
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.

Book Title: Qualitative Research – a practical guide for health and social care researchers and practitioners
Authors: Darshini Ayton; Tess Tsindos; and Danielle Berkovic
Download this book
- Digital PDF
- Pressbooks XML
- WordPress XML
- OpenDocument
- Common Cartridge (Web Links)
Book Description: This guide is designed to support health and social care researchers and practitioners to conduct qualitative research. (Published 2023)
Book Information
Book description.
This guide is designed to support health and social care researchers and practitioners to integrate qualitative research into the evidence base of health and social care research. Qualitative research designs are diverse and each design has a different focus that will inform the approach undertaken and the results that are generated. The aim is to move beyond the “what” of qualitative research to the “how”, by (1) outlining key qualitative research designs for health and social care research – descriptive, phenomenology, action research, case study, ethnography, and grounded theory; (2) a decision tool of how to select the appropriate design based on a guiding prompting question, the research question and available resources, time and expertise; (3) an overview of mixed methods research and qualitative research in evaluation studies; (4) a practical guide to data collection and analysis; (5) providing examples of qualitative research to illustrate the scope and opportunities; and (6) tips on communicating qualitative research.
Cover design by Les Thomas
Qualitative Research – a practical guide for health and social care researchers and practitioners Copyright © 2023 by Darshini Ayton; Tess Tsindos; Danielle Berkovic is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Research methods: general
Darshni Ayton, Tess Tsindos, and Danielle Berkovic assert their right to be known as the authors of this work.
This book was published via the Council of Australian University Librarians Open Educational Resources Collective in 2023. The online version is available at https://oercollective.caul.edu.au/qualitative-research/
Disclaimer: Note that corporate logos (and the logos of any other company represented) and branding are specifically excluded from the Creative Commons Attribution NonCommercial Licence 4.0 of this work, and may not be reproduced under any circumstances without the express written permission of the copyright holders.
- Research article
- Open access
- Published: 21 February 2022
A qualitative study of how COVID-19 impacts on Australians’ hopes and dreams
- Quincy F. Huang ORCID: orcid.org/0000-0003-0572-1387 1 , 2 ,
- Floraidh Rolf ORCID: orcid.org/0000-0001-7183-2953 3 ,
- Lauren A. Booker ORCID: orcid.org/0000-0002-0533-3715 4 ,
- Taleah Moore 1 &
- Sandra C. Thompson ORCID: orcid.org/0000-0003-0327-7155 1
BMC Public Health volume 22 , Article number: 367 ( 2022 ) Cite this article
7257 Accesses
4 Citations
10 Altmetric
Metrics details
Although beginning in 2019, it was early in 2020 that the global community began to comprehend the significant impact that a pandemic of a new coronavirus might have on their own lives. This study was undertaken 6–9 months after significant public health restrictions were introduced within Australia and examined the impact of the COVID-19 on individuals’ hopes and dreams for their future.
Community members who responded to a survey about COVID-19 were invited to participate in follow up interviews if they reported living with a chronic condition. Participants across Australia who consented were interviewed between August and December in 2020 over telephone or videoconferencing. A specific question was included regarding the impact of COVID-19 on their hopes and dreams for the future. Rapid identification of themes with an audio recordings technique was used to generate themes from the data.
The 90 participants were predominantly female (77%) and ranged in age from 20 to 81 years with a mean age of 50 years and lived in several Australian states. Following immersive analysis of interviews, the identified common themes impacting people’s hopes and dreams revealed: concerns for their own and others’ job stability and future work; the impact on travel both for holidays, business and reconnecting with family; reassessing of personal and social values; and the intergenerational impact of such a profound pandemic, with concern for younger people particularly prominent in those concerns. Participants reflected on their loss of future dreams, with possibilities they had planned and worked towards not possible in the short term.
Conclusions
The responses provide a window into how people view their future goals and aspirations during a time of global and local instability and highlights the potential future impacts of the COVID-19 pandemic.
Peer Review reports
Since the emergence of the COVID-19 pandemic in December of 2019, Australia has been proactive in controlling community transmission of the virus aiming for the goal of national control of pandemic impact. The first case of COVID-19 in Australia was diagnosed on 25 January 2020 [ 1 ]. As of 30 April 2021, Australia had a total of 29,801 cases of COVID-19 including 910 deaths [ 2 ]. Most cases (20,518) occurred in Victoria, followed by New South Wales (5477) and Queensland (1559). Most deaths due to COVID-19 have occurred in Victoria (820), New South Wales (54), and Tasmania (13) [ 2 ].
Over half (55%) of all COVID-19 cases have occurred in those aged 20 to 49 years, with the proportion of cases relatively similar for males and females. Most (94%) COVID-19 related deaths have occurred in individuals over the age of 70 years [ 2 ]. In comparison with the 150 million cases and over 3.1 million deaths from COVID-19 globally recorded on 30 April 2021, Australia makes up only a tiny proportion of both cases and deaths which is a testament to the effectiveness of the government’s mitigation plan for the virus, in addition to the advantage of the unique geography of Australia as an island nation at the bottom of the Southern Hemisphere [ 3 ]. The main pillars surrounding Australia’s COVID-19 pandemic response measures have been threefold: (1) surveillance, quarantine, and isolation, (2) testing and contact tracing, and (3) outbreak responsiveness [ 4 ]. The Australian government also closed the national borders and banned Australians from traveling overseas, a measure which was aimed at reducing transmission and infection [ 5 ].
While Australia saw benefits from the timely enactment of effective public health measures to control the spread of COVID-19, the pandemic’s effects on daily life of individuals and the communities in which they live have triggered profound changes. Emergency public health powers were enacted by state and territory governments in response to epidemiology and cases in the state at the time; restrictions on people’s liberties with respect to travel locally, within Australia and internationally, changed rapidly and so there were a patchwork of different arrangements at different times across Australia, with people expected to find up to date advice by visiting government websites ( https://interstatequarantine.org.au/state-and-territory-border-closures/ ). While those in more densely populated cities had the greatest exposure to the virus, residents living in cross border areas were particularly impacted by the response to containing the virus [ 6 ]. People’s trajectory of the future and their long-term hope and dreams were impacted due to uncertainty and the restrictions imposed.
While pandemics are not a new phenomenon, this extraordinary time of global change in a connected digital age provides a distinctive context in which to examine the changes to people’s hopes and dreams during a major negative global shock such as the COVID-19 pandemic. The impact of pandemics on individuals’ hopes and dreams for the future is somewhat limited in research literature. Yet, whether it was the loss of a loved one, the loss of a job, or the loss of the sense of normalcy, people and communities experienced an impact on their lives because of the COVID-19 pandemic which warrants further understanding. Recognizing the impact, not just on the short term but on the long-term vision of people, is important to provide understanding and knowledge for future pandemic responses.
This qualitative research project was conducted as part of a national collaborative effort spearheaded by a university department of rural health to collect data on individual and community experiences of the COVID-19 pandemic. The first phase of this project involved a survey of 677 people located across various states and territories in Australia, recruited through professional networks and social media. All survey members were asked if they would be willing to be contacted for a follow up interview and 416 responded positively. The original project was approved by the University of Queensland Human Research Ethics Committee (Approval number 2020000800) and amended for the qualitative approach with further reciprocal human ethics approvals were acquired from the investigators’ respective institutions before data collection and analysis. Out of the participants that expressed interest for a follow-up interview, 172 of those respondents identified themselves in the survey as living with a chronic illness. Details of the approach taken are available elsewhere [ 7 ]. Ninety of the original 172 participants across various Australian states ended up completing interviews, undertaken by phone by a team of researchers at institutions across Australia over 4 months (August to December 2020). Participants had to be 18 years or over, reside in Australia and have responded in the initial survey that they had a chronic illness.
Following carefully documented verbal informed consent, interviews were recorded, and field notes taken during the interviews. An interview guide was specifically developed for this research and is available as a Supplementary file (Interview Guide Attitudes and practices towards the COVID-19 pandemic in Australia. The interviews were semi-structured, with prompts centered on issues for exploration that included social distancing, handwashing, cleaning and disinfecting community behavior, leaving the house, government guidelines on social distancing, changes to daily life, vulnerability to COVID-19, impact on physical health, feeling safe, impact on mental health, risk of infection in one’s community. A specific question was included on how COVID-19 had affected their hopes and dreams for the future. While these themes served as a guide for interviews, investigators were encouraged to let the participants take control of the conversation to see what additional topics arose.
From the unique identifier in the data repository and using the demographic information collected during the initial survey, a participant number and identifier was constructed for each interview, linked with the unique identifier to support an audit trail. The interview identifier consisted of <Participant ID numbers _age _MM > in which the 90 interviews were labelled with a participant ID number from 1 to 90. The MM stands for Modified Monash [Model] and is a measure of rurality based on a model which measures remoteness and population size on a scale MM 1 to MM 7 where MM 1 is a major city and MM 7 is very remote.
The researchers used digital tagging to ascribe emergent themes and create a searchable dataset out of original field notes. The interviews asked specifically about participants’ hopes and dreams for the future and responses were reviewed to identify major themes common across multiple participants.
The authors used an inductive approach through immersion with the interview notes, return to and immersion in the digital recordings as needed, and establishment of links between codes to develop emergent themes, discussion of connections to identify the main themes on hopes and dreams for the future aggregated across multiple interviews. Further discussion occurred amongst the five researchers who then reviewed the relevant notes and interview recordings in greater detail.
Participants were predominantly female (77%), and individuals ranged in age from 20 to 81 years with a mean age of 50 years. The interviews covered many aspects of participants’ psychosocial wellbeing including dealing with the uncertainly of the future with participants commenting on a range of issues relevant to their future wellbeing. Four main themes emerged from the data specific to hopes and dreams for the future: job stability, travel, reassessing values, and generational impact.
Job stability
For some young adults, the COVID-19 pandemic in Australia led to the loss of education and job opportunities which ultimately impacted on their hopes and dreams for the future (Walsh, 2020). Adults aged 35 years and older also experienced job insecurity, with unemployment rates rising 14.8% in the period between March and September 2020 [ 8 ]. Job stability was a common theme among interview participants, with the main concerns being losing a job and not being able to find a job in the future. A similar proportion of males and females expressed concern for their job security, and this worry was felt across all age groups. While concerns for future job security appeared widely felt at the time, whether these fears persist in the short- or long-term remains to be seen and are likely to depend on both individual and larger macro system factors. This sentiment was captured by this woman on searching for a job: “ the chances of finding a job are always fraught, but the [current] economic situation is going to make that so much more difficult ” (Participant 63_F_46_2), while an individual who was employed commented, “[the pandemic] is probably going to lose me my job ” (Participant 65_M_65_5). Depending on their type of work, some participants felt the loss of job security more acutely, “[Musicians] playing four, five nights a week is their livelihood and a big part of their income ” (Participant 3_F_49_2).
The shift to a virtual environment also impacted students’ plans and necessitated changes to accommodate a new reality. One student commented, “ I played around with my majors to make sure that I am going to be able to work from home and have more flexible working conditions ” (Participant 39_F_34_5). Young people expressed their concerns regarding education and what the future held in terms of jobs, wondering whether education would lead to a better job. As one student commented “ The risk of me having no work is that I probably will continue to study and may end up with a postgrad and in more debt for something I am not completely interested in ” (Participant 49_F_31_1). Even those with a clear future career pathway felt less confident about what lay ahead, for example a medical student recounted a fear of readiness for graduation and practice after a long break from patient contact and clinical placement. Such concerns were not unique to students with apprehension around job security extending to those currently employed and retirees. Individuals not currently in school also remarked on going back to school being a possibility if jobs were unavailable. Teachers and educational faculty members also felt the strain the pandemic put on their careers. As one academic commented, “ We’re facing a very real possibility that there will be [no jobs] to apply for, fellowships will be gone, funding to universities will drop, and the recovery for something like that is very long ” (Participant 25_F_37_1).
Concerns were also expressed surrounding the economic insecurity that resulted from loss of jobs which were recognized as disproportionately affecting some people: “ we’ve got a huge portion of the population that can’t even look after themselves if they miss a paycheck ” (Participant 53_M_36_2). Economic uncertainty and security of employment were very real concerns for many who were unemployed or unsure what their jobs would look like in the future. Even those who were employed voiced considerable apprehension for the future; “ I’m still concerned for my own work; I am not sure what the future is going to look like for my work. I hope that it looks ok and the skills that we have…are going to be supported ” (Participant 40_F_42_3).
Despite the overwhelming fears and concerns, many individuals found the changing landscape of in-person work moving to a virtual environment to be a positive thing and to be associated with other benefits: “ Working from home is not an impossible dream, and with the population pressures that we are under it would be nice if we could keep large populations working from home and put less pressure on public transportation and nature itself ” (Participant 16_F_64_5).
Of the 90 individuals interviewed, at least a quarter of them raised job security in their discussion of hopes and dreams for the future, with concerns raised equally by men and women. The age range for participants who mentioned job security was 20 years to 66 years, with the mean age being 48 years, showing that concern for job security was felt across a wide variety of job-participating age groups.
The ability to travel both domestically and internationally was greatly hindered by border closures instituted by both state and federal governments. Beginning in late March 2020, Australian borders were closed to everyone except for Australian citizens, residents, and immediate family members [ 9 ].
Uncertainty surrounding travel, frustration of cancelled plans and not being able to plan overseas trips or seeing family and friends in the future were common preoccupations for many participants. A recent retiree commented, “ COVID has made me rethink travel, I am not game enough to go overseas for a while… if we do end up travelling it will be less planned, more spontaneous ” (Participant_47_F_60_1) Similarly, another individual discussed how he was “ reluctant to plan any holidays for fear that they will be cancelled ” (Participant_89_F_56_2).
Personal travel was not the only thing impacted by the border closures. One individual encapsulated the concerns many felt when he expressed, “ I don’t know how Australia will come out of it… I don’t know what it means for future travel of products and exports and who can afford to travel ” (Participant_41_F_M_36_2). He was concerned with the movement of goods and services through the wider global economy, which was brought on by the drastic change in travel and border closures.
The impact on individual travel goals was not limited to international travel. Domestic border closures and restrictions were announced in the Northern Territory, Queensland, South Australia, Tasmania, and Western Australia, which made it difficult or impossible for individuals to travel to or from these states [ 10 ]. While these restrictions were implemented to reduce the community transmission of COVID-19 in the present, the fear of future travel restrictions being implemented is one that may persist beyond the pandemic. A woman who was an avid domestic traveler before the pandemic “ cancelled caravanning around Western Australia due to border restrictions and not feeling safe of people around you ” (Participant 47_F_60_1). In contrast, others rethought their plans for travel to keep them much closer to home, as illustrated by an individual who had decided her “future travel will be in Australia instead ” (Participant 11_F_65_2).
In addition to the change in travel plans, travel restrictions also meant missing out on family milestones for those who had relatives in different areas. An individual “ missed two weddings and a funeral in the last two months [because he] has not been able to leave the country ” (Participant 41_M_36_2). This sentiment was shared by another who said, “ we miss that in-person contact with people that you are close to…my husband’s family lives in New Zealand and he usually travels over to see them every year ” (Participant 42_F_55_2).
Travel was one of the main aspects of individuals’ future hopes and dreams that were negatively impacted by the pandemic. Out of the 90 individuals interviewed, over half mentioned future travel in their discussions of hopes and dreams, and it was more commonly mentioned by women than men and across a wide range of age groups, from 23 to 75 years.
Reassessing values
The COVID-19 pandemic changed the day-to-day lives of people all over the world in profound and drastic ways. In Australia, daily commutes and social interactions were limited, and people found themselves staying at home and spending time with smaller social circles. People from diverse points along the adult lifespan shared thoughts around making each day count and realizing the value of family above material wealth. For many participants, this change meant slowing down and appreciating the present as much as the future, “ it has made me think more about making today count ” (Participant 33_F_56_6). This sentiment was expressed by many others, including a woman who commented, “ material things are not as important as having your family and living in a [healthy] community ” (Participant 9_F_36_6).
In addition to a greater appreciation for physical health, participants made repeated mentions of improved environmental health. The positive effect the pandemic had on climate change is a theme that several participants mentioned as something they would like to see continue after the pandemic. One woman encapsulated the views of many when she observed, “ the forced lockdowns have forced the world to change, and we can see the effects of it [on the environment] ” (Participant 33_F_56_6). As another participant similarly noted “ environmentally there has been good benefits from people who have not been able to travel… hopefully it has made people a bit more conscious [of] how their lifestyle does impact the environment ” (Participant 90_F_49_2). The positive effect of fewer commuters was also noted by younger participants “ As a society we are going to be able to reduce greenhouse gas emissions by people working from home ” (Participant 39_F_34_5).
Reassessing values in occurred commonly in consideration of future hopes and dreams, and was raised more by women than men, again across a broad age range.
Generational impact
While the COVID-19 pandemic personally affected people across all age groups, another common theme across many interviews was their concern for the younger generations, with 11 women and 7 men mentioning the future impact on younger generations in their discussions about hopes and dreams. More males than females expressed concerns for younger generations, and this sentiment was predominantly found in the older age groups. This generational concern spanned issues from economic impact to mental impact and were expressed by concerned parents and grandparents. Fear for the national economy was consistently expressed when discussing generational impacts, regardless of participants having children or being child-free. Some participants who were also mothers talked about the burden of their children ultimately paying for government welfare initiatives such as unemployment assistance like JobKeeper and JobSeeker, or the impact on their children’s dreams and their employment future. Yet, child-free participants also expressed concern at generational economic burden. Perceptions of a slow recovery and long-term economic effects transcended individual impact and were positioned by many participants as a community encumbrance.
Adults without children still recognized the economic impact that would be felt in the years to come. As observed by one male, “ there are going to be long-term economic effects but not really affecting me ” (Participant 65_M_65_5), a sentiment also noted by another similarly aged woman, “ we are not going to get over what’s happened to the economy anytime soon ” (Participant_84_F_64_5).
Furthermore, mental health concerns for younger populations were noted frequently. A mother mentioned the struggles she saw in younger generations, stating, “ it’s been quite hard for young people, the resilience is disappearing from them very quickly and I think we as adults in the community are partly responsible for that ” (Participant 44_F_55_7).
The overall worry for younger generations was one that is widely recognized by Australians as they looked forward towards recovery and moving forward. From loss of jobs to heightened national debt, the impact the pandemic had on Australia and globally was recognized as one that would be felt for years to come. As one mother expressed, “ as a parent, when thinking about my hopes and dreams for the future, it is going to be the impact on my children’s hopes and dreams ” (Participant_29_F_45_1).
The pandemic created a unique situation in which people experienced a sense of powerlessness, both at the hands of the virus and at the interventions imposed by state and federal government. Individuals were limited in their capacity to change their current situation, with lack of agency known to be a contributor to stress and hopelessness [ 11 ]. Issues related to psychosocial wellbeing were evident throughout the interviews with interviewees referring to their mental health but also considering new possibilities for the future. Considerable attention has already been given to the mental health consequences of COVID-19 across a variety of different age groups [ 12 , 13 ].
‘Hopes and dreams’ was a term used to describe a participant’s outlook on the future, the desire of an improved situation (which may be about personal, professional, or other aspects of an individual’s existence), the possible fear or concern of a less-promising future, and both practical and aspirational objectives to strive for. Although ‘hopes and dreams’ are not typically qualities that may be empirically measured (that is, comparing one person’s hopes and dreams to another person’s does not validate or invalidate that of one person over another), it is reasonable to recognize that each person considers their personal hopes and dreams paramount to their individual value systems. As the participants described their feelings, optimism or concerns on their individual hopes and dreams, they were stating and sharing their assessment of their current times living during a pandemic, their predictions for the future following the pandemic, and – importantly – what their place may or may not be in the post-pandemic world.
This study was undertaken about 6–8 months after COVID-19 first reached Australia and reflects the concerns and aspirations of people at that time. Psychosocial wellbeing, job security, travel, reassessing values, and generational impact were the focal themes expressed repeatedly by participants, spanning age and sex. While individual participants recounted their own hopes and concerns for the future, these themes dominated the interviews.
Research surrounding the psychological impacts of the COVID-19 pandemic suggests that many people experience feelings of grief due to loss of loved ones, loss of a sense of normalcy, or both [ 14 ]. However, this study found that even though individuals were limited in their capacity to change their current situation, many remained optimistic with respect to their hopes and dreams for the long term.
The concern of job security was not felt equally among all individuals, depending on personal socioeconomic factors. In Australia, 13.6% of the population lives below the poverty line, a higher rate than many other Organization for Economic Cooperation and Development (OECD) countries [ 15 ] and had detrimental impacts on economies all over the world [ 16 ]. From February 2020 to August 2020, arts and recreation services employment in Australia decreased by 17.9% [ 8 ]. This was the second highest decrease in employment for any industry in Australia during the pandemic, with the highest being accommodation and food services jobs which decreased by 18.2% [ 8 ]. Individuals who were not deemed essential workers and who did not have the ability to work from home were in an especially difficult situation. By the end of 2020, 6.5% of Australians were unemployed, the highest rate since 2001 [ 17 ]. Young adults aged 15 to 34 years accounted for 57% of individuals unemployed in Australia from March 2020 to September 2020 [ 8 ]. This high level of unemployment combined with a tumultuous job market set the background for fears of limited or lack of job stability in the future.
While job concerns appeared nearly universal, these concerns were not equally experienced. By switching to a virtual environment some people found flexibility, reduced commuting, and the additional time with family that work from home allowed was an aspect of the pandemic that many wanted to see retained in the future. While some were pleased to be protected within closed borders, for others this caused major inconvenience and challenges related to the separation from loved ones and their usual way of life [ 6 ].
In addition to job concerns, travel was another major way of Australian life impacted by the pandemic. As an island nation, Australian citizens frequently travelled overseas, with the top destinations being New Zealand, Indonesia, and the United States [ 18 ]. International arrivals into Australia decreased 81% in 2020 as compared to 2019, with international travel receipts decreasing by 43% [ 19 ]. In addition to the restrictions for incoming travelers, there was a ban on overseas travel from Australia; although as of March 2021 this was amended to allow for travel to and from New Zealand [ 9 ]. Travel restrictions have affected trade and heightened risk around Australia’s economic growth and prosperity, given the country relies heavily on exports and imports. In 2019, Australia imported USD (United States Dollars) 209 billion worth of products and exported USD 284 billion worth of products [ 20 ]. While there have been no specific restrictions on imports due to the COVID-19 pandemic, there have been significant delays because of travel restrictions [ 21 ]. Australians’ perceptions of future travel were generally pessimistic, with many saying they would not travel overseas for quite a while. Some individuals saw a greater opportunity to travel domestically within Australia, but still expressed health concerns and worry crossing state lines. Females accounted for a higher proportion of individuals who expressed future concerns surrounding travel, and this fear was found most heavily in older age groups, predominantly among retirees who had planned on traveling more regularly. The shock of the pandemic and its associated restrictions and changes in everyday life, while hearing and seeing stories of high mortality elsewhere catalyzed many to reassess their values. It has been argued that there has been a psychological shift from an individualist mindset to a collectivist mindset because of the pandemic, with communities stepping up to provide support where needed [ 22 ]. Whether this reassessment of values will last post-COVID remains to be seen; however, research suggests that humans will adapt back to the world returning to its commercialized environment, the same way they adapted to the temporary shut-down of businesses and schools [ 22 ]. Within the theme of reassessing values, care for the environment was also repeatedly mentioned. The pandemic arrived in Australia shortly after a season of devastating bushfires which arose after a period of drought and had severely impacted wildlife and people, destroying many hectares of bushland, rural properties as well as homes and infrastructure [ 23 ]. People were awake to the problems of climate change and the need to do something. Because of the impact of COVID-19 on transport and industry, both in Australia and around the world there were notable positive environmental changes. Air pollution and greenhouse gas emissions were greatly reduced, with nitrogen dioxide (NO 2 ) and particulate matter (PM 2.5 ) levels lowering worldwide [ 24 ]. Additionally, noise pollution reduction and the ecological restoration of tourist hotspots made it possible for the natural ecology to temporarily recover [ 24 ]. The greater sense of community and care for the natural world were values participants verbalized in their interviews when discussing their hopes and dreams for the future. A higher proportion of females than males mentioned reassessing values, and around one-fifth of respondents discussed this theme of reassessing values.
The final theme, generational impact stood out when examining participant outlook. Generational impact primarily surrounded economic concerns. In response to the national shutdown, the Australian government supported its citizens through tax breaks, wage subsidies, and cash payments to the most vulnerable populations [ 25 ]. Federal government budget forecasting anticipated that Australia’s national debt could reach close to AUD (Australian Dollars) 1 trillion, the burden of which would primarily be felt among younger workers (Worthington, 2020). The disproportionate burden on the younger generation who do not have established financial security in in helping to rebuild Australia’s economy was the main reason behind concerns for this group. The other aspect of generational impact surrounded concerns for the mental wellbeing of younger generations. A 2020 survey found that younger generations are showing the most resilience during the COVID-19 pandemic and are committed to contributing positively to their communities and the entire world [ 26 ]. Millennials and Generation Z are defined as individuals born between 1981 and 2012 [ 27 ]. While this survey may be an indicator of the overall resilience and motivation of younger generations, there are still many concerned for the mental health of this younger age group because of the pandemic.
While the four major themes of job security, travel, reassessing values, and generational impact reflect the ways in which the COVID-19 pandemic impacted hopes and dreams for the future in both an optimistic and pessimistic way, the resilience that individuals believed themselves to exhibit during this trying time was the true indicator of the level of hope they were able to maintain for their futures.
Limitations
This study was conducted at the beginning of the pandemic and provides a good insight into the sentiments of a variety Australians at the early stages of COVID-19. It included a diversity of interviews but we acknowledge several limitations. The data collection occurred over a few months, effectively representing a one point in time. Even though the geographic coverage was broad, numbers were skewed to participants from Queensland. In addition, as common with much population-focused qualitative research, there were more female participants. Living with chronic illness was noted by the invited participants in their initial survey responses, but many did not identify the illness itself. During the interview some participants made no mention of their chronic illness, and a few indicated they did not have a chronic illness, did not consider their illness to be relevant to their experience of the pandemic, or did not disclose this information to the interviewer. Hence, no analysis was undertaken of the impact of a chronic disease on participants’ hopes and dreams for the future.
A major global event, such as the COVID-19 pandemic, has provided a window into how people view their future goals and aspirations during this time of worldwide and local instability. Initially, people were asked about their own hopes and dreams for the future, but what emerged were broader concerns about the economy, generational and travel/ border closure impacts. The exploration of such experiences provides insight and knowledge into the long-term impacts of the pandemic which will help guide future preparation and management, both for the individual and the wider community. Also, this study highlights that during a global pandemic, people’s perception of their future, while negative at times, shows hope and resilience. While hopes and dreams for the future are unique to each person, certain themes appeared commonly during the pandemic and were felt across the population, regardless of age and gender.
Availability of data and materials
The data that supports the findings of this study are available from the corresponding author [ST] upon reasonable request.
Abbreviations
Australian Dollars
Monash Modified
Organization for Economic Cooperation and Development
United States Dollars
Western Australia
World Health Organization. Australia situation 2021. https://covid19.who.int/region/wpro/country/au .
Google Scholar
Australian Government Department of Health. Coronavirus (COVID-19) current situation and case numbers. Canberra: Department of Health; 2021. https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-current-situation-and-case-numbers .
World Health Organisation. WHO coronavirus disease (COVID-19) Dashboard. 2021. https://covid19.who.int/ .
Australian Government Department of Health. Framework for national reopening. 2020.
Australian Government Department of Home Affairs. Travel restrictions and exemptions. Canberra: Department of Home Affairs; 2021. https://www.health.gov.au/health-alerts/covid-19/domestic-travel .
McCann L, Thompson S, Rolf F, Podubinski T. Police, permits and politics: navigating life on Australia’s state borders during the COVID-19 pandemic. Aust J Rural Health. 2022 (in press). https://doi.org/10.1111/ajr.12845 .
Rolf F, Campbell N, Thompson S, Argus G. Australians’ experience of the COVID-19 pandemic: advantages and challenges of scaling up qualitative Research using large-scale rapid analysis and building Research capacity across rural Australia. Int J Qual Methods. 2021;20:16094069211051937. https://doi.org/10.1177/16094069211051937 .
Article PubMed Central Google Scholar
Gilfillan G. COVID-19: labour market impacts on key demographic groups, industries and regions. In: Parliament of Australia DoPS, editor. Canberra; 2020.
Australian Government Department of Health. Coronavirus (COVID-19) domestic travel restrictions and remote area access. Canberra: Department of Health; 2020. https://www.health.gov.au/health-alerts/covid-19/domestic-travel .
Storen R, Corrigan N. COVID-19: a chronology of state and territory government announcements (up until 30 June 2020). Canberra: Parliamentary Library, Department of Parliamentary Services, Parliament of Australia; 2020.
Thoits PA. Stress, coping, and social support processes: where are we? What next? J Health Soc Behav. 1995;53–79.
Kumar A, Nayar KR. COVID 19 and its mental health consequences: Taylor & Francis; 2021. p. 1–2.
Liu JJ, Bao Y, Huang X, Shi J, Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc Health. 2020;4(5):347–9.
Article CAS Google Scholar
De Jong EM, Ziegler N, Schippers MC. From shattered goals to meaning in life: life crafting in times of the COVID-19 pandemic. Front Psychol. 2020;11(577708). https://doi.org/10.3389/fpsyg.2020.577708 .
Davidson P, Saunders PG, Bradbury B, Wong M. Poverty in Australia 2020 - part 1: overview (Australia). Sydney: University of New South Wales; 2020.
Pak A, Adegboye OA, Adekunle AI, Rahman KM, McBryde ES, Eisen DP. Economic consequences of the COVID-19 outbreak: the need for epidemic preparedness. Front Public Health. 2020;8:241.
Article Google Scholar
The World Bank. Unemployment, total (% of total labor force) (national estimate)—Australia: International Labour Organization ILOSTAT database, 2021.
Batty N. Australian international travelers: the places we go. In: Australian Government Department of Foreign Affairs and Trade, editor. Canberra; 2019.
United Nations World Trade Organization. International Tourism and COVID-19 2020. https://www.unwto.org/international-tourism-and-covid-19 .
Observatory of Economic Complexity. Australia (AUS) exports, Imports, and Trade Partners 2019. https://oec.world/en/profile/country/aus .
Australian Government Department of Agriculture Water and the Environment. Imports and COVID-19—department of agriculture. Canberra: Department of Water, Agriculture and Environment; 2020.
Evers NF, Greenfield PM, Evers GW. COVID-19 shifts mortality salience, activities, and values in the United States: big data analysis of online adaptation. Hum Behav Emerg Technol. 2021;3(1):107–26.
Filkov AI, Ngo T, Matthews S, Telfer S, Penman TD. Impact of Australia's catastrophic 2019/20 bushfire season on communities and environment. Retrospective analysis and current trends. J Saf Sci Resil. 2020;1(1):44–56.
Rume T, Islam SD-U. Environmental effects of COVID-19 pandemic and potential strategies of sustainability. Heliyon. 2020:e04965.
Worthington B. Pandemic Budget’s tax cuts, cash splash to put Australia in record debt. 2020. https://www.abc.net.au/news/2020-10-06/budget-2020-tax-cuts-deficit-coronavirus/12731914 .
Deloitte. A call for accountability and action. The Deloitte Global 2021 Millenial and Gen Z Survey 2021. https://www2.deloitte.com/global/en/pages/about-deloitte/articles/millennialsurvey.html .
Beresford Research. Age range by generation. 2021. https://www.beresfordresearch.com/age-range-by-generation/ .
Download references
Acknowledgements
The authors acknowledge the collaboration of many individuals across multiple institutions as a part of this research collaborative. Their appreciation goes out to the Georgetown University Global Health Department, in particular Dr. Bernhard Liese.
Authors FR, LB and ST are employed by University Departments of Rural Health which receive Rural Health Multidisciplinary Training program funding from the Department of Health under a rural health workforce program.
Code availability
Not applicable.
Author information
Authors and affiliations.
Western Australian Centre for Rural Health, University of Western Australia, PO Box 109, Geraldton, WA, 6531, Australia
Quincy F. Huang, Taleah Moore & Sandra C. Thompson
School of Nursing and Health Studies, Georgetown University, Washington, DC, USA
Quincy F. Huang
Southern Queensland Rural Health, Faculty of Health and Behavioural Sciences, The University of Queensland, Charleville, Queensland, Australia
Floraidh Rolf
University Department of Rural Health, La Trobe Rural Health School, La Trobe University, Bendigo, Victoria, Australia
Lauren A. Booker
You can also search for this author in PubMed Google Scholar
Contributions
QH: Writing – original draft (lead); formal analysis (lead); writing – review and editing (equal). FR: Project administration; data curation; investigation. LB: Investigation; writing – review & editing (equal). Writing – review & editing (equal). TM Moore: Investigation; writing – review & editing (equal). SCT: Investigation; conceptualization (lead); writing – original draft (supporting); review and editing (equal). All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Sandra C. Thompson .
Ethics declarations
Ethics approval and consent to participate.
The project was approved by the University of Queensland Human Research Ethics Committee (Approval number 2020000800) with reciprocal human ethics approvals were acquired from investigators’ respective institutions: Darling Downs Health Service, Flinders University, The University of Melbourne, La Trobe University, Deakin University, James Cook University, The University of Western Australia and Torrens University. The ethics committees approved verbal consent, aware that the research was being undertaken in the first year of COVID-19 when many services were not available and people were confined to their homes. Consent processes included initial email contact which included information and a participant information sheet before any contact by phone or videoconference to set up the interview. A deliberate process of informed consent occurred at the beginning of the interview and was recorded.
Potential participants were e-mailed information about the study including a plain language statement and invited to participate. They were them contacted by phone to talk about the study and arrange an appropriate time for interview. At the time on the interview the script was “ Hello X , I am Y , and I am part of the research team for the Covid-19 collaborative project. Thank you for agreeing to speak to me about your experiences of the pandemic. Before we start, I would like to cover an important point. I do need to record the interview, and I need to you to state out loud that you consent to both the interview and to being recorded. Can you do that? [Press record and obtain verbal consent] .”
Consent for publication
Competing interests, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview Guide_Attitudes and practices towards the COVID-19 pandemic.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Huang, Q.F., Rolf, F., Booker, L.A. et al. A qualitative study of how COVID-19 impacts on Australians’ hopes and dreams. BMC Public Health 22 , 367 (2022). https://doi.org/10.1186/s12889-022-12746-4
Download citation
Received : 21 July 2021
Accepted : 09 February 2022
Published : 21 February 2022
DOI : https://doi.org/10.1186/s12889-022-12746-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Aspirations
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
You're viewing this site as a domestic an international student
You're a domestic student if you are:
- a citizen of Australia or New Zealand,
- an Australian permanent resident, or
- a holder of an Australian permanent humanitarian visa.
You're an international student if you are:
- intending to study on a student visa,
- not a citizen of Australia or New Zealand,
- not an Australian permanent resident, or
- a temporary resident (visa status) of Australia.
Social Research Methods Part 1
Gathering and Analysing Qualitative Data
Delivered by Institute for Social Science Research
Learn how to design, collect, analyse and make evidence-informed decisions based on qualitative or mixed methods data (qualitative data integrated with quantitative data). During the course, you’ll be led through real-world examples of gathering and analysing qualitative data to better understand the research process. You’ll also get to practice your skills by undertaking interviews, focus groups or visual research methods and gain feedback from the ISSR trainers.
This course will only proceed if there are 6 or more participants.
For more information, download the Methods for Social Analysis and Statistics brochure.
Upcoming courses
Who should attend.
- Research and policy officers in government or private sector
- Researchers and evaluators
- PhD students
- Anyone gathering evidence from their stakeholders through interviews, observation, focus groups, or visual elicitation methods
Entry requirements
There are no entry requirements or prerequisites. You can do any Methods for Social Analysis and Statistics course in any order you wish.
What you'll learn
- Understand the impact of bias in all aspects of the research process.
- Understand the value and purpose of qualitative research and when to use these methods.
- Gain the knowledge and skills to understand, design and conduct high-quality qualitative research to inform evidence-based decisions.
- Gain the knowledge and skills to analyse and synthesise qualitative data.
- Understand the complementarity between qualitative and quantitative methods and, where appropriate, integrate qualitative and quantitative data in mixed methods research.
- Know how to critically review the quality of qualitative findings in reports, policy briefs and published papers.
- Gain the knowledge and skills to interpret, write up and present qualitative findings for a range of audiences.
Time commitment
This is an online course that will require roughly 21 hours to complete.
- Over either 3 days (9am - 5pm AEST) or 6 days (Tue to Thu from 9am -12:30pm AEST)
Course curriculum
- Appreciating how qualitative and quantitative methods can complement and enhance our understanding of a research problem.
- Understanding qualitative methods such as observation, ethnography, cognitive/retrospective interviews, visual elicitation, and online methods (including using AI to collect your data).
- Choosing the appropriate qualitative method and analytical approach for your study (including Grounded Theory Analysis, Thematic and Content Analysis, Interpretative Phenomenological Analysis and Narrative Analysis).
- Developing qualitative research questions.
- Understanding and addressing research bias.
- Understanding how to make your research accessible and inclusive.
- Planning research (including budget, ethics, sampling, participant recruitment and logistical arrangements).
- Enhancing the validity and trustworthiness of qualitative research through best practices measures such as keeping a reflective journal, creating a well-developed coding framework and engaging others in your analysis.
- Developing qualitative instruments (including interview guides, consent forms and participant information sheets).
- Interviewing with confidence (including interview and facilitation skills, interview and focus group practice and feedback opportunities).
- Understanding the analytical process (including anonymising, step-by-step guidance through a worked example of coding, practical tips for developing a coding framework and code in ‘real world’ circumstances and developing themes from the codes).
- Using computer-assisted software in qualitative analysis process (including documentation, file storage processes, transcription and analysis, thinking about how AI can assist your analyses and the ethical implications, and an introduction to NVivo and Leximancer).
- Interpreting qualitative data (including how to interpret qualitative results from peer-reviewed papers).
- Writing results for different audiences (including PhD thesis, peer-reviewed papers, reports, book chapters, participant summaries, policy briefs, podcasts, case studies and vignettes).
- Visualising and presenting qualitative data to maximise impact.
Certification and accreditation
Students who successfully complete the course will receive a Certificate of Completion to verify their skills and achievements.
Facilitators

Some really useful best-practice advice to better construct interview/survey questions and make sure that they are optimised for participants and will help to achieve the research question/outcomes. Also really great to test my analysis skills and see how the experts do it! Simon Alperstein, National Acoustic Laboratories
Registration closes 7 days before the course starts.
The course will only proceed if there are 6 or more participants.
GST is included in the cost
Discounts can't be used with other discounts, offers or special promotions.
We accept credit cards (Visa/MasterCard) for payment, including corporate credit cards. We can also invoice corporate and government clients. If you want to discuss payment options, please contact our team at [email protected].
Related courses
This course is part of the Social Research Methods suite. There are 10 courses within this suite – see the other related courses below:
- Social Research Methods 2 – Evaluating Social, Health and Human Service Programs
- Social Research Methods 3 – Social Cost-Benefit Analysis
- Social Research Methods 4 – Longitudinal Data Analysis
- Social Research Methods 5 – Data literacy, storytelling and influencing decision-makers
- Social Research Methods 6 – Survey Design
- Social Research Methods 7 – Principles of Research Design
- Social Research Methods 8 – Introduction to Quantitative Data Analysis
- Social Research Methods 9 – Introduction to regression modelling
- Social Research Methods 10 – Data Wrangling with R: An Introduction
Institute for Social Science Research
For more professional development options:
- subscribe to our training newsletter
- or ask us how we can customise our courses and offer capability training specific to your organisation.
- Help & FAQ
A qualitative descriptive study exploring clinicians’ perspectives of the management of older trauma care in rural Australia
- Epidemiology and Preventive Medicine Alfred Hospital
- Acute & Critical Care
- Department of Forensic Medicine
- Clinical Registries
Research output : Contribution to journal › Article › Research › peer-review
Background: For older trauma patients who sustain trauma in rural areas, the risk of adverse outcomes associated with advancing age, is compounded by the challenges encountered in rural healthcare such as geographic isolation, lack of resources, and accessibility. Little is known of the experience and challenges faced by rural clinicians who manage trauma in older adults. An understanding of stakeholders’ views is paramount to the effective development and implementation of a trauma system inclusive of rural communities. The aim of this descriptive qualitative study was to explore the perspectives of clinicians who provide care to older trauma patients in rural settings. Method: We conducted semi-structured interviews of health professionals (medical doctors, nurses, paramedics, and allied health professionals) who provide care to older trauma patients in rural Queensland, Australia. A thematic analysis consisting of both inductive and deductive coding approaches, was used to identify and develop themes from interviews. Results: Fifteen participants took part in the interviews. Three key themes were identified: enablers of trauma care, barriers, and changes to improve trauma care of older people. The resilience of rural residents, and breadth of experience of rural clinicians were strengths identified by participants. The perceived systemic lack of resources, both material and in the workforce, and fragmentation of the health system across the state were barriers to the provision of trauma care to older rural patients. Some changes proposed by participants included tailored education programs that would be taught in rural centres, a dedicated case coordinator for older trauma patients from rural areas, and a centralised system designed to streamline the management of older trauma patients coming from rural regions. Conclusions: Rural clinicians are important stakeholders who should be included in discussions on adapting trauma guidelines to the rural setting. In this study, participants formulated pertinent and concrete recommendations that should be weighed against the current evidence, and tested in rural centres.
- Older adults
This output contributes to the following UN Sustainable Development Goals (SDGs)
Access to Document
- 10.1186/s12913-023-09545-x Licence: CC BY
Other files and links
- Link to publication in Scopus
Projects per year
Harnessing the power of diverse data to model population impacts of injury and inform health and social policy
1/01/22 → 31/12/26
Project : Research
Optimising Emergency and Trauma Systems through evidence based pathways
Cameron, P.
1/01/18 → 31/12/22
T1 - A qualitative descriptive study exploring clinicians’ perspectives of the management of older trauma care in rural Australia
AU - Ferrah, Noha
AU - Parker, Catriona
AU - Ibrahim, Joseph
AU - Gabbe, Belinda
AU - Cameron, Peter
N1 - Funding Information: We thank the Jamieson Trauma Institute, the Statewide Trauma Clinical Network, and the Australian Paramedics Association Queensland, for their considerable assistance in advertising this project and recruiting participants. Funding Information: NF was supported by the 2022 MAIC-RACS Trauma Research Scholarship (IMIS 204805). BG was supported by a National Health and Medical Research Council of Australia Investigator Grant (ID 2009998). PC supported by MRFF Practitioner Fellowship (MRF1139686). Publisher Copyright: © 2023, The Author(s).
PY - 2023/12
Y1 - 2023/12
N2 - Background: For older trauma patients who sustain trauma in rural areas, the risk of adverse outcomes associated with advancing age, is compounded by the challenges encountered in rural healthcare such as geographic isolation, lack of resources, and accessibility. Little is known of the experience and challenges faced by rural clinicians who manage trauma in older adults. An understanding of stakeholders’ views is paramount to the effective development and implementation of a trauma system inclusive of rural communities. The aim of this descriptive qualitative study was to explore the perspectives of clinicians who provide care to older trauma patients in rural settings. Method: We conducted semi-structured interviews of health professionals (medical doctors, nurses, paramedics, and allied health professionals) who provide care to older trauma patients in rural Queensland, Australia. A thematic analysis consisting of both inductive and deductive coding approaches, was used to identify and develop themes from interviews. Results: Fifteen participants took part in the interviews. Three key themes were identified: enablers of trauma care, barriers, and changes to improve trauma care of older people. The resilience of rural residents, and breadth of experience of rural clinicians were strengths identified by participants. The perceived systemic lack of resources, both material and in the workforce, and fragmentation of the health system across the state were barriers to the provision of trauma care to older rural patients. Some changes proposed by participants included tailored education programs that would be taught in rural centres, a dedicated case coordinator for older trauma patients from rural areas, and a centralised system designed to streamline the management of older trauma patients coming from rural regions. Conclusions: Rural clinicians are important stakeholders who should be included in discussions on adapting trauma guidelines to the rural setting. In this study, participants formulated pertinent and concrete recommendations that should be weighed against the current evidence, and tested in rural centres.
AB - Background: For older trauma patients who sustain trauma in rural areas, the risk of adverse outcomes associated with advancing age, is compounded by the challenges encountered in rural healthcare such as geographic isolation, lack of resources, and accessibility. Little is known of the experience and challenges faced by rural clinicians who manage trauma in older adults. An understanding of stakeholders’ views is paramount to the effective development and implementation of a trauma system inclusive of rural communities. The aim of this descriptive qualitative study was to explore the perspectives of clinicians who provide care to older trauma patients in rural settings. Method: We conducted semi-structured interviews of health professionals (medical doctors, nurses, paramedics, and allied health professionals) who provide care to older trauma patients in rural Queensland, Australia. A thematic analysis consisting of both inductive and deductive coding approaches, was used to identify and develop themes from interviews. Results: Fifteen participants took part in the interviews. Three key themes were identified: enablers of trauma care, barriers, and changes to improve trauma care of older people. The resilience of rural residents, and breadth of experience of rural clinicians were strengths identified by participants. The perceived systemic lack of resources, both material and in the workforce, and fragmentation of the health system across the state were barriers to the provision of trauma care to older rural patients. Some changes proposed by participants included tailored education programs that would be taught in rural centres, a dedicated case coordinator for older trauma patients from rural areas, and a centralised system designed to streamline the management of older trauma patients coming from rural regions. Conclusions: Rural clinicians are important stakeholders who should be included in discussions on adapting trauma guidelines to the rural setting. In this study, participants formulated pertinent and concrete recommendations that should be weighed against the current evidence, and tested in rural centres.
KW - Interview
KW - Older adults
KW - Trauma
UR - http://www.scopus.com/inward/record.url?scp=85163626140&partnerID=8YFLogxK
U2 - 10.1186/s12913-023-09545-x
DO - 10.1186/s12913-023-09545-x
M3 - Article
C2 - 37381004
AN - SCOPUS:85163626140
SN - 1472-6963
JO - BMC Health Services Research
JF - BMC Health Services Research
- Open access
- Published: 15 January 2022
The qualitative experience of telehealth access and clinical encounters in Australian healthcare during COVID-19: implications for policy
- Jennifer White ORCID: orcid.org/0000-0003-1235-0916 1 ,
- Julie Byles 1 &
- Tom Walley 2
Health Research Policy and Systems volume 20 , Article number: 9 ( 2022 ) Cite this article
11k Accesses
21 Citations
2 Altmetric
Metrics details
Adaptive models of healthcare delivery, such as telehealth consultations, have rapidly been adopted to ensure ongoing delivery of essential healthcare services during the COVID-19 pandemic. However, there remain gaps in our understanding of how clinicians have adapted to telehealth. This study aims to explore the telehealth experiences of specialists, based at a tertiary hospital in the Hunter Region, and general practitioners (GP), including barriers, enablers and opportunities.
An interpretative qualitative study involving in-depth interviews explored the telehealth experiences of specialists, based at a tertiary hospital in the Hunter Region of Australia, and GPs, including barriers, enablers and opportunities. Data were analysed using an inductive thematic approach with constant comparison.
Individual interviews were conducted with 10 specialists and five GPs. Key themes were identified: (1) transition to telehealth has been valuable but challenging; (2) persisting telehealth process barriers need to be addressed; (3) establishing when face-to-face consults are essential; (4) changes in workload pressures and potential for double-up; (5) essential modification of work practices; and (6) exploring what is needed going forward.
Conclusions
While there is a need to rationalize and optimize health access during a pandemic, we suggest that more needs to be done to improve telehealth going forward. Our results have important policy implications. Specifically, there is a need to effectively train clinicians to competently utilize and be confident using this telehealth and to educate patients on necessary skills and etiquette.
Peer Review reports
Adaptive models of telehealth (via telephone consultation, email or videoconferencing) have been rapidly adopted to ensure ongoing delivery of essential healthcare services during the COVID-19 pandemic [ 1 ]. Telehealth is the use of information and communication technology applications to provide health services, expertise and information over distance, geographic, time, and social and cultural barriers [ 2 ]. The increase in the uptake of telehealth has been unprecedented during COVID-19, and there is wide scope to consider how to integrate telehealth into routine practice going forward.
Telehealth consultations are likely to continue while we live with COVID-19 and the risk of other pandemics. Beyond these emergencies, telehealth may also have a role in providing timely care for people with multiple chronic complex conditions and people in hard-to-reach communities [ 3 ]. Changing to a telehealth delivery mode requires clinicians to navigate a different environment to attend to clinical tasks. Telehealth consults necessitate a greater emphasis on communication and skilled information exchange to effectively engage, activate and facilitate patient self-management [ 4 ]. Known challenges to the uptake of telehealth have included changes to professional roles, workflow and relationships [ 5 , 6 ]. Additional barriers to telehealth include assessing a patient’s needs, technical/legal issues related to sharing protected health information, equipment limitations and integrating telehealth into existing healthcare processes [ 7 ]. Clinical concern stems from evidence that a lack of confidence in telehealth and associated technology creates a barrier to its effective use among home health nurses [ 8 ], physicians [ 9 ] and counsellors [ 10 ]. Further, the diversity of platforms and providers has led to documented inconsistencies in care [ 11 ].
Central to the context of this study is evidence of a threefold increase in the number of outpatient telehealth consultations at the John Hunter Hospital, a tertiary hospital in the Hunter Region, in March 2020 compared to the equivalent quarter in 2019. Data also highlight that, despite the Australian Department of Health recommendation that video consults be used as the primary mode of contact and that telephone should be used only when video consults are not possible [ 12 ], approximately 90% of Australian telehealth consultations in 2020 took place over the telephone [ 13 ]. In order to understand the complexity of a rapid transition to telehealth management and how clinicians have approached clinical interactions and decision-making, this study aimed to explore the telehealth experiences of specialists and general practitioners (GP). Such understanding is critical if we are to improve and sustain quality service delivery to patients using telehealth, translating telehealth into a broader system of care with the methods and tools required to support it.
Qualitative research investigates the subjective nature of social reality and the relationships between individuals and the institutions and society in which they live [ 14 ]. This qualitative study employed the use of semi-structured interviews and was informed by the Consolidated criteria for reporting qualitative research (COREQ) checklist [ 15 ]. Hunter New England Local Health District specialists based at the John Hunter Hospital (JHH) and John Hunter Children’s Hospital (JHCH) and GPs who provided outpatient and community-based services were eligible for inclusion. Representation of the different outpatient speciality clinics at the JHH and JHCH was sought. Participants were invited to participate by response to an email distributed by their heads of department and the director of a large, local general practice, including detailed study information. All participants provided written informed consent. Recruitment occurred between August and November 2020. Approval for this project was obtained from the Hunter New England Health Human Research Ethics Committee (2020/ETH01732).
Data collection
Semi-structured interviews (specialist n = 10, GPs n = 5) were conducted by a single interviewer (JW) using an interview schedule [ 16 ]. Interviews began by asking participants to share their “story” of transition to telehealth, and subsequent questions explored their experience of clinical interactions and decision-making using telehealth, including perceptions of benefits, barriers and opportunities (see Table 1 ). The semi-structured nature permitted flexibility for participants to elaborate upon or cover important topics that would not have otherwise surfaced [ 17 ]. Identified themes informed continuing data collection, and sampling continued until thematic saturation (two co-coders agreeing that no new themes were emerging) was achieved.
Data analysis
Semi-structured interviews, ranging from 30 to 60 minutes, were recorded with the participant’s permission and transcribed verbatim with identifying data removed. Two authors (JW, JB), one an occupational therapist and the other a gerontologist, coded data using an inductive thematic approach [ 18 ]. At the level of initial coding, both authors read the transcripts multiple times and made notes. Transcripts were then coded line by line, describing and interpreting emerging categories and searching for differences and similarities. Following team discussion, the primary author developed a single codebook, and each code was issued with a four-letter label or code to facilitate data retrieval between the transcripts (for example, symptoms of confidence was labelled “CONF”). The next step involved examining the relationship between codes in the context of the research question in order to form themes. Consistency of findings was upheld through discussion of interpretations between researchers to confirm codes and categories. Any differences in researcher perspectives were resolved by negotiation and, if necessary, regrouped and recoded until consensus was reached. New codes were then fed back into the analysis to cross-check codes and themes and develop an overall interpretation of the data [ 19 ]. Trustworthiness of our data was achieved using several strategies, including immersion in data, reflexive analysis and peer debriefing [ 20 , 21 ]. These strategies ensured that the researchers remained open to the data and did not demonstrate bias during the data analysis as a result of preconceptions inherent in the researchers’ clinical status and experience [ 20 , 21 ]. Coders captured exemplary quotes supporting each theme.
Clinician demographics are outlined in Table 1 . Ten specialists including geriatricians, interventional cardiologists, general physicians, neurologists, endocrinologists, paediatric specialists and five GPs participated in this study. Limited participant characteristics are given to protect anonymity.
This programme of research identified key findings across six areas:
Transition to telehealth has been valuable but challenging.
Persisting telehealth process barriers need to be addressed.
Establishing when face-to-face consults are essential.
Changes in workload pressures and potential for double-up.
Essential modification of work practices.
Exploring what is needed going forward.
Transition to telehealth has been valuable but challenging
The experience of transition to telehealth varied among participants. As this was a tertiary referral hospital, many specialists already provided telehealth services to designated rural and remote local government areas. Likewise, GPs reported that telehealth “is something that we have always done… [we were] just never reimbursed for it. There has always been calls at the end of the day, conversations discussing results, follow-ups that aren’t face to face but are urgent. You know, there is a role for those” (Participant [P] 13, GP).
However, many participants reported feelings of “heightened anxiety” (P4) when trying to monitor and implement “constantly changing” (P10, GP) government directives in response to COVID-19. Specific challenges related to reading and responding to large amounts of communication received from the workplace and government about required work practice changes.
Right from the beginning … multiple, multiple emails and sort of communications about what should and shouldn’t happen, protocols to become up to date with, exposures to new terminology. (P2, specialist [S])
For most participants, the transition to telehealth reportedly happened “overnight” (P4, S) and with limited forewarning, which meant that essential processes and infrastructure were not in place. Participants reported a lack of access to essential equipment, including phones with a speaker option, computers with video capacity or multiple screens, and adequate outgoing phone lines. In many cases participants ended up buying and using their own equipment.
Most participants experimented with different modes of communication during the transition to telehealth. Over time, most participants opted to conduct phone consults, as videoconferencing modes were considered unreliable and required extra time to set up, and often failed, which often led to swapping to the phone.
Me and my colleagues did experiment with using some of the video formats, but …so much time was lost trying to get things to operate or work. Eventually I think everybody abandoned it [and used the phone]. (P12, GP)
Patient familiarity with different telehealth modes was perceived to vary, irrespective of age. Participants indicated that transition to successful telehealth consults was closely linked with patients’ familiarity with and access to the various modes of telecommunication using video features.
Most of our patients don’t have mobile phones or are confident managing of them…or a lot of them don’t have somebody that can help them to set it up. (P2, S) What has astonished me is how really poor the tech-savvy [aware] people are [with telehealth] … even 19- and 20-year-olds. (P8, S)
Persisting telehealth process barriers need to be addressed
Numerous factors were identified as barriers to engaging with telehealth. Most notable was the significant time required for staff, typically administrative staff, to schedule appointments in both hospitals and GP practices. This required knowledge of the modes of telehealth that patients had access to, as well as the correct patient contact details to enable login. Participants often spent extra time helping people access programmes and problem-solve telehealth access issues.
One of the main constraints is technology… the patient needs to be primed, and that person may or may not have the ability to prime themselves to get on [telehealth]. It takes about 10 minutes for us to get the person prepared, and 10 minutes is a long time for us to waste on, and in a busy clinic, when you have 30 patients coming, a lot of people are waiting. We are running late by an hour and a half, I then have to invest 10 minutes of my time to get this person prepared. It was very unsatisfactory re coordination aspects. (P15, S)
The initial nature of the booking system was ad hoc and “not clearly defined” (P5, S), reportedly leading to errors and confusion. Scheduling of appointments and dealing with a virtual waiting room was confusing and problematic for both participants and patients, and the absence of a system to keep patients updated regarding their appointment meant that patients were often not available at the negotiated time, especially if participants were running late or early.
Internet connection issues were common to participants and patients, which had the potential to create significant delays. Overall, patients were more likely to lack enough data or bandwidth. There was a perceived reliance on family or carers to facilitate a consult and help provide data, which was considered less than ideal and likely to create additional financial burdens. However, government directives often meant that “family members weren’t there [to help], as they would have been normally” (P1, S).
A lot of [older] people don’t have internet, so we have to access it from the son or daughter’s phone. I am not sure whether they were wanting to do that—just thinking how much data you can use in a 45-minute consultation. I am not sure whether family members would have wanted to use all their data in that way. (P1, S)
Telehealth procedures and etiquette
In contrast to the commitment and preparation required from patients to attend a face-to-face appointment, participants expressed frustration that patients appeared to place less importance on preparing for and attending telehealth consults, for example, by adhering to appointment times and environments that were free of distractions.
Yeah, it is such a waste of time, you know. You have opened the notes, you have read the notes, now you want to deal with the problem. If they are not there and you ring back 2 hours later, you then have to reopen the notes, refresh your mind with that patient. Yeah, that was a really big challenge, and also I just feel like people probably do not value it all that much. I do not think our patients value it all that much. (P10, GP)
Several clinics had existing or had developed processes/education to help patients set up and engage with a telehealth appointment, such as how to download programmes, who to call for support, and ensuring a quiet space/room with few distractions. However, participant reports suggested that patient responsiveness to this support, which aimed to facilitate a quality consult, was variable. Furthermore, many patients did not come prepared for their telehealth appointment by obtaining essential pathology or scans before a scheduled consult, as they would do in a face-to-face consult. This not only created significant delays and double-up when appointments needed to be rescheduled, but also placed patients at risk when areas of concern were not investigated in a timely manner.
I have had a lot of people not attending their blood tests or not attending their ultrasound scans or their surveillance colonoscopy. So, there certainly has been delay in some things. I haven't had a sinister outcome from that yet… touch wood. (P13, GP) [Many patients have] nothing prepared for this consultation. So, I wasted all my time and effort, no decisions could be made on that day…. I am actually quite disappointed that there is not a system of coordination before a telehealth happens. Someone needs to tell them what the expectation of the doctor is. (P15, S)
Similarly, many patients “would not pick up the phone” (P11, GP) at the scheduled time, which required participants to make multiple calls. Alternatively, patients expected participants to call when it suited them.
[Patients may say] I have just come out of shower, can you wait for 5 minutes. That is completely unacceptable. I mean we are wasting our precious time. (P15, S)
Many patients also attempted to participate in a consult when distractions—which were previously minimized during a face-to-face consult—were present. Distractions were wide-ranging, such as when children were present at home or in a car, or when in a busy/noisy environment such as a shopping centre. In these scenarios, clinicians often terminated and rescheduled the appointment, especially when issues concerning confidentiality were evident.
I had a consultation with someone who was in the middle of a paddock and, you know, we have had conversations with people that were shopping … we are not going to have this conversation. This is, you know, confidential stuff. (P8, GP)
Establishing when face-to-face consults are essential
Assessment accuracy.
All participants preferred to see new and complex clients face to face due to the imperative for obtaining a clear history, undertaking physical examinations and establishing rapport. Participant confidence in dealing with an incomplete picture varied such that some experienced greater anxiety. Most participants arranged for a patient to come in for an in-person consult if there were any concerns; however, the waiting list was often more prolonged for specialists.
It [incomplete assessment] gave me a lower threshold to bring them in [for an in-person consult]. (P10, GP)
For some, concern stemmed from putting interim measures in place or delaying treatment until a patient could be seen in person.
You may decide not to embark on treatment straightway, to see how they went, whereas if you had seen them in person, you would likely start a treatment more immediately. (P1, S)
Participants also expressed concern that patients were minimizing their issues over telehealth consults which was often linked to them not wanting to be a burden during a challenging time.
I do think a number of people minimize their symptoms because they didn’t really want to bother me. (P6)
High-risk patients
Some participants expressed concern at the potential to miss aspects of an assessment, since telehealth relied on patient self-report of symptoms rather than observation.
Yes, very early on I missed a cerebellar stroke, so that was a bit unpleasant for me. You just do not pick up from those cues of seeing them in the waiting room, standing up, walking in, where you get [visual information] …. The consultation starts in the waiting room, so you are missing out on that completely [in a telehealth consult]. (P10, GP)
Observation and physical assessment were integral to a consult, including noting social aspects, unusual neurological presentations (eye movements) and movement disorders, sensation and movements that caused patients to be at risk of falls, insulin injection sites, joints (rheumatology) and allergies.
I am fearful that I may have missed things that could be important…for example, I was talking to a woman, and by the end of the consultation the penny dropped that she was morbidly obese [which impacted clinical advice]. But nowhere on the GP referral or within her conversation or conversation with her husband had that been described. (P1, S)
Face-to-face communication was also deemed more beneficial when treating people who were deaf, brain-injured or cognitively impaired. Similarly, participants noted that providing education and supporting patients in understanding and adhering to education regarding chronic disease management was also made difficult when face-to-face communication was not possible. In these clinical scenarios, participants preferred to offer an in-person consult.
If you really want to reinforce exercise, diet, alcohol, not smoking, that kind of thing, if you really want to motivate the patient to make some change, get them in. (P12, GP)
Several critical care scenarios were noted where the inability to see someone face to face had the potential for overlooking patients at risk, particularly children and the elderly.
I gauge a lot from seeing the patient’s face and seeing how they move …. I mean, it’s just simple things like looking at their skin or their feet, the condition of their feet. You can tell a lot about how somebody is being cared for ,you know… things like vulnerability [to abuse]. (P2, S)
Specifically, there was a need to assess patients at risk of abuse and to be able to create a separate time and space where the patient and family could be spoken to separately.
Concerns around the patient’s vulnerability in the setting of family disharmony, a lot of tension in the household and things. Normally I would separate the patient from the family members with my community intervention nurse separately and see them separately, and so we could sort of gauge some aspects of the consultation in private. (P2, S)
Adequately dealing with abused patients and patients with mental health issues reportedly required a close therapeutic relationship and the time/opportunity to adequately deal with any emergent distress. All participants acknowledged the difficulty in detecting patient distress and providing support through telehealth, especially telephone, and that this was a potential barrier to telehealth.
So, they often get quite distressed, and you need to be able to manage that safely, because normally if they are going to transition from the clinic room through the corridors and social environments back to the car, etc., that allows a bit of processing. But if they go to their lounge room with no transition at all … they can end up going back to crying for a long time if you haven’t helped them kind of resolve their emotion in the session. (P7, S) Sometimes I hear silence, I don’t know this person is upset until I hear them crying. But if they come to me, I can make out very easily this person is getting upset, anxious, then we can really get into the issues that has prevented them from engaging in a proactive healthcare. It may be distress regarding the diagnosis, it may be denial about their condition, so unless we address those aspects properly, you do not actually make a clinical outcome better. (P15, S)
Therapeutic relationship
Developing a therapeutic relationship through telehealth was problematic and a key barrier reported by all participants, although not insurmountable. Telehealth, even with video capacity, made it difficult or delayed the ability to engage with a patient, read body language, respond to communication cues, and engage in conversation that allowed for a relationship to develop as well as elicit helpful supporting informative, for example, regarding socialization. In most scenarios, however, patients were seldom given the choice of telephone or video.
Well, a telehealth consult is really a conversation to try and get out what it is you need to know. One of the problems is you cannot read body cues—you have got to be quite concise in what you ask because it is not easy to interrupt, whereas in an interview there are other cues that will allow them to know that you are ready to ask another question or perhaps to ask something more on that subject. You cannot easily do that on phone. (P6, S)
Participants also felt that patients were more likely to provide additional, valuable information during an in-person consult, often when talking informally. Many GPs perceived that patients “feel more at ease to bring up other complaints they might not have thought were a big deal, and sometimes they are not. But other times, you know, it might be something that concerns us more than the patient. Mental health is a big one as well. There are a lot of times where people will come in face to face for a script or some other condition, and then you end up having a good chat about their mental health. I would not get that over the phone at all” (P11, GP).
Changes in workload pressures and potential for double-up
Telehealth was reportedly a time-consuming process, and extra time was taken in the initial stages to accommodate new processes and workflow issues. For example, administrative staff needed extra time to set up appointments, problem-solve patient access issues or rebook appointments. Participants indicated that while telehealth appointments were shorter in length, it was common to spend additional time before and after a consult. For example, a significant amount of time was spent compensating for a lack of information, thus requiring time to review reports and referrals prior to a consult. Similarly, additional work in the early transition to telehealth often required participants to spend extra time, for example, writing lengthy letters to GPs to ensure adequate follow-up and to outline any assessment omissions, ordering/faxing tests and scripts, and emailing or phoning GPs or other staff with instructions or for verification.
I finish a consultation and I am definitely not as confident as I would be when I am assessing face to face, but I guess I make it clear in my communications it is a limited assessment in some respects. (P2, S) That is a disappointing aspect of this whole coordination of telehealth that we have to ring the pharmacy, we have to ring the GP practice, we have to ring the pathology, we have to then send the scripts to this place, ring and tell them that the fax is coming. (P15, GP)
Shorter consults that were not face to face also had the potential for errors if concentration was lost during a busy clinic, especially when trying to take in information from various modalities.
It is far easier to make a mistake on telephone conversation, because the information that is coming is far less. So, I think telephone consultations are pretty hopeless. For instance, once I got the medications wrong. I must have been concentrating on something else. And they are much quicker… telephone conversations are like a quarter of the time. (P3, S) We might also make mistakes. I have seen that sometimes you call the wrong person and you go through the consultation and then you realize you are in the wrong folder. (P15, S)
Overall, many felt that telehealth resulted in a doubling up of their time and efforts.
I need to see this guy, it has been two appointments I have seen him on a telephone basis. I really do not know what is happening. I need to bring him back and see him. It does create extra work. (P5, S)
Essential modification of work practices
All clinicians readily modified their work practice and communication style through trial and error in response to adopting a telehealth practice. For some this meant modifying standardized assessments for use over the phone such as abbreviating the Mini-Mental State Exam (MMSE) cognitive assessment to obtain some semblance of a cognitive screen, because “there aren’t many validated tools for cognitive assessment over the phone” (P2, S). Other strategies reportedly included asking more detailed questions in order to elicit correct information and compensate for a lack of visual cues or relying on family and carers for clarification.
I ask them specific questions: what happened about your blood sugars, what happened with your blood tests. I am looking for answers. We need to have clear questions, as not all patients have clear questions to give clear answers. We should try to explore their questions and their concerns. (P5, S)
One clinician with extensive experience with telehealth reportedly increased the number of pauses to allow a patient to speak, since the nature of telehealth often meant that people spoke overtop each other.
[Face to face] I can pick up on subtleties in body language and I can see or hear [a patient trying to speak] and I know now it is my turn to stop talking. … I stop talking a lot earlier [during telehealth] than I would normally stop talking and check if you have got anything that you want to say. (P8, S)
Participants spent additional time seeking verification from patients such as encouraging patients to write things down or asking them to repeat what had been said.
When I think I am not sure if my patient is able to understand exactly what I am saying, then I ask them to please, get a pen and paper, and write this down. (P4, S)
Exploring what is needed going forward
All clinicians reported that telehealth was inferior to face-to-face consults but had a role going forward. Telehealth was considered most appropriate for patients where there was an existing therapeutic relationship, and for “follow-up things or for things where it is a very easy diagnosis, you know” (P8, S). Participants greatly appreciated being remunerated for time spent on the phone providing follow-up, confirming an ongoing treatment plan or writing scripts. Likewise, there was a perceived benefit for an initial consult where blood work, scans, and so on were requested prior to further assessments or prior to a well-defined procedure. These had a mutual benefit for patients in not requiring them to travel, wait for long periods and pay for parking. Specific benefits were noted for children at risk of missing a day of school at a time, significantly disabled patients where transport was difficult, and older people who had the potential to experience fatigue and confusion.
We are trying to keep kids in school, so if they have to have a day off to travel, that’s a problem. If we can telehealth to a computer at school, then that is better. (P8, S)
Some participants felt that efficiency could be improved by triaging patients ahead of time. In this way it could be determined whether it was essential that they attend in person, to ensure that care was maintained and not delayed.
I know this month I have been triaging patients, we get about 30 to 40 referrals a week in diabetes. I can easily say which one needs to come definitely and which one does not need to come. We can triage it and then that is not the problem. (P15, S)
However, participants emphasized that if increased telehealth services were expected, then more infrastructure was needed regarding equipment and staffing.
We are just expected to absorb it. That is the difficult part if you expand telehealth because telehealth can go anywhere, but at this end somebody needs to enhance us, and we have not had any enhancement. (P15, S)
Telehealth also provided the scope to provide continuity of care by streamlining services in facilities for the aged, supporting palliative care and other complex care and social issues, such as busy mums.
I think the mum was anxious, there was nothing wrong with the baby. But for her it was really good doing a video call, just reassure. Reassure is part of follow-up anyway. (P10, GP)
Participants noted the potential benefit in establishing telehealth clinics separate from in-person clinics in order reduce the demand experienced by each clinic. For example, some participants reported feeling greater cognitive fatigue with telehealth consults, due to the need to anticipate problems, check and double-check information sources or monitor different screens (such as electronic records and video).
It is the constancy of, you know, the next time that you contact someone, are they going to be there, what technical issues …I am trying to describe something to someone, you know, or have a lot of images to show them. [When they are face to face] it is easy to show them images. (P8, S)
As with other countries, telehealth has enabled Australians to stay connected with the healthcare system during COVID-19. Participant reports highlighted that the use of telehealth has increased dramatically. Consistent with international reports, convenience benefits were noted in maintaining health access for patients and reducing the burden of travel and waiting times [ 22 ]. Likewise, participants were reimbursed for essential work they were already conducting over the phone [ 23 ]. Echoing previous research, this study identified limitations of telehealth which resulted in the delivery of care where participants experienced challenges with booking processes and internet connection, and poor patient computer literacy [ 24 , 25 ]. These may be magnified in patients from low socioeconomic and culturally and linguistically diverse backgrounds [ 26 , 27 ]. Overall, participants were required to compensate for a deficient clinical history, struggled to establish a therapeutic relationship, and spent extra time post-consult to follow up on referrals and scripts.
Communication barriers due to the lack of nonverbal communication and information exchange in telehealth have been well established [ 28 ]. Evidence shows that up to 55% of the impact of consultation is attributed to visual and nonverbal communication [ 29 ]. In addition, evidence shows that patients frequently misunderstand health information given by phone [ 30 ]. Poor health literacy is exacerbated in people with mental health issues [ 31 ] and sensory conditions such as altered vision and hearing [ 32 ]. A key finding of this study was that participants self-initiated modification of work practice to ameliorate for potential communication deficits, such as more detailed questioning and seeking verification. However, clinicians accepted that clinical care given to patients using telehealth was different, and often delayed, in comparison to care given face to face and that it was difficult to establish a therapeutic relationship. Therapeutic relationships are complex and subjective, requiring patient and therapist collaboration to optimize outcomes, and previous research highlights the need for training [ 33 , 34 ]. Furthermore, while telehealth competencies exist in the provision of telehealth across various professional groups [ 35 ], few clinicians are formally trained to deliver their professional services using telehealth [ 36 ]. Consistent with growing evidence, we posit that the effective use of telehealth requires appropriate education of patients and clinicians about the safe and effective use of telehealth for the provision of high-quality patient-centred healthcare [ 37 , 38 , 39 ].
Previous research has demonstrated that patients are often satisfied with telehealth, the quality of care and convenience [ 40 , 41 ]. A recent systematic review identified barriers and facilitators to telemedicine [ 42 ], with key barriers including access to and quality of technology, lack of seriousness, difficulty expressing difficult emotions, poor body language, and communication and scheduling conflicts [ 42 ]. However, results from our study suggest there was a perceived lack of respect for and preparation before a telehealth consult among patients, which led to unnecessary duplication of consults and delayed assessment. Indeed, previous research suggests that people from rural areas, those with low literacy or low socioeconomic status, or those from culturally and linguistically diverse backgrounds find telehealth the least accessible and may benefit from education [ 43 ].
All participants acknowledged that a telehealth appointment was better than no appointment at all. However, going forward, telehealth services were deemed to require improved software which provided booking efficiency, data security and data transfer. With greater expectations of seeing people who lived in closer proximity came the need for more staffing and infrastructure to support this. As supported by a recent systematic review of the role of telehealth during COVID-19, improved administrative processes, such as having a triage system, would allow for more accurate identification of people who needed to be seen person [ 44 ].
Strengths and limitations
While our approach provided the opportunity to obtain diverse perspectives on what current and future telehealth services should look like, the use of purposive sample may have resulted in an invested sample. Likewise, our sample was small and selected from a single urban location. We also did not capture the patient perspective. Future research should explore the patient perspective, including people from culturally and linguistically diverse populations. In addition, research should be prioritized to ensure the consistent quality of telehealth consultation.
With the unprecedented increase in the uptake of telehealth, there is an opportunity to integrate telehealth into routine practice, potentially improving inequities and inefficiencies in the delivery of care for patients. This study highlights barriers to establishing a therapeutic relationship using telehealth, which was compounded by the lack of visual and nonverbal communication, internet connectivity and computer literacy. A further challenge was a perceived lack of respect for and preparation before a consult by patients, which led to further delays in the provision of timely care, such as the need to rebook appointments.
Our results suggest several policy areas for attention to support telehealth, including further investment in information technology infrastructure across health services administrative support to facilitate changes in practice and workflow. Effective communication is paramount to delivering patient-centred care, and cultivating this skill is a vital component of telehealth. Given that the use of telehealth, both phone and video, is increasing and is likely to continue while we live with COVID-19 and the risk of other pandemics, we would point to the importance of promoting communication competency through training of health professionals and patients in the use of telehealth.
Availability of data and materials
The qualitative data used and/or analysed during the current study are available from the corresponding author on reasonable request.
Keesara S, Jonas A, Schulman K. Covid-19 and health care’s digital revolution. N Engl J Med. 2020;382(23):e82.
Article CAS Google Scholar
Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154–61.
Article Google Scholar
Moffatt JJ, Eley DS. The reported benefits of telehealth for rural Australians. Aust Health Rev. 2010;34(3):276–81.
Souza-Junior VD, Mendes IAC, Mazzo A, Godoy S. Application of telenursing in nursing practice: an integrative literature review. Appl Nurs Res. 2016;29:254–60.
Plsek P. Complexity and the adoption of innovation in health care. Accelerating quality improvement in health care: strategies to accelerate the diffusion of evidence-based innovations Washington, DC: National Institute for Healthcare Management Foundation and National Committee for Quality in Health Care. 2003.
Coiera E. Why system inertia makes health reform so difficult. Bmj. 2011;342:d3693.
Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12.
Courtney-Pratt H, Cummings E, Turner P, Cameron-Tucker H, Wood-Baker R, Walters EH, et al. Entering a world of uncertainty: community nurses’ engagement with information and communication technology. CIN. 2012;30(11):612–9.
PubMed Google Scholar
Demiris G, Edison K, Vijaykumar S. A comparison of communication models of traditional and video-mediated health care delivery. Int J Med Informatics. 2005;74(10):851–6.
Ford T, Avey J, DeRuyter J, Whipple JL, Rivkin I. Providers’ voices on telebehavioral health: survey of an outpatient counseling agency in Alaska. Psychol Serv. 2012;9(3):316.
Schoenfeld AJ, Davies JM, Marafino BJ, Dean M, DeJong C, Bardach NS, et al. Variation in quality of urgent health care provided during commercial virtual visits. JAMA Intern Med. 2016;176(5):635–42.
Australian Government DoH. Temporary COVID-19 MBS telehealth services–488 factsheet. Medicare benefits schedule. 2020; 1–16.
Mehrotra A, Bhatia RS, Snoswell CL. Paying for telemedicine after the pandemic. JAMA. 2021;325(5):431–2.
Bernard HR, Bernard HR. Social research methods: qualitative and quantitative approaches. Thousand Oaks: Sage; 2013.
Google Scholar
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Patton M, editor. Qualitative evaluation and research methods, 2nd ed. Newbury Park: Sage Publications, Inc; 1990.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Braun V, Clarke V, Terry G. Thematic analysis. Qual Res Clin Health Psychol. 2014;24:95–114.
Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. 2nd ed. Thousand Oaks: Sage Publications; 1998.
Krefting L. Rigor in qualitative research: the assessment of trustworthiness. Am J Occup Therapy. 1991;45(3):214.
Pandit N. The creation of theory: a recent application of the grounded theory method. Qual Rep. 1996;2(4):1–13.
Kichloo A, Albosta M, Dettloff K, Wani F, El-Amir Z, Singh J, et al. Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Family Med Commun Health. 2020;8(3):e000530.
Henry BW, Block DE, Ciesla JR, McGowan BA, John V. Clinician behaviors in telehealth care delivery: a systematic review. Adv Health Sci Educ. 2017;1(22):869–88.
Triana AJ, Gusdorf RE, Shah KP, Horst SN. Technology literacy as a barrier to telehealth during COVID-19. Telemed Health. 2020;26(9):1118–9.
Hargittai E, Piper AM, Morris MR. From internet access to internet skills: digital inequality among older adults. Univ Access Inf Soc. 2019;18(4):881–90.
Chowdhury SR, Sunna TC, Ahmed S. Telemedicine is an important aspect of healthcare services amid COVID-19 outbreak: its barriers in Bangladesh and strategies to overcome. Int J Health Plann Manage. 2021;36(1):4–12.
Nouri S, Khoong EC, Lyles CR, Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catalyst Innovations in Care Delivery. 2020;1(3).
Kessels RP. Patients’ memory for medical information. J R Soc Med. 2003;96(5):219–22.
PubMed PubMed Central Google Scholar
Car J, Sheikh A. Telephone consultations. BMJ. 2003;326(7396):966–9.
Leclerc BS, Dunnigan L, Côté H, Zunzunegui MV, Hagan L, Morin D. Callers’ ability to understand advice received from a telephone health-line service: comparison of self-reported and registered data. Health Serv Res. 2003;38(2):697–710.
Kizilbash AH, Vanderploeg RD, Curtiss G. The effects of depression and anxiety on memory performance. Arch Clin Neuropsychol. 2002;17(1):57–67.
Kindig DA, Panzer AM, Nielsen-Bohlman L. Health literacy: a prescription to end confusion. Washington D.C.: National Academies Press; 2004.
Sabesan S, Allen D, Caldwell P, Loh P, Mozer R, Komesaroff PA, et al. Practical aspects of telehealth: doctor–patient relationship and communication. Intern Med J. 2014;44(1):101–3.
Simpson S, Richardson L, Pietrabissa G, Castelnuovo G, Reid C. Videotherapy and therapeutic alliance in the age of COVID-19. Clin Psychol Psychother. 2020;28:409.
Hilty DM, Maheu MM, Drude KP, Hertlein KM, Wall K, Long RP, et al. Telebehavioral health, telemental health, e-Therapy and e-Health competencies: the need for an interprofessional framework. J Technol Behav Sci. 2017;2(3–4):171–89.
Slovensky DJ, Malvey DM, Neigel AR. A model for mHealth skills training for clinicians: meeting the future now. Mhealth. 2017;3:52.
Gifford V, Niles B, Rivkin I, Koverola C, Polaha J. Continuing education training focused on the development of behavioral telehealth competencies in behavioral healthcare providers. Rural Remote Health. 2012;12(4):2108.
Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J Am College Surg. 2020;231(2):216-22.e2.
Esper GJ, Sweeney RL, Winchell E, Duffell JM, Kier SC, Lukens HW, et al. Rapid systemwide implementation of outpatient telehealth in response to the COVID-19 pandemic. J Healthc Manag. 2020;65(6):443–52.
Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31(3):269–75.
Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ open. 2017;7(8):e016242.
Almathami HKY, Win KT, Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J Med Internet Res. 2020;22(2):e16407.
Hawley CE, Genovese N, Owsiany MT, Triantafylidis LK, Moo LR, Linsky AM, et al. Rapid integration of home telehealth visits amidst COVID-19: what do older adults need to succeed? J Am Geriatr Soc. 2020;68(11):2431–9.
Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20(1):1–9.
Download references
Acknowledgements
The authors thank the participants.
There was no funding for this study. This study was supported by the Hunter Medical Research Institute.
Author information
Authors and affiliations.
Centre for Women’s Health Research, College of Health, Medicine and Wellbeing, University of Newcastle, Locked Bag 1000, New Lambton, NSW, 2305, Australia
Jennifer White & Julie Byles
Hunter Medical Research Institute, Newcastle, NSW, Australia
You can also search for this author in PubMed Google Scholar
Contributions
JW completed data analysis with support from JB and TW. JW drafted the manuscript for publication, and JB and TW contributed to the content and revision of the manuscript. JW managed revisions, literature and checking of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jennifer White .
Ethics declarations
Ethics approval and consent to participate.
This project received approval from Hunter New England Health Human Research Ethics Committee (2020/ETH01732). All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
White, J., Byles, J. & Walley, T. The qualitative experience of telehealth access and clinical encounters in Australian healthcare during COVID-19: implications for policy. Health Res Policy Sys 20 , 9 (2022). https://doi.org/10.1186/s12961-021-00812-z
Download citation
Received : 25 February 2021
Accepted : 21 December 2021
Published : 15 January 2022
DOI : https://doi.org/10.1186/s12961-021-00812-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Find My Rep
You are here
Qualitative Research
Preview this book.
- Description
- Aims and Scope
- Editorial Board
- Abstracting / Indexing
- Submission Guidelines
Qualitative Research publishes papers with a clear methodological focus. We invite scholarship that has multi-disciplinary appeal, that debates and enlivens qualitative methods, and that pushes at the boundaries of established ways of doing qualitative research. We are interested in papers that are attentive to a wide audience, that are alive to new and diverse ways of thinking about qualitative methods, and that contribute to discussions within the pages of this journal. These discussions can be brought to life through empirical studies and research encounters, but we do not accept papers that focus on reporting the findings from qualitative research studies.
We see our journal as contributing to the community of academics across different fields who use qualitative methods as a way of making sense of the world. We understand methods and methodology as a practice and as a perspective, and welcome contributions that reflect on and critically engage with both aspects. Qualitative Research is a space where ideas and understandings are used to open up methodological issues for reflection and debate, and we work hard to provide a supportive environment to foster this ethos.
- Academic Search Premier
- Anthropological Index Online
- Anthropological Literature
- Applied Social Sciences Index & Abstracts (ASSIA)
- British Education Index
- Business Source Corporate
- CD-ROM - International Bibliography of Book Reviews of Scholarly Literature in the Humanities and Social Sciences
- CD-ROM - International Bibliography of Book Reviews of Scholarly Lterature on the Humanities and Social S
- CD-ROM International Bibliography of Periodical Literature in the Humanities and Social Sciences
- CD-ROM International Bibliography of Periodical Literature on the Humanities and Social Sciences
- Caredata CD (Discontinued)
- Combined Health Information Database (CHID)
- Contents Pages in Education
- Criminal Justice Abstracts
- Cumulative Index to Nursing and Allied Health Literature CINAHL
- Current Contents / Social and Behavioral Sciences
- Current Contents/ Social and Behavioral Sciences
- Current Index To Statistics
- EBSCO: Human Resources Abstracts
- Educational Research Abstracts Online - e-Psyche
- Family Index
- Family Index Database
- IBZ: International Bibliography of Periodical Literature
- IBZ: International Bibliography of Periodical Literature in the Humanities and Social Sciences
- International Bibliography of Book Reviews of Scholarly Literature in the Humanities and Social Sciences
- International Bibliography of Book Reviews of Scholarly Literature on the Humanities and Social Sciences
- International Bibliography of the Social Sciences
- Journal Citation Reports Social Sciences
- Journal Citation Reports/Social Sciences Edition
- MasterFILE Premier
- Online - International Bibliography of Book Reviews of Scholarly Literature in the Humanities and Social Sciences
- Online - International Bibliography of Book Reviews of Scholarly Literature on the Humanities and Social
- Online - International Bibliography of Periodical Literature in the Humanities and Social Sciences
- Online - International Bibliography of Periodical Literature on the Humanities and Social Sciences
- PAIS Bulletin
- Psychological Abstracts
- Public Administration Abstracts
- Research Alert
- Research Into Higher Education Abstracts
- Social Care Online
- Social SciSearch
- Social Sciences Citation Index (SSCI)
- Social Sciences Index
- Social Services Abstracts
- Social Work Abstracts
- Sociological Abstracts
- Sociology of Education Abstracts
- Worldwide Political Science Abstracts
Manuscript Submission Guidelines: Qualitative Research
This Journal is a member of the Committee on Publication Ethics
Please read the guidelines below then visit the Journal’s submission site http://mc.manuscriptcentral.com/qrj to upload your manuscript. Please note that manuscripts not conforming to these guidelines may be returned.
Only manuscripts of sufficient quality that meet the aims and scope of Qualitative Research will be reviewed.
There are no fees payable to submit or publish in this Journal. Open Access options are available - see section 3.3 below.
As part of the submission process you will be required to warrant that you are submitting your original work, that you have the rights in the work, and that you have obtained and can supply all necessary permissions for the reproduction of any copyright works not owned by you, that you are submitting the work for first publication in the Journal and that it is not being considered for publication elsewhere and has not already been published elsewhere. Please see our guidelines on prior publication and note that the journal may accept submissions of papers that have been posted on pre-print servers; please alert the Editorial Office when submitting (contact details are at the end of these guidelines) and include the DOI for the preprint in the designated field in the manuscript submission system. Authors should not post an updated version of their paper on the preprint server while it is being peer reviewed for possible publication in the journal. If the article is accepted for publication, the author may re-use their work according to the journal's author archiving policy. If your paper is accepted, you must include a link on your preprint to the final version of your paper.
- What do we publish? 1.1 Aims & Scope 1.2 Article types 1.3 Writing your paper
- Editorial policies 2.1 Peer review policy 2.2 Authorship 2.3 Acknowledgements 2.4 Funding 2.5 Declaration of conflicting interests 2.6 Research Data
- Publishing policies 3.1 Publication ethics 3.2 Contributor's publishing agreement 3.3 Open access and author archiving
- Preparing your manuscript 4.1 Formatting 4.2 Artwork, figures and other graphics 4.3 Supplemental material 4.4 Reference style 4.5 English language editing services
- Submitting your manuscript 5.1 ORCID 5.2 Information required for completing your submission 5.3 Permissions
- On acceptance and publication 6.1 Sage Production 6.2 Online First publication 6.3 Access to your published article 6.4 Promoting your article
- Further information
1. What do we publish?
1.1 Aims & Scope
Qualitative Research publishes papers with a clear methodological focus. We invite scholarship that has multi-disciplinary appeal, that debates and enlivens qualitative methods, and that pushes at the boundaries of established ways of doing qualitative research. We are interested in papers that are attentive to a wide audience, that are alive to new and diverse ways of thinking about qualitative methods, and that contribute to discussions within the pages of this journal. These discussions can be brought to life through empirical studies and research encounters, but we do not accept papers that focus on reporting the findings from qualitative research studies.
We see our journal as contributing to the community of academics across different fields who use qualitative methods as a way of making sense of the world. We understand methods and methodology as a practice and as a perspective, and welcome contributions that reflect on and critically engage with both aspects. QR is a space where ideas and understandings are used to open up methodological issues for reflection and debate, and we work hard to provide a supportive environment to foster this ethos.
1.2 Article Types
Qualitative Research publishes articles, notes and reviews. Most of our submissions follow formal academic publishing guidelines, but we welcome creative and imaginative ways to explore qualitative methods and are open to conversations about the format and presentation of submissions.
We publish articles that are original, critical and creative engagements with qualitative methods. Articles must have a clear methodological focus, and not simply present findings from qualitative studies. They should be between 7,500 and 8,500 words, excluding references. Any articles that fall below or above that range will be returned.
Notes is a new format for short, engaging and imaginative submissions. It offers a more playful space for critical reflection on the craft of qualitative research. Authors are encouraged to experiment with styles of writing, and submissions can take the form of stories, anecdotes, or lessons that impart original methodological insights. Submissions should be between 2,000 and 4,000 words, excluding references.
Reviews are an important contribution to Qualitative Research. We welcome proposals that connect with the aims and the scope of our journal by offering reflective readings of key contributions to methodological debates and discussions in qualitative research. Specifically, we invite traditional book reviews that critically engage with titles and identify connections to wider literature, as well as provide a more descriptive account of content. Here, reviewers should not be afraid to (kindly) consider the significance and clarity of the contribution.
While our book reviews are usually around 800 to 1000 words and tend to focus on a single title, we also welcome longer review essays that explore two or three publications. If you would like to submit a proposal for a book review on the latest contribution or a classic of the genre, please get in touch with the editors, [email protected] . Your proposal should include a statement on why you would like to review the title(s) and how the piece relates to your own interests and expertise.
Beyond the traditional book review, we also invite reviews of events, cultural artifacts, and other dissemination platforms. Here we welcome reviews of relevant conferences and colloquia, podcasts and radio programmes, novels, and documentary series. As with the book review, the word count should be 800 to 1000 words and explicitly relate to how the event/artifact furthers debates in qualitative research. Again, please contact the editors at [email protected] with an outline of your proposal.
Please note that Qualitative Research does not accept unsolicited reviews.
1.3 Writing your paper
The Sage Author Gateway has some general advice and on how to get published , plus links to further resources. Sage Author Services also offers authors a variety of ways to improve and enhance their article including English language editing, plagiarism detection, and video abstract and infographic preparation.
1.3.1 Make your article discoverable
For information and guidance on how to make your article more discoverable, visit our Gateway page on How to Help Readers Find Your Article Online
Back to top
2. Editorial policies
2.1 Peer review policy
Sage does not permit the use of author-suggested (recommended) reviewers at any stage of the submission process, be that through the web-based submission system or other communication. Reviewers should be experts in their fields and should be able to provide an objective assessment of the manuscript. Our policy is that reviewers should not be assigned to a paper if:
• The reviewer is based at the same institution as any of the co-authors
• The reviewer is based at the funding body of the paper
• The author has recommended the reviewer
• The reviewer has provided a personal (e.g. Gmail/Yahoo/Hotmail) email account and an institutional email account cannot be found after performing a basic Google search (name, department and institution).
2.2 Authorship
All parties who have made a substantive contribution to the article should be listed as authors. Principal authorship, authorship order, and other publication credits should be based on the relative scientific or professional contributions of the individuals involved, regardless of their status. For any multiple-authored publication that substantially derives from the student’s dissertation or thesis the student should normally be named as first author.
Please note that AI chatbots, for example ChatGPT, should not be listed as authors. For more information see the policy on Use of ChatGPT and generative AI tools .
2.3 Acknowledgements
All contributors who do not meet the criteria for authorship should be listed in an Acknowledgements section. Examples of those who might be acknowledged include a person who provided purely technical help, or a department chair who provided only general support.
2.3.1 Third party submissions
Where an individual who is not listed as an author submits a manuscript on behalf of the author(s), a statement must be included in the Acknowledgements section of the manuscript and in the accompanying cover letter. The statements must:
- Disclose this type of editorial assistance – including the individual’s name, company and level of input
- Identify any entities that paid for this assistance
- Confirm that the listed authors have authorized the submission of their manuscript via third party and approved any statements or declarations, e.g. conflicting interests, funding, etc.
Where appropriate, Sage reserves the right to deny consideration to manuscripts submitted by a third party rather than by the authors themselves .
2.4 Funding
Qualitative Research requires all authors to acknowledge their funding in a consistent fashion under a separate heading. Please visit the Funding Acknowledgements page on the Sage Journal Author Gateway to confirm the format of the acknowledgment text in the event of funding, or state that: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
2.5 Declaration of conflicting interests
Qualitative Research encourages authors to include a declaration of any conflicting interests and recommends you review the good practice guidelines on the Sage Journal Author Gateway
2.6 Research Data
At Sage we are committed to facilitating openness, transparency and reproducibility of research. Where relevant, the journal encourages authors to share their research data in a suitable public repository subject to ethical and methodological considerations and where data is included, to add a data accessibility statement in their manuscript file. Authors should also follow data citation principles. For more information please visit the Sage Author Gateway , which includes information about Sage’s partnership with the data repository Figshare. For more information, including FAQs please visit the Sage Research Data policy pages .
We acknowledge this practice is not always relevant or appropriate for ethically sound qualitative inquiry, and so would encourage you to consider the unfolding ethical, legal and moral obligations linked to your research data on a case by case basis.
3. Publishing Policies
3.1 Publication ethics
Sage is committed to upholding the integrity of the academic record. We encourage authors to refer to the Committee on Publication Ethics’ International Standards for Authors and view the Publication Ethics page on the Sage Author Gateway .
3.1.1 Plagiarism
Qualitative Research and Sage take issues of copyright infringement, plagiarism or other breaches of best practice in publication very seriously. We seek to protect the rights of our authors and we always investigate claims of plagiarism or misuse of published articles. Equally, we seek to protect the reputation of the journal against malpractice. Submitted articles may be checked with duplication-checking software. Where an article, for example, is found to have plagiarised other work or included third-party copyright material without permission or with insufficient acknowledgement, or where the authorship of the article is contested, we reserve the right to take action including, but not limited to: publishing an erratum or corrigendum (correction); retracting the article; taking up the matter with the head of department or dean of the author's institution and/or relevant academic bodies or societies; or taking appropriate legal action.
3.1.2 Prior publication
If material has been previously published it is not generally acceptable for publication in a Sage journal. However, there are certain circumstances where previously published material can be considered for publication. Please refer to the guidance on the Sage Author Gateway or if in doubt, contact the Editor at the address given below.
3.2 Contributor's publishing agreement
Before publication, Sage requires the author as the rights holder to sign a Journal Contributor’s Publishing Agreement. Sage’s Journal Contributor’s Publishing Agreement is an exclusive licence agreement which means that the author retains copyright in the work but grants Sage the sole and exclusive right and licence to publish for the full legal term of copyright. Exceptions may exist where an assignment of copyright is required or preferred by a proprietor other than Sage. In this case copyright in the work will be assigned from the author to the society. For more information please visit the Sage Author Gateway
3.3 Open access and author archiving
Qualitative Research offers optional open access publishing via the Sage Choice programme and Open Access agreements, where authors can publish open access either discounted or free of charge depending on the agreement with Sage. Find out if your institution is participating by visiting Open Access Agreements at Sage . For more information on Open Access publishing options at Sage please visit Sage Open Access . For information on funding body compliance, and depositing your article in repositories, please visit Sage’s Author Archiving and Re-Use Guidelines and Publishing Policies .
4. Preparing your manuscript for submission
4.1 Formatting
- Attach to every submission a letter confirming that all authors have agreed to the submission and that the article is not currently being considered for publication by any other journal.
- Include a title page with full title and subtitle (if any). For the purposes of blind refereeing, full name of each author with current affiliation and full address/phone/fax/email details plus short biographical note should be supplied on a separate sheet. The editors will not inspect the manuscript until this information is given.
- Also for the purposes of blind refereeing, authors should replace all self-citations in the text and reference list with anonymous citations, in the style (Author, 2009), etc.
- Any citation that includes any of the authors should be replaced with (Author A and others, 2003) in the text, and in the reference list at 'Au' put 'Author A and others (2003), details withheld for peer review' followed by Author B and others, if necessary.
- Abstract of 100-150 words.
- Up to 10 key words.
- All authors must provide a full word count for their paper. The minimum word count is 7500 and the maximum is 8500 words excluding all references. Papers under the minimum and over the maximum word count will be unsubmitted.
- The journal uses notes where necessary. Historical, documentary or archival sources should be cited in endnotes. Discursive endnotes are also allowed. Endnotes are signalled in the text by superscript numbers.
- References in both the text and in any endnotes should follow Sage Harvard style. References are cited in the text thus: (author, date: page).
- An alphabetical References section should follow the text (and endnotes, if any) using the Sage Harvard system.
- All artwork, graphics, line diagrams and photographs are termed 'Figures' and should be referred to as such in the manuscript. They should be numbered consecutively. All figures should have short descriptive captions at the end of the document.
- Articles must be written in English. Use a clear, readable style, avoiding jargon. If technical terms or acronyms must be included, define them when first used.
- Non-discriminatory language is mandatory
- UK or US spellings may be used with '-ize' spellings as given in the Oxford English Dictionary (e.g. organize, recognize).
- Use single quotation marks with double quotes inside single quotes.
- Dates should be presented in the form 1 May 2010. Do not use points in abbreviations, contractions or acronyms (e.g. AD, USA, Dr, PhD)
- Qualitative Research adheres to the Sage Harvard reference style. View the Sage Harvard guidelines to ensure your manuscript conforms to this reference style.
- If you use EndNote to manage references, you can download the Sage Harvard EndNote output file .
4.2 Artwork, figures and other graphics
Qualitative Research welcomes the inclusion of figures. There is no word count equivalent for figures, but images should be carefully selected and will be reviewed for their quality and suitability.
For guidance on the preparation of illustrations, pictures and graphs in electronic format, please visit Sage’s Manuscript Submission Guidelines .
Figures supplied in colour will appear in colour online regardless of whether or not these illustrations are reproduced in colour in the printed version. For specifically requested colour reproduction in print, you will receive information regarding the costs from Sage after receipt of your accepted article.
4.3 Supplemental material
This journal does not currently accept supplemental files.
4.4 Reference style
Qualitative Research adheres to the Sage Harvard reference style. View the Sage Harvard guidelines to ensure your manuscript conforms to this reference style.
If you use EndNote to manage references, you can download the Sage Harvard EndNote output file ..
4.5 English language editing services
Authors seeking assistance with English language editing, translation, or figure and manuscript formatting to fit the journal’s specifications should consider using Sage Language Services. Visit Sage Language Services on our Journal Author Gateway for further information.
5. Submitting your manuscript
Qualitative Research is hosted on Sage Track, a web based online submission and peer review system powered by ScholarOne™ Manuscripts. Visit http://mc.manuscriptcentral.com/qrj to login and submit your article online.
IMPORTANT: Please check whether you already have an account in the system before trying to create a new one. If you have reviewed or authored for the journal in the past year it is likely that you will have had an account created. For further guidance on submitting your manuscript online please visit ScholarOne Online Help .
As part of our commitment to ensuring an ethical, transparent and fair peer review process Sage is a supporting member of ORCID, the Open Researcher and Contributor ID . ORCID provides a unique and persistent digital identifier that distinguishes researchers from every other researcher, even those who share the same name, and, through integration in key research workflows such as manuscript and grant submission, supports automated linkages between researchers and their professional activities, ensuring that their work is recognized.
The collection of ORCID IDs from corresponding authors is now part of the submission process of this journal. If you already have an ORCID ID you will be asked to associate that to your submission during the online submission process. We also strongly encourage all co-authors to link their ORCID ID to their accounts in our online peer review platforms. It takes seconds to do: click the link when prompted, sign into your ORCID account and our systems are automatically updated. Your ORCID ID will become part of your accepted publication’s metadata, making your work attributable to you and only you. Your ORCID ID is published with your article so that fellow researchers reading your work can link to your ORCID profile and from there link to your other publications.
If you do not already have an ORCID ID please follow this link to create one or visit our ORCID homepage to learn more.
5.2 Information required for completing your submission
You will be asked to provide contact details and academic affiliations for all co-authors via the submission system and identify who is to be the corresponding author. These details must match what appears on your manuscript. The affiliation listed in the manuscript should be the institution where the research was conducted. If an author has moved to a new institution since completing the research, the new affiliation can be included in a manuscript note at the end of the paper. At this stage please ensure you have included all the required statements and declarations and uploaded any additional supplementary files (including reporting guidelines where relevant).
5.3 Permissions
Please also ensure that you have obtained any necessary permission from copyright holders for reproducing any illustrations, tables, figures or lengthy quotations previously published elsewhere. For further information including guidance on fair dealing for criticism and review, please see the Copyright and Permissions page on the Sage Author Gateway .
6. On acceptance and publication
6.1 Sage Production
Your Sage Production Editor will keep you informed as to your article’s progress throughout the production process. Proofs will be made available to the corresponding author via our editing portal Sage Edit or by email, and corrections should be made directly or notified to us promptly. Authors are reminded to check their proofs carefully to confirm that all author information, including names, affiliations, sequence and contact details are correct, and that Funding and Conflict of Interest statements, if any, are accurate.
6.2 Online First publication
Online First allows final articles (completed and approved articles awaiting assignment to a future issue) to be published online prior to their inclusion in a journal issue, which significantly reduces the lead time between submission and publication. Visit the Sage Journals help page for more details, including how to cite Online First articles.
6.3 Access to your published article
Sage provides authors with online access to their final article.
6.4 Promoting your article
Publication is not the end of the process! You can help disseminate your paper and ensure it is as widely read and cited as possible. The Sage Author Gateway has numerous resources to help you promote your work. Visit the Promote Your Article page on the Gateway for tips and advice.
7. Further information
Any correspondence, queries or additional requests for information on the manuscript submission process should be sent to the Qualitative Research editorial office. Please email: [email protected]
- Read Online
- Sample Issues
- Current Issue
- Email Alert
- Permissions
- Foreign rights
- Reprints and sponsorship
- Advertising
Individual Subscription, Print Only
Institutional Subscription, E-access
Institutional Subscription, Print Only
Institutional Subscription, Combined (Print & E-access)
Individual, Single Print Issue
Institutional, Single Print Issue
Subscription Information
To purchase a non-standard subscription or a back issue, please contact SAGE Customer Services for availability.
[email protected] +44 (0) 20 7324 8701
- Open access
- Published: 13 October 2023
A qualitative exploration of young people’s mental health needs in rural and regional Australia: engagement, empowerment and integration
- Christiane Klinner ORCID: orcid.org/0000-0001-9313-6799 1 ,
- Nick Glozier 1 , 2 ,
- Margaret Yeung 1 ,
- Katrina Conn ORCID: orcid.org/0000-0002-0476-9146 1 , 3 &
- Alyssa Milton ORCID: orcid.org/0000-0002-4326-0123 1 , 2
BMC Psychiatry volume 23 , Article number: 745 ( 2023 ) Cite this article
2161 Accesses
1 Citations
Metrics details
Australian rural and regional communities are marked by geographic isolation and increasingly frequent and severe natural disasters such as drought, bushfires and floods. These circumstances strain the mental health of their inhabitants and jeopardise the healthy mental and emotional development of their adolescent populations. Professional mental health care in these communities is often inconsistent and un-coordinated. While substantial research has examined the barriers of young people’s mental health and help-seeking behaviours in these communities, there is a lack of research exploring what adolescents in rural and regional areas view as facilitators to their mental health and to seeking help when it is needed. This study aims to establish an in-depth understanding of those young people’s experiences and needs regarding mental health, what facilitates their help-seeking, and what kind of mental health education and support they want and find useful.
We conducted a qualitative study in 11 drought-affected rural and regional communities of New South Wales, Australia. Seventeen semi-structured (14 group; 3 individual) interviews were held with 42 year 9 and 10 high school students, 14 high school staff, and 2 parents, exploring participants’ experiences of how geographical isolation and natural disasters impacted their mental health. We further examined participants’ understandings and needs regarding locally available mental health support resources and their views and experiences regarding mental illness, stigma and help-seeking.
Thematic analysis highlighted that, through the lens of participants, young people’s mental health and help-seeking needs would best be enabled by a well-coordinated multi-pronged community approach consisting of mental health education and support services that are locally available, free of charge, engaging, and empowering. Participants also highlighted the need to integrate young people’s existing mental health supporters such as teachers, parents and school counselling services into such a community approach, recognising their strengths, limitations and own education and support needs.
Conclusions
We propose a three-dimensional Engagement, Empowerment, Integration model to strengthen young people’s mental health development which comprises: 1) maximising young people’s emotional investment (engagement); 2) developing young people’s mental health self-management skills (empowerment); and, 3) integrating mental health education and support programs into existing community and school structures and resources (integration).
Peer Review reports
Mental health service use is considerably lower in rural and regional communities than in urban areas in both Australia [ 1 , 2 ] and internationally [ 3 , 4 , 5 ]. Young people (YP) in particular have been reluctant to seek formal mental health support, which has been attributed to stigma and negative beliefs towards mental health services and professionals [ 6 , 7 ]. Such reluctance is particularly pronounced in rural and regional communities where mental health stigma rapidly spreads through social networks and “sticks” to the individual [ 3 ]. This phenomenon has been associated with higher levels of socio-economic disadvantage [ 8 ], social conservatism [ 9 ] and social visibility in these communities resulting in reduced privacy [ 10 , 11 ], with lack of confidentiality cited as a major concern of YP when considering accessing mental health services [ 8 ]. Professional mental health care in rural and regional areas is often inconsistent and un-coordinated [ 3 , 12 ], with help-seekers being required to travel large distances [ 13 ] and experiencing lengthy service waitlist [ 14 ]. The wellbeing of these communities is also more affected by increasingly severe and prevalent natural disasters. Prolonged drought, for example, coupled with feelings of isolation has been shown to impact YP’s mental health, making them feel overwhelmed and worry about their families, friends, money and their futures [ 15 , 16 ].
While there is substantial research examining the barriers of YP’s mental health help-seeking behaviour in drought-affected rural and regional areas, less is known about what types of supports, programs and education facilitates their help-seeking [ 17 ]. In a recent systematic review on the barriers, facilitators and interventions for mental health help-seeking behaviours in adolescents, only 19 of 56 studies identified help-seeking facilitators [ 6 ]. These included previous positive experience with health services and higher levels of mental health literacy. Most research examining enablers of YP’s help-seeking is from the perspective of adults, parents and teachers (e.g., [ 14 , 18 , 19 , 20 , 21 , 22 ]). There is a lack of research examining what YP in rural and regional areas view as facilitators to seeking help when it is needed. The few studies that have examined help-seeking facilitators report that confidentiality and accessibility of mental health services [ 23 ], for the availability of more school counselling services [ 24 ], and YP desire to develop mental health self-management skills [ 15 ] to support the mental health help-seeking process.
This research program had 2 overarching aims. The first aim, which is reported in this article, was to establish a more in-depth understanding of YP’s experiences and needs regarding their mental health help-seeking, and explore mental health education, support and programs in rural and regional communities, complemented by the views of their teachers and parents. The second aim, which is reported elsewhere [ 25 ], was to evaluate the batyr@school program which was to be delivered at the participating schools within the year. The schools were selected to participate in the program by the New South Wales Department of Education as they were identified as communities which had, at the time of establishing the research, been experiencing severe drought — a recurring natural event in Australia that has been linked to adverse mental health outcomes in the affected communities [ 26 , 27 ]. The primary research question for the research reported in this article was: What are the attitudes and needs of young people, their teachers and parents regarding mental health and help-seeking in drought affected r ural and regional areas of Australia?
Study design
This study used qualitative pre- and post-intervention data from an evaluation of the batyr@school intervention [ 28 ] delivered to YP, teachers and parents in drought affected communities in Australia [ 25 ]. Semi-structured interviews (group and individual) were conducted to enable an in-depth exploration of participants’ views, experiences and needs about this sensitive topic [ 29 , 30 ]. While acknowledging its limitations [ 31 ], we used the COnsolidated criteria for REporting Qualitative research checklist (COREQ checklist [ 32 ], See Supplementary File ).
Ethical approval for this study was provided by the University of Sydney Human Research Ethics Committee (Protocol number 2020/607). Subsequent approval was provided via the NSW State Education Research Applications Process (SERAP Number 2020373).
Setting, participants and recruitment
The participants comprised three stakeholder groups: high school students aged 14–15 years (grade 9 and 10 in Australia; n = 42; 24 females, 18 males), high school staff (primarily teachers but also administrators and Wellbeing Officers) ( n = 14; 10 females, 4 males) and two parents of high school students ( n = 2; females). Detailed participant demographics and inclusion criteria are available as a Supplementary File . Participants were recruited through 11 participating high schools who were willing to take part in the qualitative research component of the wider batyr@school evaluation. In total, 26 rural and regional school communities from drought-affected areas of New South Wales were invited to participate in focus groups or individual interviews. Focus groups were selected as the main form of data collection as this reduced the administrative burden on schools in supporting the research. Individual interviews were also offered depending on the needs of the participant (eg. time constraints, unable to attend a focus group, personal preference, accessibility issues). Of these schools, 20 participated in the mixed methods evaluation, and 11 consented to conducting the qualitative research component. Of the six schools that did not participate, 5 cited that they were under too much administrative burden to take part, and one school had experienced a recent mental health trauma so felt the timing was not appropriate.
Participants for the focus groups and interviews were recruited through a combination of passive recruitment (via distribution of info sheets through the participating schools’ communication channels to staff, parents and students) [ 33 ] and snowball sampling [ 34 ]. The intention was to minimise perceived pressure to participate whilst utilising the schools’ social networks [ 35 ]. Written informed consent was obtained from all participants.
Data collection
From June 2021 to June 2022, the chief investigator (a qualitative researcher and psychologist), supported by a postgraduate student, conducted 14 group and three individual interviews with a total of 57 participants. The group interview size ranged from 2 to 5 participants. Of the 11 student interviews, three included the active participation of a teacher. Some schools considered the presence of a teacher necessary because the student interviews were conducted during school hours. Sixteen interviews were held via Zoom, and one parent interview via telephone. The sessions lasted between 20 and 115 min (mean duration 50 min). All interviews were audio-recorded, transcribed verbatim, de-identified and checked for accuracy. One teacher who was unable to participate in an interview provided a one-page written feedback on the interview questions, which was included in the data set.
Two of the research team members, both with extensive experience in qualitative research, reviewed the transcripts alongside data gathering and adapted the interview guide for further interviews as initial themes evolved and the need for more data in particular topic areas emerged [ 36 ]. This reflexive iteration between data gathering and analysis also served to refine focus and understanding of the data, and to determine when theme saturation was achieved [ 37 ]. The interviews explored 4 questions: 1) participants’ views on how drought impacted their local community from a mental health perspective, 2) participants’ understanding of locally available mental health support resources, 3) YP’s help-seeking experiences including what participants would do if a(nother) YP reached out to them for mental health support, and 4) participants’ views on their communities’ attitudes and beliefs about mental ill health, stigma and help-seeking. Participants were also asked for improvement suggestions in all 4 focus areas. The final interview guide is available as a Supplementary File .
In the process of reviewing the interview transcripts and listening to the audio files, one qualitative researcher developed an extensive analytical memo. This memo initially contained rich descriptions of preliminary themes identified inductively as important relative to the research question, interspersed reflexive comments on their potential meaning and relationships to each other [ 38 ]. This expansive phase of memo-writing followed a process of structuring and abstraction of the data in which themes and sub-themes were consolidated in team discussions, using a critical realist approach [ 39 ]. As a result of this process, the analytic memo had transformed into a framework that was used to report the results. The authors (who had a diverse mix of backgrounds including: qualitative researchers, mental health professionals, a teacher, a university student and an expert by experience; two of the research team were young people themselves (i.e. aged under 25 years [ 40 ]) and one was residing in a regional community) collaboratively refined the written results in several rounds of discussion and editing. The findings were also triangulated with the initial qualitative findings of an internal batyr @school baseline evaluation report [ 25 ], which had previously been analysed, interpreted and iteratively refined by the same team excluding one qualitative researcher who led this study’s analysis. This collaborative approach to analysis encourages high levels of reflexivity based on comparisons between the multiple personal and professional perspectives of all involved.
Terminology
This study was set in a high school environment. Therefore, the term ‘student’ is used when referring to the YP who participated in this study and the term ‘young person/people (YP)’ in reference to adolescents generally. The term ‘participants’ is used when referring to all three study participant groups. Otherwise, the participant group is specified; for example, ‘Students said…’.
In the following results section YP’s perspectives, experiences and needs regarding mental health help-seeking, stigma, and education and support services in drought-affected rural and regional communities are described. This is complemented by the views of their teachers and parents. The participants’ descriptions of the barriers to each of these above areas relating to their community, family, school, peers and individuals are provided. Importantly, these barriers are followed by their suggested solutions and facilitators to help-seeking and support. The most salient participant quotes are included in the text and ancillary quotes illustrating the findings further are presented in a Supplementary File .
Barriers to mental wellbeing and coping mechanisms
Community level.
Students vividly described their communities’ existential stressors caused by drought and other recurring natural events such as floods, bushfires and mice plagues, all straining the community’s mental wellbeing (See Supplementary File , Quote 1). In some communities these stressors coincided with high levels of social disadvantage, substance abuse and domestic violence (Quote 2). Participants described how these existential and economic stressors affected YPs’ mental health (Quote 3). Long distances to the nearest healthcare services (GPs, specialists, hospitals), long wait times to obtain an appointment and a lack of local youth mental health services made it difficult for YP and their families to access professional help when they needed it (Quote 4a-4b). Both students and teachers summarised the, at times, complete absence of accessible mental health services and contrasted them to those perceived to be available in urban areas (Quote 5 and below):
In [capital city], there was a lot of resources; and when I come here, there's nothing […] There's a whole lot of issues with suicide and attempted suicide. I think there's a headspace, but I don't know where that is. I think it might be in [nearest city, two hours’ drive away]. Which is nowhere near here. We're in the middle of nowhere. It seems to me like there's a really high, a lot higher incidence of sexual assault and suicidal ideation here. I mean, it's really hard to compare these two populations, but it does seem that way to me. And there's no services. [Teacher_B4]
Mental health services that were provided as one-off visits to rural and regional schools were seen as lacking coordination and continuity, impacting their effectiveness (Quote 6). Students also emphasised the absence of suitable places outside of home and school where they could socialise and informally support each other’s mental health. Community events that provided social opportunities were limited, and youth and community centres were perceived as lacking essential infrastructure and personnel (Quote 7–8), and were not viewed as desirable for 14–15-year-olds to attend – being more suited to pre-adolescent children (Quotes 7–8).
Family level
With limited access to professional mental health and youth support services in the community, good relationships with parents were pivotal to students’ mental wellbeing (Quote 9). Some students valued talking with their parents about mental health, and felt understood and supported when a parent with lived experience of mental ill health shared their experience with them (Quote 10). However, participants described parents, especially fathers, often as time-poor, absent from home, and/or struggling with their own mental health in the face of the rural challenges (Quotes 11–13). Students (and one parent) highlighted that as parents were often lacking mental health literacy and skills, they tended to ignore or dismiss their children’s mental health concerns (Quote 14–16). This lack of knowledge was attributed to stigma, open conversations about mental health being a relatively new phenomenon, fear of appearing weak, stress, or hoping the issue would just go away (Quote 14–16). Students also reported how, at times, mental health issues entrusted to their parents leaked into the community (Quote 17). Others described how parents acted out their mental health struggles via physical aggression, which was viewed as role-modelling unhelpful behaviours to their children:
S1: I've seen parents who have engaged in their children's, like, dramas […] And it's so hard, because a lot of the behavioural issues do come from parents. Like, it often stems from like your roots […] S2: And how their parents deal with their own issues, there’s like, a lot of physical fighting in our community too. I definitely notice. [Female Student_B1]
Some students described situations where they or their friends had felt invalidated by their parents (or carers) when trying to share. YP withdrew from sharing their mental health issues with their parents due to negative experiences with it. This also put up a barrier for some students to access online mental health support in case it was witnessed by their parents (Quotes 18–19). Other YP described that this feeling of reluctance, combined with a lack of local mental health services, made it difficult for YP to seek non-local professional help as they relied on parental support to physically get to an appointment (Quotes 20–22). One teacher also described some parents’ lack of cooperation regarding their adolescent children’s mental health treatment in situations when it was initiated by the school (Quote 23).
School level
Students reported strongly valuing the educational mental health programs that had been provided at school by visiting services (e.g., batyr@school [an interactive mental health program for high school students in years 9 to 12 delivered by facilitators and young people with lived experience of mental ill health that aims to reduce stigma, and educate and empower students to reach out for help when needed ( www.batyr.com.au )]; Tomorrow Man, Tomorrow Woman [a mental health program for year 10 high school students that aims to cultivate awareness among emerging young women and men of the pressures that come from gender stereotypes. The program aims to grow emotional literacy and develops skills around cultivating mental wellbeing for themselves and others ( https://leonsec.vic.edu.au/tomorrow-man-tomorrow-woman/ )]; Elephant Ed [a sex education workshops for year 5 to year 12 students ( www.elephanted.com.au )]), but considered this to be a drop in the ocean. Participants felt that a whole-of-community approach was needed, which extended to including educating parents and other adults in the community (Quote 35 and 35a). Some students had not experienced any school-based mental health programs (noting a batyr@school program was scheduled for delivery at their school over the following months as it was part of the research evaluation).
The majority of schools had local school counselling services which provided what was described by students and school staff as essential and sought-after mental health support for students. School counselling, however, was extremely under resourced and not meeting demand — as it was commonly only available one day per week, was often booked out for weeks in advance, and follow up appointments were difficult to obtain (Quote 36 and below):
We've actually got massive waiting lists at the moment for students to see people with mental health training, counsellors, we've got, we've got an undersupply. We've got a school psychologist who's got waiting lists, we got a school counsellor who's got waiting lists and we've got a student support officer who's got a waiting list. [Teacher_F6]
A teacher described how their school self-funded a psychologist whose work had markedly improved the mental wellbeing of students over years (Quote 37). As part of this, parents were included in the counselling services to YP and given support how to parent YP with mental health issues which was also viewed as effective approach (Quote 37). Other teachers commented on their school counsellors’ limits and, at times, inadequate qualifications (Quote 38–39). A minority of students were unaware that their school provided a counselling service (“ Do we even have a school counsellor?” [Male Student_F3]); some students were reluctant to visit their school counsellor out of fear of being singled out by the school community (Quote 40).
Both students and teachers described teachers as essential for YPs’ mental wellbeing. Students trusted their teachers and relied on their ability to help. Teachers were highly committed, and often proud, to provide mental health support to their students (Quotes 42–44). Teachers —particularly those with student wellbeing support briefs in their roles like Physical Education teachers, Wellbeing Officers, Year Advisors and Principals — provided mental health counselling to students when school counselling services were unavailable or when approached by students, both formally and informally (Quotes 45–46). They also provided emergency mental health services for students to support and bridge gaps in the chain of professional and home care (Quotes 47–48), and they supported and educated parents (Quotes 49–50). At the same time, teachers expressed feeling overwhelmed by the extent to which a growing number of students needed acute mental health support. They described this as navigating on the edge between feeling obliged, and wanting, to provide mental health support on one hand and being at their limits on the other. These limits, as reported by teachers, included feeling overstretched and often unable to balance the time to fit mental health education and support in with their multiple teaching responsibilities (Quotes 51–53 and below):
[Teachers] have got so much on their plate with what they've got to do in learning outcomes and all that sort of stuff. They don't really have time to think about these things [referring to students’ mental health] as well. [Teacher_F11]
Teachers also emphasised that they sometimes felt ill-equipped regarding their mental health knowledge and skills to help students with complex mental health needs (Quotes 55 and below):
I feel on edge when I try to give the kids advice because I'm not trained in that, like I know myself, I've raised three kids, you know. I've done heaps in my life experience. But at the end of the day, I'm not a counsellor, I'm not a psychologist […] and yet we’re expected to be. [Teacher_B5]
Teachers felt uncertain where to draw the line between YPs’ privacy versus their caring responsibility as teachers (Quote 56); and also reported that, despite their best intentions, their own patience and empathy was challenged in regard to students with behavioural disorders:
We’ll have empathy for kids that have got really obvious issues, but then there's the other sort of kids that’ll be in your class, that exhibit disruptive sort of behaviour, and there might be some sort of issue behind that. And people are much less understanding of that, I mean, I find myself I’m much less understanding of that sort of behaviour than I was previously. [Teacher_B4]
Peer friendship and mutual support were of utmost importance to students (Quote 67). One student, for example, enthusiastically spoke of the mental health benefits of having initiated a boys social media chat group for the purpose of mutual support (Quote 68). Concurrently, students were acutely aware of their limitations regarding supporting each other’s mental health. They felt weighted down by the responsibility that came with giving, offering, or even just intending to support their friends, and were extremely keen to learn how to help each other more effectively (Quotes 69–71). A parent described YP’s attempts to help each other as “ the blind leading the blind ” (Quote 72).
Individual level
Participants reported above-mentioned existential stressors on the community, stretched and insufficiently equipped parents and teachers, a collective silencing (i.e., not talking about) of mental health issues, and a lack of local mental health support weighed on YP at an individual level. This culminated in students knowing when ‘something’ was wrong with their mental health, but often did not know how to describe let alone deal with ‘it’ effectively (Quotes 58–59). Participants described a variety of unhelpful mental health coping mechanisms that they had used themselves or observed in peers. These included: accepting mental health issues as normal (Quote below) and suppressing negative feelings (Quote 60).
Our feelings are so normalized that it's OK to be sad a lot of the time. It's OK to be angry all the time, which you don't want to be angry and sad all the time. That's not, it's OK to be sad and angry sometimes, but we don't want to do it all the time. And I think that's another issue. We don't register that something is wrong, you know […] it kind of doesn't process that it's not that's not how it has to be, like you can get help. But I don't think we realize that we need it. [Female Student_B1]
When the weight of bottling up mental health issues became overwhelming, some YP relieved their mental stress in maladaptive ways, making their social surroundings obscurely yet acutely aware that they were not coping. Such ‘concealed cries for help’ ranged from attention seeking behaviour (Quote 61), physical aggression against teachers (Quote 62), towards each other (Quote 63), and towards themselves in form of self-harm and suicide, with self-harm incidents at times being shared with peers on social media. The latter was described by students and teachers as concealed cries for attention and/or support:
Suicidal self-harm, which self-harm just seems to periodically go with depression and anxiety, now, that's just how this coping strategy that young people have developed like they don't know what else to do that puts them in this next level. [Teacher_F8]
YPs’ maladaptive stress relief behaviours further increased the mental stress load on other YP and their social circles. Examples given by participants were students’ and teachers’ anxiety coming to school out of fear of being the target of physical aggression (Quote 64), and getting distressed by seeing peers’ self-harm stories on social media (Quote 65). Posted self-harm stories were also perceived as problematic by some participating YP as they thought to be normalising self-harm as a legitimate means of mental stress relief:
The whole idea of social media has become kind of destroyed by that image that like to have depression, you've got to be self-harming. [Female Student_B1]
However, participants also reported YPs’ constructive attempts of dealing with mental distress where parental and professional support were lacking, or unwanted out of concern of being dismissed or singled out. These attempts centred around YP helping (and seeking help from) each other as described in section ‘ Peer level ’. Several students knew of the availability of online mental health resources from school advertisements (Quote 41). The uptake of these online mental health services, however, was mixed. Some students valued the anonymity that online help offered; others hesitated to use it because of “ the security risk associated with putting stuff out on the internet” [MS_B3], or because they preferred talking face-to-face with someone (MS_B3). Others hadn’t considered accessing online help at all for themselves (M + FS_F12).
Impact of COVID-19 compared to other stressors and major events
While the data gathering for this study was conducted during the height of the COVID pandemic (June 2021 to June 2022), and the impact of the pandemic was touched on in the occasional interview/focus group (mostly prompted by the interviewer), we found that the pandemic did not significantly impact, exacerbate, or otherwise change the nature of young people’s mental health needs. Geographic remoteness, long-term drought, and other natural disasters such as floods and bush fires were together much deeper and complex existential stressors on rural and regional YP and their mental health than the comparatively shorter restrictions to urban areas that came with COVID-19. Social distancing and lockdown restrictions for example were viewed as a non-issue in communities without COVID cases. Moreover, remoteness, social distance and isolation were well-known factors that all participants reported to navigate long before the pandemic started, with its restrictions not incurring a substantial difference to day-to-day life.

Mental health stigma
In all interviews, participants described the presence of stigma in the community limiting addressing mental health issues and accessing appropriate support, including in the school playground and at home. Mental health self-stigma was characterised by (a fear of) being seen as weird or weak – the latter more so among boys and men; being ashamed to be different; and being (scared of getting) judged negatively (Quotes 24–28). Students and teachers reported how fear-based negative connotations around mental ill health prevented YP and their families from talking about their feelings and seeking mental health support, especially in smaller communities where everyone knew each other (Quotes 29–32 and below):
They don’t feel comfortable but yeah, or they think oh, that's a shame. I'm not going to be going to ask for help, like, people might tease me. [Female Student_B1]
Students described how a lack of mental health awareness in the community perpetuated the mental health stigma (Quote 33), and noted that being educated about “awkward” themes made it easier for them to talk about them (Quote 34).
Mental health solutions
Multi-pronged approach to mental health education.
All participant groups emphasised the need to take a multi-pronged approach to mental health education and support, with programs and services not only for YP, but also for parents and teachers and the community as a whole (Quote 73-74a), to tackle the communal mental health stigma and enable managing mental health issues without shame (Quote 75). Students in particular stressed the importance of educating parents and teachers (Quote 76). They wanted their parents to gain more mental health awareness, know how to identify mental ill health, act appropriately when their adolescent child displayed signs of mental ill health, know where to get help and how to keep mental health issues confidential (Quotes 77–80). Indeed, students yearned for their parents’ mental health understanding and appropriate behaviour (Quote 81). It was rare for students to report that their parents already had “ a really good idea of what to do ” (FS_F5). Educating parents was also a high priority for teacher and parent participants (Quotes 82–83). All participant groups also stressed the need to upskill teachers on how to identify and support YP with mental health issues (Quotes 84–86). Several teachers wanted mental health education to be part of the core teacher training (Quote 87).
Local, face-to-face, free of charge mental health services
Participants wanted mental health services to be offered locally, that is, in their community, to overcome the access barrier and to get personal face-to-face support. They wanted mental health services to be offered free of charge, especially during times of financial hardship caused by recurring natural events (Quotes 88–93). Some participants also emphasised a need to review how school counselling services operate including how well their training addressed the needs of school communities (Quotes 94–95). One teacher considered mental health education as the foundation for other learning to happen and suggested implementing it into the school curriculum (Quote 96).
Relatable, engaging, and inspiring mental health programs
Relatability was the desired mental health intervention characteristic that participants referred to most often and most passionately. Specifically, students wanted mental health programs to be tailored to their local circumstances, with demonstrations of empathy and understanding for them (Quote 97). More importantly, participants found programs extremely relatable and effective when they portrayed the perspective of YP with lived mental ill health experience, as in the batyr @school program (Quotes 98–99 and below).
I think it was really good that [Y9 students] heard […] the story of that young girl […] she wasn't going anywhere. She had no money. She was homeless, living in a car […]. But the kids, really, they were captivated by her. I remember looking around when she was speaking and they were just staring at her, like, in awe, yeah. And a lot of kids, when they had to write a message about the program, wrote about her on their piece of paper. [Teacher_F10]
Students contrasted this with mental health programs that only consisted of standard lecture format presentations, rated these as “ disengaging ” (Quote 100–101). Students also opened up when mental health programs included interactive elements such as group discussions and physical activity games. They found these highly engaging as they could contribute their opinions and experiences, release stress while physically engaging in fun activities, and maintain focus (Quotes 102–104). Group discussions were most accepted when the groups were small and homogenous regarding YPs’ age, gender and mental health needs (Quotes 105–108).
Empowering YP
Students highly valued peer friendships, if not depending on them in the face of the rural and regional challenges. They often preferred providing mental health support to each other over approaching their parents or teachers or accessing professional mental health support (Quotes 109–110), especially mental health services with whom they had no pre-existing relationship (see next section). Obtaining practical strategies how to help each other and increasing their confidence in talking about mental health were therefore top priorities for students, rarely addressed by the existing mental health support options available to them (Quotes 111–113). Some of the more outspoken students, and students with a lived experience of mental ill health, also valued opportunities where they could act as mental health ambassadors to give their peers “ that little push to come out ” (MS_B3), pass on their experiences and inspire other YP (Quotes 114–115).
Confidentiality and trust
Confidentiality around using mental health support was extremely important to students. Many of them were deeply afraid of being identified as in need of mental health support (due to the stigma identified above); they were only prepared to open up if they felt it was absolutely safe to do so and they could trust their helper (Quotes 116–117). Trust, confidentiality and safety for them developed with knowing the helper, preferably in person, being able to relate to them, and having a positive personal relationship with them. For the students who participated in our study, these criteria tended to be met mostly by peers and teachers, less so by parents and school counselling services, and least by health professionals and online helplines not previously known to students. Face-to-face contact, relatability, engagement and empowerment of YP all contributed to enhancing YP’s trust, as detailed in the earlier parts of this section.
Early and ongoing preventative mental health education
All participant groups emphasised that mental health education for YP should start early and be taught throughout all high school years, with some participants wanting mental health education to start in primary school (Quotes 118–122). Similar to the mental health education goals for parents and teachers (see section Multi-pronged approach above), participants suggested that mental health programs for YP should raise mental health awareness, teach how to recognise mental ill health, develop mental health self-help strategies, and address and break through stigma and stereotypes that were detrimental to YP’s mental health (Quotes 123–127).
This was the first known Australian qualitative study to explore the barriers, needs and solutions of 14 to 15 year-old YP in drought-affected rural and regional communities regarding MH education, help-seeking and support, specifically focussing on how to facilitate help-seeking. The key findings through the lens of YP, their teachers and parents were that help-seeking would best be enabled by a multi-pronged community approach to mental health education and support. More specifically, they wanted such mental health education and support to be locally available to all community members, free of charge, relatable, engaging, and empowering. Participants felt the need for mental health education to take a preventative approach, emphasise the development of mental health self-management skills, start in early school years, and be offered throughout all high school years to both YP and parents. For teachers in rural and regional areas, facilitating help-seeking for YP with mental health problems led to a tension between being students’ trusted, first point of call for mental health support on one hand and feeling overwhelmed and under-skilled regarding providing this support on the other. Following, a three-dimensional approach to improving the MH situation for YP in rural and regional communities in Australia by facilitating Engagement, Empowerment and Integration is discussed in context with existing literature (See Supplementary File : Principles and Facilitators).
Emotional engagement is crucial in the effectiveness of mental health programs, as for example shown by the literature on contact-based interventions [ 41 , 42 ]. Our study adds to this literature by demonstrating how relatability facilitates emotional engagement and, at least temporarily, this can break through stigma in rural and regional communities and improve YPs’ mental health help-seeking behaviour. Hearing the lived experience mental health stories of other YP, a contact-based intervention and core component of the batyr @school program [ 28 ], was by YP, their teachers and parents perceived as particularly relatable, engaging and meaningful. Our findings demonstrate how the perceived relatability of this intervention emotionally opened up YP towards sharing their own mental health stories. Given the high acceptance of this type of interventions from this sample, more research needs be conducted into how lived experience storytelling can be harnessed as a tool to make mental health programs relatable, and thus maximise YPs engagement and help-seeking behaviour. Further research into this area could be a valuable contribution to the currently inconclusive literature in the field of contact-based interventions [ 43 ].
An important variable in the relatability of lived experience storytelling and, more broadly, a mental health education intervention as a whole, is the delivery mode. While in this study, participants preferred face-to-face over online delivery, citing trust, confidentiality and interactivity as limiting factors of online programs, systematic review evidence suggests that online interventions can provide similarly effective anti-stigma results as face-to-face sessions [ 44 ]. More studies are needed to consolidate these findings. In any case, digital delivery has a potential to add extra scaffolding to face-to-face, providing further information and support to those who want it or don’t have access to face-to-face programs, for example, due to their geographical remoteness.
Another variable relating to emotional engagement in this sample of YP was the depth of insight mental health program facilitators had of the local communities they worked with. This included insight into the specific economic and environmental challenges rural and regional communities faced and how these challenges impacted their members. YP for example connected better with counsellors who “ understood drought ” [ 15 ] or who had experienced bushfires. Following this rationale, it seems advantageous to deliver locally tailored mental health education and support by professionals who are familiar with the culture and needs of individual communities [ 10 , 24 ]. Further research into the importance of this aspect is indicated.
Empowerment
While emotionally engaging YP is important, it is not enough. Corroborating with existing literature, the present study found that YP wanted to feel a sense of empowerment and active participation in the process of learning about and managing their mental health, and seeking help [ 10 , 45 , 46 ]. This sample of YP asked to be equipped with more confidence and skills around talking about and managing their mental health. They described wanting to feel a sense of choice and self-determination. Further, a desire for empowerment was raised by YP alongside their preference for informal, especially peer-based mental health support, which is also a common theme in the literature [ 11 , 45 , 47 , 48 ] as is the finding that such informal sources are notoriously under-resourced and under-qualified (e.g., [ 11 ]). Further investigation into whether (and how) YPs’ desire for self-determination and peer-based mental health support can be harnessed is warranted. For example, in the context of developing mental health youth ambassadors — as done in the Student Chapter of the batyr @school program [ 28 ] and the Canadian Stop Now and Plan (SNAP®) Boys (e.g., [ 49 ]). This could be especially useful in rural and regional communities where professional mental health services are scarce and YP rely on strong peer friendships. With appropriate professional guidance, there is potential for YP to grow into role models for ‘good’ mental health management, building from the bottom up a positive mental health culture in their social networks including on social media to reshape current, often maladaptive, mental ill health models and discourses [ 50 , 51 ]. YP’s desire for more educated parents also speaks to a bottom-up empowerment approach to tackling mental health issues in rural and regional communities where parents are often found to feel helpless when it comes to understanding and supporting their children’s mental health [ 14 , 19 , 20 ]. Clearly, empowerment is unlikely to result from one-off interventions. It rather needs a systematic, well-coordinated and integrated mental health approach as outlined following.
Integration
In line with existing literature, our findings highlight the need for a multi-dimensional integration and coordination approach to the provision of mental health education and support in rural and regional communities. An integrated approach requires first and foremost better coordination between school- and non-school-based mental health services so that YP are offered seamless and ongoing mental health education and support solutions rather than uncoordinated or one-off piecemeal [ 3 , 12 ]. The current findings also show that embedding mental health education in school curricula earlier, more prominently and consistently throughout schooling years was requested by participants as a way to equip YP with mental health knowledge and management skills before mental health issues arise. While this may not be unique to rural and regional areas, it could be an important avenue to tackling mental health stigma and increasing help-seeking when needed, particularly because these communities can be underpinned by social conservatism and lack anonymity [ 9 , 10 , 11 ].
Intensifying school-based mental health education and support, however, has its own issues. Teachers, including welfare officers, have been shown to increasingly navigate at the edge of their time availability and mental health competence, calling for training and resources on how to identify and provide early mental health support for students [ 18 , 21 , 52 , 53 , 54 ]. Recent nation-wide surveys of teachers and the public have shown a link between teachers’ mental health care role and burnout: as teachers assume an increasingly influential role in developing YPs’ social and emotional development, with the public relying on them to do so [ 55 ], teacher burnout and exodus of the profession is rising [ 56 ]. Furthermore, school counselling services cannot completely meet the burgeoning demands for students’ mental health support in rural and regional Australia. Frequently covering multiple rural and regional communities, school counselling services often operate on a one-day-per week basis, are booked out well in advance and, regularly stretched for time, experience concerning levels of burnout [ 57 , 58 ]. We recommend more research be done on the role that external/visiting mental health programs can play in rural and regional areas and thus build on selective studies that have shown that such programs can relieve school staff and emotionally engage YP in unique and novel ways that cannot easily be replicated by schools who are bound to rather uniform structures, curricula and lesson formats [ 25 ]. There might also be a place for the integration of social workers into a multi-pronged mental health approach with the aim to strengthen social connections and support between YP and their families, schools and communities [ 59 , 60 ].
Whichever integration model is chosen, attention must be given to the careful coordination of school-based with community-based and visiting services to ensure smooth transitions, consistency and continuation of mental health education and support for YP throughout their formative high school years and beyond [ 17 ]. Co-design, also known as participatory design, with key stakeholders including YP, teachers, parents and mental health organisations, could be an important way of ensuring mental health education and support programs meet the needs and wants of (school) communities and the YP they are targeting. Participatory design places stakeholders at the centre of the design process and is part of a paradigm shift towards collaborative bottom-up engagement whereby stakeholders jointly explore and create solutions to program design and service delivery [ 61 ]. Recommendations for best practice in clinical mental health service design already emphasise the need to involve YP in the planning, implementation and evaluation of services [ 62 ] and this must be extended to community-based interventions [ 63 , 64 , 65 ].
Strengths and limitations
A key strength of this study was the recruitment of a large sample of YP from a diverse range of rural and regional areas of Australia. Their perspectives were complemented and triangulated with those of rural and regional teachers and two parents. However, due to the conservative recruitment methods we used, our sample was likely biased towards participants with a certain familiarity with, and confidence in talking about, mental health issues. Other limitations of this study relating to the participants include the presence of a teacher in 4 out of 7 student interviews, possibly inducing some students to say different things to what they would have shared had they been interviewed without the presence of their teacher. Further to this, three adult participants were interviewed individually, as they needed to be conducted at a time that was convenient to them in order to participate. It is acknowledged that these interviews may glean more information and depth, compared to the focus groups. Further, although we followed processes to establish theme saturation [ 37 ], it is acknowledged that only two parents participated, and their views were not drastically distinct to other participating adults. Given the constraints of the evaluation, a greater focus on student recruitment was prioritised, however more diverse set of parent voices could have consolidated our finding on parental support of YP in drought affected rural and regional Australia.
The design of the evaluation research was such that some of the focus groups were conducted prior to the implementation of the batyr @school program to address the first research aim (i.e. to understand experiences and needs regarding mental health help-seeking, and explore mental health education, support and programs in rural and regional communities) and some were conducted after the batyr @school program was implemented as part of the program evaluation’s second aim. As both sets of focus groups were used in data analysis, results are interpreted through a lens of school-based mental health programs. This is important as although eco-systemic enablers to help-seeking (such as service provision models, family environment, community attitudes) are addressed in the findings and elsewhere in research focusing on rural and regional areas (e.g., [ 14 , 18 , 19 , 20 , 21 , 22 ]), the solutions presented in this discussion centre around what schools and the schooling systems can do in practice to enable better mental health education, programs and support. Further to this, topic guide development was influenced by the evaluation questions, not necessarily the literature concerning young people's help-seeking or general mental health and help-seeking when impacted by drought.
Another limitation is that for the focus groups that were conducted after batyr @school program implementation, the voices of students who had not attended the batyr @school program, and YP outside of the school system were lacking. There is evidence that such unheard voices form a significant portion of YP who need but don’t reach out for mental health support [ 47 , 66 , 67 ]. There is a need for further research into understanding how to engage and support these “silent” adolescent populations to best identify how to facilitate and support help-seeking. Further to this, future studies should consider investigating the needs of young people outside the 14–15 year age range, and seek to compare perspectives based on different demographics including young people who identify with minority groups such as young people with an Aboriginal and Torres Strait Islander background, LGBTQIA + young people, and young people who have a non-English speaking background, particularly those who have arrived as refugees.
Our study highlights important facilitators of mental health education and support for YP in drought-affected rural and regional areas of Australia. These include a multi-pronged, preventative, local community approach with an emphasis on early and ongoing development of YP’s self-management skills. We propose a three-dimensional Engagement, Empowerment, Integration approach which comprises: 1) maximising YP’s emotional engagement; 2) empowering YP to manage their mental health through developing practical coping skills; and, 3) integrating MH education and support programs into existing community and school structures and resources. Integration needs to be well coordinated in respect to time, place and capacity-related factors. Particular regard should be given to the important support roles teachers, school counselling services, social workers and parents can and already do play in the social and emotional development of YP.
Terms and abbreviations used
YP: Young person or young people. This term is used interchangeably with ‘adolescents’ and refers in this study to 14–15 year-old students who are enrolled in the high school years 9 and 10. The cited literature (Background and Discussion sections) refers to adolescents using a variety of age groups, ranging from age 10 to 19 years (reference [ 6 ]), to 14–18 years (reference [ 7 ]) and 12–18 years (reference [ 8 ]).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Handley TE, Kay-Lambkin FJ, Inder KJ, Lewin TJ, Attia JR, Fuller J, et al. Self-reported contacts for mental health problems by rural residents: predicted service needs, facilitators and barriers. BMC Psychiatry. 2014;14(1):249.
PubMed PubMed Central Google Scholar
Bowman S, McKinstry C, McGorry P. Youth mental ill health and secondary school completion in Australia: time to act. Early Interv Psychiatry. 2017;11(4):277–89.
PubMed Google Scholar
Gamm L, Stone S, Pittman S. Mental health and mental disorders—a rural challenge: a literature review. Rural Healthy People. 2010;2(1):97–114.
Google Scholar
Morales DA, Barksdale CL, Beckel-Mitchener AC. A call to action to address rural mental health disparities. J Clin Transl Sci. 2020;4(5):463–7.
Anderson JK, Howarth E, Vainre M, Jones P, Humphrey A. A scoping literature review of service-level barriers for access and engagement with mental health services for children and young people. Child Youth Serv Rev. 2017;77:164–76.
Aguirre Velasco A, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? a systematic review. BMC Psychiatry. 2020;20(1):293.
Hudson J, Ingram V. Stigma-reduction & help-seeking in Australian classrooms. Sydney: Macquarie University, Centre for Emotional Health; 2017.
Quine S, Bernard D, Booth M, Kang M, Usherwood T, Alperstein G, et al. Health and access issues among Australian adolescents: a rural-urban comparison. Rural Remote Health. 2003;3(4):1–11.
Vanderbeck RM, Dunkley CM. Young people’s narratives of rural-urban difference. Child Geogr. 2003;1(2):241–59.
Waid C, Steven S, Sinclair L, Priest L, Petrie S, Carson DB, Peter, P. Report: Interventions for Rural and Remote Youth Mental Health. Carlton University; 2019. p. 1–9. https://doi.org/10.22215/sdhlab/2019.4 .
Francis K, Boyd C, Aisbett D, Newnham K, Newnham K. Rural adolescents’ attitudes to seeking help for mental health problems. Youth Stud Aust. 2006;25(4):42–9.
Salinas-Perez JA, Gutierrez-Colosia MR, Furst MA, Suontausta P, Bertrand J, Almeda N, et al. Patterns of mental health care in remote areas: Kimberley (Australia), Nunavik (Canada), and Lapland (Finland): Modèles de soins de santé mentale dans les régions éloignées: Kimberley (Australie), Nunavik (Canada) et Laponie (Finlande). Can J Psychiatr. 2020;65(10):721–30.
Aisbett D, Boyd CP, Francis KJ, Newnham K. Understanding barriers to mental health service utilization for adolescents in rural Australia. Rural Remote Health. 2007;7(1):1–10.
Salamone-Violi GM, Chur-Hansen A, Winefield HR. In this day and age why is it still so hard to find the right type of help? Carers’ perspectives regarding child and adolescent mental health services: a qualitative study. Adv Ment Health. 2017;15(1):58–70.
Carnie TL, Berry HL, Blinkhorn SA, Hart CR. In their own words: young people’s mental health in drought-affected rural and remote NSW. Aust J Rural Health. 2011;19(5):244–8.
Dean JG, Stain HJ. Mental health impact for adolescents living with prolonged droughtajr_1107 32.. 37. Aust J Rural Health. 2010;18:32–7.
Perkins A, Clarke J, Smith A, Oberklaid F, Darling S. Barriers and enablers faced by regional and rural schools in supporting student mental health: a mixed-methods systematic review. Aust J Rural Health. 2021;29(6):835–49.
Graham A, Phelps R, Maddison C, Fitzgerald R. Supporting children’s mental health in schools: teacher views. Teach Teach. 2011;17(4):479–96.
Boydell KM, Pong R, Volpe T, Tilleczek K, Wilson E, Lemieux S. Family perspectives on pathways to mental health care for children and youth in rural communities. J Rural Health. 2006;22(2):182–8.
Reardon T, Harvey K, Baranowska M, O’Brien D, Smith L, Creswell C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? a systematic review of qualitative and quantitative studies. Eur Child Adolesc Psychiatr. 2017;26(6):623–47.
Trudgen M, Lawn S. What is the threshold of teachers’ recognition and report of concerns about anxiety and depression in students? an exploratory study with teachers of adolescents in regional Australia. J Psychol Couns Sch. 2011;21(2):126–41.
Jorm AF, Kitchener BA, Sawyer MG, Scales H, Cvetkovski S. Mental health first aid training for high school teachers: a cluster randomized trial. BMC Psychiatry. 2010;10(1):51.
Ivancic L, Cairns K, Shuttleworth L, Welland L, Fildes J, Nicholas M. Lifting the weight: Understanding young people’s mental health and service needs in regional and remote Australia. 2018.
Boyd CP, Hayes L, Nurse S, Aisbett D, Francis K, Newnham K, et al. Preferences and intention of rural adolescents toward seeking help for mental health problems. Rural Remote Health. 2011;11(1):122–34.
Milton A, Yeung M, Conn K, Glozier N. batyr@school in Drought Affected Regional School Communities. Sydney: University of Sydney; 2021.
Vins H, Bell J, Saha S, Hess JJ. The mental health outcomes of drought: a systematic review and causal process diagram. Int J Environ Res Public Health. 2015;12(10):13251–75.
Edwards B, Gray M, Hunter B. The impact of drought on mental health in rural and regional Australia. Soc Indic Res. 2015;121(1):177–94.
batyr. batyr@school info pack. online at https://www.batyr.com.au/batyr-school/ : batyr; 2019.
Fielding N. Qualitative interviewing. In: Gilbert. N, editor. Researching social life (2nd edition). London: Sage; 2001. p. 123–44.
Brinkmann S. Qualitative interviewing: Oxford university press; 2013.
Buus N, Perron A. The quality of quality criteria: Replicating the development of the Consolidated Criteria for Reporting Qualitative Research (COREQ). Int J Nurs Stud. 2020;102: 103452.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Khatamian FP. Challenges of recruitment and retention of university students as research participants: lessons learned from a pilot study. J Aust Libr Inf Assoc. 2018;67(3):278–92.
Biernacki P, Waldorf D. Snowball sampling: problems and techniques of chain referral sampling. Sociol Methods Res. 1981;10(2):141–63.
Miller WE, Kreiner DS. Student perception of coercion to participate in psychological research. N Am J Psychol. 2008;10(1).
Srivastava P, Hopwood N. A practical iterative framework for qualitative data analysis. Int J Qual Methods. 2009;8(1):76–84.
Francis JJ, Johnston M, Robertson C, Glidewell L, Entwistle V, Eccles MP, et al. What is an adequate sample size? operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–45.
Birks M, Chapman Y, Francis K. Memoing in qualitative research: probing data and processes. J Res Nurs. 2008;13(1):68–75.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Gao CX, Filia KM, Bedi G, Menssink JM, Brown E, Rickwood DJ, et al. Understanding the complexity, patterns, and correlates of alcohol and other substance use among young people seeking help for mental ill-health. Soc Psychiatry Psychiatr Epidemiol. 2023:1–11.
Cooper J, Hunter C, Owen-Smith A, Gunnell D, Donovan J, Hawton K, et al. “Well it’s like someone at the other end cares about you.” a qualitative study exploring the views of users and providers of care of contact-based interventions following self-harm. Gen Hosp Psychiatry. 2011;33(2):166–76.
Chen S-P, Sargent E, Stuart H. Effectiveness of school-based interventions on mental health stigmatization. Handbook of school-based mental health promotion: Springer; 2018. p. 201–12.
Jorm AF. Effect of contact-based interventions on stigma and discrimination: a critical examination of the evidence. Psychiatr Serv. 2020;71(7):735–7.
Janoušková M, Tušková E, Weissová A, Trančík P, Pasz J, Evans-Lacko S, et al. Can video interventions be used to effectively destigmatize mental illness among young people? a systematic review. Eur Psychiatry 2017;41(1):1–9.
Martínez-Hernáez A, DiGiacomo SM, Carceller-Maicas N, Correa-Urquiza M, Martorell-Poveda MA. Non-professional-help-seeking among young people with depression: a qualitative study. BMC Psychiatr. 2014;14(1):124.
Orlowski S, Lawn S, Antezana G, Venning A, Winsall M, Bidargaddi N, et al. A rural youth consumer perspective of technology to enhance face-to-face mental health services. J Child Fam Stud. 2016;25(10):3066–75.
Rothì DM, Leavey G. Mental health help-seeking and young people: a review. Pastor Care Educ. 2006;24(3):4–13.
Rickwood D, Deane FP, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. Aust E-J Adv Mental Health. 2005;4(3):218–51.
Sewell KM, Fredericks K, Mohamud A, Kallis J, Augimeri LK. Youth experiences in evaluating the Canadian SNAP® Boys youth leadership program. Child Adolesc Soc Work J. 2020;37(3):301–14.
Jadayel R, Medlej K, Jadayel JJ. Mental disorders: a glamorous attraction on social media. J Teach Educ. 2017;7(1):465–76.
O’Reilly M, Dogra N, Whiteman N, Hughes J, Eruyar S, Reilly P. Is social media bad for mental health and wellbeing? exploring the perspectives of adolescents. Clin Child Psychol Psychiatry. 2018;23(4):601–13.
Rothì DM, Leavey G, Best R. On the front-line: Teachers as active observers of pupils’ mental health. Teach Teach Educ. 2008;24(5):1217–31.
Shelemy L, Harvey K, Waite P. Supporting students’ mental health in schools: what do teachers want and need? Emot Behav Diffic. 2019;24(1):100–16.
Loades ME, Mastroyannopoulou K. Teachers’ recognition of children’s mental health problems. Child Adolesc Mental Health. 2010;15(3):150–6.
Heffernan A, Bright D, Longmuir F, Magyar B. Perceptions of Australian schooling: What matters in 2021. Monash University; 2021.
Longmuir F, Gallo Cordoba B, Phillips M, Allen KA, Moharami M. Australian Teachers’ Perceptions of their Work in 2022. Monash University, https://bridges.monash.edu/articles/report/Australian_Teachers_Perceptions_of_their_Work_in_2022/21212891 ; 2022.
Earle K-M. Burnout in NSW school counsellors: relationships between mindfulness, career-sustaining practices and work setting. J Stud Engagem Educ Matters. 2017;7(1):71–96.
King C, Subotic-Kerry M, O’Dea B. An exploration of the factors associated with burnout among NSW secondary school counsellors. J Psychol Couns Sch. 2018;28(2):131–42.
Maple M, Pearce T, Gartshore S, MacFarlane F, Wayland S. Social work in rural New South Wales school settings: addressing inequalities beyond the school gate. Aust Soc Work. 2019;72(2):219–32.
Smith J. Locational disadvantage and the role of school counsellors and social workers: “Doing whatever it takes” to support children, families and communities. Commun Child Fam Aus. 2018;12(1):43–63.
Milton AC, Stewart E, Ospina-Pinillos L, Davenport T, Hickie IB. Participatory design of an activities-based collective mentoring program in after-school care settings: connect, promote, and protect program. JMIR Pediatr Parent. 2021;4(2):e22822.
Early Psychosis Guidelines Working Group. Australian clinical guidelines for early psychosis. Melbourne, Australia: Orygen The National Centre of Excellence in Youth Mental Health; 2016.
Corrigan P. Effect of contact-based interventions on stigma and discrimination. Psychiatr Serv. 2020;71(12):1324–5.
Freebairn L, Occhipinti J-A, Song YJC, Skinner A, Lawson K, Lee GY, et al. Participatory methods for systems modeling of youth mental health: implementation protocol. JMIR Res Protoc. 2022;11(2):e32988.
Milton A, Zelalem M, Ballesteros K, McClean T, Hartog S, Bray-Rudkin L, et al. Supporting children’s social connection and well-being in school-age care: mixed methods evaluation of the connect, promote, and protect program. JMIR Pediatr Parent. 2023;6:e44928.
O’Connor PJ, Martin B, Weeks CS, Ong L. Factors that influence young people’s mental health help-seeking behaviour: a study based on the health belief model. J Adv Nurs. 2014;70(11):2577–87.
Rickwood DJ, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? Med J Aust. 2007;187(S7):S35–9.
Download references
Acknowledgements
We thank the students, staff and families from the participating NSW public schools. We also thank batyr and their enthusiastic team who have helped on this project including.
Amy Brown, India Smith, Zoe Dunnill, Sarah Morris and Tom Riley. We would also like to extend our thanks the Department of Education team for their ongoing support of this research.
This study was funded by a grant from the Australian Department of Education and batyr, and was partially supported by the Australian Government through the Australian Research Council's Centre of Excellence for Children and Families over the Life Course (Project ID CE200100025).
Author information
Authors and affiliations.
Central Clinical School, Faculty of Medicine and Health, The University of Sydney, Sydney, Australia
Christiane Klinner, Nick Glozier, Margaret Yeung, Katrina Conn & Alyssa Milton
Australian Research Council (ARC), Centre of Excellence for Children and Families over the Life Course, Sydney, Australia
Nick Glozier & Alyssa Milton
NSW Department of Education, NSW, Australia
Katrina Conn
You can also search for this author in PubMed Google Scholar
Contributions
AM conceived this study. AM and NG designed this study. AM conducted the interviews oversaw the interpretation of the data at all stages. MY supported the interviews and conducted a preliminary analysis of data with AM, KC and NG. CK analysed the data and drafted the manuscript. CK and AM refined and revised the manuscript with the help of NG, MY and KC.
Corresponding author
Correspondence to Alyssa Milton .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was provided by the University of Sydney Human Research Ethics Committee (Protocol number 2020/607). Subsequent approval was provided via the NSW State Education Research Applications Process (SERAP Number 2020373). All participants provided written informed consent. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., additional file 4., additional file 5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Klinner, C., Glozier, N., Yeung, M. et al. A qualitative exploration of young people’s mental health needs in rural and regional Australia: engagement, empowerment and integration. BMC Psychiatry 23 , 745 (2023). https://doi.org/10.1186/s12888-023-05209-6
Download citation
Received : 12 April 2023
Accepted : 21 September 2023
Published : 13 October 2023
DOI : https://doi.org/10.1186/s12888-023-05209-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Youth mental health
- High school students
- Help-seeking
- Mental health education and support
- Rural and regional Australia
- Qualitative research
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

- Twitter (X)
Qualitative Research Methods (PHCM9120)
This course introduces a range of qualitative research methods and techniques, including participant observation, in-depth interviews and focus groups and their application to public health and health promotion.
This course aims to provide students with introductory skills for developing, conducting, documenting and analysing interviews as a method and understanding how people interpret health and illness and the contexts in which they occur. Recommended as an introduction to this approach for students including those wishing to undertake research projects using qualitative methods.
This course is an elective course for the Masters of Public Health, Health Leadership and Management and Global Health programs, comprising 6 units of credit. It is open to students doing other postgraduate programs at UNSW, or studying at other institutions by arrangement.
Face-to-face classes on-campus for Internal students & fully online for Distance External students
A/Prof Sally Nathan (external course) Course Convenor +61 (2) 9385 1061 [email protected]
Dr Husna Razee (internal course) Course Convenor +61 (2) 9385 8317 [email protected]
Who should do this course?
Course outcomes, learning & teaching, assessments.
- Readings & resources
There are no prerequisites, however, this course assumes familiarity with basic public health research and prior studies in general research and evaluation methods or epidemiology are desirable.
The overall aim of this course is to enable you to critically evaluate the use of qualitative methods in public health research – both research which informs practitioners’ work and research in which you may be involved in planning, designing, conducting and writing up for publication.
At the end of this course you should be able to:
- discuss and debate the contribution and characteristics of qualitative research in public health
- identify criteria by which to assess qualitative studies and apply these criteria in reviewing research
- demonstrate an understanding of a wide range of techniques for qualitative data collection and the ethical issues involved
- discriminate between different methods and their application
- demonstrate an ability to collect, manage and undertake thematic analysis of qualitative interview data.
The course is taught using a variety of teaching strategies matched to desired learning outcomes. Firstly, there is an emphasis on practical skills such as data collection and analysis in the classroom, and online (for external students) and through the written assignments. This will provide you with an introduction to a range of approaches employed by qualitative researchers. The overall course is designed to develop your capacity to make informed decisions about your own study designs and execution, as well as the chance to hone your skills in the critical analysis of others’ research.
Assessment Task 1 – Rigour quiz (formative assessment) Weighting: N/A Length: N/A
Assessment Task 2 – Paper critique Weighting: 25% Length: 1200 words
Assessment Task 3 – Participation: online or in-class activities Weighting: 25% Length: N/A
Assessment Task 4 – Interview assignment Weighting: 50% Length: 2500 words
Readings & resources
Learning resources for this course consist of the following (available in Moodle):
- course notes and readings
- lecture slides
- supplementary resources such as videos and podcasts.
Qualitative research videos
Nsw academics speak about qualitative research.
This video showcases various academics at UNSW Sydney talking about how they use qualitative methodologies and approaches in their research and their advice for people wanting to learn and use qualitative research methods. The videos showcase the many applications of qualitative research across disciplines.
Sally Nathan's qualitative research profile
This video provides details about the qualitative research experiences and expertise of Dr Sally Nathan who convenes Qualitative Research Methods online in the School of Public Health at UNSW Sydney. Dr Nathan's varied experiences with qualitative methods and population groups provide students with a rich and grounded learning environment to begin to master qualitative research methods.
Husna Razee's qualitative research profile
In this video Dr Husna Razee, who convenes the Qualitative Research Methods course in the face-to-face mode, speaks about her experiences and expertise in qualitative research. She has several years of experience in undertaking qualitative research as well, mentoring higher degree research students and training postgraduate students to use qualitative research. She has used creative methods of data collection throughout her teaching and research career.
Indigenous People and Qualitative Research - Making It Work
Research output : Contribution to journal › Article › peer-review
Other files and links
- Link to publisher version
Fingerprint
- Qualitative Research Psychology 100%
- Indigenous Nursing and Health Professions 100%
- Indigenous People Computer Science 100%
- Research Psychology 82%
- Researcher Nursing and Health Professions 17%
- Research Experience Nursing and Health Professions 17%
- Methodology Psychology 11%
- Qualitative Research Method Psychology 11%
T1 - Indigenous People and Qualitative Research - Making It Work
AU - Roman, Curtis
N2 - Indigenous people currently comprise 26.8 % of the Northern Territory population. The Federal Government has recently embarked on a closing the gap campaign to improve the lives of Indigenous people and to address the disadvantage that exits in the lives of Indigenous people. This paper is designed to provide Indigenous and nonindigenous people working in research with some practical advice on how to improve the research experience for Indigenous people and how to develop culturally appropriate research methodologies. The paper proposes that qualitative research methods are practical, useful, beneficial and culturally appropriate for research on and with Indigenous people. The paper also provides practical advice on how to ensure that Indigenous people are represented in research to ensure that their voices are clearly heard. It is hoped that this paper creates awareness among researchers so that they can use this awareness in their research on Indigenous people. The methodology used to write the paper is based on the author's own research experiences as an Indigenous researcher. In the main, the data used in this paper has been gathered from qualitative research textbooks and from personal experiences in research and based on the author's personal experiences of delivering post graduate research courses on Indigenous research issues. The paper shows that qualitative research methods can be useful, productive and culturally appropriate for Indigenous people and can be used to enrich data and to encourage Indigenous people to participate in research. The paper shows that through qualitative research techniques, Indigenous people are able to express themselves and identify issues themselves, which means that researchers are able to gather more data while at the same time, providing Indigenous research participants with a feeling of cultural safety. This is important for those in the area of Indigenous research as Indigenous people have had a long history of negative research experiences.
AB - Indigenous people currently comprise 26.8 % of the Northern Territory population. The Federal Government has recently embarked on a closing the gap campaign to improve the lives of Indigenous people and to address the disadvantage that exits in the lives of Indigenous people. This paper is designed to provide Indigenous and nonindigenous people working in research with some practical advice on how to improve the research experience for Indigenous people and how to develop culturally appropriate research methodologies. The paper proposes that qualitative research methods are practical, useful, beneficial and culturally appropriate for research on and with Indigenous people. The paper also provides practical advice on how to ensure that Indigenous people are represented in research to ensure that their voices are clearly heard. It is hoped that this paper creates awareness among researchers so that they can use this awareness in their research on Indigenous people. The methodology used to write the paper is based on the author's own research experiences as an Indigenous researcher. In the main, the data used in this paper has been gathered from qualitative research textbooks and from personal experiences in research and based on the author's personal experiences of delivering post graduate research courses on Indigenous research issues. The paper shows that qualitative research methods can be useful, productive and culturally appropriate for Indigenous people and can be used to enrich data and to encourage Indigenous people to participate in research. The paper shows that through qualitative research techniques, Indigenous people are able to express themselves and identify issues themselves, which means that researchers are able to gather more data while at the same time, providing Indigenous research participants with a feeling of cultural safety. This is important for those in the area of Indigenous research as Indigenous people have had a long history of negative research experiences.
UR - http://search.informit.com.au/documentSummary;dn=787614138844049;res=IELAPA
M3 - Article
SN - 1037-3403
JO - Aboriginal and Torres Strait Islander Health Worker Journal
JF - Aboriginal and Torres Strait Islander Health Worker Journal
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- What Is Qualitative Research? | Methods & Examples
What Is Qualitative Research? | Methods & Examples
Published on June 19, 2020 by Pritha Bhandari . Revised on June 22, 2023.
Qualitative research involves collecting and analyzing non-numerical data (e.g., text, video, or audio) to understand concepts, opinions, or experiences. It can be used to gather in-depth insights into a problem or generate new ideas for research.
Qualitative research is the opposite of quantitative research , which involves collecting and analyzing numerical data for statistical analysis.
Qualitative research is commonly used in the humanities and social sciences, in subjects such as anthropology, sociology, education, health sciences, history, etc.
- How does social media shape body image in teenagers?
- How do children and adults interpret healthy eating in the UK?
- What factors influence employee retention in a large organization?
- How is anxiety experienced around the world?
- How can teachers integrate social issues into science curriculums?
Table of contents
Approaches to qualitative research, qualitative research methods, qualitative data analysis, advantages of qualitative research, disadvantages of qualitative research, other interesting articles, frequently asked questions about qualitative research.
Qualitative research is used to understand how people experience the world. While there are many approaches to qualitative research, they tend to be flexible and focus on retaining rich meaning when interpreting data.
Common approaches include grounded theory, ethnography , action research , phenomenological research, and narrative research. They share some similarities, but emphasize different aims and perspectives.
Note that qualitative research is at risk for certain research biases including the Hawthorne effect , observer bias , recall bias , and social desirability bias . While not always totally avoidable, awareness of potential biases as you collect and analyze your data can prevent them from impacting your work too much.
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
Each of the research approaches involve using one or more data collection methods . These are some of the most common qualitative methods:
- Observations: recording what you have seen, heard, or encountered in detailed field notes.
- Interviews: personally asking people questions in one-on-one conversations.
- Focus groups: asking questions and generating discussion among a group of people.
- Surveys : distributing questionnaires with open-ended questions.
- Secondary research: collecting existing data in the form of texts, images, audio or video recordings, etc.
- You take field notes with observations and reflect on your own experiences of the company culture.
- You distribute open-ended surveys to employees across all the company’s offices by email to find out if the culture varies across locations.
- You conduct in-depth interviews with employees in your office to learn about their experiences and perspectives in greater detail.
Qualitative researchers often consider themselves “instruments” in research because all observations, interpretations and analyses are filtered through their own personal lens.
For this reason, when writing up your methodology for qualitative research, it’s important to reflect on your approach and to thoroughly explain the choices you made in collecting and analyzing the data.
Qualitative data can take the form of texts, photos, videos and audio. For example, you might be working with interview transcripts, survey responses, fieldnotes, or recordings from natural settings.
Most types of qualitative data analysis share the same five steps:
- Prepare and organize your data. This may mean transcribing interviews or typing up fieldnotes.
- Review and explore your data. Examine the data for patterns or repeated ideas that emerge.
- Develop a data coding system. Based on your initial ideas, establish a set of codes that you can apply to categorize your data.
- Assign codes to the data. For example, in qualitative survey analysis, this may mean going through each participant’s responses and tagging them with codes in a spreadsheet. As you go through your data, you can create new codes to add to your system if necessary.
- Identify recurring themes. Link codes together into cohesive, overarching themes.
There are several specific approaches to analyzing qualitative data. Although these methods share similar processes, they emphasize different concepts.
Qualitative research often tries to preserve the voice and perspective of participants and can be adjusted as new research questions arise. Qualitative research is good for:
- Flexibility
The data collection and analysis process can be adapted as new ideas or patterns emerge. They are not rigidly decided beforehand.
- Natural settings
Data collection occurs in real-world contexts or in naturalistic ways.
- Meaningful insights
Detailed descriptions of people’s experiences, feelings and perceptions can be used in designing, testing or improving systems or products.
- Generation of new ideas
Open-ended responses mean that researchers can uncover novel problems or opportunities that they wouldn’t have thought of otherwise.
Prevent plagiarism. Run a free check.
Researchers must consider practical and theoretical limitations in analyzing and interpreting their data. Qualitative research suffers from:
- Unreliability
The real-world setting often makes qualitative research unreliable because of uncontrolled factors that affect the data.
- Subjectivity
Due to the researcher’s primary role in analyzing and interpreting data, qualitative research cannot be replicated . The researcher decides what is important and what is irrelevant in data analysis, so interpretations of the same data can vary greatly.
- Limited generalizability
Small samples are often used to gather detailed data about specific contexts. Despite rigorous analysis procedures, it is difficult to draw generalizable conclusions because the data may be biased and unrepresentative of the wider population .
- Labor-intensive
Although software can be used to manage and record large amounts of text, data analysis often has to be checked or performed manually.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Chi square goodness of fit test
- Degrees of freedom
- Null hypothesis
- Discourse analysis
- Control groups
- Mixed methods research
- Non-probability sampling
- Quantitative research
- Inclusion and exclusion criteria
Research bias
- Rosenthal effect
- Implicit bias
- Cognitive bias
- Selection bias
- Negativity bias
- Status quo bias
Quantitative research deals with numbers and statistics, while qualitative research deals with words and meanings.
Quantitative methods allow you to systematically measure variables and test hypotheses . Qualitative methods allow you to explore concepts and experiences in more detail.
There are five common approaches to qualitative research :
- Grounded theory involves collecting data in order to develop new theories.
- Ethnography involves immersing yourself in a group or organization to understand its culture.
- Narrative research involves interpreting stories to understand how people make sense of their experiences and perceptions.
- Phenomenological research involves investigating phenomena through people’s lived experiences.
- Action research links theory and practice in several cycles to drive innovative changes.
Data collection is the systematic process by which observations or measurements are gathered in research. It is used in many different contexts by academics, governments, businesses, and other organizations.
There are various approaches to qualitative data analysis , but they all share five steps in common:
- Prepare and organize your data.
- Review and explore your data.
- Develop a data coding system.
- Assign codes to the data.
- Identify recurring themes.
The specifics of each step depend on the focus of the analysis. Some common approaches include textual analysis , thematic analysis , and discourse analysis .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Bhandari, P. (2023, June 22). What Is Qualitative Research? | Methods & Examples. Scribbr. Retrieved April 15, 2024, from https://www.scribbr.com/methodology/qualitative-research/
Is this article helpful?

Pritha Bhandari
Other students also liked, qualitative vs. quantitative research | differences, examples & methods, how to do thematic analysis | step-by-step guide & examples, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Public Health

A systematic review of studies evaluating Australian indigenous community development projects: the extent of community participation, their methodological quality and their outcomes
Mieke snijder.
National Drug and Alcohol Research Centre (NDARC), UNSW, Randwick, NSW 2052 Sydney, Australia
Anthony Shakeshaft
Annemarie wagemakers.
Public Health and Society, Department of Social Sciences, Wageningen University and Research Centre (WUR), Wageningen, The Netherlands
Anne Stephens
The Northern Research Futures Collaborative Research Network, The Cairns Institute, James Cook University (JCU), Cairns, Australia
Bianca Calabria
National Centre for Epidemiology and Population Health, Research School of Population Health, College of Medicine, Biology and Environment, Australian National University, Canberra, Australia
Community development is a health promotion approach identified as having great potential to improve Indigenous health, because of its potential for extensive community participation. There has been no systematic examination of the extent of community participation in community development projects and little analysis of their effectiveness. This systematic review aims to identify the extent of community participation in community development projects implemented in Australian Indigenous communities, critically appraise the qualitative and quantitative methods used in their evaluation, and summarise their outcomes.
Ten electronic peer-reviewed databases and two electronic grey literature databases were searched for relevant studies published between 1990 and 2015. The level of community participation and the methodological quality of the qualitative and quantitative components of the studies were assessed against standardised criteria.
Thirty one evaluation studies of community development projects were identified. Community participation varied between different phases of project development, generally high during project implementation, but low during the evaluation phase. For the majority of studies, methodological quality was low and the methods were poorly described. Although positive qualitative or quantitative outcomes were reported in all studies, only two studies reported statistically significant outcomes.
Partnerships between researchers, community members and service providers have great potential to improve methodological quality and community participation when research skills and community knowledge are integrated to design, implement and evaluate community development projects.
The methodological quality of studies evaluating Australian Indigenous community development projects is currently too weak to confidently determine the cost-effectiveness of community development projects in improving the health and wellbeing of Indigenous Australians. Higher quality studies evaluating community development projects would strengthen the evidence base.
The health gap between Indigenous and non-Indigenous Australians has been well documented [ 1 – 3 ]. Systematic literature reviews, however, have consistently concluded that evaluations of interventions aimed at reducing this health gap lack methodological rigour [ 4 – 12 ]. In addition to improving the methodological quality of the evidence-base, the need for greater community participation in, and control of, Indigenous health promotion research have been advocated [ 13 – 15 ].
Community participation has long been argued as being an essential factor in successful health promotion initiatives [ 16 – 18 ]. A recent meta-analysis concluded that community participation is effective when used in health promotion projects because it engenders greater community motivation and increases the sustainability of projects [ 19 ]. Although the review did not include Indigenous communities, the principle of community participation is highly relevant to Indigenous Australians and has great potential to improve Indigenous health. The history of dispossession and disempowerment experienced by Indigenous people highlights the importance of the full and active participation of community members to develop plausible solutions to the problems they themselves have identified [ 9 , 20 – 25 ]. The community development approach strives to empower Indigenous communities to develop and utilise skills that will enable them to more directly address the risk factors that determine their health status [ 26 ].
Despite the potential of community development approaches for improving Indigenous health outcomes, there has been no systematic examination of the extent to which they have engendered community participation and little analysis of their effectiveness. The only existing systematic review of Indigenous community development, published in 2007, evaluated 17 projects implemented in Indigenous communities in Australia, Canada, New Zealand and the United States [ 9 ]. This review emphasised that high levels of community participation were a critical factor in the success with which community development projects were implemented, however, it did not assess the level of community participation nor systematically assessed the methodological qualities of the studies. This lack of project evaluation has made it difficult to confidently estimate the extent to which community development projects have improved the health and life expectancy of Indigenous People.
This systematic review aims to identify the extent of community participation in community development projects implemented in Australian Indigenous communities, critically appraise the qualitative and quantitative methods used in their evaluation, and summarise their outcomes.
Identification of publications
The peer-reviewed and grey literature were searched to identify studies evaluating Indigenous community development projects in Australia, published between 1990 and 2015. Twenty-five years of community development projects was judged to be sufficient to provide an overview of the most recent projects. Figure 1 summarises the databases searched, the search terms used, the eligibility criteria and the classification process based on the PRISMA flow diagram [ 27 ].

PRISMA flow diagram: systematic search identifying evaluation studies of Australian Indigenous Community Development projects
Ten peer-reviewed databases were searched: Health and Society, Aboriginal and Torres Strait Islander Health Bibliography (ATSIHealth), AIATSIS, APAIS-AIATSIS, FAMILY-ATSIS, ProQuest, Scopus, CINAHL, PsychINFO, and Medline/Pubmed. Two grey literature databases were searched: Health Infonet and Closing the Gap Clearinghouse. The electronic database search identified 3623 publications and 411 duplicates were removed. Reference lists of the identified publications were scanned which identified an additional 20 publications. Another 11 publications were received from researchers in the field. The resulting 3243 publications were organised in Reference Manager Endnote [ 28 ].
Screening and eligibility
The titles and abstracts of the identified 3243 publications were read to determine their eligibility for inclusion against three criteria: 1) relevance to a community development project, including: projects focusing on community ownership, empowerment, local leadership and decision making, adopting a long-term strategy, having a focus on sustainability or having a bottom up approach (i.e. starting from the community) [ 29 , 30 ]; 2) published between 1990 and 2015; and 3) a primary focus on Indigenous communities in Australia. A total of 231 publications met all three criteria. The full text versions of these 231 publications were sought for detailed review, of which 112 were available and relevant to this review.
Classification
One hundred and twelve publications were classified into four categories derived from previous research reviewing Indigenous health initiatives [ 4 , 10 , 31 ], defined as follows. Measurement research: the development, testing or evaluation of measurement tools. Evaluation research: an evaluation of an Indigenous community development project or policy. Review: including summaries, critical or systematic reviews and/or meta-analysis; and Discussion paper: general discussion of Indigenous community development. Thirty one publications identified as studies evaluating community development projects in Indigenous Australian communities were critically appraised.
Extent of community participation
Replicating previous analyses [ 32 , 33 ], the extent of community participation was assessed using Pretty’s participation typology, which describes seven levels of community participation ranging from no participation to self-mobilisation (i.e. completely top-down to completely bottom-up) [ 32 , 34 ]. Given community participation can vary during the lifetime of a project, the extent of participation was assessed separately for four phases of project development: diagnosis (identifying a community’s priorities); development (of appropriate strategies to address the priorities); implementation (of the strategies); and evaluation (of the effectiveness of the project) [ 32 , 35 , 36 ]. The level of community participation in the 31 studies were assigned a score between 1 and 7 for each phase of project development. Detailed descriptions of different levels of community participation in relation to scores 1 to 7, and with respect to all four phases, are provided in Table 1 and are summarised as follows: no participation (score 1); passive participation (score 2 – the community was only informed about the project); participation by information (score 3 – information was collected from the community without their participation and without providing feedback); participation by consultation (score 4 – information was collected from the community, feedback was given and further inclusion of community was sought); functional participation (score 5 – community collaboration, but on outsiders’ terms); interactive participation (score 6 – collaboration on mutually defined terms); and self-mobilisation (score 7 – outsider’s work in community on community’s terms). This scoring was independently conducted by two of the authors (MS and AW), which resulted in agreement for 22 studies (71 %). The nine studies on which authors disagreed were blindly reviewed by a third author (ASt). For four studies, the score allocated by the third reviewer was the same as the score allocated by one of the first two reviewers and so that score was used, increasing the agreement rate to 84 % for 26 of the 31 studies. For the five studies where there was no agreement, the scores allocated by the first author (MS) were used.
Definitions of the seven levels of community participation in the four phases of project development
Source: adapted from Pretty (1995) and Wagemakers et al. (2008)
Critical appraisal of methodology
Qualitative methods.
The methodological quality of the qualitative study components was assessed by adapting Long and Godfrey’s qualitative study evaluation tool, which was developed to appraise evaluations of health and social care interventions [ 37 ]. This tool has 4 sections: 1) phenomenon studied and context; 2) ethics; 3) data collection, analysis and potential research bias; and 4) policy and practical implications. The latter two were used in this review because they relate specifically to evaluation issues. Data collection includes the need for clear descriptions of the data collection process (e.g. recruitment strategies, data collection procedures, specifying the interview questions, methods of recording data and the extent to which the data collection process was tailored to specific communities). Data analysis includes the description of the data analysis, the provision of adequate evidence to support the analysis (including data extracts, triangulations and descriptions of reliability) and whether the findings are interpreted in line with existing theories and literature. Potential researchers’ bias assesses whether the position of the researcher is outlined in the study and its potential influence on the data collection and analysis. The policy and practical implications include an analysis of the populations and settings to which the findings are generalisable, the implications for policy or practice, and the extent to which the methods justify the conclusions.
Quantitative methods
The methodological quality of the quantitative study components was appraised using the Dictionary for Effective Public Health Practice Project Quality Assessment tool for Quantitative studies [ 38 ], which was developed to review public health studies and has been used in other systematic reviews in the Australian Indigenous health field [ 4 , 10 ]. Sections A-F (A - selection bias, B - study design, C - confounders, D - blinding, E - data collection methods, F - withdrawals and drop-out) are rated categorically as strong, moderate or weak. Sections G (intervention integrity) and H (analysis appropriateness) comprise summaries of the relevant information rather than categorical ratings. In addition to sections A-H, this tool advocates a summary rating defined as weak (two or more weak scores are given), moderate (1 weak score is given) or strong (no weak scores are given).
Scoring for critical appraisal of methodology
Scores against both the qualitative and quantitative evaluation criteria were allocated by author MS. A random selection of 25 % of studies were assessed by a blinded coder (ASt). There was agreement for 70 % of these studies. Disagreements were resolved in consultation between the two coders.
Outcomes of the studies
The outcomes of the studies evaluating Indigenous community development projects are summarised.
Thirty-one studies evaluating Indigenous community development projects in Australia were identified. Ten (32 %) were published in the peer reviewed literature [ 39 – 48 ].
Table 2 summarises the level of community participation across the four phases of project development for each study. Table 3 summarises the number of studies relevant to each of the seven levels of community participation, separately for the four phases of project development. The highest levels of participation (level 5 to level 7), were found in the Diagnosis phase for ten studies (32 %) [ 39 , 43 , 44 , 48 – 54 ], in the Development phase for 13 studies (42 %) [ 39 – 44 , 46 , 49 – 52 , 54 , 55 ], in the Implementation phase for 17 studies (55 %) [ 39 – 44 , 46 , 48 – 54 , 56 – 58 ] and in the Evaluation phase for 7 studies (22 %) [ 39 , 40 , 43 , 44 , 50 , 53 , 59 ]. Four studies (13 %) had at least level 5 participation in all phases of the project [ 39 , 43 , 44 , 50 ]. The participation of the community was described with insufficient detail to be assessed (unknown category) for ten studies in the Diagnosis phase (32 %) [ 42 , 45 , 57 , 58 , 60 – 65 ], seven in the Development phase (23 %) [ 47 , 48 , 57 , 60 , 61 , 64 , 66 ], four (12.9 %) in the Implementation phase [ 47 , 61 , 63 , 66 ] and two (7 %) in the Evaluation phase [ 46 , 67 ].
Level of community participation in each phase of project development for each study
a Possible scores range from 1 to 7: 1 = no participation; 2 = passive participation; 3 = participation by information; 4 = participation by consultation; 5 = functional participation; 6 = interactive participation; 7 = self-mobilisation, UNK = unknown [ 32 , 34 ]
b Participation varied within the phase
c Participation was somewhere in between these levels
Number of studies across the levels of community participation and phases of project development
Note: No participation = community did not participate
Passive participation = the community was only informed about the project
Participation by information = information was collected from the community without their participation and without providing feedback. Participation by consultation = information was collected from the community, feedback was given and further inclusion of community was sought
Functional participation = community collaboration on outsider’s terms
Interactive participation = collaboration on mutually defined terms
Self-mobilisation = outsider’s work in community on community’s terms [ 32 , 34 ]
Methods used in studies
Twenty-one studies (67 %) used qualitative methods only [ 39 – 41 , 48 , 49 , 51 , 52 , 55 – 57 , 59 – 69 ], two (7 %) used quantitative methods only [ 46 , 47 ], and eight (26 %) used mixed methods [ 42 – 45 , 53 , 54 , 58 , 59 ]. Qualitative data were collected using semi-structured interviews in 24 studies [ 39 , 40 , 42 , 43 , 45 , 49 – 53 , 55 – 58 , 60 – 69 ], document analysis ( n = 15 [ 42 , 49 , 51 , 52 , 55 – 57 , 60 – 66 , 68 ]), focus groups ( n = 9 [ 39 , 40 , 43 , 45 , 48 – 50 , 53 , 58 ]), participant observation ( n = 6 [ 42 , 43 , 53 , 54 , 58 , 69 ]) and photovoice [ 70 ] ( n = 2 [ 50 , 53 ]). Quantitative data collection methods included surveys in three studies [ 45 , 48 , 58 ], hospital/clinical records ( n = 4 [ 43 , 44 , 47 , 53 ]), school records ( n = 2 [ 42 , 58 ]), police records ( n = 1 [ 42 ]), store records ( n = 1 [ 43 ]) and ABS census data ( n = 1 [ 46 ]).
Methodological quality of studies with a qualitative component
All 29 studies with a qualitative component (including mixed methods studies) provided some description of the evaluation methods used (Table 4 ). Twelve studies (41 %) gave detailed descriptions of the data collection process, including participant recruitment, focus group procedures and a clear description of which data were recorded [ 39 , 41 , 49 – 51 , 53 , 58 , 60 – 63 , 67 ]. Four of these twelve studies (14 %) provided the interview questions [ 51 , 58 , 60 , 67 ] and one study (4 %) described in detail how the data collection methods were tailored to ensure their cultural appropriateness [ 49 ]. The data analysis methods were described in detail in seven studies (24 %) [ 39 , 42 , 50 , 54 , 58 , 67 , 69 ]. The potential for researcher bias was described in seven studies (24 %) [ 39 , 44 , 45 , 49 , 53 , 58 , 69 ]. Three studies (10 %) did not discuss the implications of their findings [ 52 , 59 , 65 ].
Critical appraisal of qualitative components of studies evaluating Indigenous community development projects ( n = 29)
Methodological quality of studies with a quantitative component
The summary ratings for all ten studies with a quantitative component were classified as weak (Table 5 ). The likely extent of selection bias was unclear for six studies (60 %) because description of the participant and community selection procedures was absent or insufficiently detailed [ 42 – 44 , 46 , 47 , 59 ]. Five studies (50 %) used a cohort design without a control group [ 43 – 45 , 53 , 54 ], one study (10 %) used a time series design [ 47 ] and the evaluation design of the remaining four studies (40 %) was unclear [ 42 , 46 , 58 , 59 ]. No study adequately controlled for confounding variables. None of the studies used blinding procedures. Two studies (20 %) used validated outcome measures [ 45 , 58 ]. No study discussed the validity or reliability of their outcome measures.
Critical appraisal of quantitative component of studies evaluating Indigenous community development projects ( n = 10)
Note: Appraised using the Dictionary for Effective Public Health Practice Project Quality Assessment tool [ 38 ]
a Published in peer-reviewed literature
One study (10 %) described withdrawals and drop outs at the community level [ 46 ]. One study (10 %) described withdrawals and drop outs at the participant level [ 53 ]. Drop outs at the participant level were not applicable for the six studies (60 %) that used either routinely collected data or a one-off survey [ 42 – 44 , 47 , 54 , 58 ]. Two studies (20 %) did not report drop outs [ 45 , 59 ]. No study described the fidelity of the project. Three studies (30 %) reported on the exposure of participants to the project [ 45 , 54 , 58 ]. Inferential statistical analyses were reported by four studies (40 %) [ 42 , 47 , 53 , 58 ].
A summary of the aims and key outcomes for each study is provided in Table 6 . All studies using qualitative methods concluded that community members reported positive project impacts for their community. Two studies (7 %) reported quantitative outcomes that were statistically significant: a reduction in injuries [ 47 ] and a reduction in cannabis use among females aged 13–36 and males aged over 16 years [ 42 ].
Aims and outcomes of studies evaluating Indigenous community development project ( n = 31)
This study systematically reviewed the peer-reviewed and grey literature on community development projects in Australian Indigenous communities. One hundred and twelve relevant and available publications were identified, 31(28 %) studies were evaluations, 21of these evaluation studies (68 %) were published in grey literature. There were no marked differences observed between evaluations published in the grey and peer-reviewed literature in terms of the detailed descriptions of the qualitative methods used, the quality of the quantitative methods or the reported levels of community participation. This high comparability reflects the generally low quality of all the evaluations published in both the peer-review and the grey literature. It would be an asset to the community development field to increase the publication rate of higher-quality evaluation studies in the peer reviewed literature, especially in open access journals, to utilise peer review as a quality assurance mechanism and to optimise the transparency of study results.
Community participation in community development projects
Community participation was assessed as moderate in most of the studies evaluating Indigenous community development projects (87 %). The wide variation in community participation between projects and project phases, and within project phases, in these Australian Indigenous studies is reflected in the international literature [ 32 , 36 ]. For half of the studies included in this review, the intent for community participation was clearly described, but the actual level of participation was not reported for at least one of the phases of project development. Documenting the community participation strategies and processes used, including details about how the community was engaged and who in the community participated, would allow the more successful community participation strategies to be identified and replicated in subsequent projects [ 36 ].
Although the unique characteristics of each community will lead to variation in their capacity to participate in each phase of a project [ 36 , 71 ], the extent and nature of community participation can be optimised by careful planning and the utilisation of appropriate frameworks to guide the development, implementation and evaluation of community-based projects. An approach like participatory action research provides practical guidelines to achieve this [ 72 , 73 ].
Quality of evaluation methodology
In line with previous research [ 4 – 12 ], the methodological quality of the studies identified in this review are poor, or they are difficult to assess because their methods are inadequately described. It is acknowledged that issues specific to Indigenous community-based research can impact on the research quality, including time needed to engage with the community, difficulties with recruiting enough participants, high staff turn-over at service providers and culturally-specific delays (e.g. ceremonies or celebrations) [ 14 ]. Careful and flexible planning is therefore needed in community development projects to address these issues to reduce their impact on the quality of the research. The complex interventions framework, for example, provides one mechanism to carefully plan projects to maintain methodological rigour [ 74 , 75 ]. The methodological quality of qualitative studies could also be improved by using appropriate analysis methods, multiple coders, and describing the extent of potential bias attributable to the researcher [ 37 ].
The methodological rigour of both the qualitative and the quantitative studies could further be improved by using measures with demonstrated reliability and validity: only two studies identified by this review reported that they had used such measures [ 45 , 58 ]. Using reliable and valid measures increases confidence in the accuracy of the study outcomes [ 76 ]. Such measures should be validated specifically for the Indigenous population, because of their holistic concept of health and wellbeing [ 77 ]. Existing studies show that it is possible to develop reliable and valid measures that are culturally appropriate and acceptable to Indigenous Australians [ 78 – 83 ], but the lack of measurement studies specifically related to community projects identified in this review (one study, see Fig. 1 ) clearly indicates that more of this measurement research is urgently needed [ 80 ].
Only three studies (10 %) reported on intervention integrity, which includes the level of exposure to the project, and the consistency and frequency with which project components were delivered in practice. Studies evaluating community development projects would be improved by routinely including process measures, to allow an examination of the extent to which outcomes are a consequence of the project components, as opposed to reflecting the extent to which the project components were implemented [ 74 ].
Eight studies (26 %) evaluated a community development project using a mixed methods design. Increasing the use of mixed methods is likely to optimally improve the effectiveness of future community-based evaluations because they provide a greater range of relevant data [ 11 , 84 ]: quantitative analysis can provide rigorous methods to evaluate the effectiveness and costs of projects, while qualitative data can capture community members’ experiences [ 85 ] and help identify the project elements that are most acceptable to community members [ 11 ].
The critical appraisal also identified a lack of detailed reporting of the methodologies used, especially in relation to the qualitative evaluations. Only 41 % of the qualitative studies reported on their data collection process, for example, and only 24 % reported the data analysis methods that were used. Future Indigenous community development evaluations would benefit from more detailed reporting using established guidelines, such as the COREQ criteria for qualitative research [ 86 ] or the guidelines recommended by the Equator Network [ 87 ]. In addition to improving reporting standards, using these guidelines in the development, implementation and evaluation phases of community development projects would most likely improve the quality of the interventions and their evaluation [ 37 , 38 ].
Outcomes of indigenous community development projects
There is currently insufficient evidence about the impact of community development projects on health and wellbeing outcomes for Indigenous Australians. Although all reviewed studies reported positive outcomes for the communities, they are not methodologically rigorous enough to support clear conclusions about their cost-effectiveness, and no studies have undertaken an economic analysis to weigh the benefits of community development against its costs. This finding is highly consistent with the conclusions of similar reviews of international Indigenous community development studies, where generally positive outcomes are difficult to interpret because of the relatively poor quality of their evaluation designs and reporting [ 9 , 19 , 88 ]. Published results of community-based evaluations with greater methodological quality are required to provide evidence of cost-effective community development projects [ 9 , 74 ]. Ideally, future studies would use rigorous evaluation designs, reliable, valid and culturally appropriate measures, economic analysis and a complex intervention framework to balance standardisation and tailoring.
Strengths and limitations
To ensure that qualitative and quantitative study components were assessed against appropriate criteria the Dictionary for Effective Public Health Practice Project Quality Assessment tool [ 38 ] was used to assess the methodological quality of quantitative components and an adaptation of the qualitative study appraisal tool, developed by Long and Godfrey [ 37 ] was used for the qualitative study components. The methodological quality of the studies and extent of community participation may have been misclassified, however the high level of agreement between blinded coders suggest not. Of the 231 full-text articles sought for detailed review, 40 (17 %) were excluded because the full text version of these papers were unable to be accessed. Excluding these 40 papers is unlikely to have compromised the comprehensiveness of this review for three reasons: 1) they only represent 17 % of the full-text articles; 2) the majority were older studies or reports that were not publically available; and 3) the references lists of identified publications were hand searched and researchers in the field were consulted to identify publications not found by the electronic database search.
This systematic review identified that levels of community participation fluctuate across community development project phases: moderate in the Diagnosis and Development phases, high in the Implementation phase, but low in the Evaluation phase. It also identified that the methodological quality of studies evaluating Australian Indigenous community development projects is too weak to confidently determine the cost-effectiveness of these projects in improving the health and wellbeing of Indigenous Australians. Studies of greater methodological quality are required to accurately assess the impact of community development projects. Partnerships combining researchers’ expertise and community members’ skills and knowledge have great potential to improve methodological quality and community participation in Indigenous community development projects [ 9 , 11 , 89 ].
Acknowledgements
The authors gratefully acknowledge the NDARC Education Trustees for funding the PhD candidature of MS. We thank New South Wales Health for funding the Maldahnalanga project, of which this review is a part. We also gratefully acknowledge the Post-Doctoral Research funding from the Northern Research Futures Collaborative Research Network of ASt. We also gratefully acknowledge the input from the Aboriginal community-based partners who are part of the Maldahnalanga project.
Competing interests
None reported.
Authors’ contributions
MS conducted the literature review and drafted the paper. AS, AW and BC supervised MS in conducting the review and reviewed drafts of the paper. AW assisted in the assessment of the level of community participation. ASt assisted in the appraisal of the quality of methodologies used and the level of community participation, helped design the literature review, consulted on the initial searches and revised drafts of the paper. All authors gave approval for the paper to be published.
Contributor Information
Mieke Snijder, Phone: + 61-2-9385-0333, Email: [email protected] .
Anthony Shakeshaft, Email: [email protected] .
Annemarie Wagemakers, Email: [email protected] .
Anne Stephens, Email: [email protected] .
Bianca Calabria, Email: [email protected] .
Development of Patient and Caregiver Conceptual Models Investigating the Health-Related Quality of Life Impacts of Malignant Pleural Mesothelioma
- Original Research Article
- Published: 15 April 2024
Cite this article
- Adam E. J. Gibson 1 ,
- Waqas Ahmed 1 ,
- Louise Longworth 1 ,
- Bryan Bennett 2 ,
- Melinda Daumont 3 &
- Liz Darlison 4
Malignant pleural mesothelioma (MPM) is a rare and usually fatal malignancy frequently linked to occupational asbestos exposures and associated with poor prognosis and considerable humanistic burden. The study aimed to develop conceptual models of the health-related quality of life (HRQoL) impact on patients with and receiving treatment for MPM, and the burden on their caregivers.
This multi-country study (Australia and United Kingdom) adopted a qualitative methodology to conduct semi-structured, independent interviews with people with MPM ( n = 26), current caregivers ( n = 20), and caregivers of people who had recently died because of MPM ( n = 4). Participants were recruited using a purposive sampling approach and interviews conducted via telephone between January 2021 and January 2022. Transcripts were analysed using thematic analysis and used to construct conceptual models.
Patient analysis yielded four overarching themes: (1) debilitating burden of breathlessness and fatigue; (2) physical mesothelioma symptoms experienced by patients; (3) distress of MPM on the self and family; and (4) treatment is worth ‘having a go’ despite the potential impact on symptoms. Caregiver analysis yielded five core themes: (1) daily life limited by caregiving duties; (2) emotional well-being and the need for support; (3) the relational role shift to caregiver; (4) time spent providing care negatively impacts work and productivity; and (5) positive aspects and outcomes of caregiving.
Conclusions
This study highlights the substantial daily and emotional HRQoL impact that MPM symptoms have on patients and caregivers. Both groups reduced work, productivity, and social and leisure activities. There was evidence of positive HRQoL impacts as a result of immunotherapy and radiotherapy, but less for chemotherapy. Caregiver impacts were intensified during the end-of-life period and persisted following patient death. Evident is a need for increased psychological support, information, and advice for caregivers, increased during the end-of-life period.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
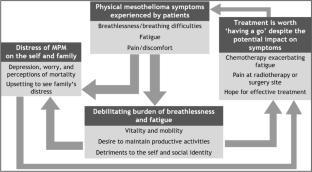
Availability of data and materials
Participant data are not available for distribution due to confidentiality. Interview discussion guide and coding inquiries can be directed to [email protected].
Hamra G, Loomis D, Dement J. Examining the association of lung cancer and highly correlated fibre size-specific asbestos exposures with a hierarchical Bayesian model. Occup Environ Med. 2014;71:353–7.
Article PubMed Google Scholar
Røe OD, Stella GM. Malignant pleural mesothelioma: history, controversy, and future of a man-made epidemic. Eur Respir Rev. 2017;24:115–31.
Article Google Scholar
Van Zandwijk N, Clarke, C., Henderson, D., Musk, W., Fong, K, Penman, A. Guidelines for the diagnosis and treatment of malignant pleural mesothelioma. J Thorac Dis. 2013;5(6):E254-E307.
Ettinger D. NCCN guidelines insights: malignant pleural mesothelioma, version 3.2016. Off J Natl Comprehen Cancer Netw. 2016;14(7):825-36.
Cavone D, Caputi A, De Maria L, Cannone ESS, Mansi F, Vimercati L. Epidemiology of mesothelioma. Environments 2019;6(7):76.
Bianchi C, Bianchi T. Global mesothelioma epidemic: trend and features. Indian J Occupat Environ Med. 2014;18(2):82-8.
Krówczyńska M, Wilk E. Asbestos Exposure and the Mesothelioma Incidence in Poland. Int J Environ Res Public Health. 2018;15(8):1741.
Article PubMed PubMed Central Google Scholar
Musk ABW, de Klerk N, Brims FJ. Mesothelioma in Australia: a review. Med J Aust. 2017;207(10):449–52.
Shah N, Williams, A. Surviving the asbestos epidemic. Insurance Digest (European). 2001:14-8.
Tsao A, Wistuba I, Roth JA, Kindler HL. Malignant pleural mesothelioma. J Clin Oncol. 2009;27(12):2081–90.
Article CAS PubMed PubMed Central Google Scholar
Baas P, Scherpereel A, Nowak AK, Fujimoto N, Peters S, Zalcman G. First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): a multicentre, randomised, open-label, phase 3 trial. The Lancet. 2021;397(10272):375-86.
Nakajima E, Vellanki, J., Larkins, E., Chatterjee, Mishra-Kalyani, PS, Donoghue, M. FDA approval summary: nivolumab in combination with ipilimumab for the treatment of unresectable malignant pleural mesothelioma. Clin Cancer Res. 2022;28(3):446-51.
EMA. Assessment report: ipilimumab/nivolumab (EMA/CHMP/260350/2021). EMA; 2021:1–164.
PBS. Submission: nivolumab plus ipilimumab. Retrieved from: https://wwwpbsgovau/industry/listing/elements/pbac-meetings/psd/2021-03/files/nivolumab-plus-ipilimumab-psd-mar-2021docx. 24th June 2022. 2021:1-42.
Kondola S, Manners D, Nowak AK. Malignant pleural mesothelioma: an update on diagnosis and treatment options. Ther Adv Respir Dis. 2016;10(3):275–88.
Girgis S, Smith AB, Lamber S, Waller A, Girgis A. ‘It sort of hit me like a baseball bat between the eyes’: a qualitative study of the psychosocial experiences of mesothelioma patients and carers. Support Care Cancer. 2019;27(2):631–8.
Sturges J, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note. Qual Res. 2004;4(1):107–18.
NHMRC. National Statement on Ethical Conduct in Human Research 2007 (Updated 2018). www.nhmrc.gov.au/guidelines/publications/e72 : National Health and Medical Research Council; 2018.
Clarke V, Braun, V. Thematic analysis. In: Michalos AC (ed) Encyclopaedia of quality of life and well-being research. Springer, Dordrecht. 2014.
Coast J. Qualitative methods for health economics: rowan and littlefield international; 2017.
Silverman D. Doing qualitative research: a practical handbook. London: SAGE; 2010.
Google Scholar
Guest G, Bunce A, Johnson L. An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Moore S, Darlison L, Tod AM. Living with mesothelioma: a literture review European. J Cancer Care. 2010;19:458–68.
Article CAS Google Scholar
Brims F, Gunatilake, S., Lawrie, I., Marshall, L., Fogg, C, Chauhan, AJ. Early specialist palliative care on quality of life for malignant pleural mesothelioma: a randomised controlled trial. Thorax. 2019;74:354-61.
Arber A, Spener L. ‘It’s all bad news’: the first 3 months following a diagnosis of malignant pleural mesothelioma. Psychooncology. 2013;22(7):1528–33.
Hughes N, Arber A. The lived eperience of patients with pleural mesothelioma. Int J Palliat Nurs. 2009;14(2):66–71.
Ejegi-Memeg S, Sherborne, V., Harrison, M., Taylor, B., Senek, M, Gardiner, C. Patients’ and informal carers’ experience of living with mesothelioma: a systematic rapid review and synthesis of the literature. Eur J Oncol Nurs. 2022;58:102122.
Harrison M, Gardiner C, Taylor B, Ejegi-Memeh S, Darlison L. Understanding the palliative care needs and experiences of people with mesothelioma and their family carers: an integrative systematic review. Palliat Med. 2021;35(6):1039–51.
Warby A, Dhillon HM, Kao S, Vardy JL. A survey of patient and caregiver experience with malignant pleural mesothelioma. Support Care Cancer. 2019;27:4675–86.
Henson K, Wickramasinghe B, Pitman A. Risk of suicide after cancer diagnosis in England. JAMA Psychiatry. 2019;76(1):51–60.
Download references
Acknowledgements
The authors would like to thank the patients and caregivers who participated for their valuable contributions and without whom this research would not have been possible.
This study was funded by Bristol-Myers Squibb.
Author information
Authors and affiliations.
Putnam Associates, 22-24 Torrington Place, Fitzrovia, London, WC1E 7HJ, UK
Adam E. J. Gibson, Waqas Ahmed & Louise Longworth
Bristol Myers Squibb (formerly), Sanderson Rd, Denham, Uxbridge, UB8 1DH, UK
Bryan Bennett
Bristol Myers Squibb (formerly), Avenue de Finlande 8, Building F – 1st Floor, 1420, Braine-l’Alleud, Belgium
Melinda Daumont
Mesothelioma UK, 235 Loughborough Road, Mountsorrel, Loughborough, Leicestershire, LE12 7AS, UK
Liz Darlison
You can also search for this author in PubMed Google Scholar
Contributions
AG contributed to the conception and design, data acquisition, data analysis, and data interpretation. WA contributed to data analysis and data interpretation. LL, BB, MD, and LD contributed to the conception and design, as well as data interpretation. All authors reviewed the manuscript.
Corresponding author
Correspondence to Adam E. J. Gibson .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Ethical approval
The study design and conduct were reviewed and received ethical approval prior to commencement by an independent ethical review board, WIRB (WCG IRB, www.wcgirb.com ). All interviewees provided recorded consent to participate and for use of their data in this research and publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 133 kb)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Gibson, A.E.J., Ahmed, W., Longworth, L. et al. Development of Patient and Caregiver Conceptual Models Investigating the Health-Related Quality of Life Impacts of Malignant Pleural Mesothelioma. Patient (2024). https://doi.org/10.1007/s40271-024-00690-x
Download citation
Accepted : 11 March 2024
Published : 15 April 2024
DOI : https://doi.org/10.1007/s40271-024-00690-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Understanding the provision of goal-concordant care in the intensive care unit: A sequential two-phase qualitative descriptive study
Affiliations.
- 1 Intensive Care Unit, Epworth HealthCare, Richmond, VIC, Australia; School of Nursing and Midwifery, Deakin University, Geelong, VIC, Australia. Electronic address: [email protected].
- 2 School of Nursing and Midwifery, Deakin University, Geelong, VIC, Australia; Centre for Quality and Patient Safety Research - Epworth HealthCare, Richmond, VIC, Australia.
- 3 School of Nursing and Midwifery, Griffith University, Nathan, QLD, Australia; Intensive Care Unit, Princess Alexandra Hospital, Metro South Health, Woolloongabba, QLD, Australia; Menzies Health Institute Queensland, Griffith University, Gold Coast, QLD, Australia. Electronic address: https://twitter.com/@MelissaJBloomer.
- PMID: 38600007
- DOI: 10.1016/j.aucc.2024.02.012
Background: Goal-concordant care in intensive care is care that aligns with the patient's expressed goals, values, preferences and beliefs. Communication and shared decision-making are key to ensuring goal-concordant care.
Aims: The aims of his study were to explore (i) critical care clinicians' perspectives on how patient goals of care were communicated between clinicians, patients, and family in the intensive care unit; (ii) critical care nurses' role in this process; and (iii) how goals of care were used to guide care.
Method: Sequential two-phase qualitative descriptive design. Data were collected from February to June 2022 in a level-3 intensive care unit in a private hospital in Melbourne, Australia. In Phase One, individual interviews were conducted with critical care nurse participants (n = 11). In Phase Two, the findings were presented to senior clinical leaders (n = 2) to build a more comprehensive understanding. Data were analysed using Braun and Clarke's six step reflexive thematic analysis.
Findings: There was poor consensus on the term 'goals of care', with some participants referring to daily treatment goals or treatment limitations and others to patients' wishes and expectations beyond the ICU. Critical care nurses perceived themselves as information brokers and patient advocates responsible for ensuring patient goals of care were respected, but engaging in goals-of-care conversations was challenging. A lack of role clarity, poor team communication, and inadequate processes to communicate patient goals impeded goal-concordant care. Senior clinical leaders affirmed these views, emphasising the need to utilise critical care nurses' insight for practical solutions to improve patient care.
Conclusions: Clarity in both, the term 'goals of care' and the critical care nurses' role in these conversations, are the essential first steps to ensuring patients' values, preferences, and beliefs to guide shared-decision-making and goal-concordant care. Improved verbal and written communication that is inclusive of all members of the treating team is key to addressing these issues.
Keywords: Communication; Critical care; Critical care nursing; Decision making; Goals of care; Intensive care units; Interviews; Nursing; Qualitative research.
Copyright © 2024 Australian College of Critical Care Nurses Ltd. Published by Elsevier Ltd. All rights reserved.
Environmental Qualitative Research at EPA

Oak Ridge Associated Universities
- Posted 5 days ago
- Application deadline: 2024-04-18
As a team member, you will assist in the provision of data collection, transcription, and qualitative analysis services to support social science research. The social science research conducted at the EPA’s Great Lakes Toxicology and Ecology Division (GLTED) utilizes case study methods that apply both theory-testing and theory-building approaches. Data collection methods document the behavior and decisions of different stakeholder groups through participant observation, document analysis, and social media mining. The research goal is to understand the decision-making process and how context shapes behavior and preferences related to the environment.
The team member will also have the opportunity to learn about and contribute to environmental decision-making for a real-world problem revolving around ecological outcomes and socioeconomic benefits of restoration and redevelopment of an urban river through a study of how actors navigate the process. The team member will work with other members of GLTED’s Sustainable and Healthy Communities team to conduct participatory community research. Responsibilities include but are not limited to attending meetings, preparing meeting and/or interview transcripts, coding and analyzing interview data, and assisting in background research, writing, and dissemination of results.
To apply for this job please visit www.zintellect.com .

IMAGES
VIDEO
COMMENTS
Section 1.1: What are the are the main strengths & advantages of qualitative research? Qualitative research uses open -ended questions and probing, which gives participants the opportunity to respond in their own words, rather than forcing them to choose from fixed responses, as quantitative methods do.
The aim is to move beyond the "what" of qualitative research to the "how", by (1) outlining key qualitative research designs for health and social care research - descriptive, phenomenology, action research, case study, ethnography, and grounded theory; (2) a decision tool of how to select the appropriate design based on a guiding ...
Background Although beginning in 2019, it was early in 2020 that the global community began to comprehend the significant impact that a pandemic of a new coronavirus might have on their own lives. This study was undertaken 6-9 months after significant public health restrictions were introduced within Australia and examined the impact of the COVID-19 on individuals' hopes and dreams for ...
Abstract. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions ...
The research described demonstrates the value of applying qualitative methods to the study of AMS implementation across the One Health continuum in Australia and of co-locating researchers in one centre to effectively share learnings. Table 1 summarizes the qualitative research projects undertaken by NCAS researchers and collaborators.
During the course, you'll be led through real-world examples of gathering and analysing qualitative data to better understand the research process. You'll also get to practice your skills by undertaking interviews, focus groups or visual research methods and gain feedback from the ISSR trainers. This course will only proceed if there are 6 ...
The declining wellbeing of Australian teachers is a longstanding problem, with much attention on retention, stress, burnout, and poor resourcing and conditions that impact wellbeing. Additionally, the COVID-19 pandemic has further illuminated these challenges. This qualitative study aimed to explore Australian teachers' perceptions of their wellbeing needs with a focus on asking the ...
Standards for reporting qualitative research: A synthesis of recom-mendations. Acad Med. 2014;89(9):1245-1251. 21. Smith GD, Gelling L, Haigh C, Barnason S, Allan HT, Jackson D. The position of reporting guidelines in qualitative nursing research. J Clin Nurs. 2018;27(5-6):889-891. 22. Bell E. Rethinking quality in qualitative research. Aust J ...
Background: Previous research has demonstrated the importance of search engines, websites, online discussion groups and social media groups for women in developed countries looking for health and medical information, but few studies have focused on Australian women. The Australian Women and Digital Health Project was designed to investigate how Australian women from a range of age groups and ...
Qualitative educational research in Australia has been characterized since the early 1970s by vitality and interest in reconstructing in cultural terms the best research practices, particularly those observed in the UK and USA. The former's influence is best demonstrated in case study method and participatory action research in the 1980s.
Literature. Denzin and Lincoln (2017) argue that qualitative research is currently in a stage of transition; comfortable paradigms are in flux and several accepted methodological conventions overlap and jostle for position among increasing positivist approaches. This postmodern turn has introduced technology to qualitative data management and stimulated debate about how to honour a tradition ...
A qualitative descriptive study exploring clinicians' perspectives of the management of older trauma care in rural Australia. BMC Health Services Research. 2023 Dec;23(1):704. doi: 10.1186/s12913-023-09545-x
Using computer software in qualitative analysis. Day 4. Data analysis: inductive logic, generating meaning. Coding systems and cycles. Thematic analysis. Discourse analysis. Day 5. Writing up: The purpose of qualitative writing. Presenting data: audience and purpose/voice and style. Criteria for assessing good qualitative research. One-on-one ...
An interpretative qualitative study involving in-depth interviews explored the telehealth experiences of specialists, based at a tertiary hospital in the Hunter Region of Australia, and GPs, including barriers, enablers and opportunities. Data were analysed using an inductive thematic approach with constant comparison.
Qualitative Research was established in 2001 by Sara Delamont and Paul Atkinson. The journal was founded to offer a critical and reflective gaze on methodological approaches, understandings and engagements, and worked to counter tendencies that imagined qualitative research could become a taken for granted set of precepts and procedures.
Study design. This study used qualitative pre- and post-intervention data from an evaluation of the batyr@school intervention [] delivered to YP, teachers and parents in drought affected communities in Australia [].Semi-structured interviews (group and individual) were conducted to enable an in-depth exploration of participants' views, experiences and needs about this sensitive topic [29, 30].
In this article, we discuss the current state of psychological research with Indigenous peoples, with a specific focus on research including Aboriginal and Torres Strait Islander peoples of Australia and the Māori people of Aotearoa (New Zealand). We identify how the mental health of Indigenous people is often significantly poorer than non-Indigenous people and could be contributing to the ...
identify criteria by which to assess qualitative studies and apply these criteria in reviewing research; ... who convenes the Qualitative Research Methods course in the face-to-face mode, speaks about her experiences and expertise in qualitative research. ... Sydney NSW 2052 Australia Telephone: +61 2 93851000. UNSW CRICOS Provider Code: 00098G
Traditional qualitative inquiry research methods exhort us to look for the 'good' story tellers who use metaphors to describe their experiences, emotions, and events. ... The Australian study of 18 deafblind participants with wide ranging communication needs, shared in-depth narrative inquiry stories told in: 'snapshots' of moments of ...
This paper is designed to provide Indigenous and nonindigenous people working in research with some practical advice on how to improve the research experience for Indigenous people and how to develop culturally appropriate research methodologies. The paper proposes that qualitative research methods are practical, useful, beneficial and ...
1. Introduction. This report documents the background, methodology and findings from the Access to Early Childhood Education (AECE): Qualitative Study, undertaken by the Australian Institute of Family Studies (AIFS) and commissioned by the then Department of Education, Employment and Workplace Relations (DEEWR; now the Department of Education) on behalf of the Early Childhood Data Subgroup ...
Qualitative research involves collecting and analyzing non-numerical data (e.g., text, video, or audio) to understand concepts, opinions, or experiences. It can be used to gather in-depth insights into a problem or generate new ideas for research. Qualitative research is the opposite of quantitative research, which involves collecting and ...
Conversely, in our recent qualitative research addressing communication about sexuality with young people with cerebral palsy who use communication methods other than speech (augmentative and alternative communication), we found that constructive collaboration between researchers and committee members yielded novel insights. ... Insights from ...
The methodological quality of the quantitative study components was appraised using the Dictionary for Effective Public Health Practice Project Quality Assessment tool for Quantitative studies , which was developed to review public health studies and has been used in other systematic reviews in the Australian Indigenous health field [4, 10 ...
2.1 Study Design and Recruitment. This multi-country study adopted a qualitative approach using semi-structured, one-to-one telephone interviews conducted with 50 adult volunteers including patients with MPM (n = 26), current caregivers of patients with MPM (n = 20), and individuals that provided care for a person diagnosed with MPM who had died over 6 months and less than 2 years ago ...
Background: Goal-concordant care in intensive care is care that aligns with the patient's expressed goals, values, preferences and beliefs. Communication and shared decision-making are key to ensuring goal-concordant care. Aims: The aims of his study were to explore (i) critical care clinicians' perspectives on how patient goals of care were communicated between clinicians, patients, and ...
Application deadline: 2024-04-18. As a team member, you will assist in the provision of data collection, transcription, and qualitative analysis services to support social science research. The social science research conducted at the EPA's Great Lakes Toxicology and Ecology Division (GLTED) utilizes case study methods that apply both theory ...