We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Chapter 7: 10 Real Cases on Transient Ischemic Attack and Stroke: Diagnosis, Management, and Follow-Up
Jeirym Miranda; Fareeha S. Alavi; Muhammad Saad
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion, clinical symptoms.
- Radiologic Findings
- Full Chapter
- Supplementary Content
Case 1: Management of Acute Thrombotic Cerebrovascular Accident Post Recombinant Tissue Plasminogen Activator Therapy
A 59-year-old Hispanic man presented with right upper and lower extremity weakness, associated with facial drop and slurred speech starting 2 hours before the presentation. He denied visual disturbance, headache, chest pain, palpitations, dyspnea, dysphagia, fever, dizziness, loss of consciousness, bowel or urinary incontinence, or trauma. His medical history was significant for uncontrolled type 2 diabetes mellitus, hypertension, hyperlipidemia, and benign prostatic hypertrophy. Social history included cigarette smoking (1 pack per day for 20 years) and alcohol intake of 3 to 4 beers daily. Family history was not significant, and he did not remember his medications. In the emergency department, his vital signs were stable. His physical examination was remarkable for right-sided facial droop, dysarthria, and right-sided hemiplegia. The rest of the examination findings were insignificant. His National Institutes of Health Stroke Scale (NIHSS) score was calculated as 7. Initial CT angiogram of head and neck reported no acute intracranial findings. The neurology team was consulted, and intravenous recombinant tissue plasminogen activator (t-PA) was administered along with high-intensity statin therapy. The patient was admitted to the intensive care unit where his hemodynamics were monitored for 24 hours and later transferred to the telemetry unit. MRI of the head revealed an acute 1.7-cm infarct of the left periventricular white matter and posterior left basal ganglia. How would you manage this case?
This case scenario presents a patient with acute ischemic cerebrovascular accident (CVA) requiring intravenous t-PA. Diagnosis was based on clinical neurologic symptoms and an NIHSS score of 7 and was later confirmed by neuroimaging. He had multiple comorbidities, including hypertension, diabetes, dyslipidemia, and smoking history, which put him at a higher risk for developing cardiovascular disease. Because his symptoms started within 4.5 hours of presentation, he was deemed to be a candidate for thrombolytics. The eligibility time line is estimated either by self-report or last witness of baseline status.
Ischemic strokes are caused by an obstruction of a blood vessel, which irrigates the brain mainly secondary to the development of atherosclerotic changes, leading to cerebral thrombosis and embolism. Diagnosis is made based on presenting symptoms and CT/MRI of the head, and the treatment is focused on cerebral reperfusion based on eligibility criteria and timing of presentation.
Symptoms include alteration of sensorium, numbness, decreased motor strength, facial drop, dysarthria, ataxia, visual disturbance, dizziness, and headache.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Image courtesy of uofmhealthblogs.org.
D.B. is a 72 year old African American female who presented to the ED with complaints of headache, altered mental status as evidenced by confusion and lethargy, slurred speech, right sided weakness, and a facial droop. Symptoms were first noted when patient woke up from a nap approximately one hour ago. Patient’s daughter is at bedside. Vital signs on arrival: HR 92 irregular, RR 12, BP 172/91, Temp 99.3, blood glucose 163.
Past Medical History
- Hypertension-diagnosed at 50 years old
- Diabetes Mellitus, Type II-diagnosed at 50 years old
- Hypercholesterolemia- diagnosed at 60 years old
- Chronic A-fib- diagnosed last year
- Sleep apnea, non-compliant with CPAP
- Frequent falls
- TIA-approximately 2 months ago
Surgical History
- Total hysterectomy, 58 years old
Pertinent Family History
- Mother, deceased at 75 years old- CVA, heart disease
- Father, deceased at 62 years old- diabetes, heart disease
- Brother- HTN
- Sister, deceased at 68 years old- heart disease
Pertinent Social History
- Smoker, 1-2 packs per day for approximately 50 years
- Sedentary lifestyle
- Poor diet, high in sodium
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
This case study presents a 68-year old “right-handed” African-American man named Randall Swanson. He has a history of hypertension, hyperlipidemia and a history of smoking one pack per day for the last 20 years. He is prescribed Atenolol for his HTN, and Simvastatin for Hyperlipidemia (but he has a history of not always taking his meds). His father had a history of hypertension and passed away from cancer 10 years ago. His mother has a history of diabetes and is still alive.
Randall was gardening with his wife on a relaxing Sunday afternoon. Out of nowhere, Randall fell to the ground. When his wife rushed to his side and asked how he was doing, he answered with garbled and incoherent speech. It was then that his wife noticed his face was drooping on the right side. His wife immediately called 911 and paramedics arrived within 6 minutes. Upon initial assessment, the paramedics reported that Randall appeared to be experiencing a stroke as he presented with right-sided facial droop and weakness and numbness on the right side of his body. Fortunately, Randall lived nearby a stroke center so he was transported to St. John’s Regional Medical Center within 17 minutes of paramedics arriving to his home.
Initial Managment
Upon arrival to the Emergency Department, the healthcare team was ready to work together to diagnose Randall. He was placed in bed with the HOB elevated to 30 degrees to decrease intracranial pressure and reduce any risks for aspiration. Randall’s wife remained at his side and provided the care team with his brief medical history which as previously mentioned, consists of hypertension, hyperlipidemia and smoking one pack per day for the last 20 years. He had no recent head trauma, never had a stroke, no prior surgeries, and no use of anticoagulation medications.
Physical Assessment
Upon first impression, Nurse Laura recognized that Randall was calm but looked apprehensive. When asked to state his name and date of birth, his speech sounded garbled at times and was very slow, but he could still be understood. He could not recall the month he was born in but he was alert and oriented to person, time, and situation. When asked to state where he was, he could not recall the word hospital. He simply pointed around the room while repeating “here.”
Further assessment revealed that his pupils were equal and reactive to light and that he presented with right-sided facial paralysis. Randall was able to follow commands but when asked to move his extremities, he could not lift his right arm and leg. He also reported that he could not feel the nurse touch his right arm and leg. Nurse Laura gathered the initial vital signs as follows: BP: 176/82, HR: 93, RR: 20, T:99.4, O2: 92% RA and a headache with pain of 3/10.
Doctor’s Orders
The doctor orders were quickly noted and included:
-2L O2 (to keep O2 >93%)
– 500 mL Bolus NS
– VS Q2h for the first 8 hrs.
-Draw labs for: CBC, INR, PT/INR, PTT, and Troponin
-Get an EKG
-Chest X ray
-Glucose check
-Obtain patient weight
-Perform a National Institute of Health Stroke Scale (also known as NIHSS) Q12h for the first 24 hours, then Q24h until he is discharged
-Notify pharmacy of potential t-PA preparation.
Nursing Actions
Nurse Laura started an 18 gauge IV in Randall’s left AC and started him on a bolus of 500 mL of NS. A blood sample was collected and quickly sent to the lab. Nurse Laura called the Emergency Department Tech to obtain a 12 lead EKG.
Pertinent Lab Results for Randall
The physician and the nurse review the labs:
WBC 7.3 x 10^9/L
RBC 4.6 x 10^12/L
Plt 200 x 10^9/L
LDL 179 mg/dL
HDL 43 mg/dL
Troponin <0.01 ng/mL
EKG and Chest X Ray Results
The EKG results and monitor revealed Randall was in normal sinus rhythm; CXR was negative for pulmonary or cardiac pathology
CT Scan and NIHSS Results
The NIH Stroke Scale was completed and demonstrated that Randall had significant neurological deficits with a score of 13. Within 20 minutes of arrival to the hospital, Randall had a CT-scan completed. Within 40 minutes of arrival to the hospital, the radiologist notified the ED physician that the CT-scan was negative for any active bleeding, ruling our hemorrhagic stroke.
The doctors consulted and diagnosed Randall with a thrombotic ischemic stroke and determined that that plan would include administering t-PA. Since Randall’s CT scan was negative for a bleed and since he met all of the inclusion criteria he was a candidate for t-PA. ( Some of the inclusion criteria includes that the last time the patient is seen normal must be within 3 hours, the CT scan has to be negative for bleeding, the patient must be 18 years or older, the doctor must make the diagnosis of an acute ischemic stroke, and the patient must continue to present with neurological deficits.)
Since the neurologist has recommended IV t-PA, the physicians went into Randall’s room and discussed what they found with him and his wife. Nurse Laura answered and addressed any remaining concerns or questions.
Administration
Randall and his wife decided to proceed with t-PA therapy as ordered, therefore Nurse Laura initiated the hospital’s t-PA protocol. A bolus of 6.73 mg of tPA was administered for 1 minute followed by an infusion of 60.59 mg over the course of 1 hour. ( This was determined by his weight of 74.8 kg). After the infusion was complete, Randall was transferred to the ICU for close observation. Upon reassessment of the patient, Randall still appeared to be displaying neurological deficits and his right-sided paralysis had not improved. His vital signs were assessed and noted as follows: BP: 149/79 HR: 90 RR: 18 T:98.9 O2: 97% 2L NC Pain: 2/10.
Randall’s wife was crying and he appeared very scared, so Nurse John tried to provide as much emotional support to them as possible. Nurse John paid close attention to Randall’s blood pressure since he could be at risk for hemorrhaging due to the medication. Randall was also continually assessed for any changes in neurological status and allergic reactions to the t-PA. Nurse John made sure that Stroke Core Measures were followed in order to enhance Randall’s outcome.
In the ICU, Randall’s neurological status improved greatly. Nurse Jan noted that while he still garbled speech and right-sided facial droop, he was now able to recall information such as his birthday and he could identify objects when asked. Randall was able to move his right arm and leg off the bed but he reported that he was still experiencing decreased sensation, right-sided weakness and he demonstrated drift in both extremities.
The nurse monitored Randall’s blood pressure and noted that it was higher than normal at 151/83. She realized this was an expected finding for a patient during a stroke but systolic pressure should be maintained at less than 185 to lower the risk of hemorrhage. His vitals remained stable and his NIHSS score decreased to an 8. Labs were drawn and were WNL with the exception of his LDL and HDL levels. His vital signs were noted as follows: BP 151/80 HR 92 RR 18 T 98.8 O2 97% RA Pain 0/10
The Doctor ordered Physical, Speech, and Occupational therapy, as well as a swallow test.
Swallowing Screen
Randall remained NPO since his arrival due to the risks associated with swallowing after a stroke. Nurse Jan performed a swallow test by giving Randall 3 ounces of water. On the first sip, Randall coughed and subsequently did not pass. Nurse Jan kept him NPO until the speech pathologist arrived to further evaluate Randall. Ultimately, the speech pathologist determined that with due caution, Randall could be put on a dysphagia diet that featured thickened liquids
Physical Therapy & Occupational Therapy
A physical therapist worked with Randall and helped him to carry out passive range of motion exercises. An occupational therapist also worked with Randall to evaluate how well he could perform tasks such as writing, getting dressed and bathing. It was important for these therapy measures to begin as soon as possible to increase the functional outcomes for Randall. Rehabilitation is an ongoing process that begins in the acute setting.
Day 3- third person
During Day 3, Randall’s last day in the ICU, Nurse Jessica performed his assessment. His vital signs remained stable and WNL as follows: BP: 135/79 HR: 90 RR: 18 T: 98.9 O2: 97% on RA, and Pain 0/10. His NIHSS dramatically decreased to a 2. Randall began showing signs of improved neurological status; he was able to follow commands appropriately and was alert and oriented x 4. The strength in his right arm and leg markedly improved. he was able to lift both his right arm and leg well and while he still reported feeling a little weakness and sensory loss, the drift in both extremities was absent.
Rehabilitation Therapies
Physical, speech, and occupational therapists continued to work with Randall. He was able to call for assistance and ambulate with a walker to the bathroom and back. He was able to clean his face with a washcloth, dress with minimal assistance, brush his teeth, and more. Randall continued to talk with slurred speech but he was able to enunciate with effort.
On day 4, Randall was transferred to the med-surg floor to continue progression. He continued to work with physical and occupational therapy and was able to perform most of his ADLs with little assistance. Randall could also ambulate 20 feet down the hall with the use of a walker.
Long-Term Rehabilitation and Ongoing Care
On day 5, Randall was discharged to a rehabilitation facility and continued to display daily improvement. The dysphagia that he previously was experiencing resolved and he was discharged home 1.5 weeks later. Luckily for Randall, his wife was there to witness his last known well time and she was able to notify first responders. They arrived quickly and he was able to receive t-PA in a timely manner. With the help of the interdisciplinary team consisting of nurses, therapists, doctors, and other personnel, Randall was put on the path to not only recover from the stroke but also to quickly regain function and quality of life very near to pre-stroke levels. It is now important that Randall continues to follow up with his primary doctor and his neurologist and that he adheres to his medication and physical therapy regimen.
Case Management
During Randall’s stay, Mary the case manager played a crucial role in Randall’s path to recovery. She determined that primary areas of concern included his history of medical noncompliance and unhealthy lifestyle. The case manager consulted with Dietary and requested that they provide Randall with education on a healthy diet regimen. She also provided him with smoking cessation information. Since Randall has been noncompliant with his medications, Mary determined that social services should consult with him to figure out what the reasons were behind his noncompliance. Social Services reported back to Mary that Randall stated that he didn’t really understand why he needed to take the medication. It was apparent that he had not been properly educated. Mary also needed to work with Randall’s insurance to ensure that he could go to the rehab facility as she knew this would greatly impact his ultimate outcome. Lastly, throughout his stay, the case manager provided Randall and his wife with resources on stroke educational materials. With the collaboration of nurses, education on the benefits of smoking cessation, medication adherence, lifestyle modifications, and stroke recognition was reiterated to the couple. After discharge, the case manager also checked up with Randall to make sure that he complied with his follow up appointments with the neurologist and physical and speech therapists,
- What risk factors contributed to Randall’s stroke?
- What types of contraindications could have prevented Randall from receiving t-PA?
- What factors attributed to Randall’s overall favorable outcome?
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Case Presentation
Statement of ethics, conflict of interest statement, funding sources, author contributions, ischemic stroke in a 29-year-old patient with covid-19: a case report.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Christian Avvantaggiato , Loredana Amoruso , Maria Pia Lo Muzio , Maria Assunta Mimmo , Michelina Delli Bergoli , Nicoletta Cinone , Luigi Santoro , Lucia Stuppiello , Antonio Turitto , Chiara Ciritella , Pietro Fiore , Andrea Santamato; Ischemic Stroke in a 29-Year-Old Patient with COVID-19: A Case Report. Case Rep Neurol 2 September 2021; 13 (2): 334–340. https://doi.org/10.1159/000515457
Download citation file:
- Ris (Zotero)
- Reference Manager
Increasing evidence reports a greater incidence of stroke among patients with Coronavirus disease 2019 (COVID-19) than the non-COVID-19 population and suggests that SARS-CoV-2 infection represents a risk factor for thromboembolic and acute ischemic stroke. Elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events, and advanced age is strongly associated with severe COVID-19 and death. We reported, instead, a case of an ischemic stroke in a young woman during her hospitalization for COVID-19-related pneumonia. A 29-year-old woman presented to the emergency department of our institution with progressive respiratory distress associated with a 2-day history of fever, nausea, and vomiting. The patient was transferred to the intensive care unit (ICU) where she underwent a tracheostomy for mechanical ventilation due to her severe clinical condition and her very low arterial partial pressure of oxygen. The nasopharyngeal swab test confirmed SARS-CoV-2 infection. Laboratory tests showed neutrophilic leucocytosis, a prolonged prothrombin time, and elevated D-dimer and fibrinogen levels. After 18 days, during her stay in the ICU after suspension of the medications used for sedation, left hemiplegia was reported. Central facial palsy on the left side, dysarthria, and facial drop were present, with complete paralysis of the ipsilateral upper and lower limbs. Computed tomography (CT) of the head and magnetic resonance imaging of the brain confirmed the presence of lesions in the right hemisphere affecting the territories of the anterior and middle cerebral arteries, consistent with ischemic stroke. Pulmonary and splenic infarcts were also found after CT of the chest. The age of the patient and the absence of serious concomitant cardiovascular diseases place the emphasis on the capacity of SARS-CoV-2 infection to be an independent cerebrovascular risk factor. Increased levels of D-dimer and positivity to β2-glycoprotein antibodies could confirm the theory of endothelial activation and hypercoagulability, but other mechanisms – still under discussion – should not be excluded.
Coronavirus disease 2019 (COVID-19), caused by the novel coronavirus SARS-CoV-2, is characterized by a wide range of symptoms, most of which cause acute respiratory distress syndrome [1, 2], associated with intensive care unit (ICU) admission and high mortality [3]. On March 11, 2020, the large global outbreak of the disease led the World Health Organization (WHO) to declare COVID-19 a pandemic, with 11,874,226 confirmed cases and 545,481 deaths worldwide (July 9, 2020) [4]. In many cases, the clinical manifestations of COVID-19 are characteristic of a mild disease that may, however, worsen to a critical lower respiratory infection [2]. At the onset of the disease, the most frequent symptoms are fever, dry cough, fatigue, and shortness of breath as the infection progresses may appear signs and symptoms of respiratory failure that require ICU admission [5, 6]. Although acute respiratory distress syndrome is the most important cause of ICU admission for COVID-19 patients, several studies have underlined the presence of neurological symptoms such as confusion, dizziness, impaired consciousness, ataxia, seizure, anosmia, ageusia, vision impairment, and stroke [7, 8]. In particular, the state of hypercoagulability in patients affected by COVID-19 favors the formation of small and/or large blood clots in multiple organs, including the brain, potentially leading to cerebrovascular disease (ischemic stroke but also intracranial hemorrhage) [9, 10 ].
We found an interesting case of stroke following a SARS-CoV-2 infection in a young patient. A 29-year-old woman, during her ICU hospitalization for COVID-19-related pneumonia, was diagnosed with ischemic stroke of the right hemisphere, without other cardiac/cerebrovascular risk factors except hypertension. The young age of the patient and the absence of higher cerebrovascular risk factors make the present case very interesting as it can help demonstrate that COVID-19 is an independent risk factor for acute ischemic stroke. In a case series of 214 patients with COVID-19 (mean [SD] age, 52.7 [15.5] years), neurologic symptoms were more common in patients with severe infection who were older than the others [ 11 ]. New-onset CVD was more common in COVID-19 patients who had underlying cerebrovascular risk factors, such as older age (>65 years) [ 12 ], and very few cases of stroke in patients younger than 50 years have been reported [ 12, 13 ]. Our case seems to be the only one younger than 30 years.
On the night between March 19 and 20, 2020, a 29-year-old woman was referred to our hospital “Policlinico Riuniti di Foggia” due to a progressive respiratory distress associated with a 2-day history of fever, nausea, and vomiting. At presentation, the heart rate was 128 bpm, the blood oxygen saturation measured by means of the pulse oximeter was 27%, the respiratory rate was 27 breaths per minute, and the blood pressure was 116/77 mm Hg. The arterial blood gas test showed a pH of 7.52, pO 2 20 mm Hg, and pCO 2 34 mm Hg. The patient was immediately transferred to the ICU where she underwent tracheostomy and endotracheal intubation for mechanical ventilation due to her severe clinical condition and deteriorated pulmonary gas exchange. The diagnosis of COVID-19 was confirmed by PCR on a nasopharyngeal swab.
The family medical history was normal, and the only known pre-existing medical conditions were polycystic ovary syndrome (diagnosed 3 years earlier), conversion disorder, and hypertension (both diagnosed 2 years earlier). Ramipril and nebivolol were prescribed for the high blood pressure treatment, and sertraline was prescribed for the conversion disorder treatment. Drug therapy adherence was inconstant. The patient had no history of diabetes, cardiac pathologies, strokes, transient ischemic attacks, thromboembolic, or other vascular pathologies.
Laboratory tests showed neutrophilic leukocytosis (white blood cell count 14.79 × 10 3 , neutrophil percentage 89.8%, and neutrophil count 13.29 × 10 3 ), a prolonged prothrombin time (15.3 s) with a slightly elevated international normalized ratio (1.38), and elevated D-dimer (6,912 ng/mL) and fibrinogen levels (766 mg/dL). Other findings are shown in Table 1 .
Laboratory test

This pharmacological therapy was set as follows: enoxaparin 6,000 U.I. once a day, piperacillin 4 g/tazobactam 0.5 g twice a day; Kaletra, a combination of lopinavir and ritonavir indicated for human immunodeficiency virus (HIV) infection treatment, 2 tablets twice a day; hydroxychloroquine 200 mg once a day; and furosemide 250 mg, calcium gluconate, and aminophylline 240 mg 3 times a day. No adverse events were reported.
On April 7, 2020, during her stay in the ICU and after suspension of the medications used for sedation, left hemiplegia was reported. The same day, the patient underwent a computed tomography examination of the head, which showed areas of hypodensity in the right hemisphere due to recent cerebral ischemia.
On April 16, 2020, the patient was oriented to time, place, and person. Central facial palsy on the left side, dysarthria, and facial drop were present, with complete paralysis of the ipsilateral upper and lower limbs. The power of all the muscles of the left limbs was grade 0 according to the Medical Research Council (MRC) scale. Deep tendon reflexes were reduced on the left upper limb but hyperactive on the ipsilateral lower limb, with a slight increase in the muscle tonus. The senses of touch, vibration, and pain were reduced on the left side of the face and body.
On the same day, the patient underwent magnetic resonance imaging (MRI) of the brain (Fig. 1 a), showing lesions on the right hemisphere affecting the territories of the anterior and middle cerebral arteries. On May 5, 2020, magnetic resonance angiography showed an early duplication of the sphenoidal segment of the right middle cerebral artery, the branches of which are irregular with rosary bead-like aspects (Fig. 1 d, e); on the same day, the second MRI (Fig. 1 b) confirmed the lesions. Computed tomography of the chest (Fig. 1 c) and abdomen (Fig. 1 f), performed 5 days after the MRI of the brain, showed not only multifocal bilateral ground-glass opacities but also a basal subpleural area of increased density within the left lung (4 × 4 × 3 cm), consistent with a pulmonary infarction. In addition, a vascular lesion, consistent with a splenic infarct, was found in the inferior pole of the spleen. Doppler echocardiography of the hearth showed regular right chambers and left atrium and a slightly hypertrophic left ventricle with normal size and kinetics (ejection fraction: 55%). The age of the patient and the absence of serious concomitant cardiovascular diseases place the emphasis on the capacity of SARS-CoV-2 infection to be an independent cerebrovascular risk factor.

Imaging. a April 16, 2020; MRI of the brain: lesions in the right hemisphere affecting the territories of the anterior and the middle cerebral arteries. b May 5, 2020; MRI of the brain: same lesions in the right hemisphere shown in the previous image. d , e May 5, 2020; MRA showed an early duplication of the sphenoidal segment of the right middle cerebral artery, the branches of which are irregular with rosary bead-like aspect and reduction of blood flow in the middle cerebral artery. c April 20, 2020; CT of the abdomen: vascular lesion, consistent with a splenic infarct, found in the inferior pole of the spleen. f April 20, 2020; CT of the chest: basal subpleural area of increased density within the left lung (4 × 4 × 3 cm), consistent with a pulmonary infarction. MRA, magnetic resonance angiography; CT, computed tomography; MRI, magnetic resonance imaging.
The pandemic outbreak of novel SARS-CoV-2 infection has caused great concern among the services and authorities responsible for public health due to not only the mortality rate but also the danger of filling up hospital capacities in terms of ICU beds and acute non-ICU beds. In this regard, the nonrespiratory complications of COVID-19 should also be taken into great consideration, especially those that threaten patients’ lives and extend hospitalization times. Stroke is one of these complications, since a greater incidence of stroke among patients with COVID-19 than the non-COVID-19 population has been reported, and a preliminary case-control study demonstrated that SARS-CoV-2 infection represents a risk factor for acute ischemic stroke [ 14 ].
We found that the reported case is extremely interesting, since the woman is only 29 years old and considering how stroke in a young patient without other known risk factors is uncommon. Not only elderly people have higher risk factors associated with acute ischemic stroke or embolization vascular events [ 15 ], but it is also true that advanced age is strongly associated with severe COVID-19 and death. The severity of the disease is directly linked to immune dysregulation, cytokine storm, and acute inflammation state, which in turn are more common in patients who present immunosenescence [6].
Inflammation plays an important role in the occurrence of cardiovascular and cerebrovascular diseases since it favors atherosclerosis and affects plaque stability [ 16 ]. The ischemic stroke of the 29-year-old woman does not appear to be imputable to emboli originating a pre-existing atheromatous plaque, both for the age of the patient and for the absence of plaques at the Doppler ultrasound study of the supra-aortic trunks.
Most likely, COVID-19-associated hypercoagulability and endothelial dysfunction are the causes of ischemic stroke, as suggested by other studies and case reports [ 10, 13, 17 ]. Although the mechanisms by which SARS-CoV-2 infection leads to hypercoagulability are still being studied, current knowledge suggests that cross talk between inflammation and thrombosis has a crucial role [ 18 ]. The release of inflammatory cytokines leads to the activation of epithelial cells, monocytes, and macrophages. Direct infection of endothelial cells through the ACE2 receptor also leads to endothelial activation and dysfunction, expression of tissue factor, and platelet activation and increased levels of VWF and FVIII, all of which contribute to thrombin generation and fibrin clot formation [ 17 ]. The 29-year-old patient showed an increased level of D-dimer, which is a degradation product of cross-linked fibrin, indicating a global activation of hemostasis and fibrinolysis and conforming to the hypothesis of COVID-19-associated hypercoagulability. Endothelial activation and hypercoagulability are also confirmed by positivity to β2 glycoprotein antibodies. Anticardiolipin antibody and/or β2 glycoprotein antibody positivity has been reported in a few studies [ 17, 19, 20 ]. In addition, widespread thrombosis in SARS-CoV-2 infection could also be caused by neutrophil extracellular traps (NETs). Neutrophilia [ 21 ] and an elevated neutrophil-lymphocyte ratio [ 22 ] have been reported by numerous studies as predictive of worse disease outcomes, and recently, the contribution of NETs in the pathophysiology of COVID-19 was reported [ 23 ]. Thrombogenic involvement of NETs has been described in various settings of thrombosis, including stroke, myocardial infarction, and deep vein thrombosis [ 24 ]. The high neutrophil count found in our case does not exclude the hypothesis that NETs are involved in the pathogenesis of ischemic stroke.
Ischemic stroke in young patients without pre-existing cerebrovascular risk factors is very unusual. In this regard, our case of an ischemic stroke, reported in a 29-year-old woman, is very interesting. Although it is not possible to determine precisely when the thromboembolic event occurred, our case of stroke during COVID-19-related pneumonia seems to confirm that COVID-19 is an independent risk factor for acute ischemic stroke. The mechanisms by which coronavirus disease leads to stroke are still under study, but it is clear that hypercoagulability and endothelial activation play a key role. Testing for SARS-CoV-2 infection should be considered for patients who develop neurologic symptoms, but it is equally important to monitor COVID-19 patients during their hospitalization to find any neurological sign or symptom in a timely manner. Our case suggests that discovering neurological deficits in sedated patients promptly can be very difficult; for this reason, sedation in mechanically ventilated patients has to be considered only if strictly necessary. Performing serial laboratory testing and waking up the patient as soon as clinical conditions allow are strategies that should be taken into account.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
No funding was received for the publication of this case report.
All authors agree with the contents of the manuscript and were fully involved in the study and preparation of the manuscript. All authors read and approved the final version of the manuscript. M.A. Mimmo, M.P. Lo Muzio, M. Delli Bergoli, and L. Amoruso collected the data. C. Avvantaggiato wrote the manuscript with support of N. Cinone, L. Santoro, and C. Ciritella. C. Avvantaggiato, A. Turitto, and L. Stuppiello researched and discussed the neurophysiological principles of this study. P. Fiore and A. Santamato supervised the project.

Email alerts
Citing articles via, suggested reading.
- Online ISSN 1662-680X
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Contact: Front Office
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Explore prestigious scientific journals and award and funding opportunities to advance your research.
Access practice-improvement tools, including guidelines, measures, Axon Registry, and practice management resources.
Learn to effectively advocate on behalf of neurologists and their patients, and access AAN position and policy statements.
Loading... please wait
We’re experiencing unusually high levels of traffic. Thank you for your patience.
Inpatient Stroke Case Studies
Inpatient e/m case studies.
Case study of a stroke patient at varying visit levels to better understand code selection for inpatient encounters under the revised guidelines for 2024.
67-year-old Female with Stroke
Total time* for Inpatient E/M in 2023
Refer to the following tables for correct code selection when billing based on time for inpatient E/M Services:
*Total time includes non face-to-face time on the date of service
Day 1: Critical Care (99291)
A 67-year-old woman with hypertension and diabetes presents to the emergency department with abrupt onset of left hemiparesis 45 minutes ago.
Pre-evaluation : Discussed presentation and vital signs with ED provider (3 mins).
Face-to-face evaluation : Performed medically appropriate history and exam. She has a dense left hemiparesis and an NIH Stroke Scale score of 8. Thrombolysis safety criteria reviewed (7 mins).
Post-evaluation : Non-contrast head CT, CTA of head and neck, and lab results reviewed in the ED. Case discussed with ED provider and thrombolysis recommended. Consultation documented in the ED (25 mins).
Total time : 35 minutes.
Critical Care Coding
According to the 2024 CPT code set, a provider may bill for critical care when the following requirements are met:
- A critical condition: one that acutely impairs a vital organ system with a high probability of imminent or life-threatening deterioration. This includes, for example, central nervous system failure.
- Direct delivery of critical care: high complexity decision-making to assess, manipulate, and support vital systems to treat organ system failure or prevent further life-threatening deterioration.
- At least 30 minutes of time spent solely in the care of the patient. It does not need to be continuous, and it includes both time at the bedside and time spent on the same floor or unit engaged in work directly related to the patient’s care (e.g., documenting critical care, reviewing test results, discussing care with other providers, obtaining history, or discussing treatments or treatment limitations with surrogates when the patient lacks the capacity to do so).
Specific critical care credentials are not required to bill critical care. Critical care is usually provided in a critical care area such as an intensive care unit or emergency department, but this is not always the case (for example, critical care provided to a deteriorating patient in a non-critical care unit).
Other examples of critical care might include:
- Evaluating a patient with status epilepticus and prescribing anti-epileptic drugs or sedative infusions,
- Evaluating a patient with acute respiratory failure from neuromuscular disease and prescribing plasmapheresis,
- Evaluating a patient with coma after cardiac arrest and discussing prognosis, treatment, and goals of care with surrogates (documenting the patient’s lack of capacity to participate)
Critical care, 30-74 minutes CPT 99291 is justified based on the above documentation, although E&M codes (e.g., 99223) associated with fewer wRVUs and lower reimbursement could be used as well.
Day 2: Subsequent Hospital Inpatient Care
Pre-rounds : Reviewed vitals, labs, and studies (LDL, Hemoglobin A1c, EKG, TTE). Review and document independent interpretation of MRI (8 mins).
On Rounds : Performed medically appropriate history and exam. The patient’s symptoms and findings improved somewhat overnight. Patient counseled about stroke evaluation and secondary prevention (10 mins).
Post-rounds : Order atorvastatin, order diabetes consult for management of diabetes. Document discussion with case management possible need for acute inpatient rehabilitation. Documentation completed (10 mins).
Total time : 28 minutes
In this situation, billing according to MDM would be associated with higher reimbursement.
Day 3: Discharge Day Management (By Primary Service)
Pre-rounds : Reviewed vitals, daily CBC and BMP, nursing notes and PT/OT notes (5 mins).
On Rounds : Performed medically appropriate history and exam. The patient reports continued slight improvement in symptoms and requests counseling on how complementary and alternative medicine might help manage her chronic conditions (15 mins).
Post-rounds : Prescribe antiplatelet agent, antidiabetic medications, and antihypertensives. Prepare discharge paperwork and document discharge summary (15 mins).
Total time : 35 minutes
Discharge Day Management Coding (Inpatient or Observation)
Discharge CPTs are selected based on total (face-to-face and non-face-to-face) time, not MDM:
- 99238: 30 minutes or less
- 99239: 31 minutes or more
Discharge CPTs would be used by the primary attending service (e.g., a Neurohospitalist service). Consulting services would continue to choose Subsequent Day codes based on time or MDM.
Discharge Day Management, 31 minutes or more CPT 99239
Disclaimer: The billing and coding information provided by the American Academy of Neurology and its affiliates (collectively, “Academy”) are assessments of clinical information provided as an educational service. The information (1) is not clinical advice; (2) does not account for how private payers cover and reimburse procedures or services*; (3) is not continually updated and may not reflect the most current clinical information (new clinical information may emerge between the time information is developed and when it is published or read); and (4) is not a substitute for the independent professional judgment of the treating provider, who is responsible for correctly coding procedures and services.
Using this information is voluntary. The Academy is providing the information on an “as is” basis and makes no warranty, expressed or implied, regarding the information. The Academy specifically disclaims any warranties of merchantability or fitness for a particular use or purpose. The Academy assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this information or for any errors or omissions.
*The Academy recommends always checking private payer policies before rendering procedures or services
Ischemic Stroke
Author: Cynthia Leung MD PhD, The Ohio State University College of Medicine.
Editor: Rahul Patwari, MD, Rush University, Chicago, Illinois.
Last Update: November 2019
A 68-year-old female, with a history of hypertension and diabetes mellitus, presented to the ED after acute onset of speech difficulty and right-sided weakness. Her symptoms began 3 hours ago. On physical exam, the patient was found to have severe expressive aphasia, right hemiplegia, and right hemi-sensory loss.
Upon completion of this module, the student will be able to:
- Recognize signs and symptoms of stroke
- Identify clinical features suggestive of common stroke mimics
- Describe the initial management of acute stroke
- Discuss the treatment options for acute ischemic stroke
Introduction
Stroke is the fifth leading cause of death and the leading cause of disability in the US with estimated direct and indirect costs of roughly 70 billion dollars per year. Based on current estimates, the prevalence of stroke is expected to increase by twenty percent by the year 2030. Advancements in the diagnosis and treatment of stroke must continue to compensate for the increasing stroke burden on our society.
Stroke is characterized by the acute onset of neurologic deficit caused by disruption of cerebral blood flow to a localized region of the brain. The reversibility and extent of symptoms in stroke is critically dependent on the duration of this disruption. Therefore, early recognition and treatment is the key to reducing morbidity and mortality associated with stroke. As the first physician to see the patient with acute stroke, the actions of the Emergency Physician can have a profound impact on the outcome of stroke patients.
Acute stroke most commonly results from occlusion of an intracranial artery by thrombosis within the artery, thromboembolism from an extracranial source, or hemorrhage. Eighty seven percent of strokes are ischemic in etiology, with the remainder caused by intracerebral or subarachnoid hemorrhage. This module will focus exclusively on the evaluation and treatment of acute ischemic stroke. The evaluation and treatment of hemorrhagic stroke can be found in the intracranial hemorrhage module.
Patients with stroke may present with a variety of neurologic symptoms including changes in vision, changes in speech, focal numbness or weakness, disequilibrium or alteration in level of consciousness. There are many alternate diagnoses that can mimic the symptoms of stroke.
The differential diagnosis includes:
- Structural brain lesion (tumor, AVM, aneurysm, hemorrhage)
- Infection (cerebral abscess, septic emboli)
- Seizure Disorder and post-seizure neurologic deficit (Todd’s paralysis)
- Peripheral Neuropathy (Bell’s palsy)
- Complicated Migraine
- Toxic-metabolic disorders (Hypoglycemia and Hyponatremia)
- Conversion Disorder
Initial Actions and Primary Survey
The initial actions in the evaluation of a patient with suspected stroke begin with emergent stabilization of the patient. As with any emergent patient, the primary survey includes assessment of the patient’s airway, breathing and circulation. Hypoxemia and hypotension due to stroke or co-morbid conditions may worsen stroke symptoms and lead to death. Therefore, treatment of any critical conditions found on primary survey must be initiated prior to continuing the evaluation. Next, a focused H&P is performed to assess level of neurologic dysfunction, exclude alternate diagnoses, and determine the patient’s eligibility for therapy.
Presentation
The initial diagnosis of acute stroke is based on clinical findings. Part of the challenge in making the diagnosis is that there is no “textbook” presentation of stroke. The signs and symptoms of stroke are highly variable and depend not only on the particular blood vessel occluded, but also the extent of occlusion and amount of circulation provided by collateral vessels. Presentations may vary from multiple profound neurologic deficits in a large vessel occlusion to very subtle isolated deficits when smaller vessels are occluded.
The single most important component of the history is the exact time of onset of symptoms. This is defined as the time when the patient was last known to be symptom-free, commonly referred to as the “last known well”. In cases where the patient’s last known well time is unclear, focused questions should be deployed to help narrow down the time window as much as possible. For example, if the patient awakens from sleep with symptoms, questioning the patient about waking in the middle of the night to walk to the restroom or kitchen may help to determine a more accurate last known well time. In patients who were awake during symptom onset, asking about specific activities such as phone calls or television shows may help to further focus the timeframe of onset. Friends and family should also be asked to provide collateral information when possible.
The remainder of the history should focus on factors which may help differentiate a stroke mimic from a true stroke. The HPI should include a detailed history of the onset, time course and pattern of symptoms to help distinguish between stroke and alternate diagnoses. Symptoms which achieve maximal intensity within seconds to minutes of onset and simultaneously affect multiple different systems at once are typical of stroke. In contrast, symptoms which progress slowly over time or progress from one area of the body to another are more suggestive of stroke mimic. The past medical history should include assessment of stroke risk factors as well as risk factors for stroke mimics. Stroke risk factors include hypertension, diabetes, hyperlipidemia, tobacco abuse, advanced age, atrial fibrillation or prosthetic heart valve, and prior stroke. In patients receiving thrombolytic therapy, the most common stroke mimics include complicated migraine, seizure and conversion disorder. A past medical history which includes any of these disorders should heighten suspicion of these alternate diagnoses.
Once the primary survey is complete, a thorough neurologic exam should be performed. This should include assessment of level of consciousness, cranial nerves, strength, sensation, cerebellar function and gait.
Common Stroke Syndromes
Signs and symptoms of stroke should follow a vascular distribution of the brain. Knowledge of the functional areas supplied by each of the major intracranial blood vessels helps to predict signs and symptoms associated with occlusion of that particular vessel.
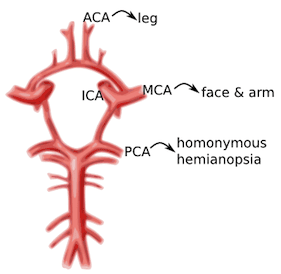
Image 1. Circle of Willis and the primary cerebral vessels. Labels added. Contect accessed from https://medlineplus.gov/ency/imagepages/18009.htm
Anterior Cerebral Artery (ACA): unilateral weakness and/or sensory loss of contralateral lower extremity greater than upper extremity
Middle Cerebral Artery (MCA): unilateral weakness and/or sensory loss of contralateral face and upper extremity greater than lower extremity with either aphasia (if dominant hemisphere) or neglect (if non-dominant hemisphere)
Posterior Cerebral Artery (PCA): unilateral visual field deficit in both eyes (homonymous hemianopsia).
Vertebrobasilar syndromes have multiple deficits which typically include contralateral weakness and/or sensory loss in combination with ipsilateral cranial nerve palsies. Suspicion for posterior circulation stroke is heightened if the patient exhibits one of these signs or symptoms beginning with “D”: diplopia, dysarthria, dysphagia, droopy face, dysequilibrium, dysmetria, and decreased level of consciousness. Nausea and vomiting are also frequently associated with brainstem stroke.
Lacunar infarcts are small strokes (measuring less than 1.5 cm) caused by occlusion of one of the deep perforating arteries which supplies the subcortical structures and brainstem. Lacunar infarcts can produce a large variety of clinical deficits depending on their location within the brainstem and have been characterized by more than 70 different clinical syndromes. However, the vast majority of lacunar strokes are described by the 5 most common lacunar syndromes: pure motor hemiparesis, sensorimotor stroke, ataxic hemiparesis, pure sensory stroke, and dysarthria-clumsy hand syndrome.
Diagnostic Testing
Rapid evaluation of patients with suspected stroke is critical because there is a very narrow time window in which stroke patients are eligible for treatment. A panel of experts convened by the National Institute of Neurological Disorders and Stroke (NINDS) has established several critical events in the identification, evaluation, and treatment of stroke patients in the ED. The most important of these time goals include a door to head CT time less than 25 minutes and a door to drug administration time of less than 60 minutes.
The diagnosis of stroke is based primarily on clinical presentation. The NIH Stroke Scale (NIHSS) provides a standardized clinical assessment which is generalizable from one physician to another and allows monitoring of the patient’s neurologic deficits over time. The NIHSS can serve as a measure of stroke severity and has been shown to be a predictor of both short and long term outcome of stroke patients. Many Emergency physicians find it convenient to keep an App on their phone to aid in rapidly calculating the NIHSS. There are also a variety of on-line NIHSS calculators available, such as the one found on MDcalc.com
The remainder of the diagnostic workup is focused on excluding alternative diagnoses, assessing for comorbid conditions and determining eligibility for therapy. The diagnostic workup includes:
Brain Imaging
Head CT without contrast should be performed on all patients to exclude intracranial hemorrhage. Unenhanced head CT is often able to identify other structural brain lesions and may detect early signs of stroke. Because radiologic changes associated with stroke are usually not visible on CT for several hours, the most common CT finding in acute ischemic stroke is normal brain. However, multiple subtle findings associated with acute ischemic stroke may be present in the first 3 hours after symptom onset. The earliest finding that may be seen on CT is hyperdensity representing acute thrombus or embolus in a major intracranial vessel. This is most frequently seen in the MCA (“hyperdense MCA sign”, see Image 2) and basilar arteries (“hyperdense basilar artery sign”). Subsequent findings include subtle hypo-attentuation causing obscuration of the nuclei in the basal ganglia and loss of gray/white differentiation in the cortex. Frank hypodensity on CT is indicative of completed stroke and may be a contraindication to thrombolytic therapy.
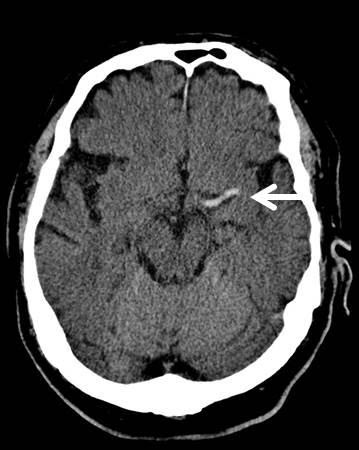
Image 2. MCA sign on CT head. Case courtesy of A.Prof Frank Gaillard, <a href=" https://radiopaedia.org/ ">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/7150">rID: 7150</a>
At specialized stroke centers, alternative testing such as diffusion weighted MRI (DWI) or CT angiography/CT perfusion studies may also be performed as these modalities are more sensitive for detecting early or evolving infarct and may help determine the most appropriate therapy.
Serum Glucose
Hypoglycemia may cause alteration in level of consciousness and any variety of neurologic symptoms. Point of care blood glucose level must be performed to exclude hypoglycemia prior to initiation of thrombolytic therapy.
EKG should be performed to exclude contemporaneous acute MI or atrial fibrillation as these conditions are frequently associated with thromboembolic stroke.
Additional laboratory studies
CBC, chemistries, PT/INR, aPTT, and cardiac markers are recommended to assess for serious comorbid conditions and aid in selection of therapy. Treatment should not be delayed for results of these additional studies unless a bleeding disorder is suspected.
The main goal of therapy in acute ischemic stroke is to remove occlusion from the involved vessel and restore blood flow to the affected area of the brain. The AHA/ASA currently recommends two forms of treatment for eligible patients with acute ischemic stroke: intravenous thrombolytic agents and mechanical thrombectomy.
Intravenous Thrombolytic Therapy
Intravenous recombinant Tissue Plasminogen Activator (rtPA) is a fibrinolytic agent that catalyzes the conversion of plasminogen to plasmin, the major enzyme responsible for clot breakdown. Treatment with IV rtPA has been shown to increase the percentage of patients with good functional outcome at 3 months and 1 year after stroke onset.
rtPA has been FDA approved for use in adult patients with symptoms attributable to ischemic stroke up to 3hrs after symptom onset. In addition, the American Heart Association has recommended rtPA for use up to 4.5 hours after symptom onset in a select subgroup of patients. Good functional outcomes are most likely to be achieved if rtPA is administered within 90 minutes of symptom onset. The likelihood of a good outcome decreases with increasing time from onset of symptoms. Therefore, every effort should be made to ensure that there are no delays in administration of thrombolytic therapy to eligible patients.
The major complication of rtPA administration in stroke is symptomatic intracranial hemorrhage. Careful selection of patients with an appropriate risk/benefit ratio is imperative to reduce the risk of symptomatic ICH. Exclusion criteria most commonly reflect factors that may increase likelihood of ICH including uncontrolled severe hypertension, coagulopathies, recent intracranial or spinal surgery, recent head trauma or stroke and history of prior ICH. The full list of inclusion and exclusion criteria for intravenous rtPA therapy can be found in the most recent version of the AHA Guidelines for the Early Management of Patients with Acute Ischemic Stroke (see references below).
In addition, strict adherence to the NINDS recommended protocol for administration of rtPA is critical to successful treatment in stroke patients. This protocol specifies important aspects of care during and after administration of rtPA. Admission to an ICU or stroke unit, frequent reassessment of the patient’s neurologic status and careful blood pressure monitoring are all vital in the first 24 hours after administration of rtPA. Most importantly, any patient who develops acute severe headache, acute severe hypertension, intractable nausea and vomiting, altered mental status or other evidence of neurologic deterioration during or after rtPA administration should have emergent noncontrast head CT to evaluate for ICH. In addition, rtPA infusion should be discontinued immediately if it has not already been completed.
Mechanical Thrombectomy
Mechanical thrombectomy is recommended for adult patients with ischemic stroke caused by occlusion of the internal carotid or proximal middle cerebral (M1) arteries and an NIHSS greater than 6, presenting within 6 hours of symptom onset. Thrombectomy is also recommended for a select group of patients presenting up to 16 hours after symptom onset if they have demonstrated perfusion mismatch on MRI or CTP and meet additional eligibility requirements. This recommendation was based on pooled analysis of 5 studies which demonstrated lower degree of disability at 3 months in patients undergoing mechanical thrombectomy compared to those undergoing thrombolytic therapy alone. This effect was most pronounced when the time from symptom onset to thrombectomy was under 2 hours, but persisted up to 7 hours after symptom onset.
Supportive Care
Unfortunately, only a small percentage of stroke patients present to the ED within the time limit to receive specialized therapy. In stroke patients not receiving rtPA or mechanical thrombectomy, the goal of care is to prevent or treat acute complications by providing supportive care. This includes ventilatory support and oxygenation if needed, prevention of hyperthermia, cardiac monitoring, and control of blood pressure and blood glucose.
Goals for Blood Pressure Control
In patients receiving intravenous rtPA, the rate of symptomatic ICH is directly related to increasing blood pressure. Therefore, strict guidelines for blood pressure control must be enforced in these patients to prevent ICH. Blood pressure should be maintained below 180/105 mm Hg in the first 24 hours after receiving thrombolytic therapy.
In contrast, the ideal blood pressure range for acute stroke patients not receiving thrombolytic therapy has not yet been determined. The current recommendations stress the importance of an individualized approach to blood pressure control with avoidance of hypotension or large fluctuations in blood pressure. For patients who do not have other medical conditions requiring aggressive blood pressure control, antihypertensive treatment should not be initiated unless blood pressure exceeds 220/120 mm Hg.
Antiplatelet Therapy
Administration of Aspirin within 48 hours after stroke has been shown to improve outcomes by reducing the rate of early recurrent stroke. In stroke patients not receiving rtPA, oral administration of aspirin within 24 – 48 hours of stroke onset is recommended. The safety of antiplatelet agents in combination with thrombolytic therapy has not been established. Therefore, aspirin should not be administered for at least 24 hours after administration of rtPA
Pearls and Pitfalls
- Use creative questioning to establish time of onset.
- Consider common conditions which may mimic the symptoms of stroke including seizure, complicated migraine, hypoglycemia, and conversion disorder. All adult patients presenting with neurologic deficit attributable to ischemic stroke within 3 hours of symptom onset should be considered for thrombolytic therapy.
- Minimum workup prior to thrombolytic therapy includes focused H&P, CT Head to exclude intracranial hemorrhage and point of care blood glucose level to exclude hypoglycemia.
- Time is brain! Do not delay administration of thrombolytic therapy to eligible patients.
- Adult patients presenting with acute ischemic stroke due to large vessel occlusion within 16 hours of symptom onset should be considered for mechanical thrombectomy.
- Patients that do not receive thrombolytic therapy should receive aspirin within 24 hours of symptom onset.
Case Study Resolution
The patient’s initial NIHSS was 11. Noncontrast CT of the head did not show any evidence of ICH. CT angiography revealed left M1 occlusion. The patient underwent mechanical thrombectomy with marked improvement in symptoms. Repeat NIHSS was 3. The patient was transferred to the neurologic critical care unit for further monitoring.
Guidelines for the Early Management of Patients with Acute Ischemic Stroke. Powers WJ, et al. Stroke 2018 Mar;49(3): e46-e99. PMID:29367334
Heart disease and StrokeStatistics—2018 Update: a report from the American Heart Association. Benjamin ES, et al. Circulation. 2018 Mar 1;137(12):e67-e493. PMID:29386200
Safety of thrombolysis in stroke mimics: results from a multicenter cohort study. Zinkstok SM, et al. Stroke. 2013 Apr;44(4):1080-4. PMID:23444310
Time to Treatment with Endovascular Thrombectomy and Outcomes from Ischemic Stroke: A Meta-analysis. Saver JL, et al. JAMA 2016; 316(12):1279-1288. PMID:
Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lees KR, et al. Lancet. 2010 May 15;375(9727):1695-1703. PMID:20472172
- Open access
- Published: 06 September 2022
Stroke in young adults, stroke types and risk factors: a case control study
- Priscilla Namaganda 1 ,
- Jane Nakibuuka 2 ,
- Mark Kaddumukasa 3 &
- Elly Katabira 4
BMC Neurology volume 22 , Article number: 335 ( 2022 ) Cite this article
10k Accesses
13 Citations
Metrics details
Stroke is the second leading cause of death above the age of 60 years, and the fifth leading cause in people aged 15 to 59 years old as reported by the World Health Organization global burden of diseases. Stroke in the young is particularly tragic because of the potential to create long-term disability, burden on the victims, their families, and the community at large. Despite this, there is limited data on stroke in young adults, and its risk factors in Uganda. Therefore, we determined the frequency and risk factors for stroke among young adults at Mulago hospital.
A case control study was conducted among patients presenting consecutively to the general medical wards with stroke during the study period September 2015 to March 2016. A brain Computerized Tomography scan was performed to confirm stroke and classify the stroke subtype. Controls were patients that presented to the surgical outpatient clinic with minor surgical conditions, matched for age and sex. Social demographic, clinical and laboratory characteristics were assessed for both cases and controls. Descriptive statistics including frequencies, percentages, means, and standard deviation were used to describe the social demographics of case and controls as well as the stroke types for cases. To determine risk factors for stroke, a conditional logistic regression, which accounts for matching (e.g., age and sex), was applied. Odds ratio (with 95% confidence interval) was used as a measure for associations.
Among 51 patients with stroke, 39(76.5%) had ischemic stroke and 12(23.5%) had hemorrhagic stroke. The mean age was 36.8 years (SD 7.4) for stroke patients (cases) and 36.8 years (SD 6.9) for controls. Female patients predominated in both groups 56.9% in cases and 52.9% in controls. Risk factors noted were HIV infection, OR 3.57 (95% CI 1.16–10.96), elevated waist to hip ratio, OR 11.59(95% CI 1.98–68.24) and sickle cell disease, OR 4.68 (95% CI 1.11–19.70). This study found a protective effect of oral contraceptive use for stroke OR 0.27 95% CI 0.08–0.87. There was no association between stroke and hypertension, diabetes, and hyperlipidemia.
Among young adults with stroke, ischemic stroke predominated over hemorrhagic stroke. Risk factors for stroke were HIV infection, elevated waist to hip ratio and sickle cell disease.
Peer Review reports
Stroke is the second leading cause of death above the age of 60 years, and the fifth leading cause in people aged 15 to 59 years old as reported by the World Health Organization (WHO) global burden of diseases [ 1 ]. The severity of stroke in the young is relatively low in developed countries ranging from 2 -7% in Italy and USA respectively [ 2 , 3 ]. In Africa, on the other hand the prevalence of stroke among young adults is 12.9% in Nigeria [ 4 ], 31% in South Africa [ 5 ], 28.9% in Morocco [ 6 ]. The incidence of ischemic stroke in the young has been increasing globally over the last 2–3 decades. From the Danish National Patient Register, the incidence rates of first‐time hospitalizations for ischemic stroke and transient ischemic attack (TIA) in young adults have increased substantially since the mid 1990s while the incidences of hospitalizations for intracerebral hemorrhage and subarachnoid hemorrhage remained stable during the study period [ 7 ].
In Uganda, literature on stroke in young adults is limited however results of a study done among acute stroke patients admitted to the national referral hospital (Mulago hospital) showed a 30-day mortality of 43.8%. Out of 133 patients, 32 patients (25%) were less than 51 years old. Out of the 56 patients that died, 13 patients (23%) were less than 51 years [ 8 ].
Rapid western cultural adaption (sedentary lifestyle, deleterious health behavior like consumption of tobacco and alcohol and high fat/cholesterol diet) and Human immunodeficiency syndrome/ Acquired immunodeficiency syndrome (HIV/AIDS) that is highly prevalent in Africa has accelerated risk factors and increased the burden of stroke [ 9 ].
Most literature indicates that the traditional risk factors i.e., hypertension, diabetes mellitus and dyslipidemia are still the commonest risk factors with hypertension having the highest frequency. Other risk factors common to the young include smoking, excessive alcohol intake, illicit drug use, oral contraceptive use and migraine [ 10 ].
Although stroke is predominantly a disease of the middle age and the elderly, its occurrence in younger age groups is not rare. Stroke in young adults seems to be increasing and is particularly tragic because of the potential to create long-term disability, burden on the victims, their families, and the community at large such as Uganda. Despite the huge socioeconomic impact of stroke in this age group, there is a scarcity of data regarding stroke in young adults in sub-Saharan Africa including Uganda. Effective stroke prevention strategies in the young require comprehensive information on risk factors and possible causes. Although case reports and etiologic investigations of possible causes of stroke in the young have been identified especially in developed countries, there is limited data on risk factors in Africa Uganda inclusive. Information obtained from this study will fill the knowledge gap in this area of stroke in the young which will inform institutional strategies on prevention and management of stroke in this age group. This study, therefore, seeks to determine the frequency of stroke types and risk factors for this population.
The aims of the study were:
To determine the frequency of stroke types among young adults on the general medical wards in Mulago hospital between September 2015 and March 2016.
To determine the risk factors for stroke (i.e., ischemic, and hemorrhagic stroke) among young adults on the general medical wards in Mulago hospital between September and March 2016.
This was a case control study. Cases were defined as patients with a confirmed diagnosis of stroke by brain computerized tomography (CT) scan that met the inclusion criteria. Controls were defined as patients with minor surgical conditions that met the inclusion criteria. The study was carried out in Mulago hospital which is the national referral hospital in Uganda as well as the teaching hospital of Makerere University College of health sciences. It has a bed capacity of 1500 beds and has both inpatient wards, outpatient departments both for medical and surgical specialties. It has a radiological department with CT scan and highly trained personnel and a well-equipped laboratory. Cases were recruited consecutively from the medical wards specifically on the neurology ward of Mulago hospital. Patients on the neurology ward are managed by physicians that have had additional training in the management of neurological conditions.
Controls were recruited from general surgical outpatient departments from Mulago hospital. They were matched for age and sex. Eligible patients were patients aged 15–45 years, confirmed diagnosis of stroke on brain CT scan and with a written informed consent or assent for patients less than 18 years. These included patients with intracranial hemorrhages and ischemic stroke, none had subarachnoid hemorrhage. Patients were excluded if they were unconscious and with no valid surrogate (next of kin) and HIV positive with opportunistic infections. Patients eligible as control were, patient aged 15–45 years, minor surgical condition, written informed consent or assent for patients less than 18 years. Patients with features of stroke secondary to non-vascular causes like trauma, tumors were excluded as controls. For controls, we chose patients with minor surgical conditions because we wanted controls to be hospital patients but with non-medical conditions that could confound our findings. Such conditions included lacerations, hernias, lipomas, ingrown toenails, circumcision.
Based on the catchment area of Mulago, patients with minor surgical conditions are likely to have similar social economic status and come from similar neighborhoods as would health controls living in the catchment areas as patients with stroke.
The best alternative would have been healthy controls from the neighborhoods of the patients with stroke, but this would have been resource consuming.
The sample size was calculated assuming a prevalence of 62.2% of hypertension among the stroke patients as was indicated in a similar study among the young Thai adults in Bangkok, Thailand (Bandasak et al., 2011) [ 11 ]. We also assumed that the risk for stroke is higher among the hypertensive with an OR of 3. With this sample size, we were powered to detect associations with other risk factors like smoking (OR 2.6) [ 12 ], diabetes (OR 13.2 for black men and 22.1 for black women) [ 13 ].
With these assumptions, a sample size of 51 cases and 51 controls was found sufficient with 80% power and 0.05 level of significance.
Sampling procedure
All young patients admitted on the general medical wards suspected of having stroke were screened and brain CT scan done. Once a diagnosis of stroke was confirmed on CT scan, participants who consented to participate in the study were recruited consecutively, a standardized questionnaire administered by the research team for those patients able to communicate. For patients not able to communicate, consent and information were obtained through the care givers. Controls were selected from the general surgical outpatient clinic using consecutive sampling method. This was done after we had obtained all the cases. These were matched for age and sex until the sample size was accrued.
Information was collected on:
Social demographic characteristics i.e., age, sex, level of education, occupation, religion, history of smoking and alcohol consumption, history of illicit drug use, history of oral contraceptive use.
Clinical examination included general physical examination, blood pressure using a digital blood pressure machine. For patients who were too weak to sit up, blood pressure measurement was taken in supine position. For those able to sit, it was taken in the sitting position. The two blood pressure measurements were taken at an interval of 5 min and the average blood pressure recorded as the final blood pressure.
Physical measurements for the weight and hip were taken using a stretchable tape measure. Waist measurements were taken at the narrowest point-umbilicus and hip measurements at the widest point- buttocks. A waist to hip ratio was obtained and recorded on the questionnaire.
Blood was drawn for laboratory tests; high density lipoprotein, low density lipoprotein (HDL/LDL), fasting blood sugar, full blood count, Hb electrophoresis, prothrombin time/ international normalization ratio (PT/INR), HIV serology, Treponema pallidum hemagglutination (TPHA).
Other information obtained was history and family history of diabetes and hypertension.
The general surgical outpatient clinic runs every Tuesday, and Thursday in Old Mulago hospital Participants were identified at the surgical outpatient clinic. Those matching the age and sex of the cases were recruited, written consent/assent obtained, and questionnaire was administered by the PI. The procedure as explained above was followed for the controls.
Data collection
A pre-tested and standardized questionnaire was used as a data collection tool. The principal investigator administered the questionnaire to the participants in data collection. Data on socio demographics and past medical history was collected.
Results from imaging and laboratory investigations were also recorded into the questionnaire.
Data collected was double entered into the computer using EPI-DATA (version 3.1) software to minimize data entry errors. Data was then backed up and archived in both soft and hard copy to avoid losses. Confidentiality was ensured using code numbers instead of patients’ names. Questionnaires were stored in a lockable cabinet for safety.
Data analysis
Data was analyzed using STATA Version 12 (StataCorp. 2011. Stata Statistical Software: Release 12 . College Station, TX: StataCorp LP). Descriptive statistics were used to describe characteristics of the study participants and the stroke subtypes which included frequencies, percentages, means and standard deviation. To determine factors associated with stroke, a conditional logistic regression, which accounts for matching (e.g., age and sex), was applied. Odds ratio (with 95% confidence interval) was used as a measure for associations. Factors with p -values < 0.2 at a bi-variable analysis were entered into a multiple conditional logistic regression to obtain the adjusted estimates. Factors whose 95% confidence interval for the odds ratio that excludes a 1 or whose p -value < 0.05, were considered statistically significant at the adjusted level. Post-hoc power calculation was performed for the adjusted analysis to check if there was enough power to detect a difference between cases and controls.
Quality control
To ensure quality of results several measures were undertaken, these included:
The questionnaires were pre-tested and standardized before study commenced.
The research team administered the structured, pre- coded and pre-tested questionnaire to enrolled participants on a face-to-face basis and brain CT scans were done by competent and well-trained radiology technicians and interpretation done by a specialist radiologist at the Radiology Department of Mulago hospital.
The questionnaires were checked for completeness at the end of every interview. The two files were compared, and any discordance corrected against data recorded with the questionnaire. The data were then backed up.
Ethical consideration
Written informed consent/ assent was obtained from all participants or their parent/guardian or legal authorized representative to participate in the study. Ethical approval was obtained from Makerere University, school of medicine research and ethics committee (SOMREC) (reference number #REC REF 2015–105).
Confidentiality was ensured using code numbers instead of patients’ names. Questionnaires were stored in a lockable cabinet for safety.
Profile of the study
Enrollment of study participants was carried out between September 2015 to March 2016 in Mulago hospital. The patient flow diagram for cases and controls is as shown in Fig. 1 .
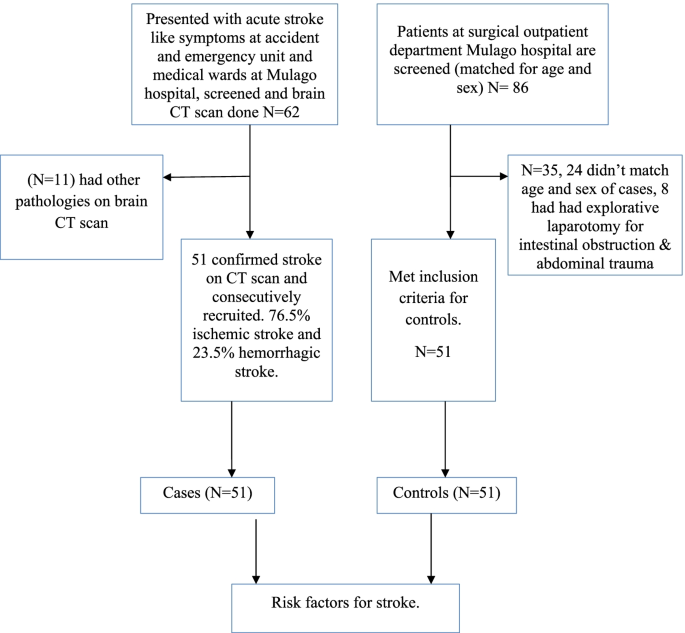
Patient flow diagram
Social demographic characteristics of the study population
A total of 51 cases aged 18 to 45 years and the same number of hospital control matched for age and sex were identified. The mean age of cases was 36.8 years (standard deviation (SD) 7.4) and the control was 36.8 years (SD 6.9). Females predominated in both groups with 56.9% in cases and 52.9% in controls. There was no significant difference in other baseline characteristics between cases and controls except in oral contraceptive use, waist to hip ratio, HIV status and sickle cell disease. Details of the social demographic characteristics are shown in Table 1 .
Clinical characteristics of the study participants
The mean fasting blood sugar was 6.6 (SD 3.9) for cases and 5.3 (SD 0.7) for controls. This was statistically significant with a p value of 0.015. Waist to hip ratio was also statistically significant with a p value of 0.007. Cases with an elevated wait to hip ratio were 14 (27.5%) and controls were 3 (5.9%). Table 2 shows the baseline clinical characteristics of the study participants.
Laboratory characteristics of the study participants
HIV serology and Hb electrophoresis were statistically significant with a p value of 0.076 and 0.023 respectively. 18 patients (35.3%) were reactive for HIV among cases and controls 10 (19.6%). 12 patients (23.5%) had abnormal Hb electrophoresis among cases controls 3 (5.9%). Table 3 shows the laboratory characteristics of the study participants.
Stroke types
Stroke types by social demographic characteristics of cases.
Among 62 patients, who had brain CT scan done, 11 patients had non stroke pathologies (4 had brain abscesses, 7 patients had ring enhancing lesions suggestive of toxoplasmosis). Among 51 patients with stroke confirmed on CT scan, the frequency of ischemic stroke was 76.5% and hemorrhagic stroke was 23.5%.
Most participants with ischemic or hemorrhagic stroke were in the age group 36–45 years. Females predominated in both ischemic and hemorrhagic stroke. Details of the social demographic characteristics by stroke types are shown in Table 4 .
Clinical and laboratory characteristics by stroke types
Majority of patients with hemorrhagic stroke were hypertensive (91.7%) compared to only 25.6% among patients with ischemic stroke. Details of the clinical and laboratory characteristics of the study participants by stroke subtypes are shown in Table 5 .
Risk factors for stroke at univariate analysis
Social demographic characteristics at univariate analysis.
Oral contraceptive use showed a significant difference with an unadjusted OR of 0.27 (95% CI 0.08–0.87) case subjects 23.3% and control subjects 56.5%. Belonging to other religion (seventh day advent, Pentecostal) was statistically significant with a p value of 0.009, OR 0.17. These findings are detailed in Table 6 below.
Clinical characteristics at univariate analysis
There was a significant difference in waist to hip ratio between cases (27.5%) and controls (5.9%), with unadjusted OR 6.85 (CI 1.70–27.62). HIV serology with an unadjusted OR of 2.64 (95% CI 1.03–6.82). Hb electrophoresis with an unadjusted OR of 4.31 (95% CI- 1.15–16.17). Fasting blood sugar with an unadjusted OR of 1.64 (95% CI 1.02–2.62). Details of the above findings are shown in Table 7 below.
Risk factors for stroke at multivariate analysis
At multivariate analysis, HIV serology (OR 3.72, 95% CI 1.16–10.96), waist to hip ratio (OR 11.26 95% CI 1.98–68.24) and sickle cell disease OR 4.78 95% CI 1.11–19.70) were independent risk factors for stroke in young adults. Table 8 shows risk factors at multivariate analysis. None of the patients with HIV met the definition of AIDS as defined by the occurrence of any of the more than 20 life-threatening cancers or “opportunistic infections”, by WHO.
This case–control study showed that the frequency of ischemic stroke was higher than that of hemorrhagic stroke in young Ugandan population. We showed that positive HIV serology, elevated waist to hip ratio and sickle cell disease were independent risk factors for stroke in this population.
This is consistent with several studies that have been done and found ischemic stroke to be more prevalent than hemorrhagic stroke. Studies done in Africa, in Libya reported 77% ischemic stroke and 23% hemorrhagic stroke (these included both intracerebral and subarachnoid hemorrhagic stroke) [ 14 ], in Morocco, 87.3% ischemic stroke and 12.7% hemorrhagic (study did not specify on the subtypes of hemorrhagic stroke) [ 6 ]. In a study from Bosnia and Herzegovina, Subarachnoid hemorrhage was more frequent in young adults compared with older patients (> 45 years of age) (22% vs. 3.5%), intracerebral hemorrhage (ICH) was similar in both groups (16.9% vs. 15.8%), but ischemic stroke (IS) was predominant stroke type in the older group (61% vs. 74%) [ 15 ]. On the other hand, studies focusing on all young stroke patients and including also subarachnoid hemorrhages have found much higher proportion of hemorrhagic strokes in younger vs. older individuals. Population-based studies have reported as low as 57% prevalence for ischemic stroke in those aged > 45, as reported by a recent narrative review [ 16 ]. This difference in occurrence of stroke subtypes could be due to the low prevalence of hypertension in this population in our setting given that hypertension has been reported to be the commonest risk factor for hemorrhagic stroke.
Most previous studies of HIV and stroke have been retrospective, but the prospective studies in Africa and East Africa have reported the importance of HIV as a risk factor for stroke [ 17 ]. A recently published study done in Malawi, with defined cases and population controls and 99% ascertainment of HIV status, reported HIV infection as an independent risk factor for stroke. This study further found that patients who had started standard HIV treatment in the previous six months had a higher risk of stroke (OR 15.6 95% CI 4.21–46.6). This was probably due to an immune reconstitution inflammatory syndrome (IRIS) like process [ 18 ]. A variety of mechanisms have been implicated in the association of HIV and stroke, these include HIV associated vasculopathy, vasculitis which causes abnormality of the intracranial or extracranial cerebral blood vessels and neoplastic involvement. Indirectly through cardioembolic, coagulopathy in association with protein C and protein S deficiency. Some infections are well established causes of stroke, such as Mycobacterium tuberculosi s , syphilis, and varicella zoster virus through increased susceptibility to acquisition or reactivation of these infections [ 19 , 20 ]. Combined antiretroviral therapy (cART) might unmask occult opportunistic infections that subsequently cause a stroke. This possibility should be considered in all patients who have had an acute stroke or have worsening of stroke symptoms after initiation of cART [ 21 ].
An elevated waist to hip ratio (WHR) was associated with 12 times increased risk of stroke among young adults in Mulago hospital compared to individuals with a normal waist to hip ratio. Abdominal obesity (measured as waist–hip ratio) is associated with an increased risk of myocardial infarction, stroke, and premature death [ 22 ]. This agrees with a few studies that have assessed the association of stroke with waist to hip ratio. Aaron et al. 1990, assessed the relation between body fat distribution, and the 2-year incidences of hypertension and stroke in a cohort of 41,837 women aged 55–69 years. Women who developed stroke were 2.1 (95% CI 1.5–2.9) times more likely to have an elevated ratio than those who did not [ 23 ]. Md Habib et al. 2011 assessed high waist to hip ratio as a risk factor for ischemic stroke for overall stroke and he found 64% of the ischemic stroke patient had abnormal WHR in Bangladesh [ 24 ]. Abdominal obesity measured with WHR was an independent risk factor for cryptogenic ischemic stroke (CIS) in young adults after rigorous adjustment for concomitant risk factors in the Revealing the Etiology, Triggers, and Outcome (SECRETO; NCT01934725) study, a prospective case–control study that included patients aged 18–49 years with a first ever CIS at 19 European university centers [ 25 ].
Sickle cell disease was also associated with increased risk of stroke among young adults in Mulago hospital. This agrees with several studies that have associated sickle cell disease with stroke. Ohene et al. 1998 assessed cerebrovascular accidents (CVA) in sickle cell disease, found the highest rates of prevalence of 4.01% and incidence of 0.61 per 100 patient-years. The incidence of hemorrhagic stroke was highest among patients aged 20 to 29 years [ 26 ].
In our study, the unadjusted OR for oral contraceptive use was 0.26 95% CI 0.08–0.87 with a p value of 0.028. This observation at the unadjusted level is significant but could be due to another variable which is a confounder to OC use such as higher socioeconomic status and better control of other possible risk factors.
In our study, we found no association between hypertension and stroke in young adults though it’s an independent risk factor for stroke in the older population. This finding is different from the multinational interstroke study which attributed most strokes among young adults in low- and middle-income countries to hypertension. In that study, only one fifth of the patients were from wealthier African countries where hypertension, diabetes and hypercholesterolemia are likely to occur with higher prevalence than in Mulago hospital [ 27 ]. Other studies have also reported the role of hypertension as a risk factor for stroke in young adults, low physical activity and hypertension were the most important risk factors, accounting for 59.7% and 27.1% of all strokes, respectively among a German nationwide case–control study based on patients enrolled in the SIFAP1 study (Stroke in Young Fabry Patients) 2007 to 2010 and controls from the population-based GEDA study (German Health Update) 2009 to 2010 [ 28 ]. A study that used population-based controls for hospitalized young patients with ischemic stroke demonstrated that independent risk factors for stroke were atrial fibrillation (OR 10.43; cardiovascular disease (OR, 8.01; type 1 diabetes mellitus (OR, 6.72; type 2 diabetes mellitus (OR, 2.31, low high‐density lipoprotein cholesterol (OR, 1.81; current smoking status (OR, 1.81; hypertension (OR, 1.43, and a family history of stroke (OR, 1.37) [ 29 ].
This finding could be explained by the high prevalence of hypertension in the general peri urban Ugandan population among young adults as reported by Kayima et al. 2015. He found a prevalence of 15% (95% CI 14.2 – 19.6%) % for young adults aged 18–44 years [ 30 ].
The study was conducted at Mulago hospital which is a national referral hospital in Uganda situated in central Uganda. Mulago hospital received patients both referred patients from all over Uganda and those from its catchment area. This is generally representative of the whole Ugandan population.
Uganda has a young population and with an HIV prevalence comparable to most countries in Sub-Saharan Africa, so the findings of this study are generalizable to other Sub-Saharan African populations.
Ischemic stroke is more prevalent than hemorrhagic stroke among young adults in Mulago hospital. Independent risk factors for stroke among young adults in Mulago hospital were HIV infection, elevated waist to hip ratio and sickle cell disease. Oral contraceptive use was found to be protective of stroke among young adults in Mulago hospital. There was no significant association between stroke among young adults and hypertension, diabetes, hyperlipidemia, smoking, alcohol use and illicit use.
Study limitations
The sample size was too small to detect all but the strongest associations with common exposures. When designing the study, we based on hypertension as a significant driver for strokes in this population based on other studies done to calculate the sample size, however based on our findings, hypertension was not a big driver of stroke in this population. Secondly the nature of stroke type associated with hypertension is hemorrhagic which were less common in this study. This was an unexpected finding and needs more evaluation.
Consecutive sampling methods has selection bias in which a variable that is associated with the outcome under investigation may occur more frequently or less in those sampled in this period as compared to the general population.
The use of a combined ischemic stroke and intracerebral hemorrhage group may have obscured relationships specific to one group, i.e., the risk factors for stroke were not stratified for type of stroke.
The best alternative for controls would have been healthy controls from the neighborhoods of the patients with stroke, but this would have been resource consuming hence the choice of hospital controls with different medical conditions from cases.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Turner MB. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245.
PubMed Google Scholar
Griffiths D, Sturm J. Epidemiology and etiology of young stroke. Stroke research and treatment, 2011. 2011.
Google Scholar
Bevan HS, Sharma K, Bradley W. Stroke in young adults. Stroke. 1990;21(3):382–6.
Article CAS Google Scholar
Mustapha AF, Sanya EO, Bello TO. Stroke among young adults at the LAUTECH Teaching Hospital, Osogbo, Nigeria. Nig Q J Hosp Med. 2012;22(3):177–80.
CAS PubMed Google Scholar
Hoffmann M. Stroke in the young: the multiethnic prospective Durban stroke data bank results. J Stroke Cerebrovasc Dis. 1998;7(6):404–13.
Chraa M, Louhab N, Kissani N. Stroke in young adults: about 128 cases. Pan Afr Med J. 2014;17(37).
Tibæk M, Dehlendorff C, Jørgensen HS, Forchhammer HB, Johnsen SP, Kammersgaard LP. Increasing incidence of hospitalization for stroke and transient ischemic attack in young adults: a registry-based study. J Am Heart Assoc. 2016;5(5):e003158. https://doi.org/10.1161/JAHA.115.003158 .
Article PubMed PubMed Central Google Scholar
Kwarisima L, Mukisa R, Nakibuuka J, Matovu S, Katabira E. Thirty-day stroke mortality and associated clinical and laboratory factors among adult stroke patients admitted at Mulago Hospital (Uganda). Afr J Neurol Sci. 2014;33(1):79–86.
Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2(1):43–53.
Article Google Scholar
Katsnelson MJ, Della-Morte D, Rundek T. Stroke in the young. Period Biol. 2012;114(3):347–53.
Bandasak R, Narksawat K, Tangkanakul C, Chinvarun Y, Siri S. Association between hypertension and stroke among young Thai adults in Bangkok, Thailand. Southeast Asian J Trop Med Public Health. 2011;42(5):1241–8 PMID: 22299451.
Bhat VM, Cole JW, Sorkin JD, Wozniak MA, Malarcher AM, Giles WH, Stern BJ, Kittner SJ. Dose-response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39(9):2439–43. https://doi.org/10.1161/STROKEAHA.107.510073 . Epub 2008 Aug 14. PMID: 18703815; PMCID: PMC3564048.
Rohr J, Kittner S, Feeser B, Hebel JR, Whyte MG, Weinstein A, Sherwin R. Traditional risk factors and ischemic stroke in young adults: the Baltimore-Washington Cooperative Young Stroke Study. Arch Neurol. 1996;53(7):603–7.
Radhakrishnan K, Ashok PP, Sridharan R, Mousa ME. Stroke in the young: incidence and pattern in Benghazi. Libya. 1986;73(4):434–8.
CAS Google Scholar
Smajlović D, Salihović D, Ibrahimagić OĆ, Sinanović O. Characteristics of stroke in young adults in Tuzla Canton Bosnia and Herzegovina. Coll Antropol. 2013;37(2):515–9.
Tatlisumak, et al. Nontraumatic intracerebral haemorrhage in young adults. Nat Rev Neurol. 2018;14:237–50. https://doi.org/10.1038/nrneurol.2018.17 .
Article PubMed Google Scholar
O’Donnell M, Yusuf S. Risk factors for stroke in Tanzania. Lancet Glob Health. 2013;1:e241–2.
Benjamin LA, Corbett EL, Connor MD, et al. HIV, antiretroviral treatment, hypertension, and stroke in Malawian adults, a case control study. Neurology. 2016;86:324–33. https://doi.org/10.1212/WNL.0000000000002278 .
Article CAS PubMed PubMed Central Google Scholar
Benjamin LA, Bryer A, Emsley HCA, Khoo S, Solomon T, Connor MD. HIV infection and stroke: current perspectives and future directions. Lancet Neurol. 2012;11(10):878–90. https://doi.org/10.1016/S1474-4422(12)70205-3 .
Lammie GA, Hewlett RH, Schoeman JF, Donald PR. Tuberculous cerebrovascular disease: a review. J Infect. 2009;59:156–66.
Berger JR. AIDS and stroke risk. Lancet Neurol. 2004;3:206–7 [PubMed: 15039031].
Nejtek V, Talari D. Novel Risk Factors for TIA and Stroke in Young Adults. 2016.
Folsom AR, Prineas RJ, Kaye SA, Munger RG. Incidence of hypertension and stroke in relation to body fat distribution and other risk factors in older women. Stroke. 1990;21:701–6.
Khan MH, Chakraborty SK, Biswas RSR. High Waist to Hip Ratio as a Risk Factor for Ischemic Stroke Patients Admitted in a Tertiary Care Hospital. Bangladesh J Anat. 2011;9(1):30–4.
JJaakonmäki N, Zedde M, Sarkanen T, Martinez-Majander N, Tuohinen S, Sinisalo J, SECRETO Study Group. Obesity and the risk of cryptogenic ischemic stroke in young adults. J Stroke Cerebrovasc Dis. 2022;31(5):106380.
Rothman SM, Fulling KH, Nelson JS. Sickle cell anemia and central nervous system infarction: a neuropathological study. Ann Neurol. 1986;20:684–90.
O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischemic and intracerebral hemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–23.
Aigner A, Grittner U, Rolfs A, Norrving B, Siegerink B, Busch MA. Contribution of established stroke risk factors to the burden of stroke in young adults. Stroke. 2017;48(7):1744–51.
Kivioja R, Pietilä A, Martinez-Majander N, Gordin D, Havulinna AS, Salomaa V, Putaala J. Risk factors for Early-Onset ischemic stroke: a Case-Control study. J Am Heart Assoc. 2018;7(21):e009774.
Kayima J, Nankabirwa J, Sinabulya I, Nakibuuka J, Zhu X, Rahman M, Kamya MR. Determinants of hypertension in a young adult Ugandan population in epidemiological transition—the MEPI-CVD survey. BMC Public Health. 2015;15(1):1–9.
Download references
Acknowledgements
We acknowledge the patients of Mulago hospital who gave us consent to obtain this information.
This study was funded with funds from the MEPI-Neurology program under Makerere University. The funding project had no role in the design of the study and collection, analysis, and interpretation of data and no role in writing the manuscript.
Author information
Authors and affiliations.
Kiruddu National Referral Hospital, P.O. Box 6553, Kampala, Uganda
Priscilla Namaganda
Mulago National Referral Hospital, Mulago Hospital Complex, P.O. Box 7272, Kampala, Uganda
Jane Nakibuuka
Department of Medicine, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda
Mark Kaddumukasa
Infectious Diseases Institute, Makerere University, Kampala, Uganda
Elly Katabira
You can also search for this author in PubMed Google Scholar

Contributions
PN– conception, design of work, acquisition, analysis, interpretation of data, drafted and substantively revised the manuscript, JN– analysis, interpretation of data, drafted and substantively revised the manuscript, MK – analysis, interpretation of data, drafted and substantively revised the manuscript, EK– design of work, acquisition, analysis, interpretation of data, drafted and substantively revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Priscilla Namaganda .
Ethics declarations
Ethics approval and consent to participate.
Written informed consent/ assent was obtained from all participants or their parent/guardian or legal authorized representative to participate in the study. Ethical approval was obtained from Makerere University, school of medicine research and ethics committee (SOMREC) (reference number #REC REF 2015–105). All methods and procedures were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Namaganda, P., Nakibuuka, J., Kaddumukasa, M. et al. Stroke in young adults, stroke types and risk factors: a case control study. BMC Neurol 22 , 335 (2022). https://doi.org/10.1186/s12883-022-02853-5
Download citation
Received : 18 March 2022
Accepted : 23 August 2022
Published : 06 September 2022
DOI : https://doi.org/10.1186/s12883-022-02853-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Young adults
- Risk factors
BMC Neurology
ISSN: 1471-2377
- General enquiries: [email protected]
This presents an analysis of a case of Ischemic stroke in terms of possible etiology, pathophysiology, drug analysis and nursing care
New? Questions? Start Here!
- Information Hub
- Important Notices
- Need Access to Evidence
- Communities & Collections
- Publication Date
- Posting Date
- Subject(CINAHL)
- Item Format
- Level of Evidence
- Research Approach
- Sigma Chapters
- Author Affiliations
- Review Type
Ischemic stroke: A case study
View file(s).
Author Information
- Martinez, Rudolf Cymorr Kirby P. ;
- Sigma Affiliation
Item Information
Item link - use this link for citations and online mentions..
Clinical Focus: Adult Medical/Surgical
Repository Posting Date
Type information, category information, original publication info, conference information, rights holder.
All rights reserved by the author(s) and/or publisher(s) listed in this item record unless relinquished in whole or part by a rights notation or a Creative Commons License present in this item record.
All permission requests should be directed accordingly and not to the Sigma Repository.
All submitting authors or publishers have affirmed that when using material in their work where they do not own copyright, they have obtained permission of the copyright holder prior to submission and the rights holder has been acknowledged as necessary.
- Article Information
A, Crude stroke prevalence estimates were applied to the 1999 to 2002 Current Population Survey (CPS), 2003 to 2006 CPS, 2007 to 2010 CPS and American Community Survey–Public Use Microdata Sample (ACS-PUMS), 2011 to 2014 ACS-PUMS, and 2015 to 2018 ACS-PUMS to calculate the number of affected individuals with stroke in each 4-year epoch. B, Stroke prevalence estimates were age-standardized to the 2017-2018 ACS-PUMS using the following age categories: 20 to 39 years, 40 to 59 years, and 60 years and older. Age-standardized stroke prevalence estimates were then applied to the 2017-2018 ACS-PUMS to calculate the age-standardized number of affected individuals with stroke in each 4-year epoch. Error bars indicate 95% CIs.
Data Sharing Statement
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Andres W , Rothstein A , Elser H, et al. Trends in the Prevalence of Stroke Among Community-Dwelling Individuals in the US, 1999-2018. JAMA Neurol. 2023;80(6):646–648. doi:10.1001/jamaneurol.2023.0742
Manage citations:
© 2024
- Permissions
Trends in the Prevalence of Stroke Among Community-Dwelling Individuals in the US, 1999-2018
- 1 Department of Neurology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia
- 2 Stroke Branch, National Institute of Neurologic Disorders and Stroke Intramural Research Program, Bethesda, Maryland
- 3 Department of Biostatistics, Epidemiology, and Informatics, Perelman School of Medicine at the University of Pennsylvania, Philadelphia
Representative estimates of stroke prevalence inform public health interventions and guide resource allocation. There is a need for updated data on stroke prevalence among community-dwelling individuals in the US. We present data from the 1999 to 2018 National Health and Nutrition Examination Surveys (NHANES) to estimate trends in stroke prevalence representative of the noninstitutionalized civilian population of US adults 20 years and older.
The NHANES is a series of nationally representative cross-sectional surveys administered biennially. 1 Participants are selected from among the noninstitutionalized US population using a complex, stratified, multistage, probability-clustered sampling design. This analysis includes all (n = 2197) participants from the 1999-2018 survey cycles 20 years and older who self-reported a history of stroke, ascertained using the question, “Has a doctor or other health professional ever told you that you had a stroke?” 2 The NHANES are approved by the National Center for Health Statistics Ethics Review Board.
Data were grouped into 4-year epochs to improve the precision of estimates. 1 Within each epoch, stroke prevalence was calculated overall and stratified by sex, self-reported race and ethnicity, and age group. Prevalence estimates were age-standardized to the 2017 to 2018 American Community Survey–Public Use Microdata Sample (ACS-PUMS) using the following age categories: 20 to 39 years, 40 to 59 years, and 60 years or older. We applied our stroke prevalence estimates to the Current Population Surveys and the ACS-PUMS to calculate the number of affected individuals with stroke. P values for linear trend over time were calculated using logistic regression models. In accordance with NHANES recommendations, analyses incorporated survey weights to account for the sampling design and the Taylor series (linearization) method was used to obtain standard errors. 1 A 2-tailed P value less than .05 was considered statistically significant, and all analyses were performed using Stata SE version 17 (StataCorp).
From 1999 to 2018, the overall crude and age-standardized prevalence of stroke was 2.84% (95% CI, 2.67-3.02) and 3.10% (95% CI, 2.92-3.29), respectively. This corresponds to an estimated 7.3 million (95% CI, 6.9 million-7.8 million) affected individuals. The overall prevalence of stroke was stable from 1999-2002 to 2015-2018 ( Table ). Crude estimates of the number of affected individuals with stroke increased over time, while age-standardized estimates were stable ( Figure ).
The age-standardized prevalence of stroke was higher among non-Hispanic Black individuals compared with other racial and ethnic groups and was similar by sex. The prevalence was higher among older compared with younger individuals. The prevalence of stroke in each age and racial and ethnic group was stable from 1999-2002 to 2015-2018 but increased over time among men (from 2.29% [95% CI, 1.94-2.71] in 1999-2002 to 2.94% [95% CI, 2.50-3.46] in 2015-2018; P for trend = .04) ( Table ).
Using a nationally representative sample of community-dwelling adults, we show that the prevalence of self-reported stroke remained stable in the US between 1999 and 2018 overall and by racial and ethnic group and age group and increased among men. Estimates herein underestimate the total burden of stroke in the US as NHANES does not include individuals residing in rehabilitation, long-term care, or other institutional settings. Stroke was self-reported in NHANES, which has high negative predictive value but modest positive predictive value 3 , 4 ; it is possible that the validity of self-reported stroke has changed over time. Importantly, we presented both crude and age-standardized prevalence estimates to account for changes in the age structure of the US population over the study period.
We report a crude stroke prevalence of 2.8% and an age-standardized stroke prevalence of 3.1% from 1999 to 2018, which is slightly higher than the 2006 to 2010 prevalence data from the Behavioral Risk Factor Surveillance System (BRFSS; 2.6% to 2.7%). 5 Both prevalence estimates, that of our study and BRFSS, are higher than the 1973 to 1991 NHANES estimates, which showed that prevalence increased from 1.41% to 1.87%. 6 Taken together, although the burden of stroke has increased since 1973 to 1991, it has stabilized in recent years.
Accepted for Publication: February 6, 2023.
Published Online: April 24, 2023. doi:10.1001/jamaneurol.2023.0742
Corresponding Author: Andrea L. C. Schneider, MD, PhD, Department of Neurology, Perelman School of Medicine at the University of Pennsylvania, 51 N 39th St, Andrew Mutch Building 416, Philadelphia, PA 19104 ( [email protected] ).
Author Contributions: Drs Rothstein and Schneider had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Drs Andres and Rothstein are co–first authors and contributed equally.
Study concept and design : Rothstein, Gottesman, Schneider.
Acquisition, analysis, or interpretation of data : Andres, Rothstein, Elser, Sloane, Kasner, Schneider.
Drafting of the manuscript : Andres.
Critical revision of the manuscript for important intellectual content : All authors.
Statistical analysis : Rothstein, Schneider.
Administrative, technical, or material support : Sloane.
Study supervision : Schneider.
Conflict of Interest Disclosures: Dr Kasner has received grants from Genentech and Diamedica as well as personal fees from Bristol Myers Squibb, Medtronic, and AstraZeneca outside the submitted work. Dr Schneider has received grants from the US Department of Defense and is Associate Editor of Neurology outside the submitted work. No other disclosures were reported.
Funding/Support: Dr Schneider is supported by grant K23NS123340 from the National Institute of Neurological Disorders and Stroke. Dr Rothstein is supported by grant T32NS061779 from the National Institute of Neurological Disorders and Stroke. Dr Gottesman is supported by the National Institute of Neurological Disorders and Stroke Intramural Research Program.
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Meeting Presentation: This paper was presented at AAN 2023 Annual Meeting; April 24, 2023; Boston, Massachusetts.
Data Sharing Statement: See the Supplement .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 01 May 2024
Triglyceride-glucose index as a potential predictor for in-hospital mortality in critically ill patients with intracerebral hemorrhage: a multicenter, case–control study
- Yang Yang 1 na1 ,
- Shengru Liang 2 na1 ,
- Jiangdong Liu 1 na1 ,
- Minghao Man 3 ,
- Dengfeng Jia 1 ,
- Jianwei Li 1 ,
- Xiaoxi Tian 1 na2 &
- Lihong Li 1 na2
BMC Geriatrics volume 24 , Article number: 385 ( 2024 ) Cite this article
174 Accesses
Metrics details
The correlation between the triglyceride-glucose index (TyG) and the prognosis of ischemic stroke has been well established. This study aims to assess the influence of the TyG index on the clinical outcomes of critically ill individuals suffering from intracerebral hemorrhage (ICH).
Patients diagnosed with ICH were retrospectively retrieved from the Medical Information Mart for Intensive Care (MIMIC-IV) and the eICU Collaborative Research Database (eICU-CRD). Various statistical methods, including restricted cubic spline (RCS) regression, multivariable logistic regression, subgroup analysis, and sensitivity analysis, were employed to examine the relationship between the TyG index and the primary outcomes of ICH.
A total of 791 patients from MIMIC-IV and 1,113 ones from eICU-CRD were analyzed. In MIMIC-IV, the in-hospital and ICU mortality rates were 14% and 10%, respectively, while in eICU-CRD, they were 16% and 8%. Results of the RCS regression revealed a consistent linear relationship between the TyG index and the risk of in-hospital and ICU mortality across the entire study population of both databases. Logistic regression analysis revealed a significant positive association between the TyG index and the likelihood of in-hospital and ICU death among ICH patients in both databases. Subgroup and sensitivity analysis further revealed an interaction between patients' age and the TyG index in relation to in-hospital and ICU mortality among ICH patients. Notably, for patients over 60 years old, the association between the TyG index and the risk of in-hospital and ICU mortality was more pronounced compared to the overall study population in both MIMIC-IV and eICU-CRD databases, suggesting a synergistic effect between old age (over 60 years) and the TyG index on the in-hospital and ICU mortality of patients with ICH.
Conclusions
This study established a positive correlation between the TyG index and the risk of in-hospital and ICU mortality in patients over 60 years who diagnosed with ICH, suggesting that the TyG index holds promise as an indicator for risk stratification in this patient population.
Peer Review reports
Introduction
Spontaneous, nontraumatic, intracerebral hemorrhage (ICH) is a catastrophic disease making up approximately 10–20% of all types of stroke [ 1 ]. Epidemiological data indicate that 30% of ICH patients requiring intensive care unit (ICU) management and 40% of them die within 30 days [ 2 ]. Despite ongoing research and advancements in this medical field, effective therapeutic options for improving the prognosis of patients with ICH are still lacking [ 3 ]. Consequently, there is an urgent need to identify remediable factors that may impact the outcomes of ICH, as this information could potentially lead to the development of new therapeutic targets.
Insulin resistance (IR), a pathological condition where tissue does not respond normally to insulin stimulation, plays a crucial role in the development of metabolic disorders [ 4 ]. More importantly, studies have revealed that compared with peripheral tissue, IR appears earlier in the central nervous system, indicating that brain is more vulnerable to IR, especially under various pathological states such as ICH and ischemic stroke (IS) [ 5 ]. Therefore, the indicators associated with IR may be closely related to the initiation of ICH and its prognosis.
The triglyceride-glucose (TyG) index, consisting of fasting triglyceride (FTG) and fasting blood glucose (FBG), is a valuable tool for analyzing lipid and glucose metabolism [ 6 , 7 ]. It is also recognized as an accurate indicator of IR [ 8 , 9 ]. Some researchers have observed a positive correlation between the TyG index and the incidence and mortality rates of progressed coronary artery disease [ 10 , 11 ]. Additional studies have indicated that the TyG index may have the potential to forecast negative cardiovascular events in individuals with coronary artery disease [ 12 ]. Moreover, multiple studies have demonstrated the predictive ability of the TyG index for the onset and mortality of IS [ 13 , 14 ]. These findings collectively highlight the association of the TyG index with cardiovascular and cerebrovascular diseases. However, the relationship between ICH and the TyG index, as well as the prognostic role of the TyG index in this condition, remains unexplored.
Therefore, the objective of this study is to evaluate the impact of the TyG index on the prognosis of critically ill patients with ICH, which may establish its potential utility as a risk stratification tool in ICH cases.
Data sources
Data used in this study were extracted from the Medical Information Mart for Intensive Care (MIMIC-IV version 2.2) and the eICU Collaborative Research Database (eICU-CRD) [ 15 , 16 ]. MIMIC-IV consists of medical records between 2008 and 2019 from over 190,000 patients who were treated in various types of ICU of the Beth Israel Deaconess Medical Center. The eICU-CRD included medical records of over 200,000 patients receiving clinical management in ICUs from over 200 medical centers between 2014 and 2015. Since data in these two databases are de-identified to hide patients’ information, the informed consent and ethics approval are not essential.
Data extraction
Structure query language (SQL), executed on the PostgresSQL (version 13.7.2), was utilized for data extraction from MIMIC-IV and eICU-CRD. One researcher (Yang Yang) with authorization to access both databases (Record ID: 48,776,647) conducted the data extraction. Inclusive criteria encompassed patients who were (1) aged 18 years and above; (2) diagnosed with ICH in accordance with International Classification of Diseases, 9th and 10th Revision (ICD9 and ICD10). Exclusion criteria included: (1) patients with multiple hospitalization entries, only data from the initial hospitalization due to ICH were considered; (2) patients lacking data of FTG and FBG on the first day of ICU admittance were omitted; (3) individuals who expired or were released within 24 h of ICU admission were excluded due to their significant missing data for key variables used in the regression analysis. Therefore, excluding this group of patients was necessary to ensure the reliability of the results of the regression analysis.
The following information was extracted for the final study cohort: (1) patients’ age and gender; (2) comorbidities identified by ICD-9 and ICD-10 codes; (3) initial FBG and FTG results within 24 h post-ICU admission; (4) average values of laboratory parameters within 24 h of ICU admittance; (5) minimum Glasgow Coma Scale (GCS) score on the first day of ICU admittance; (6) maximum Acute Physiology Score III (APSIII) and Sequential Organ Failure Assessment (SOFA) scores on the first day of ICU management; (7) treatment-related data that may impact the prognosis of ICH patients were extracted, which includes invasive mechanical ventilation, the use of anticoagulants, and the use of antiplatelet agents during hospitalization.
Assessment of the TyG index
The TyG index is calculated using the formula: TyG index = ln [FTG (mg/dl) × FBG (mg/dl)/2], where FTG and FBG represent the first recorded values of FBG and FTG since ICU admission [ 17 , 18 ]. In the subsequent statistical analysis, the TyG index was considered both as a continuous and categorical variable. When treated as a categorical variable, it was divided into four groups based on quartiles. The data extraction process is illustrated in Fig. 1 .
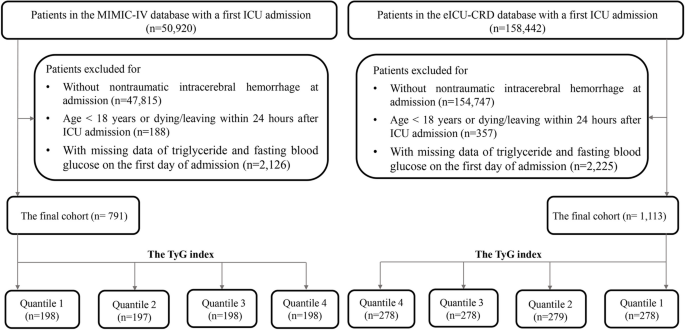
The flow chart for extracting data from the MIMIC-IV and eICU databases
Primary outcomes
The primary outcomes of interest were all-cause in-hospital mortality and ICU mortality, which were defined as deaths occurring during hospitalization and ICU staying, respectively.
Statistical analysis
Continuous variables were expressed as median (interquartile ranges) and categorical variables were described as number (percentages). Comparisons between groups were performed by Mann–Whitney U or Kruskal–Wallis test for continuous variables, and chi-squared or Fisher’s exact test for categorical ones.
In order to investigate the relationship between the TyG index and the primary outcomes, an initial analysis utilizing restricted cubic splines (RCS) with four knots was carried out to assess any potential non-linear associations between the TyG index and the risk of in-hospital and ICU mortality. If a non-linear relationship was not detected, logistic regression analysis were performed using three different models: model 1 included only the TyG index, model 2 adjusted for age and gender, and model 3 further adjusted for various potential confounders relevant to the clinical outcomes of ICH, including GCS, hypertension, congestive heart failure, white blood cell count (WBC), serum urea nitrogen (BUN), serum creatinine, red cell distribution width (RDW), serum bilirubin, serum aspartate aminotransferase (AST), prothrombin time (PT), use of anticoagulants, and use of antiplatelet agents. Additionally, to check for multicollinearity in the logistic regression analysis, a Spearman rank correlation test was carried out and the square root of the variance inflation factor (VIF) was calculated.
To explore potential variations within specific populations, subgroup analysis was conducted by stratifying patients according to gender, age (> 60 vs. ≤ 60 years), diabetes, hypertension, use of anticoagulants, and use of antiplatelet agents. The interaction between the TyG index and the other variables utilized for stratification in subgroup analysis was evaluated through likelihood ratio test. Finally, a sensitivity analysis was performed by using Cox proportional hazard regression to verify the relationship between the TyG index and in-hospital and ICU mortality. The follow-up period was measured from the date of hospital or ICU admission to the date of death during the hospitalization or ICU stay. The Cox regression model was adjusted for possible confounders as outlined in the fully adjusted model (model 3) of logistic regression mentioned above.
All statistical analysis were performed using R software (version 4.3.1). The“VIM”package was used to visualize the distribution of missing values, from which we can see that all variables had missing ratio less than 20% (Additional file 1 : Figure S1). The “mice” package was adopted to address missing values by multiple imputation to obtain 5 imputation datasets in the process of logistic regression. Besides, the “corrplot” package was used to visualize the associations between continuous variables. The“plotRCS” package was used to perform RCS. The“forestploter” package was adopted to visualized the results of subgroup analysis. The “survminer” package was used to conduct Cox regression analysis. Statistically significant was set as a two tailed P < 0.05 .
Baseline characteristics
A total of 791 patients from MIMIC-IV and 1,113 from eICU-CRD were included in the final analysis. Among them, 418 (53%) individuals in MIMIC-IV and 627 (56%) in eICU-CRD were male. The in-hospital mortality rates were 14% in MIMIC-IV and 16% in eICU-CRD, with ICU mortality rates of 10% and 8% respectively. The median age was 72.25 (60.63, 82.59) years in MIMIC-IV and 66 (55, 77) years in eICU-CRD. Besides, the average value of TyG index was 8.72 (8.38, 9.17) in MIMIC-IV and 8.76 (8.33, 9.21) in eICU-CRD.
When dividing participants into groups based on the quartiles of the TyG index, patients in the upper quartiles had significantly higher APSIII scores, and higher proportion of invasive ventilation than those in the lower quartiles ( P < 0.001 for all ). Furthermore, hospital stay time, ICU stay time, in-hospital mortality, and ICU mortality all exhibited a gradual increase from the first to the fourth quartile of the TyG index. However, there was no significant difference in the mean hospital and ICU survival time of patients who died in the hospital or ICU across the quartiles of the TyG index. (Table 1 and Additional file 2 : Table S1).
Baseline data of participants divided by the hospital and ICU outcomes are presented in Table 2 and Additional file 3 : Table S2, respectively. Compared to in-hospital and ICU survivors, non-survivors in both the MIMIC-IV and eICU-CRD databases showed significantly higher APSIII and SOFA scores, shorter hospital stays, and a higher proportion of invasive ventilation. However, compared to in-hospital and ICU survivors, ICU stay time was shorter in non-survivors from eICU-CRD and longer in non-survivors from MIMIC-IV. Furthermore, GCS scores were lower in in-hospital and ICU non-survivors compared to survivors in eICU-CRD, but there was no significant difference in GCS scores between in-hospital and ICU survivors and non-survivors in MIMIC-IV. Interestingly, despite the potential risk of secondary hemorrhage associated with antiplatelet agents, their usage was more common among in-hospital and ICU non-survivors than survivors in MIMIC-IV. Moreover, the TyG index was notably higher in the in-hospital non-survivors compared to survivors (MIMIC-IV: 8.94 (8.51–9.48) vs. 8.70 (8.36–9.09); P < 0.001 . eICU-CRD: 8.98 (8.51–9.49) vs. 8.70 (8.31–9.16); P < 0.001 ). Similarly, the TyG index was significantly elevated in ICU non-survivors in contrast to ICU survivors (MIMIC-IV: 9.00 (8.51–9.48) vs. 8.70 (8.36–9.10); P < 0.001. eICU-CRD: 9.09 (8.76–9.65) vs. 8.71 (8.31–9.17); P < 0.001) (Additional file 4 : Figure S2).
Association between the TyG index and the primary outcomes
We initially conducted a nonlinear correlation analysis between the TyG index and the primary outcomes using RCS. Findings suggested no significant nonlinear correlation between the TyG indicator and the likelihood of either in-hospital or ICU mortality (In-hospital mortality: P for nonlinear = 0.751 in MIMIC-IV , P for nonlinear = 0.562 in eICU-CRD. ICU mortality: P for nonlinear = 0.986 in MIMIC-IV , P for nonlinear = 0.431 in eICU-CRD) (Fig. 2 ). Subsequently, logistic regression analysis was conducted to assess the linear relationship between the TyG index and the primary outcomes. In the fully adjusted model (model 3) that adjusted for various potential confounders related to the clinical outcomes of ICH, a positive correlation was found between the TyG index and the risk of in-hospital mortality (MIMIC-IV: OR 1.75 [95%CI 1.20–2.52], P = 0.003 . eICU-CRD: OR 1.37 [95%CI 1.05–1.80], P < 0.001 ) and ICU mortality (MIMIC-IV: OR 2.15 [95%CI 1.45–3.17], P < 0.001. eICU-CRD: OR 1.61 [95%CI 1.13–2.27], P < 0.001 ). Moreover, compared to the first quartile (Q1) of the TyG index, the results of model 3 indicated that the fourth quartile (Q4) was linked to a higher risk of in-hospital mortality (MIMIC-IV: OR 2.31 [95%CI 1.18–4.67], P = 0.017 . eICU-CRD: 1.73 [95%CI 1.02–3.06], P = 0.036 ) and ICU mortality (MIMIC-IV: OR 3.24 [95%CI 1.54–7.11], P = 0.002 . eICU-CRD: 2.30 [95%CI 1.09–5.16], P = 0.034 ) (Table 3 , Additional file 5 : Table S3).
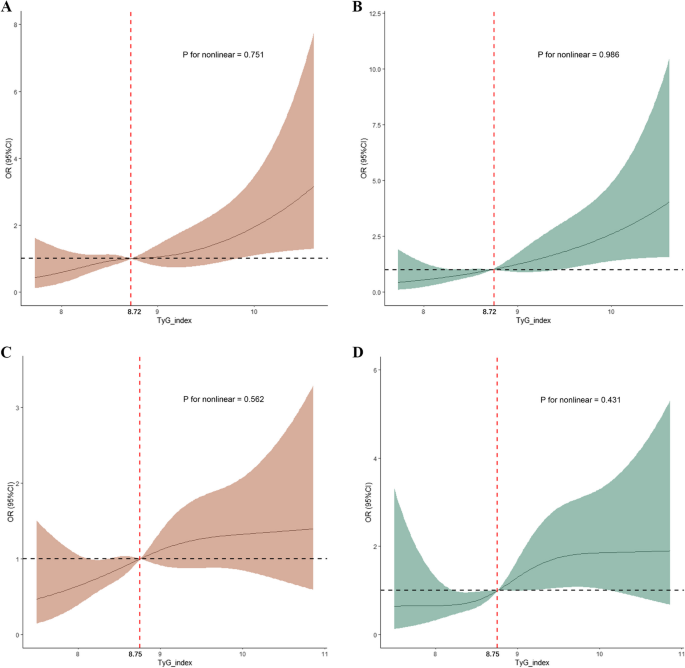
Restricted cubic spline analysis for the nonlinear association between the TyG index and the risk of, A in-hospital mortality of ICH patients from MIMIC-IV; B ICU mortality of ICH patients from MIMIC-IV; C in-hospital mortality of ICH patients from eICU-CRD; D ICU mortality of ICH patients from eICU-CRD
To assess multicollinearity in the logistic regression model, the Spearman rank correlation coefficient and VIF were calculated, respectively. Findings revealed that there was no linear correlation between the TyG index and the other continuous variables incorporated in model 3 (Additional file 6 : Figure S3). Additionally, none of the variables in model 3 exhibited a square root of VIF ≥ 2 (data not shown). Taken together, these results suggest that there is no multicollinearity present in the logistic regression model, indicating the reliability of the results.
Subgroup analysis
To investigate potential variations within specific populations, logistic regression analysis was conducted across various subgroups, including gender, age, diabetes, hypertension, use of anticoagulant agents, and use of antiplatelet agents. The forest plot revealed a significant positive correlation between the TyG index and in-hospital mortality among participants over 60 years (MIMIC-IV: OR 2.58 [95%CI 1.92–4.27], P = 0.005 . eICU-CRD: OR 1.56 [95%CI 1.10–2.22], P = 0.019 ), those without diabetes (MIMIC-IV: OR 2.20 [95%CI 1.34–3.57], P = 0.002 . eICU-CRD: OR 1.69 [95%CI 1.18–2.41], P = 0.004 ), and those with hypertension (MIMIC-IV: OR 1.97 [95%CI 1.28–3.01], P = 0.002 . eICU-CRD: OR 1.84 [95%CI 1.28–2.99], P = 0.014 ). Similarly, there was a positive association for ICU mortality in patients over 60 years (MIMIC-IV: OR 3.86 [95%CI 1.31–6.99], P < 0.001 . eICU-CRD: OR 1.70 [95%CI 1.23–2.90], P = 0.036 ), those without diabetes (MIMIC-IV: OR 2.62 [95%CI 1.56–4.40], P < 0.001 . eICU-CRD: OR 2.10 [95%CI 1.34–3.32], P = 0.001 ), and those with hypertension (MIMIC-IV: OR 2.44 [95%CI 1.54–3.84], P < 0.001 . eICU-CRD: OR 1.83 [95%CI 1.13–2.97], P = 0.013 ). Furthermore, in both MIMIC-IV and eICU-CRD, significant interactions were found between the TyG index and patients' age, diabetic status, and history of hypertension concerning in-hospital and ICU outcomes of individuals with ICH ( P for interaction < 0.05 for all) (Figs. 3 and 4 ).
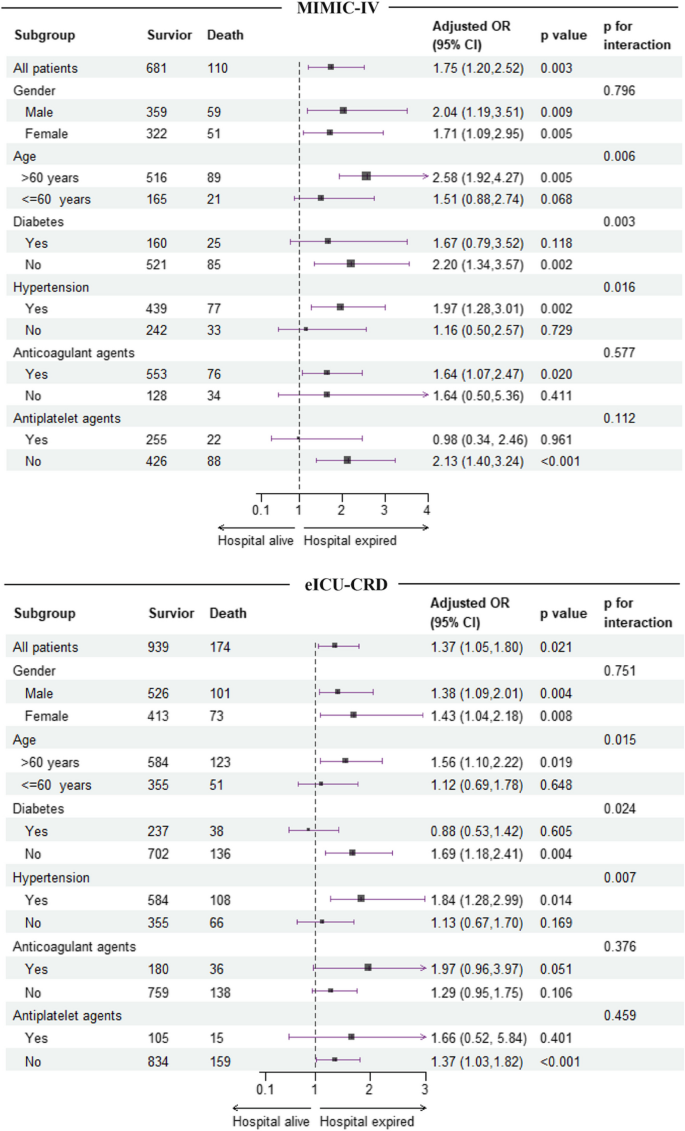
Subgroup analysis for the correlation between the TyG index and the risk of in-hospital mortality in patients with ICH from MIMIC-IV and eICU-CRD databases
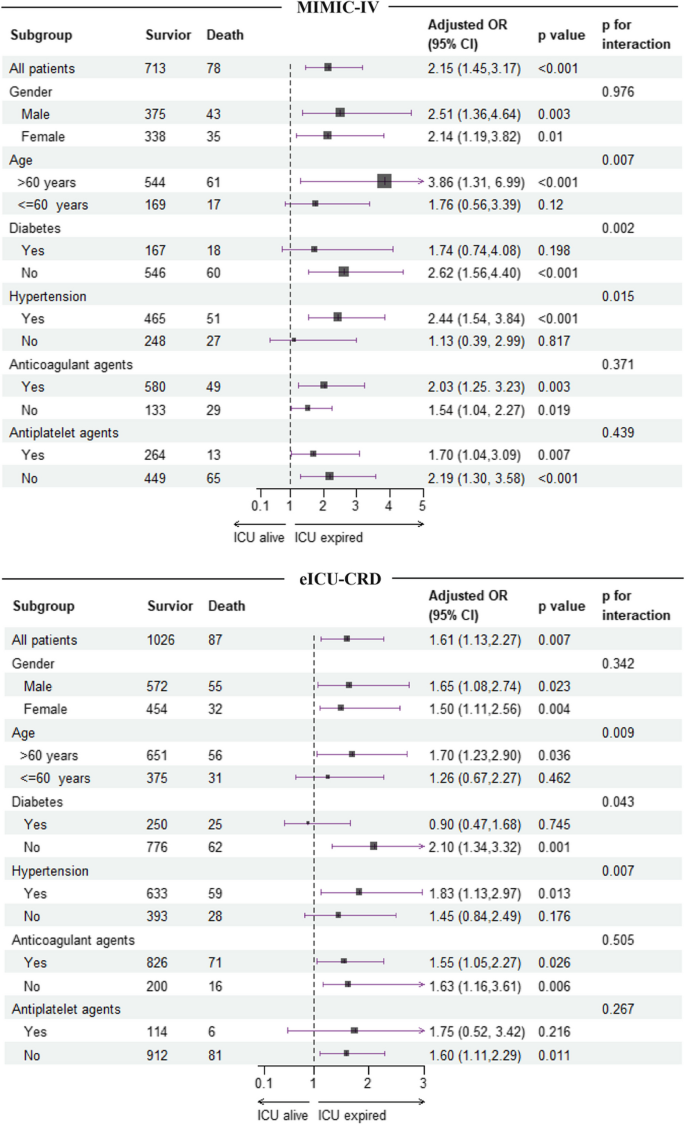
Subgroup analysis for the correlation between the TyG index and the risk of ICU mortality in patients with ICH from MIMIC-IV and eICU-CRD databases
Sensitivity analysis
To further verify the association between the TyG index and in-hospital and ICU mortality, as well as the significant interactions between the TyG index and patients' age regarding in-hospital and ICU outcomes, a sensitivity analysis was performed using Cox proportional hazard regression. Following fully adjusted, a positive correlation was observed between the TyG index and the risk of in-hospital mortality in ICH patients from both MIMI-IV and eICU-CRD datasets. The positive association between the TyG index and in-hospital and ICU mortality was also present in patients over 60 years old, those without diabetes, and those with hypertension in both databases. Importantly, significant interactions were only found between patients' age and the TyG index concerning in-hospital and ICU outcomes of ICH patients in both MIMIC-IV and eICU-CRD datasets (Table 4 and Additional file 7 : Table S4). These findings collectively suggest that the TyG index has the potential to serve as a prognostic indicator for ICH in patients over 60 years of age.
In this retrospective multicenter study, the impact of the TyG index on the prognosis of critically ill patients with ICH was evaluated, uncovering two important findings. Firstly, a positive correlation was found between the TyG index and the risk of in-hospital and ICU all-cause mortality in ICH patients. Secondly, this correlation was notably stronger in patients over 60 years old, especially in those with hypertension or lacking diabetes.
The association between the TyG index and the course of IS has been extensively studied. Wang et al. reported that individuals in the highest quartile of the TyG index face a 1.45 times greater risk of developing IS compared to those in the lowest quartile [ 19 ]. Results from a 9-year prospective study showed that keeping TyG index elevated was strongly related to an increased morbidity of IS, suggesting that monitoring and regulating the TyG index at an appropriate level could be beneficial in preventing IS [ 20 ]. Additionally, various studies have explored the capability of the TyG index in predicting the outcome of IS. Lee and colleagues found that the TyG index could forecast an adverse functional outcome three months post-reperfusion in IS patients [ 21 ]. Yang et al. noted a correlation between higher TyG index and elevated rates of both recurrence and mortality within one year following an IS event [ 22 ]. In critically ill patients, Cai W et al. found that the TyG index may assist in identifying IS patients at high risk of all-cause mortality [ 14 ]. Despite these findings highlight the significant relationship between the TyG index and IS as well as its prognosis, research on the association between the TyG index and ICH remains scarce.
To address this gap in knowledge, we conducted this study and found a positive correlation between the TyG index and the likelihood of either in-hospital or ICU mortality in individuals with ICH. The positive correlation persisted even after adjusting for potential confounders, suggesting that the TyG index could serve as an independent predictor of hospitalization outcomes in patients with ICH, potentially aiding clinicians in their decision-making process. More importantly, subgroup analysis revealed that there is a synergistic effect of old age (over 60 years), hypertension, and non-diabetic status on the TyG index’s impact on hospitalization outcomes in patients with ICH. Sensitivity analysis using Cox regression model further confirmed the synergistic effect between old age (over 60 years) and the TyG index on the in-hospital and ICU mortality of ICH patients in both MIMIC-IV and eICU-CRD databases. These results underscored the population-specific influence of the TyG index on ICH prognosis, highlighting the importance of focusing on elderly patients with ICH.
The exact mechanisms connecting the TyG index with the poor prognosis of ICH are still unclear, but evidence supports a key role of IR in this process. Patients with IR are more susceptible to hyperglycemia. A study has found that hyperglycemia could inhibit the expression of Aquaporin-4, resulting in the aggravation of vasogenic brain edema and blood–brain barrier (BBB) destruction [ 23 ]. Autophagy is a vital cellular process for maintaining homeostasis, but hyperglycemia can decrease autophagic activity in the brain during ICH, leading to the accumulation of macromolecular debris and damaged cells, ultimately causing neuronal injury [ 24 ]. In stoke rat treated with type plasminogen activator, hyperglycemia could enhance superoxide production in brain tissue and blood vessels, increasing BBB permeability in the peri-ischemic area and leading to a 3- to fivefold rise in the volume of secondary hemorrhage after thrombolysis [ 25 ]. This finding establishes a link between hyperglycemia-induced superoxide production and the increased risk of hematoma expansion in IS. The generation of reactive oxygen species has been demonstrated during ICH [ 26 , 27 ]. Moreover, studies have shown that an increase in blood glucose can exacerbate hematoma expansion in a rat model of ICH [ 28 ]. Therefore, it is plausible to infer that IR related hyperglycemia may result in poor outcomes of ICH by promoting superoxide production, thereby increasing the risk of hematoma expansion.
Adequate cerebral perfusion is crucial for determining the prognosis of patients with ICH. The automatic regulation ability of cerebral blood vessels plays a significant role in maintaining appropriate cerebral perfusion during cerebral hemorrhage. Studies have indicated that elevated intracranial pressure in patients with acute ICH can impair cerebrovascular autoregulation within a two-week period [ 29 ]. The myogenic response, which refers to the ability of smooth muscle cells to react to changes in blood pressure, is essential for preserving cerebrovascular autoregulation [ 30 ]. Animal studies have proved that IR can heighten the tension of cerebrovascular myogenic response, leading to a reduction in the diameter of the cerebrovascular lumen, subsequently causing brain tissue ischemia and nerve cell injury [ 31 ]. In addition, the smooth muscle activity of distal cerebral arteries is notably higher than that of proximal ones, making them more vulnerable to IR and resulting in impaired cerebral circulation function [ 30 ].
Chronic inflammatory response is one pathogenesis of IR, and IR in turn can reflect the level of systemic inflammation in the body [ 32 ]. Interestingly, our study revealed a gradual increase in WBC across quartile intervals of the TyG index, with values exceeding the upper limit of the reference range in the fourth quartile, suggesting an escalation of systemic inflammation during the course of ICH in patients with IR. Furthermore, the integrity of BBB was compromised during ICH, allowing the infiltration of peripheral immune cells and pro-inflammatory cytokines into the central nervous system. This heightened inflammatory response in the brain can further compromise the BBB, creating a detrimental cycle [ 33 ]. In addition, study has shown that dysregulation of the insulin signaling pathway can activate NF-κB, leading to the transcription and expression of inflammatory factors in the brain, thereby exacerbating neuroinflammation [ 34 ].
Intriguingly, although the evidence presented supports the significant role of IR in linking the TyG index to the unfavorable prognosis of intracerebral hemorrhage (ICH), our study found no correlation between the TyG index and either in-hospital or ICU mortality in ICH patients with a history of diabetes, a group known to have a higher risk of IR compared to non-diabetic individuals. Explaining the cause of this paradox is challenging. One potential reason could be reverse causality [ 14 , 35 ], where patients diagnosed with diabetes may be more likely to accept appropriate treatment or adopt healthy lifestyle habits. This could lead to their analytical parameters being similar to or even lower than those of non-diabetic counterparts. Consistent to this theory, in our study, no significant differences were observed in FBG, FTC, and TyG indexes between diabetic and non-diabetic individuals in both the MIMC-IV and eICU-CRD study cohorts (TyG index: 8.71 (8.38, 9.17) vs 8.77 (8.39, 9.14), P = 0.673 for MIMIC-IV. 8.75 (8.34, 9.22) vs 8.78 (8.3, 9.17), P = 0.925 for eICU-CRD). Additionally, as diabetic patients may have adopted a healthier lifestyle than their non-diabetic counterparts, their prognosis might be improved in subgroup analyses stratified by diabetes status.
The hyper-insulinemic-euglycemic clamp is considered the most accurate method for detecting IR, but its practicality is limited due to high costs, time-consuming procedures, and invasiveness. The homeostasis model assessment index for IR (HOMA-IR) is commonly used in clinical settings to assess beta-cell function and detect IR [ 36 ]. Nevertheless, its applicability is restricted in patients undergoing insulin therapy or those with ineffective beta cells [ 37 ]. Besides, HOMA-IR relies on measuring insulin levels, which are not routinely checked in clinical practice. Therefore, researchers have introduced the TyG index as a potentially reliable and cost-effective alternative marker for IR. Using hyper-insulin-normoglycemia clamp technique as the gold standard, a study showed excellent predictive efficiency of the TyG index for IR, with sensitive and specificity of 96.5% and 85.0%, respectively [ 8 ]. David and colleagues also demonstrated that the TyG index outperforms FBG and FTG in diagnosing type 2 diabetes and monitoring its progression [ 38 ]. Given that FBG and FTG measurements are available in most healthcare facilities, the TyG index has the potential to be widely utilized in blood glucose management and could serve as a valuable tool for risk assessment in patients with ICH.
The study has several limitations. First, the location and volume of hemorrhage, which are crucial factors influencing the prognosis of ICH, could not be extracted from the databases. Therefore, future research should incorporate these indicators to further validate the current findings. Secondly, specific population such as the Chinese or African are scarce in the study cohort. Consequently, the conclusions derived from this study should be cautiously interpreted in these population. Thirdly, the impact of dynamic changes in the TyG index on the prognosis of ICH patients was not assessed in this study. Given that variability in the TyG index has been linked to the incidence of IS [ 20 ], further studies are needed to investigate the cumulative effect of the TyG index on the incidence and outcome of ICH. Fourthly, exclusion of patients without FTG and FBG data on the first day of ICU admission may introduce bias if the missing data pattern is not completely random. Last but not the least, the utilization of propofol, fibrate, and glucose, along with insulin infusion prior to hospitalization, could have a notable effect on FTG and FBG levels. Nevertheless, neither MIMIC-IV nor eICU-CRD databases contains information on pre-hospitalization medications. Therefore, further investigation is required to confirm the current findings by incorporating these treatment-related information before ICU admission.
This study identified a positive correlation between the TyG index and in-hospital as well as ICU all-cause mortality in patients with ICH, particularly among individuals aged over 60 years with a history of hypertension. The findings indicate that the TyG index may be a useful tool for risk stratification in elderly patients with ICH, assisting clinicians in identifying high-risk individuals and providing timely intervention.
Availability of data and materials
The available data for MIMIC-IV can be accessed from the website https://mimic.physionet.org/ . The available data for eICU-CRD can be accessed from the website https://eicu-crd.mit.edu/ . The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Acute Physiology Score III
Serum aspartate aminotransferase
Blood–brain barrier
Serum urea nitrogen
The eICU Collaborative Research Database
Fasting blood glucose
Fasting triglyceride
Glasgow coma scale
The homeostasis model assessment index for IR
International Classification of Diseases
- Intensive care unit
- Intracerebral hemorrhage
Insulin resistance
Ischemic stroke
The Medical Information Mart for Intensive Care
Odds ratios
Prothrombin time
Restricted cubic spline
Red cell distribution width
Sequential Organ Failure Assessment
Structure Query Language
Triglyceride glucose index
Variance inflation factor
Qureshi A, Mendelow A, Hanley D. Intracerebral haemorrhage. Lancet (London, England). 2009;373(9675):1632–44.
Article PubMed Google Scholar
van Asch C, Luitse M, Rinkel G, van der Tweel I, Algra A, Klijn C. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. The Lancet Neurology. 2010;9(2):167–76.
Keep R, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. The Lancet Neurology. 2012;11(8):720–31.
Article CAS PubMed Google Scholar
Lee S, Park S, Choi C. Insulin Resistance: From Mechanisms to Therapeutic Strategies. Diabetes Metab J. 2022;46(1):15–37.
Scherer T, Sakamoto K, Buettner C. Brain insulin signalling in metabolic homeostasis and disease. Nat Rev Endocrinol. 2021;17(8):468–83.
Gui J, Li Y, Liu H, et al. Obesity- and lipid-related indices as a predictor of obesity metabolic syndrome in a national cohort study. Front Public Health. 2023;11:1073824.
Article PubMed PubMed Central Google Scholar
Kim J, Kim J, Roh E, et al. Triglyceride and glucose index and the risk of gestational diabetes mellitus: A nationwide population-based cohort study. Diabetes Res Clin Pract. 2021;171:108533.
Guerrero-Romero F, Simental-Mendía L, González-Ortiz M, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metabol. 2010;95(7):3347–51.
Article CAS Google Scholar
Irace C, Carallo C, Scavelli F, et al. Markers of insulin resistance and carotid atherosclerosis. A comparison of the homeostasis model assessment and triglyceride glucose index. Int J Clin Prac. 2013;67(7):665–72.
Li J, Ren L, Chang C, Luo L. Triglyceride-Glukose Index Predicts Adverse Events in Patients with Acute Coronary Syndrome: A Meta-Analysis of Cohort Studies. Horm Metabol Res. 2021;53(9):594–601.
Ding X, Wang X, Wu J, Zhang M, Cui M. Triglyceride-glucose index and the incidence of atherosclerotic cardiovascular diseases: a meta-analysis of cohort studies. Cardiovasc Diabetol. 2021;20(1):76.
Article CAS PubMed PubMed Central Google Scholar
Jin J, Cao Y, Wu L, et al. Triglyceride glucose index for predicting cardiovascular outcomes in patients with coronary artery disease. J Thorac Dis. 2018;10(11):6137–46.
Liu D, Yang K, Gu H, Li Z, Wang Y, Wang Y. Predictive effect of triglyceride-glucose index on clinical events in patients with acute ischemic stroke and type 2 diabetes mellitus. Cardiovasc Diabetol. 2022;21(1):280.
Cai W, Xu J, Wu X, et al. Association between triglyceride-glucose index and all-cause mortality in critically ill patients with ischemic stroke: analysis of the MIMIC-IV database. Cardiovasc Diabetol. 2023;22(1):138.
Pollard T, Johnson A, Raffa J, Celi L, Mark R, Badawi O. The eICU Collaborative Research Database, a freely available multi-center database for critical care research. Scientific data. 2018;5:180178.
Johnson A, Bulgarelli L, Shen L, et al. MIMIC-IV, a freely accessible electronic health record dataset. Scientific data. 2023;10(1):1.
Liao Y, Zhang R, Shi S, et al. Triglyceride-glucose index linked to all-cause mortality in critically ill patients: a cohort of 3026 patients. Cardiovasc Diabetol. 2022;21(1):128.
Zhang R, Shi S, Chen W, et al. Independent effects of the triglyceride-glucose index on all-cause mortality in critically ill patients with coronary heart disease: analysis of the MIMIC-III database. Cardiovasc Diabetol. 2023;22(1):10.
Wang A, Wang G, Liu Q, et al. Triglyceride-glucose index and the risk of stroke and its subtypes in the general population: an 11-year follow-up. Cardiovasc Diabetol. 2021;20(1):46.
Wang X, Feng B, Huang Z, et al. Relationship of cumulative exposure to the triglyceride-glucose index with ischemic stroke: a 9-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2022;21(1):66.
Lee M, Kim C, Kim Y, et al. High Triglyceride Glucose Index Is Associated with Poor Outcomes in Ischemic Stroke Patients after Reperfusion Therapy. Cerebrovasc Dis. 2021;50(6):691–9.
Yang X, Wang G, Jing J, et al. Association of triglyceride-glucose index and stroke recurrence among nondiabetic patients with acute ischemic stroke. BMC Neurol. 2022;22(1):79.
Chiu C, Chen C, Shen C, et al. Hyperglycemia exacerbates intracerebral hemorrhage via the downregulation of aquaporin-4: temporal assessment with magnetic resonance imaging. Stroke. 2013;44(6):1682–9.
Liu R, Wang J, Qiu X, Wu J. Acute hyperglycemia together with hematoma of high-glucose blood exacerbates neurological injury in a rat model of intracerebral hemorrhage. Neurosci Bull. 2014;30(1):90–8.
Won S, Tang X, Suh S, Yenari M, Swanson R. Hyperglycemia promotes tissue plasminogen activator-induced hemorrhage by Increasing superoxide production. Ann Neurol. 2011;70(4):583–90.
Zhu F, Zi L, Yang P, et al. Efficient Iron and ROS Nanoscavengers for Brain Protection after Intracerebral Hemorrhage. ACS Appl Mater Interfaces. 2021;13(8):9729–38.
Ding R, Chen Y, Yang S, et al. Blood-brain barrier disruption induced by hemoglobin in vivo: Involvement of up-regulation of nitric oxide synthase and peroxynitrite formation. Brain Res. 2014;1571:25–38.
Liu J, Gao B, Clermont A, et al. Hyperglycemia-induced cerebral hematoma expansion is mediated by plasma kallikrein. Nat Med. 2011;17(2):206–10.
Ma H, Guo Z, Liu J, Xing Y, Zhao R, Yang Y. Temporal Course of Dynamic Cerebral Autoregulation in Patients With Intracerebral Hemorrhage. Stroke. 2016;47(3):674–81.
Coucha M, Abdelsaid M, Ward R, Abdul Y, Ergul A. Impact of Metabolic Diseases on Cerebral Circulation: Structural and Functional Consequences. Compr Physiol. 2018;8(2):773–99.
Butcher J, Goodwill A, Stanley S, Frisbee J. Differential impact of dilator stimuli on increased myogenic activation of cerebral and skeletal muscle resistance arterioles in obese zucker rats. Microcirculation. 2013;20(7):579–89.
Glass C, Olefsky J. Inflammation and lipid signaling in the etiology of insulin resistance. Cell Metab. 2012;15(5):635–45.
de la Monte S. Insulin Resistance and Neurodegeneration: Progress Towards the Development of New Therapeutics for Alzheimer’s Disease. Drugs. 2017;77(1):47–65.
Akhtar A, Sah S. Insulin signaling pathway and related molecules: Role in neurodegeneration and Alzheimer’s disease. Neurochem Int. 2020;135:104707.
Laura S, David N, Alejandro F, et al. The TyG index may predict the development of cardiovascular events. Eur J Clin Invest. 2015;46:189–97.
Google Scholar
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Minh H, Tien H, Sinh C, et al. Assessment of preferred methods to measure insulin resistance in Asian patients with hypertension. J Clin Hypertens (Greenwich). 2021;23(3):529–37.
Navarro-González D, Sánchez-Íñigo L, Pastrana-Delgado J, Fernández-Montero A, Martinez J. Triglyceride-glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: The Vascular-Metabolic CUN cohort. Prev Med. 2016;86:99–105.
Download references
Acknowledgements
The present study utilized data from the MIMIC-IV and eICU database. We express our gratitude to all the staff and patients who contributed to the development of the MIMIC-IV and eICU database.
This research was supported by Innovation Science Fund of Tangdu hospital, China (No. 2023BTDQN001), Shaanxi Province Key Research and Development Plan Project (2024SF-YBXM-210), and Air Force Medical University Clinical Research Program (2023LC2319).
Author information
Yang Yang, Shengru Liang and Jiangdong Liu contribute equally to this work and are co-first authors.
Lihong Li and Xiaoxi Tian contributed equally to this work and are co-corresponding authors.
Authors and Affiliations
Department of Emergency, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, China
Yang Yang, Jiangdong Liu, Yue Si, Dengfeng Jia, Jianwei Li, Xiaoxi Tian & Lihong Li
Department of Endocrinology, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, China
Shengru Liang
Department of Neurosurgery, Tangdu Hospital, Fourth Military Medical University, Xi’an, 710038, China
Minghao Man
You can also search for this author in PubMed Google Scholar
Contributions
YY extracted data from MIMIC-IV and eICU-database, analyzed the data, and wrote the original draft. SL conducted literature review, analyzed the data, and wrote the original draft. JDL conducted literature review, and operated software. MM and DJ organized the data and checked the integrity of the data. YS and JWL assisted in statistical analysis. XT designed the study, and checked the final results. LL designed the study, conceptualized the research aims, and revised the paper. All authors have made an intellectual contribution to the manuscript and approved the final submission.
Corresponding author
Correspondence to Lihong Li .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the guidelines of the Helsinki Declaration. As the MIMIC-IV and the eICU-CRD database are publicly available and all data are de-identified to remove patients’ information, the requirement for informed consent of patients is not essential.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: figure s1..
The proportion and distribution of missing data for variables in (A) MIMIC-IV database and (B) eICU-CRD database.
Additional file 2.
Additional file 3., additional file 4: figure s2..
The boxplot of the TyG index stratified by the in-hospital and ICU outcomes. (A) The level of the TyG index in hospital survivors and non-survivors from the MIMIC-IV database. (B) The level of the TyG index in hospital survivors and non-survivors from the eICU-CRD database. (C) The level of the TyG index in ICU survivors and non-survivors from the MIMIC-IV database. (D) The level of the TyG index in ICU survivors and non-survivors from the eICU-CRD database.
Additional file 5.
Additional file 6: figure s3..
The correlation between continuous variables in the cohort derived from (A) MIMIC-IV and (B) eICU-CRD.
Additional file 7.
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yang, Y., Liang, S., Liu, J. et al. Triglyceride-glucose index as a potential predictor for in-hospital mortality in critically ill patients with intracerebral hemorrhage: a multicenter, case–control study. BMC Geriatr 24 , 385 (2024). https://doi.org/10.1186/s12877-024-05002-4
Download citation
Received : 07 March 2024
Accepted : 22 April 2024
Published : 01 May 2024
DOI : https://doi.org/10.1186/s12877-024-05002-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Triglyceride-glucose index
- All-cause mortality
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
A blood test for stroke risk? Biomarker for risk of future cerebrovascular disease
Quantitative assessments for potential stroke, cognitive decline.
A simple blood test could allow doctors to determine whether a person may be at higher risk for stroke or cognitive decline during their lifetime, according to a new UCLA Health study.
The study, published in the journal Stroke , found that measuring concentrations of a network of inflammatory molecules in the blood could allow doctors to calculate a risk score for susceptibility for cerebral small vessel disease -- a common cause of stroke and a contributor to cognitive decline found especially among the elderly.
Currently, the only way to determine a person's risk for cerebral vascular diseases has been to use a combination of imaging such as an MRI scan, family history, demographic variables and other risk factor evaluations, said study lead author Dr. Jason Hinman of the UCLA Comprehensive Stroke and Center and the Mary S. Easton Center for Alzheimer's Research and Care at UCLA. In clinical practice, neurologists may only find a patient is at risk after they have had a stroke or a cerebral event that warns of one, Hinman said.
The new study found that by measuring the concentrations of this network of inflammatory molecules in the blood of patients who have not had a cerebrovascular event, medical providers may be able to quantitatively assess a person's risk for cerebral small vessel disease and future stroke.
"The same way one uses cholesterol tests to evaluate one's future risk for heart attack, we don't have such a thing to estimate future risk for stroke," Hinman said. "I believe we can do that by something as simple as a blood test which in theory can enable broader access to the best level of care and not lock it behind advanced imaging studies and specialist evaluations."
The study focused on a biologically-connected network of inflammatory molecules known as the interleukin-18, or IL-18, network, which includes proteins and signaling molecules used to fight various infections.
Past studies have linked individual molecules in the IL-18 network to cerebral small vessel disease and stroke risk. However, the concentration of these individual molecules can fluctuate in response to other ailments such as the flu or autoimmune disorders, making them unreliable predictors of stroke risk at an individual level, Hinman said.
In 2020, University of California researchers including Hinman found that six molecules in the IL-18 network were associated with the presence of vascular brain injuries during MRI scans.
Building off these findings, Hinman sought to determine in this latest publication whether IL-18 network could be used to assess a person's susceptibility to stroke risk or cognitive decline.
To test this, the researchers used health data from a generations-long study known as the Framingham Heart Study. This study has tracked the medical history of thousands of residents in the city of Framingham, Massachusetts, throughout their lives since launching in 1948. Blood samples taken from participants had been tested for five of the six molecules later identified as being in the IL-18 network.
By using the blood samples and medical histories of the Framingham participants, Hinman and his coauthor were able to create a mathematical model that generates a risk score based on the concentrations of the IL-18 network molecules. Of the more than 2,200 Framingham residents included in Hinman's study, those whose risk scores were in the top 25% had an 84% chance of having a stroke during their lifetime. Overall, elevated risk scores were associated with a 51% increased risk of stroke and resulted in diagnostic prediction compared to existing risk assessment tools.
What remains unclear and requires further study is how or if a person's risk score can be modified or reduced, Hinman said.
"The real challenge is in the primary care space. Are you at risk before you have an event?" Hinman said. "That's what we're all interested in doing is preventing a stroke before it even happens."
- Heart Disease
- Stroke Prevention
- Brain Injury
- Disorders and Syndromes
- Cognitive neuroscience
- Blood transfusion
- COX-2 inhibitor
- Intelligence quotient
Story Source:
Materials provided by University of California - Los Angeles Health Sciences . Original written by Will Houston. Note: Content may be edited for style and length.
Journal Reference :
- Richard A. Martirosian, Crystal D. Wiedner, Jasmin Sanchez, Katherine T. Mun, Kiran Marla, Cristina Teran, Marissa Thirion, David S. Liebeskind, Emer R. McGrath, Jared M. Zucker, Rebecca Bernal, Alexa S. Beiser, Charles DeCarli, Jayandra J. Himali, Sudha Seshadri, Jason D. Hinman. Association of Incident Stroke Risk With an IL-18-Centered Inflammatory Network Biomarker Composite . Stroke , 2024; DOI: 10.1161/STROKEAHA.123.044719
Cite This Page :
Explore More
- New-To-Nature Enzyme Containing Boron Created
- New Target for Potential Leukemia Therapy
- 'Wraparound' Implants for Spinal Cord Injuries
- Climate May Influence Seismic Activity
- Atmosphere Surrounding Super-Earth?
- How Continents Stabilized
- Pressure to Be 'Perfect' Causing Burnout
- New Type of Memory State
- Mini-Robots to Clean Up Microplastics, Microbes
- Sound-Suppressing Silk Can Create Quiet Spaces
Trending Topics
Strange & offbeat.

IMAGES
VIDEO
COMMENTS
CASE STUDY 1 & 2. Courtesy of: Mitchell S.V. Elkind, MD, Columbia University and Shadi Yaghi, MD. Brown University. CASE 1. CASE 1. A 20 year old man with no past medical history presented to a primary stroke center with sudden left sided weakness and imbalance followed by decreased level of consciousness.
A 66-year-old man was admitted to hospital with a right frontal cerebral infarct producing left-sided weakness and a deterioration in his speech pattern. The cerebral infarct was confirmed with CT imaging. The only evidence of respiratory symptoms on admission was a 2 L oxygen requirement, maintaining oxygen saturations between 88% and 92%. In a matter of hours this patient developed a greater ...
Dr. Lee H. Schwamm: This patient with acute stroke benefited from an integrated system of care, 2 which was implemented at a state-certified stroke center 3 and followed stroke-specific dispatch ...
Read chapter 7 of Patient Management in the Telemetry/Cardiac Step-Down Unit: A Case-Based Approach online now, exclusively on AccessMedicine. AccessMedicine is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine.
Patient Case Presentation. Image courtesy of uofmhealthblogs.org. D.B. is a 72 year old African American female who presented to the ED with complaints of headache, altered mental status as evidenced by confusion and lethargy, slurred speech, right sided weakness, and a facial droop. Symptoms were first noted when patient woke up from a nap ...
A PFO has been demonstrated in 10%-26% of healthy adults. 14 In young patients who have had a cryptogenic stroke, however, the prevalence is thought to be much higher, for example, 40% in one study. 15 It is thought that a PFO allows microemboli to pass into the systemic circulation leading to a stroke.
In Uganda, literature on stroke in young adults is limited however results of a study done among acute stroke patients admitted to the national referral hospital (Mulago hospital) showed a 30-day mortality of 43.8%. Out of 133 patients, 32 patients (25%) were less than 51 years old. Out of the 56 patients that died, 13 patients (23%) were less ...
This case study presents a 68-year old "right-handed" African-American man named Randall Swanson. He has a history of hypertension, hyperlipidemia and a history of smoking one pack per day for the last 20 years. ... She realized this was an expected finding for a patient during a stroke but systolic pressure should be maintained at less ...
Stroke is one of these complications, since a greater incidence of stroke among patients with COVID-19 than the non-COVID-19 population has been reported, and a preliminary case-control study demonstrated that SARS-CoV-2 infection represents a risk factor for acute ischemic stroke .
Inpatient Stroke Case Studies Inpatient E/M Case Studies. Case study of a stroke patient at varying visit levels to better understand code selection for inpatient encounters under the revised guidelines for 2024. 67-year-old Female with Stroke. Total time* for Inpatient E/M in 2023.
IVT has been demonstrated to improve outcomes in patients with acute ischemic stroke within the first 4.5-h. 14, 15, 20-22 In 1996, the Food and Drug Administration (FDA) approved intravenous-tPA (IV-tPA) for treating acute ischemic stroke, based on successful outcomes in the National Institute of Neurological Disorders and Stroke study. 23, 24 ...
Case Study. A 68-year-old female, with a history of hypertension and diabetes mellitus, presented to the ED after acute onset of speech difficulty and right-sided weakness. Her symptoms began 3 hours ago. On physical exam, the patient was found to have severe expressive aphasia, right hemiplegia, and right hemi-sensory loss.
A case control study was conducted among patients presenting consecutively to the general medical wards with stroke during the study period September 2015 to March 2016. ... literature on stroke in young adults is limited however results of a study done among acute stroke patients admitted to the national referral hospital (Mulago hospital ...
Approximately 800,000 people in the United States experience a stroke each year. Stroke ranks as the fifth leading cause of death and the leading cause of disability, with over $40 billion annual cost.1 The nurse practitioner (NP) may significantly impact patient outcomes during the prehospital, acute, and posthospital phase of care. This article addresses preischemic stroke, acute, and ...
Case report. We present a case of a 69 - old patient admitted in the Neurological Ward of "St. George Hospital in Plovdiv in 2015, Bulgaria with right hemiparesis due to ischemic stroke in the basin of the left middle cerebral artery. This was a patient with sensory aphasia and paralysis facials in the right side.
Methods and Results. We compared 961 patients with a first‐ever IS at 25 to 49 years to 1403 frequency‐matched stroke‐free controls from a population‐based cohort study (FINRISK).Assessed risk factors included an active malignancy, atrial fibrillation, cardiovascular disease, current smoking status, a family history of stroke, high low‐density lipoprotein cholesterol, high ...
Abstract. This presents an analysis of a case of Ischemic stroke in terms of possible etiology, pathophysiology, drug analysis and nursing care.
The acute inflammatory state COVID-19 is known to produce had the potential to create a prothrombotic environment, culminating in an ischaemic stroke. Some early case studies produced in Wuhan describe patients in the sixth decade of life that had not been previously noted to have antiphospholipid antibodies, contain the antibodies in blood ...
This case study focuses on the comprehensive physiotherapy management of Ram Sagar, a 59-year-old patient who experienced a stroke. The study outlines the assessment, treatment plan, and interventions employed to aid Ram's functional recovery following a cerebrovascular accident (CVA). The case study highlights the
Importantly, we presented both crude and age-standardized prevalence estimates to account for changes in the age structure of the US population over the study period. We report a crude stroke prevalence of 2.8% and an age-standardized stroke prevalence of 3.1% from 1999 to 2018, which is slightly higher than the 2006 to 2010 prevalence data ...
Liz Tremayne-Ward, team lead for the trust's stroke and neurological rehabilitation service, said the study was really exciting. "We rarely get studies that focus on people with strokes further ...
Acute ischemic stroke (AIS) was diagnosed in 5% of the cases ( 2 ). However, a much lower rate of only 0.9% imaging confirmed AIS i.e., 32/3,556 total patients case number with COVID-19 was reported in New York USA ( 3 ). Subsequent retrospective reports from Europe have also confirmed AIS as a common neurovascular complications of SARS-CoV2 ...
The correlation between the triglyceride-glucose index (TyG) and the prognosis of ischemic stroke has been well established. This study aims to assess the influence of the TyG index on the clinical outcomes of critically ill individuals suffering from intracerebral hemorrhage (ICH). Patients diagnosed with ICH were retrospectively retrieved from the Medical Information Mart for Intensive Care ...
The study, published in the journal Stroke, found that measuring concentrations of a network of inflammatory molecules in the blood could allow doctors to calculate a risk score for susceptibility ...
Under the previous ICD coding rationale, clinical data generated from stroke patients were included as part of the cardiovascular diseases chapter, greatly misrepresenting the severity and specific disease burden of stroke. ... A case study conducted in the US showed that people with high financial status had better stroke treatment options ...