The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.

How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
You are using an outdated browser
Unfortunately Ausmed.com does not support your browser. Please upgrade your browser to continue.
Cultivating Critical Thinking in Healthcare
Published: 06 January 2019

Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).
Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught , assessed and integrated into the design and development of staff and nurse education and training programs (Papp et al. 2014).
So, what exactly is critical thinking and how can healthcare educators cultivate it amongst their staff?
What is Critical Thinking?
In general terms, ‘ critical thinking ’ is often used, and perhaps confused, with problem-solving and clinical decision-making skills .
In practice, however, problem-solving tends to focus on the identification and resolution of a problem, whilst critical thinking goes beyond this to incorporate asking skilled questions and critiquing solutions .
Several formal definitions of critical thinking can be found in literature, but in the view of Kahlke and Eva (2018), most of these definitions have limitations. That said, Papp et al. (2014) offer a useful starting point, suggesting that critical thinking is:
‘The ability to apply higher order cognitive skills and the disposition to be deliberate about thinking that leads to action that is logical and appropriate.’
The Foundation for Critical Thinking (2017) expands on this and suggests that:
‘Critical thinking is that mode of thinking, about any subject, content, or problem, in which the thinker improves the quality of his or her thinking by skillfully analysing, assessing, and reconstructing it.’
They go on to suggest that critical thinking is:
- Self-directed
- Self-disciplined
- Self-monitored
- Self-corrective.

Key Qualities and Characteristics of a Critical Thinker
Given that critical thinking is a process that encompasses conceptualisation , application , analysis , synthesis , evaluation and reflection , what qualities should be expected from a critical thinker?
In answering this question, Fortepiani (2018) suggests that critical thinkers should be able to:
- Formulate clear and precise questions
- Gather, assess and interpret relevant information
- Reach relevant well-reasoned conclusions and solutions
- Think open-mindedly, recognising their own assumptions
- Communicate effectively with others on solutions to complex problems.
All of these qualities are important, however, good communication skills are generally considered to be the bedrock of critical thinking. Why? Because they help to create a dialogue that invites questions, reflections and an open-minded approach, as well as generating a positive learning environment needed to support all forms of communication.
Lippincott Solutions (2018) outlines a broad spectrum of characteristics attributed to strong critical thinkers. They include:
- Inquisitiveness with regard to a wide range of issues
- A concern to become and remain well-informed
- Alertness to opportunities to use critical thinking
- Self-confidence in one’s own abilities to reason
- Open mindedness regarding divergent world views
- Flexibility in considering alternatives and opinions
- Understanding the opinions of other people
- Fair-mindedness in appraising reasoning
- Honesty in facing one’s own biases, prejudices, stereotypes or egocentric tendencies
- A willingness to reconsider and revise views where honest reflection suggests that change is warranted.
Papp et al. (2014) also helpfully suggest that the following five milestones can be used as a guide to help develop competency in critical thinking:
Stage 1: Unreflective Thinker
At this stage, the unreflective thinker can’t examine their own actions and cognitive processes and is unaware of different approaches to thinking.
Stage 2: Beginning Critical Thinker
Here, the learner begins to think critically and starts to recognise cognitive differences in other people. However, external motivation is needed to sustain reflection on the learners’ own thought processes.
Stage 3: Practicing Critical Thinker
By now, the learner is familiar with their own thinking processes and makes a conscious effort to practice critical thinking.
Stage 4: Advanced Critical Thinker
As an advanced critical thinker, the learner is able to identify different cognitive processes and consciously uses critical thinking skills.
Stage 5: Accomplished Critical Thinker
At this stage, the skilled critical thinker can take charge of their thinking and habitually monitors, revises and rethinks approaches for continual improvement of their cognitive strategies.
Facilitating Critical Thinking in Healthcare
A common challenge for many educators and facilitators in healthcare is encouraging students to move away from passive learning towards active learning situations that require critical thinking skills.
Just as there are similarities among the definitions of critical thinking across subject areas and levels, there are also several generally recognised hallmarks of teaching for critical thinking . These include:
- Promoting interaction among students as they learn
- Asking open ended questions that do not assume one right answer
- Allowing sufficient time to reflect on the questions asked or problems posed
- Teaching for transfer - helping learners to see how a newly acquired skill can apply to other situations and experiences.
(Lippincott Solutions 2018)
Snyder and Snyder (2008) also make the point that it’s helpful for educators and facilitators to be aware of any initial resistance that learners may have and try to guide them through the process. They should aim to create a learning environment where learners can feel comfortable thinking through an answer rather than simply having an answer given to them.
Examples include using peer coaching techniques , mentoring or preceptorship to engage students in active learning and critical thinking skills, or integrating project-based learning activities that require students to apply their knowledge in a realistic healthcare environment.
Carvalhoa et al. (2017) also advocate problem-based learning as a widely used and successful way of stimulating critical thinking skills in the learner. This view is echoed by Tsui-Mei (2015), who notes that critical thinking, systematic analysis and curiosity significantly improve after practice-based learning .
Integrating Critical Thinking Skills Into Curriculum Design
Most educators agree that critical thinking can’t easily be developed if the program curriculum is not designed to support it. This means that a deep understanding of the nature and value of critical thinking skills needs to be present from the outset of the curriculum design process , and not just bolted on as an afterthought.
In the view of Fortepiani (2018), critical thinking skills can be summarised by the statement that 'thinking is driven by questions', which means that teaching materials need to be designed in such a way as to encourage students to expand their learning by asking questions that generate further questions and stimulate the thinking process. Ideal questions are those that:
- Embrace complexity
- Challenge assumptions and points of view
- Question the source of information
- Explore variable interpretations and potential implications of information.
To put it another way, asking questions with limiting, thought-stopping answers inhibits the development of critical thinking. This means that educators must ideally be critical thinkers themselves .
Drawing these threads together, The Foundation for Critical Thinking (2017) offers us a simple reminder that even though it’s human nature to be ‘thinking’ most of the time, most thoughts, if not guided and structured, tend to be biased, distorted, partial, uninformed or even prejudiced.
They also note that the quality of work depends precisely on the quality of the practitioners’ thought processes. Given that practitioners are being asked to meet the challenge of ever more complex care, the importance of cultivating critical thinking skills, alongside advanced problem-solving skills , seems to be taking on new importance.
Additional Resources
- The Emotionally Intelligent Nurse | Ausmed Article
- Refining Competency-Based Assessment | Ausmed Article
- Socratic Questioning in Healthcare | Ausmed Article
- Carvalhoa, D P S R P et al. 2017, 'Strategies Used for the Promotion of Critical Thinking in Nursing Undergraduate Education: A Systematic Review', Nurse Education Today , vol. 57, pp. 103-10, viewed 7 December 2018, https://www.sciencedirect.com/science/article/abs/pii/S0260691717301715
- Fortepiani, L A 2017, 'Critical Thinking or Traditional Teaching For Health Professionals', PECOP Blog , 16 January, viewed 7 December 2018, https://blog.lifescitrc.org/pecop/2017/01/16/critical-thinking-or-traditional-teaching-for-health-professions/
- Jacob, E, Duffield, C & Jacob, D 2017, 'A Protocol For the Development of a Critical Thinking Assessment Tool for Nurses Using a Delphi Technique', Journal of Advanced Nursing, vol. 73, no. 8, pp. 1982-1988, viewed 7 December 2018, https://onlinelibrary.wiley.com/doi/10.1111/jan.13306
- Kahlke, R & Eva, K 2018, 'Constructing Critical Thinking in Health Professional Education', Perspectives on Medical Education , vol. 7, no. 3, pp. 156-165, viewed 7 December 2018, https://link.springer.com/article/10.1007/s40037-018-0415-z
- Lippincott Solutions 2018, 'Turning New Nurses Into Critical Thinkers', Lippincott Solutions , viewed 10 December 2018, https://www.wolterskluwer.com/en/expert-insights/turning-new-nurses-into-critical-thinkers
- Papp, K K 2014, 'Milestones of Critical Thinking: A Developmental Model for Medicine and Nursing', Academic Medicine , vol. 89, no. 5, pp. 715-720, https://journals.lww.com/academicmedicine/Fulltext/2014/05000/Milestones_of_Critical_Thinking___A_Developmental.14.aspx
- Snyder, L G & Snyder, M J 2008, 'Teaching Critical Thinking and Problem Solving Skills', The Delta Pi Epsilon Journal , vol. L, no. 2, pp. 90-99, viewed 7 December 2018, https://dme.childrenshospital.org/wp-content/uploads/2019/02/Optional-_Teaching-Critical-Thinking-and-Problem-Solving-Skills.pdf
- The Foundation for Critical Thinking 2017, Defining Critical Thinking , The Foundation for Critical Thinking, viewed 7 December 2018, https://www.criticalthinking.org/pages/our-conception-of-critical-thinking/411
- Tsui-Mei, H, Lee-Chun, H & Chen-Ju MSN, K 2015, 'How Mental Health Nurses Improve Their Critical Thinking Through Problem-Based Learning', Journal for Nurses in Professional Development , vol. 31, no. 3, pp. 170-175, viewed 7 December 2018, https://journals.lww.com/jnsdonline/Abstract/2015/05000/How_Mental_Health_Nurses_Improve_Their_Critical.8.aspx
Anne Watkins View profile
Help and feedback, publications.
Ausmed Education is a Trusted Information Partner of Healthdirect Australia. Verify here .

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Developing critical thinking skills for delivering optimal care
Scott IA, Hubbard RE, Crock C, et al. Developing critical thinking skills for delivering optimal care. Intern Med J. 2021;51(4):488-493. doi: 10.1111/imj.15272
Sound critical thinking skills can help clinicians avoid cognitive biases and diagnostic errors. This article describes three critical thinking skills essential to effective clinical care – clinical reasoning, evidence-informed decision-making, and systems thinking – and approaches to develop these skills during clinician training.
Medication use and cognitive impairment among residents of aged care facilities. June 23, 2021
COVID-19 pandemic and the tension between the need to act and the need to know. October 14, 2020
Choosing wisely in clinical practice: embracing critical thinking, striving for safer care. April 6, 2022
Scoping review of studies evaluating frailty and its association with medication harm. June 22, 2022
Countering cognitive biases in minimising low value care. June 7, 2017
'More than words' - interpersonal communication, cognitive bias and diagnostic errors. August 11, 2021
A partially structured postoperative handoff protocol improves communication in 2 mixed surgical intensive care units: findings from the Handoffs and Transitions in Critical Care (HATRICC) prospective cohort study. February 6, 2019
Enabling a learning healthcare system with automated computer protocols that produce replicable and personalized clinician actions. August 4, 2021
Analysis of lawsuits related to diagnostic errors from point-of-care ultrasound in internal medicine, paediatrics, family medicine and critical care in the USA. June 24, 2020
Developing and aligning a safety event taxonomy for inpatient psychiatry. July 13, 2022
Changes in unprofessional behaviour, teamwork, and co-operation among hospital staff during the COVID-19 pandemic. September 28, 2022
Pharmacists reducing medication risk in medical outpatient clinics: a retrospective study of 18 clinics. March 8, 2023
Prevalence and causes of diagnostic errors in hospitalized patients under investigation for COVID-19. April 12, 2023
Barriers to accessing nighttime supervisors: a national survey of internal medicine residents. March 17, 2021
Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016 March 3, 2017
Seroprevalence of SARS-CoV-2 among frontline health care personnel in a multistate hospital network--13 academic medical centers, April-June 2020. September 23, 2020
Transforming the medication regimen review process using telemedicine to prevent adverse events. December 16, 2020
The MedSafer study-electronic decision support for deprescribing in hospitalized older adults: a cluster randomized clinical trial. February 2, 2022
Perceived patient safety culture in a critical care transport program. July 31, 2013
Video-based communication assessment of physician error disclosure skills by crowdsourced laypeople and patient advocates who experienced medical harm: reliability assessment with generalizability theory. May 18, 2022
Implementation of the I-PASS handoff program in diverse clinical environments: a multicenter prospective effectiveness implementation study. November 16, 2022
Patient harm from cardiovascular medications. August 25, 2021
Delays in diagnosis, treatment, and surgery: root causes, actions taken, and recommendations for healthcare improvement. June 1, 2022
Influence of opioid prescription policy on overdoses and related adverse effects in a primary care population. May 19, 2021
Evaluation of a second victim peer support program on perceptions of second victim experiences and supportive resources in pediatric clinical specialties using the second victim experience and support tool (SVEST). November 3, 2021
Diagnostic errors in hospitalized adults who died or were transferred to intensive care. January 17, 2024
Estimation of breast cancer overdiagnosis in a U.S. breast screening cohort. March 16, 2022
Multiple meanings of resilience: health professionals' experiences of a dual element training intervention designed to help them prepare for coping with error. March 31, 2021
Care coordination strategies and barriers during medication safety incidents: a qualitative, cognitive task analysis. March 10, 2021
TRIAD IX: can a patient testimonial safely help ensure prehospital appropriate critical versus end-of-life care? September 15, 2021
An act of performance: exploring residents' decision-making processes to seek help. April 14, 2021
Preventing home medication administration errors. March 14, 2022
A randomized trial of a multifactorial strategy to prevent serious fall injuries. July 29, 2020
Clinical predictors for unsafe direct discharge home patients from intensive care units. October 21, 2020
Association between limiting the number of open records in a tele-critical care setting and retract-reorder errors. July 21, 2021
Standardized assessment of medication reconciliation in post-acute care. April 27, 2022
Estimating the economic cost of nurse sensitive adverse events amongst patients in medical and surgical settings. June 16, 2021
Survey of nurses' experiences applying The Joint Commission's medication management titration standards. November 3, 2021
Effectiveness of acute care remote triage systems: a systematic review. February 5, 2020
Physician task load and the risk of burnout among US physicians in a national survey. December 2, 2020
Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. September 23, 2020
Patient and physician perspectives of deprescribing potentially inappropriate medications in older adults with a history of falls: a qualitative study. May 5, 2021
We asked the experts: the WHO Surgical Safety Checklist and the COVID-19 pandemic: recommendations for content and implementation adaptations. March 17, 2021
Association between surgeon technical skills and patient outcomes. September 9, 2020
Influence of psychological safety and organizational support on the impact of humiliation on trainee well-being. June 8, 2022
Developing the Safer Dx Checklist of Ten Safety Recommendations for Health Care Organizations to address diagnostic errors. October 12, 2022
Comparison of health care worker satisfaction before vs after implementation of a communication and optimal resolution program in acute care hospitals. April 5, 2023
Not overstepping professional boundaries: the challenging role of nurses in simulated error disclosures. September 21, 2011
Temporal associations between EHR-derived workload, burnout, and errors: a prospective cohort study. July 20, 2022
Adherence to national guidelines for timeliness of test results communication to patients in the Veterans Affairs health care system. May 4, 2022
Deferral of care for serious non-COVID-19 conditions: a hidden harm of COVID-19. November 18, 2020
An observational study of postoperative handoff standardization failures. June 23, 2021
Content analysis of patient safety incident reports for older adult patient transfers, handovers, and discharges: do they serve organizations, staff, or patients? January 8, 2020
Exploring the impact of employee engagement and patient safety. September 14, 2022
Deprescribing for community-dwelling older adults: a systematic review and meta-analysis. September 16, 2020
The abrupt expansion of ambulatory telemedicine: implications for patient safety. February 9, 2022
Nurse's Achilles Heel: using big data to determine workload factors that impact near misses. April 14, 2021
A diagnostic time-out to improve differential diagnosis in pediatric abdominal pain. July 14, 2021
What safety events are reported for ambulatory care? Analysis of incident reports from a patient safety organization. October 21, 2020
Expert consensus on currently accepted measures of harm. September 9, 2020
The July Effect in podiatric medicine and surgery residency. July 14, 2021
The calm before the storm: utilizing in situ simulation to evaluate for preparedness of an alternative care hospital during COVID-19 pandemic. June 2, 2021
Missed nursing care in the critical care unit, before and during the COVID-19 pandemic: a comparative cross-sectional study. June 22, 2022
The association between nurse staffing and omissions in nursing care: a systematic review. July 11, 2018
Creating a learning health system for improving diagnostic safety: pragmatic insights from US health care organizations. June 22, 2022
Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. June 8, 2016
Impact of the initial response to COVID-19 on long-term care for people with intellectual disability: an interrupted time series analysis of incident reports. October 14, 2020
Pediatric surgical errors: a systematic scoping review. July 20, 2022
Racial bias in pulse oximetry measurement. December 20, 2020
Accuracy of practitioner estimates of probability of diagnosis before and after testing. May 5, 2021
Recommendations for the safe, effective use of adaptive CDS in the US healthcare system: an AMIA position paper. April 21, 2021
Impact of interoperability of smart infusion pumps and an electronic medical record in critical care. September 23, 2020
Decreased incidence of cesarean surgical site infection rate with hospital-wide perioperative bundle. September 29, 2021
Association of diagnostic stewardship for blood cultures in critically ill children with culture rates, antibiotic use, and patient outcomes: results of the Bright STAR Collaborative. May 18, 2022
Second victim experiences of nurses in obstetrics and gynaecology: a Second Victim Experience and Support Tool Survey December 23, 2020
Understanding the second victim experience among multidisciplinary providers in obstetrics and gynecology. May 19, 2021
eSIMPLER: a dynamic, electronic health record-integrated checklist for clinical decision support during PICU daily rounds. June 16, 2021
Treatment patterns and clinical outcomes after the introduction of the Medicare Sepsis Performance Measure (SEP-1). May 5, 2021
Organizational safety climate and job enjoyment in hospital surgical teams with and without crew resource management training, January 26, 2022
Evaluation of effectiveness and safety of pharmacist independent prescribers in care homes: cluster randomised controlled trial. March 1, 2023
The Critical Care Safety Study: the incidence and nature of adverse events and serious medical errors in intensive care. August 24, 2005
Safety II behavior in a pediatric intensive care unit. August 1, 2018
Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. October 21, 2020
The working hours of hospital staff nurses and patient safety. January 9, 2005
Effects of tall man lettering on the visual behaviour of critical care nurses while identifying syringe drug labels: a randomised in situ simulation. April 20, 2022
Family Input for Quality and Safety (FIQS): using mobile technology for in-hospital reporting from families and patients. March 2, 2022
Bundle interventions including nontechnical skills for surgeons can reduce operative time and improve patient safety. December 9, 2020
COVID-19: an emerging threat to antibiotic stewardship in the emergency department. October 21, 2020
Improving self-reported empathy and communication skills through harm in healthcare response training. January 26, 2022
Association between in-clinic opioid administration and discharge opioid prescription in urgent care: a retrospective cohort study. February 17, 2021
Predicting avoidable hospital events in Maryland. December 1, 2021
Specificity of computerized physician order entry has a significant effect on the efficiency of workflow for critically ill patients. April 21, 2005
Why do hospital prescribers continue antibiotics when it is safe to stop? Results of a choice experiment survey. September 2, 2020
COVID-19: patient safety and quality improvement skills to deploy during the surge. June 24, 2020
Patient safety skills in primary care: a national survey of GP educators. February 4, 2015
Implementing human factors in anaesthesia: guidance for clinicians, departments and hospitals: Guidelines from the Difficult Airway Society and the Association of Anaesthetists. March 1, 2023
Can an electronic prescribing system detect doctors who are more likely to make a serious prescribing error? June 8, 2011
Training in safe opioid prescribing and treatment of opioid use disorder in internal medicine residencies: a national survey of program directors. October 12, 2022
Diagnostic discordance, health information exchange, and inter-hospital transfer outcomes: a population study. June 20, 2018
Systematic review and meta-analysis of interventions for operating room to intensive care unit handoffs. March 10, 2021
All in Her Head. The Truth and Lies Early Medicine Taught Us About Women's Bodies and Why It Matters Today. March 20, 2024
The racial disparities in maternal mortality and impact of structural racism and implicit racial bias on pregnant Black women: a review of the literature. December 6, 2023
A scoping review exploring the confidence of healthcare professionals in assessing all skin tones. October 4, 2023
Patient safety in palliative care at the end of life from the perspective of complex thinking. August 16, 2023
Only 1 in 5 people with opioid addiction get the medications to treat it, study finds. August 16, 2023
Factors influencing in-hospital prescribing errors: a systematic review. July 19, 2023
Introducing second-year medical students to diagnostic reasoning concepts and skills via a virtual curriculum. June 28, 2023
Context matters: toward a multilevel perspective on context in clinical reasoning and error. June 21, 2023
The good, the bad, and the ugly: operative staff perspectives of surgeon coping with intraoperative errors. June 14, 2023
Explicitly addressing implicit bias on inpatient rounds: student and faculty reflections. June 7, 2023
The time is now: addressing implicit bias in obstetrics and gynecology education. May 17, 2023
Listen to the whispers before they become screams: addressing Black maternal morbidity and mortality in the United States. May 3, 2023
Annual Perspective
Formalizing the hidden curriculum of performance enhancing errors. March 22, 2023
Implicit racial bias, health care provider attitudes, and perceptions of health care quality among African American college students in Georgia, USA. January 18, 2023
Structural racism and impact on sickle cell disease: sickle cell lives matter. January 11, 2023
The REPAIR Project: a prospectus for change toward racial justice in medical education and health sciences research: REPAIR project steering committee. January 11, 2023
Using the Assessment of Reasoning Tool to facilitate feedback about diagnostic reasoning. January 11, 2023
Exploring the intersection of structural racism and ageism in healthcare. December 7, 2022
Calibrate Dx: A Resource to Improve Diagnostic Decisions. October 19, 2022
Improved Diagnostic Accuracy Through Probability-Based Diagnosis. September 28, 2022
Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. September 21, 2022
A state-of-the-art review of speaking up in healthcare. August 24, 2022
Skin cancer is a risk no matter the skin tone. But it may be overlooked in people with dark skin. August 17, 2022
Oxford Professional Practice: Handbook of Patient Safety. July 27, 2022
Narrowing the mindware gap in medicine. July 20, 2022
From principles to practice: embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. June 15, 2022
A call to action: next steps to advance diagnosis education in the health professions. June 8, 2022
Does a suggested diagnosis in a general practitioners' referral question impact diagnostic reasoning: an experimental study. April 27, 2022
WebM&M Cases

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What Is Critical Thinking In Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical Thinking in medical education: When and How?
Rapid response to:
Critical thinking in healthcare and education
- Related content
- Article metrics
- Rapid responses
Rapid Response:
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from that of general cognitive abilities [1].
People cannot think critically about topics for which they have little knowledge. Critical thinking should be viewed as a domain-specific construct that evolves as an individual acquires domain-specific knowledge [1]. For instance, most common people have no basis for prioritizing patients in the emergency department to be shifted to the only bed available in the intensive care unit. Medical professionals who could thinking critically in their own discipline would have difficulty thinking critically about problems in other fields. Therefore, ‘domain-general’ critical thinking training and evaluation could be non-specific and might not benefit the targeted domain i.e. medical profession.
Moreover, the literature does not demonstrate that it is possible to train universally effective critical thinking skills [1]. As medical teachers, we can start building up student’s critical thinking skill by contingent teaching-learning environment wherein one should encourage reasoning and analytics, problem solving abilities and welcome new ideas and opinions [2]. But at the same time, one should continue rather tapering the critical skills as one ascends towards a specialty, thereby targeting ‘domain-specific’ critical thinking.
For the benefit of healthcare, tools for training and evaluating ‘domain-specific’ critical thinking should be developed for each of the professional knowledge domains such as doctors, nurses, lab technicians and so on. As the Authors rightly pointed out, this humongous task can be accomplished only with cross border collaboration among cognitive neuroscientists, psychologists, medical education experts and medical professionals.
References 1. National Research Council. (2011). Assessing 21st Century Skills: Summary of a Workshop. J.A. Koenig, Rapporteur. Committee on the Assessment of 21st Century Skills. Board on Testing and Assessment, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. 2. Mafakheri Laleh M, Mohammadimehr M, Zargar Balaye Jame S. Designing a model for critical thinking development in AJA University of Medical Sciences. J Adv Med Educ Prof. 2016 Oct;4(4):179–87.
Competing interests: No competing interests
Medical Student Guide For Critical Thinking

Critical thinking is an essential cognitive skill for every individual but is a crucial component for healthcare professionals such as doctors, nurses and dentists. It is a skill that should be developed and trained, not just during your career as a doctor, but before that when you are still a medical student.
To be more effective in their studies, students must think their way through abstract problems, work in teams and separate high quality from low quality information. These are the same qualities that today's medical students are supposed to possess regardless of whether they graduate in the UK or study medicine in Europe .
In both well-defined and ill-defined medical emergencies, doctors are expected to make competent decisions. Critical thinking can help medical students and doctors achieve improved productivity, better clinical decision making, higher grades and much more.
This article will explain why critical thinking is a must for people in the medical field.
Definition of Critical Thinking
You can find a variety of definitions of Critical Thinking (CT). It is a term that goes back to the Ancient Greek philosopher Socrates and his teaching practice and vision. Critical thinking and its meaning have changed over the years, but at its core always will be the pursuit of proper judgment.
We can agree on one thing. Critical thinkers question every idea, assumption, and possibility rather than accepting them at once.
The most basic definition of CT is provided by Beyer (1995):
"Critical thinking means making reasoned judgements."
In other words, it is the ability to think logically about what to do and/or believe. It also includes the ability to think critically and independently. CT is the process of identifying, analysing, and then making decisions about a particular topic, advice, opinion or challenge that we are facing.
Steps to critical thinking
There is no universal standard for becoming a critical thinker. It is more like a unique journey for each individual. But as a medical student, you have already so much going on in your academic and personal life. This is why we created a list with 6 steps that will help you develop the necessary skills for critical thinking.
1. Determine the issue or question
The first step is to answer the following questions:
- What is the problem?
- Why is it important?
- Why do we need to find a solution?
- Who is involved?
By answering them, you will define the situation and acquire a deeper understanding of the problem and of any factors that may impact it.
Only after you have a clear picture of the issue and people involved can you start to dive deeper into the problem and search for a solution.
2. Research
Nowadays, we are flooded with information. We have an unlimited source of knowledge – the Internet.
Before choosing which medical schools to apply to, most applicants researched their desired schools online. Some of the areas you might have researched include:
- If the degree is recognised worldwide
- Tuition fees
- Living costs
- Entry requirements
- Competition for entry
- Number of exams
- Programme style
Having done the research, you were able to make an informed decision about your medical future based on the gathered information. Our list may be a little different to yours but that's okay. You know what factors are most important and relevant to you as a person.
The process you followed when choosing which medical school to apply to also applies to step 2 of critical thinking. As a medical student and doctor, you will face situations when you have to compare different arguments and opinions about an issue. Independent research is the key to the right clinical decisions. Medical and dentistry students have to be especially careful when learning from online sources. You shouldn't believe everything you read and take it as the absolute truth. So, here is what you need to do when facing a medical/study argument:
- Gather relevant information from all available reputable sources
- Pay attention to the salient points
- Evaluate the quality of the information and the level of evidence (is it just an opinion, or is it based upon a clinical trial?)
Once you have all the information needed, you can start the process of analysing it. It’s helpful to write down the strong and weak points of the various recommendations and identify the most evidence-based approach.
Here is an example of a comparison between two online course platforms , which shows their respective strengths and weaknesses.
When recommendations or conclusions are contradictory, you will need to make a judgement call on which point of view has the strongest level of evidence to back it up. You should leave aside your feelings and analyse the problem from every angle possible. In the end, you should aim to make your decision based on the available evidence, not assumptions or bias.
4. Be careful about confirmation bias
It is in our nature to want to confirm our existing ideas rather than challenge them. You should try your best to strive for objectivity while evaluating information.
Often, you may find yourself reading articles that support your ideas, but why not broaden your horizons by learning about the other viewpoint?
By doing so, you will have the opportunity to get closer to the truth and may even find unexpected support and evidence for your conclusion.
Curiosity will keep you on the right path. However, if you find yourself searching for information or confirmation that aligns only with your opinion, then it’s important to take a step back. Take a short break, acknowledge your bias, clear your mind and start researching all over.
5. Synthesis
As we have already mentioned a couple of times, medical students are preoccupied with their studies. Therefore, you have to learn how to synthesise information. This is where you take information from multiple sources and bring the information together. Learning how to do this effectively will save you time and help you make better decisions faster.
You will have already located and evaluated your sources in the previous steps. You now have to organise the data into a logical argument that backs up your position on the problem under consideration.
6. Make a decision
Once you have gathered and evaluated all the available evidence, your last step is to make a logical and well-reasoned conclusion.
By following this process you will ensure that whatever decision you make can be backed up if challenged
Why is critical thinking so important for medical students?
The first and most important reason for mastering critical thinking is that it will help you to avoid medical and clinical errors during your studies and future medical career.
Another good reason is that you will be able to identify better alternative options for diagnoses and treatments. You will be able to find the best solution for the patient as a whole which may be different to generic advice specific to the disease.
Furthermore, thinking critically as a medical student will boost your confidence and improve your knowledge and understanding of subjects.
In conclusion, critical thinking is a skill that can be learned and improved. It will encourage you to be the best version of yourself and teach you to take responsibility for your actions.
Critical thinking has become an essential for future health care professionals and you will find it an invaluable skill throughout your career.
We’ll keep you updated
- Open access
- Published: 24 May 2023
Embracing critical thinking to enhance our practice
- Luis Martí-Bonmatí ORCID: orcid.org/0000-0002-8234-010X 1
Insights into Imaging volume 14 , Article number: 97 ( 2023 ) Cite this article
3587 Accesses
1 Citations
2 Altmetric
Metrics details
Miguel de Cervantes, the great Spanish writer, once wrote that those “who read much and walk much, go far and know much" [ 1 ]. The same is true in medicine; reading and gathering experience are the main pillars on which one should develop the knowledge of solving clinical problems in the ever-changing field of healthcare. If properly done, these newly acquired skills will continuously enhance our critical thinking strategies with which we try to identify the best possible improvements in the clinical pathway of radiology. As gaps in knowledge are always present, medicine is rooted in consolidated knowledge based on validated scientific studies and clinical experience reproducibility and accuracy [ 2 ]. This represents our best approach to evidence-based decisions. Medical knowledge must be well-established before it can be considered as the basis for decision making and patients guidance in daily practice.
The practice of critical thinking helps us understand the disease manifestations and the related processes and actions that might be relevant to prevent, diagnose and treat diseases. To critically appraise the way we perform evidence-based practice, we must combine best quality research with clinical expertise. This link between exploration and practice will allow radiologists and related disciplines to impact the way medicine is practiced.
These concepts are the cornerstones of Insights into Imaging , and it is my privilege as editor-in-chief to describe in this editorial how the journal, and each author, can contribute quality through critical thinking, and hence improve the way we practice radiology by re-shaping our understandings.
It is universally recognized that, in medical imaging, strong levels of evidence are needed to assess the results of the different possible actions and to guide decisions (i.e., to demonstrate a sufficient causal relationship between a specific diagnostic criterion and a disease grading, or a given radiological intervention versus another option in a given condition) toward the most effective or safe outcome considering the benefit of patients and value-based healthcare pathways. Consequently, solid levels of evidence are required to assess the results of different possible actions derived from imaging findings. And, in doing so, we continuously generate more data in our diagnostic and therapeutic activities, whether they are processes or outcomes. This new information will then be transformed into new evidence, real world evidence. In this way, the observed relationship between action and outcome generates causality course actions that will improve our understanding of the best clinical pathways, eliminating the many confounding thoughts that we unconsciously carry during the process of learning and implementing our clinical practice.
Socratic inquiry and Skepticism as foundation. Critical thinking can be understood as the process of analyzing and questioning existing and established knowledge with the intention of improving it. Previous knowledge, either eminence- or evidence-based, should continuously be critically reconsidered and reevaluated for the benefit of the patients, as knowledge is always changing in Precision Medicine. In the real world of medical imaging, this critical thinking must be focused on the evaluation of the effectiveness and clinical impact of all those processes in which images are involved, from the acquisition with different modalities to the processing of the data, from the biological correlation of radiomics as an image biomarker to the therapeutic orientation, and finally in image-guided interventional treatments. Developing critical thinking helps to improve any medical discipline by asking ourselves how to establish better and more precise processes based on existing accumulated evidence, how to recognize and control the biases when approaching a clinical problem, and how to adapt the new clinical information in service of the best solutions. Socratic inquiry and a skeptic attitude can be used to consolidate the best knowledge and construct new associations to be more efficient and to approach excellence in our daily work. Critical thinking is therefore necessary to improve both clinical practice and research in radiology, avoiding disruptive uncertainties and wrong assumptions.
These “questioning and solving” skills require learning, practice, and experience [ 3 ], but mainly a recognition of the many uncertainties we do have despite the important scientific advances. Precisely, a good example of the importance of critical thinking is its contribution to Precision Medicine through medical imaging data and information. In daily practice, we should ask ourselves why should we accept a reliable diagnostic method that fails 15% of the time, or an appropriate treatment that is not effective in almost 25% of patients? As scientists, we can improve these clinical decisions in the daily practice. Artificial intelligence (AI) solutions integrating different imaging, clinical, molecular, and genetic data as inputs are being implemented as a suitable pathway to solve clinical problems. The design and methodology of these AI algorithms must allow for their explainability and critical thinking evaluation before they are implemented in clinical practice [ 4 ].
In summary, critical thinking develops evidence-based knowledge, provides continuous improvements, and avoids spurious technical and clinical misconceptions. Insights into Imaging is dedicated to manuscripts with a clear critical approach, focusing on excellence in clinical practice, evidence-based knowledge and causal reasoning in radiology. Science is based on long-lived critiques and authors are encouraged to systematically identify, analyze, and solve problems by identifying inconsistencies and correcting errors.
To foster this, Insights into Imaging welcomes critical thinking papers and will incorporate a new “Critical Relevance Statement” in all their publications, where authors are asked to summarize in one sentence the question they are trying to answer and the improvement they are providing to the issue at hand.
Availability of data and materials
Not applicable.
De Cervantes M (1986) The adventures of don Quixote de la Mancha. New York, Farrar, Straus, Giroux
Martí-Bonmatí L (2021) Evidence levels in radiology: the insights into imaging approach. Insights Imaging 12(1):45. https://doi.org/10.1186/s13244-021-00995-7
Article PubMed PubMed Central Google Scholar
Ho YR, Chen BY, Li CM (2023) Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students. BMC Med Educ 23(1):173. https://doi.org/10.1186/s12909-023-04134-2
Cerdá-Alberich L, Solana J, Mallol P et al (2023) MAIC-10 brief quality checklist for publications using artificial intelligence and medical images. Insights Imaging 14(1):11. https://doi.org/10.1186/s13244-022-01355-9
Download references
Acknowledgements
To the Insights into Imaging ’s Office for their help in preparing this editorial.
Author information
Authors and affiliations.
Medical Imaging Department and Biomedical Imaging Research Group, Hospital Universitario y Politécnico La Fe and Health Research Institute, Valencia, Spain
Luis Martí-Bonmatí
You can also search for this author in PubMed Google Scholar
Contributions
LBM is the only author.The author have read and approved the final version of the manuscript.
Corresponding author
Correspondence to Luis Martí-Bonmatí .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
LMB is the Editor in Chief of Insights into Imaging . He has not taken part in the review or selection process of this article.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Martí-Bonmatí, L. Embracing critical thinking to enhance our practice. Insights Imaging 14 , 97 (2023). https://doi.org/10.1186/s13244-023-01435-4
Download citation
Received : 05 April 2023
Accepted : 24 April 2023
Published : 24 May 2023
DOI : https://doi.org/10.1186/s13244-023-01435-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Critical thinking
- Precision medicine
- Reproducibility
- Causal inference
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 6 clinical reasoning, decisionmaking, and action: thinking critically and clinically.
Patricia Benner ; Ronda G. Hughes ; Molly Sutphen .
Affiliations
This chapter examines multiple thinking strategies that are needed for high-quality clinical practice. Clinical reasoning and judgment are examined in relation to other modes of thinking used by clinical nurses in providing quality health care to patients that avoids adverse events and patient harm. The clinician’s ability to provide safe, high-quality care can be dependent upon their ability to reason, think, and judge, which can be limited by lack of experience. The expert performance of nurses is dependent upon continual learning and evaluation of performance.
- Critical Thinking
Nursing education has emphasized critical thinking as an essential nursing skill for more than 50 years. 1 The definitions of critical thinking have evolved over the years. There are several key definitions for critical thinking to consider. The American Philosophical Association (APA) defined critical thinking as purposeful, self-regulatory judgment that uses cognitive tools such as interpretation, analysis, evaluation, inference, and explanation of the evidential, conceptual, methodological, criteriological, or contextual considerations on which judgment is based. 2 A more expansive general definition of critical thinking is
. . . in short, self-directed, self-disciplined, self-monitored, and self-corrective thinking. It presupposes assent to rigorous standards of excellence and mindful command of their use. It entails effective communication and problem solving abilities and a commitment to overcome our native egocentrism and sociocentrism. Every clinician must develop rigorous habits of critical thinking, but they cannot escape completely the situatedness and structures of the clinical traditions and practices in which they must make decisions and act quickly in specific clinical situations. 3
There are three key definitions for nursing, which differ slightly. Bittner and Tobin defined critical thinking as being “influenced by knowledge and experience, using strategies such as reflective thinking as a part of learning to identify the issues and opportunities, and holistically synthesize the information in nursing practice” 4 (p. 268). Scheffer and Rubenfeld 5 expanded on the APA definition for nurses through a consensus process, resulting in the following definition:
Critical thinking in nursing is an essential component of professional accountability and quality nursing care. Critical thinkers in nursing exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, openmindedness, perseverance, and reflection. Critical thinkers in nursing practice the cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting, and transforming knowledge 6 (Scheffer & Rubenfeld, p. 357).
The National League for Nursing Accreditation Commission (NLNAC) defined critical thinking as:
the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research 7 (p. 8).
These concepts are furthered by the American Association of Colleges of Nurses’ definition of critical thinking in their Essentials of Baccalaureate Nursing :
Critical thinking underlies independent and interdependent decision making. Critical thinking includes questioning, analysis, synthesis, interpretation, inference, inductive and deductive reasoning, intuition, application, and creativity 8 (p. 9).
Course work or ethical experiences should provide the graduate with the knowledge and skills to:
- Use nursing and other appropriate theories and models, and an appropriate ethical framework;
- Apply research-based knowledge from nursing and the sciences as the basis for practice;
- Use clinical judgment and decision-making skills;
- Engage in self-reflective and collegial dialogue about professional practice;
- Evaluate nursing care outcomes through the acquisition of data and the questioning of inconsistencies, allowing for the revision of actions and goals;
- Engage in creative problem solving 8 (p. 10).
Taken together, these definitions of critical thinking set forth the scope and key elements of thought processes involved in providing clinical care. Exactly how critical thinking is defined will influence how it is taught and to what standard of care nurses will be held accountable.
Professional and regulatory bodies in nursing education have required that critical thinking be central to all nursing curricula, but they have not adequately distinguished critical reflection from ethical, clinical, or even creative thinking for decisionmaking or actions required by the clinician. Other essential modes of thought such as clinical reasoning, evaluation of evidence, creative thinking, or the application of well-established standards of practice—all distinct from critical reflection—have been subsumed under the rubric of critical thinking. In the nursing education literature, clinical reasoning and judgment are often conflated with critical thinking. The accrediting bodies and nursing scholars have included decisionmaking and action-oriented, practical, ethical, and clinical reasoning in the rubric of critical reflection and thinking. One might say that this harmless semantic confusion is corrected by actual practices, except that students need to understand the distinctions between critical reflection and clinical reasoning, and they need to learn to discern when each is better suited, just as students need to also engage in applying standards, evidence-based practices, and creative thinking.
The growing body of research, patient acuity, and complexity of care demand higher-order thinking skills. Critical thinking involves the application of knowledge and experience to identify patient problems and to direct clinical judgments and actions that result in positive patient outcomes. These skills can be cultivated by educators who display the virtues of critical thinking, including independence of thought, intellectual curiosity, courage, humility, empathy, integrity, perseverance, and fair-mindedness. 9
The process of critical thinking is stimulated by integrating the essential knowledge, experiences, and clinical reasoning that support professional practice. The emerging paradigm for clinical thinking and cognition is that it is social and dialogical rather than monological and individual. 10–12 Clinicians pool their wisdom and multiple perspectives, yet some clinical knowledge can be demonstrated only in the situation (e.g., how to suction an extremely fragile patient whose oxygen saturations sink too low). Early warnings of problematic situations are made possible by clinicians comparing their observations to that of other providers. Clinicians form practice communities that create styles of practice, including ways of doing things, communication styles and mechanisms, and shared expectations about performance and expertise of team members.
By holding up critical thinking as a large umbrella for different modes of thinking, students can easily misconstrue the logic and purposes of different modes of thinking. Clinicians and scientists alike need multiple thinking strategies, such as critical thinking, clinical judgment, diagnostic reasoning, deliberative rationality, scientific reasoning, dialogue, argument, creative thinking, and so on. In particular, clinicians need forethought and an ongoing grasp of a patient’s health status and care needs trajectory, which requires an assessment of their own clarity and understanding of the situation at hand, critical reflection, critical reasoning, and clinical judgment.
Critical Reflection, Critical Reasoning, and Judgment
Critical reflection requires that the thinker examine the underlying assumptions and radically question or doubt the validity of arguments, assertions, and even facts of the case. Critical reflective skills are essential for clinicians; however, these skills are not sufficient for the clinician who must decide how to act in particular situations and avoid patient injury. For example, in everyday practice, clinicians cannot afford to critically reflect on the well-established tenets of “normal” or “typical” human circulatory systems when trying to figure out a particular patient’s alterations from that typical, well-grounded understanding that has existed since Harvey’s work in 1628. 13 Yet critical reflection can generate new scientifically based ideas. For example, there is a lack of adequate research on the differences between women’s and men’s circulatory systems and the typical pathophysiology related to heart attacks. Available research is based upon multiple, taken-for-granted starting points about the general nature of the circulatory system. As such, critical reflection may not provide what is needed for a clinician to act in a situation. This idea can be considered reasonable since critical reflective thinking is not sufficient for good clinical reasoning and judgment. The clinician’s development of skillful critical reflection depends upon being taught what to pay attention to, and thus gaining a sense of salience that informs the powers of perceptual grasp. The powers of noticing or perceptual grasp depend upon noticing what is salient and the capacity to respond to the situation.
Critical reflection is a crucial professional skill, but it is not the only reasoning skill or logic clinicians require. The ability to think critically uses reflection, induction, deduction, analysis, challenging assumptions, and evaluation of data and information to guide decisionmaking. 9 , 14 , 15 Critical reasoning is a process whereby knowledge and experience are applied in considering multiple possibilities to achieve the desired goals, 16 while considering the patient’s situation. 14 It is a process where both inductive and deductive cognitive skills are used. 17 Sometimes clinical reasoning is presented as a form of evaluating scientific knowledge, sometimes even as a form of scientific reasoning. Critical thinking is inherent in making sound clinical reasoning. 18
An essential point of tension and confusion exists in practice traditions such as nursing and medicine when clinical reasoning and critical reflection become entangled, because the clinician must have some established bases that are not questioned when engaging in clinical decisions and actions, such as standing orders. The clinician must act in the particular situation and time with the best clinical and scientific knowledge available. The clinician cannot afford to indulge in either ritualistic unexamined knowledge or diagnostic or therapeutic nihilism caused by radical doubt, as in critical reflection, because they must find an intelligent and effective way to think and act in particular clinical situations. Critical reflection skills are essential to assist practitioners to rethink outmoded or even wrong-headed approaches to health care, health promotion, and prevention of illness and complications, especially when new evidence is available. Breakdowns in practice, high failure rates in particular therapies, new diseases, new scientific discoveries, and societal changes call for critical reflection about past assumptions and no-longer-tenable beliefs.
Clinical reasoning stands out as a situated, practice-based form of reasoning that requires a background of scientific and technological research-based knowledge about general cases, more so than any particular instance. It also requires practical ability to discern the relevance of the evidence behind general scientific and technical knowledge and how it applies to a particular patient. In dong so, the clinician considers the patient’s particular clinical trajectory, their concerns and preferences, and their particular vulnerabilities (e.g., having multiple comorbidities) and sensitivities to care interventions (e.g., known drug allergies, other conflicting comorbid conditions, incompatible therapies, and past responses to therapies) when forming clinical decisions or conclusions.
Situated in a practice setting, clinical reasoning occurs within social relationships or situations involving patient, family, community, and a team of health care providers. The expert clinician situates themselves within a nexus of relationships, with concerns that are bounded by the situation. Expert clinical reasoning is socially engaged with the relationships and concerns of those who are affected by the caregiving situation, and when certain circumstances are present, the adverse event. Halpern 19 has called excellent clinical ethical reasoning “emotional reasoning” in that the clinicians have emotional access to the patient/family concerns and their understanding of the particular care needs. Expert clinicians also seek an optimal perceptual grasp, one based on understanding and as undistorted as possible, based on an attuned emotional engagement and expert clinical knowledge. 19 , 20
Clergy educators 21 and nursing and medical educators have begun to recognize the wisdom of broadening their narrow vision of rationality beyond simple rational calculation (exemplified by cost-benefit analysis) to reconsider the need for character development—including emotional engagement, perception, habits of thought, and skill acquisition—as essential to the development of expert clinical reasoning, judgment, and action. 10 , 22–24 Practitioners of engineering, law, medicine, and nursing, like the clergy, have to develop a place to stand in their discipline’s tradition of knowledge and science in order to recognize and evaluate salient evidence in the moment. Diagnostic confusion and disciplinary nihilism are both threats to the clinician’s ability to act in particular situations. However, the practice and practitioners will not be self-improving and vital if they cannot engage in critical reflection on what is not of value, what is outmoded, and what does not work. As evidence evolves and expands, so too must clinical thought.
Clinical judgment requires clinical reasoning across time about the particular, and because of the relevance of this immediate historical unfolding, clinical reasoning can be very different from the scientific reasoning used to formulate, conduct, and assess clinical experiments. While scientific reasoning is also socially embedded in a nexus of social relationships and concerns, the goal of detached, critical objectivity used to conduct scientific experiments minimizes the interactive influence of the research on the experiment once it has begun. Scientific research in the natural and clinical sciences typically uses formal criteria to develop “yes” and “no” judgments at prespecified times. The scientist is always situated in past and immediate scientific history, preferring to evaluate static and predetermined points in time (e.g., snapshot reasoning), in contrast to a clinician who must always reason about transitions over time. 25 , 26
Techne and Phronesis
Distinctions between the mere scientific making of things and practice was first explored by Aristotle as distinctions between techne and phronesis. 27 Learning to be a good practitioner requires developing the requisite moral imagination for good practice. If, for example, patients exercise their rights and refuse treatments, practitioners are required to have the moral imagination to understand the probable basis for the patient’s refusal. For example, was the refusal based upon catastrophic thinking, unrealistic fears, misunderstanding, or even clinical depression?
Techne, as defined by Aristotle, encompasses the notion of formation of character and habitus 28 as embodied beings. In Aristotle’s terms, techne refers to the making of things or producing outcomes. 11 Joseph Dunne defines techne as “the activity of producing outcomes,” and it “is governed by a means-ends rationality where the maker or producer governs the thing or outcomes produced or made through gaining mastery over the means of producing the outcomes, to the point of being able to separate means and ends” 11 (p. 54). While some aspects of medical and nursing practice fall into the category of techne, much of nursing and medical practice falls outside means-ends rationality and must be governed by concern for doing good or what is best for the patient in particular circumstances, where being in a relationship and discerning particular human concerns at stake guide action.
Phronesis, in contrast to techne, includes reasoning about the particular, across time, through changes or transitions in the patient’s and/or the clinician’s understanding. As noted by Dunne, phronesis is “characterized at least as much by a perceptiveness with regard to concrete particulars as by a knowledge of universal principles” 11 (p. 273). This type of practical reasoning often takes the form of puzzle solving or the evaluation of immediate past “hot” history of the patient’s situation. Such a particular clinical situation is necessarily particular, even though many commonalities and similarities with other disease syndromes can be recognized through signs and symptoms and laboratory tests. 11 , 29 , 30 Pointing to knowledge embedded in a practice makes no claim for infallibility or “correctness.” Individual practitioners can be mistaken in their judgments because practices such as medicine and nursing are inherently underdetermined. 31
While phronetic knowledge must remain open to correction and improvement, real events, and consequences, it cannot consistently transcend the institutional setting’s capacities and supports for good practice. Phronesis is also dependent on ongoing experiential learning of the practitioner, where knowledge is refined, corrected, or refuted. The Western tradition, with the notable exception of Aristotle, valued knowledge that could be made universal and devalued practical know-how and experiential learning. Descartes codified this preference for formal logic and rational calculation.
Aristotle recognized that when knowledge is underdetermined, changeable, and particular, it cannot be turned into the universal or standardized. It must be perceived, discerned, and judged, all of which require experiential learning. In nursing and medicine, perceptual acuity in physical assessment and clinical judgment (i.e., reasoning across time about changes in the particular patient or the clinician’s understanding of the patient’s condition) fall into the Greek Aristotelian category of phronesis. Dewey 32 sought to rescue knowledge gained by practical activity in the world. He identified three flaws in the understanding of experience in Greek philosophy: (1) empirical knowing is the opposite of experience with science; (2) practice is reduced to techne or the application of rational thought or technique; and (3) action and skilled know-how are considered temporary and capricious as compared to reason, which the Greeks considered as ultimate reality.
In practice, nursing and medicine require both techne and phronesis. The clinician standardizes and routinizes what can be standardized and routinized, as exemplified by standardized blood pressure measurements, diagnoses, and even charting about the patient’s condition and treatment. 27 Procedural and scientific knowledge can often be formalized and standardized (e.g., practice guidelines), or at least made explicit and certain in practice, except for the necessary timing and adjustments made for particular patients. 11 , 22
Rational calculations available to techne—population trends and statistics, algorithms—are created as decision support structures and can improve accuracy when used as a stance of inquiry in making clinical judgments about particular patients. Aggregated evidence from clinical trials and ongoing working knowledge of pathophysiology, biochemistry, and genomics are essential. In addition, the skills of phronesis (clinical judgment that reasons across time, taking into account the transitions of the particular patient/family/community and transitions in the clinician’s understanding of the clinical situation) will be required for nursing, medicine, or any helping profession.
Thinking Critically
Being able to think critically enables nurses to meet the needs of patients within their context and considering their preferences; meet the needs of patients within the context of uncertainty; consider alternatives, resulting in higher-quality care; 33 and think reflectively, rather than simply accepting statements and performing tasks without significant understanding and evaluation. 34 Skillful practitioners can think critically because they have the following cognitive skills: information seeking, discriminating, analyzing, transforming knowledge, predicating, applying standards, and logical reasoning. 5 One’s ability to think critically can be affected by age, length of education (e.g., an associate vs. a baccalaureate decree in nursing), and completion of philosophy or logic subjects. 35–37 The skillful practitioner can think critically because of having the following characteristics: motivation, perseverance, fair-mindedness, and deliberate and careful attention to thinking. 5 , 9
Thinking critically implies that one has a knowledge base from which to reason and the ability to analyze and evaluate evidence. 38 Knowledge can be manifest by the logic and rational implications of decisionmaking. Clinical decisionmaking is particularly influenced by interpersonal relationships with colleagues, 39 patient conditions, availability of resources, 40 knowledge, and experience. 41 Of these, experience has been shown to enhance nurses’ abilities to make quick decisions 42 and fewer decision errors, 43 support the identification of salient cues, and foster the recognition and action on patterns of information. 44 , 45
Clinicians must develop the character and relational skills that enable them to perceive and understand their patient’s needs and concerns. This requires accurate interpretation of patient data that is relevant to the specific patient and situation. In nursing, this formation of moral agency focuses on learning to be responsible in particular ways demanded by the practice, and to pay attention and intelligently discern changes in patients’ concerns and/or clinical condition that require action on the part of the nurse or other health care workers to avert potential compromises to quality care.
Formation of the clinician’s character, skills, and habits are developed in schools and particular practice communities within a larger practice tradition. As Dunne notes,
A practice is not just a surface on which one can display instant virtuosity. It grounds one in a tradition that has been formed through an elaborate development and that exists at any juncture only in the dispositions (slowly and perhaps painfully acquired) of its recognized practitioners. The question may of course be asked whether there are any such practices in the contemporary world, whether the wholesale encroachment of Technique has not obliterated them—and whether this is not the whole point of MacIntyre’s recipe of withdrawal, as well as of the post-modern story of dispossession 11 (p. 378).
Clearly Dunne is engaging in critical reflection about the conditions for developing character, skills, and habits for skillful and ethical comportment of practitioners, as well as to act as moral agents for patients so that they and their families receive safe, effective, and compassionate care.
Professional socialization or professional values, while necessary, do not adequately address character and skill formation that transform the way the practitioner exists in his or her world, what the practitioner is capable of noticing and responding to, based upon well-established patterns of emotional responses, skills, dispositions to act, and the skills to respond, decide, and act. 46 The need for character and skill formation of the clinician is what makes a practice stand out from a mere technical, repetitious manufacturing process. 11 , 30 , 47
In nursing and medicine, many have questioned whether current health care institutions are designed to promote or hinder enlightened, compassionate practice, or whether they have deteriorated into commercial institutional models that focus primarily on efficiency and profit. MacIntyre points out the links between the ongoing development and improvement of practice traditions and the institutions that house them:
Lack of justice, lack of truthfulness, lack of courage, lack of the relevant intellectual virtues—these corrupt traditions, just as they do those institutions and practices which derive their life from the traditions of which they are the contemporary embodiments. To recognize this is of course also to recognize the existence of an additional virtue, one whose importance is perhaps most obvious when it is least present, the virtue of having an adequate sense of the traditions to which one belongs or which confront one. This virtue is not to be confused with any form of conservative antiquarianism; I am not praising those who choose the conventional conservative role of laudator temporis acti. It is rather the case that an adequate sense of tradition manifests itself in a grasp of those future possibilities which the past has made available to the present. Living traditions, just because they continue a not-yet-completed narrative, confront a future whose determinate and determinable character, so far as it possesses any, derives from the past 30 (p. 207).
It would be impossible to capture all the situated and distributed knowledge outside of actual practice situations and particular patients. Simulations are powerful as teaching tools to enable nurses’ ability to think critically because they give students the opportunity to practice in a simplified environment. However, students can be limited in their inability to convey underdetermined situations where much of the information is based on perceptions of many aspects of the patient and changes that have occurred over time. Simulations cannot have the sub-cultures formed in practice settings that set the social mood of trust, distrust, competency, limited resources, or other forms of situated possibilities.
One of the hallmark studies in nursing providing keen insight into understanding the influence of experience was a qualitative study of adult, pediatric, and neonatal intensive care unit (ICU) nurses, where the nurses were clustered into advanced beginner, intermediate, and expert level of practice categories. The advanced beginner (having up to 6 months of work experience) used procedures and protocols to determine which clinical actions were needed. When confronted with a complex patient situation, the advanced beginner felt their practice was unsafe because of a knowledge deficit or because of a knowledge application confusion. The transition from advanced beginners to competent practitioners began when they first had experience with actual clinical situations and could benefit from the knowledge gained from the mistakes of their colleagues. Competent nurses continuously questioned what they saw and heard, feeling an obligation to know more about clinical situations. In doing do, they moved from only using care plans and following the physicians’ orders to analyzing and interpreting patient situations. Beyond that, the proficient nurse acknowledged the changing relevance of clinical situations requiring action beyond what was planned or anticipated. The proficient nurse learned to acknowledge the changing needs of patient care and situation, and could organize interventions “by the situation as it unfolds rather than by preset goals 48 (p. 24). Both competent and proficient nurses (that is, intermediate level of practice) had at least two years of ICU experience. 48 Finally, the expert nurse had a more fully developed grasp of a clinical situation, a sense of confidence in what is known about the situation, and could differentiate the precise clinical problem in little time. 48
Expertise is acquired through professional experience and is indicative of a nurse who has moved beyond mere proficiency. As Gadamer 29 points out, experience involves a turning around of preconceived notions, preunderstandings, and extends or adds nuances to understanding. Dewey 49 notes that experience requires a prepared “creature” and an enriched environment. The opportunity to reflect and narrate one’s experiential learning can clarify, extend, or even refute experiential learning.
Experiential learning requires time and nurturing, but time alone does not ensure experiential learning. Aristotle linked experiential learning to the development of character and moral sensitivities of a person learning a practice. 50 New nurses/new graduates have limited work experience and must experience continuing learning until they have reached an acceptable level of performance. 51 After that, further improvements are not predictable, and years of experience are an inadequate predictor of expertise. 52
The most effective knower and developer of practical knowledge creates an ongoing dialogue and connection between lessons of the day and experiential learning over time. Gadamer, in a late life interview, highlighted the open-endedness and ongoing nature of experiential learning in the following interview response:
Being experienced does not mean that one now knows something once and for all and becomes rigid in this knowledge; rather, one becomes more open to new experiences. A person who is experienced is undogmatic. Experience has the effect of freeing one to be open to new experience … In our experience we bring nothing to a close; we are constantly learning new things from our experience … this I call the interminability of all experience 32 (p. 403).
Practical endeavor, supported by scientific knowledge, requires experiential learning, the development of skilled know-how, and perceptual acuity in order to make the scientific knowledge relevant to the situation. Clinical perceptual and skilled know-how helps the practitioner discern when particular scientific findings might be relevant. 53
Often experience and knowledge, confirmed by experimentation, are treated as oppositions, an either-or choice. However, in practice it is readily acknowledged that experiential knowledge fuels scientific investigation, and scientific investigation fuels further experiential learning. Experiential learning from particular clinical cases can help the clinician recognize future similar cases and fuel new scientific questions and study. For example, less experienced nurses—and it could be argued experienced as well—can use nursing diagnoses practice guidelines as part of their professional advancement. Guidelines are used to reflect their interpretation of patients’ needs, responses, and situation, 54 a process that requires critical thinking and decisionmaking. 55 , 56 Using guidelines also reflects one’s problem identification and problem-solving abilities. 56 Conversely, the ability to proficiently conduct a series of tasks without nursing diagnoses is the hallmark of expertise. 39 , 57
Experience precedes expertise. As expertise develops from experience and gaining knowledge and transitions to the proficiency stage, the nurses’ thinking moves from steps and procedures (i.e., task-oriented care) toward “chunks” or patterns 39 (i.e., patient-specific care). In doing so, the nurse thinks reflectively, rather than merely accepting statements and performing procedures without significant understanding and evaluation. 34 Expert nurses do not rely on rules and logical thought processes in problem-solving and decisionmaking. 39 Instead, they use abstract principles, can see the situation as a complex whole, perceive situations comprehensively, and can be fully involved in the situation. 48 Expert nurses can perform high-level care without conscious awareness of the knowledge they are using, 39 , 58 and they are able to provide that care with flexibility and speed. Through a combination of knowledge and skills gained from a range of theoretical and experiential sources, expert nurses also provide holistic care. 39 Thus, the best care comes from the combination of theoretical, tacit, and experiential knowledge. 59 , 60
Experts are thought to eventually develop the ability to intuitively know what to do and to quickly recognize critical aspects of the situation. 22 Some have proposed that expert nurses provide high-quality patient care, 61 , 62 but that is not consistently documented—particularly in consideration of patient outcomes—and a full understanding between the differential impact of care rendered by an “expert” nurse is not fully understood. In fact, several studies have found that length of professional experience is often unrelated and even negatively related to performance measures and outcomes. 63 , 64
In a review of the literature on expertise in nursing, Ericsson and colleagues 65 found that focusing on challenging, less-frequent situations would reveal individual performance differences on tasks that require speed and flexibility, such as that experienced during a code or an adverse event. Superior performance was associated with extensive training and immediate feedback about outcomes, which can be obtained through continual training, simulation, and processes such as root-cause analysis following an adverse event. Therefore, efforts to improve performance benefited from continual monitoring, planning, and retrospective evaluation. Even then, the nurse’s ability to perform as an expert is dependent upon their ability to use intuition or insights gained through interactions with patients. 39
Intuition and Perception
Intuition is the instant understanding of knowledge without evidence of sensible thought. 66 According to Young, 67 intuition in clinical practice is a process whereby the nurse recognizes something about a patient that is difficult to verbalize. Intuition is characterized by factual knowledge, “immediate possession of knowledge, and knowledge independent of the linear reasoning process” 68 (p. 23). When intuition is used, one filters information initially triggered by the imagination, leading to the integration of all knowledge and information to problem solve. 69 Clinicians use their interactions with patients and intuition, drawing on tacit or experiential knowledge, 70 , 71 to apply the correct knowledge to make the correct decisions to address patient needs. Yet there is a “conflated belief in the nurses’ ability to know what is best for the patient” 72 (p. 251) because the nurses’ and patients’ identification of the patients’ needs can vary. 73
A review of research and rhetoric involving intuition by King and Appleton 62 found that all nurses, including students, used intuition (i.e., gut feelings). They found evidence, predominately in critical care units, that intuition was triggered in response to knowledge and as a trigger for action and/or reflection with a direct bearing on the analytical process involved in patient care. The challenge for nurses was that rigid adherence to checklists, guidelines, and standardized documentation, 62 ignored the benefits of intuition. This view was furthered by Rew and Barrow 68 , 74 in their reviews of the literature, where they found that intuition was imperative to complex decisionmaking, 68 difficult to measure and assess in a quantitative manner, and was not linked to physiologic measures. 74
Intuition is a way of explaining professional expertise. 75 Expert nurses rely on their intuitive judgment that has been developed over time. 39 , 76 Intuition is an informal, nonanalytically based, unstructured, deliberate calculation that facilitates problem solving, 77 a process of arriving at salient conclusions based on relatively small amounts of knowledge and/or information. 78 Experts can have rapid insight into a situation by using intuition to recognize patterns and similarities, achieve commonsense understanding, and sense the salient information combined with deliberative rationality. 10 Intuitive recognition of similarities and commonalities between patients are often the first diagnostic clue or early warning, which must then be followed up with critical evaluation of evidence among the competing conditions. This situation calls for intuitive judgment that can distinguish “expert human judgment from the decisions” made by a novice 79 (p. 23).
Shaw 80 equates intuition with direct perception. Direct perception is dependent upon being able to detect complex patterns and relationships that one has learned through experience are important. Recognizing these patterns and relationships generally occurs rapidly and is complex, making it difficult to articulate or describe. Perceptual skills, like those of the expert nurse, are essential to recognizing current and changing clinical conditions. Perception requires attentiveness and the development of a sense of what is salient. Often in nursing and medicine, means and ends are fused, as is the case for a “good enough” birth experience and a peaceful death.
- Applying Practice Evidence
Research continues to find that using evidence-based guidelines in practice, informed through research evidence, improves patients’ outcomes. 81–83 Research-based guidelines are intended to provide guidance for specific areas of health care delivery. 84 The clinician—both the novice and expert—is expected to use the best available evidence for the most efficacious therapies and interventions in particular instances, to ensure the highest-quality care, especially when deviations from the evidence-based norm may heighten risks to patient safety. Otherwise, if nursing and medicine were exact sciences, or consisted only of techne, then a 1:1 relationship could be established between results of aggregated evidence-based research and the best path for all patients.
Evaluating Evidence
Before research should be used in practice, it must be evaluated. There are many complexities and nuances in evaluating the research evidence for clinical practice. Evaluation of research behind evidence-based medicine requires critical thinking and good clinical judgment. Sometimes the research findings are mixed or even conflicting. As such, the validity, reliability, and generalizability of available research are fundamental to evaluating whether evidence can be applied in practice. To do so, clinicians must select the best scientific evidence relevant to particular patients—a complex process that involves intuition to apply the evidence. Critical thinking is required for evaluating the best available scientific evidence for the treatment and care of a particular patient.
Good clinical judgment is required to select the most relevant research evidence. The best clinical judgment, that is, reasoning across time about the particular patient through changes in the patient’s concerns and condition and/or the clinician’s understanding, are also required. This type of judgment requires clinicians to make careful observations and evaluations of the patient over time, as well as know the patient’s concerns and social circumstances. To evolve to this level of judgment, additional education beyond clinical preparation if often required.
Sources of Evidence
Evidence that can be used in clinical practice has different sources and can be derived from research, patient’s preferences, and work-related experience. 85 , 86 Nurses have been found to obtain evidence from experienced colleagues believed to have clinical expertise and research-based knowledge 87 as well as other sources.
For many years now, randomized controlled trials (RCTs) have often been considered the best standard for evaluating clinical practice. Yet, unless the common threats to the validity (e.g., representativeness of the study population) and reliability (e.g., consistency in interventions and responses of study participants) of RCTs are addressed, the meaningfulness and generalizability of the study outcomes are very limited. Relevant patient populations may be excluded, such as women, children, minorities, the elderly, and patients with multiple chronic illnesses. The dropout rate of the trial may confound the results. And it is easier to get positive results published than it is to get negative results published. Thus, RCTs are generalizable (i.e., applicable) only to the population studied—which may not reflect the needs of the patient under the clinicians care. In instances such as these, clinicians need to also consider applied research using prospective or retrospective populations with case control to guide decisionmaking, yet this too requires critical thinking and good clinical judgment.
Another source of available evidence may come from the gold standard of aggregated systematic evaluation of clinical trial outcomes for the therapy and clinical condition in question, be generated by basic and clinical science relevant to the patient’s particular pathophysiology or care need situation, or stem from personal clinical experience. The clinician then takes all of the available evidence and considers the particular patient’s known clinical responses to past therapies, their clinical condition and history, the progression or stages of the patient’s illness and recovery, and available resources.
In clinical practice, the particular is examined in relation to the established generalizations of science. With readily available summaries of scientific evidence (e.g., systematic reviews and practice guidelines) available to nurses and physicians, one might wonder whether deep background understanding is still advantageous. Might it not be expendable, since it is likely to be out of date given the current scientific evidence? But this assumption is a false opposition and false choice because without a deep background understanding, the clinician does not know how to best find and evaluate scientific evidence for the particular case in hand. The clinician’s sense of salience in any given situation depends on past clinical experience and current scientific evidence.
Evidence-Based Practice
The concept of evidence-based practice is dependent upon synthesizing evidence from the variety of sources and applying it appropriately to the care needs of populations and individuals. This implies that evidence-based practice, indicative of expertise in practice, appropriately applies evidence to the specific situations and unique needs of patients. 88 , 89 Unfortunately, even though providing evidence-based care is an essential component of health care quality, it is well known that evidence-based practices are not used consistently.
Conceptually, evidence used in practice advances clinical knowledge, and that knowledge supports independent clinical decisions in the best interest of the patient. 90 , 91 Decisions must prudently consider the factors not necessarily addressed in the guideline, such as the patient’s lifestyle, drug sensitivities and allergies, and comorbidities. Nurses who want to improve the quality and safety of care can do so though improving the consistency of data and information interpretation inherent in evidence-based practice.
Initially, before evidence-based practice can begin, there needs to be an accurate clinical judgment of patient responses and needs. In the course of providing care, with careful consideration of patient safety and quality care, clinicians must give attention to the patient’s condition, their responses to health care interventions, and potential adverse reactions or events that could harm the patient. Nonetheless, there is wide variation in the ability of nurses to accurately interpret patient responses 92 and their risks. 93 Even though variance in interpretation is expected, nurses are obligated to continually improve their skills to ensure that patients receive quality care safely. 94 Patients are vulnerable to the actions and experience of their clinicians, which are inextricably linked to the quality of care patients have access to and subsequently receive.
The judgment of the patient’s condition determines subsequent interventions and patient outcomes. Attaining accurate and consistent interpretations of patient data and information is difficult because each piece can have different meanings, and interpretations are influenced by previous experiences. 95 Nurses use knowledge from clinical experience 96 , 97 and—although infrequently—research. 98–100
Once a problem has been identified, using a process that utilizes critical thinking to recognize the problem, the clinician then searches for and evaluates the research evidence 101 and evaluates potential discrepancies. The process of using evidence in practice involves “a problem-solving approach that incorporates the best available scientific evidence, clinicians’ expertise, and patient’s preferences and values” 102 (p. 28). Yet many nurses do not perceive that they have the education, tools, or resources to use evidence appropriately in practice. 103
Reported barriers to using research in practice have included difficulty in understanding the applicability and the complexity of research findings, failure of researchers to put findings into the clinical context, lack of skills in how to use research in practice, 104 , 105 amount of time required to access information and determine practice implications, 105–107 lack of organizational support to make changes and/or use in practice, 104 , 97 , 105 , 107 and lack of confidence in one’s ability to critically evaluate clinical evidence. 108
When Evidence Is Missing
In many clinical situations, there may be no clear guidelines and few or even no relevant clinical trials to guide decisionmaking. In these cases, the latest basic science about cellular and genomic functioning may be the most relevant science, or by default, guestimation. Consequently, good patient care requires more than a straightforward, unequivocal application of scientific evidence. The clinician must be able to draw on a good understanding of basic sciences, as well as guidelines derived from aggregated data and information from research investigations.
Practical knowledge is shaped by one’s practice discipline and the science and technology relevant to the situation at hand. But scientific, formal, discipline-specific knowledge are not sufficient for good clinical practice, whether the discipline be law, medicine, nursing, teaching, or social work. Practitioners still have to learn how to discern generalizable scientific knowledge, know how to use scientific knowledge in practical situations, discern what scientific evidence/knowledge is relevant, assess how the particular patient’s situation differs from the general scientific understanding, and recognize the complexity of care delivery—a process that is complex, ongoing, and changing, as new evidence can overturn old.
Practice communities like individual practitioners may also be mistaken, as is illustrated by variability in practice styles and practice outcomes across hospitals and regions in the United States. This variability in practice is why practitioners must learn to critically evaluate their practice and continually improve their practice over time. The goal is to create a living self-improving tradition.
Within health care, students, scientists, and practitioners are challenged to learn and use different modes of thinking when they are conflated under one term or rubric, using the best-suited thinking strategies for taking into consideration the purposes and the ends of the reasoning. Learning to be an effective, safe nurse or physician requires not only technical expertise, but also the ability to form helping relationships and engage in practical ethical and clinical reasoning. 50 Good ethical comportment requires that both the clinician and the scientist take into account the notions of good inherent in clinical and scientific practices. The notions of good clinical practice must include the relevant significance and the human concerns involved in decisionmaking in particular situations, centered on clinical grasp and clinical forethought.
The Three Apprenticeships of Professional Education
We have much to learn in comparing the pedagogies of formation across the professions, such as is being done currently by the Carnegie Foundation for the Advancement of Teaching. The Carnegie Foundation’s broad research program on the educational preparation of the profession focuses on three essential apprenticeships:
To capture the full range of crucial dimensions in professional education, we developed the idea of a three-fold apprenticeship: (1) intellectual training to learn the academic knowledge base and the capacity to think in ways important to the profession; (2) a skill-based apprenticeship of practice; and (3) an apprenticeship to the ethical standards, social roles, and responsibilities of the profession, through which the novice is introduced to the meaning of an integrated practice of all dimensions of the profession, grounded in the profession’s fundamental purposes. 109
This framework has allowed the investigators to describe tensions and shortfalls as well as strengths of widespread teaching practices, especially at articulation points among these dimensions of professional training.
Research has demonstrated that these three apprenticeships are taught best when they are integrated so that the intellectual training includes skilled know-how, clinical judgment, and ethical comportment. In the study of nursing, exemplary classroom and clinical teachers were found who do integrate the three apprenticeships in all of their teaching, as exemplified by the following anonymous student’s comments:
With that as well, I enjoyed the class just because I do have clinical experience in my background and I enjoyed it because it took those practical applications and the knowledge from pathophysiology and pharmacology, and all the other classes, and it tied it into the actual aspects of like what is going to happen at work. For example, I work in the emergency room and question: Why am I doing this procedure for this particular patient? Beforehand, when I was just a tech and I wasn’t going to school, I’d be doing it because I was told to be doing it—or I’d be doing CPR because, you know, the doc said, start CPR. I really enjoy the Care and Illness because now I know the process, the pathophysiological process of why I’m doing it and the clinical reasons of why they’re making the decisions, and the prioritization that goes on behind it. I think that’s the biggest point. Clinical experience is good, but not everybody has it. Yet when these students transition from school and clinicals to their job as a nurse, they will understand what’s going on and why.
The three apprenticeships are equally relevant and intertwined. In the Carnegie National Study of Nursing Education and the companion study on medical education as well as in cross-professional comparisons, teaching that gives an integrated access to professional practice is being examined. Once the three apprenticeships are separated, it is difficult to reintegrate them. The investigators are encouraged by teaching strategies that integrate the latest scientific knowledge and relevant clinical evidence with clinical reasoning about particular patients in unfolding rather than static cases, while keeping the patient and family experience and concerns relevant to clinical concerns and reasoning.
Clinical judgment or phronesis is required to evaluate and integrate techne and scientific evidence.
Within nursing, professional practice is wise and effective usually to the extent that the professional creates relational and communication contexts where clients/patients can be open and trusting. Effectiveness depends upon mutual influence between patient and practitioner, student and learner. This is another way in which clinical knowledge is dialogical and socially distributed. The following articulation of practical reasoning in nursing illustrates the social, dialogical nature of clinical reasoning and addresses the centrality of perception and understanding to good clinical reasoning, judgment and intervention.

Clinical Grasp *
Clinical grasp describes clinical inquiry in action. Clinical grasp begins with perception and includes problem identification and clinical judgment across time about the particular transitions of particular patients. Garrett Chan 20 described the clinician’s attempt at finding an “optimal grasp” or vantage point of understanding. Four aspects of clinical grasp, which are described in the following paragraphs, include (1) making qualitative distinctions, (2) engaging in detective work, (3) recognizing changing relevance, and (4) developing clinical knowledge in specific patient populations.
Making Qualitative Distinctions
Qualitative distinctions refer to those distinctions that can be made only in a particular contextual or historical situation. The context and sequence of events are essential for making qualitative distinctions; therefore, the clinician must pay attention to transitions in the situation and judgment. Many qualitative distinctions can be made only by observing differences through touch, sound, or sight, such as the qualities of a wound, skin turgor, color, capillary refill, or the engagement and energy level of the patient. Another example is assessing whether the patient was more fatigued after ambulating to the bathroom or from lack of sleep. Likewise the quality of the clinician’s touch is distinct as in offering reassurance, putting pressure on a bleeding wound, and so on. 110
Engaging in Detective Work, Modus Operandi Thinking, and Clinical Puzzle Solving
Clinical situations are open ended and underdetermined. Modus operandi thinking keeps track of the particular patient, the way the illness unfolds, the meanings of the patient’s responses as they have occurred in the particular time sequence. Modus operandi thinking requires keeping track of what has been tried and what has or has not worked with the patient. In this kind of reasoning-in-transition, gains and losses of understanding are noticed and adjustments in the problem approach are made.
We found that teachers in a medical surgical unit at the University of Washington deliberately teach their students to engage in “detective work.” Students are given the daily clinical assignment of “sleuthing” for undetected drug incompatibilities, questionable drug dosages, and unnoticed signs and symptoms. For example, one student noted that an unusual dosage of a heart medication was being given to a patient who did not have heart disease. The student first asked her teacher about the unusually high dosage. The teacher, in turn, asked the student whether she had asked the nurse or the patient about the dosage. Upon the student’s questioning, the nurse did not know why the patient was receiving the high dosage and assumed the drug was for heart disease. The patient’s staff nurse had not questioned the order. When the student asked the patient, the student found that the medication was being given for tremors and that the patient and the doctor had titrated the dosage for control of the tremors. This deliberate approach to teaching detective work, or modus operandi thinking, has characteristics of “critical reflection,” but stays situated and engaged, ferreting out the immediate history and unfolding of events.
Recognizing Changing Clinical Relevance
The meanings of signs and symptoms are changed by sequencing and history. The patient’s mental status, color, or pain level may continue to deteriorate or get better. The direction, implication, and consequences for the changes alter the relevance of the particular facts in the situation. The changing relevance entailed in a patient transitioning from primarily curative care to primarily palliative care is a dramatic example, where symptoms literally take on new meanings and require new treatments.
Developing Clinical Knowledge in Specific Patient Populations
Extensive experience with a specific patient population or patients with particular injuries or diseases allows the clinician to develop comparisons, distinctions, and nuanced differences within the population. The comparisons between many specific patients create a matrix of comparisons for clinicians, as well as a tacit, background set of expectations that create population- and patient-specific detective work if a patient does not meet the usual, predictable transitions in recovery. What is in the background and foreground of the clinician’s attention shifts as predictable changes in the patient’s condition occurs, such as is seen in recovering from heart surgery or progressing through the predictable stages of labor and delivery. Over time, the clinician develops a deep background understanding that allows for expert diagnostic and interventions skills.
Clinical Forethought
Clinical forethought is intertwined with clinical grasp, but it is much more deliberate and even routinized than clinical grasp. Clinical forethought is a pervasive habit of thought and action in nursing practice, and also in medicine, as clinicians think about disease and recovery trajectories and the implications of these changes for treatment. Clinical forethought plays a role in clinical grasp because it structures the practical logic of clinicians. At least four habits of thought and action are evident in what we are calling clinical forethought: (1) future think, (2) clinical forethought about specific patient populations, (3) anticipation of risks for particular patients, and (4) seeing the unexpected.
Future think
Future think is the broadest category of this logic of practice. Anticipating likely immediate futures helps the clinician make good plans and decisions about preparing the environment so that responding rapidly to changes in the patient is possible. Without a sense of salience about anticipated signs and symptoms and preparing the environment, essential clinical judgments and timely interventions would be impossible in the typically fast pace of acute and intensive patient care. Future think governs the style and content of the nurse’s attentiveness to the patient. Whether in a fast-paced care environment or a slower-paced rehabilitation setting, thinking and acting with anticipated futures guide clinical thinking and judgment. Future think captures the way judgment is suspended in a predictive net of anticipation and preparing oneself and the environment for a range of potential events.
Clinical forethought about specific diagnoses and injuries
This habit of thought and action is so second nature to the experienced nurse that the new or inexperienced nurse may have difficulty finding out about what seems to other colleagues as “obvious” preparation for particular patients and situations. Clinical forethought involves much local specific knowledge about who is a good resource and how to marshal support services and equipment for particular patients.
Examples of preparing for specific patient populations are pervasive, such as anticipating the need for a pacemaker during surgery and having the equipment assembled ready for use to save essential time. Another example includes forecasting an accident victim’s potential injuries, and recognizing that intubation might be needed.
Anticipation of crises, risks, and vulnerabilities for particular patients
This aspect of clinical forethought is central to knowing the particular patient, family, or community. Nurses situate the patient’s problems almost like a topography of possibilities. This vital clinical knowledge needs to be communicated to other caregivers and across care borders. Clinical teaching could be improved by enriching curricula with narrative examples from actual practice, and by helping students recognize commonly occurring clinical situations in the simulation and clinical setting. For example, if a patient is hemodynamically unstable, then managing life-sustaining physiologic functions will be a main orienting goal. If the patient is agitated and uncomfortable, then attending to comfort needs in relation to hemodynamics will be a priority. Providing comfort measures turns out to be a central background practice for making clinical judgments and contains within it much judgment and experiential learning.
When clinical teaching is too removed from typical contingencies and strong clinical situations in practice, students will lack practice in active thinking-in-action in ambiguous clinical situations. In the following example, an anonymous student recounted her experiences of meeting a patient:
I was used to different equipment and didn’t know how things went, didn’t know their routine, really. You can explain all you want in class, this is how it’s going to be, but when you get there … . Kim was my first instructor and my patient that she assigned me to—I walked into the room and he had every tube imaginable. And so I was a little overwhelmed. It’s not necessarily even that he was that critical … . She asked what tubes here have you seen? Well, I know peripheral lines. You taught me PICC [peripherally inserted central catheter] lines, and we just had that, but I don’t really feel comfortable doing it by myself, without you watching to make sure that I’m flushing it right and how to assess it. He had a chest tube and I had seen chest tubes, but never really knew the depth of what you had to assess and how you make sure that it’s all kosher and whatever. So she went through the chest tube and explained, it’s just bubbling a little bit and that’s okay. The site, check the site. The site looked okay and that she’d say if it wasn’t okay, this is what it might look like … . He had a feeding tube. I had done feeding tubes but that was like a long time ago in my LPN experiences schooling. So I hadn’t really done too much with the feeding stuff either … . He had a [nasogastric] tube, and knew pretty much about that and I think at the time it was clamped. So there were no issues with the suction or whatever. He had a Foley catheter. He had a feeding tube, a chest tube. I can’t even remember but there were a lot.
As noted earlier, a central characteristic of a practice discipline is that a self-improving practice requires ongoing experiential learning. One way nurse educators can enhance clinical inquiry is by increasing pedagogies of experiential learning. Current pedagogies for experiential learning in nursing include extensive preclinical study, care planning, and shared postclinical debriefings where students share their experiential learning with their classmates. Experiential learning requires open learning climates where students can discuss and examine transitions in understanding, including their false starts, or their misconceptions in actual clinical situations. Nursing educators typically develop open and interactive clinical learning communities, so that students seem committed to helping their classmates learn from their experiences that may have been difficult or even unsafe. One anonymous nurse educator described how students extend their experiential learning to their classmates during a postclinical conference:
So for example, the patient had difficulty breathing and the student wanted to give the meds instead of addressing the difficulty of breathing. Well, while we were sharing information about their patients, what they did that day, I didn’t tell the student to say this, but she said, ‘I just want to tell you what I did today in clinical so you don’t do the same thing, and here’s what happened.’ Everybody’s listening very attentively and they were asking her some questions. But she shared that. She didn’t have to. I didn’t tell her, you must share that in postconference or anything like that, but she just went ahead and shared that, I guess, to reinforce what she had learned that day but also to benefit her fellow students in case that thing comes up with them.
The teacher’s response to this student’s honesty and generosity exemplifies her own approach to developing an open community of learning. Focusing only on performance and on “being correct” prevents learning from breakdown or error and can dampen students’ curiosity and courage to learn experientially.
Seeing the unexpected
One of the keys to becoming an expert practitioner lies in how the person holds past experiential learning and background habitual skills and practices. This is a skill of foregrounding attention accurately and effectively in response to the nature of situational demands. Bourdieu 29 calls the recognition of the situation central to practical reasoning. If nothing is routinized as a habitual response pattern, then practitioners will not function effectively in emergencies. Unexpected occurrences may be overlooked. However, if expectations are held rigidly, then subtle changes from the usual will be missed, and habitual, rote responses will inappropriately rule. The clinician must be flexible in shifting between what is in background and foreground. This is accomplished by staying curious and open. The clinical “certainty” associated with perceptual grasp is distinct from the kind of “certainty” achievable in scientific experiments and through measurements. Recognition of similar or paradigmatic clinical situations is similar to “face recognition” or recognition of “family resemblances.” This concept is subject to faulty memory, false associative memories, and mistaken identities; therefore, such perceptual grasp is the beginning of curiosity and inquiry and not the end. Assessment and validation are required. In rapidly moving clinical situations, perceptual grasp is the starting point for clarification, confirmation, and action. Having the clinician say out loud how he or she is understanding the situation gives an opportunity for confirmation and disconfirmation from other clinicians present. 111 The relationship between foreground and background of attention needs to be fluid, so that missed expectations allow the nurse to see the unexpected. For example, when the background rhythm of a cardiac monitor changes, the nurse notices, and what had been background tacit awareness becomes the foreground of attention. A hallmark of expertise is the ability to notice the unexpected. 20 Background expectations of usual patient trajectories form with experience. Tacit expectations for patient trajectories form that enable the nurse to notice subtle failed expectations and pay attention to early signs of unexpected changes in the patient's condition. Clinical expectations gained from caring for similar patient populations form a tacit clinical forethought that enable the experienced clinician to notice missed expectations. Alterations from implicit or explicit expectations set the stage for experiential learning, depending on the openness of the learner.
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses’ continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
This section of the paper was condensed and paraphrased from Benner, Hooper-Kyriakidis, and Stannard. 23 Patricia Hooper-Kyriakidis wrote the section on clinical grasp, and Patricia Benner wrote the section on clinical forethought.
- Cite this Page Benner P, Hughes RG, Sutphen M. Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinically. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 6.
- PDF version of this page (147K)
In this Page
- Clinical Grasp
Other titles in this collection
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Nurses' reasoning process during care planning taking pressure ulcer prevention as an example. A think-aloud study. [Int J Nurs Stud. 2007] Nurses' reasoning process during care planning taking pressure ulcer prevention as an example. A think-aloud study. Funkesson KH, Anbäcken EM, Ek AC. Int J Nurs Stud. 2007 Sep; 44(7):1109-19. Epub 2006 Jun 27.
- Registered nurses' clinical reasoning skills and reasoning process: A think-aloud study. [Nurse Educ Today. 2016] Registered nurses' clinical reasoning skills and reasoning process: A think-aloud study. Lee J, Lee YJ, Bae J, Seo M. Nurse Educ Today. 2016 Nov; 46:75-80. Epub 2016 Aug 15.
- Combining the arts: an applied critical thinking approach in the skills laboratory. [Nursingconnections. 2000] Combining the arts: an applied critical thinking approach in the skills laboratory. Peterson MJ, Bechtel GA. Nursingconnections. 2000 Summer; 13(2):43-9.
- Review About critical thinking. [Dynamics. 2004] Review About critical thinking. Hynes P, Bennett J. Dynamics. 2004 Fall; 15(3):26-9.
- Review The 'five rights' of clinical reasoning: an educational model to enhance nursing students' ability to identify and manage clinically 'at risk' patients. [Nurse Educ Today. 2010] Review The 'five rights' of clinical reasoning: an educational model to enhance nursing students' ability to identify and manage clinically 'at risk' patients. Levett-Jones T, Hoffman K, Dempsey J, Jeong SY, Noble D, Norton CA, Roche J, Hickey N. Nurse Educ Today. 2010 Aug; 30(6):515-20. Epub 2009 Nov 30.
Recent Activity
- Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinical... Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinically - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- Brooklyn, NY
- Jamaica, NY
- Phoenix, AZ
- Medical Assistant Program – Jamaica, Queens
- Medical Assistant Program – Brooklyn, NY
- Medical Assistant Program – Phoenix, AZ
- Nursing Assistant Training in Queens, NY
- Brooklyn Campus
- Phoenix Campus
- Financial Aid
- History of the School
- Career Services
- Institution For HOPE
How Critical Thinking Skills Apply to Healthcare
Critical Thinking Includes
- The skill to draw conclusions.
- The skill to troubleshoot and problem-solve.
- The capability to use skills or knowledge in a variety of situations.
Examples of Everyday Critical Thinking
- Thinking about what steps should to be taken to avoid an accident.
- Creating a list that gives ability to accomplish every task efficiently and effectively.
- Thinking through the process and dealing with issues that might arise. (missing an ingredient needed for a dish or finding out that the vacuum cleaner is broken)
Examples of Work-Related Critical Thinking
- Deciding how to deal with a customer who is upset over service or bill to ensure a happy customer.
- Handling a disagreement with another coworker.
- Presenting an issue or proposal to the supervisor.
Examples of Work-Related Critical Thinking Situations
- If you have worked in customer service then the same critical thinking skills that are used to deal with customers will be used to deal with patients in the medical field .
- If you have worked in a fast-paced environment requiring prioritizing then you will carry that skill over to the medical field.
Leave a Reply
Click here to cancel reply.
Name (required)
Email (will not be published) (required)
XHTML: You can use these tags: <a href="" title=""> <abbr title=""> <acronym title=""> <b> <blockquote cite=""> <cite> <code> <del datetime=""> <em> <i> <q cite=""> <s> <strike> <strong>
Constructing critical thinking in health professional education
- Original Article
- Open access
- Published: 04 April 2018
- Volume 7 , pages 156–165, ( 2018 )
Cite this article
You have full access to this open access article

- Renate Kahlke ORCID: orcid.org/0000-0002-4473-5039 1 &
- Kevin Eva 1
8849 Accesses
31 Citations
6 Altmetric
Explore all metrics
Introduction
Calls for enabling ‘critical thinking’ are ubiquitous in health professional education. However, there is little agreement in the literature or in practice as to what this term means and efforts to generate a universal definition have found limited traction. Moreover, the variability observed might suggest that multiplicity has value that the quest for universal definitions has failed to capture. In this study, we sought to map the multiple conceptions of critical thinking in circulation in health professional education to understand the relationships and tensions between them.
We used an inductive, qualitative approach to explore conceptions of critical thinking with educators from four health professions: medicine, nursing, pharmacy, and social work. Four participants from each profession participated in two individual in-depth semi-structured interviews, the latter of which induced reflection on a visual depiction of results generated from the first set of interviews.
Three main conceptions of critical thinking were identified: biomedical, humanist, and social justice-oriented critical thinking. ‘Biomedical critical thinking’ was the dominant conception. While each conception had distinct features, the particular conceptions of critical thinking espoused by individual participants were not stable within or between interviews.
Multiple conceptions of critical thinking likely offer educators the ability to express diverse beliefs about what ‘good thinking’ means in variable contexts. The findings suggest that any single definition of critical thinking in the health professions will be inherently contentious and, we argue, should be. Such debates, when made visible to educators and trainees, can be highly productive.
Similar content being viewed by others

Teachers’ Beliefs About Inclusive Education and Insights on What Contributes to Those Beliefs: a Meta-analytical Study

A Medical Science Educator’s Guide to Selecting a Research Paradigm: Building a Basis for Better Research

Ethical dilemmas and reflexivity in qualitative research
Avoid common mistakes on your manuscript.
What this paper adds
‘Critical thinking’ is a term commonly used across health professional education, though there is little agreement on what this means in the literature or in practice. We depart from previous work, which most often attempts to create a common definition. Instead, we offer a description of the different conceptions of critical thinking held in health professional education, illustrate their dynamic use, and discuss the tensions and affordances that this diversity brings to the field. We argue that diversity in conceptions of critical thinking can allow educators to express unique and often divergent beliefs about what ‘good thinking’ means in their contexts.
Even though the term critical thinking is ubiquitous in educational settings, there is significant disagreement about what it means to ‘think critically’ [ 1 ]. Predominantly, authors have attempted to develop consensus definitions of critical thinking that would finally put these disagreements to rest (e. g. [ 2 , 3 , 4 , 5 ]). They define critical thinking variously, but tend to focus on a rational process involving (for example) ‘interpretation, analysis, evaluation, inference, explanation, and self-regulation’ [ 2 ]. Other authors have challenged this perspective by arguing that critical thinking is a more subjective process, emphasizing the role of emotion and relationships [ 6 , 7 , 8 , 9 ]. In the tradition of critical pedagogy, critical thinking has meant critiquing ideology [ 10 , 11 , 12 ]. Last, still others have argued that critical thinking is discipline or subject-specific, meaning that critical thinking is not universal, but does have a relatively stable meaning within different disciplines [ 13 , 14 , 15 , 16 , 17 , 18 ]. However, none of these attempts to clarify the ambiguity that surrounds critical thinking have led to agreement, suggesting that each of these perspectives offers, at best, a partial explanation for the persistence of disagreements.
This is problematic in health professional education (HPE) because professional programs are mandated to educate practitioners who have a defined knowledge base and skill set. When curriculum designers, educators, researchers, or policy-makers all agree that we should teach future professionals to ‘think critically’, resting on the assumption that they also agree on what that means, they may find themselves working at cross-purposes. Moreover, the focus on a stable meaning for critical thinking, whether within a discipline or across disciplines, cannot account for the potential value of the multiplicity of definitions that exist. That is, the availability of diverse conceptions of critical thinking likely enables educators to express diverse elements of and beliefs about their work, thereby suggesting a need to explore the conceptions of critical thinking held in HPE, and the contexts that inform those conceptions.
With the historical focus on developing broad definitions of critical thinking and delineating its component skills and dispositions, little has been done either to document the diverse conceptions of this term in circulation amongst active HPE practitioners or, perhaps more importantly, to illuminate the beliefs about what constitutes ‘good thinking’ that lie behind them and the relationships between them. Perhaps clarity in our understanding of critical thinking lies in the flexibility with which it is conceptualized. This study moves away from attempting to create universal definitions of critical thinking in order to explore the tensions that surround different, converging, and competing beliefs about what critical thinking means.
In doing so, we map out conceptions of critical thinking across four health professions along with the beliefs about professional practice that underpin those conceptions. Some of these beliefs may be tied to a profession’s socialization processes and many will be tied to beliefs about ‘good thinking’ that are shared across professions, since health professionals work within shared systems [ 19 ] toward the same ultimate task of providing patient care. It is the variety of ways in which critical thinking is considered by practitioners on the whole that we wanted to understand, not the formal pronouncements of what might be listed as competencies or components of critical thinking within any one profession.
Hence, with this study, we sought to ask:
How do educators in the health professions understand critical thinking?
What values or beliefs inform that understanding?
To explore these questions, we adopted a qualitative research approach that focuses on how people interpret and make meaning out of their experiences and actively construct their social worlds [ 20 ].
This study uses an emergent, inductive design in an effort to be responsive to the co-construction of new and unexpected meaning between participants and researchers. While techniques derived from constructivist grounded theory [ 21 ] were employed, methods like extensive theoretical sampling (that are common to that methodology) were not maintained because this study was intended to be broadly exploratory. This ‘borrowing’ of techniques offers the ability to capitalize on the open and broad approach offered by interpretive qualitative methodology [ 20 ] while engaging selectively with the more specific tools and techniques available from constructivist grounded theory [ 22 , 23 ].
The first author has a background in sociocultural and critical theory. Data collection and early analyses were carried out as part of her dissertation in Educational Policy Studies. As a result of her background in critical theory, there was a need for reflexivity focused on limiting predisposition toward participant interpretations of critical thinking that aligned with critical theory. The senior author was trained in cognitive psychology, and contributed to the questioning of results and discussion required to ensure this reflexivity. The first author’s dissertation supervisor also provided support in this way by questioning assumptions made during the initial stages of this work.
Participants were recruited through faculty or departmental listservs for educators. Senior administrators were consulted to ensure that they were aware of and comfortable with this research taking place in their unit. In some cases, administrators identified a few key individuals who were particularly interested in education. These educators were contacted directly by the first author to request participation.
The purposive sample includes four educators from each of four diverse health professional programs ( n = 16 in total): medicine, nursing, pharmacy, and social work. All participants self-identified as being actively involved in teaching in their professional program and all were formally affiliated with either the University of Alberta (Medicine, Nursing, and Pharmacy) or the University of Calgary (Social Work). These four professions were selected to maximize diversity in approaches to critical thinking given that these professions have diverse perspectives and roles with respect to patient care. However, participants all worked in Alberta, Canada, within the same broad postsecondary education and healthcare contexts.
In addition, sampling priority was given to recruiting participants practising in a diverse range of specialties: primary care, geriatrics, paediatrics, mental health, critical care, and various consulting specialties. Specific specialties within each profession are not provided here in an effort to preserve participant anonymity. The goal was not to make conclusions about the perspective of any one group; rather, diversity in profession, practice context, gender, and years in practice was sought to increase the likelihood of illuminating diverse conceptions of critical thinking.
Data generation
Participants were invited to participate in two in-person semi-structured interviews conducted by the first author. All but one participant completed both interviews. Interviews were audio-recorded and interview guides are included in the online Electronic Supplementary Material. The first was about 1 hour in length and discussed how participants think about critical thinking in their teaching, professional practice, and other contexts. Participants were invited to bring a teaching artefact that represented how they teach critical thinking to the interview. Artefacts were used as a visual elicitation strategy to prompt discussion from a new angle [ 24 ]. Questions focused on what the participant thought about teaching critical thinking using the artefact and how they identified critical thinking (or lack thereof) in their students. Artefacts were not analyzed independently of the discussion they produced [ 25 ].
Interview 1 data were analyzed to produce a visual depiction of the aggregate terms, ideas, and relationships described by participants. The visual depiction took the form of a ‘mind map’ (see Appendix C of the Electronic Supplementary Material) that was generated using MindMup free online software [ 26 ]. In developing the mind map, we sought descriptions of participants’ views that remained as close to the data as possible, limiting interpretations and inferences. The ‘clusters’ that appear in the mind map (e. g., the cluster around ‘characteristics of the critical thinker’) represent relationships or categories commonly described when participants discussed those terms. Terms were not weighted or emphasized based on frequency of use (through font size or bolding) in an effort to allow individual participants to emphasize or deemphasize terms as they thought appropriate during the second interview.
Where there was no clear category or relationship, terms were left at the first level of the mind map, connected directly to ‘critical thinking’ at the centre. Including more connections and inferences would likely have improved the readability of the map for participants; however, we chose to include connections and exact language used by participants (even in cases where terms seemed similar) as often as possible, in an effort to limit researcher interpretation. That said, any attempt to aggregate data or to represent relationships is an act of interpretation and some inferences were made in the process, such as the distinction between descriptions about ‘characteristics’ of the critical thinker (the top left hand corner of the map) and ‘processes’ such as ‘reasoning’ or ‘examining assumptions’ (on the right side of the map). The second interview lasted approximately 45 minutes during which a visual elicitation approach invited participants to respond to the mind map.
Visual elicitation involves employing visual stimuli to generate verbal interview data. Participant-generated mind maps are often used in qualitative data collection [ 27 ], but the literature on using researcher-generated diagrams for visual elicitation is relatively thin [ 25 , 28 ]. In this study, using a researcher-generated mind map for visual elicitation offered several advantages. First, as with other forms of visual elicitation, diagrams of this kind can help participants develop candid responses and avoid rehearsed narratives [ 24 , 29 ]. For example, we used mind maps as one mechanism to reduce the tendency for participants who were familiar with the literature on critical thinking to get stuck on narrating seemingly rehearsed definitions of critical thinking. Second, we chose to use a mind map because it provided a social setting through which participants could react to language generated by others. Doing so does not allow the same degree of social negotiation inherent in focus groups, but it avoids the difficulty involved in attempts to disentangle individual from group views [ 30 ]. Third, the visual elicitation method was chosen because it offered a form of member check [ 31 ] that allowed researchers to understand the evolving nature of participants’ conceptions of critical thinking, rather than assuming that participants offer a single true conception during each and every discussion [ 32 ]. In other words, the mind map was used to prompt participants to elaborate their conception of critical thinking and locate it relative to other participants.
In interview 2, participants were asked to begin by discussing areas or terms on the mind map that resonated most with their own conception of critical thinking; they were then asked to discuss terms or concepts on the map that resonated less or with which they disagreed. They were also asked to comment on how relationships between ideas were represented through the map so that researchers could get a sense of the extent to which the relationships between the concepts depicted reflected the participants’ understanding of those relationships [ 28 ]. Participants were encouraged to disagree with portions of the map and most did actively disagree with some of the terms and relationships depicted, suggesting that the map did not come to dictate more than elicit individual interpretations [ 28 ]. Although participants were encouraged to ‘mark up’ the mind map, and the ‘marked up’ mind maps were treated as data, the primary data sources for this study were the audio-recorded interviews [ 25 ].
Participants were aware that the mind map represented aggregate data from the four health professions in the study, but were not initially told whether any of the responses came predominantly from any one profession; they did not generally seem to be attempting to associate terms with other professions. Nonetheless, interview 2 data are a mix of participants’ reactions to the ideas of others and their elaborations of their own understandings. Naturally, these data build on data generated in interview 1, and represent reactions to both the researcher interpretation of the data and to the conceptions of critical thinking offered by others. Interview 1 data tended to offer an initial, open impression of how participants think about critical thinking in their contexts. Because of these different approaches to data generation, quotes from interview 1 and 2 are labelled as ‘INT1’ or ‘INT2’, respectively.
Data analysis
Data were coded through an iterative cycle of initial and focused coding [ 33 ] with NVivo software. Initial line-by-line coding was used to develop codes that were close to the data, involving minimal abstraction. Initial codes were reviewed by the first author and dissertation supervisor to abstract categories (conceptions of critical thinking), sub-categories (features of those conceptions), and themes related to the relationships between those categories. Focused coding involved taking these categories and testing them against the data using constant comparison techniques derived from constructivist grounded theory [ 21 ]. Category development continued during the framing of this paper, and authors engaged in ongoing conversations to modify categories to better fit the data. In this process, we returned to the data to look for exceptions that did not fit any category, as well as contradictions and overlap between categories.
Interpretive sufficiency [ 34 ], in this study, occurred when no new features illustrating participants’ conceptions of critical thinking were identified. Memos were kept to track the development or elimination of initial insights or impressions. Institutional ethics approval was obtained from the University of Alberta.
Participant identities have been masked to preserve anonymity. The abbreviation ‘MD’ refers to educators in medical education, ‘NURS’ to nursing, ‘PHARM’ to pharmacy, and ‘SW’ to social work. Participants within each group were then assigned a number. For example, the code NURS3 is a unique identifier for a single participant.
Three main conceptions of critical thinking were identified, each of which will be elaborated in greater detail below: biomedical critical thinking, humanist critical thinking, and social justice-oriented critical thinking. It is important to note that these categories focus on the process and purpose of critical thinking, as defined by participants. Participant comments also spoke to the ‘characteristics’ or ‘dispositions’ of critical thinkers, such as ‘open-mindedness’ or ‘creativity’. The focus of this study, however, was on uncovering what critical thinking looks like as opposed to what a ‘critical thinker’ looks like.
The results below interweave responses from different professional groups in order to emphasize the way in which each of the three core conceptions that we have identified crosses professional boundaries. We then provide a brief discussion of the relationships between these three conceptions, emphasizing the limited extent to which these conceptions were profession-specific, and the tensions that we observed between these conceptions. In general, we also interweave results from both interviews because the discussion in interview 2 tended to reinforce the themes arising from interview 1, especially with respect to indications that different conceptions were used fluidly by individuals over time and dependent on the context being discussed. The interview from which data arose is marked after each quote and we have mentioned explicitly whenever a comment was made in specific response to the mind map presented during interview 2.
In this way, our data extend the literature on critical thinking by offering an appreciation of how each of these conceptions provide educators a different way of thinking, talking, and teaching about their work in HPE. We found that even individual participants’ conceptions of critical thinking shifted from time to time. That is, they often articulated more than one understanding of critical thinking over the course of an interview or between interviews 1 and 2. Some of these conceptions were shared by multiple participants but individual constellations of beliefs about what critical thinking means were unique and somewhat idiosyncratic. Thus, while participants’ conceptions of critical thinking were both idiosyncratic and common, they were also flexible and contextual; the meaning of critical thinking was continuously reconstructed and contested. In this way, critical thinking offered a window through which to explore how beliefs about what constitutes ‘good thinking’ in a profession are challenged in educational settings.
Biomedical critical thinking
Participants articulating a biomedical approach saw critical thinking and clinical reasoning as nearly synonymous. They emphasized a process that was rational, logical, and systematic. One participant articulated that critical thinking is ‘ to be able to reason logically’ (NURS4 INT1). Another related:
You have to kind of pull together data that’s relevant to the subject you’re dealing with. You have to interpret it, you have to analyse it, and you have to come up with some type of conclusions at the end as to how you deal with it. (PHARM3 INT1)
Participants discussing this approach agreed that critical thinking involved a systematic process of gathering and analyzing data: ‘I think [critical thinking and clinical reasoning] are the same. I think clinical reasoning is basically taking the data you have on a patient and interpreting it, and offering a treatment plan’ (MD1 INT1).
In keeping with an emphasis on the rational and logical, participants espousing this view often reacted negatively when they saw references to emotion on the mind map in interview 2: ‘as soon as you bring your emotions into the room, you’re no longer applying what I think is critical thinking’ (MD4 INT2). Participants also noted that decision-making was an important component of critical thinking: ‘ you have to make a decision. I think it’s a really important part of it’ (MD2 INT2).
For participants from pharmacy, in particular, critical thinking often meant departing from ‘rules’ that guide clinical practice in order to engage in reasoning and make situationally nuanced decisions. One pharmacist, describing a student not engaging in critical thinking, related that the student asked:
‘Have you ever seen Victoza given at 2.4 milligrams daily?’ … It’s very, you know, it’s very much yes or no. But at a deeper level, it’s actually missing things. … [There are] all these other factors that change the decision, right? … On paper there might be a regular set of values for the dose, … [but] without the rest of the background, that’s a very secondary thing. (PHARM4 INT1)
This perspective was identified as the dominant conception of critical thinking because the terms and concepts falling under this broad approach were most frequently discussed by participants; moreover, when participants discussed other conceptions of critical thinking, they were often explicitly drawing contrast to the biomedical view. While the biomedical perspective was dominant in all four groups (although primarily as a contrasting case for social workers), participants tended to occupy more than one perspective over the course of an interview. They might talk primarily about biomedical critical thinking, but also explicitly modify that perspective by drawing on the other two approaches identified: humanist critical and social justice-oriented critical thinking.
Humanist critical thinking
Participants, when adopting this view, described critical thinking as directed toward social good and oriented around positive human relationships. Humanist conceptions of critical thinking were often positioned as an alternative to the dominant biomedical perspective: ‘having to think of somebody else, at their most vulnerable, makes you know that knowledge alone, science alone, won’t get that patient to the place you want the patient to be. It won’t provide the best care’ (NURS1 INT1). In being so positioned, the humanist conception of critical thinking explicitly departed from the biomedical, which emphasized ‘setting aside’ emotion and de-emphasized the role of relationships in healthcare. In the humanist perspective, participants often discussed the purpose of critical thinking as:
Thinking about something for the betterment of yourself and the betterment of others. We’re social beings as human beings. … I think [critical thinking] has a higher purpose. … But I think that [if] critical thinking … [is] a human trait that we have or hope to have, then it has to have those components of what we are as humans. (NURS1 INT1)
Another participant emphasized that: ‘a great part of critical thinking is that human element and the consideration of ultimately what’s a good thing, a common good’ (NURS2 INT1).
In addressing the relational aspects of humanist critical thinking, participants argued that the focus on ‘hard’ sources of data, such as lab tests or imaging, in biomedical critical thinking was limiting. They were concerned that ‘hard data’ tend to be perceived as more objective and thus more important in biomedical critical thinking, compared with subjective patient narratives. They argued that the patient’s story is essential to critical thinking:
I think it doesn’t matter what kind of expert you are, you have to be able to think about patients in the context that they’re in and consider what the patient has to say, and really hear them. So I think that’s an important—that was a total lack of critical thinking in a totally, ‘I’m just going to get through this next patient to the next one’ . (MD1 INT1)
Taken together, these perspectives suggest that biomedical approaches to critical thinking fail to address the complex relational and psychosocial aspects of professional practice.
Social justice-oriented critical thinking
In social justice-oriented approaches to critical thinking participants articulated a process of examining the assumptions and biases embedded in their world. They often explicitly rejected biomedical conceptions of critical thinking as ‘ reductionistic ’ (SW3 INT1) because, in their view, these approaches fail to address the thinker’s own biases. Educators taking a social justice approach felt that: ‘critical thinking … is around things like … recognizing your own bias and recognizing the bias in the world’ (SW1 INT1). In this perspective, participants saw critical thinking as a process of analyzing and addressing the ways in which individual and societal assumptions limit possible actions and access to resources for individuals and social groups.
Unlike biomedical critical thinking and similar to the humanist view, participants articulating this conception tended to make the values and goals of critical thinking, as they conceived of it, explicit. They often contrasted their articulation of values in critical thinking with the ‘assumed’ and unarticulated values present in the biomedical perspective:
If you are not orientated in a social justice position, [critical thinking is] more about the mechanics, which is valuable as well, but … if we don’t understand the values associated with what we think, it seems to not be meaningless but there’s a piece missing or it’s assumed. The values are assumed. (SW3 INT1)
When taking this perspective, participants argued that it is necessary to understand social systems in order to think critically about individual patient cases. One educator questioned:
Why are there a disproportionate number of aboriginal inpatients than any other group? … When you start critically thinking about seeing the whole patient … there are issues related with all of society and that’s why people have more diabetes. (PHARM1 INT1)
Other participants had measured responses to this approach. One participant added to their primarily biomedical approach in order to accommodate perspectives encountered in the mind map, relating that behind their diagnostic work all physicians:
Certainly see a wide spectrum of social and economic status and cultures and things and recognizing that our system is kind of biased against certain groups as it is and knowing that but really not having a good sense of knowing even where to start deconstructing it. (MD2 INT2)
Relationships between conceptions of critical thinking
Results of this study suggest that critical thinking means a variety of things in different contexts and to different people. It might be tempting to see the three approaches outlined above as playing out along professional boundaries. Certainly, the social justice-oriented conception was more common among social work educators; the humanist approach was most common among participants from nursing; perspectives held by physician educators frequently aligned with dominant biomedical conceptions. In pharmacy, educators seemed to straddle all three perspectives, though they commonly emphasized a biomedical approach. Several participants suggested that their faculty or profession has a common understanding of critical thinking: ‘ critical thinking, for me and maybe for our faculty, is around things like … ’ (SW1 INT1).
However, while the disciplinary tendencies discussed above do appear in the data, these tendencies were not stable; participants often held more than one view on what critical thinking meant simultaneously, or shifted between perspectives. Participants also articulated approaches that were not common in their profession at certain moments, positioning themselves as ‘an outlier’, or positioning their specialty as having a different perspective than the profession as a whole, such that critical thinking might mean ‘thinking like a nurse’, or ‘thinking in geriatrics’. Further, participants’ perspectives shifted depending on the context in which they imagined critical thinking occurring.
This type of positioning and re-positioning occurred in both interviews, although they were particularly pronounced in interview 2, where participants were explicitly asked to react to different viewpoints by responding to the mind map. Examples of shifting perspectives in interview 1 occurred especially when participants from medicine shifted between biomedical and humanist conceptions. These shifts suggested a persistent tension and negotiation between characterizations of critical thinking as a rational process of data collection and analysis, and a more humanist approach that accounts for emotion and the relationship between professional and patient or family. Where participants sought to extend their notion of data beyond ‘hard data’ there is a sense of blending humanism with biomedical approaches to critical thinking. In the quote below, the participant brings together a call for a humanist relationship building with a need to gather and analyze all of the data, including important data about the patient’s experience:
I have colleagues who’ll say [to their patients]: ‘just say yes or no.’ … And it’s not very good and they’re missing stuff. So, critical thinking is—I guess it’s sort of dynamic in that you have to have time and you also have to have an interaction. (MD1 INT1)
While the participants described above negotiated between biomedical and humanist perspectives, participants primarily espousing a social justice-oriented conception of critical thinking responded to the ‘assumed’ values of the biomedical model. In talking about a problem solving-oriented biomedical approach, one participant argued that ‘ it’s important as well to have that, those foundational elements of how we think about what we think, but if we don’t understand the values associated … there’s a piece missing’ (SW3 INT1). Another stated that ‘critical thinking seems to be a neutral kind of process or—no, that can’t be true, can it?’ (SW1 INT2) with the mid-sentence shift indicating that two ways of conceptualizing critical thinking had come into conflict. This participant primarily discussed a social justice-oriented conception of critical thinking, which is not neutral, but at this moment also articulated a neutral, clinical reasoning-oriented or biomedical conception.
These relatively organic moments of negotiation certainly demonstrate a sense of conflicting values, of toggling between one perspective and another. However, they also suggest that there are ways in which these contradictions can be productively sustained. In negotiating between humanist and biomedical perspectives, educators effectively modify the dominant perspective.
In interview 2, when discussing the mind map, participants often encountered views that differed from their own. They responded either by making sense of and accommodating the new perspective, or by rejecting it. As an example of the former approach, one physician reacted to the ‘social justice-oriented’ corner of the mind map (specifically ‘examining assumptions’) by explaining how there are:
Assumptions in the background that come up for me all the time in terms of the different ways people live and want to live and how we run into it all the time … it’s always in the background and actually influencing you and until someone challenges the way you approached something, you don’t know what your assumptions are. (MD1 INT2)
As an example of a participant disagreeing with a perspective encountered in the mind map, one participant rejected social justice as an important component of critical thinking in medicine. They related that critical thinking has ‘got everything to do with reasoning, which makes sense. … Social justice has nothing to do with critical thinking’ (MD4 INT2). Interestingly, this participant also spoke at length about the link between social justice and critical thinking in the first interview, suggesting that a conception might seem ‘wrong’ when an individual is thinking and talking about it in one context, and entirely ‘right’ in another context.
Such results demonstrate that individual conceptions of critical thinking are multiple and flexible, not predetermined or stable. Educators bring certain values or perspectives into the foreground as they relate to the context under discussion, while others recede into the background. Though many participants seemed to have a primary perspective, multiple perspectives on critical thinking can co-exist and are actively negotiated by the individual.
In overview, the three broad conceptions of critical thinking offered here (biomedical, humanist, and social justice-oriented) echo approaches to critical thinking found in the critical thinking literature [ 11 , 35 , 36 , 37 ]. However, this study extends the literature in two key ways. First, our data point to ways in which different conceptions of critical thinking conflict and coalesce, within the field, within each profession, and even within individuals. Second, this tension offers an early empirical account of critical thinking in the health professions that suggests there may be benefits to maintaining flexibility in how one conceives of the concept.
The diverse conceptions of critical thinking identified all appear to have some value in HPE. It might be tempting to view each conception as a unique but stable perspective, reflecting thinking skills that are used within a particular context or value orientation. However, the multiplicity and flexibility of participants’ conceptions in this study offers some explanation as to why previous attempts to develop either generic (e. g. [ 2 , 3 , 5 ]) or discipline-specific [ 13 , 15 , 16 , 17 ] definitions and delineations of critical thinking have failed to stick.
Conceptions of critical thinking are not stable within a context or for a single educator. Educators’ conceptions of critical thinking shift within and between contexts as they navigate overlapping sets of values and beliefs. When educators take up different conceptions of critical thinking, the shifts they make are not just pragmatic; they actively negotiate the values and practices of the different communities in which they participate. Although we certainly saw hints of differences between professions, the strength of this study is that it captured the ways in which conceptions of critical thinking are not stably tied to any given profession. Critical thinking is connected to a broader idea of what ‘good thinking’—and, by extension, the ‘good professional’—looks like for each educator [ 38 ] within a given context or community.
These observations lead one to speculate about what purpose fluidity in conceptions of critical thinking might serve. Educators often have different values and goals for their profession, and, thus, it is not surprising that the meaning of critical thinking would be contested both within and across professions. Through their conceptions of critical thinking, participants contest ideas about what thinking is for in their profession—whether it should be focused on individual patient ‘problems’ or broader social issues, and the extent to which humanism is an important component of healthcare.
It is understandable that so much of the literature on critical thinking has sought to clarify a single ‘right’ definition; there is an argument for making a collective decision about what ‘good thinking’ means. Such a decision might offer clarity to interprofessional teaching and practice, or provide a foundation on which educational policy can be based. However, the critical thinking literature has long sought such a universal agreement and disagreements persist. Results of this study suggest a new approach, one that can account for multiple conceptions of critical thinking within and across health professions and practice contexts. The visual elicitation approach employed, asking participants to respond to the mind map, offered a unique perspective on the data that illuminated contradictions between conceptions held by individual participants, between participants, and between the conceptions themselves.
Such an approach offers a vehicle for thinking and talking about what kind of thinking is valued, both within and between professions. When conceptions of critical thinking are understood as flexible instead of stable, these acts of modification and contestation can be viewed as potential moments for critical self-reflection for individuals and for professional groups on the whole. Moreover, through their discussions of critical thinking, educators actively intervened to consider and assert what they value in their work.
These different conceptions might be complementary as often as they are incompatible. In fact, we would argue that ‘good thinking’ is inherently contentious (and should be) because it is such struggles over what ‘the good’ means in HPE that allow for challenges to the status quo. Advances at the heart of HPE and practice have been hard-won through deliberate reflection, discussion, action, and (often) conflict. For example, the ongoing movement toward relationship-oriented care has arguably occurred as a result of unexpected pushback regarding the limits of considering good healthcare as being entirely patient-centred. Thus, there is a need to bring unarticulated assumptions about important topics into the light so that the goals and values of educators and policy-makers can be openly discussed, even though they are unlikely to ever be fully resolved.
Strengths and limitations
This study offered a broad sample of educators from four different professions, who practised in a range of disciplinary contexts. Given that the sampling approach taken sought breadth rather than depth, the results explore a range of conceptions of critical thinking across HPE, rather than allowing strong claims about any one profession or context. The sample also focussed on conceptions of critical thinking within health professions education at specific institutions in Edmonton, Alberta. A multi-institutional study might build on these results to elaborate the extent to which each health profession has a core shared conception of critical thinking that translates across institutional settings. We expect that there may be significant differences between settings, given that what is meant by critical thinking seems to be highly contextual, even from moment to moment. Mapping aspects of context that impact how individuals and groups think about critical thinking would tell us much more about the values on which these conceptions are based.
Subsequent studies might also explore the extent to which conceptions of critical thinking among those identifying as ‘educators’ are comparable to those identifying as primarily ‘clinicians’. Although the boundary is definitely blurry, these groups engage in different kinds of work and participate in different communities, which we suspect may result in differences in how they conceive of critical thinking.
Conclusions
Rather than attempting to ‘solve’ the debate about what critical thinking should mean, this study maps the various conceptions of this term articulated by health professional educators. Educators took up biomedical, humanist, and social justice-oriented conceptions of critical thinking, and their conceptions often shifted from moment to moment or from context to context. The ‘mapping’ approach adopted to study this issue allowed for an appreciation of the ways in which educators actively modify and contest educational and professional values, even within their own thinking. Because critical thinking appears to be both value and context driven, arriving at a single right definition or taxonomy of critical thinking is unlikely to resolve deep tensions around what ‘good thinking’ in HPE means. Moreover, such an approach is unlikely to be productive. Such tensions produce challenges for shared understanding at the same time that they produce a productive space for discussion about core issues in HPE.
Abrami PC, Bernard RM, Borokhovski E, et al. Instructional interventions affecting critical thinking skills and dispositions: a stage 1 meta-analysis. Rev Educ Res. 2008;78:1102–34.
Article Google Scholar
Facione PA. Critical thinking: a statement of expert consensus for purposes of educational assessment and instruction. Millbrae: California Academic Press; 1990.
Google Scholar
Black B. Critical thinking—a definition and taxonomy for Cambridge Assessment: supporting validity arguments about critical thinking assessments administered by Cambridge Assessment. 34 th IAEA Annual Conference; 09.9.2008; Cambridge; 2008.
Fischer SC, Spiker VA, Riedel SL. Critical thinking training for army officers volume two: a model of critical thinking. Arlington: US Army Research Institute; 2009.
Ennis RH. Critical thinking: a streamlined conception. In: Davies M, Barnett R, editors. The Palgrave handbook of critical thinking in higher education. New York: Palgrave MacMillan; 2015. pp. 31–47.
Chapter Google Scholar
Thayer-Bacon B. Transforming critical thinking: thinking constructively. New York: Teachers College Press; 2000.
Thayer-Bacon B. Caring and its relationship to critical thinking. Educ Theory. 1993;43:323–40.
Walters KS. Critical thinking, rationality, and the vulcanization of students. In: Walters KS, editor. Re-thinking reason: new perspectives on critical thinking. Albany: State University of New York Press; 1994. pp. 61–80.
Warren KJ. Critical thinking and feminism. In: Walters KS, editor. Re-thinking reason: new perspectives on critical thinking. Albany: State University of New York Press; 1994. pp. 199–204.
Brookfield SD. Speaking truth to power: teaching critical thinking in the critical theory tradition. In: Davies M, Barnett R, editors. The Palgrave handbook of critical thinking in higher education. New York: Palgrave MacMillan; 2015. pp. 529–43.
McLaren PL. Forward: critical thinking as a political project. In: Walters KS, editor. Re-thinking reason: new perspectives on critical thinking. Albany: State University of New York Press; 1994. pp. ix–xv.
Giroux H. Toward a pedagogy of critical thinking. In: Walters KS, editor. Re-thinking reason: new perspectives on critical thinking. Albany: State University of New York Press; 1994. pp. 199–204.
McPeck JE. Critical thinking and the ‘Trivial Pursuit’ theory of knowledge. In: Walters KS, editor. Re-thinking reason: new perspectives on critical thinking. Albany: State University of New York Press; 1994. pp. 101–18.
Chan ZC. A systematic review of critical thinking in nursing education. Nurse Educ Today. 2013;33:236–40.
Scheffer BK, Rubenfeld MG. A consensus statement on critical thinking in nursing. J Nurs Educ. 2000;39:352–9.
Krupat E, Sprague JM, Wolpaw D, Haidet P, Hatem D, O’Brien B. Thinking critically about critical thinking: ability, disposition or both? Med Educ. 2011;45:625–35.
Jones A. A disciplined approach to critical thinking. In: Davies M, Barnett R, editors. The Palgrave handbook of critical thinking in higher education. New York: Palgrave MacMillan; 2015. pp. 169–82.
Papp KK, Huang GC, Lauzon Clabo LM, et al. Milestones of critical thinking: a developmental model for medicine and nursing. Acad Med. 2014;89:715–20.
Grace S, Innes E, Joffe B, East L, Coutts R, Nancarrow S. Identifying common values among seven health professions: an interprofessional analysis. J Interprof Care. 2017;31(3):1–10. https://doi.org/10.1080/13561820.2017.1288091 .
Merriam SB. Qualitative research: a guide to design and implementation. San Francisco: Jossey-Bass; 2009.
Charmaz K. Constructing grounded theory. 2nd ed. Thousand Oaks: SAGE; 2014.
Kahlke RM. Generic qualitative approaches: pitfalls and benefits of methodological mixology. Int J Qual Methods. 2014;13:37–52.
Varpio L, Martimianakis MA, Mylopoulos M. Qualitative research methodologies: embracing methodological borrowing, shifting and importing. In: Cleland J, Durning SJ, editors. Researching medical education. Chichester: John Wiley & Sons; 2015. pp. 245–55. https://doi.org/10.1002/9781118838983.ch21 .
Wheeldon J. Is a picture worth a thousand words? Using mind maps to facilitate participant recall in qualitative research. Qual Rep. 2011;16:509–22.
Umoquit MJ, Tso P, Tünde V‑A, O’brien M, Wheeldon J. Diagrammatic elicitation: defining the use of diagrams in data collection. Qual Rep. 2013;18(60):1–12.
MindMup 2. Available from: https://www.mindmup.com/ . Accessed: 1 March 2018
Wheeldon J, Framing Experience FJ. Concept maps, mind maps, and data collection in qualitative research. Int J Qual Methods. 2009;8:68–83.
Crilly N, Blackwell A, Clarkson PJ. Graphic elicitation: using research diagrams as interview stimuli. Qual Res. 2006;6:341–66.
Hathaway AD, Atkinson M. Active interview techniques in research on public deviants: exploring the two-cop personas. Field methods. 2003;15:161–85.
Onwuegbuzie AJ, Dickinson WB, Leech NL, Zoran AG. A qualitative framework for collecting and analyzing data in focus group research. Int J Qual Methods. 2009;8:1–21.
Kinchin IM, Streatfield D, Hay DB. Using concept mapping to enhance the research interview. Int J Qual Methods. 2010;9:52–68.
Varpio L, Ajjawi R, Monrouxe L, O’Brien B, Rees C. Shedding the cobra effect: problematizing thematic emergence, triangulation, saturation and member checking. Med Educ. 2017;51:40–50.
Saldaña J. The coding manual for qualitative researchers. 2nd ed. Thousand Oaks: SAGE; 2013.
Christians CG. Ethics and politics in qualitative research. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative research. 2nd ed. Thousand Oaks: SAGE; 2000. pp. 133–55.
Kahlke RM, White J. Critical thinking in health sciences education: considering ‘three waves’. Creat Educ. 2014;4:21–9.
Introduction WKS. beyond logicism in critical thinking. In: Walters KS, editor. Re-thinking reason: new perspectives on critical thinking. Albany: State University of New York Press; 1994. pp. 1–22.
Barnett R. A curriculum of critical being. In: Davies M, Barnett R, editors. The Palgrave handbook of critical thinking in higher education. New York: Palgrave MacMillan; 2015. pp. 63–76.
Pithers RT, Soden R. Critical thinking in education: a review. Educ Res. 2000;42:237–49.
Download references
Acknowledgements
We thank Dr. Paul Newton for his contributions to the analysis of these data, in his role as supervisor of the dissertation work on which this manuscript is based. Thanks also to Dr. Dan Pratt for his help and support in developing this manuscript.
Support for this work was provided by the Government of Alberta (Queen Elizabeth II Graduate Scholarship), by the Social Sciences and Humanities Research Council (Doctoral Fellowship), and by the University of British Columbia (Postdoctoral Fellowship).
Author information
Authors and affiliations.
Centre for Health Education Scholarship, University of British Columbia, Vancouver, Canada
Renate Kahlke & Kevin Eva
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Renate Kahlke .
Ethics declarations
Conflict of interest.
R. Kahlke and K. Eva declare that they have no competing interests.
Caption Electronic Supplementary Material
Appendix a: interview guide for initial interview, appendix b: interview guide for second interview, appendix c: mind map, rights and permissions.
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Kahlke, R., Eva, K. Constructing critical thinking in health professional education. Perspect Med Educ 7 , 156–165 (2018). https://doi.org/10.1007/s40037-018-0415-z
Download citation
Published : 04 April 2018
Issue Date : June 2018
DOI : https://doi.org/10.1007/s40037-018-0415-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Critical thinking
- Clinical reasoning
- Health professions education
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 20 March 2023
Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students
- Yueh-Ren Ho 1 , 2 ,
- Bao-Yu Chen 3 &
- Chien-Ming Li 2 , 4
BMC Medical Education volume 23 , Article number: 173 ( 2023 ) Cite this article
11k Accesses
7 Citations
7 Altmetric
Metrics details
In medicine, critical thinking is required for managing and tolerating medical uncertainty, as well as solving professional problems and treating diseases. However, the core of Confucianism, teacher-centered and exam-oriented settings in middle and high school education may pose challenges to developing critical thinking in Han Chinese or Taiwanese students. Students may be adversely affected by these pedagogies since student-centered settings were more effective in stimulating their critical and reflective thinking, as well as a sense of responsibility, in the ever-changing world. Therefore, guiding students with less stable foundations of critical thinking might require a different approach. A review article highlighted the potential utility of the Socratic method as a tool for teaching critical thinking in the healthcare field. The method involves posing a series of questions to students. More importantly, medical students and residents in clinical teaching are familiar with the method. Almost all healthcare students must complete a biochemistry laboratory course as part of their basic science training. Thus, we aimed to train students to develop critical thinking in the biochemistry laboratory course by using learning sheets and teacher guidance based on the Socratic method and questioning.
We recruited second-year students from a medical school, of whom 32 had medical science and biotechnology majors (MSB), 27 had pharmaceutical science majors (PS), and 85 were medical undergraduate (MU) students. An exercise in critical thinking was conducted during a biochemistry laboratory course, which consisted of five different biochemical experiments, along with learning sheets that contained three or four critical thinking questions. Then, the teacher evaluated the students’ ability to think critically based on nine intellectual dimensions (clarity, accuracy, precision, relevance, depth, breadth, logic, fairness, and significance) based on the universal intellectual standards developed by Prof. Linda Elder and Richard Paul. In the following analysis, regression models and multivariate analysis were used to determine how students improved over time, and trajectory analysis were carried out in order to observe the trends in students’ critical thinking skills construction.
Clarity and logic dimensions were identified as the key elements to facilitate the development of critical thinking skills through learning sheets and teacher guidance in students across all three different healthcare majors. The results showed that metacognitive monitoring via Socratic questioning learning sheets have demonstrated potential encourage students to develop critical thinking skills in all dimensions. Another unique contribution of current study was present the heterogeneous learning patterns and progress trajectories of clarity and logic dimensions within classes.
Using the Socratic learning model could effectively develop students’ critical thinking skills so they can more effectively care for their patients.
Peer Review reports
Introduction
Emerging trends in information technology requires that the new generation of medical students become critical thinkers [ 1 ]. The General Medical Council (GMC) of the United Kingdom encourages teachers to facilitate the acquisition of critical thinking skills by students in the medical and health professions [ 2 ]. Decades of research have proven that critical thinkers can present dispositions like flexibility, persistence, and willingness when faced with a range of tasks; they display meta-cognitive monitoring and a willingness to self-correct to seek long-term consensus[ 3 ]. Although, critical thinking is constructed from childhood in most Western countries and are valued by higher education as a necessary skill for coping with society [ 4 ]. However, critical thinking constructing and teaching has attracted little attention in Eastern education systems until recently [ 5 , 6 ].
Aside from the development of critical thinking skills is a key component of educational systems, recent educational philosophy also emphasizes both thinking processes as well as metacognitive integration skills [ 7 ]. Metacognitive monitoring includes making ease-of-learning judgments (i.e., processing fluency and beliefs), judgments of learning, feeling-of-knowing judgments (i.e., assessing the familiarity of the cue and the question itself or the domain of the question), and having confidence in the retrieved answers [ 8 , 9 ]. It is an adaptive skill of personal insight that health-profession students need to succeed in the rapidly changing and challenging healthcare industry [ 2 , 10 ]. Despite this, higher education curriculum does not emphasize on teaching these skills [ 7 ]. Additionally, any attempts to change the standards in higher education are generally met with resistance and challenges since they are require to encourage teachers to create new curriculum and change the current teaching content by researchers in current study who have more than 40 years’ teaching experience observaions. Healthcare curriculum, in general, remains conservative; Taiwan is not an exception.
Critical thinking is a fundamental component of innovative thinking and has thus become the fundamental skill for cultivating innovative talents in Western education [ 11 ]. Western scholars have asserted that teaching critical thinking should start at an early age and that its foundations should be laid in elementary and secondary schools. There are many ways to define critical thinking. A leading educational expert, Prof. Dewey, defined critical thinking as inclusive of reflective thinking and argued that the thinking process should also be taken as one of the objectives of education [ 12 ]. There are a few general dispositions that an ideal critical thinker would present according to Prof. Ennis’ observation of the constitutive abilities, such as (1) provide a clear statement of the conclusion or question; (2) provide clear reasons and be specific about their relationships with each other; (3) try to be well informed; (4) always seek and use credible sources, observations and mention them frequently; (5) consider the entire situation; (6) be mindful of the context’s primary concern; (7) be aware of alternative options; (8) be open-minded toward other points of view and refrain from making a judgment when there are insufficient evidence and reasons; (9) be willing to change your position when sufficient evidence and reasons support it; (10) seek as much precision as the nature of the subject admits; (11) whenever possible, seek the truth, and more broadly, strive to “get it right”; and (12) utilize their critical thinking abilities and dispositions [ 13 , 14 , 15 , 16 ]. In the eyes of Profs. Dewey and Ennis, critical thinking is a process of careful thought and reflection before a decision is made [ 17 ].
Nevertheless, the measurement or evaluation of critical thinking skills and abilities does not seem easy. Based on another perspective on critical thinking, intellectual standards are evolving [ 18 ]. According to Profs. Elder and Paul, critical thinking is the ability to use the most appropriate reasoning in any situation [ 18 ]. To evaluate these abilities, they established nine dimensions of critical thinking to represent different aspects of critical thinking: clarity, accuracy, precision, relevance, depth, breadth, logic, significance, and fairness [ 18 ]. As Profs. Elder and Paul concluded, those who possess discipline and critical thinking skills would make use of intellectual standards every day; thus, people should target these standards when they ask questions during the thinking process [ 18 , 19 ]. As a result of teachers’ regular introduction of the tools of critical thinking in their classrooms, the Socratic questioning and discussions become more productive and disciplined, thereby enabling students to realize the significance of questioning during the learning process [ 20 , 21 , 22 ].
According to a review article, teaching critical thinking to healthcare students (primarily medical and pharmacy students) through Socratic methods is more effective in developing critical thinking for a number of reasons [ 23 ]. In particular, Socratic questioning provides students with the opportunity to justify their own preconceived beliefs and thoughts after a series of specific, targeted inquiries [ 24 ]. Using Socratic questioning can also assist healthcare students, interns, or residents in thinking critically by understanding the “deep structure” of the question, i.e., deconstructing the question and understanding its true meaning [ 23 ]. The effectiveness of Socratic questioning lies in ascertaining the current knowledge of the students [ 25 ] and establishing a foundation for teaching at their level [ 26 ]. The teacher can accomplish this probing by asking progressively more challenging questions until the limits of the students’ knowledge are discovered [ 25 , 27 , 28 ], as well as by allowing students to express their existing knowledge, which in turn will allow them to synthesize new knowledge [ 26 ], and the dialogue represents the Socratic method [ 29 ]. Alternatively, a critical thinker is more likely to engage in certain established metacognitive strategies under the Socratic paradigm and/or channel the intellectual dimensions of critical thinking [ 17 ].
Unfortunately, Han Chinese students have struggled with learning critical thinking, which is thought to be part of their characterological profile [ 30 ]. This struggle has been faced by students studying abroad [ 11 ] and in students enrolled in the Han Chinese education system, which mainly cultivates Confucianism [ 31 ]. There are at least two types of problems with developing critical thinking in Han Chinese or Taiwanese education. The first involves the core of Confucianism, where foreign teachers have tried to promote critical thinking in elementary and high schools but sensed ethical concerns from the students who refused to participate. This is likely because if they chose to participate, they would have felt obligated to express disagreement and negative feelings to the instructor. The Han Chinese culture values harmony and “not losing face,” emphasizing a holistic perspective and collective good. Thus, students would feel uncomfortable because disagreeing with someone’s opinion in public is consciously or often avoided [ 30 ]. Therefore, encouraging the student to participate in healthy discussions and respectfully challenge their teachers is the starting point for promoting critical thinking in students enrolled in the Han Chinese educational system.
Second, in the Western education approach, learners take an active role in and are responsible for their learning process. On the contrary, the Han Chinese and Taiwan education systems are teacher-centered and exam-oriented; students are expected to follow their teachers’ instructions and perform well in class. More importantly, the textbook or teacher-centered framework lacks half of Ennis’s twelve constitutive abilities for critical thinking [ 13 , 14 , 15 ], such as judging the credibility of a source, observing and judging observation reports, drawing explanatory conclusions (including hypotheses), making and judging value judgments, and attributing unstated assumptions. As a result, Han Chinese students may find it difficult to develop critical thinking skills and present key traits and dispositions that are indicative of an ideal critical thinker. Hence, guiding and evaluating critical thinking in students might not be implemented through the same approach in Eastern educational circumstances as in the West. By understanding the difficulties that Han Chinese students face in developing critical thinking, the current study aims to design a set of critical thinking models that are suitable for Han Chinese students as a starting point for reform teaching.
Research questions, hypotheses and objectives
Research has shown that the laboratory class is not just limited to a step-wise approach to experimentation. It also allows students to develop their critical thinking skills by repeatedly engaging a simple learning framework [ 32 ]. To explore this further, the current study’s primary purpose is to use Socratic questioning in a biochemistry laboratory course with specifically designed learning sheets and feedback from teacher to guide students to improve their critical thinking skills. The learning sheets were evaluated following the universal intellectual standards for critical thinking developed by Prof. Elder and Paul [ 19 , 33 ]. For this study, we hypothesized that students with different healthcare majors might present different improvement trajectories in their intellectual dimensions according to the years of teaching observations in the three healthcare majors. Based on the research and rationale described above, the intervention effect of Socratic questioning in a biochemistry laboratory course was hypothesized as follows (see Fig. 1 ):
Pre-intervention critical thinking abilities are different amongst students of different healthcare majors, especially in each intellectual dimension (H1a). Post-intervention critical thinking abilities would develop in students from each healthcare major after using the Socratic method (H1b).
Critical thinking abilities differs significantly between pre- and post-assessments of the intellectual dimensions of students with the three different healthcare majors (H2).
After clarifying the relation of Socratic method interventions in the class, we aim to scrutinize the trajectories of students between majors further to understand the learning style in class (Aim 1). Furthermore, we also aim to identify the key intellectual dimensions that could lead to an overall improvement in the critical thinking of students in each major (Aim 2). Additionally, we observed improvement trajectories of specific intellectual dimensions within major (Aim 3).
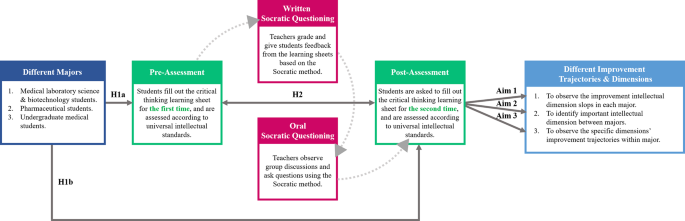
Socratic method framework and structure of the research hypotheses behind the biochemistry laboratory course
Literature review
Critical thinking engagement in the eastern and western medical education.
Over the last decade, medical education has been undergoing a variety of approaches for effectiveness teaching and transformation [ 34 ]. Many paradigms of active teaching/learning methodologies have been adopted in both Eastern and Western medical education systems, some of which are used partially (actual or conceptual similar) Socratic questioning to challenge students’ critical thinking. In this regard, the primary philosophy of case-based learning (CBL) established in the 1920s by Harvard Medical School is to guide students to apply their acquired knowledge base via critical thinking to make clinical decisions to solve the problems that they may encounter in the healthcare environment [ 35 ]. A meta-analysis study of China’s dental education reported that the CBL was a practical pedagogical method across the Chinese dental education system [ 36 ]. The results showed that the CBL method significantly increased knowledge scores, skill scores, comprehensive ability scores, and teaching satisfaction compared with the traditional lecture-based learning (LBL) mode in 2,356 dental students. Hence, there is an urgent need to change the traditional didactic lecture or teacher-centered classroom setting in which students are passive listeners instead of active participants.
Healthcare professionals are also required to solve complex problems and efficiently integrate didactic preclinical knowledge into actual clinical application in patient care [ 35 ]. On the other hand, the design thinking process may enhance both creativity and innovation so that healthcare professionals can respond to clinical problems effectively [ 37 , 38 ]. Problem-based learning (PBL) is a pedagogical approach widely accepted in medical education. It promotes active learning and results in better outcomes [ 39 , 40 , 41 ]. PBL focuses on active lifelong learning by triggering problems, directing student focus, and facilitating tutor involvement [ 39 , 42 , 43 , 44 ]. However, it is noteworthy that some hybrid PBL models have become less effective over time, as well as less aligned with the intended philosophy of student-centered learning [ 45 ]. Another alternative blended learning approach of PBL is team-based learning (TBL), which allows medical educators to provide students with pre-class work, in-class initial tests with immediate feedback, and real clinical problem-solving activities [ 46 ]. In the year-one studies of the Sydney Medical Program, a greater level of engagement in learning, a deeper understanding of concepts, and a sense of responsibility were shown among the medical students working in a TBL setting than among those in a PBL setting [ 47 , 48 ].
Medical educators face another significant challenge with the millennial generation, which has ubiquitous information technology access throughout its education. Thus, it is extremely important to improve students’ motivation to learn through hands-on instruction or teacher–student interaction and then stimulate students’ thinking and learning. In recent years, gamification has been successfully integrated into medical and scientific endeavors, enhancing motivation, participation, and time commitment across a variety of settings [ 49 , 50 , 51 ]. Another healthcare curriculum reform to stimulate active learning is flipped classroom (FC), which assigns learners didactic material, creating opportunities of longitudinal and interprofessional learning experiences for students during class participation [ 52 ] to encourage extracurricular learning, such as critical thinking. As part of the FC model, medical educators also develop formative and diagnostic assessments to identify learning gaps. According to these teaching modules, encouraging students to participate, emphasizing their learning, and observing their development trajectory are the core ideas in recent educational designs [ 53 ].
Although most of above-mentioned studies have been performed in the Eastern and Western education systems, however, without mentioning the differences between cultures and learning styles. Most importantly, the cultivation and foundations of critical thinking neglect the fact that Eastern and Western education systems emerged from very different learning and thinking patterns. Moreover, clinical reasoning and decision achievements depend on established critical thinking skills, therefore, it becomes more important to construct critical thinking early and comprehensively [ 54 ]. While Han Chinese students are not familiar with the core of critical thinking, the most effective approach to teaching critical thinking is still a highly debated topic in medical schools. Taken Taiwan medical education as an example, most clinical courses focuses on professional skills, problem solving, and disease treatment rather than construct critical mindset and metacognitive skills. Education strategies often emphasize the outcome while neglecting the process. Nevertheless, medical educators should also emphasize the process of forming students’ critical thinking when instructing and guiding them in this regard. Consequently, using metacognitive monitoring to enhance critical thinking in healthcare education would be appropriate, especially for Han Chinese systems with a Confucianist outlook. Thus, critical thinking via metacognitive monitoring is important in healthcare education, especially in Han Chinese systems with a Confucianist background.
Proficiency in the art of socratic questioning to enhance students’ critical thinking
Socratic questioning is a disciplined method of engaging in content-driven discourse that can be applied for various purposes: analyzing concepts, finding out the truth, examining assumptions, uncovering assumptions, understanding concepts, distinguishing knowledge from ignorance, and following the logical implications of thought. The scholars who established the intellectual standards of critical thinking have consistently indicated that “The key to distinguishing it from other types of questioning is that the Socratic questioning is systemic, disciplined, and deep and usually focus on foundational concepts, principles, theories, issues, or problems [ 20 , 21 , 22 ].” In short, the Socratic method is a questioning method that stimulates personal understanding. More importantly, the core principle of learning from the unknown fits best within healthcare environments.
Numerous studies have consistently urged teachers to develop Socratic dialogue in their classrooms, regardless of their learning stages and situations [ 55 , 56 , 57 ]. Using enhancement exercises in an elementary school, a study introduced a Socratic questioning strategy to provide guidance and hints to students so that they could think more deeply about an issue or problem before sharing their thoughts [ 55 ]. The lecturer of a speech course in higher education demonstrated how Socratic questioning could help students learn when confronted with a series of questions [ 56 ]. The process improves students’ ability to ask and answer questions and helps them overcome some obstacles related to their lack of self-confidence. In the book Socratic circles: Fostering critical and creative thinking in middle and high school , Dr. Matt Copeland stated that, in middle and high schools, teachers must facilitate discussions by asking questions [ 58 ]. Furthermore, this method could be applied not only to elementary school, middle school, high school but also to higher education classes [ 59 ]. During the Covid-19 pandemic, synchronous discussions in online learning demonstrated that the Socratic questioning strategy successfully improves students’ critical thinking skills [ 57 ].
The incorporation of Socratic questioning in healthcare education curriculum is under development, including for general medical education [ 60 ], medical [ 61 ], pharmacy [ 54 , 62 ], and nursing students [ 63 ]. A review article of revisiting the Socratic method as a tool for teaching critical thinking in healthcare professions revels few advantages of Socratic questioning [ 23 ]. Three type of Socratic questions were mention and could commonly used in different clinical situations [ 23 ], such as procedure question would use in those with correct answers (e.g., Which of the following medications has antithrombotic function? ); preference question can apply in those with no correct answers (e.g., What type of consultation is most suitable for this patient? ); judgment question would be the most challenge critical thinking within a Socratic paradigm by integrating different domain knowledge and skills (e.g., Does this patient require antibiotic treatment? ). It is necessary to apply and analyze information in a logical manner as well as self-regulate and use critical thinking in order to achieve the best outcome for patients. For medical doctors, pharmacists or clinical laboratory technicians to provide high quality health care across all disciplines, critical thinking is inherently required.
In medical school, the emphasis is laid on training learners in meta-capabilities, such as self-driven pattern recognition, ideally as part of an apprenticeship under the supervision of an expert diagnostician [ 61 ]. An in-depth study of the current trends in developing critical thinking amongst medical students demonstrated the use of dialogue for proper questioning and how it directs the learner’s thinking [ 64 ]. Moreover, another study confirmed that critical thinking occurs only when students are motivated and challenged to engage in higher-level thought processes [ 65 ]. In the pharmacy classroom, educators can play a significant role in influencing their students’ mindsets. Growth mindsets can be cultivated through the creation of an environment that encourages it. [ 62 ]. The Socratic questioning method can facilitate critical thinking in nursing education. One study showed that problem solving using critical thinking skills can be facilitated in both educational and practice settings by using Socratic inquiry [ 63 ].
The Socratic method has been adapted in different ways to different domains, but it has become closely associated with many areas, such as basic scientific thinking training, legal dialectical guidance, and clinical teaching. Some adaptations are helpful, some are not. The adaptations can be looked at through reasoning-focused lenses with varying degrees of magnification —a high-magnification adaptation rigorously and precisely tracks or guides the path of reasoning. Thus, how to use the Socratic method to direct students onto the path of critical thinking with appropriate guidance, but not revealing answers becomes an art that tests instructors’ teaching experience and proficiency in questioning.
Critical thinking and reflection exercises in the laboratory course
Medical schools have increasingly encouraged students to become life-long, self-directed learners because of the continual changes in the evidence-based healthcare environment. Science is often applied in everyday life, including translating knowledge from scholarly fields [ 66 ]. However, there is a vast gap between what is taught in medical schools and what is actually required in practice has increasingly widened in this information era. The majority of healthcare professionals are not considered to be real scientists. [ 2 ]. Nevertheless, they need to know how to apply scientific knowledge to their practice. Therefore, a science curriculum in medical school, such as a biochemistry laboratory course, should provide an opportunity to learn scientific methods and conceptual frameworks. It should also promote critical reasoning, providing healthcare students with problem-solving skills.
Medical educators need to accept that critical thinking is important for healthcare students and know how to teach it effectively [ 67 ]. Medical educators are now faced with a dilemma: should they develop a new course or adapt old course to develop critical thinking skills? An effective learning model should promote and stimulate students’ development of such skills [ 67 ]. One of the most common compulsory courses for healthcare students is the biochemistry laboratory course [ 68 , 69 ]. These courses are specifically designed to introduce students to prescribed experiments, requiring them to complete stepwise protocols by themselves [ 68 , 70 ]. The students are expected to understand the concepts behind the methods, procedures, and assays. However, this type of curriculum construction often fails to provide students with adequate opportunities to monitor their critical thinking and thus reduces the chances of developing problem-solving skills [ 70 ]. In order to provide students with more opportunities to think critically, previous studies have also adapted laboratory, basic science, and science fusion courses to help students develop critical thinking skills [ 67 , 68 , 71 , 72 , 73 ].
Several studies have demonstrated that students need critical thinking skills to interpret data and formulate arguments. Thus, science education, particularly in the laboratory setting, is designed to teach quantitative critical thinking (i.e. interpretation and critical evaluation of statistical reports), but the evidence has suggested that this is seldom, if ever, achieved [ 74 , 75 , 76 , 77 , 78 , 79 ]. By providing multiple opportunities for students to participate in critical thinking in the physics laboratory classes at Stanford University, scholars engaged the students to improve the experiment and modify the model repeatedly [ 32 ]. Additionally, a simple learning framework using decision-making cycles and demonstrating experts’ critical thinking significantly improved students’ critical thinking. We thus argue that students should engage in critical thinking exercises with repeated comparisons, decisions, and teacher guidance that are meant to construct their critical thinking in each of their disciplines.
Participants
This research was conducted during the 2017–2018 academic year. The participants were second-year students in the College of Medicine at the National Cheng Kung University (NCKU) of Taiwan. A total of 144 students participated in this study, of whom 32 had medical science and biotechnology majors (hereafter, MSB), 27 had pharmaceutical science majors (hereafter, PS), and 85 were medical undergraduate (hereafter, MU) students. The biochemistry laboratory course was compulsory for these three majors.
For each biochemistry laboratory class, the teacher assembled five to six groups of four to five students each. The course contained five different biochemical experiments: (1) Plasmid DNA (deoxyribonucleic acid) extraction and purification; (2) restriction enzyme digestion and electrophoresis of plasmid DNA; (3) polymerase chain reaction (PCR) amplification of plasmid DNA; (4) recombinant protein expression in Escherichia coli ; and (5) quantification of recombinant protein. The experimental learning sheets included three or four critical thinking questions (Table S1 ), encouraging students to explore experimental principles and alternative explanations further. To facilitate discussion, students were organized into small groups of four to five students seated around a single table, discussing and answering the questions. At this time, the students would pen down their first answers to the critical thinking questions, and the teacher would grade them based on the universal intellectual standards (learning sheets, first evaluation).
Furthermore, according to the students’ answers, the teacher offered a response by asking more questions according to the Socratic method to encourage students to think deeper rather than provide the correct answers. At the following week’s class, the teacher returned the learning sheet and supervised the ongoing activity, clarifying any questions raised by students and encouraging them to re-discuss and re-answer the critical thinking questions according to the teacher’s suggestions. The objective was to create a highly interactive environment to engage students in learning the relevant principles of each laboratory, including troubleshooting experiments and formulating critical concepts and skills. After the discussion, the teacher reexamined the students’ responses and assessed them based on the universal intellectual standards for subsequent grading (learning sheets, second evaluation).
The biochemistry laboratory courses and the Socratic method in current study are performed and taught by a senior biochemistry teacher (PhD in Institute of Basic Medical Science, NCKU) who has 40 years teaching experience. The teacher has long focused on teaching critical thinking skills to students, and also offers four senior clinical case related courses by practicing the Socratic method, such as clinical concept, critical thinking in medicine, clinical reasoning and special topics in clinical reasoning with more than 20 years of experience. Therefore, in the course, teacher will often ask a series of questions for students to think about the relevance of biochemical science and clinical practice.
Assessment development
The research team designed the learning sheets to guide discussion on the key issues concerning five biochemical experiments. The learning sheets were assessed according to the universal intellectual standards for critical thinking [ 33 ]. However, the assessment was adapted to include nine intellectual dimensions to assess student reasoning [ 19 , 33 ]: clarity, accuracy, precision, relevance, depth, breadth, logic, fairness, and significance (Table S2 ). Each dimension was evaluated using a binary score (0 = does not present the skill; 1 = presents the skill) for each question in the learning sheets for both the first and second evaluations. The students received the teacher’s guidance following the first evaluation, providing them with the opportunity to reconsider their reasoning and revise their answers. Our goal was to improve our students’ learning by stimulating the teaching process; at the same time, we were committed to allowing students to speak freely so that we could more effectively facilitate prospective discussions. Thus, the critical thinking scoring system based on nine intellectual dimensions was only for the purpose of the research, without consequences on students’ study progress. In this regard, students were not able to know their intellectual scores. As a result, their course grades were not determined by the learning sheets; rather, they were determined by the general operation, experiment report, and the learning attitude demonstrated during the experiments.
Statistical analysis
Descriptive statistics and variable tests.
We calculated the differences between the performance means for the first and second evaluations using paired t -tests. The mean differences between the students from the three majors were analyzed using a one-way analysis of variance (ANOVA). For the improvement slope for each universal intellectual dimension, we used the second evaluation scores of each experiment as the point with which to construct a quadratic equation curve in one variable (dimension) and then access the slope to represent the students’ improvement. The higher the slope score, the greater the students’ progress on that dimension.
Multivariate analysis
We used traditional analytical methods to observe and analyze the students’ improvement in the five experiments. Data from the second evaluation scores of each experiment served as the multi-time point measurement data. The Cox regression model for multivariate analysis was used to investigate the effect of several variables upon the time during which a specified outcome happened [ 80 ]. For each dimension, the model’s outcome determined that a student’s improvement slope was defined as minor progress if it was lower than the improvement slopes of their peers in the same major overall. However, if the student’s improvement slope was higher than the overall progress intercept of their peers, then it was defined as greater progress. The Cox regression models’ outcomes for each dimension were divided into two groups: minor and more progress. For this model’s outcome, (1) we calculated all dimensions’ slopes mean from each major (MSB: 0.369; PS: 0.405; MU: 0.401); (2) then compared the mean slope of the individual students with the mean slope of major; (3) if the student’s individual improvement slope was lower than mean slope of major, then defined as minor progress; if the student’s individual improvement slope was higher than mean slope of major, then defined as greater progress. From the analysis at this point, we understood that teacher could help students from different majors develop the different dimensions of critical thinking with the use of Socratic methods and simple repeated thinking framework practice. Additionally, we wanted to represent the improvement of intellectual dimensions between the students of different majors and their heterogeneity in critical thinking.
Dimension identification and comparison
To understand which intellectual dimensions were most representative of student improvement across majors, the analysis was divided into three sections: (1) to identify the progress percentage of all nine intellectual dimensions; (2) to identify the progress percentage of statistically significant intellectual dimensions; (3) to compare the differences among all nine dimensions, the significant dimensions, and the reciprocal dimensions. This analysis offered a better understanding of what dimensions represented the overall improvement of students’ critical thinking. Our first step was to calculate the percentage of improvement for each experiment by determining the results of the first and second evaluations for each intellectual dimension. Second, we took average percentage of improvements for each dimension. Finally, we used Student’s t -test to compare the differences among the average of all nine dimensions, the significant dimensions, and the reciprocal dimensions.
Trajectory analysis
In this study, we also hypothesized that each student’s learning and progress trajectories were heterogeneous across different majors. Depending on the major, there may also be differences between students in the same class. To focus our observations on the students’ use of the clarity and logic dimensions, we used a trajectory-tracking analysis [ 81 , 82 ] and categorized the students into two groups based on the participants’ improvement levels within the same major.
Descriptive data
We recruited 144 second-year students from three majors in the College of Medicine, among which 32 were MSB, 27 were PS, and 85 were MU students. All participants’ first and second evaluations were compared in all five biochemistry experiments. The statistically significant between-group differences in the mean initial evaluation results for each dimension are presented in Table 1 .
Overall improvement from the initial to second evaluations throughout the five experiments (H1, H2, and Aim 1)
Table 1 presents the mean results of the first and second evaluations; the five experiments exhibited statistically significant differences ( p < 0.05) across all study groups and dimensions. More detailed analyses revealed significant differences in performance in the second evaluation between the groups after all five biochemistry experiments in the clarity ( p = 0.0019), depth ( p = 0.0097), breadth ( p < 0.0001), logic ( p = 0.0371), and significance ( p = 0.0037) dimensions. However, for some of the dimensions (clarity, accuracy, precision, logic, and fairness), the initial evaluation results differ significantly between the MU and the MSB students, but this was not the case for the secondary evaluation results. The MSB students exhibited the best progress (2nd mean score minus 1st mean score) in the clarity dimension across all experiments. The PS students exhibited the best performance in the logic dimension ( p < 0.05) in the second evaluation after the five experiments.
The results of the MSB students improved steeply in most dimensions in the five experiments, especially depth (slope: 0.472), logic (0.455), and clarity (0.410) (Table 2 ). Time had a stronger effect on several of the dimensions in the multivariate analysis, specifically clarity ( p = 0.0012), relevance ( p = 0.0007), and logic ( p < 0.0001). By contrast, the PS students showed a significant overall improvement in the clarity (slope: 0.212, p < 0.0001), accuracy (0.539, p = 0.0063), precision (0.381, p = 0.0085), relevance (0.216, p < 0.0001), breadth (0.426, p = 0.0045), and logic (0.515, p = 0.0027) dimensions over the observation period (Table 3 ). Finally, the MU students showed a significant overall improvement in six dimensions: clarity (slope: 0.277, p < 0.0001), accuracy (0.520, p = 0.0003), depth (0.459, p = 0.0092), breadth (0.356, p = 0.0100), logic (0.544, p = 0.0190), and significance (0.327, p = 0.0225) (Table 4 ).
Trajectory tracking of the overall, significant, and reciprocal dimensions (Aim 2 and Aim 3)
Figure 2 a illustrates the overall improvement of students across the three majors in all nine dimensions, as assessed via trajectory analysis. The trajectory-tracking algorithm revealed that the significant dimensions for each group were as follows: MSB students—clarity, relevance, and logic; PS students—clarity, accuracy, precision, relevance, breadth, and logic; and MU students—clarity, accuracy, depth, breadth, logic, and significance (Tables 2 , 3 and 4 ; Fig. 2 b). The comparison of each group’s average percentage of improvement between the nine dimensions, the significant dimensions, and the reciprocal dimensions (clarity and logic) is summarized in Fig. 2 c. Figure 2 d–i depicts the students’ improvement in clarity and logic within the different majors using group-based trajectory modeling.
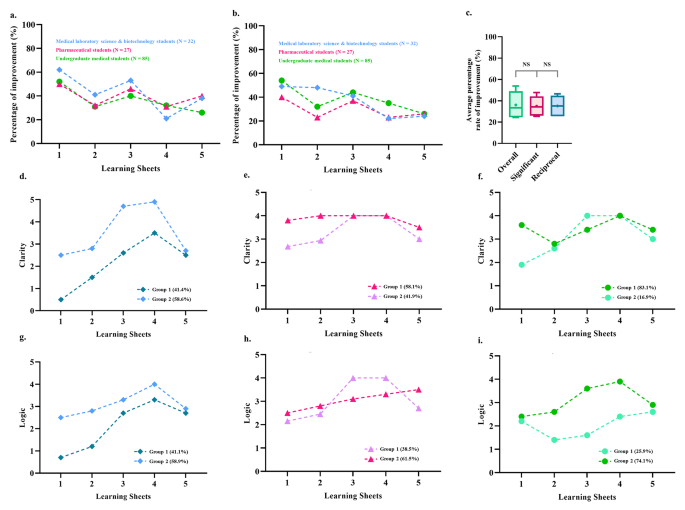
Overall improvement comparison between the students of three majors using a trajectory-tracking analysis approach . ( a ) The mean evaluation scores from the second evaluation minus those from the first evaluation for the nine dimensions were considered an improvement. They were converted to percentages to compare them to the performance in the first evaluation. ( b ) The mean evaluation scores from the second evaluation minus those from the first evaluation for the significant dimensions (within the students of each major, Tables 2 – 4 ) were considered to represent improvement and were converted to percentages to compare them to the performance in the first evaluation. ( c ) Comparison of the average percentage improvement among all nine dimensions, the significant dimensions, and the reciprocal dimensions (i.e., clarity and logic). ( d ) Trajectory analysis to assess the progress of the two subgroups of medical laboratory science and biotechnology students in the clarity dimension. ( e ) Trajectory analysis to assess the progress of the two subgroups of pharmaceutical students in the clarity dimension. ( f ) Trajectory analysis to assess the progress of the two subgroups of undergraduate medical students in the clarity dimension. ( g ) Trajectory analysis to identify the progress of the two subgroups of medical laboratory science and biotechnology students in the logic dimension. ( h ) Trajectory analysis to assess the progress of the two subgroups of pharmaceutical students in the logic dimension. ( i ) Trajectory analysis to assess the progress of the two subgroups of undergraduate medical students in the logic dimension
Empirical contributions
The Han Chinese educational system relies on the passive transmission of knowledge, as evidenced by the years of preparation by students’ through paper-based exams. By adopting this approach during teaching and learning, students do not develop a critical thinking mindset. Our experience has shown that when we encounter first-year students who have just graduated from high school, their previous education failed to develop critical thinking skills. Many foreign and Western teachers have the same experience when they encounter Asian students studying abroad for the first time. Thus, this research aims to provide clinical teachers with guidance on reducing the blind spots that students face when introduced to critical thinking. Moreover, this research aims to provide teachers with a simple teaching model and structure to guide students with less stable foundations in critical thinking. For the teaching structure and process, please refer to the procedure paragraph in the methods section and the teaching flow chart in Fig. 1 . Furthermore, the scoring system shown in the assessment development paragraph in the methods, as well as the scoring rubric is presented in Table S1 .
To our knowledge, this is the first study that uses the Socratic method and the universal intellectual standards to assess and improve critical thinking skills in biochemistry laboratory courses across different healthcare majors. We also used a novel design for teaching critical thinking, with multi-timepoint assessments and trajectory-tracking analysis to observe the students’ process and the improvement intheir critical thinking. This Socratic method, combined with critical thinking-based learning sheets, significantly improved the students’ critical thinking in all nine dimensions of the universal intellectual standards, according to the first and second evaluations conducted in each of the five sessions. Another unique contribution of this study is that it analyzed the progression results at multiple time points in the critical thinking performance of students across different majors. According to the results of comparing the average percentage improvement between all nine dimensions, the significant and reciprocal dimensions (i.e., clarity and logic) do not significantly differ from each other statistically speaking. By reducing the nine intellectual dimensions scoring system, medical educators can focus more on establishing clarity and logic skills in students. In sum, our most important finding was the identification of the clarity and logic dimensions as key elements that facilitate the development of critical thinking skills via the Socratic method in students across three different healthcare majors.
The trajectories of outcomes for students of medical science and biotechnology majors
Understanding what we learn has been identified as the starting point in the professional-development journey [ 2 ]. In principle, if thinking and decision making can be taught, educational intervention is possible. Nevertheless, for a science class like biochemistry, abductive reasoning requires a deep understanding of knowledge, and thinking must be inspired through stimulation.
In this study, the evaluation scores for MSB students did not improve significantly in almost any dimension at the beginning of the course. At first, most students felt uncomfortable with criticizing others, disagreeing with others, or challenging teacher’s knowledge and authority when they spoke their minds. Other MSB students believed that their ability to find answers and make decisions was inadequate and expected the teacher to provide the correct answers. However, preclinical medical technologists must gradually develop their critical thinking skills. Thus, the teacher provided critical thinking cues during the class and monitored the group discussions.
On the other hand, teachers must encourage these types of students, enabling them to accomplish simpler learning goals by providing them with easier-to-attempt clues. The joy of discovering answers on their own rather than the frustration of not achieving high goals should be encouraged. This coaching process improved the MSB students’ willingness to think and explore, leading to greater relevance and breadth of coverage.
The teacher used generation, conceptualization, optimization, and implementation [ 33 ] with the Socratic method to stimulate critical thinking in a four-step cycle in the five experiments. When the spontaneous discussion started in the generation phase, they tried to clarify their knowledge of the theme and identify the problem from the learning sheet. The following step was to conceptualize the problem, and the students drafted all of the possibilities and problems. Teacher frequently asked the students, ‘ What are other possible reasons? ’ Finally, the teacher provided feedback to help the MSB students reach a proper solution and implement it. The teacher would also ask the students leading questions like ‘ What relevant theories can be confirmed more precisely? ’ These guiding processes sharpened their logic and helped them better understand what they had learned. In sum, the benefits of this process included an enhanced ability to think logically, clarification of questions and knowledge gaps, and improvements in the thought process about the theme discussed.
The steady improvement of critical thinking in the students of pharmaceutical science
Currently, pharmacists are seeing their roles and responsibilities shift to becoming patient counselors and educators on the rational use of medicine. Pharmacists are trained to focus on patient-centered care and resolve current and potential drug-related problems [ 83 , 84 ]. Critical thinking, clinical reasoning, and decision-making skills are needed to solve these problems. Nowadays, pharmacists are not just responsible for carrying out doctor’s orders, while there are always alternative treatment options available for them to recommend. Teacher therefore repeatedly emphasized the link between critical thinking and pharmacist practice and encouraged students to ask questions and find out the best alternative through Socratic method in the classroom.
During class, the PS students were required to exert considerable mental effort to conduct an inquiry to solve the learning sheet questions. Instead of providing students with clues or information to help them solve the problems, the teacher guided the PS students on how to seek the information they needed for themselves. The question for the PS students was be ‘ What are the possibly executable strategies? ’ The teacher also joined the students in discussion, using the Socratic method to stimulate critical thinking and draw out ideas and underlying suppositions. In high-quality cooperative argumentative dialogue, teacher should not direct or refer learning, nor should they ask students for the correct answers as in a traditional classroom. The hints that teacher would provide were more like ‘ The narrative explanation can be more precise. ’ Thus, asking high-quality questions and providing feedback also challenges the instructors’ teaching experience.
The PS students were guided not only toward the development of critical thinking skills but also toward solving problems using evidence-based knowledge and decision-making skills. The Socratic method process meets the student where they are on the educational spectrum and encourages and helps them advance. Using this method, the PS students engaged in student-to-student interaction to build knowledge as a group and individually. The course of five experiments conducted via the learning sheets improved many aspects of the students’ critical thinking, including their clarity, relevance, breadth, and logic. In sum, the abilities that they developed in the course should help them focus more on the possible outcomes of pharmacotherapy, medication surveillance, and proper communication and therefore improve the quality of their professional future.
The advanced construction of critical thinking skills in undergraduate medical students
In medical education, “ better thinking and learning skills grounded in understanding ” are recommended for future doctors [ 2 ]. Practicing medicine requires an ability to address current and future diseases using new diagnostic and therapeutic methods [ 10 ]. Therefore, problem solving is not the only core medical skill; the ability to deal with complex, insoluble health issues is also required [ 83 ]. In this domain, critical thinking skills have proven essential in tackling difficult, complex, interdisciplinary health problems [ 10 ].
In our study, the MU students began with high-performance scores in almost all dimensions. As a result, teachers needed to create a more challenging and thought-provoking learning environment to encourage them to think more broadly and deeply. Thus, the teacher would give students advice like ‘ Searching for more relevant information can increase the breadth of knowledge ’ and ‘ If the result is true, what is the relevant theory? ’ Most MU students were faster than other majors at defining and constructing critical thinking. However, another phenomenon often observed in the classroom was that the MU students were more reluctant to express their reasoning than the students of other majors. In other words, MU students were afraid to speak openly about their reasoning and thinking, probably due to the excessive pursuit of the correct answer. In sum, the course of five experiments conducted via the learning sheets enhanced abilities of clarity, accuracy, depth, breadth, logic, and significance in MU students.
Apart from providing structure for their critical thinking, as was done with the other preclinical students, the teacher guided the MU students to use advanced critical thinking skills by regularly analyze their thinking processes, reflecting on the decision-making and thinking process [ 84 ]. Researchers have suggested that reflective practice is key to successful medical professionalism [ 85 ] and humanism [ 86 , 87 ]; but more importantly, it may help medical professionals develop better physician–patient relationships [ 88 ]. Therefore, to advance the critical thinking experience of the MU students, teacher should encourage them to gather ideas, analyze, evaluate, and synthesize information. The teacher guided them to reflect on their plan and solve the questions on the learning sheets using their thoughts and words. These reflective practices could involve various biases in the thinking process and outcome, such as the base-rate fallacy, bias blind spot, or choice-supportive bias. The Socratic debate is a common way to model a complex thinking situation and may help teachers inspire students to become critical thinkers. MU students improved their abilities in the clarity, accuracy, depth, breadth, logic, and significance dimensions in the five experiments. This kind of training in thinking should help preclinical students constantly challenge and critically appraise evidence within their context, as well as their patients’ and their own belief and value systems.
Limitations
This study provides a model for developing a specific learning environment like a biochemistry laboratory class into one that will help students develop their critical thinking skills through inquiry. Our results have shown this method to be feasible and effective. However, there were a few limitations to this study. First, although it included students from three different majors, there was no interdisciplinary collaboration that would have simulated collaborations and communication among other healthcare professionals from different fields, as occurs in clinical practice. Introducing such collaboration may have produced more exciting and comprehensive ideas for solving the problems. Training in these professions is specialized to a considerable extent, so inter-professional collaboration should improve therapeutic outcomes and optimize patient care. Second, the original scoring system was time-consuming. However, one of our study objectives was to modify and reduce the nine intellectual dimensions scoring system into the clarity and logic dimensions. Based on the analysis in the current study, the clarity and logic dimensions were sufficient for monitoring the growth of students’ critical thinking.
The present curriculum innovation aimed to teach critical thinking skills to preclinical students in various medical majors using a Socratic questioning learning model instead of a cookbook approach to learning in laboratory courses. The development of problem-solving and critical thinking skills, in addition to process-related skills, in biochemistry laboratory courses supplements traditional curriculum in a helpful way. The curriculum innovation that we described and proposed may represent an incremental step forward for the discipline; it is a novel educational approach for promoting critical thinking skills, fostering an appreciation of the affective domain, and enabling reflective practice by using small-group processing skill instruction and one-on-one Socratic questioning. The current study results are based on training critical thinking skills that should enable students to engage in the “reflection-on-action” process, which might provide an additional bridge between basic medical knowledge and clinical practice. More importantly, reconstructive mental reviews may indirectly shape preclinical students’ future actions in the challenging healthcare industry characterized by uncertainty and novel circumstances.
Data Availability
Due to conditions on participant consent and other ethical restrictions, the datasets used and analysed in the current study are not publicly available. If you have any database data requirements, please contact the corresponding author of this study.
Art-in S. Current situation and need in learning management for developing the analytical thinking of teachers in basic education of Thailand. Procedia-Social and Behavioral Sciences. 2015;197:1494–500.
Article Google Scholar
Maudsley G, Strivens J. Science’,‘critical thinking’and ‘competence’for tomorrow’s doctors. A review of terms and concepts. Med Educ. 2000;34:53–60.
Halpern DF. Thought and knowledge: an introduction to critical thinking. Psychology Press;2013.
Davies M, Barnett R. The Palgrave handbook of critical thinking in higher education. Springer;2015.
Sit HHW. Characteristics of Chinese students’ learning styles. Int Proc Econ Dev Res. 2013;62:36.
He Y. The roles of thinking styles in learning and achievement among Chinese university students.The University of Hong Kong Libraries.
Nordin S, Yunus K. Exploring Metacognitive Awareness among Teachers. Int J Acad Res Progress Educ Dev. 2020;9:462–72
Nelson TO, Narens L. Why investigate metacognition. Metacognition: Knowing about knowing. 1994;13:1–25.
Google Scholar
Dinsmore DL. Examining the ontological and epistemic assumptions of research on metacognition, self-regulation and self-regulated learning. Educational Psychol. 2017;37:1125–53.
Maudsley G, Strivens J. Promoting professional knowledge, experiential learning and critical thinking for medical students. Med Educ. 2000;34:535–44.
Zhong W, Cheng M. Developing critical thinking: experiences of Chinese International Students in a Post-1992 University in England. Chin Educ Soc. 2021;54:95–106.
Dewey J. How we think. In.: D C Heath; 1910.
Book Google Scholar
Ennis R. Critical thinking: a streamlined conception. Teach Philos. 1991;14:5–24.
Ennis RH. Is critical thinking culturally biased? Teach Philos. 1998;21:15–33.
Ennis R. Critical thinking: reflection and perspective part II. Inquiry: Crit Think Disciplines. 2011;26:5–19.
Ennis RH. A taxonomy of critical thinking dispositions and abilities. 1987. https://education.illinois.edu/docs/default-source/faculty-documents/robert-ennis/thenatureofcriticalthinking_51711_000.pdf
Zare P, Mukundan J. The use of socratic method as a teaching/learning tool to develop students’ critical thinking: a review of literature. Lang India. 2015;15:256–65.
Elder L, Paul R. Critical thinking: Tools for taking charge of your professional and personal life. The Foundation for Critical Thinking;2005.
Paul R, Elder L. Critical thinking: intellectual Standards essential to reasoning well within every domain of human thought, part two. J Dev Educ. 2013;37:32.
Elder L, Paul R. Critical thinking: the art of socratic questioning, part II. J Dev Educ. 2007;31:32.
Paul R, Elder L. Critical thinking: the art of socratic questioning. J Dev Educ. 2007;31:36.
Paul R, Elder L. Critical thinking: the art of socratic questioning, part III. J Dev Educ. 2008;31:34–5.
Oyler DR, Romanelli F. The Fact of Ignorance Revisiting the Socratic Method as a Tool for Teaching Critical Thinking. Am J Pharm Educ. 2014;78.
Paul R, Elder L, Bartell T. A Brief History of the Idea of Critical Thinking, The Critical Thinking Community. In.; 1997.
Tofade T, Elsner J, Haines ST. Best practice strategies for effective use of questions as a teaching tool. Am J Pharm Educ. 2013;77:1–7.
Vygotsky L. Zone of proximal development. Mind in society: The development of higher psychological processes 1987;5291:157.
Rud AG Jr. The Use and Abuse of Socrates in Present Day Teaching;1990.
Oh RC. The socratic method in medicine-the labor of delivering medical truths. For the Office-based Teacher of Family Medicine. 2005;37:537–9.
Stoddard HA, O’Dell DV. Would Socrates have actually used the “Socratic Method” for clinical teaching? J Gen Intern Med. 2016;31:1092–6.
Ku KY, Ho IT. Dispositional factors predicting chinese students’ critical thinking performance. Pers Indiv Differ. 2010;48:54–8.
Liu OL, Shaw A, Gu L, Li G, Hu S, Yu N, Ma L, Xu C, Guo F, Su Q. Assessing college critical thinking: preliminary results from the chinese HEIghten ® critical thinking assessment. High Educ Res Dev. 2018;37:999–1014.
Holmes NG, Wieman CE, Bonn D. Teaching critical thinking. Proc Natl Acad Sci. 2015, 112(36):11199–11204.
Elder L, Paul R. The aspiring thinker’s guide to critical thinking. Rowman & Littlefield; 2019.
Cooke M, Irby DM, Sullivan W, Ludmerer KM. American Medical Education 100 years after the Flexner Report. N Engl J Med. 2006;355:1339–44.
Behar-Horenstein LS, Catalanotto FA, Nascimento MM. Anticipated and actual implementation of case-based learning by Dental Faculty Members during and after training. J Dent Educ. 2015;79:1049–60.
Dong H, Guo C, Zhou L, Zhao J, Wu X, Zhang X, Zhang X. Effectiveness of case-based learning in chinese dental education: a systematic review and meta-analysis. BMJ Open. 2022;12:e048497–7.
Sandars J, Goh P-S. Design thinking in Medical Education: the key features and practical application. J Med Educ Curric Dev. 2020;7:2382120520926518–8.
Khan S, Vandermorris A, Shepherd J, Begun JW, Lanham HJ, Uhl-Bien M, Berta W. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18:192–2.
Preeti B, Ashish A, Shriram G. Problem based learning (PBL)-an effective approach to improve learning outcomes in medical teaching. J Clin Diagn research: JCDR. 2013;7:2896–7.
Ibrahim ME, Al-Shahrani AM, Abdalla ME, Abubaker IM, Mohamed ME. The effectiveness of problem-based learning in Acquisition of Knowledge, soft skills during basic and preclinical sciences: medical students’ points of view. Acta Informatica Medica. 2018;26:119–24.
Servant-Miklos VF. Problem solving skills versus knowledge acquisition: the historical dispute that split problem-based learning into two camps. Adv Health Sci Educ. 2019;24:619–35.
Bjork RA, Dunlosky J, Kornell N. Self-regulated learning: beliefs, techniques, and illusions. Ann Rev Psychol. 2013;64:417–44.
Colliver JA. Effectiveness of problem-based learning curricula: research and theory. Acad Med. 2000;75:259–66.
Bate E, Hommes J, Duvivier R, Taylor DC. Problem-based learning (PBL): Getting the most out of your students–Their roles and responsibilities: AMEE Guide No. 84. Medical teacher 2013.
Lim WK. Dysfunctional problem-based learning curricula: resolving the problem. BMC Med Educ. 2012;12:89–9.
Burgess AW, McGregor DM. Use of established guidelines when reporting on Interprofessional Team-Based learning in Health Professions Student Education: a systematic review. Acad Med. 2021;97:143–51.
Burgess A, Bleasel J, Haq I, Roberts C, Garsia R, Robertson T, Mellis C. Team-based learning (TBL) in the medical curriculum: better than PBL? BMC Med Educ. 2017;17:243.
Burgess A, Ayton T, Mellis C. Implementation of team-based learning in year 1 of a PBL based medical program: a pilot study. BMC Med Educ. 2016;16:49–9.
Schrope M. Solving tough problems with games. Proc Natl Acad Sci. 2013;110:7104–6.
Nessler M. Three Ways virtual Technologies are making a difference in HR. Employ Relations Today. 2014;40:47–52.
Nevin CR, Westfall AO, Rodriguez JM, Dempsey DM, Cherrington A, Roy B, Patel M, Willig JH. Gamification as a tool for enhancing graduate medical education. Postgrad Med J. 2014;90:685–93.
Technologies in Medical Education. In. The SAGE Encyclopedia of Educational Technology. edn.: SAGE Publications, Inc.; 2015.
Hurtubise L, Hall E, Sheridan L, Han H. The Flipped Classroom in Medical Education: Engaging Students to Build Competency. J Med Educ Curric Dev. 2015;2:JMECD.S23895.
Persky AM, Medina MS, Castleberry AN. Developing critical thinking skills in pharmacy students. Am J Pharm Educ. 2019;83.
Chew SW, Lin I-H, Chen N-S. Using Socratic questioning strategy to enhance critical thinking skill of elementary school students. In: 2019 IEEE 19th International Conference on Advanced Learning Technologies (ICALT): 2019 : IEEE; 2019;290–294.
Manurung YH, Siregar FS. Developing students’ critical thinking on speaking through socratic questioning method. Adv Social Sci Educ Humanit Res. 2018;263:212–6.
Wediyantoro PL, Lailiyah M, Yustisia KK. Synchronous discussion in online learning: investigating students’ critical thinking. En Jour Me. (English Journal of Merdeka): Culture Language and Teaching of English. 2020;5:196–203.
Copeland M. Socratic circles: fostering critical and creative thinking in middle and high school. Stenhouse Publishers; 2005.
Tweed RG, Lehman DR. Learning considered within a cultural context: confucian and socratic approaches. Am Psychol. 2002;57:89–99.
Wilberding E. Socratic methods in the classroom: encouraging critical thinking and problem solving through dialogue. Routledge; 2021.
Sanchez-Lara PA, Grand K, Haanpää MK, Curry CJ, Wang R, Ezgü F, Rose CM, D’Cunha Burkardt D, Conway RL, Relan A. Thinking outside “The Box”: Case‐based didactics for medical education and the instructional legacy of Dr John M. Graham, Jr. Am J Med Genet Part A. 2021;185:2636–45.
Cooley JH, Larson S. Promoting a growth mindset in pharmacy educators and students. Curr Pharm Teach Learn. 2018;10:675–9.
Makhene A. The use of the Socratic inquiry to facilitate critical thinking in nursing education. Health SA Gesondheid. 2019;24.
Harasym PH, Tsai T-C, Hemmati P. Current trends in developing medical students’ critical thinking abilities. Kaohsiung J Med Sci. 2008;24:341–55.
Roberts TG, Dyer JE. The relationship of self-efficacy, motivation, and critical thinking disposition to achievement and attitudes when an illustrated web lecture is used in an online learning environment. J agricultural Educ. 2005;46:12–23.
Chalmers AF. What is this thing called science? Hackett Publishing; 2013.
Zain AR. Effectiveness of guided inquiry based on blended learning in physics instruction to improve critical thinking skills of the senior high school student. In: Journal of Physics: Conference Series : 2018: IOP Publishing; 2018: 012015.
Goodey NM, Talgar CP. Guided inquiry in a biochemistry laboratory course improves experimental design ability. Chem Educ Res Pract. 2016;17:1127–44.
Talgar CP, Goodey NM. Views from academia and industry on skills needed for the modern research environment. Biochem Mol Biol Educ. 2015;43:324–32.
Handelsman J, Ebert-May D, Beichner R, Bruns P, Chang A, DeHaan R, Gentile J, Lauffer S, Stewart J, Tilghman SM. Education. Scientific teaching. Science. 2004;304:521-2.
Thaiposri P, Wannapiroon P. Enhancing students’ critical thinking skills through teaching and learning by inquiry-based learning activities using social network and cloud computing. Procedia-Social and Behavioral Sciences. 2015;174:2137–44.
Hirschberg CB. A course in critical thinking for PhD students in biomolecular sciences and biotechnology: classical experiments in biochemistry;2016.
Van Winkle LJ, Cornell S, Fjortoft N, Bjork BC, Chandar N, Green JM, La Salle S, Viselli SM, Burdick P, Lynch SM. Critical thinking and reflection exercises in a biochemistry course to improve prospective health professions students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2013;77.
Kanari Z, Millar R. Reasoning from data: how students collect and interpret data in science investigations. J Res Sci Teach. 2004;41:748–69.
Kumassah E, Ampiah J, Adjei E. An investigation into senior high school (shs3) physics students understanding of data processing of length and time of scientific measurement in the Volta region of Ghana. Int. J. Educ. Technol. High. Educ. 2014;37–61.
Kung RL, Linder C. University students’ ideas about data processing and data comparison in a physics laboratory course. Nordic Stud Sci Educ. 2006;2:40–53.
Ryder J, Leach J. Interpreting experimental data: the views of upper secondary school and university science students. Int J Sci Educ. 2000;22:1069–84.
Ryder J. Data interpretation activities and students’ views of the epistemology of science during a university earth sciences field study course. Teaching and Learning in the Science Laboratory.edn. Springer;2002. p.151–162.
Séré MG, Journeaux R, Larcher C. Learning the statistical analysis of measurement errors. Int J Sci Educ. 1993;15:427–38.
Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;524–532.
Haviland A, Nagin DS, Rosenbaum PR. Combining propensity score matching and group-based trajectory analysis in an observational study. Psychol Methods. 2007;12:247–67.
Helland-Hansen W, Hampson G. Trajectory analysis: concepts and applications. Basin Res. 2009;21:454–83.
Barrows HS, Tamblyn RM. Problem-based learning: an approach to medical education. Volume 1. Springer;1980.
Jensen G, Denton B. Teaching physical therapy students to reflect: a suggestion for clinical education. J Phys Therapy Educ. 1991;5:33–8.
Stern DT, Papadakis M. The developing physician—becoming a professional. N Engl J Med. 2006;355:1794–9.
Gracey CF, Haidet P, Branch WT, Weissmann P, Kern DE, Mitchell G, Frankel R, Inui T. Precepting humanism: strategies for fostering the human dimensions of care in ambulatory settings. Acad Med. 2005;80:21–8.
Branch WT Jr, Kern D, Haidet P, Weissmann P, Gracey CF, Mitchell G, Inui T. Teaching the human dimensions of care in clinical settings. JAMA. 2001;286:1067–74.
Wald HS, Davis SW, Reis SP, Monroe AD, Borkan JM. Reflecting on reflections: enhancement of medical education curriculum with structured field notes and guided feedback. Acad Med. 2009;84:830–7.
Download references
Acknowledgements
The authors wish to thank Chi-Her Lin, MD for their encouragement and support in the writing of this manuscript, and Prof. Woei-Jer Chuang, Hung-Chi Cheng, Chang-Shi Chen, Po-Hsin J. Huang, Chien-hung Yu, and Wen-Tsan Chang for their help with the experimental design. Special thanks to Tanvi Gupta for her help with the improving reading fluency.
This work was supported by the Teaching Practice Research Program, Ministry of Education, Taiwan (Grant No: PMN1110350, PMN1100853, PMN1090364, PMN108075, PMN107018).
Author information
Authors and affiliations.
Department of Biochemistry and Molecular Biology, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Yueh-Ren Ho
School of Medicine, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Yueh-Ren Ho & Chien-Ming Li
Institute of Clinical Medicine, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Bao-Yu Chen
Division of Infectious Diseases, Department of Internal Medicine, Chi Mei Medical Center, Zhonghua Raod No.901, Yongkang District 710, Tainan City, Taiwan (R.O.C.)
Chien-Ming Li
You can also search for this author in PubMed Google Scholar
Contributions
Yueh-Ren Ho: substantially contributed to the conception, data curation, interpretation, drafting and critical revision of the paper. She has given final approval to the manuscript and agrees to be accountable for the work. Bao-Yu Chen: substantially contributed to the conception, formal analysis, methodology, visualization, and writing and editing the manuscript. Chien-Ming Li: substantially contributed to the conception, data curation, review and editing the manuscript.
Corresponding author
Correspondence to Yueh-Ren Ho .
Ethics declarations
Ethics approval and consent to participate.
Students participating in this course will be informed before the class begins that their results will be used for educational academic research, and their written informed consent were obtained. The methodology of the study including the content analysis of literature on data curation activities were approved and funded by Teaching Practice Research Program, Ministry of Education, Taiwan. Throughout the study, all methods followed the approved methodology and adhered to the relevant guidelines and regulations. According to Human Subjects Research Act, Chap. 2, article 5: The Ministry of Education review current study nature and announced the principal investigator shall not submit the research protocol for review and approval by the Institutional Review Board. Please refer to the source of law in the website of Laws & Regulations Database of The Republic of China (Taiwan) ( https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=L0020176 ).
Consent for publication
Not applicable.
Competing interests
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ho, YR., Chen, BY. & Li, CM. Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students. BMC Med Educ 23 , 173 (2023). https://doi.org/10.1186/s12909-023-04134-2
Download citation
Received : 20 September 2022
Accepted : 02 March 2023
Published : 20 March 2023
DOI : https://doi.org/10.1186/s12909-023-04134-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Biochemistry experiment
- Critical thinking
- Socratic method
- Medical education
- Metacognition
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
Critical thinking is connected to a broader idea of what 'good thinking'—and, by extension, the 'good professional'—looks like for each educator [ 38] within a given context or community. These observations lead one to speculate about what purpose fluidity in conceptions of critical thinking might serve.
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Critical thinking skills have been linked to improved patient outcomes, better quality patient care and improved safety outcomes in healthcare (Jacob et al. 2017).. Given this, it's necessary for educators in healthcare to stimulate and lead further dialogue about how these skills are taught, assessed and integrated into the design and development of staff and nurse education and training ...
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
This article describes three critical thinking skills essential to effective clinical care - clinical reasoning, evidence-informed decision-making, and systems thinking - and approaches to develop these skills during clinician training. ... Implicit racial bias, health care provider attitudes, and perceptions of health care quality among ...
The development of critical thinking skills in healthcare is somewhat unique. In chess, students can start playing using the same tools employed by the experts (the chess board); however, in healthcare, allowing students to make medical decisions is ethically inappropriate and irresponsible. Simulations centers allow students to gain needed ...
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from ...
The authors examine the role of critical thinking in medicine and healthcare, arguing that critical thinking skills are essential for doctors and patients. They describe an international project that involves collaboration between education and health. ... The author uses academic rank, field of specialization, and university affiliation to ...
the need for fostering critical thinking amongmedical practitioners. This article attempts to provide a conceptual analysis of critical thinking with reference to medical education along with measures to foster critical thinking through relevant teaching learning and assessment methods. Key words: Critical thinking, medical education, quality
Critical thinking can help medical students and doctors achieve improved productivity, better clinical decision making, higher grades and much more. This article will explain why critical thinking is a must for people in the medical field. Definition of Critical Thinking. You can find a variety of definitions of Critical Thinking (CT). It is a ...
Abstract Healthcare systems across the world are challenged with problems of misdiagnosis, non-beneficial care, unwarranted practice variation and inefficient or unsafe practice. ... Three critical thinking skills underpin effective care: clinical reasoning, evidence-informed decision-making and systems thinking. It is important to define these ...
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. Without critical thinking, physicians, and particularly residents, are prone to cognitive errors, which can lead to diagnostic errors, especially in a high ...
The practice of critical thinking helps us understand the disease manifestations and the related processes and actions that might be relevant to prevent, diagnose and treat diseases. To critically appraise the way we perform evidence-based practice, we must combine best quality research with clinical expertise.
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
Critical thinking is the ability to analyze, evaluate, and apply information in a logical and systematic way. It is a crucial skill for healthcare professionals, who face complex and dynamic ...
It makes you a well-rounded individual, one who has looked at all of their options and possible solutions before making a choice. According to the University of the People in California, having critical thinking skills is important because they are [ 1 ]: Universal. Crucial for the economy. Essential for improving language and presentation skills.
If you have worked in customer service then the same critical thinking skills that are used to deal with customers will be used to deal with patients in the medical field. If you have worked in a fast-paced environment requiring prioritizing then you will carry that skill over to the medical field. The examples listed above are just a few of ...
Instead, we offer a description of the different conceptions of critical thinking held in health professional education, illustrate their dynamic use, and discuss the tensions and affordances that this diversity brings to the field. We argue that diversity in conceptions of critical thinking can allow educators to express unique and often ...
A review article highlighted the potential utility of the Socratic method as a tool for teaching critical thinking in the healthcare field. The method involves posing a series of questions to students. More importantly, medical students and residents in clinical teaching are familiar with the method. Almost all healthcare students must complete ...