills" emerge almost every year.
60+ Addiction Topics to Inspire You for a Great Paper. There are many forms of addictions that afflict humanity today. People who suffer from drug abuse, alcohol, or another type of addiction deserve to speak about their issues. Students among world-recognized universities unite to explore this problem, so the topic of drug addiction is ...
About Addiction Science. Many people don't understand why or how other people become addicted to drugs. They may mistakenly think that those who use drugs lack moral principles or willpower and that they could stop their drug use simply by choosing to. In reality, drug addiction is a complex disease, and quitting usually takes more than good ...
This charge has two critical components. The first is the strategic support and conduct of research across a broad range of disciplines. The second is ensuring the rapid and effective dissemination and use of the results of that research to significantly improve prevention and treatment and to inform policy as it relates to drug abuse and ...
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that ...
Internet usage has seen a stark global rise over the last few decades, particularly among adolescents and young people, who have also been diagnosed increasingly with internet addiction (IA). IA impacts several neural networks that influence an adolescent's behaviour and development. This article issued a literature review on the resting-state and task-based functional magnetic resonance ...
Abstract. Problematic computer use is a growing social issue which is being debated worldwide. Internet Addiction Disorder (IAD) ruins lives by causing neurological complications, psychological disturbances, and social problems. Surveys in the United States and Europe have indicated alarming prevalence rates between 1.5 and 8.2% [1].
The data suggested a high level of endorsement across all groups—greater than 60 percent, even among those reporting no overdose loss—that addiction is an extremely or very important policy issue. Respondents who reported overdose loss had 37 percent greater odds of viewing addiction as a very or extremely important policy priority.
The findings are from a review, published Tuesday in the journal PLOS Mental Health, of 12 neuroimaging studies of a few hundred adolescents ages 10 to 19 between 2013 and 2022. Ad Feedback ...
Jon Lampley, a veteran of Stephen Colbert's talk show, releases his debut album. by D. Parvaz, Ayesha Rascoe, Ryan Benk. 7 min. Searching for a song you heard between stories?
My research colleagues and I looked at 20 years' worth of data for our January paper in the journal Diabetologia, and found that in diabetes-related clinical trials, there is a clear difference ...