Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

Patient Case Presentation

Figure 1. Blue and silver stethoscope (Pixabay, N.D.)
Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness. She also noticed other changes about herself, including decreased appetite, insomnia, fatigue, and poor ability to concentrate. The things that used to bring Ms. S.W. joy, such as gardening and listening to podcasts, are no longer bringing her the same happiness they used to. She became especially concerned as within the past two weeks she also started experiencing feelings of worthlessness, the perception that she is a burden to others, and fleeting thoughts of death/suicide.
Ms. S.W. acknowledges that she has numerous stressors in her life. She reports that her daughter’s grades have been steadily declining over the past two semesters and she is unsure if her daughter will be attending college anymore. Her relationship with her son is somewhat strained as she and his father are not on good terms and her son feels Ms. S.W. is at fault for this. She feels her career has been unfulfilling and though she’d like to go back to school, this isn’t possible given the family’s tight finances/the patient raising a family on a single income.
Ms. S.W. has experienced symptoms of depression previously, but she does not think the symptoms have ever been as severe as they are currently. She has taken antidepressants in the past and was generally adherent to them, but she believes that therapy was more helpful than the medications. She denies ever having history of manic or hypomanic episodes. She has been unable to connect to a mental health agency in several years due to lack of time and feeling that she could manage the symptoms on her own. She now feels that this is her last option and is looking for ongoing outpatient mental health treatment.
Past Medical History
- Hypertension, diagnosed at age 41
Past Surgical History
- Wisdom teeth extraction, age 22
Pertinent Family History
- Mother with history of Major Depressive Disorder, treated with antidepressants
- Maternal grandmother with history of Major Depressive Disorder, Generalized Anxiety Disorder
- Brother with history of suicide attempt and subsequent inpatient psychiatric hospitalization,
- Brother with history of Alcohol Use Disorder
- Father died from lung cancer (2012)
Pertinent Social History
- Works full-time as an enrollment specialist for Columbus City Schools since 2006
- Has two children, a daughter age 17 and a son age 14
- Divorced in 2015, currently single
- History of some emotional abuse and neglect from mother during childhood, otherwise denies history of trauma, including physical and sexual abuse
- Smoking 1/2 PPD of cigarettes
- Occasional alcohol use (approximately 1-2 glasses of wine 1-2 times weekly; patient had not had any alcohol consumption for the past year until two weeks ago)

Mental Health Case Study: Understanding Depression through a Real-life Example
Imagine feeling an unrelenting heaviness weighing down on your chest. Every breath becomes a struggle as a cloud of sadness engulfs your every thought. Your energy levels plummet, leaving you physically and emotionally drained. This is the reality for millions of people worldwide who suffer from depression, a complex and debilitating mental health condition.
Understanding depression is crucial in order to provide effective support and treatment for those affected. While textbooks and research papers provide valuable insights, sometimes the best way to truly comprehend the depths of this condition is through real-life case studies. These stories bring depression to life, shedding light on its impact on individuals and society as a whole.
In this article, we will delve into the world of mental health case studies, using a real-life example to explore the intricacies of depression. We will examine the symptoms, prevalence, and consequences of this all-encompassing condition. Furthermore, we will discuss the significance of case studies in mental health research, including their ability to provide detailed information about individual experiences and contribute to the development of treatment strategies.
Through an in-depth analysis of a selected case study, we will gain insight into the journey of an individual facing depression. We will explore their background, symptoms, and initial diagnosis. Additionally, we will examine the various treatment options available and assess the effectiveness of the chosen approach.
By delving into this real-life example, we will not only gain a better understanding of depression as a mental health condition, but we will also uncover valuable lessons that can aid in the treatment and support of those who are affected. So, let us embark on this enlightening journey, using the power of case studies to bring understanding and empathy to those who need it most.
Understanding Depression
Depression is a complex and multifaceted mental health condition that affects millions of people worldwide. To comprehend the impact of depression, it is essential to explore its defining characteristics, prevalence, and consequences on individuals and society as a whole.
Defining depression and its symptoms
Depression is more than just feeling sad or experiencing a low mood. It is a serious mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities that were once enjoyable. Individuals with depression often experience a range of symptoms that can significantly impact their daily lives. These symptoms include:
1. Persistent feelings of sadness or emptiness. 2. Fatigue and decreased energy levels. 3. Significant changes in appetite and weight. 4. Difficulty concentrating or making decisions. 5. Insomnia or excessive sleep. 6. feelings of guilt, worthlessness, or hopelessness. 7. Loss of interest or pleasure in activities.
Exploring the prevalence of depression worldwide
Depression knows no boundaries and affects individuals from all walks of life. According to the World Health Organization (WHO), an estimated 264 million people globally suffer from depression. This makes depression one of the most common mental health conditions worldwide. Additionally, the WHO highlights that depression is more prevalent among females than males.
The impact of depression is not limited to individuals alone. It also has significant social and economic consequences. Depression can lead to impaired productivity, increased healthcare costs, and strain on relationships, contributing to a significant burden on families, communities, and society at large.
The impact of depression on individuals and society
Depression can have a profound and debilitating impact on individuals’ lives, affecting their physical, emotional, and social well-being. The persistent sadness and loss of interest can lead to difficulties in maintaining relationships, pursuing education or careers, and engaging in daily activities. Furthermore, depression increases the risk of developing other mental health conditions, such as anxiety disorders or substance abuse.
On a societal level, depression poses numerous challenges. The economic burden of depression is significant, with costs associated with treatment, reduced productivity, and premature death. Moreover, the social stigma surrounding mental health can impede individuals from seeking help and accessing appropriate support systems.
Understanding the prevalence and consequences of depression is crucial for policymakers, healthcare professionals, and individuals alike. By recognizing the significant impact depression has on individuals and society, appropriate resources and interventions can be developed to mitigate its effects and improve the overall well-being of those affected.
The Significance of Case Studies in Mental Health Research
Case studies play a vital role in mental health research, providing valuable insights into individual experiences and contributing to the development of effective treatment strategies. Let us explore why case studies are considered invaluable in understanding and addressing mental health conditions.
Why case studies are valuable in mental health research
Case studies offer a unique opportunity to examine mental health conditions within the real-life context of individuals. Unlike large-scale studies that focus on statistical data, case studies provide a detailed examination of specific cases, allowing researchers to delve into the complexities of a particular condition or treatment approach. This micro-level analysis helps researchers gain a deeper understanding of the nuances and intricacies involved.
The role of case studies in providing detailed information about individual experiences
Through case studies, researchers can capture rich narratives and delve into the lived experiences of individuals facing mental health challenges. These stories help to humanize the condition and provide valuable insights that go beyond a list of symptoms or diagnostic criteria. By understanding the unique experiences, thoughts, and emotions of individuals, researchers can develop a more comprehensive understanding of mental health conditions and tailor interventions accordingly.
How case studies contribute to the development of treatment strategies
Case studies form a vital foundation for the development of effective treatment strategies. By examining a specific case in detail, researchers can identify patterns, factors influencing treatment outcomes, and areas where intervention may be particularly effective. Moreover, case studies foster an iterative approach to treatment development—an ongoing cycle of using data and experience to refine and improve interventions.
By examining multiple case studies, researchers can identify common themes and trends, leading to the development of evidence-based guidelines and best practices. This allows healthcare professionals to provide more targeted and personalized support to individuals facing mental health conditions.
Furthermore, case studies can shed light on potential limitations or challenges in existing treatment approaches. By thoroughly analyzing different cases, researchers can identify gaps in current treatments and focus on areas that require further exploration and innovation.
In summary, case studies are a vital component of mental health research, offering detailed insights into the lived experiences of individuals with mental health conditions. They provide a rich understanding of the complexities of these conditions and contribute to the development of effective treatment strategies. By leveraging the power of case studies, researchers can move closer to improving the lives of individuals facing mental health challenges.
Examining a Real-life Case Study of Depression
In order to gain a deeper understanding of depression, let us now turn our attention to a real-life case study. By exploring the journey of an individual navigating through depression, we can gain valuable insights into the complexities and challenges associated with this mental health condition.
Introduction to the selected case study
In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane’s case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
Background information on the individual facing depression
Before the onset of depression, Jane led a fulfilling and successful life. She had a promising career, a supportive network of friends and family, and engaged in hobbies that brought her joy. However, a series of life stressors, including a demanding job, a breakup, and the loss of a loved one, began to take a toll on her mental well-being.
Jane’s background highlights a common phenomenon – depression can affect individuals from all walks of life, irrespective of their socio-economic status, age, or external circumstances. It serves as a reminder that no one is immune to mental health challenges.
Presentation of symptoms and initial diagnosis
Jane began noticing a shift in her mood, characterized by persistent feelings of sadness and a lack of interest in activities she once enjoyed. She experienced disruptions in her sleep patterns, appetite changes, and a general sense of hopelessness. Recognizing the severity of her symptoms, Jane sought help from a mental health professional who diagnosed her with major depressive disorder.
Jane’s case exemplifies the varied and complex symptoms associated with depression. While individuals may exhibit overlapping symptoms, the intensity and manifestation of those symptoms can vary greatly, underscoring the importance of personalized and tailored treatment approaches.
By examining this real-life case study of depression, we can gain an empathetic understanding of the challenges faced by individuals experiencing this mental health condition. Through Jane’s journey, we will uncover the treatment options available for depression and analyze the effectiveness of the chosen approach. The case study will allow us to explore the nuances of depression and provide valuable insights into the treatment landscape for this prevalent mental health condition.
The Treatment Journey
When it comes to treating depression, there are various options available, ranging from therapy to medication. In this section, we will provide an overview of the treatment options for depression and analyze the treatment plan implemented in the real-life case study.
Overview of the treatment options available for depression
Treatment for depression typically involves a combination of approaches tailored to the individual’s needs. The two primary treatment modalities for depression are psychotherapy (talk therapy) and medication. Psychotherapy aims to help individuals explore their thoughts, emotions, and behaviors, while medication can help alleviate symptoms by restoring chemical imbalances in the brain.
Common forms of psychotherapy used in the treatment of depression include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic therapy. These therapeutic approaches focus on addressing negative thought patterns, improving relationship dynamics, and gaining insight into underlying psychological factors contributing to depression.
In cases where medication is utilized, selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed. These medications help rebalance serotonin levels in the brain, which are often disrupted in individuals with depression. Other classes of antidepressant medications, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) or tricyclic antidepressants (TCAs), may be considered in specific cases.
Exploring the treatment plan implemented in the case study
In Jane’s case, a comprehensive treatment plan was developed with the intention of addressing her specific needs and symptoms. Recognizing the severity of her depression, Jane’s healthcare team recommended a combination of talk therapy and medication.
Jane began attending weekly sessions of cognitive-behavioral therapy (CBT) with a licensed therapist. This form of therapy aimed to help Jane identify and challenge negative thought patterns, develop coping strategies, and cultivate more adaptive behaviors. The therapeutic relationship provided Jane with a safe space to explore and process her emotions, ultimately helping her regain a sense of control over her life.
In conjunction with therapy, Jane’s healthcare provider prescribed an SSRI medication to assist in managing her symptoms. The medication was carefully selected based on Jane’s specific symptoms and medical history, and regular follow-up appointments were scheduled to monitor her response to the medication and adjust the dosage if necessary.
Analyzing the effectiveness of the treatment approach
The effectiveness of treatment for depression varies from person to person, and it often requires a period of trial and adjustment to find the most suitable intervention. In Jane’s case, the combination of cognitive-behavioral therapy and medication proved to be beneficial. Over time, she reported a reduction in her depressive symptoms, an improvement in her overall mood, and increased ability to engage in activities she once enjoyed.
It is important to note that the treatment journey for depression is not always linear, and setbacks and challenges may occur along the way. Each individual responds differently to treatment, and adjustments might be necessary to optimize outcomes. Continuous communication between the individual and their healthcare team is crucial to addressing any concerns, monitoring progress, and adapting the treatment plan as needed.
By analyzing the treatment approach in the real-life case study, we gain insights into the various treatment options available for depression and how they can be tailored to meet individual needs. The combination of psychotherapy and medication offers a holistic approach, addressing both psychological and biological aspects of depression.
The Outcome and Lessons Learned
After undergoing treatment for depression, it is essential to assess the outcome and draw valuable lessons from the case study. In this section, we will discuss the progress made by the individual in the case study, examine the challenges faced during the treatment process, and identify key lessons learned.
Discussing the progress made by the individual in the case study
Throughout the treatment process, Jane experienced significant progress in managing her depression. She reported a reduction in depressive symptoms, improved mood, and a renewed sense of hope and purpose in her life. Jane’s active participation in therapy, combined with the appropriate use of medication, played a crucial role in her progress.
Furthermore, Jane’s support network of family and friends played a significant role in her recovery. Their understanding, empathy, and support provided a solid foundation for her journey towards improved mental well-being. This highlights the importance of social support in the treatment and management of depression.
Examining the challenges faced during the treatment process
Despite the progress made, Jane faced several challenges during her treatment journey. Adhering to the treatment plan consistently proved to be difficult at times, as she encountered setbacks and moments of self-doubt. Additionally, managing the side effects of the medication required careful monitoring and adjustments to find the right balance.
Moreover, the stigma associated with mental health continued to be a challenge for Jane. Overcoming societal misconceptions and seeking help required courage and resilience. The case study underscores the need for increased awareness, education, and advocacy to address the stigma surrounding mental health conditions.
Identifying the key lessons learned from the case study
The case study offers valuable lessons that can inform the treatment and support of individuals with depression:
1. Holistic Approach: The combination of psychotherapy and medication proved to be effective in addressing the psychological and biological aspects of depression. This highlights the need for a holistic and personalized treatment approach.
2. Importance of Support: Having a strong support system can significantly impact an individual’s ability to navigate through depression. Family, friends, and healthcare professionals play a vital role in providing empathy, understanding, and encouragement.
3. Individualized Treatment: Depression manifests differently in each individual, emphasizing the importance of tailoring treatment plans to meet individual needs. Personalized interventions are more likely to lead to positive outcomes.
4. Overcoming Stigma: Addressing the stigma associated with mental health conditions is crucial for individuals to seek timely help and access the support they need. Educating society about mental health is essential to create a more supportive and inclusive environment.
By drawing lessons from this real-life case study, we gain insights that can improve the understanding and treatment of depression. Recognizing the progress made, understanding the challenges faced, and implementing the lessons learned can contribute to more effective interventions and support systems for individuals facing depression.In conclusion, this article has explored the significance of mental health case studies in understanding and addressing depression, focusing on a real-life example. By delving into case studies, we gain a deeper appreciation for the complexities of depression and the profound impact it has on individuals and society.
Through our examination of the selected case study, we have learned valuable lessons about the nature of depression and its treatment. We have seen how the combination of psychotherapy and medication can provide a holistic approach, addressing both psychological and biological factors. Furthermore, the importance of social support and the role of a strong network in an individual’s recovery journey cannot be overstated.
Additionally, we have identified challenges faced during the treatment process, such as adherence to the treatment plan and managing medication side effects. These challenges highlight the need for ongoing monitoring, adjustments, and open communication between individuals and their healthcare providers.
The case study has also emphasized the impact of stigma on individuals seeking help for depression. Addressing societal misconceptions and promoting mental health awareness is essential to create a more supportive environment for those affected by depression and other mental health conditions.
Overall, this article reinforces the significance of case studies in advancing our understanding of mental health conditions and developing effective treatment strategies. Through real-life examples, we gain a more comprehensive and empathetic perspective on depression, enabling us to provide better support and care for individuals facing this mental health challenge.
As we conclude, it is crucial to emphasize the importance of continued research and exploration of mental health case studies. The more we learn from individual experiences, the better equipped we become to address the diverse needs of those affected by mental health conditions. By fostering a culture of understanding, support, and advocacy, we can strive towards a future where individuals with depression receive the care and compassion they deserve.
Similar Posts

Exploring the World of Bipolar Bingo: Understanding the Game and Its Connection to Bipolar Disorder
Imagine a world where a game of chance holds the power to bring solace and support to individuals affected by bipolar disorder. A seemingly unlikely connection, but one that exists nonetheless. Welcome to the world of…

Can Anxiety Disorders be Genetic? Exploring the Hereditary Aspects of Anxiety Disorders
Introduction to Genetic Factors in Anxiety Disorders Understanding anxiety disorders Anxiety disorders are a common mental health condition that affect millions of individuals worldwide. People with anxiety disorders experience overwhelming feelings of fear, worry, and unease…

Understanding the Abbreviations and Acronyms for Bipolar Disorder
Living with bipolar disorder can be a challenging journey. The constant rollercoaster of emotions, the highs and lows, can take a toll on a person’s mental and emotional well-being. But what if there was a way…

The Connection Between Ice Cream and Depression: Can Ice Cream Really Help?
Ice cream has long been hailed as a delightful treat, bringing joy to people of all ages. It is often associated with carefree summer days, laughter, and moments of pure bliss. But what if I told…

Understanding the Relationship Between Bipolar Disorder and PTSD
Imagine living with extreme mood swings that can range from feeling on top of the world one day to plunging into the depths of despair the next. Now add the haunting memories of a traumatic event…

The Connection Between Meth and Bipolar: Understanding the Link and Seeking Treatment
It’s a tangled web of interconnectedness – the world of mental health and substance abuse. One doesn’t often think of them as intertwined, but for those battling bipolar disorder, the link becomes all too clear. And…
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
4 Treatment of Depression
- Published: February 2013
- Cite Icon Cite
- Permissions Icon Permissions
Chapter 4 covers the treatment of depression, and discusses popular myths regarding depression, its frequency, characteristics and diagnosis, and includes case studies, assessment, case conceptualization, intervention development and course of treatment, problems that may arise in therapy, ethical considerations, common mistakes in the course of treatment, relapse prevention, and cultural factors.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
April 23, 2024
Research in Context: Treating depression
Finding better approaches.
While effective treatments for major depression are available, there is still room for improvement. This special Research in Context feature explores the development of more effective ways to treat depression, including personalized treatment approaches and both old and new drugs.

Everyone has a bad day sometimes. People experience various types of stress in the course of everyday life. These stressors can cause sadness, anxiety, hopelessness, frustration, or guilt. You may not enjoy the activities you usually do. These feelings tend to be only temporary. Once circumstances change, and the source of stress goes away, your mood usually improves. But sometimes, these feelings don’t go away. When these feelings stick around for at least two weeks and interfere with your daily activities, it’s called major depression, or clinical depression.
In 2021, 8.3% of U.S. adults experienced major depression. That’s about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain. People with major depression may become unable to meet their responsibilities at work or home. Depression can also lead people to use alcohol or drugs or engage in high-risk activities. In the most extreme cases, depression can drive people to self-harm or even suicide.
The good news is that effective treatments are available. But current treatments have limitations. That’s why NIH-funded researchers have been working to develop more effective ways to treat depression. These include finding ways to predict whether certain treatments will help a given patient. They're also trying to develop more effective drugs or, in some cases, find new uses for existing drugs.
Finding the right treatments
The most common treatments for depression include psychotherapy, medications, or a combination. Mild depression may be treated with psychotherapy. Moderate to severe depression often requires the addition of medication.
Several types of psychotherapy have been shown to help relieve depression symptoms. For example, cognitive behavioral therapy helps people to recognize harmful ways of thinking and teaches them how to change these. Some researchers are working to develop new therapies to enhance people’s positive emotions. But good psychotherapy can be hard to access due to the cost, scheduling difficulties, or lack of available providers. The recent growth of telehealth services for mental health has improved access in some cases.
There are many antidepressant drugs on the market. Different drugs will work best on different patients. But it can be challenging to predict which drugs will work for a given patient. And it can take anywhere from 6 to 12 weeks to know whether a drug is working. Finding an effective drug can involve a long period of trial and error, with no guarantee of results.
If depression doesn’t improve with psychotherapy or medications, brain stimulation therapies could be used. Electroconvulsive therapy, or ECT, uses electrodes to send electric current into the brain. A newer technique, transcranial magnetic stimulation (TMS), stimulates the brain using magnetic fields. These treatments must be administered by specially trained health professionals.
“A lot of patients, they kind of muddle along, treatment after treatment, with little idea whether something’s going to work,” says psychiatric researcher Dr. Amit Etkin.
One reason it’s difficult to know which antidepressant medications will work is that there are likely different biological mechanisms that can cause depression. Two people with similar symptoms may both be diagnosed with depression, but the causes of their symptoms could be different. As NIH depression researcher Dr. Carlos Zarate explains, “we believe that there’s not one depression, but hundreds of depressions.”
Depression may be due to many factors. Genetics can put certain people at risk for depression. Stressful situations, physical health conditions, and medications may contribute. And depression can also be part of a more complicated mental disorder, such as bipolar disorder. All of these can affect which treatment would be best to use.
Etkin has been developing methods to distinguish patients with different types of depression based on measurable biological features, or biomarkers. The idea is that different types of patients would respond differently to various treatments. Etkin calls this approach “precision psychiatry.”
One such type of biomarker is electrical activity in the brain. A technique called electroencephalography, or EEG, measures electrical activity using electrodes placed on the scalp. When Etkin was at Stanford University, he led a research team that developed a machine-learning algorithm to predict treatment response based on EEG signals. The team applied the algorithm to data from a clinical trial of the antidepressant sertraline (Zoloft) involving more than 300 people.

EEG data for the participants were collected at the outset. Participants were then randomly assigned to take either sertraline or an inactive placebo for eight weeks. The team found a specific set of signals that predicted the participants’ responses to sertraline. The same neural “signature” also predicted which patients with depression responded to medication in a separate group.
Etkin’s team also examined this neural signature in a set of patients who were treated with TMS and psychotherapy. People who were predicted to respond less to sertraline had a greater response to the TMS/psychotherapy combination.
Etkin continues to develop methods for personalized depression treatment through his company, Alto Neuroscience. He notes that EEG has the advantage of being low-cost and accessible; data can even be collected in a patient’s home. That’s important for being able to get personalized treatments to the large number of people they could help. He’s also working on developing antidepressant drugs targeted to specific EEG profiles. Candidate drugs are in clinical trials now.
“It’s not like a pie-in-the-sky future thing, 20-30 years from now,” Etkin explains. “This is something that could be in people's hands within the next five years.”
New tricks for old drugs
While some researchers focus on matching patients with their optimal treatments, others aim to find treatments that can work for many different patients. It turns out that some drugs we’ve known about for decades might be very effective antidepressants, but we didn’t recognize their antidepressant properties until recently.
One such drug is ketamine. Ketamine has been used as an anesthetic for more than 50 years. Around the turn of this century, researchers started to discover its potential as an antidepressant. Zarate and others have found that, unlike traditional antidepressants that can take weeks to take effect, ketamine can improve depression in as little as one day. And a single dose can have an effect for a week or more. In 2019, the FDA approved a form of ketamine for treating depression that is resistant to other treatments.
But ketamine has drawbacks of its own. It’s a dissociative drug, meaning that it can make people feel disconnected from their body and environment. It also has the potential for addiction and misuse. For these reasons, it’s a controlled substance and can only be administered in a doctor’s office or clinic.
Another class of drugs being studied as possible antidepressants are psychedelics. These include lysergic acid diethylamide (LSD) and psilocybin, the active ingredient in magic mushrooms. These drugs can temporarily alter a person’s mood, thoughts, and perceptions of reality. Some have historically been used for religious rituals, but they are also used recreationally.
In clinical studies, psychedelics are typically administered in combination with psychotherapy. This includes several preparatory sessions with a therapist in the weeks before getting the drug, and several sessions in the weeks following to help people process their experiences. The drugs are administered in a controlled setting.
Dr. Stephen Ross, co-director of the New York University Langone Health Center for Psychedelic Medicine, describes a typical session: “It takes place in a living room-like setting. The person is prepared, and they state their intention. They take the drug, they lie supine, they put on eye shades and preselected music, and two therapists monitor them.” Sessions last for as long as the acute effects of the drug last, which is typically several hours. This is a healthcare-intensive intervention given the time and personnel needed.
In 2016, Ross led a clinical trial examining whether psilocybin-assisted therapy could reduce depression and anxiety in people with cancer. According to Ross, as many as 40% of people with cancer have clinically significant anxiety and depression. The study showed that a single psilocybin session led to substantial reductions in anxiety and depression compared with a placebo. These reductions were evident as soon as one day after psilocybin administration. Six months later, 60-80% of participants still had reduced depression and anxiety.
Psychedelic drugs frequently trigger mystical experiences in the people who take them. “People can feel a sense…that their consciousness is part of a greater consciousness or that all energy is one,” Ross explains. “People can have an experience that for them feels more ‘real’ than regular reality. They can feel transported to a different dimension of reality.”
About three out of four participants in Ross’s study said it was among the most meaningful experiences of their lives. And the degree of mystical experience correlated with the drug’s therapeutic effect. A long-term follow-up study found that the effects of the treatment continued more than four years later.
If these results seem too good to be true, Ross is quick to point out that it was a small study, with only 29 participants, although similar studies from other groups have yielded similar results. Psychedelics haven’t yet been shown to be effective in a large, controlled clinical trial. Ross is now conducting a trial with 200 people to see if the results of his earlier study pan out in this larger group. For now, though, psychedelics remain experimental drugs—approved for testing, but not for routine medical use.
Unlike ketamine, psychedelics aren’t considered addictive. But they, too, carry risks, which certain conditions may increase. Psychedelics can cause cardiovascular complications. They can cause psychosis in people who are predisposed to it. In uncontrolled settings, they have the risk of causing anxiety, confusion, and paranoia—a so-called “bad trip”—that can lead the person taking the drug to harm themself or others. This is why psychedelic-assisted therapy takes place in such tightly controlled settings. That increases the cost and complexity of the therapy, which may prevent many people from having access to it.
Better, safer drugs
Despite the promise of ketamine or psychedelics, their drawbacks have led some researchers to look for drugs that work like them but with fewer side effects.
Depression is thought to be caused by the loss of connections between nerve cells, or neurons, in certain regions of the brain. Ketamine and psychedelics both promote the brain’s ability to repair these connections, a quality called plasticity. If we could understand how these drugs encourage plasticity, we might be able to design drugs that can do so without the side effects.

Dr. David Olson at the University of California, Davis studies how psychedelics work at the cellular and molecular levels. The drugs appear to promote plasticity by binding to a receptor in cells called the 5-hydroxytryptamine 2A receptor (5-HT2AR). But many other compounds also bind 5-HT2AR without promoting plasticity. In a recent NIH-funded study, Olson showed that 5-HT2AR can be found both inside and on the surface of the cell. Only compounds that bound to the receptor inside the cells promoted plasticity. This suggests that a drug has to be able to get into the cell to promote plasticity.
Moreover, not all drugs that bind 5-HT2AR have psychedelic effects. Olson’s team has developed a molecular sensor, called psychLight, that can identify which compounds that bind 5-HT2AR have psychedelic effects. Using psychLight, they identified compounds that are not psychedelic but still have rapid and long-lasting antidepressant effects in animal models. He’s founded a company, Delix Therapeutics, to further develop drugs that promote plasticity.
Meanwhile, Zarate and his colleagues have been investigating a compound related to ketamine called hydroxynorketamine (HNK). Ketamine is converted to HNK in the body, and this process appears to be required for ketamine’s antidepressant effects. Administering HNK directly produced antidepressant-like effects in mice. At the same time, it did not cause the dissociative side effects and addiction caused by ketamine. Zarate’s team has already completed phase I trials of HNK in people showing that it’s safe. Phase II trials to find out whether it’s effective are scheduled to begin soon.
“What [ketamine and psychedelics] are doing for the field is they’re helping us realize that it is possible to move toward a repair model versus a symptom mitigation model,” Olson says. Unlike existing antidepressants, which just relieve the symptoms of depression, these drugs appear to fix the underlying causes. That’s likely why they work faster and produce longer-lasting effects. This research is bringing us closer to having safer antidepressants that only need to be taken once in a while, instead of every day.
—by Brian Doctrow, Ph.D.
Related Links
- How Psychedelic Drugs May Help with Depression
- Biosensor Advances Drug Discovery
- Neural Signature Predicts Antidepressant Response
- How Ketamine Relieves Symptoms of Depression
- Protein Structure Reveals How LSD Affects the Brain
- Predicting The Usefulness of Antidepressants
- Depression Screening and Treatment in Adults
- Serotonin Transporter Structure Revealed
- Placebo Effect in Depression Treatment
- When Sadness Lingers: Understanding and Treating Depression
- Psychedelic and Dissociative Drugs
References: An electroencephalographic signature predicts antidepressant response in major depression. Wu W, Zhang Y, Jiang J, Lucas MV, Fonzo GA, Rolle CE, Cooper C, Chin-Fatt C, Krepel N, Cornelssen CA, Wright R, Toll RT, Trivedi HM, Monuszko K, Caudle TL, Sarhadi K, Jha MK, Trombello JM, Deckersbach T, Adams P, McGrath PJ, Weissman MM, Fava M, Pizzagalli DA, Arns M, Trivedi MH, Etkin A. Nat Biotechnol. 2020 Feb 10. doi: 10.1038/s41587-019-0397-3. Epub 2020 Feb 10. PMID: 32042166. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. J Psychopharmacol . 2016 Dec;30(12):1165-1180. doi: 10.1177/0269881116675512. PMID: 27909164. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, Bossis AP, Grigsby J, Fischer S, Ross S. J Psychopharmacol . 2020 Feb;34(2):155-166. doi: 10.1177/0269881119897615. Epub 2020 Jan 9. PMID: 31916890. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE. Science . 2023 Feb 17;379(6633):700-706. doi: 10.1126/science.adf0435. Epub 2023 Feb 16. PMID: 36795823. Psychedelic-inspired drug discovery using an engineered biosensor. Dong C, Ly C, Dunlap LE, Vargas MV, Sun J, Hwang IW, Azinfar A, Oh WC, Wetsel WC, Olson DE, Tian L. Cell . 2021 Apr 8: S0092-8674(21)00374-3. doi: 10.1016/j.cell.2021.03.043. Epub 2021 Apr 28. PMID: 33915107. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. Nature . 2016 May 26;533(7604):481-6. doi: 10.1038/nature17998. Epub 2016 May 4. PMID: 27144355.
Connect with Us
- More Social Media from NIH
- Research article
- Open access
- Published: 22 April 2024
Impact of COVID-19 pandemic on depression incidence and healthcare service use among patients with depression: an interrupted time-series analysis from a 9-year population-based study
- Vivien Kin Yi Chan 1 na1 ,
- Yi Chai 1 , 2 na1 ,
- Sandra Sau Man Chan 3 ,
- Hao Luo 4 ,
- Mark Jit 5 , 7 ,
- Martin Knapp 4 , 6 ,
- David Makram Bishai 7 ,
- Michael Yuxuan Ni 7 , 8 , 9 ,
- Ian Chi Kei Wong 1 , 10 , 11 , 13 &
- Xue Li ORCID: orcid.org/0000-0003-4836-7808 1 , 10 , 12 , 13
BMC Medicine volume 22 , Article number: 169 ( 2024 ) Cite this article
800 Accesses
29 Altmetric
Metrics details
Most studies on the impact of the COVID-19 pandemic on depression burden focused on the earlier pandemic phase specific to lockdowns, but the longer-term impact of the pandemic is less well-studied. In this population-based cohort study, we examined the short-term and long-term impacts of COVID-19 on depression incidence and healthcare service use among patients with depression.
Using the territory-wide electronic medical records in Hong Kong, we identified all patients aged ≥ 10 years with new diagnoses of depression from 2014 to 2022. We performed an interrupted time-series (ITS) analysis to examine changes in incidence of medically attended depression before and during the pandemic. We then divided all patients into nine cohorts based on year of depression incidence and studied their initial and ongoing service use patterns until the end of 2022. We applied generalized linear modeling to compare the rates of healthcare service use in the year of diagnosis between patients newly diagnosed before and during the pandemic. A separate ITS analysis explored the pandemic impact on the ongoing service use among prevalent patients with depression.
We found an immediate increase in depression incidence (RR = 1.21, 95% CI: 1.10–1.33, p < 0.001) in the population after the pandemic began with non-significant slope change, suggesting a sustained effect until the end of 2022. Subgroup analysis showed that the increases in incidence were significant among adults and the older population, but not adolescents. Depression patients newly diagnosed during the pandemic used 11% fewer resources than the pre-pandemic patients in the first diagnosis year. Pre-existing depression patients also had an immediate decrease of 16% in overall all-cause service use since the pandemic, with a positive slope change indicating a gradual rebound over a 3-year period.
Conclusions
During the pandemic, service provision for depression was suboptimal in the face of increased demand generated by the increasing depression incidence during the COVID-19 pandemic. Our findings indicate the need to improve mental health resource planning preparedness for future public health crises.
Peer Review reports
The COVID-19 pandemic that began in 2020 has resulted in an unprecedented public health crisis, with 771 million confirmed cases and over 6 million deaths across the globe as of September 2023 [ 1 ]. To curb the spread and reduce the mortality of SARS-CoV-2 infections, governments worldwide enacted stringent measures to contain its spread, including social mobility restrictions, mask-wearing, massive screenings, and lockdowns. Despite their effectiveness in limiting viral spread, these measures may have created a macro-environment of fear, social exclusion of individuals who contracted the virus, and reduced community cohesion [ 2 , 3 , 4 ]. The pandemic and the ensuing measures also led to economic disruption and created financial hardship for millions of families [ 4 , 5 ]. The combined pandemic stresses may have exacerbated the risk factors for mental health conditions including depression. Among patients with pre-existing depression, the government effort re-prioritized for outbreak control may have also led to disrupted non-emergency services and unmet care need in mental health [ 6 ].
A meta-analysis estimated an additional 53 million cases of depression and a 27.6% increase in its global prevalence in 2020 due to COVID-19-related illnesses and reduced mobility [ 7 ], which affected individuals across age groups [ 8 , 9 , 10 ]. In Hong Kong, a survey showed a consistent mental health crisis with a two-fold increase in depression symptoms and a 28.3% rise in the stress level even during the well-managed small-scale outbreaks [ 11 ]. Conversely, other studies reported that the pandemic reduced the risk of depression and self-harm because of the emotional security provided by timely government intervention, but these findings were confounded by increased barriers to seek medical help [ 12 , 13 , 14 ]. In the emergency phase of the pandemic, it was reported that lockdowns significantly reduced healthcare service use for both outpatient and inpatient services [ 15 , 16 , 17 ]. Studies also found an elevated risk of depression relapse and use of antidepressants [ 18 , 19 ].
Literature exploring pandemic impact on depression has mostly focused on the earlier phase of the pandemic (2020–2021) when short-term lockdown orders were in place. There are fewer studies and more mixed results for the post-emergency phase. Hong Kong followed the “dynamic zero-COVID policy” of China with strict border control, contact tracing, and quarantine before cases spread until the end of 2022 and so recorded a low number of SARS-CoV-2 cases for most of the time before a major Omicron outbreak [ 20 ]. It did not experience full lockdown, although stringent infection control and social measures were deployed for an entire 3-year-long period. This context thus enables us to evaluate the longer-term pandemic impact apart from a focus on lockdowns. In the late pandemic period, it is also useful to understand any potential decline in depression incidence and rebound in health service utilization. Using interrupted time series (ITS) analysis with a cohort study, we examined the changes in depression incidence and healthcare service use due to the pandemic, aiming to measure both the short-term (immediately after pandemic onset) and long-term (3 years since the outbreak) impacts on the burden of depression. We aimed to facilitate better preparedness in mental health resource planning for future public health crises.
Data source
We analyzed the Clinical Data Analysis and Reporting System (CDARS), the territory-wide routine electronic medical record (EMR) developed by the Hospital Authority, which manages all public healthcare services in Hong Kong and provides publicly funded healthcare services to all eligible residents (> 7.6 million). CDARS covers real-time anonymized patient-level data, including demographics, deaths, attendances, and all-cause diagnoses coded based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM), since 1993 across outpatient, inpatient, and emergency settings for research and auditing purposes in the public sector. The quality and accuracy of CDARS have been demonstrated in population-based studies on COVID-19 [ 21 , 22 ] and depression [ 23 , 24 ]. In Hong Kong, the public healthcare is heavily subsidized at a highly affordable price, while the private sector is financed mainly by non-compulsory medical insurance and out-of-pocket payments. The Hospital Authority thus manages 76% of chronic medical conditions including mental health illnesses despite a dual-track public and private system [ 25 ].
Study design and participants
This study consisted of both a quasi-experimental design with ITS analyses and a population-based retrospective study. We first identified all patients who received new clinical diagnoses of major depressive disorder or dysthymia (ICD-9-CM codes: 296.2, 300.4, 311) between January 2014 and December 2022. Patients aged below 10 were excluded to avoid confusion with maternal depression in the coding system. We performed an ITS analysis to evaluate changes in medically attended depression incidence during 36 quarters of data observations. The data cut point was the first quarter of 2020, leaving 24 quarters as pre-cut points and 12 quarters as post-cut points. ITS analysis is a valuable tool to assess the impact of population-level interventions or major macro-environmental changes and widely used in various health policy assessments [ 26 ]. Since patients who received incident diagnoses in different years could have different disease durations and care needs, we divided all patients into nine “incident cohorts” (2014 to 2022 cohorts) based on year of depression incidence. All patients were followed up until the end of 2022 for their service use patterns across outpatient, inpatient, and emergency settings.
An exploratory trend analysis showed that use of healthcare resources was the greatest at the beginning of the disease course before stabilizing. Recognizing this feature, we separately investigated the pandemic impact on the (1) initial and (2) ongoing healthcare service use. Respectively, we compared the rates of healthcare service use during the first calendar year following diagnosis, which potentially represents the most care-demanding phase, among patients newly diagnosed during the pandemic (2020 to 2022, the exposure groups) with those diagnosed before the pandemic (2014 to 2019, the reference groups) using a generalized linear model. To study the ongoing resource utilization among the relatively stable prevalent patients, defined as having a disease duration for at least 3 years by the start of the pandemic (i.e., represented by all patients in the 2014–2016 cohorts), we conducted another ITS analysis to compare their rates of service use before and during the pandemic until the end of 2022. The data points before the third calendar year of diagnosis were excluded in the analysis. The linkage between the three parts of analyses is illustrated in Additional file 1 : Figure S1.
Exposure and outcomes of interest
Our study defined the exposure as the macro-environment with the implementation of containment measures in response to the pandemic. Based on the COVID-19 Stringency Index by the Oxford COVID-19 Government Response Tracker, the Hong Kong government introduced relevant policies since January 2020 and announced the lifting of most mandates by December 2022 [ 27 ]. With quarterly data, we operationally defined the exposure period starting from the first quarter of 2020 until December 2022 (the intervention period). The reference period (the pre-pandemic period) was between the first quarter of 2014 and the last quarter of 2019.
The first outcome of interest was quarterly incidence of medically attended depression, defined as the number of patients who received depression diagnosis in the current quarter but without history of depression divided by the local eligible population, with age standardization using 5-year age bands based on the 2021 mid-year population. The second outcome was quarterly or yearly rates of attendance episodes or bed-days by incident cohort and service setting, defined by the total visit episodes or bed-days in the current period divided by the number of patients with depression whose observation period (from their first diagnosis to death or end of study) fell within the same period. We further stratified the outpatient attendance into “all-cause” (all outpatient services) and “psychiatric-related” (psychiatric specialist clinic, day hospital, and community nursing) use. Stratified data were unavailable in the inpatient and emergency settings.
Statistical analysis
In the ITS analyses, we applied segmented quasi-Poisson regression models since the data showed signs of overdispersion [ 28 ]. We included a continuous time variable in quarters, a binary indicator for the pandemic period (the exposure period) to represent level change (immediate effect) and the interaction of the two to measure slope change (gradual effect) [ 29 ], offsetting the logarithm of the local population or patients with depression. We adjusted the quarters of the data points to account for seasonality. Residual plots, autocorrelation function, and partial autocorrelation function suggested very little evidence of autocorrelation [ 28 , 30 ]. We then used Newey-West method to obtain robust standard errors and address autocorrelation up to the largest lag [ 31 , 32 ]. In the comparison of the initial healthcare service use between patients newly diagnosed during and before the pandemic, we fitted the rates of service use in the year of diagnosis between cohorts using a generalized linear model with negative binomial log link function. The model adjusted for a binary indicator of whether the diagnosis year occurred before or during the pandemic (the exposure period) and offset the logarithm of incident patients with depression in each cohort. In all analyses, we excluded data points related to major local social movements in 2014 and 2019 to address confounding due to changes in socio-political environment [ 33 , 34 , 35 ].
Subgroup and sensitivity analyses
In the ITS analysis to evaluate changes in depression incidence, we further stratified the analysis into three age groups: adolescents (10–24), adults (25–64), and the older population (65 +) to explore whether these population subgroups were differentially susceptible to a new depression diagnosis as a result of the pandemic.
During the first quarter of 2022, there was an unprecedented abrupt increase of SARS-CoV-2 cases due to the Omicron variant, marking the start of “fifth-wave outbreak” in Hong Kong [ 20 ]. In contrast to the earlier waves of smaller-scale outbreaks (below 13,000 cumulative cases before 2022), the public healthcare services were overwhelmed at the beginning of this wave, which possibly strained diagnostic capacity and caused the number of depression diagnoses to be lower than usual. We therefore performed sensitivity analyses for the ITS analyses for depression incidence and healthcare service use by adjusting a variable indicating the relevant quarter to validate the results. In addition, since outpatient service reception may be subject to long waiting time, we conducted an additional sensitivity analysis with a 6-month lag for the pandemic period by adding a binary indicator for the transition period and re-defining the pandemic to start from the third quarter of 2020. Lastly, we also performed sensitivity analyses for the pandemic impact on ongoing healthcare resource utilization by changing the defined disease duration of 3 years as stable patients into 2 years.
All data were analyzed using R version 4.0.3 and cross-validated by two investigators.
Over the 9-year study period, we identified 85,111 patients with new depression diagnosis, who generated 4,433,558 attendance or admission episodes across all diagnosis settings and 1,327,424 inpatient bed-days. For these patients, the mean age was 48.6 (SD:19.8) with 71.6% being female. Detailed demographic characteristics of the patients diagnosed in each year are summarized in Additional file 2 : Table S1.
Incidence of medically attended depression
Figure 1 illustrates the trends of the observed and model-implied quarterly incidence of medically attended depression between 2014 and 2022. The average quarterly incidence rates were 3.44 and 3.59 per 10,000 population before and during the pandemic (Additional file 2 : Table S2), respectively. After adjusting for major social movements, ITS analysis showed a small but marginally significant decline in the population incidence in the pre-pandemic period (risk ratio, RR = 0.995, 95% CI: 0.99–1.00, p = 0.042). Since the pandemic, however, there was a significant immediate increase in incidence indicated by level change (RR = 1.21, 95% CI: 1.10–1.33, p < 0.001), with a non-significant slope change (Fig. 1 A).
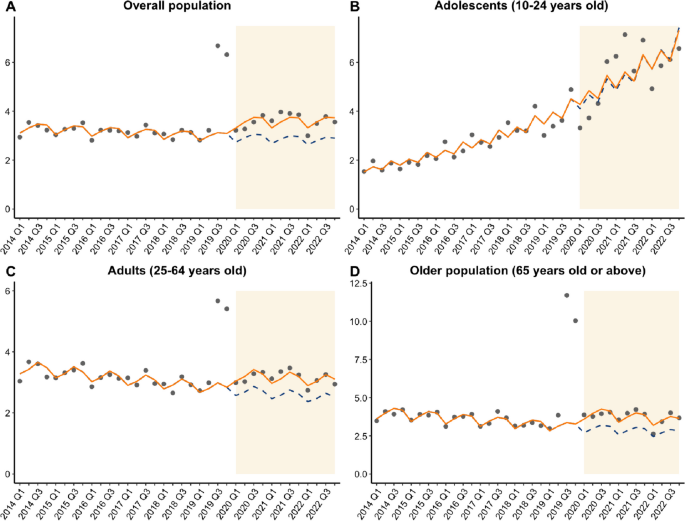
Interrupted time series analysis plot of pandemic impact on depression incidence
Stratifying by age groups, ITS analysis showed a slow but significant decline in incidence in the pre-pandemic period among adults and the older population (RR = 0.99, 95% CI: 0.99–0.99) but a significant increase over the time among adolescents (RR = 1.04, 95% CI: 1.04–1.05) before the pandemic. Since the pandemic, we found significant level increases indicating immediate effects of the pandemic among adults (RR = 1.19, 95% CI: 1.09–1.29) and the older population (RR = 1.33, 95% CI: 1.29–1.38, all p < 0.001), but not adolescents. The slope changes remained non-significant in all subgroups (Fig. 1 B–D).
In the sensitivity analysis which accounted for the fifth-wave outbreak, we found a similar level change (RR = 1.20, 95% CI: 1.10–1.32, p < 0.001) as the main analysis, with a significant but slowly declining pre-pandemic trend (RR = 0.995, 95% CI: 0.990–0.999, p = 0.039). Using a 6-month transition window showed a consistent level change (RR = 1.28, 95% CI: 1.22–1.34, p < 0.001) and pre-pandemic trend (RR = 0.995, 95% CI: 0.994–0.996, p < 0.001). The slope changes in both sensitivity analyses remained non-significant.

Healthcare service use
In each incident cohort, the patterns followed the natural disease history such that the greatest service demand consistently occurred within the first 2 years of a depression diagnosis, followed by gradual decline subsequently (Fig. 2 ). During the pandemic, service utilization appeared to decrease further across all diagnosis settings except for inpatient bed-days. All counts and rates of healthcare service use are listed in Additional file 2 : Tables S3–S12.
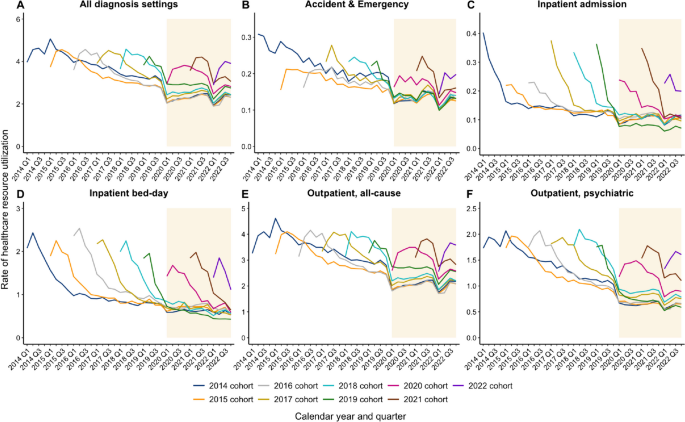
Trend of healthcare resource utilization from 2014 to 2022
Pandemic impact on initial healthcare service use
Table 1 details the rates of healthcare service use in the year of diagnosis stratified by incident cohort and the regression results across diagnosis settings. Annual rates of overall all-cause visits per patient in the year of diagnosis were 10.5 to 10.8 episodes among patients diagnosed between 2015 and 2018, in contrast to 9.0 to 10.2 episodes among those diagnosed between 2020 and 2022. Adjusting for major social movements, the negative binomial model showed that the pandemic was associated with significantly reduced utilization in inpatient bed-days (RR = 0.78, 95% CI: 0.70–0.85), outpatient all-cause visits (RR = 0.89, 95% CI: 0.85–0.93), outpatient psychiatric visits (RR = 0.82, 95% CI: 0.76–0.88), and overall all-cause visits (RR = 0.89, 95% CI: 0.85–0.94, all p < 0.001). Being diagnosed during the pandemic was not significantly associated with changes in rates of emergency and inpatient admission episodes.
Pandemic impact on ongoing healthcare service use
For the combined 2014–2016 cohorts, the mean rate of overall all-cause visits counting from their third year of diagnosis was 3.38 episodes per patient in the pre-pandemic period, which dropped to 2.25 episodes per patient in the pandemic period. Adjusting for social movements, the ITS analysis showed significant decreases in the original trends of ongoing service use in all diagnosis settings (RRs ranged from 0.96 to 0.99, all p < 0.01) before the pandemic (Table 2 and Fig. 3 ). When the pandemic began, there were immediate decreases in service use indicated by significant level changes in inpatient admission episodes (RR = 0.91, 95% CI: 0.83–0.99, p = 0.024), inpatient bed-days (RR = 0.87, 95% CI: 0.78–0.96, p = 0.017), outpatient all-cause visits (RR = 0.83, 95% CI: 0.76–0.91, p < 0.001), outpatient psychiatric visits (RR = 0.77, 95% CI: 0.74–0.83, p < 0.001), and overall all-cause visits (RR = 0.84, 95% CI: 0.76–0.92, p < 0.001), but not emergency visits. Regarding gradual effects, there were significant but small slope changes during the pandemic across all diagnosis settings except inpatient bed-days, with RRs ranging from 1.02 to 1.03, indicating a gradual rebound over time (Table 2 and Fig. 3 ).
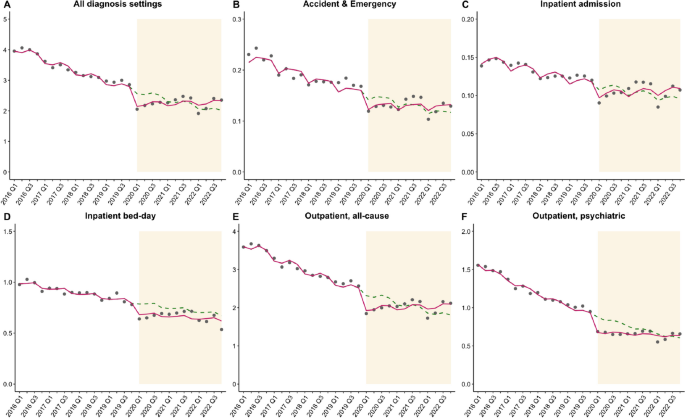
Impact of the pandemic on the ongoing healthcare resource utilization among the 2014–2016 cohorts
In the sensitivity analyses accounting for the fifth-wave outbreak and changing definition of disease duration prior to the pandemic, effect sizes were largely consistent with those in the main analysis (Additional file 2 : Tables S13–S14).
Using a 9-year population-based study with a quasi-experimental design, we present the immediate and long-term impacts of 3 years of the pandemic on depression burden. We found a 21% immediate increase in incidence of medically attended depression, with 19% and 33% increases among adults and the older population during the 3-year period. There was no significant slope change during the pandemic, indicating a sustained effect towards the end of 2022. Though the pandemic did not affect incidence among adolescents, the incidence had been rising significantly in this subgroup over time even before the pandemic. Despite the increasing overall incidence, patients newly diagnosed during the pandemic used 11% fewer resources in their year of diagnosis than the pre-pandemic patients. Patients with pre-existing depression also had an immediate decrease by 16% in overall all-cause visits, with a positive slope change which suggests a gradual rebound over 3 years.
Rising incidence of medically attended depression
Our findings are largely consistent with the previous literature that has reported an increased prevalence of depressive mood during the pandemic [ 7 , 8 , 9 , 10 , 11 ]. However, the results from EMR-based studies that focused on clinically confirmed incident diagnoses were mixed. A cohort study based on the UK Biobank reported a 2.0- to 3.1-fold increase in new diagnoses of depressive or anxiety disorders compared to the pre-pandemic period, especially in the first 6 months of the pandemic [ 36 ]. Another Israeli time-series analysis observed a 36% increase in depression incidence among youth [ 37 ]. Conversely, population-based time-series and cohort studies in the UK found a 28% to 43% decline in recorded depression incidence with a gradual return towards pre-pandemic rates [ 38 , 39 ]. One explanation for such discrepancies is service disruption during lockdowns that led to under-diagnoses in primary care systems. Alternatively, the nature of social measures may have contributed to the trends differently. Costa-Font et al. highlighted that a “preventive lockdown” when there was low mortality appeared to increase depressive symptoms, but it was the opposite when lockdowns were in a high-mortality context [ 40 ]. This echoes with our findings in Hong Kong, where control measures were mostly preventive following the “dynamic zero-COVID” approach while maintaining low case load most of the time.
In our subgroup analysis, we found that adults and the older population were prone to developing depression due to the pandemic, but adolescents were not. However, prior studies tend to report consistent risks across age groups: adults were likely to suffer from job insecurity and increased caregiver responsibilities, older adults were susceptible to prolonged isolation, fear of illness, and grief of losing the loved ones, while adolescents faced school closures, reduced peer interactions, and outdoor activities [ 37 , 41 , 42 , 43 , 44 ]. Between 2014 and 2019, we found the incidence among Hong Kong adolescents was already increasing, with rates doubling within 5 years and overtaking the incidence among adults and the older population. This pre-existing rising trend might explain why the pandemic, despite being an additional risk factor, did not have as comparable impact as in other age groups due to a potential diminishing marginal effect. The earlier rise in adolescent depression may have stemmed from existing contextual forces including social unrest and other unknown stressors [ 35 ]. Our findings suggest that resources for depression care among adults and the older population are needed to prepare for future pandemic threats. However, policymakers should be aware of the worrying mental health situation in adolescents. As the rising incidence was minimally linked to the pandemic in this subgroup, it implies that the mental health crisis could persist in the future regardless of the pandemic. Further investigation is needed to confirm the stressors behind the recent trend and ways to reverse the deterioration in adolescent mental health.
Declining use of healthcare resources
Given the increased demand for depression care during the pandemic, evaluating the pattern in healthcare service use in this critical period is important to identify potential unmet care needs, optimize strategies of service provision, and strengthen the preparedness for future pandemics. Despite the rising incidence, we found that the pandemic substantially reduced the use of inpatient and outpatient services among both newly diagnosed and pre-existing patients. This is consistent with the previous studies in South Africa, South Korea, the United States, and the UK, which estimated 15% to 51% reductions in healthcare resource utilization depending on diagnosis settings [ 15 , 17 , 45 , 46 ]. Most of them were conducted during the early phase of the pandemic with a focus on lockdowns. This may explain the generally greater decline in service use compared with our observations for Hong Kong. Among the pre-existing patients, the reductions in service use were unlikely to represent an immediate improvement in depression outcomes but rather the limited capacity of the system even without mobility restriction to access. This also affected the care delivery for the rising number of new patients during the pandemic, who need the greatest care in the first years of diagnosis but accessed less care than historical controls. The findings therefore revealed a suboptimal service provision in response to the extra care demand generated by the pandemic.
In our study, the service types most impacted by the pandemic were the inpatient bed-days for newly diagnosed patients and outpatient psychiatric visits for pre-existing patients. This is consistent with the observation that most inpatient care occurred at the beginning of the disease course, while outpatient follow-ups became more common as patients stabilized. During the pandemic, however, inpatient resources were reserved for outbreak control, leaving the new patients with inadequate service access. Among pre-existing patients, reluctance to visit clinics owing to fear of getting infected may have discouraged them from attending regular appointments [ 47 ]. Video consultations for SARS-CoV-2 infected cases have been initiated since July 2022, which led to 214,900 consultations for quarantined patients [ 48 ]. “Tele-psychiatry” in the post-pandemic era is worth investigation for its feasibility and effectiveness in extending continuity of care, as it enables follow-ups after hospital discharge and ensures ongoing patient access even without physical attendance.
Strengths and limitations
One of the major strengths of our study is the use of territory-wide longitudinal data with a large sample size, which allowed a quasi-experimental study design. This enabled us to investigate the population-level impact of the pandemic and validate prior findings from smaller community-based studies. The context of Hong Kong also enabled us to study the longer-term impact of the entire pandemic apart from a focus on lockdowns. When studying healthcare service use, our study differed from previous studies by separating patients into nine incident cohorts before analyzing their rates of service use during the follow-up. This allowed us to differentiate the pandemic impact more clearly on new and pre-existing patients, unlike most of the previous studies.
There are also limitations to our study. Firstly, patients’ decision to seek treatment mediates whether their condition is recorded. Systematic differences between age groups in the propensity to seek treatment during different periods rather than differences in the underlying population-level burden may have driven the trends before and after 2020. Secondly, we were unable to stratify the patterns of service use into all-cause and psychiatric-related use in the emergency and inpatient settings since such information was not available in the raw data. Thirdly, though the public sector provides the majority of local healthcare services, patients may have sought help from private doctors especially when the public healthcare system was overwhelmed at the start of the fifth-wave outbreak, possibly leading to underestimated incidence and healthcare service use. Patients who were diagnosed in private clinics before seeking care in the public sector may also be labeled as incident cases later than actual diagnosis date. We therefore performed sensitivity analyses but found no change in the conclusion. Lastly, the findings represent the mixed overall effect of the pandemic macro-environment, but the current time-series study was unable to disentangle the effects of specific contributing factors.
Using ITS analyses from a 9-year cohort study, we found a persistent increase in incidence of medically attended depression over the pandemic period in the overall population, adults, and the older population. However, patients newly diagnosed during the pandemic used fewer resources in their first year of diagnosis than pre-pandemic patients. Pre-existing patients also had immediate decreases in healthcare service use following the pandemic in all diagnosis settings, with a gradual rebound over 3 years. Our findings highlight the need to improve the preparedness in mental health resource planning for future public health crises.
Availability of data and materials
We are unable to directly share the data used in this study since the data custodian, the Hong Kong Hospital Authority who manages the Clinical Data Analysis and Reporting System (CDARS), has not given permission. However, CDARS data can be accessed via the Hospital Authority Data Sharing Portal for research purpose. The relevant information can be found online ( https://www3.ha.org.hk/data ).
Abbreviations
Clinical Data Analysis and Reporting System
- Electronic medical records
Interrupted time-series
World Health Organization. WHO Coronavirus (COVID-19) dashboard. https://covid19.who.int . Published 2023. Accessed 29 Mar 2023.
Borkowska M, Laurence J. Coming together or coming apart? Changes in social cohesion during the COVID-19 pandemic in England. Eur Soc. 2021;23(sup1):S618–36.
Article Google Scholar
Chew CC, Lim XJ, Chang CT, Rajan P, Nasir N, Low WY. Experiences of social stigma among patients tested positive for COVID-19 and their family members: a qualitative study. BMC Public Health. 2021;21(1):1623.
Article CAS PubMed PubMed Central Google Scholar
ElTohamy A, Hyun S, Macaranas AR, Chen JA, Stevens C, Liu CH. Testing positive, losing a loved one, and financial hardship: real-world impacts of COVID-19 on US college student distress. J Affect Disord. 2022;314:357–64.
Article PubMed PubMed Central Google Scholar
Beland LP, Brodeur A, Wright T. The short-term economic consequences of COVID-19: exposure to disease, remote work and government response. PLoS ONE. 2023;18(3):e0270341.
World Health Organization. Third round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report—November-December 2021. Geneva: World Health Organisation; 2022.
Covid-Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–12.
Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2022;52(14):3222–30.
Article PubMed Google Scholar
Kim SJ, Sohn S, Choi YK, et al. Time-series trends of depressive levels of Korean adults during the 2020 COVID-19 pandemic in South Korea. Psychiatry Investig. 2023;20(2):101–8.
Mooldijk SS, Dommershuijsen LJ, de Feijter M, Luik AI. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. 2022;149:274–80.
Zhao SZ, Wong JYH, Luk TT, Wai AKC, Lam TH, Wang MP. Mental health crisis under COVID-19 pandemic in Hong Kong, China. Int J Infect Dis. 2020;100:431–3.
Lee Y, Lui LMW, Chen-Li D, et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J Affect Disord. 2021;290:364–77.
Zhai Y, Du X. Trends and prevalence of suicide 2017–2021 and its association with COVID-19: interrupted time series analysis of a national sample of college students in the United States. Psychiatry Res. 2022;316:114796.
Steeg S, Bojanic L, Tilston G, et al. Temporal trends in primary care-recorded self-harm during and beyond the first year of the COVID-19 pandemic: time series analysis of electronic healthcare records for 2.8 million patients in the Greater Manchester Care Record. EClinicalMedicine. 2021;41:101175.
Liberman JN, Bhattacharjee S, Rui P, et al. Impact of the COVID-19 pandemic on healthcare resource utilization in individuals with major depressive disorder. Health Serv Res Manag Epidemiol. 2022;9:23333928221111864.
PubMed PubMed Central Google Scholar
Lear-Claveras A, Claveria A, Couso-Viana S, Nabbe P, Olivan-Blazquez B. Analysis of drug and health resource use before and after COVID-19 lockdown in a population undergoing treatment for depression or anxiety. Front Psychol. 2022;13:861643.
Wettstein A, Tlali M, Joska JA, et al. The effect of the COVID-19 lockdown on mental health care use in South Africa: an interrupted time-series analysis. Epidemiol Psychiatr Sci. 2022;31:e43.
MacNeil A, Birk S, Villeneuve PJ, Jiang Y, de Groh M, Fuller-Thomson E. Incident and recurrent depression among adults aged 50 years and older during the COVID-19 pandemic: a longitudinal analysis of the Canadian longitudinal study on aging. Int J Environ Res Public Health. 2022;19(22):15032.
Frangou S, Travis-Lumer Y, Kodesh A, et al. Increased incident rates of antidepressant use during the COVID-19 pandemic: interrupted time-series analysis of a nationally representative sample. Psychol Med. 2023;53(11):4943–51.
Burki T. Hong Kong’s fifth COVID-19 wave-the worst yet. Lancet Infect Dis. 2022;22(4):455–6.
Luo H, Lau WCY, Chai Y, et al. Rates of antipsychotic drug prescribing among people living with dementia during the COVID-19 pandemic. JAMA Psychiat. 2023;80(3):211–9.
Huang C, Wei Y, Yan VKC, et al. Vaccine effectiveness of BNT162b2 and CoronaVac against SARS-CoV-2 omicron infection and related hospital admission among people with substance use disorder in Hong Kong: a matched case-control study. Lancet Psychiatry. 2023;10(6):403–13.
Chan VK, Cheung EC, Chan SS, et al. Mortality-causing mechanisms and healthcare resource utilisation of treatment-resistant depression: a six-year population-based cohort study. Lancet Reg Health West Pac. 2022;22:100426.
Chan VKY, Luo H, Chan SSM, et al. Treatment-resistant depression and risk of autoimmune diseases: evidence from a population-based cohort and nested case-control study. Transl Psychiatry. 2023;13(1):76.
Census and Statistics Department. Thematic household survey report - report no. 58 - health status of Hong Kong residents. https://www.censtatd.gov.hk/en/data/stat_report/product/B1130201/att/B11302582015XXXXB0100.pdf . Published 2015. Accessed 21 Dec 2023.
Lagarde M. How to do (or not to do) … Assessing the impact of a policy change with routine longitudinal data. Health Policy Plan. 2012;27(1):76–83.
Hale T, Angrist N, Goldszmidt R, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav. 2021;5(4):529–38.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–55.
PubMed Google Scholar
Xiao H, Augusto O, Wagenaar BH. Reflection on modern methods: a common error in the segmented regression parameterization of interrupted time-series analyses. Int J Epidemiol. 2021;50(3):1011–5.
Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42(4):1187–95.
Bottomley C, Scott JA, Isham V. Analysing interrupted time series with a control. Epidemiol Methods. 2019;8(1):20180010.
Newey WK, West KD. Automatic lag selection in covariance-matrix estimation. Rev Econ Stud. 1994;61(4):631–53.
Wan KM, Ka-Ki Ho L, Wong NWM, Chiu A. Fighting COVID-19 in Hong Kong: the effects of community and social mobilization. World Dev. 2020;134:105055.
Hou WK, Li TW, Liang L, et al. Trends of depression and anxiety during massive civil unrest and COVID-19 in Hong Kong, 2019–2020. J Psychiatr Res. 2021;145:77–84.
Ni MY, Yao XI, Leung KSM, et al. Depression and post-traumatic stress during major social unrest in Hong Kong: a 10-year prospective cohort study. Lancet. 2020;395(10220):273–84.
Wang Y, Ge F, Wang J, et al. Trends in incident diagnoses and drug prescriptions for anxiety and depression during the COVID-19 pandemic: an 18-month follow-up study based on the UK Biobank. Transl Psychiatry. 2023;13(1):12.
Bilu Y, Flaks-Manov N, Bivas-Benita M, et al. Data-driven assessment of adolescents’ mental health during the COVID-19 pandemic. J Am Acad Child Adolesc Psychiatry. 2023;62:920–37.
Qi C, Osborne T, Bailey R, et al. Effect of the COVID-19 pandemic on incidence of long-term conditions in Welsh residents: a population linkage study. Lancet. 2022;400 Suppl 1:S69.
Carr MJ, Steeg S, Webb RT, et al. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. Lancet Public Health. 2021;6(2):e124–35.
Costa-Font J, Knapp M, Vilaplana-Prieto C. The ‘welcomed lockdown’ hypothesis? Mental wellbeing and mobility restrictions. Eur J Health Econ. 2023;24(5):679–99.
Grolli RE, Mingoti MED, Bertollo AG, et al. Impact of COVID-19 in the mental health in elderly: psychological and biological updates. Mol Neurobiol. 2021;58(5):1905–16.
de Figueiredo CS, Sandre PC, Portugal LCL, et al. COVID-19 pandemic impact on children and adolescents’ mental health: biological, environmental, and social factors. Prog Neuropsychopharmacol Biol Psychiatry. 2021;106:110171.
Webb LM, Chen CY. The COVID-19 pandemic’s impact on older adults’ mental health: Contributing factors, coping strategies, and opportunities for improvement. Int J Geriatr Psychiatr. 2022;37:1–7.
Bafail DA. Mental health issues associated with COVID-19 among the elderly population: a narrative review. Cureus. 2022;14(12):e33081.
Seo JH, Kim SJ, Lee M, Kang JI. Impact of the COVID-19 pandemic on mental health service use among psychiatric outpatients in a tertiary hospital. J Affect Disord. 2021;290:279–83.
Mansfield KE, Mathur R, Tazare J, et al. Indirect acute effects of the COVID-19 pandemic on physical and mental health in the UK: a population-based study. Lancet Digit Health. 2021;3(4):e217–30.
Einav S, Tankel J. The unseen pandemic: treatment delays and loss to follow-up due to fear of COVID. J Anesth Analg Crit Care. 2022;2(1):5.
The Government of the Hong Kong Special Administrative Region. LCQ19: Designated clinics and tele-consultation service under the Hospital Authority [Press release]. https://www.info.gov.hk/gia/general/202302/15/P2023021500405.htm . Assessed 21 Dec 2023.
Download references
Acknowledgements
We thank Ms. Qiwen Fang and Ms. Yin Zhang for assistance in data retrieval; Dr. Deliang Yang and Ms. Jin Lee for statistical advice and support; we also thank Ms. Lisa Lam for English proofreading.
The study was jointly supported by the Collaborative Research Fund (ACESO, C7154-20GF), the Research Impact Fund (SCAN-2030, R7007-22) granted by the Research Grant Council, University Grants Committee, and the Health and Medical Research Fund (COVID19F04; COVID19F11) granted by the Health Bureau, The Government of the Hong Kong Special Administrative Region, and the Laboratory of Data Discovery for Health (D 2 4H) funded by the Innovation and Technology Commission for data during the pandemic, modeling depression burden between 2014 and 2022. The funders had no active role in the design and conduct of the work and in the analysis, interpretation, and preparation of study reports.
Author information
Vivien Kin Yi Chan and Yi Chai are co-first authors with equal contribution.
Authors and Affiliations
Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
Vivien Kin Yi Chan, Yi Chai, Ian Chi Kei Wong & Xue Li
The Hong Kong Jockey Club Centre for Suicide Research and Prevention, The University of Hong Kong, Hong Kong SAR, China
Department of Psychiatry, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
Sandra Sau Man Chan
Department of Social Work and Social Administration, Faculty of Social Sciences, The University of Hong Kong, Hong Kong SAR, China
Hao Luo & Martin Knapp
Department of Infectious Disease Epidemiology, London School of Hygiene & Tropical Medicine, London, UK
Care Policy and Evaluation Centre, Department of Health Policy, London School of Economics and Political Science, London, UK
Martin Knapp
School of Public Health, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
Mark Jit, David Makram Bishai & Michael Yuxuan Ni
The State Key Laboratory of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong SAR, China
Michael Yuxuan Ni
Urban Systems Institute, The University of Hong Kong, Hong Kong SAR, China
Laboratory of Data Discovery for Health (D24H), Hong Kong SAR, China
Ian Chi Kei Wong & Xue Li
School of Pharmacy, Aston University, London, UK
Ian Chi Kei Wong
Department of Medicine, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
Advanced Data Analytics for Medical Science (ADAMS) Limited, Hong Kong SAR, China
You can also search for this author in PubMed Google Scholar
Contributions
X Li and ICK Wong conceived the study idea and study design. VKY Chan and Y Chai gathered the data and performed data analyses. All authors provided clinical, statistical, and epidemiological advice and interpreted the results. VKY Chan and X Li wrote and revised the drafts with all authors’ critical comments and revisions. All authors agree to be accountable for all aspects of the work. X Li and ICK Wong obtained the funding and supervised the study conduct. The corresponding authors confirm that all co-authors meet authorship criteria. All authors read and approved the final manuscript.
Authors’ Twitter handles
Vivien Kin Yi Chan: @vivienkinyichan
Martin Knapp: @knappem
Hao Luo: @HaoLuo429
Ian Chi Kei Wong: @Ian_HKU
Xue Li: @snowly12191
HKU Pharmacy: @HkuPharm
Corresponding authors
Correspondence to Ian Chi Kei Wong or Xue Li .
Ethics declarations
Ethics approval and consent to participate.
This study received ethics approval from the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong Western Cluster (UW 20-218). Informed consent has been waived as the study utilized de-identified data.
Consent for publication
Not applicable.
Competing interests
X Li received research grants from the Hong Kong Health and Medical Research Fund (HMRF, HMRF Fellowship Scheme, HKSAR), Research Grants Council Early Career Scheme (RGC/ECS, HKSAR), Janssen, and Pfizer; internal funding from the University of Hong Kong; and consultancy fees from Merck Sharp & Dohme and Pfizer; she is also a non-executive director of Advanced Data Analytics for Medical Science (ADAMS) Limited Hong Kong; all are unrelated to this work. ICK Wong received research funding outside the submitted work from Amgen, Bristol-Myers Squibb, Pfizer, Janssen, Bayer, GSK, Novartis, Takeda, the Hong Kong Research Grants Council, the Hong Kong Health and Medical Research Fund, National Institute for Health Research in England, European Commission, National Health and Medical Research Council in Australia, and the European Union’s Seventh Framework Programme for research and technological development. He has also received consulting fees from IQVIA, the WHO, and expert testimony for Appeal Court in Hong Kong over the past 3 years. He is an advisory member of Pharmacy and Poisons Board, Expert Committee on Clinical Events Assessment Following COVID-19 Immunization, and the Advisory Panel on COVID-19 Vaccines of the Hong Kong Government. He is also a non-executive director of Jacobson Medical Hong Kong, Advanced Data Analytics for Medical Science (ADAMS) Limited, and OCUS Innovation Limited (Hong Kong, Ireland, and UK), and the founder and a director of Therakind Limited (UK). Other authors declared no competing interests related to this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: figure s1..
Study schema to illustrate the linkage between analyses.
Additional file 2: Table S1.
Age and sex distribution of patients newly diagnosed with depression between 2014 and 2022. Table S2. Quarterly age-standardized incidence and counts of patients newly diagnosed with depression between 2014 to 2022. Table S3. Quarterly counts of accident & emergency visit among incident cohorts between 2014 and 2022. Table S4. Quarterly counts of inpatient admission among incident cohorts between 2014 and 2022. Table S5. Quarterly counts of inpatient stay among incident cohorts between 2014 and 2022. Table S6. Quarterly counts of outpatient all-cause visit among incident cohorts between 2014 and 2022. Table S7. Quarterly counts of outpatient psychiatric-related visit among incident cohorts between 2014 and 2022. Table S8. Quarterly rates of accident & emergency visit among incident cohorts between 2014 and 2022. Table S9. Quarterly rates of inpatient admission among incident cohorts between 2014 and 2022. Table S10. Quarterly rates of inpatient stay among incident cohorts between 2014 and 2022. Table S11. Quarterly rates of outpatient all-cause visit among incident cohorts between 2014 and 2022. Table S12. Quarterly rates of outpatient psychiatric-related visit among incident cohorts between 2014 and 2022. Table S13. Sensitivity analysis results of ITS analysis of pandemic impact on the ongoing healthcare resource utilization among the 2014-2016 cohorts by adjusting for the fifth-wave outbreak. Table S14. Sensitivity analysis results of ITS analysis of pandemic impact on the ongoing healthcare resource utilization among the 2014-2017 cohorts (changing the defined disease duration prior to the pandemic from 3 years to 2 years).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chan, V.K.Y., Chai, Y., Chan, S.S.M. et al. Impact of COVID-19 pandemic on depression incidence and healthcare service use among patients with depression: an interrupted time-series analysis from a 9-year population-based study. BMC Med 22 , 169 (2024). https://doi.org/10.1186/s12916-024-03386-z
Download citation
Received : 04 December 2023
Accepted : 09 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s12916-024-03386-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health resource utilization
- Health service use
- Interrupted time series
- Cohort study
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 29 April 2024
Cognitive profile in multiple sclerosis and post-COVID condition: a comparative study using a unified taxonomy
- Cristina Delgado-Alonso 1 ,
- Alfonso Delgado-Alvarez 1 ,
- María Díez-Cirarda 1 ,
- Silvia Oliver-Mas 1 ,
- Constanza Cuevas 1 ,
- Paloma Montero-Escribano 1 ,
- Ana Maria Ramos-Leví 2 ,
- María José Gil-Moreno 1 ,
- Juan Ignacio López-Carbonero 1 ,
- Bruce P. Hermann 3 ,
- Jorge Matias-Guiu 1 &
- Jordi A. Matias-Guiu ORCID: orcid.org/0000-0001-5520-2708 1
Scientific Reports volume 14 , Article number: 9806 ( 2024 ) Cite this article
538 Accesses
49 Altmetric
Metrics details
- Central nervous system infections
- Multiple sclerosis
Post-COVID condition (PCC) and multiple sclerosis (MS) share some clinical and demographic features, including cognitive symptoms and fatigue. Some pathophysiological mechanisms well-known in MS, such as autoimmunity, neuroinflammation and myelin damage, have also been implicated in PCC. In this study, we aimed to compare the cognitive phenotypes of two large cohorts of patients with PCC and MS, and to evaluate the relationship between fatigue and cognitive performance. Cross-sectional study including 218 patients with PCC and 218 with MS matched by age, sex, and years of education. Patients were evaluated with a comprehensive neuropsychological protocol and were categorized according to the International Classification of Cognitive Disorders system. Fatigue and depression were also assessed. Cognitive profiles of PCC and MS largely overlapped, with a greater impairment in episodic memory in MS, but with small effect sizes. The most salient deficits in both disorders were in attention and processing speed. The severity of fatigue was greater in patients with PCC. Still, the correlations between fatigue severity and neuropsychological tests were more prominent in the case of MS. There were no differences in the severity of depression among groups. Our study found similar cognitive profiles in PCC and MS. Fatigue was more severe in PCC, but was more associated with cognitive performance in MS. Further comparative studies addressing the mechanisms related to cognitive dysfunction and fatigue may be of interest to advance the knowledge of these disorders and develop new therapies.
Similar content being viewed by others

An autoantibody signature predictive for multiple sclerosis

Prasinezumab slows motor progression in rapidly progressing early-stage Parkinson’s disease

Long COVID: plasma levels of neurofilament light chain in mild COVID-19 patients with neurocognitive symptoms
Introduction.
Cognitive dysfunction and fatigue are commonly reported after the acute phase of SARS-CoV-2 infection and have been emphasized as the most frequent symptoms by the World Health Organization in the post-COVID condition or Long-COVID (PCC) 1 . Several studies have confirmed the presence of objective cognitive deficits in neuropsychological assessments 2 , 3 . PCC occurs mainly in middle and working age, and women are predominant 4 , 5 , 6 , 7 . Cognitive deficits are more prominent in attention and processing speed, episodic memory and executive function and have been linked to structural and functional brain changes in neuroimaging studies 8 , 9 , 10 , 11 , 12 , 13 . A longitudinal study showed greater reductions in cortical thickness and brain volumes in patients after COVID-19 than in healthy controls compared with neuroimaging acquired before the pandemic 14 . A recent study has also associated fatigue in PCC with structural imaging changes in the thalamus and basal ganglia 15 .
Similarly, most patients with Multiple Sclerosis (MS) also report fatigue and cognitive deficits. Cognitive deficits are especially focused on attention and processing speed impairment, followed by executive function and episodic memory. MS is a recognized autoimmune disorder, and cognitive deficits have been linked to cortical and subcortical structural and functional brain damage 16 , 17 .
Although the pathophysiology of PCC and the neurological symptoms of PCC is still unknown, several studies suggest mechanisms of neuroinflammation, autoimmune disorders, myelin dysregulation, and reactivation of another virus (such as Epstein-Barr infection) 18 , 19 . Although in a different clinical course and extent, these mechanisms are at least partially shared with MS. Besides, the role of Epstein-Barr virus or other viral infections in the development of MS and/or disease activity is supported by some studies 20 . Overall, this suggests an interest in evaluating the similarities and differences in the cognitive profiles of patients with PCC and MS. Comparative studies may also be useful to contextualize the cognitive deficits found in PCC, which have important socioeconomic consequences 21 . However, to our knowledge, there are no studies comparing cognitive dysfunction associated with PCC and MS. In addition, the relationship between fatigue and cognitive performance is still unclear. Previous studies in MS have found that cognitive tests assessing vigilance and alertness are more related to fatigue, which could be caused by shared mechanisms associated with brain atrophy and neurochemical dysfunction 22 . In PCC, fatigue has also correlated with some attentional tests 23 , 24 . Thus, this study aimed to compare the cognitive phenotypes of two large cohorts of patients with PCC and MS that were examined with the same neuropsychological protocol. We also aimed to evaluate the relationships between fatigue, and cognitive performance in the two cohorts. We also compared the frequency of depression, which is a relevant factor in both MS and PCC 25 , 26 , 27 .
Study design and participants
We conducted a cross-sectional investigation including patients with PCC and MS involved in previous research studies evaluating the cognitive characteristics of these disorders 28 , 29 . Patients were recruited from specific clinical programs dedicated to diagnosing and treating individuals with PCS and MS, where comprehensive neuropsychological assessment were integrated into the clinical protocol. The research protocol was approved by the Ethics Committee of our center (Comité de Ética de la Investigación con Medicamentos del Hospital Clínico San Carlos). Written informed consent was obtained from all participants.
Patients with PCC met the following criteria: (a) Diagnosis of COVID-19 confirmed by RT-PCR; (b) cognitive complaints or fatigue in close relationship with SARS-CoV-2 infection; (c) WHO criteria for Post-COVID-19 condition 1 . Exclusion criteria were as follows: (a) any cognitive complaint before COVID-19; (b) any medical, systemic, neurological or developmental comorbidity potentially linked to cognitive dysfunction; (c) history of alcohol or drug abuse; (d) neuropsychiatric disorders not attributable to PCC; (e) any sensory or motor disorder potentially biasing assessments.
Patients with MS met the following criteria: (a) diagnosis of MS according to the 2010 McDonald criteria 30 ; (2) age between 18 and 80 years. Exclusion criteria were as follows: (a) a relapse within the previous two months or active treatment with corticosteroids; (b) any other medical, systemic, neurological or developmental comorbidity potentially causing cognitive impairment; (c) history of alcohol or drug abuse; (d) neuropsychiatric disorders not attributable to MS; (e) sensory or motor disorder biasing assessments.
From an initial sample of 240 patients with PCC (mean age 48.42 ± 10.84 years, 77.9% of women, mean time since the acute infection of 17.48 ± 8.43 months), and 298 patients with MS (mean age 48.09 ± 9.84 years, 69.8% of women, mean duration of disease of 15.87 ± 7.85 years), a matched sample of 436 participants (218 per group) was obtained. The main clinical and demographic characteristics of each group and the vaccination status are presented in Table 1 . Time of SARS-CoV-2 infection (month and year) leading to PCC and time of assessments is shown in Supplementary Fig. 1 .
Neuropsychological and behavioral assessments
Patients were evaluated with a comprehensive neuropsychological protocol that is mainly based on the cognitive tests included in the Neuronorma battery. This was a set of neuropsychological tests co-normed in our country in older and young people 31 , 32 and has been validated in several diseases 33 . Previous works by our group implemented this battery to describe the cognitive profile in patients with MS and recently in PCC 28 , 29 . This battery was administered by trained neuropsychologists. The following tests were shared in the assessment of patients with PCC and MS and were included in the present study: forward and backward digit span, Corsi block-tapping test, Symbol Digit Modalities Test, Boston Naming Test (BNT), Judgment Line Orientation (JLO), Rey-Osterrieth Complex Figure (ROCF) (copy and recall at 3, 30 min, and recognition), Free and Cued Selective Reminding Test (FCSRT) (total free recall, total recall, delayed free recall, and delayed total recall), verbal fluencies (animals and words beginning with “ p ” and “m” in 1 min each one), Stroop Color-Word Interference Test.
Furthermore, patients were evaluated with the Modified Fatigue Impact Scale (MFIS) 34 . MFIS contains 21 items related to cognitive, physical, and psychosocial dimensions of fatigue, which are scored using a Likert-type scale. The assessment evaluates the impact of fatigue in the past 4 weeks. Additionally, depression was assessed with the Beck Depression Inventory-II 32 . Following previous literature, we used a cut-off of ≥ 38 to delineate fatigue and ≥ 19 to define moderate to severe depression 34 , 35 .
Statistical analysis
Statistical analysis was conducted using IBM(R) SPSS v26.0, JASP v0.16.1 and R software 36 . Figures were prepared using the ggplot2 package (v3.4.1). Using MedCalc 20.218, patients with MS and PCC were matched 1:1 according to sex, age (± 3 years), and years of education (± 3 years). The two independent samples t-test was used to compare the two groups. Effect sizes were estimated with Cohen’s d, and were classified as small (d = 0.2–0.49), moderate (d = 0.5–0.79), and large (d ≥ 0.8).
We calculated the percentage of impairment of each test according to the normative data correcting by age, years of education, and sex when needed. Normative data are based on a multicenter study conducted in Spain before the pandemic 31 , 32 . In addition, we used the criteria proposed by IC-CoDiMS and IC-CoDi-COVID groups to describe the cognitive phenotypes in patients with MS and PCC, respectively 37 , 38 . In this taxonomy, initially developed for epilepsy as IC-CoDE 39 , 40 , a domain is considered impaired when two tests within the same domain fall below the cutoff. For this study, we used -1 S.D as the cutoff to define impairment, according to the findings of the previous studies in both MS and PCC using these criteria 37 , 38 . Five cognitive domains are considered: attention/processing speed, executive function, language, visuospatial, and episodic memory. Then, according to the number of domains impaired, the patients are classified as: cognitively intact, single-domain impairment, bi-domain impairment, or multi-domain impairment (≥ 3 impaired domains). The tests specified in Table 2 were used to describe each cognitive domain. The chi-squared test was used to compare cognitive phenotypes between MS and PCC.
Pearson’s coefficient was used to estimate the correlations between fatigue and neuropsychological tests in PCC and MS. Coefficients < 0.40 were interpreted as a weak correlation, 0.40–0.69 as moderate, and > 0.69 as strong. Fisher r-to-z transformation was calculated to compare between correlation coefficients.
A p -value < 0.05 was considered statistically significant. Due to the number of cognitive tests in the neuropsychological protocol, we also specified those contrasts statistically significant after False-Discovery Rate (FDR) correction in the comparison of cognitive performance between PCC and MS.
Ethical approval
This study was approved by the Ethics and Research Committee from our centre and was performed according to the Declaration of Helsinki and its later amendments.
Comparison between PCC and MS
Patients with MS showed lower raw scores compared to PCC in Corsi forward and backwards, FCSRT (total free recall), ROCF memory at 3 and 30 min, and semantic verbal fluency. Conversely, PCC showed greater fatigue severity measured with MFIS. There were no statistically significant differences in the other neuropsychological tests and depressive symptoms. Effect size was moderate for fatigue, and low for the other significant neuropsychological tests. All results are shown in Table 3 .
Cognitive phenotypes
There were no statistically significant differences in the cognitive phenotypes (χ 2 3.014, p = 0.389). Specifically, 127 (58.25%) of PCC patients were regarded as cognitively intact, and 91 (41.74%) as cognitively impaired, 43 (19.72%) showed single-domain, 27 (12.38%) bi-domain, and 21 (9.63%) generalized impairment. Patients with MS were classified as cognitively intact in 112 cases (51.37%), and cognitively impaired in 106 (48.62%). Of those with impairment, 44 (20.18%) showed single-domain, 38 (17.43%) bi-domain, and 24 (11.00%) generalized impairment (Fig. 1 ).
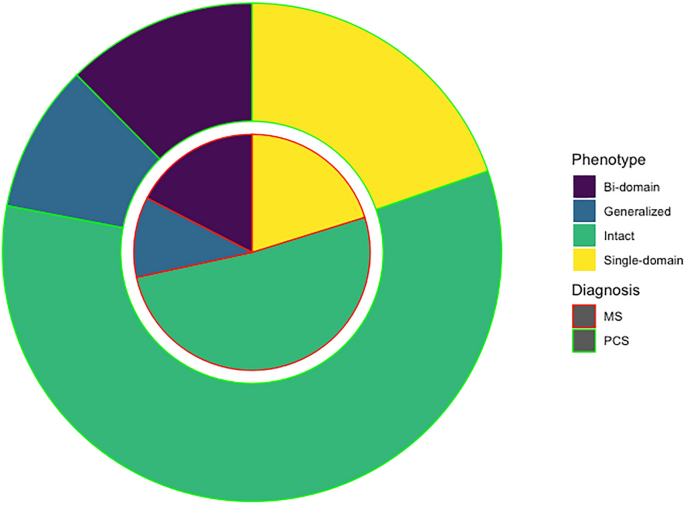
Circle chart representing the cognitive phenotypes in PCC and MS.
Regarding the specific cognitive domains, 63 (28.89%) of PCC and 81 (37.15%) of MS showed impairment in attention/processing speed (χ 2 = 3.36, p = 0.067); 24 (11.00%) and 37 (16.97%) in episodic memory (χ 2 = 3.22, p = 0.073); 41 (18.8%) and 46 (21.10%) in executive function (χ 2 = 0.359, p = 0.549); 14 (6.42%) and 16 (7.33%) in visuospatial function (χ 2 = 0.143, p = 0.705); and 22 (10.09%) and 26 (11.92%) in language (χ 2 = 0.375, p = 0.541). The frequency of impairment of each individual test is shown in Supplementary Fig. 2 . Patients with MS showed higher frequency of impairment in Stroop trial 1 (χ 2 = 6.29, p = 0.012), semantic fluency (χ 2 = 9.86, p = 0.002), letter fluency (χ 2 = 9.42, p = 0.002), ROCF at 3 and 30 min (χ 2 = 6.12, p = 0.013 and χ 2 = 13.28, p < 0.001, respectively), and FCSRT total free recall (χ 2 = 7.20, p = 0.007). The other tests, including SDMT, showed no statistically significant differences ( p > 0.05).
Comparison of cognitive profiles within the groups with cognitive impairment
We also compared those patients meeting the criteria for cognitive impairment with PCC and MS. Patients with MS showed lower scores in ROCF memory at 3 min and 30 min and semantic fluency in age- and education-adjusted scaled scores (Supplementary Table 1 ). Patients with PCC showed greater severity of fatigue (59.95 ± 14.98 vs 54.47 ± 20.89, t = 2.13, p = 0.034). As depicted in Fig. 2 , the represented cognitive profile showed a more prominent impairment in those tests associated with attention and information processing speed.
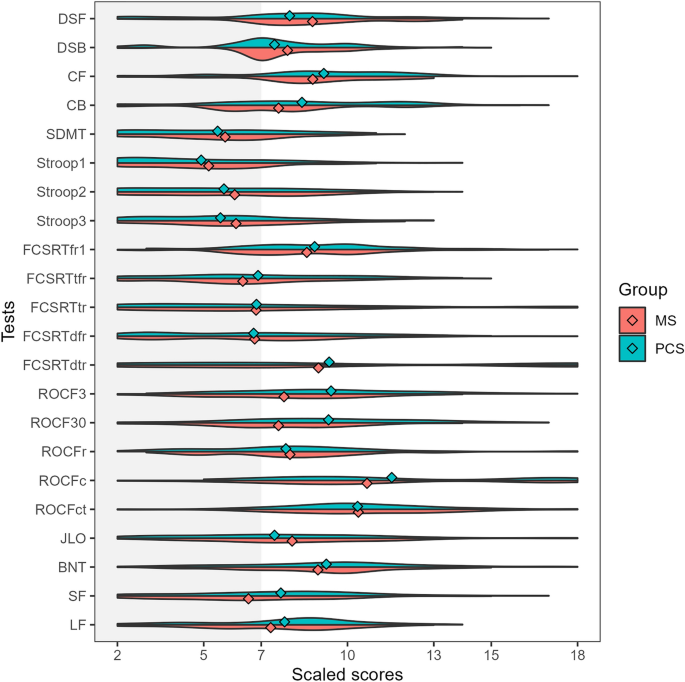
Violin plots representing the adjusted scaled scores (mean 10, standard deviation 3) in each cognitive test in patients with PCC (green) and MS (red) classified as cognitively impaired. The dots represent the mean of each group. DSF digit span forward, DSB digit span backward, CF Corsi forward, CB Corsi backward, SDMT symbol digit modalities test, FCSRT (free and cued selective reminding test, fr1 free recall 1, tfr total free recall, tr total recall, dfr delayed free recall, dtr delayed total recall, ROCF3 Rey-Osterrieth complex figure (memory at 3 min), ROCF30 Rey-Osterrieth complex figure (memory at 30 min), ROCFr Rey-Osterrieth complex figure (memory recognition), ROCFc Rey-Osterrieth complex figure (copy accuracy), ROCFct Rey-Osterrieth complex figure (copy time), JLO judgment line orientation, BNT Boston naming test, SF semantic fluency (animals), LF letter fluency (words beginning with “ p ”).
Correlations between fatigue and neuropsychological tests
All correlations are shown in Fig. 3 . In PCC, MFIS (total score) showed weak correlations with SDMT, FCSRT (total free recall and total recall), Stroop (parts 1, 2, and 3) and semantic and letter fluency. In MS, MFIS (total score) showed moderate correlations with SDMT, FCSRT (free delayed recall and total delayed recall), Stroop test (parts 1 and 2); and weak correlations were found with almost all the other tests.
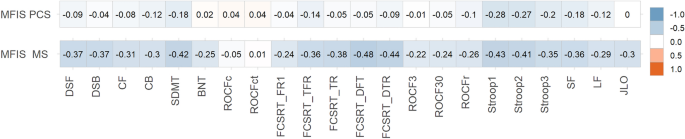
Heatmap showing correlations between MFIS (total score) and neuropsychological tests scores in PCC and MS. The size and direction of the correlation are shown in the right vertical label. DSF digit span forward, DSB digit span backward, CF Corsi forward, CB Corsi backward, SDMT symbol digit modalities test, FCSRT (free and cued selective reminding test), fr1 free recall 1, tfr total free recall, tr total recall, dfr delayed free recall, dtr delayed total recall, ROCF3 Rey-Osterrieth complex figure (memory at 3 min), ROCF30 Rey-Osterrieth complex figure (memory at 30 min), ROCFr Rey-Osterrieth complex figure (memory recognition), ROCFc Rey-Osterrieth complex figure (copy accuracy), ROCFct Rey-Osterrieth complex figure (copy time), JLO judgment line orientation, BNT Boston naming test, SF semantic fluency (animals), LF letter fluency (words beginning with “ p ”).
Patients with MS showed higher correlations than PCC in the following tests: digit span forward (z = 3.02, p = 0.002), digit span backward (r = 3.53, p < 0.001), Corsi forward (Z = 2.45, p = 0.014), SDMT (z = 2.82, p = 0.004), Boston Naming Test (z = 2.81, p = 0.005), FCSRT recall trial 1 (Z = 2.15, p = 0.015), FCSRT total free recall (Z = 2.38, p = 0.017), FCSRT total recall (z = 3.63, p < 0.001), FCSRT delayed free recall (Z = 4.94, p < 0.001), FCSRT delayed total recall (Z = 3.93, p < 0.001), ROCF (memory at 3 min) (Z = 2.26, p = 0.011), ROCF (memory at 30 min) (z = 2.1, p = 0.035), semantic fluency (Z = 2.03, p = 0.04), letter fluency (M-words) (z = 2.64, p = 0.008), letter fluency (R-words) (z = 3.02, p = 0.002), Judgment Line Orientation (Z = 3.26, p = 0.001). There were no statistically significant differences ( p > 0.05) in the comparison of correlation coefficients in Stroop (trials 1, 2, and 3), Corsi backward, ROCF (copy accuracy and time), ROCF (memory recognition), and letter fluency ( P -words).
In this study, we examined the existence of differences in cognitive characteristics between PCC and MS, and the relationship between cognitive function and fatigue. We used two large cohorts of patients that were evaluated with a common neuropsychological protocol. Our study found a significant overlap in cognitive profile between both diseases. Importantly, attention and processing speed were the most pronounced deficits in both disorders, which is consistent with previous studies 2 , 37 , 41 , 42 . Few differences were found in episodic memory tests, which were more impaired in the group of patients with MS than PCC. Similarly, semantic fluency was also more impaired, which could also be linked to the greater impairment of episodic memory 43 . However, effect sizes for these tests were small, confirming that MS and PCC present a very similar cognitive profile.
We applied a novel approach using an international classification of cognitive disorders that is being implemented across several disease groups 37 , 38 , 40 , 44 . This classification system is based on a five-domain cognitive model (attention/processing speed, executive function, episodic memory, visuospatial function, and language) and provides a working definition of impairment to identify cognitive phenotypes and improve cognitive diagnostics. This taxonomy has found reproducible findings across several independent cohorts examined with different neuropsychological batteries in epilepsy 40 , multiple sclerosis 37 and PCC 38 . It has also shown favorable cross-cultural properties in diverse settings 36 . Our study also supports the use of this taxonomy as a valid method for comparative research across disorders.
By comparing both disorders, the similarities in the cognitive characteristics and the severity of deficits contribute to contextualizing the cognitive dysfunction in PCC. In this regard, our findings suggest that cognitive deficits in PCC are almost as pronounced and prevalent as in MS, and fatigue is even more severe, supporting the mounting evidence that fatigue and cognitive dysfunction are associated with occupational issues and socioeconomic consequences 45 , 46 .
The severity and frequency of fatigue was greater in patients with PCC. Interestingly, correlations between MFIS total score (evaluating fatigue impact in the last 4 weeks) and neuropsychological tests were larger in the case of MS. However, the cognitive tests that showed stronger correlations with MFIS were similar in both disorders (e.g., Stroop). This may suggest common mechanisms and neural underpinnings in fatigue and cognitive dysfunction in both disorders, as has been recently described 9 . This opens the way to test new therapies for fatigue based on their association with functional brain changes, such as non-invasive brain stimulation, which have shown positive effects in two clinical trials 47 , 48 . However, at the same time, the lower correlation with neuropsychological tests and the greater severity of fatigue in PCC suggest the existence of other mechanisms (probably not dependent on the central nervous system and including systemic processes such as immune mechanisms, mitochondrial dysfunction or muscle abnormalities) involved in the pathophysiology of fatigue in PCC 24 , 49 , 50 . In contrast, fatigue in MS would be more dependent on central mechanisms.
Another interesting result is the lack of significant differences in the severity and frequency of depressive symptoms. Although neuropsychiatric symptoms have been especially emphasized in PCC, most studies did not include a control group 51 . The prevalence of depression is higher in MS than in the general population, and has been associated with several factors, including genetic and immunological factors, brain changes, and psychosocial factors 52 . Similarly, in PCC, proinflammatory factors and psychosocial factors have been hypothesized, but clear evidence about the pathophysiology of depression is still lacking.
Our study has some limitations. First, although the protocol includes several tests of the main cognitive domains, we acknowledge the possibility of differences between groups if other specific tests are used. In this regard, a more thorough analysis of attention and executive function subdomains may be of interest to further characterize the cognitive mechanisms impaired in each disorder. In this study, we selected only those tests shared by both cohorts to avoid potential differences in the frequency of impairment to the length of the battery or the number of neuropsychological tests and scores. Second, fatigue was only assessed with MFIS, which mainly evaluates the impact of fatigue in daily living. More comprehensive questionnaires may be of interest to evaluate potential differences in the clinical characteristics of fatigue across disorders. Additionally, it could also be of interest to evaluate the feeling of fatigue on the same day of the examination because MFIS considers the fatigue severity in the 4 weeks before the assessment. Third, our study is performed in a single center. However, demographic characteristics and degree of impairment in both PCC and MS are consistent with previous studies of the literature, suggesting that both cohorts are representative of these disorders. In this regard, the most important proportion were infected during the first waves (especially the first in March 2020) and before vaccines were available. Furthermore, we must acknowledge the possibility of selection bias, particularly concerning MS, where individuals with more pronounced motor and cognitive impairments may be less inclined to undergo extensive neuropsychological evaluations. Nevertheless, our study was conducted within a framework where comprehensive neuropsychological assessments are standard practice for both MS and PCS. Additionally, the demographic characteristics of our participants closely resemble those of other large-scale studies published in the field 53 , 54 .
In conclusion, our study finds similar cognitive profiles in PCC and MS, which are mainly characterized by attention and processing speed deficits. Fatigue was more severe in PCC, but the relationship between fatigue and cognitive function was greater in the case of MS. Further comparative studies addressing the mechanisms associated with cognitive dysfunction and fatigue may be of interest to advance the knowledge of these disorders and develop new therapies.
Data availability
The datasets generated and analyzed are available from the corresponding author on reasonable request.
Soriano, J. B., Murthy, S., Marshall, J. C., Relan, P. & Diaz, J. V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 22 , e102–e107 (2022).
Article CAS PubMed Google Scholar
Bertuccelli, M. et al. Cognitive impairment in people with previous COVID-19 infection: A scoping review. Cortex 154 , 212–230 (2022).
Article PubMed PubMed Central Google Scholar
Ceban, F. et al. Brain behavior and immunity fatigue and cognitive impairment in Post-COVID-19 syndrome: A systematic review and meta-analysis. Brain Behav. Immun. 101 , 93–135 (2022).
Article ADS CAS PubMed Google Scholar
Crook, H., Raza, S., Nowell, J., Young, M. & Edison, P. Long covid—mechanisms, risk factors, and management. BMJ 374 , 1–18 (2021).
Google Scholar
Peter, R. S. et al. Post-acute sequelae of covid-19 six to 12 months after infection: Population based study. BMJ 379 , e071050 (2022).
Article PubMed Google Scholar
Bai, F. et al. Female gender is associated with long COVID syndrome: A prospective cohort study. Clin. Microbiol. Infect. 28 , 611 (2022).
Article Google Scholar
Bahmer, T. et al. Severity, predictors and clinical correlates of Post-COVID syndrome (PCS) in Germany: A prospective, multi-centre, population-based cohort study. EClinicalMedicine 51 , 101549 (2022).
Caroli, A. et al. Brain diffusion alterations in patients with COVID-19 pathology and neurological manifestations. NeuroImage Clin. 37 , 103338 (2023).
Díez-Cirarda, M. et al. Multimodal neuroimaging in post-COVID syndrome and correlation with cognition. Brain 146 , 2142–2152 (2023).
Lu, Y. et al. Cerebral micro-structural changes in COVID-19 patients–an MRI-based 3-month follow-up study. EClinicalMedicine 25 , 100484 (2020).
Ajcevic, M. et al. Cerebral hypoperfusion in post-COVID-19 cognitively impaired subjects revealed by arterial spin labeling MRI. Sci. Rep. 13 , 5808 (2023).
Article ADS CAS PubMed PubMed Central Google Scholar
Paolini, M. et al. Brain correlates of subjective cognitive complaints in COVID-19 survivors: A multimodal magnetic resonance imaging study. Eur. Neuropsychopharmacol. 68 , 1–10 (2023).
Zhao, S., Toniolo, S., Hampshire, A. & Husain, M. Effects of COVID-19 on cognition and brain health. Trends Cognit. Sci. 27 , 1053–1067 (2023).
Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature https://doi.org/10.1038/s41586-022-04569-5 (2022).
Heine, J. et al. Articles structural brain changes in patients with post-COVID fatigue: A prospective observational study. eClinicalMedicine 58 , 101874 (2023).
Matías-Guiu, J. A. et al. Identification of cortical and subcortical correlates of cognitive performance in multiple sclerosis using voxel-based morphometry. Front. Neurol. 9 , 1–12 (2018).
Petracca, M. et al. Neuroimaging correlates of cognitive dysfunction in adults with multiple sclerosis. Brain Sci. 11 , 346 (2021).
Article CAS PubMed PubMed Central Google Scholar
Fernández-Castañeda, A. et al. Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. BioRxiv (2022).
Gold, J. E., Okyay, R. A., Licht, W. E. & Hurley, D. J. Investigation of long covid prevalence and its relationship to epstein-barr virus reactivation. Pathogens 10 , 1–15 (2021).
Aloisi, F., Giovannoni, G. & Salvetti, M. Epstein–Barr virus as a cause of multiple sclerosis: Opportunities for prevention and therapy. Lancet. Neurol. 22 , 338–349 (2023).
Perlis, R. H. et al. Association of Post-COVID-19 condition symptoms and employment status. JAMA Netw. Open 6 , e2256152 (2023).
Hanken, K., Eling, P. & Hildebrandt, H. Is there a cognitive signature for MS-related fatigue?. Multiple Scler. 21 , 376–381 (2015).
Calabria, M. et al. Post-COVID-19 fatigue: The contribution of cognitive and neuropsychiatric symptoms. J. Neurol. 269 , 3990–3999 (2022).
Matias-Guiu, J. A. et al. Neuropsychological predictors of fatigue in Post-COVID syndrome. J. Clin. Med. 11 , 1–13 (2022).
Leavitt, V. M. et al. Dissociable cognitive patterns related to depression and anxiety in multiple sclerosis. Multiple Scler 26 , 1247–1255 (2020).
Article CAS Google Scholar
Premraj, L. et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID syndrome: A meta-analysis. J. Neurol. Sci. 434 , 120162 (2022).
Delgado-Alonso, C. et al. Unraveling brain fog in post-COVID syndrome: Relationship between subjective cognitive complaints and cognitive function, fatigue, and neuropsychiatric symptoms. Eur. J. Neurol. https://doi.org/10.1111/ene.16084 (2023).
Delgado-Alonso, C. et al. Cognitive dysfunction associated with COVID-19: A comprehensive neuropsychological study. J. Psychiatr. Res. 150 , 40–46 (2022).
Matías-Guiu, J. A. et al. Validation of the Neuronorma battery for neuropsychological assessment in multiple sclerosis. Multiple Scler. Relat. Disord. 42 , 102070 (2020).
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 69 , 292–302 (2011).
Peña-Casanova, J. et al. Spanish multicenter normative studies (NEURONORMA project): Methods and sample characteristics. Arch. Clin. Neuropsychol. 24 , 307–319 (2009).
Peña-Casanova, J. et al. Estudios normativos españoles en población adulta joven (Proyecto NEURONORMA jóvenes): Métodos y características de la muestra. Neurologia 27 , 253–260 (2012).
Sánchez-Benavides, G. et al. Cognitive and neuroimaging profiles in mild cognitive impairment and Alzheimer’s disease: Data from the Spanish Multicenter Normative Studies (NEURONORMA Project). J. Alzheimer’s Dis. 41 , 887–901 (2014).
Kos, D. et al. Evaluation of the modified fatigue impact scale in four different European countries. Multiple Scler. 11 , 76–80 (2005).
Beck, A. T. Manual for the beck depression inventory-II. (No Title) (1996).
R Core Team. R: A Language and Environment for Statistical Computing. (2022).
Hancock, L. M. et al. A proposed new taxonomy of cognitive phenotypes in multiple sclerosis: The International Classification of Cognitive Disorders in MS (IC-CoDiMS). Multiple Scler. J. 29 , 615–627 (2022).
Matias-Guiu, J. A. et al. Development of criteria for cognitive dysfunction in post-COVID syndrome: The IC-CoDi-COVID approach. Psychiatry Res. 319 , 115006 (2023).
Norman, M. et al. Addressing neuropsychological diagnostics in adults with epilepsy: Introducing the International Classification of Cognitive Disorders in Epilepsy: The IC CODE Initiative. Epilepsia Open 6 , 266–275 (2021).
McDonald, C. R. et al. Development and application of the International Classification of Cognitive Disorders in Epilepsy (IC-CoDE): Initial results from a multi-center study of adults with temporal lobe epilepsy. Neuropsychology 37 , 301–314 (2022).
Gonzalez-Fernandez, E. & Huang, J. Cognitive aspects of COVID-19. Curr. Neurol. Neurosci. Rep. 23 , 531–538 (2023).
Benedict, R. H. B., Amato, M. P., DeLuca, J. & Geurts, J. J. G. Cognitive impairment in multiple sclerosis: Clinical management, MRI, and therapeutic avenues. Lancet Neurol 19 , 860–871 (2020).
Delgado-Álvarez, A. et al. Cognitive processes underlying verbal fluency in multiple sclerosis. Front. Neurol. 11 , 1–11 (2021).
Reyes, A. et al. Establishing the cross-cultural applicability of a harmonized approach to cognitive diagnostics in epilepsy: Initial results of the International Classification of Cognitive Disorders in Epilepsy in a Spanish-speaking sample. Epilepsia 64 , 728–741 (2023).
Delgado-Alonso, C. et al. Fatigue and cognitive dysfunction are associated with occupational status in post-COVID syndrome. Int. J. Environ. Res. Public Health 19 , 13368 (2022).
Moccia, M. et al. Determinants of early working impairments in multiple sclerosis. Front. Neurol. 13 , 1062847 (2022).
Oliver-Mas, S. et al. Transcranial direct current stimulation for post-COVID fatigue: A randomized, double-blind, controlled pilot study. Brain Commun. https://doi.org/10.1093/braincomms/fcad117 (2023).
Santana, K. et al. Non-invasive brain stimulation for fatigue in post-acute sequelae of SARS-CoV-2 (PASC). Brain Stimul. 16 , 100–107 (2023).
Paul, B. D., Lemle, M. D., Komaroff, A. L. & Snyder, S. H. Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome. Proc. Natl. Acad. Sci. 118 , e2024358118 (2021).
Ramakrishnan, R. K., Kashour, T., Hamid, Q., Halwani, R. & Tleyjeh, I. M. Unraveling the mystery surrounding post-acute sequelae of COVID-19. Front. Immunol. 12 , 686029 (2021).
Renaud-Charest, O. et al. Onset and frequency of depression in post-COVID-19 syndrome: A systematic review. J. Psychiatr. Res. 144 , 129–137 (2021).
Solaro, C., Gamberini, G. & Masuccio, F. G. Depression in multiple sclerosis: Epidemiology, aetiology, diagnosis and treatment. CNS Drugs 32 , 117–133 (2018).
Strober, L. et al. Symbol digit modalities test: A valid clinical trial endpoint for measuring cognition in multiple sclerosis. Multiple Scler 25 , 1781–1790 (2019).
Crivelli, L. et al. Changes in cognitive functioning after COVID-19: A systematic review and meta-analysis. Alzheimers Dement. 18 , 1047–1066 (2022).
Download references
Acknowledgements
The authors acknowledge all the participants in this study, and specifically the association of patients with long-COVID “Asociación Madrileña de Covid Persistente (AMACOP)” for their support.
This research has received funding from the Nominative Grant FIBHCSC 2020 COVID-19 (Department of Health, Community of Madrid) and Fundación para el Conocimiento Madri + d (Healthstart plus program, Community of Madrid, REACT-EU funds) through project G63-HEALTHSTARPLUS-HSP4. Jordi A Matias-Guiu is supported by Instituto de Salud Carlos III through the project INT20/00079 and INT23/00017 (co-funded by European Regional Development Fund “A way to make Europe”). María Valles-Salgado is supported by the Instituto de Salud Carlos III through a predoctoral contract (FI20/000145) (co-funded by European Regional Development Fund “A way to make Europe”). Maria Diez-Cirarda is funded by a Sara Borrell postdoctoral fellowship from the Instituto de Salud Carlos III (CD22/00043) (co-funded by European Regional Development Fund “A way to make Europe”). Silvia Mas-Oliver is supported by Fundación para el Conocimiento madri + d through project G63-HEALTHSTARPLUS-HSP4.
Author information
Authors and affiliations.
Department of Neurology, Hospital Clínico San Carlos, Instituto de Investigacion Sanitaria “San Carlos” (IdISSC), C/Profesor Martín Lagos, 28040, Madrid, Spain
Cristina Delgado-Alonso, Alfonso Delgado-Alvarez, María Díez-Cirarda, Silvia Oliver-Mas, Constanza Cuevas, Paloma Montero-Escribano, María José Gil-Moreno, Juan Ignacio López-Carbonero, Jorge Matias-Guiu & Jordi A. Matias-Guiu
Department of Endocrinology, Hospital Clínico San Carlos, Instituto de Investigacion Sanitaria “San Carlos” (IdISSC), Madrid, Spain
Ana Maria Ramos-Leví
Department of Neurology, School of Medicine and Public Health, University of Wisconsin, Madison, WI, USA
Bruce P. Hermann
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: C.D.A., J.M.G., J.A.M.G. Methodology: C.D.A., M.D.C., B.P.H., J.A.M.G. Data curation: all. Investigation: all. Formal analysis: C.D.A., A.M.R.L., J.A.M.G. Project administration: J.M.G., J.A.M.G. Writing original draft: C.D.A., J.A.M.G. Writing – review & editing: A.D.A., M.D.C., J.M.G., B.P.H.
Corresponding author
Correspondence to Jordi A. Matias-Guiu .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary legends., supplementary table 1., supplementary figure 1., supplementary figure 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Delgado-Alonso, C., Delgado-Alvarez, A., Díez-Cirarda, M. et al. Cognitive profile in multiple sclerosis and post-COVID condition: a comparative study using a unified taxonomy. Sci Rep 14 , 9806 (2024). https://doi.org/10.1038/s41598-024-60368-0
Download citation
Received : 29 June 2023
Accepted : 22 April 2024
Published : 29 April 2024
DOI : https://doi.org/10.1038/s41598-024-60368-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Assessing quality of direct-to-consumer telemedicine in China: a cross-sectional study using unannounced standardised patients
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Zhen Zeng 1 ,
- Dong (Roman) Xu 2 ,
- Yiyuan Cai 3 ,
- http://orcid.org/0000-0002-7943-4041 Wenjie Gong 1 , 4 , 5
- 1 HER Team and Department of Maternal and Child Health, Xiangya School of Public Health , Central South University , Changsha , China
- 2 SMU Institute for Global Health (SIGHT), School of Health Management and Dermatology Hospital , Southern Medical University (SMU) , Guangzhou , China
- 3 Department of Epidemiology and Health Statistics, School of Public Health , Guizhou Medical University , Guiyang , China
- 4 Institute of Applied Health Research , University of Birmingham , Birmingham B15 2TT , UK
- 5 Department of Psychiatry , University of Rochester , Rochester , New York , USA
- Correspondence to Professor Wenjie Gong, HER Team and Department of Maternal and Child Health, Xiangya School of Public Health, Central South University, Changsha, Hunan, 410078, China; gongwenjie{at}csu.edu.cn
Direct-to-onsumer telemedicine (DTCT) has become popular as an alternative to traditional care. However, uncertainties about the potential risks associated with the lack of comprehensive quality evaluation could influence its long-term development. This study aimed to assess the quality of care provided by DTCT platforms in China using unannounced standardised patients (USP) between July 2021 and January 2022. The study assessed consultation services on both hospital and enterprise-sponsored platforms using the Institute of Medicine quality framework. It employed 10 USP cases, covering conditions such as diabetes, asthma, common cold, gastritis, angina, low back pain, child diarrhoea, child dermatitis, stress urinary incontinence and postpartum depression. Descriptive and regression analyses were employed to examine platform characteristics and compare quality across platform types. The results showed that of 170 USP visits across 107 different telemedicine platforms, enterprise-sponsored platforms achieved a 100% success in access, while hospital-sponsored platforms had a success rate of only 47.5% (56/118). Analysis highlighted a low overall correct diagnosis rate of 45% and inadequate adherence to clinical guidelines across all platforms. Notably, enterprise-sponsored platforms outperformed in accessibility, response time and case management compared with hospital-sponsored platforms. This study highlights the suboptimal quality of DTCT platforms in China, particularly for hospital-sponsored platforms. To further enhance DTCT services, future studies should compare DTCT and in-person care, aiming to identify gaps and potential risks associated with using DTCT as alternatives or supplements to traditional care. The potential of future development in enhancing DTCT services may involve exploring the integration of hospital resources with the technology and market capabilities of enterprise-sponsored platforms.
- Health services research
- Quality measurement
- Performance measures
- Patient-centred care
https://doi.org/10.1136/bmjqs-2024-017072
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Direct-to-consumer telemedicine (DTCT) signifies a revolutionary global healthcare delivery model. It involves patients independently initiating medical services remotely, engaging directly with healthcare providers through text messaging or video/phone calls. By bypassing traditional intermediaries like referral clinicians or facilitators, DTCT empowers patients to access medical care swiftly and efficiently. 1 In China, DTCT is burgeoning, boasting over 1700 registered platforms, 2 each serving as an individual website or application for DTCT services. These platforms are categorised into two main types: hospital sponsored and enterprise sponsored. Hospital-sponsored platforms, associated with single physical hospitals, primarily use in-house medical staff and offer streamlined functions due to resource limitations. In contrast, enterprise-sponsored platforms, supported by larger corporations, provide access to a wider network of licensed physicians and offer a diverse range of functions with sophisticated user interfaces. 3 Despite enhanced accessibility and convenience compared with in-person care, DTCT faces quality challenges, such as communication difficulties and antibiotic misuse. 4 5 However, research on DTCT quality remains limited, especially in the context of China. To address this gap, our study employs unannounced standardised patients (USPs)—individuals trained and validated to portray specific medical conditions in a consistent and standardised manner 6 7 —to assess DTCT quality in China across different platform types based on the Institute of Medicine (IOM) quality framework.
This cross-sectional study examined both types of DTCT platforms that offered Chinese language services. The study was conducted between July 2021 and January 2022. Prior informed consent was waived due to minimal risk, and all analyses were performed on fully deidentified aggregated data. 8
To assess consultation service quality, we employed 10 different USP cases, each representing a specific medical condition (details in online supplemental eMethods and online supplemental example of a USP case ). Following thorough training and assessment, we selected 15 qualified USPs from the initial pool of 25 candidates. Each case was assigned at least one USP. As USPs’ initial requests for physician consultations could be denied for various reasons, mirroring real-world scenarios, each case made consultation requests until they completed at least five consultations on each platform type. The USPs captured screenshots and recorded the consultation process, including any failed attempts and reasons for failure. We evaluated the access success rate and assessed consultation quality using the IOM quality framework 9 ( table 1 ).
Supplemental material
- View inline
Quality outcome indicators
We conducted descriptive and regression analyses to evaluate platform characteristics and quality outcomes. Regression analyses compared quality differences using ordinary least squares and logistic regressions, with hospital-sponsored platforms as the benchmark and controlling for patient case fixed effects. Adjusted differences and 95% CIs were reported, adjusted for platform-level clustering. Statistical significance was set at α=0.05. Stata SE (V.16.0) was used for all analyses.
Our study involved 170 visits, with 52 visits on 10 enterprise-sponsored platforms and 118 visits on 97 hospital-sponsored platforms (summarised in online supplemental eTable 1 ). The overall access rate was 63.5% (108/170). Enterprise-sponsored platforms achieved a 100% access rate (52/52), significantly higher than hospital-sponsored ones (56/118, 47.5%) (p<0.001). Common reasons for unsuccessful consultations included incomplete functions, like platforms claiming to offer DTCT services but lacking an accessible feature for initiating online consultations with physicians (25/62, 40.3%), and no response (13/62, 21.0%).
Of 108 successful consultations, 49 consultations (45%) received a correct diagnosis, while adherence to published guidelines was low for consultation (15%) and management decisions (31%). On average, physicians took 3 hours and 47 min to respond, with the total interaction time spanning 12 hours and 19 min. After controlling for disease case fixed effects and adjusting SEs for clustering at platform level, enterprise-sponsored platforms had higher rates of completed management decisions, shorter response times and higher costs ( table 2 ).
Comparison on main quality outcomes between platform types for successful consultations
In this study, we rigorously evaluated the quality of care across two types of DTCT platforms in China using USPs. With 108 successful visits out of 170 attempts, we found a diagnostic accuracy of approximately 45%, along with a decline in completion rates for recommended management decisions to 31%. This may be linked to the limited inquiries during USP encounters, with clinicians asking only about 15% of recommended consultation questions per visit. Besides traditional quality metrics, the timeliness of DTCT services is concerning, with a response time of 3 hours and 47 min and an overall interaction time of 12 hours and 19 min. In China, DTCT predominantly operates asynchronously, leading to these extended durations. Despite offering a more flexible alternative to in-person counselling by eliminating the need for travel, prolonged waiting times may still impact user satisfaction and the perceived effectiveness of DTCT platforms. Future research should prioritise enhancing the timeliness of DTCT services to ensure prompt access and timely interactions. The patient-centredness score averaging 2.4, indicating a medium to low level of patient-centred care, 10 is potentially influenced by less satisfactory outcomes discussed earlier in terms of effectiveness, safety and timeliness. These findings raise concerns about how effective DTCT services are. Further evaluation, including a direct comparison with in-person care, is needed for a clearer understanding of their quality. This can guide improvement measures, especially when DTCT services act as alternatives or supplements to traditional in-person care.
Notably, enterprise-sponsored platforms achieved 100% access success, surpassing hospital-sponsored ones at 47.5%. They exhibited superior performance in response times and completion rates for management decisions. Despite recent growth and policy support, 3 hospital-sponsored platforms seem to be in early developmental stages, potentially limiting medical resource accessibility. These findings challenge a marketing survey suggesting a preference for hospital-sponsored platforms, 11 emphasising higher access denial risks and less timely responses for consumers on these platforms.
This study was limited by the use of a uniform USP for each case. Using standardised scenarios with different USPs potentially allows for a comprehensive assessment of equity. However, due to constraints imposed by scripted scenarios in our study, this aspect was not explored.
Our study highlights the suboptimal quality of DTCT in China, specifically disparities between hospital-sponsored and enterprise-sponsored platforms. These findings likely echo broader challenges and principles inherent in DTCT globally. As DTCT gains momentum after COVID-19, future research becomes critical to effectively address these issues.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by Xiangya School of Public Health (IRB No XYGW-2021-37). Prior informed consent was waived due to minimal risk and no individually identifiable information on physicians.
Acknowledgments
We sincerely thank Xiaohui Wang, Yaolong Chen, Yun Lu, Xiaojing Fan, Zhongliang Zhou, Jay Pan, and Chengxiang Tang for their unwavering leadership in development and management the SP cases. We also apperciate Lu Liu, Chunping Li, and Huanyu Hu for their their diligent efforts as project assistants, as well as all the standardized patients and study coordinators for their hard work.
- Elliott T ,
- iiMedia Report
- Resneck JS ,
- Steuer M , et al
- Gidengil CA , et al
- Peabody JW ,
- Glassman P , et al
- Colliver JA ,
- Rhodes KV ,
- Institute of Medicine (US) Committee on Quality of Health Care in America
- Tu J , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors WG conceived the study. ZZ coordinated the daily implementation of this study under the supervision of DRX, YC and WG. ZZ carried out data analysis and composed the initial manuscript draft, receiving guidance from WG and DRX. All authors contributed to critical review of the manuscript and approved the final draft.
Funding This study was funded by China Medical Board (20-368), Swiss Agency for Development and Cooperation (81067392) and the National Natural Science Foundation of China (82273643).
Competing interests None declared.
Provenance and peer review Not commissioned; internally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:

IMAGES
VIDEO
COMMENTS
Sara, a 35-year-old married female. Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks. Bleiberg, K.L., & Markowitz, J.C. (2008).
In a study of 239 outpatients diagnosed with major depressive disorder in a NIMH. 16-week multi-center clinical trial, participants were assigned to interpersonal therapy, CBT, imipramine with clinical management, or placebo with clinical management. One. hundred sixty-two patients completed the trial.
Dr. SooJeong Youn: This case highlights the importance of attending to the intricate, multilevel, systemic factors that affect the mental health experience and clinical presentation of patients ...
Patient Case Presentation. Figure 1. Blue and silver stethoscope (Pixabay, N.D.) Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness.
This clinical case study explores the characteristics associated with treatment response in a Puerto Rican adolescent and illustrates the challenges and variability inherent in CBT treatment for major depressive disorder (MDD) in youth. Methods: The patient is a 15-year- old adolescent female who at pretreatment presented a diagnosis of MDD ...
Diagnosis of depression can be made using the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) or the 10th revision of the International Statistical Classification of Disease and Related Health Problems (ICD-10). 5 (Refer to Appendix 3 and 4, pages 73-76 in CPG.) 6,7
When a patient with depression is feeling sleepy, be aware of sleep apnoea. A 67-year-old man was referred to an outpatient clinic of geriatric psychiatry because of persistent symptoms of depression and anxiety, accompanied by sleepiness. The latter had been evaluated multiple times in the general practice over several years; each time it was ...
Key Clinical Message. We present an evolutionary-driven cognitive-behavioral intervention for a moderately depressed patient. Standard cognitive and behavioral therapy techniques focused on the patient's perfectionistic and self-downing beliefs, while novel, evolutionary-informed techniques were used to guide behavioral activation and conceptualize secondary emotional problems related to anger.
European Archives of Psychiatry and Clinical Neuroscience (2024) Treatment outcomes for major depressive disorder (MDD) need to be improved. Presently, no clinically relevant tools have been ...
CBT for difficult-to-treat depression: single complex case - Volume 15. ... this case study is a good example of naturalistic practice-based evidence, with a high level of collaboration and participation from the service user. ... Early intervention for adults at high risk of recurrent/chronic depression: cognitive model and clinical case series.
Introduction to the selected case study. In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane's case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
Chapter 4 covers the treatment of depression, and discusses popular myths regarding depression, its frequency, characteristics and diagnosis, and includes case studies, assessment, case conceptualization, intervention development and course of treatment, problems that may arise in therapy, ethical considerations, common mistakes in the course ...
depression (e.g., avoidance, difficulty concentrating and making decisions, and fatigue) as additional signs of incompetence. Once he became depressed, he interpreted many of his experiences through the lens of his core belief of incompetence or failure. Three of these situations are noted at the bottom of the Case Conceptualization Diagram.
This clinical case is part of a feasibility study assessing the acceptability of Be a Mom Coping with Depression, and to our knowledge, this is the first blended CBT intervention developed for the treatment of PPD. In this case study, the intervention was effective in reducing anxiety and depressive symptoms.
Aim and Objectives: The present case study aimed to assess psychosocial problems and to provide psychiatric social work intervention based on cognitive behaviour therapy (CBT) to the client. Methods and materials: The single-subject case study design was used and the pre-post baseline assessment was done. Semi-structured clinical and
Background: There is ample evidence of the efficacy of cognitive-behavioral therapy (CBT) for depression in adolescents, including Puerto Rican adolescents. However, there is still a high percentage of adolescents who do not respond to a standard "dose" of 12 sessions of CBT. This clinical case study explores the characteristics associated with treatment response in a Puerto Rican ...
In 2021, 8.3% of U.S. adults experienced major depression. That's about 21 million people. Among adolescents, the prevalence was much greater—more than 20%. Major depression can bring decreased energy, difficulty thinking straight, sleep problems, loss of appetite, and even physical pain.
Depression is a highly prevalent and severely disabling disease. The treatment effects, intensity and onset time of antidepressants have been highlighted in many studies. Recent studies on the rapid-onset of antidepressant response focused on the effect of a single low dose of intravenous ketamine.
This case study illustrates the efectiveness of Cognitive Behavior Therapy (CBT) in the management of depression in 15 years old boy. M.F. presented with complaints of social withdrawal, low mood, loss of interest, decreased appetite, and weight loss and decreased sleep from last one year. He was assessed using HTP and Beck Depression Inventory ...
Clinical case scenarios: Common mental health disorders in primary care (May 2012) Page 4 of 85 . Introduction . NICE clinical case scenarios . Clinical case scenarios are an educational resource that can be used for individual or group learning. Each question should be considered by the individual or group before referring to the answers.
current issue. current issue; browse recently published; browse full issue index; learning/cme
Most studies on the impact of the COVID-19 pandemic on depression burden focused on the earlier pandemic phase specific to lockdowns, but the longer-term impact of the pandemic is less well-studied. In this population-based cohort study, we examined the short-term and long-term impacts of COVID-19 on depression incidence and healthcare service use among patients with depression.
Evidence-Based Case Review ... Although research on the treatment of adolescent depression is limited, recent clinical trials have identified promising interventions, both pharmacologic and psychotherapeutic. ... Although research has clearly documented the use of antidepressant medication for adults with depression, 19 far fewer studies have ...
Post-COVID condition (PCC) and multiple sclerosis (MS) share some clinical and demographic features, including cognitive symptoms and fatigue. Some pathophysiological mechanisms well-known in MS ...
Direct-to-onsumer telemedicine (DTCT) has become popular as an alternative to traditional care. However, uncertainties about the potential risks associated with the lack of comprehensive quality evaluation could influence its long-term development. This study aimed to assess the quality of care provided by DTCT platforms in China using unannounced standardised patients (USP) between July 2021 ...