Featured Topics
Featured series.
A series of random questions answered by Harvard experts.

Explore the Gazette
Read the latest.

Women rarely die from heart problems, right? Ask Paula.

When will patients see personalized cancer vaccines?
A molecular ‘warhead’ against disease
“When my son was diagnosed [with Type 1], I knew nothing about diabetes. I changed my research focus, thinking, as any parent would, ‘What am I going to do about this?’” says Douglas Melton.
Kris Snibbe/Harvard Staff Photographer
Breakthrough within reach for diabetes scientist and patients nearest to his heart
Harvard Correspondent
100 years after discovery of insulin, replacement therapy represents ‘a new kind of medicine,’ says Stem Cell Institute co-director Douglas Melton, whose children inspired his research
When Vertex Pharmaceuticals announced last month that its investigational stem-cell-derived replacement therapy was, in conjunction with immunosuppressive therapy, helping the first patient in a Phase 1/2 clinical trial robustly reproduce his or her own fully differentiated pancreatic islet cells, the cells that produce insulin, the news was hailed as a potential breakthrough for the treatment of Type 1 diabetes. For Harvard Stem Cell Institute Co-Director and Xander University Professor Douglas Melton, whose lab pioneered the science behind the therapy, the trial marked the most recent turning point in a decades-long effort to understand and treat the disease. In a conversation with the Gazette, Melton discussed the science behind the advance, the challenges ahead, and the personal side of his research. The interview was edited for clarity and length.
Douglas Melton
GAZETTE: What is the significance of the Vertex trial?
MELTON: The first major change in the treatment of Type 1 diabetes was probably the discovery of insulin in 1920. Now it’s 100 years later and if this works, it’s going to change the medical treatment for people with diabetes. Instead of injecting insulin, patients will get cells that will be their own insulin factories. It’s a new kind of medicine.
GAZETTE: Would you walk us through the approach?
MELTON: Nearly two decades ago we had the idea that we could use embryonic stem cells to make functional pancreatic islets for diabetics. When we first started, we had to try to figure out how the islets in a person’s pancreas replenished. Blood, for example, is replenished routinely by a blood stem cell. So, if you go give blood at a blood drive, your body makes more blood. But we showed in mice that that is not true for the pancreatic islets. Once they’re removed or killed, the adult body has no capacity to make new ones.
So the first important “a-ha” moment was to demonstrate that there was no capacity in an adult to make new islets. That moved us to another source of new material: stem cells. The next important thing, after we overcame the political issues surrounding the use of embryonic stem cells, was to ask: Can we direct the differentiation of stem cells and make them become beta cells? That problem took much longer than I expected — I told my wife it would take five years, but it took closer to 15. The project benefited enormously from undergraduates, graduate students, and postdocs. None of them were here for 15 years of course, but they all worked on different steps.
GAZETTE: What role did the Harvard Stem Cell Institute play?
MELTON: This work absolutely could not have been done using conventional support from the National Institutes of Health. First of all, NIH grants came with severe restrictions and secondly, a long-term project like this doesn’t easily map to the initial grant support they give for a one- to three-year project. I am forever grateful and feel fortunate to have been at a private institution where philanthropy, through the HSCI, wasn’t just helpful, it made all the difference.
I am exceptionally grateful as well to former Harvard President Larry Summers and Steve Hyman, director of the Stanley Center for Psychiatric Research at the Broad Institute, who supported the creation of the HSCI, which was formed specifically with the idea to explore the potential of pluripotency stem cells for discovering questions about how development works, how cells are made in our body, and hopefully for finding new treatments or cures for disease. This may be one of the first examples where it’s come to fruition. At the time, the use of embryonic stem cells was quite controversial, and Steve and Larry said that this was precisely the kind of science they wanted to support.
GAZETTE: You were fundamental in starting the Department of Stem Cell and Regenerative Biology. Can you tell us about that?
MELTON: David Scadden and I helped start the department, which lives in two Schools: Harvard Medical School and the Faculty of Arts and Science. This speaks to the unusual formation and intention of the department. I’ve talked a lot about diabetes and islets, but think about all the other tissues and diseases that people suffer from. There are faculty and students in the department working on the heart, nerves, muscle, brain, and other tissues — on all aspects of how the development of a cell and a tissue affects who we are and the course of disease. The department is an exciting one because it’s exploring experimental questions such as: How do you regenerate a limb? The department was founded with the idea that not only should you ask and answer questions about nature, but that one can do so with the intention that the results lead to new treatments for disease. It is a kind of applied biology department.
GAZETTE: This pancreatic islet work was patented by Harvard and then licensed to your biotech company, Semma, which was acquired by Vertex. Can you explain how this reflects your personal connection to the research?
MELTON: Semma is named for my two children, Sam and Emma. Both are now adults, and both have Type 1 diabetes. My son was 6 months old when he was diagnosed. And that’s when I changed my research plan. And my daughter, who’s four years older than my son, became diabetic about 10 years later, when she was 14.
When my son was diagnosed, I knew nothing about diabetes and had been working on how frogs develop. I changed my research focus, thinking, as any parent would, “What am I going to do about this?” Again, I come back to the flexibility of Harvard. Nobody said, “Why are you changing your research plan?”
GAZETTE: What’s next?
MELTON: The stem-cell-derived replacement therapy cells that have been put into this first patient were provided with a class of drugs called immunosuppressants, which depress the patient’s immune system. They have to do this because these cells were not taken from that patient, and so they are not recognized as “self.” Without immunosuppressants, they would be rejected. We want to find a way to make cells by genetic engineering that are not recognized as foreign.
I think this is a solvable problem. Why? When a woman has a baby, that baby has two sets of genes. It has genes from the egg, from the mother, which would be recognized as “self,” but it also has genes from the father, which would be “non-self.” Why does the mother’s body not reject the fetus? If we can figure that out, it will help inform our thinking about what genes to change in our stem cell-derived islets so that they could go into any person. This would be relevant not just to diabetes, but to any cells you wanted to transplant for liver or even heart transplants. It could mean no longer having to worry about immunosuppression.
Share this article
You might like.
New book traces how medical establishment’s sexism, focus on men over centuries continues to endanger women’s health, lives

Sooner than you may think, says researcher who recently won Sjöberg Prize for pioneering work in field
Approach attacks errant proteins at their roots
Harvard announces return to required testing
Leading researchers cite strong evidence that testing expands opportunity
Yes, it’s exciting. Just don’t look at the sun.
Lab, telescope specialist details Harvard eclipse-viewing party, offers safety tips
For all the other Willie Jacks
‘Reservation Dogs’ star Paulina Alexis offers behind-the-scenes glimpse of hit show, details value of Native representation

- April 11, 2024 | Double Trouble: Decoding the Pain-Depression Feedback Loop
- April 11, 2024 | Elemental Surprise: Physicists Discover a New Quantum State
- April 11, 2024 | A Real Life Eye of Sauron? New Technology To Detect Airborne Threats Instantly
- April 11, 2024 | This Math Problem Stumped Scientists for Almost a Century – Two Mathematicians Have Finally Solved It
- April 11, 2024 | Galactic Genesis Unveiled: JWST Witnesses the Dawn of Starlight
Beyond Blood Sugar Control: New Target for Curing Diabetes Unveiled
By Helmholtz Munich March 22, 2024
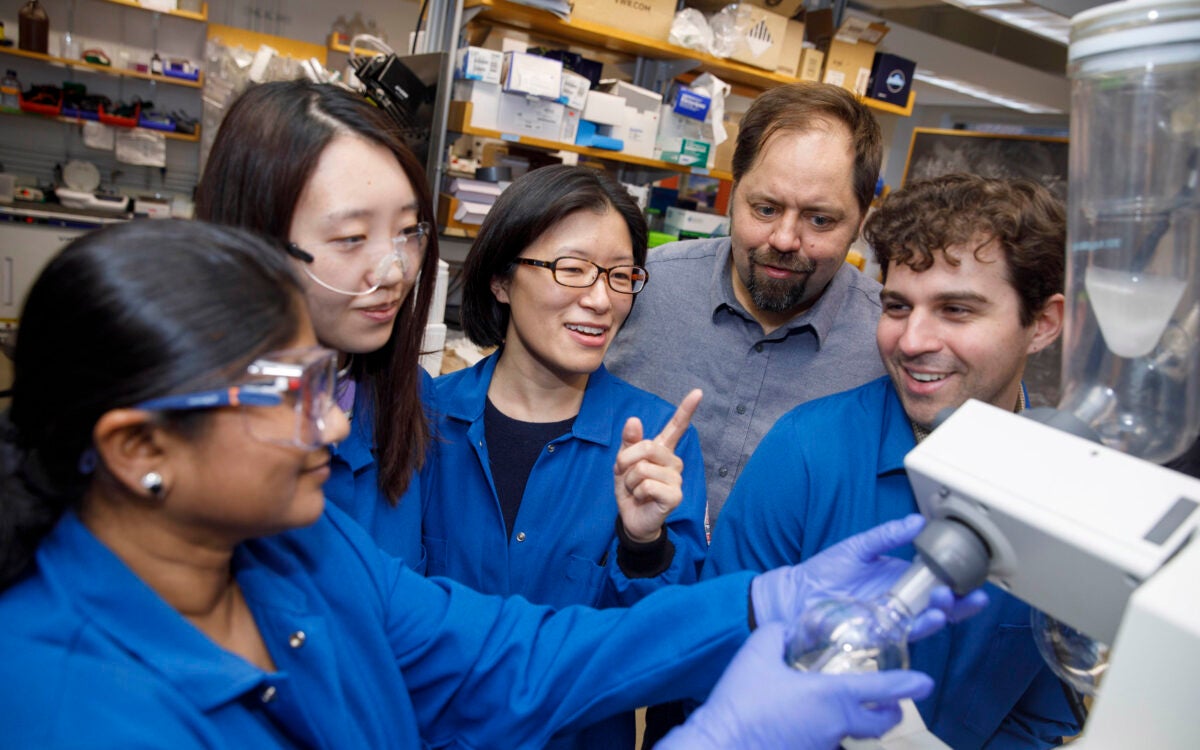
Targeting the inceptor receptor could lead to breakthrough treatments for diabetes by protecting beta cells and improving blood sugar control, with German research institutions leading this promising discovery. Insulin-producing beta cells in the islet of Langerhans. Credit: Helmholtz Munich | Erik Bader
Research focusing on the insulin -inhibitory receptor, known as inceptor, has revealed promising paths for protecting beta cells, providing optimism for therapy that directly addresses diabetes. A groundbreaking study involving mice with obesity caused by diet shows that eliminating inceptor improves glucose management. This finding encourages further investigation into inceptor as a potential therapeutic target for treating type 2 diabetes.
These findings, led by Helmholtz Munich in collaboration with the German Center for Diabetes Research, the Technical University of Munich, and the Ludwig-Maximilians-University Munich, drive advancements in diabetes research.
Targeting Inceptor to Combat Insulin Resistance in Beta Cells
Insulin resistance, often linked to abdominal obesity, presents a significant healthcare dilemma in our era. More importantly, the insulin resistance of beta cells contributes to their dysfunction and the transition from obesity to overt type 2 diabetes. Currently, all pharmacotherapies, including insulin supplementation, focus on managing high blood sugar levels rather than addressing the underlying cause of diabetes: beta cell failure or loss. Therefore, research into beta cell protection and regeneration is crucial and holds promising prospects for addressing the root cause of diabetes, offering potential avenues for causal treatment.
With the recent discovery of inceptor, the research group of beta cell expert Prof. Heiko Lickert has uncovered an interesting molecular target. Upregulated in diabetes, the insulin-inhibitory receptor inceptor may contribute to insulin resistance by acting as a negative regulator of this signaling pathway. Conversely, inhibiting the function of the inceptor could enhance insulin signaling – which in turn is required for overall beta cell function, survival, and compensation upon stress.
In collaboration with Prof. Timo Müller, an expert in molecular pharmacology in obesity and diabetes, the researchers explored the effects of inceptor knock-out in diet-induced obese mice. Their study aimed to determine whether inhibiting inceptor function could also enhance glucose tolerance in diet-induced obesity and insulin resistance, both critical pre-clinical stages in the progression toward diabetes. The results were now published in Nature Metabolism .
Removing Inceptor Improves Blood Sugar Levels in Obese Mice
The researchers delved into the effects of removing inceptor from all body cells in diet-induced obese mice. Interestingly, they found that mice lacking inceptor exhibited improved glucose regulation without experiencing weight loss, which was linked to increased insulin secretion in response to glucose. Next, they investigated the distribution of inceptor in the central nervous system and discovered its widespread presence in neurons. Deleting inceptor from neuronal cells also improved glucose regulation in obese mice. Ultimately, the researchers selectively removed the inceptor from the mice’s beta cells, resulting in enhanced glucose control and a slight increase in beta cell mass.
Research for Inceptor-Blocking Drugs
“Our findings support the idea that enhancing insulin sensitivity through targeting inceptor shows promise as a pharmacological intervention, especially concerning the health and function of beta cells,” says Timo Müller. Unlike intensive early-onset insulin treatments, utilizing inceptor to enhance beta cell function offers promise in alleviating the detrimental effects on blood sugar and metabolism induced by diet-induced obesity. This approach avoids the associated risks of hypoglycemia-associated unawareness and unwanted weight gain typically observed with intensive insulin therapy.
“Since inceptor is expressed on the surface of pancreatic beta cells, it becomes an accessible drug target. Currently, our laboratory is actively researching the potential of several inceptor-blocking drug classes to enhance beta cell health in pre-diabetic and diabetic mice. Looking forward, inceptor emerges as a novel and intriguing molecular target for enhancing beta cell health, not only in prediabetic obese individuals but also in patients diagnosed with type 2 diabetes,” explains Heiko Lickert.
Reference: “Global, neuronal or β cell-specific deletion of inceptor improves glucose homeostasis in male mice with diet-induced obesity” by Gerald Grandl, Gustav Collden, Jin Feng, Sreya Bhattacharya, Felix Klingelhuber, Leopold Schomann, Sara Bilekova, Ansarullah, Weiwei Xu, Fataneh Fathi Far, Monica Tost, Tim Gruber, Aimée Bastidas-Ponce, Qian Zhang, Aaron Novikoff, Arkadiusz Liskiewicz, Daniela Liskiewicz, Cristina Garcia-Caceres, Annette Feuchtinger, Matthias H. Tschöp, Natalie Krahmer, Heiko Lickert and Timo D. Müller, 28 February 2024, Nature Metabolism . DOI: 10.1038/s42255-024-00991-3
More on SciTechDaily

Quantum Breakthrough Reveals Superconductor’s Hidden Nature

Novel Molecules Discovered to Combat Asthma and COVID-Related Lung Diseases

Orbital Engineering, Yale Engineers Change Electron Trajectories

Finding and Erasing Quantum Computing Errors in Real-Time

“Glow-in-the-Dark” Proteins: The Future of Viral Disease Detection?
A black hole – a million times as bright as our sun – offers potential clue to reionization of universe.

Risk Factors for Falls in Older Americans Identified – A Growing Public Health Concern

Common Fireworks Emit Toxic Metals Into the Air – Damage Human Cells and Animal Lungs
1 comment on "beyond blood sugar control: new target for curing diabetes unveiled".
Interesting study and hopefully another tool which will apply to diabetic patients.
Leave a comment Cancel reply
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Experimental Treatments for Type 2 Diabetes
- Drug Treatments
- Diet and Nutrition
Artificial Pancreas
Pancreas transplant, frequently asked questions.
Lifestyle changes such as eating a diabetes-friendly diet , exercising more, and maintaining a healthy body weight combined with existing treatment options are the best way to prevent or manage type 2 diabetes .
However, for people with type 2 diabetes who have trouble controlling their blood sugar by making healthier lifestyle choices or taking medications, experimental treatments could help.
This article provides an overview of type 2 diabetes experimental treatments and explains how the latest type 2 diabetes research has led to new Food and Drug Administration (FDA)–approved pharmacological treatments and devices like the "artificial pancreas."
Read on to learn more about other experimental treatments for type 2 diabetes that show promise but haven't been approved by the FDA yet.
fotograzia / Getty Images
Pharmacological Treatments
Only about half of all U.S. adults with type 2 diabetes achieve good blood sugar level targets based on the A1c test , a simple blood test measuring blood sugar levels averaged over the past three months.
Fortunately, advances in type 2 diabetes research have led to some groundbreaking experimental treatments and drug combinations that show promise in preliminary studies.
Mounjaro (Tirzepatide)
The latest pharmacological treatment approved by the FDA for type 2 diabetes combines glucagon-like peptide-1 ( GLP-1 ) agonists and glucose-dependent insulinotropic polypeptides (GIP).
In May 2022, the FDA approved the novel type 2 diabetes injectable medication called Mounjaro (tirzepatide). Mounjaro is the first and only FDA-approved dual GIP and GLP-1 agonist medication for type 2 diabetes.
Sodium-glucose cotransporter-2 (SGLT2) inhibitors, also known as a glifozins , are another state-of-the-art class of drugs approved by the FDA to lower blood sugar in adults with type 2 diabetes. SGLT2 inhibitors are prescribed along with lifestyle changes like diet and exercise. Glifozins are not FDA-approved for patients with type 1 diabetes.
Accumulating evidence suggests that SGLT2 inhibitors have other health benefits such as promoting weight loss and improving cardiac functions. A meta-analysis (a formal assessment of previous research) of 10 clinical trials found that the use of SGLT2 inhibitors was associated with a 33% lower risk of life-threatening cardiovascular disease.
Wegovy (Semaglutide)
In June 2021, the FDA approved Wegovy, a weight-loss prescription drug, for people diagnosed with obesity and a weight-related condition such as high blood pressure or high cholesterol . In September 2022, researchers announced that weekly injections of this drug may reduce the risk of type 2 diabetes risk by 61%.
Tesaglitazar
Tesaglitazar is an experimental drug that showed promise as a treatment for type 2 diabetes in early studies. However, its development was put on hold by AstraZeneca in May 2006 before all of the phase 3 trials were completed. But this experimental treatment might be making a comeback.
In August 2022, a study in mice showed that combining tesaglitazar with GLP-1 agonists reduced the drug's adverse effects while increasing its positive effects on sugar metabolism. Still, human studies are needed.
Special Dietary and Nutritional Treatments
Eating a diet to help type 2 diabetes is one of the most effective ways for people with type 2 diabetes to control blood sugar. If you have diabetes, it's important to educate yourself about different types of carbohydrates and to monitor your blood sugar levels using a glucometer .
Research on supplements for type 2 diabetes has had mixed results. After years of research, a study of 2,423 people concluded that vitamin D supplements don't prevent type 2 diabetes and may not have long-term benefits. That said, a 2019 meta-analysis of other peer-reviewed studies concluded that vitamin D supplements may help people with type 2 diabetes control their blood sugar levels in the short term.
Over-the-counter (OTC) nutritional supplements that lower blood sugar can carry potential risks and are not intended to replace diabetes medications . Always use common sense and speak with a healthcare provider before making dietary changes or using nutritional supplements.
The "artificial pancreas" is a portable external device that controls blood glucose levels using a closed-loop insulin pump system. A 2021 study found that closed-loop artificial pancreas therapy helped people with type 2 diabetes safely manage their blood sugar levels and reduced the risk of severe hypoglycemia (low blood sugar) events.
Bariatric Surgery for Type 2 Diabetes
Bariatric weight-loss surgery is an effective treatment for many people with type 2 diabetes. Among bariatric procedures, a 2019 randomized trial found that gastric bypass surgery (creating and attaching a small pouch directly to the small intestine, bypassing the stomach) is superior to gastric sleeve surgery (removing a portion of the stomach) for remission of type 2 diabetes.
Although a pancreas transplant can benefit people with type 1 diabetes by restoring insulin production and improving blood sugar control, it's an extreme measure and isn't typically a treatment option for those with type 2 diabetes.
However, in certain patients with type 2 diabetes who have both a low production of insulin (hormone created by your pancreas that controls the sugar in your bloodstream) and insulin resistance (when cells stop responding to the insulin you make), a pancreas transplant may be considered.
However, the United Network for Organ Sharing (UNOS) eligibility criteria strictly limit access to pancreas transplantation in patients with type 2 diabetes.
Islet Transplant Surgery for Diabetics
Islet cell transplantation is a treatment option for some patients with type 1 diabetes but isn't currently an FDA-approved option for those with type 2 diabetes.
Diabetes research has led to some groundbreaking new treatment options. In May 2022, the FDA approved a potentially game-changing new drug called Mounjaro (tirzepatide) that targets both GLP-1 and GIP. In September 2022, researchers announced that another experimental drug, tesaglitazar, which didn't initially succeed in clinical trials, shows renewed promise when combined with a GLP-1 antagonist.
Other new treatments, like SGLT2 inhibitors, are effective for type 2 diabetes when combined with lifestyle changes related to diet and exercise. For people who have trouble losing weight, bariatric surgery and weight-loss drugs like Wegovy (semaglutide) can help people maintain a healthy weight and lower their risk of type 2 diabetes.
Experimental treatments for type 2 diabetes carry risks. Always speak to a healthcare provider before making changes to your diet or taking nutritional supplements.
No. There is no cure for type 2 diabetes. Losing weight, eating healthier, and exercising more can help to prevent and manage this type 2 diabetes. If diet, exercise, and weight loss fail to control blood sugar, antidiabetic medications or insulin therapy can help achieve glycemic targets.
If you have diabetes and want to take something other than metformin , speak to a healthcare provider about your options. Some alternatives to metformin that people with type 2 diabetes can use to control high blood sugar include, Farxiga (dapagliflozin), Invokana (canagliflozin), Jardiance (empagliflozin), and Nesina (alogliptin).
There's little to no evidence-based research showing that specific vitamins are helpful to people with diabetes in the long term. Vitamin D may help people with diabetes in the short term, but a yearslong National Institutes of Health–funded trial ultimately found that vitamin D supplements do not prevent type 2 diabetes.
ElSayed NA, Aleppo G, Aroda VR, et al. 5. Facilitating positive health behaviors and well-being to improve health outcomes: Standards of care in diabetes—2023 . Diabetes Care . 2023;46(Suppl 1):S68-S96. doi:10.2337/dc23-S005
Carls G, Huynh J, Tuttle E, Yee J, Edelman SV. Achievement of glycated hemoglobin goals in the us remains unchanged through 2014. Diabetes Ther . 2017;8(4):863-873. doi:10.1007/s13300-017-0280-5
ElSayed NA, Aleppo G, Aroda VR, et al. 9. Pharmacologic approaches to glycemic treatment: Standards of care in diabetes—2023 . Diabetes Care . 2023;46(Suppl 1):S140-S157. doi:10.2337/dc23-S009
Gasbjerg LS, Gabe MBN, Hartmann B, et al. Glucose-dependent insulinotropic polypeptide (GIP) receptor antagonists as anti-diabetic agents. Peptides . 2018;100:173-181. doi:10.1016/j.peptides.2017.11.021
Food and Drug Administration. MOUNJAROTM (tirzepatide) injection, for subcutaneous use [drug label].
FDA. Sodium-glucose Cotransporter-2 (SGLT2) Inhibitors.
Pharmacy Practice News. Evidence mounts for benefits of SGLT2 inhibitors and GLP-1 RAs .
Bhattarai M, Salih M, Regmi M, et al. Association of sodium-glucose cotransporter 2 inhibitors with cardiovascular outcomes in patients with type 2 diabetes and other risk factors for cardiovascular disease: a meta-analysis. JAMA Netw Open . 2022;5(1):e2142078. doi:10.1001/jamanetworkopen.2021.42078
FDA. FDA Approves New Drug Treatment for Chronic Weight Management, First Since 2014.
UAB News. Who will benefit from new ‘game-changing’ weight-loss drug semaglutide?
Hellmold H, Zhang H, Andersson U, et al. Tesaglitazar, a pparα/γ agonist, induces interstitial mesenchymal cell dna synthesis and fibrosarcomas in subcutaneous tissues in rats . Toxicological Sciences . 2007;98(1):63-74. doi:10.1093/toxsci/kfm094
Quarta C, Stemmer K, Novikoff A, et al. GLP-1-mediated delivery of tesaglitazar improves obesity and glucose metabolism in male mice . Nat Metab . 2022;4(8):1071-1083. doi:10.1038/s42255-022-00617-6
Tufts Medical Center. D2d (Vitamin D and Type 2 Diabetes) results .
Hu Z, Chen J, Sun X, Wang L, Wang A. Efficacy of vitamin D supplementation on glycemic control in type 2 diabetes patients: A meta-analysis of interventional studies . Medicine . 2019;98(14):e14970. doi:10.1097/MD.0000000000014970
Zhou K, Isaacs D. Closed-loop artificial pancreas therapy for type 1 diabetes . Curr Cardiol Rep . 2022;24(9):1159-1167. doi:10.1007/s11886-022-01733-1
Boughton CK, Tripyla A, Hartnell S, et al. Fully automated closed-loop glucose control compared with standard insulin therapy in adults with type 2 diabetes requiring dialysis: An open-label, randomized crossover trial . Nat Med . 2021;27(8):1471-1476. doi:0.1038/s41591-021-01453-z
ElSayed NA, Aleppo G, Aroda VR, et al. 8. Obesity and weight management for the prevention and treatment of type 2 diabetes: Standards of care in diabetes—2023 . Diabetes Care . 2023;46(Suppl 1):S128-S139. doi:10.2337/dc23-S008
Hofsø D, Fatima F, Borgeraas H, et al. Gastric bypass versus sleeve gastrectomy in patients with type 2 diabetes (Oseberg): A single-centre, triple-blind, randomised controlled trial . The Lancet Diabetes & Endocrinology . 2019;7(12):912-924. doi:10.1016/S2213-8587(19)30344-4
Kandaswamy R, Stock PG, Gustafson SK, et al. Optn/srtr 2016 annual data report: Pancreas . Am J Transplant . 2018;18:114-171. doi:10.1111/ajt.14558
Bleskestad KB, Nordheim E, Lindahl JP, et al. Insulin secretion and action after pancreas transplantation. A retrospective single-center study . Scandinavian Journal of Clinical and Laboratory Investigation . 2021;81(5):365-370. doi:10.1080/00365513.2021.1926535
Stratta RJ, Farney AC, Fridell JA. Analyzing outcomes following pancreas transplantation: Definition of a failure or failure of a definition . American J Transplantation . 2022;22(6):1523-1526. doi:10.1111/ajt.17003
Pullen LC. Islet cell transplantation hits a milestone . Am J Transplant . 2021;21(8):2625-2626. doi:10.1111/ajt.16039
diaTribe Learn. What are my choices for metformin alternatives?
NIH. NIH-funded trial finds vitamin D does not prevent type 2 diabetes in people at high risk .
By Christopher Bergland Christopher Bergland is a retired ultra-endurance athlete turned medical writer and science reporter.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Pharmacological Reviews

New Aspects of Diabetes Research and Therapeutic Development
Both type 1 and type 2 diabetes mellitus are advancing at exponential rates, placing significant burdens on health care networks worldwide. Although traditional pharmacologic therapies such as insulin and oral antidiabetic stalwarts like metformin and the sulfonylureas continue to be used, newer drugs are now on the market targeting novel blood glucose–lowering pathways. Furthermore, exciting new developments in the understanding of beta cell and islet biology are driving the potential for treatments targeting incretin action, islet transplantation with new methods for immunologic protection, and the generation of functional beta cells from stem cells. Here we discuss the mechanistic details underlying past, present, and future diabetes therapies and evaluate their potential to treat and possibly reverse type 1 and 2 diabetes in humans.
Significance Statement
Diabetes mellitus has reached epidemic proportions in the developed and developing world alike. As the last several years have seen many new developments in the field, a new and up to date review of these advances and their careful evaluation will help both clinical and research diabetologists to better understand where the field is currently heading.
I. Introduction
Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020 ). Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing pancreatic beta cells. The much more prevalent T2D arises in conjunction with peripheral tissue insulin resistance and beta cell failure and is estimated to increase to 21%–33% of the US population by the year 2050 (Boyle et al., 2010 ). To combat this growing health threat and its cardiac, renal, and neurologic comorbidities, new and more effective diabetes drugs and treatments are essential. As the last several years have seen many new developments in the field of diabetes pharmacology and therapy, we determined that a new and up to date review of these advances was in order. Our aim is to provide a careful evaluation of both old and new therapies ( Fig. 1 ) in a manner that we hope will be of interest to both clinical and bench diabetologists. Instead of the usual encyclopedic approach to this topic, we provide here a targeted and selective consideration of the underlying issues, promising new treatments, and a re-examination of more traditional approaches. Thus, we do not discuss less frequently used diabetes agents, such as alpha-glucosidase inhibitors; these were discussed in other recent reviews (Hedrington and Davis, 2019 ; Lebovitz, 2019 ).

Pharmacologic targeting of numerous organ systems for the treatment of diabetes. Treatment of diabetes involves targeting of various organ systems, including the kidney by SGLT2 inhibitors; the liver, gut, and adipose tissue by metformin; and direct actions upon the pancreatic beta cell. Beta cell compounds aim to increase secretion or mass and/or to protect from autoimmunity destruction. Ultimately, insulin therapy remains the final line of diabetes treatment with new technologies under development to more tightly regulate blood glucose levels similar to healthy beta cells. hESC, human embryonic stem cell.
II. Diabetes Therapies
A. metformin.
Metformin is a biguanide originally based on the natural product galegine, which was extracted from the French lilac (Bailey, 1992 ; Rojas and Gomes, 2013 ; Witters, 2001 ). A closely related biguanide, phenformin, was also used initially for its hypoglycemic actions. Based on its successful track record as a safe, effective, and inexpensive oral medication, metformin has become the most widely prescribed oral agent in the world in treating T2D (Rojas and Gomes, 2013 ; He and Wondisford, 2015 ; Witters, 2001 ), whereas phenformin has been largely bypassed due to its unacceptably high association with lactic acidosis (Misbin, 2004 ). Unlike sulfonylureas, metformin lowers blood glucose without provoking hypoglycemia and improves insulin sensitivity (Bailey, 1992 ). Despite these well known beneficial metabolic actions, metformin’s mechanism of action and even its main target organ remain controversial. In fact, metformin has multiple mechanisms of action at the organ as well as the cellular level, which has hindered our understanding of its most important molecular effects on glucose metabolism (Witters, 2001 ). Adding to this, a specific receptor for metformin has never been identified. Metformin has actions on several tissues, although the primary foci of most studies have been the liver, skeletal muscle, and the intestine (Foretz et al., 2014 ; Rena et al., 2017 ). Metformin and phenformin clearly suppress hepatic glucose production and gluconeogenesis, and they improve insulin sensitivity in the liver and elsewhere (Bailey, 1992 ). The hepatic actions of metformin have been the most exhaustively studied to date, and there is little doubt that these actions are of some importance. However, several of the studies remain highly controversial, and there are still open questions.
One of the first reported specific molecular targets of metformin was mitochondrial complex I of the electron transport chain. Inhibition of this complex results in reduced oxidative phosphorylation and consequently decreased hepatic ATP production (El-Mir et al., 2008 ; Evans et al., 2005 ; Owen et al., 2000 ). As is the case in many other studies of metformin, however, high concentrations of the drug were found to be necessary to depress metabolism at this site (El-Mir et al., 2000 ; He and Wondisford, 2015 ; Owen et al., 2000 ). Also controversial is whether metformin works by activating 5′ AMP-activated protein kinase (AMPK), a molecular energy sensor that is known to be a major metabolic sensor in cells, or if not AMPK directly, then one of its upstream regulators such as liver kinase B2 (Zhou et al., 2001 ). Although metformin was shown to activate AMPK in several excellent studies, other studies directly contradicted the AMPK hypothesis. Most dramatic were studies showing that metformin’s actions to suppress hepatic gluconeogenesis persisted despite genetic deletion of the AMPK’s catalytic domain (Foretz et al., 2010 ). More recent studies identified additional or alternative targets, such as cAMP signaling in the liver (Miller et al., 2013 ) or glycogen synthase kinase-3 (Link, 2003 ). Other work showed that the phosphorylation of acetyl-CoA carboxylase and acetyl-CoA carboxylase 2 are involved in regulating lipid homeostasis and improving insulin sensitivity after exposure to metformin (Fullerton et al., 2013 ).
Although there are strong data to support each of these pathways, it is not entirely clear which signaling pathway(s) is most essential to the actions of metformin in hepatocytes. Metformin clearly inhibits complex I and concomitantly decreases ATP and increases AMP. The latter results in AMPK activation, reduced fatty acid synthesis, and improved insulin receptor activation, and increased AMP has been shown to inhibit adenylate cyclase to reduce cAMP and thus protein kinase A activation. Downstream, this reduces the expression of phosphoenolpyruvate carboxykinase and glucose 6-phosphatase via decreased cAMP response element-binding protein, the cAMP-sensitive transcription factor. Decreased PKA also promotes ATP-dependent 6-phosphofructokinase, liver type activity via fructose 2,6-bisphosphate and reduces gluconeogenesis, as fructose-bisphosphatase 1 is inhibited by fructose 2,6-bisphosphate, along with other mechanisms (Rena et al., 2017 ; Pernicova and Korbonits, 2014 ).
More recent work has shown that metformin at pharmacological rather than suprapharmacological doses increases mitochondrial respiration and complex 1 activity and also increases mitochondrial fission, now thought to be critical for maintaining proper mitochondrial density in hepatocytes and other cells. This improvement in respiratory activity occurs via AMPK activation (Wang et al., 2019 ).
Although the liver has historically been the major suspected site of metformin action, recent studies have suggested that the gut instead of the liver is a major target, a concept supported by the increased efficacy of extended-release formulations of metformin that reside for a longer duration in the gut after their administration (Buse et al., 2016 ). An older, but in our view an important observation, is that the intravenous administration of metformin has little or no effect on blood glucose, whereas, in contrast, orally administered metformin is much more effective (Bonora et al., 1984 ). Recent imaging studies using labeled glucose have shown directly that metformin stimulates glucose uptake by the gut in patients with T2D to reduce plasma glucose concentrations (Koffert et al., 2017 ; Massollo et al., 2013 ). Additionally, it is possible that metformin may exert its effect in the gut by inducing intestinal glucagon-like peptide-1 (GLP-1) release (Mulherin et al., 2011 ; Preiss et al., 2017) to potentiate beta cell insulin secretion and by stimulating the central nervous system (CNS) to exert control over both blood glucose and liver function. Indeed, CNS effects produced by metformin have been proposed to occur via the local release of GLP-1 to activate intestinal nerve endings of ascending nerve pathways that are involved in CNS glucose regulation (Duca et al., 2015 ). Lastly, several papers have now implicated that metformin may act by altering the gut microbiome, suggesting that changes in gut flora may be critical for metformin’s actions (McCreight et al., 2016 ; Wu et al., 2017 ; Devaraj et al., 2016 ). A new study proposed that activation of the intestinal farnesoid X receptor may be the means by which microbiota alter hyperglycemia (Sun et al., 2018 ). However, these studies will require more mechanistic detail and confirmation before they can be fully accepted by the field. In addition to the action of metformin on gut flora, the production of imidazole propionate by gut microbes in turn has been shown to interfere with metformin action through a p38-dependent mechanism and AMPK inhibition. Levels of imidazole propionate are especially higher in patients with T2D who are treated with metformin (Koh et al., 2020 ).
In summary, the combined contribution of these various effects of metformin on multiple cellular targets residing in many tissues may be key to the benefits of metformin treatment on lowering blood glucose in patients with type 2 diabetes (Foretz et al., 2019 ). In contrast, exciting new work showing metformin leads to weight loss by increasing circulating levels of the peptide hormone growth differentiation factor 15 and activation of brainstem glial cell-derived neurotropic factor family receptor alpha like receptors to reduce food intake and energy expenditure works independently of metformin’s glucose-lowering effect (Coll et al., 2020 ).
B. Sulfonylureas and Beta Cell Burnout
The class of compounds known as sulfonylureas includes one of the oldest oral antidiabetic drugs in the pharmacopoeia: tolbutamide. Tolbutamide is a “first generation” oral sulfonylurea secretagogue whose clinical usefulness is due to its prompt stimulation of insulin release from pancreatic beta cells. “Second generation” sulfonylureas include drugs such as glyburide, gliclazide, and glipizide. Sulfonylureas act by binding to a high affinity sulfonylurea binding site, the sulfonylurea receptor 1 subunit of the K(ATP) channel, which closes the channel. These drugs mimic the physiologic effects of glucose, which closes the K(ATP) channel by raising cytosolic ATP/ADP. This in turn provokes beta cell depolarization, resulting in increased Ca 2+ influx into the beta cell (Ozanne et al., 1995 ; Ashcroft and Rorsman, 1989 ; Nichols, 2006 ). Importantly, sulfonylureas, and all drugs that directly increase insulin secretion, are associated with hypoglycemia, which can be severe, and which limits their widespread use in the clinic (Yu et al., 2018 ). Meglitinides are another class of oral insulin secretagogues that, like the sulfonylureas, bind to sulfonylurea receptor 1 and inhibit K(ATP) channel activity (although at a different site of action). The rapid kinetics of the meglitinides enable them to effectively blunt the postprandial glycemic excursions that are a hallmark (along with elevated fasting glucose) of T2D (Rosenstock et al., 2004). However, the need for their frequent dosing (e.g., administration before each meal) has limited their appeal to patients.
The efficacy of sulfonylureas is known to decrease over time, leading to failure of the class for effective long-term treatment of T2D (Harrower, 1991 ). More broadly, it is now widely accepted that the number of functional beta cells in humans declines during the progression of T2D. Thus, one would expect that due to this decline, all manner of oral agents intended to target the beta cell and increase its cell function (and especially insulin secretion) will fail over time (RISE Consortium, 2019 ), a process referred to as “beta cell failure” (Prentki and Nolan, 2006 ). Currently, treatments that can expand beta cell mass or improve beta cell function or survival over time are not yet available for use in the clinic. As a result, treatments that may be able to help patients cope with beta cell burnout such as islet cell transplantation, insulin pumps, or stem cell therapy are alternatives that will be discussed below.
C. Ca 2+ Channel Blockers and Type 1 Diabetes
Strategies to treat and prevent T1D have historically focused on ameliorating the toxic consequences of immune dysregulation resulting in autoimmune destruction of pancreatic beta cells. More recently, a concerted focus on alleviating the intrinsic beta cell defects (Sims et al., 2020 ; Soleimanpour and Stoffers, 2013 ) that also contribute to T1D pathogenesis have been gaining traction at both the bench and the bedside. Several recent preclinical studies suggest that Ca 2+ -induced metabolic overload induces beta cell failure (Osipovich et al., 2020 ; Stancill et al., 2017 ; Xu et al., 2012 ), with the potential that excitotoxicity contributes to beta cell demise in both T1D and T2D, similar to the well known connection between excitotoxicity and, concomitantly, increased Ca 2+ loading of the cells and neuronal dysfunction. Indeed, the use of the phenylalkylamine Ca 2+ channel blocker verapamil has been successful in ameliorating beta cell dysfunction in preclinical models of both T1D and T2D (Stancill et al., 2017 ; Xu et al., 2012 ). Verapamil is a well known blocker of L-type Ca 2+ channels, and, in normally activated beta cells, it limits Ca 2+ entry into the beta cell (Ohnishi and Endo, 1981 ; Vasseur et al., 1987 ). This would be expected to, in turn, alter the expression of many Ca 2+ influx–dependent beta cell genes (Stancill et al., 2017 ), and the evidence to date suggests it is likely that verapamil preserves beta cell function in diabetes models by repressing thioredoxin-interacting protein (TXNIP) expression and thus protecting the beta cell. This is somewhat surprising given the physiologic role of Ca 2+ is to acutely trigger insulin secretion; this process would be expected to be inhibited by L-type Ca 2+ channel blockers (Ashcroft and Rorsman, 1989 ; Satin et al., 1995 ).
Hyperglycemia is a well known inducer of TXNIP expression, and a lack of TXNIP has been shown to protect against beta cell apoptosis after inflammatory stress (Chen et al., 2008a ; Shalev et al., 2002 ; Chen et al., 2008b ). Excitingly, the use of verapamil in patients with recent-onset T1D improved beta cell function and improved glycemic control for up to 12 months after the initiation of therapy, suggesting there is indeed promise for targeting calcium and TXNIP activation in T1D. Use of verapamil for a repurposed indication in the preservation of beta cell function in T1D is attractive due its well known safety profile as well as its cardiac benefits (Chen et al., 2009 ). Although the long-term efficacy of verapamil to maintain beta cell function in vivo is unclear, a recently described TXNIP inhibitor may also show promise in suppressing the hyperglucagonemia that also contributes to glucose intolerance in T2D (Thielen et al., 2020 ). As there is a clear need for increased Ca 2+ influx into the beta cell to trigger and maintain glucose-dependent insulin secretion (Ashcroft and Rorsman, 1990 ; Satin et al., 1995 ), it remains to be seen how well regulated insulin secretion is preserved in the presence of L-type Ca 2+ channel blockers like verapamil in the system. One might speculate that reducing but not fully eliminating beta cell Ca 2+ influx might reduce TXNIP levels while preserving enough influx to maintain glucose-stimulated insulin release. Alternatively, these two phenomena may operate on entirely different time scales. At present, these issues clearly will require further investigation.
D. GLP-1 and the Incretins
Studies dating back to the 1960s revealed that administering glucose in equal amounts via the peripheral circulation versus the gastrointestinal tract led to dramatically different amounts of glucose-induced insulin secretion (Elrick et al., 1964 ; McIntyre et al., 1964 ; Perley and Kipnis, 1967 ). Gastrointestinal glucose administration greatly increased insulin secretion versus intravenous glucose, and this came to be known as the “incretin effect” (Nauck et al., 1986a ; Nauck et al., 1986b ). Subsequent work showed that release of the gut hormone GLP-1 mediated this effect such that food ingestion induced intestinal cell hormone secretion. GLP-1 so released would then circulate to the pancreas via the blood to prime beta cells to secrete more insulin when glucose became elevated because these hormones stimulated beta cell cAMP formation (Drucker et al., 1987 ). The discovery that a natural peptide corresponding to GLP-1 could be found in the saliva of the Gila monster, a desert lizard, hastened progress in the field, and ample in vitro studies subsequently confirmed that GLP-1 potentiated insulin secretion in a glucose-dependent manner. GLP-1 has little or no significant action on insulin secretion in the absence of elevated glucose (such as might typically correspond to the postprandial case or during fasting), thus minimizing the likelihood of hypoglycemia provoked by GLP-1 in treated patients (Kreymann et al., 1987 ). Although not completely understood, the glucose dependence of GLP-1 likely reflects the requirement for adenine nucleotides to close glucose-inhibited K(ATP) channels and thus subsequently activate Ca 2+ influx–dependent insulin exocytosis. Besides potentiating GSIS at the level of the beta cell, glucagon-like peptide-1 receptor (GLP-1R) agonists also decrease glucagon secretion from pancreatic islet alpha cells, reduce gastric emptying, and may also increase beta cell proliferation, among other cellular actions (reviewed in Drucker, 2018 ; Muller et al., 2019).
Intense interest in the incretins by basic scientists, clinicians, and the pharma community led to the rapid development of new drugs for treating primarily T2D. These drugs include a range of GLP-1R agonists and inhibitors of the incretin hormone degrading enzyme dipeptidyl peptidase 4 (DPP4), whose targeting increases the half-lives of GLP-1 and gastric inhibitory polypeptide (GIP) and thereby increases protein hormone levels in plasma. GLP-1R agonists have been associated with not only a lowering of plasma glucose but also weight loss, decreased appetite, reduced risk of cardiovascular events, and other favorable outcomes (Gerstein et al., 2019; Hernandez et al., 2018; Husain et al., 2019; Marso et al., 2016a; Marso et al., 2016b ; Buse et al., 2004). Regarding their untoward actions, although hypoglycemia is not a major concern, there have been reports of pancreatitis and pancreatic cancer from use of GLP-1R agonists. However, a recent meta-analysis covering four large-scale clinical trials and over 33,000 participants noted no significantly increased risk for pancreatitis/pancreatic cancer in patients using GLP-1R agonists (Bethel et al., 2018).
Ongoing and future developments in the use of proglucagon-derived peptides such as GLP-1 and glucagon include the use of combined GLP-1/GIP, glucagon/GLP-1, and agents targeting all three peptides in combination (reviewed in Alexiadou and Tan, 2020 ). Although short-term infusions of GLP-1 with GIP failed to yield metabolic benefits beyond those seen with GLP-1 alone (Bergmann et al., 2019 ), several GLP-1/GIP dual agonists are currently in development and have shown promising metabolic results in clinical trials (Frias et al., 2017 ; Frias et al., 2020 ; Frias et al., 2018 ). At the level of the pancreatic islet, beneficial effects of dual GLP-1/GIP agonists may be related to imbalanced and biased preferences of these agonists for the gastric inhibitory polypeptide receptor over the GLP-1R (Willard et al., 2020 ) and possibly were not simply to dual hormone agonism in parallel. Dual glucagon/GLP-1 agonist therapy has also been shown to have promising metabolic effects in humans (Ambery et al., 2018 ; Tillner et al., 2019 ). Oxyntomodulin is a natural dual glucagon/GLP-1 receptor agonist and proglucagon cleavage product that is also secreted from intestinal enteroendocrine cells, which has beneficial effects on insulin secretion, appetite regulation, and body weight in both humans and rodents (Cohen et al., 2003 ; Dakin et al., 2001 ; Dakin et al., 2002 ; Shankar et al., 2018 ; Wynne et al., 2005 ). Interestingly, alpha cell crosstalk to beta cells through the combined effects of glucagon and GLP-1 is necessary to obtain optimal glycemic control, suggesting a potential pathway for therapeutic dual glucagon/GLP-1 agonism within the islets of patients with T2D (Capozzi et al., 2019a ; Capozzi et al., 2019b ). Although the early results appear promising, more studies will be necessary to better understand the mechanistic and clinical impacts of these multiagonist agents.
E. DPP4 Inhibitors
Inhibition of DPP4, the incretin hormone degrading enzyme, is one of the most common T2D treatments to increase GLP-1 and GIP plasma hormone levels. These DPP4 inhibitors or “gliptins” are generally used in conjunction with other T2D drugs such as metformin or sulfonylureas to obtain the positive benefits discussed above (Lambeir et al., 2008 ). DPP4 is a primarily membrane-bound peptidase belonging to the serine peptidase/prolyl oligopeptidase gene family, which cleaves a large number of substrates in addition to the incretin hormones (Makrilakis, 2019 ). DPP4 inhibitors provide glucose-lowering benefits while being generally well tolerated, and the variety of available drugs (including sitagliptin, saxagliptin, vildagliptin, alogliptin, and linagliptin) with slightly different dosing frequency, half-life, and mode of excretion/metabolism allows for use in multiple patient populations (Makrilakis, 2019 ). This includes the elderly and individuals with renal or hepatic insufficiency (Makrilakis, 2019 ).
Although hypoglycemia is not a concern for DPP4 inhibitor use, other considerations should be made. DPP4 inhibitors tend to be more expensive than metformin or other second-line oral drugs in addition to having more modest glycemic effects than GLP-1R agonists (Munir and Lamos, 2017 ). Finally, meta-analysis of randomized and observational studies concluded that heart failure in patients with T2D was not associated with use of DPP4 inhibitors; however, this study was limited by the short follow-up and lack of high-quality data (Li et al., 2016 ). Thus, the US Food and Drug Administration (FDA) did recommend assessing risk of heart failure hospitalization in patients with pre-existing cardiovascular disease, prior heart failure, and chronic kidney disease when using saxagliptin and alogliptin (Munir and Lamos, 2017 ).
F. Sodium Glucose Cotransporter 2 Inhibitors
A recent development in the field of T2D drugs are sodium glucose cotransporter 2 (SGLT2) inhibitors, which have an interesting and very different mechanism of action. Within the proximal tubule of the nephron, SGLT2 transports ingested glucose into the lumen of the proximal tubule between the epithelial layers, thereby reclaiming glucose by this reabsorption process (reviewed in Vallon, 2015 ). SGLT2 inhibitors target this transporter and increase glucose in the tubular fluid and ultimately increase it in the urine. In patients with diabetes, SGLT2 inhibition results in a lowering of plasma glucose with urine glucose content rising substantially (Adachi et al., 2000 ; Vallon, 2015 ). These drugs, although they are relatively new, have become an area of great interest for not only patients with T2D (Grempler et al., 2012 ; Imamura et al., 2012 ; Meng et al., 2008 ; Nomura et al., 2010 ) but also for patients with T1D (Luippold et al., 2012 ; Mudaliar et al., 2012 ). Part of their appeal also rests on reports that their use can lead to a statistically significant decline in cardiac events that are known to occur secondarily to diabetes, possibly independently of plasma glucose regulation (reviewed in Kurosaki and Ogasawara, 2013 ). Although the long-term consequences of their clinical use cannot yet be determined, raising the glucose content of the urogenital tract leads to an increased risk of urinary tract infections and other related infections in some patients (Kurosaki and Ogasawara, 2013 ).
Another recent concern about the use of SGLT2 inhibitors has been the development of normoglycemic diabetic ketoacidosis (DKA). Despite the efficacy of SGLT2 inhibitors, observations of hyperglucagonemia in patients with euglycemic DKA has led to a number of recent studies focused on SGLT2 actions on pancreatic islets. Initial studies of isolated human islets treated with small interfering RNA directed against SGLT2 and/or SGLT2 inhibitors demonstrated increased glucagon release. These studies were complemented by the finding of elevations in glucagon release in mice that were administered SGLT2 inhibitors in vivo (Bonner et al., 2015 ). Insights into the possible mechanistic links between SGLT2 inhibition, DKA frequency, and glucagon secretion in humans may relate to the observation of heterogeneity in SGLT2 expression, as SGLT2 expression appears to have a high frequency of interdonor and intradonor variability (Saponaro et al., 2020 ). More recently, both insulin and GLP-1 have been demonstrated to modulate SGLT2-dependent glucagon release through effects on somatostatin release from delta cells (Vergari et al., 2019 ; Saponaro et al., 2019 ), suggesting potentially complex paracrine effects that may affect the efficacy of these compounds.
On the other hand, several recent studies question that the development of euglycemic DKA after SGLT2 inhibitor therapy may be through alpha cell–dependent mechanisms. Three recent studies found no effect of SGLT2 inhibitors to promote glucagon secretion in mouse and/or rat models and could not detect SGLT2 expression in human alpha cells (Chae et al., 2020 ; Kuhre et al., 2019 ; Suga et al., 2019 ). A fourth study demonstrated only a brief transient effect of SGLT2 inhibition to raise circulating glucagon concentrations in immunodeficient mice transplanted with human islets, which returned to baseline levels after longer exposures to SGLT2 inhibitors (Dai et al., 2020 ). Furthermore, SGLT2 protein levels were again undetectable in human islets (Dai et al., 2020 ). These results could suggest alternative islet-independent mechanisms by which patients develop DKA, including alterations in ketone generation and/or clearance, which underscore the additional need for further studies both in molecular models and at the bedside. Nevertheless, SGLT2 inhibitors continue to hold promise as a valuable therapy for T2D, especially in the large segment of patients who also have superimposed cardiovascular risk (McMurray et al., 2019; Wiviott et al., 2019; Zinman et al., 2015).
G. Thiazolidinediones
Once among the most commonly used oral agents in the armamentarium to treat T2D, thiazolidinediones (TZDs) were clinically popular in their utilization to act specifically as insulin sensitizers. TZDs improve peripheral insulin sensitivity through their action as peroxisome proliferator-activated receptor (PPAR) γ agonists, but their clinical use fell sharply after studies suggested a connection between cardiovascular toxicity with rosiglitazone and bladder cancer risk with pioglitazone (Lebovitz, 2019 ). Importantly, an FDA panel eventually removed restrictions related to cardiovascular risk with rosiglitazone in 2013 (Hiatt et al., 2013 ). Similarly, concerns regarding use of bladder cancer risk with pioglitazone were later abated after a series of large clinical studies found that pioglitazone did not increase bladder cancer (Lewis et al., 2015 ; Schwartz et al., 2015 ). However, usage of TZDs had already substantially decreased and has not since recovered.
Although concerns regarding edema, congestive heart failure, and fractures persist with TZD use, there have been several studies suggesting that TZDs protect beta cell function. In the ADOPT study, use of rosiglitazone monotherapy in patients newly diagnosed with T2D led to improved glycemic control compared with metformin or sulfonylureas (Kahn et al., 2006). Later analyses revealed that TZD-treated subjects had a slower deterioration of beta cell function than metformin- or sulfonylurea-treated subjects (Kahn et al., 2011). Furthermore, pioglitazone use improved beta cell function in the prevention of T2D in the ACT NOW study (Defronzo et al., 2013; Kahn et al., 2011). Mechanistically, it is unclear if TZDs lead to beneficial beta cell function through direct effects or through indirect effects of reduced beta cell demand due to enhanced peripheral insulin sensitivity. Indeed, a beta cell–specific knockout of PPAR γ did not impair glucose homeostasis, nor did it impair the antidiabetic effects of TZD use in mice (Rosen et al., 2003 ). However, other reports demonstrated PPAR-responsive elements within the promoters of both glucose transporter 2 and glucokinase that enhance beta cell glucose sensing and function, which could explain beta cell–specific benefits for TZDs (Kim et al., 2002 ; Kim et al., 2000 ). Furthermore, TZDs have been shown to improve beta cell function by upregulating cholesterol transport (Brunham et al., 2007 ; Sturek et al., 2010 ). Additionally, use of TZDs in the nonobese diabetic (NOD) mouse model of T1D augmented the beta cell unfolded protein response and prevented beta cell death, suggesting potential benefits for TZDs in both T1D and T2D (Evans-Molina et al., 2009 ; Maganti et al., 2016 ). With a now refined knowledge of demographics in which to avoid TZD treatment due to adverse effects, together with genetic approaches to identify candidates more likely to respond effectively to TZD therapy (Hu et al., 2019 ; Soccio et al., 2015 ), it remains to be seen if TZD therapy will return to more prominent use in the treatment of diabetes.
H. Insulin and Beyond: The Use of “Smart” Insulin and Closed Loop Systems in Diabetes Treatment
Due to recombinant DNA technology, numerous insulin analogs are now available in various forms ranging from fast acting crystalline insulin to insulin glargine; all of these analogs exhibit equally effective insulin receptor binding. Most are generated by altering amino acids in the B26–B30 region of the molecule (Kurtzhals et al., 2000 ). The American Diabetes Association delineates these insulins by their 1) onset or time before insulin reaches the blood stream, 2) peak time or duration of maximum blood glucose–lowering efficacy, and 3) the duration of blood glucose–lowering time. Insulin administration is independent of the residuum of surviving and/or functioning beta cells in the patient and remains the principal pharmacological treatment of both T1D and T2D. The availability of multiple types of delivery methods, i.e., insulin pens, syringes, pumps, and inhalants, provides clinicians with a solid and varied tool kit with which to treat diabetes. The downsides, however, are that 1) hypoglycemia is a constant threat, 2) proper insulin doses are not trivial to calculate, 3) compliance can vary especially in children and young adults, and 4) there can be side effects of a variety of types. Nonetheless, insulin therapy remains a mainstay treatment of diabetes.
To eliminate the downsides of insulin therapy, research in the past several decades has worked toward generating glucose-sensitive or “smart” insulin molecules. These molecules change insulin bioavailability and become active only upon high blood glucose using glucose-binding proteins such as concanavalin A, glucose oxidase to alter pH sensitivity, and phenylboronic acid (PBA), which forms reversible ester linkages with diol-containing molecules including glucose itself (reviewed in Rege et al., 2017 ). Indeed, promising recent studies included various PBA moieties covalently bonded to an acylated insulin analog (insulin detemir, which contains myristic acid coupled to Lys B29 ). The detemir allows for binding to serum albumin to prolong insulin’s half-life in the circulation, and PBA provided reversible glucose binding (Chou et al., 2015 ). The most promising of the PBA-modified conjugates showed higher potency and responsiveness in lowering blood glucose levels compared with native insulin in diabetic mouse models and decreased hypoglycemia in healthy mice, although the molecular mechanisms have not yet been determined (Chou et al., 2015 ).
An additional active area of research includes structurally defining the interaction between insulin and the insulin receptor ectodomain. Importantly, a major conformational change was discovered that may be exploited to impair insulin receptor binding under hypoglycemic conditions (Menting et al., 2013 ; Rege et al., 2017 ). Challenges in the design, testing, and execution of glucose-responsive insulins may be overcome by the adaptation of novel modeling approaches (Yang et al., 2020 ), which may allow for more rapid screening of candidate compounds.
Technologies have also progressed in the field of artificial pancreas design and development. Currently two “closed loop” systems are now available: Minimed 670G from Medtronic and Control-IQ from Tandem Diabetes Care. Both systems use a continuous glucose monitor, insulin pump, and computer algorithm to predict correct insulin doses and administer them in real time. Such algorithm systems also take into account insulin potency, the rate of blood glucose increase, and the patient’s heart rate and temperature to adjust insulin delivery levels during exercise and after a meal. In addition, so-called “artificial pancreas” systems have also been clinically tested, which use both insulin and glucagon and as such result in fewer reports of hypoglycemic episodes (El-Khatib et al., 2017 ). These types of systems will continue to become more popular as the development of room temperature–stable glucagon analogs continue, such as GVOKE by Xeris Pharmaceuticals (currently available in an injectable syringe) and Baqsimi, a nasally administered glucagon from Eli Lilly.
I. Present and Future Therapies: Beta Cell Transplantation, Replication, and Immune Protection
1. islet transplantation.
The idea to use pancreatic allo/xenografts to treat diabetes remarkably dates back to the late 1800s (Minkowski, 1892 ; Pybus, 1924 ; Williams, 1894 ). Before proceeding to the discovery of insulin (together with Best, MacLeod, and Collip), Frederick Banting also postulated the potential for transplantation of pancreatic tissue emulsions to treat diabetes in dog models in a notebook entry in 1921 (Bliss, 1982 ). Decades later, Paul Lacy, David Scharp, and colleagues successfully isolated intact functional pancreatic islets and transplanted them into rodent models (Kemp et al., 1973 ). These studies led to the initial proof of concept studies for humans, with the first successful islet transplant in a patient with T1D occurring in 1977 (Sutherland et al., 1978 ). A rapid expansion of islet transplantation, inspired by these original studies led to key observations of successfully prolonged islet engraftment by the “Edmonton protocol” whereby corticosteroid-sparing immunosuppression was applied, and islets from at least two allogeneic donors were used to achieve insulin independence (Shapiro et al., 2000 ). More recent work has focused on improving upon the efficiency and long-term engraftment of allogeneic transplants leading to more prolonged graft function (to the 5-year mark) and successful transplantation from a single islet donor (Hering et al., 2016; Hering et al., 2005 ; Rickels et al., 2013 ). Critical to these efforts to improve the success rate was the recognition that the earlier generation of immunosuppressive agents to counter tissue rejection was toxic to islets (Delaunay et al., 1997 ; Paty et al., 2002 ; Soleimanpour et al., 2010 ) and that more appropriate and less toxic agents were needed (Hirshberg et al., 2003 ; Soleimanpour et al., 2012 ).
Certainly, islet transplantation as a therapeutic approach for patients with T1D has been scrutinized due to several challenges, including (but not limited to) the lack of available donor supply to contend with demand, limited long-term functional efficacy of islet allografts, the potential for re-emergence of autoimmune islet destruction and/or metabolic overload-induced islet failure, and significant adverse effects of prolonged immunosuppression (Harlan, 2016 ). Furthermore, although islet transplantation is not currently available for individuals with T2D, simultaneous pancreas-kidney transplantation in T2D had similar favorable outcomes to simultaneous pancreas-kidney transplantation in T1D; therefore, islet-kidney transplantation may eventually be a feasible option to treat T2D, as patients will already be on immunosuppressors (Sampaio et al., 2011 ; Westerman et al., 1983 ). An additional significant obstacle is the tremendous expense associated with islet transplantation therapy. Indeed, the maintenance, operation, and utilization of an FDA-approved and Good Manufacturing Practice–compliant islet laboratory can lead to operating costs at nearly $150,000 per islet transplant, which is not cost effective for the vast majority of patients with T1D (Naftanel and Harlan, 2004 ; Wallner et al., 2016 ). At present, the focus has been to obtain FDA approval for islet allo-transplantation as a therapy for T1D to allow for insurance compensation (Hering et al., 2016; Rickels and Robertson, 2019 ). In the interim, the islet biology, stem cell, immunology, and bioengineering communities have continued the development of cell-based therapies for T1D by other approaches to overcome the challenges identified during the islet transplantation boom of the 1990s and 2000s.
2. Pharmacologic Induction of Beta Cell Replication
Besides transplantation, progress in islet cell biology and especially in developmental biology of beta cells over several decades raised the additional possibility that beta cell mass reduction in diabetes might be countered by increasing beta cell number through mitogenic means. A key method to expand pancreatic beta cell mass is through the enhancement of beta cell replication. Although the study of pancreatic beta cell replication has been an area of intense focus in the beta cell biology field for several decades, only recently has this seemed truly feasible. Seminal studies identified that human beta cells are essentially postmitotic, with a rapid phase of growth occurring in the prenatal period that dramatically tapers off shortly thereafter (Gregg et al., 2012 ; Meier et al., 2008 ). The plasticity of rodent beta cells is considerably higher than that of human beta cells (Dai et al., 2016 ), which has led to a renewed focus on validation of pharmacologic agents to enhance rodent beta cell replication using isolated and/or engrafted human islets (Bernal-Mizrachi et al., 2014 ; Kulkarni et al., 2012 ; Stewart et al., 2015 ). Indeed, a large percentage of agents that were successful when applied to rodent systems were largely unsuccessful at inducing replication in human beta cells (Bernal-Mizrachi et al., 2014 ; Kulkarni et al., 2012 ; Stewart et al., 2015 ). However, several recent studies have begun to make significant progress on successfully pushing human beta cells to replicate.
Several groups have reported successful human beta cell proliferation, both in vitro and in vivo, in response to inhibitors of the dual specificity tyrosine phosphorylation-regulated kinase 1A (DYRK1A). These inhibitors include harmine, INDY, GNF4877, 5-iodotubericidin, leucettine-42, TG003, AZ191, CC-401, and more specific, recently developed DYRK1A inhibitors (Ackeifi et al., 2020 ). Although DYRK1A is conclusively established as the important mediator of human beta cell proliferation, comprehensively determining other cellular targets and if additional gene inhibition amplifies the proliferative response is still in process. New evidence from Wang and Stewart shows dual specificity tyrosine phosphorylation-regulated kinase 1B to be an additional mitogenic target and also describes variability in the range of activated kinases within cells and/or levels of inhibition for the many DYRK1A inhibitors listed above (Ackeifi et al., 2020 ). Interestingly, opposite to these human studies, earlier mouse studies from the Scharfmann group demonstrated that Dyrk1a haploinsufficiency leads to decreased proliferation and loss of beta cell mass (Rachdi et al., 2014b ). In addition, overexpression of Dyrk1a in mice led to beta cell mass expansion with increased glucose tolerance (Rachdi et al., 2014a ).
Although important differences in beta cell proliferative capacity have been shown between human and rodent species, there are also significant differences in the mitogenic capacity of beta cells from juvenile, adult, and pregnant individuals. This demonstrates that proliferative stimuli appear to act within the complex islet, pancreas, and whole-body environments unique to each time point. For example, the administration of the hormones platelet-derived growth factor alpha or GLP-1 result in enhanced proliferation in juvenile human beta cells yet are ineffective in adult human beta cells (Chen et al., 2011 ; Dai et al., 2017 ). This has been shown to be due to a loss of platelet-derived growth factor alpha receptor expression as beta cells age but appears to be unrelated to GLP-1 receptor expression levels (Chen et al., 2011 ). Indeed, the GLP-1 receptor is highly expressed in adult beta cells, and GLP-1 secretion increases insulin secretion, as detailed previously; however, the induction of proliferative factors such as nuclear factor of activated T cells, cytoplasmic 1; forkhead box protein 1; and cyclin A1 is only seen in juvenile islets (Dai et al., 2017 ). Human studies using cadaveric pancreata from pregnant donors also showed increased beta cell mass, yet lactogenic hormones from the pituitary or placenta (prolactin, placental lactogen, or growth hormone) are unable to stimulate proliferation in human beta cells despite their ability to produce robust proliferation in mouse beta cells (reviewed in Baeyens et al., 2016 ). Experiments overexpressing mouse versus human signal transducer and activator of transcription 5, the final signaling factor inducing beta cell adaptation, in human beta cells allows for prolactin-mediated proliferation revealing fundamental differences in prolactin pathway competency in human (Chen et al., 2015 ). Overcoming the barrier of recapitulating human pregnancy’s effect on beta cells through isolating placental cells or blood serum during pregnancy may result in the discovery of a factor(s) that facilitates the increase in beta cell mass observed during human pregnancy.
Mechanisms that stimulate beta cell proliferation have also been discovered from studying genetic mutations that result in insulinomas, spontaneous insulin-producing beta cell adenomas. The most common hereditary mutation occurs in the multiple endocrine neoplasia type 1 (MEN1) gene. Indeed, administration of a MEN1 inhibitor in addition to a GLP-1 agonist (which cannot induce proliferation alone) is able to increase beta cell proliferation in isolated human islets through synergistic activation of KRAS proto-oncogene, GTPase downstream signals (Chamberlain et al., 2014 ). Interestingly, MEN1 mutations are uncommon in sporadic insulinomas, yet assaying genomic and epigenetic changes in a large cohort of non-MEN1 insulinomas found alterations in trithorax and polycomb chromatin modifying genes that were functionally related to MEN1 (Wang et al., 2017 ). Stewart and colleagues hypothesized that changes in histone 3 lysine 27 and histone 3 lysine 4 methylation status led to increased enhancer of zeste homolog 2 and lysine demethylase 6A, decreased cyclin-dependent kinase inhibitor 1C, and thereby increased beta cell proliferation, among other phenotypes. They also proposed that these findings help to explain why increased proliferation always occurs despite broad heterogeneity of mutations found between individual insulinomas (Wang et al., 2017 ).
Although factors that induce proliferation are continuing to be discovered, there are drawbacks that still limit their clinical application. Harmine and other DYRK1A inhibitors are not beta cell specific, nor have all their cellular targets been determined (Ackeifi et al., 2020 ). Targeting other pathways to induce human beta cell proliferation such as modulation of prostaglandin E2 receptors (i.e., inhibition of prostaglandin E receptor 3 alone or in combination with prostaglandin E receptor 4 activation) showed promising increases in proliferative rate yet suffers from the same lack of specificity (Carboneau et al., 2017 ). Induction of proliferation may also come at the expense of glucose sensing as in insulinomas, which have an increased expression of “disallowed genes” and alterations in glucose transporter and hexokinase expression (Wang et al., 2017 ). A further untoward consequence that must be avoided is the production of cancerous cells through unchecked proliferation. Finally, increasing beta cell mass through low rates of proliferation may increase the pool of functional insulin-secreting cells in T2D, but without additional measures, these beta cells will still ultimately be targeted for immune cell destruction in T1D.
3. Beta Cell Stress Relieving Therapies
Metabolic, inflammatory, and endoplasmic reticulum (ER) stress contribute to beta cell dysfunction and failure in both T1D and T2D. Although reduction of metabolic overload of beta cells by early exogenous insulin therapy or insulin sensitizers can temporarily reduce loss of beta cell mass/function early in diabetes, a focus on relieving ER and inflammatory stress is also of interest to preserve beta cell health.
ER stress is a well known contributor to beta cell demise both in T1D and T2D (Laybutt et al., 2007 ; Marchetti et al., 2007 ; Marhfour et al., 2012 ; Tersey et al., 2012 ) and a target of interest in the prevention of beta cell loss in both diseases. Preclinical studies suggest that the use of chemical chaperones, including 4-phenylbutyric acid and tauroursodeoxycholic acid (TUDCA), to alleviate ER stress improves beta cell function and insulin sensitivity in mouse models of T2D (Cnop et al., 2017 ; Ozcan et al., 2006 ). Furthermore, TUDCA has been shown to preserve beta cell mass and reduce ER stress in mouse models of T1D (Engin et al., 2013 ). Interestingly, TUDCA has shown promise at improving insulin action in obese nondiabetic human subjects, yet beta cell function and insulin secretion were not assessed (Kars et al., 2010 ). A clinical trial regarding the use of TUDCA for humans with new-onset T1D is also ongoing ( {"type":"clinical-trial","attrs":{"text":"NCT02218619","term_id":"NCT02218619"}} NCT02218619 ). However, a note of caution regarding use of ER chaperones is that they may prevent low level ER stress necessary to potentiate beta cell replication during states of increased insulin demand (Sharma et al., 2015 ), suggesting that the broad use of ER chaperone therapies should be carefully considered.
The blockade of inflammatory stress has long been an area of interest for treatments of both T1D and T2D (Donath et al., 2019 ; Eguchi and Nagai, 2017 ). Indeed, use of nonsteroidal anti-inflammatory drugs (NSAIDs), which block cyclooxygenase, have been observed to improve metabolic control in patients with diabetes since the turn of the 20th century (Williamson, 1901 ). Salicylates have been shown to improve insulin secretion and beta cell function in both obese human subjects and those with T2D (Fernandez-Real et al., 2008; Giugliano et al., 1985 ). However, another NSAID, salsalate, has not been shown to improve beta cell function while improving other metabolic outcomes (Kim et al., 2014 ; Penesova et al., 2015 ), possibly suggesting distinct mechanisms of action for anti-inflammatory compounds. The regular use of NSAIDs to enhance metabolic outcomes is also often limited to the tolerability of long-term use of these agents due to adverse effects. Recently, golilumab, a monoclonal antibody against the proinflammatory cytokine tumor necrosis factor alpha, was demonstrated to improve beta cell function in new-onset T1D, suggesting that targeting the underlying inflammatory milieu may have benefits to preserve beta cell mass and function in T1D (Quattrin et al., 2020). Taken together, both new and old approaches to target beta cell stressors still remain of long-term interest to improve beta cell viability and function in both T1D and T2D.
3. New Players to Induce Islet Immune Protection
Countless researchers have expended intense industry to determine T1D disease etiology and treatments focused on immunotherapy and tolerogenic methods. Multiple, highly comprehensive reviews are available describing these efforts (Goudy and Tisch, 2005 ; Rewers and Gottlieb, 2009 ; Stojanovic et al., 2017 ). Here we will focus on the protection of beta cells through programmed cell death protein-1 ligand (PD-L1) overexpression, major histocompatibility complex class I, A, B, C (HLA-A,B,C) mutated human embryonic stem cell–derived beta cells, and islet encapsulation methods.
Cancer immunotherapies that block immune checkpoints are beneficial for treating advanced stage cancers, yet induction of autoimmune diseases, including T1D, remains a potential side effect (Stamatouli et al., 2018 ; Perdigoto et al., 2019 ). A subset of these drugs target either the programmed cell death-1 protein on the surface of activated T lymphocytes or its receptor PD-L1 (Stamatouli et al., 2018 ; Perdigoto et al., 2019 ). PD-L1 expression was found in insulin-positive beta cells from T1D but not insulin-negative islets or nondiabetic islets, leading to the hypothesis that PD-L1 is upregulated in an attempt to drive immune cell attenuation (Osum et al., 2018 ; Colli et al., 2018 ). Adenoviral overexpression of PD-L1 specifically in beta cells rescued hyperglycemia in the NOD mouse model of T1D, but these animals eventually succumbed to diabetes by the study’s termination (El Khatib et al., 2015 ). A more promising report from Ben Nasr et al. ( 2017 ) demonstrated that pharmacologically or genetically induced overexpression of PD-L1 in hematopoietic stem and progenitor cells inhibited beta cell autoimmunity in the NOD mouse as well as in vitro using human hematopoietic stem and progenitor cells from patients with T1D.
As mentioned above, islet transplantation to treat T1D is limited by islet availability, cost, and the requirement for continuous immunosuppression. Islet cells generated by differentiating embryonic or induced pluripotent stem (iPS) cells could circumvent these limitations. Ideally, iPS-derived beta cells could be manipulated to eliminate the expression of polymorphic HLA-A,B,C molecules, which were found to be upregulated in T1D beta cells (Bottazzo et al., 1985 ; Richardson et al., 2016 ). These molecules allow peptide presentation to CD8+ T cells or cytotoxic T lymphocytes and may lead to beta cell removal. Interestingly, remaining insulin-positive cells in T1D donor pancreas are not HLA-A,B,C positive (Nejentsev et al., 2007; Rodriguez-Calvo et al., 2015 ). However, current differentiation protocols are still limited in their ability to produce fully glucose-responsive beta cells without transplantation into animal models to induce mature characteristics. Additionally, use of iPS-derived beta cells will still lead to concerns regarding DNA mutagenesis resulting from the methods used to obtain pluripotency or teratoma formation from cells that have escaped differentiation.
Encapsulation devices would protect islets or stem cells from immune cell infiltration while allowing for the proper exchange of nutrients and hormones. Macroencapsulation uses removable devices that would help assuage fears surrounding mutation or tumor formation; indeed, the first human trial using encapsulated hESC-derived beta cells will be completed in January 2021 ( {"type":"clinical-trial","attrs":{"text":"NCT02239354","term_id":"NCT02239354"}} NCT02239354 ). Macroencapsulation of islets prior to transplantation using various alginate-based hydrogels has historically been impeded by a strong in vivo foreign body immune response (Desai and Shea, 2017 ; Doloff et al., 2017 ; Pueyo et al., 1993 ). More recently, chemically modified forms of alginate that avoid macrophage recognition and fibrous deposition have been successfully used in rodents and for up to 6 months in nonhuman primates (Vegas et al., 2016 ). Indeed, Bochenek et al. ( 2018 ) successfully transplanted alginate protected islets for 4 months without immunosuppression in the bursa omentalis of nonhuman primates demonstrating the feasibility for this approach to be extended to humans. It remains to be seen if these devices will be successful for long-term use, perhaps decades, in patients with diabetes.
III. Summary
Although existing drug therapies using classic oral antidiabetic drugs like sulfonylureas and metformin or injected insulin remain mainstays of diabetes treatment, newer drugs based on incretin hormone actions or SGLT2 inhibitors have increased the pharmacological armamentarium available to diabetologists ( Fig. 1 ). However, the explosion of progress in beta cell biology has identified potential avenues that can increase beta cell mass in sophisticated ways by employing stem cell differentiation or enhancement of beta cell proliferation. Taken together, there should be optimism that the increased incidence of both T1D and T2D is being matched by the creativity and hard work of the diabetes research community.
Abbreviations
Authorship contributions.
Wrote and contributed to the writing of the manuscript: Satin, Soleimanpour, Walker
This work was supported by the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) [Grant R01-DK46409] (to L.S.S.), [Grant R01-DK108921] (to S.A.S.), and [Grant P30-DK020572 pilot and feasibility grant] (to S.A.S.), the Juvenile Diabetes Research Foundation (JDRF) [Grant CDA-2016-189] (to L.S.S. and S.A.S.), [Grant SRA-2018-539] (to S.A.S.), and [Grant COE-2019-861] (to S.A.S.), and the US Department of Veterans Affairs [Grant I01 BX004444] (to S.A.S.). The JDRF Career Development Award to S.A.S. is partly supported by the Danish Diabetes Academy and the Novo Nordisk Foundation.
https://doi.org/10.1124/pharmrev.120.000160
- Ackeifi C, Swartz E, Kumar K, Liu H, Chalada S, Karakose E, Scott DK, Garcia-Ocaña A, Sanchez R, DeVita RJ, et al. (2020) Pharmacologic and genetic approaches define human pancreatic β cell mitogenic targets of DYRK1A inhibitors . JCI Insight 5 :e132594. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Adachi T, Yasuda K, Okamoto Y, Shihara N, Oku A, Ueta K, Kitamura K, Saito A, Iwakura I, Yamada Y, et al. (2000) T-1095, a renal Na+-glucose transporter inhibitor, improves hyperglycemia in streptozotocin-induced diabetic rats . Metabolism 49 :990–995. [ PubMed ] [ Google Scholar ]
- Alexiadou K, Tan TM (2020) Gastrointestinal peptides as therapeutic targets to mitigate obesity and metabolic syndrome . Curr Diab Rep 20 :26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ambery P, Parker VE, Stumvoll M, Posch MG, Heise T, Plum-Moerschel L, Tsai LF, Robertson D, Jain M, Petrone M, et al. (2018) MEDI0382, a GLP-1 and glucagon receptor dual agonist, in obese or overweight patients with type 2 diabetes: a randomised, controlled, double-blind, ascending dose and phase 2a study . Lancet 391 :2607–2618. [ PubMed ] [ Google Scholar ]
- Ashcroft FM, Rorsman P (1989) Electrophysiology of the pancreatic beta-cell . Prog Biophys Mol Biol 54 :87–143. [ PubMed ] [ Google Scholar ]
- Ashcroft FM, Rorsman P (1990) ATP-sensitive K+ channels: a link between B-cell metabolism and insulin secretion . Biochem Soc Trans 18 :109–111. [ PubMed ] [ Google Scholar ]
- Baeyens L, Hindi S, Sorenson RL, German MS (2016) β-Cell adaptation in pregnancy . Diabetes Obes Metab 18 ( Suppl 1 ):63–70. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bailey CJ (1992) Biguanides and NIDDM . Diabetes Care 15 :755–772. [ PubMed ] [ Google Scholar ]
- Ben Nasr M, Tezza S, D’Addio F, Mameli C, Usuelli V, Maestroni A, Corradi D, Belletti S, Albarello L, Becchi G, et al. (2017) PD-L1 genetic overexpression or pharmacological restoration in hematopoietic stem and progenitor cells reverses autoimmune diabetes . Sci Transl Med 9 :eaam7543. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bergmann NC, Lund A, Gasbjerg LS, Meessen ECE, Andersen MM, Bergmann S, Hartmann B, Holst JJ, Jessen L, Christensen MB, et al. (2019) Effects of combined GIP and GLP-1 infusion on energy intake, appetite and energy expenditure in overweight/obese individuals: a randomised, crossover study . Diabetologia 62 :665–675. [ PubMed ] [ Google Scholar ]
- Bernal-Mizrachi E, Kulkarni RN, Scott DK, Mauvais-Jarvis F, Stewart AF, Garcia-Ocaña A (2014) Human β-cell proliferation and intracellular signaling part 2: still driving in the dark without a road map . Diabetes 63 :819–831. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bethel MA, Patel RA, Merrill P, Lokhnygina Y, Buse JB, Mentz RJ, Pagidipati NJ, Chan JC, Gustavson SM, Iqbal N, et al.; EXSCEL Study Group (2018) Cardiovascular outcomes with glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: a meta-analysis . Lancet Diabetes Endocrinol 6 :105–113. [ PubMed ] [ Google Scholar ]
- Bliss M (1982) Banting’s, Best’s, and Collip’s accounts of the discovery of insulin . Bull Hist Med 56 :554–568. [ PubMed ] [ Google Scholar ]
- Bochenek MA, Veiseh O, Vegas AJ, McGarrigle JJ, Qi M, Marchese E, Omami M, Doloff JC, Mendoza-Elias J, Nourmohammadzadeh M, et al. (2018) Alginate encapsulation as long-term immune protection of allogeneic pancreatic islet cells transplanted into the omental bursa of macaques . Nat Biomed Eng 2 :810–821. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bonner C, Kerr-Conte J, Gmyr V, Queniat G, Moerman E, Thévenet J, Beaucamps C, Delalleau N, Popescu I, Malaisse WJ, et al. (2015) Inhibition of the glucose transporter SGLT2 with dapagliflozin in pancreatic alpha cells triggers glucagon secretion . Nat Med 21 :512–517. [ PubMed ] [ Google Scholar ]
- Bonora E, Cigolini M, Bosello O, Zancanaro C, Capretti L, Zavaroni I, Coscelli C, Butturini U (1984) Lack of effect of intravenous metformin on plasma concentrations of glucose, insulin, C-peptide, glucagon and growth hormone in non-diabetic subjects . Curr Med Res Opin 9 :47–51. [ PubMed ] [ Google Scholar ]
- Bottazzo GF, Dean BM, McNally JM, MacKay EH, Swift PG, Gamble DR (1985) In situ characterization of autoimmune phenomena and expression of HLA molecules in the pancreas in diabetic insulitis . N Engl J Med 313 :353–360. [ PubMed ] [ Google Scholar ]
- Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF (2010) Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence . Popul Health Metr 8 :29. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brunham LR, Kruit JK, Pape TD, Timmins JM, Reuwer AQ, Vasanji Z, Marsh BJ, Rodrigues B, Johnson JD, Parks JS, et al. (2007) Beta-cell ABCA1 influences insulin secretion, glucose homeostasis and response to thiazolidinedione treatment . Nat Med 13 :340–347. [ PubMed ] [ Google Scholar ]
- Buse JB, DeFronzo RA, Rosenstock J, Kim T, Burns C, Skare S, Baron A, Fineman M (2016) The primary glucose-lowering effect of metformin resides in the gut, not the circulation: results from short-term pharmacokinetic and 12-week dose-ranging studies . Diabetes Care 39 :198–205. [ PubMed ] [ Google Scholar ]
- Buse JB, Henry RR, Han J, Kim DD, Fineman MS, Baron AD; Exenatide-113 Clinical Study Group (2004) Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes . Diabetes Care 27 :2628–2635. [ PubMed ] [ Google Scholar ]
- Capozzi ME, Svendsen B, Encisco SE, Lewandowski SL, Martin MD, Lin H, Jaffe JL, Coch RW, Haldeman JM, MacDonald PE, et al. (2019a) β Cell tone is defined by proglucagon peptides through cAMP signaling . JCI Insight 4 :e126742. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Capozzi ME, Wait JB, Koech J, Gordon AN, Coch RW, Svendsen B, Finan B, D’Alessio DA, Campbell JE (2019b) Glucagon lowers glycemia when β-cells are active . JCI Insight 5 :e129954. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Carboneau BA, Allan JA, Townsend SE, Kimple ME, Breyer RM, Gannon M (2017) Opposing effects of prostaglandin E 2 receptors EP3 and EP4 on mouse and human β-cell survival and proliferation . Mol Metab 6 :548–559. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chae H, Augustin R, Gatineau E, Mayoux E, Bensellam M, Antoine N, Khattab F, Lai BK, Brusa D, Stierstorfer B, et al. (2020) SGLT2 is not expressed in pancreatic α- and β-cells, and its inhibition does not directly affect glucagon and insulin secretion in rodents and humans . Mol Metab 42 :101071. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chamberlain CE, Scheel DW, McGlynn K, Kim H, Miyatsuka T, Wang J, Nguyen V, Zhao S, Mavropoulos A, Abraham AG, et al. (2014) Menin determines K-RAS proliferative outputs in endocrine cells . J Clin Invest 124 :4093–4101. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen H, Gu X, Liu Y, Wang J, Wirt SE, Bottino R, Schorle H, Sage J, Kim SK (2011) PDGF signalling controls age-dependent proliferation in pancreatic β-cells . Nature 478 :349–355. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen H, Kleinberger JW, Takane KK, Salim F, Fiaschi-Taesch N, Pappas K, Parsons R, Jiang J, Zhang Y, Liu H, et al. (2015) Augmented Stat5 signaling bypasses multiple impediments to lactogen-mediated proliferation in human β-cells . Diabetes 64 :3784–3797. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen J, Cha-Molstad H, Szabo A, Shalev A (2009) Diabetes induces and calcium channel blockers prevent cardiac expression of proapoptotic thioredoxin-interacting protein . Am J Physiol Endocrinol Metab 296 :E1133–E1139. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen J, Hui ST, Couto FM, Mungrue IN, Davis DB, Attie AD, Lusis AJ, Davis RA, Shalev A (2008a) Thioredoxin-interacting protein deficiency induces Akt/Bcl-xL signaling and pancreatic beta-cell mass and protects against diabetes . FASEB J 22 :3581–3594. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen J, Saxena G, Mungrue IN, Lusis AJ, Shalev A (2008b) Thioredoxin-interacting protein: a critical link between glucose toxicity and beta-cell apoptosis . Diabetes 57 :938–944. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chou DH, Webber MJ, Tang BC, Lin AB, Thapa LS, Deng D, Truong JV, Cortinas AB, Langer R, Anderson DG (2015) Glucose-responsive insulin activity by covalent modification with aliphatic phenylboronic acid conjugates . Proc Natl Acad Sci USA 112 :2401–2406. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cnop M, Toivonen S, Igoillo-Esteve M, Salpea P (2017) Endoplasmic reticulum stress and eIF2α phosphorylation: the Achilles heel of pancreatic β cells . Mol Metab 6 :1024–1039. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cohen MA, Ellis SM, Le Roux CW, Batterham RL, Park A, Patterson M, Frost GS, Ghatei MA, Bloom SR (2003) Oxyntomodulin suppresses appetite and reduces food intake in humans . J Clin Endocrinol Metab 88 :4696–4701. [ PubMed ] [ Google Scholar ]
- Coll AP, Chen M, Taskar P, Rimmington D, Patel S, Tadross JA, Cimino I, Yang M, Welsh P, Virtue S, et al. (2020) GDF15 mediates the effects of metformin on body weight and energy balance . Nature 578 :444–448. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Colli ML, Hill JLE, Marroquí L, Chaffey J, Dos Santos RS, Leete P, Coomans de Brachène A, Paula FMM, Op de Beeck A, Castela A, et al. (2018) PDL1 is expressed in the islets of people with type 1 diabetes and is up-regulated by interferons-α and-γ via IRF1 induction . EBioMedicine 36 :367–375. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- RISE Consortium (2019) Lack of durable improvements in β-cell function following withdrawal of pharmacological interventions in adults with impaired glucose tolerance or recently diagnosed type 2 diabetes . Diabetes Care 42 :1742–1751. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dai C, Hang Y, Shostak A, Poffenberger G, Hart N, Prasad N, Phillips N, Levy SE, Greiner DL, Shultz LD, et al. (2017) Age-dependent human β cell proliferation induced by glucagon-like peptide 1 and calcineurin signaling . J Clin Invest 127 :3835–3844. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dai C, Kayton NS, Shostak A, Poffenberger G, Cyphert HA, Aramandla R, Thompson C, Papagiannis IG, Emfinger C, Shiota M, et al. (2016) Stress-impaired transcription factor expression and insulin secretion in transplanted human islets . J Clin Invest 126 :1857–1870. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dai C, Walker JT, Shostak A, Bouchi Y, Poffenberger G, Hart NJ, Jacobson DA, Calcutt MW, Bottino R, Greiner DL, et al. (2020) Dapagliflozin does not directly affect human α or β cells . Endocrinology 161 :bqaa080. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dakin CL, Gunn I, Small CJ, Edwards CM, Hay DL, Smith DM, Ghatei MA, Bloom SR (2001) Oxyntomodulin inhibits food intake in the rat . Endocrinology 142 :4244–4250. [ PubMed ] [ Google Scholar ]
- Dakin CL, Small CJ, Park AJ, Seth A, Ghatei MA, Bloom SR (2002) Repeated ICV administration of oxyntomodulin causes a greater reduction in body weight gain than in pair-fed rats . Am J Physiol Endocrinol Metab 283 :E1173–E1177. [ PubMed ] [ Google Scholar ]
- Defronzo RA, Tripathy D, Schwenke DC, Banerji M, Bray GA, Buchanan TA, Clement SC, Gastaldelli A, Henry RR, Kitabchi AE, et al.; ACT NOW Study (2013) Prevention of diabetes with pioglitazone in ACT NOW: physiologic correlates . Diabetes 62 :3920–3926. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Delaunay F, Khan A, Cintra A, Davani B, Ling ZC, Andersson A, Ostenson CG, Gustafsson J, Efendic S, Okret S (1997) Pancreatic beta cells are important targets for the diabetogenic effects of glucocorticoids . J Clin Invest 100 :2094–2098. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Desai T, Shea LD (2017) Advances in islet encapsulation technologies . Nat Rev Drug Discov 16 :338–350. [ PubMed ] [ Google Scholar ]
- Devaraj S, Venkatachalam A, Chen X (2016) Metformin and the gut microbiome in diabetes . Clin Chem 62 :1554–1555. [ PubMed ] [ Google Scholar ]
- Doloff JC, Veiseh O, Vegas AJ, Tam HH, Farah S, Ma M, Li J, Bader A, Chiu A, Sadraei A, et al. (2017) Colony stimulating factor-1 receptor is a central component of the foreign body response to biomaterial implants in rodents and non-human primates . Nat Mater 16 :671–680. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Donath MY, Dinarello CA, Mandrup-Poulsen T (2019) Targeting innate immune mediators in type 1 and type 2 diabetes . Nat Rev Immunol 19 :734–746. [ PubMed ] [ Google Scholar ]
- Drucker DJ (2018) Mechanisms of action and therapeutic application of glucagon-like peptide-1 . Cell Metab 27 :740–756. [ PubMed ] [ Google Scholar ]
- Drucker DJ, Philippe J, Mojsov S, Chick WL, Habener JF (1987) Glucagon-like peptide I stimulates insulin gene expression and increases cyclic AMP levels in a rat islet cell line . Proc Natl Acad Sci USA 84 :3434–3438. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Duca FA, Côté CD, Rasmussen BA, Zadeh-Tahmasebi M, Rutter GA, Filippi BM, Lam TK (2015) Metformin activates a duodenal Ampk-dependent pathway to lower hepatic glucose production in rats . Nat Med 21 :506–511. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Eguchi K, Nagai R (2017) Islet inflammation in type 2 diabetes and physiology . J Clin Invest 127 :14–23. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- El Khatib MM, Sakuma T, Tonne JM, Mohamed MS, Holditch SJ, Lu B, Kudva YC, Ikeda Y (2015) β-Cell-targeted blockage of PD1 and CTLA4 pathways prevents development of autoimmune diabetes and acute allogeneic islets rejection . Gene Ther 22 :430–438. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- El-Khatib FH, Balliro C, Hillard MA, Magyar KL, Ekhlaspour L, Sinha M, Mondesir D, Esmaeili A, Hartigan C, Thompson MJ, et al. (2017) Home use of a bihormonal bionic pancreas versus insulin pump therapy in adults with type 1 diabetes: a multicentre randomised crossover trial . Lancet 389 :369–380. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- El-Mir MY, Detaille D, R-Villanueva G, Delgado-Esteban M, Guigas B, Attia S, Fontaine E, Almeida A, Leverve X (2008) Neuroprotective role of antidiabetic drug metformin against apoptotic cell death in primary cortical neurons . J Mol Neurosci 34 :77–87. [ PubMed ] [ Google Scholar ]
- El-Mir MY, Nogueira V, Fontaine E, Avéret N, Rigoulet M, Leverve X (2000) Dimethylbiguanide inhibits cell respiration via an indirect effect targeted on the respiratory chain complex I . J Biol Chem 275 :223–228. [ PubMed ] [ Google Scholar ]
- Elrick H, Stimmler L, Hlad CJ Jr, Arai Y (1964) Plasma Insulin Response to Oral and Intravenous Glucose Administration . J Clin Endocrinol Metab 24 :1076–1082. [ PubMed ] [ Google Scholar ]
- Engin F, Yermalovich A, Nguyen T, Hummasti S, Fu W, Eizirik DL, Mathis D, Hotamisligil GS (2013) Restoration of the unfolded protein response in pancreatic β cells protects mice against type 1 diabetes [published correction appears in Sci Transl Med (2013) 5 :214er11] . Sci Transl Med 5 :211ra156. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD (2005) Metformin and reduced risk of cancer in diabetic patients . BMJ 330 :1304–1305. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Evans-Molina C, Robbins RD, Kono T, Tersey SA, Vestermark GL, Nunemaker CS, Garmey JC, Deering TG, Keller SR, Maier B, et al. (2009) Peroxisome proliferator-activated receptor gamma activation restores islet function in diabetic mice through reduction of endoplasmic reticulum stress and maintenance of euchromatin structure . Mol Cell Biol 29 :2053–2067. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fernández-Real JM, López-Bermejo A, Ropero AB, Piquer S, Nadal A, Bassols J, Casamitjana R, Gomis R, Arnaiz E, Pérez I, et al. (2008) Salicylates increase insulin secretion in healthy obese subjects . J Clin Endocrinol Metab 93 :2523–2530. [ PubMed ] [ Google Scholar ]
- Foretz M, Guigas B, Bertrand L, Pollak M, Viollet B (2014) Metformin: from mechanisms of action to therapies . Cell Metab 20 :953–966. [ PubMed ] [ Google Scholar ]
- Foretz M, Guigas B, Viollet B (2019) Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus . Nat Rev Endocrinol 15 :569–589. [ PubMed ] [ Google Scholar ]
- Foretz M, Hébrard S, Leclerc J, Zarrinpashneh E, Soty M, Mithieux G, Sakamoto K, Andreelli F, Viollet B (2010) Metformin inhibits hepatic gluconeogenesis in mice independently of the LKB1/AMPK pathway via a decrease in hepatic energy state . J Clin Invest 120 :2355–2369. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Frias JPBastyr EJ 3rd, Vignati L, Tschöp MH, Schmitt C, Owen K, Christensen RHDiMarchi RD (2017) The sustained effects of a dual GIP/GLP-1 receptor agonist, NNC0090-2746, in patients with type 2 diabetes . Cell Metab 26 :343–352.e2. [ PubMed ] [ Google Scholar ]
- Frias JP, Nauck MA, Van J, Benson C, Bray R, Cui X, Milicevic Z, Urva S, Haupt A, Robins DA (2020) Efficacy and tolerability of tirzepatide, a dual glucose-dependent insulinotropic peptide and glucagon-like peptide-1 receptor agonist in patients with type 2 diabetes: A 12-week, randomized, double-blind, placebo-controlled study to evaluate different dose-escalation regimens . Diabetes Obes Metab 22 :938–946. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Frias JP, Nauck MA, Van J, Kutner ME, Cui X, Benson C, Urva S, Gimeno RE, Milicevic Z, Robins D, et al. (2018) Efficacy and safety of LY3298176, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial . Lancet 392 :2180–2193. [ PubMed ] [ Google Scholar ]
- Fullerton MD, Galic S, Marcinko K, Sikkema S, Pulinilkunnil T, Chen ZP, O’Neill HM, Ford RJ, Palanivel R, O’Brien M, et al. (2013) Single phosphorylation sites in Acc1 and Acc2 regulate lipid homeostasis and the insulin-sensitizing effects of metformin . Nat Med 19 :1649–1654. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, Probstfield J, Riesmeyer JS, Riddle MC, Rydén L, et al.; REWIND Investigators (2019) Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial . Lancet 394 :121–130. [ PubMed ] [ Google Scholar ]
- Giugliano D, Ceriello A, Saccomanno F, Quatraro A, Paolisso G, D’Onofrio F (1985) Effects of salicylate, tolbutamide, and prostaglandin E2 on insulin responses to glucose in noninsulin-dependent diabetes mellitus . J Clin Endocrinol Metab 61 :160–166. [ PubMed ] [ Google Scholar ]
- Goudy KS, Tisch R (2005) Immunotherapy for the prevention and treatment of type 1 diabetes . Int Rev Immunol 24 :307–326. [ PubMed ] [ Google Scholar ]
- Gregg BE, Moore PC, Demozay D, Hall BA, Li M, Husain A, Wright AJ, Atkinson MA, Rhodes CJ (2012) Formation of a human β-cell population within pancreatic islets is set early in life . J Clin Endocrinol Metab 97 :3197–3206. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Grempler R, Thomas L, Eckhardt M, Himmelsbach F, Sauer A, Sharp DE, Bakker RA, Mark M, Klein T, Eickelmann P (2012) Empagliflozin, a novel selective sodium glucose cotransporter-2 (SGLT-2) inhibitor: characterisation and comparison with other SGLT-2 inhibitors . Diabetes Obes Metab 14 :83–90. [ PubMed ] [ Google Scholar ]
- Harlan DM (2016) Islet transplantation for hypoglycemia unawareness/severe hypoglycemia: caveat emptor . Diabetes Care 39 :1072–1074. [ PubMed ] [ Google Scholar ]
- Harrower AD (1991) Efficacy of gliclazide in comparison with other sulphonylureas in the treatment of NIDDM . Diabetes Res Clin Pract 14 ( Suppl 2 ):S65–S67. [ PubMed ] [ Google Scholar ]
- He L, Wondisford FE (2015) Metformin action: concentrations matter . Cell Metab 21 :159–162. [ PubMed ] [ Google Scholar ]
- Hedrington MS, Davis SN (2019) Considerations when using alpha-glucosidase inhibitors in the treatment of type 2 diabetes . Expert Opin Pharmacother 20 :2229–2235. [ PubMed ] [ Google Scholar ]
- Hering BJ, Clarke WR, Bridges ND, Eggerman TL, Alejandro R, Bellin MD, Chaloner K, Czarniecki CW, Goldstein JS, Hunsicker LG, et al.; Clinical Islet Transplantation Consortium (2016) Phase 3 trial of transplantation of human islets in type 1 diabetes complicated by severe hypoglycemia . Diabetes Care 39 :1230–1240. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hering BJ, Kandaswamy R, Ansite JD, Eckman PM, Nakano M, Sawada T, Matsumoto I, Ihm SH, Zhang HJ, Parkey J, et al. (2005) Single-donor, marginal-dose islet transplantation in patients with type 1 diabetes . JAMA 293 :830–835. [ PubMed ] [ Google Scholar ]
- Hernandez AFGreen JBJanmohamed SD’Agostino RB Sr , Granger CB, Jones NP, Leiter LA, Rosenberg AE, Sigmon KN, Somerville MCet al.; Harmony Outcomes committees and investigators (2018) Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial . Lancet 392 :1519–1529. [ PubMed ] [ Google Scholar ]
- Hiatt WR, Kaul S, Smith RJ (2013) The cardiovascular safety of diabetes drugs--insights from the rosiglitazone experience . N Engl J Med 369 :1285–1287. [ PubMed ] [ Google Scholar ]
- Hirshberg B, Preston EH, Xu H, Tal MG, Neeman Z, Bunnell D, Soleimanpour S, Hale DA, Kirk AD, Harlan DM (2003) Rabbit antithymocyte globulin induction and sirolimus monotherapy supports prolonged islet allograft function in a nonhuman primate islet transplantation model . Transplantation 76 :55–60. [ PubMed ] [ Google Scholar ]
- Hu W, Jiang C, Guan D, Dierickx P, Zhang R, Moscati A, Nadkarni GN, Steger DJ, Loos RJF, Hu C, et al. (2019) Patient adipose stem cell-derived adipocytes reveal genetic variation that predicts antidiabetic drug response . Cell Stem Cell 24 :299–308.e6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Husain M, Birkenfeld AL, Donsmark M, Dungan K, Eliaschewitz FG, Franco DR, Jeppesen OK, Lingvay I, Mosenzon O, Pedersen SD, et al.; PIONEER 6 Investigators (2019) Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes . N Engl J Med 381 :841–851. [ PubMed ] [ Google Scholar ]
- Imamura M, Nakanishi K, Suzuki T, Ikegai K, Shiraki R, Ogiyama T, Murakami T, Kurosaki E, Noda A, Kobayashi Y, et al. (2012) Discovery of Ipragliflozin (ASP1941): a novel C-glucoside with benzothiophene structure as a potent and selective sodium glucose co-transporter 2 (SGLT2) inhibitor for the treatment of type 2 diabetes mellitus . Bioorg Med Chem 20 :3263–3279. [ PubMed ] [ Google Scholar ]
- Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, Kravitz BG, Lachin JM, O’Neill MC, Zinman B, et al.; ADOPT Study Group (2006) Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy . N Engl J Med 355 :2427–2443. [ PubMed ] [ Google Scholar ]
- Kahn SE, Lachin JM, Zinman B, Haffner SM, Aftring RP, Paul G, Kravitz BG, Herman WH, Viberti G, Holman RR; ADOPT Study Group (2011) Effects of rosiglitazone, glyburide, and metformin on β-cell function and insulin sensitivity in ADOPT . Diabetes 60 :1552–1560. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kars M, Yang L, Gregor MF, Mohammed BS, Pietka TA, Finck BN, Patterson BW, Horton JD, Mittendorfer B, Hotamisligil GS, et al. (2010) Tauroursodeoxycholic acid may improve liver and muscle but not adipose tissue insulin sensitivity in obese men and women . Diabetes 59 :1899–1905. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kemp CB, Knight MJ, Scharp DW, Lacy PE, Ballinger WF (1973) Transplantation of isolated pancreatic islets into the portal vein of diabetic rats . Nature 244 :447. [ PubMed ] [ Google Scholar ]
- Kim HI, Cha JY, Kim SY, Kim JW, Roh KJ, Seong JK, Lee NT, Choi KY, Kim KS, Ahn YH (2002) Peroxisomal proliferator-activated receptor-gamma upregulates glucokinase gene expression in beta-cells . Diabetes 51 :676–685. [ PubMed ] [ Google Scholar ]
- Kim HI, Kim JW, Kim SH, Cha JY, Kim KS, Ahn YH (2000) Identification and functional characterization of the peroxisomal proliferator response element in rat GLUT2 promoter . Diabetes 49 :1517–1524. [ PubMed ] [ Google Scholar ]
- Kim SH, Liu A, Ariel D, Abbasi F, Lamendola C, Grove K, Tomasso V, Ochoa H, Reaven G (2014) Effect of salsalate on insulin action, secretion, and clearance in nondiabetic, insulin-resistant individuals: a randomized, placebo-controlled study . Diabetes Care 37 :1944–1950. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Koffert JP, Mikkola K, Virtanen KA, Andersson AD, Faxius L, Hällsten K, Heglind M, Guiducci L, Pham T, Silvola JMU, et al. (2017) Metformin treatment significantly enhances intestinal glucose uptake in patients with type 2 diabetes: Results from a randomized clinical trial . Diabetes Res Clin Pract 131 :208–216. [ PubMed ] [ Google Scholar ]
- Koh A, Mannerås-Holm L, Yunn NO, Nilsson PM, Ryu SH, Molinaro A, Perkins R, Smith JG, Bäckhed F (2020) Microbial imidazole propionate affects responses to metformin through p38γ-dependent inhibitory AMPK phosphorylation . Cell Metab 32 :643–653.e4. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kreymann B, Williams G, Ghatei MA, Bloom SR (1987) Glucagon-like peptide-1 7-36: a physiological incretin in man . Lancet 2 :1300–1304. [ PubMed ] [ Google Scholar ]
- Kuhre RE, Ghiasi SM, Adriaenssens AE, Wewer Albrechtsen NJ, Andersen DB, Aivazidis A, Chen L, Mandrup-Poulsen T, Ørskov C, Gribble FM, et al. (2019) No direct effect of SGLT2 activity on glucagon secretion . Diabetologia 62 :1011–1023. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kulkarni RN, Mizrachi EB, Ocana AG, Stewart AF (2012) Human β-cell proliferation and intracellular signaling: driving in the dark without a road map . Diabetes 61 :2205–2213. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kurosaki E, Ogasawara H (2013) Ipragliflozin and other sodium-glucose cotransporter-2 (SGLT2) inhibitors in the treatment of type 2 diabetes: preclinical and clinical data . Pharmacol Ther 139 :51–59. [ PubMed ] [ Google Scholar ]
- Kurtzhals P, Schäffer L, Sørensen A, Kristensen C, Jonassen I, Schmid C, Trüb T (2000) Correlations of receptor binding and metabolic and mitogenic potencies of insulin analogs designed for clinical use . Diabetes 49 :999–1005. [ PubMed ] [ Google Scholar ]
- Lambeir AM, Scharpé S, De Meester I (2008) DPP4 inhibitors for diabetes--what next? Biochem Pharmacol 76 :1637–1643. [ PubMed ] [ Google Scholar ]
- Laybutt DR, Preston AM, Akerfeldt MC, Kench JG, Busch AK, Biankin AV, Biden TJ (2007) Endoplasmic reticulum stress contributes to beta cell apoptosis in type 2 diabetes . Diabetologia 50 :752–763. [ PubMed ] [ Google Scholar ]
- Lebovitz HE (2019) Thiazolidinediones: the forgotten diabetes medications . Curr Diab Rep 19 :151. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lewis JD, Habel LA, Quesenberry CP, Strom BL, Peng T, Hedderson MM, Ehrlich SF, Mamtani R, Bilker W, Vaughn DJ, et al. (2015) Pioglitazone use and risk of bladder cancer and other common cancers in persons with diabetes . JAMA 314 :265–277. [ PubMed ] [ Google Scholar ]
- Li L, Li S, Deng K, Liu J, Vandvik PO, Zhao P, Zhang L, Shen J, Bala MM, Sohani ZN, et al. (2016) Dipeptidyl peptidase-4 inhibitors and risk of heart failure in type 2 diabetes: systematic review and meta-analysis of randomised and observational studies . BMJ 352 :i610. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Link JT (2003) Pharmacological regulation of hepatic glucose production . Curr Opin Investig Drugs 4 :421–429. [ PubMed ] [ Google Scholar ]
- Luippold G, Klein T, Mark M, Grempler R (2012) Empagliflozin, a novel potent and selective SGLT-2 inhibitor, improves glycaemic control alone and in combination with insulin in streptozotocin-induced diabetic rats, a model of type 1 diabetes mellitus . Diabetes Obes Metab 14 :601–607. [ PubMed ] [ Google Scholar ]
- Maganti AV, Tersey SA, Syed F, Nelson JB, Colvin SC, Maier B, Mirmira RG (2016) Peroxisome proliferator-activated receptor-γ activation augments the β-cell unfolded protein response and rescues early glycemic deterioration and β cell death in non-obese diabetic mice . J Biol Chem 291 :22524–22533. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Makrilakis K (2019) The role of DPP-4 inhibitors in the treatment algorithm of type 2 diabetes mellitus: when to select, what to expect . Int J Environ Res Public Health 16 :2720. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Marchetti P, Bugliani M, Lupi R, Marselli L, Masini M, Boggi U, Filipponi F, Weir GC, Eizirik DL, Cnop M (2007) The endoplasmic reticulum in pancreatic beta cells of type 2 diabetes patients . Diabetologia 50 :2486–2494. [ PubMed ] [ Google Scholar ]
- Marhfour I, Lopez XM, Lefkaditis D, Salmon I, Allagnat F, Richardson SJ, Morgan NG, Eizirik DL (2012) Expression of endoplasmic reticulum stress markers in the islets of patients with type 1 diabetes . Diabetologia 55 :2417–2420. [ PubMed ] [ Google Scholar ]
- Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, Lingvay I, Rosenstock J, Seufert J, Warren ML, et al.; SUSTAIN-6 Investigators (2016a) Semaglutide and cardiovascular outcomes in patients with type 2 diabetes . N Engl J Med 375 :1834–1844. [ PubMed ] [ Google Scholar ]
- Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, Nissen SE, Pocock S, Poulter NR, Ravn LS, et al.; LEADER Steering Committee; LEADER Trial Investigators (2016b) Liraglutide and cardiovascular outcomes in type 2 diabetes . N Engl J Med 375 :311–322. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Massollo M, Marini C, Brignone M, Emionite L, Salani B, Riondato M, Capitanio S, Fiz F, Democrito A, Amaro A, et al. (2013) Metformin temporal and localized effects on gut glucose metabolism assessed using 18F-FDG PET in mice . J Nucl Med 54 :259–266. [ PubMed ] [ Google Scholar ]
- McCreight LJ, Bailey CJ, Pearson ER (2016) Metformin and the gastrointestinal tract . Diabetologia 59 :426–435. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McIntyre N, Holdsworth CD, Turner DS (1964) New interpretation of oral glucose tolerance . Lancet 2 :20–21. [ PubMed ] [ Google Scholar ]
- McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Bělohlávek J, et al.; DAPA-HF Trial Committees and Investigators (2019) Dapagliflozin in patients with heart failure and reduced ejection fraction . N Engl J Med 381 :1995–2008. [ PubMed ] [ Google Scholar ]
- Meier JJ, Butler AE, Saisho Y, Monchamp T, Galasso R, Bhushan A, Rizza RA, Butler PC (2008) Beta-cell replication is the primary mechanism subserving the postnatal expansion of beta-cell mass in humans . Diabetes 57 :1584–1594. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meng W, Ellsworth BA, Nirschl AA, McCann PJ, Patel M, Girotra RN, Wu G, Sher PM, Morrison EP, Biller SA, et al. (2008) Discovery of dapagliflozin: a potent, selective renal sodium-dependent glucose cotransporter 2 (SGLT2) inhibitor for the treatment of type 2 diabetes . J Med Chem 51 :1145–1149. [ PubMed ] [ Google Scholar ]
- Menting JG, Whittaker J, Margetts MB, Whittaker LJ, Kong GK, Smith BJ, Watson CJ, Záková L, Kletvíková E, Jiráček J, et al. (2013) How insulin engages its primary binding site on the insulin receptor . Nature 493 :241–245. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miller RA, Chu Q, Xie J, Foretz M, Viollet B, Birnbaum MJ (2013) Biguanides suppress hepatic glucagon signalling by decreasing production of cyclic AMP . Nature 494 :256–260. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Minkowski O (1892) Weitere Mitteilungen über den Diabetes mellitus nach Extirpation des Pankreas . Berliner Klinische Wochenschrift 29 :90–93. [ Google Scholar ]
- Misbin RI (2004) The phantom of lactic acidosis due to metformin in patients with diabetes . Diabetes Care 27 :1791–1793. [ PubMed ] [ Google Scholar ]
- Mudaliar S, Armstrong DA, Mavian AA, O’Connor-Semmes R, Mydlow PK, Ye J, Hussey EK, Nunez DJ, Henry RR, Dobbins RL (2012) Remogliflozin etabonate, a selective inhibitor of the sodium-glucose transporter 2, improves serum glucose profiles in type 1 diabetes . Diabetes Care 35 :2198–2200. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mulherin AJ, Oh AH, Kim H, Grieco A, Lauffer LM, Brubaker PL (2011) Mechanisms underlying metformin-induced secretion of glucagon-like peptide-1 from the intestinal L cell . Endocrinology 152 :4610–4619. [ PubMed ] [ Google Scholar ]
- Müller TD, Finan B, Bloom SR, D’Alessio D, Drucker DJ, Flatt PR, Fritsche A, Gribble F, Grill HJ, Habener JF, et al. (2019) Glucagon-like peptide 1 (GLP-1) . Mol Metab 30 :72–130. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Munir KM, Lamos EM (2017) Diabetes type 2 management: what are the differences between DPP-4 inhibitors and how do you choose? Expert Opin Pharmacother 18 :839–841. [ PubMed ] [ Google Scholar ]
- Naftanel MA, Harlan DM (2004) Pancreatic islet transplantation . PLoS Med 1 :e58. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nauck M, Stöckmann F, Ebert R, Creutzfeldt W (1986a) Reduced incretin effect in type 2 (non-insulin-dependent) diabetes . Diabetologia 29 :46–52. [ PubMed ] [ Google Scholar ]
- Nauck MA, Homberger E, Siegel EG, Allen RC, Eaton RP, Ebert R, Creutzfeldt W (1986b) Incretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses . J Clin Endocrinol Metab 63 :492–498. [ PubMed ] [ Google Scholar ]
- Nejentsev S, Howson JM, Walker NM, Szeszko J, Field SF, Stevens HE, Reynolds P, Hardy M, King E, Masters J, et al.; Wellcome Trust Case Control Consortium (2007) Localization of type 1 diabetes susceptibility to the MHC class I genes HLA-B and HLA-A . Nature 450 :887–892. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nichols CG (2006) KATP channels as molecular sensors of cellular metabolism . Nature 440 :470–476. [ PubMed ] [ Google Scholar ]
- Nomura S, Sakamaki S, Hongu M, Kawanishi E, Koga Y, Sakamoto T, Yamamoto Y, Ueta K, Kimata H, Nakayama K, et al. (2010) Discovery of canagliflozin, a novel C-glucoside with thiophene ring, as sodium-dependent glucose cotransporter 2 inhibitor for the treatment of type 2 diabetes mellitus . J Med Chem 53 :6355–6360. [ PubMed ] [ Google Scholar ]
- Ohnishi ST, Endo M, editors. (1981) The Mechanism of Gated Calcium Transport Across Biological Membranes , Academic Press, New York. [ Google Scholar ]
- Osipovich AB, Stancill JS, Cartailler JP, Dudek KD, Magnuson MA (2020) Excitotoxicity and overnutrition additively impair metabolic function and identity of pancreatic β-cells . Diabetes 69 :1476–1491. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Osum KC, Burrack AL, Martinov T, Sahli NL, Mitchell JS, Tucker CG, Pauken KE, Papas K, Appakalai B, Spanier JA, et al. (2018) Interferon-gamma drives programmed death-ligand 1 expression on islet β cells to limit T cell function during autoimmune diabetes . Sci Rep 8 :8295. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Owen MR, Doran E, Halestrap AP (2000) Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain . Biochem J 348 :607–614. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ozanne SE, Guest PC, Hutton JC, Hales CN (1995) Intracellular localization and molecular heterogeneity of the sulphonylurea receptor in insulin-secreting cells . Diabetologia 38 :277–282. [ PubMed ] [ Google Scholar ]
- Ozcan U, Yilmaz E, Ozcan L, Furuhashi M, Vaillancourt E, Smith RO, Görgün CZ, Hotamisligil GS (2006) Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes . Science 313 :1137–1140. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Paty BW, Harmon JS, Marsh CL, Robertson RP (2002) Inhibitory effects of immunosuppressive drugs on insulin secretion from HIT-T15 cells and Wistar rat islets . Transplantation 73 :353–357. [ PubMed ] [ Google Scholar ]
- Penesova A, Koska J, Ortega E, Bunt JC, Bogardus C, de Courten B (2015) Salsalate has no effect on insulin secretion but decreases insulin clearance: a randomized, placebo-controlled trial in subjects without diabetes . Diabetes Obes Metab 17 :608–612. [ PubMed ] [ Google Scholar ]
- Perdigoto AL, Quandt Z, Anderson M, Herold KC (2019) Checkpoint inhibitor-induced insulin-dependent diabetes: an emerging syndrome . Lancet Diabetes Endocrinol 7 :421–423. [ PubMed ] [ Google Scholar ]
- Perley MJ, Kipnis DM (1967) Plasma insulin responses to oral and intravenous glucose: studies in normal and diabetic subjects . J Clin Invest 46 :1954–1962. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pernicova I, Korbonits M (2014) Metformin--mode of action and clinical implications for diabetes and cancer . Nat Rev Endocrinol 10 :143–156. [ PubMed ] [ Google Scholar ]
- Preiss D, Dawed A, Welsh P, Heggie A, Jones AG, Dekker J, Koivula R, Hansen TH, Stewart C, Holman RR, et al.; DIRECT consortium group (2017) Sustained influence of metformin therapy on circulating glucagon-like peptide-1 levels in individuals with and without type 2 diabetes . Diabetes Obes Metab 19 :356–363. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Prentki M, Nolan CJ (2006) Islet beta cell failure in type 2 diabetes . J Clin Invest 116 :1802–1812. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pueyo ME, Darquy S, Capron F, Reach G (1993) In vitro activation of human macrophages by alginate-polylysine microcapsules . J Biomater Sci Polym Ed 5 :197–203. [ PubMed ] [ Google Scholar ]
- Pybus F (1924) Notes on suprarenal and pancreatic grafting . Lancet 204 :550–551. [ Google Scholar ]
- Quattrin T, Haller MJ, Steck AK, Felner EI, Li Y, Xia Y, Leu JH, Zoka R, Hedrick JA, Rigby MR, et al.; T1GER Study Investigators (2020) Golimumab and Beta-Cell Function in Youth with New-Onset Type 1 Diabetes . N Engl J Med 383 :2007–2017. [ PubMed ] [ Google Scholar ]
- Rachdi L, Kariyawasam D, Aïello V, Herault Y, Janel N, Delabar JM, Polak M, Scharfmann R (2014a) Dyrk1A induces pancreatic β cell mass expansion and improves glucose tolerance . Cell Cycle 13 :2221–2229. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rachdi L, Kariyawasam D, Guez F, Aïello V, Arbonés ML, Janel N, Delabar JM, Polak M, Scharfmann R (2014b) Dyrk1a haploinsufficiency induces diabetes in mice through decreased pancreatic beta cell mass . Diabetologia 57 :960–969. [ PubMed ] [ Google Scholar ]
- Rege NK, Phillips NFB, Weiss MA (2017) Development of glucose-responsive ‘smart’ insulin systems . Curr Opin Endocrinol Diabetes Obes 24 :267–278. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rena G, Hardie DG, Pearson ER (2017) The mechanisms of action of metformin . Diabetologia 60 :1577–1585. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rewers M, Gottlieb P (2009) Immunotherapy for the prevention and treatment of type 1 diabetes: human trials and a look into the future . Diabetes Care 32 :1769–1782. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Richardson SJ, Rodriguez-Calvo T, Gerling IC, Mathews CE, Kaddis JS, Russell MA, Zeissler M, Leete P, Krogvold L, Dahl-Jørgensen K, et al. (2016) Islet cell hyperexpression of HLA class I antigens: a defining feature in type 1 diabetes . Diabetologia 59 :2448–2458. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rickels MR, Liu C, Shlansky-Goldberg RD, Soleimanpour SA, Vivek K, Kamoun M, Min Z, Markmann E, Palangian M, Dalton-Bakes C, et al. (2013) Improvement in β-cell secretory capacity after human islet transplantation according to the c7 protocol . Diabetes 62 :2890–2897. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rickels MR, Robertson RP (2019) Pancreatic islet transplantation in humans: recent progress and future directions . Endocr Rev 40 :631–668. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rodriguez-Calvo T, Suwandi JS, Amirian N, Zapardiel-Gonzalo J, Anquetil F, Sabouri S, von Herrath MG (2015) Heterogeneity and lobularity of pancreatic pathology in type 1 diabetes during the prediabetic phase . J Histochem Cytochem 63 :626–636. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rojas LB, Gomes MB (2013) Metformin: an old but still the best treatment for type 2 diabetes . Diabetol Metab Syndr 5 :6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rosen ED, Kulkarni RN, Sarraf P, Ozcan U, Okada T, Hsu CH, Eisenman D, Magnuson MA, Gonzalez FJ, Kahn CR, et al. (2003) Targeted elimination of peroxisome proliferator-activated receptor gamma in beta cells leads to abnormalities in islet mass without compromising glucose homeostasis . Mol Cell Biol 23 :7222–7229. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rosenstock J, Hassman DR, Madder RD, Brazinsky SA, Farrell J, Khutoryansky N, Hale PM; Repaglinide Versus Nateglinide Comparison Study Group (2004) Repaglinide versus nateglinide monotherapy: a randomized, multicenter study . Diabetes Care 27 :1265–1270. [ PubMed ] [ Google Scholar ]
- Sampaio MS, Kuo HT, Bunnapradist S (2011) Outcomes of simultaneous pancreas-kidney transplantation in type 2 diabetic recipients . Clin J Am Soc Nephrol 6 :1198–1206. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Saponaro C, Gmyr V, Thévenet J, Moerman E, Delalleau N, Pasquetti G, Coddeville A, Quenon A, Daoudi M, Hubert T, et al. (2019) The GLP1R agonist liraglutide reduces hyperglucagonemia induced by the SGLT2 inhibitor dapagliflozin via somatostatin release . Cell Rep 28 :1447–1454.e4. [ PubMed ] [ Google Scholar ]
- Saponaro C, Mühlemann M, Acosta-Montalvo A, Piron A, Gmyr V, Delalleau N, Moerman E, Thévenet J, Pasquetti G, Coddeville A, et al. (2020) Interindividual heterogeneity of SGLT2 expression and function in human pancreatic islets . Diabetes 69 :902–914. [ PubMed ] [ Google Scholar ]
- Satin LS, Tavalin SJ, Kinard TA, Teague J (1995) Contribution of L- and non-L-type calcium channels to voltage-gated calcium current and glucose-dependent insulin secretion in HIT-T15 cells . Endocrinology 136 :4589–4601. [ PubMed ] [ Google Scholar ]
- Schwartz AV, Chen H, Ambrosius WT, Sood A, Josse RG, Bonds DE, Schnall AM, Vittinghoff E, Bauer DC, Banerji MA, et al. (2015) Effects of TZD use and discontinuation on fracture rates in ACCORD Bone Study . J Clin Endocrinol Metab 100 :4059–4066. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shalev A, Pise-Masison CA, Radonovich M, Hoffmann SC, Hirshberg B, Brady JN, Harlan DM (2002) Oligonucleotide microarray analysis of intact human pancreatic islets: identification of glucose-responsive genes and a highly regulated TGFbeta signaling pathway . Endocrinology 143 :3695–3698. [ PubMed ] [ Google Scholar ]
- Shankar SS, Shankar RR, Mixson LA, Miller DL, Pramanik B, O’Dowd AK, Williams DM, Frederick CB, Beals CR, Stoch SA, et al. (2018) Native oxyntomodulin has significant glucoregulatory effects independent of weight loss in obese humans with and without type 2 diabetes . Diabetes 67 :1105–1112. [ PubMed ] [ Google Scholar ]
- Shapiro AM, Lakey JR, Ryan EA, Korbutt GS, Toth E, Warnock GL, Kneteman NM, Rajotte RV (2000) Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen . N Engl J Med 343 :230–238. [ PubMed ] [ Google Scholar ]
- Sharma RB, O’Donnell AC, Stamateris RE, Ha B, McCloskey KM, Reynolds PR, Arvan P, Alonso LC (2015) Insulin demand regulates β cell number via the unfolded protein response . J Clin Invest 125 :3831–3846. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sims EK, Mirmira RG, Evans-Molina C (2020) The role of beta-cell dysfunction in early type 1 diabetes . Curr Opin Endocrinol Diabetes Obes 27 :215–224. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Soccio RE, Chen ER, Rajapurkar SR, Safabakhsh P, Marinis JM, Dispirito JR, Emmett MJ, Briggs ER, Fang B, Everett LJ, et al. (2015) Genetic variation determines PPARγ function and anti-diabetic drug response in vivo . Cell 162 :33–44. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Soleimanpour SA, Crutchlow MF, Ferrari AM, Raum JC, Groff DN, Rankin MM, Liu C, De León DD, Naji A, Kushner JA, et al. (2010) Calcineurin signaling regulates human islet beta-cell survival . J Biol Chem 285 :40050–40059. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Soleimanpour SA, Hirshberg B, Bunnell DJ, Sumner AE, Ader M, Remaley AT, Rother KI, Rickels MR, Harlan DM (2012) Metabolic function of a suboptimal transplanted islet mass in nonhuman primates on rapamycin monotherapy . Cell Transplant 21 :1297–1304. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Soleimanpour SA, Stoffers DA (2013) The pancreatic β cell and type 1 diabetes: innocent bystander or active participant? Trends Endocrinol Metab 24 :324–331. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stamatouli AM, Quandt Z, Perdigoto AL, Clark PL, Kluger H, Weiss SA, Gettinger S, Sznol M, Young A, Rushakoff R, et al. (2018) Collateral damage: insulin-dependent diabetes induced with checkpoint inhibitors . Diabetes 67 :1471–1480. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stancill JS, Cartailler JP, Clayton HW, O’Connor JT, Dickerson MT, Dadi PK, Osipovich AB, Jacobson DA, Magnuson MA (2017) Chronic β-cell depolarization impairs β-cell identity by disrupting a network of Ca 2+ -regulated genes . Diabetes 66 :2175–2187. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stewart AF, Hussain MA, García-Ocaña A, Vasavada RC, Bhushan A, Bernal-Mizrachi E, Kulkarni RN (2015) Human β-cell proliferation and intracellular signaling: part 3 . Diabetes 64 :1872–1885. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stojanovic I, Dimitrijevic M, Vives-Pi M, Mansilla MJ, Pujol-Autonell I, Rodríguez-Fernandez S, Palova-Jelínkova L, Funda DP, Gruden-Movsesijan A, Sofronic-Milosavljevic L, et al. (2017) Cell-based tolerogenic therapy, experience from animal models of multiple sclerosis, type 1 diabetes and rheumatoid arthritis . Curr Pharm Des 23 :2623–2643. [ PubMed ] [ Google Scholar ]
- Sturek JM, Castle JD, Trace AP, Page LC, Castle AM, Evans-Molina C, Parks JS, Mirmira RG, Hedrick CC (2010) An intracellular role for ABCG1-mediated cholesterol transport in the regulated secretory pathway of mouse pancreatic beta cells . J Clin Invest 120 :2575–2589. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Suga T, Kikuchi O, Kobayashi M, Matsui S, Yokota-Hashimoto H, Wada E, Kohno D, Sasaki T, Takeuchi K, Kakizaki S, et al. (2019) SGLT1 in pancreatic α cells regulates glucagon secretion in mice, possibly explaining the distinct effects of SGLT2 inhibitors on plasma glucagon levels . Mol Metab 19 :1–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sun L, Xie C, Wang G, Wu Y, Wu Q, Wang X, Liu J, Deng Y, Xia J, Chen B, et al. (2018) Gut microbiota and intestinal FXR mediate the clinical benefits of metformin . Nat Med 24 :1919–1929. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sutherland DE, Matas AJ, Najarian JS (1978) Pancreatic islet cell transplantation . Surg Clin North Am 58 :365–382. [ PubMed ] [ Google Scholar ]
- Tersey SA, Nishiki Y, Templin AT, Cabrera SM, Stull ND, Colvin SC, Evans-Molina C, Rickus JL, Maier B, Mirmira RG (2012) Islet β-cell endoplasmic reticulum stress precedes the onset of type 1 diabetes in the nonobese diabetic mouse model . Diabetes 61 :818–827. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thielen LA, Chen J, Jing G, Moukha-Chafiq O, Xu G, Jo S, Grayson TB, Lu B, Li P, Augelli-Szafran CE, et al. (2020) Identification of an anti-diabetic, orally available small molecule that regulates TXNIP expression and glucagon action . Cell Metab 32 :353–365.e8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tillner J, Posch MG, Wagner F, Teichert L, Hijazi Y, Einig C, Keil S, Haack T, Wagner M, Bossart M, et al. (2019) A novel dual glucagon-like peptide and glucagon receptor agonist SAR425899: Results of randomized, placebo-controlled first-in-human and first-in-patient trials . Diabetes Obes Metab 21 :120–128. [ PubMed ] [ Google Scholar ]
- Vallon V (2015) The mechanisms and therapeutic potential of SGLT2 inhibitors in diabetes mellitus . Annu Rev Med 66 :255–270. [ PubMed ] [ Google Scholar ]
- Vasseur M, Debuyser A, Joffre M (1987) Sensitivity of pancreatic beta cell to calcium channel blockers. An electrophysiologic study of verapamil and nifedipine . Fundam Clin Pharmacol 1 :95–113. [ PubMed ] [ Google Scholar ]
- Vegas AJ, Veiseh O, Doloff JC, Ma M, Tam HH, Bratlie K, Li J, Bader AR, Langan E, Olejnik K, et al. (2016) Combinatorial hydrogel library enables identification of materials that mitigate the foreign body response in primates . Nat Biotechnol 34 :345–352. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vergari E, Knudsen JG, Ramracheya R, Salehi A, Zhang Q, Adam J, Asterholm IW, Benrick A, Briant LJB, Chibalina MV, et al. (2019) Insulin inhibits glucagon release by SGLT2-induced stimulation of somatostatin secretion . Nat Commun 10 :139. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wallner K, Shapiro AM, Senior PA, McCabe C (2016) Cost effectiveness and value of information analyses of islet cell transplantation in the management of ‘unstable’ type 1 diabetes mellitus . BMC Endocr Disord 16 :17. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang H, Bender A, Wang P, Karakose E, Inabnet WB, Libutti SK, Arnold A, Lambertini L, Stang M, Chen H, et al. (2017) Insights into beta cell regeneration for diabetes via integration of molecular landscapes in human insulinomas . Nat Commun 8 :767. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang Y, An H, Liu T, Qin C, Sesaki H, Guo S, Radovick S, Hussain M, Maheshwari A, Wondisford FE, O’Rourke B, He L (2019) Metformin improves mitochondrial respiratory activity through activation of AMPK . Cell Rep 29 :1511–1523.e5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Westerman J, Wirtz KW, Berkhout T, van Deenen LL, Radhakrishnan R, Khorana HG (1983) Identification of the lipid-binding site of phosphatidylcholine-transfer protein with phosphatidylcholine analogs containing photoactivable carbene precursors . Eur J Biochem 132 :441–449. [ PubMed ] [ Google Scholar ]
- World Health Organization (2020) World Health Organization Diabetes Fact Sheet . [ Google Scholar ]
- Willard FS, Douros JD, Gabe MB, Showalter AD, Wainscott DB, Suter TM, Capozzi ME, van der Velden WJ, Stutsman C, Cardona GR, et al. (2020) Tirzepatide is an imbalanced and biased dual GIP and GLP-1 receptor agonist . JCI Insight 5 :e140532. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams P (1894) Notes on diabetes treated with extract and by grafts of sheep’s pancreas . BMJ 2 :1303–1304. [ Google Scholar ]
- Williamson RT (1901) On the treatment of glycosuria and diabetes mellitus with sodium salicylate . BMJ 1 :760–762. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Witters LA (2001) The blooming of the French lilac . J Clin Invest 108 :1105–1107. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, et al.; DECLARE–TIMI 58 Investigators (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes . N Engl J Med 380 :347–357. [ PubMed ] [ Google Scholar ]
- Wu H, Esteve E, Tremaroli V, Khan MT, Caesar R, Mannerås-Holm L, Ståhlman M, Olsson LM, Serino M, Planas-Fèlix M, et al. (2017) Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug . Nat Med 23 :850–858. [ PubMed ] [ Google Scholar ]
- Wynne K, Park AJ, Small CJ, Patterson M, Ellis SM, Murphy KG, Wren AM, Frost GS, Meeran K, Ghatei MA, et al. (2005) Subcutaneous oxyntomodulin reduces body weight in overweight and obese subjects: a double-blind, randomized, controlled trial . Diabetes 54 :2390–2395. [ PubMed ] [ Google Scholar ]
- Xu G, Chen J, Jing G, Shalev A (2012) Preventing β-cell loss and diabetes with calcium channel blockers . Diabetes 61 :848–856. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yang JF, Gong X, Bakh NA, Carr K, Phillips NFB, Ismail-Beigi F, Weiss MA, Strano MS (2020) Connecting rodent and human pharmacokinetic models for the design and translation of glucose-responsive insulin . Diabetes 69 :1815–1826. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yu O, Azoulay L, Yin H, Filion KB, Suissa S (2018) Sulfonylureas as initial treatment for type 2 diabetes and the risk of severe hypoglycemia . Am J Med 131 :317.e11–317.e22. [ PubMed ] [ Google Scholar ]
- Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, et al. (2001) Role of AMP-activated protein kinase in mechanism of metformin action . J Clin Invest 108 :1167–1174. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al.; EMPA-REG OUTCOME Investigators (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes . N Engl J Med 373 :2117–2128. [ PubMed ] [ Google Scholar ]
Melbourne researchers' diabetes breakthrough could reduce need for insulin injections
Diabetes researchers say they have made a breakthrough that could pave the way to eliminating the need for daily insulin injections.
Key points:
- The Monash University team was able to get pancreatic cells to produce insulin
- If the research leads to animal studies then clinical trials, it could reduce the need for insulin injections
- It could be a "game changer" in treatment for the chronic disease, an independent researcher says
The Monash University research, published in the Nature journal Signal Transduction and Targeted Therapy , could lead to the regeneration of insulin in pancreatic stem cells.
Insulin is a hormone, made by what are known as beta cells in the pancreas, which helps to regulate blood sugar levels.
Broadly, people with diabetes do not naturally produce enough insulin, or their bodies do not use the hormone as they should. The beta cells in many people with diabetes are unable to produce insulin at all.
"There are different forms of diabetes and it's a disease that requires relentless attention," said Keith Al-Hasani, a Monash University researcher and one of the study's authors.
Type 1 diabetes generally first presents when patients are children, which Dr Al-Hasani said often meant up to five insulin injections per day as young people adjusted to the disease. Adult sufferers can administer up to 100 shots a month to manage the illness.
After the death of a 13-year-old with type 1 diabetes, the researchers studied donated pancreatic cells and used a compound to trigger insulin production.
"We're reprogramming cells that don't generally produce insulin, to express insulin now," researcher and study co-author Ishant Khurana said.
The compound GSK126 is approved for use to treat another condition by the US Food and Drug Administration, but has not been used for diabetes treatment in Australia or elsewhere.
"This is a big breakthrough in the diabetes realm," Dr Khurana said.
While the researchers studied stem cells, they did not genetically alter the cells to get their results.
The authors acknowledged there was still a long way to go before the potential treatment could be used in humans.
They next want to collect more pancreatic cell samples from a bigger range of people, then move to animal trials before possibly beginning human clinical trials.
The end goal, Dr Khurana said, was to eliminate the need for daily injections and pancreatic transplants.
It would affect most people with Type 1 diabetes, and the about 30 per cent of people with Type 2 diabetes who are insulin dependent.
According to Diabetes Australia, about 1.8 million Australians have diabetes and it is the fastest-growing illness in the country. About 500 million have the disease worldwide.
Simon McCrudden, 46, has been administering his own insulin since he was seven years old and said removing the burden of daily injections would be "massive".
"I'd have to re-learn just how to just do daily life, but it'd be great," he said.
Associate professor Neale Cohen, the director of diabetes clinical research at the Baker Heart and Diabetes Institute, said the Monash research was still in its early days but showed great potential.
"There are a number of attempts to find ways of replacing beta cells, which are all tremendously important. And if that is possible, what it would mean it would be a cure for people with Type 1 diabetes," he said.
Dr Cohen, who was not involved in the study, said research over a number of decades had found "it seems to be remarkably difficult to reprogram cells to become insulin-producing cells.
"So if you can cure these people from this very difficult chronic condition, that's a game changer," he said.
"People will no longer need to inject insulin, and they won't have the burden of this chronic illness."
- X (formerly Twitter)
- Medical Research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Type 2 diabetes articles from across Nature Portfolio
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). It arises from a resistance to and relative deficiency of the pancreatic β-cell hormone insulin.

Macrophage vesicles in antidiabetic drug action
Thiazolidinediones (TZDs) are potent insulin-sensitizing drugs, but their use is accompanied by adverse side-effects. Rohm et al. now report that TZD-stimulated macrophages release miR-690-containing vesicles that improve insulin sensitization and bypass unwanted side-effects.
- Rinke Stienstra
- Eric Kalkhoven

Metformin induces a Lac-Phe gut–brain signalling axis
The mechanism by which metformin affects food intake remains controversial. Now, two studies link metformin treatment with the induction of the appetite-suppressing metabolite N -lactoyl-phenylalanine, which is produced by the intestine.
- Tara TeSlaa
Latest Research and Reviews

Adipose tissue macrophages secrete small extracellular vesicles that mediate rosiglitazone-induced insulin sensitization
Rohm et al. show that small extracellular vesicles from adipose tissue macrophages from obese rosiglitazone-treated mice ameliorate glucose tolerance and insulin sensitivity in obese mice, while circumventing the adverse effects of rosiglitazone.
- Theresa V. Rohm
- Felipe Castellani Gomes Dos Reis
- Jerrold M. Olefsky
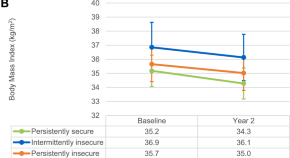
Association of food insecurity with changes in diet quality, weight, and glycemia over two years in adults with prediabetes and type 2 diabetes on medicaid
- Kristine D. Gu
- Jessica Cheng
- Anne N. Thorndike

Characterization of the gut bacterial and viral microbiota in latent autoimmune diabetes in adults
- Casper S. Poulsen
- Mette K. Andersen
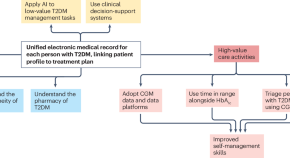
Continuous glucose monitoring for the routine care of type 2 diabetes mellitus
Continuous glucose monitoring (CGM) is an effective tool in the management of diabetes mellitus. This Perspective discusses the potential benefits of widespread adoption of CGM in people with type 2 diabetes mellitus at different stages of disease progression and treatment intensification.
- Ramzi A. Ajjan
- Tadej Battelino
- Samuel Seidu

Comparative impact of Roux-en-Y gastric bypass, sleeve gastrectomy or diet alone on beta-cell function in insulin-treated type 2 diabetes patients
- Matthias Lannoo
- Caroline Simoens
- Bart Van der Schueren
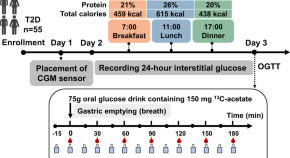
Gastric emptying of a glucose drink is predictive of the glycaemic response to oral glucose and mixed meals, but unrelated to antecedent glycaemic control, in type 2 diabetes
- Chunjie Xiang
News and Comment
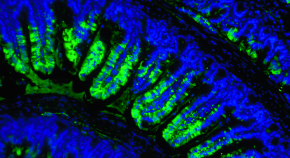
Metformin acts through appetite-suppressing metabolite: Lac-Phe
- Shimona Starling
Slowly progressive insulin-dependent diabetes mellitus in type 1 diabetes endotype 2
- Tetsuro Kobayashi
- Takashi Kadowaki
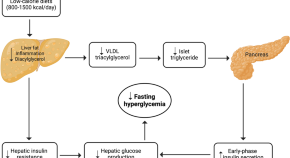
Low-calorie diets for people with isolated impaired fasting glucose
Thirunavukkarasu et al. discuss how standard lifestyle interventions prove ineffective in preventing type 2 diabetes in individuals with isolated impaired fasting glucose, a highly prevalent prediabetes phenotype globally. They propose low-calorie diets as a promising strategy for diabetes prevention in this high-risk population.
- Sathish Thirunavukkarasu
- Jonathan E. Shaw
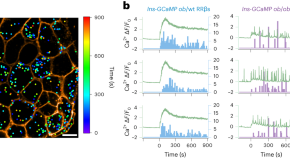
Functionally heterogeneous β cells regulate biphasic insulin secretion
Here, we reveal functional heterogeneity among β cells and discover that readily releasable β cells (RRβs) are a subpopulation that disproportionally contributes to biphasic glucose-stimulated insulin secretion. We further show that the dysfunction of RRβs has a crucial role in the progression of diabetes.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Changing our Future Through Research
The ADA is committed to innovation and breakthrough research that will improve the lives of all people living with diabetes.

ADA Research: Science. Progress. Hope.
ADA research provides critical funding for diabetes research. With 100% of donations directed to research, our goal is to ensure adequate financial resources to support innovative scientific discovery that will translate to life-changing treatments and eventual cures.
of our funded researchers remain dedicated to careers in diabetes science
publications per grant, cited an average of 28 times, proving expertise and credibility
Every $1 the ADA invests in diabetes research leads to $12.47 in additional research funding
ADA Research Impact
Explore some of the latest innovations and discoveries and see how the ADA continues to advance science, leverage investments and retain scientists.

Research Funds at Work
Imagine what 290 scientists, each working on a unique project at 117 institutions across the U.S. can do. Learn about the research we fund to move the diabetes fight forward.

Helping People Thrive
Uncover inspiring patient stories and find out how our research is transforming lives.

Discover programs on research, career development, training, and more.
Learn more about the current opportunities for 2024 research funding.
Pathway to Stop Diabetes ®
A bold initiative dedicated to bringing 100 brilliant scientists to diabetes research.
Explore Research Projects
As part of our mission, ADA’s Research Programs invest in projects that have the potential to prevent the development of diabetes and help people living with diabetes.

Type 1 Diabetes Research
Project topics span technology, islet transplantation, immunology, improving transition to self-management, and more.

Type 2 Diabetes Research
Project topics include support for potential new treatments, a better understating of genetic factors, addressing disparities, and more.

Prediabetes/Insulin Resistance Research
Projects include understanding the role of exercise, novel therapies, and more.

Gestational Diabetes Research
Projects focus on advancing the prevention of gestational diabetes and to properly diagnose and treat it when it occurs.

Research on Obesity
Projects include studying the biology of appetite regulation and metabolism, identification of new treatment targets, and trials exploring interventions for weight loss.
Donate Today and Change Lives!
This Outdated Diabetes Drug Still Has Something to Offer
By learning how an old diabetes drug works, researchers are discovering new, safer treatment options.
- Miles Martin - [email protected]
Published Date
- Insulin-Resistance
- Type 2 Diabetes
Share This:
Article content.
Thiazolidinediones (TZDs) are a class of drug that can be used to treat type 2 diabetes by reversing insulin resistance, one of the main hallmarks of the disease. While TZDs were extremely popular in the 1990’s and early 2000’s, they have fallen out of use among physicians in recent decades because they were discovered to cause unwanted side effects, including weight gain and excess fluid accumulation in body tissues.
Now, researchers at University of California San Diego School of Medicine are exploring how to isolate the positive effects of these drugs, which could help yield new treatments that don’t come with the old side effects. In a new study published in Nature Metabolism , the researchers discovered how one of the most well-known TZD drugs works at the molecular level and were able to replicate its positive effects in mice without giving them the drug itself.
“For decades, TZDs have been the only drugs we have that can reverse insulin resistance, but we seldom use them anymore because of their side effects profile,” said Jerrold Olefsky, M.D. , a professor of medicine and assistant vice chancellor for integrative research at UC San Diego Health Sciences. “Impaired insulin sensitivity is the root cause of type 2 diabetes, so any treatment we can develop to safely restore this would be a major step forward for patients.”
The main driver of insulin resistance in type 2 diabetes is obesity, which currently affects more than 40 percent of Americans and in 2021 bore an annual medical cost of nearly $173 billion. In addition to causing adipose tissue (fat) to expand, obesity also causes low levels of inflammation. This inflammation causes immune cells, called macrophages, to accumulate in adipose tissue, where they can comprise up to 40 percent of the total number of cells in the tissue.
When adipose tissue is inflamed, these macrophages release tiny nanoparticles containing instructions for surrounding cells in the form of microRNAs, small fragments of genetic material that help regulate gene expression. These microRNA-containing capsules, called exosomes, are released into the circulation and can travel through the bloodstream to be absorbed by other tissues, such as the liver and muscles. This can then lead to the varied metabolic changes associated with obesity, including insulin resistance. For the current study, the researchers wanted to understand how TZD drugs, which restore insulin resistance, affect this exosome system.
The researchers treated a group of obese mice with rosiglitazone, a type of TZD drug. Those mice became more sensitive to insulin, but they also gained weight and retained excess fluid, known side effects of rosiglitazone. However, by isolating exosomes from the adipose tissue macrophages of the mice who had received the drug and injecting them into another group of obese mice that had not received it, the researchers were able to deliver the positive effects of rosiglitazone without transferring the negative effects.
“For decades, TZDs have been the only drugs we have that can reverse insulin resistance, but we seldom use them anymore because of their side effects profile. Impaired insulin sensitivity is the root cause of type 2 diabetes, so any treatment we can develop to safely restore this would be a major step forward for patients.”
“The exosomes were just as effective in reversing insulin resistance as the drug itself but without the same side effects,” said Olefsky. “This indicates that exosomes can ultimately link obesity-related inflammation and insulin resistance to diabetes. It also tells us that we may be able to leverage this system to boost insulin sensitivity.”
The researchers were also able to identify the specific microRNA within the exosomes that was responsible for the beneficial metabolic effects of rosiglitazone. This molecule, called miR-690, could eventually be leveraged into new therapies for type 2 diabetes.
“It’s likely not practical to develop exosomes themselves as a treatment because it would be difficult to produce and administer them, but learning what drives the beneficial effects of exosomes at the molecular level makes it possible to develop drugs that can mimic these effects,” said Olefsky. “There’s also plenty of precedent for using microRNAs themselves as drugs, so that’s the possibility we’re most excited about exploring for miR-690 going forward.”
Additional authors on the study include: Theresa V. Rohm, Felipe Castellani Gomes Dos Reis, Roi Isaac, Cairo Murphy, Karina Cunha e Rocha, Gautam Bandyopadhyay, Hong Gao, Avraham M. Libster, Rizaldy C. Zapata, Yun Sok Lee, Wei Ying, Charlene Miciano and Allen Wang, all at UC San Diego.
This study was funded, in part, by the National Institutes of Health (grants P30DK063491, R01DK101395, DK124298, R00DK115998, R21HD107516, R01DK125560, DK099205, AA028550, DK101737, AA011999, DK120515, AA029019, DK091183), the Swiss National Science Foundation (grant P2BSP3_200177), the Larry L. Hillblom Foundation (grants 2023-D-012-FEL and 2023-D-011-FEL), UCLA LIFT-UP, and Janssen Pharmaceuticals.
Disclosures: Wei Ying and Jerrold Olefsky are co-inventors on a provisional patent covering the use of miR-690 as an insulin sensitizer.
You May Also Like
Opening portals to the underworld, servicenow developer david loo returns to his roots to accept cse’s distinguished alumni award, take 10 with a triton: carrie metzgar is chasing stars, medical innovator: farah sheikh, stay in the know.
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.
You have been successfully subscribed to the UC San Diego Today Newsletter.
Campus & Community
Arts & culture, visual storytelling.
- Media Resources & Contacts
Signup to get the latest UC San Diego newsletters delivered to your inbox.
Award-winning publication highlighting the distinction, prestige and global impact of UC San Diego.
Popular Searches: Covid-19 Ukraine Campus & Community Arts & Culture Voices
- Patient Care & Health Information
- Diseases & Conditions
- Type 2 diabetes
Type 2 diabetes is usually diagnosed using the glycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months. Results are interpreted as follows:
- Below 5.7% is normal.
- 5.7% to 6.4% is diagnosed as prediabetes.
- 6.5% or higher on two separate tests indicates diabetes.
If the A1C test isn't available, or if you have certain conditions that interfere with an A1C test, your health care provider may use the following tests to diagnose diabetes:
Random blood sugar test. Blood sugar values are expressed in milligrams of sugar per deciliter ( mg/dL ) or millimoles of sugar per liter ( mmol/L ) of blood. Regardless of when you last ate, a level of 200 mg/dL (11.1 mmol/L ) or higher suggests diabetes, especially if you also have symptoms of diabetes, such as frequent urination and extreme thirst.
Fasting blood sugar test. A blood sample is taken after you haven't eaten overnight. Results are interpreted as follows:
- Less than 100 mg/dL (5.6 mmol/L ) is considered healthy.
- 100 to 125 mg/dL (5.6 to 6.9 mmol/L ) is diagnosed as prediabetes.
- 126 mg/dL (7 mmol/L ) or higher on two separate tests is diagnosed as diabetes.
Oral glucose tolerance test. This test is less commonly used than the others, except during pregnancy. You'll need to not eat for a certain amount of time and then drink a sugary liquid at your health care provider's office. Blood sugar levels then are tested periodically for two hours. Results are interpreted as follows:
- Less than 140 mg/dL (7.8 mmol/L ) after two hours is considered healthy.
- 140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L ) is diagnosed as prediabetes.
- 200 mg/dL (11.1 mmol/L ) or higher after two hours suggests diabetes.
Screening. The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 35 or older and in the following groups:
- People younger than 35 who are overweight or obese and have one or more risk factors associated with diabetes.
- Women who have had gestational diabetes.
- People who have been diagnosed with prediabetes.
- Children who are overweight or obese and who have a family history of type 2 diabetes or other risk factors.
After a diagnosis
If you're diagnosed with diabetes, your health care provider may do other tests to distinguish between type 1 and type 2 diabetes because the two conditions often require different treatments.
Your health care provider will test A1C levels at least two times a year and when there are any changes in treatment. Target A1C goals vary depending on age and other factors. For most people, the American Diabetes Association recommends an A1C level below 7%.
You also receive tests to screen for complications of diabetes and other medical conditions.
More Information
- Glucose tolerance test
Management of type 2 diabetes includes:
- Healthy eating.
- Regular exercise.
- Weight loss.
- Possibly, diabetes medication or insulin therapy.
- Blood sugar monitoring.
These steps make it more likely that blood sugar will stay in a healthy range. And they may help to delay or prevent complications.
Healthy eating
There's no specific diabetes diet. However, it's important to center your diet around:
- A regular schedule for meals and healthy snacks.
- Smaller portion sizes.
- More high-fiber foods, such as fruits, nonstarchy vegetables and whole grains.
- Fewer refined grains, starchy vegetables and sweets.
- Modest servings of low-fat dairy, low-fat meats and fish.
- Healthy cooking oils, such as olive oil or canola oil.
- Fewer calories.
Your health care provider may recommend seeing a registered dietitian, who can help you:
- Identify healthy food choices.
- Plan well-balanced, nutritional meals.
- Develop new habits and address barriers to changing habits.
- Monitor carbohydrate intake to keep your blood sugar levels more stable.
Physical activity
Exercise is important for losing weight or maintaining a healthy weight. It also helps with managing blood sugar. Talk to your health care provider before starting or changing your exercise program to ensure that activities are safe for you.
- Aerobic exercise. Choose an aerobic exercise that you enjoy, such as walking, swimming, biking or running. Adults should aim for 30 minutes or more of moderate aerobic exercise on most days of the week, or at least 150 minutes a week.
- Resistance exercise. Resistance exercise increases your strength, balance and ability to perform activities of daily living more easily. Resistance training includes weightlifting, yoga and calisthenics. Adults living with type 2 diabetes should aim for 2 to 3 sessions of resistance exercise each week.
- Limit inactivity. Breaking up long periods of inactivity, such as sitting at the computer, can help control blood sugar levels. Take a few minutes to stand, walk around or do some light activity every 30 minutes.
Weight loss
Weight loss results in better control of blood sugar levels, cholesterol, triglycerides and blood pressure. If you're overweight, you may begin to see improvements in these factors after losing as little as 5% of your body weight. However, the more weight you lose, the greater the benefit to your health. In some cases, losing up to 15% of body weight may be recommended.
Your health care provider or dietitian can help you set appropriate weight-loss goals and encourage lifestyle changes to help you achieve them.
Monitoring your blood sugar
Your health care provider will advise you on how often to check your blood sugar level to make sure you remain within your target range. You may, for example, need to check it once a day and before or after exercise. If you take insulin, you may need to check your blood sugar multiple times a day.
Monitoring is usually done with a small, at-home device called a blood glucose meter, which measures the amount of sugar in a drop of blood. Keep a record of your measurements to share with your health care team.
Continuous glucose monitoring is an electronic system that records glucose levels every few minutes from a sensor placed under the skin. Information can be transmitted to a mobile device such as a phone, and the system can send alerts when levels are too high or too low.
Diabetes medications
If you can't maintain your target blood sugar level with diet and exercise, your health care provider may prescribe diabetes medications that help lower glucose levels, or your provider may suggest insulin therapy. Medicines for type 2 diabetes include the following.
Metformin (Fortamet, Glumetza, others) is generally the first medicine prescribed for type 2 diabetes. It works mainly by lowering glucose production in the liver and improving the body's sensitivity to insulin so it uses insulin more effectively.
Some people experience B-12 deficiency and may need to take supplements. Other possible side effects, which may improve over time, include:
- Abdominal pain.
Sulfonylureas help the body secrete more insulin. Examples include glyburide (DiaBeta, Glynase), glipizide (Glucotrol XL) and glimepiride (Amaryl). Possible side effects include:
- Low blood sugar.
- Weight gain.
Glinides stimulate the pancreas to secrete more insulin. They're faster acting than sulfonylureas. But their effect in the body is shorter. Examples include repaglinide and nateglinide. Possible side effects include:
Thiazolidinediones make the body's tissues more sensitive to insulin. An example of this medicine is pioglitazone (Actos). Possible side effects include:
- Risk of congestive heart failure.
- Risk of bladder cancer (pioglitazone).
- Risk of bone fractures.
DPP-4 inhibitors help reduce blood sugar levels but tend to have a very modest effect. Examples include sitagliptin (Januvia), saxagliptin (Onglyza) and linagliptin (Tradjenta). Possible side effects include:
- Risk of pancreatitis.
- Joint pain.
GLP-1 receptor agonists are injectable medications that slow digestion and help lower blood sugar levels. Their use is often associated with weight loss, and some may reduce the risk of heart attack and stroke. Examples include exenatide (Byetta, Bydureon Bcise), liraglutide (Saxenda, Victoza) and semaglutide (Rybelsus, Ozempic, Wegovy). Possible side effects include:
SGLT2 inhibitors affect the blood-filtering functions in the kidneys by blocking the return of glucose to the bloodstream. As a result, glucose is removed in the urine. These medicines may reduce the risk of heart attack and stroke in people with a high risk of those conditions. Examples include canagliflozin (Invokana), dapagliflozin (Farxiga) and empagliflozin (Jardiance). Possible side effects include:
- Vaginal yeast infections.
- Urinary tract infections.
- Low blood pressure.
- High cholesterol.
- Risk of gangrene.
- Risk of bone fractures (canagliflozin).
- Risk of amputation (canagliflozin).
Other medicines your health care provider might prescribe in addition to diabetes medications include blood pressure and cholesterol-lowering medicines, as well as low-dose aspirin, to help prevent heart and blood vessel disease.

Insulin therapy
Some people who have type 2 diabetes need insulin therapy. In the past, insulin therapy was used as a last resort, but today it may be prescribed sooner if blood sugar targets aren't met with lifestyle changes and other medicines.
Different types of insulin vary on how quickly they begin to work and how long they have an effect. Long-acting insulin, for example, is designed to work overnight or throughout the day to keep blood sugar levels stable. Short-acting insulin generally is used at mealtime.
Your health care provider will determine what type of insulin is right for you and when you should take it. Your insulin type, dosage and schedule may change depending on how stable your blood sugar levels are. Most types of insulin are taken by injection.
Side effects of insulin include the risk of low blood sugar — a condition called hypoglycemia — diabetic ketoacidosis and high triglycerides.
Weight-loss surgery
Weight-loss surgery changes the shape and function of the digestive system. This surgery may help you lose weight and manage type 2 diabetes and other conditions related to obesity. There are several surgical procedures. All of them help people lose weight by limiting how much food they can eat. Some procedures also limit the amount of nutrients the body can absorb.
Weight-loss surgery is only one part of an overall treatment plan. Treatment also includes diet and nutritional supplement guidelines, exercise and mental health care.
Generally, weight-loss surgery may be an option for adults living with type 2 diabetes who have a body mass index (BMI) of 35 or higher. BMI is a formula that uses weight and height to estimate body fat. Depending on the severity of diabetes or the presence of other medical conditions, surgery may be an option for someone with a BMI lower than 35.
Weight-loss surgery requires a lifelong commitment to lifestyle changes. Long-term side effects may include nutritional deficiencies and osteoporosis.
People living with type 2 diabetes often need to change their treatment plan during pregnancy and follow a diet that controls carbohydrates. Many people need insulin therapy during pregnancy. They also may need to stop other treatments, such as blood pressure medicines.
There is an increased risk during pregnancy of developing a condition that affects the eyes called diabetic retinopathy. In some cases, this condition may get worse during pregnancy. If you are pregnant, visit an ophthalmologist during each trimester of your pregnancy and one year after you give birth. Or as often as your health care provider suggests.
Signs of trouble
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar. This condition also is called hyperglycemia. Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Symptoms include:
- Frequent urination.
- Increased thirst.
- Blurred vision.
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L ). HHNS may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Symptoms include:
- Extreme thirst.
- Drowsiness.
- Dark urine.
Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medicines — including the diabetes medicines called SGLT2 inhibitors.
The toxicity of the acids made by diabetic ketoacidosis can be life-threatening. In addition to the symptoms of hyperglycemia, such as frequent urination and increased thirst, ketoacidosis may cause:
- Shortness of breath.
- Fruity-smelling breath.
Low blood sugar. If your blood sugar level drops below your target range, it's known as low blood sugar. This condition also is called hypoglycemia. Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physically active than usual. Symptoms include:
- Irritability.
- Heart palpitations.
- Slurred speech.
If you have symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level. Examples include fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, eat or drink another source of sugar. Eat a meal after your blood sugar level returns to normal.
If you lose consciousness, you need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
- Medications for type 2 diabetes
- GLP-1 agonists: Diabetes drugs and weight loss
- Bariatric surgery
- Endoscopic sleeve gastroplasty
- Gastric bypass (Roux-en-Y)
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Careful management of type 2 diabetes can reduce the risk of serious — even life-threatening — complications. Consider these tips:
- Commit to managing your diabetes. Learn all you can about type 2 diabetes. Make healthy eating and physical activity part of your daily routine.
- Work with your team. Establish a relationship with a certified diabetes education specialist, and ask your diabetes treatment team for help when you need it.
- Identify yourself. Wear a necklace or bracelet that says you are living with diabetes, especially if you take insulin or other blood sugar-lowering medicine.
- Schedule a yearly physical exam and regular eye exams. Your diabetes checkups aren't meant to replace regular physicals or routine eye exams.
- Keep your vaccinations up to date. High blood sugar can weaken your immune system. Get a flu shot every year. Your health care provider also may recommend the pneumonia vaccine. The Centers for Disease Control and Prevention (CDC) also recommends the hepatitis B vaccination if you haven't previously received this vaccine and you're 19 to 59 years old. Talk to your health care provider about other vaccinations you may need.
- Take care of your teeth. Diabetes may leave you prone to more-serious gum infections. Brush and floss your teeth regularly and schedule recommended dental exams. Contact your dentist right away if your gums bleed or look red or swollen.
- Pay attention to your feet. Wash your feet daily in lukewarm water, dry them gently, especially between the toes, and moisturize them with lotion. Check your feet every day for blisters, cuts, sores, redness and swelling. Contact your health care provider if you have a sore or other foot problem that isn't healing.
- Keep your blood pressure and cholesterol under control. Eating healthy foods and exercising regularly can go a long way toward controlling high blood pressure and cholesterol. Take medication as prescribed.
- If you smoke or use other types of tobacco, ask your health care provider to help you quit. Smoking increases your risk of diabetes complications. Talk to your health care provider about ways to stop using tobacco.
- Use alcohol sparingly. Depending on the type of drink, alcohol may lower or raise blood sugar levels. If you choose to drink alcohol, only do so with a meal. The recommendation is no more than one drink daily for women and no more than two drinks daily for men. Check your blood sugar frequently after drinking alcohol.
- Make healthy sleep a priority. Many people with type 2 diabetes have sleep problems. And not getting enough sleep may make it harder to keep blood sugar levels in a healthy range. If you have trouble sleeping, talk to your health care provider about treatment options.
- Caffeine: Does it affect blood sugar?
Alternative medicine
Many alternative medicine treatments claim to help people living with diabetes. According to the National Center for Complementary and Integrative Health, studies haven't provided enough evidence to recommend any alternative therapies for blood sugar management. Research has shown the following results about popular supplements for type 2 diabetes:
- Chromium supplements have been shown to have few or no benefits. Large doses can result in kidney damage, muscle problems and skin reactions.
- Magnesium supplements have shown benefits for blood sugar control in some but not all studies. Side effects include diarrhea and cramping. Very large doses — more than 5,000 mg a day — can be fatal.
- Cinnamon, in some studies, has lowered fasting glucose levels but not A1C levels. Therefore, there's no evidence of overall improved glucose management.
Talk to your health care provider before starting a dietary supplement or natural remedy. Do not replace your prescribed diabetes medicines with alternative medicines.
Coping and support
Type 2 diabetes is a serious disease, and following your diabetes treatment plan takes commitment. To effectively manage diabetes, you may need a good support network.
Anxiety and depression are common in people living with diabetes. Talking to a counselor or therapist may help you cope with the lifestyle changes and stress that come with a type 2 diabetes diagnosis.
Support groups can be good sources of diabetes education, emotional support and helpful information, such as how to find local resources or where to find carbohydrate counts for a favorite restaurant. If you're interested, your health care provider may be able to recommend a group in your area.
You can visit the American Diabetes Association website to check out local activities and support groups for people living with type 2 diabetes. The American Diabetes Association also offers online information and online forums where you can chat with others who are living with diabetes. You also can call the organization at 800-DIABETES ( 800-342-2383 ).
Preparing for your appointment
At your annual wellness visit, your health care provider can screen for diabetes and monitor and treat conditions that increase your risk of diabetes, such as high blood pressure, high cholesterol or a high BMI .
If you are seeing your health care provider because of symptoms that may be related to diabetes, you can prepare for your appointment by being ready to answer the following questions:
- When did your symptoms begin?
- Does anything improve the symptoms or worsen the symptoms?
- What medicines do you take regularly, including dietary supplements and herbal remedies?
- What are your typical daily meals? Do you eat between meals or before bedtime?
- How much alcohol do you drink?
- How much daily exercise do you get?
- Is there a history of diabetes in your family?
If you are diagnosed with diabetes, your health care provider may begin a treatment plan. Or you may be referred to a doctor who specializes in hormonal disorders, called an endocrinologist. Your care team also may include the following specialists:
- Certified diabetes education specialist.
- Foot doctor, also called a podiatrist.
- Doctor who specializes in eye care, called an ophthalmologist.
Talk to your health care provider about referrals to other specialists who may be providing care.
Questions for ongoing appointments
Before any appointment with a member of your treatment team, make sure you know whether there are any restrictions, such as not eating or drinking before taking a test. Questions that you should regularly talk about with your health care provider or other members of the team include:
- How often do I need to monitor my blood sugar, and what is my target range?
- What changes in my diet would help me better manage my blood sugar?
- What is the right dosage for prescribed medications?
- When do I take the medications? Do I take them with food?
- How does management of diabetes affect treatment for other conditions? How can I better coordinate treatments or care?
- When do I need to make a follow-up appointment?
- Under what conditions should I call you or seek emergency care?
- Are there brochures or online sources you recommend?
- Are there resources available if I'm having trouble paying for diabetes supplies?
What to expect from your doctor
Your health care provider is likely to ask you questions at your appointments. Those questions may include:
- Do you understand your treatment plan and feel confident you can follow it?
- How are you coping with diabetes?
- Have you had any low blood sugar?
- Do you know what to do if your blood sugar is too low or too high?
- What's a typical day's diet like?
- Are you exercising? If so, what type of exercise? How often?
- Do you sit for long periods of time?
- What challenges are you experiencing in managing your diabetes?
- Professional Practice Committee: Standards of Medical Care in Diabetes — 2020. Diabetes Care. 2020; doi:10.2337/dc20-Sppc.
- Diabetes mellitus. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetes-mellitus-dm. Accessed Dec. 7, 2020.
- Melmed S, et al. Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 3, 2020.
- Diabetes overview. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/all-content. Accessed Dec. 4, 2020.
- AskMayoExpert. Type 2 diabetes. Mayo Clinic; 2018.
- Feldman M, et al., eds. Surgical and endoscopic treatment of obesity. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Oct. 20, 2020.
- Hypersmolar hyperglycemic state (HHS). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hyperosmolar-hyperglycemic-state-hhs. Accessed Dec. 11, 2020.
- Diabetic ketoacidosis (DKA). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetic-ketoacidosis-dka. Accessed Dec. 11, 2020.
- Hypoglycemia. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hypoglycemia. Accessed Dec. 11, 2020.
- 6 things to know about diabetes and dietary supplements. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/tips/things-to-know-about-type-diabetes-and-dietary-supplements. Accessed Dec. 11, 2020.
- Type 2 diabetes and dietary supplements: What the science says. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/providers/digest/type-2-diabetes-and-dietary-supplements-science. Accessed Dec. 11, 2020.
- Preventing diabetes problems. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/all-content. Accessed Dec. 3, 2020.
- Schillie S, et al. Prevention of hepatitis B virus infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recommendations and Reports. 2018; doi:10.15585/mmwr.rr6701a1.
- Diabetes prevention: 5 tips for taking control
- Hyperinsulinemia: Is it diabetes?
Associated Procedures
News from mayo clinic.
- Mayo study uses electronic health record data to assess metformin failure risk, optimize care Feb. 10, 2023, 02:30 p.m. CDT
- Mayo Clinic Minute: Strategies to break the heart disease and diabetes link Nov. 28, 2022, 05:15 p.m. CDT
- Mayo Clinic Q and A: Diabetes risk in Hispanic people Oct. 20, 2022, 12:15 p.m. CDT
- The importance of diagnosing, treating diabetes in the Hispanic population in the US Sept. 28, 2022, 04:00 p.m. CDT
- Mayo Clinic Minute: Managing Type 2 diabetes Sept. 28, 2022, 02:30 p.m. CDT
Products & Services
- A Book: The Essential Diabetes Book
- A Book: The Mayo Clinic Diabetes Diet
- Assortment of Health Products from Mayo Clinic Store
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Clinical Trials
Type 2 diabetes.
Displaying 96 studies
The purpose of this study is to identify changes to the metabolome (range of chemicals produced in the body) and microbiome (intestine microbe environment) that are unique to Roux-en-Y gastric bypass surgery and assess the associated effect on the metabolism of patients with type 2 diabetes.
The purpose of this study is to evaluate the impact of a digital storytelling intervention derived through a community-based participatory research (CBPR) approach on type 2 diabetes mellitus (T2D) outcomes among Hispanic adults with poorly controlled type 2 diabetes mellitus (T2D) in primary care settings through a randomized clinical trial.
The purpose of this study is to assess the impact of a whole food plant-based diet on blood sugar control in diabetic patients versus a control group on the American Diabetics Association diet before having a total hip, knee, or shoulder replacement surgery.
The purpose of this study is to learn more about if the medication, Entresto, could help the function of the heart and kidneys.
The primary aim of this study is to compare the outcome measures of adult ECH type 2 diabetes patients who were referred to onsite pharmacist services for management of their diabetes to similar patients who were not referred for pharmacy service management of their diabetes. A secondary aim of the study is to assess the Kasson providers’ satisfaction level and estimated pharmacy service referral frequency to their patients. A tertiary aim of the study is to compare the hospitalization rates of type 2 diabetes rates who were referred to onsite pharmacist services for management of their diabetes to similar patients ...
To explore the feasibility of conducting a family centered wellness coaching program for patients at high risk for developing diabetes, in a primary care setting.
To determine engagement patterns.
To describe characteristics of families who are likely to participate.
To identify barriers/limitations to family centered wellness coaching.
To assess whether a family centered 8 week wellness coaching intervention for primary care patients at high risk for diabetes will improve self-care behaviors as measured by self-reported changes in physical activity level and food choices.
This study is being done to understand metformin's mechanisms of action regarding glucose production, protein metabolism, and mitochondrial function.
The purpose of this study is to assess the effectiveness of Revita® DMR for improving HbA1c to ≤ 7% without the need of insulin in subjects with T2D compared to sham and to assess the effectiveness of DMR versus Sham on improvement in Glycemic, Hepatic and Cardiovascular endpoints.
The purpose of this study is to evaluate 6 weeks of home use of the Control-IQ automated insulin delivery system in individuals with type 2 diabetes.
This study will evaluate whether bile acids are able to increase insulin sensitivity and enhance glycemic control in T2DM patients, as well as exploring the mechanisms that enhance glycemic control. These observations will provide the preliminary data for proposing future therapeutic as well as further mechanistic studies of the role of bile acids in the control of glycemia in T2DM.
The purpose of this study is to determine if Inpatient Stress Hyperglycemia is an indicator of future risk of developing type 2 Diabetes Mellitus.
The purpose of this study is to assess the effectiveness of a digital storytelling intervention derived through a community based participatory research (CBPR) approach on self-management of type 2 diabetes (T2D) among Somali adults.
The GRADE Study is a pragmatic, unmasked clinical trial that will compare commonly used diabetes medications, when combined with metformin, on glycemia-lowering effectiveness and patient-centered outcomes.
The overall goal of this proposal is to determine the effects of acute hyperglycemia and its modulation by Glucagon-like Peptide-1 (GLP-1) on myocardial perfusion in type 2 diabetes (DM). This study plan utilizes myocardial contrast echocardiography (MCE) to explore a) the effects of acute hyperglycemia on myocardial perfusion and coronary flow reserve in individuals with and without DM; and b) the effects of GLP-1 on myocardial perfusion and coronary flow reserve during euglycemia and hyperglycemia in DM. The investigators will recruit individuals with and without DM matched for age, gender and degree of obesity. The investigators will measure myocardial perfusion ...
The purpose of this study is to test the hypothesis that patients with T2DM will have greater deterioration in BMSi and in cortical porosity over 3 yrs as compared to sex- and age-matched non-diabetic controls; and identify the circulating hormonal (e.g., estradiol [E2], testosterone [T]) and biochemical (e.g., bone turnover markers, AGEs) determinants of changes in these key parameters of bone quality, and evaluate the possible relationship between existing diabetic complications and skeletal deterioration over time in the T2DM patients.
The purpose of this study is to determine the effect of endogenous GLP-1 secretion on islet function in people with Typr 2 Diabetes Mellitus (T2DM).
GLP-1 is a hormone made by the body that promotes the production of insulin in response to eating. However, there is increasing evidence that this hormone might help support the body’s ability to produce insulin when diabetes develops.
The purpose of this study is to assess whether psyllium is more effective in lowering fasting blood sugar and HbA1c, and to evaluate the effect of psyllium compared to wheat dextrin on the following laboratory markers: LDL-C, inflammatory markers such as ceramides and hsCRP, and branch chain amino acids which predict Diabetes Mellitus (DM).
This trial is a multi-center, adaptive, randomized, double-blind, placebo- and active- controlled, parallel group, phase 2 study in subjects with Type 2 Diabetes Mellitus to evaluate the effect of TTP399 on HbA1c following administration for 6 months.
The purpose of this study is to find the inheritable changes in genetic makeup that are related to the development of type 2 diabetes in Latino families.
The objective of this early feasibility study is to assess the feasibility and preliminary safety of the Endogenex Divice for endoscopic duodenal mucosal regeneration in patients with type 2 diabetes (T2D) inadequately controlled on 2-3 non-insulin glucose-lowering medications.
The purpose of this study is to evaluate if breathing pure oxygen overnight affects insulin sensitivity in participants with diabetes.
The purpose of this study is to determine the impact of patient decision aids compared to usual care on measures of patient involvement in decision-making, diabetes care processes, medication adherence, glycemic and cardiovascular risk factor control, and use of resources in nonurban practices in the Midwestern United States.
This mixed methods study aims to answer the question: "What is the work of being a patient with type 2 diabetes mellitus?" .
The purpose of this study is to assess penile length pre- and post-completion of RestoreX® traction therapy compared to control groups (no treatment) among men with type II diabetes.
This observational study is conducted to determine how the duodenal layer thicknesses (mucosa, submucosa, and muscularis) vary with several factors in patients with and without type 2 diabetes.
The study is being undertaken to understand how a gastric bypass can affect a subject's diabetes even prior to their losing significant amounts of weight. The hypothesis of this study is that increased glucagon-like peptide-1 (GLP-1) secretion explains the amelioration in insulin secretion after Roux-en-Y Gastric Bypass (RYGB) surgery.
The purpose of this study is to estimate the risk of diabetes related complications after total pancreatectomy. We will contact long term survivors after total pancreatectomy to obtain data regarding diabetes related end organ complications.
The purpose of this study is to understand nighttime glucose regulation in humans and find if the pattern is different in people with Type 2 diabetes
The study purpose is to understand patients’ with the diagnosis of Diabetes Mellitus type 1 or 2 perception of the care they receive in the Diabetes clinic or Diabetes technology clinic at Mayo Clinic and to explore and to identify the healthcare system components patients consider important to be part of the comprehensive regenerative care in the clinical setting.
However, before we can implement structural changes or design interventions to promote comprehensive regenerative care in clinical practice, we first need to characterize those regenerative practices occurring today, patients expectations, perceptions and experiences about comprehensive regenerative care and determine the ...
The investigators will determine whether people with high muscle mitochondrial capacity produce higher amount of reactive oxygen species (ROS) on consuming high fat /high glycemic diet and thus exhibit elevated cellular oxidative damage. The investigators previously found that Asian Indian immigrants have high mitochondrial capacity in spite of severe insulin resistance. Somalians are another new immigrant population with rapidly increasing prevalence of diabetes. Both of these groups traditionally consume low caloric density diets, and the investigators hypothesize that when these groups are exposed to high-calorie Western diets, they exhibit increased oxidative stress, oxidative damage, and insulin resistance. The investigators will ...
The purpose of this research is to find out how genetic variations in GLP1R, alters insulin secretion, in the fasting state and when blood sugars levels are elevated. Results from this study may help us identify therapies to prevent or reverse type 2 diabetes mellitus.
It is unknown how patient preferences and values impact the comparative effectiveness of second-line medications for Type 2 diabetes (T2D). The purpose of this study is to elicit patient preferences toward various treatment outcomes (e.g., hospitalization, kidney disease) using a participatory ranking exercise, use these rankings to generate individually weighted composite outcomes, and estimate patient-centered treatment effects of four different second-line T2D medications that reflect the patient's value for each outcome.
The purpose of this mixed-methods study is to deploy the tenets of Health and Wellness Coaching (HWC) through a program called BeWell360 model , tailored to the needs of Healthcare Workers (HCWs) as patients living with poorly-controlled Type 2 Diabetes (T2D). The objective of this study is to pilot-test this novel, scalable, and sustainable BeWell360 model that is embedded and integrated as part of primary care for Mayo Clinic Employees within Mayo Clinic Florida who are identified as patients li)ving with poorly-controlled T2D.
To determine if the EndoBarrier safely and effectively improves glycemic control in obese subjects with type 2 diabetes.
Can QBSAfe be implemented in a clinical practice setting and improve quality of life, reduce treatment burden and hypoglycemia among older, complex patients with type 2 diabetes?
Questionnaire administered to diabetic patients in primary care practice (La Crosse Mayo Family Medicine Residency /Family Health Clinic) to assess patient’s diabetic knowledge. Retrospective chart review will also be done to assess objective diabetic control based on most recent hemoglobin A1c.
The purpose of this study is to assess key characteristics of bone quality, specifically material strength and porosity, in patients who have type 2 diabetes. These patients are at an unexplained increased risk for fractures and there is an urgent need to refine clinical assessment for this risk.
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM). It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking is responsible for muscle insulin resistance, although it has been shown that raising FFA with Intralipid can cause muscle insulin resistance within 4 hours. We do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. We propose to alter the profile and concentrations of FFA of healthy, non-obese adults using an overnight, intra-duodenal palm oil infusion vs. ...
The objectives of this study are to identify circulating extracellular vesicle (EV)-derived protein and RNA signatures associated with Type 2 Diabetes (T2D), and to identify changes in circulating EV cargo in patients whose T2D resolves after sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB).
This research study is being done to develop educational materials that will help patients and clinicians talk about diabetes treatment and management options.
Assessment of glucose metabolism and liver fat after 12 week dietary intervention in pre diabetes subjects. Subjects will be randomized to either high fat (olive oil supplemented),high carb/high fiber (beans supplemented) and high carb/low fiber diets. Glucose metabolism will be assessed by labeled oral glucose tolerance test and liver fat by magnetic resonance spectroscopy pre randomization and at 8 and 12 week after starting dietary intervention.
To study the effect of an ileocolonic formulation of ox bile extract on insulin sensitivity, postprandial glycemia and incretin levels, gastric emptying, body weight and fasting serum FGF-19 (fibroblast growth factor) levels in overweight or obese type 2 diabetic subjects on therapy with DPP4 (dipeptidyl peptidase-4) inhibitors (e.g. sitagliptin) alone or in combination with metformin.
The purpose of this study is to evaluate whether or not a 6 month supply (1 meal//day) of healthy food choices readily available in the patient's home and self management training including understanding of how foods impact diabetes, improved food choices and how to prepare those foods, improve glucose control. In addition, it will evaluate whether or not there will be lasting behavior change modification after the program.
The purpose of this study evaluates a subset of people with isolated Impaired Fasting Glucose with Normal Glucose Tolerance (i.e., IFG/NGT) believed to have normal β-cell function in response to a glucose challenge, suggesting that – at least in this subset of prediabetes – fasting glucose is regulated independently of glucose in the postprandial period. To some extent this is borne out by genetic association studies which have identified loci that affect fasting glucose but not glucose tolerance and vice-versa.
The purpose of this study is to learn more about how the body stores dietary fat. Medical research has shown that fat stored in different parts of the body can affect the risk for diabetes, heart disease and other major health conditions.
The purpose of this study is to see why the ability of fat cells to respond to insulin is different depending on body shape and how fat tissue inflammation is involved.
The purpose of this study is to determine the mechanism(s) by which common bariatric surgical procedures alter carbohydrate metabolism. Understanding these mechanisms may ultimately lead to the development of new interventions for the prevention and treatment of type 2 diabetes and obesity.
The purpose of this study is to compare the rate of progression from prediabetes at 4 months to frank diabetes at 12 months (as defined by increase in HbA1C or fasting BS to diabetic range based on the ADA criteria) after transplantation in kidney transplant recipients on Exenatide SR + SOC vs. standard-of-care alone.
The purpose of this study is to evaluate the effects of improving glycemic control, and/or reducing glycemic variability on gastric emptying, intestinal barrier function, autonomic nerve functions, and epigenetic changes in subjects with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) who are switched to intensive insulin therapy as part of clinical practice.
This study is designed to compare an intensive lifestyle and activity coaching program ("Sessions") to usual care for diabetic patients who are sedentary. The question to be answered is whether the Sessions program improves clinical or patient centric outcomes. Recruitment is through invitiation only.
A research study to enhance clinical discussion between patients and pharmacists using a shared decision making tool for type 2 diabetes or usual care.
While the potential clinical uses of pulsed electromagnetic field therapy (PEMF) are extensive, we are focusing on the potential benefits of PEMF on vascular health. We are targeting, the pre diabetic - metabolic syndrome population, a group with high prevalence in the American population. This population tends to be overweight, low fitness, high blood pressure, high triglycerides and borderline high blood glucose.
This is a study to evaluate a new Point of Care test for blood glucose monitoring.
This protocol is being conducted to determine the mechanisms responsible for insulin resistance, obesity and type 2 diabetes.
The purpose of this study is to assess the effects of a nighttime rise in cortisol on the body's glucose production in type 2 diabetes.
The goal of this study is to evaluate a new format for delivery of a culturally tailored digital storytelling intervention by incorporating a facilitated group discussion following the videos, for management of type II diabetes in Latino communities.
The purpose of this study is to determine the metabolic effects of Colesevelam, particularly for the ability to lower blood sugar after a meal in type 2 diabetics, in order to develop a better understanding of it's potential role in the treatment of obesity.
The purpose of this study is to test whether markers of cellular aging and the SASP are elevated in subjects with obesity and further increased in patients with obesity and Type 2 Diabetes Mellitus (T2DM) and to relate markers of cellular aging (senescence) and the SASP to skeletal parameters (DXA, HRpQCT, bone turnover markers) in each of these groups.
Integration of Diabetes Prevention Program (DPP) and Diabetes Self Management Program (DSMP) into WellConnect.
Using stem cell derived intestinal epithelial cultures (enteroids) derived from obese (BMI> 30) patients and non-obese and metabolically normal patients (either post-bariatric surgery (BS) or BS-naïve with BMI < 25), dietary glucose absorption was measured. We identified that enteroids from obese patients were characterized by glucose hyper-absorption (~ 5 fold) compared to non-obese patients. Significant upregulation of major intestinal sugar transporters, including SGLT1, GLU2 and GLUT5 was responsible for hyper-absorptive phenotype and their pharmacologic inhibition significantly decreased glucose absorption. Importantly, we observed that enteroids from post-BS non-obese patients exhibited low dietary glucose absorption, indicating that altered glucose absorption ...
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM). It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking is responsible for the abnormal response to insulin. Likewise, we do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. We will measure muscle FFA storage into intramyocellular triglyceride, intramyocellular fatty acid trafficking, activation of the insulin signaling pathway and glucose disposal rates under both saline control (high overnight FFA) and after an overnight infusion of intravenous ...
The purpose of this study is to improve our understanding of why gastrointestinal symptoms occur in diabetes mellitus patients and identify new treatment(s) in the future.
These symptoms are often distressing and may impair glycemic control. We do not understand how diabetes mellitus affects the GI tracy. In 45 patients undergoing sleeve gastrectomy, we plan to compare the cellular composition of circulating peripheral mononuclear cells, stomach immune cells, and interstitial cells of Cajal in the stomach.
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM), whereas lower body obesity (LBO) is characterized by near-normal insulin sensitivity. It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking differs between different obesity phenotypes. Likewise, we do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. By measuring muscle FFA storage into intramyocellular triglyceride, intramyocellular fatty acid trafficking, activation of the insulin signaling pathway and glucose disposal rates we will provide the first integrated examination ...
The goal of this study is to evaluate the presence of podocytes (special cells in the kidney that prevent protein loss) in the urine in patients with diabetes or glomerulonephritis (inflammation in the kidneys). Loss of podocyte in the urine may be an earlier sign of kidney injury (before protein loss) and the goal of this study is to evaluate the association between protein in the urine and podocytes in the urine.
The purpose of this study is to create a prospective cohort of subjects with increased probability of being diagnosed with pancreatic cancer and then screen this cohort for pancreatic cancer
The purpose of this study is to evaluate the effects of multiple dose regimens of RM-131 on vomiting episodes, stomach emptying and stomach paralysis symptoms in patients with Type 1 and Type 2 diabetes and gastroparesis.
The purpose of this study is assess the feasibility, effectiveness, and acceptability of Diabetes-REM (Rescue, Engagement, and Management), a comprehensive community paramedic (CP) program to improve diabetes self-management among adults in Southeast Minnesota (SEMN) treated for servere hypoglycemia by the Mayo Clinic Ambulance Services (MCAS).
The purpose of this study is to determine if a blood test called "pancreatic polypeptide" can help distinguish between patients with diabetes mellitus with and without pancreatic cancer.
The purpose of this study is to evaluate the effectiveness and safety of brolucizumab vs. aflibercept in the treatment of patients with visual impairment due to diabetic macular edema (DME).
Women with gestational diabetes mellitus (GDM) are likely to have insulin resistance that persists long after pregnancy, resulting in greater risk of developing type 2 diabetes mellitus (T2DM). The study will compare women with and without a previous diagnosis of GDM to determine if women with a history of GDM have abnormal fatty acid metabolism, specifically impaired adipose tissue lipolysis. The study will aim to determine whether women with a history of GDM have impaired pancreatic β-cell function. The study will determine whether women with a history of GDM have tissue specific defects in insulin action, and also identify the effect of a ...
Although vitreous hemorrhage (VH) from proliferative diabetic retinopathy (PDR) can cause acute and dramatic vision loss for patients with diabetes, there is no current, evidence-based clinical guidance as to what treatment method is most likely to provide the best visual outcomes once intervention is desired. Intravitreous anti-vascular endothelial growth factor (anti-VEGF) therapy alone or vitrectomy combined with intraoperative PRP each provide the opportunity to stabilize or regress retinal neovascularization. However, clinical trials are lacking to elucidate the relative time frame of visual recovery or final visual outcome in prompt vitrectomy compared with initial anti-VEGF treatment. The Diabetic Retinopathy Clinical Research ...
The purpose of this study is to demonstrate feasibility of dynamic 11C-ER176 PET imaging to identify macrophage-driven immune dysregulation in gastric muscle of patients with DG. Non-invasive quantitative assessment with PET can significantly add to our diagnostic armamentarium for patients with diabetic gastroenteropathy.
The purpose of this study is to assess the safety and tolerability of intra-arterially delivered mesenchymal stem/stromal cells (MSC) to a single kidney in one of two fixed doses at two time points in patients with progressive diabetic kidney disease.
Diabetic kidney disease, also known as diabetic nephropathy, is the most common cause of chronic kidney disease and end-stage kidney failure requiring dialysis or kidney transplantation. Regenerative, cell-based therapy applying MSCs holds promise to delay the progression of kidney disease in individuals with diabetes mellitus. Our clinical trial will use MSCs processed from each study participant to test the ...
The purpose of this study is to evaluate whether or not semaglutide can slow down the growth and worsening of chronic kidney disease in people with type 2 diabetes. Participants will receive semaglutide (active medicine) or placebo ('dummy medicine'). This is known as participants' study medicine - which treatment participants get is decided by chance. Semaglutide is a medicine, doctors can prescribe in some countries for the treatment of type 2 diabetes. Participants will get the study medicine in a pen. Participants will use the pen to inject the medicine in a skin fold once a week. The study will close when ...
The purpose of this study is to look at how participants' daily life is affected by their heart failure. The study will also look at the change in participants' body weight. This study will compare the effect of semaglutide (a new medicine) compared to "dummy" medicine on body weight and heart failure symptoms. Participants will either get semaglutide or "dummy" medicine, which treatment participants get is decided by chance. Participants will need to take 1 injection once a week.
This study aims to measure the percentage of time spent in hyperglycemia in patients on insulin therapy and evaluate diabetes related patient reported outcomes in kidney transplant recipients with type 2 diabetes. It also aimes to evaluate immunosuppression related patient reported outcomes in kidney transplant recipients with type 2 diabetes.
The objectives of this study are to evaluate the safety of IW-9179 in patients with diabetic gastroparesis (DGP) and the effect of treatment on the cardinal symptoms of DGP.
The purpose of this study is to understand why patients with indigestion, with or without diabetes, have gastrointestinal symptoms and, in particular, to understand where the symptoms are related to increased sensitivity to nutrients.Subsequently, look at the effects of Ondansetron on these patients' symptoms.
The purpose of this study is to evaluate the safety, tolerability, pharmacokinetics, and exploratory effectiveness of nimacimab in patients with diabetic gastroparesis.
The purpose of this study is to prospectively assemble a cohort of subjects >50 and ≤85 years of age with New-onset Diabetes (NOD):
- Estimate the probability of pancreatic ductal adenocarcinoma (PDAC) in the NOD Cohort;
- Establish a biobank of clinically annotated biospecimens including a reference set of biospecimens from pre-symptomatic PDAC and control new-onset type 2 diabetes mellitus (DM) subjects;
- Facilitate validation of emerging tests for identifying NOD subjects at high risk for having PDAC using the reference set; and
- Provide a platform for development of an interventional protocol for early detection of sporadic PDAC ...
The purpose of this study is to look at the relationship of patient-centered education, the Electronic Medical Record (patient portal) and the use of digital photography to improve the practice of routine foot care and reduce the number of foot ulcers/wounds in patients with diabetes.
Diabetes mellitus is a common condition which is defined by persistently high blood sugar levels. This is a frequent problem that is most commonly due to type 2 diabetes. However, it is now recognized that a small portion of the population with diabetes have an underlying problem with their pancreas, such as chronic pancreatitis or pancreatic cancer, as the cause of their diabetes. Currently, there is no test to identify the small number of patients who have diabetes caused by a primary problem with their pancreas.
The goal of this study is to develop a test to distinguish these ...
The purpose of this study is to demonstrate the performance of the Guardian™ Sensor (3) with an advanced algorithm in subjects age 2 - 80 years, for the span of 170 hours (7 days).
The primary purpose of this study is to evaluate the impact of dapagliflozin, as compared with placebo, on heart failure, disease specific biomarkers, symptoms, health status and quality of life in patients with type 2 diabetes or prediabetes and chronic heart failure with preserved systolic function.
The primary purpose of this study is to prospectively assess symptoms of bloating (severity, prevalence) in patients with diabetic gastroparesis.
The purpose of this study is to track the treatment burden experienced by patients living with Type 2 Diabetes Mellitus (T2DM) experience as they work to manage their illness in the context of social distancing measures.
To promote social distancing during the COVID-19 pandemic, health care institutions around the world have rapidly expanded their use of telemedicine to replace in-office appointments where possible.1 For patients with diabetes, who spend considerable time and energy engaging with various components of the health care system,2,3 this unexpected and abrupt transition to virtual health care may signal significant changes to ...
The purpose of this study is to evaluate the safety and efficacy of oral Pyridorin 300 mg BID in reducing the rate of progression of nephropathy due to type 2 diabetes mellitus.
The purpose of this study is to evaluate the effect of Aramchol as compared to placebo on NASH resolution, fibrosis improvement and clinical outcomes related to progression of liver disease (fibrosis stages 2-3 who are overweight or obese and have prediabetes or type 2 diabetes).
The purpose of this study is to evaluate the ability of appropriately-trained family physicians to screen for and identify Diabetic Retinopathy using retinal camera and, secondarily, to describe patients’ perception of the convenience and cost-effectiveness of retinal imaging.
The primary purpose of this study is to evaluate the impact of dapagliflozin, as compared with placebo, on heart failure disease-specific biomarkers, symptoms, health status, and quality of life in patients who have type 2 diabetes and chronic heart failure with reduced systolic function.
Hypothesis: We hypothesize that patients from the Family Medicine Department at Mayo Clinic Florida who participate in RPM will have significantly reduced emergency room visits, hospitalizations, and hospital contacts.
Aims, purpose, or objectives: In this study, we will compare the RPM group to a control group that does not receive RPM. The primary objective is to determine if there are significant group differences in emergency room visits, hospitalizations, outpatient primary care visits, outpatient specialty care visits, and hospital contacts (inbound patient portal messages and phone calls). The secondary objective is to determine if there are ...
The purpose of this research is to determine if CGM (continuous glucose monitors) used in the hospital in patients with COVID-19 and diabetes treated with insulin will be as accurate as POC (point of care) glucose monitors. Also if found to be accurate, CGM reading data will be used together with POC glucometers to dose insulin therapy.
The purpose of this study is to evaluate the effect of fenofibrate compared with placebo for prevention of diabetic retinopathy (DR) worsening or center-involved diabetic macular edema (CI-DME) with vision loss through 4 years of follow-up in participants with mild to moderately severe non-proliferative DR (NPDR) and no CI-DME at baseline.
The purpose of this study is to assess painful diabetic peripheral neuropathy after high-frequency spinal cord stimulation.
The purpose of this study is to examine the evolution of diabetic kindey injury over an extended period in a group of subjects who previously completed a clinical trial which assessed the ability of losartan to protect the kidney from injury in early diabetic kidney disease. We will also explore the relationship between diabetic kidney disease and other diabetes complications, including neuropathy and retinopathy.
The purpose of this study is to evaluate the effietiveness of remdesivir (RDV) in reducing the rate of of all-cause medically attended visits (MAVs; medical visits attended in person by the participant and a health care professional) or death in non-hospitalized participants with early stage coronavirus disease 2019 (COVID-19) and to evaluate the safety of RDV administered in an outpatient setting.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 8, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Study finds remote care approach improves therapy adherence and uptake in patients with type 2 diabetes
by Brigham and Women’s Hospital

A new study by investigators from Mass General Brigham demonstrated that a remote team focused on identifying, educating and prescribing therapy can improve guideline-directed-medical-therapy (GDMT) adherence in patients with type 2 diabetes and high cardiovascular and/or kidney risk.
The research team observed that patients who received education simultaneously with medication management demonstrated a higher rate of medication uptake and initiated treatment earlier compared to patients who received education over two months prior to medication management. Their results were presented at the 2024 American College of Cardiology's Annual Scientific Session and simultaneously published in Circulation .
"Our results suggest that patients are more inclined to adhere to therapy when approached with education and treatment simultaneously and immediately," said corresponding author Alexander J. Blood, MD, MSc, who presented the results. Blood serves as an attending physician in the Division of Cardiovascular Medicine as well as the Heart and Vascular Center at Brigham and Women's Hospital.
"Providers should 'strike while the iron is hot.' If a patient is already interested in investing in their health and willing to meet with you, that's the time to initiate treatment while providing educational resources."
Type 2 diabetes, which increases an individual's risk of cardiovascular and kidney events, affects millions of adults in the United States. Medications such as SGLT2 inhibitors and GLP-1 receptor agonists can improve cardiovascular and kidney outcomes in patients with type 2 diabetes, but data from clinical trials and society recommendations have not led to widespread adoption and utilization of these therapies.
To investigate the impact of patient education on prescription acceptance and therapy uptake, the research team conducted a parallel, randomized, open label clinical trial. They enrolled 200 adult patients with type 2 diabetes at Mass General Brigham, who were at elevated risk of cardiac and/or kidney complications.
Patients were randomly assigned to one of two groups. The "education-first" group received a dedicated two-month period of education, consisting of curated patient-centric videos on disease management and medication, prior to treatment initiation via an online portal. The second "simultaneous" group had access to the educational videos but received patient education concurrently with the initiation of their treatment.
Both groups received treatment through a research and clinical care management platform designed and created by the Accelerator for Clinical Transformation at Brigham and Women's Hospital and Mass General Brigham, which facilitated care coordination among patient navigators, pharmacists, nurse practitioners and physicians. These health care professionals guided patients through every step of their engagement with health care and streamlined communication. The platform is part of Mass General Brigham's larger efforts to transform health care delivery by helping patients access services and monitor health from home, especially at a time when hospitals are regularly operating over capacity.
Patients were followed for six months from enrollment or one month after medication initiation, whichever duration was longer.
While patients in both groups experienced benefits such as weight loss and reductions in blood glucose levels by the end of the study, those who received simultaneous education demonstrated a higher retention rate. Specifically, 60% of patients in this group were confirmed to have taken their prescribed therapy, compared to 44% in the "education-first" group. Additionally, contrary to initial predictions, patients in the "education-first" group did not engage more with the educational platform than those in the simultaneous group.
While the findings suggest that a pre-treatment education period may not be the solution to medication adherence issues, they underscore the potential of remote, team-based care delivery. This approach holds promise in facilitating the implementation of new therapies, bridging care quality disparities, and enhancing health care outcomes across diverse populations.
The authors describe how the flexibility inherent in remote treatment may extend access to care, particularly benefiting traditionally underserved populations or individuals with busy schedules. Moreover, the inclusion of a patient navigation team fosters ongoing patient-provider communication, providing the personalized support necessary for sustained patient engagement in their care.
"We strongly believe that remote care programs that leverage non-licensed navigators, clinical pharmacists, and team-based care, together with a care delivery platform, will improve operational efficiencies and communication and thereby address many of the persistent problems in health care," said Benjamin M. Scirica, MD, MPH, principal investigator of the DRIVE study and director of the Accelerator for Clinical Transformation.
"On a broader scale, programs like this enhance access, elevate patient outcomes, reduce physician burden, and promote the appropriate utilization of guideline-recommended medications."
Explore further
Feedback to editors

Researchers demonstrate miniature brain stimulator in humans
15 hours ago

Study reveals potential to reverse lung fibrosis using the body's own healing technique
Apr 12, 2024

Researchers discover cell 'crosstalk' that triggers cancer cachexia

Study improves understanding of effects of household air pollution during pregnancy

Wearable sensors for Parkinson's can improve with machine learning, data from healthy adults

New insights on B cells: Researchers explore building better antibodies and curbing autoimmune diseases

Grieving pet owners comforted by 'supernatural' interactions

Study shows AI improves accuracy of skin cancer diagnoses

Cell's 'garbage disposal' may have another role: Helping neurons near skin sense the environment

Chlamydia vaccine shows promise in early trial
Related stories.

Remote health care delivery program improves blood pressure and cholesterol levels
Nov 9, 2022

Remotely delivered program improves blood pressure, cholesterol control in 5,000 patients
Nov 17, 2020

Diabetes medication class tied to lower risk of kidney stones
Jan 31, 2024

Algorithm-driven digital program helped lower patients' cholesterol, blood pressure

Remote blood pressure management program enhanced care during pandemic, finds research
Mar 13, 2023

New study finds virtual care team strategy improves treatment for heart failure patients
Mar 6, 2023
Recommended for you

Study suggests light physical activity as a child is key to reducing risk of type 2 diabetes
Apr 9, 2024

Electronic sock detects unhealthy walking style linked to cardiovascular and diabetic complications
Apr 8, 2024

New insights into adult-onset type 1 diabetes
Apr 1, 2024

Researchers report clear shift in arterial diseases in diabetes
Mar 28, 2024

Risk prediction using genes and gut bacteria can improve early detection of diseases like type 2 diabetes
Mar 26, 2024

Insulin copayment caps not associated with an increase in insulin use among commercially insured populations
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Institute Trustees
- History & Legacy
- Publications
- About Research
- Research Areas
- Research Departments
- Core Technologies and Services
- Postdoctoral Program
- Collaborations
- Technologies and Tools
- Research Internships
- Research Board of Trustees & External Scientific Advisory Board
- About the Graduate School
- VAI Graduate School Board of Directors
- Doctoral Program
- Leadership and Staff
- Current Students
- Student Life
- Outcome Data
- About K-12 Education
- For Families
- For Educators
- Inquiry Insider
- About Support
- Ways to Give
- Ways to Support
- Purple Community
- Donor Stories
Get the latest stories right in your inbox.
- Clinical Trials
- Department of Neurodegenerative Science
- International Linked Clinical Trials (iLCT)
- Parkinson's Disease
Phase 2 clinical trial of Type 2 diabetes drug for treatment of Parkinson’s shows positive and promising results
April 3, 2024
LONDON (April 3, 2024) — Results from a one-year, phase 2 clinical trial of the Type 2 diabetes drug lixisenatide suggest that the treatment may slow the progression of motor symptoms in Parkinson’s disease. The study published today in The New England Journal of Medicine and was supported by Cure Parkinson’s and Van Andel Institute (VAI) through the International Linked Clinical Trials (iLCT) program.
About the trial
The LixiPark study involved 156 people who had been recently diagnosed with Parkinson’s. Participants were treated with either lixisenatide or a placebo in addition to their usual Parkinson’s medication. The results of the randomized, double-blinded study showed that the progression of motor symptoms in those receiving the lixisenatide treatment slowed, while motor symptoms in participants receiving the placebo continued to progress. The difference between the two groups was statistically significant, indicating that lixisenatide may be able to delay the progression of motor symptoms in people with Parkinson’s. The findings were consistent at the end of the 12-month treatment period and two months after treatment stopped.
Led by Professors Olivier Rascol and Wassilios Meissner at the University Hospital of Toulouse and University Hospital of Bordeaux, respectively, the LixiPark trial involved 21 different research centers of the NS-Park Network across France. The study, sponsored by the Toulouse University Hospital, was co-funded by UK charity Cure Parkinson’s, with Van Andel Institute, and the French Ministry of Health, with drug and placebo support from pharmaceutical company Sanofi.
Lixisenatide was prioritized for clinical testing through Cure Parkinson’s and VAI’s International Linked Clinical Trials program, an initiative that brings together leading Parkinson’s experts and advocates to prioritize potentially disease modifying treatments for clinical evaluation. Many of the drugs prioritized by the iLCT Committee have been approved to treat other conditions.
About GLP-1R agonists
Lixisenatide belongs to a group of medicines called glucagon-like peptide 1 receptor agonists (or GLP-1R agonists) that work by mimicking the action of a natural gut hormone that is produced after eating food. This gut hormone stimulates insulin release from the pancreas, which helps cells in the body to absorb glucose that is eventually turned into energy. GLP-1R agonists are clinically approved for the treatment of Type 2 diabetes.
Related: Learn more about GLP-1R agonists ➔
The LixiPark clinical trial results are important as they represent the second clinical trial of a drug in this class that has demonstrated a positive outcome on motor symptom progression in people with Parkinson’s at phase 2.[1] The first GLP-1R agonist to show potential to slow the progression of motor symptoms in Parkinson’s is exenatide, another iLCT prioritized drug currently being evaluated in large-scale, phase 3 clinical testing. Results from the exenatide trial are expected in 2024.
There is a known link between Parkinson’s and Type 2 diabetes, with research suggesting that people with Type 2 diabetes have a higher risk of developing Parkinson’s.[2] Insulin resistance is common among people with Parkinson’s, and individuals with Parkinson’s who are Type 2 diabetic often experience a more rapid progression of their symptoms.[3] It has also been reported that people with diabetes who are treated with GLP-1R agonists have a reduced risk of developing Parkinson’s.[4]
While these results show exciting potential, further testing is required before this drug can be approved for clinical use in Parkinson’s. This phase 2 study has laid excellent groundwork for future testing, and Cure Parkinson’s is working with the investigators to plan the next phase of development.
It is important to note that there are a wide range of subtle differences between the broader class of GLP-1R agonists and they have not all been tested in Parkinson’s. Some GLP-1R agonists do not cross the blood brain barrier very well, and therefore are not able to affect the brains of people with Parkinson’s. More research is required to better understand these differences in the context of a potential treatment for Parkinson’s.
Professors Wassilios Meissner and Olivier Rascol, Principal Investigators of the study, jointly said:
“For 30 years, we have been trying to understand how to slow the decline associated with Parkinson’s disease over time. In this context, the positive results of the LixiPark phase 2 trial showing less progression of motor symptoms of Parkinson’s disease over a year constitute a significant step forward in the future management of the disease. We look forward to confirming these encouraging results in the future, in order to translate such findings into clinical practice.”
Dr. Simon Stott, Director of Research at Cure Parkinson’s, said:
“This is a very encouraging result for us here at Cure Parkinson’s. Along with our funding partners at Van Andel institute, we have been championing the repurposing of GLP-1 receptor agonists for Parkinson’s since 2010. This is the second phase 2 clinical trial indicating that this class of diabetes drugs is doing something interesting in Parkinson’s. We congratulate the investigators who conducted this study, and we are truly grateful to the participants and their families for helping to advance the research into disease modifying therapies for Parkinson’s.”
Dr. Richard Wyse, MBE, Director of Clinical Development at Cure Parkinson’s, added:
“I am thrilled to see the extremely positive, groundbreaking clinical outcome of the lixisenatide trial, which could have real meaning for people living with Parkinson’s. Cure Parkinson’s originally identified lixisenatide as a potential treatment and has been championing and supporting this work, prioritizing it for trial through our International Linked Clinical Trials program. It has been a great pleasure working with the investigators, and we look forward to future clinical developments as we continue to pursue this exciting field of disease-modifying therapeutics to help treat Parkinson’s disease.”
Dr. Darren Moore , Chair of Van Andel Institute’s Department of Neurodegenerative Science and a member of the iLCT Committee, said:
“Today’s findings are a promising step forward in our exploration of GLP-1 receptor agonists as potential ways to slow or stop Parkinson’s progression. This important work would not be possible without collaboration and a shared commitment to finding therapies that impede Parkinson’s and improve quality of life. We are deeply grateful to our partners, the trial investigators and the trial participants and their families.”
[1] Read more about exenatide and Parkinson’s: cureparkinsons.org.uk/exenatide
[2] Rhee SY et al. 2020. Association between glycemic status and the risk of Parkinson disease: A nationwide population-based study . Diabetes Care. Deischinger et al. 2021. Diabetes mellitus is associated with a higher relative risk for Parkinson’s disease in women than in men . Journal of Parkinson’s Disease.
[3] Athauda et al. 2022. The impact of type 2 diabetes in Parkinson’s disease . Movement Disorders.
[4] Brauer et al. 2020. Diabetes medications and risk of Parkinson’s disease: a cohort study of patients with diabetes . Brain.
ABOUT CURE PARKINSON’S
Cure Parkinson’s funds and facilitates curative research across the globe. Our funding and innovation through our International Linked Clinical Trials Programme has enabled the world’s leading Parkinson’s researchers to collaborate in prioritising the next generation of drugs for clinical trial. In 2022, nearly 30% of all drugs that were being tested in clinical trials as possible cures for Parkinson’s had been evaluated by the iLCT Committee.
Together we will cure Parkinson’s.
Further information at www.cureparkinsons.org.uk
ABOUT VAN ANDEL INSTITUTE
Van Andel Institute (VAI) is committed to improving the health and enhancing the lives of current and future generations through cutting-edge biomedical research and innovative educational offerings. Established in Grand Rapids, Michigan, in 1996 by the Van Andel family, VAI is now home to more than 500 scientists, educators and support staff, who work with a growing number of national and international collaborators to foster discovery. The Institute’s scientists study the origins of cancer, Parkinson’s and other diseases and translate their findings into breakthrough prevention and treatment strategies. Our educators develop inquiry-based approaches for K-12 education to help students and teachers prepare the next generation of problem-solvers, while our Graduate School offers a rigorous, research-intensive Ph.D. program in molecular and cellular biology. Learn more at vai.org.
ABOUT THE NS-PARK/F-CRIN NETWORK
The NS-PARK network (F-CRIN), which received F-CRIN accreditation in 2014, is a national French clinical research network specialising in Parkinson’s disease and movement disorders. It brings together investigators and clinical researchers from 27 French centres, including the 25 Parkinson’s expert centres in France. It is governed by an executive board consisting of a coordinator, Professor Olivier Rascol (Toulouse), a co-coordinator, Professor Jean-Christophe Corvol (Paris, Pitié Salpêtrière), and associates Professor David Devos (Lille) and Professor Stéphane Thobois (Lyon). NS-PARK’s goal is to facilitate clinical research into Parkinson’s disease and movement disorders and contribute to the development of innovative therapies to improve the care of patients suffering from these diseases. The network is accredited and funded by the F-CRIN national clinical research infrastructure. It also receives annual financial support from Inserm and the Ministry of Health as part of the Neurodegenerative Diseases Plan (MND Plan) of the General Directorate for Healthcare Services (DGOS).
This outdated diabetes drug still has something to offer
By learning how an old diabetes drug works, researchers are discovering new, safer treatment options.
Thiazolidinediones (TZDs) are a class of drug that can be used to treat type 2 diabetes by reversing insulin resistance, one of the main hallmarks of the disease. While TZDs were extremely popular in the 1990's and early 2000's, they have fallen out of use among physicians in recent decades because they were discovered to cause unwanted side effects, including weight gain and excess fluid accumulation in body tissues.
Now, researchers at University of California San Diego School of Medicine are exploring how to isolate the positive effects of these drugs, which could help yield new treatments that don't come with the old side effects. In a new study published in Nature Metabolism , the researchers discovered how one of the most well-known TZD drugs works at the molecular level and were able to replicate its positive effects in mice without giving them the drug itself.
"For decades, TZDs have been the only drugs we have that can reverse insulin resistance, but we seldom use them anymore because of their side effects profile," said Jerrold Olefsky, M.D., a professor of medicine and assistant vice chancellor for integrative research at UC San Diego Health Sciences. "Impaired insulin sensitivity is the root cause of type 2 diabetes, so any treatment we can develop to safely restore this would be a major step forward for patients."
The main driver of insulin resistance in type 2 diabetes is obesity, which currently affects more than 40 percent of Americans and in 2021 bore an annual medical cost of nearly $173 billion. In addition to causing adipose tissue (fat) to expand, obesity also causes low levels of inflammation. This inflammation causes immune cells, called macrophages, to accumulate in adipose tissue, where they can comprise up to 40 percent of the total number of cells in the tissue.
When adipose tissue is inflamed, these macrophages release tiny nanoparticles containing instructions for surrounding cells in the form of microRNAs, small fragments of genetic material that help regulate gene expression. These microRNA-containing capsules, called exosomes, are released into the circulation and can travel through the bloodstream to be absorbed by other tissues, such as the liver and muscles. This can then lead to the varied metabolic changes associated with obesity, including insulin resistance. For the current study, the researchers wanted to understand how TZD drugs, which restore insulin resistance, affect this exosome system.
The researchers treated a group of obese mice with rosiglitazone, a type of TZD drug. Those mice became more sensitive to insulin, but they also gained weight and retained excess fluid, known side effects of rosiglitazone. However, by isolating exosomes from the adipose tissue macrophages of the mice who had received the drug and injecting them into another group of obese mice that had not received it, the researchers were able to deliver the positive effects of rosiglitazone without transferring the negative effects.
"The exosomes were just as effective in reversing insulin resistance as the drug itself but without the same side effects," said Olefsky. "This indicates that exosomes can ultimately link obesity-related inflammation and insulin resistance to diabetes. It also tells us that we may be able to leverage this system to boost insulin sensitivity."
The researchers were also able to identify the specific microRNA within the exosomes that was responsible for the beneficial metabolic effects of rosiglitazone. This molecule, called miR-690, could eventually be leveraged into new therapies for type 2 diabetes.
"It's likely not practical to develop exosomes themselves as a treatment because it would be difficult to produce and administer them, but learning what drives the beneficial effects of exosomes at the molecular level makes it possible to develop drugs that can mimic these effects," said Olefsky. "There's also plenty of precedent for using microRNAs themselves as drugs, so that's the possibility we're most excited about exploring for miR-690 going forward."
- Personalized Medicine
- Colon Cancer
- Pharmacology
- Diet and Weight Loss
- HIV and AIDS
- Diseases and Conditions
- Diabetes mellitus type 1
- Drug discovery
- Pharmaceutical company
- Diabetes mellitus type 2
- Nocebo - Placebo
- Erectile dysfunction
Story Source:
Materials provided by University of California - San Diego . Original written by Miles Martin. Note: Content may be edited for style and length.
Journal Reference :
- Theresa V. Rohm, Felipe Castellani Gomes Dos Reis, Roi Isaac, Cairo Murphy, Karina Cunha e Rocha, Gautam Bandyopadhyay, Hong Gao, Avraham M. Libster, Rizaldy C. Zapata, Yun Sok Lee, Wei Ying, Charlene Miciano, Allen Wang, Jerrold M. Olefsky. Adipose tissue macrophages secrete small extracellular vesicles that mediate rosiglitazone-induced insulin sensitization . Nature Metabolism , 2024; DOI: 10.1038/s42255-024-01023-w
Cite This Page :
Explore More
- Quantum Effects in Electron Waves
- Star Trek's Holodeck Recreated Using ChatGPT
- Cloud Engineering to Mitigate Global Warming
- Detecting Delayed Concussion Recovery
- Genes for Strong Muscles: Healthy Long Life
- Brightest Gamma-Ray Burst
- Stellar Winds of Three Sun-Like Stars Detected
- Fences Causing Genetic Problems for Mammals
- Ozone Removes Mating Barriers Between Fly ...
- Parkinson's: New Theory On Origins and Spread
Trending Topics
Strange & offbeat.

Living With Diabetes
Warning signs of diabetes, types of diabetes, type 1 vs type 2 diabetes, type 1 diabetes, type 1 diabetes causes, type 1 diabetes symptoms, is there a cure for type 1 diabetes, type 2 diabetes, type 2 diabetes treatment.

Educate teachers, school personnel and other child care providers about taking care of your child with type 1 diabetes. Download this helpful guide now.
Type 2 Diabetes is a serious condition which causes higher than normal blood sugar levels. It affects people from all social, economic, and ethnic backgrounds.
It is estimated that more than 34 million Americans have diabetes, including approximately 7 million who have the disease but have not yet been diagnosed. Worldwide, it is estimated that over 463 million people are living with some form of the disease.
Diabetes mellitus (type 2 diabetes), the medical term for the condition, occurs when the body cannot make or effectively use its own insulin, a hormone produced by special cells in the pancreas called islet (eye-let) cells. Insulin is like a key that opens the door of a cell so that food, or glucose, can enter. Without insulin, this glucose builds up in the blood and leads to starvation of the body’s cells, as well as dehydration and break down of body tissue.
There are multiple forms of diabetes. Type 2 diabetes is the most common form. Approximately 90 percent of those with diabetes have type 2. Unlike type 1 diabetes, in which all the insulin-producing cells are destroyed, people with type 2 diabetes are able to produce some of their own insulin, but their bodies are unable to use this insulin to completely control blood sugar levels. This is known as insulin resistance.
Who gets type 2 diabetes?
Type 2 diabetes usually develops after the age of 35, although it can occur in younger people as well, especially if they are overweight and have a sedentary lifestyle.
Commonly referred to as “adult onset” diabetes, 80% of those with this form of diabetes are overweight and have a family history of type 2 diabetes.
Certain ethnic groups have a higher risk of developing this form of the disease, including African Americans, Hispanics and American Indians. In addition, women who had diabetes during pregnancy (gestational diabetes) are also at greater risk of developing type 2 diabetes later in life.
What are the symptoms of type 2 diabetes?
Knowing the warning signs of type 2 diabetes is helpful for early diagnosis. Symptoms can include:
- Increased thirst
- Increased urination
- Unexplained weight loss
- Extreme hunger
- Extreme weakness or fatigue
- Blurred vision
- Infections which are slow or difficult to heal
The symptoms of type 2 diabetes usually happen over time, unlike the symptoms of type 1 diabetes which are sudden and often too severe to overlook. That’s why many people mistakenly overlook the warning signs of type 2, and often think the symptoms are signs of other conditions, such as aging, overworking, or hot weather. Because these symptoms are often ignored, it is estimated that more than seven million people in the United States have diabetes and are not aware of it.
Individuals who have undiagnosed or untreated diabetes for several years may develop some complications, such as nerve damage, pain or numbness in their hands and feet, or changes in their eyes or kidneys. People who are over 35, overweight, have a family history of diabetes, or who belong to a high-risk group should be checked at least once a year to detect diabetes at its earliest stages.
What is the treatment for type 2 diabetes?
The treatment for type 2 diabetes focuses on improving the person’s ability to more effectively use the insulin his/her own body produces to normalize blood sugar levels. A treatment program including diet, exercise, and weight loss will help decrease insulin resistance and, in turn, lower blood sugar levels. If blood sugar levels are still high, there are many medications which can help to either stimulate more insulin production in the pancreas or help the body better use the insulin it makes. Insulin injections may be needed if these oral medications, along with diet and exercise, do not lower blood sugar levels enough.
What are the problems associated with type 2 diabetes?
New advances in research and treatment methods are helping people with type 2 diabetes live full, active and healthy lives. However, it is important to remember that diabetes is a serious, chronic condition with potential short-term and long-term complications. Frequent self-monitoring of blood sugar levels and carefully following an individualized meal and exercise program is a good course of action.
People with undiagnosed, untreated or long-term diabetes are at risk of developing complications, including nerve and blood vessel damage. These potential complications, which can affect the eyes, kidneys, limbs, heart, brain, and stomach, may occur after many years of living with diabetes. Early detection, improved medications, and new technologies may help prevent or minimize diabetes-related complications.
Can type 2 diabetes be prevented?
The key to success is in preventing pre-diabetes and type 2 diabetes. Identifying risk means asking yourself the following key questions:
- Am I aged 35 years or older?
- Am I overweight?
- Do I have high blood pressure or cholesterol?
- Do I have a family history of diabetes?
- Am I African American, Hispanic, American Indian or Asian?
- Do I have a history of diabetes occurring during pregnancy?
- Did I deliver a baby weighing more than 9 pounds?
If you answered “yes” to any of these questions, then you should make an appointment with your physician to be screened. To lower your risk of pre-diabetes and type 2 diabetes try the following:
- Look for opportunities to move more during the day
- Exercise 30 minutes at least five times per week
- Eat a healthy meal plan including grains, cereals, fresh fruit and vegetables, low fat dairy and lean meat
- Reduce fat intake
- Reduce food portions
- Maintain an ideal body weight

Get more answers to your questions about type 1 diabetes, type 2 diabetes and gestational diabetes symptoms and treatments. (In Spanish: ¿Que es La Diabetes?).

Educate teachers, school personnel and other child care providers about taking care of your child with type 1 diabetes.

Get news about research toward a cure, diabetes management tips, information for parents of children with type 1 diabetes and more. Sign up and become a DRI Insider today!
Keep Up With Our Progress Toward A Cure & More
Deciphering America's Type 2 diabetes dilemma
With so much know about the prevention of diabetes, why do rates across the united states continue to rise.
Type 2 diabetes rates continue to climb in the United States, despite well-known treatments and prevention approaches. To better understand why, USA TODAY's health team traveled across the country, talking to researchers, clinicians and patients. They found people with diabetes often must fend for themselves against systemic barriers and a difficult disease.
We tell the story of America's Type 2 diabetes dilemma in five parts:
If Type 2 diabetes is preventable, why is the problem getting worse?
In the first story , we profile three people grappling with Type 2 diabetes, by far the most common form of the disease. One, a chef, manages to take control of her disease by changing the way she cooks. Another, an executive, puts his financial advantages to good use by stepping up his exercise routine and getting excellent medical care. A third struggles more without those outward assets, relying instead on his and his wife's optimism and perseverance.
Diabetes runs deep in rural Mississippi. Residents band together to make change.
The second story journeys to the Mississippi Delta, a land with rich soil that used to grow healthy produce. Now It's hard to find nutritious food here and diabetes is rampant. So, local residents have taken it upon themselves to help their neighbors and themselves.
Colorado's diabetes rate is the lowest in the US. But that's only half the story.
Then we travel to Colorado , the state with the lowest rate of Type 2 diabetes, which offers another way of looking at how zip code affects health in America. The state has prioritized diabetes care, built hiking trails and devoted its tobacco settlement money to prevention efforts. Still, there are pockets where diabetes remains a problem.
Managing Type 2 diabetes is complicated. And it’s likely to get worse.
Next, we spend a few days with a Philadelphia resident whose life is regimented by her diabetes and the many doctors' appointments needed to manage it. Doctors, too, are frustrated by the lack of time and resources they're given to adequately help their patients with diabetes and other chronic diseases.
Type 2 diabetes crisis can be controlled. These solutions are how we get there.
In the last piece, we explore what it will take to solve the problem of diabetes in America. No single approach will be enough, experts told us. Instead, a combination of existing food and education programs, medication, devices and a focus on prevention rather than treatment could begin to finally make a difference in the diabetes dilemma.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diabetes Overview
Healthy Living with Diabetes
- Español
On this page:
How can I plan what to eat or drink when I have diabetes?
How can physical activity help manage my diabetes, what can i do to reach or maintain a healthy weight, should i quit smoking, how can i take care of my mental health, clinical trials for healthy living with diabetes.
Healthy living is a way to manage diabetes . To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products.
Healthy living may help keep your body’s blood pressure , cholesterol , and blood glucose level, also called blood sugar level, in the range your primary health care professional recommends. Your primary health care professional may be a doctor, a physician assistant, or a nurse practitioner. Healthy living may also help prevent or delay health problems from diabetes that can affect your heart, kidneys, eyes, brain, and other parts of your body.
Making lifestyle changes can be hard, but starting with small changes and building from there may benefit your health. You may want to get help from family, loved ones, friends, and other trusted people in your community. You can also get information from your health care professionals.
What you choose to eat, how much you eat, and when you eat are parts of a meal plan. Having healthy foods and drinks can help keep your blood glucose, blood pressure, and cholesterol levels in the ranges your health care professional recommends. If you have overweight or obesity, a healthy meal plan—along with regular physical activity, getting enough sleep, and other healthy behaviors—may help you reach and maintain a healthy weight. In some cases, health care professionals may also recommend diabetes medicines that may help you lose weight, or weight-loss surgery, also called metabolic and bariatric surgery.
Choose healthy foods and drinks
There is no right or wrong way to choose healthy foods and drinks that may help manage your diabetes. Healthy meal plans for people who have diabetes may include
- dairy or plant-based dairy products
- nonstarchy vegetables
- protein foods
- whole grains
Try to choose foods that include nutrients such as vitamins, calcium , fiber , and healthy fats . Also try to choose drinks with little or no added sugar , such as tap or bottled water, low-fat or non-fat milk, and unsweetened tea, coffee, or sparkling water.
Try to plan meals and snacks that have fewer
- foods high in saturated fat
- foods high in sodium, a mineral found in salt
- sugary foods , such as cookies and cakes, and sweet drinks, such as soda, juice, flavored coffee, and sports drinks
Your body turns carbohydrates , or carbs, from food into glucose, which can raise your blood glucose level. Some fruits, beans, and starchy vegetables—such as potatoes and corn—have more carbs than other foods. Keep carbs in mind when planning your meals.
You should also limit how much alcohol you drink. If you take insulin or certain diabetes medicines , drinking alcohol can make your blood glucose level drop too low, which is called hypoglycemia . If you do drink alcohol, be sure to eat food when you drink and remember to check your blood glucose level after drinking. Talk with your health care team about your alcohol-drinking habits.

Find the best times to eat or drink
Talk with your health care professional or health care team about when you should eat or drink. The best time to have meals and snacks may depend on
- what medicines you take for diabetes
- what your level of physical activity or your work schedule is
- whether you have other health conditions or diseases
Ask your health care team if you should eat before, during, or after physical activity. Some diabetes medicines, such as sulfonylureas or insulin, may make your blood glucose level drop too low during exercise or if you skip or delay a meal.
Plan how much to eat or drink
You may worry that having diabetes means giving up foods and drinks you enjoy. The good news is you can still have your favorite foods and drinks, but you might need to have them in smaller portions or enjoy them less often.
For people who have diabetes, carb counting and the plate method are two common ways to plan how much to eat or drink. Talk with your health care professional or health care team to find a method that works for you.
Carb counting
Carbohydrate counting , or carb counting, means planning and keeping track of the amount of carbs you eat and drink in each meal or snack. Not all people with diabetes need to count carbs. However, if you take insulin, counting carbs can help you know how much insulin to take.
Plate method
The plate method helps you control portion sizes without counting and measuring. This method divides a 9-inch plate into the following three sections to help you choose the types and amounts of foods to eat for each meal.
- Nonstarchy vegetables—such as leafy greens, peppers, carrots, or green beans—should make up half of your plate.
- Carb foods that are high in fiber—such as brown rice, whole grains, beans, or fruits—should make up one-quarter of your plate.
- Protein foods—such as lean meats, fish, dairy, or tofu or other soy products—should make up one quarter of your plate.
If you are not taking insulin, you may not need to count carbs when using the plate method.

Work with your health care team to create a meal plan that works for you. You may want to have a diabetes educator or a registered dietitian on your team. A registered dietitian can provide medical nutrition therapy , which includes counseling to help you create and follow a meal plan. Your health care team may be able to recommend other resources, such as a healthy lifestyle coach, to help you with making changes. Ask your health care team or your insurance company if your benefits include medical nutrition therapy or other diabetes care resources.
Talk with your health care professional before taking dietary supplements
There is no clear proof that specific foods, herbs, spices, or dietary supplements —such as vitamins or minerals—can help manage diabetes. Your health care professional may ask you to take vitamins or minerals if you can’t get enough from foods. Talk with your health care professional before you take any supplements, because some may cause side effects or affect how well your diabetes medicines work.
Research shows that regular physical activity helps people manage their diabetes and stay healthy. Benefits of physical activity may include
- lower blood glucose, blood pressure, and cholesterol levels
- better heart health
- healthier weight
- better mood and sleep
- better balance and memory
Talk with your health care professional before starting a new physical activity or changing how much physical activity you do. They may suggest types of activities based on your ability, schedule, meal plan, interests, and diabetes medicines. Your health care professional may also tell you the best times of day to be active or what to do if your blood glucose level goes out of the range recommended for you.

Do different types of physical activity
People with diabetes can be active, even if they take insulin or use technology such as insulin pumps .
Try to do different kinds of activities . While being more active may have more health benefits, any physical activity is better than none. Start slowly with activities you enjoy. You may be able to change your level of effort and try other activities over time. Having a friend or family member join you may help you stick to your routine.
The physical activities you do may need to be different if you are age 65 or older , are pregnant , or have a disability or health condition . Physical activities may also need to be different for children and teens . Ask your health care professional or health care team about activities that are safe for you.
Aerobic activities
Aerobic activities make you breathe harder and make your heart beat faster. You can try walking, dancing, wheelchair rolling, or swimming. Most adults should try to get at least 150 minutes of moderate-intensity physical activity each week. Aim to do 30 minutes a day on most days of the week. You don’t have to do all 30 minutes at one time. You can break up physical activity into small amounts during your day and still get the benefit. 1
Strength training or resistance training
Strength training or resistance training may make your muscles and bones stronger. You can try lifting weights or doing other exercises such as wall pushups or arm raises. Try to do this kind of training two times a week. 1
Balance and stretching activities
Balance and stretching activities may help you move better and have stronger muscles and bones. You may want to try standing on one leg or stretching your legs when sitting on the floor. Try to do these kinds of activities two or three times a week. 1
Some activities that need balance may be unsafe for people with nerve damage or vision problems caused by diabetes. Ask your health care professional or health care team about activities that are safe for you.

Stay safe during physical activity
Staying safe during physical activity is important. Here are some tips to keep in mind.
Drink liquids
Drinking liquids helps prevent dehydration , or the loss of too much water in your body. Drinking water is a way to stay hydrated. Sports drinks often have a lot of sugar and calories , and you don’t need them for most moderate physical activities.
Avoid low blood glucose
Check your blood glucose level before, during, and right after physical activity. Physical activity often lowers the level of glucose in your blood. Low blood glucose levels may last for hours or days after physical activity. You are most likely to have low blood glucose if you take insulin or some other diabetes medicines, such as sulfonylureas.
Ask your health care professional if you should take less insulin or eat carbs before, during, or after physical activity. Low blood glucose can be a serious medical emergency that must be treated right away. Take steps to protect yourself. You can learn how to treat low blood glucose , let other people know what to do if you need help, and use a medical alert bracelet.
Avoid high blood glucose and ketoacidosis
Taking less insulin before physical activity may help prevent low blood glucose, but it may also make you more likely to have high blood glucose. If your body does not have enough insulin, it can’t use glucose as a source of energy and will use fat instead. When your body uses fat for energy, your body makes chemicals called ketones .
High levels of ketones in your blood can lead to a condition called diabetic ketoacidosis (DKA) . DKA is a medical emergency that should be treated right away. DKA is most common in people with type 1 diabetes . Occasionally, DKA may affect people with type 2 diabetes who have lost their ability to produce insulin. Ask your health care professional how much insulin you should take before physical activity, whether you need to test your urine for ketones, and what level of ketones is dangerous for you.
Take care of your feet
People with diabetes may have problems with their feet because high blood glucose levels can damage blood vessels and nerves. To help prevent foot problems, wear comfortable and supportive shoes and take care of your feet before, during, and after physical activity.

If you have diabetes, managing your weight may bring you several health benefits. Ask your health care professional or health care team if you are at a healthy weight or if you should try to lose weight.
If you are an adult with overweight or obesity, work with your health care team to create a weight-loss plan. Losing 5% to 7% of your current weight may help you prevent or improve some health problems and manage your blood glucose, cholesterol, and blood pressure levels. 2 If you are worried about your child’s weight and they have diabetes, talk with their health care professional before your child starts a new weight-loss plan.
You may be able to reach and maintain a healthy weight by
- following a healthy meal plan
- consuming fewer calories
- being physically active
- getting 7 to 8 hours of sleep each night 3
If you have type 2 diabetes, your health care professional may recommend diabetes medicines that may help you lose weight.
Online tools such as the Body Weight Planner may help you create eating and physical activity plans. You may want to talk with your health care professional about other options for managing your weight, including joining a weight-loss program that can provide helpful information, support, and behavioral or lifestyle counseling. These options may have a cost, so make sure to check the details of the programs.
Your health care professional may recommend weight-loss surgery if you aren’t able to reach a healthy weight with meal planning, physical activity, and taking diabetes medicines that help with weight loss.
If you are pregnant , trying to lose weight may not be healthy. However, you should ask your health care professional whether it makes sense to monitor or limit your weight gain during pregnancy.
Both diabetes and smoking —including using tobacco products and e-cigarettes—cause your blood vessels to narrow. Both diabetes and smoking increase your risk of having a heart attack or stroke , nerve damage , kidney disease , eye disease , or amputation . Secondhand smoke can also affect the health of your family or others who live with you.
If you smoke or use other tobacco products, stop. Ask for help . You don’t have to do it alone.
Feeling stressed, sad, or angry can be common for people with diabetes. Managing diabetes or learning to cope with new information about your health can be hard. People with chronic illnesses such as diabetes may develop anxiety or other mental health conditions .
Learn healthy ways to lower your stress , and ask for help from your health care team or a mental health professional. While it may be uncomfortable to talk about your feelings, finding a health care professional whom you trust and want to talk with may help you
- lower your feelings of stress, depression, or anxiety
- manage problems sleeping or remembering things
- see how diabetes affects your family, school, work, or financial situation
Ask your health care team for mental health resources for people with diabetes.
Sleeping too much or too little may raise your blood glucose levels. Your sleep habits may also affect your mental health and vice versa. People with diabetes and overweight or obesity can also have other health conditions that affect sleep, such as sleep apnea , which can raise your blood pressure and risk of heart disease.

NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for healthy living with diabetes?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of healthy living for people with diabetes, such as
- how changing when you eat may affect body weight and metabolism
- how less access to healthy foods may affect diabetes management, other health problems, and risk of dying
- whether low-carbohydrate meal plans can help lower blood glucose levels
- which diabetes medicines are more likely to help people lose weight
Find out if clinical trials are right for you .
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for healthy living with diabetes are looking for participants?
You can view a filtered list of clinical studies on healthy living with diabetes that are federally funded, open, and recruiting at www.ClinicalTrials.gov . You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Elizabeth M. Venditti, Ph.D., University of Pittsburgh School of Medicine.

IMAGES
VIDEO
COMMENTS
MELTON: The first major change in the treatment of Type 1 diabetes was probably the discovery of insulin in 1920. Now it's 100 years later and if this works, it's going to change the medical treatment for people with diabetes. Instead of injecting insulin, patients will get cells that will be their own insulin factories.
Apr. 29, 2022 — A novel therapy ameliorates obesity and Type 2 diabetes in mice fed a high-fat diet. The therapy acts through sustained release of nitric oxide, a gaseous signaling chemical ...
Researchers believe the liver may hold the key to new, preventative Type 2 diabetes treatments. This year marks the 100th anniversary of the discovery of insulin, a scientific breakthrough that ...
St. Petersburg, Fla. - September 12, 2023 - Scientists at Johns Hopkins All Children's Hospital, along with an international team of researchers, are shedding new light on the causes of Type 2 diabetes. The new research, published in the journal Nature Communications, offers a potential strategy for developing new therapies that could restore dysfunctional pancreatic beta-cells or ...
Yesterday's research, tomorrow's treatment. ... What a cure looks like. People with Type 2 diabetes make up 90 per cent of all people living with the disease. And unlike Type 1 diabetes, Type 2 can be prevented. In the past 30 years, Type 2 diabetes among children has doubled, according to medical journal The Lancet. ...
This finding encourages further investigation into inceptor as a potential therapeutic target for treating type 2 diabetes. These findings, led by Helmholtz Munich in collaboration with the German Center for Diabetes Research, the Technical University of Munich, and the Ludwig-Maximilians-University Munich, drive advancements in diabetes research.
For Immediate Release: May 13, 2022. Today, the U.S. Food and Drug Administration approved Mounjaro (tirzepatide) injection to improve blood sugar control in adults with type 2 diabetes, as an ...
Despite the successful development of new therapies for the treatment of type 2 diabetes, such as glucagon-like peptide-1 (GLP-1) receptor agonists and sodium-glucose cotransporter-2 inhibitors, the search for novel treatment options that can provide better glycaemic control and at reduce complications is a continuous effort. The present Review aims to present an overview of novel targets and ...
In people with obesity, bariatric surgery can cause remission of type 2 diabetes, and therapeutic alternatives are being sought to achieve levels of weight loss comparable to surgery 2. Insulin ...
In a potential game changer for patients with type 2 diabetes, a team of researchers at the Diabetes, Obesity, and Metabolism Institute (DOMI) at the Icahn School of Medicine at Mount Sinai has identified a therapeutic target for the preservation and regeneration of beta cells (β cells)—cells in the pancreas that produce and distribute insulin.
By Andrew Stewart, MD, as told to Hallie Levine. Type 2 diabetes is one of the world's greatest health problems. It affects about 400 million people globally. If it's uncontrolled, it can lead ...
Introduction. Diabetes mellitus (DM) is a global epidemic posing a significant health threat to people around the world. According to the International Diabetes Federation (IDF) estimates in 2019, 463 million people aged 20-79 years suffered from DM worldwide, which is projected to rise to a staggering 700 million in the next 25 years 1 (Figure 1).DM is the fastest growing health challenge ...
Type 2 diabetes (T2D) is an archetypical chronic condition of significant prevalence. Yet the concept of cure in the context of T2D reveals an interplay between the medical imagination and clinical realities that can shift the course of a patient's care. There are two domains in which cure is sociologically constructed: the professional domain ...
Tesaglitazar. Tesaglitazar is an experimental drug that showed promise as a treatment for type 2 diabetes in early studies. However, its development was put on hold by AstraZeneca in May 2006 before all of the phase 3 trials were completed. But this experimental treatment might be making a comeback.
The downsides, however, are that 1) hypoglycemia is a constant threat, 2) proper insulin doses are not trivial to calculate, 3) compliance can vary especially in children and young adults, and 4) there can be side effects of a variety of types. Nonetheless, insulin therapy remains a mainstay treatment of diabetes.
This research will provide insights into the role of the brain in the control of blood sugar levels and has potential to facilitate the development of novel approaches to diabetes treatment." The problem: Type 2 diabetes (T2D) is among the most pressing and costly medical challenges confronting modern society. Even with currently available ...
Adult sufferers can administer up to 100 shots a month to manage the illness. Study co-author Keith Al-Hasani says the research could lead to a cost-effective treatment. (ABC News: Rosanne Maloney ...
Towards a cure: promising research in 2023 Conclusion References ... Type 2 diabetes accounts for 90% of all diabetes cases, with social risk factors such as high BMI, poor diet, environmental ...
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). ... two studies link metformin treatment with the ...
Type 2 Diabetes Research Project topics include support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. See Project Examples ... Projects include studying the biology of appetite regulation and metabolism, identification of new treatment targets, and trials exploring interventions for ...
The main driver of insulin resistance in type 2 diabetes is obesity, which currently affects more than 40 percent of Americans and in 2021 bore an annual medical cost of nearly $173 billion. In addition to causing adipose tissue (fat) to expand, obesity also causes low levels of inflammation.
Treatment. Management of type 2 diabetes includes: Healthy eating. Regular exercise. Weight loss. Possibly, diabetes medication or insulin therapy. ... Research has shown the following results about popular supplements for type 2 diabetes: Chromium supplements have been shown to have few or no benefits. Large doses can result in kidney damage ...
A Comparative Effectiveness Study of Major Glycemia-lowering Medications for Treatment of Type 2 Diabetes Rochester, MN. The GRADE Study is a pragmatic, unmasked clinical trial that will compare commonly used diabetes medications, when combined with metformin, on glycemia-lowering effectiveness and patient-centered outcomes.
Type 2 diabetes, which increases an individual's risk of cardiovascular and kidney events, affects millions of adults in the United States. ... Both groups received treatment through a research ...
LONDON (April 3, 2024) — Results from a one-year, phase 2 clinical trial of the Type 2 diabetes drug lixisenatide suggest that the treatment may slow the progression of motor symptoms in Parkinson's disease. The study published today in The New England Journal of Medicine and was supported by Cure Parkinson's and Van Andel Institute (VAI) through the International Linked Clinical Trials ...
The main driver of insulin resistance in type 2 diabetes is obesity, which currently affects more than 40 percent of Americans and in 2021 bore an annual medical cost of nearly $173 billion.
Type 2 Diabetes is a serious condition which causes higher than normal blood sugar levels. It affects people from all social, economic, and ethnic backgrounds. ... New advances in research and treatment methods are helping people with type 2 diabetes live full, active and healthy lives. However, it is important to remember that diabetes is a ...
In the first story, we profile three people grappling with Type 2 diabetes, by far the most common form of the disease. One, a chef, manages to take control of her disease by changing the way she ...
To assess the association between glucagon-like peptide-1 receptor agonists (GLP-1RA) treatment and the risk of suicide attempts in people with type 2 diabetes (T2D), with a focus on subgroups with and without a history of depression or suicide attempts. Methods. This retrospective cohort study utilized TriNetX, a federated network of real ...
DKA is a medical emergency that should be treated right away. DKA is most common in people with type 1 diabetes. Occasionally, DKA may affect people with type 2 diabetes who have lost their ability to produce insulin. Ask your health care professional how much insulin you should take before physical activity, whether you need to test your urine ...