5 Emergency Medicine Personal Statement Samples
Looking at emergency medicine personal statement samples can be very useful when preparing your residency applications. Your personal statement is one of the most challenging components of the ERAS or CaRMS residency applications, but it is also one of the most important ones. Especially when you consider the fact that emergency medicine is one of the most competitive residencies . Your residency personal statement is a one-page essay that is supposed to tell the residency directors who you are, why you've chosen to pursue your chosen medical specialty - which in this case is emergency medicine - and why you are a good fit it. This blog will give you some tips for writing a strong personal statement and share five different winning emergency medicine personal statement samples that you can use as a frame of reference as you prepare for residency applications .
>> Want us to help you get accepted? Schedule a free strategy call here . <<

Article Contents 19 min read
What is the purpose of a personal statement .
If you want to write a compelling residency personal statement , you need to understand what this document is supposed to achieve. Your personal statement should highlight the "why" behind your decision to apply to a particular residency program. Essentially, you want your statement to answer the following three questions:
Imagine that you've been called for your residency interview, and the interviewer has asked \" How Will You Contribute to Our Program? \" or \u201cwhat kind of doctor will you be?\u201d. When they ask these questions, they are trying to find out what you have to offer as a candidate, and that's one of the things that your personal statement should tell them. Talk about your reasons for choosing the specialty, how your values align with theirs, your strengths and abilities, and what makes you unique as a candidate. ","label":"What will you bring to the program?","title":"What will you bring to the program?"}]" code="tab2" template="BlogArticle">
We know that it sounds like a lot of information to fit in a one-page essay. It can be challenging to get right, but it is doable. Take a look at the emergency medicine personal statement samples below and pay attention to the way that the candidates answer these questions in their essays.
On the second day of my medical school rotations, one of the attendings pointed at me and said, "Now he looks like an ER doc." I laughed because I was not surprised at all. I have always gravitated toward Emergency Medicine because it fits my personality. I am naturally energetic and drawn to a high-paced environment.
I have been convinced that Emergency Medicine is the right fit for me since my first year of medical school, and I got to put my theory to the test during my Emergency Medicine rotation. In the space of a week, we saw gunshot wounds, infections, overdoses, broken bones, common colds, and motor vehicle accidents. At first, I wasn't sure I would be able to keep up with the pace of the trauma bay, but I thrived on it.
A few weeks ago, I celebrated my upcoming medical school graduation by purchasing a 7500-piece jigsaw puzzle. It is the biggest puzzle I have ever attempted to solve, and I can't wait to get started. See, the thing is that solving puzzles of any sort makes me happy. It is one of the many reasons I hope to have a long and rewarding career as an emergency physician.
As a third-year medical student, several factors motivated me to choose a residency in emergency medicine. During my clerkship, I got to experience the fast-paced, unpredictable nature of the emergency room. I quickly found a mentor in one of the attendings that I worked with. His breadth of knowledge, enthusiasm, and calm efficiency - even when all hell seemed to be breaking loose around us - showed me how challenging emergency medicine could be. My interest was certainly piqued, and the more I learned, the more I wanted to know.
I especially enjoyed the challenges of the undifferentiated patient. Often in the emergency room, you are the first to assess and treat a patient who's come in with little more than a chief complaint. You, therefore, have to start the process of diagnosing them from the very beginning. I loved the challenge of being faced with a set of symptoms and having to identify their common etiology.
That said, the most gratifying part for me was the interactions that I had with my patients. Behind all the symptoms that I was presented with were real people from all walks of life. I specifically remember a 62-year-old man who had been brought in after losing consciousness, falling in his kitchen, and getting a deep laceration on his forehead. He was presenting with vertigo and showing symptoms of malnutrition. While I attended to his bleeding forehead, we got to talking, and he explained to me how he had recently lost his wife and had been on a juice fast so that he could try to live longer. I was able to have a conversation with him and advise him on the kind of diet that was better suited for him.
I pride myself on my ability to quickly build rapport with people, especially patients. It is a skill that has always served me well, but it had never felt so useful as it did in the emergency room. Every patient has a story, and sometimes part of treating them is taking a few minutes to ask the right questions and make them feel heard. I was honestly surprised to learn that immersing myself in the unpredictable nature of the emergency room did not mean that I had to interact less with patients. On the contrary, I feel like I got a chance to connect with more people during my emergency medicine rotation than on any other service.
It taught me that emergency physicians wear many different hats throughout the day, and depending on the situation, they can call on various aspects of their medical training. Some cases require the kind of patience and bedside manner that people typically associate with internal and family medicine, while others need a physician who is as quick, decisive, and creative as a trauma surgeon. You never know which hat you will need to wear until your patient is in front of you, and then you simply have to adapt so that you can provide them with the best care possible.
For these reasons, a career in emergency medicine would satisfy my curiosity, constant need to be challenged, and need to connect with patients. I know that I have the skills and the drive required to pursue my training and become a competent emergency physician. Leading a musical band has taught me the importance of communication and shown me that while I am capable of working on my own, I enjoy being a part of a team, and I know how to reach out for assistance when need be.
I look forward to joining a residency program that will help me develop my medical skills and that values patient care and will help me achieve my goal of becoming a caring, competent emergency physician.
When I was a child, my mother often asked me what I wanted to become when I grew up, and up until high school, the answer was never a doctor. My parents are both family physicians, as are my grandmother and my oldest sister. No one ever said anything to me, but I always assumed they wanted me to follow in their footsteps. And I felt like although I didn't want to be, I was different from them because I had no desire to pursue a career in medicine at all.
That said, when you grow up in a house full of physicians, you learn a few things without knowing it. I found that out during a camping trip with my 7th-grade class when one of my friends had an allergic reaction, and we couldn't find an adult to help. Ms. XY was in the bathroom for a maximum of five minutes, but it felt like hours for us as we watched our friend break out in hives and struggle to breathe. I decided to call my mum instead of waiting for our teacher. Whenever she tells this story, she insists that I sounded like an intern on her first day when she picked up, and I said: "X seems to be reacting to something, we are not sure what it is, but she has raised patches of skin all-over her neck and her pulse feels slower than it should be. She needs Epi, right?"
This was not a ground-breaking diagnosis, by any means but it was my first time dealing with someone who was having an allergic reaction. I remember feeling a sense of pride at the fact that I had been level-headed enough to take note of the symptoms that my friend was having and seek help and communicate effectively. After confirming that my classmate did indeed need a shot from an epi-pen, so I went to get one from Ms. X, and she administered the shot.
Even though I had a few experiences of this nature, I was still going back and forth between four different professions, and I could not decide on one. First, I wanted to be a chemist, then a teacher, then a therapist, and then a police officer, and back and forth. It was my guidance counselor in high school that helped me figure out that the right medical career could combine all the things that I love about the professions I grappled with.
I didn't believe her at first, but she was right. After a few conversations with her on the topic, I finally started looking into the different fields that medical doctors can work in. I read an article describing emergency physicians as decisive jacks of all trades, who thrive in high-energy, fast-paced environments, and it felt like they were describing me. That was when my interest in emergency medicine was piqued.
It turned into a mission during my first week of clinical rotations when I worked in the emergency room and loved every minute of it. Every single day in the x general hospital emergency department, I saw at least one gunshot wound, a person with one or multiple broken bones, a motor vehicle accident, and a person whose medical condition is nonurgent. On many days, we had to treat several of those cases simultaneously.
My time at X general hospital confirmed that emergency medicine could give me a platform to do everything I love about the other professions I had considered. As an emergency physician, I get to be on the front lines and occasionally provide preventive care. I also have to listen to my patients and make sure they feel heard and understood, all while teaching them how to take care of their bodies in order to heal correctly.
Now, I can think of no better place to spend my professional career than the emergency department, and I know that with the right training, I will be able to provide my patients with the best care possible because that is exactly what every single patient deserves.
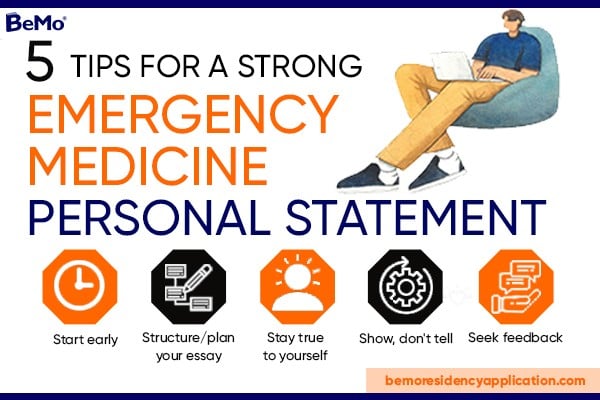
Want an overview of the tips that we cover later in this blog? Check out this infographic:
I didn't always want to be an emergency medicine physician. Actually, when I was in elementary school, I remember telling my dad that I wanted to be an engineer because someone had said to me that they fixed broken things, and I thought that was the coolest thing in the world. I wanted to fix broken things and make people happy. It wasn't until much later that I realized that medicine allows you to do something far cooler, in my opinion: fix people's bodies.
While in college, I got the opportunity to explore the intense, fast-paced world of critical care through an internship. Within a few months of working as a scribe at the X medical center emergency department, I fell in love with emergency medicine. I worked the same hours as some doctors and saw the same number of patients they saw. As I transcribed their medical decision-making, I would imagine myself in their shoes and wonder how I would react to similar situations. The time that I spent in that emergency department gave me an in-depth look at what being an emergency room physician means daily. I got to see them be radiologists, intensivists, orthopedists, and so much more. I admired the physicians who worked in the Emergency Department and loved that they got to wear so many different hats on a given day.
Some days were busy from the moment I came in for my shift to when I would leave to go home. Other days were so quiet that I could actually study for my MCAT right in the middle of the emergency room. The calm rarely lasted long, though, and I always looked forward to the next patient because you never knew what to expect. Sometimes it was a child with a broken bone or a pregnant woman with vaginal bleeding and abdominal pain. Other times it was a drunken man who wanted to tackle everybody in his way or a police officer with a gunshot wound. I found myself excited to get to work, and I just knew that emergency medicine was the perfect specialty for me. It promised to give me a platform to make medical decisions, use the full breadth of the skills I would have as a doctor, be hands-on with my patients, and experience something different every day.
There was no doubt in my mind that emergency medicine was right for me, but I was yet to figure out whether I was a good fit for emergency medicine. When I finally got into medical school, I spent a lot of time reflecting on the qualities that I was told a good emergency physician should have. I knew that I was a good team player because I have been part of a team my whole life. As one of the founding members of a small African dance group in my city, I have always taken the opportunity to be both a leader and a team member in great stride, and we have danced together for thirteen years now. My time as president of the Pre-med Student Union at X university taught me that sometimes you have to take control, and other times, you have to ask for help and work with others. I now know how o recognize those times, and I feel comfortable in both situations.
By my third year of medical school, I was more confident in my skills, and I started to believe that I am well suited to be an emergency physician. On one particular day, I was in the residence cafeteria when a small fire broke out, and chaos erupted around me. I didn't have to think about my actions; I just knew that I needed to remain calm, look for the nearest exit, and help as many people as possible get there. One of my classmates thanked me when we got outside and told me that I was very calm under pressure, a quality that I did not realize I possessed but looking back, I could see right away that she was right. I have always thrived under pressure. I can keep a level head in busy, fast-paced environments and focus on the task I have in front of me.
This theory was tested when I saw my first patient on the first shift of my first emergency medicine rotation. I had arrived five minutes before my shift to get acclimated to the department that I would be working in that day. Right behind me were paramedics, bringing in a two-month-old male who was hypothermic, hypotensive, and barely breathing. I watched in awe as the entire medical team coordinated to intubate, place a peripheral line, administer medications, and work to save this infant's life. Everyone worked together like it was a choreographed dance, and I was able to step back, look for the place where I'd be most helpful, and jump in. I helped one of the residents run the labs, and within an hour, the little boy was stabilized and on his way to the intensive care unit.
I went home many hours and patients later, still thinking about that little boy and how the emergency team's quick and coordinated efforts potentially saved his life. Each day after that, I continued to learn. I learned during my rotations on other services and in medical school. Now, I hope to get the chance to learn from one of the best residency programs in the country so that one day, I, too, can be a part of a coordinated effort to save lives as a skilled emergency medicine physician.
Use a Residency Match Calculator will to assess your match chances this year. It's a quick and easy way to find out how competitive you are for your chosen medical specialty! ","label":"Bonus tip:","title":"Bonus tip:"}]" code="tab3" template="BlogArticle">
I am the youngest of nine children and my parent’s only daughter, so I am used to commotion, and I have learned to thrive within it. When I was growing up, our house was only quiet in the dead of night, and even then, my older brothers would sometimes be playing around in the basement. By the time I was in high school, I'd gotten so used to the chaos around me that very little could break my concentration. I am very aware of my surroundings, but I've learned to decipher what requires my attention and what doesn't. My partner often refers to it as my superpower, and I guess it is in some ways.
This superpower served me well when I first moved to the United States at the age of sixteen and had to spend most of my free time studying. I was able to study in the busy cafeteria during lunch period and in loud classrooms during free periods. I even managed to do my homework in the stands at football games while my brother was playing on a few occasions. I grew up in France, so moving to America meant learning a new curriculum in a language that I did not speak very well at the time. The first few weeks were challenging, but once I figured out how to use my superpower to put in more study hours, I started making progress. Eventually, I graduated in the top 25% of my class.
I approach everything that I do with this same dedication and work ethic. I did it throughout my undergrad years, when I worked as a teacher's assistant, ran track for the school team, and completed my degree in biotechnology. I also did it in medical school, where I discovered that I genuinely enjoy teaching by offering tutoring lessons. I plan to continue in this way during my residency and during what I will work to ensure is a long and fulfilling career.
I believe that my perseverance and passion will help me along the way as I train to become a doctor, but it is because of my curiosity, compassion, and love for the field that I know that with the proper training, I can be a great emergency physician. When I was in primary school, we had a career day, and one of my classmates' friends came in and told us all about his work as an ER doctor. He talked about how he got to heal kids and adults who were hurting, and then he gave us lollipops and told us that if we worked hard, we could do it too. I was sold! At the dinner table that evening, I explained to my family that I was going to become a doctor. They all assumed it was because of the lollipop, but my interest had just been piqued, and the more I've learned about medicine since then, the more I've wanted to know.
I had always been drawn to emergency medicine because of the fast-paced and unpredictable nature of the emergency room. During my clerkship, I got to learn more about the core specialties in medicine, and I confirmed that emergency medicine was perfect for me. One of the attendings that I worked with in the ER told me that "emergency doctors are people who just like doing things, all the time." She told me that she knew it was right for her when she realized that she was just as comfortable around big scary things like traumas and codes as when dealing with children with appendicitis.
Her words stayed with me because they described precisely how I felt during my time in the emergency room. I loved the diversity in patients' presentations—surgical, medical, social, psychiatric, etc. I loved being required to think on my feet and act quickly to provide lifesaving or limb-saving care at a moment's notice.
Emergency medicine is the perfect platform for me to utilize my superpower, work ethic, and passion for medicine to provide patient care in an environment that is almost reminiscent of the home I grew up in. I cannot imagine a more fulfilling career path for myself.
Five Tips for a strong personal statement
1. start early.
Writing a residency personal statement, especially for a competitive field like emergency medicine, is not something that you can rush through. We recommend that you give yourself at least six to eight weeks to brainstorm, write, edit and polish your personal statement. The earlier you start, the more time you will have to review your statement and get a second pair of eyes to look at it to ensure it is as compelling as possible. You do not want to be scrambling at the last minute and end up with a subpar essay because you waited until the last minute to get the job done.
The key to an excellent personal statement is preparation. You should take the time to brainstorm and plan the structure of your essay for two reasons: First, because having a structure will guide you and keep you on track as you write. Secondly, because we tend to get attached to our work, and if we get to a point where we realize that the flow of the personal statement is off, it is harder to delete a whole paragraph than it is to just rewrite a few sentences. We suggest that you brainstorm first. Think about the questions that we mentioned earlier and write down your answers to those questions, as well as any memorable experiences that have contributed to your decision to become a physician.
4. Stay true to yourself
Students often make the mistake of writing what they think the program directors want to hear instead of the truth. This usually backfires because it can end up sounding cliché and generic, but also because it will likely not be consistent with the rest of your application. Your personal statement should be about you and your suitability for the residency program. So, be honest and don't try to fabricate your statement or exaggerate your experiences. Instead, tell the residency program directors about your exposure to medicine, what you've learned, and how your experiences led to you wanting to pursue this vocation.
Have you started preparing for your residency interviews? This video is for you:
5. Seek feedback
It's not enough to make statements about yourself. If you want to write a compelling statement, you need to back your claims up with specific examples or short anecdotes. Not only do people tend to remember such things more, but it is just a more impactful way to write. For example, instead of saying, "I am good at handling stress," you could say, "My role as the oldest sister of five children has often tested my ability to handle stressful situations." The second sentence is more memorable, and if you followed it up with an anecdote about one of those stressful situations, it would be even more impactful. It shows the directors that you have experience dealing with stressful situations, and it also gives them some new information about your background.
Your residency personal statement shouldn't be longer than one page unless otherwise specified. You should aim for an essay that is between 650 and 800 words.
Your personal statement should tell the program directors why you've chosen to pursue your specialty, why you're suited for it, and their program.
They are an essential part of your residency application as they give you a chance to tell the program directors why you are a good fit for your chosen field and their program in your own words. You should definitely not underestimate their importance.
While you can certainly send different versions of your personal statement to different programs, we do not recommend that you address them to any program in particular because this would mean writing several different personal statements. Instead, focus on writing personal statements that are tailored to specific specialties.
That depends on the concern in question. You should only discuss issues that you haven't addressed in other application components and that are relevant to the rest of your statement. If you address any red flags, make sure you demonstrate maturity and honesty by taking ownership of the problem and explaining how you've learned and grown from your mistakes.
Yes. Emergency medicine is one of the most competitive residencies, so you need to ensure your residency application is compelling if you want to secure a spot in a top program.
No, you do not. Most students apply to 15 - 30 residency programs in one application cycle, so writing a letter for each one is simply not feasible. Instead, you should write a letter for each specialty that you are considering.
You can write a strong personal statement if you take the time to brainstorm and plan for your essay early, use specific examples in your writing, and seek feedback from experts.
Want more free tips? Subscribe to our channels for more free and useful content!
Apple Podcasts
Like our blog? Write for us ! >>
Have a question ask our admissions experts below and we'll answer your questions, get started now.
Talk to one of our admissions experts
Our site uses cookies. By using our website, you agree with our cookie policy .
FREE Training Webinar:
How to make your residency application stand out, (and avoid the top 5 reasons most applicants don't match their top choice program).
Quick Links
- UW HR Resources
Impressing: Personal Statement
Personal statement, personal statements usually fall into 3 categories:.
- The top 5% are works of writing wonder which is appreciated by all who read them but add only a little to your interview chances.
- The middle 85% are not necessarily memorable but they are well written and get a sense of you across; these may not add a whole lot to your interview chances but they don’t detract and they will hopefully create a memorable image that will be yours for the season.
- The bottom 10% are poorly written with grammatical mistakes, spelling errors, a lack of organization, or some combination of the three; these will truly hurt your chances for an interview – some committees have a zero-tolerance policy for spelling or grammar errors.
Those who write papers in the bottom 10% are often the ones who are shooting for the top 5%; we, therefore, recommend that your goal should be the middle 85%. The goal of your statement should be to explain why you want to go into emergency medicine and why you think emergency medicine is the right specialty for you.
Overarching theme
Look over your CV and think about the experiences before and during medical school that might inform what kind of emergency physician you will become. Often there is a common thread that holds together even the most disparate of experiences – this common thread is usually one of your core values as a person. This may be a good theme to weave throughout and hold together your personal statement.
Experiences to highlight
Use your experiences to give programs an idea of who you are. Be specific – talking about the aspects of care that you like in emergency medicine is good but it’s even better when programs can see how your personal experiences reinforce aspects of emergency medicine that resonate with you as a person. It’s OK to include patient vignettes and talk about your accomplishments, but be sure to relate them back to yourself. How did the experience impact you? What did you learn about yourself? How will the experience make you a better family physician? What about the experience demonstrates your commitment to the discipline of emergency medicine, your ability to work with others, and your ability to work with patients? Often choosing one experience and telling the story is a good way to open your statement, develop your theme, and make it memorable.
Commitment to specialty
Talk about why you are choosing emergency medicine. What experiences convince you that this is the right field for you?
Strengths that you bring
What do you bring to a program? What are you naturally good at? What specific skills do you have that will serve you well in residency? Give examples.
Future plans/what you are looking for in a residency program
At the end of this long road of school and training, what kind of work do you see yourself doing? This is not necessary but if you do have a sense then you should bring it up – it will help paint a better picture of you and give you something to discuss during the interviews.
Organizing your statement
There are many ways to organize your statement to get these points across. One common way of organizing the personal statement is a three to five-paragraph form reminiscent of those essays you had to write in high school. To use this approach the first paragraph tells a story to open the theme, the middle paragraph(s) fleshes out other experiences that highlight the theme and discuss your commitment to emergency medicine and what you have to bring to it, and the third paragraph reviews your strengths and future plans/training desires. However, this is a personal statement and you are free to write and organize it as you desire.
- Write in complete sentences.
- Have transitions between paragraphs
- Use the active voice.
- Make your writing interesting – use a thesaurus and vary sentence length.
- Have at least two other people (one who knows you well and one who knows the process of applying to EM residency well) read your personal statement and give feedback.
- Give yourself plenty of time to work on your statement and revise it based on feedback.
- Rehash your CV or write an autobiography.
- Discuss research or experiences that you can’t expand significantly on in an interview.
- Be overly creative ‐‐ no poems or dioramas.
- Use abbreviations – spell things out.
- Say “emergency room” or “emergency room doctor” – use the emergency department and emergency physician
- Start every sentence with “I”.
- Make it longer than one page, in single‐spaced, 12-point font.
- Have ANY spelling or grammatical errors.
- Write a statement that could be used for several different specialties (i.e. one that talks about wanting a primary care career but not specifically emergency medicine). If you are still deciding on a specialty and applying to different fields, write two different statements.
- End your essay speaking to the reader (e.g., thanking them for their time).
- Be arrogant or overly self‐deprecating.
- Focus on lifestyle issues or what you will do with all your free time as an EP.
- Focus on your being an adrenalin junkie.
- Use hackneyed stories of growth, travel, or adventure unless it really is personal and you can express that.
Adapted with permission from the copyrighted career advising resources developed by Amanda Kost, MD, and the University of Washington Department of Family Medicine
2 Med School Essays That Admissions Officers Loved
Here are tips on writing a medical school personal statement and examples of essays that stood out.
2 Great Med School Personal Statements

Getty Images
A compelling medical school admissions essay can address nearly any topic the applicant is interested in, as long as it conveys the applicant's personality.
A personal statement is often a pivotal factor in medical school admissions decisions.
"The essay really can cause me to look more deeply at the entire application," Dr. Stephen Nicholas, former senior associate dean of admissions with the Columbia University Vagelos College of Physicians and Surgeons , told U.S. News in 2017. "So I do think it's pretty important."
A compelling medical school admissions essay can address nearly any topic the applicant is interested in, as long as it conveys the applicant's personality, according to Dr. Barbara Kazmierczak, director of the M.D.-Ph.D. Program and a professor of medicine and microbial pathogenesis with the Yale School of Medicine.
“The passion that the writer is bringing to this topic tells us about the individual rather than the topic that they’re describing, and the essay is the place for us to learn about the applicant – who they are and what experiences have brought them to this point of applying to medical school,” she told U.S. News in 2017.
Rachel Rudeen, former admissions coordinator for the University of Minnesota Medical School , says personal statements help medical schools determine whether applicants have the character necessary to excel as a doctor. "Grit is something we really look for," she says.
Evidence of humility and empathy , Rudeen adds, are also pluses.
Why Medical Schools Care About Personal Statements
The purpose of a personal statement is to report the events that inspired and prepared a premed to apply to medical school, admissions experts say. This personal essay helps admissions officers figure out whether a premed is ready for med school, and it also clarifies whether a premed has a compelling rationale for attending med school, these experts explain.
When written well, a medical school personal statement conveys a student's commitment to medicine and injects humanity into an admissions process that might otherwise feel cold and impersonal, according to admissions experts.
Glen Fogerty, associate dean of admissions and recruitment with the medical school at the University of Arizona—Phoenix , put it this way in an email: "To me, the strongest personal statements are the ones that share a personal connection. One where a candidate shares a specific moment, the spark that ignited their passion to become a physician or reaffirmed why they chose medicine as a career."
Dr. Viveta Lobo, an emergency medicine physician with the Stanford University School of Medicine in California who often mentors premeds, says the key thing to know about a personal statement is that it must indeed be personal, so it needs to reveal something meaningful. The essay should not be a dry piece of writing; it should make the reader feel for the author, says Lobo, director of academic conferences and continuing medical education with the emergency medicine department at Stanford.
A great personal statement has an emotional impact and "will 'do' something, not just 'say' something," Lobo wrote in an email. Admissions officers "read hundreds of essays – so before you begin, think of how yours will stand out, be unique and different," Lobo suggests.
How to Write a Personal Statement for Medical School
Lobo notes that an outstanding personal statement typically includes all of the following ingredients:
- An intriguing introduction that gets admissions officers' attention.
- Anecdotes that illustrate what kind of person the applicant is.
- Reflections about the meaning and impact of various life experiences .
- A convincing narrative about why medical school is the logical next step.
- A satisfying and optimistic conclusion.
"You should sound excited, and that passion should come through in your writing," Lobo explains.
A personal statement should tie together an applicant's past, present and future by explaining how previous experiences have led to this point and outlining long-term plans to contribute to the medical profession, Lobo said during a phone interview. Medical school admissions officers want to understand not only where an applicant has been but also the direction he or she is going, Lobo added.
When premeds articulate a vision of how they might assist others and improve society through the practice of medicine, it suggests that they aren't self-serving or simply interested in the field because of its prestige, Lobo says. It's ideal when premeds can eloquently describe a noble mission, she explains.
Elisabeth Fassas, author of "Making Pre-Med Count: Everything I Wish I'd Known Before Applying (Successfully) to Medical School," says premeds should think about the doctors they admire and reflect on why they admire them. Fassas, a first-year medical student at the University of Maryland , suggests pondering the following questions:
- "Why can you really only see yourself being a physician?"
- "What is it about being a doctor that has turned you on to this field?"
- "What kind of doctor do you imagine yourself being?"
- "Who do you want to be for your patients?"
- "What are you going to do specifically for your patients that only you can do?"
Fassas notes that many of the possible essay topics a med school hopeful can choose are subjects that other premeds can also discuss, such as a love of science. However, aspiring doctors can make their personal statements unique by articulating the lessons they learned from their life experiences, she suggests.
Prospective medical students need to clarify why medicine is a more suitable calling for them than other caring professions, health care fields and science careers, Fassas notes. They should demonstrate awareness of the challenges inherent in medicine and explain why they want to become doctors despite those difficulties, she says.
Tips on Crafting an Excellent Medical School Personal Statement
The first step toward creating an outstanding personal statement, Fassas says, is to create a list of significant memories. Premeds should think about which moments in their lives mattered the most and then identify the two or three stories that are definitely worth sharing.
Dr. Demicha Rankin, associate dean for admissions at the Ohio State University College of Medicine , notes that a personal statement should offer a compelling portrait of a person and should not be "a regurgitation of their CV."
The most outstanding personal statements are the ones that present a multifaceted perspective of the applicant by presenting various aspects of his or her identity, says Rankin, an associate professor of anesthesiology.
For example, a premed who was a swimmer might explain how the discipline necessary for swimming is analogous to the work ethic required to become a physician, Rankin says. Likewise, a pianist or another type of musician applying to medical school could convey how the listening skills and instrument-tuning techniques cultivated in music could be applicable in medicine, she adds.
Rankin notes that it's apparent when a premed has taken a meticulous approach to his or her personal statement to ensure that it flows nicely, and she says a fine essay is akin to a "well-woven fabric." One sign that a personal statement has been polished is when a theme that was explored at the beginning of the essay is also mentioned at the end, Rankin says, explaining that symmetry between an essay's introduction and conclusion makes the essay seem complete.
Rankin notes that the author of an essay might not see flaws in his or her writing that are obvious to others, so it's important for premeds to show their personal statement to trusted advisers and get honest feedback. That's one reason it's important to begin the writing process early enough to give yourself sufficient time to organize your thoughts, Rankin says, adding that a minimum of four weeks is typically necessary.
Mistakes to Avoid in a Medical School Personal Statement
One thing premeds should never do in an admissions essay is beg, experts say. Rankin says requests of any type – including a plea for an admissions interview – do not belong in a personal statement. Another pitfall to avoid, Rankin says, is ranting about controversial political subjects such as the death penalty or abortion.
If premeds fail to closely proofread their personal statement, the essay could end up being submitted with careless errors such as misspellings and grammar mistakes that could easily have been fixed, according to experts. Crafting a compelling personal statement typically necessitates multiple revisions, so premeds who skimp on revising might wind up with sloppy essays, some experts say.
However, when fine-tuning their personal statements, premeds should not automatically change their essays based on what others say, Fogerty warns.
"A common mistake on personal statements is having too many people review your statement, they make recommendations, you accept all of the changes and then – in the end – the statement is no longer your voice," Fogerty wrote in an email. It's essential that a personal statement sound like the applicant and represent who he or she is as a person, Fogerty says.
Dr. Nicholas Jones, a Georgia-based plastic and reconstructive surgeon, says the worst error that someone can make in the personal statement is to be inauthentic or deceptive.
"Do not lie. Do not fabricate," he warns.
Jones adds that premeds should not include a story in their personal statement that they are not comfortable discussing in-depth during a med school admissions interview . "If it's something too personal or you're very emotional and you don't want to talk about that, then don't put it in a statement."
Medical School Personal Statement Examples
Here are two medical school admissions essays that made a strong, positive impression on admissions officers. The first is from Columbia and the second is from the University of Minnesota. These personal statements are annotated with comments from admissions officers explaining what made these essays stand out.
Searching for a medical school? Get our complete rankings of Best Medical Schools.
Tags: medical school , education , students , graduate schools
Popular Stories
Paying for Graduate School

Applying to College

Best Global Universities

Best Colleges

You May Also Like
How to win a fulbright scholarship.
Cole Claybourn and Ilana Kowarski April 26, 2024
What to Ask Law Students and Alumni
Gabriel Kuris April 22, 2024

Find a Strong Human Rights Law Program
Anayat Durrani April 18, 2024

Environmental Health in Medical School
Zach Grimmett April 16, 2024

How to Choose a Law Career Path
Gabriel Kuris April 15, 2024

Questions Women MBA Hopefuls Should Ask
Haley Bartel April 12, 2024

Law Schools With the Highest LSATs
Ilana Kowarski and Cole Claybourn April 11, 2024

MBA Programs That Lead to Good Jobs
Ilana Kowarski and Cole Claybourn April 10, 2024

B-Schools With Racial Diversity
Sarah Wood April 10, 2024

Law Schools That Are Hardest to Get Into
Sarah Wood April 9, 2024


International Emergency Medicine Education Project
We promote emergency medicine and provide free, reusable education resources for medical students and educators
Why Emergency Medicine? A medical student’s reflection

As the Canadian Resident Matching Service (CaRMS) application cycle approaches for the Class of 2020 in Canada, I have been reflecting on the common question of “Why Emergency Medicine (EM)?” This has encouraged me to consider all aspects of the specialty that I love, as well as some of the perceived challenges of pursuing EM residency training. Additionally, I have been asked about advice for medical students interested in exploring EM, mainly from those beginning medical school or clerkship this month. So, in an attempt at a personal reflection exercise, I am also hoping to provide some practical points for consideration for any medical student thinking about exploring this wonderful specialty.
Some of the reasons why I love Emergency Medicine:
Versatility.
From the clinical presentations and various procedures, to the patients and team members working in the emergency department, I am constantly drawn to the multifaceted and dynamic nature of EM. Speaking to well-seasoned staff physicians, this versatility has them constantly learning and encountering new things. During my first EM shift of clerkship, the first patient of the day came in with atrial fibrillation, the second was hypothermic and without vital signs, the third had lower back pain, and the fourth presented with a COPD exacerbation. The range in presentations and levels of acuity are something that greatly appeal to me and allow for constant growth in Medicine. This diversity provides endless opportunities to learn new things in the setting of, at times, very limited information and time.

Opportunities for subspecialization
EM offers several formal opportunities to find your niche within the specialty, in the form of fellowships. These areas include ultrasound, trauma, resuscitation and reanimation, critical care, toxicology, pediatric EM, disaster medicine, and medical education. This is not an exhaustive list and will vary depending on where you are training. The Canadian Association of Emergency Physicians has developed an accessible directory for enhanced competencies: https://caep.ca/em-community/resident-section/enhanced-competency-directory/ .

Portability
One long-standing interest of mine throughout my post-secondary education has been Population and Global Health. Therefore, something that I really appreciate about EM is its portability. EM is present in an array of settings, from rural to large academic centers. This flexibility allows you to tailor your practice to your interests, both within and outside of Medicine. In a recent post by one of iEM’s blog authors, Dr. Ibrahim Sarbay, 82 countries were identified as recognizing EM as a primary specialty. See “Countries Recognize Emergency Medicine as a Specialty” for a breakdown of countries: https://iem-student.org/2019/05/13/countries-recognize-emergency-medicine/ )

Working with vulnerable populations
This is something that continues to draw me to EM, as the emergency department serves as an entry point into the healthcare system for some individuals. Throughout my rotations, I have been privileged to work with various patients, and have found myself constantly inspired from learning about their unique challenges within the healthcare system, as well as the various interventions that have been developed to target social determinants of health at institutional and systemic levels. While there is considerable work that still needs to be done to address these disparities, I continue being fascinated with the various advancements that are underway. This has additionally expanded my understanding of humanity and has forced me to reflect on how I approach clinical interactions. Overall, it has allowed for considerable growth within Medicine and on a personal level. This continues to be one of the aspects of EM that I truly value most.

Perceived challenges
I need to preface this by saying that it may be difficult to truly appreciate challenges of any specialty from solely experiencing it through the role of a medical student. However, these are points that I consider challenges of EM-based on my personal experiences during several EM rotations, as well as through discussion with residents and staff physicians.
Physician burnout
A recent study in JAMA by Dyrbye et al. (2018) surveyed second-year resident physicians in the United States. Their findings indicated a burnout prevalence (based on the Maslach Burnout Inventory ) of 53.8% of surveyed EM residents. While EM did not exhibit the highest burnout rate (Urology, 63.8%; Neurology, 61.6%; Ophthalmology, 55.8%), it was on the higher end for specialties that were assessed. [1] The topics of burnout and wellness promotion have become fairly pronounced in the EM community. EM Cases released an episode in 2017 regarding burnout prevention and wellness during EM training, that featured Dr. Sara Gray and Chris Trevelyan. Link: https://emergencymedicinecases.com/preventing-burnout-promoting-wellness-emergency-medicine/

Practicing “fishbowl medicine”
I have heard this term thrown around quite a bit, alluding to the fact that specialties are observing the way that EM physicians are managing patients. The fishbowl effect reflects the tendency of a specialist in other disciplines to compare the actions of EM physicians to the standards of practice that are held in the setting of those specialists (e.g., the operating room, the specialty clinics, etc.). [2] While I recognize that this can occasionally cause conflict between groups, I personally love the multidisciplinary nature of EM and view the collaborative efforts with other specialties as further opportunities for growth regarding my understanding of various disease processes and overall management of patients. Dr. Sheldon Jacobson published an interesting reflection of how this concept can actually be viewed positively within the practice of EM [2].

Everyone has personal reasons for pursuing any specialty, and for many, the reasons for pursuing EM run deeper than those listed above. However, these are just some of the factors that I believe to be basic and practical considerations for this specialty. EM makes me excited to expand upon my knowledge base in Medicine, to constantly learn and better my understanding of the human condition, and to be a part of the supportive environment that multidisciplinary EM teams create. It is an ever-expanding field and I hope to one day be able to contribute to it in a meaningful way. I could go on and on about why I love the specialty, well beyond the limits of a blog post – I may be a little biased, but EM is pretty great!
References and Further Reading
- Dyrbye LN, Burke SE, Hardeman RR et al. Association of Clinical Specialty with Symptoms of Burnout and Career Choice Regret Among US Resident Physicians. JAMA. 2018 Sep;320(11):1114-1130.
- Jacobson S. The Fishbowl Effect. Acad Emerg Med, 2015 Oct;12(10):956-957.
If you liked this story, you may like these too!

Emergency Medicine: A Unique Specialty
R. Rogers, et al.
The Importance of The Emergency Medicine Clerkship

Thinking Like an Emergency Physician

Choosing the Emergency Medicine As A Career
J. Holliman.
Sharing is caring
- Click to share on Twitter (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
Published by Nada Radulovic, Canada
I am senior medical student at Queen’s University in Canada. Aside from having a longstanding interest in Emergency Medicine and Global Health, I have really enjoyed being involved in international collaborations and initiatives aimed at promoting free open access medical education (FOAMed). Outside of Medicine, I enjoy running, spending time outdoors and discovering new coffee shops! View all posts by Nada Radulovic, Canada
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Discover more from International Emergency Medicine Education Project
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- West J Emerg Med
- v.23(3); 2022 May
Emergency Medicine History and Expansion into the Future: A Narrative Review
Martin r. huecker.
* University of Louisville School of Medicine, Department of Emergency Medicine, Louisville, Kentucky
Jacob Shreffler
Melissa platt, dan o’brien, ryan stanton.
† Central Emergency Physicians
Terrence Mulligan
‡ University of Maryland School of Medicine, Department of Emergency Medicine, Baltimore, Maryland
Jeremy Thomas
Introduction.
Emergency medicine (EM) has advanced profoundly since its specialty recognition in 1979. As diagnosis and treatment changes, payment restructures and best practices evolve. 1 We drive these changes, impacting hospital throughput and revenue to ensure quality emergency care. Our impact on the practice of medicine depends on a body of knowledge, the “biology” of emergency medicine. 2 From 2000 to 2010 the number of emergency physicians (EP) increased more than in any other specialty. 3 With estimates of over 48,000 EPs practicing in the United States currently and continued opening of new residency programs, multiple sources expect a 20–30% surplus of board-certified emergency physicians by 2030. 4 , 5 Presciently, a 1997 paper by Holliman et al predicted that the supply of emergency doctors would equal demand in about 2020. 6
In 2020, multiple EM organizations created a taskforce to study the projected EM workforce oversupply. 4 The considerations address issues related to who practices emergency medicine (advanced practice providers, non-board-certified physicians) and who manages emergency clinicians (contract management groups, academic and hospital systems). Only two offer non-zero sum approaches: broaden the umbrella to expand emergency physician scope of practice and expand the reach of emergency medicine to ensure that no community is left behind. 4 This review aims to provide context for the workforce dilemma by describing the evolution of the scope of EM and possible future directions.
EMERGENCY MEDICINE PAST AND PRESENT
Care for the acutely ill and injured patient traces its roots back thousands of years, but organized emergency medical care blossomed in the late 20th century ( Figure ). Emergency medicine became a medical specialty in response to several factors, chief among them the presence of patients with increased mobility who required unscheduled care that the current system could not accommodate (and increased financial support for these visits). A group of pioneers founded the Emergency College of American Physicians in 1968 in response to the need for physicians skilled in managing emergency patients. 7 In 1970 Cincinnati opened the first EM residency. In 1976, the American Board of Emergency Medicine (ABEM) and the Society for Academic Emergency Medicine originated. After the American Board of Medical Specialties (ABMS) first voted 100 to 5 against our application for specialty status (1977), emergency medicine was approved as the 23 rd specialty in 1979. 8 , 9

A timeline of Emergency Medicine Milestones.
Leaders in EM have displayed innovation in approaching challenges related to patient care and organizational structure. The Rape of Emergency Medicine (1992) brought light onto the problem of patient and physician harm by management abuses. 10 Decades later we contend with business interests often superseding patient care and education, with the explosion of hospitals and residency programs run by for-profit entities. We have struggled to maintain the commitment to quality training and patient care in a world of financial and economic motivation.
The field of EM adapted to medical and technological advances, resulting in diverse areas of focus that developed from the bottom-up into ABEM subspecialities: 1990s, Pediatric Emergency Medicine, Sports Medicine and Medical Toxicology; 2000s, Undersea and Hyperbaric Medicine, and Hospice and Palliative Care Medicine; 2010s, Anesthesiology Critical Care Medicine, Emergency Medical Services (EMS), Internal Medicine-Critical Care Medicine, Pain Medicine, and the focused practice designation in Advanced EM Ultrasonography. 11 Subspecialities available to ABEM-certified physicians via other ABMS boards include Addiction Medicine, Brain Injury Medicine, Clinical Informatics, and Surgical Critical Care.
As the scope of EM continues to expand, our leaders can directly modulate the trajectory of the specialty. In 2011, Brian Zink wrote that EM “does not manage a specific disease, but the time dependent exploration of and intervention in the acute physical and/or psychological crises of humans.” 9 Emergency physicians have increasingly become the expert acute diagnosticians. As the Model of the Clinical Practice of EM has expanded, from 22 12 pages to 42, 13 we retain our focus on the full spectrum of patient acuity, treating (a) critical, (b) emergent, and (c) lower acuity patients. 13
Many factors have driven the successful growth of EM: the rise of hospital medicine; medical advances; improved transport; specialization of workforce; effective emergency treatments; efficiency and safety; and evidence-based medicine. 14 Emergency medicine is now practiced in greater than 50 countries using many different models. 15 Where our specialty has strong representation, outcomes improve for many illnesses: cardiac arrest; stroke; early analgesia; geriatric care; substance use treatment; psychiatric emergency care; and overall system efficiency. 14 , 16 As Peter Cameron asserts, “EM is a specialty for the 21 st century 14 ” because of our strengths in systems thinking and evidence-based medicine.
FUTURE OF EMERGENCY MEDICINE
We agree with the ACEP Taskforce regarding the potential to “broaden the umbrella” and “expand the reach” – not to solve a workforce issue, but to embrace and deliberately shape the natural history of our specialty. Emergency physicians should continue to leverage our unique training to take ownership of undifferentiated patients. This includes “owning more of what we already do” (observation medicine, critical care, sports medicine, emergency psychiatric care, ultrasound, pediatrics, EMS, public health, etc) while also entering into new realms (proceduralist medicine, correctional care, pandemic preparedness, disaster medicine, rural medicine, pain/addiction, informatics and more). 4 Below we offer a brief selection of possibilities for expansion and new frontiers in EM ( Table 1 ).
Emergency Medicine Subspecialties and New Frontiers.
ABEM , American Board of Emergency Medicine; ABMS , American Board of Medical Specialties; EM , emergency medicine.
Education and Research
One cannot understate the importance of the academic development of EM with residency education, clinical quality assurance, and research. To discover and engage new frontiers, we need qualified individuals, valued as educators and researchers rather than solely for clinical revenue generation. Although EM researchers gain a small percentage of overall National Institutes of Health awards, our principal investigators received almost $90 billion from 2008 to 2017. 17 Beyond growing and ensuring quality education in EM, academic emergency physicians should use their skills to educate and lead research in undergraduate and graduate medical education. We can participate in preclinical course instruction, simulation, academic administration, and clerkships to provide foundational EM knowledge to future physicians. Academic leaders in international EM devote time and energy to the development of EM training programs and health systems around the world.
Public Health
Emergency physicians represent the first and sometimes only point of contact for large numbers of vulnerable individuals in the US healthcare system. The ED’s original role as the safety net in a complex medical system has sadly become more prominent and important. Simple public-health interventions in the ED include the standard screening for depression, 18 domestic violence, 19 and sex and human trafficking. 20 The ED has for years attempted to reach individuals in need of immunization, 21 and now can play a key role in COVID-19 vaccination. 22
A 2009 EM publication called for more research, removal of barriers, innovation based on local needs, and legislation to improve incentives for large-scale community changes. 23 Since then, research has covered screening for frailty and fall risk in the elderly, 24 hypertension (with counseling/education), 25 and motivation to provide the many material needs to address social determinants of health and disease (housing, food insecurity, unemployment, etc.). 26
In the US, preventive healthcare in general receives embarrassingly scant incentives ($1 of preventive care for every $4 of treatment care). 27 Focused training in public health represents an EM niche with almost unlimited value and reach. The COVID-19 pandemic has shown the potential for emergency physicians to successfully influence the public with health messaging and advising of government officials.
The COVID-19 pandemic has brought telehealth to the forefront of medical innovation. Emergency medicine will continue to embrace new technology both in clinical practice and in training future physicians. 28 Telehealth improves access to medical services and has rapidly increased in EDs throughout the US. 29 While cost barriers exist, investment in these technologies will have clear downstream benefits to patients. 30 Specific telehealth certification for EPs would help confront the legislative and litigative challenges. A 2015 systematic review of telehealth applications in the ED found “overwhelmingly positive” results in outcomes of technical quality, user satisfaction, clinical processes, throughput, and disposition. 31

Administration
Emergency physicians thrive in stressful clinical environments, managing unpredictability and making important decisions with limited data. We work closely with other physicians, understand patient flow into and out of the hospital, implement strategies for efficient patient care, understand technology and informatics, and can rapidly determine what does and does not work at individual and organizational levels. Who better to serve as leaders in healthcare than those with knowledge and experiences from the ground floor?
Emergency Geriatric Medicine
As the number of US residents aged 65 years and older continues to grow, geriatric ED visits will continue to increase. 32 , 33 Development and optimization of guidelines, physician training programs, and standards aimed at improving care for geriatric patients must be prioritized. 33 Special training in Geriatric Emergency Medicine would incorporate clinical skills related to injury prevention/fall assessment, indwelling devices, medication management, delirium and dementia, and palliative care. 34
Emergency Medical Services
Well-established in medical direction roles with EMS, EPs now experiment with paramedicine to reach patients (for vaccination, buprenorphine treatment, preventive medicine) who have difficulty obtaining transport to healthcare services that are often completely absent in their communities. The role of EMS in addressing geographical healthcare disparities and social determinants of disease will expand in the next 10 years.
Emergency Hospitalist Medicine
Internal Medicine-trained hospitalists manage hospital observation units, which optimize resource utilization. 35 Despite overlap in clinical duties, internal medicine hospitalists and EM physicians do not regularly collaborate, missing the potential for enhanced patient care and even revenue generation. 36 Emergency physicians and hospitalists could collaborate to manage short-stay patients and even train EM residents who have interest in observation or inpatient medicine. 37 By improving patient care quality and streamlining hospital flow, we could solve the crowding issue from within our specialty.
Rural Medicine
The physician oversupply issue predominates in urban areas, where 92% of EPs are employed, leaving rural EDs still largely underserved. 38 Rural hospitals are closing at an alarming rate, potentially leaving 60 million people without adequate care. 39 As clinicians who manage rural EDs age and retire, more rural areas will become “emergency physician deserts.” 38 One-fifth of the US population resides in rural areas, but EM residents receive very little dedicated training. 40 As Hill et al noted in the Journal of Emergency Medicine , “It is commonplace for programs not based in a Level I trauma center to send residents to an off-site rotation for trauma education. Why aren’t we doing the same for rural education?” 40 Emergency medicine-primary care partnership models could address rural populations’ health needs. 41 Increased presence of EPs in rural communities could alleviate our workforce concerns and treat the impending shortage of primary care physicians.
Substance Use Disorder and Homelessness
As the healthcare gateway and often only point of contact, EPs should have optimal training to identify, treat, and refer patients with substance use disorder. 42 Facing all-time highs in overdose deaths, 43 EPs well connected with addiction services can combat the opioid and polysubstance use crises. Current fellowships in toxicology, pain control, and addiction medicine provide training for proficiency. The over three million homeless US residents 44 are under-recognized in the ED and have unique needs unmet within the current models of emergency care. 45 Having frequent encounters with homeless individuals, 44 EPs can manage medical concerns while attempting to connect them with community resources.
Wellness/Lifestyle Medicine
Emergency physicians are satirically portrayed as the “healthy doctors,” with multiple, often physically demanding habits and hobbies. We may be the ideal specialty to practice Lifestyle Medicine (which now has an active American Board of Lifestyle Medicine 46 ). Entrepreneurial EPs already provide health optimization care in many locations in the country. Patients lost in the US “sick-care system” crave physicians who take care of their own health. Emergency physicians are clear candidates to assume wellness leadership roles in organizations (eg, Chief Wellness Officer).
We were voted down on our first application for board status and our first application for primary board status. As EM continues its expansion, leaders will meet more challenges. Medicine represents a “wicked domain” where, unlike predictable rule-based domains (golf, chess), there is no causal structure, and we encounter tradeoffs. Generalists or “integrators” can step outside of the model more easily, grafting insights from one domain to use in another. 47
Emergency medicine was not created by individual physicians, scientists, or health professionals. It was pulled into existence by the public itself and by the pathologies that for decades had fallen through the cracks in our system. Our success in the past 50 years reveals that EM is truly a different paradigm in medical practice and scientific thinking. Every new paradigm emerges from the pressure of unexplained, untreated, undescribed phenomena that the old one cannot explain.
We have now become the safety net not just for patients, not just for specialists, not just for the holes in our medical system, not just for the holes in our entire socioeconomic model, but also for the holes in our entire medical philosophy. By thoughtfully expanding into new niches, we broaden, rather than narrow, our scope. We discover obstacles to quality patient care and provide the missing components. As we overcome challenges, we must maintain balance: expand our abilities but on the foundation of fundamentals. It would be a mistake to let economics and workforce oversupply drive the evolution of our specialty.
A career in EM provides a rewarding balance of risk, decision-making, and compassionate care for patients. 48 As integrators constructing the future of EM, we can recognize limitations and look ahead with hope to an intelligent expansion. An early critic of EM said, “Emergency medicine is not a specialty, it is a location.” 49 Let’s prove him wrong with a willingness to define ourselves not by the location in which we practice, but by the special, generalist care we deliver. While we contemplate expansion beyond the department, we must call for increased resources within the walls of the ED, with optimal staffing, reimbursement, and empowerment. Years ago, another critic said, “Emergency medicine is pointing in a very wrong direction which is bound to fail.” 49 Whatever direction we are heading, let’s work together to guarantee success.
Section Editor: Leon Sanchez, MD, MPH
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest : By the West JEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
The Essay as a Literary Model for the Trials of Emergency Medicine
In spring 2020, near the end of my intern year, I spoke with the mother of a 24-year-old man who had been brought in unresponsive to our resuscitation bay. “He was trying,” his mother told me. Hearing her own words out loud, she was struggling to believe what happened. “He had just finished rehab and promised he would stop,” she explained.
You Might Also Like
- New Resident Fellow Brings a Literary Perspective to Medicine
- ACEP Section of Careers in Emergency Medicine To Recognize Longevity, Tenure in Specialty
- ACEP Seeking Nominations for Emergency Medicine Longevity, Tenure Awards
Explore This Issue
Medics wheeled him into our emergency department while performing chest compressions. Earlier that evening, after saying good night to his parents, the young man had climbed the stairs to his bedroom and closed the door. Twenty minutes later, his mother found him lying on the floor without a heartbeat. She tried using naloxone, once in each nostril, but he never woke up. Twenty more minutes passed before he arrived at our emergency department, still pulseless.
As an intern, I had some experience informing patients of serious new diagnoses, including the news of metastatic cancer, but this was the first time I was going to tell a mother her son had died.
I did not know what to expect.
How the Essay and Emergency Medicine Are Related
In the 1570s, at the age of 38, the French aristocrat Michel de Montaigne set out to write a series of trials, or essais in French , on an encyclopedic range of topics to figure out, through writing, how he felt and how those feelings made him who he was. In his trials, he experimented with ideas of friendship, cruelty, fashion, death, and even cannibalism. In doing so, he invented a new literary form: the essay.
His essays often deviated from their point, improvised, and evolved into an articulation of an opinion that was not always obvious at the outset of his writing. But that was part of the exercise. His aim was to challenge himself with a variety of experiences and situations, to test himself in real time by putting pen to paper in order to discover his true feelings.
Like the field of emergency medicine, the essay arrived late as a literary form, long after the poem, the play, or the earliest forms of prose. Like the essay, emergency medicine is a series of trials where we must sometimes treat diseases before making the final diagnosis. We improvise until the outcome is known.
The Combined Roles of Improvisation and Practice

Chris Whissen & Shutterstock.com
Now in the second year of my residency program, I am placed in a new role at the center of the resuscitation bay, taking care of the sickest patients in Brooklyn for brief moments in time. And I’ve found that despite all my studying and pre-reading, I never feel completely prepared. There is no shortcut around improvisation. As in our simulation center, I grow and learn by working through cases in real time.
Despite all the algorithms and mnemonics, the unique details of each trauma, cardiac arrest, or intubation are different. Slowly but surely (and perhaps more slowly than I’d like), the experience has become easier, mostly through practicing the practice of medicine. As Montaigne wrote, “When we consider through what mists and how gropingly we are led to our knowledge of most of the things within our grasp, we shall assuredly conclude that it is familiarity rather than knowledge that takes away their strangeness.” 1
“Essayons,” or “Let’s Try” in French, is the motto of the United States Army Corps of Engineers, and it does not refer to a lukewarm, half-hearted “try.” The motto recognizes that when failure lurks around every corner and when resignation would be easier, trying can be the greatest act of courage.
It seems strange to advance in my training before feeling that I’ve mastered my first year. From what I’ve heard from senior physicians, I may feel this way for a while, even as a third-year resident, a fellow, or a new attending. However, as the form of the essay teaches us, it’s the trial itself that helps us to grow.
All We Can Do Is Try
As I spoke with the mother about her 24-year-old son, her grief took the form of a series of questions. I was not entirely sure I could answer them. She said that she had checked on her son 20 minutes after he had said good night. What if she had checked on him sooner? How much time would she have had to save his life? If he had been unconscious for five or 10 minutes, would the naloxone have been enough? Was there any way to tell from signs on his body how late she had been to rescuing him?
I thought of all the cardiac arrests I had seen in my short time in training. Each time I wondered whether their lives could have been saved by someone more qualified than me or if my team could have done anything differently, if we had placed the central line faster or drawn the blood tests sooner or called anesthesia instead of attempting the intubation ourselves. I thought, on the other hand, what if I hadn’t tried at all? How would I ever become independent enough to take care of patients on my own? How would I ever get used to the feeling of possibly falling short?
No doubt, this mother had been dealing with her son’s opioid addiction for years. She had the naloxone ready. No doubt, she had rehearsed the scenario in her mind—first one nostril, then the other. However, nothing could have prepared her for the reality of what unfolded that evening. I told her that in administering the naloxone and calling 911, she had done all that she could do. She had tried. With that, she had done the best that any of us can ever do.

- Montaigne M. Essays . Ringwood, Victoria, Australia: Penguin Books; 1966:87.
Pages: 1 2 | Single Page
Topics: Opioid Crisis Resident

How to Manage Elderly Patient Pain without Opioids

Are Opiates Futile in Low Back Pain?

September 2023 News from the College
Current issue.

ACEP Now: Vol 43 – No 04 – April 2024
Download PDF
2 Responses to “The Essay as a Literary Model for the Trials of Emergency Medicine”
January 29, 2022
Excellent analysis, thank you for this fantastic piece!
January 24, 2023
Beautifully written and full of insight into one of the heaviest topics of our day. I’m proud to have been a small part of your path of discovery.
Leave a Reply Cancel Reply
Your email address will not be published. Required fields are marked *

Don't have an Account?
Register Now!

- International Student
- Essay Writing Center
- Sample Essays
Sample Medical School Essays
Applying to medical school is an exciting decision, but the application process is very competitive. This means when it comes to your application you need to ensure you’ve put your best foot forward and done everything you can to stand out from other applicants. One great way to provide additional information on why you have decided to pursue a career in medicine and why you’re qualified, is your medical school essay. Read these samples to get a good idea on how you can write your own top-notch essay.
This section contains five sample medical school essays
- Medical School Sample Essay One
- Medical School Sample Essay Two
- Medical School Sample Essay Three
- Medical School Sample Essay Four
- Medical School Sample Essay Five
Medical School Essay One
When I was twelve years old, a drunk driver hit the car my mother was driving while I was in the backseat. I have very few memories of the accident, but I do faintly recall a serious but calming face as I was gently lifted out of the car. The paramedic held my hand as we traveled to the hospital. I was in the hospital for several weeks and that same paramedic came to visit me almost every day. During my stay, I also got to know the various doctors and nurses in the hospital on a personal level. I remember feeling anxiety about my condition, but not sadness or even fear. It seemed to me that those around me, particularly my family, were more fearful of what might happen to me than I was. I don’t believe it was innocence or ignorance, but rather a trust in the abilities of my doctors. It was as if my doctors and I had a silent bond. Now that I’m older I fear death and sickness in a more intense way than I remember experiencing it as a child. My experience as a child sparked a keen interest in how we approach pediatric care, especially as it relates to our psychological and emotional support of children facing serious medical conditions. It was here that I experienced first-hand the power and compassion of medicine, not only in healing but also in bringing unlikely individuals together, such as adults and children, in uncommon yet profound ways. And it was here that I began to take seriously the possibility of becoming a pediatric surgeon.
My interest was sparked even more when, as an undergraduate, I was asked to assist in a study one of my professors was conducting on how children experience and process fear and the prospect of death. This professor was not in the medical field; rather, her background is in cultural anthropology. I was very honored to be part of this project at such an early stage of my career. During the study, we discovered that children face death in extremely different ways than adults do. We found that children facing fatal illnesses are very aware of their condition, even when it hasn’t been fully explained to them, and on the whole were willing to fight their illnesses, but were also more accepting of their potential fate than many adults facing similar diagnoses. We concluded our study by asking whether and to what extent this discovery should impact the type of care given to children in contrast to adults. I am eager to continue this sort of research as I pursue my medical career. The intersection of medicine, psychology, and socialization or culture (in this case, the social variables differentiating adults from children) is quite fascinating and is a field that is in need of better research.
Although much headway has been made in this area in the past twenty or so years, I feel there is a still a tendency in medicine to treat diseases the same way no matter who the patient is. We are slowly learning that procedures and drugs are not always universally effective. Not only must we alter our care of patients depending upon these cultural and social factors, we may also need to alter our entire emotional and psychological approach to them as well.
It is for this reason that I’m applying to the Johns Hopkins School of Medicine, as it has one of the top programs for pediatric surgery in the country, as well as several renowned researchers delving into the social, generational, and cultural questions in which I’m interested. My approach to medicine will be multidisciplinary, which is evidenced by the fact that I’m already double-majoring in early childhood psychology and pre-med, with a minor in cultural anthropology. This is the type of extraordinary care that I received as a child—care that seemed to approach my injuries with a much larger and deeper picture than that which pure medicine cannot offer—and it is this sort of care I want to provide my future patients. I turned what might have been a debilitating event in my life—a devastating car accident—into the inspiration that has shaped my life since. I am driven and passionate. And while I know that the pediatric surgery program at Johns Hopkins will likely be the second biggest challenge I will face in my life, I know that I am up for it. I am ready to be challenged and prove to myself what I’ve been telling myself since that fateful car accident: I will be a doctor.
Tips for a Successful Medical School Essay
- If you’re applying through AMCAS, remember to keep your essay more general rather than tailored to a specific medical school, because your essay will be seen by multiple schools.
- AMCAS essays are limited to 5300 characters—not words! This includes spaces.
- Make sure the information you include in your essay doesn't conflict with the information in your other application materials.
- In general, provide additional information that isn’t found in your other application materials. Look at the essay as an opportunity to tell your story rather than a burden.
- Keep the interview in mind as you write. You will most likely be asked questions regarding your essay during the interview, so think about the experiences you want to talk about.
- When you are copying and pasting from a word processor to the AMCAS application online, formatting and font will be lost. Don’t waste your time making it look nice. Be sure to look through the essay once you’ve copied it into AMCAS and edit appropriately for any odd characters that result from pasting.
- Avoid overly controversial topics. While it is fine to take a position and back up your position with evidence, you don’t want to sound narrow-minded.
- Revise, revise, revise. Have multiple readers look at your essay and make suggestions. Go over your essay yourself many times and rewrite it several times until you feel that it communicates your message effectively and creatively.
- Make the opening sentence memorable. Admissions officers will read dozens of personal statements in a day. You must say something at the very beginning to catch their attention, encourage them to read the essay in detail, and make yourself stand out from the crowd.
- Character traits to portray in your essay include: maturity, intellect, critical thinking skills, leadership, tolerance, perseverance, and sincerity.
Medical School Essay Two
If you had told me ten years ago that I would be writing this essay and planning for yet another ten years into the future, part of me would have been surprised. I am a planner and a maker of to-do lists, and it has always been my plan to follow in the steps of my father and become a physician. This plan was derailed when I was called to active duty to serve in Iraq as part of the War on Terror.
I joined the National Guard before graduating high school and continued my service when I began college. My goal was to receive training that would be valuable for my future medical career, as I was working in the field of emergency health care. It was also a way to help me pay for college. When I was called to active duty in Iraq for my first deployment, I was forced to withdraw from school, and my deployment was subsequently extended. I spent a total of 24 months deployed overseas, where I provided in-the-field medical support to our combat troops. While the experience was invaluable not only in terms of my future medical career but also in terms of developing leadership and creative thinking skills, it put my undergraduate studies on hold for over two years. Consequently, my carefully-planned journey towards medical school and a medical career was thrown off course. Thus, while ten-year plans are valuable, I have learned from experience how easily such plans can dissolve in situations that are beyond one’s control, as well as the value of perseverance and flexibility.
Eventually, I returned to school. Despite my best efforts to graduate within two years, it took me another three years, as I suffered greatly from post-traumatic stress disorder following my time in Iraq. I considered abandoning my dream of becoming a physician altogether, since I was several years behind my peers with whom I had taken biology and chemistry classes before my deployment. Thanks to the unceasing encouragement of my academic advisor, who even stayed in contact with me when I was overseas, I gathered my strength and courage and began studying for the MCAT. To my surprise, my score was beyond satisfactory and while I am several years behind my original ten-year plan, I am now applying to Brown University’s School of Medicine.
I can describe my new ten-year plan, but I will do so with both optimism and also caution, knowing that I will inevitably face unforeseen complications and will need to adapt appropriately. One of the many insights I gained as a member of the National Guard and by serving in war-time was the incredible creativity medical specialists in the Armed Forces employ to deliver health care services to our wounded soldiers on the ground. I was part of a team that was saving lives under incredibly difficult circumstances—sometimes while under heavy fire and with only the most basic of resources. I am now interested in how I can use these skills to deliver health care in similar circumstances where basic medical infrastructure is lacking. While there is seemingly little in common between the deserts of Fallujah and rural Wyoming, where I’m currently working as a volunteer first responder in a small town located more than 60 miles from the nearest hospital, I see a lot of potential uses for the skills that I gained as a National Guardsman. As I learned from my father, who worked with Doctors Without Borders for a number of years, there is quite a bit in common between my field of knowledge from the military and working in post-conflict zones. I feel I have a unique experience from which to draw as I embark on my medical school journey, experiences that can be applied both here and abroad.
In ten years’ time, I hope to be trained in the field of emergency medicine, which, surprisingly, is a specialization that is actually lacking here in the United States as compared to similarly developed countries. I hope to conduct research in the field of health care infrastructure and work with government agencies and legislators to find creative solutions to improving access to emergency facilities in currently underserved areas of the United States, with an aim towards providing comprehensive policy reports and recommendations on how the US can once again be the world leader in health outcomes. While the problems inherent in our health care system are not one-dimensional and require a dynamic approach, one of the solutions as I see it is to think less in terms of state-of-the-art facilities and more in terms of access to primary care. Much of the care that I provide as a first responder and volunteer is extremely effective and also relatively cheap. More money is always helpful when facing a complex social and political problem, but we must think of solutions above and beyond more money and more taxes. In ten years I want to be a key player in the health care debate in this country and offering innovative solutions to delivering high quality and cost-effective health care to all our nation’s citizens, especially to those in rural and otherwise underserved areas.
Of course, my policy interests do not replace my passion for helping others and delivering emergency medicine. As a doctor, I hope to continue serving in areas of the country that, for one reason or another, are lagging behind in basic health care infrastructure. Eventually, I would also like to take my knowledge and talents abroad and serve in the Peace Corps or Doctors Without Borders.
In short, I see the role of physicians in society as multifunctional: they are not only doctors who heal, they are also leaders, innovators, social scientists, and patriots. Although my path to medical school has not always been the most direct, my varied and circuitous journey has given me a set of skills and experiences that many otherwise qualified applicants lack. I have no doubt that the next ten years will be similarly unpredictable, but I can assure you that no matter what obstacles I face, my goal will remain the same. I sincerely hope to begin the next phase of my journey at Brown University. Thank you for your kind attention.
Additional Tips for a Successful Medical School Essay
- Regardless of the prompt, you should always address the question of why you want to go to medical school in your essay.
- Try to always give concrete examples rather than make general statements. If you say that you have perseverance, describe an event in your life that demonstrates perseverance.
- There should be an overall message or theme in your essay. In the example above, the theme is overcoming unexpected obstacles.
- Make sure you check and recheck for spelling and grammar!
- Unless you’re very sure you can pull it off, it is usually not a good idea to use humor or to employ the skills you learned in creative writing class in your personal statement. While you want to paint a picture, you don’t want to be too poetic or literary.
- Turn potential weaknesses into positives. As in the example above, address any potential weaknesses in your application and make them strengths, if possible. If you have low MCAT scores or something else that can’t be easily explained or turned into a positive, simply don’t mention it.
Medical School Essay Three
The roots of my desire to become a physician are, thankfully, not around the bedside of a sick family member or in a hospital, but rather on a 10-acre plot of land outside of a small town in Northwest Arkansas. I loved raising and exhibiting cattle, so every morning before the bus arrived at 7 a.m. I was in the barn feeding, checking cattle for any health issues and washing the show heifers. These early mornings and my experiences on a farm not only taught me the value of hard work, but ignited my interest in the body, albeit bovine at the time. It was by a working chute that I learned the functions of reproductive hormones as we utilized them for assisted reproduction and artificial insemination; it was by giving vaccinations to prevent infection that I learned about bacteria and the germ theory of disease; it was beside a stillborn calf before the sun had risen that I was exposed to the frailty of life.
Facing the realities of disease and death daily from an early age, I developed a strong sense of pragmatism out of necessity. There is no place for abstractions or euphemisms about life and death when treating a calf’s pneumonia in the pouring rain during winter. Witnessing the sometimes harsh realities of life on a farm did not instill within me an attitude of jaded inevitability of death. Instead, it germinated a responsibility to protect life to the best of my abilities, cure what ailments I can and alleviate as much suffering as possible while recognizing that sometimes nothing can be done.
I first approached human health at the age of nine through beef nutrition and food safety. Learning the roles of nutrients such as zinc, iron, protein and B-vitamins in the human body as well as the dangers of food-borne illness through the Beef Ambassador program shifted my interest in the body to a new species. Talking with consumers about every facet of the origins of food, I realized that the topics that most interested me were those that pertained to human health. In college, while I connected with people over samples of beef and answered their questions, I also realized that it is not enough simply to have adequate knowledge. Ultimately knowledge is of little use if it is not digestible to those who receive it. So my goal as a future clinical physician is not only to illuminate the source of an affliction and provide treatment for patients, but take care to ensure the need for understanding by both patient and family is met.
I saw this combination of care and understanding while volunteering in an emergency room, where I was also exposed to other aspects and players in the medical field. While assisting a nurse perform a bladder scan and witnessing technicians carry out an echocardiogram or CT scan, I learned the important roles that other professionals who do not wear white coats have in today’s medical field. Medicine is a team sport, and coordinating the efforts of each of these players is crucial for the successful execution of patient care. It is my goal to serve as the leader of this healthcare unit and unify a team of professionals to provide the highest quality care for patients. Perhaps most importantly my time at the VA showed me the power a smile and an open ear can have with people. On the long walk to radiology, talking with patients about their military service and families always seemed to take their mind off the reason for their visit, if only for a few minutes. This served as a reminder that we are helping people with pasts and dreams, rather than simply remedying patients’ symptoms.
Growing up in a small town, I never held aspirations of world travel when I was young. But my time abroad revealed to me the state of healthcare in developing countries and fostered a previously unknown interest in global health. During my first trip abroad to Ghana, my roommate became ill with a severe case of traveler’s diarrhea. In the rural north of the country near the Sahara, the options for healthcare were limited; he told me how our professor was forced to bribe employees to bypass long lines and even recounted how doctors took a bag of saline off the line of another patient to give to him. During a service trip to a rural community in Nicaragua, I encountered patients with preventable and easily treatable diseases that, due to poverty and lack of access, were left untreated for months or years at a time. I was discouraged by the state of healthcare in these countries and wondered what could be done to help. I plan to continue to help provide access to healthcare in rural parts of developing countries, and hopefully as a physician with an agricultural background I can approach public health and food security issues in a multifaceted and holistic manner.
My time on a cattle farm taught me how to work hard to pursue my interests, but also fueled my appetite for knowledge about the body and instilled within me a firm sense of practicality. Whether in a clinic, operating room or pursuing public and global health projects, I plan to bring this work ethic and pragmatism to all of my endeavors. My agricultural upbringing has produced a foundation of skills and values that I am confident will readily transplant into my chosen career. Farming is my early passion, but medicine is my future.
Medical School Essay Four
I am a white, cisgender, and heterosexual female who has been afforded many privileges: I was raised by parents with significant financial resources, I have traveled the world, and I received top-quality high school and college educations. I do not wish to be addressed or recognized in any special way; all I ask is to be treated with respect.
As for my geographic origin, I was born and raised in the rural state of Maine. Since graduating from college, I have been living in my home state, working and giving back to the community that has given me so much. I could not be happier here; I love the down-to-earth people, the unhurried pace of life, and the easy access to the outdoors. While I am certainly excited to move elsewhere in the country for medical school and continue to explore new places, I will always self-identify as a Mainer as being from Maine is something I take great pride in. I am proud of my family ties to the state (which date back to the 1890’s), I am proud of the state’s commitment to preserving its natural beauty, and I am particularly proud of my slight Maine accent (we don’t pronounce our r’s). From the rocky coastline and rugged ski mountains to the locally-grown food and great restaurants, it is no wonder Maine is nicknamed, "Vacationland.” Yet, Maine is so much more than just a tourist destination. The state is dotted with wonderful communities in which to live, communities like the one where I grew up.
Perhaps not surprisingly, I plan to return to Maine after residency. I want to raise a family and establish my medical practice here. We certainly could use more doctors! Even though Maine is a terrific place to live, the state is facing a significant doctor shortage. Today, we are meeting less than half of our need for primary care providers. To make matters worse, many of our physicians are close to retirement age. Yet, according to the AAMC, only 53 Maine residents matriculated into medical school last year! Undoubtedly, Maine is in need of young doctors who are committed to working long term in underserved areas. As my primary career goal is to return to my much adored home state and do my part to help fill this need, I have a vested interest in learning more about rural medicine during medical school.
I was raised in Cumberland, Maine, a coastal town of 7,000 just north of Portland. With its single stoplight and general store (where it would be unusual to visit without running into someone you know), Cumberland is the epitome of a small New England town. It truly was the perfect place to grow up. According to the most recent census, nearly a third of the town’s population is under 18 and more than 75% of households contain children, two statistics which speak to the family-centric nature of Cumberland’s community. Recently rated Maine's safest town, Cumberland is the type of place where you allow your kindergartener to bike alone to school, leave your house unlocked while at work, and bring home-cooked food to your sick neighbors and their children. Growing up in such a safe, close-knit, and supportive community instilled in me the core values of compassion, trustworthiness, and citizenship. These three values guide me every day and will continue to guide me through medical school and my career in medicine.
As a medical student and eventual physician, my compassion will guide me to become a provider who cares for more than just the physical well-being of my patients. I will also commit myself to my patients’ emotional, spiritual, and social well-being and make it a priority to take into account the unique values and beliefs of each patient. By also demonstrating my trustworthiness during every encounter, I will develop strong interpersonal relationships with those whom I serve. As a doctor once wisely said, “A patient does not care how much you know until he knows how much you care.”
My citizenship will guide me to serve my community and to encourage my classmates and colleagues to do the same. We will be taught in medical school to be healers, scientists, and educators. I believe that, in addition, as students and as physicians, we have the responsibility to use our medical knowledge, research skills, and teaching abilities to benefit more than just our patients. We must also commit ourselves to improving the health and wellness of those living in our communities by participating in public events (i.e by donating our medical services), lobbying for better access to healthcare for the underprivileged, and promoting wellness campaigns. As a medical student and eventual physician, my compassion, trustworthiness, and citizenship will drive me to improve the lives of as many individuals as I can.
Cumberland instilled in me important core values and afforded me a wonderful childhood. However, I recognize that my hometown is not perfect. For one, the population is shockingly homogenous, at least as far as demographics go. As of the 2010 census, 97.2% of the residents of Cumberland were white. Only 4.1% of residents speak a language other than English at home and even fewer were born in another country. Essentially everybody who identified with a religion identified as some denomination of Christian. My family was one of maybe five Jewish families in the town. Additionally, nearly all the town’s residents graduated from high school (98.1%), are free of disability (93.8%), and live above the poverty line (95.8%). Efforts to attract diverse families to Cumberland is one improvement that I believe would make the community a better place in which to live. Diversity in background (and in thought) is desirable in any community as living, learning, and working alongside diverse individuals helps us develop new perspectives, enhances our social development, provides us with a larger frame of reference, and improves our understanding of our place in society.
Medical School Essay Five
“How many of you received the flu vaccine this year?” I asked my Bricks 4 Kidz class, where I volunteer to teach elementary students introductory science and math principles using Lego blocks. “What’s a flu vaccine?” they asked in confusion. Surprised, I briefly explained the influenza vaccine and its purpose for protection. My connection to children and their health extends to medical offices, clinics and communities where I have gained experience and insight into medicine, confirming my goal of becoming a physician.
My motivation to pursue a career in medicine developed when my mother, who was diagnosed with Lupus, underwent a kidney transplant surgery and suffered multiple complications. I recall the fear and anxiety I felt as a child because I misunderstood her chronic disease. This prompted me to learn more about the science of medicine. In high school, I observed patients plagued with acute and chronic kidney disease while briefly exploring various fields of medicine through a Mentorship in Medicine summer program at my local hospital. In addition to shadowing nephrologists in a hospital and clinical setting, I scrubbed into the operating room, viewed the radiology department, celebrated the miracle of birth in the delivery room, and quietly observed a partial autopsy in pathology. I saw many patients confused about their diagnoses. I was impressed by the compassion of the physicians and the time they took to reassure and educate their patients.
Further experiences in medicine throughout and after college shaped a desire to practice in underserved areas. While coloring and reading with children in the patient area at a Family Health Center, I witnessed family medicine physicians diligently serve patients from low-income communities. On a medical/dental mission trip to the Philippines, I partnered with local doctors to serve and distribute medical supplies to rural schools and communities. At one impoverished village, I held a malnourished two-year old boy suffering from cerebral palsy and cardiorespiratory disease. His family could not afford to take him to the nearest pediatrician, a few hours away by car, for treatment. Overwhelmed, I cried as we left the village. Many people were suffering through pain and disease due to limited access to medicine. But this is not rare; there are many people suffering due to inadequate access/accessibility around the world, even in my hometown. One physician may not be able to change the status of underserved communities, however, one can alleviate some of the suffering.
Dr. X, my mentor and supervisor, taught me that the practice of medicine is both a science and an art. As a medical assistant in a pediatric office, I am learning about the patient-physician relationship and the meaningful connection with people that medicine provides. I interact with patients and their families daily. Newborn twins were one of the first patients I helped, and I look forward to seeing their development at successive visits. A young boy who endured a major cardiac surgery was another patient I connected with, seeing his smiling face in the office often as he transitioned from the hospital to his home. I also helped many excited, college-bound teenagers with requests for medical records in order to matriculate. This is the art of medicine – the ability to build relationships with patients and have an important and influential role in their lives, from birth to adulthood and beyond.
In addition, medicine encompasses patient-centered care, such as considering and addressing concerns. While taking patient vitals, I grew discouraged when parents refused the influenza vaccine and could not understand their choices. With my experience in scientific research, I conducted an informal yet insightful study. Over one hundred families were surveyed about their specific reasons for refusing the flu vaccine. I sought feedback on patients’ level of understanding about vaccinations and its interactions with the human immune system. Through this project, I learned the importance of understanding patient’s concerns in order to reassure them through medicine. I also learned the value of communicating with patients, such as explaining the purpose of a recommended vaccine. I hope to further this by attending medical school to become a physician focused on patient-centered care, learning from and teaching my community.
Children have been a common thread in my pursuit of medicine, from perceiving medicine through child-like eyes to interacting daily with children in a medical office. My diverse experiences in patient interaction and the practice of medicine inspire me to become a physician, a path that requires perseverance and passion. Physicians are life-long learners and teachers, educating others whether it is on vaccinations or various diseases. This vocation also requires preparation, and I eagerly look forward to continually learning and growing in medical school and beyond.
To learn more about what to expect from the study of medicine, check out our Study Medicine in the US section.
Related Content:
Get the international student newsletter.
Career mentorship, clinical and technology skills
- See us on facebook
- See us on youtube
- See us on instagram
APPLICATION GUIDE Clinical Science, Technology and Medicine Summer Internship
Applications Now Open
Applications open for the 2020 Clinical Science, Technology and Medicine Summer Internship program. Program application deadline is February 14, 2020.
How to write "the change you want to see in health care" essay

By SeventyFourImages via EnvatoElements
By Urvi Gupta
There are many ways of approaching an essay such as this one. Here are some methods that we find useful, and we hope they will be helpful to you as well.
The most powerful essays are those which could not be written by anyone other than yourself. Keep this in mind as you begin your brainstorm. Finding stories which are personal and teach the reader something about you is crucial.
Pull out some pen and paper. Set a 5-minute timer on your phone. Use this time to jot down every thought that comes into mind about the ways you wish our health care system was better. Try to keep your pen to the paper and keep writing throughout the 5 minutes.
Look over your list. Which ones stick out to you as the most compelling? Through your interactions with healthcare, have any of the challenges you brainstormed impacted you personally? Have you had any experiences where you worked towards any of these goals? Use these questions to pick 1-3 topics from your list.
Begin outlining your essay. For each of your topics, try to include answers to the following questions:
Briefly describe the topic/issue.
Why is this topic important to you specifically? How has it affected you/the people around you/the world? Give concrete examples.
How do you propose you can make it better? Again, be specific and try to draw inspiration from your own life.
Begin writing!
Read your draft out loud to yourself or a friend/family member to look for areas that are unclear or that could be improved.
Remember that it is less important as to what you pick for the change you want to see in health care and more important that you have something compelling and personal to say about it. We want to learn about you!
The views expressed here are the authors and they do not necessarily reflect the views and opinions of Stanford University School of Medicine. External websites are shared as a courtesy. They are not endorsed by the Stanford University School of Medicine.
The most powerful essays are those which could not be written by anyone other than yourself.
Urvi Gupta, BS SASI Teaching Assistant
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
The following represent additions to UpToDate from the past six months that were considered by the editors and authors to be of particular interest. The most recent What's New entries are at the top of each subsection.
ADULT RESUSCITATION
Effectiveness of introducer (bougie) for tracheal intubation (January 2024)
While the tracheal tube introducer (commonly referred to as a "bougie") is widely considered an important tool for emergency intubation, high-quality evidence supporting its role has been limited. In a new systematic review and meta-analysis of 18 studies involving over 9000 adult patients, use of an introducer was associated with a higher overall rate of successful first-pass intubation compared with no introducer (in most cases an tracheal tube with a stylet) [ 1 ]. First-pass success rates were higher using an introducer regardless of the method of intubation (ie, direct versus video laryngoscopy) or where intubation was performed (eg, emergency department, intensive care unit, prehospital). The introducer was most effective in patients (n = 585 in five studies) with a Cormack-Lehane III or IV view. We consider the introducer an essential tool for difficult airway management that should be readily available in the emergency department. (See "Endotracheal tube introducers (gum elastic bougie) for emergency intubation", section on 'Evidence of effectiveness' .)
Extracorporeal cardiopulmonary resuscitation (December 2023)
Extracorporeal cardiopulmonary resuscitation (ECPR) is being increasingly used, but data are limited and the benefits are uncertain. In a recent meta-analysis of 11 studies (10,000 patients) who underwent CPR, compared with standard CPR, ECPR was associated with decreased in-hospital mortality and increased long-term favorable neurologic outcome and survival at one year [ 2 ]. The benefit of ECPR was confined to patients with in-hospital cardiac arrest. These data support the growing practice of ECPR in select patients likely to benefit. (See "Extracorporeal life support in adults: Management of venoarterial extracorporeal membrane oxygenation (V-A ECMO)", section on 'Sudden cardiac arrest (extracorporeal cardiopulmonary resuscitation)' .)
Heart rate control in septic shock (December 2023)
Beta blockade has the potential to limit harm from the adrenergic overdrive that occurs in septic shock. However, data to support heart rate control in patients with septic shock are limited. In a recent, unblinded randomized trial of 126 patients with septic shock-related tachycardia (heart rate ≥95/min) who were receiving norepinephrine, the beta blocker landiolol did not reduce organ failure as measured by the sequential organ failure assessment score [ 3 ]. Furthermore, landiolol was associated with increased 28-day mortality compared with standard care (37 versus 25 percent). We continue to avoid the routine use of beta blockers in patients with septic shock. (See "Investigational and ineffective pharmacologic therapies for sepsis", section on 'Heart rate control' .)
Aerosol generation during noninvasive respiratory support modalities (October 2023)
Studies have reported conflicting data as to whether high levels of aerosols are generated when noninvasive ventilation (NIV) or high-flow nasal oxygen (HFNO) is used. In a 2023 systematic review including 12 studies in patients with respiratory infections and 15 studies in healthy volunteers, use of NIV or HFNO was not associated with increased generation of pathogen-laden aerosols compared with controls with unsupported normal or labored breathing, low-flow nasal oxygen, or oxygen or nonrebreather mask [ 4 ]. Inconsistency among studies may reflect differences in sampling and detection methodologies and operating room ventilation. Notably, the National Health Service in the United Kingdom has removed mask ventilation, intubation, and extubation from its list of aerosol-generating procedures. (See "Overview of infection control during anesthetic care", section on 'Considerations during aerosol-generating procedures' .)
ENVIRONMENTAL EMERGENCIES
Supraglottic airway for out-of-hospital cardiac arrest from drowning (April 2024)
In a drowning victim with cardiac arrest, ventilation is generally considered the most important initial treatment since the arrest is typically due to hypoxemia. Few studies have evaluated the optimal pre-hospital airway management technique specifically for drowning victims with out-of-hospital cardiac arrest. A propensity score-matched pre-hospital registry study with nearly 12,000 patients found that compared with use of a supraglottic airway (SGA), tracheal intubation was associated with a slightly higher rate of return of spontaneous circulation (5.8 versus 4.7 percent), but there was no difference in one-month survival or good neurologic outcomes [ 5 ]. These results suggest that even though pre-hospital tracheal intubation may be the optimal approach, an SGA is an acceptable alternative. (See "Drowning (submersion injuries)", section on 'Bystander interventions and prehospital care' .)
GENERAL ADULT EMERGENCY MEDICINE
Unchanged emergency department discharge rates for pulmonary embolism (April 2024)
Outpatient anticoagulation to avoid hospitalization is safe for a select group of patients with acute pulmonary embolism (PE). However, a recent study of over 1.6 million emergency department (ED) visits for PE in the United States reported that ED discharge rates for PE were unchanged between 2012 and 2020 (38 versus 33 percent) [ 6 ]. Among low-risk patients, only one third were discharged from the ED. However, this study was unable to determine whether other factors may have prevented discharge such as drug accessibility, concurrent deep vein thrombosis, and right ventricular burden. Although not conclusive, this study suggests that increased physician awareness is needed to encourage safe ED discharge of low-risk patients with PE. (See "Treatment, prognosis, and follow-up of acute pulmonary embolism in adults" .)
Ensitrelvir for mild to moderate COVID-19 (March 2024)
Although nirmatrelvir-ritonavir reduces hospitalization and death from COVID-19,drug interactions preclude its use in some patients. Ensitrelvir is an oral protease inhibitor that prevents SARS-CoV-2 replication and has fewer drug interactions. In a randomized, double-blinded trial of over 1800 patients with mild to moderate COVID-19 (majority vaccinated) in Asia in early 2022, five days of ensitrelvir reduced time to symptom resolution by one day compared with placebo [ 7 ]. Since only two participants (one in each arm) had a COVID-19-related hospitalization within the 28-day study period, it is unknown whether the drug prevents hospitalizations or death from COVID-19. Ensitrelvir is approved for emergency use in Japan; it is undergoing US Food and Drug Administration approval process in the United States. (See "COVID-19: Management of adults with acute illness in the outpatient setting", section on 'Therapies of limited or uncertain benefit' .)
Emergency physician-performed point-of-care ultrasound for cholecystitis (February 2024)
Emergency physician-performed point-of-care ultrasound can be helpful when evaluating an adult with right upper quadrant pain, but test characteristics vary depending on the operator and indication. A meta-analysis with over 1700 patients found that the sensitivity and specificity of point-of-care ultrasound for acute cholecystitis was 71 and 94 percent, respectively [ 8 ]. These findings suggest this rapid, bedside imaging modality can help expedite care if cholecystitis is identified but may not be sufficient to rule out the diagnosis. (See "Evaluation of the adult with nontraumatic abdominal or flank pain in the emergency department", section on 'Role of point-of-care ultrasound' .)
Guidelines on management of acute respiratory distress syndrome (February 2024)
The American Thoracic Society recently updated their guidelines on the management of patients ventilated for acute respiratory distress syndrome (ARDS) [ 9 ]. Compared with previous recommendations, emphasis was placed on the value of systemic corticosteroid administration, early use of extracorporeal membrane oxygenation, and use of neuromuscular blockade, particularly in patients with severe ARDS. Recommendations also focus on the avoidance of recruitment maneuvers, especially prolonged maneuvers. We agree with these recommendations. (See "Acute respiratory distress syndrome: Ventilator management strategies for adults", section on 'Introduction' .)
Time window to start dual antiplatelet therapy for high-risk TIA or minor ischemic stroke (January 2024)
There is evidence from several randomized trials that early initiation of short-term dual antiplatelet therapy (DAPT) for select patients with high-risk transient ischemic attack (TIA) or minor ischemic stroke reduces the risk of recurrent ischemic stroke. The evidence comes from trials that started DAPT within 12 to 24 hours of symptom onset. Results from the recent INSPIRES trial suggest that DAPT is still beneficial when started up to 72 hours after symptom onset [ 10 ]. Although the time window is extended by the results from INSPIRES, we start DAPT as soon as possible for patients with high-risk TIA or minor ischemic stroke. (See "Early antithrombotic treatment of acute ischemic stroke and transient ischemic attack", section on 'High-risk TIA and minor ischemic stroke' .)
Timing of appendectomy for uncomplicated appendicitis (November 2023)
Appendectomy is traditionally performed urgently to reduce the risk of perforation. However, a large randomized trial showed that patients with uncomplicated appendicitis (including those with appendicolith on computed tomography) who had an in-hospital delay of up to 24 hours before surgery had no increased risk of perforation or other complications compared with those who underwent surgery within 8 hours [ 11 ]. Given these data and general acceptance of antibiotic management of these patients, we suggest performing appendectomy within 24 hours of presentation in patients with uncomplicated appendicitis who elect to undergo surgery. (See "Management of acute appendicitis in adults", section on 'Timing of appendectomy' .)
Low-dose dexamethasone for severe migraine in adults (October 2023)
Parenteral dexamethasone is used along with short-acting abortive therapies to reduce migraine recurrence for patients with severe symptoms, but optimal dosing is uncertain. Prior trials have reported benefit at doses ranging from 8 to 24 mg. In a recent trial of 209 adults with moderate to severe migraine presenting to the emergency department treated with metoclopramide and intravenous (IV) dexamethasone, rates of sustained relief at 48 hours were similar between groups randomly assigned to 4 versus 16 mg of dexamethasone [ 12 ]. Rates of immediate headache relief and medication use in the week following discharge were also similar. These results support our preference for adjunctive dexamethasone at a dose of 4 mg IV to reduce migraine recurrence. (See "Acute treatment of migraine in adults", section on 'Abortive therapy plus parenteral dexamethasone' .)
GENERAL PEDIATRIC EMERGENCY MEDICINE
Concussion and mental health disorders in children and adolescents (March 2024)
Ongoing research continues to examine the complex relationship between concussion and mental health disorders. In a recent case-control study of over 18,000 children (≤17 years old) with concussion and over 37,000 matched controls, concussion was associated with an increased risk for a new diagnosis of a behavior disorder at two and four years after injury [ 13 ]. For most diagnoses, the absolute numbers were low. Confidence in a causal relationship is limited by risk of confounding and reliance on an electronic medical record for establishing lack of baseline behavioral problems prior to injury. Whether pediatric concussion is an independent risk factor for new behavioral problems after recovery remains unclear. (See "Concussion in children and adolescents: Management", section on 'Mental health disorders' .)
Increasing exposure to illicit fentanyl in young children in the United States (March 2024)
The potent opioid fentanyl is commonly implicated in fatal adult and pediatric poisonings, but there are limited data on accidental nonfatal exposures in young children. In the United States between 2013 and 2023, calls to poison control centers for children ≤6 years of age exposed to illicit fentanyl increased from 5 to 539 annually [ 14 ]. More than 80 percent were children ≤2 years old or were exposed at home. Most patients had severe effects and half received naloxone . These data confirm the seriousness of the presence of illicit fentanyl in the households of young children and suggest it as a focus for prevention measures. (See "Opioid intoxication in children and adolescents", section on 'Epidemiology' .)
Short-course antibiotic therapy in children with febrile UTI (February 2024)
In children with urinary tract infection (UTI) without suspected kidney involvement, there is controversy about the duration of empiric antibiotic therapy. In an unblinded trial from Italy of amoxicillin-clavulanate to treat UTI, 142 children three months to five years of age were randomly assigned to a 10-day course (standard) or a 5-day course (short) of antibiotics [ 15 ]. Fewer children assigned to the short course had recurrent UTI within 30 days of antibiotic completion (2.8 versus 14.3 percent [difference -11.5 percent, 95% CI -20.5 to -2.5]). Rates of resistance to amoxicillin-clavulanate within 5 days following completion of antibiotics (1.4 versus 4.3 percent) and within 30 days (1.4 versus 0 percent) were similar. This trial lends further support for a 5-day course of antibiotics to treat UTI when kidney involvement is not suspected. (See "Urinary tract infections in infants older than one month and children less than two years: Acute management, imaging, and prognosis", section on 'Preferred empiric oral regimens' .)
PRIMARY CARE ORTHOPEDICS AND SPORTS MEDICINE
Avulsion fractures of hip and pelvis in children (October 2023)
There are few large-scale studies of pelvic avulsion fractures in children. A retrospective review of over 700 children with pelvic or hip avulsion fractures from a single tertiary care hospital reported the average patient age was just over 14 years and nearly 80 percent were sustained by males [ 16 ]. The anterior-superior and inferior iliac spines and ischial tuberosity were the most common sites, accounting for over 80 percent of fractures. Most injuries were sustained while the patient was running or kicking during sport, most often football (soccer). The incidence of avulsion fracture rose substantially during the study period, 2005 to 2020. (See "Pelvic trauma: Initial evaluation and management", section on 'Epidemiology and mechanism' .)
New guidelines for airway management in infants (January 2024)
Very young children are at higher risk of complications of airway management than children in older age groups; however, guidelines for infants have been lacking. In 2024, the European Society of Anesthesiology and Intensive Care and the British Journal of Anesthesia published joint guidelines for airway management in neonates and infants [ 17 ]. A summary of their recommendations appears in the following table ( table 1 ). (See "Airway management for pediatric anesthesia", section on 'Pediatric airway management guidelines' .)
Videolaryngoscopy for endotracheal intubation in critically ill children (January 2024)
Use of videolaryngoscopy (VL) in children provides a shared view during emergency endotracheal intubation (ETI) that permits an experienced physician observer to give assistance to the proceduralist. In a multicenter quality study of VL during ETI in pediatric intensive care units with standardized coaching by an attending, over 3500 ETIs were performed with VL, and use of VL increased from 30 percent to 89 percent of ETIs over four years [ 18 ]. Compared with direct laryngoscopy, VL was associated with lower adverse events (9 versus 15 percent). The majority of proceduralists were residents or fellows. These findings and prior studies confirm the safety of VL during emergency ETI in children and demonstrate the value of standardized coaching during the procedure for less experienced clinicians. (See "Technique of emergency endotracheal intubation in children", section on 'Video versus direct laryngoscopy' .)
Multiple-dose activated charcoal for amatoxin-containing mushroom poisoning (March 2024)
Ingesting mushrooms that contain amatoxins can cause acute liver injury, liver and multisystem organ failure, and death. Multiple-dose activated charcoal (MDAC), which increases elimination of amatoxins by blocking enterohepatic recirculation, is a frequently used therapy, typically combined with other antidotes. A systematic review that included nearly 1200 patients (665 received MDAC, 2 received single-dose activated charcoal) with amatoxin-containing mushroom poisoning found that activated charcoal administration was associated with higher transplant-free survival (83 versus 75 percent) [ 19 ]. These findings support our recommendation to administer MDAC to patients with suspected amatoxin-containing mushroom ingestion. (See "Amatoxin-containing mushroom poisoning (eg, Amanita phalloides): Clinical manifestations, diagnosis, and treatment", section on 'Elimination enhancement' .)
Delta-8 tetrahydrocannabinol use by United States adolescents (March 2024)
Delta-8 tetrahydrocannabinol (THC) is typically a minor cannabinoid found in cannabis, but can also be synthesized. It is increasingly found in United States (US) cannabis products, often marketed as low delta-9 THC. A survey of US twelfth graders in 2023 found that 11 percent reported using delta-8 THC within the past 12 months, compared with 30 percent reporting marijuana use [ 20 ]. Delta-8 THC use was lower in states with cannabis legalization (8 versus 14 percent) or delta-8 THC regulation (6 versus 14 percent). These findings suggest that delta-8 THC is a public health concern in adolescents, particularly in states that do not regulate it and have not legalized marijuana for adult use. (See "Cannabis (marijuana): Acute intoxication", section on 'Cannabis formulations' .)
Xylazine and fentanyl detection in overdose deaths (March 2024)
Xylazine (street name "Tranq") is an alpha-2 adrenergic agonist increasingly found as an adulterant in or co-administered with illicit fentanyl ; whether the combined use of xylazine with fentanyl or other opioids increases the risk of overdose death is unclear. In a retrospective study of over 3000 fentanyl-related overdose fatalities over four years, the median postmortem fentanyl concentration was higher in the 148 cases that also had xylazine detected; significantly more decedents with xylazine detected had very high fentanyl concentrations (>40 mcg/L) [ 21 ]. This finding suggests that co-administration of xylazine may permit tolerance to higher doses of fentanyl and may be associated with decreased, rather than increased, lethality. The mechanism of this effect is not clear and requires further study. (See "Clonidine, xylazine, and related imidazoline poisoning", section on 'Epidemiology' .)
Diethylene glycol poisoning outbreak in Indonesia (February 2024)
Diethylene glycol (DEG) ingestion causes gastrointestinal symptoms followed by an elevated anion gap metabolic acidosis, acute kidney injury (AKI), and delayed neurologic toxicity in survivors. Outbreaks continue to occur when DEG is substituted for the more expensive propylene glycol in liquid/syrup medications. In Indonesia in 2022, 52 previously healthy children who had taken a syrup-based antipyretic or cough medication were treated for rapidly progressing AKI [ 22 ]. DEG and/or ethylene glycol were identified in 16 out of 17 patients who had toxicology testing performed. Most children required kidney replacement therapy and 34 died. DEG and/or ethylene glycol poisoning must be on the differential diagnosis of any child with a rapidly progressing AKI. (See "Methanol and ethylene glycol poisoning: Management", section on 'Diethylene glycol' .)
Insulin-euglycemia therapy for phosphide poisoning (January 2024)
The metallic phosphide rodenticides, zinc and aluminum phosphide, cause shock, cardiac dysfunction, dysrhythmias, respiratory failure, and metabolic acidosis. In acute poisoning, mortality is very high, treatment is primarily supportive (including vasopressors, bicarbonate, and magnesium infusion), and no antidote exists. In a trial of 108 patients with aluminum phosphide poisoning and hypotension or acidosis, compared with supportive care and norepinephrine, insulin-euglycemia therapy reduced mortality (65 versus 96 percent) and tracheal intubation (61 versus 82 percent), and improved mean arterial pressure six hours after poisoning (65 versus 13 mmHg) [ 23 ]. These findings suggest that insulin-euglycemia therapy may be beneficial in critically ill patients poisoned with phosphide poisoning. (See "Overview of rodenticide poisoning", section on 'Zinc and aluminum phosphide' .)
Photobiomodulation therapy for local tissue damage from snake envenoming (January 2024)
Photobiomodulation therapy (also called low-level laser therapy [LLLT]) may decrease inflammation and enhance healing following envenoming by snake species that cause local tissue damage or myonecrosis. In a trial of 60 patients with Bothrops snakebites all of whom received antivenom, LLLT decreased pain intensity scores, extent of edema, and extremity circumference compared with no LLLT [ 24 ]. LLLT is a promising adjunct to antivenom, but more trials and access to equipment are needed before it can be recommended for routine use. (See "Snakebites worldwide: Management", section on 'Photobiomodulation' .)
National practice guidelines not associated with increased MOUD prescribing in the ED (January 2024)
In emergency department (ED) patients who survive an opioid overdose, initiation of medications for opioid use disorder (MOUD) is associated with decreased one-year mortality (approximately 5 percent without MOUD). However, prescribing rates are low and multiple barriers exist. A study of more than 20,000 ED visits for opioid toxicity in Canada found that even though MOUD prescribing increased between 2013 and 2020, it was still relatively low (<6 percent) and was not improved by the publication of Canadian clinical practice guidelines in 2018 [ 25 ]. These findings suggest that EDs and health systems need to make systematic efforts to implement and maintain MOUD-initiation programs that directly engage clinicians to overcome barriers and increase rates of prescribing. (See "Acute opioid intoxication in adults", section on 'Prevention of recurrent opioid overdose' .)
Methemoglobinemia in infants due to contaminated hospital water supply (January 2024)
Methemoglobinemia is a potentially life-threatening condition in which heme iron becomes oxidized, preventing oxygen delivery. A report from a hospital in Japan described methemoglobinemia in 10 neonates who were fed infant formula prepared with tap water from the general hospital water supply [ 26 ]. The cause was identified as high levels of nitrites, and the source was traced to contamination by an anticorrosion agent from the heating system that entered the water supply due to a malfunctioning valve. All 10 survived, although 3 required methylene blue therapy. Infants are especially susceptible to methemoglobinemia because they have lower baseline levels of the enzyme that converts heme iron back to its normal state. (See "Methemoglobinemia", section on 'Nitrates and nitrites (from foods, drugs, preservatives, and chemicals)' .)
Avoiding intubation in acutely poisoned but stable, unresponsive adults (December 2023)
In unresponsive patients with trauma or undifferentiated coma, tracheal intubation is generally recommended to protect the airway and prevent aspiration. However, the benefit of intubation is unclear in stable poisoned patients who have decreased level of consciousness but are oxygenating and ventilating adequately. In a randomized trial of 225 adults with acute poisoning and coma (GCS score ≤8), compared with airway management at the physician’s discretion, individuals not intubated unless hypoxia, seizure, vomiting, or hypotension developed had a lower likelihood of mechanical ventilation (18 versus 60 percent), intensive care unit admission (40 versus 66 percent), or adverse events from intubation (6 versus 15 percent); they also had a lower risk of pneumonia [ 27 ]. These findings support avoiding intubation solely for a GCS score ≤8 in stable, unresponsive poisoned patients who are expected not to deteriorate based upon the suspected poison (eg, ingestion of a short-acting sedative such as ethanol). (See "Initial management of the critically ill adult with an unknown overdose", section on '"A": Airway stabilization' .)
High blood lead levels in US children after eating cinnamon applesauce pouches (November 2023)
The Centers for Disease Control and Prevention have issued a health alert following reports of high blood lead levels from several states for a total of 22 children who were fed cinnamon-containing applesauce pouches that were subsequently found to contain extremely high concentrations of lead [ 28 ]. Children who have eaten a recalled product should undergo blood lead testing. Clinicians should advise parents, primary caregivers, and guardians to not buy specific cinnamon-containing apple puree or applesauce products named in the US Food and Drug Administration announcement and to discard any recalled products that they have purchased. (See "Childhood lead poisoning: Exposure and prevention", section on 'Food' and "Childhood lead poisoning: Clinical manifestations and diagnosis", section on 'Laboratory evaluation' and "Childhood lead poisoning: Management" .)
Validation of an enzymatic assay for ethylene glycol poisoning in humans (November 2023)
Serum ethylene glycol (EG) concentrations are usually measured by gas chromatography, which is not widely offered by hospital clinical laboratories, leading to diagnostic uncertainty, need for empiric treatment, and delays in confirmation. Some hospitals have adopted an EG enzyme-based glycerol dehydrogenase (GDH) assay modified from a veterinary assay and run on automated chemistry analyzers. A study of 118 patient blood samples found that using a 9 mg/dL threshold (well below a toxic concentration), the GDH assay had a 100 percent positive and negative predictive value compared with gas chromatography [ 29 ]. This assay may provide a screening tool for possible EG poisoning that is associated with reduced costs and time of diagnostic uncertainty. (See "Methanol and ethylene glycol poisoning: Pharmacology, clinical manifestations, and diagnosis", section on 'Testing for methanol and ethylene glycol' .)
Skin preparation prior to fracture repair (March 2024)
The optimal preparation of contaminated or dirty wounds and whether any skin preparation can influence surgical site infection (SSI) independent of other factors (eg, prophylactic systemic antibiotics) are unknown. In a multiple-period, cluster-randomized, crossover trial comparing skin preparation with iodine povacrylex in alcohol versus chlorhexidine gluconate in alcohol in 1700 open fracture repairs, the incidence of superficial or deep SSI was similar for both approaches [ 30 ]. Based on these findings, which are consistent with those from a previous trial, either chlorhexidine- or iodine-based skin preparations can be used prior to surgery for open, traumatic lower extremity wounds. (See "Surgical management of severe lower extremity injury", section on 'Limb preparation and skin antisepsis' .
Whole blood transfusion for severe traumatic hemorrhage (January 2024)
For severe traumatic hemorrhage, whole blood transfusion is an alternative to balanced component transfusion (1:1:1 ratio of packed red blood cells/plasma/platelets). In an observational study comparing these two approaches, low titer group O whole blood transfusion was associated with lower 24-hour mortality (8 versus 19 percent) and lower volume of blood products received at 72 hours (48 versus 82 mL/kg) [ 31 ]. The survival benefit was greatest in patients with shock or coagulopathy. While this study suggests improved outcomes for whole blood transfusion, randomized trials are needed to determine which transfusion strategy might be superior and which patients would benefit the most. (See "Ongoing assessment, monitoring, and resuscitation of the severely injured patient", section on 'Whole blood transfusion' .)
Impact of pediatric trauma centers on clinical outcomes (October 2023)
Level 1 pediatric trauma centers (PTC) ( table 2 ) are the preferred sites for initial resuscitation and ongoing management of critically injured children. In a meta-analysis of 34 studies that evaluated children hospitalized for traumatic injury, treatment in a PTC was associated with lower mortality than in an adult trauma center (ATC, odds ratio 0.59) [ 32 ]. Compared with an ATC, care of children with blunt trauma in a PTC was also associated with a lower likelihood of computed tomography or operative management for blunt solid organ injury. For seriously injured infants, children, and adolescents, these findings support treatment in a PTC. When a level 1 PTC is not available, these children should receive care at a hospital that has the highest level of pediatric trauma expertise and resources. (See "Trauma management: Approach to the unstable child", section on 'Definitive care' .)
- von Hellmann R, Fuhr N, Ward A Maia I, et al. Effect of Bougie Use on First-Attempt Success in Tracheal Intubations: A Systematic Review and Meta-Analysis. Ann Emerg Med 2024; 83:132.
- Low CJW, Ramanathan K, Ling RR, et al. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with cardiac arrest: a comparative meta-analysis and trial sequential analysis. Lancet Respir Med 2023; 11:883.
- Whitehouse T, Hossain A, Perkins GD, et al. Landiolol and Organ Failure in Patients With Septic Shock: The STRESS-L Randomized Clinical Trial. JAMA 2023; 330:1641.
- Zhang MX, Lilien TA, van Etten-Jamaludin FS, et al. Generation of Aerosols by Noninvasive Respiratory Support Modalities: A Systematic Review and Meta-Analysis. JAMA Netw Open 2023; 6:e2337258.
- Yoshimura S, Kiguchi T, Nishioka N, et al. Association of pre-hospital tracheal intubation with outcomes after out-of-hospital cardiac arrest by drowning comparing to supraglottic airway device: A nationwide propensity score-matched cohort study. Resuscitation 2024; 197:110129.
- Watson NW, Carroll BJ, Krawisz A, et al. Trends in Discharge Rates for Acute Pulmonary Embolism in U.S. Emergency Departments. Ann Intern Med 2024; 177:134.
- Yotsuyanagi H, Ohmagari N, Doi Y, et al. Efficacy and Safety of 5-Day Oral Ensitrelvir for Patients With Mild to Moderate COVID-19: The SCORPIO-SR Randomized Clinical Trial. JAMA Netw Open 2024; 7:e2354991.
- Wilson SJ, Thavanathan R, Cheng W, et al. Test Characteristics of Emergency Medicine-Performed Point-of-Care Ultrasound for the Diagnosis of Acute Cholecystitis: A Systematic Review and Meta-analysis. Ann Emerg Med 2024; 83:235.
- Qadir N, Sahetya S, Munshi L, et al. An Update on Management of Adult Patients with Acute Respiratory Distress Syndrome: An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med 2024; 209:24.
- Gao Y, Chen W, Pan Y, et al. Dual Antiplatelet Treatment up to 72 Hours after Ischemic Stroke. N Engl J Med 2023; 389:2413.
- Jalava K, Sallinen V, Lampela H, et al. Role of preoperative in-hospital delay on appendiceal perforation while awaiting appendicectomy (PERFECT): a Nordic, pragmatic, open-label, multicentre, non-inferiority, randomised controlled trial. Lancet 2023; 402:1552.
- Friedman BW, Solorzano C, Kessler BD, et al. Randomized Trial Comparing Low- vs High-Dose IV Dexamethasone for Patients With Moderate to Severe Migraine. Neurology 2023; 101:e1448.
- Delmonico RL, Tucker LY, Theodore BR, et al. Mild Traumatic Brain Injuries and Risk for Affective and Behavioral Disorders. Pediatrics 2024; 153.
- Temple C, Hendrickson RG. Increasing Exposure of Young Children to Illicit Fentanyl in the United States. N Engl J Med 2024; 390:956.
- Montini G, Tessitore A, Console K, et al. Short Oral Antibiotic Therapy for Pediatric Febrile Urinary Tract Infections: A Randomized Trial. Pediatrics 2024; 153.
- Ferraro SL, Batty M, Heyworth BE, et al. Acute Pelvic and Hip Apophyseal Avulsion Fractures in Adolescents: A Summary of 719 Cases. J Pediatr Orthop 2023; 43:204.
- Disma N, Asai T, Cools E, et al. Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. Br J Anaesth 2024; 132:124.
- Giuliano J Jr, Krishna A, Napolitano N, et al. Implementation of Video Laryngoscope-Assisted Coaching Reduces Adverse Tracheal Intubation-Associated Events in the PICU. Crit Care Med 2023; 51:936.
- Varekamp J, Tan JL, Stam J, et al. Effects of interrupting the enterohepatic circulation in amatoxin intoxications. Clin Toxicol (Phila) 2024; 62:69.
- Harlow AF, Miech RA, Leventhal AM. Adolescent Δ8-THC and Marijuana Use in the US. JAMA 2024; 331:861.
- Hays HL, Spiller HA, DeRienz RT, et al. Evaluation of the relationship of xylazine and fentanyl blood concentrations among fentanyl-associated fatalities. Clin Toxicol (Phila) 2024; 62:26.
- Hidayati EL, Fahlevi R, Puspitasari HA, et al. Emerging progressive atypical acute kidney injury in young children linked to ethylene glycol and diethylene glycol intoxication. Pediatr Nephrol 2024; 39:897.
- Adel B, Elgharbawy NM, Shahin MM, et al. Insulin-euglycemia therapy in acute aluminum phosphide poisoning: a randomized clinical trial. Clin Toxicol (Phila) 2023; 61:1032.
- Carvalho ÉDS, Souza ARDN, Melo DFC, et al. Photobiomodulation Therapy to Treat Snakebites Caused by Bothrops atrox: A Randomized Clinical Trial. JAMA Intern Med 2024; 184:70.
- Hu T, McCormack D, Juurlink DN, et al. Initiation of opioid agonist therapy after hospital visits for opioid poisonings in Ontario. CMAJ 2023; 195:E1709.
- Takahashi S, Ishige T, Takizawa T. Methemoglobinemia Outbreak in a Neonatal ICU and Maternity Ward. N Engl J Med 2023; 389:2395.
- Freund Y, Viglino D, Cachanado M, et al. Effect of Noninvasive Airway Management of Comatose Patients With Acute Poisoning: A Randomized Clinical Trial. JAMA 2023; 330:2267.
- Health Alert Network: High Blood Lead Levels in Children Consuming Recalled Cinnamon Applesauce Pouches. HAN00500. Centers for Disease Control and Prevention. . Atlanta, GA, November 13, 2023. https://emergency.cdc.gov/han/2023/han00500.asp?ACSTrackingID=USCDC_511-DM117142&ACSTrackingLabel=HAN%20500%20-%20General%20Public&deliveryName=USCDC_511-DM117142 (Accessed on November 14, 2023).
- Filip AB, Farnsworth CW, Mullins ME, et al. Accuracy of a Glycerol Dehydrogenase Assay for Ethylene Glycol Detection. J Med Toxicol 2023; 19:362.
- PREP-IT Investigators, Sprague S, Slobogean G, et al. Skin Antisepsis before Surgical Fixation of Extremity Fractures. N Engl J Med 2024; 390:409.
- Shea SM, Mihalko EP, Lu L, et al. Doing more with less: low-titer group O whole blood resulted in less total transfusions and an independent association with survival in adults with severe traumatic hemorrhage. J Thromb Haemost 2024; 22:140.
- Moore L, Freire G, Turgeon AF, et al. Pediatric vs Adult or Mixed Trauma Centers in Children Admitted to Hospitals Following Trauma: A Systematic Review and Meta-Analysis. JAMA Netw Open 2023; 6:e2334266.
A Hospital Emergency Room Essay
Most people go to a hospital emergency room when they have been in a serious accident. They also do so when they have broken bones or other body parts that are out of place. Regardless of their justification for visiting an emergency room, most patients require immediate attention in order to capitalize on the opportunity window that can save their lives.
General processes in the emergency room are kept at a minimum in order to attend to patients as soon as possible. Usually, three processes are undertaken, and they include triage, treatment and transfer. An emergency room is not a place for chronic issues or follows ups.
It only handles those matters that are out of control. However, some patients may visit the emergency room more than once because of the nature of their condition or inability of previous procedures to deal with the ailment completely. The staff members in the emergency room have special training to deal with such a high-stakes environment. Their goal is to stabilize the patient, after which they send them to other hospital units. Sometimes these individuals may be admitted in the hospital or may be fortune enough to go home.
Patients in emergency rooms are likely to exhibit certain characteristics that justify the need for emergency treatment. Some of them could be unconscious while others may exhibit signs of a heart attack. Such instances include chest tightness, light headedness, pressure and severe chest pains.
Alternatively, people may visit the emergency room with cases of poison ingestion. Sometimes these individuals may be having a severe reaction to a previous intervention like medicine. In other scenarios, it may be brought on by a sting or bite. Patients in the emergency room are likely to have severe head injury and may even be physically or mentally disoriented. Some of the subjects may experience severe pain in a certain body part.
If the complication is lung-related, then they could have shortness of breath. Nonstop breathing as well as continuous bleeding may also be some of the symptoms that patients have in the emergency room. Others could lose sensory abilities like hearing, speech, vision and body movement. These patients may also exude body fluids from unusual places such as blood from the mouth or could have mucous-like discharge from injured parts of the body.
Inside the emergency room, patients may undergo treatment in various forms. For instance, if someone is suffering from a cardiac arrest, he or she will receive advanced life support. A person with a heart attack will enter the resuscitation room where they will receive oxygen and be subjected to an ECG test.
They will receive nitroglycerin as well as morphine for pain. A person with trauma must go through an x-ray within the shortest time possible. Once the nature of the broken bone is established, then reperfusion or surgery will take place. Such persons must receive treatment within an hour of the accident so as to increase chances of survival.
Emergency rooms come in different varieties and forms depending on the nature of the injury, trauma or condition. One such emergency room is the resuscitation room. Here, very ill patients are admitted. The facility only contains equipment that deals with emergency situations.
Even the number and type of staff members must reflect this goal. In the room, one will have an attending physician as well as two nurses. Sometimes these staff members may be permanently located in the room. Alternatively, they could be available on call whenever an ambulance service enters the hospital. In resuscitation, other medical experts like technicians, medical students and pharmacists can also handle their cases.
Pediatric and mental health emergency rooms also exist in hospitals. These locations are different from the conventional ones because the groups under consideration do not share the same characteristics with conventional patients. In pediatric emergency rooms, one may find an additional staff member whose role is to ensure that children are at ease.
In the psychiatric emergency room, one is likely to find specialists who can handle dire mental health conditions. Psychiatrists, social workers as well as nurses may be in these facilities. Their work is to ensure that their patients do not become a risk to themselves as well as to their environment.
Workers in the emergency room must think on their feet and do the right thing with limited resources. Life and death situations are quite common, so none of the employees take their work lightly. Sometimes, emergencies may occur in large proportions.
For instance, a terrorist attack may take place or a bombing may occur. In this regard, emergency rooms may need to operate beyond their capacity. When such events arise, it is sometimes necessary to divert more resources towards emergency care. Staff members, from other parts of the hospital, need to set aside their usual responsibilities and focus on urgent cases first.
As mentioned earlier, most emergency rooms have a triage component that allows them to assess patients as soon as they come. Imaging technologies are one of several tests that can be administered in the medical settings. The right radiography equipment needs to be available in order to foster fast responses to an emergency situation.
Radiographers must also ensure that they use high-speed tests, which allow them to carry out an imaging procedure in the fastest way possible. Therefore, choice of equipment and tests has a profound effect on how effectively the radiography function contributes towards the goals in an emergency room. A case in point is a person who is experiencing severe chest pain. When the person enters the emergency room, he or she needs to undergo a chest x-ray so as to establish possible causes of the problem.
The radiographer on duty must examine this patient’s chest as fast as possible and convey the results to the radiologist in charge or the concerned medical specialist. Sometimes if a patient experiences a cardiac arrest, the radiographer will have to carry out a CT scan in order to determine what is wrong with the patient.
However, because this is an emergency situation, then the radiographer should use cutting edge technologies to save on time. Some new forms of the procedure like CT angiography would be required as a diagnostic tool. Therefore, radiographers in the emergency room must be well-versed with the latest developments in their fields in order to accelerate service provision.
Radiographers within the emergency room also tend to do fewer tests than the ones in other hospital units. In conventional hospital departments, physicians will focus on protecting themselves against liability. In order to achieve this, many of them request for several unnecessary diagnostic tests.
Radiographers have found that their work is overwhelming in these units because of such a different approach. However, the converse is true in the emergency unit. All the attention must be dedicated to the patient. Decisions on possible diagnostics need to be minimized as much as possible so as to avail more time for treatment. As a consequence, radiographers tend to do fewer tests, per patient, in this unit.
In certain circumstances, the emergency room physician may want to perform the radiographic tests himself. Here, the radiographer may need to communicate effectively with the concerned doctor to establish which task will be done and which one will not. Usually, many ER doctors will expect radiographers to perform MRI or CT scans.
However, in the event that a patient requires an ultrasound, then chances are that the physician will want to perform the test on his own. Because of the high-risk nature of the emergency room, most specialists prefer to receive training in a range of diagnostic procedures, including radiography. This may cause professionals in the latter community to be maligned during certain procedures.
Staff members in the emergency room usually work in a shift system. Emergencies may arise during off hours, so they need to be within reach. Radiographers frequently use shifts while other specialist medical professionals may need to be available on call. Their services are more difficult to substitute so they must carry on with routine work irrespective of how busy they happen to be.
New developments in radiography have enabled radiologists and radiographers to perform tests and transmit information using high band width to the medical practitioners who need them. Therefore, radiographers need to familiarize themselves with this approach if they work in emergency rooms.
Emergency rooms can make the difference between life and death. Therefore, staff members need to respond as swiftly and professionally as possible. Conservative use of tests and right decisions can increase a person’s chances of survival.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, December 23). A Hospital Emergency Room. https://ivypanda.com/essays/a-hospital-emergency-room/
"A Hospital Emergency Room." IvyPanda , 23 Dec. 2018, ivypanda.com/essays/a-hospital-emergency-room/.
IvyPanda . (2018) 'A Hospital Emergency Room'. 23 December.
IvyPanda . 2018. "A Hospital Emergency Room." December 23, 2018. https://ivypanda.com/essays/a-hospital-emergency-room/.
1. IvyPanda . "A Hospital Emergency Room." December 23, 2018. https://ivypanda.com/essays/a-hospital-emergency-room/.
Bibliography
IvyPanda . "A Hospital Emergency Room." December 23, 2018. https://ivypanda.com/essays/a-hospital-emergency-room/.
- Medical Ethics in Radiography
- Ethical Issues at the Radiology Department
- Adapting the Dominican Culture in the Radiology Department
- Radiologic Technologists Responsibilities
- Radiography Stereotypes and Emotional Intelligence
- Providers' Role in Quality Assurance in Breast Cancer Screening
- Radiology and Radiography: Research Paper
- Witnessed Resuscitation: Benefits and Disadvantages
- Ergonomics and Work-Related Issues in Sonographers
- Development of Cardiopulmonary Resuscitation
- The Concept of Medical Terminology
- Medical terminology errors
- Medical terminologies for dummies
- Medical Professionals Exam
- Patient Care Improvement: System-Based Practice
- Study protocol
- Open access
- Published: 26 April 2024
The skåne emergency medicine (SEM) cohort
- Ulf Ekelund ORCID: orcid.org/0000-0002-0951-1582 1 ,
- Bodil Ohlsson 2 ,
- Olle Melander 2 ,
- Jonas Björk 3 , 4 ,
- Mattias Ohlsson 6 , 7 ,
- Jakob Lundager Forberg 5 ,
- Pontus Olsson de Capretz 1 ,
- Axel Nyström ORCID: orcid.org/0000-0001-6657-5681 3 , 6 &
- Anders Björkelund 6
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine volume 32 , Article number: 37 ( 2024 ) Cite this article
17 Accesses
Metrics details
In the European Union alone, more than 100 million people present to the emergency department (ED) each year, and this has increased steadily year-on-year by 2–3%. Better patient management decisions have the potential to reduce ED crowding, the number of diagnostic tests, the use of inpatient beds, and healthcare costs.
We have established the Skåne Emergency Medicine (SEM) cohort for developing clinical decision support systems (CDSS) based on artificial intelligence or machine learning as well as traditional statistical methods. The SEM cohort consists of 325 539 unselected unique patients with 630 275 visits from January 1st, 2017 to December 31st, 2018 at eight EDs in the region Skåne in southern Sweden. Data on sociodemographics, previous diseases and current medication are available for each ED patient visit, as well as their chief complaint, test results, disposition and the outcome in the form of subsequent diagnoses, treatments, healthcare costs and mortality within a follow-up period of at least 30 days, and up to 3 years.
The SEM cohort provides a platform for CDSS research, and we welcome collaboration. In addition, SEM’s large amount of real-world patient data with almost complete short-term follow-up will allow research in epidemiology, patient management, diagnostics, prognostics, ED crowding, resource allocation, and social medicine.
All over the world, emergency departments (ED) are struggling with an increasing inflow of patients, and especially elderly patients with complex pathology that is difficult to assess due to simultaneous chronic diseases, risk factors and/or polypharmacy [ 1 , 2 ]. ED clinicians need to make fast and accurate risk estimates, and optimal management from the start is crucial for good patient outcomes. At the same time, the amount of available clinical information in electronic medical records is also increasing, as is the total body of medical knowledge. Often the ED physician can no longer grasp and process all available information, making it impossible for an individual clinician to provide the theoretically best possible care.
Artificial intelligence (AI) and machine learning (ML) are now developing fast, and most industries will likely be fundamentally changed by AI in the coming years [ 3 ]. In medicine, AI and ML provide new possibilities when applied to extensive electronic health records and registers [ 4 ]. The most impressive advances have occurred in radiology and pathology, where ML accuracy of image classifications now exceeds that of humans [ 5 ]. In emergency medicine, AI/ML-driven decision support tools have the potential to improve diagnostic accuracy [ 5 ], alleviate ED crowding [ 6 , 7 ], and decrease the use of inpatient beds and healthcare costs [ 8 ]. The Swedish Board of Health and Welfare has therefore emphasized the great potential of AI/ML in emergency medicine [ 9 ]. So far however, there have been few AI/ML studies in the ED setting, and practically no implementation in routine ED care. The creation of ML-based decision support for ED use requires large amounts of high-quality clinical data, preferably from representative unselected ED patients in routine care.
In the present paper we describe the rationale for, and construction of, the Skåne Emergency Medicine (SEM) cohort and outline possible studies. The SEM cohort is a recently established data platform for developing clinical decision support systems (CDSS) based on traditional statistical methods or AI/ML, to be used in ED triage or later in the management of specific patient conditions. Specific aims include the prediction of diagnoses, critical interventions (e.g. defibrillation of cardiac arrest, thrombolysis in stroke) or inpatient care within 30 days of the ED visit, and mortality up to 1 year after the ED visit. We describe in this paper the process of building the SEM dataset with careful consideration of ethics, data protection, and bias. With the SEM cohort, we hope to create CDSS that can be tested in randomized trials in routine emergency care.
Methods/design
The formation of the SEM cohort was an initiative within the Artificially Intelligent use of Registers at Lund University (AIR Lund) research environment [ 10 ], which is a multidisciplinary collaboration between Lund University (Emergency medicine, Internal medicine, Epidemiology and biostatistics, Computational biology, Technology and society/ethics, and Law), Halmstad University (Information technology), and the Swedish health care regions Skåne and Halland.
Skåne is Sweden’s southernmost region and has some 1.4 million inhabitants. Healthcare is publicly financed with a small copayment at every visit. Patients in region Skåne almost always go to the nearest ED, and in general do not seek care outside the region. The SEM cohort includes data from patients presenting at eight general EDs in Skåne from January 1st, 2017 to December 31st, 2018. The characteristics of these EDs are described in Table 1 . Five EDs are open 24/7/365 (Skåne university hospital at Lund and Malmö, Helsingborg general hospital, Kristianstad central hospital and Ystad hospital) and three EDs are open during office hours (Landskrona, Trelleborg and Hässleholm hospitals). There are very few patients with psychiatric disorders, problems related to obstetrics/ gynecology, ophthalmology, and pediatric patients without orthopedic problems at these EDs, since there are specialized EDs for these patients in the region. Table 1 describes that the yearly ED census ranges between 80000 (Malmö) and 5000 (Landskrona) patient cases, and that admission rates to in-hospital care range between 20% (Helsingborg) and 32% (Hässleholm or Landskrona). All EDs use the rapid emergency triage and treatment system (RETTS [ 11 ]) that includes five priority levels: Highest priority 1 (Red); Priority 2 (Orange); Priority 3 (Yellow); Lowest priority 4 (Green); and Priority primary care (Blue). The RETTS set of chief complaints are thus common for all EDs in the SEM cohort. All EDs have similar access to patient testing, and clinical guidelines are generally the same in the entire region.
During and after the data collection period, the patients were informed of the purpose and structure of the SEM cohort in writing via public advertising on a website, and that they could decline participation at any time, for any reason, by contacting a research nurse or the first author at Lund. The creation of the SEM cohort and its use for AI/ML research and cross-sectional analyses has been approved by the Swedish Ethical Review Authority (Dnr 2019–05783), and by Region Skåne (302 − 19). There is no approval for commercial use of the data.
Data collection
During the study period, all patients at the eight EDs were included in the SEM cohort by default via identification in the common ED patient log system (Patientliggaren™, Tietoevry [ 12 ]), and data from the other registers (below) were then linked by each patient’s unique Swedish identification (ID) number, which is universally used in Swedish healthcare and all government registers. After collection and linkage, all data were pseudonymized with patient study ID numbers and kept on secure servers behind firewalls at Lund University where access is logged. The key between personal and study IDs is kept separately on a Region Skåne server with standard healthcare data security.
The data sources include healthcare databases and registers with complete national or regional coverage, which should ensure close to complete data on all patient visits. As much as possible, we used well described high-quality data sources (see e.g. references [ 13 , 14 , 15 , 16 ]) to collect the SEM data in order to decrease bias and data errors. The number of missing data varies across the sources but is generally very low. Data variables were chosen based on importance in the emergency care process as well as availability in the source registers. The collected data were the same as used in clinical care, and there was no major change in data labelling during 2017–2018. The SEM cohort was not designed with a specific CDSS or study in mind, but the size of the cohort (below) and the number of variables and data included was chosen to ensure sufficient statistical power for most CDSS research projects.
Data from the source registers were kept in their exported form with no deletion or curation, and software scripts are used to extract data to form tailor-made new datasets for each specific research project. Data curation or deletion will generally take place in each CDSS project, and only as needed in the original SEM cohort data.
As shown in Table 2 , the available data for each patient visit include the patient’s baseline data, data on the ED visit, and the outcome within 30 days up to three years after the ED visit: diagnoses, ED returns, hospital admissions, death, and healthcare costs. In total, the SEM data include several hundred variables for each patient, and many more that can be calculated from the original variables, such as ED crowding or boarding data, return visits, and mortality at different times after ED arrival. Detailed variable lists are available on reasonable request.
The SEM cohort is thus mainly based on register data and does not include free text information such as the patient’s detailed symptom history, findings at the physical examination, reasons for decisions and preliminary assessments. Also missing are the initial ED vital signs (blood oxygen saturation, respiratory rate, pulse rate, blood pressure, consciousness level and body temperature) and pharmacological treatment in the ED, since these data are primarily recorded on paper in the region. However, all this missing information can be obtained as needed by manual review of the individual patient records. As for diagnostic tests, ECG data are available as the raw signal, amplitude/interval measurements as well as the machine interpretation, and imaging and functional test data are available as the free text results. The images are not part of the SEM cohort data but can be obtained in specific projects.
Basic cohort characteristics
The SEM cohort is briefly described in Table 3 and includes 325 539 unique patients with 630 275 ED visits during 2017 and 2018. Fewer than five patients declined participation which makes the cohort almost 100% complete. The mean age was 55 years, 49% were male and 23.5% of all patients arrived by ambulance. The most common triage category was 3, Yellow, and 15.0% of the patients had no registered triage category mostly due to immediate referral from the ED to external primary care or self-care. 11% of the patients had previous diagnoses of diabetes, 10% of cancer, 8% of pulmonary disease, and 1.7% suffered from dementia.
Table 4 shows that the most common chief complaint in SEM was abdominal pain, followed by chest pain, dyspnea, hand injury and unspecific disorder. (The term “unspecific disorder” is used when the triage nurse is unable to classify the patient’s problem using the more specific terms in the system.) Some 9% of all visits had no registered chief complaint, again mostly because of immediate referral to primary or self-care. The median time to doctor was 70 min and the median length of stay was 206 min. In 24% percent of all ED visits the patient was admitted to in-hospital care.
As can be seen in Table 5 , the most common discharge diagnoses were bacterial pneumonia, cerebrovascular incident, and acute myocardial infarction. The mortality at the ED was 0.2%, it was 0.9% within 7 days, and 2.2% within 30 days.
In addition to CDSS development, SEM’s large amount of real-world ED patient data with almost complete follow-up will allow research in many fields of emergency medicine: Epidemiology, patient management, diagnostics, prognostics, ED crowding, resource allocation, and social medicine. Some of these studies may need supplementary ethics approval. The SEM cohort is currently being used to analyze cases of missed acute aortic syndrome, for prediction of venous thromboembolism, mapping of characteristics and outcomes in patients with dizziness or with head trauma, and for the evaluation of emergency care for adult patients with congenital heart disease.
Studies of the epidemiology of ED patients may be beneficial for public health surveillance, resource planning, evaluating healthcare delivery and for facilitating research, e.g. sample size calculations for prospective studies. Epidemiological information supports clinical evidence-based decision-making and enables the ED to organize according to the needs of the population. The SEM cohort includes almost all patients presenting at eight EDs in southern Sweden during two years, and it should therefore be possible to obtain reasonably accurate and generalizable data on chief complaints and underlying disease states in the entire population as well as in subgroups based on age, sex, comorbidities or sociodemographics. Also, diurnal, weekly, and seasonal variations may be described.
ED patient management and its impact on outcomes may be studied in the SEM cohort by analyzing e.g. waiting times, length of ED stay, admissions to intensive care, as well as patients who left without being seen by a physician or who returned to the ED. These analyses may also be made in the absence or presence of ED crowding. As mentioned, pharmaceutical treatment at the ED is not immediately available but can be extracted for all patients from the digitized (scanned) ED patient paper records.
The SEM cohort allows analysis of the accuracy of diagnostic and functional testing by comparing pre-test probability with short or medium-term outcomes such as diagnoses or death.
The utilization and costs of diagnostic testing, hospital admission and care at specific wards in each patient up to 30 days in the cohort can be used to analyze resource use in all patients and in specific subgroups. Also, the SEM cohort may be used to evaluate ED care and acute healthcare consumption in different socioeconomic and demographic groups, as well as inequalities and possible discrimination.
Strengths and limitations
SEM includes real-world clinical data from consecutive patients presenting to eight different EDs during two years. The large number of patient visits, variables, and clinical events should be sufficient for most analyses of interest. Data were collected in regular care and there are several general advantages with using routine care data when building CDSS. Firstly, it provides access to large amounts of data from a diverse and unselected patient population, which is crucial for developing CDSS that work across different patient demographics. Secondly, routine care data may be immediately available, reducing the cost and time required to collect data. Finally, routine care data collection will often allow simple tracking of patient outcomes and evaluation of the effectiveness of the CDSS, especially in a country with comprehensive healthcare databases like Sweden. In the future, it may be possible to use native, uncurated electronic health records directly for medical research [ 17 ]. Another strength of the multimodal SEM cohort is its potential utility in developing CDSS that provide relative risks of multiple diagnoses, in contrast to algorithms based on a single type of input and output (e.g. radiology algorithms detecting cancer), and current clinical decision support tools which often serve merely as rule-out tests, e.g. the PERC rule for pulmonary embolism.
SEM includes data from ED patient visits in one Swedish region, and the data may therefore not be generalizable to other populations or healthcare settings. There are few patients in the SEM cohort with problems related to psychiatry, obstetrics/gynecology, and ophthalmology, as well as few pediatric patients without orthopedic problems. Some clinical variables are missing or less readily available in SEM, e.g. free text imaging results that require manual review, and this will of course prevent or complicate the creation of some types of CDSS, as well as some data disaggregation. Missing data in SEM are rare, but there may of course be errors in the data, which can lead to biased or inaccurate CDSS. Since SEM data were registered as part of regular care, bias may also arise from different patient evaluation and management based on previous clinical findings (verification bias) or based on patients’ ethnic or socioeconomic background. Also, historical bias will exist in any clinical database, i.e. when the data no longer accurately reflect a new healthcare reality.
Several variables in the SEM database were originally manually entered or determined subjectively, such as time stamps in the ED and discharge diagnoses and may therefore contain errors or bias. Diagnoses might also have been registered several times for the same care episode. Bias or errors in the training data will cause a high risk of bias in the final CDSS, but the size and impact of the problem will vary in different CDSS. The optimal approach to the potential problem with bias is therefore best determined in each use case and CDSS. Before clinical implementation, any CDSS based on SEM data should be carefully reviewed and prospectively tested in a clinical trial in the specific healthcare setting.
On the other hand, it should be noted that if a CDSS is intended to operate in real time with standard register data as input, it is preferable that the underlying ML model is developed using this type of data rather than curated data that do not reflect the “dirty” truth of day-to-day operations. With sufficiently large training data, current ML algorithms can cope with a fair amount of noise and navigate between varying levels of noise in different types of input data.
In addition to algorithm quality, several barriers to successful implementation and use of AI/ML-based CDSS must be considered: IT problems, low model transparency (black box algorithms), proprietary code, lack of trust and knowledge among physicians and decision-makers, legal framework (oversight, malpractice issues) and ethical issues, integrity risks and financial challenges [ 18 , 19 , 20 ]. However, the size and implications of these barriers will vary in different use cases.
In conclusion, the SEM cohort provides a platform for collaborative CDSS research. SEM’s large amount of real-world patient data with almost complete follow-up will also allow research in epidemiology, patient management, diagnostics, prognostics, ED crowding, resource allocation, and social medicine.
SEM cohort access
So far, collaborations have been established with other research groups at Lund and Halmstad Universities in Sweden. We welcome initiatives on international collaborative projects using the SEM cohort. Anonymized parts of the SEM database will be available for sharing on reasonable request, as will detailed variable lists. Please contact the corresponding author via email ([email protected]).
Data availability
Anonymized parts of the SEM database will be available for sharing on reasonable request. Please send an email to [email protected].
Abbreviations
artificial intelligence
clinical decision support system
emergency department
machine learning
rapid emergency triage and treatment system
Skåne emergency medicine cohort
Muth C, Blom JW, Smith SM, et al. Evidence supporting the best clinical management of patients with multimorbidity and polypharmacy: a systematic guideline review and expert consensus. J Intern Med. 2019;285(3):272–88. https://doi.org/10.1111/joim.12842
Article CAS PubMed Google Scholar
Socialstyrelsen. Väntetider och patientflöden på akutmottagningar. 2015:1–80. ( http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19990/2015-12-11.pdf ).
Lynch S. Andrew Ng: Why AI Is the New Electricity. Stanford Graduate School of Business. ( https://www.gsb.stanford.edu/insights/andrew-ng-why-ai-new-electricity)
Obermeyer Z, Emanuel EJ. Predicting the Future - Big Data, Machine Learning, and Clinical Medicine. N Engl J Med. 2016;375(13):1216–9. https://doi.org/10.1056/NEJMp1606181
Article PubMed PubMed Central Google Scholar
Tang X. The role of artificial intelligence in medical imaging research. BJR Open. 2020;2(1):20190031. https://doi.org/10.1259/bjro.20190031
Article PubMed Google Scholar
Harrou F, Dairi A, Kadri F, Sun Y. Forecasting emergency department overcrowding: a deep learning framework. Chaos Solitons Fractals. 2020;139:110247. https://doi.org/10.1016/j.chaos.2020.110247
Sudarshan VK, Brabrand M, Range TM, Wiil UK. Performance evaluation of Emergency Department patient arrivals forecasting models by including meteorological and calendar information: a comparative study. Comput Biol Med. 2021;135:104541. https://doi.org/10.1016/j.compbiomed.2021.104541
NHS using AI to. Reduce ‘avoidable’ hospital admissions this winter. The Independent: Nov 14; 2023. https://www.independent.co.uk/
Google Scholar
Socialstyrelsen. Digitala vårdtjänster och artificiell intelligens i hälso- och sjukvården. Swedish National Board of Health and Welfare (Socialstyrelsen); 2019.
AIR Lund– Artificially Intelligent use of Registers at Lund University. Lund University. ( https://portal.research.lu.se/en/projects/air-lund-artificially-intelligent-use-of-registers ).
Predicare. The RETTS system. ( https://predicare.com/ ).
TietoEvry. Patientliggaren. ( https://www.tietoevry.com/ ).
Statistics Sweden. ( https://www.scb.se/en/ ).
Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. https://doi.org/10.1186/1471-2458-11-450
Wettermark B, Hammar N, Fored CM, et al. The new Swedish prescribed Drug Register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16(7):726–35. https://doi.org/10.1002/pds.1294
Brooke HL, Talback M, Hornblad J, et al. The Swedish cause of death register. Eur J Epidemiol. 2017;32(9):765–73. https://doi.org/10.1007/s10654-017-0316-1
Article CAS PubMed PubMed Central Google Scholar
Khan MS, Usman MS, Talha KM et al. Leveraging electronic health records to streamline the conduct of cardiovascular clinical trials. Eur Heart J 2023. https://doi.org/10.1093/eurheartj/ehad171
Stewart J, Lu J, Goudie A, et al. Applications of machine learning to undifferentiated chest pain in the emergency department: a systematic review. PLoS ONE. 2021;16(8):e0252612. https://doi.org/10.1371/journal.pone.0252612
Panch T, Mattie H, Celi LA. The inconvenient truth about AI in healthcare. NPJ Digit Med. 2019;2:77. https://doi.org/10.1038/s41746-019-0155-4
Goodman KE, Rodman AM, Morgan DJ. Preparing Physicians for the clinical algorithm era. N Engl J Med. 2023;389(6):483–7. https://doi.org/10.1056/NEJMp2304839
Welch S, Augustine J, Camargo CA Jr., Reese C. Emergency department performance measures and benchmarking summit. Acad Emerg Med. 2006;13(10):1074-80. (In eng). DOI: j.aem.2006.05.026 [pii] https://doi.org/10.1197/j.aem.2006.05.026
The American College of Surgeons CoT. Resources for Optimal Care of the injured patient. The American College of Surgeons; 2006.
National Prescribed Drug Register. National Board of Health and Wellfare. Jan 14. 2022 ( https://www.socialstyrelsen.se/en/statistics-and-data/registers/national-prescribed-drug-register/ ).
National Patient Register, Swedish National Board of Health and Welfare. ( https://www.socialstyrelsen.se/en/statistics-and-data/registers/national-patient-register/ ).
National Cause of Death Register. National Board of Health and Welfare. ( https://www.socialstyrelsen.se/en/statistics-and-data/registers/ ).
Letterstal A, Ekelund U, Castren M, Lindmarker P, Safwenberg U, Kurland L. [SVAR–a unique Swedish emergency registry]. Lakartidningen. 2010;107(43):2659–60. http://www.ncbi.nlm.nih.gov/pubmed/21137537
PubMed Google Scholar
Ekelund U, Kurland L, Eklund F, et al. Patient throughput times and inflow patterns in Swedish emergency departments. A basis for ANSWER, A National SWedish Emergency Registry. Scand J Trauma Resusc Emerg Med. 2011;19:37. https://doi.org/10.1186/1757-7241-19-37
The Swedish Emergency Care Registry. SVAR. ( https://www.ucr.uu.se/svar/ ).
Siemens Healthineers. ( https://www.siemens-healthineers.com/en-uk ).
Healthcare G. ( https://www.gehealthcare.com/ ).
SECTRA. ( https://sectra.com/ ).
Download references
Acknowledgements
We are grateful for the excellent help and project coordination by Cecilia Åkesson Kotsaris, and for the invaluable data management by Paul Söderholm, both at Region Skåne. We also thank the patients for their participation, and the research assistants and the emergency department staff in Region Skåne for their kind help.
The study was supported by an ALF research grant at Skåne University Hospital and by a grant from Region Skåne. This study was part of the AIR Lund (Artificially Intelligent use of Registers at Lund University) research environment and received funding from the Swedish Research Council (VR; grant no. 2019 − 00198). There was no industry involvement. Funding organizations had no role in the planning, design, or conduct of the study, collection, analysis or interpretation of data, or preparation, review or approval of the manuscript.
Open access funding provided by Lund University.
Author information
Authors and affiliations.
Emergency medicine, Department of Clinical Sciences Lund, Lund University, Department of Emergency Medicine, Skåne University Hospital, Lund, Sweden
Ulf Ekelund & Pontus Olsson de Capretz
Department of Clinial Sciences Malmö, Lund University, Department of Internal Medicine, Skåne University Hospital, Malmö, Sweden
Bodil Ohlsson & Olle Melander
Occupational and Environmental Medicine, Department of Laboratory Medicine, Lund University, Lund, Sweden
Jonas Björk & Axel Nyström
Forum South, Clinical Studies Sweden, Skåne University Hospital, Lund, Sweden
Jonas Björk
Emergency medicine, Department of Clinical Sciences Lund, Lund University, Department of Emergency Medicine, Helsingborg Hospital, Helsingborg, Sweden
Jakob Lundager Forberg
Centre for Environmental and Climate Science, Lund University, Lund, Sweden
Mattias Ohlsson, Axel Nyström & Anders Björkelund
Center for Applied Intelligent Systems Research (CAISR), Halmstad University, Halmstad, Sweden
Mattias Ohlsson
You can also search for this author in PubMed Google Scholar
Contributions
UE, BO, and OM conceived the cohort, were responsible for the ethics approval, and generated funding together with JB. JB, MO, JLF and POC provided expert opinion in the design of the cohort and the database. AB led the data management together with AN and made the general data analyses. UE and AB drafted the manuscript. All authors critically revised and approved the final manuscript and meet the criteria for authorship established by the ICMJE.
Corresponding author
Correspondence to Ulf Ekelund .
Ethics declarations
Ethics approval and consent to participate.
The creation of the SEM cohort and its use for AI/ML research and cross-sectional analyses has been approved by the Swedish Ethical Review Authority (Dnr 2019–05783) and Region Skåne (KVB 302 − 19). There is no approval for commercial use of the data. All included patients had access to written information on the SEM cohort and its purpose, and had the possibility to decline participation at any time, for any reason.
Consent for publication
Not applicable.
Competing interests
None of the authors declare competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ekelund, U., Ohlsson, B., Melander, O. et al. The skåne emergency medicine (SEM) cohort. Scand J Trauma Resusc Emerg Med 32 , 37 (2024). https://doi.org/10.1186/s13049-024-01206-0
Download citation
Received : 18 October 2023
Accepted : 11 April 2024
Published : 26 April 2024
DOI : https://doi.org/10.1186/s13049-024-01206-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency medicine
- Emergency department
- Decision-making
- Artificial intelligence
- Machine learning
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine
ISSN: 1757-7241
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essay Examples >
- Essays Topics >
- Essay on Literature
Short Story Emergency Essay Examples
Type of paper: Essay
Topic: Literature , Psychology , Environment , Medicine , Nursing , Nature , Surrealism , Drugs
Published: 12/16/2019
ORDER PAPER LIKE THIS
Emergency is set in the emergency department of a hospital. In this interesting and unique tale, readers are introduced to an unreliable narrator and his equally questionable friend. Both in reality and as a result of drug induced hallucination, Johnson exploits the use of place in both setting up and accentuating the themes of the story.
The narrator has been working in the hospital as a clerk for the last few weeks. He had his friend, Georgie, abuse drugs, and Georgie takes them illegally from the medical supplies in the hospital. The nature of the story lends itself to being set in a hospital as, clearly, this makes the drug use both easier to fashion and more dire as the stoned men are caring for sick and vulnerable people. The concept of an orderly and a clerk being under the influence of drugs while at work in a hospital setting is both unsettling and dark. Although at times amusing, this is a dire situation. The same could be said about the emergency department of a hospital; both unpredictable and surreal, the place literally holds life and death within its grasp.
Through the setting of the emergency department of the hospital, the story verges on the surreal. As the narrator is on drugs it is possible that his account of events is unreliable. It is also feasible that many of the happenings are part of a drug fuelled trip. Johnson uses the place of the emergency department as an appropriate backdrop for the various characters and incidents that he introduces to his readers. The constantly changing environment of his kind of hospital ward serves to accentuate the randomness experienced by the characters throughout the story.
Based on the information in the story itself, it is set in the summer. However, conversation between the two friends moved into winter during the narrative. Clearly, here is a difference between the reality of the situation and the narrator's hallucination of being close to nature. Moving between such contrasting seasons demonstrates the state of mind of the narrator. If something as fundamental and scientific as the seasons can be interpreted as fluid, it is possible that everything in the story is equally so. In this respect, the author has used setting and place to demonstrate the interior and exterior world of the unreliable narrator.
The story is based upon two hospital staff members which experiment illegally with the drugs used by medical professionals. The nature of this concept allows the author to use place to his advantage in all ways. Firstly, the hospital is an ever changing, unique environment and therefore lends itself to random happenings, and events that could seem surreal even to someone who was not under the influence of drugs. Secondly, however, the hallucinations experienced by the narrator mean that the place can be as fluid as his state of mind.
Johnson has both well-chosen and well-developed the sense of place in this story. The fluid and random nature of an emergency department perfectly reflects the state of mind and the experiences of the narrator. Both on a literal level and a metaphorical one, the hospital setting provides a backdrop for the main themes of the story.
Johnson, D. (2002). Emergency. Jesus’ Son. Reclam Philipp Jun

Cite this page
Share with friends using:
Removal Request

Finished papers: 914
This paper is created by writer with
ID 272799898
If you want your paper to be:
Well-researched, fact-checked, and accurate
Original, fresh, based on current data
Eloquently written and immaculately formatted
275 words = 1 page double-spaced

Get your papers done by pros!
Other Pages
Impotence research papers, crude oil research papers, carpentry research papers, oratory research papers, minimum wage research papers, gourmet research papers, airfoil research papers, fairy tales argumentative essays, the cultivation analysis theory essay sample, vitamins and minerals assignment course work examples, free essay on sustainable environment, organizational development and change critical thinking, example of biography on ayn rand, example of other creative writing, name term paper examples, example of research paper on law enforcement management, a review of current and evolving trends in terrorism financing article review example, learning a second language research paper sample, good essay about jerry perezs profile, counterarguments argumentative essay sample, example of difference between noir and ne noir essay, free report on performance management 2, example of engaging class motivation in second language learning essay, good example of essay on human emotion of guilt, good example of essay on machine learning perceptron, good example of omega house management conflicts essay, following the american psychological associations guidelines research papers examples, example of preface 3 essay, free research paper on east asia, military psychology research paper sample, sample movie review on the twilight samurai, investment proposal case study example, maxima essays, roger ebert essays, charlize theron essays, edward heath essays, sanak essays, clint mansell essays, mohamed bouazizi essays, packwood essays, oak ridge essays, jean fouquet essays, louis renault essays.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline

COMMENTS
Emergency Medicine Personal Statement Sample #1. On the second day of my medical school rotations, one of the attendings pointed at me and said, "Now he looks like an ER doc." I laughed because I was not surprised at all. I have always gravitated toward Emergency Medicine because it fits my personality.
Those who write papers in the bottom 10% are often the ones who are shooting for the top 5%; we, therefore, recommend that your goal should be the middle 85%. The goal of your statement should be to explain why you want to go into emergency medicine and why you think emergency medicine is the right specialty for you. Overarching theme
Type of paper: Admission Essay. Topic: Medicine, Teaching, Nursing, God, Students, Life, Patient, Doctor. Pages: 4. Words: 1100. Published: 12/02/2019. It is said that the best healers are the wounded ones. I didn't understand what that meant until I became wounded, myself. My passion for emergency medicine goes way back to my own personal crisis.
Rachel Rudeen, former admissions coordinator for the University of Minnesota Medical School, says personal statements help medical schools determine whether applicants have the character necessary ...
Elevating the capability of early identification, appropriate treatment, and life support for severe or critical patients will always be the core topics of emergency medicine. Emergency medicine in the future will be characterized by continuous advances in practices, research, technologies, and so forth. In terms of clinical practices, problems ...
Aside from having a longstanding interest in Emergency Medicine and Global Health, I have really enjoyed being involved in international collaborations and initiatives aimed at promoting free open access medical education (FOAMed). Outside of Medicine, I enjoy running, spending time outdoors and discovering new coffee shops! ...
INTRODUCTION. Emergency medicine (EM) has advanced profoundly since its specialty recognition in 1979. As diagnosis and treatment changes, payment restructures and best practices evolve. 1 We drive these changes, impacting hospital throughput and revenue to ensure quality emergency care. Our impact on the practice of medicine depends on a body of knowledge, the "biology" of emergency ...
Ringwood, Victoria, Australia: Penguin Books; 1966:87. ACEP Now offers real-time clinical news, news from the American College of Emergency Physicians, and news on practice trends and health care reform for the emergency medicine physician. ACEP Now is an official publication of the American College of Emergency Physicians.
Get your free examples of research papers and essays on Emergency Medicine here. Only the A-papers by top-of-the-class students. Learn from the best! ... with several success factors such as development of a vision for the future and establishment of key targets for the short and long-term. Health policies enable organizations, institutes ...
Principles of Emergency Medicine 3 Approach to the emergency patient be prepared to act and react to prevent morbidity and, when possible, mortality. EPs must maintain a healthy skepticism towards patient's answers to common ques-tions. Considering worst-case scenarios is fundamental to emergency medicine (EM) practice. Most importantly,
A Brief History of Emergency Medical Services in the United States. 3/22/2016 Joshua Bucher, MD , Hashim Zaidi, MD. Pre-hospital emergency care in the modern age is often described as a "hierarchy" of human and physical resources utilized in the acute setting to provide the best possible patient care until definitive care can be established.
AMCAS essays are limited to 5300 characters—not words! ... In ten years' time, I hope to be trained in the field of emergency medicine, which, surprisingly, is a specialization that is actually lacking here in the United States as compared to similarly developed countries. ... In short, I see the role of physicians in society as ...
There are many ways of approaching an essay such as this one. Here are some methods that we find useful, and we hope they will be helpful to you as well. ... Dial 911 in the event of a medical emergency; Explore Health Care. Learn how we are healing patients through science & compassion . Back. ... Technology and Medicine Summer Internship ...
GENERAL ADULT EMERGENCY MEDICINE. Unchanged emergency department discharge rates for pulmonary embolism (April 2024) Outpatient anticoagulation to avoid hospitalization is safe for a select group of patients with acute pulmonary embolism (PE). However, a recent study of over 1.6 million emergency department (ED) visits for PE in the United ...
It is often difficult to keep up with all of the highest impact papers in emergency medicine. ... Clinical cure occurred in 88.6% in the short group and 90.8% in the control group (risk difference, -0.016; 97.5% confidence limit, -0.087). In pediatric patients who are otherwise healthy presenting with community-acquired pneumonia, it is ...
Patients in emergency rooms are likely to exhibit certain characteristics that justify the need for emergency treatment. Some of them could be unconscious while others may exhibit signs of a heart attack. Such instances include chest tightness, light headedness, pressure and severe chest pains. Alternatively, people may visit the emergency room ...
1048 Words. 5 Pages. 7 Works Cited. Open Document. Emergency room physicians are on the front lines in a crisis, caring for everyone from trauma victims to sick kids. An ability to think quickly and care for a wide variety of patients makes them valuable assets at every hospital. It also brings some perks.
Emergency: Stories about urgent situations. This week we present two stories from people who deal with emergencies. Part 1: As a first-generation pre-med student with no financial aid, Brooke Dolecheck takes a job as a 911 operator to support herself. Brooke Dolecheck graduated from Boise State University in 2019 with a Bachelor of Arts in ...
1. Emergency Medicine Admission Essay Emergency Medicine became a potential career option for me after I obtained my Emergency Medical Technician Basic Certification the year before I entered medical school. I worked full-time in the emergency department as a patient transporter, which gave me the privilege of witnessing and participating in the daily work of the physicians and nurses.
Mayhem and Medicine. Every day in the United States, an average of 100 people are killed with guns and hundreds more are injured. One consequence is that U.S. physicians have been drafted to serve ...
For a preview of our questions, read on for two free Emergency Medicine questions written by leading medical practitioners. Question 1. A 50 y/o man is brought into the ER by coworkers following an accidental splash into his eyes with chemicals. The workers don't know what the liquid was but they work in a factory where they etch glass.
gaging way to enhance your emergency medicine learning journey. These ebooks are intended to be an adjunct to the EmergencyMedicineCases.com podcasts, as well as to existing emergency medicine curricula and resources. For optimal learning, we suggest EM Cases Digest be used in conjunction with the podcasts for spaced, repetitive learning,
Background In the European Union alone, more than 100 million people present to the emergency department (ED) each year, and this has increased steadily year-on-year by 2-3%. Better patient management decisions have the potential to reduce ED crowding, the number of diagnostic tests, the use of inpatient beds, and healthcare costs. Methods We have established the Skåne Emergency Medicine ...
Published: 12/16/2019. Emergency is set in the emergency department of a hospital. In this interesting and unique tale, readers are introduced to an unreliable narrator and his equally questionable friend. Both in reality and as a result of drug induced hallucination, Johnson exploits the use of place in both setting up and accentuating the ...