- Whooping cough

On this page
When to see a doctor, risk factors, complications.
Whooping cough (pertussis) is a highly contagious respiratory tract infection. In many people, it's marked by a severe hacking cough followed by a high-pitched intake of breath that sounds like "whoop."
Before the vaccine was developed, whooping cough was considered a childhood disease. Now whooping cough primarily affects children too young to have completed the full course of vaccinations and teenagers and adults whose immunity has faded.
Deaths associated with whooping cough are rare but most commonly occur in infants. That's why it's so important for pregnant women — and other people who will have close contact with an infant — to be vaccinated against whooping cough.
Once you become infected with whooping cough, it takes about seven to 10 days for signs and symptoms to appear, though it can sometimes take longer. They're usually mild at first and resemble those of a common cold:
- Nasal congestion
- Red, watery eyes
After a week or two, signs and symptoms worsen. Thick mucus accumulates inside your airways, causing uncontrollable coughing. Severe and prolonged coughing attacks may:
- Provoke vomiting
- Result in a red or blue face
- Cause extreme fatigue
- End with a high-pitched "whoop" sound during the next breath of air
However, many people don't develop the characteristic whoop. Sometimes, a persistent hacking cough is the only sign that an adolescent or adult has whooping cough.
Infants may not cough at all. Instead, they may struggle to breathe, or they may even temporarily stop breathing.
Call your doctor if prolonged coughing spells cause you or your child to:
- Turn red or blue
- Seem to be struggling to breathe or have noticeable pauses in breathing
- Inhale with a whooping sound
From Mayo Clinic to your inbox
Whooping cough is caused by a type of bacteria called Bordetella pertussis. When an infected person coughs or sneezes, tiny germ-laden droplets are sprayed into the air and breathed into the lungs of anyone who happens to be nearby.
The whooping cough vaccine you receive as a child eventually wears off. This leaves most teenagers and adults susceptible to the infection during an outbreak — and there continue to be regular outbreaks.
Infants who are younger than age 12 months who are unvaccinated or haven't received the full set of recommended vaccines have the highest risk for severe complications and death.
Teens and adults often recover from whooping cough with no problems. When complications occur, they tend to be side effects of the strenuous coughing, such as:
- Bruised or cracked ribs
- Abdominal hernias
- Broken blood vessels in the skin or the whites of your eyes
In infants — especially those under 6 months of age — complications from whooping cough are more severe and may include:
- Slowed or stopped breathing
- Dehydration or weight loss due to feeding difficulties
- Brain damage
Because infants and toddlers are at greatest risk of complications from whooping cough, they're more likely to need treatment in a hospital. Complications can be life-threatening for infants younger than 6 months old.
The best way to prevent whooping cough is with the pertussis vaccine, which doctors often give in combination with vaccines against two other serious diseases — diphtheria and tetanus. Doctors recommend beginning vaccination during infancy.
The vaccine consists of a series of five injections, typically given to children at these ages:
- 15 to 18 months
- 4 to 6 years
Vaccine side effects
Side effects of the vaccine are usually mild and may include a fever, crankiness, headache, fatigue or soreness at the site of the injection.
Booster shots
- Adolescents. Because immunity from the pertussis vaccine tends to wane by age 11, doctors recommend a booster shot at that age to protect against whooping cough (pertussis), diphtheria and tetanus.
- Adults. Some varieties of the every-10-year tetanus and diphtheria vaccine also include protection against whooping cough (pertussis). This vaccine will also reduce the risk of your transmitting whooping cough to infants.
- Pregnant women. Health experts now recommend that pregnant women receive the pertussis vaccine between 27 and 36 weeks of gestation. This may also give some protection to the infant during the first few months of life.
Preventive medications
If you've been exposed to someone who has whooping cough, your doctor may recommend antibiotics to protect against infection if you:
- Are a health care provider
- Are pregnant
- Are younger than age 12 months
- Have a health condition that could put you at risk of severe illness or complications, such as a weakened immune system or asthma
- Live with someone who has whooping cough
- Live with someone who is at high risk of developing severe illness or complications from a whooping cough infection
Feb 11, 2022
- Pertussis frequently asked questions. Centers for Disease Control and Prevention. https://www.cdc.gov/pertussis/about/faqs.html. Accessed Nov. 2, 2017.
- Kasper DL, et al., eds. Pertussis and other Bordatella infections. In: Harrison's Principles of Internal Medicine. 19th ed. New York, N.Y.: McGraw-Hill Education; 2015. http://accessmedicine.mhmedical.com. Accessed Nov. 2, 2017.
- Cornia P, et al. Pertussis infection in adolescents and adults: Clinical manifestations and diagnosis. https://www.uptodate.com/contents/search. Accessed Nov. 2, 2017.
- Yeh S. et al. Pertussis infection in infants and children: Clinical features and diagnosis. https://www.uptodate.com/contents/search. Accessed Nov. 2, 2017.
- Yeh S. Pertussis infection in infants and children: Treatment and prevention. https://www.uptodate.com/contents/search. Accessed Nov. 2, 2017.
- Tdap (Tetanus, Diphtheria, Pertussis) vaccine information statements. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/tdap.html. Accessed Nov. 2, 2017.
- Postexposure antimicrobial prophylaxis. Centers for Disease Control and Prevention. https://www.cdc.gov/pertussis/outbreaks/pep.html. Accessed Nov. 13, 2017.
- Steckelberg JM (expert opinion). Mayo Clinic, Rochester, Minn. Nov. 20, 2017.
- Diseases & Conditions
- Whooping cough symptoms & causes
News from Mayo Clinic

More Information
Associated procedures.
- Chest X-rays
CON-XXXXXXXX
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

JONATHAN M. KLINE, PharmD, ELEANOR A. SMITH, MD, AND ADRIENNE ZAVALA, MD
Am Fam Physician. 2021;104(2):186-192
Pertussis, also known as whooping cough, remains a public health concern despite expanded immunization recommendations over the past three decades. The presentation of pertussis, which is variable and evolves over the course of the disease, includes nonspecific symptoms in the catarrhal stage, coughing with the classic whooping in the paroxysmal stage, and persistent cough in the convalescent stage. When there is clinical suspicion for pertussis, the diagnosis should be confirmed using polymerase chain reaction testing, which has replaced culture as the preferred confirmatory test. Recent evidence has confirmed a waning of acquired immunity following pertussis immunization or infection, leading to changes in tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) immunization recommendations. Patients 11 years or older should receive at least one dose of Tdap, although Tdap may replace any dose of the tetanus and diphtheria toxoids (Td) vaccine. All pregnant patients should receive Tdap between 27 and 36 weeks' gestation with each pregnancy to convey immunity to the newborn. Cocooning (vaccinating close contacts of high-risk individuals) is no longer recommended because immunized patients can still contract and transmit pertussis. A history of seizure or hypotonic-hyporesponsive episodes after a prior pertussis vaccination is no longer a contraindication to immunization. Antibiotic treatment is intended to prevent transmission of pertussis to others and does not shorten the disease course or improve symptoms. Antibiotic prophylaxis is recommended for household contacts of someone with pertussis and for those exposed to pertussis who are at high risk of severe illness (e.g., infants, people who are immunocompromised or in the third trimester of pregnancy) or in close contact with someone at high risk. Azithromycin is the preferred antibiotic for treatment or prophylaxis.
Pertussis, or whooping cough, is an acute respiratory tract infection that continues to affect a significant portion of the global population, with more than 24 million estimated cases in 2014. 1 Pertussis, a Centers for Disease Control and Prevention (CDC) reportable disease, is caused by Bordetella pertussis . The disease can lead to substantial complications in infants, such as apnea, pneumonia, seizures, other hypoxic complications, hospitalization, or death. 2 , 3 Bordetella parapertussis and rarely Bordetella bronchiseptica can also cause a pertussis-like syndrome.
The incidence of pertussis in the United States decreased with universal childhood immunization, but it has rebounded steadily in recent years, from a low of 1,010 reported cases in 1976 to a peak of 48,277 cases in 2012. 4 The most recent available data show 15,609 reported cases in 2018. 5
What Is the Typical Presentation and Progression of Pertussis?
There are three stages of pertussis (catarrhal, paroxysmal, and convalescent), each with a different clinical presentation ( Table 1 ). 6 – 8 However, clinical presentation varies widely depending on age and immunization status, and not every patient has the classic stage progression. 9
EVIDENCE SUMMARY
The key clinical features of the initial catarrhal stage are difficult to distinguish from a viral upper respiratory tract infection and include malaise, rhinorrhea, dry cough, and lacrimation. Fever is usually mild or absent. After one to two weeks, the paroxysmal stage may manifest. Typical features of this stage include paroxysmal coughing, whooping on inspiration after coughing, and posttussive emesis.
Other common features of the paroxysmal stage include periods of apnea associated with paroxysms, chest and abdominal soreness from prolonged coughing, and scleral hemorrhage. In between paroxysms, the patient may be asymptomatic. The paroxysmal stage typically lasts up to six weeks before transitioning to the convalescent stage. In this stage, the coughing lessens but typically persists for an additional two to four weeks, with some patients experiencing symptoms for a longer period (e.g., “100-day cough”). 7 , 10 – 12
Can Pertussis Be Diagnosed with Clinical Signs and Symptoms Alone, or Is Laboratory Testing Required?
The diagnosis of pertussis requires laboratory confirmation. Because early detection and treatment are critical to reducing transmission, accurate identification of the clinical features of pertussis is important to prompt testing .
No validated, accepted clinical decision rule has been established for diagnosing pertussis. 13 However, the key clinical features of the infection are included in CDC and World Health Organization (WHO) case definitions. The CDC case definition of pertussis includes coughing of any duration and at least one sign or symptom (i.e., paroxysmal coughing, inspiratory whooping, posttussive emesis, or apnea) and contact with a laboratory-confirmed case of pertussis, or at least two weeks of coughing and one of these signs or symptoms. 14 The WHO definition adds the clinical suspicion of pertussis and specifies that apnea is a criterion only in infants younger than one year. 15 Although sensitive, the CDC and WHO criteria lack specificity. 13
Two 2017 systematic reviews evaluated the clinical features used in the diagnosis of pertussis ( Table 2 ) . 13 , 16 One found that the best clinical predictors of pertussis in adults were the presence of whooping (positive likelihood ratio [LR+] = 1.45) and posttussive emesis (LR+ = 1.46), and the best negative predictors were a lack of paroxysmal coughing (negative likelihood ratio [LR−] = 0.33) and presence of fever (LR− = 0.97). 16 However, the second systematic review reported minimal value of individual signs and symptoms, with the clinician's overall impression having the highest likelihood ratio out of both reviews (LR+ = 3.3). 13
According to a 2019 guideline, pertussis should be considered likely in adults who have posttussive emesis or inspiratory whooping and unlikely if the patient has fever or lack of paroxysmal coughing. 17 In children, pertussis should be considered likely if the patient has posttussive emesis, paroxysmal coughing, or inspiratory whooping. 17
What Is the Preferred Diagnostic Laboratory Test for Pertussis?
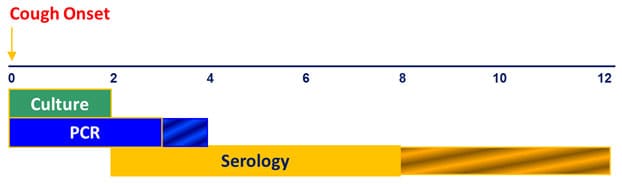
Polymerase chain reaction (PCR) is the most accurate test to confirm pertussis (LR+ = 13; LR− = 0.03) and is the diagnostic test of choice in most cases. 18 Culture should be used to confirm a positive PCR result during pertussis outbreaks for strain identification or if PCR is not available. 7 Serology can be a helpful adjunct late in the course of illness (more than three weeks) but only in patients older than six months who have not been vaccinated in the past year. 19 , 20
The sensitivities of culture and PCR are highest during the catarrhal and early paroxysmal phase, whereas the sensitivity of serology (immunoglobulin G) does not peak until late in the paroxysmal and convalescent phases ( Table 3 ) . 18 , 19 , 21 , 22 PCR is the preferred test because it provides rapid and accurate results, whereas cultures are limited by antibiotic use and prior immunization, they are challenging to grow, and results take seven to 10 days. 7
Serology is primarily used for epidemiology but could be useful in patients who present late in the course of illness because it can help confirm the diagnosis as late as 12 weeks after symptom onset. 6 , 23 Serology is not useful in patients who would be expected to have circulating antibodies (e.g., those who were recently vaccinated). 24 Direct fluorescent antibody assays are no longer used because of low sensitivity and specificity. 19
In infants younger than three months with a typical clinical presentation, leukocytosis (leukocyte level higher than 20,000 per μL [20.00 × 10 9 per L]) with greater than 50% lymphocytes can be virtually diagnostic for pertussis. 19 , 20
Why Does Pertussis Remain a Common Disease Despite High Vaccination Rates?
Some strains have shifted away from displaying the acellular vaccine antigens (i.e., pertussis toxin, pertactin, fimbriae 2 or 3, and filamentous hemagglutinin). These are known as vaccine antigen deficient strains or escape mutants . 4 , 25 , 26 Even without this shift, immunity wanes in most patients because of uncertain causes .
Unlike with other vaccines, there is not a standardized antibody titer to confirm protection against pertussis. 27 Although pertussis vaccines were initially whole cell, the high reactogenicity of the vaccine caused frequent adverse effects (e.g., local reaction, seizure, pain, fever sometimes leading to febrile seizure), resulting in the adoption of acellular vaccines in the 1990s.
Immunity typically wanes two to four years after administration of the acellular pertussis vaccine, although this can occur as early as one year postvaccination. 28 Individuals with natural infection also experience waning immunity, including children with a history of pertussis. 4 , 29 Because of this rapid decrease in immunity, it is not considered an effective public health strategy to continue recurrent tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) boosters. 4
Why Did the Vaccine Recommendations Change for Adolescents in 2005 and Pregnant Patients in 2012?
Despite high pertussis vaccination rates in infants and children, there was a significant increase in the incidence of pertussis in the 1990s and early 2000s, especially among adolescents. Infants younger than two months have the highest risk of hospitalization and death; therefore, a passive immunity strategy (placental transmission of maternal antibodies) was adopted to protect this group. 4
Because of the increasing incidence of pertussis in the United States and an observed waning immunity regardless of the source of inoculation (whole cell or acellular vaccine or infection), the CDC's Advisory Committee on Immunization Practices (ACIP) published updated pertussis vaccination guidelines in 2005, including introducing a booster of Tdap, rather than tetanus and diphtheria toxoids (Td), at 11 to 12 years of age or once as an adult if not previously received. 4 Table 4 summarizes current pertussis vaccine guidelines. 4 , 28
Because more than 85% of pertussis deaths occur in infants too young to receive pertussis vaccination, it is recommended that pregnant patients receive the Tdap vaccine between 27 and 36 weeks' gestation with each pregnancy. 4 , 30 This timing was recommended because of rapid waning of antipertussis antibodies and optimal timing of placental antibody transfer. 30 , 31 If the third-trimester booster is missed, ACIP recommends not vaccinating patients with Tdap postpartum if they have ever received Tdap. 4
Should Nonmaternal Caretakers of Infants or Close Contacts of Health Care Workers Be Given Tdap Boosters?
No, unless otherwise overdue for the Tdap vaccine. The target is for all individuals to receive a Tdap booster once. 28 Although ACIP's 2020 recommendation allows for either Td or Tdap formulations for tetanus prophylaxis or booster, the change is essentially for the convenience of the clinician and patient because there is no identified risk of extra Tdap administrations. 28
There is no difference in adverse effects in patients given Td or Tdap at an interval of five to 10 years, and data in pregnant patients given multiple doses in shorter time spans also have not shown an increase in adverse effects. 28 , 32 Cocooning (vaccinating close contacts of infants and others at high risk) was based on a faulty assumption that vaccinated individuals could not transmit the disease. 4 It is now known that immunized patients can contract and transmit pertussis, although the vaccine reduces disease severity in the vaccinated individual. 27 Models have since shown that household siblings are more significant carriers of pertussis than the mother. 4 Therefore, passive immunity through immunization of the mother during pregnancy is the primary public health goal.
If a Patient Has a Seizure After Administration of Any Dose of DTaP or Tdap, Are Additional Doses Contraindicated?
Seizure after pertussis vaccination was previously a contraindication for receiving further doses, but the risk of repeat seizure or a complicated neurologic event after subsequent diphtheria and tetanus toxoids and acellular pertussis (DTaP) or Tdap administration is low (0.5 cases of encephalopathy per 10 million doses), and further pertussis vaccination should not be avoided. 4 , 28 Safety concerns with DTaP and Tdap are summarized in eTable A .
Immunization should be temporarily delayed in a patient who has uncontrolled seizure disorder or a progressing neurologic disorder, such as infantile spasms, until the disorder is stabilized. Patients with a history of seizures that are currently controlled and patients who had a seizure with previous pertussis vaccines without prolonged symptoms of coma or encephalopathy do not have a contraindication to receiving additional doses of DTaP or Tdap vaccines. 4 Children who have had persistent crying or hypotonic-hyporesponsive episodes with DTaP are unlikely to have repeat episodes with further doses; therefore, these are not contraindications to receiving DTaP or Tdap boosters. 4
What Antibiotic Should Be Used to Treat Patients with Pertussis?
Antibiotics are intended to prevent transmission of pertussis to others and do not shorten the disease course or improve symptoms. Azithromycin (Zithromax) is the preferred treatment for pertussis because of its favorable safety profile, but use of other macrolides (erythromycin, clarithromycin) or trimethoprim/sulfamethoxazole is an acceptable alternative. 2 , 33 , 34
EVIDENCE REVIEW
Antibiotics for pertussis have been shown to provide a microbiologic cure and are prescribed to prevent the spread of the disease within 21 days of cough onset. 2 , 33 – 35 A Cochrane review did not show that antibiotics significantly reduce mortality, symptom duration, or complications in patients with pertussis. 2
Azithromycin has replaced erythromycin as the preferred treatment because of its daily dosing, shorter course, and fewer gastrointestinal adverse effects. 2 , 33 , 36 In adults, azithromycin can be given as a dosage of 500 mg for three days or 500 mg on day 1, then 250 mg on days 2 to 5. In children, it can be given as a dosage of 10 mg per kg for three days or 10 mg per kg on day 1, then 5 mg per kg on days 2 to 5. 2 , 33 , 36
Should Pertussis-Related Cough Be Treated with Adjunct Therapies?
Treatments aimed at reducing cough, including corticosteroids, antihistamines, beta-2 agonists, and pertussis immune globulin, have not been associated with improved symptoms in patients with pertussis. 37
A 2014 Cochrane review evaluating symptomatic treatments for pertussis, including one or two poor-quality studies per intervention, found no benefit in the reduction of coughing episodes or length of hospitalization. 37 The use of symptomatic treatments is not recommended.
Who Should Receive Antibiotic Prophylaxis?
Postexposure prophylaxis should be initiated in household contacts of someone with pertussis and in those exposed to pertussis who are at high risk of severe illness or in close contact with someone who is at high risk of severe illness. 38 Postexposure prophylaxis should be initiated within 21 days of exposure. 38
The CDC recommends postexposure prophylaxis within 21 days of exposure in household contacts of someone with pertussis and in those exposed to pertussis who are at high risk of severe illness or in close contact with someone at high risk. 38 Those at highest risk of severe illness include infants and people who are in their third trimester of pregnancy, are immunocompromised, or who have comorbidities that increase the risk of severe illness (e.g., respiratory disorders). The CDC has limited prophylaxis to only these groups because placebo-controlled studies of erythromycin have not demonstrated effectiveness, and a Cochrane review found no benefit of postexposure prophylaxis in those older than six months who are not in contact with an infant. 2 , 39
Azithromycin is the preferred agent for prophylaxis, at the same dosage as pertussis treatment. 2 , 33 Tdap should no longer be administered for postexposure prophylaxis. 4
This article updates previous articles on this topic by Kline, et al. , 10 and Gregory . 40
Data Sources: The primary resources used to identify literature were PubMed and the Cochrane database. Primary search terms included pertussis (free text) or pertussis (MeSH) and one of the following terms: treatment, complications, diagnosis, prevention, vaccination. Limits were used to identify primary literature. Essential Evidence Plus and article reference lists were reviewed to identify further sources. The CDC website was also searched using the terms above and the additional term ACIP. Search dates: April 30, 2020; June 2, 2020; July 7, 2020; October 8, 2020; and March 16, 2021.
Yeung KHT, Duclos P, Nelson EAS, et al. An update of the global burden of pertussis in children younger than 5 years: a modelling study. Lancet Infect Dis. 2017;17(9):974-980.
Altunaiji S, Kukuruzovic R, Curtis N, et al. Antibiotics for whooping cough (pertussis). Cochrane Database Syst Rev. 2007(3):CD004404.
Centers for Disease Control and Prevention. Pertussis (whooping cough). Clinical complications. Accessed July 19, 2020. https://www.cdc.gov/pertussis/clinical/complications.html
Liang JL, Tiwari T, Moro P, et al. Prevention of pertussis, tetanus, and diphtheria with vaccines in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2018;67(2):1-44.
Centers for Disease Control and Prevention. Pertussis (whooping cough). Pertussis cases by year (1922–2018). Accessed October 25, 2020. https://www.cdc.gov/pertussis/surv-reporting/cases-by-year.html
Cornia PB, Hersh AL, Lipsky BA, et al. Does this coughing adolescent or adult patient have pertussis?. JAMA. 2010;304(8):890-896.
Daniels HL, Sabella C. Bordetella pertussis (pertussis). Pediatr Rev. 2018;39(5):247-257.
Mattoo S, Cherry JD. Molecular pathogenesis, epidemiology, and clinical manifestations of respiratory infections due to Bordetella pertussis and other Bordetella subspecies. Clin Microbiol Rev. 2005;18(2):326-382.
Tozzi AE, Ravà L, Ciofi degli Atti ML, et al. Clinical presentation of pertussis in unvaccinated and vaccinated children in the first six years of life. Pediatrics. 2003;112(5):1069-1075.
Kline JM, Lewis WD, Smith EA, et al. Pertussis: a reemerging infection [published correction appears in Am Fam Physician . 2014;89(5):317]. Am Fam Physician. 2013;88(8):507-514. Accessed February 11, 2021. https://www.aafp.org/afp/2013/1015/p507.html
Centers for Disease Control and Prevention. Pertussis (whooping cough). Clinical features. Accessed September 10, 2020. https://www.cdc.gov/pertussis/clinical/features.html
Liang Y, Salim AM, Wu W, et al. Chao Yuanfang: imperial physician of the Sui dynasty and an early pertussis observer?. Open Forum Infect Dis. 2016;3(1) ):ofw017.
Ebell MH, Marchello C, Callahan M. Clinical diagnosis of Bordetella pertussis infection: a systematic review. J Am Board Fam Med. 2017;30(3):308-319.
Centers for Disease Control and Prevention. Pertussis (whooping cough) ( Bordetella pertussis ) 2020 case definition. Accessed June 2, 2020. https://wwwn.cdc.gov/nndss/conditions/pertussis/case-definition/2020/
World Health Organization. Pertussis. Vaccine-preventable diseases: surveillance standards. Accessed June 2, 2020. https://www.who.int/publications/m/item/vaccine-preventable-diseases-surveillance-standards-pertussis
Moore A, Ashdown HF, Shinkins B, et al. Clinical characteristics of pertussis-associated cough in adults and children: a diagnostic systematic review and meta-analysis. Chest. 2017;152(2):353-367.
Moore A, Harnden A, Grant CC, et al. Clinically diagnosing pertussis-associated cough in adults and children: CHEST Guideline and Expert Panel report. Chest. 2019;155(1):147-154.
Dragsted DM, Dohn B, Madsen J, et al. Comparison of culture and PCR for detection of Bordetella pertussis and Bordetella parapertussis under routine laboratory conditions. J Med Microbiol. 2004;53(pt 8):749-754.
van der Zee A, Schellekens JFP, Mooi FR. Laboratory diagnosis of pertussis. Clin Microbiol Rev. 2015;28(4):1005-1026.
Cherry JD, Tan T, Wirsing von König CH, et al. Clinical definitions of pertussis: summary of a global pertussis initiative roundtable meeting, February 2011. Clin Infect Dis. 2012;54(12):1756-1764.
Templeton KE, Scheltinga SA, van der Zee A, et al. Evaluation of real-time PCR for detection of and discrimination between Bordetella pertussis , Bordetella parapertussis , and Bordetella holmesii for clinical diagnosis [published correction appears in J Clin Microbiol . 2004;42(4):1860]. J Clin Microbiol. 2003;41(9):4121-4126.
André P, Caro V, Njamkepo E, et al. Comparison of serological and real-time PCR assays to diagnose Bordetella pertussis infection in 2007. J Clin Microbiol. 2008;46(5):1672-1677.
Nguyen VTN, Simon L. Pertussis: the whooping cough. Prim Care. 2018;45(3):423-431.
Gopal DP, Barber J, Toeg D. Pertussis (whooping cough). BMJ. 2019;364:I401.
Barkoff AM, He Q. Molecular epidemiology of Bordetella pertussis . Adv Exp Med Biol. 2019;1183:19-33.
Poolman JT. Shortcomings of pertussis vaccines: why we need a third generation vaccine. Expert Rev Vaccines. 2014;13(10):1159-1162.
Magpantay FMG, Domenech DE, Cellès M, et al. Pertussis immunity and epidemiology: mode and duration of vaccine-induced immunity. Parasitology. 2016;143(7):835-849.
Havers FP, Moro PL, Hunter P, et al. Use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccines: updated recommendations of the Advisory Committee on Immunization Practices—United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(3):77-83.
Wendelboe AM, Van Rie A, Salmaso S, et al. Duration of immunity against pertussis after natural infection or vaccination. Pediatr Infect Dis J. 2005;24(5 suppl):S58-S61.
Healy CM, Rench MA, Baker CJ. Importance of timing of maternal combined tetanus, diphtheria, and acellular pertussis (Tdap) immunization and protection of young infants. Clin Infect Dis. 2013;56(4):539-544.
Munoz FM, Bond NH, Maccato M, et al. Safety and immunogenicity of tetanus diphtheria and acellular pertussis (Tdap) immunization during pregnancy in mothers and infants: a randomized clinical trial [published correction appears in JAMA . 2017;317(4):441–442]. JAMA. 2014;311(17):1760-1769.
Fortner KB, Swamy GK, Broder KR, et al. Reactogenicity and immunogenicity of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) in pregnant and nonpregnant women. Vaccine. 2018;36(42):6354-6360.
Langley JM, Halperin SA, Boucher FD, et al.; Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC). Azithromycin is as effective as and better tolerated than erythromycin estolate for the treatment of pertussis. Pediatrics. 2004;114(1):e96-e101.
Tiwari T, Murphy TV, Moran J National Immunization Program, CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC guidelines. MMWR Recomm Rep. 2005;54(RR-14):1-16.
Wood N, McIntyre P. Pertussis: review of epidemiology, diagnosis, management and prevention. Paediatr Respir Rev. 2008;9(3):201-211.
Cherry JD. Treatment of pertussis-2017. J Pediatric Infect Dis Soc. 2018;7(3):e123-e125.
Wang K, Bettiol S, Thompson MJ, et al. Symptomatic treatment of the cough in whooping cough. Cochrane Database Syst Rev. 2014(9):CD003257.
Centers for Disease Control and Prevention. Pertussis (whooping cough). Postexposure antimicrobial prophylaxis. Accessed July 20, 2020. https://www.cdc.gov/pertussis/pep.html
Halperin SA, Bortolussi R, Langley JM, et al. A randomized, placebo-controlled trial of erythromycin estolate chemoprophylaxis for household contacts of children with culture-positive Bordetella pertussis infection. Pediatrics. 1999;104(4):e42.
Gregory DS. Pertussis: a disease affecting all ages. Am Fam Physician. 2006;74(3):420-426. Accessed February 11, 2021. https://www.aafp.org/afp/2006/0801/p420.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Pertussis. Presentation, investigation and management
Affiliation.
- 1 Paediatric Infectious Diseases Unit, Department of General Medicine, Royal Children's Hospital, Melbourne, Victoria.
- PMID: 15227860
Background: Pertussis (whooping cough) is a highly infectious, preventable disease, which causes significant morbidity and mortality.
Objective: This article discusses the presentations, investigations and management of cases and their contacts.
Discussion: Maternal antibody does not confer protection to the infant so babies are particularly at risk of infection and complications until they have completed the primary course of vaccinations at 2, 4 and 6 months of age. Diagnosis is primarily clinical, but can be confirmed with immunofluorescence on nasopharyngeal aspirate or nasal swab. Recent changes to the Australian Standard Vaccination Schedule include the removal of the 18 month dose of DTPa and the addition of an adult formulation booster vaccination at 15-17 years of age.
Publication types
- Anti-Bacterial Agents / therapeutic use
- Bordetella pertussis / isolation & purification
- Child, Preschool
- Family Practice / methods*
- Family Practice / standards
- Immunization Schedule
- Patient Isolation / standards
- Pertussis Vaccine / therapeutic use
- Practice Guidelines as Topic
- Whooping Cough / diagnosis*
- Whooping Cough / drug therapy
- Whooping Cough / microbiology
- Whooping Cough / prevention & control*
- Anti-Bacterial Agents
- Pertussis Vaccine
Chapter 10: Pertussis
Disease description, importance of rapid case identification, importance of surveillance, disease reduction goals, case definitions, laboratory testing, vaccination, enhancing surveillance, case investigation, outbreak control, manual for the surveillance of vaccine-preventable diseases.
Authors: Amy Blain, MPH; Tami Skoff, MS; Pam Cassiday, MS; Maria Lucia Tondella, PhD; Anna Acosta, MD
Pertussis, more commonly known as whooping cough, is a contagious, respiratory disease caused by the bacterium Bordetella pertussis . The illness is typically characterized by a prolonged paroxysmal cough that is often accompanied by an inspiratory whoop. Disease presentation can vary with age and history of previous exposure or vaccination. Young infants may present to a clinic or hospital with apnea and no other disease symptoms. Adults and adolescents with some immunity may exhibit only mild symptoms or have the typical prolonged paroxysmal cough. In all persons, cough can continue for months.
Pertussis rarely causes severe complications among healthy, vaccinated persons. Infants, however, are at greatest risk for pertussis-related complications and mortality. Pneumonia is the most common complication in all age groups; seizures and encephalopathy are rare and generally occur only among very young infants. Death is infrequent and most likely to occur in unvaccinated infants, although fatalities are occasionally reported among older children and adults with serious underlying health conditions. [1]
In addition to B. pertussis , 3 other Bordetella species can cause disease in humans: B. parapertussis , B. holmesii , and B. bronchiseptica . B. parapertussis causes a pertussis-like illness that is generally milder than pertussis, likely because the bacteria do not produce pertussis toxin. Co-infection of B. pertussis and B. parapertussis can occur but is uncommon. Disease attributable to Bordetella species other than B. pertussis is not reportable to the Centers for Disease Control and Prevention (CDC).
In the pre-vaccine era, pertussis was a common childhood disease and a major cause of child and infant mortality in the United States. Routine childhood vaccination led to a reduction in disease incidence from an average of 150 reported cases per 100,000 persons between 1922 and 1940, to 0.5 cases per 100,000 persons in 1976. [2] The incidence of reported pertussis began increasing in the 1980s, however, and significant peaks in disease have been observed in recent years. In 2012, 48,277 cases were reported nationwide, exceeding levels observed since 1955. Reported pertussis cases have decreased since 2012, with 18,975 cases reported during 2017; however, levels remain significantly increased compared to those observed during the 1990s and early 2000s. Multiple factors have likely contributed to the increase, including waning immunity from acellular pertussis vaccines, heightened provider and public awareness, improved diagnostic testing, and possibly molecular changes within the pertussis bacterium. The incidence of pertussis remains highest among young infants. From 2012 through 2017, 66.7%, of all pertussis-related deaths (n = 72) reported to CDC were among infants less than two months of age, who were too young to have received DTaP vaccine. As of 2017, the second highest incidence of pertussis continues to occur among school-aged children and adolescents. [3–5]
Early diagnosis and treatment of pertussis might limit its spread to other susceptible people. When pertussis is strongly suspected, attempts to identify and provide chemoprophylaxis to household and other close contacts at high risk should proceed without waiting for laboratory confirmation. When suspicion of pertussis is low, the investigation can be delayed until there is laboratory confirmation of the diagnosis. However, chemoprophylaxis of pregnant women and infants, as well as their household contacts, should not be delayed.
Surveillance data collected through case investigations are used to assess the impact of disease and monitor changes in epidemiology over time. Surveillance data are also used to guide public health policy and development of prevention and control strategies. CDC uses surveillance data to monitor national trends in pertussis and identify populations at risk. Local and state health departments use surveillance data to identify clusters of related cases that might indicate an outbreak.
Laboratory surveillance to monitor changes in the B. pertussis organism is also important. Isolates of B. pertussis collected through routine surveillance have provided researchers with the resources necessary to identify such changes, including recent changes in the organism at the molecular level. [6–9] This information is vital to understanding the evolution of B. pertussis and how those changes may impact the current pertussis vaccination program and other prevention strategies. See Section VII, “Laboratory Testing” for more details.
As part of the Healthy People 2020 project, disease reduction goals of 2,500 indigenous pertussis cases per year in children <1 year of age and 2,000 cases per year among adolescents 11 through 18 years of age were proposed. [10] In 2017, 2,276 cases were reported among infants less than 1 year of age, while 6,171 cases were observed among adolescents 11 through 18 years of age. [5]
Top of Page
The following case definition for pertussis was approved by the Council of State and Territorial Epidemiologists (CSTE) in June 2019 and went into effect January 1, 2020. [11]
Clinical case definition
In the absence of a more likely diagnosis, a cough illness lasting ≥2 weeks with at least one of the following signs or symptoms:
- Paroxysms of coughing, OR
- Inspiratory “whoop,” OR
- Posttussive vomiting, OR
- Apnea (with or without cyanosis)
Laboratory criteria for diagnosis
- Isolation of B. pertussis from a clinical specimen
- Positive polymerase chain reaction (PCR) for B. pertussis
Epidemiologic linkage
- Contact with a laboratory-confirmed case of pertussis.
Case classification
- In the absence of a more likely diagnosis, illness meeting the clinical criteria,OR
- Paroxysms of coughing, or
- Inspiratory “whoop”, or
- Posttussive vomiting, or
- Apnea (with or without cyanosis) AND
- Contact with a laboratory confirmed case (epidemiologic linkage)
- Isolation of B. pertussis from a clinical specimen, OR
- PCR positive for B. pertussis
Collection of epidemiologic and clinical data is essential for reporting cases that meet the clinical case definition. Investigators should make every attempt to collect information on paroxysms of cough, whoop, posttussive vomiting, apnea, and duration of cough, as these variables are required to determine whether an individual meets the pertussis clinical case definition. When feasible, case investigations initiated shortly after cough onset should include follow-up calls to collect information on cough duration of at least 14 days. Follow-up is essential regardless of confirmatory test results so that cases meeting the clinical case definition can be reported. Both probable and confirmed pertussis cases should be reported to the National Notifiable Diseases Surveillance System (NNDSS) by the state health department via the National Electronic Telecommunications System for Surveillance (NETSS) or National Electronic Disease Surveillance System (NEDSS).
Laboratory confirmation of pertussis is important because other pathogens can cause symptoms similar to pertussis. All patients with cough and a positive B. pertussis culture or PCR should be reported as confirmed, even those with cough lasting less than 14 days.
Refer to Chapter 22, “ Laboratory Support for Surveillance of Vaccine-Preventable Diseases ” for detailed information on laboratory testing for pertussis and for specific information on specimen collection and shipment.
Specimen collection
Specimen collection and shipping are important steps in obtaining laboratory diagnosis or disease confirmation. Guidelines have been published for specimen collection and handling of microbiologic agents . Information is also available on using CDC laboratories as support for reference and disease surveillance ; this includes
- a central website for requesting lab testing,
- the form [2 pages, 2.80 MB] required for submitting specimens to CDC (See Appendix 23, Form # CDC 50.34 ),
- information on general requirements for shipment of etiologic agents ( Appendix 24 [4 pages] ) — although written to guide specimen submission to CDC, this information may be applicable to submission of specimens to other laboratories; and
- the CDC Infectious Diseases Laboratories Test Directory , which not only contains a list of orderable tests for that institution, but also detailed information on appropriate specimen types, collection methods, specimen volume, and points of contact.
Determining who has pertussis and who does not can be difficult. Whenever possible, a nasopharyngeal swab or aspirate should be obtained from all persons with suspected pertussis. A properly obtained nasopharyngeal swab or aspirate is essential for optimal laboratory diagnosis. Health department personnel and other healthcare practitioners who are asked to obtain these specimens should receive training and supervision from persons experienced in collection of nasopharyngeal specimens. CDC has developed two short training videos for collection of nasopharyngeal aspirate and swab specimens, which can be accessed on the CDC pertussis website .
Reporting and Case Notification
Case reporting within a jurisdiction.
Each state and territory (jurisdiction) has regulations or laws governing the reporting of diseases and conditions of public health importance. [12] These regulations and laws list the diseases to be reported and describe those persons or institutions responsible for reporting, including healthcare providers, hospitals, laboratories, schools, daycare and childcare facilities, and other institutions. Persons reporting should contact the jurisdiction/state health department for jurisdiction-specific reporting requirements.
Case notification to CDC
Notifications by jurisdiction/state health departments of all probable and confirmed pertussis cases should be sent to CDC using event code 10190 through NNDSS via NETSS or NEDSS. When provisional information is reported to NNDSS, NETSS and NEDSS reports can be updated as additional information is collected. NETSS and NEDSS accept information about clinical symptoms, laboratory confirmation, and vaccination history; this information is included in the Pertussis Surveillance Worksheet ( Appendix 11 [2 pages] ) available for reference and use in case investigation. Case notifications should not be delayed because of incomplete information or lack of confirmation. Data can be updated electronically as more information becomes available.
Information to collect
Case investigation should include collection of the epidemiologic information listed on the CDC pertussis surveillance worksheet (see Appendix 11 ). State health departments often supplement the suggested CDC investigation questions with additional information relevant to cases in their communities. The jurisdiction in which the patient resides at the time of diagnosis should submit the case notification to CDC.
Comments on reporting
When laboratory testing is not completed or is negative, but the individual has symptoms consistent with pertussis, it is important to determine duration of cough—specifically, whether it lasts 14 days or longer—in order to determine if a person’s illness meets the definition of a clinical case. If the first interview is conducted within 14 days of cough onset and cough is still present at the time of interview, it is important to follow up at 14 days or later after cough onset.
Pertussis case investigation methods vary across state and local health jurisdictions; CDC is committed to helping improve standardization of surveillance practices for pertussis. Please refer to Appendix 11 for a detailed instruction sheet describing each data element outlined in the pertussis surveillance worksheet.
For specific information about the use of pertussis vaccines, refer to The Pink Book , which provides general recommendations, including vaccine use and scheduling, immunization strategies for providers, vaccine content, adverse events and reactions, vaccine storage and handling, and contraindications and precautions.
A number of surveillance activities can improve detection and reporting of cases as well as the completeness and accuracy of the case report form information reported. In addition to those outlined below, Chapter 19, “Enhancing Surveillance ,” lists activities that might be applicable to pertussis surveillance.
Assuring regular and appropriate diagnostic testing
It is important that available diagnostic tests are used appropriately. To ensure pertussis diagnosis and reporting is optimized, reporting jurisdictions should assess the timing of diagnostic testing relative to cough onset for cases identified through routine surveillance. Bacterial culture for pertussis is most useful during the first 2 weeks of cough and prior to antibiotic use. PCR may effectively diagnose pertussis from 2–4 weeks of cough onset, although sensitivity declines after 3 weeks. Appropriate serologic assays are most useful in the 2–8 weeks following cough onset; however, this testing is not confirmatory for the purpose of case reporting. Diagnostic testing at inappropriate times may result in both false-positive and false-negative results, reducing the overall quality of pertussis diagnosis, and ultimately, pertussis surveillance.
Optimal Timing in Weeks for Diagnostic Testing
Unlike many other vaccine-preventable diseases of childhood, pertussis remains endemic in the United States. Cases are expected to occur in all communities; a period of several years in which no cases are reported from a jurisdiction likely reflects failures to diagnose and/or report disease rather than an absence of disease. The level of diagnostic testing being undertaken can be evaluated by reviewing the number of pertussis diagnostic tests (e.g., cultures or PCR results) ordered by physicians within a jurisdiction.
Monitoring surveillance indicators
Regular monitoring of surveillance indicators might identify specific areas of the surveillance and reporting system that need improvement. Some suggested surveillance indicators to monitor include:
- Completeness of key data elements collected during pertussis case investigations. Information on clinical presentation, antibiotic treatment, vaccination history, and epidemiologic data are of particular importance and should be collected to the fullest extent possible.
- The proportion of cases reported among infants, children, adolescents, and adults. Jurisdictions with reported pertussis cases heavily weighted toward infants are likely missing a significant proportion of pertussis disease in their community.
- The proportion of cases diagnosed solely with DFA or serologic assays. A high proportion of non-confirmatory laboratory testing for pertussis may be an indication of the need for increased education and promotion of proper pertussis diagnostic testing practices.
- The median interval between onset of cough and notification of state or local public health authorities in probable and confirmed cases.
Expanding pertussis data collection
CDC has partnered with 7 states (CO, CT, GA, MN, NM, NY, and OR) participating in the Emerging Infections Program (EIP) Network to conduct enhanced surveillance of pertussis (EPS) and other Bordetella species. EPS is characterized by enhanced case ascertainment and augmented data collection that goes beyond what is requested nationally through NNDSS. Participating sites collect isolates and specimens, when available, for further characterization at the CDC Pertussis and Diphtheria Laboratory. EPS sites also provide the infrastructure for conducting pertussis special studies including those aimed at evaluating pertussis prevention and control strategies.
Other states interested in collecting additional pertussis surveillance information may consider adding the following data elements that are not currently included on the national pertussis surveillance worksheet:
- Cyanosis (Did the patient experience cyanosis during his/her pertussis infection?)
- Healthcare personnel status (Was the patient employed as healthcare personnel during his/her pertussis infection?)
- Pregnancy status of female patient at cough onset (Was the patient pregnant or post-partum at time of cough onset?)
- Mother’s Tdap vaccination history (Did the mother receive Tdap prior to, during, or after her pregnancy with the infant case-patient?)
- Gestational age (in weeks) at time of birth
Completing the pertussis death worksheet
- At present, there are no standard reporting guidelines for pertussis-related deaths. To improve understanding of the characteristics associated with fatal pertussis infections, CDC developed a Pertussis Death Worksheet during 2018. The worksheet is intended to capture clinical, laboratory, and epidemiologic information for all laboratory diagnosed or epidemiologically linked pertussis cases that resulted in death, whether or not the decedent meets the CSTE pertussis case definition requirements for reporting. Reporting jurisdictions with cases of fatal pertussis should ensure that the CDC Pertussis Death Worksheet is completed and returned via fax to Amy Blain at 404-235-1822. Detailed instructions are provided in the Manual for Surveillance of VPDs Appendices.
Streamlining reporting using electronic methods
Although many surveillance systems still rely on paper and pencil for data collection, use of data from sources such as electronic medical records, electronic case reporting [13–19] , and clinical laboratory information systems (LIMS) can significantly improve reporting speed, enhance data quality, and reduce workload.
Case investigations generally include reviews of laboratory, hospital, and clinic records, as well as immunization registries, which are the best sources for information about diagnoses and immunization histories. Investigations also include interviews of patients, which are necessary to identify sources of infections and contacts at risk. Investigations can include treatment of patients and chemoprophylaxis and or vaccination of contacts.
Treatment and chemoprophylaxis
Antimicrobial treatment does not generally lessen the severity of disease unless it is begun early in the course of illness, prior to paroxysmal coughing. [20] Early treatment reduces transmission and is essential for disease control. The spread of pertussis can be limited by decreasing the infectivity of the patient and by protecting close contacts.[ 21 ] Persons with pertussis are infectious from the onset of symptoms through the third week after the onset of paroxysms or until 5 days after the start of effective antimicrobial treatment. The recommended antimicrobial agents and doses are the same for treatment and chemoprophylaxis. [20]
Three macrolides (azithromycin, erythromycin, clarithromycin) are recommended for treatment of pertussis. Azithromycin is most popular because it is given in a short, simple regimen of 1 dose each day for 5 days. It is the preferred antimicrobial for use in infants younger than 1 month of age. For infants younger than 1 month of age, macrolides should be used with caution: some studies have demonstrated an association between erythromycin and azithromycin with infantile hypertrophic pyloric stenosis (IHPS). However, infants younger than 1 month of age are at increased risk of developing severe pertussis and life-threatening complications. These risks outweigh the potential risk of IHPS that has been associated with macrolide use. Resistance of B. pertussis to macrolides is rare, and antimicrobial susceptibility testing is not routinely recommended. Testing is appropriate in some circumstances and is recommended when treatment failure is suspected. Refer to Section VII, “Laboratory Testing” for information on how to contact the CDC Pertussis and Diphtheria Laboratory to discuss susceptibility testing. If resistance to macrolides is suspected or if their use is contraindicated, it is recommended to treat with trimethoprim–sulfamethoxazole (TMP-SMZ). TMP-SMZ should not be used to treat infants younger than 2 months of age. [20]
CDC recommends administration of chemoprophylaxis to contacts at high risk and household members of a pertussis patient. For more specific information on chemoprophylaxis, please see the Outbreak Control section below.
Limited available data suggest B. parapertussis is less susceptible to antibiotics than pertussis, although some studies indicate that erythromycin, azithromycin, clarithromycin, TMP-SMZ, and ciprofloxacin have activity against B. parapertussis . [20-29] Because data on the clinical effectiveness of antibiotic treatment are limited, treatment decisions should be based on clinical judgment with particular attention towards special populations, including infants, elderly, and immunocompromised persons; treatment may be warranted to prevent severe outcomes and decrease duration of illness.
During the course of a pertussis investigation, under-vaccinated contacts of pertussis cases may be identified. Contacts who have not received the recommended number of pertussis-containing vaccinations (i.e., DTaP, Tdap) should follow the age appropriate catch-up immunization schedule. [30,31] Vaccination is not a substitute for chemoprophylaxis and is unlikely to prevent illness in a person who has already been infected with B. pertussis . [30-33]
Pertussis outbreaks can be difficult to identify and manage. Other respiratory pathogens often cause clinical symptoms similar to pertussis, and co-circulation with other pathogens does occur. To respond appropriately (e.g., provide appropriate chemoprophylaxis), it is important to confirm that B. pertussis is circulating in the outbreak setting and to determine whether other pathogens are contributing to the outbreak. Because culture is the most specific test for pertussis, confirmation by culture for at least one suspected pertussis case is recommended any time there is suspicion of a pertussis outbreak.
To reduce the risk of pertussis in new mothers and their infants, especially those too young to be vaccinated, ACIP recommends that pregnant women receive a dose of Tdap vaccine during each pregnancy. During outbreaks, prevention measures should focus on efforts to improve Tdap coverage during pregnancy to reduce severe illness and possible deaths in vulnerable infants.
Pertussis incidence remains elevated in the United States, and community transmission is widespread. Thus, extensive contact tracing and broad-scale use of chemoprophylaxis among contacts may not be an effective use of limited public health resources. While antibiotics may prevent pertussis disease if given prior to symptom onset, there are no data to indicate that widespread use of chemoprophylaxis among contacts effectively controls or limits the scope of pertussis outbreaks. Another important consideration is the overuse of antibiotics; CDC promotes the judicious use of antibiotics among healthcare providers and patients. [34] Given these considerations, CDC supports targeting chemoprophylaxis through the following measures to persons at high risk of developing severe pertussis and to persons who will have close contact with those at high risk of developing severe pertussis:
- Providing chemoprophylaxis to all household contacts of a pertussis case. Within families, secondary attack rates have been demonstrated to be high, even when household contacts are up-to-date with immunizations. [35] Administration of antimicrobial prophylaxis to asymptomatic household contacts within 21 days of cough onset in the index patient can prevent symptomatic infection.
- Infants and women in their third trimester of pregnancy—severe and sometimes fatal pertussis-related complications occur in infants <12 months of age, especially among infants <4 months of age. Women in their third trimester of pregnancy may be a source for transmission of pertussis to their newborn infant.
- All persons with pre-existing health conditions that may be exacerbated by a pertussis infection (e.g., immunocompromised persons and patients with moderate to severe medically treated asthma).
- Contacts who themselves have close contact with either infants <12 months of age, pregnant women, or individuals with pre-existing health conditions at risk for severe illness or complications.
- All contacts in high-risk settings that include infants <12 months of age or women in the third trimester of pregnancy, which include but are not limited to, neonatal intensive care units, childcare settings, and maternity wards.
A broader use of chemoprophylaxis may be appropriate in limited closed settings, when the number of identified cases is small, and when a community-wide outbreak is not ongoing. However, when continued transmission of pertussis is evident, multiple rounds of antibiotics would not be recommended. Rather than repeating a course of antibiotics, contacts should be monitored for onset of signs and symptoms of pertussis for 21 days.
Active screening for symptomatic patients with suspected pertussis can be considered during outbreaks in settings such as schools, daycare centers, and hospitals. Active screening for suspected cases potentially reduces exposure to persons with pertussis, encourages timely medical evaluation and treatment of cases, and promotes prompt administration of antibiotics to close contacts at high risk for infection or complications due to infection. [35-42]
- Vitek CR, Pascual FB, Baughman AL, Murphy TV. Increase in deaths from pertussis among young infants in the United States in the 1990s. Pediatr Infect Dis J 2003;22(7):628–34.
- Davis SF, Strebel PM, Cochi SL, Zell ER, Hadler SC. Pertussis surveillance—United States, 1989–1991. MMWR Surveill Summ 1992;41(SS-8):11–19.
- CDC. Pertussis—United States, 2001–2003 . MMWR Morb Mortal Wkly Rep 2005;54(50):1283–6.
- Guris D, Strebel PM, Bardenheier B, , et al. Changing epidemiology of pertussis in the United States: increasing reported incidence among adolescents and adults, 1990–1996. Clin Infect Dis 1999;28(6):1230–7. DOI: 10.1086/514776.
- National Notifiable Diseases Surveillance System, 1990–2015. Division of Health Informatics and Surveillance , Center for Surveillance, Epidemiology, and Laboratory Services, Office of Public Health Scientific Services, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, Atlanta, GA 30329.
- Schmidtke AJ, Boney KO, Martin SW, Skoff TH, Tondella ML, Tatti KM. Population diversity among Bordetella pertussis isolates, United States, 1935–2009. Emerg Infect Dis 2012;18(8):1248–55. DOI: 10.3201/eid1808.120082.
- Pawloski LC, Queenan AM, Cassiday PK, et al. Prevalence and molecular characterization of pertactin-deficient Bordetella pertussis in the United States. Clin Vaccin Immunol 2014;21:119–25. DOI: 10.1128/CVI.00717-13
- Martin SW, Pawloski L, Williams M, Weening K, DeBolt C, Qin X, et al. Pertactin-negative B. pertussis strains: evidence for a possible selective advantage. Clin Infect Dis 2015;60(2):223–7. DOI: 10.1093/cid/ciu788.
- Cassiday PK, Skoff TH, Jawahir S, Tondella ML. Changes in predominance of pulsed-field gel electrophoresis profiles of Bordetella pertussis isolates, United States, 2000–2012. Emerg Infect Dis 2016;22(3):442–8. DOI: 10.3201/eid2203.151136
- U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020 . Washington, DC.
- CSTE. Revision to the case definition for national pertussis surveillance . CSTE position statement 19-ID-08: Atlanta, GA: CSTE; 2019.
- Adams DA, Thomas KR, Jajosky R, et al. Summary of notifiable infectious diseases and conditions—United States, 2014. MMWR Morb Mortal Wkly Rep 2016;63(54):1–152 DOI: 10.15585/mmwr.mm6354a1
- CDC. Progress in improving state and local disease surveillance—United States, 2000–2005 . MMWR Morb Mortal Wkly Rep 2005;54(33):822–5.
- CSTE. Improving public health practice by enhancing the public health community’s capability for electronic information exchange using HL7 CDA [5 pages] . CSTE position statement 13-SI-03; Atlanta, GA: CSTE; 2013.
- CSTE. Common data structure for national notifiable diseases. CSTE position statement 15-EB-01 [6 pages] . Atlanta, GA: CSTE; 2015.
- Smith PF, Hadler JL, Stanbury M, Rolfs RT, Hopkins RS; CSTE Surveillance Strategy Group. “Blueprint version 2.0”: updating public health surveillance for the 21st century. J Public Health Manag Pract 2013 May–Jun;19(3):231–9. doi: 10.1097/PHH.0b013e318262906e
- CSTE. Review of and recommendations for the National Notifiable Disease Surveillance System: a state and local health department perspective [49 pages] .
- CSTE. 2004–2010 National assessments of electronic laboratory reporting in health departments: findings and recommendations [4 pages] . [assessment brief]. Atlanta, GA: CSTE; 2012.
- Mac Kenzie WR, Davidson AJ, Wiesenthal A, et al. The promise of electronic case reporting. Public Health Rep 2016;131(6):742–6. https://journals.sagepub.com/doi/10.1177/0033354916670871
- CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines . MMWR Recomm Rep 2005;54(RR-14):1–16.
- American Academy of Pediatrics. Pertussis (Whooping Cough). In: Kimberlin DW, editor. Red Book: 2015 Report of the Committee on Infectious Diseases. Elk Grove Village, IL: American Academy of Pediatrics ;2015:608–21.
- Mastrantonio P, Stefanelli P, Giuliano M, et al. Bordetella parapertussis infection in children: epidemiology, clinical symptoms, and molecular characteristics of isolates. J Clin Microbiol 1998;36(4):999–1002.
- Hoppe JE, Tschirner T. Comparison of media for agar dilution susceptibility testing of Bordetella pertussis and Bordetella parapertussis . Eur J Clin Microbiol Infect Dis 1995;14(9):775–9.
- Hoppe JE, Bryskier A. In vitro susceptibilities of Bordetella pertussis and Bordetella parapertussis to two ketolides (HMR 3004 and HMR 3647), four macrolides (azithromycin, clarithromycin, erythromycin A, and roxithromycin), and two ansamycins (rifampin and rifapentine). Antimicrob Agents Chemother 1998;42:965–6.
- Hoppe JE, Tschirner T. Comparison of Etest and agar dilution for testing the activity of three macrolides against Bordetella parapertussis . Diagn Microbiol Infect Dis 1997;28(1):49–51. DOI: 10.1016/S0732-8893(97)89160-2
- Hoppe JE, Rahimi-Galougahi E, Seibert G. In vitro susceptibilities of Bordetella pertussis and Bordetella parapertussis to four fluoroquinolones (levofloxacin, d-ofloxacin, ofloxacin, and ciprofloxacin), cefpirome, and meropenem. Antimicrob Agents Chemother 1996;40(3):807–8.
- Hoppe JE, Simon CG. In vitro susceptibilities of Bordetella pertussis and Bordetella parapertussis to seven fluoroquinolones. Antimicrob Agents Chemother 1990;34(11):2287–8. DOI: 10.1128/AAC.34.11.2287
- Hoppe JE, Eichhorn A. Activity of new macrolides against Bordetella pertussis and Bordetella parapertussis . Eur J Clin Microbiol Infect Dis 1989;8(7):653–4. DOI: 10.1007/BF01968151
- Watanabe M, Haraguchi Y. In vitro susceptibility of Bordetella parapertussis to various antimicrobial agents. Antimicrob Agents Chemother 1989;33(6):968–9. DOI: 10.1128/AAC.33.6.968
- CDC. Catch-up immunization schedule for persons aged 4 months through 18 years who start late or who are more than 1 month behind—United States, 2017 [8 pages] . [updated 2017 Feb 6; cited 2017 Mar 14].
- CDC. Recommended immunization schedule for adults aged 19 years or older, by vaccine and age group—United States, 2017 [6 pages] . [updated 2017 Feb 6; cited 2017 Mar 14].
- Bisgard KM, Christie CD, Reising SF, Sanden GM, Cassiday PK, Gomersall C, et al. Molecular epidemiology of Bordetella pertussis by pulsed-field gel electrophoresis profile: Cincinnati, 1989–1996. J Infect Dis 2001;183:1360–7. DOI: 10.1086/319858
- Kurzynski TA, Boehm DM, Rott-Petri JA, et al. Antimicrobial susceptibilities of Bordetella species isolated in a Multicenter Pertussis Surveillance Project. Antimicrob Agents Chemother 1988;32(1):137–40. DOI: 10.1128/AAC.32.1.137
- CDC. Get smart: know when antibiotics work . Atlanta GA [updated: 2013 Oct 23; cited 2014 Jan 20].
- Sprauer MA, Cochi SL, Zell ER. Prevention of secondary transmission of pertussis in households with early use of erythromycin. Am J Dis Child 1992;146(2):177–81. DOI: 10.1001/archpedi.1992.02160140043018
- Dodhia H, Miller E. Review of the evidence for the use of erythromycin in the management of persons exposed to pertussis. Epidemiol Infect 1998;120(2):143–9.
- Halperin SA, Bortolussi R, Langley JM, et al. A randomized, placebo-controlled trial of erythromycin estolate chemoprophylaxis for household contacts of children with culture-positive Bordetella pertussis infection. Pediatrics 1999;104(4):e42
- von König CH. Use of antibiotics in the prevention and treatment of pertussis. Pediatr Infect Dis J 2005;24(5 Suppl):S66–8.
- Alexander EM, Travis S, Booms C, Kaiser A, Fry NK, Harrison TG, et al. Pertussis outbreak on a neonatal unit: identification of a healthcare worker as the likely source. J Hosp Infect 2008;69(2):131–4. DOI: 10.1016/j.jhin.2008.02.011
- Elumogo TN, Booth D, Enoch DA, Kuppuswamy A, Tremlett C, Williams CJ, et al. Bordetella pertussis in a neonatal intensive care unit: identification of the mother as the likely source. J Hosp Infect 2012;82(2):133–5. DOI: 10.1016/j.jhin.2012.07.012
- CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC guidelines. MMWR Recomm Rep 2005;54(RR14):1–16.
- Clark TA. Responding to pertussis. J Pediatr 2012;161(6):980–2.
- Webcast related to this manual
- CDC pertussis web site
- Pertussis vaccination
To receive email updates about this page, enter your email address:
- Vaccines & Immunizations
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

11 templates

66 templates

teacher appreciation
9 templates

memorial day
12 templates

pediatrician
27 templates
Respiratory Infections: Whooping Cough
Respiratory infections: whooping cough presentation, free google slides theme and powerpoint template.
Discover the profound impact of presenting well-researched data with this fully customizable Google Slides and PowerPoint template. The minimalist design with white text on a deep blue background allows each point to shine, enabling you to present your research on whooping cough convincingly. The clean layout helps you to translate complex medical information into digestible content, easing the way for the panel, symposium, or conference attendees. Download this design to cause true ripples in the scientific community!
Features of this template
- 100% editable and easy to modify
- 20 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access


European Centre for Disease Prevention and Control
An agency of the European Union
Increase of pertussis cases in the EU/EEA
After a few years of limited circulation in the EU/EEA, particularly during the COVID-19 pandemic, more than 25 000 cases of pertussis were reported in 2023, and more than 32 000 between January and March 2024. Similar numbers were observed in 2016 (41 026) and 2019 (34 468).
Executive summary
Epidemiological situation.
Pertussis is an endemic disease in the EU/EEA and worldwide. Every three to five years, larger epidemics are expected even with high vaccination coverge.
During 2023-24, in 17 EU/EEA countries, infants (those under the age of one year) represented the group with the highest reported incidence, whereas in six countries, the highest incidence is reported in adolescents 10-19 years. The majority of deaths occurred in infants. These surveillance data need to be interpreted with caution due to known differences in Member State surveillance systems, availability of laboratory methods, testing practices, as well as vaccination schedules. Furthermore, case ascertainment can vary by age group. In many countries, maternal vaccination programmes are used to protect infants in the first months of life. However coverage data, where available for such programmes, appears to be sub-optimal.
The observed epidemiological picture can be ascribed to a number of factors, which include: expected epidemic peaks, presence of unvaccinated or not up to date vaccinated individuals, waning immunity, decreased contribution of natural boosting in the overall population during the COVID-19 pandemic period.
Risk assessment
The risk from pertussis was assessed for four different population groups as a product of the probability of infection and its impact. The overall risk is assessed as high for unimmunised or partially immunised infants<6 months of age , as they represent the group with the highest morbidity and mortality from pertussis.
Infants >6 months and children up to 15 years of age have a moderate risk if they are unimmunised or partially immunised and have a low risk if they are fully vaccinated according to national immunisation schedules.
Older adolescents >16 years and adults up to 64 years of age have a moderate risk which is reduced to low if they have recently received a booster dose.
Finally, older adults (≥65 years of age) and persons of any age with underlying conditions such as asthma, chronic obstructive pulmonary disease (COPD) or immunosuppression, have an overall moderate risk from pertussis, having a moderate probability of infection and moderate impact (i.e. a higher probability of experiencing severe illness than individuals in the younger age/group).
Recommendations
The primary objective of national pertussis immunisation programmes in EU/EEA countries should be to curb morbidity and mortality in newborn infants. To this end, and in view of the ongoing pertussis outbreaks, ECDC encourages EU/EEA public health authorities to focus on the following areas:
- Achieve and sustain high vaccination coverage through timely and full completion of pertussis primary immunisation series and subsequent boosters recommended nationally.
- In addition to the routine programme, maternal immunisation is a highly effective approach to prevent disease and death in young infants. There is a need to bolster interventions to improve access and implementation of childhood and maternal immunisation policies. Review and, if needed, upgrade of immunisation information systems will enable a follow-up of vaccination status across different providers and life stages to strategically inform vaccination programmes.
- Increase the awareness of health professionals about the epidemiological situation of pertussis in their geographical area, the clinical presentation of pertussis, and prevention through vaccination: if needed, develop protocols for the management of cases with protracted cough and laboratory confirmed pertussis. Pertussis can occur in persons of all ages with varying clinical picture, and clinical suspicion is often low. If needed, testing options should be outlined for the confirmation of the disease.
- Continue surveillance of pertussis and ensure public health capacity for early detection, diagnosis, response to and control of outbreaks , including appropriate contact tracing around the cases to protect close contacts at risk of severe disease. Monitoring and reporting of B. pertussis resistance to macrolides is important.
- Employ risk communication on the disease and the importance of vaccination , and strategies to promote vaccine acceptance and uptake. Information on pertussis should stress that this is a highly transmissible disease, and there is a need to protect infants . Healthcare providers’ recommendations are very important for uptake of maternal vaccination, in countries that have such programmes, and for timely completion of the primary immunisation series and boosters. Factors that affect acceptance of the pertussis vaccine should be explored.


Pertussis (whooping cough)
Pertussis, also known as whooping cough, is a highly contagious acute respiratory infection, caused by the bacterium Bordetella pertussis. The disease is characterised by a severe cough, which can last two months or even longer.
Threats and outbreaks of pertussis
Disease threats and outbreaks reports; Communicable disease threats report, Risk assessments.
Factsheet about pertussis
Pertussis, also known as whooping cough, is a highly contagious acute respiratory infection, caused by the bacterium Bordetella pertussis.
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Balance transfer cards
- Cash back cards
- Rewards cards
- Travel cards
- Online checking
- High-yield savings
- Money market
- Home equity loan
- Personal loans
- Student loans
- Options pit
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
Whooping cough: Richhill family's 'frightening experience'
A County Armagh woman whose husband and eight-year-daughter had whooping cough has said it has been "a really frightening experience" for the family.
There have been 769 laboratory confirmed cases of the infection in Northern Ireland from the start of the year to 5 May.
Five babies have died from whooping cough in England.
Adam McCrory and his daughter Emily from Richhill have had whooping cough.
His wife Sharon McCrory told BBC News NI: "It's very scary watching your family go through this.
"We haven't had a full night's sleep in six weeks.
"Emily still gets an attack maybe once or twice a night."
Hundreds of cases of whooping cough in NI
Whooping cough cases up again as five babies die
What can people do to protect themselves
Mrs McCrory said Emily started coughing at the start of the Easter holidays and after it worsened and after Adam also became ill, they both went to the doctor.
Two weeks later whooping cough was diagnosed.
The doctor took a swab.
"The swab went away, came back and I got a phone call from the PHA (Public Health Agency)," she said.
The family was put on antibiotics.
Neither Mrs McCrory nor the couple's seven and 10-year-old sons contracted the disease.
'You thought you were suffocating'
Adam McCrory said he had pneumonia in the past "and I thought that was bad, but it was nothing like this."
"This one's different, it won't let you get a breath at all - it expels all your air and then it won't let you bring it back in again.
"It was definitely scary, you thought you were suffocating."
"It can just come on you unexpectantly," he added.
Mrs McCrory said she remains concerned about her daughter.
"It's been extremely frightening from a mother's point of view - it's given me weeks of desperate anxiety," she said.
"I won't sleep because I'm afraid of Emily maybe struggling when I'm asleep, so I'm going to her room and checking on her and watching her - it's desperate," she added.
What is whooping cough?
The first signs are similar to a cold, with a runny nose and sore throat.
After about a week, the infection can develop into coughing bouts that last a few minutes and are typically worse at night.
Young babies may make a distinctive "whoop" or have difficulty breathing after a bout of coughing.
The bacterial infection spreads through coughs and sneezes.
People of all ages can catch whooping cough, but it is most serious for young children and babies.
Cases are also on the rise in the rest of the UK and have caused the death of five babies in England .
Known as pertussis or "100-day cough", the infection is a cyclical disease with peaks seen every three to five years.
On Thursday, the PHA said an increases in cases of the illness was due in 2020 but was prevented by Covid lockdown measures.
'It's here and it's very serious'
Mrs McCrory said she would fear what could happen to vulnerable people if they got the illness.
"Emily's a strong wee girl and she's never had anything really in her life and Adam would be strong and never really gets too sick and I've seen how it affects those two," she said.
"I would dread to see an older person or anybody with anything underlying," she added.
She urged anyone with symptoms to get them checked out.
"I would urge anyone if they've got a cough and it's a wheeze and a gasp - don't hesitate, go straight away and get the swab," she said.
"It's very distinguishable, it's very unique as a cough," she added.
Recommended Stories
Chaotic brawl breaks out, punching allegations surface after nycfc’s 3-2 win over toronto fc.
Toronto alleged on Saturday that NYCFC’s head coach cornered and punched one of their players at the last match between the two clubs.
Max Fried, Braves' bullpen come one out shy of combined no-hitter vs. Mets
J.D. Martinez's homer in the bottom of the 9th inning ended the Braves' no-hit bid.
UFC St. Louis: Esteban Ribovics delivers wild head-kick KO to beat Terrance McKinney seconds into their fight
It took Esteban Ribovics only 37 seconds to get the win Saturday night.
Why are social media users blocking celebrities and influencers on TikTok? A look at the #Blockout movement
Here's why some social media users are blocking stars from their feeds after the Met Gala.
Why Apple’s ‘Crush’ ad is so misguided
This week Apple unveiled new iPad models at its Let Loose event, including a new 13-inch display for the iPad Air, as well as Tandem OLED and a new M4 chip for the iPad Pro. For Apple completionists, we compiled all of the new announcements in case you missed it. In the world of EVs, the embattled Fisker Ocean is facing yet another federal safety probe.
Q&A with Maddy Dychtwald: What the longevity revolution means for women
Women are living longer than men, but they often spend the last decade or so in "a cascade of poor health,” author Maddy Dychtwald said.
28 Years Later is coming to theaters next summer
Fans have been waiting a long, long time for another installment in the 28 Days Later franchise, and we now know when the next followup is coming out: June 20, 2025. 28 Years Later will be directed by Danny Boyle and written by Alex Garland.
SAP’s chief sustainability officer isn’t interested in getting your company to do the right thing
SAP chief sustainability officer Sophia Mendelsohn has been on the job since September, but her career really goes back to her undergraduate years at Harvard when she studied sustainability. Ever since her first job working in China, she observed the connection between prosperity and sustainability. “I've been in sustainability a minute, before it was cool,” Mendelsohn told TechCrunch.
Lions' Terrion Arnold said he'd jam his mother into the dirt if they lined up against each other
Detroit Lions rookie cornerback Terrion Arnold gave a memorable quote about his mother and how important she has been in his development as a player.
Northern lights dazzle Maine, California, New Hampshire and other states during rare solar storm: See the photos
The largest solar storm in nearly 20 years is hitting Earth this weekend.
Junkyard Gem: 2005 Honda Accord, Hello Kitty Edition
A heavily customized 2005 Honda Accord sedan with many Hello Kitty items, found in a Denver self-service wrecking yard.
The 40+ best Amazon deals this weekend: Save up to 80% on vacuums, gardening tools, tech goodies and more
We've got our eye on a viral Bissell carpet cleaner on rare sale for $99, plus an Apple iPad marked down by $80, to name a few.
The No. 1 bestselling Hanes hoodie is on sale for just $15 on Amazon
Make this your everywhere hoodie for the rest of spring and into summer — it's nearly 40% off.
Amazon shoppers can't stop raving about this $17 tank top — 'I get tons of compliments every time I wear it!'
Not only is it on sale, but it comes in 40 dynamite colors and prints as well.
This No. 1 bestselling whitening pen 'worked better than a visit to my dentist,' and it's down to $15 for three
More than 14,000 shoppers give this genius tool a five-star rating: 'No tingling, discomfort or negative side effects. Just gorgeous white teeth.'
Courteney Cox uses this popular anti-aging tool anywhere and everywhere — and it's on sale for $8
Roll your wrinkles away with this deal on a centuries-old skin-care secret.
'Lumps and crepey skin are gone': Grab this anti-aging body lotion for just $10
The Gold Bond favorite has earned over 20,000 flawless reviews on Amazon.
Mortgage rates today, May 11, 2024: Rates tick down after a 5-week climb
These are today's mortgage rates. Rates are trending downward after rising for five straight weeks, which indicates it could be a good time to buy. Lock in your rate today.
CD rates today, May 11, 2024 (best account provides 5.15% APY)
If you’re searching for today’s best CD rates, we’ve narrowed down some of the top offers. Learn more about CD rates today.
'Very flattering if you have a tummy': this flowy top is just $23
With charming floral prints, flattering silhouette and flowy comfort, you'll be living in this top until the end of the summer.
What's the difference between whooping cough and a normal cough?
- Whooping cough
- Thursday 9 May 2024 at 12:16pm

Words by Olivia Mustafa
The UK is experiencing a rapid rise in whooping cough , with almost 3,000 cases confirmed between January and March 2024.
New figures from the UK Health Security Agency (UKHSA) show 1,319 cases of the illness were detected in March, up from 918 in February and 556 in January. This compares to just 858 cases of whooping cough for the whole of 2023.
Five infants are also known to have died in between January and March 2024.
Dr Michael Head, Senior Research Fellow in Global Health told ITV News these figures are significant - but not unprecedented.
"The data is definitely concerning," he said.
"We do see large outbreaks of whooping cough on a cycle every few years but the one we're seeing at the moment is big."
But what has caused this most recent spike in cases, and how simple is it to tell the difference between whooping cough and a regular cough?
What is whooping cough?
Whooping cough is a infection of the lungs and airways. It is caused by bacteria called Bordetella pertussis, and is very contagious.
What are the symptoms?
The first signs of whooping cough are similar to those of a cold, such as a runny nose and a sore throat.
Symptoms then progress after about a week into coughing bouts lasting a few minutes, which might get worse at night. Coughing can last for weeks or months.
Those with the illness may make a 'whoop' sound, caused by gasping for breath between coughs - but this does not happen everyone with whooping cough.
It can cause breathing difficulties, with young infants turning blue or grey and adults becoming red in the face after coughing bouts.
Whooping cough may also bring up thick mucus, which can cause vomiting.
How is it different to a normal cough?
Dr Head explained whooping cough is similar to other kinds of respiratory illness in the early stages.
He said: "You'll have some kind of cough, and perhaps a runny nose or a fever. It is very, very hard to tell the difference at that stage between whooping cough and anything else.
"You can only really notice it's whooping cough later on in the presentation when that distinctive 'hoop' sound kicks in."
Given not everyone experiences this symptom, the illness is difficult to accurately diagnose without laboratory testing, according to Dr Head.
"That's another reason why it is hard to get outbreaks under control and why vaccination is vital," he said.
How serious is it?
Whooping cough can lead to serious and sometimes deadly complications in babies and young children.
Around a third of babies under the age of one with whooping cough will need hospital care.
Complications can include apnea (life-threatening pauses in breathing), pneumonia, convulsions and encephalopathy (disease of the brain).
Teenagers and adults can also experience complications, but they are generally less serious in those who are older.
What has caused this recent outbreak?
According to Dr Head, outbreaks of whooping cough happen every few years.
He said: "The reasons are not totally clear but will be related to drops in vaccine uptake and probably waning of immunity in older children and younger adults.
"Once you get to that sort of nine or ten years of age, the immunity from the vaccines does start to wear off. Waning of immunity and any lower vaccine uptake does mean the vulnerable populations like children and pregnant women are more likely to be exposed."
Dr Head believes the time of year could explain the uptick in cases across the past few months.
"The reason why we see respiratory infections during the winter is that people will cluster indoors. If it's cold and wet, if you're indoors with little ventilation, the window shut, then there's many opportunities for that bacteria to spread," he said.
How is it treated?
Those with severe whooping cough, or babies under 6 months with the illness, will need hospital treatment. It is treated with antibiotics.
How contagious is it?
People with whooping cough are contagious from about six days after the start of cold-like symptoms to three weeks after the coughing starts.
Starting antibiotics within three weeks of starting to cough can reduce the time someone is contagious for.
Dr Head explained whooping cough is about as contagious as measles, which is one of the most infectious diseases around.
"It has an R number of 15 to 17, so one infected person can potentially infect 15 to 17 other separable people," he said.
"It's also mostly in the upper respiratory tract meaning it is easier to spread because the bacteria are nearer the the the mouth and nose."
Is there a vaccine?
All babies are offered a whooping cough vaccination as part of routine NHS vaccines. It is given as part of the six-in-one vaccine for babies at eight, 12, and 16 weeks old.
It's also administered in the four-in-one pre-school booster, for children aged three years and four months old.
The NHS recommends all pregnant women are vaccinated against whooping cough between 16 and 32 weeks.
Dr Head said: "High vaccine coverage is vital to maintain each and every year to protect pregnant women and babies. Otherwise, we get outbreaks like we're seeing this year.
"If you are recommended for vaccine, then do take up the offer for you or your child."
What should those worried about whooping cough do?
Ask for an urgent GP appointment or call NHS 111 if:
a baby under six months old has symptoms
you have a very bad cough that is getting worse
if you've been in contact with someone with whooping cough and you're pregnant
you or your child has been in contact with someone with whooping cough and have a weakened immune system
Call 999 or go to A&E if:
you or your child turn blue or grey (on black or brown skin this may be easier to see on the palms of the hands or the soles of the feet)
the sufferer is experiencing breathing difficulties, seizures or chest pain
Visit the NHS website for more advice.
Want a quick and expert briefing on the biggest news stories? Listen to our latest podcasts to find out What You Need To Know…

COMMENTS
Pertussis - Download as a PDF or view online for free. 9. Paroxysmal Stage ( 2-4 wks) * Cough is first dry & intermittent * Inexorable paroxysm * Machine-gun burst of uninterrupted cough * Series of coughing in single expiration * Eyes bulging—watering * Chin & Chest held forward * Tongue protruding maximally
Whooping cough is a highly contagious disease caused by pertussis bacteria and may lead to death, particularly in infants less than 12 months of age. Whooping cough is preventable but Although it can be prevented by routine vaccination, it still affects many people, it can have serious complications including death. Management is only supportive.
Whooping cough is a contagious respiratory tract infection. Ten days after patients become infected, they begin to show symptoms such as nasal congestion, fever or a characteristic cough (which sounds like "whoop"). In order for you to answer all the frequently asked questions about this disease, we bring you this watercolor-style template.
While anyone can get pertussis, adults living with asthma are at increased risk of infection and complications. Whooping Cough Symptoms. Besides the iconic cough that has a 'whooping' sound, other symptoms include runny nose, nasal congestion, sneezing, fever and fatigue. Symptoms usually develop within five to 10 days after you are exposed.
Pertussis, or whooping cough, is an acute infectious disease caused by the bacterium Bordetella pertussis. Outbreaks of pertussis were first described in the 16th century by Guillaume de Baillou. The organism was first isolated by Jules Bordet and Octave Gengou in 1906. In the 20th century, pertussis was one of the most common
Pertussis PP Presentation. 1|Summary of Key Points from WHO Position Paper, PT Vaccines,August 2015. Summary(of(Key(Points. WHOPositionPaperonVaccines( againstPertussis September(2015. 2|Summary of Key Points from WHO Position Paper, PT Vaccines,August 2015. Background.
Pertussis (whooping cough), caused by Bordetella pertussis, is endemic in all countries. Globally, it is estimated that there were 24.1 million pertussis cases and 160 700 deaths from pertussis in children < 5 years of age in 2014 (1), with periodic epidemics occurring every two to five years. Pertussis is transmitted from
Whooping cough (pertussis) is a highly contagious respiratory tract infection. In many people, it's marked by a severe hacking cough followed by a high-pitched intake of breath that sounds like "whoop." Before the vaccine was developed, whooping cough was considered a childhood disease. Now whooping cough primarily affects children too young to ...
• 4:48 to the point where she has a whooping cough, • 4:51 or any cough at all. • 4:52 For the same reason of having the body primed, • 4:54 previous exposure to pertussis can also • 4:56 be a modifying factor. • 4:58 So, for example, if grandpa recently had • 5:00 a pertussis infection, his body's primed • 5:03 to fight a re ...
Pertussis diagnosis and treatment. 0:06of the stages that occur during the bacterial infection. 0:15is in the upper respiratory tract. 0:19and inflammation in the airways. 0:27with whooping when breathing in, and vomiting after fits. 0:35which tag the bacteria for destruction by the immune system.
Pertussis. (whooping cough) is a bacterial respiratory infection caused by the organism, Bordetella pertussis (Figure 1), a fastidious, Gram negative bacillus. It is highly infectious and is spread by respiratory droplets to 70-100% of susceptible household contacts and 50-80% of susceptible school contacts.1 Pertussis infection occurs ...
Pertussis, also known as whooping cough, remains a public health concern despite expanded immunization recommendations over the past three decades. The presentation of pertussis, which is variable ...
Clinical Features. Educate parents to consider pertussis when their child has a cough or apnea. Let them know that it can be a severe illness, especially for infants, and they should seek immediate treatment. Inquire about contact with infants and pregnant women when you suspect a case in an older child, adolescent, or adult.
Video transcript. - [Voiceover] We've learned that pertussis is caused by a contagious bacterial infection that causes damage to the upper respiratory tract. In this picture, the infection would be here in the main airway leading to the lungs, and this airway is called the trachea. The bacteria that damages this airway during an infection is ...
Background: Pertussis (whooping cough) is a highly infectious, preventable disease, which causes significant morbidity and mortality. Objective: This article discusses the presentations, investigations and management of cases and their contacts. Discussion: Maternal antibody does not confer protection to the infant so babies are particularly at risk of infection and complications until they ...
Bordetella pertussis is the causative agent of whooping cough, a major cause of childhood morbidity and mortality. An estimated 50 million cases and 300 000 deaths occur every year; case-fatality rates in developing countries may be as high as 4% in ... Clinical presentation and severity of pertussis in different age groups - ...
Best way to prevent is to get vaccinated (Pertussis vaccination) Start at 2 months for kids. Then doses at 4 and 6 months. A booster at 15-18 months. Another booster at 4-6 months. Anyone who is 11-12 years and has not gotten the vaccine can get it, as well as any adult who has never had it. See full transcript.
Because of this, there is currently much discussion in the pertussis field on the development of new vaccines and vaccination strategies [ 4 - 9 ]. The scope of this review is more basic aspects of B. pertussis virulence and disease pathogenesis and treatment. B. pertussis is transmitted by aerosols and infects the ciliated epithelium of the ...
Pertussis, more commonly known as whooping cough, is a contagious, respiratory disease caused by the bacterium Bordetella pertussis. The illness is typically characterized by a prolonged paroxysmal cough that is often accompanied by an inspiratory whoop. Disease presentation can vary with age and history of previous exposure or vaccination.
Bordetella pertussis by Nicole Madden on Prezi. Blog. April 18, 2024. Use Prezi Video for Zoom for more engaging meetings. April 16, 2024. Understanding 30-60-90 sales plans and incorporating them into a presentation.
Template available for Google Slides and PowerPoint you can use in your presentations. Got any suggestions? We want to hear from you! Send us a message and help improve Slidesgo. Send suggestions ... Pertussis Clinical Case Presentation . Medical . Free Google Slides theme and PowerPoint template . FAQs ...
Discover the profound impact of presenting well-researched data with this fully customizable Google Slides and PowerPoint template. The minimalist design with white text on a deep blue background allows each point to shine, enabling you to present your research on whooping cough convincingly. The clean layout helps you to translate complex ...
Pertussis is an endemic disease in the EU/EEA and worldwide. Every three to five years, larger epidemics are expected even with high vaccination coverge. After a few years of limited circulation in the EU/EEA, particularly during the COVID-19 pandemic, more than 25 000 cases of pertussis were reported in 2023, and more than 32 000 between ...
Pertussis continues to be a significant public health concern. We aimed to examine the epidemiological characteristics of pertussis in Vojvodina, which accounts for almost a third of Serbia's population. Our aim was to determine the overall and age-specific incidence and mortality rates of pertussis in Vojvodina from 1948 to 2023, as well as the coverage of immunization against pertussis ...
Whooping Cough Presentation by Nathaly Mendoza on Prezi. Blog. April 18, 2024. Use Prezi Video for Zoom for more engaging meetings. April 16, 2024. Understanding 30-60-90 sales plans and incorporating them into a presentation. April 13, 2024. How to create a great thesis defense presentation: everything you need to know.
Fri, May 10, 2024, 5:44 PM EDT · 3 min read. A County Armagh woman whose husband and eight-year-daughter had whooping cough has said it has been "a really frightening experience" for the family ...
The first signs of whooping cough are similar to those of a cold, such as a runny nose and a sore throat. Symptoms then progress after about a week into coughing bouts lasting a few minutes, which ...