- TheFreeDictionary
- Word / Article
- Starts with
- Free toolbar & extensions
- Word of the Day
- Free content
- presentation

pre·sen·ta·tion
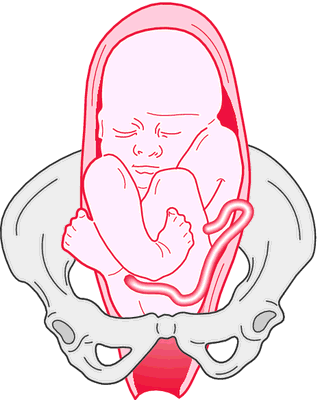
- breech presentation
- brow presentation
cephalic presentation
Compound presentation, face presentation, footling presentation, funic presentation, longitudinal presentation, oblique presentation, pelvic presentation, placental presentation, shoulder presentation, transverse presentation, vertex presentation, patient discussion about presentation.
Q. What are the presenting signs of ALS? Are the upper or lower extremeties affected initialilly? A. The most common presenting sign of ALS is asymmetric limb weakness, usually starting with the hands (problems with pinching, writing, holding things etc.) shoulders (lifting arms above head etc.) or legs (problems walking). Other presenting signs may be problems with speaking or swallowing, although these are less common. You may read more here: www.nlm.nih.gov/medlineplus/amyotrophiclateralsclerosis.html
Q. Iam a bipolar and presently on tegretol medication.I found this to be the best way to get my doubt clarified. I am a bipolar and presently on tegretol medication. My doctor frequently changes the meds and he has tried variety of medicines before prescribing tegretol. He changes the meds every time when I visit him for routine check-up. I am bit confused and obviously cannot question my doctor as I repose faith and confidence in him. I found this to be the best way to get my doubt clarified. A. Are you being treated by your GP? I would suggest if you are having trouble finding the right combinations it might be a good time to ask to be referred to a Psychaitrist. GP's will do their best but like anything specialized they only have a certain amount of knowledge and a specialist in the field could be more help. I also think that other treatments along with The medications like theropy and group theropy, excercise, good diet, plenty of sleep etc helps a lot too... Try to be patient it is a process to get everything in place that will work the best for you... everyone is different and the .mmedications and treatments that work for one may not work for another...
- 21-hydroxylase deficiency
- abnormal presentation
- anterior presentation
- antigen presentation
- asynclitism
- atypical GERD
- bacterial meningitis
- Baudelocque method
- Baudelocque, Jean-Louis
- bimanual version
- bipolar version
- cardinal points
- case report
- prescribing
- prescribing cascade
- prescribing error
- prescribing information
- prescribing nurse
- prescription
- prescription abandonment
- prescription drug
- prescription exemption certificate
- Prescription Medicines Code of Practice Authority
- prescription monitoring program
- prescription only medicine
- Prescription Pre-payment Certificate
- Prescription Pricing Authority
- Prescription Pricing Division
- prescriptive authority
- presence of mind
- presenile dementia
- presenile spontaneous gangrene
- presenilin gene
- presenility
- presentative
- presenteeism
- presenting part
- presenting symptom
- preseptal cellulitis
- preservation
- preservative
- presinusoidal
- presomite embryo
- presphenoid
- presphenoid bone
- presphygmic
- presphygmic interval
- presphygmic period
- presplenic fold
- prespondylolisthesis
- pressed juice
- pressor base
- pressor fiber
- Present Worth
- Present Worth of Capital Expenditures
- present you as
- present you with
- present yourself
- Present, The
- present-day
- Present-Day English
- Present-Minded Individualism
- present-worth factor
- presentability
- presentable
- presentablely
- presentableness
- presentably
- Presentance Report
- Presentaneous
- Presentasi Pemikiran Kritis Mahasiswa
- Presentation Accept
- Presentation and Personalization Management
- Presentation Brothers College, Cork
- Presentation client
- Presentation Connect
- Presentation Connection Endpoint
- Presentation Connection Endpoint Identifier
- Presentation Context Definition List
- Presentation Context Identifier
- Presentation Controller Mediator Entity Foundation
- Presentation Convent Kodaikanal
- Presentation copy
- Presentation Data Value
- Presentation Department
- Presentation Departments
- Présentation des Normes Européennes
- presentation drawing
- Presentation du Systeme de Planification et de Gestion de Frequence
- Presentation Element Parser, YACC
- Presentation Environment for Multimedia Objects
- Presentation File
- Presentation Function
- Présentation Générale Lex Persona
- presentation graphics
- presentation graphics program
- Facebook Share
Presentation Skills Toolkit for Medical Students
New section.
The ability to design and deliver an effective presentation is an important skill for all learners to develop. The Undergraduate Medical Education Section of the Group on Educational Affairs developed this toolkit as a resource for medical students and health professions trainees as you learn to create and give effective presentations in the classroom, in the clinical setting, and at academic meetings and conferences. In this toolkit, you’ll find helpful resources on developing and delivering formal lectures and presentations, poster and oral abstract presentations, patient presentations, and leading small group sessions.
Please note: Availability of resources may change over time. To suggest edits or updates, email [email protected] .
On this page:
Formal lectures and presentations, posters and abstracts, patient presentations.
- Leading Small Groups
Traditional academic presentations in medicine and the biomedical sciences are necessarily dense with complex content. Thus, slides tend to be wordy, and presenters may use their slides as cue cards for themselves rather than as tools to facilitate learning for their audience. With the necessary resources, medical students (and presenters at all levels) can better identify appropriate learning objectives and develop presentations that help learners meet those objectives. Organization of content, clarity of slide design, and professional delivery are all essential components to designing and giving effective formal presentations.
Achieving all of these elements can make creating and delivering a formal presentation challenging. The strategies and resources below can help you develop a successful formal presentation.

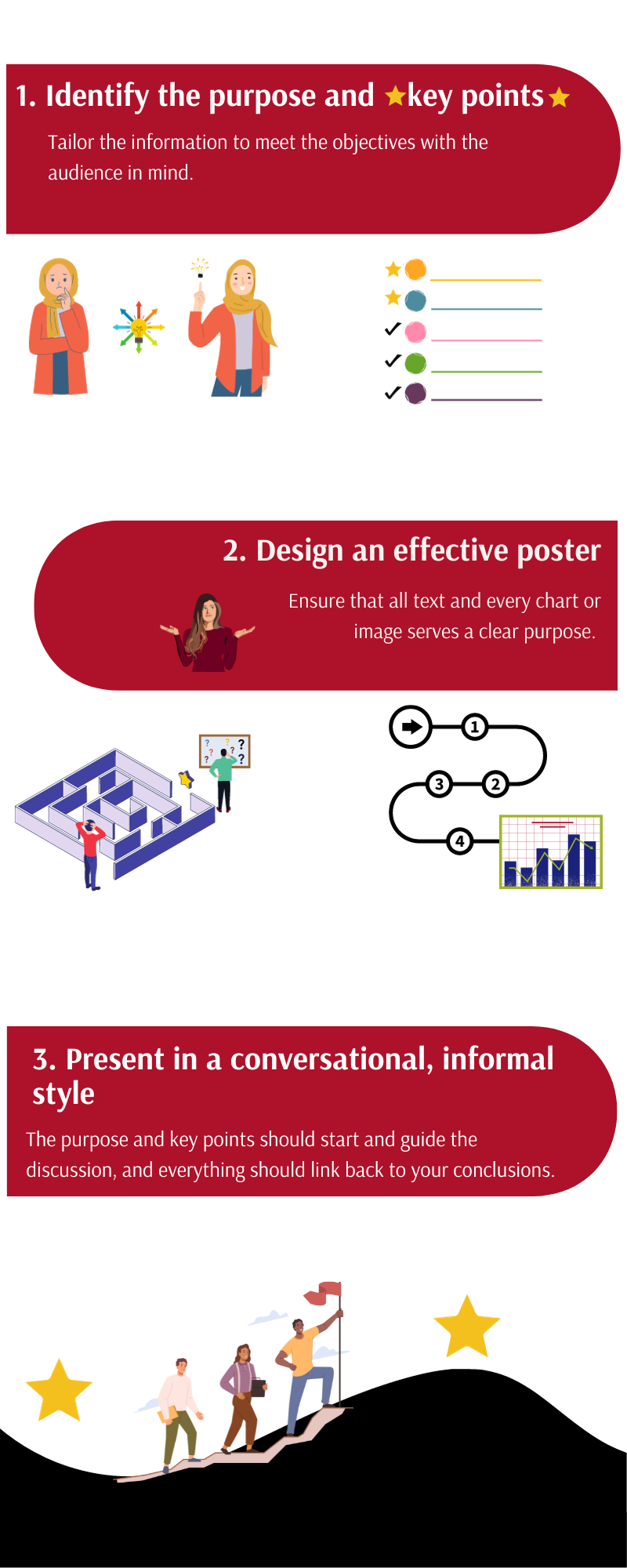
View long description of infographic .
Strategies for success
- Define the objectives of the presentation. Always define learning objectives for each of your lectures to make it clear what knowledge or skills the audience should acquire from your presentation. The best learning objectives define specific, measurable, or observable knowledge or skill gains. Furthermore, consider how to communicate the importance of the topic to your audience and how information should be arranged to best communicate your key points.
- Design an effective slide set. You should begin creating your slides only after defining your objectives and key points. The slides should support your talk but not be your talk. Keep slides simple. The audience should be able to review a slide and grasp key points quickly. Avoid lengthy text and distracting decorative fonts, clip art, graphs, and pictures. If additional wording or images are necessary, consider handouts or alternative methods of sharing this information. Lastly, design your slide deck to emphasize the key points, revisiting your outline as necessary, and summarize concepts at regular intervals throughout your presentation to strengthen knowledge gains.
- Practice your performance. Effective public speaking starts with preparation and practice. Ensure there is enough time to create your lecture and a supporting slide deck. Know your lecture material and slides without prompts! Understand the audience and learning climate (the size and knowledge level of your audience) and be prepared for the venue (virtual, in-person, or both, lecture hall or classroom). Think about what effective audience engagement may look like and how to incorporate audience response systems, polling, etc., into the lecture.
- Create a positive learning environment. Anticipate questions and allocate sufficient time to answer them. Always repeat the questions being asked for the audience’s benefit and to ensure your understanding. Some questions may be challenging, so be prepared and answer honestly. It is acceptable not to know an answer.
- Demonstrate professionalism in presenting. Exhibit professionalism by being punctual and having appropriate time management. Remember that mistakes happen; be kind to yourself and remain calm and collected. Be enthusiastic: If you can enjoy the experience, so will your audience. Finally, be open to feedback following your presentation.
Additional resources
Below is a collection of resources that further address the elements of creating and delivering a formal presentation. Each resource addresses a specific presentation skill or set of skills listed above and can be used to develop your understanding further.
- Healthy Presentations: How to Craft Exceptional Lectures in Medicine, the Health Professions, and the Biomedical Sciences (requires purchase, book). This illustrated book is a practical guide for improving scientific presentations. It includes specific, practical guidance on crafting a talk, tips on incorporating interactive elements to facilitate active learning, and before-and-after examples of improved slide design. (Skills addressed: 1-3)
- American College of Physicians: Giving the Podium Presentation (freely available, website). This guide includes recommendations related to presentation delivery, including tips on what to wear, how to prepare, answering questions, and anticipating the unexpected. (Skills addressed: 3-5)
- The 4 Ps of Giving a Good Presentation (freely available, PDF). This simple guide on public speaking from the University of Hull covers such topics as positive thinking, preparing, practice, and performing. (Skills addressed: 3-5)
- Zoom Guides (freely available, website). This website from the University of California, San Francisco is one of many great resources created by universities for presenting on a virtual platform, specifically Zoom. (Skills addressed: 3-5)
- Writing Learning Objectives (freely available, PDF). This excellent resource from the AAMC defines Bloom’s Taxonomy and provides verbiage for creating learning objectives. (Skill addressed: 1)
- Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83 (freely available, article). This AMEE Guide explains and explores the more commonly used adult learning theories and how they can be used to enhance learning. It presents a model that combines many of the theories into a flow diagram that can be followed by those planning a presentation. (Skill addressed: 1)
- Assertion-Evidence Approach (freely available, website). This approach to slide design incorporates clear messaging and the strategic combination of text and images. (Skill addressed: 2)
- Multimedia Learning (requires purchase, book). This book outlines the learning theories that should guide all good slide design. It is an accessible resource that will help presenters of all levels create slide decks that best facilitate learning. (Skill addressed: 2)
- Collaborative Learning and Integrated Mentoring in the Biosciences (CLIMB) (freely available, website). This website from Northwestern University shares slide design tips for scientific presentations. Specific tips include simplifying messages and annotating images and tables to facilitate learning. (Skill addressed: 2)
- Clear and to the Point (freely available, online book). This book describes 8 psychological principles for constructing compelling PowerPoint presentations. (Skill addressed: 2)
Return to top ↑
Presenting the results of the research projects, innovations, and other work you have invested in at regional and national meetings is a tremendous opportunity to advance heath care, gain exposure to thought leaders in your field, and put your evidence-based medicine and communication skills into practice in a different arena. Effective scientific presentations at meetings also provide a chance for you to interact with an engaged audience, receive valuable feedback, be exposed to others’ projects, and expand your professional network. Preparation and practice are integral to getting the most out of these experiences.
The strategies and resources below will help you successfully present both posters and abstracts at scientific meetings.
Strategies for success
- Identify a poster’s/abstract’s purpose and key points . Determine the purpose of sharing your work (feedback vs. sharing a new methodology vs. disseminating a novel finding) and tailor the information in your poster or abstract to meet that objective. Identify one to three key points. Keep in mind the knowledge and expertise of the intended audience; the amount of detail that you need to provide at a general vs. specialized meeting may vary.
- Design an effective poster . Design your poster to follow a logical flow and keep it uncluttered. The methods and data should support your conclusions without extraneous information; every chart or image should serve a purpose. Explicitly outline the key takeaways at the beginning or end.
- Present in a conversational, informal style . Imagine you are explaining your project to a colleague. The purpose of your work and key points should guide your presentation, and your explanation of the methods and data should link to your conclusions. Be prepared to discuss the limitations of your project, outline directions for future research, and receive feedback from your audience. Treat feedback as an opportunity to improve your project prior to producing a manuscript.
Additional resources
These resources support the development of the skills mentioned above, guiding you through the steps of developing a poster that frames your research in a clear and concise manner. The videos provide examples that can serve as models of effective poster and abstract presentations.
- How to design an outstanding poster (freely available, article). This article outlines key items for laying out an effective poster, structuring it with the audience in mind, practicing your presentation, and maximizing your work’s impact at meetings. (Skills addressed: 1-3)
- Giving an Effective Poster Presentation (freely available, video). This video shows medical students in action presenting their work and shares strategies for presenting your poster in a conversational style, preparing for questions, and engaging viewers. (Skills addressed: 2,3)
- Better Scientific Poster (freely available, toolkit). This toolkit includes strategies and templates for creating an effective and visually interesting scientific poster. Virtual and social media templates are also available. (Skill addressed: 2)
As with all presentations, it can be very helpful to practice with colleagues and/or mentors before the meeting. This will allow you to get feedback on your project, style, and poster design prior to sharing it with others outside of your institution. It can also help you prepare for the questions you may get from the audience.
Patient presentation skills are valuable for medical students in the classroom and in the care of patients during clinical rotations. Patient presentations are an integral part of medical training because they combine communication skills with knowledge of disease manifestations and therapeutic strategies in a clinical scenario. They are used during active learning in both the preclinical and clinical phases of education and as students advance in training and interact with diverse patients.
Below are strategies for delivering effective patient presentations.

- Structure the presentation appropriately . The structure of your narrative is important; a concise, logical presentation of the relevant information will create the most impact. In the clinical setting, preferences for presentation length and style can vary between specialties and attendings, so understanding expectations is vital.
- Synthesize information from the patient encounter . Synthesis of information is integral for effective and accurate delivery that highlights relevant points. Being able to select pertinent information and present it in an efficient manner takes organization and practice, but it is a skill that can be learned.
- Deliver an accurate, engaging, and fluent oral presentation . In delivering a patient presentation, time is of the essence. The overall format for the presentation is like a written note but usually more concise. Succinctly convey the most essential patient information in a way that tells the patient’s story. Engage your listeners by delivering your presentation in an organized, clear, and professional manner with good eye contact. Presentations will go more smoothly with careful crafting and practice.
- Adjust presentations to meet team, patient, and setting needs . Adaptability is often required in the clinical setting depending on attending preferences, patient needs, and location, making it imperative that you are mindful of your audience.
The resources below provide samples of different types of patient presentations and practical guides for structuring and delivering them. They include tips and tricks for framing a case discussion to deliver a compelling story. Resources that help with adjusting patient presentations based on the setting, such as bedside and outpatient presentations, are also included.
- A Guide to Case Presentations (freely available, document). This practical guide from the Ohio State University discusses basic principles of presentations, differences between written and oral communication of patient information, organization, and common pitfalls to avoid. (Skills addressed: 1-3)
- Verbal Case Presentations: A Practical Guide for Medical Students (freely available, PDFs). This resource from the Augusta University/University of Georgia Medical Partnership provides a practical guide to crafting effective case presentations with an explanation of the goals of each section and additional tips for framing the oral discussion. It also provides a full sample initial history and physical examination presentation. (Skills addressed: 1-4)
- Patient Presentations in Emergency Medicine (freely available, video). This training video for medical students from the Society for Academic Emergency Medicine demonstrates how to tell a compelling story when presenting a patient’s case. The brief video offers handy dos and don'ts that will help medical students understand how best to communicate in the emergency department efficiently and effectively. These skills can also be applied to patient presentations in other specialties. (Skills addressed: 1-4)
Additional information and support on effectively constructing and delivering a case presentation can be found through various affinity support and mentorship groups, such as the Student National Medical Association (SNMA), Latino Medical Student Association (LMSA), and Building the Next Generation of Academic Physicians (BNGAP).
Leading Small Groups
For physicians, working within and leading small groups is an everyday practice. Undergraduate medical education often includes small group communication as well, in the form of problem-based learning groups, journal clubs, and study groups. Having the skills to form, maintain, and help small groups thrive is an important tool for medical students.
Below are strategies to provide effective small group leadership.
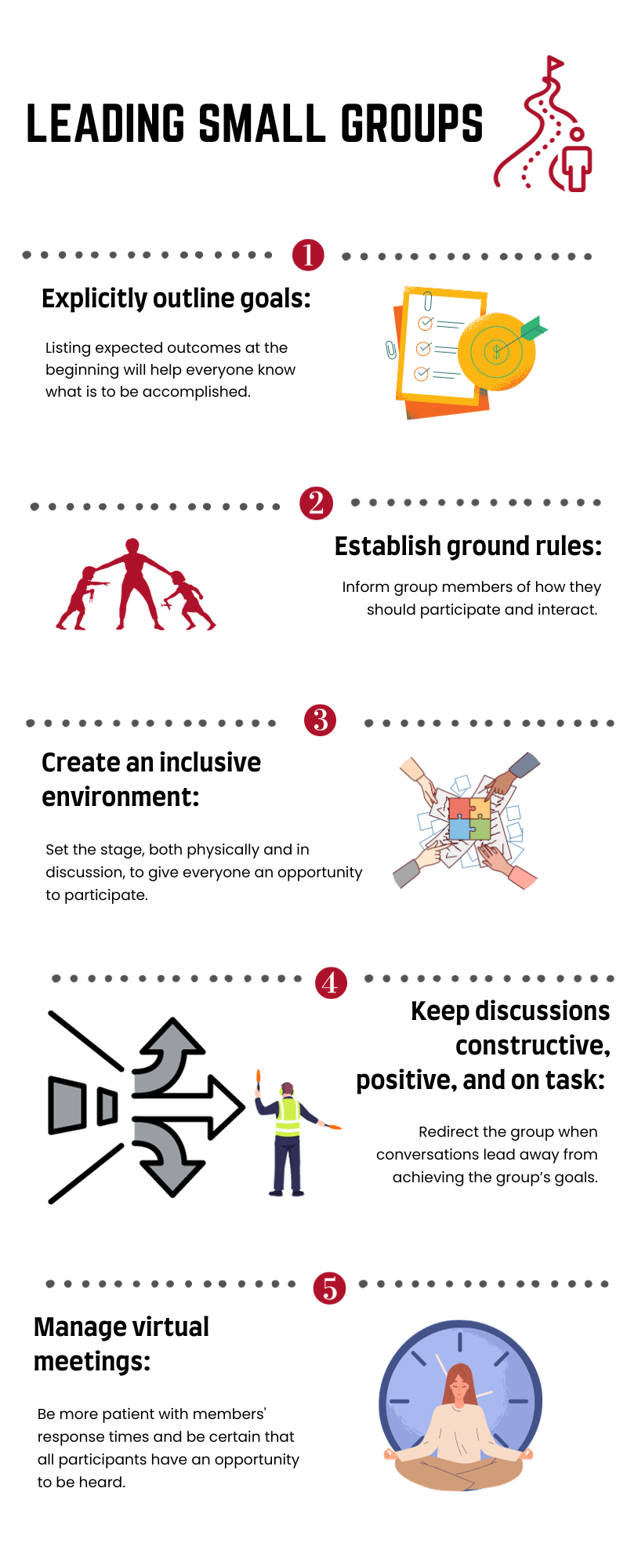
- Outline goals/outcomes . Delineating the goals of a meeting ensures that everyone understands the outcome of the gathering and can help keep conversations on track. Listing goals in the agenda will help all participants understand what is to be accomplished.
- Establish ground rules . Establishing explicit procedural and behavioral expectations serves to solidify the framework in which the conversation will take place. These include items such as attendance and how people are recognized as well as the way group members should treat each other.
- Create an inclusive environment . In addition to setting expectations, group leaders can take steps to help all participants feel that their perspectives are valuable. Setting up the room so that everyone sits around a table can facilitate conversations. Having individuals introduce themselves can let the group understand everyone’s background and expertise. In addition, running discussions in a “round-robin style” (when possible) may help every person have an opportunity to express themselves.
- Keep discussions constructive, positive, and on task . As meetings evolve, it can be easy for conversations to drift. Reminding the group of goals and frequently summarizing the discussion in the context of the planned outcomes can help redirect meetings when needed.
- Manage virtual meetings . Online meetings present their own challenges. Adequate preparation is key, particularly working through technological considerations in advance. Explicitly discussing goals and ground rules is even more important in the virtual environment. Group leaders should be more patient with members’ response times and be especially diligent that all participants have an opportunity to be heard.
The resources listed below outline additional helpful points, expanding on the skills described above and providing additional perspectives on managing small group meetings of different types.
- Communication in the Real World: Small Group Communication (freely available, online module). This chapter includes an overview of managing small groups, including understanding the types and characteristics, group development, and interpersonal dynamics. (Skills addressed: 3,4)
- Conversational Leadership (freely available, online book chapter). This short online resource provides guidance for determining group size and seating to best facilitate participation by all group members. (Skill addressed: 4)
- Tips on Facilitating Effective Group Discussion (freely available, PDF). This resource from Brown University provides tips for effective group facilitation, creating an environment conducive for discussions, keeping conversations positive, and managing common problems. Also included is a valuable list of references for further exploration. (Skills addressed: 1-4)
- Facilitating Effective Discussions: Self-Checklist (freely available, online checklist). This checklist from Brown University provides an easy-to-use, practical framework for preparing for, performing, and reflecting on small group facilitation. (Skills addressed: 1-4)
- Sample Guidelines for Classroom Discussion Agreements (freely available, PDF). These guidelines from Brown University give useful tips for managing classroom discussions, including when disagreements occur among group participants. (Skill addressed: 2)
- Fostering and assessing equitable classroom participation (freely available, online article). This online resource from Brown University includes methods to maximize group members’ participation in discussions and to communicate expectations. Also included is a valuable list of references for further exploration. (Skill addressed: 3)
- Facilitating small group learning in the health professions (freely available, online article). The aim of this paper published in BMC Medical Education is to provide students involved in peer/near peer teaching with an overview of practical approaches and tips to improve learner engagement when facilitating small groups. It includes a discussion of the roles of facilitators, strategies for fostering interactions among the group, and methods for resolving common problems. (Skills addressed: 1-4)
- Facilitating a Virtual Meeting (freely available, PDF). This infographic from the University of Nebraska Medical Center includes key points to consider when facilitating an online meeting, including technical considerations, preparation, and follow-up. (Skill addressed: 5)
- Most universities have a communication department with faculty who specialize in small group communication. You may also find that these individuals are a valuable resource.
This toolkit was created by a working group of the Undergraduate Medical Education (UME) Section of the Group on Educational Affairs (GEA).
Working Group Members
- Geoffrey Talmon, MD, University of Nebraska Medical Center
- Jason Kemnitz, EdD, University of South Dakota Sanford School of Medicine
- Lisa Coplit, MD, Frank H. Netter School of Medicine at Quinnipiac University
- Rikki Ovitsh, MD, SUNY Downstate College of Medicine
- Susan Nofziger, MD, Northeast Ohio Medical University
- Amy Moore, MEd, Cleveland Clinic Lerner College of Medicine
- Melissa Cellini, MD, New York Medical College
- Richard Haspel, MD, Harvard Medical School
- Christine Phillips, MD, Boston University School of Medicine
- Arvind Suresh, Geisel School of Medicine at Dartmouth
- Emily Green, PhD, MA, Warren Alpert Medical School of Brown University
- Holly Meyer, PhD, MS, Uniformed Services University of the Health Sciences
- Karina Clemmons, EdD, University of Arkansas for Medical Sciences
- Shane Puckett, EdD, University of South Florida
- Angela Hairrell, PhD, Burnett School of Medicine at Texas Christian University
- Arkene Levy Johnston, PhD, Kiran C. Patel College of Allopathic Medicine
- Sarah Collins, PhD, UT Southwestern Medical Center
- Patrick Fadden, MD, Virginia Commonwealth University School of Medicine
- Lia Bruner, MD, Augusta University - University of Georgia Medical Partnership
- Jasna Vuk, MD, PhD, University of Arkansas for Medical Sciences
- Pearl Sutter, University of Connecticut School of Medicine
- Kelly Park, Baylor University Medical Center
Overview and General Information about Oral Presentation
- Daily Presentations During Work Rounds
- The New Patient Presentation
- The Holdover Admission Presentation
- Outpatient Clinic Presentations
- The structure of presentations varies from service to service (e.g. medicine vs. surgery), amongst subspecialties, and between environments (inpatient vs. outpatient). Applying the correct style to the right setting requires that the presenter seek guidance from the listeners at the outset.
- Time available for presenting is rather short, which makes the experience more stressful.
- Individual supervisors (residents, faculty) often have their own (sometimes quirky) preferences regarding presentation styles, adding another layer of variability that the presenter has to manage.
- Students are evaluated/judged on the way in which they present, with faculty using this as one way of gauging a student’s clinical knowledge.
- Done well, presentations promote efficient, excellent care. Done poorly, they promote tedium, low morale, and inefficiency.
General Tips:
- Practice, Practice, Practice! Do this on your own, with colleagues, and/or with anyone who will listen (and offer helpful commentary) before you actually present in front of other clinicians. Speaking "on-the-fly" is difficult, as rapidly organizing and delivering information in a clear and concise fashion is not a naturally occurring skill.
- Immediately following your presentations, seek feedback from your listeners. Ask for specifics about what was done well and what could have been done better – always with an eye towards gaining information that you can apply to improve your performance the next time.
- Listen to presentations that are done well – ask yourself, “Why was it good?” Then try to incorporate those elements into your own presentations.
- Listen to presentations that go poorly – identify the specific things that made it ineffective and avoid those pitfalls when you present.
- Effective presentations require that you have thought through the case beforehand and understand the rationale for your conclusions and plan. This, in turn, requires that you have a good grasp of physiology, pathology, clinical reasoning and decision-making - pushing you to read, pay attention, and in general acquire more knowledge.
- Think about the clinical situation in which you are presenting so that you can provide a summary that is consistent with the expectations of your audience. Work rounds, for example, are clearly different from conferences and therefore mandate a different style of presentation.
- Presentations are the way in which we tell medical stories to one another. When you present, ask yourself if you’ve described the story in an accurate way. Will the listener be able to “see” the patient the same way that you do? Can they come to the correct conclusions? If not, re-calibrate.
- It's O.K. to use notes, though the oral presentation should not simply be reduced to reading the admission note – rather, it requires appropriate editing/shortening.
- In general, try to give your presentations on a particular service using the same order and style for each patient, every day. Following a specific format makes it easier for the listener to follow, as they know what’s coming and when they can expect to hear particular information. Additionally, following a standardized approach makes it easier for you to stay organized, develop a rhythm, and lessens the chance that you’ll omit elements.
Specific types of presentations
There are a number of common presentation-types, each with its own goals and formats. These include:
- Daily presentations during work rounds for patients known to a service.
- Newly admitted patients, where you were the clinician that performed the H&P.
- Newly admitted patients that were “handed off” to the team in the morning, such that the H&P was performed by others.
- Outpatient clinic presentations, covering several common situations.
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics.
Note that there is an acceptable range of how oral presentations can be delivered. Ultimately, your goal is to tell the correct story, in a reasonable amount of time, so that the right care can be delivered. Nuances in the order of presentation, what to include, what to omit, etc. are relatively small points. Don’t let the pursuit of these elements distract you or create undue anxiety.
Daily presentations during work rounds of patients that you’re following:
- Organize the presenter (forces you to think things through)
- Inform the listener(s) of 24 hour events and plan moving forward
- Promote focused discussion amongst your listeners and supervisors
- Opportunity to reassess plan, adjust as indicated
- Demonstrate your knowledge and engagement in the care of the patient
- Rapid (5 min) presentation of the key facts
Key features of presentation:
- Opening one liner: Describe who the patient is, number of days in hospital, and their main clinical issue(s).
- 24-hour events: Highlighting changes in clinical status, procedures, consults, etc.
- Subjective sense from the patient about how they’re feeling, vital signs (ranges), and key physical exam findings (highlighting changes)
- Relevant labs (highlighting changes) and imaging
- Assessment and Plan : Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
Example of a daily presentation for a patient known to a team:
- Opening one liner: This is Mr. Smith, a 65 year old man, Hospital Day #3, being treated for right leg cellulitis
- MRI of the leg, negative for osteomyelitis
- Evaluation by Orthopedics, who I&D’d a superficial abscess in the calf, draining a moderate amount of pus
- Patient appears well, states leg is feeling better, less painful
- T Max 101 yesterday, T Current 98; Pulse range 60-80; BP 140s-160s/70-80s; O2 sat 98% Room Air
- Ins/Outs: 3L in (2 L NS, 1 L po)/Out 4L urine
- Right lower extremity redness now limited to calf, well within inked lines – improved compared with yesterday; bandage removed from the I&D site, and base had small amount of purulence; No evidence of fluctuance or undrained infection.
- Creatinine .8, down from 1.5 yesterday
- WBC 8.7, down from 14
- Blood cultures from admission still negative
- Gram stain of pus from yesterday’s I&D: + PMNS and GPCs; Culture pending
- MRI lower extremity as noted above – negative for osteomyelitis
- Continue Vancomycin for today
- Ortho to reassess I&D site, though looks good
- Follow-up on cultures: if MRSA, will transition to PO Doxycycline; if MSSA, will use PO Dicloxacillin
- Given AKI, will continue to hold ace-inhibitor; will likely wait until outpatient follow-up to restart
- Add back amlodipine 5mg/d today
- Hep lock IV as no need for more IVF
- Continue to hold ace-I as above
- Wound care teaching with RNs today – wife capable and willing to assist. She’ll be in this afternoon.
- Set up follow-up with PMD to reassess wound and cellulitis within 1 week
The Brand New Patient (admitted by you)
- Provide enough information so that the listeners can understand the presentation and generate an appropriate differential diagnosis.
- Present a thoughtful assessment
- Present diagnostic and therapeutic plans
- Provide opportunities for senior listeners to intervene and offer input
- Chief concern: Reason why patient presented to hospital (symptom/event and key past history in one sentence). It often includes a limited listing of their other medical conditions (e.g. diabetes, hypertension, etc.) if these elements might contribute to the reason for admission.
- The history is presented highlighting the relevant events in chronological order.
- 7 days ago, the patient began to notice vague shortness of breath.
- 5 days ago, the breathlessness worsened and they developed a cough productive of green sputum.
- 3 days ago his short of breath worsened to the point where he was winded after walking up a flight of stairs, accompanied by a vague right sided chest pain that was more pronounced with inspiration.
- Enough historical information has to be provided so that the listener can understand the reasons that lead to admission and be able to draw appropriate clinical conclusions.
- Past history that helps to shed light on the current presentation are included towards the end of the HPI and not presented later as “PMH.” This is because knowing this “past” history is actually critical to understanding the current complaint. For example, past cardiac catheterization findings and/or interventions should be presented during the HPI for a patient presenting with chest pain.
- Where relevant, the patient's baseline functional status is described, allowing the listener to understand the degree of impairment caused by the acute medical problem(s).
- It should be explicitly stated if a patient is a poor historian, confused or simply unaware of all the details related to their illness. Historical information obtained from family, friends, etc. should be described as such.
- Review of Systems (ROS): Pertinent positive and negative findings discovered during a review of systems are generally incorporated at the end of the HPI. The listener needs this information to help them put the story in appropriate perspective. Any positive responses to a more inclusive ROS that covers all of the other various organ systems are then noted. If the ROS is completely negative, it is generally acceptable to simply state, "ROS negative.”
- Other Past Medical and Surgical History (PMH/PSH): Past history that relates to the issues that lead to admission are typically mentioned in the HPI and do not have to be repeated here. That said, selective redundancy (i.e. if it’s really important) is OK. Other PMH/PSH are presented here if relevant to the current issues and/or likely to affect the patient’s hospitalization in some way. Unrelated PMH and PSH can be omitted (e.g. if the patient had their gall bladder removed 10y ago and this has no bearing on the admission, then it would be appropriate to leave it out). If the listener really wants to know peripheral details, they can read the admission note, ask the patient themselves, or inquire at the end of the presentation.
- Medications and Allergies: Typically all meds are described, as there’s high potential for adverse reactions or drug-drug interactions.
- Family History: Emphasis is placed on the identification of illnesses within the family (particularly among first degree relatives) that are known to be genetically based and therefore potentially heritable by the patient. This would include: coronary artery disease, diabetes, certain cancers and autoimmune disorders, etc. If the family history is non-contributory, it’s fine to say so.
- Social History, Habits, other → as relates to/informs the presentation or hospitalization. Includes education, work, exposures, hobbies, smoking, alcohol or other substance use/abuse.
- Sexual history if it relates to the active problems.
- Vital signs and relevant findings (or their absence) are provided. As your team develops trust in your ability to identify and report on key problems, it may become acceptable to say “Vital signs stable.”
- Note: Some listeners expect students (and other junior clinicians) to describe what they find in every organ system and will not allow the presenter to say “normal.” The only way to know what to include or omit is to ask beforehand.
- Key labs and imaging: Abnormal findings are highlighted as well as changes from baseline.
- Summary, assessment & plan(s) Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- The assessment and plan typically concludes by mentioning appropriate prophylactic considerations (e.g. DVT prevention), code status and disposition.
- Chief Concern: Mr. H is a 50 year old male with AIDS, on HAART, with preserved CD4 count and undetectable viral load, who presents for the evaluation of fever, chills and a cough over the past 7 days.
- Until 1 week ago, he had been quite active, walking up to 2 miles a day without feeling short of breath.
- Approximately 1 week ago, he began to feel dyspneic with moderate activity.
- 3 days ago, he began to develop subjective fevers and chills along with a cough productive of red-green sputum.
- 1 day ago, he was breathless after walking up a single flight of stairs and spent most of the last 24 hours in bed.
- Diagnosed with HIV in 2000, done as a screening test when found to have gonococcal urethritis
- Was not treated with HAART at that time due to concomitant alcohol abuse and non-adherence.
- Diagnosed and treated for PJP pneumonia 2006
- Diagnosed and treated for CMV retinitis 2007
- Became sober in 2008, at which time interested in HAART. Started on Atripla, a combination pill containing: Efavirenz, Tonofovir, and Emtricitabine. He’s taken it ever since, with no adverse effects or issues with adherence. Receives care thru Dr. Smiley at the University HIV clinic.
- CD4 count 3 months ago was 400 and viral load was undetectable.
- He is homosexual though he is currently not sexually active. He has never used intravenous drugs.
- He has no history of asthma, COPD or chronic cardiac or pulmonary condition. No known liver disease. Hepatitis B and C negative. His current problem seems different to him then his past episode of PJP.
- Review of systems: negative for headache, photophobia, stiff neck, focal weakness, chest pain, abdominal pain, diarrhea, nausea, vomiting, urinary symptoms, leg swelling, or other complaints.
- Hypertension x 5 years, no other known vascular disease
- Gonorrhea as above
- Alcohol abuse above and now sober – no known liver disease
- No relevant surgeries
- Atripla, 1 po qd
- Omeprazole 20 mg, 1 PO, qd
- Lisinopril 20mg, qd
- Naprosyn 250 mg, 1-2, PO, BID PRN
- No allergies
- Both of the patient's parents are alive and well (his mother is 78 and father 80). He has 2 brothers, one 45 and the other 55, who are also healthy. There is no family history of heart disease or cancer.
- Patient works as an accountant for a large firm in San Diego. He lives alone in an apartment in the city.
- Smokes 1 pack of cigarettes per day and has done so for 20 years.
- No current alcohol use. Denies any drug use.
- Sexual History as noted above; has sex exclusively with men, last partner 6 months ago.
- Seated on a gurney in the ER, breathing through a face-mask oxygen delivery system. Breathing was labored and accessory muscles were in use. Able to speak in brief sentences, limited by shortness of breath
- Vital signs: Temp 102 F, Pulse 90, BP 150/90, Respiratory Rate 26, O2 Sat (on 40% Face Mask) 95%
- HEENT: No thrush, No adenopathy
- Lungs: Crackles and Bronchial breath sounds noted at right base. E to A changes present. No wheezing or other abnormal sounds noted over any other area of the lung. Dullness to percussion was also appreciated at the right base.
- Cardiac: JVP less than 5 cm; Rhythm was regular. Normal S1 and S2. No murmurs or extra heart sounds noted.
- Abdomen and Genital exams: normal
- Extremities: No clubbing, cyanosis or edema; distal pulses 2+ and equal bilaterally.
- Skin: no eruptions noted.
- Neurological exam: normal
- WBC 18 thousand with 10% bands;
- Normal Chem 7 and LFTs.
- Room air blood gas: pH of 7.47/ PO2 of 55/PCO2 of 30.
- Sputum gram stain remarkable for an abundance of polys along with gram positive diplococci.
- CXR remarkable for dense right lower lobe infiltrate without effusion.
- Monitored care unit, with vigilance for clinical deterioration.
- Hypertension: given significant pneumonia and unclear clinical direction, will hold lisinopril. If BP > 180 and or if clear not developing sepsis, will consider restarting.
- Low molecular weight heparin
- Code Status: Wishes to be full code full care, including intubation and ICU stay if necessary. Has good quality of life and hopes to return to that functional level. Wishes to reconsider if situation ever becomes hopeless. Older brother Tom is surrogate decision maker if the patient can’t speak for himself. Tom lives in San Diego and we have his contact info. He is aware that patient is in the hospital and plans on visiting later today or tomorrow.
- Expected duration of hospitalization unclear – will know more based on response to treatment over next 24 hours.
The holdover admission (presenting data that was generated by other physicians)
- Handoff admissions are very common and present unique challenges
- Understand the reasons why the patient was admitted
- Review key history, exam, imaging and labs to assure that they support the working diagnostic and therapeutic plans
- Does the data support the working diagnosis?
- Do the planned tests and consults make sense?
- What else should be considered (both diagnostically and therapeutically)?
- This process requires that the accepting team thoughtfully review their colleagues efforts with a critical eye – which is not disrespectful but rather constitutes one of the main jobs of the accepting team and is a cornerstone of good care *Note: At some point during the day (likely not during rounds), the team will need to verify all of the data directly with the patient.
- 8-10 minutes
- Chief concern: Reason for admission (symptom and/or event)
- Temporally presented bullets of events leading up to the admission
- Review of systems
- Relevant PMH/PSH – historical information that might affect the patient during their hospitalization.
- Meds and Allergies
- Family and Social History – focusing on information that helps to inform the current presentation.
- Habits and exposures
- Physical exam, imaging and labs that were obtained in the Emergency Department
- Assessment and plan that were generated in the Emergency Department.
- Overnight events (i.e. what happened in the Emergency Dept. and after the patient went to their hospital room)? Responses to treatments, changes in symptoms?
- How does the patient feel this morning? Key exam findings this morning (if seen)? Morning labs (if available)?
- Assessment and Plan , with attention as to whether there needs to be any changes in the working differential or treatment plan. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- Chief concern: 70 yo male who presented with 10 days of progressive shoulder pain, followed by confusion. He was brought in by his daughter, who felt that her father was no longer able to safely take care for himself.
- 10 days ago, Mr. X developed left shoulder pain, first noted a few days after lifting heavy boxes. He denies falls or direct injury to the shoulder.
- 1 week ago, presented to outside hospital ER for evaluation of left shoulder pain. Records from there were notable for his being afebrile with stable vitals. Exam notable for focal pain anteriorly on palpation, but no obvious deformity. Right shoulder had normal range of motion. Left shoulder reported as diminished range of motion but not otherwise quantified. X-ray negative. Labs remarkable for wbc 8, creat 2.2 (stable). Impression was that the pain was of musculoskeletal origin. Patient was provided with Percocet and told to see PMD in f/u
- Brought to our ER last night by his daughter. Pain in shoulder worse. Also noted to be confused and unable to care for self. Lives alone in the country, home in disarray, no food.
- ROS: negative for falls, prior joint or musculoskeletal problems, fevers, chills, cough, sob, chest pain, head ache, abdominal pain, urinary or bowel symptoms, substance abuse
- Hypertension
- Coronary artery disease, s/p LAD stent for angina 3 y ago, no symptoms since. Normal EF by echo 2 y ago
- Chronic kidney disease stage 3 with creatinine 1.8; felt to be secondary to atherosclerosis and hypertension
- aspirin 81mg qd, atorvastatin 80mg po qd, amlodipine 10 po qd, Prozac 20
- Allergies: none
- Family and Social: lives alone in a rural area of the county, in contact with children every month or so. Retired several years ago from work as truck driver. Otherwise non-contributory.
- Habits: denies alcohol or other drug use.
- Temp 98 Pulse 110 BP 100/70
- Drowsy though arousable; oriented to year but not day or date; knows he’s at a hospital for evaluation of shoulder pain, but doesn’t know the name of the hospital or city
- CV: regular rate and rhythm; normal s1 and s2; no murmurs or extra heart sounds.
- Left shoulder with generalized swelling, warmth and darker coloration compared with Right; generalized pain on palpation, very limited passive or active range of motion in all directions due to pain. Right shoulder appearance and exam normal.
- CXR: normal
- EKG: sr 100; nl intervals, no acute changes
- WBC 13; hemoglobin 14
- Na 134, k 4.6; creat 2.8 (1.8 baseline 4 m ago); bicarb 24
- LFTs and UA normal
- Vancomycin and Zosyn for now
- Orthopedics to see asap to aspirate shoulder for definitive diagnosis
- If aspiration is consistent with infection, will need to go to Operating Room for wash out.
- Urine electrolytes
- Follow-up on creatinine and obtain renal ultrasound if not improved
- Renal dosing of meds
- Strict Ins and Outs.
- follow exam
- obtain additional input from family to assure baseline is, in fact, normal
- Since admission (6 hours) no change in shoulder pain
- This morning, pleasant, easily distracted; knows he’s in the hospital, but not date or year
- T Current 101F Pulse 100 BP 140/80
- Ins and Outs: IVF Normal Saline 3L/Urine output 1.5 liters
- L shoulder with obvious swelling and warmth compared with right; no skin breaks; pain limits any active or passive range of motion to less than 10 degrees in all directions
- Labs this morning remarkable for WBC 10 (from 13), creatinine 2 (down from 2.8)
- Continue with Vancomycin and Zosyn for now
- I already paged Orthopedics this morning, who are en route for aspiration of shoulder, fluid for gram stain, cell count, culture
- If aspirate consistent with infection, then likely to the OR
- Continue IVF at 125/h, follow I/O
- Repeat creatinine later today
- Not on any nephrotoxins, meds renaly dosed
- Continue antibiotics, evaluation for primary source as above
- Discuss with family this morning to establish baseline; possible may have underlying dementia as well
- SC Heparin for DVT prophylaxis
- Code status: full code/full care.
Outpatient-based presentations
There are 4 main types of visits that commonly occur in an outpatient continuity clinic environment, each of which has its own presentation style and purpose. These include the following, each described in detail below.
- The patient who is presenting for their first visit to a primary care clinic and is entirely new to the physician.
- The patient who is returning to primary care for a scheduled follow-up visit.
- The patient who is presenting with an acute problem to a primary care clinic
- The specialty clinic evaluation (new or follow-up)
It’s worth noting that Primary care clinics (Internal Medicine, Family Medicine and Pediatrics) typically take responsibility for covering all of the patient’s issues, though the amount of energy focused on any one topic will depend on the time available, acuity, symptoms, and whether that issue is also followed by a specialty clinic.
The Brand New Primary Care Patient
Purpose of the presentation
- Accurately review all of the patient’s history as well as any new concerns that they might have.
- Identify health related problems that need additional evaluation and/or treatment
- Provide an opportunity for senior listeners to intervene and offer input
Key features of the presentation
- If this is truly their first visit, then one of the main reasons is typically to "establish care" with a new doctor.
- It might well include continuation of therapies and/or evaluations started elsewhere.
- If the patient has other specific goals (medications, referrals, etc.), then this should be stated as well. Note: There may well not be a "chief complaint."
- For a new patient, this is an opportunity to highlight the main issues that might be troubling/bothering them.
- This can include chronic disorders (e.g. diabetes, congestive heart failure, etc.) which cause ongoing symptoms (shortness of breath) and/or generate daily data (finger stick glucoses) that should be discussed.
- Sometimes, there are no specific areas that the patient wishes to discuss up-front.
- Review of systems (ROS): This is typically comprehensive, covering all organ systems. If the patient is known to have certain illnesses (e.g. diabetes), then the ROS should include the search for disorders with high prevalence (e.g. vascular disease). There should also be some consideration for including questions that are epidemiologically appropriate (e.g. based on age and sex).
- Past Medical History (PMH): All known medical conditions (in particular those requiring ongoing treatment) are listed, noting their duration and time of onset. If a condition is followed by a specialist or co-managed with other clinicians, this should be noted as well. If a problem was described in detail during the “acute” history, it doesn’t have to be re-stated here.
- Past Surgical History (PSH): All surgeries, along with the year when they were performed
- Medications and allergies: All meds, including dosage, frequency and over-the-counter preparations. Allergies (and the type of reaction) should be described.
- Social: Work, hobbies, exposures.
- Sexual activity – may include type of activity, number and sex of partner(s), partner’s health.
- Smoking, Alcohol, other drug use: including quantification of consumption, duration of use.
- Family history: Focus on heritable illness amongst first degree relatives. May also include whether patient married, in a relationship, children (and their ages).
- Physical Exam: Vital signs and relevant findings (or their absence).
- Key labs and imaging if they’re available. Also when and where they were obtained.
- Summary, assessment & plan(s) presented by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic. This typically concludes with a “health care maintenance” section, which covers age, sex and risk factor appropriate vaccinations and screening tests.
The Follow-up Visit to a Primary Care Clinic
- Organize the presenter (forces you to think things through).
- Accurately review any relevant interval health care events that might have occurred since the last visit.
- Identification of new symptoms or health related issues that might need additional evaluation and/or treatment
- If the patient has no concerns, then verification that health status is stable
- Review of medications
- Provide an opportunity for listeners to intervene and offer input
- Reason for the visit: Follow-up for whatever the patient’s main issues are, as well as stating when the last visit occurred *Note: There may well not be a “chief complaint,” as patients followed in continuity at any clinic may simply be returning for a visit as directed by their doctor.
- Events since the last visit: This might include emergency room visits, input from other clinicians/specialists, changes in medications, new symptoms, etc.
- Review of Systems (ROS): Depth depends on patient’s risk factors and known illnesses. If the patient has diabetes, then a vascular ROS would be done. On the other hand, if the patient is young and healthy, the ROS could be rather cursory.
- PMH, PSH, Social, Family, Habits are all OMITTED. This is because these facts are already known to the listener and actionable aspects have presumably been added to the problem list (presented at the end). That said, these elements can be restated if the patient has a new symptom or issue related to a historical problem has emerged.
- MEDS : A good idea to review these at every visit.
- Physical exam: Vital signs and pertinent findings (or absence there of) are mentioned.
- Lab and Imaging: The reason why these were done should be mentioned and any key findings mentioned, highlighting changes from baseline.
- Assessment and Plan: This is most clearly done by individually stating all of the conditions/problems that are being addressed (e.g. hypertension, hypothyroidism, depression, etc.) followed by their specific plan(s). If a new or acute issue was identified during the visit, the diagnostic and therapeutic plan for that concern should be described.
The Focused Visit to a Primary Care Clinic
- Accurately review the historical events that lead the patient to make the appointment.
- Identification of risk factors and/or other underlying medical conditions that might affect the diagnostic or therapeutic approach to the new symptom or concern.
- Generate an appropriate assessment and plan
- Allow the listener to comment
Key features of the presentation:
- Reason for the visit
- History of Present illness: Description of the sequence of symptoms and/or events that lead to the patient’s current condition.
- Review of Systems: To an appropriate depth that will allow the listener to grasp the full range of diagnostic possibilities that relate to the presenting problem.
- PMH and PSH: Stating only those elements that might relate to the presenting symptoms/issues.
- PE: Vital signs and key findings (or lack thereof)
- Labs and imaging (if done)
- Assessment and Plan: This is usually very focused and relates directly to the main presenting symptom(s) or issues.
The Specialty Clinic Visit
Specialty clinic visits focus on the health care domains covered by those physicians. For example, Cardiology clinics are interested in cardiovascular disease related symptoms, events, labs, imaging and procedures. Orthopedics clinics will focus on musculoskeletal symptoms, events, imaging and procedures. Information that is unrelated to these disciples will typically be omitted. It’s always a good idea to ask the supervising physician for guidance as to what’s expected to be covered in a particular clinic environment.
- Highlight the reason(s) for the visit
- Review key data
- Provide an opportunity for the listener(s) to comment
- 5-7 minutes
- If it’s a consult, state the main reason(s) that the patient was referred as well as who referred them.
- If it’s a return visit, state the reasons why the patient is being followed in the clinic and when the last visit took place
- If it’s for an acute issue, state up front what the issue is Note: There may well not be a “chief complaint,” as patients followed in continuity in any clinic may simply be returning for a return visit as directed
- For a new patient, this highlights the main things that might be troubling/bothering the patient.
- For a specialty clinic, the history presented typically relates to the symptoms and/or events that are pertinent to that area of care.
- Review of systems , focusing on those elements relevant to that clinic. For a cardiology patient, this will highlight a vascular ROS.
- PMH/PSH that helps to inform the current presentation (e.g. past cardiac catheterization findings/interventions for a patient with chest pain) and/or is otherwise felt to be relevant to that clinic environment.
- Meds and allergies: Typically all meds are described, as there is always the potential for adverse drug interactions.
- Social/Habits/other: as relates to/informs the presentation and/or is relevant to that clinic
- Family history: Focus is on heritable illness amongst first degree relatives
- Physical Exam: VS and relevant findings (or their absence)
- Key labs, imaging: For a cardiology clinic patient, this would include echos, catheterizations, coronary interventions, etc.
- Summary, assessment & plan(s) by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic.
- Reason for visit: Patient is a 67 year old male presenting for first office visit after admission for STEMI. He was referred by Dr. Goins, his PMD.
- The patient initially presented to the ER 4 weeks ago with acute CP that started 1 hour prior to his coming in. He was found to be in the midst of a STEMI with ST elevations across the precordial leads.
- Taken urgently to cath, where 95% proximal LAD lesion was stented
- EF preserved by Echo; Peak troponin 10
- In-hospital labs were remarkable for normal cbc, chem; LDL 170, hdl 42, nl lfts
- Uncomplicated hospital course, sent home after 3 days.
- Since home, he states that he feels great.
- Denies chest pain, sob, doe, pnd, edema, or other symptoms.
- No symptoms of stroke or TIA.
- No history of leg or calf pain with ambulation.
- Prior to this admission, he had a history of hypertension which was treated with lisinopril
- 40 pk yr smoking history, quit during hospitalization
- No known prior CAD or vascular disease elsewhere. No known diabetes, no family history of vascular disease; He thinks his cholesterol was always “a little high” but doesn’t know the numbers and was never treated with meds.
- History of depression, well treated with prozac
- Discharge meds included: aspirin, metoprolol 50 bid, lisinopril 10, atorvastatin 80, Plavix; in addition he takes Prozac for depression
- Taking all of them as directed.
- Patient lives with his wife; they have 2 grown children who are no longer at home
- Works as a computer programmer
- Smoking as above
- ETOH: 1 glass of wine w/dinner
- No drug use
- No known history of cardiovascular disease among 2 siblings or parents.
- Well appearing; BP 130/80, Pulse 80 regular, 97% sat on Room Air, weight 175lbs, BMI 32
- Lungs: clear to auscultation
- CV: s1 s2 no s3 s4 murmur
- No carotid bruits
- ABD: no masses
- Ext; no edema; distal pulses 2+
- Cath from 4 weeks ago: R dominant; 95% proximal LAD; 40% Cx.
- EF by TTE 1 day post PCI with mild Anterior Hypokinesis, EF 55%, no valvular disease, moderate LVH
- Labs of note from the hospital following cath: hgb 14, plt 240; creat 1, k 4.2, lfts normal, glucose 100, LDL 170, HDL 42.
- EKG today: SR at 78; nl intervals; nl axis; normal r wave progression, no q waves
- Plan: aspirin 81 indefinitely, Plavix x 1y
- Given nitroglycerine sublingual to have at home.
- Reviewed symptoms that would indicate another MI and what to do if occurred
- Plan: continue with current dosages of meds
- Chem 7 today to check k, creatinine
- Plan: Continue atorvastatin 80mg for life
- Smoking cessation: Doing well since discharge without adjuvant treatments, aware of supports.
- Plan: AAA screening ultrasound
3 types of medical presentations (and how to give them)
Here are some tips for presenting the top three types of medical presentations: lectures, research presentations, and case reports.
Derek Murray
Building presentations

With your long to-do list as a medical professional, giving presentations is probably not a high priority. Yet, medical presentations are inevitable. Are you ready to give them when your job requires it? If so, where do you even start?
We want to make it a little easier for you to present data-heavy medical topics in an easy-to-understand way.
So, let’s dive right in with the top three types of medical presentations.
Key Takeaways:
- Structure your medical presentation into a story to make it memorable.
- Medical presentations can be lectures, research, or case presentations.
- Customize the presentation based on the type and goal.
1. Lectures
Medical lectures educate an audience about a medical topic. They’re one of the most challenging presentations. According to the Learning Pyramid , lectures are the most passive learning techniques, which is also why they have the lowest retention rates.

There are several settings for educational lectures, including:
- Conferences
- University or school lectures
Medical lectures help students or an audience comprehend complex medical information and then turn what they learned into actionable strategies.
For example, you may teach students with little medical knowledge about a new medical concept. But they must understand the topic and be able to recall it for examinations.
Tips for giving medical lectures
How can you turn one of the most challenging presentations into an engaging, memorable lecture? Here are a few tips to ace your educational medical lectures:
- Be interactive : Use Q&As, activities, and open discussions.
- Hand out resources: Give physical booklets students can review after the presentation.
- Use multimedia: Add audio-visual elements like images, video, and audio clips.
- Use simple language: Your audience is learning, so they need simple language and plenty of definitions to understand the topic.
- Make it entertaining: Keep your audience’s attention with a more engaging and entertaining presentation.
UnitedHealth Group incorporated imagery and movement to show rather than tell about mental health in 2022 to boost their engagement on the topic.

2. Research presentations
The most information-heavy medical presentation is the research presentation. Research presentations share findings with experienced medical professionals, usually in conference settings. Some of the audience includes:
- Investigators
- Ph.D. students
- Medical professionals and experienced doctors
Research presentations can also be part of healthcare marketing . You may have to introduce a new process, pharmaceutical, or device to encourage other healthcare professionals to adopt it in their practices.
Tips for giving research presentations
Use these tips to improve your research presentations :
- Speak on a higher level: You’re talking to a knowledgeable audience, so they expect a higher level of research.
- Back all facts with data: Use statistics and research to back all claims.
- Use power poses: Build authority with a confident presentation.
- Grab the audience’s attention: Start your presentation by giving your audience a reason to care, like a problem you want to solve.
- Build up the conclusion: Structure the research in a natural, progressive order that builds up to your conclusion.
- Look at the future: Conclude with how the research findings will impact the future of medicine.
- Visualize data : Simplify findings and data with visuals and charts.
Cardinal Health transformed the complex research for Smart Compression into understandable slides using a mix of graphics and storytelling in their medical presentation.
3. Case reports
Medical professionals must give oral case reports when transferring information between providers or a team. These presentations are very brief and often don’t require visuals.
Sometimes a case is especially unique and offers educational value to others. In that case, presenters should transform their quick oral case reports into a longer presentation that incorporates data and visuals.
Tips for giving case reports
Case reports use a similar structure to oral patient presentations, except with more details about each point. You’ll still want to pack as much information in a short presentation as possible.
- Begin the presentation with a patient overview: Start by introducing the patient, including all relevant demographic details in summarized graphics and lists.
- Present the history of the patient: Describe the patient’s history, why they sought care, and the symptoms they presented in charts and visuals.
- Explore medical information: Dive into the medical details, like treatment and history, using a storytelling structure to connect the information.
- Offer a plan: Outline a treatment plan alongside proof.
Summarize details in charts: You’ll pack a large amount of information in a concise presentation, so use plenty of charts and diagrams to summarize data and simplify outcomes.
Tips for preparing engaging medical presentations
Your medical presentations have highly complex topics rich with data. These topics can easily feel overwhelming or even boring if they don’t have the right structure and appearance.
Here are three medical presentation tips we’ve learned to help you prepare and present high-quality medical presentations that engage AND inform.
Know your audience’s knowledge level
Before building and presenting a medical topic, you must know your audience’s knowledge level. A lecture to a class of first-year college students will sound far different from a presentation to doctors with 10+ years of industry experience.
Build a presentation around your audience’s knowledge, so it’s understandable yet challenging. By taking this extra step, you’ll know what points need more explanation and what topics you can dig deeper into based on your audience’s experience.
Build a structured story
A complex topic becomes easy to understand and follow if you use a storytelling structure . You might ask, “How can a lecture on a new treatment be a story?”
Any time you communicate, it’s a story: You have the challenge to solve, potential solutions to try, and a final winner (like when presenting medical research). You can structure that story in a progressive order or by announcing one primary outcome and providing a list of proofs (like with patient case studies).
Focus on a goal
The goal of medical presentations can be educating, training, or persuading the audience, depending on the type of medical presentation. Knowing your goal guides which data is most relevant to bring your desired outcome.
Communicate at the speed of healthcare with Prezent
Whether you’re preparing a lecture, research presentation, or case report, creating presentation slides is probably far down your priority list. The fast-paced healthcare industry has enough duties vying for attention. So how are you supposed to squeeze in hours to build an engaging presentation?
Prezent has your back. No need to sweat the details as we have already developed leading presentation templates perfect for data-driven presentations. Personalize to your audience’s knowledge and presentation preferences with AI-powered technology. Save time and energy with access to 35,000+ custom-built slide templates designed with key business and pharma storylines in mind.
You’ll have an engaging and clear presentation deck in minutes rather than hours. Take back your time and communicate efficiently with Prezent so you can focus on turning your ideas and insights into action.
Our proof is in our results. Schedule a demo to see the platform in action.
Get the latest from prezent community.
Join thousands of subscribers who receive our best practices on communication, storytelling, presentation design, and more. New tips weekly. (No spam, we promise!)
Tools for the Patient Presentation
The formal patient presentation.
- Posing the Clinical Question
- Searching the Medical Literature for EBM
Sources & Further Reading
First Aid for the Wards
Lingard L, Haber RJ. Teaching and learning communications in medicine: a rhetorical approach . Academic Medicine. 74(5):507-510 1999 May.
Lingard L, Haber RJ. What do we mean by "relevance"? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format . Academic Medicine. 74(10):S124-S127.
The Oral Presentation (A Practical Guide to Clinical Medicine, UCSD School of Medicine) http://meded.ucsd.edu/clinicalmed/oral.htm
"Classically, the formal oral presentation is given in 7 minutes or less. Although it follows the same format as a written report, it is not simply regurgitation. A great presentation requires style as much as substance; your delivery must be succinct and smooth. No time should be wasted on superfluous information; one can read about such matters later in your admit note. Ideally, your presentation should be formulated so that your audience can anticipate your assessment and plan; that is, each piece of information should clue the listener into your thinking process and your most likely diagnosis." [ Le, et al, p. 15 ]
Types of Patient Presentations
New Patient
New patients get the traditional H&P with assessment and plan. Give the chief complaint and a brief and pertinent HPI. Next give important PMH, PSH, etc. The ROS is often left out, as anything important was in the HPI. The PE is reviewed. Only give pertinent positives and negatives. The assessment and plan should include what you think is wrong and, briefly, why. Then, state what you plan to do for the patient, including labs. Be sure to know why things are being done: you will be asked.
The follow-up presentation differs from the presentation of a new patient. It is an abridged presentation, perhaps referencing major patient issues that have been previously presented, but focusing on new information about these issues and/or what has changed. Give the patient’s name, age, date of admission, briefly review the present illness, physical examination and admitting diagnosis. Then report any new finding, laboratory tests, diagnostic procedures and changes in medications.
The attending physician will ask the patient’s permission to have the medical student present their case. After making the proper introductions the attending will let the patient know they may offer input or ask questions at any point. When presenting at bedside the student should try to involve the patient.
Preparing for the Presentation
There are four things you must consider before you do your oral presentation
- Occasion (setting and circumstances)
Ask yourself what do you want the presentation to do
- Present a new patient to your preceptor : the amount of detail will be determined by your preceptor. It is also likely to reflect your development and experience, with less detail being required as you progress.
- Present your patient at working or teaching rounds : the amount of detail will be determined by the customs of the group. The focus of the presentation will be influenced by the learning objectives of working responsibilities of the group.
- Request a consultant’s advice on a clinical problem : the presentation will be focused on the clinical question being posed to the consultant.
- Persuade others about a diagnosis and plan : a shorter presentation which highlights the pertinent positives and negatives that are germane to the diagnosis and/or plan being suggested.
- Enlist cooperation required for patient care : a short presentation focusing on the impact your audience can have in addressing the patient’s issues.
Preparation
- Patient evaluation : history, physical examination, review of tests, studies, procedures, and consultants’ recommendations.
- Selected reading : reference texts; to build a foundational understanding.
- Literature search : for further elucidation of any key references from selected reading, and to bring your understanding up to date, since reference text information is typically three to seven years old.
- Write-up : for oral presentation, just succinct notes to serve as a reminder or reference, since you’re not going to be reading your presentation.
Knowledge (Be prepared to answer questions about the following)
- Pathophysiology
- Complications
- Differential diagnosis
- Course of conditions
- Diagnostic tests
- Medications
- Essential Evidence Plus
Template for Oral Presentations
Chief Complaint (CC)
The opening statement should give an overview of the patient, age, sex, reason for visit and the duration of the complaint. Give marital status, race, or occupation if relevant. If your patient has a history of a major medical problem that bears strongly on the understanding of the present illness, include it. For ongoing care, give a one sentence recap of the history.
History of Present Illness (HPI)
This will be very similar to your written HPI. Present the most important problem first. If there is more than one problem, treat each separately. Present the information chronologically. Cover one system before going onto the next. Characterize the chief complaint – quality, severity, location, duration, progression, and include pertinent negatives. Items from the ROS that are unrelated to the present problem may be mentioned in passing unless you are doing a very formal presentation. When you do your first patient presentation you may be expected to go into detail. For ongoing care, present any new complaints.
Review of Systems (ROS)
Most of the ROS is incorporated at the end of the HPI. Items that are unrelated to the present problem may be briefly mentioned. For ongoing care, present only if new complaints.
Past Medical History (PMH)
Discuss other past medical history that bears directly on the current medical problem. For ongoing care, have the information available to respond to questions.
Past Surgical History
Provide names of procedures, approximate dates, indications, any relevant findings or complications, and pathology reports, if applicable. For ongoing care, have the information available to respond to questions.
Allergies/Medications
Present all current medications along with dosage, route and frequency. For the follow-up presentation just give any changes in medication. For ongoing care, note any changes.
Smoking and Alcohol (and any other substance abuse)
Note frequency and duration. For ongoing care, have the information available to respond to questions.
Social/Work History
Home, environment, work status and sexual history. For ongoing care, have the information available to respond to questions.
Family History Note particular family history of genetically based diseases. For ongoing care, have the information available to respond to questions.
Physical Exam/Labs/Other Tests
Include all significant abnormal findings and any normal findings that contribute to the diagnosis. Give a brief, general description of the patient including physical appearance. Then describe vital signs touching on each major system. Try to find out in advance how thorough you need to be for your presentation. There are times when you will be expected to give more detail on each physical finding, labs and other test results. For ongoing care, mention only further positive findings and relevant negative findings.
Assessment and Plan
Give a summary of the important aspects of the history, physical exam and formulate the differential diagnosis. Make sure to read up on the patient’s case by doing a search of the literature.
- Include only the most essential facts; but be ready to answer ANY questions about all aspects of your patient.
- Keep your presentation lively.
- Do not read the presentation!
- Expect your listeners to ask questions.
- Follow the order of the written case report.
- Keep in mind the limitation of your listeners.
- Beware of jumping back and forth between descriptions of separate problems.
- Use the presentation to build your case.
- Your reasoning process should help the listener consider a differential diagnosis.
- Present the patient as well as the illness .
- << Previous: Home
- Next: Posing the Clinical Question >>
- Last Updated: Jul 19, 2023 10:52 AM
- URL: https://rowanmed.libguides.com/tools
Medical Presentations: How to Present Effectively on Urgent Topics

In the face of the pandemic that consumed 2020, we saw an uptick in medical presentations. And rightfully so. The world was in a state of panic over the unknown of a new virus, people were craving information, and organizations like the World Health Organization (WHO) were scrambling to provide data and resources to help address questions and concerns. Whether it was news stories, or medical research, the world needed to understand what we were up against with COVID-19. Naturally, presentations helped to deliver that information. But this isn’t the first time a virus or disease has rattled communities, and it’s certainly not the first time professionals have used medical presentations to educate the masses. Medical presentations are a helpful tool for medical professionals, research clinics, and organizations to help inform and educate their communities on a wide variety of urgent topics. This can include patient treatment, clinical trial research and results, training for medical staff, general education, medical research, or important data regarding diseases.
While medical presentations tend to be fundamentally different from normal presentations in that they include critical and sensitive information, there are still design best practices just like any other deck. That said, what works for a sales pitch might not resonate well with a medical presentation.
Keep these five things in mind when you want to present effectively on urgent medical presentation topics.
Consider your audience
You may be presenting to a group of doctors within your organization to get the team up to speed on new practices, sharing treatment plans with a patient, or educating the community on new health threats. How you structure your medical presentation is not a one-size-fits-all situation. How you talk to internal staff, versus how you would deliver information to a scared patient is not the same. When you’re crafting your message, consider your audience, and tailor the narrative to their overarching concerns and needs.
Keep things straightforward
Unless you’re presenting to third year residents, your audience probably won’t be able to digest complicated medical terminology. It’s important to avoid medical jargon, complex definitions, or overcomplicated explanations that will confuse your audience. Instead, break things down in layman's terms and relate the information back to your audience and how it will affect them. Keeping things straightforward, and clear, will help your audience digest and process the information quicker. The end goal is that your audience leaves with clarity, feeling more educated on the topic and its urgency.
Use icons to reflect the urgency of the situation
The use of visual aids, such as compelling images or meaningful icons, can help paint the picture of urgency in any presentation. Things like clocks, alarms, lightning bolts, or exclamation points can depict emergencies and symbolize something significant in your presentation. The use of impactful visuals will help engage your audience and let them know what they absolutely need to pay attention to. It helps you control the narrative, and highlight any pertinent information or key takeaways.
Beautiful.ai’s free library of hundreds of thousands of images and icons can help take your presentation to the next level. Our custom icons were thoughtfully created by one of our in-house designers, and are a great way to compliment your data and add urgency to your slide .
Hit them with the facts
In most medical presentations, factual data carries the slides. Whether it’s a survey, research results, or statistics about a particular disease, numerical data will help people understand the urgency or severity of the topic. For example, it was common for nearly every COVID-19 presentation or article to include statistics of the percentage of the population infected, which regions were seeing the greatest spikes in cases, death tolls by county, and data relevant to high-risk individuals. While the numbers may not always be fun— especially as they pertain to a pandemic— they paint a clear picture of what the audience needs to understand. Seeing scary statistics can put into perspective just how real the situation is.
Using the proper charts, graphs , or infographics allows you to dictate exactly what information the audience is consuming. Data visualization with infographics can also help the audience understand and retain otherwise complicated data. However, even with the best charts, you can still overwhelm the audience with information. Opt to include only the most relevant info and useful data.
Allow time to process
Regardless of what you’re presenting— big or small— you should leave time at the end for questions. Medical presentations can be paralyzing, and your audience will likely be seeking more answers. Give your audience a minute or two following the presentation to process what they learned, and then give them a chance to ask questions. You may need to elaborate on specific slides, or revisit a piece of data, to help provide clarification. When it comes to urgent topics, you want your audience to leave feeling more knowledgeable and at ease than they were prior to tuning in.

Jordan Turner
Jordan is a Bay Area writer, social media manager, and content strategist.
Recommended Articles
What is the 10/20/30 rule for presentations and why it's important for your team, team building presentation tips that inspire instead of bore, why your team needs presentation management, lightning talks and ignite talks: a beginners guide.
Effective Presentations: Optimize the Learning Experience With Evidence-Based Multimedia Principles [Incl. Seminar]
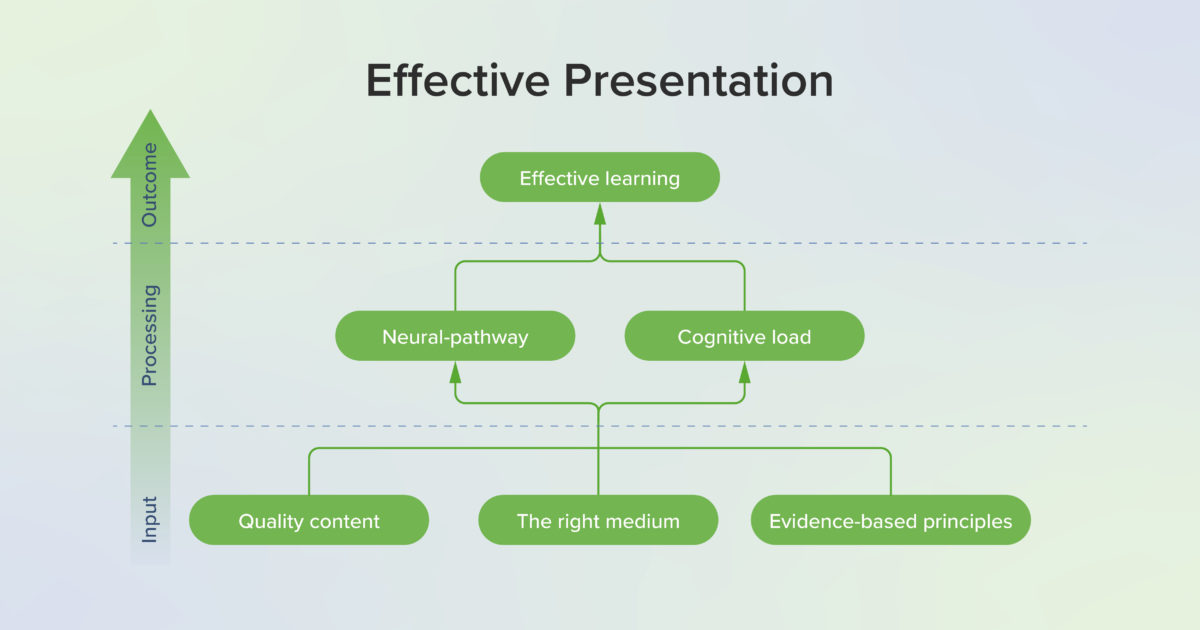
TABLE OF CONTENTS
What is an effective presentation.
Professional education requires presentations, from a small discussion or a short video to speaking to a lecture hall with an audience of hundreds. In fact, presentations are at the core of the educational process. With the effort to view all our educational efforts through an evidence-based lens, the construction of an effective presentation needs to undergo the same scrutiny. Whether a presenter intends to share plans, teach educational information, give updates on project progress, or convey the results of research, the extent to which the audience understands and remembers the presentation relies not only on the quality of the content but also the manner in which that content is presented. While the medium of the presentation may range from written content to graphics, videos, live presentations, or any combination of these and more, each of these mediums can be enhanced and made more effective by the use of evidence-based practices for presenting. Regardless of the medium, effective presentations have the same key features: they are appealing, engaging, informative, and concise. Effective presentations gain attention and captivate the audience, but most importantly, they convey information and ideas memorably.
With the integration of technology and online learning, educators have more opportunities than ever to present rich content that enhances and supports student learning. However, these opportunities can be intimidating to educators striving to engage students, as it can be daunting to create visually appealing and informative materials. Additionally, many educators feel pressured by the continued myth of learning styles: the widespread misconception that learning materials should match students’ visual, auditory, or kinesthetic “styles” to optimize learning (1). Despite being featured in many articles and discussions, there is no compelling evidence that matching educational content to learner’s style preferences increases educational outcomes. However, using multiple modes of delivery such as visuals, audio, and active learning has been shown to benefit all learners. In other words, no matter their stated preference, all learners benefit from a variety of media. Using evidence-based principles for multimedia content such as the principles found in Richard Mayer’s multimedia learning as well as the principles of graphic design and universal design supports learning and increases educational outcomes.
Why effective presentations work
What makes a presentation effective? Is an appealing and engaging presentation also an effective one? Research from cognitive science provides a foundation for understanding how verbal and pictorial information are processed by the learner’s mind during a presentation.
Mayer’s cognitive theory of multimedia learning
Based in cognitive science research, Mayer’s evidence-based approach to multimedia and cognition has greatly influenced both instructional design and the learning sciences. Mayer’s cognitive theory of multimedia learning comprises three learning principles: the dual channel principle, the limited capacity principle, and the active processing principle. Mayer’s cognitive theory of multimedia learning lays the theoretical foundation that underlies the practical applications to boost cognitive processes (2).
The dual channel principle proposes that learners process verbal and pictorial information via two separate channels (see figure below). Within each channel, learners can process limited amounts of information simultaneously due to limits in working memory, a phenomenon known as the limited capacity principle . In addition to these principles describing learning via the verbal and pictorial channels, the active processing principle proposes deeper learning occurs when learners are actively engaged in cognitive processing, such as attending to relevant information, creating mental schema to organize the material cognitively, and then relating to prior knowledge (3). These three principles work in tandem to describe the learning process that occurs when an audience of learners experiences a multimedia presentation.
Cognitive Load Theory, Adapted from Mayer (3) . Depicting how verbal and visual information is processed in dual channels through sensory, working, and long-term memory to create meaningful learning.
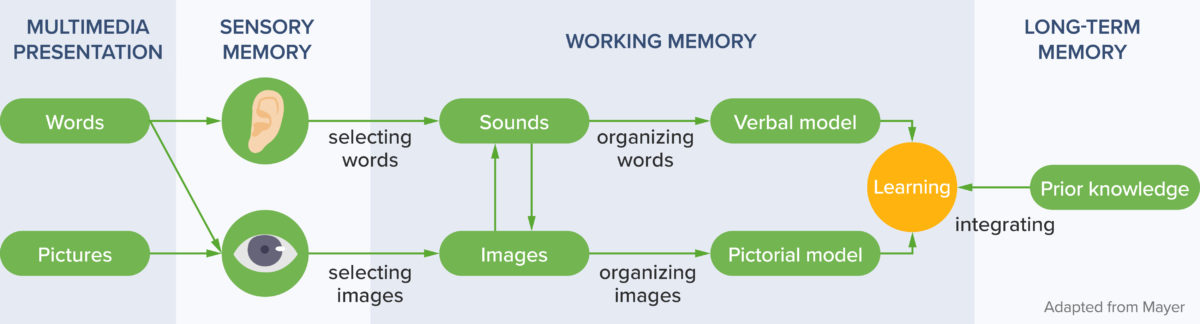
As learners listen to a lecture or watch a video, words and images are detected in the sensory memory and held for a very brief period of time. As the learners attend to relevant information, they are selecting words and images , which allows the selected information to move into the working memory where it may be held for a short period of time. However, working memory is limited to about 30 seconds and can only hold a few bits of information at a time. Organizing the words and images creates a coherent cognitive representation (schema) of these bits of information in the working memory. After the words and images are selected and then organized into schema, integrating these bits of information with prior knowledge from long term memory creates meaningful learning.
Cognitive Capacity . Three types of processing combine to determine cognitive capacity. To improve essential processing and generative processing, extraneous processing should be limited as much as possible .
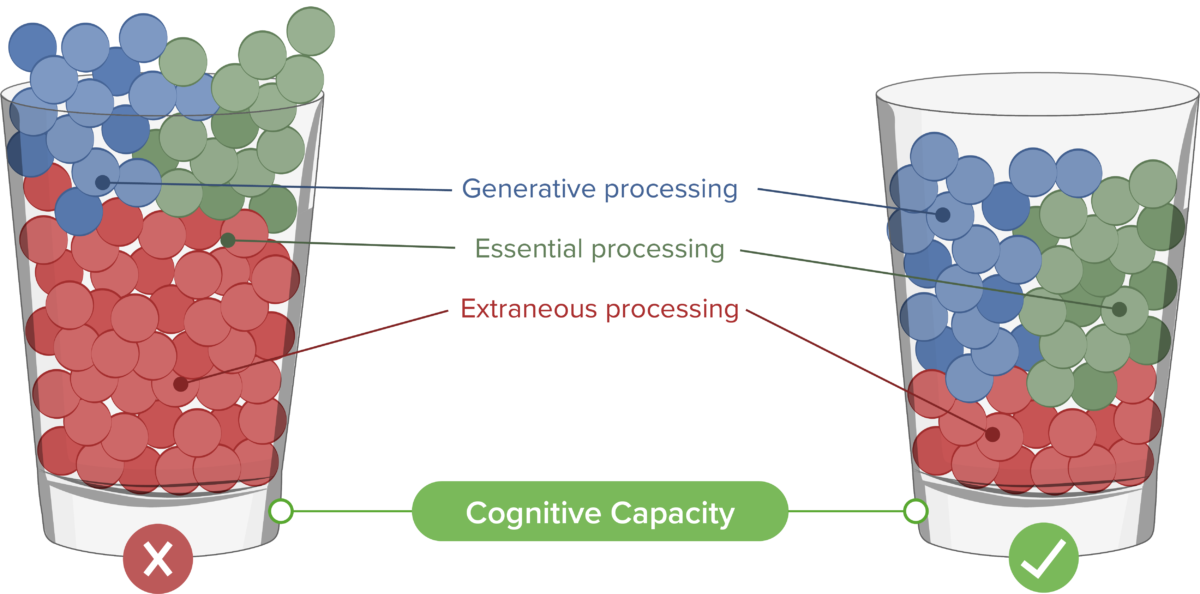
No matter how important the content may be, the capacity of learners to retain ideas from a single presentation is limited. The amount of information a learner can process as they select, organize, and integrate the ideas in a presentation relates to the cognitive load, which includes Essential, Extraneous, and Generative cognitive processing. Essential cognitive processing is required for the learner to create a cognitive representation of necessary and relevant information. This is the desired part of processing but should be managed to not overload the cognitive process. Extraneous processing refers to cognitive processing that does not contribute to learning and is often caused by poor design. Extraneous processing should be eliminated whenever possible to free up cognitive resources. Generative cognitive processing gives meaning to the material and creates deep learning. Learners must be motivated to engage and understand the information for this type of processing to occur.
Foundations in neuroscience
What we know about cognition and learning has been supported and informed by research in neuroscience (4). Neuroscience advances have also allowed us to gain deeper understanding into cognitive science principles, including those on multimedia learning. Researchers have been increasingly tracking learner eye movements to study learners’ attention and interest as a method of validating the impact of multimedia principles, and the results have supported the benefits of proper multimedia design on learner performance (5). Another avenue of research with great potential includes functional MRI (fMRI) readings or electroencephalography (EEG) (6). It has long been established that verbal and pictorial data is processed in different parts of the brain. More recently however, by examining changes in blood flow in different regions of the brain, researchers in Sweden were able to demonstrate that increased extraneous load could impact the effectiveness of learning, in line with the dual channel principle (7).
Evidence for effective presentations
Mayer’s multimedia principles.
Mayer’s Multimedia Principles.
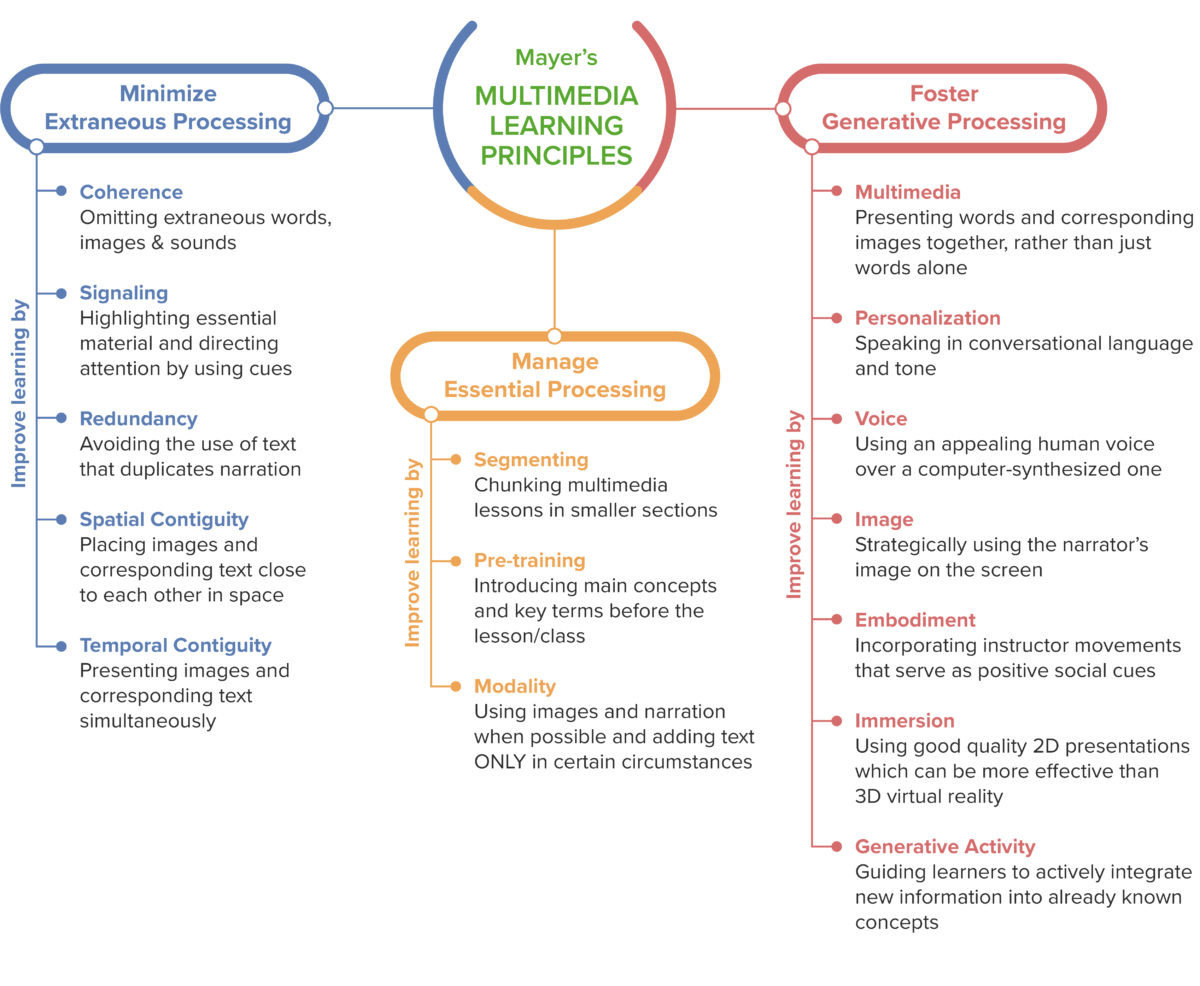
Mayer’s multimedia principles are a set of evidence-based guidelines for producing multimedia based on facilitating essential processing, reducing extraneous processing, and promoting generative processing (8). Mayer’s list of principles often includes fifteen principles, some of which have changed over time, and in a study conducted with medical students, the following nine principles were found to be particularly effective (3). The first three of these principles are used to reduce extraneous processing.
Principles for reducing extraneous processing:
- Coherence principle: eliminate extraneous material
- Signaling principle: highlight essential material
- Spatial contiguity principle: place printed words near corresponding graphics
To illustrate these principles, we will use a lesson about the kidneys. The instructor wants to make diagrams of the anatomy to use during discussion. The coherence principle says to only include the information necessary to the lesson. Graphics such as clip art, information that does not relate to anatomy, or unnecessary music reduces cognitive capacity. The signaling principle says to highlight essential material; this might include putting important content in bold or larger font. Or, if the kidney is shown in situ , the rest of the anatomy may be shown in grayscale or a much lighter color to de-emphasize it. The spatial contiguity principle says to place printed words, such as the labels, near the graphics.
Reduce extraneous processing . Do : keep labels next to diagrams, use only essential material, highlight essential material such as titles. Don’t: separate labels from diagrams, include extra facts, or have excessive text on a slide, especially with no indication of what is most important.
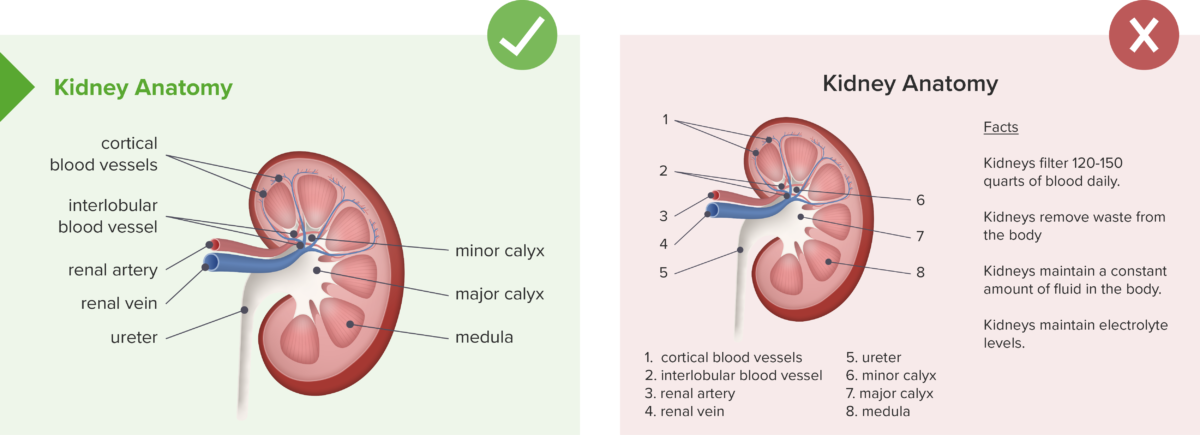
Principles for managing essential processing:
- Pre-training principle: provide pre-training in names and characteristics of key concepts
- Segmenting principle: break lessons into learner-controlled segments
- Modality principle: present words in spoken form
The next three principles are used to manage essential processing. If the kidney lesson moves into diseased states or diagnostics, the pre-training principle says that learners should be given information on any unfamiliar terminology before the lesson begins. To satisfy the segmenting principle , the learner should be able to control each piece of the lesson. For example, a “next” button may allow them to progress from pre-training to anatomy to diseased states and then diagnostics. The modality principle says that words should be spoken when possible. Voice-over can be used and text can be limited to essential material such as key definitions or lists.
Manage essential processing. Do: Present terms and key concepts first, break lessons into user-controlled segments, and present words in spoken form. Don’t: Give long blocks of text for students to read without priming students for key concepts.
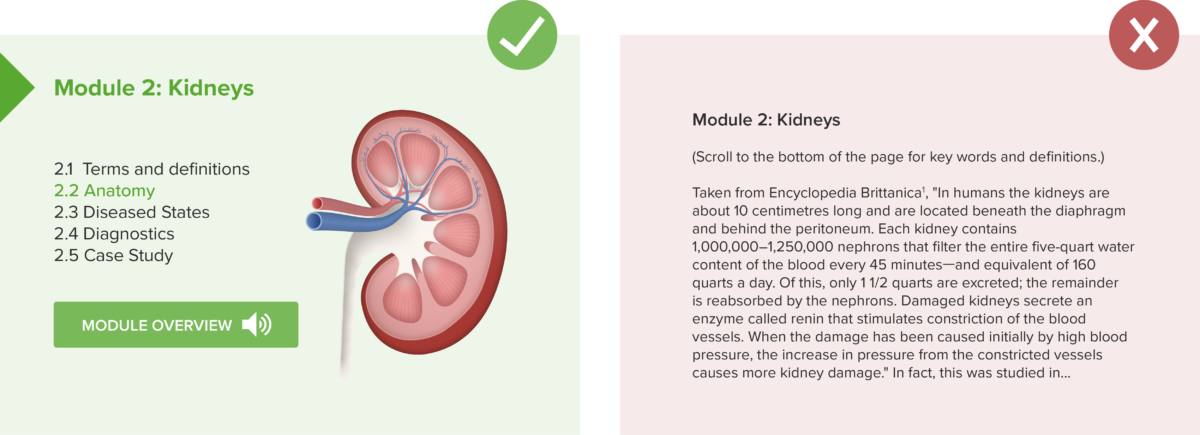
Principles for fostering generative processing:
- Multimedia principle: present words and pictures rather than words alone
- Personalization principle: present words in conversational or polite style
- Voice principle: use a human voice rather than a machine voice
Mayer’s work also includes principles to increase generative processing. The multimedia principle is a direct result of the dual channel principle and limited capacity principle. Words and pictures together stimulate both channels and allow the memory to process more information than words alone. To adhere to the personalization principle to promote deeper learning, a case study is better presented as a story than a page of diagnostics and patient demographics. Finally, the voice principle says that a human voice is more desirable, so it is better to use the instructor’s voice when doing voice-overs rather than auto-generated readers.
Foster generative processing. Do: Present words and pictures, present words in conversational style, and use a human voice. Don’t: Present text only, present words as a list of facts or overly technical language, or use a computer-generated voice.
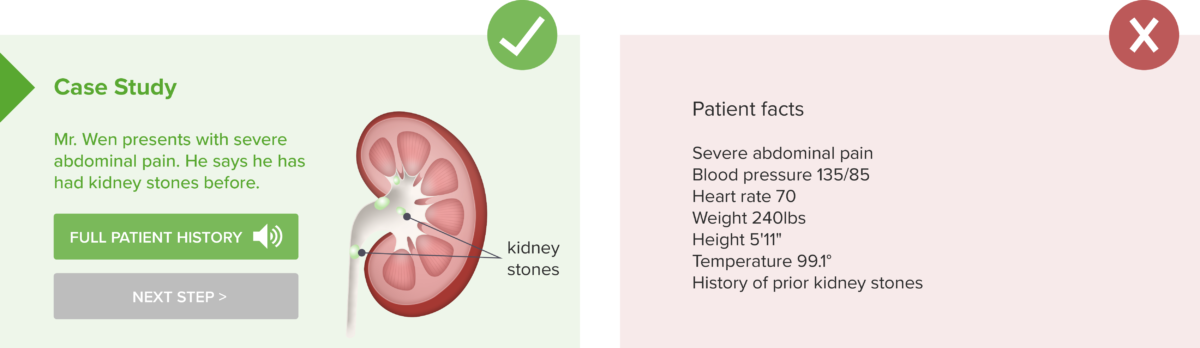
Additional multimedia principles:
- Temporal contiguity principle: present words and pictures simultaneously rather than successively
- Redundancy principle: for a fast paced lesson, people learn better from graphics and narration rather than graphics, narration, and text
- Image principle: people do not learn better if a static image of the instructor is added to the presentation
Additional principles include the temporal contiguity principle , which states that words and pictures should be shown simultaneously rather than successively. This also includes narration and images or animation. For example, if an animation demonstrates normal cell division, the narration should be given during the animation, not after. The redundancy principle states that people do not necessarily learn better if text is added to graphics and narration. The duplication of information creates extraneous processing as learners try to process print and spoken text. The image principle states that learners do not learn better if a static image of the instructor is added to a presentation. For example, if students are watching an animation with normal cell division, they do not learn better if an image of their instructor is placed next to the animation.
Additional principles for fostering generative processing:
- Embodiment principle: onscreen instructors should display high embodiment not low
- Immersion principle: 3D virtual reality is not necessarily better than 2D presentations
- Generative activity principle: use generative learning activities during learning
In the newest edition of Mayer’s Multimedia Learning (8), three additional principles have been added. The embodiment principle states that onscreen instructors should display high embodiment rather than low embodiment, meaning they should use natural gestures, look at the camera as if making eye contact, and if drawing, show the image being drawn. If demonstrating something like a surgical procedure, a first-person perspective should be used so the learner sees the perspective of the person performing. Low embodiment would include standing still, lack of eye contact, and using a third-person perspective. The immersion principle states that 3D immersive virtual reality is not necessarily more effective than 2D presentations, such as on a computer screen. This is thought to be caused by the cognitive load on the learning involved in using 3D immersive technology but more studies are needed. Lastly, the generative activity principle states that learners should use generative learning activities while learning such as summarizing, mapping, drawing, imagining, self-testing, self-explaining, teaching, and enacting. These activities help learners cognitively select and organize new material and then integrate with prior knowledge.
Other Design Principles
Mayer’s design principles are functional but do not address aesthetics per se . Anyone can master the basic graphic design principles as discussed by Reynolds (9) to captivate and engage an audience.
- Create graphics that are designed for the back of the room. Whatever the venue, the person in the back needs to be able to see and gather information from the graphics. Ensure font size is appropriate, image size and clarity is sufficient, and that font type and spacing allow words to be seen clearly from a distance. For online materials, this principle may mean designing for the person who will be viewing on the smallest screen (such as a phone) rather than assuming viewers will use a large monitor (10).
- Limit the types of fonts. Too many fonts or fonts that don’t coordinate well can make graphics seem jarring and unpleasant. Some programs will suggest font families that are appealing, and a safe guideline is to limit to two or three fonts maximum per graphic.
- Use contrasting colors. Colors that are too similar or using type on top of images that lack contrast can make type difficult to read. Color family suggestions can be found online or in software such as Powerpoint.
Graphic design principles. Do: Use coordinating fonts and color schemes with contrasting colors. Don’t: use multiple fonts, excessive colors, and/or non-contrasting colors that may be difficult to distinguish.
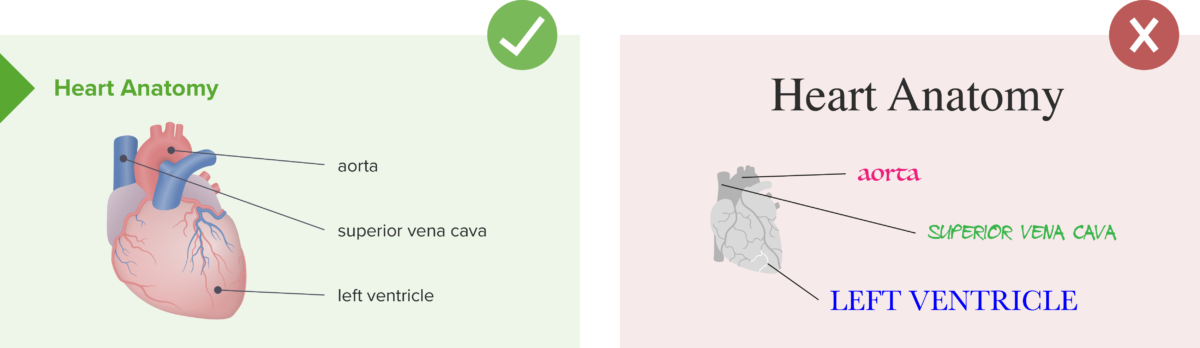
In addition to singular graphics or presentations, online course presentation makes a difference in how learners perceive and utilize a course. When designing online learning experiences, consider using guidelines such as Quality Matters to assess the functionality. Quality Matters rubrics look at key components that have been proven to facilitate learning by making navigation and presentation of course elements explicit. Key components include providing information on how to get started, including learning objectives, allowing learners to track their progress, and using learning activities and technology tools that support active learning. Navigation among course components should facilitate access to materials.
In addition to all of these principles, accessibility must be considered in all forms of presentation. In education, designing for accessibility can be guided by universal design principles . Some schools may even require all courses and materials to be fully accessible. Providing accessible options has been shown to benefit all learners, not just those with a documented need for accommodations (11). Some basic accommodations that should be offered in any class include offering media in multiple modes. For example, videos should have the option of captioning and/or access to a transcript, and photos and graphics should have captions that describe the image. Many learning management systems and software programs now have options to check for accessibility. Additionally, most schools can provide assistance in assessing and developing accessible materials.
Practical Applications for Presentations in Health Professions Education
Implementation in the classroom.
When planning how to present materials in the classroom, first consider the most effective form of presentation for the given information. It may be a Powerpoint, a video, a graphic, or a handout. Consider using a variety of media appropriate for the intended outcomes. Creating high quality materials may seem daunting, but quality content can be reused, shared, and has been shown to enhance student learning.
Powerpoint has been much maligned for overuse and abuse, but well-designed presentations can be remarkably effective (12). When designing in Powerpoint, limit the amount of text per slide. One rule to remember is the 5/5/5 rule: Use no more than 5 lines of text with 5 words each or 5 text-heavy slides in a row and try to avoid bullets (13). Graphics are preferable to text or tables when representing data, but graphs and labels should be kept as simple as possible using 2D graphics and simplified labels that are easy for viewers to see (14). When presenting, refrain from reading from the slides. Slides should highlight important concepts and provide visual aids, not present everything. In addition, keep Powerpoint and video presentations short; most listeners will lose attention in 6–10 minutes (15,16). Whenever possible, engage the audience by interspersing active learning elements. Between sections or topics, transition slides can be used to indicate pauses for activity or reflection or to cue students to changes in topic (14).
When planning a presentation, consider presenting some of the information online before class for students to review. This flipped classroom technique allows for more class to be spent using active learning and facilitates the presentation of multiple forms of media and accessible options.
Implementation online
Videos often become an integral part of the online learning experience. To facilitate learning, consider the following tips for your own video production (17,18):
- Align the video with learning objectives and course outcomes. Focus on pertinent instructional points to reduce extraneous processing and thereby reduce cognitive load.
- Limit the length of videos and use interactive elements to promote active learning. To help maintain student engagement and deepen learning, include interactive elements such as discussions, quizzes or embedded questions to maintain student attention.
- Limit extraneous information, graphics, and sounds that do not pertain to the learning goals (19). Busy backgrounds, music, or animations that don’t contribute to understanding concepts unnecessarily add to a learner’s cognitive load.
- When using existing videos, ensure the source is reliable and the video is high quality. Video production can take time, so using professional videos can be beneficial if they come from credible sources that target the learning objectives with up-to-date and accurate information.
Additionally, Schooley et al. (18) have proposed a 25-item quality checklist that can help educators create and curate high-quality videos. Many of the items in the checklist have been discussed here such as length, captioning, using relevant graphics, and self-assessment opportunities, but also included are other points an educator should consider, such as the offering learners the ability to download files and adjust playback speed as well as providing them with recommendations for further reading.
For a course in any modality, creating and curating content online can save time and facilitate student learning. As you consider what material to create and use for your courses, assess existing material using the guidelines above to determine if it could be made more beneficial to learners. Does it follow Mayer’s principles? Does it follow graphic design principles and universal design principles? Consider using a Quality Matters rubric to check the course design for best practices.
Recommendations
Educator’s perspective.
- Use Mayer’s multimedia design principles to revise existing presentations and review new creations for simple changes that can make a big difference (12).
- When delivering a presentation, start by discussing an unusual case, presenting an interesting story or an unexpected statistic, or explain how the topic impacts the listeners. This personalization will help gain their attention from the start (13).
- When designing your own materials and graphics, “less is more” is often a good guideline: limit the amount of information on slides, limit the types of fonts, and limit the excessive use of colors (9,12).
- Videos should be limited to 5–6 minutes when possible and avoid exceeding 10 minutes. Break up longer videos and intersperse interactive elements to keep students engaged (15–17).
- When using technology and online delivery, universal design and accessibility considerations can be complicated. See if your school has an expert that can review your materials to ensure all students will benefit.
Student perspective
- When creating presentations, reports, and charts, follow Mayer’s multimedia design principles to ensure your audience gets the most from your presentation.
- Avoid copy/pasting but rather try and present concepts in an original way in order to augment your understanding of the material.
- When looking at materials online, look for options such as captioning, transcripts, or audio buttons for accessing additional media output.
- If a presentation is lengthy, pause and insert your own activities to help yourself stay focused. Taking notes, pausing for reflection, and self-quizzing can help deepen your learning and keep your mind from wandering.
- If a variety of media aren’t offered, consider finding your own to supplement your learning. Credible sources with learning objectives that align with your course can augment your learning experience.
(Please select all that apply)
1. When creating a graphic about the current status of heart disease in the US, which of the following would align with best practices?
a. Gaining the audience’s attention with a picture of your dog.
b. Using 3 colors that coordinate well on a contrasting background.
c. A 2D graph with simple labels rather than a table of data.
d. An image on the left with labels listed separately on the right.
e. An image next to a paragraph of text that you will read for the audience.
2. Which of the following are true about educational videos?
a. They need to be created by professionals to be high-quality.
b. They should be less than 10 minutes.
c. There should be an option for closed captioning or a written transcript.
d. Longer videos may be used but should be broken up with active learning elements.
e. Videos don’t need to align to objectives as long as they’re well-made.
3. Which of the following would be examples of Mayer’s multimedia principles?
a. Using a human voice rather than a machine voice.
b. Using formal language instead of conversational language.
c. Playing soothing music in the background of a video.
d. Providing new words and definitions before the presentation begins.
e. Putting important words in bold for emphasis.
4. Which of these would follow best practices for online content?
a. Creating a module where all the material is on one page for easy access.
b. Adding buttons for next, back, and table of contents options for students to navigate.
c. Breaking material into 7-minute videos with practice questions between them.
d. Adding fun clip art and cool images to the pages even if it doesn’t directly relate to the content.
e. Having text only because images are distracting.
Answers: (1) b,c. (2) b,c,d. (3) a,d,e. (4) b,c.
Online Seminar
This online seminar and its accompanying article will focus on the topic of Effective Presentations, which have a set of key qualities: they are appealing, engaging, informative, and concise. Effective presentations gain attention and captivate the audience, but most importantly, they convey information and ideas memorably and efficiently. Using evidence-based principles in educational multimedia can ensure the development of high-quality learning experiences. Our host, Dr. Peter Horneffer will be sharing with us some key multimedia concepts that can help facilitate the development and implementation of effective multimedia into the educational process.
Watch the seminar recording:
Would you like to learn more? Explore the Pulse Seminar Library.
Share this page:

Meredith Ratliff is a doctoral student in Instructional Design and Technology at the University of Central Florida. Her research interests include evidence-based medical education, branching scenarios, and faculty development. She has received her B.S. and M.A.T. in Mathematics at the University of Florida and her MA in Instructional Design and Technology from UCF. She has been an Associate Faculty member in the mathematics department at Valencia College in Kissimmee, Florida for the past nine years. As part of the Learning Science team at Lecturio, she serves as an educational consultant helping to design and develop materials for medical educators.
Satria Nur Sya’ban is a doctor from Indonesia who graduated from Universitas Airlangga. While a student, he served as the president of CIMSA, a national medical student NGO, working on a diverse range of issues that included medical education and curriculum advocacy by medical students. Before graduating, he took two gap years to serve as a Regional Director, and subsequently as Vice-President, of the International Federation of Medical Students’ Associations (IFMSA)*, working on and developing various initiatives to better empower medical student organizations to make a change at the national level. At Lecturio, he serves as a Medical Education Consultant, supporting Lecturio in developing and maintaining partnerships with student organizations and universities in Asia, as well as providing counsel on how Lecturio can fit in existing teaching models and benefit students’ learning experience.
*IFMSA has been one of the leading global health organizations worldwide since 1951, representing over 1.3 million medical students as members spanning over 123 countries.

Adonis is a doctor from Lebanon who graduated from the University of Balamand. He was a research fellow at the Department of Emergency Medicine at the American University of Beirut Medical Center and has worked with the World Health Organization Regional Office of the Eastern Mediterranean. During his studies, Adonis served as the president of the Lebanese Medical Students’ International Committee (LeMSIC), a national medical student organization in Lebanon, and moved on to serve as the Regional Director of the Eastern Mediterranean Region of the IFMSA*. Among his roles as Regional Director, he focused on medical education advocacy, oversaw collaborations with external partners, and undertook several medical education projects and initiatives around the region. As a Medical Education Consultant at Lecturio, he advises the Lecturio team on how the platform can fit in existing teaching models and benefit students’ learning experience, develops and maintains partnerships with student organizations and universities in the MENA region, and conducts research on learning science and evidence-based strategies.

Sarah Haidar is an educator and educational specialist from Lebanon who has graduated with a BA in English Linguistics and a Secondary Teaching Diploma (T.D.) from Haigazian University in Beirut, Lebanon. She has received her M.Ed. in Teaching English as a Second Language (TESOL) from the Lebanese International University. She has been teaching ESL classrooms at the Deutsche Internationale Schule for four years. As part of the administrative team at the All American Institute of Medical Sciences (AAIMS), she is working on the design and implementation of a set of academic and administrative reforms that can help both faculty and students in their professional and academic endeavors. She has joined Lecturio to support the Learning Science team in the writing and communication based tasks that might be needed to announce and market their services and events that are targeted at medical educators. She is also supporting the Learning Science team with her perspective on educational and pedagogical topics that will inform the general audience of educators.

Sara Keeth is a Ph.D. and certified PMP (Project Management Professional) who graduated from the University of Texas at Dallas. As an educator, she has worked as a Teaching Fellow at the University of Texas at Dallas, as a full-time professor at Richland College (now Dallas College’s Richland Campus), and has also taught at Austin College. Dr. Keeth has also worked as a consultant for Parker University’s Research Center and has a decade of experience as an operations manager for an advertising agency. As Senior Learning Science and Research Project Manager at Lecturio, she manages the Learning Science department’s activities, shares her education expertise and best practices for medical educators, and develops evidence-based content for both students and faculty.
- Newton PM. The Learning Styles Myth is Thriving in Higher Education. Front Psychol [Internet]. 2015 [cited 2022 Jun 3];6. Available from: https://www.frontiersin.org/article/10.3389/fpsyg.2015.01908
- Mayer R, Mayer RE. The Cambridge Handbook of Multimedia Learning. Cambridge University Press; 2005. 688 p.
- Mayer RE. Applying the science of learning to medical education. Med Educ [Internet]. 2010 [cited 2022 Mar 23];44(6):543–9. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2923.2010.03624.x
- Ng B, Ong AKK. Neuroscience and digital learning environment in universities: What do current research tell us? J Scholarsh Teach Learn [Internet]. 2018 Oct 2 [cited 2022 Jun 4];18(3). Available from: https://scholarworks.iu.edu/journals/index.php/josotl/article/view/22651
- Alemdag E, Cagiltay K. A systematic review of eye tracking research on multimedia learning. Comput Educ [Internet]. 2018 Oct 1 [cited 2022 Jun 9];125:413–28. Available from: https://www.sciencedirect.com/science/article/pii/S0360131518301660
- Dan A, Reiner M. Real Time EEG Based Measurements of Cognitive Load Indicated Mental States During Learning. 2017;9(2):14.
- Sörqvist P, Dahlström Ö, Karlsson T, Rönnberg J. Concentration: The Neural Underpinnings of How Cognitive Load Shields Against Distraction. Front Hum Neurosci [Internet]. 2016 [cited 2022 Jun 9];10. Available from: https://www.frontiersin.org/article/10.3389/fnhum.2016.00221
- Mayer RE. Multimedia Learning. 3rd ed. Cambridge University Press; 2021. 450 p.
- Reynolds G. Presentation Zen: Simple Ideas on Presentation Design and Delivery. New Riders; 2011. 462 p.
- Elias T. Universal instructional design principles for mobile learning. Int Rev Res Open Distrib Learn [Internet]. 2011 Feb 28 [cited 2022 Jun 15];12(2):143. Available from: http://www.irrodl.org/index.php/irrodl/article/view/965
- Shimoni R, Barrington G, Wilde R, Henwood S. Addressing the needs of diverse distributed students. Int Rev Res Open Distrib Learn [Internet]. 2013 Jul 5 [cited 2022 Jun 10];14(3):134–57. Available from: https://www.irrodl.org/index.php/irrodl/article/view/1413
- Grech V. The application of the Mayer multimedia learning theory to medical PowerPoint slide show presentations. J Vis Commun Med [Internet]. 2018 Jan 2 [cited 2022 Jun 10];41(1):36–41. Available from: https://doi.org/10.1080/17453054.2017.1408400
- Vogel WH, Viale PH. Presenting With Confidence. J Adv Pract Oncol [Internet]. 2018 [cited 2022 Jun 10];9(5):545–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6505544/
- Lenz PH, McCallister JW, Luks AM, Le TT, Fessler HE. Practical Strategies for Effective Lectures. Ann Am Thorac Soc [Internet]. 2015 Apr [cited 2022 Jun 6];12(4):561–6. Available from: http://www.atsjournals.org/doi/10.1513/AnnalsATS.201501-024AR
- Guo P, Kim J, Rubin R. How video production affects student engagement: An empirical study of MOOC videos. 2014. 41 p.
- Carmichael M, Reid AK, Karpicke JD. Assessing the Impact of Educational Video on Student Engagement, Critical Thinking and Learning: :24. Available from: https://us.sagepub.com/sites/default/files/hevideolearning.pdf
- Dong C, Goh PS. Twelve tips for the effective use of videos in medical education. Med Teach [Internet]. 2015 Feb 1 [cited 2022 Jun 6];37(2):140–5. Available from: https://doi.org/10.3109/0142159X.2014.943709
- Schooley SP, Tackett S, Peraza LR, Shehadeh LA. Development and piloting of an instructional video quality checklist (IVQC). Med Teach [Internet]. 2022 Mar 4 [cited 2022 Jun 10];44(3):287–93. Available from: https://doi.org/10.1080/0142159X.2021.1985099
- Brame CJ. Effective educational videos [Internet]. Vanderbilt University. [cited 2022 Jun 10]. Available from: https://cft.vanderbilt.edu/guides-sub-pages/effective-educational-videos/
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Next Online Event
Never miss a pulse.
Get our insights direct to your inbox
- Wednesday, 17 April
- 9:00 PT | 12:00 ET | 18:00 CEST
- Wednesday Jan 24 at 09:00am ET
- Thursday Jan 25 at 12:00pm ET
Sign up for emails on new Lecturio Pulse content.
Never miss a pulse. We’ll email you when new content is published.
User Reviews
Get premium to test your knowledge.
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to present...
How to present clinical cases
- Related content
- Peer review
- Ademola Olaitan , medical student 1 ,
- Oluwakemi Okunade , final year medical student 1 ,
- Jonathan Corne , consultant physician 2
- 1 University of Nottingham
- 2 Nottingham University Hospitals
Presenting a patient is an essential skill that is rarely taught
Clinical presenting is the language that doctors use to communicate with each other every day of their working lives. Effective communication between doctors is crucial, considering the collaborative nature of medicine. As a medical student and later as a doctor you will be expected to present cases to peers and senior colleagues. This may be in the setting of handovers, referring a patient to another specialty, or requesting an opinion on a patient.
A well delivered case presentation will facilitate patient care, act a stimulus for timely intervention, and help identify individual and group learning needs. 1 Case presentations are also used as a tool for assessing clinical competencies at undergraduate and postgraduate level.
Medical students are taught how to take histories, examine, and communicate effectively with patients. However, we are expected to learn how to present effectively by observation, trial, and error.
Principles of presentation
Remember that the purpose of the case presentation is to convey your diagnostic reasoning to the listener. By the end of your presentation the examiner should have a clear view of the patient’s condition. Your presentation should include all the facts required to formulate a management plan.
There are no hard and fast rules for a perfect presentation, rather the content of each presentation should be determined by the case, the context, and the audience. For example, presenting a newly admitted patient with complex social issues on a medical ward round will be very different from presenting a patient with a perforated duodenal ulcer who is in need of an emergency laparotomy.
Whether you’re presenting on a busy ward round or during an objective structured clinical examination (OSCE), it is important that you are concise yet get across all the important points. Start by introducing patients with identifiers such as age, sex, and occupation, and move on to the complaint that they presented with or the reason that they are in hospital. The presenting complaint is an important signpost and should always be clearly stated at the start of the presentation.
Presenting a history
After you’ve introduced the patient and stated the presenting complaint, you can proceed in a chronological approach—for example, “Mr X came in yesterday with worsening shortness of breath, which he first noticed four days ago.” Alternatively you can discuss each of the problems, starting with the most pertinent and then going through each symptom in turn. This method is especially useful in patients who have several important comorbidities.
The rest of the history can then be presented in the standard format of presenting complaint, history of presenting complaint, medical history, drug history, family history, and social history. Strictly speaking there is no right or wrong place to insert any piece of information. However, in some instances it may be more appropriate to present some information as part of the history of presenting complaints rather than sticking rigidly to the standard format. For example, in a patient who presents with haemoptysis, a mention of relevant risk factors such as smoking or contacts with tuberculosis guides the listener down a specific diagnostic pathway.
Apart from deciding at what point to present particular pieces of information, it is also important to know what is relevant and should be included, and what is not. Although there is some variation in what your seniors might view as important features of the history, there are some aspects which are universally agreed to be essential. These include identifying the chief complaint, accurately describing the patient’s symptoms, a logical sequence of events, and an assessment of the most important problems. In addition, senior medical students will be expected to devise a management plan. 1
The detail in the family and social history should be adapted to the situation. So, having 12 cats is irrelevant in a patient who presents with acute appendicitis but can be relevant in a patient who presents with an acute asthma attack. Discerning the irrelevant from the relevant is not always easy, but it comes with experience. 2 In the meantime, learning about the diseases and their associated features can help to guide you in the things you need to ask about in your history. Indeed, it is impossible to present a good clinical history if you haven’t taken a good history from the patient.

Presenting examination findings
When presenting examination findings remember that the aim is to paint a clear picture of the patient’s clinical status. Help the listener to decide firstly whether the patient is acutely unwell by describing basics such as whether the patient is comfortable at rest, respiratory rate, pulse, and blood pressure. Is the patient pyrexial? Is the patient in pain? Is the patient alert and orientated? These descriptions allow the listener to quickly form a mental picture of the patient’s clinical status. After giving an overall picture of the patient you can move on to present specific findings about the systems in question. It is important to include particular negative findings because they can influence the patient’s management. For example, in a patient with heart failure it is helpful to state whether the patient has a raised jugular venous pressure, or if someone has a large thyroid swelling it is useful to comment on whether the trachea is displaced. Initially, students may find it difficult to know which details are relevant to the case presentation; however, this skill becomes honed with increasing knowledge and clinical experience.
Presenting in an exam
Although the same principles as presenting in other situations also apply in an exam setting, the exam situation differs in the sense that its purpose is for you to show your clinical competence to the examiner.
It’s all about making a good impression. Walk into the room confidently and with a smile. After taking the history or examining the patient, turn to the examiner and look at him or her before starting to present your findings. Avoid looking back at the patient while presenting. A good way to avoid appearing fiddly is to hold your stethoscope behind your back. You can then wring to your heart’s content without the examiner sensing your imminent nervous breakdown.
Start with an opening statement as you would in any other situation, before moving on to the main body of the presentation. When presenting the main body of your history or examination make sure that you show the examiner how your findings are linked to each other and how they come together to support your conclusion.
Finally, a good summary is just as important as a good introduction. Always end your presentation with two or three sentences that summarise the patient’s main problem. It can go something like this: “In summary, this is Mrs X, a lifelong smoker with a strong family history of cardiovascular disease, who has intermittent episodes of chest pain suggestive of stable angina.”
Improving your skills
The RIME model (reporter, interpreter, manager, and educator) gives the natural progression of the clinical skills of a medical student. 3 Early on in clinical practice students are simply reporters of information. As the student progresses and is able to link together symptoms, signs, and investigation results to come up with a differential diagnosis, he or she becomes an interpreter of information. With further development of clinical skills and increasing knowledge students are actively able to suggest management plans. Finally, managers progress to become educators. The development from reporter to manager is reflected in the student’s case presentations.
The key to improving presentation skills is to practise, practise, and then practise some more. So seize every opportunity to present to your colleagues and seniors, and reflect on the feedback you receive. 4 Additionally, by observing colleagues and doctors you can see how to and how not to present.
Remember the purpose of the presentation
Be flexible; the context should dictate the content of the presentation
Always include a presenting complaint
Present your findings in a way that shows understanding
Have a system
Use appropriate terminology
Additional tips for exams
Start with a clear introductory statement and close with a brief summary
After your summary suggest a working diagnosis and a management plan
Practise, practise, practise, and get feedback
Present with confidence, and don’t be put off by an examiner’s poker face
Be honest; do not make up signs to fit in with your diagnosis
Originally published as: Student BMJ 2010;18:c1539
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
See “Medical ward rounds” ( Student BMJ 2009;17:98-9, http://archive.student.bmj.com/issues/09/03/life/98.php ).
- ↵ Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: Opinions of internal medicine clerkship directors. J Gen Intern Med 2009 ; 24 : 370 -3. OpenUrl CrossRef PubMed Web of Science
- ↵ Lingard LA, Haber RJ. What do we mean by “relevance”? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format. Acad Med 1999 ; 74 : S124 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med 1999 ; 74 : 1203 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Haber RJ, Lingard LA. Learning oral presentation skills: a rhetorical analysis with pedagogical and professional implications. J Gen Intern Med 2001 ; 16 : 308 -14. OpenUrl CrossRef PubMed Web of Science

- Free Study Planner
- Residency Consulting
- Free Resources
- Med School Blog
- 1-888-427-7737
The Ultimate Patient Case Presentation Template for Med Students
- by Neelesh Bagrodia
- Apr 06, 2024
- Reviewed by: Amy Rontal, MD

Knowing how to deliver a patient presentation is one of the most important skills to learn on your journey to becoming a physician. After all, when you’re on a medical team, you’ll need to convey all the critical information about a patient in an organized manner without any gaps in knowledge transfer.
One big caveat: opinions about the correct way to present a patient are highly personal and everyone is slightly different. Additionally, there’s a lot of variation in presentations across specialties, and even for ICU vs floor patients.
My goal with this blog is to give you the most complete version of a patient presentation, so you can tailor your presentations to the preferences of your attending and team. So, think of what follows as a model for presenting any general patient.
Here’s a breakdown of what goes into the typical patient presentation.

7 Ingredients for a Patient Case Presentation Template
1. the one-liner.
The one-liner is a succinct sentence that primes your listeners to the patient.
A typical format is: “[Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y].
2. The Chief Complaint
This is a very brief statement of the patient’s complaint in their own words. A common pitfall is when medical students say that the patient had a chief complaint of some medical condition (like cholecystitis) and the attending asks if the patient really used that word!
An example might be, “Patient has chief complaint of difficulty breathing while walking.”
3. History of Present Illness (HPI)
The goal of the HPI is to illustrate the story of the patient’s complaint.
I remember when I first began medical school, I had a lot of trouble determining what was relevant and ended up giving a lot of extra details. Don’t worry if you have the same issue. With time, you’ll learn which details are important.
The OPQRST Framework
In the beginning of your clinical experience, a helpful framework to use is OPQRST:
Describe when the issue started, and if it occurs during certain environmental or personal exposures.
P rovocative
Report if there are any factors that make the pain better or worse. These can be broad, like noting their shortness of breath worsened when lying flat, or their symptoms resolved during rest.
Relay how the patient describes their pain or associated symptoms. For example, does the patient have a burning versus a pressure sensation? Are they feeling weakness, stiffness, or pain?
R egion/Location
Indicate where the pain is located and if it radiates anywhere.
Talk about how bad the pain is for the patient. Typically, a 0-10 pain scale is useful to provide some objective measure.
Discuss how long the pain lasts and how often it occurs.
A Case Study
While the OPQRST framework is great when starting out, it can be limiting.
Let’s take an example where the patient is not experiencing pain and comes in with altered mental status along with diffuse jaundice of the skin and a history of chronic liver disease. You will find that certain sections of OPQRST do not apply.
In this event, the HPI is still a story, but with a different framework. Try to go in chronological order. Include relevant details like if there have been any changes in medications, diet, or bowel movements.
Pertinent Positive and Negative Symptoms
Regardless of the framework you use, the name of the game is pertinent positive and negative symptoms the patient is experiencing.
I’d like to highlight the word “pertinent.” It’s less likely the patient’s chronic osteoarthritis and its management is related to their new onset shortness of breath, but it’s still important for knowing the patient’s complete medical picture. A better place to mention these details would be in the “Past Medical History” section, and reserve the HPI portion for more pertinent history.
As you become exposed to more illness scripts, experience will teach you which parts of the history are most helpful to state. Also, as you spend more time on the wards, you will pick up on which questions are relevant and important to ask during the patient interview.
By painting a clear picture with pertinent positives and negatives during your presentation, the history will guide what may be higher or lower on the differential diagnosis.
Some other important components to add are the patient’s additional past medical/surgical history, family history, social history, medications, allergies, and immunizations.
The HEADSSS Method
Particularly, the social history is an important time to describe the patient as a complete person and understand how their life story may affect their present condition.
One way of organizing the social history is the HEADSSS method:
– H ome living situation and relationships – E ducation and employment – A ctivities and hobbies – D rug use (alcohol, tobacco, cocaine, etc.) Note frequency of use, and if applicable, be sure to add which types of alcohol consumption (like beer versus hard liquor) and forms of drug use. – S exual history (partners, STI history, pregnancy plans) – S uicidality and depression – S piritual and religious history
Again, there’s a lot of variation in presenting social history, so just follow the lead of your team. For example, it’s not always necessary/relevant to obtain a sexual history, so use your judgment of the situation.
4. Review of Symptoms
Oftentimes, most elements of this section are embedded within the HPI. If there are any additional symptoms not mentioned in the HPI, it’s appropriate to state them here.
5. Objective
Vital signs.
Some attendings love to hear all five vital signs: temperature, blood pressure (mean arterial pressure if applicable), heart rate, respiratory rate, and oxygen saturation. Others are happy with “afebrile and vital signs stable.” Just find out their preference and stick to that.
Physical Exam
This is one of the most important parts of the patient presentation for any specialty. It paints a picture of how the patient looks and can guide acute management like in the case of a rigid abdomen. As discussed in the HPI section, typically you should report pertinent positives and negatives. When you’re starting out, your attending and team may prefer for you to report all findings as part of your learning.
For example, pulmonary exam findings can be reported as: “Regular chest appearance. No abnormalities on palpation. Lungs resonant to percussion. Clear to auscultation bilaterally without crackles, rhonchi, or wheezing.”
Typically, you want to report the physical exams in a head to toe format: General Appearance, Mental Status, Neurologic, Eyes/Ears/Nose/Mouth/Neck, Cardiovascular, Pulmonary, Breast, Abdominal, Genitourinary, Musculoskeletal, and Skin. Depending on the situation, additional exams can be incorporated as applicable.
Now comes reporting pertinent positive and negative labs. Several labs are often drawn upon admission. It’s easy to fall into the trap of reading off all the labs and losing everyone’s attention. Here are some pieces of advice:
You normally can’t go wrong sticking to abnormal lab values.
One qualification is that for a patient with concern for acute coronary syndrome, reporting a normal troponin is essential. Also, stating the normalization of previously abnormal lab values like liver enzymes is important.
Demonstrate trends in lab values.
A lab value is just a single point in time and does not paint the full picture. For example, a hemoglobin of 10g/dL in a patient at 15g/dL the previous day is a lot more concerning than a patient who has been stable at 10g/dL for a week.
Try to avoid editorializing in this section.
Save your analysis of the labs for the assessment section. Again, this can be a point of personal preference. In my experience, the team typically wants the raw objective data in this section.
This is also a good place to state the ins and outs of your patient (if applicable). In some patients, these metrics are strictly recorded and are typically reported as total fluid in and out over the past day followed by the net fluid balance. For example, “1L in, 2L out, net -1L over the past 24 hours.”
6. Diagnostics/Imaging
Next, you’ll want to review any important diagnostic tests and imaging. For example, describe how the EKG and echo look in a patient presenting with chest pain or the abdominal CT scan in a patient with right lower quadrant abdominal pain.
Try to provide your own interpretation to develop your skills and then include the final impression. Also, report if a diagnostic test is still pending.
7. Assessment/Plan
This is the fun part where you get to use your critical thinking (aka doctor) skills! For the scope of this blog, we’ll review a problem-based plan.
It’s helpful to begin with a summary statement that incorporates the one-liner, presenting issue(s)/diagnosis(es), and patient stability.
Then, go through all the problems relevant to the admission. You can impress your audience by casting a wide differential diagnosis and going through the elements of your patient presentation that support one diagnosis over another.
Following your assessment, try to suggest a management plan. In a patient with congestive heart failure exacerbation, initiating a diuresis regimen and measuring strict ins/outs are good starting points.
You may even suggest a follow-up on their latest ejection fraction with an echo and check if they’re on guideline-directed medical therapy. Again, with more time on the clinical wards you’ll start to pick up on what management plan to suggest.
One pointer is to talk about all relevant problems, not just the presenting issue. For example, a patient with diabetes may need to be put on a sliding scale insulin regimen or another patient may require physical/occupational therapy. Just try to stay organized and be comprehensive.
A Note About Patient Presentation Skills
When you’re doing your first patient presentations, it’s common to feel nervous. There may be a lot of “uhs” and “ums.”
Here’s the good news: you don’t have to be perfect! You just need to make a good faith attempt and keep on going with the presentation.
With time, your confidence will build. Practice your fluency in the mirror when you have a chance. No one was born knowing medicine and everyone has gone through the same stages of learning you are!
Practice your presentation a couple times before you present to the team if you have time. Pull a resident aside if they have the bandwidth to make sure you have all the information you need.
One big piece of advice: NEVER LIE. If you don’t know a specific detail, it’s okay to say, “I’m not sure, but I can look that up.” Someone on your team can usually retrieve the information while you continue on with your presentation.
Example Patient Case Presentation Template
Here’s a blank patient case presentation template that may come in handy. You can adapt it to best fit your needs.
Chief Complaint:
History of Present Illness:
Past Medical History:
Past Surgical History:
Family History:
Social History:
Medications:
Immunizations:
Vital Signs : Temp ___ BP ___ /___ HR ___ RR ___ O2 sat ___
Physical Exam:
General Appearance:
Mental Status:
Neurological:
Eyes, Ears, Nose, Mouth, and Neck:
Cardiovascular:
Genitourinary:
Musculoskeletal:
Most Recent Labs:
Previous Labs:
Diagnostics/Imaging:
Impression/Interpretation:
Assessment/Plan:
One-line summary:
#Problem 1:
Assessment:
#Problem 2:
Final Thoughts on Patient Presentations
I hope this post demystified the patient presentation for you. Be sure to stay organized in your delivery and be flexible with the specifications your team may provide.
Something I’d like to highlight is that you may need to tailor the presentation to the specialty you’re on. For example, on OB/GYN, it’s important to include a pregnancy history. Nonetheless, the aforementioned template should set you up for success from a broad overview perspective.
Stay tuned for my next post on how to give an ICU patient presentation. And if you’d like me to address any other topics in a blog, write to me at [email protected] !
Looking for more (free!) content to help you through clinical rotations? Check out these other posts from Blueprint tutors on the Med School blog:
- How I Balanced My Clinical Rotations with Shelf Exam Studying
- How (and Why) to Use a Qbank to Prepare for USMLE Step 2
- How to Study For Shelf Exams: A Tutor’s Guide
About the Author
Hailing from Phoenix, AZ, Neelesh is an enthusiastic, cheerful, and patient tutor. He is a fourth year medical student at the Keck School of Medicine of the University of Southern California and serves as president for the Class of 2024. He is applying to surgery programs for residency. He also graduated as valedictorian of his high school and the USC Viterbi School of Engineering, obtaining a B.S. in Biomedical Engineering in 2020. He discovered his penchant for teaching when he began tutoring his friends for the SAT and ACT in the summer of 2015 out of his living room. Outside of the academic sphere, Neelesh enjoys surfing at San Onofre Beach and hiking in the Santa Monica Mountains. Twitter: @NeeleshBagrodia LinkedIn: http://www.linkedin.com/in/neelesh-bagrodia

Related Posts

How to Approach Step 1 Dedicated in 2024
How to Study For Shelf Exams: A Tutor’s Guide

The Ultimate ICU Patient Presentation Template for Med Students
Search the blog, try blueprint med school study planner.
Create a personalized study schedule in minutes for your upcoming USMLE, COMLEX, or Shelf exam. Try it out for FREE, forever!
Could You Benefit from Tutoring?
Sign up for a free consultation to get matched with an expert tutor who fits your board prep needs
Find Your Path in Medicine
A side by side comparison of specialties created by practicing physicians, for you!
Popular Posts

Need a personalized USMLE/COMLEX study plan?
Example sentences clinical presentation
Definition of 'clinical' clinical.

Definition of 'present' present
Cobuild collocations clinical presentation.
Browse alphabetically clinical presentation
- clinical pharmacology
- clinical phenotype
- clinical practice
- clinical presentation
- clinical professional
- clinical psychologist
- clinical psychology
- All ENGLISH words that begin with 'C'
Quick word challenge
Quiz Review
Score: 0 / 5
Wordle Helper

Scrabble Tools
- More from M-W
- To save this word, you'll need to log in. Log In
presentation
Definition of presentation
- fairing [ British ]
- freebee
- largess
Examples of presentation in a Sentence
These examples are programmatically compiled from various online sources to illustrate current usage of the word 'presentation.' Any opinions expressed in the examples do not represent those of Merriam-Webster or its editors. Send us feedback about these examples.
Word History
15th century, in the meaning defined at sense 1a
Phrases Containing presentation
- breech presentation
Dictionary Entries Near presentation
present arms
presentation copy
Cite this Entry
“Presentation.” Merriam-Webster.com Dictionary , Merriam-Webster, https://www.merriam-webster.com/dictionary/presentation. Accessed 11 May. 2024.
Kids Definition
Kids definition of presentation, medical definition, medical definition of presentation, more from merriam-webster on presentation.
Nglish: Translation of presentation for Spanish Speakers
Britannica English: Translation of presentation for Arabic Speakers
Britannica.com: Encyclopedia article about presentation
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
More commonly misspelled words, your vs. you're: how to use them correctly, every letter is silent, sometimes: a-z list of examples, more commonly mispronounced words, how to use em dashes (—), en dashes (–) , and hyphens (-), popular in wordplay, the words of the week - may 10, a great big list of bread words, 10 scrabble words without any vowels, 8 uncommon words related to love, 9 superb owl words, games & quizzes.

Unit 1 What is Medicine?
Jan 05, 2020
400 likes | 427 Views
Unit 1 What is Medicine?. Skills focus Listening preparing for a lecture predicting lectures content from the introduction understanding lecture organization choosing an appropriate form of notes making lecture notes Speaking speaking from notes. Vocabulary focus
Share Presentation
- delivery room
- tree diagram
- making lecture notes
- making perfect lecture notes

Presentation Transcript
Skills focus Listening • preparing for a lecture • predicting lectures content from the introduction • understanding lecture organization • choosing an appropriate form of notes • making lecture notes Speaking • speaking from notes Vocabulary focus • words from general English with a special meaning in medical studies • prefixes and suffixes
Vocabulary bank Guessing words in context Using related words Sometimes a word in general English has a special meaning in medicine. Examples: patient, dressing, theatre If you recognize a word but don’t understand it in context, think: • What is the basic meaning of the word? • Does that help me understand the special meaning?
Vocabulary bank Guessing words in context Examples: Water can drip from a tap. A drip means a tiny flow of liquid. If a doctor puts a patient on a drip, it means that the patient receive a tiny flow of some type of liquid, usually in the form of a drug, such as an antibiotic.
1.1 Vocabulary A Read the e-mail. What do the word in blue mean in medical English? Hi Beth Hope you’re having a good time on holiday. I’m stuck in front of my computer again, trying to finish my history essay. It’s 11:30 a.m. and I’m not even dressed yet. Actually, we’ve got a leak in the bathroom and I’m waiting for the plumber to come and fix the valves, or whatever’s wrong with it. He’s waiting for a delivery of the parts, apparently. I’m trying to be patient, but every ten seconds I can hear a drip from the bathroom and it’s starting to drive me crazy! Some of the girls invited me to see a play at the theatre last night. It’s not my kind of thing normally, but I have to admit the cast were excellent, even if the storyline was not that great. I tried to take a photo of them for you, but my finger was covering the camera lens, so it hasn’t come out very well. Anyway – back to my history essay. See you next week. Sophie
part of speech changed from verb to noun notes about the patient’s previous and present medical problem(s) works in a similar way to a valve in plumbing protective covering for a wound to avoid infection during the healing process feature of the heart that enables it to function by opening and closing, allowing blood to pass through part of speech changed from adjective to noun delivery room – room in hospital where babies are born/delivered part of speech changed from verb to noun person who receives care from a doctor, nurse or other healthcare professional liquid passed slowly into patient’s blood through a tube part of speech changed from verb to noun room in a hospital where operations are performed department in hospital where patients register on arrival made of plaster of Paris to aid in the healing of broken bones by keeping the body part stiff works in a similar way to a camera lens part of the eye located behind the pupil that focuses light
1.1 Vocabulary B Complete each sentence with one of the words in red from Exercise A. Change the form if necessary. 1 It’s only fairly recently that ‘birthing partners’ have been allowed to be present in the _________ room. 2 Behind the iris is the soft, elastic _____ that widens or contracts under different lighting conditions. 3 The ________ will need to take the prescription to the pharmacist in order to get his medication. 4 The heart is a muscular pump, dependent on a series of four _______ that enable it to function. 5 Take the patient’s ________ by asking him or her about their past and current medical problems. 6 You will be taken down to _________ for your operation once you have been seen by the anaesthetist. 7 The patient was ___________ to the Emergency Unit following a near-fatal car accident, and is currently on a ______. 8 The nurse will change the __________ on your wound now, but the ________ on your leg won’t come off for another week or so. delivery lens patient valves history theatre admitted drip dressing cast
1.1 Vocabulary C&D Study box a and box b. suffix extra letters at the end a base word extra letters at the beginning a base word prefix
anti-inflammatory against anti related to human life bio biology lack of disability dis PREFIX implant im not insomnia in not ir not irreversible malformed mal bad/wrong micro very small microscope outbreak out exterior pre pre-existing before from one place to another trans transplant ultra excessive ultraviolet un not/ opposite unconscious
dialysis sis noun radiologist specialist in the study of ist SUFFIX genetic ic adjective conditioning noun ing tasteful ful verb → adjective make into fy modify treatment verb → noun ment adjective → noun ity immunity organism noun ism
al noun → adjective chemical ion verb → noun investigation SUFFIX ian related to person’s job title paediatrician ogy study of histology er related to person’s job title driver ate to make procreate ance verb → noun acquaintance ness weakness adjective → noun to cause/ to become ize hospitalize
1.1 Vocabulary E Describe the following pictures delivery room, delivering a baby admissions, admit a patient history of a patient, take the patient’s history
1.1 Vocabulary E Describe the following pictures the operation is taking place in theatre, operating theatre the leg is in a cast, a plaster cast being on a drip dressing for a wound
1.1 Vocabulary E Describe the following pictures the valve helps the heart to function effectively, aortic valve lens (of an eye) the joint of a knee, knee joint
1.2 Listening A You are a student in the Faculty of Medicine at Hadford University. The title of the first lecture is What is medicine? 1 Write a definition of medicine. 2 What other ideas will be in this lecture? Make some notes. See Skills bank.
Skills bank Making the most of lectures 4 Ps
Skills bank Before a lecture… Plan • Find out the topic of the lecture. • Research the topic. • Check the pronunciation of names and key words in English.
Skills bank Before a lecture… Prepare • Get to the lecture room early. • Sit where you can see and hear clearly. • Bring any equipment you may need. • Write the date, topic and name of the lecturer at the top of a sheet of paper.
Skills bank During a lecture… Predict • Listen carefully to the introduction. Think: What kind of lecture is this? • Write an outline. Leave space for notes. • Think of possible answers/solutions/effects, etc., while the lecturer is speaking.
Skills bank During a lecture… Produce • Write notes/copy from the board. • Record sources – books/websites/names. • At the end, ask the lecturer/other students for missing information.
1.2 Listening B Listen to Part 1 of the talk. What does the lecturer say about medicine? Tick one or more of the following. √ a It is about dissecting bodies. ____ b It is about understanding physiology. ____ c It is about becoming healers. ____ d It is about a lot of studying. ____ 请将本单元的音频和本PPT放在一个单独的文件夹中,点击小喇叭即可播放音频(下同)
1.2 Listening C In Part 2 of the talk, what core subjects will a medical student study?
1.2 Listening D In Part 3 of the talk, the lecturer mentions cell and scan. What do these words mean in general and medical English? smallest unit of living organism place of imprisonment use of ultrasound to visualize internal organs and body tissue look round or read quickly
1.2 Listening E In Part 4 of the talk, the lecturer provides more detail on what is covered by human anatomy.
1.2 Listening F Write a definition of anatomy The study of the outward appearance of the structures of the human body.
1.2 Listening G Look back at your notes from Exercise A. Did you predict: • the main ideas? • most of the special vocabulary? • the order of information?
A In a medical context, what can you … a disease, a condition, cancer a patient, a condition, diabetes patient history, observations, results 1.3 Extending skills results of a test, findings, compounds, samples medicine, dentistry, veterinary medicine, oncology an operation, an experiment, an ultrasound scan medicine, tablets, exercise, drugs, medication, treatment drugs, an injection, a dose results of a test, an x-ray, an ultrasound [scan]
B How can you organize information in a lecture? Match the beginnings and endings. question and contrast problem and definition 1.3 Extending skills classification and disadvantages advantages and effect comparison and events cause and supporting information sequence of process stages of a solution theories or opinions then answer
Skills bank Making perfect lecture notes two columns advantages and disadvantages pros cons spidergram cause and effect classification and definition tree diagram comparison and contrast table
Skills bank Making perfect lecture notes table facts and figures 18th 19th 1920 timeline sequence of events flowchart stages of process question and answer headings and notes
E Listen to five lecture introductions. Choose a possible way to take notes from Exercise C in each case. Example You hear: In the lecture today, I’m going to talk about the different stages of Alzheimer’s and how these can be recognized in the patient … You choose: flowchart 1.3 Extending skills
E Listen to five lecture introductions. Choose a possible way to take notes from Exercise C in each case. Lecture 1 Lecture 2 Lecture 3 Lecture 4 Lecture 5 advantages and disadvantages (two columns) classification and definition (tree diagram) 1.3 Extending skills process of stages (flowchart) problem and solution (headings and notes/two columns) cause and effect (spidergram)
A Study pictures 1-5. What do they show? Match the following words. scalpel 1.4 Extending skills stagnant water antiseptic vaccination laser surgery
B What does each diagram (a-c) show? 1.4 Extending skills the thyroid gland brain scans comparing a healthy patient with a patient suffering from Alzheimer’s the chemical breakdown of penicillin
C Listen to the lecture introductions from lesson 1.3 again. Make an outline of your notes. 1.4 Extending skills D Look at your outline for each lecture. What do you expect the lecture to talk about in the lecture? In what order?
E Listen to the next part each lecture. Complete your notes. Lecture 1 Lecture 2 Lecture 3 Lecture 4 Lecture 5 1.4 Extending skills 请将本单元的音频和本PPT放在一个单独的文件夹中,点击超链接即可播放音频
F Uncover the opposite page. Check your notes against the model notes. Are yours the same or different? 1.4 Extending skills G Work in pair. 1 Use the notes on the opposite page. Reconstruct one lecture. 2 Give the lecture to another pair.
Tips for Reference 1.1 Vocabulary部分,可以先让学生课前通过查阅词典等完成A、B、C、D的练习;接着,课堂上讲解vocabulary bank中的“Guessing words in context”技能;E部分的图片可以请学生课堂讨论。 1.2 Listening部分,按次序听完,并将skills bank中“Making the most of lectures”技能融入听力训练中。 1.3 Extending skills部分,重点讲解如何通过学术讲座的开头介绍,设计笔记的类型。 1.4 Extending skills部分,可以作为学生课后操练的练习;由学生听完整的讲座内容,并做好笔记;课堂上请学生根据笔记讲述内容。
- More by User
Folk Medicine
Folk Medicine. By Diana, Lisa, Mariana, Marlene. Folk Medicine. Folk Medicine is an herb that was used in the past. Folk medicine was here before any other medicine. Midwives used folk medicine when they needed to deliver babies. Herbs. Saw Palmetto is good for stomachaches and diarrhea
1.26k views • 8 slides
In Science and Medicine, We use the Metric System!
In Science and Medicine, We use the Metric System!. Dimensions. Unit of length: meter Unit of mass: gram Unit of volume: liter. SI Base Units of Measurement. Mass = the gram; g 1 gram ≈ 1/28 ounce Length = the meter; m 1 meter ≈ 1.094 yard Volume = the liter; l
985 views • 13 slides
Pathogenesis of Sepsis
Pathogenesis of Sepsis. Arzu TOPELI-ISKIT, MD Hacettepe University Faculty of Medicine Department of Internal Medicine Medical Intensive Care Unit Ankara 21 April 2006.
1.02k views • 34 slides
ALTERNATIVE MEDICINE THREATENS EXTINCTION
What is Alternative Medicine?. Alternative Medicine, stated in Wikepedia as, any of various systems of healing or treating disease not included in the traditional medical curricula taught in the U.S. and Britain. . TCM. Traditonal Chinese Medicine (TCM), a type of Alternative Medicine, is a 5,000 y
484 views • 15 slides

The Bridge Dancers Open Court - Unit 3- Mystery to Medicine - Lesson 3 Vocabulary
The Bridge Dancers Open Court - Unit 3- Mystery to Medicine - Lesson 3 Vocabulary. gorge enchained pitches herb medicines poultice lulling. gorge . When we reach the edge of the gorge , the path levels off and we run alongside it.
179 views • 17 slides
Breaking Bad News
Breaking Bad News. KHALED FAHAD ALKETHIRI 433103220 TARIQ KHALID ALMATRUDI 433100521 SULIMAN ALAA AL-BATNIJI 431101485. Objectives. Brainstorming stations. Definition of bad news and its importance. Methods and advices about breaking bad news.
831 views • 27 slides
Medicine: Past and Present
Medicine: Past and Present. plague infected microbes antibodies bacteria vaccine epidemic immune dispel sterilize. Open Court 4 th Grade Unit 3 From Mystery to Medicine Lesson 1 Medicine: Past and Present Melissa Lape – Wilson Elementary. plague “Use context clues”.
443 views • 14 slides

Randy S. Wax, MD, FRCP(C) Technology Application Unit and Critical Care Unit, Department of Medicine, Mount Sinai Hospi
Simulation technology in critical care: 1000 deaths for medical education Technology for teaching and evaluating critical care knowledge, skills and attitudes. Randy S. Wax, MD, FRCP(C) Technology Application Unit and Critical Care Unit, Department of Medicine, Mount Sinai Hospital
664 views • 49 slides
Illinois Medical Bill Reviewer Training
Illinois Medical Bill Reviewer Training. Unit 1: Professional Services Module 7: Physical Medicine Guidelines. Overview. Hi! In this module, you will learn about physical medicine, acupuncture, and manipulation. Part I: Physical Medicine Physical Medicine Guidelines Patient Evaluation
292 views • 19 slides
Ancient Greek Medicine
Abdulwahab Al-Qurtas 7-4. Ancient Greek Medicine. Table of Contents. Introduction. Ancient Greek Medicine. Asclepieia . Hippocrates “Father of Medicine.” The Hippocratic Oath. Other Contributors to Greek Medicine. Greek Contribution to Modern Medicine. Conclusion. Bibliography.
2.57k views • 14 slides
Integration of a medicine dispenser unit to the ThereGate system
Integration of a medicine dispenser unit to the ThereGate system. Matthias Füller Viktor Kovács 28. 09. 2010. Introduction. Problem of aging society Elderly people with dementia Forget to take medicine Leaving home without any reasons Everyday activities get difficult
131 views • 6 slides
War and medicine
Medicine, Disease and Society in Britain, 1750 - 1950. War and medicine. Lecture 17. Roger Cooter, ‘Medicine in war’, in Deborah Brunton (ed.), Medicine Transformed (Manchester, MUP), pp. 331-333:.
415 views • 21 slides
Mind-Body Medicine
Mind-Body Medicine. Unit 4 Seminar Dr. Melissa Dengler, ND Kaplan University. Interconnectedness.
624 views • 32 slides
Value of PDAs in Clinical Practice and Education My Internal Medicine Perspective
Value of PDAs in Clinical Practice and Education My Internal Medicine Perspective. Lorenzo Di Francesco, MD, FACP Assistant Professor of Medicine Associate Program Director, GMH Co-Director, Hospital Medicine Unit Emory University School of Medicine March 27, 2003. Outline.
481 views • 27 slides
THE ORIGINS OF FAMILY MEDICINE
THE ORIGINS OF FAMILY MEDICINE. DEPT . OF PUBLIC HEALTH & PREVENTIVE MEDICINE FACULTY OF MEDICINE-PADJADJARAN UNIVERSITY 2013. Specific Learning Objectives. Understand family medicine as a discipline (C1) Recognize the changes in paradigm in medicine (C1)
1.53k views • 36 slides
Interchange Book 1 Units 1-16. Click on a unit. Unit 4. Unit 1. Unit 2. Unit 3. Unit 5. Unit 6. Unit 7. Unit 8. Unit 9. Unit 10. Unit 11. Unit 12. Unit 13. Unit 14. Unit 15. Unit 16. Interchange Book 1 Unit 1 Please call me Beth. Student ’ s Book 1, unit 1, page 3
2.15k views • 46 slides

The Best Medicine
The Best Medicine. KEY WORDS in Unit 1 (page 8). Unit 1. Sum-up activity: VOCABULARY. AFTER Previous knowledge vocabulary activity …. KEY WORDS (page 8) Make sure you understand these terms!. Listen to the pronunciation at http://dictionary.cambridge.org.
219 views • 9 slides

Unit 4 Astronomy: the science of the stars
Unit 4 Astronomy: the science of the stars. brainstorming. What subjects do you learn at school?. Chinese English mathematics physics history. geography physics biology chemistry. geophysics. biochemistry. astronomy biochemistry geophysics medicine. medicine.
369 views • 24 slides
英语 (新目标)B. 七年级下册. 新课标( RJ ). 单元复习. Unit 1 My name’s Gina. Unit 2 This is my sister. Unit 3 Is this your pencil? Unit 4 Where’s my schoolbag?. Unit 5 Do you have a soccer ball? Unit 6 Do you like bananas? Unit 7 How much are these socks? Unit 8 When is your birthday?
4.45k views • 348 slides
Table of Contents – pages iv-v
Table of Contents – pages iv-v. Unit 1: What is Biology? Unit 2: Ecology Unit 3: The Life of a Cell Unit 4: Genetics Unit 5: Change Through Time Unit 6: Viruses, Bacteria, Protists, and Fungi Unit 7: Plants Unit 8: Invertebrates Unit 9: Vertebrates Unit 10: The Human Body.
1.77k views • 154 slides

IMAGES
VIDEO
COMMENTS
This definition of medical jargon appears to be a dictionary definition. ... In medicine, a presentation is the appearance in a patient of illness or disease—or signs or symptoms thereof—before a medical professional. In practice, one usually speaks of a patient as presenting with this or that. Examples include:
presentation. (prĕz′ən-tā′shən, prē′zən-) n. Medicine. a. The position of the fetus in the uterus at birth with respect to the mouth of the uterus. b. A symptom or sign or a group of symptoms or signs that is evident during a medical examination: The patient's presentation was consistent with a viral illness. c.
The ability to design and deliver an effective presentation is an important skill for all learners to develop. The Undergraduate Medical Education Section of the Group on Educational Affairs developed this toolkit as a resource for medical students and health professions trainees as you learn to create and give effective presentations in the classroom, in the clinical setting, and at academic ...
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics. Note that there is an acceptable range of how oral presentations can be delivered.
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Delivery. It is important to dress appropriately, stand up straight, and project your voice towards the back of the room. Practise using a microphone, or any other presentation aids, in advance. If you don't have your own presenting style, think of the style of inspirational scientific speakers you have seen and imitate it.
To prepare most effectively for your presentation, you might find considering four main areas particularly useful: planning, preparation, phrasing, and projection. Planning —A good presentation begins with the early stage of planning. Common complaints about ineffectual and dull presentations revolve around the apparent lack of structure ...
And this pause can be delivered in a number of ways. First, you can separate your presentation into several sections, thereby helping your audience navigate the overall flow of what you're saying. For example: 'Key findings', 'What this means for the medical world', and 'Next steps'.
adjective. pre· sent· ing pri-ˈzent-iŋ. : of, relating to, or being a symptom, condition, or sign which is evident or disclosed by a patient on physical examination. may be the presenting sign of a severe systemic disease H. H. Roenigk, Jr.
12.4 Disorders of purine and pyrimidine metabolism. Notes. Notes. 12.5 The porphyrias. Notes. Notes. AbstractThis chapter provides concise details of the clinical features, immediate management, key investigations, and further management of all of the comm.
Structure your medical presentation into a story to make it memorable. Medical presentations can be lectures, research, or case presentations. Customize the presentation based on the type and goal. 1. Lectures. Medical lectures educate an audience about a medical topic. They're one of the most challenging presentations.
Teaching and learning communications in medicine: a rhetorical approach. Academic Medicine. 74(5):507-510 1999 May. Lingard L, Haber RJ. What do we mean by "relevance"? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format. Academic Medicine. 74(10):S124-S127.
Medical presentations can be paralyzing, and your audience will likely be seeking more answers. Give your audience a minute or two following the presentation to process what they learned, and then give them a chance to ask questions. You may need to elaborate on specific slides, or revisit a piece of data, to help provide clarification. ...
Generative cognitive processing gives meaning to the material and creates deep learning. Learners must be motivated to engage and understand the information for this type of processing to occur. ... The application of the Mayer multimedia learning theory to medical PowerPoint slide show presentations. J Vis Commun Med [Internet]. 2018 Jan 2 ...
Presenting a patient is an essential skill that is rarely taught Clinical presenting is the language that doctors use to communicate with each other every day of their working lives. Effective communication between doctors is crucial, considering the collaborative nature of medicine. As a medical student and later as a doctor you will be expected to present cases to peers and senior colleagues ...
The art of presenting. The oral case presentation is a time-honoured tradition whereby a trainee presents a new admission to the attending physician. We describe the presentation styles of students, residents and staff physicians and offer pointers on how to present like stereotypical members of each group. Although the case presentation occurs ...
Enlist cooperation required for patient care: A short presentation focusing on the impact your audience can have in addressing the patient's issues. Preparation: Patient evaluation: history, physical examination, review of tests, studies, procedures, and consultants' recommendations. Selected reading: reference texts; to build a ...
7 Ingredients for a Patient Case Presentation Template. 1. The One-Liner. The one-liner is a succinct sentence that primes your listeners to the patient. A typical format is: " [Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y]. 2.
Only 12 (35.29%) of them thought that the CP curriculum system should be the sole leading teaching and learning system in clinical medicine, meaning more faculty preferred a hybrid system of both the CP curriculum and the traditional system. However, these differences were not statistically significant (p-value > 0.05).
CLINICAL PRESENTATION definition | Meaning, pronunciation, translations and examples
Discover Medical Abbreviations: Dive deeper into a comprehensive list of top-voted Medical Acronyms and Abbreviations. Explore PPT Definitions: Discover the complete range of meanings for PPT, beyond just its connections to Medical. Expand Your Knowledge: Head to our Home Page to explore and understand the meanings behind a wide range of acronyms and abbreviations across diverse fields and ...
presentation: [noun] the act of presenting. the act, power, or privilege especially of a patron of applying to the bishop or ordinary for instituting someone into a benefice.
Unit 1 What is Medicine? Skills focus Listening • preparing for a lecture • predicting lectures content from the introduction • understanding lecture organization • choosing an appropriate form of notes • making lecture notes Speaking • speaking from notes Vocabulary focus • words from general English with a special meaning in ...