- Open access
- Published: 23 March 2023

Quality of care in the context of universal health coverage: a scoping review
- Bernice Yanful ORCID: orcid.org/0000-0002-6824-6694 1 ,
- Abirami Kirubarajan 2 ,
- Dominika Bhatia 2 ,
- Sujata Mishra 2 ,
- Sara Allin 2 &
- Erica Di Ruggiero 1 , 2 , 3
Health Research Policy and Systems volume 21 , Article number: 21 ( 2023 ) Cite this article
7971 Accesses
2 Citations
6 Altmetric
Metrics details
Introduction
Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries. The primary objective of this scoping review was to summarize the existing conceptual and empirical literature on quality of care within the context of UHC and identify knowledge gaps.
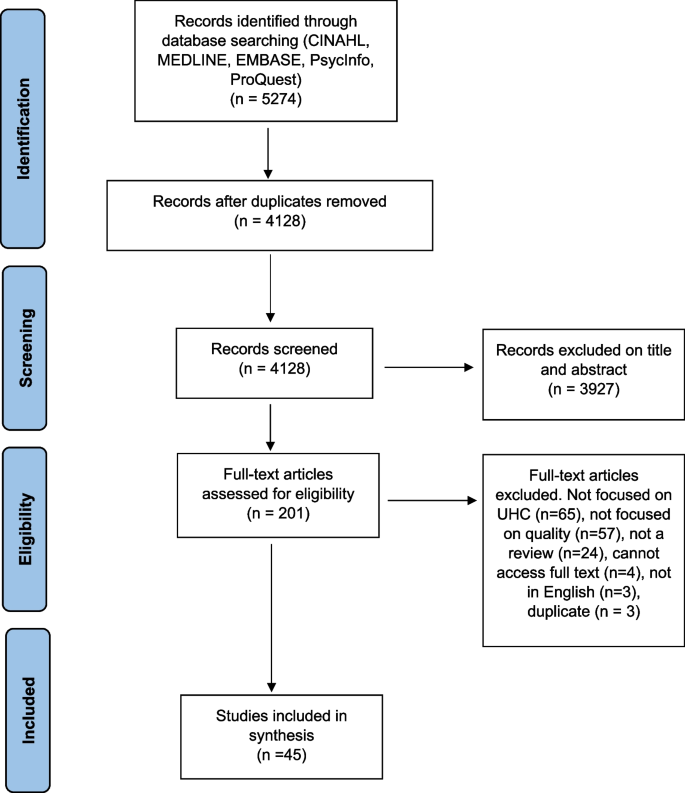
We conducted a scoping review using the Arksey and O’Malley framework and further elaborated by Levac et al. and applied the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews reporting guidelines. We systematically searched MEDLINE, EMBASE, CINAHL-Plus, PAIS Index, ProQuest and PsycINFO for reviews published between 1 January 1995 and 27 September 2021. Reviews were eligible for inclusion if the article had a central focus on UHC and discussed quality of care. We did not apply any country-based restrictions. All screening, data extraction and analyses were completed by two reviewers.
Of the 4128 database results, we included 45 studies that met the eligibility criteria, spanning multiple geographic regions. We synthesized and analysed our findings according to Kruk et al.’s conceptual framework for high-quality systems, including foundations, processes of care and quality impacts. Discussions of governance in relation to quality of care were discussed in a high number of studies. Studies that explored the efficiency of health systems and services were also highly represented in the included reviews. In contrast, we found that limited information was reported on health outcomes in relation to quality of care within the context of UHC. In addition, there was a global lack of evidence on measures of quality of care related to UHC, particularly country-specific measures and measures related to equity.
There is growing evidence on the relationship between quality of care and UHC, especially related to the governance and efficiency of healthcare services and systems. However, several knowledge gaps remain, particularly related to monitoring and evaluation, including of equity. Further research, evaluation and monitoring frameworks are required to strengthen the existing evidence base to improve UHC.
Peer Review reports
According to the World Health Organization, universal health coverage (UHC) is achieved when ‘all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship’ [ 1 ]. UHC has gained renewed attention from researchers and policymakers following its inclusion in the 2030 Agenda for Sustainable Development (SDGs). SDG target 3.8 calls for achieving ‘universal health coverage, including financial risk protection, access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all’ [ 2 ].
While there is growing evidence linking UHC to different health, economic and social outcomes, recent estimates suggest that about 800 million people globally still do not have access to full financial coverage of essential health services, including but not limited to high-income countries [ 3 ]. The WHO’s well-established UHC cube identifies three dimensions of UHC: (1) population (who is covered); (2) services (services that are covered); (3) direct costs (the proportion of the costs that are covered) [ 4 ]. Absent from the cube is the explicit inclusion of quality of care. However, without attention to the quality of care provided, increasing service coverage alone is unlikely to produce better health outcomes. As such, quality of care is critical to the achievement of UHC. A high-quality health system has been defined as one ‘that optimises health care in a given context by consistently delivering care that improves or maintains health outcomes, by being valued and trusted by all people, and by responding to changing population needs’ [ 5 , p. e1200].
Current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries (LMICs) [ 6 ]. While the era of the Millennium Development Goals (MDGs) expanded access to essential health services in LMICs, poor quality of care remains a significant problem, and explains persistently high levels of maternal and child mortality [ 6 ]. In addition, poor quality of care is estimated to cause between 5.7 and 8.4 million deaths yearly in LMICs [ 7 ]. Low-quality services are also an issue in high-income countries (HICs), particularly for disadvantaged populations such as immigrant and Indigenous groups [ 6 , 8 ].
As such, efforts to achieve UHC focused solely on expanding access to care are insufficient. Achieving UHC will require a more deliberate focus on quality of care across its various dimensions including effectiveness, safety, people-centredness, timeliness, equity, integration of care and efficiency [ 6 ]. However, existing literature synthesizing evidence on the quality of care within the context of UHC is more limited.
The primary objective of this scoping review is to synthesize and analyse the existing conceptual and empirical literature on quality of care within the context of UHC. The secondary objective is to identify knowledge gaps on quality of care within the context of advancing UHC and highlight areas for further inquiry.
We conducted a scoping review using the five-stage scoping review framework proposed by Arksey and O’Malley [ 9 ] and further elaborated by Levac et al. with the following stages [ 10 ]: (1) formulating the research question; (2) searching for relevant studies; (3) selection of eligible studies; (4) data extraction and (5) analysing and describing the results. In addition, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews reporting guidelines [ 11 ]. In accordance with the guidelines, our protocol is publicly available through Open Science Forum [ 12 ]. The scoping review methodology was selected due to its relevance to both identifying emerging and established content areas, and integration of diverse study methodologies [ 13 ]. As such, our methodology was well-aligned with the exploratory aims of our study.
To synthesize the existing knowledge on quality of care within the context of UHC, we focused on retrieving and analysing relevant reviews (as opposed to primary research studies). Bennett et al. [ 14 ] applied this overview of reviews approach in identifying health policy and system research priorities for the SDGs.
Information sources and search strategy
We developed the search strategy in consultation with a research librarian with expertise in public health and health systems. After finalizing our search in MEDLINE (Ovid) through an iterative process involving pilot tests, we completed a systematic search of MEDLINE (Ovid), EMBASE (Ovid), CINAHL-Plus (EBSCO), PAIS Index, ProQuest and PsycINFO (Ovid) for articles published from 1 January 1995 to 27 September 2021. The date cut-off of 1995 was selected to capture articles published during the period leading up to the adoption of the MDGs. We applied adapted search filters from the InterTASC Information Specialists’ Subgroup Search Filter Resource for each database [ 15 ].
Our searches combined terms related to the concepts of (1) UHC (e.g. universal health insurance, universal coverage) and (2) quality of care and its seven dimensions (e.g. equity, safety, people-centredness). Our search strategy is available in Appendix A. Figure 1 outlines the eligibility criteria we used to assess studies for inclusion in the review.
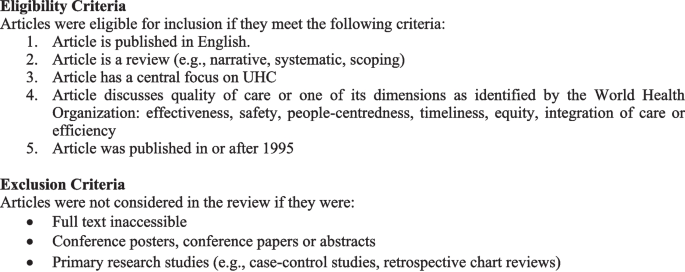
Eligibility and exclusion criteria
Data management
Results from database searches were managed through Covidence ( www.covidence.org ) for deduplication and screening.
Study selection
Two reviewers (BY&AK) independently assessed studies against the eligibility criteria in two phases: (1) titles and abstracts and (2) full-text articles. A pilot test of the title and abstract screening was completed for approximately the first 100 search results. The two reviewers discussed disagreements to revise eligibility criteria as required. Any disagreements were resolved via consensus and in consultation with senior co-authors.
Data extraction
BY & AK independently completed data extraction for the first 10 articles using a standardized form. Following the pilot, the full data extraction was completed by the two reviewers in parallel. We extracted data on key study characteristics and according to each domain and subcomponent identified in Kruk et al.’s [ 5 ] framework described in the following section. The process of data extraction was iterative, with the form subject to revisions. Geographic regions were classified either by WHO regions [ 16 ] or through self-identification by the articles, such as a global focus, LMICs, HICs, ‘developing’ or ‘developed’.
Data synthesis
We synthesized the results through both a descriptive summary and a qualitative, narrative synthesis. We anchored our narrative synthesis in Kruk et al.’s [ 5 ] conceptual framework for high-quality health systems. The framework draws from Donabedian’s well-known conceptual model of quality of care, which was first developed in the 1960s and identifies structures, processes and outcomes as three components of quality of care. Kruk et al. [ 5 ] offer a new evidence-based framework relevant to present-day health systems, recognizing the heterogeneity of health systems across HIC and LMIC contexts.
They define three key domains of a high-quality health system, which they argue should be at the core of implementing and advancing UHC: foundations, processes of care and quality impacts. Foundations refer to the context and resources required to lead a high-quality health system. Processes of care include competent care and systems, relating to evidence-based effective care and health systems’ ability to respond to patient needs. Quality impacts include both patient and provider-reported health outcomes and client confidence in the health system, as well as economic benefits such as a reduction of resource waste and financial risk protection. The Kruk et al. [ 5 ] framework does not explicitly address equity; however, the authors state that equity in the quality of healthcare is critical, which they define as ‘the absence of disparities in the quality of health services between individuals and groups with different levels of underlying social disadvantage [p. e1214].’ When compared with Donabedian’s model for evaluating the quality of care [ 17 ], Kruk et al. [ 5 ] offer a much more elaborated framework that explicitly names a range of subcomponents to guide quality measurement and improvement (e.g. governance, positive user experience, etc.).
As our scoping review examines the existing literature on quality of care within the context of UHC and identifies knowledge gaps, Kruk et al.’s [ 5 ] framework provided a useful analytic tool by which to organize and interpret our findings.
We organized the results from our narrative synthesis according to each component of the framework (foundations, processes of care and quality impacts), addressing equity as a cross-cutting theme across these components. Table 1 summarizes the components and subcomponents of the framework.
Description of included reviews
The database searches yielded 4128 results after deduplication. Following screening, 45 articles that met eligibility criteria were included in the review. The search results are shown in Appendix A and a summary of each article is presented in Table 2 . Narrative reviews comprised 40.0% of the studies ( n = 18), 35.6% were systematic reviews (n = 16), while 20.0% were scoping reviews ( n = 9), and 4.4% were overviews of systematic reviews ( n = 2). Of the 45 reviews, 28 covered multiple WHO regions (62.2%). This included reviews with a broad global focus, reviews focused on LMICs, ‘developing’ or ‘developed’ countries, as well as reviews with an explicit focus on more than one of six WHO regions. Regarding the dimensions of quality of care, equity was the most well represented, examined by 40 of the studies (88.9%). Integration of care and safety were the least represented across the studies, each examined by 11 of the reviews (24.4%). We did not formally appraise the quality of studies included in our review, which is not required for a scoping review given its overarching aim to map the scope and size of the available literature on a given topic.
Narrative synthesis of results
Conceptualizing universal healthcare/coverage and quality of care.
The included studies highlighted varying definitions of UHC and quality of care. A common definition of UHC was that all people who require any essential healthcare services, including but not limited to promotion, prevention and treatment, are able to access services without financial stress [ 18 , 19 , 20 ]. One study further expanded this definition to include that UHC was the desired outcome of health system performance [ 18 ]. Some studies specified the definition was outlined in the Alma Ata declaration [ 21 , 22 ].
Definitions of quality of care also varied. One study distinguished between service quality (e.g. patient satisfaction, responsiveness) and technical quality (e.g. adherence to clinical guidelines) [ 23 ]. Another study defined high-quality healthcare as ‘providing the highest possible level of health with the available resources’ [ 24 , p. 142]. However, most studies did not provide a working definition of quality of care, and instead used proxy indicators such as infant mortality [ 25 ] to highlight quality-related outcomes.
Synthesis according to Kruk et al. Conceptual framework
Below, we synthesize findings from the studies according to the components of Kruk et al.’s [ 5 ] conceptual framework (foundations, processes of care and impacts). We highlight the most common themes that we identified in the literature for each domain and provide illustrative examples. Unless specified, findings were not specific to LMIC or HIC contexts.
Foundations
Governance: leaders, policies, processes and procedures providing direction and oversight of health system(s).
A common theme across the literature was health system governance at local, regional and national scales, and its relationship to quality of care within the context of UHC. Naher et al. [ 26 ] identified transparency, accountability, laws and regulations, and citizen engagement as critical components of governance. The articles discussed both poor and good governance, their underlying determinants and drivers, as well as interventions to improve governance and thus quality of care [ 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ].
The literature suggests that poor governance is a common issue across health systems, and is both a cause and indicator of poor-quality care. Causes and forms of poor governance include weak supervision of, and inadequate incentives and remuneration for healthcare providers; lack of transparency and accountability in decision-making; and insufficient financial capacity; in addition to fragmented regulations and policies. Poor governance has also been found to result in low patient trust and confidence in the health system, wasted resources and poor patient outcomes [ 26 , 40 , 44 ]. In contrast, the reviewed literature described strong governance as critical to effective healthcare services [ 26 ] and the basis for achieving UHC [ 32 ].
Interventions to improve governance described by the reviewed literature include decentralization, social accountability mechanisms, such as social audits, and policy reforms to strengthen provider incentives and service integration [ 26 , 28 , 31 , 45 , 47 , 53 ]. However, the evidence regarding the effectiveness of these interventions on governance and quality of care was largely inconclusive. Regarding integration, White [ 45 ] noted the need to ensure adequate leadership and organizational capacity before integrating services, as a key determinant of success.
Quality of care measures
Six studies identified measures and/or measurement instruments to assess quality of care or its various dimensions within the context of UHC [ 19 , 22 , 27 , 30 , 42 , 51 ]. These measures differed based on their service areas of focus (e.g. family planning, primary care), the geographic contexts for which they are intended and whether they assessed foundations, processes of care or quality impacts. The reviewed literature identified a lack of standardized quality assessment tools as a significant barrier to the realization of UHC [ 22 , 42 ]. However, researchers also noted the need for country-specific indicators reflective of a country’s unique social, political and economic circumstances, and population needs and expectations [ 18 , 22 , 30 , 39 , 51 ]. Studies also emphasized the importance of integrating equity as an explicit component in the measurement and monitoring of UHC through for example, disaggregation of data by key socioeconomic and demographic variables including place of residence, occupation, religion, ethnicity and migration status [ 18 , 27 , 30 , 35 ]. Table 3 maps the measures identified in the studies according to the domains and subdomains of Kruk et al.’s framework.
Skills and availability of health system workers
Several studies also identified critical health workforce shortages and inequities in the distribution of appropriately qualified staff between urban and rural areas as significant constraints to the provision of high-quality, equitable care within the context of UHC, particularly in LMIC contexts [ 21 , 23 , 25 , 29 , 31 , 38 , 40 , 43 , 44 , 46 , 47 , 48 , 49 , 50 , 53 ]. Strategies discussed to address these concerns included (i) improving recruitment and retention of health system staff for rural and remote areas [ 21 , 46 , 47 , 50 ]; (ii) recruiting and training community health workers, while increasing the skills of lay health workers [ 21 ]; (iii) training traditional medicine practitioners in conventional medicine and utilizing them as community health workers [ 49 ]; and (iv) increasing task shifting, through delegating tasks to less specialized health workers [ 21 , 31 ], for which supportive supervision and adequate training is required [ 21 ].
Processes of care
Access to competent care and systems, incentives to improve quality of care delivery.
Evidence from the reviewed studies suggests that poor provider competence across a range of health services remains an ongoing issue, particularly in LMICs, posing a considerable barrier to the provision of timely, safe and effective quality of care [ 22 , 23 , 29 , 31 , 33 , 39 , 40 , 46 , 47 , 49 ]. For example, in China, a study with standardized patients found that providers in village hospitals provided correct treatment for tuberculosis only 28% of the time [ 47 ].
Within health systems seeking to provide UHC, significant inequities remain in both LMICs and HICs regarding the quality of care received by different populations. Vulnerable populations, who are more likely to receive care from lower-level health facilities, such as health centres, are disproportionately impacted by incompetent care and systems, having already constrained access to care [ 26 ], fewer options regarding providers and being more likely to receive inappropriate referrals [ 40 ], all indicators of lower-quality care.
Four studies described organizational factors influencing provider competence, including performance appraisal, continuing education, incentives, and remuneration and payment mechanisms [ 27 , 31 , 40 , 46 ]. For example, Sanogo et al. [ 40 ] discussed how delays in provider reimbursement as observed in Ghana, can demotivate healthcare providers, which Agarwal et al. [ 27 ] noted may decrease providers’ willingness to exert maximum effort on assigned tasks, compromising the quality of care.
Regarding incentives to improve motivation and quality of care delivery, Yip et al. [ 47 ] suggested a pay-for-performance system in China, as physicians are traditionally incentivized for treatment-based care through fee-for-service. However, the systematic review from Wiysonge et al. [ 46 ] noted a lack of evidence to support whether financial incentives for healthcare providers would improve quality of care in low-income countries.
User experience: wait times and people centredness
Wait times, a core component of quality of care, were noted as ongoing concerns in HICs and LMICs [ 21 , 23 , 33 , 39 , 40 , 47 , 48 , 55 , 56 ]. In HICs such as Norway and the United Kingdom, long wait times have been found to increase the demand for duplicative voluntary private health insurance, which Kiil argues may threaten the overall quality of public-sector driven UHC and exacerbate inequities [ 56 ]. In LMICs, evidence has shown that service quality is often superior in the private sector compared with the public sector, defined in relation to shorter wait times, better hospitality and increased time spent with providers [ 23 ].
Several studies described the relationship between positive user experience and people-centred care, which focuses on the needs and preferences of populations served while engaging them in shaping health policies and services. In addition, people centredness has been linked to improved mental and physical health, and reduced health inequities among other outcomes [ 20 , 22 , 31 , 35 , 57 ].
One study presented a people-centred care partnership model intended to support the work of advanced practice nurses in sustaining UHC, identifying nine attributes of people centredness including mutual trust and shared decision-making [ 20 ].
Several studies also discussed strategies aimed at increasing patient/community voice and engagement and the people centredness of health systems. These strategies included citizenship endorsement groups in Mexico [ 34 ] and various public forums to foster accountability and transparency [ 26 ]. However, McMichael et al. [ 35 ] cautioned that approaches to increase the voice of patients and communities risk excluding the most vulnerable, as those facing the greatest barriers to participation in such initiatives are often the most disadvantaged in their access and use of health services.
Quality impacts
Quality of care outcomes.
A few of the reviewed articles reported on empirical studies that analyzed patient and population health outcomes in relation to quality of care in the context of UHC. Where reported, these outcomes were discussed in reference to (i) specific programmes intended to improve quality of care and advance UHC, (ii) the impacts of health insurance schemes or health system reforms, (iii) private versus public sector provision of healthcare and/or (iv) the effects of specific service delivery models.
Regarding programmes intended to improve the quality of care, a community health extension programme in Ethiopia was associated with increased perinatal survival and decreased prevalence of communicable diseases. Though resource constraints such as inadequate medical supplies and limited supervision of health extension workers were noted as challenges, a key success factor included strong community engagement [ 29 ].
Another six studies examined health outcomes in relation to health insurance schemes or health system reforms [ 25 , 40 , 46 , 47 , 48 , 55 ]. Some improvements in health outcomes were noted. For example, in China, health system reforms aimed at achieving UHC have been associated with decreased maternal mortality rates [ 25 ]. However, the burden of noncommunicable diseases such as diabetes is rising amid significant gaps in their detection and treatment [ 47 ].
Studies also compared patient outcomes in relation to private versus public sector healthcare provision [ 24 , 56 , 58 ]. How the private sector was conceptualized varied across the studies, both in terms of how it was categorized (e.g. for-profit versus not-for-profit), as well as its role in healthcare financing and delivery. Given this heterogeneity, whether the public or private sector leads to higher-quality care and consequently, better health outcomes, is unclear in the reviewed literature. However, the private sector, when financed through out-of-pocket payments, is more likely to exacerbate inequities in access to healthcare.
Finally, two studies examined integrated models of care and their relationship to health outcomes [ 52 , 54 ]. According to these studies, different forms of service integration may positively impact health, for example, through slowed disease progression [ 54 ] and decreased preterm births [ 52 ].
Patient-reported satisfaction and trust in health system
Reports of poor perceived quality of care and low patient satisfaction as barriers to healthcare uptake and enrollment in health insurance schemes were common across the reviewed studies [ 26 , 28 , 36 , 40 , 44 , 47 , 55 , 56 ]. For instance, Alhassan et al. [ 28 ] found that perceived low quality of care, long wait times and poor treatment by healthcare providers reduced clients’ trust in Ghana’s National Health Insurance Scheme, reducing subsequent re-enrollment rates. In Ghana, perceived quality of care was found to exert a greater influence on men’s decisions regarding care uptake than on women’s decisions [ 36 , 44 ]. O’Connell et al. [ 36 ] suggested this gendered difference may be due to men’s care being more likely to be prioritized within household financial decisions, affording them the opportunity to be more discerning regarding the quality of care.
Several studies also discussed the effects of health system reforms and different service delivery models on patient satisfaction and trust in healthcare systems [ 23 , 28 , 29 , 31 , 38 , 43 , 47 , 54 , 57 ]. Yip et al. noted that despite reforms aimed at expanding access to care across China, many patients have chosen to forgo care at primary healthcare facilities altogether due to a lack of trust and dissatisfaction with quality of care [ 47 ]. Similarly, Ravaghi et al. identified contradictory results regarding the effects of hospital autonomy reforms on patient satisfaction. Two studies in Indonesia cited in Ravaghi’s review reported improvements, while others noted decreased or no change in patient satisfaction [ 38 ]. In contrast, four reviews found that integrated, people-centred health services may positively impact patient satisfaction [ 29 , 31 , 54 , 57 ].
Efficiency of healthcare services and systems
Twenty-seven studies addressed the efficiency of healthcare systems and services, which the review by Morgan et al., defined as ‘the extent to which resources are used effectively or are wasted’ [ 23 , p. 608]. These studies discussed inefficiencies in health systems [ 22 , 26 , 28 , 29 , 44 , 48 ], the possible effects of health reforms and other interventions on efficiency [ 21 , 25 , 31 , 37 , 38 , 41 , 44 , 45 , 46 , 47 , 50 , 53 , 54 , 55 , 58 , 59 ], efficiency as a criterion in health policymaking [ 32 ], and the measurement of efficiency [ 22 , 30 , 42 , 51 ], an example of which, as cited in Rezapour et al.’s study, was the percentage of prescriptions including antibiotics in health centres and health posts [ 51 ].
Additionally, some studies compared the efficiency of public and private sector healthcare provision, reporting mixed results [ 23 , 24 , 48 , 58 , 61 ]. For example, higher overhead costs and lower quality of care outcomes, including higher death rates, have been observed in private hospitals compared with public hospitals in the United States [ 24 ]. In contrast, research on the National Health Service in England has suggested that privatization and market-oriented reforms have improved the efficiency of hospital care through cost cutting without evidence of reduced quality [ 58 ].
In LMICs, the private sector has been linked to increased service costs related to overprescribing and use of unnecessary and expensive procedures [ 23 ]. However, Morgan et al. noted that studies assessing private sector performance in LMICs have often focused on unqualified or informal small private providers, such as small drug shops, operating amid weak public health systems and poor regulation, providing an incomplete picture of the role of the private sector in progress towards UHC [ 23 ]. Table 4 captures a high-level overview of the key highlights related to each domain and subdomain of Kruk et al.’s [ 5 ] framework discussed in the studies.
Identified evidence gaps and priorities for future research
Substantial evidence gaps that were identified in the reviewed literature are grouped thematically below. Themes are ordered by how frequently they were discussed by the reviewed studies.
Gap 1: How to measure and monitor UHC, with particular attention to quality of care and equity
Several studies identified the need for additional research to inform the development, selection and use of monitoring and evaluation frameworks and measures to assess quality of care and equity in relation to UHC in various geographic contexts at multiple levels of the health system, including facility and institutional levels [ 22 , 30 , 31 , 34 , 39 , 42 ]. For example, Rodney et al. stressed that countries should select contextually relevant indicators, and pay particular attention to the measurement of equity within UHC, cautioning that measuring equity based solely on wealth quintiles may mask inequities related to other factors such as race or disability [ 39 ]. In addition, two studies discussed the lack of client-reported measurements and advocated for further research to integrate data from household surveys and user-experience surveys [ 22 , 30 ].
Gap 2: Comparative information on the efficiency and effectiveness of public and private health provision and appropriate mix of public and private healthcare
Researchers noted the need for more conclusive evidence comparing the efficiency and effectiveness of public and private health sector provision, and the role of the private sector in contributing to UHC [ 21 , 23 , 56 , 57 , 62 ]. For example, Morgan et al. highlighted the need for greater evidence on how system-level influences such as regulations, may be used to create a public–private healthcare mix that promotes high-quality care and supports the achievement of UHC [ 23 ].
Gap 3: Effects of financial and insurance schemes on quality-of-care delivery and patient outcomes
The reviewed literature identified a lack of evidence regarding the impacts of different financial and insurance schemes on quality-of-care delivery and patient outcomes, particularly for vulnerable groups including women-headed households, children with special needs and migrants [ 34 , 46 , 55 , 62 ]. For example, van Hees et al. noted a lack of evidence regarding the impacts of financial schemes, such as pooling of funds and cost sharing, on equity [ 55 ].
Gap 4: Effects of integrated service delivery models
Studies identified the need for more robust evidence related to the effects of integrated service delivery models on access to quality care, as well as patient and population health outcomes [ 22 , 37 , 52 , 54 ]. Lê et al. specifically highlighted the lack of evidence on equity outcomes related to service integration, suggesting the need for further research in this area [ 54 ].
Gap 5: Mechanisms and contexts that enable and hinder implementation of quality-related interventions
Finally, researchers called for additional evidence regarding the mechanisms and contextual factors such as societal stigma that influence the effectiveness of interventions related to quality of care in the context of UHC [ 34 , 37 , 55 ]. To this aim, van Hees et al. recommended realist evaluations to surface what works, for whom, and in what contextual circumstances [ 55 ]. For example, Palagyi et al. identified a need for further research on task shifting, particularly how the skills gained by health workers can be maintained, and its implications for team dynamics and the delivery of existing programmes [ 37 ].
This scoping review aimed to characterize the existing conceptual and empirical literature on quality of care within the context of UHC. As noted in our results, in the reviewed literature, quality of care was often ill defined or defined inconsistently. A lack of conceptual clarity compromises the development of a robust evidence base able to inform the design and implementation of effective quality-related policies and interventions.
The 45 articles we reviewed for our study reveal a heterogeneous body of literature when compared with Kruk et al.’s quality of care framework. While some framework components including governance and the efficiency of healthcare services and systems were highly represented in the included literature, others were less represented such as physical and technological resources and tools, and patient and population health outcomes.
We also noted in the reviewed literature a lack of clarity regarding how the studies distinguished between private sector involvement in financing and/or delivery of care. This lack of clarity limits our understanding of the implications of private sector engagement for the quality of care and the achievement of UHC in various geographical contexts. Research is required to provide greater clarity of the role and impacts of private sector involvement in financing and/or delivery of health services, to help inform countries’ decision-making regarding private sector engagement. In addition, further research is needed regarding the interactions between the public and private sector and their effects on the sustainability of UHC. For example, studies have noted a concern that the availability of concierge services can create downstream implications for people who cannot afford private insurance, such as an imbalance in resource distribution [ 57 ].
Overall, the identified evidence gaps pointed to the need to build a stronger evidence base about what works, for whom, and under what contextual circumstances, and with what effects on equity to improve quality of care in LMICs and HICs. This includes a need for further evidence on the effects of integrated service delivery models, as well as how regulation can be used to create a public–private healthcare mix promoting high-quality and equitable care. The literature further highlighted the urgent need for additional research to inform the creation of robust monitoring and evaluation frameworks prioritizing equity that could support improvements to quality of care. This includes further research to help support the inclusion and use of disaggregated data, such as by wealth, sex and ethnicity to monitor and inform efforts to increase equity in access, utilization and outcomes for vulnerable populations. Beyond the above-noted research priorities, we also recommend additional research comparing quality related outcomes before and after UHC implementation, and how they intersect with health equity.
Strengths of our scoping review include the use of a broad search methodology and validated search filters in consultation with an expert librarian, and the use of a conceptual framework to guide analysis of findings. Further, our search was not constrained based on country of origin. In our search of the literature, we did not find other published reviews of similar scope about quality of care within the context of UHC.
The primary limitation of our review is the small number of included studies that met our eligibility criteria. This highlights that quality-related research in UHC remains an emerging field. In addition, many of the included studies were narrative reviews, which may not have captured the full breadth of the literature. Another limitation of our review is that we included only English-language studies. Future reviews should attempt to search and synthesize evidence in additional languages to provide more global relevance. Further, the conceptual framework we applied to the analysis of findings does not consider various factors that render health systems more fragile such as pandemics, disasters and conflicts, which may compromise the quality of care and realization of UHC. As our study did not include search terms for specific vulnerable populations such as Indigenous or racialized groups, there is also need for future research related to LMICs and communities experiencing marginalization and discrimination within HICs.
In addition, there may be limited applicability of findings across studies to different geographic regions. Finally, due to the heterogeneity and qualitative nature of the included studies, meta-analysis and synthesis beyond thematic analysis were not feasible.
This review summarized the existence of available evidence on quality of care within the context of UHC, identifying strategies aimed at improving quality of care as well as diverse knowledge gaps. Further research, evaluation and monitoring frameworks including those that attend to equity are required to strengthen the existing evidence base.
Availability of data and materials
This work analyzed secondary sources, which are cited and are publicly accessible or with academic institutional credentials. Authors can confirm that all other relevant data are included in the article and/or its additional files.
Abbreviations
African Region
Region of the Americas
Community Health Worker
Eastern Mediterranean Region
European Region
High-Income Countries
Low- and Middle-Income Countries
Millennium Development Goals
National Health Insurance Scheme
National Health Service
Primary Healthcare
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Sustainable Development Goals
South-East Asian Region
Universal Health Coverage
Western Pacific Region
World Health Organization. Regional Office for the Eastern Mediterranean. Universal health coverage. WHO; 2023. Available from: https://www.emro.who.int/health-topics/uhc/index.html .
United Nations. SDG indicators. Metadata repository. UN; 2023. Available from: https://unstats.un.org/sdgs/metadata/?Text=&Goal=3&Target=3.8SDG .
World Health Organization. Primary health care on the road to universal health coverage. WHO; 2019. Available from: https://www.who.int/docs/default-source/documents/2019-uhc-report-executive-summary .
World Health Organization. The world health report: health systems financing: the path to universal coverage. WHO; 2010. Available from: https://apps.who.int/iris/handle/10665/44371 .
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6(11):e1196–252. https://doi.org/10.1016/S2214-109X(18)30386-3 .
Article PubMed PubMed Central Google Scholar
World Health Organization, OECD, International Bank for Reconstruction and Development/The World Bank. Delivering quality health services: a global imperative for universal health coverage. WHO, OECD, World Bank Group; 2018. Available from: https://www.worldbank.org/en/topic/universalhealthcoverage/publication/delivering-quality-health-services-a-global-imperative-for-universal-health-coverage .
National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Care Services, Board on Global Health, Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: improving health care worldwide. National Academies Press; 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535653/ .
Canadian Institute for Health Information. Hospital care for heart attacks among First Nations, Inuit and Métis. CIHI; 2013. Available from: https://publications.gc.ca/site/eng/439389/publication.html .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616 .
Article Google Scholar
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. https://doi.org/10.1186/1748-5908-5-69 .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7);467–73. https://doi.org/10.7326/M18-0850 .
Yanful B, Kirubarajan A, Mishra S, Bhatia D, Allin S, Di Ruggiero E. Quality in universal health coverage: protocol for a scoping review. Open Science Framework; 2020. Available from: https://osf.io/f8vb6/ .
Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4. https://doi.org/10.1016/j.jclinepi.2014.03.013 .
Article PubMed Google Scholar
Bennett S, Jessani N, Glandon D, Qiu M, Scott K, Meghani A, et al. Understanding the implications of the Sustainable Development Goals for health policy and systems research: results of a research priority setting exercise. Global Health. 2020;16(1):5. https://doi.org/10.1186/s12992-019-0534-2 .
The InterTASC Information Specialists’ Sub-Group. The ISSG search filter resource. ISSG; 2022. Available from: https://sites.google.com/a/york.ac.uk/issg-search-filters-resource/home .
World Health Organization. WHO regional offices. WHO; 2023. Available from: https://www.who.int/about/who-we-are/regional-offices .
Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(3):166. https://doi.org/10.1111/j.1468-0009.2005.00397.x .
Boerma T, Eozenou P, Evans D, Evans T, Kieny MP, Wagstaff A. Monitoring progress towards universal health coverage at country and global levels. PLoS Med. 2014;11(9):e1001731. https://doi.org/10.1371/journal.pmed.1001731 .
Gupta RD, Shahabuddin A. Measuring progress toward universal health coverage: does the monitoring framework of Bangladesh need further improvement? Cureus. 2018; 10(1):e2041. https://doi.org/10.7759/cureus.2041 .
Kamei T, Takahashi K, Omori J, Arimori N, Hishinuma M, Asahara K, et al. Toward advanced nursing practice along with people-centered care partnership model for sustainable universal health coverage and universal access to health. Rev Lat Am Enfermagem. 2017; 25:1–10. https://doi.org/10.1590/1518-8345.1657.2839 .
Blanchet K, Gordon I, Gilbert CE, Wormald R, Awan H. How to achieve universal coverage of cataract surgical services in developing countries: lessons from systematic reviews of other services. Ophthalmic Epidemiol. 2012;19(6):329–39. https://doi.org/10.3109/09286586.2012.717674 .
Bresick G, Christians F, Makwero M, Besigye I, Malope S, Dullie L. Primary health care performance: a scoping review of the current state of measurement in Africa. BMJ Glob Health. 2019;4(Suppl 8):e001496. https://doi.org/10.1136/bmjgh-2019-001496 .
Morgan R, Ensor T, Waters H. Performance of private sector health care: implications for universal health coverage. Lancet. 2016;388(10044):606–12. https://doi.org/10.1016/s0140-6736(16)00343-3 .
Petrou P, Samoutis G, Lionis C. Single-payer or a multipayer health system: a systematic literature review. Public Health. 2018;163:141–52. https://doi.org/10.1016/j.puhe.2018.07.006 .
Article CAS PubMed Google Scholar
Li H, Liu K, Gu J, Zhang Y, Qiao Y, Sun X. The development and impact of primary health care in China from 1949 to 2015: a focused review. Int J Health Plann Manage. 2017;32(3):339–50. https://doi.org/10.1002/hpm.2435 .
Naher N, Hoque R, Hassan MS, Balabanova D, Adams AM, Ahmed SM. The influence of corruption and governance in the delivery of frontline health care services in the public sector: a scoping review of current and future prospects in low and middle-income countries of south and south-east Asia. BMC Public Health. 2020;20(1), 880. https://doi.org/10.1186/s12889-020-08975-0 .
Agarwal S, Sripad P, Johnson C, Kirk K, Bellows B, Ana J, et al. A conceptual framework for measuring community health workforce performance within primary health care systems. Hum Resour Health. 2019;17(1):86. https://doi.org/10.1186/s12960-019-0422-0 .
Alhassan RK, Nketiah-Amponsah E, Arhinful DK. A review of the national health insurance scheme in Ghana: what are the sustainability threats and prospects? PLoS ONE. 2016;11(11):e0165151. https://doi.org/10.1371/journal.pone.0165151 .
Article CAS PubMed PubMed Central Google Scholar
Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15(1):24. https://doi.org/10.1186/s12992-019-0470-1 .
Báscolo E, Houghton N, del Riego A. Construcción de un marco de monitoreo para la salud universal. Rev Panam Salud Pública. 2018. https://doi.org/10.26633/rpsp.2018.81 .
Bitton A, Fifield J, Ratcliffe H, Karlage A, Wang H, Veillard JH, et al. Primary healthcare system performance in low-income and middle-income countries: a scoping review of the evidence from 2010 to 2017. BMJ Glob Health. 2019;4(Suppl 8):e001551. https://doi.org/10.1136/bmjgh-2019-001551 .
Farzaneh A, Ravaghi H. Fanaei A. The ethical framework for policy-making of universal health coverage: a systematic review. J Clin Diagn Res. 2020;14(3):IE01–6. https://doi.org/10.7860/jcdr/2019/43038.13589 .
Ansu-Mensah M, Danquah FI, Bawontuo V, Ansu-Mensah P, Kuupiel D. Maternal perceptions of the quality of care in the free maternal care policy in sub-Sahara Africa: a systematic scoping review. BMC Health Serv Res. 2020;20(1):911. https://doi.org/10.1186/s12913-020-05755-9 .
Mate KS, Sifrim ZK, Chalkidou K, Cluzeau F, Cutler D, Kimball M, et al. Improving health system quality in low- and middle-income countries that are expanding health coverage: a framework for insurance. Int J Qual Health Care. 2013;25(5):497–504. https://doi.org/10.1093/intqhc/mzt053 .
McMichael C, Healy J. Health equity and migrants in the Greater Mekong Subregion. Glob Health Action. 2017;10(1):1271594. https://doi.org/10.1080/16549716.2017.1271594 .
O’Connell TS, Bedford KJA, Thiede M, McIntyre D. Synthesizing qualitative and quantitative evidence on non-financial access barriers: implications for assessment at the district level. Int J Equity Health. 2015;14(1):54. https://doi.org/10.1186/s12939-015-0181-z .
Palagyi A, Dodd R, Jan S, Nambiar D, Joshi R, Tian M, et al. Organisation of primary health care in the Asia-Pacific region: developing a prioritised research agenda. BMJ Glob Health. 2019;4(Suppl 8):e001467. https://doi.org/10.1136/bmjgh-2019-001467 .
Ravaghi H, Foroughi Z, Nemati A, Bélorgeot VD. A holistic view on implementing hospital autonomy reforms in developing countries: a systematic review. Health Policy Plan. 2018;33(10):1118–27. https://doi.org/10.1093/heapol/czy095 .
Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health. 2014;13(1):72. https://doi.org/10.1186/s12939-014-0072-8 .
Sanogo NA, Fantaye AW, Yaya S. Universal health coverage and facilitation of equitable access to care in Africa. Front Public Health. 2019;26(7):102. https://doi.org/10.3389/fpubh.2019.00102 .
Sehngelia L, Pavlova M, Groot W. Impact of healthcare reform on universal coverage in Georgia: a systematic review. Divers Equal Health Care. 2016;13:5. https://doi.org/10.21767/2049-5471.100074 .
Sprockett A. Review of quality assessment tools for family planning programmes in low- and middle-income countries. Health Policy Plan. 2017;32(2):292-302. https://doi.org/10.1093/heapol/czw123 .
Teerawattananon Y, Luz A, Pilasant S, Tangsathitkulchai S, Chootipongchaivat S, Tritasavit N, et al. How to meet the demand for good quality renal dialysis as part of universal health coverage in resource-limited settings? Health Res Policy Syst. 2016;14(1):21. https://doi.org/10.1186/s12961-016-0090-7 .
Umeh CA. Challenges toward achieving universal health coverage in Ghana, Kenya, Nigeria, and Tanzania. Int J Health Plann Manage. 2018;33(4):794–805. https://doi.org/10.1002/hpm.2610 .
White F. Primary health care and public health: foundations of universal health system. Med Princ Pract. 2015;24(2):103–16. https://doi.org/10.1159/000370197 .
Wiysonge CS, Paulsen E, Lewin S, Ciapponi A, Herrera CA, Opiyo N, et al. Financial arrangements for health systems in low-income countries: an overview of systematic reviews. Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.CD011084.pub2 .
Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. 2019;394(10204):1192–204. https://doi.org/10.1016/s0140-6736(19)32136-1 .
Christmals CD, Aidam K. Implementation of the National Health Insurance Scheme (NHIS) in Ghana: lessons for South Africa and low- and middle-income countries. Risk Manag Healthc Policy. 2020;13:1879–904. https://doi.org/10.2147/rmhp.s245615 .
Kim JK, Kim KH, Shin YC, Jang BH, Ko SG. Utilization of traditional medicine in primary health care in low- and middle-income countries: a systematic review. Health Policy Plan. 2020; 35(8):1070–83. https://doi.org/10.1093/heapol/czaa022 .
Mumghamba EG, Joury E, Fatusi O, Ober-Oluoch J, Onigbanjo RJ, Honkala S. Capacity building and financing oral health in the African and Middle East Region. Adv Dent Res. 2015;27(1):32–42. https://doi.org/10.1177/0022034515578909 .
Rezapour R, Tabrizi JS, Farahbakhsh M, Saadati M, Abdolahi HM. Developing Iranian primary health care quality framework: a national study. BMC Public Health. 2019;19(1):911. https://doi.org/10.1186/s12889-019-7237-8 .
Schmied V, Mills A, Kruske S, Kemp L, Fowler C, Homer C. The nature and impact of collaboration and integrated service delivery for pregnant women, children and families: collaboration in universal child and family health services. J Clin Nurs. 2010;19(23–24):3516–26. https://doi.org/10.1111/j.1365-2702.2010.03321.x .
Victora CG, Hanson K, Bryce J, Vaughan JP. Achieving universal coverage with health interventions. Lancet. 2004;364(9444):1541–8. https://doi.org/10.1016/s0140-6736(04)17279-6 .
Lê G, Morgan R, Bestall J, Featherstone I, Veale T, Ensor T. Can service integration work for universal health coverage? Evidence from around the globe. Health Policy. 2016;120(4):406–19. https://doi.org/10.1016/j.healthpol.2016.02.007 .
van Hees SGM, O’Fallon T, Hofker M, Dekker M, Polack S, Banks LM, et al. Leaving no one behind? Social inclusion of health insurance in low- and middle-income countries: a systematic review. Int J Equity Health. 2019;18(1):134. https://doi.org/10.1186/s12939-019-1040-0 .
Kiil A. What characterises the privately insured in universal health care systems? A review of the empirical evidence. Health Policy. 2012;106(1):60–75. https://doi.org/10.1016/j.healthpol.2012.02.019 .
Palumbo R. Keeping candles lit: the role of concierge medicine in the future of primary care. Health Serv Manage Res. 2017;30(2):121–8. https://doi.org/10.1177/0951484816682397 .
Almeida ÁS. The role of private non-profit healthcare organizations in NHS systems: implications for the Portuguese hospital devolution program. Health Policy. 2017;121(6):699–707. https://doi.org/10.1016/j.healthpol.2017.03.016 .
Hayati R, Bastani P, Kabir MJ, Kavosi Z, Sobhani G. Scoping literature review on the basic health benefit package and its determinant criteria. Glob Health. 2018;14(1):26. https://doi.org/10.1186/s12992-018-0345-x .
Schveitzer MC, Zoboli ELCP, Vieira MM da S. Nursing challenges for universal health coverage: a systematic review. Rev Lat Am Enfermagem. 2016(24):e2676. https://doi.org/10.1590/1518-8345.0933.2676 .
Fallah R, Bazrafshan A. Participation of delivering private hospital services in universal health coverage: a systematic scoping review of the developing countries’ evidence. J Educ Health Promot. 2021;31(10):113. https://doi.org/10.4103/jehp.jehp_957_20 .
Nandi S, Schneider H. Using an equity-based framework for evaluating publicly funded health insurance programmes as an instrument of UHC in Chhattisgarh State, India. Health Res Policy Syst. 2020;18(1):50. https://doi.org/10.1186/s12961-020-00555-3 .
Download references
Acknowledgements
Thank you to Vincci Lui from Gerstein Science Information Centre at the University of Toronto for her guidance and advice regarding the search strategy. We also would like to acknowledge Garry Aslanyan, Beverley Essue, Miguel Ángel González Block, Greg Marchildon and Jeremy Veillard, for their guidance.
This research was funded by the Canadian Institutes of Health Research (CIHR) (#407149) for the project titled ‘Towards Equitable Universal Health Coverage in a Globalized Era: A Research Agenda-Setting Workshop’.
Author information
Authors and affiliations.
Division of Social and Behavioural Health Sciences, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Bernice Yanful & Erica Di Ruggiero
Institute of Health Policy, Management and Evaluation, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Abirami Kirubarajan, Dominika Bhatia, Sujata Mishra, Sara Allin & Erica Di Ruggiero
Centre for Global Health, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Erica Di Ruggiero
You can also search for this author in PubMed Google Scholar
Contributions
All listed authors were involved in the study design. BY and AK performed title/abstract and full-text screening, data extraction, and data synthesis, as well as drafting the manuscript. All authors contributed to subsequent revisions. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Bernice Yanful .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sara Allin and Erica Di Ruggiero are co-senior authors.
APPENDIX A: Appendix: Search Strategy
Database: ovid medline: epub ahead of print, in-process & other non-indexed citations, ovid medline® daily and ovid medline®, 1946: september 27, 2021, appendix b: study selection.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yanful, B., Kirubarajan, A., Bhatia, D. et al. Quality of care in the context of universal health coverage: a scoping review. Health Res Policy Sys 21 , 21 (2023). https://doi.org/10.1186/s12961-022-00957-5
Download citation
Received : 21 June 2022
Accepted : 28 December 2022
Published : 23 March 2023
DOI : https://doi.org/10.1186/s12961-022-00957-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality of care
- Universal health coverage
- Health systems
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Frontiers in Oncology
- Cancer Epidemiology and Prevention
- Research Topics
Universal Health Coverage and Global Health in Oncology
Total Downloads
Total Views and Downloads
About this Research Topic
Cancer is a global burden and has been acknowledged as a dedicated sustainable development goal (SDG) by the WHO. Worldwide cancer care in all its aspects reaching from prevention and early detection up to palliative care is still characterized by extensive inequalities in accessibility, availability, ...
Keywords : low and middle income countries, vulnerable groups, universal health coverage, global health, inequalities, accessibility, availability, acceptability, affordability
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Research Topics & Ideas: Healthcare
100+ Healthcare Research Topic Ideas To Fast-Track Your Project

Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you’ve landed on this post, chances are you’re looking for a healthcare-related research topic , but aren’t sure where to start. Here, we’ll explore a variety of healthcare-related research ideas and topic thought-starters across a range of healthcare fields, including allopathic and alternative medicine, dentistry, physical therapy, optometry, pharmacology and public health.
NB – This is just the start…
The topic ideation and evaluation process has multiple steps . In this post, we’ll kickstart the process by sharing some research topic ideas within the healthcare domain. This is the starting point, but to develop a well-defined research topic, you’ll need to identify a clear and convincing research gap , along with a well-justified plan of action to fill that gap.
If you’re new to the oftentimes perplexing world of research, or if this is your first time undertaking a formal academic research project, be sure to check out our free dissertation mini-course. In it, we cover the process of writing a dissertation or thesis from start to end. Be sure to also sign up for our free webinar that explores how to find a high-quality research topic.
Overview: Healthcare Research Topics
- Allopathic medicine
- Alternative /complementary medicine
- Veterinary medicine
- Physical therapy/ rehab
- Optometry and ophthalmology
- Pharmacy and pharmacology
- Public health
- Examples of healthcare-related dissertations
Allopathic (Conventional) Medicine
- The effectiveness of telemedicine in remote elderly patient care
- The impact of stress on the immune system of cancer patients
- The effects of a plant-based diet on chronic diseases such as diabetes
- The use of AI in early cancer diagnosis and treatment
- The role of the gut microbiome in mental health conditions such as depression and anxiety
- The efficacy of mindfulness meditation in reducing chronic pain: A systematic review
- The benefits and drawbacks of electronic health records in a developing country
- The effects of environmental pollution on breast milk quality
- The use of personalized medicine in treating genetic disorders
- The impact of social determinants of health on chronic diseases in Asia
- The role of high-intensity interval training in improving cardiovascular health
- The efficacy of using probiotics for gut health in pregnant women
- The impact of poor sleep on the treatment of chronic illnesses
- The role of inflammation in the development of chronic diseases such as lupus
- The effectiveness of physiotherapy in pain control post-surgery
Topics & Ideas: Alternative Medicine
- The benefits of herbal medicine in treating young asthma patients
- The use of acupuncture in treating infertility in women over 40 years of age
- The effectiveness of homoeopathy in treating mental health disorders: A systematic review
- The role of aromatherapy in reducing stress and anxiety post-surgery
- The impact of mindfulness meditation on reducing high blood pressure
- The use of chiropractic therapy in treating back pain of pregnant women
- The efficacy of traditional Chinese medicine such as Shun-Qi-Tong-Xie (SQTX) in treating digestive disorders in China
- The impact of yoga on physical and mental health in adolescents
- The benefits of hydrotherapy in treating musculoskeletal disorders such as tendinitis
- The role of Reiki in promoting healing and relaxation post birth
- The effectiveness of naturopathy in treating skin conditions such as eczema
- The use of deep tissue massage therapy in reducing chronic pain in amputees
- The impact of tai chi on the treatment of anxiety and depression
- The benefits of reflexology in treating stress, anxiety and chronic fatigue
- The role of acupuncture in the prophylactic management of headaches and migraines
Topics & Ideas: Dentistry
- The impact of sugar consumption on the oral health of infants
- The use of digital dentistry in improving patient care: A systematic review
- The efficacy of orthodontic treatments in correcting bite problems in adults
- The role of dental hygiene in preventing gum disease in patients with dental bridges
- The impact of smoking on oral health and tobacco cessation support from UK dentists
- The benefits of dental implants in restoring missing teeth in adolescents
- The use of lasers in dental procedures such as root canals
- The efficacy of root canal treatment using high-frequency electric pulses in saving infected teeth
- The role of fluoride in promoting remineralization and slowing down demineralization
- The impact of stress-induced reflux on oral health
- The benefits of dental crowns in restoring damaged teeth in elderly patients
- The use of sedation dentistry in managing dental anxiety in children
- The efficacy of teeth whitening treatments in improving dental aesthetics in patients with braces
- The role of orthodontic appliances in improving well-being
- The impact of periodontal disease on overall health and chronic illnesses
Tops & Ideas: Veterinary Medicine
- The impact of nutrition on broiler chicken production
- The role of vaccines in disease prevention in horses
- The importance of parasite control in animal health in piggeries
- The impact of animal behaviour on welfare in the dairy industry
- The effects of environmental pollution on the health of cattle
- The role of veterinary technology such as MRI in animal care
- The importance of pain management in post-surgery health outcomes
- The impact of genetics on animal health and disease in layer chickens
- The effectiveness of alternative therapies in veterinary medicine: A systematic review
- The role of veterinary medicine in public health: A case study of the COVID-19 pandemic
- The impact of climate change on animal health and infectious diseases in animals
- The importance of animal welfare in veterinary medicine and sustainable agriculture
- The effects of the human-animal bond on canine health
- The role of veterinary medicine in conservation efforts: A case study of Rhinoceros poaching in Africa
- The impact of veterinary research of new vaccines on animal health
Topics & Ideas: Physical Therapy/Rehab
- The efficacy of aquatic therapy in improving joint mobility and strength in polio patients
- The impact of telerehabilitation on patient outcomes in Germany
- The effect of kinesiotaping on reducing knee pain and improving function in individuals with chronic pain
- A comparison of manual therapy and yoga exercise therapy in the management of low back pain
- The use of wearable technology in physical rehabilitation and the impact on patient adherence to a rehabilitation plan
- The impact of mindfulness-based interventions in physical therapy in adolescents
- The effects of resistance training on individuals with Parkinson’s disease
- The role of hydrotherapy in the management of fibromyalgia
- The impact of cognitive-behavioural therapy in physical rehabilitation for individuals with chronic pain
- The use of virtual reality in physical rehabilitation of sports injuries
- The effects of electrical stimulation on muscle function and strength in athletes
- The role of physical therapy in the management of stroke recovery: A systematic review
- The impact of pilates on mental health in individuals with depression
- The use of thermal modalities in physical therapy and its effectiveness in reducing pain and inflammation
- The effect of strength training on balance and gait in elderly patients
Topics & Ideas: Optometry & Opthalmology
- The impact of screen time on the vision and ocular health of children under the age of 5
- The effects of blue light exposure from digital devices on ocular health
- The role of dietary interventions, such as the intake of whole grains, in the management of age-related macular degeneration
- The use of telemedicine in optometry and ophthalmology in the UK
- The impact of myopia control interventions on African American children’s vision
- The use of contact lenses in the management of dry eye syndrome: different treatment options
- The effects of visual rehabilitation in individuals with traumatic brain injury
- The role of low vision rehabilitation in individuals with age-related vision loss: challenges and solutions
- The impact of environmental air pollution on ocular health
- The effectiveness of orthokeratology in myopia control compared to contact lenses
- The role of dietary supplements, such as omega-3 fatty acids, in ocular health
- The effects of ultraviolet radiation exposure from tanning beds on ocular health
- The impact of computer vision syndrome on long-term visual function
- The use of novel diagnostic tools in optometry and ophthalmology in developing countries
- The effects of virtual reality on visual perception and ocular health: an examination of dry eye syndrome and neurologic symptoms
Topics & Ideas: Pharmacy & Pharmacology
- The impact of medication adherence on patient outcomes in cystic fibrosis
- The use of personalized medicine in the management of chronic diseases such as Alzheimer’s disease
- The effects of pharmacogenomics on drug response and toxicity in cancer patients
- The role of pharmacists in the management of chronic pain in primary care
- The impact of drug-drug interactions on patient mental health outcomes
- The use of telepharmacy in healthcare: Present status and future potential
- The effects of herbal and dietary supplements on drug efficacy and toxicity
- The role of pharmacists in the management of type 1 diabetes
- The impact of medication errors on patient outcomes and satisfaction
- The use of technology in medication management in the USA
- The effects of smoking on drug metabolism and pharmacokinetics: A case study of clozapine
- Leveraging the role of pharmacists in preventing and managing opioid use disorder
- The impact of the opioid epidemic on public health in a developing country
- The use of biosimilars in the management of the skin condition psoriasis
- The effects of the Affordable Care Act on medication utilization and patient outcomes in African Americans
Topics & Ideas: Public Health
- The impact of the built environment and urbanisation on physical activity and obesity
- The effects of food insecurity on health outcomes in Zimbabwe
- The role of community-based participatory research in addressing health disparities
- The impact of social determinants of health, such as racism, on population health
- The effects of heat waves on public health
- The role of telehealth in addressing healthcare access and equity in South America
- The impact of gun violence on public health in South Africa
- The effects of chlorofluorocarbons air pollution on respiratory health
- The role of public health interventions in reducing health disparities in the USA
- The impact of the United States Affordable Care Act on access to healthcare and health outcomes
- The effects of water insecurity on health outcomes in the Middle East
- The role of community health workers in addressing healthcare access and equity in low-income countries
- The impact of mass incarceration on public health and behavioural health of a community
- The effects of floods on public health and healthcare systems
- The role of social media in public health communication and behaviour change in adolescents
Examples: Healthcare Dissertation & Theses
While the ideas we’ve presented above are a decent starting point for finding a healthcare-related research topic, they are fairly generic and non-specific. So, it helps to look at actual dissertations and theses to see how this all comes together.
Below, we’ve included a selection of research projects from various healthcare-related degree programs to help refine your thinking. These are actual dissertations and theses, written as part of Master’s and PhD-level programs, so they can provide some useful insight as to what a research topic looks like in practice.
- Improving Follow-Up Care for Homeless Populations in North County San Diego (Sanchez, 2021)
- On the Incentives of Medicare’s Hospital Reimbursement and an Examination of Exchangeability (Elzinga, 2016)
- Managing the healthcare crisis: the career narratives of nurses (Krueger, 2021)
- Methods for preventing central line-associated bloodstream infection in pediatric haematology-oncology patients: A systematic literature review (Balkan, 2020)
- Farms in Healthcare: Enhancing Knowledge, Sharing, and Collaboration (Garramone, 2019)
- When machine learning meets healthcare: towards knowledge incorporation in multimodal healthcare analytics (Yuan, 2020)
- Integrated behavioural healthcare: The future of rural mental health (Fox, 2019)
- Healthcare service use patterns among autistic adults: A systematic review with narrative synthesis (Gilmore, 2021)
- Mindfulness-Based Interventions: Combatting Burnout and Compassionate Fatigue among Mental Health Caregivers (Lundquist, 2022)
- Transgender and gender-diverse people’s perceptions of gender-inclusive healthcare access and associated hope for the future (Wille, 2021)
- Efficient Neural Network Synthesis and Its Application in Smart Healthcare (Hassantabar, 2022)
- The Experience of Female Veterans and Health-Seeking Behaviors (Switzer, 2022)
- Machine learning applications towards risk prediction and cost forecasting in healthcare (Singh, 2022)
- Does Variation in the Nursing Home Inspection Process Explain Disparity in Regulatory Outcomes? (Fox, 2020)
Looking at these titles, you can probably pick up that the research topics here are quite specific and narrowly-focused , compared to the generic ones presented earlier. This is an important thing to keep in mind as you develop your own research topic. That is to say, to create a top-notch research topic, you must be precise and target a specific context with specific variables of interest . In other words, you need to identify a clear, well-justified research gap.
Need more help?
If you’re still feeling a bit unsure about how to find a research topic for your healthcare dissertation or thesis, check out Topic Kickstarter service below.

You Might Also Like:


15 Comments
I need topics that will match the Msc program am running in healthcare research please
Hello Mabel,
I can help you with a good topic, kindly provide your email let’s have a good discussion on this.
Can you provide some research topics and ideas on Immunology?
Thank you to create new knowledge on research problem verse research topic
Help on problem statement on teen pregnancy
This post might be useful: https://gradcoach.com/research-problem-statement/
can you provide me with a research topic on healthcare related topics to a qqi level 5 student
Please can someone help me with research topics in public health ?
Hello I have requirement of Health related latest research issue/topics for my social media speeches. If possible pls share health issues , diagnosis, treatment.
I would like a topic thought around first-line support for Gender-Based Violence for survivors or one related to prevention of Gender-Based Violence
Please can I be helped with a master’s research topic in either chemical pathology or hematology or immunology? thanks
Can u please provide me with a research topic on occupational health and safety at the health sector
Good day kindly help provide me with Ph.D. Public health topics on Reproductive and Maternal Health, interventional studies on Health Education
may you assist me with a good easy healthcare administration study topic
May you assist me in finding a research topic on nutrition,physical activity and obesity. On the impact on children
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Achieving Universal Health Insurance Coverage in the United States: Addressing Market Failures or Providing a Social Floor?
The United States spends substantially more on health care than most developed countries, yet leaves a greater share of the population uninsured. We suggest that incremental insurance expansions focused on addressing market failures will propagate inefficiencies and are not likely to facilitate active policy decisions that align with societal coverage goals. By instead defining a basic bundle of services that is publicly financed for all, while allowing individuals to purchase additional coverage, policymakers could both expand coverage and maintain incentives for innovation, fostering universal access to innovative care in an affordable system.
Katherine Baicker is dean and Emmett Dedmon Professor, University of Chicago Harris School of Public Policy, Chicago, Illinois. Amitabh Chandra is Ethel Zimmerman Wiener Professor of Public Policy, Harvard Kennedy School, and Henry and Allison McCance Professor of Business Administration, Harvard Business School, Cambridge, Massachusetts. Mark Shepard is Associate Professor, Harvard Kennedy School, Cambridge, Massachusetts. Their email addresses are [email protected], [email protected], and [email protected]. This paper is based on a manuscript prepared for the Journal of Economic Perspectives. The authors thank the editors and Joe Newhouse for helpful feedback and suggestions, and Jason Furman and Matt Fiedler for sharing historical data on US uninsured rates. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research.
Baicker serves on the boards of Eli Lilly, the Mayo Clinic, the Urban Institute, the Chicago Council on Global Affairs, and NORC. Baicker and Chandra serve on the CBO Panel of Health Advisers.
Amitabh Chandra Disclosures
Congressional Budget Office (Federal Government). Panel of Health Advisors. Unpaid. Leigh Speakers Bureau, Speakers Bureau Washington Speakers Bureau, Speakers Bureau Analysis Group, Academic Affiliate Kyruus, Advisor Health Engine, Advisor SmithRx, Advisor
MARC RIS BibTeΧ
Download Citation Data
Published Versions
Katherine Baicker & Amitabh Chandra & Mark Shepard, 2023. " Achieving Universal Health Insurance Coverage in the United States: Addressing Market Failures or Providing a Social Floor?, " Journal of Economic Perspectives, vol 37(2), pages 99-122.
Mentioned in the News
More from nber.
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .

Filed under:
- Health Care
Dylan Scott answers 9 key questions about universal health care around the world
Vox policy reporter Dylan Scott traveled to Taiwan, Australia, and the Netherlands to see their health systems.
/cdn.vox-cdn.com/uploads/chorus_image/image/66226566/MW_Vox_DutchHealthcare2019_118.0.jpg)
Share this story
- Share this on Facebook
- Share this on Twitter
- Share this on Reddit
- Share All sharing options
Share All sharing options for: Dylan Scott answers 9 key questions about universal health care around the world
Vox policy reporter Dylan Scott traveled the world last fall to explore what the US can learn from other countries’ health systems , visiting Taiwan, Australia, and the Netherlands. His trips were the foundation for Everybody Covered , a Vox series on health care that also reported on health systems in the United Kingdom and Maryland .
Dylan did a Reddit Ask Me Anything session on Wednesday, January 29, discussing everything from how countries pay for universal health care to what it will take to achieve further health care reform in America. Here’s a roundup of some of the most interesting questions and answers, lightly edited for clarity.
1) How do countries pay for public health insurance?
Icantnotthink: Where does the payment for public health care come from in other countries?
Dylan: Most of these countries use some mix of 1) payroll taxes for individuals, 2) employer contributions, and 3) general government revenue and progressive/sin taxes. To be honest, there isn’t one model to follow. Each country had its own health funding plan that has since been reformed to meet the needs of their current system, just as the US would. But other countries are looking for health care dollars in many of the same places Medicare-for-all supporters think we should here.
2) When it comes to covering everyone, is a country’s population density important?
Verybalnduser: How important would you say a country’s population density is to keeping total cost down?
Dylan Scott: It’s a huge asset. Taiwan has been able to keep its overall spending low — people on the left would say their single-payer program is actually underfunded — and cost sharing low for patients in large part because its urbanized nature makes it easier for a smaller workforce to meet the needs of its patient population. The Netherlands has been very innovative in delivery reforms, meant to keep costs in check, something that’s clearly been aided by its density. Australia , on the other hand, even with a universal public insurance plan, has still struggled with access in its more rural areas.
3) Is there a lot of paperwork in a single-payer system?
ZenBacle: How much paperwork do patients in single-payer systems have to fill out? And how much time do those patients have to spend fighting with health care providers to get them to honor their coverage?
Dylan Scott: One of the benefits of single-payer is there’s a lot less administration. We visited a hospital in Taipei, Taiwan, and while all the clinic lobbies were full, the cashier’s desk was basically empty. One survey finding that stuck out to me showed the doctors in the Netherlands (with private insurance) are more annoyed about paperwork than their peers in more socialized systems. So while I wouldn’t want to try to quantify it off the top of my head, there seems to be less of a paperwork headache.
Everybody Covered
What the US can learn from other countries’ health systems
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/19653153/0Q1A6670__1_.jpg)
- Taiwan’s single-payer success story — and its lessons for America
- Two sisters. Two different journeys through Australia’s health care system.
- The Netherlands has universal health insurance — and it’s all private
- The answer to America’s health care cost problem might be in Maryland
- In the UK’s health system, rationing isn’t a dirty word
4) Between Taiwan, Australia, and the Netherlands, which policy would translate most easily to the US?
Doctor_YOOOOU: Which of these universal health care systems is “closest” in terms of the amount of reform required to the United States?
Dylan: This is a tricky one — no country looks much like the US status quo. The Netherlands does have a lot of the same features as Obamacare (ban on preexisting conditions, individual mandate, government assistance to cover the costs), but it’s available to everybody and it’s stricter. The mandate penalty is harsher, the government rules on cost sharing are more stringent, and the government actually helps set prices and an overall budget for health care. So it’s much more involved than the US government is in administering that private health insurance. And almost all of the insurers are nonprofits.
So we’re talking about huge changes to move the US system to something that looks more like the Dutch — and that’s one I’d name as closest (along with Japan) to what we have right now.
5) Do solutions exist within the US that can be applied to the rest of the country?
Blakestonefeather: You traveled the world to explore what the US can learn, but did you also travel the US to learn if the US can learn? [In other words,] what are the barriers we in America face to learning/being able to learn?
Dylan Scott: We actually did one story in the US, on Maryland’s unique system for paying hospitals . (Every insurer — private, Medicare and Medicaid — pays the same rates for the same services.)
But there is a huge challenge in translating policies from abroad to the US. Taiwan and Australia have about the same population as Texas, but Taiwan’s is contained to a tiny island off the coast of China and Australia is a continent. The Netherlands is one of the most densely populated countries in the world; the United States is one of the least.
Then you’ve got political differences; Princeton economist Uwe Reinhardt famously didn’t believe single-payer could work in the US, not because it’s not a good idea but because the government was too beholden to corporate interests. The recent failure of surprise billing legislation in Congress in the face of industry opposition is certainly a warning sign to any aspiring reformers.
So the dissatisfying answer to “so what can the US learn from these other countries’ successes?” is: It’s complicated. But my hope for this series is it would speak to the kinds of values and strategies, if less the specific policies, that are necessary to achieve universal health care.
6) What does the American health care system get right?
taksark: What’s something good about the American health care system that could be kept and improved on in a better version?
Dylan Scott: The geographic immensity of the US has forced a lot of experimentation with telemedicine, and that is both a necessity and an area where other countries have tried to draw from what the US has done. I heard a lot from doctors about coming to the US to learn the latest on best practices for delivering care.
I think the US is still seen as a leader in innovative medicine — the question is why can’t we give more people access to it?
7) Besides America, what other countries have private health insurance?
To_Much_Too_Soon: How many other countries besides America have private health insurance?
Dylan: The US relies much more on private health insurance than any other country I’m aware of. About half of US citizens depend on private insurance as their primary coverage, and about 8 percent of our GDP is private health spending; most other developed economies don’t top 4 percent of GDP for private spending.
There are countries like the Netherlands with universal private insurance. But their private insurance is a lot different than ours: Almost all of the insurers are nonprofits, the government sets rules about premiums and cost sharing, there is a global budget for health care costs, etc.
Some countries with single-payer programs, like Australia, allow private insurance as a supplement — so you can get more choice in doctor or can skip the line for surgery. But no developed economy I know of is so dependent on private insurance as the US and with comparatively few regulations about its benefits.
8) What surprised you the most throughout your reporting?
JoseyGunner: What shocked you the most during your travels?
Dylan Scott: I was surprised how often people I talked to were shocked by the worst parts of US health care. The uninsured rates, the deductibles we have to pay, the very idea of a surprise medical bill — all of it was unfathomable to many of the people I met.
9) What are the biggest hurdles to any future health reforms in the US?
Flogopickles: What do you see as America’s biggest hurdle to achieving any sort of movement in affordable care for our citizens?
Dylan Scott: The status quo is powerful for two reasons: One, it’s good enough for enough people that big change feels like a risky proposition to a lot of the population and, two, health industry interests are so influential in Washington, DC. Overcoming those two things — people’s inherent aversion to risk in health care and the power of industry to constrain policymaking, especially price constraints for medical care — are the biggest hurdles to any future health reforms.
Join the conversation
• Read Dylan Scott’s full Reddit AMA
• Sign up for VoxCare, Vox’s health policy newsletter
• Join Vox’s health policy Facebook group
• Listen to the Impact episode about Taiwan’s single-payer system
Will you support Vox today?
We believe that everyone deserves to understand the world that they live in. That kind of knowledge helps create better citizens, neighbors, friends, parents, and stewards of this planet. Producing deeply researched, explanatory journalism takes resources. You can support this mission by making a financial gift to Vox today. Will you join us?
We accept credit card, Apple Pay, and Google Pay. You can also contribute via
Biden’s surprise proposal to debate Trump early, explained
Make “free speech” a progressive rallying cry again, the silver lining in a very bad poll for biden, sign up for the newsletter today, explained, thanks for signing up.
Check your inbox for a welcome email.
Oops. Something went wrong. Please enter a valid email and try again.
Point Turning Point: the Case for Universal Health Care
An argument that the COVID-19 pandemic might be the turning point for universal health care.
Why the U.S. Needs Universal Health Care
As we all grapple with our new reality, it's difficult to think of anything beyond the basics. How do we keep our families safe? Are we washing our hands enough ? Do we really have to sanitize the doorknobs and surfaces every day? How do we get our cats to stop videobombing our Zoom meetings? Do we have enough toilet paper?

Win McNamee | Getty Images
The more we read the headlines, the more we feel the need to do something, or at least say something. Change is happening – ready or not. Maybe talking about some of these important issues can lead to action that will help us steer out of this skid.
Historically, Americans have found ways to meet their circumstances with intention, moving in mass to make heretofore unimaginable change that has sustained and improved our lives to this day. The Great Depression lead to the creation of the New Deal and Social Security. The Triangle Shirtwaist Factory fire brought about change in labor conditions. The Cuyahoga River fire lead to the founding of the Environmental Protection Agency.
Could the COVID-19 pandemic be the turning point for universal health care? We can't think of a more propitious time. In the first two weeks of April, 5.2 million Americans filed for unemployment. Economists believe that 30% unemployment is possible by fall. For most Americans, our health care is tied to our employment, and because of this, millions of Americans are losing their health care just when they may need it the most. Economists predict that health insurance premiums will likely increase by 40% in the next year due to less payers and more who are in need of care and the eventual collapse of private health care insurance .
Our current circumstances have illustrated the need for universal health care in a way that is obvious and undeniable. Below we have listed the most frequent arguments in opposition followed by an evidence-based rebuttal.
1. Point: "Governments are wasteful and shouldn't be in charge of health care."
Counterpoint: In 2017, the U.S. spent twice as much on health care (17.1% of GDP) as comparable Organization for Economic Co-Operation and Development countries (OECD) (8.8% of GDP), all of whom have universal health care. The country with the second highest expenditure after the U.S. is Switzerland at 12.3%, nearly 5% less. Of all these countries, the U.S. has the highest portion of private insurance. In terms of dollars spent, the average per capita health care spending of OECD countries is $3,558, while in the U.S. it's $10,207 – nearly three times as costly.
Bottom line: Among industrialized countries with comparable levels of economic development, government-provided health care is much more efficient and more economical than the U.S. system of private insurance.
2. Point: "U.S. health care is superior to the care offered by countries with universal health care."
Counterpoint: According to the Commonwealth Health Fund , in the U.S., infant mortality is higher and the life span is shorter than among all comparable economies that provide universal health care. Maternal mortality in the U.S. is 30 per 100,000 births and 6.4 per 100,000 births on average in comparable countries, which is nearly five times worse.
In addition, the U.S. has the highest chronic disease burden (e.g., diabetes, hypertension) and an obesity rate that is two times higher than the OECD average. In part due to these neglected conditions, in comparison to comparable countries, the U.S. (as of 2016) had among the highest number of hospitalizations from preventable causes and the highest rate of avoidable deaths.
The Peterson-Kaiser Health System Tracker , which is a collaborative effort to monitor the quality and cost of U.S. health care, shows that among comparable countries with universal health care, mortality rate is lower across the board on everything from heart attacks to child birth. The U.S. also has higher rates of medical, medication and lab errors relative to similar countries with universal health care.
Bottom line: With our largely privately funded health care system, we are paying more than twice as much as other countries for worse outcomes.
3. Point: "Universal health care would be more expensive."
Counterpoint: The main reason U.S. health care costs are so high is because we don't have universal health care. Unlike other first world countries, the health care system in the U.S. is, to a great extent, run through a group of businesses. Pharmaceutical companies are businesses. Insurance companies are businesses. Hospital conglomerates are businesses. Even doctors' offices are businesses.
Businesses are driven to streamline and to cut costs because their primary goal is to make a profit. If they don't do this, they can't stay in business. It could mean that in the process of "streamlining," they would be tempted to cut costs by cutting care. Under the current system, a share of our health care dollars goes to dividends rather than to pay for care, hospitals are considered a "financial asset" rather than a public service entity and a large portion of their budgets are dedicated to marketing rather than patient care.
Given all these business expenses, it shouldn't be surprising that the business-oriented privately funded health care system we have is more expensive and less effective than a government provided universal system. In addition, for the health care system as a whole, universal health care would mean a massive paperwork reduction. A universal system would eliminate the need to deal with all the different insurance forms and the negotiations over provider limitations. As a result, this would eliminate a large expense for both doctors and hospitals.
The economist Robert Kuttner critiques the system this way: "For-profit chains … claim to increase efficiencies by centralizing administration, cutting waste, buying supplies in bulk at discounted rates, negotiating discounted fees with medical professionals, shifting to less wasteful forms of care and consolidating duplicative facilities." As he points out, "using that logic, the most efficient 'chain' of all is a universal national system."
Evidence to support these points can be found in a recent Yale University study that showed that single-payer Medicare For All would result in a 13% savings in national health-care expenditures. This would save the country $450 billion annually.
Bottom line: Universal health care would be less expensive overall, and an added benefit would be that health care decisions would be put in the hands of doctors rather than insurance companies, which have allegiances to shareholders instead of patient care.
4. Point: "I have to take care of my own family. I can't afford to worry about other people."
Counterpoint: It is in all of our best interests to take care of everyone. Aside from the fact that it is the compassionate and moral thing to do, viruses do not discriminate. When people don't have insurance, they won't go to the doctor unless they're gravely ill. Then, they're more likely to spread illness to you and your family members while they delay getting the care they need.
In addition, when people wait for care or don't get the prophylactic care then need, they end up in the emergency room worse off with more costly complications and requiring more resources than if they had been treated earlier. Taxpayers currently cover this cost. This affects everyone, insured or not. Why not prevent the delay upfront and make it easy for the patient to get treatment early and, as an added bonus, cost everyone less money?
In addition, the health of the economy impacts everyone. Healthy workers are essential to healthy businesses and thus a healthy economy. According to the Harvard School of Public Health , people who are able to maintain their health are more likely to spend their money on goods and services that drive the economy.
Bottom line: The health of others is relevant to the health of our families either through containment of infectious diseases such as COVID-19 or through the stability of the economy. Capitalism works best with a healthy workforce.
5. Point: "Entrepreneurship and innovation is what makes the U.S. a world leader."
Counterpoint: Imagine how many people in the U.S. could start their own businesses or bring their ideas to market if they didn't have to worry about maintaining health care for their families. So many people stay tethered to jobs they hate just so their family has health care. With workers not needing to stay in jobs they don't like in order to secure health insurance, universal healthcare would enable people to acquire jobs where they would be happier and more productive. Workers who wanted to start their own business could more easily do so, allowing them to enter the most creative and innovative part of our economy – small businesses.
In his book, "Everything for Sale," economist Robert Kuttner asserts that it's important to understand that businesses outside of the U.S. don't have to provide health care for their employees, which makes them more competitive. From a business point of view, American companies, released from the burden of paying employee insurance, would be more competitive internationally. They would also be more profitable as they wouldn't have to do all the paperwork and the negotiating involved with being the intermediary between employees and insurance companies.
Bottom line: Unburdening businesses from the responsibility of providing health insurance for their employees would increase competitiveness as well as encourage entrepreneurship and innovation, and allow small businesses room to thrive.
6. Point: "The wait times are too long in countries with universal health care."
Counterpoint: The wait times on average are no longer in countries with universal healthcare than they are in the U.S., according to the Peterson-Kaiser Health System Tracker . In some cases, the wait times are longer in the U.S., with insurance companies using valuable time with their requirements to obtain referrals and approvals for sometimes urgently needed treatments. On average, residents of Germany, France, UK, Australia, and the Netherlands reported shorter wait times relative to the U.S.
Bottom line: Wait times are longer in the U.S. when compared with many countries with a universal health care system.
7. Point: "My insurance is working just fine, so why change anything?"
Counterpoint: A comprehensive study conducted in 2018 found that 62% of bankruptcies are due to medical bills and, of those, 75% were insured at the time. Most people who have insurance are insufficiently covered and are one accident, cancer diagnosis or heart attack away from going bankrupt and losing everything. The U.S. is the only industrialized country in the world whose citizens go bankrupt due to medical bills. And, if you survive a serious illness and don't go bankrupt, you may end up buried in bills and paperwork from your insurance company and medical providers. All of this takes time and energy that would be better spent healing or caring for our loved ones. Besides, we don't need to abolish private health insurance. Some countries like Germany have a two-tiered system that provides basic non-profit care for all but also allows citizens to purchase premium plans through private companies.
Bottom line: Private insurance does not protect against medical bankruptcy, but universal health care does. The residents of countries with universal health care do not go bankrupt due to medical bills.
8. Point: "I don't worry about losing my insurance because if I lose my job, I can just get another one."
Counterpoint: We can't predict what will happen with the economy and whether another job will be available to us. This pandemic has proven that it can all go bad overnight. In addition, if you lose your job, there is less and less guarantee that you will find a new job that provides insurance . Providing insurance, because it is so expensive, has become an increasingly difficult thing for companies to do. Even if you're able to find a company that provides health care when you change jobs, you would be relying on your employer to choose your health plan. This means that the employee assumes that the company has his or her best interests in mind when making that choice, rather than prioritizing the bottom line for the benefit of the business. Even if they're not trying to maximize their profit, many companies have been forced to reduce the quality of the insurance they provide to their workers, simply out of the need to be more competitive or maintain solvency.
Bottom line: There are too many factors beyond our control (e.g., pandemic, disability, economic recession) to ensure anyone's employment and, thus, health care. Universal health care would guarantee basic care. Nobody would have to go without care due to a job loss, there would be greater control over costs and businesses would not have to fold due to the exorbitant and rising cost of providing health insurance to their employees.
9. Point: "Pharmaceutical companies need to charge so much because of research and development."
Counterpoint: It's usually not the pharmaceutical companies developing new drugs. They develop similar drugs that are variations on existing drugs, altered slightly so that they can claim a new patent. Or they buy out smaller companies that developed new drugs, thus minimizing their own R&D costs. Most commonly, they manufacture drugs developed under funding from the National Institutes of Health, and thus, the tax payers are the greatest funder of drug development via NIH grants provided to university labs.
Oddly, this investment in R&D does not appear to extend any discount to the tax payers themselves. In "The Deadly Costs of Insulin, " the author writes that insulin was developed in a university lab in 1936. In 1996, the cost of a vial of insulin was $21. Today, the cost of a vial of insulin could be as much as $500, causing some without insurance to risk their lives by rationing or going without. The cost of manufacturing the drug has not gone up during that time. So, what accounts for the huge increase in price? In " The Truth About Drug Companies ," the author demonstrates that drug companies use the bulk of their profits for advertising, not R&D or manufacturing. A universal health care system would not only not need to advertise, but would also be more effective at negotiating fair drug prices. Essentially, the government as a very large entity could negotiate price much more effectively as one large system with the government as the largest purchaser.
Bottom line: Taxpayers contribute most of the money that goes into drug development. Shouldn't they also reap some of the benefits of their contribution to R&D? Americans should not have to decide between their heart medication and putting food on the table when their tax dollars have paid for the development of many of these medications.
10. Point: "I don't want my taxes to go up."
Counterpoint: Health care costs and deductibles will go down to zero and more than compensate for any increase in taxes, and overall health care needs will be paid for, not just catastrophic health events. According to the New York Times , “…when an American family earns around $43,000, half of the average compensation when including cash wages plus employer payroll tax and premium contributions, 37% of that ends up going to taxes and health care premiums. In high-tax Finland, the same type of family pays 23% of their compensation in labor taxes, which includes taxes they pay to support universal health care. In France, it’s 2%. In the United Kingdom and Canada, it is less than 0% after government benefits.”
Bottom line: With a universal health care system, health care costs and deductibles will be eliminated and compensate for any increase in taxes.
11. Point: "I don't want to have to pay for health care for people making bad choices or to cover their pre-existing conditions."
Counterpoint: Many of the health problems on the pre-existing conditions list are common, genetically influenced and often unavoidable. One estimate indicates that up to 50% – half! – of all (non-elderly) adults have a pre-existing condition. Conditions on the list include anxiety, arthritis, asthma, cancer, depression, heart defect, menstrual irregularities, stroke and even pregnancy. With universal health care, no one would be denied coverage.
It's easy to assume that your health is under your control, until you get into an accident, are diagnosed with cancer or have a child born prematurely. All of a sudden, your own or your child's life may rely on health care that costs thousands or even millions of dollars. The health insurance that you once thought of as "good enough" may no longer suffice, bankruptcy may become unavoidable and you (or your child) will forever have a pre-existing condition. Some people may seem careless with their health, but who's to judge what an avoidable health problem is, vs. one that was beyond their control?
For the sake of argument, let's say that there are some folks in the mix who are engaging in poor health-related behaviors. Do we really want to withhold quality care from everyone because some don't take care of their health in the way we think they should? Extending that supposition, we would withhold public education just because not everyone takes it seriously.
Bottom line: In 2014, protections for pre-existing conditions were put in place under the Affordable Care Act. This protection is under continuous threat as insurance company profits are placed above patient care. Universal health care would ensure that everyone was eligible for care regardless of any conditions they may have.
And, if universal health care is so awful, why has every other first-world nation implemented it? These countries include: Australia, Austria, Bahrain, Belgium, Brunei, Canada, Cyprus, Denmark, Finland, France, Germany, Greece, Hong Kong, Iceland, Ireland, Israel, Italy, Japan, Kuwait, Luxembourg, Netherlands, New Zealand, Norway, Portugal, Singapore, Slovenia, South Korea, Spain, Sweden, Switzerland, United Arab Emirates and the U.K.
Changing collective minds can seem impossible. But there is precedent. Once unimaginable large-scale change has happened in our lifetime (e.g. legalization of gay marriage, election of the first black president of the U.S. and the #MeToo movement), and support for universal health care has never been higher (71% in favor, according to a 2019 Hill-HarrisX survey ).
Point: As Chuck Pagano said, "If you don't have your health, you don't have anything."
Counterpoint: If good health is everything, why don't we vote as if our lives depended on it? This pandemic has taught us that it does.
Bottom line: Launching universal health care in the U.S. could be a silver lining in the dark cloud of this pandemic. Rather than pay lip service to what really matters, let's actually do something by putting our votes in service of what we really care about: the long-term physical and economic health of our families, our communities and our country.
Photos: Hospital Heroes

Tags: health insurance , health care , Coronavirus , pandemic , New Normal
Most Popular

Patient Advice

health disclaimer »
Disclaimer and a note about your health ».
Sign Up for Our 3-Day Guide to Medicare
Confused about Medicare? We can help you understand the different Medicare coverage options available to help you choose the best Medicare coverage for you or a loved one.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
5 types of primary care doctors.
Elaine K. Howley May 15, 2024
How to Tell You Have a Hernia?
Claire Wolters May 14, 2024
How to Treat Seasonal Allergies
Shanley Chien May 13, 2024
Questions to Ask About Diabetes
Toby Smithson and Elaine K. Howley May 13, 2024
ER, Urgent Care or Primary Physician?
Elaine K. Howley May 10, 2024

IUI vs. IVF
Christine Comizio May 9, 2024

Navigating Insurance and Costs at ASCs
Paul Wynn May 9, 2024

ASC vs. Hospital Outpatient Department
Shanley Chien May 9, 2024

How to Prepare for a Colonoscopy
Ruben Castaneda and Payton Sy May 9, 2024

How to Find the Best Spinal Surgeon
Elaine K. Howley May 6, 2024

Healthcare Thesis Statement: Examples of Universal Healthcare Pros and Cons
Every citizen of every country in the world should be provided with free and high-quality medical services. Health care is a fundamental need for every human, regardless of age, gender, ethnicity, religion, and socioeconomic status.
Universal health care is the provision of healthcare services by a government to all its citizens (insurancespecialists.com). This means each citizen can access medical services of standard quality. In the United States, about 25% of its citizens are provided with healthcare funded by the government. These citizens mainly comprise the elderly, the armed forces personnel, and the poor (insurancespecialists.com).
Introduction
Thesis statement.
- Universal Healthcare Pros
- Universal Healthcare Cons
Works Cited
In Russia, Canada, and some South American and European countries, the governments provide universal healthcare programs to all citizens. In the United States, the segments of society which do not receive health care services provided by the government usually pay for their health care coverage. This has emerged as a challenge, especially for middle-class citizens. Therefore, the universal health care provision in the United States is debatable: some support it, and some oppose it. This assignment is a discussion of the topic. It starts with a thesis statement, then discusses the advantages of universal health care provision, its disadvantages, and a conclusion, which restates the thesis and the argument behind it.
The government of the United States of America should provide universal health care services to its citizens because health care is a basic necessity to every citizen, regardless of age, gender, ethnicity, religion, and socioeconomic status.
Universal Healthcare Provision Pros
The provision of universal health care services would ensure that doctors and all medical practitioners focus their attention only on treating the patients, unlike in the current system, where doctors and medical practitioners sped a lot of time pursuing issues of health care insurance for their patients, which is sometimes associated with malpractice and violation of medical ethics especially in cases where the patient is unable to adequately pay for his or her health care bills (balancedpolitics.org).
The provision of universal health care services would also make health care service provision in the United States more efficient and effective. In the current system in which each citizen pays for his or her health care, there is a lot of inefficiency, brought about by the bureaucratic nature of the public health care sector (balancedpolitics.org).
Universal health care would also promote preventive health care, which is crucial in reducing deaths as well as illness deterioration. The current health care system in the United States is prohibitive of preventive health care, which makes many citizens to wait until their illness reach critical conditions due to the high costs of going for general medical check-ups. The cost of treating patients with advanced illnesses is not only expensive to the patients and the government but also leads to deaths which are preventable (balancedpolitics.org).
The provision of universal health care services would be a worthy undertaking, especially due to the increased number of uninsured citizens, which currently stands at about 45 million (balancedpolitics.org).
The provision of universal health care services would therefore promote access to health care services to as many citizens as possible, which would reduce suffering and deaths of citizens who cannot cater for their health insurance. As I mentioned in the thesis, health care is a basic necessity to all citizens and therefore providing health care services to all would reduce inequality in the service access.
Universal health care would also come at a time when health care has become seemingly unaffordable for many middle income level citizens and business men in the United States. This has created a nation of inequality, which is unfair because every citizen pays tax, which should be used by the government to provide affordable basic services like health care. It should be mentioned here that the primary role of any government is to protect its citizens, among other things, from illness and disease (Shi and Singh 188).
Lastly not the least, the provision of universal health care in the United States would work for the benefit of the country and especially the doctors because it would create a centralized information centre, with database of all cases of illnesses, diseases and their occurrence and frequency. This would make it easier to diagnose patients, especially to identify any new strain of a disease, which would further help in coming up with adequate medication for such new illness or disease (balancedpolitics.org).
Universal Healthcare Provision Cons
One argument against the provision of universal health care in the United States is that such a policy would require enormous spending in terms of taxes to cater for the services in a universal manner. Since health care does not generate extra revenue, it would mean that the government would either be forced to cut budgetary allocations for other crucial sectors of general public concern like defense and education, or increase the taxes levied on the citizens, thus becoming an extra burden to the same citizens (balancedpolitics.org).
Another argument against the provision of universal health care services is that health care provision is a complex undertaking, involving varying interests, likes and preferences.
The argument that providing universal health care would do away with the bureaucratic inefficiency does not seem to be realistic because centralizing the health care sector would actually increase the bureaucracy, leading to further inefficiencies, especially due to the enormous number of clientele to be served. Furthermore, it would lead to lose of business for the insurance providers as well as the private health care practitioners, majority of whom serve the middle income citizens (balancedpolitics.org).
Arguably, the debate for the provision of universal health care can be seen as addressing a problem which is either not present, or negligible. This is because there are adequate options for each citizen to access health care services. Apart from the government hospitals, the private hospitals funded by non-governmental organizations provide health care to those citizens who are not under any medical cover (balancedpolitics.org).
Universal health care provision would lead to corruption and rent seeking behavior among policy makers. Since the services would be for all, and may sometimes be limited, corruption may set in making the medical practitioners even more corrupt than they are because of increased demand of the services. This may further lead to deterioration of the very health care sector the policy would be aiming at boosting through such a policy.
The provision of universal health care would limit the freedom of the US citizens to choose which health care program is best for them. It is important to underscore that the United States, being a capitalist economy is composed of people of varying financial abilities.
The provision of universal health care would therefore lower the patients’ flexibility in terms of how, when and where to access health care services and why. This is because such a policy would throw many private practitioners out of business, thus forcing virtually all citizens to fit in the governments’ health care program, which may not be good for everyone (Niles 293).
Lastly not the least, the provision of universal health care would be unfair to those citizens who live healthy lifestyles so as to avoid lifestyle diseases like obesity and lung cancer, which are very common in America. Many of the people suffering from obesity suffer due to their negligence or ignorance of health care advice provided by the government and other health care providers. Such a policy would therefore seem to unfairly punish those citizens who practice good health lifestyles, at the expense of the ignorant (Niles 293).
After discussing the pros and cons of universal health care provision in the United States, I restate my thesis that “The government of United States of America should provide universal health care to its citizens because health care is a basic necessity to every citizen, regardless of age, sex, race, religion, and socio economic status”, and argue that even though there are arguments against the provision of universal health care, such arguments, though valid, are not based on the guiding principle of that health care is a basic necessity to all citizens of the United States.
The arguments are also based on capitalistic way of thinking, which is not sensitive to the plight of many citizens who are not able to pay for their insurance health care cover.
The idea of providing universal health care to Americans would therefore save many deaths and unnecessary suffering by many citizens. Equally important to mention is the fact that such a policy may be described as a win win policy both for the rich and the poor or middle class citizens because it would not in any way negatively affect the rich, because as long as they have money, they would still be able to customize their health care through the employment family or personal doctors as the poor and the middle class go for the universal health care services.
Balanced politics. “Should the Government Provide Free Universal Health Care for All Americans?” Balanced politics: universal health . Web. Balanced politics.org. 8 august https://www.balancedpolitics.org/universal_health_care.htm
Insurance specialists. “Growing Support for Universal Health Care”. Insurance information portal. Web. Insurance specialists.com 8 august 2011. https://insurancespecialists.com/
Niles, Nancy. Basics of the U.S. Health Care System . Sudbury, MA: Jones & Bartlett Learning, 2010:293. Print.
Shi, Leiyu and Singh, Douglas. Delivering Health Care in America: A Systems Approach . Sudbury, MA: Jones & Bartlett Learning, 2004:188. Print.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, October 11). Healthcare Thesis Statement: Examples of Universal Healthcare Pros and Cons. https://ivypanda.com/essays/pros-and-cons-of-universal-health-care-provision-in-the-united-states/
"Healthcare Thesis Statement: Examples of Universal Healthcare Pros and Cons." IvyPanda , 11 Oct. 2018, ivypanda.com/essays/pros-and-cons-of-universal-health-care-provision-in-the-united-states/.
IvyPanda . (2018) 'Healthcare Thesis Statement: Examples of Universal Healthcare Pros and Cons'. 11 October.
IvyPanda . 2018. "Healthcare Thesis Statement: Examples of Universal Healthcare Pros and Cons." October 11, 2018. https://ivypanda.com/essays/pros-and-cons-of-universal-health-care-provision-in-the-united-states/.
1. IvyPanda . "Healthcare Thesis Statement: Examples of Universal Healthcare Pros and Cons." October 11, 2018. https://ivypanda.com/essays/pros-and-cons-of-universal-health-care-provision-in-the-united-states/.
Bibliography
IvyPanda . "Healthcare Thesis Statement: Examples of Universal Healthcare Pros and Cons." October 11, 2018. https://ivypanda.com/essays/pros-and-cons-of-universal-health-care-provision-in-the-united-states/.
- Affordable Care Act Medicaid Expansion Pros & Cons
- The Pros and Cons of Using Pie Charts in Healthcare
- A Company Having Healthcare Insurance for Workers: Pros and Cons
- Substandard Patient Care or Health Care Delivery
- Health Care Communication Methods
- Hospice and Pain Management
- Evolution of Hospice Care
- Home Based and Community Based Services (HCBS)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Gates Foundation Open Access

The promise and peril of universal health care
David e. bloom.
1 Department of Global Health and Population, Harvard T. H. Chan School of Public Health, Boston, MA 02115, USA
Alexander Khoury
Ramnath subbaraman.
2 Center for Global Public Health and the Department of Public Health and Community Medicine, Tufts University School of Medicine, Boston, MA 02111, USA
Universal health care (UHC) is garnering growing support throughout the world, a reflection of social and economic progress and of the recognition that population health is both an indicator and an instrument of national development. Substantial human and financial resources will be required to achieve UHC in any of the various ways it has been conceived and defined. Progress toward achieving UHC will be aided by new technologies, a willingness to shift medical tasks from highly trained to appropriately well-trained personnel, a judicious balance between the quantity and quality of health care services, and resource allocation decisions that acknowledge the important role of public health interventions and nonmedical influences on population health.
The September 1978 Alma- Ata Declaration is a landmark event in the history of global health. The declaration raised awareness of “health for all” as a universal human right,whose fulfillment reduces human misery and suffering, advances equality, and safeguards human dignity. It also recognized economic and social development and international security as not only causes, but also consequences, of better health. In addition, it highlighted the power of primary health care and international cooperation to advance the protection and promotion of health in resource-constrained settings.
Building on the achievement of Alma-Ata and gaining further traction from the Millenium Development Goals and the Sustainable Development Goals set by the United Nations, universal health care (UHC) has emerged in recent years as a central imperative of the World Health Organization (WHO), the United Nations and most of its member states, and much of civil society. UHC characterizes national health systems in which all individuals can access quality health services without individual or familial financial hardship. More broadly, UHC covers social systems that provide medical and nonmedical services and infrastructure that are vital to promoting public health.
Although there are numerous articulations of the UHC agenda, the WHO and World Bank offer a relatively simple UHC service-coverage index that is useful for intercountry comparison. This index focuses on four categories of health indicators: reproductive, maternal, and child health; infectious disease control; noncommunicable diseases; and service capacity and access. Comparison of UHC index values for 129 countries reveals that country index scores are positively correlated with income per capita, though there is considerable variation in scores among countries with similar incomes. These variations presumably reflect differentials in income inequality, commitment to public health infrastructure, and the quality and reach of human resources for health. The WHO and World Bank also offer multiple measures of health spending–related financial hardship in assessing UHC, which do not increase monotonically with increasing income, health spending per capita, or coverage of health services. Rather, catastrophic health expenditures tend to be lower in countries that channel health spending through public social security or insurance programs, rather than private insurance schemes.

Bangkok, Thailand. A nurse keeps records of a blood donor at the Thai National Blood Centre on 14 June 2017.
The financial cost of massively expanding access to health care globally is a formidable barrier to achieving UHC. For example, the Disease Control Priorities Network estimates that low- and lower-middle-income countries would, on average, need to raise their respective annual per capita health expenditures by U.S.$53 and U.S.$61 per person to achieve coveragewith the essential UHC package of 218 core interventions, a sizable burden in relation to average expenditure increases in recent years. Wealthy industrial countries are much further along the path to achieving UHC, though they also face challenges involving rising costs of new health care technologies and the growing share of their populations at the older (and more health care–intensive) ages.
Technically and economically efficient approaches to the achievement of UHC may include the use of electronic medical records, telemedicine systems, digital monitors for drug adherence, and clinical decision–support applications; expansion of the quantity and quality of human resources for health at the physician, nurse, and community health worker levels; improvements in inventory systems and supply chains for the delivery of vaccines, drugs, diagnostics, and medical devices; screening for risk factors and early signs of disease; and focusing on the often neglected domains of surgical care, reproductive health, and mental health. Also key will be efforts to ensure universal access to proven public health interventions that address social and environmental determinants of health, such as health education campaigns; access to safe water; regulation of excessive sugar and salt in the food supply; control of tobacco and the unsafe consumption of alcohol; road traffic safety; walkable city designs; expanding enrollment in high-quality primary and secondary schools; and more equitable distributions of income and wealth.
Achieving UHC is an ambitious aspiration and a powerful indicator of human progress. Fortunately, it may be expected to deliver myriad health, economic, and social welfare benefits along the way, helping to mobilize the substantial political and financial resources needed for its continued future expansion.
Universal health care (UHC) characterizes national health systems wherein all individuals can access quality health services without individual or familial financial hard ship. More broadly, UHC covers social systems that provide medical and nonmedical services and infrastructure that are vital to promoting public health.
ThenotionofUHCdates toOtto vonBismarck, who established the world’s first national social health insurance system in Germany in 1883 ( 1 ). More recently, the September 1978 Alma-Ata Declaration raised global awareness of “health for all” as a universal human right and of the power of primary health care to advance its achievement ( 2 ). During the 20th century, many industrialized countries extended UHC to their citizens. Although progress in expanding UHC slowed in the 1980s—mainly because of economic slowdowns, fiscal stress, and structural adjustment programs—achieving UHC in all countries is currently among the central imperatives of the World Health Organization (WHO), the United Nations (UN) and most of its member states, and much of civil society.
As the Alma-AtaDeclaration’s 40th anniversary approaches, we examine the rationale, progress, consequences, and prospects for achieving UHC globally. We first explore the rationale for UHC, the scope of what UHC encompasses, and its operational definitions at the international level. We then report statistics on current measures of UHC attainment, highlighting patterns by country income level. We go on to review evidence on three key premises of UHC: that it promotes longer, healthier lives; that it does so efficiently; and that it confers social, economic, and political benefits above and beyond the utilitarian value of living healthier lives. Finally, we discuss prospects for further expansion of UHC.
We argue that UHC has considerable potential to improve the trajectory of human progress. To achieve UHC, however, governments and the public health community will have to mobilize substantial human, financial, and technological resources and avoid pitfalls in implementation.
Rationale and scope
Four sets of arguments are commonly advanced in support of UHC. The first set appeals to ethics and morality and the notion that safeguarding everyone’s physical and mental health is just, fair, and consistent with principles of right conduct and distributive justice. The second argument, rooted in international law, relates to the acceptance of health as a fundamental human right ( 3 ). The third set of arguments is pragmatic, relating to the observation that healthy populations tend to be more socially cohesive and politically stable. The final set of arguments is economic in nature: UHC corrects health-related market failures, such as those related to the social benefits of disease prevention among individuals, and good health may promote economic well-being not just among healthy individuals but also at the macroeconomic level ( 4 ). These economic arguments are bolstered by evidence that committing resources to health care is associated with a high return on investment, rivaling, or even surpassing, other high-return investments like those in primary and secondary education ( 5 – 8 ).
Although there is a strong rationale for the possible benefits of UHC, there are also numerous challenges to its realization. A central challenge preceding any realization of UHC is defining its scope and boundaries. Although precise definitions of UHC vary widely among sources, the WHO’s definition is a typical formulation of the concept as a system in which “all individuals and communities receive the health services they need without suffering financial hardship. It includes the full spectrum of essential, quality health services, from health promotion to prevention, treatment, rehabilitation, and palliative care” ( 9 ).
This definition highlights many of the ambiguities involved in conceptualizing UHC. What levels of reduced mortality risk, increases to quality of living, or other thresholds must be crossed before a health service is considered needed or essential? Should financial hardship be defined by the amount of money spent relative to income, the amount of income that households retain after health spending, or some other criteria? Should these criteria shift or remain constant across settings? Given this definition’s emphasis on health services, does UHC also imply a commitment to addressing social and environmental health determinants beyond the traditional purview of health service delivery?
As discussed below, the answer to this last question may have considerable implications for UHC’s effectiveness in improving health outcomes. It is widely accepted that most health outcomes are associated with social and environmental factors, including wealth, income inequality, discrimination, education, occupation, diet, substance use, violence and conflict, air pollution, and water and sanitation access ( 10 , 11 ). Addressing these factors is central to emerging public health agendas such as One Health (which views human, animal, and environmental health holistically) and Planetary Health (which focuses on the economic and social systems that shape human and environmental health). Deficiencies in the availability and quality of medical services are important but, nonetheless, contribute less to premature mortality than these nonmedical determinants ( 11 ). But even though UHC definitions that address nonmedical health determinants have greater potential to improve health outcomes, operationalizing a UHC agenda that addresses these determinants would require wide-ranging interventions in sectors outside of health care, which may be more politically, socially, and technically challenging.
Given the ambiguities in defining UHC, there are several possible approaches to put the concept into practice. These approaches vary according to intended use, such asmaking comparisons across countries, tracking progress over time, or delineating a roadmap for achieving UHC. The WHO and World Bank offer a relatively simple UHC service-coverage index (hereafter, “the WHO– World Bank index”), which is useful for intercountry comparisons. They define this index in terms of 16 indicators, grouped into four categories: reproductive, maternal, newborn, and child health; infectious-disease control; noncommunicable diseases; and service capacity and access ( 9 ).
This relatively small number of indicators allows 129 countries to be included in the UHC service-coverage index. The indicators are meant to serve as a proxy for the overall coverage of the health care system, which should ideally provide many more health services than those represented.
However, although measurement of a handful of tracer conditions and services has often been used as a proxy for overall health system quality, many public health experts have concerns that only indicators that get measured actually get implemented in practice. In addition, the health services included in the index are fairly basic—in terms of the medical conditions covered, skill levels required by health care personnel, and technological capacity required—limiting this metric’s value for comparing high income countries with well-funded health systems. Some of the indicators, such as access to insecticide-treated bed nets for malaria prevention, have minimal relevance in most high-income countries. In addition, these indicators do not comprehensively capture many of the high burden diseases that could be successfully addressed with health services in high income countries, such as treatment for most types of cancer.
The WHO and World Bank also describe multiple approaches for measuring health spending–related financial hardship in assessing UHC. They suggest two thresholds for annual health spending— equal to 10 and 25% of total household expenditures—as alternative metrics for routinely measuring catastrophic health spending, which refers to out-of-pocket expenses exceeding a household’s ability to pay without imposing considerable financial hardship. Two additional metrics aim to more directly assess impoverishment resulting from health expenditures, by measuring the percentage of households whose average daily non health consumption expenditures would have placed its members above the U.S.$1.90 and U.S. $3.20 per capita poverty lines but for the household’s spending on healthcare ( 12 ). Given the very low thresholds for impoverishing health expenditures, these metrics are primarily relevant in low and middle-income countries (LMICs).
More comprehensive UHC priority descriptions exist. For example, the Disease Control Priorities (DCP) Network has compiled 218 distinct cost-effective interventions, which they argue should form a standard of essential services for LMICs because they address a substantial burden of disease. Unlike the indicators in the WHO– World Bank index, more than one-third of the DCP Network’s essential interventions—including tobacco taxes, air pollution reduction, and road safety improvements—focus on broader social or environmental determinants and would require non–health care sector involvement. ( 13 ). A subset of 108 interventions, termed the highest-priority package, avert death or disability while also scoring highly on a financial risk protection index. Comprehensive data are not available on population coverage for many interventions included in the DCP Network’s UHC package, limiting its use in making comparisons among countries. Measurement and inclusion of many of these evidence-based services should be considered in future iterations of the global UHC agenda. coverage increase with rising income levels ( 14 ), it is also likely that the higher country incomes are, at least in part, the result of better health care coverage and health ( 4 ). Disparities in UHC service coverage by income level are even more apparent when looking at groups of countries together: The average service-coverage score for low-income countries is roughly half that of high income countries ( Table 1 ). Sub-Saharan Africa and South Asia feature the lowest index scores, whereas the Latin American and Caribbean and the East Asia and Pacific regions have index scores comparable to those in North America and in Europe and Central Asia.
Population, income, health expenditure, and UHC index score by income group and geographic region . Figures are weighted according to population size. Source: World Bank (2018) ( 15 ), with UHC service-coverage index scores and catastrophic health expenditure data from World Bank (2017) ( 9 ). All data are for 2016, except for the health expenditure data, which are for 2015, and the catastrophic health spending data, which are for 2010.
Also notable are the instances of similar income countries having highly disparate index scores. For example, Nigeria and Vietnam both have per capita GDPs around U.S.$2200, but Vietnam’s UHC index score is 34 points higher than Nigeria’s. This reflects the fact that Vietnam outperforms Nigeria on several indicators, including reported rates of three-dose diphtheriatetanus- pertussis infant vaccination coverage (94 versus 42%), births attended by skilled professionals (94 versus 35%), and households with access to basic sanitation (78 versus 32%). Dissimilar income distributions in the two countries offer a plausible partial explanation for the coverage discrepancies. An estimated 78% of Nigeria’s population lives on less than U.S.$3.20 per day in 2017 dollars, compared with only 32% of Vietnam’s population ( 15 , 16 ). Poverty imposes constraints on accessing health services, particularly in LMICs ( 17 ). Furthermore, less-comprehensive health service coverage reinforces poverty by failing to protect individuals from illnesses that have high treatment costs or that limit their ability to work or learn ( 18 ).
Unlike the association between UHC service coverage and GDP per capita ( Fig. 1 ), protection from catastrophic health expenditures is not clearly correlated with GDP per capita. In aggregate, middle-income countries have higher rates of catastrophic health expenditures than low- and high-income countries ( Table 1 ). However, the variation in catastrophic expenditure rates within these income groups is greater than the variation among them. Furthermore, protection from catastrophic health expenditures does not systematically improve with increasing UHC service-coverage index score or with increasing percentage of GDP spent on health care ( 19 ). Thus, protection from health care–related financial ruin does not directly follow from GDP growth, improved essential health service coverage, or increased total health care spending. Rather, catastrophic health expenditures may be associated with the pathways through which health care spending occurs. Countries in which much of health spending is prepaid through public social security or insurance programs tend to have lower catastrophic health expenditure rates than countries that mostly rely on private insurance schemes ( 19 ).

WHO–World Bank UHC index score versus the natural logarithm of GDP per capita. The plot captures absolute changes in UHC index scores (maximum of 80) relative to percentage changes in GDP per capita. Source: UHC index scores from World Bank (2017) ( 9 ) and GDP per capita from World Bank (2018) ( 15 ). R 2 , coefficient of determination.
Even among countries attaining the maximum UHC index score of 80, there is substantial heterogeneity in health outcomes, health spending, and the proportion of the population protected from catastrophic health spending. Comparing the UHC records of two high-income countries with perfect index scores, the United States and Japan, illustrates these disparities.
The United States is the only high-income country that does not explicitly provide UHC for its citizens, although its relative expenditures on health care—15% of GDP in 2008 and 17% of GDP in 2017—are much higher than those of any other Organisation for Economic Cooperation and Development country ( 20 ). Unlike the United States, Japan expanded health insurance coverage to its entire population in 1961. This change coincided with a massive improvement in the health of Japan’s population, which, by 1983, had the highest life expectancy of any country (and also now, at 84 years) ( 15 ). Japan’s health system has been lauded for its role in promoting a world-leading level of population health and for maintaining relatively low health care costs historically. However, these health expenditures have risen from 8% of GDP in 2008 to 11% in 2017 ( ), and the Japanese health care system must adapt to a continually increasing elder share of the population while constrained by an economy that has performed relatively poorly since the 1990s.
Consequences of expanding UHC
The premise that UHC could lead to longer, healthier lives has a strong underlying rationale. For most indicators in the WHO–World Bank index, achieving high coverage could benefit individuals through reduced disability, increased longevity, improved nutritional status, increased economic productivity, or decreased health-related financial hardship ( Table 2 ).
UHC essential services as defined by the WHO and World Bank and the rationale for their impact on health and social outcomes.
Increased coverage of services can also have a population-level health impact, especially for leading infectious causes of death, such as tuberculosis (TB), HIV/AIDS, and malaria. For these diseases, early treatment of affected individuals can terminate the chain of transmission, thereby reducing disease incidence. For example, over a 7-year time period, HIV-uninfected individuals living in areas with high antiretroviral therapy coverage in Kwa Zulu Natal, South Africa, were 38% less likely to acquire HIV than those in areas with low coverage ( 21 ). Similarly, in China during the 1990s, TB prevalence declined only in provinces where the directly observed therapy short-course (DOTS) strategy—which involves provision of free or subsidized TB testing and treatment—was rolled out with high coverage ( 22 ).
Similarly, expanding vaccine coverage through the UHC agenda—especially for leading causes of child mortality such as Streptococcus pneumoniae, Haemophilus influenzae, and rotavirus—would have a population-level health impact in a highly cost-effective manner. The full societal benefits of disease prevention through vaccination include increased schooling and labor productivity, slowing of the pace at which antimicrobial resistance develops, and reductions in health and economic risk, all magnified by the value of improved health outcomes among non vaccinated community members owing to herd effects ( 23 ).
Regarding the potential impacts of UHC on both health and financial hardship, some compelling evidence is found in the Oregon Health Insurance Experiment ( 24 ). In 2008, the U.S. state of Oregon randomly selected about 30,000 individuals to be eligible to apply for Medicaid from among the roughly 90,000 who had expressed interest in applying to the newly expanded program providing low-cost health coverage for low-income adults. Through comparisons of individuals who were not selected to those who applied and were accepted, researchers found that receiving Medicaid virtually eliminated catastrophic medical spending, reduced medical debt, increased use of preventive medical care, reduced depressive symptoms, and improved subjective perception of overall health status. Measures of physical health—including control of high blood pressure, high cholesterol, and diabetes—did not significantly improve among individuals who received Medicaid; however, the 2-year follow-up time for individuals may have been too short to detect meaningful improvements in these outcome indicators.
Other literature on the impact of increased coverage and density of primary care and hospital based services on health outcomes is generally of weaker quality. Nevertheless, examples from Costa Rica and Cuba suggest a strong association between the universal expansion of public sector primary care services and rapid reductions in child and adult mortality and increases in life expectancy ( 25 , 26 ). In addition, a systematic review highlights the consistency, across a variety of LMIC contexts, of the positive association between large-scale primary care initiatives and lower child mortality ( 27 ). In other LMIC settings, increased hospital access is associated with reduced maternal mortality ( 28 ). In high-income countries, a higher density of primary care providers is associated with lower all-cause mortality ( 29 ).
Beyond improving health, expanding UHC could potentially promote economic well-being, reduce economic inequalities, and bolster social and political stability ( 5 , 30 ). Improving population health could accelerate economic growth by improving labor productivity, school attendance, educational attainment, cognitive function, capital accumulation, and fertility control ( 31 , 32 ). Rigorous microeconomic evidence supports the impact of health improvements on individual or House hold economic circumstances. Interventions with demonstrated effects on education and earnings include iodine supplementation ( 33 ), iron supplementation ( 34 ), deworming ( 35 , 36 ), and malaria eradication campaigns ( 37 ). These benefits may also have an appreciable macroeconomic impact ( 38 ): On average, a 10-year life expectancy gain is associated with up to a 1% increase in annual income per capita growth ( 5 ).
The impact of better health on economic growth may be particularly powerful in LMICs, where children, adolescents, and prime-age adults are the chief beneficiaries of health gains, leading to improvements in productivity across the life course ( 37 ). Ensuring access to basic health care, especially for the prevention and treatment of infectious diseases, may be essential for escaping poverty traps in settings where extreme poverty has historically been persistent ( 39 , 40 ). But benefits of health on economic growth are also manifest in high-income countries, where gains in longevity tend to accrue disproportionately to older adults. The social and economic value resulting from these gains in longevity for older adults may not be well represented in national GDP because the value created is often related to the enabling effect of health on nonmarket activities such as child-rearing, caretaking of other individuals, and community volunteer work ( 41 ).
Expanding UHC also reduces health disparities because poor members of society are less likely to receive adequate health care than wealthier individuals where UHC systems are lacking. Increased access to primary care is associated with reduced wealth- and race-based mortality disparities in both LMICs ( 27 ) and high-income countries ( 29 ). As noted, decreasing health inequality may also reduce income, wealth, and education disparities. As with investments in education, expansion of health care coverage is one of the rare policies that simultaneously promotes equitable distribution of income while also increasing economic growth ( 6 , 42 ). Reducing disparities through improved public health and social welfare systems may help to minimize the risk of political and social instability, though empirical evidence of this association is not especially robust ( 43 ). Through these various pathways, UHC serves important functions that support a healthy, prosperous, and cohesive society.
Although the potential benefits of UHC are numerous, possible pitfalls in implementation could undermine its impact and prevent UHC from fulfilling its promise. Rapid scale-up of UHC without sufficient concern for the quality of implementation could have unintended adverse consequences, as delivery of health services will not be effective in improving health outcomes if the delivered care is not of reasonable quality. Deficiencies in quality of care such as medical errors, spread of infection in health care settings, and poor retention of patients across sequential steps of care (also known as the cascade of care) could undermine the benefits of expanded service coverage. Even though existing UHC frameworks allude to this problem, quality-related indicators can be hard to measure, and achieving high quality of care will be especially challenging with large-scale expansion of coverage ( 44 ).
The recent history of TB care delivery illustrates limitations of focusing on coverage of health services without ensuring that the services offered are of sufficient quality to be effective. In 1991, the World Health Assembly adopted the DOTS strategy, which included comprehensive coverage of free or subsidized TB testing and treatment as a key objective. Over the next two decades, high-burden countries such as India and China achieved high DOTS coverage nationally, leading to reductions in disease prevalence or TB-related mortality ( 22 , 45 ). However, despite high global DOTS coverage, TB incidence is declining slowly (<1.5% per year); the disease remains the leading infectious cause of death, resulting in nearly 1.7 million deaths annually, one-third of which occur in India. Poor quality of care may in part explain these disappointing public health outcomes ( 46 ). For example, in India, considerable numbers of patients are lost across sequential steps of the care cascade; as a result, only about 39% of prevalent TB patients were estimated to have achieved an optimal outcome in the government program in 2013 ( Fig. 2 ) ( 47 ). Similarly, in Rwanda, improved rates of maternal institutional delivery have not translated into reductions in newborn mortality, likely owing to gaps in care quality ( 48 ).

Cascade of care for patients with any form of TB in India in 2013. Patient losses at each stage of care represent shortcomings in quality of care that undermine the effectiveness of TB services, despite a high level of population coverage. Source: Subbaraman et al. ( 47 ).
As these examples suggest, poorly functioning health systems are a central challenge to realizing the benefits of UHC. Health systems in LMICs commonly suffer from a variety of weaknesses, including absenteeism and insufficient training among health care workers, mistreatment of patients by health care workers, corruption, poorly functioning inventory systems and supply chains, electricity cuts and outages, and lack of clean water. These shortcomings in health care delivery often reflect higher-level problems in governance and market failures. Achieving UHC will therefore require innovations in the structure and operation of health systems to ensure that rapid expansion in coverage is not undermined by shortcomings in delivery and quality of care.
With regard to the scope of UHC, it is entirely appropriate for countries to prioritize different health interventions in their UHC agendas to address local needs and constraints. It is also reasonable to expect the number of health services considered essential in each setting to undergo progressive expansion over time to reflect changing resource availability and to address new or emerging health concerns. For example, the WHO–World Bank index—perhaps the most prominent articulation of the UHC agenda— mostly focuses on health service coverage for conditions that have been long-standing global health priorities, such as maternal health, HIV, and TB. The index does not emphasize measurement of service coverage for other conditions that contribute substantially to the global burden of disability or death, such as depression and anxiety (the leading causes of disability globally) and conditions that require basic surgical care (inaccessible to about 5 billion people) ( 49 , 50 ).
In addition, the WHO–World Bank index includes a measure of access to essential medicines but does not cover access to essential diagnostic tests, which are crucial to address population level threats to health, such as antimicrobial resistance ( 51 ). Rising rates of antimicrobial resistance could be a major unintended consequence of UHC if increasing health care coverage does not go hand-in-hand with expanded access to diagnostic tests that facilitate judicious use of antibiotics. As suggested by these examples, if countries adhere to an overly narrow set of UHC priorities, they could miss out on opportunities to address conditions for which there is a dearth of health care providers and institutional capacity in LMICs.
The relatively limited inclusion of measures of nonmedical health determinants in most UHC frameworks represents another, more fundamental, limitation in scope. The WHO–World Bank index focuses on assessing delivery of medical services, with the exception of access to adequate sanitation and insecticide-treated bed nets. The UHC scope thus defined largely avoids the question of ensuring universal access to many public health interventions that could lead to healthier lives—including health education campaigns, in-home piped water supplies, regulation of excessive sugar and salt in the food supply, tobacco control, road traffic safety, construction of walkable cities, high quality primary and secondary education, and equitable distribution of wealth.
Two examples illustrate the limitations of a UHC approach that avoids addressing underlying nonmedical health determinants. In the United States, the dramatic rise in mortality among middle-aged white people in recent years occurred during a time of increasing health insurance coverage in the general population. These “deaths of despair”—largely attributable to mortality from substance use, suicide, and injuries—are thought to be driven by social determinants, such as lack of employment opportunities for blue-collar workers and increasing wealth inequality ( 52 ).
Another example is stunting owing to chronic child undernutrition, which is associated with poor health outcomes, cognitive development, and educational attainment. Most factors that contribute to stunting—poverty, lack of maternal education, poor maternal nutrition, lack of dietary diversity, and lack of sanitation—reflect failures to address nonmedical health determinants ( 53 , 54 ). In India, which accounts for 40% of the world’s stunted children, social inequalities such as gender and caste discrimination drive deficiencies in maternal education and sanitation access, thereby impeding progress in reducing stunting ( 53 , 54 ). As these examples suggest, UHC that narrowly focuses on health service delivery alone is necessary, but insufficient, to bring about wide-ranging health and social benefits. UHC will be implemented within the wider context of the Sustainable Development Goals (SDG) set by the UN, which includes targets related to some of these nonmedical determinants; however, embedding these SDG targets within a UHC-related public health framework could shape the approach and intensity with which these targets are achieved.
The financial cost of massively expanding access to health care globally is a formidable barrier to achieving UHC. The cost of attaining UHC partly hinges on a population’s existing health, which is influenced by factors such as age structure, levels of physical activity, pollution, water and sanita sanitation infrastructure, vaccination coverage, and diet. Using their broad operationalization of UHC described above, the DCP et work estimates that low- and lower-middle-income countries would, on average, need to raise their respective annual per capita health expenditures by U.S.$26 and U.S.$31 per person to achieve coverage with the highest priority package (108 core interventions); achieving coverage with the essential UHC package (218 core interventions) would require an annual spending increase of U.S.$53 and U.S.$61 per person on average ( 13 ).
However, the authors caution that achievement of even the essential UHC package would not be sufficient to reach the SDG target of reducing deaths of individuals less than 70 year sold by 40% by 2030. Achieving the highest-priority and essential UHC package would accomplish around half and two-thirds of this goal, respectively ( 13 ). Presumably, covering the essential health services in the WHO–World Bank index would require lower per capita health expenditure but would be expected to fall even shorter in reaching the SDG targets
As Table 3 shows, the health expenditure growth needed to achieve essential UHC in LMICs by 2030 is comparable to the rate of health spending increases that these countries experienced in recent years. However, these raw estimates of recent growth in health spending could paint an overly optimistic picture. A recent study from the Global Burden of Disease Health Financing Collaborator Network uses data from a similar period (1995–2015) and an ensemble of models that include covariates associated with GDP and health expenditure growth (such as fertility rates and mean years of education) to project health expenditure growth through 2030 ( 55 ). The Network projects that the difference between the number of individuals covered by UHC in the “worst-case” and “best-case” health financing scenarios would be about 871 million people ( 55 ).
Health expenditures needed to attain the highest-priority package (HPP) and essential UHC (EUHC) package by income. Source: Watkins et al. (2017) ( 13 ), with public health expenditure data and average growth (2000–2015) calculated from WHO (2018) ( 15 ).
Given the sizable expenditure increases necessary to achieve UHC, rolling out UHC programsin stages will be necessary. The Lancet Commission on Investing in Health advocates a “progressive universalist” approach to funding these efforts, whereby selected health services are offered broadly and affordably to all citizens by the government, even if this necessitates offeringa smaller package of interventions. The authors argue that this approach is more efficient and equitable than a system that covers more interventions but necessitates higher out-of-pocket expenditures or restricts coverage to fewer individuals ( 56 ).
In light of expected health expenditure increases required to achieve UHC, physicians and public health practitioners may have to radically rethink strategies for health care delivery to simultaneously improve efficiency and health outcomes. For example, lack of trained health care personnel, especially in LMICs, is arguably the most serious hurdle to scaling up UHC ( 57 ). In many countries—such as India, Bangladesh, and Uganda—most health care personnel are informal providers who lack formal medical training ( 58 ). Informal providers are often assumed to deliver low-quality care; however, a recent randomized trial found that intensive training sessions with these providers can improve the quality of care that they deliver to a level that is, in some cases, on par with formal providers ( 59 ). Careful and constructive engagement with these informal providers may therefore be one strategy for bridging the substantial health care workforce gaps that threaten to undermine progress toward UHC in LMICs. Stemming outmigration of physicians from LMICs through bonding schemes (such as conditional scholarships) or enforcement of ethical recruitment policies in high-income countries may also help to reduce health care worker shortages ( 60 ).
Programs to recruit and train community health workers (CHWs) offer another, more widely accepted, strategy for expanding the health care workforce and increasing the coverage and effectiveness of primary health care. Growing evidence suggests that these programs can contribute to improved outcomes in child nutrition, maternal health, HIV, and TB ( 61 ). Moreover, CHW programs could potentially expand the reach of health care provision to the household level. This would be especially beneficial in the context of a rapidly increasing global burden of chronic disease. Primary and secondary prevention of chronic diseases requires early screening for risk factors and lifelong treatment of those risks (e.g., medications for hypertension), and many chronic diseases and risk factors cluster within households ( 62 ). CHWs may also have an important role in tracking newborns at the household level from the first to the last vaccination during infancy. By extending screening, monitoring, and treatment of medical conditions to the household level, CHW programs could have substantial effects on preventing disease, increasing rates of health screening, and improving treatment outcomes, thus improving UHC coverage, efficiency, and impact.
Integrating innovative technologies into health systems—including electronic medical records, clinical decision–support applications, telemedicine, digital medication-adherence technologies, and point-of-care diagnostic tests—could also facilitate UHC by improving the reach, timeliness, efficiency, and quality of clinical care and public health monitoring. These technologies could improve the quality and coverage of longitudinal clinical records, facilitate health care providers’ use of evidence-based clinical care algorithms, extend access to specialized medical knowledge to rural communities, reduce time delays for diagnosis and treatment, and enable real-time monitoring of medication adherence. Artificial intelligence and machine learning have the potential to perform some tasks—such as interpreting x-rays, electrocardiograms, and electroencephalograms— that currently require highly trained and specialized health care workers.
Technological innovations will not obviate the need to dramatically increase the health care workforce in LMICs, but they could still prove to be game changers as the global community tries to rapidly scale up health service delivery to achieve UHC. The ambitious scope of the UHC agendamay provoke physicians and public health experts to reimagine how to deliver health services. New frontline health care personnel (such as CHWs and nonhealth professionals receiving appropriate training) and innovative technologies could help to move care provision into nontraditional spaces, such as homes or workplaces, extending the existing health system’s effective reach.
The bottom line
Four decades after the Alma-Ata Declaration articulated primary care for all as being a most important worldwide social goal, the global community is striving to achieve UHC with renewed interest and ambition. A central motivation of the UHC agenda is the belief that access to health care—with the goals of extending longevity, minimizing disability, and diminishing suffering—is a fundamental human right that advances equality and safeguards human dignity. Achieving UHC would represent one of the most ambitious ventures in the area of human rights, even if UHC were defined narrowly as universal delivery of essential health services. In addition, evidence suggests that well-implemented universal coverage of essential health services could improve welfare more broadly, by reducing economic inequalities, promoting economic well-being, and, perhaps, improving social and political stability.
A broader UHC conception that aims to also address the nonmedical determinants that most strongly shape human health would have even greater implications for society and would require broader social transformations. Addressing cross-cutting social and environmental determinants that contribute to ill health—such as wealth inequality; race, gender, and caste discrimination; air pollution; and lack of water and sanitation facilities—could lead the UHC agenda to intersect more closely with the human rights, One Health, and Planetary Health agendas in the coming decades.
Numerous potential pitfalls could impede UHC expansion or undermine its positive impact on health and well-being. Most challenging, perhaps, is the need to increase health financing rapidly enough to facilitate universal coverage of essential health services among LMIC populations that are simultaneously growing in size and aging. For example, for the world’s less-developed regions, an increase of roughly 1 billion people isprojected from 2018 through 2030, with the percentage aged 60 years or older projected to increase from 10.6 to 14.2%( 63 ). In addition, a UHC agenda that fails to address social determinants of health could limit its impact on health outcomes. Finally, focusing too much on coverage alone, rather than on ensuring the quality of health services, ould undermine UHC effectiveness. Addressing these challenges may require radical transformations in the way that health services are delivered, potentially by expanding the use of frontline health personnel and incorporating innovative technologies into care delivery.
Ultimately, the path to UHC and the interventions prioritized in this process will be unique to each country pursuing universal coverage. Although achieving full UHC is a daunting task, incremental steps toward fulfilling this goal also offer myriad health, economic, and social welfare benefits. cognizing these benefits should help mobilize the resources needed for continued future expansion of UHC.
ACKNOWLEDGMENTS
We are grateful for feedback from K. Prettner, T. Bärnighausen, R. Steinglass, D. Cadarette, R. Glass, M. A. Pate, and two anonymous reviewers.
Research by D.E.B. reported in this manuscript was supported by the National Institute on Aging of the National Institutes of Health under award number P30AG024409. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. D.E.B.’s research on this manuscript was also made possible by a grant fromthe Carnegie Corporation of New York. R.S. acknowledges support from a grant from the Bill and Melinda Gates Foundation via the Arcady Group (OPP1154665) and a Doris Duke Clinical Scientist Development Award. This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ . This license does not apply to figures/photos/artwork or other content included in the article that is credited to a third party; obtain authorization from the rights holder before using such material.
Competing interests
D.E.B. has been in receipt of grants, travel grants, and/or personal fees from Merck, Pfizer, GSK, Sanofi Pasteur, and Sanofi Pasteur–MSD (all related to his research on the value of vaccination) and Gilead Life Sciences (related to his work on the value of treatment for hepatitis C in India). The authors declare no other competing interests.
REFERENCES AND NOTES
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Universal Health Care Research Paper

Related Papers
International Journal of Health Care Finance & Economics
gayatri khanal
Compared to other industrialized countries, the U.S. spends most of all on health care. Nonetheless, the U.S. ranks relatively low on health care indicators. This paradox has been already known for decades. For example, the turning point comparing the U.S. and Canada was in 1972. Health expenditure as a percentage of GDP was higher in Canada than in the USA from 1960 until 1972. Since 1972 expenditure on health care has been higher in the U.S. than in Canada (OECD 2005a, Health data 2005, fourteenth OECD electronic database on health systems, date of release June 2005, last update 04/26/2005). The present study integrates the dispersed literature on spending and health care rankings and adds some statistical analysis to these studies. The evaluation of different factors influencing health care expenditure in the U.S. relative to other countries is restricted to a comparison with Canada. The U.S. and Canada are two countries that are sufficiently similar to make comparisons useful. The comparison of factors influencing health care expenditure in the U.S. and Canada in 2002 reveals that health care expenditure in the U.S. is higher than in Canada mainly due to administration costs, Baumol’s cost disease and pharmaceutical prices. It is not primarily inefficiency in health care production but the dominant prevalence for free choice and own responsibility that explains the paradox of high expenditure on health care and low ranking on health care indicators.
Franak Viacorka
The purpose of this paper is to show both positive and negative effects of further socialization of American health care system, including externalities. We also try to answer why European or Canadian models of universal or single-payer medicine may fail in the United States. As an alternative, we present a range of steps to liberalize health care, based on the publication by Gail Wilensky, James C. Capretta, Joseph Antos. We assume that these steps should stimulate the market, make it more competitive and transparent, and this, as we believe, should normalize prices and make healthcare affordable for different social groups without raising taxes.
Sarah Horton , Jessica Mulligan
The Affordable Care Act (ACA) of 2010—the U.S.'s first major health care reform in over half a century—has sparked new debates in the United States about individual responsibility, the collective good, and the social contract. Although the ACA aims to reduce the number of the uninsured through the simultaneous expansion of the private insurance industry and government-funded Medicaid, critics charge it merely expands rather than reforms the existing fragmented and costly employer-based health care system. Focusing in particular on the ACA's individual mandate and its planned Medicaid expansion, this statement charts a course for ethnographic contributions to the on-the-ground impact of the ACA while showcasing ways critical medical anthropologists can join the debate. We conclude with ways that anthropologists may use critiques of the ACA as a platform from which to denaturalize assumptions of “cost” and “profit” that underpin the global spread of market-based medicine more broadly.
Oroma Nwanodi
Background: The United States spends 18% of gross domestic product, the largest proportion globally, on healthcare. American healthcare administration costs two to five times more than other high-income nations, which is transferred to the public as health insurance premium price difference. Improved healthcare access is an underlying tenet of the Affordable Care Act (ACA), however inflated health insurance premiums could reduce healthcare access.
Journal of Health Care Finance
Sarah Horton
Tyler Kinch
In this paper, I explore how knowledge about Canada’s health care system was constructed by both opponents and proponents of American health care reform, and how this knowledge was subsequently used. I use a constructivist social problems theoretical framework in order to guide a qualitative content analysis of articles from top-circulating American newspapers. Constructivist social problems theory is relevant to this study, because different knowledges about Canada emerged out of the problematization of American health care. Proponents of American health care reform grounded their claims in a knowledge that praised Canada, while opponents of American health care reform grounded their claims in a knowledge that was critical of Canada.
Mitchell Rice
Michael Millenson
Karen Lasser
Results. Among all participants, 3.1% (95% confidence interval (CI)=2.5%, 3.7%) died. The hazard ratio for mortality among the uninsured compared with the insured, with adjustment for age and gender only, was 1.80 (95% CI=1.44, 2.26). After additional adjustment for race/ethnicity, income, education, self- and physician-rated health status, body mass index, leisure exercise, smoking, and regular alcohol use, the uninsured were more likely to die (hazard ratio=1.40; 95% CI=1.06, 1.84) than those with insurance. Conclusions. Uninsurance is associated with mortality. The strength of that association appears similar to that from a study that evaluated data from the mid-1980s, despite changes in medical therapeutics and the demography of the uninsured since that time. (Am J Public Health. 2009;99:jjj-jjj. doi:10.2105/
RELATED PAPERS
Hugh Waters
Lawrence Gostin
Annals of Medicine and Surgery
Mahiben Maruthappu
Journal of Pediatric Surgery
Jean-martin Laberge
Stephen Schoenbaum
Bradley Hall
Californian Journal of …
Lisa Cacari Stone
Saint Louis University Law Journal
The Journal of Rural Health
Political Economy Research Institute, UMASS-Amherst
Peter S Arno
BMC health services research
Liana Bruce
Peter S Arno , Jeannette Wicks-Lim
Kamran Nayeri
International Journal of Health Services
Wayne Nealis
Medical Anthropology Quarterly
Carolyn Sargent
Journal of Public Health Management and Practice
Carleen Stoskopf
Peter Muennig , Marthe Gold
Health Affairs
Pamela Nadash
The American Journal of Surgery
bahar deniz
Law and Contemporary Problems
Frank Pasquale
Steve Schoenbaum
Adam Glaser
Peter Muennig
Bonnie Duran
Jose Cuchilla
Rachel Nardin
Journal of health and social behavior
Stefan Timmermans
Milena A Melo , Jessica Mulligan
Molly Cooke
Journal of Public Economics
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Home — Essay Samples — Nursing & Health — Health Care — Universal Health Care
Universal Health Care Essay Examples
Writing an essay about Universal Health Care can help you understand the issues and come up with solutions to improve healthcare for all. It's a hot topic that needs attention, so why not dive into it and make a difference with your words?
So, you want to write an essay about Universal Health Care, but you're not sure where to start? Don't worry, I've got your back. When choosing a topic for your essay, think about what aspect of Universal Health Care interests you the most. It could be the ethical implications, the economic impact, or the accessibility for all. Once you've found your focus, you can start brainstorming ideas for your essay.
Now, let's talk about the different types of essays you can write about Universal Health Care. If you're into debating and presenting different viewpoints, an argumentative essay might be right up your alley. For those who like to explore the causes and effects of an issue, a cause and effect essay could be a great choice. If you want to express your personal thoughts and feelings, an opinion essay might be the way to go. And if you're all about providing facts and information, an informative essay could be your best bet.
Let's say you're ready to dive into writing your essay. You might be wondering how to structure it and what to include. Well, let me give you a few examples. For a thesis statement on Universal Health Care, you could focus on topics like the impact of Universal Health Care on the economy, the ethical implications of providing healthcare for all, or the importance of accessibility to healthcare services. And when it comes to the , you could start by discussing the current state of healthcare and then lead into your thesis statement. Finally, for the , you could summarize your main points and reiterate the importance of Universal Health Care for the well-being of society. With these examples, you'll be well on your way to writing a stellar essay on Universal Health Care.
The Impact of Household Cleaning Products on Health and The Environment
Combatting health care disparities, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Universal Health Care: Persuasive Speech Outline
The benefits of universal health care for the united states, a discussion on universal health care, financial factors that influence healthcare, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Mental Health Promotion
Health programe and its model, universal healthcare around the world and the opportunities it brings, how america benefits from joining the universal healthcare, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
The Debate Over Free Healthcare Ans Universal Healthcare in America
Having a healthier lifestyle, possible effect of changes in the aca on the market power of healthcare providers, health and social care, the negative effects of the current health care reform bill, investigation of the universal definition of health, patient satisfaction survey, the social determinants of health and its influence on indigenous people’s health in canada, health monitoring and disease prediction system, new medical policy & people's health, current developments in diagnostic methods of concussions, healthcare finance cost allocation, why and how healthcare marketing should develop patient personas, typical errors on the part of doctors, how to solve the problem of nursing turnover within the american healthcare system, impact of telemedicine in the health sector, the need to raise more awareness about mental health, enhancing healthcare access: a south african perspective, foundations of responsive caregiving: infants, toddlers, and twos, ecommerce on healthcare sector, relevant topics.
- Affordable Care Act
- Healthcare Crisis
- Nursing Care Plan
- Health Care Policy
- Eating Disorders
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

IMAGES
VIDEO
COMMENTS
The goal of universal health coverage (UHC) from the United Nations (UN) has metamorphized from its early phase of primary health care (PHC) to the recent sustainable development goal (SDG). In this context, we aimed to document theoretical and philosophical ...
UHC is built on the foundations of human rights and equity, with health services allocated according to people's needs and funded according to their ability to pay. With its commitment to decrease inequalities and provide "health for all", UHC aims to help fulfil the 2030 SDG agenda's pledge to leave no-one behind.
Introduction Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries. The primary objective of this scoping review was to summarize ...
The financial cost of massively expanding access to health care globally is a formidable barrier to achieving UHC. For example, the Disease Control Priorities Network estimates that low- and lower-middle-income countries would, on average, need to raise their respective annual per capita health expenditures by U.S.$53 and U.S.$61 per person to achieve coverage with the essential UHC package of ...
Universal health care would ensure access to health care services for the entire population, improving health outcomes regardless of gender, race, age, employment status, geographic location, or other factors. The economic benefits of universal health care are widely shared and support growth. Universal health care would reduce health care ...
As of the 23rd of June 2021, over 178 million people across the world have been infected by the novel coronavirus SARS-CoV-2, causing 3,880,450 deaths. The pandemic of novel coronavirus disease (COVID-19) has had far-reaching consequences for all parts of society, causing unprecedented disruption of health services as national authorities struggle to cope. Stringent public health and social ...
4.4 Primary health care cost and impact methodology 96 4.5 Examples of interventions provided by primary care services, by platform 97 4.6 Primary health care cost estimates in Indonesia 98 4.7 Illustration of potential increase of public spending on primary health care 99 4.8 Increasing primary health care spending at a given GDP level 100
The UN has declared universal health coverage an urgent global goal. Efforts to achieve this goal have been supported by rigorous research on the scientific, technical, and administrative aspects of health systems design. Yet a substantial portion of the world's population does not have access to essential health services. There is growing recognition that achieving universal health coverage ...
Universal health coverage means that all people have access to the full range of quality health services they need, when and where they need them, without financial hardship. It covers the full continuum of essential health services, from health promotion to prevention, treatment, rehabilitation and palliative care.
Therefore, the Research Topic "Universal Health Coverage and Global Health in Oncology" will focus on research approaches and results of cancer care implementation and its barriers that can be transferred to other countries. Low and Middle-Income Countries (LMICs) as well as industrial countries face intensive and frequently increasing ...
Here, we'll explore a variety of healthcare-related research ideas and topic thought-starters across a range of healthcare fields, including allopathic and alternative medicine, dentistry, physical therapy, optometry, pharmacology and public health. NB - This is just the start….
The United States spends substantially more on health care than most developed countries, yet leaves a greater share of the population uninsured. We suggest that incremental insurance expansions focused on addressing market failures will propagate inefficiencies and are not likely to facilitate active policy decisions that align with societal ...
Dylan Scott answers 9 key questions about universal health care around the world. Vox policy reporter Dylan Scott traveled to Taiwan, Australia, and the Netherlands to see their health systems ...
Background: The Universal Health Coverage (UHC) is a very important and effective policy in the health system of countries worldwide.Using the experiences and learning from the best practices of successful countries in the UHC can be very helpful. Therefore, the aim of the present study is to provide a scoping review of successful global interventions and practices in achieving UHC.
Bottom line: With our largely privately funded health care system, we are paying more than twice as much as other countries for worse outcomes. 3. Point: "Universal health care would be more ...
Universal health care is the provision of healthcare services by a government to all its citizens (insurancespecialists.com). This means each citizen can access medical services of standard quality. In the United States, about 25% of its citizens are provided with healthcare funded by the government. These citizens mainly comprise the elderly ...
OUTLOOK. The financial cost of massively expanding access to health care globally is a formidable barrier to achieving UHC. For example, the Disease Control Priorities Network estimates that low- and lower-middle-income countries would, on average, need to raise their respective annual per capita health expenditures by U.S.$53 and U.S.$61 per person to achieve coveragewith the essential UHC ...
Franak Viacorka. The purpose of this paper is to show both positive and negative effects of further socialization of American health care system, including externalities. We also try to answer why European or Canadian models of universal or single-payer medicine may fail in the United States.
universal healthcare. PAGES 2 WORDS 621. Universal healthcare is a political policy based on the premises of universal human rights, fairness, justice, and equity. The United States was also founded on ethical principles like justice and equity. Therefore, programs like Obamacare that promote universal healthcare are essential for upholding the ...
Investigation of The Universal Definition of Health. 3 pages / 1162 words. They say beauty is in the eye of the beholder. This means beauty does not really exist on its own but it is, instead, produced in the eyes of the observer. In the same way, happiness, justice and peace are all subject to opinion.
Essay on Universal Healthcare in Spain. The Spanish healthcare system covers 99.7 percent of its citizens, however, the American healthcare system leaves around 9 percent of its citizens uninsured ("Key Facts About the Uninsured" 9). Both the United States and Spain's healthcare industry differs greatly.