
Beyond the pages of academic medicine


10 Tips for Reviewing a Qualitative Paper

Editor’s Note: The following post is part of a series of Peer Reviewer Resources written by some of Academic Medicine ‘s top peer reviewers. Read other peer review posts .
By: Carol-anne Moulton, MD, FRACS, MEd, PhD, Department of Surgery, University of Toronto, and Priyanka Patel, MSc, Wilson Center, University Health Network, University of Toronto
This is a tough task. Let us say that off the bat. We have been involved in qualitative research for a long time now and the complexity of it never ceases to amaze us…so there is no “how to” guide that will suit all qualitative research.
Having said that, we think there are some guiding principles that can help us begin to understand the rigor of qualitative research and consequently the review process.
- Question/Purpose : This should be clearly stated, as in all research studies. There are generally no hypotheses statements in qualitative research as we are not testing but rather exploring. Ideally, the questions are framed around how and why type questions, rather than how often, is there a difference, or what are the factors type questions.
- Rationale of study : We like to make sure that the study was built upon a well justified and referenced rationale. It may not be our area of study but we think it is important for the authors to provide rationale for their study by building up the arguments from the literature. Theories or pre-existing frameworks that informed the research question should be described up front. Some work claims to be atheoretical. Traditionally, grounded theorists claimed their work to be atheoretical, but nowadays many grounded theorists are acknowledging being informed by particular perspectives, frameworks, or theories. This should be made explicit.
- Methodology described : What type of research was this? Ethnography? Grounded theory? Phenomenology? Discourse analysis? It’s important that the researchers describe their research journey in a clear and detailed enough way to give the readers an understanding for how the analyses evolved. This should include an explanation of why the methodological approach was used, as well as the key principles from the methodology that guided the study.
- Epistemology : Researchers come from all paradigms and it is important to identify within which paradigm the authors are situated. Sometimes they might state deliberately “We have used constructivist grounded theory,” but it might be a matter of reading between the lines to figure it out. If from the positivist paradigm, authors might use the terms valid or verified to imply they are making statements of truth. The paradigm helps us understand what the authors mean by “truth” and informs how they went about creating knowledge and constructing meaning from their results.
- Context described satisfactorily : Qualitative research is not meant to imply generalizability. In fact, we celebrate the importance of context. We recognize that the phenomena we study are often different in meaningful ways when taken to a different context. For example, the experiences of physicians coping with burnout may be unique based on specialty and/or institution (i.e. type of systems-level support available, differing demands in academic or community institutions). A good qualitative study should therefore describe sufficient details of context (i.e. physical, cultural, social, and/or environmental context) in which the research was conducted to allow the reader to make judgments of whether the results might be transferable to another (possibly their own) setting.
- Data collection and analysis : Do they provide enough information to understand the collection and analysis process? As reviewers, we often ask ourselves whether the data collection and analyses are clear and detailed enough for us to gain a sense of how the analysis of the phenomena evolved. For example, who made up the research team? Because most knowledge is viewed as a co-construction between researcher and participants, each individual (e.g. a sociologist versus a surgeon) will analyze the results differently, but both meaningfully, based on their unique position and perspective.
- Sampling strategies : These are very important to understand whether the question was aligned with the data collection process. The sample reflects the type of results achieved and helps the reader understand from which perspective the data was collected. Some common sampling strategies include theoretical sampling and negative case sampling. Researchers may theoretically sample by selecting participants that in someway inform their understanding of an emergent theme or idea. Negative case sampling may be used to search for instances that may challenge the emergent patterns from the data for the purpose of refining the analysis. Negative case sampling is used to ensure that the researchers are not specifically selecting cases that confirm their findings.
- Analysis elevated beyond description : Results might be descriptive in nature (e.g. “One surgeon felt upset and isolated after he experienced a hernia complication in his first month of independent practice”) or they might be elevated to create more abstract concepts and ideas removed from the primary dataset (e.g. characterizing the phases of surgeons’ reactions to complications). In either case, the researcher should ensure that the way they present their findings are aligned with principles of the methodology used.
- Proof of an iterative process : Qualitative research is usually done in an iterative manner where ideas and concepts are built up over time and occur through cycles of data collection and data analysis. This is demonstrated through statements like “Our interview template was altered over time to reflect the emergent ideas through the analysis process,” or “As we became interested in this concept, we began to sample for…”.
- Reflexivity : This is tough to understand, especially for those of us who come from the positivist paradigm where it is of utmost importance to “prove” that the results are “true” and untainted by bias. The aim of qualitative research is to understand meaning rather than assuming that there is a singular truth or reality. A good qualitative researcher recognizes that the way they make sense of and attach meaning to the data is partly shaped by the characteristics of the researcher (i.e. age, gender, social class, ethnicity, professional status, etc.) and the assumptions they hold. The researcher should make explicit the perspectives they are coming from so that the readers can interpret the data appropriately. Consider a study exploring the pressures surgical trainees experience in residency conducted by a staff surgeon versus a non-surgical anthropologist. You can imagine the findings may differ based on the types of questions the two interviewers decide to ask, what they each find interesting or important, or how comfortable the resident feels discussing sensitive information with an outsider (anthropologist) as opposed to an insider (surgeon). We like to see that a researcher has reflected on how her or his unique position, preconceptions, and biases influenced the findings.
19 thoughts on “ 10 Tips for Reviewing a Qualitative Paper ”
Pingback: Qualitative Review in Nursing - Nursing Papers 247
Pingback: Qualitative Review in Nursing - Essay Don
Pingback: Qualitative Review in Nursing - Assignmentnerds.net
Pingback: Qualitative Review in Nursing - Academia Essays
Pingback: qualitative review in nursing - Superb Papers
Pingback: Qualitative Review in Nursing - Allessaysexpert
Pingback: Qualitative Review in Nursing - Chip Writers
Pingback: Science - Technical Assignments
Pingback: Qualitative Review in Nursing – fastwriting
Pingback: Qualitative Review in Nursing – EssaySolutions.net
Pingback: Qualitative Review in Nursing - Homework Market
Pingback: Qualitative Review in Nursing - Midterm Essays
Pingback: Qualitative Review in Nursing - Tutoring Beast
Pingback: Qualitative Review in Nursing - StudyCore
Pingback: Qualitative Review in Nursing - Custom Nursing Essays
Pingback: qualitative review in nursing - Gradesmine.com
Pingback: Qualitative Review in Nursing - Master My Course
Pingback: Qualitative Review in Nursing - Proficient Essay Help
Pingback: Qualitative Review in Nursing - Eliteprofessionalwriters.com
Comments are closed.
Discover more from AM Rounds
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 22, Issue 1
- How to appraise qualitative research
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Calvin Moorley 1 ,
- Xabi Cathala 2
- 1 Nursing Research and Diversity in Care, School of Health and Social Care , London South Bank University , London , UK
- 2 Institute of Vocational Learning , School of Health and Social Care, London South Bank University , London , UK
- Correspondence to Dr Calvin Moorley, Nursing Research and Diversity in Care, School of Health and Social Care, London South Bank University, London SE1 0AA, UK; Moorleyc{at}lsbu.ac.uk
https://doi.org/10.1136/ebnurs-2018-103044
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
In order to make a decision about implementing evidence into practice, nurses need to be able to critically appraise research. Nurses also have a professional responsibility to maintain up-to-date practice. 1 This paper provides a guide on how to critically appraise a qualitative research paper.
What is qualitative research?
- View inline
Useful terms
Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis. The data collection methods used in qualitative research include in depth interviews, focus groups, observations and stories in the form of diaries or other documents. 3
Authenticity
Title, keywords, authors and abstract.
In a previous paper, we discussed how the title, keywords, authors’ positions and affiliations and abstract can influence the authenticity and readability of quantitative research papers, 4 the same applies to qualitative research. However, other areas such as the purpose of the study and the research question, theoretical and conceptual frameworks, sampling and methodology also need consideration when appraising a qualitative paper.
Purpose and question
The topic under investigation in the study should be guided by a clear research question or a statement of the problem or purpose. An example of a statement can be seen in table 2 . Unlike most quantitative studies, qualitative research does not seek to test a hypothesis. The research statement should be specific to the problem and should be reflected in the design. This will inform the reader of what will be studied and justify the purpose of the study. 5
Example of research question and problem statement
An appropriate literature review should have been conducted and summarised in the paper. It should be linked to the subject, using peer-reviewed primary research which is up to date. We suggest papers with a age limit of 5–8 years excluding original work. The literature review should give the reader a balanced view on what has been written on the subject. It is worth noting that for some qualitative approaches some literature reviews are conducted after the data collection to minimise bias, for example, in grounded theory studies. In phenomenological studies, the review sometimes occurs after the data analysis. If this is the case, the author(s) should make this clear.
Theoretical and conceptual frameworks
Most authors use the terms theoretical and conceptual frameworks interchangeably. Usually, a theoretical framework is used when research is underpinned by one theory that aims to help predict, explain and understand the topic investigated. A theoretical framework is the blueprint that can hold or scaffold a study’s theory. Conceptual frameworks are based on concepts from various theories and findings which help to guide the research. 6 It is the researcher’s understanding of how different variables are connected in the study, for example, the literature review and research question. Theoretical and conceptual frameworks connect the researcher to existing knowledge and these are used in a study to help to explain and understand what is being investigated. A framework is the design or map for a study. When you are appraising a qualitative paper, you should be able to see how the framework helped with (1) providing a rationale and (2) the development of research questions or statements. 7 You should be able to identify how the framework, research question, purpose and literature review all complement each other.
There remains an ongoing debate in relation to what an appropriate sample size should be for a qualitative study. We hold the view that qualitative research does not seek to power and a sample size can be as small as one (eg, a single case study) or any number above one (a grounded theory study) providing that it is appropriate and answers the research problem. Shorten and Moorley 8 explain that three main types of sampling exist in qualitative research: (1) convenience (2) judgement or (3) theoretical. In the paper , the sample size should be stated and a rationale for how it was decided should be clear.
Methodology
Qualitative research encompasses a variety of methods and designs. Based on the chosen method or design, the findings may be reported in a variety of different formats. Table 3 provides the main qualitative approaches used in nursing with a short description.
Different qualitative approaches
The authors should make it clear why they are using a qualitative methodology and the chosen theoretical approach or framework. The paper should provide details of participant inclusion and exclusion criteria as well as recruitment sites where the sample was drawn from, for example, urban, rural, hospital inpatient or community. Methods of data collection should be identified and be appropriate for the research statement/question.
Data collection
Overall there should be a clear trail of data collection. The paper should explain when and how the study was advertised, participants were recruited and consented. it should also state when and where the data collection took place. Data collection methods include interviews, this can be structured or unstructured and in depth one to one or group. 9 Group interviews are often referred to as focus group interviews these are often voice recorded and transcribed verbatim. It should be clear if these were conducted face to face, telephone or any other type of media used. Table 3 includes some data collection methods. Other collection methods not included in table 3 examples are observation, diaries, video recording, photographs, documents or objects (artefacts). The schedule of questions for interview or the protocol for non-interview data collection should be provided, available or discussed in the paper. Some authors may use the term ‘recruitment ended once data saturation was reached’. This simply mean that the researchers were not gaining any new information at subsequent interviews, so they stopped data collection.
The data collection section should include details of the ethical approval gained to carry out the study. For example, the strategies used to gain participants’ consent to take part in the study. The authors should make clear if any ethical issues arose and how these were resolved or managed.
The approach to data analysis (see ref 10 ) needs to be clearly articulated, for example, was there more than one person responsible for analysing the data? How were any discrepancies in findings resolved? An audit trail of how the data were analysed including its management should be documented. If member checking was used this should also be reported. This level of transparency contributes to the trustworthiness and credibility of qualitative research. Some researchers provide a diagram of how they approached data analysis to demonstrate the rigour applied ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Example of data analysis diagram.
Validity and rigour
The study’s validity is reliant on the statement of the question/problem, theoretical/conceptual framework, design, method, sample and data analysis. When critiquing qualitative research, these elements will help you to determine the study’s reliability. Noble and Smith 11 explain that validity is the integrity of data methods applied and that findings should accurately reflect the data. Rigour should acknowledge the researcher’s role and involvement as well as any biases. Essentially it should focus on truth value, consistency and neutrality and applicability. 11 The authors should discuss if they used triangulation (see table 2 ) to develop the best possible understanding of the phenomena.
Themes and interpretations and implications for practice
In qualitative research no hypothesis is tested, therefore, there is no specific result. Instead, qualitative findings are often reported in themes based on the data analysed. The findings should be clearly linked to, and reflect, the data. This contributes to the soundness of the research. 11 The researchers should make it clear how they arrived at the interpretations of the findings. The theoretical or conceptual framework used should be discussed aiding the rigour of the study. The implications of the findings need to be made clear and where appropriate their applicability or transferability should be identified. 12
Discussions, recommendations and conclusions
The discussion should relate to the research findings as the authors seek to make connections with the literature reviewed earlier in the paper to contextualise their work. A strong discussion will connect the research aims and objectives to the findings and will be supported with literature if possible. A paper that seeks to influence nursing practice will have a recommendations section for clinical practice and research. A good conclusion will focus on the findings and discussion of the phenomena investigated.
Qualitative research has much to offer nursing and healthcare, in terms of understanding patients’ experience of illness, treatment and recovery, it can also help to understand better areas of healthcare practice. However, it must be done with rigour and this paper provides some guidance for appraising such research. To help you critique a qualitative research paper some guidance is provided in table 4 .
Some guidance for critiquing qualitative research
- ↵ Nursing and Midwifery Council . The code: Standard of conduct, performance and ethics for nurses and midwives . 2015 https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf ( accessed 21 Aug 18 ).
- Barrett D ,
- Cathala X ,
- Shorten A ,
Patient consent for publication Not required.
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- How to Write a Literature Review | Guide, Examples, & Templates
How to Write a Literature Review | Guide, Examples, & Templates
Published on January 2, 2023 by Shona McCombes . Revised on September 11, 2023.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research that you can later apply to your paper, thesis, or dissertation topic .
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates, and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarize sources—it analyzes, synthesizes , and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
What is the purpose of a literature review, examples of literature reviews, step 1 – search for relevant literature, step 2 – evaluate and select sources, step 3 – identify themes, debates, and gaps, step 4 – outline your literature review’s structure, step 5 – write your literature review, free lecture slides, other interesting articles, frequently asked questions, introduction.
- Quick Run-through
- Step 1 & 2
When you write a thesis , dissertation , or research paper , you will likely have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and its scholarly context
- Develop a theoretical framework and methodology for your research
- Position your work in relation to other researchers and theorists
- Show how your research addresses a gap or contributes to a debate
- Evaluate the current state of research and demonstrate your knowledge of the scholarly debates around your topic.
Writing literature reviews is a particularly important skill if you want to apply for graduate school or pursue a career in research. We’ve written a step-by-step guide that you can follow below.
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research problem and questions .
Make a list of keywords
Start by creating a list of keywords related to your research question. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list as you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some useful databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can also use boolean operators to help narrow down your search.
Make sure to read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
You likely won’t be able to read absolutely everything that has been written on your topic, so it will be necessary to evaluate which sources are most relevant to your research question.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models, and methods?
- Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible , and make sure you read any landmark studies and major theories in your field of research.
You can use our template to summarize and evaluate sources you’re thinking about using. Click on either button below to download.
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It is important to keep track of your sources with citations to avoid plagiarism . It can be helpful to make an annotated bibliography , where you compile full citation information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
The only proofreading tool specialized in correcting academic writing - try for free!
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Try for free
To begin organizing your literature review’s argument and structure, be sure you understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly visual platforms like Instagram and Snapchat—this is a gap that you could address in your own research.
There are various approaches to organizing the body of a literature review. Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarizing sources in order.
Try to analyze patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organize your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text , your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, you can follow these tips:
- Summarize and synthesize: give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: don’t just paraphrase other researchers — add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically evaluate: mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: use transition words and topic sentences to draw connections, comparisons and contrasts
In the conclusion, you should summarize the key findings you have taken from the literature and emphasize their significance.
When you’ve finished writing and revising your literature review, don’t forget to proofread thoroughly before submitting. Not a language expert? Check out Scribbr’s professional proofreading services !
This article has been adapted into lecture slides that you can use to teach your students about writing a literature review.
Scribbr slides are free to use, customize, and distribute for educational purposes.
Open Google Slides Download PowerPoint
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a thesis, dissertation , or research paper , in order to situate your work in relation to existing knowledge.
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarize yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your thesis or dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
A literature review is a survey of credible sources on a topic, often used in dissertations , theses, and research papers . Literature reviews give an overview of knowledge on a subject, helping you identify relevant theories and methods, as well as gaps in existing research. Literature reviews are set up similarly to other academic texts , with an introduction , a main body, and a conclusion .
An annotated bibliography is a list of source references that has a short description (called an annotation ) for each of the sources. It is often assigned as part of the research process for a paper .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, September 11). How to Write a Literature Review | Guide, Examples, & Templates. Scribbr. Retrieved April 9, 2024, from https://www.scribbr.com/dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, what is a theoretical framework | guide to organizing, what is a research methodology | steps & tips, how to write a research proposal | examples & templates, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
About Journal
American Journal of Qualitative Research (AJQR) is a quarterly peer-reviewed academic journal that publishes qualitative research articles from a number of social science disciplines such as psychology, health science, sociology, criminology, education, political science, and administrative studies. The journal is an international and interdisciplinary focus and greatly welcomes papers from all countries. The journal offers an intellectual platform for researchers, practitioners, administrators, and policymakers to contribute and promote qualitative research and analysis.
ISSN: 2576-2141
Call for Papers- American Journal of Qualitative Research
American Journal of Qualitative Research (AJQR) welcomes original research articles and book reviews for its next issue. The AJQR is a quarterly and peer-reviewed journal published in February, May, August, and November.
We are seeking submissions for a forthcoming issue published in February 2024. The paper should be written in professional English. The length of 6000-10000 words is preferred. All manuscripts should be prepared in MS Word format and submitted online: https://www.editorialpark.com/ajqr
For any further information about the journal, please visit its website: https://www.ajqr.org
Submission Deadline: November 15, 2023
Announcement
Dear AJQR Readers,
Due to the high volume of submissions in the American Journal of Qualitative Research , the editorial board decided to publish quarterly since 2023.
Volume 8, Issue 1
Current issue.
Social distancing requirements resulted in many people working from home in the United Kingdom during the COVID-19 pandemic. The topic of working from home was often discussed in the media and online during the pandemic, but little was known about how quality of life (QOL) and remote working interfaced. The purpose of this study was to describe QOL while working from home during the COVID-19 pandemic. The novel topic, unique methodological approach of the General Online Qualitative Study ( D’Abundo & Franco, 2022a), and the strategic Social Distancing Sampling ( D’Abundo & Franco, 2022c) resulted in significant participation throughout the world (n = 709). The United Kingdom subset of participants (n = 234) is the focus of this article. This big qual, large qualitative study (n >100) included the principal investigator-developed, open-ended, online questionnaire entitled the “Quality of Life Home Workplace Questionnaire (QOLHWQ)” and demographic questions. Data were collected peak-pandemic from July to September 2020. Most participants cited increased QOL due to having more time with family/kids/partners/pets, a more comfortable work environment while being at home, and less commuting to work. The most cited issue associated with negative QOL was social isolation. As restrictions have been lifted and public health emergency declarations have been terminated during the post-peak era of the COVID-19 pandemic, the potential for future public health emergencies requiring social distancing still exists. To promote QOL and work-life balance for employees working remotely in the United Kingdom, stakeholders could develop social support networks and create effective planning initiatives to prevent social isolation and maximize the benefits of remote working experiences for both employees and organizations.
Keywords: qualitative research, quality of life, remote work, telework, United Kingdom, work from home.
(no abstract)
This essay reviews classic works on the philosophy of science and contemporary pedagogical guides to scientific inquiry in order to present a discussion of the three logics that underlie qualitative research in political science. The first logic, epistemology, relates to the essence of research as a scientific endeavor and is framed as a debate between positivist and interpretivist orientations within the discipline of political science. The second logic, ontology, relates to the approach that research takes to investigating the empirical world and is framed as a debate between positivist qualitative and quantitative orientations, which together constitute the vast majority of mainstream researchers within the discipline. The third logic, methodology, relates to the means by which research aspires to reach its scientific ends and is framed as a debate among positivist qualitative orientations. Additionally, the essay discusses the present state of qualitative research in the discipline of political science, reviews the various ways in which qualitative research is defined in the relevant literature, addresses the limitations and trade-offs that are inherently associated with the aforementioned logics of qualitative research, explores multimethod approaches to remedying these issues, and proposes avenues for acquiring further information on the topics discussed.
Keywords: qualitative research, epistemology, ontology, methodology
This paper examines the phenomenology of diagnostic crossover in eating disorders, the movement within or between feeding and eating disorder subtypes or diagnoses over time, in two young women who experienced multiple changes in eating disorder diagnosis over 5 years. Using interpretative phenomenological analysis, this study found that transitioning between different diagnostic labels, specifically between bulimia nervosa and anorexia nervosa binge/purge subtype, was experienced as disempowering, stigmatizing, and unhelpful. The findings in this study offer novel evidence that, from the perspective of individuals diagnosed with EDs, using BMI as an indicator of the presence, severity, or change of an ED may have adverse consequences for well-being and recovery and may lead to mischaracterization or misclassification of health status. The narratives discussed in this paper highlight the need for more person-centered practices in the context of diagnostic crossover. Including the perspectives of those with lived experience can help care providers working with individuals with eating disorders gain an in-depth understanding of the potential personal impact of diagnosis changing and inform discussions around developing person-focused diagnostic practices.
Keywords: feeding and eating disorders, bulimia nervosa, diagnostic labels, diagnostic crossover, illness narrative
Often among the first witnesses to child trauma, educators and therapists are on the frontline of an unfolding and multi-pronged occupational crisis. For educators, lack of support and secondary traumatic stress (STS) appear to be contributing to an epidemic in professional attrition. Similarly, therapists who do not prioritize self-care can feel depleted of energy and optimism. The purpose of this phenomenological study was to examine how bearing witness to the traumatic narratives of children impacts similar helping professionals. The study also sought to extrapolate the similarities and differences between compassion fatigue and secondary trauma across these two disciplines. Exploring the common factors and subjective individual experiences related to occupational stress across these two fields may foster a more complete picture of the delicate nature of working with traumatized children and the importance of successful self-care strategies. Utilizing Constructivist Self-Development Theory (CSDT) and focus group interviews, the study explores the significant risk of STS facing both educators and therapists.
Keywords: qualitative, secondary traumatic stress, self-care, child trauma, educators, therapists.
This study explored the lived experiences of residents of the Gulf Coast in the USA during Hurricane Katrina, which made landfall in August 2005 and caused insurmountable destruction throughout the area. A heuristic process and thematic analysis were employed to draw observations and conclusions about the lived experiences of each participant and make meaning through similar thoughts, feelings, and themes that emerged in the analysis of the data. Six themes emerged: (1) fear, (2) loss, (3) anger, (4) support, (5) spirituality, and (6) resilience. The results of this study allude to the possible psychological outcomes as a result of experiencing a traumatic event and provide an outline of what the psychological experience of trauma might entail. The current research suggests that preparedness and expectation are key to resilience and that people who feel that they have power over their situation fare better than those who do not.
Keywords: mass trauma, resilience, loss, natural disaster, mental health.
Women from rural, low-income backgrounds holding positions within the academy are the exception and not the rule. Most women faculty in the academy are from urban/suburban areas and middle- and upper-income family backgrounds. As women faculty who do not represent this norm, our primary goal with this article is to focus on the unique barriers we experienced as girls from rural, low-income areas in K-12 schools that influenced the possibilities for successfully transitioning to and engaging with higher education. We employed a qualitative duoethnographic and narrative research design to respond to the research questions, and we generated our data through semi-structured, critical, ethnographic dialogic conversations. Our duoethnographic-narrative analyses revealed six major themes: (1) independence and other benefits of having a working-class mom; (2) crashing into middle-class norms and expectations; (3) lucking and falling into college; (4) fish out of water; (5) overcompensating, playing middle class, walking on eggshells, and pushing back; and (6) transitioning from a working-class kid to a working class academic, which we discuss in relation to our own educational attainment.
Keywords: rurality, working-class, educational attainment, duoethnography, higher education, women.
This article draws on the findings of a qualitative study that focused on the perspectives of four Indian American mothers of youth with developmental disabilities on the process of transitioning from school to post-school environments. Data were collected through in-depth ethnographic interviews. The findings indicate that in their efforts to support their youth with developmental disabilities, the mothers themselves navigate multiple transitions across countries, constructs, dreams, systems of schooling, and services. The mothers’ perspectives have to be understood against the larger context of their experiences as citizens of this country as well as members of the South Asian diaspora. The mothers’ views on services, their journey, their dreams for their youth, and their interpretation of the ideas anchored in current conversations on transition are continually evolving. Their attempts to maintain their resilience and their indigenous understandings while simultaneously negotiating their experiences in the United States with supporting their youth are discussed.
Keywords: Indian-American mothers, transitioning, diaspora, disability, dreams.
This study explored the influence of yoga on practitioners’ lives ‘off the mat’ through a phenomenological lens. Central to the study was the lived experience of yoga in a purposive sample of self-identified New Zealand practitioners (n=38; 89.5% female; aged 18 to 65 years; 60.5% aged 36 to 55 years). The study’s aim was to explore whether habitual yoga practitioners experience any pro-health downstream effects of their practice ‘off the mat’ via their lived experience of yoga. A qualitative mixed methodology was applied via a phenomenological lens that explicitly acknowledged the researcher’s own experience of the research topic. Qualitative methods comprised an open-ended online survey for all participants (n=38), followed by in-depth semi-structured interviews (n=8) on a randomized subset. Quantitative methods included online outcome measures (health habits, self-efficacy, interoceptive awareness, and physical activity), practice component data (tenure, dose, yoga styles, yoga teacher status, meditation frequency), and socio-demographics. This paper highlights the qualitative findings emerging from participant narratives. Reported benefits of practice included the provision of a filter through which to engage with life and the experience of self-regulation and mindfulness ‘off the mat’. Practitioners experienced yoga as a self-sustaining positive resource via self-regulation guided by an embodied awareness. The key narrative to emerge was an attunement to embodiment through movement. Embodied movement can elicit self-regulatory pathways that support health behavior.
Keywords: embodiment, habit, interoception, mindfulness, movement practice, qualitative, self-regulation, yoga.
Historically and in the present day, Black women’s positionality in the U.S. has paradoxically situated them in a society where they are both intrinsically essential and treated as expendable. This positionality, known as gendered racism, manifests commonly in professional environments and results in myriad harms. In response, Black women have developed, honed, and practiced a range of coping styles to mitigate the insidious effects of gendered racism. While often effective in the short-term, these techniques frequently complicate Black women’s well-being. For Black female clinicians who experience gendered racism and work on the frontlines of community mental health, myriad bio-psycho-social-spiritual harms compound. This project provided an opportunity for Black female clinicians from across the U.S. to share their experiences during the dual pandemics of COVID-19 and anti-Black violence. I conducted in-depth interviews with clinicians (n=14) between the ages of 30 and 58. Using the Listening Guide voice-centered approach to data generation and analysis, I identified four voices to help answer this project’s central question: How do you experience being a Black female clinician in the U.S.? The voices of self, pride, vigilance, and mediating narrated the complex ways participants experienced their workplaces. This complexity seemed to be context-specific, depending on whether the clinicians worked in predominantly White workplaces (PWW), a mix of PWW and private practice, or private practice exclusively. Participants who worked only in PWW experienced the greatest stress, oppression, and burnout risk, while participants who worked exclusively in private practice reported more joy, more authenticity, and more job satisfaction. These findings have implications for mentoring, supporting, and retaining Black female clinicians.
Keywords: Black female clinicians, professional experiences, gendered racism, Listening Guide voice-centered approach.
The purpose of this article is to speak directly to the paucity of research regarding Dominican American women and identity narratives. To do so, this article uses the Listening Guide Method of Qualitative Inquiry (Gilligan, et al., 2006) to explore how 1.5 and second-generation Dominican American women narrated their experiences of individual identity within American cultural contexts and constructs. The results draw from the emergence of themes across six participant interviews and showed two distinct voices: The Voice of Cultural Explanation and the Tides of Dominican American Female Identity. Narrative examples from five participants are offered to illustrate where 1.5 and second-generation Dominican American women negotiate their identity narratives at the intersection of their Dominican and American selves. The article offers two conclusions. One, that participant women use the Voice of Cultural Explanation in order to discuss their identity as reflected within the broad cultural tensions of their daily lives. Two, that the Tides of Dominican American Female Identity are used to express strong emotions that manifest within their personal narratives as the unwanted distance from either the Dominican or American parts of their person.
Keywords: Dominican American, women, identity, the Listening Guide, narratives
- Open access
- Published: 02 April 2022
A qualitative study of rural healthcare providers’ views of social, cultural, and programmatic barriers to healthcare access
- Nicholas C. Coombs 1 ,
- Duncan G. Campbell 2 &
- James Caringi 1
BMC Health Services Research volume 22 , Article number: 438 ( 2022 ) Cite this article
22k Accesses
19 Citations
10 Altmetric
Metrics details
Ensuring access to healthcare is a complex, multi-dimensional health challenge. Since the inception of the coronavirus pandemic, this challenge is more pressing. Some dimensions of access are difficult to quantify, namely characteristics that influence healthcare services to be both acceptable and appropriate. These link to a patient’s acceptance of services that they are to receive and ensuring appropriate fit between services and a patient’s specific healthcare needs. These dimensions of access are particularly evident in rural health systems where additional structural barriers make accessing healthcare more difficult. Thus, it is important to examine healthcare access barriers in rural-specific areas to understand their origin and implications for resolution.
We used qualitative methods and a convenience sample of healthcare providers who currently practice in the rural US state of Montana. Our sample included 12 healthcare providers from diverse training backgrounds and specialties. All were decision-makers in the development or revision of patients’ treatment plans. Semi-structured interviews and content analysis were used to explore barriers–appropriateness and acceptability–to healthcare access in their patient populations. Our analysis was both deductive and inductive and focused on three analytic domains: cultural considerations, patient-provider communication, and provider-provider communication. Member checks ensured credibility and trustworthiness of our findings.
Five key themes emerged from analysis: 1) a friction exists between aspects of patients’ rural identities and healthcare systems; 2) facilitating access to healthcare requires application of and respect for cultural differences; 3) communication between healthcare providers is systematically fragmented; 4) time and resource constraints disproportionately harm rural health systems; and 5) profits are prioritized over addressing barriers to healthcare access in the US.
Conclusions
Inadequate access to healthcare is an issue in the US, particularly in rural areas. Rural healthcare consumers compose a hard-to-reach patient population. Too few providers exist to meet population health needs, and fragmented communication impairs rural health systems’ ability to function. These issues exacerbate the difficulty of ensuring acceptable and appropriate delivery of healthcare services, which compound all other barriers to healthcare access for rural residents. Each dimension of access must be monitored to improve patient experiences and outcomes for rural Americans.
Peer Review reports
Unequal access to healthcare services is an important element of health disparities in the United States [ 1 ], and there remains much about access that is not fully understood. The lack of understanding is attributable, in part, to the lack of uniformity in how access is defined and evaluated, and the extent to which access is often oversimplified in research [ 2 ]. Subsequently, attempts to address population-level barriers to healthcare access are insufficient, and access remains an unresolved, complex health challenge [ 3 , 4 , 5 ]. This paper presents a study that aims to explore some of the less well studied barriers to healthcare access, particularly those that influence healthcare acceptability and appropriateness.
In truth, healthcare access entails a complicated calculus that combines characteristics of individuals, their households, and their social and physical environments with characteristics of healthcare delivery systems, organizations, and healthcare providers. For one to fully ‘access’ healthcare, they must have the means to identify their healthcare needs and have available to them care providers and the facilities where they work. Further, patients must then reach, obtain, and use the healthcare services in order to have their healthcare needs fulfilled. Levesque and colleagues critically examined access conceptualizations in 2013 and synthesized all ways in which access to healthcare was previously characterized; Levesque et al. proposed five dimensions of access: approachability, acceptability, availability, affordability and appropriateness [ 2 ]. These refer to the ability to perceive, seek, reach, pay for, and engage in services, respectively.
According to Levesque et al.’s framework, the five dimensions combine to facilitate access to care or serve as barriers. Approachability indicates that people facing health needs understand that healthcare services exist and might be helpful. Acceptability represents whether patients see healthcare services as consistent or inconsistent with their own social and cultural values and worldviews. Availability indicates that healthcare services are reached both physically and in a timely manner. Affordability simplifies one’s capacity to pay for healthcare services without compromising basic necessities, and finally, appropriateness represents the fit between healthcare services and a patient’s specific healthcare needs [ 2 ]. This study focused on the acceptability and appropriateness dimensions of access.
Before the novel coronavirus (SARS-CoV-2; COVID-19) pandemic, approximately 13.3% of adults in the US did not have a usual source of healthcare [ 6 ]. Millions more did not utilize services regularly, and close to two-thirds reported that they would be debilitated by an unexpected medical bill [ 7 , 8 , 9 ]. Findings like these emphasized a fragility in the financial security of the American population [ 10 ]. These concerns were exacerbated by the pandemic when a sudden surge in unemployment increased un- and under-insurance rates [ 11 ]. Indeed, employer-sponsored insurance covers close to half of Americans’ total cost of illness [ 12 ]. Unemployment linked to COVID-19 cut off the lone outlet to healthcare access for many. Health-related financial concerns expanded beyond individuals, as healthcare organizations were unequipped to manage a simultaneous increase in demand for specialized healthcare services and a steep drop off for routine revenue-generating healthcare services [ 13 ]. These consequences of the COVID-19 pandemic all put additional, unexpected pressure on an already fragmented US healthcare system.
Other structural barriers to healthcare access exist in relation to the rural–urban divide. Less than 10% of US healthcare resources are located in rural areas where approximately 20% of the American population resides [ 14 ]. In a country with substantially fewer providers per capita compared to many other developed countries, persons in rural areas experience uniquely pressing healthcare provider shortages [ 15 , 16 ]. Rural inhabitants also tend to have lower household income, higher rates of un- or under-insurance, and more difficulty with travel to healthcare clinics than urban dwellers [ 17 ]. Subsequently, persons in rural communities use healthcare services at lower rates, and potentially preventable hospitalizations are more prevalent [ 18 ]. This disparity often leads rural residents to use services primarily for more urgent needs and less so for routine care [ 19 , 20 , 21 ].
The differences in how rural and urban healthcare systems function warranted a federal initiative to focus exclusively on rural health priorities and serve as counterpart to Healthy People objectives [ 22 ]. The rural determinants of health, a more specific expression of general social determinants, add issues of geography and topography to the well-documented social, economic and political factors that influence all Americans’ access to healthcare [ 23 ]. As a result, access is consistently regarded as a top priority in rural areas, and many research efforts have explored the intersection between access and rurality, namely within its less understood dimensions (acceptability and appropriateness) [ 22 ].
Acceptability-related barriers to care
Acceptability represents the dimension of healthcare access that affects a patient’s ability to seek healthcare, particularly linked to one’s professional values, norms and culture [ 2 ]. Access to health information is an influential factor for acceptable healthcare and is essential to promote and maintain a healthy population [ 24 ]. According to the Centers for Disease Control and Prevention, health literacy or a high ‘health IQ’ is the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others, which impacts healthcare use and system navigation [ 25 ]. The literature indicates that lower levels of health literacy contribute to health disparities among rural populations [ 26 , 27 , 28 ]. Evidence points to a need for effective health communication between healthcare organizations and patients to improve health literacy [ 24 ]. However, little research has been done in this area, particularly as it relates to technologically-based interventions to disseminate health information [ 29 ].
Stigma, an undesirable position of perceived diminished status in an individual’s social position, is another challenge that influences healthcare acceptability [ 30 ]. Those who may experience stigma fear negative social consequences in relation to care seeking. They are more likely to delay seeking care, especially among ethnic minority populations [ 31 , 32 ]. Social media presents opportunities for the dissemination of misleading medical information; this runs further risk for stigma [ 33 ]. Stigma is difficult to undo, but research has shown that developing a positive relationship with a healthcare provider or organization can work to reduce stigma among patients, thus promoting healthcare acceptability [ 34 ].
A provider’s attempts to engage patients and empower them to be active decision-makers regarding their treatment has also been shown to improve healthcare acceptability. One study found that patients with heart disease who completed a daily diary of weight and self-assessment of symptoms, per correspondence with their provider, had better care outcomes than those who did not [ 35 ]. Engaging with household family members and involved community healers also mitigates barriers to care, emphasizing the importance of a team-based approach that extends beyond those who typically provide healthcare services [ 36 , 37 ]. One study, for instance, explored how individuals closest to a pregnant woman affect the woman’s decision to seek maternity care; partners, female relatives, and community health-workers were among the most influential in promoting negative views, all of which reduced a woman’s likelihood to access care [ 38 ].
Appropriateness-related barriers to care
Appropriateness marks the dimension of healthcare access that affects a patient’s ability to engage, and according to Levesque et al., is of relevance once all other dimensions (the ability to perceive, seek, reach and pay for) are achieved [ 2 ]. The ability to engage in healthcare is influenced by a patient’s level of empowerment, adherence to information, and support received by their healthcare provider. Thus, barriers to healthcare access that relate to appropriateness are often those that indicate a breakdown in communication between a patient with their healthcare provider. Such breakdown can involve a patient experiencing miscommunication, confrontation, and/or a discrepancy between their provider’s goals and their own goals for healthcare. Appropriateness represents a dimension of healthcare access that is widely acknowledged as an area in need of improvement, which indicates a need to rethink how healthcare providers and organizations can adapt to serve the healthcare needs of their communities [ 39 ]. This is especially true for rural, ethnic minority populations, which disproportionately experience an abundance of other barriers to healthcare access. Culturally appropriate care is especially important for members of minority populations [ 40 , 41 , 42 ]. Ultimately, patients value a patient-provider relationship characterized by a welcoming, non-judgmental atmosphere [ 43 , 44 ]. In rural settings especially, level of trust and familiarity are common factors that affect service utilization [ 45 ]. Evidence suggests that kind treatment by a healthcare provider who promotes patient-centered care can have a greater overall effect on a patient’s experience than a provider’s degree of medical knowledge or use of modern equipment [ 46 ]. Of course, investing the time needed to nurture close and caring interpersonal connections is particularly difficult in under-resourced, time-pressured rural health systems [ 47 , 48 ].
The most effective way to evaluate access to healthcare largely depends on which dimensions are explored. For instance, a population-based survey can be used to measure the barrier of healthcare affordability. Survey questions can inquire directly about health insurance coverage, care-related financial burden, concern about healthcare costs, and the feared financial impacts of illness and/or disability. Many national organizations have employed such surveys to measure affordability-related barriers to healthcare. For example, a question may ask explicitly about financial concerns: ‘If you get sick or have an accident, how worried are you that you will not be able to pay your medical bills?’ [ 49 ]. Approachability and availability dimensions of access are also studied using quantitative analysis of survey questions, such as ‘Is there a place that you usually go to when you are sick or need advice about your health?’ or ‘Have you ever delayed getting medical care because you couldn’t get through on the telephone?’ In contrast, the remaining two dimensions–acceptability and appropriateness–require a qualitative approach, as the social and cultural factors that determine a patient’s likelihood of accepting aspects of the services that are to be received (acceptability) and the fit between those services and the patient’s specific healthcare needs (appropriateness) can be more abstract [ 50 , 51 ]. In social science, qualitative methods are appropriate to generate knowledge of what social events mean to individuals and how those individuals interact within them; these methods allow for an exploration of depth rather than breadth [ 52 , 53 ]. Qualitative methods, therefore, are appropriate tools for understanding the depth of healthcare providers’ experiences in the inherently social context of seeking and engaging in healthcare.
In sum, acceptability- and appropriateness-related barriers to healthcare access are multi-layered, complex and abundant. Ensuring access becomes even more challenging if structural barriers to access are factored in. In this study, we aimed to explore barriers to healthcare access among persons in Montana, a historically underserved, under-resourced, rural region of the US. Montana is the fourth largest and third least densely populated state in the country; more than 80% of Montana counties are classified as non-core (the lowest level of urban/rural classification), and over 90% are designated as health professional shortage areas [ 54 , 55 ]. Qualitative methods supported our inquiry to explore barriers to healthcare access related to acceptability and appropriateness.
Participants
Qualitative methods were utilized for this interpretive, exploratory study because knowledge regarding barriers to healthcare access within Montana’s rural health systems is limited. We chose Montana healthcare providers, rather than patients, as the population of interest so we may explore barriers to healthcare access from the perspective of those who serve many persons in rural settings. Inclusion criteria required study participants to provide direct healthcare to patients at least one-half of their time. We defined ‘provider’ as a healthcare organization employee with clinical decision-making power and the qualifications to develop or revise patients’ treatment plans. In an attempt to capture a group of providers with diverse experience, we included providers across several types and specialties. These included advanced practice registered nurses (APRNs), physicians (MDs and DOs), and physician assistants (PAs) who worked in critical care medicine, emergency medicine, family medicine, hospital medicine, internal medicine, pain medicine, palliative medicine, pediatrics, psychiatry, and urgent care medicine. We also included licensed clinical social workers (LCSWs) and clinical psychologists who specialize in behavioral healthcare provision.
Recruitment and Data Collection
We recruited participants via email using a snowball sampling approach [ 56 ]. We opted for this approach because of its effectiveness in time-pressured contexts, such as the COVID-19 pandemic, which has made healthcare provider populations hard to reach [ 57 ]. Considering additional constraints with the pandemic and the rural nature of Montana, interviews were administered virtually via Zoom video or telephone conferencing with Zoom’s audio recording function enabled. All interviews were conducted by the first author between January and September 2021. The average length of interviews was 50 min, ranging from 35 to 70 min. There were occasional challenges experienced during interviews (poor cell phone reception from participants, dropped calls), in which case the interviewer remained on the line until adequate communication was resumed. All interviews were included for analysis and transcribed verbatim into NVivo Version 12 software. All qualitative data were saved and stored on a password-protected University of Montana server. Hard-copy field notes were securely stored in a locked office on the university’s main campus.
Data analysis included a deductive followed by an inductive approach. This dual analysis adheres to Levesque’s framework for qualitative methods, which is discussed in the Definition of Analytic Domains sub-section below. Original synthesis of the literature informed the development of our initial deductive codebook. The deductive approach was derived from a theory-driven hypothesis, which consisted of synthesizing previous research findings regarding acceptability- and appropriateness-related barriers to care. Although the locations, patient populations and specific type of healthcare services varied by study in the existing literature, several recurring barriers to healthcare access were identified. We then operationalized three analytic domains based on these findings: cultural considerations, patient-provider communication, and provider-provider communication. These domains were chosen for two reasons: 1) the terms ‘culture’ and ‘communication’ were the most frequently documented characteristics across the studies examined, and 2) they each align closely with the acceptability and appropriateness dimensions of access to healthcare, respectively. In addition, ‘culture’ is included in the definition of acceptability and ‘communication’ is a quintessential aspect of appropriateness. These domains guided the deductive portion of our analysis, which facilitated the development of an interview guide used for this study.
Interviews were semi-structured to allow broad interpretations from participants and expand the open-ended characterization of study findings. Data were analyzed through a flexible coding approach proposed by Deterding and Waters [ 58 ]. Qualitative content analysis was used, a method particularly beneficial for analyzing large amounts of qualitative data collected through interviews that offers possibility of quantifying categories to identify emerging themes [ 52 , 59 ]. After fifty percent of data were analyzed, we used an inductive approach as a formative check and repeated until data saturation, or the point at which no new information was gathered in interviews [ 60 ]. At each point of inductive analysis, interview questions were added, removed, or revised in consideration of findings gathered [ 61 ]. The Standards for Reporting Qualitative Research (SRQR) was used for reporting all qualitative data for this study [ 62 ]. The first and third authors served as primary and secondary analysts of the qualitative data and collaborated to triangulate these findings. An audit approach was employed, which consisted of coding completed by the first author and then reviewed by the third author. After analyses were complete, member checks ensured credibility and trustworthiness of findings [ 63 ]. Member checks consisted of contacting each study participant to explain the study’s findings; one-third of participants responded and confirmed all findings. All study procedures were reviewed and approved by the Human Subjects Committee of the authors’ institution’s Institutional Review Board.
Definitions of Analytic Domains
Cultural considerations.
Western health systems often fail to consider aspects of patients’ cultural perspectives and histories. This can manifest in the form of a providers’ lack of cultural humility. Cultural humility is a process of preventing imposition of one’s worldview and cultural beliefs on others and recognizing that everyone’s conception of the world is valid. Humility cultivates sensitive approaches in treating patients [ 64 ]. A lack of cultural humility impedes the delivery of acceptable and appropriate healthcare [ 65 ], which can involve low empathy or respect for patients, or dismissal of culture and traditions as superstitions that interfere with standard treatments [ 66 , 67 ]. Ensuring cultural humility among all healthcare employees is a step toward optimal healthcare delivery. Cultural humility is often accomplished through training that can be tailored to particular cultural- or gender-specific populations [ 68 , 69 ]. Since cultural identities and humility have been marked as factors that can heavily influence patients’ access to care, cultural considerations composed our first analytic domain. To assess this domain, we asked participants how they address the unique needs of their patients, how they react when they observe a cultural behavior or attitude from a patient that may not directly align with their treatment plan, and if they have received any multicultural training or training on cultural considerations in their current role.
Patient-provider communication
Other barriers to healthcare access can be linked to ineffective patient-provider communication. Patients who do not feel involved in healthcare decisions are less likely to adhere to treatment recommendations [ 70 ]. Patients who experience communication difficulties with providers may feel coerced, which generates disempowerment and leads patients to employ more covert ways of engagement [ 71 , 72 ]. Language barriers can further compromise communication and hinder outcomes or patient progress [ 73 , 74 ]. Any miscommunication between a patient and provider can affect one’s access to healthcare, namely affecting appropriateness-related barriers. For these reasons, patient-provider communication composed our second analytic domain. We asked participants to highlight the challenges they experience when communicating with their patients, how those complications are addressed, and how communication strategies inform confidentiality in their practice. Confidentiality is a core ethical principle in healthcare, especially in rural areas that have smaller, interconnected patient populations [ 75 ].
Provider-Provider Communication
A patient’s journey through the healthcare system necessitates sufficient correspondence between patients, primary, and secondary providers after discharge and care encounters [ 76 ]. Inter-provider and patient-provider communication are areas of healthcare that are acknowledged to have some gaps. Inconsistent mechanisms for follow up communication with patients in primary care have been documented and emphasized as a concern among those with chronic illness who require close monitoring [ 68 , 77 ]. Similar inconsistencies exist between providers, which can lead to unclear care goals, extended hospital stays, and increased medical costs [ 78 ]. For these reasons, provider-provider communication composed our third analytic domain. We asked participants to describe the approaches they take to streamline communication after a patient’s hospital visit, the methods they use to ensure collaborative communication between primary or secondary providers, and where communication challenges exist.
Healthcare provider characteristics
Our sample included 12 providers: four in family medicine (1 MD, 1 DO, 1 PA & 1 APRN), three in pediatrics (2 MD with specialty in hospital medicine & 1 DO), three in palliative medicine (2 MDs & 1 APRN with specialty in wound care), one in critical care medicine (DO with specialty in pediatric pulmonology) and one in behavioral health (1 LCSW with specialty in trauma). Our participants averaged 9 years (range 2–15) as a healthcare provider; most reported more than 5 years in their current professional role. The diversity of participants extended to their patient populations as well, with each participant reporting a unique distribution of age, race and level of medical complexity among their patients. Most participants reported that a portion of their patients travel up to five hours, sometimes across county- or state-lines, to receive care.
Theme 1: A friction exists between aspects of patients’ rural identities and healthcare systems
Our participants comprised a collection of medical professions and reported variability among health-related reasons their patients seek care. However, most participants acknowledged similar characteristics that influence their patients’ challenges to healthcare access. These identified factors formed categories from which the first theme emerged. There exists a great deal of ‘rugged individualism’ among Montanans, which reflects a self-sufficient and self-reliant way of life. Stoicism marked a primary factor to characterize this quality. One participant explained:
True Montanans are difficult to treat medically because they tend to be a tough group. They don’t see doctors. They don’t want to go, and they don’t want to be sick. That’s an aspect of Montana that makes health culture a little bit difficult.
Another participant echoed this finding by stating:
The backwoods Montana range guy who has an identity of being strong and independent probably doesn’t seek out a lot of medical care or take a lot of medications. Their sense of vitality, independence and identity really come from being able to take care and rely on themselves. When that is threatened, that’s going to create a unique experience of illness.
Similar responses were shared by all twelve participants; stoicism seemed to be heavily embedded in many patient populations in Montana and serves as a key determinant of healthcare acceptability. There are additional factors, however, that may interact with stoicism but are multiply determined. Stigma is an example of this, presented in this context as one’s concern about judgement by the healthcare system. Respondents were openly critical of this perception of the healthcare system as it was widely discussed in interviews. One participant stated:
There is a real perception of a punitive nature in the medical community, particularly if I observe a health issue other than the primary reason for one’s hospital visit, whether that may be predicated on medical neglect, delay of care, or something that may warrant a report to social services. For many of the patients and families I see, it’s not a positive experience and one that is sometimes an uphill barrier that I work hard to circumnavigate.
Analysis of these factors suggest that low use of healthcare services may link to several characteristics, including access problems. Separately, a patient’s perceived stigma from healthcare providers may also impact a patient’s willingness to receive services. One participant put it best by stating
Sometimes, families assume that I didn’t want to see them because they will come in for follow up to meet with me but end up meeting with another provider, which is frustrating because I want to maintain patients on my panel but available time and resource occasionally limits me from doing so. It could be really hard adapting to those needs on the fly, but it’s an honest miss.
When a patient arrives for a healthcare visit and experiences this frustration, it may elicit a patient’s perceptions of neglect or disorganization. This ‘honest miss’ may, in turn, exacerbate other acceptable-related barriers to care.
Theme 2: Facilitating access to healthcare requires application of and respect for cultural differences
The biomedical model is the standard of care utilized in Western medicine [ 79 , 80 ]. However, the US comprises people with diverse social and cultural identities that may not directly align with Western conceptions of health and wellness. Approximately 11.5% of the Montana population falls within an ethnic minority group. 6.4% are of American Indian or Alaska Native origin, 0.5% are of Black or African American origin, 0.8% are of Asian origin and 3.8% are of multiple or other origins. [ 81 ]. Cultural insensitivity is acknowledged in health services research as an active deterrent for appropriate healthcare delivery [ 65 ]. Participants for this study were asked how they react when a patient brings up a cultural attitude or behavior that may impact the proposed treatment plan. Eight participants noted a necessity for humility when this occurs. One participant conceptualized this by stating:
When this happens, I learn about individuals and a way of life that is different to the way I grew up. There is a lot of beauty and health in a non-patriarchal, non-dominating, non-sexist framework, and when we can engage in such, it is really expansive for my own learning process.
The participants who expressed humility emphasized that it is best to work in tandem with their patient, congruently. Especially for those with contrasting worldviews, a provider and a patient working as a team poses an opportunity to develop trust. Without it, a patient can easily fall out of the system, further hindering their ability to access healthcare services in the future. One participant stated:
The approach that ends up being successful for a lot of patients is when we understand their modalities, and they have a sense we understand those things. We have to show understanding and they have to trust. From there, we can make recommendations to help get them there, not decisions for them to obey, rather views based on our experiences and understanding of medicine.
Curiosity was another reaction noted by a handful of participants. One participant said:
I believe patients and their caregivers can be engaged and loving in different ways that don’t always follow the prescribed approach in the ways I’ve been trained, but that doesn’t necessarily mean that they are detrimental. I love what I do, and I love learning new things or new approaches, but I also love being surprised. My style of medicine is not to predict peoples’ lives, rather to empower and support what makes life meaningful for them.
Participants mentioned several other characteristics that they use in practice to prevent cultural insensitivity and support a collaborative approach to healthcare. Table 1 lists these facilitating characteristics and quotes to explain the substance of their benefit.
Consensus among participants indicated that the use of these protective factors to promote cultural sensitivity and apply them in practice is not standardized. When asked, all but two participants said they had not received any culturally-based training since beginning their practice. Instead, they referred to developing skills through “on the job training” or “off the cuff learning.” The general way of medicine, one participant remarked, was to “throw you to the fire.” This suggested that use of standardized cultural humility training modules for healthcare providers was not common practice. Many attributed this to time constraints.
Individual efforts to gain culturally appropriate skills or enhance cultural humility were mentioned, however. For example, three participants reported that they attended medical conferences to discuss cultural challenges within medicine, one participant sought out cultural education within their organization, and another was invited by Native American community members to engage in traditional peace ceremonies. Participants described these additional efforts as uncommon and outside the parameters of a provider’s job responsibilities, as they require time commitments without compensation.
Additionally, eight participants said they share their personal contact information with patients so they may call them directly for medical needs. The conditions and frequency with which this is done was variable and more common among providers in specialized areas of medicine or those who described having a manageable patient panel. All who reported that they shared their personal contact information described it as an aspect of rural health service delivery that is atypical in other, non-rural healthcare systems.
Theme 3: Communication between healthcare providers is systematically fragmented
Healthcare is complex and multi-disciplinary, and patients’ treatment is rarely overseen by a single provider [ 82 ]. The array of provider types and specialties is vast, as is the range of responsibilities ascribed to providers. Thus, open communication among providers both within and between healthcare systems is vital for the success of collaborative healthcare [ 83 ]. Without effective communication achieved between healthcare providers, the appropriate delivery of healthcare services may be become compromised. Our participants noted that they face multiple challenges that complicate communication with other providers. Miscommunication between departments, often implicating the Emergency Department (ED), was a recurring point noted among participants. One participant who is a primary care physician said:
If one of my patients goes to the ER, I don’t always get the notes. They’re supposed to send them to the patient’s primary care doc. The same thing happens with general admissions, but again, I often find out from somebody else that my patient was admitted to the hospital.
This failure to communicate can negatively impact the patient, particularly if time sensitivity or medical complexity is essential to treatment. A patient’s primary care physician is the most accurate source of their medical history; without an effective way to obtain and synthesize a patient’s health information, there may be increased risk of medical error. One participant in a specialty field stated:
One of the biggest barriers I see is obtaining a concise description of a patient’s history and needs. You can imagine if you’re a mom and you’ve got a complicated kid. You head to the ER. The ER doc looks at you with really wide eyes, not knowing how to get information about your child that’s really important.
This concern was highlighted with a specific example from a different participant:
I have been unable to troubleshoot instances when I send people to the ER with a pretty clear indication for admission, and then they’re sent home. For instance, I had an older fellow with pretty severe chronic kidney disease. He presented to another practitioner in my office with shortness of breath and swelling and appeared to have newly onset decompensated heart failure. When I figured this out, I sent him to the ER, called and gave my report. The patient later came back for follow up to find out not only that they had not been admitted but they lost no weight with outpatient dialysis . I feel like a real opportunity was missed to try to optimize the care of the patient simply because there was poor communication between myself and the ER. This poor guy… He ended up going to the ER four times before he got admitted for COVID-19.
In some cases, communication breakdown was reported as the sole cause of a poor outcome. When communication is effective, each essential member of the healthcare team is engaged and collaborating with the same information. Some participants called this process ‘rounds’ when a regularly scheduled meeting is staged between a group of providers to ensure access to accurate patient information. Accurate communication may also help build trust and improve a patient’s experience. In contrast, ineffective communication can result in poor clarity regarding providers’ responsibilities or lost information. Appropriate delivery of healthcare considers the fit between providers and a patient’s specific healthcare needs; the factors noted here suggest that provider-provider miscommunication can adversely affect this dimension of healthcare access.
Another important mechanism of communication is the sharing of electronic medical records (EMRs), a process that continues to shift with technological advances. Innovation is still recent enough, however, for several of our study participants to be able to recall a time when paper charts were standard. Widespread adoption and embrace of the improvements inherent in electronic medical records expanded in the late 2000’s [ 84 ]. EMRs vastly improved the ability to retain, organize, safeguard, and transfer health information. Every participant highlighted EMRs at one point or another and often did so with an underlying sense of anger or frustration. Systematic issues and problems with EMRs were discussed. One participant provided historical context to such records:
Years back, the government aimed to buy an electronic medical record system, whichever was the best, and a number of companies created their own. Each were a reasonable system, so they all got their checks and now we have four completely separate operating systems that do not talk to each other. The idea was to make a router or some type of relay that can share information back and forth. There was no money in that though, so of course, no one did anything about it. Depending on what hospital, clinic or agency you work for, you will most likely work within one of these systems. It was a great idea; it just didn’t get finished.
Seven participants confirmed these points and their impacts on making coordination more difficult, relying on outdated communication strategies more often than not. Many noted this even occurs between facilities within the same city and in separate small metropolitan areas across the state. One participant said:
If my hospital decides to contract with one EMR and the hospital across town contracts with another, correspondence between these hospitals goes back to traditional faxing. As a provider, you’re just taking a ‘fingered crossed’ approach hoping that the fax worked, is picked up, was put in the appropriate inbox and was actually looked at. Information acquisition and making sure it’s timely are unforeseen between EMRs.
Participants reported an “astronomic” number of daily faxes and telephone calls to complete the communication EMRs were initially designed to handle. These challenges are even more burdensome if a patient moves from out of town or out of state; obtaining their medical records was repeatedly referred to as a “chore” so onerous that it often remains undone. Another recurring concern brought up by participants regarded accuracy within EMRs to lend a false sense of security. They are not frequently updated, not designed to be family-centered and not set up to do anything automatically. One participant highlighted these limitations by stating:
I was very proud of a change I made in our EMR system [EPIC], even though it was one I never should have had to make. I was getting very upset because I would find out from my nursing assistant who read the obituary that one of my patients had died. There was a real problem with the way the EMR was notifying PCP’s, so I got an EPIC-level automated notification built into our EMR so that any time a patient died, their status would be changed to deceased and a notification would be sent to their PCP. It’s just really awful to find out a week later that your patient died, especially when you know these people and their families really well. It’s not good care to have blind follow up.
Whether it be a physical or electronic miscommunication between healthcare providers, the appropriate delivery of healthcare can be called to question
Theme 4: Time and resource constraints disproportionately harm rural health systems
Several measures of system capacity suggest the healthcare system in the US is under-resourced. There are fewer physicians and hospital beds per capita compared to most comparable countries, and the growth of healthcare provider populations has stagnated over time [ 15 ]. Rural areas, in particular, are subject to resource limitations [ 16 ]. All participants discussed provider shortages in detail. They described how shortages impact time allocation in their day-to-day operations. Tasks like patient intakes, critical assessments, and recovering information from EMRs take time, of which most participants claimed to not have enough of. There was also a consensus in having inadequate time to spend on medically complex cases. Time pressures were reported to subsequently influence quality of care. One participant stated:
With the constant pace of medicine, time is not on your side. A provider cannot always participate in an enriching dialogue with their patients, so rather than listen and learn, we are often coerced into the mindset of ‘getting through’ this patient so we can move on. This echoes for patient education during discharge, making the whole process more arduous than it otherwise could be if time and resources were not as sparse.
Depending on provider type, specialty, and the size of patient panels, four participants said they have the luxury of extending patient visits to 40 + minutes. Any flexibility with patient visits was regarded as just that: a luxury. Very few providers described the ability to coordinate their schedules as such. This led some study participants to limit the number of patients they serve. One participant said:
We simply don’t have enough clinicians, which is a shame because these people are really skilled, exceptional, brilliant providers but are performing way below their capacity. Because of this, I have a smaller case load so I can engage in a level of care that I feel is in the best interest of my patients. Everything is a tradeoff. Time has to be sacrificed at one point or another. This compromise sets our system up to do ‘ok’ work, not great work.
Of course, managing an overly large number of patients with high complexity is challenging. Especially while enduring the burden of a persisting global pandemic, participants reflected that the general outlook of administering healthcare in the US is to “do more with less.” This often forces providers to delegate responsibilities, which participants noted has potential downsides. One participant described how delegating patient care can cause problems.
Very often will a patient schedule a follow up that needs to happen within a certain time frame, but I am unable to see them myself. So, they are then placed with one of my mid-level providers. However, if additional health issues are introduced, which often happens, there is a high-risk of bounce-back or need to return once again to the hospital. It’s an inefficient vetting process that falls to people who may not have specific training in the labs and imaging that are often included in follow up visits. Unfortunately, it’s a forlorn hope to have a primary care physician be able to attend all levels of a patient’s care.
Several participants described how time constraints stretch all healthcare staff thin and complicate patient care. This was particularly important among participants who reported having a patient panel exceeding 1000. There were some participants, however, who praised the relationships they have with their nurse practitioners and physician’s assistants and mark transparency as the most effective way to coordinate care. Collectively, these clinical relationships were built over long standing periods of time, a disadvantage to providers at the start of their medical career. All but one participant with over a decade of clinical experience mentioned the usefulness of these relationships. The factors discussed in Theme 4 are directly linked to the Availability dimension of access to healthcare. A patient’s ability to reach care is subject to the capacity of their healthcare provider(s). Additionally, further analysis suggests these factors also link to the Appropriateness dimension because the quality of patient-provider relationships may be negatively impacted if a provider’s time is compromised.
Theme 5: Profits are prioritized over addressing barriers to healthcare access in the US.
The US healthcare system functions partially for-profit in the public and private sectors. The federal government provides funding for national programs such as Medicare, but a majority of Americans access healthcare through private employer plans [ 85 ]. As a result, uninsurance rates influence healthcare access. Though the rate of the uninsured has dropped over the last decade through expansion of the Affordable Care Act, it remains above 8 percent [ 86 ]. Historically, there has been ethical criticism in the literature of a for-profit system as it is said to exacerbate healthcare disparities and constitute unfair competition against nonprofit institutions. Specifically, the US healthcare system treats healthcare as a commodity instead of a right, enables organizational controls that adversely affect patient-provider relationships, undermines medical education, and constitutes a medical-industrial complex that threatens influence on healthcare-related public policy [ 87 ]. Though unprompted by the interviewer, participants raised many of these concerns. One participant shared their views on how priorities stand in their practice:
A lot of the higher-ups in the healthcare system where I work see each patient visit as a number. It’s not that they don’t have the capacity to think beyond that, but that’s what their role is, making sure we’re profitable. That’s part of why our healthcare system in the US is as broken as it is. It’s accentuated focus on financially and capitalistically driven factors versus understanding all these other barriers to care.
Eight participants echoed a similar concept, that addressing barriers to healthcare access in their organizations is largely complicated because so much attention is directed on matters that have nothing to do with patients. A few other participants supported this by alluding to a “cherry-picking” process by which those at the top of the hierarchy devote their attention to the easiest tasks. One participant shared an experience where contrasting work demands between administrators and front-line clinical providers produces adverse effects:
We had a new administrator in our hospital. I had been really frustrated with the lack of cultural awareness and curiosity from our other leaders in the past, so I offered to meet and take them on a tour of the reservation. This was meant to introduce them to kids, families and Tribal leaders who live in the area and their interface with healthcare. They declined, which I thought was disappointing and eye-opening.
Analysis of these factors suggest that those who work directly with patients understand patient needs better than those who serve in management roles. This same participant went on to suggest an ulterior motive for a push towards telemedicine, as administrators primarily highlight the benefit of billing for virtual visits instead of the nature of the visits themselves.
This study explored barriers and facilitators to healthcare access from the perspective of rural healthcare providers in Montana. Our qualitative analysis uncovered five key themes: 1) a friction exists between aspects of patients’ rural identities and healthcare systems; 2) facilitating access to healthcare requires application of and respect for cultural differences; 3) communication between healthcare providers is systematically fragmented; 4) time and resource constraints disproportionately harm rural health systems; and 5) profits are prioritized over addressing barriers to healthcare access in the US. Themes 2 and 3 were directly supported by earlier qualitative studies that applied Levesque’s framework, specifically regarding healthcare providers’ poor interpersonal quality and lack of collaboration with other providers that are suspected to result from a lack of provider training [ 67 , 70 ]. This ties back to the importance of cultural humility, which many previous culture-based trainings have referred to as cultural competence. Cultural competence is achieved through a plethora of trainings designed to expose providers to different cultures’ beliefs and values but induces risk of stereotyping and stigmatizing a patient’s views. Therefore, cultural humility is the preferred idea, by which providers reflect and gain open-ended appreciation for a patient’s culture [ 88 ].
Implications for Practice
Perhaps the most substantial takeaway is how embedded rugged individualism is within rural patient populations and how difficult that makes the delivery of care in rural health systems. We heard from participants that stoicism and perceptions of stigma within the system contribute to this, but other resulting factors may be influential at the provider- and organizational-levels. Stoicism and perceived stigma both appear to arise, in part, from an understandable knowledge gap regarding the care system. For instance, healthcare providers understand the relations between primary and secondary care, but many patients may perceive both concepts as elements of a single healthcare system [ 89 ]. Any issue experienced by a patient when tasked to see both a primary and secondary provider may result in a patient becoming confused [ 90 ]. This may also overlap with our third theme, as a disjointed means of communication between healthcare providers can exacerbate patients’ negative experiences. One consideration to improve this is to incorporate telehealth programs into an existing referral framework to reduce unnecessary interfacility transfers; telehealth programs have proven effective in rural and remote settings [ 91 ].
In fact, telehealth has been rolled out in a variety of virtual platforms throughout its evolution, its innovation matched with continued technological advancement. Simply put, telehealth allows health service delivery from a distance; it allows knowledge and practice of clinical care to be in a different space than a patient. Because of this, a primary benefit of telehealth is its impact on improving patient-centered outcomes among those living in rural areas. For instance, text messaging technology improves early infant diagnosis, adherence to recommended diagnostic testing, and participant engagement in lifestyle change interventions [ 92 , 93 , 94 ]. More sophisticated interventions have found their way into smartphone-based technology, some of which are accessible even without an internet connection [ 95 , 96 ]. Internet accessibility is important because a number of study participants noted internet connectivity as a barrier for patients who live in low resource communities. Videoconferencing is another function of telehealth that has delivered a variety of health services, including those which are mental health-specific [ 97 ], and mobile health clinics have been used in rural, hard-to-reach settings to show the delivery of quality healthcare is both feasible and acceptable [ 98 , 99 , 100 ]. While telehealth has potential to reduce a number of healthcare access barriers, it may not always address the most pressing healthcare needs [ 101 ]. However, telehealth does serve as a viable, cost-effective alternative for rural populations with limited physical access to specialized services [ 102 ]. With time and resource limitations acknowledged as a key theme in our study, an emphasis on expanding telehealth services is encouraged as it will likely have significant involvement on advancing healthcare in the future, especially as the COVID-19 pandemic persists [ 103 ].
Implications for Policy
One could argue that most of the areas of fragmentation in the US healthcare system can be linked to the very philosophy on which it is based: an emphasis on profits as highest priority. Americans are, therefore, forced to navigate a health service system that does not work solely in their best interests. It is not surprising to observe lower rates of healthcare usage in rural areas, which may be a result from rural persons’ negative views of the US healthcare system or a perception that the system does not exist to support wellness. These perceptions may interact with ‘rugged individualism’ to squelch rural residents’ engagement in healthcare. Many of the providers we interviewed for this study appeared to understand this and strived to improve their patients’ experiences and outcomes. Though these efforts are admirable, they may not characterize all providers who serve in rural areas of the US. From a policy standpoint, it is important to recognize these expansive efforts from providers. If incentives were offered to encourage maximum efforts be made, it may lessen burden due to physician burnout and fatigue. Of course, there is no easy fix to the persisting limit of time and resources for providers, problems that require workforce expansion. Ultimately, though, the current structure of the US healthcare system is failing rural America and doing little to help the practice of rural healthcare providers.
Implications for Future Research
It is important for future health systems research efforts to consider issues that arise from both individual- and system-level access barriers and where the two intersect. Oftentimes, challenges that appear linked to a patient or provider may actually stem from an overarching system failure. If failures are critically and properly addressed, we may refine our understanding of what we can do in our professional spaces to improve care as practitioners, workforce developers, researchers and advocates. This qualitative study was exploratory in nature. It represents a step forward in knowledge generation regarding challenges in access to healthcare for rural Americans. Although mental health did not come up by design in this study, future efforts exploring barriers to healthcare access in rural systems should focus on access to mental healthcare. In many rural areas, Montana included, rates of suicide, substance use and other mental health disorders are highly prevalent. These characteristics should be part of the overall discussion of access to healthcare in rural areas. Optimally, barriers to healthcare access should continue to be explored through qualitative and mixed study designs to honor its multi-dimensional stature.
Strengths and Limitations
It is important to note first that this study interviewed healthcare providers instead of patients, which served as both a strength and limitation. Healthcare providers were able to draw on numerous patient-provider experiences, enabling an account of the aggregate which would have been impossible for a patient population. However, accounts of healthcare providers’ perceptions of barriers to healthcare access for their patients may differ from patients’ specific views. Future research should examine acceptability- and appropriateness-related barriers to healthcare access in patient populations. Second, study participants were recruited through convenience sampling methods, so results may be biased towards healthcare providers who are more invested in addressing barriers to healthcare access. Particularly, the providers interviewed for this study represented a subset who go beyond expectations of their job descriptions by engaging with their communities and spending additional uncompensated time with their patients. It is likely that a provider who exhibits these behavioral traits is more likely to participate in research aimed at addressing barriers to healthcare access. Third, the inability to conduct face-to-face interviews for our qualitative study may have posed an additional limitation. It is possible, for example, that in-person interviews might have resulted in increased rapport with study participants. Notwithstanding this possibility, the remote interview format was necessary to accommodate health risks to the ongoing COVID-19 pandemic. Ultimately, given our qualitative approach, results from our study cannot be generalizable to all rural providers’ views or other rural health systems. In addition, no causality can be inferred regarding the influence of aspects of rurality on access. The purpose of this exploratory qualitative study was to probe research questions for future efforts. We also acknowledge the authors’ roles in the research, also known as reflexivity. The first author was the only author who administered interviews and had no prior relationships with all but one study participant. Assumptions and pre-dispositions to interview content by the first author were regularly addressed throughout data analysis to maintain study integrity. This was achieved by conducting analysis by unique interview question, rather than by unique participant, and recoding the numerical order of participants for each question. Our commitment to rigorous qualitative methods was a strength for the study for multiple reasons. Conducting member checks with participants ensured trustworthiness of findings. Continuing data collection to data saturation ensured dependability of findings, which was achieved after 10 interviews and confirmed after 2 additional interviews. We further recognize the heterogeneity in our sample of participants, which helped generate variability in responses. To remain consistent with appropriate means of presenting results in qualitative research however, we shared minimal demographic information about our study participants to ensure confidentiality.
The divide between urban and rural health stretches beyond a disproportionate allocation of resources. Rural health systems serve a more complicated and hard-to-reach patient population. They lack sufficient numbers of providers to meet population health needs. These disparities impact collaboration between patients and providers as well as the delivery of acceptable and appropriate healthcare. The marker of rurality complicates the already cumbersome challenge of administering acceptable and appropriate healthcare and impediments stemming from rurality require continued monitoring to improve patient experiences and outcomes. Our qualitative study explored rural healthcare providers’ views on some of the social, cultural, and programmatic factors that influence access to healthcare among their patient populations. We identified five key themes: 1) a friction exists between aspects of patients’ rural identities and healthcare systems; 2) facilitating access to healthcare requires application of and respect for cultural differences; 3) communication between healthcare providers is systematically fragmented; 4) time and resource constraints disproportionately harm rural health systems; and 5) profits are prioritized over addressing barriers to healthcare access in the US. This study provides implications that may shift the landscape of a healthcare provider’s approach to delivering healthcare. Further exploration is required to understand the effects these characteristics have on measurable patient-centered outcomes in rural areas.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to individual privacy could be compromised but are available from the corresponding author on reasonable request.
Ethics approval and consent to participate.
All study procedures and methods were carried out in accordance with relevant guidelines and regulations from the World Medical Association Declaration of Helsinki. Ethics approval was given by exempt review from the Institutional Review Board (IRB) at the University of Montana (IRB Protocol No.: 186–20). Participants received oral and written information about the study prior to interview, which allowed them to provide informed consent for the interviews to be recorded and used for qualitative research purposes. No ethical concerns were experienced in this study pertaining to human subjects.
Consent for publication.
The participants consented to the publication of de-identified material from the interviews.
Riley WJ. Health Disparities: Gaps in Access, Quality and Affordability of Medical Care. Trans Am Clin Climatol Assoc. 2012;123:167–74.
PubMed PubMed Central Google Scholar
Levesque J, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. https://doi.org/10.1186/1475-9276-12-18 .
Article PubMed PubMed Central Google Scholar
Serban N. A Multidimensional Framework for Measuring Access. In: Serban N. Healthcare System Access: Measurement, Inference, and Intervention. New Jersey: John Wiley & Sons; 2019. p. 13–59.
Google Scholar
Roncarolo F, Boivin A, Denis JL, et al. What do we know about the needs and challenges of health systems? A scoping review of the international literature. BMC Health Serv Res. 2017;17:636. https://doi.org/10.1186/s12913-017-2585-5 .
Cabrera-Barona P, Blaschke T. Kienberger S. Explaining Accessibility and Satisfaction Related to Healthcare: A Mixed-Methods Approach. Soc Indic Res. 2017;133,719–739. https://doi.org/10.1007/s11205-016-1371-9 .
Coombs NC, Meriwether WE, Caringi J, Newcomer SR. Barriers to healthcare access among U.S. adults with mental health challenges: A population-based study. SSM Popul Health. 2021;15:100847. https://doi.org/10.1016/j.ssmph.2021.100847 .
Farietta TP, Lu B, Tumin R. Ohio’s Medicaid Expansion and Unmet Health Needs Among Low-Income Women of Reproductive Age. Matern Child Health. 2018;22(12):1771–9. https://doi.org/10.1007/s10995-018-2575-1 .
Article Google Scholar
Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance. JAMA Intern Med. 2016;1;176(10):1501–1509. https://doi.org/10.1001/jamainternmed.2016.4419 .
National Alliance on Mental Illness: The Doctor is Out. Continuing Disparities in Access to Mental and Physical Health Care. 2017. https://www.nami.org/Support-Education/Publications-Reports/Public-Policy-Reports/The-Doctor-is-Out . Accessed 29 Aug 2021.
Pollitz K, Lopes L, Kearney A, Rae M, Cox C, Fehr F, Rousseau D, Kaiser Family Foundation. US Statistics on Surprise Medical Billing. JAMA. 2020;323(6):498. https://doi.org/10.1001/jama.2020.0065 .
Kahraman C, Orobello C, Cirella GT. hanging Dynamics with COVID-19: Future Outlook. In: XX Cirella GT, editor. Human Settlements: Urbanization, Smart Sector Development, and Future Outlook. Singapore: Springer; 2022. p. 235–52.
Book Google Scholar
Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19 — Implications for the Health Care System. N Engl J Med. 2020;383(15):1483–8. https://doi.org/10.1056/NEJMsb2021088 .
Article CAS PubMed Google Scholar
Defêche J, Azarzar S, Mesdagh A, Dellot P, Tytgat A, Bureau F, Gillet L, Belhadj Y, Bontems S, Hayette M-P, Schils R, Rahmouni S, Ernst M, Moutschen M, Darcis G. In-Depth Longitudinal Comparison of Clinical Specimens to Detect SARS-CoV-2. Pathogens. 2021;10(11):1362. https://doi.org/10.3390/pathogens10111362 .
Article CAS PubMed PubMed Central Google Scholar
Rosenblatt RA, Hart LG. Physicians and rural America. West J Med. 2000;173(5):348–51. https://doi.org/10.1136/ewjm.173.5.348 .
Kaiser Family Foundation Analysis of OECD Data. 2020. https://www.healthsystemtracker.org/chart-collection/u-s-health-care-resources-compare-countries/#item-physicians-density-per-1000-population-2000-2018 . Accessed 31 Oct 2021.
Government Accounting Office. Physician Workforce: Locations and Types of Graduate Training Were Largely Unchanged, and Federal Efforts May Not Be Sufficient to Meet Needs. 2017. https://www.gao.gov/assets/gao-17-411.pdf . Accessed 31 Oct 2021.
The Kaiser Family Foundation: The Uninsured in Rural America. 2003. https://www.kff.org/wp-content/uploads/2013/01/the-uninsured-in-rural-america-update-pdf.pdf . Accessed 15 Sept 2021.
Wright B, Potter AJ, Trivedi AN, Mueller KJ. The Relationship Between Rural Health Clinic Use and Potentially Preventable Hospitalizations and Emergency Department Visits Among Medicare Beneficiaries. J Rural Health. 2018;34(4):423–30. https://doi.org/10.1111/jrh.12253 .
Article PubMed Google Scholar
Weichelt B, Bendixsen C, Patrick T. A Model for Assessing Necessary Conditions for Rural Health Care’s Mobile Health Readiness: Qualitative Assessment of Clinician-Perceived Barriers. JMIR Mhealth Uhealth. 2019;7(11): e11915. https://doi.org/10.2196/11915 .
Mangundu M, Roets L, Janse van Rensberg E. Accessibility of healthcare in rural Zimbabwe: The perspective of nurses and healthcare users. Afr J Prim Health Care Fam Med. 2020;12(1):e1-e7. https://doi.org/10.4102/phcfm.v12i1.2245 .
Rahayu YYS, Araki T, Rosleine D. Factors affecting the use of herbal medicines in the universal health coverage system in Indonesia. J Ethnopharmacol. 2020;260: 112974. https://doi.org/10.1016/j.jep.2020.112974 .
Bolin JN, Bellamy GR, Ferdinand AO, et al. Rural Healthy People 2020: New Decade, Same Challenges. Journal of Rural Health. 2015;31(3):326–33.
Reid S. The rural determinants of health: using critical realism as a theoretical framework. Rural Remote Health. 2019;19(3):5184. https://doi.org/10.22605/RRH5184 .
Wynia MK, Osborn CY. Health literacy and communication quality in health care organizations. J Health Commun. 2010;15 Suppl 2(Suppl 2):102–115. https://doi.org/10.1080/10810730.2010.499981 .
Centers for Disease Control and Prevention. What is Health Literacy? 2022. https://www.cdc.gov/healthliteracy/learn/index.html . Accessed 25 Feb 2022.
Davis TC, Arnold CL, Rademaker A, et al. Differences in barriers to mammography between rural and urban women. J Womens Health (Larchmt). 2012;21(7):748–55. https://doi.org/10.1089/jwh.2011.3397 .
Halverson J, Martinez-Donate A, Trentham-Dietz A, et al. Health literacy and urbanicity among cancer patients. J Rural Health. 2013;29(4):392–402. https://doi.org/10.1111/jrh.12018 .
Zahnd WE, Scaife SL, Francis ML. Health literacy skills in rural and urban populations. Am J Health Behav. 2009;33(5):550–7. https://doi.org/10.5993/ajhb.33.5.8 .
Dogba MJ, Dossa AR, Breton E, Gandonou-Migan R. Using information and communication technologies to involve patients and the public in health education in rural and remote areas: a scoping review. BMC Health Serv Res. 2019;19(1):128. https://doi.org/10.1186/s12913-019-3906-7 .
Committee on the Science of Changing Behavioral Health Social Norms, Board on Behavioral, Cognitive, and Sensory Sciences, Division of Behavioral and Social Sciences and Education; National Academies of Sciences, Engineering, and Medicine. In: Ending Discrimination Against People with Mental and Substance Use Disorders: The Evidence for Stigma Change. Washington: National Academics Press; 2016. p. 33–52.
Wu Y, Zhou H, Wang Q, Cao M, Medina A, Rozelle S. Use of maternal health services among women in the ethnic rural areas of western China. BMC Health Serv Res. 2019;19(1):179. https://doi.org/10.1186/s12913-019-3996-2 .
Meyer E, Hennink M, Rochat R, et al. Working Towards Safe Motherhood: Delays and Barriers to Prenatal Care for Women in Rural and Peri-Urban Areas of Georgia. Matern Child Health J. 2016;20(7):1358–65. https://doi.org/10.1007/s10995-016-1997-x .
Heinrich S. Medical science faces the post-truth era: a plea for the grassroot values of science. Curr Opin Anaesthesiol. 2020;33(2):198–202. https://doi.org/10.1097/ACO.0000000000000833 .
Esquivel MM, Chen JC, Woo RK, et al. Why do patients receive care from a short-term medical mission? Survey study from rural Guatemala. J Surg Res. 2017;215:160–6. https://doi.org/10.1016/j.jss.2017.03.056 .
Park LG, Dracup K, Whooley MA, et al. Symptom Diary Use and Improved Survival for Patients With Heart Failure [published correction appears in Circ Heart Fail. 2017 Dec;10(12):]. Circ Heart Fail. 2017;10(11):e003874. https://doi.org/10.1161/CIRCHEARTFAILURE.117.003874 .
Taleb F, Perkins J, Ali NA, et al. Transforming maternal and newborn health social norms and practices to increase utilization of health services in rural Bangladesh: a qualitative review. BMC Pregnancy Childbirth. 2015;15:75. https://doi.org/10.1186/s12884-015-0501-8 .
Billah SM, Hoque DE, Rahman M, et al. Feasibility of engaging “Village Doctors” in the Community-based Integrated Management of Childhood Illness (C-IMCI): experience from rural Bangladesh. J Glob Health. 2018;8(2): 020413. https://doi.org/10.7189/jogh.08.020413 .
Kaiser JL, Fong RM, Hamer DH, et al. How a woman’s interpersonal relationships can delay care-seeking and access during the maternity period in rural Zambia: An intersection of the Social Ecological Model with the Three Delays Framework. Soc Sci Med. 2019;220:312–21. https://doi.org/10.1016/j.socscimed.2018.11.011 .
Rao KD, Sheffel A. Quality of clinical care and bypassing of primary health centers in India. Soc Sci Med. 2018;207:80–8. https://doi.org/10.1016/j.socscimed.2018.04.040 .
Lee YT, Lee YH, Kaplan WA. Is Taiwan’s National Health Insurance a perfect system? Problems related to health care utilization of the aboriginal population in rural townships. Int J Health Plann Manage. 2019;34(1):e6–10. https://doi.org/10.1002/hpm.2653 .
Lyford M, Haigh MM, Baxi S, Cheetham S, Shahid S, Thompson SC. An Exploration of Underrepresentation of Aboriginal Cancer Patients Attending a Regional Radiotherapy Service in Western Australia. Int J Environ Res Public Health. 2018;15(2):337. https://doi.org/10.3390/ijerph15020337 .
Article PubMed Central Google Scholar
Rohr JM, Spears KL, Geske J, Khandalavala B, Lacey MJ. Utilization of Health Care Resources by the Amish of a Rural County in Nebraska. J Community Health. 2019;44(6):1090–7. https://doi.org/10.1007/s10900-019-00696-9 .
Johnston K, Harvey C, Matich P, et al. Increasing access to sexual health care for rural and regional young people: Similarities and differences in the views of young people and service providers. Aust J Rural Health. 2015;23(5):257–64. https://doi.org/10.1111/ajr.12186 .
Legido-Quigley H, Naheed A, de Silva HA, et al. Patients’ experiences on accessing health care services for management of hypertension in rural Bangladesh, Pakistan and Sri Lanka: A qualitative study. PLoS ONE. 2019;14(1): e0211100. https://doi.org/10.1371/journal.pone.0211100 .
Shaw B, Amouzou A, Miller NP, Bryce J, Surkan PJ. A qualitative exploration of care-seeking pathways for sick children in the rural Oromia region of Ethiopia. BMC Health Serv Res. 2017;17(1):184. https://doi.org/10.1186/s12913-017-2123-5 .
Larson E, Vail D, Mbaruku GM, Kimweri A, Freedman LP, Kruk ME. Moving Toward Patient-Centered Care in Africa: A Discrete Choice Experiment of Preferences for Delivery Care among 3,003 Tanzanian Women. PLoS ONE. 2015;10(8): e0135621. https://doi.org/10.1371/journal.pone.0135621 .
Spleen AM, Lengerich EJ, Camacho FT, Vanderpool RC. Health care avoidance among rural populations: results from a nationally representative survey. J Rural Health. 2014;30(1):79–88. https://doi.org/10.1111/jrh.12032 .
Weisgrau S. Issues in rural health: access, hospitals, and reform. Health Care Financ Rev. 1995;17(1):1–14.
CAS PubMed PubMed Central Google Scholar
National Center for Health Statistics. 2018. https://www.cdc.gov/nchs/surveys.htm . Accessed 29 Aug 2021.
Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):88. https://doi.org/10.1186/s12913-017-2031-8 .
Dyer TA, Owens J, Robinson PG. The acceptability of healthcare: from satisfaction to trust. Community Dent Health. 2016;33(4):242–51. https://doi.org/10.1922/CDH_3902Dyer10 .
Padgett DK. Qualitative and Mixed Methods in Public Health. Thousand Oaks, California: SAGE Publications Inc.; 2012.
Tolley EE, Ulin PR, Mack N, Robinson ET, Succop SM. Qualitative Methods in Public Health: A Field Guide for Applied Research. 2nd ed. San Francisco, California: John Wiley & Sons, Inc.; 2016.
Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. In: National Center for Health Statistics: Vital Health Statistics. 2014. https://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf . Accessed 31 Oct 2021.
Health Resources & Services Administration. Health Professional Shortage Area Find. 2021. https://data.hrsa.gov/tools/shortage-area/hpsa-find . Accessed 31 Oct 2021.
Shaghaghi A, Bhopal RS, Sheikh A. Approaches to Recruiting “Hard-To-Reach” Populations into Re-search: A Review of the Literature. Health Promot Perspect. 2011;1(2):86–94. https://doi.org/10.5681/hpp.2011.009 .
Sadler GR, Lee HC, Lim RS, Fullerton J. Recruitment of hard-to-reach population subgroups via adaptations of the snowball sampling strategy. Nurs Health Sci. 2010;12(3):369–74. https://doi.org/10.1111/j.1442-2018.2010.00541.x .
Deterding NM, Waters MC. Flexible Coding of In-depth Interviews: A Twenty-first-century Approach. Sociological Methods & Research. 2021;50(2):708–39. https://doi.org/10.1177/0049124118799377 .
Schreier M, Stamann C, Janssen M, Dahl T, Whittal A. Qualitative Content Analysis: Conceptualizations and Challenges in Research Practice-Introduction to the FQS Special Issue" Qualitative Content Analysis I". InForum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2019;20:26 DEU.
Guest G, Namey E, Chen M. A simple method to assess and report thematic saturation in qualitative research. PLoS ONE. 2020;15(5): e0232076. https://doi.org/10.1371/journal.pone.0232076 .
Mayring P. Qualitative Content Analysis. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2000;1(2). https://doi.org/10.17169/fqs-1.2.1089 .
O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Academic Medicine, Vol. 89, No. 9 / Sept 2014. https://doi.org/10.1097/ACM.0000000000000388 .
Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. 2014;41(5):545–7. https://doi.org/10.1188/14.ONF.545-547 .
Miller S. Cultural humility is the first step to becoming global care providers. J Obstet Gynecol Neonatal Nurs. 2009;38(1):92–3. https://doi.org/10.1111/j.1552-6909.2008.00311.x .
Prasad SJ, Nair P, Gadhvi K, Barai I, Danish HS, Philip AB. Cultural humility: treating the patient, not the illness. Med Educ Online. 2016;21:30908. https://doi.org/10.3402/meo.v21.30908 .
George MS, Davey R, Mohanty I, Upton P. “Everything is provided free, but they are still hesitant to access healthcare services”: why does the indigenous community in Attapadi, Kerala continue to experience poor access to healthcare? Int J Equity Health. 2020;19(1):105. https://doi.org/10.1186/s12939-020-01216-1 .
Romanelli M, Hudson KD. Individual and systemic barriers to health care: Perspectives of lesbian, gay, bisexual, and transgender adults. Am J Orthopsychiatry. 2017;87(6):714–28. https://doi.org/10.1037/ort0000306 .
Bailie J, Schierhout G, Laycock A, et al. Determinants of access to chronic illness care: a mixed-methods evaluation of a national multifaceted chronic disease package for Indigenous Australians. BMJ Open. 2015;5(11): e008103. https://doi.org/10.1136/bmjopen-2015-008103 .
Reeve C, Humphreys J, Wakerman J, Carter M, Carroll V, Reeve D. Strengthening primary health care: achieving health gains in a remote region of Australia. Med J Aust. 2015;202(9):483–7. https://doi.org/10.5694/mja14.00894 .
Swan LET, Auerbach SL, Ely GE, Agbemenu K, Mencia J, Araf NR. Family Planning Practices in Appalachia: Focus Group Perspectives on Service Needs in the Context of Regional Substance Abuse. Int J Environ Res Public Health. 2020;17(4):1198. https://doi.org/10.3390/ijerph17041198 .
Kabia E, Mbau R, Oyando R, et al. “We are called the et cetera”: experiences of the poor with health financing reforms that target them in Kenya. Int J Equity Health. 2019;18(1):98. https://doi.org/10.1186/s12939-019-1006-2 .
Ho JW, Kuluski K, Im J. “It’s a fight to get anything you need” - Accessing care in the community from the perspectives of people with multimorbidity. Health Expect. 2017;20(6):1311–9. https://doi.org/10.1111/hex.12571 .
Latif A, Mandane B, Ali A, Ghumra S, Gulzar N. A Qualitative Exploration to Understand Access to Pharmacy Medication Reviews: Views from Marginalized Patient Groups. Pharmacy (Basel). 2020;8(2):73. https://doi.org/10.3390/pharmacy8020073 .
Tschirhart N, Diaz E, Ottersen T. Accessing public healthcare in Oslo, Norway: the experiences of Thai immigrant masseuses. BMC Health Serv Res. 2019;19(1):722. https://doi.org/10.1186/s12913-019-4560-9 .
Ireland S, Belton S, Doran F. “I didn’t feel judged”: exploring women’s access to telemedicine abortion in rural Australia. J Prim Health Care. 2020;12(1):49–56. https://doi.org/10.1071/HC19050 .
Stokes T, Tumilty E, Latu ATF, et al. Improving access to health care for people with severe chronic obstructive pulmonary disease (COPD) in Southern New Zealand: qualitative study of the views of health professional stakeholders and patients. BMJ Open. 2019;9(11): e033524. https://doi.org/10.1136/bmjopen-2019-033524 .
Jafar TH, Ramakrishnan C, John O, et al. Access to CKD Care in Rural Communities of India: a qualitative study exploring the barriers and potential facilitators. BMC Nephrol. 2020;21(1):26. https://doi.org/10.1186/s12882-020-1702-6 .
Doetsch J, Pilot E, Santana P, Krafft T. Potential barriers in healthcare access of the elderly population influenced by the economic crisis and the troika agreement: a qualitative case study in Lisbon, Portugal. Int J Equity Health. 2017;16(1):184. https://doi.org/10.1186/s12939-017-0679-7 .
Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–36. https://doi.org/10.1126/science.847460 .
Risberg G, Hamberg K, Johansson E.E. Gender perspective in medicine: a vital part of medical scientific rationality. A useful model for comprehending structures and hierarchies within medical science. BMC Med. 2006;4(1):1.
Montana Census & Economic Information Center. 2021. https://ceic.mt.gov/ . Accessed 18 Sept 2021.
Smith M, Saunders R, Stuckhardt L, McGinnis JM, Committee on the Learning Health Care System in America, Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington: National Academies Press; 2013.
O’Daniel M, Rosenstein AH, Professional Communication and Team Collaboration. In: Hughes RG, editor. Chapter 33: Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality: Rockville; 2008.
Evans RS. Electronic Health Records: Then, Now, and in the Future. Yearb Med Inform. 2016;Suppl 1(Suppl 1):S48-S61. https://doi.org/10.15265/IYS-2016-s006 .
Tikkanen R, Osborn R, Mossialos E, Djordjevic A, Wharton GA. International Health Care System Profiles: United States. The Commonwealth Fund. 2020. https://www.commonwealthfund.org/international-health-policy-center/countries/united-states . Accessed 19 Sept 2021.
Berchick ER, Barnett JC, Upton RD. Health Insurance Coverage in the United States. Washington: United States Census Bureau; 2018.
Brock DW, Buchanan A. Ethical Issues in For-Profit Health Care. In: Gray BH, editor. For-Profit Enterprise in Health Care. Washington: National Academics Press; 1986.
Lekas HM, Pahl K, Fuller Lewis C. Rethinking Cultural Competence: Shifting to Cultural Humility. Health Serv Insights. 2020;13:1178632920970580. https://doi.org/10.1177/1178632920970580 .
Beaulieu MD. Primary and secondary care: Breaking down barriers for our patients with chronic diseases. Can Fam Physician. 2013;59(2):221.
Crafford L, Jenkins LS. Why seek a second consultation at an emergency centre? A qualitative study. Afr J Prim Health Care Fam Med. 2017;9(1):e1–8. https://doi.org/10.4102/phcfm.v9i1.1397 .
Sorensen MJ, von Recklinghausen FM, Fulton G, et al. Secondary overtriage: The burden of unnecessary interfacility transfers in a rural trauma system. JAMA Surg. 2013;148:763–8.
Sutcliffe CG, Thuma PE, van Dijk JH, et al. Use of mobile phones and text messaging to decrease the turnaround time for early infant HIV diagnosis and notification in rural Zambia: an observational study. BMC Pediatr. 2017;17(1):66. https://doi.org/10.1186/s12887-017-0822-z .
Baldwin LM, Morrison C, Griffin J, et al. Bidirectional Text Messaging to Improve Adherence to Recommended Lipid Testing. J Am Board Fam Med. 2017;30(5):608–14. https://doi.org/10.3122/jabfm.2017.05.170088 .
Albright K, Krantz MJ, Backlund Jarquín P, DeAlleaume L, Coronel-Mockler S, Estacio RO. Health Promotion Text Messaging Preferences and Acceptability Among the Medically Underserved. Health Promot Pract. 2015;16(4):523–32. https://doi.org/10.1177/1524839914566850 .
Cramer ME, Mollard EK, Ford AL, Kupzyk KA, Wilson FA. The feasibility and promise of mobile technology with community health worker reinforcement to reduce rural preterm birth. Public Health Nurs. 2018;35(6):508–16. https://doi.org/10.1111/phn.12543 .
Gbadamosi SO, Eze C, Olawepo JO, et al. A Patient-Held Smartcard With a Unique Identifier and an mHealth Platform to Improve the Availability of Prenatal Test Results in Rural Nigeria: Demonstration Study. J Med Internet Res. 2018;20(1): e18. https://doi.org/10.2196/jmir.8716 .
Trondsen MV, Tjora A, Broom A, Scambler G. The symbolic affordances of a video-mediated gaze in emergency psychiatry. Soc Sci Med. 2018;197:87–94. https://doi.org/10.1016/j.socscimed.2017.11.056 .
Schwitters A, Lederer P, Zilversmit L, et al. Barriers to health care in rural Mozambique: a rapid ethnographic assessment of planned mobile health clinics for ART. Glob Health Sci Pract. 2015;3(1):109–16. https://doi.org/10.9745/GHSP-D-14-00145 .
Kojima N, Krupp K, Ravi K, et al. Implementing and sustaining a mobile medical clinic for prenatal care and sexually transmitted infection prevention in rural Mysore, India. BMC Infect Dis. 2017;17(1):189. https://doi.org/10.1186/s12879-017-2282-3 .
Gorman SE, Martinez JM, Olson J. An assessment of HIV treatment outcomes among utilizers of semi-mobile clinics in rural Kenya. AIDS Care. 2015;27(5):665–8. https://doi.org/10.1080/09540121.2014.986053 .
Lee S, Black D, Held ML. Factors Associated with Telehealth Service Utilization among Rural Populations. J Health Care Poor Underserved. 2019;30(4):1259–72. https://doi.org/10.1353/hpu.2019.0104 .
Agha Z, Schapira RM, Maker AH. Cost effectiveness of telemedicine for the delivery of outpatient pulmonary care to a rural population. Telemed J E Health. 2002;8(3):281–91. https://doi.org/10.1089/15305620260353171 .
Doraiswamy S, Abraham A, Mamtani R, Cheema S. Use of Telehealth During the COVID-19 Pandemic: Scoping Review. J Med Internet Res. 2020;22(12): e24087. https://doi.org/10.2196/24087 .
Download references
Acknowledgements
This research was supported by the Center for Biomedical Research Excellence award (P20GM130418) from the National Institute of General Medical Sciences of the National Institute of Health. The first author was also supported by the University of Montana Burnham Population Health Fellowship. We would like to thank Dr. Christopher Dietrich, Dr. Jennifer Robohm and Dr. Eric Arzubi for their contributions on determining inclusion criteria for the healthcare provider population used for this study.
This research did not receive any specific grant from funding agencies in the public, commercial, and not-for-profit sectors.
Author information
Authors and affiliations.
School of Public & Community Health Sciences, University of Montana, 32 Campus Dr, Missoula, MT, 59812, USA
Nicholas C. Coombs & James Caringi
Department of Psychology, University of Montana, 32 Campus Dr, Missoula, MT, 59812, USA
Duncan G. Campbell
You can also search for this author in PubMed Google Scholar
Contributions
The authors confirm contribution to the paper as follows: study conception and design: NC and JC; data collection: NC; analysis and interpretation of results: NC and JC; draft manuscript preparation: NC, DC and JC; and manuscript editing: NC, DC and JC. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Correspondence to Nicholas C. Coombs .
Ethics declarations
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Coombs, N.C., Campbell, D.G. & Caringi, J. A qualitative study of rural healthcare providers’ views of social, cultural, and programmatic barriers to healthcare access. BMC Health Serv Res 22 , 438 (2022). https://doi.org/10.1186/s12913-022-07829-2
Download citation
Received : 11 January 2022
Accepted : 21 March 2022
Published : 02 April 2022
DOI : https://doi.org/10.1186/s12913-022-07829-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Access to healthcare
- Rural health
- Qualitative methods
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Pediatr Psychol

Commentary: Writing and Evaluating Qualitative Research Reports
Yelena p. wu.
1 Division of Public Health, Department of Family and Preventive Medicine, University of Utah,
2 Cancer Control and Population Sciences, Huntsman Cancer Institute,
Deborah Thompson
3 Department of Pediatrics-Nutrition, USDA/ARS Children’s Nutrition Research Center, Baylor College of Medicine,
Karen J. Aroian
4 College of Nursing, University of Central Florida,
Elizabeth L. McQuaid
5 Department of Psychiatry and Human Behavior, Brown University, and
Janet A. Deatrick
6 School of Nursing, University of Pennsylvania
Objective To provide an overview of qualitative methods, particularly for reviewers and authors who may be less familiar with qualitative research. Methods A question and answer format is used to address considerations for writing and evaluating qualitative research. Results and Conclusions When producing qualitative research, individuals are encouraged to address the qualitative research considerations raised and to explicitly identify the systematic strategies used to ensure rigor in study design and methods, analysis, and presentation of findings. Increasing capacity for review and publication of qualitative research within pediatric psychology will advance the field’s ability to gain a better understanding of the specific needs of pediatric populations, tailor interventions more effectively, and promote optimal health.
The Journal of Pediatric Psychology (JPP) has a long history of emphasizing high-quality, methodologically rigorous research in social and behavioral aspects of children’s health ( Palermo, 2013 , 2014 ). Traditionally, research published in JPP has focused on quantitative methodologies. Qualitative approaches are of interest to pediatric psychologists given the important role of qualitative research in developing new theories ( Kelly & Ganong, 2011 ), illustrating important clinical themes ( Kars, Grypdonck, de Bock, & van Delden, 2015 ), developing new instruments ( Thompson, Bhatt, & Watson, 2013 ), understanding patients’ and families’ perspectives and needs ( Bevans, Gardner, Pajer, Riley, & Forrest, 2013 ; Lyons, Goodwin, McCreanor, & Griffin, 2015 ), and documenting new or rarely examined issues ( Haukeland, Fjermestad, Mossige, & Vatne, 2015 ; Valenzuela et al., 2011 ). Further, these methods are integral to intervention development ( Minges et al., 2015 ; Thompson et al., 2007 ) and understanding intervention outcomes ( de Visser et al., 2015 ; Hess & Straub, 2011 ). For example, when designing an intervention, qualitative research can identify patient and family preferences for and perspectives on desirable intervention characteristics and perceived needs ( Cassidy et al., 2013 ; Hess & Straub, 2011 ; Thompson, 2014 ), which may lead to a more targeted, effective intervention.
Both qualitative and quantitative approaches are concerned with issues such as generalizability of study findings (e.g., to whom the study findings can be applied) and rigor. However, qualitative and quantitative methods have different approaches to these issues. The purpose of qualitative research is to contribute knowledge or understanding by describing phenomenon within certain groups or populations of interest. As such, the purpose of qualitative research is not to provide generalizable findings. Instead, qualitative research has a discovery focus and often uses an iterative approach. Thus, qualitative work is often foundational to future qualitative, quantitative, or mixed-methods studies.
At the time of this writing, three of six current calls for papers for special issues of JPP specifically note that manuscripts incorporating qualitative approaches would be welcomed. Despite apparent openness to broadening JPP’s emphasis beyond its traditional quantitative approach, few published articles have used qualitative methods. For example, of 232 research articles published in JPP from 2012 to 2014 (excluding commentaries and reviews), only five used qualitative methods (2% of articles).
The goal of the current article is to present considerations for writing and evaluating qualitative research within the context of pediatric psychology to provide a framework for writing and reviewing manuscripts reporting qualitative findings. The current article may be especially useful to reviewers and authors who are less familiar with qualitative methods. The tenets presented here are grounded in the well-established literature on reporting and evaluating qualitative research, including guidelines and checklists ( Eakin & Mykhalovskiy, 2003 ; Elo et al., 2014 ; Mays & Pope, 2000 ; Tong, Sainsbury, & Craig, 2007 ). For example, the Consolidated Criteria for Reporting Qualitative Research checklist describes essential elements for reporting qualitative findings ( Tong et al., 2007 ). Although the considerations presented in the current manuscript have broad applicability to many fields, examples were purposively selected for the field of pediatric psychology.
Our goal is that this article will stimulate publication of more qualitative research in pediatric psychology and allied fields. More specifically, the goal is to encourage high-quality qualitative research by addressing key issues involved in conducting qualitative studies, and the process of conducting, reporting, and evaluating qualitative findings. Readers interested in more in-depth information on designing and implementing qualitative studies, relevant theoretical frameworks and approaches, and analytic approaches are referred to the well-developed literature in this area ( Clark, 2003 ; Corbin & Strauss, 2008 ; Creswell, 1994 ; Eakin & Mykhalovskiy, 2003 ; Elo et al., 2014 ; Mays & Pope, 2000 ; Miles, Huberman, & Saldaña, 2013 ; Ritchie & Lewis, 2003 ; Saldaña, 2012 ; Sandelowski, 1995 , 2010 ; Tong et al., 2007 ; Yin, 2015 ). Researchers new to qualitative research are also encouraged to obtain specialized training in qualitative methods and/or to collaborate with a qualitative expert in an effort to ensure rigor (i.e., validity).
We begin the article with a definition of qualitative research and an overview of the concept of rigor. While we recognize that qualitative methods comprise multiple and distinct approaches with unique purposes, we present an overview of considerations for writing and evaluating qualitative research that cut across qualitative methods. Specifically, we present basic principles in three broad areas: (1) study design and methods, (2) analytic considerations, and (3) presentation of findings (see Table 1 for a summary of the principles addressed in each area). Each area is addressed using a “question and answer” format. We present a brief explanation of each question, options for how one could address the issue raised, and a suggested recommendation. We recognize, however, that there are no absolute “right” or “wrong” answers and that the most “right” answer for each situation depends on the specific study and its purpose. In fact, our strongest recommendation is that authors of qualitative research manuscripts be explicit about their rationale for design, analytic choices, and strategies so that readers and reviewers can evaluate the rationale and rigor of the study methods.
Summary of Overarching Principles to Address in Qualitative Research Manuscripts
What Is Qualitative Research?
Qualitative methods are used across many areas of health research, including health psychology ( Gough & Deatrick, 2015 ), to study the meaning of people’s lives in their real-world roles, represent their views and perspectives, identify important contextual conditions, discover new or additional insights about existing social and behavioral concepts, and acknowledge the contribution of multiple perspectives ( Yin, 2015 ). Qualitative research is a family of approaches rather than a single approach. There are multiple and distinct qualitative methodologies or stances (e.g., constructivism, post-positivism, critical theory), each with different underlying ontological and epistemological assumptions ( Lincoln, Lynham, & Guba, 2011 ). However, certain features are common to most qualitative approaches and distinguish qualitative research from quantitative research ( Creswell, 1994 ).
Key to all qualitative methodologies is that multiple perspectives about a phenomenon of interest are essential, and that those perspectives are best inductively derived or discovered from people with personal experience regarding that phenomenon. These perspectives or definitions may differ from “conventional wisdom.” Thus, meanings need to be discovered from the population under study to ensure optimal understanding. For instance, in a recent qualitative study about texting while driving, adolescents said that they did not approve of texting while driving. The investigators, however, discovered that the respondents did not consider themselves driving while a vehicle was stopped at a red light. In other words, the respondents did approve of texting while stopped at a red light. In addition, the adolescents said that they highly valued being constantly connected via texting. Thus, what is meant by “driving” and the value of “being connected” need to be considered when approaching the issue of texting while driving with adolescents ( McDonald & Sommers, 2015 ).
Qualitative methods are also distinct from a mixed-method approach (i.e., integration of qualitative and quantitative approaches; Creswell, 2013b ). A mixed-methods study may include a first phase of quantitative data collection that provides results that inform a second phase of the study that includes qualitative data collection, or vice versa. A mixed-methods study may also include concurrent quantitative and qualitative data collection. The timing, priority, and stage of integration of the two approaches (quantitative and qualitative) are complex and vary depending on the research question; they also dictate how to attend to differing qualitative and quantitative principles ( Creswell et al., 2011 ). Understanding the basic tenets of qualitative research is preliminary to integrating qualitative research with another approach that has different tenets. A full discussion of the integration of qualitative and quantitative research approaches is beyond the scope of this article. Readers interested in the topic are referred to one of the many excellent resources on the topic ( Creswell, 2013b ).
What Are Typical Qualitative Research Questions?
Qualitative research questions are typically open-ended and are framed in the spirit of discovery and exploration and to address existing knowledge gaps. The current manuscript provides exemplar pediatric qualitative studies that illustrate key issues that arise when reporting and evaluating qualitative studies. Example research questions that are contained in the studies cited in the current manuscript are presented in Table 2 .
Example Qualitative Research Questions From the Pediatric Literature
What Are Rigor and Transparency in Qualitative Research?
There are several overarching principles with unique application in qualitative research, including definitions of scientific rigor and the importance of transparency. Quantitative research generally uses the terms reliability and validity to describe the rigor of research, while in qualitative research, rigor refers to the goal of seeking to understand the tacit knowledge of participants’ conception of reality ( Polanyi, 1958 ). For example, Haukeland and colleagues (2015) used qualitative analysis to identify themes describing the emotional experiences of a unique and understudied population—pediatric siblings of children with rare medical conditions such as Turner syndrome and Duchenne muscular dystrophy. Within this context, the authors’ rendering of the diverse and contradictory emotions experienced by siblings of children with these rare conditions represents “rigor” within a qualitative framework.
While debate exists regarding the terminology describing and strategies for strengthening scientific rigor in qualitative studies ( Guba, 1981 ; Morse, 2015a , 2015b ; Sandelowski, 1993a ; Whittemore, Chase, & Mandle, 2001 ), little debate exists regarding the importance of explaining strategies used to strengthen rigor. Such strategies should be appropriate for the specific study; therefore, it is wise to clearly describe what is relevant for each study. For example, in terms of strengthening credibility or the plausibility of data analysis and interpretation, prolonged engagement with participants is appropriate when conducting an observational study (e.g., observations of parent–child mealtime interactions; Hughes et al., 2011 ; Power et al., 2015 ). For an interview-only study, however, it would be more practical to strengthen credibility through other strategies (e.g., keeping detailed field notes about the interviews included in the analysis).
Dependability is the stability of a data analysis protocol. For instance, stepwise development of a coding system from an “a priori” list of codes based on the underlying conceptual framework or existing literature (e.g., creating initial codes for potential barriers to medication adherence based on prior studies) may be essential for analysis of data from semi-structured interviews using multiple coders. But this may not be the ideal strategy if the purpose is to inductively derive all possible coding categories directly from data in an area where little is known. For some research questions, the strategy may be to strengthen confirmability or to verify a specific phenomenon of interest using different sources of data before generating conclusions. This process, which is commonly referred to in the research literature as triangulation, may also include collecting different types of data (e.g., interview data, observational data), using multiple coders to incorporate different ways of interpreting the data, or using multiple theories ( Krefting, 1991 ; Ritchie & Lewis, 2003 ). Alternatively, another investigator may use triangulation to provide complementarity data ( Krefting, 1991 ) to garner additional information to deepen understanding. Because the purpose of qualitative research is to discover multiple perspectives about a phenomenon, it is not necessarily appropriate to attain concordance across studies or investigators when independently analyzing data. Some qualitative experts also believe that it is inappropriate to use triangulation to confirm findings, but this debate has not been resolved within the field ( Ritchie & Lewis, 2003 ; Tobin & Begley, 2004 ). More agreement exists, however, regarding the value of triangulation to complement, deepen, or expand understanding of a particular topic or issue ( Ritchie & Lewis, 2003 ). Finally, instead of basing a study on a sample that allows for generalizing statistical results to other populations, investigators in qualitative research studies are focused on designing a study and conveying the results so that the reader understands the transferability of the results. Strategies for transferability may include explanations of how the sample was selected and descriptive characteristics of study participants, which provides a context for the results and enables readers to decide if other samples share critical attributes. A study is deemed transferable if relevant contextual features are common to both the study sample and the larger population.
Strategies to enhance rigor should be used systematically across each phase of a study. That is, rigor needs to be identified, managed, and documented throughout the research process: during the preparation phase (data collection and sampling), organization phase (analysis and interpretation), and reporting phase (manuscript or final report; Elo et al., 2014 ). From this perspective, the strategies help strengthen the trustworthiness of the overall study (i.e., to what extent the study findings are worth heeding; Eakin & Mykhalovskiy, 2003 ; Lincoln & Guba, 1985 ).
A good example of managing and documenting rigor and trustworthiness can be found in a study of family treatment decisions for children with cancer ( Kelly & Ganong, 2011 ). The researchers describe how they promoted the rigor of the study and strengthening its credibility by triangulating data sources (e.g., obtaining data from children’s custodial parents, stepparents, etc.), debriefing (e.g., holding detailed conversations with colleagues about the data and interpretations of the data), member checking (i.e., presenting preliminary findings to participants to obtain their feedback and interpretation), and reviewing study procedure decisions and analytic procedures with a second party.
Transparency is another key concept in written reports of qualitative research. In other words, enough detail should be provided for the reader to understand what was done and why ( Ritchie & Lewis, 2003 ). Examples of information that should be included are a clear rationale for selecting a particular population or people with certain characteristics, the research question being investigated, and a meaningful explanation of why this research question was selected (i.e., the gap in knowledge or understanding that is being investigated; Ritchie & Lewis, 2003 ). Clearly describing recruitment, enrollment, data collection, and data analysis or extraction methods are equally important ( Dixon-Woods, Shaw, Agarwal, & Smith, 2004 ). Coherency among methods and transparency about research decisions adds to the robustness of qualitative research ( Tobin & Begley, 2004 ) and provides a context for understanding the findings and their implications.
Study Design and Methods
Is qualitative research hypothesis driven.
In contrast to quantitative research, qualitative research is not typically hypothesis driven ( Creswell, 1994 ; Ritchie & Lewis, 2003 ). A risk associated with using hypotheses in qualitative research is that the findings could be biased by the hypotheses. Alternatively, qualitative research is exploratory and typically guided by a research question or conceptual framework rather than hypotheses ( Creswell, 1994 ; Ritchie & Lewis, 2003 ). As previously stated, the goal of qualitative research is to increase understanding in areas where little is known by developing deeper insight into complex situations or processes. According to Richards and Morse (2013) , “If you know what you are likely to find, … you should not be working qualitatively” (p. 28). Thus, we do not recommend that a hypothesis be stated in manuscripts presenting qualitative data.
What Is the Role of Theory in Qualitative Research?
Consistent with the exploratory nature of qualitative research, one particular qualitative method, grounded theory, is used specifically for discovering substantive theory (i.e., working theories of action or processes developed for a specific area of concern; Bryant & Charmaz, 2010 ; Glaser & Strauss, 1967 ). This method uses a series of structured steps to break down qualitative data into codes, organize the codes into conceptual categories, and link the categories into a theory that explains the phenomenon under study. For example, Kelly and Ganong (2011) used grounded theory methods to produce a substantive theory about how single and re-partnered parents (e.g., households with a step-parent) made treatment decisions for children with childhood cancer. The theory of decision making developed in this study included “moving to place,” which described the ways in which parents from different family structures (e.g., single and re-partnered parents) were involved in the child’s treatment decision-making. The resulting theory also delineated the causal conditions, context, and intervening factors that contributed to the strategies used for moving to place.
Theories may be used in other types of qualitative research as well, serving as the impetus or organizing framework for the study ( Sandelowski, 1993b ). For example, Izaguirre and Keefer (2014) used Social Cognitive Theory ( Bandura, 1986 ) to investigate self-efficacy among adolescents with inflammatory bowel disease. The impetus for selecting the theory was to inform the development of a self-efficacy measure for adolescent self-management. In another study on health care transition in youth with Type 1 Diabetes ( Pierce, Wysocki, & Aroian, 2016 ), the investigators adapted a social-ecological model—the Socio-ecological Model of Adolescent and Young Adult Transition Readiness (SMART) model ( Schwartz, Tuchman, Hobbie, & Ginsberg, 2011 )—to their study population ( Pierce & Wysocki, 2015 ). Pierce et al. (2016) are currently using the adapted SMART model to focus their data collection and structure the preliminary analysis of their data about diabetes health care transition.
Regardless of whether theory is induced from data or selected in advance to guide the study, consistent with the principle of transparency , its role should be clearly identified and justified in the research publication ( Bradbury-Jones, Taylor, & Herber, 2014 ; Kelly, 2010 ). Methodological congruence is an important guiding principle in this regard ( Richards & Morse, 2013 ). If a theory frames the study at the outset, it should guide and direct all phases. The resulting publication(s) should relate the phenomenon of interest and the research question(s) to the theory and specify how the theory guided data collection and analysis. The publication(s) should also discuss how the theory fits with the finished product. For instance, authors should describe how the theory provided a framework for the presentation of the findings and discuss the findings in context with the relevant theoretical literature.
A study examining parents’ motivations to promote vegetable consumption in their children ( Hingle et al., 2012 ) provides an example of methodological congruence. The investigators adapted the Model of Goal Directed Behavior ( Bagozzi & Pieters, 1998 ) for parenting practices relevant to vegetable consumption (Model of Goal Directed Vegetable Parenting Practices; MGDVPP). Consistent with the adapted theoretical model and in keeping with the congruence principle, interviews were guided by the theoretical constructs contained within the MGDVPP, including parents’ attitudes, subjective norms, and perceived behavioral control related to promoting vegetable consumption in children ( Hingle et al., 2012 ). The study discovered that the adapted model successfully identified parents’ motivations to encourage their children to eat more vegetables.
The use of the theory should be consistent with the basic goal of qualitative research, which is discovery. Alternatively stated, theories should be used as broad orienting frameworks for exploring topical areas without imposing preconceived ideas and biases. The theory should be consistent with the study findings and not be used to force-fit the researcher’s interpretation of the data ( Sandelowski, 1993b ). Divergence from the theory when it does not fit the study findings is illustrated in a qualitative study of hypertension prevention beliefs in Hispanics ( Aroian, Peters, Rudner, & Waser, 2012 ). This study used the Theory of Planned Behavior as a guiding theoretical framework but found that coding separately for normative and control beliefs was not the best organizing schema for presenting the study findings. When divergence from the original theory occurs, the research report should explain and justify how and why the theory was modified ( Bradbury-Jones et al., 2014 ).
What Are Typical Sampling Methods in Qualitative Studies?
Qualitative sampling methods should be “purposeful” ( Coyne, 1997 ; Patton, 2015 ; Tuckett, 2004 ). Purposeful sampling is based on the study purpose and investigator judgments about which people and settings will provide the richest information for the research questions. The logic underlying this type of sampling differs from the logic underlying quantitative sampling ( Patton, 2015 ). Quantitative research strives for empirical generalization. In qualitative studies, generalizability beyond the study sample is typically not the intent; rather, the focus is on deriving depth and context-embedded meaning for the relevant study population.
Purposeful sampling is a broad term. Theoretical sampling is one particular type of purposeful sampling unique to grounded theory methods ( Coyne, 1997 ). In theoretical sampling, study participants are chosen according to theoretical categories that emerge from ongoing data collection and analyses ( Bryant & Charmaz, 2010 ). Data collection and analysis are conducted concurrently to allow generating and testing hypotheses that emerge from analyzing incoming data. The following example from the previously mentioned qualitative interview study about transition from pediatric to adult care in adolescents with type 1 diabetes ( Pierce et al., 2016 ) illustrates the process of theoretical sampling: An adolescent study participant stated that he was “turned off” by the “childish” posters in his pediatrician’s office. He elaborated that he welcomed transitioning to adult care because his diabetes was discovered when he was 18, an age when he reportedly felt more “mature” than most pediatric patients. These data were coded as “developmental misfit” and prompted a tentative hypothesis about developmental stage at entry for pediatric diabetes care and readiness for health care transition. Examining this hypothesis prompted seeking study participants who varied according to age or developmental stage at time of diagnosis to examine the theoretical relevance of an emerging theme about developmental fit.
Not all purposeful sampling, however, is “theoretical.” For example, ethnographic studies typically seek to understand a group’s cultural beliefs and practices ( Creswell, 2013a ). Consistent with this purpose, researchers conducting an ethnographic study might purposefully select study participants according to specific characteristics that reflect the social roles and positions in a given group or society (e.g., socioeconomic status, education; Johnson, 1990 ).
Random sampling is generally not used in qualitative research. Random selection requires a sufficiently large sample to maximize the potential for chance and, as will be discussed below, sample size is intentionally small in qualitative studies. However, random sampling may be used to verify or clarify findings ( Patton, 2015 ). Validating study findings with a randomly selected subsample can be used to address the possibility that a researcher is inadvertently giving greater attention to cases that reinforce his or her preconceived ideas.
Regardless of the sampling method used, qualitative researchers should clearly describe the sampling strategy and justify how it fits the study when reporting study findings (transparency). A common error is to refer to theoretical sampling when the cases were not chosen according to emerging theoretical concepts. Another common error is to apply sampling principles from quantitative research (e.g., cluster sampling) to convince skeptical reviewers about the rigor or validity of qualitative research. Rigor is best achieved by being purposeful, making sound decisions, and articulating the rationale for those decisions. As mentioned earlier in the discussion of transferability , qualitative researchers are encouraged to describe their methods of sample selection and descriptive characteristics about their sample so that readers and reviewers can judge how the current sample may differ from others. Understanding the characteristics of each qualitative study sample is essential for the iterative nature of qualitative research whereby qualitative findings inform the development of future qualitative, quantitative, or mixed-methods studies. Reviewers should evaluate sampling decisions based on how they fit the study purpose and how they influence the quality of the end product.
What Sample Size Is Needed for Qualitative Research?
No definitive rules exist about sample size in qualitative research. However, sample sizes are typically smaller than those in quantitative studies ( Patton, 2015 ). Small samples often generate a large volume of data and information-rich cases, ultimately leading to insight regarding the phenomenon under study ( Patton, 2015 ; Ritchie & Lewis, 2003 ). Sample sizes of 20–30 cases are typical, but a qualitative sample can be even smaller under some circumstances ( Mason, 2010 ).
Sample size adequacy is evaluated based on the quality of the study findings, specifically the full development of categories and inter-relationships or the adequacy of information about the phenomenon under study ( Corbin & Strauss, 2008 ; Ritchie & Lewis, 2003 ). Small sample sizes are of concern if they do not result in these outcomes. Data saturation (i.e., the point at which no new information, categories, or themes emerge) is often used to judge informational adequacy ( Morgan, 1998 ; Ritchie & Lewis, 2003 ). Although enough participants should be included to obtain saturation ( Morgan, 1998 ), informational adequacy pertains to more than sample size. It is also a function of the quality of the data, which is influenced by study participant characteristics (e.g., cognitive ability, knowledge, representativeness) and the researcher’s data-gathering skills and analytical ability to generate meaningful findings ( Morse, 2015b ; Patton, 2015 ).
Sample size is also influenced by type of qualitative research, the study purpose, the sample, the depth and complexity of the topic investigated, and the method of data collection. In general, the more heterogeneous the sample, the larger the sample size, particularly if the goal is to investigate similarities and differences by specific characteristics ( Ritchie & Lewis, 2003 ). For instance, in a study to conduct an initial exploration of factors underlying parents’ motivations to use good parenting practices, theoretical saturation (i.e., the point at which no new information, categories, or themes emerge) was obtained with a small sample ( n = 15), most likely because the study was limited to parents of young children ( Hingle et al., 2012 ). If the goal of the study had been, for example, to identify racial/ethnic, gender, or age differences in food parenting practices, a larger sample would likely be needed to obtain saturation or informational adequacy.
Studies that seek to understand maximum variation in a phenomenon might also need a larger sample than one that is seeking to understand extreme or atypical cases. For example, a qualitative study of diet and physical activity in young Australian men conducted focus groups to identify perceived motivators and barriers to healthy eating and physical activity and examine the influence of body weight on their perceptions. Examining the influence of body weight status required 10 focus groups to allow for group assignment based on body mass index ( Ashton et al., 2015 ). More specifically, 61 men were assigned to a healthy-weight focus group ( n = 3), an overweight/obese focus group ( n = 3), or a mixed-weight focus group ( n = 4). Had the researcher not been interested in whether facilitators and barriers differed by weight status, its likely theoretical saturation could have been obtained with fewer groups. Depth of inquiry also influences sample size ( Sandelowski, 1995 ). For instance, an in-depth analysis of an intervention for children with cancer and their families included 16 family members from three families. Study data comprised 52 hrs of videotaped intervention sessions and 10 interviews ( West, Bell, Woodgate, & Moules, 2015 ). Depth was obtained through multiple data points and types of data, which justified sampling only a few families.
Authors of publications describing qualitative findings should show evidence that the data were “saturated” by a sample with sufficient variation to permit detailing shared and divergent perspectives, meanings, or experiences about the topic of inquiry. Decisions related to the sample (e.g., targeted recruitment) should be detailed in publications so that peer reviewers have the context for evaluating the sample and determining how the sample influenced the study findings ( Patton, 2015 ).
Qualitative Data Analysis
When conducting qualitative research, voluminous amounts of data are gathered and must be prepared (i.e., transcribed) and managed. During the analytic process, data are systematically transformed through identifying, defining, interpreting, and describing findings that are meant to comprehensively describe the phenomenon or the abstract qualities that they have in common. The process should be systematic ( dependability ) and well-documented in the analysis section of a qualitative manuscript. For example, Kelly and Ganong (2011) , in their study of medical treatment decisions made by families of children with cancer, described their analytic procedure by outlining their approach to coding and use of memoing (e.g., keeping careful notes about emerging ideas about the data throughout the analytic process), comparative analysis (e.g., comparing data against one another and looking for similarities and differences), and diagram drawing (e.g., pictorially representing the data structure, including relationships between codes).
How Should Researchers Document Coding Reliability?
Because the intent of qualitative research is to account for multiple perspectives, the goal of qualitative analysis is to comprehensively incorporate those perspectives into discernible findings. Researchers accustomed to doing quantitative studies may expect authors to quantify interrater reliability (e.g., kappa statistic) but this is not typical in qualitative research. Rather, the emphasis in qualitative research is on (1) training those gathering data to be rigorous and produce high-quality data and on (2) using systematic processes to document key decisions (e.g., code book), clear direction, and open communication among team members during data analysis. The goal is to make the most of the collective insight of the investigative team to triangulate or complement each other’s efforts to process and interpret the data. Instead of evaluating if two independent raters came to the same numeric rating, reviewers of qualitative manuscripts should judge to what extent the overall process of coding, data management, and data interpretation were systematic and rigorous. Authors of qualitative reports should articulate their coding procedures for others to evaluate. Together, these strategies promote trustworthiness of the study findings.
An example of how these processes are described in the report of a qualitative study is as follows:
The first two authors independently applied the categories to a sample of two interviews and compared their application of the categories to identify lack of clarity and overlap in categories. The investigators created a code book that contained a definition of categories, guidelines for their application, and excerpts of data exemplifying the categories. The first two authors independently coded the data and compared how they applied the categories to the data and resolved any differences during biweekly meetings. ATLAS.ti, version 6.2, was used to document and accommodate ongoing changes and additions to the coding structure ( Palma et al., 2015 , p. 224).
Do I Need to Use a Specialized Qualitative Data Software Program for Analysis?
Multiple computer software packages for qualitative data analysis are currently available ( Silver & Lewins, 2014 ; Yin, 2015 ). These packages allow the researcher to import qualitative data (e.g., interview transcripts) into the software program and organize data segments (e.g., delineate which interview excerpts are relevant to particular themes). Qualitative analysis software can be useful for organizing and sorting through data, including during the analysis phase. Some software programs also offer sophisticated coding and visualization capabilities that facilitate and enhance interpretation and understanding. For example, if data segments are coded by specific characteristics (e.g., gender, race/ethnicity), the data can be sorted and analyzed by these characteristics, which may contribute to an understanding of whether and/or how a particular phenomenon may vary by these characteristics.
The strength of computer software packages for qualitative data analysis is their potential to contribute to methodological rigor by organizing the data for systematic analyses ( John & Johnson, 2000 ; MacMillan & Koenig, 2004 ). However, the programs do not replace the researchers’ analyses. The researcher or research team is ultimately responsible for analyzing the data, identifying the themes and patterns, and placing the findings within the context of the literature. In other words, qualitative data analysis software programs contribute to, but do not ensure scientific rigor or “objectivity” in, the analytic process. In fact, using a software program for analysis is not essential if the researcher demonstrates the use of alternative tools and procedures for rigor.
Presentation of Findings
Should there be overlap between presentation of themes in the results and discussion sections.
Qualitative papers sometimes combine results and discussion into one section to provide a cohesive presentation of the findings along with meaningful linkages to the existing literature ( Burnard, 2004 ; Burnard, Gill, Stewart, Treasure, & Chadwick, 2008 ). Although doing so is an acceptable method for reporting qualitative findings, some journals prefer the two sections to be distinct.
When the journal style is to distinguish the two sections, the results section should describe the findings, that is, the themes, while the discussion section should pull the themes together to make larger-level conclusions and place the findings within the context of the existing literature. For instance, the findings section of a study of how rural African-American adolescents, parents, and community leaders perceived obesity and topics for a proposed obesity prevention program, contained a description of themes about adolescent eating patterns, body shape, and feedback on the proposed weight gain prevention program according to each subset of participants (i.e., adolescents, parents, community leaders). The discussion section then put these themes within the context of findings from prior qualitative and intervention studies in related populations ( Cassidy et al., 2013 ). In the Discussion, when making linkages to the existing literature, it is important to avoid the temptation to extrapolate beyond the findings or to over-interpret them ( Burnard, 2004 ). Linkages between the findings and the existing literature should be supported by ample evidence to avoid spurious or misleading connections ( Burnard, 2004 ).
What Should I Include in the Results Section?
The results section of a qualitative research report is likely to contain more material than customary in quantitative research reports. Findings in a qualitative research paper typically include researcher interpretations of the data as well as data exemplars and the logic that led to researcher interpretations ( Sandelowski & Barroso, 2002 ). Interpretation pertains to the researcher breaking down and recombining the data and creating new meanings (e.g., abstract categories, themes, conceptual models). Select quotes from interviews or other types of data (e.g., participant observation, focus groups) are presented to illustrate or support researcher interpretations. Researchers trained in the quantitative tradition, where interpretation is restricted to the discussion section, may find this surprising; however, in qualitative methods, researcher interpretations represent an important component of the study results. The presentation of the findings, including researcher interpretations (e.g., themes) and data (e.g., quotes) supporting those interpretations, adds to the trustworthiness of the study ( Elo et al., 2014 ).
The Results section should contain a balance between data illustrations (i.e., quotes) and researcher interpretations ( Lofland & Lofland, 2006 ; Sandelowski, 1998 ). Because interpretation arises out of the data, description and interpretation should be combined. Description should be sufficient to support researcher interpretations, and quotes should be used judiciously ( Morrow, 2005 ; Sandelowski, 1994 ). Not every theme needs to be supported by multiple quotes. Rather, quotes should be carefully selected to provide “voice” to the participants and to help the reader understand the phenomenon from the participant’s perspective within the context of the researcher’s interpretation ( Morrow, 2005 ; Ritchie & Lewis, 2003 ). For example, researchers who developed a grounded theory of sexual risk behavior of urban American Indian adolescent girls identified desire for better opportunities as a key deterrent to neighborhood norms for early sexual activity. They illustrated this theme with the following quote: “I don’t want to live in the ‘hood and all that…My sisters are stuck there because they had babies. That isn’t going to happen to me” ( Saftner, Martyn, Momper, Loveland-Cherry, & Low, 2015 , p. 372).
There is no precise formula for the proportion of description to interpretation. Both descriptive and analytic excess should be avoided ( Lofland & Lofland, 2006 ). The former pertains to presentation of unedited field notes or interview transcripts rather than selecting and connecting data to analytic concepts that explain or summarize the data. The latter pertains to focusing on the mechanics of analysis and interpretation without substantiating researcher interpretations with quotes. Reviewer requests for methodological rigor can result in researchers writing qualitative research papers that suffer from analytic excess ( Sandelowski & Barroso, 2002 ). Page limitations of most journals provide a safeguard against descriptive excess, but page limitations should not circumvent researchers from providing the basis for their interpretations.
Additional potential problems with qualitative results sections include under-elaboration, where themes are too few and not clearly defined. The opposite problem, over-elaboration, pertains to too many analytic distinctions that could be collapsed under a higher level of abstraction. Quotes can also be under- or over-interpreted. Care should be taken to ensure the quote(s) selected clearly support the theme to which they are attached. And finally, findings from a qualitative study should be interesting and make clear contributions to the literature ( Lofland & Lofland, 2006 ; Morse, 2015b ).
Should I Quantify My Results? (e.g., Frequency With Which Themes Were Endorsed)
There is controversy over whether to quantify qualitative findings, such as providing counts for the frequency with which particular themes are endorsed by study participants ( Morgan, 1993 ; Sandelowski, 2001 ). Qualitative papers usually report themes and patterns that emerge from the data without quantification ( Dey, 1993 ). However, it is possible to quantify qualitative findings, such as in qualitative content analysis. Qualitative content analysis is a method through which a researcher identifies the frequency with which a phenomenon, such as specific words, phrases, or concepts, is mentioned ( Elo et al., 2014 ; Morgan, 1993 ). Although this method may appeal to quantitative reviewers, it is important to note that this method only fits specific study purposes, such as studies that investigate the language used by a particular group when communicating about a specific topic. In addition, results may be quantified to provide information on whether themes appeared to be common or atypical. Authors should avoid using imprecise language, such as “some participants” or “many participants.” A good example of quantification of results to illustrate more or less typical themes comes from a manuscript describing a qualitative study of school nurses’ perceived barriers to addressing obesity with students and their families. The authors described that all but one nurse reported not having the resources they needed to discuss weight with students and families whereas one-quarter of nurses reported not feeling competent to discuss weight issues ( Steele et al., 2011 ). If quantification of findings is used, authors should provide justification that explains how quantification is consistent with the aims or goals of the study ( Sandelowski, 2001 ).
Conclusions
This article highlighted key theoretical and logistical considerations that arise in designing, conducting, and reporting qualitative research studies (see Table 1 for a summary). This type of research is vital for obtaining patient, family, community, and other stakeholder perspectives about their needs and interests, and will become increasingly critical as our models of health care delivery evolve. For example, qualitative research could contribute to the study of health care providers and systems with the goal of optimizing our health care delivery models. Given the increasing diversity of the populations we serve, qualitative research will also be critical in providing guidance in how to tailor health interventions to key characteristics and increase the likelihood of acceptable, effective treatment approaches. For example, applying qualitative research methods could enhance our understanding of refugee experiences in our health care system, clarify treatment preferences for emerging adults in the midst of health care transitions, examine satisfaction with health care delivery, and evaluate the applicability of our theoretical models of health behavior changes across racial and ethnic groups. Incorporating patient perspectives into treatment is essential to meeting this nation’s priority on patient-centered health care ( Institute of Medicine Committee on Quality of Health Care in America, 2001 ). Authors of qualitative studies who address the methodological choices addressed in this review will make important contributions to the field of pediatric psychology. Qualitative findings will lead to a more informed field that addresses the needs of a wide range of patient populations and produces effective and acceptable population-specific interventions to promote health.
Acknowledgments
The authors thank Bridget Grahmann for her assistance with manuscript preparation.
This work was supported by National Cancer Institute of the National Institutes of Health (K07CA196985 to Y.W.). This work is a publication of the United States Department of Agriculture/Agricultural Research Center (USDA/ARS), Children’s Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine, Houston, Texas. It is also a publication of the USDA/ARS, Children’s Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine, Houston, Texas, and funded in part with federal funds from the USDA/ARS under Cooperative Agreement No. 58‐6250‐0‐008 (to D.T.). The contents of this publication do not necessarily reflect the views or policies of the USDA, nor does mention of trade names, commercial products, or organizations imply endorsement from the U.S. government. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of interest : None declared.
- Aroian K. J., Peters R. M., Rudner N., Waser L. (2012). Hypertension prevention beliefs of hispanics . Journal of Transcultural Nursing , 23 , 134–142. doi:10.1177/1043659611433871. [ PubMed ] [ Google Scholar ]
- Ashton L. M., Hutchesson M. J., Rollo M. E., Morgan P. J., Thompson D. I., Collins C. E. (2015). Young adult males’ motivators and perceived barriers towards eating healthily and being active: A qualitative study . The International Journal of Behavioral Nutrition and Physical Activity , 12 , 93 doi:10.1186/s12966‐015‐0257‐6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bagozzi R., Pieters R. (1998). Goal-directed emotions . Cognition & Emotion , 12 ( 1 ), 1–26. [ Google Scholar ]
- Bandura A. (1986). Social foundations of thought and action: A social cognitive theory . Englewood Cliffs, NJ: Prentice-Hall Inc. [ Google Scholar ]
- Bevans K. B., Gardner W., Pajer K., Riley A. W., Forrest C. B. (2013). Qualitative development of the PROMIS ® pediatric stress response item banks . Journal of Pediatric Psychology , 38 , 173–191. doi:10.1093/jpepsy/jss107. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bradbury-Jones C., Taylor J., Herber O. (2014). How theory is used and articulated in qualitative research: Development of a new typology . Social Science and Medicine , 120 , 135–141. doi:10.1016/j.socscimed.2014.09.014. [ PubMed ] [ Google Scholar ]
- Bryant A., Charmaz K. (2010). The Sage handbook of grounded theory . Thousand Oaks, CA: Sage. [ Google Scholar ]
- Burnard P. (2004). Writing a qualitative research report . Nurse Education Today , 24 , 174–179. doi:10.1016/j.nedt.2003.11.005. [ PubMed ] [ Google Scholar ]
- Burnard P., Gill P., Stewart K., Treasure E., Chadwick B. (2008). Analysing and presenting qualitative data . British Dental Journal , 204 , 429–432. doi:10.1038/sj.bdj.2008.292. [ PubMed ] [ Google Scholar ]
- Cassidy O., Sbrocco T., Vannucci A., Nelson B., Jackson-Bowen D., Heimdal J., Heimdal J., Mirza N., Wilfley D. E., Osborn R., Shomaker L. B., Young J. F., Waldron H., Carter M., Tanofsky-Kraff M., (2013). Adapting interpersonal psychotherapy for the prevention of excessive weight gain in rural African American girls . Journal of Pediatric Psychology , 38 , 965–977. doi:10.1093/jpepsy/jst029. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Clark J. (2003). How to peer review a qualitative manuscript . Peer Review in Health Sciences , 2 , 219–235. [ Google Scholar ]
- Corbin S., Strauss A. (2008). Basics of qualitative research (3rd ed.). Los Angeles, CA: Sage Publications. [ Google Scholar ]
- Coyne I. T. (1997). Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? Journal of Advanced Nursing , 26 , 623–630. doi:10.1046/j.1365‐2648.1997.t01‐25‐00999.x. [ PubMed ] [ Google Scholar ]
- Creswell J. W. (1994). Research design: Qualitative & quantitative approaches . Journal of Marketing Research , 33 , 252 doi:10.2307/3152153. [ Google Scholar ]
- Creswell J. W. (2013a). Qualitative inquiry and research design: Choosing among five approaches . Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Creswell J. W. (2013b). Research design: Qualitative, quantitative, and mixed methods approaches (4th ed.). Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Creswell J. W., Klassen A. C., Plano Clark V. L., Smith K. C.;for the Office of Behavioral and Social Sciences Research. (2011). Best practices for mixed methods research in the health sciences . Retrieved from National Institutes of Health: http://obssr.od.nih.gov/mixed_methods_research .
- de Visser R. O., Graber R., Hart A., Abraham C., Scanlon T., Watten P., Memon A. (2015). Using qualitative methods within a mixed-methods approach to developing and evaluating interventions to address harmful alcohol use among young people . Health Psychology , 34 , 349–360. doi:10.1037/hea0000163. [ PubMed ] [ Google Scholar ]
- Dey I. (1993). Qualitative data analysis: A user-friendly guide for social scientists . New York, NY: Routledge. [ Google Scholar ]
- Dixon-Woods M., Shaw R. L., Agarwal S., Smith J. A. (2004). The problem of appraising qualitative research . Quality and Safety in Health Care , 13 , 223–225. doi:10.1136/qhc.13.3.223. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Eakin J. M., Mykhalovskiy E. (2003). Reframing the evaluation of qualitative health research: Reflections on a review of appraisal guidelines in the health sciences . Journal of Evaluation in Clinical Practice , 9 , 187–194. doi:10.1046/j.1365‐2753.2003.00392.x. [ PubMed ] [ Google Scholar ]
- Elo S., Kääriäinen M., Kanste O., Pölkki T., Utriainen K., Kyngäs H. (2014). Qualitative content analysis: A focus on trustworthiness . SAGE Open , 4 ( 1 ), 1–10. doi:10.1177/2158244014522633. [ Google Scholar ]
- Glaser B., Strauss A. (1967). The discovery grounded theory: Strategies for qualitative inquiry . Nursing Research , 17 , 364 doi:10.1097/00006199‐196807000‐00014. [ Google Scholar ]
- Gough B., Deatrick J. A. (2015). Qualitative health psychology research: Diversity, power, and impact . Health Psychology , 34 , 289–292. doi:10.1037/hea0000206. [ PubMed ] [ Google Scholar ]
- Guba E. G. (1981). Criteria for assessing the trustworthiness of naturalistic inquiries . Educational Communication and Technology , 29 , 75–91. doi:10.1007/BF02766777. [ Google Scholar ]
- Haukeland Y. B., Fjermestad K. W., Mossige S., Vatne T. M. (2015). Emotional experiences among siblings of children with rare disorders . Journal of Pediatric Psychology , 40 , 12–20. doi:10.1093/jpepsy/jsv022. [ PubMed ] [ Google Scholar ]
- Hess J. S., Straub D. M. (2011). Brief report: Preliminary findings from a pilot health care transition education intervention for adolescents and young adults with special health care needs . Journal of Pediatric Psychology , 36 , 172–178. doi:10.1093/jpepsy/jsq091. [ PubMed ] [ Google Scholar ]
- Hingle M., Beltran A., O’Connor T., Thompson D., Baranowski J., Baranowski T. (2012). A model of goal directed vegetable parenting practices . Appetite , 58 , 444–449. doi:10.1016/j.appet.2011.12.011. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hughes S. O., Power T. G., Papaioannou M. A., Cross M. B., Nicklas T. A., Hall S. K., Shewchuk R. M. (2011). Emotional climate, feeding practices, and feeding styles: An observational analysis of the dinner meal in Head Start families . The International Journal of Behavavioral Nutrition and Physical Activity , 8 , 60 doi:10.1186/1479‐5868‐8‐60. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Institute of Medicine Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: A new health system for the 21st century . National Academies Press. Washington, DC. [ Google Scholar ]
- Izaguirre M. R., Keefer L. (2014). Development of a self-efficacy scale for adolescents and young adults with inflammatory bowel disease . Journal of Pediatric Gastroenterology and Nutrition , 59 , 29–32. doi:10.1097/mpg.0000000000000357. [ PubMed ] [ Google Scholar ]
- John W. S., Johnson P. (2000). The pros and cons of data analysis software for qualitative research . Journal of Nursing Scholarship , 32 , 393–397. [ PubMed ] [ Google Scholar ]
- Johnson J. C. (1990). Selecting ethnographic informants . Sage Publications. Thousand Oaks, CA. [ Google Scholar ]
- Kars M. C., Grypdonck M. H., de Bock L. C., van Delden J. J. (2015). The parents’ ability to attend to the “voice of their child” with incurable cancer during the palliative phase . Health Psychology , 34 , 446–452. doi:10.1037/hea0000166. [ PubMed ] [ Google Scholar ]
- Kelly K., Ganong L. (2011). Moving to place: Childhood cancer treatment decision making in single-parent and repartnered family structures . Qualitative Health Research , 21 , 349–364. doi:10.1177/1049732310385823. [ PubMed ] [ Google Scholar ]
- Kelly M. (2010). The role of theory in qualitative health research . Family Practice , 27 , 285–290. doi:10.1093/fampra/cmp077. [ PubMed ] [ Google Scholar ]
- Krefting L. (1991). Rigor in qualitative research: The assessment of trustworthiness . The American Journal of Occupational Therapy , 45 , 214–222. doi:10.5014/ajot.45.3.214. [ PubMed ] [ Google Scholar ]
- Lincoln Y. S., Guba E. G. (1985). Naturalistic inquiry . Newbury Park, CA: Sage Publications. [ Google Scholar ]
- Lincoln Y. S., Lynham S. A., Guba E. G. (2011). Paradigmatic controversies, contradictions, and emerging confluences, revisited . In Denzin N. K., Lincoln Y. S. (Eds.), The Sage handbook of qualitative research (4th ed., pp. 97–128). Thousand Oaks, CA: Sage. [ Google Scholar ]
- Lofland J., Lofland L. H. (2006). Analyzing social settings: A guide to qualitative observation and analysis . Belmont, CA: Wadsworth Publishing Company. [ Google Scholar ]
- Lyons A. C., Goodwin I., McCreanor T., Griffin C. (2015). Social networking and young adults’ drinking practices: Innovative qualitative methods for health behavior research . Health Psychology , 34 , 293–302. doi:10.1037/hea0000168. [ PubMed ] [ Google Scholar ]
- MacMillan K., Koenig T. (2004). The wow factor: Preconceptions and expectations for data analysis software in qualitative research . Social Science Computer Review , 22 , 179–186. doi:10.1177/0894439303262625. [ Google Scholar ]
- Mason M. (Producer). (2010). Sample size and saturation in PhD studies using qualitative interviews . Forum: Qualitative Social Research . Retrieved from http://nbn-resolving.de/urn:nbn:de:0114-fqs100387 .
- Mays N., Pope C. (2000). Qualitative research in health care: Assessing quality in qualitative research . British Medical Journal , 320 , 50 doi:10.1136/bmj.320.7226.50. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McDonald C. C., Sommers M. S. (2015). Teen drivers’ perceptions of inattention and cell phone use while eriving . Traffic Injury Prevention , 16 ( Suppl 2 ), S52–S58. doi:10.1080/15389588.2015.1062886. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miles M. B., Huberman A. M., Saldaña J. (2013). Qualitative data analysis: A methods sourcebook (3rd ed.). Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Minges K. E., Owen N., Salmon J., Chao A., Dunstan D. W., Whittemore R. (2015). Reducing youth screen time: Qualitative metasynthesis of findings on barriers and facilitators . Health Psychology , 34 , 381–397. doi:10.1037/hea0000172. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morgan D. L. (1993). Qualitative content analysis: A guide to paths not taken . Qualitative Health Research , 3 , 112–121. doi:10.1177/104973239300300107. [ PubMed ] [ Google Scholar ]
- Morgan D. L. (1998). Planning Focus Groups: Focus Group Kit #2 . Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Morrow S. (2005). Quality and trustworthiness in qualitative research in counseling psychology . Journal of Counseling Psychology , 52 , 250–260. doi:10.1037/0022‐0167.52.2.250. [ Google Scholar ]
- Morse J. M. (2015a). Critical analysis of strategies for determining rigor in qualitative inquiry . Qualitative Health Research , 25 , 1212–1222. doi:10.1177/1049732315588501. [ PubMed ] [ Google Scholar ]
- Morse J. M. (2015b). Data were saturated . Qualitative Health Research , 25 , 587–588. doi:10.1177/1049732315576699. [ PubMed ] [ Google Scholar ]
- Palermo T. M. (2013). New guidelines for publishing review articles in JPP: Systematic reviews and topical reviews . Journal of Pediatric Psychology , 38 , 5–9. doi:10.1093/jpepsy/jss124. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Palermo T. M. (2014). Evidence-based interventions in pediatric psychology: Progress over the decades . Journal of Pediatric Psychology , 39 , 753–762. doi:10.1093/jpepsy/jsu048. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Palma E., Deatrick J., Hobbie W., Ogle S., Kobayashi K., Maldonado L. (2015). Maternal caregiving demands for adolescent and young adult survivors of pediatric brain tumors . Oncology Nursing Forum , 42 , 222–229. doi:10.1188/15.ONF.. [ PubMed ] [ Google Scholar ]
- Patton M. Q. (2015). Qualitative research & evaluation methods: Integrating theory and practice (4th ed.). Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Pierce J. S., Wysocki T. (2015). Topical Review: Advancing research on the transition to adult care for type 1 diabetes . Journal of Pediatric Psychology , 40 , 1041–1047. doi:10.1093/jpepsy/jsv064. [ PubMed ] [ Google Scholar ]
- Pierce J. S., Wysocki T., Aroian K. (2016). Multiple stakeholder perspectives on health care transition outcomes in Type 1 Diabetes . Unpublished data. [ Google Scholar ]
- Polanyi M. (1958). Personal knowledge . New York, NY: Harper & Row. [ Google Scholar ]
- Power T. G., Hughes S. O., Goodell L. S., Johnson S. L., Duran J. A., Williams K., Beck A. D., Frankel L. A. (2015). Feeding practices of low-income mothers: How do they compare to current recommendations? The International Journal of Behavioral Nutrition and Physical Activity , 12 , 34 doi:10.1186/s12966‐015‐0179‐3. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Richards L., Morse J. M. (2013). Readdme first for a user’s guide to qualitative methods (3rd ed.). Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Ritchie J., Lewis J. (Eds.). (2003). Qualitative research practice: A guide for social science students and researchers . Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Saftner M. A., Martyn K. K., Momper S. L., Loveland-Cherry C. J., Low L. K. (2015). Urban American Indian adolescent girls framing sexual risk behavior . Journal of Transcultural Nursing , 26 , 365–375. doi:10.1177/1043659614524789. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Saldaña J. (2012). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage Publications. [ Google Scholar ]
- Sandelowski M. (1993a). Rigor or rigor mortis: The problem of rigor in qualitative research revisited . Advances in Nursing Science , 16 , 1–8. [ PubMed ] [ Google Scholar ]
- Sandelowski M. (1993b). Theory unmasked: The uses and guises of theory in qualitative research . Research in Nursing & Health , 16 , 213–218. doi:10.1002/nur.4770160308. [ PubMed ] [ Google Scholar ]
- Sandelowski M. (1994). The use of quotes in qualitative research . Research in Nursing and Health , 17 , 479–482. [ PubMed ] [ Google Scholar ]
- Sandelowski M. (1995). Sample size in qualitative research . Research in Nursing and Health , 18 , 179–183. [ PubMed ] [ Google Scholar ]
- Sandelowski M. (1998). Writing a good read: Strategies for re-presenting qualitative data . Research in Nursing and Health , 21 , 375–382. doi:10.1016/s1361‐3111(98)80052‐6. [ PubMed ] [ Google Scholar ]
- Sandelowski M. (2001). Real qualitative researchers do not count: The use of numbers in qualitative research . Research in Nursing and Health , 24 , 230–240. [ PubMed ] [ Google Scholar ]
- Sandelowski M. (2010). What’s in a name? Qualitative description revisited . Research in Nursing and Health , 33 , 77–84. doi:10.1002/nur.20362.. [ PubMed ] [ Google Scholar ]
- Sandelowski M., Barroso J. (2002). Finding the findings in qualitative studies . Journal of Nursing Scholarship , 34 , 213–219. [ PubMed ] [ Google Scholar ]
- Schwartz L. A., Tuchman L. K., Hobbie W. L., Ginsberg J. P. (2011). A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions . Child: Care, Health, and Development , 37 , 883–895. doi:10.1111/j.1365‐2214.2011.01282.x. [ PubMed ] [ Google Scholar ]
- Silver C., Lewins A. (2014). Using software in qualitative research: A step-by-step guide (2nd ed.). London: Sage Publications. [ Google Scholar ]
- Steele R. G., Wu Y. P., Jensen C. D., Pankey S., Davis A. M., Aylward B. S. (2011). School nurses’ perceived barriers to discussing weight with children and their families: A qualitative approach . Journal of School Health , 81 , 128–137. doi:10.1111/j.1746‐1561.2010.00571.x. [ PubMed ] [ Google Scholar ]
- Thompson D. (2014). Talk to me, please!: The importance of qualitative research to games for health . Games for Health: Research, Development, and Clinical Applications , 3 , 117–118. doi:10.1089/g4h.2014.0023. [ PubMed ] [ Google Scholar ]
- Thompson D., Baranowski T., Buday R., Baranowski J., Juliano M., Frazior M., Wilsdon J., Jago R. (2007). In pursuit of change: Youth response to intensive goal setting embedded in a serious video game . Journal of Diabetes Science and Technology , 1 , 907–917. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thompson D., Bhatt R., Watson K. (2013). Physical activity problem-solving inventory for adolescents: Development and initial validation . Pediatric Exercise Science , 25 , 448–467. [ PubMed ] [ Google Scholar ]
- Tobin G. A., Begley C. M. (2004). Methodological rigour within a qualitative framework . Journal of Advanced Nursing , 48 , 388–396. doi:10.1111/j.1365‐2648.2004.03207.x. [ PubMed ] [ Google Scholar ]
- Tong A., Sainsbury P., Craig J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups . International Journal for Quality in Health Care , 19 , 349–357. doi:10.1093/intqhc/mzm042. [ PubMed ] [ Google Scholar ]
- Tuckett A. G. (2004). Qualitative research sampling: The very real complexities . Nurse Researcher , 12 , 47–61. doi:10.7748/nr2004.07.12.1.47.c5930. [ PubMed ] [ Google Scholar ]
- Valenzuela J. M., Buchanan C. L., Radcliffe J., Ambrose C., Hawkins L. A., Tanney M., Rudy B. J. (2011). Transition to adult services among behaviorally infected adolescents with HIV—a qualitative study . Journal of Pediatric Psychology , 36 , 134–140. doi:10.1093/jpepsy/jsp051. [ PubMed ] [ Google Scholar ]
- West C. H., Bell J. M., Woodgate R. L., Moules N. J. (2015). Waiting to return to normal: An exploration of family systems intervention in childhood cancer . Journal of Family Nursing , 21 , 261–294. doi:10.1177/1074840715576795. [ PubMed ] [ Google Scholar ]
- Whittemore R., Chase S. K., Mandle C. L. (2001). Validity in qualitative research . Qualitative Health Research , 11 , 522–537. doi:10.1177/104973201129119299. [ PubMed ] [ Google Scholar ]
- Yin R. K. (2015). Qualitative research from start to finish (2nd ed.). New York, NY: Guilford Press. [ Google Scholar ]
- Open access
- Published: 05 January 2024
Acceptability, values, and preferences of older people for chronic low back pain management; a qualitative evidence synthesis
- Heather Ames 1 ,
- Christine Hillestad Hestevik 1 &
- Andrew M. Briggs 2 , 3
BMC Geriatrics volume 24 , Article number: 24 ( 2024 ) Cite this article
956 Accesses
4 Altmetric
Metrics details
Chronic primary low back pain (CPLBP) and other musculoskeletal conditions represent a sizable attribution to the global burden of disability, with rates greatest in older age. There are multiple and varied interventions for CPLBP, delivered by a wide range of health and care workers. However, it is not known if these are acceptable to or align with the values and preferences of care recipients. The objective of this synthesis was to understand the key factors influencing the acceptability of, and values and preferences for, interventions/care for CPLBP from the perspective of people over 60 and their caregivers.
We searched MEDLINE, CINAHL and OpenAlex, for eligible studies from inception until April 2022. We included studies that used qualitative methods for data collection and analysis; explored the perceptions and experiences of older people and their caregivers about interventions to treat CPLBP; from any setting globally. We conducted a best fit framework synthesis using a framework developed specifically for this review. We assessed our certainty in the findings using GRADE-CERQual.
All 22 included studies represented older people’s experiences and had representation across a range of geographies and economic contexts. No studies were identified on caregivers. Older people living with CPLBP express values and preferences for their care that relate to therapeutic encounters and the importance of therapeutic alliance, irrespective of the type of treatment, choice of intervention, and intervention delivery modalities. Older people with CPLBP value therapeutic encounters that validate, legitimise, and respect their pain experience, consider their context holistically, prioritise their needs and preferences, adopt a person-centred and tailored approach to care, and are supported by interprofessional communication. Older people valued care that provided benefit to them, included interventions beyond analgesic medicines alone and was financially and geographically accessible.

Conclusions
These findings provide critical context to the implementation of clinical guidelines into practice, particularly related to how care providers interact with older people and how components of care are delivered, their location and their cost. Further research is needed focusing on low- and middle-income settings, vulnerable populations, and caregivers.
Peer Review reports
Low back pain (LBP) and other musculoskeletal conditions represent a sizable contribution to the global burden of disability [ 1 , 2 , 3 , 4 , 5 ]. While the prevalence and impact of LBP are relevant across the life-course, global estimates for prevalence and disability show rates to be greatest in older age. The high prevalence of LBP in older people accounts for frequent care seeking for LBP [ 6 ], particularly among older adults experiencing recurrent LBP [ 7 ]. The number of older people experiencing and seeking care for LBP is expected to increase due to population ageing and an increasing prevalence of risk factors for noncommunicable diseases [ 8 ]. Despite this, intervention trials and clinical guidelines for LBP disproportionately underrepresent older people [ 9 , 10 ], potentially leaving an important knowledge gap for optimal care of LBP in older people.
Clinical management of LBP is characterized by multiple and varied interventions, delivered by a wide range of health and care workers [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 ]. In many contexts the interventions delivered may not be aligned with best evidence leading to unwarranted care variation and potential harm. Further, interventions may not be aligned with the values, preferences and acceptability attitudes among care recipients (and/or their carers), substantiating the need for global guidelines in this area [ 21 ]. Importantly, values and preferences of older people likely differ to younger adults. From the perspective of healthy ageing, carers are an essential workforce for supporting functional ability in older people and enabling ageing in place. The perspectives of carers are therefore critical to ensure care planning and delivery for any health condition experienced by an older people is feasible and acceptable and does not negatively impact on the quality of life of the carer [ 22 , 23 ] . For example, recent work has also identified the need to sample perspectives of carers related to delivery of care for people living with chronic pain [ 24 ].
In response to this context and the priority to support healthy ageing, the World Health Organization (WHO) initiated the development of standard clinical guideline for the non-surgical management of chronic primary LBP (CPLBP) in adults, including older people, in primary and community care settings in 2020 [ 21 ]. The guidelines were published in December 2023 [ 25 ].
This qualitative evidence synthesis was commissioned in parallel to several systematic reviews of evidence of benefits and harms of prioritized interventions for the Guideline, synthesized from randomized controlled trials (RCTs) [ 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ]. These interventions were broad in scope, intensity and setting for delivery (reflected in the inclusion criteria for this synthesis). The aim of all the interventions is to improve health and wellbeing outcomes for people living with CPLBP. However, it is important to explore how this broad variation in interventions is perceived and experienced by older people with CPLBP and/or their caregivers (formal or informal, family members). Are some interventions more accepted than others? Are there differences between the interventions and/or access to them related to equity (gender, culture, place of residence, socio economic status) or setting (geographic or health care setting)? These important context questions can only be comprehensively answered using qualitative research methods. These contextual data are intended to support the development of the WHO guideline and complement additional perspectives brought to the development process by other stakeholders involved in the guideline development, consistent with WHO guideline development methods [ 45 ].
It is important to consider people’s preferences around interventions when formulating and implementing clinical management guidelines. In this paper we use the concept of person-centred care, in order to encompass a broader perspective than those related to being a patient. We have adopted the definition of person-centred care that is used in the WHO Guideline, that is “Person-centred care means eliciting an individual’s values, preferences and priorities: once expressed, they should guide all aspects of that person’s health care, supporting their personalized health and life goals” [ 46 , 47 ].
An intervention may be proven effective but if it is not accepted by people living with the condition (and/or their carers) or they feel it causes burden or harm, it will not be adopted. An important step in a WHO guidelines development process is to consider what people living with CPLBP and their caregivers find acceptable? Feasible? Valued? [ 45 ] For example, there is a need to understand preferences and perspectives concerning accessibility, availability, affordability, perceived quality, burden [time, distance, frequency of visits], stigma, duration of therapeutic effect, person/patient’s role (passive or active role), immediacy of treatment effect, configuration of the care team– single practitioner or team approach, influence on comorbid health conditions, and symptoms related to the treatment. Some of these dimensions of value, preference and acceptability have been identified as previously as important to decision-making around treatments among older adults with osteoarthritis [ 48 ]. To date there has been some research conducted that considers people’s preferences for treatment for CPLBP [ 49 , 50 , 51 , 52 , 53 , 54 , 55 ]. However, to our knowledge, there has been no synthesis of primary qualitative research exploring the key factors influencing the implementation, uptake, and experience of interventions designed to manage CPLBP from the perspective of people aged over 60 and their caregivers.
The objective of this qualitative evidence synthesis (QES) was to understand the key factors influencing the acceptability of, and values and preferences/perspectives for, interventions/care for CPLBP from the perspective of people over 60 and their caregivers. The purpose of the QES was to inform the development of the WHO guideline [ 25 ].
This QES followed the best practice as described by the Cochrane collaboration in their handbook [ 56 , 57 ]. The protocol was registered on PROSPERO at inception ( https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=328469 ).
We included primary studies with qualitative study designs. We included mixed-methods studies when it was possible to extract the data that were collected and analysed using qualitative methods. The inclusion criteria are described in Table 1 .
We searched in two databases (MEDLINE and CINAHL powered by Ovid) (April 28, 2022) and supplemented the search with a search in an open-source dataset, OpenAlex [ 59 , 60 ] (May 3, 2022) through the EPPI-Reviewer platform [ 59 ]. We also screened the references of the included studies. Finally, we asked members of the WHO Guideline Development Group to recommend any relevant research they were aware of.
To maximise efficiency of the study selection process, we used the machine learning function “priority screening” in the systematic review software EPPI-reviewer [ 61 ].
Two review authors (HA and CHH) independently assessed eligibility of the titles and abstracts. We retrieved the full text of all the papers identified as potentially relevant. Two authors (HA and CHH) then assessed the eligibility of these papers independently. Discrepancies in decisions were resolved by discussion among the authors.
Data extraction was performed using a data extraction form designed specifically for this review. One author performed the data extraction and a second author checked for accuracy against the source paper and any discordances were resolved through consensus discussion. We extracted the following information from the studies; author, year of publication, geographic setting, description of context, data collection methods (sampling, collection, and analysis), description of participants covering the aspects named in the inclusion table (see Table 1 ) and if ethics approval was given for the study.
We assessed the methodological limitations of the included studies using a list of domains iteratively developed by the Cochrane EPOC group [ 62 , 63 , 64 , 65 ]. We did not exclude studies based on our assessment of methodological limitations but used the information about methodological limitations to assess our confidence in the review findings.
We analysed the data by conducting a best fit framework synthesis [ 66 , 67 , 68 , 69 ]. Best fit framework synthesis is a qualitative synthesis method that blends deductive and inductive synthesis and analysis processes. As part of the synthesis method, review authors identify a conceptual framework that fits at least 50% of the data. After data extraction, data that does not fit within the framework is further analysed in order to develop a new framework that includes all of the data. We used the themes identified in the scoping review on older adults’ perceptions and experiences of integrated care by Lawless et al. [ 70 ], a conceptual framework from Chua et al. on choosing interventions for hip or knee osteoarthritis [ 48 ] as well as the PROGRESS Plus framework that addresses issues related to equity [ 71 ] to generate an a priori theoretical framework. We chose these frameworks as they were relevant to the topic we were exploring and expected to cover at least 50% of the data. The PROGRESS+ framework [ 71 ] was added to address the specific needs of the WHO guidelines process around equity, gender and human rights. HA moved the extracted data into the framework and CHH checked the data. We then analysed the data within each framework section and developed our findings. Relevant data that did not fit into the framework were analysed thematically. We used a thematic analysis approach as described by Miles and Huberman [ 72 ] as referred to in Carroll 2013 [ 66 ] in their paper on best fit framework synthesis. New themes were generated based on our interpretation of the evidence and constant comparison of the new themes across the included studies. In accordance with best fit framework synthesis methods, we inductively expanded the a priori framework to include a section on person-centred care and communication to reflect the breadth of all our findings.
Findings were then organized according to the domains defined in the WHO Handbook for Guideline Development that inform the determination of a recommendation, derived from qualitative evidence, including values and preferences, resource implications, equity and human rights, acceptability and feasibility (See Table 2 ).
Finally, we assessed our confidence in the findings using GRADE-CERQual [ 73 ]. We present detailed descriptions of our confidence assessment in Evidence Profile(s) [ 74 ].
In each section we present the summary of findings table and a summary of the main points discussed in the findings. For specific findings and our confidence in them please refer to Tables 4 - 9 (Summary of Qualitative Evidence Tables).
Review author reflexivity
Neither Heather Ames (HA), Christine Hillestad Hestevik (CHH) or Andrew Briggs (AMB) have reached the age of 60, so we do not understand the lived experience of being an older adult. HA is a previous elite athlete who has experience with chronic musculoskeletal pain and interventions due to injury and AMB has experience of chronic musculoskeletal pain. Both HA and AMB’s parents are over 60, have experienced chronic pain and have discussed their treatments with them. All authors support an evidence-based medicine approach to care. AMB is a clinician, researcher, and health systems professional in the field of chronic musculoskeletal pain. CHH does not have personal experience with chronic musculoskeletal pain or treatment interventions. She did her PhD on healthcare provided to older people from the perspectives of older persons, their family caregivers and healthcare professionals and has some experience with older persons experiences with encounters when in need of healthcare. These prior experiences, particularly a lived experience of chronic musculoskeletal pain, lead us to believe in the difficulties older people are facing. It also felt like the topics that were being raised were familiar from the perspective of personal and research experience.
From a yield of 1878 unique citations, 22 studies were included in this review, reflected in 24 reports. See Fig. 1 for the study selection process. For a description of the included studies see Table 3 .
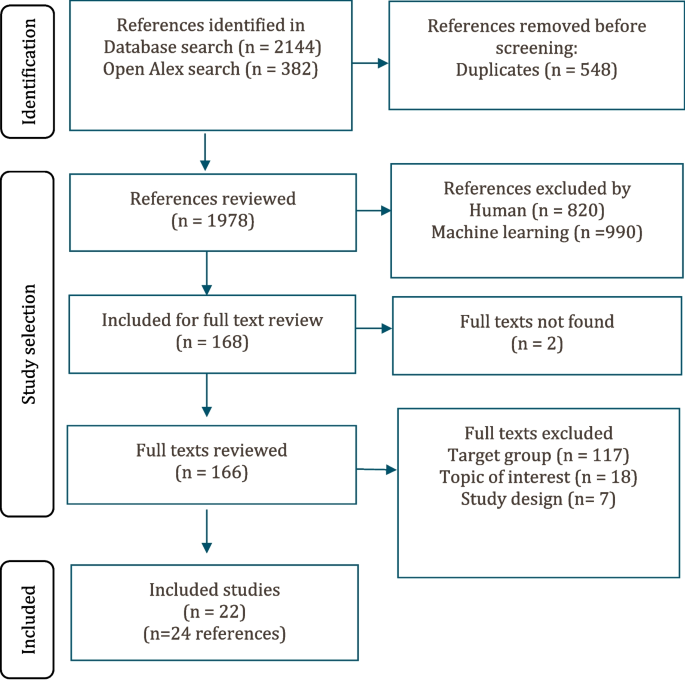
Study selection flowchart
The included studies were conducted in the United States ( n = 8) [ 53 , 54 , 78 , 90 , 91 , 93 , 94 , 96 ], United Kingdom ( n = 3) [ 77 , 79 , 92 ], Germany ( n = 2) [ 85 , 86 ], Sweden ( n = 2) [ 75 , 87 ], Australia ( n = 2) [ 84 , 88 , 89 ], Canada ( n = 1) [ 80 ], Chile ( n = 1) [ 95 ], Brazil ( n = 1) [ 76 ], and Nigeria ( n = 2) [ 81 , 82 , 83 ]. One study focused on Aboriginal Australians, a vulnerable population [ 88 , 89 ]. In 14 of the studies all participants were aged 60 or older [ 53 , 54 , 77 , 80 , 84 , 85 , 86 , 87 , 90 , 91 , 93 , 94 , 95 , 96 ]. In five, the mean or median age of the participants were 60 or older [ 75 , 76 , 78 , 79 , 92 ]. Three studies were included under the inclusion criteria for age for a low or middle-income country or identified vulnerable population [ 75 , 81 , 82 , 83 , 88 , 89 ]. In these studies, the age of the participants ranged from 26 to 72 years, but we only used disaggregated results from participants aged 40 or above.
In 16 of the studies, the participants were community-dwelling older adults [ 53 , 54 , 76 , 77 , 78 , 80 , 81 , 82 , 83 , 87 , 88 , 89 , 90 , 91 , 93 , 94 , 95 , 96 ]. Three of the studies were conducted in a primary health care setting but the residence of the participants was not discussed [ 75 , 85 , 86 ]. In three studies, the setting was unclear so we could not define the residence of the participants [ 79 , 84 , 92 ]. Nine of the studies were nested in a trial or a larger feasibility study [ 53 , 54 , 84 , 86 , 90 , 91 , 92 , 93 , 94 ].
We did not identify any studies that explored the perceptions or experiences of caregivers (formal or informal, family members).
Acceptability, values, and preferences
Since there was a large overlap in evidence related to values and preferences and acceptability, the findings are presented pooled. Values and preferences extended to interactions with health care providers, interventions for CPLBP and the modes of care delivery for CPLBP. Sixteen studies from 11 countries contributed to these findings (USA, Germany, Australia, United Kingdom, England, Scotland, Canada, Nigeria, Sweden, Brazil, and Chile). Participants in nine studies were all over 60 [ 54 , 77 , 80 , 85 , 87 , 91 , 93 , 95 , 96 ]. Four studies had participants with a mean or average age of 60 or older [ 75 , 76 , 79 , 92 ] and four studies were from LMICs or vulnerable populations [ 76 , 81 , 82 , 83 , 88 , 89 ] of which three were included based on a lowered age threshold [ 81 , 82 , 83 , 88 , 89 ]. In 13 of the studies most of the participants were women (53–83%) [ 54 , 75 , 76 , 77 , 79 , 80 , 81 , 82 , 85 , 87 , 91 , 93 , 95 , 96 ]. In two studies [ 83 , 92 ] there was an equal distribution of men and women. In one study most participants were men (52–66% men) [ 88 , 89 ].
Interactions with health care providers
Most participants wanted their health care providers to collaborate and work together to provide holistic care for their CPLBP. There was a preference among participants for providers who were respectful, caring, person-centred, collaborative, open to discussing treatment options and provided individualized care. They preferred health care providers who recognized them and their pain as individual and unique. This type of care allowed them to feel safe and feel they had meaningful relationships. When this was lacking, they could feel frustrated, vulnerable and experience a sense of aloneness (high confidence) [ 75 , 79 , 83 , 88 , 89 , 91 , 93 , 95 , 96 ].
Participants generally emphasized the care should be person-centred and provide continuity. They also identified a preference for a collaborative communication style which meant involving the older person in discussions about diagnosis and treatment options and viewing them as the expert on their own body (low confidence) [ 77 , 79 , 80 , 88 , 91 ].
Participants wanted collaboration and communication across their care teams to ensure co-ordinated care delivery and avoid duplication in care or diagnostics (moderate confidence) [ 75 , 88 , 91 ]. Some participants felt that they often received conflicting advice or information from health care providers. Participants valued receiving a diagnosis as this influenced their treatment decisions. The way the diagnosis was communicated could also shape their beliefs and responses to pain (moderate confidence) [ 76 , 79 , 81 , 83 , 85 , 89 , 91 , 92 , 95 ]. Some participants expressed dissatisfaction with health care providers for being unwilling to discuss treatment options other than medication (low confidence) [ 75 , 93 , 96 ]. The summary of findings is presented in Table 4 .
Values and preferences for CPLBP interventions in older people
Participants had clear values and preferences for how they chose a specific treatment for CPLBP. A choice of treatment could be influenced by previous experiences. Participants valued treatments that they viewed as effective, beneficial, and credible and fit them as individuals (high confidence) [ 53 , 54 , 79 , 80 , 81 , 82 , 84 , 85 , 86 , 87 , 93 , 95 , 96 ].
Most participants used and valued medication for its ability to provide short-term pain relief. However, many participants did not like the side effects associated with medications or the way the medication(s) made them feel (moderate confidence) [ 53 , 78 , 79 , 91 , 93 , 96 ]. Many also feared addiction, especially in relation to opioid analgesics. In some cases, participants adjusted or stopped medication without consulting their health care provider because of fears of adverse events (moderate confidence) [ 53 , 79 , 91 , 96 , 97 ].
Mindfulness and meditation encouraged participants to examine, assess, understand, and accept their pain rather than avoid it. Participants were able to use mindfulness and meditation for pain management and coping to varying degrees (moderate confidence) [ 54 , 90 , 94 ]. The summary of the findings is presented in Table 5 .
Format of interventions and educational materials for CPLBP in older people
Participants discussed their experiences with, and views of, organized and unorganized physical therapies and activities. Specific physical interventions were rarely mentioned. For many participants, physical activity was an important aspect of coping with their CPLBP. Many participants preferred a group format for physical exercises as it facilitated social support, collaboration and encouraged increased attendance (moderate confidence) [ 54 , 79 , 80 , 81 , 82 , 85 ]. Some participants also expressed preferences for educational material for physical interventions which had drawings and descriptions of the exercises. This made them more comprehensible, easier to follow and helpful for present and future reference (low confidence) [ 79 , 81 , 82 , 85 , 86 ].
Peer support interventions appeared to be acceptable and valued by some older people. They were seen as an acceptable way of gaining support and sharing information or advice. Participants mostly viewed peer support as feasible as it could be delivered through several different modalities (for example, face to face, in groups or online) that would fit individual preferences and lifestyles. However, it was clear that peer support was difficult to find and access in some settings, although appeared to be valued as a component of overall self-management of a CPLBP experience (low confidence) [ 77 , 78 , 80 , 92 , 96 ] [ 77 , 78 , 80 , 92 , 96 ].. The summary of the findings is presented in Table 6 .
Cost/resources related to CPLBP care in older people
Seven studies from five countries contributed to these findings (USA, Australia, England, Nigeria, and Sweden). Participants in three studies were all over 60 [ 53 , 84 , 91 ], two studies had participants with a mean or average age of 60 or older [ 75 , 79 ] and two studies were from LMICs or vulnerable populations of which both were included based on a lowered age threshold [ 83 , 88 , 89 ]. In five of the studies most of the participants where women (55–100%) [ 53 , 75 , 79 , 84 , 91 ]. In one study there was an equal distribution between men and women [ 83 ]. In one study most participants were men (66%) [ 88 , 89 ].
We found that cost and resources could be a barrier to accessing care for CPLBP for some participants. High costs (financial, time and travel) could render treatments inaccessible to participants or acts as a deterrent (moderate confidence) [ 53 , 79 , 83 , 91 ]. Many also preferred health care providers near where they lived to minimise travel burden. However, some participants were willing to travel if a trusted or favoured provider relocated, or they wanted to explore new treatment options. Others chose to find a new practitioner closer to them in this situation (moderate confidence) [ 53 , 75 , 79 , 83 , 84 , 88 , 91 ]. The summary of the findings is presented in Table 7 .
Feasibility
Twelve studies from eight countries contributed to these findings (USA, Canada, UK, Australia, England, Scotland, Nigeria, Chile). Participants in seven studies were all over 60 [ 53 , 77 , 80 , 84 , 91 , 95 , 96 ]. Three studies had participants with a mean or average age of 60 or older [ 78 , 79 , 92 ] and two studies were from LMICs or vulnerable populations of which both were included based on a lowered age threshold [ 81 , 82 , 83 ]. In 10 of the studies most of the participants where women (62–100%) [ 53 , 77 , 78 , 79 , 80 , 81 , 82 , 84 , 91 , 95 , 96 ]. In two studies there was about an equal distribution between men and women [ 83 , 92 ].
Some participants found information about treatments difficult to access and wanted help finding it or navigating the information from a health or care worker or through a peer support system. They felt that this could help them make decisions (low confidence) [ 78 , 79 , 84 , 92 , 96 ].
Physical activity and/or exercise was used a part of a self-management strategy for many participants. Activities such as swimming and walking were often mentioned as being done in their own time and when it fit their schedule. Some participants adopted physical exercise, assistive products, or alternative forms of treatment to supplement the conventional treatments they were receiving or when they felt “conventional treatments” failed. However, some did not inform their health care providers about their self-management strategies or changes they had made (moderate confidence). The summary of findings is presented in Table 8 .
Equity and human rights
Seven studies from six countries contributed to this finding (USA, Canada, UK, England, Scotland, and Sweden, Brazil). Participants in four studies were all over 60 [ 77 , 80 , 91 , 93 ] and three studies had participants with a mean or average age of 60 or older [ 75 , 79 , 92 ]. In six of the studies most of the participants were women [ 75 , 77 , 79 , 80 , 91 , 93 ]. In one study there was an equal distribution of men and women [ 92 ].
Some participants perceived age-related stigma or bias when accessing healthcare for their CPLBP. They reported feeling that they were treated differently, dismissed, or discriminated against because of their age. They felt they were not taken seriously. This perceived stigma could deter them from seeking further treatment. However, in other cases participants believed that they were taken more seriously as they aged (Low confidence). The summary of the finding is presented in Table 9 .
Additions to the framework
To incorporate all the data we analysed we expanded the framework to include a section we labelled person centred care.
Main findings
Based on this synthesis of qualitative evidence derived from more than 650 older participants across 22 studies with representation across a range of geographies and economic contexts, we identified that older people living with CPLBP express values and preferences for their care that relate to therapeutic encounters and the importance of therapeutic alliance, irrespective of the type of treatment offered or delivered, choice of intervention, and intervention delivery modalities. Older people with CPLBP value therapeutic encounters that validate, legitimise, and respect their pain experience; that consider their context holistically and prioritise their needs and preferences; that adopt a person-focused and tailored approach to care; and that are supported by interprofessional communication. Older people value care that provides benefit to them, that includes a suite of interventions beyond analgesic medicines alone, and that is financially and geographically accessible. These findings provide critical context to service delivery models for older people; formulation of recommendations for guidelines that relate to older people; and service considerations for the implementation of clinical guidelines into practice, particularly related to how health care workers interact with older people, with attention to potential age-related bias, and how components of care are delivered.
Person-centred care for older adults living with CPLBP
Many older people felt that healthcare providers did not legitimise their pain and that pain was deprioritised relative to other health conditions. Musculoskeletal pain, including CPLBP, is a common experience in older people [ 98 , 99 ] and a very frequent co-morbidity with other noncommunicable diseases [ 100 ]. Therefore, pain assessment is a key component of the WHO Integrated Care for Older People (ICOPE) assessment and care pathway [ 101 ]. Comorbidities more strongly associated with mortality or acute health declines can make it difficult for health professionals to prioritise symptoms of CPLBP in time-limited clinical encounters. There seems to be a difference between patient and care provider priorities when it comes to pain management and our findings point to the need to legitimise and respond to pain as this clearly is a priority for older people, consistent with recently reported evidence [ 55 ]. Our findings point to the importance of the therapeutic relationship and communication between older people and care providers to understand the impact of, and preference for, CPLBP care. Older people also experienced issues linked to equity during the therapeutic encounter. These could be expressed through ageism and stigma associated with CPLBP. Being told to ‘just live with it’, or the idea that CPLBP was an inevitable part of ageing were common and suggest a potential age-related bias among healthcare providers. Being aware of potential clinician bias related to chronic pain in older people is important, since ageism is associated with poorer health outcomes, particularly in low resource settings [ 102 ].
The needs and priorities of older people may well differ to younger adults (e.g. return to work, taking care of dependents, intensity of everyday activities or sport may be less important for older people). There are previous findings of the perceived needs of adult groups with CPLBP [ 103 , 104 ]. Consistent with other reviews among adults, we identified that older people value clear and consistent information, a clear diagnosis, prognosis, and a communication style that is meaningful and avoids jargon [ 105 ]. Communication that emphasises disability or impairments can be unhelpful to fostering pain self-efficacy, contribute to fear, unhelpful care seeking and further compound disability [ 106 , 107 , 108 , 109 ], which will foster healthy ageing. Rather, providing empowering and positive communication that is validating, helping to make sense of pain and the likelihood of a positive prognosis, providing cognitive reassurance and clear information about benefits and harms of interventions (in particular, medicines) can support shared decision-making, positive behaviour change towards effective self-management, and better engagement in meaningful activities [ 110 ]; all important for supporting healthy ageing.
We identified a preference for integrated and coordinated CPLBP care across care providers and facilities, consistent with the WHO ICOPE model [ 101 ]. This includes holistic care planning with comprehensive assessments and care plans aligned with the person’s values, priorities and preferences concerning their care. The older person should be involved with decision-making and goal-setting from the the start of their care journey. The care should be regular and include sustained follow-up, with integration and communication across different levels of care. This approach to care can help to avoid unnecessary treatments, polypharmacy and other potential harms [ 47 , 110 ]. Our findings about fears of side effects, dependency and medicine withdrawal or non-adherence also points to the need for clinicians to take time to explain risk-benefits of different medicines so that older people understand what medicines are for and how to use them safely.
Values and preferences were largely agnostic to intervention modality, other than values relating to medicines, where specific issues related to fear of adverse events were observed. Although analgesic medicines were considered important for CPLBP care, older people preferred care packages that extend beyond analgesia so that care is more holistic and considers safety (e.g. issues of dependency for opioid analgesics) and that were meaningful and personally enjoyable – such as social benefits of group exercise. Recent evidence points to the importance of considering pharmacologic and non-pharmacologic therapies for CPLBP care, consistent with the experiences, values and preferences of older people [ 97 ]. Other evidence highlights care needs also extend beyond biomedical domains [ 24 , 103 ]. Specifcally, tailoring components of care that addresses pain, emotional and social wellbeing, consistent with WHO ICOPE [ 101 ] model for improving functional ability, is important.
Implementing and delivering care for older people living with CPLBP
When developing, implementing, and delivering interventions for older people who experience functional disability related to musculoskeletal pain (or other co-morbidities), consideration of economic, social, and cultural contexts is critical. Many experienced financial and geographic barriers to care. Access to care that is expensive (or not included in UHC or insurance rebates), that requires travel, or accessing buildings that are not adapted for people experiencing functional disability can be problematic. This threat is more severe for those living in poverty without access to healthcare or who cannot afford to access healthcare near them, such as in low-resource settings. This lack of access may lead to worse outcomes for older people living in these settings, widening inequities in access to health care and health outcomes. Services also need to consider the user’s social context [ 111 ]. If not taken into account, pain care is likely to be inequitable and inaccessible. Support needs to go beyond the purely biomedical (especially focusing on medication) and encompass interventions that address peer support and socialization as well as issues around acceptability and stigma. Interventions should be tailored to local contexts to increase social and cultural approval. Some of the interventions included in this synthesis, such as exercise, were stigmatized in some settings [ 81 , 82 , 83 ]. Other research has also found that stigma can be associated with gender [ 112 ] or with interventions targeted at older people [ 113 ].
Older people also wanted support for the implementation of interventions such as guidance on how to perform exercises in the form of drawings and text. None of the studies we included talked about digital supports except for those related to peer support where digital meetings were discussed. While some formative evidence exists around the role of digital technologies to support healthy ageing [ 114 , 115 , 116 ], further research is required to understand users’ perspectives, benefits and harms in different contexts and among different population groups. Other research has also shown the acceptability of peer support in older adults with CPLBP [ 117 ]. Research on older people has found that they access digital tools but may face barriers such as physical mobility, sight and hearing impairment and low digital literacy when trying to use them [ 118 , 119 , 120 ]. Studies examining the use of digital tools for interventions for low back pain not limited to older people have found that users value models that are easily understandable, provide an opening to further communication with health care providers, family and colleagues and can provide prompts, reassurance, ongoing support and interaction with other users [ 121 , 122 ].
These empirical findings hold direct relevance to the formulation of recommendations in guidelines and implementation of recommended care within service models and local care pathways. In this context, the current QES has informed the development of the WHO Guideline for non-surgical management of chronic primary low back pain in adults in primary and community care settings [ 25 ]. Without consideration of the fundamental EtD factors (Table 2 ) and the evidence underpinning each when formulating recommendations for guidelines or implementation plans for service models, as presented in our QES, care recipients (and in some cases, care providers) may not accept or be able to access care, manifesting as an enduring disease burden and inequity in health outcomes. The QES findings, when coupled with evidence for benefit, harm, cost effectiveness and implementation feasibility and lived experience perspectives that contribute to co-creation of solutions (care recommendations, service models, care pathways) that are more likely to be implemented, sustainable and acceptable [ 123 ]. Indeed, consideration of qualitative evidence anchored to EtD domains is common practice for WHO guidelines [ 45 ].
Implications for research
There was a clear lack of research from low- and middle-income settings as well as vulnerable populations in all settings. Most of the included studies explored the perceptions of community dwelling older adults. More research on the experiences of older adults living in residential care or other settings could help to broaden our understanding. Very few of the studies explored perceptions of specific interventions. Most looked at treatment across interventions and participants did not differentiate between interventions in the same way a health care provider would. For example, participants viewed the visit to the physiotherapist as the intervention whereas health care providers would view each of the treatments received as individual interventions. One topic not frequently discussed in the included studies was cost and out of pocket expenses. This may be because several studies were conducted as part of a trial where participants did not pay to access the intervention. Cost was also rarely discussed in studies taking place in publicly funded health care systems. Understanding affordability of care, willingness to pay and inequities in access to care due to cost will be important in planning implementation of health services for CPLBP care for older people. Further research is also needed on the perspectives and experiences of caregivers as there were no studies identified that explored this topic of interest.
Implications for practice
The questions that form our implications for practice are derived from our findings with moderate or high confidence. They may help health system or program managers to plan, implement or manage interventions for CPLBP. It is important to consider local contextual factors including gender, age, cultural group, and education when implementing interventions.
Is the burden to access services low (financial, time and travel)? Have issues related to burden and equity of access been considered?
When planning, implementing, or managing an intervention for CPLBP or communicating with people over 60 with CPLBP:
◦ have participants values and preferences been explored and taken into consideration?
◦ are participants informed about the physical exercise or physical supports available to them?
When communicating with adults over 60 with CPLBP, have values and preferences been considered, regarding:
◦ communication, cultural preferences, and health care provider collaboration?
◦ receiving a diagnosis and preferences for information?
When prescribing medication, do health care workers provide open and honest communication with their patients about medications, the risk of side effects, and the risk of dependency, inviting them to return with concerns and informing of the importance of working together to manage their medications?
Older people with CPLBP value therapeutic encounters that legitimise and respect their pain experience, that consider their context holistically and prioritises their needs and preferences, that is tailored, and that is supported by interprofessional communication. Older people value care that provides benefit, that includes interventions beyond analgesic medicines alone, and that is financially and geographically accessible. These findings provide critical context to the implementation of clinical guidelines and service models into practice, particularly related to how care providers interact with older people and how components of care are delivered and their accessibility.
Availability of data and materials
All the studies in this synthesis are published and available. The data that is in each finding is available in an interactive Summary of Qualitative Findings table. For access to this tool please send an email to the corresponding author.
Abbreviations
Chronic primary low back pain
- Low back pain
- Qualitative evidence synthesis
Randomised controlled trial
Universal health coverage
Integrated care for older people
World health organization
Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10267):2006–17.
Article CAS PubMed PubMed Central Google Scholar
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–22.
Article Google Scholar
Ferreira ML, de Luca K, Haile LM, Steinmetz JD, Culbreth GT, Cross M, et al. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. 2023;5(6):e316-ee29.
Article CAS Google Scholar
Gill TK, Mittinty MM, March LM, Steinmetz JD, Culbreth GT, Cross M, et al. Global, regional, and national burden of other musculoskeletal disorders, 1990–2020, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. 2023;5(11):e670-ee82.
Black RJ, Cross M, Haile LM, Culbreth GT, Steinmetz JD, Hagins H, et al. Global, regional, and national burden of rheumatoid arthritis, 1990–2020, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. 2023;5(10):e594–610.
Beyera GK, O’Brien J, Campbell S. Health-care utilisation for low back pain: a systematic review and meta-analysis of population-based observational studies. Rheumatol Int. 2019;39(10):1663–79.
Article PubMed Google Scholar
Vigdal ØN, Storheim K, Killingmo RM, Småstuen MC, Grotle M. Characteristics of older adults with back pain associated with choice of first primary care provider: a cross-sectional analysis from the BACE-N cohort study. BMJ Open. 2021;11(9):e053229.
Article PubMed PubMed Central Google Scholar
Wong AY, Karppinen J, Samartzis D. Low back pain in older adults: risk factors, management options and future directions. Scoliosis Spinal Disord. 2017;12(1):1–23.
Paeck T, Ferreira ML, Sun C, Lin CWC, Tiedemann A, Maher CG. Are older adults missing from low back pain clinical trials? A systematic review and meta-analysis. Arthritis Care Res. 2014;66(8):1220–6.
Carvalho do Nascimento PR, Ferreira ML, Poitras S, Bilodeau M. Exclusion of older adults from ongoing clinical trials on low back pain: a review of the WHO trial registry database. J Am Geriatr Soc. 2019;67(3):603–8.
Rittweger J, Just K, Kautzsch K, Reeg P, Felsenberg D. Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise: a randomized controlled trial. Spine. 2002;27(17):1829–34.
Hutchinson AJ, Ball S, Andrews JC, Jones GG. The effectiveness of acupuncture in treating chronic non-specific low back pain: a systematic review of the literature. J Orthop Surg Res. 2012;7(1):1–8.
Yerlikaya M, Saracoglu İ. The attitudes and beliefs of physiotherapists, family physicians and physiatrists concerning chronic low back pain. J Health Sci Med. 5(2):393–8.
La Touche R, Escalante K, Linares MT. Treating non-specific chronic low back pain through the Pilates method. J Bodyw Mov Ther. 2008;12(4):364–70.
Senderovich H, Wagman H, Zhang D, Vinoraj D, Waicus S. The effectiveness of Cannabis and Cannabis derivatives in treating lower Back pain in the aged population: a systematic review. Gerontology. 2021;68:1–13.
Google Scholar
Netchanok S, Wendy M, Marie C. The effectiveness of Swedish massage and traditional Thai massage in treating chronic low back pain: a review of the literature. Complement Ther Clin Pract. 2012;18(4):227–34.
Wu L-C, Weng P-W, Chen C-H, Huang Y-Y, Tsuang Y-H, Chiang C-J. Literature review and meta-analysis of transcutaneous electrical nerve stimulation in treating chronic back pain. Reg Anesth Pain Med. 2018;43(4):425–33.
Owen PJ, Miller CT, Mundell NL, Verswijveren SJ, Tagliaferri SD, Brisby H, et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2020;54(21):1279–87.
Kolber MR, Ton J, Thomas B, Kirkwood J, Moe S, Dugré N, et al. PEER systematic review of randomized controlled trials: management of chronic low back pain in primary care. Can Fam Physician. 2021;67(1):e20–30.
Pillastrini P, Gardenghi I, Bonetti F, Capra F, Guccione A, Mugnai R, et al. An updated overview of clinical guidelines for chronic low back pain management in primary care. Joint Bone Spine. 2012;79(2):176–85.
World Health Organization. Development of WHO Guideline on management of chronic primary low back pain in adults. 2022. Available from: https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/ageing-and-health/integrated-care-for-older-people-icope/development-of-who-guideline-on-management-of-chronic-primary-low-back-pain-in-adults . Accessed 1 Sept 2023.
Cesari M, Sumi Y, Han ZA, Perracini M, Jang H, Briggs A, et al. Implementing care for healthy ageing. BMJ Glob Health. 2022;7(2):e007778.
Lee D-CA, Burton E, Slatyer S, Jacinto A, Oliveira D, Bryant C, et al. Understanding the role, quality of life and strategies used by older carers of older people to maintain their own health and well-being: a national Australian survey. Clin Interv Aging. 2022;17:1549–67.
Slater H, Jordan JE, O’Sullivan PB, Schütze R, Goucke R, Chua J, et al. ‘Listen to me, learn from me’: a priority setting partnership for shaping interdisciplinary pain training to strengthen chronic pain care. Pain. 2022;163.
WHO guideline for non-surgical management of chronic primary low back pain in adults in primary and community care settings. Geneva: World Health Organization; 2023. https://www.who.int/publications/i/item/9789240081789 . Licence: CC BY-NC-SA 3.0 IGO.
Cancelliere C, Hincapié C, Bussières A, Gross D, Pereira P, Mior S, et al. Education or advice for chronic primary low back pain in adults; A systematic review protocol. PROSPERO; 2022.
Cancelliere C, Hayden J, Ogilvie R, Hincapié C, Bussières A, Gross D, et al. Exercise therapy for chronic primary low back pain in adults; A systematic review protocol. PROSPERO; 2022.
Rubinstein S, de Zoete A, Innocenti T, Maas E, Pellekooren S, Chiarotto A, et al. Systematic review on the effect of spinal manipulative therapy in people with chronic primary low back pain (protocol). PROSPERO; 2022.
Maas E, Pellekooren S, Ostelo R, Innocenti T, Chiarotto A, de Zoete A, et al. Systematic review on the effect of massage therapy in people with chronic primary low back pain (protocol). PROSPERO; 2022.
Pellekooren S, Maas E, Wegner I, Ostelo R, Innocenti T, Chiarotto A, et al. Systematic review on the effect of traction in people with chronic primary low back pain (protocol). PROSPERO; 2022.
Cancelliere C, Hincapié C, Bussières A, Gross D, Pereira P, Mior S, et al. Acupuncture for chronic primary low back pain in adults (protocol). PROSPERO; 2022.
Cancelliere C, Hincapié C, Bussières A, Gross D, Pereira P, Mior S, et al. Transcutaneous electrical nerve stimulation (TENS) for chronic primary low back pain in adults (protocol). PROSPERO; 2022.
Probyn K, Petkovic J, Cogo E, Bergman H, Arienti C, Negrini S, et al. Protocolfor a systematic review on therapeutic ultrasound for chronic primary low back painin adults. Open science framework; 2022.
Probyn K, Villannueva G, Cogo E, Bergman H, Petkovic J, Conde M, et al. Protocolfor a systematic review on psychosocial therapies for chronic primary low back painin adults. Open science framework; 2022.
Chou R, Dana T. Pharmacotherapies for chronic primary low back pain: systematic review to inform the WHO global guideline on chronic primary low back pain in adults (protocol). PROSPERO; 2022.
Wewege M, Bagg M, Jones M, McAuley J. Analgesic medicines for adults with low back pain: a systematic review and network meta-analysis (protocol). PROSPERO.; 2019.
Chou R, Hartung D, Turner J, Blazina I, Chan B, Levander X, et al. Opioid treatments for chronic pain. Comparative Effectiveness Review No. 229. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2015-00009-I.) 2020.
McDonagh MS, Selph SS, Buckley DI, Holmes RS, Mauer K, Ramirez S, et al. Nonopioid pharmacologic treatments for chronic pain. Comparative Effectiveness Review No. 228.; 2020.
Chou R, Pinto RZ, Fu R, Lowe RA, Henschke N, McAuley JH, et al. Systemic corticosteroids for radicular and non-radicular low back pain. Cochrane Database Syst Rev. 2022;10.
Probyn K, Villannueva G, Cogo E, Bergman H, Conde M, Negrini S, et al. Protocolfor a systematic review on localanaesthetic agents for chronic primary lowback painin adults. Open science framework; 2022.
McDonagh M, Wagner J, Ahmed AY, Fu R, Morasco B, Kansagara D, et al. Living systematic review on Cannabis and other plant-based treatments for chronic pain. Comparative Effectiveness Review No. 250. . 2021.
Probyn K, Villannueva G, Chi Y, Cogo E, Conde M, Berman B, et al. Protocolfor a systematic review on herbal medicinesfor chronic primary low back painin adults. Open science framework; 2022.
Williams C, Tutty A, Cashin A, McAuley J, Kamper S, Michaleff Z, et al. Effectiveness of weight management intervention for chronic primary low back pain care: protocol for a systematic review and meta-analysis to inform the WHO global guideline on low back pain in adults. PROSPERO; 2022.
Probyn K, Villannueva G, Bergman H, Arienti C, Minozzi S, Lazzarini SG, et al. Protocolfor a systematic review on biopsychosocial rehabilitationfor chronic primary low back painin adults. Open science framework; 2022.
World Health Organization. WHO handbook for guideline development. World Health Organization; 2014.
Care AGSEPoPC, Brummel-Smith K, Butler D, Frieder M, Gibbs N, Henry M, et al. Person-centered care: a definition and essential elements. J Am Geriatr Soc. 2016;64(1):15–8.
Hutting N, Caneiro J, Ong'wen OM, Miciak M, Roberts L. Person-centered care for musculoskeletal pain: Putting principles into practice. Musculoskelet Sci Pract.. 2022:102663.
Chua J, Briggs AM, Hansen P, Chapple C, Abbott JH. Choosing interventions for hip or knee osteoarthritis-what matters to stakeholders? A mixed-methods study. Osteoarthr Cartil Open. 2020;2(3):100062.
Kløjgaard ME, Manniche C, Pedersen LB, Bech M, Søgaard R. Patient preferences for treatment of low back pain—a discrete choice experiment. Value Health. 2014;17(4):390–6.
Staats P, Deer T, Ottestad E, Erdek M, Spinner D, Gulati A. Understanding the role of patient preference in the treatment algorithm for chronic low back pain: results from a survey-based study. Pain Manag. 2021;12.
Walsh DA, Boeri M, Abraham L, Atkinson J, Bushmakin AG, Cappelleri JC, et al. Exploring patient preference heterogeneity for pharmacological treatments for chronic pain: a latent class analysis. Eur J Pain. 2022;26(3):648–67.
Rutgers KM. Shared decision making in physical therapy treatments of people with intermittent claudication, before and after the implementation of KomPas; a pre-post study. 2021. Master's Thesis.
Stensland M. Managing the incurable: older pain clinic Patients’ experiences of managing treatment-resistant chronic low Back pain. J Gerontol Soc Work. 2021;64(4):405–22.
Lee TLSK, Hawkes RJ, Phelan EA, Turner JA. The benefits of T'ai Chi for older adults with chronic Back pain: a qualitative study. J Altern Complement Med. 2020;26(6):456–62.
Slater H, Jordan JE, O'Sullivan PB, Schütze R, Goucke R, Chua J, et al. “Listen to me, learn from me”: a priority setting partnership for shaping interdisciplinary pain training to strengthen chronic pain care. Pain. 2022;10(1097).
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2019.
Book Google Scholar
Noyes J, Booth A, Cargo M, Flemming K, Harden A, Harris J, et al. Qualitative evidence. Cochrane Handbook for systematic reviews of interventions; 2019. p. 525–45.
Nicholas M, Vlaeyen JW, Rief W, Barke A, Aziz Q, Benoliel R, et al. The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain. 2019;160(1):28–37.
OpenAlex. OpenAlex documentation 2022 [Available from: https://docs.openalex.org/ .
Priem J, Piwowar H, Orr R. OpenAlex: A fully-open index of scholarly works, authors, venues, institutions, and concepts. arXiv preprint arXiv:220501833. 2022.
Thomas J, Brunton J, Graziosi S. EPPI-reviewer 4: software for research synthesis. EPPI-Centre software. London: Social Science Research Unit, UCL Institute of Education; 2010.
Ames HM, Glenton C, Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database Syst Rev. 2017;2.
Ames HM, Glenton C, Lewin S, Tamrat T, Akama E, Leon N. Clients’ perceptions and experiences of targeted digital communication accessible via mobile devices for reproductive, maternal, newborn, child, and adolescent health: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2019;10.
Munabi-Babigumira S, Glenton C, Lewin S, Fretheim A, Nabudere H. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low-and middle-income countries: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2017;11.
Glenton C, Carlsen B, Lewin S, Wennekes MD, Winje BA, Eilers R. Healthcare workers’ perceptions and experiences of communicating with people over 50 years of age about vaccination: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2021;7.
Carroll C, Booth A, Leaviss J, Rick J. “Best fit” framework synthesis: refining the method. BMC Med Res Methodol. 2013;13(1):1–16.
Booth A, Carroll C. How to build up the actionable knowledge base: the role of ‘best fit’framework synthesis for studies of improvement in healthcare. BMJ Qual Saf. 2015;24(11):700–8.
Carroll C, Booth A, Cooper K. A worked example of" best fit" framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. 2011;11(1):1–9.
Brunton G, Oliver S, Thomas J. Innovations in framework synthesis as a systematic review method. Res Synth Methods. 2020;11(3):316–30.
Lawless MT, Marshall A, Mittinty MM, Harvey G. What does integrated care mean from an older person’s perspective? A scoping review. BMJ Open. 2020;10(1):e035157.
O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol. 2014;67(1):56–64.
Huberman M, Miles MB. The qualitative researcher’s companion. Sage; 2002.
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. BioMed Central; 2018.
Lewin S, Bohren M, Rashidian A, Munthe-Kaas H, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings—paper 2: how to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implement Sci. 2018;13(1):11–23.
Allvin R, Fjordkvist E, Blomberg K. Struggling to be seen and understood as a person - chronic back pain patients’ experiences of encounters in health care: an interview study. Nurs Open. 2019;6(3):1047–54.
Bonfim IDS, Correa LA, Nogueira LAC, Meziat-Filho N, Reis FJJ, de Almeida RS. Your spine is so worn out - the influence of clinical diagnosis on beliefs in patients with non-specific chronic low back pain - a qualitative study. Braz J Phys Ther. 2021;25(6):811–8.
Cooper K, Schofield P, Klein S, Smith BH, Jehu LM. Exploring peer-mentoring for community dwelling older adults with chronic low back pain: a qualitative study. Physiotherapy. 2017;103(2):138–45.
Cummings EC, van Schalkwyk GI, Grunschel BD, Snyder MK, Davidson L. Self-efficacy and paradoxical dependence in chronic back pain: a qualitative analysis. Chronic Illness. 2017;13(4):251–61.
Dima A, Lewith GT, Little P, Moss-Morris R, Foster NE, Bishop FL. Identifying patients’ beliefs about treatments for chronic low back pain in primary care: a focus group study. Br J Gen Pract. 2013;63(612):e490–8.
Hay ME, Connelly DM. Exploring the experience of exercise in older adults with chronic Back pain. J Aging Phys Act. 2020;28(2):294–305.
Igwesi-Chidobe CN, Godfrey EL, Kitchen S, Onwasigwe CN, Sorinola IO. Community-based self-management of chronic low back pain in a rural African primary care setting: a feasibility study. Primary Health Care Res Dev. 2019;20:e45.
Igwesi-Chidobe CN, Kitchen S, Sorinola IO, Godfrey EL. Evidence, theory and context: using intervention mapping in the development of a community-based self-management program for chronic low back pain in a rural African primary care setting - the good back program. BMC Public Health. 2020;20(1):343.
Igwesi-Chidobe CN, Kitchen S, Sorinola IO, Godfrey EL. “a life of living death”: the experiences of people living with chronic low back pain in rural Nigeria. Disabil Rehabil. 2017;39(8):779–90.
Kirby ER, Broom AF, Adams J, Sibbritt DW, Refshauge KM. A qualitative study of influences on older women’s practitioner choices for back pain care. BMC Health Serv Res. 2014;14:131.
Kuss K, Leonhardt C, Quint S, Seeger D, Pfingsten M, Wolf P, et al. Graded activity for older adults with chronic low Back pain: program development and mixed methods feasibility cohort study. Pain Med. 2016;17(12):2218–29.
Leonhardt C, Kuss K, Becker A, Basler H-D, de Jong J, Flatau B, et al. Graded exposure for chronic low Back pain in older adults: a pilot study. J Geriatr Phys Ther. 2017;40(1):51–9.
Lilje SC, Olander E, Berglund J, Skillgate E, Anderberg P. Experiences of older adults with Mobile phone text messaging as reminders of home exercises after specialized manual therapy for recurrent low Back pain: a qualitative study. JMIR MHealth UHealth. 2017;5(3):e39.
Lin I, O’Sullivan P, Coffin J, Mak DB, Toussaint S, Straker L. “I can sit and talk to her”: Aboriginal people, chronic low back pain and healthcare practitioner communication. Aust Fam Physician. 2014;43(5):320–4.
Lin IB, O'Sullivan PB, Coffin JA, Mak DB, Toussaint S, Straker LM. Disabling chronic low back pain as an iatrogenic disorder: a qualitative study in Aboriginal Australians. BMJ Open. 2013;3(4).
Luiggi-Hernandez JG, Woo J, Hamm M, Greco CM, Weiner DK, Morone NE. Mindfulness for chronic low Back pain: a qualitative analysis. Pain Med. 2018;19(11):2138–45.
Lyons Kevin J, Salsbury Stacie A, Hondras Maria A, Hondras Maria A, Jones Mark E, Andresen Andrew A, et al. Perspectives of older adults on co-management of low back pain by doctors of chiropractic and family medicine physicians: a focus group study. BMC Complement Altern Med. 2013;13(1):225.
MacKichan F, Paterson C, Britten N. GP support for self-care: the views of people experiencing long-term back pain. Fam Pract. 2013;30(2):212–8.
Makris Una E, Makris Una E, Higashi Robin T, Marks Emily G, Fraenkel L, Fraenkel L, et al. Ageism, negative attitudes, and competing co-morbidities – why older adults may not seek care for restricting back pain: a qualitative study. Bmc Geriatrics. 2015;15(1):39.
Morone NE, Lynch CS, Greco CM, Tindle HA, Weiner DK. “I felt like a new person” the effects of mindfulness meditation on older adults with chronic pain: qualitative narrative analysis of diary entries. J Pain. 2008;9(9):841–8.
Rodriguez I, Abarca E, Herskovic V, Campos M. Living with chronic pain: a qualitative study of the daily life of older people with chronic pain in Chile. Pain Res Manag. 2019;2019:8148652.
Teh Carrie F, Karp Jordan F, Kleinman Arthur M, Reynolds Charles F, Weiner Debra L, Cleary PD. Older People’s experiences of patient-centered treatment for chronic pain: a qualitative study. Pain Med. 2009;10(3):521–30.
Makris UE, Higashi RT, Marks EG, Fraenkel L, Gill TM, Friedly JL, et al. Physical, emotional, and social impacts of restricting back pain in older adults: a qualitative study. Pain Med. 2016;18(7):1225–35.
PubMed Central Google Scholar
Wong CK, Mak RY, Kwok TS, Tsang JS, Leung MY, Funabashi M, et al. Prevalence, incidence, and factors associated with non-specific chronic low back pain in community-dwelling older adults aged 60 years and older: a systematic review and meta-analysis. J Pain. 2022;23(4):509–34.
De Souza IMB, Sakaguchi TF, Yuan SLK, Matsutani LA, do Espírito-Santo AdS, Pereira CAdB, et al. Prevalence of low back pain in the elderly population: a systematic review. Clinics. 2019;74.
Simões D, Araújo FA, Severo M, Monjardino T, Cruz I, Carmona L, et al. Patterns and consequences of multimorbidity in the general population: there is no chronic disease management without rheumatic disease management. Arthritis Care Res. 2017;69(1):12–20.
World Health Organization. Integrated care for older people (ICOPE): guidance for person-centred assessment and pathways in primary care. World Health Organization; 2019.
Chang ES, Kannoth S, Levy S, Wang SY, Lee JE, Levy BR. Global reach of ageism on older persons’ health: a systematic review. PLoS One. 2020;15(1):e0220857.
Chou L, Cicuttini FM, Urquhart DM, Anthony SN, Sullivan K, Seneviwickrama M, et al. People with low back pain perceive needs for non-biomedical services in workplace, financial, social and household domains: a systematic review. J Phys. 2018;64(2):74–83.
Van Rysewyk S, Blomkvist R, Chuter A, Crighton R, Hodson F, Roomes D, et al. Understanding the lived experience of chronic pain: a systematic review and synthesis of qualitative evidence syntheses. Br J Pain. 2023;17:20494637231196424.
Lim YZ, Chou L, Au RT, Seneviwickrama KMD, Cicuttini FM, Briggs AM, et al. People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: a systematic review. J Physiother. 2019;65(3):124–35.
O’Keeffe M, Ferreira GE, Harris IA, Darlow B, Buchbinder R, Traeger AC, et al. Effect of diagnostic labelling on management intentions for non-specific low back pain: a randomized scenario-based experiment. Eur J Pain. 2022;26(7):1532–45.
O’Keeffe M, Michaleff ZA, Harris IA, Buchbinder R, Ferreira GE, Zadro JR, et al. Public and patient perceptions of diagnostic labels for non-specific low back pain: a content analysis. Eur Spine J. 2022;31(12):3627–39.
Sloan TJ, Walsh DA. Explanatory and diagnostic labels and perceived prognosis in chronic low Back pain. Spine. 2010;35(21).
Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain. 2012;16(1):3–17.
Article CAS PubMed Google Scholar
Belton J, Birkinshaw H, Pincus T. Patient-centered consultations for persons with musculoskeletal conditions. Chiropr Man Ther. 2022;30(1):53.
Ashton-James CE, Anderson SR, Mackey SC, Darnall BD. Beyond pain, distress, and disability: the importance of social outcomes in pain management research and practice. Pain. 2022;163(3):e426-ee31.
Ruissen GR, Liu Y, Schmader T, Lubans DR, Harden SM, Wolf SA, et al. Effects of group-based exercise on flourishing and stigma consciousness among older adults: findings from a randomised controlled trial. Appl Psychol: Health Well-Being. 2020;12(2):559–83.
PubMed Google Scholar
Bunn F, Dickinson A, Barnett-Page E, Mcinnes E, Horton K. A systematic review of older people’s perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing Soc. 2008;28(4):449–72.
Ienca M, Schneble C, Kressig RW, Wangmo T. Digital health interventions for healthy ageing: a qualitative user evaluation and ethical assessment. BMC Geriatr. 2021;21:1–10.
De Santis KK, Mergenthal L, Christianson L, Busskamp A, Vonstein C, Zeeb H. Digital Technologies for Health Promotion and Disease Prevention in older people: scoping review. J Med Internet Res. 2023;25:e43542.
Pan American Health Organization and International Telecommunication Union. The role of digital Technologies in Aging and Health. Washington, D.C.; 2023.
Cooper K, Schofield P, Smith BH, Klein S. PALS: peer support for community dwelling older people with chronic low back pain: a feasibility and acceptability study. Physiotherapy. 2020;106:154–62.
Terp R, Kayser L, Lindhardt T. Older patients’ competence, preferences, and attitudes toward digital technology use: explorative study. JMIR Hum Factors. 2021;8(2):e27005.
Fenge L-A, Melacca D, Lee S, Rosenorn-Lanng E. Older peoples’ preferences and challenges when using digital technology: a systematic review with particular reference to digital games. Int J Educ Ageing. 2019;5(1):61–78.
Airola E. Learning and use of eHealth among older adults living at home in rural and nonrural settings: systematic review. J Med Internet Res. 2021;23(12):e23804.
Svendsen MJ, Wood KW, Kyle J, Cooper K, Rasmussen CDN, Sandal LF, et al. Barriers and facilitators to patient uptake and utilisation of digital interventions for the self-management of low back pain: a systematic review of qualitative studies. BMJ Open. 2020;10(12):e038800.
Geraghty AW, Roberts LC, Stanford R, Hill JC, Yoganantham D, Little P, et al. Exploring patients’ experiences of internet-based self-management support for low back pain in primary care. Pain Med. 2020;21(9):1806–17.
Belton JL, Slater H, Ravindran TS, Briggs AM. Harnessing People’s lived experience to strengthen health systems and support equitable musculoskeletal health care. J Orthop Sports Phys Ther. 2023;53(4):162–71.
Download references
Acknowledgements
We would like to acknowledge our search specialist Elisabet Hafstad for her expertise in developing and conducting the search for this synthesis.
Open access funding provided by Norwegian Institute of Public Health (FHI) This synthesis was commissioned and funded by the WHO to contribute to a guidelines process. The lead authors (HA and CHH) discussed the synthesis objectives and inclusion criteria with the commissioner. HA and CHH independently conducted the synthesis and came to the findings.
Author information
Authors and affiliations.
The Norwegian Institute of Public Health, PO Box 222, 0213, Oslo, Skøyen, Norway
Heather Ames & Christine Hillestad Hestevik
Ageing and Health Unit, Department of Maternal, Newborn, Child & Adolescent Health and Ageing, World Health Organization, Avenue Appia 20, 1211, Geneva, Switzerland
Andrew M. Briggs
Faculty of Health Sciences, Curtin University, PO Box U1987, Perth, 6845, Western Australia
You can also search for this author in PubMed Google Scholar
Contributions
All authors conceptualised the synthesis and wrote the protocol. HA and CHH conducted the search, study selection, analysis, and decision on findings. AMB was not involved in data extraction or synthesis. AMB acted as a subject expert during the synthesis process and connecting the findings of the synthesis to the broader field. All authors were involved in drafting this manuscript.
Authors’ information
HA is an anthropologist and health systems research who has been working with qualitative evidence synthesis since 2013. She is a senior researcher at the Norwegian Institute of Public Health and an Associate convener with the Cochrane Qualitative and Implementation Methods Group.
CHH is a health systems researcher with a speciality within nutrition. She has been working with qualitative evidence synthesis since 2018. She is a senior advisor at the Norwegian Institute of Public Health where she specialises in conducting systematic reviews.
AMB is a consultant to the WHO, supporting the development of the WHO Guideline on chronic primary low back pain in adults. He is also a health systems and services researcher and practicing physiotherapist.
Corresponding author
Correspondence to Heather Ames .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
HA and CHH declare that they have no competing interests. AMB declares he works as a consultant to the WHO.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search strategy.
Additional file 2.
Machine learning plan.
Additional file 3.
Excluded full text studies with reason.
Additional file 4.
Evidence profile table.
Additional file 5.
Final adapted framework.
Additional file 6.
ENTREQ Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ames, H., Hestevik, C.H. & Briggs, A.M. Acceptability, values, and preferences of older people for chronic low back pain management; a qualitative evidence synthesis. BMC Geriatr 24 , 24 (2024). https://doi.org/10.1186/s12877-023-04608-4
Download citation
Received : 29 March 2023
Accepted : 16 December 2023
Published : 05 January 2024
DOI : https://doi.org/10.1186/s12877-023-04608-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Interventions
- Older adults
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 01 April 2024
Paramedic attitudes and experiences working as a community paramedic: a qualitative survey
- Aarani Paramalingam 1 ,
- Andrea Ziesmann 1 ,
- Melissa Pirrie 1 ,
- Francine Marzanek 1 ,
- Ricardo Angeles 1 &
- Gina Agarwal 1 , 2
BMC Emergency Medicine volume 24 , Article number: 50 ( 2024 ) Cite this article
118 Accesses
3 Altmetric
Metrics details
Community paramedicine (CP) is an extension of the traditional paramedic role, where paramedics provide non-acute care to patients in non-emergent conditions. Due to its success in reducing burden on hospital systems and improving patient outcomes, this type of paramedic role is being increasingly implemented within communities and health systems across Ontario. Previous literature has focused on the patient experience with CP programs, but there is lack of research on the paramedic perspective in this role. This paper aims to understand the perspectives and experiences, both positive and negative, of paramedics working in a CP program towards the community paramedic role.
An online survey was distributed through multiple communication channels (e.g. professional organizations, paramedic services, social media) and convenience sampling was used. Five open-ended questions asked paramedics about their perceptions and experiences with the CP role; the survey also collected demographic data. While the full survey was open to all paramedics, only those who had experience in a CP role were included in the current study. The data was qualitatively analyzed using a comparative thematic analysis.
Data was collected from 79 respondents who had worked in a CP program. Three overarching themes, with multiple sub-themes, were identified. The first theme was that CP programs fill important gaps in the healthcare system. The second was that they provide paramedics with an opportunity for lateral career movement in a role where they can have deeper patient connections. The third was that CP has created a paradigm shift within paramedicine, extending the traditional scope of the practice. While paramedics largely reported positive experiences, there were some negative perceptions regarding the slower pace of work and the “soft skills” required in the role that vary from the traditional paramedic identity.
Conclusions
CP programs utilize paramedic skills to fill a gap in the healthcare system, can improve paramedic mental health, and also provide a new pathway for paramedic careers. As a new role, there are some challenges that CP program planners should take into consideration, such as additional training needs and the varying perceptions of CP.
Peer Review reports
Community paramedicine (CP) is an emerging professional role where paramedics use their training and skills in emergency response to respond to individuals with non-acute needs who do not require transport to hospital [ 1 ]. In Ontario, Canada, CP programs have begun to garner attention as an innovative approach to support independent living in an aging older adult population with complex health conditions [ 2 ]. Although there were some very early adopters of CP programs in Ontario, these programs began to gain momentum in 2013 [ 3 ]. By 2014, 13 Paramedic Services in Ontario reported having CP programs [ 2 ]. Community paramedicine programs can be diverse in scope, and can include paramedics completing home visits to frequent 911 callers, supporting clients with healthcare navigation, providing community-based education, and conducting drop-in clinic style wellness programs [ 1 ]. The structure, mandate, and resources required for CP programs tend to vary by paramedic service and local contexts. Staffing and training arrangements can also vary, with some programs designating full-time ‘community paramedics’ while others deploy paramedics on modified duties to staff programs.
Our literature review found that few studies have sought to understand how paramedics experience and view these programs. Evaluations of CP tend to focus on patient experiences, such as their health outcomes and health service utilization [ 4 , 5 , 6 ]. While participants have generally expressed support for and acceptance of CP [ 5 , 6 ], it is unclear exactly how paramedics perceive CP programs, particularly as it relates to their understanding of paramedic professional identity and their mental health.
As the CP role becomes a more permanent part of paramedic practice, it is expected to redefine and broaden the paramedic identity beyond its traditional boundaries. Historically, service users and healthcare providers have defined paramedics as thrill seekers who provide transport, emergency response, and trauma care [ 7 ]. However, as the delivery of healthcare has become more complex and integrated, paramedic identity has also shifted. Paramedics in Canada have already adopted broad professional identities such as ‘clinician,’ ‘educator,’ ‘team member,’ and ‘patient advocate’ [ 8 ]. This expansion of the paramedic identity is expected to accelerate as CP programs are increasingly adopted in Ontario. CP programs require paramedics to work with individuals on a repeat basis, provide chronic disease management services, and use ‘soft’ skills such as motivational interviewing and advocacy. How paramedics feel about these changes to their professional identity as a result of CP has yet to be understood.
Additionally, participation in the CP role may alter paramedics’ mental health experience. Paramedics in traditional emergency response roles tend to experience Occupational Stress Injury (OSI) due to demanding work environments and exposure to traumatic incidents [ 9 , 10 ]. Occupational Stress Injury refers to any form of psychological stress resulting from the duties one performs on the job [ 9 ]. While OSI is common for all public safety personnel, some studies suggest a higher incidence of post traumatic stress disorder for paramedics when compared to police officers and firefighters [ 11 , 12 ]. Paramedics are estimated to be at higher risk of screening positive for a DSM-IV mental disorder than municipal or provincial police services, firefighters, and dispatchers [ 12 ]. While some preliminary research in one CP program suggests that paramedics who practice CP experience reduced stress and a greater quality of work life [ 9 ], it is unclear how working in CP programs in different capacities may alter paramedics’ exposure to OSI and affect one’s overall mental health.
This paper seeks to describe the positive and negative experiences of paramedics working in a CP program and assess CP’s impacts on paramedic professional identity and paramedic’s mental health experience. As paramedic experiences may not be aligned with the experiences of CP program participants or even paramedic leadership, this paper also seeks to identify workplace elements (e.g., training, supports, paramedic leadership and culture) that may promote or hinder the expansion of CP programs in Ontario.
A survey tool was developed and distributed by the McMaster Community Paramedicine Research Team in 2016, using the online platform FluidSurveys, to assess paramedics’ perceptions and experiences working in a CP role. The survey was developed based on recurring themes and insights from a focus group and three key informant interviews with paramedics. The survey drafts were also reviewed and approved by a paramedic and a paramedic superintendent with research experience. The survey tool used open-ended questions to have paramedics describe their perception of the CP role prior to, and after working in a CP program, including both positive and negative aspects.
Population and recruitment
Paramedics were invited to participate in a survey that was distributed through social media by the Ontario Paramedic Association and the CP@clinic program. On Twitter, the invitation to complete the survey was re-tweeted by multiple accounts including paramedic services, paramedic staff, and other accounts. In addition, some Paramedic Services in Ontario delivering CP programs emailed the survey link to their paramedic staff. All paramedics (with and without CP experience) were invited to complete the full survey, but only those who indicated that they had worked in a CP role were included in this study (screening question in the survey). Respondents were informed about the purpose of the research study and informed consent was obtained. This study was approved by the Hamilton Integrated Research Ethics Board (Project #13-466).
Data collection
A convenience sample was collected using an online survey. The survey was available for 16 weeks from October 2016 to January 2017, to provide ample time to gather responses from all potential participants. Data from the open-ended questions were collated into a single transcript.
The survey collected the following demographic information: age, sex, years of service, type of paramedic training (i.e., primary care, advanced care, critical care), whether the paramedic was on modified duty while working in a CP program (i.e., awaiting return to regular duties), length of time working in CP programs, and types of programs they worked in. Fivetypes of CP programs were provided as options: home visit program, clinic style program, paramedic navigator style program, triage program, and other.
The following open-ended questions were asked to elicit responses about paramedics’ experience of the CP role:
What was your opinion of community paramedicine before working a community paramedicine role?
Please explain how your opinion of community paramedicine has changed since working in a community paramedic role?
What was positive about your experience working in a community paramedic role? What did you enjoy about this role?
What were the negative aspects in your experience working as a community paramedic?
Would you like to change anything about the community paramedic role?
A comparative thematic analysis was used to describe the experiences of community paramedics before and after working in a CP role. Two members of the research team (AP, AZ) independently coded responses and identified emergent themes. Using a phenomenological approach during secondary coding, coders grounded the emergent themes within paramedics’ lived experience of the community paramedicine role, finding explanations for their experience within the context of the data itself. Responses with thick narrative descriptions were retained for analysis. Incomplete or partial responses were included in the qualitative analysis. Themes were then synthesized, refined, and were validated and triangulated by research team members (GA, AZ, MP, FM, RA). The demographic data was analyzed using descriptive analysis.
Demographics
Of the total survey respondents ( n =434), 79 reported working in a CP role. These respondents were predominantly male (57.0%), had 10 or more years of experience in a paramedic role (77.2%), and were not on modified duty while working in a CP role (86.1%). Respondents reported experience with working in multiple types of CP programs, with the most common type being clinic style programs (68.4%) (see Table 1 ). While the survey was open to all paramedics, the majority of respondents report working in Ontario ( n =61, 77.2%) and 16 respondents (20.3%) did not provide the province in which they worked.
A number of themes and sub-themes emerged from the analysis. Before having worked in a CP program, paramedics broadly identified three unique opportunities and impacts of the CP role: 1) filling gaps in emergency response and the healthcare system at large, 2) providing opportunity for lateral career movement, and 3) creating practice paradigm shifts. After working in a CP role, respondents were able to describe in detail the positive and negative aspects of these three opportunities and impacts. These themes are conceptualized in Fig. 1 .
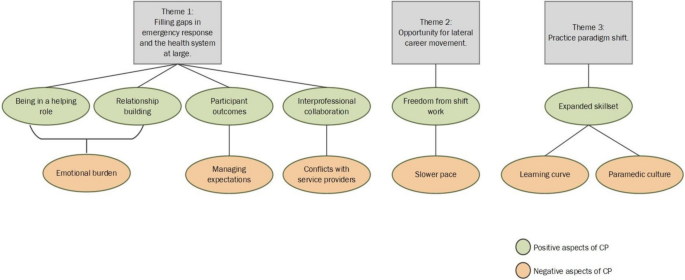
Diagram depicting the major themes and the positive and negative experiences of paramedics working in a CP role
Theme 1: CP programs can fill important gaps in emergency response and the healthcare system at large, but come with new professional challenges
Before working in a CP role, the majority of respondents viewed the CP role positively. CP was thought to fill important gaps in emergency response and the health system at large. It offered paramedics an opportunity to practice continuity of care by providing prevention and disease management support to older adults who were often inappropriately accessing emergency care services. Paramedics felt that the needs of these individuals were not being fulfilled through traditional emergency response.
There are several individuals I have come across in my career who would have benefitted from a regularly scheduled home visit. ...There are a lot of individuals who require that [health] maintenance… it greatly reduces the workload of Emergency Services and frees them up for what they are actually required for – emergencies. (P.24)
[I thought] it was a vital service that filled gaps in the health care sector that was having excellent results where implemented (P.43)
After working in a CP program, respondents expanded on these initial sentiments. They described delivering a different level of care to their communities that involved stepping into a novel helping role, building relationships with participants and their families, supporting participant health outcomes, and taking part in interprofessional collaboration. This new level of care also came with new professional challenges such as increased emotional burden, managing participant expectations, and conflicts with other health and social service providers.
Sub-theme 1A: being in a helping role
Helping program participants in a CP role was described as novel and different when compared to the emergency response role. Community paramedics worked with participants on a long-term basis and witnessed their health and quality of life improvements. Paramedics enjoyed helping participants who were part of vulnerable or underserved communities. By taking time to listen to these participants and hear their stories, paramedics were able to exercise more compassion and felt less judgemental about participants’ situations. This was a rewarding aspect of the CP role, even having a powerful positive effect on paramedics’ own mental health.
Making a difference in people's lives ... often the people in the community who are ignored and shunned by others. I enjoyed going out in the community, solving problems, working with other services, having the time to LISTEN to patients rather than be worried about my scene time...this is one of the most important things for Paramedic mental health as well. (P.46)
...the knowledge that community paramedics, with sometimes very simple interventions/strategies can make all the difference in people's lives, preventing people from falling through the cracks, or helping them out of that situation…(P.61)
Sub-theme 1B: relationship building with program participants
Paramedics enjoyed building relationships with participants and getting to know them on a personal level, which was not possible in an emergency response role due to limited time on scene during acute calls. Building rapport with participants in the comfort of their homes created a sense of trust that fostered into natural friendships, with some paramedics describing themselves as building a ‘family’ with participants. Others noted that this trust allowed participants to share more details about their health and medical history, allowing paramedics to better assist in their care. Paramedics felt it was important to build these strong social relationships with participants in order to encourage and affect health behaviour changes for participants. Strong relationships with participants allow paramedics to thoroughly follow-up after initial visits and engage in conversations about participants’ short- and long-term health goals. Additionally, although the CP role lacked the adrenaline rush, this increased socialization was described as filling this gap.
The paramedics have built a rapport with [participants] and have really built a family with them.(P.19)
Getting to know [participants] beyond the 30 minutes to an hour we’re used to being with [them in an emergency capacity]. I found as they got to know me, they were more willing to share health concerns they were having and trusted me more. (P.26)
I realized that community paramedicine can be more enjoyable than I thought…where it lacks in adrenaline it makes up for in a social aspect. (P.10)
Seeing how much they trust us and tell us some of their most intimate issues. (P.49)
Sub-theme 1C: emotional burden
While paramedics enjoyed the rapport and relationships built with participants, they also felt they were making greater emotional investments in participants who were in poor health, may have been in a palliative state or dealing with addictions issues. Burnout, attachment fatigue, and difficulty dealing with participant deaths were common experiences. For some paramedics, having built rapport with certain participants meant that they were the primary contact for follow-up care even on their days off, leading to poor work-life balance. Similar to other clinical practitioners who work one-on-one with individuals over a long period of time (e.g., physicians, social workers), one respondent emphasized the need for paramedics in a CP role to be trained to reflect on their experience and make adjustments to how they work with participants.
Can be emotionally draining working over the long term with [participants]... who are very sick, some are palliative, difficult personalities, addictions, etc. Paramedics historically aren’t used to becoming emotionally involved with [people] … but this is difficult not to do when you are seeing people over and over again, and getting involved with their families and other circles of care as well. (P.5)
Couldn't just leave work behind at work like a traditional paramedic could - had to field phone calls on my vacation to help make arrangements for a [participant]... because no other community paramedics were available or as familiar with [them]. (P. 9)
Paramedics are not usually trained, educated, or encouraged to engage in self-reflective or reflective practice and it’s essential for a role like community paramedicine. (P. 34)
Sub-theme 1D: participant outcomes
Paramedics reported a better understanding of the impact of CP programing on participants’ health and well-being. Identifying ‘silent’ health issues before they resulted in emergency transport, making appropriate referrals and reducing 911 calls were some of the positive outcomes. For some, their CP training had become an integral part of their role as a paramedic overall, providing valuable transferable skills that could also be used during an emergency response to further improve health outcomes and close gaps in care. Additionally, beyond identifying health issues and making appropriate referrals, some paramedics felt that CP programs help build a sense of community, which may in turn also improve participant health and well-being. Paramedics particularly appreciated being able to witness these positive outcomes first-hand.
I have realized that community paramedicine has a very broad impact in the community. It is very underappreciated ... It has improved the livelihood of many [participants], and can (with the aid of other resources), assist them [with] their healthcare needs. (P.9)
Seeing them get proper treatment for an illness they did not know they had (i.e. hypertension, diabetes). (P.62)
Seeing the direct benefit of timely and appropriate interventions; having a big impact on people's quality of life, even when palliative (P. 60)
I see that most [people] don't want to go to the hospital and really don't need to. The issue is [that in] our current system people expect to be taken as they think that's the only way a doctor will see them. When they realised someone could see them at home and then refer them to the required service less 911 calls were made. (P.10)
I'm fortunate enough to work in a service that has integrated some aspects of community paramedicine into every response. Being trained to recognize signs in a [participant]'s home that indicate a higher need for home care and offering ways for them to access more care is deeply satisfying. The relief on a person's face when told they could get some home care, or help with day to day chores makes me feel like I made a difference to their quality of life. (P.36)
Seeing how much change we were able to create in a short period of time. Watching the sense of community flourish in the buildings while we were there. (P.49)
Sub-theme 1E: managing participant expectations
Managing the expectations of program participants and trying to elicit health behaviour change was a challenging aspect of the CP role. While seeing positive improvements in participants' lives motivated community paramedics and likely provided them with increased job satisfaction, working with participants who were not able to achieve these positive outcomes in some participants despite working to identify their health issues, and referring and connecting them to services, was a frustrating aspect of the role. Paramedics experienced frustration when participants did not follow their health advice, did not experience improvements in their health, or when participants expressed dissatisfaction with the help they received. Some of this frustration was also directed towards referral agencies who were not able to help the participant.
Some people are noncompliant with their medications or taking the advice of their physicians. It can be frustrating having people come to you for help for the same problems but not be receptive to the advice that you give. (P. 42)
There have been moments of frustration when patients don't follow through or even attempt to follow advice given to them by myself or the agency that has been tasked with giving them assistance. (P. 42)
[Some] clients who are out of the normal scope of practice for a paramedic who are better served by other agencies but those agencies failing the client. Even when you help put services in place for a client they are not happy and want more. (P.7)
Sub-theme 1F: interprofessional collaboration
Paramedics enjoyed working with differenthealthcare providers in their community. Collaboration with different services and providers was felt by paramedics to benefit program participants and improve their career satisfaction. Collaboration with different healthcare providers outside of an emergency paramedicine context made paramedics feel respected and part of a valued healthcare team that was centred around improving participant health. This collaboration provided better coordinated care and also showcased paramedics’ clinical skills beyond that of transport and ambulance-driving to other healthcare professions.
The integration, collaboration, and cooperation with health care and with allied health care providers. We truly make a difference in people's lives, keeping them in their homes longer, safer, and healthier. (P. 67)
Building relationships and pathways with community health care providers and showing them that paramedics are more than just ambulance drivers. (P. 13)
Interacting with the [primary care provider] as we caught early onset [urinary tract infections (UTIs)] and [upper respiratory tract infections] with treatment started based solely on our assessment and conversation via cell phone with [the provider] saving [the participant] stress and cost of travelling to their office. (P. 49)
...Enjoy working more closely with physicians to develop treatment plans.(P.56)
Sub-theme 1G: conflicts with other service providers
While paramedics appreciated the interprofessional collaboration offered by the CP role, they also described conflicts and challenges working with other service providers in the health and social work sector. Paramedics described some service providers as failing and unable to meet participant needs. Overlap between CP activities and other healthcare roles also led to tensions regarding professional boundaries, including physician concerns about CPs diagnosing their patients.
Some doctors did not like paramedics assessing and diagnosing issues (e.g. chest infections, UTIs, and muscular-skeletal injuries). (P. 39)
Don't know if referrals are getting back to [participants]…[There are] already programs in place that have [the] same mandate as CP, like Health Link, forcing medics to do home visits when [participants] don’t need them any more. (P. 12)
Oftentimes, navigating the system was a challenge and often wait times with family doctors or other services were unavoidable. (P. 29)
Theme 2: CP offers paramedics an opportunity for lateral career movement that is free from the demands of shift work and allows them to be connected to the community in a clinical capacity that is slower paced.
Some respondents viewed CP as a new opportunity for lateral career movement within the paramedic profession, ideal for paramedics in the late-stage of their career as it offered less physically demanding work. It was also noted that CP could help keep aging paramedics in the service for a longer period of time and the community could continue benefiting from their skill set.
After having worked in the new role, paramedics described CP as offering greater freedoms compared to the demands of shift work in traditional emergency response roles. CP offered freedom from the demands of shift work by providing better hours, increased autonomy, reduced physical demands, and reduced paramedic stress. For paramedics with longer years of service, this was a welcomed change of pace, with some reporting mental and physical health improvements. Others noted the importance of still being connected to the community in this new role. For others, adjustment to the slower pace of the CP role was difficult due to their preference for emergency work..
I enjoyed being still involved with the community but not having to have the daily physical demands of responding to 911 calls. The role is less stressful and after being a paramedic on the road for 14 years it is an amazing and a welcome change of pace both mentally and physically. (P. 58)
The autonomy to structure my day without the oversight of dispatch or supervisors. (P.63)
[It] would be great for light duty/modified work, could keep aging medics on for [a] longer period of time, good idea for last years of work. (P.51)
I prefer a higher paced environment dealing with acute injuries…(P.30)
Theme 3: Paramedics viewed and experienced the CP role as a practice paradigm shift
Before working in a CP role, paramedics viewed ed CP to be a practice paradigm shift for the profession. For some, this shift in practice was thought to be in opposition to the traditional emergency care role while others felt it was a natural extension of paramedic practice.
I did not feel that was something I would enjoy as it does not have the same adrenaline rush you get when on emergency calls. (P. 13)
[I] felt it was long overdue and a natural extension of what we were already doing in an emergency capacity. (P. 43)
I thought that it would be the next step in emergency medicine, our next frontier. Fire has prevention, we should have health promotion. (P. 26)
After working in a CP role and experiencing the practice paradigm shift first-hand, paramedics noted being largely satisfied by their newly expanded skill set, but also felt that it was a significant learning curve. Paramedics experienced negative sentiments from their peers in traditional emergency response regarding the CP role, highlighting the diverging paradigms between the two roles.
Sub-theme 3A: expanded skill set
The CP program expanded paramedics’ skill set to provide better care to program participants. Some of the new clinical skills described included medication provision, suturing, catheterization, point-of-care testing. Paramedics felt these skills improved their overall ability to perform when returning to emergency response duties. Others felt these new clinical skills were not used or required for the CP role because participants were mainly looking to socialize and interact.
I very much enjoyed the increased scope of practice. I believe that it allows me to provide better care and assist people in the community more than I have before. Moreover, I feel that the additional training has made me a better, and more well-rounded medic overall. (P.34)
I enjoyed the expanded roles (phlebotomy, catheterization, suturing etc)...(P.25).
Sub-theme 3B: learning curve
Working in a CP role was a significant learning curve for some paramedics. Challenges included learning soft skills such as communication, confidence leading sessions with older adults, and learning administrative tasks such as new documentation and computer skills. For paramedics working in both emergency response and CP roles, it was difficult to shift between emergency response protocols and CP protocols. This may have been due to competing priorities between emergency response and CP protocols, such as deciding whether to transport an individual to hospital or keeping an individual at home.
It is a difficult shift in frame of mind to go from 911 assessments to CP assessments and having to switch back into 911 mode when necessary...It can be tough to play the role of both emerg[ency] response and CP. (P.18)
Adapting to new ways, changing the way you do calls, learning the CP documentation and computer programs, being confident with [program participants] and visits, knowing when to communicate with the providers and how. (P. 2)
Much more patient advocacy & health teaching then I had expected. (P.14)
Sub-theme 3C: negative paramedic culture
Community paramedics described a negative paramedic culture that is unaccepting of the CP role and its softer skill set. Lack of buy-in from paramedics in traditional emergency response roles, along with poor understanding of the positive impacts of CP programming, have led to negative perceptions of the role in the paramedic workforce. Community paramedics felt that their emergency response colleagues did not respect their role and felt misunderstood by the profession at large.
Paramedic culture that needs to be educated and changed on the value of CP work. (P.32)
Misunderstood by co-workers and some management. Labeled the tea and cookie brigade. (P.24)
I also found that EMS crews treated CP with very little mutual respect and understanding... (P. 41)
There were a number of positive and negative aspects of the CP role identified by paramedic respondents. While the majority of respondents felt that working in a CP program was a largely positive experience, some expressed dissatisfaction and difficulty adapting to the role. Many positive aspects of the CP role also had unintended negative aspects, particularly as it related to paramedics’ sense of professional identity and their mental health experience when working in the CP role. In order to ensure paramedic job satisfaction and understand the future state of CP programs, these opposing experiences need to be further examined and addressed.
Paramedic professional identity
While many paramedics felt CP was an extension of the paramedic identity, some felt it was a threat to the traditional paramedic identity, removing the defining element of ‘emergency response’ and blurring professional boundaries with other health and social service roles. These diverging experiences and attitudes towards the CP role and its place in the paramedicine profession suggest that there are different fractional identities within the paramedic workforce. Donelley et al. found that emergency service workers often define their role using four domains: caregiving (helping individuals in need), thrill seeking (the adrenaline rush experienced during critical incidents), capacity (having the knowledge, skills, and training to act), and duty (obligation to one’s community and service) [ 7 ]. Paramedics who understand their professional identity as falling within the ‘caregiving’ or ‘duty’ domain may be more accepting of the CP role and understand its fit within their existing paramedic mandates. However, paramedics who understand their professional identity as falling within the ‘thrill seeking’ and ‘capacity to conduct an emergency response’ domain may view CP as not only redefining and expanding the profession, but a threat to the professional identity. Expansion and further resourcing of CP programs may exacerbate divisions and tensions between staff who have different professional motivations if these concerns are not addressed.
Paramedic mental health
Working in a CP role may have also led to some improvements in paramedic mental health. In the traditional emergency response role, paramedics take on shift work, are often exposed to traumatic emergency response incidents, and are limited in their interactions with individuals in their care (single touchpoint and limited time). In contrast, community paramedics experienced more freedom to structure their day, new opportunities to build relationships with program participants due to multiple touchpoints and they experienced reduced physical demands. These experiences likely contributed to a less stressful, flexible work environment which in turn improved mental health for some.
However, increased socialization with participants also introduced new emotional burdens and stressors for some community paramedics. Increased attachment to program participants often made it difficult to deal with their deaths. Participants are often vulnerable populations who face complex health and social issues, such as poverty and addiction. Increased contact with vulnerable populations may increase paramedics’ exposure to vicarious trauma or ‘compassion fatigue,’ which refers to the secondary trauma experienced by working closely with individuals who have experienced trauma first-hand [ 13 , 14 , 15 ]. Vicarious trauma and compassion fatigue can have similar negative impacts on paramedic mental health as first-hand trauma, leading to emotional disturbances, stress, intrusive thoughts, and reduced productivity [ 15 ]. Particularly for community paramedics with a strong orientation towards empathy and caregiving, compassion fatigue may be experienced as a negative or challenging consequence of the role [ 15 ].
Considerations for CP programming
The experiences of paramedics working in a CP program suggests the CP role comes with new opportunities and challenges for staff and the profession at large. Paramedics have broad and diverse understandings of their professional identity, leading some to view CP as a natural fit within the profession while others view it as extending too far beyond the boundaries of paramedicine. This suggests the need for paramedic leaders to clearly define the purpose, mandate, and function of the CP role within the paramedic workforce. Paramedic services interested in implementing and expanding on CP programs to achieve program outcomes such as a reduction in emergency calls and improving participant health outcomes should reflect on their workplace culture and consider the role of their leadership in promoting this role. Champions of CP programming may be identified to better support the workforce’s understanding of this role and how it fits within larger paramedic mandates and objectives. Paramedic leaders who are championing the CP role should consider what factors may contribute to a paramedic feeling alienated in a CP role and how staff are selected to fill this role. In addition, negative perceptions of the CP role as ‘soft’ or ‘easy’ in comparison to emergency response roles needs to be dispelled if community paramedics are to feel valued for their efforts and contributions.
In addition, a number of training supports may need to be provided that take into consideration the new emotional burdens of the CP role. While the CP role may contribute to good mental health by providing a flexible work environment, reducing exposure to traumatic incidents, and allowing paramedics to socialize with individuals in their care, it may also put some paramedics at risk for vicarious trauma and compassion fatigue. Drawing from professions such as social work and counselling, a number of training and professional development supports can be provided to reduce compassion fatigue. Examining compassion fatigue in community paramedics, Cornelius et al. suggests that paramedics should establish boundaries when working with program participants, ensuring that participants recognize the relationship between them and the paramedic is time limited [ 15 ]. Additionally, the caseload of community paramedics should be examined and managed by supervisors in terms of size and complexity of cases [ 15 ]. Other paramedic supports could include resiliency training, counselling services, and stress management workshops [ 15 ]. Training provided should match the type and scope of the CP program the paramedic is working in and their work environment.
Limitations
A limitation of this study is that it used an online survey with predefined open-ended questions to extract information on lived experience rather than a semi-structured interview. This approach prevented researchers from prompting paramedics on their responses and engaging in discussion to obtain a deeper description of their experiences. However, the survey approach allowed the research team to obtain responses from a large number of paramedics and collect responses from across Ontario. Another limitation is that due to the inherent nature of the survey link, it cannot be guaranteed that unique responses were captured. However, multiple entries from respondents are unlikely.
Future research should attempt to engage paramedics on the issues described in this paper and should consider how the relative impacts of working in different types of CP programs (e.g., clinic style programs, at home visits, etc.) may affect paramedic experiences. This approach may provide more detailed data to inform future CP training and program design.
This paper found paramedics who have worked in a CP role, reported that the role offered opportunities to fill a gap in the healthcare system, to move laterally within the paramedic profession, and to create a practice paradigm shift within the profession. Most described having positive perceptions of their professional identity after working as a CP, as they were able to fulfill stepping into a helping role to a greater extent. In contrast, some came out of the experience with negative perceptions. It is important for CP program planners to consider these diverse experiences when planning for the expansion of these programs. A workforce culture that views CP programming negatively and as potentially eroding the traditional paramedic identity may work to hinder the program’s ability to achieve positive outcomes such as a reduction in emergency calls and an improvement in participant health outcomes. Incorporating the CP role within larger paramedic mandates and objectives by paramedic leadership may support this work, as well as CP champions who clarify the role and impacts of CP to staff.
Availability of data and materials
The data that support the findings of this study are not publicly available due to them containing information that could compromise participant privacy. De-identified, limited data will be shared by the corresponding author upon reasonable request.
Abbreviations
- Community Paramedicine
Occupational Stress Injury
Chan J, Griffith LE, Costa AP, Leyenaar MS, Agarwal G. Community paramedicine: a systematic review of program descriptions and training. CJEM. 2019;21(6):749–61. https://doi.org/10.1017/cem.2019.14 .
Article PubMed Google Scholar
Ministry of Health and Long-Term Care. Ontario Expanding Community Role for Paramedics. Ontario Newsroom. January 21, 2014 published. Accessed 9 Feb 2023. https://news.ontario.ca/mohltc/en/2014/01/ontario-expanding-community-role-for-paramedics.html.
County of Renfrew. About Us. Community Paramedic. Accessed 9 Feb 2023. http://www.communityparamedic.ca/pages/home/about-us.php.
Agarwal G, Angeles R, Pirrie M, et al. Effectiveness of a community paramedic-led health assessment and education initiative in a seniors’ residence building: the Community Health Assessment Program through Emergency Medical Services (CHAP-EMS). BMC Emerg Med. 2017;17:8. https://doi.org/10.1186/s12873-017-0119-4 .
Article CAS PubMed PubMed Central Google Scholar
Brydges M, Denton M, Agarwal G. The CHAP-EMS health promotion program: a qualitative study on participants’ views of the role of paramedics. BMC Health Serv Res. 2016;16:9. https://doi.org/10.1186/s12913-016-1687-9 .
Article Google Scholar
Martin A, O’Meara P, Farmer J. Consumer perspectives of a community paramedicine program in rural Ontario. Aust J Rural Health. 2016;24(4):278–83. https://doi.org/10.1111/ajr.12259 .
Donnelly EA, Siebert D, Siebert C. Development of the Emergency Medical Services Role Identity Scale (EMS-RIS). Soc Work Health Care. 2015;54(3):212–33. https://doi.org/10.1080/00981389.2014.999979 .
Tavares W, Bowles R, Donelon B. Informing a Canadian paramedic profile: framing concepts, roles and crosscutting themes. BMC Health Serv Res. 2016;16:1–16. https://doi.org/10.1186/s12913-016-1739-1 .
Nixon J. Paramedic perspectives of community paramedicine and quality of work life in Northern Ontario, Canada. Master's Thesis. Laurentian University; 2019. Accessed February 09, 2023. https://zone.biblio.laurentian.ca/bitstream/10219/3241/1/Nixon%20-%20Thesis%20Document%20-%20April25-2019-FINAL.pdf.
Ad-hoc Committee on Operational Stress Injury. Operational Stress Injury in Paramedic Services: A Briefing to the Paramedic Chiefs of Canada. Paramedic Chiefs of Canada; 2014. Accessed 9 Feb 2023. https://www.paramedicchiefs.ca/docs/PCC%20Ad%20hoc%20Committee%20on%20Stress%20Injury%20Report.doc.
Drewitz-Chesney C. Posttraumatic stress disorder among paramedics: exploring a new solution with occupational health nurses using the Ottawa Charter as a framework. Workplace Health Saf. 2012;60(6):257–63. https://doi.org/10.1177/216507991206000605 .
Carleton RN, Afifi TO, Turner S, et al. Mental disorder symptoms among public safety personnel in Canada. Can J Psychiatry. 2018;63(1):54–64. https://doi.org/10.1177/0706743717723825 .
Figley CR. Compassion fatigue: Toward a new understanding of the costs of caring. In B. H. Stamm, ed. Secondary traumatic stress: Self-care issues for clinicians, researchers, and educators. The Sidran Press; 1995: 3-28.
Figley CR. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in those who Treat the Traumatized. Brunner/Routledge; 1995.
Cornelius, C. Compassion Fatigue: A Hidden Stress in Providers of Mobile-Integrated Healthcare. J Emerg Med Serv. 40(8). Retrieved from https://www.jems.com/2015/08/17/compassion-fatigue-a-hidden-stress-in-providers-of-mobile-integrated-healthcare/ .
Download references
Acknowledgements
We would like to acknowledge the assistance of Brent McLeod and the OPA (Ontario Paramedic Association).
Not applicable.
Author information
Authors and affiliations.
Department of Family Medicine, McMaster University, 100 Main St W, Hamilton, ON, L8P 1H6, Canada
Aarani Paramalingam, Andrea Ziesmann, Melissa Pirrie, Francine Marzanek, Ricardo Angeles & Gina Agarwal
Department of Health Research Methods, Evidence, and Impact, McMaster University, 1280 Main Street West, Hamilton, Ontario, L8S 4L8, Canada
Gina Agarwal
You can also search for this author in PubMed Google Scholar
Contributions
The study was conceived of by GA, RA, FM and AP, AZ, GA, RA, FM and MP analysed the data. AP drafted the article under the supervision of GA and all authors were involved in editing to produce a final draft. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Gina Agarwal .
Ethics declarations
Ethics approval and consent to participate.
Respondents were informed about the purpose of the research study and informed consent was obtained. This study was conducted in accordance with the Declaration of Helsinki and was approved by the Hamilton Integrated Research Ethics Board (Project #13-466).
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Paramalingam, A., Ziesmann, A., Pirrie, M. et al. Paramedic attitudes and experiences working as a community paramedic: a qualitative survey. BMC Emerg Med 24 , 50 (2024). https://doi.org/10.1186/s12873-024-00972-5
Download citation
Received : 15 February 2023
Accepted : 21 March 2024
Published : 01 April 2024
DOI : https://doi.org/10.1186/s12873-024-00972-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Professional identity
- Mental health
- Thematic analysis
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]
Retirement planning – a systematic review of literature and future research directions
- Published: 28 October 2023
Cite this article
- Kavita Karan Ingale ORCID: orcid.org/0000-0003-3570-4211 1 &
- Ratna Achuta Paluri 2
506 Accesses
Explore all metrics
Rising life expectancy and an aging population across nations are leading to an increased need for long-term financial savings and a focus on the financial well-being of retired individuals amidst changing policy framework. This study is a systematic review based on a scientific way of producing high-quality evidence based on 191 articles from the Scopus and Web of Science databases. It adopts the Theory, Context, Characteristics, and Method (TCCM) framework to analyze literature. This study provides collective insights into financial decision-making for retirement savings and identifies constructs for operationalizing and measuring financial behavior for retirement planning. Further, it indicates the need for an interdisciplinary approach. Though cognitive areas were studied extensively, the non-cognitive areas received little attention. Qualitative research design is gaining prominence in research over other methods, with the sparse application of mixed methods design. The study’s TCCM framework explicates several areas for further research. Furthermore, it guides the practice and policy by integrating empirical evidence and concomitant findings. Coherent synthesis of the extant literature reconciles the highly fragmented field of retirement planning. No research reports prospective areas for further analysis based on the TCCM framework on retirement planning, which highlights the uniqueness of the study.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

A Research Proposal to Examine Psychological Factors Influence on Financial Planning for Retirement in China
Domains and determinants of retirement timing: A systematic review of longitudinal studies
Micky Scharn, Ranu Sewdas, … Allard J. van der Beek

Reinventing Retirement
Deanna L. Sharpe
Data Availability
The research data will be made available on request.
Acknowledgment.
Elderly population is defined as a population aged 65 years and over.
Defined benefit plan guarantees benefits to the employee, while defined contribution plan requires employees to decide on their own investment and bear the financial risks identified with it.
“The old-age dependency ratio is defined as the number of individuals aged 65 and over per 100 people of working age defined as those at ages 20 to 64”(OECD 2023 ).
Adams GA, Rau BL (2011) Putting off tomorrow to do what you want today: planning for Retirement. Am Psychol 66(3):180–192. https://doi.org/10.1037/a0022131
Article Google Scholar
Aegon Cfor, Longevity, Retirement ICR (2016) The Aegon Retirement Readiness Survey 2016. In The Aegon Retirement Readiness Survey 2016 . https://www.aegon.com/contentassets/c6a4b1cdded34f1b85a4f21d4c66e5d3/2016-aegon-retirement-readiness-report-india.pdf
Agarwalla SK, Barua SK, Jacob J, Varma JR (2015) Financial Literacy among Working Young in Urban India. World Development , 67 (2013), 101–109. https://doi.org/10.1016/j.worlddev.2014.10.004
Ajzen I (1991) The theory of Planned Behavior. Organ Behav Hum Decis Process 50:179–211. https://doi.org/10.47985/dcidj.475
Anderson A, Baker F, Robinson DT (2017) Precautionary savings, retirement planning, and misperceptions of financial literacy. J Financ Econ 126(2):383–398. https://doi.org/10.1016/j.jfineco.2017.07.008
Atkinson A, Messy FA (2011) Assessing financial literacy in 12 countries: an OECD/INFE international pilot exercise. J Pension Econ Finance 10(4):657–665. https://doi.org/10.1017/S1474747211000539`
Aydin AE, Akben Selcuk E (2019) An investigation of financial literacy, money ethics, and time preferences among college students: a structural equation model. Int J Bank Mark 37(3):880–900. https://doi.org/10.1108/IJBM-05-2018-0120
Bapat D (2020) Antecedents to responsible financial management behavior among young adults: the moderating role of financial risk tolerance. Int J Bank Mark 38(5):1177–1194. https://doi.org/10.1108/IJBM-10-2019-0356
Beckett A, Hewer P, Howcroft B (2000) An exposition of consumer behaviour in the financial services industry. Int J Bank Mark 18(1):15–26. https://doi.org/10.1108/02652320010315325
Białowolski P (2019) Economic sentiment as a driver for household financial behavior. J Behav Experimental Econ 80(August 2017):59–66. https://doi.org/10.1016/j.socec.2019.03.006
Binswanger J, Carman KG (2012) How real people make long-term decisions: the case of retirement preparation. J Economic Behav Organ 81(1):39–60. https://doi.org/10.1016/j.jebo.2011.08.010
Brounen D, Koedijk KG, Pownall RAJ (2016) Household financial planning and savings behavior. J Int Money Finance 69:95–107. https://doi.org/10.1016/j.jimonfin.2016.06.011
Brown R, Jones M (2015) Mapping and exploring the topography of contemporary financial accounting research. Br Acc Rev 47(3):237–261. https://doi.org/10.1016/j.bar.2014.08.006
Brown S, Gray D (2016) Household finances and well-being in Australia: an empirical analysis of comparison effects. J Econ Psychol 53:17–36. https://doi.org/10.1016/j.joep.2015.12.006
Brown S, Taylor K (2014) Household finances and the big five personality traits. J Econ Psychol 45:197–212. https://doi.org/10.1016/j.joep.2014.10.006
Brown S, Taylor K (2016) Early influences on saving behaviour: analysis of British panel data. J Bank Finance 62:1–14. https://doi.org/10.1016/j.jbankfin.2015.09.011
Brüggen EC, Post T, Schmitz K (2019) Interactivity in online pension planners enhances engagement with retirement planning – but not for everyone. J Serv Mark 33(4):488–501. https://doi.org/10.1108/JSM-02-2018-0082
Bruggen E, Post T, Katharina S (2019) Interactivity in online pension planners enhances engagement with retirement planning but not for everyone. J Serv Mark 33(4):488–501
Calcagno R, Monticone C (2015) Financial literacy and the demand for financial advice. J Bank Finance 50:363–380. https://doi.org/10.1016/j.jbankfin.2014.03.013
Campbell JY (2006) Household finance. J Finance 61(4):1553–1604. https://doi.org/10.1111/j.1540-6261.2006.00883.x
Choudhury K (2015) Service quality and customers’ behavioural intentions: class and mass banking and implications for the consumer and society. Asia Pac J Mark Logistics 27(5):735–757
Chowdhry N, Jung J, Dholakia U (2018) Association for consumer research. Adv Consum Res 42:42–46
Google Scholar
Clark GL, Knox-Hayes J, Strauss K (2009) Financial sophistication, salience, and the scale of deliberation in UK retirement planning. Environ Plann A 41(10):2496–2515. https://doi.org/10.1068/a41265
Clark R, Lusardi A, Mitchell OS (2017) Employee Financial Literacy and Retirement Plan Behavior: a case study. Econ Inq 55(1):248–259. https://doi.org/10.1111/ecin.12389
Collins JM, Urban C (2016) The role of information on Retirement Planning: evidence from a field study. Econ Inq 54(4):1860–1872. https://doi.org/10.1111/ecin.12349
Creswell J (2009) Research Design Qualitative Quantitative and Mixed Methods Approaches. In Sage Publishing: Vol. Third edit . https://doi.org/10.1002/tl.20234
Csorba L (2020) The determining factors of financial culture, financial literacy, and financial behavior. Public Finance Q 65:67–83. https://doi.org/10.35551/PFQ_2020_1_6
Davidoff T, Gerhard P, Post T (2017) Reverse mortgages: what homeowners (don’t) know and how it matters. J Economic Behav Organ 133:151–171. https://doi.org/10.1016/j.jebo.2016.11.007
Davis FD (1989) Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly: Management Information Systems 13(3):319–339. https://doi.org/10.2307/249008
Devlin J (2001) Consumer evaluation and competitive advantage in retail financial services - a research agenda. Eur J Mark 35(5/6):639–660
Dholakia U, Tam L, Yoon S, Wong N (2016) The ant and the grasshopper: understanding personal saving orientation of consumers. J Consum Res 43(1):134–155. https://doi.org/10.1093/jcr/ucw004
Dolls M, Doerrenberg P, Peichl A, Stichnoth H (2018) Do retirement savings increase in response to information about retirement and expected pensions? J Public Econ 158(July 2017):168–179. https://doi.org/10.1016/j.jpubeco.2017.12.014
Dragos SL, Dragos CM, Muresan GM (2020) From intention to the decision in purchasing life insurance and private pensions: different effects of knowledge and behavioural factors. J Behav Experimental Econ 87(March):101555. https://doi.org/10.1016/j.socec.2020.101555
Drever AI, Odders-white E, Kalish CW, Hoagland EM, Nelms EN, Drever AI, Odders-white E, Charles W, Else-quest NM, Hoagland EM, Nelms EN (2015) Foundations of Financial Weil-Being: Insights into the Role of Executive Function, Financial Socialization, and Experience-Based Learning in Childhood and Youth Source : The Journal of Consumer Affairs, Vol. 49, No. 1, Special Issue on Starting Ea. The Journal of Consumer Affairs , 49 (1)
Duflo E, Saez E (2002) Participation and investment decisions in a retirement plan: the influence of colleagues’ choices. J Public Econ 85(1):121–148. https://doi.org/10.1016/S0047-2727(01)00098-6
Duxbury D, Summers B, Hudson R, Keasey K (2013) How people evaluate defined contribution, annuity-based pension arrangements: a behavioral exploration. J Econ Psychol 34:256–269. https://doi.org/10.1016/j.joep.2012.10.008
Earl J, Bednall T, Muratore A (2015) A matter of time: why some people plan for retirement and others do not. Work Aging and Retirement 1(2):181–189. https://doi.org/10.1093/workar/wau005
Employees Benefits Research Institute (2020) EBRI Retirement Confidence Survey Report (Issue 202)
Engel JF, Kollat DT, Blackwell RD (1968) A model of consumer motivation and behavior. In: Research in consumer behavior. Holt, Rinehart and Winston, Inc., New York, pp 3–20
Erasmus A, Boshoff E, Rousseau G (2001) Consumer decision-making models within the discipline of consumer science: a critical approach. J Family Ecol Consumer Sci /Tydskrif Vir Gesinsekologie En Verbruikerswetenskappe 29(1):82–90. https://doi.org/10.4314/jfecs.v29i1.52799
Farrell L, Fry TRL, Risse L (2016) The significance of financial self-efficacy in explaining women’s personal finance behaviour. J Econ Psychol 54:85–99
Fernandes D, Lynch JG, Netemeyer RG (2014) Financial literacy, financial education, and downstream financial behaviors. Manage Sci 60(8):1861–1883. https://doi.org/10.1287/mnsc.2013.1849
Filbec G, Ricciardi V, Evensky H, Fan S, Holzhauer H, Spieler A (2017) Behavioral finance: a panel discussion. J Behav Experimental Finance 15:52–58. https://doi.org/10.1016/j.jbef.2015.07.003
Fishbein M (1979) A theory of reasoned action: some applications and implications. Nebraska Symposium on Motivation 27:65–116
Fisher PJ, Montalto CP (2010) Effect of saving motives and horizon on saving behaviors. J Econ Psychol 31(1):92–105. https://doi.org/10.1016/j.joep.2009.11.002
Flores SAM, Vieira KM (2014) Propensity toward indebtedness: an analysis using behavioral factors. J Behav Exp Finance 3:1–10
Foxall GR, Pallister JG (1998) Measuring purchase decision involvement for financial services: comparison of the Zaichkowsky and Mittal scales. Int J Bank Mark 16(5):180–194. https://doi.org/10.1108/02652329810228181
Friedman M (1957) Introduction to “A theory of the consumption function”. In: A theory of the consumption function. Princeton University Press, pp 1–6
Frydman C, Camerer CF (2016) The psychology and neuroscience of financial decision making. Trends Cogn Sci 20(9):661–675. https://doi.org/10.1016/j.tics.2016.07.003
Gardarsdóttir RB, Dittmar H (2012) The relationship of materialism to debt and financial well-being: the case of Iceland’s perceived prosperity. J Econ Psychol 33(3):471–481. https://doi.org/10.1016/j.joep.2011.12.008
Gathergood J (2012) Self-control, financial literacy and consumer over-indebtedness. J Econ Psychol 33(3):590–602
Gerhard P, Gladstone JJ, Hoffmann AOI (2018) Psychological characteristics and household savings behavior: the importance of accounting for latent heterogeneity. J Economic Behav Organ 148:66–82. https://doi.org/10.1016/j.jebo.2018.02.013
Gibbs PT (2009) Time, temporality, and
Goedde-Menke M, Lehmensiek-Starke M, Nolte S (2014) An empirical test of competing hypotheses for the annuity puzzle. J Econ Psychol 43:75–91
Gough O, Nurullah M (2009) Understanding what drives the purchase decision in pension and investment products. J Financial Serv Mark 14(2):152–172. https://doi.org/10.1057/fsm.2009.14
Griffin B, Loe D, Hesketh B (2012) Using Proactivity, Time Discounting, and the theory of Planned Behavior to identify predictors of Retirement Planning. Educ Gerontol 38(12):877–889. https://doi.org/10.1080/03601277.2012.660857
Gritten A (2011) New insights into consumer confidence in financial services. Int J Bank Mark 29(2):90–106. https://doi.org/10.1108/02652321111107602
Grohmann A (2018) Financial literacy and financial behavior: Evidence from the emerging Asian middle class. Pacific Basin Finance Journal , 48 (November 2017), 129–143. https://doi.org/10.1016/j.pacfin.2018.01.007
Grohmann A, Kouwenberg R, Menkhoff L (2015) Childhood roots of financial literacy. J Econ Psychol 51:114–133. https://doi.org/10.1016/j.joep.2015.09.002
Hair JF, Sarstedt M, Ringle CM, Mena JA (2012) An assessment of the use of partial least squares structural equation modeling in marketing research . 414–433. https://doi.org/10.1007/s11747-011-0261-6
Hanna SD, Kim KT, Chen SCC (2016) Retirement savings. In: Handbook of consumer finance research, pp 33–43
Harrison T, Waite K, White P (2006) Analysis by paralysis: the pension purchase decision process. Int J Bank Mark 24(1):5–23. https://doi.org/10.1108/02652320610642317
Hastings J, Mitchell O (2011) How financial literact and impatience shape retirement wealth and investment behaviors. Pengaruh Harga Diskon Dan Persepsi Produk Terhadap Nilai Belanja Serta Perilaku Pembelian Konsumen, NBER Working paper, 1–28
Hauff J, Carlander A, Amelie G, Tommy G, Holmen M (2016) Breaking the ice of low financial involvement: does narrative information format from a trusted sender increase savings in mutual funds? Int J Bank Mark 34(2):151–170
Hentzen JK, Hoffmann A, Dolan R, Pala E (2021) Artificial intelligence in customer-facing financial services: a systematic literature review and agenda for future research. Int J Bank Mark. https://doi.org/10.1108/IJBM-09-2021-0417
Hershey DA, Mowen JC (2000) Psychological determinants of financial preparedness for retirement. Gerontologist 40(6):687–697. https://doi.org/10.1093/geront/40.6.687
Hershey DA, Henkens K, Van Dalen HP (2007) Mapping the minds of retirement planners: a cross-cultural perspective. J Cross-Cult Psychol 38(3):361–382. https://doi.org/10.1177/0022022107300280
Hershey DA, Jacobs-Lawson JM, McArdle JJ, Hamagami F (2007b) Psychological foundations of financial planning for retirement. J Adult Dev 14(1–2):26–36. https://doi.org/10.1007/s10804-007-9028-1
Hershey DA, Jacobs-Lawson JM, McArdle JJ, Hamagami F (2008) Psychological foundations of financial planning for retirement. J Adult Dev 14(1–2):26–36. https://doi.org/10.1007/s10804-007-9028-1
Hershfield H, Goldstein D, Sharpe W, Fox J, Yeykelis L, Carstensen L, Bailenson J (2011) Increasing saving behavior through age-progressed renderings of the future self. J Mark Res 48:23–37
Hoffmann AOI, Broekhuizen TLJ (2009) Susceptibility to and impact of interpersonal influence in an investment context. J Acad Mark Sci 37:488–503
Hoffmann AOI, Broekhuizen TLJ (2010) Understanding investors’ decisions to purchase innovative products: drivers of adoption timing and range. Int J Res Mark 27(4):342–355. https://doi.org/10.1016/j.ijresmar.2010.08.002
Hoffmann AOI, Plotkina D (2020a) Positive framing when assessing the personal resources to manage one’s finances increases consumers’ retirement self-efficacy and improves retirement goal clarity. Psychol Mark 38(12):2286–2304. https://doi.org/10.1002/mar.21563
Hoffmann AOI, Plotkina D (2020b) Why and when does financial information affect retirement planning intentions and which consumers are more likely to act on them? Journal of Business Research , 117 (September 2019), 411–431. https://doi.org/10.1016/j.jbusres.2020.06.023
Hoffmann AOI, Plotkina D (2021) Let your past define your future. How recalling successful financial experiences can increase beliefs of self-efficacy in financial planning. J Consum Aff 55(3):847–871. https://doi.org/10.1111/joca.12378
Hoffmann AOI, Risse L (2020) Do good things come in pairs? How personality traits help explain individuals’ simultaneous pursuit of a healthy lifestyle and financially responsible behavior. J Consum Aff 54(3):1082–1120. https://doi.org/10.1111/joca.12317
Hsiao YJ, Tsai WC (2018) Financial literacy and participation in the derivatives markets. J Bank Finance 88:15–29
Huhmann BA, McQuitty S (2009) A model of consumer financial numeracy. Int J Bank Mark 27(4):270–293. https://doi.org/10.1108/02652320910968359
Huston SJ (2010) Measuring financial literacy. J Consum Aff 44(2):296–316. https://doi.org/10.1111/j.1745-6606.2010.01170.x
Ijevleva K, Arefjevs I (2014) Analysis of the Aggregate Financial Behaviour of customers using the Transtheoretical Model of Change. Procedia - Social and Behavioral Sciences 156(April):435–438. https://doi.org/10.1016/j.sbspro.2014.11.217
Ingale KK, Paluri RA (2020) Financial literacy and financial behavior: a bibliometric analysis. Rev Behav Finance. https://doi.org/10.1108/RBF-06-2020-0141
Jacobs-Lawson J, Hershey D (2005) Influence of future time perspective, financial knowledge, and financial risk tolerance on retirement savings behavior. Financial Serv Rev 14:331–344. https://doi.org/10.1088/1751-8113/44/8/085201
Jappelli T, Padula M (2013) Investment in financial literacy and saving decisions. J Bank Finance 37(8):2779–2792. https://doi.org/10.1016/j.jbankfin.2013.03.019
Kadoya Y, Rahim Khan MS (2020) Financial literacy in Japan: new evidence using financial knowledge, behavior, and attitude. Sustain (Switzerland) 12(9). https://doi.org/10.3390/su12093683
Kamil NSSN, Musa R, Sahak SZ (2014) Examining the Role of Financial Intelligence Quotient (FiQ) in explaining credit card usage behavior: a conceptual Framework. Procedia - Social and Behavioral Sciences 130:568–576. https://doi.org/10.1016/j.sbspro.2014.04.066
Kerry MJ (2018) Psychological antecedents of retirement planning: a systematic review. Front Psychol 9(OCT). https://doi.org/10.3389/fpsyg.2018.01870
Kerry MJ, Embretson SE (2018) An experimental evaluation of competing age predictions of future time perspective between workplace and retirement domains. Front Psychol 8(JAN):1–9. https://doi.org/10.3389/fpsyg.2017.02316
Kiliyanni AL, Sivaraman S (2016) The perception-reality gap in financial literacy: evidence from the most literate state in India. Int Rev Econ Educ 23:47–64. https://doi.org/10.1016/j.iree.2016.07.001
Kimiyaghalam F, Mansori S, Safari M, Yap S (2017) Parents’ influence on retirement planning in Malaysia. Family Consumer Sci Res J 45(3):315–325
Klapper L, Lusardi A, Panos GA (2013) Financial literacy and its consequences: evidence from Russia during the financial crisis. J Bank Finance 37(10):3904–3923
Koehler DJ, Langstaff J, Liu WQ (2015) A simulated financial savings task for studying consumption and retirement decision-making. J Econ Psychol 46:89–97. https://doi.org/10.1016/j.joep.2014.12.004
Kramer MM (2016) Financial literacy, confidence, and financial advice seeking. Journal of Economic Behavior and Organization , 131 (June 2015), 198–217. https://doi.org/10.1016/j.jebo.2016.08.016
Kumar S, Tomar S, Verma D (2019) Women’s financial planning for retirement: systematic literature review and future research agenda. Int J Bank Mark 37(1):120–141. https://doi.org/10.1108/IJBM-08-2017-0165
Kwon KN, Lee J (2009) The effects of reference point, knowledge, and risk propensity on the evaluation of financial products. J Bus Res 62(7):719–725. https://doi.org/10.1016/j.jbusres.2008.07.002
Landerretche OM, Martínez C (2013) Voluntary savings, financial behavior, and pension finance literacy: evidence from Chile. J Pension Econ Finance 12(3):251–297. https://doi.org/10.1017/S1474747212000340
Lee T (2017) (David). Clear, conspicuous, and improving: US corporate websites for critical financial literacy in retirement. International Journal of Bank Marketing , 35 (5), 761–780. https://doi.org/10.1108/IJBM-01-2016-0010
Liang C-J, Wang Wen‐Hung, Farquhar JD (2009) (2009). The influence of customer perceptions on financial performance in financial services. International Journal of Bank Marketing , 27 (2), 129–149
Liberman N, Trope Y (2003) Construal level theory of intertemporal judgment and decision. In: Loewenstein G, Read D, Baumeister R (eds) Time and decision: economic and psychological perspectives on intertemporal choice, pp 245–276
Lim KL, Soutar GN, Lee JA (2013) Factors affecting investment intentions: a consumer behaviour perspective. J Financ Serv Mark 18:301–315
Lin C, Hsiao YJ, Yeh CY (2017) Financial literacy, financial advisors, and information sources on demand for life insurance. Pac Basin Finance J 43(March):218–237. https://doi.org/10.1016/j.pacfin.2017.04.002
Lown JM (2011) Development and validation of a Financial Self-Efficacy Scale. J Financial Couns Plann 22(2):54–63
Lusardi A, Mitchell OS (2007) Baby Boomer retirement security: the roles of planning, financial literacy, and housing wealth. J Monet Econ 54(1):205–224. https://doi.org/10.1016/j.jmoneco.2006.12.001
Maloney M, McCarthy A (2017) Understanding pension communications at the organizational level: insights from bounded rationality theory & implications for HRM. Hum Resource Manage Rev 27(2):338–352. https://doi.org/10.1016/j.hrmr.2016.08.001
Marjanovic Z, Fiksenbaum L, Greenglass E (2018) Financial threat correlates with acute economic hardship and behavioral intentions that can improve one’s personal finances and health. J Behav Experimental Econ 77(April):151–157. https://doi.org/10.1016/j.socec.2018.09.012
Marques S, Mariano J, Lima ML, Abrams D (2018) Are you talking to the future me? The moderator role of future self-relevance on the effects of aging salience in retirement savings. J Appl Soc Psychol 48(7):360–368. https://doi.org/10.1111/jasp.12516
McKechnie S (1992) Consumer buying behaviour in financial services: an overview. Int J Bank Mark 10(5):5–39. https://doi.org/10.1108/02652329210016803
Milner T, Rosenstreich D (2013a) A review of consumer decision-making models and development of a new model for financial services. J Financial Serv Mark 18(2):106–120. https://doi.org/10.1057/fsm.2013.7
Milner T, Rosenstreich D (2013b) Insights into mature consumers of financial services. J Consumer Mark 30(3):248–257. https://doi.org/10.1108/07363761311328919
Mitchell OS, Mukherjee A (2017) Assessing the demand for micro pensions among India’s poor. J Econ Ageing 9:30–40. https://doi.org/10.1016/j.jeoa.2016.05.004
Mitchell O, Utkus S (2003) Lessons from Behavioral Finance for Retirement Plan Design (PRC WP 2003-6). http://prc.wharton.upenn.edu/prc/prc.html
Modigliani F, Brumberg RH (1954) Utility analysis and the consumption function: an interpretation of cross-section data. In: Kurihara KK (ed) Post-Keynesian economics. Rutgers University Press, New Brunswick, pp 388–436
Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, Atkins D, Barbour V, Barrowman N, Berlin JA, Clark J, Clarke M, Cook D, D’Amico R, Deeks JJ, Devereaux PJ, Dickersin K, Egger M, Ernst E, …, Tugwell P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7). https://doi.org/10.1371/journal.pmed.1000097
Monti M, Pelligra V, Martignon L, Berg N (2014) Retail investors and financial advisors: new evidence on trust and advice taking heuristics. J Bus Res 67(8):1749–1757. https://doi.org/10.1016/j.jbusres.2014.02.022
Mouna A, Anis J (2017) Financial literacy in Tunisia: its determinants and its implications on investment behavior. Res Int Bus Finance 39:568–577
Mullainathan S, Thaler R (2000) Massachusetts Institute of Technology Department of Economics Working Paper Series . September
Nga KH, Yeoh KK (2018) An exploratory model on retirement savings behaviour: a Malaysian study. Int J Bus Soc 19(3):637–659
OECD (2023) Old-age dependency ratio (indicator). https://doi.org/10.1787/e0255c98-en . Accessed 13 Oct 2023
Onwuegbuzie AJ, Collins KM (2007) A typology of mixed methods sampling designs in social science research. Qualitative Rep 12(2):474–498
Pallister JG, Wang HC, Foxall GR (2007) An application of the style/involvement model to financial services. Technovation 27(1–2):78–88. https://doi.org/10.1016/j.technovation.2005.10.001
Pan L, Pezzuti T, Lu W, Pechmann C (2019) Hyperopia and frugality: different motivational drivers and yet similar effects on consumer spending. J Bus Res 95(August 2018):347–356
Parise G, Peijnenburg K (2017) Understanding the Determinants of Financial Outcomes and Choices: The Role of Noncognitive Abilities. BIS Working Papers
Paul J, Rosado-Serrano A (2019) Gradual internationalization vs Born-Global/International new venture models: a review and research agenda. Int Mark Rev 36(6):830–858. https://doi.org/10.1108/IMR-10-2018-0280
Paul J, Criado AR (2020) The art of writing literature review: what do we know and what do we need to know? Int Bus Rev 29(4):101717. https://doi.org/10.1016/j.ibusrev.2020.101717
Paul J, Khatri P, Kaur Duggal H (2023) Frameworks for developing impactful systematic literature reviews and theory building: what, why and how? J Decis Syst 00(00):1–14. https://doi.org/10.1080/12460125.2023.2197700
Petkoska J, Earl JK (2009) Understanding the influence of demographic and psychological variables on Retirement Planning. Psychol Aging 24(1):245–251. https://doi.org/10.1037/a0014096
Piotrowska M (2019) The importance of personality characteristics and behavioral constraints for retirement saving. Econ Anal Policy 64:194–220
Plath DA, Stevenson TH (2005) Financial services consumption behavior across Hispanic American consumers. J Bus Res 58(8):1089–1099. https://doi.org/10.1016/j.jbusres.2004.03.003
Poterba JM (2015) Saver heterogeneity and the challenge of assessing retirement saving adequacy. Natl Tax J 68(2):377–388. https://doi.org/10.17310/ntj.2015.2.06
Potrich ACG, Vieira KM, Kirch G (2018) How well do women do when it comes to financial literacy? Proposition of an indicator and analysis of gender differences. J Behav Experimental Finance 17:28–41. https://doi.org/10.1016/j.jbef.2017.12.005
Rai D, Lin CW (2019) (Wilson). The influence of implicit self-theories on consumer financial decision making. Journal of Business Research , 95 (August 2018), 316–325. https://doi.org/10.1016/j.jbusres.2018.08.016
Ramalho TB, Forte D (2019) Financial literacy in Brazil – do knowledge and self-confidence relate with behavior? RAUSP Manage J 54(1):77–95. https://doi.org/10.1108/RAUSP-04-2018-0008
Rana J, Paul J (2017) Consumer behavior and purchase intention for organic food: a review and research agenda. J Retailing Consumer Serv 38(June):157–165. https://doi.org/10.1016/j.jretconser.2017.06.004
Ranyard R, McNair S, Nicolini G, Duxbury D (2020) An item response theory approach to constructing and evaluating brief and in-depth financial literacy scales. J Consum Aff 54(3):1121–1156. https://doi.org/10.1111/joca.12322
RBI Household Finance Committee (2017) Indian household finance. Reserve Bank of India, Mumbai
Ruefenacht M, Schlager T, Maas P, Puustinen P (2015) Drivers of long-term savings behavior from consumer’s perspective. Electron Libr 34(1):1–5
Scholz JK, Seshadri A, Khitatrakun S (2006) Are Americans saving “optimally” for retirement? J Polit Econ 114(4):607–643
Schuabb T, França LH, Amorim SM (2019) Retirement savings model tested with Brazilian private health care workers. Front Psychol 10(JULY):1–11. https://doi.org/10.3389/fpsyg.2019.01701
Schuhen M, Schurkmann S (2014) International Review of Economics Education. Int Rev Econ Educ 16:1–11
Segel-Karpas D, Werner P (2014) Perceived financial retirement preparedness and its correlates: a national study in Israel. Int J Aging Hum Dev 79(4):279–301. https://doi.org/10.1177/0091415015574177
Seth H, Talwar S, Bhatia A, Saxena A, Dhir A (2020) Consumer resistance and inertia of retail investors: Development of the resistance adoption inertia continuance (RAIC) framework. Journal of Retailing and Consumer Services , 55 (August 2019), 102071. https://doi.org/10.1016/j.jretconser.2020.102071
Sewell M (2008) Behavioural finance. Economist 389(8604):1–13. https://doi.org/10.1057/9780230280786_5
Shefrin HM, Thaler RH (1988) The behavioral life‐cycle hypothesis. Econ Inq 26(4):609–643
Shim S, Serido J, Tang C (2012) The ant and the grasshopper revisited: the present psychological benefits of saving and future oriented financial behavior. J Econ Psychol 33(1):155–165
Simon HA (1978) Information-processing theory of human problem solving. In: Handbook of learning and cognitive processes, vol 5, pp 271–295
Sivaramakrishnan S, Srivastava M, Rastogi A (2017) Attitudinal factors, financial literacy, and stock market participation. Int J Bank Mark 34(1):1–5
Snyder H (2019) Literature review as a research methodology: an overview and guidelines. J Bus Res 104(August):333–339. https://doi.org/10.1016/j.jbusres.2019.07.039
Stawski RS, Hershey DA, Jacobs-Lawson JM (2007) Goal clarity and financial planning activities as determinants of retirement savings contributions. Int J Aging Hum Dev 64(1):13–32. https://doi.org/10.2190/13GK-5H72-H324-16P2
Steinert JI, Zenker J, Filipiak U, Movsisyan A, Cluver LD, Shenderovich Y (2018) Do saving promotion interventions increase household savings, consumption, and investments in Sub-saharan Africa? A systematic review and meta-analysis. World Dev 104:238–256. https://doi.org/10.1016/j.worlddev.2017.11.018
Steinhart Y, Mazursky D (2010) Purchase availability and involvement antecedents among financial products. Int J Bank Mark 28(2):113–135. https://doi.org/10.1108/02652321011018314
Strömbäck C, Lind T, Skagerlund K, Västfjäll D, Tinghög G (2017) Does self-control predict financial behavior and financial well-being? J Behav Experimental Finance 14:30–38. https://doi.org/10.1016/j.jbef.2017.04.002
Strömbäck C, Skagerlund K, Västfjäll D, Tinghög G (2020) Subjective self-control but not objective measures of executive functions predict financial behavior and well-being. Journal of Behavioral and Experimental Finance , 27 . https://doi.org/10.1016/j.jbef.2020.100339
Tam L, Dholakia U (2014) Saving in cycles: how to get people to save more money. Psychol Sci 25(2):531–537. https://doi.org/10.1177/0956797613512129
Tang N, Baker A (2016) Self-esteem, financial knowledge and financial behavior. J Econ Psychol 54:164–176
Tate M, Evermann J, Gable G (2015) An integrated framework for theories of individual attitudes toward technology. Inform Manage 52(6):710–727. https://doi.org/10.1016/j.im.2015.06.005
Taylor MP, Jenkins SP, Sacker A (2011) Financial capability and psychological health. J Econ Psychol 32(5):710–723. https://doi.org/10.1016/j.joep.2011.05.006
Tennyson S, Yang HK (2014) The role of life experience in long-term care insurance decisions. Journal of Economic Psychology , 42 (2014), 175–188. https://doi.org/10.1016/j.joep.2014.04.002
Thaler BRH (1994) Psychology and savings policies. Am Econ Rev 84(2):175–179. http://www.jstor.org/stable/3132220
Thaler R (1980) Toward a positive theory of consumer choice. J Econ Behav Organ 1:39–60
Thaler RH (2005) Advances in behavioral finance. Adv Behav Finance 2:1–694. https://doi.org/10.2307/2329257
Thaler R, Shefrin H (1981) An economic theory of self-control. J Polit Econ 89(2):392–406
Tomar S, Kent Baker H, Kumar S, Hoffmann AOI (2021) Psychological determinants of retirement financial planning behavior. Journal of Business Research , 133 (November 2020), 432–449. https://doi.org/10.1016/j.jbusres.2021.05.007
Topa G, Moriano JA, Depolo M, Alcover CM, Morales JF (2009) Antecedents and consequences of retirement planning and decision-making: a meta-analysis and model. J Vocat Behav 75(1):38–55. https://doi.org/10.1016/j.jvb.2009.03.002
Topa G, Moriano JA, Depolo M, Alcover CM, Moreno A (2011) Retirement and wealth relationships: Meta-analysis and SEM. Res Aging 33(5):501–528. https://doi.org/10.1177/0164027511410549
Tranfield D, Denyer D, Smart P (2003) Towards a methodology for developing evidence-informed management knowledge by means of systematic review. Br J Manag 14(3):207–222. https://doi.org/10.1111/1467-8551.00375
Ülkümen G, Cheema A (2011) Framing goals to influence personal savings: the role of specificity and construal level. J Mark Res 48(6):958–969. https://doi.org/10.1509/jmr.09.0516
United Nations, Department of Economic and Social, Affairs PD (2020) (2019). World Population Ageing 2019. In United Nations . http://link.springer.com/chapter/10.1007/ 978-94-007-5204-7_6
Utkarsh, Pandey A, Ashta A, Spiegelman E, Sutan A (2020) Catch them young: impact of financial Socialization, financial literacy and attitude towards money on the financial well-being of young adults. Int J Consumer Stud 44(6):531–541. https://doi.org/10.1111/ijcs.12583
Valente TW, Paredes P, Poppe P (1998) Matching the message to the process: the relative ordering of knowledge, attitudes, and practices in behavior change research. Hum Commun Res 24(3):366–385
Van Rooij M, Teppa F (2014) Personal traits and individual choices: taking action in economic and non-economic decisions. J Econ Behav Organ 100:33–43
van Rooij M, Lusardi A, Alessie R (2011) Financial literacy and stock market participation. J Financ Econ 101(2):449–472. https://doi.org/10.1016/j.jfineco.2011.03.006
Van Rooij MCJ, Lusardi A, Alessie RJM (2011a) Financial literacy and retirement planning in the Netherlands. J Econ Psychol 32(4):593–608. https://doi.org/10.1016/j.joep.2011.02.004
van Schie RJG, Dellaert BGC, Donkers B (2015) Promoting later planned retirement: construal level intervention impact reverses with age. J Econ Psychol 50:124–131. https://doi.org/10.1016/j.joep.2015.06.010
Venkatesh V, Morris M, Davis G, Davis F (2003) Factors influencing the Use of M-Banking by academics: Case Study sms-based M-Banking. MIS Q 27(3):425–478
Vitt LA (2004) Consumers’ financial decisions and the psychology of values. J Financial Service Professionals 58(November):68–77. http://search.ebscohost.com/login.aspx?direct=true &db=bth&AN=14888952&site=ehost-live
Wang L, Lu W, Malhotra NK (2011) Demographics, attitude, personality, and credit card features correlate with credit card debt: a view from China. J Econ Psychol 32(1):179–193. https://doi.org/10.1016/j.joep.2010.11.006
World Economic Forum (2019) Investing in (and for) our future. Issue June. www.weforum.org
Xia T, Wang Z, Li K (2014) Financial literacy overconfidence and stock market participation. Soc Indic Res 119(3):1233–1245. https://doi.org/10.1007/s11205-013-0555-9
Xiao JJ, Chen C, Chen F (2014) Consumer financial capability and financial satisfaction. Soc Indic Res 118(1):415–432. https://doi.org/10.1007/s11205-013-0414-8
Yeung DY, Zhou X (2017) Planning for retirement: longitudinal effect on retirement resources and post-retirement well-being. Front Psychol 8:1300
Zhou R, Pham MT (2004) Promotion and prevention across mental accounts: when financial products dictate consumers’ investment goals. J Consum Res 31(1):125–135. https://doi.org/10.1086/383429
Download references
Acknowledgements
Authors would like to acknowledge the academicians and researchers who guided the search of the article and would like to thank the experts for the valuable inputs to refine the work.
There is no funding received for this research.
Author information
Authors and affiliations.
Symbiosis International (Deemed University), Pune, India
Kavita Karan Ingale
Symbiosis Institute of Operations Management, Symbiosis International (Deemed) University, Pune, India
Ratna Achuta Paluri
You can also search for this author in PubMed Google Scholar
Contributions
Both authors contributed to the conceptualization, research design, methodology, analysis of the data,writing of the manuscript and its revision.
Corresponding author
Correspondence to Kavita Karan Ingale .
Ethics declarations
Conflict of interest.
The authors declare that there is no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Ingale, K.K., Paluri, R.A. Retirement planning – a systematic review of literature and future research directions. Manag Rev Q (2023). https://doi.org/10.1007/s11301-023-00377-x
Download citation
Received : 14 December 2022
Accepted : 04 October 2023
Published : 28 October 2023
DOI : https://doi.org/10.1007/s11301-023-00377-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Retirement planning
- Systematic literature review
- Financial behavior
- Household finance
- Long-term savings
- Pension plan
- Financial literacy
- TCCM framework
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
This review aims to synthesize a published set of evaluative criteria for good qualitative research. The aim is to shed light on existing standards for assessing the rigor of qualitative research encompassing a range of epistemological and ontological standpoints. Using a systematic search strategy, published journal articles that deliberate criteria for rigorous research were identified. Then ...
While many books and articles guide various qualitative research methods and analyses, there is currently no concise resource that explains and differentiates among the most common qualitative approaches. We believe novice qualitative researchers, students planning the design of a qualitative study or taking an introductory qualitative research course, and faculty teaching such courses can ...
A qualitative systematic review brings together research on a topic, systematically searching for research evidence from primary qualitative studies and drawing the findings together. There is a debate over whether the search needs to be exhaustive. 1 , 2 Methods for systematic reviews of quantitative research are well established and explicit ...
Abstract. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions ...
Current methodological issues in qualitative case study research. The future of qualitative research will be influenced and constructed by the way research is conducted, and by what is reviewed and published in academic journals (Morse, Citation 2011).If case study research is to further develop as a principal qualitative methodological approach, and make a valued contribution to the field of ...
quality of qualitative research in different epistemological and ontological perspectives. This review is also intended to provide guidelines for the acceleration of future devel-opments and dialogues among qualitative researchers in the context of assessing the qualitative research. The rest of this review article is structured in the fol-
Qualitative research is a type of research that explores and provides deeper insights into real-world problems.[1] Instead of collecting numerical data points or intervene or introduce treatments just like in quantitative research, qualitative research helps generate hypotheses as well as further investigate and understand quantitative data. Qualitative research gathers participants ...
Qualitative Research is a peer-reviewed international journal that has been leading debates about qualitative methods for over 20 years. The journal provides a forum for the discussion and development of qualitative methods across disciplines, publishing high quality articles that contribute to the ways in which we think about and practice the craft of qualitative research.
Review. is multidisciplinary, we encourage authors to consult the debates and articles on qualitative research standards and transparency discussed in their own disciplinary associations and journals. Ethics . Papers should report if they received ethical approval from an Institutional Review Board (or similar body). We note that transparency ...
The first review (Culver et al., Citation 2003) examined the publication of qualitative research across three sport psychology journals from 1990 to 1999 and found that 17.3% of all published articles were qualitative studies.
A good qualitative researcher recognizes that the way they make sense of and attach meaning to the data is partly shaped by the characteristics of the researcher (i.e. age, gender, social class, ethnicity, professional status, etc.) and the assumptions they hold. The researcher should make explicit the perspectives they are coming from so that ...
Systematic reviews have become an important component of evidence-based health care. To date, these reviews have focused predominantly on randomized controlled trials to determine the effectiveness of treatments. However, there is a growing interest in reviews of qualitative research to summarize research addressing a phenomenon of interest or ...
Qualitative research relies on nuanced judgements that require researcher reflexivity, yet reflexivity is often addressed superficially or overlooked completely during the research process. In this AMEE Guide, we define reflexivity as a set of continuous, collaborative, and multifaceted practices through which researchers self-consciously ...
As mentioned previously, there are a number of existing guidelines for literature reviews. Depending on the methodology needed to achieve the purpose of the review, all types can be helpful and appropriate to reach a specific goal (for examples, please see Table 1).These approaches can be qualitative, quantitative, or have a mixed design depending on the phase of the review.
Those doing qualitative research cannot "opt out" of knowing their relevant scholarly conversations. Undertaking a qualitative systematic review provides a vital means to know and tune into the past conversation in your topic area that allows the researcher to position themselves and their work substantively, ontologically, theoretically, and methodologically in this landscape.
Useful terms. Some of the qualitative approaches used in nursing research include grounded theory, phenomenology, ethnography, case study (can lend itself to mixed methods) and narrative analysis. The data collection methods used in qualitative research include in depth interviews, focus groups, observations and stories in the form of diaries ...
Qualitative research involves the studied use and collection of a variety of empirical materials - case study, personal experience, introspective, life story, interview, observational, historical, interactional, and visual texts - that describe routine and problematic moments and meanings in individuals' lives.
Look at what results have emerged in qualitative versus quantitative research; Discuss how the topic has been approached by empirical versus theoretical scholarship; Divide the literature into sociological, historical, and cultural sources; Theoretical. A literature review is often the foundation for a theoretical framework. You can use it to ...
American Journal of Qualitative Research (AJQR) is a quarterly peer-reviewed academic journal that publishes qualitative research articles from a number of social science disciplines such as psychology, health science, sociology, criminology, education, political science, and administrative studies.The journal is an international and interdisciplinary focus and greatly welcomes papers from all ...
Thus, to capture a snapshot of the current state of qualitative research and qualitative data analysis practices in HRD, we conducted a review of Human Resource Development Quarterly (HRDQ) between 1990 and the current issue (Volume 33, Issue 3) in 2019 and identified 59 qualitative articles. The types of qualitative research included: 24 case ...
Ensuring access to healthcare is a complex, multi-dimensional health challenge. Since the inception of the coronavirus pandemic, this challenge is more pressing. Some dimensions of access are difficult to quantify, namely characteristics that influence healthcare services to be both acceptable and appropriate. These link to a patient's acceptance of services that they are to receive and ...
For example, of 232 research articles published in JPP from 2012 to 2014 (excluding commentaries and reviews), only five used qualitative methods (2% of articles). The goal of the current article is to present considerations for writing and evaluating qualitative research within the context of pediatric psychology to provide a framework for ...
This qualitative evidence synthesis was commissioned in parallel to several systematic reviews of evidence of benefits and harms of prioritized interventions for the Guideline, synthesized from randomized controlled trials (RCTs) [26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44]. These interventions were broad in scope, intensity and ...
Responses with thick narrative descriptions were retained for analysis. Incomplete or partial responses were included in the qualitative analysis. Themes were then synthesized, refined, and were validated and triangulated by research team members (GA, AZ, MP, FM, RA). The demographic data was analyzed using descriptive analysis.
Writing a literature review requires a range of skills to gather, sort, evaluate and summarise peer-reviewed published data into a relevant and informative unbiased narrative. Digital access to research papers, academic texts, review articles, reference databases and public data sets are all sources of information that are available to enrich ...
Rising life expectancy and an aging population across nations are leading to an increased need for long-term financial savings and a focus on the financial well-being of retired individuals amidst changing policy framework. This study is a systematic review based on a scientific way of producing high-quality evidence based on 191 articles from the Scopus and Web of Science databases. It adopts ...
Narrative reviews have many strengths. They are flexible and practical, and ideally provide a readable, relevant synthesis of a diverse literature. Narrative reviews are often helpful for teaching or learning about a topic because they deliver a general overview. They are also useful for setting the stage for future research, as they offer an ...
In this review, only articles using this latter approach are included. Both empirical and non-empirical articles were included as long as fictional narratives were used in a substantive way. ... Initial analysis also demonstrates that the use of fiction in research articles continues to increase . The ... Qualitative Research in Psychology, 3(2 ...