MINI REVIEW article
Childhood immunization and covid-19: an early narrative review.

- MPH Program, School of Pharmacy and Health Sciences, Fairleigh Dickinson University, Madison, NJ, United States
The COVID-19 pandemic has evolved into arguably the largest global public health crisis in recent history—especially in the absence of a safe and effective vaccine or an effective anti-viral treatment. As reported, the virus seems to less commonly infect children and causing less severe symptoms among infected children. This narrative review provides an inclusive view of scientific hypotheses, logical derivation, and early analyses that substantiate or refute such conjectures. At the completion of a relatively less restrictive search of this evolving topic, 13 articles—all published in 2020, were included in this early narrative review. Directional themes arising from the identified literature imply the potential relationship between childhood vaccination and COVID-19—either based on the potential genomic and immunological protective effects of heterologous immunity, or based on observational associations of cross-immunity among vaccines and other prior endemic diseases. Our review suggests that immune response to the SARS-CoV-2 virus in children is different than in adults, resulting in differences in the levels of severity of symptoms and outcomes of the disease in different age groups. Further clinical investigations are warranted of at least three childhood vaccines: BCG, MMR, and HEP-A for their potential protective role against the SARS-CoV-2 virus.

Introduction
The novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has infected close to 9.5 million people and has claimed nearly 762,000 lives globally, as of August 16, 2020 ( 1 ). This pandemic has evolved into arguably the largest global public health crisis in recent history—especially in the absence of a safe and effective vaccine or an effective anti-viral treatment. This virus has demonstrated a high attack rate, a broad gamut of identifiable symptoms, and viability among a potentially massive number of infected silent carriers.
Unlike many infectious diseases, such as endemic malaria and common flu where children are known to have the highest mortality rates and to drive transmission in households and communities—it appears as it could be that SARS-CoV-2 just does not translate into severe disease as frequently in children, specifically for young children, below 10 years of age. Moreover, infected children suffer milder symptoms of COVID-19, with much lower case-fatality rates (CFR), and recover quickly from the infection ( 2 – 7 ). In an initial assessment from Wuhan, China, among 50 children identified with COVID-19, the severity varied between asymptomatic and mild in 96% of the patients ( 8 ). While diagnostic findings were similar to those of adults, fewer children developed severe pneumonia. Neonates, on the other hand, have developed symptomatic and more severe COVID-19 ( 2 , 7 ).
Data obtained from the Chinese Center for Disease Control and Prevention as of February 17, Spanish Ministry of Health as of March 24, Korea's Centers for Disease Control and Prevention as of March 24, and the Italian National Institute of Health as of March 17—suggests that the CFR for COVID-19 for children are disproportionately lower compared to any other age group ( 9 ). The CFR was 0% for all four countries for the age group “0–9 years.” Singh et al., suggest that milder symptomatology implies potential immunologic protective factors in children and the direction for a design of interventions for all age groups ( 2 ). While it is likely that early publication of reports from countries with generally more equipped healthcare systems may not be fully indicative of the long-term overall potential impact in less developed nations—current observations do not suggest such trends yet.
Propositions for such lower observed rate of fatality and symptomatic illness have included the potential protective effect of global active viral immunization of children from birth till 6 years of age ( 10 ). It is suggested that childhood vaccines for mumps, rubella, poliomyelitis, Hepatitis B, and varicella may impart transient immunity against SARS-CoV-2 that protects their lung cells from contracting COVID-19 ( 10 ). Subsequently, aging, immunosuppression, and co-morbid states reduce the adaptability of the immune system ( 5 ).
The rates of heterologous immunity have been studied in some of the common childhood vaccinations including measles and Bacillus Calmette-Guerin (BCG) vaccines. African American girls who received the measles vaccine demonstrated 47% reduced mortality from other diseases. Similarly, the BCG vaccine has demonstrated a 25% reduction in mortality to other diseases ( 11 ). Previous research has supported that live vaccines have increased resistance to other vaccine unrelated diseases. Thus, they have specific effects by preventing the targeted disease but also non-specific effects on non-targeted infections as well. It is theorized that vaccines boost immune responses, offering additional resistance to viruses other than the ones they are intended to prevent ( 12 ). It should also be noted that research only suggests there is a correlation between vaccines and non-specific responses, not causation.
Such hypothesis of cross-immunogenicity of existing childhood vaccines with the novel coronavirus, if proven true, could have far reaching implications for public health immunization policies across the globe. However, no broad assessment of this topic has thus far been undertaken to the best of our knowledge at the time of this writing.
In this narrative review, we provide an inclusive view of scientific hypotheses, logical derivation, and early analyses that substantiate or refute such conjectures. The goal of this study is not to establish a comprehensive, systematic understanding of the link between childhood vaccination and COVID-19 outcomes. Instead we attempt to offer a robust starting point to facilitate further development of relevant hypotheses and designing of studies to test this promising public health opportunity.
Given the early stage in the evolving literature on this topic, our attempt at a systematic search of health sciences databases such as PubMed using keywords and search strategies such as: “coronavirus OR COVID-19 OR nCoV OR SARS-CoV-2) AND (child OR children OR childhood OR pediatric OR infant OR babies OR baby OR neonates) AND (immunization OR vaccination OR vaccine)” limited to English language articles published in between June 2019 and April 2020 did not yield sufficiently relevant publications. While there may have been articles that were published in other languages during the review period, those were not included unless an English translation was available. Given the importance of this topic, we believe that such non-English articles, if any, will be included in future assessments as there is broader presence of the data in global literature.
As such, given the broader base of sources accessed by its search function, we performed a plain language search using the same keywords listed above on Google Scholar, which includes journal and conference papers, theses and dissertations, academic books, pre-prints, abstracts, technical reports, and other scholarly literature from all broad areas of research ( 13 ). All types of study and countries of origin were eligible for inclusion. In addition, any relevant articles that were identified during and outside the formal search process were also included if their content were relevant to our study. Four reviewers extracted relevant data into a cloud-based spreadsheet. We recorded the country of origin, study design, type of data, results, and conclusions. As this was intended to be a rapid review, each article was reviewed by one reviewer.
At the completion of the quick search and identification process, 14 out of 30 identified articles were included in this early narrative review ( Table 1 ). Included papers were all published in 2020 following the early release of data on COVID-19, presenting hypotheses about the potential relationship between childhood vaccination and COVID-19—either based on the protective effects of heterologous immunity, or based on observational associations of cross-immunity among vaccines and other prior endemic diseases.
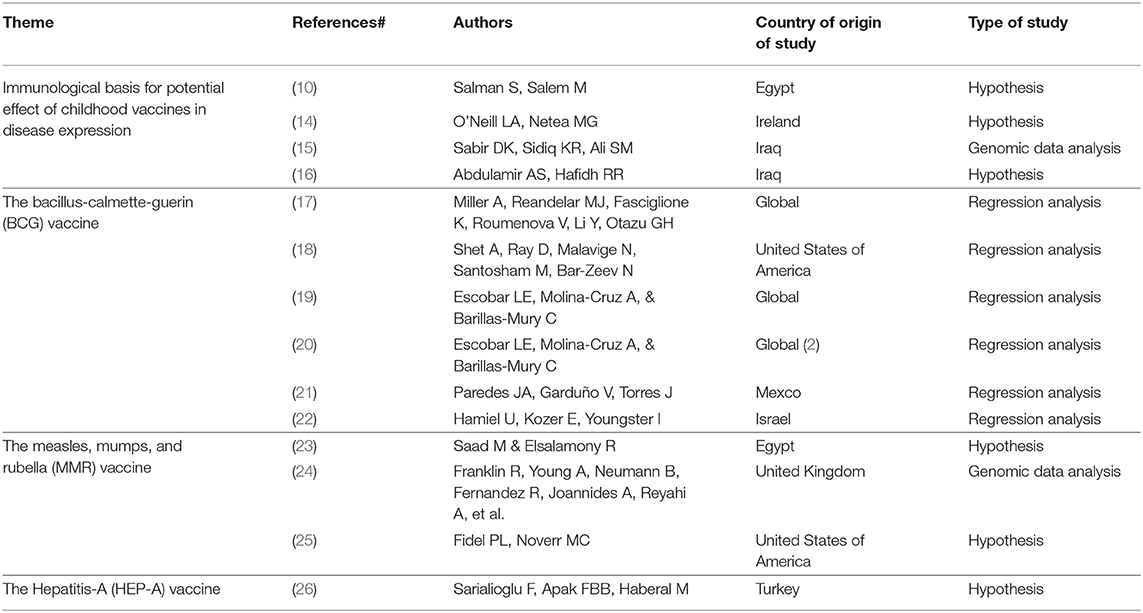
Table 1 . Summary of studies included in the narrative review.
The Immunological Basis for Potential Effect of Childhood Vaccines in Disease Expression
In many countries, children are routinely vaccinated against a number of bacterial and viral diseases. Vaccines may have non-specific physiologic effects when they alter the immune response to unrelated organisms, called heterologous immunity. The non-specific effects of vaccines are usually more pronounced in girls and appear to be maximal in the first 6 months of life ( 11 )—when passed maternal immunity is further supplemented by newly introduced vaccines, starting at 2 months. There are several theories as to why heterologous immunity may occur.
Salman and Salem suggest that cross-immunogenicity of childhood vaccines for multiple viruses could potentially be a reason for the relatively milder infection and severity of COVID-19 among children ( 10 ). Most routine viral vaccines are either inactivated or killed viruses that stimulate T Helper 1 cells (CD4+) to secrete many different types of cytokines as interferon gamma, interleukin-2 (IL-2), and IL-12, improving the cytotoxicity of natural killer cells to recognize and destroy cells infected with new cross-reactive viruses. For example, warts that are caused by human papilloma virus (HPV) could be ameliorated using intralesional MMR vaccine ( 10 ).
Furthermore, neutralizing antibodies produced against the foregoing vaccine-preventable microbes might cross-react with the antigenic epitopes of the spike (S) and nucleocapsid (N) proteins and prevent COVID-19 in children ( 15 ). An investigation of this hypothesis, using the BLAST search tool, showed no significant sequence similarity between these proteins and those in the childhood vaccine-preventable microbes, inferring that memory T-cells, rather than vaccine neutralizing antibodies, may be involved in the protection of children against COVID-19 owing to them having a larger number of naive T-cells that can be programmed to protect them against the disease ( 27 ).
Potentially, the low immunity in children that doesn't exaggerate the immune response against the virus as in the case of adults, could explain the lesser severity of SARS-CoV-2 in this age group. Children have less adults-like memory cells specific to other circulating coronaviruses and therefore, are less capable to mount a devastating and vigorous cell-mediated attack on alveoli and interstitial tissue of the lung upon new infection ( 16 ).
The Bacille Calmette–Guérin (BCG) Vaccine
The Bacille Calmette-Guérin (BCG) vaccine is given in infancy for prevention of severe forms of tuberculosis and has the widest use, and a strongest safety profile among all childhood vaccines ( 28 ). Epidemiological and randomized trial evidence suggest a protective effect of BCG on infant mortality via non-specific heterologous protection against other infections possibly through innate immune epigenetic mechanisms ( 29 ).
O'Neil and Netea suggest that induction of trained immunity by BCG vaccine could provide protection against COVID-19, and the use of oral polio vaccine and new recombinant BCG-based vaccine VPM1002 may be some of the approaches to induce resistance to SARS-CoV-2 ( 14 ). The authors hypothesize that induction of trained immunity is at least partly the mechanism through which BCG vaccination induces its beneficial effects and might protect against SARS-CoV-2.
A retrospective study compared countries that do not have BCG vaccination policies (Italy, USA, Lebanon, the Netherlands, and Belgium), to countries that have such policies ( 17 ). The results showed that while middle-high and high-income countries with current universal BCG policies had 0.78 COVID-19 deaths per million, those without such policies had 16.39 COVID-19 deaths per million people—and the difference was statistically significant. Further analysis of 28 countries found a positive significant correlation ( p = 0.02) between the year of the universal vaccination policy and mortality rate—suggesting that if the policy to vaccinate was adopted at an earlier year, more of the elderly population in these countries would have been vaccinated, thus potentially offering them more protection. In countries, such as Italy, where BCG vaccine was never given, the mortality rate was significantly higher compared to Japan where BCG vaccination has been implemented since 1947. In countries, such as Iran, with BCG vaccination starting in 1984, mortality was higher since today's elderly population did not receive the vaccination.
In order to mitigate the bias centered around the differential epidemic time curves experienced by different countries, Shet et al., calculated days from the 100th COVID-19-positive case to align countries on a more comparable time curve ( 18 ). A log-linear regression model was built with crude COVID-19-attributable mortality data per 1 million population for each country as outcome, BCG vaccine inclusion in the national immunization schedule as exposure, and adjusted for the effects of: country-specific GDP per capita, the percentage of population 65 years and above, and the relative position of each country on the epidemic timeline. COVID-19-attributable mortality among BCG-using countries was 5.8 times lower ( P = 0.006) than in non-BCG-using countries. Sensitivity analysis run excluding China as the majority case contributor from the model resulted in no appreciable change in the protective effect of BCG.
Escobar et al., in a study that carefully controlled for confounding variables found that there was an inverse correlation between countries/locations with a stronger BCG vaccination policy and COVID-19 related mortality ( 19 ). COVID-19 mortality rates in New York, Illinois, Alabama and Florida—states without BCG-vaccination policies in the US, were significantly higher than locations with BCG-vaccine policies, namely Pernambuco, Rio de Janeiro, and Sao Paulo in Brazil, or Mexico State and Mexico City in Mexico.
In a more recent study, the same authors demonstrate a strong correlation between the BCG index and COVID-19 mortality in different socially similar European countries ( r 2 = 0.88; P = 8 × 10–7), indicating that every 10% increase in the BCG index was associated with a 10.4% reduction in COVID-19 mortality ( 20 ).
However, evidence suggesting a protective effect of the BCG vaccine was not found to be universally consistent and only demonstrated association not causality. There indeed are a myriad of factors apart from the effect of a childhood vaccine that could impact the findings of association, and such caution in interpretation would be recommended—especially this early in our understanding of the COVID-19 disease.
Paredes et al., showed that when confounders such as under-reporting, SARS-CoV-2 capability testing and differing lockdown measures were considered, the differential impact of BCG vaccination on COVID-19 related mortality rate was not significant ( 21 ). Among high-income countries, the mean number of deaths per 1 million population for countries with no universal BCG vaccination (223.2 ± 166.1) was not statistically significant from countries with current or previous BCG vaccination programs (55 ± 82.5; P = 0.85). No statistically significant difference was noted in mean number of deaths at the 1,000th case in these three groups either.
Hamiel et al., compared infection rates and proportions with severe COVID-19 disease in 2 cohorts: individuals born during 3 years before and 3 years after cessation of the universal BCG vaccine program in Israel ( 22 ). There was no statistically significant difference in the proportion of positive reverse transcriptase-polymerase chain reaction tests for SARS-CoV-2 in the BCG vaccinated group compared to the unvaccinated group (11.7 vs. 10.4%, p = 0.09). There also was no statistically significant difference in positivity rates per 100,000 (121 vs. 100, p = 0.15).
The Measles, Mumps, and Rubella (MMR) Vaccine
Saad at al., suggested two potential mechanisms for higher COVID-19 cases per population ratio and higher death rate in Italy (no MMR vaccine) compared to China: ( 1 ) by generating bystander immunity the measles vaccine increases ability of immune system to combat non-measles pathogens, including coronaviruses, and ( 2 ) due to shared structural similarities between measles and coronavirus the cross-reactivity and immunity between the measles vaccine and coronavirus leads to partial protection against COVID-19 ( 23 ).
Franklin et al., identified that the macro domains of SARS-CoV-2 and rubella virus and the MMR vaccine, share 29% amino acid sequence identity ( 24 ). This finding suggests the viruses possess the same protein fold. Patients with high illness severity had high levels of rubella IgG (161.9 + 147.6 IU/ml) compared to patients with a moderate severity of disease (74.5 + 57.7 IU/ml). The authors suggest the MMR vaccine could result in potentially reduced severe outcomes with COVID-19.
In their commentary, Fidel and Noverr support the use of live attenuated MMR vaccine as a preventive measure against the pathological inflammation and sepsis associated with COVID-19 infection ( 25 ). While they emphasize the strictly preventive nature of the suggestion, the basis of such suggestion is the induction of non-specific effects by live attenuated vaccines that represent “trained innate immunity” delivered by leukocyte precursors in the bone marrow more effectively functioning against broader infectious attacks. On the basis of data from prior BCG trials in infants, the vaccine-induced trained innate cells are expected to remain in the circulation for roughly 1 year, which should see people through the most severe waves of COVID-19 infection.
The Hepatitis-A (HEP-A) Vaccine
Sarialioglu et al., reported on the differences in the rate in which COVID-19 had affected some countries such as China, US, Italy, Spain, France, England, the Netherlands, and Belgium more severely than some others such as India, Pakistan, countries of the African continent, and South America which had lower rates of infection and mortality at the time of their study ( 26 ). The authors hypothesize that routine vaccination for hepatitis A virus (HAV) causing high seroprevalence among populations in countries in the low COVID-19 prevalence group, while it is rather low in the industrialized countries.
In addition, the authors point to the COVID-19 experience in the Diamond Princess cruise ship, which after arriving in Yokohama, Japan on February 3rd 2020, was placed under quarantine for the disease based on another passenger who had disembarked in Hong Kong a couple of days earlier and has tested positive for the virus ( 30 ). A report ( 31 ) showed that by February 20th over 18% of the 700 infected among the 3,700 people showed no symptoms. The low frequency of symptomatic disease on the ship, may be explained by stimulated immunity before passengers started the cruise trip when HEP-A vaccine was recommended for international travel in areas with high HAV endemicity. However, no publicly available information on the HEP-A vaccination status of the passengers were found.
While there does not seem to be any objective evidence to support this yet, the authors further contemplate that the severity of COVID-19 and vulnerability of very young children, particularly infants <1 year of age, may be attributed to the eventual decrease of maternal anti-HAV antibodies toward age 1 year—as HEP-A vaccine is not administered until after 1 year of age.
The authors conclude that immune response caused by the hepatitis A vaccine may be protective against COVID-19 infection by a possible adaptive immune cross-reaction. Patients with asymptomatic COVID-19 disease could indirectly indicate those with protection from HAV seropositivity. The HEP-A vaccine may help to keep the COVID-19 infection at mucosal colonization levels and prevent lower respiratory tract involvement and fatality ( 26 ).
At the time of this writing, the pandemic of COVID-19 continues to be a global public health emergency, claiming the lives of hundreds, and infecting millions all over the world. While the trend thus far shows a relatively less severe morbidity and mortality profile of the disease among children, the reason behind such a trend is not yet well-understood. While several theories for such welcome relief have been proposed, we present available insights and hypotheses on the potential link between childhood vaccination and the less severe expression of COVID-19 in this early narrative review.
Although it is relatively early in the process of the scientific community's gaining full understanding of the SARS-CoV-2 virus and characterization of its infection, known virus-prevention strategies from past pandemics that could lead to potential attenuation of the currently ongoing disaster, are of high interest. Public health emergencies, by their nature, often do not have the luxury of time needed for well-researched remedies, and that is why hypotheses and theories are relevant—even if with the possibility of bridging current patients and populations to the time when treatment and vaccination for COVID-19 are available.
Our narrative review finds that there indeed is a potential scientifically-based possibility of heterologous immunity from common childhood vaccines to be imparting a protective effect on COVID-19 infections in children. While not unequivocal, population-level differences found in several studies in the rate of infection and severity of expression of COVID-19 between countries with and without certain common childhood vaccination policies suggest the need for deeper and more well-structured investigation, in the minimum. Although prevalence of some target diseases and organisms may have been eradicated in certain parts of the world, the reinstitution of relatively inexpensive vaccines for those diseases into the currently recommended childhood vaccination regimen may merit careful re-evaluation. Our review found suggestions from the medical community of such promise in at least three of the most common vaccines given to children—BCG, MMR, and HEP-A.
However, it is indeed not recommended that such practices be instituted without establishing a reasonable scientific evidence to validate some of these hypotheses—especially when children are involved. Pragmatic randomized controlled trials designed to time- and cost-efficiently test feasible primary endpoints of cross-immunogenicity with existing childhood vaccines should be initiated alongside focused global efforts to develop effective treatment for COVID-19, and a safe and effective SARS-CoV-2 vaccine. At least, rapid testing and eventual use of promising, non-COVID-19 vaccines could be explored for help with avoiding large patient casualties in the meantime, until adequate treatment and vaccines are developed.
Certainly, routine pediatric vaccination for other conditions needs to be maintained even in the face of parental fear of potential exposure to COVID-19 during well child visits. Parents need to be reminded of the increased risks for outbreaks of vaccine-preventable diseases that children and their communities may face upon lifting of social distancing guidelines—unless children are vaccinated appropriately.
Based on our review, it may be concluded that although controlled clinical trials may be time and resource intensive, those may be justificable in investigating further and confirming the value of at least three childhood vaccines: BCG, MMR, and HEP-A as possible explanations for lower incidence of COVID-19, and less severe expression of the disease in children. Currently hypothesized explanations for an evidently less severe impact of COVID-19 on children globally includes the protective cross-immunity provided by other common childhood vaccines. There is a strong basis to hypothesize that immune response to the SARS-CoV-2 virus in children is different than in adults, resulting in differences in the levels of severity of symptoms and outcomes of the disease in different age groups.
Author Contributions
Upon initial suggestion of the topic by the BB-S, JK-H, DR, and SR participated equally in generating the research question, conducting library search, and writing the manuscript and selected articles were divided equally for review and data entering into the common spread sheet. All authors participated in revising and editing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. World Health Organization. Coronavirus Disease (COVID-19) Situation Report – 209 . (2020) Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200816-covid-19-sitrep-209.pdf?sfvrsn=5dde1ca2_2 (accessed August 31, 2020)
Google Scholar
2. Singh T, Hesto SM, Langel SN, Blasi M, Hurst JH, Fouda GG, et al. Lessons from COVID-19 in children: key hypotheses to guide preventative and therapeutic strategies. Clin Infect Dis. (2020) ciaa547. doi: 10.1093/cid/ciaa547
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR. Are children less susceptible to COVID-19? J Microbiol Immunol Infect. (2020) 53:371–2. doi: 10.1016/j.jmii.2020.02.011
4. Brodin P. Why is COVID-19 so mild in children? Acta Paediatrica. (2020) 109:1082–3. doi: 10.1111/apa.15271
5. Carsetti R, Quintarelli C, Quinti I, Mortari EP, Zumla A, Ippolito G Locatelli F. The immune system of children: the key to understanding SARS-CoV-2 susceptibility? Lancet Child Adolescent Health. (2020) 4:414–6. doi: 10.1016/S2352-4642(20)30135-8
6. Mehta NS, Mytton OT, Mullins EWS, Fowler TA, Falconer CL, Murphy OB, et al. SARS-CoV-2 (COVID-19): what do we know about children? A systematic review. Clin Infect Dis. ciaa556. doi: 10.1093/cid/ciaa556. [Epub ahead of print].
7. Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica. (2020) 109:1088–95. doi: 10.1111/apa.15270
8. Ma H, Hu J, Tian J, Zhou X, Li H, Laws M et al. Visualizing the novel coronavirus (COVID-19) in children: what we learn from patients at wuhan children's hospital. SSRN Electron J. (2020). doi: 10.2139/ssrn.3556676
CrossRef Full Text | Google Scholar
9. Roser M, Ritchie H, Ortiz-Ospina E, Hasell J. Our World in Data: Mortality Risk of COVID-19 . Available online at: https://ourworldindata.org/mortality-risk-covid (accessed June 1, 2020)
10. Salman S, Salem M. Routine childhood immunization may protect against COVID-19. Med Hypotheses. (2020). doi: 10.1016/j.mehy.2020.109689. [Epub ahead of print].
11. Shann F. The non-specific effects of vaccines. Arch Dis Childhood. (2010) 95:662–7. doi: 10.1136/archdischild-2015-310282
12. Aaby P, Benn CS, Flanagan KL, Klein SL, Kollmann TR, Lynn DJ, et al. The non-specific and sex-differential effects of vaccines. Nat Rev Immunol. (2020) 20:464–70. doi: 10.1038/s41577-020-0338-x
13. Google Scholar (2020). Available at: https://scholar.google.co.uk/intl/en/scholar/help.html#coverage (accessed June 1, 2020)
14. O'Neill LA, Netea MG. BCG-induced trained immunity: can it offer protection against COVID-19? Nat Rev Immunol. (2020) 20:335–7. doi: 10.1038/s41577-020-0337-y
15. Sabir DK, Sidiq KR, Ali SM. Current speculations on the low incidence rate of the COVID-19 among children. Int. J. School. Health. (2020) 7:61–2. doi: 10.30476/intjsh.2020.85997.1066
16. Abdulamir AS, Hafidh RR. The possible immunological pathways for the variable immunopathogenesis of covid-−19 infections among healthy adults, elderly and children. Electron J Gen Med. (2020) 17:em202. doi: 10.29333/ejgm/7850
17. Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, Otazu GH. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiological study. medRxiv [Preprint]. (2020). doi: 10.1101/2020.03.24.20042937
18. Shet A, Ray D, Malavige N, Santosham M, Bar-Zeev N. Differential COVID-19-attributable mortality and BCG vaccine use in countries. medRxiv [Preprint]. (2020). doi: 10.1101/2020.04.01.20049478
19. Escobar LE, Molina-Cruz A, Barillas-Mury C. BCG vaccine-induced protection from COVID-19 infection, wishful thinking or a game changer? medRxiv [Preprint] . (2020). doi: 10.1101/2020.05.05.20091975
20. Escobar LE, Molina-Cruz A, Barillas-Mury C. BCG vaccine protection from severe coronavirus disease 2019 (COVID-19). Proc Natl Acad Sci USA. (2020) 117:17720–6. doi: 10.1073/pnas.2008410117
21. Paredes JA, Garduño V, Torres J. COVID-19 related mortality: is the BCG vaccine truly effective? medRxiv [Preprint]. (2020). doi: 10.1101/2020.05.01.20087411
22. Hamiel U, Kozer E, Youngster I. SARS-CoV-2 rates in bCG-vaccinated and unvaccinated young adults. JAMA. (2020) 23:2340–1. doi: 10.1001/jama.2020.8189
23. Saad M, Elsalamony R. Measles vaccines may provide partial protection against COVID-19. Int J Cancer Biomed Res. (2020) 5:14-19. doi: 10.21608/jcbr.2020.26765.1024
24. Franklin R, Young A, Neumann B, Fernandez R, Joannides A, Reyahi A, et al. Homologous protein domains in SARS-CoV-2 and measles, mumps and rubella viruses: Preliminary evidence that MMR vaccine might provide protection against COVID-19. medRxiv [Preprint]. (2020) doi: 10.1101/2020.04.10.20053207
25. Fidel PL, Noverr MC. Could an unrelated live attenuated vaccine serve as a preventive measure to dampen septic inflammation associated with covid-19 infection? mBio. (2020) 11:e00907–20. doi: 10.1128/mBio.00907-20
26. Sarialioglu F, Apak FBB, Haberal M. Can hepatitis a vaccine provide protection against covid-19? Exp Clin Transpl. (2020) 2:141–3. doi: 10.6002/ect.2020.0109
27. Ahmadpoor PL, Rostaing L. Why the immune system fails to mount an adaptive immune response to a COVID-19 infection. Transpl Int. (2020) 33:824–5. doi: 10.1111/tri.13611
28. Revised BCG vaccination guidelines for infants at risk for HIV infection. Weekly Epidemiol Rec . (2007) 82:193–6.
29. Butkeviciute E, Jones CE, Smith SG. Heterologous effects of infant BCG vaccination: potential mechanisms of immunity. Future Microbiol. (2018) 13:1193–208. doi: 10.2217/fmb-2018-0026
30. Mallapaty S. What the cruise-ship outbreaks reveal about COVID-19. Nature. (2020) 580:18. doi: 10.1038/d41586-020-00885-w
31. Mizumoto K, Kagaya K, Zarebski A, and Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance . (2020). 25:180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180
PubMed Abstract | CrossRef Full Text
Keywords: children, vaccines, COVID-19, SARS-CoV-2, immunization
Citation: Beric-Stojsic B, Kalabalik-Hoganson J, Rizzolo D and Roy S (2020) Childhood Immunization and COVID-19: An Early Narrative Review. Front. Public Health 8:587007. doi: 10.3389/fpubh.2020.587007
Received: 24 July 2020; Accepted: 10 September 2020; Published: 28 October 2020.
Reviewed by:
Copyright © 2020 Beric-Stojsic, Kalabalik-Hoganson, Rizzolo and Roy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bojana Beric-Stojsic, bstojsic@fdu.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Essay: Vaccination is key to beat COVID-19

Now that COVID-19 vaccines have been developed the question becomes, should I get the vaccine?
While most Rochesterians will get vaccinated , about 30% stated that they would not get the vaccine or were unsure that they would. Underlying diseases, allergies and lack of knowledge on long-term effects were some of the reasons why people were unsure or unwilling to get the vaccine.
More: NY expected to get 170,000 COVID-19 vaccine doses Dec. 15. What to know about who gets it
Here are answers to why getting vaccinated is key to beating COVID-19 and helping us move into a post-pandemic world:
What exactly are the COVID-19 candidate vaccines?
Both the Pfizer and Moderna vaccine candidates are messenger RNA (mRNA) vaccines, and considered to be new technology. While mRNA vaccines have never been utilized before, a decade's worth of work and research has gone into this technology to make it efficient and safe for humans.
The AstraZeneca’s vaccine candidate is an adenovirus-based vaccine. The only other adenovirus-based vaccine that has gained FDA approval is the recent Ebola vaccine produced by Merck. Adenovirus was originally isolated from chimpanzees and modified so that it no longer could replicate within human cells, meaning that it could no longer cause a cold.
What is mRNA?
Most cells have an in depth, very detailed code book which is the DNA. The final product of this code book would be the physical products, proteins, made by the code book. mRNA in this case, would be the summary of the code book, where all the unnecessary words are taken out. In terms of an mRNA vaccine, the mRNA would be the very small, concise and specific code for a part of the virus that your cells would make.
Production of this small part of the virus would trigger an immune reaction, allowing for your body to create the antibodies needed against the virus without every introducing the virus itself into your body. Most importantly, your body would never create the entire COVID-19 virus because of the vaccine.
How do the vaccine candidates work?
Both the Pfizer and Moderna COVID-19 vaccine candidates function the same. They introduce mRNA into your cells that produces a protein "spike" that is found on the surface of the virus. Your cells then read the code for this protein and produce it.
Once the “spike” proteins are produced, your immune system reacts to this foreign object and trains itself to remove the intruder by producing antibodies.
The AstraZeneca vaccine candidate also functions similarly. Instead of asking your cells to produce the spike protein, the adenovirus itself contains that protein. Once introduced to your system, the adenovirus containing the spike protein triggers the immune system to create antibodies so that it can fight against the slight insult to the immune system.
In both cases, once your immune system has made the antibody against the “spike” protein, it retains memory of this and can re-produce the same antibodies needed to fight the virus if you were ever exposed to the actual virus.
Isn’t it bad for your cells to do this long term though?
Long term, most likely. However, the beauty of mRNA that is introduced into your system is that it’s very fragile and has a one-time use typically. Your cells would make the protein “spike” and then the mRNA would be degraded, so your cells would never make the “spike” again.
What about long-term effects?
Long term effects and how long the vaccines will provide immunity are unknown at this point. However, initial data has shown that there are minimal initial effects to the vaccine thus far. The symptoms that were seen, such as a sore arm or feeling unwell for a few days, are typical reactions to vaccines when first given and is a response of your body cranking up productivity to fight against the intrusion.
Long-term effects of the vaccine will be made available once enough time has passed, but generally there is little to fear.
Should I get the vaccine even if I’m unsure or I don’t want to?
Yes, absolutely and emphatically yes.
The science behind the vaccines are sound and initial data suggest that there are no long-term effects to be majorly concerned about. Transparency in science is key and as long as vaccine producers are transparent there is nothing to fear.
Nazish Jeffery is a Rochester native who is pursuing her Ph.D. in biochemistry and molecular biology at the University of Rochester. She is president of the UR Science Policy Initiative.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 12, Issue 4
- Intervention studies to encourage vaccination using narrative: a systematic scoping review protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-6251-3587 Tsuyoshi Okuhara ,
- Hiroko Okada ,
- Eiko Goto ,
- Takahiro Kiuchi
- Department of Health Communication, School of Public Health , The University of Tokyo , Bunkyo-ku , Japan
- Correspondence to Dr Tsuyoshi Okuhara; okuhara-ctr{at}umin.ac.jp
Introduction Vaccine hesitancy is a global problem, impeding uptake of vaccines against measles, mumps, and rubella and those against human papillomavirus and COVID-19. Effective communication strategy is needed to address vaccine hesitancy. To guide the development of research in the field and the development of effective strategies for vaccine communication, this scoping review aims to analyse studies of interventions using narrative to encourage vaccination.
Methods and analysis We will search the following databases: MEDLINE, CINAHL, PsycINFO and PsycARTICLES. We will identify additional literature by searching the reference lists of eligible studies. Eligible studies will be those that quantitatively examined the persuasiveness of narrative to encourage vaccination. Two independent reviewers will screen the titles, abstracts and full texts of all studies identified. Two independent reviewers will share the responsibility for data extraction and verification. Discrepancies will be resolved through consensus. Data such as study characteristics, participant characteristics, methodology, main results and theoretical foundation will be extracted. The findings will be synthesised in a descriptive and a narrative review.
Ethics and dissemination This work does not warrant any ethical or safety concerns. This scoping review will be presented at a relevant conference and published in a peer-reviewed journal.
- INFECTIOUS DISEASES
- Infection control
- Public health
- PUBLIC HEALTH
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2021-053870
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
We use the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews checklist, the most current guidance on conducting scoping reviews, in order to ensure a systematic approach to searching, screening and reporting.
As this is a scoping review, formal quality assessment and risk of bias assessment will not be conducted.
This review may miss important literature published in languages other than English.
Introduction
Vaccines have long been lauded as one of the most important public health achievements of the past century. In the past decade, however, a growing number of individuals have begun to perceive vaccination as risky. Vaccine hesitancy, defined as ‘delay in acceptance or refusal of vaccines despite availability of vaccination service’, is a problem attracting growing attention and concern. 1 Vaccine hesitancy impeding uptake of vaccines against measles, mumps, and rubella and COVID-19 vaccines is a global problem. 2–5 Communication can be an effective tool, if used in a planned and integrated strategy, to counteract vaccine hesitancy and promote optimal vaccine uptake. 6
Using narrative to motivate health behaviour is an emerging form of persuasion in public health communication. 7 8 Narrative refers to the use of case stories or examples to support the argument offered by the communicator, 8 such as ‘I suffered greatly from the COVID-19. Therefore, I recommend you receive the COVID-19 vaccine to prevent severe illness due to infection’. Especially in vaccination promotion, using narrative is proposed to counter antivaccination messages in mass media and on the internet, which propagate doubt, fear and opposition to vaccination. 9 These antivaccination messages often use an emotional narrative of alleged victims of a vaccine’s side effects. 10 Scholars of vaccine communication have recently directed their interest to using narrative effectively as well, such as describing people feeling secure at recognising that they and their loved ones are protected by vaccination, or describing an experience of a person whose health suffered because of a preventable disease. 11 12
However, health-related narrative persuasion research is still emerging. Published studies remain relatively small in number, and few studies have measured health-behaviour outcomes in non-student participants. 13 To our knowledge, no study has reviewed previous studies of interventions aimed at encouraging vaccination using narrative to determine which vaccines have been targeted, what study designs have been adopted (eg, participant background, sample size, randomisation), and what outcomes have been measured (eg, vaccination behaviour, behavioural intentions, attitudes). Reviewing them will be important for developing the field of study to encourage vaccination using narrative, for critically examining the results of previous studies, and for applying them to vaccine communication practice.
Recent studies on vaccine communication have shown that narrative messages that recount personal experiences with disease increase an audience’s perception of the risk of developing disease, intention to vaccinate and likelihood of changing behaviour to prevent infectious disease, compared with didactic messages. 14 However, communication scholars have not yet reached consensus regarding the persuasiveness of narrative versus didactic messages, and the optimal usage thereof. 15 No studies have reviewed what form of intervention (eg, statistics) previous studies have adopted to quantify the persuasiveness of narrative to encourage vaccination, and what results those studies have shown.
Although theoretical developments in understanding the mechanisms and processes involved in narrative persuasion remain limited, 16 several theoretical perspectives have been proposed to explain how and why narrative communication may contribute to attitudinal and behavioural changes. The earliest studies applied models of behaviour change—the most representative being social cognitive theory. 17 Then, theories of persuasion in psychology—the most representative being the extended elaboration likelihood model 18 and the transportation-imagery model 19 —were proposed and evaluated. However, no studies have reviewed which theories and models formed the basis for previous intervention studies of encouraging vaccination using narrative.
The objective of this review is to create an overview of studies of interventions aimed at encouraging vaccination using narrative, and to identify the content and gaps in these studies. This scoping review will serve as a useful reference for researchers who plan future intervention studies on vaccine communication using narrative, speeding up their research and helping them to conduct better-designed intervention studies. This work will be useful in guiding the development of research in the field and the development of effective strategies for vaccine communication and addressing vaccine hesitancy. Our research questions will be as follows. These wide review objectives and questions will be best achieved and answered through a scoping review.
RQ1: What study designs have previous intervention studies adopted to examine the persuasiveness of narrative approaches in encouraging vaccination?
RQ2: What outcomes have previous intervention studies measured to examine the persuasiveness of narrative approaches in encouraging vaccination?
RQ3: What forms of intervention other than using narrative have previous intervention studies adopted to compare and combine with the persuasiveness of narrative in encouraging vaccination?
RQ4: What results have previous intervention studies shown about the persuasiveness of narrative approaches in encouraging vaccination including comparisons and combinations with other forms of intervention than using narrative?
RQ5: Which theories and models have been used in previous intervention studies to explain the persuasiveness of narrative in encouraging vaccination?
Methods and analysis
This systematic scoping review protocol is prepared according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews checklist (see online supplemental file 1 ). 20 The planned start date for the study is 1 April 2022, and the planned end date is 31 March 2023.
Supplemental material
Literature search.
Using the EBSCOhost Search Platform, we will search the following databases: MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO, PsycARTICLES. We will search the abstracts using the combination of keywords: (vaccine OR vaccination OR immunization) AND (narrative OR story OR storytelling). We will search the reference lists of identified eligible studies to identify any additional potentially eligible literature.
Eligibility criteria
We seek to include all intervention studies in these databases that quantitatively examined the persuasiveness of narrative to encourage vaccination, both experimental (eg, randomised controlled trials, quasi-randomised controlled trials, non-randomised trials) and quasi-experimental research (eg, pretest–post-test design, post-test design). All comparators will be eligible (ie, any forms of intervention other than using narrative). Studies without a comparator will also be eligible. Grey literature (information produced outside of traditional publishing and distribution channels, such as conference proceedings) will be included if it provides enough information to assess its eligibility. Qualitative studies will be excluded.
Studies assessing any outcomes such as behaviour, behavioural intention and attitude will be eligible, as will studies of any kind of vaccination. Studies on participants of any age, gender, ethnicity and countries will be eligible, and we will not filter by year. Only papers written in English will be included; studies not published in full text will be excluded.
Study selection
Two independent reviewers including the first author (TO) will screen the titles and abstracts of all studies initially identified, according to the eligibility criteria. Disagreements will be resolved by consensus; the opinion of a third reviewer will be sought if necessary. The full text versions of potentially relevant studies will be retrieved and screened independently by two reviewers including the first author (TO). Consensus will be reached through discussion, and if no consensus can be reached on any study, a third reviewer will arbitrate. All studies not meeting the eligibility criteria will be excluded. The results will be displayed in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Data extraction and reporting the results
A customised data extraction form will be created to extract all relevant data from each study. The data extraction form will be piloted in a sample of the eligible studies to assess its reliability in extracting the targeted study data. The first author (TO) will conduct data extraction, and another author will check the extracted data against the full texts of the studies to ensure that there are no omissions or errors. Consensus will be reached through discussion, and if no consensus can be reached on any study, a third reviewer will arbitrate. The following data will be extracted: study characteristics (author, year of publication, type of paper and country), participant characteristics (student or non-student, gender, age and other demographic information), methodology (study design, sample size and outcome), comparators and combinations (forms of intervention other than using narrative), main results of the intervention including comparison and combination with other forms of intervention than using narrative, and theoretical foundation of the intervention. The findings will be summarised in a concise table and synthesised in a descriptive and narrative review. We will discuss the findings and their implications for future research and practice as we answer each of the research questions.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Ethics and dissemination
This work does not warrant any ethical or safety concerns. We intend to present the results of this review at a relevant conference and publish them in a peer-reviewed journal.
Ethics statements
Patient consent for publication.
Not applicable.
Acknowledgments
We thank John Daniel from Edanz ( https://jp.edanz.com/ac ) for editing a draft of this manuscript.
- MacDonald NE , SAGE Working Group on Vaccine Hesitancy
- Robinson E ,
- Lesser I , et al
- Bankamp B ,
- Hickman C ,
- Icenogle JP , et al
- Wilder-Smith AB ,
- Goldstein S ,
- MacDonald NE ,
- Guirguis S , et al
- Hinyard LJ ,
- Braddock K ,
- Brewer NT ,
- Brocard P , et al
- MacDonald NE
- de Graaf A ,
- Sanders J ,
- Pietrantoni L ,
- Winterbottom A ,
- Bekker HL ,
- Conner M , et al
- Moyer-Gusé E
- Slater MD ,
- Tricco AC ,
- Zarin W , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors All authors have made substantive intellectual contributions to the development of this protocol. TO was involved in conceptualising this review and in writing this protocol. HO, EG and TK commented critically on several drafts of the manuscript.
Funding This work was supported by the Japan Society for the Promotion of Science KAKENHI (grant number 19K10615, 19K22743).
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
A Narrative Review of COVID-19 Vaccines
Affiliation.
- 1 Sydney Pharmacy School, Faculty of Medicine and Health, The University of Sydney, Sydney 2006, Australia.
- PMID: 35062723
- PMCID: PMC8779282
- DOI: 10.3390/vaccines10010062
The COVID-19 pandemic has shaken the world since early 2020 and its health, social, economic, and societal negative impacts at the global scale have been catastrophic. Since the early days of the pandemic, development of safe and effective vaccines was judged to be the best possible tool to minimize the effects of this pandemic. Drastic public health measures were put into place to stop the spread of the virus, with the hope that vaccines would be available soon. Thanks to the extraordinary commitments of many organizations and individuals from around the globe and the collaborative effort of many international scientists, vaccines against COVID-19 received regulatory approval for emergency human use in many jurisdictions in less than a year after the identification of the viral sequence. Several of these vaccines have been in use for some time; however, the pandemic is still ongoing and likely to persist for the foreseeable future. This is due to many reasons including reduced compliance with public health restrictions, limited vaccine manufacturing/distribution capacity, high rates of vaccine hesitancy, and the emergence of new variants with the capacity to spread more easily and to evade current vaccines. Here we discuss the discovery and availability of COVID-19 vaccines and evolving issues around mass vaccination programs.
Keywords: COVID-19; COVID-19 vaccines; SARS-CoV-2; vaccination; vaccine hesitancy.
Publication types

- High contrast
- About UNICEF
- Children in South Asia
- Where we work
- Regional Director
- Goodwill ambassador
- Work with us
- Press centre
Search UNICEF
My covid-19 vaccination experience, interview with an educator.

Photo: (Left to right) Hasina pictured with her three daughters, Nafisa (19), Lamia (29) and Maliha (30).
Children in Bangladesh have faced some of the worst disruption to their education in the whole world.
Schools have been completely closed since March 2020 — shutting 42 million children off from their education and the support networks many rely on to stay safe and thrive, for over a year.
Hasina Saki is part of this support network for children in Chittagong, Bangladesh. She works as Head Assistant of Administration at a government high school.
Across the world, many educators, especially younger ones, are not being prioritized for COVID-19 vaccines — putting them, and the children who rely on them, at risk.
At fifty-seven-year-old, Hasina was prioritised for a COVID-19 vaccination in Bangladesh because of her age, and on March 1st she received her first dose of the vaccine.
Ahead of her second dose at the end of this month, she tells us about her vaccination, the impact it’s had so far on her work with children (and life with her own) — and why she won’t stop taking actions to protect herself and others now that she’s been vaccinated.
How do you feel about getting the first dose of the COVID-19 vaccine?
It was definitely mixed feelings at first. It was relief with some hesitance.
But, as soon as the vaccination process started throughout the country all my questions vanished at once. The amazingly efficient and systematic vaccination procedure felt like a festival; a festival of life, a festival of hope.
So, the biggest emotion that I associate with being vaccinated is most definitely hope!
How has being vaccinated changed your daily life?
Schools have not reopened for children in Bangladesh, but I’m in the administrative department of the school, which is considered an office — and these are open. I need to go into school to complete administrative duties.
I am definitely feeling much more at peace after getting vaccinated.
But of course, we all have to be patient and strong until we all make it through this pandemic together.
As much as I hope that the vaccine protects me physically, I am still very much trying to abide by all the basic hygiene and safety measures that COVID taught us.
What does your vaccination mean to your family?
This means a lot to us. Being a working mother, COVID has been quite a challenge for me.
So, me getting vaccinated is hopefully providing my whole family with some reassurance.
What does your vaccination mean for your community?
Bangladesh is a heavily populated country, so COVID-19 makes for a very fragile and risky situation.
This smooth and fast vaccination program is vital for our country. We are very grateful to receive the vaccine now, when we really need it.

What does COVID-19 vaccination mean for the children at your school?
I’m optimistic that ongoing COVID-19 vaccinations will spell good news for the children of the school.
As more people get vaccinated, hopefully schools will reopen soon.
I hope that all the staff at work are able to get vaccinated as soon as possible.
What advice would you give to others about being vaccinated for COVID-19?
I suggest to everyone who gets the opportunity to be vaccinated, to keep a positive, hopeful and grateful attitude.
Surely the world will get through this stronger. We all have to do our part. Together, we’re stronger.
UNICEF South Asia would like to extend huge thanks to Hasina for taking the time to talk to us about COVID-19 vaccines.
We must do everything in our power to safeguard the future of the next generation. This begins by safeguarding those responsible for opening that future up for them — regardless of their age or institution.
The more educators, health workers and social workers who are vaccinated against COVID-19, the more opportunities and protection for the children who rely on them.
If you have an upcoming COVID-19 vaccination, read up on tips from our health experts on what to expect and how to prepare .
After being vaccinated, it’s important you continue the behaviours that protect yourself and others against COVID-19 by:
Washing your hands with soap and water for a minimum of 20 seconds, or hand sanitizer — as often as you can.
Keeping at least 1 metre distance between yourself and others.
Meeting people in well ventilated, or outdoor spaces
Wearing a mask when you can’t keep your distance from others, or are inside a public space.
This is because COVID-19 vaccines have proven effective at stopping people from developing the virus, but we don't yet know whether they prevent people from passing the infection onto others.
This is especially important until two weeks after your second dose of the vaccine. During this period, your body is still building protection against the virus — and while it is you could still get sick.
Related topics
More to explore, refrigerated trucks for vaccines handed over.
The trucks, which can carry four million vaccine doses each, will support the government’s efforts to strengthen its immunisation programme.
Poor Diets Damaging Children’s Health
Dr. naznin akter’s journey in safeguarding special girl chil.
n the battle against cervical cancer, a determined mother and doctor diligently works to protect girls against this deadly disease
Testing Fun Ways to Interest Children in Climate Change
Schools in Bangladesh are testing fun ways to interest children in climate change and nature issues from an early age

- Coronavirus Disease 2019
Defining the COVID-19 Narrative
The story we tell about this pandemic will shape our preparedness for the next..
Posted July 6, 2021 | Reviewed by Vanessa Lancaster
- The core narrative of the pandemic, and arguably the central one, is the presence of inequities.
- COVID-19 exposed inequities in morbidity and mortality, who bears the burden of steps we have taken to mitigate the virus, and vaccine uptake.
- The effects of these inequities will likely be with us for some time, shaping the story of the pandemic and the lives of those who lived it.

What story will we tell about COVID-19 ? The events of the past year and a half were more than just a story of the emergence and behavior of a virus. It was also a story of the social, economic, scientific, and political context into which the virus emerged and the intersection of these forces within complex, dynamic systems. Given this complexity, it can be challenging to predict which stories will rise to the surface of the overarching story of the pandemic. Yet, we need to try. The stories we tell about health shape how we engage with the present moment to support a better future—or how we fail to do so.
With this in mind, I suggest four critical narratives that emerged from the broader story of the pandemic and which can help define the overall COVID-19 narrative in the years to come. Next week, I will address the perhaps deeper issue of why we remember what we remember.
The first narrative which has come to define the COVID-19 moment is that of scientific excellence. The speed with which a COVID-19 vaccine was developed, supported by mRNA technology, reflects a new era in cutting -edge science. This narrative of scientific excellence is powerful for two key reasons.
First, because this latest vaccine technology is unique and impressive and has begun the long-awaited process of helping return us to our families, friends, colleagues, lives. Second, it is powerful because of how closely it aligns with how we already think about health. We often think about health in terms of treatment—doctors and medicines—which can cure us when we are sick, rather than in terms of the structural forces in society which shape whether or not we get sick, to begin with. We tend to confuse health (the state of not being sick) with healthcare (what we turn to once sickness strikes), which has led us to invest vast sums in healthcare at the expense of the core forces that shape health. The success of vaccines reflects that this investment is indeed core to supporting scientific excellence. Still, our story of health and COVID-19 is incomplete if it is confined to science and treatment alone.
This leads to the following core narrative of the pandemic and arguably the central one—the presence of inequities. These include, centrally, inequities in morbidity and mortality, who bears the burden of the steps we have taken to mitigate the virus and vaccine uptake. When COVID-19 struck, it quickly became apparent that certain groups—such as Black Americans, people over 65, and people with underlying health conditions—were more vulnerable to the virus than others. This vulnerability was shaped by longstanding health inequities informed by marginalization, social and economic injustice, and other foundational forces in our society. The story of COVID-19 is, in large part, the level of these forces.
These inequities have also come to define who has most felt the consequences of our efforts to mitigate the pandemic. COVID-19 caused us to embrace extraordinary measures, shut down society, and incur severe economic costs in the process. The pandemic led to significant job losses , which most affected low-income, minority workers. When the economy began to recover, with higher-wage workers bouncing back relatively quickly, lower-wage minority workers recovered at a far slower rate. The effects of this inequity will likely be with us for some time, shaping the story of the pandemic and the lives of those who lived it.
Third, the story of COVID-19 would be incomplete without an honest reckoning with widespread loss of trust in institutions and the consequences of this for public health. The most prominent example of this was how the inconsistent, often dishonest, words of former President Trump informed a lack of trust in guidance from the White House throughout the crisis. It is also true that seeming inconsistencies occasionally characterized public health efforts, perhaps most clearly in our field’s widespread embrace of civic protests last summer, in apparent contrast with our guidance on social distancing and masks. Given that COVID-19 emerged at a time when trust in institutions was already declining , the story of the pandemic may well be, in large part, a story of how this trend accelerated, making it harder for anyone to speak with a widely-heeded, authoritative voice on matters core to health.
Finally, a core narrative of the pandemic, one which could well characterize our future memory of this time, is that, as bad as COVID-19 was, it could have been far worse. I realize that this may seem strange, even unfeeling, in the context of mass death and suffering. But it is nevertheless true. COVID-19 has been a disaster. Yet, the virus itself, compared to past pandemics, is nowhere near as lethal as it might have been. A future pandemic could combine the high transmissibility of COVID-19 with the lethality of, say, SARS or even of the Black Death. While the latter may seem historically remote, there is no reason why we could not see something as deadly strike in our own time. The better we understand this, the more the story we tell about COVID-19 can help inform our efforts to build a world that is no longer vulnerable to contagion.
Each of these stories represents a vital part of the broader narrative of COVID-19. It is also the case that one or two of these narratives may rise even further to the top of our minds to conclusively define this era. Only time will tell for sure what will happen. However, I would argue several factors contribute to making stories stick when we think back on critical events, which increases the chance that the stories I have presented here will long outlast this moment. I will explore these factors and how we come to believe what we believe in our narratives next week.
This piece was also posted on Substack.

Sandro Galea, M.D., is the Robert A. Knox professor and dean of the Boston University School of Public Health
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Affective Forecasting
- Neuroscience
Persuasive Essay Guide
Persuasive Essay About Covid19
How to Write a Persuasive Essay About Covid19 | Examples & Tips
11 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Free Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About Covid19
- 3. Examples of Persuasive Essay About Covid-19 Vaccine
- 4. Examples of Persuasive Essay About Covid-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences, evidence, and analysis. Here's an example:
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About Covid19
When writing a persuasive essay about the Covid-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About Covid-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of Covid-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the Covid-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About Covid-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!

Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
Choose a Specific Angle
Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make your essay more persuasive and manageable. For example, you could focus on vaccination, public health measures, the economic impact, or misinformation.
Provide Credible Sources
Support your arguments with credible sources such as scientific studies, government reports, and reputable news outlets. Reliable sources enhance the credibility of your essay.
Use Persuasive Language
Employ persuasive techniques, such as ethos (establishing credibility), pathos (appealing to emotions), and logos (using logic and evidence). Use vivid examples and anecdotes to make your points relatable.
Organize Your Essay
Structure your essay involves creating a persuasive essay outline and establishing a logical flow from one point to the next. Each paragraph should focus on a single point, and transitions between paragraphs should be smooth and logical.
Emphasize Benefits
Highlight the benefits of your proposed actions or viewpoints. Explain how your suggestions can improve public health, safety, or well-being. Make it clear why your audience should support your position.
Use Visuals -H3
Incorporate graphs, charts, and statistics when applicable. Visual aids can reinforce your arguments and make complex data more accessible to your readers.
Call to Action
End your essay with a strong call to action. Encourage your readers to take a specific step or consider your viewpoint. Make it clear what you want them to do or think after reading your essay.
Revise and Edit
Proofread your essay for grammar, spelling, and clarity. Make sure your arguments are well-structured and that your writing flows smoothly.
Seek Feedback
Have someone else read your essay to get feedback. They may offer valuable insights and help you identify areas where your persuasive techniques can be improved.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You have read good sample essays and got some helpful tips. You now have the tools you needed to write a persuasive essay about Covid-19. So don't let the doubts stop you, start writing!
If you need professional writing help, don't worry! We've got that for you as well.
MyPerfectWords.com is a professional essay writing service that can help you craft an excellent persuasive essay on Covid-19. Our experienced essay writer will create a well-structured, insightful paper in no time!
So don't hesitate and get in touch with our persuasive essay writing service today!
Frequently Asked Questions
Are there any ethical considerations when writing a persuasive essay about covid-19.
Yes, there are ethical considerations when writing a persuasive essay about COVID-19. It's essential to ensure the information is accurate, not contribute to misinformation, and be sensitive to the pandemic's impact on individuals and communities. Additionally, respecting diverse viewpoints and emphasizing public health benefits can promote ethical communication.
What impact does COVID-19 have on society?
The impact of COVID-19 on society is far-reaching. It has led to job and economic losses, an increase in stress and mental health disorders, and changes in education systems. It has also had a negative effect on social interactions, as people have been asked to limit their contact with others.

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading


Vaccine Hesitancy Narratives
Article sidebar.

Main Article Content
Photo by Hush Naidoo Jade Photography on Unsplash
INTRODUCTION
In this collection of narratives, the authors describe their own experiences with and reflections on healthcare worker vaccine hesitancy. The narratives explore each author’s engagement with different communities experiencing vaccine hesitancy, touching on reasons for hesitancy, proposed solutions, and legal aspects. Author’s names appear above their narratives.
l. Johanna T. Crane
Vaccine hesitancy, defined as “a delay of acceptance or refusal of vaccination despite the availability of vaccination services,” [1] is a worldwide but locally shaped phenomenon that pre-dates the COVID-19 pandemic. [2] Contrary to some portrayals, vaccine hesitancy is not the same as the more absolute antivaccination stance, or what some call “anti-vax.” Many people who are hesitant are not ideologically opposed to vaccines. Hesitancy is also sometimes framed as anti-science, yet reluctance to vaccinate is often about managing risk, trustworthiness, and doubt in the context of uncertainty; it represents an effort to “talk back to science” about unaddressed needs and concerns. [3]
In the US, the newness of the vaccines, the unprecedented speed at which they were developed, and their remaining under emergency use authorization at first complicated public confidence. Political polarization and racial and social inequality shape vaccine acceptance and public distrust as well. While vaccine acceptance has increased in the months since the vaccines first became available, many eligible individuals have not yet been vaccinated, including a significant number of healthcare workers. [4]
Vaccine hesitancy among healthcare workers may seem surprising, especially given their frontline experience – I confess that it surprised me at first. But when I began interviewing health care workers for a study on COVID vaccine roll-out at community health centers, I learned to take a more complex view. Although the study was focused on patient vaccine access, [5] many of the frontline health care workers we spoke with also described hesitancy among some of their colleagues (and, in a few cases, themselves). From these conversations, I learned that these “healthcare heroes” are also regular people and members of communities. Their concerns about COVID vaccination often reflect the prevailing concerns advanced in their communities, such as worries about vaccine side effects and safety. Like other workers, some fear missing work and losing income, as not all healthcare employers offer paid time off for vaccination or recovery. (Importantly, reluctance to vaccinate is highest among healthcare workers in lower-paid positions with little job security, such as clerks, housekeepers, patient care assistants, and home health aides.) [6] For some healthcare workers of color, the protection offered by the vaccine sits in tension with both current and historical experiences of medical abuse and neglect. Some interviewees, fully vaccinated themselves, rejected the framework of “hesitancy” entirely, arguing that Black and Brown reluctance to be vaccinated first should be understood through the lens of “self-protection”.
Due to the nature of their work, healthcare workers have faced great social pressure to vaccinate and vaccinate first. This is understandable, given that vaccination against COVID-19 protects not only workers themselves but aligns with the ethical duty to prevent harm to patients by reducing the risk of transmission in healthcare settings. When the FDA approved COVID-19 vaccines under emergency use authorization in December 2020, many healthcare workers were extremely grateful to be designated “1a” – the first group prioritized to receive the shots. [7] For many bioethicists, prioritization of healthcare workers represented a recognition of the extreme risks that many front-line workers had endured since the onset of the pandemic, including critical shortages in PPE. But it is important to remember that for some workers, going first may have felt like serving as guinea pigs for new vaccines that had yet to be granted full FDA approval. For these individuals, the expectation that they would vaccinate first may have felt like an additional risk rather than a reward.
Healthcare workers who are hesitant to vaccinate may feel ashamed or be subject to shaming by others; [8] this may make it difficult to discuss their concerns in the workplace. Throughout the pandemic, healthcare workers have been lauded as “heroes”, and some healthcare employers have promoted vaccination among their workforce as a “heroic” action. This messaging implies that waiting to vaccinate is shameful or cowardly and is echoed in opinion pieces and op-eds describing unvaccinated people as “selfish” or “free riders.” [9]
By fostering the proper dialogue, we can respond respectfully to hesitancy among healthcare workers while still working towards the goal of increased vaccination. We in the bioethics and medical community should be willing to listen to our colleagues’ concerns with respect. Top-down approaches aimed at “correcting” hesitancy cannot address the more fundamental issues of trust that are often at stake. Instead, there must be dialogue over time. Conversations with a trusted healthcare provider have a crucial role. [10] Blaming and shaming rhetoric, whether explicit or implicit, gets us nowhere – in fact, it likely moves us backward by likely exacerbating any existing distrust or resentment that workers may hold toward their employers. [11] Lastly, the onus of trust must be with institutions, not individuals. There is a lot of talk about getting communities of color, and Black people, particularly, to "trust" healthcare institutions and the COVID vaccines. This racializes trust and puts the burden on harmed communities rather than on institutions acting in trustworthy ways. [12]
Dialogue, respect, and trustworthiness must guide us even in the new era of workplace mandates. Mandates make these strategies even more important as we look toward an uncertain future. As Heidi Larson, founder of the Vaccine Confidence Project, recently said, “We should not forget that we are making people's future history now. Are people going to remember that they were treated respectfully and engaged?” [13]
ll. Kara Simpson
Since the release of the vaccine for COVID-19 in late 2020, there have been robust discussions within the medical community, the media, and political arenas about vaccine hesitancy among healthcare workers. The public became aware that healthcare workers, the first group to become eligible for the vaccine, were not rushing to “take the shot.”
Many people’s opinions were aligned by race, ethnicity, socioeconomic status, and political affiliation. People of color were one of the first groups to be labeled vaccine hesitant as our experiences of distrust of the medical community and the politicization of the vaccine explained the low turnout. [14] It was not uncommon to hear, “this vaccine just came out; let’s wait and see if there are side effects.” Interestingly, many people in the healthcare community and in the public did not understand why healthcare workers of color remained hesitant.
Trust is a vital component of any viable relationship, especially in the clinical realm. To have successful health outcomes, it is essential for clinicians to build trusting relationships with their patients and peers. Many people of color are distrustful towards the medical institution due to the years of systemic racism and abuses that they have experienced, witnessed, or learned about. Healthcare workers of color are not excluded from the experiences of their communities outside of work. In fact, I assert that healthcare of color may have an additional burden of hesitation because of their lived experiences of distrust in receiving care and inequality within their professional environment. These dual traumas can work in tandem to strengthen hesitancy. I assert that building trusting clinical relationships will address hesitancy over time.
Currently, many healthcare workers are worried about vaccine mandates. For a group of people that have experienced intergenerational enslavement and marginalization, mandates feel coercive and serve as a reminder of how “lesser” bodies are considered unworthy of voice, fundamental human rights, independent decision making. To call the vaccine mandate paternalistic would be an understatement.
An unintended result of vaccine mandates will be the reinforcement of hesitancy and distrust of the medical institution as trust and coercion cannot coexist. This mandate will give more power to the conspiracy theories and harm those who already do not seek or receive adequate health care because of systemic inequalities. Furthermore, mandates can also dissuade people of color from becoming healthcare workers, and others may leave the field.
In essence, vaccine hesitancy is a symptom of a much larger problem: the distrust of the medical establishment. As bioethicists, our mission should be to support interventions that foster “trustworthiness” of the institutions rather than those that cause trauma. Several organizations have proposed mask mandates and weekly testing as a measure to protect the population at large and still respect the autonomy of the unvaccinated. [15]
lll. Jennifer Breznay
I work in a very large community teaching hospital in Brooklyn, and we were extremely hard hit by COVID in March 2020. I worked on inpatient medical units and witnessed a lot of suffering. And after nine months of fear and despair about COVID’s toll, I felt tremendous frustration in December when I heard that many healthcare workers would reject the vaccine. As the co-chair of the Bioethics Committee, I drafted a statement recommending vaccination for all employees. When the draft was revised and approved by the Bioethics Committee, I began to discuss it with employees, and I appreciated different perspectives I had not heard before. In the end, rather than releasing the statement, we directed our efforts at creating a dialogue.
I also volunteer at a not-for-profit which operates seven early childhood education centers in Northern Brooklyn. The Executive Director invited me to collaborate on strategies to encourage staff vaccination, and we decided to offer a Zoom conference to 20 members of the staff. I was extremely nervous about how the audience would perceive me, a white doctor whom they did not know. I felt awkward about coming to them with an agenda. And there was also the question of whether I was an appropriate messenger compared to a person of color.
Yet, I felt like I shouldn't back away from this. So, I chose to simply disclose my discomfort at the beginning of the Zoom. I said, “Thanks for having me. You know, as a white physician, I understand you might have concerns about trusting what I say. Four hundred years of inequity and abuse by the healthcare system can create a lot of mistrust, but I’m here to try to answer your questions.” Ultimately the Executive Director reported that the Zoom was successful in stimulating a lot of conversation among the staff about the vaccine. I think the critical piece is the intimate but open conversation, where you can elicit values.
lV. Ashley L. Stewart
In the rural areas of our state, healthcare institutions are inextricably tied to their communities. Rural hospitals hire from, serve, and function in the community where they are located. Successful implementation of a vaccine roll-out in such rural areas requires explicit recognition of the role and influence of the community. After identifying issues common to the area, rural institutions can address them. Even when rural institutions find that healthcare worker concerns seem to be unique or personal, they are often related to the larger concerns of the community. [16]
Community-based increased vaccine hesitancy may coincide with an underlying issue, such as lack of information rather than principled or experience-based resistance. [17] When the vaccines became available, rural vaccination coordinators encountered a wealth of misinformation that left many people initially undecided. Compounding this lack of information, workers expressed a sense of fear about the professional consequences of voicing concerns, especially in tight-knit communities. Many workers expressed concern about being judged merely for sharing their questions or decisions. [18] They also felt that saying or doing something to promote the value of vaccination might change their relationship with members of the community where they live and work. [19] As there was a fear of engaging in productive conversations, it was difficult for them to find valuable information, and the lack of information discouraged them from being vaccinated. Vaccine coordinators wanted to get information to the entire community based on the most current research and release unbiased, consistent, and timely information from sources all people in the community could trust, including from multiple sources at once. Communication must focus on answering many types of questions, which must often be done in private or anonymously.
Where poorly supported or incorrect information is widely available, sharing objective information is crucial to turning the tide of distrust. If the healthcare community dismisses concerns or assumes that answering questions based on misinformation is a waste of time, the community-based institutions will further the distrust. Some may feel that vaccine coordinators should not address misinformation directly, yet avoidance has been widely unsuccessful. [20] Being respectful and non-judgmental in answering questions posed by people who do not know what is true can be hard, but in rural communities, answering completely and honestly without judgment is a critical component of any effort to inform people. Telling people to get vaccinated “for the greater good” can sound the same as being told not to get a vaccine because it is “bad” if both sources of information fail to back up their claims. Ultimately rural institutions are respected because they are a resource to their communities, a priority we must preserve.
It is also critical to treat everyone respectfully regardless of vaccine status. [21] People may perceive mandates, divisive policies, or disrespectful treatment of people based on vaccination status as discriminatory or coercive, weakening the appeal of vaccination. Such practices may make people less trusting and more anchored to their position as they come to see vaccination proponents as untrustworthy or authoritarian. We must work to maintain respect for human autonomy. Using unethical means to achieve even a just end will not lead to a “greater good” but rather to the perception that people in positions of authority would achieve a result “by any means necessary.”
V. David N. Hoffman
The central moral quandary that arises whenever vaccine hesitancy among healthcare workers is discussed is whether workers who refuse to get vaccinated should or could be fired. We should clarify that we are applying a definition of mandate in the employment context for private employers, the violation of which results in loss of employment. Government-controlled provider organizations are just now weighing in on this topic and are generally pursuing strategies that impose periodic, usually weekly, testing requirements for those workers who decline to get vaccinated.
In the private sector, employers can require their employees to do a great many things as a condition of employment, and one of them is to get vaccinated against COVID -19. In the most prominent case to date, just such a mandate gave rise to a lawsuit in Texas involving Houston Methodist Hospital. In that case, 170 employees asserted that an employer should not be allowed to force them to get vaccinated. The judge held that, while no employer can force an employee to get vaccinated, no employer is obligated to continue the employment of any employee who declines to follow rules established by that employer, including the obligation to get vaccinated. [22]
In Texas, what the judge said is you are not being forced to get vaccinated, but your employer is allowed to set limits and conditions on employment, including vaccination. Employees do not have an obligation to get vaccinated, but they also have no right to their jobs. That is because of a widely misunderstood legal concept: “employment at will.” Employment at will sounds like a rule that employees can do what they want at work, but in fact, employment at will means only that you can quit your job whenever you want (we do not permit indentured servitude). At the same time, your employer can fire you at any time, for any reason or no reason, unless the reason is a pretext and involves one of the protected statuses (race, color, religion, sex, or national origin, and in some jurisdictions gender orientation, gender identity).
Generally, any employers, including hospitals, can decide that if someone is not willing to get a vaccination, or if they are not willing to complete sexual harassment training or participate in the hospital’s infection control program, that is the employee’s right, but it will mean that an employer can similarly decline to continue providing employment.
The evolution of this hesitancy discussion will be influenced by the narrower debate playing out in the court of public opinion, and the courts of law, over the enforceability of New York’s recently enacted vaccine mandate. Regardless of whether that mandate survives, with or without medical and religious exemptions, healthcare employers will be left with a profound ethical dilemma. At the end of all the litigation, if there is a religious exemption, employers will always be burdened with the responsibility to determine whether an individual employee has asserted a genuine and sincere religious objection to vaccination and whether the employer is able to provide an accommodation that is safe and effective in protecting the interests of co-workers and patients. The anticipated federal mandate, which reportedly will have a test/mask alternative, will only make this ethical task more challenging.
This leads to the final point in this analysis, which is that while private employers, including hospitals, can deprive an individual of their employment if those individuals refuse to get vaccinated, just because an employer can do so does not mean it should do so. [23]
[1] MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine . 2015;33(34):4161-4164. doi:10.1016/j.vaccine.2015.04.036
[2] Larson HJ, de Figueiredo A, Xiahong Z, et al. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine . 2016;12:295-301. doi:10.1016/j.ebiom.2016.08.042
[3] Larson H. Stuck: How Vaccine Rumors Start - and Why They Don’t Go Away . Oxford University Press; 2020; Benjamin R. Informed Refusal: Toward a Justice-based Bioethics. Sci Technol Hum Values . 2016;41(6):967-990. doi:10.1177/0162243916656059
[4] Deepa Shivaram, In The Fight Against COVID, Health Workers Aren't Immune To Vaccine Misinformation
September 18, 2021. NPR Special Series: The Coronavirus. https://www.npr.org/2021/09/18/1037975289/unvaccinated-covid-19-vaccine-refuse-nurses-heath-care-workers
[5] Crane JT, Pacia D, Fabi R, Neuhaus C, and Berlinger N. Advancing Covid vaccination equity at Federally Qualified Health Centers: A rapid qualitative review. Accepted and awaiting publication at JGIM.
[6] Ashley Kirzinger. “KFF/The Washington Post Frontline Health Care Workers Survey - Vaccine Intentions.” KFF , 22 Apr. 2021, https://www.kff.org/report-section/kff-washington-post-frontline-health-care-workers-survey-vaccine-intentions/.
[7] Johanna Crane, Samuel Reis-Dennis and Megan Applewhite. “Prioritizing the ‘1a’: Ethically Allocating Scarce Covid Vaccines to Health Care Workers.” The Hastings Center , 21 Dec. 2020, https://www.thehastingscenter.org/prioritizing-the-1a-ethically-allocating-covid-vaccines-to-health-care-workers/.
[8] “'I'm Not an Anti-Vaxxer, but...' US Health Workers' Vaccine Hesitancy Raises Alarm.” The Guardian , Guardian News and Media, 10 Jan. 2021, https://www.theguardian.com/world/2021/jan/10/coronavirus-covid-19-vaccine-hesitancy-us-health-workers.
[9] Gerson M. If you are healthy and refuse to take the vaccine, you are a free-rider. Washington Post . April 15, 2021.
[10] Crane JT, Pacia D, Fabi R, Neuhaus C, and Berlinger N. Advancing Covid vaccination equity at Federally Qualified Health Centers: A rapid qualitative review. Accepted and awaiting publication at JGIM.
[11] Larson H. Stuck : How Vaccine Rumors Start - and Why They Don’t Go Away . Oxford University Press; 2020.
[12] Benjamin R. Race for Cures: Rethinking the Racial Logics of ‘Trust’ in Biomedicine. Sociology Compass . 2014;8(6):755-769. doi:10.1111/soc4.12167; Warren RC, Forrow L, David Augustin Hodge S, Truog RD. Trustworthiness before Trust — Covid-19 Vaccine Trials and the Black Community. N Engl J Med . Published online October 16, 2020. doi:10.1056/NEJMp2030033
[13] Offri D. Heidi Larson, Vaccine Anthropologist. New Yorker . Published online June 12, 2021. Accessed August 11, 2021. https://www.newyorker.com/science/annals-of-medicine/heidi-larson-vaccine-anthropologist
[14] Razai M S, Osama T, McKechnie D G J, Majeed A. Covid-19 Vaccine Hesitancy Among Ethnic Minority Groups. BMJ 2021; 372 :n513 doi:10.1136/bmj.n513
[15] Dasgupta, Sharoda, et al. “Differences in Rapid Increases in County-Level COVID-19 Incidence by Implementation of Statewide Closures and Mask Mandates — United States, June 1–September 30, 2020.” Annals of Epidemiology , vol. 57, Sept. 2021, pp. 46–53., https://doi.org/10.1016/j.annepidem.2021.02.006.
[16] Do, Tuong Vi C et al. “COVID-19 Vaccine Acceptance Among Rural Appalachian Healthcare Workers (Eastern Kentucky/West Virginia): A Cross-Sectional Study.” Cureus vol . 13,8 e16842. 2 Aug. 2021, doi:10.7759/cureus.16842;
Danabal, K.G.M., Magesh, S.S., Saravanan, S. et al. Attitude towards COVID 19 vaccines and vaccine hesitancy in urban and rural communities in Tamil Nadu, India – a community-based survey. BMC Health Serv Res 21, 994 (2021). https://doi.org/10.1186/s12913-021-07037-4
[17] Scott C. Ratzan MD, MPA, MA, Lawrence O. Gostin JD, Najmedin Meshkati PhD, CPE, Kenneth Rabin PhD & Ruth M. Parker MD (2020) COVID-19: An Urgent Call for Coordinated, Trusted Sources to Tell Everyone What They Need to Know and Do, Journal of Health Communication, 25:10, 747-749, DOI: 10.1080/10810730.2020.1894015
[18] Huang, Pien. “Some Health Care Workers Are Wary of Getting COVID-19 Vaccines.” NPR , NPR, 1 Dec. 2020, https://www.npr.org/sections/health-shots/2020/12/01/940158684/some-health-care-workers-are-wary-of-getting-covid-19-vaccines .
Portnoy, Jenna. “Several Hundred Virginia Health-Care Workers Have Been Suspended or Fired over Coronavirus Vaccine Mandates.” The Washington Post , WP Company, 4 Oct. 2021, https://www.washingtonpost.com/local/covid-vaccine-mandate-hospitals-virginia/2021/10/01/b7976d16-21ff-11ec-8200-5e3fd4c49f5e_story.html.
[19] Jennifer A. Lueck & Alaina Spiers (2020) Which Beliefs Predict Intention to Get Vaccinated against COVID-19? A Mixed-Methods Reasoned Action Approach Applied to Health Communication, Journal of Health Communication , 25:10, 790-798, DOI: 10.1080/10810730.2020.1865488
[20] Lockyer, Bridget, et al. “Understanding Covid-19 Misinformation and Vaccine Hesitancy in Context: Findings from a Qualitative Study Involving Citizens in Bradford, UK.” Health Expectations , vol. 24, no. 4, 4 May 2021, pp. 1158–1167., https://doi.org/10.1101/2020.12.22.20248259.
Scott C. Ratzan & Ruth M. Parker (2020) Vaccine Literacy—Helping Everyone Decide to Accept Vaccination, Journal of Health Communication , 25:10, 750-752, DOI: 10.1080/10810730.2021.1875083.
[21] Zimmerman, Anne. Columbia Academic Commons, 2020, Toward a Civilized Vaccination Discussion: Abandoning the False Assumption That Scientific Goals Are Shared by All , https://academiccommons.columbia.edu/doi/10.7916/d8-rzh0-1f73.
[22] Bridges, et al v. Houston Methodist Hospital et al, https://docs.justia.com/cases/federal/districtcourts/texas/txsdce/4:2021cv01774/1830373/18
[23] David N. Hoffman, “Vaccine Mandates for Health Care Workers Raise Several Ethical Dilemmas,” Hasting Center Bioethics Forum. August 2021. https://www.thehastingscenter.org/vaccine-mandates-for-health-care-workers-raise-several-ethical-dilemmas/
David N. Hoffman
JD, Lecturer in Bioethics, Columbia University. General Counsel, Claxton Hepburn Medical Center
Ashley L. Stewart
Infection Prevention Coordinator, Carthage Area Hospital
Jennifer Breznay
MD MPH, Program Director, Division of Geriatrics, Co-Chair, Bioethics Committee, Maimonides Medical Center, Brooklyn, NY
Kara Simpson
LCSW-R, Director of Social Work, Behavioral Health Service, NYC H+H Jacobi
Johanna T. Crane
Ph.D. Anthropologist, Associate Professor, Alden March Bioethics Institute
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License .
Most read articles by the same author(s)
- David N. Hoffman, Emily Beer, Have Arguments For and Against Medical Aid in Dying Stood the Test of Time? , Voices in Bioethics: Vol. 9 (2023)
- David Hoffman, HIPAA Insanity , Voices in Bioethics: Archives (2014-2015)
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Exploring parents’ views of the use of narratives to promote childhood vaccination online
Roles Funding acquisition, Methodology, Writing – review & editing
* E-mail: [email protected]
Affiliations Department of Anthropology, Laval University, Quebec, Quebec, Canada, Department of Biohazard, Quebec National Institute of Public Health, Quebec, Quebec, Canada
Roles Formal analysis, Investigation, Writing – original draft
Affiliation Department of Biohazard, Quebec National Institute of Public Health, Quebec, Quebec, Canada
Roles Investigation, Writing – review & editing
Roles Conceptualization, Writing – review & editing
Affiliation Department of Pediatrics, Vaccine Evaluation Center, BC Children’s Hospital Research Institute, University of British Columbia, Vancouver, British Columbia, Canada
Affiliation Department of Pediatrics, Dalhousie University, Halifax, Nova Scotia, Canada
Affiliation Faculty of Nursing, University, University of Alberta, Edmonton, Alberta, Canada
Affiliation School of Public Health Sciences, University of Waterloo, Waterloo, Ontario, Canada
Affiliation Department of Family Medicine, Laval University, Quebec, Quebec, Canada
Affiliation Department of Community Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada
- Eve Dubé,
- Marie-Eve Trottier,
- Dominique Gagnon,
- Julie A. Bettinger,
- Devon Greyson,
- Janice Graham,
- Noni E. MacDonald,
- Shannon E. MacDonald,
- Samantha B. Meyer,

- Published: July 19, 2023
- https://doi.org/10.1371/journal.pone.0284107
- Peer Review
- Reader Comments
Negative information about vaccines that spreads online may contribute to parents’ vaccine hesitancy or refusal. Studies have shown that false claims about vaccines that use emotive personal narratives are more likely to be shared and engaged with on social media than factual evidence-based public health messages. The aim of this study was to explore parents’ views regarding the use of positive narratives to promote childhood vaccination.
We identified three ∼4-minute video narratives from social media that counter frequent parental concerns about childhood vaccination: parents and informed decision-making (online misinformation about vaccines); a paediatrician’s clinical experience with vaccine-preventable diseases (prevention of still existing diseases); and a mother’s experience with vaccine-preventable disease (risks of the disease). Focus group discussions were held with parents of children aged 0 to 5 years to assess their views on these three narratives and their general opinion on the use of narratives as a vaccine promotion intervention.
Four focus groups discussions were virtually held with 15 parents in December 2021. In general, parents trusted both health care provider’s and parent’s narratives, but participants identified more with stories having a parent as the main character. Both narratives featuring personal stories with vaccine-preventable diseases were preferred by parents, while the story about informed decision-making was perceived as less influential. Parents expressed the need for reliable and nuanced information about vaccines and diseases and felt that a short video format featuring a story was an efficient vaccine promotion intervention. However, many mentioned that they generally are not watching such videos while navigating the Web.
While vaccine-critical stories are widely shared online, evidence on how best public health could counter these messages remains scarce. The use of narratives to promote vaccination was well-perceived by parents. Future studies are needed to assess reach and impact of such an intervention.
Citation: Dubé E, Trottier M-E, Gagnon D, Bettinger JA, Greyson D, Graham J, et al. (2023) Exploring parents’ views of the use of narratives to promote childhood vaccination online. PLoS ONE 18(7): e0284107. https://doi.org/10.1371/journal.pone.0284107
Editor: Asrat Genet Amnie, City University of New York, UNITED STATES
Received: August 30, 2022; Accepted: March 23, 2023; Published: July 19, 2023
Copyright: © 2023 Dubé et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: This research was funded by the Canadian Institutes of Health Research Catalyst Grant. ED received the grant. https://cihr-irsc.gc.ca/f/193.html The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
In Canada and elsewhere, an increasing number of parents are choosing to delay or refuse some or all recommended vaccines for their children, leading to declining community protection and subsequent outbreaks of vaccine-preventable diseases [ 1 – 8 ]. The ubiquity of anti-vaccine discourse on the Internet, particularly on social media sites, is considered by many experts to be a key driver of vaccine hesitancy [ 9 ].
The Internet and social media have provided multiple avenues for parents to “talk” about their children’s health with other parents and medical experts, but also with pseudo-scientists and alternative care providers. Stories shared online are often powerful and can impact parents’ decision-making [ 10 , 11 ]. Evidence suggests vaccine-related stories often present “anti-vaccine” views in more compelling ways than public health “pro-vaccine” messaging. It is also increasingly recognized that parental vaccination decisions can be affected by a small number of vaccination stories or narratives [ 10 , 12 – 14 ].
A narrative is defined as “a representation of connected events and characters that has an identifiable structure, is bounded in space and time, and contains implicit or explicit messages about the topic being addressed” [ 15 p. 222]. Recent meta-analyses have concluded that narratives are more effective than traditional educational or informational messages at increasing the intention to adopt specific health behaviours [ 16 – 18 ]. Narrative messages are more persuasive because people become absorbed in the story and can identify with characters, reducing resistance to persuasion [ 18 , 19 ]. However, little is known about how to optimally use stories as a public health strategy to promote vaccines [ 12 , 20 ]. Two interventions using narratives about HPV and COVID-19 vaccinations have been recently evaluated and positively influenced vaccine attitudes and vaccine uptake [ 21 , 22 ].
The aim of this project was to explore parents’ views on the use of narratives to promote childhood vaccination.
Materials and methods
This article presents the findings of the first qualitative phase of a larger study aiming to develop and test narratives promoting childhood vaccination.
Identification of narratives
First, we investigated different social media platforms (Facebook, Twitter, Instagram, TikTok, forums) and conducted Google searches to identify narratives about childhood vaccines (videos and written posts) that Canadian parents could view online. We then conducted a content analysis among this corpus of online stories to identify patterns. Our analysis focused on creating a ‘story map’ of recurring topics, beliefs about vaccination (e.g., ‘vaccines cause autism’, ‘vaccines are made for profit’, ‘vaccine-preventable diseases are mild’, etc.), characters involved (e.g., parents, friends, partners, children, doctors, nurses, public health experts, pharmaceutical companies, etc.), events (e.g., medical consultation, illness episode, discussion with relatives, etc.) and type of message (e.g., warning, question, support, etc.). This exploratory phase allowed us to identify frequent parental concerns about childhood vaccination shared online ( Table 1 ). Every narrative had a parent (mostly mothers) or an expert (e.g., health care provider, researcher) as the main character.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0284107.t001
Subsequently, for expediency an online search was conducted to identify narratives (in video format) that counter the most recurrent negative themes that were identified, as described in Table 1 . Furthermore, we searched for videos that were public and available on YouTube and Facebook in both French and English, the two official languages in Canada. For the paediatrician story video, we found a French video and an English video with a similar story. For the informed decision-making video featuring parents, the video was in English and we added French subtitles with the help of a bilingual PhD student and an undergraduate student. English sub titles were already available for the video of the mother’s experience with vaccine preventable disease. Since the research team is bilingual, we did not need the help of a translator for data analysis or verbatim transcriptions. The story plot and main characters of these videos are described below (see S1 File for more information about the videos).
Narrative #1: Parent’s informed decision making [ 23 ].
A mother and a father shared that they did not get their first child vaccinated because others in their social network shared negative comments about vaccines, which made them hesitant. They later searched for more information about vaccines online and looked at both “anti-vaccination” websites and official sources (e.g., government, public health) and felt that official websites were more credible and trustworthy. The parents noted that, as they became better informed about childhood vaccinations, they made an informed decision and decided to have both their sons immunized as the best way to protect their health. The video ends with parents recommending looking for evidence-based information about vaccination and warning other parents about online misinformation.
Narrative #2: A paediatrician’s story [ 24 , 25 ].
A paediatrician and infectious diseases specialist explain the importance of vaccines and their role in preventing many infectious diseases worldwide. He recounts difficult cases he had to handle with young children suffering and eventually dying of vaccine-preventable diseases. The video ends with the paediatrician reminding of the importance of vaccinating children.
Narrative #3: A mother’s story [ 26 ].
A mother is recounting the story of her son’s illness and hospitalization due to a meningococcal disease (with a strain not covered by the available vaccines at that time). The video also features her child, now older, suffering from serious complications and permanently disabled. The mother shares the challenges of living with a child with severe disabilities. The video ends with a call to vaccinate by the mother, who wants to make sure that parents choose to vaccinate their children to avoid living the same difficult issues.
Exploration of parents’ views on the three narratives
Once narratives were selected, online focus groups discussions were held to assess parents’ views on the three stories and to obtain general opinions regarding this type of vaccine promotion intervention (see S2 File for focus group guide).
Recruitment.
Participants were recruited through a sample of parents who participated in an online panel survey on COVID-19 pandemic and agreed to be recontacted for other studies in Québec, Canada [ 27 ]. We purposely excluded parents who expressed very positive attitudes about vaccines, as identified on an auto-evaluated 5-item vaccine hesitancy scale (“ Generally speaking , how hesitant about vaccines do you consider yourself to be ?”). Email invitations to participate in virtual focus groups discussion were sent to parents of at least one child under the age of 5, who considered themselves somewhat or very hesitant towards vaccination, who lived in Québec, Canada. The repartition of English and French focus group discussion reflects Quebec’s language demographic as the majority use French as their main language (86 . 3%) . Although the majority of Quebecers speak French , we conducted focus group discussion with anglophones to explore potential cultural–linguistic differences . To participate, parents needed to have access to a computer and a webcam and to be fluent in English or French.
Data collection.
A focus group guide was developed by the research team to assess parents’ views about the three narratives (see Fig 1 ). During focus groups, each narrative was presented, followed by questions to assess parents’ views on each video. The second part aimed to collect general comments on parents’ perceptions of this type of interventions and suggestions about how to use such strategies as a public health intervention.
https://doi.org/10.1371/journal.pone.0284107.g001
All focus group discussions were recorded and transcribed verbatim. A deductive thematic analysis was conducted with NVivo12 using the main themes of the focus group guide as conceptual categories.
This study has been approved by the ethics committee of Centre Hospitalier Universitaire de Québec (2022–5680). Incentives of 50$ were given to each participant of the focus group for their time and involvement. An online informed consent form was signed before the focus groups.
In total, 101 invitations were sent to parents and 20 agreed to participate. Out of those, 5 dropped out after the reminder of the focus group because they were no longer available. Four focus groups with 3 to 5 participants each were conducted ( Table 2 ). Level of hesitancy was determined according to self-evaluation using a 10-point scale. Three groups were conducted with French-speaking parents and one with English-speaking parents. Focus group length was between 45 and 90 minutes, depending on the number of people attending.
https://doi.org/10.1371/journal.pone.0284107.t002
Parents’ opinions about childhood vaccination in general
Although we purposely excluded parents with very positive attitudes toward vaccines, the majority of participants had positive views about vaccination. Many participants were highly trusting of information about vaccines from healthcare providers and other medical sources (e.g. “If the information comes from [name of a paediatric hospital] , I would trust it completely”) . Most parents intended to or had already accepted routine vaccines for their child, and protection against infectious diseases was the most recurrent reason (e.g., “When I think about vaccines , I think about protection and prevention”) . However, some parents did not feel that they need to vaccinate their children and expressed a preference for natural immunity (e.g. “we have to let our kids develop their immune system by itself”) .
Parents’ views of the three narratives.
For the paediatrician’s story, the majority of parents noted that when a doctor or a nurse talks about their experience, they usually trusted the information (e.g. “I think the doctor is credible” , “no matter if it’s a nurse or a doctor , I would listen to them because it’s their speciality”) . However, this narrative was not well-perceived by the majority. This was mainly due to the context of the video (e.g. The paediatrician was outside of the clinic, in a park and provided information in a factual tone without much personal touch or emotions). Many participants noted that the health care provider wearing a “smock” or a “doctor’s outfit” and including his professional affiliations (e.g., name of the association or the hospital) would have enhanced his credibility and increased trust.
Half of the parents liked the informed decision-making video featuring parents. These parents felt they could identify with other parents and shared similar concerns (e.g., “I think the parents they do … provide a different perspective . They do show that’s what they lived through , and they shared their own experiences . For sure , we can relate to them more as parents ). Others shared that they too have had difficulties to decide about vaccination for their children with all the contradictory information online. Parents who did not like the video were mainly thinking that having difficulties to find information online was not an important issue and noted that it’s not that hard to find good information online (or to spot misinformation). Some parents also mentioned that a health care providers’ call to vaccinate was likely to be more effective to move unsure parents toward vaccine acceptance (e.g., “I think they also do need to introduce a doctor or a nurse in that video , maybe towards the end , in order to draw a conclusion or a shout out to action ‘‘ get your kids vaccinated” or something , in the very end”) .
For the last video featuring a mother’s experience with vaccine-preventable disease, the majority of participants identified with the mother and felt like the testimony was real, emotive and very powerful to move vaccine-hesitant parents (e.g., “ I think it is important to remind what vaccines are for because we don’t see those diseases often” , ”I think this video is sad , I think it shows the effect of the vaccines and I would vaccinate my child , yes”) . A few participants thought that it was too dramatic and played on guilt. These parents were worried about the potential for a backfire effect (e.g.,” I think there is a limit that should not be crossed (…) the only thing that is does is that it scares the population (…) if people against vaccination saw that , it would give them fuel to go more against it”) . In one of the focus groups, this situation created a debate. Some parents thought it was fair to show a video “playing on emotions” (i.e., guilt, fear) as this is how information is spread among “anti-vaccination” forums and websites whereas others considered that this was not the role of public health to do so. Table 3 summarizes the main themes that emerged from the focus group discussions for each narrative.
https://doi.org/10.1371/journal.pone.0284107.t003
Parents’ opinions about use of narratives to promote vaccination.
In general, participants mentioned the need for more detailed and nuanced information to make a decision about their child’s vaccination. Among information needs, parents mentioned information on brands and pharmaceutical information, vaccine preventable diseases and their consequences, nuanced information on the potential risks and benefits of vaccines. Many parents suggested adding information on sources of accurate information about vaccines (weblinks) at the end of the narratives.
All participants agreed that the narratives should be presented in a shorter video format (between ~20 seconds and one minute), but opinions about which social media platform to use were diverse (i.e., not one preferred one platform). In general, parents mainly mentioned using Facebook or YouTube to watch videos, but they mostly said that they did not watch those kinds of videos unless they are “forced” to, similar to a commercial on TV, radio or on the web before videos or between a music playlist (e.g., “For me , it’s sad to say , but I think the only way I would see that kind of video would be if it was a commercial that I have no choice to see . Because if it was on Facebook , I would not stop to look at it”) . Some parents suggested presenting such narratives in waiting rooms of medical clinics to prompt further discussion about vaccination with healthcare providers. Others noted that these narratives could complement written information on governmental or hospital web pages. Parents felt that testimony from other parents were better because they could relate more to their experiences, but many felt that health care providers were more trustworthy. Finally, there were no strong opinions on the specific vaccine-preventable diseases that should be featured in the narratives, but some parents expressed that it would be more relevant, and of interest to them, if there was an epidemic or an outbreak of the specific disease at the moment they watched the video.
The use of emotive testimonies from parents of children that are believed to have been harmed by vaccination is a common tactic of vaccine-critical groups [ 28 ]. However, the use of similar approaches to promote vaccination is uncommon in health authorities’ communication strategies due to concerns that this would be fearmongering and even unethical [ 29 , 30 ]. Still, emerging evidence indicates that narratives are powerful communication tools that should be more widely used in public health communication interventions for behaviour change [ 18 ]. In this study, we explored perceptions of Canadian parents of young children about use of narratives to promote vaccination.
Findings of the focus groups’ discussions indicate that parents are more likely to identify with other parents’ stories. However, health care providers’ advice and information about vaccines were perceived as more trustworthy. This is aligned with findings of other studies; the messenger is as important as the information that the narrative is trying to convey and trust in the main character(s) is needed to believe the story [ 31 , 32 ]. During the discussion, parents also expressed the need for balanced or nuanced information (e.g., on the risks and benefits of vaccines, on vaccine-preventable diseases, on the role of the pharmaceutical industry, etc.), which is also a common request in other studies on vaccine acceptance [ 33 , 34 ]. Although the search of nuanced information is frequently invoked by parents in order to make an informed decision about vaccines, it is still unclear what exactly type of information parents are considering “nuanced”, as often public health material is considered “too pro-vaccine” while vaccine critical websites are seen as “too anti-vaccine” [ 35 ].
While invoking negative emotions, guilt or fear in vaccine promotion interventions could create a backfire effect and be counter productive, most participants thought it was a good strategy to counterbalance vaccine critical stories that are shared online [ 36 , 37 ]. In addition, parents all agreed that the video format on the web was the best way to reach them. The advantages of audio or video messages over print and written messages is well recognized in health communication literature [ 18 , 31 , 38 ]. However, most parents that participated in our study noted that they would be unlikely to watch such videos. Optimizing the benefits of using videos for vaccine promotion, it is of critical importance to ensure to have a captive audience when designing the intervention. It is still unclear in the literature if promoting vaccination through narratives has more impact when using negative (e.g., emphasis on the risk of vaccine-preventable diseases) or positive (e.g., emphasis on the safety, efficacy and usefulness of vaccines) framing. Some studies found that negative information is more convincing while others concluded that positive messages were more credible [ 36 , 39 , 40 ]. Findings of our qualitative study indicated that parents want to be informed about the benefits and risks about vaccines and found that messages focused only on benefits of vaccination were less credible and trustworthy [ 41 , 42 ]. This indicates that narratives should not over emphasize the benefits of vaccines (e.g., no vaccine is 100% effective and 100% safe) and should include information about the potential risks of vaccines (e.g., mild, and common adverse events after immunization, rare risk of severe adverse events).
Limitations
This qualitative study is exploratory, and findings may not be generalizable to other contexts. In addition, we were not able to achieve data saturation with regards to the preferred narrative. This may be because we were not able to interview all recruited participants, as some did not show up for the online focus group sessions, even if two email reminders were sent. As for all qualitative studies, desirability bias was also inevitable. Some participants that had a high level of vaccine hesitancy in the survey expressed more positive views about vaccines during the focus group discussion. The fact that most participants were positive about vaccination and that majority of their children were already immunized is a major limitation to understand views of hesitant parents about the videos. Two participants overtly expressed vaccine hesitancy during the focus group discussions and their opinions on the narratives were different. It is thus not possible to make comparisons with the views of other participants with more positive opinions about vaccination. In addition, we were not able to recruit many very hesitant parents. Perhaps these parents are less willing to participate in a study that aimed to develop positive messages about vaccines. Recruitment via social media using a question to filter non-hesitant parents has been shown to be an effective way of recruiting vaccine hesitant parents [ 43 ]. Finally, during the first two focus group discussions, the first narrative was the most disliked. To limit this bias, we rotated the order of presentation of the narratives for the last two focus group discussions.
Childhood vaccination is a thorny issue that poses “wicked” risk communication problems for public health authorities. Wicked problems are by their very nature persistent and hard-to-resolve because they do not lend themselves to a scientific consensus about the best means for resolving the problem [ 44 ]. While scientific consensus on the public health benefits of vaccination are unequivocal, there is no such agreement on how best to use communication to respond and guide efforts to address vaccine hesitancy. With the public’s growing use of social media to inform health decisions, it is vital for public health experts to understand these platforms and how they could be mobilized for vaccine promotion interventions [ 45 ]. Although recent studies have shown positive impact of debunking myths on vaccination acceptance, these approaches can backfire for the highly hesitant [ 46 , 47 ]. By promoting messages on the importance of vaccination to prevent disease instead of focusing on specific myths, the use of narratives is a promising approach. In this qualitative study, the use of narratives to promote vaccination was well-perceived by parents. As some participants suggested, it could be beneficial for online narratives in a video format to feature on governmental pages about vaccine information to make a decision. This could facilitate dissemination of narratives-based vaccine promotion strategies. The feasibility of this avenue should be explored as past analysis have highlighted that official websites are generally not using such approaches [ 42 ]. Larger quantitative studies are needed to assess the reach and impact of such an intervention.
Supporting information
https://doi.org/10.1371/journal.pone.0284107.s001
https://doi.org/10.1371/journal.pone.0284107.s002
https://doi.org/10.1371/journal.pone.0284107.s003
Acknowledgments
We would like to thank Mélissa Picard-Filiatrault biomedical undergraduate and Laurie-Ann Carrier, anthropology student, who helped us with the exploratory phase and during focus groups.
- 1. Attitudes et croyances des parents québécois sur la vaccination–Enquête sur la couverture vaccinale des enfants de 1 an et 2 ans au Québec en 2014 [Internet]. INSPQ. [June 13 2022]. Disponible sur: https://www.inspq.qc.ca/publications/2125
- View Article
- PubMed/NCBI
- Google Scholar
- 23. What made this vaccine-hesitant couple change…—I Boost Immunity [Internet]. [August 3 2022]. Avalable: https://www.facebook.com/iboostimmunity/posts/1432957773404880/
- 24. Hib Vaccine—Vaccines and Your Baby—The Children’s Hospital of Philadelphia (8 of 14) [Internet]. 2009 [August 3 2022]. Avalable: https://www.youtube.com/watch?v=xNbVjCdvrdA
- 25. Arnaud Gagneur—L’importance de la vaccination [Internet]. 2011 [August 3 2022]. Avalable: https://www.youtube.com/watch?v=B_kpGPZeShI
- 26. Stop the Spread of Meningococcal Disease [Internet]. 2014 [August 3 2022]. Avalable: https://www.youtube.com/watch?v=mWPZGYAdcnc
- 27. COVID-19—Sondages sur les attitudes et comportements des adultes québécois [Internet]. INSPQ. [Dec 20 2021]. Avalable: https://www.inspq.qc.ca/covid-19/sondages-attitudes-comportements-quebecois
- 45. Global Vaccine Action Plan [Internet]. [June 23 2022]. Disponible sur: https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/global-vaccine-action-plan
- 46. The COVID-19 Vaccine Communication Handbook | CANVax [Internet]. [Oct 6 2022]. Disponible sur: https://canvax.ca/covid-19-vaccine-communication-handbook
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
- PMC10211334
What we talk about when we talk about COVID-19 vaccination campaign impact: a narrative review
Horácio n. hastenreiter filho.
1 Department of Industrial Engineering, Pontifical Catholic University of Rio de Janeiro, Rio de Janeiro, Brazil
2 School of Management, Federal University of Bahia, Salvador, Brazil
Igor T. Peres
Lucas g. maddalena, fernanda a. baião, otavio t. ranzani.
3 Barcelona Institute for Global Health, Barcelona, Spain
4 Pulmonary Division, Heart Institute, Faculty of Medicine, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brazil
Silvio Hamacher
Paula m. maçaira, fernando a. bozza.
5 National Institute of Infectious Disease Evandro Chagas, Oswaldo Cruz Foundation, Rio de Janeiro, Brazil
6 D'Or Institute for Research and Education, Rio de Janeiro, Brazil
Associated Data
The lack of precise definitions and terminological consensus about the impact studies of COVID-19 vaccination leads to confusing statements from the scientific community about what a vaccination impact study is.
The present work presents a narrative review, describing and discussing COVID-19 vaccination impact studies, mapping their relevant characteristics, such as study design, approaches and outcome variables, while analyzing their similarities, distinctions, and main insights.
The articles screening, regarding title, abstract, and full-text reading, included papers addressing perspectives about the impact of vaccines on population outcomes. The screening process included articles published before June 10, 2022, based on the initial papers’ relevance to this study’s research topics. The main inclusion criteria were data analyses and study designs based on statistical modelling or comparison of pre- and post-vaccination population.
The review included 18 studies evaluating the vaccine impact in a total of 48 countries, including 32 high-income countries (United States, Israel, and 30 Western European countries) and 16 low- and middle-income countries (Brazil, Colombia, and 14 Eastern European countries). We summarize the main characteristics of the vaccination impact studies analyzed in this narrative review.
Although all studies claim to address the impact of a vaccination program, they differ significantly in their objectives since they adopt different definitions of impact, methodologies, and outcome variables. These and other differences are related to distinct data sources, designs, analysis methods, models, and approaches.
1. Introduction
Since 2020, epidemiological studies related to the effects of vaccination against COVID-19 have been gaining prominence in leading international journals, reaching more than 700 studies in the Scopus database in June 2022. These papers apply distinct study designs and address different measures of vaccine performance. Clinical trials first stood out in the search to present the efficacy of the vaccines during their phase-3 periods before licensing for application in the general population.
With the beginning of the vaccination roll-outs worldwide, several researchers were dedicated to evaluating the vaccine’s effects on individuals or populations. Vaccine efficacy is determined by randomized controlled trials, and vaccine effectiveness is estimated from post-introduction observational studies. While effectiveness and efficacy of vaccination measure the direct effect of a vaccine on the vaccinated individuals and aim to describe an individual’s risk reduction after vaccination, studies on vaccine impact address the outcome of a vaccination program in a community. These studies are typically ecological or modeling analyses that compare disease outcomes from pre- and post-vaccine introduction. The reductions in disease outcomes are estimated through the direct effects of vaccination in vaccinated participants and indirect effects due to reduced transmission within a community ( 1 ).
Most vaccination efficacy studies assess an individual’s risk reduction after being vaccinated compared with those unvaccinated, thus inevitably addressing vaccine effectiveness ( 2–4 ). Vaccination impact studies are typically more feasible since individualized data are not always available in many scenarios. Only aggregated or deidentified data about the vaccination progress is often publicly available to infer how the vaccination roll-out impacts the population. While vaccine effectiveness studies are more consistent in study design and estimates ( 5 ), the existing impact studies differ significantly in many perspectives, including different study designs, estimated community outcomes, confounder variables, data sources, methods and models.
Moreover, there are literature works that address the impact of COVID-19 vaccination but should be characterized as vaccine effectiveness studies instead. For example, while the title of the work by Pritchard et al. ( 6 ) mentions vaccine impact, it presented the reduction of individual infections in vaccinated people. In the same way, the main results shown in Tande et al. ( 7 ) refer to the relative risks between vaccinated and non-vaccinated individuals, and Moghadas et al. ( 8 ) presented a theoretical simulation addressing individual outcomes.
The lack of precise definitions and terminological consensus leads to confusing statements from the scientific community about what a vaccination impact study is. In addition, there is a myriad of possible study designs in the literature that address the impact of vaccination programs on distinct populations. Difficulties in comparing study results reduce the understanding of the potential impact of a COVID-19 vaccination program on a specific population.
The present work presents a narrative review describing and discussing COVID-19 vaccine impact studies, mapping their relevant characteristics, such as study design, approach and outcome variables, while analyzing their similarities, distinctions, and main insights. Our search approach not only aims to make explicit the real distinction between vaccination impact studies and vaccination efficacy and effectiveness studies, but also presents a range of possibilities of scope and methods, among other variables. The methodology applied here, followed by other recent publications ( 9–13 ), can be used to explain the impact of a vaccination roll-out in a community, guiding and equipping other researchers interested in the subject.
2. Materials and methods
We performed the electronic search using the PubMed and Google Scholar databases. The search included literature published before November 30, 2021, using the keywords “covid-19,” “SARS-CoV-2,” “vaccine*” and “impact*.” The articles’ screening included studies addressing the impact of COVID-19 vaccines on population outcomes. The study selection was conducted by: (i) formulating the eligibility criteria; (ii) reading the abstract and selecting for full-text reading; (iii) reading the full-texts and selecting for study inclusion; and (iv) conducting a snowballing process including other studies by forward and backward search ( 14–17 ).
We considered the following eligibility criteria for study inclusion: articles covering the vaccine impact research topic, with a design of statistical modeling and/or comparison between pre- and post-vaccination population, and written in English. We excluded articles not covering the topic of COVID-19 vaccination impact, lacking a detailed description, using unclear methods, addressing vaccine effectiveness rather than impact, or related to vaccine acceptance and health impacts. Among those who focused on the vaccine’s effect on preventing COVID-19 cases, most presented the impact from the individual perspective of those vaccinated (effectiveness) and not the effect of the vaccination process on the entire population (vaccine impact). We further conducted a snowballing process from the first set of articles, including the literature before June 10, 2022. The snowballing search is a backward and forward screening, looking at the reference list of the included articles (backward) and the papers citing the included studies (forward) ( 18 ). We extracted the following research characteristics to be discussed: author, year, country, period of analysis, data source, design, outcomes and methods/models/approaches applied.
The database search found 741 articles, which were screened following the eligibility criteria. From the title and abstract reading, we excluded 704 papers presenting unclear methods lacking a detailed description or not covering the topic of COVID-19 vaccination impact, and 25 studies analyzing vaccine effectiveness rather than vaccine impact. This first study selection process yielded a set of 12 articles. From the full-text reading, we excluded four papers that did not perform statistical modelling or comparisons between pre- and post-vaccination, leaving a total of eight articles. From the selected papers, we further conducted a snowballing search, finding 269 additional articles citing or being cited by those that composed the initial set. These additional articles were screened with the criteria described before, and 10 new articles were selected, totaling 18 articles. Figure 1 illustrates the flowchart of the whole screening process. As the objective was not to conduct a systematic review, articles with similar approaches covering the same countries whose titles did not cover the vaccine impact theme were not analyzed.

Flowchart of the screening process.
The selected papers presented a diversity of methods, models, and approaches to address the impact of vaccines. Table 1 presents the characteristics of each article in terms of country, period, data source, design, outcomes and methods/models/approaches. The periods of reference for most studies involve 5 months or more. In some cases, the periods of reference for the used data start before the beginning of the vaccination to assess the evolution of cases before and after vaccination. There are studies from Latin America (Brazil and Colombia), North America (United States), Europe (England, Italy, Portugal, and other European countries) and Asia (Israel).
Main characteristics of included studies.
3.1. Summary of studies
Although the selected studies address the impact of a vaccination program, they differ significantly in their objective since they adopt different definitions of impact and methodologies. For instance, some studies have compared COVID-19 outcomes during different periods of the pandemic roll-out (specifically, the pre- and post-vaccination). In contrast, other studies perform a counterfactual analysis to calculate the vaccination program’s impact on a population, estimating what could have been the COVID-19 outcome if either no vaccination program existed, or vaccination uptake had lower levels on the studied population.
Cot et al. ( 19 ) built an epidemic Renormalization Group (eRG) framework to reproduce and predict the diffusion of the pandemic in the U.S., taking human mobility across the U.S. and the influence of social distancing into account. Human mobility is monitored using open-source flight data among U.S. states. The eRG framework provides a single first-order differential equation that describes the time-evolution of the cumulative number of infected cases in an isolated region. Meslé et al. ( 20 ) estimated the number of deaths directly averted in the population of older adults (60 years and older) due to COVID-19 vaccination in the WHO European Region from December 2020 to November 2021. The authors simulated COVID-19 outcomes in a scenario without vaccination. The simulation parameters were based on information from previous studies of COVID-19 vaccine effectiveness in preventing deaths, thus calculating the number of directly averted deaths for each country. The analysis also applied an adapted formula used by Machado et al. ( 21 ) to measure the influenza vaccine program impact, which calculates the number of deaths averted with one dose and with full vaccination through two different equations. The equations associate death numbers with vaccine effectiveness and vaccination uptake.
McNamara et al. ( 22 ) estimated the national-level impact of the initial phases of the COVID-19 vaccination program in the US. The authors compared relative changes in four different outcomes considering pre- and post-vaccination periods for the whole population and age groups. The authors applied a difference-in-differences framework to evaluate whether outcomes declined rapidly after vaccination roll-out in age groups with earlier vaccine eligibility. McNamara et al. ( 22 ) is mentioned by Ortiz and Neuzil ( 1 ) as an example of a COVID-19 vaccination program impact study. Victora et al. ( 23 ) investigated whether vaccination impacts the mortality of older individuals in a context of SARS-CoV-2 gamma variant (P.1 lineage) dominance in Brazil. The study analyzed the changes in COVID-19 proportionate mortality and mortality rate ratio in different age groups during the increase of vaccination coverage. First, they obtained proportionate mortality for older individuals (i.e., the ratio between the number of COVID-19 deaths at ages 70–79 and 80+ years and total number of COVID-19 deaths). Second, they calculated COVID-19 age-specific mortality rates by dividing the numbers of weekly deaths by the estimated population by age group. Mortality rates at ages 70–79 and 80+ years were then divided by rates for the age range 0–9 years in the same week, resulting in mortality rate ratios.
Rossman et al. ( 24 ) analyzed the temporal dynamics of new COVID-19 cases and hospitalizations after the vaccination campaign to distinguish the possible impact of vaccination from other factors, including a third lockdown implemented in Israel in January 2021. The authors performed several comparisons: individuals aged 60 years and older were prioritized to receive the vaccine first versus younger age groups; the January 2021 lockdown versus the September 2020 lockdown; and early vaccinated versus late-vaccinated cities. Galvani et al. ( 25 ) estimated the impact of the US COVID-19 vaccination campaign in controlling the virus’s transmission and deaths. The authors compared COVID-19 outcomes on the current scenario with two counterfactuals: 50% of vaccination coverage and without a vaccination campaign. They estimated the averted number of COVID-19 deaths and hospitalizations, and calculated the adjusted odds ratios for vaccination impact, stratified by vaccine platform and previous SARS-COV-2 infection. To evaluate the vaccination program impact in the US, the researchers expanded their COVID-19 age-stratified agent-based model to include transmission dynamics of the different variants. They also used the population demographics, the contact network accounting for pandemic mobility patterns, and age-specific risks of severe health outcomes due to COVID-19 as model parameters.
Andrews et al. ( 26 ) estimated the number of deaths prevented by vaccination in England between the start of the vaccination program and the end of March 2021. Assessments are made to compare the COVID-19 mortality in the current scenario with an estimated counterfactual scenario without a vaccination program. Machado et al. ( 27 ) analyzed the impact of vaccination on the control of the pandemic. They investigated the relationship between vaccine coverage and non-pharmacological interventions (NPIs), developing different scenarios for the fade-out of NPIs as vaccine coverage increases in the population. The analysis is based on developing a standard mathematical model for assessing the population-level impact of a COVID-19 vaccine in a community. A SEIR model is created by splitting the total human population into mutually exclusive compartments: unvaccinated susceptible vaccinated, susceptible, early exposed, pre-symptomatic infected, symptomatically infected, asymptomatically-infected, hospitalized and recovered.
Haas et al. ( 28 ) analyzed the number of averted COVID-19 infections, hospitalizations, and deaths in Israel due to the nationwide vaccination campaign using the Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine. The authors estimated the direct effects of the immunization program for all susceptible individuals who were at least with one dose of COVID-19 vaccine compared to unvaccinated individuals. Moreover, Milman et al. ( 29 ) analyzed the community-level evidence for SARS-CoV-2 vaccine protection of unvaccinated individuals using a correlation analysis to test results collected during the rapid vaccine rollout in a large population from 177 Israeli communities. To control for the spatiotemporally dynamic nature of the epidemic, they focused on relative changes in the proportion of positive tests within each community between fixed time intervals.
Miłobedzki et al. ( 30 ) estimated the number of confirmed new deaths based on infections and vaccinations for the European Union countries. They computed the long-run marginal death effect concerning confirmed infections and compared it with respect to confirmed vaccinations. The authors also calculated the minimal weekly number of new vaccinations per million population in a European country to keep the number of new deaths per million population at a certain level. Liu et al. ( 31 ) applied a dynamic transmission model to analyze possible dosing interval strategies for two-dose COVID-19 vaccination in thirteen European middle-income countries and compared their impacts in terms of mortality. A vaccine with similar characteristics to AstraZeneca (AZD1222) was used in the base scenario. The authors also included sensitivity analyses considering different values for vaccine efficacy.
Caetano et al. ( 32 ) estimated the COVID-19 averted deaths in Portugal using a SEIR model to measure the impact of vaccination strategy. The authors adapted an age-structured SEIR deterministic model and used hospitalization data for the model calibration to measure the impact of the COVID-19 Portuguese vaccination strategy on the effective reproduction number. They also explored three scenarios for vaccine effectiveness waning: the no-immunity-loss, 1-year and 3-year immunity duration scenarios. Rojas-Botero et al. ( 33 ) estimated the number of directly averted deaths due to COVID-19 vaccination among older adults in Colombia. The authors calculated the full vaccination coverage of older adults, for each epidemiological week and age group, from March to December 2021. A sensitivity analysis considered variations in vaccine effectiveness by age group. Sacco et al. ( 34 ) estimated the number of averted COVID-19 cases, hospitalizations, intensive care unit admissions, and deaths by COVID-19 vaccination in Italy. The authors applied a method widely used in the study of vaccination impact during the influenza season ( 21 , 35 ).
Mattiuzzi et al. ( 36 ) measure the association between the percentage of averted deaths of older people and the percentage of vaccine uptake in each corresponding European country. The authors used data on vaccine uptake and efficacy to perform univariate (Spearman’s correlation) and multivariate (multiple linear regression analysis) correlations to determine the association of the percentage of averted deaths with vaccine uptake and the type of vaccine administered. Shoukat et al. ( 37 ) applied an age-stratified agent-based model of COVID-19 in US data to estimate the averted COVID-19 hospitalizations and deaths due to the vaccination roll-out. The model was calibrated using reported incidence in New York City (NYC), considering the relative transmissibility of each variant and vaccination coverage. The authors simulated the COVID-19 outbreak in NYC under the counterfactual scenario of no-vaccination and compared the resulting disease burden using the number of cases, hospitalizations, and deaths reported under the actual vaccination status. Also in US, Suthar et al. ( 38 ) used generalized linear mixed models assuming a negative binomial outcome distribution to analyze the impact of vaccines in reducing COVID-19 incidence and mortality. The authors also included a first-order autoregressive correlation structure to account for multiple observations per municipality and to identify potential autocorrelation.
The set of studies herein described sought to establish causal relationships between the vaccination process and different outcomes related to COVID-19. However, in Cot et al. ( 19 ) and Rossman et al. ( 24 ), there is the intermediation of confounders variables such as mobility and non-pharmacological interventions (NPI). Studies based exclusively on simulations, such as the one from Iboi et al. ( 39 ), were not included. Although all studies aimed to estimate the impact of the vaccination roll-out in a population-level, they used different analysis methods, which implies diverse models and tools, to achieve their established objectives. For instance, while Meslé et al. ( 20 ) estimated vaccination campaigns’ impact by calculating the number of averted deaths, the study by McNamara et al. ( 22 ) estimated by comparing pre-vaccination COVID-19 outcomes with post-vaccination outcomes. In this sense, the study by Fang et al. ( 40 ) used the association between the vaccination coverage and the incidences and deaths caused by COVID-19 to calculate the impact of each percentage increase in population vaccination rates in the reduction of county-wide COVID-19 incidence and mortality. Often, the analysis method explained how the explanatory and outcome variables were associated. The differences among the analysed studies regarding their objectives lead to significant contrasts in the analysis methods, tools, and variables considered.
3.2. Data sources
The most important data for the studies are those related to the COVID-19 vaccination campaign, the confirmed cases and their outcomes. Usually, the National Ministry of Health and the Centers for Diseases Control are the main sources of these data. Nonetheless, depending on the approaches applied, other sources (secondary data) are also considered, as in Mattiuzzi et al. ( 36 ), which used the data produced by Meslé et al. ( 20 ).
3.3. Study design
By analyzing the populational level of the data used in the studies and their observational nature, we can say that all the studies follow an ecological study design, according to Levin et al. ( 41 ). More specifically, and according to Hanquet et al. ( 42 ), the impact of a vaccination program is estimated by comparing the population with access to a vaccination program with a reference population without the program, and vaccination program impact studies may follow mainly three different designs, which are specific subtypes of an ecological study:
- Comparison of pre- and post-vaccination population. According to this design, the two populations being assessed are separated by time, and the study outcome is compared between the pre- and post-vaccination periods. In this design, it is important to consider the different control measures (or non-pharmaceutical interventions) imposed by governments to the population being analysed in these two periods. Some initiatives such as the Oxford Covid-19 Government Response Tracker – OxCGRT ( 43 ) systematically collects daily data on policy measures enforced by governments (e.g., school closures, travel restrictions, vaccination policy, lockdowns) to tackle COVID-19 since the beginning of the pandemic and across more than 180 countries, and define indicators which may help leverage the impact of a vaccination program taking into account the different stringency levels applied to the pre- and post-vaccination populations.
- Cluster randomized vaccination trials. This design is based on generating comparable social units called clusters by randomization. The outcome is compared between placebo and vaccine clusters. Cluster-randomized trials are usually conducted to quantify a treatment or intervention effect. In cluster-randomized trials, individuals are grouped based on specific characteristics (e.g., neighbourhood of residence), and the entire cluster is randomized to treatment or control. The process of randomization ensures that the treatment and control groups are exchangeable. This approach is useful when it is impractical or infeasible to randomize at the individual level. The randomized clusters can be compared to assess the overall impact of an intervention, which is particularly important in settings where intervention may have indirect effects ( 44 ).
- Statistical modelling. This design is normally associated with an outcome prediction (e.g., disease occurrence) without vaccination. It compares it to the population’s occurrence with vaccination programs, henceforward named “epidemiological statistical modelling.” This design can adjust for differences between populations, such as annual variations and secular disease trends or changes in health care use.
As shown in Table 1 , none of the analysed articles followed the cluster-randomized vaccination trial study design. This is possibly due to the urge brought by the pandemic to vaccinate the worldwide population with vaccines which effectiveness has already been attested ( 45 ).
Nine out of the eighteen studies followed the epidemiological, statistical modelling study design, aiming to predict the impact on a community outcome by simulating scenarios with and without a vaccination roll-out. Meslé et al. ( 20 ), Galvani et al. ( 25 ), and Andrews et al. ( 26 ) estimated the number of either averted deaths or averted hospitalisations or both. To make these estimations possible, vaccine efficacy and effectiveness against deaths and hospitalisations studies were considered input variables of the impact study. In particular, Meslé et al. ( 20 ) proposed a standard approach to compare the estimated direct impact of the differential roll-out of COVID-19 vaccination programs across 33 countries in the WHO European Region, from December 2020 to November 2021. They calculated the weekly number of deaths averted per country taking the number of confirmed cases, vaccine coverage, and vaccine effectiveness in the given locality and time range into account, following Machado et al. ( 21 ). They also differed the vaccine coverage and effectiveness with at least one dose (which they called VU1 and VE1) from the vaccine coverage and effectiveness for those with complete vaccination schemas (VU2 and VE2), understanding that the number of vaccine doses influences the development of a full immune response individually, and consequently the protection from severe infection and death. Lower and upper bounds used for VE1 and VE2 were chosen based on observational studies for the vaccines most frequently used in the countries of that study. In their study, Meslé et al. ( 20 ) confirmed that both speed and extent of the vaccination in some eligible groups were determinants of vaccination impact with regard to averted deaths. Galvani et al. ( 25 ) also acknowledged the effectiveness of the different COVID-19 vaccine types administered in the US from October 2020 to June 2021 in preventing severe diseases, hospitalizations, and deaths due to COVID-19, which in turn contributed to increasing the impact of the vaccination program, potentially because of the vaccine’s ability to reduce transmission of the virus.
The remaining studies followed the pre- and post-vaccination population comparison design. In McNamara et al. ( 22 ) and Rossman et al. ( 24 ), there were clear rules to define when a specific age group goes from pre-vaccination status to post-vaccination status. However, there is no such specification in Victora et al. ( 23 ), which analyses COVID-19 community outcomes over time, while vaccination coverage rises for the age groups studied.
Meslé et al. ( 20 ) applied the same formula to measure the averted deaths due to vaccination for all the populations from the 33 countries covered by their study. Even though all analyzed countries are from the WHO European region, they differ in many aspects, including geographical, sociodemographic, and vaccination programs, since each country applied vaccines from different manufacturers, which is even pointed out in the study. Moreover, the analysis described by Meslé et al. ( 20 ) also assumes that populations with and without vaccination programs (a.k.a. pre- and post-vaccination populations) have similar baseline transmission (hence the clustered populations are similar), which does not hold. Milman et al. ( 29 ) presented the relative change in the positive test fraction according to the change in the proportion of vaccinated individuals. Finally, data completeness is also essential for ecological studies. Complete and accurate data is fostered in the different health systems, but huge variation in quality and validity remains across organizations ( 46 ).
3.4. COVID-19 community outcomes analyzed
Although all articles address the impact of vaccination programs, the outcomes differ significantly. The results from the studies compare the dynamics of the pandemic based on different outcomes, with or without an ongoing vaccination program, and even simulating different vaccination scenarios. They calculate the variations in the disease outcome, which may refer to the reduction in cases, hospitalizations, deaths, or the number of deaths averted. It is important to note that a comparative analysis between studies is hampered by the different ways the impacts of vaccination processes are presented. Most studies estimated the impact in terms of averted COVID-19 deaths ( 20 , 25 , 26 , 28 , 32–34 , 36 , 37 ), and some of them also analyzed the averted hospitalizations (and severe hospitalizations) ( 24–26 , 28 , 34 , 37 ). Other studies investigated the COVID-19 incidence seeking to estimate the reduction in the number of cases ( 19 , 21 , 28 , 29 , 34 , 38 ).
There could be a more specific interest in low- and middle-income countries (LMICs) in view of the considerable obstacles in both receiving and distributing doses, especially at the beginning of the vaccination roll-out when vaccines were scarcer. In the three studies related to countries with disparities in access to healthcare and potential discrimination in vaccine distribution, the results are in line with those of developed countries in terms of impact. In both South American countries (Brazil and Colombia) and thirteen European countries (Albania, Armenia, Azerbaijan, Belarus, Bosnia and Herzegovina, Bulgaria, Georgia, Republic of Moldova, Russian Federation, Serbia, North Macedonia, Turkey, and Ukraine), they successfully adopted strategies based on staggering vaccination in age groups, prioritizing older adults. All studies point to significant and relevant impacts of vaccine campaigns on the analyzed populations, whether due to the variation in the proportion of deaths in different age groups, the declines observed for the prioritized groups in the curves of cases and deaths, or the number of deaths avoided. The findings of each study are presented in Supplementary Table S1 .
4. Discussion
The impact studies included in the present narrative review show significant differences in how they are developed and the main achieved outcomes. The analysis methods and tools are also quite different. We only selected articles based on actual vaccination data (even if combined with hypothetical vaccination scenarios) and those presented due to vaccine impact on the entire population. The selected studies covered European, Latin American, North American and Asian countries. The reviewed studies used data collected between December 2020 and June 2022.
Most COVID-19 vaccination campaigns worldwide have multiple vaccine platforms available to immunize a population. Therefore, the vaccination impact is not often associated with a vaccine from a single manufacturer. However, Israel exclusively used the Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine. Thus, works from Rossman et al. ( 24 ), Milman et al. ( 29 ) and Haas et al. ( 28 ) could address the impact of a single platform vaccination campaign.
Cot et al. ( 19 ) established the relationship between the weekly percentage of the vaccinated population and the number of infections. The number of deaths averted by the vaccine is the main result of Meslé et al. ( 20 ), covering 33 European countries. Works from Rossman et al. ( 24 ), Andrews et al. ( 26 ), Galvani et al. ( 25 ), and Victora et al. ( 23 ) make use of temporal differences in the vaccination rate of different age groups to show a reduction in deaths, contamination, and/or hospitalizations for distinct age groups.
Regarding confounders, Rossman et al. ( 24 ), Andrews et al. ( 26 ), Galvani et al. ( 25 ), and Victora et al. ( 23 ) adjusted their results by age group. In Galvani et al. ( 25 ), the mobility rate was considered in the model. Notably, Victora et al. ( 23 ) and Galvani et al. ( 25 ) mentioned different variants of concern (VoCs) of the SARS-Cov virus; however, these VoCs should not be characterized as confounders of these studies since they were not explicitly taken into account in the models. Thus, pre- and post-vaccination populations were assumed to have similar baseline transmission. These studies only mentioned the VoCs that were dominant in the studied populations: Victora et al. ( 23 ) study was conducted when gamma was the dominant VoC, while Galvani et al. ( 25 ) was conducted during the dominance of the Alpha, Gamma, Delta, and the original Wuhan-1 variants. Likewise, vaccine manufacturers were not explicitly addressed in the models to calculate the impact and should not be considered confounder variables.
The studies also differ in outcomes, involving deaths, hospital admissions, incidences, non-ICU hospitalizations, ICU hospitalizations, and symptomatic cases. Machado et al. ( 27 ), Cot et al. ( 19 ), and Rossman et al. ( 24 ) addressed the impact of other interventions or occurrences used as parameters; the following interventions or occurrences were mentioned: pre-existing immunity, self-isolation of infected individuals, state stay-home order, state facemask police or proportions of members of public who wear masks in public and, finally, lockdowns. Rossman et al. ( 24 ) and Machado et al. ( 27 ) used the impact of lockdown as a model parameter.
The way of presenting the results is also quite different. Most articles present the number of cases, hospitalizations or deaths averted. In some studies, the asymmetry in the temporality of the vaccination process between different age groups is used to point out how it affects the relative participation of these groups in the total number of cases, deaths or hospitalizations. There are approaches that establish comparisons between countries and territories. In these cases, the different vaccination rates observed are related to different declines in the numbers of cases, hospitalizations or deaths. There is a specific article that studies the differentiated impact determined by the different intervals between doses. Finally, there is a study in which the authors identify the minimum weekly vaccination rate to guarantee a specific value for the number of deaths.
Several of the reviewed articles made use of epidemiological models such as SEIR, which can be seen as simplistic, that is, using a few compartments instead of thousands of compartments to represent the real complexity of the system. In an epidemic, several phenomena are difficult to understand, caused by the interaction of a huge number of agents which, even when acting locally, are capable of influencing results elsewhere ( 47 ). However, SEIR models proved robust enough to be applied in different geographic locations and in populations of different ethnic origins, enabling and recommending their use in territories with a lack of viral testing. Barbosa et al. ( 48 ) applied the SEIR model using epidemiological data from Marabá, a poor municipality in the state of Pará in Brazil, with estimated values of latency time and infectious time obtained in Chinese populations and these proved to be useful for predicting the evolution of COVID-19 cases, a more complex process than the estimation of the vaccine impact. One last important consideration concerning the presented models is that they do not recognize the prolonged duration of the pandemic and the representative rate of deaths during a given period, since they do not use the number of deaths and births in the most active period of the pandemic as parameters, thus, disregarding its vital dynamics, foreseen in the complex systems applied to epidemiological models presented by Lima ( 47 ).
Figure 2 synthesizes the main characteristics of the vaccination impact studies analyzed in this narrative review. Although the lack of systematicity in the review process does not allow the complete range of designs, methods, variables, and results of vaccine impact studies to be presented, it is understood that the outline of its characteristics is broad enough to give those interested in the subject the breadth of possibilities available.

The main characteristics of the vaccination impact studies analysed in this review. As visually represented, a vaccination impact study is distinguished by four perspectives: Input variables, Community outcome, Study design, and Analysis methods, models, and approaches.
5. Conclusion
The articles analyzed in this Narrative Review, regardless of the methods applied and country(ies) covered, share in their results the significant population impact brought by the vaccination process. Although the pandemic is cooling down at the moment, its permanence has required new booster doses to be administered. In addition, the possibilities for the emergence of new variants of concern can alter vaccine efficacy, establishing new levels of vaccine impact. Studying the impact of COVID-19 vaccines will remain the slogan of the day for some time. The present work contributed to the research on this theme, offering a broad and structured view of the methodological possibilities, models, approaches and designs. Furthermore, it aims to contribute to a broader view of the possible studies, as it also brings together the different possibilities of input variables adopted and different outcome variables that may represent the vaccination impact.
There is, however, an approach to vaccine impact that remains underexplored. In addition to disparities in the application of COVID-19 tests and in the supply of protective equipment, LMICs suffered from problems related to the availability of vaccines ( 49 ). In none of the analyzed studies, the discussion on the superiority of the strategy, adopted by the richest countries, in terms of vaccine impact, of protecting them-selves other than globally controlling the COVID-19 pandemic, was privileged. In one of the studies, Louden ( 50 ) says that careful consideration of vaccine production, pricing, allocation, and distribution must be taken into account to ensure equitable access to COVID-19 vaccines scaling up the global COVID-19 vaccination program but in this study vaccine impact was not the approach. Ali et al. ( 51 ) discussed the problem of vaccine equity in LMICs. They found that inequalities in wealth, education, and geographic access can affect vaccine impact and vaccination dropout which demands more attention in countries where the level of inequality is considerably higher. The analysis of global vaccination rollouts comparing LMIC to rich countries should include each country demography (and the age groups approved to be vaccinated). LMICs with low proportion of population older than 60 years cannot be direct compared to some European countries with high proportion of population older than 60 years. Furthermore, the propensity of young adults to get vaccinated in a country with a young population is different than in one with an old population. The assessment of the benefits of potentially protecting older adults to the risks of the vaccine is dependent on demography.
Another study alternative, which was not observed, would be to evaluate the vaccine impact in terms of the relative dynamics of cases and deaths after the consolidation of the vaccination process, comparing the results between countries before and after vaccination, as a function of the percentage of vaccinated and the number of doses administered. Brazil, for example, a LMIC, due to the greater adherence of its population to vaccination, after being the eighth country in deaths by COVID-19 in the world in the period of 2020–2021, already occupies the 17th position in October of 2022, considering the entire pandemic period, registering fewer deaths per capita , bearing in mind only the year 2022, than the United States and many European developed countries. Finally, the impact of vaccination campaigns could be analyzed in terms of compliance with COVID-19 regulations, mobility and contact behavior in communities, the likelihood of transmission at a potentially infectious contact, human behavior (and mental health), and health care costs.
Author contributions
HF, LM, FBa, and IP: conceptualization, formal analysis, investigation, and visualization. HF, LM, FBa, and IP: methodology and writing—original draft preparation. FBa, IP, OR, SH, PM, and FBo: validation. HF, LM, and IP: data curation. IP, OR, SH, PM, and FBa: writing—review and editing. OR, SH, and FBo: supervision. All authors contributed to the article and approved the submitted version.
This work was performed as part of the Grand Challenges ICODA pilot initiative (INV-017293), funded by the Minderoo Foundation and the Bill & Melinda Gates Foundation. The research was also supported by the National Council for Scientific and Technological Development (CNPq) [grant numbers 310940/2019-2 and 403863/2016-3 to SH; 422810/2021-5 and 312059/2022-1 to FBa; and 422470/2021-0 and 311519/2022-9 to PM], Carlos Chagas Filho Foundation for Research Support of the State of Rio de Janeiro (FAPERJ) [grant numbers 211.308/2019 to FBa; and 211.086/2019, 211.645/2021, and 201.348/2022 to PM], and the Pontifical Catholic University of Rio de Janeiro (PUC-Rio). OTR is funded by Sara Borrell from Instituto de Salud Carlos III (CD19/00110).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
This research was conducted in the Center for Healthcare Operations and Intelligence - NOIS (www.nois.ind.puc-rio.br) in PUC-Rio. The authors thank all NOIS participants for their collaborative production of scientific analyses of the COVID-19 pandemic in Brazil. OTR acknowledges the support from the Generalitat de Catalunya through the CERCA Program and from the Spanish Ministry of Science and Innovation and State Research Agency through the “Centro de Excelencia Severo Ochoa 2019-2023” Program (CEX2018- 000806-S).
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1126461/full#supplementary-material
- Share full article

Four Wild Ways to Save the Koala (That Just Might Work)
To protect Australia’s iconic animals, scientists are experimenting with vaccine implants, probiotics, tree-planting drones and solar-powered tracking tags.
A veterinary nurse treats a koala infected with chlamydia at Currumbin Wildlife Hospital in Currumbin, Australia. Credit...
Supported by

By Emily Anthes
Photographs and Video by Chang W. Lee
This story is part of a series on wildlife conservation in Australia, which Emily Anthes reported from Australia and New York.
- April 15, 2024
It was spring in Queensland, Australia, a season when many wild animals find themselves in trouble, and the Currumbin Wildlife Hospital was a blur of fur and feathers.
A groggy black swan emerged from the X-ray room, head swaying on its long neck. A flying fox wore a tiny anesthetic mask. An injured rainbow lorikeet squawked in its cage. (“Very angry,” a sign warned.)
“We see everything,” Dr. Michael Pyne, the hospital’s senior veterinarian. Also on the schedule for the day: three eagles, two carpet pythons, a blue-faced honeyeater, a short-eared brushtail possum and, Dr. Pyne said, “a whole heap of koalas.”
More than a dozen koalas were convalescing in open-air enclosures, wrapping their woolly arms around the trunks of eucalyptus trees. The wards were often full; in 2023, the hospital admitted more than 400 koalas, a fourfold increase from 2010.
The surge has been driven largely by the spread of chlamydia , a devastating bacterial infection. But the hospital was also seeing more koalas with traumatic injuries, including those caused by cars and dogs. Starving, dehydrated koalas came in during droughts; burned koalas appeared after wildfires. Occasionally, koalas even turned up with injuries caused by cows.
“That’s why they’re endangered,” Dr. Pyne said. “Everything’s against them.”

The koala, long an Australian icon, has become an unfortunate emblem of the country’s biodiversity crisis. The animals are threatened by deforestation, climate change and infectious disease. Together, these forces put the koala at the real risk of extinction . Although koalas are notoriously difficult to count, populations in some places have plummeted by as much as 80 percent , scientists estimate.
“We don’t know what the threshold is where there’s a point of no return,” said Tanya Pritchard, the senior manager for species recovery and landscape restoration at the World Wide Fund for Nature-Australia. “So we do need to act pretty urgently.”
Scientists and conservation groups are giving the koala everything they’ve got. Some are pursuing traditional time-tested strategies, including the protection of koala habitats and the advocacy of tougher conservation laws.
Others are trying more experimental approaches, from koala probiotics to tree-planting drones. Many of these projects are in the early stages, and none represent a complete solution. But given the wide array of threats that koalas are facing, saving them might require deploying every available tool.
“At this point,” Ms. Pritchard said, “every koala counts.”
Here are some of the tools in development.

Put shots in arms
Chlamydia, a common sexually transmitted infection in humans, is also widespread in the animal kingdom. How koalas were first infected is unknown, but one possibility is that the marsupials picked up chlamydia from the feces of livestock.
The disease, which can spread through sexual contact and from mothers to joeys, has become staggeringly widespread in parts of Australia. Chlamydia can cause urinary tract infections, blindness and infertility, suggesting that koalas could be in even worse shape than their declining numbers would indicate. “How many of those koalas that are out there can’t breed anymore because chlamydia has made them sterile?” Dr. Pyne said.
Scientists are now collaborating with the Currumbin Wildlife Hospital in Currumbin, Australia, to test a new chlamydia vaccine in wild koalas. So far, the vaccine is producing “quite spectacular results,” said Ken Beagley, an immunologist at the Queensland University of Technology who led the development of the vaccine.
Across two ongoing studies, more than 300 wild koalas have been vaccinated, and many vaccinated females have gone on to have healthy joeys, some of which have now had joeys of their own, Dr. Beagley said. “It was far better than we expected,” he said of the outcome.
Still, it will be challenging to inoculate thousands of wild koalas with the current vaccine, which requires two shots given 30 days apart. So Dr. Beagley and his colleagues are developing a delayed-release vaccine implant , which could be injected under the skin when a koala receives its first shot. Over the course of several weeks, the small capsule would slowly absorb water and then burst, thus delivering the second dose.
Give them the good microbes

Koalas are notoriously picky eaters with highly unusual tastes. “They feed on a really unpalatable diet of eucalyptus leaves, which is high in fiber, low in protein, high in toxins,” said Michaela Blyton, a molecular ecologist and microbiologist at the University of Queensland.
Living on eucalyptus requires a cooperative community of gut microbes, which help digest the leaves. Dr. Blyton’s work suggests that these microbial communities are so finely tuned that they may dictate which eucalyptus species, of the many that dot Australia, an individual koala can eat. That microbial specificity could explain why koalas are sometimes unable to diversify their diets, even in the face of starvation.
In a 2019 study, Dr. Blyton showed that she could shift koalas’ microbiomes, and expand their diets , by giving them fecal transplants from koalas that dined on a different type of eucalyptus. (To perform the transplant, Dr. Blyton packaged fecal samples from donor koalas in small capsules, which were administered orally.)
Now, she is hoping to use the same approach to maintain microbial equilibrium in koalas taking antibiotics, which are the frontline treatment for chlamydia. The drugs can throw the gut microbiome out of whack, prompting koalas to stop eating altogether, with sometimes fatal results. “It’s a hard ask to get the animal going again, and a lot of the time we just can’t,” said Dr. Blyton, who collaborates with Currumbin and other wildlife hospitals.
Dr. Blyton has developed a technique for freeze-drying fecal samples from healthy koalas, yielding shelf-stable capsules that can be given to koalas with chlamydia as a sort of oral probiotic. Unfortunately, early trial results suggested that administering the capsules was stressful for sick koalas. So Dr. Blyton is now trying to turn the freeze-dried fecal samples into a powder that could be added to other nutritional supplements the animals already receive.
Deploy the drones
Koalas — sedentary, tree-dwelling animals — are tricky to spot in the wild, adding to the challenges of tracking how their populations are faring, identifying critical habitats and safeguarding the animals from threats.
Grant Hamilton, a quantitative ecologist at the Queensland University of Technology, has developed a new koala-spotting system that is powered by artificial intelligence. A drone equipped with a thermal camera flies over the treetops, looking for pockets of body heat hidden under the canopy. Machine learning algorithms can quickly process this footage, tallying the koalas. The scientists then use statistical models to estimate the total koala population in a given area.
The scientists are now teaching local conservation groups how to fly the drones in their own neighborhoods. Dr. Hamilton and his colleagues will then analyze the data to help these organizations identify critical koala habitats that might benefit from protection or restoration. “We can use A.I. to help people to manage their backyards or their parks,” he said. “That’s a really exciting idea.”
The World Wide Fund for Nature-Australia, which is currently running a campaign to save or plant two billion trees by 2030, is experimenting with using drones for habitat restoration. Over the course of eight hours, a single tree-planting drone can rain some 40,000 seeds across the landscape.
Drones aren’t suited for all environments, but they offer a way to “scale up this work,” Ms. Pritchard said. “To me, it’s a little bit symbolic of our own plight,” she added. “If we can’t save the koala, as our most important and most loved species, what does that mean for our own situation and the health of our own habitats?”
Harness solar (and people) power
Despite the threats they face, koalas do have one thing going for them. “They are one of the cutest animals on Earth,” said Dr. Romane Cristescu, a conservation ecologist at the University of the Sunshine Coast.
To harness the public’s natural affection for koalas, she and her colleagues are developing a suite of technological tools, including solar-powered, location-tracking ear tags, which send data to a mobile app. The app, which is still undergoing testing, aims to help Australians get to know the koalas that live in their neighborhoods — “where they go, who they meet, their children, their boyfriend,” Dr. Cristescu said. “We’re going to tell people, ‘Hey, look, that koala’s got a life.’”
Dr. Cristescu hopes that people who develop attachments to their local koalas will be more inclined to support conservation efforts and change their own behaviors, like choosing not to cut down the trees in their yards. “We have a lot more empathy for a koala that has a name and a story,” she said.
The app also encourages users to log koala sightings and to report sick koalas, data that can be sent to scientists and wildlife care teams, she said.
The ear tags could be used for other purposes, too, said Dr. Cristescu, who also leads a research program that uses trained dogs to sniff out koalas and koala scat. After Australia’s catastrophic wildfires in 2019 and 2020, her team used dogs and drones to find and rescue injured koalas. The location-tracking ear tags could provide a quicker way to find koalas in danger, she said.

Emily Anthes is a science reporter, writing primarily about animal health and science. She also covered the coronavirus pandemic. More about Emily Anthes
Chang W. Lee has been a photographer for The Times for 30 years, covering events throughout the world. He is currently based in Seoul. Follow him on Instagram @nytchangster . More about Chang W. Lee
Explore the Animal Kingdom
A selection of quirky, intriguing and surprising discoveries about animal life..
Two periodical cicada broods are appearing in a 16-state area in the Midwest and Southeast for the first time in centuries. Can you get rid of them? Do they bite? We answer your questions .
Aside from chimps and humans, researchers have found clear evidence of menopause in only five species — all of them whales. A new study looks at the possible causes for it .
Scientists never imagined that the blind cave salamanders called olms willingly left their caves. Then, they discovered several at aboveground springs in northern Italy .
According to a common narrative that male mammals tend to be larger than female ones. A new study paints a more complex picture .
Daddy longlegs, the group of splendidly leggy arachnids also known as harvestmen, have been thought to have just two eyes. New research has uncovered four more vestigial ones .
The means by which some whales sing underwater has long been a mystery. A contraption that forced air through the larynxes of three carcasses puts forth an explanation .
Advertisement

COMMENTS
An additional aspect of vaccines many parents are troubled with is the increase in suggested vaccines for young children. "Today, the CDC recommends that children receive vaccines for 10 diseases — plus the flu vaccine — by age 6, which can mean up to 37 separate shots. That compares to five vaccines for the same age group in 1995 ...
The effects of scientific messages and narratives about vaccination. In 2018-19, the U.S. experienced the largest measles outbreak in over a quarter-century, a disease for which, like COVID-19, an effective and safe vaccine exists [].The increasing number of measles cases, largely driven by inadequate vaccination rates in several mostly-religious communities [], prompted news attention ...
Abstract. The COVID-19 pandemic has shaken the world since early 2020 and its health, social, economic, and societal negative impacts at the global scale have been catastrophic. Since the early days of the pandemic, development of safe and effective vaccines was judged to be the best possible tool to minimize the effects of this pandemic.
Fighting against COVID-19 is the top priority for all the countries and nations. The development of a safe and effective COVID-19 vaccine is considered the optimal way of ending the pandemic. Three hundred and 44 vaccines were in development, with 149 undergoing clinical research and 35 authorized for emergency use as to March 15 of 2022.
Amid the staggering amount of suffering and death during this historic pandemic of COVID-19, a remarkable success story stands out. The development of several highly efficacious vaccines against a previously unknown viral pathogen, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), in less than 1 year from the identification of the virus is unprecedented in the history of vaccinology.
At the completion of the quick search and identification process, 14 out of 30 identified articles were included in this early narrative review . Included papers were all published in 2020 following the early release of data on COVID-19, presenting hypotheses about the potential relationship between childhood vaccination and COVID-19—either ...
Nazish Jeffery, a University of Rochester graduate student who writes occasionally on science and public policy, explains why vaccinations are the key to stopping the scourge of the COVID-19 pandemic.
Introduction Vaccine hesitancy is a global problem, impeding uptake of vaccines against measles, mumps, and rubella and those against human papillomavirus and COVID-19. Effective communication strategy is needed to address vaccine hesitancy. To guide the development of research in the field and the development of effective strategies for vaccine communication, this scoping review aims to ...
Please use one of the following formats to cite this article in your essay, paper or report: APA. Moore, Sarah. (2022, January 17). The Importance of Global COVID-19 Vaccination.
A Narrative Review of COVID-19 Vaccines Vaccines (Basel). 2021 Dec 31;10(1):62. doi: 10.3390/vaccines10010062. ... Several of these vaccines have been in use for some time; however, the pandemic is still ongoing and likely to persist for the foreseeable future. This is due to many reasons including reduced compliance with public health ...
The Polio vaccine was originally created by a man named Jonas Salk in 1955 and was replaced by Bruce Sabin in 1960. A discussion was held in Chicago on May 26, 1960, critiquing the Polio vaccine. Two Doctors of the panels Dr. Ratner and Dr. Kleinman have been critics of Salk's Polio vaccine since it was created.
Yes, vaccines prevent 33000 children in the U.S, and prevent 2 and 3 million deaths worldwide, prevent 8500 child hospitalization in Colorado. Vaccines are an important part to health, today many diseases can travel easily. Anyone can carry disease and pass it to an unvaccinated person.
Nearly every 100 years, humans collectively face a pandemic crisis. After the Spanish flu, now the world is in the grip of coronavirus disease 2019 (COVID-19). First detected in 2019 in the Chinese city of Wuhan, COVID-19 causes severe acute respiratory distress syndrome. Despite the initial evidence indicating a zoonotic origin, the contagion ...
After being vaccinated, it's important you continue the behaviours that protect yourself and others against COVID-19 by: Washing your hands with soap and water for a minimum of 20 seconds, or hand sanitizer — as often as you can. Keeping at least 1 metre distance between yourself and others. Meeting people in well ventilated, or outdoor spaces.
During the COVID-19 pandemic, medicine and public health have grappled with challenges related to individual behaviour and decision making, both in terms of infection and more recently concerning the uptake of COVID-19 vaccines. Social theory has long pointed to the role of narrative when trying to grasp the complexity of understanding and decision making in times of crisis.
The speed with which a COVID-19 vaccine was developed, supported by mRNA technology, reflects a new era in cutting-edge science. This narrative of scientific excellence is powerful for two key ...
Examples of Persuasive Essay About Covid-19 Vaccine. Covid19 vaccines are one of the ways to prevent the spread of Covid-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your ...
Photo by Hush Naidoo Jade Photography on Unsplash INTRODUCTION In this collection of narratives, the authors describe their own experiences with and reflections on healthcare worker vaccine hesitancy. The narratives explore each author's engagement with different communities experiencing vaccine hesitancy, touching on reasons for hesitancy, proposed solutions, and legal aspects.
A fundamental challenge complicates news decisions about covering vaccine side effects: although serious vaccine side effects are rare, less severe ones do occur occasionally. The study was designed to test whether a side effect message could induce vaccine hesitancy and whether that could be countered by pro-vaccine messages about vaccine safety. A large (N = 2,345), nationally representative ...
Background Negative information about vaccines that spreads online may contribute to parents' vaccine hesitancy or refusal. Studies have shown that false claims about vaccines that use emotive personal narratives are more likely to be shared and engaged with on social media than factual evidence-based public health messages. The aim of this study was to explore parents' views regarding the ...
Objective. The present work presents a narrative review, describing and discussing COVID-19 vaccination impact studies, mapping their relevant characteristics, such as study design, approaches and outcome variables, while analyzing their similarities, distinctions, and main insights.
It is a testament to human ingenuity and collective effort in advancing healthcare. Vaccination remains a key pillar in pursuing a healthier, more resilient world. 500 Words Essay on Vaccination. Vaccination, a triumph of modern medicine, has significantly altered the landscape of public health.
The Covid 19 pandemic has affected many aspects of school life, all in order to prevent any further spread of the disease. Our school is working hard to go back to the normal school life we used to have before the global pandemic. Yet, parents are still worried about their kids, and teachers about their students.
To protect Australia's iconic animals, scientists are experimenting with vaccine implants, probiotics, tree-planting drones and solar-powered tracking tags.