- Introduction to Genomics
- Educational Resources
- Policy Issues in Genomics
- The Human Genome Project
- Funding Opportunities
- Funded Programs & Projects
- Division and Program Directors
- Scientific Program Analysts
- Contact by Research Area
- News & Events
- Research Areas
- Research investigators
- Research Projects
- Clinical Research
- Data Tools & Resources
- Genomics & Medicine
- Family Health History
- For Patients & Families
- For Health Professionals
- Jobs at NHGRI
- Training at NHGRI
- Funding for Research Training
- Professional Development Programs
- NHGRI Culture
- Social Media
- Broadcast Media
- Image Gallery
- Press Resources
- Organization
- NHGRI Director
- Mission & Vision
- Policies & Guidance
- Institute Advisors
- Strategic Vision
- Leadership Initiatives
- Diversity, Equity, and Inclusion
- Partner with NHGRI
- Staff Search

Genetic Disorders
Many human diseases have a genetic component. Some of these conditions are under investigation by researchers at or associated with the National Human Genome Research Institute (NHGRI).
A genetic disorder is a disease caused in whole or in part by a change in the DNA sequence away from the normal sequence. Genetic disorders can be caused by a mutation in one gene (monogenic disorder), by mutations in multiple genes (multifactorial inheritance disorder), by a combination of gene mutations and environmental factors, or by damage to chromosomes (changes in the number or structure of entire chromosomes, the structures that carry genes). As we unlock the secrets of the human genome (the complete set of human genes), we are learning that nearly all diseases have a genetic component. Some diseases are caused by mutations that are inherited from the parents and are present in an individual at birth, like sickle cell disease. Other diseases are caused by acquired mutations in a gene or group of genes that occur during a person's life. Such mutations are not inherited from a parent, but occur either randomly or due to some environmental exposure (such as cigarette smoke). These include many cancers, as well as some forms of neurofibromatosis.
List of Genetic Disorders
This list of genetic, orphan and rare diseases is provided for informational purposes only and is by no means comprehensive.

Featured Content
Last updated: May 18, 2018

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

8.6: Genetic Disorders
- Last updated
- Save as PDF
- Page ID 16765

- Suzanne Wakim & Mandeep Grewal
- Butte College
Each hand in Figure \(\PageIndex{1}\) has an extra pinky finger. This is a condition called polydactyly, which literally means "many digits." People with polydactyly may have extra fingers and/or toes, and the condition may affect just one hand or foot or both hands and feet. Polydactyly is often genetic in origin and may be part of a genetic disorder that is associated with other conditions.

What Are Genetic Disorders?
Genetic disorders are diseases, syndromes, or other conditions that are caused by mutations in one or more genes or by chromosomal alterations. Genetic disorders are typically present at birth, but they should not be confused with congenital disorders, which are any disorders, regardless of cause, that are present at birth. Some congenital disorders are not caused by genetic mutations or chromosomal alterations. Instead, they are caused by problems that arise during embryonic or fetal development or during the process of birth. An example of a nongenetic congenital disorder is fetal alcohol syndrome. This is a collection of birth defects, including facial anomalies and intellectual disability, caused by maternal alcohol consumption during pregnancy.
Genetic Disorders Caused by Mutations
Table \(\PageIndex{1}\) lists several genetic disorders caused by mutations in just one gene. Some of the disorders are caused by mutations in autosomal genes, others by mutations in X-linked genes. Which disorders would you expect to be more common in males than females?
Very few genetic disorders are controlled by dominant mutant alleles. A dominant allele is expressed in every individual who inherits even one copy of it. If it causes a serious disorder, affected people may die young and fail to reproduce. Therefore, the mutant dominant allele is likely to die out of the population.
A recessive mutant allele, such as the allele that causes sickle cell anemia or cystic fibrosis, is not expressed in people who inherit just one copy of it. These people are called carriers. They do not have the disorder themselves, but they carry the mutant allele and their offspring can inherit it. Thus, the allele is likely to pass on to the next generation rather than die out.
Genetic Disorders Caused by Chromosomal Alterations
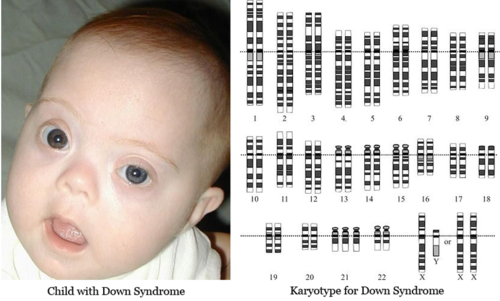
As we learned in the Cell Reproduction chapter , mistakes may occur during meiosis that results in nondisjunction . This is the failure of replicated chromosomes to separate properly during meiosis. Some of the resulting gametes will be missing all or part of a chromosome, while others will have an extra copy of all or part of the chromosome. If such gametes are fertilized and form zygotes, they usually do not survive. If they do survive, the individuals are likely to have serious genetic disorders.
Table \(\PageIndex{2}\) lists several genetic disorders that are caused by atypical numbers of chromosomes. Most chromosomal disorders involve the X chromosome. The X and Y chromosomes are the only chromosome pair in which the two chromosomes are very different in size. This explains why nondisjunction of the sex chromosomes tends to occur more frequently than nondisjunction of autosomes.
Diagnosing and Treating Genetic Disorders
A genetic disorder that is caused by a mutation can be inherited. Therefore, people with a genetic disorder in their family may be concerned about having children with the disorder. A genetic counselor can help them understand the risks of their children being affected. If they decide to have children, they may be advised to have prenatal (“before birth”) testing to see if the fetus has any genetic disorders. One method of prenatal testing is amniocentesis. In this procedure, a few fetal cells are extracted from the fluid surrounding the fetus in utero , and the fetal chromosomes are examined. Down syndrome and other chromosomal alterations can be detected in this way.
The symptoms of genetic disorders can sometimes be treated or prevented. For example, in the genetic disorder called phenylketonuria (PKU) , the amino acid phenylalanine builds up in the body to harmful levels. PKU is caused by a mutation in a gene that normally codes for an enzyme needed to break down phenylalanine. The buildup of PKU can lead to serious health problems, such as intellectual disability and delayed development, among other serious problems. Babies in the United States and many other countries are screened for PKU soon after birth. If PKU is diagnosed, the infant can be fed a low-phenylalanine diet. This prevents the buildup of phenylalanine and the health problems associated with it. With a low phenylalanine diet, most symptoms of the disorder can be prevented.
Curing Genetic Disorders
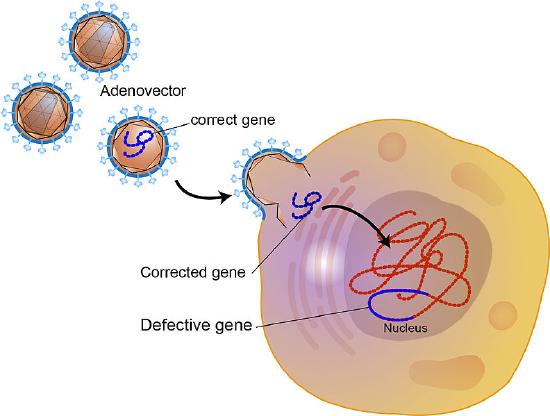
Cures for genetic disorders are still in the early stages of development. One potential cure is gene therapy. Gene therapy is an experimental technique that uses genes to treat or prevent disease. In gene therapy, normal genes are introduced into cells to compensate for mutated genes. If a mutated gene causes a necessary protein to be nonfunctional or missing, gene therapy may be able to introduce a normal copy of the gene to produce the needed functional protein.
A gene that is inserted directly into a cell usually does not function, so a carrier called a vector is genetically engineered to deliver the gene (Figure \(\PageIndex{3}\)). Certain viruses, such as adenoviruses , are often used as vectors. They can deliver the new gene by infecting cells. The viruses are modified so they do not cause disease when used in people. If the treatment is successful, the new gene delivered by the vector will allow the synthesis of a functioning protein.
Feature: Human Biology in the News
Down syndrome is the most common genetic cause of intellectual disability. It occurs in about 1 in every 700 live births, and it currently affects nearly half a million Americans. Until recently, scientists thought that the changes leading to intellectual disability in people with Down syndrome all happen before birth.
Researchers recently discovered a genetic disorder that affects brain development in people with Down Syndrome throughout childhood and into adulthood. The newly discovered genetic disorder changes communication between nerve cells in the brain, resulting in the slower transmission of nerve impulses. This finding may eventually allow the development of strategies to promote brain functioning in Down syndrome patients and may also be applicable to other developmental disabilities such as autism.
- Define genetic disorder.
- Identify three genetic disorders caused by mutations in a single gene.
- Why are single-gene genetic disorders more commonly controlled by recessive than dominant mutant alleles?
- What is nondisjunction? Why may it cause genetic disorders?
- Explain why genetic disorders caused by a number of chromosomes most often involve the X chromosome.
- How is Down syndrome detected in utero ?
- Use the example of PKU to illustrate how the symptoms of a genetic disorder can sometimes be prevented.
- Explain how gene therapy works.
- Compare and contrast genetic disorders and congenital disorders.
- Explain why parents that do not have Down syndrome can have a child with Down syndrome.
- Hemophilia A and Turner’s syndrome both involve problems with the X chromosome. What is the major difference between these two types of disorders in terms of how the X chromosome is affected?
- Can you be a carrier of Marfan syndrome and not have the disorder? Explain your answer.
- True or False. It is impossible for people to have more than three copies of one chromosome.
- True or False. The gene for sickle cell anemia is on a sex chromosome.
Explore More
Scientists have promised that gene therapy will be the next big leap for medicine, but what is it exactly? Learn more here:
Attributions
- Polydactyly by Baujat G, Le Merrer M. CC BY 2.0 via Wikimedia Commons
- Down Syndrome Karyotype by National Human Genome Research Institute, public domain via Wikimedia Commons
- Brushfield eyes by Erin Ryan, public domain via Wikimedia Commons
- Virus by Darryl Leja at NHGRI public domain via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0
Genetics Basics
- Glossary of Genomic Terms
Genetics research studies how individual genes or groups of genes are involved in health and disease. Understanding genetic factors and genetic disorders is important in learning more about promoting health and preventing disease.
Some genetic changes have been associated with an increased risk of having a child with a birth defect or developmental disability or developing diseases such as cancer or heart disease. Genetics also can help us understand how medical conditions happen.
How We Get Our Genes
People get (inherit) their chromosomes , which contain their genes , from their parents. Chromosomes come in pairs and humans have 46 chromosomes, in 23 pairs. Children randomly get one of each pair of chromosomes from their mother and one of each pair from their father. The chromosomes that form the 23rd pair are called the sex chromosomes. They decide if a person is born a male or female. A female has two X chromosomes, and a male has one X and one Y chromosome. Each daughter gets an X from her mother and an X from her father. Each son gets an X from his mother and a Y from his father.
Genetic Disorders
Genetic disorders can happen for many reasons. Genetic disorders often are described in terms of the chromosome that contains the gene that is changed in people who have the disorder. If the gene is on one of the first 22 pairs of chromosomes, called the autosomes, the genetic disorder is called an autosomal condition. If the gene is on the X chromosome, the disorder is called X-linked.
Genetic disorders also are grouped by how they run in families. Disorders can be dominant or recessive, depending on how they cause conditions and how they run in families.
Dominant diseases can be caused by only one copy of a gene having a DNA mutation . If one parent has the disease, each child has a 50% chance of inheriting the mutated gene.
For recessive diseases, both copies of a gene must have a DNA mutation in order to get one of these diseases. If both parents have one copy of the mutated gene, each child has a 25% chance of having the disease, even though neither parent has it. In such cases, each parent is called a carrier of the disease. They can pass the disease on to their children, but do not have the disease themselves.
Single Gene Disorders

Chapter 6. Genetic Disorders
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
- Autosomal Dominant Disorders
- Autosomal Recessive Disorders
- Lysosomal Storage Disorders
- Glycogen Storage Disorders
- Genetic Conditions with X-Linked Inheritance Pattern
- Genetic Conditions with Mixed Inheritance Patterns
- Additional Genetic Abnormalities
- Sex Chromosome Abnormalities
- Diseases of Genomic Imprinting
- Sexual Differentiation Disorders
- Full Chapter
- Supplementary Content
There are three major types of mutations: (1) genome mutations, which involve loss or gain of an entire chromosome; (2) chromosomal mutations, which involve alterations in one or more chromosomes that are usually identifiable by karyotyping; and (3) gene mutations, which are partial or complete deletion of the gene or alteration of the base. Genome mutations usually result in death of the fetus, or death during infancy or early childhood.
Many diseases have a genetic component, albeit without a specific identifiable gene mutation. Such conditions are said to have a multifactorial inheritance pattern. Examples of such diseases include coronary artery disease, hypertension, gout, and diabetes mellitus.
When discussing genetic diseases, some definitions are important to remember: (1) hereditary or familial, a condition derived from parents (i.e., a condition that is transmitted in the germ line); and (2) congenital, a condition that is present at birth. Not all hereditary conditions are congenital, and not all congenital conditions are hereditary. Some hereditary conditions are manifested at the time of birth or shortly thereafter, and many manifest later in life.
The overall effects of the mutation of a single gene include (1) an enzyme defect; (2) defects in membrane receptors and/or transport system; (3) alterations in structure, function, or quantity of nonenzymatic protein; or (4) mutations resulting in unusual reactions to drugs. An enzyme defect can cause accumulation of substrate, a metabolic block resulting in a decreased amount of needed end product, or failure to inactivate a tissue-damaging substrate.
Overview: In general, autosomal dominant disorders have reduced penetrance and variable expressivity. They usually do not encode enzymes because a loss of up to 50% of an enzyme's activity can be compensated for by activity of the enzyme encoded by the normal allele ( Table 6-1 ).
LDL, low-density lipoprotein; APC, adenomatous polyposis coli.
Familial Hypercholesterolemia
Mutation: Low-density lipoprotein receptor gene ( LDL ); there are more than 100 known mutations.
Mechanism: The LDL receptor recognizes apolipoprotein B100 or apolipoprotein E; therefore, a mutation of the receptor results in impaired uptake of cholesterol into cells.
Manifestations of familial hypercholesterolemia
- Elevated cholesterol level: Heterozygotes have half the normal amount of LDL receptors and two to three times the normal level of cholesterol; homozygotes have five or more times the normal level of cholesterol.
- Tendon sheath xanthomas, corneal arcus, and xanthelasma.
- Early atherosclerosis and its consequences; homozygotes usually die of cardiovascular disease before the age of 30 years.
Familial Polyposis ...
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
infertility
30 templates
linguistics
89 templates
15 templates

28 templates

public health
35 templates

holy spirit
38 templates
Genetic Diseases
Genetic diseases presentation, free google slides theme, powerpoint template, and canva presentation template.
Download the "Genetic Diseases" presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking medical attention. This Google Slides theme and PowerPoint template is editable and can be used to teach the general public or medical students about a certain disease.
Features of this template
- 100% editable and easy to modify
- Different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

Register for free and start editing online
- Open access
- Published: 12 April 2024
Dual rare genetic diseases in five pediatric patients: insights from next-generation diagnostic methods
- Yupeng Liu 1 na1 ,
- Xue Ma 2 na1 ,
- Zhehui Chen 2 ,
- Ruxuan He 3 ,
- Yao Zhang 2 ,
- Hui Dong 2 ,
- Yanyan Ma 4 ,
- Tongfei Wu 2 ,
- Qiao Wang 5 ,
- Yuan Ding 5 ,
- Xiyuan Li 6 ,
- Dongxiao Li 7 ,
- Jinqing Song 2 ,
- Mengqiu Li 2 ,
- Ying Jin 2 ,
- Jiong Qin 1 &
- Yanling Yang ORCID: orcid.org/0000-0002-0034-0123 2
Orphanet Journal of Rare Diseases volume 19 , Article number: 159 ( 2024 ) Cite this article
69 Accesses
4 Altmetric
Metrics details
Clinicians traditionally aim to identify a singular explanation for the clinical presentation of a patient; however, in some cases, the diagnosis may remain elusive or fail to comprehensively explain the clinical findings. In recent years, advancements in next-generation sequencing, including whole-exome sequencing, have led to the incidental identification of dual diagnoses in patients. Herein we present the cases of five pediatric patients diagnosed with dual rare genetic diseases. Their natural history and diagnostic process were explored, and lessons learned from utilizing next-generation diagnostic technologies have been reported.
Five pediatric cases (3 boys, 2 girls) with dual diagnoses were reported. The age at diagnosis was from 3 months to 10 years. The main clinical presentations were psychomotor retardation and increased muscular tension, some accompanied with liver dysfunction, abnormal appearance, precocious puberty, dorsiflexion restriction and varus of both feet, etc. After whole-exome sequencing, nine diseases were confirmed in these patients: Angelman syndrome and Krabbe disease in case 1, Citrin deficiency and Kabuki syndrome in case 2, Homocysteinemia type 2 and Copy number variant in case 3, Isolated methylmalonic acidemia and Niemann-Pick disease type B in case 4, Isolated methylmalonic acidemia and 21-hydroxylase deficiency in case 5. Fifteen gene mutations and 2 CNVs were identified. Four novel mutations were observed, including c.15292de1A in KMT2D , c.159_164inv and c.1427G > A in SLC25A13 , and c.591 C > G in MTHFR .
Conclusions
Our findings underscore the importance of clinicians being vigilant about the significance of historical and physical examination. Comprehensive clinical experience is crucial for identifying atypical clinical features, particularly in cases involving dual rare genetic diseases.
In the realm of rare genetic diseases, ensuring effective medical management and genetic counseling hinges on providing precise diagnoses. However, clinical evaluations and conventional genetic testing bring about the diagnosis in < 50% patients [ 1 ]. The capacity to offer molecular diagnostics to patients has witnessed a substantial improvement, rapidly emerging as the most suitable method for those with rare diseases. Consequently, it has become an indispensable process for identifying various genetic diseases in a single patient [ 2 ].
A distinctive facet of the dual molecular diagnostic process is the occurrence of a unique or overlapping clinical diagnosis involving > 1 independently genetically separated locus. Medical literature intermittently features reports on patients with concomitant diagnoses of ≥ 2 genetically related disorders, colloquially known as “double trouble” [ 3 ]. The identification of a significant number of cases with dual genetic diseases is incidental, often occurring during next-generation or whole sequencing procedures [ 2 , 3 , 4 ]. Whole-exome sequencing data indicate that the prevalence of dual molecular diagnosis, contrary to previous assumptions, may be higher, readily detectable in approximately 7% cases [ 2 ]. Herein we present a description of the clinical evaluation of five patients with dual molecular diagnoses of genetic diseases.
From 2013 to 2022, 1,659 patients were diagnosed at our hospitals with inherited metabolic disorders via gene sequencing. In this retrospective study, we aimed to evaluate five pediatric patients exhibiting dual rare genetic diseases observed in our outpatient clinics. The comprehensive data collection encompassed age at onset and diagnosis, clinical manifestations, family history, treatment, and outcomes. In addition, routine blood and urine examination was performed to assess liver, renal, and heart functions.
Dried blood spots were collected for further analyses. As previously described, liquid chromatography–mass spectrometry (Waters MS/MS system A, 1445–002; API3200, Applied Biosystems, CA, USA) was employed to analyze blood amino acids, free carnitine, and acylcarnitines [ 5 , 6 , 7 ]. Metabolite concentrations were computed using ChemoView software. Urinary organic acids were analyzed using gas chromatography–mass spectrometry, which was performed on a Shimadzu GCMS-QP2010 system (Kyoto, Japan) [ 8 , 9 , 10 ]. Fluorescence polarization immunoassay was utilized to analyze plasma total homocysteine levels. Lysosomal enzyme activity in peripheral blood leukocytes was determined using a synthetic fluorescent substrate based on a standard curve.
Genomic DNA from peripheral blood samples was extracted, purified, and subsequently sent to Euler Genomics (Beijing, China), Berry Genomics Corporation (Beijing, China), and GrandOmics (Beijing, China) for next-generation or whole-exon sequencing for variant screening. DNA samples were sequenced on Illumina HiSeq 2500 (Illumina, San Diego, USA). Each variant was compared with information from 1000 Genomics ( www.1000genomes.org ), the ExAC database ( http://exac.broadinstitute.org/ ), and the gnomAD database ( http://gnomad.broadinstitute.org/ ). In silico analysis of variants to predict pathogenicity also involved Mutation Taster, PolyPhen-2, and SIFT. Interpretation of the variants was based on the Human Gene Mutation Database ( http://www.hgmd.cf.ac.uk/ac/index.php ). Pathogenicity assessment followed the American College of Medical Genetics and Genomics guidelines, classifying variants as pathogenic, likely pathogenic, variants of uncertain significance, likely benign, or benign.
Before research commencement, a consent form was signed by all patients or their caregivers, indicating their approval for all aspects of the clinical assessment, including genetic testing, and all ancillary testing (e.g., bone marrow aspiration).
Clinical reports
Case 1: angelman syndrome and krabbe disease.
Case 1, a 7-year-old boy, presented with general developmental delay, irritability, and a distinctive giggle. Physical assessment revealed muscle tension, limb stiffness, thumb buckling, and substandard comprehension proficiency. Brain MRI revealed myelin dysplasia, while blood amino acid and acylcarnitine profiles were normal. Electroencephalogram data indicated slow wave emission from bilateral occipital and temporal spines. Chromosome G banding was 46, XY. Whole-exome sequencing identified a 4.88 Mb deletion in 15q11.2q13.1 (copy number variation, CNV) and compound heterozygous variants, c.1963G > A (p.V655M) and c.1511T > C (p.L504P), in the GALC gene. The CNV was associated with Angelman syndrome, while the two GALC variants were found to originate from his parents (Tables 1 , 2 and 3 ). Peripheral leukocyte galactose cerebrosidase activity showed a significant decrease (3.8 nmol/g/h, normal range 33.4–123.9 nmol/g/h), confirming the diagnosis of Krabbe disease.
Case 2: Citrin deficiency and kabuki syndrome
Case 2, a girl, visited us with developmental delay and liver dysfunction. Born at term (weight, 3.3 kg) after an uncomplicated pregnancy, she exhibited persistent jaundice until 3 months of age. Elevated levels of serum alpha-fetoprotein and blood citrulline (110 µmol/L, normal range 10–50 µmol/L) were observed, along with mild liver dysfunction and hyperammonemia. Ultrasound of the abdomen revealed hepatomegaly, but brain MRI was normal. Treatment with a lactose-free diet led to gradual improvement, with liver function and blood citrulline level returning to normal after 6 months.
Physical examination revealed distinctive features, such as a long cleft on the eyelid, elongated lateral canthus, heavy eyebrows, cleft palate, and increased muscle tension. Chromosome G banding was 46, XX. Whole-exome sequencing identified a de novo variant c.15292de1A (p.T5098Lfs*49) in the KMT2D gene, supporting the diagnosis of Kabuki syndrome. Besides, compound heterozygous variants in the SLC25A13 gene, c.159_164inv (p.N54delinsD*) and c.1427G > A (p.R476Q), were identified. Her parents were heterozygous carriers at the same mutation site in SLC25A13. These findings confirmed the second diagnosis of citrin deficiency.
Case 3: homocysteinemia type 2 and copy number variant
A 10-year-old boy visited our hospital with psychomotor retardation and seizures. He exhibited normalcy during the newborn period. However, developmental delays in major motor skills surfaced after one month of age, with independent walking achieved at 3 years. A progressive deterioration in motor functions emerged at the age of 8 years, characterized by dysarthria, increased muscular tension in both lower limbs, dorsiflexion restriction, and varus of both feet, which were identified upon physical assessment. MRI indicated brain atrophy. Urinary organic acid, blood amino acid, and acylcarnitine profiles were normal, but plasma total homocysteine level was increased to 108.5 µmol/L (normal range 0–15 µmol/L) and 5-methyltetrahydrofolate level in cerebrospinal fluid was significantly decreased to 19.8 nmol/L (normal range 60–210 nmol/L), indicative of secondary cerebral folate deficiency. Compound heterozygous variants, c.591C > G (p.Y197*) and c.584G > A (p.A195V), in the MTHFR gene confirmed the diagnosis of homocysteinemia type 2 due to methylenetetrahydrofolate reductase deficiency. Simultaneously, whole-exome sequencing identified a 0.648 Mb deletion in 16p11.2, confirming the diagnosis of 16p11.2 deletion syndrome. Both parents were found to carry heterozygous MTHFR variants without the deletion in 16p11.2.
Case 4: Isolated methylmalonic acidemia and niemann-pick disease type B
A 3-year-old girl visited our hospital with general developmental delay. Initially considered for cerebral palsy at 1 year of age, she underwent physical rehabilitation. Routine blood test results were normal, but significantly increased levels of urine methylmalonate and methylcitrate were observed. Blood propionyl carnitine level was increased to 15.2 µmol/L (normal range 1.0–5.0 µmol/L), and propionylcarnitine/acetylcarnitine ratio was high at 0.53 (normal range 0.03–0.25). Plasma total homocysteine level was normal. These findings led to the diagnosis of isolated methylmalonic aciduria (MMA). Whole-exome sequencing identified compound heterozygous variants in methylmalonyl-CoA mutase (MMUT, c.1540C > A and c.323G > A), confirming the diagnosis of MMUT deficiency.
Clinical examination also revealed liver abnormalities. Serum alanine aminotransferase (59.4 IU/L) and aspartate aminotransferase (73.7 IU/L) levels showed a slight increase. Abdominal ultrasonography revealed significant enlargement of the liver (lower edge 3.1 cm below the right costal margin) and spleen (lower edge 2.2 cm below the left costal margin). Whole-exome sequencing identified compound heterozygous variants (c.1144C > T and c.1675G > T) in SMPD1 gene. Niemann-Pick cells were found in her bone marrow. Further, peripheral leukocyte acid sphingomyelinase activity was significantly decreased (80.8 nmol/g/min, normal value 216.1–950.9 nmol/g/min), confirming the diagnosis of Niemann-Pick disease type B.
Case 5: Isolated methylmalonic acidemia and 21-hydroxylase deficiency
A boy, aged 1 year and 8 months, visited us with feeding difficulties, diarrhea, metabolic acidosis, and psychomotor retardation following vaccination against polio at 3 months of age. He exhibited a significant increase in urine methylmalonate (34.4 mmol/mol creatinine, normal range 0.2–3.6 mmol/mol creatinine) and methylcitrate levels, while plasma total homocysteine level was normal. Two pathogenic variants (c.866G > C and c.2179C > T) in MMUT gene supported the diagnosis of methylmalonyl-CoA mutase deficiency. Treatment with cobalamin intramuscular injection and L-carnitine supplementation improved his clinical picture. Mental development and upper limb motor function normalized, but spastic paralysis persisted in the lower limbs, necessitating the use of a brace.
At 5 years of age, signs of precocious puberty emerged. His left wrist bone age was 13 years. Serum growth hormone level was normal. Upon gonadotropin-releasing hormone stimulation, the luteinizing hormone/follicle stimulating hormone peak value was < 0.6. Plasma adrenocorticotropic hormone levels showed a marked increase (309 pg/mL, normal range 0–46 pg/mL), while plasma cortisol levels were normal (7.9 µg/dL, normal range 5–25 µg/dL). Testosterone and 17-α-hydroxyprogesterone levels were increased to 5.77 ng/mL (normal range 0.27–0.90 ng/mL) and 495 nmol/L (normal control < 30 nmol/L), respectively. Estradiol level was normal at < 20 pg/mL (normal range 0–56 pg/mL). Aldosterone level was 32.29 ng/dL (normal range 5–17.5 ng/dL in horizontal position and 6.5–30 ng/dL in vertical position). MRI revealed no abnormalities in the pituitary and hypothalamus. Notably, double adrenal ultrasound, along with CT enhancement, depicted bilateral adrenal thickening, particularly on the left. Endocrine examination results indicated congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Two pathogenic variants (c.188A > T and c.518T > A) were found in CYP21A2 gene, confirming the diagnosis.
In clinical training, clinicians are traditionally oriented toward identifying a single explanation for the clinical presentation of a patient. The concept of multiple genetic diseases in a single patient is perceived as complex and challenging [ 1 ]. Conventionally, clinicians abstract a specific phenotype to recognize Mendelian disease patterns, forming the basis for adequate diagnosis. Clinical attributes not aligning with this genetic etiology pattern may be considered phenotypic expressions. However, literature reports several cases of co-occurring genetic disorders [ 2 , 3 , 4 ]. Posey et al. indicated that the occurrence of molecular “double trouble” is not as rare as previously assumed, suggesting up to 7% patients diagnosed by whole-exome sequencing possess a dual or triple genetic diagnosis [ 2 ]. This challenges the hypothesis that a single diagnosis concludes genetic investigations. Complete diagnosis in such cases is challenging, as distinguishing whether atypical clinical features represent a novel primary disease phenotype or a second genetic or acquired disease poses difficulty.
Herein all five patients exhibited clinical features that overlapped with their primary diagnoses. However, the presence of atypical clinical features prompted secondary diagnoses. For instance, in Case 1, a distinctive giggle and general developmental delay could be attributed to Angelman syndrome, but irritability and skeletal/muscle presentations were untypical. In addition to Angelman syndrome, whole-exome sequencing and CNV analyses identified a compound heterozygous variant in the GALC gene; moreover, a significant decrease was observed in galactose cerebrosidase activity. These findings confirmed the diagnosis of Krabbe disease. Similar methods were applied in Cases 2, 3, and 4 for addressing non-specific presentations. As indicated in Table 1 , the examination of a secondary disease for atypical features of the primary disease was systematically initiated. In Case 5, however, because of a variation in clinical symptomatology and a less specific physical assessment, secondary disease examination was relatively complex. At 3 months of age, Case 5 presented with feeding difficulties, diarrhea, metabolic acidosis, and psychomotor retardation following vaccination against polio. Elevated levels of urine methylmalonate and methylcitrate were observed, while total homocysteine level was normal. The diagnosis of isolated MMA was confirmed by Sanger sequencing of the MMUT gene. Clinical condition of this patient improved post-treatment. The emergence of precocious puberty at age 5 raised questions about whether it represented a new phenotype of isolated MMA or resulted from a second genetic or acquired disease. To address this, whole-exome sequencing was employed for a second diagnosis, confirming 21-hydroxylase deficiency. The significance of conducting accurate diagnoses is paramount for patients, families, and caregivers as precise diagnosis offers insights into patient condition from the perspective of natural history and prognosis, enabling the application of tailored therapeutic strategies. In the context of genetic conditions, this also ensures the provision of genetic counseling. When faced with an indistinct phenotype or possibility of various etiologies, comprehensive investigations become imperative. Employing advanced genome-wide techniques, such as chromosomal microarray analysis, can facilitate CNV identification; moreover, whole-exome sequencing can be applied to detect mutations in protein-coding genes.
MMA, a rare inherited disorder, is the most common organic aciduria in Mainland China [ 11 , 12 ]. MMAs encompass a group of genetically heterogeneous autosomal recessive disorders stemming from defective metabolic pathways involving MMUT or its cofactor, cobalamin [ 13 ]. The clinical manifestation of MMA is intricate, ranging from asymptomatic disease to severe multisystem injuries and even death. MMAs tend to occur at any age, from prenatal to adult life [ 14 , 15 ]. From June 1998 to December 2020, our hospital diagnosed 1,266 cases of MMA in Mainland China [ 11 , 16 , 17 ]. Predominant clinical presentations included psychomotor retardation and metabolic crisis [ 11 , 18 ]. Multiorgan damage, including hematological abnormalities, pulmonary hypertension, kidney damage, eye disease, and skin lesion, was evident. Notably, megaloblastic anemia was a primary hematological abnormality [ 11 , 16 ]. Cases 3 and 5 exhibited additional complexities, including liver function abnormalities and precocious puberty. Unfortunately, dual diagnoses were identified in these cases through whole-exome sequencing, underscoring the necessity for detailed history and physical examination in clinical practice.
It is conceivable that clinical signs and symptoms of multiple appropriately characterized disorders may exhibit similar biochemical and radiological attributes. This can lead to the masking and/or overlooking of one disorder if another affecting a similar system is present. Even if an atypical feature or pattern is identified, it is often attributed to the primary diagnosis, with secondary diagnoses potentially being overlooked. Consequently, the atypical feature of one disease may inaccurately reflect another undiagnosed condition, emphasizing the need for careful consideration of the complete assessment.
In cases where the clinical picture is atypical or exhibits more severity than expected, the possibility of a dual diagnosis (“double trouble”) should be contemplated [ 3 ]. Recent cases highlight the ongoing necessity for meticulous clinical evaluation, including a thorough physical examination, particularly in patients with atypical clinical features. The identification of another condition can significantly influence genetic management and counseling [ 2 , 3 ].
In conclusion, this study reports five pediatric cases with dual diagnoses confirmed through whole-exome sequencing. Our findings underscore the importance of considering the possibility of genetic diseases when the overall clinical picture does not align with a single unifying diagnosis. Clinicians are urged to be cognizant of the significance of physical examination and history, drawing on their extensive experience in identifying atypical clinical features.
Data availability
All data generated or analyzed during this study are included in this article.
Boycott KM, Innes AM. When one diagnosis is not enough. N Engl J Med. 2017;376(1):83–5.
Article PubMed Google Scholar
Posey JE, Harel T, Liu P, Rosenfeld JA, James RA, Coban Akdemir ZH, et al. Resolution of Disease Phenotypes resulting from Multilocus genomic variation. N Engl J Med. 2017;376(1):21–31.
Article CAS PubMed Google Scholar
Hannah-Shmouni F, Al-Shahoumi R, Brady LI, Wu L, Frei J, Tarnopolsky MA. Dual molecular diagnoses in a neurometabolic specialty clinic. Am J Med Genet A. 2021;185(3):766–73.
Kurolap A, Orenstein N, Kedar I, Weisz Hubshman M, Tiosano D, Mory A, et al. Is one diagnosis the whole story? Patients with double diagnoses. Am J Med Genet A. 2016;170(9):2338–48.
Wilcken B, Wiley V, Hammond J, Carpenter K. Screening newborns for inborn errors of metabolism by tandem mass spectrometry. N Engl J Med. 2003;348(23):2304–12.
Weisfeld-Adams JD, Morrissey MA, Kirmse BM, Salveson BR, Wasserstein MP, McGuire PJ, et al. Newborn screening and early biochemical follow-up in combined methylmalonic aciduria and homocystinuria, cblC type, and utility of methionine as a secondary screening analyte. Mol Genet Metab. 2010;99(2):116–23.
Nelson D, Xu N, Carlson J. Semi-automated quantification of methylmalonic acid in human serum by LC-MS/MS. Scand J Clin Lab Invest. 2012;72(6):441–6.
Kimura M, Yamamoto T, Yamaguchi S. Automated metabolic profiling and interpretation of GC/MS data for organic acidemia screening: a personal computer-based system. Tohoku J Exp Med. 1999;188(4):317–34.
Fu X, Iga M, Kimura M, Yamaguchi S. Simplified screening for organic acidemia using GC/MS and dried urine filter paper: a study on neonatal mass screening. Early Hum Dev. 2000;58(1):41–55.
Hori D, Hasegawa Y, Kimura M, Yang Y, Verma IC, Yamaguchi S. Clinical onset and prognosis of Asian children with organic acidemias, as detected by analysis of urinary organic acids using GC/MS, instead of mass screening. Brain Dev. 2005;27(1):39–45.
Liu Y, Liu YP, Zhang Y, Song JQ, Zheng H, Dong H, et al. Heterogeneous phenotypes, genotypes, treatment and prevention of 1 003 patients with methylmalonic acidemia in the mainland of China. Zhonghua Er Ke Za Zhi. 2018;56(6):414–20.
CAS PubMed Google Scholar
Liu MY, Liu TT, Yang YL, Chang YC, Fan YL, Lee SF, et al. Mutation Profile of the MUT Gene in Chinese Methylmalonic Aciduria patients. JIMD Rep. 2012;6:55–64.
Article PubMed PubMed Central Google Scholar
Yu HC, Sloan JL, Scharer G, Brebner A, Quintana AM, Achilly NP, et al. An X-linked cobalamin disorder caused by mutations in transcriptional coregulator HCFC1. Am J Hum Genet. 2013;93(3):506–14.
Carrillo-Carrasco N, Chandler RJ, Venditti CP. Combined methylmalonic acidemia and homocystinuria, cblC type. I. Clinical presentations, diagnosis and management. J Inherit Metab Dis. 2012;35(1):91–102.
Carrillo-Carrasco N, Venditti CP. Combined methylmalonic acidemia and homocystinuria, cblC type. II. Complications, pathophysiology, and outcomes. J Inherit Metab Dis. 2012;35(1):103–14.
Yang Y, Sun F, Song J, Hasegawa Y, Yamaguchi S, Zhang Y, et al. Clinical and biochemical studies on Chinese patients with methylmalonic aciduria. J Child Neurol. 2006;21(12):1020–4.
Kang L, Liu Y, Shen M, Liu Y, He R, Song J, et al. A study on a cohort of 301 Chinese patients with isolated methylmalonic acidemia. J Inherit Metab Dis. 2020;43(3):409–23.
He R, Mo R, Shen M, Kang L, Song J, Liu Y, et al. Variable phenotypes and outcomes associated with the MMACHC c.609G > A homologous mutation: long term follow-up in a large cohort of cases. Orphanet J Rare Dis. 2020;15(1):200.
Download references
Acknowledgements
We would like to thank all the patients and their families who participated in this study. We thank the Euler Genomics (Beijing, China), Berry Genomics Corporation (Beijing, China), and GrandOmics (Beijing, China) for their invaluable support in genetic sequencing and analysis. We are greatly indebted to the team of Professor Seiji Yamaguchi (Department of Pediatrics, Shimane Medical University, Japan) for their expert technical assistance in the diagnosis and treatment of methylmalonic acidemia.
This work was supported by grants from the National Key Research and Development Program of China [grant numbers 2021YFC2700903, 2022YFC2703401]; the Beijing Municipal Science and Technology Commission [grant numbers Z141107004414036, Z151100003915126]; and the Foundation of 2018 Beijing Key Clinical Specialty Construction Project-Pediatrics [grant number 2199000726].
Author information
Yupeng Liu and Xue Ma contributed equally.
Authors and Affiliations
Department of Pediatrics, Peking University People’s Hospital, Beijing, China
Yupeng Liu & Jiong Qin
Department of Pediatrics, Peking University First Hospital, Beijing, China
Xue Ma, Zhehui Chen, Yao Zhang, Hui Dong, Tongfei Wu, Jinqing Song, Mengqiu Li, Ying Jin & Yanling Yang
Department of Respiration, Beijing Children’s Hospital, Capital Medical University, Beijing, China
Department of Pediatrics, Qinghai University Affiliated Hospital, Xining, China
Department of Endocrinology, Genetics and Metabolism, Beijing Children’s Hospital, Capital Medical University, Beijing, China
Qiao Wang & Yuan Ding
Department of Precise Medicine, General Hospital of Tianjin Medical University, Tianjin, China
Children’s Hospital Affiliated to Zhengzhou University, Zhengzhou, China
Dongxiao Li
You can also search for this author in PubMed Google Scholar
Contributions
YYL and QJ conceived the study. LYP and MX drafted the manuscript. CZH, HRX, ZY, DH, MYY, WTF, WQ, DY, LDX, SJQ, LMQ, JY participated in the clinical management and patient data collection. LXY checked the genetic data. All authors read and approved the final version of the manuscript.

Corresponding authors
Correspondence to Jiong Qin or Yanling Yang .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Hospital Institutional Ethics Committee and was performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from the parents of the patients for collection of samples and publication of medical data.
Consent for publication
Not applicable.
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Liu, Y., Ma, X., Chen, Z. et al. Dual rare genetic diseases in five pediatric patients: insights from next-generation diagnostic methods. Orphanet J Rare Dis 19 , 159 (2024). https://doi.org/10.1186/s13023-024-03148-3
Download citation
Received : 03 August 2022
Accepted : 24 March 2024
Published : 12 April 2024
DOI : https://doi.org/10.1186/s13023-024-03148-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Genetic disease
- Dual molecular diagnoses
- Whole-exome sequencing
- Methylmalonic acid
Orphanet Journal of Rare Diseases
ISSN: 1750-1172
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
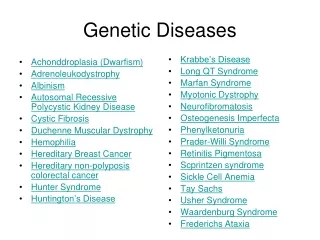
Genetic Diseases
Oct 10, 2014
510 likes | 1.49k Views
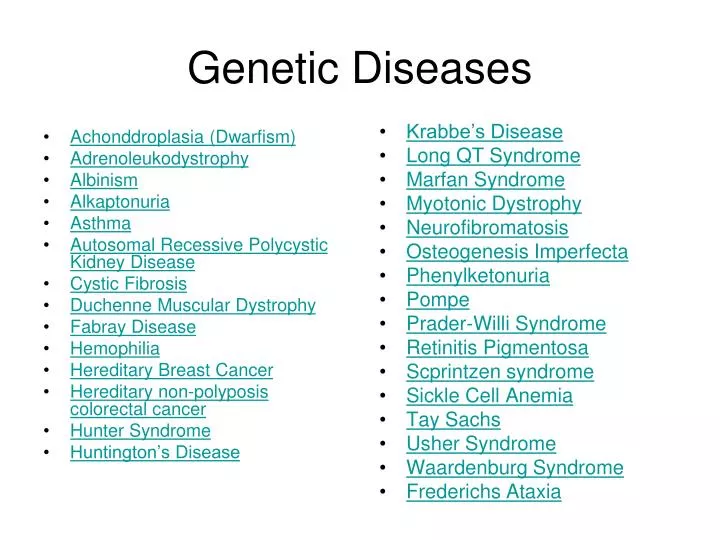
Achonddroplasia (Dwarfism) Adrenoleukodystrophy Albinism Alkaptonuria Asthma Autosomal Recessive Polycystic Kidney Disease Cystic Fibrosis Duchenne Muscular Dystrophy Fabray Disease Hemophilia Hereditary Breast Cancer Hereditary non-polyposis colorectal cancer Hunter Syndrome
Share Presentation
- association
- breast cancer
- mayo clinic
- cystic fibrosis
- national gaucher foundation
- hereditary colon cancer association

Presentation Transcript
Achonddroplasia (Dwarfism) Adrenoleukodystrophy Albinism Alkaptonuria Asthma Autosomal Recessive Polycystic Kidney Disease Cystic Fibrosis Duchenne Muscular Dystrophy Fabray Disease Hemophilia Hereditary Breast Cancer Hereditary non-polyposis colorectal cancer Hunter Syndrome Huntington’s Disease Krabbe’s Disease Long QT Syndrome Marfan Syndrome Myotonic Dystrophy Neurofibromatosis Osteogenesis Imperfecta Phenylketonuria Pompe Prader-Willi Syndrome Retinitis Pigmentosa Scprintzen syndrome Sickle Cell Anemia Tay Sachs Usher Syndrome Waardenburg Syndrome Frederichs Ataxia Genetic Diseases
Achondroplasia (Dwarfism) • Associations • Little People of America • Human Growth Foundation • March of Dimes • Books • Human Diseases and Conditions • Diseases • World of Health • Resource File (a folder of information gathered from the Public Library’s database) • Web pages • Short Stature • Mayo Clinic • MedLine Plus • Web MD
Associations The ARC of the United States Australian Leukodystrophy Group CLIMB ELA Fight ALD NIH Office of Rare Diseases United Leukodystrophy Foundation ) Resource File (a folder of information gathered from the Public Library’s database Books World of Health Web pages MedLine Plus Leukodystrophy types Mayo Clinic Adrenoleukodystrophy
Albinism • Associations • NOAH • Books • Diseases • World of Health • Human Diseases and Conditions • Resource Files (a file of articles from the public library’s database) • Web pages • MedLine plus • Mayo Clinic • Scientific American • National Institutes of Health
Alkaptonuria • Associations • Children living with inherited metabolic diseases (CLIMB) • National Institute of diabetes and digestive and kidney diseases • National Organization for rare disorders (NORD) • Books • Human Diseases and Conditions • World of Health • Diseases • Sick • Resource File (a folder of information gathered from the Public Library’s database) • Web pages • National Institutes of Health • Medline Plus
Associations Asthma and Allergy Foundation of America American Lung Association American Academy of Allergy, Asthma, and Immunology Books World of Health Diseases Sick Coping with Asthma Human Diseases and Conditions Resource File (a folder of information from the public library’s database) Web Sites National Heart Blood and Lung Institute MedLine Plus Web MD CDC Mayo Clinic Asthma
Autosomal Recessive Polycystic Kidney Disease • Associations • ARPKD / CHF Alliance • CAGS • Rare Diseases organization • Books • World of Health • Diseases • Kidney Disorders • Human Diseases and Conditions • Resource File (a folder of information from the public library’s database) • Web sites: • National Institutes of Health • NIH • Web MD
Associations Cystic Fibrosis Foundation Boomer Esiason Foundation Kids Health Canadian Cystic Fibrosis Foundation Books World of Health Diseases Sick Genetics and Human Health Human Diseases and Conditions Web sites Medline Mayo Clinic National Heart lung and Blood Institute Genetics Home Reference Resource File (a folder of information from the public library’s database) Cystic Fibrosis
Duchenne Muscular Dystrophy • Organizations • Muscular Dystrophy Association • Parent Project Muscular Dystrophy • Your Genes your health • Books • World of Health • Diseases • Sick • Human Diseases and Conditions • Resource File (a folder of information from the public library’s database) • Web Sites • Medline PlusCDCMayo Clinic • National Institute of Neurological Disorders and Stroke
Fabry Disease • Associations • Alliance of Genetic support groups • Mount Sinai Medical center • Fabry support and information group • National Organization for Rare Disorders • Books • World of Health • Diseases • Sick • Human Diseases and Conditions • Resource File (a folder of information gathered from the Public Library’s database) • Web pages • National Institute for Neurological disorders and stroke • National Institutes of Health • Overview
Gaucher’s Disease • Associations • Center for Jewish diseases, department of Human genetics, Mount Sinai Medical center. • Children’s Gaucher Research Fund • National Gaucher Foundation • Books • World of Health • Diseases • Sick • Human Diseases and Conditions • Genetics and Human Health • Resource File (a folder of information gathered from the Public Library’s database) • Web pages • Mayo Clinic • Medline Plus • National Institute of Neurological Disorders and Stroke
Associations National Hemophilia Organization Bleeding Disorders Association Hemophilia Organization of America Books World of Health Diseases Sick Human Diseases and Conditions Genetics and Human Health Resource File (a folder of information from the public library’s database) Web Sites Medline Plus National Heart lung and blood Institute Mayo Clinic E Medicine Hemophilia
Associations National Breast Cancer Foundation American Cancer Society Susan G. Komen Books World of Health Diseases Sick Breast Cancer The Cancer Dictionary Web Sites National Cancer Institute Medicine Net Web MD Mayo Clinic Resource File (a folder of information from the public library’s database) Hereditary Breast Cancer
Hereditary non-polyposis colorectal cancer • Organizations • Colon Cancer Alliance • Colorectal Cancer Network • Hereditary Colon Cancer Association • Books • World of Health • Sick • The Cancer Dictionary • Human Diseases and Conditons • Resource File (a folder of information from the public library’s database) • Web Sites • Cleveland ClinicNational Institutes of Health • National Cancer InstituteWeb MDMayo Clinic
Hunter Syndrome • Organizations • Rare Diseases • Brave Community • Resource File (a folder of information from the public library’s database) • Web Sites • A list of links • Mayo Clinic • Medline Plus • Web MD • Shire
Huntington’s Disease • Organizations • Hereditary Disease Foundation • Huntington’s Disease Society of America • National Institute of Neurological Disorders and Stroke • Books • World of Health • Disease • Human Diseases and Conditions • Resource File (a folder of information from the public library’s database) • Web Sites • Mayo Clinic • Medline Plus • NCBI • Web MD
Krabbe’s Disease • Organizations • United Leukodystrophy Foundation • Hunter’s Hope Foundation • National Organization for Rare Disorders • Resource File (a folder of information from the public library’s database) • Web Sites • Mayo Clinic • Medline Plus • National Institute of Neurological Disorders and Stroke • University of Maryland Medical Center
Long QT Syndrome • Organizations • CARE • American Heart Association • Heart rhythm Society • Resource File (a folder of information from the public library’s database) • Web sites • Mayo Clinic • Cleveland Clinic • National Heart Lung and Blood Institute
Marfan Syndrome • Organizations • National Marfan Foundation • A list of Associations from around the world • Books • Diseases • Human Diseases and Conditions • Resource File (a folder of information from the public library’s database) • Web sites • Mayo Clinic • Medline Plus • Web MD
Myotonic Dystrophy • Organizations • Muscular Dystrophy Association • Mytonic Dystrophy Foundation • Books • World of Health • Diseases • Sick • Human Diseases and Conditions • Resource File (a folder of information from the public library’s database) • Web sites • Genetics Home Reference • Mayo Clinic • NCBI
Neurofibromatosis • Organizations • Acoustic Neuroma Association • Acoustic Neuroma Association of Canada • Books • World of Health • Human Diseases and Conditions • Resource File (a folder of information from the public library’s database) • Web Sites • National Institute for Neurological Disorders and Stroke • Kids Health • Medline Plus • Mayo Clinic
Osteogenesis Imperfecta • Organizations • Children’s Brittle Bone Foundation • Resource File (a folder of information from the public library’s database) • Books • World of Health • Diseases (Look under bone diseases) • Web Sites • Medline Plus • Web MD • Net Doctor • University of Maryland Medical Center
Phenylketonuria • Resource File (a folder of information from the public library’s database) • Books • World of Health • Human Diseases and Conditions • Web Sites • Mayo Clinic • Medline Plus • Web MD • Rare Diseases
Pompe • Associations • Acid Maltase Deficiency Association (ADMA) • Association for Glycogen Storage Disease • Books • World of Health • Diseases • Sick • Human Diseases and Conditions • Resource File (a folder of information gathered from the Public Library’s database) • Web pages • National Association for Neurological disorders and stroke • National Institutes of Health
Prader-Willi Syndrome • Resource File (a folder of information from the public library’s database) • Organizations • Prader-Willi Association • Books • World of Health • Web sites • Medline Plus • University of Michigan • Mayo Clinic • Rare Diseases
Retinitis Pigmentosa • Resource File (a folder of information from the public library’s database) • Organizations • Foundation Fighting Blindness • Low Vision Organization • American Optometric Association • Books • World of Health • Diseases • Web Sites • Medline Plus • Web MD • Natural Eye Care
Shprintzen Syndrome • Resource File (a folder of information from the public library’s database) • Organizations • Coalition for Heritable Disorders of Connective Tissue • Hydrocephalus Association • Web sites • Genetics Home Reference • CCDD • Web MD
Sickle Cell Anemia • Resource File (a folder of information from the public library’s database) • Organizations • Sickle Cell Disease Association • Sickle Cell Information Center • Books • Sickle Cell Anemia • Sick • Diseases • World of Health • Human Diseases and Conditions • Web Sites • Mayo ClinicMedline PlusWeb MD • Kids HealthCDC
Tay Sachs • Resource File (a folder of information from the public library’s database) • Organizations • National Institute of Neurological Disorders and Stroke • National Tay Sachs and Allied Diseases • Rare Diseases • Books • Diseases • World of Health • Human Diseases and Conditions • Web sites • Genetics Home Reference • Mayo Clinic • Medline Plus
Usher Syndrome • Resource File (a folder of information from the public library’s database) • Organizations • Usher Syndrome Foundation • American Council of the Blind • Foundation Fighting Blindness • Helen Keller National Center for Deaf-Blind youths and Adults • Web Sites • NIDCD • Genetics Home Reference • National Institutes for Health • Web MD
Waardenburg Syndrome • Resource File (a folder of information from the public library’s database) • Organizations • National Organization of Rare Diseases • Web Sites • Medline Plus • Web MD • Rare diseases
Frederichs Ataxia • Web sites: • Mayo Clinic • Medline Plus • Web MD • Organizations • The Frederichs Ataxia Research Alliance • Muscular Dystrophy Association
- More by User
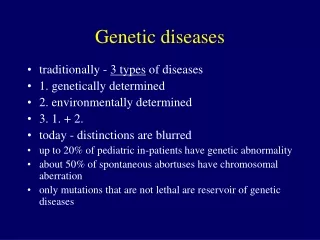
Genetic diseases
Genetic diseases. traditionally - 3 types of diseases 1. genetically determined 2. environmentally determined 3. 1. + 2. today - distinctions are blurred up to 20% of pediatric in-patients have genetic abnormality about 50% of spontaneous abortuses have chromosomal aberration
1.71k views • 43 slides
Genetic Diseases. By: Mr. Hunter. What is a genetic disorders?. A genetic disorder is a disease caused by a different form of a gene called a variation or an alteration of a gene called a mutation. Mutations. Mutations can occur randomly or because of an environmental exposure.
367 views • 9 slides
Complex Genetic Diseases
Functional genomic approach to ion channels as targets in complex polygenic disease J. Jay Gargus, MD, PhD Division of Human Genetics, Department of Pediatrics, and Department of Physiology & Biophysics University of California, Irvine. Complex Genetic Diseases.
468 views • 29 slides
Objectives. Develop a basic understanding of the genetic apparatus Comprehend definitions of major genetic abnormalities Correlate molecular abnormalities and genetic defects . Outline. I. DefinitionsGenetic codeChromosomes, Genes, Cell DivisionMolecular mechanismsII. Abnormal fetal de
1.3k views • 113 slides
Lifestyle diseases, Genetic diseases, Chronic diseases
Lifestyle diseases, Genetic diseases, Chronic diseases . Cardiovascular Diseases. These diseases affect the heart or blood vessels. These diseases are responsible for more than 40% of all deaths in the US. Types of Cardio Diseases. Hypertension: high blood pressure and can occur at any age.
953 views • 16 slides
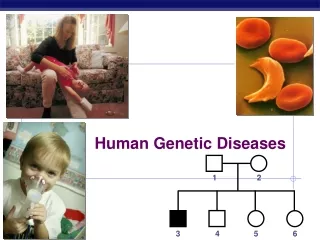
Human Genetic Diseases
1. 2. 3. 4. 5. 6. Human Genetic Diseases. = male. = female. = male w/ trait. = female w/ trait. Pedigree analysis. Pedigree analysis reveals Mendelian patterns in human inheritance data mapped on a family tree. Genetic counseling.
230 views • 13 slides
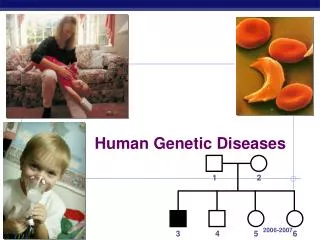
1. 2. 3. 4. 5. 6. Human Genetic Diseases. = male. = female. = male w/ trait. = female w/ trait. Pedigree analysis. Pedigree analysis reveals Mendelian patterns in human inheritance data mapped on a family tree. 1. 2. 1. 2. 3. 4. 5. 6. 3. 4. 5. 6.
341 views • 21 slides
Genetic Diseases. Objectives. To recap genetic inheritance To identify four genetic diseases To review key factors to study To propose research. Reproduction:. The gametes (sex cells of humans each contain 23 chromosomes . This is half the number of all other cells .
431 views • 23 slides
Genetic Diseases. Genetic Diseases. Genetic Diseases can result from many things such as mutations in the gene or mutations in chromsome number First lets recall a view facts…. A female will have an two ____ chromosomes A male will have an ___ and ___ chromosom
457 views • 20 slides

Genetic Diseases. How they are caused and why they can be beneficial. What kind of genetic disease?. Can be of two kinds: Caused by environmental factors Hereditary
235 views • 10 slides
Genetic diseases. Recessive alleles & carriers. Amniocentesis. Sex-linked traits.
169 views • 4 slides
Genetic Diseases. Lecture 51 Thursday, May 3, 2007 Ref. Basic Pathology Chapter 7. Ocular Genetics Review Article. Ocular Genetics: Current understanding. Ian M. MacDonald, Mai Tran, and Maria A. Musarella. Survey of Ophthalmology, 40 (2):159-196, 2004
519 views • 21 slides
Genetic Diseases Woot!
Genetic Diseases Woot!. Adult Polycystic Kidney Disease. Sx : Path: Mutation? Associated with: Inheritance? Juvenile polycystic kidney disease is AR!. Pain, hematuria , HTN, renal fail. Bilaterally large, cystic kidneys 90% APKD 1 (Chromosome 16)
285 views • 14 slides

Genetic Diseases. Syllabus Notes (1-16-08). 3.1.1 Chromosomes are made of DNA and proteins. 3.1.2 Karyotyping: chromosomes are arranged in pairs according to their structure.
591 views • 34 slides
Genetic Diseases. All human diseases can be divided into three categories: - genetically determined - environmentally determined - combination of both (both genetic and environmental factors play a role)
642 views • 39 slides
Autosomal Genetic Diseases
Autosomal Genetic Diseases. Biology. Autosomal Genetic Diseases. The majority of human genetic disorders, are carried on the autosomes, which are all the chromosomes except the sex chromosomes
445 views • 14 slides
Genetic Diseases. Genetic Diseases. ALBINISM. THALASSEMIA. SCID [bubble boy syndrome]. AGAMMAGLOBULINEMIA. SICKLE CELL ANAEMIA. HUNTINGTON’S CHOREA. . Sickle-Cell Anaemia.
347 views • 22 slides
Genetic Diseases. 1.Sickle Cell Anemia 2. Malaria and its link with Sickle Cell 3. Cystic Fibrosis 4. Huntington's 5. Tay-Sachs 6. Phenylketonuria 7. Hemophilia 8. Color blindness.
843 views • 30 slides
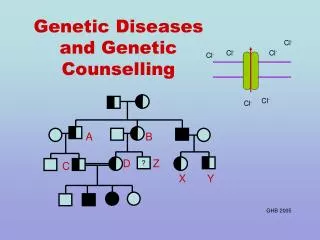
Genetic Diseases and Genetic Counselling
A. B. D. Z. ?. C. X. Y. Cl -. Cl -. Cl -. Cl -. Cl -. Cl -. Genetic Diseases and Genetic Counselling. GHB 2005. Every gene carries information telling the body how to make a particular. protein. Adult cells have two copies of each gene, so….
446 views • 23 slides
435 views • 43 slides
Achonddroplasia (Dwarfism) Adrenoleukodystrophy Albinism Autosomal Recessive Polycystic Kidney Disease Cystic Fibrosis Duchenne Muscular Dystrophy Hemophilia Hereditary Breast Cancer Hereditary non-polyposis colorectal cancer Hunter Syndrome Huntington’s Disease. Krabbe’s Disease
326 views • 28 slides
242 views • 21 slides
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- RESEARCH BRIEFINGS
- 10 April 2024
Genetic risk variants lead to type 2 diabetes development through different pathways
This is a summary of: Suzuki, K. et al . Genetic drivers of heterogeneity in type 2 diabetes pathophysiology. Nature 627 , 347–357 (2024) .
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
doi: https://doi.org/10.1038/d41586-024-00440-x
Figure 1 is published under a CC BY 4.0 licence.
Ahmad, E., Lim, S., Lasmptey, R., Webb, D. R. & Davies, M. J. Lancet 400 , 1803–1820 (2022).
Article PubMed Google Scholar
Uffelmann, E. et al. Nature Rev. Methods Primers 1 , 59 (2021).
Article Google Scholar
Download references
Reprints and permissions
Related Articles

Cell-type-resolved mosaicism reveals clonal dynamics of the human forebrain
Article 10 APR 24

AI can help to tailor drugs for Africa — but Africans should lead the way
Comment 09 APR 24

Advanced CRISPR system fixes a deadly mutation in cells
Research Highlight 04 APR 24
Diabetes drug slows development of Parkinson’s disease
News 03 APR 24

Stealthy stem cells to treat disease
Spotlight 28 FEB 24

Genetic drivers of heterogeneity in type 2 diabetes pathophysiology
Article 19 FEB 24
Computational Postdoctoral Fellow with a Strong Background in Bioinformatics
Houston, Texas (US)
The University of Texas MD Anderson Cancer Center
Locum Associate or Senior Editor (Immunology), Nature Communications
The Editor in Immunology at Nature Communications will handle original research papers and work on all aspects of the editorial process.
London, Beijing or Shanghai - Hybrid working model
Springer Nature Ltd
Assistant Professor - Cell Physiology & Molecular Biophysics
Opportunity in the Department of Cell Physiology and Molecular Biophysics (CPMB) at Texas Tech University Health Sciences Center (TTUHSC)
Lubbock, Texas
Texas Tech University Health Sciences Center, School of Medicine
Postdoctoral Associate- Curing Brain Tumors
Baylor College of Medicine (BCM)
Energy AI / Grid Modernization / Hydrogen Energy / Power Semiconductor Concentration / KENTECH College
21, Kentech-gil, Naju-si, Jeollanam-do, Republic of Korea(KR)
Korea Institute of Energy Technology
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diabetes Overview
Healthy Living with Diabetes
- Español
On this page:
How can I plan what to eat or drink when I have diabetes?
How can physical activity help manage my diabetes, what can i do to reach or maintain a healthy weight, should i quit smoking, how can i take care of my mental health, clinical trials for healthy living with diabetes.
Healthy living is a way to manage diabetes . To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products.
Healthy living may help keep your body’s blood pressure , cholesterol , and blood glucose level, also called blood sugar level, in the range your primary health care professional recommends. Your primary health care professional may be a doctor, a physician assistant, or a nurse practitioner. Healthy living may also help prevent or delay health problems from diabetes that can affect your heart, kidneys, eyes, brain, and other parts of your body.
Making lifestyle changes can be hard, but starting with small changes and building from there may benefit your health. You may want to get help from family, loved ones, friends, and other trusted people in your community. You can also get information from your health care professionals.
What you choose to eat, how much you eat, and when you eat are parts of a meal plan. Having healthy foods and drinks can help keep your blood glucose, blood pressure, and cholesterol levels in the ranges your health care professional recommends. If you have overweight or obesity, a healthy meal plan—along with regular physical activity, getting enough sleep, and other healthy behaviors—may help you reach and maintain a healthy weight. In some cases, health care professionals may also recommend diabetes medicines that may help you lose weight, or weight-loss surgery, also called metabolic and bariatric surgery.
Choose healthy foods and drinks
There is no right or wrong way to choose healthy foods and drinks that may help manage your diabetes. Healthy meal plans for people who have diabetes may include
- dairy or plant-based dairy products
- nonstarchy vegetables
- protein foods
- whole grains
Try to choose foods that include nutrients such as vitamins, calcium , fiber , and healthy fats . Also try to choose drinks with little or no added sugar , such as tap or bottled water, low-fat or non-fat milk, and unsweetened tea, coffee, or sparkling water.
Try to plan meals and snacks that have fewer
- foods high in saturated fat
- foods high in sodium, a mineral found in salt
- sugary foods , such as cookies and cakes, and sweet drinks, such as soda, juice, flavored coffee, and sports drinks
Your body turns carbohydrates , or carbs, from food into glucose, which can raise your blood glucose level. Some fruits, beans, and starchy vegetables—such as potatoes and corn—have more carbs than other foods. Keep carbs in mind when planning your meals.
You should also limit how much alcohol you drink. If you take insulin or certain diabetes medicines , drinking alcohol can make your blood glucose level drop too low, which is called hypoglycemia . If you do drink alcohol, be sure to eat food when you drink and remember to check your blood glucose level after drinking. Talk with your health care team about your alcohol-drinking habits.

Find the best times to eat or drink
Talk with your health care professional or health care team about when you should eat or drink. The best time to have meals and snacks may depend on
- what medicines you take for diabetes
- what your level of physical activity or your work schedule is
- whether you have other health conditions or diseases
Ask your health care team if you should eat before, during, or after physical activity. Some diabetes medicines, such as sulfonylureas or insulin, may make your blood glucose level drop too low during exercise or if you skip or delay a meal.
Plan how much to eat or drink
You may worry that having diabetes means giving up foods and drinks you enjoy. The good news is you can still have your favorite foods and drinks, but you might need to have them in smaller portions or enjoy them less often.
For people who have diabetes, carb counting and the plate method are two common ways to plan how much to eat or drink. Talk with your health care professional or health care team to find a method that works for you.
Carb counting
Carbohydrate counting , or carb counting, means planning and keeping track of the amount of carbs you eat and drink in each meal or snack. Not all people with diabetes need to count carbs. However, if you take insulin, counting carbs can help you know how much insulin to take.
Plate method
The plate method helps you control portion sizes without counting and measuring. This method divides a 9-inch plate into the following three sections to help you choose the types and amounts of foods to eat for each meal.
- Nonstarchy vegetables—such as leafy greens, peppers, carrots, or green beans—should make up half of your plate.
- Carb foods that are high in fiber—such as brown rice, whole grains, beans, or fruits—should make up one-quarter of your plate.
- Protein foods—such as lean meats, fish, dairy, or tofu or other soy products—should make up one quarter of your plate.
If you are not taking insulin, you may not need to count carbs when using the plate method.

Work with your health care team to create a meal plan that works for you. You may want to have a diabetes educator or a registered dietitian on your team. A registered dietitian can provide medical nutrition therapy , which includes counseling to help you create and follow a meal plan. Your health care team may be able to recommend other resources, such as a healthy lifestyle coach, to help you with making changes. Ask your health care team or your insurance company if your benefits include medical nutrition therapy or other diabetes care resources.
Talk with your health care professional before taking dietary supplements
There is no clear proof that specific foods, herbs, spices, or dietary supplements —such as vitamins or minerals—can help manage diabetes. Your health care professional may ask you to take vitamins or minerals if you can’t get enough from foods. Talk with your health care professional before you take any supplements, because some may cause side effects or affect how well your diabetes medicines work.
Research shows that regular physical activity helps people manage their diabetes and stay healthy. Benefits of physical activity may include
- lower blood glucose, blood pressure, and cholesterol levels
- better heart health
- healthier weight
- better mood and sleep
- better balance and memory
Talk with your health care professional before starting a new physical activity or changing how much physical activity you do. They may suggest types of activities based on your ability, schedule, meal plan, interests, and diabetes medicines. Your health care professional may also tell you the best times of day to be active or what to do if your blood glucose level goes out of the range recommended for you.

Do different types of physical activity
People with diabetes can be active, even if they take insulin or use technology such as insulin pumps .
Try to do different kinds of activities . While being more active may have more health benefits, any physical activity is better than none. Start slowly with activities you enjoy. You may be able to change your level of effort and try other activities over time. Having a friend or family member join you may help you stick to your routine.
The physical activities you do may need to be different if you are age 65 or older , are pregnant , or have a disability or health condition . Physical activities may also need to be different for children and teens . Ask your health care professional or health care team about activities that are safe for you.
Aerobic activities
Aerobic activities make you breathe harder and make your heart beat faster. You can try walking, dancing, wheelchair rolling, or swimming. Most adults should try to get at least 150 minutes of moderate-intensity physical activity each week. Aim to do 30 minutes a day on most days of the week. You don’t have to do all 30 minutes at one time. You can break up physical activity into small amounts during your day and still get the benefit. 1
Strength training or resistance training
Strength training or resistance training may make your muscles and bones stronger. You can try lifting weights or doing other exercises such as wall pushups or arm raises. Try to do this kind of training two times a week. 1
Balance and stretching activities
Balance and stretching activities may help you move better and have stronger muscles and bones. You may want to try standing on one leg or stretching your legs when sitting on the floor. Try to do these kinds of activities two or three times a week. 1
Some activities that need balance may be unsafe for people with nerve damage or vision problems caused by diabetes. Ask your health care professional or health care team about activities that are safe for you.

Stay safe during physical activity
Staying safe during physical activity is important. Here are some tips to keep in mind.
Drink liquids
Drinking liquids helps prevent dehydration , or the loss of too much water in your body. Drinking water is a way to stay hydrated. Sports drinks often have a lot of sugar and calories , and you don’t need them for most moderate physical activities.
Avoid low blood glucose
Check your blood glucose level before, during, and right after physical activity. Physical activity often lowers the level of glucose in your blood. Low blood glucose levels may last for hours or days after physical activity. You are most likely to have low blood glucose if you take insulin or some other diabetes medicines, such as sulfonylureas.
Ask your health care professional if you should take less insulin or eat carbs before, during, or after physical activity. Low blood glucose can be a serious medical emergency that must be treated right away. Take steps to protect yourself. You can learn how to treat low blood glucose , let other people know what to do if you need help, and use a medical alert bracelet.
Avoid high blood glucose and ketoacidosis
Taking less insulin before physical activity may help prevent low blood glucose, but it may also make you more likely to have high blood glucose. If your body does not have enough insulin, it can’t use glucose as a source of energy and will use fat instead. When your body uses fat for energy, your body makes chemicals called ketones .
High levels of ketones in your blood can lead to a condition called diabetic ketoacidosis (DKA) . DKA is a medical emergency that should be treated right away. DKA is most common in people with type 1 diabetes . Occasionally, DKA may affect people with type 2 diabetes who have lost their ability to produce insulin. Ask your health care professional how much insulin you should take before physical activity, whether you need to test your urine for ketones, and what level of ketones is dangerous for you.
Take care of your feet
People with diabetes may have problems with their feet because high blood glucose levels can damage blood vessels and nerves. To help prevent foot problems, wear comfortable and supportive shoes and take care of your feet before, during, and after physical activity.

If you have diabetes, managing your weight may bring you several health benefits. Ask your health care professional or health care team if you are at a healthy weight or if you should try to lose weight.
If you are an adult with overweight or obesity, work with your health care team to create a weight-loss plan. Losing 5% to 7% of your current weight may help you prevent or improve some health problems and manage your blood glucose, cholesterol, and blood pressure levels. 2 If you are worried about your child’s weight and they have diabetes, talk with their health care professional before your child starts a new weight-loss plan.
You may be able to reach and maintain a healthy weight by
- following a healthy meal plan
- consuming fewer calories
- being physically active
- getting 7 to 8 hours of sleep each night 3
If you have type 2 diabetes, your health care professional may recommend diabetes medicines that may help you lose weight.
Online tools such as the Body Weight Planner may help you create eating and physical activity plans. You may want to talk with your health care professional about other options for managing your weight, including joining a weight-loss program that can provide helpful information, support, and behavioral or lifestyle counseling. These options may have a cost, so make sure to check the details of the programs.
Your health care professional may recommend weight-loss surgery if you aren’t able to reach a healthy weight with meal planning, physical activity, and taking diabetes medicines that help with weight loss.
If you are pregnant , trying to lose weight may not be healthy. However, you should ask your health care professional whether it makes sense to monitor or limit your weight gain during pregnancy.
Both diabetes and smoking —including using tobacco products and e-cigarettes—cause your blood vessels to narrow. Both diabetes and smoking increase your risk of having a heart attack or stroke , nerve damage , kidney disease , eye disease , or amputation . Secondhand smoke can also affect the health of your family or others who live with you.
If you smoke or use other tobacco products, stop. Ask for help . You don’t have to do it alone.
Feeling stressed, sad, or angry can be common for people with diabetes. Managing diabetes or learning to cope with new information about your health can be hard. People with chronic illnesses such as diabetes may develop anxiety or other mental health conditions .
Learn healthy ways to lower your stress , and ask for help from your health care team or a mental health professional. While it may be uncomfortable to talk about your feelings, finding a health care professional whom you trust and want to talk with may help you
- lower your feelings of stress, depression, or anxiety
- manage problems sleeping or remembering things
- see how diabetes affects your family, school, work, or financial situation
Ask your health care team for mental health resources for people with diabetes.
Sleeping too much or too little may raise your blood glucose levels. Your sleep habits may also affect your mental health and vice versa. People with diabetes and overweight or obesity can also have other health conditions that affect sleep, such as sleep apnea , which can raise your blood pressure and risk of heart disease.

NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for healthy living with diabetes?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of healthy living for people with diabetes, such as
- how changing when you eat may affect body weight and metabolism
- how less access to healthy foods may affect diabetes management, other health problems, and risk of dying
- whether low-carbohydrate meal plans can help lower blood glucose levels
- which diabetes medicines are more likely to help people lose weight
Find out if clinical trials are right for you .
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for healthy living with diabetes are looking for participants?
You can view a filtered list of clinical studies on healthy living with diabetes that are federally funded, open, and recruiting at www.ClinicalTrials.gov . You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Elizabeth M. Venditti, Ph.D., University of Pittsburgh School of Medicine.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(8); 2023 Aug
- PMC10494960

Unraveling Huntington’s Disease: A Report on Genetic Testing, Clinical Presentation, and Disease Progression
Moutushi ahmed.
1 Internal Medicine, Khulna Medical College, Khulna, BGD
Debasish Mridha
2 Neurology, Michigan Advanced Neurology Center, Saginaw, USA
This study presents the clinical features and disease progression of a 39-year-old male patient diagnosed with Huntington's disease (HD). The diagnosis was confirmed by direct genetic testing, using DNA obtained from a blood sample that revealed expanded cytosine-adenine-guanine (CAG) repeats in the huntingtin gene (HD gene). The patient exhibited motor symptoms, including chorea, muscle rigidity, coordination difficulties, and speech and swallowing impairments. Cognitive symptoms comprised impaired judgment, planning difficulties, slowed thinking, memory lapses, and attention problems. The patient's progressive deterioration resulted in wheelchair dependency and increased reliance on supportive care. This report highlights the significance of genetic testing in confirming HD diagnosis and emphasizes the need for a multidisciplinary approach to manage the symptoms and improve the patient's quality of life.
Introduction
Huntington's disease (HD) is a neurodegenerative disorder characterized by motor, cognitive, and psychiatric symptoms [ 1 ]. It arises from an abnormal amplification of CAG trinucleotide repeats in the huntingtin gene. This genetic anomaly gives rise to mutant huntingtin protein, instigating a gradual breakdown of various areas within the brain [ 2 ]. Huntington's disease (HD) is a severe condition that causes significant challenges for patients and their families. It requires comprehensive and compassionate care to manage the various symptoms and functional limitations caused by the disease.
HD typically becomes symptomatic in mid-adulthood; however, in some cases, the disease can manifest much earlier in life, known as Juvenile Huntington's disease (JHD). JHD refers to the onset of symptoms before the age of 20 years and accounts for approximately 5-10% of all HD cases. Juvenile HD presents unique challenges compared to the adult-onset form of the disease, with a more aggressive and rapidly progressive disease course. Children with JHD may experience a more severe decline in motor and cognitive functions, leading to profound disability and increased reliance on supportive care [ 3 ].
The clinical presentation of HD includes a wide range of motor symptoms, such as involuntary jerky movements, muscle stiffness, and walking difficulties, which significantly impact daily activities and mobility. Additionally, cognitive impairments, including forgetfulness, trouble concentrating, challenges in planning and organizing, and difficulties in decision-making, ultimately add to the burden of the disease. Psychiatric symptoms, such as mood swings, restlessness, irritability, apathy, lack of interest, impulsivity, and lack of emotion, further contribute to the complexity of managing HD [ 4 - 6 ].
This study aimed to describe HD’s clinical presentation and disease progression in a 39-year-old male patient diagnosed with confirmed expanded CAG repeats in the huntingtin gene through genetic testing.
Case presentation
This study involves a 39-year-old married male who was diagnosed with Huntington's disease (HD) in his late 20s after undergoing genetic testing. The patient has a significant family history of HD, as both his father and sister tragically lost their lives to this devastating condition. His father succumbed to HD, while his sister experienced Juvenile HD and passed away. These familial occurrences highlight the genetic nature of HD and underscore the crucial role of genetic testing in confirming the diagnosis.
The patient married at the age of 25 years, had no children, and worked as an accountant. As time passed, he developed symptoms that affected his concentration and experienced abnormal, uncontrollable movements. His coordination deteriorated, and irritability became a constant struggle. Upon undergoing genetic testing, the diagnosis was confirmed, and his condition continued to worsen. Regrettably, the progression of the disease forced him to give up his job, as its impact on his daily life became too significant to manage. As the disease progressed, the patient's motor symptoms worsened, leading to severe disability, complete wheelchair dependency, and eventual loss of speech.
The patient's neurological examination revealed prominent chorea, generalized rigidity, and dystonia, confirming the motor manifestations of HD. Alongside these motor symptoms, significant cognitive impairments were evident, including attention difficulties, memory lapses, and executive function deficits. Behavioral changes, such as irritability, apathy, and impulsivity, further complicated the disease presentation. Due to the progressive nature of HD, the patient requires constant monitoring and assistance from two caregivers, and he relies on a liquid nutritional supplement (Ensure) with a daily intake of eight servings. The patient has been taking antiepileptic medications, valproic acid (250 mg/5 mL twice daily) and levetiracetam (500 mg twice daily), but the seizures persist, necessitating ongoing management. In addition, he has been taking Austedo (12 mg twice daily), Seroquel (50 mg thrice daily), and Ativan (1 mg) as needed. He has been seeing a psychiatrist, as regular psychiatric follow-up is crucial to address the associated mental health challenges. The patient also undergoes physical therapy (PT) and occupational therapy (OT) thrice a week to manage functional limitations. The family, especially the patient's mother and wife, experiences distress witnessing the continual decline in his health. This study underscores the intricate nature of comprehensive HD management, highlighting the importance of a multidisciplinary approach in managing diverse symptoms and enhancing the patient's overall well-being.
Depending on the patient's family history and any associated signs or symptoms, there are different types of tests used to detect HD, including prenatal, pre-symptomatic, and confirmatory. The diagnosis of HD in this patient was confirmed through confirmatory genetic testing, specifically the detection of expanded CAG repeats in the huntingtin gene.
HD is an autosomal dominant neurodegenerative disorder caused by abnormal expansion of CAG trinucleotide repeats in the huntingtin gene on chromosome 4p16.3. The expanded CAG repeats result in the production of mutant huntingtin protein, leading to progressive neurodegeneration in various regions of the brain.
Genetic testing for HD plays a crucial role in identifying at-risk individuals, confirming the diagnosis, and providing genetic counseling. The most common method for genetic testing involves polymerase chain reaction (PCR) amplification of the CAG repeat region in the huntingtin gene, followed by fragment analysis or DNA sequencing to determine the number of CAG repeats. In individuals with HD, the CAG repeat expansion typically exceeds 36 repeats, whereas a normal allele generally has 10 to 35 CAG repeats (Figure 1 ).

The image is adapted from New NIST SRM helps improve diagnosis of Huntington's disease (April 12, 2011) (https://shorturl.at/gIZ23; public domain).
The number of CAG repeats in the huntingtin gene can provide valuable information about disease prognosis and age of onset. There is an inverse correlation between the number of CAG repeats and the age at which symptoms first appear, known as the age of onset. Individuals with a higher number of CAG repeats tend to experience an earlier onset of symptoms. However, it is important to note that there can be considerable variability in the age of onset, even among individuals with a similar number of CAG repeats [ 7 ].
Conclusions
This study provides crucial insights into the clinical features and progression of Huntington's disease (HD) in a patient diagnosed through genetic testing. It emphasizes the pivotal role of genetic testing in confirming HD diagnosis, especially for individuals with a family history of the disease. Early detection is highlighted, underscoring the importance of timely intervention and comprehensive symptom management to enhance the overall quality of life for affected individuals. An interdisciplinary approach involving specialists from neurology, psychiatry, physical therapy, and occupational therapy is essential in addressing the diverse manifestations of this debilitating neurodegenerative disorder. Through collaboration, healthcare professionals can optimize symptom control, provide support for the patient's well-being, and offer understanding and assistance to families facing the challenges of HD. Ultimately, this collaborative approach aimed to improve HD management and the quality of life for patients and their loved ones, offering hope and compassion throughout the journey of dealing with HD.
Acknowledgments
This study was conducted under the supervision of Debasish Mridha, M.D., and Michigan Advanced Neurology Center.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study

IMAGES
VIDEO
COMMENTS
Genetic disorders occur when a mutation affects your genes or chromosomes. Some disorders cause symptoms at birth, while others develop over time. Genetic testing can help you learn more about the likelihood of experiencing a genetic disorder. If you or a loved one have a genetic disorder, it's important to seek care from an experienced ...
human genetic disease, any of the diseases and disorders that are caused by mutations in one or more genes.. With the increasing ability to control infectious and nutritional diseases in developed countries, there has come the realization that genetic diseases are a major cause of disability, death, and human tragedy. Rare, indeed, is the family that is entirely free of any known genetic disorder.
Definition. Mutations in DNA can result in genetic disorders. Genetic disorders are conditions that occur as a result of changes to or mutations in DNA within the body's cells. Most cells in the ...
A genetic disorder is a disease caused in whole or in part by a change in the DNA sequence away from the normal sequence. Genetic disorders can be caused by a mutation in one gene (monogenic disorder), by mutations in multiple genes (multifactorial inheritance disorder), by a combination of gene mutations and environmental factors, or by damage to chromosomes (changes in the number or ...
Genetic disorders are caused by mutations or chromosomal alterations that affect the normal functioning of cells. In this chapter, you will learn about the types, causes, symptoms, and treatments of some common genetic disorders, such as cystic fibrosis, Down syndrome, and hemophilia. You will also explore how genetic testing and gene therapy can help diagnose and prevent these disorders. Read ...
All diseases have a genetic component. However, the extent to which genes contribute to disease varies and much remains to be learned. Advances in understanding the genetic mechanisms behind these disease enables the development of early diagnostic tests, new treatments, or interventions to prevent disease onset or minimize disease severity. This chapter provides information about the ...
When most people consider the genetic basis of disease, they might think about the rare, single gene disorders, such as cystic fibrosis (CF), phenylketonuria or haemophilia, or perhaps even cancers with a clear heritable component (for example, inherited predisposition to breast cancer). ... In conclusion, the presentation and severity of ...
Genetics Basics. Genetics research studies how individual genes or groups of genes are involved in health and disease. Understanding genetic factors and genetic disorders is important in learning more about promoting health and preventing disease. Some genetic changes have been associated with an increased risk of having a child with a birth ...
The start of 2022 is an inflection point in the development of diagnostics and treatments for rare genetic diseases in prenatal, pediatric, and adult individuals-the theme of this special issue. ... Phenotype expansion and its antecedent—very incomplete knowledge of the breadth of clinical presentations of childhood genetic diseases—are ...
These estimates can help programs choose the diseases to target. The sum of the frequencies for the 380 genes is ~1 in 50 (1,989 per 100,000) births. If the 16 adult disorders are removed, the sum of the frequencies of the remaining 364 genes is ~1 in 190 (527 per 100,000) births. One in 190 is obviously an underestimate for the 614 genes that ...
Chapter 6. Genetic Disorders. There are three major types of mutations: (1) genome mutations, which involve loss or gain of an entire chromosome; (2) chromosomal mutations, which involve alterations in one or more chromosomes that are usually identifiable by karyotyping; and (3) gene mutations, which are partial or complete deletion of the gene ...
Infectious diseases are an ever-present global threat. In this Review, Kwok, Mentzer and Knight discuss our latest understanding of how human genetics influence susceptibility to disease ...
A primary goal of human genetics is to identify DNA sequence variants that influence biomedical traits, particularly those related to the onset and progression of human disease. Over the past 25 ...
Genetics Presentation templates ... Genetic Diseases Download the "Genetic Diseases" presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise ...
Download the "Genetic Diseases" presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking medical attention. This Google Slides ...
7. Some common Genetic Diseases Thalassemia • Thalassemia is an inherited blood disorder in which the body makes an abnormal form of hemoglobin. Hemoglobin is the protein molecule in red blood cells that carries oxygen. •Frequency: Thalassemia affects approximately 4.4 of every 10,000 live births throughout the world.
The prevalence of genetic disease ranged from 4.5% to 12% of total admis-sions.1,2,5,6 A prevalence of 30% to 40% was documented by Hall et al4 and Scriver et al3 by using a broad definition of genetic conditions. Hall7 has emphasized the relevance of these data and their application in providing improved.
Genetic disorder. Jun 28, 2014 •. 272 likes • 155,684 views. AI-enhanced description. Chhabi Acharya. This document discusses genetic disorders, which are illnesses caused by abnormalities in a person's genome. It begins by introducing genetic disorders and explaining that most are rare. It then discusses the history of genetics research.
Abstract. Genetic diseases cause numerous complex and intractable pathologies. DNA sequences encoding each human's complexity and many disease risks are contained in the mitochondrial genome, nuclear genome, and microbial metagenome. Diagnosis of these diseases has unified around applications of next-generation DNA sequencing.
In the realm of rare genetic diseases, ensuring effective medical management and genetic counseling hinges on providing precise diagnoses. However, clinical evaluations and conventional genetic testing bring about the diagnosis in < 50% patients [].The capacity to offer molecular diagnostics to patients has witnessed a substantial improvement, rapidly emerging as the most suitable method for ...
Genetic Diseases. Genetic Diseases. Genetic Diseases. Genetic Diseases can result from many things such as mutations in the gene or mutations in chromsome number First lets recall a view facts…. A female will have an two ____ chromosomes A male will have an ___ and ___ chromosom. 457 views • 20 slides
The clinical presentations of genetic disorders vary widely, from an isolated (major) congenital anomaly (CA) or multiple malformations (MCA) to more subtle clinical signs or symptoms. The diagnostic pathway is often long and requires extensive evaluations that may be invasive and costly . Diagnosis of most genetic disorders in neonatal and ...
The largest genome-wide association study for type 2 diabetes so far, which included several ancestry groups, led to the identification of eight clusters of genetic risk variants. The clusters ...
Comorbidities are prevalent in digestive cancers, intensifying patient discomfort and complicating prognosis. Identifying potential comorbidities and investigating their genetic connections in a systemic manner prove to be instrumental in averting additional health challenges during digestive cancer management. Here, we investigated 150 diseases across 18 categories by collecting and ...
Healthy living is a way to manage diabetes. To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products. Healthy living may help keep your body's blood pressure, cholesterol, and blood glucose level, also called blood sugar level, in the ...
This study presents the clinical features and disease progression of a 39-year-old male patient diagnosed with Huntington's disease (HD). The diagnosis was confirmed by direct genetic testing, using DNA obtained from a blood sample that revealed expanded cytosine-adenine-guanine (CAG) repeats in the huntingtin gene (HD gene).