- General Nursing
- Nursing Specialties
- Nursing Students
- United States Nursing
- World Nursing
- Boards of Nursing
- Breakroom / Clubs
- Nurse Q&A
- Student Q&A
- Fastest BSN
- Most Affordable BSN
- Fastest MSN
- Most Affordable MSN
- Best RN to BSN
- Fastest RN to BSN
- Most Affordable RN to BSN
- Best LPN/LVN
- Fastest LPN/LVN
- Most Affordable LPN/LVN
- Fastest DNP
- Most Affordable DNP
- Medical Assistant
- Best Online Medical Assistant
- Best Accelerated Medical Assistant
- Most Affordable Medical Assistant
- Nurse Practitioner
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Emergency NP
- Best RN to NP
- Psychiatric-Mental Health NP
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Best NP Jobs and Salaries
- Family NP (FNP)
- Orthopedic NP
- Psychiatric-Mental Health NP (PMHNP)
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Best Free Online NCLEX-RN Study Guide
- The Nursing Process
- Question Leveling
- NCLEX-RN Question Identification
- Expert NCLEX-RN Test-Taking Strategies
- Best Scrubs for Nurses
- Best Shoes for Nurses
- Best Stethoscopes for Nurses
- Best Gifts for Nurses
- Undergraduate
- How to Become an LPN/LVN
- How to Earn an ADN
- Differences Between ADN, ASN, AAS
- How to Earn a BSN
- Best MSN Concentrations
- Is an MSN Worth It?
- How to Earn a DNP
- MSN vs. DNP

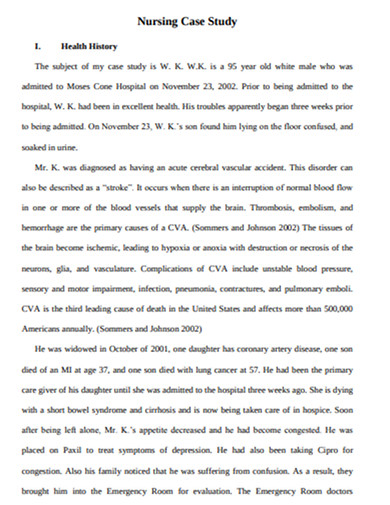
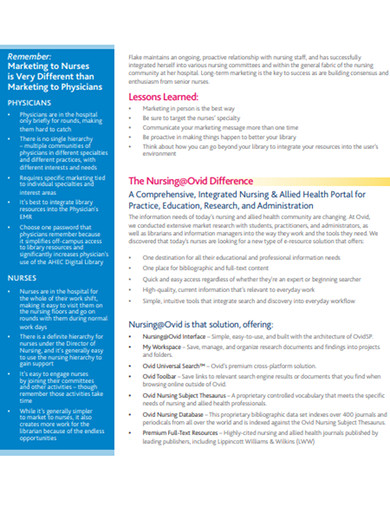
Nursing Case Studies: Diagnosis, Rationales, Fundamentals
Test your knowledge and clinical investigative skills in trying to diagnose what is going on with the patients presented in each of the Case Study Investigations. Can you come up with the right diagnosis? Case Studies Articles
Case Study: Child With Altered Mental Status
In this Case Study, an 11-year-old child with autism presents by ambulance to the children's hospital with altered mental status, bizarre behavior and fever....
Four Days of Nausea, Vomiting and Fever
What is most important in this case study in which an older Vietnamese woman presents to the ER with fever, nausea and vomiting?
I'm Dizzy, Tired and Can't Remember What I Ate for Lunch
A 74-year-old white male presents to the ED with confusion, fatigue, dizziness, headache and distal right arm paresthesia. Experienced nurses, model your...
Agonizing Pelvic Pain: What's Going On with this 17-year-old? | Ca…
A new case study in which the patient, a 17-yr-old African American female, is having ongoing, excruciating pelvic pain. This case study is based upon the very...
A Fracture from a Fall: What's Going on Here?
A new case study in which a 77 yo white female arrives to the emergency room by taxi with a suspected skull fracture. This topic was suggested by a reader –...
Breathless, Coughing and Run-down: What's Going On? | Case Study
A new case study in which the patient, a 32-yr-old white male presents to a local free clinic with fatigue, moderate dyspnea, and a persistent and...
Suicidal Ideation and Muscle Twitches | Case Study
A new case study in which the patient, a 40 yr-old mixed-race woman presents to her primary care physician with concerns about suicidal ideation. She has some...
Unexplained Diarrhea and Weight Loss: What's going on? | Case Stud…
A new case study in which the patient, a 28 y/o white female presents to a primary care clinic complaining of recurrent diarrhea. She first experienced diarrhea...
Repeat After Me... What's the problem here? | Case Study
A homeless man is brought to the ER by the local police after he is found sitting at a bus stop with a bloody rag pressed to his left knee. The temperature...
Wild Mood Swings and Outbursts of Anger: What's Wrong with this M…
A new case study in which the patient, a 50-yr-old male of mixed race visits his primary care physician with concerns about wild mood swings and outbursts of...
Case Study: Does this Cherokee Woman Have Dementia?
An 85-yr-old Cherokee woman living in a skilled nursing facility has lost weight since admission and won’t socialize or join in activities. She won't...

Case Study: It's a Lump, but is it Breast Cancer?
I am so excited about this Case Study because I feel it will be useful to so many of you! Welcome to a new Case Study in which the patient, a 45-yr-old, white,...

Case Study: Newborn with Vomiting and Diarrhea
A three-day old male infant is brought to the ER by his 22-yr-old mother with vomiting and diarrhea. Diagnostic results will be released upon request, with the...
Case Study: Joint Pain, Rash, Hair Loss - What's Going On?
A new case study in which R.W. presents to her PCP with a cough, mild fever, joint stiffness and pain and a history of rashes, anemia and hair loss.

Case Study: An OB Catastrophe
The following is a case simulation involving a patient initially encountered in Labor and Delivery. While the initial encounter occurred in a specific setting,...
Differential Case Study: Lyme Disease or Covid-19?
Lakeith, a 35-year-old black man living in New York State, presents with a fever of 101 degrees F. He is concerned he might have contracted Covid-19. Based upon...
Case Study: Sudden Severe Pain
A new case study in which the patient, D.C., a 52-year-old, white, married college professor wakes up to severe and intensifying pain. Though the coronavirus...

Case Study: Unexplained Bruises
Karen brings her daughter, Ann into the pediatric clinic stating, "She's just been so tired lately. All she wants to do is sleep and she’s got no appetite....
Case Study: What's Causing This Cough?
A new case study in which the patient, H.T. an 82-year-old Hispanic man presents to his primary care clinic with cough, malaise and confusion. How well do you...

Case Study(CSI): Stomach flu? Anxiety? What's Going on Here?
A new case study in which the patient, A.W. a 65-year-old African American woman presents to her primary care clinic with unspecified complaints. She told the...

Case Study: I'm too tired to walk the dog...
A new case study in which the patient, T.K. a 51-year-old woman who has finally taken a staycation, doesn’t have enough energy to walk her dog. You’re the...

Case Study: My Stomach Hurts
It's late in the day on a beautiful Saturday in late summer. You are finishing up your shift at a local urgent care clinic when a 28-year-old, white male comes...

Case Study: Trust Your Gut? A Fecal Transplant Could Change Your L…
Fecal Microbial Transplant (FMT) is a well-accepted practice for the treatment of C. diff, however in the U.S. it is still typically used only after multiple...

Case Study: Magic Mushrooms as Medicine? Mind-Body Connection Pt. …
Can "tripping" cure depression? Can LSD reduce chronic anxiety? This article explores the use of psychedelics to treat mental illness. Read on to find links for...
Case Study: Does Childhood Abuse Prevent Weight Loss? Pt. 2
This is an important topic for nurses. We need to understand the connection between childhood trauma and mind/body issues to build trust with patients and...
The Nursing Process: A Comprehensive Guide

In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse’s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
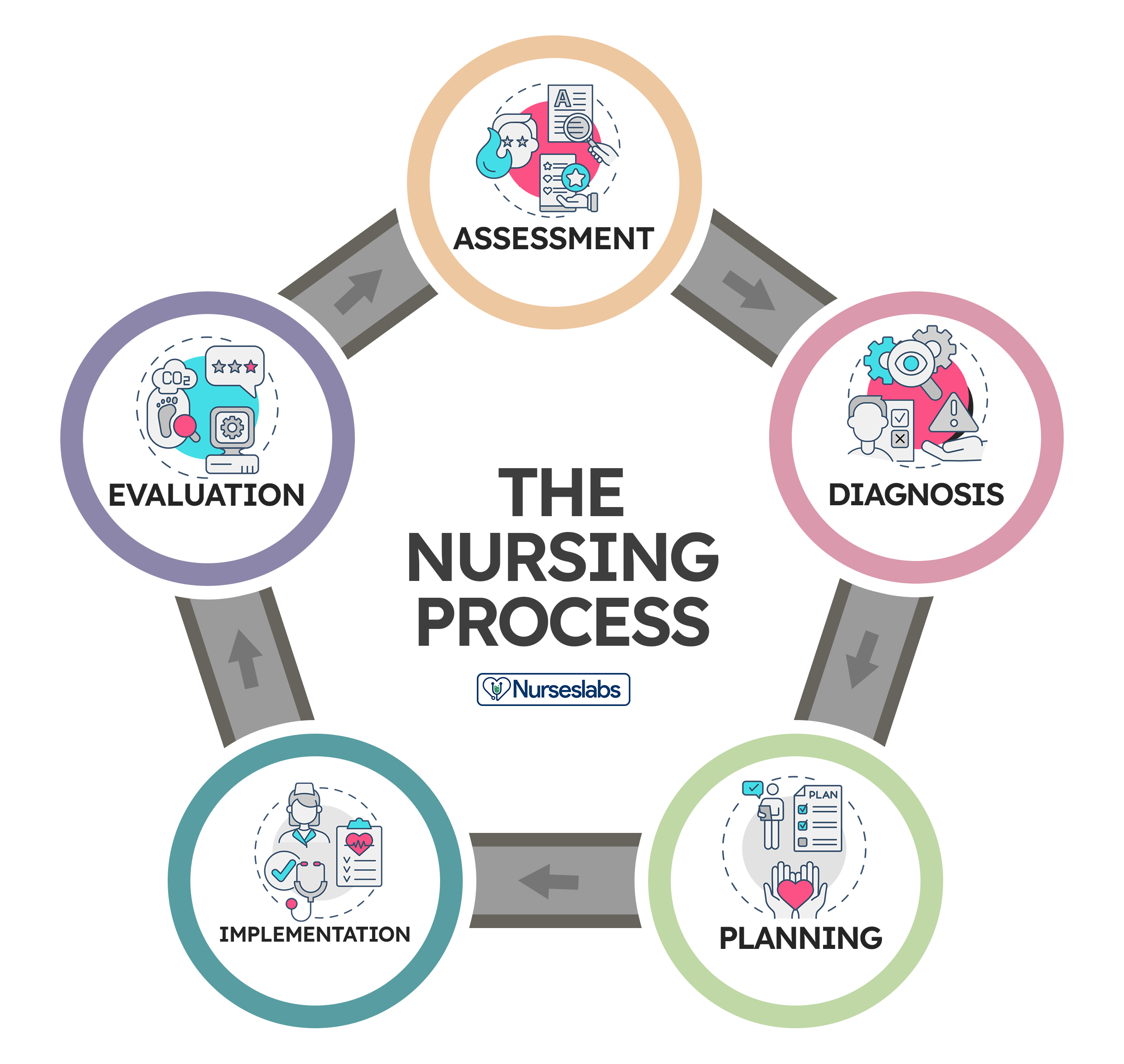
Application of the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data, 2. diagnosis: “what is the problem” , initial planning, ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care.
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation. The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch, smell, or hearing, and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature, pulse, and respiratory rates, blood pressure, vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance, facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members, support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history, which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation.
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature.
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care.
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions. When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement, and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation: “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration , educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking, to reduce the patient’s anxiety, anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing, administering an injection, manipulating equipment, bandaging, moving, lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non-RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.
3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory , nursing practice, and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation: “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan, and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan.
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.
39 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Very helpful Thank you
Leave a Comment Cancel reply

7 steps to successful nursing case study writing.
A nursing case study is a detailed study of a patient that is encountered during a nurse’s daily practice. They are usually written by nurses in training as part of their coursework, but they can also be written by experienced nurses as a way of sharing best practice.
Case studies are an important part of the nursing curriculum as they provide students with a real-life insight into the complexities of patient care. They also allow nurses to reflect on their own practice and identify areas where they could make improvements.
When writing a nursing case study, it is important to follow the instructions provided by your tutor. This will ensure that your case study is relevant and meets the required academic standards. It is also important to be clear and concise in your writing, and to use evidence-based sources to support your claims.
If you are struggling to write a nursing case study, there are a number of resources that can help you. The following books are all recommended reading for anyone wanting to write a case study:
- The Complete Guide to Case Study Research by Elaine M. Hubbell
- Nursing Case Studies: A Guide to Understanding and Writing Them by Jennifer R. Gray
- Writing Nursing Case Studies by Sally G. Reed
Once you have a good understanding of how to write a nursing case study, you will be able to produce high-quality studies that will be of benefit to both yourself and your patients.
Importance of nursing case study writing.
Nursing case studies are an important part of your nursing education. They provide you with the opportunity to apply the knowledge and skills you have learned in the classroom to real-world scenarios. Nursing case studies also allow you to develop critical thinking and problem-solving skills.
The nursing case study should be a detailed and accurate account of the care that was provided to the patient. It should be used to evaluate the outcome of that care and to identify any areas where improvements can be made.
Steps when writing a nursing case study paper.
There are various steps you should keep in mind in order to help you write a successful nursing case study.
These important steps include:
- Define the problem.
- Gathering information.
- Developing alternatives.
- Analyzing the alternatives.
- Selecting the best alternative.
- Implementing the solution.
- Evaluating the outcome.
Defining the Problem
When writing a nursing case study, it is important to first define the problem. The problem should be something that can be solved through nursing interventions. Once the problem is defined, the nursing case study can be written to discuss the interventions that were used to solve the problem.
Nursing case studies are a great way to learn about different nursing interventions and how they can be used to solve problems. By reading nursing case studies, nurses can learn about different diseases and conditions and how to treat them. Nursing case studies can also be used to teach other nurses about different interventions.
Gathering Information
When it comes to writing a nursing case study, the first and most important step is gathering information. This is where you will need to do your research and collect data from a variety of sources. Once you have all of the information you need, you can begin to write your case study.
It is crucial to gather information before starting to write your nursing case study. This ensures that you include all of the relevant information. This means including details about the patient’s medical history, symptoms, and treatment.
Developing Alternatives
Once you have all of the necessary information, you can begin developing alternatives for the patient’s treatment. This will involve looking at the different options and deciding which is best based on the specific case. You will need to consider the risks and benefits of each option before making a recommendation.
Once you have developed a few different options, you can then start writing the case study. This should include an overview of the patient’s history, their current condition, and the different treatment options that were considered. Be sure to explain why you ultimately recommended the chosen course of treatment.
Analyzing the Alternatives
When you are given a nursing case study to write, the first step is to read the case thoroughly. Make sure you understand the situation and the patient’s history. Once you have a good understanding of the case, you can start to analyze the alternatives.
There are usually three alternatives in a nursing case study: nursing intervention, medical intervention, and no intervention. You will need to evaluate each alternative and decide which is best for the patient.
Nursing intervention is usually the first choice because it is the least invasive and has the least risk. Medical intervention is usually the next choice because it is more invasive but has a higher chance of success. No intervention is usually the last choice because it means doing nothing and letting the patient’s condition worsen.
Once you have evaluated the alternatives, you can start to write your case study. Remember to include all of the important information, such as the patient’s history, the alternatives you considered, and your recommendation.
Selecting the Best Alternative
When you are presented with a nursing case study, the first thing you need to do is identify the problem. Once you have identified the problem, you need to gather information about the patient. This information will help you to develop a plan of care. Once you have developed a plan of care, you need to select the best alternative.
The best alternative is the one that will best meet the needs of the patient. When selecting the best alternative, you need to consider the patient’s preferences, the severity of the problem, the risks and benefits of each alternative, and the resources available.
Implementing the Solution
Once you have selected the best alternative, you need to implement the plan of care. After you have implemented the plan of care, you need to evaluate the patient’s response. If the patient’s condition improves, you need to continue the plan of care. If the patient’s condition does not improve, you need to reevaluate the plan of care and select a different alternative.
Evaluating the Outcome
A nursing case study is a detailed account of a patient’s medical history and treatment. It is used to evaluate the outcome of a patient’s care and to identify any areas where improvements can be made.
When writing a nursing case study, it is important to include a detailed description of the patient’s symptoms and medical history. The case study should also include a discussion of the treatment that was provided and the outcome of that treatment.
It is also important to discuss any areas where improvements could be made in the care that was provided. This could include changes to the treatment plan, changes to the way that the patient was monitored, or changes to the way that the patient’s symptoms were managed.
Conclusion.
Writing a successful nursing case study can be a challenging task. However, by following the steps provided in this blog that is, first defining the problem, gathering information, developing alternatives., analyzing the alternatives, selecting the best alternative, implementing the solution and evaluating the outcome. You will be able to write a top-notch nursing case study that meets your requirements.
If you need professional assistance, place your order right here to get help from expert nursing paper writers.

Work with professional online writers

- Affordable Nursing Papers
- Nursing Coursework Writing
- Nursing Essay Writing Service
- Nursing Essay Assignments
- Nursing Assignment Writing
- Nursing Case Study Writing
- Nursing Process Essay Writing
- Nursing Capstone Project
- BSN Capstone Project
- Reliable Nursing Writers
- PICO Question Examples
- Nursing Speeches
- Nursing PowerPoint Presentations
- Online Nursing Essay Writers
- Nursing Thesis
- Nursing Coursework
- Nursing Term Papers
- Legit Nursing Writers
- Best Nursing Writing Company
- Nursing Students Writing Help
- Cheap Nursing Term Paper

- Refund Guarantee
- On time delivery
- Plagiarism-free papers
- Safe and Confidential
- Trained Writers
- Nursing Essay Writing
- Nursing Coursework Help
- Nursing Dissertations
- Nursing Case Studies
- Nursing Assignment Help
Contact Info
- 123 Fifth Ave, New York, NY 12004, United States.
- +1(413) 798-7210
- [email protected]
An Example of the Nursing Process

The nursing process can be a confusing concept for nursing students to grasp. Below is an example of the process from start to finish in a story like fashion:
Implementation
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 1
- What is a case study?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Roberta Heale 1 ,
- Alison Twycross 2
- 1 School of Nursing , Laurentian University , Sudbury , Ontario , Canada
- 2 School of Health and Social Care , London South Bank University , London , UK
- Correspondence to Dr Roberta Heale, School of Nursing, Laurentian University, Sudbury, ON P3E2C6, Canada; rheale{at}laurentian.ca
https://doi.org/10.1136/eb-2017-102845
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
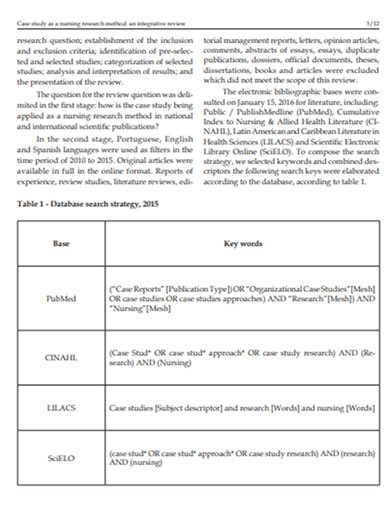
What is it?
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research. 1 However, very simply… ‘a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units’. 1 A case study has also been described as an intensive, systematic investigation of a single individual, group, community or some other unit in which the researcher examines in-depth data relating to several variables. 2
Often there are several similar cases to consider such as educational or social service programmes that are delivered from a number of locations. Although similar, they are complex and have unique features. In these circumstances, the evaluation of several, similar cases will provide a better answer to a research question than if only one case is examined, hence the multiple-case study. Stake asserts that the cases are grouped and viewed as one entity, called the quintain . 6 ‘We study what is similar and different about the cases to understand the quintain better’. 6
The steps when using case study methodology are the same as for other types of research. 6 The first step is defining the single case or identifying a group of similar cases that can then be incorporated into a multiple-case study. A search to determine what is known about the case(s) is typically conducted. This may include a review of the literature, grey literature, media, reports and more, which serves to establish a basic understanding of the cases and informs the development of research questions. Data in case studies are often, but not exclusively, qualitative in nature. In multiple-case studies, analysis within cases and across cases is conducted. Themes arise from the analyses and assertions about the cases as a whole, or the quintain, emerge. 6
Benefits and limitations of case studies
If a researcher wants to study a specific phenomenon arising from a particular entity, then a single-case study is warranted and will allow for a in-depth understanding of the single phenomenon and, as discussed above, would involve collecting several different types of data. This is illustrated in example 1 below.
Using a multiple-case research study allows for a more in-depth understanding of the cases as a unit, through comparison of similarities and differences of the individual cases embedded within the quintain. Evidence arising from multiple-case studies is often stronger and more reliable than from single-case research. Multiple-case studies allow for more comprehensive exploration of research questions and theory development. 6
Despite the advantages of case studies, there are limitations. The sheer volume of data is difficult to organise and data analysis and integration strategies need to be carefully thought through. There is also sometimes a temptation to veer away from the research focus. 2 Reporting of findings from multiple-case research studies is also challenging at times, 1 particularly in relation to the word limits for some journal papers.

Examples of case studies
Example 1: nurses’ paediatric pain management practices.
One of the authors of this paper (AT) has used a case study approach to explore nurses’ paediatric pain management practices. This involved collecting several datasets:
Observational data to gain a picture about actual pain management practices.
Questionnaire data about nurses’ knowledge about paediatric pain management practices and how well they felt they managed pain in children.
Questionnaire data about how critical nurses perceived pain management tasks to be.
These datasets were analysed separately and then compared 7–9 and demonstrated that nurses’ level of theoretical did not impact on the quality of their pain management practices. 7 Nor did individual nurse’s perceptions of how critical a task was effect the likelihood of them carrying out this task in practice. 8 There was also a difference in self-reported and observed practices 9 ; actual (observed) practices did not confirm to best practice guidelines, whereas self-reported practices tended to.
Example 2: quality of care for complex patients at Nurse Practitioner-Led Clinics (NPLCs)
The other author of this paper (RH) has conducted a multiple-case study to determine the quality of care for patients with complex clinical presentations in NPLCs in Ontario, Canada. 10 Five NPLCs served as individual cases that, together, represented the quatrain. Three types of data were collected including:
Review of documentation related to the NPLC model (media, annual reports, research articles, grey literature and regulatory legislation).
Interviews with nurse practitioners (NPs) practising at the five NPLCs to determine their perceptions of the impact of the NPLC model on the quality of care provided to patients with multimorbidity.
Chart audits conducted at the five NPLCs to determine the extent to which evidence-based guidelines were followed for patients with diabetes and at least one other chronic condition.
The three sources of data collected from the five NPLCs were analysed and themes arose related to the quality of care for complex patients at NPLCs. The multiple-case study confirmed that nurse practitioners are the primary care providers at the NPLCs, and this positively impacts the quality of care for patients with multimorbidity. Healthcare policy, such as lack of an increase in salary for NPs for 10 years, has resulted in issues in recruitment and retention of NPs at NPLCs. This, along with insufficient resources in the communities where NPLCs are located and high patient vulnerability at NPLCs, have a negative impact on the quality of care. 10
These examples illustrate how collecting data about a single case or multiple cases helps us to better understand the phenomenon in question. Case study methodology serves to provide a framework for evaluation and analysis of complex issues. It shines a light on the holistic nature of nursing practice and offers a perspective that informs improved patient care.
- Gustafsson J
- Calanzaro M
- Sandelowski M
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
Registered Nurse RN
Registered Nurse, Free Care Plans, Free NCLEX Review, Nurse Salary, and much more. Join the nursing revolution.
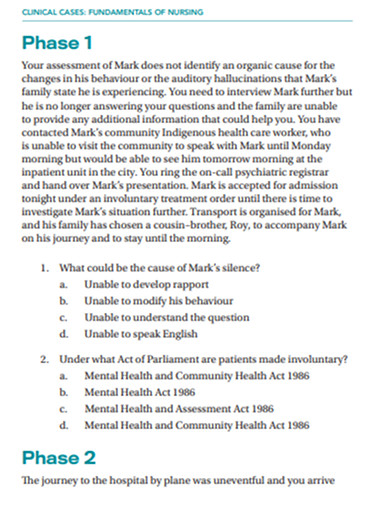
Next Generation NCLEX Case Study Sample Questions
One of the big changes on the Next Generation NCLEX exam is a shift toward case studies. Case studies often require a deeper level of critical thinking, and understanding diseases on a more in-depth level (especially the pathophysiology) will make these types of questions easier to answer.
In this article, you’ll be able to watch a free video to help you prepare for the new Next Generation NCLEX case study format. Nurse Sarah will walk you step-by-step through each scenario and help you understand how to use critical thinking and nursing knowledge to answer these types of questions.
Next Generation NCLEX Case Study Review Questions Video
NGN Case Study Sample Questions and Answers
First, let’s take a look at our case study summary below:
Case Study Summary:
A 68-year-old male is admitted with shortness of breath. He reports difficulty breathing with activity, lying down, or while sleeping. He states that in order to “breathe easier,” he has had to sleep in a recliner for the past week. The patient has a history of hypertension, myocardial infarction (2 years ago), and cholecystectomy (10 years ago). The patient is being transferred to a cardiac progressive care unit for further evaluation and treatment.
Question 1 of 6: The nurse receives the patient admitted with shortness of breath. What findings are significant and require follow-up? The options are listed below. Select all that apply.
To answer this first question in the NGN case study, let’s look at the information provided in the nursing notes and vital signs tabs provided:

This question is asking us to identify findings that are significant and require the nurse to follow-up. In other words, what is presenting that we can’t ignore but need to investigate further.
Therefore, let’s comb through the nursing notes and vital signs to see what is abnormal and requires follow-up.
First, the patient arrived to the room via stretcher. That’s fine and doesn’t necessarily require follow-up.
Next, the patient is alert and oriented x 4 (person, place, time, event). This tells us that the patient’s neuro status is intact so far. Therefore, the shortness of breath isn’t affecting the patient’s mental function yet (we have enough oxygen on board right now for brain activity).
However, the nurse has noticed the shortness of breath with activity and talking, which should not normally happen. This tells us something is wrong and is significant enough to require follow-up. We want to know why is this happening, is it going to get worse, etc.
The patient’s weight and vital signs were collected (this is good). Weight is 155 lbs. and BMI is within a healthy range (doesn’t tell us too much but may be useful later). The patient is also connected to a bedside monitor, so they need to be monitored constantly like on a progressive care unit.
The monitor shows sinus tachycardia . This is significant because it seems the patient’s shortness of breath is causing the heart to compensate by increasing the heart rate to provide more oxygen (hence the lungs may be compromised).
Then we find out that the lungs are indeed compromised because crackles are heard in both lungs , and this may be why our patient is short of breath. This is significant (could the patient have pulmonary edema?)
Then we find out the nurse has noted an S3. This is an extra heart sound noted after S2. And what jumps out to me about this is that it is usually associated with volume overload in the heart like in cases of heart failure . However, S3 may be normal in some people under 40 or during pregnancy, but that’s not the case with our patient based on what we read in the case summary.
Therefore, based on everything I’m reading in this case study, I’m thinking this patient may have heart failure, but we need those test results back (especially the echo and chest x-ray, and hopefully a BNP will be in there too).
We are also told that the patient has an 18 gauge IV inserted (which is good thing to have so we can give medications if required), orders have been received, labs drawn, and testing results are pending.

Now let’s look at the “Vital Signs” tab above, and ask yourself what is normal vs. abnormal for this patient (adult male).
- The heart rate is high at 112 (tachycardia), and should normally be 60-100 bpm (see heart rhythms ).
- Blood pressure is higher than normal (normal is 120/80), which indicates hypertension.
- Oxygen saturation is 94% (this is on the low side as we’d normally want around 95% or higher, and the patient is on 4 L nasal cannula, which tells us the lungs are not okay).
- Respiratory rate is increased (26 breaths per minute)…normal is 12-20 breaths per minute.
Based on the information we were provided, I’ve selected the answers below. These findings are significant and definitely require follow-up by the nurse.

When answering these NGN case study questions, it’s helpful to think of the ABCDE (airway, breathing, circulation, etc.) as all of these fall into that category. If we don’t follow-up on the shortness of breath, crackles, respiratory rate, o2 saturation (94% on 4 L nasal cannula), the respiratory system can further decline.
In addition, the sinus tachycardia, S3 gallop, and hypertension could indicate fluid overload in the heart. This may cause the heart to tire out and lead the lethal rhythm. On the other hand, temperature, pain, weight, and BMI are not abnormal and do not require follow-up.
See the Complete Next Generation NCLEX Case Study Review
Each question in the case study builds on the previous question. To see how these questions evolve based on the patient’s condition and labs, watch the entire Next Generation NCLEX Case Study Review video on our YouTube Channel (RegisteredNurseRN).
NCLEX Practice Quizzes
We’ve developed many free NCLEX review quizzes to test your knowledge on nursing topics and to help you prepare for the Next Generation NCLEX exam.
Nurse Sarah’s Notes and Merch
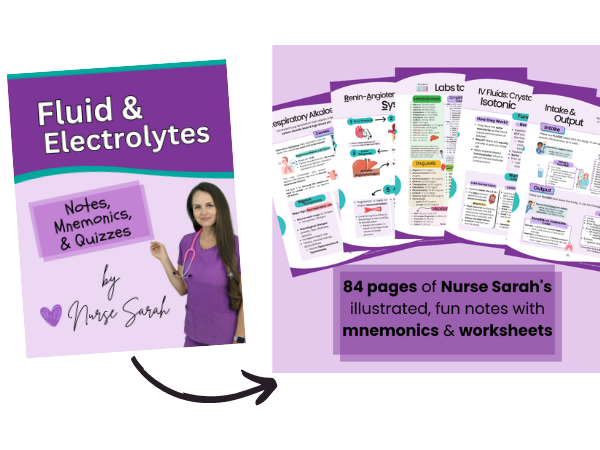
Just released is “ Fluid and Electrolytes Notes, Mnemonics, and Quizzes by Nurse Sarah “. These notes contain 84 pages of Nurse Sarah’s illustrated, fun notes with mnemonics, worksheets, and 130 test questions with rationales.
You can get an eBook version here or a physical copy of the book here.
Please Share:
- Click to print (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
Disclosure and Privacy Policy
Important links, follow us on social media.
- Facebook Nursing
- Instagram Nursing
- TikTok Nurse
- Twitter Nursing
- YouTube Nursing
Copyright Notice

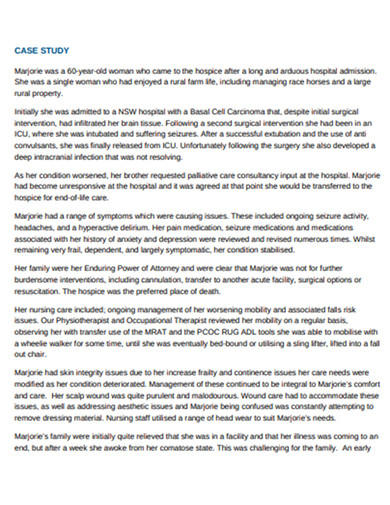
Nursing Case Study
ScienceDirect posted a nursing ethics case study where an end-stage prostate cancer patient, Mr. Green, confided to nursing staff about his plan to commit suicide. The patient asked the nurse to keep it a secret. The ethical problem is whether the nurse should tell the health care team members about the patient’s thought without his permission. The best ethical decision for this nursing case study was to share this critical information with other health care professionals, which was the action the nurse took. The team adhered to the proper self-harm and suicide protocol. The appropriate team performed a palliative therapy. As a result, the patient didn’t harm himself and died peacefully a few months after he was discharged.
What Is a Nursing Case Study? A nursing case study is a detailed study of an individual patient. Through this type of research, you can gain more information about the symptoms and the medical history of a patient. It will also allow you to provide the proper diagnoses of the patient’s illness based on the symptoms he or she experienced and other affecting factors. Nursing students usually perform this study as part of their practicum, making it an essential experience because, through this research methodology , they can apply the lessons they have learned from school. The situation mentioned above was an excellent example of a nursing case study.
Nursing Case Study Format
1. introduction.
Purpose: Briefly introduces the case study, including the main health issue or condition being explored. Background: Provides context for the patient scenario, outlining the significance of the case in nursing practice. Objectives: Lists the learning objectives or goals that the case study aims to achieve.
2. Patient Information
Demographics: Age, gender, ethnicity, and relevant personal information. Medical History: Past medical history, including any chronic conditions, surgeries, or significant health events. Current Health Assessment: Presents the patient’s current health status, including symptoms, vital signs, and results from initial examinations.
3. Case Description
Clinical Presentation: Detailed description of the patient’s presentation, including physical examination findings and patient-reported symptoms. Diagnostic Findings: Summarizes diagnostic tests that were performed, including lab tests, imaging studies, and other diagnostic procedures, along with their results. Treatment Plan: Outlines the initial treatment provided to the patient, including medications, therapies, surgeries, or other interventions.
4. Nursing Care Plan
Nursing Diagnoses: Identifies the nursing diagnoses based on the assessment data. Goals and Outcomes: Establishes short-term and long-term goals for the patient’s care, including expected outcomes. Interventions: Describes specific nursing interventions planned or implemented to address each nursing diagnosis and achieve the stated goals. Evaluation: Discusses the effectiveness of the nursing interventions, including patient progress and any adjustments made to the care plan.
5. Analysis
Critical Analysis: Analyzes the case in depth, considering different aspects of patient care, decision-making processes, and the application of nursing theories and principles. Reflection: Reflects on the nursing practice, lessons learned, and how the case study has impacted the understanding and application of nursing knowledge.
6. Conclusion
Summary: Provides a concise summary of the key points from the case study, including the patient outcome and the nursing care impact. Implications for Practice: Discusses the implications of the case for nursing practice, including any changes to practice or policy that could improve patient care. Recommendations: Offers recommendations for future care or areas for further study based on the case study findings.
Examples of Nursing Case Study
Management of Acute Myocardial Infarction (AMI) Introduction: A 58-year-old male with a history of hypertension and smoking presents to the emergency department with chest pain. This case study explores the nursing management for patients with AMI. Patient Information: Demographics: 58-year-old male, smoker. Medical History: Hypertension, no previous diagnosis of heart disease. Current Health Assessment: Reports severe chest pain radiating to his left arm, sweating, and nausea. Case Description: Clinical Presentation: Patient appeared in distress, clutching his chest. Diagnostic Findings: ECG showed ST-elevation in anterior leads. Troponin levels were elevated. Treatment Plan: Immediate administration of aspirin, nitroglycerin, and morphine for pain. Referred for emergency coronary angiography. Nursing Care Plan: Nursing Diagnoses: Acute pain related to myocardial ischemia. Goals: Relieve pain and prevent further myocardial damage. Interventions: Monitoring vital signs, administering prescribed medications, and providing emotional support. Evaluation: Pain was managed effectively, and the patient was stabilized for angiography. Analysis: The timely nursing interventions contributed to stabilizing the patient’s condition, showcasing the critical role nurses play in acute care settings. Conclusion: This case highlights the importance of quick assessment and intervention in patients with AMI, emphasizing the nurse’s role in pain management and support.
Managing Type 1 Diabetes in a Pediatric Patient Introduction: A 10-year-old female diagnosed with type 1 diabetes presents for a routine check-up. This case study focuses on the nursing care plan for managing diabetes in pediatric patients. Patient Information: Demographics: 10-year-old female. Medical History: Diagnosed with type 1 diabetes six months ago. Current Health Assessment: Well-controlled blood glucose levels, but expresses difficulty with frequent insulin injections. Case Description: Clinical Presentation: Patient is active, engaging in school activities but struggles with diabetes management. Diagnostic Findings: HbA1c is 7.2%, indicating good control. Treatment Plan: Insulin therapy, carbohydrate counting, and regular blood glucose monitoring. Nursing Care Plan: Nursing Diagnoses: Risk for unstable blood glucose levels. Goals: Maintain blood glucose within target range and increase patient comfort with diabetes management. Interventions: Education on insulin pump use, dietary advice, and coping strategies. Evaluation: Patient showed interest in using an insulin pump and understood dietary recommendations. Analysis: This case emphasizes the importance of education and emotional support in managing chronic conditions in pediatric patients. Conclusion: Effective management of type 1 diabetes in children requires a comprehensive approach that includes education, technological aids, and psychological support.
Elderly Care for Alzheimer’s Disease Introduction: An 82-year-old female with Alzheimer’s disease presents with increased confusion and agitation. This case study examines the complexities of caring for elderly patients with Alzheimer’s. Patient Information: Demographics: 82-year-old female. Medical History: Alzheimer’s disease, osteoarthritis. Current Health Assessment: Increased confusion, agitation, and occasional aggression. Case Description: Clinical Presentation: Patient exhibits signs of advanced Alzheimer’s with memory loss and disorientation. Diagnostic Findings: Cognitive tests confirm the progression of Alzheimer’s. Treatment Plan: Non-pharmacological interventions for agitation, memory aids, and safety measures in the home. Nursing Care Plan: Nursing Diagnoses: Impaired memory related to Alzheimer’s disease. Goals: Reduce agitation and prevent harm. Interventions: Use of calming techniques, establishing a routine, and environmental modifications. Evaluation: Agitation was reduced, and the patient’s safety was improved through environmental adjustments. Analysis: The case underscores the need for tailored interventions to manage Alzheimer’s symptoms and improve the quality of life for the elderly. Conclusion: Nursing care for Alzheimer’s patients requires a multifaceted approach focusing on safety, symptom management, and patient dignity.
Nursing Case Study Topics with Samples to Edit & Download
- Telehealth Nursing
- Mental Health and Psychiatric Nursing
- Geriatric Nursing Care
- Palliative and End-of-Life Care
- Pediatric Nursing
- Emergency and Critical Care Nursing
- Chronic Disease Management
- Nursing Ethics and Patient Rights
- Infection Control and Prevention
- Oncology Nursing
- Nursing Leadership and Management
- Cultural Competence in Nursing
- Substance Abuse and Addiction Nursing
- Technological Innovations in Nursing
- Nursing Education and Training
Nursing Case Study Examples & Templates
1. nursing case study template.
2. Free Nursing Student Care Plan Template
3. Nursing Action Case Study Example
4. Hospital Nursing Care Case Study Example
5. Printable Nursing Health Case Study Example
professays.com
6. Fundamentals of Nursing Case Study Example
secure-ecsd.elsevier.com
7. Sample Nursing Case Study Example
caresearch.com.au
8. Nursing Research Case Study Example
9. Standard Nursing Case Study Example
resourcecenter.ovid.com
10. Nursing Disability Case Study Example
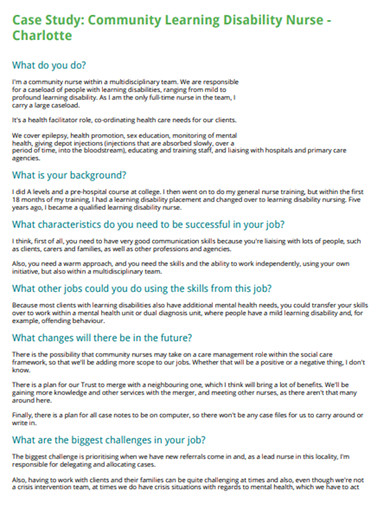
careerswales.com
11. Nursing care Patients Case Study Example

12. School of Nursing Case Study Example

ebn.bmj.com
13. Evaluation of Nursing Care Case Study Example
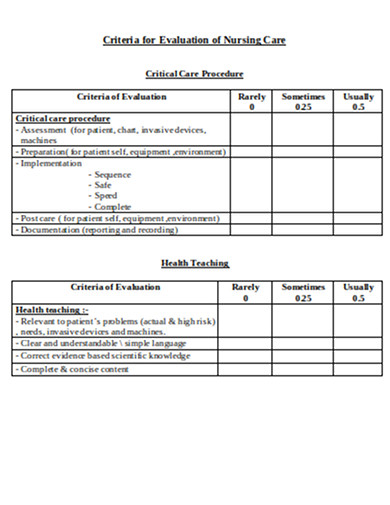
philadelphia.edu
Nursing Case Study Segments
Typically, a nursing case study contains three main categories, such as the items below.
1. The Status of a Patient
In this section, you will provide the patient’s information, such as medical history, and give the current patient’s diagnosis, condition, and treatment. Always remember to write down all the relevant information about the patient. Other items that you can collect in this stage are the reasons for the patient to seek medical care and the initial symptoms that he or she is experiencing. After that, based on the gathered information, you will explain the nature and cause of the illness of the patient.
2. The Nursing Assessment of the Patient
In this stage, you will need to prepare your evaluation of the patient’s condition. You should explain each observation that you have collected based on the vital signs and test results. You will also explain each nursing diagnosis that you have identified and determine the proper nursing care plan for the patient.
3. The Current Care Plan and Recommendations
Describe the appropriate care plan that you can recommend to the patient based on the diagnosis, current status, and prognosis in detail, including how the care plan will affect his or her life quality. If needed, you can also evaluate the patient’s existing care plan and give recommendations to enhance it. It is also crucial to cite relevant authoritative sources that will support your recommendations .
Objectives of Nursing Case Study
Nursing case studies are integral educational tools that bridge theoretical knowledge with practical application in patient care. They serve several key objectives essential for the development of nursing students and professionals. Here are the primary objectives of nursing case studies:
1. Enhance Critical Thinking and Clinical Reasoning
Case studies encourage nurses to analyze complex patient scenarios, make informed decisions, and apply critical thinking skills to solve problems. They simulate real-life situations, requiring nurses to evaluate data, consider multiple outcomes, and choose the best course of action.
2. Improve Diagnostic Skills
Through the detailed analysis of patient information, symptoms, and diagnostic results, nursing case studies help improve diagnostic skills. They allow nurses to practice interpreting clinical data to identify patient conditions and understand the underlying causes of symptoms.
3. Facilitate Application of Theoretical Knowledge
Nursing case studies provide a direct bridge between classroom learning and clinical practice. They offer a practical venue for applying theoretical knowledge about anatomy, physiology, pharmacology, and nursing theories to real-world patient care situations.
4. Promote Understanding of Comprehensive Patient Care
These studies emphasize the importance of holistic care, considering the physical, emotional, social, and psychological aspects of patient well-being. Nurses learn to develop comprehensive care plans that address all facets of a patient’s health.
5. Encourage Reflective Practice and Self-Assessment
Reflecting on case study outcomes enables nurses to evaluate their own decision-making processes, clinical judgments, and actions. This self-assessment promotes continuous learning and professional growth by identifying areas for improvement.
6. Foster Interdisciplinary Collaboration
Case studies often involve scenarios that require collaboration among healthcare professionals from various disciplines. They teach nurses the value of teamwork, communication, and the integration of different expertise to achieve optimal patient outcomes.
7. Enhance Patient Education and Advocacy Skills
By working through case studies, nurses improve their ability to educate patients and families about health conditions, treatment plans, and preventive measures. They also learn to advocate for their patients’ needs and preferences within the healthcare system.
8. Prepare for Real-Life Challenges
Nursing case studies prepare students and new nurses for the unpredictability and challenges of real-life clinical settings. They provide safe, controlled environments to practice responses to emergencies, ethical dilemmas, and complex patient needs without the risk of actual harm.
Steps in Nursing Process
Whether you are handling a patient with schizophrenia, pneumonia, diabetes, appendicitis, hypertension, COPD, etc, you will need to follow specific steps to ensure that you are executing the critical nursing process.
1. Assess the Patient
The first step of the nursing process requires critical thinking skills as it involves gathering both subjective and objective data. Subjective data includes verbal statements that you can collect from the patient or caregiver. In contrast, objective information refers to measurable and tangible data, such as vital signs, height, weight, etc. You can also use other sources of information, such as electronic health records, and friends that are in direct contact with the patient.
2. Diagnose the Patient
This critical step will help you in the next steps, such as planning and implementation of patient care. In this step, you will formulate a nursing diagnosis by applying clinical judgment. As a nurse, the North American Nursing Diagnosis Association (NANDA) will give you an up-to-date nursing diagnosis list, which will allow you to form a diagnosis based on the actual health problem.
3. Plan for a Proper Patient Care Plan
This part is where you will plan out the appropriate care plan for the patient. You will set this goal following the evidence-based practice (EDP) guidelines. The goal you will set should be specific, measurable, attainable, realistic, and timely ( SMART ).
4. Implement the Plan
In this stage, you can execute the plan that you have developed in the previous step. The implementation may need interventions such as a cardiac monitor, medication administration, etc.
5. Evaluate the Results
It is crucial to remember that every time the team does an intervention, you must do a reassessment to ensure that the process will lead to a positive result. You may need to reassess the patient depending on his progress, and the care plan may be modified based on the reassessment result.
Where to find nursing case studies?
Nursing case studies can be found in a variety of academic, professional, and medical resources. Here are some key places to look for nursing case studies:
- Academic Journals : Many academic journals focus on nursing and healthcare and publish case studies regularly. Examples include the “Journal of Clinical Nursing,” “Nursing Case Studies,” and “American Journal of Nursing.”
- University and College Libraries : Many academic institutions provide access to databases and journals that contain nursing case studies. Libraries often have subscriptions to these resources.
- Online Medical Libraries : Websites like PubMed, ScienceDirect, and Wiley Online Library offer a vast collection of nursing and medical case studies.
- Professional Nursing Organizations : Organizations such as the American Nurses Association (ANA) and the National League for Nursing (NLN) often provide resources, including case studies, for their members.
- Nursing Education Websites : Websites dedicated to nursing education, such as Lippincott NursingCenter and Nurse.com, often feature case studies for educational purposes.
- Government Health Websites : The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) sometimes publish case studies related to public health nursing and disease outbreaks.
- Nursing Textbooks and eBooks : Many nursing textbooks and eBooks include case studies to illustrate key concepts and scenarios encountered in practice.
- Online Nursing Forums and Communities : Forums and online communities for nursing professionals may share or discuss case studies as part of their content.
- Conference Proceedings : Nursing and healthcare conferences often include presentations of case studies. Many of these are published in the conference proceedings, which may be accessible online.
Carrying out a nursing case study can be a delicate task since it puts the life of a person at stake. Thus, it requires a thorough investigation. With that said, it is essential to gain intensive knowledge about this type of study. Today, we have discussed an overview of how to conduct a nursing case study. However, if you think that you are having problems with your writing skills , we recommend you to consider looking for an essay writing service from the experts in the nursing department to ensure that the output follows the appropriate writing style and terminology.
AI Generator
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Akhtar N, Lee L Utilization and complications of central venous access devices in oncology patients. Current Oncology.. 2021; 28:(1)367-377 https://doi.org/10.3390/curroncol28010039
BD ChloraPrep: summary of product characteristics.. 2021; https://www.bd.com/en-uk/products/infection-prevention/chloraprep-patient-preoperative-skin-preparation/chloraprep-smpc-pil-msds
Chloraprep 10.5ml applicator.. 2022a; https://www.bd.com/en-uk/products/infection-prevention/chloraprep-patient-preoperative-skin-preparation/chloraprep-patient-preoperative-skin-preparation-product-line/chloraprep-105-ml-applicator
Chloraprep 3ml applicator.. 2022b; https://www.bd.com/en-uk/products/infection-prevention/chloraprep-patient-preoperative-skin-preparation/chloraprep-patient-preoperative-skin-preparation-product-line/chloraprep-3-ml-applicator
Website.. 2021; https://www.cdc.gov/cancer/preventinfections/providers.htm
Ceylan G, Topal S, Turgut N, Ozdamar N, Oruc Y, Agin H, Devrim I Assessment of potential differences between pre-filled and manually prepared syringe use during vascular access device management in a pediatric intensive care unit. https://doi.org/10.1177/11297298211015500
Clare S, Rowley S Best practice skin antisepsis for insertion of peripheral catheters. Br J Nurs.. 2021; 30:(1)8-14 https://doi.org/10.12968/bjon.2021.30.1.8
Caguioa J, Pilpil F, Greensitt C, Carnan D HANDS: standardised intravascular practice based on evidence. Br J Nurs.. 2012; 21:(14)S4-S11 https://doi.org/10.12968/bjon.2012.21.Sup14.S4
Easterlow D, Hoddinott P, Harrison S Implementing and standardising the use of peripheral vascular access devices. J Clin Nurs.. 2010; 19:(5-6)721-727 https://doi.org/10.1111/j.1365-2702.2009.03098.x
Florman S, Nichols RL Current approaches for the prevention of surgical site infections. Am J Infect Dis.. 2007; 3:(1)51-61 https://doi.org/10.3844/ajidsp.2007.51.61
Gorski LA, Hadaway L, Hagle M Infusion therapy standards of practice. J Infus Nurs.. 2021; 44:(S1)S1-S224 https://doi.org/10.1097/NAN.0000000000000396
Guenezan J, Marjanovic N, Drugeon B Chlorhexidine plus alcohol versus povidone iodine plus alcohol, combined or not with innovative devices, for prevention of short-term peripheral venous catheter infection and failure (CLEAN 3 study): an investigator-initiated, openlabel, single centre, randomised-controlled, two-by-two factorial trial [published correction appears in Lancet Infect Dis. 2021 Apr 6]. Lancet Infect Dis.. 2021; 21:(7)1038-1048 https://doi.org/10.1016/S1473-3099(20)30738-6
Gunka V, Soltani P, Astrakianakis G, Martinez M, Albert A, Taylor J, Kavanagh T Determination of ChloraPrep® drying time before neuraxial anesthesia in elective cesarean delivery: a prospective observational study. Int J Obstet Anesth.. 2019; 38:19-24 https://doi.org/10.1016/j.ijoa.2018.10.012
Ishikawa K, Furukawa K Staphylococcus aureus bacteraemia due to central venous catheter infection: a clinical comparison of infections caused by methicillin-resistant and methicillin-susceptible strains. Cureus.. 2021; 13:(7) https://doi.org/10.7759/cureus.16607
Loveday HP, Wilson JA, Pratt RJ Epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect.. 2014; 86:(S1)S1-70 https://doi.org/10.1016/S0195-6701(13)60012-2
Promoting safer use of injectable medicines.. 2007; https://healthcareea.vctms.co.uk/assets/content/9652/4759/content/injectable.pdf
Standards for infusion therapy. 4th edn.. 2016; https://www.rcn.org.uk/clinical-topics/Infection-prevention-and-control/Standards-for-infusion-therapy
Taxbro K, Chopra V Appropriate vascular access for patients with cancer. Lancet.. 2021; 398:(10298)367-368 https://doi.org/10.1016/S0140-6736(21)00920-X
Case Studies
Gema munoz-mozas.
Vascular Access Advanced Nurse Practitioner—Lead Vascular Access Nurse, The Royal Marsden NHS Foundation Trust
View articles · Email Gema
Colin Fairhurst
Vascular Access Advanced Clinical Practitioner, University Hospitals Plymouth NHS Trust
View articles
Simon Clare
Research and Practice Development Director, The Association for Safe Aseptic Practice
View articles · Email Simon
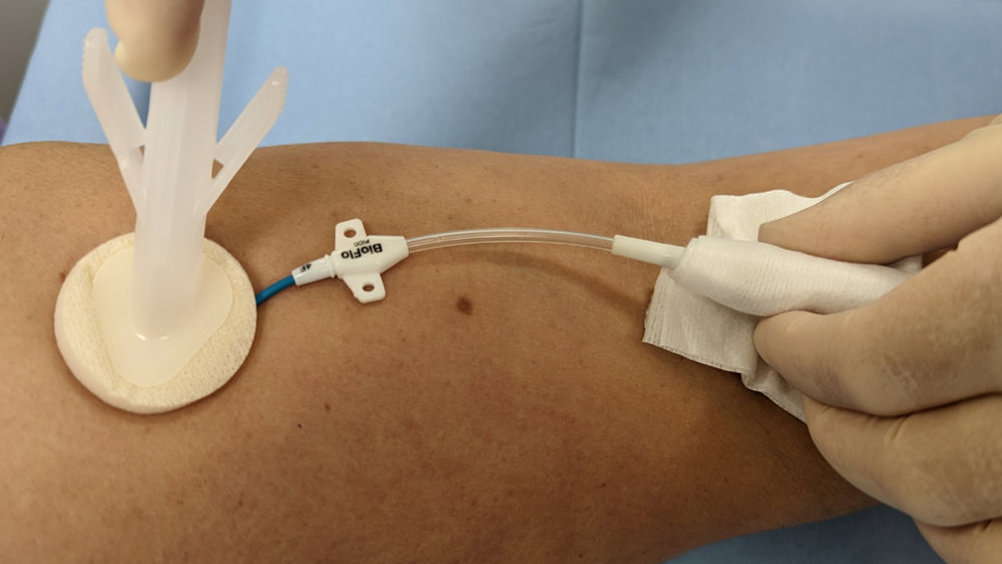
Intravenous (IV) access, both peripheral and central, is an integral part of the patient care pathways for diagnosing and treating cancer. Patients receiving systemic anticancer treatment (SACT) are at risk for developing infections, which may lead to hospitalisation, disruptions in treatment schedules and even death ( Centers for Disease Control and Prevention, 2021 ). However, infection rates can be reduced and general patient outcomes improved with the evidence-based standardisation of IV practice, and the adoption of the appropriate equipment, such as peripheral IV cannulas, flushing solutions and sterile IV dressings ( Easterlow et al, 2010 ).
Cancer treatment frequently involves the use of central venous catheters (CVCs)-also referred to as central venous access devices (CVADs)—which can represent a lifeline for patients when used to administer all kinds of IV medications, including chemotherapy, blood products and parenteral nutrition. They can also be used to obtain blood samples, which can improve the patient’s quality of life by reducing the need for peripheral stabs from regular venepunctures ( Taxbro and Chopra, 2021 ). CVCs are relatively easy to insert and care for; however, they are associated with potential complications throughout their insertion and maintenance.
One serious complication of CVC use is catheter-related bloodstream infections (CRBSIs), which can increase morbidity, leading to prolonged hospitalisation and critical use of hospital resources ( Akhtar and Lee, 2021 ). Early-onset CRBSIs are commonly caused by skin pathogens, and so a cornerstone of a CRBSI prevention is skin antisepsis at the time of CVC insertion. Appropriate antisepsis (decontamination/preparation) of the site for CVC insertion can prevent the transmission of such skin pathogens during insertion, while reducing the burden of bacteria on the CVC exit site ( Loveday et al, 2014 ).
Evidence-based practice for the prevention of a CRBSIs and other healthcare-associated infections recommends skin antisepsis prior to insertion of a vascular-access device (VAD) using a 2% chlorhexidine gluconate and 70% isopropyl alcohol solution. This is recommended in guidelines such as epic3 ( Loveday et al, 2014 ), the Standards for Infusion Therapy ( Royal College of Nursing, 2016 ) and the Infusion Therapy Standards of Practice ( Gorski et al, 2021 ). A strong evidenced-backed product such as BD ChloraPrep™ ( Figure 1 ) has a combination of 2% chlorhexidine gluconate in 70% isopropyl alcohol that provides broad-spectrum rapid-action antisepsis, while the applicators facilitate a sterile, single-use application that eliminates direct hand-to-patient contact, helping to reduce cross-contamination and maintaining sterile conditions ( BD, 2021 ). The BD ChloraPrep™ applicator’s circular head allows precise antisepsis of the required area, and the sponge head helps to apply gentle friction in back-and-forth motion to penetrate the skin layers ( BD, 2021 ). BD ChloraPrep’s rapidacting, persistent and broad-spectrum characteristics and proven applicator system ( Florman and Nichols, 2007 ) make it a vital part of the policy and protocol for insertion, care and maintenance of CVCs in specialist cancer centres such as the Royal Marsden. Meanwhile, the use of BD PosiFlush™ Prefilled Saline Syringe ( Figure 2 ), a prefilled normal saline (0.9% sodium choride) syringe, is established practice for the flushing regime of VADs in many NHS Trusts.
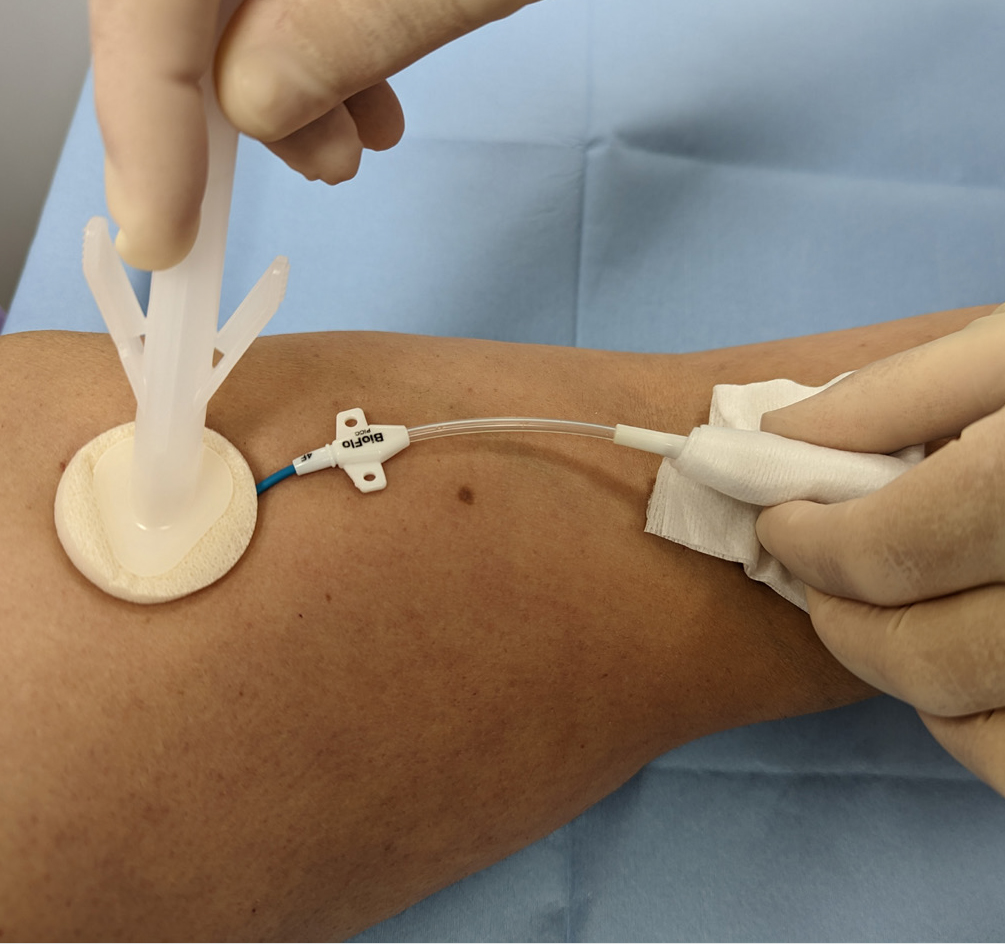
The following five case studies present examples from personal experience of clinical practice that illustrate how and why clinicians in oncology and other disciplines use BD ChloraPrep ™ and BD PosiFlush ™ Prefilled Saline Syringe in both adult and paediatric patients.
Case study 1 (Andy)
Andy was a 65-year-old man being treated for metastatic colorectal cancer at the Royal Marsden NHS Foundation Trust specialist cancer service, which provides state-of-the-art treatment to over 60 000 patients each year.
Andy had a peripherally inserted central catheter (PICC) placed at the onset of his chemotherapy treatment to facilitate IV treatment. While in situ, PICCs require regular maintenance to minimise associated risks. This consists of a weekly dressing change to minimise infection and a weekly flush to maintain patency, if not in constant use. For ambulatory patients, weekly PICC maintenance can be carried out either in the hospital outpatient department or at home by a district nurse or family member trained to do so. Patients, relatives, carers and less-experienced nurses involved in PICC care (flushing and dressing) can watch a video on the Royal Marsden website as an aide memoir.
Initially, Andy decided to have his weekly PICC maintenance at the hospital’s nurse-led clinic for the maintenance of CVCs. At the clinic, Andy’s PICC dressing change and catheter flushing procedures were performed by a nursing associate (NA), who, having completed the relevant competences and undergone supervised practise, could carry out weekly catheter maintenance and access PICC for blood sampling.
In line with hospital policy, the PICC dressing change was performed under aseptic non-touch technique (ANTT) using a dressing pack and sterile gloves. After removal of the old dressing, the skin around the entry site and the PICC was cleaned with a 3 ml BD ChloraPrep™ applicator, using back-andforth strokes for 30 seconds and allowing the area to air dry completely before applying the new dressing. As clarified in a recent article on skin antisepsis (Clare and Rowley, 2020), BD ChloraPrep™ applicator facilitated a sterile, single-use application that eliminates direct hand-to-patient contact, which help reduce cross-contamination and maintaining ANTT. Its circular head allowed precise antisepsis around the catheter, and the sponge head helped to apply gentle friction in back-and-forth strokes to penetrate the skin layers.
Once the new dressing was applied, the NA continued to clean the catheter hub and change the needle-free connector. Finally, the catheter lumen was flushed with 10 ml of normal saline (0.9% sodium chloride) with a pre-filled saline syringe (BD PosiFlush™ Prefilled Saline Syringe). This involved flushing 1 ml at a time, following a push-pause technique, with positive pressure disconnection to ensure catheter patency. The classification of these syringes as medical devices enables NAs and other nonregistered members of the clinical team to support nursing staff with the care and maintenance of PICCs and other CVCs, within local policies and procedures. Using pre-filled syringes can save time and minimise the risk of contamination of the solution ( Ceylan et al, 2021 ).
The use of pre-filled 0.9% sodium chloride syringes facilitates home maintenance of PICCs for patients. When Andy did not need to attend hospital, his PICC maintenance could be performed by a family member. Patients and relatives could access the necessary equipment and training from the day-case unit or outpatient department. Home PICC maintenance is extremely beneficial, not just to providers, but also to patients, who may avoid unnecessary hospital attendance and so benefit from more quality time at home and a reduced risk of hospital-acquired infections. Many patients and relatives have commented on the convenience of having their PICC maintenance at home and how easy they found using the ChloraPrep™ and BD PosiFlush™ Prefilled Saline Syringe ‘sticks’.
Case study 2 (Gail)
Gail was as a 48-year-old woman being treated for bladder cancer with folinic acid, fluorouracil and oxaliplatin (FOLOX). She was admitted for a replacement PICC, primarily for continuous cytotoxic intravenous medication via infusion pump in the homecare setting. Her first PICC developed a reaction thought to be related to a sutureless securement device (SSD) anchoring the PICC. The device was removed, but this resulted in displacement of the PICC and incorrect positioning in the vessel (superior vena cava). Now unsafe, the PICC was removed, awaiting replacement, which resulted in a delayed start for the chemotherapy.
A second PICC placement was attempted by a nurse-led CVC placement team, and a line attempt was made in Gail’s left arm. Skin antisepsis was undertaken using a 2% chlorhexidine gluconate and 70% isopropyl alcohol solution (ChloraPrep™). A BD ChloraPrep ™ 10 ml applicator was selected, using manufacturer’s recommendations, as per best practice guidance for CVC placement ( Loveday et al, 2014 ) and to comply with local policy for the use of ANTT. The BD ChloraPrep™ applicator allowed improved non-touch technique and helped facilitate good key-part and key-site protection, in line with ANTT ( Clare and Rowley, 2021 ).
The inserting clinician failed to successfully position the PICC in Gail’s left arm and moved to try on the right. On the second attempt, Gail noted the use of BD ChloraPrep™ and stated that she was allergic to the product, reporting a severe skin rash and local discomfort. The line placer informed the Gail that she had used BD ChloraPrep™ on the failed first attempt without issue, and she gave her consent to continue the procedure. No skin reaction was noted during or after insertion of the PICC.
BD ChloraPrep™ has a rapid-acting broad-spectrum antiseptic range and ability to keep fighting bacteria for at least 48 hours ( BD, 2021 ). These were tangible benefits during maintenance of the CVC insertion site, in the protection of key sites following dressing change and until subsequent dressing changes. There are reported observations of clinicians not allowing the skin to fully dry and applying a new dressing onto wet skin after removing old dressings and disinfecting the exit site with BD ChloraPrep™. This has been reported to cause skin irritation, which can be mistaken for an allergic reaction and lead the patient to think that they have an allergy to chlorhexidine. In our centre’s general experience, very few true allergic reactions have ever been reported by the insertion team. Improved surveillance might better differentiate between later reported reactions, possibly associated with a delayed response to exposure to BD ChloraPrep ™ at insertion, and local skin irritation caused by incorrect management at some later point during hospitalisation.
Staff training is an important consideration in the safe and correct use of BD ChloraPrep™ products and the correct use of adhesive dressings to avoid irritant contact dermatitis (ICD). It is worth noting that it can be difficult to differentiate between ICD and allergic contact dermatitis (ACD). Education and training should be multifaceted (such as with training videos and study days), allowing for different ways of learning, and monitored with audit. Local training in the benefits of using BD ChloraPrep™ correctly have been reinforced by adding simple instructions to ANTT procedure guidelines for CVC insertion and maintenance. Education on its own is often limited to a single episode of training, the benefit of using ANTT procedure guidelines is that they are embedded in a programme of audits and periodic competency reassessment. This makes sure that, as an integral part of good practice, skin antisepsis with BD ChloraPrep ™ is consistently and accurately retrained and assessed.
Gail’s case illustrates the importance of correct application of BD ChloraPrep ™ and how good documentation and surveillance are vital in monitoring skin health during the repeated use skindisinfection products. Care should be taken when recording ICD and ACD reactions, and staff should take steps to confirm true allergy versus temporary skin irritation.
Case study 3 (Beata)
Beata was a 13-year-old teenage girl being treated for acute myeloid leukaemia. Although Beata had a dual-lumen skin-tunnelled catheter in situ, a peripheral intravenous cannula (PIVC) was required for the administration of contrast media for computed tomography (CT) scanning. However, Beata had needlephobia, and so the lead vascular access nurse was contacted to insert the cannula, following ultrasound guidance and the ANTT. After Beata and her mother gave their consent to the procedure, the nurse gathered and prepared all the equipment, including a cannulation pack, single-use tourniquet, skin-antisepsis product, appropriate cannula, PIVC dressing, 0.9% sodium chloride BD PosiFlush ™ Prefilled Saline Syringe, sterile gel, sterile dressing to cover ultrasound probe and personal protective equipment.
Prior to PIVC insertion, a 4x5 cm area of skin underwent antisepsis with a 1.5 ml BD ChloraPrep ™ Frepp applicator, with back-and-forth strokes for 30 seconds, and was allowed to air-dry. The vascular access team prefer to use BD ChloraPrep ™ Frepp over single-use wipes, as the former is faster acting and provides the right volume to decontaminate the indicated area using ANTT ( Clare and Rowley, 2021 ).
Following insertion, the PIVC was flushed with a 10 ml BD PosiFlush ™ Prefilled Saline Syringe syringe, using a pushpause pulsatile technique, with positive pressure disconnection. Local policy recommends the use of pre-filled saline syringes, as they save time and minimise infection risk compared with manually drawn saline flushes ( Ceylan et al, 2021 ). The Trust also permits competent non-registered members of staff to perform PIVC insertion, which is more cost-effective than depending on registered nurses.
In Beata’s case, the team considered the use of BD ChloraPrep™ and BD PosiFlush™ Prefilled Saline Syringe to be essential for the prevention of VAD-associated infections, as well as increasing the quality of nursing care by saving time in the day-case and inpatient settings alike.
Case study 4 (Emma)
Emma, a 43-year-old woman diagnosed with acute lymphoblastic leukaemia, was scheduled for an allogenic stem-cell transplant and associated chemotherapy. To facilitate this, she attended the vascular access service at University Hospitals Plymouth NHS Trust for the insertion of a triple-lumen skin-tunnelled catheter. This was identified as the best VAD for her needs, because of its longevity, multiple points of access and decreased infection risk compared with other devices, such as PICCs.
This was Emma’s second advanced VAD insertion, having previously received an apheresis line due to poor peripheral venous access, to facilitate the prior stem-cell harvest. She was yet to receive any treatment, and, therefore, no immunodeficiency had been identified prior to the insertion procedure.
Trust policy for skin disinfection prior to the insertion or removal of PICC lines is a 2% chlorhexidine gluconate and 70% isopropyl alcohol solution, BD ChloraPrep™. There is an exception for patient history of allergy or sensitivity to BD ChloraPrep™, where 10% povidone iodine is used instead. Emma had received BD ChloraPrep™ before, with no sign allergy or sensitivity, and so the vascular access team decided to use this product again for insertion. BD Chloraprep™ was used, in preference of other skin antisepsis options, due to the applicator’s ability to effectively penetrate the layers of the epidermis, as well as the ability to eliminate direct hand-to-skin contact between the operator and patient ( Clare and Rowley, 2021 ).
Insertion of a skin-tunnelled catheter first requires disinfection of a large area, including the neck and upper chest. Following the manufacturer’s coverage recommendations, a 10.5 ml BD ChloraPrep™ applicator was selected as most suitable to cover an area of 25x30 cm ( BD, 2022 a).
The applicator was activated by pinching the wings to allow the antiseptic solution to properly load onto the sponge. To ensure proper release of the solution, the applicator was held on the skin against the anticipated site of insertion until the sponge pad became saturated. Then, a back-and-forth rubbing motion was undertaken for a minimum of 30 seconds, ensuring that the full area to be used was covered. The solution was then left to dry completely, prior to full-body draping, leaving the procedural area exposed for the procedure. Generally, drying time takes from 30 to 60 seconds, but local policy is not restrictive, as allowing the solution to fully dry is of paramount importance ( Gunka et al, 2019 ). BD Chloraprep™ is effective against a wide variety of microorganisms and has a rapid onset of action ( Florman and Nichols, 2007 ). Therefore, it was felt to be the best option for procedural and ongoing care skin asepsis in a patient anticipated to be immunocompromised during treatment.
It is the normal policy of the Trust’s vascular access service to flush VADs using BD PosiFlush™ Prefilled Saline Syringes with 0.9% sodium chloride. Likewise, BD PosiFlush™ Prefilled Saline Syringes Sterile Pathway (SP) are used to prime all VADs prior to insertion and to check for correct patency once inserted. BD PosiFlush ™ Prefilled Saline Syringe were used in preference of other options, such as vials or bags, due to the absence of requirement for a prescription in the local organisation. They are treated as a medical device and, therefore, can be used without prescription. The advantage of this is that flushes can be administered in a nurse-led clinic, where prescribers are not always available. Aside from the logistical advantages, the use of pre-filled syringes reduces the risk of microbial contamination through preparation error and administration error through correct labelling ( National Patient Safety Agency, 2007 ) In Emma’s case, three BD PosiFlush™ SP Prefilled Saline Syringes were used to check patency and/or ascertain venous location following the insertion of the skin-tunnelled catheter.
In this case, both BD ChloraPrep ™ and BD PosiFlush ™ Prefilled Saline Syringe proved simple to use and helped achieve a successful procedural outcome for the patient.
Case study 5 (Frank)
Frank was a 47-year-old man who had been diagnosed with infective endocarditis following a trans-oesophageal echo. A few days later, to facilitate his planned treatment of 6 weeks of intravenous antibiotics to be administered 4-hourly every day, he was referred to the vascular access service for insertion of longterm IV access. To facilitate this administration, the decision was made to place a PICC.
Frank’s referral included a history of illegal intravenous drug use and details of the consequent difficulty the ward-based team had in finding suitable veins to obtain vascular access. His medical history also included infected abscesses in the left groin and methicillin-resistant Staphylococcus aureus (MRSA) colonisation.
First, Frank was administered suppression therapy for MRSA decolonisation. Following this and prior to PICC insertion, the skin antisepsis procedure was undertaken using a 2% chlorhexidine gluconate and 70% isopropyl alcohol solution, BD ChloraPrep™, in adherence to Trust policy ( Loveday et al, 2014 ). Specifically, BD ChloraPrep™ applicators are selected for their single-use application. They have been demonstrated to reduce the risk of infectious complications (catheter colonisation and local infection) by 92% compared with 5% povidone iodine (PVI) 69% ethanol ( Guenezan et al, 2021 ). A 3 ml BD ChloraPrep™ applicator was considered suitable to decontaminate an area sufficient for the intended PICC insertion procedure, as recommended by the manufacturer ( BD, 2022 b). It was applied using a back-and-forth motion for a minimum of 30 seconds and left to fully dry ( Loveday et al, 2014 ). Staphylococcus aureus bacteraemia’s have a mortality rate of 20-40% and are predominantly caused by VAD insertion ( Ishikawa and Furukawa, 2021 ), and, therefore, the need to reduce this risk was of particular importance for this patient due to the history of MRSA colonisation.
In Frank’s case, the use of BD ChloraPrep™ during the insertion procedure and for each subsequent dressing change episode participated in an uneventful period of treatment. The clinical challenges posed by the patients’ presentation of MRSA colonisation meant the risk of infection was increased but, through correct antisepsis, no adverse events were noted, and the full course of treatment was successfully administered through the PICC.

IMAGES
VIDEO
COMMENTS
6 Steps to Replace Clinical Using Case Studies. 1. Watch the intro video as a group. Gather the entire class together and view the intro video. This video lays out the scenario for the given case study and helps them begin to consider the disease process. 2.
Nursing Case Studies: Diagnosis, Rationales, Fundamentals. Test your knowledge and clinical investigative skills in trying to diagnose what is going on with the patients presented in each of the Case Study Investigations. Can you come up with the right diagnosis?
A nursing case study can be described as a student-learning activity that tells a story about a patient/family (clinical scenario) and requires thinking to translate knowledge into nursing practice through the use of questions related to the story (Oermann & Gaberson, 2017; Ignatavicius, 2019). Billings and Halstead (2020) state that completing ...
The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care. Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
Using a problem-solving approach as a basis for nursing practice requires the use of critical thinking and decision-making. Some experts have referred to that thinking more recently as clinical reasoning. The 2020 NCLEX-RN® Test Plan identifies the nursing process as one of five integrated processes which is defined as "a scientific ...
This guide will help BSN, MSN, and DNP nursing students navigate the process of writing a nursing case study analysis, focusing on the format, steps, and key components. How do you analyze a case study in nursing? A nursing case study is an in-depth examination of a single individual. It is usually used to identify new areas of knowledge or to ...
This is an important issue for the quality of case study research, since description of the process of refining case study parameters, establishing clear boundaries of the case, articulating propositions based on existing literature, identifying the sources of data (people, records, policies, etc.) and the ways in which data would be captured ...
In this insightful white paper, nurse education expert Donna Ignatavicius offers practical advice on how to effectively use single-episode case studies, unfolding case studies, and debriefing to promote student learning and critical thinking. Find out how you can put her valuable tips and strategies to work in your program to help strengthen ...
case studies and reading materials, with the nursing process as a framework. Questioning Strategies A skillfully asked questioncan help students see relationships and fill gaps from the unknown to the known. DeTornyay and Thompson's (1982) classic work encouraged the use of higher order questions.
Writing a successful nursing case study can be a challenging task. However, by following the steps provided in this blog that is, first defining the problem, gathering information, developing alternatives., analyzing the alternatives, selecting the best alternative, implementing the solution and evaluating the outcome.
Formulating client goals for prioritized problems is a component of planning, which is the third step in the nursing process. Study with Quizlet and memorize flashcards containing terms like A nurse is caring for a group of clients. Which of the following actions by the nurse demonstrates the use of critical thinking skills?, A nurse is ...
Want more case studies with full-answer rationales tailored to you and your budget? Try Smart'n for free. Nursing Case Study: Mich's chest pain Background of Mich's chest pain. Mich is a 15-year-old male who was brought to the emergency department by his parents due to complaints of chest pain and shortness of breath.
The nursing process can be a confusing concept for nursing students to grasp. Below is an example of the process from start to finish in a story like fashion: Assessment John visits his general physician on Monday because he was feeling sick over the weekend. When he is called back from the waiting room, the nurse on staff takes his temperature ...
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1 However, very simply… 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units'.1 A case study has also been described as an intensive, systematic investigation of a ...
August 17, 2023. Nursing Paper Solutions. NursingStudy.org is your ultimate resource for nursing case study examples and solutions. Whether you're a nursing student, a seasoned nurse looking to enhance your skills, or a healthcare professional seeking in-depth case studies, our comprehensive collection has got you covered.
NGN Case Study Sample Questions and Answers. First, let's take a look at our case study summary below: Case Study Summary: A 68-year-old male is admitted with shortness of breath. He reports difficulty breathing with activity, lying down, or while sleeping. He states that in order to "breathe easier," he has had to sleep in a recliner for ...
The nursing process and care planning provide a common language for nurses and improve the profession through evidence-based protocols (Patiraki et al., 2017). Nursing students make more mistakes than are acceptable because they cannot clarify the nursing diagnosis while performing the nursing process (Andsoy et al., 2013). A common language ...
Part 1 The nurse and the patient: nursing - a skill-related practice patient services - the focus of nursing health - the goal of nursing the nursing process - the model for nursing patient ...
Quiz yourself with questions and answers for Case Study- Nursing Process Exam, so you can be ready for test day. ... The nurse is evaluating, which is the final step of the nursing process, to determine if the pain medication administered to the client is effective. Evaluation is the same as assessment; however, to determine the client's status ...
A nursing case study is a detailed study of an individual patient, which allows you to gain more information about the symptoms and the medical history of a patient and provide the proper diagnoses of the patient's illness based on the symptoms he or she experienced and other affecting factors. Learn more about this type of research by reading the article.
Case Studies. 02 April 2023. Case Studies. Gema Munoz-Mozas. Colin Fairhurst. Simon Clare. References. Intravenous (IV) access, both peripheral and central, is an integral part of the patient care pathways for diagnosing and treating cancer. Patients receiving systemic anticancer treatment (SACT) are at risk for developing infections, which may ...
ScholarWorks@UMass Amherst
Ask the client when the condition started. Assessment is the first step of the nursing process, where the nurse gathers subjective and objective information about the client's condition. Study with Quizlet and memorize flashcards containing terms like A nurse is caring for a group of clients. Which of the following actions by the nurse ...