Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 05 July 2022

A meta-review of psychological resilience during COVID-19
- Katie Seaborn ORCID: orcid.org/0000-0002-7812-9096 1 ,
- Kailyn Henderson 2 ,
- Jacek Gwizdka ORCID: orcid.org/0000-0003-2273-3996 3 &
- Mark Chignell ORCID: orcid.org/0000-0001-8120-6905 2
npj Mental Health Research volume 1 , Article number: 5 ( 2022 ) Cite this article
3836 Accesses
4 Citations
7 Altmetric
Metrics details
- Health care
- Public health
- Quality of life
- Research data
- Scientific community
Psychological resilience has emerged as a key factor in mental health during the global COVID-19 pandemic. However, no work to date has synthesised findings across review work or assessed the reliability of findings based on review work quality, so as to inform public health policy. We thus conducted a meta-review on all types of review work from the start of the pandemic (January 2020) until the last search date (June 2021). Of an initial 281 papers, 30 were included for review characteristic reporting and 15 were of sufficient review quality for further inclusion in strategy analyses. High-level strategies were identified at the individual, community, organisational, and governmental levels. Several specific training and/or intervention programmes were also identified. However, the quality of findings was insufficient for drawing conclusions. A major gap between measuring the psychological resilience of populations and evaluating the effectiveness of strategies for those populations was revealed. More empirical work, especially randomised controlled trials with diverse populations and rigorous analyses, is strongly recommended for future research.
Similar content being viewed by others

Psycho-social factors associated with mental resilience in the Corona lockdown
Ilya M. Veer, Antje Riepenhausen, … Raffael Kalisch

Interrelations of resilience factors and their incremental impact for mental health: insights from network modeling using a prospective study across seven timepoints
Sarah K. Schäfer, Jessica Fritz, … Tanja Michael
COVIDiSTRESS diverse dataset on psychological and behavioural outcomes one year into the COVID-19 pandemic
Angélique M. Blackburn, Sara Vestergren & the COVIDiSTRESS II Consortium
Introduction
The COVID-19 pandemic has disrupted many aspects of life at a global scale. Mental health and psychological well-being have subsequently emerged as key research foci in healthcare and public health during the pandemic 1 , 2 , 3 , 4 . Most countries have endorsed interventions with known or foreseen effects on psychological well-being, such as social distancing, physical isolation, and self-quarantine. Given what is already known about the relationship between mental health and psychological interventions 5 , this has further motivated questions on the assessment, management, and prevention of negative psychological outcomes 1 , 2 , 3 , 6 , 7 , 8 . Psychological resilience plays an essential role in times of crisis. As a behavioural characteristic, it can be framed as positive adaptability: the ability to “bounce back” when confronted with unusual and negative circumstances involving adversity, stress, and trauma 9 , 10 . Psychological resilience may be affected by socio-economic status 11 , cultural factors 12 , and other sources of influence. In pandemics, psychological resilience may dramatically affect outcomes. External offerings, such as social support systems, may reduce levels of depression 1 , while internal orientations related to psychological stress 2 , coping skills 2 , positive mood 7 , and positivity, especially “finding the good in the bad,” 9 are all facets of psychological resilience that subdue or prevent negative outcomes. The extent to which it is achieved, and how, may be a fundamental determinant of a population’s ability to combat mental health difficulties resulting from stressors related to the COVID-19 global pandemic.
A meta-review is a standard way of assessing the state of affairs. Meta-reviews, also termed umbrella reviews or overviews of reviews, are systematic reviews of extant review work that aim to achieve clarity and consensus on a specific research question or topic while considering factors such as review quality and bias 13 , 14 . Intended beneficiaries are decision-makers, the academic community, and the public. Meta-reviews synthesise systematic reviews and meta-analyses of primary studies, which typically represent the highest achievable level of evidence 13 . As such, assessing the quality of the body of review work is a key component of meta-reviews 13 . However, the COVID-19 pandemic has resulted in a unique set of circumstances. Indeed, the ongoing, pressing need for answers has led to a large number of submitted manuscripts, as well as greater leniency in publishing criteria 15 . Emerging from this “paperdemic” are crucial questions regarding scientific integrity during COVID-19 15 . The collection of review work on psychological resilience may be subject to the same pressures of time and demand. Yet, as indicated by citation counts and media coverage, this work is being relied upon to inform our understanding of the situation and make public health decisions. A rigorous evaluation is necessary to reach consensus for healthcare governance and identify current inadequacies that must be accounted for in future editorial policies and publishing requirements.
This meta-review addresses an urgent need to both assess what is known about psychological resilience during COVID-19 and appraise the quality of research and review work being conducted on this topic. Our research objectives were: (RQ1) to summarise the nature and quality of this body of work and (RQ2) to derive a consensus on strategies implemented to evaluate, maintain, and cultivate psychological resilience throughout the COVID-19 pandemic. While our objective was to provide a reliable overview of the review work along with the means for building knowledge and taking action, we were largely limited by the state of the literature. In short, we cannot offer strong evidence for or against the strategies gathered across the corpus of survey work. Indeed, the severe limitations in this body of work are alarming and undermine the recommendations offered by specific reviews, however highly cited. We map out a series of psychological resilience factors, measures, and strategies gathered from these reviews that, while having potential validity, urgently need high quality empirical work on their efficacy within the context of the COVID-19 pandemic.
Review sample and characteristics
From an initial total of 281 reviews retrieved across three databases in two phases, 97 were screened and 30 were selected for analysis (Fig. 1 ). Excluded reviews and reasons for their exclusion are presented in Supplementary Table 4 .
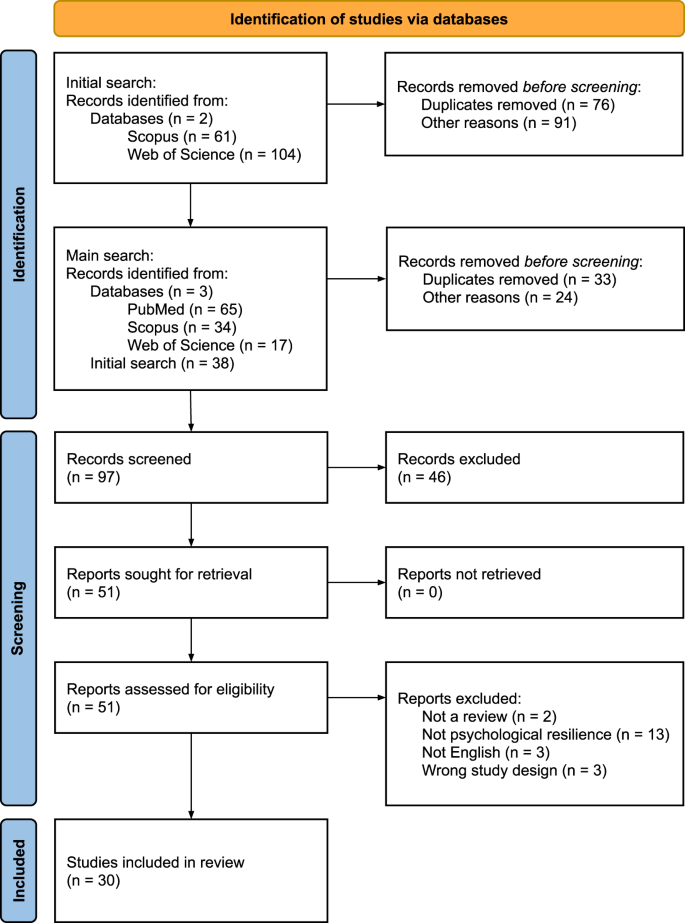
PRISMA flow chart showing study inclusion and exclusion at the identification, screening, and included stages. The identification stage featured an initial search of two databases and a main search of three databases. The screening stage involved screening records, retrieving reports, and assessing their eligibility. Of these, 30 were included in the final stage.
General characteristics of the included reviews are presented in Supplementary Table 5 . Study characteristics were extracted from the 30 included reviews, all of which were published in 2020 or 2021. The review types included narrative (7), rapid (8), systematic (2), scoping (4), mini (1), and mixed methods (1). Only ten (33%) reviews used protocols: four pre-registered with PROSPERO, two with OSF (one in parallel), one with Cochrane Reviews, and three available but unregistered. Of these, one was available from the authors upon request, one was uploaded to an institutional website, and one explained “any discrepancies from the study as planned (and, if relevant, registered)” 11 , 16 . Three reviews were highly cited (50 or more citations) but had no registered protocol and were deemed of low quality; three had registered protocols and were highly cited but of low quality; and five highly cited reviews, deemed of sufficient quality, had no registered protocol.
Participants were from the general population (all ages), as well as subset populations such as individuals working in healthcare (e.g., nurses, doctors, medical staff, social workers, etc.). Specific settings included hospitals, clinics, medical centres, and workplaces. Specific contexts mostly pertained to specific outbreak and pandemic situations, such as SARS, COVID-19, Ebola, H1N1, and MERS (Table 1 ). Twenty-five (83%) studies reported the number of databases searched, which ranged between 1 and 14 (M = 4.84, SD = 2.56, MD = 4, IQR = 3), with the earliest search being carried out on November 17, 2019, and the latest search on March 15, 2021. Twenty-three reviews (77%) reported the number of studies included, which ranged from 2 to 139 (M = 36.65, SD = 32.09, MD = 25, IQR = 31). These included qualitative and quantitative study designs: cross-sectional (surveys, observational), longitudinal, randomised controlled trials (RCTs), descriptive, cohort (prospective, retrospective), interviews, reviews, case-control, and mixed-methods. These studies were conducted in and across six continents: Asia, Africa, North America, South America, Europe, and Australia. Frequent countries of origin of the studies included China, UK, USA, Canada, India, Hong Kong, Italy, and Taiwan. Many of the outcomes reported pertained to the psychological and mental health impacts, e.g., anxiety, stress, depression, posttraumatic stress disorder (PTSD), insomnia, of COVID-19, and risk factors for these impacts.
Risk of bias across reviews
Full details of the risk of bias assessments are presented in Table 2 . The mean SANRA scores for qualitative reviews was 0.74 (SD = 0.12) and the mean JBI score for all other reviews was 0.78 (SD = 0.21). Based on the cut-off of 0.8, 15 reviews were determined to be of sufficient quality to answer RQ2: psychological resilience strategies.
Measures of psychological resilience
Reviews provided 31 unique positive measures (Table 3 ) and 55 unique negative measures (Table 4 ) to assess individuals’ psychological resilience status. Most also covered risk (with respect to negative measures) and protective (with respect to positive measures) factors and status results. A total of 14 risk factors (Table 5 ) and 7 protective factors (Table 6 ) were identified. Half of the factors received a GRADE score of moderate (7/14 for risk factors and 3/7 for protective factors). Counterpoints were included where possible to highlight patterns in how factors were framed and indicate where gaps and possibilities exist.
Strategies for psychological resilience
A corpus of 19 high-level strategies were gathered (Table 7 ). Most (17/19 or 89%) could not be given a GRADE score due to insufficient evidence, and the two remaining received very low GRADE scores. A further 15 specific training and/or intervention programmes were identified. Most were only identified by one review. The programmes were: Psychological first aid (PFA) 17 , 18 , 19 , trauma risk management (TRiM) 17 , 18 , eye movement desensitisation and reprocessing (EMDR) 17 , 18 , cognitive behavioural therapy (CBT) 18 , 20 , 21 , cognitive behavioural therapy for insomnia (CBTi) 18 mindfulness-based cognitive therapy (MBCT) 21 , mindfulness-based stress reduction (MBSR) 18 , occupation therapy (OT) 18 , Motivational Interviewing (MI) 20 , resilience and coping for the healthcare community (RCHC) 17 , anticipate, plan, and deter (APD) 17 , resilience at work (RAW) 17 , mindfulness training 19 , 21 , 22 , 23 , hardiness training 21 , 22 , and crisis intervention 20 .
Almost none of the high-level strategies or specific programmes were evaluated for their effectiveness, within or outside of COVID-19. Moreover, only one review 24 focused on longitudinal work, while also including and merging together non-longitudinal work, such as naturalistic studies. Indeed, 8 of the 15 reviews (53%) called for longitudinal research as future work. One exception was a significant effect of the number of protective measures and equipment provided within work contexts on reducing psychological distress, according to the reporting of Giorgi et al. 20 on 6 of 42 papers. However, no risk of bias or quality assessment was conducted, limiting our ability to draw conclusions on the strength or generalisability of this strategy. The other exception was PFA. Pollock and colleagues 18 reported on a cluster-randomised study by Sijbrandij et al. 25 in which PFA was evaluated through a measure of burnout against a control (no intervention) at baseline, post-assessment, and follow-up stages with 408 participants. Results for completers and intention-to-treat groups indicated that there was no significant difference between groups or over time (95% CI). However, Pollock et al. noted risk of bias due to insufficient reporting, use of single items from a multi-item measure, and weak statistical analyses. Subsequently, we are not confident that there is sufficient evidence to draw conclusions about the efficacy of PFA. Indeed, we are not confident to recommend any of these high-level strategies or specific programmes, based on the review work so far.
Review work, especially systematic surveys, are considered the gold standard of evidence 13 . A wide range of professionals rely on review syntheses to make decisions on policy, practice, and research 26 . In global pandemics, psychological health and resilience are key variables that impact the ability of individuals and populations to recover and carry on. As such, recognition of resilience factors, methods of measuring resilience, and strategies to build and maintain resilience are essential. Unfortunately, this meta-review indicates that the present body of review work is severely limited, leaving us unable to confidently summarise or synthesise knowledge for public health. The implications are grave, particularly given that some of this research has already been used to inform decision-making and justify subsequent research. Additionally, it is difficult to advocate for or against measures and guidance in terms of clinical practice.
Assessing review quality is one of the main objectives of meta-review work 13 . The quality of this corpus was very low overall. Furthermore, a large portion of the work could not be assessed due to insufficiency in reporting and weaknesses in review methodology. The intended main target—strategies for psychological resilience—was particularly impacted. The narrative reviews were notably biased, characterised by opinions and claims without literature backing or reasoning. The quality of most of these reviews was subsequently too low to meet the standard for inclusion in our analyses. The other types of reviews were also insufficient to draw conclusions. Meta-analyses were not possible due to the sheer variety of measures (i.e., heterogeneity) and disconnect between these measures and the strategies reported. Indeed, we found a preponderance of instruments for a relatively short list of measures, with little reasoning behind this diversity. Moreover, most of the strategies reported were mere suggestions rather than options grounded in evidence-based sources. The two strategies that did have some evidentiary support—namely, providing PPE and training or intervention programmes—were nevertheless deemed by ourselves and the original reviewers as very low in quality. In short, we have found clear and widespread evidence that the review work on psychological resilience has been subject to the COVID-19 “paperdemic” phenomenon 15 . This leaves us unable to provide recommendations with confidence. Yet, some of these reviews, notably Preti et al. 27 ( c = 269), Etkind et al. 28 ( c = 171), and Heath et al. 29 ( c = 128), have received a lot of attention via citations, news outlets, and social media. In light of their quality, reliance on these papers to inform policy and practice is inadvisable. At best, these reviews signal a keen interest and urgent need for rigorous, empirical work on matters pertaining to psychological resilience.
Synthesising the nature of the review work revealed several biases and gaps. Most of the reviews were focused on frontline healthcare workers (HCWs) and women. Yet, the literature points to several other groups for whom psychological resilience and/or well-being may be integral within the context of COVID-19, including older adults 30 , people with disabilities 31 , LGBTQ + folk 32 , people with pre-existing mental health conditions 7 , 30 , racialized groups and ethnic minorities 33 , 34 , and people living in low-income and/or isolated areas 35 . A certain level of bias in focus is a natural and common feature of many areas of study 36 . Yet, it cannot be allowed to influence review work, once discovered. We encourage researchers and practitioners to consider work focused on these overlooked populations. Additionally, the way that psychological resilience has been approached needs reconsideration. We found a negative bias in factors and measures. Most measures defined resilience as the absence of mental health problems rather than the presence of fortitude, flexibility, growth, and so on. We also found a concerted focus on risk, rather than protective, factors. While identifying who may be more susceptible and in what contexts is important, it is equally important to determine what characteristics and conditions are favourable to higher rates of psychological resilience. Mental health and well-being stressors may be unavoidable in a pandemic, which this negative bias highlights. Yet, without knowledge of additive and protective factors, it is difficult to make suggestions for clinical practice. Our tables highlight these gaps and can be used to guide future research. Finally, the gap between psychological resilience measures and strategies needs to be addressed, with strategies assessed via these measures in longitudinal studies within the context of COVID-19. Clinical practice and public health would be well-served by a direct link between negative or positive outcomes and the various strategies offered. Without this work and the consensus that a review of it could offer, we cannot make recommendations with confidence.
Methodologically, there was some consistency in the limitations observed in the surveyed review work. Most reviews were not associated with a registered protocol, such as on PROSPERO or Covidence. This created undue repetition in the corpus. It is strongly encouraged that all review protocols be registered in advance; with a hot topic like COVID-19, it is likely that review work is already being undertaken. Additionally, most works included research conducted outside of the COVID-19 pandemic and did not distinguish which results were particular to COVID-19. As such, we cannot draw conclusions on whether there are any special features of the COVID-19 context relevant to psychological resilience. Future work should focus on research conducted during COVID-19 or should delineate between studies conducted during COVID-19 and other contexts, including other pandemics.
This meta-review is limited in a few ways. The heterogeneity in the corpus made it difficult to find and extract data for synthesis and comparison. For example, some reviews reported on sample size in terms of the number of people, while others reported on the number of hospitals or used another population metric. Additionally, finding a “one size fits all” tool for quality and risk of bias assessment proved challenging. This may be a matter of the topic (i.e., a feature of work on psychological resilience) or the breadth of review types included. As with most meta-reviews, included reviews sometimes reported on the same studies, and so certain characteristics that appear to be common across reviews may actually reflect multiple citations of the same study. This issue also limits the accuracy of estimating the number of studies (aggregated across the reviews) that were surveyed. While it is beyond the scope of the present work, this may be addressed by extracting the studies from all reviews, eliminating duplicates, and re-conducting the analyses for each review—a significant effort that may not yield findings equivalent in value to the time and labour required.
The original search was conducted in June 2021, and more reviews are likely to have been published since that time. A retrospective covering the “last waves” of the pandemic will be a necessary future complement to the present meta-review. In the meantime, we briefly comment on a few relevant papers that speak to the issue of longitudinal changes during the pandemic. Riehm et al. 37 noted that time as a factor of resilience is severely understudied. Their findings from over 6000 adults in the Understanding America Study showed that mental distress varied markedly by resilience level during the early months of the COVID-19 pandemic, with low-resilience adults reporting the largest increases in mental distress. Bäuerle et al 38 . evaluated the impact of the “CoPE It” e-mental health intervention designed to improve resilience to mental distress during the pandemic. However, while they found a significant net gain between baseline and post-intervention, they relied on data obtained at only two time points and did not use a control group. There remains an urgent need for longitudinal studies of the effectiveness of interventions to increase psychological resilience during pandemics. A recently published study protocol by Godara et al. 39 exemplifies the type of research that is needed in this area. The planned study on a mindfulness intervention would last ten weeks, involve 300 participants, include a control group, and cover a range of key outcomes, such as levels of stress, loneliness, depression and anxiety, resilience, prosocial behaviour, empathy, and compassion. This proposed study and others like it could provide the needed information on the effectiveness of interventions to improve psychological resilience that is currently lacking.
We conclude with a sober reflection on the state of affairs. As this meta-review has shown, there is insufficient high-quality evidence to inform policy and practice. The silver lining is that a way forward can be mapped through the gaps and weaknesses that characterise this body of work. We urgently recommend the following:
Systematic reviews that follow international standards for methodology (e.g., Cochrane, JBI) and register their protocol through PROSPERO or an equivalent independent body.
Empirical work that uses a common means of measuring positive and negative states and traits related to psychological resilience.
Empirical work that evaluates the proposed psychological resilience strategies, including training interventions and programmes, during COVID-19.
Empirical and review work that targets a range of population subsets beyond frontline HCWs in a broader range of geographical locations and cultural contexts.
Empirical work that involves experimental control, longitudinal designs, naturalistic settings, and other rigorous approaches.
We conducted a systematic meta-review of literature reviews on psychological resilience during the COVID-19 pandemic. We followed the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA) guidelines 40 with modifications for meta-reviews based on Aromataris et al. 13 . Our PRISMA checklist for the abstract is in Supplementary Table 1 and our PRISMA checklist for the article is in Supplementary Table 2 . We used the protocol available in Seaborn et al. 6 . This protocol was registered in advance of data collection with PROSPERO on February 17, 2021 under registration ID CRD42021235288.
Eligibility criteria
All types of reviews that summarised empirical work on psychological resilience in relation to the COVID-19 pandemic were included. We aimed to source only the highest quality of work available. As such, included reviews needed to be published in an academic or medical trade venue and peer reviewed as a basic criterion for quality. Publications from the start of the pandemic (January 2020) until the start of the review (June 2021) were included. Only reviews written in English were included, as this was the language known by all of the authors and the current international standard. Theory and opinion papers were not included, as they would not provide the type of summarised evidence sought for public health decision making. Inaccessible and unpublished literature reviews, including papers posted to archival websites and grey literature, were excluded because a minimum of quality could not be guaranteed.
Information sources, search strategy, and study selection
Three databases, PubMed, Scopus, and Web of Science, were searched between January 16 and 19, 2021, with an update on June 9, 2021. Full search terms and queries can be found in Supplementary Table 3 . A1, A3, and A2 conducted the searches, saving the results to Zotero and removing duplicates there. The combined list was then uploaded to Covidence. A1, A4, and A2 independently screened the papers in two phases: first based on the titles, keywords, and abstracts, and then based on the full text. A list of reviews excluded at the full text stage is available in Supplementary Table 4 . A1 and A4 divided the work and A2 screened all papers. Conflicts were resolved by involving the other reviewer.
Data collection and extraction
A1, A3, and A2 independently extracted data into a Google Sheet. A1 and A3 extracted data for about 50% of the total papers each, and A2 extracted data from all papers. A4 was assigned to resolve conflicts between the sets of data extractions. Data extraction variables were decided based on an extension of PICOS 41 for meta-reviews 13 . These included: article title, authors, year of publication, objectives, type of review, participant demographics (population subset, setting), number of databases searched, date ranges of database searches, publication date ranges of reviewed articles, number of studies, types of studies, country of origin of studies, study risk of bias/quality assessment tool used, protocol registration, citation count via Google Scholar, outcomes reported, method/s of analysis, measures of psychological resilience, their instruments, whether they were tested in COVID-19, how they were assessed (i.e., statistically), CIs, measures used to evaluate strategies, their instruments, whether they were tested in COVID-19, how they were assessed (i.e., statistically), CIs, thematic frameworks, and major finding.
Risk of bias and confidence assessments
Risk of bias and quality assessments were independently conducted by A1, A4, and A2 using a Google Form and Sheet. A1 and A4 were each responsible for about 50% of the papers, and A2 assessed all papers. We used the Scale for the Assessment of Narrative Review Articles (SANRA) 42 for qualitative reviews and the JBI Critical Appraisal Checklist for Systematic Reviews and Research Synthesis 13 for the rest. In contrast to the protocol, we did not use the AMSTAR-2 because there were too few reviews that met the characteristics required for that tool. Sums were averaged across the reviewers. Cut-offs were determined after evaluating and comparing the reviews in a weighted fashion; for both, the cut-off was set at 0.8. Only the data of reviews that met the standard of quality were used to answer RQ2. Confidence in the quality of evidence was assessed by A1 and A2 using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system 43 .
Data analysis
The planned meta-synthesis could not be conducted due to the nature of the reviews captured. As such, measures of effect, variability (i.e., heterogeneity), and other inferential statistics could not be generated. Instead, a combination of descriptive statistics and thematic analyses were generated to identify meaningful patterns across the data 44 , 45 . A3 was responsible for the descriptives. A1, A4, and A2 conducted the thematic analyses. High-level themes were inductively derived as a means of “seeing across” the corpus of review work, while most sub-themes were semantically derived, using the words found within the reviews. All thematic analyses involved a standard, rigorous process of familiarisation with the data, initial coding by one reviewer, generation of initial themes by that reviewer, independent application of those themes by two reviewers, discussion and re-review until conflicts were resolved or themes discarded, and finalisation of themes by the first reviewer. A4 was the first reviewer for the measures data. A1 was the first reviewer for the strategies and risk/protective factors data. A2 was the second reviewer in all cases. We used Google Sheets for all analyses.
Data availability
Most of the data is included in this paper and/or the Supplementary Information. All other data can be made available by the authors upon request.
Giebel, C. et al. COVID-19-related social support service closures and mental well-being in older adults and those affected by dementia: A UK longitudinal survey. BMJ Open 11 , e045889 (2021).
Article PubMed PubMed Central Google Scholar
Robillard, R. et al. Social, financial and psychological stress during an emerging pandemic: Observations from a population survey in the acute phase of COVID-19. BMJ Open 10 , e043805 (2020).
Ranieri, V. et al. COVID-19 welbeing study: A protocol examining perceived coercion and psychological well-being during the COVID-19 pandemic by means of an online survey, asynchronous virtual focus groups, and individual interviews. BMJ Open 11 , e043418 (2021).
Article PubMed Google Scholar
da Silva Júnior, F. J. G. et al. Impact of COVID-19 pandemic on mental health of young people and adults: A systematic review protocol of observational studies. BMJ Open 10 , e039426 (2020).
van Agteren, J. et al. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat. Hum. Behav. 5 , 631–652 (2021).
Seaborn, K., Chignell, M. & Gwizdka, J. Psychological resilience during COVID-19: A meta-review protocol. BMJ Open 11 , e051417 (2021).
Jia, R. et al. Mental health in the UK during the COVID-19 pandemic: Cross-sectional analyses from a community cohort study. BMJ Open 10 , e040620 (2020).
Feroz, A. S. et al. Impact of the COVID-19 pandemic on mental health and well-being of communities: an exploratory qualitative study protocol. BMJ Open 10 , e041641 (2020).
Tugade, M. M. & Fredrickson, B. L. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J. Pers. Soc. Psychol. 86 , 320–333 (2004).
American Psychological Association. Building your resilience. https://www.apa.org . https://www.apa.org/topics/resilience (2012).
Wu, X., Li, X., Lu, Y. & Hout, M. Two tales of one city: Unequal vulnerability and resilience to COVID-19 by socioeconomic status in Wuhan, China. Res. Soc. Stratif. Mobil. 72 , 100584 (2021).
PubMed PubMed Central Google Scholar
Braun-Lewensohn, O., Abu-Kaf, S. & Kalagy, T. Hope and resilience during a pandemic among three cultural groups in Israel: The second wave of Covid-19. Front. Psychol . 12 , 637349 (2021).
Aromataris, E. et al. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. JBI Evid. Implement. 13 , 132–140 (2015).
Google Scholar
Higgins, J. (eds) Cochrane Handbook for Systematic Reviews of Interventions (John Wiley & Sons, 2019).
Dinis-Oliveira, R. J. COVID-19 research: Pandemic versus “paperdemic”, integrity, values and risks of the “speed science”. Forensic Sci. Res. 5 , 174–187 (2020).
Rieckert, A. et al. How can we build and maintain the resilience of our health care professionals during COVID-19? recommendations based on a scoping review. BMJ Open 11 , e043718 (2021).
Hooper, J. J., Saulsman, L., Hall, T. & Waters, F. Addressing the psychological impact of COVID-19 on healthcare workers: Learning from a systematic review of early interventions for frontline responders. BMJ Open 11 , e044134 (2021).
Pollock, A. et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst. Rev. 11 , CD013779 (2020).
PubMed Google Scholar
Kunzler, A. M. et al. Mental health and psychosocial support strategies in highly contagious emerging disease outbreaks of substantial public concern: A systematic scoping review. PLoS One 16 , e0244748 (2021).
Article CAS PubMed PubMed Central Google Scholar
Giorgi, G. et al. COVID-19-related mental health effects in the workplace: A narrative review. Int. J. Environ. Res. Public. Health 17 , 7857 (2020).
Labrague, L. J. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies. J. Nurs. Manag. 29 , 1893–1905 (2021).
Batra, K., Singh, T. P., Sharma, M., Batra, R. & Schvaneveldt, N. Investigating the psychological impact of COVID-19 among healthcare workers: A meta-analysis. Int. J. Environ. Res. Public. Health 17 , 9096 (2020).
Article CAS PubMed Central Google Scholar
Muller, A. E. et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res . 293 , 113441 (2020).
Prati, G. & Mancini, A. D. The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 51 , 201–211 (2021).
Sijbrandij, M. et al. The effect of psychological first aid training on knowledge and understanding about psychosocial support principles: A cluster-randomized controlled trial. Int. J. Environ. Res. Public. Health 17 , 484 (2020).
Article PubMed Central Google Scholar
Pettman, T. L. et al. Communicating with decision-makers through evidence reviews. J. Public Health 33 , 630–633 (2011).
Article CAS Google Scholar
Preti, E. et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Curr. Psychiatry Rep. 22 , 43 (2020).
Etkind, S. N. et al. The role and response of palliative care and hospice services in epidemics and pandemics: A rapid review to inform practice during the COVID-19 pandemic. J. Pain Symptom Manage. 60 , e31–e40 (2020).
Heath, C., Sommerfield, A. & von Ungern-Sternberg, B. S. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: A narrative review. Anaesthesia 75 , 1364–1371 (2020).
Article CAS PubMed Google Scholar
Steptoe, A. & Gessa, G. D. Mental health and social interactions of older people with physical disabilities in England during the COVID-19 pandemic: A longitudinal cohort study. Lancet Public Health 6 , e365–e373 (2021).
Armitage, R. & Nellums, L. B. The COVID-19 response must be disability inclusive. Lancet Public Health 5 , e257 (2020).
Salerno, J. P., Williams, N. D. & Gattamorta, K. A. LGBTQ populations: Psychologically vulnerable communities in the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 12 , S239–S242 (2020).
Article Google Scholar
Poole, L., Ramasawmy, M. & Banerjee, A. Digital first during the COVID-19 pandemic: Does ethnicity matter? Lancet Public Health 6 , e628–e630 (2021).
Patel, P., Hiam, L., Sowemimo, A., Devakumar, D. & McKee, M. Ethnicity and covid-19. BMJ 369 , m2282 (2020).
Patel, J. A. et al. Poverty, inequality and COVID-19: The forgotten vulnerable. Public Health 183 , 110–111 (2020).
Whiting, P. et al. Sources of variation and bias in studies of diagnostic accuracy. Ann. Intern. Med. 140 , 189–202 (2004).
Riehm, K. E. et al. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J. Affect. Disord. 282 , 381–385 (2021).
Bäuerle, A. et al. Mental health burden of the COVID-19 outbreak in Germany: Predictors of mental health impairment. J. Prim Care Community Health 11 , 2150132720953682 (2020).
Godara, M. et al. Investigating differential effects of socio-emotional and mindfulness-based online interventions on mental health, resilience, and social capacities during the COVID-19 pandemic: The study protocol. PLoS One 16 , e0256323 (2021).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372 , n71 (2021).
Tacconelli, E. Systematic reviews: CRD’s guidance for undertaking reviews in health care. Lancet Infect. Dis. 10 , 226 (2010).
Baethge, C., Goldbeck-Wood, S. & Mertens, S. SANRA—a scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 4 , 5 (2019).
Guyatt, G. H. et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336 , 924–926 (2008).
Guest, G., MacQueen, K. M. & Namey, E. E. Applied Thematic Analysis (Sage, 2012).
Braun, V. & Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 3 , 77–101 (2006).
De Kock, J. H. et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 21 , 104 (2021).
Article PubMed PubMed Central CAS Google Scholar
Varghese, A. et al. Decline in the mental health of nurses across the globe during COVID-19: a systematic review and meta-analysis. J. Glob. Health 11 , 05009 (2021).
Hughes, M. C., Liu, Y. & Baumbach, A. Impact of COVID-19 on the health and well-being of informal caregivers of people with dementia: A rapid systematic review. Gerontol. Geriatr. Med. 7 , 23337214211020164 (2021).
Gilan, D. et al. Psychomorbidity, resilience, and exacerbating and protective factors during the SARS-CoV-2-pandemic’a systematic literature review and results from the German COSMO-PANEL. Dtsch. Arzteblatt Int. 117 , 625–632 (2020).
Jans-Beken, L. A perspective on mature gratitude as a way of coping with COVID-19. Front. Psychol. 12 , 632911 (2021).
Blanc, J. et al. Addressing psychological resilience during the coronavirus disease 2019 pandemic: A rapid review. Curr. Opin. Psychiatry 34 , 29–35 (2021).
Sterina, E., Hermida, A. P., Gerberi, D. J. & Lapid, M. I. Emotional resilience of older adults during COVID-19: A systematic review of studies of stress and well-being. Clin. Gerontol . https://doi.org/10.1080/07317115.2021.1928355 (2021).
De Brier, N., Stroobants, S., Vandekerckhove, P. & De Buck, E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): a rapid systematic review. PLoS One 15 , e0244052 (2020).
Sirois, F. M. & Owens, J. Factors associated with psychological distress in health-care workers during an infectious disease outbreak: A rapid systematic review of the evidence. Front. Psychiatry 11 , 589545 (2020).
Chew, Q. H., Wei, K. C., Vasoo, S. & Sim, K. Psychological and coping responses of health care workers toward emerging infectious disease outbreaks: A rapid review and practical implications for the COVID-19 pandemic. J. Clin. Psychiatry 81 , 20r13450 (2020).
Balcombe, L. & de Leo, D. Psychological screening and tracking of athletes and digital mental health solutions in a hybrid model of care: Mini review. JMIR Form. Res . 4 , e22755 (2020).
Berger, E., Jamshidi, N., Reupert, A., Jobson, L. & Miko, A. Review: The mental health implications for children and adolescents impacted by infectious outbreaks—a systematic review. Child Adolesc. Ment. Health 26 , 157–166 (2021).
Ho, C. Y. et al. The impact of death and dying on the personhood of medical students: A systematic scoping review. BMC Med. Educ. 20 , 516 (2020).
Seifert, G. et al. The relevance of complementary and integrative medicine in the COVID-19 pandemic: A qualitative review of the literature. Front. Med. 7 , 587749 (2020).
Schwartz, R., Sinskey, J. L., Anand, U. & Margolis, R. D. Addressing postpandemic clinician mental health: A narrative review and conceptual framework. Ann. Intern. Med. 173 , 981–988 (2020).
Wright, E. M., Carson, A. M. & Kriebs, J. Cultivating resilience among perinatal care providers during the covid-19 pandemic. J. Perinat. Neonatal Nurs. 35 , 105–109 (2021).
Davis, B. E., Lakin, L., Binns, C. C., Currie, K. M. & Rensel, M. R. Patient and provider insights into the impact of multiple sclerosis on mental health: A narrative review. Neurol. Ther . https://doi.org/10.1007/s40120-021-00240-9 (2021).
Kaur, T. & Som, R. R. The predictive role of resilience in psychological immunity: A theoretical review. Int. J. Curr. Res. Rev. 12 , 139–143 (2020).
Download references
Author information
Authors and affiliations.
Department of Industrial Engineering and Economics, Tokyo Institute of Technology, Tokyo, Japan
Katie Seaborn
Department of Mechanical and Industrial Engineering, The University of Toronto, Toronto, ON, Canada
Kailyn Henderson & Mark Chignell
School of Information, The University of Texas at Austin, Austin, TX, USA
Jacek Gwizdka
You can also search for this author in PubMed Google Scholar
Contributions
All authors had full access to the data and were responsible for the decision to submit this manuscript for publication. All authors accessed and verified the final data. All were involved in data collection and analysis. K.S., J.G., and M.C. were responsible for conceptualising the research. K.S. was responsible for methodology and project administration. K.S. and M.C. were responsible for supervision. K.S., K.H., and J.G. handled data curation. K.S., M.C., and K.H. were responsible for data screening and verification. K.S., J.G., and K.H. were responsible for data extraction. J.G. was responsible for descriptive analysis. K.S., M.C., and K.H. were responsible for qualitative analysis. K.S. wrote the first draft of the paper with input from the rest. K.H. and K.S. were responsible for data visualisation and the supplemental material. Each author wrote the part of the results section relevant to their data analysis.
Corresponding author
Correspondence to Katie Seaborn .
Ethics declarations
Competing interests.
All authors declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Seaborn, K., Henderson, K., Gwizdka, J. et al. A meta-review of psychological resilience during COVID-19. npj Mental Health Res 1 , 5 (2022). https://doi.org/10.1038/s44184-022-00005-8
Download citation
Received : 25 January 2022
Accepted : 17 March 2022
Published : 05 July 2022
DOI : https://doi.org/10.1038/s44184-022-00005-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
ORIGINAL RESEARCH article
Cross-sectional study of resilience, positivity and coping strategies as predictors of engagement-burnout in undergraduate students: implications for prevention and treatment in mental well-being.

- 1 School of Education and Psychology, University of Navarra, Pamplona, Spain
- 2 School of Psychology, University of Almería, Almería, Spain
- 3 UCD School of Psychology, University College Dublin, Dublin, Ireland
- 4 Konrad Lorenz University Foundation, Bogota, Colombia
- 5 Stress Prevention Unit, University of Sassari, Sassari, Italy
- 6 Department of Biomedical Sciences, University of Sassari, Sassari, Italy
- 7 STEM Unit and Centre for Workplace Excellence, University of South Australia, Adelaide, SA, Australia
In a population of young adults, this study analyzes possible linear relations of resilience and positivity to coping strategies and engagement-burnout. The aim was to establish a model with linear, associative, and predictive relations, to identify needs and make proposals for therapeutic intervention in different student profiles. A population of 1,126 undergraduate students with different student profiles gave their informed, written consent, and completed validated questionnaires (CD-RISC Scale; Positivity; Coping Strategies of Stress; Engagement, and Burnout). An ex post-facto design involved bivariate association analyses, multiple regression and structural predictions. The results offered evidence of associations and predictive relationships between resilience factors, positivity, coping strategies and engagement-burnout. The factors of resilience and positivity had significant differential associations (positive and negative) with factors of coping strategies. Their negative relationship to burnout factors, and positive relation to engagement factors, is especially important. Results of structural analysis showed an acceptable model of relationships between variables. We conclude with practical implications for therapeutic intervention: (1) the proactive factors of resilience reflect a perception of self-efficacy and the ability to change adaptively; (2) the reactive factors of resilience are usually associated with withstanding experiences of change, uncertainty or trauma.
Introduction
The problem of academic stress in the University context and the demands of therapeutic response in this context has had great relevance in recent times. Numerous recent investigations have analyzed mental health prevention strategies in young University students, in order to minimize the psychological effects of this situation ( 1 , 2 ). To do this, they have focused their interest on the role of resilience and well-being. An example of this is the Monographic, in which this research is inserted ( 3 ).
The analysis of resilience, as a psychological variable in the sphere of preventive and therapeutic intervention, is important from both the structural and functional points of view ( 4 – 6 ). The distinction between structural and functional analysis of resilience is not often reflected in the previous literature, despite the importance of this distinction. Structural analysis of resilience makes it possible to reach a precise understanding of the role of each behavioral component of the theoretical construct, in order to infer therapeutic adjustment strategies for each person ( 7 , 8 ). Questions that illustrate structural analysis could be: Do all components of resilience have the same functionality? Is it possible to identify certain components of resilience that have a proactive value and others that are more reactive in nature? In complementary fashion, Functional analysis contributes to a procedural view of the behaviors associated with each component of resilience, in relation to other variables ( 9 ). In this case, questions may refer to the most likely possible relationship between components of resilience and a given variable: What factors in resilience will be strongest in predicting the psychological variable positivity, or coping strategies? Positivity and coping strategies were selected as important behavioral factors that can help predict states of engagement vs. burnout, in the context of academic stress, just as previous research has suggested ( 10 , 11 ). From an understanding of these structural and functional relationships, preventive and therapeutic intervention strategies can be plausibly established. The present study, therefore, offers a new model of evidence of plausible predictive relationships between the proactive and reactive components of resilience, positivity, coping strategies and state of engagement-burnout.
Resilience and Mental Well-Being in Young Adults
Over the past 50 years, the psychological study of stress and resilience to adversity has been plentiful ( 12 ). With the influence of Positive Psychology, resilience has become a very popular topic in the field of psychopathology as well, where there is growing interest in positive adaptation in response to stress ( 13 ).
A recent meta-analysis by Grossman ( 14 ) has identified more than 10,000 articles that include the term resilience, relating it negatively to physical health complaints, and positively to overall well-being. Moreover, resilience has been positively associated with the experience of positive emotions and the use of adaptive coping strategies, that is, problem-focused coping ( 15 ). Most researchers agree on the general definition of resilience as the ability to withstand adversity or recover from stress and negative experiences ( 12 , 14 – 17 ). Refining this definition, it can further be said that resilience is also the ability to move forward and grow in response to difficulties and challenges, that is, to become stronger through adversity ( 18 ).
The role of resilience, whether in protecting against stress, or in generating well-being, has been analyzed from several perspectives ( 19 ). Research also reports its value in personal recovery after health accidents ( 20 ), as well as in prevention of psychopathological symptoms, especially when resilience is worked on clinically within a cognitive-behavioral methodology ( 21 ). Additionally, recent studies have shown a connection between resilience and well-being, and between resilience and mental health ( 22 ), mediated by the relationship between optimism and subjective well-being ( 23 , 24 ).
Resilience and Behavioral Positivity as Protective Factors Against Stress
Resilience, as a personal characteristic, has been considered in Positive Psychology to be a factor that protects against stress ( 25 ). There is broad agreement that it is a complex, multidimensional construct ( 26 ). There is also consensus that two important aspects must be present to speak of resilience: an experience of adversity and a subsequent positive adaptation ( 13 , 27 – 29 ). These two underlying aspects of resilient experience help us implicitly understand two types of resilient behavior: (1) reactive , bearing up under negative events, or the ability to withstand ( 30 ); recall as coined by Persius: “he conquers who endures”; and (2) proactive , or a reaction to events that actively seeks to restore well-being ( 31 , 32 ); “look for the silver lining of the cloud” alludes to this type of behavior.
This positive adaptation brings benefits in terms of skills (hidden skills that are discovered and appreciated), relationships (which are selected, strengthened and improved), and changes in priorities and life philosophy, both toward the present and future ( 33 ). Moreover, scholars agree that resilience is an ability that can be the object of learning. Previous research points to the ability to bounce back as a relatively common phenomenon that does not stem from extraordinary qualities but from “ordinary magic” ( 34 ). Consequently, resilience improves with life experiences ( 35 , 36 ). On the other hand, there is still much debate about its nature. There is no clear understanding or consensus in the scientific community about its structure or its components ( 14 , 15 ), about the mechanisms that are implicit in the construct, or whether the processes and products of resilence should be considered traits or states ( 27 , 37 – 41 ). Several recent studies have established the connection between resilience and mental health, through positivity ( 42 ). Yet to be established are the precise behavioral mechanisms by which resilience takes shape as behavior. The present study seeks to contribute toward this end.
Resilience and Coping Strategies
Resilience has been associated with coping strategies, which have been identified as emotional meta-strategies ( 43 , 44 ). Accordingly, resilience has been found to be associated with a positive predictor of self-regulation, learning approaches and coping strategies ( 45 – 47 ). A relationship has also been established with effective learning ( 48 ). The literature is clear in that resilience reflects successful management of stress events ( 49 ), moderating their negative effects, and promoting adaptation and psychological well-being ( 14 , 29 , 50 ).
Certain previous studies have established specific relationships between resilience and coping ( 39 , 47 ). Resilience and coping are often used interchangeably, although there is growing evidence to suggest that they are conceptually distinct constructs, though related ( 37 ). Flecher and Srkar ( 27 ) indicate that “Resilience influences how an event is appraised whereas coping refers to the strategies employed following the appraisal of a stressful encounter” (p. 16). The message that emerges from the literature, according to these authors, is that resilience consists of various factors that promote personal assets and protect the individual from the negative appraisal of stressors; recovery and coping, then, are conceived as conceptually different from resilience.
Recent studies have shown that resilience and coping strategies are associated with and linearly predict well-being ( 51 , 52 ), as well as different diseases and health problems ( 53 , 54 ). Taking this consistent relationship further, the present study aims to show the mediational role of coping strategies between resilience and the motivational states of engagement-burnout.
Resilience and the Emotional States of Engagement vs. Burnout
Resilience has appeared as a protective variable against stress, and a negative predictor (or protective) of burnout ( 55 ). In the sphere of employment, numerous studies have indicated a negative relationship between resilience and burnout ( 56 ), as well as a positive relationship with engagement ( 57 ). Other research studies have shown that emotional skills mediate in the states of engagement-burnout ( 58 ).
In the academic context, resilience has been considered as an attitudinal or meta-motivational variable, within the Competence for Studing, learning and Performance with Stress , a CSLS model of competence for managing academic stress [( 59 ); in review]. Given its high degree of relationship with self-regulatory behavior, it has been conceptualized as a meta-ability that can determine the motivational state of students, in situations of academic stress. Therefore, it is possible to assume that it is a positive predictor of the motivational state of engagement and a negative predictor of the motivational state of burnout in University students. Several studies have reported the negative mediational role of resilience with respect to a state of burnout, and a positive mediational role in engagement ( 60 , 61 ).
Aims and Hypotheses
Yet to be established, however, are the specific mechanisms of how each component of resilience acts on the two motivational states (engagement vs. burnout), through coping strategies. This is the aim of the present study. Linear relations between resilience, coping strategies and engagement-burnout were applied to infer needs and proposals for intervening in different profiles of students. Based on prior evidence, the following hypotheses were posed: (H1) resilience would be associated with the personal variable of positivity, acting as a positive predictor; (H2) both variables, jointly, would be associated with and would be significantly positive predictors of problem-focused strategies and the motivational state of engagement; (H3) both would also be negative predictors of emotion-focused strategies and the motivational state of burnout.
Participants
An initial 1,126 undergraduate students participated in this study. The response rate was 95%, for a total of 1,069 students. This sample corresponds to a population of inference of 1,376 University students, with 99% total confidence and 0.1 percentage. The sample contained students enrolled in Psychology, Primary Education, and Educational Psychology; 85.5% were women and 14.5% were men. The age range was 19–25, and mean age was 21.33 years (sd = 2,73). Two Spanish public universities with similar characteristics were represented; 324 students attended one University and the remainder attended the other. The study design was incidental and non-randomized. The Guidance Department at each University invited teacher participation, and the teachers invited their own students to participate, on an anonymous, voluntary basis. Each course (subject) was considered one specific teaching-learning process.
Instruments
A validated Spanish version ( 62 ) of the Connor-Davidson Resilience scale , CD-RISC Scale ( 63 ) was used to measure resilience. Answers range from 1 (“Not true at all”) to 5 (“True nearly all the time”). Adequate reliability and validity values had been obtained in Spanish samples, and a five-factor structure emerged [Chi-square = 1,619, 170; Degrees of freedom (350-850) = 265; p < 0.001; Ch/Df = 6,110; SRMR (Standarized Root Mean-Square) = 0.062; NFI (Normed Fit Index) = 0.957; RFI (Relative Fix Index) = 0.948; IFI (Incremental Fix Index) = 0.922; TLI (Tucker Lewis index) = 0.980; CFI (Comparative fit index) = 0.920; RMSEA (Root Mean Square Error) = 0.063; HOELTER = 240 ( p < 0.05) and 254 ( p < 0.01)]. F1: Persistence/tenacity and strong sense of self-efficacy (TENACITY; alpha = 0.80); F2: Emotional and cognitive control under pressure (STRESS; alpha = 0.80); F3: Adaptability/ability to bounce back (CHANGE; alpha = 0.77); F4: Perceived Control (CONTROL; alpha = 0.77), and F5: Spirituality (alpha = 0.71).
The positivity scale Escala de Positividad , by Caprara et al. ( 64 ), was used to measure this variable. Ten items are to be answered on a 5-point Likert scale. Acceptable values were obtained in our sample from the Spanish validation data [Chi-square = 208.992; Degrees of freedom (58-20) = 38; p < 0.001; Ch/Df = 5,499; SRMR (Standarized Root Mean-Square) = 0.062; NFI (Normed Fit Index) = 0.901; RFI (Relative Fix Index) = 0.894; IFI (Incremental Fix Index) = 0.912; TLI (Tucker Lewis index) = 0.923, CFI (Comparative fit index) = 0.916; RMSEA (Root Mean Square Error) = 0.085; HOELTER = 260 ( p < 0.05) and 291 ( p < 0.01)]. Good internal consistency was also found (Alpha = 0.893; Part 1 = 0.832, Part 2 = 0.813; Spearman-Brown = 0.862; Guttman = 0.832).
Coping Strategies
This variable was measured using the Escala Estrategias de Coping (Coping Strategies Scale), EEC, in its original version ( 65 ), validated for University students ( 66 ). Theoretical-rational criteria were used in constructing this scale, taking the Lazarus and Folkman questionnaire ( 67 ) and coping assessment studies by Moos and Billings ( 68 ) as foundational. Validation of the original, 90-item instrument produced a first-order structure with 64 items and a second-order structure with 10 factors and two dimensions, both of them significant. Answers range from 1 (“Not true at all”) to 5 (“True nearly all the time”). The second-order structure showed adequate fit values (Chi-square = 378.750; Degrees of freedom (87-34) = 53, p < 0.001; Ch/Df = 7,146; SRMR = 0.071; NFI = 0.901; RFI = 0.945; IFI = 0.903, TLI = 0.951, CFI = 0.903). Reliability was confirmed with the following measures: Cronbach alpha values of 0.93 (complete scale), 0.93 (first half) and 0.90 (second half), Spearman-Brown of 0.84 and Guttman 0.80. There are eleven factors and two dimensions: (1) Dimension: emotion-focused coping, F1. Fantasy distraction; F6. Help for action; F8. Preparing for the worst; F9. Venting and emotional isolation; F11. Resigned acceptance. (2) Dimension: problem-focused coping, F2. Help seeking and family counsel; F5. Self-instructions; F10. Positive reappraisal and firmness; F12. Communicating feelings and social support; F13. Seeking alternative reinforcement.
Engagement-Burnout
Adequate reliability and construct validity indices for this construct have been found in cross-cultural investigations. Engagement was assessed using a validated Spanish version of the Utrecht Work Engagement Scale for Students ( 69 ). Satisfactory psychometric properties were found with a sample of students from Spain. The model obtained good fit indices, and the second-order structure had three factors: vigor, dedication, and absorption. Answers range from 1 (“Not true at all”) to 5 (“True nearly all the time”). Scale unidimensionality and metric invariance were also confirmed in the samples assessed (Chi Square = 592.526, df = 74, p < 0.001; Ch/Df = 8,007; SRMR = 0.057; CFI = 0.954, TLI = 0.976, IFI = 0.954, TLI = 0.979, and CFI = 0.923; RMSEA = 0.083; HOELTER = 153, p < 0.05; 170 p < 0.01). The Cronbach alpha for this sample was 0.900 (14 items), with 0.856 (7 items) and 0.786 (7 items) for the two parts.
The Maslach Burnout Inventory, MBI ( 70 ), in its validated, open format Spanish version ( 69 ), was used to assess Burnout. Answers range from 1 (“Not true at all”) to 5 (“True nearly all the time”). Psychometric properties for this version were satisfactory in students from Spain. Good fit indices were obtained in this sample, and a second-order structure of three factors: exhaustion or depletion, cynicism, and lack of effectiveness. Scale unidimensionality and metric invariance were also confirmed in the samples assessed (Chi Square = 667.885, df = 87, p < 0.001; Ch/Df = 7,67; CFI = 0.956, TLI = 0.964, IFI = 0.951, TLI = 0.951, and CFI = 0.953; RMSEA = 0.071; HOELTER = 224, p < 0.05; 246 p < 0.01). The Cronbach alpha for this sample was 0.874 (15 items); the two parts of the scale showed 0.853 (8 items) and 0.793 (7 items), respectively.
In a single study, after signing their informed consent, students completed the validated questionnaires on an online platform. Scale completion was voluntary ( 71 ); students reported on five specific teaching-learning processes, each one representing a different University subject they took during a 2-year academic period. Presage variables were assessed in September-October of 2018 and 2019, Process variables in February-March of 2018 and 2019, and Product variables in May-June of 2018 and 2019. The respective Ethics Committees of the two universities approved the procedure, in the context of an R&D Project (2018-2021).
Data Analyses
The ex post-facto design ( 72 ) of this cross-sectional study involved bivariate association analyses, multiple regresion and structural predictions (SEM). The preliminary analyzes were carried out to guarantee the adequacy in the use of the parametric analyzes carried out: normal distribution (Kolmogoroff-Sminorf), skewness and kurtosis (±0.05).
Correlation Analysis
In order to test the association hypotheses in H1, H2, and H3, we correlated positivity with the variable resilience, coping strategies, and engagement-burnout variables (Pearson bivariate correlation), using SPSS (v.25). The assumptions assumed and contrasted for the Pearson correlation were: (1) The data must have a linear relationship, this was determined through a scatter plot; (2) The variables must have a normal distribution; (3) The observations used for the analysis should be collected randomly from the reference population.
Prediction Analysis
For the prediction hypotheses of H1, H2, and H3, multiple regression analyses were carried out, and Beta indices of prediction and significance were calculated, using SPSS (v.25). The correlation and prediction factors were calculated using the factors originating from the exploratory factor analysis, prior to the confirmatory factor analysis.
Structural Equation Model
Two different Structural Equation Models (SEM) models were tested. In the first model, the effect of gender and the mediating prediction of engagement-burnout as predictors of coping strategies (Resilience → Positivity → Engagament-Burnout → Coping strategies) was evaluated; in the second model, the prediction presented in the graph and significantly valid (Resilience → Positivity → Coping strategies → Engagament-Burnout). Model fit was assessed by first examining the chi-square to degrees of freedom ratio as well as the Comparative Fit Index (CFI) and Normed Fit Index (NFI), Incremental Fit Index (IFI), and Relative Fit Index (RFI). These should ideally be >0.90. The Hoelter Index was also used to determine sample size adequacy ( 73 ). AMOS (v.26) was used for these analyses. Indirect effects values were assumed to be: the regression coefficients for small (0.14), medium (0.39), and large (0.59) effects are interpreted under the assumption that the error variances of the mediator and the dependent variable are both 1.0 ( 74 ). Direct, indirect and total effects, their significance levels and confidence intervals ( 75 , 76 ) were calculated by bootstrapping (1,000 samples), using the maximum likelihood method ( 77 ). For the specific calculation of the confidence intervals of the indirect effects (Specific Indirect Effects mediation AMOS plugin, V.26) were used.
Descriptive Preliminary Results
The direct and statistical values found in the preliminary sampling normality and adequacy tests showed acceptable values for the subsequent linear analysis of association and structural prediction carried out. See Table 1 .
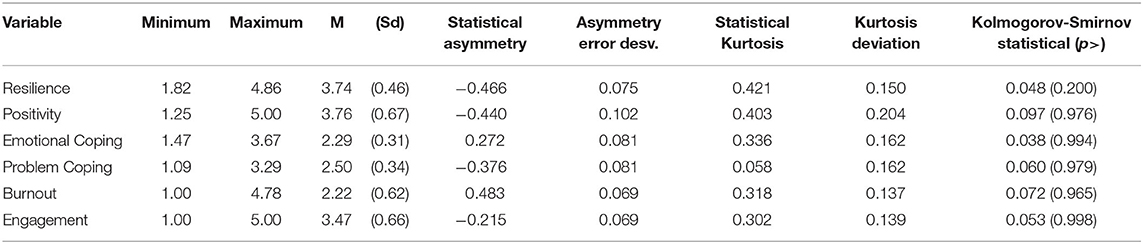
Table 1 . Descriptive values of the analyzed variables.
Bivariate Association Relations
Resilience and positivity.
The bivariate correlational analyses between resilience (total and factors) and positivity showed a significant positive association between the two, with particular associative strength for perceived control and tenacity. See Table 2 .
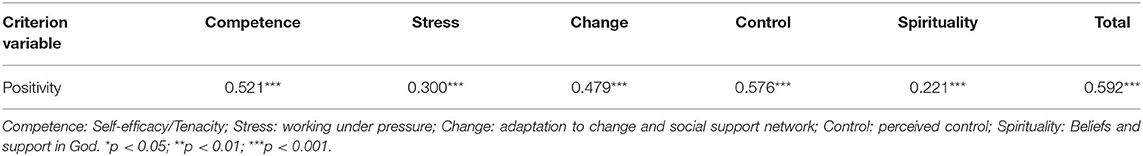
Table 2 . Bivariate correlations between resilience and positivity ( n = 1,069).
Bivariate correlational analyses between resilience (total and factors) and coping strategies showed several significant relationships. On one hand, the total resilience score was positively associated with total coping strategies ( r = 0.245, p < 0.001). In general, all the factors or components of resilience appeared to be associated positively with coping strategies focused on the problem and negatively with factors focused on emotion, except for spirituality, which appeared positively associated with both. Specifically, this association was positive with problem-focused strategies (CF2. Seeking help and family advice; CF5. Self-Instructions; CF10. Positive reappraisal and firmness; CF12. Communicating feelings and social support; CF13. Seeking alternative reinforcement), and negative with emotion-focused strategies (CF8. Preparing for the worst; CF9. Emotional venting and isolation; CF11. Resigned acceptance). Three resilience factors followed this tendency, namely: perceived control (control), acceptance of change (change) and tenacity and perception of competence (competence). The tolerance to stress factor (stress) was low related to emotion-focused strategies (only with CF9. Emotional venting and isolation; CF11. Resigned acceptance). The only factor that was positively associated both with emotion-focused strategies and with problem-focused strategies was spirituality (CF1. Avoidant distraction; CF8. Preparing for the worst; CF11. Resigned acceptance). Of special interest is the negative association between the components of resilience and the CF9 factor (Emotional venting and isolation), as a precursor coping factor for health problems. See Table 3 .
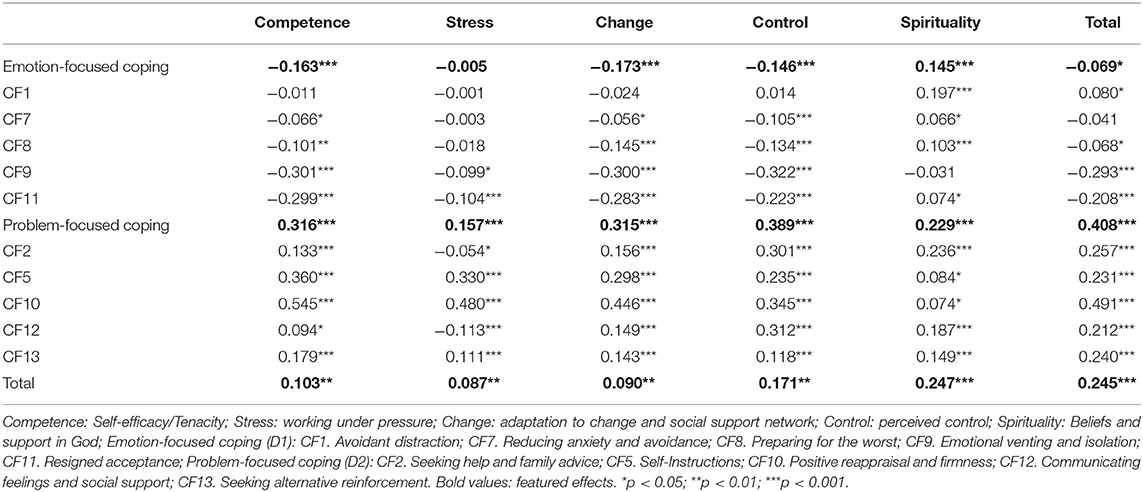
Table 3 . Bivariate association of resilience with specific strategies for coping with stress ( n = 1,069).
Resilience and Engagement vs. Burnout
Total resilience was found to be consistently, significantly, and positively associated with engagement ( r = 0.346 ; p < 0.001) and its components, and negatively with burnout ( r = −0.372 ; p < 0.001) and its components, with particular associative strength for the component lack of effectiveness . Certain resilience factors were significantly associated with engagement and burnout, positively for the former, negatively for the latter: tenacity and perceived competence ( competence ), adaptation to change (change) , perceived control (control) , and stress tolerance (stress) were found to be positively associated with engagement; the component with the least associative strength was spiritual beliefs (spirituality) . Complementarily, the resilience factors that appeared negatively associated with burnout were tenacity and perceived competence (competence) , perceived control (control) , and adaptation to change ( change ). Moreover, the resilience factors that appeared negatively associated with burnout were the tenacity and perceived competence (competence) , perceived control (control) , and adaptation to change (change); with a lower associative force, the stress tolerance (stress) and spiritual beliefs (spirituality) . See Table 4 .
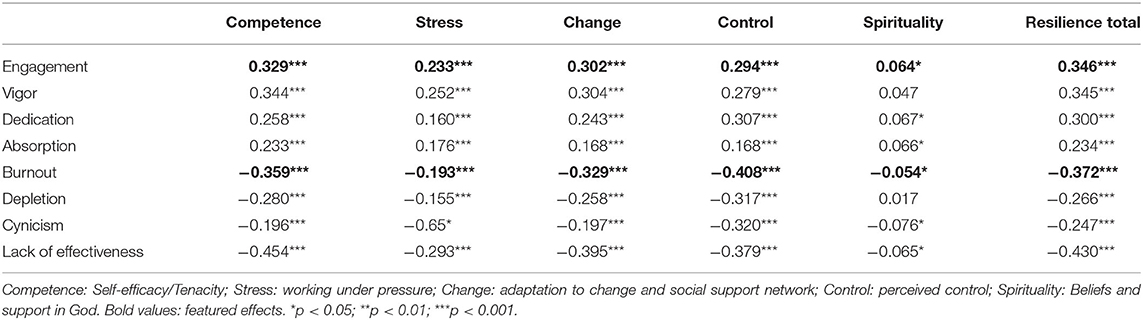
Table 4 . Bivariate associations of resilience and engagement-burnout ( n = 1,069).
Multiple Prediction Relations
The multiple regression analysis showed a significant prediction effect of resilience factors on positivity. The resilience factors with the greatest positive predictive statistical effect were Perceived competence, Perceived control, and Spirituality. However, Tolerance to stress (stress) was not predictive of positivity. See Table 5 .
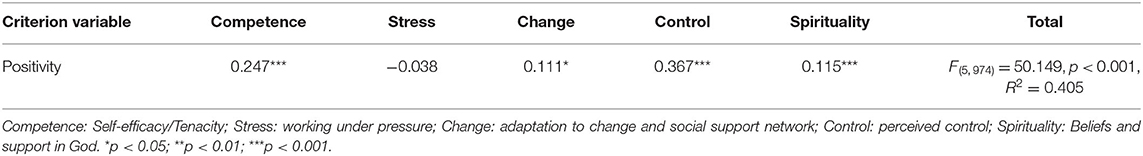
Table 5 . Regression relations between resilience components and positivity ( n = 1,069).
Results of multiple regression showed three types of relations between resilience factors and coping strategies: (1) factors that negatively predicted the use of emotion-focused strategies and positively predicted problem-focused strategies: perceived control, adaptation to change , and perceived competence ; (2) one factor that positively predicted the use of emotion-focused strategies and negatively predicted problem-focused strategies: stress management ; (3) one factor that predicted the combined use of both strategy types: Spirituality .
It should be noted that in the case of emotion-focused strategies, the factors that were predicted with the most statistical force -significant and moderate correlation- were CF9 ( Emotional venting and isolation ) and CF11 (Resigned acceptance ), while in problem-focused strategies, they were CF10 (Positive reappraisal and firmness), CF12 (Communicating feelings and social support), and CF5 (Self-Instructions). Of special note is Factor CF9, which was negatively predicted by the factors perceived competence, perceived control and adaptation to change . However, it was positively predicted by the stress management factor and unassociated with spirituality . See Table 6 .
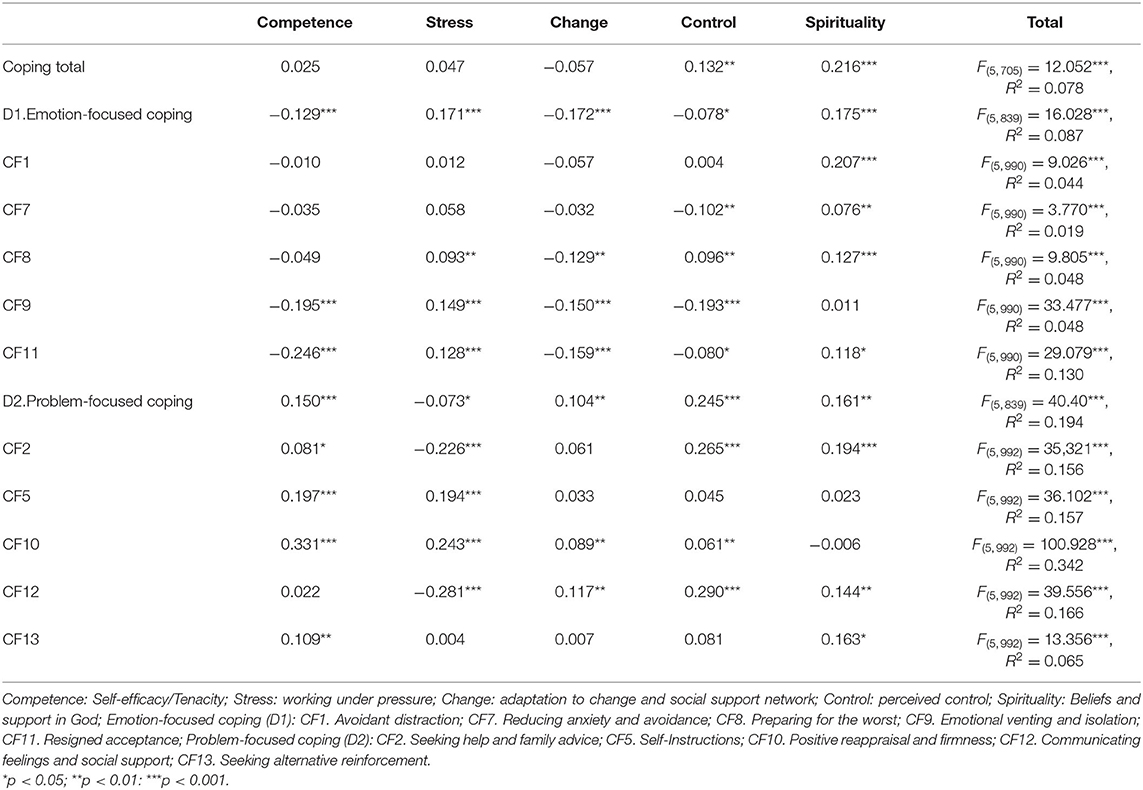
Table 6 . Multiple regression of resilience to dimensions and factors of coping strategies ( n = 1,069).
Resilience and Engagement-Burnout
Results of multiple regression showed three types of relations between resilience factors and the motivational state of engagement-burnout: (1) factors that negatively predicted burnout, and positively predicted engagement, as well as its components: perceived competence, perceived control , and adaptation to change . Perceived competence positively predicted, with greater strength, the components of vigor, dedication and absorption; perceived control was a significant negative predictor of the emotional state of depletion, cynicism and lack of effectiveness; adaptation to change had the same tendency, but with less strength; (2) two factors that did not significantly predict burnout and engagement: tolerance of stress and spirituality . The only factor that positively and significantly predicted depletion was spirituality . See Table 7 .

Table 7 . Multiple regression of resilience to engagement-burnout ( n = 1,069).
Structural Prediction Model
Evidence was obtained of association and prediction relationships between resilience factors, coping strategies and engagement-burnout. Different significant associations (positive or negative) appeared between resilience factors and factors of coping strategies. The negative relationship to burnout factors, and positive relation to engagement factors, was especially important. The SEM results showed an acceptable relationship model. See Table 8 and Figure 1 .
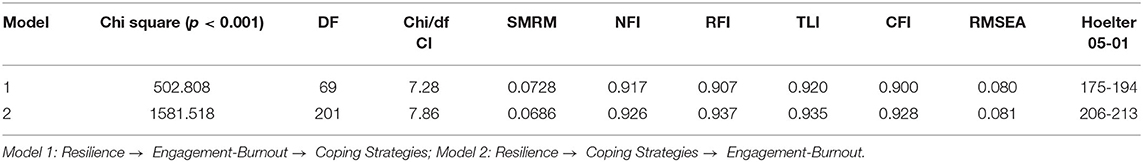
Table 8 . Models of structural linear results of the variables ( n = 1,069).
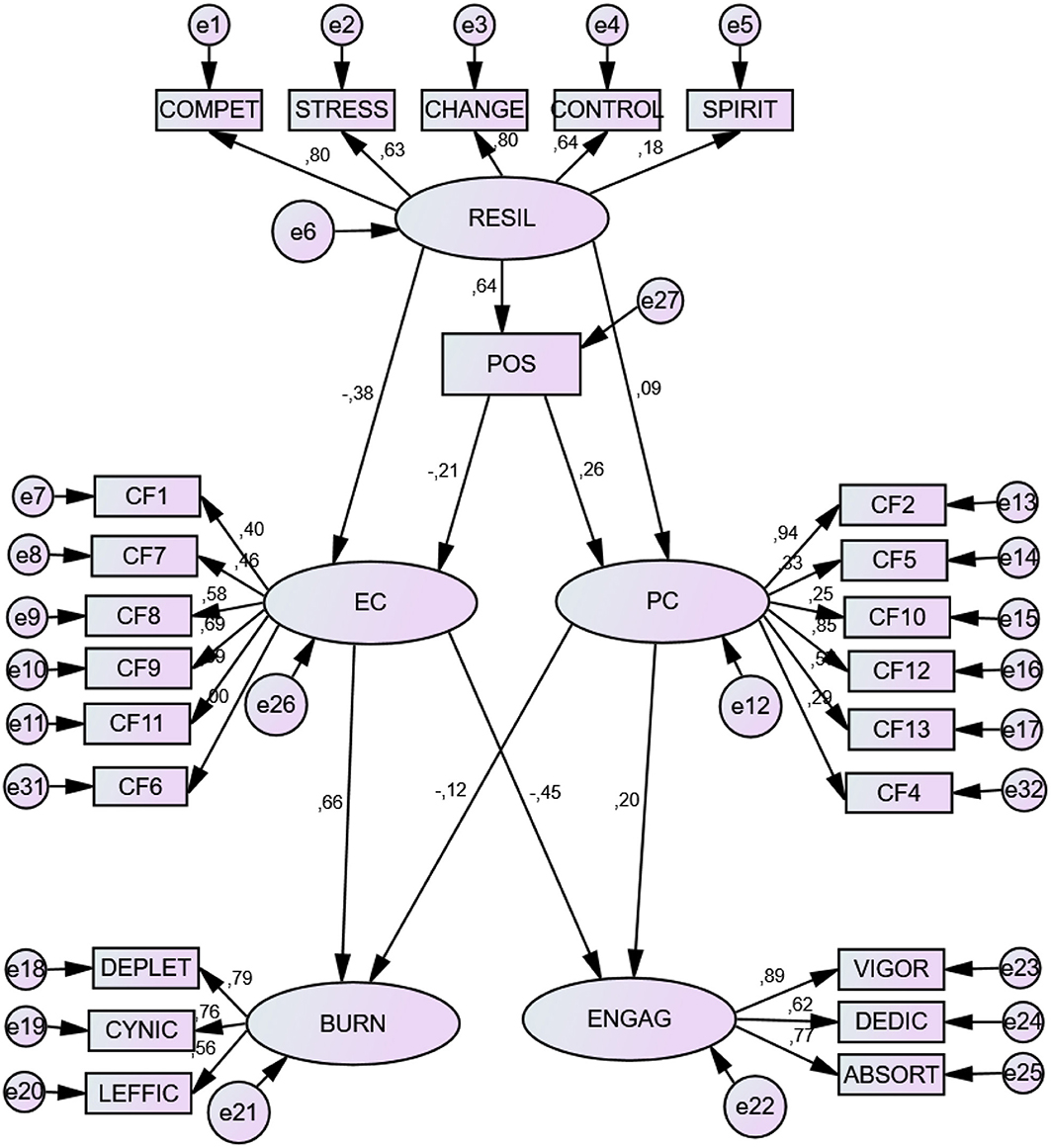
Figure 1 . Structural prediction model. RESIL, resilience; POS, Positivity; EC, Emotional Coping; PC, Problem Coping; BURN, Burnout; ENGAG, Engagement. COMPET, Persistence/tenacity and strong sense of self-efficacy; STRESS, Emotional and cognitive control under pressure; CHANGE, Adaptability/ability to bounce back; CONTROL, Perceived Control; SPIRIT, Spirituality. Emotion-focused coping: F1. Avoidant distraction; F7. Reducing anxiety and avoidance; F8. Preparing for the worst; F9. Emotional venting and isolation; F11. Resigned acceptance; Problem-focused coping: F2. Seeking help and family advice; F5. Self-Instructions; F10. Positive reappraisal and firmness; F12. Communicating feelings and social support; F13. Seeking alternative reinforcement. DEPLET, depletion; CYNIC, Cynicism; LEFFIC, Lack of effectiveness; VIGOR, vigor; DEDIC, Dedication; ABSORT, Absorption.
Direct Effects
There were several significant, direct prediction effects. Resilience showed a significant predictive effect on positivity. These two in conjunction appeared as positive predictors of problem-focused coping and negative predictors of emotion-focused coping . While resilience was the best negative predictor of emotion-focused coping, positivity was the best predictor of problem-focused coping . The factors that appeared with the most weight in the construct were perceived competence, ability to adapt to change , and perceived control .
Problem-focused coping was a positive predictor of engagement and negative predictor of burnout, while emotion-focused coping was a positive predictor burnout and negative predictor of engagement . F2 (Seeking help and family advice) and F12 (Communicating feelings and social support) were the factors with most weight in problem-focused coping , referring to social support; F11 (Resigned acceptance) and F9 (Emotional venting and isolation) had the most weight in emotion-focused coping .
Absorption and vigor were the factors with most weight in engagement; depletion; and cynicism had the most weight in burnout (See Table 9 ). Specific partial direct effects are shown in Table 10 .
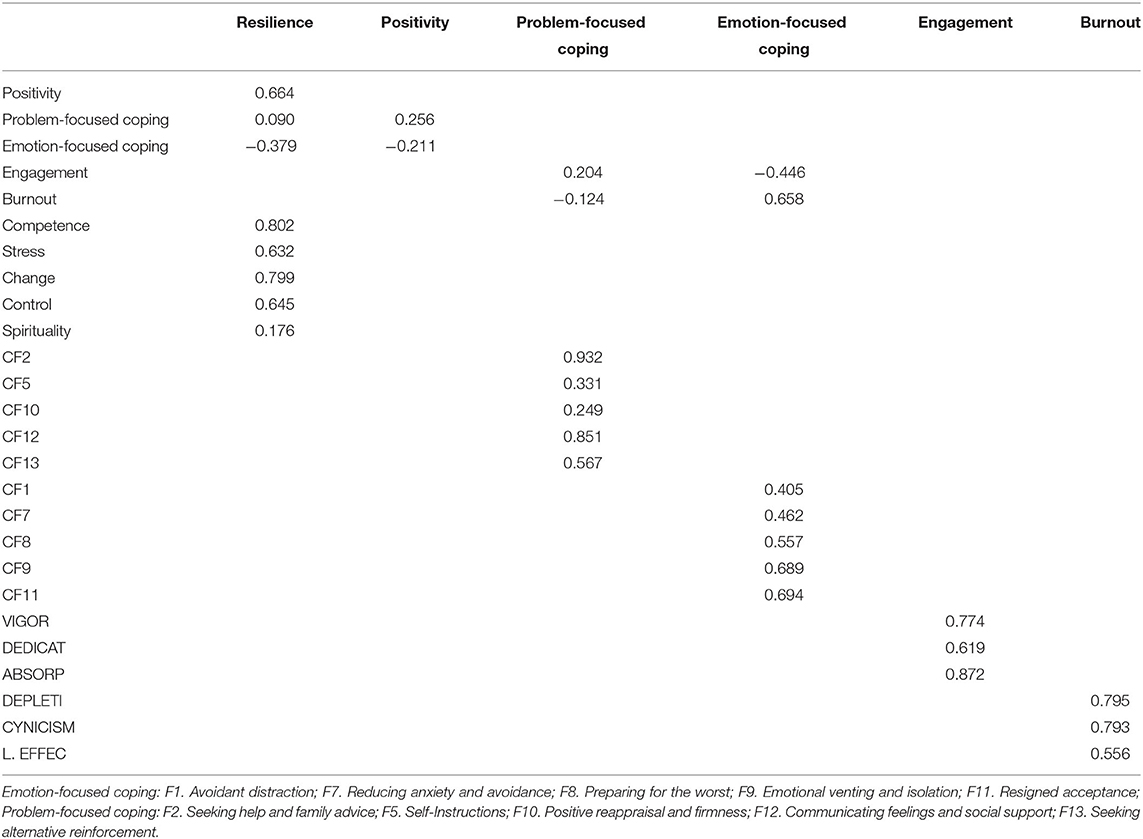
Table 9 . Standardized direct effects (default model).
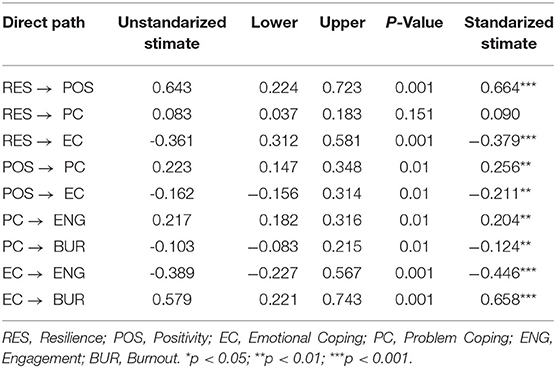
Table 10 . Direct effects specific and partial standardized values (95% B-CCI).
Indirect Effects
There were several indirect positive effects of Resilience and Positivity. Both variables showed multiple predictive indirect effects, in the same direction as the direct effects. Likewise, Coping Strategies had indirect effects on the components of Engagement and of Burnout: problem-focused strategies showed positive effects on Engagement and negative effects on Burnout, while emotion-focused strategies had inverse effects. Specifically, Resilience indirectly and positively predicted F2 (Seeking help and family advice) and F12 (Communicating feelings and social support), and negatively F9 (Emotional venting and isolation) and F11 (Resigned acceptance). It also positively and indirectly predicted the components of engagement and negatively the components of burnout. In a complementary way, Positivity indirectly and positively predicted F2 (Seeking help and family advice) and F12 (Communicating feelings and social support), and negatively F8 (Preparing for the worst). Finally, the strategies focused on the problem had an indirect and positive predictive effect on the engagement factors and negative on the burnout factors; however, the strategies focused on emotion had the reverse, that is, an indirect positive prediction on burnout and negative on engagement (see Table 11 ). Specific partial indirect effects are shown in Table 12 .
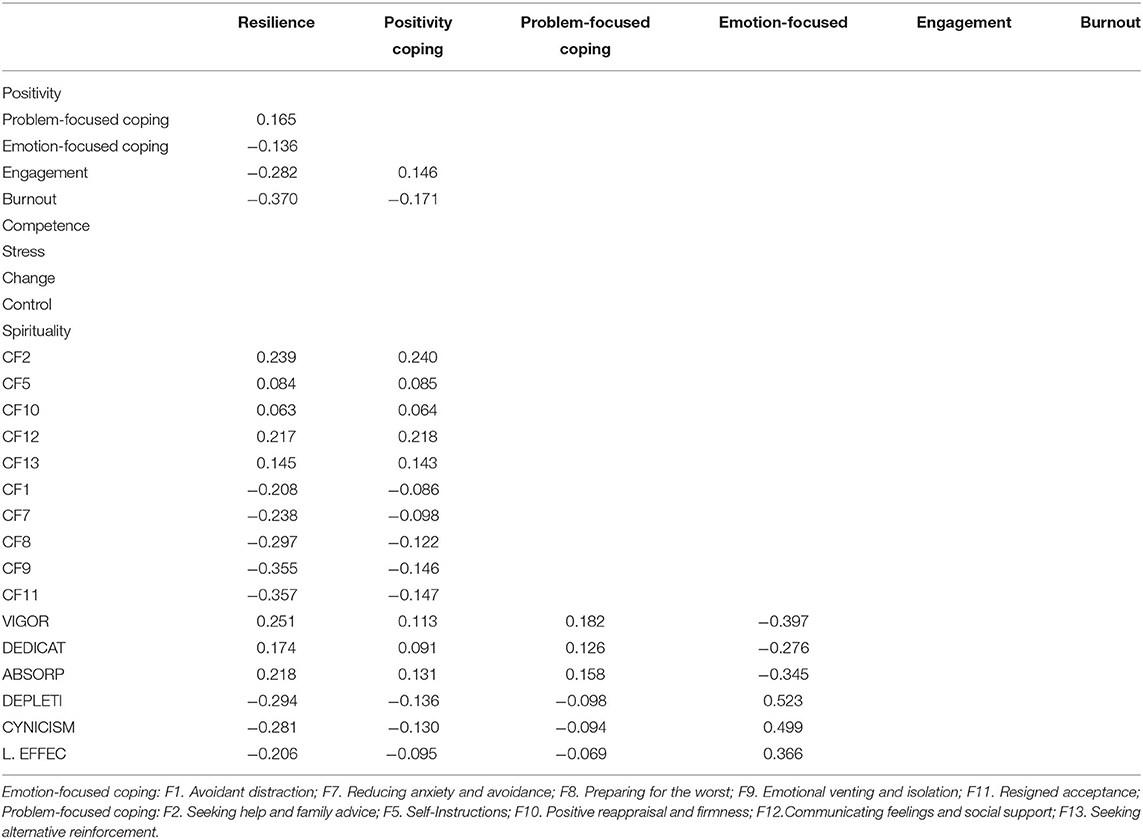
Table 11 . Standardized indirect effects (default model).
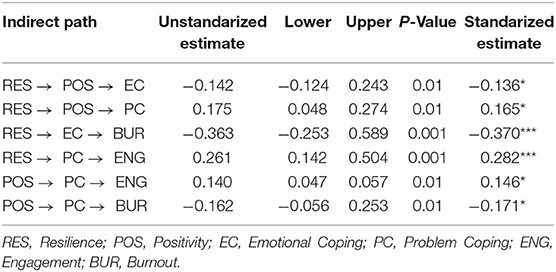
Table 12 . Indirect effects specific and partial standardized values (95% B-CCI).
This study aimed to show the relationship between resilience, positivity, coping strategies and the emotional state of burnout or engagement in undergraduate students. This relationship has not been reported previously, and, furthermore, it allows us to infer various implications for therapeutic intervention in mental health. The results referring to bivariate linear associations (Hypothesis 1) gave empirical evidence that resilience and positivity scores maintain a significant, positive association ( 78 – 80 ), especially in the case of the components perceived competence (tenacity and self-efficacy) and perceived control . These results reinforce the idea that resilience involves an important perception of self-efficacy and self-control ( 25 , 81 – 86 ). The results also agree with previous research that has shown a consistent relationship between self-regulation and resilience ( 10 , 45 , 87 , 88 ). In other words, an outlook of positivity seems more likely when a person's learning history has equipped them with positive achievement experiences, based on a perception of ability when facing adversity ( 29 , 89 , 90 ).
In the case of the association between resilience and coping strategies , the results showed that resilience is associated with a greater number of coping strategies –positive association with problem-focused strategies and negative with emotion-focused– especially in the case of perceived control, acceptance of change and perceived competence . These results expand on and refine those found in prior evidence ( 84 , 91 – 98 ), since the three behavioral factors would make the use of emotional management strategies less necessary; a higher level of self-regulation allows situations to be perceived with a lower level of stress ( 1 , 10 , 83 – 87 , 89 , 90 , 93 – 100 , 104 , 105 , 113 – 116 , 122 – 125 , 143 – 145 , 148 ). It is noteworthy that the stress tolerance factor (stress) was less related to emotion-focused strategies, which also implies a lower level of perceived stress ( 101 – 103 ). Also worth mentioning is the spirituality factor, which was the only factor associated with both emotion-focused strategies and problem-focused strategies ( 104 , 105 ). This would make it a kind of catalyst to other components which tend toward one type of strategy or another ( 106 – 108 ). Previous research has suggested the possibility that there are two different types of resilience profiles, with and without the spirituality factor ( 109 – 111 ).
The association between resilience and the motivational state of engagement-burnout appeared in the same direction as reported by previous research. In other words, there was a positive association with the state of engagement and a negative association with burnout , giving empirical value to resilience as a protective factor against stress ( 58 , 112 ), by means of students' emotional state ( 11 , 113 – 116 ).
In the case of multivariate prediction relationships ( Hypothesis 2 ), the results allow us to refine previous association relationships. The resilience factors that best predicted positivity were perceived competence, perceived control, and spirituality, while tolerance of stress did not appear as a significant predictor of positivity. This relationship might suggest that resilience includes proactive factors (based on positivity) and reactive factors (stress tolerance). It is not the same to be proactively positive in the face of stress than to bear with it in a reactive way ( 117 – 121 ).
Predictive relationships in relation to coping strategies have reinforced a consistent view of their directionality ( 122 – 125 ). Once again, the factors of perceived control, adaptation to change , and perceived competence negatively predicted the use of emotion-focused strategies and positively predicted problem-focused strategies ( 47 ). The factor tolerance to stress positively predicted the use of emotion-focused strategies and negatively predicted problem-focused strategies. Special attention must be given to the use of strategy F9 (Emotional venting and isolation), due to its harmful effect on physical and psychological health ( 126 ). This might suggest that the resilience factor tolerance to stress , as a passive or reactive factor in stress management, may involve harmful components from the behavioral point of view ( 127 ). The spirituality factor, however, predicted the combined use of problem- and emotion-focused strategies, making it a factor that adds value to the previous resilience factors ( 110 , 128 ).
Overall, the multivariate, linear predictive structural relationships ( Hypothesis 3 ) confirmed the predictions proposed. Resilience was found to positively predict positivity, and these two together predict a double path of influence: (1) positively predicting the use of problem-focused strategies and engagement, (2) negatively predicting the use of emotion-focused strategies and burnout. These novel results identify the specific coping mechanisms in the direct and indirect influence of resilience on engagement and on burnout, complementing previous research ( 57 , 129 ). However, identification of this relationship does not exhaust the possibilities of other influences and factors, which future research should establish.
It is also necessary to recognize certain limitations of the present investigation. First, there is the cross-sectional nature of the study. Second, the search for general models of relationships between these variables—already complex in itself- has meant setting aside the analysis of certain potentially mediating variables, such as gender and cultural diversity; previous research has established that both factors play a role ( 130 , 131 ). Third, the use of self-report tools for collecting data is always a well-known risk of bias. Future research should combine different evaluation systems ( 132 ). Fourth, the sample is University standardized and not clinical; results should therefore be taken with caution, and any inferences toward the clinical population must be done in a contextualized way. Fifth, the sample is composed predominantly of women. Consequently, all these limitations should be resolved in future research studies, expanding the sample type and analyzing different profiles or clusters of resilience types ( 133 ). The connection to other important variables, such as socioeconomic status and personal strengths, should also be clarified and delimited, considering their importance in current research. It would therefore be of interest to establish relationships between character strengths and resilience ( 84 , 134 – 136 ).
Conclusions
The above results confirm prior evidence and add new detail regarding to the structure and functionality of the construct of resilience. The structural analyses allow us to state that there are different profiles of factors: (1) proactive factors of resilience , its core components, with greater positive, proactive value, such as perceived competence, perceived control, and adaptation to change. In all three cases, they reflect a perception of self-efficacy and the ability to adapt in changing environments ( 31 , 137 ). (2) reactive factors of resilience , bearing with the negative emotion and maintaining the positive emotion that is usually associated with experiences of change, uncertainty or trauma ( 138 ); (3) the catalyzing factor of resilience , referring to spirituality , which adds value to the above factors, and may be considered a type of personal strength ( 139 ). This diversity of factors might indicate that there are different profiles of resilient persons, depending on the combination of the different factors in each person. Future research should inquire further into these complementary profiles.
Implications
Regarding implications for the practice of assessment and intervention in mental health, one can reasonably infer that these variables ought to be assessed in processes of post-traumatic stress or traumatic experiences. These variables convey crucial information about relevant factors to understanding and that can be protective for young adults, making it possible to predict successful outcomes from such situations ( 107 , 140 ). They also allow us to start from a previous explanatory model, and to infer factors for intervening at a molecular (clinical) level and at a molar (educational and contextualized) level of analysis ( 141 ).
Regarding implications for the promotion of mental health in higher education settings, in the Health, Counseling and Disability Services blog at Finders University, Garth Furber ( 142 ) indicates that Resilience is not an optional extra, not something that is nice to have, but something essential to build ( 143 – 145 ). The competency model for studying, learning, and performing under stress (SLPS competency) has considered resilience a meta-motivational variable, coping strategies to be meta-emotional variables, and engagement-burnout an emotional state that favors or hinders learning and academic achievement. The emotional fragility of students has become a serious problem in the university. Developing the capacity of resilience to stress is a precursor of student well-being ( 146 , 147 ). Universities are recognizing its importance and are beginning to invest in research and services designed to build resilience. The specific relationships that have been demonstrated between these variables make it possible to design specific University intervention programs, all universities should have centers that offer counseling and psychological support for students ( 148 ). Also, the pandemic could represent an extra burden in this equation that is not accounted in this paper.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Comité de Ética de la Universidad de Navarra; http://www.estres.investigacion-psicopedagogica.org/lib/pdf/CERTIFICADO_COMITE_DE_ETICA_UNAV.pdf . The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JF: director of the project, conceptualization, data analysis, and first draft. FS and SP: critical review and writing. AG-U and SF: data collection, data analysis, and project support. GS: technical support for the project. All authors: contributed to the article and approved the submitted version.
This work was supported by R&D Project PGC2018-094672-B-I00, University of Navarra (Ministry of Science and Education, Spain), and R&D Project UAL18-SEJ-DO31-A-FEDER (University of Almería, Spain), and the European Social Fund.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. de la Fuente J, Paoloni PV, Vera-Martínez MM, Garzón-Umerenkova A. Effect of levels of self-regulation and situational stress on achievement emotions in undergraduate students: class, study and testing. Int J Environ Res Public Health. (2020) 17:4293. doi: 10.3390/ijerph17124293
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Nahum M, Afek A, Ben-Avraham R, Davidov A, Cohen NB, Yehuda AB, et al. Psychological resilience, mental health and inhibitory control among youth and young adults under stress. Front Psychol . (2021) 10:446. doi: 10.3389/fpsyg.2019.00446
CrossRef Full Text | Google Scholar
3. Gabrielli S, Robis D, Cefai C. Promoting resilience interventions for mental well-being in youth: research topic. Front Psychol . (2020). Available online at: https://www.frontiersin.org/research-topics/13113/promoting-resilience-interventions-for-mental-well-being-in-youth#articles
4. Frangou S. Brain structural and functional correlates of resilience to bipolar disorder. Front Hum Neurosci. (2012) 5:184. doi: 10.3389/fnhum.2011.00184
5. Matheson K, Asokumar A, Anisman H. Resilience: safety in the aftermath of traumatic stressor experiences. Front Behav Neurosci . (2020) 14:596919. doi: 10.3389/fnbeh.2020.596919
6. Moreno-López L, Ioannidis K, Askelund AD, Smith AJ, Schueler K, Van Harmelen AL. The resilient emotional brain: a scoping review of the medial prefrontal cortex and limbic structure and function in resilient adults with a history of childhood maltreatment. Biol Psychiatry Cogn Neurosci Neuroimaging. (2020) 5:392–402. doi: 10.1016/j.bpsc.2019.12.008
7. Askeland KG, Hysing M, Sivertsen B, Breivik K. Factor structure and psychometric properties of the resilience scale for adolescents (READ). Assessment. (2020) 27:1575–87. doi: 10.1177/1073191119832659
8. Briganti G, Linkowski P. Item and domain network structures of the resilience scale for adults in 675 University students. Epidemiol Psychiatr Sci . (2020) 29:1–9. doi: 10.1017/S2045796020000323
9. Kasyanova E, Vinogradova N. Resilience as a factor of professional development of railway engineering students. In: International Session of Factors of Regional Extensive Development (FRED-2019) . Atlantis Press (2020). doi: 10.2991/fred-19.2020.1
10. de la Fuente J, Amate J, González-Torres MC, Artuch R, García-Torrecillas JM, Fadda S. Effects of levels of self-regulation and regulatory teaching on strategies for coping with academic stress in undergraduate students. Front Psychol . (2020) 11:22. doi: 10.3389/fpsyg.2020.00022
11. de la Fuente J, Lahortiga-Ramos F, Laspra-Solís C, Maestro-Martín C, Alustiza I, Aubá E, et al. Structural equation model of achievement emotions, coping strategies and engagement-burnout in undergraduate students: a possible underlying mechanism in facets of perfectionism. Int J Environ Res Public Health. (2020) 17:2106. doi: 10.3390/ijerph17062106
12. Prince-Embury K, Keefer KV, Saklofske DH. Psychosocial skills: school-based promotion of resiliency in children and adolescents. In: Lipnevich AA, Preckel F, Roberts RD, editors. Psychosocial Skills and School Systems in the 21st Century . Cham: Springer (2016). p. 301–24.
Google Scholar
13. O'Dougherty Wright M, Masten AS, Narayan AJ. Resilience processes in development: four waves of research on positive adaptation in the context of adversity. In: Goldstein S,Brooks RB, editors. Handbook of Resilience in Children . New York, NY: Springer (2013). p.15–37.
14. Grossman MR. Clarifying the Nature of Resilience: A Meta-Analytic Approach (Graduate theses and dissertations) (2014). Available online at: http://scholarcommons.usf.edu/etd/5031 (accessed June 10, 2020).
15. Grossman MR. The Structure of Resilience: An Empirical Examination of Resilience Factors (Graduate theses and dissertations). University of South Florida (2017). Retrieved from: https://scholarcommons.usf.edu/etd/6851 (accessed June 10, 2020).
16. Gerson M, Fernandez N. PATH: a program to build resilience and thriving in undergraduates. J Appl Soc Psychol. (2013) 43:2169–84. doi: 10.1111/jasp.12168
17. Petway KT, Brenneman MW, Kyllonen PC. Conecting noncognitive development to the Educational Pipeline. In: Khine MS, Areepattamannil S, editors. Non-cognitive Skills and Factors in Educational Attainment . Dordrecht: Sense Publishers (2016).
18. Ryan J, Jones S, Hayes P, Turner M. Building student resilience for graduate work readiness. In: Diver A, editor. Employability via Higher education: Sustainabilility as Scholars . Liverpool: Springer (2019).
19. Aburn G, Gott M, Hoare K. What is resilience? An integrative review of the empirical literature. J Adv Nurs. (2016) 72:980–1000. doi: 10.1111/jan.12888
20. Rapport LJ, Wong CG, Hanks RA. Resilience and well-being after traumatic brain injury. Disabil Rehabil. (2020) 42:2049–55. doi: 10.1080/09638288.2018.1552327
21. Chmitorz A, Kunzler A, Helmreich I, Tüscher O, Kalisch R, Kubiak T, et al. Intervention studies to foster resilience-a systematic review and proposal for a resilience framework in future intervention studies. Clin Psychol Rev. (2018) 59:78–100. doi: 10.1016/j.cpr.2017.11.002
22. Wu Y, Sang Z, Zhang X-C, Margraf J. The relationship between resilience and mental health in Chinese college students: a longitudinal cross-lagged analysis. Front Psychol . (2020) 11:108. doi: 10.3389/fpsyg.2020.00108
23. He F, Cao R, Feng Z, Guan H, Peng J. The impacts of dispositional optimism and psychological resilience on the subjective well-being of burn patients: a structural equation modelling analysis. PLoS ONE. (2013) 8:8–12. doi: 10.1371/journal.pone.0082939
24. Miranda JO, Cruz RNC. Resilience mediates the relationship between optimism and well-being among Filipino University students. Curr Psychol . (2020) 39:1–10. doi: 10.1007/s12144-020-00806-0
25. Hernandez AL, González-Escobar S, González NI, López-Fuentes A, Barcelata BE. Stress, self-efficacy, academic achievement and resilience in emerging adults. Electron J Res Educ Psychol . (2019) 17:129–48. doi: 10.25115/ejrep.v17i47.2226
26. Wu G, Feder A, Cohen H, Kim JJ, Calderon S, Charney DS, et al. Understanding resilience. Front Behav Neurosci. (2013) 7:10. doi: 10.3389/fnbeh.2013.00010
27. Fletcher D, Sarkar M. Psychological resilience: a review and critique of definitions, concepts, and theory. Eur Psychol. (2013) 18:12–23. doi: 10.1027/1016-9040/a000124
28. Masten AS. Resilience in developing systems: progress and promise as the fourth wave rises. Dev Psychopathol. (2007) 19:921–30. doi: 10.1017/S0954579407000442
29. Denovan A, Crust L, Clough PJ. Resilience at work. In: Oades LG, Steger M, Fave AD, Passmore J, editors. The Wiley Blackwell Handbook of the Psychology of Positivity and Strengths-Based Approaches at Work . Hoboken, NJ: John Wiley and Sons (2017). p. 132–49.
30. Obradović J. How can the study of physiological reactivity contribute to our understanding of adversity and resilience processes in development? Dev Psychopathol. (2012) 24:371. doi: 10.1017/S0954579412000053
31. Holguin-Alvarez JA, Rodríguez-Castillo MF. Proactividad y resiliencia en estudiantes emprendedores de Lima (Proactivity and resilience in entrepreneurial students from Lima). Propósitos y Representaciones. (2020) 8:1–20. doi: 10.20511/pyr2020.v8n2.367
32. Sierra MTC. Resiliencia, bienestar y aprendizaje a lo largo de la vida (Resilience, wellness and lifelong learning). Revista INFAD de Psicología. Int J Dev Educ Psychol. (2016) 1:161–70. doi: 10.17060/ijodaep.2016.n2.v1.501
33. Haidt J. The Happiness Hypothesis: Finding Modern Truth in Ancient Wisdom . New York, NY: Basic Books (2006).
34. Masten AS. Ordinary Magic: Resilience in Development . New York, NY: Guilford Publications (2015).
PubMed Abstract | Google Scholar
35. APA. The Road to Resilience . American Psychological Association (2014). Retrieved from: https://studentsuccess.unc.edu/files/2015/08/The-Road-to-Resiliency.pdf (accessed June 10, 2020).
36. APA. The Road to Resilience . (2020). Retrieved from: https://www.apa.org/centrodeapoyo/resiliencia-camino (accessed June 10, 2020).
37. Alonso-Tapia J, Rodríguez-Rey R, Garrido E, Saiz H, Ruiz M, Nieto C. Coping, personality, and resilience: prediction of subjective resilience from coping strategies and protective personality factors. Behav Psychol Psicolog í a Conductual . (2019) 27:375–89.
38. Denovan A, Dagnalla N, Dhingrab K, Grogana S. Evaluating the perceived stress scale among UK University students: implications for stress measurement and management. Stud Higher Educ. (2019) 44:120–33. doi: 10.1080/03075079.2017.1340445
39. Tamannaeifar M, Shahmirzaei S. Prediction of academic resilience based on coping styles and personality traits. Pract Clin Psychol. (2019) 7:1–10. doi: 10.32598/jpcp.7.1.1
40. Johnson ML, Taasoobshirazi G, Kestler JL, Cordova JR. Models and messengers of resilience: a theoretical model of college students' resilience, regulatory strategy use, and academic achievement. Educ Psychol. (2015) 35:869–85. doi: 10.1080/01443410.2014.893560
41. Liu H, Zhang J, Ji Y, Yang L. Biological and psychological perspectives of resilience: is it possible to improve stress resistance? Front Hum Neurosci . (2018) 12:326. doi: 10.3389/fnhum.2018.00326
42. Ungar M, Theron L. Resilience and mental health: how multisystemic processes contribute to positive outcomes. Lancet Psychiatry. (2020) 7:441–8. doi: 10.1016/S2215-0366(19)30434-1
43. Ben-Zur H. The effectiveness of coping meta-strategies: perceived eficiency, emotional correlates and cognitive performance. Pers Individ Diff. (1999) 26:923–39. doi: 10.1016/S0191-8869(98)00198-6
44. de la Fuente J. Competency for Studying, Learning and Performing under Stress: Self-help guide for University students, graduates and professional examination candidates . Almería: Education and Psychology I+D+I: e-publishing RandDandI Series (2015).
45. Artuch-Garde R, González-Torres Md C, de la Fuente J, Vera MM, Fernández-Cabezas M, López-García M. Relationship between resilience and self-regulation: a study of Spanish youth at risk of social exclusion. Front Psychol . (2017) 8:612. doi: 10.3389/fpsyg.2017.00612
46. de la Fuente J, Zapata L, Vera MM, González-Torres MC, Artuch-Garde R. Bullying, personal self-gulations, resilience, coping strategies and engagement-burnout: implications for intervention with universities students. In: Triggs P, editor. Handbook of Bullying . New York, NY: Nova Science Publisher (2014). p. 91–107.
47. de la Fuente J, Fernández-Cabezas M, Cambil M, Vera MM, González-Torres MC, Artuch-Garde R. Linear relationship between resilience, learning approaches, and coping strategies to predict achievement in undergraduate students. Front Psychol . (2017) 8:1039. doi: 10.3389/fpsyg.2017.01039
48. Prickett T, Walters J, Yang L, Harvey M, Crick T. Effective learning and resilience in first year undergraduate computer science. In: Proceedings of the 2020 ACM Conference on Innovation and Technology in Computer Science Education . New York, NY: Association for Computing Machinery (ACM) (2020). doi: 10.1145/3341525.3387372
49. Sarrionandia A, Ramos-Díaz E, Fernández-Lasarte O. Resilience as a mediator of emotional intelligence and perceived stress: a cross-country study. Front Psychol . (2018) 9:2653. doi: 10.3389/fpsyg.2018.02653
50. Pidgeon AE, Rowe NF, Stapleton P, Magyar HB, Lo BC. Examining characteristics of resilience among University students: an international study. Open J Soc Sci. (2014) 2:14–22. doi: 10.4236/jss.2014.211003
51. Palma-Gómez A, Herrero R, Baños R, García-Palacios A, Castañeiras C, Fernandez GL, et al. Efficacy of a self-applied online program to promote resilience and coping skills in University students in four Spanish-speaking countries: study protocol for a randomized controlled trial. BMC Psychiatry. (2020) 148:1–15. doi: 10.1186/s12888-020-02536-w
52. Tomás JM, Sancho P, Melendez JC, Mayordomo T. Resilience and coping as predictors of general well-being in the elderly: a structural equation modeling approach. Aging Mental Health. (2012) 16:317–26. doi: 10.1080/13607863.2011.615737
53. Lai HL, Hung CM, Chen CI, Shih ML, Huang CY. Resilience and coping styles as predictors of health outcomes in breast cancer patients: a structural equation modelling analysis. Eur J Cancer Care. (2020) 29:e13161. doi: 10.1111/ecc.13161
54. Tu PC, Yeh DC, Hsieh HC. Positive psychological changes after breast cancer diagnosis and treatment: the role of trait resilience and coping styles. J Psychosoc Oncol. (2020) 38:156–70. doi: 10.1080/07347332.2019.1649337
55. Fiorilli C, Farina E, Buonomo I, Costa S, Romano L, Larcan R, et al. Trait emotional intelligence and school burnout: the mediating role of resilience and academic anxiety in high school. Int J Environ Res Public Health. (2020) 17:3058. doi: 10.3390/ijerph17093058
56. Anasori E, Bayighomog SW, Tanova C. Workplace bullying, psychological distress, resilience, mindfulness, and emotional exhaustion. Serv Ind J. (2020) 40:65–89. doi: 10.1080/02642069.2019.1589456
57. Malik P, Garg P. Learning organization and work engagement: the mediating role of employee resilience. Int J Hum Resour Manag. (2020) 31:1071–94. doi: 10.1080/09585192.2017.1396549
58. Salmela-Aro K, Upadyaya K. School engagement and school burnout profiles during high school-The role of socio-emotional skills. Eur J Dev Psychol . (2020) 17:1–22. doi: 10.1080/17405629.2020.1785860
59. de la Fuente J. A structural equation model of protection and risk factors for University academic stress: analysis and implications for the COVID-19 emergency. Front Psychol . (in review).
60. Oyoo SA. Academic resilience as a predictor of academic burnout among form four students in Homa-Bay County, Kenya. Int J Educ Res. (2018) 6:187–200.
61. Yu J, Chae S. The mediating effect of resilience on the relationship between the academic burnout and psychological well-being of medical students. Korean J Med Educ. (2020) 32:13. doi: 10.3946/kjme.2020.149
62. Manzano-García G, Ayala-Calvo JC. New perspectives: towards an integration of the concept “burnout” and its explanatory models. Anal Psicol . (2013) 29:800–9. doi: 10.6018/analesps.29.3.145241
63. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress Anxiety . (2003) 18:76–82. doi: 10.1002/da.10113
64. Caprara GV, Alessandri G, Eisenberg N, Kupfer A, Steca P, Caprara MG, et al. The positivity scale. Psychol Assess . (2012) 24:701–12. doi: 10.1037/a0026681
65. Chorot P, Sandín B. Escalas de Estrategias de Coping [Scales of Coping Strategies] . Madrid: UNED (1987).
66. de la Fuente J. Competence for Studying, Learning and Performance Under Stress: Self-Help Guide for University Students, Graduates and Professional Examination Candidades . Almería: Education and Psychology I+D+I (2015).
67. Lazarus RS, Folkman S. Stress, Appraisal, and Coping . New York, NY: Springer (1984).
68. Billings AC, Moos RH. Psychosocial theory and research on depression: an integrative framework and review. Clin Psychol Rev . (1982) 2:213–37. doi: 10.1016/0272-7358(82)90013-7
69. Schaufeli WB, Salanova M, González-Romá V, Bakker AB. The measurement of engagement and burnout: a two sample confirmatory factor analytic approach. J Happiness Stud. (2002) 3:71–92. doi: 10.1023/A:1015630930326
70. Maslach C, Jackson SE, Leiter MP. MBI: Maslach Burnout Inventory . Sunnyvale, CA: CPP (1996).
71. de la Fuente J, López M, Zapata L, Sollinas G, Fadda S. Improving mental health trough and online self-assessment and self-help e-Utility in university students. In: Nata RV, editor. Progress in Education , Vol. 33. New York, NY: Nova Publisher (2015). p. 63–74.
72. Ato M, Ato López J, Benavente A. Un sistema de clasificación de los diseños de investigación en psicología (A classification system for research designs in psychology). Anales de Psicolog í a . (2013) 29:1038–59. doi: 10.6018/analesps.29.3.178511
73. Tabachnick BG, Fidell LS. SAS for Windows Workbook for Tabachnick and Fidell Using Multivariate Statistics . Allyn and Bacon1 (2001).
74. Cheung MW-L. Comparison of methods for constructing confidence intervals of standardized indirect effects. Behav Res Methods. (2009) 41:425–38. doi: 10.3758/BRM.41.2.425
75. MacKinnon D, Fairchild A, Fritz M. Mediation analysis. Ann Rev Psychol. (2007) 58:593–614. doi: 10.1146/annurev.psych.58.110405.085542
76. Preacher KJ, Zhang Z, Zyphur MJ. Alternative methods for assessing mediation in multilevel data: the advantages of multilevel SEM. Struct Equ Model. (2011) 18:161–82. doi: 10.1080/10705511.2011.557329
77. Rucker D, Preacher K, Tormala Z, Petty R. Mediation analysis in social psychology: current practices and new recommendations. Soc Pers Psychol Compass. (2011) 5:359–71. doi: 10.1111/j.1751-9004.2011.00355.x
78. Bingöl TY, Batik MV, Hosoglu R, Firinci Kodaz A. Psychological resilience and positivity as predictors of self-efficacy. Asian J Educ Train. (2019) 5:63–9. doi: 10.20448/journal.522.2019.51.63.69
79. Chambers C, Ryder E. Supporting Compassionate Healthcare Practice: Understanding the Role of Resilience, Positivity and Wellbeing . Abingdon: Routledge. (2018).
80. Milioni M, Alessandri G, Eisenberg N, Caprara GV. The role of positivity as predictor of ego-resiliency from adolescence to young adulthood. Pers Ind Diff. (2016) 101:306–11. doi: 10.1016/j.paid.2016.06.025
81. Gomez-Baya D, Tomé G, Reis M, Gaspar de Matos M. Long-term self-regulation moderates the role of internal resources for resilience in positive youth development in Portugal. J Genet Psychol. (2020) 181:127–49. doi: 10.1080/00221325.2020.1735986
82. Lin M, Wolke D, Schneider S, Margraf J. Bullying history and mental health in University students: the mediator roles of social support, personal resilience, and self-efficacy. Front Psychiatry. (2020) 10:960. doi: 10.3389/fpsyt.2019.00960
83. Freire C, del Mar Ferradás M, Regueiro B, Rodríguez S, Valle A, Núñez JC. Coping strategies and self-efficacy in University students: a person-centered approach. Front Psychol. (2020) 11:841. doi: 10.3389/fpsyg.2020.00841
84. Smith KJ, Haight TD, Emerson DJ, Mauldin S, Wood BG. Resilience as a coping strategy for reducing departure intentions of accounting students. Account Educ. (2020) 29:77–108. doi: 10.1080/09639284.2019.1700140
85. Bonanno GA, Burton CL. Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspect Psychol Sci . (2013) 8:591–612. doi: 10.1177/1745691613504116
86. Freire C, Ferradás MM, Núñez JC, Valle A, Vallejo G. Eudaimonic well-being and coping with stress in University students: the mediating/moderating role of self-efficacy. Int J Environ Res Public Health . (2019) 16:48. doi: 10.3390/ijerph16010048
87. de la Fuente J, Mañas I, Franco C, Cangas AJ, Soriano E. Differential effect of level of self-regulation and mindfulness training on coping strategies used by University students. Int J Environ Res Public Health. (2018) 15:E2230. doi: 10.3390/ijerph15102230
88. Freire C, Ferradás MM, Núñez JC, Valle A. Coping flexibility and eudaimonic well-being in University students. Scand J Psychol . (2018) 59:433–42. doi: 10.1111/sjop.12458
89. DeRosier ME, Frank E, Schwartz V, Leary KA. The potential role of resilience education for preventing mental health problems for college students. Psychiatr Ann . (2013) 43:538–44. doi: 10.3928/00485713-20131206-05
90. KarimiJozestani L, Faramarzi S, Yarmohammadian A. The effectiveness of training metacognition-based study skill on the students' achievement motivation, self-efficacy, satisfaction with school and resilience. Interdiscip J Virtual Learn Med Sci. (2020) 7:98–109. doi: 10.5812/ijvlms.12151
91. Secades XG, Molinero O, Salguero A, Barquín RR, de la Vega R, Márquez S. Relationship between resilience and coping strategies in competitive sport. Percept Motor Skills. (2016) 122:336–49. doi: 10.1177/0031512516631056
92. Shing EZ, Jayawickreme E, Waugh CE. Contextual positive coping as a factor contributing to resilience after disasters. J Clin Psychol. (2016) 72:1287–306. doi: 10.1002/jclp.22327
93. Zimmer-Gembeck MJ, Skinner EA. The development of coping: implications for psychopathology and resilience. In: Cicchetti D, editor. Developmental Psychology: Risk, Resilience, and Intervention . New York, NY: Hoboken, NJ: John Wiley and Sons (2016). p. 485–545.
94. Bettis AH, Coiro MJ, England J, Murphy LK, Zelkowitz RL, Dejardins L, et al. Comparison of two approaches to prevention of mental health problems in college students: enhancing coping and executive function skills. J Am Coll Health. (2017) 65:313–22. doi: 10.1080/07448481.2017.1312411
95. Chou P-C, Chao Y-MY, Yang H-J, Yeh G-L, Lee TS-H. Relationships between stress, coping and depressive symptoms among overseas University preparatory Chinese students: a cross-sectional study. BMC AQQ22Public Health. (2011) 11:352. doi: 10.1186/1471-2458-11-352
PubMed Abstract | CrossRef Full Text
96. Houston JB, First J, Spialek ML, Sorenson ME, Mills-Sandoval T, Lockett M, et al. Randomized controlled trial of the resilience and coping intervention (RCI) with undergraduate University students. J Am Coll Health. (2017) 65:1–9. doi: 10.1080/07448481.2016.1227826
97. Howard DE, Schiraldi G, Pineda A, Campanella R. Stress and mental health among college students: overview and promising prevention interventions. In: Landow MV, editor. Stress and Mental Health of College Students . New York, NY: Nova Science Publishers (2006). p. 91–124.
98. Prince-Embury S, Saklofske DH, Keefer KV. Three-factor model of personal resiliency. In: Kumar U, editor. Routledge International Handbooks. The Routledge International Handbook of Psychosocial Resilience. Abingdon: Routledge/Taylor and Francis Group (2017). p. 34–45.
99. Cheng C, Kogan A, Chio JH. The effectiveness of a new, coping flexibility intervention as compared with a cognitive-behavioural intervention in managing work stress. Work Stress. (2012) 26:272–88. doi: 10.1080/02678373.2012.710369
100. Kobylińska D, Kusev P. Flexible emotion regulation: how situational demands and individual differences influence the effectiveness of regulatory strategies. Front Psychol . (2019) 10:72. doi: 10.3389/fpsyg.2019.00072
101. Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M, Aslaksen PM, Flaten MA. Resilience as a moderator of pain and stress. J Psychosom Res. (2006) 61:213–9. doi: 10.1016/j.jpsychores.2005.12.007
102. Lee CM, Watson REB, Kleyn CE. The impact of perceived stress on skin ageing. J Eur Acad Dermatol Venereol. (2020) 34:54–8. doi: 10.1111/jdv.15865
103. Shi X, Wu J. Chronic stress and anticipatory event-related potentials: the moderating role of resilience. Stress. (2020) 23:607–13. doi: 10.1080/10253890.2020.1766019
104. Mpofu S, Mabvurira V, Chirimambowa T. Religion, spirituality and resilience of HIV positive children in Zimbabwe. Can Soc Sci. (2020) 16:1–10.
105. Martínez-Rodríguez RDC, Benítez-Corona L. Resilient coping strategies for physical therapy classes in Pachuca. In: Mazurek H, editor. Pratiques Basées sur la Résilience. Hidalgo: AMU, IRD, LED. (2020). pp. 485–492.
106. Borji M, Memaryan N, Khorrami Z, Farshadnia E, Sadighpour M. Spiritual health and resilience among University students: the mediating role of self-esteem. Pastoral Psychol. (2020) 69:1–10. doi: 10.1007/s11089-019-00889-y
107. Sadeghifard YZ, Veisani Y, Mohamadian F, Azizifar A, Naghipour S, Aibod S. Relationship between aggression and individual resilience with the mediating role of spirituality in academic students-a path analysis. J Educ Health Promot. (2020) 9:2. doi: 10.4103/jehp.jehp_324_19
108. Schulenberg SE, editor. Positive Psychological Approaches to Disaster: Meaning, Resilience, and Posttraumatic Growth . London: Springer Nature (2020).
109. González-Torres MC, Artuch R. Perfiles de resiliencia y estrategias de afrontamiento en la universidad: variables contextuales y demográficas [Resilience profiles and coping strategies at university: contextual and demographic variables]. Electron J Res Educ Psychol . (2014) 12:621–48. doi: 10.14204/ejrep.34.14032
110. Mujib A, Rena S. The Moderating Effect of Spirituality on the Relationship Between Academic Life Stressors and Perceived Stress in Medical Undergraduate Students . Jakarta: ICRMH (2019).
111. Shrivastava A. Spiritual and non spiritual practices for work stress coping: a comparative study among academic faculties in india. Int J Indian Psychol . (2020) 8:1055–60. doi: 10.25215/0801.133
112. Smith NA, Brown JL, Tran T, Suárez-Orozco C. Parents, friends and immigrant youths' academic engagement: a mediation analysis. Int J Psychol . (2020) 55:743–53. doi: 10.1002/ijop.12672
113. Turner J, Bartlett D, Andiappan M, Cabot L. Students' perceived stress and perception of barriers to effective study: impact on academic performance in examinations. Br Dent J . (2015) 219:453–8. doi: 10.1038/sj.bdj.2015.850
114. Gustems-Carnicer J, Calderón C, Calderón-Garrido D. Stress, coping strategies and academic achievement in teacher education students. Eur J Teach Educ . (2019) 42:375–90. doi: 10.1080/02619768.2019.1576629
115. Vizoso CM, Arias O. Estresores académicos percibidos por estudiantes universitarios y su relación con el burnout y el rendimiento académicos (Academic stressors perceived by University students and their relationship with academic burnout, efficacy and performance). Anu Psicol . (2016) 46:90–7. doi: 10.1016/j.anpsic.2016.07.006
116. González-Cabanach R, Souto-Gestal A, González-Doniz L, Franco V. Perfiles de afrontamiento y estrés académico en estudiantes universitarios (Profiles of coping and academic stress among University students). Rev Invest Educ . (2018) 36:421–433. doi: 10.6018/rie.36.2.290901
117. Arampatzi E, Burger M, Stavropoulos S, Tay L. The role of positive expectations for resilience to adverse events: subjective well-being before, during and after the Greek bailout referendum. J Happiness Stud. (2020) 21:965–95. doi: 10.1007/s10902-019-00115-9
118. Cruickshank N. He who defends everything, defends nothing: proactivity in organizational resilience. Transnational Corporations Rev . (2020) 12:1–11. doi: 10.1080/19186444.2020.1764326
119. Galiana DR. Análisis de la felicidad, resiliencia y optimismo como factores emocionales en la inserción laboral de los universitarios (tesis doctoral) . España: Universidad Miguel Hernández De Elche (2015)
120. Hadi S. New perspective on the resilience of SMEs proactive, adaptive, reactive from business turbulence: a systematic review. J Xi'an Univ Arch Technol . (2020) 12:1265–75.
121. Jia X, Chowdhury M, Prayag G, Chowdhury MMH. The role of social capital on proactive and reactive resilience of organizations post-disaster. Int J Disaster Risk Reduct. (2020) 48:101614. doi: 10.1016/j.ijdrr.2020.101614
122. Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord . (2015) 173:90–6. doi: 10.1016/j.jad.2014.10.054
123. Ethridge P, Ali N, Racine SE, Pruessner J, Weinberg A. Risk and resilience in an acute stress paradigm: evidence from salivary cortisol and time-frequency analysis of the reward positivity. Clin Psychol Sci . (2020) 8:872–89. doi: 10.1177/2167702620917463
124. Cabanach RG, Valle A, Rodríguez S, Piñeiro I, Freire C. Escala de Afrontamiento del Estrés Académico (A-CEA) (The coping scale of academic stress questionnaire (A-CEA)). Rev Iberoam Psicol Salud . (2010) 1:51–64.
125. Tavolacci MP, Ladner J, Grigioni S, Richard L, Villet H, Dechelotte P. Prevalence and association of perceived stress, substance use and behavioral addictions: a cross-sectional study among University students in France, 2009-2011. BMC Public Health. (2013) 13:724. doi: 10.1186/1471-2458-13-724
126. Shoua-Desmarais N, von Harscher H, Rivera M, Felix T, Havas N, Rodriguez P, et al. First year burnout and coping in one US medical school. Acad Psychiatry . (2020) 44:394–8. doi: 10.1007/s40596-020-01198-w
127. Jiang H, Jiang X, Sun P, Li X. Coping with workplace ostracism: the roles of emotional exhaustion and resilience in deviant behavior. Manag Decis. (2020) 59:358–71. doi: 10.1108/MD-06-2019-0848
128. Wiese-Bjornstal DM, Wood KN, Wambach AJ, White AC, Rubio VJ. Exploring religiosity and spirituality in coping with sport injuries. J Clin Sport Psychol. (2020) 14:68–87. doi: 10.1123/jcsp.2018-0009
129. Holliday KN. An Examination of the Impact of Mentoring on Girls Academic Engagement and Resilience (doctoral thesis), Texas State University, San Marcos, TX, United States (2020). Available online at: https://digital.library.txstate.edu/handle/10877/9871
130. Verrochi D. Building resilience in gender and sexual minority youth. Creat Nurs. (2020) 26:109–13. doi: 10.1891/CRNR-D-19-00047
131. Alessi EJ, Greenfield B, Manning D, Dank M. Victimization and resilience among sexual and gender minority homeless youth engaging in survival sex. J Interpers Violence. (2020) 36:1–24. doi: 10.1177/0886260519898434
132. Didkowsky N, Ungar M, Liebenberg L. Using visual methods to capture embedded processes of resilience for youth across cultures and contexts. J Can Acad Child Adolesc Psychiatry . (2010) 19:12–8.
133. Yu N. Using systemizing-empathizing theory to explore individual differences in resilience by brain types. In: International Conference on Mental Health and Humanities Education (ICMHHE 2020) . Wuhan: Atlantis Press (2020). p. 68–78. doi: 10.2991/assehr.k.200425.015
134. Botha T. Flourishing Beyond Borders: Character Strengths, Resilience and Self-Perceived Well-Being of the Accompanying Expatriate Partner During International Relocation (doctoral dissertation). Potchefstroom: North-West University (2020).
135. Florin M, Schrimmer L, McCargo S, Bohn T, Caton C. Fostering Hope and Enhancing Resilience through Character Strengths Interventions . (2020). Available online at: https://repository.upenn.edu/mapp_slp/35 (accessed July 15, 2020).
136. Karris-Bachik MA, Carey G, Craighead WE. VIA character strengths among US college students and their associations with happiness, well-being, resiliency, academic success and psychopathology. J Posit Psychol . (2020) 15:1–14. doi: 10.1080/17439760.2020.1752785
137. Dehnad V. A proactive model to control reactive behaviors. World J Educ. (2017) 7:24–31. doi: 10.5430/wje.v7n4p24
138. Chen C. The role of resilience and coping styles in subjective well-being among Chinese University students. Asia Pacific Educ Res. (2016) 25:377–87. doi: 10.1007/s40299-016-0274-5
139. Porobić S. Long-term adaptation among naturalised bosnian refugees in sweden-existential preoccupation, spirituality and resilience. In: Forced Migration and Resilience . Wiesbaden: Springer (2020). p. 71–97.
140. Gibbs LAL, Anderson MI, Simpson GK, Jones KF. Spirituality and resilience among family caregivers of survivors of stroke: a scoping review. NeuroRehabilitation. (2020) 46:41–52. doi: 10.3233/NRE-192946
141. de la Fuente J, González-Torres MC, Aznárez-Sanado M, Martínez-Vicente JM, Peralta-Sánchez FJ, Vera MM. Implications of unconnected micro, molecular, and molar level research in psychology: the case of executive functions, self-regulation, and external regulation. Front Psychol . (2019) 10:1919. doi: 10.3389/fpsyg.2019.01919
142. Furber G. Disability Services blog at Finders University , (2018). Available online at: https://blogs.flinders.edu.au/student-health-and-well-being/2018/01/22/disability-services-seeking-mentors-new-students-disabilities/ (accessed December 6, 2020).
143. Scharp KM, Dorrance Hall E. Examining the relationship between undergraduate student parent social support-seeking factors, stress, and somatic symptoms: a two-model comparison of direct and indirect effects. Health Commun . (2019) 34:54–64. doi: 10.1080/10410236.2017.1384427
144. Cheng C, Lau H-PB, Chan MPS. Coping flexibility and psychological adjustment to stressful life changes: a meta-analytic review. Psychol Bull . (2014) 140:1582–607. doi: 10.1037/a0037913
145. Deasy C, Coughlan B, Pironom J, Jourdan D, Mannix-McNamara P. Psychological distress and coping amongst higher education students: a mixed method enquiry. PLoS ONE . (2014) 9:e115193. doi: 10.1371/journal.pone.0115193
146. Beerten-Duijkers JC, Vissers CTW, Rinck M, Barkley RA, Egger OI. Self-directedness positively contributes to resilience and quality of life: findings from a mixed psychiatric sample. J Soc Clin Psychol. (2020) 39:59–76. doi: 10.1521/jscp.2020.39.01.002
147. Turner M, Holdsworth S, Scott-Young C. Resilience at University: the development and testing of a new measure. Higher Educ Res Dev. (2017) 36:386–400 doi: 10.1080/07294360.2016.1185398
148. de la Fuente J, Martínez-Vicente JM, Peralta-Sánchez FJ, González-Torres MC, Artuch R, Garzón-Umerenkova A. Satisfaction with the self-assessment of University students through e-Coping with academic stress Utility TM. Front Psychol . (2018) 9:1932. doi: 10.3389/fpsyg.2018.01932
Keywords: resilience, positivity, coping strategies, engagement-burnout, structural equation model, young adults
Citation: de la Fuente J, Santos FH, Garzón-Umerenkova A, Fadda S, Solinas G and Pignata S (2021) Cross-Sectional Study of Resilience, Positivity and Coping Strategies as Predictors of Engagement-Burnout in Undergraduate Students: Implications for Prevention and Treatment in Mental Well-Being. Front. Psychiatry 12:596453. doi: 10.3389/fpsyt.2021.596453
Received: 19 August 2020; Accepted: 18 January 2021; Published: 16 February 2021.
Reviewed by:
Copyright © 2021 de la Fuente, Santos, Garzón-Umerenkova, Fadda, Solinas and Pignata. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jesús de la Fuente, jdlfuente@unav.es ; jfuente@ual.es
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
The Secret to Building Resilience
- Karen Dillon,
- Danna Greenberg

It’s a team sport.
The ability to bounce back from setbacks is often described as the difference between successful and unsuccessful people. Resilience has been shown to positively influence work satisfaction and engagement, as well as overall well-being, and can lower depression levels. But resilience isn’t just a kind of solitary internal “grit” that allows us to bounce back. New research shows that resilience is also heavily enabled by strong relationships and networks. We can nurture and build our resilience through a wide variety of interactions with people in our personal and professional lives. These interactions can help us to alter the magnitude of the challenge we’re facing. They can help crystalize the meaningful purpose in what we are doing or help us see a path forward to overcome a setback — these are the kinds of interactions that motivate us to persist. Are your relationships broad and deep enough to help support you when you hit setbacks? Here’s an exercise to help you think that through.
An anesthesiologist we’ll call Jacob used to describe his job as “90% boredom, 10% horror.” With a few exceptions of challenging surgeries and managing a department of several hundred physicians and nurses, most of the time, Jacob’s role was routine. But that was before the Covid-19 pandemic. Since anesthesiology is not a specialty that can resort to remote “telemedicine,” Jacob and his team entered an overwhelmed hospital day after day. “For two months, I wasn’t sleeping at night,” he shared with us. “I was sending my team into battle with inadequate protection, not even really knowing how many of them might get sick.” The burden of being responsible for both a team he cared deeply about and the lives of a huge volume of patients affected by the pandemic was crushing. Routinely putting in 16-hour days, Jacob was having to determine how and when his team would work in these trying circumstances. “There were nights and weekends when some [colleagues] called me and were crying on the phone. Let’s face it, they were scared for their lives.” And Jacob was, too.
But Jacob didn’t break. He and his team have held together as they continued to do their work throughout the pandemic. So what allowed Jacob to endure this period of extraordinary stress? Resilience.
The ability to bounce back from setbacks is often described as the difference between successful and unsuccessful people. Resilience has been shown to positively influence work satisfaction and engagement , as well as overall well-being , and can lower depression levels. There is even evidence that resilience can help protect us from physical illness . But resilience, conventional thinking assumes, is something we find within ourselves only when we are tested — a kind of solitary internal “grit” that allows those of us who are strong to bounce back.
But that’s not necessarily true. Our research (which is not yet published) shows that resilience is not purely an individual characteristic, but is also heavily enabled by strong relationships and networks. We can nurture and build our resilience through a wide variety of interactions with people in our personal and professional lives. These interactions can help us to shift or push back on work demands and alter the magnitude of the challenge we’re facing. They can help crystalize the meaningful purpose in what we are doing or help us see a path forward to overcome a setback — these are the kinds of interactions that motivate us to persist. People in our support systems can provide empathy or simply help us laugh and bolster our resilience by shifting perspective and reminding us we are not alone in the fight. In short, resilience is not something we need to find deep down inside ourselves: we can actually become more resilient in the process of connecting with others in our most challenging times.
Based on in-depth interviews with 150 leaders (five men and five women from 15 different organizations who were considered to be among their “most successful” leaders), we have defined how connections can help us become more resilient when we encounter major life or professional challenges. A well-developed network of relationships can help us rebound from setbacks by:
- Helping us shift work or manage surges
- Helping us to make sense of people or politics in a given situation
- Helping us find the confidence to push back and self advocate
- Helping us see a path forward
- Providing empathic support so we can release negative emotions
- Helping us to laugh at ourselves and the situation
- Reminding us of the purpose or meaning in our work
- Broadening us as individuals so that we maintain perspective when setbacks happen
As Jacob (who was among those we interviewed) learned in what was unquestionably the toughest period of his entire career, resilience is a team sport.
While, clearly, a portion of Jacob’s fortitude came from personal strength, our discussion with him revealed a number of ways that relationships bolstered his resilience. A patchwork of different people in his network collectively played a critical role in helping Jacob navigate and survive this extraordinary period — each offering a different perspective or helping hand in some way. First, his boss was a continual source of input and validation, boosting Jacob’s confidence as he faced unprecedented medical and leadership challenges. “She always made herself available and these interactions helped me quit worrying endlessly about different decisions.” In addition, he tapped into the strong working relationship he had with another department head to jointly manage surges in workload. The resources he was able to “borrow” from this colleague enabled him to push back on non-essential work, as well as bypass typical bureaucratic gridlock to secure resources. “At a couple of really important junctures, this helped us from getting over-run.” And a very strong chief of staff stepped in and took ownership of several work-streams put in place to help deal with Covid. For Jacob, knowing that this reliable person had those domains in hand “took stress from a 10 to an 8 many times.” Even his daily exchanges with his office manager played a critical role — she was able to find ways to laugh with him even under this stress. “It wasn’t gallows humor, but sarcastic comments about difficult people or situations that lightened things for us and made us feel on the same team,” he recalled.
Jacob was also lucky in that his home was a critical refuge for him through this time. His wife, who also had a medical background, provided an outlet to vent that yielded both empathy and possible solutions. His children even played a role that he did not realize until past the early crisis: “They were proud of me. They would tell me this, and it was better than anything else to help me buckle down and keep pushing through.”
In short, Jacob shows us that resilience is found not just in having a network of supporters, but in truly connecting with them when you need them most. It’s in the actual interactions themselves — the conversations that validate your plans, reframe your perspective on a situation, help you laugh and feel authentic with others, or just encourage you to get back up and try again because the battle is a worthy one — that we become resilient. Yes, we’re all told to build a network to help further our careers, but what’s important to understand is how essential these relationships can also be to our day-to-day emotional well-being — if we are building these relationships in the right way as we progress through our careers. Relationships may be our most undervalued resources.
But such a network won’t materialize overnight. When we talk to people who have shown exceptional resilience, it’s clear that they often have cultivated and maintained authentic connections that come from many parts of their life — not only through work, but through athletic pursuits, volunteer work, civic or religious communities, book or dinner clubs, communities of parents they’ve met through their children, and so on. Interactions in these spheres provide critical “dimensionality”, broadening their identity and “opening the aperture” on how they look at their lives. We become more (or less) resilient through our interactions with others.
Are your relationships broad and deep enough to help support you when you hit setbacks? Here’s an exercise to help you think that through.
Step 1: Identify your top resilience needs .
Below are eight common relational sources of resilience, the same ones we noted above. Our research shows that these sources are not universally or equally important to everyone. For example, some people value laughter, while others prefer empathy. In short, our resilience needs are personal and are shaped by our unique history, personality, and professional/personal context. But collectively, the relationships we develop are a toolbox that we can turn to in our most difficult times, which we can rely upon to help us navigate day-to-day life challenges.
Using the framework below, identify the top three sources of resilience that you would most like to strengthen in your life . Make a note of those that are most important for you to work on developing.

Step 2: Plan how to expand your network .
Reflecting on the top three resilience needs you indicated, place the names of people or groups that you could invest in to further cultivate sources of resilience. Connections that yield resilience can be intentionally cultivated in two ways. First, we can broaden existing relationships by, for example, exploring non-work interests with a teammate or strengthening mutually beneficial relationships with influential work colleagues that help us push back. Second, we can initiate engagement with new groups or people to cultivate important elements of resilience — for example spiritual groups that remind us of our purpose, or affinity groups that allow us to laugh. Broadening our network helps us develop dimensionality in our lives — a rich variety of relationships and connections that help us grow, that can provide perspective on our struggles, and that can offer us a stronger sense of purpose.
These groups may come from any and all walks of life — athletic pursuits, spiritual associations, nonprofit board work, community organizing groups around social, environmental, or political issues, etc. Engaging in nonwork groups (particularly board work, social action, and community organizing groups) helps us develop resilience in our work life as well. Exposure to a diverse group of people allows us to learn different ways of managing, leading, and handling crises, and helps us develop different relational skills such as negotiating with various stakeholders. It also helps us cultivate empathy and perspective that we carry back into our work, among other benefits. In summary, meaningful investment in non-work relationships broadens the toolkit one can rely upon to manage setbacks when they arise.
One critical insight from our interviews is that relying on your network in times of transition matters a great deal. When people told us stories of significant transitions — moves, job losses, role expansions, or family changes — they tended to separate into one of two groups. One group tended to lean into the transition and relied on existing relationships to work through the ambiguity and anxiety they were experiencing. This group also used the transition to reach out to one or two new groups such as a working parents group, a newcomers group, or a work-based coaching circle. In contrast, the second group operated with a mindset that they just needed to absorb the transition and closed in on their circle. They felt overwhelmed and said they would lean into activities when they had time in the future. Over the ensuing 18 months, this group became a smaller version of themselves and often drifted away from the connections that had been so important to their lives.
Covid has created a significant transition for us all. The importance of building and maintaining your connections has never been clearer. For most of us, the challenges and setbacks we are experiencing in work and life during this pandemic have been relentless. But you’re not alone in this battle. You can build resilience. Start by understanding the critical importance of growing, maintaining, and tapping a diverse network to help you ride out the storm.
Support and funding for the research behind this article was received from the Innovation Resource Center for Human Resources.
- Rob Cross is the Edward A. Madden Professor of Global Leadership at Babson College in Wellesley, Massachusetts, and a senior vice president of research at the Institute for Corporate Productivity. He is the coauthor of The Microstress Effect: How Little Things Add Up—and What to Do About It (Harvard Business Review Press, 2023) and author of Beyond Collaboration Overload (Harvard Business Review Press, 2021).
- Karen Dillon is a former editor of Harvard Business Review and coauthor of The Microstress Effect: How Little Things Pile Up and Create Big Problems — and What to Do About It (Harvard Business Review Press, 2023). She is also coauthor of three books with Clayton Christensen, including the New York Times best-seller How Will You Measure Your Life?
- DG Danna Greenberg is the Walther H. Carpenter Professor of Management and Organizations at Babson College. Her latest book, Maternal Optimism: Forging Positive Paths through Work and Motherhood , explores the uniqueness of each working mother’s journey to integrate career and family.
Partner Center
Resilience Theory: A Summary of the Research (+PDF)

Resilience theory argues that it’s not the nature of adversity that is most important, but how we deal with it.
When we face adversity, misfortune, or frustration, resilience helps us bounce back. It helps us survive, recover, and even thrive in the face and wake of misfortune, but that’s not all there is to it.
Read on to learn about resilience theory in a little more depth, including its relationship with shame, organizations, and more.
But first, we thought you might like to download our three Resilience Exercises for free . These engaging, science-based exercises will help you to effectively deal with difficult circumstances and give you the tools to improve the resilience of your clients, students or employees.
This Article Contains:
What is resilience theory.
- 6 Impactful Articles on Resilience and Mental Toughness
What Research in Positive Psychology Shows
Resilience theory in social work, family resilience theory, shame resilience theory, community resilience theory, organizational resilience theory, the ‘science of resilience’, norman garmezy’s main findings and contribution, seligman’s 3ps model of resilience, a take-home message.
Resilience has been defined in numerous ways.
Defining resilience
The following definitions abound:
“the ability to bounce back from adversity, frustration, and misfortune”
Ledesma, 2014, p.1
“the developable capacity to rebound or bounce back from adversity, conflict, and failure or even positive events, progress, and increased responsibility”
Luthans, 2002a, p. 702
“a stable trajectory of healthy functioning after a highly adverse event”
Bonanno, 2004; Bonanno, Westphal, & Mancini, 2011
“the capacity of a dynamic system to adapt successfully”
Masten, 2014; Southwick, Bonanno, Masten, Panter-Brick, & Yehuda, 2014
When a panel discussion asked researchers to debate the nature of resilience , all agreed that resilience is complex. As a construct, it can have a different meaning between people, companies, cultures, and society. They also agreed that people could be more resilient at one point in their lives and less during another, and that they may be more resilient in some aspects of their lives than others (Southwick et al., 2014).
In case you’re interested, the table below from Greene, Galambos, and Lee (2004) shows even more ways resilience has been described.
Resilience theory
Resilience as a concept is not necessarily straightforward, and there are many operational definitions in existence. Resilience theory, according to van Breda (2018, p. 1), is the study of the things that make this phenomenon whole:
Its definition; What ‘adversity’ and ‘outcomes’ actually mean, and; The scope and nature of resilience processes.
6 Impactful Resilience Articles on Resilience and Mental Toughness
Ready to learn a bit more about resilience theory? For those who are keen to dig into the literature, this list demonstrates precisely how widely the concept can be applied: in social work, organizations, childhood development contexts, and more. You’ll find the full citations for these papers in the Reference section at the end of this article.
1. A Critical Review of Resilience Theory and Its Relevance for Social Work
In this literature review, Adrian van Breda (2018) considers peer-reviewed articles on resilience in the field of social work, discussing the evolution of an (as-yet to be established) consensus on its definition. He considers how it works and developments in the theory, looking at the study of resilience in South African cultures and societies.
2. Resilience Theory and Research on Children and Families: Past, Present, and Promise
Masten is known for her work on resilience and its role in helping families and children deal with adversity . In this article, she defines resilience as “the capacity of a system to adapt successfully to significant challenges that threaten its function, viability, or development” (Masten, 2018, p. 1).
Masten delves into the theory’s history and its research in this field in an attempt to integrate applications, models, and knowledge that may help children and their families grow and adjust.
3. Family Resilience: A Developmental Systems Framework
Professor Froma Walsh, cofounder of the Chicago Center for Family Health, has written extensively on family resilience and the positive adaptation of family units. In Family Resilience: A Developmental Systems Framework , Walsh (2016) considers the key processes in family resilience and gives a great overview of the concept from a family systems perspective.
4. Community Resilience: Toward an Integrated Approach
Berkes and Ross (2013) examined two distinct approaches to understanding community resilience: a social-ecological approach and a mental health and developmental psychology perspective. This article, which we unpack a little more further on, is a great read for anyone with an academic interest in the growing research on resilience at the community level.
5. Organizational Resilience: Towards a Theory and Research Agenda
Vogus and Sutcliffe (2007) attempted to define organizational resilience and examine its underpinning mechanisms. Their paper considers the relational, cognitive, structural, and affective elements of the construct before proposing some research questions for those with an academic interest in the topic.
6. Are Adolescents With High Mental Toughness Levels More Resilient Against Stress?
Download 3 Free Resilience Exercises (PDF)
These detailed, science-based exercises will equip you or your clients to recover from personal challenges and turn setbacks into opportunities for growth.
Download 3 Free Resilience Tools Pack (PDF)
By filling out your name and email address below.
Resilience and positive psychology are often closely related. Both are concerned with how promotive factors work, and both look at how a beneficial construct can facilitate our wellbeing (Luthar, Lyman, & Crossman, 2014).
Resilience theory and positive psychology are both applied fields of study, meaning that we can use them in daily life to benefit humanity, and both are very closely concentrated on the importance of social relationships (Luthar, 2006; Csikszentmihalyi & Nakamura, 2011).
So let’s look at what positive psychology research shows on resilience.
Character strengths and resilience
Strengths such as gratitude, kindness, hope, and bravery have been shown to act as protective factors against life’s adversities, helping us adapt positively and cope with difficulties such as physical and mental illness (Fletcher & Sarkar, 2013).
Some character strengths can also be significant predictors of resilience, with particular correlations between resilience and emotional, intellectual, and restraint-related strengths (Martínez-Martí & Ruch, 2017).
In their 2017 study, Martínez-Martí and Ruch found that hope, bravery, and zest had the most extensive relationship with positive adaptation in the face of challenge. This led the researchers to speculate that processes such as determination, social connectedness, emotional regulation , and more were at play.
From this particular cross-sectional study, however, no causal relationship was determined. In other words, we don’t know whether resilience impacts our strengths or vice versa.
The effect may work the other way around with adversity, and post-traumatic growth helps us build character strengths, but nonetheless, it’s an example of resilience and positive psychology’s interconnection (Tedeschi & Calhoun, 1995; Peterson, Park, Pole, D’Andrea, & Seligman, 2008).
Resilience and positive emotions
Most people think of happiness whenever positive psychology is mentioned, so are happiness and resilience related? Cohn, Fredrickson, Brown, Mikels, and Conway (2009) suggested that they may well be. To be specific, happiness is a positive emotion.
According to the broaden-and-build theory of positive emotions, happiness is one emotion that helps us become more explorative and adaptable in our thoughts and behaviors. We create enduring resources that help us live well (Fredrickson, 2004).
Cohn et al. (2009) found that participants who frequently experienced positive emotions such as happiness grew more satisfied with their lives by creating resources, such as ego resilience, that helped them tackle a wide variety of challenges.
These results correspond with other evidence that positive emotions can facilitate resource growth and findings that link psychological resilience with physical health, psychological wellbeing, and positive affect (Lyubomirsky, King, & Diener, 2005; Nath & Pradhan, 2012).
Its role in positive organizational behavior
Other studies have looked at resilience as one of numerous coping positive psychological resources, alongside optimism and hope.
Positive organizational behavior has been defined by Luthans (2002b, p. 59) as “the study and application of positively oriented human resource strengths and psychological capacities that can be measured, developed, and effectively managed for performance improvement in today’s workplace.”
Can training employees help encourage positive organizational behavior? The jury is still out (Robertson, Cooper, Sarkar, & Curran, 2015).

Some of the reasons for this are the central role of community relationships to both academic fields and the key social work principle that people should accept responsibility for one another’s wellbeing (International Federation of Social Workers, 2014).
One of the main drivers for more resilience theory research in social work contexts is the idea that identifying resilience-building factors can help at-risk clients in the following ways (Greene et al., 2004):
Promoting their competence and improving their health Helping them overcome adversity and navigate life stressors Boosting their ability to grow and survive
Concerning social workers, key issues in the field include:
Identifying protective factors and using them to inform interventions Using practical applications to promote the capacity and strength of individual clients, societies, and communities Understanding how social work policy and services promote or hinder wellbeing and social and economic injustice
Social work strategies for building client resilience
Greene et al.’s (2004) research also investigated the strategies and skills social workers relied on to boost the resilience of their clients. Some of these included:
Providing clients with safety and necessities when faced with adversity or traumatic events; for example, talking calmly with distressed individuals, reassuring them of their capabilities and ability to get through their troubles.
Listening, being present and honest, and learning from individuals’ stories while acknowledging their pain.
Promoting interpersonal relationships, attachments, and connections between people in a community or society.
Encouraging them to view themselves as a valued member of society.
Modeling resilient behaviors, such as dealing with work stress in healthy ways.
Realizing Resilience Masterclass
For social workers, therapists, and educators, an immense benefit can be gained from being able to boost your client’s resilience. To do so, enrolling in our Realizing Resilience Masterclass course would equip you to strengthen others, guide them, and teach them the six pillars of resilience.
This masterclass, based on scientific techniques, will provide you with all the material you need to deliver exceptional resilience training sessions. It is the ultimate shortcut to help others become more resilient. For more information, view our Realizing Resilience Masterclass page.

Shame resilience – Noor Pinna
Family resilience has been defined in several ways. One way of viewing the construct is as the “characteristics, dimensions, and properties of families which help families to be resistant to disruption in the face of change and adaptive in the face of crisis situations’’ (McCubbin & McCubbin, 1988, p. 247).
Another more recent definition describes it as the “capacity of the family, as a functional system, to withstand and rebound from stressful life challenges – emerging strengthened and more resourceful’’ (Walsh, 1996; 2003; 2016).
Both of these definitions take the concept of individual psychological or emotional resilience and apply it at a broader level; one of the key areas that interests researchers is how families respond immediately when faced with challenges and over the longer term (Walsh, 2016).
Family resilience processes
In a meta-analysis on family resilience, Walsh (2003) proposed that the concept involves nine dynamic processes that interact with one another and help families strengthen their ties while developing more resources and competencies.
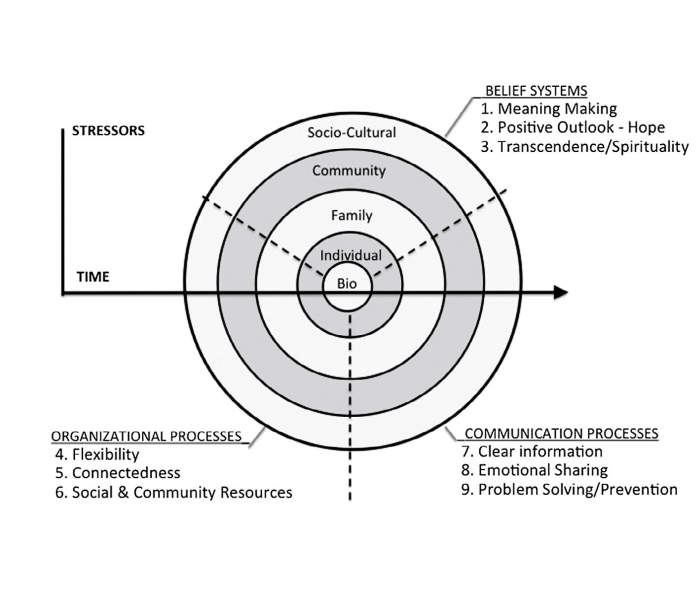
- Making sense of adversity – e.g., normalizing distress and contextualizing it, viewing crises as manageable and meaningful
- Having a positive outlook – e.g., focusing on potential, having hope and optimism
- Spirituality and transcendence – e.g., growing positively from adversity and connecting with larger values
- Flexibility – e.g., reorganizing and restabilizing to provide predictability and continuity
- Connectedness – e.g., providing each other with mutual support and committing to one another
- Mobilizing economic and social resources – e.g., creating financial security and seeking support from the community at large
- Clarity – e.g., providing one another with information and consistent messages
- Sharing emotions openly – including positive and painful feelings
- Solving problems collaboratively – e.g., through joint decision-making, a goal-focus, and building on successes

The theory attempts to study how we respond to and defeat shame, an emotion we all experience. Brown (2008) describes shame resilience theory as the ability to recognize this negative emotion when we feel it and overcome it constructively in such a way that we can “retain our authenticity and grow from our experiences.”
Read more about shame resilience theory in this excellent article: Shame Resilience Theory : How to Respond to Feelings of Shame .

A community resilience concept
Magis (2010, p. 401) defined community resilience as the ”existence, development and engagement of community resources by community members to thrive in an environment characterized by change, uncertainty, unpredictability, and surprise.”
In other words, one approach to defining community resilience emphasizes the importance of individual mental health and personal development on a social system’s capacity to unite and collaborate toward a shared goal or objective (Berkes & Ross, 2013).
The key focus of community resilience is on identifying and developing both individual and community strengths and establishing the processes that underpin resilience-promoting factors (Buikstra et al., 2010). Its goals also include understanding how communities leverage these strengths together to facilitate self-organization and agency, which then contributes to a collective process of overcoming challenges and adversity (Berkes & Ross, 2013).
Community resilience is considered an ongoing process of personal development in dealing with adversity through adaptation and understandably plays a vital role in social work contexts (Almedom, Tesfamichael, Mohammed, Mascie-Taylor, & Alemu, 2007).
Relevant research questions related to community resilience theory include (Berkes & Ross, 2013):
- What are the characteristics of individual and community resilience, and how can these be fostered (Buikstra et al., 2010)?
- How is community resilience related to health, and how are health professionals able to help (Kulig, 2000; Kulig, Edge, & Joyce, 2008; Kulig, Hegney, & Edge, 2010)?
- How can community resilience improve readiness for disaster (Norris, Stevens, Pfefferbaum, Wyche, & Pfefferbaum, 2008)?
Community strengths promoting resilience
While community strengths vary between groups, Berkes and Ross (2013) identified a few characteristics that have a central role in helping communities develop resilience. These strengths, processes, and attributes include:
- Social networks and support
- Early experience
- People–place connections
- Engaged governance
- Community problem-solving
- Ability to cope with divisions
Just as people can develop their resilience, organizations can learn to rebound from and adapt after facing challenges. Organizational resilience can be thought of as “a ‘culture of resilience,’ which manifests itself as a form of ‘psychological immunity’” to incremental and transformational changes, according to Boston Consulting Group Fellow Dr. George Stalk, Jr. (Everly, 2011).
With a host of factors contributing to a dynamic and sometimes turbulent business environment, organizational resilience has gained incredible salience in recent years. And at the heart of it, Everly argues, are optimism and perceived self-efficacy.
How to build organizational resilience
A culture of organizational resilience relies heavily on role-modeling behaviors. Even a few credible and high-profile individuals in a company demonstrating resilient behaviors may encourage others to do the same (Everly, 2011).
These behaviors include:
- Persisting in the face of adversity
- Putting effort into dealing with challenges
- Practicing and demonstrating self-aiding thought patterns
- Providing support to and mentoring others
- Leading with integrity
- Practicing open communication
- Showing decisiveness
Read more about Positive Organizations here.
InBrief: the science of resilience
Are some people born more resilient than others? Southwick and Charney (2012) discussed human biological responses to trauma and looked at a sample of high-risk individuals to understand why some are more able to cope even in the face of life-changing adversity.
They examined three samples of participants to investigate whether these individuals had a genetic predisposition toward being more resilient:
- Special Forces instructors
- Vietnam prisoners of war
- Individuals who had suffered considerable trauma
Southwick and Charney (2012) looked at the psychological factors of these individuals; their genetic factors; and their spiritual, social, and biological factors.
The results:
Risk and protective factors generally have additive and interactive effects… having multiple genetic, developmental, neurobiological, and/or psychosocial risk factors will increase allostatic load or stress vulnerability, whereas having and enhancing multiple protective factors will increase the likelihood of stress resilience.
Put succinctly, genetic factors do have an important influence on our responses to trauma and stress. The image below gives a good overview of their findings.
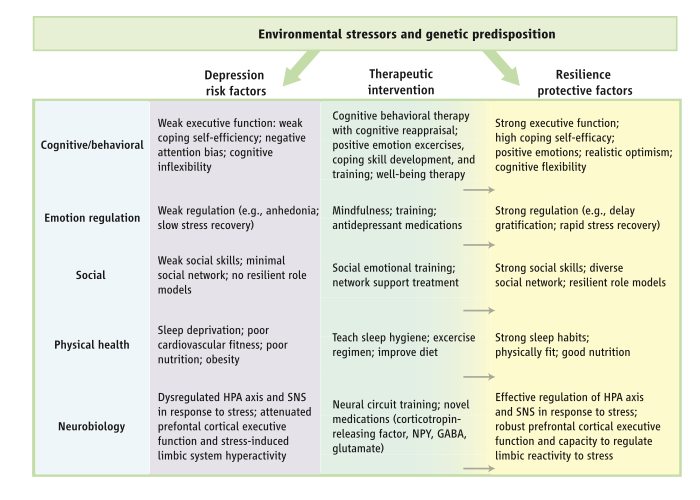
Source: Southwick & Charney, 2012, p. 81
In the article , mentioned in our References section, you can learn more about two key concepts that are central to resilience theory:
- Learned helplessness – where individuals believe they are incapable of changing or controlling their circumstances after repeatedly experiencing a stressful event
- Stress inoculation – whereby they can develop an “adaptive stress response and become more resilient than normal to the negative effects of future stressors” (Southwick & Charney, 2012, p. 80)
University of Minnesota developmental psychologist Norman Garmezy is one of the best-known contributors to resilience theory as we know it. His seminal work on resilience focused on how we could prevent mental illness through protective factors such as motivation, cognitive skills, social change, and personal ‘voice’ (Garmezy, 1992).
His pioneering work included the Project Competence Longitudinal Study (PCLS), which contributed operational definitions, frameworks, measures, and more to the study of competence and resilience. Started around 1974, the PCLS was developed to enable more structured and rigorous resilience research and look into protective buffers that help children overcome adversity (Masten & Tellegen, 2012).
One of its more impactful discoveries was that resilience is a dynamic construct that changes over time; another was the concept of developmental cascades, which describe how functioning in one domain can influence other levels of adaptive function.
If you’re curious to find out more about the work of Norman Garmezy, Masten and Tellegen’s (2012) paper is a great read: Resilience in Developmental Psychopathology: Contributions of the Project Competence Longitudinal Study .
17 Tools To Build Resilience and Coping Skills
Empower others with the skills to manage and learn from inevitable life challenges using these 17 Resilience & Coping Exercises [PDF] , so you can increase their ability to thrive.
Created by Experts. 100% Science-based.
The best-known positive psychology framework for resilience is Seligman’s 3Ps model.
These three Ps – personalization, pervasiveness, and permanence – refer to three emotional reactions that we tend to have to adversity. By addressing these three, often automatic, responses, we can build resilience and grow, developing our adaptability and learning to cope better with challenges.
Seligman’s (1990) 3Ps are:
Personalization – a cognitive distortion that’s best described as the internalization of problems or failure. When we hold ourselves accountable for bad things that happen, we put a lot of unnecessary blame on ourselves and make it harder to bounce back.
Pervasiveness – assuming negative situations spread across different areas of our life; for example, losing a contest and assuming that all is doom and gloom in general. By acknowledging that bad feelings don’t impact every life domain, we can move forward toward a better life.
Permanence – believing that bad experiences or events last forever, rather than being transient or one-off events. Permanence prevents us from putting effort into improving our situation, often making us feel overwhelmed and as though we can’t recover.
These three perspectives help us understand how our thoughts, mindset, and beliefs affect our experiences. By recognizing their role in our ability to adapt positively, we can start becoming more resilient and learn to bounce back from life’s challenges.
Resilience is something we can all develop, whether we want to grow as individuals, as a family, or as a society more broadly. If you’re interested in developing your psychological resilience, our Realizing Resilience Masterclass uses science-based tools and techniques to help you understand the concept better and cultivate more “bounce-back.”
Or, if you’re hoping to read more about the topic in general, we’ve got a vast range of blog posts, worksheets, and activities in our Resilience & Coping section on this site. Before you go, though, tell us, what interests you most about resilience theory and what fields have you been applying it in professionally?
We hope you enjoyed reading this article. Don’t forget to download our three Resilience Exercises for free .
- Almedom, A. M., Tesfamichael, B., Mohammed, Z. S., Mascie-Taylor, C. G. N., & Alemu, Z. (2007). Use of ‘ sense of coherence (SOC)’ scale to measure resilience in Eritrea: Interrogating both the data and the scale. Journal of Biosocial Science , 39 (1), 91–107.
- Bonanno, G. A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely adverse events? American Psychologist , 59 (1), 20–28.
- Bonanno G. A., Westphal, M., & Mancini, A. D. (2011). Resilience to loss and potential trauma. Annual Review of Clinical Psychology, 7 , 511–535.
- Berkes, F., & Ross, H. (2013). Community resilience: Toward an integrated approach. Society & Natural Resources , 26 (1), 5–20.
- Brown, B. (2006). Shame resilience theory: A grounded theory study on women and shame. Families in Society: The Journal of Contemporary Social Services , 87 (1), 43–52.
- Brown, B. (2008). I thought it was just me (but it isn’t). Avery.
- Buikstra, E., Ross, H., King, C. A., Baker, P. G., Hegney, D., McLachlan, K., & Rogers-Clark, C. (2010). The components of resilience: Perceptions of an Australian rural community. Journal of Community Psychology, 38 , 975–991.
- Cohn, M. A., Fredrickson, B. L., Brown, S. L., Mikels, J. A., & Conway, A. M. (2009). Happiness unpacked: Positive emotions increase life satisfaction by building resilience. Emotion, 9 (3), 361–368.
- Csikszentmihalyi, M., & Nakamura, J. (2011). Positive psychology: Where did it come from, where is it going? In K. M. Sheldon, T. B. Kashdan, & M. F. Steger (Eds.), Designing positive psychology: Taking stock and moving forward (pp. 3–8). Oxford University Press.
- Everly, G. S. (2011). Building a resilient organizational culture. Harvard Business Review, 10 (2), 109–138.
- Fletcher, D., & Sarkar, M. (2013). Psychological resilience. European Psychologist , 18 , 12–23.
- Fredrickson, B. (2004). The broaden-and-build theory of positive emotions. Philosophical Transaction of the Royal Society B , 359(1449), 1367–1377.
- Garmezy, N. (1992). Risk and protective factors in the development of psychopathology . Cambridge University Press.
- Gerber, M., Kalak, N., Lemola, S., Clough, P. J., Perry, J. L., Pühse, U., … Brand, S. (2013). Are adolescents with high mental toughness levels more resilient against stress? Stress and Health , 29 (2), 164–171.
- Greene, R. R., Galambos, C., & Lee, Y. (2004). Resilience theory: Theoretical and professional conceptualizations. Journal of Human Behavior in the Social Environment , 8 (4), 75–91.
- International Federation of Social Workers. (2014). Global definition of social work: Principles. Retrieved from https://www.ifsw.org/what-is-social-work/global-definition-of-social-work/
- Kulig, J. C. (2000). Community resiliency: The potential for community health nursing theory development. Public Health Nursing , 17 , 374–385.
- Kulig, J. C., Edge, D. S., & Joyce, B. (2008). Understanding community resiliency in rural communities through multimethod research. Journal of Rural Community Development , 3 , 76–94.
- Kulig, J. C., Hegney, D., & Edge, D. S. (2010). Community resiliency and rural nursing: Canadian and Australian perspectives. In C. A. Winters & H. J. Lee (Eds.), Rural nursing: Concepts, theory and practice (3rd ed.) (pp. 385–400). Springer.
- Ledesma, J. (2014). Conceptual frameworks and research models on resilience in leadership. Sage Open , 4 (3), 1–8.
- Luthar, S. S. (2006). Resilience in development: A synthesis of research across five decades. In D. Cicchetti & D. J. Cohen (Eds.), Developmental psychopathology , Vol. 3: Risk, disorder, and adaptation (2nd ed.) (pp. 739–795). Wiley.
- Luthar, S. S., Lyman, E. L., & Crossman, E. J. (2014). Resilience and positive psychology. In M. Lewis & K. D. Rudolph (Eds.), Handbook of developmental psychopathology (pp. 125–140). Springer Science + Business Media.
- Luthans, F. (2002a). The need for and meaning of positive organizational behavior. Journal of Organizational Behavior , 23 , 695–706.
- Luthans, F. (2002b). Positive organizational behavior. Developing and managing psychological strengths. Academy of Management Executive , 16 (1), 57–72.
- Lyubomirsky, S. L., King, L., & Diener, E. (2005). The benefits of frequent positive affect: Does happiness lead to success? Psychological Bulletin , 14 , 803–855.
- Magis, K. (2010). Community resilience: An indicator of social sustainability. Society & Natural Resources , 23 , 401–416.
- Martínez-Martí, M. L., & Ruch, W. (2017). Character strengths predict resilience over and above positive affect, self-efficacy, optimism, social support, self-esteem, and life satisfaction. The Journal of Positive Psychology , 12 (2), 110–119.
- Masten A. S. (2014). Global perspectives on resilience in children and youth. Child Development , 85 , 6–20.
- Masten, A. S. (2018). Resilience theory and research on children and families: Past, present, and promise. Journal of Family Theory & Review , 10 (1), 12–31.
- Masten, A. S., & Tellegen, A. (2012). Resilience in developmental psychopathology: Contributions of the project competence longitudinal study. Development and Psychopathology , 24 (2), 345–361.
- McCubbin, L. D., & McCubbin, H. I. (1988). Typologies of resilient families: Emerging roles of social class and ethnicity. Family Relations , 37 (3), 247–254.
- Nath, P., & Pradhan, R. K. (2012). Influence of positive affect on physical health and psychological well-being: Examining the mediating role of psychological resilience. Journal of Health Management , 14 (2), 161–174.
- Norris, F. H., Stevens, S. P., Pfefferbaum, B., Wyche, K. F., & Pfefferbaum, R. L. (2008). Community resilience as a metaphor, theory, set of capabilities, and strategy for disaster readiness. American Journal of Community Psychol ogy, 41 , 127–150.
- Peterson, C., Park, N., Pole, N., D’Andrea, W., & Seligman, M. E. P. (2008). Strengths of character and posttraumatic growth. Journal of Traumatic Stress , 21 , 214–217.
- Robertson, I. T., Cooper, C. L., Sarkar, M., & Curran, T. (2015). Resilience training in the workplace from 2003 to 2014: A systematic review. Journal of Occupational and Organizational Psychology , 88 (3), 533–562.
- Seligman, M. (1990). Learned optimism. Pocket Books.
- Southwick, S. M., & Charney, D. S. (2012). The science of resilience: implications for the prevention and treatment of depression. Science , 338 (6103), 79–82.
- Southwick, S. M., Bonanno, G. A., Masten, A. S., Panter-Brick, C., & Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology , 5 (1), 25338.
- Tedeschi, R. G., & Calhoun, L. G. (1995). Trauma & transformation: Growing in the aftermath of suffering . Sage.
- Van Breda, A. D. (2018). A critical review of resilience theory and its relevance for social work. Social Work, 54 (1), 1–18.
- Vogus, T. J., & Sutcliffe, K. M. (2007). Organizational resilience: Towards a theory and research agenda. In 2007 IEEE International Conference on Systems, Man and Cybernetics (pp. 3418–3422). IEEE.
- Walsh, F. (1996). The concept of family resilience: Crisis and challenge. Family Process , 35 , 261–281.
- Walsh, F. (2003). Family resilience: A framework for clinical practice. Family Process , 42 , 1–18.
- Walsh, F. (2016). Family resilience: a developmental systems framework. European Journal of Developmental Psychology , 13 (3), 313–324.
Share this article:
Article feedback
What our readers think.
This article seems very interesting and explains a lot of theory. For my PhD, I am seeking a suggestion regarding which theory or model would be particularly fit for a topic that addresses individual and organisational resilience to adapt in a disrupted labor market.
intresting PhD topic! Here are a few suggestions: – Resilience Theory : Explores how individuals and organizations withstand and adapt to adversity, offering insights into bouncing back from labor market challenges. – Psychological Capital (PsyCap) Theory : Investigates the role of an individual’s positive psychological state (hope, efficacy, resilience, optimism) in fostering adaptability and resilience.
I hope this helps and all the best with your research 🙂 Warm regards, Julia | Community Manager
Very good and interesting………….
This is a terrific summary of a complex area. Connect with me on LinkedIn please – I’m writing in this field also.
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Expanding the Window of Tolerance: 6 PDFs & Worksheets
In 2019, 970 million people worldwide were struggling with stress, anxiety, and mental health issues (World Health Organization, n.d.). Given these soaring numbers, many individuals [...]

Boosting Mental Toughness in Young Athletes & 20 Strategies
Mental toughness is not about being the loudest and brashest athlete on the sports field, pitch, track, or in the pool. Instead, mental toughness is [...]

10 Most Common Unhealthy Coping Mechanisms: A List
Life entails a wide tapestry of different experiences. Some of those are pleasant, some sad, others challenging. Coping mechanisms are the ways we respond to [...]
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (28)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (18)
- Positive Parenting (4)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (36)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (31)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
3 Resilience Exercises Pack

Reviewed by Psychology Today Staff
Resilience is the psychological quality that allows some people to be knocked down by the adversities of life and come back at least as strong as before. Rather than letting difficulties, traumatic events, or failure overcome them and drain their resolve, highly resilient people find a way to change course, emotionally heal, and continue moving toward their goals .
- What Creates Resilience
- How to Build Resilience
- Why Failure Can Help Us

Psychologists have identified some of the factors that appear to make a person more resilient, such as a positive attitude, optimism , the ability to regulate emotions, and the ability to see failure as a form of helpful feedback.
Optimism, for instance, has been shown to help blunt the impact of stress on the mind and body in the wake of disturbing experiences. That gives people access to their own cognitive resources, enabling cool-headed analysis of what might have gone wrong and consideration of behavioral paths that might be more productive.
Other aspects of resilience’s roots remain under study. There does appear to be a genetic predisposition for resilience , for instance; but early environments and life circumstances play a role in how resilient genes are ultimately expressed.
Not necessarily; people who have undergone trauma can be—and often are— highly resilient . In some cases, however, traumatized individuals may develop maladaptive coping skills, such as substance use, that negatively impact them and may reduce their ability to cope with future challenges.
Many factors that determine resilience—such as genetics , early life experiences, and luck—can’t be modified. But specific resilience-building skills can be learned. These include breaking out of negative thought cycles , pushing back against catastrophizing , and looking for upsides when faced with setbacks.
After experiencing trauma, many people find deeper psychological and spiritual meaning in their lives , known as post- traumatic growth. It doesn’t always occur immediately after the trauma, and the individual may still experience symptoms of anxiety , depression , or flashbacks.

Getting through pain and disappointment without letting them become overwhelming isn’t necessarily easy for anyone. But researchers have begun to uncover what more resilient people do to emotionally and mentally carry on after the death of a loved one, a job loss, chronic or acute illness, or another setback. What they’ve learned may help others become more resilient themselves.
For instance, do you attribute personal and professional setbacks solely to your own inadequacy—or are you able to identify contributing factors that are specific and temporary? Do you demand a perfect streak—or are you able to accept that life is a mix of losses and wins? In each case, the latter quality has been tied to greater levels of resilience.
Healthy habits—getting enough sleep, eating well, and exercising—can reduce stress, which may, in turn, boost resilience. Similarly, being sure to nurture close relationships can help an individual find support when trouble arises. Regularly thinking about morals and actively living according to one’s values have been linked to higher resilience.
Any crisis, such as the coronavirus pandemic, can test resilience. Looking to loved ones for help and emotional support , increasing self-care, and focusing on the aspects of the situation that are under your control can help you weather almost any storm.
A locus of control can be internal—meaning that an individual perceives that they are in control of what happens to them—or external, meaning that an individual attributes all that happens to them to external factors. An internal locus of control is tied to greater resilience .
Yes. For many, bringing an external locus of control inward requires a significant mindset change; like any skill, it takes practice and repetition. In the short term, it helps to work on being decisive and taking concrete actions when faced with adversity , rather than responding passively.
Living through a traumatic childhood can leave deep scars, but healing is possible . Talking to a loved one or therapist can help immensely. Research has found that reframing trauma—accepting that you were not to blame for abuse, for instance—can help adults feel empathy for their younger self and recognize their many strengths.

To fail is deeply human; everyone, no matter their background, skillset, or life story, will fail spectacularly at least once in their life. Its commonplace nature, however, doesn’t mean that experiencing a major loss or setback is easy or fun—or that it’s widely accepted in a winner-takes-all culture that prioritizes success at all costs.
But learning to be okay with making mistakes, big or small, is a critical skill—one tied not only to resilience but also, perhaps, to future success. One recent study, for example, found that young scientists who experienced a significant setback early in their career actually went on to greater success than scientists who had seen early wins.
You don’t have to pretend that it’s pleasant to fail or ignore the frustration that arises when a goal falls out of reach. Instead, accepting the emotions that came with the setback, being curious about why things went wrong and how you can improve in the future, and practicing self-compassion can help .
Becoming okay with making mistakes helps build better emotional regulation , which can benefit someone in a wide variety of domains from relationships to the workplace. Further, analyzing and accepting a setback can provide lessons that will stop the failure from repeating itself in the future .
Many successful people—from Steve Jobs to J.K. Rowling—report that they moved past major early failures by evading "the rumination trap ” and avoiding a spiral into negative thinking .

Young adults develop skills and resources when they are single. For men especially, experience living single is also helpful emotionally after a romantic relationship ends.
A Personal Perspective: Bill's early HIV diagnosis loomed large, but as death neared, the love and loyalty between us outshined the painful memories.

A Personal Perspective: A counselor may suggest a sober sibling write a letter to someone who has passed away. You may be surprised at what you get from it.

One of the greatest wins in emotional growth might be realizing that you are handling situations better than before.

Drop common thought fallacies related to adverse childhood experiences to reduce needless suffering and begin to heal.

Discover how great leaders blend achievement, purpose, and joy to not just succeed, but truly thrive.

Six skills highlight the human capacity for well-being by cultivating body literacy and leveraging positive life experiences to foster balance.

When we tune into these insights and meet feelings with curiosity and compassion, we can find inner strength and resolve that will serve us well.

Perfectionism can negatively affect your well-being. Here's how to avoid that outcome.

What if we celebrated the growth mindset and skill set harnessed in youth athletics? Let's look beyond wins. Character thrives in the chase
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Recommended pages
- Undergraduate open days
- Postgraduate open days
- Accommodation
- Information for teachers
- Maps and directions
- Sport and fitness
Research themes
The research that we conduct is focussed around several distinct themes.
Social Neuroscience

The more neuroscience based aspects of our work encompass the application of artificial intelligence and agent based modelling across research topics. Ongoing research also focuses on resilience in human cognition and ageing.
Researchers: Dr Julie Christian, Dr Dietmar Heinke
Resilience within forensic settings
Our research in this area focuses on resilient responses in relation to the experience or witnessing of aggression, violence and other offender behaviours. We undertake this work with both adult and child participants. In addition we also carry out research examining resilience among workers in the criminal justice system, including adaptive behaviours in response to threats and coping with other people’s traumatic experiences.
Researchers: Dr Stephane De Brito , Dr Jessica Woodhams
Resilience among children

Researchers: Dr Stephane De Brito , Dr Gary Law , Dr Elizabeth Newton
Resilience and health-related outcomes

Our work is also concerned with how individuals demonstrate resilience following periods of ill-health or health threats. In particular we examine factors that predict recovery (including outcomes such as wound-healing), survivorship issues and benefit finding and the impact of long-term psychological and physical sequela following treatment in relation to resilience-based outcomes. For example, recent work has examined benefit finding and the demonstration of resilience among survivors of breast cancer.
Researchers: Dr Theresa Powell , Dr Biza Stenfert Kroese , Dr Gerard Riley
How does redundant capacity aid resilience in biological, physical and social systems? Redundant capacity may provide an excess capacity, a form of functional redundancy enabling functional compensation and a redundant element on which evolution can act. Redundant capacity consequently enables systems to withstand, recover and adapt to disturbances. Such information could help to establish how redundancy can be built into biological, physical and social systems to aid resilience in an uncertain future.
Researcher: Dr Julie Christian
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

Psychological resilience, coping behaviours and social support among health care workers during the COVID‐19 pandemic: A systematic review of quantitative studies
Leodoro j. labrague.
1 Sultan Qaboos University, Muscat Oman
Associated Data
The data that support the findings of this study are available from the corresponding author upon reasonable request.
To appraise and synthesize studies examining resilience, coping behaviours and social support among health care workers during the coronavirus pandemic.
A wide range of evidence has shown that health care workers, currently on the frontlines in the fight against COVID‐19, are not spared from the psychological and mental health‐related consequences of the pandemic. Studies synthesizing the role of coping behaviours, resilience and social support in safeguarding the mental health of health care workers during the pandemic are largely unknown.
This is a systematic review with a narrative synthesis. A total of 31 articles were included in the review.
Health care workers utilized both problem‐centred and emotion‐centred coping to manage the stress associated with the coronavirus pandemic. Coping behaviours, resilience and social support were associated with positive mental and psychological health outcomes.
Substantial evidence supports the effectiveness of coping behaviours, resilience and social support to preserve psychological and mental health among health care workers during the COVID‐19 pandemic.
Implications for Nursing Management
In order to safeguard the mental health of health care workers during the pandemic, hospital and nursing administrators should implement proactive measures to sustain resilience in HCWs, build coping skills and implement creative ways to foster social support in health care workers through theory‐based interventions, supportive leadership and fostering a resilient work environment.
1. INTRODUCTION
The COVID‐19 pandemic is an urgent health concern worldwide that greatly affects the mental health, well‐being and possibly work effectiveness of health care workers. Mounting evidence indicates that health care workers have suffered a deterioration in their mental and psychological health during the coronavirus pandemic, with reports from individual and review studies showing higher prevalence rates of anxiety, burnout, depression, PTSD and psychological distress among health care workers compared to the general public (Chew et al., 2020 ; Shechter et al., 2020 ). In a systematic meta‐analysis by Serrano‐Ripoll et al., ( 2020 ), the pooled prevalence rate of stress among health care workers during the pandemic was 40%; furthermore, 30% of health care workers in the pooled analysis had anxiety, 28% experienced burnout, 24% had depression, and 13% had post‐traumatic stress disorder. Hence, hospital administrators should pay attention to the mental well‐being of health care workers as poorer mental health may put them at greater risk for PTSD and even suicide (Reger et al., 2020 ).
Evidence suggests that during stressful events (including disasters, calamities and disease outbreak), individuals are more likely to suffer adverse mental and psychological consequences when they are not equipped with sufficient levels of resilience and coping abilities (Duncan, 2020 ; Labrague et al., 2018 ). Support from peers, colleagues, family and friends has also been shown to help individuals sustain emotional balance in the face of threats and stress‐inducing events (Nowicki et al., 2020 ). Earlier studies conducted during other infectious disease outbreaks such as SARS, Ebola and MERS‐CoV identified a protective role for psychological resilience, coping behaviours and social support in health care workers against the psychological and mental health burden of caring for infected patients (Baduge et al., 2018 ; De Brier et al., 2020 ). Studies conducted during the COVID‐19 pandemic have shown a similar pattern: psychological resilience, coping behaviours and social support safeguard mental health and well‐being among health care workers who are on the frontlines of the fights against this deadly virus (Blanco‐Donoso et al., 2021 ; Chew et al., 2020 ; Labrague & De los Santos, 2020a , 2020b ).
Despite the abundance of empirical studies on the topic, no studies have systematically synthesized and integrated the results. A broader perspective on the topic of protective factors for psychological and mental health among health care workers is vital for the formulation of effective organisational strategies to better support the mental health of health care workers on the frontlines of the COVID‐19 pandemic. Hence, this systematic review was conducted to synthesize and integrate evidence pertaining to health care workers’ psychological resilience, coping behaviours and social support during the coronavirus pandemic.
2.1. Design
This is a systematic review with a narrative synthesis with results reported according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) protocol.
2.2. Data sources and search strategies
Relevant studies were identified through electronic database searches using PubMed, CINAHL, SCOPUS, MEDLINE and PsychINFO from August 2020 to October 2020. The following MeSH and search terms (‘psychological resilience’, ‘psychological adaptation’ OR ‘coping’, ‘mental health’, ‘health personnel’ OR ‘healthcare workers’, ‘social support’, and ‘2019‐nCoV’ OR ‘COVID‐19’ OR ‘SARS‐CoV‐2’ OR ‘severe acute respiratory syndrome coronavirus 2’) were used individually and in combination using Boolean operators (AND, OR and NOT). In addition, cited literature in the articles reviewed were also checked for potentially relevant studies (Figure 1 ).

Diagram of the process used to identify references for the review
2.3. Inclusion criteria
This review included primary studies assessing psychological resilience, coping and social support among health care professionals during the COVID‐19 pandemic. The inclusion criteria were as follows: study participants were health care workers, study was peer‐reviewed, published since the onset of the pandemic and published in the English language. In this review, health care workers are defined as people who work in health care settings to provide health care services to patients—including doctors, nurses, midwives, nursing assistants, radiologists, physiotherapists, pharmacists, health care assistants and psychologists. Only studies with quantitative designs were included in this review to facilitate homogeneity of the included papers.
2.4. Search outcomes
The initial search yielded 478 articles, from which 121 duplicates were removed. After the removal of duplicates, 357 residual references were reviewed for relevance based on the title and abstract. After screening titles and abstracts based on the inclusion criteria, 239 articles were excluded, resulting in 118 articles. After full‐text reading of the articles, 87 articles were excluded due to various reasons (e.g. used different study participants, irrelevant to the objective, did not meet the eligibility criteria and poor quality score (<5). Finally, a total of 31 articles were deemed relevant to the review. The data abstraction process is shown in Figure 1 .
2.5. Appraisal of methodological quality
Two independent researchers appraised the quality of the articles using the Joanna Briggs Institute (JBI) Critical Appraisal for Analytical Cross‐Sectional Studies in order to avoid selection bias. The JBI appraisal checklist consisted of eight items examining inclusion criteria, subjects and settings, measurement exposure, use of objective and standard criteria for measurement conditions, confounding variables, management of confounding variables, outcomes measurement and data analysis. Studies that fulfilled at least five assessment criteria were included in the review.
2.6. Data extraction and synthesis
Extraction and appraisal of data were completed by two independent researchers. Using a data matrix template, the following data were extracted from the studies: authors, year of publication, country, research approach, samples, measures, key findings and quality score (Table 1 ). Due to heterogeneity in the scales used and in the findings of the included studies, statistical pooling was not possible. As such, we used a narrative synthesis to describe the findings. In particular, constant comparison analysis (Miles & Huberman, 1994 ) was performed to compare findings across studies and to identify patterns and commonalities between studies.
Summary of Included Studies
Abbreviations: BRCS, Brief Resilient Coping Scale; BRS, Brief Resilience Scale; CD‐RISC, Connor‐Davidson Resilience Scale; CISS, Coping Inventory for Stressful Situations; COPE, Coping Orientation to Problems Experienced; CSCQ, Simplified Coping Style Questionnaire; CSES, Coping Self‐Efficacy Scale; CSES‐SF, Coping Self‐Efficacy Scale—Short Form; DRS, Dispositional Resilience Scale; MSPSS, Multidimensional Scale of Perceived Social Support; PSSQ, Perceived Social Support Questionnaire; PSSQ, Perceived Social Support Scale; RD‐CBQ, Researcher‐designed Coping Behaviours Questionnaire; RS, Resilience Scale; RSA, Resilience Scale for Adults; SIQ, Stressor and Incidence Questionnaire; SSRS, Social Support Rate Scale; SSW, Social Support at Work.
2.7. Study characteristics
Thirty‐one articles were included in the review. A majority of studies were conducted in China (14), with the remaining studies conducted in Italy (5), Philippines (2), the United States (2), Turkey (2), Spain (2), Israel (1), Palestine (1), Pakistan (1) and Egypt (1). Sample sizes ranged from 10 to 4,618 participants. Most of the health care workers included in the studies were nurses, doctors, nursing assistants, midwives, radiologists, physiotherapists, pharmacists, health care assistants or psychologists.
Most studies had a cross‐sectional research design ( n = 30), mostly using online surveys, and one study had longitudinal research design. Most studies utilized standardized scales to measure psychological resilience, coping skills and social support in health care workers. Six studies utilized research‐designed questionnaires/items to identify coping skills in health care workers. Cronbach's alphas ranged from 0.81 to 0.96 in studies that reported internal consistency.
2.8. Methodological quality score
Using the Joanna Briggs Institute critical appraisal checklist, the majority of the studies were rated as moderate in quality (26/31) and five were rated high. Issues related to identification of potential confounding variables and how these confounders were managed and controlled were common in the included articles.
2.9. Major findings
Study results were classified into the following categories: (1) levels of resilience and coping, (2) specific coping skills, (3) coping in relation to mental health, (4) resilience in relation to mental health, (5) social support in relation to mental health and (6) strategies to enhance resilience, coping behaviours and social support.
2.10. Levels of psychological resilience and coping
Six studies reported data on level of psychological resilience (Bozdağ & Ergün, 2020 ; Huang et al., 2020 , 2020 , 2020 , 2020 ; Khalaf et al., 2020 ; Labrague & De los Santos, 2020a ; Lin et al., 2020 ) and three studies described level of coping behaviours in health care workers (Lin et al., 2020 ; Mi et al., 2020 ; Nie et al., 2020 ). High levels of psychological resilience were reported in three studies (Bozdağ & Ergün, 2020 ; Huang et al., 2020a ; Lin et al., 2020 ) and moderate levels of psychological resilience were reported in four studies (Huang et al., 2020b ; Khalaf et al., 2020 ; Labrague & De los Santos, 2020a ; Luceño‐Moreno et al., 2020 ). In one cross‐sectional study of health care workers assigned to radiology units in China, online survey data indicated that 83.8% of participants reported higher psychological resilience (Huang et al., 2020a ). Similarly, a study by Lin et al. ( 2020 ) reported high levels of resilience in Chinese health care workers; however, among them, nurses were found to have lower resilience when compared to doctors and other medical staff. In a study from Turkey, health care workers scored 18.43 points out of a possible 30 points on the brief resilience scale (BRS), indicating a greater capability to rebound from the adversity associated with the coronavirus pandemic. On the other hand, four cross‐sectional studies reported moderate levels of psychological resilience among physicians (Khalaf et al., 2020 ), medical staff (Huang et al., 2020b ) and hospital nurses (Labrague & De los Santos, 2020a ) who were on the frontlines during the pandemic. In another study, health care workers in Spain obtained a mean score of 3.02 on the Brief Resilience Scale (BRS), indicating a moderate capacity to bounce back to a healthy state in the face of adversity (Luceño‐Moreno et al., 2020 ).
With regard to coping mechanisms, three studies measured ways of coping among health care workers using the Simplified Coping Style Questionnaire (Lin et al., 2020 ; Nie et al., 2020 ) and a researcher‐designed coping behaviour scale (Mi et al., 2020 ). The three studies reported higher scores for positive versus. negative coping mechanisms, suggesting that when confronted with stress‐inducing events such as the COVID‐19 pandemic, health care workers are able to utilize positive coping mechanisms.
2.11. Specific coping skills
Fourteen studies identified specific coping mechanisms employed by health care workers during the pandemic (Blanco‐Donoso et al., 2021 ; Cai, 2020 ; Chen et al., 2020 ; Chew et al., 2020 ; Dong et al., 2020 ; Giusti et al., 2020 ; Labrague & De los Santos, 2020a , 2020b ; Maraqa et al., 2020 ; Mi et al., 2020 ; Nie et al., 2020 ; Salman et al., 2020 ; Shechter et al., 2020 ; Vagni et al., 2020 ; Xiao et al., 2020 ). Among these fourteen studies reporting specific coping styles among health care workers during the pandemic, eleven quantitative studies (Blanco‐Donoso et al., 2021 ; Chen et al., 2020 ; Cai, 2020 ; Chew et al., 2020 ; Dong et al., 2020 ; Giusti et al., 2020 ; Labrague & De los Santos, 2020a , 2020b ; Maraqa et al., 2020 ; Nie et al., 2020 ; Vagni et al., 2020 ; Xiao et al., 2020 ) indicated that health care workers use support from and communication with family, friends and colleagues as their primary coping mechanisms to manage the adverse mental health consequences of the COVID‐19 pandemic. Religious coping mechanisms such as praying were reported as an important coping mechanism in three cross‐sectional studies. For instance, in two separate studies involving health care workers in Pakistan (Salman et al., 2020 ) and Palestine (Maraqa et al., 2020 ), praying and other religious activities were the highest‐ranked coping mechanisms. In the United States, where prevalence of COVID‐19 is highest, frontline emergency health care workers identified religious coping mechanisms such as praying as one of the most important ways to combat the mental and psychological burden of the pandemic (Shechter et al., 2020 ).
Involvement in distraction activities (such as engaging in sports, exercise, music, yoga or meditation) was also identified as an important coping mechanisms utilized by health care workers during the height of the pandemic (Chen et al., 2020 ; Dong et al., 2020 ; Maraqa et al., 2020 ; Mi et al., 2020 ; Shechter et al., 2020 ). Other coping mechanisms identified by health care workers included learning about COVID‐19 and its prevention (Cai, 2020 ; Chen et al., 2020 ) and adherence to infection control guidelines (Cai, 2020 ; Dong et al., 2020 ; Maraqa et al., 2020 ).
2.12. Coping in relation to mental health
Nine studies described the interaction between coping skills and mental health in health care workers during the COVID‐19 pandemic (Babore et al., 2020 ; Chew et al., 2020 ; Di Monte et al., 2020 ; Hou et al., 2020 ; Maiorano et al., 2020 ; Mi et al., 2020 ; Nie et al., 2020 ; Vagni et al., 2020 ; Zhu et al., 2020 ). The use of positive coping mechanisms such as seeking social support, positive thinking and problem solving was associated with lower levels of traumatic stress, stigma (Chew et al., 2020 ), psychological distress (Babore et al., 2020 ), stress symptoms (Nie et al., 2020 ), anxiety and depression (Mi et al., 2020 ; Zhu et al., 2020 ). On the other hand, utilization of negative coping skills, such as avoidance, was strongly linked with increased levels of emotional stress (Chew et al., 2020 ), PTSD symptoms (Hou et al., 2020 ), psychological distress (Babore et al., 2020 ; Nie et al., 2020 ) and fatigue (Hou et al., 2020 ). In one study, the use of emotion‐centred and avoidant coping styles was associated with increased levels of emotional exhaustion, while problem‐centred coping styles were strongly associated with decreased scores on the depersonalization subscale and increased scores on the personal accomplishment subscale of the MBI (Di Monte et al., 2020 ). Interestingly, unlike previous studies, two separate studies in Italy found that the use of a negative coping style—specifically, the blocking of unpleasant emotions and thoughts—was found to effectively reduce psychological distress (Vagni et al., 2020 ) and PTSD (Maiorano et al., 2020 ). Maiorano et al. ( 2020 ) and Vagni et al., ( 2020 ) both argued that by blocking negative emotions, health care workers are able to continue their work and experience lower perceived levels of stress.
2.13. Resilience in relation to mental health
A number of papers examined the effects of psychological resilience on the mental health of health care workers (12/31) (Di Monte et al., 2020 ; Huang et al., 2020a ; Khalaf et al., 2020 ; Labrague & De los Santos, 2020a , 2020b ; Li et al., 2020 ; Lin et al., 2020 ; Lucero‐Moreno et al., 2020; Maiorano et al., 2020 ; Mosheva et al., 2020 ; Tam et al., 2020 ; Yörük & Güler, 2020 ). Of these, eight studies reported a protective role of psychological resilience against coronavirus‐related anxiety. Increased psychological resilience in health care workers was associated with lower incidence of pandemic‐related anxiety among nurses working in hospitals (Labrague & De los Santos, 2020a ) and public health centres (Labrague & De los Santos, 2020b ). Results obtained from Israel and Egypt showed a similar pattern in which lower levels of coronavirus‐related anxiety were associated with higher levels of resilience (Khalaf et al., 2020 ; Mosheva et al., 2020 ). In two separate studies from China, health care workers with higher scores on psychological resilience measures reported significantly lower levels of anxiety than those who obtained lower scores on psychological resilience measures (Huang et al., 2020a ; Lin et al., 2020 ). In a study involving 720 health care workers in the United States, resilient participants were more likely than non‐resilient participants to report reduced levels of anxiety, stress, fatigue and insomnia (Huffman et al., 2021 ).
Four studies reported a strong link between personal resilience and depression (Khalaf et al., 2020 ; Lin et al., 2020 ; Luceño‐Moreno et al., 2020 ; Yörük & Güler, 2020 ), suggesting that interventions to enhance resilience among health care workers may help prevent or reduce the occurrence of depression in this population during the COVID‐19 pandemic. In addition to depression and anxiety, a few more studies confirmed the protective role of psychological resilience against psychological stress (Khalaf et al., 2020 ; Luceño‐Moreno et al., 2020 ; Tam et al., 2020 ;), emotional exhaustion (Di Monte et al., 2020 ) and PTSD symptoms (Li et al., 2020 ; Lucero‐Moreno et al., 2020; Maiorano et al., 2020 ;). In one study, resilience partially mediated the association between institutional support and coronavirus‐related distress (Tam et al., 2020 ).
2.14. Social support in relation to mental health
Seven studies explored the causal relationship between social support and mental health outcomes in health care workers during the pandemic (Blanco‐Donoso et al., 2021 ; Chew et al., 2020 ; Dong et al., 2020 ; Giusti et al., 2020 ; Labrague & De los Santos, 2020a , 2020b ; Nie et al., 2020 ; Xiao et al., 2020 ). Mental health outcomes examined in relation to social support included traumatic stress, emotional distress, psychological distress, burnout, anxiety and stress. Adequate managerial and supervisorial support and support extended by colleagues, peers, friends and family were associated with reduced levels of traumatic stress (Blanco‐Donoso et al., 2021 ; Chew et al., 2020 ) and emotional distress (Dong et al., 2020 ).
In an online cross‐sectional study involving nurses in China, higher perceptions of social support explained significant variance in the psychological distress measure (Nie et al., 2020 ), while in Italy, health care workers who perceived greater support from family and friends reported a significant reduction in burnout symptoms (Giusti et al., 2020 ). A study involving Filipino nurses showed a similar pattern: frontline nurses who perceived higher social support were less likely to demonstrate dysfunctional anxiety related to the coronavirus (Labrague & De los Santos, 2020a , 2020b ). In addition, adequate social support for health care workers was associated with a significant reduction in stress and an improvement in self‐efficacy during the pandemic (Xiao et al., 2020 ).
2.15. Strategies to enhance resilience, coping behaviours and social support
Several recommendations to enhance resilience, coping behaviours and social support in HCWs were offered in the literature. Many authors suggested the development and implementation of interventions geared towards enhancing resilience in HCWs through evidence‐based education and training to strengthen HCWs' defences against various mental and psychological consequences of the pandemic (Babore et al., 2020 ; Blanco‐Donoso et al., 2021 ; Dong et al., 2020 ; Labrague & De los Santos, 2020b ; Shanafelt et al., 2020 ). A few authors suggested individual and group skill training programmes to foster resilience and coping skills in HCWs including online cognitive behaviour therapy or mindfulness‐based therapy (Dong et al., 2020 ; Giusti et al., 2020 ; Shanafelt et al., 2020 ). Huffman et al. ( 2021 ) suggested the implementation of mindfulness‐based stress reduction and cognitive framing to improve coping abilities in HCWs, while Maiorano et al. ( 2020 ) identified hardiness training to effectively enhance the ability of HCWs to withstand the burden of the pandemic and cope effectively with the stress associated with it. In addition, reinforcement of positive coping strategies through coping skills trainings was seen beneficial for strengthening the psychological well‐being of health care providers during the pandemic (Di Monte et al., 2020 ; Khalaf et al., 2020 ; Mi et al., 2020 ).
Effective leadership was seen as vital in the promotion of mental health in HCWs and in the promotion of a resilient work environment (Chen et al., 2020 ; Shechter et al., 2020 ). By being attentive to the psychological, mental and psychosocial needs of the HCWs hospital administrators can effectively offer support and foster resilience and coping (Blanco‐Donoso et al., 2021 ; Chew et al., 2020 ; Dong et al., 2020 ). Effective leadership and organisational support through the implementation of a safe and resilient work environment, provision of complete and quality PPE and supplies to prevent infection, provision of updated and evidence‐based guidelines for infection prevention, provision of accurate and timely information regarding the disease and implementation of trainings relevant to COVID‐19 were seen vital to support the needs of HCWs and improve their mental well‐being (Labrague & De los Santos, 2020a ; Maraqa et al., 2020 ).
3. DISCUSSION
This systematic review is the first to examine psychological resilience, social support and coping behaviours among health care workers during the COVID‐19 pandemic and their effects on mental and psychological health. Despite the threat caused by the new virus and the pandemic's mental health consequences, HCWs reported having moderate to high levels of psychological resilience. In explaining this occurrence, it is important to note that the studies included in the review were conducted during the first wave of the pandemic. Therefore, HCWs are still equipped with substantial personal resources (e.g. coping, self‐efficacy, resilience) to combat the psychological burden caused by the coronavirus pandemic (Chen & Bonanno, 2020 ). However, with the increasing cases of infected patients, increasing patients’ death, increased workload due to increasing COVID‐19 admissions and lack of personal protective equipment, HCWs’ resilience, or ability to bounce back from stressful events, may eventually decline or deteriorate in the long run (Ferreira et al., 2020 ). Additionally, the lack of social connectedness and the seemingly no definite end in sight for social restrictions may contribute to this decline. As the virus continues to spread along with the threat of the new COVID‐19 variants, it is imperative that proactive measures to sustain resilience in HCWs are continuously instituted. These measures may include limiting shift hours, providing adequate hospital supplies, providing rest areas in the hospitals and providing timely updates and accurate information to HCWs regarding the virus.
Coping strategies—that is, mechanisms that an individual can employ to manage the impacts of potential threats—have been long considered an important personal resource to effectively reduce the impact of stress and its accompanying adverse consequences (Lazarus & Folkman, 1987 ). It was evident in this review that health care workers utilized both positive (e.g. use of social support and praying) and negative (e.g. use of distraction activities) coping strategies to effectively manage the stress associated with the COVID‐19 pandemic. Interestingly, the use of religious coping mechanisms—such as reading the Bible for Christians or reciting the Quran for Muslims—has been identified as an effective strategy to reduce stress, anxiety and their adverse effects during the height of the pandemic. As a coping strategy, prayer provides context, social connection and inner strength, making an individual capable of managing stress more effectively. This type of coping is not only practical, but also safe during the pandemic as it does not require contact with someone. A substantial amount of studies have established a positive link between religious coping mechanisms and reduced anxiety, aggression, psychological distress and depressive symptoms as well as enhanced optimism, hope, quality of life and psychological health (O'Brien et al., 2019 ; Solaimanizadeh et al., 2020 ).
Seeking social support as a means of coping with adversity has been categorized as a problem‐focused coping strategy (Samios et al., 2020 ) and has been found to effectively reduce stress. Mounting evidence has strongly linked adequate support from managers, co‐workers, family and friends with positive mental health outcomes for both health care and non‐health care professionals during stressful and traumatic events such as calamities, accidents, disasters and disease outbreaks (Baduge et al., 2018 ; Labrague et al., 2018 ). During the pandemic, when stress and anxiety are elevated, adequate social support may help health care workers maintain healthy emotional states. However, the different restrictions to combat the virus, including social distancing, lockdown and quarantine measures, may prevent HCWs from engaging in activities previously learned to effectively cope with stress. For instance, studies conducted before the pandemic identified social support (from friends, peers, family and even the community) and involvement of outdoor distraction activities (e.g. outdoor exercise) as important coping skills to combat stress among nurses (Ha & Sung, 2018 ; Lim et al., 2010 ). However, with the ongoing pandemic, utilizing these coping strategies can be more challenging. Because promoting social connectedness is of vital importance (as social isolation is what makes this crisis unique compared to other crises), it is essential to find creative ways to foster relationships (e.g. online social connection), to ensure that HCWs are socially and emotionally connected with their families and friends, without the risk of being infected or of infecting them. Other alternative ways to effectively cope with the mental health burden of the pandemic included formulating a new routine that incorporates healthy and optimistic behaviours, such as exercising, journaling and writing in a gratitude journal (Huang et al., 2020b ).
Psychological resilience, like social support, has long been considered a protective factor against the adverse psychological effects of stressful or traumatic situations (Hart et al., 2014 ). In the context of pandemic, a wide range of evidence has demonstrated that resilient health care workers are more likely to rebound effectively and endure the pandemic‐associated psychological burden than non‐resilient health care workers (Foster et al., 2020 ). The role of psychological resilience in protecting individuals against the mental health consequences of an emergency or disaster situation has also been confirmed in previous studies (Duncan, 2020 ; Labrague et al., 2018 ). Our finding also adds support to earlier research conducted prior to the pandemic in which higher resilience in health care workers was strongly linked to reduced burnout, compassion fatigue, anxiety, depression and psychological distress (Mealer et al., 2017 ).
3.1. Limitations of the study
Although this study provided current understanding of resilience, coping behaviours and social support among HCWs, a few limitations of the review were identified. Potentially relevant research published in other languages were excluded as this review included only articles published in English language. Further, it is worth noting that this review included articles published during the first wave of the pandemic; therefore, ongoing investigations are needed to explore how resilience, coping behaviours and social support among HCWs change through the different waves of the pandemic.
4. IMPLICATIONS FOR NURSING MANAGEMENT
This review suggests that building resilience and increasing coping skills and social support among health care workers may protect them against the adverse mental and psychological health consequences of the coronavirus pandemic. As such, hospital administrators should foster psychological resilience and reinforce positive coping strategies among health care workers by implementing theory‐tested interventions or programmes. Due to restrictions including social distancing and lockdown measures, these interventions could be delivered in innovative ways, such as webinars, online workshops and on‐demand videos. Interprofessional, web‐based nightly debriefing programmes (Azizoddin et al., 2020 ) and online cognitive behavioural therapy (Weiner et al., 2020 ) have been demonstrated to enhance resilience and morale in health care workers and improve clinical processes for quality patient care. Furthermore, increasing social support may provide a sense of greater emotional security among health care workers, thereby reducing their apprehensions and anxiety so they can function effectively during the pandemic. If health care workers are encouraged to express their feelings and concerns and openly discuss their experiences and challenges in the care and management of COVID‐19 patients, their morale will improve and their mental health will be sustained.
As positive coping strategies were seen to improve mental health in health care workers, providing training in the development of self‐efficacy and effective coping skills may help health care workers better manage the increased work pressures that have accompanied the COVID‐19 pandemic. Hospital administrators should consider increasing health care workers’ access to mental health professionals during the pandemic in to support their mental health needs.
5. CONCLUSIONS
The review findings suggest that health care workers manage their stress during the height of the COVID‐19 pandemic by utilizing both problem‐focused (e.g. use of social support and religious practice) and emotion‐focused (e.g. use of diversionary activities) coping strategies. Furthermore, this review found substantial evidence on the value and effectiveness of coping mechanisms, psychological resilience and social support in preserving the mental health and psychological well‐being of health care workers during disease outbreaks such as the coronavirus pandemic. Considering the global extent of the pandemic, this review is of interest to international readers—particularly hospital administrators.
CONFLICT OF INTEREST
The author declares no conflict of interest.
AUTHOR CONTRIBUTIONS
The author is qualified for authorship according to the following criteria:
- Have made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data;
- Been involved in drafting the manuscript or revising it critically for important intellectual content;
- Given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content; and
- Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ETHICAL APPROVAL
This review study does not require ethical approval since human samples were not included.
ACKNOWLEDGEMENT
The expertise of Dr. Anthony Monnae is acknowledged.
Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID‐19 pandemic: A systematic review of quantitative studies . J Nurs Manag . 2021; 29 :1893–1905. 10.1111/jonm.13336 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
DATA AVAILABILITY STATEMENT
- Azizoddin, D. R. , Vella Gray, K. , Dundin, A. , & Szyld, D. (2020). Bolstering clinician resilience through an interprofessional, web‐based nightly debriefing program for emergency departments during the COVID‐19 pandemic . Journal of Interprofessional Care , 34 ( 5 ), 711–715. [ PubMed ] [ Google Scholar ]
- Babore, A. , Lombardi, L. , Viceconti, M. L. , Pignataro, S. , Marino, V. , Crudele, M. , Candelori, C. , Bramanti, S. M. , & Trumello, C. (2020). Psychological effects of the COVID‐2019 pandemic: Perceived stress and coping strategies among healthcare professionals . Psychiatry Research , 293 , 113366. 10.1016/j.psychres.2020.113366 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baduge, M. S. P. , Morphet, J. , & Moss, C. (2018). Emergency nurses' and department preparedness for an ebola outbreak: A (narrative) literature review . International Emergency Nursing , 38 , 41–49. 10.1016/j.ienj.2017.12.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bozdağ, F. , & Ergün, N. (2020). Psychological resilience of healthcare professionals during COVID‐19 pandemic . Psychological Reports . Ahead of Print. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blanco‐Donoso, L. M. , Moreno‐Jiménez, J. , Amutio, A. , Gallego‐Alberto, L. , Moreno‐Jiménez, B. , & Garrosa, E. (2021). Stressors, job resources, fear of contagion, and secondary traumatic stress among nursing home workers in face of the COVID‐19: The case of Spain . Journal of Applied Gerontology , 40 ( 3 ), 244–256. 10.1177/0733464820964153 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cai, Y. (2020). Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID 19) in Hubei, China . Medical Science Monitor , 26 , e924171. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen, S. , & Bonanno, G. A. (2020). Psychological adjustment during the global outbreak of COVID‐19: A resilience perspective . Psychological Trauma: Theory, Research, Practice, and Policy , 12 ( S1 ), S51–S54. [ PubMed ] [ Google Scholar ]
- Chen, H. , Sun, L. , Du, Z. , Zhao, L. , & Wang, L. (2020). A cross‐sectional study of mental health status and self‐psychological adjustment in nurses who supported Wuhan for fighting against the COVID‐19 . Journal of Clinical Nursing , 29 ( 21–22 ), 4161–4170. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chew, Q. H. , Chia, F.‐A. , Ng, W. K. , Lee, W. C. I. , Tan, P. L. L. , Wong, C. S. , Puah, S. H. , Shelat, V. G. , Seah, E.‐J. , Huey, C. W. T. , Phua, E. J. , & Sim, K. (2020). Perceived stress, stigma, traumatic stress levels and coping responses amongst residents in training across multiple specialties during COVID‐19 pandemic—A longitudinal study . International Journal of Environmental Research and Public Health , 17 ( 18 ), 6572. 10.3390/ijerph17186572 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Brier, N. , Stroobants, S. , Vandekerckhove, P. , & De Buck, E. (2020). Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID‐19): A rapid systematic review . PLoS One , 15 ( 12 ), e0244052. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Di Monte, C. , Monaco, S. , Mariani, R. , & Di Trani, M. (2020). From resilience to burnout: Psychological features of Italian general practitioners during COVID‐19 emergency . Frontiers in Psychology , 11 , 2476. 10.3389/fpsyg.2020.567201 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dong, Z. Q. , Ma, J. , Hao, Y. N. , Shen, X. L. , Liu, F. , Gao, Y. , & Zhang, L. (2020). The social psychological impact of the COVID‐19 pandemic on medical staff in China: A cross‐sectional study . European Psychiatry , 63 ( 1 ), E65. 10.1192/j.eurpsy.2020.59 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duncan, D. L. (2020). What the COVID‐19 pandemic tells us about the need to develop resilience in the nursing workforce . Nursing Management , 27 ( 3 ), 22–27. 10.7748/nm.2020.e1933 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ferreira, R. J. , Buttell, F. , & Cannon, C. (2020). COVID‐19: Immediate predictors of individual resilience . Sustainability , 12 ( 16 ), 6495. 10.3390/su12166495 [ CrossRef ] [ Google Scholar ]
- Foster, K. , Roche, M. , Giandinoto, J. , & Furness, T. (2020). Workplace stressors, psychological well‐being, resilience, and caring behaviours of mental health nurses: A descriptive correlational study . International Journal of Mental Health Nursing , 29 ( 1 ), 56–68. 10.1111/inm.12610 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Giusti, E. M. , Pedroli, E. , D'Aniello, G. E. , Stramba Badiale, C. , Pietrabissa, G. , Manna, C. , Stramba Badiale, M. , Riva, G. , Castelnuovo, G. , & Molinari, E. (2020). The psychological impact of the COVID‐19 outbreak on health professionals: A cross‐sectional study . Frontiers in Psychology , 11 . 10.3389/fpsyg.2020.01684 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ha, D. G. , & Sung, M. H. (2018). Impact of job stress, coping behavior, hardiness on burnout in nurses in the emergency department . Korean Journal of Occupational Health Nursing , 27 ( 4 ), 215–223. [ Google Scholar ]
- Hart, P. L. , Brannan, J. D. , & De Chesnay, M. (2014). Resilience in nurses: An integrative review . Journal of Nursing Management , 22 ( 6 ), 720–734. 10.1111/j.1365-2834.2012.01485.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hou, T. , Dong, W. , Zhang, R. , Song, X. , Zhang, F. , Cai, W. , … Deng, G. (2020). Self‐efficacy and fatigue among health care workers during COVID‐19 outbreak: A moderated mediation model of posttraumatic stress disorder symptoms and negative coping . Researchsquare . 10.21203/rs.3.rs-23066/v1. Pre‐print. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huang, L. , Wang, Y. , Liu, J. , Ye, P. , Chen, X. , Xu, H. , … Ning, G. (2020). Factors influencing anxiety of health care workers in the radiology department with high exposure risk to COVID‐19 . Medical Science Monitor: International Medical Journal of Experimental and Clinical Research , 26 , e926008–e926011. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Huang, L. , Wang, Y. , Liu, J. , Ye, P. , Cheng, B. , Xu, H. , Qu, H. , & Ning, G. (2020). Factors associated with resilience among medical staff in radiology departments during the outbreak of 2019 Novel coronavirus disease (COVID‐19): A cross‐sectional study . Medical Science Monitor , 26 , e925669‐1–e925669‐10. 10.12659/MSM.925669 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huffman, E. M. , Athanasiadis, D. I. , Anton, N. E. , Haskett, L. A. , Doster, D. L. , Stefanidis, D. , & Lee, N. K. (2021). How resilient is your team? Exploring healthcare providers’ well‐being during the COVID‐19 pandemic . The American Journal of Surgery , 221 ( 2 ), 277–284. 10.1016/j.amjsurg.2020.09.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Khalaf, O. O. , Khalil, M. A. , & Abdelmaksoud, R. (2020). Coping with Depression and Anxiety in Egyptian Physicians during COVID‐19 Pandemic . Middle East Current Psychiatry , 27 ( 1 ), 1–7. [ Google Scholar ]
- Labrague, L. J. , & De los Santos, J. A. A. (2020a). COVID‐19 anxiety among front‐line nurses: Predictive role of organisational support, personal resilience and social support . Journal of Nursing Management , 28 ( 7 ), 1653–1661. 10.1111/jonm.13121 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Labrague, L. J. , & De los Santos, J. A. A. (2020b). Prevalence and predictors of coronaphobia among frontline hospital and public health nurses . Public Health Nursing . 10.1111/phn.12841. Ahead of Print. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Labrague, L. J. , Hammad, K. , Gloe, D. S. , McEnroe‐Petitte, D. M. , Fronda, D. C. , Obeidat, A. A. , Leocadio, M. C. , Cayaban, A. R. , & Mirafuentes, E. C. (2018). Disaster preparedness among nurses: A systematic review of literature . International Nursing Review , 65 ( 1 ), 41–53. 10.1111/inr.12369 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lazarus, R. S. , & Folkman, S. (1987). Transactional theory and research on emotions and coping . European Journal of Personality , 1 ( 3 ), 141–169. 10.1002/per.2410010304 [ CrossRef ] [ Google Scholar ]
- Li, X. , Zhou, Y. , & Xu, X. (2020). Factors associated with the psychological well‐being among front‐line nurses exposed to COVID‐2019 in China: A predictive study . Journal of Nursing Management , 29 ( 2 ), 240–249. [ PubMed ] [ Google Scholar ]
- Lim, J. , Bogossian, F. , & Ahern, K. (2010). Stress and coping in Singaporean nurses: A literature review . Nursing & Health Sciences , 12 ( 2 ), 251–258. 10.1111/j.1442-2018.2010.00514.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lin, J. , Ren, Y. , Gan, H. , Chen, Y. , Huang, Y. , & You, X. (2020). Factors Influencing Resilience of Medical Workers from Other Provinces to Wuhan Fighting Against 2019 Novel Coronavirus Pneumonia . Researchsquare . https://dx.doi.org/10.21203/rs.3.rs‐17931/v1 [ Google Scholar ]
- Luceño‐Moreno, L. , Talavera‐Velasco, B. , García‐Albuerne, Y. , & Martín‐García, J. (2020). Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID‐19 pandemic . International Journal of Environmental Research and Public Health , 17 ( 15 ), 5514. 10.3390/ijerph17155514 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Maiorano, T. , Vagni, M. , Giostra, V. , & Pajardi, D. (2020). COVID‐19: Risk factors and protective role of resilience and coping strategies for emergency stress and secondary trauma in medical staff and emergency workers—An online‐based inquiry . Sustainability , 12 ( 21 ), 9004. 10.3390/su12219004 [ CrossRef ] [ Google Scholar ]
- Maraqa, B. , Nazzal, Z. , & Zink, T. (2020). Palestinian health care workers’ stress and stressors during COVID‐19 pandemic: A cross‐sectional study . Journal of Primary Care & Community Health , 11 . 10.1177/2F2150132720955026. Ahead of Print. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mealer, M. , Jones, J. , & Meek, P. (2017). Factors affecting resilience and development of posttraumatic stress disorder in critical care nurses . American Journal of Critical Care , 26 ( 3 ), 184–192. 10.4037/ajcc2017798 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mi, T. , Yang, X. , Sun, S. , Li, X. , Tam, C. C. , Zhou, Y. , & Shen, Z. (2020). Mental health problems of HIV healthcare providers during the COVID‐19 pandemic: The interactive effects of stressors and coping . AIDS and Behavior , 25 ( 1 ), 18–27. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miles, M. B. , & Huberman, M. (1994). Qualitative data analysis: A sourcebook of new methods . 2nd ed. Sage Publications. [ Google Scholar ]
- Mosheva, M. , Hertz‐Palmor, N. , Dorman Ilan, S. , Matalon, N. , Pessach, I. M. , Afek, A. , Ziv, A. , Kreiss, Y. , Gross, R. , & Gothelf, D. (2020). Anxiety, pandemic‐related stress and resilience among physicians during the COVID‐19 pandemic . Depression and Anxiety , 37 ( 10 ), 965–971. 10.1002/da.23085 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nie, A. , Su, X. , Zhang, S. , Guan, W. , & Li, J. (2020). Psychological impact of COVID‐19 outbreak on frontline nurses: A cross‐sectional survey study . Journal of Clinical Nursing , 29 ( 21–22 ), 4217–4226. 10.1111/jocn.15454 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nowicki, G. J. , Ślusarska, B. , Tucholska, K. , Naylor, K. , Chrzan‐Rodak, A. , & Niedorys, B. (2020). The severity of traumatic stress associated with COVID‐19 pandemic, perception of support, sense of security, and sense of meaning in life among nurses: Research protocol and preliminary results from Poland . International Journal of Environmental Research and Public Health , 17 ( 18 ), 6491. 10.3390/ijerph17186491 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O'Brien, B. , Shrestha, S. , Stanley, M. A. , Pargament, K. I. , Cummings, J. , Kunik, M. E. , Fletcher, T. L. , Cortes, J. , Ramsey, D. , & Amspoker, A. B. (2019). Positive and negative religious coping as predictors of distress among minority older adults . International Journal of Geriatric Psychiatry , 34 ( 1 ), 54–59. 10.1002/gps.4983 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reger, M. A. , Piccirillo, M. L. , & Buchman‐Schmitt, J. M. (2020). COVID‐19, mental health, and suicide risk among health care workers: Looking beyond the crisis . The Journal of Clinical Psychiatry , 81 ( 5 ), 1–2. 10.4088/JCP.20com13381 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Salman, M. , Raza, M. H. , Mustafa, Z. U. , Khan, T. M. , Asif, N. , Tahir, H. , Shehzadi, N. , & Hussain, K. (2020). The psychological effects of COVID‐19 on frontline healthcare workers and how they are coping: A web‐based, cross‐sectional study from Pakistan . medRxiv . 10.1101/2020.06.03.20119867 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Samios, C. , Catania, J. , Newton, K. , Fulton, T. , & Breadman, A. (2020). Stress, savouring, and coping: The role of savouring in psychological adjustment following a stressful life event . Stress and Health , 36 ( 2 ), 119–130. 10.1002/smi.2914 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Serrano‐Ripoll, M. J. , Meneses‐Echavez, J. F. , Ricci‐Cabello, I. , Fraile‐Navarro, D. , Fiol‐deRoque, M. A. , Pastor‐Moreno, G. , Castro, A. , Ruiz‐Pérez, I. , Zamanillo Campos, R. , & Gonçalves‐Bradley, D. C. (2020). Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta‐analysis . Journal of Affective Disorders , 277 , 347–357. 10.1016/j.jad.2020.08.034 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shanafelt, T. , Ripp, J. , & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID‐19 pandemic . JAMA , 323 ( 21 ), 2133–2134. 10.1001/jama.2020.5893 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shechter, A. , Diaz, F. , Moise, N. , Anstey, D. E. , Ye, S. , Agarwal, S. , Birk, J. L. , Brodie, D. , Cannone, D. E. , Chang, B. , Claassen, J. , Cornelius, T. , Derby, L. , Dong, M. , Givens, R. C. , Hochman, B. , Homma, S. , Kronish, I. M. , Lee, S. A. J. , … Abdalla, M. (2020). Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID‐19 pandemic . General Hospital Psychiatry , 66 , 1–8. 10.1016/j.genhosppsych.2020.06.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Solaimanizadeh, F. , Mohammadinia, N. , & Solaimanizadeh, L. (2020). The relationship between spiritual health and religious coping with death anxiety in the elderly . Journal of Religion and Health , 59 ( 4 ), 1925–1932. 10.1007/s10943-019-00906-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tam, C. C. , Sun, S. , Yang, X. , Li, X. , Zhou, Y. , & Shen, Z. (2020). Psychological distress among HIV healthcare providers during the COVID‐19 pandemic in China: Mediating roles of institutional support and resilience . AIDS and Behavior , 25 ( 1 ), 9–17. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vagni, M. , Maiorano, T. , Giostra, V. , & Pajardi, D. (2020). Coping with COVID‐19: Emergency stress, secondary trauma and self‐efficacy in healthcare and emergency workers in Italy . Frontiers in Psychology , 11.566912. https://dx.doi.org/10.3389%2Ffpsyg.2020.566912 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Weiner, L. , Berna, F. , Nourry, N. , Severac, F. , Vidailhet, P. , & Mengin, A. C. (2020). Efficacy of an online cognitive behavioral therapy program developed for healthcare workers during the COVID‐19 pandemic: The REduction of STress (REST) study protocol for a randomized controlled trial . Trials , 21 ( 1 ), 1–10. 10.1186/s13063-020-04772-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Xiao, H. , Zhang, Y. , Kong, D. , Li, S. , & Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID‐19) in January and February 2020 in China . Medical Science Monitor: International Medical Journal of Experimental and Clinical Research , 26 , e923549–e923551. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yörük, S. , & Güler, D. (2020). The relationship between psychological resilience, burnout, stress, and sociodemographic factors with depression in nurses and midwives during the COVID‐19 pandemic: A cross‐sectional study in Turkey . Perspectives in Psychiatric Care , 57 ( 1 ), 390‐398. [ PubMed ] [ Google Scholar ]
- Zhu, J. , Sun, L. , Zhang, L. , Wang, H. , Fan, A. , Yang, B. , & Xiao, S. (2020). Prevalence and influencing factors of anxiety and depression symptoms in the first‐line medical staff fighting against COVID‐19 in Gansu . Frontiers in Psychiatry , 11 , 386. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Data, AI, & Machine Learning
- Managing Technology
- Social Responsibility
- Workplace, Teams, & Culture
- AI & Machine Learning
- Diversity & Inclusion
- Big ideas Research Projects
- Artificial Intelligence and Business Strategy
- Responsible AI
- Future of the Workforce
- Future of Leadership
- All Research Projects
- AI in Action
- Most Popular
- The Truth Behind the Nursing Crisis
- Work/23: The Big Shift
- Coaching for the Future-Forward Leader
- Measuring Culture

The spring 2024 issue’s special report looks at how to take advantage of market opportunities in the digital space, and provides advice on building culture and friendships at work; maximizing the benefits of LLMs, corporate venture capital initiatives, and innovation contests; and scaling automation and digital health platform.
- Past Issues
- Upcoming Events
- Video Archive
- Me, Myself, and AI
- Three Big Points

The Top 10 Findings on Resilience and Engagement
From the ADP Research Institute, the 10 most intriguing discoveries from a global study of resilience and engagement.
- Workplace, Teams, & Culture
- Managing Your Career
- Organizational Behavior
- Remote Work

The challenges of the past year have threatened people’s physical and psychological well-being, both personally and professionally. But if business leaders and their teams are able to better discern where they currently stand in terms of their own physical and mental health, they will be better able to determine which actions to take to survive and ultimately thrive through current and future challenges.
My colleagues and I at the ADP Research Institute recently finished conducting a global study of resilience and engagement , looking at levels of both across 25 countries in 2020. We surveyed a minimum of 1,000 people per country, for a total of over 26,000 participants. Our hope in conducting this research was twofold: first, to help leaders become more engaged and resilient in their own lives, despite the deeply unsettling events of the past year; and second, to identify ways that leaders can build engagement and resilience in their employees.
Get Updates on Transformative Leadership
Evidence-based resources that can help you lead your team more effectively, delivered to your inbox monthly.
Please enter a valid email address
Thank you for signing up
Privacy Policy
Before we dive in, it’s important to note that we define engagement as the emotional state of mind that causes people to do their best work sustainably, and resilience as the capacity of an individual to withstand, bounce back from, and work through challenging circumstances or events. Our validated survey instrument enabled us to calculate which employees were fully engaged — highly committed and willing to give their all to their team and organization. Fully engaged employees are dedicated to an organization’s purpose, certain in their definition of excellence, confident in the support of their teammates, and excited by their organization’s future. In contrast, we designated those employees who were not fully engaged as “just coming to work.”
Similarly, through the 10 items that measure and predict resilience, we were able to identify highly resilient employees who demonstrated agency and the ability to compartmentalize, felt psychologically safe, and demonstrated trust in their leaders’ abilities to anticipate the future, communicate, and follow through on commitments. 1 Those employees who were not highly resilient were designated as vulnerable . (See “The Relationship Between Engagement and Resilience” for more details on how engagement and resilience are correlated.)
Engagement is a proactive state of mind. We measured engagement levels by asking respondents questions such as how clear their expectations were, whether they got to use their strengths every day, whether they felt they would be recognized for doing excellent work, and whether someone at work was encouraging them to grow. Resilience, in contrast, is a reactive capacity , describing how people will respond when challenges arise.
Given the world events of the past year — and our previous research on engagement, which has been conducted for more than a decade — some of our findings were predictable, such as the low levels of engagement and resilience we found around the world: Only 14% of workers were fully engaged, and only 15% of workers were highly resilient. Many of the results, however, did surprise us. What follows are our 10 most intriguing discoveries .
1. Trust is everything. The most powerful driver of both engagement and resilience is trust. Employees who said they completely trust their team leader were 14 times more likely to be fully engaged. Those lucky enough to completely trust their colleagues, team leader, and senior leaders, selecting 5 on a trust scale ranging from 1 to 5, were 42 times more likely to be highly resilient. Psychologically, it’s easier to engage in our best work when we don’t have to expend mental resources looking over our shoulders or protecting ourselves against dysfunctional workplace practices that erode trust, like bullying or micromanaging. When it comes to building engagement and resilience, trust is everything.
2. One is the loneliest number. It is almost impossible to be either engaged or resilient if you do not feel like part of a team. Those who said they are on a team were 2.6 times more likely to be fully engaged and 2.7 times more likely to be highly resilient than those who didn’t identify as team members. For millennia, humans have experienced psychological well-being only when they feel connected to and supported by a small group of people around them — whether that group is a family unit, a small band of hunters and gatherers, or a hyperlocal team at work. Human flourishing happens through team flourishing — and if there’s no team to be had, engagement, resilience, and excellence are nowhere to be found.
3. Office space isn’t essential. Virtual workers are both more engaged and more resilient than those who are physically in an office or shared workspace. This was true before the pandemic and is even more true now. Before the pandemic, our research had found the most engaged people around the world were working from home four days a week and working in an office one day a week. These workers reported having both more freedom to set their own schedules and more opportunities to do what they love. In 2020, well into the pandemic, 20% of virtual workers were fully engaged and 18% were highly resilient — a stark contrast to the 11% of fully engaged and 9% of highly resilient office-based workers during the same period. How the work is done and with whom people work are both important, but organizations can stop worrying about whether virtual work is detrimental to teamwork. Feeling like part of a team is a state of mind, not a state of place. Engagement and resilience are about who you work with, not where you’re working.
4. It’s good to be in tech. The most engaged industry is technology — perhaps because tech workers already had a greater reliance on technology to connect and collaborate before the pandemic. These employees are still doing their best work, sustainably, and are able to use their strengths at work each day. For many in tech, working from home and connecting exclusively virtually with coworkers may feel more familiar than for the rest of us: 20% of technology workers are fully engaged, followed by those in the finance and professional services industries, at around 16% and 15%, respectively. The industries with the smallest percentage of fully engaged workers are app-based task employment and manufacturing, hovering around only 12%.
5. Nurses and teachers are suffering most. Our study found that the least resilient professions are in health care, health care support, and education. Undoubtedly, there are many potential causes for this beyond the coronavirus pandemic, such as inherently stressful work and comparatively lower wages. However, since our data revealed the strong link between resilience and the feeling of being on a team, one of the most powerful causes of this limited resiliency is likely that neither the teaching nor nursing profession is organized around teams.
Most hospitals are organized around parallel processes, such as nursing, therapy, or physician care, which rarely come together to create organized teams. Instead, nurses “live” in departments where one nurse supervisor manages 50 or more individual nurses. For the most part, teachers work not in teams but in classrooms, where they are individual contributors by default rather than team members.
Interestingly enough, one of the benefits of the pandemic for teachers is that many school districts have encouraged teachers to organize themselves into mutually supportive, dynamic “teaching pods” — in other words, teams. The teaching profession — along with many other professions — may want to explore how these pandemic-induced changes could usefully outlast the pandemic.
6. The unknown is scarier than change. Though people talk a lot about how each of us fears change and needs our hands tightly held through any transformation, this study challenged those assumptions. We asked people how many workplace changes they had experienced as a result of COVID-19 — such as promotions placed on hold, more virtual work, changed hours, or social distancing at work, to name a few. Surprisingly, the people who reported five or more changes at work were 13 times more likely to be highly resilient. This suggests that we humans fear the unknown more than we fear change. Company leaders shouldn’t rush employees back to normalcy when so much of the danger inherent in this current “normalcy” remains unknown and unknowable. Instead, leaders should tell their teams specifically what changes they are making to their work and why in order to increase their overall level of resilience.
7. The honeymoon (effect) is over. Pre-pandemic, we consistently found that the most engaged employees were those who had been with the company less than one year. This was not due to the quality of the work environment in the first year but was instead caused by the honeymoon effect: New employees are much more likely to rate their experience positively, just as newlyweds are much more likely to bask in the warm glow of new love. The honeymoon effect is partially explained by the fact that people want to confirm to themselves that they made a wise decision to join a new company.
But now, for the first time ever, this effect has vanished. People on the job less than a year are now less likely to be highly resilient or fully engaged (14% for each), and people who took a new job during COVID-19 are even less so (with 11% highly resilient and 8% fully engaged). Workers who have taken on new roles during the pandemic were two times less likely to be fully engaged than others.
These findings have two troubling implications. The first is that many workers have not chosen their current job but instead were forced to take it out of necessity. The second implication is that after the pandemic eases and the pressure on the job market lifts, companies will have to be extremely intentional and intelligent in order to retain those millions of workers who took on their current role under duress.
8. Members of Gen Z are no less resilient than their elders. Contrary to conventional wisdom, young people in Generation Z (aged 18 to 24) are not less engaged and less resilient than older generations. Our data contradicts the notion that younger generations are superficially confident but emotionally vulnerable: Age does not predict resilience. Resilience is much more a function of exposure to challenges, being on a team, and trusting one’s colleagues than it is of age.
9. Relationships boost resilience. Women are not more resilient than men, or vice versa. However, around the world, married people are more resilient than singles — and this holds true whether or not a couple has kids. Going into this study, we thought that having children might increase employees’ stress and therefore reduce their resilience, but this did not prove to be true. In fact, married people with kids were slightly more resilient than any other category. That said, do not imagine that children are an unmitigated blessing — because if you are single with children, you are two times less likely to be resilient. This data strongly suggests that it is much harder to summon and sustain one’s resilience when going through life alone.
10. Resilience and engagement levels rise with your role. The higher up in the organization someone is, the more resilient and engaged they are likely to feel. Those in upper management are over three times more likely to be fully engaged compared with individual contributors, and over four times more likely to be highly resilient. In one sense, this is positive news: We need those who have been given great responsibility to have the psychological well-being to exercise that responsibility wisely over time.
However, this strong relationship between role level and both resilience and engagement is also deeply worrying: In today’s working world, in virtually all professions, the real value to our customers, our patients, our children, and our communities is delivered by the folks on the front lines of organizations. They are the ones who have to make the most decisions — and the best decisions — for our companies, schools, hospitals, cities, and towns to thrive. The data reveals that at present, we haven’t yet figured out how to give these workers what they truly need, at scale, to contribute their best in the face of life’s many challenges.
Related Articles
Many of these issues, such as the lack of teams in certain industries and the disconnect between senior leadership and front-line workers, predate the pandemic and have grown even more prevalent since it began. With COVID-19 and virtual work testing everyone’s engagement and resilience daily, people are better able to discern and highlight these long-standing systemic concerns — which better enables leaders to tackle them.
As this data reveals, leaders must remember that people don’t fear change so much as they fear the unknown, so employees need clarity and specificity from leaders, not sugarcoated enthusiasm. People function best in teams, so anything leaders do to help them feel a part of a small, high-performing team — whether or not they are colocated — will boost workers’ engagement and resilience. Leaders need to see their employees not as “labor” but as the messy, complex, emotional beings they are — dealing with real-world human challenges, just like they are. The more that leaders can infuse these findings in their organizations’ policies and practices, the more likely we will all be to flourish, both during these difficult times and beyond.
About the Author
Marcus Buckingham ( @mwbuckingham ) is a New York Times bestselling author, a global researcher, and head of ADP Research Institute — People + Performance.
1. You can see the eight engagement questions on p. 6 of ADP Research Institute’s “ Global Workplace Study 2020 .”
More Like This
Add a comment cancel reply.
You must sign in to post a comment. First time here? Sign up for a free account : Comment on articles and get access to many more articles.
Comments (5)
Jen stevens, narayan kamath.
A Systematic Review of the Association between Psychological Resilience and Improved Psychosocial Outcomes in Prostate Cancer Patients. Could Resilience Training Have a Potential Role?
Affiliations.
- 1 GenesisCare, Tugun, Australia.
- 2 Brain-Behaviour Research Group, University of New England, Armidale, Australia. [email protected].
- 3 Brain-Behaviour Research Group, University of New England, Armidale, Australia.
- PMID: 38606864
- DOI: 10.5534/wjmh.230319
Purpose: A high incidence of psychosocial problems in prostate cancer patients has been reported including anxiety, depression and distress. These can add to the patients' disease burden and have been associated with unfavorable cancer treatment outcomes. Interventions designed to address them have found limited success, but psychological resilience (PR) training has never been formally tested. The measurement of PR in prostate cancer patients has been described and has been associated with more favorable psychosocial outcomes in these patients but it has never been systematically reviewed. The aim of this study was to conduct the first systematic review of those studies that have measured it using standardized scales and to determine the potential for resilience training to help overcome the significant psychosocial problems faced by prostate cancer patients.
Materials and methods: We searched the literature to identify articles that measured PR among prostate cancer patients.
Results: Of 384 articles identified by the search criteria, there were 19 studies suitable for inclusion regarding 5,417 patients. The most commonly-used scale was the original Connor-Davidson Resilience Scale, or an abbreviated version of it. Possible scores range from 0 to 100, mean scores from these studies ranged from 72.9 to 87.1 (standard deviations varied between 13.2 and 16.3). PR was consistently associated with improved psychological outcomes including depression, anxiety and distress, although these were measured with a wide variety of methods making it difficult to quantify the effects. There was also evidence of PR mediating the physical effects of prostate cancer and treatment including urinary symptoms, fatigue and insomnia.
Conclusions: As resilience training has been successful in other cancer settings, it seems likely that it could improve the significant adverse psychosocial outcomes that have been reported in prostate cancer patients and trials designed to objectively test it should be encouraged.
Keywords: Cancer survivors; Neoplasms; Prostate; Prostatic neoplasms; Resilience, psychological.
Copyright © 2024 Korean Society for Sexual Medicine and Andrology.
The effect of alexithymia on distress disclosure among nurses: the mediating role of resilience
- Published: 20 April 2024
Cite this article
- Qianru Liu ORCID: orcid.org/0000-0003-4735-0932 1 , 2 ,
- Xuetai Jian 1 , 2 ,
- Fangyu Peng 1 ,
- Meng Wang 1 , 2 ,
- Jiaxin Li 1 , 3 ,
- Xinru Deng 1 , 2 ,
- Yinglu Wan 1 &
- Li Geng ORCID: orcid.org/0000-0001-5882-4641 1
Distress disclosure has been proven to enhance the mental health of nurses. Although previous research has identified a negative association between alexithymia and distress disclosure, studies on their relationship are limited, particularly regarding their potential mediators. Therefore, this study aimed to investigate whether alexithymia is a negative predictor of distress disclosure among nurses and to explore the mediating effects of resilience between distress disclosure and alexithymia. A multicenter cross-sectional study was conducted in five hospitals in China, involving 828 nurses. Multiple linear regression was used to identify the predictors of distress disclosure, and structural equation modeling (SEM) analysis was used to analyze the mediating effect. Hierarchical multiple regression revealed that alexithymia and resilience significantly influenced distress disclosure among nurses. Based on SEM analysis, resilience served as a partial mediator of the effects of alexithymia and distress disclosure. The findings of this study suggest that interventions that aim to reduce alexithymia and increase psychological resilience may be beneficial in promoting distress disclosure among nurses.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price excludes VAT (USA) Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
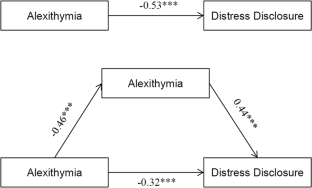
Data availability
The data that support the findings of this study are available from the corresponding author, Li Geng, upon reasonable request.
Aldaz, E., Aritzeta, A., & Galdona, N. (2019). The association between alexithymia, emotional intelligence and burnout among nursing assistants working in nursing home settings: A cross-sectional study. Journal of Advanced Nursing, 75 (11), 2786–2796. https://doi.org/10.1111/jan.14153
Article PubMed Google Scholar
Bagby, R. M., Parker, J. D. A., & Taylor, G. J. (1994). The twenty-item Toronto Alexithymia Scale-I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research , 38 (1), 23–32. https://doi.org/10.1016/0022-3999(94)90005-1
Ben-Zur, H. (2019). Transactional model of stress and coping. In V. Zeigler-Hill & T. K. Shackelford (Eds.), Encyclopedia of personality and individual differences . Springer International Publishing. https://doi.org/10.1007/978-3-319-28099-8_2128-1
Bui, M. V., McInnes, E., Ennis, G., & Foster, K. (2023). Resilience and mental health nursing: An integrative review of updated evidence. International Journal of Mental Health Nursing, 32 (4), 1055–1071. https://doi.org/10.1111/inm.13132
Caulfield, R., Wiseman, T., Gullick, J., & Ogilvie, R. (2023). Factors preceding occupational distress in emergency nurses: An integrative review. Journal of Clinical Nursing, 32 (13–14), 3341–3360. https://doi.org/10.1111/jocn.16461
Dalokay, E. B., & Aydin, A. (2023). The relationship between alexithymia, communication skills and mental well-being of nurses in Turkey: A cross-sectional study. Archives of Psychiatric Nursing, 43 , 81–86. https://doi.org/10.1016/j.apnu.2022.12.020
Dere, J., Tang, Q. P., Zhu, X. Z., Cai, L., Yao, S. Q., & Ryder, A. G. (2013). The cultural shaping of alexithymia: Values and externally oriented thinking in a Chinese clinical sample. Comprehensive Psychiatry, 54 (4), 362–368. https://doi.org/10.1016/j.comppsych.2012.10.013
Durmaz, O., & Baykan, H. (2020). Mentalizing self and others: A controlled study investigating the relationship between alexithymia and theory of mind in major depressive disorder. Indian Journal of Psychiatry, 62 (5), 559–565. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_554_19
Article PubMed PubMed Central Google Scholar
Gao, R. C., Wu, L., Shi, P. L., Sang, N., Hao, M., & Wu, G. C. (2022). The impact of distress disclosure and anxiety on the association between social support and quality of life among Chinese women with systemic lupus erythematosus. Frontiers in Psychiatry , 13, 893235. https://doi.org/10.3389/fpsyt.2022.893235
Gherman, M. A., Arhiri, L., Holman, A. C., & Soponaru, C. (2022). Protective factors against morally injurious memories from the COVID-19 pandemic on nurses' occupational wellbeing: A cross-sectional experimental study. International Journal of Environmental Research and Public Health , 19 (18), 11817. https://doi.org/10.3390/ijerph191811817
Gonsalves, P. P., Nair, R., Roy, M., Pal, S., & Michelson, D. (2023). A systematic review and lived experience synthesis of self-disclosure as an active ingredient in interventions for adolescents and young adults with anxiety and depression. Administration and Policy in Mental Health and Mental Health Services Research, 50 (3), 488–505. https://doi.org/10.1007/s10488-023-01253-2
Keum, B. T., Oliffe, J. L., Rice, S. M., Kealy, D., Seidler, Z. E., Cox, D. W.,... Ogrodniczuk, J. S. (2023). Distress disclosure and psychological Distress among men: the role of feeling understood and loneliness. Current Psychology , 42 (13), 10533–10542. https://doi.org/10.1007/s12144-021-02163-y
Khatatbeh, H., Pakai, A., Al-Dwaikat, T., Onchonga, D., Amer, F., Prémusz, V., & Olah, A. (2022). Nurses’ burnout and quality of life: A systematic review and critical analysis of measures used. Nursing Open, 9 (3), 1564–1574. https://doi.org/10.1002/nop2.936
Kim, K., Lee, J., & Yoon, J. (2023). Effects of emotional regulation, resilience, and distress disclosure on post-traumatic growth in nursing students. International Journal of Environmental Research and Public Health , 20(4). https://doi.org/10.3390/ijerph20042782
Kinnaird, E., Stewart, C., & Tchanturia, K. (2019). Investigating alexithymia in autism: A systematic review and meta-analysis. European Psychiatry, 55 , 80–89. https://doi.org/10.1016/j.eurpsy.2018.09.004
Labrague, L. J. (2021). Influence of nurse managers’ toxic leadership behaviours on nurse-reported adverse events and quality of care. Journal of Nursing Management, 29 (4), 855–863. https://doi.org/10.1111/jonm.13228
Li, L., Wang, X., Tan, J. H., Li, J. J., & Yuan, Y. G. (2022). Influence of sleep difficulty on post-traumatic stress symptoms among frontline medical staff during COVID-19 pandemic in China. Psychology, Health & Medicine, 27 (9), 1924–1936. https://doi.org/10.1080/13548506.2021.1981411
Article Google Scholar
Liu, X., Yang, H. J., Hu, Y. L., Zhou, Y. J., Wang, J. H., Dong, L. L.,... Liang, T. (2022). Incidence of workplace violence against nurses among Chinese hospitals: A meta-analysis. Journal of Nursing Management , 30 (6), 1490–1501. https://doi.org/10.1111/jonm.13427
Liu, Y. F., Zou, L., Yan, S. J., Zhang, P., Zhang, J., Wen, J.,... Fu, W. N. (2023). Burnout and post-traumatic stress disorder symptoms among medical staff two years after the COVID-19 pandemic in Wuhan, China: Social support and resilience as mediators. Journal of Affective Disorders , 321 , 126–133. https://doi.org/10.1016/j.jad.2022.10.027
Mersin, S., Ibrahimoglu, Ö., Kiliç, H. S., & Kahraman, B. B. (2020). Social media usage and alexithymia in nursing students. Perspectives in Psychiatric Care, 56 (2), 401–408. https://doi.org/10.1111/ppc.12448
Nan, R. L., Ma, L., Yan, H., Zhang, Y. B., Pei, J. H., Chen, H. X.,... Dou, X. M. (2023). Prevalence and associated factors of alexithymia in intensive care unit nurses. Nursing Open , 10 (7), 4471–4479. https://doi.org/10.1002/nop2.1689
Norouzi, M., Vajargah, P. G., Falakdami, A., Mollaei, A., Takasi, P., Ghazanfari, M. J.,... Karkhah, S. (2022). A systematic review of death anxiety and related factors among nurses. OMEGA - Journal of Death and Dying , Advance online publication. https://doi.org/10.1177/00302228221095710
O’Loughlin, J. I., Cox, D. W., Kahn, J. H., & Wu, A. D. (2018). Attachment avoidance, alexithymia, and gender: Examining their associations with distress disclosure tendencies and event-specific disclosure. Journal of Counseling Psychology, 65 (1), 65–73. https://doi.org/10.1037/cou0000245
Pei, J. H., Wang, X. L., Chen, H. X., Zhang, H. C., Nan, R. L., Zhang, J., & Dou, X. M. (2021). Alexithymia, social support, depression, and burnout among emergency nurses in China: A structural equation model analysis. BMC Nursing, 20 (1), 194. https://doi.org/10.1186/s12912-021-00702-3
Pirlott, A. G., & MacKinnon, D. P. (2016). Design approaches to experimental mediation. Journal of Experimental Social Psychology, 66 , 29–38. https://doi.org/10.1016/j.jesp.2015.09.012
Preece, D. A., Mehta, A., Petrova, K., Sikka, P., Bjureberg, J., Becerra, R., & Gross, J. J. (2023). Alexithymia and emotion regulation. Journal of Affective Disorders, 324 , 232–238. https://doi.org/10.1016/j.jad.2022.12.065
Puckett, J. A., Mereish, E. H., Levitt, H. M., Horne, S. G., & Hayes-Skelton, S. A. (2018). Internalized heterosexism and psychological distress: The moderating effects of decentering. Stigma and Health, 3 (1), 9–15. https://doi.org/10.1037/sah0000065
Rutter, M. (1990). Psychosocial resilience and protective mechanisms. The American Journal of Orthopsychiatry, 57 (3), 316–331. https://doi.org/10.1111/j.1939-0025.1987.tb03541.x
Sagar, R., Talwar, S., Desai, G., & Chaturvedi, S. K. (2021). Relationship between alexithymia and depression: A narrative review. Indian Journal of Psychiatry, 63 (2), 127–133. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_738_19
Saikkonen, S., Karukivi, M., Vahlberg, T., & Saarijärvi, S. (2018). Associations of social support and alexithymia with psychological distress in Finnish young adults. Scandinavian Journal of Psychology, 59 (6), 602–609. https://doi.org/10.1111/sjop.12478
Sharafkhani, R., Nukpezah, R. N., Lathabhavan, R., Kallmen, H., Fournier, A., & Marznaki, Z. H. (2023). Factors that affect levels of alexithymia, empathy and communication skills of nursing students in northern Iran. Nursing Open, 10 (6), 3936–3945. https://doi.org/10.1002/nop2.1652
Song, Y. Y., Liu, H., Wang, S., & Jiang, X. L. (2022). Dyadic effects of rumination and self-disclosure on posttraumatic growth in newly diagnosed gynecological cancer couples: An actor-partner interdependence modeling approach. Supportive Care in Cancer, 30 (6), 5167–5174. https://doi.org/10.1007/s00520-022-06869-y
Tang, S., Wang, M., Bao, Y. M., Hu, S. W., Kong, X. L., & Chen, D. (2022). Characteristics and independent predictors of self-disclosure among male patients undergoing in vitro fertilization: A cross-sectional study. Perspectives in Psychiatric Care, 58 (4), 2286–2293. https://doi.org/10.1111/ppc.13058
Troy, A. S., Willroth, E. C., Shallcross, A. J., Giuliani, N. R., Gross, J. J., & Mauss, I. B. (2023). Psychological resilience: An affect-regulation framework. Annual Review of Psychology, 74 , 547–576. https://doi.org/10.1146/annurev-psych-020122-041854
Tsuchiya, M., Adachi, K., Kumagai, K., Kondo, N., & Kimata, A. (2022). Cancer disclosure to friends: Survey on psychological distress and perceived social support provision. European Journal of Cancer Care (English Language Edition) , 31 (5), e13332. https://doi.org/10.1111/ecc.13332
Ungar, M., & Theron, L. (2020). Resilience and mental health: How multisystemic processes contribute to positive outcomes. Lancet Psychiatry, 7 (5), 441–448. https://doi.org/10.1016/S2215-0366(19)30434-1
Wang, L., Shi, Z. B., Zhang, Y. Q., & Zhang, Z. (2010). Psychometric properties of the 10-item Connor-Davidson Resilience Scale in Chinese earthquake victims. Psychiatry and Clinical Neurosciences, 64 (5), 499–504. https://doi.org/10.1111/j.1440-1819.2010.02130.x
Wen, J., Wu, Y., Peng, L. X., Chen, S. Y., Yuan, J. Y., Wang, W. H., & Cong, L. (2022). Constructing and verifying an alexithymia risk-prediction model for older adults with chronic diseases living in nursing homes: A cross-sectional study in china. Geriatrics , 7 (6), 139. https://doi.org/10.3390/geriatrics7060139
Wu, M. (2010). Structural equation modeling: Operation and application of AMOS (1st ed.). Chongqing University Press.
Xu, Y. R., Yang, L., Ma, L. X., Huang, X., & Gan, J. M. (2023). Analysis of the mediating effect of self–representation in alexithymia and fear of disease progression in patients with nasopharyngeal carcinoma. Chinese Journal of Oncology Prevention and Treatment, 15 (1), 70–74. https://doi.org/10.3969/j.issn.1674-5671.2023.01.11
Yeo, H. J., & Park, H. S. (2020). The structural analysis of variables related to posttraumatic growth among psychiatric nurses. Journal of Korean Academy of Nursing, 50 (1), 26–38. https://doi.org/10.4040/jkan.2020.50.1.26
Yim, J. Y., & Kim, J. A. (2022). Factors influencing posttraumatic growth among nurses caring for COVID-19 patients: A path analysis. Journal of Nursing Management, 30 (6), 1940–1948. https://doi.org/10.1111/jonm.13660
Zhang, Y. Q., Wang, T. Y., Jin, S. J., Zhang, H., Chen, L. X., & Du, S. Z. (2023). Resilience mediates the association between alexithymia and stress in Chinese medical students during the COVID-19 pandemic. General Psychiatry , 36 (1), e100926. https://doi.org/10.1136/gpsych-2022-100926
Zhao, P. F., Lapierre, M. A., Rains, S. A., & Segrin, C. (2021). When and why we disclose distress on SNSs: Perceived affordances, disclosure goals, and anticipated negative evaluations. Computers in Human Behavior , 125 , 106964. https://doi.org/10.1016/j.chb.2021.106964
Zhu, X. Z., Yi, J. Y., Yao, S. Q., Ryder, A. G., Taylor, G. J., & Bagby, M. (2007). Cross-cultural validation of a chinese translation of the 20-item Toronto Alexithymia scale. Comprehensive Psychiatry, 48 (5), 489–496. https://doi.org/10.1016/j.comppsych.2007.04.007
Download references
Acknowledgements
We would particularly like to acknowledge my research participants, for their wonderful collaboration and support.
This study was supported by the National Key R&D Program of China [ grant numbers: 2020YFC2006000].
Author information
Authors and affiliations.
Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Qianru Liu, Xuetai Jian, Fangyu Peng, Meng Wang, Jiaxin Li, Xinru Deng, Yinglu Wan & Li Geng
School of Nursing, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Qianru Liu, Xuetai Jian, Meng Wang & Xinru Deng
School of Nursing, Yangtze University, Jingzhou, China
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Yinglu Wan or Li Geng .
Ethics declarations
Ethics approval and informed consent.
All subjects were given informed consent and volunteered to participate in this study. The study was approved by the ethics committee of Tongji Medical College, Huazhong University Science and Technology [numbers: 2023-S092].
Conflicts of interest
The author(s) report no conflicts of interest in this work.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Qianru Liu, Xuetai Jian contributed equally to this work and share the first authorship. Yinglu Wan and Li Geng contributed equally to this work and share the corresponding authorship.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Liu, Q., Jian, X., Peng, F. et al. The effect of alexithymia on distress disclosure among nurses: the mediating role of resilience. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06004-6
Download citation
Accepted : 11 April 2024
Published : 20 April 2024
DOI : https://doi.org/10.1007/s12144-024-06004-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Alexithymia
- Distress disclosure
- Find a journal
- Publish with us
- Track your research

- < Previous
UKnowledge > College of Nursing > DNP Projects > 447
DNP Projects
The effect of a community resiliency model education on resilience, psychological empowerment, and well-being in behavioral health nurses.
Lorrie Smith-Esterle , University of Kentucky Follow
Date Available
Year of publication, degree name.
Doctor of Nursing Practice
Committee Chair
Dr. Andrew Makowski
Clinical Mentor
Dr. Julie Perry
Committee Member
Dr. Debra Hampton
Background: Resilience, well-being, and psychological empowerment are associated with improvement in job satisfaction and nurse retention rates. The Community Resiliency Model (CRM) can promote emotional regulation, well-being, and create an internal state of balance in response to work-related stressors. Educating nurses on how to use CRM enables the recognition of changes in thoughts, emotions, sensations, and internal or external stimuli, which can promote resilience, well-being, and psychological empowerment.
Purpose: The purpose of this project was to evaluate evaluate the effect of a resiliency education using the Community Resiliency Model (CRM) on resilience, psychological empowerment, and well-being of behavioral health nurses.
Methodology: The project employed a quasi-experimental one-group pretest/post-test design and included behavioral health nurse participants. A pretest and post-test survey and an intervention involving a 20-minute web based educational session and use of the iChill application were used. The CD-RISC-10, Spreitzer Psychological Empowerment Scale, and WHO-5 were used to evaluate the impact of the intervention and changes after the intervention.
Results: Behavioral health nurses found CRM skills helpful in coping with stress. Nurses also found CRM skills valuable enough to share with others. Well-being scores increased post intervention. Overall, there was not significant increase in mean scores post-intervention compared to pre-intervention for the CD-RISC-10 (p = .11; see Table 2), Spreitzer Psychological Empowerment Scale (p = .53; see Table 3), and the WHO-5 (p = .39; see Table 4).
Conclusion: The educational video presentation was effective in helping behavioral health nurses use CRM skills to cope with stress. These results suggest that a 20-minute video is an effective method for delivering CRM education to nurses in a busy healthcare environment. Further research with larger matched samples and longitudinal studies can provide better insight into the impact of CRM on resilience, psychological empowerment, and well-being in this population.
Recommended Citation
Smith-Esterle, Lorrie, "The Effect of a Community Resiliency Model Education on Resilience, Psychological Empowerment, and Well-being in Behavioral Health Nurses" (2023). DNP Projects . 447. https://uknowledge.uky.edu/dnp_etds/447
Since April 18, 2024
Included in
Psychiatric and Mental Health Commons , Psychiatric and Mental Health Nursing Commons , Somatic Psychology Commons
Advanced Search
- Notify me via email or RSS
Browse by Author
- Collections
- Disciplines
Author Corner
- Submit Research
New Title Here
Below. --> connect.
- Law Library
- Special Collections
- Copyright Resource Center
- Graduate School
- Scholars@UK

- We’d like your feedback
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
University of Kentucky ®
An Equal Opportunity University Accreditation Directory Email Privacy Policy Accessibility Disclosures

IMAGES
VIDEO
COMMENTS
Psychological resilience: an update on definitions, a critical appraisal, and research recommendations ... developmental psychiatry, and psychiatric epidemiology discussed complex and dynamic current topics in resilience research. Four core themes emerged including (1) considerations related to the definitions of resilience, (2) approaches to ...
Resilience is the process and outcome of successfully adapting to difficult or challenging life experiences, especially through mental, emotional, and behavioral flexibility and adjustment to external and internal demands. ... Topics in Psychology. ... Psychological research demonstrates that the resources and skills associated with resilience ...
Topics in Psychology. Explore how scientific research by psychologists can inform our professional lives, family and community relationships, emotional wellness, and more. ... The ability to learn resilience is one reason research has shown that resilience is ordinary, not extraordinary. One example is the response of many Americans to the ...
Results: While different definitions emerged, all shared a focus on conceptualizing resilience at multiple levels, from the biological to the social structural level, a focus on the dynamic nature of resilience, and a move away from conceptualizing resilience as only an individual trait. Critical areas for future research included 1) focused ...
Building Resilience: The Conceptual Basis and Research Evidence for Resilience Training Programs. Sarah Forbes [email protected] and Deniz Fikretoglu View all authors and affiliations. ... and the impact of resilience and psychological training on outcome measures across a variety of settings. The results of our review show that the quality of ...
Psychological resilience showed only a weak relationship with Germ Aversion. ... the field should move on to addressing other topics. Resilience is a dynamic process by which individuals utilize ...
Psychological resilience allows one to cope successfully with adversities occurring during stressful periods, which may otherwise trigger mental illness. ... This article is part of the Research Topic Promoting Resilience Interventions for Mental Well-being in Youth View all 21 articles. Psychological Resilience, Mental Health, and Inhibitory ...
Background: The ability to resist adverse outcomes, or demonstrate resilience after exposure to trauma is a thriving field of study. Yet ongoing debate persists regarding definitions of resilience, generalizability of the extant literature, neurobiological correlates, and a consensus research agenda. Objectives: To address these pressing questions, Drs. Christy Denckla and Karestan Koenen (co ...
Research into psychological resilience originated in studies of the development of mental health or mental disorder through child and adolescent development (Rutter, 1993, 2006). The construct has been invoked to explain how some children are able to overcome early life adversity and disadvantage, and avoid mental disorders (e.g., Lee, Cheung ...
Scientific community. Psychological resilience has emerged as a key factor in mental health during the global COVID-19 pandemic. However, no work to date has synthesised findings across review ...
This article is part of the Research Topic Promoting Resilience Interventions for Mental Well-being in Youth View all 21 articles. ... Davidov A, Cohen NB, Yehuda AB, et al. Psychological resilience, mental health and inhibitory control among youth and young adults under stress. Front Psychol. (2021) 10:446. doi: 10.3389/fpsyg.2019.00446.
Psychological resilience has been studied for decades, and many researchers have reviewed the literatures on psychological resilience to further sort out the research content and direction, however, there is still a lack of summary and evaluation on the literature features, research direction, research depth, hot topics and other aspects of ...
To clarify the point through an example of psychological resilience, there is a long research tradition in individual or psychological resilience, which embarks from the child and adolescent development literature (Masten & Reed, 2002) and has increasingly been adopted to general psychology. In this research tradition, psychological resilience ...
Step 1: Identify your top resilience needs. Below are eight common relational sources of resilience, the same ones we noted above. Our research shows that these sources are not universally or ...
Resilience theory and positive psychology are both applied fields of study, meaning that we can use them in daily life to benefit humanity, and both are very closely concentrated on the importance of social relationships (Luthar, 2006; Csikszentmihalyi & Nakamura, 2011). So let's look at what positive psychology research shows on resilience.
List of figures and boxes Figures Figure 1: Visualisation of resilience research: intersections with related disciplines in psychology 8 Figure 2: Resilience is related to, but not the linear opposite of, concepts such as depression, anxiety or PTSD 11 Figure 3: Visualisation of protective mechanisms 12 Boxes Box 1: Principles of brief interventions: What can (and cannot) be learned from ...
Resilience is the psychological quality that allows some people to be knocked down by the adversities of life and come back at least as strong as before. Rather than letting difficulties ...
Our research in this area focuses on how children, young people and families demonstrate resilience following adversity, and how this impacts on future outcomes. It also examines the relational context of successful coping by looking at the role of peer relationships, or belonging and commitment. For example, current work examines resilience ...
Implications for Nursing Management. In order to safeguard the mental health of health care workers during the pandemic, hospital and nursing administrators should implement proactive measures to sustain resilience in HCWs, build coping skills and implement creative ways to foster social support in health care workers through theory‐based interventions, supportive leadership and fostering a ...
1. Trust is everything. The most powerful driver of both engagement and resilience is trust. Employees who said they completely trust their team leader were 14 times more likely to be fully engaged. Those lucky enough to completely trust their colleagues, team leader, and senior leaders, selecting 5 on a trust scale ranging from 1 to 5, were 42 ...
Psychological resilience is the ability to cope mentally and emotionally with a crisis, or to return to pre-crisis status quickly. ... As of 2006 little research had been done on the topic of family resilience in the wake of the death of a family member. Clinical attention to bereavement has focused on the individual mourning process rather ...
We have opened this call to include research on such topics as: Methodological considerations and best practices in measuring resilience and growth in historically marginalized or under-resourced communities. Theoretical approaches to the study of resilience and growth amidst social disadvantage. Longitudinal studies on resilience and growth to ...
Purpose: A high incidence of psychosocial problems in prostate cancer patients has been reported including anxiety, depression and distress. These can add to the patients' disease burden and have been associated with unfavorable cancer treatment outcomes. Interventions designed to address them have found limited success, but psychological resilience (PR) training has never been formally tested.
Psychological Resilience - Science topic. The human ability to adapt in the face of tragedy, trauma, adversity, hardship, and ongoing significant life stressors. Questions (72) Publications ...
The research items consist of 10 items of general information, 4 dimensions of the Nurses' Moral Courage Scale (NMCS), 4 dimensions of the Resilience Scale, and 5 dimensions of the Practice Environment Scale (PES), including a total of 23 statistical analysis variables. ... and was related to five factors. Psychological resilience and nursing ...
Consistent with prior research (Kim et al., 2023; Wen et al., 2022), this study found a negative correlation between alexithymia and psychological resilience, but a positive correlation between psychological resilience and distress disclosure. Moreover, resilience was identified as a mediator of the association between distress disclosure and ...
The study used the Relational Scanning Model Comparison Types to compare the psychological resilience of children who received Montessori education with those who did not. The research involved 99 children aged 3-6 years who received regular preschool and Montessori education during the 2021-2022 academic year.
Background: Resilience, well-being, and psychological empowerment are associated with improvement in job satisfaction and nurse retention rates. The Community Resiliency Model (CRM) can promote emotional regulation, well-being, and create an internal state of balance in response to work-related stressors. Educating nurses on how to use CRM enables the recognition of changes in thoughts ...
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022. Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this ...
Midwifery practice inevitably includes miscarriages, stillbirths, and neonatal deaths. The aim of the present study was to investigate the relationship between attitudes toward death and emotional intelligence, personality, resilience, and justice beliefs among midwives in Greece. A descriptive cross-sectional study was conducted from 2020 to 2022 among 348 midwives employed in public ...