- Open access
- Published: 26 August 2020

Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis
- Cassie M. Hazell ORCID: orcid.org/0000-0001-5868-9902 1 ,
- Laura Chapman 2 ,
- Sophie F. Valeix 3 ,
- Paul Roberts 4 ,
- Jeremy E. Niven 5 &
- Clio Berry 6
Systematic Reviews volume 9 , Article number: 197 ( 2020 ) Cite this article
13k Accesses
58 Citations
81 Altmetric
Metrics details
Data from studies with undergraduate and postgraduate taught students suggest that they are at an increased risk of having mental health problems, compared to the general population. By contrast, the literature on doctoral researchers (DRs) is far more disparate and unclear. There is a need to bring together current findings and identify what questions still need to be answered.
We conducted a mixed methods systematic review to summarise the research on doctoral researchers’ (DRs) mental health. Our search revealed 52 articles that were included in this review.
The results of our meta-analysis found that DRs reported significantly higher stress levels compared with population norm data. Using meta-analyses and meta-synthesis techniques, we found the risk factors with the strongest evidence base were isolation and identifying as female. Social support, viewing the PhD as a process, a positive student-supervisor relationship and engaging in self-care were the most well-established protective factors.
Conclusions
We have identified a critical need for researchers to better coordinate data collection to aid future reviews and allow for clinically meaningful conclusions to be drawn.
Systematic review registration
PROSPERO registration CRD42018092867
Peer Review reports
Student mental health has become a regular feature across media outlets in the United Kingdom (UK), with frequent warnings in the media that the sector is facing a ‘mental health crisis’ [ 1 ]. These claims are largely based on the work of regulatory authorities and ‘grey’ literature. Such sources corroborate an increase in the prevalence of mental health difficulties amongst students. In 2013, 1 in 5 students reported having a mental health problem [ 2 ]. Only 3 years later, however, this figure increased to 1 in 4 [ 3 ]. In real terms, this equates to 21,435 students disclosing mental health problems in 2013 rising to 49,265 in 2017 [ 4 ]. Data from the Higher Education Statistics Agency (HESA) demonstrates a 210% increase in the number of students terminating their studies reportedly due to poor mental health [ 5 ], while the number of students dying by suicide has consistently increased in the past decade [ 6 ].
This issue is not isolated to the UK. In the United States (US), the prevalence of student mental health problems and use of counselling services has steadily risen over the past 6 years [ 7 ]. A large international survey of more than 14,000 students across 8 countries (Australia, Belgium, Germany, Mexico, Northern Ireland, South Africa, Spain and the United States) found that 35% of students met the diagnostic criteria for at least one common mental health condition, with highest rates found in Australia and Germany [ 8 ].
The above figures all pertain to undergraduate students. Finding equivalent information for postgraduate students is more difficult, and where available tends to combine data for postgraduate taught students and doctoral researchers (DRs; also known as PhD students or postgraduate researchers) (e.g. [ 4 ]). The latest trend analysis based on data from 36 countries suggests that approximately 2.3% of people will enrol in a PhD programme during their lifetime [ 9 ]. The countries with the highest number of DRs are the US, Germany and the UK [ 10 ]. At present, there are more than 281,360 DRs currently registered across these three countries alone [ 11 , 12 ], making them a significant part of the university population. The aim of this systematic review is to bring attention specifically to the mental health of DRs by summarising the available evidence on this issue.
Using a mixed methods approach, including meta-analysis and meta-synthesis, this review seeks to answer three research questions: (1) What is the prevalence of mental health difficulties amongst DRs? (2) What are the risk factors associated with poor mental health in DRs? And (3) what are the protective factors associated with good mental health in DRs?
Literature search
We conducted a search of the titles and abstracts of all article types within the following databases: AMED, BNI, CINAHL, Embase, HBE, HMIC, Medline, PsycInfo, PubMed, Scopus and Web of Science. The same search terms were used within all of the databases, and the search was completed on the 13th April 2018. Our search terms were selected to capture the variable terms used to describe DRs, as well as the terms used to describe mental health, mental health problems and related constructs. We also reviewed the reference lists of all the papers included in this review. Full details of the search strategy are provided in the supplementary material .
Inclusion criteria
Articles meeting the following criteria were considered eligible for inclusion: (1) the full text was available in English; (2) the article presented empirical data; (3) all study participants, or a clearly delineated sub-set, were studying at the doctoral level for a research degree (DRs or equivalent); and (4) the data collected related to mental health constructs. The last of these criteria was operationalised (a) for quantitative studies as having at least one mental health-related outcome measure, and (b) for qualitative studies as having a discussion guide that included questions related to mental health. We included university-published theses and dissertations as these are subjected to a minimum level of peer-review by examiners.
Exclusion criteria
In order to reduce heterogeneity and focus the review on doctoral research as opposed to practice-based training, we excluded articles where participants were studying at the doctoral level, but their training did not focus on research (e.g. PsyD doctorate in Clinical Psychology).
Screening articles
Papers were screened by one of the present authors at the level of title, then abstract, and finally at full text (Fig. 1 ). Duplicates were removed after screening at abstract. At each level of screening, a random 20% sub-set of articles were double screened by another author, and levels of agreement were calculated (Cohen’s kappa [ 13 ]). Where disagreements occurred between authors, a third author was consulted to decide whether the paper should or should not be included. All kappa values evidence at least moderate agreement between authors [ 14 ]—see Fig. 1 for exact kappa values.
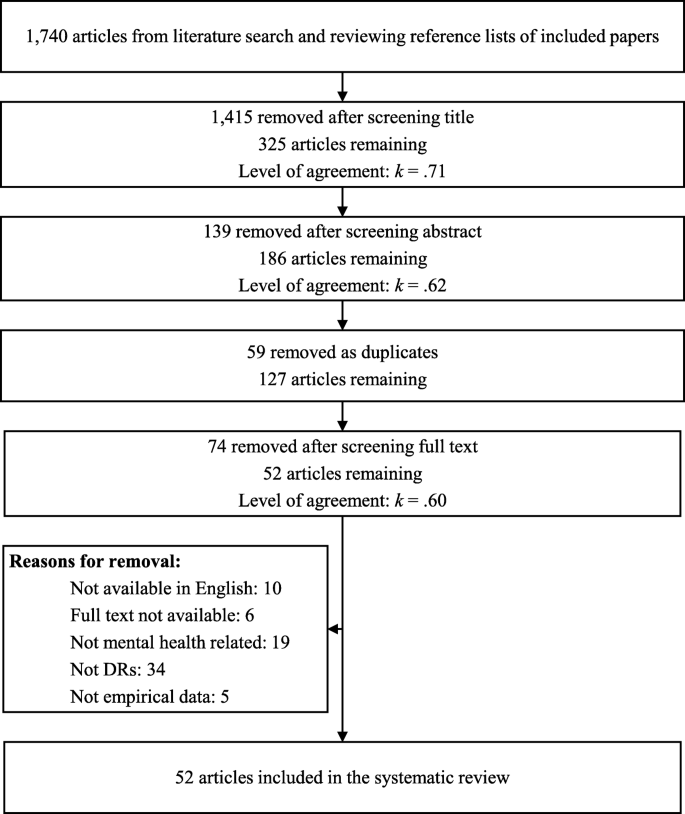
PRISMA diagram of literature review process
Data extraction
This review reports on both quantitative and qualitative findings, and separate extraction methods were used for each. Data extraction was performed by authors CH, CB, SV and LC.
Quantitative data extraction
The articles in this review used varying methods and measures. To accommodate this heterogeneity, multiple approaches were used to extract quantitative data. Where available, we extracted (a) descriptive statistics, (b) correlations and (c) a list of key findings. For all mental health outcome measures, we extracted the means and standard deviations for the DR participants, and where available for the control group (descriptive statistics). For studies utilising a within-subjects study design, we extracted data where a mental health outcome measure was correlated with another construct (correlations). Finally, to ensure that we did not lose important findings that did not use descriptive statistics or correlations, we extracted the key findings from the results sections of each paper (list of key findings). Key findings were identified as any type of statistical analysis that included at least one mental health outcome.
Qualitative data extraction
In line with the meta-ethnographic method [ 15 ] and our interest in the empirical data as well as the authors’ interpretations thereof, i.e. the findings of each article [ 16 ], the data extracted from the articles comprised both results/findings and discussion/conclusion sections. For articles reporting qualitative findings, we extracted the results and discussion sections from articles verbatim. Where articles used mixed methods, only the qualitative section of the results was extracted. Methodological and setting details from each article were also extracted and provided (see Appendix A) in order to contextualise the studies.
Data analysis
Quantitative data analysis, descriptive statistics.
We present frequencies and percentages of the constructs measured, the tools used and whether basic descriptive statistics ( M and SD ) were reported. The full data file is available from the first author upon request.
Effect sizes
Where studies had a control group, we calculated a between-group effect size (Cohen’s d ) using the formula reported by Wilson [ 17 ], and interpreted using the standard criteria [ 13 ]. For all other studies, we sought to compare results with normative data where the following criteria were satisfied: (a) at least three studies reported data using the same mental health assessment tool; (b) empirical normative data were available; and (c) the scale mean/total had been calculated following original authors’ instructions. Only the Perceived Stress Scale (PSS) 10- [ 18 ] and 14-item versions [ 19 ] met these criteria. Normative data were available from a sample of adults living in the United States: collected in 2009 for the 10-item version ( n = 2000; M = 15.21; SD = 7.28) [ 20 ] and in 1983 for the 14-item version ( n = 2355; M = 19.62; SD = 7.49) [ 18 ].
The meta-analysis of PSS data was conducted using MedCalc [ 21 ], and based on a random effects model, as recommended by [ 22 ]. The between-group effect sizes (DRs versus US norms) were calculated comparing PSS means and standard deviations in the respective groups. The effect sizes were weighted using the variable variances [ 23 ].
Correlations
Where at least three studies reported data reflecting a bivariate association between a mental health and another variable, we summarised this data into a meta-analysis using the reported r coefficients and sample sizes. Again, we used MedCalc [ 21 ] to conduct the analysis using a random effects model, based on the procedure outlined by Borenstein, Hedges, Higgins and Rothstein [ 24 ]. This analysis approach involves converting correlation coefficients into Fisher’s z values [ 25 ], calculating the summary of Fisher’s z , and then converting this to a summary correlation coefficient ( r ). The effect sizes were weighted in line with the Hedges and Ollkin [ 23 ] method. Heterogeneity was assessed using the Q statistic, and I 2 value—both were interpreted according to the GRADE criteria [ 26 ]. Where correlations could not be summarised within a meta-analysis, we have reported these descriptively.
Due to the heterogenous nature of the studies, the above methods could not capture all of the quantitative data. Therefore, additional data (e.g. frequencies, statistical tests) reported in the identified articles was collated into a single document, coded as relating to prevalence, risk or protective factors and reported as a narrative review.
Qualitative data analysis
We used thematic analytic methods to analyse the qualitative data. We followed the thematic synthesis method [ 16 , 27 ] and were informed by a thematic analysis approach [ 28 , 29 ]. We took a critical realist epistemological stance [ 30 , 31 ] and aimed to bring together an analysis reflecting meaningful patterns amongst the data [ 29 ] or demi-regularities, and identifying potential social mechanisms that might influence the experience of such phenomena [ 31 ]. The focus of the meta-synthesis is interpretative rather than aggregative [ 32 ].
Coding was line by line, open and complete. Following line-by-line coding of all articles, a thematic map was created. Codes were entered on an article-by-article basis and then grouped and re-grouped into meaningful patterns. Comparisons were made across studies to attempt to identify demi-regularities or patterns and contradictions or points of departure. The thematic map was reviewed in consultation with other authors to inductively create and refine themes. Thematic summaries were created and brought together into a first draft of the thematic structure. At this point, each theme was compared against the line-by-line codes and the original articles in order to check its fit and to populate the written account with illustrative quotations.
Research rigour
The qualitative analysis was informed by independent coding by authors CB and SV, and analytic discussions with CH, SV and LC. Our objective was not to capture or achieve inter-rater reliability, rather the analysis was strengthened through involvement of authors from diverse backgrounds including past and recent PhD completion, experiences of mental health problems during PhD completion, PhD supervision experience, experience as employees in a UK university doctoral school and different nationalities. In order to enhance reflexivity, CB used a journal throughout the analytic process to help notice and bracket personal reflections on the data and the ways in which these personal reflections might impact on the interpretation [ 29 , 33 ]. The ENTREQ checklist [ 34 ] was consulted in the preparation of this report to improve the quality of reporting.
Quality assessment
Quantitative data.
The quality of the quantitative papers was assessed using the STROBE combined checklist [ 35 ]. A random 20% sub-sample of these studies were double-coded and inter-rater agreement was 0.70, indicating ‘substantial’ agreement [ 14 ]. The maximum possible quality score was 23, with a higher score indicating greater quality, with the mean average of 15.97, and a range from 0 to 22. The most frequently low-scoring criteria were incomplete reporting regarding the management of missing data, and lack of reported efforts to address potential causes of bias.
Qualitative data
There appeared to be no discernible pattern in the perceived quality of studies; the highest [ 36 , 37 , 38 , 39 , 40 ] and lowest scoring [ 41 , 42 , 43 , 44 , 45 , 46 ] studies reflected both theses and journal publications, a variety of locations and settings and different methodologies. The most frequent low-scoring criteria were relating to the authors’ positions and reflections thereof (i.e. ‘Qualitative approach and research paradigm’, ‘Researcher characteristics and reflexivity’, ‘Techniques to enhance trustworthiness’, ‘Limitations’, ‘Conflict of interest and Funding’). Discussions of ethical issues and approval processes was also frequently absent. We identified that we foregrounded higher quality studies in our synthesis in that these studies appeared to have greater contributions reflected in the shape and content of the themes developed and were more likely to be the sources of the selected illustrative quotes.
Mixed methods approach
The goal of this review is to answer the review questions by synthesising the findings from both quantitative and/or qualitative studies. To achieve our goal, we adopted an integrated approach [ 47 ], whereby we used both quantitative and qualitative methods to answer the same review question, and draw a synthesised conclusion. Different analysis approaches were used for the quantitative and qualitative data and are therefore initially reported separately within the methods. A separate synthesised summary of the findings is then provided.
Overview of literature
Of the 52 papers included in this review (Table 1 ), 7 were qualitative, 29 were quantitative and 16 mixed methods. Most articles (35) were peer-reviewed papers, and the minority were theses (17). Only four of the articles included a control group; in three instances comprising students (but not DRs) and in the other drawn from the general population.
Quantitative results
Thirty-five papers reported quantitative data, providing 52 reported sets of mental health related data (an average of 1.49 measures per study): 24 (68.57%) measured stress, 10 (28.57%) anxiety, 9 (25.71%) general wellbeing, 5 (14.29%) social support, 3 (8.57%) depression and 1 (2.86%) self-esteem. Five studies (9.62%) used an unvalidated scale created for the purposes of the study. Fifteen studies (28.85%) did not report descriptive statistics.
Of the four studies that included a control group, only two of these reported descriptive statistics for both groups on a mental health outcome [ 66 , 69 ]. There is a small (Cohen’s d = 0.27) and large between-group effect (Cohen’s d = 1.15) when DRs were compared to undergraduate and postgraduate clinical psychology students respectively in terms of self-reported stress.
The meta-analysis of DR scores on the PSS (both 10- and 14-item versions) compared to population normative data produced a large and significant between-group effect size ( d = 1.12, 95% CI [0.52, 1.73]) in favour of DRs scoring higher on the PSS than the general population (Fig. 2 ), suggesting DRs experience significantly elevated stress. However, these findings should be interpreted in light of the significant between-study heterogeneity that can be classified as ‘considerable’ [ 26 ].
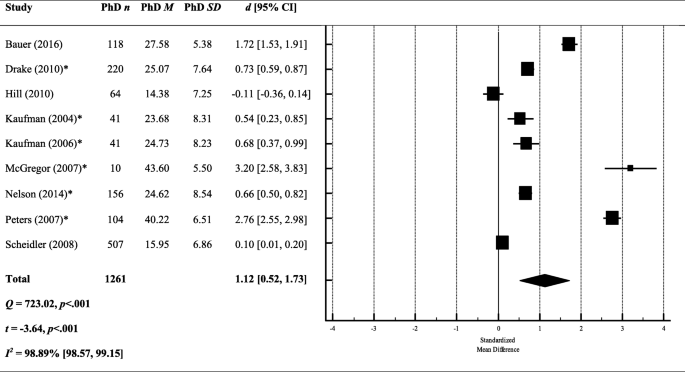
A meta-analysis of between-group effect sizes (Cohen’s d ) comparing PSS scores (both 10- and 14-item versions) from DRs and normative population data. *Studies using the 14 item version of the PSS; a positive effect size indicates DRs had a higher score on the PSS; a negative effect size indicates that the normative data produced a higher score on the PSS; black diamond = total effect size (based on random effects model); d = Cohen’s d ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
To explore this heterogeneity, we re-ran the meta-analysis separately for the 10- and 14-item versions. The effect size remained large and significant when looking only at the studies using the 14-item version ( k = 6; d = 1.41, 95% CI [0.63, 2.19]), but was reduced and no longer significant when looking at the 10-item version only ( k = 3; d = 0.57, 95% CI [− 0.51, 1.64]). However, both effect sizes were still marred by significant heterogeneity between studies (10-item: Q = 232.02, p < .001; 14-item: Q = 356.76, p < .001).
Studies reported sufficient correlations for two separate meta-analyses; the first assessing the relationship between stress (PSS [ 18 , 19 ]) and perceived support, and the second between stress (PSS) and academic performance.
Stress x support
We included all measures related to support irrespective of whom that support came from (e.g. partner support, peer support, mentor support). The overall effect size suggests a small and significant negative correlation between stress and support ( r = − .24, 95% CI [− 0.34, − 0.13]) (see Fig. 3 ), meaning that low support is associated with greater perceived stress. However, the results should be interpreted in light of the significant heterogeneity between studies. The I 2 value quantifies this heterogeneity as almost 90% of the variance being explained by between-study heterogeneity, which is classified as ‘substantial’ (26).
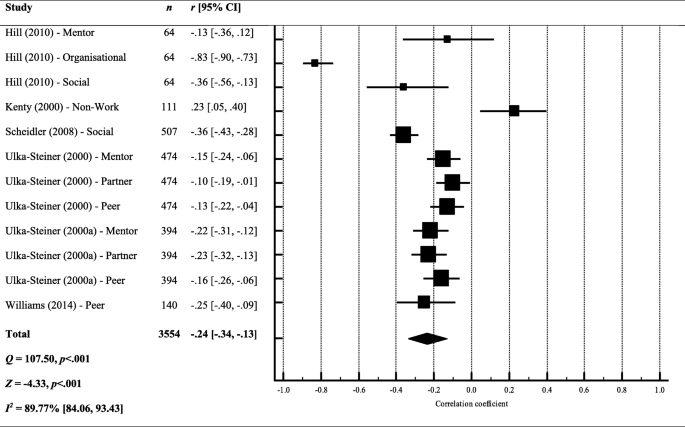
Forest plot and meta-analysis of correlation coefficients testing the relationship between stress and perceived support. Black diamond = total effect size (based on random effects model); r = Pearson’s r ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
Stress x performance
The overall effect size suggests that there is no relationship between stress and performance in their studies ( r = − .07, 95% CI [− 0.19, 0.05]) (see Fig. 4 ), meaning that DRs perception of their progress was not associated with their perceived stress This finding suggests that the amount of progress that DRs were making during their studies was not associated with stress levels.
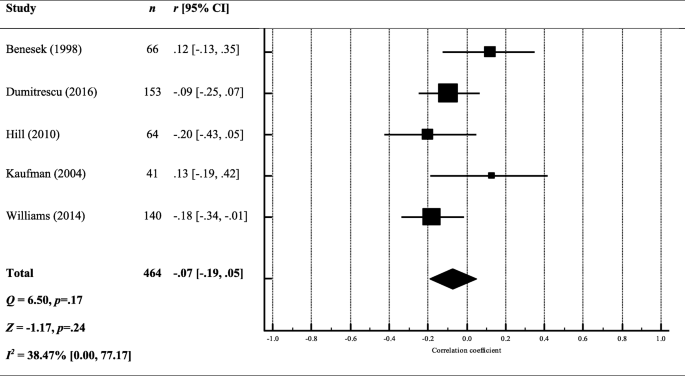
Forest plot and meta-analysis of correlation coefficients testing the relationship between stress and performance. Black diamond = total effect size (based on random effects model); r = Pearson’s r ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
Other correlations
Correlations reported in less than three studies are summarised in Fig. 5 . Again, stress was the most commonly tested mental health variable. Self-care and positive feelings towards the thesis were consistently found to negatively correlate with mental health constructs. Negative writing habits (e.g. perfectionism, blocks and procrastination) were consistently found to positively correlate with mental health constructs. The strongest correlations were found between stress, and health related quality of life ( r = − .62) or neuroticism ( r = .59), meaning that lower stress was associated with greater quality of life and reduced neuroticism. The weakest relationships ( r < .10) were found between mental health outcomes and: faculty concern, writing as knowledge transformation, innate writing ability (stress and anxiety), years married, locus of control, number of children and openness (stress only).
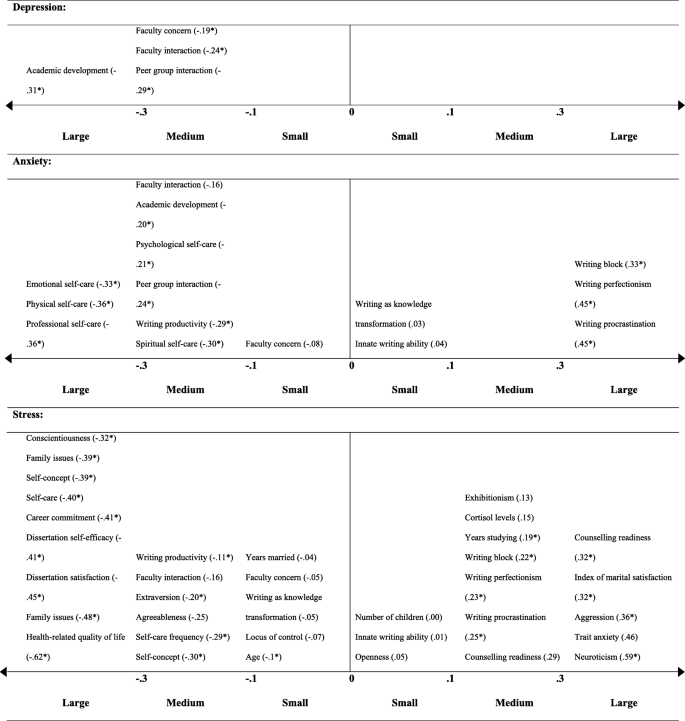
Correlation coefficients testing the relationship between a mental health outcome and other construct. Correlation coefficients are given in brackets ( r ); * p < .05; each correlation coefficient reflects the results from a single study
Several studies reported DR mental health problem prevalence and this ranged from 36.30% [ 54 ] to 55.9% [ 67 ]. Using clinical cut-offs, 32% were experiencing a common psychiatric disorder [ 64 ]; with another study finding that 53.7% met the questionnaire cut-off criteria for depression, and 41.9% for anxiety [ 67 ]. One study compared prevalence amongst DRs and the general population, employees and other higher education students; in all instances, DRs had higher levels of psychological distress (non-clinical), and met criteria for a clinical psychiatric disorder more frequently [ 64 ].
Risk factors
Demographics Two studies reported no significant difference between males and females in terms of reported stress [ 57 , 73 ], but the majority suggested female DRs report greater clinical [ 80 ], and non-clinical problems with their mental health [ 37 , 64 , 79 , 83 , 89 ].
Several studies explored how mental health difficulties differed in relation to demographic variables other than gender, suggesting that being single or not having children was associated with poorer mental health [ 64 ] as was a lower socioeconomic status [ 71 ]. One study found that mental health difficulties did not differ depending on DRs’ ethnicity [ 51 ], but another found that Black students attending ‘historically Black universities’ were significantly more anxious [ 87 ]. The majority of the studies were conducted in the US, but only one study tested for cross-cultural differences: reporting that DRs in France were more psychologically distressed than those studying in the UK [ 67 ].
Work-life balance Year of study did not appear to be associated with greater subjective stress in a study involving clinical psychology DRs (Platt and Schaefer [ 75 ]), although other studies suggested greater stress reported by those in the latter part of their studies [ 89 ], who viewed their studies as a burden [ 81 ], or had external contracts, i.e. not employed by their university [ 85 ]. Regression analyses revealed that a common predictor of poor mental health was uncertainty in DR studies; whether in relation to uncertain funding [ 64 ] or uncertain progress [ 80 ]. More than two-thirds of DRs reported general academic pressure as a cause of stress, and a lack of time as preventing them from looking after themselves [ 58 ]. Being isolated was also a strong predictor of stress [ 84 ].
Protective factors
DRs who more strongly endorsed all of the five-factor personality traits (openness, conscientiousness, extraversion, agreeableness and neuroticism) [ 66 ], self-reported higher academic achievement [ 40 ] and viewed their studies as a learning process (rather than a means to an end) [ 82 ] reported fewer mental health problems. DRs were able to mitigate poor mental health by engaging in self-care [ 72 ], having a supervisor with an inspirational leadership style [ 64 ] and building coping strategies [ 56 ]. The most frequently reported coping strategy was seeking support from other people [ 37 , 58 ].
Qualitative results
Meta-synthesis.
Four higher-order themes were identified: (1) Always alone in the struggle, (2) Death of personhood, (3) The system is sick and (4) Seeing, being and becoming. The first two themes reflect individual risk/vulnerability factors and the processes implicated in the experience of mental distress, the third represents systemic risk and vulnerability factors and the final theme reflects individual and systemic protective mechanisms and transformative influences. See Table 2 for details of the full thematic structure with illustrative quotes.
Always alone in the struggle
‘Always alone in the struggle’ reflects the isolated nature of the PhD experience. Two subthemes reflect different aspects of being alone; ‘Invisible, isolated and abandoned’ represents DRs’ sense of physical and psychological separation from others and ‘It’s not you, it’s me’ represents DRs’ sense of being solely responsible for their PhD process and experience.
Invisible, isolated and abandoned
Feeling invisible and isolated both within and outside of the academic environment appears a core DR experience [ 39 , 43 , 81 ]. Isolation from academic peers seemed especially salient for DRs with less of a physical presence on campus, e.g. part-time and distance students, those engaging in extensive fieldwork, outside employment and those with no peer research or lab group [ 36 , 52 , 68 ]. Where DRs reported relationships with DR peers, these were characterised as low quality or ‘not proper friendships’ and this appeared linked to a sense of essential and obvious competition amongst DRs with respect to current and future resources, support and opportunities [ 39 ], in which a minority of individuals were seen to receive the majority share [ 36 , 74 ]. Intimate sharing with peers thus appeared to feel unsafe. This reflected the competitive environment but also a sense of peer relationships being predicated on too shared an experience [ 39 ].
In addition to poor peer relations, a mismatch between the expected and observed depth of supervisor interest, engagement and was evident [ 40 , 81 ]. This mismatch was clearly associated with disappointment and anger, and a sense of abandonment, which appeared to impact negatively on DR mental health and wellbeing [ 42 ] (p. 182). Moreover, DRs perceived academic departments as complicit in their isolation; failing to offer adequate opportunities for academic and social belonging and connections [ 42 , 81 ] and including PGRs only in a fleeting or ‘hollow’ sense [ 37 ]. DRs identified this isolation as sending a broader message about academia as a solitary and unsupported pursuit; a message that could lead some DRs to self-select out of planning for future in academia [ 37 , 42 ]. DRs appeared to make sense of their lack of belonging in their department as related to their sense of being different, and that this difference might suggest they did not ‘fit in’ with academia more broadly [ 74 ]. In the short-term, DRs might expend more effort to try and achieve a social and/or professional connection and equitable access to support, opportunities and resources [ 74 ]. However, over the longer-term, the continuing perception of being professionally ‘other’ also seemed to undermine DRs’ sense of meaning and purpose [ 81 ] and could lead to opting out of an academic career [ 62 , 74 ].
Isolation within the PhD was compounded by isolation from one’s personal relationships. This personal isolation was first physical, in which the laborious nature of the PhD acted as a catalyst for the breakdown of pre-existing relationships [ 76 ]. Moreover, DRs also experienced a sense of psychological detachment [ 45 , 74 ]. Thus, the experience of isolation appeared to be extremely pervasive, with DRs feeling excluded and isolated physically and psychologically and across both their professional and personal lives.
It’s not you, it’s me
‘It’s not you, it’s me’ reflects DRs’ perfectionism as a central challenge of their PhD experience and a contributor to their sense of psychological isolation from other people. DRs’ perfectionism manifested in four key ways; firstly, in the overwhelming sense of responsibility experienced by DRs; secondly, in the tendency to position themselves as inadequate and inferior; thirdly, in cycles of perfectionist paralysis; and finally, in the tendency to find evidence which confirms their assumed inferiority.
DRs positioned themselves as solely responsible for their PhD and for the creation of a positive relationship with their supervisor [ 36 , 52 , 81 ]. DRs expressed a perceived need to capture their supervisors’ interest and attention [ 36 , 52 , 74 ], feeling that they needed to identify and sell to their supervisors some shared characteristic or interest in order to scaffold a meaningful relationship. DRs appeared to feel it necessary to assume sole responsibility for their personal lives and to prohibit any intrusion of the personal in to the professional, even in incredibly distressing circumstances [ 42 ].
DRs appeared to compare themselves against an ideal or archetypal DR and this comparison was typically unfavourable [ 37 ], with DRs contrasting the expected ideal self with their actual imperfect and fallible self [ 37 , 42 , 52 ]. DRs’ sense of inadequacy appeared acutely and frequently reflected back to them by supervisors in the form of negative or seemingly disdainful feedback and interactions [ 41 , 76 ]. DRs framed negative supervisor responses as a cue to work harder, meaning they were continually striving, but never reaching, the DR ideal [ 76 ]. This ideal-actual self-discrepancy was associated with a tendency towards punitive self-talk with clear negative valence [ 38 ].
DRs appear to commonly use self-castigation as a necessary (albeit insufficient) means to motivate themselves to improve their performance in line with perfectionistic standards [ 38 , 41 ]. The oscillation between expectation and actuality ultimately resulted in increased stress and anxiety and reduced enjoyment and motivation. Low motivation and enjoyment appeared to cause procrastination and avoidance, which lead to a greater discrepancy between the ideal and actual self; in turn, this caused more stress and anxiety and further reduced enjoyment and motivation leading to a sense of stuckness [ 76 ].
The internalisation of perceived failure was such that DRs appeared to make sense of their place, progress and possible futures through a lens of inferiority, for example, positioning themselves as less talented and successful compared to their peers [ 37 ]. Thus, instances such as not being offered a job, not receiving funding, not feeling connected to supervisors, feeling excluded by academics and peers were all made sense of in relation to DRs’ perceived relative inadequacy [ 36 ].
Death of personhood
The higher-order theme ‘Death of personhood’ reflects DRs’ identity conflict during the PhD process; a sense that DRs’ engage in a ‘Sacrifice of personal identity’ in which they feel they must give up their pre-existing self-identity, begin to conceive of themselves as purely ‘takers’ personally and professionally, thus experiencing the ‘Self as parasitic’, and ultimately experience a ‘Death of self-agency’ in relation to the thesis, the supervisor and other life roles and activities.
A sacrifice of personal identity
The sacrifice of personal identity first manifests as an enmeshment with the PhD and consequent diminishment of other roles, relationships and activities that once were integral to the DRs’ sense of self [ 59 , 76 ]. DRs tended to prioritise PhD activities to the extent that they engaged in behaviours that were potentially damaging to their personal relationships [ 76 ]. DRs reported a sense of never being truly free; almost physically burdened by the weight of their PhD and carrying with them a constant ambient guilt [ 37 , 38 , 44 , 76 ]. Time spent on non-PhD activities was positioned as selfish or indulgent, even very basic activities of living [ 76 ].
The seeming incompatibility of aspects of prior personal identity and the PhD appears to result in a sense of internal conflict or identity ‘collision’ [ 59 ]. Friends and relatives often provided an uncomfortable reflection of the DR’s changing identity, leaving DRs feeling hyper-visible and carrying the burden of intellect or trailblazer status [ 74 ]; providing further evidence for the incompatibility of their personal and current and future professional identities. Some DRs more purposefully pruned their relationships and social activities; to avoid identity dissonance, to conserve precious time and energy for their PhD work, or as an acceptance of total enmeshment with academic work as necessary (although not necessarily sufficient) for successful continuation in academia [ 40 , 52 , 77 ]. Nevertheless, the diminishment of the personal identity did not appear balanced by the development of a positive professional identity. The professional DR identity was perceived as unclear and confusing, and the adoption of an academic identity appeared to require DRs to have a greater degree of self-assurance or self-belief than was often the case [ 37 , 81 ].
Self as parasitic
Another change in identity manifested as DRs beginning to conceive of themselves as parasitic. DRs spoke of becoming ‘takers’, feeling that they were unable to provide or give anything to anyone. For some DRs, being ‘parasitic’ reflected them being on the bottom rung of the professional ladder or the ‘bottom of the pile’; thus, professionally only able to receive support and assistance rather than to provide for others. Other DRs reported more purposefully withdrawing from activities in which they were a ‘giver’, for example voluntary work, as providing or caring for others required time or energy that they no longer had [ 38 , 44 ]. Furthermore, DRs appeared to conceive of themselves as also causing difficulty or harm to others [ 81 ], as problems in relation to their PhD could lead them to unwillingly punishing close others, for example, through reducing the duration or quality of time spent together [ 38 ].
Feeling that close others were offering support appeared to heighten the awareness of the toll of the PhD on the individual and their close relationships, emphasising the huge undertaking and the often seemingly slow progress, and actually contributing to the sense of ambient guilt, shame, anger and failure [ 38 ]. Moreover, DRs spoke of feeling extreme guilt in perceiving that they had possibly sacrificed their own, and possibly family members’, current wellbeing and future financial security [ 49 ].
Death of self-agency
In addition to their sense of having to sacrifice their personal identity, DRs also expressed a loss of their sense of themselves as agentic beings. DRs expressed feeling powerless in various domains of their lives. First, DRs positioned the thesis as a powerful force able to overwhelm or swallow them [ 46 , 52 , 59 ]. Secondly, DRs expressed a sense of futility in trying to retain any sense of personal power in the climate of academia. An acute feeling of powerlessness especially in relation to supervisors was evident, with many examples provided of being treated as means to an end, as opposed to ends in themselves [ 39 , 42 , 62 ]. Supervisors did not interact with DRs in a holistic way that recognised their personhood and instead were perceived as prioritising their own will, or the will of other academics, above that of the DR [ 39 , 62 ].
Furthermore, DRs reported feeling as if they were used as a means for research production or furthering their supervisors’ reputations or careers [ 62 ]. DRs perceived that holding on to a sense of personal agency sometimes felt incompatible with having a positive supervisor relationship [ 42 ]. Thus whilst emotional distress, anger, disappointment, sadness, jealousy and resentment were clearly evident in relation to feeling excluded, used or over-powered by supervisors [ 37 , 42 , 52 , 62 ], DRs usually felt unable to change supervisor irrespective of how seriously this relationship had degraded [ 37 , 62 ]. Instead, DRs appeared to take on a position of resignation or defensive pessimism, in which they perceived their supervisors as thwarting their personhood, personal goals and preferences, but typically felt compelled to accept this as the status quo and focus on finishing their PhDs [ 42 ]. DRs resignation was such that they internalised this culture of silence and silenced themselves; tending to share litanies of problems with supervisors whilst prefacing or ending the statements with some contradictory or undermining phrase such as ‘but that’s okay’ [ 42 , 52 ].
The apparent lack of self-agency extended outward from the PhD into DRs not feeling able to curate positive life circumstances more generally [ 76 ]. A lack of time was perhaps the key struggle across both personal and professional domains, yet DRs paradoxically reported spending a lot of time procrastinating and rarely (if ever) mentioned time management as a necessary or desired coping strategy for the problem of having too little time [ 46 ]. The lack of self-agency was not only current but also felt in reference to a bleak and uncertain future; DRs lack of surety in a future in academia and the resultant sense of futility further undermined their motivation to engage currently with PhD tasks [ 38 , 40 ].
The system is sick
The higher-order theme ‘The system is sick’ represents systemic influences on DR mental health. First, ‘Most everyone’s mad here’ reflects the perceived ubiquity mental health problems amongst DRs. ‘Emperor’s new clothes’ reflects the DR experience of engaging in a performative piece in which they attempt to live in accordance with systemic rather than personal values. Finally, ‘Beware the invisible and visible walls’ reflects concerns with being caught between ephemeral but very real institutional divides.
Most everyone’s mad here
No studies focused explicitly on experiences of DRs who had been given diagnoses of mental health problems. Some study participants self-disclosed mental health problems and emphasised their pervasive impact [ 50 ]. Further lived experiences of mental distress in the absence of explicit disclosure were also clearly identifiable. The ‘typical’ presentation of DRs with respect to mental health appeared characterised as almost unanimous [ 39 ] accounts of chronic stress, anxiety and depression, emotional distress including frustration, anger and irritability, lack of mental and physical energy, somatic problems including appetite problems, headaches, physical pain, nausea and problems with drug and alcohol abuse [ 39 , 46 , 59 , 76 ]. Health anxiety, concerns regarding perceived new and unusual bodily sensations and perceived risks of developing stress-related illnesses were also common [ 46 , 59 , 76 ]. A PhD-specific numbness and hypervigilance was also reported, in which DRs might be less responsive to personal life stressors but develop an extreme sensitivity and reactivity to PhD-relevant stimuli [ 39 ].
An interplay of trait and state factors were suggested to underlie the perceived ubiquity of mental health problems amongst DRs. Etiological factors associated with undertaking a PhD specifically included the high workload, high academic standards, competing personal and professional demands, social isolation, poor resources in the university, poor living conditions and poverty, future and career uncertainty [ 36 , 41 , 43 , 46 , 49 , 76 ]. The ‘nexus’ of these factors was such that the PhD itself acted as a crucible; a process of such intensity that developing mental health problems was perhaps inevitable [ 39 ].
The perceived inevitability of mental health problems was such that DRs described people who did not experience mental health problems during a PhD as ‘lucky’ [ 39 ]. Supervisors and the wider academic system were seen to promote an expectation of suffering, for example, with academics reportedly normalising drug and alcohol problems and encouraging unhealthy working practices [ 39 ]. Furthermore, DRs felt that academics were uncaring with respect to the mental challenge of doing a PhD [ 39 ]. Nevertheless, academics were suggested to deny any culpability or accountability for mental health problems amongst DRs [ 39 , 59 , 74 ]. The cycle of indigenousness was further maintained by a lack of mental health literacy and issues with awareness, availability and access to help-seeking and treatment options amongst DRs and academics more widely [ 39 ]. Thus, DRs appeared to feel they were being let down by a system that was almost set up to cause mental distress, but within which there was a widespread denial of the size and scope of the problem and little effort put into identifying and providing solutions [ 39 , 59 ]. DRs ultimately felt that the systemic encouragement of unhealthy lifestyles in pursuit of academic success was tantamount to abuse [ 62 ].
A performance of optimum suffering
Against a backdrop of expected mental distress, DRs expressed their PhD as a performative piece. DRs first had to show just the right amount of struggle and difficulty; feeling that if they did not exhibit enough stress, distress and ill-health, their supervisors or the wider department might not believe they were taking their PhD seriously enough [ 40 ]. At the same time, DRs felt that their ‘researcher mettle’ was constantly being tested and they must rise to this challenge. This included first guarding against presenting oneself as intellectually inferior [ 36 ]. Yet it also seemed imperative not to show vulnerability more broadly [ 74 ]. Disclosing mental or physical health problems might lead not only to changed perceptions of the DR but to material disadvantage [ 74 ]. The poor response to mental health disclosures suggested to some DRs that universities might be purposefully trying to dissuade or discourage DRs with mental health problems or learning disabilities from continuing [ 74 ]. The performative piece is thus multi-layered, in that DRs must experience extreme internal psychological struggles, exhibit some lower-level signs of stress and fatigue for peer and faculty observance, yet avoid expressing any real academic or interpersonal weakness or the disclosure of any diagnosable disability or disease.
Emperor’s new clothes
DRs described feeling beholden to the prevailing culture in which it was expected to prioritise above all else developing into a competitive, self-promoting researcher in a high-performing research-active institution [ 39 , 42 ]. Supervisors often appeared the conduit for transmission of this academic ideal [ 74 ]. DRs felt reticent to act in any way which suggested that they did not personally value the pursuit of a leading research career above all else. For example, DRs felt that valuing teaching was non-conformist and could endanger their continuing success within their current institution [ 55 ]. Many DRs thus exhibited a sense of dissonance as their personal values often did not align with the institutional values they identified [ 74 ]. Yet DRs expressed a sense of powerlessness and a feeling of being ‘caught up’ in the values of the institution even when such values were personally incongruent [ 74 ]. The psychological toll of this sense of inauthenticity seemed high [ 55 ]. Where DRs acted in ways which ostensibly suggested values other than prioritising a research career, for example becoming pregnant, they sensed disapproval [ 76 ]. DRs also felt unable to challenge other ‘institutional myths’ for example, the perceived institutional denial of the duration of and financial struggle involved in completing a PhD [ 49 ]. There was a perceived tendency of academics to locate problems within DRs as opposed to acknowledging institutional or systemic inequalities [ 49 ]. DRs expressed strongly a sense in which there is inequity in support, resources and opportunities, yet universities were perceived as ignoring such inequity or labelling such divisions as based on meritocracy [ 36 , 74 ].
Beware the invisible and visible walls
DRs described the reality of working in academia as needing to negotiate a maze of invisible and visible walls. In the former case, ‘invisible walls’ reflect ephemeral norms and rules that govern academia. DRs felt that a big part of their continuing success rested upon being able to negotiate such rules [ 39 ]. Where rules were violated and explicit or implicit conflicts occurred, DRs were seen to be vulnerable to being caught in the ‘crossfire’ [ 36 ]. DRs identified academic groups and departments as being poor in explicitly identifying, discussing and resolving conflicts [ 37 ]. The intangibility of the ‘invisible walls’ gave rise to a sense of ambient anxiety about inadvertently transgressing norms and divides, such that some DRs reported behaving in ways that surprised even themselves [ 37 ].
Gendered and racial micropolitics of academic institutions were seen to manifest as more visible walls between people, with institutions privileging those with ‘insider’ status [ 36 ]. Women and people of colour typically felt excluded or disadvantaged in a myriad of observable and unobservable ways, with individuals able to experience both insider and outsider statuses simultaneously [ 36 , 37 ], for example when a male person of colour [ 36 ]. Female DRs suggested that not only must women prove themselves to a greater extent than men to receive equal access to resources, opportunities and acclaim but also are typically under additional pressure in both their professional and personal lives [ 37 , 52 , 76 ]. Women also felt that they had to take on more additional roles and responsibilities and encountered more conflicts in their personal lives compared to men [ 52 ]. Examples of professionally successful women in DRs’ departments were described as those who had crossed the divide and adopted a more traditionally male role [ 40 ]. Thus, being female or non-White were considered visible characteristics that would disadvantage people in the competitive academic environment and could give rise to a feeling of increased stress, pressure, role conflicts, and a feeling of being unsafe.
Seeing, being and becoming
The higher-order theme of ‘Seeing, being and becoming’ reflects protective and transformative influences on DR mental health. ‘De-programming’ refers to the DRs disentangling their personal beliefs and values from systemic values and also from their own tendency towards perfectionism. ‘The power of being seen’ reflects the positive impact on DR mental health afforded by feeling visible to personal and professional others. ‘Finding hope, meaning and authenticity’ refers to processes by which DRs can find or re-locate their own self-agency, purpose and re/establish a sense of living in accordance with their values. ‘The importance of multiple goals, roles and groups’ represents the beneficial aspects of accruing and sustaining multiple aspects to one’s identity and connections with others and activities outside the PhD. Finally, ‘The PhD as a process of transcendence’ reflects how the struggles involved in completing a PhD can be transformative and self-actualising.
De-programming
DRs reported being able to protect their mental health by ‘de-programming’ and disentangling their attitudes and practices from social and systemic values and norms. This disentangling helped negate DRs’ adopting unhealthy working practices and offered some protection against experiencing inauthenticity and dissonance between personal and systemic values.
First, DRs spoke of rejecting the belief that they should sacrifice or neglect personal relationships, outside interests and their self-identity in pursuit of academic achievement. DRs could opt-out entirely by choosing a ‘user-friendly’ programme [ 44 ] which encouraged balance between personal and professional goals, or else could psychologically reject the prevailing institutional discourse [ 40 ]. Rather than halting success, de-programming from the prioritisation of academia above all else was seen to be associated not only with reduced stress but greater confidence, career commitment and motivation [ 40 , 50 ]. It was also suggested possible to ‘de-programme’ in the sense of choosing not to be preoccupied by the ‘invisible walls’ of academia and psychologically ‘opt out’ of being concerned by potential conflicts, norms and rules governing academic workplace conduct [ 36 ]. Interaction with people outside of academia was seen to scaffold de-programming, by helping DRs to stay ‘grounded’ and offering a model what ‘normal’ life looks like. People outside of academia could also help DRs to see the truth by providing unbiased opinions regarding systemic practices [ 39 ].
A further way in which de-programming manifested was in DRs challenging their perfectionist beliefs. This include re-framing the goal as not trying to be the archetype of a perfect DR, and accepting that multiple demands placed on one individual invariably requires compromise [ 40 , 76 ]. DRs spoke of the need to conceptualise the PhD as a process, rather than just a product [ 46 , 82 ]. The process orientation facilitated framing of the PhD as just one-step in the broader process of becoming an academic as opposed to providing discrete evidence of worth [ 82 ]. Within this perspective, uncertainty itself could be conceived as a privilege [ 81 ]. The PhD was then seen as an opportunity rather than a test [ 37 , 46 ]. Moreover, the process orientation facilitated viewing the PhD as a means of growing into a contributing member of the research community, as opposed to needing to prove oneself to be accepted [ 82 ]. Remembering the temporary nature of the PhD was advised [ 45 ] as was holding on to a sense that not completing the PhD was also a viable life choice [ 76 ]. DRs also expressed, implicitly or explicitly, a decision to change their conceptualisation of themselves and their progress; choosing not to perceive themselves as stuck, but planning, learning and progressing [ 38 , 39 , 81 , 82 ]. This new perspective appeared to be helpful in reducing mental distress.
The power of being seen
DRs described powerful benefits to feeling seen by other people, including a sense of belonging and mattering, increased self-confidence and a sense of positive progress [ 37 ]. Being seen by others seems to provoke the genesis of an academic identity; it brings DRs into existence as academics. Being seen within the academic institution also supports mental health and can buffer emotional exhaustion [ 37 , 52 , 55 , 81 ]. DRs expressed a need to feel that supervisors, academics and peers were interested in them as people, their values, goals, struggles and successes; yet they also needed to feel that they and their research mattered and made a difference within and outside of the institution [ 42 , 52 , 81 ]. It was clear that DRs could find in their disciplinary communities the sense of belonging that often eluded them within their immediate departments [ 42 ]. Feeling a sense of belonging to the academic community seemed to buffer disengagement and amotivation during the PhD [ 81 ]. Positive engagement with the broader community was scaffolded by a sense of trust in the supervisor [ 81 ]. DRs often felt seen and supported by postdocs, especially where supervisors appeared absent or unsupportive [ 50 ].
Spending time with peers could be beneficial when there was a sense of shared experience and walking alongside each other [ 39 ]. Friendship was seen to buffer stress and protect against mental health problems through the provision of social and emotional support and help in identifying struggles [ 39 , 43 ]. In addition to relational aspects, the provision of designated physical spaces on campus or in university buildings also seemed important to being seen [ 37 ]. Peers in the university could provide DRs with further physical embodiments of being seen, for example, gift-giving in response to their birthdays or returning from leave [ 37 , 50 ]. Outside of the academic institution, DRs described how being seen by close others could support DRs to be their authentic selves, providing an antidote to the invisible walls of academia [ 50 ]. Good quality friendships within or outside academia could be life-changing, providing a visceral sense of connection, belonging and authenticity that can scaffold positive mental health outcomes during the PhD [ 39 ]. Pets could also serve to help DRs feel seen but without needing to extend too much energy into maintaining social relationships [ 50 ].
Finally, DRs also needed to see themselves, i.e. to begin to see themselves as burgeoning academics as opposed to ‘just students’ [ 81 ]. Feeling that the supervisor and broader academic community were supportive, developing one’s own network of process collaborators and successfully obtaining grant funding seemed tangible markers that helped DRs to see themselves as academics [ 37 , 81 ]. Seeing their own work published was also helpful in providing a boost in confidence and being a joyful experience [ 42 ]. Moreover, with sufficient self-agency, DRs can not only see themselves but render themselves visible to other people [ 37 ].
Multiple goals, roles and groups
In antidote to the diminished personal identity and enmeshment with the PhD, DRs benefitted from accruing and sustaining multiple goals, roles, occupations, activities and social group memberships. Although ‘costly’ in terms of increased stress and role conflicts, sustaining multiple roles and activities appeared essential for protecting against mental health problems [ 50 , 68 ].
Leisure activities appeared to support mental health through promoting physical health, buffering stress, providing an uplift to DRs’ mood and through the provision of another identity other than as an academic [ 44 , 50 , 76 ]. Furthermore, engagement in activities helped DRs to find a sense of freedom, allowing them to carve up leisure and work time and psychologically detach from their PhD [ 68 , 76 ]. Competing roles, especially family, forced DRs to distance themselves from the PhD physically which reinforced psychological separation [ 50 , 59 ]. Engaging in self-care and enjoyable activities provided a sense of balance and normalcy [ 39 , 44 , 68 ]. This normalcy was a needed antidote to abnormal pressure [ 59 ]. Even in the absence of fiercely competing roles and priorities, DRs still appeared to benefit from treating their PhD as if it is only one aspect of life [ 59 ]. Additional roles and activities reduced enmeshment with the PhD to the extent that considering not completing the PhD was less averse [ 40 ]. This position appeared to help DRs to be less overwhelmed and less sensitive to perceived and anticipated failures.
Finding hope, meaning and authenticity
Finding hopefulness and meaning within the PhD can scaffold a sense of living a purposeful, enjoyable, important and authentic life. Hopefulness is predicated on the ability to identify a goal, i.e. to visualise and focus on the desired outcome and to experience both self-agency and potential pathways towards the goal. Hopefulness was enhanced by the ability to break down tasks into smaller goals and progress in to ‘baby steps’ [ 38 , 59 ]. In addition, DRs benefitted from finding explicit milestones against which they can compare their progress [ 59 ], as this appeared to feed back into the cycle of hopeful thinking and spur further self-agency and goal pursuit.
The experience of meaning manifested in two main ways; first as the more immediate lived experience of passion in action [ 76 ]. Secondly, DRs found meaning in feeling that in their PhD and lives more broadly they were living in accordance with their values, for example, experiencing their own commitment in action through continuing to work on their PhD even when it was difficult to do so [ 76 ]. DRs who were able to locate their PhD within a broader sense of purpose appeared to derive wellbeing benefits. There was a need to ensure that values were in alignment, for example, finding homeostasis between emotional, intellectual, social and spiritual parts of the self [ 46 , 59 , 90 ].
The processes of finding hopefulness and meaning appear to be largely relational. Frequent contact with supervisors in person and social and academic contact with other DRs were basic scaffolds for hope and meaning [ 52 ]. DRs spoke of how a sense that their supervisors believed in them inspired their self-agency and motivation [ 42 , 62 , 76 ]. Partners, friends and family could also inspire motivation for continuing in PhD tasks [ 44 , 76 ]. Other people also could help instil a sense of motivation to progress and complete the PhD; a sense of being seen is to be beholden to finish [ 39 ]. Meaning appeared to be scaffolded by a sense of contribution, belonging and mattering [ 81 ] and could arise from the perception of putting something into the collective pot, inspiring hopefulness and helping others [ 39 , 42 ]. Moreover, hopefulness, meaning and authenticity also appeared mutually reinforcing [ 81 ]. Finding meaning and working on a project which is in accordance with personal values, preferences and interests is also helpful in completing the PhD and provides a feedback loop into hope, motivation and agentic thinking [ 39 , 81 ]. Furthermore, DRs could use agentic action to source a community of people who share their values, enabling them to engage in collective authenticity [ 39 ].
The PhD as a process of transcendence
The immense challenge of the PhD could be a catalyst for growth, change and self-actualisation, involving empowerment through knowledge, self-discovery, and developing increased confidence, maturity, capacity for self-direction and use of one’s own autonomy [ 44 , 82 ]. The PhD acted as a forge in which DRs were tested and became remoulded into something greater than they had been before [ 44 , 82 , 90 ]. The struggles endured during the PhD caused DRs to reconsider their sense of their own capacities, believing themselves to be more able than they previously would have thought [ 50 ]. The struggles endured added to the sense of accomplishment. A trusted and trusting supervisor appears to aid in the PhD being a process of transcendence [ 62 ].
More broadly, the PhD also helped DRs to transcend personal tragedy, allowing immersion in a meaningful activity which begins as a means of coping and becomes something completely [ 39 ]. The PhD could also serve as a transformative selection process for DRs’ social relationships, with some relationships cast aside and yet others formed anew [ 39 ]. Overall, therefore, the very aspects of the PhD which were challenging, and distressing could allow DRs to transcend their former selves and, through the struggle, become something more.
Summation of results
The findings regarding the risk and protective factors associated with DR mental health have been summarised in Table 3 in relation to (1) the type of research evidencing the factor (i.e. whether the evidence is quantitative only, part of the meta-synthesis only, or evident in both results sections); and (2) the volume of evidence (i.e. whether the factor was found in a single study or across multiple studies). The factors in the far-right column (i.e. the factors found across multiple research studies utilising both qualitative and quantitative methods) are the ones with the strongest evidence at present.
This systematic review summarises a heterogeneous research area, with the aim of understanding the mental health of DRs, including possible risk and protective factors. The qualitative and quantitative findings presented here suggest that poor mental health is a pertinent problem facing DRs; stress appears to be a key issue and significantly in excess of that experienced in the general population. Several risk and protective factors at the individual, interpersonal and systemic levels emerged as being important in determining the mental health of DRs. The factors with the strongest evidence-base (i.e. those supported by multiple studies using qualitative and quantitative findings) denote that being female and isolated increases the risk of the mental health problems, whereas seeing the PhD as a process, feeling socially supported, having a positive supervisor relationship and engaging in self-care is protective.
Results in context
Stress can be defined as (1) the extent to which a stimulus exerts pressure on an individual, and their propensity to bear the load; (2) the duration of the response to an aversive stimuli, from initial alert to exhaustion; or (3) a dynamic (im)balance between the demands and personal resource to manage those demands [ 91 ]. The Perceived Stress Scale (PSS) [ 18 , 19 ] used in our meta-analysis is aligned with the third of these definitions. As elaborated upon within the Transactional Model of Stress [ 92 ], stress is conceptualised as a persons’ appraisal of the internal and external demands put upon them, and whether these exceed their available resources. Thus, our results suggest that, when compared to the general population, PhD students experience a greater maladaptive imbalance between their available resources and the demands placed upon them. Stress in itself is not a diagnosable mental health problem, yet chronic stress is a common precipitant to mental health difficulties such as depression and posttraumatic stress disorder [ 93 , 94 ]. Therefore, interventions should seek to bolster DRs’ resources and limit demands placed on them to minimise the risks associated with acute stress and limit its chronicity.
Individual factors
Female DRs were identified as being at particular risk of developing mental health difficulties. This may result from additional hurdles when studying in a male-dominated profession [ 95 , 96 , 97 ], and the expectation that in addition to their doctoral studies, females should retain sole or majority responsibility for the domestic and/or caring duties within their family [ 52 , 76 ]. It may also be that females are more willing to disclose and seek help for mental health difficulties [ 98 ]. Nevertheless, the World Health Organisation (WHO) mental health survey results indicate that whilst anxiety and mood disorders are more prevalent amongst females, externalising disorders are more common in males [ 99 ]. As the vast majority of studies in this review focussed on internalising problems (e.g. stress, anxiety and depression) [ 37 , 64 , 79 , 80 , 83 , 89 ], this may explain the gender differences found in this review. Further research is needed to explore which perspective, if any, may explain gender gap in our results.
Perhaps unsurprisingly, self-care was associated with reduced mental health problems. The quantitative findings suggest that all types of self-care are likely to be protective of mental health (i.e. physical, emotional, professional and spiritual self-care). Self-care affords DRs the opportunity to take time away from their studies and nurture their non-PhD identities. However, the results from our meta-synthesis suggest that DRs are not attending to their most basic needs much less engaging in self-care behaviours that correspond to psychological and/or self-fulfilment needs [ 100 ]. Consequently, an important area for future enquiry will be identifying the barriers preventing DRs from engaging in self-care.
Interpersonal factors
Across both quantitative and qualitative studies, interpersonal factors emerged as the most salient correlate of DR mental health. That is, isolation was a risk factor, whereas connectedness to others was a protective factor. There was some variability in how these constructs were conceptualised across studies, i.e. (1) isolation: a lack of social support, having fewer social connections, feeling isolated or being physically separate from others; and (2) social connectedness: multiple group membership, academic relationships or non-academic relationships; but there was no indication that effects varied between concepts. The relationship between isolation and negative health consequences is well-established, for example both physical and mental health problems [ 101 ], and even increased mortality [ 102 ]. Conversely, social support is associated with reduced stress in the workplace [ 103 , 104 ]. Reducing isolation is therefore a promising interventional target for improving DRs’ mental health.
The findings regarding isolation are even more alarming when considered alongside the findings from several studies that PhD studies are consistently reported to dominate the lives of DRs, resulting in poor ‘work-life balance’ and losing non-PhD aspects of their identities. The negative impact of having fewer identities [ 105 ] can be mitigated by having a strong support network [ 106 ], and increasing multiple group memberships [ 107 ]. But for DRs, it is perhaps the absence of this social support, combined with identity impoverishment, which can explain the higher than average prevalence of stress found in our meta-analysis.
Systemic factors
DRs’ attitudes towards their studies may be a product of top-down systemic issues in academia more broadly. Experiencing mental health problems was reported as being the ‘norm’, but also appeared to be understood as a sign of weakness. The meta-synthesis results suggest that DRs believed their respective universities prioritise academic success over workplace wellbeing and encourage unhealthy working habits. Working in an unsupportive and pressured environment is strongly associated with negative psychological outcomes, including increased depression, anxiety and burnout [ 108 ]. The supervisory relationship appeared a particularly important aspect of the workplace environment. The quantitative analysis found a negative correlation between inspirational supervision and mental health problems. Meta-synthetic finding suggested toxic DR-supervisor relationships characterised by powerlessness and neglect, as well as relationships where DRs felt valued and respected—the former of these being associated with poor mental health, and the latter being protective. The association between DR-supervisor relationship characteristics needs to be verified using quantitative methods. Furthermore, DRs’ sense that they needed to exhibit ‘optimum suffering’, which appears to reflect a PhD-specific aspect of a broader academic performativity [ 109 ], is an important area for consideration. An accepted narrative around DRs needing to experience a certain level of dis/stress would likely contribute to poor mental health and as an impediment to the uptake and effectiveness of proffered interventions. Although further research is needed, it is apparent that individual interventions alone are not sufficient to improve DR mental health, and that a widespread culture shift is needed in order to prevent the transmission of unhealthy work attitudes and practices.
Limitations of the literature
Although we found a respectable number of articles in this area, the focus and measures used varied to the extent that typical review analysis procedures could not be used. That is, there was much heterogeneity in terms of how mental health was conceptualised and measured, as well as the range of risk and protective factors explored. Similarly, the quality of the studies was hugely variable. Common flaws amongst the literature include small sample sizes, the use of unvalidated tools and the incomplete reporting of results. Furthermore, for qualitative studies specifically, there appeared to be a focus on breadth instead of depth, particularly in relation to studies using mixed methods.
The generalisability of our findings is limited largely due to the lack of research conducted outside of the US, but also because we limited our review to papers written in English only. The nature of doctoral studies varies in important ways between studies. For example, in Europe, PhD studies usually apply for funding to complete their thesis within 3–4 years and must know their topic of interest at the application stage. Whereas in the US, PhD studies usually take between 5 and 6 years, involve taking classes and completing assignments, and the thesis topic evolves over the course of the PhD. These factors, as well as any differences in the academic culture, are likely to affect the prevalence of mental health problems amongst DRs and the associated risk and protective factors. More research is needed outside of the US.
‘Mental health’ in this review was largely conceptualised as a type of general wellbeing rather than a clinically meaningful construct. None of the studies were ostensibly focused on sampling DRs who were currently experiencing or had previously experienced mental health problems per se, meaning the relevance of the risk, vulnerability and protective factors identified in the meta-synthesis may be more limited in this group. Few studies used clinically meaningful measures. Where clinical measures were used, they captured data on common mental health problems only (i.e. anxiety and depression). Due to these limitations, we are unable to make any assertions about the prevalence of clinical-level mental health problems amongst DRs.
Limitations of this review
As a result of the heterogeneity in this research area, some of the results presented within this review are based on single studies (e.g. correlation data; see Fig. 5 ) rather than the amalgamation of several studies (e.g. meta-analysis/synthesis). To aid clarity when interpreting the results of this review, we have (Table 3 ) summarised the volume of evidence supporting risk and protective factors. Moreover, due to the small number of studies eligible for inclusion in this review, we were unable to test whether any of our findings are related to the study characteristics (e.g. year of publication, country of origin, methodology).
We were able to conduct three meta-analyses, one of which aimed to calculate the between-group effect size on the PSS [ 18 , 19 ] between DRs and normative population data. Comparing these data allowed us to draw some initial conclusions about the prevalence of stress amongst DRs, yet we were unable to control for other group differences which might moderate stress levels. For example, the population data was from people in the United States (US) in 1 year, whereas the DR data was multi-national at a variety of time points; and self-reported stress levels may vary with nationality [ 110 ] or by generation [ 111 , 112 ]. Moreover, two of the three meta-analyses showed significant heterogeneity. This heterogeneity could be explained by differences in the sample characteristics (e.g. demographics, country of origin), doctoral programme characteristics (e.g. area of study, funding status, duration of course) or research characteristics (e.g. study design, questionnaires used). However, due to the small number of studies included in these meta-analyses, we were unable to test any of these hypotheses and are therefore unable to determine the cause of this heterogeneity. As more research is conducted on the mental health of DRs, we will be able to conduct larger and more robust meta-analyses that have sufficient power and variance to statistically explore the causes of this heterogeneity. At present, our findings should be interpreted in light of this limitation.
Practice recommendations
Although further research is clearly needed, we assert that this review has identified sufficient evidence in support of several risk and protective factors to the extent that they could inform prevention and intervention strategies. Several studies have evidenced that isolation is toxic for DRs, and that social support can protect against poor mental health. Initiatives that provide DRs with the opportunity to network and socialise both in and outside of their studies are likely to be beneficial. Moreover, there is support for psychoeducation programmes that introduce DRs to a variety of self-care strategies, allow them to find the strategies that work for them and encourage DRs to make time to regularly enact their chosen strategies. Finally, the supervisory relationship was identified as an important correlate of DR mental health. Positive supervision was characterised as inspirational and inclusive, whereas negative supervision productised DRs or neglected them altogether. Supervisor training programmes should be reviewed in light of these findings to inform how institutions shape supervisory practices. Moreover, the initial findings reported here evidence a culture of normalising and even celebrating suffering in academia. It is imperative therefore that efforts to improve and protect the mental health of DRs are endorsed by the whole institution.
Research recommendations
First, we encourage further large-scale mental health prevalence studies that include a non-PhD comparison group and use validated clinical tools. None of the existing studies focused on the presence of serious mental health problems—this should be a priority for future studies in this area. Mixed-methods explorations of the experiences of DRs who have mental health problems, including serious problems, and in accessing mental health support services would be a welcome addition to the literature. More qualitative studies involving in-depth data collection, for example interview and focus group techniques, would be useful in further supplementing findings from qualitative surveys. Our review highlights a need for better communication and collaboration amongst researchers in this field with the goal of creating a level of consistency across studies to strengthen any future reviews on this subject.
The results from this systematic review, meta-analysis and meta-synthesis suggest that DRs reported greater levels of stress than the general population. Research regarding the risk and protective factors associated with the mental health of DRs is heterogenous and disparate. Based on available evidence, robust risk factors appear to include being isolated and being female, and robust protective factors include social support, viewing the PhD as a process, a positive DR-supervisor relationship and engaging in self-care. Further high-quality, controlled research is needed before any firm statements can be made regarding the prevalence of clinically relevant mental health problems in this population.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Confidence intervals
Doctoral researchers
Higher Education Statistics Agency
Perceived Stress Scale
Standard deviation
United Kingdom
United States
Baron E. Eleven sketches inspired by the university mental health crisis—in pictures. The Guardian. 2017. Available from: https://www.theguardian.com/education/gallery/2017/jun/27/eleven-sketches-university-mental-health-crisis . Cited 2017 Oct 6.
Google Scholar
National Union of Students. 20 per cent of students consider themselves to have a mental health problem: National Union of Students; 2013. Available from: https://www.nus.org.uk/en/news/20-per-cent-of-students-consider-themselves-to-have-a-mental-health-problem/ . Cited 2017 Oct 6.
YouGov. One in four students suffer from mental health problems. 2016. Available from: https://d25d2506sfb94s.cloudfront.net/cumulus_uploads/document/obtomdatp4/Survey_Results.pdf . Cited 2017 Oct 6.
Universities UK. Minding Our Future: starting a conversation about the support of student mental health. London: Universities UK; 2017. Available from: https://www.universitiesuk.ac.uk/minding-our-future .
The Guardian. Number of university dropouts due to mental health problems trebles. The Guardian. 2017. Available from: https://www.theguardian.com/society/2017/may/23/number-university-dropouts-due-to-mental-health-problems-trebles . Cited 2017 Oct 6.
Thorley C. Not By Degrees: Improving student mental health in the UK’s universities. London; 2017. Available from: www.ippr.org . Cited 2017 Oct 6.
Oswalt SB, Lederer AM, Chestnut-Steich K, Day C, Halbritter A, Ortiz D. Trends in college students’ mental health diagnoses and utilization of services, 2009–2015. J Am Coll Health. 2018;68:41–51.
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–38.
PubMed PubMed Central Google Scholar
OECD. Education at a Glance 2019. Education at a Glance: OECD Indicators: OECD; 2019. (Education at a Glance). Available from: http://gpseducation.oecd.org/Content/EAGCountryNotes/BRA.pdf . Cited 2020 Mar 26.
OECD. OECD Science, Technology and Innovation Outlook 2016. OECD Science, technology and innovation outlook 2016. 2016. Available from: http://www.oecd.org/sti/STIO 10 key technology trends for the future.pdf. Cited 2020 Mar 26.
Higher Education Statistics Agency (HESA). Higher education student statistics: UK, 2016/17: HESA; 2018. Available from: https://www.hesa.ac.uk/news/11-01-2018/sfr247-higher-education-student-statistics/numbers .
NCES. Number of doctoral degrees earned in the United States from 1949/50 to 2028/29, by gender. 2019. Available from: https://www.statista.com/statistics/185167/number-of-doctoral-degrees-by-gender-since-1950/ .
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46 Available from: http://psycnet.apa.org/index.cfm?fa=search.displayRecord&uid=1960-06759-001 .
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159 Available from: http://www.jstor.org/stable/2529310?origin=crossref . Cited 2017 Mar 8.
CAS PubMed Google Scholar
Noblit GW, Hare RD. Meta-ethnography: Synthesizing qualitative studies: Sage Publications; 1988. p. 88.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45.
Wilson DB. Meta-analysis stuff. 2011. Available from: http://mason.gmu.edu/~dwilsonb/ma.html . Cited 2017 Dec 3.
Cohen S, Williamson GM. Perceived stress in a probability sample of the U.S. In: Spacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Cohen S, Janicki-Deverts D. Who’s Stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42(6):1320–34.
MedCalc Software bvba. MedCalc Statistical Software. Belgium: Ostend; 2016.
Viechtbauer W. Bias and efficiency of Meta-analytic variance estimators in the random-effects model. J Educ Behav Stat. 2005;30(3):261–93 Available from: http://jeb.sagepub.com/cgi/doi/10.3102/10769986030003261 . Cited 2017 Mar 8.
Hedges LV, Ollkin L. Statistical methods for meta-analysis. New York: Academic Press; 1985. Available from:. https://doi.org/10.1002/9780470743386.refs .
Book Google Scholar
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester: Wiley; 2009. Cited 2019 Jan 10. Available from. https://doi.org/10.1002/9780470743386 .
Fisher RA. Frequency distribution of the values of the correlation coefficient in samples from an indefinitely large population. Biometrika. 1915;10(4):507–21 Available from: https://www.statista.com/statistics/185167/number-of-doctoral-degrees-by-gender-since-1950/ .
Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach: GRADE Working Group; 2013. Available from: gdt.guidelinedevelopment.org/app/handbook/handbook.html .
Lachal J, Revah-Levy A, Orri M, Moro MR. Metasynthesis: an original method to synthesize qualitative literature in psychiatry. Front Psychiatry. 2017;8:269.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. London: Sage Publications Ltd; 2013.
Bhaskar R. The possibility of naturalism: a philosophical critique of the contemporary human sciences. London: Routledge; 2014.
Fletcher AJ. Applying critical realism in qualitative research: methodology meets method. Int J Soc Res Methodol. 2017;20(2):181–94.
Walsh D, Downe S. Meta-synthesis method for qualitative research: a literature review. J Adv Nurs. 2005;50(2):204–11.
PubMed Google Scholar
Maton K. Reflexivity, relationism, & research: Pierre Bourdieu and the epistemic conditions of social scientific knowledge. Sp Cult. 2003;6(1):52–65.
Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for Reporting Observational Studies. Ann Intern Med. 2007;147(8):573. Cited 2019 Sep 27. Available from. https://doi.org/10.7326/0003-4819-147-8-200710160-00010 .
Article Google Scholar
Acker S, Haque E. The struggle to make sense of doctoral study. High Educ Res Dev. 2015;34(2):229–41. Available from. https://doi.org/10.1080/07294360.2014.956699 .
Appel ML, Dahlgren LG. Swedish doctoral students’ experiences on their journey towards a PhD: obstacles and opportunities inside and outside the academic building. Scand J Educ Res. 2003;47(1):89–110. Available from. https://doi.org/10.1080/00313830308608 .
Devonport TJ, Lane AM. In it together: Dyadic coping among doctoral students and partners. J Hosp Leis Sport Tour Educ. 2014;15:124–34. Available from. https://doi.org/10.1016/j.jhlste.2014.08.002 .
Enzor J. Friendship, mental health, and doctoral education: a generic qualitative thematic analysis: Capella University; 2017.
Kurtz-Costes B, Helmke LA, Ülkü-Steiner B. Gender and doctoral studies: the perceptions of Ph.D. students in an American university. Gend Educ. 2006;18(2):137–55.
Bazrafkan L, Shokrpour N, Yousefi A, Yamani N. Management of stress and anxiety among PhD students during thesis writing: a qualitative study. The Health Care Manager. 2016;35:231–40.
Cotterall S. More than just a brain: emotions and the doctoral experience. High Educ Res Dev. 2013;32(2):174–87.
Kaufman JA. Personal perceptions of stress and self-perceived need for social support among doctoral psychology students in a distance education university sample: Capella University; 2004.
Kenty JR. Stress management strategies for women doctoral students. Nurse Educ. 2000;25(5):251–4 Available from: http://pesquisa.bvsalud.org/portal/resource/pt/mdl-16646205 .
Scrubb MM. An examination of the doctoral student stress survey (DSSS) as an instrument for measuring the effects of stress as perceived by doctoral students in a distance learning university: Walden University; 1997.
Usman Yousaf S, Akram M, Usman B. Exploring the causes of stress and coping with it amongst doctoral level students: highlighting the importance of information collection and management. Pakistan J Inf Manag Libr. 2016;18(2):12–25 Available from: https://search.proquest.com/openview/68246cbba8a9da0ec067d56631b479f1/1?pq-origsite=gscholar&cbl=54989 .
Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis Studies. Res Sch. 2006;13(1):29 Available from: http://www.ncbi.nlm.nih.gov/pubmed/20098638%0A http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2809982 .
Bauer J. Personality factors, self-care, and perceived stress levels on counselor education and counseling psychology doctoral students. Dissertations: Western Michigan University; 2016.
Begun AL, Carter JR. Career Implications of Doctoral Social Work Student Debt Load. J Soc Work Educ. 2017;53(2):161–73. Available from. https://doi.org/10.1080/10437797.2016.1243500 .
Benjamin S, Williams J, Maher MA. Focusing the lens to share the story: using photographs and interviews to explore doctoral students’ sense of well-being. Int J Dr Stud. 2017;12:197–217.
Benesek JP. Stress and coping among psychology doctoral students: a comparison of self-reported stress levels and coping styles of PhD and PsyD students: University of Hartford; 1998.
Bireda AD. Challenges to the doctoral journey: a case of female doctoral students from Ethiopia. Open Prax. 2015;7(4):287–97.
Bolliger DU, Halupa C. Student perceptions of satisfaction and anxiety in an online doctoral program. Distance Educ. 2012;33(1):81–98.
Cole LJ. Academic worry and frequent mental distress among online doctoral students: Walden University; 2008.
Devine K, Hunter KH. PhD student emotional exhaustion: the role of supportive supervision and self-presentation behaviours. Innov Educ Teach Int. 2017;54(4):335–44.
Drake KL. Psychology graduate student well-being: the relationship between stress, coping, and health outcomes: University of Cincinnati; 2010.
Dumitrescu GA. Self-efficacy, locus of control , perceived stress and student satisfaction as correlates of dissertation completion: Andrews University; 2016.
El-Ghoroury NH, Galper DI, Sawaqdeh A, Bufka LF. Stress, coping, and barriers to wellness among psychology graduate students. Train Educ Prof Psychol. 2012;6(2):122–34.
Haynes C, Bulosan M, Citty J, Grant-Harris M, Hudson J, Koro-Ljungberg M. My world is not my doctoral program…Or is it?: Female students’ perceptions of well-being. Int J Dr Stud. 2012;7:001–17.
Hill LM. Perceived stress, academic support, social support, and professional support factors as predictors of student success in distributed-learning doctoral education: Fielding Graduate University; 2010.
Holahan CK. Stress experienced by women doctoral students, need for support, and occupational sex typing: An interactional view. Sex Roles. 1979;5(4):425–36.
Hunter KH, Devine K. Doctoral students’ emotional exhaustion and intentions to leave academia. Int J Doctoral Stud. 2016;11.
Kaufman JA. Stress and social support among online doctoral psychology students. J College Stud Psychother. 2006;20(3):79–88 Available from: http://search.proquest.com/docview/57185202?accountid=12253%5Cn http://man-fe.hosted.exlibrisgroup.com/openurl/44MAN/44MAN_services_page?url_ver=Z39.88-2004&rft_val_fmt=journal&genre=unknown&sid=ProQ:ProQ%3Aeducation&atitle=Stress+and+Social+Support+among +.
Levecque K, Anseel F, De Beuckelaer A, Van Der Heyden J, Gisle L. Work organization and mental health problems in PhD students. Res Policy. 2017;46:868–79.
Lonka K, Chow A, Keskinen J, Hakkarainen K, Sandström N, Pyhältö K. How to measure PhD students’ conceptions of academic writing - and are they related to wellbeing? J Writ Res. 2014;5(3):245–69.
Lowe RL. The relationship between personality, self-care, stress, and perceived wellness in psychology doctoral students: Tennessee University; 2015.
Marais GAB, Shankland R, Haag P, Fiault R, Juniper B. A survey and a positive psychology intervention on French PhD student well-being. Int J Dr Stud. 2018;13:109–38.
Martinez E, Ordu C, Sala MRD, McFarlane A. Striving to obtain a school-work-life balance: The full-time doctoral student. Int J Dr Stud. 2013;8:39–59.
McGregor BA, Antoni MH, Ceballos R, communication BBBS. very low CD19+ B-lymphocyte percentage is associated with high levels of academic stress among healthy graduate students. Stress Heal. 2008;24(5):413–8.
Nelson K. Academic progress in doctoral students: Levels of hope, subjective well-being, and stress: Walden University; 2014. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc12&NEWS=N&AN=2015-99151-189 .
Nottingham K. A predictive analysis of the psychosocial outcomes of doctoral students: Capella University; 2017.
Orozco AB. Self-care effects on anxiety in doctoral students: Fielding Graduate University; 2014. p. 35–61.
Peters BM. The relationships among physiological and perceived stress, quality of life, self-care and impairment in doctoral students: State University of New York at Buffalo; 2007.
Pifer MJ, Baker VL. “It could be just because I’m different”: Otherness and its outcomes in doctoral education. J Divers High Educ. 2014;7(1):14–30.
Platt J, Schaefer C. Clinical psychological students’ subjective stress ratings during their doctoral training. Psychol Rep. 1995;76:994 Available from: http://www.ncbi.nlm.nih.gov/pubmed/7568619 .
Pychyl TA. Personal projects, subjective well-being and the lives of doctoral students. Ottawa: Carleton University; 1995.
Pychyl TA, Little BR. Dimensional specificity in the prediction of subjective well-being: Personal projects in pursuit of the PhD. Soc Indic Res. 1998;45(1–3):423–73 Available from: file://d/d/Texte/Guenter/Literatu/Original/Journals/SIR98-45-423-473.pdf.
Rocha-Singh IA. Perceived stress among graduate students: development and validation of the Graduate Stress Inventory. Educ Psychol Meas. 1994;54(3):714–27.
Scheidler JA. Effects of perceived stress and perceived social support on marital satisfaction in doctoral students: Walden University. 2008;20.
Sekas G, Wile MZ. Stress-related illnesses and sources of stress: comparing M.D., Ph.D., M.D. and Ph.D. students. J Med Educ. 1980;55:440–6 Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L10000589%5Cn http://sfx.library.uu.nl/utrecht?sid=EMBASE&issn=00222577&id=doi:&atitle=Stress-related+illnesses+and+sources+of+stress%3A+comparing+M.D.-Ph.D.%2C+M.D.+and+Ph.D.+student .
Stubb J, Pyhältö K, Lonka K. Balancing between inspiration and exhaustion: PhD students’ experienced socio-psychological well-being. Stud Contin Educ. 2011;33(1):33–50.
Stubb J, Pyhältö K, Lonka K. The experienced meaning of working with a PhD thesis. Scand J Educ Res. 2012;56(4):439–56.
Ülkü-Steiner B, Kurtz-Costes B, Kinlaw CR. Doctoral student experiences in gender-balanced and male-dominated graduate programs. J Educ Psychol. 2000;92(2):296–307.
Volkert D, Candela L, Bernacki M. Student motivation, stressors, and intent to leave nursing doctoral study: a national study using path analysis. Nurse Educ Today. 2018;61:210–5. Available from. https://doi.org/10.1016/j.nedt.2017.11.033 .
Article PubMed Google Scholar
Waaijer CJF, Heyer A, Kuli S. Effects of appointment types on the availability of research infrastructure, work pressure, stress, and career attitudes of PhD candidates of a Dutch university. Res Eval. 2016;25(4):349–57.
Wang C-H, Chen Y-W, Wu T-Y. Self-guided bibliotherapy: a case study of a Taiwanese doctoral student. Int J Humanties. 2010;8(1):413–22.
Williams MD. HBCU vs. PWI: institutional integration at PWIs and Black doctoral student depression, anxiety, and stress: University of Minnesota; 2014.
Wright T. Issues in brief counselling with postgraduate research students. Couns Psychol Q. 2006;19(4):357–72.
Scrubb MM. An examination of the Doctoral Student Stress Survey (DSSS) as an instrument for measuring the effects of stress as perceived by doctoral students in a distance learning university, vol. 58: Walden University; 1998. p. 3041. Dissertation Abstracts International Section A: Humanities and Social Sciences. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc3&NEWS=N&AN=1998-95003-070 .
Hadden BW, Smith CV. I gotta say, today was a good (and meaningful) day: daily meaning in life as a potential basic psychological need. J Happiness Stud. 2017:1–18.
Butler G. Definitions of stress. Occas Pap R Coll Gen Pract. 1993;(61):1–5 Available from: http://www.ncbi.nlm.nih.gov/pubmed/8199583%0A http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2560943 .
Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Publishing Company; 1984.
Siegrist J. Chronic psychosocial stress at work and risk of depression: evidence from prospective studies. Eur Arch Psychiatry Clin Neurosci. 2008;258(SUPPL. 5):115–9.
Marin MF, Lord C, Andrews J, Juster RP, Sindi S, Arsenault-Lapierre G, et al. Chronic stress, cognitive functioning and mental health. Neurobiol Learn Mem. 2011;96(4):583–95. Available from. https://doi.org/10.1016/j.nlm.2011.02.016 .
Ward M. The gender salary gap in British academia. Appl Econ. 2001;33(13):1669–81. Cited 2019 May 23. Available from. https://doi.org/10.1080/00036840010014445 .
Howe-Walsh L, Turnbull S. Barriers to women leaders in academia: tales from science and technology. Stud High Educ. 2016;41(3):415–28. Cited 2019 May 23. Available from. https://doi.org/10.1080/03075079.2014.929102 .
Gardiner M, Tiggemann M. Gender differences in leadership style, job stress and mental health in male- and female-dominated industries. J Occup Organ Psychol. 1999;72(3):301–15.
Mackenzie CS, Gekoski WL, Knox VJ. Age, gender, and the underutilization of mental health services: the influence of help-seeking attitudes. Aging Ment Health. 2006;10(6):574–82 Cited 2017 May 12. Available from: http://www.tandfonline.com/action/journalInformation?journalCode=camh20 .
Seedat S, Scott KM, Sampson NA, Williams D, Kessler RC. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Pschiatry. 2013;66(7):785–95.
Maslow AH. A theory of human motivation. Psychol Rev. 1943;50(4):370–96 Available from: http://content.apa.org/journals/rev/50/4/370 . Cited 2019 Jun 10.
Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–71 Available from: https://doi.org/10.1016/j.puhe.2017.07.035 .
Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality. Perspect Psychol Sci. 2015;10(2):227–37. Available from. https://doi.org/10.1177/1745691614568352 .
Viswesvaran C, Sanchez JI, Fisher J. The role of social support in the process of work stress: a meta-analysis. J Vocat Behav. 1999;54(2):314–34.
Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med. 2003;60(1):3–9.
CAS PubMed PubMed Central Google Scholar
Brook AT, Garcia J, Fleming M. The effects of multiple identities on psychological well-being. Personal Soc Psychol Bull. 2008;34(12):1588–600.
Thoits PA. Self, Identity, Stress, and Mental Health. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the Sociology of Mental Health. Dordrecht: Springer; 2012. p. 357–77.
Haslam C, Jetten J, Cruwys T, Dingle G, Haslam A. The new psychology of health: Unlocking the social cure. New York: Routledge; 2018.
Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: a meta-analysis. Occup Environ Med. 2005;62(2):105–12.
Macfarlane B. Student performativity in higher education: converting learning as a private space into a public performance. High Educ Res Dev. 2015;34(2):338–50.
Daniels K. Perceived risk from occupational stress: a survey of 15 European countries. Occup Environ Med. 2004;61(5):467–70.
American Psychiatric Association (APA). Stress in America: missing the health care connection. Washington: American Psychiatric Association (APA). 2013.
Twenge JM. Time period and birth cohort differences in depressive symptoms in the U.S., 1982–2013. Soc Indic Res. 2015;121(2):437–54.
Download references
Acknowledgements
Thank you to the Office for Students for their funding to support this work; and thank you to the University of Sussex Doctoral school and our steering group for championing and guiding the ‘Understanding the mental health of Doctoral Researchers (U-DOC)’ project.
The present project was supported by the Office for Students Catalyst Award. The funder had no involvement in the design of the study, the collection, analysis or interpretation of the data, nor the writing of this manuscript.
Author information
Authors and affiliations.
School of Social Sciences, University of Westminster, 115 New Cavendish Street, London, W1W 6UW, UK
Cassie M. Hazell
School of Psychology, University of Sussex, Falmer, Brighton, BN1 9QJ, UK
Laura Chapman
Research and Enterprise, University of Sussex, Falmer, Brighton, BN1 9RH, UK
Sophie F. Valeix
Centre for Higher Education and Equity Research, University of Sussex, Falmer, Brighton, BN1 9RH, UK
Paul Roberts
School of Life Sciences, University of Sussex, Falmer, Brighton, BN1 9QG, UK
Jeremy E. Niven
Primary Care and Public Health, Brighton and Sussex Medical School and School of Psychology, University of Sussex, Falmer, Brighton, BN1 9PH, UK
You can also search for this author in PubMed Google Scholar
Contributions
CH contributed to the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, visualisation, writing—original draft preparation and writing—review and editing of this paper. LC contributed to the data curation, investigation, project administration, validation and writing—review and editing of this paper. SV contributed to the data curation, formal analysis, investigation, project administration, validation and writing—review and editing of this paper. PR contributed to the funding acquisition, project administration, supervision and writing—review and editing of this paper. JN contributed to the conceptualisation, funding acquisition, methodology, project administration, supervision, validation, writing—original draft preparation and writing—review and editing of this paper. CB contributed to the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, visualisation, writing—original draft preparation and writing—review and editing of this paper. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Clio Berry .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not needed for the present study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hazell, C.M., Chapman, L., Valeix, S.F. et al. Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis. Syst Rev 9 , 197 (2020). https://doi.org/10.1186/s13643-020-01443-1
Download citation
Received : 15 June 2020
Accepted : 31 July 2020
Published : 26 August 2020
DOI : https://doi.org/10.1186/s13643-020-01443-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- PhD students
- doctoral researchers
- Postgraduate researchers
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Mental Health, PhD
Bloomberg school of public health, phd program description.
The PhD program is designed to provide key knowledge and skill-based competencies in the field of public mental health. To gain the knowledge and skills, all PhD students will be expected to complete required coursework, including courses that meet the CEPH competency requirements and research ethics; successfully pass the departmental comprehensive exam; select and meet regularly with a Thesis Advisory Committee (TAC) as part of advancing to doctoral candidacy; present a public seminar on their dissertation proposal; successfully pass the departmental and school-wide Preliminary Oral Exams; complete a doctoral thesis followed by a formal school-wide Final Oral Defense; participate as a Teaching Assistant (TA); attend Grand Rounds in the Department of Psychiatry; and provide a formal public seminar on their own research. Each of these components is described in more detail below. The Introduction to Online Learning course is taken before the start of the first term.
Department Organization
The PhD Program Director, Dr. Rashelle Musci ( [email protected] ), works with the Vice-Chair for Education, Dr. Judy Bass ( [email protected] ), to support new doctoral students, together with their advisers, to formulate their academic plans; oversee their completion of ethics training; assist with connections to faculty who may serve as advisers or sources for data or special guidance; provide guidance to students in their roles as teaching assistants; and act as a general resource for all departmental doctoral students. The Vice-Chair also leads the Department Committee on Academic Standards and sits on the School Wide Academic Standards Committee. Students can contact Drs. Musci or Bass directly if they have questions or concerns.
Within the department structure, there are several standing and ad-hoc committees that oversee faculty and student research, practice and education. For specific questions on committee mandate and make-up, please contact Dr. Bass or the Academic Program Administrator, Patty Scott, [email protected] .
Academic Training Programs
The Department of Mental Health houses multiple NIH-funded doctoral and postdoctoral institutional training programs:
Psychiatric Epidemiology Training (PET) Program
This interdisciplinary doctoral and postdoctoral program is affiliated with the Department of Epidemiology and with the Department of Psychiatry and Behavioral Sciences at the School of Medicine. The Program is co-directed by Dr. Peter Zandi ( [email protected] ) and Dr. Heather Volk ( [email protected] ). The goal of the program is to increase the epidemiologic expertise of psychiatrists and other mental health professionals and to increase the number of epidemiologists with the interest and capacity to study psychiatric disorders. Graduates are expected to undertake careers in research on the etiology, classification, distribution, course, and outcome of mental disorders and maladaptive behaviors. The Program is funded with a training grant from the National Institute of Mental Health.
Pre-doctoral trainees are required to take the four-term series in Epidemiologic Methods (340.751-340.754), as well as the four-term series in Biostatistics (140.621-624). In addition to the other departmental requirements for the doctoral degree, pre-doctoral trainees must also take four advanced courses in one of the domains of expertise they have selected to pursue: Genetic and Environmental Etiology of Mental Disorders, Mental Health Services and Outcomes, Mental Health and Aging, and Global Mental Health. Pre-doctoral trainees should consult with their adviser and the program director to select courses consistent with their training goals.
Postdoctoral fellows take some courses, depending on background and experience, and engage in original research under the supervision of a faculty member. They are expected to have mastery of the basic principles and methods of epidemiology and biostatistics. Thus, fellows are required to take 340.721 Epidemiologic Inference in Public Health, 330.603 Psychiatric Epidemiology, and some equivalent of 140.621 Statistical Methods in Public Health I and 140.622 Statistical Methods in Public Health II. They may be waived from these requirements by the program director if they can demonstrate equivalent prior coursework.
Drug Dependence Epidemiology Training (DDET) Program
This training program is co-led by Dr. Renee M. Johnson ( [email protected] ) and Dr. Brion Maher ( [email protected] ). The DDET program is designed to train scientists in the area of substance use and substance use disorders. Research training within the DDET Program focuses on: (1) genetic, biological, social, and environmental factors associated with substance use, (2) medical and social consequences of drug use, including HIV/AIDS and violence, (3) co-morbid mental health problems, and (4) substance use disorder treatment and services. The DDET program is funded by the NIH National Institute on Drug Abuse.
The program supports both pre-doctoral and postdoctoral trainees. Pre-doctoral trainees have a maximum of four years of support on the training grant. After completing required coursework, pre-doctoral trainees are expected to complete original research under the supervision of a faculty member affiliated with the DDET program. Postdoctoral trainees typically have two years of support on the training grant. They are required to engage in original research on a full-time basis, under the supervision of a DDET faculty member. Trainees’ research projects must be relevant to the field of substance use.
All trainees are required to attend a weekly seminar series focused on career development and substance use research. The DDET program supports trainees’ attendance at relevant academic meetings, including the Annual Meeting of the College on Problems of Drug Dependence (CPDD) each June. Training grant appointments are awarded annually and are renewable given adequate progress in the academic program, successful completion of program and departmental requirements, and approval of the training director.
Pre-doctoral trainees are required to take the required series in epidemiology and biostatistics, as well as The Epidemiology of Substance Use and Related Problems (330.602). In addition, they must take three advanced courses that enhance skills or content expertise in substance use and related problems: one in epidemiology (e.g., HIV/AIDS epidemiology), one in biostatistics, and one in social and behavioral science or health policy. The most appropriate biostatistics course will provide instruction on a method the trainee will use during the thesis research (e.g., survival analysis, longitudinal analysis methods). (Course requirements for trainees from other departments will be decided on a case-by-case basis.)
Postdoctoral trainees are expected to enter the program with mastery of the basic principles and methods of epidemiology and biostatistics. They are required to take The Epidemiology of Substance Use and Related Problems in their first year (330.602), as well as required ethics courses. Postdoctoral trainees are encouraged to take courses in scientific writing and grant writing.
Global Mental Health Training (GMH) Program
The Global Mental Health Training (GMH) Program is a training program to provide public health research training in the field of Global Mental Health. It is housed in the Department of Mental Health , in collaboration with the Departments of International Health and Epidemiology. The GMH Program is supported by a T32 research training grant award from the National Institute of Mental Health (NIMH). Dr. Judy Bass ( [email protected] ) is the training program director.
As part of this training program, trainees will undertake a rigorous program of coursework in epidemiology, biostatistics, public mental health and global mental health, field-based research experiences, and integrative activities that will provide trainees with a solid foundation in the core proficiencies of global mental health while giving trainees the opportunity to pursue specialized training in one of three concentration areas that are recognized as high priority: (1) Prevention Research; (2) Intervention Research; or (3) Integration of Mental Health Services Research.
Pre-doctoral trainees are required to take the required series in epidemiology and biostatistics and department of mental health required courses. In addition, they must take three courses that will enhance skills and content expertise in global mental health: 330.620 Qualitative and Quantitative Methods for Mental Health and Psychosocial Research in Low Resource Settings, 224.694 Mental Health Intervention Programming in Low and Middle Income Countries, and 330.680 Promoting Mental Health and Preventing Mental Disorder in Low and Middle Income Countries.
The Mental Health Services and Systems (MHSS) Program
The Mental Health Services and Systems (MHSS) program is an NIMH-funded T32 training program run jointly by the Department of Mental Health and the Department of Health Policy and Management and also has a close affiliation with the Johns Hopkins School of Medicine. Drs. Elizabeth Stuart ( [email protected] ) and Ramin Mojtabai ( [email protected] ) are the training program co-directors.
The goal of the MHSS Program is to train scholars who will become leaders in mental health services and systems research. This program focuses on producing researchers who can address critical gaps in knowledge with a focus on: (1) how healthcare services, delivery settings, and financing systems affect the well-being of persons with mental illness; (2) how cutting-edge statistical and econometric methods can be used in intervention design, policies, and programs to improve care; and (3) how implementation science can be used to most effectively disseminate evidence-based advances into routine practice. The program strongly emphasizes the fundamental principles of research translation and dissemination throughout its curriculum.
Pre-doctoral trainees in the MHSS program are expected to take a set of core coursework in epidemiology and biostatistics, 5 core courses related to the core elements of mental health services and systems (330.662: Public Mental Health, 330.664: Introduction to Mental Health Services, 140.664: Causal Inference in Medicine and Public Health, 550.601: Implementation Research and Practice, and 306.665: Research Ethics and Integrity), and to specialize in one of 3 tracks: (1) health services and economics; (2) statistics and methodology; or (3) implementation science applied to mental health. Trainees are also expected to participate in a biweekly training grant seminar every year of the program and take a year-long practicum course exposing them to real-world mental health service systems and settings.
For more details see this webpage: http://www.jhsph.edu/research/centers-and-institutes/center-for-mental-health-and-addiction-policy-research/training-opportunities/
Epidemiology and Biostatistics of Aging
This program offers training in the methodology and conduct of significant clinical- and population-based research in older adults. This training grant, funded by the National Institute on Aging, has the specific mission to prepare epidemiologists and biostatisticians who will be both leaders and essential members of the multidisciplinary research needed to define models of healthy, productive aging and the prevention and interventions that will accomplish this goal. The Associate Director of this program is Dr. Michelle Carlson ( [email protected]) .
The EBA training grant has as its aims:
- Train pre- and post-doctoral fellows by providing a structured program consisting of: a) course work, b) seminars and working groups, c) practica, d) directed multidisciplinary collaborative experience through a training program research project, and e) directed research.
- Ensure hands-on participation in multidisciplinary research bringing trainees together with infrastructure, mentors, and resources, thus developing essential skills and experience for launching their research careers.
- Provide in-depth knowledge in established areas of concentration, including a) the epidemiology and course of late-life disability, b) the epidemiology of chronic diseases common to older persons, c) cognition, d) social epidemiology, e) the molecular, epidemiological and statistical genetics of aging, f) measurement and analysis of complex gerontological outcomes (e.g, frailty), and g) analysis of longitudinal and survival data.
- Expand the areas of emphasis to which trainees are exposed by developing new training opportunities in: a) clinical trials; b) causal inference; c) screening and prevention; and d) frailty and the integration of longitudinal physiologic investigation into epidemiology.
- Integrate epidemiology and biostatistics training to form a seamless, synthesized approach whose result is greater than the sum of its parts, to best prepare trainees to tackle aging-related research questions.
These aims are designed to provide the fields of geriatrics and gerontology with epidemiologists and biostatisticians who have an appreciation for and understanding of the public health and scientific issues in human aging, and who have the experience collaborating across disciplines that is essential to high-quality research on aging. More information can be found at: https://coah.jhu.edu/graduate-programs-and-postdoctoral-training/epidemiology-and-biostatistics-of-aging/ .
Aging and Dementia Training Program
This interdisciplinary pre- and post-doctoral training program is an interdisciplinary program, funded by the National Institute on Aging, affiliated with the Department of Neurology and the Department of Psychiatry at the School of Medicine, the Department of Mental Health at the School of Public Health and the Department of Psychology and Brain Sciences at the School of Arts and Sciences. The Department of Mental Health contact is Dr. Michelle Carlson ( [email protected] ). The goal of this training program is to train young investigators in age-related cognitive and neuropsychiatric disorders.
Program Requirements
Course location and modality is found on the BSPH website .
Residence Requirements
All doctoral students must complete and register for four full-time terms of a regular academic year, in succession, starting with Term 1 registration in August-September of the academic year and continuing through Term 4 ending in May of that same academic year. Full-time registration entails a minimum of 16 credits of registration each term and a maximum of 22 credits per term.
Full-time residence means more than registration. It means active participation in department seminars and lectures, research work group meetings, and other socializing experiences within our academic community. As such, doctoral trainees are expected to be in attendance on campus for the full academic year except on official University holidays and vacation leave.
Course Requirements
Not all courses are required to be taken in the first year alone; students typically take 2 years to complete all course requirements.
Students must obtain an A or B in all required courses. If a grade of C or below is received, the student will be required to repeat the course. An exception is given if a student receives a C (but not a D) in either of the first two terms of the required biostatistics series, but then receives a B or better in both of the final two terms of the series; then a student will not be required to retake the earlier biostatistics course. However, the student cannot have a cumulative GPA lower than 3.0 to remain in good academic standing. Any other exceptions to this grade requirement must be reviewed and approved by the departmental CAS and academic adviser.
Below are the required courses for the PhD; further Information can be found on the PhD in Mental Health webpage.
BIOSTATISTICS
Must be completed to be eligible to sit for the departmental written comprehensive exams.
EPIDEMIOLOGY
Department of mental health courses.
For Department of Mental Health doctoral students, a research paper is required entailing one additional course credit. PH.330.840 Special Studies and Research Mental Health listing Dr. Eaton as the mentor.
COURSE REQUIREMENTS OUTSIDE THE DEPARTMENT OF MENTAL HEALTH
The School requires that at least 18 credit units must be satisfactorily completed in formal courses outside the student's primary department. Among these 18 credit units, no fewer than three courses (totaling at least 9 credits) must be satisfactorily completed in two or more departments of the Bloomberg School of Public Health. The remaining outside credit units may be earned in any department or division of the University. This requirement is usually satisfied with the biostatistics and epidemiology courses required by the department.
Candidates who have completed a master’s program at the Bloomberg School of Public Health may apply 12 credits from that program toward this School requirement. Contact the Academic Office for further information.
SCHOOL-WIDE COURSES
Introduction to Online Learning taken before the first year.
ETHICS TRAINING
PH.550.860 Academic & Research Ethics at BSPH (0 credit - pass/fail) required of all students in the first term of registration.
Responsible Conduct of Research (RCR) connotes a broad range of career development topics that goes beyond the more narrowly focused “research ethics” and includes issues such as conflict of interest, authorship responsibilities, research misconduct, animal use and care, and human subjects research. RCR training requirements for JHPSH students are based on two circumstances: their degree program and their source of funding, which may overlap.
- All PhD students are required to take one of two courses in Responsible Conduct of Research, detailed below one time, in any year, during their doctoral studies.
- All students, regardless of degree program, who receive funding from one of the federal grant mechanisms outlined in the NIH notice below, must take one of the two courses listed below to satisfy the 8 in-person hours of training in specific topic areas specified by NIH (e.g., conflict of interest, authorship, research misconduct, human and animal subject ethics, etc.).
The two courses that satisfy either requirement are:
- PH.550.600 Living Science Ethics - Responsible Conduct of Research [1 credit, Evans]. Once per week, 1st term.
- PH.306.665 Research Ethics and integrity [3 credits, Kass]. Twice per week, 3rd term.
Registration in either course is recorded on the student’s transcript and serves as documentation of completion of the requirement.
- If a non-PhD or postdoctoral student is unsure whether or not their source of funding requires in-person RCR training, they or the PI should contact the project officer for the award.
- Students who have conflicts that make it impossible for them to take either course can attend a similar course offered by Sharon Krag at Homewood during several intensive sessions (sequential full days or half days) that meet either on weekends in October or April, a week in June, or intersessions in January. Permission is required. Elizabeth Peterson ( [email protected] ) can provide details on dates and times.
- Students who may have taken the REWards course (Research Ethics Workshops About Responsibilities and Duties of Scientists) in the SOM can request that this serve as a replacement, as long as they can provide documentation of at least 8 in-person contact hours.
- Postdoctoral students are permitted to enroll in either course but BSPH does not require them to take RCR training. However, terms of their funding might require RCR training and it is their obligation to fulfill the requirement.
- The required Academic Ethics module is independent of the RCR training requirement. It is a standalone module that must be completed by all students at the Bloomberg School of Public Health. This module covers topics associated with maintaining academic integrity, including plagiarism, proper citations, and cheating.
PhD in Mental Health
Department of Mental Health candidates for the degree Doctor of Philosophy (PhD) must fulfill all University and School requirements. These include, but are not limited to, a minimum of four consecutive academic terms at the School in full-time residency (some programs require 6 terms), continuous registration throughout their tenure as a PhD student, satisfactory completion of a Departmental Written Comprehensive Examination, satisfactory performance on a University Preliminary Oral Examination, readiness to undertake research, and preparation and successful defense of a thesis based upon independent research.
PhD Students are required to be registered full-time for a minimum of 16 credits per term and courses must be taken for letter grade or pass/fail. Courses taken for audit do not count toward the 16-credit registration minimum.
Students having already earned credit at BSPH from a master's program or as a Special Student Limited within the past three years for any of the required courses may be able to use them toward satisfaction of doctoral course requirements.
For a full list of program policies, please visit the PhD in Mental Health page where students can find more information and links to our handbook.
Completion of Requirements
The University places a seven-year maximum limit upon the period of doctoral study. The Department of Mental Health students are expected to complete all requirements in an average of 4-5 years.
Learning Outcomes
The PhD program is designed to provide key knowledge and skill-based competencies in the field of public mental health. Upon successful completion of the PhD in Mental Health, students will have mastered the following competencies:
- Evaluate the clinical presentations, incidence, prevalence, course and risk/protective factors for major mental and behavioral health disorders.
- Differentiate important known biological, psychological and social risk and protective factors for major mental and behavioral disorders and assess how to advance understanding of the causes of these disorders in populations.
- Evaluate and explain factors associated with resiliency and recovery from major mental and behavioral disorders.
- Evaluate, select, and implement effective methods and measurement strategies for assessment of major mental and behavioral disorders across a range of epidemiologic settings.
- Critically evaluate strategies for the prevention and treatment of major mental and behavioral disorders as well as utilization and delivery of mental health services over the life course, across a range of settings, and in a range of national contexts.
- Assess preventive and treatment interventions likely to prove effective in optimizing mental health of the population, reducing the incidence of mental and behavioral disorders, raising rates of recovery from disorders, and reducing risk of later disorder recurrence.
According to the requirements of the Council on Education for Public Health (CEPH), all BSPH degree students must be grounded in foundational public health knowledge. Please view the list of specific CEPH requirements by degree type .
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Research disruption during PhD studies and its impact on mental health: Implications for research and university policy
Contributed equally to this work with: Maria Aristeidou, Angela Aristidou
Roles Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Institute for Educational Technology, The Open University, Milton Keynes, Buckinghamshire, United Kingdom
Roles Conceptualization, Investigation, Resources, Writing – original draft, Writing – review & editing
Affiliation UCL School of Management, London, United Kingdom
- Maria Aristeidou,
- Angela Aristidou

- Published: October 18, 2023
- https://doi.org/10.1371/journal.pone.0291555
- Reader Comments
Research policy observers are increasingly concerned about the impact of the disruption caused by the Covid-19 pandemic on university research. Yet we know little about the effect of this disruption, specifically on PhD students, their mental health, and their research progress. This study drew from survey responses of UK PhD students during the Covid-19 pandemic. We explored evidence of depression and coping behaviour (N = 1780) , and assessed factors relating to demographics, PhD characteristics, Covid-19-associated personal circumstances, and significant life events that could explain PhD student depression during the research disruption (N = 1433) . The majority of the study population (86%) reported a negative effect on their research progress during the pandemic. Results based on eight mental health symptoms (PHQ-8) showed that three in four PhD students experienced significant depression. Live-in children and lack of funding were among the most significant factors associated with developing depression. Engaging in approach coping behaviours (i.e., those alleviating the problem directly) related to lower levels of depression. By assessing the impact of research disruption on the UK PhD researcher community, our findings indicate policies to manage short-term risks but also build resilience in academic communities against current and future disruptions.
Citation: Aristeidou M, Aristidou A (2023) Research disruption during PhD studies and its impact on mental health: Implications for research and university policy. PLoS ONE 18(10): e0291555. https://doi.org/10.1371/journal.pone.0291555
Editor: Yadeta Alemayehu, Mettu University, ETHIOPIA
Received: January 23, 2023; Accepted: August 31, 2023; Published: October 18, 2023
Copyright: © 2023 Aristeidou, Aristidou. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The raw dataset on PhD students' patient health questionnaire scale and coping mechanisms is available from the Open Research Data Online (ORDO) database: https://doi.org/10.21954/ou.rd.22794203 .
Funding: This work was supported by the Institute of Educational Technology at The Open University (MA) and the University College London (UCL) School of Management (AA). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The abrupt outbreak in January 2020 and the global proliferation of a novel virus (Covid-19) has created a crisis for many sectors, including the international higher education (HE) sector [ 1 ] that continues during the ‘post-pandemic’ period. A point of particular alarm for HE leaders, policy observers, and governments is the disruption to the typical flow and pace of university research activity. While research related to Covid-19 is still in overdrive, other research was slowed or stopped due to worldwide physical distancing measures to contain the virus’ spread (e.g., sudden campus and laboratory closures, mobility restrictions, stay-at-home orders) [ 2 ]. The resulting ‘drop in research work’ is suggested to have a detrimental impact on the HE sector on the ‘research and innovation pipeline’ [ 3 ], and on ‘research capacity, innovation and research impact’ [ 4 ].
As research and university policies internationally are being (re)shaped at a rapid pace in efforts to meet the challenge of university research disruption [ 5 ], we contribute to academic and policy conversations by examining the effect of the research disruption on the mental health of PhD students. A considerable body of research acknowledges the role of PhD students in the innovation process, in knowledge creation and diffusion (e.g., [ 6 ]) and further posits that the period of one’s PhD program is key to early career success and research productivity (e.g., [ 7 ]). These outcomes, which matter to research policy, have been linked to PhD student mental health [ 8 – 10 ]. In those times of relative stability, research had additionally demonstrated the higher prevalence of mental health issues amongst the PhD student population across research disciplines, as compared to other students within academia [ 9 ] and the general population [ 9 , 11 , 12 ]. In the period since Covid-19 disrupted our social and economic lives, depression levels in the general population have been exacerbated globally [ 13 , 14 ]. These trends suggested that the already high prevalence of poor mental health in PhD students is likely to be further exacerbated during the pandemic. Indeed, as reported in early studies on research students’ experience of the Covid-19 pandemic (e.g., [ 15 ]) and the post-pandemic period (e.g., [ 16 ]) the impact on students’ mental wellbeing has been significant, with students suggesting a number of support measures at institutional and national level.
Ignoring, at this critical moment, the increased likelihood of poor mental health in PhD students may jeopardize research capacity and HE competitiveness for years to come. Therefore, there is a pressing need to identify–within the PhD student population–those whose mental health is more affected by the research disruption, so that policies and assistance can be timelier and more targeted. Additionally, by understanding more clearly the factors that may contribute to poor mental health, and their interrelationships (presented in Methods), policymakers and HE leaders may be better placed to tackle, and ultimately overcome, this and future research disruptions.
Motivated by the current lack of an empirical basis for insights into PhD students’ mental health during the pandemic-induced disruption, we collected survey data contemporaneously during July 2020. Our 1780 survey respondents are PhD students in 94 UK Universities, across the natural and social sciences and across PhD stages. Our study has three objectives: first, to explore mental health prevalence (depression) and coping behaviour in a large-scale representative sample of PhD students in the UK (O1); second, to evaluate the relationships among mental health prevalence and coping behaviour (O2); third, to identify factors that increase the likelihood of poor PhD student mental health during the period of research disruption (O3). Our study extends previous research on mental health in the HE sector by considering the dynamics of severe disruption, as opposed to the dynamics of relative stability, on PhD students’ mental health, performance satisfaction, and coping behaviours.
Background and literature review
Uk phd students’ mental health in times of disruption.
In the UK, there are approximately 100,000 postgraduate students completing doctoral research [ 17 ]. Since 2018, significant government funding has been targeted at developing insights into supporting UK PhD students’ mental health [ 18 ]. Still, with the exception of Byrom et al. [ 11 ], published research on PhD students’ mental health in the UK exhibits the same limitations as the international research: It reflects discipline- or institution-related specificity (e.g., [ 19 ]) or utilizes samples of early career researchers in general (e.g., [ 20 ]).
Early findings on postgraduate research students’ wellbeing during the pandemic showed that only a small proportion of them are in good mental health wellbeing (28%) while the rest demonstrate possible or probable depression or anxiety [ 15 ]. Goldstone and Zhang [ 15 ] further highlight the differences among student groups with, for example, students with disabilities or caring responsibilities or female students having lower levels of mental wellbeing. The post-pandemic findings have been more promising, as only about one in four students were at risk of experiencing mental health issues [ 16 ].
In response to the Covid-19 research disruption, substantive actions have been taken by the HE sector and the UK Government to disseminate approaches deployed by UK universities to support student mental health (e.g., [ 18 ]) and to update mental health frameworks for UK universities (e.g., [ 4 ]), but so far, mitigation activities have been targeting mental health for UK university students broadly, not UK PhD students specifically.
Overcoming the paucity of evidence on UK PhD students’ mental health during the pandemic is a crucial first step to drawing strong conclusions on the prevalence and determinants of mental health issues and ways to mitigate them specific to the PhD population. For example, policy recommendations by UK postgraduate respondents during the pandemic [ 15 ] focused mainly on financial support, such as extensions to their funded period of study and tuition and visa fee support (including waivers to fees). To develop an overarching framework specific to the Objectives of our study, we synthesize insights from the international literature on PhD student mental health conducted in the period before the research disruption.
International research on PhD student mental health in times of relative stability
In the international literature examining mental health specifically for PhD students (see the systematic review in [ 21 ], the issue of mental health for PhD students is acknowledged to be multidimensional and complex [ 10 ]. In this growing research area, some address mental health as an aspect of the broader ‘health’ of the PhD students (e.g., [ 22 ]), some focus on psychological distress [ 23 ], while others take depression as a specific manifestation of distress [ 9 , 24 ]. The latter is particularly interesting because depression within the PhD population in these studies is often assessed with standardised questionnaires (e.g., PHQ, see below) that allow for developing comparative insights. It is also the approach adopted by the only global survey of PhD students’ mental health by Evans et al. [ 12 ], showing that 39% of PhD students report moderate-to-severe depression, significantly more than the general population.
Literature on PhD student’s mental health determinants in times of relative stability
Past literature on PhD students’ mental health offers insights into the determinants of PhD students’ mental health in times of stability, which may help understand the relationships we want to examine between PhD mental health, performance satisfaction and coping in times of research disruption.
First, past studies evidence the influence of PhD students’ personal lives on poor mental health. PhD students with children or with partners are less likely to have or develop psychological distress [ 9 ]. The normalcy of family roles is a much-needed antidote to the known pressures of a PhD program [ 25 ] and might even protect against mental health problems [ 22 , 26 ]. Other aspects of PhD students’ personal lives, such as significant life events (e.g., severe problems in personal relationships or severe illness of the student or someone close to them), have been linked to dissatisfaction with their research progress [ 24 ]. Research progress is defined as students’ perception of their progress in the completion of their degree [ 27 ] and is linked to their mental health. Dissatisfaction is tied to negative outcomes, such as attrition and delay [ 28 ], but also to lower productivity and mental health problems, such as worry, anxiety, exhaustion, and stress [ 29 ]. Related to this, Levecque and colleagues [ 9 ] observed that PhD students expressing a high interest in an academic career are in better mental health than those with no or little interest in remaining in academia.
Second, gender was the key personal factor that emerged as a determinant for mental health in past studies: PhD students who self-identify as female report greater clinical [ 9 , 30 ] and non-clinical problems with their mental health [ 23 , 31 ]. This is explained through the additional pressure women report on their professional and personal lives [ 23 ].
Third, past studies argue that each PhD phase presents PhD students with specific sets of challenges and should thus be explored discreetly in relation to mental health [ 32 ]. Still, the evidence on the link between the PhD phase (or the year of study as a proxy for the PhD phase) and mental health is inconclusive. Barry et al.’s [ 33 ] survey reports no connection between the PhD phase and depression levels in an Australian PhD population. However, Levecque et al. [ 9 ] report high degrees of depression in the early PhD stage of students in Belgium, and a global survey of PhD students across countries and disciplines shows that depression likelihood increases as the PhD program progresses [ 32 ].
Fourth, past research offers strong evidence that financial concerns impact PhD students’ mental health negatively. In a study by El-Ghoroury et al. [ 34 ], 63.9% of PhD students cited debt or financial issues as a cause for poor wellbeing and cited financial constraints as the major barrier to improving their wellness (through social interactions, outside-PhD activities, etc). Even uncertainty about funding was shown to predict poor mental health [ 9 ]. To this end, Geven et al. [ 35 ] explored packages of reforms in a pre-pandemic graduate school programme, including an extension of the grant period, and indicated that such policies can increase students’ completion rates to up to 20%.
Finally, age is not shown to be associated with mental health [ 9 ], but numerous studies found that having children, particularly for female PhD students and in Science-Technology-Engineering-Maths (STEM) disciplines [ 36 ], consistently corresponds with heightened stress [ 37 ]. However, a specific examination of the relationship between children and mental health indicates that PhD students with one or more children in the household showed significantly lower odds of having or developing a common psychiatric disorder [ 9 ]. Further, parenting and, in particular, motherhood during doctorate studies contribute to the development of students’ coping mechanisms that allows them to succeed in a balance in both worlds [ 38 ].
Past research insights into PhD mental health and coping
Past research explored how PhD students may “cope” with stressors and thus mitigate poor mental health [ 39 ]. Studies identify the importance of social interactions (e.g., [ 22 ]); balancing life demands (e.g., [ 16 ]), reaching out for social support (e.g., [ 40 ]) sometimes through peer relationships (e.g., [ 10 , 39 ]); and ‘planning’ (e.g., [ 22 ]); As invaluable as these insights are, drawing comparisons between these findings is difficult because often the identification of coping styles or strategies was not the focus of these studies, making it difficult to draw fine-grained conclusions as to their effect on PhD students’ mental health.
There is, however, a long tradition of research on coping for physiological wellbeing that provides standardised measures for individuals’ coping and their link to mental health [ 41 ]. The most widely used measurement instrument in the literature reviewed is the COPE Inventory, which allows researchers to assess how people cope in a variety of stressful situations, including in HE for students [ 42 – 44 ], making it particularly relevant to the context and sample under investigation in our study of PhD students. Additionally, COPE allows for the identification of consistent ways of coping, which provides predictive validity across a range of situations. Predictive validity is desired when examining the role of coping in relation to mental health. Indeed, multiple studies have linked the COPE measurement to mental health outcomes (e.g., [ 45 , 46 ]), including depression [ 43 ], which is a focus of our study.
Data and methods
Participants.
For the current study, we recruited participants that were active PhD students from March to July 2020 at any stage of their research to take part in an online survey. The survey ran between the 31st of July and the 23rd of August 2020, with the aim of capturing the potential impact of the Covid-19 disruption during the first lockdown on their research progress and mental health. The use of online surveys to assess the scope of mental health problems is particularly appropriate during the Covid-19 outbreak [ 47 ]. The current study has been reviewed by, and received a favourable opinion, from The Open University Human Research Ethics Committee (reference number: HREC/3605/Aristeidou), http://www.open.ac.uk/research/ethics/ . For the recruitment of a diverse audience, we followed a snowball sampling method, forwarding our invitation to PhD student groups in a number of UK-based universities, but also exploited the reach of PhD social media channels and online PhD groups, and we invited academics and respondents to recruit other participants. Vouchers were provided as an incentive for participation to the first 300 respondents. Before completing the survey, the respondents were provided with an online information sheet and were asked to provide their written consent through a digital consent form. They reported their email addresses to be identifiable and contactable for validation, consent issues, potential withdrawal, and incentive processing. The dataset was anonymized on the 30th of August 2020, prior to initiating data analysis.
Exclusion criteria included survey respondents who ‘straight-lined’ (chose the same answer option repeatedly), gave inconsistent responses to similar questions, or did not use their institution emails (rendering them unidentifiable). Finally, there were 1790 PhD students in the study from 94 different HE institutions across all four UK nations (England, Scotland, Northern Ireland and Wales). The majority of the study population (86%) reported that their research progress had been impacted in a negative way. The dataset [ 48 ] included 44.4% male and 55.4% female participants, while the doctoral students in the UK consist of 51% male and 49% female students [ 17 ]. Weighting adjustments were made to correct the sample representativeness. The majority of the survey respondents were 25–34 years old (80.4%), with live-in children (71%). Most respondents (86.7%) were conducting their PhDs full-time, and almost two-thirds (64.4%) were funded by a research council or a charitable body in the UK. At the time of the survey, a large proportion of the survey respondents were in the ‘executing’ phase of their research (i.e., data collection/analysis). Finally, a natural science-related PhD was being pursued by slightly over two-thirds of the respondents (68.8%). According to data sourced from HESA [ 17 ], the likelihood of individuals embarking on a research postgraduate degree at a younger age (such as 18–20) appears to be relatively low. This is evident from the fact that only 90–130 students within this age group register for such programs each year. More details on the demographics and characteristics of the sample can be found in Table 1 and below.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0291555.t001
Variables and instruments
Brief cope inventory (bci)..
The BCI [ 49 ] is a 28-item self-report questionnaire designed to measure effective and ineffective ways to cope with a stressful life event, and it is the abbreviated version of the original 60-item COPE inventory developed by [ 42 ]. The BCI has a 4-point Likert scale with options on each item ranging from 0 (I usually do not do this at all) to 3 (I usually do this a lot). Coping in this study is categorised in two overarching coping behaviours, as per Eisenberg et al. [ 50 ]: (a) the approach behaviours that attempt to reduce stress by alleviating the problem directly, which include 12 items related to active coping, positive reframing, planning, acceptance, seeking emotional support, and seeking informational support; and (b) the avoidant coping behaviours that attempt to reduce stress by distancing oneself from the problem, which include 12 items related to denial, substance use, venting, behavioural disengagement, self-distraction, and self-blame. Items that belong to neither overarching behaviour are coping related to humour and religion. These were included in the overall coping score but excluded from the analysis based on the two overarching behaviours. A higher score indicates frequent use of that coping behaviour. Cronbach’s alpha for the BCI was .88. Further, both the approach and avoidant scales have shown very good internal consistency in this sample, with Cronbach’s alpha equal to 0.83 and 0.80, respectively.
Patient health questionnaire eight-item depression scale (PHQ-8).
PHQ-8 [ 57 ] is an eight-item version of the Patient Health Questionnaire (PHQ-9). PHQ is a popular measure for assessing depression and is frequently used for PhD mental health (e.g., [ 12 , 51 ]), making it an ideal choice for our study. PHQ-9 has been validated as both a diagnostic and severity measure [ 52 , 53 ] in population-based settings [ 54 ] and self-administered modes [ 55 , 56 ], and it was recently used in a global survey of PhD students’ depression prevalence [ 12 ]. PHQ-8 omits the ninth question that assesses suicidal or self-injurious thoughts, and it was deemed more appropriate for our research because researchers in web-based interviews/surveys are unable to provide adequate interventions remotely. The PHQ-8 items employ a 4-point Likert scale with options on each item ranging from 0 (not at all) to 3 (nearly every day). Then, the scores are summed to give a total score between 0 and 24 points, where 0–4 represent no significant depressive symptoms, 5–9 mild depressive symptoms, 10–13 moderate, 15–19 moderately severe, and 20–24 severe [ 55 ]. Evidence from a large-scale validation study [ 57 ] indicates that a PHQ-8 score ≥ 10 represents clinically significant depression. In this study, Cronbach’s alpha for the PHQ-8 was 0.71, indicating a good internal consistency.
Performance satisfaction.
Performance satisfaction is an 8-item self-report scale designed to measure the students’ self-perceived progress in their PhD research, their confidence in being able to finish on time, and their satisfaction. The scale was successfully used in a PhD student well-being study at the university of Groningen [ 24 ] prior to the Covid-19 pandemic. The performance satisfaction 5-point Likert scale responses range from 1 (completely disagree) to 5 (completely agree). The score for each respondent equals the mean score of the 8-item responses. A reliability analysis was carried out on the performance satisfaction scale. Cronbach’s alpha showed the scale to reach acceptable reliability, α = 0.86.
Significant life events Significant Life events is a questionnaire designed to capture whether PhD students had experienced any significant life events in the 12 months prior to the survey. This was successfully used in studying PhD students’ mental health at the university of Groningen [ 24 ] prior to the Covid-19 pandemic research disruption. Events include the death of someone close, severe problems in personal relationships, financial problems, severe illness of oneself or someone close, being in the process of buying a house, getting married, expecting a child, none of these events, and prefer not to say. Significant life events were used as an incident control variable in this study.
Statistical analyses
SPSS (Version 25) was used for statistical analysis. In the first phase, descriptive statistics were used to describe the PHQ-8 Depression and coping behaviours of the sample and the distribution of these three variables among demographics, PhD characteristics, and Covid-19-related circumstances (O1). We used a weighting adjustment for gender to correct the survey representativeness for descriptive analysis; females were given a ‘corrective’ weight of 0.88 and males of 1.15.
In relation to O2, Spearman rank correlations were used to examine the degree of association between all of the 28 coping behaviours and PHQ-8 Depression scores. This finding contributed to our understanding of how individual coping behaviours could relate to lower or higher depressive symptoms.
To assess whether the behaviours significant to our study (i.e., those with a negative or the strongest positive PHQ-8 Depression association) were used more frequently by students of a particular demographic group (O2), we used independent-samples t-test and ANOVA. Before assessing the relationship between our variables, outliers, and groups with a sample size smaller than 15 for each group were removed from the tests (e.g., Gender = other; Funding = partially funded; Likelihood in HE = already employed in academia).
In relation to O3, a binary logistic regression analysis was performed to examine whether Covid-19-related circumstances explain significant depression in PhD students, while controlling for demographics, PhD characteristics, and external incidents. Prior to performing the regression analysis, PHQ-8 Depression score outliers, as well as groups with fewer than 10 events per variable (e.g., gender = other; age = 55–64; Impact reason = mental health), were detected and excluded from the dataset. The dichotomous dependent variable was calculated based on PHQ-8 Depression scores smaller than 10 for non-significant depression, and equal or larger than 10 for significant depression. Associations between Depression in PhD students and the independent variables in our dependency model were estimated using odds ratios (ORs) as produced by the logistic regression procedure in SPSS (Version 25). The ORs were used to explain the strength of the presence or absence of significant depression. Wald tests were used to assess the significance of each predictor. A test of the full model against a constant only model was statistically significant, indicating that the predictors as a set reliably distinguished between PhD students who are having or developing significant depression and those who are not ( Χ 2 (25) = 405.258, p < . 001 ). A Nagelkerke R 2 of .798 indicated a good to substantial relationship between prediction and grouping (68% of variance explained by the proposed model in completion rates). Table 2 presents response percentages about the categorical variables entered in the model, including the two dependent variables (significant depression and non-significant depression).
https://doi.org/10.1371/journal.pone.0291555.t002
Exploring depression prevalence and coping behaviours
The average PHQ-8 Depression score was 10.13 ( SD = 3.23) on a scale of 0–24 (weighted cases). Importantly, this highlights that the majority of survey respondents are facing moderate depression symptoms ( Fig 1 ). The PHQ-8 item with the highest score, in a range of 0–4, was ‘having trouble to concentrate on things, such as reading the newspaper or watching television’ ( M = 1.45; SD = 0.84), and the item with the lowest score was ‘moving or speaking so slowly that other people could have noticed; or the opposite–being so fidgety or restless that have been moving around a lot more than usual’ ( M = 1.10; SD = 0.75). Of the study population, 75% self-reported significant depression (moderate, moderately severe, or severe major).
https://doi.org/10.1371/journal.pone.0291555.g001
The coping behaviours that the majority of PhD students used in a medium or large amount to overcome the Covid-19 disruption were “accepting the reality of the fact that it has happened” (84%), followed by “thinking hard about what steps to make” (76%) ( Fig 2 ). Both are approaching coping behaviours. Other coping behaviours used to a great extent were “praying or meditating” (73%) , “blaming myself for things that happened” (avoidant) (71%) , and “expressing my negative feelings” (avoidant) (69%). On the other hand, coping behaviours that were used the least were all avoidant ones: “giving up attempting to cope” ( 13%) , “refusing to believe that it has happened” (15%) , “using alcohol or other drugs to make myself feel better” (17%) , and “giving up trying to deal with it” (17%) . Overall, approach coping behaviours were used to a greater extent ( M = 26.43, SD = 5.15) than avoidant coping behaviours ( M = 23.97, SD = 4.90).
https://doi.org/10.1371/journal.pone.0291555.g002
The Spearman correlations between coping behaviours and PHQ-8 scores ( Table 3 ), which included outliers, suggested that only two items have significant negative (very weak) associations with depression: Item 15, “getting comfort and understanding from someone” ( r s (1780) = -.107, p < .01); and Item 7, “taking action to try to make the situation better” ( r s (1762) = -.077, p < .01). The majority of the coping behaviours had a significant positive relationship with higher scores in depressive symptoms. The coping behaviours with the largest effect and a moderate to strong association were Item 13, “criticizing myself” ( r s (1762) = .452, p < .01), followed by Item 11 “using alcohol or other drugs to help me go through it” ( r s (1762) = .387, p < .01).
https://doi.org/10.1371/journal.pone.0291555.t003
Table 4 shows the relationship among approach and avoidant coping behaviours, and demographics. Our analyses indicated that both approach and avoidant coping behaviours had been significantly used to a greater extent by the female over male PhD students, by students without a live-in partner than those with a live-in partner, and by those without live-in children than those with live-in children. There is no evidence that the students of a particular age group were using avoidant coping more than those of another age group. However, students aged 25–34 were using approach coping behaviours less than other groups, and those aged 45–54 more ( Table 5 ).
https://doi.org/10.1371/journal.pone.0291555.t004
https://doi.org/10.1371/journal.pone.0291555.t005
Our analyses indicated that female PhD students, who had significantly lower PHQ-8 Depression scores, were using Table 3 ‘s Items 15 ( t [1778] = 14.61, p < .001) and Item 7 ( t [480] = 15.11, p < .001) significantly more than male students. Also, those without live-in partners were getting comfort and understanding from someone to a significantly greater extent than those without ( t [702] = 20.09, p < .001). PhD students without live-in children were taking action to try to make the situation better significantly more than those who have them ( t [894] = 25.21, p < .001).
Predictors of depression and relative influence
Covid-19-related circumstances (receiving an extension, impact reasons, and impact results), performance satisfaction, and coping behaviours (approach and avoidant) were entered together as predictors of depression. Demographics (gender, age, live-in partner, and live-in children), PhD characteristics (discipline, PhD phase, PhD mode, funding, interest in HE, and likelihood in HE) and external incidents were used as control variables. Table 6 reports the findings of the analyses.
https://doi.org/10.1371/journal.pone.0291555.t006
Prediction success overall was 95.3% (83.1% for not significant depression and 98.0% for significant depression). The Wald criterion demonstrated that not having an extension ( p = .014), having caring responsibilities ( p < .001), and using approach ( p < .001) or avoidant ( p < .001) coping behaviours made significant contributions to prediction. The OR value indicated that in the case that PhD students were not receiving an extension amid the Covid-19 disruption, or they did not know whether they were receiving one yet, they were 5.4 times more likely to experience significant depression. For the impact reason, our findings showed that–compared to those who experienced personal illness–PhD students who had caring responsibilities (e.g., childcare or other) showed slightly lower depressive symptoms (OR = 0.10). The OR for approach and avoidant coping behaviours were 0.13 and 43.73, respectively. This finding indicates that when approach coping is raised by one unit (e.g., +1 to the score), we see evidence for better mental health, while when avoidant coping is raised by one unit, a PhD student is very likely (44 times) to experience significant depression.
Turning to our control variables, PhD students with children in the household and with live-in partners showed significantly higher odds (about 14 and 7 times more, respectively) of having or developing depressive symptoms than those without. The latter can be explained by the fact that 88% of the participants with live-in partners also reported having live-in children. Also, male students were slightly more likely than female students to experience significant depression (with a borderline p-value), but this might be explained by the significantly increased use of coping approaches by female students. This gender-related finding that shows nearly no difference between the two categories slightly differs from Goldstone and Zhang’s model [ 15 ] which highlights a difference between female and male participants’ mental wellbeing. This difference can be explained by the fact that the research instruments used in the two studies were different, as well as the survey period.
Some PhD characteristics that made significant contributions to prediction were the discipline of PhD studies and the interest of students to remain in academia after finishing their PhD projects. The risk of experiencing significant depression in PhD students in social sciences (OR = 9.68) was lower than in students conducting a PhD in natural sciences. In contrast to findings by Levecque et al. [ 9 ], we observed that PhD students expressing a high interest in an academic career were 3.5 times more likely to develop depressive symptoms than those with no or only little interest in remaining in academia. Further, those considering having a high likelihood of remaining in academia were slightly more depressed (OR = 3.73), as well as those who were in the executing phase of their PhD research (OR = 3.33). No differences between funded and self-funded students were detected. Finally, the OR for the external incident variable was 6.13, indicating that for each incident unit (e.g., one more incident), we see evidence for depressive symptoms that are six times worse.
Our study contributes new empirical data and new insights needed to develop knowledge on the effect of university research disruption on the PhD student population. In turn, new knowledge may provide the evidence base for university and research policy.
Exploring mental health and coping behaviours
Our first contribution is to provide empirical estimates for the performance satisfaction, prevalence of mental health problems, and coping behaviours of PhD students during the pandemic-induced research disruption, on the basis of representative data across disciplines and across universities in the UK.
Our findings show that most UK PhD students across universities and disciplines report that their research progress has been affected negatively (86%). By contrast, in pre-pandemic periods, 79% of UK PhD students across Universities and disciplines had indicated excellent research progress [ 11 ]. This shift within the same population is important to reveal because of its potential implications for PhDs’ careers and university research capacity and innovation, as we know that dissatisfaction about the PhD trajectory is tied to negative outcomes such as attrition and delay [ 24 , 28 ], but also to lower productivity [ 58 ].
We found that during the period of severe research disruption caused by the Covid-19 pandemic, 75% of the UK students surveyed from 94 universities and across disciplines self-reported in the moderate-severe range for depression. This is at least three times more compared to the reported prevalence of depression among the general population internationally during the Covid-19 outbreak (16–28%, [ 59 ]). Our findings are also in line with findings in Goldstone and Zhang’s study [ 15 ] on UK postgraduate students’ mental wellbeing during the pandemic, in which 72% of the surveyed students were found to demonstrate possible or probable depression or anxiety.
By adopting widely used standardised questionnaires, our findings provide an accessible benchmark for the comparison with studies that took place among PhD student populations in periods of HE stability (pre-2020), thereby providing the empirical basis to accurately estimate the issue of poor mental health among PhD students during a period of research disruption. Using the same questionnaire as in our survey (PHQ-9) and drawing on a sample of PhD students from multiple universities and across research disciplines, a pre-pandemic global survey reported that 39% of PhD students scored in the moderate-severe range for depression [ 12 ]. Pre-pandemic national surveys of PhD students across institutions and disciplines report similar rates of depression, between 32% (in Belgium, Levecque et al. [ 9 ] and 38% (in the Netherlands, Van der Weijden et al. [ 60 ]. In a pre-pandemic (2018–2019) survey of UK PhD students across 48 universities and disciplines, only 25% reported levels that would indicate probable depression or anxiety [ 11 ]. These comparisons indicate that the prevalence of depression among the UK PhD student population of our study during the pandemic-induced period of research disruption is two-to-three times more than that which was reported in periods of stability for the UK PhD student population, for PhD student populations of other countries, and the global PhD population.
Our findings on PhD students’ mental health and PhD students’ coping advance past literature [ 22 , 23 , 34 ] in two significant ways. First, by using a highly reliable coping measure (COPE), we are able to demonstrate the relationship between coping styles and mental health outcomes in PhD students in a way that allows for comparisons and to build further research in this area. Second, we identify specific coping behaviours amongst the UK PhD students that are associated with lower depression scores and some that have a negative association with depression (i.e., getting comfort and understanding from someone and taking action to try to make the situation better ). Both are ‘coping approach’ behaviours (i.e., attempts to reduce stress by alleviating the problem directly; [ 50 ]). Studies using COPE in other populations have also linked coping-approach behaviours to fewer symptoms of psychological distress [ 45 ], more physical and psychological well-being at work [ 46 ], and an absence of anxiety and depression [ 61 ].
Factors explaining PhD students’ depression
Our second contribution is to explain–within the UK PhD population–whose mental health is more affected by the pandemic-induced research disruption. We find that several factors have a significant impact on PhD students to have or develop mental health issues during a period of research disruption.
Consistent with past research on PhD students’ mental health, our findings reveal the significant influence of their personal lives on poor mental health. The relationships we observed during a period of research disruption, however, differ from those suggested in studies conducted in periods of stability (e.g., [ 9 , 22 , 25 , 26 , 62 ]). We found that PhD students with live-in children or with a live-in partner and PhDs with caring responsibilities are more likely to have or develop significant depression compared to those without. This difference can be explained by the closure of schools that resulted in parents home-schooling their children, a greater demand for devices and the internet in households, and parents going through emotional hardship [ 63 ]. We additionally find six times worse depressive symptoms for each ‘external life incident’ (e.g., childbirth, moving home) that occurred in the PhD students’ lives. A larger number of external incidents were found to be associated with students with live-in partners and students with live-in children, which may explain these as reinforcing negative effects. These new insights explain that–although most of these realities in PhD students’ personal lives existed besides the research disruption—when combined with the research disruption, their mental health can spiral downward.
Our findings also address the role of structural PhD characteristics (PhD discipline and PhD phase) in predicting whether a student might present mental health issues in times of research disruption. We find that in a period of research disruption, the risk of significant depression is higher in the execution phase of the PhD compared to the beginning or extension phases, contrary to Levecque and colleagues’ findings [ 9 ]. Because there is very limited research on the PhD stage and mental health, our findings contribute insights to a broader community of scholars who advocate for the further study of the challenges in each PhD stage discreetly (e.g., [ 32 ]). Furthermore, we find that the risk of experiencing significant depression in PhD students in social sciences was lower than students conducting a PhD in natural sciences. Our survey respondents offered explanations on the role of PhD discipline in mental health during the pandemic in the open text responses. These converge on the fact that natural sciences often require being physically in a laboratory, which is probably unfeasible when university facilities are closed.
In tune with past research on finances and mental health in PhD students [ 9 , 64 ], we found those without funded extensions are more likely to have or develop significant depression (moderate, moderately severe, and severe) compared to those with them. We reveal the size of this association (about 5.5 times more) and link PhD funding extensions to standardized assessments of depression prevalence, thus uniquely providing new evidence for policy scholars.
Implications for research and higher education policy
Our findings show an alarming increase in self-reported depression levels among the UK PhD student population. The long-term mental health impact of Covid-19 may take years to become fully apparent, and managing this impact requires concerted effort not just from the healthcare system at large [ 59 ] but also from the HE sector specifically. With mental illness a cause for PhD student attrition, loss of research capacity and productivity, data from our survey should prompt consideration of immediate intervention strategies.
For research and education policy scholars, our findings contribute directly to the development of evidence-based research and university policies on support for targeted groups of PhD students in times of disruption. Specifically, our findings show that institutional and funder support should not only be in the form of PhD-funded extensions–which are nevertheless shown in our study and other studies (e.g., [ 15 ]) to be very significant. But also, in the form of providing expedited alternatives to the changes evoked by the pandemic for PhD students, such as new and adjusted policies that explicitly consider those PhDs with caring responsibilities, since 77% of our respondents reported that childcare and other caring responsibilities are the reason for dissatisfaction with their PhD progress. If not, the Covid-19 research disruption could erase decades of progress towards equality in academia [ 65 ].
Our main contribution is that we offer insights into how to mitigate mental health consequences for PhD students in times of research disruption. Individual-driven coping behaviours are suggested to be of equal importance to those promoted by the PhD students’ institutions [ 66 ]. In this study, approach coping behaviours were found to associate with lower depression levels, which may eventually contribute to PhD completion. The importance of developing coping mechanisms has also been highlighted in pre-pandemic studies, with, for instance, mothers finding ways to combine academic work and family responsibilities and succeed in both roles [ 38 ]. Still, institutions may play a crucial role in offering training for PhD students on coping and wellbeing through, for instance, a virtual platform to comply with social distancing policies. Such efforts may include mental health support and coping behaviour guidance, so that students are guided on how to successfully deal with disruptions (for example, to avoid avoidant coping behaviours that may lead them to higher levels of depression). Pre-pandemic reforms have previously shown that a well-structured programme and well-timed financial support can facilitate and uphold PhD completion, alongside student efforts [ 35 ]. As the future generation of academics, PhD students would be better equipped to handle the current and future disruptions and better cope with other disruptions in their academic journeys.
Limitations and implications for further research
Although our study has gone some way towards enhancing our understanding of Covid-19-related effects on UK PhD students’ mental health, it is plausible that a number of limitations could have influenced the results obtained. First, while our research attracted a representative number of students from different age groups, PhD modes, phases and funding, there was a very strong presence of students in natural sciences [ 17 ]. Second, as this was a cross-sectional study, we did not follow the UK PhD population longitudinally, and we may not offer insights into the trajectory of the relationships we articulate in our findings. Nevertheless, our adoption of standardized questionnaires allows for a platform for comparisons with past and future research efforts. Third, findings in this survey are based on self-report and may be subject to unconscious biases (e.g., PhD students assessing themselves or the situation inaccurately). Fifth, the research undertaken employed the PHQ-8 with a specific emphasis on assessing aspects related to depression. It is important to acknowledge that while these questionnaires offer valuable insights into depression, they may not comprehensively encompass the broader spectrum of general mental health. Therefore, the findings of the study should be interpreted within the context of its targeted focus on depression, recognizing the potential existence of other dimensions of mental health that were not directly addressed within this research framework. Finally, despite the high percentage of prediction in our findings (80%), additional factors may likely explain variabilities in our study outcomes, such as leadership factors or supervision styles in the 94 UK Universities whose PhD students participated in our survey.
As our study strongly demonstrates, juxtaposing findings from studies conducted during periods of relative HE stability with those conducted during periods of disruption is a fruitful approach for advancing research and university policy. By identifying which insights that would have been invaluable during periods of stability are less so during a period of disruption, scholars can provide significant advancements to existing research and new insights for policy, research and HE leadership.
Conclusions
Our study extends previous research on mental health in the HE sector by considering the dynamics of a severe disruption as opposed to the dynamics of relative stability in PhD mental health and coping behaviours. Drawing on our insights into these interrelationships, we suggest extensions to the literature on PhD students’ mental health, research and university policy. With our findings, HE leaders and policymakers may be better placed to tackle and ultimately overcome this and future research disruptions.
Acknowledgments
The authors would like to thank all the PhD students who committed time for taking part in this study and their responses informed the writing of this paper.
- View Article
- Google Scholar
- 3. O’Malley B. 180 congressmen support call for US$26bn research support. University World News [Internet]. 2020 [cited 2023 Jan 15]; Available from: https://www.universityworldnews.com/post.php?story=20200502080814674
- PubMed/NCBI
- 39. Drake KL. Psychology Graduate Student Well-being: The Relationship between Stress, Coping, and Health Outcomes. University of Cincinnati; 2010.
- 40. Pychyl T. Personal projects, subjective well-being and the lives of doctoral students. | CURVE [Internet]. Carleton University; 1995 [cited 2023 Jan 15]. Available from: https://curve.carleton.ca/d330c15c-eeaa-459c-afea-4bf841b7daa0
- 48. Aristeidou M, Aristidou A. PhDMentalHealth_UKDataset [Internet]. The Open University; 2023 [cited 2023 May 10]. Available from: https://ordo.open.ac.uk/articles/dataset/PhDMentalHealth_UKDataset/22794203/0 .
- 65. Malisch JL, Harris BN, Sherrer SM, Lewis KA, Shepherd SL, McCarthy PC, et al. Opinion: In the wake of COVID-19, academia needs new solutions to ensure gender equity [Internet]. Vol. 117, Proceedings of the National Academy of Sciences of the United States of America. National Academy of Sciences; 2020 Jul [cited 2023 Jan 15]. Available from: https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2010636117/-/DCSupplemental .

‘You have to suffer for your PhD’: poor mental health among doctoral researchers – new research
Lecturer in Social Sciences, University of Westminster
Disclosure statement
Cassie Hazell has received funding from the Office for Students.
University of Westminster provides funding as a member of The Conversation UK.
View all partners
PhD students are the future of research, innovation and teaching at universities and beyond – but this future is at risk. There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.
My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were more likely to meet the criteria for clinical levels of depression and anxiety. They were also more likely to have significantly more severe symptoms than the working-professional control group.
We surveyed 3,352 PhD students, as well as 1,256 working professionals who served as a matched comparison group . We used the questionnaires used by NHS mental health services to assess several mental health symptoms.
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety.
The groups reported an equally high risk of suicide. Between 33% and 35% of both PhD students and working professionals met the criteria for “suicide risk”. The figures for suicide risk might be so high because of the high rates of depression found in our sample.
We also asked PhD students what they thought about their own and their peers’ mental health. More than 40% of PhD students believed that experiencing a mental health problem during your PhD is the norm. A similar number (41%) told us that most of their PhD colleagues had mental health problems.
Just over a third of PhD students had considered ending their studies altogether for mental health reasons.
There is clearly a high prevalence of mental health problems among PhD students, beyond those rates seen in the general public. Our results indicate a problem with the current system of PhD study – or perhaps with academic more widely. Academia notoriously encourages a culture of overwork and under-appreciation.
This mindset is present among PhD students. In our focus groups and surveys for other research , PhD students reported wearing their suffering as a badge of honour and a marker that they are working hard enough rather than too much. One student told us :
“There is a common belief … you have to suffer for the sake of your PhD, if you aren’t anxious or suffering from impostor syndrome, then you aren’t doing it "properly”.
We explored the potential risk factors that could lead to poor mental health among PhD students and the things that could protect their mental health.
Financial insecurity was one risk factor. Not all researchers receive funding to cover their course and personal expenses, and once their PhD is complete, there is no guarantee of a job. The number of people studying for a PhD is increasing without an equivalent increase in postdoctoral positions .
Another risk factor was conflict in their relationship with their academic supervisor . An analogy offered by one of our PhD student collaborators likened the academic supervisor to a “sword” that you can use to defeat the “PhD monster”. If your weapon is ineffective, then it makes tackling the monster a difficult – if not impossible – task. Supervisor difficulties can take many forms. These can include a supervisor being inaccessible, overly critical or lacking expertise.
A lack of interests or relationships outside PhD study, or the presence of stressors in students’ personal lives were also risk factors.
We have also found an association between poor mental health and high levels of perfectionism, impostor syndrome (feeling like you don’t belong or deserve to be studying for your PhD) and the sense of being isolated .
Better conversations
Doctoral research is not all doom and gloom. There are many students who find studying for a PhD to be both enjoyable and fulfilling , and there are many examples of cooperative and nurturing research environments across academia.
Studying for a PhD is an opportunity for researchers to spend several years learning and exploring a topic they are passionate about. It is a training programme intended to equip students with the skills and expertise to further the world’s knowledge. These examples of good practice provide opportunities for us to learn about what works well and disseminate them more widely.
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence, offers balance, and avoids perpetuating unhelpful myths.
Indeed, in our own study, we found that the percentage of PhD students who believed their peers had mental health problems and that poor mental health was the norm, exceeded the rates of students who actually met diagnostic criteria for a common mental health problem . That is, PhD students may be overestimating the already high number of their peers who experienced mental health problems.
We therefore need to be careful about the messages we put out on this topic, as we may inadvertently make the situation worse. If messages are too negative, we may add to the myth that all PhD students experience mental health problems and help maintain the toxicity of academic culture.
- Mental health
- Academic life
- PhD research

Deputy Social Media Producer

Research Fellow /Senior Research Fellow – Implementation Science

Associate Professor, Occupational Therapy

GRAINS RESEARCH AND DEVELOPMENT CORPORATION CHAIRPERSON

Faculty of Law - Academic Appointment Opportunities

UCL Institute of Mental Health
UCL Wellcome 4-year PhD in Mental Health Science
About the programme, frequently asked questions, how to apply, supervisors and steering committee, supporting students.

This programme, funded in 2019, is the first of its kind in the UK, representing an investment of over £5m by the Wellcome Trust. It is based in the UCL Institute of Mental Health, and will recruit six students per year from 2020-2024.

Click here to access our FAQs
Contact details
Director Jonathan Roiser: [email protected]
Co-directors Alexandra Pitman: [email protected] Sunjeev Kamboj: [email protected]
For general information: [email protected]
Applications
No longer accepting applications.
Student Website
Visit our student-led website to found out more about the students on the programme:
Visit our website
Read the latest blogs written by our PhD students whilst studying on the programme:
Visit our blog site
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10584151

Research disruption during PhD studies and its impact on mental health: Implications for research and university policy
Maria aristeidou.
1 Institute for Educational Technology, The Open University, Milton Keynes, Buckinghamshire, United Kingdom
Angela Aristidou
2 UCL School of Management, London, United Kingdom
Associated Data
The raw dataset on PhD students' patient health questionnaire scale and coping mechanisms is available from the Open Research Data Online (ORDO) database: https://doi.org/10.21954/ou.rd.22794203 .
Research policy observers are increasingly concerned about the impact of the disruption caused by the Covid-19 pandemic on university research. Yet we know little about the effect of this disruption, specifically on PhD students, their mental health, and their research progress. This study drew from survey responses of UK PhD students during the Covid-19 pandemic. We explored evidence of depression and coping behaviour (N = 1780) , and assessed factors relating to demographics, PhD characteristics, Covid-19-associated personal circumstances, and significant life events that could explain PhD student depression during the research disruption (N = 1433) . The majority of the study population (86%) reported a negative effect on their research progress during the pandemic. Results based on eight mental health symptoms (PHQ-8) showed that three in four PhD students experienced significant depression. Live-in children and lack of funding were among the most significant factors associated with developing depression. Engaging in approach coping behaviours (i.e., those alleviating the problem directly) related to lower levels of depression. By assessing the impact of research disruption on the UK PhD researcher community, our findings indicate policies to manage short-term risks but also build resilience in academic communities against current and future disruptions.
Introduction
The abrupt outbreak in January 2020 and the global proliferation of a novel virus (Covid-19) has created a crisis for many sectors, including the international higher education (HE) sector [ 1 ] that continues during the ‘post-pandemic’ period. A point of particular alarm for HE leaders, policy observers, and governments is the disruption to the typical flow and pace of university research activity. While research related to Covid-19 is still in overdrive, other research was slowed or stopped due to worldwide physical distancing measures to contain the virus’ spread (e.g., sudden campus and laboratory closures, mobility restrictions, stay-at-home orders) [ 2 ]. The resulting ‘drop in research work’ is suggested to have a detrimental impact on the HE sector on the ‘research and innovation pipeline’ [ 3 ], and on ‘research capacity, innovation and research impact’ [ 4 ].
As research and university policies internationally are being (re)shaped at a rapid pace in efforts to meet the challenge of university research disruption [ 5 ], we contribute to academic and policy conversations by examining the effect of the research disruption on the mental health of PhD students. A considerable body of research acknowledges the role of PhD students in the innovation process, in knowledge creation and diffusion (e.g., [ 6 ]) and further posits that the period of one’s PhD program is key to early career success and research productivity (e.g., [ 7 ]). These outcomes, which matter to research policy, have been linked to PhD student mental health [ 8 – 10 ]. In those times of relative stability, research had additionally demonstrated the higher prevalence of mental health issues amongst the PhD student population across research disciplines, as compared to other students within academia [ 9 ] and the general population [ 9 , 11 , 12 ]. In the period since Covid-19 disrupted our social and economic lives, depression levels in the general population have been exacerbated globally [ 13 , 14 ]. These trends suggested that the already high prevalence of poor mental health in PhD students is likely to be further exacerbated during the pandemic. Indeed, as reported in early studies on research students’ experience of the Covid-19 pandemic (e.g., [ 15 ]) and the post-pandemic period (e.g., [ 16 ]) the impact on students’ mental wellbeing has been significant, with students suggesting a number of support measures at institutional and national level.
Ignoring, at this critical moment, the increased likelihood of poor mental health in PhD students may jeopardize research capacity and HE competitiveness for years to come. Therefore, there is a pressing need to identify–within the PhD student population–those whose mental health is more affected by the research disruption, so that policies and assistance can be timelier and more targeted. Additionally, by understanding more clearly the factors that may contribute to poor mental health, and their interrelationships (presented in Methods), policymakers and HE leaders may be better placed to tackle, and ultimately overcome, this and future research disruptions.
Motivated by the current lack of an empirical basis for insights into PhD students’ mental health during the pandemic-induced disruption, we collected survey data contemporaneously during July 2020. Our 1780 survey respondents are PhD students in 94 UK Universities, across the natural and social sciences and across PhD stages. Our study has three objectives: first, to explore mental health prevalence (depression) and coping behaviour in a large-scale representative sample of PhD students in the UK (O1); second, to evaluate the relationships among mental health prevalence and coping behaviour (O2); third, to identify factors that increase the likelihood of poor PhD student mental health during the period of research disruption (O3). Our study extends previous research on mental health in the HE sector by considering the dynamics of severe disruption, as opposed to the dynamics of relative stability, on PhD students’ mental health, performance satisfaction, and coping behaviours.
Background and literature review
Uk phd students’ mental health in times of disruption.
In the UK, there are approximately 100,000 postgraduate students completing doctoral research [ 17 ]. Since 2018, significant government funding has been targeted at developing insights into supporting UK PhD students’ mental health [ 18 ]. Still, with the exception of Byrom et al. [ 11 ], published research on PhD students’ mental health in the UK exhibits the same limitations as the international research: It reflects discipline- or institution-related specificity (e.g., [ 19 ]) or utilizes samples of early career researchers in general (e.g., [ 20 ]).
Early findings on postgraduate research students’ wellbeing during the pandemic showed that only a small proportion of them are in good mental health wellbeing (28%) while the rest demonstrate possible or probable depression or anxiety [ 15 ]. Goldstone and Zhang [ 15 ] further highlight the differences among student groups with, for example, students with disabilities or caring responsibilities or female students having lower levels of mental wellbeing. The post-pandemic findings have been more promising, as only about one in four students were at risk of experiencing mental health issues [ 16 ].
In response to the Covid-19 research disruption, substantive actions have been taken by the HE sector and the UK Government to disseminate approaches deployed by UK universities to support student mental health (e.g., [ 18 ]) and to update mental health frameworks for UK universities (e.g., [ 4 ]), but so far, mitigation activities have been targeting mental health for UK university students broadly, not UK PhD students specifically.
Overcoming the paucity of evidence on UK PhD students’ mental health during the pandemic is a crucial first step to drawing strong conclusions on the prevalence and determinants of mental health issues and ways to mitigate them specific to the PhD population. For example, policy recommendations by UK postgraduate respondents during the pandemic [ 15 ] focused mainly on financial support, such as extensions to their funded period of study and tuition and visa fee support (including waivers to fees). To develop an overarching framework specific to the Objectives of our study, we synthesize insights from the international literature on PhD student mental health conducted in the period before the research disruption.
International research on PhD student mental health in times of relative stability
In the international literature examining mental health specifically for PhD students (see the systematic review in [ 21 ], the issue of mental health for PhD students is acknowledged to be multidimensional and complex [ 10 ]. In this growing research area, some address mental health as an aspect of the broader ‘health’ of the PhD students (e.g., [ 22 ]), some focus on psychological distress [ 23 ], while others take depression as a specific manifestation of distress [ 9 , 24 ]. The latter is particularly interesting because depression within the PhD population in these studies is often assessed with standardised questionnaires (e.g., PHQ, see below) that allow for developing comparative insights. It is also the approach adopted by the only global survey of PhD students’ mental health by Evans et al. [ 12 ], showing that 39% of PhD students report moderate-to-severe depression, significantly more than the general population.
Literature on PhD student’s mental health determinants in times of relative stability
Past literature on PhD students’ mental health offers insights into the determinants of PhD students’ mental health in times of stability, which may help understand the relationships we want to examine between PhD mental health, performance satisfaction and coping in times of research disruption.
First, past studies evidence the influence of PhD students’ personal lives on poor mental health. PhD students with children or with partners are less likely to have or develop psychological distress [ 9 ]. The normalcy of family roles is a much-needed antidote to the known pressures of a PhD program [ 25 ] and might even protect against mental health problems [ 22 , 26 ]. Other aspects of PhD students’ personal lives, such as significant life events (e.g., severe problems in personal relationships or severe illness of the student or someone close to them), have been linked to dissatisfaction with their research progress [ 24 ]. Research progress is defined as students’ perception of their progress in the completion of their degree [ 27 ] and is linked to their mental health. Dissatisfaction is tied to negative outcomes, such as attrition and delay [ 28 ], but also to lower productivity and mental health problems, such as worry, anxiety, exhaustion, and stress [ 29 ]. Related to this, Levecque and colleagues [ 9 ] observed that PhD students expressing a high interest in an academic career are in better mental health than those with no or little interest in remaining in academia.
Second, gender was the key personal factor that emerged as a determinant for mental health in past studies: PhD students who self-identify as female report greater clinical [ 9 , 30 ] and non-clinical problems with their mental health [ 23 , 31 ]. This is explained through the additional pressure women report on their professional and personal lives [ 23 ].
Third, past studies argue that each PhD phase presents PhD students with specific sets of challenges and should thus be explored discreetly in relation to mental health [ 32 ]. Still, the evidence on the link between the PhD phase (or the year of study as a proxy for the PhD phase) and mental health is inconclusive. Barry et al.’s [ 33 ] survey reports no connection between the PhD phase and depression levels in an Australian PhD population. However, Levecque et al. [ 9 ] report high degrees of depression in the early PhD stage of students in Belgium, and a global survey of PhD students across countries and disciplines shows that depression likelihood increases as the PhD program progresses [ 32 ].
Fourth, past research offers strong evidence that financial concerns impact PhD students’ mental health negatively. In a study by El-Ghoroury et al. [ 34 ], 63.9% of PhD students cited debt or financial issues as a cause for poor wellbeing and cited financial constraints as the major barrier to improving their wellness (through social interactions, outside-PhD activities, etc). Even uncertainty about funding was shown to predict poor mental health [ 9 ]. To this end, Geven et al. [ 35 ] explored packages of reforms in a pre-pandemic graduate school programme, including an extension of the grant period, and indicated that such policies can increase students’ completion rates to up to 20%.
Finally, age is not shown to be associated with mental health [ 9 ], but numerous studies found that having children, particularly for female PhD students and in Science-Technology-Engineering-Maths (STEM) disciplines [ 36 ], consistently corresponds with heightened stress [ 37 ]. However, a specific examination of the relationship between children and mental health indicates that PhD students with one or more children in the household showed significantly lower odds of having or developing a common psychiatric disorder [ 9 ]. Further, parenting and, in particular, motherhood during doctorate studies contribute to the development of students’ coping mechanisms that allows them to succeed in a balance in both worlds [ 38 ].
Past research insights into PhD mental health and coping
Past research explored how PhD students may “cope” with stressors and thus mitigate poor mental health [ 39 ]. Studies identify the importance of social interactions (e.g., [ 22 ]); balancing life demands (e.g., [ 16 ]), reaching out for social support (e.g., [ 40 ]) sometimes through peer relationships (e.g., [ 10 , 39 ]); and ‘planning’ (e.g., [ 22 ]); As invaluable as these insights are, drawing comparisons between these findings is difficult because often the identification of coping styles or strategies was not the focus of these studies, making it difficult to draw fine-grained conclusions as to their effect on PhD students’ mental health.
There is, however, a long tradition of research on coping for physiological wellbeing that provides standardised measures for individuals’ coping and their link to mental health [ 41 ]. The most widely used measurement instrument in the literature reviewed is the COPE Inventory, which allows researchers to assess how people cope in a variety of stressful situations, including in HE for students [ 42 – 44 ], making it particularly relevant to the context and sample under investigation in our study of PhD students. Additionally, COPE allows for the identification of consistent ways of coping, which provides predictive validity across a range of situations. Predictive validity is desired when examining the role of coping in relation to mental health. Indeed, multiple studies have linked the COPE measurement to mental health outcomes (e.g., [ 45 , 46 ]), including depression [ 43 ], which is a focus of our study.
Data and methods
Participants.
For the current study, we recruited participants that were active PhD students from March to July 2020 at any stage of their research to take part in an online survey. The survey ran between the 31st of July and the 23rd of August 2020, with the aim of capturing the potential impact of the Covid-19 disruption during the first lockdown on their research progress and mental health. The use of online surveys to assess the scope of mental health problems is particularly appropriate during the Covid-19 outbreak [ 47 ]. The current study has been reviewed by, and received a favourable opinion, from The Open University Human Research Ethics Committee (reference number: HREC/3605/Aristeidou), http://www.open.ac.uk/research/ethics/ . For the recruitment of a diverse audience, we followed a snowball sampling method, forwarding our invitation to PhD student groups in a number of UK-based universities, but also exploited the reach of PhD social media channels and online PhD groups, and we invited academics and respondents to recruit other participants. Vouchers were provided as an incentive for participation to the first 300 respondents. Before completing the survey, the respondents were provided with an online information sheet and were asked to provide their written consent through a digital consent form. They reported their email addresses to be identifiable and contactable for validation, consent issues, potential withdrawal, and incentive processing. The dataset was anonymized on the 30th of August 2020, prior to initiating data analysis.
Exclusion criteria included survey respondents who ‘straight-lined’ (chose the same answer option repeatedly), gave inconsistent responses to similar questions, or did not use their institution emails (rendering them unidentifiable). Finally, there were 1790 PhD students in the study from 94 different HE institutions across all four UK nations (England, Scotland, Northern Ireland and Wales). The majority of the study population (86%) reported that their research progress had been impacted in a negative way. The dataset [ 48 ] included 44.4% male and 55.4% female participants, while the doctoral students in the UK consist of 51% male and 49% female students [ 17 ]. Weighting adjustments were made to correct the sample representativeness. The majority of the survey respondents were 25–34 years old (80.4%), with live-in children (71%). Most respondents (86.7%) were conducting their PhDs full-time, and almost two-thirds (64.4%) were funded by a research council or a charitable body in the UK. At the time of the survey, a large proportion of the survey respondents were in the ‘executing’ phase of their research (i.e., data collection/analysis). Finally, a natural science-related PhD was being pursued by slightly over two-thirds of the respondents (68.8%). According to data sourced from HESA [ 17 ], the likelihood of individuals embarking on a research postgraduate degree at a younger age (such as 18–20) appears to be relatively low. This is evident from the fact that only 90–130 students within this age group register for such programs each year. More details on the demographics and characteristics of the sample can be found in Table 1 and below.
Variables and instruments
Brief cope inventory (bci).
The BCI [ 49 ] is a 28-item self-report questionnaire designed to measure effective and ineffective ways to cope with a stressful life event, and it is the abbreviated version of the original 60-item COPE inventory developed by [ 42 ]. The BCI has a 4-point Likert scale with options on each item ranging from 0 (I usually do not do this at all) to 3 (I usually do this a lot). Coping in this study is categorised in two overarching coping behaviours, as per Eisenberg et al. [ 50 ]: (a) the approach behaviours that attempt to reduce stress by alleviating the problem directly, which include 12 items related to active coping, positive reframing, planning, acceptance, seeking emotional support, and seeking informational support; and (b) the avoidant coping behaviours that attempt to reduce stress by distancing oneself from the problem, which include 12 items related to denial, substance use, venting, behavioural disengagement, self-distraction, and self-blame. Items that belong to neither overarching behaviour are coping related to humour and religion. These were included in the overall coping score but excluded from the analysis based on the two overarching behaviours. A higher score indicates frequent use of that coping behaviour. Cronbach’s alpha for the BCI was .88. Further, both the approach and avoidant scales have shown very good internal consistency in this sample, with Cronbach’s alpha equal to 0.83 and 0.80, respectively.
Patient health questionnaire eight-item depression scale (PHQ-8)
PHQ-8 [ 57 ] is an eight-item version of the Patient Health Questionnaire (PHQ-9). PHQ is a popular measure for assessing depression and is frequently used for PhD mental health (e.g., [ 12 , 51 ]), making it an ideal choice for our study. PHQ-9 has been validated as both a diagnostic and severity measure [ 52 , 53 ] in population-based settings [ 54 ] and self-administered modes [ 55 , 56 ], and it was recently used in a global survey of PhD students’ depression prevalence [ 12 ]. PHQ-8 omits the ninth question that assesses suicidal or self-injurious thoughts, and it was deemed more appropriate for our research because researchers in web-based interviews/surveys are unable to provide adequate interventions remotely. The PHQ-8 items employ a 4-point Likert scale with options on each item ranging from 0 (not at all) to 3 (nearly every day). Then, the scores are summed to give a total score between 0 and 24 points, where 0–4 represent no significant depressive symptoms, 5–9 mild depressive symptoms, 10–13 moderate, 15–19 moderately severe, and 20–24 severe [ 55 ]. Evidence from a large-scale validation study [ 57 ] indicates that a PHQ-8 score ≥ 10 represents clinically significant depression. In this study, Cronbach’s alpha for the PHQ-8 was 0.71, indicating a good internal consistency.
Performance satisfaction
Performance satisfaction is an 8-item self-report scale designed to measure the students’ self-perceived progress in their PhD research, their confidence in being able to finish on time, and their satisfaction. The scale was successfully used in a PhD student well-being study at the university of Groningen [ 24 ] prior to the Covid-19 pandemic. The performance satisfaction 5-point Likert scale responses range from 1 (completely disagree) to 5 (completely agree). The score for each respondent equals the mean score of the 8-item responses. A reliability analysis was carried out on the performance satisfaction scale. Cronbach’s alpha showed the scale to reach acceptable reliability, α = 0.86.
Significant life events Significant Life events is a questionnaire designed to capture whether PhD students had experienced any significant life events in the 12 months prior to the survey. This was successfully used in studying PhD students’ mental health at the university of Groningen [ 24 ] prior to the Covid-19 pandemic research disruption. Events include the death of someone close, severe problems in personal relationships, financial problems, severe illness of oneself or someone close, being in the process of buying a house, getting married, expecting a child, none of these events, and prefer not to say. Significant life events were used as an incident control variable in this study.
Statistical analyses
SPSS (Version 25) was used for statistical analysis. In the first phase, descriptive statistics were used to describe the PHQ-8 Depression and coping behaviours of the sample and the distribution of these three variables among demographics, PhD characteristics, and Covid-19-related circumstances (O1). We used a weighting adjustment for gender to correct the survey representativeness for descriptive analysis; females were given a ‘corrective’ weight of 0.88 and males of 1.15.
In relation to O2, Spearman rank correlations were used to examine the degree of association between all of the 28 coping behaviours and PHQ-8 Depression scores. This finding contributed to our understanding of how individual coping behaviours could relate to lower or higher depressive symptoms.
To assess whether the behaviours significant to our study (i.e., those with a negative or the strongest positive PHQ-8 Depression association) were used more frequently by students of a particular demographic group (O2), we used independent-samples t-test and ANOVA. Before assessing the relationship between our variables, outliers, and groups with a sample size smaller than 15 for each group were removed from the tests (e.g., Gender = other; Funding = partially funded; Likelihood in HE = already employed in academia).
In relation to O3, a binary logistic regression analysis was performed to examine whether Covid-19-related circumstances explain significant depression in PhD students, while controlling for demographics, PhD characteristics, and external incidents. Prior to performing the regression analysis, PHQ-8 Depression score outliers, as well as groups with fewer than 10 events per variable (e.g., gender = other; age = 55–64; Impact reason = mental health), were detected and excluded from the dataset. The dichotomous dependent variable was calculated based on PHQ-8 Depression scores smaller than 10 for non-significant depression, and equal or larger than 10 for significant depression. Associations between Depression in PhD students and the independent variables in our dependency model were estimated using odds ratios (ORs) as produced by the logistic regression procedure in SPSS (Version 25). The ORs were used to explain the strength of the presence or absence of significant depression. Wald tests were used to assess the significance of each predictor. A test of the full model against a constant only model was statistically significant, indicating that the predictors as a set reliably distinguished between PhD students who are having or developing significant depression and those who are not ( Χ 2 (25) = 405.258, p < . 001 ). A Nagelkerke R 2 of .798 indicated a good to substantial relationship between prediction and grouping (68% of variance explained by the proposed model in completion rates). Table 2 presents response percentages about the categorical variables entered in the model, including the two dependent variables (significant depression and non-significant depression).
Exploring depression prevalence and coping behaviours
The average PHQ-8 Depression score was 10.13 ( SD = 3.23) on a scale of 0–24 (weighted cases). Importantly, this highlights that the majority of survey respondents are facing moderate depression symptoms ( Fig 1 ). The PHQ-8 item with the highest score, in a range of 0–4, was ‘having trouble to concentrate on things, such as reading the newspaper or watching television’ ( M = 1.45; SD = 0.84), and the item with the lowest score was ‘moving or speaking so slowly that other people could have noticed; or the opposite–being so fidgety or restless that have been moving around a lot more than usual’ ( M = 1.10; SD = 0.75). Of the study population, 75% self-reported significant depression (moderate, moderately severe, or severe major).

The coping behaviours that the majority of PhD students used in a medium or large amount to overcome the Covid-19 disruption were “accepting the reality of the fact that it has happened” (84%), followed by “thinking hard about what steps to make” (76%) ( Fig 2 ). Both are approaching coping behaviours. Other coping behaviours used to a great extent were “praying or meditating” (73%) , “blaming myself for things that happened” (avoidant) (71%) , and “expressing my negative feelings” (avoidant) (69%). On the other hand, coping behaviours that were used the least were all avoidant ones: “giving up attempting to cope” ( 13%) , “refusing to believe that it has happened” (15%) , “using alcohol or other drugs to make myself feel better” (17%) , and “giving up trying to deal with it” (17%) . Overall, approach coping behaviours were used to a greater extent ( M = 26.43, SD = 5.15) than avoidant coping behaviours ( M = 23.97, SD = 4.90).

The Spearman correlations between coping behaviours and PHQ-8 scores ( Table 3 ), which included outliers, suggested that only two items have significant negative (very weak) associations with depression: Item 15, “getting comfort and understanding from someone” ( r s (1780) = -.107, p < .01); and Item 7, “taking action to try to make the situation better” ( r s (1762) = -.077, p < .01). The majority of the coping behaviours had a significant positive relationship with higher scores in depressive symptoms. The coping behaviours with the largest effect and a moderate to strong association were Item 13, “criticizing myself” ( r s (1762) = .452, p < .01), followed by Item 11 “using alcohol or other drugs to help me go through it” ( r s (1762) = .387, p < .01).
Spearman correlations between coping behaviours and PHQ-8 scores. The majority of the coping behaviours had a significant positive relationship with higher scores in depressive symptoms.
*p < .05
**p < .01, two tailed.
Table 4 shows the relationship among approach and avoidant coping behaviours, and demographics. Our analyses indicated that both approach and avoidant coping behaviours had been significantly used to a greater extent by the female over male PhD students, by students without a live-in partner than those with a live-in partner, and by those without live-in children than those with live-in children. There is no evidence that the students of a particular age group were using avoidant coping more than those of another age group. However, students aged 25–34 were using approach coping behaviours less than other groups, and those aged 45–54 more ( Table 5 ).
The relationship among approach and avoidant coping behaviours, and demographics indicated that both approach and avoidant coping behaviours have been significantly used to a greater extent by specific student groups.
The table shows the results of the ANOVA post-hoc comparisons between age groups. Students aged 25–34 were using approach coping behaviours less than other groups, and those aged 45–54 more.
Our analyses indicated that female PhD students, who had significantly lower PHQ-8 Depression scores, were using Table 3 ‘s Items 15 ( t [1778] = 14.61, p < .001) and Item 7 ( t [480] = 15.11, p < .001) significantly more than male students. Also, those without live-in partners were getting comfort and understanding from someone to a significantly greater extent than those without ( t [702] = 20.09, p < .001). PhD students without live-in children were taking action to try to make the situation better significantly more than those who have them ( t [894] = 25.21, p < .001).
Predictors of depression and relative influence
Covid-19-related circumstances (receiving an extension, impact reasons, and impact results), performance satisfaction, and coping behaviours (approach and avoidant) were entered together as predictors of depression. Demographics (gender, age, live-in partner, and live-in children), PhD characteristics (discipline, PhD phase, PhD mode, funding, interest in HE, and likelihood in HE) and external incidents were used as control variables. Table 6 reports the findings of the analyses.
Note. ref = reference category
* = p < 0.05 ** = p < 0.01 *** = p < 0.001, Model fit PHQ-8 LR = 405.258 df = 26 p < 0.001 Nagelkerke R 2 = 0.798
Prediction success overall was 95.3% (83.1% for not significant depression and 98.0% for significant depression). The Wald criterion demonstrated that not having an extension ( p = .014), having caring responsibilities ( p < .001), and using approach ( p < .001) or avoidant ( p < .001) coping behaviours made significant contributions to prediction. The OR value indicated that in the case that PhD students were not receiving an extension amid the Covid-19 disruption, or they did not know whether they were receiving one yet, they were 5.4 times more likely to experience significant depression. For the impact reason, our findings showed that–compared to those who experienced personal illness–PhD students who had caring responsibilities (e.g., childcare or other) showed slightly lower depressive symptoms (OR = 0.10). The OR for approach and avoidant coping behaviours were 0.13 and 43.73, respectively. This finding indicates that when approach coping is raised by one unit (e.g., +1 to the score), we see evidence for better mental health, while when avoidant coping is raised by one unit, a PhD student is very likely (44 times) to experience significant depression.
Turning to our control variables, PhD students with children in the household and with live-in partners showed significantly higher odds (about 14 and 7 times more, respectively) of having or developing depressive symptoms than those without. The latter can be explained by the fact that 88% of the participants with live-in partners also reported having live-in children. Also, male students were slightly more likely than female students to experience significant depression (with a borderline p-value), but this might be explained by the significantly increased use of coping approaches by female students. This gender-related finding that shows nearly no difference between the two categories slightly differs from Goldstone and Zhang’s model [ 15 ] which highlights a difference between female and male participants’ mental wellbeing. This difference can be explained by the fact that the research instruments used in the two studies were different, as well as the survey period.
Some PhD characteristics that made significant contributions to prediction were the discipline of PhD studies and the interest of students to remain in academia after finishing their PhD projects. The risk of experiencing significant depression in PhD students in social sciences (OR = 9.68) was lower than in students conducting a PhD in natural sciences. In contrast to findings by Levecque et al. [ 9 ], we observed that PhD students expressing a high interest in an academic career were 3.5 times more likely to develop depressive symptoms than those with no or only little interest in remaining in academia. Further, those considering having a high likelihood of remaining in academia were slightly more depressed (OR = 3.73), as well as those who were in the executing phase of their PhD research (OR = 3.33). No differences between funded and self-funded students were detected. Finally, the OR for the external incident variable was 6.13, indicating that for each incident unit (e.g., one more incident), we see evidence for depressive symptoms that are six times worse.
Our study contributes new empirical data and new insights needed to develop knowledge on the effect of university research disruption on the PhD student population. In turn, new knowledge may provide the evidence base for university and research policy.
Exploring mental health and coping behaviours
Our first contribution is to provide empirical estimates for the performance satisfaction, prevalence of mental health problems, and coping behaviours of PhD students during the pandemic-induced research disruption, on the basis of representative data across disciplines and across universities in the UK.
Our findings show that most UK PhD students across universities and disciplines report that their research progress has been affected negatively (86%). By contrast, in pre-pandemic periods, 79% of UK PhD students across Universities and disciplines had indicated excellent research progress [ 11 ]. This shift within the same population is important to reveal because of its potential implications for PhDs’ careers and university research capacity and innovation, as we know that dissatisfaction about the PhD trajectory is tied to negative outcomes such as attrition and delay [ 24 , 28 ], but also to lower productivity [ 58 ].
We found that during the period of severe research disruption caused by the Covid-19 pandemic, 75% of the UK students surveyed from 94 universities and across disciplines self-reported in the moderate-severe range for depression. This is at least three times more compared to the reported prevalence of depression among the general population internationally during the Covid-19 outbreak (16–28%, [ 59 ]). Our findings are also in line with findings in Goldstone and Zhang’s study [ 15 ] on UK postgraduate students’ mental wellbeing during the pandemic, in which 72% of the surveyed students were found to demonstrate possible or probable depression or anxiety.
By adopting widely used standardised questionnaires, our findings provide an accessible benchmark for the comparison with studies that took place among PhD student populations in periods of HE stability (pre-2020), thereby providing the empirical basis to accurately estimate the issue of poor mental health among PhD students during a period of research disruption. Using the same questionnaire as in our survey (PHQ-9) and drawing on a sample of PhD students from multiple universities and across research disciplines, a pre-pandemic global survey reported that 39% of PhD students scored in the moderate-severe range for depression [ 12 ]. Pre-pandemic national surveys of PhD students across institutions and disciplines report similar rates of depression, between 32% (in Belgium, Levecque et al. [ 9 ] and 38% (in the Netherlands, Van der Weijden et al. [ 60 ]. In a pre-pandemic (2018–2019) survey of UK PhD students across 48 universities and disciplines, only 25% reported levels that would indicate probable depression or anxiety [ 11 ]. These comparisons indicate that the prevalence of depression among the UK PhD student population of our study during the pandemic-induced period of research disruption is two-to-three times more than that which was reported in periods of stability for the UK PhD student population, for PhD student populations of other countries, and the global PhD population.
Our findings on PhD students’ mental health and PhD students’ coping advance past literature [ 22 , 23 , 34 ] in two significant ways. First, by using a highly reliable coping measure (COPE), we are able to demonstrate the relationship between coping styles and mental health outcomes in PhD students in a way that allows for comparisons and to build further research in this area. Second, we identify specific coping behaviours amongst the UK PhD students that are associated with lower depression scores and some that have a negative association with depression (i.e., getting comfort and understanding from someone and taking action to try to make the situation better ). Both are ‘coping approach’ behaviours (i.e., attempts to reduce stress by alleviating the problem directly; [ 50 ]). Studies using COPE in other populations have also linked coping-approach behaviours to fewer symptoms of psychological distress [ 45 ], more physical and psychological well-being at work [ 46 ], and an absence of anxiety and depression [ 61 ].
Factors explaining PhD students’ depression
Our second contribution is to explain–within the UK PhD population–whose mental health is more affected by the pandemic-induced research disruption. We find that several factors have a significant impact on PhD students to have or develop mental health issues during a period of research disruption.
Consistent with past research on PhD students’ mental health, our findings reveal the significant influence of their personal lives on poor mental health. The relationships we observed during a period of research disruption, however, differ from those suggested in studies conducted in periods of stability (e.g., [ 9 , 22 , 25 , 26 , 62 ]). We found that PhD students with live-in children or with a live-in partner and PhDs with caring responsibilities are more likely to have or develop significant depression compared to those without. This difference can be explained by the closure of schools that resulted in parents home-schooling their children, a greater demand for devices and the internet in households, and parents going through emotional hardship [ 63 ]. We additionally find six times worse depressive symptoms for each ‘external life incident’ (e.g., childbirth, moving home) that occurred in the PhD students’ lives. A larger number of external incidents were found to be associated with students with live-in partners and students with live-in children, which may explain these as reinforcing negative effects. These new insights explain that–although most of these realities in PhD students’ personal lives existed besides the research disruption—when combined with the research disruption, their mental health can spiral downward.
Our findings also address the role of structural PhD characteristics (PhD discipline and PhD phase) in predicting whether a student might present mental health issues in times of research disruption. We find that in a period of research disruption, the risk of significant depression is higher in the execution phase of the PhD compared to the beginning or extension phases, contrary to Levecque and colleagues’ findings [ 9 ]. Because there is very limited research on the PhD stage and mental health, our findings contribute insights to a broader community of scholars who advocate for the further study of the challenges in each PhD stage discreetly (e.g., [ 32 ]). Furthermore, we find that the risk of experiencing significant depression in PhD students in social sciences was lower than students conducting a PhD in natural sciences. Our survey respondents offered explanations on the role of PhD discipline in mental health during the pandemic in the open text responses. These converge on the fact that natural sciences often require being physically in a laboratory, which is probably unfeasible when university facilities are closed.
In tune with past research on finances and mental health in PhD students [ 9 , 64 ], we found those without funded extensions are more likely to have or develop significant depression (moderate, moderately severe, and severe) compared to those with them. We reveal the size of this association (about 5.5 times more) and link PhD funding extensions to standardized assessments of depression prevalence, thus uniquely providing new evidence for policy scholars.
Implications for research and higher education policy
Our findings show an alarming increase in self-reported depression levels among the UK PhD student population. The long-term mental health impact of Covid-19 may take years to become fully apparent, and managing this impact requires concerted effort not just from the healthcare system at large [ 59 ] but also from the HE sector specifically. With mental illness a cause for PhD student attrition, loss of research capacity and productivity, data from our survey should prompt consideration of immediate intervention strategies.
For research and education policy scholars, our findings contribute directly to the development of evidence-based research and university policies on support for targeted groups of PhD students in times of disruption. Specifically, our findings show that institutional and funder support should not only be in the form of PhD-funded extensions–which are nevertheless shown in our study and other studies (e.g., [ 15 ]) to be very significant. But also, in the form of providing expedited alternatives to the changes evoked by the pandemic for PhD students, such as new and adjusted policies that explicitly consider those PhDs with caring responsibilities, since 77% of our respondents reported that childcare and other caring responsibilities are the reason for dissatisfaction with their PhD progress. If not, the Covid-19 research disruption could erase decades of progress towards equality in academia [ 65 ].
Our main contribution is that we offer insights into how to mitigate mental health consequences for PhD students in times of research disruption. Individual-driven coping behaviours are suggested to be of equal importance to those promoted by the PhD students’ institutions [ 66 ]. In this study, approach coping behaviours were found to associate with lower depression levels, which may eventually contribute to PhD completion. The importance of developing coping mechanisms has also been highlighted in pre-pandemic studies, with, for instance, mothers finding ways to combine academic work and family responsibilities and succeed in both roles [ 38 ]. Still, institutions may play a crucial role in offering training for PhD students on coping and wellbeing through, for instance, a virtual platform to comply with social distancing policies. Such efforts may include mental health support and coping behaviour guidance, so that students are guided on how to successfully deal with disruptions (for example, to avoid avoidant coping behaviours that may lead them to higher levels of depression). Pre-pandemic reforms have previously shown that a well-structured programme and well-timed financial support can facilitate and uphold PhD completion, alongside student efforts [ 35 ]. As the future generation of academics, PhD students would be better equipped to handle the current and future disruptions and better cope with other disruptions in their academic journeys.
Limitations and implications for further research
Although our study has gone some way towards enhancing our understanding of Covid-19-related effects on UK PhD students’ mental health, it is plausible that a number of limitations could have influenced the results obtained. First, while our research attracted a representative number of students from different age groups, PhD modes, phases and funding, there was a very strong presence of students in natural sciences [ 17 ]. Second, as this was a cross-sectional study, we did not follow the UK PhD population longitudinally, and we may not offer insights into the trajectory of the relationships we articulate in our findings. Nevertheless, our adoption of standardized questionnaires allows for a platform for comparisons with past and future research efforts. Third, findings in this survey are based on self-report and may be subject to unconscious biases (e.g., PhD students assessing themselves or the situation inaccurately). Fifth, the research undertaken employed the PHQ-8 with a specific emphasis on assessing aspects related to depression. It is important to acknowledge that while these questionnaires offer valuable insights into depression, they may not comprehensively encompass the broader spectrum of general mental health. Therefore, the findings of the study should be interpreted within the context of its targeted focus on depression, recognizing the potential existence of other dimensions of mental health that were not directly addressed within this research framework. Finally, despite the high percentage of prediction in our findings (80%), additional factors may likely explain variabilities in our study outcomes, such as leadership factors or supervision styles in the 94 UK Universities whose PhD students participated in our survey.
As our study strongly demonstrates, juxtaposing findings from studies conducted during periods of relative HE stability with those conducted during periods of disruption is a fruitful approach for advancing research and university policy. By identifying which insights that would have been invaluable during periods of stability are less so during a period of disruption, scholars can provide significant advancements to existing research and new insights for policy, research and HE leadership.
Conclusions
Our study extends previous research on mental health in the HE sector by considering the dynamics of a severe disruption as opposed to the dynamics of relative stability in PhD mental health and coping behaviours. Drawing on our insights into these interrelationships, we suggest extensions to the literature on PhD students’ mental health, research and university policy. With our findings, HE leaders and policymakers may be better placed to tackle and ultimately overcome this and future research disruptions.
Acknowledgments
The authors would like to thank all the PhD students who committed time for taking part in this study and their responses informed the writing of this paper.
Funding Statement
This work was supported by the Institute of Educational Technology at The Open University (MA) and the University College London (UCL) School of Management (AA). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- CAREER NEWS
- 14 December 2021
Depression and anxiety ‘the norm’ for UK PhD students
- Chris Woolston 0
Chris Woolston is a freelance writer in Billings, Montana.
You can also search for this author in PubMed Google Scholar
PhD students in the United Kingdom are more likely than other educated members of the general public to report symptoms of depression or anxiety, according to a survey.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
doi: https://doi.org/10.1038/d41586-021-03761-3
Hazell, C. M. et al. Humanit. Soc. Sci. Commun. 8 , 305 (2021).
Article Google Scholar
Levecque, K., Anseel, F., de Beuckelaer, A., van der Heyden, J. & Gisle, L. Res. Pol. 46 , 868–879 (2017).
Article PubMed Google Scholar
Satinsky, E. N. et al. Sci. Rep. 11 , 14370 (2021).
Download references
Related Articles

It’s time to talk about the hidden human cost of the green transition
Correspondence 16 APR 24

Shrouded in secrecy: how science is harmed by the bullying and harassment rumour mill
Career Feature 16 APR 24
Use fines from EU social-media act to fund research on adolescent mental health
Correspondence 09 APR 24

Deadly diseases and inflatable suits: how I found my niche in virology research
Spotlight 17 APR 24

I dive for fish in the longest freshwater lake in the world
Female academics need more support — in China as elsewhere

Londoners see what a scientist looks like up close in 50 photographs
Career News 18 APR 24

How young people benefit from Swiss apprenticeships
Qiushi Chair Professor
Distinguished scholars with notable achievements and extensive international influence.
Hangzhou, Zhejiang, China
Zhejiang University
ZJU 100 Young Professor
Promising young scholars who can independently establish and develop a research direction.
Head of the Thrust of Robotics and Autonomous Systems
Reporting to the Dean of Systems Hub, the Head of ROAS is an executive assuming overall responsibility for the academic, student, human resources...
Guangzhou, Guangdong, China
The Hong Kong University of Science and Technology (Guangzhou)
Head of Biology, Bio-island
Head of Biology to lead the discovery biology group.
BeiGene Ltd.
Research Postdoctoral Fellow - MD (Cardiac Surgery)
Houston, Texas (US)
Baylor College of Medicine (BCM)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Advancing Mental Health Research, Psychiatry and Behavioral Sciences at Northwestern with Sachin Patel, MD, PhD
Sachin Patel, MD, PhD, is the new chair and Lizzie Gilman Professor of Psychiatry and Behavioral Sciences at Feinberg and psychiatrist-in-chief at Northwestern Memorial Hospital’s Norman and Ida Stone Institute of Psychiatry. In this episode, he talks about the current mental health crisis in this country, his research and vision for the department.

"Understanding the brain, understanding mental illness, will bear fruit in terms of novel treatments, better ways to treat people, better ways to give people the access to care that they need. And all that begins with the research that folks are doing here at Feinberg across the spectrum, all the way from basic neuroscience, all the way to health implementation sciences."
— Sachin Patel, MD, PhD
- Chair, Department of Psychiatry and Behavioral Sciences
- Lizzie Gilman Professor of Psychiatry and Behavioral Sciences
- Psychiatrist-in-Chief, Northwestern Memorial Hospital’s Norman and Ida Stone Institute of Psychiatry
Episode Notes
Patel is an internationally recognized expert in the field of psychiatric neuroscience, a physician-scientist who combines a deep background in cellular, molecular and behavioral neuroscience with clinical expertise in psychiatry and addiction medicine. Upon completing his clinical training in 2010, he joined the faculty at Vanderbilt University where he rose to the rank of tenured professor and director of the Division of General Psychiatry. He began his new role as chair of the Department of Psychiatry and Behavioral Sciences at Feinberg January 2022.
Topics covered:
- Patel has always been interested in the brain and decided to enter the field of psychiatry in medical school where he was exposed to neuroscience at a variety of levels. Later he was able to blend his interest in neuroscience and clinical practice as a physician scientist.
- He spent more than a decade at Vanderbilt University where he was most recently director of the Division of General Psychiatry. His research program focuses on understanding how environmental stress affects brain structure and function, and how understanding the impact of stress could potentially reveal new targets for the treatment of mental illnesses affected by stress.
- The COVID-19 pandemic has highlighted the need for mental health services in this country. Patel says the need was present before the COVID-19 pandemic, but talking more about the mental health during the pandemic has been a good thing for the field. One of the factors that drew him to Northwestern Medicine was the institution's major investments in behavioral health.
- Patel will be launching a new Center for Psychiatric Neuroscience which is aimed at bringing together basic translational neuroscientists that have a goal of understanding and deepening the understanding of physiological mechanisms that underlie mental illness with the ultimate goal of being able to reveal new molecular targets, for example, for therapeutics intervention.
- His recent research involves studying the cannabinoid system and understanding the role of this system in central stress responses and how we could leverage our understanding of the system to potentially develop new therapeutics for stress related disorders, whether that is anxiety disorders, affective disorders or post-traumatic stress disorder.
- In the next decade, Patel expects the field of psychiatry is headed toward an exponential increase in the types of treatments it can provide for patients. He encourages Northwestern, students, trainees, scientists and faculty to believe that their work and understanding the brain, understanding mental illness will bear fruit in terms of novel treatments, better ways to treat people, better ways to give people the access to care that they need.
Additional Reading:
- Article: Neurobiological Interactions Between Stress and the Endocannabinoid System
- Article: The endocannabinoid system as a target for novel anxiolytic drugs
iTunes Spotify Google Play Music
Recorded on March 28, 2022.
Read the Full Transcript
Continuing medical education credit, physicians who listen to this podcast may claim continuing medical education credit after listening to an episode of this program..
Target Audience
Academic/Research, Multiple specialties
Learning Objectives
At the conclusion of this activity, participants will be able to:
- Identify the research interests and initiatives of Feinberg faculty.
- Discuss new updates in clinical and translational research.
Accreditation Statement
The Northwestern University Feinberg School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
Credit Designation Statement
The Northwestern University Feinberg School of Medicine designates this Enduring Material for a maximum of 0.25 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Disclosure Statement
Sachin Patel, MD, PhD, has received a consulting fee from Johnson and Johnson, Jazz Pharmaceuticals, and Psy Therapeutics. Stephen Dinwiddie, MD, content reviewer, has nothing to disclose. Course director, Robert Rosa, MD, has nothing to disclose. Planning committee member, Erin Spain, has nothing to disclose. Feinberg School of Medicine's CME Leadership and Staff have nothing to disclose: Clara J. Schroedl, MD, Medical Director of CME, Sheryl Corey, Manager of CME, Allison McCollum, Senior Program Coordinator, Katie Daley, Senior Program Coordinator, Michael John Rooney, Senior RSS Coordinator, and Rhea Alexis Banks, Administrative Assistant 2.
Claim your credit
Melbourne School of Psychological Sciences
Mental Health PhD Program
A multidisciplinary PhD Program in Mental Health
This Program brings together graduate researchers addressing mental health from diverse disciplinary perspectives - psychiatry, psychology, epidemiology and community mental health, history and philosophy of psychiatry, general practice, paediatrics, psychiatric nursing and social work, among others. Launched in March 2018, the Program is a joint initiative of the University of Melbourne's School of Psychological Sciences, Centre for Mental Health and the Department of Psychiatry. These were joined in 2020 by the Centre for Youth Mental Health and the Florey Institute of Neuroscience & Mental Health.
Our goal is to provide all University of Melbourne PhD students researching mental health with a platform to connect, share and discover new disciplines so that they can become fully-rounded researchers who can approach the field of mental health from a multi-disciplinary perspective.
Host departments
The Melbourne School of Psychological Sciences is one of the most highly regarded schools of psychology in Australia. The School attracts some of the best students nationally and internationally to its broad range of APAC-accredited undergraduate, graduate, professional and research programs. The School's teaching is underpinned by excellence in research across a range of fields, including cognitive and behavioural neuroscience, quantitative psychology, social psychology, developmental psychology and clinical science.
The Centre for Mental Health is part of the Melbourne School of Population and Global Health and aims to improve mental health and mitigate the impact of mental illness at a population level. It does this through high-quality, collaborative, interdisciplinary research, academic teaching, professional and community education, and mental health system development. The Centre contributes to evidence-informed mental health policy and practice in Australia and internationally through the work of its three units:
- Global and Cultural Mental Health
- Mental Health Policy and Practice
- Population Mental Health.
The Centre's three units are involved in active and productive collaborations within the University and beyond. These relationships range from not-for-profit agencies like Mind Australia through to international NGOs such as the World Health Organization, and enables the translation of their research into policy and practice.
The Department of Psychiatry is committed to the prevention of mental illness and improved quality of life for individuals affected by mental illness, both nationally and internationally. The Department has unique strengths around biological and translational psychiatry research which are internationally recognised. Together with clinical collaborations and involvement in mental health policy and practice, this provides a stimulating environment for learning and research training programs. Their research is driven by pure and applied questions that require cross-disciplinary approaches and partnerships with diverse community organisations - especially those effected with mental illness. The research informs our teaching and clinical training and engagement with the wider community.
The Centre for Youth Mental Health brings together the experience and expertise of world leaders in the field of youth mental health and has become an internationally renowned research centre in this field. The Centre focuses on understanding the biological, psychological and social factors that influence onset, remission and relapse of mental illnesses in young people. Its research findings are actively translated into improved policy, practice and training that inform the development of better interventions, treatments and service systems for young people at different stages of mental ill-health. The multidisciplinary nature of its research provides a diverse and stimulating environment for students. The local and international collaborations with other universities and research institutes link it with a broader research community, with unique global perspectives and the opportunity for an exciting exchange of ideas.
The Florey Institute of Neuroscience & Mental Health (The Florey) is the largest brain research group in the southern hemisphere and one of the world’s top brain research centres. It is an independent medical research institute with strong connections to other research groups, globally. Our scientists are found at three research facilities, one on the grounds of the University of Melbourne in Parkville, one in the adjacent Royal Melbourne Hospital and the other at Austin Health in Heidelberg.

Program activities
Mental health is a multidisciplinary, complex and rapidly growing research domain. Your years as a graduate researcher at the University of Melbourne are the perfect time for you to broaden your skill set, build your network and expand your understanding of this dynamic field. At the moment we have over 70 graduate researchers in our community who come from over a dozen different Centres and Schools within the University and we would love for you to join us!
Our online platform
In order for you to get to know others and learn from the MHPP community's wide variety of disciplines and expertise, we have an online platform with different channels offering a host of opportunities:
- PhD Progress and Professional Development Channel: Ask any questions you might have about all aspects of your PhD, get peer support and develop your research skills by making the most of professional development opportunities such as online workshops and skills training.
- MHPP Events Channel: Find information here about the events organised by the Program , including social get-togethers, webinars and workshops.
- Members and Alumni Channel: Connect with your fellow PhD students across the many different institutes and schools represented in the Program, learn from alumni and build your research network.
- Items of Interest Channel: Be kept up to date about University of Melbourne events related to mental health and get invited to attend colloquium talks by local and visiting experts across the different academic host units, offering unparalleled access to cutting-edge research in mental health.
And more…
In addition, you can also use the MHPP as a unique opportunity to expand your CV by working on your transferable skills and help run an event or become a Mental Health PhD Program Event Coordinator ( not mandatory ).
Program structure
Mhpp co-directors team.

“This PhD Program provides currently enrolled University of Melbourne PhD students working within the domain of mental health with the opportunity to become accomplished graduate researchers who are not only prepared to engage with their own discipline, but are equipped with the capacity to place their work in a broader multidisciplinary context within mental health.”

Centre for Mental Health, Melbourne School of Population and Global Health
“A PhD position is a big commitment and this program creates a platform to support a true cohort experience and provide a network of support, aimed to help PhD candidates working within the mental health domain through their doctorate and beyond.”

Department of Psychiatry, Melbourne Medical School
“Undertaking a PhD can be one of the most rewarding experiences in your life, yet sometimes, as one buries deeper into their topic, there is risk of feeling quite isolated and disconnected. The Mental Health PhD Program provides a wonderful opportunity to share the journey, connect with others with similar interests, and gain exposure to the broader mental health research landscape.”

Centre for Youth Mental Health
“The Mental Health PhD Program is a vibrant community of post-graduate students who share a common passion and interest in creating new knowledge in the field of mental health, but who come at this through different disciplines, lenses and research methodologies. This program provides a wonderful and unique opportunity for exposure to different ways of thinking about similar problems in a supportive, collaborative and engaging way.”

Florey Institute of Neuroscience & Mental Health
“To transform our understandings into mental health and metal ill-health, we really need multifaceted complimentary approaches that span preclinical tools to clinical approaches and services. This PhD Program provides a unique opportunity for students to be exposed to this breadth of multidisciplinary research that is available within Parkville and the University of Melbourne, and to share their PhD journey with a diverse cohort that will get them thinking about all the levels at which we need to tackle research in the mental health field.”
MHPP Operations Manager

The Mental Health PhD Program now has a wonderful Operations Manager: Brendan Pearl (Department of Psychiatry). Brendan is involved in the organisation, coordination and promotion of many of our great events.
MHPP Event Coordinators
The Mental Health PhD Program has a new online platform with a team of Event Coordinators. This is a team of current MHPP PhD students who help organise events and provide a true cohort experience. The invaluable contributions of these wonderful MHPP members is what makes the Program truly great!
It is also a great way for members to work on their transferable skills, expand their CVs and create a vast multidisciplinary network with the University of Melbourne. If you would like to join the MHPP and are perhaps interested in taking on the role of Event Coordinator for some time during your PhD journey then please visit the application tab here . We would love to hear from you!

Florey Institute for Neuroscience and Mental Health

Centre for Mental Health

Department of General Practice

Melbourne Neuropsychiatry Centre, Department of Psychiatry

Department of Psychiatry
Please find below testimonials from some of our current graduate researchers about their experience of the Mental Health PhD Program.
If you are a mental health graduate researcher, this program is a fundamental building block to understanding how dynamic, complex, inspirational, positive and exciting the field of mental health can be.

Tam Dennis - Graduate Researcher at the Melbourne School of Psychological Sciences
I am very fortunate to be a part of this amazing community and highly recommend it for any PhD student in the area of mental health!

Kavisha Fernando - Graduate Researcher at the Department of Psychiatry
The Mental Health PhD Program (MHPP) is a wonderful program which promotes learning and professional development during your PhD journey.

Carra Simpson - Graduate Researcher at the Melbourne School of Psychological Sciences
What I like about the MHPP is that it provides a platform which is graduate-researcher driven and truly multidisciplinary; it provides opportunities for developing skills which we identify as useful and are above and beyond the scope of our individual departments.

Brendan Pearl - Graduate Researcher at the Department of Psychiatry
I recommend all students with a project related to mental health join the program, get involved and reap the benefits!

Hannah Savage -Graduate Researcher at the Department of Psychiatry
I highly recommend this program to any PhD students in the field of mental health research.

Phoebe Thomson - Graduate Researcher at the Department of Paediatrics
The Mental Health PhD Program creates an inspiring and supportive community of researchers who are united by a common passion for improving mental health and well-being.

Annai Charlton - Graduate Researcher at The Florey Institute of Neuroscience and Mental Health
The Mental Health PhD Program provides me with lots of different opportunities; networking, career development and the opportunity to ask experts from interdisciplinary fields for advice.

"The MHPP has helped me develop skills that I otherwise wouldn’t have developed, such as being able to communicate about research to people who work in related fields but use very different research techniques (animal work or qualitative research). It’s also a very social program, and I’ve met a lot of other very friendly PhD students. Being an off-campus PhD student, I sometimes felt a bit disconnected from the university, but this program has helped alleviate this feeling. The new online Teams platform is great, I get to check it whenever I want and there are optional events to join. I’ve found lots of them very useful and I ended spending about 1.5 hours a fortnight engaged with the program (5 minutes a day reading updates and chatting to other students and 1 hour attending an event such as an expert discussion, watching an interview or a coffee moment). I’m hoping to meet you soon and feel free to contact me if you have any questions!"
Yara Toenders - Graduate Researcher at the Centre for Youth Mental Health
Being a part of the MHPP community has been one of the best parts of my PhD.

Anna Ross, Graduate Researcher at the Centre for Mental Health, Melbourne School of Population and Global Health
How to apply?
The Mental Health PhD Program is offered by the University's School of Psychological Sciences, the Centre for Mental Health, the Department of Psychiatry, the Centre for Youth Mental Health and the Florey Institute of Neuroscience & Mental Health.
Graduate researchers at any stage of their PhD candidature and in any Department, Centre or School at the University of Melbourne are eligible to participate.
The Mental Health PhD Program is intended to be a supplement to the training graduate researchers receive in their home department. Program participants will remain enrolled in their current faculties and departments.
Eligibility
To be eligible, graduate researchers must be currently enrolled in a PhD, have their primary supervisor based at the University of Melbourne and be undertaking doctoral research on a topic related to mental health.
Prospective graduate researchers
If you are not currently enrolled, you will need to apply separately for entry to a PhD in a relevant field. This will generally involve finding an appropriate supervisor in a suitable academic Department, School or Faculty. Once you have commenced your mental health-related PhD course, you can then register to join the Mental Health PhD Program.
Check that you meet the University's eligibility and entry requirements to undertake a PhD, and find instructions on how to apply on MDHS' Graduate Research pages . You can also read more general information about the MDHS PhD course .
Applications
The application procedure is currently closed. Due to unforeseen technical issues, the opening for 2021 applications has unfortunately been delayed until February 8, 2020. Our apologies for any inconvenience.
Applications to join the Program can be submitted throughout the year and graduate researchers can join the Program at any time during their candidature.
If you meet the eligibility criteria and you are interested in meeting your peers from throughout the University of Melbourne and creating a more multidisciplinary understanding of mental health research then please apply below. We look forward to welcoming you to our community!
Apply for the Program
If you have any questions, please don’t hesitate to contact us .
Frequently Asked Questions
What will i get out of the program.
It has never been more important for PhD students to be strategic about career moves, build broad networks and master the right skills to get into their career of choice. The Mental Health PhD Program offers you a platform to:
- Increase your understanding of the multidisciplinary field of mental health
- Save you time finding support and learning about events and resources at the University of Melbourne
- Engage in professional development opportunities specific to the domain of mental health
- Expand your CV
- Present your work, to practice your conference talks or poster presentations
- Get access to extra professional development opportunities workshops, lectures and events that are organised within the University of Melbourne PhD Program Network and only advertised to PhD students who are enrolled in one of the University of Melbourne PhD Programs
- Socialise, share, reflect and learn with and from your peers.
What will the time investment be?
We understand that as a PhD student you have a busy schedule and often competing demands, so we have created an online platform that you can access when and where you like. As a member of the MHPP, we kindly ask you to meet the following time commitment of around three hours per month:
- A weekly active contribution to the online platform. This can be done by posting a question, sharing a tip with your peers, replying to a question posted by another member, liking a post, etc (5-10 minutes per week).
- Join our bi-weekly online events. We really encourage you to attend these live online events so you can ask any questions or join the discussion and share your expertise. That way we really can learn with and from each other. However, we understand you might not always be able to make it so we record most of our events so you can access them at a later point (one hour fortnightly).
- Read any emails you get from the MHPP carefully and reply promptly when needed.
Do I need formal approval from my supervisor to be part of the Mental Health PhD Program?
As of 2020, the Mental Health PhD Program has a new model and formal proof of approval from your Primary Supervisor is no longer required. However, we strongly encourage you to discuss your enrolment into this specific program, as well as your professional development in general, with your supervisor before signing up.
Does the Mental Health PhD Program offer PhD positions?
This multidisciplinary PhD Program is an academic and professional development initiative for currently-enrolled PhD students who are researching a topic within Mental Health. Therefore, this program does not directly enrol students.
Eligible students will need to apply separately for entry to a PhD in a relevant field. This will typically involve finding an appropriate supervisor in a suitable academic Department, School or Faculty. Once students have commenced their mental health-related PhD course, they can register to join the Mental Health PhD Program, which is intended to be a supplement to the training that students receive in their home department.
How can I unsubscribe?
If you need to terminate your enrolment you can do so by unsubscribing from the Mental Health PhD Program Newsletter.
Where can I go for further information?
Please email Anna Schroeder at [email protected] with any questions or feedback. I’d love to hear from you.
This interdisciplinary PhD Program provides participants with the opportunity to become accomplished graduate researchers who are not only prepared to engage with their own discipline, but are also equipped with the capacity to place their work in a broader multidisciplinary context within mental health, maximising their graduate career outcomes.
If you have any questions about the Program or our events, please contact the Program Coordinator Anna Schroeder at [email protected] .
Program Co-Directors
Professor Nick Haslam Melbourne School of Psychological Sciences
Professor Jane Pirkis Centre for Mental Health
Professor Chris Davey Department of Psychiatry
Associate Professor Kelly Allot Centre for Youth Mental Health
Professor Andrew Lawrence Florey Institute of Neuroscience & Mental Health
Operations Manager
Brendan Pearl Department of Psychiatry
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Psychedelic Therapy—A New Paradigm of Care for Mental Health
- 1 Department of Mental Health, James J. Peters VA Medical Center, Bronx, New York
- 2 Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, New York
- Original Investigation Single-Dose Psilocybin Treatment for Major Depressive Disorder Charles L. Raison, MD; Gerard Sanacora, MD, PhD; Joshua Woolley, MD, PhD; Keith Heinzerling, MD; Boadie W. Dunlop, MD, MS; Randall T. Brown, MD, PhD; Rishi Kakar, MD; Michael Hassman, DO; Rupal P. Trivedi, MD; Reid Robison, MD; Natalie Gukasyan, MD; Sandeep M. Nayak, MD; Xiaojue Hu, MD; Kelley C. O’Donnell, MD, PhD; Benjamin Kelmendi, MD; Jordan Sloshower, MD, MSc; Andrew D. Penn, RN, MS, NP; Ellen Bradley, MD; Daniel F. Kelly, MD; Tanja Mletzko, MA; Christopher R. Nicholas, PhD; Paul R. Hutson, PharmD; Gary Tarpley, PhD; Malynn Utzinger, MD; Kelsey Lenoch, BS; Kasia Warchol, BS; Theraysa Gapasin, MS, aMFT; Mike C. Davis, MD, PhD; Courtney Nelson-Douthit, BS; Steffanie Wilson, PhD; Carrie Brown, MA; William Linton, BS; Matthew W. Johnson, PhD; Stephen Ross, MD; Roland R. Griffiths, PhD JAMA
An increasing number of clinicians and researchers have become interested in the potential of psychedelic drugs for the treatment of mental health disorders, including depression, anxiety, posttraumatic stress disorder, eating disorders, and addictions. 1 , 2
Currently, most psychedelic compounds are illegal under federal law. They were placed on the most restrictive class of drugs, Schedule I, in the 1970s as part of the “war on drugs,” meaning that they were considered to have high potential for abuse with no accepted medical use. 2 However, the ever-growing global mental health crisis, coupled with the shortage of effective therapeutic strategies, has given rise to a reconsideration of the therapeutic potential of these compounds in recent years.
Classic psychedelics have rapid and profound effects on perception, cognition, and consciousness that result in part from their actions at serotonin 5-HT2 A receptors. 1 This can result in heightened awareness of one’s internal states and feelings of connectedness that last for several hours. Psychedelics can also induce challenging and difficult experiences and need to be used carefully and in the presence of facilitators or therapists who are trained to work with people experiencing nonordinary states of consciousness. But these compounds offer unique therapeutic possibilities in their ability to promote openness to engage with things that are often avoided and suppressed. In fact, before they were determined to be Schedule I drugs, psychedelics were used therapeutically to help patients open up and identify and discuss emotionally triggering material in psychotherapy. 2
The study by Raison et al provides an excellent example of the promise of this new approach using psilocybin therapy for patients with major depressive disorder. 3 Although the trial was relatively small, it demonstrated that a single dose of psilocybin in the context of a 6-week period that included active psychotherapy resulted in a rapid, robust, and sustained reduction in depressive symptoms.
Psilocybin is a naturally occurring compound belonging to a class of compounds known as tryptamines, similar to lysergic acid diethylamide (LSD), dimethyltryptamine (DMT), and mescaline. Understanding its therapeutic efficacy requires an appreciation of the context in which it is used, and not just its pharmacological profile or biological mechanism of action. The psychotherapy that occurs with the psychedelic medication is a critical component of this approach. 4
When a psychedelic is taken with the proper preparation, intention, facilitation, and therapeutic environment, the patient can use the experience to gain new insights that can catalyze healing and recovery. The psychedelic allows feelings such as self-compassion, forgiveness, understanding, and self-acceptance to surface that can be powerful antidotes to shame, guilt, anger, isolation, disconnection, or other negative emotions that patients find difficult to discuss in therapy and that do not seem to be mitigated by traditional antidepressants. 1 Furthermore, a sense of boundlessness or ego dissolution may be felt as a mystical or spiritual experience, helping people find meaning, perspective, and connection with others and the world. These experiences have been associated with symptom reduction and may represent an important mechanism of action. 4
The psychedelic approach Is radically different from traditional approaches that seek to suppress depressive symptoms by targeting presumptive underlying pathophysiology or biological dysregulation. Dysphoria, irritability, anxiety, and sleep problems can respond to classic antidepressants and help patients manage symptoms and improve functioning. But the benefits of psychopharmacotherapy and psychotherapy are often small and incremental, and true remission is generally not obtained for months or years. 5 , 6 Furthermore, psychotropic medications require chronic use, can be difficult to discontinue, and cause a variety of adverse effects, including weight gain, sexual dysfunction, and feelings of sedation or emotional numbing. Symptoms can reappear, even in stabilized patients, when the medications are discontinued, creating a heartbreaking dilemma for patients.
In contrast, psychedelic therapies address the cause of symptoms rather than merely suppressing them. Here, a medication is administered acutely for only a few sessions—sometimes even a single medication session—in the context of a therapeutic framework that provides the opportunity to integrate and synthesize the revelations that occur during the medication session. The acute pharmacological effects of the medicine, including potential adverse effects, resolve quickly and the safety profile is good. Clinically significant response rates are robust and can be maintained for weeks or months.
However, it is clear that despite the enthusiasm, psychedelic therapies do not represent a panacea for every patient. There are no silver bullets in psychiatry. In the study by Raison et al, similar to all other reports, there are a significant number of patients who did not respond to therapy. 3 , 7 It is important to analyze and understand adverse outcomes in psychedelic trials and conduct longitudinal studies to determine how sustained the effects will be and what may initiate a recrudescence of symptoms. Future studies will help identify who is most likely to benefit from psychedelics, whether booster or repeated treatment is safe and beneficial, and what the optimal dose and therapeutic frameworks are.
Nonetheless, psychedelic therapy represents a novel way of approaching mental health treatment that may benefit many people. It will also bring new knowledge regarding molecular bases of mental illness and how they relate to consciousness. Inquiries into the mechanisms of action of psychedelics will open new windows of understanding regarding neuronal plasticity and brain functioning. 1
Psychedelic therapies necessitate a rethinking of mental health care delivery in which medication is integrally paired with psychotherapy and delivered in a novel setting and framework. This will require an investment of time and resources, and it is not likely that these approaches will be broadly available to psychiatric patients except in clinical trials for the next few years. However, if the gains are strong and enduring and patients report symptom reduction and existential and spiritual transformation, the investment may be warranted. Meanwhile, clinicians should be knowledgeable about these new treatments as public interest and the empirical base grow.
The social, economic, and public health impacts of untreated mental disorders demand solutions. If psychedelic therapies do prove to have enduring effects after just a single or a few administrations in the context of a few sessions for preparation and integration, they have the potential to offer not just a new approach to mental health care, but an entirely new paradigm of care.
Corresponding Author: Rachel Yehuda, PhD, James J. Peters VA Medical Center, 130 W Kingsbridge Rd, 526 OOMH, Bronx, NY 10468 ( [email protected] ).
Published Online: August 31, 2023. doi:10.1001/jama.2023.12900
Conflict of Interest Disclosures: Dr Yehuda reported receiving nonfinancial support from MAPS PBC (Multidisciplinary Association for Psychedelic Studies Public Benefit); grants from COMPASS Pathways, Steven and Alexandra Cohen Foundation, and The Bob and Renee Parsons Foundation; and honoraria for talks at the National Institute for the Clinical Application of Behavioral Medicine, Danish Psychiatric Society, Boston Trauma Conference, and UPenn Nursing School outside the submitted work and reported consulting for TeraMind, Wesana, and the Noetic Fund. Dr. Lehrner is an investigator on a trial sponsored by MAPS PBC financially supported by the Steven and Alexandra Cohen Foundation and a trial sponsored by COMPASS Pathways and reported receiving honoraria for talks at Psychedelic Science 2023 and Philadelic 2023.
See More About
Yehuda R , Lehrner A. Psychedelic Therapy—A New Paradigm of Care for Mental Health. JAMA. 2023;330(9):813–814. doi:10.1001/jama.2023.12900
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Mental Health
The Department of Mental Health conducts research to advance the understanding of mental and behavioral disorders; develops, implements, and evaluates methods to prevent and control these disorders; and promotes mental health in the population.
- Mental Health Diversity, Equity, and Inclusion
- Origins of Mental Health
- Job Openings
- Faculty Profiles
- PET Alumni Profiles - Postdocs
- PET Alumni Profiles - Predocs
- Trainee Profiles
- NIMH T32 Mental Health Services and Systems Training Grant
- Funded Training Program in Data Integration for Causal Inference in Behavioral Health
- Aging and Dementia Funded Training Program
- COVID-19 and Mental Health Research
- Mental Health Resources During COVID-19
- News and Media
- Social Determinants of Mental and Behavioral Health
- Our Work in Action
- Global Mental Health
- Related Faculty
- Courses of Interest
- Training and Funding Opportunities
- Mental Health in the Workplace: A Public Health Summit
- Autism and Developmental Disabilities
- Alumni Newsletters
- Alumni Updates
- Postdoctoral Fellows
- Doctor of Philosophy (PhD) Students in Mental Health
- Master of Health Science (MHS) Students in Mental Health
- In the News
- Past Seminars 2020-21 AY: Wednesday Seminar Series
- Make a Gift
- Available Datasets
Mental Health Headlines
Black public health heroes who made—and are making—history.
Researchers, physicians, and activists who have inspired Bloomberg School faculty and shaped the field of public health
How Abortion Trigger Laws Impact Mental Health
New research shows symptoms of depression and anxiety ticked up in states that enacted trigger laws after Dobbs.
The Journey to Thrive
Transgender people live in an often-hostile world. Can community, research, and resilience reduce the threats to their health?
What We Do in the Department of Mental Health
Our Department—the only department dedicated to mental health in a school of public health—brings together leading researchers across multiple disciplines joined by their passion for understanding, preventing, and treating mental health and substance use disorders. Faculty, students, and community health leaders in Mental Health are dedicated to educating the next generation of public health workers and scientists about the importance of mental health, the specific skills needed to address public mental health issues, and the integration of mental and physical health.
Mental Health Highlights
One-of-a-kind department.
We are the only department dedicated to mental health in a school of public health. In 1961, we were founded as the Department of Mental Hygiene—our name has changed, but our mission remains the same.
Spanning the Life Course
Faculty, staff, and students carry out research across childhood, adulthood, and later life mental and behavioral health.
Teaching and Training Focus
We are committed to providing our students with training and mentoring to excel in a challenging but supportive way.
From Methods to Prevention
We cover a broad scope of mental and behavioral health across methods and disorders.
Mental Health Programs
The Department of Mental Health offers a doctoral program, a master's program in health science, and a combined bachelor’s/master’s program. We also offer postdoctoral training, two certificate programs, and a special Summer Institute.
Bachelor's/Master of Health Science (Bachelor's/MHS)
The Bachelor's/MHS program gives Public Health Studies majors at Johns Hopkins University an opportunity to seamlessly extend their undergraduate studies to graduate-level coursework and research.
Master of Health Science (MHS)
The MHS in Mental Health is a nine-month degree program that provides a foundation in the research methods and content-area knowledge essential to public mental health.
Doctor of Philosophy (PhD)
The PhD program provides advanced training in the application of research methods to understand and enhance public mental health.
Centers and Institutes in the Department of Mental Health
The department houses several school-based centers, and has a significant role in many others across the school. These are described below. Centers help bring together faculty, students, and community partners across multiple departments and schools to meet their particular missions in pursuit of improving public mental health.
Center for Mental Health and Addiction Policy
Johns hopkins center on aging and health, moore center for the prevention of child sexual abuse, wendy klag center for autism and developmental disabilities, judith bass, phd '04, mph, mia,.
is an implementation science researcher, with a broad background in sociology, economic development studies, and psychiatric epidemiology.

Follow Our Department
Department news, bloomberg faculty receive new grant to launch first-ever center on workplace mental health, dr. holly wilcox promoted to full professor, carlina carter named to the indispensable role of blacks at johns hopkins university project, upcoming events, dept of mental health wednesday seminar, support our department.
A gift to our department can help to provide student scholarships and internships, attract and retain faculty, and support innovation.
Request Info
- Admissions Overview
- Visit UMass Boston
- Financial Aid
- First-Year Students
- Transfer Students
- Graduate Students
- International Students
- Academics Overview
- Majors & Programs
- Online Learning
- Colleges & Schools
- Academic Calendar
- Healey Library
- Student Equity, Access & Success
- Global Programs
- Study Abroad
- Fellowships
- Campus Life Overview
- Student Groups & Activities
- Housing & Dining
- Health & Wellness
- Diversity & Inclusion
- Safety & Security
- Orientation & New Students
- Research Overview
- Community-Driven Research
- Recognizing Excellence
- Student Research
- Centers & Institutes
- Core Facilities
- Research & Sponsored Programs
- About Overview
- Leadership & Administration
- Mission & Vision
- Facts & Figures
- Accreditation & Rankings
- History of UMass Boston
- Student Consumer Information
- Athletics Overview
- Recreation at UMass Boston
- Current Students
- Parents & Families
- Faculty & Staff
UMass Boston

- Counseling Psychology PhD
Preparing counseling psychologists for advanced careers as scholars and practitioners.
Accredited by the Commission on Accreditation of the American Psychological Association since 2015, UMass Boston's PhD in Counseling Psychology prepares doctoral-level professional counseling psychologists for careers as scholars, university faculty, and practitioners.
Our scientist-practitioner training model prepares students to:
- deliver high quality, evidence-based psychological services and interventions
- employ applied research skills to improve practice and explore social and psychological issues
- serve as effective instructors and teachers
- use innovative approaches to solve problems related to educational and mental health care disparities, improve services for underrepresented populations, and employ systems-level change strategies to advance local and global social justice
Why Apply to UMass Boston's Counseling Psychology PhD Program?
The UMass Boston Counseling Psychology program prepares the next generation of counseling psychology scholars, teachers, and social justice advocates. We believe in the benefits of working with a variety of research methods and theoretical approaches, receiving guidance from multiple mentors, and understanding how to think about human rights and social justice as they apply to local and transnational contexts.
Start Your Application
Plan Your Education
How to apply.
Applicants must meet general graduate admission requirements in addition to the following program-specific requirements:
- Test Scores: Effective 2021, GRE scores are no longer required for admission to the PhD program
- Letters of Recommendation: 3
- Writing Sample: Yes
- Applied master's degree required. We are accepting applications from candidates who will have completed an applied master's program with supervised clinical experience (e.g., Mental Health Counseling, School Psychology, School Counseling, Social Work, and other programs) prior to the Fall admission.
- Minimum of five social science classes (preferably psychology, human development, and statistics)
- Completed project or academic paper
- Statement of purpose: The Statement of Purpose is your opportunity to tell the faculty why you are interested in counseling psychology, to share the reasons why you are applying to UMass Boston in particular, and to describe your training and career goals, as well as how our program may support your progress toward those goals. Many people link their interest to specific faculty expertise as that helps us match applicants to specific faculty for interviews on the interview day.
- Transcripts
- Résumé/Curriculum Vitae
Deadlines & Cost
Deadline: December 1 for fall
Application Fee: The nonrefundable application fee is $75. UMass Boston alumni and current students that plan to complete degree requirements prior to graduate enrollment can submit the application without paying the application fee.
Program Cost Information: Bursar’s Website
Graduate training at the UMass Boston Counseling Psychology Program will prepare students for taking the EPPP (Examination for Professional Practice in Psychology); however, requirements for sitting for the EPPP vary by state licensing boards. The Counseling Psychology Program has reviewed the licensing requirements for all U.S. jurisdictions to determine eligibility (see below). Please note that not all graduates choose to take the EPPP.
U.S. Boards of Psychology in Which Graduates Would Be Eligible to Sit for the EPPP Upon Completion of the Doctoral Program
Alabama, Alaska, Arizona, Arkansas, Colorado, Connecticut, Delaware, District of Columbia (DC), Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Puerto Rico, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virgin Islands, Virginia, Washington, West Virginia, Wisconsin, and Wyoming
U.S. Boards of Psychology in Which Graduates Would NOT Be Eligible to Sit for the EPPP Upon Completion of the Doctoral Program Without Additional Coursework
- California: additional coursework in human sexuality; alcohol/chemical dependency detection and treatment; child abuse assessment; spousal/partner abuse assessment, detection, and intervention strategies; aging and long-term care; and suicide risk assessment and intervention is needed.
- Maine: additional coursework in family or intimate partner violence screening and referral and intervention strategies, including knowledge of community resources, cultural factors, evidence-based risk assessment, and same-gender abuse dynamics is needed.
- New York: Unable to determine if a graduate is eligible. The doctoral program must be registered by the New York Licensing Department as licensure qualifying or determined by the department to be the substantial equivalent in accordance with the Regulations of the Commissioner. Please contact the New York Office of the Professions for specific details on the licensure requirements. Note: We have many alumni who are licensed in NY but historically this state has had additional requirements.
The program is designed to take five years of full-time study, including a full-time internship. Students who enter with a master’s degree in counseling or another applied field will have a reduction in required course credits to the extent their master’s level courses match our required courses, however, it is required that students complete a minimum of three years on campus plus internship. The majority of students have completed the program with four years on campus plus one additional year of internship.
Foundational Courses (18 Credits)
- COUNSL 608 - Psychopathology and Diagnosis 3 Credit(s)
- COUNSL 620 - Life Span Human Development 3 Credit(s)
- CSP 641 - Cognitive and Affective Foundations 3 Credit(s)
- CSP 660 - Physiological Bases of Behavior 3 Credit(s)
- CSP 680 - History & Systems in Counseling and School Psychology 3 Credit(s)
- CSP 705 - Social and Cultural Psychology 3 Credit(s)
Prevention, Assessment, and Intervention Courses (6 Credits)
- COUNSL 614 - Counseling Theory and Practice I 3 Credit(s)
Complete one of the following:
- COUNSL 613 - Vocational Development and Career Information 3 Credit(s)
- COUNSL 615 - Counseling Theory and Practice II 3 Credit(s)
- CSP 706 - Personality Assessment 3 Credit(s)
- CSP 713 - Advanced Career and Group Theory and Practice 3 Credit(s)
- CSP 717 - Advanced Theory and Practice in counseling and School Psychology 3 Credit(s)
- CSP 752 - Health Psychology: Current Theory, Research, and Interventions 3 Credit(s)
- CSP 780 - Supervision and Training in Psychology 3 Credit(s)
- CSP 783 - Practicum in Counseling Psychology I 3 Credit(s)
- CSP 784 - Practicum in Counseling Psychology II: Evidence-Based Practice 3 Credit(s)
- PSYCLN 727 - Emotion-Focused Psychotherapy 3 Credit(s)
- SPY G 602 - Standardized Assessment and Report Writing 3 Credit(s)
Research Courses (18 Credits)
- CSP 703 - Research in Counseling and School Psychology 1-6 Credit(s)
- CSP 704 - Qualitative and Quantitative Research Methods in Counseling and School Psychology 3 Credit(s)
- CSP 708 - Intermediate Statistics in CSP 3 Credit(s)
- CSP 770 - Advanced Statistics in Counseling and School Psychology 3 Credit(s)
- CSP 891 - Dissertation Seminar 3 Credit(s)
- CSP 899 - Dissertation Research 1-9 Credit(s)
Teaching Requirement Course (3 Credits)
- CSP 782 - Teaching in Counseling and School Psychology 3 Credit(s)
Social Justice & Systems Change Courses (12 Credits)
- CSP 701 - Social Justice in Counseling and School Psychology 3 Credit(s)
- CSP 702 - Foundations and Ethics in Counseling Psychology 3 Credit(s)
- CSP 787 - Advanced Practicum III in Counseling and School Psychology 3 Credit(s)
- CSP 801 - Transnational Social Justice in Counseling and School Psychology 3 Credit(s)
Graduation Criteria
Complete 73 credits from 19 courses including six foundational courses; two prevention, assessment, and intervention courses; six research courses; one teaching requirement course; and four social justice and systems change courses. Students who enter with a master’s degree in counseling or a related field will have a reduction in required course credits to the extent their master’s level courses match our required courses.
Capstone: Students starting with a Bachelor’s degree must complete a capstone project based on CSP 704 and 708 consisting of a literature review paper on a topic approved by the faculty advisor. Doctoral candidacy: Completion of a qualifying paper, a critical and synthetic review of a focused body of literature in the area in which the student plans to complete the dissertation. Dissertation: Compose and defend a research project (quantitative or qualitative) that makes a substantive contribution to the knowledge base in counseling psychology or school psychology. It is usually completed by the end of the fourth year, although students may choose to complete the dissertation during or following the internship year. Practicum: Participate in two semesters of practicum. Internship: Complete one full-year of Internship. During the fourth or fifth year after having met all course requirements. Teaching: Co-teach at least one semester. Research Team: Participate on at least one faculty-student research team for five semesters.
En Route Master’s Degree: Students may, with the approval of the program director, apply to receive an MA degree en route to the PhD. To qualify, students must complete 36 credits of course work and the capstone project.
Statute of limitations: Eight years.
Student Admissions, Outcomes, and Other Data
Counseling Psychology PhD Student Admissions, Outcomes, and Other Data
Contact & Faculty
Graduate Program Director / Director of Training Sharon Horne sharon.horne [at] umb.edu (617) 287-7495
Counseling & School Psychology Graduate Programs csp.admissions [at] umb.edu
Counseling Psychology PhD Faculty
- Gonzalo Bacigalupe
- Laura A. Hayden
- Sharon Horne
- Sharon Lamb
- Meredith Maroney
- Takuya Minami
- Kerrie Wilkins-Yel
Learn more about faculty, students, alumni, and the program with the Counseling & School Psychology newsletters .
About Our PhD Programs
Hear why our students chose UMass Boston's Counseling & School Psychology PhD programs.

Counseling & School Psychology
Learn more about UMass Boston's Counseling & School Psychology department, our research, and our faculty.

College of Education & Human Development
Learn more about the faculty, research, and programs that make up our College of Education & Human Development.
Accreditation
The Counseling Psychology Program has been continuously accredited since 2015 by the American Psychological Association Office of Program Consultation and Accreditation. Questions related to the program’s APA accreditation status should be directed to the Commission on Accreditation:
Office of Program Consultation and Accreditation American Psychological Association 750 1st Street, NE, Washington, DC 20002 Phone: (202) 336-5979 / E-mail: [email protected] / Web: www.apa.org/ed/accreditation
University of Utah Hospital
General questions.
- Billing & Insurance
- Health Care Home
- Press Releases
University of Utah announces major funding for new addiction treatment research
Media contact:.
Patricia Brandt Manager, Public Relations and Communications, Huntsman Mental Health Institute University of Utah Health Email: Patricia.Brandt @hsc.utah.edu
Salt Lake City (April 10, 2024) - Worldwide, someone dies from drug or alcohol addiction every four minutes. Now, researchers at Huntsman Mental Health Institute at the University of Utah have been selected by Wellcome Leap to research a new treatment for substance use disorder as part of a $50 million commitment to develop innovative treatments.

Brian J. Mickey, MD, PhD, professor of psychiatry at Huntsman Mental Health Institute (pictured top left), will lead the team of investigators with expertise in psychiatry, biomedical engineering, neuroscience, radiology, and social work to research a new, noninvasive treatment for addiction. Co-principal investigators include Jan Kubanek, PhD , (pictured top center), and Taylor Webb, PhD (pictured top right); co-investigators include (from left to right) Eric Garland, PhD, LCSW ; Rana Jawish, MD ; Vincent Koppelmans, PhD ; and Tom Riis, PhD.
The research will be funded by the Untangling Addiction program, which is a $50 million program founded by Wellcome Leap , to develop scalable measures to assess addiction susceptibility, quantify the risks stemming from addiction, and develop innovative treatments.
“Substance use disorder is a significant global health problem, and yet the treatment options are limited,” Mickey said. “We’re developing a non-invasive intervention for preventing and treating addiction, chronic pain, and depression. This funding will help us validate and generate the data to support the next critical step: an efficacy trial to determine the effectiveness of the intervention.”
Mickey’s team will use a novel ultrasound-based device to modulate deep brain regions and behaviors associated with opioid addiction. The goal will be to ultimately develop this approach into an individually targeted therapeutic intervention for a range of addictions. “Addictions are brain illnesses that have enormous negative impact on individuals, families, and society,” Mickey said. “A major reason that addictions have been difficult to prevent—and treat—is that they are driven by dysfunction of deep brain regions that are challenging to access. Many psychiatric problems such as depression, anxiety, and addiction are caused by malfunction of brain circuits. This project is an example of our mission to understand how these neural circuits are dysregulated and to develop novel, circuit-targeted interventions that return the brain to a healthy state.”
"We are proud to bring Wellcome Leap's innovative problem-solving and funding approach to our research enterprise at the University of Utah," said Taylor Randall, President , University of Utah. "To have our mental health researchers contributing to pioneering work on addiction treatment reaffirms our commitment to improving lives through discovery."
“What makes research like this so impactful is that it brings together a variety of disciplines to help solve complex problems in mental health,” said Mark Hyman Rapaport, MD , CEO of Huntsman Mental Health Institute. “This is particularly timely news given the groundbreaking of a new translational research building on campus focused on mental health and the brain. Our nation is in a mental health crisis, but there is hope if we can think differently and work together to change this trajectory.”
About Huntsman Mental Health Institute
Huntsman Mental Health Institute at University of Utah Health brings together 75 years of patient care, research, and education into one of the nation's leading academic medical centers focused on mental health. Nestled in the campus of University of Utah, Huntsman Mental Health Institute serves the community with 1,600 faculty and staff in 20 locations providing inpatient and outpatient services for youth, teens, and adults as well as a comprehensive crisis care model which includes the nationally recognized SafeUT app and the 988 Crisis hotline for Utah. Our mission is to advance mental health knowledge, hope, and healing for all. Learn more at: HMHI.utah.edu and join the conversation on Instagram , Facebook , TikTok , X and LinkedIn .
- huntsman mental health institute
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Mental health and the pandemic: What U.S. surveys have found
The coronavirus pandemic has been associated with worsening mental health among people in the United States and around the world . In the U.S, the COVID-19 outbreak in early 2020 caused widespread lockdowns and disruptions in daily life while triggering a short but severe economic recession that resulted in widespread unemployment. Three years later, Americans have largely returned to normal activities, but challenges with mental health remain.
Here’s a look at what surveys by Pew Research Center and other organizations have found about Americans’ mental health during the pandemic. These findings reflect a snapshot in time, and it’s possible that attitudes and experiences may have changed since these surveys were fielded. It’s also important to note that concerns about mental health were common in the U.S. long before the arrival of COVID-19 .
Three years into the COVID-19 outbreak in the United States , Pew Research Center published this collection of survey findings about Americans’ challenges with mental health during the pandemic. All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
The research behind the first item in this analysis, examining Americans’ experiences with psychological distress, benefited from the advice and counsel of the COVID-19 and mental health measurement group at Johns Hopkins Bloomberg School of Public Health.
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022.
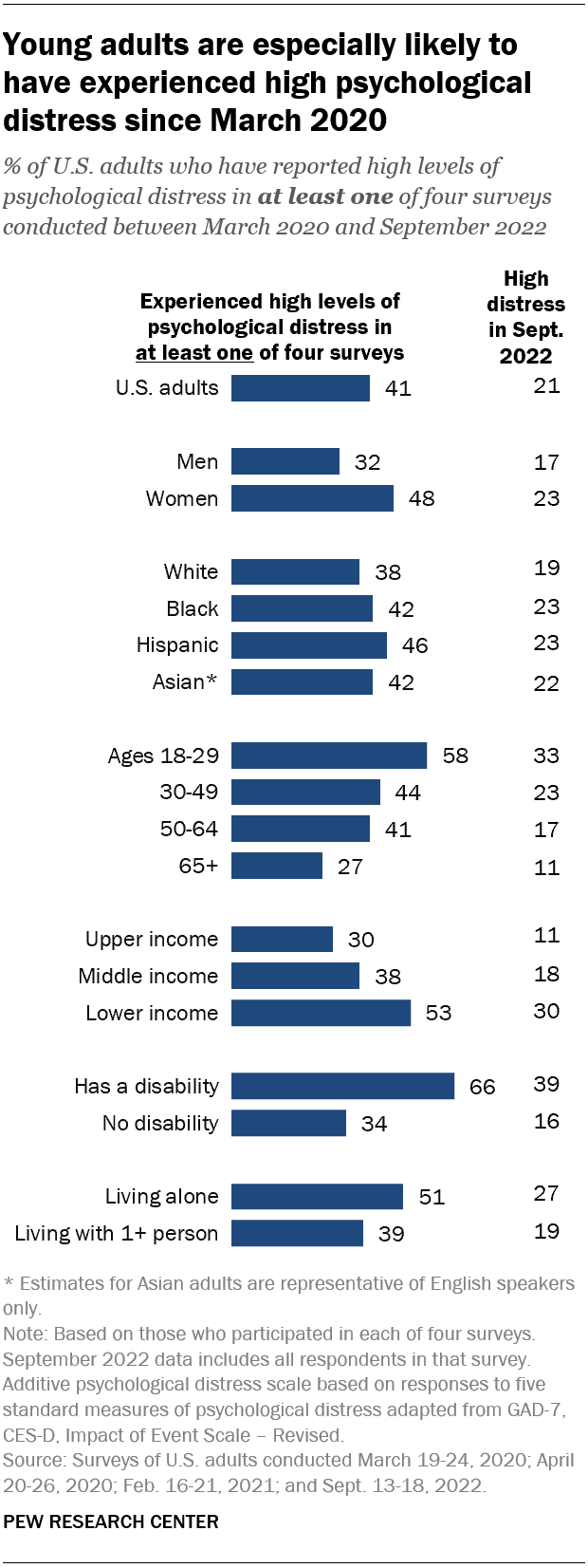
Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this category, based on their answers in at least one of these four surveys.
Women are much more likely than men to have experienced high psychological distress (48% vs. 32%), as are people in lower-income households (53%) when compared with those in middle-income (38%) or upper-income (30%) households.
In addition, roughly two-thirds (66%) of adults who have a disability or health condition that prevents them from participating fully in work, school, housework or other activities have experienced a high level of distress during the pandemic.
The Center measured Americans’ psychological distress by asking them a series of five questions on subjects including loneliness, anxiety and trouble sleeping in the past week. The questions are not a clinical measure, nor a diagnostic tool. Instead, they describe people’s emotional experiences during the week before being surveyed.
While these questions did not ask specifically about the pandemic, a sixth question did, inquiring whether respondents had “had physical reactions, such as sweating, trouble breathing, nausea, or a pounding heart” when thinking about their experience with the coronavirus outbreak. In September 2022, the most recent time this question was asked, 14% of Americans said they’d experienced this at least some or a little of the time in the past seven days.
More than a third of high school students have reported mental health challenges during the pandemic. In a survey conducted by the Centers for Disease Control and Prevention from January to June 2021, 37% of students at public and private high schools said their mental health was not good most or all of the time during the pandemic. That included roughly half of girls (49%) and about a quarter of boys (24%).
In the same survey, an even larger share of high school students (44%) said that at some point during the previous 12 months, they had felt sad or hopeless almost every day for two or more weeks in a row – to the point where they had stopped doing some usual activities. Roughly six-in-ten high school girls (57%) said this, as did 31% of boys.
On both questions, high school students who identify as lesbian, gay, bisexual, other or questioning were far more likely than heterosexual students to report negative experiences related to their mental health.
Mental health tops the list of worries that U.S. parents express about their kids’ well-being, according to a fall 2022 Pew Research Center survey of parents with children younger than 18. In that survey, four-in-ten U.S. parents said they’re extremely or very worried about their children struggling with anxiety or depression. That was greater than the share of parents who expressed high levels of concern over seven other dangers asked about.
While the fall 2022 survey was fielded amid the coronavirus outbreak, it did not ask about parental worries in the specific context of the pandemic. It’s also important to note that parental concerns about their kids struggling with anxiety and depression were common long before the pandemic, too . (Due to changes in question wording, the results from the fall 2022 survey of parents are not directly comparable with those from an earlier Center survey of parents, conducted in 2015.)
Among parents of teenagers, roughly three-in-ten (28%) are extremely or very worried that their teen’s use of social media could lead to problems with anxiety or depression, according to a spring 2022 survey of parents with children ages 13 to 17 . Parents of teen girls were more likely than parents of teen boys to be extremely or very worried on this front (32% vs. 24%). And Hispanic parents (37%) were more likely than those who are Black or White (26% each) to express a great deal of concern about this. (There were not enough Asian American parents in the sample to analyze separately. This survey also did not ask about parental concerns specifically in the context of the pandemic.)
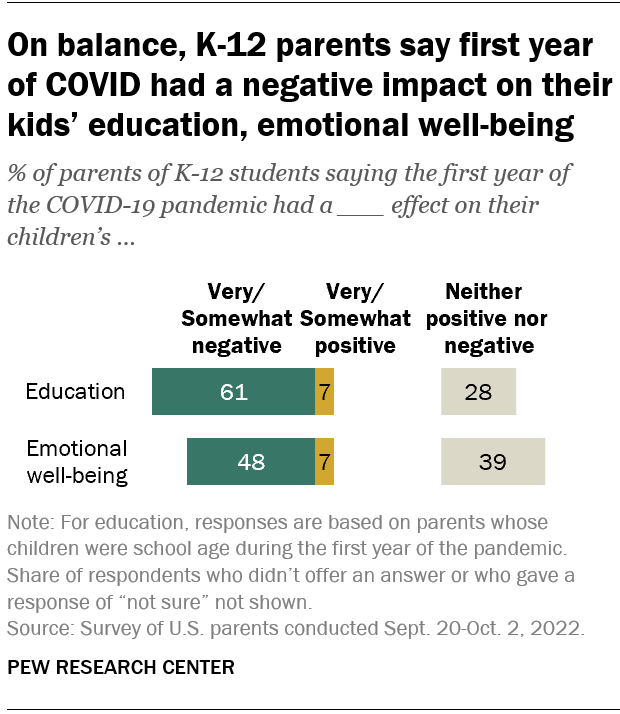
Looking back, many K-12 parents say the first year of the coronavirus pandemic had a negative effect on their children’s emotional health. In a fall 2022 survey of parents with K-12 children , 48% said the first year of the pandemic had a very or somewhat negative impact on their children’s emotional well-being, while 39% said it had neither a positive nor negative effect. A small share of parents (7%) said the first year of the pandemic had a very or somewhat positive effect in this regard.
White parents and those from upper-income households were especially likely to say the first year of the pandemic had a negative emotional impact on their K-12 children.
While around half of K-12 parents said the first year of the pandemic had a negative emotional impact on their kids, a larger share (61%) said it had a negative effect on their children’s education.
- Coronavirus (COVID-19)
- Happiness & Life Satisfaction
- Medicine & Health
- Teens & Youth
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, economy remains the public’s top policy priority; covid-19 concerns decline again, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
- All Stories
- Journalists
- Expert Advisories
- Media Contacts
- X (Twitter)
- Arts & Culture
- Business & Economy
- Education & Society
- Environment
- Law & Politics
- Science & Technology
- International
- Michigan Minds Podcast
- Michigan Stories
- 2024 Elections
- Artificial Intelligence
- Abortion Access
- Mental Health
Michigan Minds Podcast: Nursing & Mental Health: Balancing Stressors, Stigma & Health
- Morgan Sherburne
Christopher Friese , PhD, joined Michigan Minds for the National Nurses Week Special Series. Friese is a professor at the U-M School of Nursing and the director of the Center for Improving Patient and Population Health ( CIPPH ). His research focuses in two areas—measuring and enhancing the quality of cancer care delivery, and understanding and improving the delivery of nursing care to a variety of patients. His research findings were among the first to establish a significant relationship between favorable nurse practice environments and lower surgical mortality.

412 Maynard St. Ann Arbor, MI 48109-1399 Email [email protected] Phone 734-764-7260 About Michigan News
- Engaged Michigan
- Global Michigan
- Michigan Medicine
- Public Affairs
Publications
- Michigan Today
- The University Record
Office of the Vice President for Communications © 2024 The Regents of the University of Michigan

Social Welfare Alum Recounts Mental Health Journey

“Eight years ago, when I was 22 years old, I tried to kill my dad,” Cohen Miles-Rath, ‘19 MSW, began in his talk, Transforming Our Approach to Mental Health: How My Crisis Could Have Been Prevented.
Miles-Rath, now a mental health advocate for the Mental Health Association in New York State, shared the story of his long and painful journey at the School of Social Welfare on April 17, part of the class, “The Art of Storytelling for Social Justice.”
The attack, the result of a psychotic episode, is what most people learn first about him, Miles-Rath explained, since headlines such as Man bites off father’s ear in knife attack are some of the first Google results on a search for his name. But those titles are a snapshot of what Miles-Rath was experiencing, and the mental health issues he struggled with for months following an injury that sidelined his promising college track career and resulted in a disastrous final cross country meet.
During his first psychotic episode in his final undergraduate year at SUNY Geneseo, he thought that he was on a mission to save the world, and was being sent signs to proceed with the mission. A professor recognized that he was making strange drawings and acting irrationally, and referred Miles-Rath to campus mental health support services, who reached out to the police. He was then led to the psychiatric unit of the hospital where he was put on medication to curb his manic thoughts.
He was released from the hospital, promptly stopped taking the medication, and proceeded with his mission, this time creating a Facebook page to share and educate others about his theory. He was brought to the hospital by the police a second time after loitering outside a church in the early hours of the morning, where he waited for an ex-girlfriend to show up at the church to marry him — something he believed was preordained.
He was released from the hospital three days later, and again stopped taking the prescribed medication. It was only days later when he attacked his father and was incarcerated. Miles-Rath now recognizes that while they treated the immediate symptoms in the hospital, there was no plan for treatment to continue with recovery after the hospital release; no plan for therapy or check-ins to ensure that he continued with the prescribed medications.
Recovery began for Miles-Rath while incarcerated. He was put on medication, had frequent meetings with a psychiatrist, and received letters from friends and family who recognized his actions and his illness, and offered their love and support.
“When I received those letters, I finally accepted my mental illness,” he said. “And I started to embrace that treatment because I wanted those medications and that’s when I started recovering.”
Following his release, he continued with mandatory treatments and was able to complete the two remaining courses for his undergraduate degree, and decided to enroll at Stony Brook in the Master of Social Work (MSW) program to help others suffering from mental illness.
While at Stony Brook, he worked as a graduate assistant in the Office of Government and Community Relations , and found success both inside and outside of the classroom while employing the methods he learned to balance self-care and to prioritize his own mental health. Miles-Rath said the MSW program helped him to realize that his initial goal of becoming a therapist was no longer his dream.
“I went into my masters wanting to be a therapist counselor, but I came out wanting to do more macro social work, where you look at more systems policy, culture, and the bigger aspects of things that impact all our lives. What I really liked about the MSW program was that it left some doors open and I was able to find where my strengths were, and then pursue them,” he said. “I found my niche in my second year and my specialization, and that really set the tone for what I wanted to do after graduation, where I found a position that uses everything that I learned in the classroom, all those skills and knowledge that I developed while at Stony Brook.”
He identified several ways to transform the approach to mental health, including fostering social and emotional intelligence from childhood through adulthood; introducing mental health literacy to recognize the signs of mental illness; integrating health care and social care to ensure that hospital-based care will continue after release; and raising the voices of peers and the services they can provide, among others.
As a mental health advocate, Miles-Rath now works to end the stigma against mental illness. “What basis do we have to judge someone’s character when we don’t know enough about them or their situation? And what do these assumptions do for people who might actually need as much help as we can give them? My mental health crisis resulted in violence. It didn’t have to — prevention or intervention could have worked,” he said.
His memoir, Mending Reality: An Advocate’s Existential Journey with Mental Health — revealing the terror of untreated psychosis and outlining the help that could have prevented this crisis — is being considered for publication.
— Beth Squire
Related Posts

Add comment
Cancel reply.
Your Website
Save my name, email, and website in this browser for the next time I comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .

SBUH Hosting First-Ever Journey to Healing Event
Stony Brook University Hospital is hosting its first-ever Journey to Healing event on May 20 aimed at supporting, connecting and celebrating trauma survivors

Chris R. Vaccaro ’11 Incorporates Public Policy Into His Passions
Alumnus Chris R. Vaccaro, MA ’11, has incorporated his passions — civil engagement, journalism, baseball and Italian American heritage — into everything he does. And he attributes many of his professional successes to...

Central Islip High School Students Learn About Future Careers in Engineering and Applied Sciences
A team of engineers, researchers, students and entrepreneurs brought their expertise and advice to Central Islip High School on March 13. Professor Wei Yin, associate dean for diversity and outreach at the College of...
Search SBU News
Subscribe to newsletter, latest stories.

OLLI Receives Largest-Ever Individual Member Gift

Two SoCJ Students Accepted to Dow Jones News Fund Internship Program

Stony Brook Student Advocates Urge Congress to Support NSF Research and Attend Prestigious AAAS CASE Workshop in DC

Armani Awarded Luce/ACLD Dissertation Fellowship in American Art

Stony Brook Collaborative for the Earth Launches Podcast

Zamolodchikov Honored at Star-Studded Ceremony for 2024 Breakthrough Prize

Three from Stony Brook Elected AAAS Fellows for 2023

CAS Hosting First-Ever Humanities Research Day April 24

Eighth Annual Hack@CEWIT Shines a Light on AI

SBU Awarded $1M in Federal Funding for Advancing Energy Technology

Provost’s Lectures Highlight ‘Intellectual Fearlessness’ of Stony Brook

SUNY Expands Chancellor’s Summer Research Excellence Fund

Celebration of Life Honors Brooke Ellison’s Inspiring Legacy

Top Chef Triumph: Executive Chef Claims Silver Medal in Culinary Showdown

Stony Brook Medicine Makes Becker’s Healthcare List of Top Places to Work
- Find Stories
- Media Resources
- Media Relations Team
- Press Clip Archives
- Press Release Archives
Sign Up Today!
Connect with sbu.
© 2021 Stony Brook University
Subscribe to News
- OLLI Receives Largest-Ever Individual Member Gift April 18, 2024
- Two SoCJ Students Accepted to Dow Jones News Fund Internship Program April 18, 2024
- Stony Brook University Faculty Members Named AAAS Fellows April 18, 2024
- Stony Brook Student Advocates Urge Congress to Support NSF Research and Attend Prestigious AAAS CASE Workshop in DC April 18, 2024
- Social Welfare Alum Recounts Mental Health Journey April 18, 2024
- Alumni News
- Arts & Entertainment
- Awards and Honors
- College of Arts & Sciences
- College of Business
- College of Engineering & Applied Sciences
- Commencement
- Faculty/Staff
- Graduate School
- Long Island
- School of Communication and Journalism
- School of Dental Medicine
- School of Health Professions
- School of Medicine
- School of Nursing
- School of Pharmacy
- School of Professional Development
- School of Social Welfare
- Student Spotlight
- Sustainability
- Stay Informed
Get the latest word on Stony Brook news, discoveries and people.
- Events Calendar
- Strauss Health Sciences Library
- Department A-Z Directory
- Campus Directory
- Faculty & Staff Resources
- Supporter & Alumni Resources
- Student Resources
- Mental Health Resources
- University Policies
- CU Anschutz Medical Campus
- CU Colorado Springs
- School of Dental Medicine
- Graduate School
School of Medicine
- College of Nursing
- Skaggs School of Pharmacy and Pharmaceutical Sciences
- Colorado School of Public Health
- Education Admissions Current Students Academy of Medical Educators Diversity & Inclusion Continuing Medical Education Contact Us
- Research Clinical Trials Colorado Clinical & Translational Sciences Institute (CCTSI) Research Core Labs Health Data Compass Information Services Office of Grants & Contracts Office of Laboratory Animal Resources Regulatory Compliance Research Affairs Research Development Resources for Investigators Transformational Research Funding Donate
- Patient Care Clinical Affairs Advanced Practice Providers Donate
- Departments | Centers | Institutes
- Dean's Office About Us Administrative Fellowship Program Administrative Toolbox Alumni Contact Information CU Medicine Today Diversity & Inclusion The Hub Information Services Leadership University of Colorado Medicine Donate

Home News Why Do Women Have a Higher Risk of Developing Autoimmune Disorders? back to News
Why Do Women Have a Higher Risk of Developing Autoimmune Disorders?
It’s complicated, says cu associate professor of medicine kristen demoruelle, md, phd, but genetics, sex hormones, and different environmental factors are likely at play..
minute read
Kristen Demoruelle , MD, PhD, associate professor of medicine at the University of Colorado School of Medicine , is working to develop new insights and novel prevention strategies that stop immune dysregulation before rheumatoid arthritis (RA) develops – a disease that affects approximately 18 million people around the world, 70% of which are women.
Demoruelle, who works in the Division of Rheumatology , spends much of her time studying the immune system at two potential sites that are likely involved in the development of RA – the lung and female genital tract mucosa.
“The work that I do attempts to find ways to better identify who will get RA so that at some point in the future, hopefully, we can prevent it. That’s the ultimate goal,” she says.
For the 50 million people in the U.S. that live with an autoimmune disease, like RA, it’s not known exactly what causes the immune system to attack the body, but researchers hypothesize it may be a combination of genetics and other factors.
Here, Demoruelle discusses what scientists know about why women face higher rates of autoimmune disease and how research is evolving and making new treatments – and possibly prevention – possible.

What defines an autoimmune disease or disorder?
We all have an immune system that's designed to do helpful things for us, like help us fight infections. Basically in all autoimmune diseases, the immune system gets mixed up for reasons that we don't totally understand and it starts to attack the person instead of attacking an infection. Depending on how and what parts of the body the immune system attacks, we label it as different types of autoimmune diseases. Rheumatoid arthritis, for example, primarily affects the joints, whereas multiple sclerosis attacks brain and spinal cord.
There are many factors that might create the right conditions for these disorders to arise. Why do women seem to have a heightened risk?
There may be a lot of factors that play into sex disparities in autoimmune diseases. The human body is complex. We know that women have two X chromosomes and men only have one. You only need one, so that second chromosome gets silenced throughout the body’s cells. Recent research findings suggest that that protein that silences the second X chromosome may contribute to higher rates of autoimmune disease in women.
Pregnancy also impacts the immune system and even a woman’s body’s ability to become pregnant has certain unique requirements of the immune system that may contribute to the disparities we see with higher rates of autoimmune diseases in women. Finally, there are features of the female immune system that can be overly protective. In terms of evolution, that can be a good thing, because you want your body to fight off infections – but it might also raise the risk for developing an autoimmune disorder.
How is research evolving in this realm?
It’s changed quite a bit over the past decade. We have seen much more research focused on women since the National Institute of Health made a policy requirement to include both sexes in the research studies they fund. Here, at the University of Colorado, the Ludeman Center for Women’s Health Research has supported the research of many young scientists who have made novel discoveries to understand sex differences across the lifespan.
There has been a huge push to ensure that studies are done with both men and women so that we can learn what's similar, and what's different to better the wellbeing in everyone.
For example, in some clinical trials, we’ve learned that medication doses should be different for men and women. Having that kind of information is crucial, so, yes, science has changed for the better over time in this area.
With that, we’re also seeing a lot more emphasis on personalized treatments.
That’s right. There are a lot of different medications available these days to treat different diseases, and we want to get to a point where we know how to choose the right medicine, for the right person and the right time. For example, in rheumatoid arthritis, we have a lot more medications to treat rheumatoid arthritis than we did 20 years ago, and it's really been a game changer for patients. That being said, there are still 20% to 25% of patients that don't respond to the treatments that we have. We want to better understand when to target which part of the immune system in each person.
In some studies that have looked at the differences between men and women and their response to these treatments for rheumatoid arthritis, we do see, in general, that women don’t respond as well as men do. This is where personalized medicine could really become helpful.
My hope is that we get to a place of personalized medicine where a variety of factors are considered. One of those needs to be sex because there are differences in treatment response. With more research, we’re getting closer to making that a possibility.
Topics: Research , Patient Care , Autoimmune disease , DOM Newsroom

Kristen Demoruelle, MD, PhD
Related Stories
Research Education Students Mental Health Global Health
Research Shows Value of Mental Health Training for Teachers in India
Research Patient Care Autoimmune disease DOM Newsroom
Research Education Community Health Sciences
Young Researchers Serve Up Science on STEM Poster Day at the Colorado Capitol
Cu anschutz, fitzsimons building.
13001 East 17th Place
Aurora, CO 80045
303.724.5375
School of Medicine Home
Find a Doctor
Find a Researcher
Departments
School Profiles
Affiliate/Partner Hospitals
CU Medicine
Map and Parking
Health Sciences Library
Student Life
Colorado Springs Branch
- Website Feedback
- Privacy Policy
- Terms of Use
- Accessibility
- Accreditation
© 2024 The Regents of the University of Colorado , a body corporate. All rights reserved.
Accredited by the Higher Learning Commission . All trademarks are registered property of the University. Used by permission only.

Turn Your Curiosity Into Discovery
Latest facts.
11 Facts About National Numeracy Day May 22nd
9 Facts About Workers Memorial Day April 28th
40 facts about elektrostal.
Written by Lanette Mayes
Modified & Updated: 02 Mar 2024
Reviewed by Jessica Corbett

Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to captivate you.
This article will provide you with 40 fascinating facts about Elektrostal, giving you a better understanding of why this city is worth exploring. From its origins as an industrial hub to its modern-day charm, we will delve into the various aspects that make Elektrostal a unique and must-visit destination.
So, join us as we uncover the hidden treasures of Elektrostal and discover what makes this city a true gem in the heart of Russia.
Key Takeaways:
- Elektrostal, known as the “Motor City of Russia,” is a vibrant and growing city with a rich industrial history, offering diverse cultural experiences and a strong commitment to environmental sustainability.
- With its convenient location near Moscow, Elektrostal provides a picturesque landscape, vibrant nightlife, and a range of recreational activities, making it an ideal destination for residents and visitors alike.
Known as the “Motor City of Russia.”
Elektrostal, a city located in the Moscow Oblast region of Russia, earned the nickname “Motor City” due to its significant involvement in the automotive industry.
Home to the Elektrostal Metallurgical Plant.
Elektrostal is renowned for its metallurgical plant, which has been producing high-quality steel and alloys since its establishment in 1916.
Boasts a rich industrial heritage.
Elektrostal has a long history of industrial development, contributing to the growth and progress of the region.
Founded in 1916.
The city of Elektrostal was founded in 1916 as a result of the construction of the Elektrostal Metallurgical Plant.
Located approximately 50 kilometers east of Moscow.
Elektrostal is situated in close proximity to the Russian capital, making it easily accessible for both residents and visitors.
Known for its vibrant cultural scene.
Elektrostal is home to several cultural institutions, including museums, theaters, and art galleries that showcase the city’s rich artistic heritage.
A popular destination for nature lovers.
Surrounded by picturesque landscapes and forests, Elektrostal offers ample opportunities for outdoor activities such as hiking, camping, and birdwatching.
Hosts the annual Elektrostal City Day celebrations.
Every year, Elektrostal organizes festive events and activities to celebrate its founding, bringing together residents and visitors in a spirit of unity and joy.
Has a population of approximately 160,000 people.
Elektrostal is home to a diverse and vibrant community of around 160,000 residents, contributing to its dynamic atmosphere.
Boasts excellent education facilities.
The city is known for its well-established educational institutions, providing quality education to students of all ages.
A center for scientific research and innovation.
Elektrostal serves as an important hub for scientific research, particularly in the fields of metallurgy, materials science, and engineering.
Surrounded by picturesque lakes.
The city is blessed with numerous beautiful lakes, offering scenic views and recreational opportunities for locals and visitors alike.
Well-connected transportation system.
Elektrostal benefits from an efficient transportation network, including highways, railways, and public transportation options, ensuring convenient travel within and beyond the city.
Famous for its traditional Russian cuisine.
Food enthusiasts can indulge in authentic Russian dishes at numerous restaurants and cafes scattered throughout Elektrostal.
Home to notable architectural landmarks.
Elektrostal boasts impressive architecture, including the Church of the Transfiguration of the Lord and the Elektrostal Palace of Culture.
Offers a wide range of recreational facilities.
Residents and visitors can enjoy various recreational activities, such as sports complexes, swimming pools, and fitness centers, enhancing the overall quality of life.
Provides a high standard of healthcare.
Elektrostal is equipped with modern medical facilities, ensuring residents have access to quality healthcare services.
Home to the Elektrostal History Museum.
The Elektrostal History Museum showcases the city’s fascinating past through exhibitions and displays.
A hub for sports enthusiasts.
Elektrostal is passionate about sports, with numerous stadiums, arenas, and sports clubs offering opportunities for athletes and spectators.
Celebrates diverse cultural festivals.
Throughout the year, Elektrostal hosts a variety of cultural festivals, celebrating different ethnicities, traditions, and art forms.
Electric power played a significant role in its early development.
Elektrostal owes its name and initial growth to the establishment of electric power stations and the utilization of electricity in the industrial sector.
Boasts a thriving economy.
The city’s strong industrial base, coupled with its strategic location near Moscow, has contributed to Elektrostal’s prosperous economic status.
Houses the Elektrostal Drama Theater.
The Elektrostal Drama Theater is a cultural centerpiece, attracting theater enthusiasts from far and wide.
Popular destination for winter sports.
Elektrostal’s proximity to ski resorts and winter sport facilities makes it a favorite destination for skiing, snowboarding, and other winter activities.
Promotes environmental sustainability.
Elektrostal prioritizes environmental protection and sustainability, implementing initiatives to reduce pollution and preserve natural resources.
Home to renowned educational institutions.
Elektrostal is known for its prestigious schools and universities, offering a wide range of academic programs to students.
Committed to cultural preservation.
The city values its cultural heritage and takes active steps to preserve and promote traditional customs, crafts, and arts.
Hosts an annual International Film Festival.
The Elektrostal International Film Festival attracts filmmakers and cinema enthusiasts from around the world, showcasing a diverse range of films.
Encourages entrepreneurship and innovation.
Elektrostal supports aspiring entrepreneurs and fosters a culture of innovation, providing opportunities for startups and business development.
Offers a range of housing options.
Elektrostal provides diverse housing options, including apartments, houses, and residential complexes, catering to different lifestyles and budgets.
Home to notable sports teams.
Elektrostal is proud of its sports legacy, with several successful sports teams competing at regional and national levels.
Boasts a vibrant nightlife scene.
Residents and visitors can enjoy a lively nightlife in Elektrostal, with numerous bars, clubs, and entertainment venues.
Promotes cultural exchange and international relations.
Elektrostal actively engages in international partnerships, cultural exchanges, and diplomatic collaborations to foster global connections.
Surrounded by beautiful nature reserves.
Nearby nature reserves, such as the Barybino Forest and Luchinskoye Lake, offer opportunities for nature enthusiasts to explore and appreciate the region’s biodiversity.
Commemorates historical events.
The city pays tribute to significant historical events through memorials, monuments, and exhibitions, ensuring the preservation of collective memory.
Promotes sports and youth development.
Elektrostal invests in sports infrastructure and programs to encourage youth participation, health, and physical fitness.
Hosts annual cultural and artistic festivals.
Throughout the year, Elektrostal celebrates its cultural diversity through festivals dedicated to music, dance, art, and theater.
Provides a picturesque landscape for photography enthusiasts.
The city’s scenic beauty, architectural landmarks, and natural surroundings make it a paradise for photographers.
Connects to Moscow via a direct train line.
The convenient train connection between Elektrostal and Moscow makes commuting between the two cities effortless.
A city with a bright future.
Elektrostal continues to grow and develop, aiming to become a model city in terms of infrastructure, sustainability, and quality of life for its residents.
In conclusion, Elektrostal is a fascinating city with a rich history and a vibrant present. From its origins as a center of steel production to its modern-day status as a hub for education and industry, Elektrostal has plenty to offer both residents and visitors. With its beautiful parks, cultural attractions, and proximity to Moscow, there is no shortage of things to see and do in this dynamic city. Whether you’re interested in exploring its historical landmarks, enjoying outdoor activities, or immersing yourself in the local culture, Elektrostal has something for everyone. So, next time you find yourself in the Moscow region, don’t miss the opportunity to discover the hidden gems of Elektrostal.
Q: What is the population of Elektrostal?
A: As of the latest data, the population of Elektrostal is approximately XXXX.
Q: How far is Elektrostal from Moscow?
A: Elektrostal is located approximately XX kilometers away from Moscow.
Q: Are there any famous landmarks in Elektrostal?
A: Yes, Elektrostal is home to several notable landmarks, including XXXX and XXXX.
Q: What industries are prominent in Elektrostal?
A: Elektrostal is known for its steel production industry and is also a center for engineering and manufacturing.
Q: Are there any universities or educational institutions in Elektrostal?
A: Yes, Elektrostal is home to XXXX University and several other educational institutions.
Q: What are some popular outdoor activities in Elektrostal?
A: Elektrostal offers several outdoor activities, such as hiking, cycling, and picnicking in its beautiful parks.
Q: Is Elektrostal well-connected in terms of transportation?
A: Yes, Elektrostal has good transportation links, including trains and buses, making it easily accessible from nearby cities.
Q: Are there any annual events or festivals in Elektrostal?
A: Yes, Elektrostal hosts various events and festivals throughout the year, including XXXX and XXXX.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
Share this Fact:

IMAGES
VIDEO
COMMENTS
The PhD degree is a research-oriented doctoral degree. In the first two years, students take core courses in the Departments of Mental Health, Biostatistics, and Epidemiology, in research ethics, and attend weekly department seminars. Students must complete a written comprehensive exam (in January of their second year), a preliminary exam, two ...
The health of the next generation of researchers needs systemic change to research cultures. Anxiety and depression among graduate students seems to be on the rise. Systemic change is needed to ...
The MHS is a nine-month degree program that provides a foundation in the research methods and content-area knowledge essential to public mental health. Doctoral Doctor of Philosophy (PhD) in Mental Health. The PhD program provides advanced training in the application of research methods to understand and enhance public mental health. Combined
Research Areas. The Department of Mental Health covers a wide array of topics related to mental health, mental illness, and substance abuse. We emphasize ongoing research that enriches and stimulates the teaching programs. All students and fellows are encouraged to participate in at least one research group. Faculty and students from multiple ...
Background Data from studies with undergraduate and postgraduate taught students suggest that they are at an increased risk of having mental health problems, compared to the general population. By contrast, the literature on doctoral researchers (DRs) is far more disparate and unclear. There is a need to bring together current findings and identify what questions still need to be answered ...
The perceived inevitability of mental health problems was such that DRs described people who did not experience mental health problems during a PhD as 'lucky' . Supervisors and the wider academic system were seen to promote an expectation of suffering, for example, with academics reportedly normalising drug and alcohol problems and ...
Seminars in Research in Public Mental Health (all terms required for first year students) 1: PH.330.617: Psychopathology for Public Health (first term) 1: 3: ... Upon successful completion of the PhD in Mental Health, students will have mastered the following competencies: Evaluate the clinical presentations, incidence, prevalence, course and ...
Research policy observers are increasingly concerned about the impact of the disruption caused by the Covid-19 pandemic on university research. Yet we know little about the effect of this disruption, specifically on PhD students, their mental health, and their research progress. This study drew from survey responses of UK PhD students during the Covid-19 pandemic.
Mental disorder manifestation, mental health problems, and expectations related to the PhD training. Participants were asked whether they had been diagnosed with a mental disorder before or after ...
A similar number (41%) told us that most of their PhD colleagues had mental health problems. Just over a third of PhD students had considered ending their studies altogether for mental health reasons.
The UCL Wellcome 4-year PhD in Mental Health Science is an opportunity for students to train in a wide range of fields relevant to mental health research. This programme, funded in 2019, is the first of its kind in the UK, representing an investment of over £5m by the Wellcome Trust.
A new King's College London PhD programme will provide mental health research training fellowships to doctors, nurses, psychologists and allied health professionals. The eight-year programme, offering 25 fellowships, has been funded by a grant of £7.8m from Wellcome Trust, with additional funding or support from a number of partners.
UK PhD students' mental health in times of disruption. In the UK, there are approximately 100,000 postgraduate students completing doctoral research [].Since 2018, significant government funding has been targeted at developing insights into supporting UK PhD students' mental health [].Still, with the exception of Byrom et al. [], published research on PhD students' mental health in the ...
The results don't prove that pursuing a PhD directly contributes to mental-health problems, says study co-author Clio Berry, a research psychologist at Brighton and Sussex Medical School, UK.
As an PhD/MPhil researcher at City's Centre for Mental Health Research, you will be contributing to a body of knowledge and expertise.Making a direct impact on people's health and well-being. Our research on Mental Health addresses the complex links between mental and physical ill-health. We cover including some of the biggest healthcare challenges facing society, such as dementia and ...
Sachin Patel, MD, PhD, is the new chair and Lizzie Gilman Professor of Psychiatry and Behavioral Sciences at Feinberg and psychiatrist-in-chief at Northwestern Memorial Hospital's Norman and Ida Stone Institute of Psychiatry. In this episode, he talks about the current mental health crisis in this country, his research and vision for the department.
Associate Professor Kelly Allott. Centre for Youth Mental Health "The Mental Health PhD Program is a vibrant community of post-graduate students who share a common passion and interest in creating new knowledge in the field of mental health, but who come at this through different disciplines, lenses and research methodologies.
PhD. Dr. Rosmarin (pronouns: he/him), is the director of the Spirituality and Mental Health Program at McLean Hospital and an associate professor of psychology in the Department of Psychiatry at Harvard Medical School. Dr. Rosmarin's program of research examines the relevance of spiritual/religious issues to psychopathology and its treatment.
Natalie Christine Dattilo, PhD. Founder, Priority Wellness Group; Instructor, Harvard Medical School. What: Exercise is my non-negotiable self-care activity. I exercise not only for my physical health, but for my mental health, too. It helps me regulate my emotions better and reminds me that I am strong and capable.
An increasing number of clinicians and researchers have become interested in the potential of psychedelic drugs for the treatment of mental health disorders, including depression, anxiety, posttraumatic stress disorder, eating disorders, and addictions. 1,2 Currently, most psychedelic compounds are illegal under federal law.
Master of Health Science (MHS) Onsite or Online | Full-Time or Part-Time | 9 months - 2 years. The MHS in Mental Health is a nine-month degree program that provides a foundation in the research methods and content-area knowledge essential to public mental health.
Alla Kholmogorova currently works at the Moscow State University of Psychology and Education (dean of the faculty of Counseling and Clinical Psychology). Alla does research in Health Psychology ...
employ applied research skills to improve practice and explore social and psychological issues serve as effective instructors and teachers use innovative approaches to solve problems related to educational and mental health care disparities, improve services for underrepresented populations, and employ systems-level change strategies to advance ...
Worldwide, someone dies from drug or alcohol addiction every four minutes. Now, researchers at Huntsman Mental Health Institute at University of Utah have been selected by Wellcome Leap to research a new treatment for substance use disorder as part of a $50 million commitment to develop innovative treatments. Brian J. Mickey, MD, PhD, Professor of Psychiatry at Huntsman Mental Health Institute ...
Three years into the COVID-19 outbreak in the United States, Pew Research Center published this collection of survey findings about Americans' challenges with mental health during the pandemic.All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
Christopher Friese, PhD, joined Michigan Minds for the National Nurses Week Special Series.Friese is a professor at the U-M School of Nursing and the director of the Center for Improving Patient and Population Health ().His research focuses in two areas—measuring and enhancing the quality of cancer care delivery, and understanding and improving the delivery of nursing care to a variety of ...
Program Director: Shiv Pillai, M.D., Ph.D., Professor of MedicineShiv Pillai is a Professor of Medicine and Health Sciences and Technology at Harvard Medical School. He is the director of the Harvard PhD and MMSc Immunology programs and of the HMS-HST MD student research program. He is also the program director of an NIH-funded Autoimmune Center of Excellence at Massachusetts General Hospital.
"Eight years ago, when I was 22 years old, I tried to kill my dad," Cohen Miles-Rath, '19 MSW, began in his talk, Transforming Our Approach to Mental Health: How My Crisis Could Have Been Prevented. Miles-Rath, now a mental health advocate for the Mental Health Association in New York State, shared the story of his long and painful journey at the School of Social Welfare on April 17 ...
Kristen Demoruelle, MD, PhD, associate professor of medicine at the University of Colorado School of Medicine, is working to develop new insights and novel prevention strategies that stop immune dysregulation before rheumatoid arthritis (RA) develops - a disease that affects approximately 18 million people around the world, 70% of which are women.
A center for scientific research and innovation. Elektrostal serves as an important hub for scientific research, particularly in the fields of metallurgy, materials science, and engineering. ... Health Science. 12 Jan 2024 18 Neo40 Supplement Facts . Events. 17 Dec 2023 10 Mindblowing Facts About 40 Hour Famine . Celebrity.