Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines


Preparing for Gender Affirmation Surgery: Ask the Experts
Featured Expert:

Romy Smith, LMSW
Preparing for your gender affirmation surgery can be daunting. To help provide some guidance for those considering gender affirmation procedures, our team from the Johns Hopkins Center for Transgender and Gender Expansive Health (JHCTGEH) answered some questions about what to expect before and after your surgery.
What kind of care should I expect as a transgender individual?
What kind of care should I expect as a transgender individual? Before beginning the process, we recommend reading the World Professional Association for Transgender Health Standards Of Care (SOC). The standards were created by international agreement among health care clinicians and in collaboration with the transgender community. These SOC integrate the latest scientific research on transgender health, as well as the lived experience of the transgender community members. This collaboration is crucial so that doctors can best meet the unique health care needs of transgender and gender-diverse people. It is usually a favorable sign if the hospital you choose for your gender affirmation surgery follows or references these standards in their transgender care practices.
Can I still have children after gender affirmation surgery?
Many transgender individuals choose to undergo fertility preservation before their gender affirmation surgery if having biological children is part of their long-term goals. Discuss all your options, such as sperm banking and egg freezing, with your doctor so that you can create the best plan for future family building. JHCTGEH has fertility specialists on staff to meet with you and develop a plan that meets your goals.
Are there other ways I need to prepare?
It is very important to prepare mentally for your surgery. If you haven’t already done so, talk to people who have undergone gender affirmation surgeries or read first-hand accounts. These conversations and articles may be helpful; however, keep in mind that not everything you read will apply to your situation. If you have questions about whether something applies to your individual care, it is always best to talk to your doctor.
You will also want to think about your recovery plan post-surgery. Do you have friends or family who can help care for you in the days after your surgery? Having a support system is vital to your continued health both right after surgery and long term. Most centers have specific discharge instructions that you will receive after surgery. Ask if you can receive a copy of these instructions in advance so you can familiarize yourself with the information.
An initial intake interview via phone with a clinical specialist.
This is your first point of contact with the clinical team, where you will review your medical history, discuss which procedures you’d like to learn more about, clarify what is required by your insurance company for surgery, and develop a plan for next steps. It will make your phone call more productive if you have these documents ready to discuss with the clinician:
- Medications. Information about which prescriptions and over-the-counter medications you are currently taking.
- Insurance. Call your insurance company and find out if your surgery is a “covered benefit" and what their requirements are for you to have surgery.
- Medical Documents. Have at hand the name, address, and contact information for any clinician you see on a regular basis. This includes your primary care clinician, therapists or psychiatrists, and other health specialist you interact with such as a cardiologist or neurologist.
After the intake interview you will need to submit the following documents:
- Pharmacy records and medical records documenting your hormone therapy, if applicable
- Medical records from your primary physician.
- Surgical readiness referral letters from mental health providers documenting their assessment and evaluation
An appointment with your surgeon.
After your intake, and once you have all of your required documentation submitted you will be scheduled for a surgical consultation. These are in-person visits where you will get to meet the surgeon. typically include: The specialty nurse and social worker will meet with you first to conduct an assessment of your medical health status and readiness for major surgical procedures. Discussion of your long-term gender affirmation goals and assessment of which procedures may be most appropriate to help you in your journey. Specific details about the procedures you and your surgeon identify, including the risks, benefits and what to expect after surgery.
A preoperative anesthesia and medical evaluation.
Two to four weeks before your surgery, you may be asked to complete these evaluations at the hospital, which ensure that you are healthy enough for surgery.
What can I expect after gender affirming surgery?
When you’ve finished the surgical aspects of your gender affirmation, we encourage you to follow up with your primary care physician to make sure that they have the latest information about your health. Your doctor can create a custom plan for long-term care that best fits your needs. Depending on your specific surgery and which organs you continue to have, you may need to follow up with a urologist or gynecologist for routine cancer screening. JHCTGEH has primary care clinicians as well as an OB/GYN and urologists on staff.
Among other changes, you may consider updating your name and identification. This list of resources for transgender and gender diverse individuals can help you in this process.
The Center for Transgender and Gender Expansive Health Team at Johns Hopkins
Embracing diversity and inclusion, the Center for Transgender and Gender Expansive Health provides affirming, objective, person-centered care to improve health and enhance wellness; educates interdisciplinary health care professionals to provide culturally competent, evidence-based care; informs the public on transgender health issues; and advances medical knowledge by conducting biomedical research.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
Find Additional Treatment Centers at:

Request an Appointment

Facial Feminization Surgery (FFS)

Gender Affirmation: Do I Need Surgery?

Gender Affirmation Nonsurgical Services
Related Topics
Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps
Your Journey Starts Here!
There’s so much to consider when looking for a surgeon to perform your gender-affirming surgery: experience with the procedure, geographic location and the types of insurance they accept are all primary concerns. Before getting bogged down with too many details, start your journey by searching for surgeons that offer the procedures that you’re interested in. All set? Let’s go!
Search Surgeons by U.S. State
Search surgeons by country, search surgeons by name.

Global Surgeon Maps
Visually search for surgeons by geographic location.
- FFS Surgeons Map
- Vaginoplasty Surgeons Map
- Top Surgery Surgeons Map
- Metoidioplasty Surgeons Map
- Phalloplasty Surgeons Map
- Hysterectomy Surgeons Map
Featured Surgeons
Dr. drew schnitt.

Dr. Schnitt is a board certified cosmetic, plastic, reconstructive and craniofacial surgeon who has been practicing in South Florida since 2002. His experience in cosmetic and craniofacial surgery makes him an excellent choice for gender-affirming facial surgery, as well as Top Surgery, Breast Augmentation and Body Sculpting.
Dr. Adam Bonnington

Dr. Bonnington is a highly skilled obstetrician-gynecologist in San Francisco who is passionate about working with underrepresented patient populations and has a particular interest in caring for transgender and gender expansive individuals. Dr. Bonnington joined MoZaic Care as a Surgical Associate in 2020 and performs Vaginoplasty, Orchiectomy and Hysterectomy.
Dr. Angela Rodriguez

Dr. Rodriguez is a board-certified plastic surgeon in San Francisco who is dedicated full time to providing surgical care for transgender patients. Dr. Rodriguez had 14 years of craniofacial, aesthetic and pediatric plastic surgery experience before becoming a Gender Surgeon. She has a special interest in Facial Feminization and is also highly proficient in Vaginoplasty and Top Surgery.
Dr. Jeffrey B. Marvel

Dr. Marvel is a board-certified cosmetic surgeon who has developed a reputation in Nashville and Central Tennessee for his technical skills, attention to detail and natural-looking results. Since 1997, Dr. Marvel and Marvel Cosmetic Surgery’s dedicated staff have offered top-notch hospitality and care for patients seeking a wide range of cosmetic procedures and treatments. Dr. Marvel is pleased to help transgender men and women who are looking for a skilled cosmetic surgeon in Tennessee for Breast Augmentation, Facial Feminization, Hair Grafting and Top Surgery.
Dr. Paul Steinwald

Dr. Steinwald has performed FTM Top Surgery hundreds of times, and he’s well-known for having pioneered the Inverted-T procedure. Dr. Steinwald has the most experience with Top Surgery than any other surgeon in Colorado. Body Feminization and Breast Augmentation are also offered for trans feminine folks.
Dr. Dany Hanna

Dr. Hanna is a Urologist and fellowship-trained Gender Surgeon who works exclusively with transgender and non-binary patients at the Hanna Gender Center in Dallas, Texas. He completed a yearlong fellowship in gender-affirming surgery and also trained with the renowned Dr. Miroslav Djordjevic in Belgrade, Serbia. Dr. Hanna specializes in Vaginoplasty and also offers Nullification, Metoidioplasty, Top Surgery and Breast Augmentation.
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
- BOOK CONSULTATION
- The Surgical Journey
- Where do I start?
- Am I eligible for surgery?
- Preparing for Surgery
- General Recovery Info
- Risks & Safety
- Top Surgery
- Top Surgery Techniques
- Techniques Beyond the Binary
- Top Surgery Videos
- Breast Augmentation
- Facial Surgery
- Techniques & Incisions
- Body Contouring
- Body Feminization
- Body Masculinization
- Non-Binary Body Contouring
- Bottom Surgery
- “Feminizing” Techniques & Recovery
- “Masculinizing” Techniques & Recovery
- Our Services
- Currently Offered
- Outside Services
- Transition 101
- Introduction to Transitioning
- Support Services: Helpful Links
- Transitioning Later In Life
- Legal Name & Gender Change
- Transmasculine & Pregnancy
- Transgender Healthcare
- Mental Health
- Hormone Therapy
Trans Youth & Adolescents
- Mental Health Support
- Common Questions About Your Child’s Transition
- For Caregivers
- Explaining Your Child’s Identity
- Talking With Schools About Your Child
- Puberty Blockers
- Challenging Topics
- Detransition
- Adolescents
- Gatekeeping vs Empowerment
- Rapid Onset Gender Dysphoria
- Double Incision
- Periareolar
- Inverted T / Aggressive Breast Reduction
- Gynecomastia
- Facial Feminization
- Facial Masculinization
- Labiaplasty
- Vaginoplasty
- Pricing and Financing
- Insurance Approval
- Insurance Denial
- Insurance Accepted
- Referral Letters
- Advocacy Team
- Make a Payment Now
- Our Philosophy
- Meet Our Team
- Office & Facilities
- Testimonials
- Get in Touch
- For Current Patients
- For Providers
Consultation request
- Interpretation Services
- Privacy Policy

slide toggle Demystifying and Navigating Your Options: Gender Reassignment Surgery
Do you have any questions? Check our F.A.Q. section or contact us directly!
Demystifying and Navigating Your Options: Gender Reassignment Surgery
Medically reviewed by Paul Gonzales on March 25, 2024.

Previously, the term gender reassignment surgery (GRS) referred to genital reconstruction bottom surgeries like vaginoplasty, vulvoplasty, phalloplasty, or metoidioplasty. Individuals who look up this term on a search engine do so looking for information on gender-affirming procedures generally for transgender, non-binary and gender non-conforming people. This detailed guide breaks down everything you need to know about these procedures, their costs, their eligibility requirements, the potential benefits and risks and more. If you are interested in undergoing any gender-affirming or “gender reassignment” surgery, you can schedule a free, virtual consultation with one of our surgeons.
At the Gender Confirmation Center (GCC), we generally avoid using terminology like GRS in a clinical setting out of the recognition that for the vast majority of our patients, surgeries do not “reassign” anyone’s gender. Rather, surgery can help individuals experience greater alignment with their bodies and greater gender euphoria as a result.
Types of Gender “Reassignment” Surgeries: “Female to Male (FTM)”
Female to Male (FTM) is outdated terminology that the GCC does not use in our clinical practice. This abbreviation leaves out the experiences of many trans masculine and non-binary patients who do not identify with being labeled as a “woman becoming a man.”
In the past, “FTM gender confirmation surgery” was used to describe surgical procedures that reverse the effects of an initial estrogenic puberty or procedures that reconstruct a patient’s genitals. We still receive various inquiries about which “FTM” procedures we offer, so below you can find a list of surgeries that have typically been placed under this label.
Please note that patients can seek out any of these procedures regardless of their gender identity. The goal of our practice is not to make our patients “into men,” but to help them feel more comfortable, affirmed, and/or aligned with their bodies.
Chest Surgery or Top Surgery
“FTM” top surgery is an antiquated term that refers to gender-affirming chest reconstruction and/or breast reduction. Practices who use this acronym sometimes have limited experience meeting the unique needs of non-binary patients seeking top surgery . Patients who would like to remove their chest tissue to have a flatter chest can choose from a variety of incision options to reach their desired results around chest tightness, contour and/or scar shape.
Not all patients who pursue top surgery want flat chests. Whether you would like to opt for a breast reduction or a chest reconstruction with some volume left behind, the button buttonhole incision is the most commonly pursued type.
Top surgery patients who would like to maintain an erotic or a high level of sensation in their nipples can ask their surgeon about nerve-preservation techniques . Inversely, many patients who get top surgery choose to have their nipples removed .
Genital Reconstruction or Bottom Surgery
While the following bottom surgery procedures are traditionally put under the “FTM” category, we recognize that not all patients who pursue these procedures identify as men nor are they looking to “masculinize” their genitals.
Two procedures can be used to reconstruct a penis or “neophallus”: metoidioplasty and phalloplasty. Metoidioplasty or “meta” releases the ligaments around the erectile tissue (called a clitoris or penis) to extend it to about 2-4 inches in length. A phalloplasty uses a donor flap (usually from the forearm or thigh) to construct a penis of 4 inches in length or more (depending on availability of tissue). Both procedures can be specialized to allow a patient to maintain erotic sensation in their genitals (nerve preservation) and/or urinate standing up (urethroplasty).
Associated procedures include the removal of the uterus (hysterectomy), the removal of the vaginal canal (vaginectomy), the construction of a scrotum (scrotoplasty), the insertion of penile/testicular implants, and more.
Body Masculinization Surgery (BMS)
Body Masculinization Surgery (BMS) refers to a series of body contouring procedures. Most often, BMS involves liposuction of one or more of the following areas: abdomen, flanks, hips, thighs, buttocks, or arms. BMS can also involve removing unwanted, excess skin from fat loss or liposuction. Occasionally, some patients may opt for silicone pectoral implants alongside or after their top surgery results.
Facial Masculinization Surgery (FMS)
Facial Masculinization Surgery (FMS) refers to a series of procedures that patients can choose from to give their face a more angular, conventionally masculine appearance. In the bottom third of the face, the chin, jaw, or laryngeal prominence (aka Adam’s apple) can be augmented or increased in size. In the middle third of the face, the appearance of the nose and/or cheeks can be altered. In the top third of the face, the hairline’s position can be changed and the forehead can be augmented.
Types of Gender “Reassignment” Surgeries: “Male to Female (MTF)”
Male to Female (MTF) is outdated terminology that we do not use in our clinical practice. This abbreviation leaves out the experiences of many trans feminine and non-binary patients who do not identify with being labeled as a “man becoming a woman.”
In the past, “MTF gender confirmation surgery” was used to describe surgical procedures that reverse the effects of an initial androgenic (testosterone-dominant) puberty and/or reconstruct a patient’s genitals. As a practice, we still get asked by prospective patients about the “MTF” procedures we offer, which is why we have compiled a guide of surgeries that have typically been placed under this category.
Please note that patients can seek out any of these procedures regardless of their gender identity. The goal of our practice is not to make our patients turn “into women,” but to help them feel greater gender congruence with their bodies.
Breast Augmentation or “MTF” Top Surgery
Typically, for trans feminine and non-binary patients who prefer to have more volume on their chest, breast augmentation with saline or silicone implants allows for greater success in their desired outcomes. Fat grafting procedures limit the amount of volume transferred to the chest based on available body fat that can be safely removed.
Genital Reconstruction or Bottom Surgeries
The most common surgeries that are placed under this category are vaginoplasty and vulvoplasty (also called zero-depth vaginoplasty) procedures. The most common vaginoplasty uses a penile-inversion technique to reconstruct a vaginal canal. However, a penile-preserving vaginoplasty is also another option for patients. Lifelong dilation after this procedure is necessary to maintain the depth of the canal so that it can be used for penetrative sex. Labiaplasty revisions are sometimes sought out by patients wishing to adjust the size, shape and symmetry of their labia and/or clitoral hood.
Before a vaginoplasty, patients may opt to remove the testicles ( orchiectomy ). Patients of varying gender identities undergo orchiectomies for many reasons, such as chronic pain or to simplify their hormone therapy. For patients who plan to have a vaginoplasty in the future, it’s best to consider the timing of an orchiectomy procedure since scrotal tissue can be used to construct the labia.
Facial Feminization Surgery (FFS)
FFS refers to a series of procedures that a patient can choose from to give their face a softer, more conventionally feminine appearance. In the bottom third of the face, the laryngeal prominence (or Adam’s apple), chin, or jaw can be reduced in size. In the middle third of the face, the appearance of the nose and/or cheeks can be altered. In the top third of the face, the hairline’s position can be changed and the forehead can be reduced.
Body Feminization Surgery (BFS)
BFS encompasses a series of body contouring procedures. Most often, BFS involves removal of fat through liposuction of one or more of the following areas: the thighs, the abdomen/waist, or the arms. The fat removed from these areas of the body can be transferred to the buttocks and/or hip areas and is commonly referred to as a Brazilian butt lift (BBL). BFS can also involve removing unwanted excess skin from fat loss or liposuction, a procedure often referred to as a tummy tuck or abdominoplasty.
Evaluating Candidacy for Gender Affirmation Surgery
Strict guidelines evaluate patient readiness for life-altering GRS procedures.
Informed consent
The GCC follows an informed consent model for surgery because it gives patients autonomy over their health. Under this model, adults can consent to procedures if they have received adequate education about their risks, advantages, and potential effects on their health given their unique medical history. Historically, TGD people have had a difficult time accessing quality gender-affirming health care in part because of gatekeeping and discrimination based on requirements set by insurance companies. For example, letters from medical and mental health providers are a part of these requirements. We recognize that therapists and other healthcare providers are invaluable sources of support for patients undergoing a medical gender transition.
Health factors
We recommend our patients get medical clearance from their primary care provider (PCP) before surgery. If you have medical conditions that may affect your surgery, we can work with your PCP or specialist to ensure a safe recovery. Patients should inform their surgeons of any cardiovascular or respiratory issues, history of anorexia, diabetes, or use of immunosuppressant medications.
Different surgeons may consider a patient’s Body Mass Index (BMI) as part of their eligibility for surgery. You can read more about our requirements and recommendations around BMI here .
We require all our patients to stop smoking or consuming any form of nicotine for at least 3 weeks before and 3 weeks after surgery, as this can lead to significant problems with delayed wound healing. Please do not drink alcohol for at least 1 week before and 1 week after surgery or until prescription pain medications are discontinued.
Insurance requirements
Patients who wish to have their insurance cover their gender affirming surgery need to fulfill certain requirements. You will need to get a letter of support from a mental health professional to confirm that the procedure is medically necessary. If the surgeon is outside of your insurance’s in-network providers, you will need to get a referral letter from your primary care provider (PCP). Additionally, some insurance companies may require that a patient undergo gender-affirming hormone therapy to cover surgery.
Hormone Therapy Considerations
At GCC, we do not require our patients to undergo hormone therapy to access medically necessary, gender-affirming surgeries. That said, undergoing hormones before surgery can help some patients improve the appearance of post-op results.
- Facial surgery: It may take up to 1.5 years on hormone therapy before soft tissue changes can appear on the face so patients should consider waiting to undergo facial surgery until these changes have settled.
- Bottom surgery: Maximal bottom growth may take up to 2 years for patients on a standard dose of testosterone so patients should consider undergoing metoidioplasty until maximal growth is achieved for optimal outcomes.
- Breast augmentation: Maximal breast growth may take up to 1.5 to 2 years for patients on a standard dose of estrogen so patients should consider undergoing breast augmentation until maximal growth is achieved.
- Body contouring: It may take up to 1.5 years on hormone therapy before the fat redistribution process settles so patients should consider waiting until then before undergoing liposuction or fat grafting procedures.
When it comes to age and eligibility for surgery, we are typically asked about 2 populations: adolescents and seniors. The World Professional Association for Transgender Health (WPATH) has outlined in their Standards of Care (SOC), Version 8 , the need for the involvement of caregivers/parents and mental health professionals in the informed consent process for adolescents. If these protocols are followed, the only type of gender-affirming surgery that an adolescent can undergo is top surgery.
As long they are in good health and cleared for surgery, senior patients are eligible for surgery regardless of their age and can achieve good aesthetic outcomes. It’s important to consider what accommodations are necessary to support post-op recovery. You can read more about our eligibility standards here .
Weighing GRS Benefits Against Complications
The decision to undergo “gender reassignment surgery” is a highly personal one. Understanding both the pros and cons provides critical insight.
How GRS Can Transform Lives
The WPATH’s SOC 8 reviews the medical research literature around the long-term effects of gender-affirming surgery on trans and non-binary patients. Gender-affirming procedures report greater satisfaction and lower regret rates compared to similar cosmetic and reconstructive procedures performed in cisgender patients.
- Improved mental health
- Improved body-image, etc.
- Enhanced quality of life
Rates of anxiety, depression, and suicide risk all tend to decrease substantially following surgery for those who need it, which is why these procedures are considered medically necessary for many patients.
Risk Factors and Long-Term Effects
All surgeries carry risks of complications. Generally speaking, patients who optimize their health prior to surgery (e.g., do not smoke tobacco) and manage any pre-existing medical conditions can greatly reduce their risk for complications. Undergoing surgery with a board-certified surgeon who has hospital access privileges can help ensure the integrity of your surgical process. If you have specific questions about surgical complications and how to prevent them, you can consult our content library on this question.
Navigating Emotions
Surgery not only takes a physical, but also an emotional toll on the body. Experiencing pain, inflammation, discomfort and limitations on physical activity occasionally mat result in temporary postoperative depression. Likewise, having to wait weeks or months to have a sense of what your final results from surgery will look like can give some patients temporary feelings of regret during recovery. For this reason, we highly encourage patients to tap into their support networks of friends, (chosen) family and/or mental health professionals during this time. To learn more about the emotional recovery process, click here .
Conclusion: Is Gender Reassignment Surgery the Right Choice?
While gender-affirming surgery has been proven to be positively life-changing for many trans and non-binary individuals. Whether you seek surgery or not, we remain dedicated to your health, empowerment, and right to be your authentic self.
More Articles
Understanding the cost of double incision top surgery: a comprehensive guide, gatekeeping vs. empowerment: accessing gender affirming care, treating gender dysphoria in adolescents, sign up for instructions to get a virtual consultation.
The virtual consultation will be billed to your insurance company. We will accept the insurance reimbursement as payment in full.
Dr. Scott Mosser Suite 1010, 450 Sutter St San Francisco, CA 94108 Phone: (415) 780-1515 Fax: ( 628) 867-6510
Gender Journey Resources
- Trans Youth & Adolescents
Before & After
- Top surgery
- Virtual Consultations
Board Certification & Memberships

- Terms of Use
Copyright © 2023 Gender Confirmation Center. All Rights Reserved.
MTFsurgery .net
- Orchiectomy
- Penile Inversion Vaginoplasty
- Peritoneal Vaginoplasty
- Rectosigmoid Vaginoplasty
- Vulvoplasty
- Non-Binary Bottom Surgery
- Facial Feminization Surgery
- Breast Augmentation
- Breast Augmentation w/ Fat Transfer
- Body Feminization
- What Is Board Certification?
- Getting Surgery In Thailand
- Vaginoplasty Hair Removal
- Follicular Cautery vs. Hair Removal
- Vaginal Stenosis After Vaginoplasty
- Importance of Dilation
- Breast Aug & Surgeon Experience
- Browse All Surgeons
- Orchiectomy Surgeons
Vaginoplasty Surgeons
- FFS Surgeons
- Breast Augmentation Surgeons
- Body Feminization Surgeons
- MTF Breast Augmentation
- MTF Vaginoplasty
MTF Surgery » Surgeons
Surgeons Who Perform Gender-Affirming Surgery
Trans feminine Gender Affirming Surgery is becoming more and more common, but it can still be tough to find the right surgeon. The surgeons listed below are highly qualified plastic, reconstructive, urological and cosmetic surgeons who regularly perform gender-affirming procedures for those on the trans feminine spectrum. When choosing a surgeon, look for board certification, experience with transgender surgery, and a someone you feel confident and comfortable with.
Also see: Vaginoplasty Surgeons , Orchiectomy Surgeons
Featured Surgeons
Dr. Kathy Rumer
Dr. Kathy Rumer is an expert in transgender surgery, performing 200-250 MTF gender reassignment surgeries per year. Dr. Rumer also directs a 1-year gender surgery fellowship program. She offers the full range of male to female surgery procedures, including Vaginoplasty, Facial Feminization Surgery and Breast Augmentation. Read more »
Dr. Scott Mosser
Dr. Scott W. Mosser is a board certified and award-winning surgeon based in San Francisco who specializes in MTF/N Breast Augmentation and Body Feminization. He has worked with the transgender community for more than 10 years. Dr. Mosser is co-founder of the American Society of Gender Surgeons (ASGS), and Medical Director of the Gender Institute at Saint Francis Memorial Hospital. Read more »
Dr. Angela Rodriguez
Dr. Rodriguez is a board-certified plastic surgeon in San Francisco who is dedicated full time to providing surgical care for transgender patients. She is highly proficient in gender-affirming Vaginoplasty and has a special interest in Facial Feminization. Her commitment to transforming lives and passion for social justice drove her pursuance to master transgender surgery, but it's Dr. Rodriguez's surgical skills, bedside manner and results that patients love. More »
Dr. Scott W. Mosser is a board certified and award-winning surgeon based in San Francisco who specializes in MTF/N Breast Augmentation and Body Feminization. He has worked with the transgender community for more than 10 years. Dr. Mosser is co-founder of the American Society of Gender Surgeons (ASGS), and Medical Director of the Gender Institute at Saint Francis Memorial Hospital. More »
Dr. Danny Hanna
Dr. Hanna is a fellowship-trained Gender Surgeon based in Dallas, Texas. At the Hanna Gender Center, Dr. Hanna works exclusively with transgender and non-binary patients, offering gender-affirming genital surgeries as well as Breast Augmentation, Body Sculpting and Hair Grafting. More »
Newly Added Surgeons
Dr. Kenan Celtik
Dr. Celtik is a Reconstructive Urologist who specializes in gender-affirming Vaginoplasty. He is fellowship-trained in Gender Surgery and has completed 15 years of advanced medical education, including rigorous training in female pelvic reconstruction, robotic surgery and neurourology. Dr. Celtik's deep expertise and commitment to providing exceptional care and surgical outcomes make him a great choice of Vaginoplasty surgeon. He joined the Crane Center for Transgender Surgery in 2023 and is based in the San Francisco area. More »
Dr. Drew Marano
Dr. Marano is a fellowship-trained plastic and reconstructive surgeon in New York City who has deep expertise in Gender Affirmation Surgery. Dr. Marano is fellowship-trained in the full spectrum of gender-affirming procedures and is particularly passionate about Robotic Vaginoplasty and Facial Feminization Surgery. Dr. Marano's extensive training and dedication to provide the highest level of care make him a sound choice of surgeon in the New York metropolitan area. More »
Dr. Aneesh Gupta
Dr. Gupta is a triple board-certified cosmetic surgeon in Philadelphia who offers Breast Augmentation and Body Feminization surgery. Dr. Gupta's experience with gender-affirming care has informed how Jazzi Cosmetic Surgery has created a welcoming environment for all patients. Throughout your surgical journey, you can expect everyone you interact with at Jazzi to be friendly and professional. More »
Facial Feminization Experts
Dr. Joel Beck
Dr. Beck is a board certified plastic and reconstructive surgeon who has been offering gender-affirming facial surgery since 2003. Based in Charlotte, North Carolina, Dr. Beck is one of only a few FFS Surgeons in the Southeast. He also offers Breast Augmentation, Body Sculpting and Hair Grafting. More »
Dr. Gerhard Mundinger
Dr. Mundinger is a board-certified plastic surgeon with broad training and expertise in craniofacial and gender-affirming surgery. Dr. Mundinger joined the Austin branch of the Crane Center for Transgender Surgery in 2021, where he offers Facial Feminization Surgery, Vaginoplasty and Breast Augmentation. More »
Dr. Drew Schnitt
Dr. Schnitt is a board certified cosmetic, plastic, reconstructive and craniofacial surgeon based in South Florida. In practice since 2002, Dr. Schnitt's extensive experience in cosmetic and craniofacial surgery make him a great choice for Facial Feminization Surgery, as well as gender-affirming Breast Augmentation and Body Sculpting. More »
Dr. Josef Hadeed
Dr. Hadeed is a board certified, Duke University-trained surgeon who offers gender-affirming feminizing surgery in Beverly Hills, California and Miami, Florida. Dr. Hadeed's surgical offerings include Orchiectomy, Facial Feminization, Breast Augmentation and Body Sculpting. More »
Dr. Alexander Facque
Dr. Facque is a board-certified plastic surgeon in San Francisco, California who joined the Gender Confirmation Center's team in September 2020 as a full-time Associate Surgeon with deep expertise in Facial Gender Confirmation Surgery, Breast Augmentation and Body Sculpting. Dr. Facque was introduced to gender-affirming care in 2012 and now works exclusively with transgender and non-binary patients. More »
Dr. Thomas Satterwhite
Dr. Satterwhite is a Plastic Surgeon in San Francisco works exclusively with transgender and non-binary patients. Dr. Satterwhite performs Facial Feminization Surgery, Vaginoplasty, Breast and Buttock Augmentation, and Body Sculpting. More »
Dr. Toby Meltzer
Dr. Meltzer is a plastic and reconstructive surgeon who is widely recognized as one of the leading surgeons in the field of Gender Reassignment Surgery. Dr. Meltzer has been performing MTF Surgery since 1993 and has completed over 4000 gender affirming surgeries. He performs about 200 gender reassignment surgery cases per year in Scottsdale, Arizona. More »
Dr. Christopher Salgado
Dr. Salgado is a board-certified plastic surgeon in Florida who has deep expertise in Gender Affirming Surgery. In practice for more than 20 years, Dr. Salgado performs all aspects of male-to-female surgery, from Facial Feminization and Breast Augmentation to Vaginoplasty, giving patients the opportunity to experience a continuity of care throughout their surgical transition. After many years in academic practice, Dr. Salgado opened his private practice in Miami in 2019. More »
Dr. Eric Bensimon
Dr. Bensimon has dedicated his career to helping trans women seeking FFS. With over 15 years experience in FFS, Dr. Eric Bensimon is one of the world's most experienced surgeons practicing Facial Feminization Surgery. Dr. Bensimon is based in Montreal, Canada. More »
Dr. Praful Ramineni
Dr. Ramineni is a highly experienced, board-certified plastic and reconstructive surgeon who specializes in gender-affirming top and bottom surgeries. Dr. Ramineni has more than 15 years of experience as a surgeon and performs at least 600 procedures a year. He's known for not just his exceptional surgical skills and natural-looking results, but also for his caring bedside manner and great communication style. More »
Dr. Daniel J. Freet
Dr. Freet is a board certified Plastic and Reconstructive Surgeon who offers the full spectrum of MTF Surgery procedures at the University of Texas in Houston. Leading a multidisciplinary gender surgery team, Dr. Freet performs Gender Reassignment Surgery (Vaginoplasty), as well as Facial Feminization and Breast Augmentation. More »
Dr. Gabriel Del Corral
Dr. Del Corral is a double board-certified plastic and reconstructive surgeon who offers Vaginoplasty and other gender-affirming procedures at the Medstar Center for Gender Affirmation in Washington D.C. and Baltimore, Maryland. Fellowship trained in microsurgery, Dr. Del Corral also has expertise in reconstructive surgery, maxillofacial surgery and cosmetic surgery. He specializes in Gender Affirmation Surgery and has a particular interest in Vaginoplasty and Facial Feminization. More »
Dr. Heidi Wittenberg
Dr. Wittenberg is an experienced Urogynecologist in San Francisco who works exclusively with trans and non-binary patients. Dr. Wittenberg is the director of MoZaic Care, which specializes in gender affirming genital and pelvic surgeries, and a Founder Surgeon and Co-Director for the first SRC accredited Center of Excellence in Gender Confirmation Surgery, at Greenbrae Surgery Center. More »
Dr. Adam Bonnington
Dr. Bonnington is a Gender Surgeon in San Francisco who has focused his career on working with underrepresented patient populations. He joined Dr. Heidi Wittenberg at MoZaic Care as a Surgical Associate in 2020 where he works exclusively with transgender and non-binary individuals. Dr. Bonnington performs Orchiectomy and Vaginoplasty. More »
Dr. Loren Schechter
Dr. Schechter is one of the country's foremost experts on gender-affirming surgery. He is the Medical Director of the Gender Affirmation Surgery Program at Rush University Medical Center in Chicago. Dr. Schechter's outstanding surgical skills and more than 20 years experience with transgender surgery have made him an in-demand surgeon. He offers the full spectrum MTF Gender Confirmation procedures, including Breast Augmentation, single-stage Vaginoplasty, and FFS. More »
Dr. Curtis Crane
Dr. Crane is a board-certified plastic surgeon in Austin, Texas who has deep experience with the full spectrum of male-to-female Gender Reassignment Surgery procedures. Dr. Crane and his team perform approximately 130 Vaginoplasty surgeries every year, as well as Vulvoplasty, Facial Feminization and Breast Augmentation. More »
Dr. Richard Santucci
Dr. Santucci, who spent 18 years as one of the nation's most distinguished academic Reconstructive Urologists, hasn't looked back since turning his focus to Gender Affirming Surgery. Before joining the Crane Center for Transgender Surgery, Dr. Santucci served as the Director of the Center for Urologic Reconstruction and the Specialist-in-Chief for Urology at the Detroit Medical Center. Dr. Santucci's years of experience with complex genitourinary surgery uniquely qualifies him to excel at gender-affirming genital reconstruction. More »
Dr. Ashley DeLeon
Dr. DeLeon is a board-certified surgeon who specializes exclusively in Gender Affirmation Surgery. Dr. DeLeon was fellowship trained in gender-affirming procedures by Dr. Curtis Crane. Dr. DeLeon practices in Austin, Texas at the Crane Center for Transgender Surgery, one of the busiest gender surgery practices in the world. Dr. DeLeon's special focus is on male-to-female bottom surgery procedures: Orchiectomy, Vulvoplasty and Vaginoplasty. More »
Dr. Dev Gurjala
Dr. Gurjala is a board-certified plastic surgeon in San Francisco who offers the full array of male-to-female surgery. Prior to joining Align Surgical Associates in 2019, Dr. Gurjala performed gender surgery, microsurgery, and general reconstructive and aesthetic surgery for five years in the Kaiser Permanente system in California. More »
Dr. Michael Safir
Dr. Safir is a board-certified urologist in Los Angeles who specializes exclusively in gender-affirming bottom surgery procedures. With sub-specialty certification in Female Pelvic Medicine and Reconstructive Surgery (FPM-RS), Dr. Safir is one of a handful of urologists in the world with individual fellowship training and experience in both male and female genital reconstruction. He gained signicant experience performing gender-affirming genital procedures for five years at one of the highest volume gender surgery centers in the world. More »
Dr. John Henry Pang
Dr. Pang is a double board-certified plastic and reconstructive surgeon who has also completed fellowship training in Gender Affirming Surgery. Before joining Align Surgical Associates in San Francisco, Dr. Pang completed the Transgender Surgery training program at Mount Sinai in New York City. His practice is dedicated to providing the highest level of care for his transgender and non-binary patients. More »
Dr. Ellie Zara Ley
Dr. Ley is a board-certified plastic surgeon who had over 15 years of training and experience in plastic surgery, craniofacial surgery and microsurgery before completing Gender Surgery training. Now based in San Francisco, Dr. Ley provides superb surgical care for those seeking Vaginoplasty, Facial Feminization and other feminizing surgeries. More »
Dr. Kathy Rumer is an expert in transgender surgery, performing 200-250 MTF gender reassignment surgeries per year. Dr. Rumer also directs a 1-year gender surgery fellowship program. She offers the full range of male to female surgery procedures, including Vaginoplasty, Facial Feminization Surgery and Breast Augmentation. More »
Dr. John Whitehead
Dr. Whitehead offers gender affirming male-to-female surgery in Florida. Dr. Whitehead was trained in the art of gender reassignment surgery by Dr. Harold Reed, the now-retired urologist who practiced at The Reed Center for decades. Dr. Whitehead offers Orchiectomy, Vaginoplasty and Vulvoplasty. More »
Dr. Dmitriy Nikolavsky
Dr. Nikolavsky is a highly regarded Reconstructive Urologist and Gender Surgeon at SUNY Upstate Medical University in Syracuse NY. In addition to offering primary Vaginoplasty surgery, Dr. Nikolavsky is also an expert at treating post-operative urinary complications and provides long term follow-up care for patients who have had Vaginoplasty. Read more »
Dr. Jonathan Keith
Dr. Keith is a fellowship-trained Plastic Surgeon in New Jersey with expertise in Gender Reassignment Surgery. In 2018, Dr. Keith co-founded the first multidisciplinary clinical program for transgender patients in New Jersey. He is the first surgeon in New Jersey to offer the full range of gender-affirming procedures, including Facial Surgery, Vaginoplasty and Breast Augmentation. More »
Dr. Nick Esmonde
Dr. Esmonde is a Gender Surgeon in Portland, Oregon who has impeccable training in Gender Affirmation Surgery and whose practice is almost exclusively focused on helping transgender and non-binary patients. Dr. Esmonde offers the full spectrum of feminizing surgeries, from Facial Feminization to Vaginoplasty. More »
Dr. Christopher McClung
Dr. McClung is a board-certified urologist in Columbus, Ohio who specializes in gender-affirming Vaginoplasty. Dr. McClung's deep experience with complex urological reconstructions provided an ideal background for becoming a Gender Surgeon. He has now performed over 200 feminizing bottom surgeries and his practice is fully dedicated to providing gender-affirming surgical care. In addition to his urology and reconstructive expertise, Dr. McClung's patients also appreciate his gentle bedside manner. More »
Dr. Min Jun
Dr. Min Jun is an exceptionally trained Reconstructive Urologist and Gender Surgeon in San Francisco who specializes in Robotic Peritoneal Flap Vaginoplasty. Dr. Jun has completed fellowship training in both Reconstructive Urology and Gender Affirming Surgery. He worked with the Crane Center for Transgender Surgery in 2020-2023 and now has his own practice in San Francisco. More »
Surgeons in Thailand
Dr. Pichet Rodchareon
Dr. Pichet Rodchareon is a board-certified plastic surgeon in Bangkok who has extensive experience performing male-to-female Gender Reassignment Surgery. Dr. Pichet is considered one of top SRS surgeons in Thailand. His training includes plastic surgery, hand surgery, craniofacial and maxillofacial surgery. More »
Dr. Kamol Pansritum
Dr. Kamol Pansritum is recognized as one of the most experienced GRS Surgeons in the world, having completed over 5,000 gender reassignment surgeries, and more than 10,000 related surgical procedures for trans women since 1997. Dr. Kamol currently performs more than 200 MTF reassignment surgeries a year at his private hospital in Bangkok, Thailand. More »
More MTF Surgeons
Dr. Cassie Nghiem
Dr. Nghiem is an Ivy League-educated, fellowship-trained plastic surgeon in Washington, D.C. who specializes in Gender-Affirming Surgery, including Breast Augmentation and Facial Feminization. She works closely with her patients to deliver the best quality care that is aligned with their goals. Known for her advanced surgical skills, Dr. Nghiem's patients also love her friendly personality and kind demeanor. More »
Dr. Manish Champaneria
Dr. Manish Champaneria is a board-certified surgeon with extensive training and experience in plastic surgery and a special focus on reconstructive breast procedures and Facial Feminization. Dr. Champaneria practices in San Diego, California. More »
Dr. Walter Lin
Dr. Walter Lin is a fellowship-trained Plastic Surgeon in San Francisco who performs Breast Augmentation for transfeminine individuals. Dr. Lin's expertise in the areas of microsurgical reconstruction of the extremities, breast, and lymphatic systems has greatly contributed to his skill with gender-affirming Breast Augmentation. Dr. Lin joined the staff of Buncke Clinic and the San Francisco Transgender Institute in 2017. More »
Dr. Michelle Lee
Dr. Lee is a board-certified and fellowship-trained plastic surgeon with high proficiency in aesthetic and reconstructive procedures for the breast and face. Widely regarded as being one of the finest plastic surgeons in the Los Angeles area, Dr. Lee possesses the perfect combination of skill, artistry, experience and compassion, which makes her ideally suited to performing gender-affirming surgery. More »
Dr. Alvina Won
Dr. Won is a board-certified Cosmetic Surgeon who is committed to providing the highest level of compassionate care in a welcoming environment for all patients. Dr. Won gained significant experience with gender-affirming surgery during a year-long cosmetic surgery fellowship with Dr. Tony Mangubat, a 20+ year veteran of transgender surgery. Based in the Seattle area, just north of Seattle, Dr. Won now devotes part of her practice to performing MTF Breast Augmentation, Buttock Augmentation and Body Sculpting. More »
Dr. Laurel Chandler
Dr. Chandler is a Harvard fellowship-trained plastic surgeon who has received specialty training in gender-affirming breast surgery. During both her residency and fellowship training, Dr. Chandler worked with established gender surgeons to learn the aesthetic nuances of transgender Breast Augmentation. Dr. Chandler provides individualized care for a diverse range of patients, up to 90% of whom are transgender and non-binary. More »
Dr. Javad Sajan
Voted #1 Best Surgeon in Seattle in 2016 and 2017, Dr. Sajan is an internationally recognized Cosmetic & Reconstructive Plastic Surgeon whose specializations include Facial Feminization and Breast Augmentation. Dr. Sajan enjoys providing gender-affirming surgical care and is honored to play a role in his patients' transitions. More »
Dr. Daniel Jacobs
Dr. Jacobs is a board-certified plastic surgeon in San Francisco, California who joined the Gender Confirmation Center in July 2022. With more than 30 years of plastic experience and a practice that's dedicated to gender-affirming care, Dr. Jacobs is a sound choice for transfeminine and non-binary individuals seeking Breast Augmentation surgery. More »
Dr. Daniel Crane
Dr. Crane is a plastic surgeon in the Miami area who has expertise in breast, body and facial surgeries. He was one of only 30 residents selected from across the country to participate in a highly specialized aesthetic fellowship training program. In 2022, Dr. Crane joined Dr. Drew Schnitt's Inspire Aesthetics. His unique training in plastic and aesthetic surgery provides him with the knowledge and experience to help you achieve your surgery goals. More »
Dr. E. Antonio Mangubat
Dr. E. Antonio Mangubat is the Pacific Northwest's most sought-after surgeon for transgender surgery, with more than 20 years of experience performing procedures for trans women, including Facial Feminization, MTF Breast Augmentation, Body Sculpting and Hair Restoration. More »
Dr. Dustin Reid
Dr. Dustin Reid is a double board-certified plastic surgeon in Austin who offers Breast Augmentation, Body Feminization and Hair Restoration. Dr. Reid is committed to providing expert surgical care and guidance throughout your surgery experience. More »
Dr. Daniel Medalie
Dr. Daniel Medalie is a board certified plastic and reconstructive surgeon who has been performing gender-affirming surgeries since 1996. Based in the Cleveland area, he offers Breast Augmentation and Tracheal Shave procedures for transfeminine individuals. More »
Dr. Russell Sassani
Dr. Russell Sassani is a board certified plastic and reconstructive surgeon who has quickly become one of the most popular surgeons in the Southeastern United States for trans women. He performs Breast Augmentation, Facial Feminization and Body Sculpting in the Mami/Fort Lauderdale area. More »
Dr. Mark Youssef
Dr. Mark Youssef, Director of the Transgender Surgery Institute of Southern California, is a Cosmetic Surgeon in Santa Monica who helps clients on the trans feminine spectrum with Breast Augmentation, Body Feminization and Facial Feminization surgeries. He operates at his private surgery center, Younique Surgery Center in Santa Monica. More »

Dr. Hope Sherie
Dr. Hope Sherie is a board-certified cosmetic surgeon who has extensive training in MTF surgery procedures. Dr. Sherie offers trans women the highest level of surgical care at her practice in Charlotte, North Carolina. Procedures available include Orchiectomy and Breast Augmentation. More »
Dr. Charles Lee
Dr. Charles Lee is a board-certified plastic and reconstructive surgeon who has deep expertise in microsurgery and breast surgery. In practice since 2003, Dr. Lee offers MTF Top Surgery at Crane Center for Transgender Surgery in San Francisco. More »
Dr. Alan Dulin
Dr. Alan Dulin is a board-certified surgeon who has many years of experience performing Male-to-Female Surgery in the Dallas area. Dr. Dulin offers transgender women Breast Augmentation & Body Contouring, Facial Feminization Surgery and Orchiectomy. More »
Dr. Scott Harris
Dr. Scott Harris is a board-certified Surgeon with years of experience performing Male to Female Surgery in Texas. Known for his meticulous attention to detail, Dr. Harris offers a number of feminizing surgeries for trans women, including Facial Feminization Surgery, Breast Augmentation and Body Sculpting procedures. More »
Dr. Jeffrey Marvel
Dr. Marvel is a board-certified cosmetic surgeon who has developed a great reputation in Nashville and Central Tennessee for his technical skills, attention to detail and natural-looking results. Since 1997, Dr. Marvel and Marvel Cosmetic Surgery's dedicated staff have offered top-notch hospitality and care for patients seeking a wide range of cosmetic procedures, including Facial Feminization, Breast Augmentation and Hair Grafting. More »
Dr. Eric Emerson
Dr. Eric Emerson is a Board-Certified Plastic Surgeon with over 20 years experience specializing in breast surgery, body contouring and facial surgery. Dr. Emerson is a sound choice for trans women seeking breast augmentation and body and facial feminization surgery in the Carolinas and eastern United States. More »
Dr. Gregory Swank
Dr. Gregory Swank a board-certified, Duke University-trained surgeon who offers male-to-female surgery in North Carolina. Dr. Swank's surgical offerings for trans women include Breast Augmentation, and Body and Facial Feminization. More »
Dr. Michael Beckenstein
Dr. Michael Beckenstein is a double-board-certified Plastic Surgeon in Birmingham who is pleased to offer his expertise and skills in cosmetic and reconstructive surgery to the MTF community in Alabama and throughout the Southeast. Dr. Beckenstein specializes in Breast Augmentation as well as Hair Restoration. More »
Dr. Helena Guarda
Dr. Helena Guarda is a board-certified Plastic and Reconstructive Surgeon who is committed to offering Breast Augmentation and Feminization Surgeries as part of her LGBT-friendly practice in Suffolk, Virginia. Dr. Guarda is excited to work with patients from all parts of Virginia, as well as those coming from nearby states such as North Carolina, Maryland, West Virginia, Tennessee, and Kentucky. More »
Dr. Elliot Jacobs
Dr. Jacobs is a nationally-recognized, board-certified plastic surgeon in Boca Raton, Florida with more than 30 years of experience in breast and facial surgeries. Dr. Jacobs offers MTF Surgery procedures at his private, modern and fully accredited surgical suite. More »
Dr. Rex Moulton-Barrett
Dr. Rex Moulton-Barrett is a double board certified cosmetic, plastic and reconstructive surgeon in the San Francisco Bay Area who has been performing MTF Breast Augmentation surgery since 2010. Read more »
Dr. Vartan Mardirossian
Dr. Vartan Mardirossian is a surgeon in South Florida who specializes in Facial Feminization Surgery. Dr. Mardirossian has extensive training and experience performing Facial Feminization procedures, including 7 years of training under renowned FFS surgeon Dr. Jeffrey Spiegel . Read more »
Last updated: 04/03/24


Rumer Gender Surgery

Explore Other MTF Procedures
Request More Information
Gender reassignment surgery, what is mtf gender reassignment surgery.
MTF Gender Reassignment Surgery (GRS) is the male to female procedure for transgender women who wish to have the vagina they should have been born with.
What Should I Know About Gender Reassignment Surgery?
Dr. Rumer performs a One-Stage Modified Penile Inversion Vaginoplasty . Having a strong background in engineering and fine arts, she is able to design a result that has an authentic appearance with excellent depth, function and sensation – a result perfectly suited to your anatomy. In addition, Dr. Rumer’s GRS technique does not require electrolysis or laser hair removal of the genital area before surgery and there is NO regrowth.
What Does The Procedure Involve?
GRS is done while you are asleep under general anesthesia. It takes approximately four hours to perform. Following your surgery, you will be admitted to the hospital for three days of strict bed rest while your new vagina heals. After those three days of bed rest in the hospital, you will be discharged with a catheter in your bladder, some vaginal packing and two drains. One week from your surgery, you will return to the office in order to have the catheter, vaginal packing and drains removed. At that time you will be given your dilators with full instructions on the dilation schedule and lifetime instructions for the care of your new vagina.
How Long Is Recovery And When Can I Resume My Normal Activities?
Patients are asked to rest and relax for the first week after MTF Gender Reassignment Surgery. It is very important to diligently follow your dilation schedule to maximize your results. After the first follow-up visit, patients can begin to get back to normal daily activities, but strenuous activity is not recommended until six weeks after surgery.
Also see: Comparing Penile Inversion and Rectosigmoid Vaginoplasty , Breast Augmentation , Facial Feminization , Body Contouring
Rumer Cosmetic Surgery Kathy L. Rumer, DO, FACOS 105 Ardmore Avenue Ardmore, PA 19003
(855) R U A LOOKER Phone: (855) 782-5665
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, male-to-female gender-affirming surgery: 20-year review of technique and surgical results.

- 1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

Figure 1 . The initial circumferential subcoronal incision.

Figure 2 . The de-gloved penis being passed through the scrotal opening.

Figure 3 . The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.
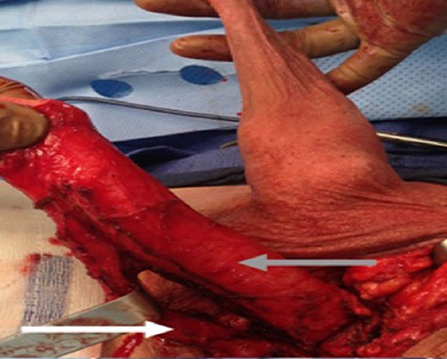
Figure 4 . The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

Figure 5 . The inverted penile skin flap.
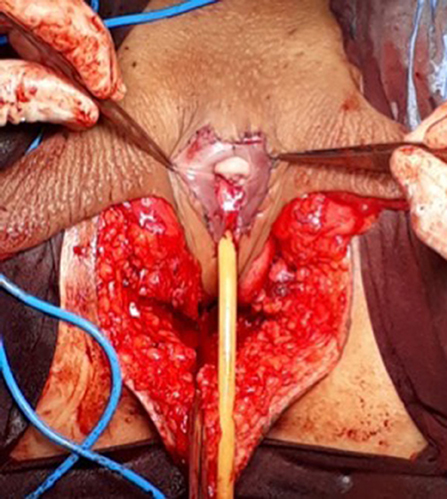
Figure 6 . The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.
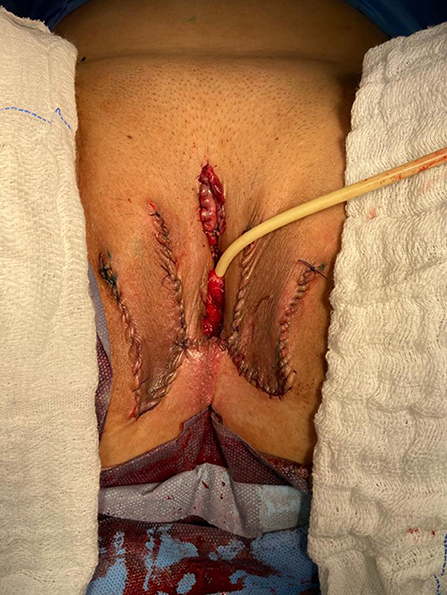
Figure 7 . The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Figure 8 . Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
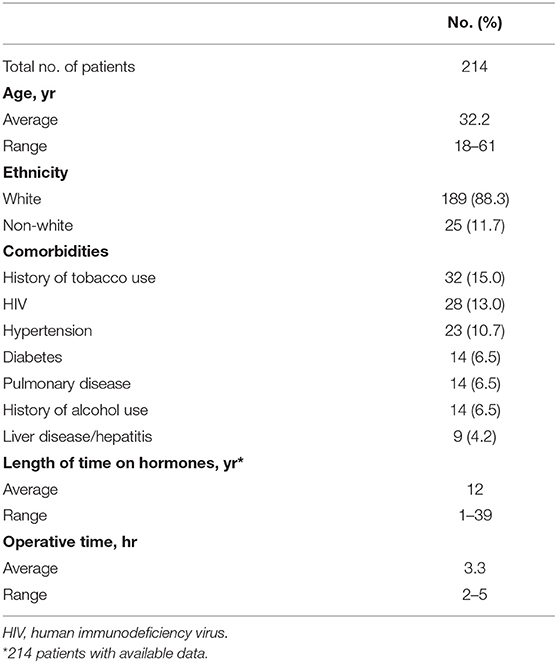
Table 1 . Patient demographics.
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
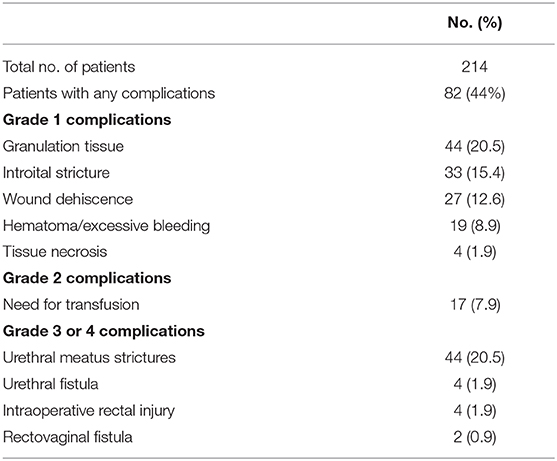
Table 2 . Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.
Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-non-conforming people, version 7. Int J Transgend. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
CrossRef Full Text | Google Scholar
2. Massie JP, Morrison SD, Maasdam JV, Satterwhite T. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstruct Surg. (2018) 141:911–921. doi: 10.1097/PRS.0000000000004427
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep . (2018) 19:62. doi: 10.1007/s11934-018-0809-9
4. Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int . (2007) 100:607–13. doi: 10.1111/j.1464-410X.2007.07017.x
5. Rossi NR, Hintz F, Krege S, Rübben H, Vom DF, Hess J. Gender reassignment surgery – a 13 year review of surgical outcomes. Eur Urol Suppl . (2013) 12:e559. doi: 10.1016/S1569-9056(13)61042-8
6. Silva RUM, Abreu FJS, Silva GMV, Santos JVQV, Batezini NSS, Silva Neto B, et al. Step by step male to female transsexual surgery. Int Braz J Urol. (2018) 44:407–8. doi: 10.1590/s1677-5538.ibju.2017.0044
7. Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender surgery in Denmark from 1994 to 2015: 20-year follow-up study. J Sex Med. (2016) 13:720–5. doi: 10.1016/j.jsxm.2016.01.012
8. Perovic SV, Stanojevic DS, Djordjevic MLJ. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. (2001) 86:843–50. doi: 10.1046/j.1464-410x.2000.00934.x
9. Krege S, Bex A, Lümmen G, Rübben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. (2001) 88:396–402. doi: 10.1046/j.1464-410X.2001.02323.x
10. Wagner S, Greco F, Hoda MR, Inferrera A, Lupo A, Hamza A, et al. Male-to-female transsexualism: technique, results and 3-year follow-up in 50 patients. Urol International. (2010) 84:330–3. doi: 10.1159/000288238
11. Reed H. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin PlasticSurg. (2011) 25:163–74. doi: 10.1055/s-0031-1281486
12. Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. (2015) 12:1837–45. doi: 10.1111/jsm.12936
13. Sigurjonsson H, Rinder J, Möllermark C, Farnebo F, Lundgren TK. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. (2015) 6:69–73. doi: 10.1016/j.jpra.2015.09.003
14. Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. (2018) 199:760–5. doi: 10.1016/j.juro.2017.10.013
15. Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr. Urol. Rep. (2018) 19:36. doi: 10.1007/s11934-018-0795-y
16. Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. (2013) 64:141–9. doi: 10.1016/j.eururo.2012.12.030
17. Horbach SER, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med . (2015) 12:1499–512. doi: 10.1111/jsm.12868
18. Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. (2018) 6:457–68.e2. doi: 10.1016/j.sxmr.2017.11.005
19. Salim A, Poh M. Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. (2018) 45:343–50. doi: 10.1016/j.cps.2018.04.001
20. Hess J, Rossi NR, Panic L, Rubben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. DtschArztebl Int. (2014) 111:795–801. doi: 10.3238/arztebl.2014.0795
21. Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. (2016) 13:988–93. doi: 10.1016/j.jsxm.2016.03.370
22. Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol . (2010) 72:214–31. doi: 10.1111/j.1365-2265.2009.03625.x
23. Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest . (2015) 38:1373–81. doi: 10.1007/s40618-015-0398-0
24. Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, et al. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J Sex Med . (2015) 12:180–8. doi: 10.1111/jsm.12758
Keywords: transsexualism, gender dysphoria, gender-affirming genital surgery, penile inversion vaginoplasty, surgical outcome
Citation: Moisés da Silva GV, Lobato MIR, Silva DC, Schwarz K, Fontanari AMV, Costa AB, Tavares PM, Gorgen ARH, Cabral RD and Rosito TE (2021) Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Front. Surg. 8:639430. doi: 10.3389/fsurg.2021.639430
Received: 17 December 2020; Accepted: 22 March 2021; Published: 05 May 2021.
Reviewed by:
Copyright © 2021 Moisés da Silva, Lobato, Silva, Schwarz, Fontanari, Costa, Tavares, Gorgen, Cabral and Rosito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Veber Moisés da Silva, veber.gabriel@gmail.com
This article is part of the Research Topic
Gender Dysphoria: Diagnostic Issues, Clinical Aspects and Health Promotion
How Gender Reassignment Surgery Works (Infographic)
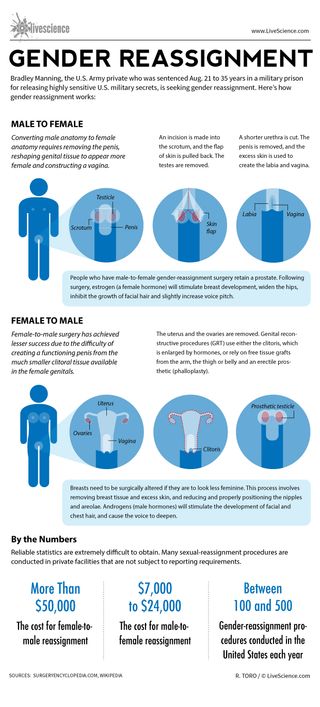
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Man's years of premature ejaculation had a rare cause
Viagra alternatives? Study of mouse erections hints at new ways to treat erectile dysfunction
Jupiter's elusive 5th moon caught crossing the Great Red Spot in new NASA images
Most Popular
- 2 China creates its largest ever quantum computing chip — and it could be key to building the nation's own 'quantum cloud'
- 3 'Quantum-inspired' laser computing is more effective than both supercomputing and quantum computing, startup claims
- 4 2,500-year-old Illyrian helmet found in burial mound likely caused 'awe in the enemy'
- 5 Papua New Guineans, genetically isolated for 50,000 years, carry Denisovan genes that help their immune system, study suggests
- 2 Sun launches strongest solar flare of current cycle in monster X8.7-class eruption
- 3 Newfound 'glitch' in Einstein's relativity could rewrite the rules of the universe, study suggests
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Plast Reconstr Surg Glob Open
- v.9(3); 2021 Mar
Regret after Gender-affirmation Surgery: A Systematic Review and Meta-analysis of Prevalence
Valeria p. bustos.
From the * Division of Plastic and Reconstructive Surgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Mass.
Samyd S. Bustos
† Department of Plastic Surgery, University of Pittsburgh, Pittsburgh, Pa.
Andres Mascaro
‡ Department of Plastic and Reconstructive Surgery, Cleveland Clinic, Weston, Fla.
Gabriel Del Corral
§ Department of Plastic and Reconstructive Surgery, MedStar Georgetown University Hospital, Washington, D.C.
Antonio J. Forte
¶ Division of Plastic and Reconstructive Surgery, Mayo Clinic, Jacksonville, Fla.
Pedro Ciudad
∥ Department of Plastic, Reconstructive and Burn Surgery, Arzobispo Loayza National Hospital, Lima, Peru
Esther A. Kim
** Division of Plastic and Reconstructive Surgery, University of California, San Francisco, Calif.
Howard N. Langstein
†† Division of Plastic and Reconstructive Surgery, University of Rochester Medical Center, Strong Memorial Hospital, Rochester, N.Y.
Oscar J. Manrique
Associated data.
Supplemental Digital Content is available in the text.
Background:
There is an unknown percentage of transgender and gender non-confirming individuals who undergo gender-affirmation surgeries (GAS) that experiences regret. Regret could lead to physical and mental morbidity and questions the appropriateness of these procedures in selected patients. The aim of this study was to evaluate the prevalence of regret in transgender individuals who underwent GAS and evaluate associated factors.
A systematic review of several databases was conducted. Random-effects meta-analysis, meta-regression, and subgroup and sensitivity analyses were performed.
A total of 27 studies, pooling 7928 transgender patients who underwent any type of GAS, were included. The pooled prevalence of regret after GAS was 1% (95% CI <1%–2%). Overall, 33% underwent transmasculine procedures and 67% transfemenine procedures. The prevalence of regret among patients undergoing transmasculine and transfemenine surgeries was <1% (IC <1%–<1%) and 1% (CI <1%–2%), respectively. A total of 77 patients regretted having had GAS. Twenty-eight had minor and 34 had major regret based on Pfäfflin’s regret classification. The majority had clear regret based on Kuiper and Cohen-Kettenis classification.
Conclusions:
Based on this review, there is an extremely low prevalence of regret in transgender patients after GAS. We believe this study corroborates the improvements made in regard to selection criteria for GAS. However, there is high subjectivity in the assessment of regret and lack of standardized questionnaires, which highlight the importance of developing validated questionnaires in this population.
Introduction
Discordance or misalignment between gender identity and sex assigned at birth can translate into disproportionate discomfort, configuring the definition of gender dysphoria. 1 – 3 This population has increased risk of psychiatric conditions, including depression, substance abuse disorders, self-injury, and suicide, compared with cis-gender individuals. 4 , 5 Approximately 0.6% of adults in the United States identify themselves as transgenders. 6 Despite advocacy to promote and increase awareness of the human rights of transgender and gender non-binary (TGNB) individuals, discrimination continue to afflict the daily life of these individuals. 4 , 7
Gender-affirmation care plays an important role in tackling gender dysphoria. 5 , 8 – 10 Gender-affirmation surgeries (GAS) aim to align the patients’ appearance with their gender identity and help achieve personal comfort with one-self, which will help decrease psychological distress. 5 , 10 These interventions should be addressed by a multidisciplinary team, including psychiatrists, psychologists, endocrinologists, physical therapists, and surgeons. 1 , 9 The number of GAS has consistently increased during the last years. In the United States, from 2017 to 2018, the number of GAS increased to 15.3%. 8 , 11 , 12
Significant improvement in the quality of life, body image/satisfaction, and overall psychiatric functioning in patients who underwent GAS has been well documented. 5 , 13 – 19 However, despite this, there is a minor population that experiences regret, occasionally leading to de-transition surgeries. 20 Both regret and de-transition may add an important burden of physical, social, and mental distress, which raises concerns about the appropriateness and effectiveness of these procedures in selected patients. Special attention should be paid in identifying and recognizing the prevalence and factors associated with regret. In the present study, we hypothesized that the prevalence of regret is less than the last estimation by Pfafflin in 1993, due to improvements in standard of care, patient selection, surgical techniques, and gender confirmation care. Therefore, the aim of this study was to evaluate the prevalence of regret and assess associated factors in TGNB patients 13-years-old or older who underwent GAS. 20
Search Methodology
Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines, a comprehensive research of several databases from each database’s inception to May 11, 2020, for studies in both English and Spanish languages, was conducted. 21 The databases included Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, and Daily, Ovid EMBASE, Ovid Cochrane Central Register of Controlled Trials, Ovid Cochrane Database of Systematic Reviews, and Scopus. The search strategy was designed and conducted by an experienced librarian, with input from the study’s principal investigator. Controlled vocabulary supplemented with keywords was used to search for studies of de-transition and regret in adult patients who underwent gender confirmation surgery. The actual strategy listing all search terms used and how they are combined is available in Supplemental Digital Content 1. ( See Supplemental Digital Content 1, which displays the search strategy. http://links.lww.com/PRSGO/B598 .)
Study Selection
Search results were exported from the database into XML format and then uploaded to Covidence. 22 The study selection was performed in a 2-stage screening process. The first step was conducted by 2 screeners (V.P.B. and S.S.B.), who reviewed titles and abstracts and selected those of relevance to the research question. Then, the same 2 screeners reviewed full text of the remaining articles and selected those eligible according to the inclusion and exclusion criteria (Fig. (Fig.1). 1 ). If disagreements were encountered, a third reviewer (O.J.M.) moderated a discussion, and a joint decision between the 3 reviewers was made for a final determination. Inclusion criteria were all the articles that included patients aged 13 years or more who underwent GAS and report regret or de-transition rates, and observational or interventional studies in English or Spanish language. Exclusion criteria were letter to the editors, case series with <10 patients, case reports correspondences, and animal studies.

PRISMA flow diagram for systematic reviews.
Data Extraction/Synthesis
After selecting the articles, we assessed study characteristics. We identified year of publication, country in which the study was conducted, population size, and number of transmasculine and transfemenine patients with their respective mean age (expressed with SD, range, or interquartile range if included in the study). In addition, we extracted information of the method of data collection (interviews versus questionnaires), number of regrets following GAS, as well as the type of surgery, time of follow-up, and de-transition procedures. We classified the type of regret based on the patient’s reasons for regret if they were mentioned in the studies. We used the Pfäfflin and Kuiper and Cohen-Kettenis classifications of regret (Table (Table1 1 ). 20 , 23
Pfäfflin and Kuiper and Cohen-Kettenis Categories of Regret
Quality Assessment
To assess the risk of bias within each study, the National Institute of Health (NIH) quality assessment tool was used. 24 This tool ranks each article as “good,” “fair,” or “poor,” and with this, we categorized each article into “low risk,” “moderate risk,” or “high risk” of bias, respectively.
Our primary outcome of interest was the prevalence of regret of transgender patients who underwent any type of GAS. Secondary outcomes of interest were discriminating the prevalence of regrets by type gender transition (transfemenine and transmasculine), and type of surgery.
Data Analysis and Synthesis
The binominal data were analyzed, and the pooled prevalence of regret was estimated using proportion meta-analysis with Stata Software/IC (version 16.1). 25 Given the heterogeneity between studies, we conducted a logistic-normal-random-effect model. The study-specific proportions with 95% exact CIs and overall pooled estimates with 95% Wald CIs with Freeman-Turkey double arcsine transformation were used. The effect size and percentage of weight were presented for each individual study. 25 , 26
To evaluate heterogeneity, I 2 statistics was used. If P < 0.05 or I 2 > 50%, significant heterogeneity was considered. A univariate meta-regression analysis was performed to assess the significance in country of origin, tools of measurement, and quality of the studies.
To assess publication bias, we used funnel plot graphic and the Egger test. If this test showed us no statistical significance ( P > 0.05), we assumed that the publication bias had a low impact on the results of our metanalysis. To assess the impact of the publication bias on our missing studies, we used the trim-and-fill method.
A sensitivity analysis was conducted to assess the influence of certain characteristics in the magnitude and precision of the overall prevalence of regret. The following characteristics were excluded: <10 participants included, and the presence of a high risk of bias.
A total of 74 articles were identified in the search, and 2 additional records were identified through other sources. After the first-step screening process, 39 articles were relevant based on the information provided in their titles and abstracts. After the second-step process, a total of 27 articles were included in the systematic review and metanalysis (Fig. (Fig.1 1 ).
Based on the NIH quality assessment tool, the majority of article ranged between “poor” and “fair” categories. 24 ( See Supplemental Digital Content 2, which displays the score of each reviewed study. http://links.lww.com/PRSGO/B599 .)
Study Characteristics
In total, the included studies pooled 7928 cases of transgender individuals who underwent any type of GAS. A total of 2578 (33%) underwent transmasculine procedures, 5136 (67%) underwent transfemenine surgeries, and 1 non-binary patient underwent surgery. In Table Table2 2 characteristics of studies are listed. Without discriminating type of surgical technique, from all transfemenine surgeries included, 772 (39.3%) were vaginoplasty, 260 (13.3%) were clitoroplasty, 107 (5.5%) were breast augmentation, 72 (3.7%) were labioplasty and vulvoplasty, and a small minority were facial feminization surgery, vocal cord surgery, thyroid cartilage reduction, and oophorectomy surgery. The rest did not specify type of surgery. In regard to transmasculine surgeries, 297 (12.4%) were mastectomies, 61 (2.6%) were phalloplasties, and 51 (2.1%) hysterectomies (Table (Table3 3 and and4). 4 ). Overall, follow-up time from surgery to the time of regret assessment ranged from 0.8 to 9 years (Table (Table2 2 ).
*Reflects the mean of both transmasculine and transfemenine.
†Includes both scheduled and completed surgery.
‡Includes both surgery and no surgery patients.
H, High; He, Heterosexual; Ho, Homosexual; I, Interview; IQR, Interquartile Range; L, Low; M, Moderate; Me, Median; NA, Not applicable; NS: Not specified, Q: Questionnaire; RAP: Radial Arterial Forearm-Flap Phalloplasty without or with cutaneous nerve to clitoral nerve anastomosis; SP: Suprapubic Pedicle-Flap Phalloplasty.
Studies Differentiating Type of Surgery among Transfemenine Patients
Studies Differentiating the Type of Surgery among Transmasculine Patients
Regrets and De-transition
Almost all studies conducted non-validated questionnaires to assess regret due to the lack of standardized questionnaires available in this topic. 15 , 19 – 33 Most of the questions evaluating regret used options such as, “ yes,” “sometimes,” “no” or “ all the time,” “sometimes,” “never,” or “most certainly, ” “very likely,” “maybe,” “rather not,” or “definitely not.” 14 , 18 , 19 , 23 , 27 – 38 Other studies used semi-structured interviews. 34 , 37 , 39 – 43 However, in both circumstances, some studies provided further specific information on reasons for regret. 14 , 20 , 23 , 29 , 32 , 36 , 41 , 44 – 46 Of the 7928 patients, 77 expressed regret (12 transmen, 57 transwomen, 8 not specified), understood by those who had “sometimes” or “always” felt it.
Reasons for Regret
The most prevalent reason for regret was the difficulty/dissatisfaction/acceptance in life with the new gender role. 23 , 29 , 32 , 36 , 44 Other less prevalent reasons were “failure” of surgery to achieve their surgical goals in an aesthetic level and psychological level. 29 , 32 , 36 , 47 Based on the reasons presented, we classified the types of regrets according to Pfäfflin’s types of regret and Kuiper and Cohen-Kettenis classification. According to Pfäfflin’s types, 28 patients had minor regret, and 34 patients had major regret. 14 , 20 , 23 , 29 , 32 , 36 , 41 , 44 , 45 Based on the Kuiper and Cohen-Kettenis regret classification, 35 patients had clear regret, 26 uncertain regret, 1 regret, and none presented with regret assumed by others. 23 In Table Table5 5 and and6, 6 , the reasons and classifications are shown.
Type of Regret
*8 mastectomies, 2 vaginectomies, 2 phalloplasties, 2 testicular implants removal, and 1 breast augmentation.
N, no; NS, not specified; Y, Yes.
Causes of Regret
NS, not specified.
Prevalence of Regret
The pooled prevalence of regret among the TGNB population after GAS was 1% (95% Confidence interval [CI] <1%–2%; I 2 = 75.1%) (Fig. (Fig.2). 2 ). The prevalence for transmasculine surgeries was <1% (CI <1%–<1%, I 2 = 28.8%), and for transfemenine surgeries, it was 1% (CI <1%–2%, I 2 = 75.5%) (Fig. (Fig.3). 3 ). The prevalence of regret after vaginoplasty was of 2% (CI <1%–4%, I 2 = 41.5%) and that after mastectomy was <1% (CI <1–<1%, I 2 = 21.8%) (Fig. (Fig.4 4 ).

Pooled prevalence of regret among TGNB individuals after gender confirmation surgery. Heterogeneity χ 2 = 104.31 (d.f. = 26), P = 0.00, I 2 [variation in effect size (ES) attributable to heterogeneity] = 75.08%, Estimate of between-study variance Ʈ 2 = 0.02, Test of ES = 0, z = 4.22, P = 0.00.

Subgroup analysis of the prevalence of regret among TGNB individuals after gender confirmation surgery based on gender. ES, effect size.

Subgroup analysis of the prevalence of regret among TGNB individuals after gender confirmation surgery based on the type of surgery. ES, effect size.
Meta-regression and Publication Bias
No covariates analyzed affected the pooled endpoint in this metanalysis. The Funnel Plot shows asymmetry between studies (Fig. (Fig.5). 5 ). The Egger test resulted in a P value of 0.0271, which suggests statistical significance for publication bias. The Trim & Fill method imputed 14 approximated studies, with limited impact of the adjusted results. The change in effect size was from 0.010 to 0.005 with no statistical significance (Fig. (Fig.6 6 ).

Funnel plot.

Funnel plot of the Trim & Fill method.
Sensitivity Analysis
When excluding studies with sample sizes less than 10 and high-risk biased studies, the pooled prevalence was similar 1% (CI <1%–3%) compared with the pooled prevalence when those studies were included 1% (CI <1%–2%).
The prevalence of regret in the TGNB population after GAS was of 1% (CI <1%–2%). The prevalence of regret for transfemenine surgeries was 1% (CI <1%–2%), and the prevalence for transmasculine surgeries was <1% (CI <1%–<1%). Traditionally, the landmark reference of regret prevalence after GAS has been based on the study by Pfäfflin in 1993, who reported a regret rate of 1%–1.5%. In this study, the author estimated the regret prevalence by analyzing two sources: studies from the previous 30 years in the medical literature and the author’s own clinical practice. 20 In the former, the author compiled a total of approximately 1000–1600 transfemenine, and 400–550 transmasculine. In the latter, the author included a total of 196 transfemenine, and 99 transmasculine patients. 20 In 1998, Kuiper et al followed 1100 transgender subjects that underwent GAS using social media and snowball sampling. 23 Ten experienced regret (9 transmasculine and 1 transfemenine). The overall prevalence of regret after GAS in this study was of 0.9%, and 3% for transmasculine and <0.12% for transfemenine. 23 Because these studies were conducted several years ago and were limited to specific countries, these estimations may not be generalizable to the entire TGNB population. However, a clear trend towards low prevalences of regret can be appreciated.
The causes and types of regrets reported in the studies are specified and shown in Table Table5 5 and and6. 6 . Overall, the most common reason for regret was psychosocial circumstances, particularly due to difficulties generated by return to society with the new gender in both social and family enviroments. 23 , 29 , 32 , 33 , 36 , 44 In fact, some patients opted to reverse their gender role to achieve social acceptance, receive better salaries, and preserve relatives and friends relationships. These findings are in line with other studies. Laden et al performed a logistic regression analysis to assess potential risk factors for regret in this population. 46 They found that the two most important risk factors predicting regret were “poor support from the family” and “belonging to the non-core group of transsexuals.” 46 In addition, a study in Italy hypothesized that the high percentage of regret was attributed to social experience when they return after the surgery. 33
Another factor associated with regret (although less prevalent) was poor surgical outcomes. 20 , 23 , 36 Loss of clitoral sensation and postoperative chronic abdominal pain were the most common reported factors associated with surgical outcomes. 14 , 36 In addition, aesthetic outcomes played an important role in regret. Two studies mentioned concerns with aesthetic outcomes. 14 , 47 Only one of them quoted a patient inconformity: “body doesn’t meet the feminine ideal.” 14 Interestingly, Lawrence et al demonstrated in their study that physical results of surgery are by far the most influential in determining satisfaction or regret after GAS than any preoperative factor. 36 Concordantly, previous studies have shown absence of regret if sensation in clitoris and vaginal is achieved and if satisfaction with vaginal width is present. 36
Other factors associated to regret were identified. Blanchard et al in 1989 noted a strong positive correlation between heterosexual preference and postoperative regret. 32 All patients in this study who experienced regret were heterosexual transmen. 32 On the contrary, Lawrence et al in 2003 did not find such correlation and attributed their findings to the increase in social tolerance in North American and Western European societies. 36 Bodlund et al found that clinically evident personality disorder was a negative prognostic factor for regret in patients undergoing GAS. 48 On the other hand, Blanchard et al did not find a correlation among patient’s education, age at surgery, and gender assigned at birth. 32
In the present review, nearly half of the patients experienced major regret (based on Pfäfflin classification), meaning that they underwent or desire de-transition surgery, that will never pass through the same process again, and/or experience increase of gender dysphoria from the new gender. One study found that 10 of 14 patients with regret underwent de-transition surgeries (8 mastectomies, 2 vaginectomies, 2 phalloplasties, 2 testicular implants removal, and 1 breast augmentation) for reasons of social regret, true regret or feeling non-binary. 23 On the other hand, based on the Kuiper and Cohen Kettenis’ classification, half of the patients in this review had clear regret and uncertain regret . This means that they freely expressed their regret toward the procedure, but some had role reversal to the former gender and others did not. Interestingly, Pfäfflin concluded that from a clinical standpoint, trangender patients suffered from many forms of minor regrets after GAS, all of which have a temporary course. 20 This is an important consideration meaning that the actual true regret rate will always remain uncertain, as temporarity and types of regret can bring a huge challenge for assessment.
Regret after GAS may result from the ongoing discrimination that afflicts the TGNB population, affecting their freely expression of gender identity and, consequently feeling regretful from having had surgery. 15 Poor social and group support, late-onset gender transition, poor sexual functioning, and mental health problems are factors associated with regret. 15 Hence, assessing all these potential factors preoperatively and controlling them if possible could reduce regret rates even more and increase postoperative patient satisfaction.
Regarding transfemenine surgery, vaginoplasty was the most prevalent. 14 , 19 , 23 , 30 – 33 , 35 , 36 , 44 , 45 Interesintgly, regret rates were higher in vaginoplasties. 14 , 36 , 44 In this study, we estimated that the overall prevalence of regret after vaginoplasty was 2% (from 11 studies reviewed). This result is slightly higher than a metanalysis of 9 studies from 2017 that reported a prevalence of 1%. 13 Moreover, vaginoplasty has shown to increase the quality of life in these patients. 13 Mastectomy was the most prevalent transmasculine surgery. Also, it showed a very low prevalence of regret after mastectomy (<1%). Olson-Kennedy et al demonstrated that chest surgery decreases chest dysphoria in both minors and young adults, which might be the major reason behind our findings. 38
In the current study, we identified a total of 7928 cases from 14 different countries. To the best of our knowledge, this is the largest attempt to compile the information on regret rates in this population. However, limitations such as significant heterogeneity among studies and among instruments used to assess regret rates, and moderate-to-high risk of bias in some studies represent a big barrier for generalization of the results of this study. The lack of validated questionnaires to evaluate regret in this population is a significant limiting factor. In addition, bias can occur because patients might restrain from expressing regrets due to fear of being judged by the interviewer. Moreover, the temporarity of the feeling of regret in some patients and the variable definition of regret may underestimate the real prevalence of “true” regret.
Based on this meta-analysis, the prevalence of regret is 1%. We believe this reflects and corroborates the increased in accuracy of patient selection criteria for GAS. Efforts should be directed toward the individualization of the patient based on their goals and identification of risk factors for regrets. Surgeons should continue to rigorously follow the current Standard of Care guidelines of the World Professional Association for Transgender Health (WATH). 49
CONCLUSIONS
Our study has shown a very low percentage of regret in TGNB population after GAS. We consider that this is a reflection on the improvements in the selection criteria for surgery. However, further studies should be conducted to assess types of regret as well as association with different types of surgical procedure.
Acknowledgments
All the authors have completed the ICMJE uniform disclosure form. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supplementary Material
Published online 19 March 2021
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com .
Gender reassignment surgery - a narrative overview of anaesthetic considerations and implications
Affiliations.
- 1 Department of Anaesthesia, All India Institute of Medical Sciences, Rishikesh, India.
- 2 Department of Burns and Plastic Surgery, AIIMS Rishikesh, India.
- 3 Department of Anaesthesia, AIIMS Bhopal, India.
- 4 Department of Burns and Plastic Surgery, VMMC Safdarjung Hospital, India.
- PMID: 34714015
- PMCID: PMC10165989
- DOI: 10.5114/ait.2021.109446
The twenty-first century, with its transforming ideology and rising acceptance, is witnessing an increased number of transgender people applying for gender reassignment surgery (GRS). The procedure of GRS is a lengthy and complex one involving the active collaboration of multiple disciplines including psychology, psychiatry, family medicine, plastic surgery, endocrinology, otolaryngology, urology, gynaecology, maxillofacial surgery, and anaesthesiology. The considerable paucity of literature regarding the management of patients presenting for GRS places health care providers at a disadvantage. It is imperative to cautiously regard the specific medical, emotional, social, and economic concerns regarding these patients. Health care providers need to be trained well to deal empathetically with such patients. The present literature about GRS deals mainly with the surgeon's perspective, while the anaesthetist's approach remains hazy. This is because GRS imposes the need for anaesthesiologists to search for better and more efficient modes of anaesthesia so as to improve prognosis and minimize the associated morbidity. Anaesthetists should understand the associated psychological aspects and effects of hormone therapy while performing an extensive and informative pre-operative evaluation to formulate an effective strategy. Providing the optimal modes for anaesthesia and keeping a cautious watch for complications along with timely intervention in the advent of the same comprise the approach for high-quality anaesthetic care. This review aims to provide a detailed overview of significant considerations and competent peri-operative outcomes in patients presenting for GRS.
Keywords: anaesthesia; concerns; peri-operative care.; gender reassignment surgery.
Publication types
- Anesthesia*
- Anesthesiology*
- Anesthetics*
- Sex Reassignment Surgery*
- Transgender Persons*
- Anesthetics

much more than surgery
The quality and safety in our care and services; Your peace of mind. Excellence is a core value that drives the decisions and actions of every member of our staff.
EXPERIENCED SURGEONS
Our surgeons have performed more than 10 000 gender-affirming surgeries over the past 12 years.
PERSONALIZED FOLLOW-UP
Care is provided in the spirit of patient support and in consideration of the uniqueness of your own experience. From the preoperative period to your postoperative follow-ups, we will be right beside you.
QUALITY FACILITIES
Surgeries are performed at the Centre Métropolitain de Chirurgie, our private hospital centre accredited with exemplary standing. For some surgeries, a stay at the Asclépiade convalescent home is necessary.
A WORRY-FREE STAY
No matter where you come from, we will help you plan your stay.

Dr Pierre Brassard, FRCSC

Dre Maud Bélanger, FRCSC

Dre Valérie J. Brousseau, FRCSC

Dr Alex Laungani, FRCSC

Dr Chen Lee, FRCSC

Dr Dru Perkins
Dr Mar Aristeo Poncio
Male to Female / MTF / MTX
Vaginoplasty, Vaginoplasty without vaginal cavity, Breast Augmentation, Adam's Apple Reduction, Voice Surgery, Facial and Body Feminization, Corrective surgeries: Secondary Vaginoplasty, Genital Scar Revision, Vulvar Reconstruction, Labioplasty, Correction of the Clitoris
Female to Male / FTM / FTX
Masculinization of the Torso or Mastectomy, Metoidioplasty, Phalloplasty, Insertion of Testicular Implant(s), Insertion of Penile Implants , Masculinization of the Face and Body surgeries, Corrective surgeries: Torso Scar Removal, Nipple Correction, Secondary Phalloplasty, Phallus Revision
- Newsletters
- Instapundit
- News & Politics
Appeals Court Finds a Constitutional Right to Gender Reassignment Surgery

The 14th Amendment to the Constitution is truly a magical amendment. It was used to justify attempts to kick Donald Trump off the 2024 ballot. Through the decades, judges who want to play at social engineering have used it frequently to justify questionable law.
It's even been invoked to bypass Congress to raise the debt limit.
Now, the Fourth Circuit Court of Appeals has decided that the amendment's "equal protection" clause means that state Medicaid programs have to cover gender reassignment surgeries.
The appeals court ruled that West Virginia's Medicaid rules on mastectomies are unconstitutional because they violate the "equal protection standard" by not covering mastectomies for gender dysphoria.
Yes, really.
The ruling also includes a North Carolina Medicaid case that the state government won't cover "sex changes." The Fourth Circuit nullified the state ban on gender change surgeries, citing the 14th Amendment’s guarantee of “equal protection of the laws.”
This was a court looking for an excuse to make law.
Judge Roger Gregory who wrote the majority opinion in Kadel v. Folwell (8-6) asked, “Is removing a patient’s breasts to treat cancer the same procedure as removing a patient’s breasts to treat gender dysphoria?” He continued, “There is no case law to ground this discussion nor obvious first principles.”
Wall Street Journal:
He is undeterred, and he concludes that gender dysphoria and transgender status are intertwined, so that such insurance exclusions are nothing more than a proxy for discriminating against gender identity. Then he goes further, finding that West Virginia’s and North Carolina’s policies also unconstitutionally discriminate based on sex. How so? Imagine, Judge Gregory says, an unidentified patient seeking a vaginoplasty. Is this a biological female with a rare birth defect? Is it a transgender patient? “By virtue of the fact that they are seeking a vaginoplasty, we know that they were born without a vagina,” he writes. “But we do not know what sex they were assigned at birth. Without that information, we cannot say whether the Plan or Program will cover the surgery.” Ergo, sex discrimination.
Gregory gets even nuttier.
The differences in coverage "is rooted in a gender stereotype: the assumption that people who have been assigned female at birth are supposed to have breasts, and that people assigned male at birth are not."
It's not a "gender stereotype." It's a biological fact.
"No doubt, the majority of those assigned female at birth have breasts, and the majority of those assigned male at birth do not. But we cannot mistake what is for what must be.”
Not just a "majority." It's a universal biological fact with a tiny number of exceptions.
Treating different things differently doesn’t violate the 14th Amendment’s Equal Protection Clause, and jurists aren’t supposed to ignore the obvious. Writing in dissent at the Fourth Circuit, Judge Julius Richardson struggles to contain his exasperation. “The states,” he says, “have chosen to cover alterations of a person’s breasts or genitalia only if the person experiences physical injury, disease, or (in West Virginia) congenital absence of genitalia.” That determination does not turn on the patient’s sex or gender. “Christopher Fain—one of the plaintiffs below—received coverage for a hysterectomy based on a diagnosis unrelated to Fain’s transgender status,” the dissent says. Likewise, males with gynecomastia qualify for surgery coverage in West Virginia only “if they have physical symptoms, like breast pain,” meaning that isn’t a procedure done merely “to affirm a patient’s biological sex.”
The ruling that opened this can of worms was Bostock v. Clayton County, a case that "held that Title VII of the Civil Rights Act of 1964 protects employees against discrimination because of sexuality or gender identity." Now, as a dissenting judge in Kadel v. Folwell, Judge J. Harvie Wilkinson III is saying that this ruling could be a Roe v Wade ruling for the transgender community.
“This is imperial judging at its least defensible,” he says, “What plaintiffs propose is nothing less than to use the Constitution to establish a nationwide mandate that States pay for emerging gender dysphoria treatments.”
He's not wrong. But getting the ruling past this Supreme Court would be a stretch.

Rick Moran has been writing for PJ Media for 18 years. His work has appeared in dozens of media outlets including the Washington Times and ABC News. He was an editor at American Thinker for 14 years. His own blog is Right Wing Nut House . For media inquiries, please contact [email protected] .
Recommended

Trending on PJ Media Videos
- The Trial Still in Search of a Crime
- Snopes Admits Ashley Biden’s Diary Is Genuine, So Let’s Talk About What It Says
- The Sailors From the Baltimore Bridge Collapse Ship Are Still on Board and That Isn't Even the Weird Part
- Search Close Search submit
Join our Journal Club this Saturday, May 18th
Female to Male Gender Reassignment Surgery (FTM GRS)
Female-to-male gender reassignment surgery (FTM GRS) is a complex and irreversible genital surgery for female transsexual who is diagnosed with gender identity disorder and has a strong desire to live as male. The procedure is to remove all female genital organs including the uterus, ovaries, and vagina with the construction of male genitalia composed of the penis and scrotum.
The patient who is fit for this surgery must strictly follow the standard of care set by the World Professional Association of Transgender Healthcare (WPATH) or equivalent criteria; Express desire or live in another gender role (Female gender) long enough, under hormonal replacement therapy, evaluated and approved by a psychiatrist or other qualified professional gender therapist.
Apart from genital surgery, the patient would seek other procedures to allow them to live as males smoothly such as breast amputation, facial surgery, body surgery, etc.
Interested in having this procedure?
Useful Information
Ensure you consider all aspects of a procedure. You can speak to your surgeon about these areas of the surgery in more detail during a consultation.
The surgery is very complicated and only a handful of surgeons are able to perform this procedure. It is a multi-staged procedure, the first stage is the removal of the uterus, ovary, and vagina. The duration of the procedure is 2-3 hours. The second and later stages are penis and scrotum reconstruction which is at least 6 months later. There are several techniques for penile reconstruction depending on the type of tissue such as skin/fat of the forearm, skin/fat of the thigh, or adjacent tissue around the clitoris. This second stage of surgical time is between 3-5 hours. A penile prosthesis can be incorporated simultaneously or at a later stage. The scrotal prosthesis is also implanted later.
The procedure is done under general anesthesia and might be combined with spinal anesthesia for faster recovery by reducing the usage of anesthetic gas.
Inpatient/Outpatient
The patient will be hospitalized as an in-patient for between 5-7 days for each stage depending on the technique and surgeon. The patient will have a urinary catheter at all times in the hospital.
Additional Information
What are the risks.
The most frequent complication of FTM GRS is bleeding, wound infection, skin flap or graft necrosis, urinary stenosis and fistula, unsightly scar, etc. The revision procedure is scar revision, hair transplant, or tattooing to camouflage unsightly scars.
What is the recovery process?
During hospitalization, the patient must be restricted in bed continuously or intermittently for several days between 3-5 days. After release from the hospital, the patients return to their normal lives but not having to do physical exercise during the first 2 months after surgery. The patient will have a urinary catheter continuously for several weeks to avoid a urinary fistula. If the patient has a penile prosthesis, it would need at least 6 months before sexual intimacy.
What are the results?
With good surgical technique, the result is very satisfying with an improved quality of life. The patient is able to live in a male role completely and happily either on their own or with their female or male partners.
- Patient Information
- Global Statistics
- Media Centre
- World Congress
- Global Sponsors
- Privacy Policy
19 Mantua Road, Mount Royal, NJ 08061 United States
Registration number: 0330131
US Office: +1-603-643-2325
UK Office: +44 20 7038 7812
© 2022 International Society of Aesthetic Plastic Surgery. All Rights Reserved.
- Create an account
Log into My ISAPS
Forgot your password? Reset it here
Join the ISAPS Community
All members will continue to receive information relevant to their membership and ISAPS events.
I confirm by clicking below I would like to receive information about:
Welcome to the ISAPS community
By creating an account, you can:.
- Register for events
- Update your personal details
- Gain access to ISAPS publications and video library
- Become a member (explore our memberships here)
ISAPS Members can also:
- Access your member benefits
- Secure discounted member rates for events
- Read the Aesthetic Plastic Surgery Journal
- Gain full access to the video library
- View the Members Directory
- Update your 'Find a Surgeon' profile details
- Renew/Upgrade your Membership
The first step to becoming a part of the community is creating an account, so join us!
Politics Analysis

How Faith Guided This Trump Aide’s Time in Government
Economy Analysis

What Stands Between US Citizens and the American Dream Today
Society Analysis

THE WPATH TAPES: Behind-Scenes Recordings Reveal What Top Gender Doctors Really Think About Sex-Change Procedures
Society Commentary

How I Rediscovered My Love of Acting on the Set of ‘Reagan’
Society Commentary

SOCIETAL ROT, Part 3: How Blue Cities’ Flouting of Federal Immigration Laws Has Proved Fatal
Security Analysis

NPR Reporter Assigned to Cover Posters Urging Illegals to Vote for Biden Won’t Answer Whether Aliens Voting Bothers Her
Politics News

DC Holds Training Sessions for Noncitizens to Vote
Law Commentary

Rural America Won’t Be Spared During Biden’s Immigration Crisis
Security Analysis

China’s Land Grab
Security News

US Is Failing to Counter Threat of Chinese Land Ownership, Report Finds
International Analysis

She Spoke Out in Defense of China’s Uyghurs, Then China Abducted Her Sister
International Commentary

Europe Must Stop Dragging Its Feet and Oppose Chinese Forced Labor
Economy News

Struggling to Keep Job, FDIC Chair Known for Berating Staff Humbled at Capitol
International News

Russian Troops Make Major Gains After Congress, Biden Greenlight Aid Package to Ukraine

A Bill to Ensure Fair Representation for American Citizens
Law News

Veteran Prosecutor Testifies Michael Cohen Admitted He Had ‘Nothing Truthful’ Implicating Trump
Politics News

House Oversight Committee Probing Biden Voter Mobilization Order
Society Analysis

EXCLUSIVE: Federal Farm Credit Agency Plows Ahead With DEI, ‘Queer’ Farming

EXCLUSIVE: DOJ’s Kristen Clarke Testified She Was Never Arrested. Court Records and Text Messages Indicate She Was.

EXCLUSIVE: She Survived a Death Camp. Facing Biden DOJ Charges, She Is Prepared to Die in Prison
Politics News

EXCLUSIVE: Congressman Calls on House to Pass Bill Banning Earmarks

Censorship: A Global Pandemic
International Commentary

Common Sense vs. Antisemitism

Charge of ‘Genocide’ Is Blood Libel of Our Time
Education Commentary

BASED: Frat Boys Cause a Sensation by Defending Old Glory

This Is the Next Generation of Marxism

Stories of Young People Whose Bodies Were Sacrificed on Altar of ‘Gender Ideology Cult’
Megan Brock / @MegEBrock / Kate Anderson / @kliseanderson / May 15, 2024
Recordings from meetings of the World Professional Association for Transgender Health reveal doctors pushing risky sex-change procedures for children, contradicting the organization's own guidelines. (Photo illustration: Anastassiya Bezhekeneva/Getty Images)

Get your FREE digital copy of The Heritage Foundation’s Founders’ Almanac.
The World Professional Association for Transgender Health , or WPATH, is the leading authority in the field of gender medicine. Its guidance is routinely used by top medical associations in the U.S. and abroad, while its standards of care inform insurance companies’ approach to coverage policies.
But behind closed doors, top WPATH doctors discussed, and at times seemed to challenge, the organization’s own published guidelines for sex-change procedures and acknowledged pushing experimental medical interventions that can have devastating and irreversible complications, according to exclusive footage obtained by the Daily Caller News Foundation.

WPATH published highly influential clinical guidance called “Standards of Care for the Health of Transgender and Gender Diverse People, Version 8,” or SOC 8, which recommends the use of invasive medical interventions such as puberty blockers, cross-sex hormones and sex change surgeries, calling them “safe and effective.”
The Daily Caller News Foundation filed a series of public records requests to the World Professional Association for Transgender Health’s SOC 8 co-authors who are employed at taxpayer-funded institutions, making their emails subject to open records laws.
Buried in more than 100 pages of responsive records from the University of Nevada was a series of emails sent in 2022 among prominent WPATH members and leaders , including WPATH Global Education Institute Co-Chair Gail Knudson.
In one email, Knudson sent a colleague the link to a folder containing nearly 30 hours of recordings from WPATH’s Global Education Institute summit in September 2022 in Montreal, Canada, which included sessions on mental health, puberty blockers, cross-sex hormones, and sex-change surgery.
These sessions provided WPATH members with in-depth education on the clinical application of topics addressed in the SOC 8 treatment guidelines. However, the footage reveals WPATH-affiliated doctors advocating that children undergo risky sex-change procedures and even pushing for these treatments for patients struggling with severe mental health issues.
Several sessions were dedicated exclusively to treating children and included recommendations for minors to receive puberty blockers, cross-sex hormones, and surgeries.
For instance, WPATH guidance recommends addressing a patient’s mental health issues before giving him or her sex-change medical interventions. However, in one recorded session, a WPATH faculty member and gender doctor claimed that mental health issues don’t necessarily affect a patient’s ability to receive cross-sex hormones.
In another video, a doctor told attendees that children should be informed that cross-sex hormones will likely make them infertile. but admitted that he would prescribe them anyway if a child says he or she wants the treatment, regardless of future consequences.
A surgeon euphemistically referred to a phalloplasty procedure, a surgical series that includes obliterating the vaginal cavity and creating a fake penis with harvested tissue, as an “adventure” for young people. He did this despite later admitting that those same procedures “definitely” will have “complications,” such as permanent issues with bladder function and tissue death.
One physician called the entire field of cross-sex hormones “off-label,” referring to the concept of drugs being used for alternative purposes than what they were approved for. The doctor went on to say that female patients might actually appreciate drug side effects that cause them to lose hair, because they’d look “more like men.”
The U.S. Food and Drug Administration says that when it approves a drug, health care providers generally may prescribe that drug for an unapproved use, or off-label, when “they judge that it is medically appropriate for their patient.”
In several other videos, doctors argued in favor of transitioning patients who experience psychotic episodes. One admitted that some of his patients with schizophrenia have to be careful how much cross-sex hormones they take or they can’t “keep the voices down.”
The Daily Caller News Foundation consulted medical professionals from respected organizations, such as Do No Harm, who all argued that the comments from WPATH-affiliated doctors show that the transgender medical industry doesn’t have patients’ best interests at heart.
While the average person, nationally and internationally, likely never has heard of the World Professional Association for Transgender Health, the modern medical industry is deeply tied to the organization and relies on it to dictate the standards of care for transgender medicine.
WPATH’s guidelines are cited as criteria for obtaining insurance coverage by both private insurance companies and tax-funded insurance plans , positioning them as a lynchpin of the sex reassignment industry.
Additionally, WPATH’s guidelines help inform policy statements from major medical and professional organizations, such as the American Academy of Pediatrics , the American Psychological Association , and the Endocrine Society .
The American Academy of Pediatrics is being sued by Isabelle Ayala, a former patient who was medically transitioned as a child and claims she was rushed through sex-change medical procedures.
There’s been an explosion in the number of young people, including children, being put on hormones and puberty blockers and getting sex-change surgeries, according to a study published in August 2023 by the JAMA Network.
This surge has been fueled, in part, by groups such as Planned Parenthood, which distributes cross-sex hormones to patients as young as 16. Planned Parenthood saw a roughly 125% jump in the number of transgender services it provided between 2020 and 2022.
Twenty-three states, however, have enacted legislation preventing doctors from performing sex-change surgeries on minors amid backlash from concerned parents and doctors who don’t subscribe to the WPATH-endorsed “gender-affirming care” model. Gender-affirming care is another euphemism used by medical professionals to describe the idea that doctors should affirm a patient’s wish to live as the opposite biological sex through social transitioning, hormone therapy, and even surgery.
The SOC 8 was released just days ahead of the 2022 symposium and contained several significant changes to how doctors and medical institutions implemented transgender medical treatment. For instance, WPATH removed minimum age requirements that established when a child can or should receive transgender medical services such as puberty blockers, cross-sex hormones, and sex-reassignment surgeries.
The World Professional Association for Transgender Health’s previous guidelines recommended that hormone therapy be given once a patient was over the age of 16, but the updated version removed this barrier and suggests hormone therapy begin at the first signs of sexual maturity.
The videos obtained by the Daily Caller News Foundation give the first glimpse at how doctors and mental health professionals discussed implementing the new guidelines. To highlight the most significant portions of the content obtained in the records requests, the foundation has decided to publish a series of articles collectively called “The WPATH Tapes.”
Following this release, the Daily Caller News Foundation intends to publish all of the videos in their entirety to provide the public with necessary information about WPATH’s approach to medical care and shine a light on an influential organization that has largely remained anonymous until now.
“The WPATH Tapes” Table of Contents
- Video Shows Prominent Doctors Acknowledging, And Even Challenging, The Experimental Nature Of Sex Change Drugs
- Top Psychiatrist Argues Schizophrenic Patients Can Consent To Sex Change Surgeries
- ‘Keep The Voices Down’: In Unearthed Video, Doctors Discuss Putting Mentally Ill Patients, Including Kids, On Hormones
- Gender Doctor Calls Genital Surgery An ‘Adventure’ For Young People While Describing Grisly Complications
- ‘No Idea About Their Fertility’: Gender Doctors Shed Light On Grim Reality Facing Kids Considering Sex Changes
- Leader Of Gender Medicine Org Says Binary Sex ‘Doesn’t Really Hold True,’ Cheers On ‘Deconstructed’ Biology
- Private Footage Reveals Leading Medical Org’s Efforts To ‘Normalize’ Gender Ideology
Originally published by the Daily Caller News Foundation
Join the millions of people who benefit from The Daily Signal’s fair, accurate, trustworthy reporting with direct access to:
- Intelligence from inside Washington
- Deep policy understanding from over 100 experts
Don’t have time to read the Washington Post or New York Times? Then get The Morning Bell, an early morning edition of the day’s most important political news, conservative commentary and original reporting from a team committed to following the truth no matter where it leads.
Ever feel like the only difference between the New York Times and Washington Post is the name? We do. Try the Morning Bell and get the day’s most important news and commentary from a team committed to the truth in formats that respect your time…and your intelligence.
N.H. Senate to vote on bills affecting LGBTQ youths
The controversial proposals on the calendar this week would affect education and health care.

Tom Huckman recalls personally thanking New Hampshire Governor Chris Sununu during a chance encounter on the slopes of the King Pine Ski Area several years ago.
Huckman, the father of a transgender daughter, said he expressed gratitude that Sununu had just signed a bill to prohibit discrimination on the basis of gender identity , and the governor replied that it was “simply the right thing to do.”
“Those words still resonate with me today,” Huckman said Tuesday, “because they encapsulate the essence of good leadership: doing what’s right, even when it’s not easy.”
Now he and other supporters of LGBTQ rights are anticipating a near-term scenario that could test Sununu’s commitment to protect transgender Granite Staters.
Advertisement
The New Hampshire Senate, where Republicans hold a 14-10 majority, is slated to vote this week on several controversial proposals that opponents said would harm trans and gender-diverse young people. And senators are expected to vote next week on House Bill 396 , which would add three carve-outs to the nondiscrimination provisions Sununu signed into law in 2018, by expressly allowing public and private entities statewide to separate bathrooms and locker rooms , sporting events and competitions, and detention facilities based on “biological sex” rather than gender identity.
Huckman, who described himself as a fiscally conservative voter who switched his registration from Republican to independent to better align with his values, called on Sununu to ready his veto pen.
“These bills threaten the safety, the privacy, the dignity of young transgender individuals like our daughter, Sarah,” said Huckman, who lives in Ossipee, N.H.. “They undermine the progress that we’ve made for more inclusivity and a more equitable society.”
Sununu has not spoken for or against these pending bills.
“They seem to keep changing in terms of what might be proposed and where they might go,” he told reporters earlier this month. “If they pass something, I’ll take a look at what comes to my desk,” he added, saying some proposals may make more sense than others.
The controversial proposals on the calendar this week would affect education and health care:
- House Bill 1312 would add sexual orientation, gender, gender identity, and gender expression to the existing law that requires schools to give parents at least two weeks’ notice before any instructional material or program about human sexuality, so parents can opt out.
- House Bill 619 would prohibit “genital gender reassignment surgery” for minors. House Bill 1660 would prohibit state Medicaid funds from covering such surgeries for minors.
- House Bill 1205 would require middle school and high school sports to be separated based on the sex listed on a student’s original birth certificate. Transgender girls would be barred from female sports. Proponents said the bill would protect girls from unfair competition.
Huckman said sports were great for the mental wellbeing of his daughter, Sarah Rose Huckman, who was featured in “Changing the Game,” a 2021 documentary about transgender high school athletes. Chris Erchull, an attorney with GLBTQ Legal Advocates & Defenders, said they remain optimistic Sununu will follow the lead of Republican governors like Mike DeWine of Ohio and Spencer Cox of Utah, who have vetoed anti-trans legislation in their states.
This story first appeared in Globe NH | Morning Report, our free newsletter focused on the news you need to know about New Hampshire, including great coverage from the Boston Globe and links to interesting articles from other places. If you’d like to receive it via e-mail Monday through Friday, you can sign up here.
Steven Porter can be reached at [email protected] . Follow him @reporterporter .

IMAGES
VIDEO
COMMENTS
Dr. Jacobs is an award-winning and board-certified plastic surgeon in San Francisco who joined The Gender Confirmation Center in July, 2022. Dr. Jacobs has more than 30 years of plastic surgery experience and provides outstanding surgical care for transmasculine, transfeminine and non-binary patients. Breast Augmentation, Top Surgery.
Male-to-female gender reassignment surgery (MTF GRS) is a complex and irreversible genital surgery for male transsexual who is diagnosed with gender identity disorder and has a strong desire to live as female. The procedure is to remove all male genital organs including the penis and testes with the construction of female genitalia composed of ...
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. To help provide guidance for those considering gender affirmation surgery, two experts from the Johns Hopkins Center for Transgender Health answer questions about what to expect before and after your surgery.
Gender Affirming Surgeries. For those patients who choose to have gender-affirming surgery, the Mount Sinai Center for Transgender Medicine and Surgery can help. These procedures may also be referred to as gender reassignment or confirmation procedures. We are among the world's leaders in this field, performing several hundred surgeries each ...
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
The Crane Center for Transgender Surgery has announced the launch of a gender-affirming hormone clinic at their transgender wellness center in Austin, Texas. The new clinic offers hormone replacement therapy for transgender and non-binary adults through an informed consent model. Both in-office and telemedicine appointments are available.
Dr. Jens Berli. Dr. Jens Berli is a board-certified plastic and reconstructive surgeon in Portland, Oregon who specializes in Gender Affirming Surgery. He joined the Transgender Health Program at Oregon Health & Science University (OHSU) in 2016. Dr. Berli is an Assistant Professor of Surgery in the Division of Plastic and Reconstructive ...
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected]. We will assist you in obtaining what you need to qualify for surgery. University of Michigan Comprehensive Gender Services Program brings ...
Previously, the term gender reassignment surgery (GRS) referred to genital reconstruction bottom surgeries like vaginoplasty, vulvoplasty, phalloplasty, or metoidioplasty. Individuals who look up this term on a search engine do so looking for information on gender-affirming procedures generally for transgender, non-binary and gender non ...
Sex and sexual health tips for transgender women after gender-affirming surgery. Sex after surgery. Achieving orgasm. Libido. Vaginal depth and lubrication. Aftercare. Contraceptions and STIs ...
Dr. Whitehead was trained in the art of gender reassignment surgery by Dr. Harold Reed, the now-retired urologist who practiced at The Reed Center for decades. Dr. ... Dr. Kamol Pansritum is recognized as one of the most experienced GRS Surgeons in the world, having completed over 5,000 gender reassignment surgeries, and more than 10,000 ...
Dr. Kathy Rumer is a Philadelphia-based surgeon who specializes in Male to Female Gender Reassignment Surgery (MTF GRS) specifically one-stage vaginoplasty. Dr. Kathy L. Rumer is trusted by her patients for ethical, high quality care. (855) R U A LOOKER Phone: (855) 782-5665. Schedule a Consultation » Rumer Gender Surgery.
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current ...
Gender reassignment surgery (GRS) has proven to be a revolutionary intervention for patients with gender dysphoria, hence playing a pivotal role in alleviating their psychological discomfort. GRS is a multidisciplinary endeavour requiring a collaborative effort of psychology, psychiatry, family medicine, plastic surgery, endocrinology ...
Here's how gender reassignment works: Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina. An incision ...
Introduction. Discordance or misalignment between gender identity and sex assigned at birth can translate into disproportionate discomfort, configuring the definition of gender dysphoria. 1-3 This population has increased risk of psychiatric conditions, including depression, substance abuse disorders, self-injury, and suicide, compared with cis-gender individuals. 4,5 Approximately 0.6% of ...
The twenty-first century, with its transforming ideology and rising acceptance, is witnessing an increased number of transgender people applying for gender reassignment surgery (GRS). The procedure of GRS is a lengthy and complex one involving the active collaboration of multiple disciplines includi …
Facial feminization surgery. Jeffrey Weinzweig, Stephen B. Baker, in Aesthetic Surgery of the Facial Skeleton, 2022. Introduction. Almost 40 years ago, Dr. Douglas Ousterhout pioneered the field of facial feminization surgery (FFS) when, in 1982, Dr. Darrell Pratt, a plastic surgeon who performed gender reassignment surgery (GRS), conveyed the request of a male-to-female transgender patient ...
Our surgeons are considered to be the most experienced in the field of gender reassignment surgery and perform more than 500 surgical procedures per year. ... GrS Montréal, much more than surgery. The quality and safety in our care and services; ... SURGEONS. Our surgeons have performed more than 10 000 gender-affirming surgeries over the past ...
The differences in coverage "is rooted in a gender stereotype: the assumption that people who have been assigned female at birth are supposed to have breasts, and that people assigned male at ...
Female-to-male gender reassignment surgery (FTM GRS) is a complex and irreversible genital surgery for female transsexual who is diagnosed with gender identity disorder and has a strong desire to live as male. The procedure is to remove all female genital organs including the uterus, ovaries, and vagina with the construction of male genitalia ...
Recordings from meetings of the World Professional Association for Transgender Health reveal doctors pushing risky sex-change procedures for children, contradicting the organization's own guidelines.
Section 3701-59-06 - Hospital quality standards for gender reassignment surgery and genital gender reassigment surgery for minors (A) As used in this rule: (1) "Biological sex," "Birth sex," and "sex" mean the biological indication of male and female, including sex chromosomes, naturally occurring sex hormones, gonads, and nonambiguous internal and external genitalia present at birth, without ...
The sex reassignment surgical industry is projected by some financial analysts to become a $5 billion industry by 2030. This rapid growth of the sex change surgery industry hinges upon insurance coverage, a topic Laungani addressed during his talk. "So something that alters the appearance just for cosmetic purposes versus having a function.
House Bill 619 would prohibit "genital gender reassignment surgery" for minors. House Bill 1660 would prohibit state Medicaid funds from covering such surgeries for minors.