

Volume 18, issue 1, December 2020
100 articles in this issue
The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression
Authors (first, second and last of 9).
- Nader Salari
- Habibolah Khazaie
- Soudabeh Eskandari
- Content type: Research
- Open Access
- Published: 17 December 2020
- Article: 100
Turnover among Australian general practitioners: a longitudinal gender analysis
Authors (first, second and last of 5).
- E. Anne Bardoel
- Grant Russell
- Margaret Kay
- Published: 09 December 2020
- Article: 99
- Research to support evidence-informed decisions on optimizing gender equity in health workforce policy and planning ,
- Research to support evidence-informed decisions on optimizing gender equity in health workforce policy and planning
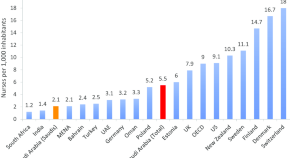
Challenges and policy opportunities in nursing in Saudi Arabia
Authors (first, second and last of 11).
- Mohammed Alluhidan
- Nabiha Tashkandi
- Mohammed G. Alghamdi
- Content type: Case study
- Published: 04 December 2020
- Article: 98
Task-shifting directly observed treatment and multidrug-resistant tuberculosis injection administration to lay health workers: stakeholder perceptions in rural Eswatini
Authors (first, second and last of 4).
- Ernest Peresu
- J. Christo Heunis
- Diana De Graeve
- Published: 03 December 2020
- Article: 97
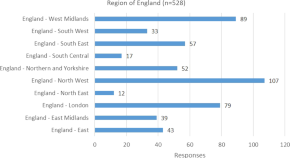
Workforce experience of the implementation of an advanced clinical practice framework in England: a mixed methods evaluation
- Jessica Lawler
- Katrina Maclaine
- Alison Leary
- Article: 96
More public health service providers are experiencing job burnout than clinical care providers in primary care facilities in China
- Liang Zhang
- Dionne Kringos
- Article: 95
Attitude of nurses and midwives towards collaborative care with physicians in Jimma University medical center, Jimma, South West Ethiopia
- Eneyew Melkamu
- Aynalem Yetwale
- Published: 02 December 2020
- Article: 94
Factors associated with increasing rural doctor supply in Asia-Pacific LMICs: a scoping review
- Likke Prawidya Putri
- Belinda Gabrielle O’Sullivan
- Rebecca Kippen
- Content type: Review
- Published: 01 December 2020
- Article: 93
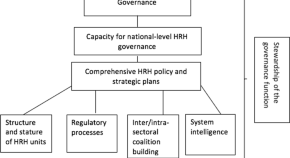
Looking back to look forward: a review of human resources for health governance in South Africa from 1994 to 2018
- Manya Van Ryneveld
- Helen Schneider
- Uta Lehmann
- Published: 26 November 2020
- Article: 92
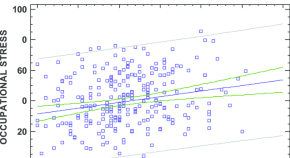
Occupational stress and burnout among physiotherapists: a cross-sectional survey in Cadiz (Spain)
Authors (first, second and last of 6).
- Ines Carmona-Barrientos
- Francisco J. Gala-León
- Jose A. Moral-Munoz
- Published: 25 November 2020
- Article: 91
The relevance of educational attainments of parents of medical students for health workforce planning: data from Guiné-Bissau
- Paulo Ferrinho
- Inês Fronteira
- Clotilde Neves
- Article: 90
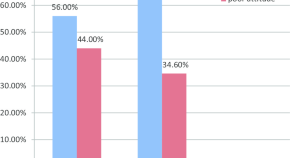
The effect of breaches of the psychological contract on the job satisfaction and wellbeing of doctors in Ireland: a quantitative study
- Aedin Collins
- Alexandra Beauregard
- Published: 12 November 2020
- Article: 89
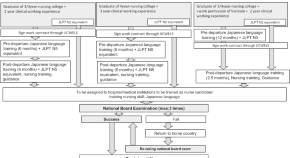
Factors associated with the recruitment of foreign nurses in Japan: a nationwide study of hospitals
- Yuko O. Hirano
- Kunio Tsubota
- Published: 10 November 2020
- Article: 88
- Research to support evidence-informed decisions on optimizing the contributions of nursing and midwifery workforces ,
- Research to support evidence-informed decisions on optimizing the contributions of nursing and midwifery workforces
Impact of Medical Doctors Global Health and Tropical Medicine on decision-making in caesarean section: a pre- and post-implementation study in a rural hospital in Malawi
Authors (first, second and last of 8).
- Wouter Bakker
- Emma Bakker
- Thomas van den Akker
- Published: 09 November 2020
- Article: 87
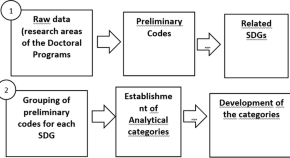
Alignment and contribution of nursing doctoral programs to achieve the sustainable development goals
Authors (first, second and last of 10).
- Isabel Amélia Costa Mendes
- Carla Aparecida Arena Ventura
- Álvaro Francisco Lopes de Sousa
- Published: 07 November 2020
- Article: 86
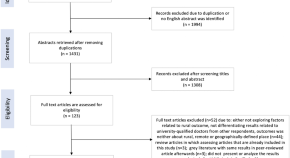
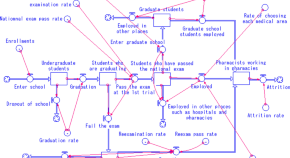
Projecting supply and demand for pharmacists in pharmacies based on the number of prescriptions and system dynamics modeling
- Yasuhiro Morii
- Seiichi Furuta
- Katsuhiko Ogasawara
- Published: 05 November 2020
- Article: 85
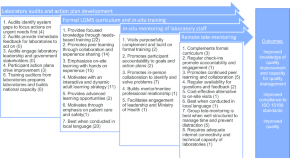
Strengthening the clinical laboratory workforce in Cambodia: a case study of a mixed-method in-service training program to improve laboratory quality management system oversight
- Siew Kim Ong
- Grant T. Donovan
- Lucy A. Perrone
- Published: 04 November 2020
- Article: 84
The COVID-19 pandemic presents an opportunity to develop more sustainable health workforces
- Ivy Lynn Bourgeault
- Claudia B. Maier
- Mohsin Sidat
- Content type: Commentary
- Published: 31 October 2020
- Article: 83
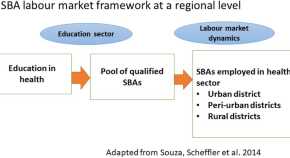
Using data to support evidence-informed decisions about skilled birth attendants in fragile contexts: a situational analysis from Democratic Republic of the Congo
- Tim Martineau
- Joanna Raven
- Published: 29 October 2020
- Article: 82
Virtual adaptation of traditional healthcare quality improvement training in response to COVID-19: a rapid narrative review
- Zuneera Khurshid
- Aoife De Brún
- Eilish McAuliffe
- Published: 28 October 2020
- Article: 81
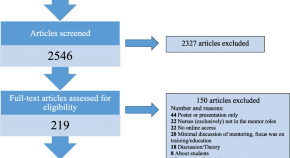
The experiences of female surgeons around the world: a scoping review
- Meredith D. Xepoleas
- Naikhoba C. O. Munabi
- Caroline A. Yao
- Article: 80
Are health care assistants part of the long-term solution to the nursing workforce deficit in Kenya?
- Louise Fitzgerald
- David Gathara
- Mike English
- Published: 20 October 2020
- Article: 79
The current status of gender equity in medicine in Korea: an online survey about perceived gender discrimination
- Hyun-Young Shin
- Hang Aie Lee
- Article: 78

Increasing access to health workers in rural and remote areas: what do stakeholders’ value and find feasible and acceptable?
- Onyema Ajuebor
- Mathieu Boniol
- Elie A. Akl
- Published: 16 October 2020
- Article: 77
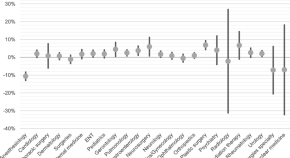
The association between the workload of general practitioners and patient experiences with care: results of a cross-sectional study in 33 countries
- Willemijn L. A. Schäfer
- Michael J. van den Berg
- Peter P. Groenewegen
- Article: 76
Maternal and newborn care during the COVID-19 pandemic in Kenya: re-contextualising the community midwifery model
- Rachel Wangari Kimani
- Sheila Shaibu
- Published: 07 October 2020
- Article: 75
Regulation, migration and expectation: internationally qualified health practitioners in Australia—a qualitative study
- Melissa Cooper
- Philippa Rasmussen
- Judy Magarey
- Article: 74
Experiences of a new cadre of midwives in Bangladesh: findings from a mixed method study
- Rashid U. Zaman
- Adiba Khaled
- Sophie Witter
- Published: 06 October 2020
- Article: 73
Health professional regulation in historical context: Canada, the USA and the UK (19th century to present)
- Tracey L. Adams
- Article: 72
- Health workforce: Accreditation of education and regulation of practice ,
- Health workforce: Accreditation of education and regulation of practice
Ensuring quality of health workforce education and practice: strengthening roles of accreditation and regulatory systems
- William Burdick
- Ibadat Dhillon
- Content type: Editorial
- Article: 71
Exploring the role of shift work in the self-reported health and wellbeing of long-term and assisted-living professional caregivers in Alberta, Canada
- Oluwagbohunmi Awosoga
- Claudia Steinke
- Sheli Murphy
- Published: 24 September 2020
- Article: 70
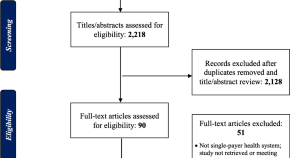
The evidence gap on gendered impacts of performance-based financing among family physicians for chronic disease care: a systematic review reanalysis in contexts of single-payer universal coverage
- Neeru Gupta
- Holly M. Ayles
- Published: 22 September 2020
- Article: 69
Work-life interface and intention to stay in the midwifery profession among pre- and post-clinical placement students in Canada
Authors (first, second and last of 7).
- Farimah HakemZadeh
- Elena Neiterman
- Article: 68
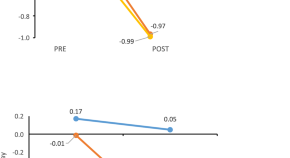
Modern work patterns of “classic” versus millennial family doctors and their effect on workforce planning for community-based primary care: a cross-sectional survey
- Lindsay Hedden
- Setareh Banihosseini
- Rita McCracken
- Published: 21 September 2020
- Article: 67

“They have been neglected for a long time”: a qualitative study on the role and recognition of rural health motivators in the Shiselweni region, Eswatini
- Caroline Walker
- Doris Burtscher
- Katherine Whitehouse
- Article: 66
Midwives’ challenges and factors that motivate them to remain in their workplace in the Democratic Republic of Congo—an interview study
- Malin Bogren
- Malin Grahn
- Published: 17 September 2020
- Article: 65
Development of competency model for family physicians against the background of ‘internet plus healthcare’ in China: a mixed methods study
- Xiaohe Wang
- Published: 11 September 2020
- Article: 64

Plan, recruit, retain: a framework for local healthcare organizations to achieve a stable remote rural workforce
Authors (first, second and last of 13).
- Birgit Abelsen
- Roger Strasser
- Published: 03 September 2020
- Article: 63

A health care professionals training needs assessment for oncology in Uganda
Authors (first, second and last of 14).
- Josaphat Byamugisha
- Ian G. Munabi
- Charles Ibingira
- Published: 01 September 2020
- Article: 62
Implementation and evaluation of a Project ECHO telementoring program for the Namibian HIV workforce
Authors (first, second and last of 37).
- Leonard Bikinesi
- Gillian O’Bryan
- Bruce Struminger
- Article: 61

Biased technical change in hospital care and the demand for physicians
- Jos L. T. Blank
- Thomas K. Niaounakis
- Vivian G. Valdmanis
- Published: 20 August 2020
- Article: 60
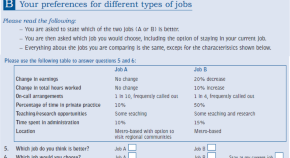
Preferences of physicians for public and private sector work
- Anthony Scott
- Jon Helgeim Holte
- Published: 10 August 2020
- Article: 59
How should community health workers in fragile contexts be supported: qualitative evidence from Sierra Leone, Liberia and Democratic Republic of Congo
- Sally Theobald
- Published: 08 August 2020
- Article: 58
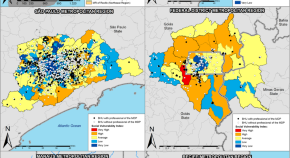
Spatial distribution of the “ Mais Médicos (More Doctors) Program” and social vulnerability: an analysis of the Brazilian metropolitan regions
- Aimê Oliveira
- Jorge Otávio Maia Barreto
- Leonor Maria Pacheco Santos
- Published: 05 August 2020
- Article: 57
Knowledge, attitude, and preparedness toward IPV care provision among nurses and midwives in Tanzania
- Joel Seme Ambikile
- Sebalda Leshabari
- Mayumi Ohnishi
- Published: 03 August 2020
- Article: 56
Involving systems thinking and implementation science in pharmacists’ emerging role to facilitate the safe and appropriate use of traditional and complementary medicines
- Joanna E. Harnett
- Shane P. Desselle
- Carolina Oi Lam Ung
- Article: 55

Measuring motivation among close-to-community health workers: developing the CTC Provider Motivational Indicator Scale across six countries
Authors (first, second and last of 12).
- Frédérique Vallières
- Miriam Taegtmeyer
- Published: 01 August 2020
- Article: 54
A cross-sectional study on preferred employment settings of final-year nursing students in Israel
- Keren Grinberg
- Rachel Nissanholtz-Gannot
- Published: 31 July 2020
- Article: 53
Mentoring the working nurse: a scoping review
- Jerilyn Hoover
- Adam D. Koon
- Krishna D. Rao
- Published: 29 July 2020
- Article: 52
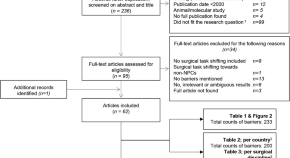
Barriers to surgery performed by non-physician clinicians in sub-Saharan Africa—a scoping review
- Phylisha van Heemskerken
- Henk Broekhuizen
- Leon Bijlmakers
- Published: 17 July 2020
- Article: 51
For authors
- Find a journal
- Publish with us
- Track your research
The abiding, hidden, and pervasive centrality of the health research workforce

- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
HR’s New Role
- Peter Cappelli
- Ranya Nehmeh

Though the human resources function was once a strong advocate for employees, in the 1980s things changed. As labor markets became slack, HR shifted its focus to relentless cost cutting. Because it was hard for employees to quit, pay and every kind of benefit got squeezed. But now the pendulum has swung the other way. The U.S. unemployment rate has been below 4% for five years (except during the Covid shutdown), and the job market is likely to remain tight. So today the priorities are keeping positions filled and preventing employees from burning out. Toward that end HR needs to focus again on taking care of workers and persuade management to change outdated policies on compensation, training and development, layoffs, vacancies, outsourcing, and restructuring.
One way to do that is to show leaders what the true costs of current practices are, creating dashboards with metrics on turnover, absenteeism, reasons for quitting, illness rates, and engagement. It’s also critical to prevent employee stress, especially by addressing fears about AI and restructuring. And when firms do restructure, they should take a less-painful, decentralized approach. To increase organizational flexibility and employees’ opportunities, HR can establish internal labor markets, and to promote a sense of belonging and win employees’ loyalty, it should ramp up DEI efforts.
In this tight labor market, cost cutting is out. Championing employee concerns is in.
Idea in Brief
The pendulum swing.
For decades, when U.S. labor markets were slack, HR focused on cost cutting, which meant squeezing employees’ pay, benefits, and training. But now that labor markets are tight, the challenge is to retain workers.
The New Priorities
HR must focus on keeping positions filled and preventing employees from burning out or becoming dissatisfied.
The HR function must educate leaders about the true costs of turnover, address employee anxiety about AI and restructuring, lobby for investments in training, rethink how contract workers and vendors are used, and strengthen diversity, equity, and inclusion efforts.
From World War II through 1980 the focus of the human resources function was advocating for workers—first as a way to keep unions out of companies and later to manage employees’ development in the era when all talent was grown from within. Then things changed. Driven by the stagflation of the 1970s, the recession of the early 1980s, and more recently the Great Recession, HR’s focus increasingly shifted to relentless cost cutting. Decades of slack labor markets made slashing HR expenses easy because it was hard for people to quit. Pay and every kind of benefit, including training and development, got squeezed. Work demands went up, and job security fell.
- Peter Cappelli is the George W. Taylor Professor of Management at the Wharton School and the director of its Center for Human Resources. He is the author of several books, including Our Least Important Asset: Why the Relentless Focus on Finance and Accounting Is Bad for Business and Employees (Oxford University Press, 2023).
- Ranya Nehmeh is an HR specialist working on topics related to people strategy, human capital, leadership development, and talent management and is the author of The Chameleon Leader: Connecting with Millennials (2019).
Partner Center
- Open access
- Published: 14 April 2003
Human resources for health policies: a critical component in health policies
- Gilles Dussault 1 &
- Carl-Ardy Dubois 2
Human Resources for Health volume 1 , Article number: 1 ( 2003 ) Cite this article
124k Accesses
185 Citations
14 Altmetric
Metrics details
In the last few years, increasing attention has been paid to the development of health policies. But side by side with the presumed benefits of policy, many analysts share the opinion that a major drawback of health policies is their failure to make room for issues of human resources. Current approaches in human resources suggest a number of weaknesses: a reactive, ad hoc attitude towards problems of human resources; dispersal of accountability within human resources management (HRM); a limited notion of personnel administration that fails to encompass all aspects of HRM; and finally the short-term perspective of HRM.
There are three broad arguments for modernizing the ways in which human resources for health are managed:
• the central role of the workforce in the health sector;
• the various challenges thrown up by health system reforms;
• the need to anticipate the effect on the health workforce (and consequently on service provision) arising from various macroscopic social trends impinging on health systems.
The absence of appropriate human resources policies is responsible, in many countries, for a chronic imbalance with multifaceted effects on the health workforce: quantitative mismatch, qualitative disparity, unequal distribution and a lack of coordination between HRM actions and health policy needs.
Four proposals have been put forward to modernize how the policy process is conducted in the development of human resources for health (HRH):
• to move beyond the traditional approach of personnel administration to a more global concept of HRM;
• to give more weight to the integrated, interdependent and systemic nature of the different components of HRM when preparing and implementing policy;
• to foster a more proactive attitude among human resources (HR) policy-makers and managers;
• to promote the full commitment of all professionals and sectors in all phases of the process.
The development of explicit human resources policies is a crucial link in health policies and is needed both to address the imbalances of the health workforce and to foster implementation of the health services reforms.
Introduction
The concern with growing inequalities in health status, problems of access and falling returns for investments in health care and the difficulty of controlling the growth of costs have prompted most countries to engage in reforms of their health sector. In low-income countries, multilateral and bilateral international organizations as well as major foundations now give a high priority to health as an essential part of the fight against poverty. Major investments are currently made by international agencies and foundations to increase vaccination rates in countries (for example, via the Global Alliance for Vaccines and Immunizations) and to combat HIV/AIDS, tuberculosis and malaria (Global Fund to Fight AIDS, Tuberculosis and Malaria; Roll Back Malaria alliance).
Concurrently, the debt relief process launched by international financial agencies is increasing the resources available for health in the poorest and most disease-ridden countries. Forty-two countries (34 in Africa alone) are eligible for debt relief under the Heavily Indebted Poor Countries initiative (HIPC), launched by the International Monetary Fund and the World Bank. A report of May 2002 estimated that the 26 countries that have reached the decision point (at which they have access to the full advantages of the initiative) would see their total debt reduced by two-thirds between the beginning of the initiative (1999) and 2005. This represents a sum of about USD 40 billion, of which 60% is expected to go to education (40%) and health (20%, not including AIDS), an average amount of USD 830 million per year to the social sector. Five more countries are expected to reach the decision point before the end of 2002 [ 1 ].
Paradoxically, the ability of poor countries to pursue actions made financially viable by access to new resources has never been so limited. This is due to major problems with regard to their health workforce, such as loss of personnel and productivity linked to the effects of AIDS, migration from the public sector to the private sector, and migration from the health sector to other sectors, as well as migration to richer or more stable countries. These problems are often caused, or at least exacerbated, by inadequate policies and practices at the levels of training, planning and deployment of staff, management of performance and definition of working conditions.
While acknowledging the fundamentally political character of human resources for health (HRH) issues, this article argues for the need for more rational health workforce policies as a sine qua non for the successful implementation of health policies. The discussion is structured into four sections. Drawing on the recent literature, Section A formulates the rationale for including explicit human resources policies in health policies, which most countries, rich and poor, have yet to do. Section B presents the specificities of the process of devising, adopting, introducing and evaluating HRH policies. Sections C and D formulate proposals on how better to develop HRH policies and discuss what is known about their conditions of success.
Why HRH policies are needed
The usefulness of health policies.
The idea of formulating health policies is relatively recent. Until the end of the 1940s, national policies tended to be a distinctive feature of planned economies. As the Marshall Plan made the drafting of national plans a condition for the financing of Europe's reconstruction [ 2 ], national policies became a normal instrument of policy.
In poor countries, the drafting of national policies also became a condition of access to aid [ 3 , 4 ]. In the health sector, it took the form of statements and plans aiming at reaching the goal of Health for All by the Year 2000 (HFA) set by the World Health Organization (WHO) in the late 1970s. Following Alma-Ata, the Member States of WHO adopted a strategy in 1981 setting objectives and priorities within the framework of HFA. Three years later, a regional strategy was adopted by 38 Member countries of the European Region of WHO. This movement was followed up nationally and in all continents, by measures taken by ministries of health aimed at devising policies in which priority-setting continues to be an essential part. Although countries have hardly come close to achieving the goal of HFA, policy-makers now agree that health policies are nonetheless crucial tools that can help in various ways (see Table 1 ):
A health policy facilitates planning. According to WHO, policies help to develop a vision of the future, to define short-, medium- and long-term references, to determine objectives, to set out priorities, to delegate roles and to define means of action and institutional arrangements [ 5 , 6 ].
A health policy can support decision-making in a context of greater public awareness of the harmful effects of incoherent policies and of greater public scrutiny of decision-makers regarding the costs and benefits of proposed options. The public expects governments to be more selective and to adopt strategies that are effective, efficient and reliably high performing [ 7 , 8 ]. An explicit framework for identifying problems, for choosing priorities and objectives, and for rational assessment of alternatives for intervention can be a tool for decision-makers to justify their choices [ 9 ]. The complexity of the health field is another argument that pleads in favour of the development of a policy framework for guiding decision-making [ 10 ]. Health problems are multifaceted and may require various sectors to work in conjunction. Actions undertaken in the health sector may have significant and long-lasting effects both on the health of individuals and on other economic and social sectors. Wrong decisions in this field may therefore have particularly disastrous effects. Thus, it is important that in the health sector, more than in any other field, the decision-making process should be anchored in solid analytical skills, based on the best available knowledge, supported by proven management techniques, and guided by a clear vision of the hoped-for future and the means needed to get there.
A health policy provides a framework for evaluating performance. By setting expectations, objectives, priorities and strategies and the resources required to achieve them, policy simultaneously sets out criteria on the basis of which actions can be evaluated while providing a frame of reference that may be used by health professionals at different levels to understand their responsibilities.
A health policy can help to rally professionals and other sectors around health problems and to legitimize actions. When it is part of a judicious planning of change, the development of health policies provides a unique opportunity for building consensus around health issues and for allowing citizens to voice their opinion, thus giving a greater degree of legitimacy to actions that will be proposed later. Critical and difficult decisions, such as new allocation of resources or rationing services, may be made more acceptable to interest groups if they are taken in the context of a political process that has brought the main players together.
Limitations of current approaches to human resources management (HRM)
It is not enough for health policies to be intrinsically good. If they remain at the planning stage and do not take economic and social realities into sufficient consideration, their influence is likely to remain minimal [ 6 ]. Their success depends heavily on how their development and implementation process is conducted. Many analysts argue that a major failing of health policies is precisely the insufficient consideration given to HRH issues [ 11 , 12 ]. In many reforms, there is discordance between the elevated attention given to issues of financing and structural transformation and the low attention given to HRH issues [ 13 ], which are often treated as just another production factor [ 14 ]. The implications of reforms for HRH are often considered only in retrospect when it emerges that proposed plans (a) cannot be implemented because of unaffordable personnel costs; (b) they are opposed by professional groups; (c) they are shown to be unrealistic in view of the baseline situation; or (d) they require modifications in the organization of work that are too difficult, in view of the current organizational capacity or of the political acceptability of the modifications [ 15 ]. The low level of interest in human resources issues is surprising if we consider the crucial role played by the health workforce in the process of achieving the objectives set by health policies [ 16 ]. But it is more easily understood when the difficulties of addressing these issues are considered, as will be illustrated later.
Even where HRH issues receive attention, the way they are addressed is usually characterized by:
A limited vision of HRM , reduced to personnel administration , i.e. operational tasks relating to recruitment, maintaining discipline and handling complaints. This lowers the status of HRH administrators and isolates them within the organization [ 17 ]. HRM of this type does not address all aspects of workforce issues.
Dispersal of accountability and lack of coordinated actions. Those responsible for HRH development in health ministries often limit their role to staff planning and allocation, and leave other, more delicate matters to political decision-makers. This practice has led to a cleavage between health policies and the HRH operations required to implement them [ 18 ]. Training programmes, for instance, may duplicate each other and not always correspond to needs. The absence of regular strategic consultations with the main actors concerned with workforce planning and development opens the door to uncoordinated, even contradictory interventions [ 19 ].
Reactive attitudes in the management of the health workforce. It has been observed, for example in Turkey [ 20 ], that governments often set very broad, annually adjusted HRH objectives outside a general policy framework and without an explicit link to health needs. Opening new schools, increasing admissions in existing schools or even temporarily easing restrictions on immigration of health personnel are often decided punctually to address problems that could easily have been anticipated [ 21 ].
Subordination of HRH decisions to economic criteria. In many instances, health workers are treated as mere production tools, such as when financial incentives are introduced to increase productivity, without taking into account other dimensions of work. As a result, these measures regularly fail to produce the expected results [ 22 ]. Governments tend to be more concerned with macroeconomic issues, such as the size of the workforce and the wage bill [ 23 ], and easily overlook other issues of importance relating to work organization, personnel motivation and individual performance.
A short-term view of HRM. This refers to the tendency to provide symptomatic responses to problems without looking at their causes or considering their long-term consequences. In Canada, nursing is in a critical situation because of difficulties in recruiting and retaining personnel. The causes of these problems are well known to be linked to conditions of practice, working conditions and the image of the profession, but little is done to address them, even when radical reactions from the nursing profession, such as long-lasting strikes, have to be faced [ 24 ]. In other cases, staff numbers have been reduced to meet fiscal constraints, which subsequently created shortages much more difficult to rectify. In Quebec, such across-the-board reductions in the mid-1990s as part of a commitment to balance the government budget led to shortages of certain professional categories, both clinical and managerial; excessive workload; disruption of performing teams; and increased psychological distress among staff and users of services [ 25 ]. This short-term management is also common among aid donors, who tend to support actions that fit their project cycle and to ignore problems that require long-term interventions, but whose impact may remain uncertain [ 19 ].
These observations give an idea of the difficulties that need to be addressed before HRH issues can be more firmly incorporated into health policy. Workforce problems are among the most complex matter on the international health reform agenda. Even in countries where national plans for the development of HRH have been made, they have been implemented only partially, and few countries evaluate policy advances in this area [ 5 ]. Hence, HRH issues remain of crucial importance and their omission from health policy agendas can only be prejudicial to health sector reforms.
Workforce issues and health policies
There are at least three arguments for giving serious attention to workforce issues in policies and even for designing specific HRH policies:
More than any other type of organization, health organizations are highly dependent on their workforce. The growth and development of any organization depend on the availability of an appropriate workforce, on its competences and level of effort in trying to perform the tasks assigned to it [ 26 , 27 ]. HR are a strategic capital in any organization (see Table 2 ), especially in service and health organizations, where the various clinical, managerial, technical and other personnel are the principal input making it possible for most health interventions to be performed. Staff diagnose problems and determine which services will be provided and when, where and how. Health interventions are knowledge-based and the providers are the "guardians" of this knowledge [ 11 ].
HR account for a high proportion of budgets assigned to the health sector [ 32 ]. The health sector is a major employer in all countries. The International Labour Organisation reckons that 35 million persons are currently employed in the health sector worldwide [ 33 ]. While health expenditure claims an increasingly important share of gross domestic product, wage costs (salaries, bonuses and other payments) account for between 65% and 80% of the recurrent health expenditure [ 34 , 35 ]. These costs are strongly linked to the ways in which HR are deployed and used [ 20 ]. In community-based health care, which relies less on equipment and advanced technology, HR have an even more prominent role and account for an even higher proportion of total costs [ 36 ]. In addition to representing direct costs, health care providers, particularly those who have the autonomy to prescribe, generate other costs. When incentives, such as payment by fee-for-service, encourage production, there is a risk of inducing demand for non-essential services. Studies of geographical variations of the use of health services show that it is often explained more by professional decisions and patterns of practice rather than by population needs [ 37 , 38 ].
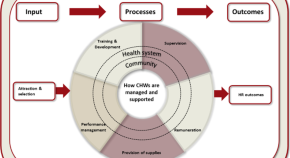
The economic and human costs of poor HRM are particularly high in the health sector. The quality of health services, their efficacy, efficiency, accessibility and viability depend primarily on the performance of those who deliver them [ 5 , 39 ] The performance of providers is, in turn, determined by the policies and practices that define number of staff, their qualifications, their deployment and their working conditions [ 40 ]. Crucial choices must therefore be made in relation to the processes that will influence the performance of the workforce, as defined in Table 3 , in terms of productivity of personnel, technical and sociocultural quality of services and organizational stability, on which the performance of health services will depend (see Fig. 1 ). Wrong choices may have harmful effects on the functioning of health services and, consequently, on the ability of these services in helping to attain health policy objectives. Also, given that they have long-term effects, these decisions are usually difficult to correct.
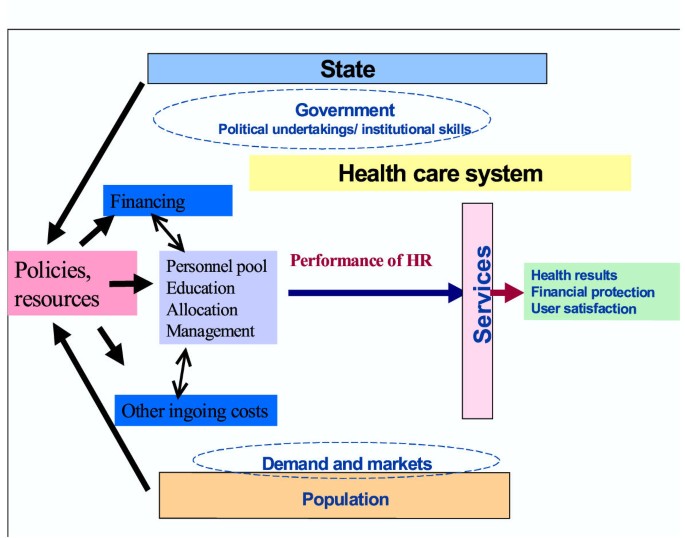
Relationship between the performance of human resources and the performance of services
The challenges of health system reforms
The challenges raised by sector reforms aiming at reducing costs, improving performance, increasing equity, decentralizing management and reviewing patterns of health care provision have a direct impact on staff, the very people on whom the success of reform depends [ 22 , 41 , 42 ]. These are illustrated here:
Reduction of costs. The response to inflation in health expenditure is often to reduce costs by stimulating efficiency. Given the proportion of the health budget absorbed by the workforce, any attempt to reduce costs or to improve efficiency calls for measures that directly affect staff. These typically include:
improved planning to avoid overstaffing . This requires more information on the staffing situation, the application of more accurate methods for determining personnel requirements, and closer coordination between supply of staff (often independently controlled by education institutions) and demand or capacity of absorption.
better distribution of personnel by categories : for example, increasing the proportion of assistants and technicians in order to improve the productivity of specialized staff in performing tasks requiring higher skills.
recognition of new categories of personnel , such as the clinical nurse, or giving official recognition to existing providers, such as midwives or traditional healers, that have been chosen in recent years.
modification of the working conditions to promote staff mobility and greater flexibility in personnel deployment or to rationalize methods of remuneration to bring them more in line with the expected performance.
The improvement of performance entails actions such as reviewing incentive systems, the development of new skills, improving work organization, and the adoption of new strategies of professional development.
The improvement of equity of access to services cannot be achieved without a more balanced redistribution of personnel between isolated and urban areas, and between rich and poor regions. It also depends on the provision of appropriate incentives for recruiting, and above all, retaining staff in the less well-served areas.
The decentralization of services , which is on the agenda of many governments, entails transfer of decision-making posts to intermediate and local levels. At the same time, it raises urgent needs for the development of HRH required to fill these new posts, particularly in management.
The proposed changes in health care models and the promotion of primary care are major challenges in terms of redefining professional roles and integrating services. They require health professionals to be more mobile, more versatile and to acquire new skills and the ability to work in multiprofessional teams. They suppose that non-medical staff will play an extended role in providing primary care services and that there will be a higher use of alternative treatment methods and a greater acceptance of non-traditional providers.
In labour-intensive sectors, the process of change entails important adjustments in the job market. Evidence suggests that these could be implemented more easily if HRH issues are dealt with at the policy development and planning stages. In Kazakhstan, the success in primary health care reform has been attributed, in large part, to the policy for mobilizing HRH, either by fostering professionalism among providers, providing adequate financial incentives or giving primary health care units more autonomy. In Chile, however, the reform of the health sector begun in the 1990s has run up against the lack of engagement of health professionals, who had a different perception of reform from that of the government [ 39 ]. The successful experience of Costa Rica is another case that illustrates the benefits of making HRH policy part of a health policy [ 16 ].
The need to anticipate the potential effects of macroscopic social trends affecting health systems on the health workforce (and consequently on the provision of services)
Health care systems are affected by a number of major trends that can have important effects on the organization of work and may consequently require adjustments if the objectives of equity, efficiency and quality are to be attained.
Technological transition. Technological innovations have already brought radical changes in how most diseases are treated. Health professionals must adjust their roles and skills accordingly. New information technologies and telecommunications have a high potential for improving productivity, by allowing health professionals to exchange clinical data over a distance in real time or to have immediate access to new knowledge. They allow greater flexibility in the organization of work, improve communication between professionals and create jobs in new sectors. At the same time, they eliminate jobs, impose new skill requirements and require new investment in terms of training.
Telemedicine, the term given to the various applications of information technology and telecommunications for health service delivery and health information over long and short distances, has the potential importance of reducing costs and injuries linked to patient transfer, of improving the provision of services in isolated regions, of giving access to distance training and of fostering development of domiciliary care [ 43 , 44 ]. On the other hand, it may require modifications in conventional modes of work organization and remuneration or new working methods (teamwork and networking, sharing of information, use of computers).
Sociodemographic transition. Demographic changes have a substantial effect both on the demand for services and on the workforce providing them. The ageing of the population in industrialized countries, likely to increase the use of health services [ 45 ], will also be accompanied by a fall in the working population. For example, 42% of public sector employees in Finland are due to retire in the next 10 years [ 46 ]. Tools for management of human resources should be adapted to this ageing workforce. Training programmes and compensation programmes ought to be adjusted to meet the specific needs of both young staff and older staff. Another aspect linked to this transition is the growing proportion of women in the job market and their desire to combine their career and their familial roles. Female doctors work fewer hours per week, retire earlier and take time off more frequently than their male colleagues, factors that affect the planning of the medical workforce [ 47 – 49 ]. The impact of the HIV epidemic is worst in the most productive age group, including the health workforce. In the low-income countries, especially African countries, which are paying the heaviest toll, the epidemic has consequences on the health workforce in the form of reduced numbers, absenteeism, reduced productivity and psychological distress [ 50 ].
Globalization of markets. At least two factors linked to globalization of markets have direct effects on the health workforce:
structural adjustment measures undertaken by states have included radical reviews of their public sectors and often led to cuts in health and social programmes, reduced numbers of staff and, in most cases, to a deterioration of working conditions [ 33 ].
the use of market mechanisms to manage health care systems has led to a redefinition of the role of the state, expected to concentrate more on its role as regulator and to give more scope to the private sector in the provision of services. The case of Nicaragua may be cited in this regard [ 51 ]. The traditional relationship between the employer-state and health personnel has been modified. Centralized negotiations between national unions and governments are supplanted by management of employment relations at the local level; the case of Great Britain illustrates this point [ 52 ]. The career structure is no longer so clearly defined, and as a consequence workers are less inclined to show loyalty to an organization that may make them redundant when it restructures.
Changes in the behaviour of consumers and in their relationships with health professionals. In rich countries, consumer demands are more diversified, more sophisticated and better informed, and consumers easily question the capacity of their governments to meet these demands [ 45 ]. As taxpayers, they are concerned about the rising costs of the health services, but as users, they want access to services of the highest quality. They expect administrators and health professionals to do better with the same resources. The same trend is seen in low-income countries when consumers become better informed about which services are available to others or should be available to them.
Mobility of the workforce and the brain drain. In industrialized countries, conditions of mobility of the workforce, in particular the highly qualified workforce, are now negotiated within the framework of regional agreements, aiming at greater standardization of qualifications between countries [ 53 ]. In developing countries, however, this mobility has often taken the form of a more brutal exodus of skills, depriving countries of rare resources crucial for the development of their health systems [ 53 ]. As the job market is rapidly changing and competition is increasing, public health care systems must also cope with difficulties of retaining personnel who are attracted by better offers from the private sector or who decide to pursue other more lucrative professional activities [ 50 ].
As a result of these major trends, vertical, pyramidal and rigid forms of work organization are replaced by more flexible structures and methods of deployment. The limited horizon of the local or regional job market expands to cater to new global economic orders. The traditional focus on products and services is supplanted by a client-centred approach that emphasizes needs and preferences. The traditional division of work that put a premium on specialization is yielding to a greater integration of health services provision and to teamwork. Production based on information and knowledge is replacing a machine-based mode of production. Stable and protected working relations, with the underlying assumption of a lifetime career, are giving way to flexibility of work and employment [ 54 , 55 ].
The arguments outlined here indicate the crucial role of HRM in improving the performance of health systems and implementing reforms and suggest that HR allocation cannot be left to the unregulated market. Strategic planning is essential to control the effects of the complex factors that affect HR. Technocratic planning as practised in the past is highly ineffective, as illustrated by the chronic imbalances (see Table 4 ) experienced by most countries [ 56 , 57 ], i.e. mismatch of numbers, qualitative disparity, unequal distribution and a lack of coherence between HRM practices and the overriding concerns of health policy (see Table 5 ). These imbalances prove to be major limiting factors to achieving the objectives of health sector reforms or to implementing health policy.
Which human resources policies?
What is a policy.
The notion of policy is not always conceived or understood in a uniform manner. Policy is sometimes perceived as a product (principles, declaration, law) that serves as a frame of reference for action; sometimes as a process that ought to lead to the attainment of certain goals [ 58 ]. The policy process itself, however, gives rise to numerous interpretations. Two major approaches can be distinguished [ 59 ].
The traditional approach understands public policy as a cyclic process, the different stages of which can be separately analysed (see Fig. 2 ). In order to resolve a problem, a policy is devised, a number of objectives are set and strategies are defined to achieve them. The operational implementation of the policy is expected to lead to resolution of the problem [ 60 – 64 ].
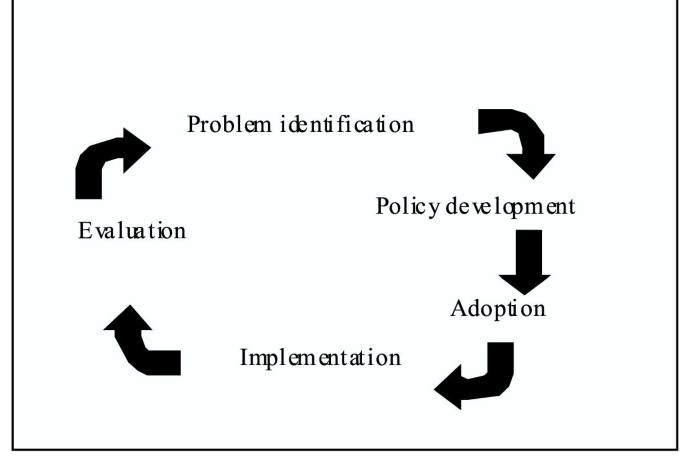
Policy cycle
Here, the policy process is assumed to be rational, to follow a logical succession of stages and to be based on an objective evaluation of different alternatives and on scientific knowledge [ 65 ]. Critics [ 61 , 66 – 68 ] have shown that to understand policy-making, account had to be taken of the uncertainty inherent in all decision-making, the limited rationality of the agents, the power relations in social systems and the ideological biases influencing the decision-makers (see Table 6 ).
The alternative approach to technical rationality, from which only a very partial explanation of policy can be derived [ 27 ], puts the emphasis on the interpersonal and contextual relations of the policy process. Policy is conceived not as a sequential process but as an integrated process in which values and differences are made explicit, consensus agreements sought, compromises made, alliances formed and action justified [ 69 – 72 ]. This is a political exercise that goes beyond technical activities and calls for a process of exchange and negotiation between various interest groups. For Kingdon [ 73 ], political changes rarely stem from a linear process, but tend to result from repeated interactions between three flows of ideas relating to defining problems, proposing solutions and obtaining policy consensus. Change happens when these flows converge, creating a window of opportunity that can be seized by policy-makers [ 73 ].
Characteristics of HR activities in the health sector
In HRM the two planning approaches are not mutually exclusive, and can even be complementary. The rational approach encourages a recognition of the role of information, of modern analytical techniques and of decision-making tools for developing coherent policies These are necessary but not sufficient conditions. The second approach brings an appraisal of the political, economic, cultural and social context in which the development and implementation of policies take place. But there are also some specifics to the health context that need to be taken into account in the process of developing and implementing HRH policies:
The intersectoral nature of issues linked to HRH and the variety of participants and sectors involved. The causes of HR problems in the health sector are various and complex. Solutions depend on many inputs (financial resources, education programmes, working conditions), which are in many instances outside the control of the health sector decision-makers or HRM administrators [ 74 , 75 ]. In most industrialized countries, such as Canada or the countries of Western Europe, central unions negotiate working conditions directly with the government and sign collective agreements that leave administrators of health organizations little room for independent decisions [ 17 , 25 ]. Responsibility for the production of personnel, for the definition of curricula and for certification criteria is usually in the hands of independent training institutions. Practice standards are generally defined by professional bodies. In other words, strategies for intervening on the health workforce cannot be decided autonomously by a single organization or single unit at the ministry of health. They have to incorporate the viewpoints of a wide variety of institutions, participants and interest groups who have a stake in the decision-making and in implementing actions.
The time-lag between decision-making and outcome. Contextual changes influencing the demand for health services and tendencies within the workforce cannot be dealt with in a short time. For a number of decisions relating to the health workforce, short-term or medium-term projections are not sufficient. Hall [ 76 ] shows that a 10% rise in the number of students registering with medical schools will produce only a 2% increase in the supply of doctors after 10 years. A substantial lapse of time is therefore required to bring about major quantitative and qualitative changes in the health workforce or to rectify the adverse effects of poor decisions [ 77 ]. Accordingly, HRH policies in reforms and attempts to expand health services should allow for the intervals needed to train and develop the workforce. They must equally anticipate the long-term impact some major trends such as ageing of the population are likely to have on the demand for services and on the workforce demand.
Strong professional dominance. Health care systems are widely influenced by the role of professionals whose training emphasizes the value of autonomy and professional self-regulation [ 78 ]. Generally speaking, professional structures are well established, supported by laws, guidelines, culture and history [ 79 ]. Various professional categories assume distinct roles and have their own training structures and regulatory mechanisms. These groups also tend to have a distinctive culture and a very pronounced identity that may complicate implementation of changes. Strong in the conviction of their cultural and symbolic power and in their ability to rally public opinion behind them, they may hinder the implementation of new policies if there is no clear understanding of the proposed changes, or if these changes are perceived as affecting them negatively [ 23 , 80 ]. All these factors indicate that the process of development and implementation of workforce policies in the health sector must be an ongoing process of adjustment, not only to the needs of the population but also to the changing expectations of the personnel, and that it should be conducted with their full participation [ 81 , 82 ].
The interdependence of the different professional categories. Most health occupations are highly interdependent when carrying out their tasks. Problems in one professional category may spill over into another. For example, a shortage of nurses resulting from inadequate planning may have adverse effects on the work of doctors.
The role of the state as the principal employer. The state remains the principal employer in the health sector, despite a tendency to give increasingly greater scope to the private sector in the provision of services [ 33 ]. HRH are expensive to produce and in terms of recurrent expenditure. Any inadequate workforce policy that encourages overproduction of personnel, excess consumption of resources or poor utilization of available personnel has a direct effect on public finances and further reduces scarce resources that could have been assigned to other sectors of the economy.
The high proportion of women employed in health services. The health sector is also recognized as being a major employer of women [ 83 ], who are increasingly active in the job market while fulfilling family responsibilities. As seen in Zimbabwe, women working in the health sector often receive lower salaries and have fewer opportunities than their male colleagues to rise to the higher echelons of the hierarchy [ 84 ]. Concentrated in specific professional categories such as nursing, they often pay the highest toll when budgets are cut [ 33 ].
The ambiguity of the relationship between health needs, service requirements and resource needs (human or material) in the supply of these services. Understanding of health needs is imperfect. Understanding of the services required to respond to needs is also imperfect. The relative contribution of health services is not well understood. The development of HRH policy has to deal with uncertainty and with many other factors – political, economic, social and cultural – that influence these relationships [ 85 ].
Deficiencies of the market. In other sectors of the economy, the job market responds to the law of supply and demand, and adjustment processes may be both more easy and less costly [ 82 ]. But in health, where there are imperfections as in any market, the state may be required to intervene in order to see through the necessary adjustments within the framework of the political process. The challenge here is to overcome the rigidity associated with certain institutional mechanisms (unions, professional regulations, etc.) that may restrain the implementation of the adjustments required or render them more costly.
The content of HRH policies
Martinez and Martineau [ 41 ] suggest four categories of issues that HRH policies should address:
Planning for the supply of personnel. This aims to ensure adequate numbers of personnel in the different employment categories and that personnel are available and distributed equitably and coherently between geographical regions, establishments and levels of care. The challenge is to deploy personnel of adequate quality in sufficient numbers at the right time and place; this includes equitable gender distribution within the limits of what the country can afford.
Education and training. This involves providing the different categories of personnel with the skills required by the objectives set by health policies. Policy actions may include: adaptation of the training curricula to health policy objectives and to service requirements; development of new teaching and learning methods; monitoring of skills and training requirements; development of training infrastructures; training of trainers; and the regulation of training institutions and programmes.
Management of performance. This relates to the optimization of the service production process and to making sure that staff are encouraged to provide effective, efficient, high-quality services that meet the needs and expectations of citizens. Guidelines regarding the organization and division of work, practice standards, payment methods, circulation of information, management practices and tools, evaluation and accountability mechanisms and, more generally, the strategies for maintaining and upgrading the quality of services provided are included here.
Working conditions. Expected policy guidelines address methods of recruiting and retaining staff, career management, mechanisms of mobility, methods and levels of remuneration incentives, management of labour relations, and systems of evaluation.
As critical choices are made in relation to objectives and defining priorities and strategies, the question arises: Which criteria can help? Two sets of considerations can help answer that question.
First, HRH-related objectives – which need to be coherent with health objectives and health needs – should be subordinated to health services [ 86 ] (see Fig. 3 ).
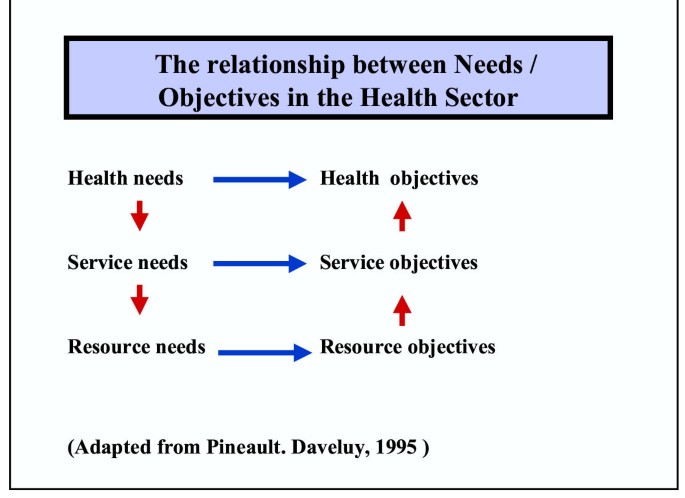
The relationship between needs and objectives in the health sector
Second, policy choices are not neutral, but are always derived from sets of values that condition their social acceptability, legitimacy and consequently the probability of success of their implementation. Accordingly, the following would help the choice of objectives, priorities and strategies:
an explicit statement of the values that will inspire policy and to which decision-makers will be bound: equity in access? the importance of the personnel as associates in the development and implementation of the policies? equality between men and women? a good balance between family and professional life?
a clear identification of service objectives to which HRH policies are expected to contribute: more balanced distribution of services, level of quality sought, continuity of services, efficiency.
quantifiable objectives, covering a specific period and covering all aspects of HR issues. The policy should be able to justify how these objectives are linked to service objectives.
strategies considered and the required means for attaining these objectives.
monitoring and evaluation.
Prescriptions for modernizing the policy process in health workforce development
The literature presents at least four "prescriptions" to adapt the policy process relating to the health workforce:
(1) : HRH policies must be comprehensive, i.e. go beyond personnel administration and incorporate all aspects of HRM. [ 11 , 18 , 41 , 87 ] HRM should be recognized as a set of trans-sectoral activities, all necessary , acting globally on the HR system so that the workforce is used in ways that effectively contribute to meeting the health needs of the population. HRM will continue to include traditional functions such as recruitment of personnel, but also others, such as negotiations with professional groups and unions, as reforms usually envisage changes in working conditions, allocation of responsibilities or training programmes. Closer relations need to be maintained with various ministries, such as that of education for training issues, or finance for matters relating to remuneration and to incentive schemes. The policy challenges, therefore, are to involve HR managers in all decisions relating to the workforce and to develop coordinated (across both jurisdictions and stakeholders) "policy packages" [ 88 , 89 ].
(2) : The development and implementation of HRH policies should reflect the integrated, interdependent and systemic nature of the different components of HRM. Acknowledging the systemic nature of HRM calls for a recognition of (1) the contribution of each of its functions and their mutual dependencies; and (2) the links between HR policy, health policy and the environment in which they are to be implemented.
The HRH subsystem brings together a number of interdependent functions working in synergy that determine the performance of any health care system: staffing, management of performance, training and definition of working conditions [ 41 , 81 , 90 ]. The challenge here is to ensure that these basic functions are dealt with in a coherent manner. Any action affecting one of them may have effects on other functions. Operations intended to balance the distribution of personnel may, for instance, have consequences on staff motivation and performance. The development of in-service training may have effects on the provision of services. Letting staff surplus build up may make it difficult to provide professional development opportunities. Reducing staff to meet cost restrictions may affect the quality of services. The internal coherence of the HR subsystem depends on balancing its different functions. Youlong et al. [ 91 ], referring to China, showed how a system of professional regulation, when not based on a systemic approach, may have an unequal impact on rich and poor regions and work against an equitable distribution of care.
The HR subsystem also has exchange and interdependency relations with other parts of the health care system. The quality of a service depends on its personnel, but also on the settings in which it develops and on the resources available to provide services. In other words, the issue of HRH cannot be dealt with or managed in isolation. HRH policy development and implementation must allow for the fact that personnel is only one input among others that contribute to a balanced health system. Steps must be taken to ensure that HR meet the objectives of health policies while concurrently ensuring that the broad thrust of health policy allows the conditions to be created for full development of the workforce.
(3) : Given the critical and strategic role of HR in health organizations, the implementation of HRH policies requires that decision-making and management be more proactive [ 23 ]. A more strategic conception of and approach to HRM require a higher degree of sensitivity to the many signals of change emanating from both inside and outside health care organizations themselves: changes in laws and other regulations; economic trends (labour market, growth rate, economic priorities of the government); organizational changes; technological progress; and sociocultural and demographic changes.
HRH managers should be capable of recognizing and interpreting these different signals, and of acting judiciously in response to them by making appropriate adjustments to the workforce [ 92 ]. Permanent monitoring of macroscopic changes and of organizational changes and their consequences for HRH is needed to identify new environmental challenges and emerging problems [ 29 ]. The recruitment and retention of high-level HRH managers, with enough autonomy to implement policies flexibly, is a correlate of this prescription and is the real test of the commitment of political leaders to a more rational and need-centred HRM.
(4) : The mobilization of all stakeholders is a key element in the development, implementation and evaluation of HRH policies. Many players influence or have the potential to influence changes in the workforce, given that they control or influence one or several of the key functions cited above [ 40 ]. Minimally, these include:
those who define and negotiate working conditions: ministries of health, finance, civil service, planning, unions, hospital boards.
those who define standards of professional practice: professional councils, governmental regulatory agencies.
those who produce health workers: training establishments, ministry of education.
those who produce services: health establishments and their staff, both private and public; professionals.
those who consume services: users, user associations.
those who finance services: governments, citizens, private insurers, donors.
Recognizing the roles of these players makes planning health workforce actions part of a political process in which the different key players express their opinions and exert their influence. Involvement of these different players in policy development, even though it will demand more energy and time, may in fact facilitate the subsequent adoption and implementation of policy and ensure that its effects are sustained.
These different prescriptions highlight a number of challenges and needed actions:
When developing policy: ensure that objectives and priorities affecting the different aspects of HRM are made explicit; ensure that objectives and priorities are consistent with the requirements of services, health needs and available resources; involve all sectors concerned in the definition of objectives and priorities.
When implementing policy: ensure that the mechanisms required for coordination of the different actions are properly in place; ensure continuing monitoring of signals from inside and outside the system; mobilize resources required for the different actions; foster synergy between the different HRM functions.
When evaluating policy: ensure wide participation in evaluation; collect relevant information on the different components of HRM; use results of evaluation for creating an evidence base and for upgrading actions.
Conditions for success of human resources policies
The success of policy remains conditional on a number of factors, of which four appear to be especially crucial in the context of HRH:
Institutional/technical capacities
The development, implementation and evaluation of HRH policies is part of a complex process relying on multiple analytical tasks: analysis of needs, planning, evaluation of programmes, economic evaluation, policy analysis, demographics and statistics, teaching methods, etc. Capacities required for their performance are essential resources. Saltman and Figueras [ 93 ] point out that countries that have had the most success in reforming their health systems are precisely those that have been able to mobilize technical capacities to design coherent and viable policies. Decision-makers who understand the specific features of the health workforce, its critical role and HRM and its importance for supporting reforms are essential. But for planning and implementing appropriate actions in relation to the many components of HRM, specialized technical capacities are needed.
Policy implementation depends also on the strength and stability of institutions. Thain [ 94 ] stresses the importance of constitutional, political, informational and technological resources that help to construct an environment that promotes sound policy formulation and implementation.
National capacities for developing and implementing HRH policies are inadequate [ 74 ] because skills are rare and institutions are weak, or the information base is deficient and good information is not available. Regularly updated statistical data are essential to the formulation of appropriate and coherent policies. This includes data on health needs, on existing services, and on personnel and their distribution (in terms of geography, sex and professional categories), their training and their working conditions.
To reinforce national capacities, Martineau and Buchan [ 95 ] suggest actions on two fronts: (1) strategic , by providing national leaders with the means to develop a clear vision of health needs, environmental constraints and options for the development of the workforce. HRH policies externally imposed, by donors or otherwise, inhibit the development of this kind of national leadership and hinder the adaptation of policies and programmes to the national context [ 96 ]; (2) operational , by developing the specific skills required by each component of HRM.
Stepping up technical capacities requires time for training and building experience. This also applies to the consolidation of institutions. These actions change the power relationship between actors, challenge old practices, and call for new regulatory mechanisms, all of which generate resistance and require long periods of adaptation.
Political feasibility
Commitment is crucial for both the development and the implementation of policies. In a climate of instability in which decision-makers are frequently replaced and priorities redefined, it may be difficult to devise policies consistent with a long-term approach. Stability of the state apparatus is a prerequisite for the credibility of the political process. Commitment is expressed when government explicitly includes the development of the workforce in its priorities and treats it as an essential public health function. It presupposes that government accepts the political risks of promoting changes likely to provoke the opposition of powerful interest groups. Benveniste [ 97 ] points out that change becomes possible only when a sufficient critical mass of stakeholders is convinced of its necessity and supports it. Mobilizing the ministries of health, education, finance and so on, and local governments, professional bodies and private organizations is not only a good strategy, but probably a necessary one [ 98 ]. Some interest groups such as doctors are particularly powerful, dominant and capable of mobilizing public opinion. Ignoring them is a recipe for failure. HR actions have more chance of being coherent if they are concerted, and of being implemented if they truly reflect the outcome of the political process, i.e. needs expressed, proposals made and compromises reached. The challenge is to identify all the key players and make their resources, interests and expectations explicit. Negotiating with them may pre-empt the development of an active and organized opposition to the proposed changes.
Social acceptability
New policies may hurt the expectations, preferences, beliefs or values of some stakeholders [ 99 ], such as when male personnel are used to deliver maternal and child care. Increasing the acceptability of reforms is possible, either by adapting the policies to the social and cultural environment, or by trying to change the latter through education or social marketing strategies, or, of course, by combining the two.
Affordability
The correction of imbalances in personnel may require substantial short-term financial commitments. Understaffing may require the opening of new training institutions or an increase of the intake of existing schools. Overstaffing may be addressed by offering financially attractive early retirement programmes. Geographical redeployment of personnel requires systems of incentives to attract workers to distant areas. Programmes for improving quality and performance require investment in infrastructure or equipment, or changes in working conditions (bonuses, salary increases, etc.). It is important, therefore, that HRH policy be based on an accurate assessment of its financial implications and of the capacity of the country to mobilize the necessary resources.
Conclusions
Attaining health objectives in a population depends to a large extent on the provision of effective, efficient, accessible, viable and high-quality services by personnel, present in sufficient numbers and appropriately allocated across different occupations and geographical regions. The lack of explicit policies for HRH development has produced, in most countries, imbalances that threaten the capacity of health care systems to attain their objectives. The workforce in the health sector has specific features that cannot be ignored. Health organizations are faced with external pressures that cannot be effectively met without appropriate adjustments to the workforce. The development of the workforce thus appears to be a crucial part of the health policy development process. Putting workforce problems on the political agenda and developing explicit HRH policies is a way to clarify objectives and priorities in this area, to rally all sectors concerned around these objectives, and to promote a more comprehensive and systematic approach to HRM. In the long term, this opens the prospect of developing health care systems more responsive to the expectations and needs of populations.
The World Bank: Financial impact of the HIPC Initiative: first 26 country cases. Washington, DC. 2002
Google Scholar
Decosas J: Planning for primary health care: the case of the Sierra Leone national action plan. Int J Health Plann Manage. 1990, 20 (1): 167-177.
CAS Google Scholar
Cassels A, K Janovsky K: Better health in developing countries: Are sector-wide approaches the way of the future?. Lancet North Am Ed. 1998, 35 (9142): 1777-1779.
Article Google Scholar
Walt G, Pavignani E, Gilson L, Buse K: Health sector development: from aid coordination to resource management. Health Policy Plan. 1999, 14: 207-218.
Article CAS PubMed Google Scholar
World Health Organization: World Health Report 2000. Health systems: improving performance. Geneva. 2000, [ http://www.who.int/m/topics/world_health_report/en/index.html ]
Cassels A: A guide to sector-wide approaches for health development. Genève, Organisation Mondiale de la Santé/DANIDA/DFID/Commission Européenne. 1997
Beaglehole R, Davis P: Setting national health goals and targets in the context of a fiscal crisis: the politics of social choice in New Zealand. Int J Health Serv. 1992, 22 (3): 417-428.
Peters BG: La capacité des pouvoirs publics d'élaborer des politiques. Centre canadien de gestion, Rapport de recherche No 18. 1996
Castley RJ: Policy-focused approach to manpower planning. Int J Manpower. 1996, 17 (3): 15-24.
Dussault G: Cadre pour l'analyse de la main-d'œuvre sanitaire. Ruptures Revue Transdisciplinaire Santé. 2001, 7 (2): 64-78.
Pan American Health Organization (PAHO): Development and strengthening of human resources management in the health sector. Washington DC, 128th Session of the Executive Committee. 2001
Buchan J: Health sector reform and human resources: lessons from the United Kingdom. Health Policy Plan. 2000, 15: 319-325.
Healy J, McKee M: Health sector reform in Central and Eastern Europe: the professional dimension. Health Policy Plan. 1997, 12 (4): 286-295.
Filmer D, Hammer JS, Pritchett LH: Weak links in the chain: a diagnosis of health policy in poor countries. World Bank Res Obs (Int). 2000, 15 (2): 199-224.
SARA: A public health workforce crisis in sub-Saharan Africa. An issues paper. Support for analysis and research in Africa (SARA). 2001
Pan American Health Organization (PAHO): Human Resources: a critical factor in health sector reform. Report of a meeting in San José. Costa Rica, 3–5 December 1997. Washington DC. 1998
Bach S: Changing public service employment relations. In: Public Service Employment Relations in Europe, Transformation, Modernization and Inertia. Edited by: Bach S, Bordogna L, Della RG, Winchester D. 1999, London: Routledge
Buchan J, Seccombe I: The changing role of the NHS personnel function. In: Evaluating the NHS Reforms. Edited by: Legrand J, Robinson R. 1994, London: Kings Fund
Biscoe G: Human resources: the political and policy context. Human Resource Devel J. 2000, 4: 3-[ http://www.moph.go.th/ops/hrdj/ ]
Ozcan S, Taranto Y, Hornby P: Shaping the health future in Turkey – a new role for human resource planning. Int J Health Plann Manage. 1995, 10 (4): 305-319.
Adams OB, Hirschfeld M: Human resources for health – challenges for the 21st century. World Health Stat Q. 1998, 51 (1): 28-32.
CAS PubMed Google Scholar
Brito P, Galin P, Novick M: Labor relations, employment conditions and participation in health sector. Annecy, World Health Organization Workshop on Global Workforce Strategy. 2000, [ http://www.who.int/health-services-delivery/human/workforce/Documents.htm ]
Bach S: HR and new approaches to public sector management: improving HRM capacity. Annecy, World Health Organization Workshop on Global Workforce Strategy. 2000, [ http://www.who.int/health-services-delivery/human/workforce/Documents.htm ]
Dussault G: The nursing labour market in Canada: review of the literature. Cahiers du groupe de recherche interdisciplinaire en santé (research paper r01–03). University of Montréal. 2001
CESSSS (Commission d'Etude sur les services de santé et les services sociaux): Rapport et recommandations – Commission d'Etude sur les services de santé et les services sociaux – Les Solutions émergentes. Gouvernement du Québec. 2000, [ http://www.cessss.gouv.qc.ca/pdf/fr/00-109.pdf ]
Evans RG: Strained mercy: the economics of Canadian health care. Toronto: Butterworth & Co. 1984
Murray VV, Dimick DE: Contextual influences on personnel policies and programs: an explanatory model. Acad Manage Rev. 1978, 750-761.
Pfeffer J: The human equation: building profits by putting people first. Boston: Harvard University Press. 1998
Zairi M: Managing human resources in healthcare: learning from world class practices – part I. Health Manpow Manage. 1998, 24 (2): 88-99.
Koch MJ, McGraith RJ: Improving labor productivity: human resource management policies do matter. Strategic Manage J. 1996, 17: 335-354.
Eaton S: Beyond unloving care: linking human resource management and patient care quality in nursing homes. Int J Hum Resour Manage. 2000, 11 (3): 591-616.
Narine L: Impact of health system factors on changes in human resource and expenditures levels in OECD countries. J Health Hum Serv Adm. 2000, 22 (3): 292-307.
International Labour Organisation: Terms of employment and working conditions in health sector reforms. Report for discussion at the Joint meeting on terms of employment and working conditions in health sector reforms. Geneva. 1998
Saltman RB, von Otter C: Implementing planned markets in health care: balancing social and economic responsibility. Ballmoor: Open University Press. 1995
Kolehamainen-Aiken RL: Decentralization and human resources: implications and impact. Human Resource Devel J. 1997, 2 (1): 1-14.
Pong RW, Saunders D, Church J, Wanke M, Cappon P: Health human resources in community-based health care: a review of the literature. Health Canada, Health Promotion and Programs Branch. 1995
Wennberg JE, Freeman JL, Shelton RM, Bubolz TA: Hospital use and mortality among Medicare beneficiaries in Boston and New Haven. N Engl J Med. 1989, 321: 1168-1173.
McPherson K, Wennberg JE, Hovind OB, Clifford P: Small-area variation in the use of common surgical procedures: an international comparison of New England, England and Norway. New Engl J Med. 1982, 307: 1310-1314.
Bennett S, Franco LM: Health worker motivation and health sector reform. PHR Primer for policy makers. Washington: PHR Project. 2000, [ http://www.phrplus.org/Pubs/pps3.pdf ]
Martineau T, Martinez J: Human resources in the health sector: guidelines for appraisal and strategic development. Brussels: EuropeanCommission, Directorate General for Development, "Health and Development Series". 1997
Martinez J, Martineau T: Rethinking human resources: an agenda for the millennium. Health Policy Plan. 1998, 13: 345-358.
Thompson D, Snape E, Stokes C: Health services reform and human resource management in Hong Kong public hospitals. Int J Health Plann Manage. 1999, 14: 19-39.
Industrie Canada: L'industrie de la télésanté. La série descadres de compétitivité sectorielle. Principales caractéristiques de l'industrie. Ottawa, Ontario. 2001, [ http://strategis.ic.gc.ca/SSGF/hs01321f.html ]
ORTECH: L'imagerie médicale: document de travail Report No. 98-X11-C06-1534-1. For Industry Canada: Ottawa: Ontario. 1999, [ http://strategis.ic.gc.ca/SSGF/hm01489f.html ]
Svehla TA, Crosier GC: Managing the mosaic. Addressing workforce diversity and managing institutional change in healthcare. Chicago: American Hospital Pub. 1994
Organisation pour la Coopération et le Développement Economique (OCDE): Récents développements et défis a venir de la gestion des ressources humaines dans les pays membres de l'OCDE. Réunion du Groupe de travail sur la gestion des ressources humaines. Paris: OCDE. 2000, [ http://www.olis.oecd.org/olis/2001doc.nsf/LinkTo/PUMA-HRM(2001)5-FINAL ]
Woodward CA, Williams AP, Ferrier B, Cojhen M: Time spent on professional activities and unwaged domestic work: is it different for male and female primary care physicians who have children at home?. Can Fam Physician. 1996, 42: 1935-1938.
Kletke PR, Marder WD, Silberger AB: The growing proportion of female physicians: implications for US physician supply. American Journal of Public Health. 1990, 80 (3): 300-304.
Article CAS PubMed PubMed Central Google Scholar
Warde CA, Gelberg L: Physician role conflict and resulting career changes: gender and generational differences. J Gen Intern Med. 1996, 12 (7): 407-411.
Tawfik L, Kinoti SN: The impact of HIV/AIDS on the health sector in sub-Saharan Africa: the issue of human resources. The SARA Project. 2001
Nigenda G, Machado MH: From state to market: the Nicaraguan labour market for health personnel. Health Policy Plan. 2000, 15: 312-318.
Chanda R: Trade in health services. Geneva:World Health Organization, Commission on Macroeconomics and Health. 2001
Chiavenato I: Advances and challenges in human resource management in the new millennium. Public Pers Manage. 2001, 30 (1): 17-25.
J Lipiec J: Human resources management perspective at the turn of the century. Public Pers Manage. 2001, 30 (2): 137-145.
Mejia A: Le déséquilibre des personnels de santé. World Health Stat Q. 1987, 40: 335-348.
Egger D, Adams O: Imbalances in human resources for health: Can policy formulation and planning make a difference?. Human Resource Devel J. 1999, 3: 1-[ http://www.moph.go.th/ops/hrdj/hrdj6/table_contents.htm ]
Wildavsky A: Speaking truth to power: the art and craft of policy analysis. Boston: Little, Brown & Co. 1979
Leppo K: Strengthening capacities for policy development and strategic management in national health systems. A background paper prepared for the Forum of senior policy-makers and managers of health systems. Geneva: World Health Organization. 2001
Siler-Wells G: An implementation model for health system reform. Soc Sci Med. 1987, 24 (10): 821-832.
Walt G: Health policy: an introduction to process and power. London: Zed Books. 1994
Pederson AP, Edwards RK, Kelner M: Coordination de la politique publique favorisant la santé. Analyse documentaire et bibliographie. Toronto: Département des Sciences du comportement, Université de Toronto. 1988
Lee K, Mills A: Policy-making and planning in the health sector. London: Croom Helm. 1982
Jones CO: An introduction to the study of public policy. California: Belmont. 1970
Ziglio E: Policy-making and planning in conditions of uncertainty: theoretical considerations for health promotion policy. Edinburgh: Research Unit in Health and Behavioural Change. 1987
Simon HA: Administrative behavior. a study of decision-making processes in administrative organization. New York: Macmillan. 1957
Friedberg E: Le pouvoir et la règle: dynamiques de l'action organisée. Paris: Editions du Seuil. 1993
Barker C: The health care policy process. Thousand Oaks: Sage Publications. 1996
Nutt PC: Planning methods: for health and related organizations. Toronto: Wiley. 1984
Linder SH, Peters BG: From social theory to policy design. J Public Policy. 1984, 4 (3): 237-259.
Roberts MJ, Hsiao W, Berman P, Gleich MR: Getting health reform right. New York: Oxford University Press.
Reich MR: Political analysis. The World Bank Flagship Course. Boston: Harvard School of Public Health. 2000
Kingdon JW: Agendas, alternatives, and public policies. Boston: Little, Brown. 1984
Egger D, Lipson D, Adams O: Achieving the right balance: the role of policy-making processes in managing human resources for health problems. Geneva: World Health Organization. 2000, [ http://www.who.int/health-services-delivery/documents/index.htm#disc_pap ]
Dovlo D: Ghana: HRD policy reform issues. In Workshop on human resources and health sector reforms. Edited by: Martinez J, Martineau T. 1996, Liverpool: Liverpool School of Tropical Medicine
Hall T: Why plan human resources for health?. Human Resource Devel J. 1998, 2 (2): 77-86.
Siddiqui J, Kleiner BH: Human resource management in the health care industry. Health Manpow Manage. 1998, 24 (4): 143-147.
Freidson E: Professional dominance: the social structure of medical care. New York: Atherton Press. 1970
Committee on Quality of Health Care in America. Institute of Medicine (IOM): Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press. 2001, [ http://www.nap.edu/catalog/10027.html ]
Collins C: Management and organization of developing health systems. Oxford: Oxford University Press. 1994
Dussault G: Human resources development: the challenge of health sector reform. Washington, DC: Latin America and the Caribbean Department, Human Development Division, World Bank. 1999
Smith DA, Preker AS: Labour market adjustment in health systems. Annecy, World Health Organization Workshop on Global Workforce Strategy. 2000
Standing H: Gender – a missing dimension in human resource policy and planning for health reforms. Human Resource Devel J. 2000, 4: 1-[ http://www.moph.go.th/ops/hrdj/hrdj9/index.htm ]
United Nations Industrial Development Organization: Human resources in zimbabwe's industrial development – the current and prospective contribution of women. Vienna: Regional and Country Studies Branch Industrial Policy and Perspectives Division PPD. 1989
Hossain B: Discussion notes. Human Resource Devel J. 1998, 2: 2-
Pineault R, Daveluy C: La planification de la santé: concepts, méthodes, stratégies. Montreal: Éditions Nouvelles. 1995
Davidson CH: Organizing a human resource function. In Human Resource Management In Health Care. Edited by: Brown M. 1992, Gaithersburg, Md: Aspen Publishers, 3-9.
Storey J: Developments in the management of human resources. Oxford: Blackwell. 1992
Barer ML, Stoddart GL: Improving access to needed medical services in rural and remote Canadian communities: recruitment and retention revisited. Canada, Discussion paper prepared for Federal/Provincial/Territorial Advisory Committee on Health Human Resources. 1999
Hernandez SR, Fottler MD, Joiner CL: Strategic management of human resources in health services organizations. In Strategic management of human resources in health services organizations. Edited by: New York: John Wiley & Sons. 1988, Fottler MD, Hernandez SR, Joiner CL, 3-19.
Youlong G, Wilkes A, Bloom G: Health human resource development in rural China. Health Policy Plan. 1997, 12: 320-328.
Thomas MA: What is a human resources strategy?. Health Manpow Manage. 1996, 22 (2): 4-11.
Saltman RB, Figueras J: European health care reform. analysis of current strategies. Copenhagen: World Health Organization Regional Office for Europe. 1997
Thain C: Implementing economic policy: an analytical framework. Policy Polit. 1987, 15 (2): 67-75.
Martineau T, Buchan J: HR and the success of health sector reform. "Eliminating health disparities". 128th Annual Meeting of the American Public Health Association. Boston. 2000
Milèn A: Que savons-nous du renforcement des capacités? Aperçu des connaissances et bonnes pratiques existantes. Geneva: World HealthOrganization. 2001
Benveniste G: Mastering the politics of planning: crafting credible plans and policies that make a difference. San Francisco: Jossey-Bass. 1990
Martinez J, Collini L: A review of the human resources issues in the health sector : a briefing paper. London: DFID Health Systems Resource Center (HSRC). 1999
Thrasher M: Exchange networks and implementation. Policy Polit. 1983, 11 (4): 375-391.
Download references
Acknowledgements
This paper was supported by the Department of Health Service Provision of the World Health Organization (Geneva). Thanks are expressed to Orvill Adams, Mario Dal Poz and the Human Resources for Health team.

Author information
Authors and affiliations.
World Bank Institute, Washington, DC, USA
Gilles Dussault
Health Services Research Unit, Department of Public Health and Policy, London School of Hygiene and Tropical Medicine and European Observatory on Health Care Systems, London, United Kingdom
Carl-Ardy Dubois
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Gilles Dussault .
Additional information
Competing interests.
None declared.
Authors' contributions
The authors contributed equally to this work.
Gilles Dussault and Carl-Ardy Dubois contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Dussault, G., Dubois, CA. Human resources for health policies: a critical component in health policies. Hum Resour Health 1 , 1 (2003). https://doi.org/10.1186/1478-4491-1-1
Download citation
Received : 28 March 2003
Accepted : 14 April 2003
Published : 14 April 2003
DOI : https://doi.org/10.1186/1478-4491-1-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health Sector
- Human Resource Management
- Health Workforce
- Professional Category
- Human Resource Policy
Human Resources for Health
ISSN: 1478-4491
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 11.4.2024 in Vol 26 (2024)
A Perspective on Crowdsourcing and Human-in-the-Loop Workflows in Precision Health
Authors of this article:

- Peter Washington, PhD
Information and Computer Sciences, University of Hawaii at Manoa, Honolulu, HI, United States
Corresponding Author:
Peter Washington, PhD
Information and Computer Sciences
University of Hawaii at Manoa
1680 East-West Road
Honolulu, HI, 96822
United States
Email: [email protected]
Modern machine learning approaches have led to performant diagnostic models for a variety of health conditions. Several machine learning approaches, such as decision trees and deep neural networks, can, in principle, approximate any function. However, this power can be considered to be both a gift and a curse, as the propensity toward overfitting is magnified when the input data are heterogeneous and high dimensional and the output class is highly nonlinear. This issue can especially plague diagnostic systems that predict behavioral and psychiatric conditions that are diagnosed with subjective criteria. An emerging solution to this issue is crowdsourcing, where crowd workers are paid to annotate complex behavioral features in return for monetary compensation or a gamified experience. These labels can then be used to derive a diagnosis, either directly or by using the labels as inputs to a diagnostic machine learning model. This viewpoint describes existing work in this emerging field and discusses ongoing challenges and opportunities with crowd-powered diagnostic systems, a nascent field of study. With the correct considerations, the addition of crowdsourcing to human-in-the-loop machine learning workflows for the prediction of complex and nuanced health conditions can accelerate screening, diagnostics, and ultimately access to care.
Introduction
Crowdsourcing, a term first coined in 2006 [ 1 ], is the use of distributed human workers to accomplish a central task. Crowdsourcing exploits the “power of the crowd” to achieve goals that are only feasible with a distributed group of humans collaborating, either explicitly or implicitly, toward a common goal. Crowdsourcing has often been applied to public health surveillance [ 2 ], such as for tracking epidemics [ 3 , 4 ], quantifying tobacco use [ 5 ], monitoring water quality [ 6 ], tracking misinformation [ 7 ], and understanding the black-market price of prescription opioids [ 8 ]. In the context of health care, crowdsourcing is most often used for public health, a domain that can clearly benefit from scalable and distributed assessments of health status. Although sampling bias can be an issue in epidemiological uses of crowdsourcing [ 9 ], approaches that account for these issues have performed quite robustly.
A smaller but potentially transformative effort to apply crowdsourcing to precision health rather than population health has recently emerged. In precision health contexts, the goal is to provide a diagnosis using information labeled by crowd workers. There are several variations to this basic setup. Crowdsourcing workflows for diagnostics can diverge with respect to the underlying task, worker motivation strategies, worker training, worker filtering, and privacy requirements.
Here, I describe the existing research in the relatively small and early but growing field of crowdsourcing for precision health. I then discuss ongoing challenges and corresponding opportunities that must be addressed as this field matures.
Existing Examples of Crowdsourcing in and Adjacent to Health Care
There are relatively few examples of crowdsourcing in precision health. The vast successes of machine learning for health [ 10 - 15 ] and the human labor costs required for crowdsourcing make purely automated approaches more appealing when they are possible and feasible. However, the crowdsourcing approaches that have been tested tend to perform well for prediction tasks that are beyond the scope of current automated approaches, especially in psychiatry and the behavioral sciences.
I want to begin by highlighting successes in science, as they can often be applied to health and have started to lead to improvements in diagnostics. Framing crowdsourcing tasks as “citizen science” opportunities can be an effective incentive mechanism [ 16 ]. Oftentimes, these projects are “gamified.” Gamification refers to the incorporation of engaging elements into traditionally burdensome workflows, and in particular game-like affordances, to foster increased participation. A combination of large crowd sizes, worker training procedures, and easy identification tasks have led to previous success in the existing gamified citizen science experiments applied to precision health. For example, in a study involving nearly 100,000 crowd workers who scored images on a citizen science platform, cancer was correctly identified with an area under the receive operating characteristic of around 95% [ 17 ]. In the BioGames app, users who performed with greater than 99% accuracy in a training tutorial were invited to diagnose malaria [ 18 , 19 ]. It was discovered that with a large crowd size, the aggregated diagnostic accuracy of nonexpert crowd workers approached that of experts [ 20 ]. Another citizen science malaria diagnosis application, MalariaSpot, resulted in 99% accuracy in the diagnosis of malaria from blood films [ 21 ]. If the annotation task is relatively simple and nonexperts can be trained with minimal onboarding efforts, then citizen science can be an effective and affordable approach.
“Gamified” crowdsourcing for citizen science has also been successful without explicitly requiring workers to undergo a formal training process. Foldit [ 22 - 25 ] and EteRNA [ 26 - 31 ] are 2 games where players with no biology or chemistry background can explore the design space of protein and RNA folding, respectively. These are both NP-hard (ie, computationally complex) problems, and human players in aggregate have designed solutions that outcompete state-of-the-art computational approaches. These solutions have been used to solve health challenges, such as finding a gene signature for active tuberculosis, which can potentially be used in tuberculosis diagnostics [ 32 ]. Other gamified experiences have been used to build training libraries for complex classification tasks in precision psychiatry. Notably, GuessWhat is a mobile charades game played between children with autism and their parents [ 33 , 34 ]. While the game provides therapeutic benefits to the child with autism [ 35 ], the game simultaneously curates automatic labels of behaviors related to autism through the metadata associated with gameplay [ 36 , 37 ]. These automatically annotated video data have been used to develop state-of-the-art computer vision models for behaviors related to the diagnosis of autism, such as facial expression evocation [ 38 - 41 ], eye gaze [ 42 ], atypical prosody [ 43 ], and atypical body movements [ 44 , 45 ].
An alternative incentive mechanism is paid crowdsourcing. The most popular paid crowdsourcing platform, by far, is Amazon Mechanical Turk (MTurk) [ 46 ]. While paid crowdsourcing specifically for precision health is a relatively nascent field, the general study of paid crowdsourcing (particularly on MTurk) is quite mature. Studies have explored worker quality management [ 47 ], understanding crowd worker demographics [ 48 ], the generation of annotations for use in the training of machine learning models [ 49 - 53 ], the rights of crowd workers [ 54 - 56 ], and understanding crowd worker communities and economics [ 57 - 59 ]. Preliminary studies of paid crowdsourcing have yielded mixed success. Around 81% of images were correctly classified on MTurk in a study involving the grading of diabetic retinopathy from images, with workers failing to correctly indicate the level of severity [ 60 ]. In a separate binary labeling task for glaucomatous optic neuropathy, workers achieved sensitivity in the 80s but reached a specificity below 50% [ 61 ].
In a broader classification task of various medical conditions, workers consistently labeled the “easy” cases while struggling to correctly label and even refusing to label more complicated and nuanced tasks [ 62 ]. Clearly, there is a need for extensive innovations to the traditional paid crowdsourcing workflow to translate this methodology to precision health.
I have extensively investigated the utility of paid crowdsourcing for the diagnosis of autism from unstructured home videos, achieving relatively high diagnostic performance [ 63 - 66 ]. In these experiments, untrained annotators watched short videos depicting children with and without autism and answered questions about the behaviors depicted within the videos. These annotations were provided as input into previously developed machine learning models, achieving binary test performance in the 90s across performance metrics due to the reduction of the complex feature space (unstructured videos) into a low-dimensional representation (vectors of a few categorical ordinal values). This pipeline combining crowdsourcing and machine learning can possibly be extended to other diagnostic domains in psychiatry where the input feature space is complex, heterogeneous, and subjective.
Ongoing Challenges and Corresponding Opportunities
Since crowdsourcing for precision health care is an emerging field of study, numerous challenges must be solved for clinical translation to develop. In the proceeding sections, I highlight several areas that are pressing for the field and for which preliminary work has been published.
Worker Identification and Training
While traditional crowdsourcing can work with minimal to no worker training, complex annotation tasks require the identification of qualified workers. I have found that worker identification can occur through the quantification of their performance on test tasks [ 67 , 68 ] and training promising workers [ 66 ]. Such crowd filtration paradigms will require domain-specific procedures. There is ample room to develop new crowdsourcing systems that inherently support natural worker identification and training procedures for crowdsourcing workflows that require well-designed training processes.
Worker Retention
Once proficient workers are identified, continually engaging and retaining these workers is critical. I have found that workers who are repeatedly encouraged by a human (or human-like chatbot) and treated as members of a broader research team tend to enjoy paid work and even ask for more tasks after the completion of the study [ 69 ]. Thus, it is possible that the guarantee of job security can lead to long-term worker retention. However, worker retention in unpaid settings that rely on intrinsic motivation will require additional innovations. For example, there exists an opportunity to explore the creation of crowd worker communities to provide a means of intrinsic motivation leading to worker retention.
Task Assignment
Certain workers perform exceptionally well on a subset of tasks while underperforming on other assigned tasks [ 70 , 71 ]. There is an opportunity to develop algorithmic innovations involving the effective and optimal assignment of workers to subtasks in a dynamic manner. Reinforcement learning could be a promising approach but has yet to be explored in such scenarios.
Privacy of Human Participants
Data in psychiatry and behavioral sciences are particularly sensitive. Ensuring that sensitive health information is handled appropriately and that workers’ privacy is maintained is essential from an ethical perspective. There are 2 general families of approaches to achieving privacy in crowd-powered health care. First, the data can be modified to obscure sensitive information without removing information required for a diagnosis. I have explored privacy-preserving alterations to video data that obfuscate the identity of participants while maximizing the capacity for workers to annotate behaviors of interest [ 70 , 71 ]. For example, in the case of video analytics on bodily movements, the face can be tracked and blurred, or the body can be converted to a stick figure using a pose-based computer vision library. Sometimes, however, it is impossible to modify the data without severely degrading the diagnostic performance. Therefore, the second family of approaches involves carefully vetting crowd workers, training them, and onboarding them into a secure computing environment. In my previous experiences with this process [ 40 ], I discovered that crowd workers were enthusiastic about the prospect of the “job security” that is implied from the thorough vetting procedure and were, therefore, willing to complete extra privacy and security training (in our case, Research, Ethics, Compliance, and Safety training). There is ample room to expand upon these methods and to develop new paradigms and systems for crowdsourcing involving identifiable and protected health information.
Ensuring Reliability and Reproducibility
An intrinsic challenge when incorporating human workers into precision health workflows is the variability in human responses, both within workers and between workers. I have found that while most crowd workers are inconsistent in their annotation patterns, there are workers who provide consistently sensitive and specific annotations across a wide spectrum of data points [ 67 ]. It is therefore critical to measure both internal consistency and consistency against a gold standard when recruiting crowd workers for precision health care workflows.
Handling Financial Constraints
The crowdsourcing method with the lowest setup barriers is paid crowdsourcing. In such scenarios, financial constraints can limit the scalability of crowdsourcing workflows. One approach is to migrate from a paid system to a gamified system or another means of providing intrinsic motivation to crowd workers. However, achieving critical mass for large-scale pipelines is likely unattainable for such unpaid solutions. Paid crowd workers who consistently perform well could be recruited as full-time or long-term part-time employees for companies and organizations providing crowd-powered services. Integrating such workflows into a Food and Drug Administration (FDA)–approved process can be challenging, but it is worth exploring if it turns out that crowd-powered solutions for digital psychiatry continue to remain superior to pure-artificial intelligence (AI) approaches in the coming years.
Translation Outside of Research Contexts
While pure machine learning approaches for precision health are beginning to translate to clinical settings through formal FDA approval procedures, the prospect of translating human-in-the-loop methods that integrate crowd workers rather than expert clinicians is daunting, especially in light of the challenges mentioned above. However, if such approaches lead to clinical-grade performance for certain conditions that are challenging to diagnose using machine learning alone, then the extra implementation and regulatory effort required to migrate these methods into production-level workflows are likely to be warranted.
While machine learning for health has enabled and will continue to enable more efficient, precise, and scalable diagnostics for a variety of conditions, such models are unlikely to generalize to more difficult scenarios such as psychiatry and the behavioral sciences, which require the ability to identify complex and nuanced social human behavior. Crowd-powered human-in-the-loop workflows have the potential to mitigate some of these current limitations while still offering a high degree of automation. I invite researchers in the fields of digital phenotyping [ 72 - 76 ], mobile sensing [ 77 - 83 ], affective computing [ 84 - 90 ], and related subjects to consider integrating crowdsourcing and human-in-the-loop approaches into their methods when pure-AI leads to suboptimal performance.
Acknowledgments
This project is funded by the NIH Director’s New Innovator Award (DP2) from the National Institutes of Health (award DP2-EB035858).
Conflicts of Interest
None declared.
- Howe J. The rise of crowdsourcing. Wired. Jun 01, 2006. URL: https://sistemas-humano-computacionais.wdfiles.com/local--files/capitulo%3Aredes-sociais/Howe_The_Rise_of_Crowdsourcing.pdf [accessed 2024-03-29]
- Brabham DC, Ribisl KM, Kirchner TR, Bernhardt JM. Crowdsourcing applications for public health. Am J Prev Med. 2014;46(2):179-187. [ CrossRef ] [ Medline ]
- Leung GM, Leung K. Crowdsourcing data to mitigate epidemics. Lancet Digit Health. 2020;2(4):e156-e157. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stockham N, Washington P, Chrisman B, Paskov K, Jung JY, Wall DP. Causal modeling to mitigate selection bias and unmeasured confounding in internet-based epidemiology of COVID-19: model development and validation. JMIR Public Health Surveill. 2022;8(7):e31306. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kraemer JD, Strasser AA, Lindblom EN, Niaura RS, Mays D. Crowdsourced data collection for public health: a comparison with nationally representative, population tobacco use data. Prev Med. 2017;102:93-99. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jakositz S, Pillsbury L, Greenwood S, Fahnestock M, McGreavy B, Bryce J, et al. Protection through participation: crowdsourced tap water quality monitoring for enhanced public health. Water Res. 2020;169:115209. [ CrossRef ] [ Medline ]
- Ghenai A, Mejova Y. Catching Zika fever: application of crowdsourcing and machine learning for tracking health misinformation on Twitter. arXiv. Preprint posted online Jul 12, 2017. [ CrossRef ]
- Dasgupta N, Freifeld C, Brownstein JS, Menone CM, Surratt HL, Poppish L, et al. Crowdsourcing black market prices for prescription opioids. J Med Internet Res. 2013;15(8):e178. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wazny K. "Crowdsourcing" ten years in: a review. J Glob Health. 2017;7(2):020602. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chen PHC, Liu Y, Peng L. How to develop machine learning models for healthcare. Nat Mater. 2019;18(5):410-414. [ CrossRef ] [ Medline ]
- Dua S, Acharya UR, Dua P, editors. Machine Learning in Healthcare Informatics, Volume 56. Berlin, Heidelberg. Springer; 2014.
- Esteva A, Robicquet A, Ramsundar B, Kuleshov V, DePristo M, Chou K, et al. A guide to deep learning in healthcare. Nat Med. 2019;25(1):24-29. [ CrossRef ] [ Medline ]
- Ghassemi M, Naumann T, Schulam P, Beam AL, Chen IY, Ranganath R. A review of challenges and opportunities in machine learning for health. AMIA Jt Summits Transl Sci Proc. 2020;2020:191-200. [ FREE Full text ] [ Medline ]
- Shailaja K, Seetharamulu B, Jabbar MA. Machine learning in healthcare: a review. 2018. Presented at: 2018 Second International Conference on Electronics, Communication and Aerospace Technology (ICECA); March 29-31, 2018;910-914; Coimbatore, India. [ CrossRef ]
- Yu KH, Beam AL, Kohane IS. Artificial intelligence in healthcare. Nat Biomed Eng. 2018;2(10):719-731. [ CrossRef ] [ Medline ]
- Das R, Keep B, Washington P, Riedel-Kruse IH. Scientific discovery games for biomedical research. Annu Rev Biomed Data Sci. 2019;2(1):253-279. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dos Reis FJC, Lynn S, Ali HR, Eccles D, Hanby A, Provenzano E, et al. Crowdsourcing the general public for large scale molecular pathology studies in cancer. EBioMedicine. 2015;2(7):681-689. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mavandadi S, Dimitrov S, Feng S, Yu F, Sikora U, Yaglidere O, et al. Distributed medical image analysis and diagnosis through crowd-sourced games: a malaria case study. PLoS One. 2012;7(5):e37245. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ozcan A. Educational games for malaria diagnosis. Sci Transl Med. 2014;6(233):233ed9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Feng S, Woo M, Chandramouli K, Ozcan A. A game-based platform for crowd-sourcing biomedical image diagnosis and standardized remote training and education of diagnosticians. In: Optics and Biophotonics in Low-Resource Settings, Volume 9314. 2015. Presented at: SPIE BIOS; February 7-12, 2015; San Francisco, CA. [ CrossRef ]
- Luengo-Oroz MA, Arranz A, Frean J. Crowdsourcing malaria parasite quantification: an online game for analyzing images of infected thick blood smears. J Med Internet Res. 2012;14(6):e167. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cooper S, Khatib F, Makedon I, Lu H, Barbero J, Baker D, et al. Analysis of social gameplay macros in the Foldit cookbook. 2011. Presented at: FDG '11: Proceedings of the 6th International Conference on Foundations of Digital Games; June 29, 2011 - July 1, 2011;9-14; Bordeaux, France. [ CrossRef ]
- Curtis V. Motivation to participate in an online citizen science game: a study of Foldit. Sci Commun. 2015;37(6):723-746. [ CrossRef ]
- Eiben CB, Siegel JB, Bale JB, Cooper S, Khatib F, Shen BW, et al. Increased Diels-Alderase activity through backbone remodeling guided by Foldit players. Nat Biotechnol. 2012;30(2):190-192. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kleffner R, Flatten J, Leaver-Fay A, Baker D, Siegel JB, Khatib F, et al. Foldit standalone: a video game-derived protein structure manipulation interface using Rosetta. Bioinformatics. 2017;33(17):2765-2767. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Andreasson JOL, Gotrik MR, Wu MJ, Wayment-Steele HK, Kladwang W, Portela F, et al. Crowdsourced RNA design discovers diverse, reversible, efficient, self-contained molecular switches. Proc Natl Acad Sci U S A. 2022;119(18):e2112979119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Krüger A, Watkins AM, Wellington-Oguri R, Romano J, Kofman C, DeFoe A, et al. Community science designed ribosomes with beneficial phenotypes. Nat Commun. 2023;14(1):961. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee J, Kladwang W, Lee M, Cantu D, Azizyan M, Kim H, et al. RNA design rules from a massive open laboratory. Proc Natl Acad Sci U S A. 2014;111(6):2122-2127. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shi J, Das R, Pande VS. SentRNA: improving computational RNA design by incorporating a prior of human design strategies. arXiv. Preprint posted online Mar 06, 2019. [ CrossRef ]
- Treuille A, Das R. Scientific rigor through videogames. Trends Biochem Sci. 2014;39(11):507-509. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wayment-Steele HK, Kladwang W, Strom AI, Lee J, Treuille A, Becka A, et al. RNA secondary structure packages evaluated and improved by high-throughput experiments. Nat Methods. 2022;19(10):1234-1242. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sweeney TE, Braviak L, Tato CM, Khatri P. Genome-wide expression for diagnosis of pulmonary tuberculosis: a multicohort analysis. Lancet Respir Med. 2016;4(3):213-224. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kalantarian H, Jedoui K, Washington P, Wall DP. A mobile game for automatic emotion-labeling of images. IEEE Trans Games. 2020;12(2):213-218. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kalantarian H, Washington P, Schwartz J, Daniels J, Haber N, Wall D. A gamified mobile system for crowdsourcing video for autism research. 2018. Presented at: 2018 IEEE International Conference on Healthcare Informatics (ICHI); June 4-7, 2018;350-352; New York, NY. [ CrossRef ]
- Penev Y, Dunlap K, Husic A, Hou C, Washington P, Leblanc E, et al. A mobile game platform for improving social communication in children with autism: a feasibility study. Appl Clin Inform. 2021;12(5):1030-1040. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kalantarian H, Washington P, Schwartz J, Daniels J, Haber N, Wall DP. Guess what? Towards understanding autism from structured video using facial affect. J Healthc Inform Res. 2019;3(1):43-66. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kalantarian H, Jedoui K, Washington P, Tariq Q, Dunlap K, Schwartz J, et al. Labeling images with facial emotion and the potential for pediatric healthcare. Artif Intell Med. 2019;98:77-86. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hou C, Kalantarian H, Washington P, Dunlap K, Wall DP. Leveraging video data from a digital smartphone autism therapy to train an emotion detection classifier. medRxiv. Preprint posted online Aug 01, 2021. [ CrossRef ]
- Kalantarian H, Jedoui K, Dunlap K, Schwartz J, Washington P, Husic A, et al. The performance of emotion classifiers for children with parent-reported autism: quantitative feasibility study. JMIR Ment Health. 2020;7(4):e13174. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Washington P, Kalantarian H, Kent J, Husic A, Kline A, Leblanc E, et al. Improved digital therapy for developmental pediatrics using domain-specific artificial intelligence: machine learning study. JMIR Pediatr Parent. 2022;5(2):e26760. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Washington P, Kalantarian H, Kent J, Husic A, Kline A, Leblanc E, et al. Training an emotion detection classifier using frames from a mobile therapeutic game for children with developmental disorders. arXiv. Preprint posted online Dec 16, 2020 . [ CrossRef ]
- Varma M, Washington P, Chrisman B, Kline A, Leblanc E, Paskov K, et al. Identification of social engagement indicators associated with autism spectrum disorder using a game-based mobile app: comparative study of gaze fixation and visual scanning methods. J Med Internet Res. 2022;24(2):e31830. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chi NA, Washington P, Kline A, Husic A, Hou C, He C, et al. Classifying autism from crowdsourced semistructured speech recordings: machine learning model comparison study. JMIR Pediatr Parent. 2022;5(2):e35406. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lakkapragada A, Kline A, Mutlu OC, Paskov K, Chrisman B, Stockham N, et al. The classification of abnormal hand movement to aid in autism detection: machine learning study. JMIR Biomed Eng. 2022;7(1):e33771. [ FREE Full text ] [ CrossRef ]
- Washington P, Kline A, Mutlu OC, Leblanc E, Hou C, Stockham N, et al. Activity recognition with moving cameras and few training examples: applications for detection of autism-related headbanging. 2021. Presented at: CHI '21: CHI Conference on Human Factors in Computing Systems; May 8-13, 2021;1-7; Yokohama, Japan. [ CrossRef ]
- Paolacci G, Chandler J, Ipeirotis PG. Running experiments on Amazon Mechanical Turk. Judgm Decis Mak. 2010;5(5):411-419. [ FREE Full text ] [ CrossRef ]
- Ipeirotis PG, Provost F, Wang J. Quality management on Amazon Mechanical Turk. 2010. Presented at: HCOMP '10: Proceedings of the ACM SIGKDD Workshop on Human Computation; July 25, 2010;64-67; Washington DC. [ CrossRef ]
- Lee YJ, Arida JA, Donovan HS. The application of crowdsourcing approaches to cancer research: a systematic review. Cancer Med. 2017;6(11):2595-2605. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ross J, Zaldivar A, Irani L, Tomlinson B. Who are the turkers? Worker demographics in Amazon Mechanical Turk. ResearchGate. 2009. URL: https://www.researchgate.net/publication/268427703_Who_are_the_Turkers_Worker_Demographics_in_Amazon_Mechanical_Turk [accessed 2024-03-22]
- Russakovsky O, Deng J, Su H, Krause J, Satheesh S, Ma S, et al. ImageNet large scale visual recognition challenge. Int J Comput Vis. 2015;115:211-252. [ CrossRef ]
- Sheng VS, Zhang J. Machine learning with crowdsourcing: a brief summary of the past research and future directions. Proc AAAI Conf Artif Intell. 2019;33(01):9837-9843. [ CrossRef ]
- Sorokin A, Forsyth D. Utility data annotation with Amazon Mechanical Turk. 2008. Presented at: 2008 IEEE Computer Society Conference on Computer Vision and Pattern Recognition Workshops; June 23-28, 2008;1-8; Anchorage, AK. [ CrossRef ]
- Xintong G, Hongzhi W, Song Y, Hong G. Brief survey of crowdsourcing for data mining. Expert Syst Appl. 2014;41(17):7987-7994. [ CrossRef ]
- Irani LC, Silberman MS. Turkopticon: interrupting worker invisibility in Amazon Mechanical Turk. 2013. Presented at: CHI '13: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; April 27, 2013 - May 2, 2013;611-620; Paris, France. [ CrossRef ]
- Irani L, Silberman MS. From critical design to critical infrastructure: lessons from turkopticon. Interactions. 2014;21(4):32-35. [ CrossRef ]
- Kummerfeld JK. Quantifying and avoiding unfair qualification labour in crowdsourcing. arXiv. Preprint posted online May 26, 2021. [ CrossRef ]
- Hansson K, Ludwig T. Crowd dynamics: conflicts, contradictions, and community in crowdsourcing. Comput Support Coop Work. 2019;28:791-794. [ FREE Full text ] [ CrossRef ]
- Shen XL, Lee MKO, Cheung CMK. Exploring online social behavior in crowdsourcing communities: a relationship management perspective. Comput Human Behav. 2014;40:144-151. [ CrossRef ]
- Wu W, Gong X. Motivation and sustained participation in the online crowdsourcing community: the moderating role of community commitment. Internet Res. 2021;31(1):287-314. [ CrossRef ]
- Brady CJ, Villanti AC, Pearson JL, Kirchner TR, Gupta OP, Shah C. Rapid grading of fundus photographs for diabetic retinopathy using crowdsourcing. J Med Internet Res. Oct 30, 2014;16(10):e233. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mitry D, Peto T, Hayat S, Blows P, Morgan J, Khaw KT, et al. Crowdsourcing as a screening tool to detect clinical features of glaucomatous optic neuropathy from digital photography. PLoS One. 2015;10(2):e0117401. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cheng J, Manoharan M, Zhang Y, Lease M. Is there a doctor in the crowd? Diagnosis needed! (For less than $5). iConference 2015 Proceedings. 2015. URL: https://www.ideals.illinois.edu/items/73844 [accessed 2024-03-22]
- Leblanc E, Washington P, Varma M, Dunlap K, Penev Y, Kline A, et al. Feature replacement methods enable reliable home video analysis for machine learning detection of autism. Sci Rep. 2020;10(1):21245. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tariq Q, Daniels J, Schwartz JN, Washington P, Kalantarian H, Wall DP. Mobile detection of autism through machine learning on home video: a development and prospective validation study. PLoS Med. 2018;15(11):e1002705. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tariq Q, Fleming SL, Schwartz JN, Dunlap K, Corbin C, Washington P, et al. Detecting developmental delay and autism through machine learning models using home videos of Bangladeshi children: development and validation study. J Med Internet Res. 2019;21(4):e13822. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Washington P, Tariq Q, Leblanc E, Chrisman B, Dunlap K, Kline A, et al. Crowdsourced privacy-preserved feature tagging of short home videos for machine learning ASD detection. Sci Rep. 2021;11(1):7620. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Washington P, Leblanc E, Dunlap K, Penev Y, Kline A, Paskov K, et al. Precision telemedicine through crowdsourced machine learning: testing variability of crowd workers for video-based autism feature recognition. J Pers Med. 2020;10(3):86. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Washington P, Leblanc E, Dunlap K, Penev Y, Varma M, Jung JY, et al. Selection of trustworthy crowd workers for telemedical diagnosis of pediatric autism spectrum disorder. Pac Symp Biocomput. 2021;26:14-25. [ FREE Full text ] [ Medline ]
- Washington P, Kalantarian H, Tariq Q, Schwartz J, Dunlap K, Chrisman B, et al. Validity of online screening for autism: crowdsourcing study comparing paid and unpaid diagnostic tasks. J Med Internet Res. 2019;21(5):e13668. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Washington P, Chrisman B, Leblanc E, Dunlap K, Kline A, Mutlu C, et al. Crowd annotations can approximate clinical autism impressions from short home videos with privacy protections. Intell Based Med. 2022;6:100056. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Insel TR. Digital phenotyping: technology for a new science of behavior. JAMA. 2017;318(13):1215-1216. [ CrossRef ] [ Medline ]
- Huckvale K, Venkatesh S, Christensen H. Toward clinical digital phenotyping: a timely opportunity to consider purpose, quality, and safety. NPJ Digit Med. 2019;2:88. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Onnela JP. Opportunities and challenges in the collection and analysis of digital phenotyping data. Neuropsychopharmacology. 2021;46(1):45-54. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Onnela JP, Rauch SL. Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health. Neuropsychopharmacology. 2016;41(7):1691-1696. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Washington P, Mutlu CO, Kline A, Paskov K, Stockham NT, Chrisman B, et al. Challenges and opportunities for machine learning classification of behavior and mental state from images. arXiv. Preprint posted online Jan 26, 2022. [ CrossRef ]
- Baumeister H, Montag C, editors. Digital Phenotyping and Mobile Sensing: New Developments in Psychoinformatics. Cham, Switzerland. Springer International Publishing; 2019.
- Laport-López F, Serrano E, Bajo J, Campbell AT. A review of mobile sensing systems, applications, and opportunities. Knowl Inf Syst. 2020;62(1):145-174. [ CrossRef ]
- Macias E, Suarez A, Lloret J. Mobile sensing systems. Sensors (Basel). 2013;13(12):17292-17321. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nazir S, Ali Y, Ullah N, García-Magariño I. Internet of things for healthcare using effects of mobile computing: a systematic literature review. Wirel Commun Mob Comput. 2019;2019:1-20. [ FREE Full text ] [ CrossRef ]
- Silva BMC, Rodrigues JJPC, de la Torre Díez I, López-Coronado M, Saleem K. Mobile-health: a review of current state in 2015. J Biomed Inform. 2015;56:265-272. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sim I. Mobile devices and health. N Engl J Med. 2019;381(10):956-968. [ CrossRef ]
- Yürür O, Liu CH, Sheng Z, Leung VCM, Moreno W, Leung KK. Context-awareness for mobile sensing: a survey and future directions. IEEE Commun Surv Tutor. 2014;18(1):68-93. [ CrossRef ]
- Picard RW. Affective Computing. Cambridge, MA. MIT Press; 2000.
- Picard RW. Affective computing: challenges. Int J Hum-Comput Stud. 2003;59(1-2):55-64. [ CrossRef ]
- Poria S, Cambria E, Bajpai R, Hussain A. A review of affective computing: from unimodal analysis to multimodal fusion. Inf Fusion. 2017;37:98-125. [ CrossRef ]
- Scherer KR, Bänziger T, Roesch E, editors. A Blueprint for Affective Computing: a Sourcebook and Manual. Oxford, United Kingdom. Oxford University Press; 2010.
- Tao J, Tan T. Affective computing: a review. In: Affective Computing and Intelligent Interaction. Berlin, Heidelberg. Springer; 2005. Presented at: First International Conference, ACII 2005; October 22-24, 2005;981-995; Beijing, China. [ CrossRef ]
- Wang Y, Song W, Tao W, Liotta A, Yang D, Li X, et al. A systematic review on affective computing: emotion models, databases, and recent advances. Inf Fusion. 2022;83-84:19-52. [ CrossRef ]
- Zhao S, Wang S, Soleymani M, Joshi D, Ji Q. Affective computing for large-scale heterogeneous multimedia data: a survey. ACM Trans Multimed Comput Commun Appl. 2019;15(3s):1-32. [ CrossRef ]
Abbreviations
Edited by A Mavragani; submitted 22.07.23; peer-reviewed by E Vashishtha, MO Khursheed, L Guo; comments to author 02.09.23; revised version received 15.11.23; accepted 30.01.24; published 11.04.24.
©Peter Washington. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 11.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Bull World Health Organ
- v.88(6); 2010 Jun 1

Language: English | Arabic | French | Spanish
Priorities for research into human resources for health in low- and middle-income countries
أولويات البحوث في الموارد البشرية الصحية في البلدان المنخفضة الدخل والمتوسطة الدخل, priorités de la recherche sur les ressources humaines pour la santé dans les pays à revenu faible ou intermédiaire, prioridades de las investigaciones sobre recursos humanos para la salud en países de ingresos bajos y medios, michael kent ranson.
a Alliance for Health Policy and Systems Research, World Health Organization, 20 avenue Appia, 1211 Geneva 27, Switzerland.
Mickey Chopra
b Health Systems Research Unit, Medical Research Council, South Africa.
Salla Atkins
Mario roberto dal poz.
c Human Resources for Health, World Health Organization, Geneva, Switzerland.
Sara Bennett
To identify the human resources for health (HRH) policy concerns and research priorities of key stakeholders in low- and middle-income countries; to assess the extent to which existing HRH research addresses these concerns and priorities; and to develop a prioritized list of core research questions requiring immediate attention to facilitate policy development and implementation.
The study involved interviews with key informants, including health policy-makers, researchers and community and civil society representatives, in 24 low- and middle-income countries in four regions, a literature search for relevant reviews of research completed to date, and the assessment of interview and literature search findings at a consultative multinational workshop, during which research questions were prioritized.
Twenty-one research questions emerged from the key informant interviews, many of which had received little or no attention in the reviewed literature. The questions ranked as most important at the consultative workshop were: (i) To what extent do incentives work in attracting and retaining qualified health workers in underserviced areas? (ii) What is the impact of dual practice and multiple employment? and (iii) How can incentives be used to optimize efficiency and the quality of health care?
There was a clear consensus about the type of HRH policy problems faced by different countries and the nature of evidence needed to tackle them. Coordinated action to support and implement research into the highest priority questions identified here could have a major impact on health worker policies and, ultimately, on the health of the poor.
الملخص
الهدف.
التعرُّف على الموارد البشرية الصحية، والشواغل في السياسات والأولويات في البحوث لدى كبار المعنيين في البلدان المنخفضة الدخل وفي البلدان المتوسطة الدخل، وتقييم تلبية البحوث الموجودة حالياً حول الموارد البشرية الصحية لهذه الشواغل والأولويات، وإعداد قائمة بالأولويات في القضايا البحثية الأساسية التي تتطلب إيلاءها أهمية فورية لتسهيل إعداد السياسات وتنفيذها.
الطريقة
شملت الطريقة إجراءات المقابلات مع المعنيين الرئيسيين بالدراسة وهم أصحاب القرار السياسي حول الصحة، والباحثون الصحيون وممثلو المجتمع المدني في 24 بلداً من البلدان المنخفضة الدخل والبلدان المتوسطة الدخل في أربعة أقاليم. حيث أجرى الباحثون بحثاً في النشريات الطبية للتعرُّف على المراجعات ذات الصلة بالبحوث بهدف استكمالها في الوقت الحاضر، مع تقييم النتائج التي أسفرت عنها المقابلات والبحث في النشريات في حلقة عملية تشاورية متعددة البلدان، خلالها وضعت أولويات القضايا البحثية.
الموجودات
اتضح للباحثين وجود 21 قضية بحثية من المقابلات مع كبار المعنيين ولم يحظ الكثير من هذه القضايا بالاهتمام في النشريات التي خضعت للمراجعة. وصنف الباحثون هذه القضايا في الفئات الأكثر أهمية ضمن الحلقة العملية التشاورية؛ وهي: (1) إلى أي مدى تنجح التحفيزات في اجتذاب العاملين الصحيين المؤهلين واستبقائهم في المناطق المحرومة من الخدمات. (2) ما أثر الممارسات المزدوجة أو المتعددة للتوظيف؟، (3) وكيف يمكن للحوافز أن تستخدم في الحصول على أفضل كفاءة وأفضل رعاية صحية ممكنة.
الاستنتاج
لقد كان هناك اتفاق واضح في الآراء حول نمط المشكلات في الموارد البشرية الصحية التي تواجه البلدان المختلفة، وحول البينات اللازمة للتصدي لهذه المشكلات. وقد يكون للإجراءات المنسقة التي تهدف لدعم وتنفيذ البحوث في القضايا ذات الأولويات الأرفع والتي تعرف عليها الباحثون في هذه الدراسة أثر كبير على السياسات الخاصة بالعاملين الصحيين، وبالتالي على صحة الفقراء.
Résumé
Identifier les sujets de préoccupation pour les politiques de gestion des ressources humaines pour la santé (RHS) et les priorités de la recherche pour les acteurs clés des pays à revenu faible ou intermédiaire ; évaluer dans quelle mesure la recherche actuelle sur les ressources humaines pour la santé répond à ces préoccupations et à ces priorités ; et élaborer une liste de thèmes de recherche essentiels, requérant une attention immédiate pour faciliter le développement et la mise en œuvre de politiques, avec les priorités associées.
Méthodes
L'étude a compris des entretiens avec des informateurs clés (notamment des décideurs politiques et des chercheurs dans le domaine de la santé et des représentants des communautés et de la société civile), qui ont été réalisés dans 24 pays à revenu faible ou intermédiaire appartenant à quatre régions, une recherche bibliographique des revues de la littérature pertinentes effectuées à ce jour et l'évaluation des résultats des entretiens et de la recherche bibliographique dans le cadre d'un atelier consultatif plurinational, au cours duquel les thèmes de recherche ont été classés par priorité.
Résultats
Vingt-et-un thèmes de recherche ont émergé des entretiens avec les informateurs clés, dont beaucoup n'avaient guère ou pas attiré l'attention d'après la littérature examinée. Les thèmes classés comme les plus importants lors de l'atelier consultatif étaient : (i) dans quelle mesure les dispositions incitatives réussissent-elles à attirer et à retenir la main d'œuvre médicale qualifiée dans les zones mal desservies ? (ii) quel est l'impact des pratiques doubles et des emplois multiples ? et (iii) Comment peut-on utiliser des mesures incitatives pour optimiser l'efficacité et la qualité des soins de santé ?
Il n'y avait pas de consensus clair sur le type de problème rencontré par les différents pays dans leur politique RHS et sur la nature des éléments nécessaires pour y faire faire face. Une action coordonnée pour appuyer et mettre en œuvre la recherche sur les thèmes identifiés comme les plus fortement prioritaires pourrait avoir un impact majeur sur les politiques en faveur des ressources humaines pour la santé et, en fin de compte, sur la santé des plus démunis.
Determinar los problemas decisionales y las prioridades de investigación en materia de recursos humanos para la salud de los principales interesados en los países de ingresos bajos y medios; evaluar en qué medida las investigaciones sobre recursos humanos para la salud abordan esas preocupaciones y prioridades; y elaborar una lista de líneas prioritarias de investigación que requieran atención inmediata para facilitar la formulación y aplicación de políticas.
Métodos
El estudio abarcó entrevistas con informantes clave, en particular con formuladores de políticas sanitarias, investigadores y representantes de la comunidad y de la sociedad civil, de 24 países de ingresos bajos y medios de cuatro regiones, una búsqueda bibliográfica de revisiones de interés de investigaciones realizadas hasta la fecha, y la evaluación de entrevistas y resultados de búsquedas bibliográficas en un taller consultivo multinacional, en el que se estableció el orden de prioridad de diversas cuestiones de investigación.
De las entrevistas a informantes clave surgieron 21 cuestiones de investigación, muchas de las cuales habían recibido poca o ninguna atención en las publicaciones revisadas. Las preguntas consideradas de mayor importancia en el taller consultivo fueron: (i) ¿En qué medida funcionan los incentivos empleados para atraer y retener a los trabajadores sanitarios cualificados en las zonas subatendidas? (ii) ¿Qué repercusiones tienen la doble práctica y el pluriempleo? (iii) ¿Cómo pueden utilizarse los incentivos para optimizar la eficiencia y la calidad de la atención sanitaria?
Conclusión
Hubo un consenso claro acerca del tipo de problemas que afrontan los diferentes países en relación con las políticas de recursos humanos para la salud, así como sobre la naturaleza de la evidencia necesaria para abordarlos. Una acción coordinada tendente a apoyar e implementar las investigaciones sobre las cuestiones más prioritarias aquí identificadas podría tener gran incidencia en las políticas sobre el personal sanitario y, en definitiva, en la salud de los pobres.
Introduction
Since human resources account for approximately 70% of recurrent expenditure in most health systems, inadequate human resource training, regulation, distribution and management can have enormous implications. 1 Many low- and middle-income countries (LMICs), particularly in sub-Saharan Africa, suffer from both a shortage of health-care providers and poor distribution of providers within the country. These problems are exacerbated by deficiencies in skill mixes and poor physical and managerial infrastructure. 2 Moreover, the failure of health system reforms has been linked to the failure to strengthen policy, planning and management of human resources for health (HRH) early in the process. 3
In a recent overview of systematic reviews, significant gaps were found in knowledge about the way training, regulatory, financial and organizational mechanisms affect the supply, distribution and performance of health-care workers. Furthermore, the data available tend to come from high-income settings and may not apply to LMICs. 4
Despite the urgent need to address these knowledge gaps and the international nature of HRH problems, there is still no consensus on research priorities. The World Health Organization’s (WHO’s) Task Force on Health Systems Research included HRH “at the district level and below” and “requirements at higher management levels” as two of the 12 research categories important for attaining the Millennium Development Goals (MDGs). 5 However, the expert group made no attempt to establish priorities among the 12 categories or the many issues within each category. The Joint Learning Initiative on HRH, 2 a consortium of more than 100 health leaders who worked together to identify strategies for strengthening HRH, concluded that “the weak knowledge base of the health workforce hampers planning, policy development, and program operations” (p. 4) and called for donors to “significantly enhance their financing of research…” (p. 139). In addition, a diverse group of participants at the first Global Forum on Human Resources for Health in 2008 called for better research on the health-care workforce. 6
This paper presents the results of an initiative that aimed to identify the HRH policy concerns and research priorities of key stakeholders in LMICs, to assess the extent to which existing HRH research addresses these concerns and priorities, and to establish immediate priorities for the research essential for policy development and implementation.
There were three steps in determining research priorities ( Fig. 1 ). First, interviews were conducted with health policy-makers, researchers and community and civil society representatives in 24 LMICs in four regions: East Africa, Latin America and the Caribbean, the Middle East and North Africa, and South-East Asia. They resulted in a series of regional reports. Second, a systematic literature review was carried out to identify completed research, which was then mapped against the needs articulated by stakeholders. Third, the findings of the first two steps were discussed at a consultative multinational workshop during which research issues were ranked and the top-ranked issues were subject to brainstorming.

The three steps in determining priorities for research on human resources for health (HRH) in low- and middle-income countries
Data from the regional reports and the systematic literature review were categorized using a predetermined conceptual framework 4 that included the main outcomes of human resource policies (i.e. appropriate supply or quantity of health workers, appropriate distribution of health workers, efficient use of health workers and good performance) and broad policy levers (i.e. training, regulatory mechanisms, financial mechanisms, organizational mechanisms, and macromechanisms or mechanisms outside the health-care sector).
Informant interviews
The WHO-based Alliance for Health Policy and Systems Research (HPSR) competitively awarded grants to four organizations in four regions, representing 24 countries, to conduct key informant interviews of policy-makers, researchers and community and civil society representatives. Table 1 lists the countries involved, the types of informant interviewed and the interview topics in each region. In all regions, informants were purposively selected by the four organizations. Between May 2007 and March 2008, informants were asked about their thoughts on policy concerns and research priorities in three areas: health financing, the non-state health sector and HRH. 1 Open-ended questions were asked and interviewers used semistructured interview guides.
NGO, nongovernmental organization.
The data were analysed in several phases by two authors (i.e. MKR and MC). First, regional reports were read and HRH policy concerns and research priorities were extracted and categorized. This process was relatively deductive insofar as the categories used were based largely on the predetermined conceptual framework. Second, policy concerns and research priorities common to at least three regional reports were identified. Third, specific policy concerns and research priorities, as expressed by individual informants, were extracted from country-level reports, which were available for the East Africa and Middle East and North Africa regions only. This last step was carried out to gain some sense of the consistency and breadth of the policy concerns and research priorities identified.
Literature review
A literature review was carried out to identify current HRH research and to assess the extent to which it addresses the priorities expressed by informants. Our review was limited to existing literature reviews on HRH topics. We searched Medline through the Ovid interface and EMBASE Ovid (Ovid Technologies Inc., New York, United States of America) for entries dated from 1979 to March 2008. The search terms used in Medline are shown, as an example, in Box 1 . We also searched the Cochrane Library, which includes the Cochrane Database of Systematic Reviews and the Database of Reviews of Effectiveness. Grey literature was identified with Google using the search terms “review” or “synthesis” with “human resources for health” or “health workforce”. The first 100 results were reviewed for each search combination. In addition, the journal Human resources for health was searched by hand from the first issue in 2003. Also searched were the Equinet web site and other web sites that came to light, and a World Bank bibliography of HRH studies.
Details of the literature search terms used in Medline to identify current research on human resources for health (HRH) a
Medline search through PubMed
Total number of hits: 1141
Dates: publication date from 1979 to 2008
Methodology:
REVIEW[Publication Type] OR “META ANALYSIS”[Publication Type] OR “META-ANALYSIS”[Publication Type] OR “SYSTEMATIC REVIEW”[Title/Abstract]
Non-state sector:
((“HEALTH PERSONNEL”[TW] OR “HEALTH CARE PERSONNEL”[TW] OR “HEALTHCARE PERSONNEL”[TW] OR “MEDICAL PERSONNEL”[TW] OR “HEALTH PROFESSIONAL*”[TW] OR “HEALTH CARE PROFESSIONAL*”[TW] OR “HEALTHCARE PROFESSIONAL*”[TW] OR “MEDICAL PROFESSIONAL*”[TW] OR “HEALTH CARE WORKER*”[TW] OR “HEALTHCARE WORKER*”[TW] OR “MEDICAL WORKER*”[TW] OR “HEALTH WORKFORCE”[TW] OR “HEALTH CARE WORKFORCE”[TW] OR “HEALTHCARE WORKFORCE”[TW] OR “MEDICAL WORKFORCE”[TW]) AND (DEMAND[TW] OR NEED*[TW] OR SUPPLY[TW] OR SHORTAGE[TW] OR CAPACITY[TW] OR EMPLOYMENT[TW] OR DISTRIBUT*[TW] OR MALDISTRIBUT*[TW] OR RECRUIT*[TW] OR ALLOCAT*[TW] OR MOBILITY[TW] OR INTERNATIONAL EDUCATIONAL EXCHANGE[MeSH Major Topic] OR HEALTH CARE RATIONING[MeSH Major Topic] OR RESOURCE ALLOCATION[MeSH Major Topic] OR “HEALTH SERVICES NEEDS AND DEMAND”[MeSH Major Topic] PERSONNEL MANAGEMENT[MeSH Major Topic:EXP] OR HEALTH PERSONNEL[MeSH Major Topic:EXP] OR “BRAIN DRAIN”[Text Word] OR “BORDER CROSSING”[Text Word] OR EMIGRATION[Text Word] OR IMMIGRATION[Text Word] OR MIGRATION[Text Word] OR (FOREIGN AND (PERSONNEL OR GRADUTE*))[TW] OR HEALTH MANPOWER[Text Word] OR HUMAN RESOURCE*[TW] OR “EMIGRATION AND IMMIGRATION”[MeSH Major Topic] OR FOREIGN MEDICAL GRADUATES[MeSH Major Topic] OR FOREIGN PROFESSIONAL PERSONNEL[MeSH Major Topic] OR HEALTH MANPOWER[MeSH Terms] OR MANPOWER[MeSH Subheading]))
Population:
INTERNATIONAL[TW] AND (COOPERATION[TW] OR “CO-OPERATION”[TW] OR “CO OPERATION”[TW]) OR AFRICA[TW] OR CARIBBEAN[TW] OR “CENTRAL AMERICA”[TW] OR “LATIN AMERICA”[TW] OR “SOUTH AMERICA”[TW] OR ASIA[TW] OR “EAST* EUROPE”[TW] OR ((DEVELOPING[TW] OR “LESS DEVELOPED”[TW] OR “UNDER DEVELOPED”[TW]) AND WORLD[TW] OR LMIC[TW] OR ((DEVELOPING[TW] OR “LESS DEVELOPED”[TW] OR “THIRD WORLD”[TW] OR “UNDER DEVELOPED”[TW] OR POOR[TW] OR “LOW* INCOME”[TW] OR “MIDDLE INCOME”[TW] OR “LOW AND MIDDLE INCOME”[TW]) AND (COUNTRIES[TW] OR COUNTRY[TW] OR “NATION*”[TW])) OR WORLD HEALTH [MeSH Major Topic] OR INTERNATIONAL COOPERATION[MeSH Major Topic] OR EUROPE, EASTERN[MH:EXP] OR ASIA[MH:EXP] OR SOUTH AMERICA[MH:EXP] OR LATIN AMERICA[MH:EXP] OR CENTRAL AMERICA[MH:EXP] OR CARIBBEAN REGION[MH:EXP] OR AFRICA[MeSH Terms:EXP] OR DEVELOPING COUNTRIES[MeSH Terms]
a Findings in the other two thematic areas, health financing and the non-state sector, are being prepared for publication elsewhere. Please contact the authors of this paper for further information.
Each review identified in the search had to satisfy two inclusion criteria: (i) it had to indicate that a literature search had been carried out, and (ii) it had to have an HRH topic as a primary focus. Multinational reviews and reviews from individual LMICs were included, but those of literature from a single, high-income country were excluded. All Medline, EMBASE and Cochrane citations were screened by two independent reviewers (SH, AS). Disagreements were resolved by consensus following retrieval of the full texts. Of the 3601 citations identified from the published literature, 40 reviews were included by consensus on initial evaluation. Thereafter, 20 additional reviews were included following discussion, plus 12 from the grey literature, resulting in a total of 72 reviews.
Consultative workshop
A workshop was organized to rank research priorities in April 2008 in Berkeley, California, USA, in conjunction with the Berkeley Global Health Workforce Conference, which focused on HRH research and targeted researchers, policy-makers and representatives of international organizations working in HRH. Following an open invitation to conference participants, two additional LMIC participants were sponsored by the research team to ensure regional diversity and a good skill mix. Ten of the 15 participants were researchers, one was a health policy-maker and the remaining four classified themselves as “other”. Seven of the 15 were based at institutions in LMICs. Before the workshop, participants were given an unranked list of emerging priority research questions and an overview of the literature reviews. At the workshop, participants: (i) discussed the list of research questions, (ii) decided on the nature and relative weighting of criteria for ranking research questions, and (iii) ranked the research questions using three criteria (described below). Each research question was scored on the three criteria using a three-point Likert scale, in which 1 = no and 3 = yes, by each of the 15 participants individually using a self-administered questionnaire. Index scores were then calculated for each individual participant and summed across individuals. The authors of this paper did not participate in the ranking.
Policy concerns
The following broad policy concerns emerged in interviews from across the regions.
Stewardship
Informants expressed concern about a lack of stewardship from the highest levels, in government ministries, to HRH management at individual facilities. In some countries (e.g. Chile, Costa Rica, Egypt, El Salvador and Jordan), informants commented on the lack of a national HRH plan. In the West Bank and Gaza Strip, as in many countries, it was felt that “the implementation of training programmes and the production of HRH is not linked to strategic planning in order to balance supply with needs and demand”. At the facility level, some informants were concerned about the shortage of managers (e.g. in Algeria), while others were concerned about management quality. In Suriname, there was a call for “accountable management of health institutions and organizations – managers who can create a positive and stimulating working environment for health workers”.
Health worker numbers
In all regions and most countries, informants thought that the number of health-care workers should be increased. In Costa Rica, for example, informants said that more “specialists, health technicians and nursing assistants” were needed. In many countries across all four regions, there was concern about the out-migration of human resources, particularly doctors and nurses. In Jordan, there was a call for a “national plan to manage and contain the migration (i.e. brain drain) of health professionals”.
Distribution of health workers
In almost all countries, there were disparities in the distribution of health workers between regions, between rural and urban areas, and between public and private sectors. One informant in Algeria commented that although only 8% of the population lives in Algiers, 24% of specialist physicians are located there. In Argentina, the “poor regional distribution” of educational centres needed to be addressed. In many countries (e.g. Algeria and Egypt), the public sector had more difficulty recruiting or retaining human resources than the private sector. In Uganda, one informant reported that workers leave the public sector for the private for-profit sector because of low salaries, heavy workloads and the absence of other incentives. It was reported in several countries that dual practice (i.e. public sector employees practising in the private sector) has had a negative impact on the quality and cost-effectiveness of services provided by the public sector. In the United Republic of Tanzania, where dual practice was identified as an important policy challenge, some informants called for clear policy and regulatory instruments to limit the number of “stolen hours”.
Efficient use
Informants expressed concerns about inappropriate ratios of health-care workers, both relative to one another and relative to the burden of illness. For example, in Argentina it was felt that there were too many specialists relative to general practitioners and too many general practitioners relative to nurses. In Algeria, there was a call to modify training curricula to take better account of the epidemiological transition and to adapt programmes targeted at “new” pathologies. In Costa Rica, it was felt that there should be increases in certain specialty HRH areas to address the needs of an ageing population. Also in Costa Rica, it was suggested that some university training programmes could be closed if they “were not aligned with the country’s needs”. In Jordan and in Peru, it was suggested that training curricula should be changed to reflect health sector needs better.
Performance
Often informants simply expressed concerns about the performance of health workers, without mentioning any related intervention. For example, in El Salvador one informant called for an increase in the quality and “warmth” of health-care workers.
In many countries, informants expressed the need to improve monetary and non-monetary incentives for health workers. In Costa Rica, informants stated that wages should be increased in the public sector to match those in the private sector, so as to reduce the flow of trained staff to the private sector. Non-monetary incentives included: in Egypt, career development opportunities; in the Dominican Republic, job “stability” and a reduction in the continuous transfer of staff from one location to another; and, in Nicaragua, the availability of appropriate equipment and instruments.
Informants also had concerns about the quality of health worker training, mechanisms for accrediting training institutions, and the licensing and re-licensing of health-care workers. In Algeria, they said that several problems at training institutions needed to be addressed, including “overload and the low quality of teaching”. In several countries (e.g. Peru), they suggested the need for accreditation or regulation of HRH education. In many locations (i.e. Costa Rica, the Dominican Republic, Egypt, Panama, the Plurinational State of Bolivia, the Syrian Arab Republic, Tunisia, and the West Bank and Gaza Strip), informants commented on the need to develop continuing medical education programmes. In Egypt, they were concerned about the absence of re-licensing programmes, while in Jordan they suggested that re-licensing should be linked to a system of continuing medical education.
Research priorities
Table 2 lists details of the research questions that emerged from key informant interviews, the quality of existing research on these questions, and any literature reviews identified that dealt with them.
LMIC, low- and middle-income country; HIC, high-income country.
Ranking the questions
Participants in the consultative workshop reviewed and refined the list of research questions before ranking them. The objective was to increase the clarity rather than change the focus of the questions. For example, question 15 on worker substitution was refined to read: “What are the conditions, regulations, and financial and other inputs required to most efficiently and optimally implement task-shifting?” Workshop participants opted to add one additional question that could be inferred from the original list but was not explicitly stated: “What are the barriers to and facilitators of the implementation of HRH plans?”
Based on a literature review of previous priority-setting exercises, Alliance HPSR staff proposed three criteria for ranking the final 22 questions:
- Can the research question be answered?
- Are the results of the research likely to improve health?
- Is there a lack of research on this topic?
Workshop participants agreed to these criteria and decided that they should be weighted equally in deriving combined scores.
Table 3 ranks the 22 research questions according to the average scores awarded by workshop participants. The question that ranked first overall – “To what extent do financial and non-financial incentives work in attracting and retaining qualified health workers in underserviced areas?” – also received the highest scores for both answerability and potential health impact. We also assessed the sensitivity of the overall ranking to a change in the weighting of the three ranking criteria: we assessed the effect of doubling the weighting of the potential health impact (i.e. the second criterion) relative to the others. The top five questions remained exactly the same, though the question – “What is the impact of dual practice?” – dropped to fourth place. Workshop participants agreed that the final ranking reflected the groups beliefs.
LIMIC, low- and middle-income countries.
In subsequent discussions, workshop participants felt that the quantity and distribution of health workers was the most critical issue and that research on improving the internal migration and distribution of existing health workers was more important than research into increasing health worker supply or international migration. Participants also thought that it was important to evaluate experience already gained at national and subnational levels with experimentation on dual practice and incentives for retaining health workers in underserved areas. Next, participants felt that improving the performance of existing health workers by reducing dual practice and examining financial incentives could have a significant impact in the short term.
A list of 21 research questions emerged from key informant interviews across 24 LMICs, with the most highly ranked concerning how to improve the distribution and efficient use of health workers. While each broad research topic was common to several countries or regions, there was considerable variation in specific sub-topics. The overview of systematic reviews provided little insight into the relative importance of research questions as many had received little or no attention and authors generally suggested that additional research was still required.
There were several limitations to this exercise. The methods were not standardized across regions. For example, it was difficult to compare findings obtained using a more quantitative and deductive approach in Latin America and the Caribbean with those obtained using a more qualitative and inductive approach in the Middle East and North Africa. In addition, since regions, countries and informants were purposively selected, the results may not be representative and generalizable. The literature review covered only English-language publications, though the exercise is being repeated for Portuguese- and Spanish-language literature. The study did not assess the extent to which research currently being carried out in LMICs might address the research questions because surveying the HRH researchers or funders involved was felt to be beyond its scope. The data collected were categorized using a predetermined conceptual framework and categories not included in the framework may have been neglected. Finally, the researchers who ranked the research questions may have scored issues of personal interest more highly, though this is unlikely, as there was no budget under discussion.
In future priority-setting exercises, how best to translate policy priorities into research questions should be more closely examined. Key informants consulted in this study had much more difficulty discussing research questions than policy concerns, and study team leaders were largely responsible for translating one into the other. This may have introduced a bias because country and regional team leaders may, for example, have neglected policy concerns they felt to be less interesting or researchable. Our study partly compensated for this possible bias by mapping policy concerns (categorized by outcomes of HRH policies) and research questions (categorized by policy interventions or levers) onto a common conceptual framework. This process required those carrying out the final data analysis to reconsider whether each outcome or intervention category had been mentioned during the interviews.
Nevertheless, this is the first study that has carefully documented the engagement of a diverse group of stakeholders, including researchers, policy-makers, civil society representatives and community members, in four geographical regions and 24 LMICs in identifying global research priorities. Because of the geographical diversity of the data, the findings are likely to be transferable to many LMICs. Further, by focusing on HRH issues, the study has produced more specific conclusions than previous, broad, priority-setting exercises.
The relatively small number of literature reviews identified ( Table 2 ) suggests that priority research questions could first be investigated through systematic, desk-based literature reviews. Thereafter, original research will probably involve a range of approaches. Large-scale quantitative work may be required to determine the effects of some HRH interventions, qualitative work may be needed to investigate implementation processes, and multinational case studies may involve both approaches. Currently, there is an active debate on establishing quality in health systems research. 35
Since many HRH policy issues are complex, policy-makers need data from several different research perspectives and research funders will have to coordinate efforts to ensure progress. Recently, the Alliance HPSR, in collaboration with the WHO Human Resources for Health Department and the Global Health Workforce Alliance, started to investigate the top-ranked research question, on the effectiveness of financial and non-financial incentives. Further, the Bulletin of the World Health Organization published a theme issue in May 2010 on increasing access to health workers in underserved areas. 36 In the United Kingdom of Great Britain and Northern Ireland, the Department for International Development has issued a request for research proposals on task-shifting and strategies for scaling-up pre-service training.
This study has demonstrated that there is considerable consensus about the type of HRH policy problems faced by different countries and the nature of evidence needed. However, little research has been carried out in LMICs. 4 Research on strategies for improving the distribution, retention, motivation and performance of health workers, as well as on controlling dual practice, is urgently needed. The results could ultimately have a major impact on the health of the poor.
Acknowledgements
Salla Atkins is also affiliated with the Division of International Health, Department of Public Health Sciences, Karolinska Institutet, Stockholm, Sweden.
The authors would like to thank Sarah Hoibak and Angus Steele for their contributions to the literature review and Taghreed Adam, Maia Ambegaokar, Fadi El-Jardali, Gilles Dussault and Felix Rigoli for commenting on the manuscript. We also wish to thank the many colleagues who contributed to the Alliance for HPSR’s priority-setting work, including: Delius Asiimwe and Gaspar Munishi (East Africa report); Gonzalo Urcullo, Rodrigo Muñoz and Ricardo Bitrán (Latin America and the Caribbean report); Soewarta Kosen (South-East Asia report); Fadi El-Jardali, Judy Makhoul, Diana Jamal and Victoria Tchaghchaghian (Middle East and North Africa report); Shirley Williams; George Gotsadze; the many country-based investigators; and participants in the workshop in Berkeley, USA.
This study was funded by the WHO Alliance for Health Policy and Systems Research.
Competing interests:
None declared.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diabetes Overview
Healthy Living with Diabetes
- Español
On this page:
How can I plan what to eat or drink when I have diabetes?
How can physical activity help manage my diabetes, what can i do to reach or maintain a healthy weight, should i quit smoking, how can i take care of my mental health, clinical trials for healthy living with diabetes.
Healthy living is a way to manage diabetes . To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products.
Healthy living may help keep your body’s blood pressure , cholesterol , and blood glucose level, also called blood sugar level, in the range your primary health care professional recommends. Your primary health care professional may be a doctor, a physician assistant, or a nurse practitioner. Healthy living may also help prevent or delay health problems from diabetes that can affect your heart, kidneys, eyes, brain, and other parts of your body.
Making lifestyle changes can be hard, but starting with small changes and building from there may benefit your health. You may want to get help from family, loved ones, friends, and other trusted people in your community. You can also get information from your health care professionals.
What you choose to eat, how much you eat, and when you eat are parts of a meal plan. Having healthy foods and drinks can help keep your blood glucose, blood pressure, and cholesterol levels in the ranges your health care professional recommends. If you have overweight or obesity, a healthy meal plan—along with regular physical activity, getting enough sleep, and other healthy behaviors—may help you reach and maintain a healthy weight. In some cases, health care professionals may also recommend diabetes medicines that may help you lose weight, or weight-loss surgery, also called metabolic and bariatric surgery.
Choose healthy foods and drinks
There is no right or wrong way to choose healthy foods and drinks that may help manage your diabetes. Healthy meal plans for people who have diabetes may include
- dairy or plant-based dairy products
- nonstarchy vegetables
- protein foods
- whole grains
Try to choose foods that include nutrients such as vitamins, calcium , fiber , and healthy fats . Also try to choose drinks with little or no added sugar , such as tap or bottled water, low-fat or non-fat milk, and unsweetened tea, coffee, or sparkling water.
Try to plan meals and snacks that have fewer
- foods high in saturated fat
- foods high in sodium, a mineral found in salt
- sugary foods , such as cookies and cakes, and sweet drinks, such as soda, juice, flavored coffee, and sports drinks
Your body turns carbohydrates , or carbs, from food into glucose, which can raise your blood glucose level. Some fruits, beans, and starchy vegetables—such as potatoes and corn—have more carbs than other foods. Keep carbs in mind when planning your meals.
You should also limit how much alcohol you drink. If you take insulin or certain diabetes medicines , drinking alcohol can make your blood glucose level drop too low, which is called hypoglycemia . If you do drink alcohol, be sure to eat food when you drink and remember to check your blood glucose level after drinking. Talk with your health care team about your alcohol-drinking habits.

Find the best times to eat or drink
Talk with your health care professional or health care team about when you should eat or drink. The best time to have meals and snacks may depend on
- what medicines you take for diabetes
- what your level of physical activity or your work schedule is
- whether you have other health conditions or diseases
Ask your health care team if you should eat before, during, or after physical activity. Some diabetes medicines, such as sulfonylureas or insulin, may make your blood glucose level drop too low during exercise or if you skip or delay a meal.
Plan how much to eat or drink
You may worry that having diabetes means giving up foods and drinks you enjoy. The good news is you can still have your favorite foods and drinks, but you might need to have them in smaller portions or enjoy them less often.
For people who have diabetes, carb counting and the plate method are two common ways to plan how much to eat or drink. Talk with your health care professional or health care team to find a method that works for you.
Carb counting
Carbohydrate counting , or carb counting, means planning and keeping track of the amount of carbs you eat and drink in each meal or snack. Not all people with diabetes need to count carbs. However, if you take insulin, counting carbs can help you know how much insulin to take.
Plate method
The plate method helps you control portion sizes without counting and measuring. This method divides a 9-inch plate into the following three sections to help you choose the types and amounts of foods to eat for each meal.
- Nonstarchy vegetables—such as leafy greens, peppers, carrots, or green beans—should make up half of your plate.
- Carb foods that are high in fiber—such as brown rice, whole grains, beans, or fruits—should make up one-quarter of your plate.
- Protein foods—such as lean meats, fish, dairy, or tofu or other soy products—should make up one quarter of your plate.
If you are not taking insulin, you may not need to count carbs when using the plate method.

Work with your health care team to create a meal plan that works for you. You may want to have a diabetes educator or a registered dietitian on your team. A registered dietitian can provide medical nutrition therapy , which includes counseling to help you create and follow a meal plan. Your health care team may be able to recommend other resources, such as a healthy lifestyle coach, to help you with making changes. Ask your health care team or your insurance company if your benefits include medical nutrition therapy or other diabetes care resources.
Talk with your health care professional before taking dietary supplements
There is no clear proof that specific foods, herbs, spices, or dietary supplements —such as vitamins or minerals—can help manage diabetes. Your health care professional may ask you to take vitamins or minerals if you can’t get enough from foods. Talk with your health care professional before you take any supplements, because some may cause side effects or affect how well your diabetes medicines work.
Research shows that regular physical activity helps people manage their diabetes and stay healthy. Benefits of physical activity may include
- lower blood glucose, blood pressure, and cholesterol levels
- better heart health
- healthier weight
- better mood and sleep
- better balance and memory
Talk with your health care professional before starting a new physical activity or changing how much physical activity you do. They may suggest types of activities based on your ability, schedule, meal plan, interests, and diabetes medicines. Your health care professional may also tell you the best times of day to be active or what to do if your blood glucose level goes out of the range recommended for you.

Do different types of physical activity
People with diabetes can be active, even if they take insulin or use technology such as insulin pumps .
Try to do different kinds of activities . While being more active may have more health benefits, any physical activity is better than none. Start slowly with activities you enjoy. You may be able to change your level of effort and try other activities over time. Having a friend or family member join you may help you stick to your routine.
The physical activities you do may need to be different if you are age 65 or older , are pregnant , or have a disability or health condition . Physical activities may also need to be different for children and teens . Ask your health care professional or health care team about activities that are safe for you.
Aerobic activities
Aerobic activities make you breathe harder and make your heart beat faster. You can try walking, dancing, wheelchair rolling, or swimming. Most adults should try to get at least 150 minutes of moderate-intensity physical activity each week. Aim to do 30 minutes a day on most days of the week. You don’t have to do all 30 minutes at one time. You can break up physical activity into small amounts during your day and still get the benefit. 1
Strength training or resistance training
Strength training or resistance training may make your muscles and bones stronger. You can try lifting weights or doing other exercises such as wall pushups or arm raises. Try to do this kind of training two times a week. 1
Balance and stretching activities
Balance and stretching activities may help you move better and have stronger muscles and bones. You may want to try standing on one leg or stretching your legs when sitting on the floor. Try to do these kinds of activities two or three times a week. 1
Some activities that need balance may be unsafe for people with nerve damage or vision problems caused by diabetes. Ask your health care professional or health care team about activities that are safe for you.

Stay safe during physical activity
Staying safe during physical activity is important. Here are some tips to keep in mind.
Drink liquids
Drinking liquids helps prevent dehydration , or the loss of too much water in your body. Drinking water is a way to stay hydrated. Sports drinks often have a lot of sugar and calories , and you don’t need them for most moderate physical activities.
Avoid low blood glucose
Check your blood glucose level before, during, and right after physical activity. Physical activity often lowers the level of glucose in your blood. Low blood glucose levels may last for hours or days after physical activity. You are most likely to have low blood glucose if you take insulin or some other diabetes medicines, such as sulfonylureas.
Ask your health care professional if you should take less insulin or eat carbs before, during, or after physical activity. Low blood glucose can be a serious medical emergency that must be treated right away. Take steps to protect yourself. You can learn how to treat low blood glucose , let other people know what to do if you need help, and use a medical alert bracelet.
Avoid high blood glucose and ketoacidosis
Taking less insulin before physical activity may help prevent low blood glucose, but it may also make you more likely to have high blood glucose. If your body does not have enough insulin, it can’t use glucose as a source of energy and will use fat instead. When your body uses fat for energy, your body makes chemicals called ketones .
High levels of ketones in your blood can lead to a condition called diabetic ketoacidosis (DKA) . DKA is a medical emergency that should be treated right away. DKA is most common in people with type 1 diabetes . Occasionally, DKA may affect people with type 2 diabetes who have lost their ability to produce insulin. Ask your health care professional how much insulin you should take before physical activity, whether you need to test your urine for ketones, and what level of ketones is dangerous for you.
Take care of your feet
People with diabetes may have problems with their feet because high blood glucose levels can damage blood vessels and nerves. To help prevent foot problems, wear comfortable and supportive shoes and take care of your feet before, during, and after physical activity.

If you have diabetes, managing your weight may bring you several health benefits. Ask your health care professional or health care team if you are at a healthy weight or if you should try to lose weight.
If you are an adult with overweight or obesity, work with your health care team to create a weight-loss plan. Losing 5% to 7% of your current weight may help you prevent or improve some health problems and manage your blood glucose, cholesterol, and blood pressure levels. 2 If you are worried about your child’s weight and they have diabetes, talk with their health care professional before your child starts a new weight-loss plan.
You may be able to reach and maintain a healthy weight by
- following a healthy meal plan
- consuming fewer calories
- being physically active
- getting 7 to 8 hours of sleep each night 3
If you have type 2 diabetes, your health care professional may recommend diabetes medicines that may help you lose weight.
Online tools such as the Body Weight Planner may help you create eating and physical activity plans. You may want to talk with your health care professional about other options for managing your weight, including joining a weight-loss program that can provide helpful information, support, and behavioral or lifestyle counseling. These options may have a cost, so make sure to check the details of the programs.
Your health care professional may recommend weight-loss surgery if you aren’t able to reach a healthy weight with meal planning, physical activity, and taking diabetes medicines that help with weight loss.
If you are pregnant , trying to lose weight may not be healthy. However, you should ask your health care professional whether it makes sense to monitor or limit your weight gain during pregnancy.
Both diabetes and smoking —including using tobacco products and e-cigarettes—cause your blood vessels to narrow. Both diabetes and smoking increase your risk of having a heart attack or stroke , nerve damage , kidney disease , eye disease , or amputation . Secondhand smoke can also affect the health of your family or others who live with you.
If you smoke or use other tobacco products, stop. Ask for help . You don’t have to do it alone.
Feeling stressed, sad, or angry can be common for people with diabetes. Managing diabetes or learning to cope with new information about your health can be hard. People with chronic illnesses such as diabetes may develop anxiety or other mental health conditions .
Learn healthy ways to lower your stress , and ask for help from your health care team or a mental health professional. While it may be uncomfortable to talk about your feelings, finding a health care professional whom you trust and want to talk with may help you
- lower your feelings of stress, depression, or anxiety
- manage problems sleeping or remembering things
- see how diabetes affects your family, school, work, or financial situation
Ask your health care team for mental health resources for people with diabetes.
Sleeping too much or too little may raise your blood glucose levels. Your sleep habits may also affect your mental health and vice versa. People with diabetes and overweight or obesity can also have other health conditions that affect sleep, such as sleep apnea , which can raise your blood pressure and risk of heart disease.

NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for healthy living with diabetes?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of healthy living for people with diabetes, such as
- how changing when you eat may affect body weight and metabolism
- how less access to healthy foods may affect diabetes management, other health problems, and risk of dying
- whether low-carbohydrate meal plans can help lower blood glucose levels
- which diabetes medicines are more likely to help people lose weight
Find out if clinical trials are right for you .
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for healthy living with diabetes are looking for participants?
You can view a filtered list of clinical studies on healthy living with diabetes that are federally funded, open, and recruiting at www.ClinicalTrials.gov . You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Elizabeth M. Venditti, Ph.D., University of Pittsburgh School of Medicine.
- Ways to Give
- Contact an Expert
- Explore WRI Perspectives
Filter Your Site Experience by Topic
Applying the filters below will filter all articles, data, insights and projects by the topic area you select.
- All Topics Remove filter
- Climate filter site by Climate
- Cities filter site by Cities
- Energy filter site by Energy
- Food filter site by Food
- Forests filter site by Forests
- Freshwater filter site by Freshwater
- Ocean filter site by Ocean
- Business filter site by Business
- Economics filter site by Economics
- Finance filter site by Finance
- Equity & Governance filter site by Equity & Governance
Search WRI.org
Not sure where to find something? Search all of the site's content.

4 Ways Ocean Health is Critical to Human Health Everywhere
The ocean has long sustained coastal communities that rely on it for their food, livelihoods and wellbeing. But these benefits don’t stop at the shoreline. New research commissioned by the Ocean Panel shows that the health of the ocean is directly linked to the health of humans everywhere.
The extent to which ocean health impacts human health is relatively unexplored in science and academia to date. This new research illustrates that a healthy ocean and its biodiversity can offer critical benefits to all people — such as new medicines and technologies, nutritious and sustainable diets and opportunities to bolster physical and mental wellbeing.
But these benefits aren’t a given. Policymakers must act swiftly to curb greenhouse gas emissions, pollution, overfishing and other practices that are degrading the health of the ocean. Otherwise, many of the ocean’s benefits to human health could be lost even as we are just beginning to realize their full potential.
1) A Healthy Ocean Enhances Physical and Mental Health and Societal Wellbeing.
Mounting research shows that access to the ocean can directly benefit human health — specifically in communities that have socioeconomic disadvantages and typically less access to nature .
Research finds coastal residents are more likely than inland dwellers to meet recommended levels of physical activity. This reduces the risk of many non-communicable diseases, such as cardiovascular disease and diabetes. The ocean also has positive impacts on mental health. For example, in Indonesia during the Covid-19 pandemic, exposure to and interaction with the ocean served as a ‘buffer’ against negatives outcomes like depression and anxiety.
These effects are so strong that some medical practitioners are starting to administer so-called “ blue prescriptions ,” which call for time spent in natural ocean and coastal spaces to promote health instead of relying on pharmaceuticals.
The ocean’s benefits aren’t reserved for coastal dwellers, either. Globally, $5 trillion is spent each year on coastal and marine tourism. This represents approximately half of all tourism, reflecting the value that visitors place on time spent near the ocean.
These human health benefits are strongest when the ocean itself is healthy. Research suggests that countries with more protected ocean areas have lower mortality rates. Conversely, increased ocean pollution has proven negative health effects. For example, a significant amount of toxic microplastic has been found in seafood. Individuals with identifiable microplastic in their arteries are at a 2.1 times higher risk of a heart attack, nonfatal stroke or death from any cause than individuals without such identifiable microplastics.

2) Ocean Biodiversity Can Inspire New Medicines and Biotechnology.
Marine species have evolved in competition with each other over millions of years to survive in diverse and sometimes extreme ocean environments. During this time, they’ve developed a wide array of adaptations that can help create new medicines and health-related biotechnologies. For example, some bryozoans (sedentary, filter-feeding aquatic invertebrates) create chemical compounds called “bryostatins” when their cells change food into energy. Certain bryostatins are currently being tested as anti-cancer drugs.
Marine-derived medicine is not a new concept. The earliest example dates back some 5,000 years, to China in 2953 BCE . The first marine-based drug approved by the U.S. Food and Drug Administration, Cytarabine , was developed in the late 1960s. To date, twenty-three marine-derived pharmaceuticals have been approved and an additional 33 are in clinical trials and development. These drugs are already used to treat inflammation, immune system disorders, skin pathologies, infectious diseases and cancers.

Advances in marine ‘green chemistry’ are also providing solutions to health issues stemming from fossil fuel-based products. For example, “bioplastics” made from seaweed are currently being produced an alternative to fossil fuel-based plastics. Unlike petroleum-based plastics, these are biodegradable. And they typically contain much lower concentrations of associated harmful chemicals that can, for example, increase the risk of certain cancers. Bioplastics from seaweed can also be molded into health devices such as inhalers or packaging for medicine or food .
These innovations are likely just the tip of the iceberg. The market for marine-derived pharmaceuticals alone is currently valued at $4.1 billion and anticipated to reach $9.1 billion by 2033. Potential new applications in both biomedicine and biotechnology are being discovered with increasing frequency as more companies invest in this area.
3) A Healthy Ocean Can Support Global Food Security.
Over 3 billion people currently depend on seafood as their main protein source. Sustainably managed, the ocean could produce enough food to nourish many more . This offers a critical pathway toward improving food security in a world where around 828 million people still suffer from hunger and more than 3.1 billion are unable to afford a healthy diet.
But ocean-based food sources are threatened on multiple fronts.
Climate change is warming the ocean , increasing its acidity and decreasing its oxygen content. This is disrupting marine food chains and shrinking certain fish populations — including some of the more nutritious and commercially important seafood species. Even if global warming is limited to below 2 degrees C (3.6 degrees F), the availability of key nutrients such as iron, calcium and omega-3 from catches is expected to fall by 10% due to species decline. Under a “business as usual” scenario, where global warming may reach 4-5 degrees C (7.2-9 degrees F) by 2100, nutrients from fisheries could decrease by 30% .
Marine pollutants, overfishing, illegal fishing and globalization also strain fishery stocks and put fishers’ livelihoods at risk. Illegal, unregulated and unreported fishing is estimated to cost low- and middle-income nations between $2 billion and $15 billion annually.
Solutions to these threats are typically most successful when they involve those most impacted: the local communities that rely on fisheries for their food and livelihoods.
In Timor-Leste, for example — a country where acute food insecurity and chronic malnutrition are widespread — the research organization WorldFish has been working with local fishers and government to improve fishery policy and management systems. This includes taking steps to maximize nutrient yields, such as by targeting more nutritious species and overcoming barriers to increased fish consumption. They’ve developed new products that extend shelf life, extended supply chains inland to reach more people and shared tips on preparing fish for children. The approach appears to be leading to increased fish consumption for malnourished groups such as children.

4) A Sustainable Ocean-based Economy Provides Opportunities to Improve Health and Address Inequity.
The ocean isn’t just a source of medicine, food and recreation. It’s a major economic driver, with ocean-based industries and activities contributing approximately $2.5 trillion to the global economy each year. Fisheries, aquaculture operations and the fishery supply chain support the work of more than 500 million people worldwide. Their incomes directly impact theirs and their families’ health through access to food, healthcare and other necessities. Intact coastal ecosystems also serve as a buffer against climate change impacts like storms and floods which can destroy homes, livelihoods and infrastructure.
These benefits are only possible if the ocean’s resources and ecosystems are managed responsibly. Unsustainable practices — such as overfishing and the degradation of coastal ecosystems — both diminish the ocean economy and increase social inequity by threatening the health and livelihoods of those that are most dependent upon it. Climate-induced declines in ocean health could cost the global economy $428 billion per year by 2050 and $1.979 trillion per year by 2100.
In some places, individuals and institutions are collaborating to drive bottom-up behavioral change toward a more equitable ocean economy. In Bangladesh, for instance, communities of fishers have started to form self-developing networks and cooperatives. Members typically contribute to a common fund which provides financial support and fishing equipment to those most in need, such as people requiring medical treatment. Such networks and cooperatives can also enhance fishers’ political strength when negotiating with government agencies and can lead to increased compliance with fishing regulations. For example, Bangladesh’s Hilsa Guard network monitors compliance of their peers with temporal fishing bans.
But top-down change is also critical. National governments must work toward a more equitable ocean economy, such as by developing and implementing Sustainable Ocean Plans (a national policy tool for holistic ocean management).
How Can Leaders Protect Ocean Health and Human Health Simultaneously?
While a healthy ocean is essential for human health, the reverse is also true: Continuing to degrade the ocean through pollution, human-induced climate change and unsustainable management poses serious threats to physical and mental health as well as food security and the global economy. Governments must act urgently to safeguard the ocean so that it can continue to support human health and wellbeing everywhere. Ocean Panel’s report presents three key actions to promote equity, sustainability, biodiversity and human flourishing:
- Protect, restore and manage marine biodiversity: The huge potential for marine medicines, biotechnology and food depends on effectively protecting and managing marine biodiversity. To achieve this, nations must work in collaboration with local resource users to ratify and implement key frameworks that can help ensure protections. These include the Global Biodiversity Framework, the WTO Fisheries Subsidies Agreement and the recent High Seas Treaty. These global actions will protect and restore the ocean, improve human health and wellbeing and reduce stressors on ocean ecosystems.
- Combat climate change and eliminate pollution: Slowing the effects of climate change and removing ocean pollutants is imperative to protecting marine ecosystems and the services they provide. National commitments to the Paris Agreement, the COP28 outcomes and the UN Global Plastics Treaty (currently in negotiation) must be upheld. To protect human health and wellbeing, the negotiators of the UN Global Plastics Treaty must ensure that it imposes strict safety requirements on the more than 10,000 synthetic chemicals added to plastics, a mandatory cap on global plastic production, and mechanisms to curb the manufacture of single-use plastics.
- Improve ocean and human health measurement to support equity: Evidence and linked indicators of ocean health and human health must be incorporated by governments and the healthcare sector into all policies and decision-making around ocean-human interactions. This data should be shared widely and made available and accessible. Through continued measurement, the effectiveness of health and ocean management policies can be assessed, unintended consequences detected, and improvements and course corrections made.
These actions should not be limited to those working in sustainability or conservation sectors, either. As trusted members of society, health professionals can play a key role in safeguarding both ocean health and human health by advocating for change, advancing equity and promoting sustained global action on responsible ocean management. A more ocean-literate health sector can also reduce the health sector’s carbon footprint and help cut medical waste and pollution.
The National Health Service (NHS) in the U.K., for example, serves a population of 67 million people and imports 80% of its goods via maritime routes, generating harmful greenhouse gas emissions. The NHS aims to tackle this through its target to reach net zero-emissions by 2045 . Similarly, some health sector professionals are already working to drive change in this area.
Taken together, these actions can ensure that the ocean is able to thrive and that we can fully harness its benefits to uplift people everywhere.
Relevant Work
Climate change poses an existential risk to ocean industries. here’s how they can respond., 5 pillars of a new ocean agenda, what is kelp and why is it vital to people and the planet, 4 sustainable ocean strategies that yield economic benefits, how you can help.
WRI relies on the generosity of donors like you to turn research into action. You can support our work by making a gift today or exploring other ways to give.
Stay Informed
World Resources Institute 10 G Street NE Suite 800 Washington DC 20002 +1 (202) 729-7600
© 2024 World Resources Institute
Join our live presentation on Jan 23rd as we present four stories that will shape 2024, followed by a live Q&A.

Together, we can unleash the positive, tangible and system-wide transformations needed to protect our planet for this and future generations.

COMMENTS
Human Resources for Health calls for papers on 'The abiding, hidden, and pervasive centrality of the health research workforce'.. This Collection calls for papers that go beyond narrow conceptual approaches and professional understandings of health care workers and the health research workforce, and requests that contributors examine important workforce issues through the broad lens of ...
With data from 194 Member States as of 2020, the global health workforce is estimated to be 65 million, reflecting growth of 29% since the adoption in 2016 of the Global Strategy on Human Resources for Health: workforce 2030, as well as improved data availability and predicted employment trends in the High-Level Commission on Health Employment and Economic Growth. This data supported ...
Background. This Commentary is a joint publication by Human Resources for Health and Health Research Policy and Systems.. Health workers are central to people-centred health systems, resilient economies and sustainable development [1, 2].Progress on these global goals depends on the effective deployment of capable and motivated health workers, in a timely manner to places where they are needed ...
We also estimate that 30-50% or about $4 billion of development assistance for health is devoted to human resources—salaries, allowances, training, education, technical assistance, and capacity building. Current spending patterns on human resources are fragmented and inefficient.
Human resource management research in healthcare: a big data bibliometric study Authors (first, second and last of 7) Xiaoping Qin ... Article: 94; The transition of human resources for health information systems from the MDGs into the SDGs and the post-pandemic era: reviewing the evidence from 2000 to 2022 Authors (first, second and last of 4 ...
The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Nader Salari. Habibolah Khazaie. Soudabeh Eskandari. Research. Open Access. Published: 17 December 2020. Article: 100.
8 A HEALTH POLICY AND SYSTEMS RESEARCH READER ON HUMAN RESOURCES FOR HEALTH Newman CJ, et al. (2011). Workplace violence and gender discrimination in Rwanda's health workforce: increasing safety and gender equality. Hum Resour Health. 9(19):1-13 ..... 395 Nigenda G, Solorzano A (1997).
It is vital to address the issues of human resources for health in all countries. While there has been much progress in this field, the challenges ahead are daunting. ... budgeting, cost control and financial management, record and information systems, health systems research, health legislation and ethics, technology assessment, accreditation ...
Human Resources for Health is calling for submissions to our Collection on The abiding, hidden, and pervasive centrality of the health research workforce. Research for health and development (R4HD) acknowledges that many of the determinants of health lie outside the boundaries of the health system. Understanding the health researchers' labor ...
The Human Resources for Health (HRH) account for all people engaged in actions whose primary aim is to enhance health. 1 The HRH are considered a key 'building block' of health systems. 2 Moreover ...
The Human Resources for Health (HRH) curricula package structures three curricula to recognize, formalize and build a critical mass of leaders and managers in the much needed area of HRH. ... analysis and intelligence; and research. The Overview document is an accompaniment to each of the three prototype curricula for a one year master's ...
This perspective article highlights the potential of underutilized health policy and systems research (HPSR) approaches for developing more effective human resources for health policy. The example of health worker motivation is used to showcase four types of HPSR (exploratory, influence, explanatory and emancipatory) that move beyond describing ...
Health workers are central to people-centred health systems, resilient economies and sustainable development. Given the rising importance of the health workforce, changing human resource for health (HRH) policy and practice and recent health policy and systems research (HPSR) advances, it is critical to reassess and reinvigorate the science behind HRH as part of health systems strengthening ...
The Fourth Global Forum on Human Resources for Health, held in Dublin, Ireland, in November 2017, brought unprecedented momentum to the intersectoral health workforce agenda and the investment case for human resources for health, culminating in the adoption of the Dublin Declaration.1 The forum leveraged the political capital built through the ...
This Commentary is a joint publication by Human Resources for Health and Health Research Policy and Systems.. Health workers are central to people-centred health systems, resilient economies and sustainable development [1, 2].Progress on these global goals depends on the effective deployment of capable and motivated health workers, in a timely manner to places where they are needed, so that ...
Background. Very few reviews exist which examine the policies and interventions adopted in high- and middle-income countries to tackle challenges related to the availability, distribution, and performance of human resources for health (HRH) [].More commonly, literature and evidence reviews have focused on low- and lower middle-income countries [2-4]; however, the challenges in higher-income ...
Given the rising importance of the health workforce, changing human resource for health (HRH) policy and practice and recent health policy and systems research (HPSR) advances, it is critical to reassess and reinvigorate the science behind HRH as part of health systems strengthening and social development more broadly. Building on the recently
The studies on Health services research discussed at the published papers can also contribute to research in the domains of Workforce, Human resources and Health policy. In addition to Health administration research, the journal articles aim to explore topics under Psychological intervention, Rural area, Job satisfaction and Family medicine.
Though the human resources function was once a strong advocate for employees, in the 1980s things changed. As labor markets became slack, HR shifted its focus to relentless cost cutting. Because ...
Join us in the Health Professions Building atrium for the 7th Annual Herbert H. and Grace A. Dow College of Health Professions Research Symposium. The symposium will feature research projects completed by faculty, staff, and students. This event has been generously sponsored by Gary Russell and Barb Anderson Russell since 2021. Date: - Time ...
The University of Alabama at Birmingham (UAB) Marnix E. Heersink School of Medicine saw great success in acquiring research funding in 2023, making significant strides in securing resources to advance human health through biomedical discovery. Multiple Departments Rank in Top 20 in NIH Funding ...
In the last few years, increasing attention has been paid to the development of health policies. But side by side with the presumed benefits of policy, many analysts share the opinion that a major drawback of health policies is their failure to make room for issues of human resources. Current approaches in human resources suggest a number of weaknesses: a reactive, ad hoc attitude towards ...
Modern machine learning approaches have led to performant diagnostic models for a variety of health conditions. Several machine learning approaches, such as decision trees and deep neural networks, can, in principle, approximate any function. However, this power can be considered to be both a gift and a curse, as the propensity toward overfitting is magnified when the input data are ...
Since human resources account for approximately 70% of recurrent expenditure in most health systems, inadequate human resource training, regulation, distribution and management can have enormous implications. 1 Many low- and middle-income countries (LMICs), particularly in sub-Saharan Africa, suffer from both a shortage of health-care providers ...
Your health care team may be able to recommend other resources, such as a healthy lifestyle coach, to help you with making changes. Ask your health care team or your insurance company if your benefits include medical nutrition therapy or other diabetes care resources. Talk with your health care professional before taking dietary supplements
U.S. Department of Veterans Affairs | 810 Vermont Avenue, NW Washington DC 20420. Updated/Reviewed: 2024-04-05
New research shows how strongly ocean health is linked to human health, and how warming seas and pollution aren't just bad for the ocean but for people, too. ... These benefits are only possible if the ocean's resources and ecosystems are managed responsibly. Unsustainable practices — such as overfishing and the degradation of coastal ...