
Unit 7: Injury Prevention and Safety Promotion
Unit 7 focuses on injury prevention and safety promotion in schools. You will find information on children’s disaster preparedness, brain injury, substance use disorder, and violence and suicide prevention. Additionally, information on sun and water safety, hearing loss, and mercury safety in schools. Lesson plans and trainings with free CEU’s are available under some topics.
Emergency Preparedness in Schools
- Children in Disasters Emergency Kit Checklists
- Easy as ABC
General Injury Prevention & Safety Promotion
- Don’t Mess with Mercury (includes lesson plans)
- Hearing Loss Prevention (includes lesson plan and accompanies the comic book issue Ask a Scientist: How Loud is Too Loud? [PDF – 5 MB] | Español [PDF – 5 MB] )
- Heat and Infants and Children
- HEADS UP to Schools
- Concussion Handout for Kids [PDF – 4 MB]
- Sun Safety Tips for Schools
- Water Safety
Violence Prevention
- Two introductory modules that provide an overview of ACEs and the public health approach to preventing them. Additionally, please find training modules for specific professions including mental health providers appropriate for school counselors.
- Coping with Stress
- Dating Matters ® : Strategies to Promote Healthy Teen Relationships is a comprehensive teen dating violence prevention model developed by CDC to stop teen dating violence before it starts. Dating Matters is an evidence-based teen dating violence prevention model that includes prevention strategies for individuals, peers, families, schools, and neighborhoods. The online module is designed for educators.
Opioids and Other Drugs
- CDC’s Response to the Opioid Overdose Epidemic
- Find free science- and standards-based classroom lessons and multimedia activities on teens and drugs – all funded or created by the National Institute on Drug Abuse for Teens (NIDA).
- Games: Drug Use and Effects
- This free fact sheet by the Substance Abuse and Mental Health Services Administration (SAMHSA) provides facts about opioids for teens. It describes short- and long-term effects, lists signs of opioid use and helps to dispel common myths about opioids.
- Youth Opioid Abuse Prevention Brochure [PDF – 3.48 MB]

Healthy Youth
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
7 Chapter Seven: Preventing Injury; Protecting Children’s Safety
Kelly McKown
Chapter 7 Learning Objectives
By the end of this chapter, you should be able to:
- Connect classroom design to safety and injury prevention.
- Discuss ways to handle unsafe behavior by understanding the function of behaviors.
- Describe how teachers can ensure the toys and materials they offer children do not present injury risks and are nontoxic.
- Explain ways adults can support safe and developmentally appropriate use of technology.
- Lists ways to protect children from choking, poisoning, burns, drowning, and falls.
- Identify how to implement safe sleep practices to protect against Sudden Infant Death Syndrome.
- Explain what active supervision is and what it might look like.
- Discuss how to create a culture of safety.
- Identify common risks that lead to injury in children.
- Describe how understanding injuries can help create a safety plan that prevents future injury.
- Summarize strategies teachers can use to help children learn about and protect their own safety.
- Recall several ways to engage family in safety education.
- Analyze the value of allowing risky play.
Introduction
Keeping children safe must be a top priority for all early care and education programs. Active Supervision is the most effective strategy for creating a safe environment and preventing injuries in young children. It transforms supervision from a passive approach to an active skill. Staff use this strategy to make sure that children of all ages explore their environments safely. Each program can keep children safe by teaching all staff how to look, listen, and engage.
What is Active Supervision?
Active supervision requires focused attention and intentional observation of children at all times. Staff position themselves so that they can observe all of the children: watching, counting, and listening at all times. During transitions, staff account for all children with name-to-face recognition by visually identifying each child. They also use their knowledge of each child’s development and abilities to anticipate what they will do, then get involved and redirect them when necessary. This constant vigilance helps children learn safely.
Strategies to Put Active Supervision in Place
The following strategies allow children to explore their environments safely. Infants, toddlers, and preschoolers must be directly supervised at all times. This includes daily routines such as sleeping, eating, and diapering or bathroom use. Programs that use active supervision take advantage of all available learning opportunities and never leave children unattended.
Set Up the Environment
Staff set up the environment so that they can supervise children and be accessible at all times. When activities are grouped together and furniture is at waist height or shorter, adults are always able to see and hear the children. Small spaces are kept clutter-free and big spaces are set up so that children have clear play spaces that staff can observe.

Position Staff
Staff carefully plan where they will position themselves in the environment to prevent children from harm. They place themselves so that they can see and hear all of the children in their care. They make sure there are always clear paths to where children are playing, sleeping, and eating so they can react quickly when necessary. Staff stay close to children who may need additional support. Their location helps them provide support, if necessary.
Scan and Count
Staff are always able to account for the children in their care. They continuously scan the entire environment to know where everyone is and what they are doing. They count the children frequently. This is especially important during transitions when children are moving from one location to another.
Specific sounds or the absence of them may signify reason for concern. Staff who are listening closely to children immediately identify signs of potential danger. Programs that think systematically implement additional strategies to safeguard children. For example, bells added to doors help alert staff when a child leaves or enters the room.
Anticipate Children’s Behavior
Staff use what they know about each child’s individual interests and skills to predict what he/she will do. They create challenges that children are ready for and support them in succeeding. But, they also recognize when children might wander, get upset, or take a dangerous risk. Information from the daily health check (e.g., illness, allergies, lack of sleep or food, etc.) informs staff’s observations and helps them anticipate children’s behavior. Staff who know what to expect are better able to protect children from harm.
Engage and Redirect
Staff use what they know about each child’s individual needs and development to offer support. Staff wait until children are unable to problem-solve on their own to get involved. They may offer different levels of assistance or redirection depending on each individual child’s needs. [2]

Active Supervision for Infants and Toddlers
Infant/toddler care is responsive, individualized care. And it’s important to think about infants and toddlers that are cared for in small groups with a primary-caregiver system of care and also to think about the flow of the day as being responsive to the individualized needs of the children. Staff work very closely with children throughout the day guiding them through individual or small-group routines and experiences. Staff are providing responsive, individualized care, and they will know each child well. That’s an important piece of both individualized care and active and responsive supervision. They have a good sense of how each child gets through the day, what their abilities are, what their temperament is. Even as they grow and change from day to day, they’re able to follow each child in their care with an understanding of how it is that they’re growing.

In center-based programs or larger family child care homes, more than one caregiver is working together in a team. And the other thing that’s important to remember is the kind of communication that develops between the two teachers in a classroom or a family-childcare provider and an assistant — a communication that supports a child’s safe movement throughout the day as well as their ability to explore and grow in a nurturing environment.
Adults provide support to each other, particularly at key times of the day, like transitions. All of those important, individualized routines require both adults to work together, such as individual sleeping times, going indoors and outdoors, changing times, feeding and eating times for infants and toddlers, and other times during the day when there may be a particular child that needs individualized care. It’s so important that the staff working with them are working together to support continuity of care.
The environment itself can be a partner in caring for infants and toddlers, particularly when it comes to keeping children safe. We want to create environments that provide places for children to play and be both together and apart but always in full view and within easy reach of a caring and attentive adult. [6]
Creating an Environment of Yes!
An environment of “yes” means that everything infants and toddlers can get their hands on is safe and acceptable for them to use. One way to ensure this is to for adults to do ongoing safety checks in group care spaces and provide families with information about doing safety checks of their own. The teacher, home visitor, and the child’s family play a vital role in making sure everything is safe, then stepping back to allow exploration.
Sometimes infants and toddlers will use materials in creative ways that surprise us! When teachers feel uncomfortable about an activity, they should stop and ask themselves two questions:
- Is it dangerous?
- What are the children learning from this experience?
If it is decided that the activity is safe with supervision, they should stay nearby. They should be thoughtful and open to what the children might be learning. If the activity is not safe, they need to consider what else might address the infants’ and toddlers’ curiosity in the same way. For example, if young toddlers are delighted to discover that by shaking their sippy cups, liquid comes out; a teacher may be worried that this water on the floor will lead to a slippery accident. Instead, they might provide squeeze bottles outside or at the water table. The adult is responsible for keeping children safe and encouraging learning through curiosity.
Saying “no” to infants and toddlers or asking them to “share” is a strategy that rarely works. One way to prevent conflict is to reflect on, and then set up, the space where children play in ways that promote “yes!”
- What areas generate the most “no’s” or require the most adult guidance?
- What do the children need and enjoy the most when it comes to playtime?
- Do you have multiples of favorite toys?
- Do you have enough places where toddlers can play alone or with a few friends?
- Do you have adequate space for active play?
- Is the room appropriately child-proofed? [7]

Classroom Design
Designing an effective and engaging classroom environment takes careful thought and planning, but it’s important. A well-organized classroom that is interesting, orderly, and attractive contributes to children’s participation and engagement with the learning materials and activities. This engagement, in turn, contributes to children’s learning. Not all early learning centers for infants provide a high-quality environment for the youngest learners. What Does a High-Quality Program for Infants Look Like?
Let’s look at it from a child’s perspective. We want children to feel safe and comfortable in the classroom. We want them to be interested in the learning activities and to take full advantage of being at school and take full advantage of the activities you’ve planned and the materials you’ve selected. It can be helpful to get down at a child’s level and take a look at the classroom. Does it feel welcoming and inviting? Is there enough room to move, make choices, and stay involved with a toy or activity or project? And does the room help the child know what to do and what’s expected?
Active Supervision
It’s important not to become complacent with safety practices. Teachers need to keep it fresh, thoughtful, and intentional. This begins with setting up the environment. Classrooms will have unique factors to consider. But some general considerations include making sure that there is a teacher responsible for every part of the space children are in, which may be referred to as zoning, and for every part of the day (including transitions).
How teachers position their bodies is really important. They should see all of the children in their care from any position in the room. And when in playing areas, their back should not be to the center of the room, but towards the wall. It is also important to move closer to children as needed (rather than staying in one place and potentially missing out on problems that may arise).
Teachers also need to talk to each other, using back-and-forth communication, so that safety information is easily spread through the room. It may seem strange at first, sometimes, for teachers to talk to each other; but, it’s incredibly helpful for active supervision – when there are either changes in staff or children’s routines, changes in roles, changes during transitions.
And one of the main purposes of zoning was created to help all children be engaged and to minimize unnecessary wait times. When all staff know their roles in the classroom with zoning and tasks are getting handled, children are engaged and the unsupervised wait time is really minimized.
During transitions or routine changes, teachers need to have a heightened awareness. Transitions are challenging times for both children and their teachers, so the risk to safety increases. One thing that teachers can think about is how they can minimize the number of changes so that there aren’t as many transitions happening in the classroom. There should be plans what adults will do, before, during, and after transition times. 10
Designing an Effective and Safe Classroom Environment
There are all sorts of classrooms. They differ by size and shape, amount of light and wall space, placement of sinks and counters, and amount of storage. Figuring out how to design the physical space and to maximize children’s interactions within the space will take some time. Make a floor plan. Move things around. Take a look at other classrooms and see what works.
Here are a few things to think about when designing your space and making it as workable as possible. Think about the number of interest areas or centers that you want or need for the group of children. Arrange the space so that noisy areas are separated from quiet areas. Locate centers next to needed storage or equipment. Use furniture or other items to provide boundaries. But, make sure that the adults can see all of the areas of the room. [2]
Factors to Consider
Space and boundaries:
· Are the centers clearly defined with furniture, rugs, or shelves?
· Is there enough space for all children to easily move about the room?
· In each defined area, is there adequate space for the number of children using it?
Proximity and distance:
· Are the quiet and noisy areas in proximity or separated?
· Are centers located near things that children need to complete projects (art center near sink, puzzle or game shelves within reach of tables, etc.)?
· Are teachers able to view children in all centers?
Home and culture:
· What home-like features are included in the classroom?
· How is(are) the culture(s) of the local community reflected in the classroom?
Flexibility and permanence:
· How does the space accommodate gross motor activity?
· What aspects of the physical space cannot be changed (cost or structural issues) and are challenging to overcome (e.g., limited access to natural light, cumbersome cubbies, etc.)?
Engagement and challenging behaviors:
· Are there areas of the classroom where challenging behaviors are more likely to occur?
· Are there areas where typically children are positively engaged in classroom activities?
Traffic patterns:
· Can children move easily from space to space?
· Is running and wandering discouraged?
Material selection:
· Are materials chosen to support development and learning?
· Are they culturally relevant and meaningful to the children?
· Is there is a sufficient variety and quantity (without overwhelming children)? [3]
Pause to Reflect
Tips for Environmental Design
Traffic patterns need to discourage running.
Use furniture, rugs, and similar items to define boundaries.
Ensure that teachers can see what is happening in all areas of the classroom.
Cultural and home-like features are present in the room.
Use spaces with as much flexibility as possible.
Quiet and noisy centers are spaced appropriately.
Ensure interesting classroom content selection is balanced with appropriate stimulation versus overstimulation.
Each center provides enough information about what to do there and how to play. [1]

[1] Presenter Notes: Designing Environments by the Office of Head Start is in the public domain.
Grouping of Children
Teachers want to be intentional about how they group children, whether it’s a decision made in the moment or as part of lesson planning. Match the size of the group with the purpose of the activity. Think about the children who will be in the group. Young children need opportunities to participate and learn with the whole group, small groups, and they will thrive with a bit of one-on-one time with an adult. [6]
Large groups are good for:
· Introducing concepts
· Building community
· Conducting routine activities
Small groups are good for:
· Maximizing back and forth interactions
· Peer modeling of skills
· Guiding instruction
One-on-one interactions are good for:
· Tasks requiring complex skills
· Instance when a child needs specific direction and assistance [7]
Every early childhood environment is full of pros and cons; it is how educators work with the many characteristics of a classroom that can make a tremendous difference. Teachers can be surprised by the results when they:
· Assess the spaces for both limitations and strengths.
· Strategize how to optimize what they have to work with in their classrooms.
· Try a different arrangement, see what happens, and then modify based on what is working and what is not.

Sometimes a modification can be minor (raising or lowering a shelf, “stop” signs over unavailable areas, masking tape to better define a space, etc.). This highlights the “work-in-progress” nature of early childhood environments. As the needs of children change, the room may need minor changes or have to be rearranged completely to meet those needs. [9]
Interpersonal Safety
Children can behave in ways that hurt themselves or others so teachers must prepared to handle unsafe behaviors in their duty to protect children from injury. An important way to think about behavior is as a form of communication. Young children let us know their wants and needs through their behavior long before they have or can use words in the heat of the moment. They give us cues to help us understand what they are trying to communicate.
Early childhood educators can help children by interpreting their cues and responding to meet their needs. The following example illustrates the importance of responding to the possible meaning behind behavior:
Javon bites Blair because he wants the block she is playing with and we remove Javon from the situation. Not only are we not responding to his want or need, but we are taking him out of the context where he can learn to communicate his feelings in a way that doesn’t hurt others.
Forms and Functions of Behavior
There are many reasons a child might use specific behaviors. This is why it is important for adults to carefully observe children, pay attention to their cues, get to know them, and know what part of the schedule gives them a hard time to better understand what they are trying to tell us through their behavior. [11]
Each behavior has a:
FORM = the behavior the child is using to communicate
AND A FUNCTION = the reason or purpose the child is using that behavior [12]
Table 7.1 – Forms and Functions of Behavior [13]
Here are some examples of form and functions of infants, toddlers, and preschoolers:
Table 7.2 – Examples of Forms and Possible Functions of Behaviors [14]
Form and function are also shaped by culture. Children are socialized to express their feelings in culturally acceptable ways. It is important to talk with families so you can look for acceptable ways that children express themselves in a culturally respectful way.
As you have probably already experienced—it is not always easy to figure out the meaning of a child’s behavior. To add to the complexity of understanding the meaning of behavior:
A single form of behavior may serve more than one function. For example, a toddler might use biting (form) for different functions (“I want the toy you have.” “I want to play with you but don’t know how to let you know.” “I’m tired.” “I’m frustrated because you don’t understand what I am trying to tell you.” “I want some attention.”)
Several forms of behavior may serve one function. For example, a child’s purpose (function) may be to build with their favorite blocks, but they use different forms of behavior (biting, yelling, grabbing, running away with the blocks, sharing) based on how they feel that day, who is playing in the block area, or based on their cultural expectations.
The meaning of behavior is shaped by culture, family, and the unique makeup and experiences of the individual child. For example, some cultures may express sadness by crying or by having a nonchalant facial expression. Some cultures may express happiness by laughing and being exuberant, while others may expect more restrained behaviors.
Some of these functions of communication become a concern for children’s safety (of the child communicating, the other children, and other people in the environment). Early childhood educators must take the time to understand a behavior’s meaning so that they can help the child replace unsafe forms of communication with forms that don’t hurt others or harm the environment. Pausing to try to figure out the meaning behind a child’s behavior—instead of just reacting to the behavior—can change the way we see a child, the way we respond to a child, and the way we teach a child. Becoming a “behavior has meaning” detective who is always on the lookout for the meaning of behavior will help you keep children safe. [15] Take a look at the following example of an unsafe behavior, what it might mean, and what an educator might do to support the child.
Taking a Closer Look at Behavior
You may also find it valuable to examine behavior much the way you would injuries and traffic patterns. Gather data about unsafe behaviors:
When are they happening? Are there specific times of day that children are finding it more challenging to behave/communicate in safe ways?
Where are they happening? Are there hot spots for challenging behavior? What in the environment might be the focus of the unsafe behavior/communication?
Why they are happening? What happened before the led up to the behavior? What happened after?
Who are the behaviors happening between? All children will have times where they communicate with unsafe behavior, but some children may need more adult support in certain contexts (time of day, activity, groupings of children, etc.).
Look for patterns. Reflect on what can be changed in the physical environment, schedule/routine, groupings, and supervision to help prevent children from hurting themselves or others when trying to communicate their needs.
Safe Toys, Materials, and Equipment
Play is a natural activity for every young child. Play provides many opportunities for children to learn and grow – physically, mentally, and socially. If play is the child’s work, then the toys, materials, and equipment in the environment are what will enable children to do their work well and safely. [19]
Protecting children from unsafe toys is the responsibility of everyone. Careful toy selection and proper supervision of children at play are still—and always will be—the best ways to protect children from toy-related injuries. [20]
It is important that educators consider both safety and durability when choosing toys for children. Toys should be constructed to withstand the uses and abuses of children in the age range for which the toy is appropriate.
The U.S. Consumer Product Safety Commission (CPSC) has safety regulations for certain toys. Manufacturers must design and manufacture their products to meet these regulations so that hazardous products are not sold (see Table 3.3).
Table 7.3 – Mandatory Toy Safety Regulations [21]
In addition to the mandatory standards, many toy manufacturers also adhere to the toy industry’s voluntary safety standards (see Table 3.4). [22]
Table 7.4 – Voluntary Standards for Toy Safety [23]
Toys should be chosen with care. Teachers should look for quality design and construction. Safety labels to look for include “Flame retardant/Flame resistant” on fabric products and “Washable/hygienic materials” on stuffed toys and dolls. Watch for the hazards listed in Table 3.5 [25] .
Table 7.5 – Hazards to Avoid in Toys [26]
Check all toys periodically for breakage and potential hazards. A damaged or dangerous toy should be thrown away or repaired immediately.
Age Appropriate Toys
Teachers must keep in mind the ages of children they are choosing toys for, including their typical interests and skill levels. The manufacturer’s age recommendation is a good starting place to ensure that toys are age-appropriate. Warnings such as “Not recommended for children under 3” should be followed. [27] See Table 3.6 for some age-appropriate toys to consider. Please note that toys appear on the list when they become appropriate and are not repeated in later ages.
Table 7.6 – Age Appropriate Toys [28]
Federal law requires that all art materials offered for sale to consumers of all ages in the United States undergo a toxicological review of the complete formulation of each product to determine the product’s potential for producing adverse chronic health effects. It also requires that the art materials be properly labeled for acute and chronic hazards, as required by the Labeling of Hazardous Art Materials Act(LHAMA) and the Federal Hazardous Substances Act (FHSA), respectively.
In addition to the LHAMA requirements, art materials – such as paintbrushes and stencils – that are designed or intended primarily for children 12 years of age or younger, are also required, like all children’s products, to comply with the requirements of the Consumer Product Safety Improvement Act of 2008 (CPSIA). [32] Under the FHSA, most children’s products that contain a hazardous substance are banned, whether the hazard is based on chronic toxicity, acute toxicity, flammability, or other hazard identified in the statute.
Children’s products that meet the FHSA’s definition of an art material include, but are not limited to, crayons, chalk, paint sets, colored pencils, and modeling clay. Non-toxic art and craft supplies intended for children are readily available. Read the labels and only purchase art and craft materials intended for children and that are labeled with the statement “Conforms to ASTM D-4236.” [33]
One such label will come from the Art and Creative Materials Institute’s (ACMI) certification program. “ACMI-certified product seals…indicate that these products have been evaluated by a qualified toxicologist and are labeled in accordance with federal and state laws… The AP (Approved Product) Seal identifies art materials that are safe and that are certified in a toxicological evaluation by a medical expert to contain no materials in sufficient quantities to be toxic or injurious to humans, including children, or to cause acute or chronic health problems.” [34]
Safety Risks from Art Materials
For certain chemicals and exposure situations, children may be especially susceptible to the risk of injury. For example, since children are smaller than adults, children’s exposures to the same amount of a chemical may result in more severe effects. Further, children’s developing bodies, including their brains, nervous systems, and lungs may make them more susceptible than adults. Differences in metabolism may also affect children’s responses to some chemicals.
Children‘s behaviors and cognitive abilities may also influence their risk. For example, children under the age of 12 are less able to remember and follow complex steps for safety procedures, and are more impulsive, making them more likely to ignore safety precautions. Children have a much higher chance of toxic exposure than adults because they are unaware of the dangers, not as concerned with cleanliness and safety precautions as adults, and are often more curious and attracted to novel smells, sights, or sounds. Children need regular and consistent reminders of safety rules, and there is no substitute for direct supervision.
Guidelines for Selecting Art and Craft Materials
Here are some helpful reminders about choosing art materials for children:
· Note that even products labeled ‘non-toxic’ when used in an unintended manner can have harmful effects.
· Products with cautionary/warning labels should not be used with children under age 12.
· Avoid solvents and solvent-based supplies, which include turpentine, paint thinner, shellac, and some glues, inks, and a few solvent-containing permanent markers.
· Avoid products or processes that produce airborne dust that can be inhaled (including powdered tempera paint).
· Avoid old supplies, unlabeled supplies, and be wary of donated supplies with cautionary/warning labels and that do not contain the statement “Conforms to ASTM D4236.”
· Look for products that are clearly labeled with information about intended uses.
· Give special attention to students with asthma or allergies, which may elevate the students’ sensitivities to fumes, dust, or products that come into contact with the skin. [41]
· Gather your supplies beforehand so that you can continue to supervise their use without needing to step away.
· Instruct children on safety practices before you begin (such as, modeling how to cut safely with scissors).
· Do activities in well-ventilated areas.
· Use protective equipment (such as smocks).
· Assume that anything you use should be safe enough that it won’t harm children if it gets on their skin or in their mouths and/or eyes. [42]
Using Technology and Media Safely
Developmentally appropriate use of technology can help young children grow and learn, especially when families and early educators play an active role. Early learners can use technology to explore new worlds, make-believe, and actively engage in fun and challenging activities. They can learn about technology and technology tools and use them to play, solve problems, and role play. But how technology is used is important to protect children’s health and safety.
Technology can be a Tool for Learning
What exactly is developmentally appropriate when it comes to technology for children? In Technology and Interactive Media as Tools in Early Childhood Programs Serving Children from Birth through Age 8 , the National Association for the Education of Young Children (NAEYC) and the Fred Rogers Center state that “appropriate experiences with technology and media allow children to control the medium and the outcome of the experience, to explore the functionality of these tools, and pretend how they might be used in real life [43] .”
Lisa Guernsey, author of Screen Time: How Electronic Media—From Baby Videos to Educational Software—Affects Your Young Child , also provides guidance for families and early educators. For example, instead of applying arbitrary, “one-size-fits-all” time limits, families and early educators should determine when and how to use various technologies based on the Three C’s: the content, the context, and the needs of the individual child. They should ask themselves the following questions:
· Content—How does this help children learn, engage, express, imagine, or explore?
· Context—What kinds of social interactions (such as conversations with families or peers) are happening before, during, and after the use of the technology? Does it complement, and not interrupt, children’s learning experiences and natural play patterns?
· The individual child—What does this child need right now to enhance his or her growth and development? Is this technology an appropriate match with this child’s needs, abilities, interests, and development stage? [44]
Early childhood educators should keep in mind the developmental levels of children when using technology for early learning. That is, they first should consider what is best for healthy child development and then consider how technology can help early learners achieve learning outcomes. Technology should never be used for technology’s sake. Instead, it should only be used for learning and meeting developmental objectives, which can include being used as a tool during play.
When technology is used in early learning settings, it should be integrated into the learning program and used in rotation with other learning tools such as art materials, writing materials, play materials, and books, and should give early learners an opportunity for self-expression without replacing other classroom learning materials. There are additional considerations for educators when technology is used, such as whether a particular device will displace interactions with teachers or peers or whether a device has features that would distract from learning. Further, early educators should consider the overall use of technology throughout a child’s day and week, and adhere to recommended guidelines from the Let’s Move initiative, in partnership with families. Additionally, if a child has special needs, specific technology may be required to meet that child’s educational and care needs. And dual language learners can use digital resources in multiple languages or translation to support both their home language and English development.

For Infants and Toddlers
Research shows that unstructured playtime is particularly important for infants and toddlers because they learn more quickly through interactions with the real world than they do through media use and, at such a young age, they have limited periods of awake time. At this age, children require “hands-on exploration and social interaction with trusted caregivers to develop their cognitive, language, motor, and social-emotional skills.”
For children under the age of 2, technology use in early learning settings is generally discouraged. But if determined appropriate by the IFSP team under Part C of the IDEA, children with disabilities in this age range may also use technology, for example, an assistive technology device to help them communicate with others, access and participate in different learning opportunities, or help them get their needs met.
Active versus Passive Engagement
Early childhood educators should understand the differences between passive and active use of technology. Passive use of technology generally occurs when children are consuming content, such as watching a program on television, a computer, or a handheld device without accompanying reflection, imagination, or participation.
Active use occurs when children use technologies such as computers, devices, and apps to engage in meaningful learning or storytelling experiences. Examples include sharing their experiences by documenting them with photos and stories, recording their own music, using video chatting software to communicate with loved ones, or using an app to guide playing a physical game. These types of uses are capable of deeply engaging the child, especially when an adult supports them. While actions such as swiping or pressing on devices may seem to be interactive, if the child does not intentionally learn from the experience, it is not considered to be active use. To be considered active use, the content should enable deep, cognitive processing, and allow intentional, purposeful learning at the child’s developmental level.
Early childhood educators also need to think of ways they can reduce the sedentary nature of most technology use. Technology can encourage and complement physical activity, such as doing yoga with a video or learning about the plants outdoors with a nature app.
The Digital Divide
Research points to a widening digital use divide, which occurs when some children have the opportunity to use technology actively while others are asked primarily to use it passively. The research showed that children from families with lower incomes are more likely to complete passive tasks in learning settings while their more affluent peers are more likely to use technology to complete active tasks.
For low-income children who may not have access to devices or the internet at home, early childhood settings provide opportunities to learn how to use these tools more actively. For example, research shows that preschool-aged children from low-income families in an urban Head Start center who received daily access to computers and were supported by an adult mentor displayed more positive attitudes toward learning, improved self-esteem and self-confidence, and increased kindergarten readiness skills than children who had computer access but did not have support from a mentor.
Co-Viewing of Technology
Most research on children’s media usage shows that children learn more from content when parents/caregivers or early educators watch and interact with children, encouraging them to make real-world connections to what they are viewing both while they are viewing and afterward.

There are many ways that adult involvement can make learning more effective for young children using technology. Adult guidance that can increase active use of more passive technology includes, but are not limited to, the following:
· Prior to the child viewing content, an adult can talk to the child about the content and suggest certain elements to watch for or pay particular attention to;
· An adult can view the content with the child and interact with the child in the moment;
· After a child views the content, an adult can engage the child in an activity that extends learning such as singing a song they learned while viewing the content or connecting the content to the world.

Safety Risks of Technology
In addition to the health risks of sedentary activity (in place of active play), there are concerns about privacy and security with any technology. The rights of children under 13 and technology in school are governed by federal laws, but looking at privacy policies is important.
Software and apps may also include advertising and in-app purchasing (generally inappropriate for young children). So early childhood educators should choose software and apps that avoid advertising and in-app purchases.
Not all technology is appropriate for young children and not every technology-based experience is good for young children’s development. To ensure that technology has a positive impact, adults who use technology with children should continually update their knowledge and equip themselves to make sophisticated decisions on how to best leverage these technology tools to enhance learning and interpersonal relationships for young children.
Access to technology for children is necessary in the 21st century but not sufficient. To have beneficial effects, it must be accompanied by strong adult support. [53]
Preventing Injuries Indoors
Some injuries that early childhood educators should be aware of and intentionally act to prevent in the last chapter were presented in the previous chapter and earlier in this chapter during the discussion about safe toys and art materials. Here is some further information about injuries that are more likely to happen indoors.
Choking occurs when an object blocks the airway, preventing breathing. [54] Infants have the highest rates of choking (140 per 100,000). That risk decreases as they get older and their airway increases in size, with 90% of fatal choking happening in children less than 4 years of age. [55]
Reducing the Risks of Choking
The main way to prevent choking is to recognize that objects that are 1½ inches or less in diameter are higher risk. [56] Foods are the most common cause of choking. Having children sit during snacks and meals at an unhurried pace, allowing time for children to properly chew their food helps prevent choking on food. Food is safest when cut into small pieces or served in small amounts. See Table 3.7 for foods that commonly cause choking.
Table 7.7 – Common Choking Hazards [57]
Toys, and other items that children may play with, are another common source of choking hazards. Ensuring children only have access to age-appropriate toys is an important step. See Table 3.7 for items that should be kept out of reach of young children.
Teachers can use a small parts tester, a commercial product commonly known as choke tube, to test whether or not an object is a choking hazard. Recognizing and responding to choking will be addressed in Chapter 5. [58]

There are many hazards that put children at risk for accidental poisoning, both indoors and outdoors. Poisoning can occur at any time a harmful substance is intentionally or unintentionally ingested. Poisons come in many forms including plants, cleaning supplies, spoiled food, and medications. Children, who are naturally curious and like to explore, are in particular at risk for poisoning.

Guidelines to Prevent Poisoning
· Keep all cleaning supplies and chemicals locked.
· All medications should be kept in a locked storage area, out of reach.
· Check medications periodically for expiration dates and properly dispose of expired medications. Some medications become toxic when they are past their expiration date.
· Do not tell children that medication is “candy” as this makes it look more attractive to them.
· Ensure all medications and chemicals are properly labeled. Childproof caps should be on medicine bottles.
· Use safe food practices. (see Chapter 15)
· Never use cans that have bulges or deep dents in them.
· Keep poisonous plants out of reach of children and pets. (see Table 3.8)
· Keep the number for Poison Control near a telephone. [61]
Table 7.8 Poisonous Plants [62]
Every day, over 300 children ages 0 to 19 are treated in emergency rooms for burn-related injuries and two children die as a result of being burned.
Younger children are more likely to sustain injuries from scald burns that are caused by hot liquids or steam, while older children are more likely to sustain injuries from flame burns that are caused by direct contact with fire. [63]
Causes of Burns
Burns can be caused by dry or wet heat, chemicals, or electricity (both indoors and outdoors).
· Burns from dry heat can occur from fire, irons, hairdryers, curling irons, and stoves (American Institute for Preventive Medicine, 2012; Leahy, Fuzy & Grafe, 2013).
· Burns from wet or moist heat occur from hot liquids, such as hot water or steam (American Institute for Preventive Medicine; Leahy, Fuzy & Grafe). These types of burns are called scalds. Scalds can occur within seconds and cause serious injury.
· Chemical burns occur from chemical sources and can also cause serious burns when exposed to skin, or if swallowed, whether intentionally or unintentionally.
· Electrical burns can cause very serious injury as they can burn both the outside and inside of the person’s body, causing injury that cannot be seen, and which can be life-threatening.
· Radiation burns can also occur from sources of radiation such as sunlight (American Institute for Preventive Medicine). [64]
Types of Burns
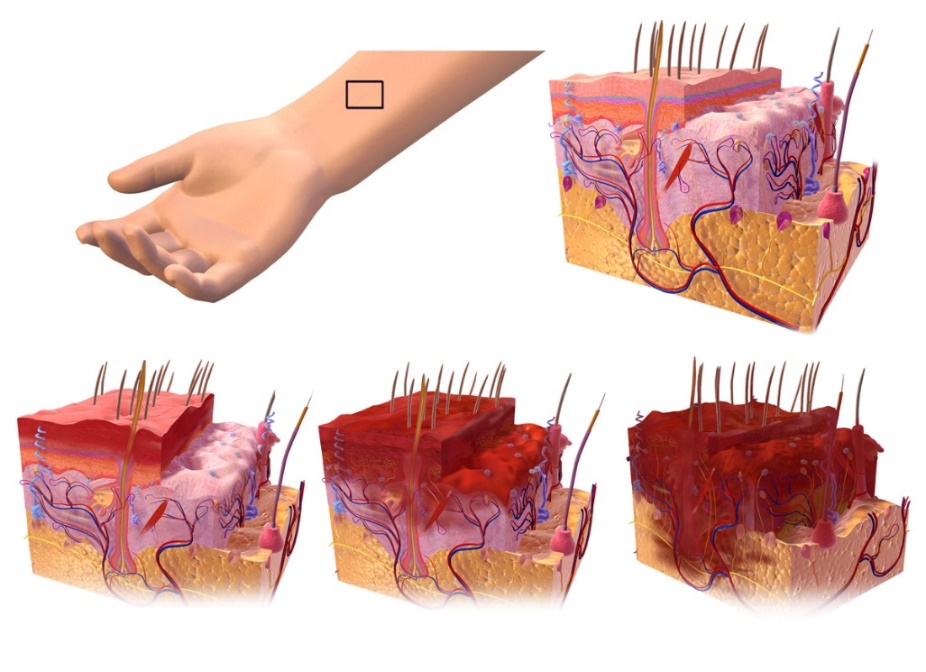
Burns are divided into first, second, and third degree burns.
First degree burns affect only the outer layer of the skin (epidermis). These types of burns are the least serious as they are only on the surface of the skin. First degree burns usually appear red, dry, and slightly swollen (MedlinePlus, 2014). Blisters do not occur with this type of burn. They should heal within a couple of days (American Institute for Preventive Medicine, 2012). A first degree burn is pictured in the bottom left of Figure 3.20.
Second degree burns affect the top layer of the skin and the second layer of skin underneath (dermis). These are more serious than first degree burns. The skin may appear very swollen, red, moist, (MedlinePlus, 2014) and may have blisters or look watery and weepy (American Institute for Preventive Medicine, 2012). A second degree burn is pictured in the bottom middle of Figure 3.20.
Third degree burns are the most serious burn. A third degree burn affects all layers of the skin and may affect the organs below the surface of the skin. The skin may appear white or black and charred (MedlinePlus, 2014). The person may deny pain because the nerve endings in their skin have been burned away (American Institute for Preventive Medicine, 2012). Third degree burns require immediate medical treatment. If teachers suspect a child has a third degree burn, they should immediately call 911. A third degree burn is pictured in the bottom right of Figure 3.20. [65]
Chemical burns can occur anytime a liquid or powder chemical comes into contact with skin or mucous membranes that line the eyes, nose, or throat. Chemical burns may also occur if a chemical is swallowed. These burns can cause serious injury and emergency services should be contacted. If a person receives a chemical burn, the chemical should be removed from the skin by using a gloved hand to brush it off and then wash the area with plenty of cool water. Electrical burns can occur if a person has been using an electrical appliance and is exposed to water or if an electrical short occurs while using the electrical appliance. Using faulty or frayed cords on electrical appliances can result in electrical burns. Electrical burns are a serious injury. Emergency medical services (EMS) should be immediately activated.
Never use oils such as butter or vegetable oil on any type of burn as this can cause further injury. For first or second degree burns flush the area with plenty of cool (not ice cold) water for about 15 minutes or until the pain decreases and cover with a clean, dry bandage. Using ice or ice-cold water can cause frostbite (American Institute for Preventive Medicine, 2012). For major burns remove any clothing that is not stuck to the skin, cover the burned area with a dry, clean cloth, and seek emergency assistance. [67]
Guidelines to Prevent Burns
· Install and regularly test smoke alarms.
· Practice fire drills. [68]
· Train staff to use fire extinguishers.
· Teach children to stop, drop, and roll. [69]
· Never allow children to use electrical appliances unsupervised.
· Never use electrical appliances near water sources.
· Never use electrical appliances in which the cord appears to be damaged or frayed.
· Never pull a plug from the cord. Always remove a cord from an outlet by holding the base of the plug.
· Cover electrical outlets with childproof plugs. Never allow children to put anything inside an electrical outlet.
· Ensure stoves and other appliances are turned off when finished with them.
· Turn pot handles inward so that a person cannot accidentally bump a handle and spill hot liquids.
· Do not use space heaters and other personal heaters.
· Check to be sure the hot water heater is not set too high. To avoid scalds from hot tap water, hot water heaters should be set to 120 degrees or less (MedlinePlus, 2014).
· Keep chemicals, cleaning solutions, and matches and lighters securely locked and out of reach of children. [70]
Safe Sleeping
Sudden Infant Death Syndrome (SIDS) is identified when the death of a healthy infant occurs suddenly and unexpectedly, and medical and forensic investigation findings (including an autopsy) are inconclusive. SIDS is the leading cause of death in infants 1 to 12 months old, and approximately 1,500 infants died of SIDS in 2013 (CDC, 2015). Because SIDS is diagnosed when no other cause of death can be determined, possible causes of SIDS are regularly researched. One leading hypothesis suggests that infants who die from SIDS have abnormalities in the area of the brainstem responsible for regulating breathing (Weekes-Shackelford & Shackelford, 2005). [71]
This is a very important topic for early childhood educators as one study found that while data suggests that only 7% of incidents of SIDS should occur while children are in child care, 20.4% actually did. [72]

Risk Factors for SIDS
Babies are at higher risk for SIDS if they:
- Sleep on their stomachs
- Sleep on soft surfaces, such as an adult mattress, couch, or chair or under soft coverings
- Sleep on or under soft or loose bedding
- Get too hot during sleep
- Are exposed to cigarette smoke in the womb or in their environment, such as at home, in the car, in the bedroom, or other areas
- The adult smokes, has recently had alcohol, or is tired.
- The baby is covered by a blanket or quilt.
- The baby sleeps with more than one bed-sharer.
- The baby is younger than 11 to 14 weeks of age.
Important Facts About SIDS
· SIDS happens in families of all social, economic and ethnic groups.
· Most SIDS deaths occur between one and four months of age.
· SIDS occurs in boys more than girls.
· The death is sudden and unexpected, often occurring during sleep. In most cases, the baby seems healthy.
· Although it is not known exactly what causes SIDS, researchers know that it is not caused by suffocation, choking, spitting up, vomiting, or immunizations.
· SIDS is not contagious. [74]
Reducing the Risks
Although the sudden and unexpected death of an infant cannot be predicted or prevented, research shows that certain infant care practices can help reduce the risk of a baby dying suddenly and unexpectedly. Early childhood educators can help lower the risk of SUID for infants less than one year of age by following these risk reduction guidelines.
Sleeping Position
The chance of an infant dying suddenly and unexpectedly in childcare is higher when a baby first starts the transition from home to care. Research shows if a baby has been placed on his/her back by the families, and the childcare provider places the baby to sleep on his/her stomach, there is a higher risk of death in the first weeks of child care. One of the most important things you can do to reduce the risk of sudden unexpected death is to place babies to sleep on their backs.
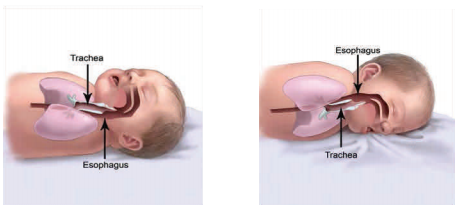
Healthy babies do not choke when placed to sleep on their backs. By reflex, babies swallow or cough up fluids to keep the airway clear. Since the windpipe (trachea) is positioned on top of the esophagus, fluids are not likely to enter the airway. (See Figure 3.21)
Babies who are able to roll back and forth between their back and tummy should be placed on their backs for sleep and allowed to assume their sleep position of choice. When infants fall asleep while playing on their tummies, move the baby to a crib onto his/her back to continue sleeping.
Cribs, Sleep Surface and Bedding
Infants should sleep in a crib, bassinet, portable crib or play yard that conforms to the safety standards of the Consumer Product Safety Commission (CPSC). The mattress should be firm, fit tightly, and be covered with a tight fitted sheet. Babies should not sleep on adult beds, waterbeds, couches, beanbag chairs or other soft surfaces. Do not use fluffy blankets or comforters under the baby, or put the baby to sleep on a sheepskin, pillow or other soft materials. Keep stuffed toys, bumper pads, loose bedding and other toys and soft objects out of the crib.
Temperature
Babies should be kept warm, not hot. Babies should be dressed with only one additional layer than you are wearing for warmth. In areas where babies sleep, keep the temperature so that it feels comfortable to you. If needed, infants can be dressed in blanket sleepers for warmth. This ensures that the baby’s head will be uncovered during sleep.
No one should smoke around children. California Child Care Licensing Regulations prohibit smoking in childcare centers. Smoke in the infants’ environment is a major risk factor for SIDS.
If the family provides a pacifier, it should be offered to the infant. If a pacifier is used, it should never be attached to a string. Infants should not be forced to take a pacifier and if it falls out during sleep it doesn’t need to be given back to the infant.
Breastfeeding
Breastfeeding has many health benefits for mother and baby, including a reduced risk of SIDS. Childcare programs should be breastfeeding friendly. [76]
Indoor Falls
While most falls occur outdoors, and this topic is addressed in Chapter 4, they can also happen indoors. Teachers (and adults at home) can prevent falls indoors by
- Installing stops on windows that prevent them from being opened more than four inches or install window guards on lower parts of windows. Removing furniture from near windows. Screens should not be relied on to prevent a fall.
- Installing safety gates at the top and bottom of staircases. Installing lower rails on stairs that children can reach and use. Making sure the surface of the stairs stays clear.
- Using safety straps and harnesses on baby equipment and furniture. Children should not be left unattended in high chairs or on changing tables.
- Baby walkers should not be used (licensing prohibits these).
- Teaching children to walk where surfaces may be slick. Preventing these surfaces as much as possible, such as wiping up spills. [78]
Indoor Water Safety
Small children are top-heavy; they tend to fall forward and headfirst when they lose their balance. They do not have enough muscle development in their upper body to pull themselves up out of a bucket, toilet or bathtub, or for that matter, any body of water. Even a bucket containing only a few inches of water can be dangerous for a small child.
It’s important that early childhood educators follow the safety practices outlined in Chapter 4 for water safety both indoors and outdoors, keep children under active supervision, and be very aware of containers of water. [79]
Active supervision is critical to keep young children safe. When programs create a culture of safety, they go beyond following regulations and policies, by making a commitment to protecting safety so that children don’t get hurt. There are some common risks to safety that educators should be aware or (and that will be covered in more depth in the next two chapters). When early care and education programs create a safety plan using data they have gathered by documenting and analyzing the injuries children get, they can make changes to help protect children’s safety.
Teachers need to create safe indoor environments in which children engage, explore, and interact. By recognizing that behavior is communication, they can help children use safe behaviors to get their needs met. Teachers should choose age-appropriate toys and materials that are well constructed, hazard-free, and nontoxic. With adult support, children can navigate media and technology safely. Teachers must work to prevent injuries that may occur indoors, such as choking, poisoning, burns, drowning, and falls. And teachers that care for infants must follow practices to reduce the risk of Sudden Infant Death Syndrome.
Chapter 7 Review
Chapter 3 Workbook
See Workbook in Chapter 4
References:
[1] Photo provided by author.
[2] Managing the Classroom: Designing Environments by the Office of Head Start is in the public domain.
[3] Assessing Your Physical Spaces and Strategizing Chances by the Office of Head Start is in the public domain.
[4] Presenter Notes: Designing Environments by the Office of Head Start is in the public domain.
[5] Photo provided by author.
[6] Managing the Classroom: Designing Environments by the Office of Head Start is in the public domain.
[7] Preparing for Intentionally Grouping Children by the Office of Head Start is in the public domain.
[8] Photo provided by author.
[9] Presenter Notes: Designing Environments by the Office of Head Start is in the public domain.
[10] Presenter Notes: Designing Environments by the Office of Head Start is in the public domain.
[11] Behavior Has Meaning: Presenter Notes by the National Center on Early Childhood Health and Wellness is in the public domain.
[12] Form and Function by the National Center on Early Childhood Health and Wellness is in the public domain.
[13] Behavior Has Meaning: Presenter Notes by the National Center on Early Childhood Health and Wellness is in the public domain.
[14] Form and Function by the National Center on Early Childhood Health and Wellness is in the public domain.
[15] Behavior Has Meaning: Presenter Notes by the National Center on Early Childhood Health and Wellness is in the public domain.
[16] Girl Playing on Plastic Inline Boards is free for commercial use.
[17] AIAN Education Manager Webinar Series: February 2013 by the U.S. Department of Health and Human Services is in the public domain
[18] Biting: A Fact Sheet for Families by the U.S. Department of Health and Human Services is in the public domain.
[19] Which Toy for Which Child by the U.S. Consumer Product Safety Commission is in the public domain.
[20] Think Toy Safety by the U.S. Consumer Product Safety Commission is in the public domain.
[21] Which Toy for Which Child by the U.S. Consumer Product Safety Commission is in the public domain.
[22] Which Toy for Which Child by the U.S. Consumer Product Safety Commission is in the public domain.
[23] Think Toy Safety by the U.S. Consumer Product Safety Commission is in the public domain.
[24] Think Toy Safety by the U.S. Consumer Product Safety Commission is in the public domain.
[25] Think Toy Safety by the U.S. Consumer Product Safety Commission is in the public domain.
[26] Think Toy Safety by the U.S. Consumer Product Safety Commission is in the public domain.
[27] Think Toy Safety by the U.S. Consumer Product Safety Commission is in the public domain.
[28] Think Toy Safety by the U.S. Consumer Product Safety Commission is in the public domain.
[29] Children Wooden Multicolored Toy Labyrinth by Marco Verch is licensed under CC BY 2.0 .
[30] Image is in the public domain.
[31] Image is in the public domain.
[32] Art Materials Business Guide by the U.S. Consumer Product Safety Commission is in the public domain.
[33] Art and Craft Safety Guide by the U.S. Consumer Product Safety Commission is in the public domain.
[34] ACMI. (2020). Home. Retrieved from https://acmiart.org/
[35] Image by The Art and Creative Materials Institute is licensed under CC BY-SA 4.0
[36] Image provided by author
[37] Image provided by author
[38] Image provided by author
[39] Image provided by author
[40] Image provided by author
[41] Art and Craft Safety Guide by the U.S. Consumer Product Safety Commission is in the public domain.
[42] Snell, S. (2018). Don’t Eat the Paint: Art Safety with Young Children. Retrieved from https://communitycarecollege.edu/early-childhood-education/tips-for-art-safety-with-young-children/
[43] National Association for the Education of Young Children & Fred Rogers Center for Early Learning and Children’s Media at Saint Vincent College (2012), page 8. (cited in: https://tech.ed.gov/earlylearning/principles/ )
[44] Guernsey, L. (2012) Screen Time: How electronic media—from baby videos to educational software—affects your young child. New York, NY: Basic Books. (cited in: https://tech.ed.gov/earlylearning/principles/ )
[45] Bilingual Pre-K Technology Integration by Professional Learning is licensed under CC BY-SA 4.0
[46] Council on Communications and Media. (2016). Media and Young Minds. Pediatrics, 138 (5). Retrieved from https://pediatrics.aappublications.org/content/138/5/e20162591
[47] AAP, APHA, & MCHB. (2011). Caring for Our Children: National Health and Safety Performance Standards: Guidelines for Early Care and Educational Programs, Third Edition. Retrieved from https://nrckids.org/files/CFOC3_updated_final.pdf
[48] California Preschool Program Guidelines by the California Department of Education is used with permission.
[49] California Preschool Program Guidelines by the California Department of Education is used with permission.
[50] Guiding Principles for Use of Technology with Early Learners by the Office of Educational Technology is in the public domain.
[51] U.S. Department of Education, Office of Educational Technology. (2015) Ed tech developer’s guide. Retrieved from https://tech.ed.gov/developers-guide/ (cited in https://tech.ed.gov/earlylearning/principles/ )
[52] Guiding Principles for Use of Technology with Early Learners by the Office of Educational Technology is in the public domain.
[53] Guiding Principles for Use of Technology with Early Learners by the Office of Educational Technology is in the public domain.
[54] Anderson, K. (2020). Choking: Knowing the Signs and What to Do. Retrieved from https://www.chla.org/blog/rn-remedies/choking-knowing-the-signs-and-what-do
[55] American Academy of Pediatrics. (2020). Safety and Injury Prevention Curriculum. Retrieved from https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/healthy-child-care/Pages/Safety-and-Injury-Prevention.aspx
[56] American Academy of Pediatrics. (2020). Safety and Injury Prevention Curriculum. Retrieved from https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/healthy-child-care/Pages/Safety-and-Injury-Prevention.aspx
[57] Anderson, K. (2020). Choking: Knowing the Signs and What to Do. Retrieved from https://www.chla.org/blog/rn-remedies/choking-knowing-the-signs-and-what-do
[58] Anderson, K. (2020). Choking: Knowing the Signs and What to Do. Retrieved from https://www.chla.org/blog/rn-remedies/choking-knowing-the-signs-and-what-do
[59] Small Parts: What Parents Need to Know , by the U.S. Consumer Product Safety Commission is in the public domain.
[60] Image by r. nial bradshaw is licensed under CC BY 2.0 .
[61] Safety and Injury Prevention by Kimberly McLain, Erin K. O’Hara-Leslie, & Andrea C. Wade is licensed under CC BY 4.0
[62] Even Plants Can Be Poisonous by from the Office of Head Start is in the public domain.
[63] Burn Prevention by the Centers for Disease Control and Prevention is in the public domain
[64] Safety and Injury Prevention by Kimberly McLain, Erin K. O’Hara-Leslie, & Andrea C. Wade is licensed under CC BY 4.0
[65] Safety and Injury Prevention by Kimberly McLain, Erin K. O’Hara-Leslie, & Andrea C. Wade is licensed under CC BY 4.0
[66] 1st, 2nd, and 3rd degree burns by Bruce Blaus is licensed under CC BY-SA 4.0 .
[67] Safety and Injury Prevention by Kimberly McLain, Erin K. O’Hara-Leslie, & Andrea C. Wade is licensed under CC BY 4.0 .
[68] Burn Prevention by the Centers for Disease Control and Prevention is in the public domain.
[69] Mayo Clinic. (2019). Burn Safety: Protect your child from burns. Retrieved from: https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/child-safety/art-20044027
[70] Safety and Injury Prevention by Kimberly McLain, Erin K. O’Hara-Leslie, & Andrea C. Wade is licensed under CC BY 4.0 .
[71] Lifespan Development: A Psychological Perspective by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0
[72] Moon, R. Y., Patel, K. M., & Shaefer, S. J. (2000). Sudden infant death syndrome in child care settings. Pediatrics , 106 (2 Pt 1), 295–300. https://doi.org/10.1542/peds.106.2.295
[73] Image by the U.S. Department of Health and Human Services is in the public domain.
[74] California Dept. of Public Health MCAH. (2014). What Child Care Providers and Other Caregivers Should Know. Retrieved from https://cchealth.org/sids/pdf/Child-Care-SIDS-Booklet.pdf.
[75] California Dept. of Public Health MCAH. (2014). What Child Care Providers and Other Caregivers Should Know. Retrieved from https://cchealth.org/sids/pdf/Child-Care-SIDS-Booklet.pdf.
[76] California Dept. of Public Health MCAH. (2014). What Child Care Providers and Other Caregivers Should Know. Retrieved from https://cchealth.org/sids/pdf/Child-Care-SIDS-Booklet.pdf.
[77] California Dept. of Public Health MCAH. (2014). What Child Care Providers and Other Caregivers Should Know. Retrieved from https://cchealth.org/sids/pdf/Child-Care-SIDS-Booklet.pdf.
[78] Mayo Clinic. (2020). Infant and toddler health. Retrieved from: https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/child-safety/art-20046124
[79] California Childcare Health Program. (2003). Prevent Drowning. Retrieved from https://cchp.ucsf.edu/sites/g/files/tkssra181/f/drownen081803_adr.pdf
[1] Community Playthings. (2020). Inspiration Gallery. Retrieved from https://www.communityplaythings.com/inspiration/room-inspirations
[2] Active Supervision from the Office of Head Start is in the public domain.
[3] California Infant/Toddler Curriculum Framework by the California Department of Education is used with permission.
[4] Active Supervision from the Office of Head Start is in the public domain.
[5] California Infant/Toddler Curriculum Framework by the California Department of Education is used with permission.
[6] Keeping Babies Safe: Active Supervision for Infants & Toddlers by the Dept. of Health and Human Services is in the public domain.
[7] Environment as Curriculum for Infants and Toddlers by the Office of Head Start is in the public domain.
[8] California Infant/Toddler Curriculum Framework by the California Department of Education is used with permission.
[9] Active Supervision for Preschoolers by the Dept. of Health and Human Services is in the public domain.
[10] Infant/Toddler Learning and Development Program Guidelines by the California Department of Education is used with permission.
[11] Creating and Enhancing a Culture of Safety Head Start Town Hall Meeting: September 12, 2018 by the Dept. of Health and Human Services is in the public domain.
[12] 10 Actions to Create a Culture of Safety by the National Center on Childhood Health and Wellness is in the public domain.
[13] Fatal Injury Reports, National, Regional and State, 1981-2018 , by the Centers for Disease Control and Prevention is in the public domain.
[14] Child Injury by the Centers for Disease Control and Prevention is in the public domain.
[15] CDC Childhood Injury Report by the Centers for Disease Control and Prevention is in the public domain.
[16]Health implications of children in child care centres Part B: Injuries and infections. (2009). Paediatrics & child health , 14 (1), 40–48. https://doi.org/10.1093/pch/14.1.40
[17] California Dept. of Public Health MCAH. (2014). What Child Care Providers and Other Caregivers Should Know. Retrieved from https://cchealth.org/sids/pdf/Child-Care-SIDS-Booklet.pdf.
[18] American Academy of Pediatrics. (2020). Safety and Injury Prevention Curriculum. Retrieved from https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/healthy-child-care/Pages/Safety-and-Injury-Prevention.aspx
[19] Anderson, K. (2020). Choking: Knowing the Signs and What to Do. Retrieved from https://www.chla.org/blog/rn-remedies/choking-knowing-the-signs-and-what-do
[20] Drowning Prevention by the Centers for Disease Control and Prevention is in the public domain.
[21] California Childcare Health Program. (n.d.). Prevent Drowning. Retrieved from https://cchp.ucsf.edu/sites/g/files/tkssra181/f/drownen081803_adr.pdf
[22] Burn Prevention by the Centers for Disease Control and Prevention is in the public domain.
[23] Safety and Injury Prevention by Kimberly McLain, Erin K. O’Hara-Leslie, & Andrea C. Wade is licensed under CC BY 4.0
[24] Fall Prevention by the Centers for Disease Control and Prevention is in the public domain.
[25] Mayo Clinic. (2020). Fall Safety for Kids: How to Prevent Falls. Retrieved from https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/child-safety/art-20046124
[26] Poisoning Prevention by the Centers for Disease Control and Prevention is in the public domain.
[27] Safety Tips for Pedestrians by the Pedestrian and Bicycle Information Center is in the public domain
[28] Child Passenger Safety: Get the Facts by the Centers for Disease Control and Prevention is in the public domain
[29] Health and Safety Screener by the Office of Head Start is in the public domain.
[30] Infant/Toddler Learning & Development Program Guidelines by the California Department of Education is used with permission.
[31]Robertson, C. (2013). Safety, nutrition, and health in early education (5th ed.). Belmont, CA: Wadsworth.
[32] Hazard Mapping for Early Care and Education Programs by the National Center on Early Childhood Health and Wellness is in the public domain.
[33] Hazard Mapping for Early Care and Education Programs by the National Center on Early Childhood Health and Wellness is in the public domain.
[34] 150917-M-UF252-286.JPG by Nathan L. Hanks Jr. is in the public domain.
[35] California Preschool Curriculum Framework Volume 2 by the California Department of Education is used with permission.
[36] California Preschool Curriculum Framework Volume 2 by the California Department of Education is used with permission.
[37] Adventure Playground Natural Free Photo by MadCabbage is in the public domain.
[38] Brussoni, M., Olsen, L. L., Pike, I., & Sleet, D. A. (2012). Risky Play and Children’s Safety: Balancing Priorities for Optimal Child Development. International Journal of Environmental Research and Public Health , 9 (9), 3134–3148. doi:10.3390/ijerph9093134. Retrieved from https://www.mdpi.com/1660-4601/9/9/3134
Chapter Seven: Preventing Injury; Protecting Children’s Safety Copyright © by Kelly McKown is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 10 fall and injury prevention.
Leanne Currie .
Affiliations
Fall and injury prevention continues to be a considerable challenge across the care continuum. In the United States, unintentional falls are the most common cause of nonfatal injuries for people older than 65 years. Up to 32 percent of community-dwelling individuals over the age of 65 fall each year, and females fall more frequently than males in this age group. 1 , 2 Fall-related injuries are the most common cause of accidental death in those over the age of 65, resulting in approximately 41 fall-related deaths per 100,000 people per year. In general, injury and mortality rates rise dramatically for both males and females across the races after the age of 85, but males older than 85 are more likely to die from a fall than females. 2–6 Unfortunately, fall-related death rates in the United States increased between 1999 and 2004, from 29 to 41 per 100,000 population. 2 , 7 Sadly, these rates are moving away from the Healthy People 2010 fall-prevention goal, which specifically seeks to reduce the number of deaths resulting from falls among those age 65 or older from the 2003 baseline of 38 per 100,000 population to no more than 34 per 100,000. 8 Thus, falls are a growing public health problem that needs to be addressed.
The sequelae from falls are costly. Fall-related injuries account for up to 15 percent of rehospitalizations in the first month after discharge from hospital. 9 Based on data from 2000, total annual estimated costs were between $16 billion and $19 billion for nonfatal, fall-related injuries and approximately $170 million dollars for fall-related deaths across care settings in the community. 10 , 11 Several factors have been implicated as causes of falls and injuries; to date, however, no definitive predictor profile has been identified. Although the underlying status of the individual who sustains a fall may contribute to the fall and subsequent injury, the trauma resulting from the fall itself is most often the cause of morbidity and mortality.
Over the past 20 years gerontology researchers, spearheaded by Mary Tinnetti from Yale University, have carried out a significant amount of research to address the problem of falls and injuries in the community. However, ubiquitous use of successful interventions is not yet in place in the community. As health care moves toward patient-centered care, and as a growing body of research provides guidance for widespread fall-prevention programs, fall- and fall-related-injury prevention now has the potential to be addressed across the care continuum.
Inpatient fall prevention has been an individual area of concern for nursing for almost 50 years. 12 , 13 Traditional hospital-based incident reports deem all inpatient falls to be avoidable, and therefore falls are classified as adverse events. Indeed, falls are the most frequently reported adverse events in the adult inpatient setting. But underreporting of fall events is possible, so injury reporting is likely a more consistent quality measure over time and organizations should consider judging the effects of interventions based on injury rates, not only fall rates. Inpatient fall rates range from 1.7 to 25 falls per 1,000 patient days, depending on the care area, with geropsychiatric patients having the highest risk. 14–18 Extrapolated hospital fall statistics indicate that the overall risk of a patient falling in the acute care setting is approximately 1.9 to 3 percent of all hospitalizations. 16–18 In the United States, there are approximately 37 million hospitalizations each year; 19 therefore, the resultant number of falls in hospitals could reach more than 1 million per year.
Injuries are reported to occur in approximately 6 to 44 percent of acute inpatient falls. 5 , 20–23 Serious injuries from falls, such as head injuries or fractures, occur less frequently, 2 to 8 percent, but result in approximately 90,000 serious injuries across the United States each year. 20 Fall-related deaths in the inpatient environment are a relatively rare occurrence. Although less than 1 percent of inpatient falls result in death, this translates to approximately 11,000 fatal falls in the hospital environment per year nationwide. Since falls are considered preventable, fatal fall-related injuries should never occur while a patient is under hospital care.
In the long-term care setting, 29 percent to 55 percent of residents are reported to fall during their stay. 24 , 25 In this group, injury rates are reported to be up to 20 percent, twice that of community-dwelling elderly. The increase in injury rates is likely because long-term care residents are more vulnerable than those who can function in the community. 26 Rubenstein 27 reported 1,800 long-term care fatal falls in the United States during1988. The current number of long-term care fatal falls has not been estimated; however, there are 16,000 nursing homes in the United States caring for 1.5 million residents in 2004. 28 This population will likely grow in the coming years, thus fall and injury prevention remains of utmost concern.
- Fall and Fall-Related Injury Reporting
Falls and related injuries have consistently been associated with the quality of nursing care in the acute care setting. They are included as a nursing-quality indicator monitored by the American Nurses Association, National Database of Nursing Quality Indicators (ANA–NDNQI) and by the National Quality Forum. 29 , 30 Participation in the ANA–NDNQI provides hospitals with the ability to view their fall and injury rates in relation to other hospitals of similar type and size. However, participation in ANA–NDNQI is voluntary; despite a rapidly growing participation rate, it is not yet ubiquitous (1,089 hospitals as of June 2007, approximately 15 percent of U.S. hospitals). The National Quality Forum also advocates for voluntary reporting of quality indicators for acute care (falls prevalence and fall-related injuries) and ambulatory care (fall-risk screening for geriatrics). 31 , 32
The Maryland Quality Indicator Project is a second voluntary national repository that provides fall and fall-related injury benchmarks for the behavioral health, long-term care, and home care settings. 33 Unfortunately, this project has a participation level of approximately 1,000 hospitals (approximately 14 percent), making national benchmarking difficult. In the home care setting, the Centers for Medicare & Medicaid Service’s Outcome and Assessment Information Set (CMS–OASIS) provides the reporting basis for the patients’ physical functioning. 34 Growing efforts to expand patient safety initiatives to the home care setting seek to include falls as a quality indicator for patients who are cared for at home, but who are not completely bed bound. 35 , 36 Collection of these data has the potential for organizations to track fall rates of vulnerable patients and to identify patients at risk for falls and injuries. However, further research is required to validate such screening and to examine which interventions are effective based on risk status.
In the nursing home setting, the long-term care minimum dataset (LTCMDS) is used for reporting all aspects of care. The LTCMDS captures fall and injury histories via assessments that are performed on admission and at regular intervals during a resident’s stay. 37 In addition, residents are evaluated for balance and for the ability to perform activities of daily living (ADLs), with the goal to apply fall-prevention measures should the patient be deficient in these areas. Recent research by Hill-Westmoreland and Gruber-Baldini 38 indicated only a 75 percent concordance between chart abstraction and minimum dataset reporting for a group of long-term care facilities. A more recent development in the long-term care setting, the Nursing Home Quality Initiative, promotes the collection of a list of enhanced quality indicators, including those that track declines in functional and cognitive status. 34 , 37 The Agency for Healthcare Research and Quality (AHRQ) has elected to monitor only postoperative hip fracture as their fall-related preventive quality indicator, which is consistent with thinking that monitoring fall-related injuries is a more dependable measure of quality. 39 , 40 However, tracking of all fractures would be of benefit. The Health Plan Employer Data and Information Set has recently added Fall Risk Assessment to its dataset, which will provide a method to benchmark the evaluation of fall risk between health insurance providers. 41 However, application of fall- and injury-prevention programs is not included as an indicator, which will make it difficult to benchmark these important measures. Increased and more accurate monitoring of these elements has the potential to reduce falls among nursing home residents; however, the effect of these efforts has yet to be established.
Definitions of Falls and Fall-Related Injuries
Falls and related injuries have had varying definitions. 42 , 43 Falls may be precipitated by intrinsic or extrinsic factors. Intrinsic factors are those that have a physiologic origin, and extrinsic factors are those precipitating from environmental or other hazards. Distinguishing between intrinsic or extrinsic risk factors can facilitate identification of preventive strategies. According to Tinetti, Speechley, and Ginter, 44 a fall in the nonhospitalized geriatric population is defined as “an event which results in a person coming to rest unintentionally on the ground or lower level, not as a result of a major intrinsic event (such as a stroke) or overwhelming hazard.” Agostini, Baker, and Bogardus 45 adapted this definition for the inpatient, acute, and long-term care areas to define a fall as “unintentionally coming to rest on the ground, floor, or other lower level, but not as a result of syncope or overwhelming external force.”
Other definitions are broader and include falls related to intrinsic events such as syncope or stroke. For example, Nevitt’s 46 definition of a fall is “falling all the way down to the floor or ground, or falling and hitting an object like a chair or stair.” The ANA–NDNQI provides an all-inclusive definition 47 (p. 26):
An unplanned descent to the floor (or extension of the floor, e.g., trash can or other equipment) with or without injury. All types of falls are included, whether they result from physiological reasons or environmental reasons.
The International Classification of Diseases 9 Clinical Modifications (ICD-9-CM) uses several codes to categorize falls, all of which have broad descriptions: Accidentally bumping against moving object caused by crowd with subsequent fall (E917.6); Fall on or from ladders or scaffolding (E881); Fall from or out of building or other structure (E882); Other fall from one level to another (E884); Fall on same level from slipping, tripping, or stumbling (E885); Fall on same level from collision, pushing, or shoving by or with another person (E886); and Other and unspecified fall (E888). 48 In the inpatient care setting, E888 is the code that is typically used to record a fall in a medical record. However, this ICD-9-CM code is not consistently used for reporting; therefore, institutions generally rely on incident reports as the method of counting fall events. 48
Fall-related injuries in the community, home care, and long-term care areas are generally characterized by ICD-9-CM diagnoses for the related injured body part. In contrast, incident reports in the acute care setting use the following ANA–NDNQI fall-related injuries categories:
- None indicates that the patient did not sustain an injury secondary to the fall.
- Minor indicates those injuries requiring a simple intervention.
- Moderate indicates injuries requiring sutures or splints.
- Major injuries are those that require surgery, casting, further examination (e.g., for a neurological injury).
- Deaths refers to those that result from injuries sustained from the fall. 29
According to Morse, 21 inpatient falls can be classified into three categories: accidental falls (derived from extrinsic factors, such as environmental considerations), anticipated physiologic falls (derived from intrinsic physiologic factors, such as confusion), and unanticipated physiologic falls (derived from unexpected intrinsic events, such as a new onset syncopal event or a major intrinsic event such as stroke). Morse asserts that using this classification, approximately 78 percent of the falls related to anticipated physiologic events can be identified early, and safety measures can be applied to prevent the fall. Research to identify precursors to unexpected intrinsic events, such as screening for predictors of syncopal events, might increase the early identification of anticipated physiologic falls, which could ultimately prevent more falls. 49–51
Falls and Fall-Related Injuries as Medical Errors
The definition of a fall is consistent with that of a medical error: “the failure of a planned action to be completed as intended” (i.e., error of execution) or “the use of a wrong plan to achieve an aim” (i.e., error of planning). 52 , 53 For example, an error of execution might be the failure to perform the planned action of placing a call light within the patient’s reach, and an error in planning might be to provide aggressive physical therapy before a patient's balance has been established. An error of commission is “an error that occurs as a result of an action taken,” for example, a fall that occurs subsequent to a behavioral health patient's electroconvulsive therapy. An error of omission, “an error which occurs as a result of an action not taken,” might occur if the patient is not assessed for fall and injury risk, which prevents appropriate interventions from being applied. Latent errors related to fall and injury prevention are those in which an agency does not apply appropriate standards, training, or support for the practice-based fall- and injury-prevention processes. Recent efforts by the Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations [JCAHO]) in its National Patient Safety Goals advocate for institution-wide risk assessment for falls and documentation of a fall-prevention program. 54 These efforts have the potential to eliminate latent errors related to falls and injuries. Monitoring errorsmight occur if the patient is not monitored to identify fall risk, or if the patient is not monitored to identify a post-fall injury such as a subdural hematoma.
This review summarizes the current research related to fall and injury prevention. The chapter is organized to present research from two perspectives: (1) community setting, and (2) acute and long-term settings. For each setting, the research that addresses risk factors, risk assessment instruments, and fall- and injury-prevention interventions are reviewed. Reports on the outcomes of fall- and injury-prevention research using experimental or quasi-experimental research design is summarized in tables at the end of the chapter.
- Research Evidence
Falls and Related Injuries in the Community
In the following section, research about falls and related injuries in the community were identified and categorized as follows: risk factor identification, risk assessment instruments, and prevention strategies.
Risk factors in the community
The pivotal research of Tinetti, Speechly and Ginter 44 related to fall and injury prevention in community-dwelling individuals older than 65 years identified the following risk factors for falling: (1) postural hypotension, (2) use of any benzodiazepine or sedative-hypnotics, (3) use of four or more prescription medications, (4) environmental hazards, and (5) muscular strength or range of motion impairments. Other researchers have identified additional patient or treatment risk factors: (1) comorbidities, including diabetes, diabetic foot ulcer, 55 stroke, 56 syncope, 57 anemia, 58 , 59 Alzheimer’s disease, 60 Parkinson’s disease, 61 vitamin D deficiency, 62 , 63 and vitamin D deficiency in combination with low creatinine clearance; 64 (2) patient characteristics, including fallophobia (also known as “fear of falling”), 65 , 66 gait problems (e.g., weakness and impaired sensation), 67 postural hypotension, inability to get out of chair, impaired ability to perform ADLs, frailty, 68–70 inability to follow instructions, 71 and inability to adapt to changing environment; 72 and (3) other characteristics, including recent hospitalization, 9 nonsupportive footwear (e.g., slippers), 73 reckless wheelchair use, 74 environmental hazards, and use of psychotropic medication. 75 , 76 Age and gender are also associated with falls and fall-related morbidity and mortality. Fall rates increase with age, 77 and in community-dwellers between 65 and 85 years of age, females are more likely to fall, but males are more likely to die from fall-related injuries than females in this group. 1 , 2
The roles of ethnicity and race in relation to falls and injury have also been studied. Reyes-Ortiz and colleagues 78 examined risk factors for Mexican-Americans and found that in the community, the risk factors are the same as for their White counterparts. Hanlon and colleagues 79 examined predictors of falls between Caucasians and African Americans and found that African Americans were 23 percent less likely to fall than Whites (odds ratio = 0.77). Faulkner and colleagues 80 explored this difference in women and found that Caucasian women were 50 percent more likely to fall than African American women, although this was not statistically significant (relative risk = 1.50, 95% confidence interval [95% CI] = 0.90–2.49). The researchers further examined situations leading to falls and found that circumstances differed by ethnicity: Caucasian women were more likely to fall outdoors versus indoors (odds ratio = 1.6, 95% CI = 1.0–2.7) and laterally versus forward (odds ratio = 2.0, 95% CI = 1.1–3.4), but less likely to fall on the hand or wrist (odds ratio = 0.6, 95% CI = 0.3–1.0). This research suggests that activities differ between older African American women and their Caucasian counterparts and should be considered when making fall- and injury-prevention plans.
Risk factors for injury in the community
Risk factors for injury in the community are increasingly well characterized. Porthouse and her research team 81 performed a comprehensive cohort study of almost 4,300 women older than 70 years and confirmed the following risk factors for various types of fall-related fractures: (1) fall in the past 12 months, (2) increasing age, (3) previous fracture, and (4) low body weight. This work also identified that smoking was not associated with fracture risk. A growing body of research is examining vitamin D deficiency as a risk factor for fracture; however, results are conflicting to date, but bear further research. 81 , 82
Colon-Emeric and colleagues 83 used data from a large community epidemiologic study to identify whether historical and functional information could help to predict fracture risk. The researchers identified nine characteristics that were predictors of fracture: (1) female sex, (2) age greater than 75 years, (3) White race, (4) body mass index (BMI) of less than 22.8 kg/m 2 , (5) history of stroke, (6) cognitive impairment, (7) one or more ADL impairments, (8) one or more Rosow-Breslau impairments (e.g., perform heavy work, walk a mile, climb stairs), and (9) antiepileptic drug use. Ohm and colleagues 84 recently identified that elderly community-dwelling individuals with traumatic head injuries were more likely to die based on the use of antiplatelet therapy (relative risk = 2.5 for those taking antiplatelet therapies; P = 0.016). A similar body of research related to chronic subdural hematomas has identified that patients on anticoagulant or antiplatelet therapy are at higher risk for chronic subdural hematoma and that many of these are first identified when a patient is evaluated after a fall. 85 Many injury risk factors are consistent with fall risk factors, accentuating the need for effective screening of elderly community-dwelling individuals. However, factors that make people more susceptible to injury, such as antiplatelet therapy, establish the need for additional safety measures for individuals at risk for injury. Table 1 lists the intrinsic and extrinsic risk factors for falls, injuries, and fall-related deaths in the community.
Risk Factors for Falls, Injuries, and Fall-Related Deaths in the Community
Risk assessment instruments for community dwellers
Tinetti 86 developed a fall risk assessment index based on the following nine risk factors: mobility, morale, mental status, distance vision, hearing, postural blood pressure, back examination, medications, and ability to perform ADLs. This instrument has been the most widely used and tested, with a reported sensitivity of 80 percent and specificity of 74 percent. 87 Other instruments used in the community include the following (with reported sensitivities and specificities in parentheses): (1) Berg Balance Test (sensitivity = 77 percent; specificity = 86 percent), (2) Elderly Fall Screening Test (sensitivity = 93 percent; specificity = 78 percent), (3) Dynamic Gait Index (sensitivity = 85 percent; specificity = 38 percent), and (4) Timed Get Up and Go test (sensitivity = 87 percent; specificity = 87 percent). 87 Aside from the Timed Get Up and Go test, which takes less than a minute for a health care provider to administer, these instruments generally take 15 to 20 minutes to complete. 87
Lord and colleagues 88 recently evaluated the effect of an exercise-related fall-prevention program, but found that the intervention was not useful in community dwellers who were not screened for risk. The researchers concluded that screening to identify individuals at high risk for falls would be necessary for a successful fall-prevention program. Further research to identify the most accurate, yet easy-to-use risk assessment instrument would be necessary to move these efforts forward.
A recent systematic review by Scott and colleagues 89 examined fall risk assessment instruments in the community. The authors concluded that, in general, risk assessment instruments are available; however, most have been tested in only one setting. Therefore, further validation studies should be conducted on fall risk assessment instruments before any specific instrument can be recommended.
A potential time point for risk assessment is in the emergency department (ED). Several researchers have examined the effect of fall- and injury-prevention interventions applied to patients who are discharged from the ED after a noninjury or nonserious-injury fall. The overarching goal of these studies is to evaluate the ability of comprehensive risk assessment followed by targeted interventions to prevent future falls and fall-related injuries. Several studies have successfully shown that screening followed by tailored management can decrease repeat falls. 42 , 90–94 Close and colleagues 42 found that fall rates were reduced by 61 percent and recurrent falls were reduced by 67 percent for patients who had comprehensive risk assessment after a fall, compared to individuals who received standard treatment. Davison and colleagues 90 found a 36 percent decrease in fall rates after 1 year for patients who received a multimodal intervention for fall prevention after being identified as a faller on admission to the ED. In addition, these researchers noted an increase in falls self-efficacy, which is a measure of an individual’s perception of their ability to manage situations where they are at high risk for falling – the higher self-efficacy, the more able a person is able to manage high risk situations. In a related study, Lee, Hurley, and colleagues 91 conducted a randomized controlled trial to examine the impact of a personal emergency response system and found that there was no difference between treatment and control groups for self-efficacy or patient anxiety. The Lee and colleagues study is informative in that emergency contact alone was not sufficient to improve a patient’s belief in their ability to manage fall risk situations. Although no standardized instrument has yet been developed for use in the ED environment, the potential for the prevention of falls and related injuries in the community would be increased with the accurate identification of patients at risk for falls while they are in the ED.
Automated risk assessment in the community setting
To date, a limited number of computer-based, community-based fall assessment instruments have been described. By far the most complex and integrated is the Fall Risk Assessment and Management System, which was developed by the Australia Family Practice Group for use in the community by family practice physicians. 95 Fall Risk Assessment and Management System includes automated recommendations after the clinician executes a thorough patient assessment. Although this system appears promising, its efficacy has not yet been reported.
Lord, Menz, and Tiedemann 96 describe an electronic fall risk assessment instrument that provides a method to measure several risk factors, including vision, peripheral sensation, muscle force, reaction time, and postural sway. Although this instrument is thorough, it is meant for use by a physical therapist or a physician, nurse practitioner, or physician assistant for a focused fall risk assessment, rather than as a triage or screening tool. The novel aspect of this instrument is the comparison of the individual’s score to the normative scores for each of the assessments, which provides the clinician with an anchor and may facilitate improved screening over time. However, the predictive validity of this instrument has not been reported, and its use may be limited to a fall-prevention clinic.
Another electronic fall risk assessment instrument, described by Dyer and colleagues, 97 is an electronic checklist in a fall-prevention clinic. Unfortunately, the researchers concluded that the clinic itself was more successful than the instrument in identifying risk factors for falling, underscoring the reality that the implementation of an instrument without associated policy and procedure changes may have limited effect.
The presence of these automated systems indicates that there is movement toward computerized fall risk assessment. Indeed, many clinical information systems have adapted paper-based assessment instruments for use in the acute care setting. However, the efficacy of these systems has not been reported, and their effectiveness is likely to be constrained by the limits of the original instrument, the system in which they are placed, and the design team in ensuring that the automated instrument accurately reflects the original instrument.
Prevention strategies in the community
To date, several reviews conducted to examine the evidence available to support practice in this area have identified the need for multimodal, interdisciplinary prevention programs; the need for more accurate risk assessment instruments; and the need for more research related to this complex and costly problem. 11 , 98–107
Cumming 100 reviewed 21 trials and concluded that exercise programs were the most promising, and reduction of antipsychotic medications should be considered. However, Cumming also concluded that none of the reviewed research studies provided a definitive prevention strategy. Chang and collaborators 99 conducted a similar review targeted at examining interventions for older adults in the community and found that multimodal assessments with targeted intervention reduced risk of falls by 37 percent, and that exercise interventions reduced fall risk by 14 percent. Hill-Westmoreland, Soeken, and Spellbring 38 conducted a recent meta-analysis, including a sensitivity analysis, which identified an improved effect on fall prevention in the community when individualized management was added to exercise interventions. They concluded that exercise interventions were not sufficient in and of themselves, and interventions needed to be tailored to address individual risk factors.
Researchers have explored several other individual prevention strategies, including fall prevention clinics, exercise interventions with leg strengthening (e.g., Tai Chi), vitamin D supplements, home visits for safety evaluations, cataract surgery, and cardiac pacing. Falls and balance clinics present a promising community-based solution to the problem of falls. 108 Perell and colleagues 109 found a 50 percent reduction in fall rates for patients who were screened at a clinic and who had tailored interventions applied; however, this study had no control group and the researchers did not report injury rates, so the results are tentative. Clinics such as these provide focused intervention planning for patients identified at risk for falling, but the success of such clinics is contingent upon accurate identification of high-risk patients.
Identification of recurrent fallers via comprehensive screening followed by tailored interventions has been successful at reducing recurrent falls. Screening and intervention done in the ED reduced recurrent falls by 36 percent in one study, 90 and a nurse-led intervention that provided home assessment and tailored interventions reduced recurrent falls by 38 percent in another study. 110 Hogan and colleagues 111 also evaluated tailored interventions for patients who had had a fall within the past 3 months. They found no significant differences between the intervention and control groups in fall rates or time to first fall; however, the intervention group had a longer time between falls ( P = 0.001). However, the Hogan and colleagues study limited inclusion criteria to patients older than 65 years of age who had fallen in the past 3 months, and these two factors alone are likely insufficient to determine risk. These recent studies add to early work in the PROFET study, which found a 61 percent decrease in falls for patients who were identified in the ED and who had subsequent detailed risk assessment and tailored interventions. 42
Exercise-related interventions are by far the most commonly studied individual community prevention strategy. Most of this research indicates that exercise is beneficial for patients, and some research demonstrates that exercise regimes that involve leg strengthening and balance training, such as Tai Chi, are most effective. 112–122 Robertson and colleagues 123 performed a meta-analysis of four studies that examined effects of home exercise programs. They found in the pooled effect analysis that both fall and injury rates decreased by 35 percent. Exercise in conjunction with cognitive behavioral therapy, where patients are taught how to increase self-awareness about risky situations, has demonstrated promising results, including a longer time to first fall and decreased injuries. 124 Unfortunately, this work did not demonstrate an effect on falls efficacy, fear of falling, or actual fall rates. More recently, balance training has been compared to general exercise, and results show that balance training can prevent falls in the nonfrail elderly, but not in the frail elderly. 125 Lin and colleagues 126 found that deployment of large scale Tai Chi training to the general community had mixed results. Luukinen and colleagues 127 found a decrease in fall and injury rates with a targeted exercise program when compared to usual care, but the results were statistically significant only in a group that was not homebound—suggesting that early intervention may be more effective. Further research to explore interventions for homebound community dwellers, particularly for the very old and frail, will be important.
Laboratory studies indicate that calcium and vitamin D reduce bone loss, 128 and a growing body of work is examining the ability for vitamin D supplementation to prevent fractures in individuals who are vitamin D deficient. A meta-analysis performed by Bischoff-Ferrari and team 129 revealed that larger doses of vitamin D supplementation (700–800 IU/deciliter) reduced the risk of fracture by up to 26 percent, whereas smaller doses of vitamin D (400 IU/deciliter) did not reduce fracture risk. However, research to date has been inconclusive, and larger, more recent studies have indicated that the use of vitamin D does not reduce fracture risk in the general community. 130 On the other hand, vitamin D supplementation may be integral in preventing falls themselves: 131 Recently, Latham and colleagues 132 , 133 demonstrated that vitamin D intake is an individual predictor for fall reduction, primarily by improving muscle strength. Bischoff-Ferrari and colleagues 134 have also identified a reduction in fall risk for women, but not for men, using vitamin D supplementation. Although these results are promising, more research is required to identify best practice recommendations related to vitamin D deficiency screening and vitamin D supplementation or other bone-supporting medication regimes.
Other researchers are exploring the ability for osteoporosis-prevention medications to reduce fracture risk. 135 Sato and colleagues 136 , 137 reported that risedronate, an oral bisphosphonate for osteoporosis prevention, was effective at preventing fracture in older females, older males who have had a stroke, and older females with Alzheimer’s disease. A recent large study by McCloskey and colleagues 138 (N = 5579) demonstrated a 20–29 percent decrease in clinical fractures in community-dwelling females older than 75 years with and without osteoporosis who were prescribed clodronate 800 mg daily. However, this study did not find a decrease in hip fractures. Recent reports of adverse side effects of large doses of bisphosphonates, including osteonecrosis of the jaw, indicate that further research is warranted and that patients should be monitored for side effects of these drugs. Other related fall prevention efforts include home assessment for risk factors with the implementation of safety devices such as handrails, nonslip surfaces on stairs, and removal of throw rugs. 139–143 Researchers who conducted a recent randomized controlled trial found that thin-soled shoes were found to be the best type of shoe for patients, rather than running shoes, which have sticky soles. 144 Research addressing syncope-related falls indicate that cardiac pacing may be appropriate for individuals with syncope. 145
Summary of community-based research on falls and related injuries
In summary, authors of several reviews have examined the efficacy of community-based fall- and injury-prevention programs. These reviewers have indicated that individualized multimodal interventions are effective at reducing falls and related injuries in the community setting. 105 However, multimodal interventions are not in place across primary care areas, which hinders their potential efficacy, and the aging community would likely benefit from large-scale implementation of these proven preventive interventions. (See Evidence Tables 1 through 9 for individual study results.)
Evidence Table 1
Reviews Examining Fall-Prevention Interventions in the Community
View in own window
Study Design Type: (1) Meta-analysis, (2) Randomized controlled trials, (3) Nonrandomized trials, (4) Cross-sectional studies, (5) Case control studies, (6) Pretest and post-test (before and after) studies, (7) Time series studies, (8) Noncomparative studies, (9) Retrospective cohort studies, (10) Prospective cohort studies, (11) Systematic literature reviews, (12) Literature reviews, nonsystematic/narrative, (13) Quality-improvement projects/research, (14) Changing-practice projects/research, (15) Case series, (16) Consensus reports, (17) Published guidelines, (18) Unpublished research, reviews, etc.
Evidence Table 2
Studies on Community-Based Fall-Prevention Screening with Tailored Interventions (listed chronologically)
Evidence Table 3
Studies Examining Exercise-Related Interventions in the Community (listed chronologically)

Evidence Table 4
Studies examining physiologic interventions in the community (listed chronologically)
Evidence Table 5
Reviews Examining Fall Prevention Interventions in Acute and Long-Term Care (listed chronologically)
Evidence Table 6
Studies Examining Environmental Interventions in Acute and Long-Term Care (listed chronologically)
Evidence Table 7
Studies Examining Physical Activity Interventions in Acute and Long-Term Care (listed chronologically)
Evidence Table 8
Studies Examining Multimodal Interventions in Acute and Long-Term Care (listed chronologically)
Evidence Table 9
Studies Examining Interventions to Prevent Injury in Acute and Long-Term Care (listed chronologically)
Falls and Related Injuries in the Acute and Long-Term Care Settings
Fall and related injury prevention is a major focus for both acute and long-term health care organizations. In 2005, the Joint Commission added the requirement for fall risk assessment and periodic reassessment as a National Patient Safety Goal in the acute care setting. 54 The goal of this requirement is to ensure that all patients are screened for falls and thus seeks to reduce harm from falls. However, the outcome is unpredictable because fall and injury risk assessment instruments have shown inconsistent reliability and validity A more promising extension of this goal starting in 2006 and continuing forward is the additional requisite of implementing and evaluating a fall-prevention program. 146 National compliance with these goals has the potential to significantly impact the problem of falls in the acute care setting. Efforts to enhance quality of care in the long-term care environment via improved reporting have the potential to reduce falls and related injuries in these particularly vulnerable patients; however, the successful implementation of fall-prevention programs will be necessary to improve the problem.
Falls in the acute and long-term care settings have several possible consequences. Recurrent falls have been identified as contributing to increases in the length of stay (LOS) in elderly psychiatric patients. 147 However, some research has suggested that LOS itself may be a predictor. A fall may also lead to a poorer quality of life because of fallophobia, a fear of future falls, which may itself contribute to fall risk. 148 Injuries occur in between 6 and 44 percent of falls in the acute care setting. 20 , 21 , 23 In the long-term care population, between 9 and 15 percent of falls result in injury, with approximately 4 percent of these falls resulting in fractures. 149 Additionally, patients who have underlying disease states are more susceptible to injuries; for example, osteoporosis can increase the risk for fracture, and bleeding disorders can increase the risk for subdural hematomas. 150 Moreover, fall-related injuries increase resource utilization: injuries from falls lead to increased LOS and an increased chance of unplanned readmission or of discharge to residential or nursing home care. 151 Furthermore, inpatients who have incurred an injury due to a fall have approximately 60 percent higher total charges than those who did not fall or those who fell and did not sustain an injury. 152
Evans and colleagues, 153 via the Joanna Briggs Institute, performed a systematic review of the evidence up to 1997 for fall and injury prevention in the acute care setting. They examined 200 studies related to identification of predictors, risk assessment instrument development and testing, and fall- and injury-prevention interventions. Of these studies, only two were randomized controlled trials (RCTs). The trial by Tideiksaar and colleagues 154 examined the use of bed alarms to notify staff when patients at high risk for falls got out of bed; however, this study had a sample size that was too small to identify an effect from using bed alarms. The other RCT examined the use of colored bracelets to identify patients at high risk for falls. Again, the study results were inconclusive. 155 Evans and colleagues concluded that the fall risk assessment instruments available were not generalizable. However, they did not adequately compare the psychometric properties of the instruments in question; rather they evaluated research related to the implementation of such instruments, which was relatively weak up to that time. In addition, Evans and colleagues concluded that individual interventions were not more useful that any of the fall-prevention programs that might be developed at a particular institution for a specific subset of patients. However, recent research has seen a growing number of RCTs, which will facilitate the ability to make stronger practice recommendations for this complex and challenging problem.
For this review, research related to falls and related injuries in the acute and long-term care settings were identified and categorized as follows: risk factor identification, risk assessment instruments, and prevention strategies. Each category of research is discussed below.
Acute care and long-term care risk factors
Factors associated with patients at risk of falling in the acute care setting have been explored extensively, particularly over the past two decades. 17 , 87 , 156–160 Evans and colleagues 161 conducted a systematic review of research and identified 28 risk factors for falling, including impaired mental status, special toileting needs, impaired physical status, and to some extent age and medications. Oliver and colleagues 159 reviewed risk factor and risk assessment literature and identified five risk factors consistent across studies: unsteady gait, increased toileting needs, confusion, sedative-hypnotics, and history of falling. In the long-term care environment, risk factors are largely the same, with the addition of inability to transfer effectively 162 and short-term memory loss. 163 Although ability to transfer and short-term memory function might be characterized by unsteady gait and confusion, these items are expressly captured via the LTCMDS.
Research has consistently demonstrated that multiple factors are associated with falling in elderly and hospitalized patients and that fall risk increases as the number of factors increases. 98 , 153 , 156–159 , 164–166 Although increased age is a strong predictor of falling in the community, increased age has not always been identified as a predictor in the acute care setting. Some studies have found increased age to be a risk factor, 17 , 165 but others have found that increased age is not a factor in acute care. 157 , 167 , 168 Comorbidities and impaired functional status may be more important predictors of falls and subsequent injury in this setting. 150 , 157 Recent work by Hendrich 169 did not support the association between increasing age (older than 65 years) and increasing risk of falling in the inpatient environment. Instead, Hendrich and colleagues 169 found that confusion was the most important risk factor associated with the risk of falling. Nevertheless, age must be considered when discussing injury associated with falls because often with age comes frailty. Several researchers have identified gender as a risk factor, with female gender being a stronger risk factor in the older population 170 and male gender a stronger factor in the younger population. 167 , 169 , 171 A recent retrospective analysis by Krauss and colleagues 170 found that altered mental status was not a factor in falls, but that patients in academic medical centers were more likely to fall. This research was limited because it did not control for patient acuity or staffing levels.
Harwood and colleagues 172 , 173 reviewed the literature related to visual problems and falls and found that uncorrected visual impairment nearly doubled the risk of falling. Cardiovascular causes of falls derive predominantly from neurally mediated disorders (e.g., vasovagal syncope) and cardiac abnormalities (e.g., arrhythmias, infarction, valvular stenosis). 174 , 175 Time of day has also been implicated; Tutuarimia and colleagues 176 identified a higher rate of falls on the night shift, but this is inconsistent with other research and may in fact be explained by staffing patterns. Association of falls to the lunar cycle has also been explored, but no association was found. 177
Vitamin D deficiency has been implicated as a risk factor for falls and fracture in the long-term care setting. 178 In addition, elevated alkaline phosphatase and low serum parathyroid hormone have been identified as predictors for falls, 179 , 180 and anemia has also been implicated. 181
A number of researchers are exploring the relationship between nurse-to-patient staffing ratios and an increase in the incidence of falls. 20 , 176 , 182–184 Some of this work has identified an inverse association between licensed nurse staffing ratios and fall rates (i.e., a higher proportion of nurses is associated with lower fall rates); 176 , 182 , 184 , 185 however, the overall the results are inconclusive. 186 In addition, a growing body of research related to failure to rescue, defined as being “based on the premise that although deaths in hospitals are sometimes unavoidable, many can be prevented,” 187–189 supports the inclusion of unanticipated physiologic events in the definition of falls since the patient’s safety issues should be addressed at all times. Other researchers examining nurse staffing ratios and fall rates suggest that fall rates are reduced by increasing the number of nurse aids rather than licensed nursing staff. 190 This is potentially supported by recent work by Krauss and colleagues; 191 of the fallers in their case-control study, 85 percent of those in need of assistance or supervision with ambulation fell while not being supervised.
Certain subgroups of patients have been identified at higher risk because of the inherent characteristics of their disease process or treatment modalities. These groups include geriatric, behavioral health, oncology, rehabilitation, stroke, and multiple sclerosis patients. In the behavioral health setting, fall rates range from 4.5 to 25 falls per 1,000 patient days. 192 , 193 Researchers have identified the typical faller in the behavioral health setting as a female with a history of falls; who was younger than 65 years of age; who was experiencing anxiety and agitation; and who was receiving a sedative, a tranquilizer, or a laxative. 194 Irvin 195 explored risk factors in the psychiatric setting and found that gait or balance problems and history of falls were the primary predictors. Although many of these characteristics are consistent with patients in the acute care setting, younger age and comorbidities such as depression and psychosis are often predictors in the behavioral health population. 196–199 In addition, treatments specific to behavioral health patients are different than those in the acute care setting. For example, patients being treated for late-life depression are at risk for falling in the first weeks of using a tricyclic antidepressant and should be monitored closely while they are adjusting to the new medication. 75 De Carle and Kohn 200 , 201 have described risk factors in behavioral health patients and have identified electroconvulsive therapy as a predictor.
Patients in rehabilitation units are also at higher risk, likely because they have suffered neurological injuries such as stroke or head injury, which precipitate muscle weakness, impaired cognition, and impulsivity. 202–205 In addition, these patients are being physically challenged, which places them in higher-risk situations and thus at greater risk for falling. 206
In the pediatric inpatient setting, fall rates range from 0 to 0.8 per 1,000 patient days. 207 These rates are very low compared to adult inpatient and long-term care rates. The factors that limit the number of falls in this population are unclear, but may be related to increased supervision of pediatric patients via higher nurse-to-patient staffing ratios and the common practice of parents staying with pediatric inpatients.
Injury risk factors in the acute and long-term care setting
In general, injury risk factors are similar across care areas. Vassallo and colleagues 208 examined the risk factors associated with injury in a group of inpatient fallers and found that three factors were associated with injuries related to falls: (1) history of falls, (2) confusion, and (3) unsafe gait. In addition to these, Rothschild and colleagues 134 identified physiological processes, such as increased bleeding tendencies and osteoporosis, as factors that increased risk for bleeding or fracture. The risk for medications or physiologic factors to precipitate injuries related to bleeding have been explored on a limited basis in the inpatient population. Contrary to results in the community, 84 Stein and team 209 found that hospitalized stroke patients who are anticoagulated are not at higher risk for injury than nonanticoagulated patients; however, this study was small and the issue warrants further research. Bond and colleagues 210 examined over a 4-year period the risk for bleeding injury among 1,600 patients who fell while hospitalized. These researchers found that half of the patients were on thrombotic therapy and that the incidence of fall-related intracranial hemorrhage was low, even in persons taking warfarin. The authors suggested that selection bias may be a factor because physicians might withhold anticoagulant therapy for patients who have a higher fall risk. More recently, Spector and colleagues 211 performed a large study of nursing homes and found that 85 percent of fractures were caused by falls, and that those with epilepsy, those with agitation, and those taking anticonvulsants had the highest risk of sustaining a fracture if they fell.
Risk Factors for Falls and Injuries in Acute and Long-Term Care
Acute care risk assessment instruments
Many tools have been developed to identify patients at highest risk for falling in the acute care setting. 21 , 159 , 167 , 169 , 212–215 Perell and colleagues 87 reviewed risk assessment tools and identified 6 functional assessment instruments and 15 fall risk assessment instruments developed by nursing. Vassallo and colleagues 216 concurrently examined the predictive validity in the acute care setting of four commonly used risk assessment instruments (STRATIFY, Downton, Tullamore, and Tinetti) and found that the STRATIFY instrument was the easiest to use, was most effective of the four at predicting falls in the first week of inpatient admission (total predictive accuracy of 66.6 percent), but had the poorest sensitivity (68.2 percent).
The most commonly reported risk assessment instrument is the Morse Falls Risk Assessment Tool. 217 In 2002, O’Connell and Myers 218 conducted psychometric testing with this tool on 1,059 patients admitted to an Australian hospital. In this study, the Morse Falls Risk tool had a sensitivity of 83 percent and a specificity of 29 percent, but a positive predictive value of only 18 percent. This resulted in a very high false-positive rate, with the tool identifying more than 70 percent of patients who did not fall at high risk for falling. This research was confounded by the fact that the interventions were applied based on the instrument’s predictions; therefore, the predictive validity cannot be conclusively stated. The STRATIFY Falls Prediction tool also had a low positive predictive value (30 percent) and relatively low sensitivity (66 percent) and specificity (47 percent). 212
The Heinrich Falls Risk Model I is reported to be more robust (sensitivity, 77 percent; specificity, 72 percent) than either of the others, and the Hendrich Falls Risk Model II demonstrated even more improvement (sensitivity, 74.9 percent; specificity 73.9, percent; positive predictive value, 75 percent). 169 The inclusion of a Get Up and Go test in the Heinrich II tool was the major change between version I and version II. The Get Up and Go test evaluates a person’s ability to rise from a chair in a single movement, which is an assessment method that has been explored in earlier fall-prediction research. It is surprising that the sensitivity and specificity of the tool increases only slightly with the addition of this factor, underscoring the complexity of predicting patient falls. In addition, prospective evaluation of the use of the Hendrich II instrument has yet to be reported.
Several studies have tested the predictive validity of fall risk assessment instruments in relation to the judgment of nurses. Myers and Nikoletti 219 concluded that neither the fall risk assessment instrument nor nurses’ clinical judgment acted as a reliable predictor. Eagle and colleagues 220 compared the Functional Reach test, the Morse Falls Scale, and nurses’ clinical judgment in the rehabilitation and geriatric environment. This study also concluded that the two standardized assessment processes were no better at predicting falls than the clinical judgment of nurses. A limitation in both of these studies was that the evaluation occurred only at one time point close to admission, which does not account for the variability of patient status throughout a patient’s hospital stay.
In the domain of rehabilitation medicine, Ruchinskas 221 compared structured assessments—including the Mini-Mental State Exam, the Geriatric Depression Scale, the Functional Intervention Model, and the clinical judgment of physical and occupational therapists—on admission and discharge. This study concluded that the clinical judgment of therapists had a positive predictive power of 33 percent and a negative predictive power of 82 percent. However, the more accurate predictors of falling for the patients in their sample were a history of falls and presence of a neurological diagnosis. In the residential care environment, Lundin-Olson and colleagues 222 found that clinical judgment can contribute to the accurate prediction of fall risk, but is not sufficient on its own as a valid predictor.
Although fall-prediction research has been performed for two decades, it is clear that fall prevention is a complex problem that cannot be solved by risk assessment alone, hence the dissatisfaction with available risk assessment instruments.
Long-term care assessment instruments
Lundin-Olson and colleagues 223 developed the Mobility Interaction Fall Chart (MIF chart), which is an instrument based on a patients’ ability to walk and talk at the same time, the ability to maintain pace while carrying a glass of water, visual impairment, and difficulty concentrating. When the predictive validity of the MIF chart was evaluated, the researchers found that the chart was helpful only when used in conjunction with clinical judgment and knowledge of a patient’s history of falls, thus making the use of this instrument on its own limited. 222
The Downton instrument, originally developed in the community setting, characterizes risk by five factors: (1) increased dependency, (2) cognitive impairment, (3) increased number of physical symptoms, (4) presence of anxiety, and (5) presence of depression. 224 This instrument has recently been prospectively evaluated in the long-term care setting with a reported sensitivity ranging from 81 to 95 percent and specificity ranging from 35 to 40 percent. 225 Although the specificity is low, this instrument might provide a standardized measure to identify those at risk in the long-term care environment.
Becker and colleagues 162 have recently described an algorithm to assess fall risk in the long-term care setting, categorizing long-term care residents into three subgroups: (1) residents requiring assistance to transfer, (2) residents able to transfer with history of falls and requiring the use of restraints, and (3) residents able to transfer and with no history of falls but with urinary incontinence and visual impairment. The researchers found that the residents with the history of falls were at highest risk for falls, which is consistent with other research in this domain, but might be useful to tailor interventions and would warrant prospective evaluation.
Acute care pediatric risk assessment instruments
Falls in the acute care pediatric setting are relatively rare; however, standardized assessment may be beneficial to reduce falls and injuries in this population. Graf 207 has recently developed an instrument for acute care pediatric risk assessment. According to Graf, factors associated with pediatric falls include (1) seizure medication (odds ratio 4.9), (2) orthopedic diagnosis, (3) not using an IV (odds ratio 3.6), (4) physical/occupational therapy ordered, and (5) LOS (odds ratio 1.84 for every 5 days). This model has a sensitivity and specificity of 69 percent and 84 percent, respectively, and is being prospectively evaluated by the investigator with the hope that standardized assessment will facilitate reduction in these already-low rates.
Automated risk assessment in the acute and long-term care settings
Recent national patient safety efforts highlight the promise of using informatics processes to manage patient safety issues such as the management of patient falls. However, to date, most automated risk assessment techniques in the acute care setting are electronic versions of existing fall risk assessment instruments, with limited use of computerized decision support. 167 , 226 , 227 Promising new work in data mining for fall prediction has demonstrated that use of the LTCMDS has the potential to use existing data to generate risk models for patients in this setting. Volrathongchai 228 has recently explored the ability to use computerized data mining techniques to identify elderly residents of long-term care facilities who were at risk for falls. Although this work has not been prospectively evaluated, the research found that the use of these data mining techniques, in conjunction with nursing knowledge, had the potential to identify fallers.
Acute and long-term care prevention strategies
The goal of any fall- and injury-prevention effort is to decrease adverse outcomes for the patients who are most vulnerable to falling. A beneficial consequence of fall- and related-injury-prevention programs is the potential to streamline resource use, with the added potential for decreased costs associated with this problem. 229–231 To date, however, a ubiquitous fall- and injury-prevention strategy has not been identified for hospitalized patients, and implementation of multifaceted strategies is often difficult to introduce in the complex clinical environment. 232
Several reviews have examined fall-prevention strategies in the acute and long-term care settings. 98 , 99 , 153 , 159 , 233 Oliver, Hopper, and Seed 234 examined 10 studies, including 3 RCTs and 7 prospective studies with historical controls. Oliver and colleagues found that the pooled effects ratio was 1.0 (95% CI = 0.60–1.68), indicating that overall the interventions were not able to prevent falls. More recently, Oliver and colleagues 235 have performed a meta-analysis of fall- and injury-prevention strategies and found a decrease in fall rates with multimodal intervention and a decrease in hip fractures with hip protectors in the long-term care setting. Agostini, Baker, and Bogardus 98 conducted a review of the literature related to fall prevention for hospitalized and institutionalized older adults. This review did not pool the results, but examined the literature related to the use of armbands, bed alarms, and restraints for fall prevention, all of which will be discussed individually below.
The use of physical restraints to prevent falls has been refuted because restraints limit mobility, contribute to injuries, and don’t prevent falls. 236 , 237 Agostini and colleagues 98 examined literature related to fall prevention via restraint and side rail use, as well as fall rates when restraints were removed. Six studies found that restraints were associated with increased injuries, and restraint and side rail removal did not increase fall rates. Evans, Wood, and Lambert 238 also examined the literature and found 16 studies that examined restraint minimization, concluding that restraint-minimization programs involving effective staff education can reduce injuries and do not increase fall rates.
Several individual fall-prevention interventions have been examined, including the use of armband identification bracelets, exercise regimen, postfall assessment, bed alarms, toileting regimen, and vitamin D supplementation. Mayo and colleagues 155 conducted a randomized controlled trial to examine if armbands would help identify high-risk patients in a rehabilitation unit and prevent falls in the high-risk group. The researchers, however, found that high-risk patients with a blue armband had higher fall rates than those without the armband. Despite widespread use, only one study from 1993 has examined bed alarms. Tideiksaar and colleagues 154 found that bed alarms were an effective method for fall prevention (relative risk = 0.32), but the intervention warrants further research. An associated intervention, a movement detector, has recently been developed. Kwok and colleagues 239 studied movement detectors and found no difference between intervention and control groups. However, a pilot study examined the use of a movement detection patch attached to the thigh, which alerts clinicians when elderly long-term care residents are moving about. 240 Kelly and colleagues found a 91 percent decrease in falls during the 1-week testing period. Although this study quality was poor, the intervention might be suitable for select patients and bears further testing. Rask and colleagues 224 and Taylor and colleagues 225 evaluated the use of a fall-prevention program with a fall coordinator in the long-term care setting; they found that the control nursing homes had increases in fall rates over 4 years, whereas the intervention nursing homes had stable fall rates during the same time period.
Mulrow and colleagues 241 examined the effects of a physical therapy exercise intervention for frail long-term care residents and found that fall rates increased in the intervention group. However, the intervention group in this study also showed an increase in general strength and a decrease in the use of assistive devices, making one wonder if the physical therapy intervention sought to decrease the use of assistive devices in inappropriate situations. Rubenstein and colleagues 242 examined the ability for post-fall assessment to identify underlying factors that could be remedied to prevent further falls. Choi and colleagues 243 examined the effect of Tai Chi in the long-term care setting and found a 38 percent decrease in falls in the Tai Chi group, but this was not statistically significant (relative risk = 0.62; 95% CI = 0.32–1.19). A larger study may demonstrate statistical significance. A more recent study by Nowalk 244 reported no difference between groups who received strength training. The authors concluded that long term care residents may require individualized training, rather than group training.
Bakarich, McMillan, and Prosser 245 examined the impact of a toileting regimen for elderly confused patients with mobility problems in the acute care units of a large metropolitan teaching hospital. The researchers found that there were 53 percent fewer falls during shifts in which the risk assessment and toileting intervention was used, but that compliance with the assessment and intervention was difficult to maintain. More recently, Klay and Marfyak 246 found that a continence specialist in the long-term care environment reduced falls by 58 percent. Vitamin D has also reduced falls in elderly females in the long-term care setting by up to 49 percent, and in both males and females by 25 percent. 129 , 134 , 178 , 247 , 248 Further investigation of the use of vitamin D in the acute care and rehabilitation setting for fall and injury prevention is warranted. Jensen and colleagues 249 examined the effect of exercise training on elderly residential care patients and found an increase in strength and balance, and a nonstatistically significant decrease in falls. This study was limited by its small sample size and unequal distribution of important risk factors such as Mini-Mental State Exam scores across groups.
As with community interventions, tailored, multipronged prevention strategies are being shown to be more effective in acute and long-term care settings than individual interventions alone. Hofmann and colleagues 250 used three concurrent interventions—staff education, an exercise program, and environmental modifications—for a frail elderly population. The concurrent use of these interventions decreased the fall rate by 38 percent and decreased the fracture rate by 50 percent. Haines and colleagues 251 also examined a multipronged intervention involving staff and patient education, an exercise program, and the use of hip protectors. Researchers found a 22 percent decrease in falls and a 28 percent decrease in injuries in the intervention group.
One of the most promising studies by Jensen and her research team 252 investigated the effects of a comprehensive fall risk assessment and tailored intervention program in the long-term care setting. The intervention included assessment via the Mobility Interaction Fall Chart, visual evaluation, medication evaluation, and delirium screening by all members of the care team—physicians, nurses, and physical and occupational therapists. This research demonstrated that the comprehensive assessment and tailored interventions reduced falls by 51 percent and injuries by 77 percent over a 34-week period. Healy and colleagues 253 also found a statistically significant reduction in falls (RR = 0.71) by applying a tailored plan of care to adult inpatients who were deemed at high risk for a fall based on having had a previous fall. In effect, this research used history of fall as a method to triage high-risk patients, who then received a comprehensive risk assessment with targeted interventions. This research did not demonstrate a decrease in injuries; however, further research using this technique will be useful. McMurdo, Millar, and Daly 254 found up to a 55-percent reduction in fall rates in a group of 133 nursing home residents with comprehensive risk assessment and balance training, but these results were not statistically significant. A larger sample size would provide a better understanding of the effect of the intervention.
Other research examining multimodal interventions have had mixed outcomes. A recent study by Vassallo and colleagues 255 in long-term care facilities found a decrease in falls was nullified when the results were controlled for LOS. However, controlling for LOS removes the ability for LOS to be identified as a predictor, which may be the case for patients who stay longer in a hospital setting. Kerse and colleagues 256 found that in a group of nursing homes, long-term care residents who were randomized to risk assessment followed by tailored interventions showed an increase in falls (incident rate ratio = 1.34; P = 0.018). Semin-Goossens, van der Helm, and Bossuyt 257 evaluated the effect of a guideline with semistructured interventions and found that fall rates in high-risk neurology and medical patients were not reduced. The researchers attributed the failure of the program to resistance by nurses to changing attitudes toward falls with the statement that nurses did not find falls troublesome enough. However, the failure was more likely due to system issues, such as ability to implement and agreement with the guideline, and training issues, which are common with guideline implementation failures. 258 , 259 In addition, the Semin-Goossens guideline did not use a standardized risk assessment instrument, which might have made it difficult to identify patients at risk. Fonda and colleagues 260 studied a multimodal process-improvement plan and found that after 3 years, fall rates were decreased by 19 percent and injuries were decreased by 77 percent. Furthermore, this effect was sustained with continued use of the multimodal intervention. Schwendimann and others 261 found a moderate, but not statistically significant decrease in fall rates, and no change in injury rates after implementing an interdisciplinary fall-prevention program. Lane 262 found no decrease in patient fall rates before and after implementation of a fall-prevention program. Although the results of multimodal studies are conflicting, it is important to note that none of the studies of multimodal interventions—whether effective or ineffective results—controlled for staffing ratios or skill mix.
An increasing number of studies are examining the prevention of injury in the acute and long-term care settings. Hip protectors have been evaluated in the long-term care environment since the early 1990s. Although early work found that hip protectors were effective in reducing hip fractures in the frail or osteoporitic elderly, 263 more recent work indicates that compliance with using hip protectors is difficult to maintain, making recommendation for hip protector use conditional. 264 , 265 Ray and colleagues 266 examined the ability of a 2-day staff safety education plan to reduce serious fall-related injuries and found that this intervention was not effective, but the result may have been confounded by lack of staff compliance with the safety plan. (See Evidence Tables 1 to 9 for individual study results.)
Summary of acute and long-term care falls and related injuries
In summary, fall prevention in the acute and long-term care settings is a complex and demanding problem with multiple patient types and risk factors to manage. Standardized risk assessment with multimodal tailored interventions appears to be the most successful method of prevention; however, implementation of comprehensive interventions across care settings can be challenging. Further research toward overcoming barriers to implementation, guideline adherence, staffing ratios, and tailored interventions for newly identified risk factors such as vitamin D deficiency and anemia are warranted. Furthermore, research must be conducted on a larger scale to demonstrate generalizability and to be able to translate evidence into practice.
- Evidence-Based Practice Implications
Screening for fall and injury risk should be performed across settings. In the community, all patients older than 65 years should be screened, and in the home care, acute care, and long-term care settings, patients of all ages should be screened. Screening needs to include injury risk, not just fall risk. The most effective interventions are multimodal ones that address specific areas of risk and work with interdisciplinary fall-prevention teams.
In the community, screening can take place with a general annual physical exam or other routine health care visit. A standardized risk assessment tool should be used, such as the Tinnetti screening tool, which has the highest sensitivity and specificity for use in the community, but screening for injury risk must be included. If a patient is seen in an emergency room because of a fall, evidence suggests that focused fall and injury risk evaluation is warranted, especially if the patient is to be discharged home, i.e., the discharge prescription should include a focused fall risk assessment by the primary care provider or by a fall-prevention clinic. Tailored interventions for elderly community dwellers can decrease fall rates. Interventions that have had the most success in the community include exercise interventions with leg strengthening and balance training (e.g., Tai Chi), medication adjustment, management of cardiac-related syncope, effective diabetes management, management of vitamin D deficiency, and home safety modifications. Interventions to prevent injury in the community include calcium with vitamin D for fracture prevention, and additional fall precautions and increased screening for patients on anticoagulant therapy.
In the acute and long-term care settings, screening should be carried out using a standardized assessment tool for all patients. The Morse tool is the most commonly used in the acute care setting, but it does not screen for injury risk. In the long-term care setting, the LTCMDS may be an effective screening tool. In both acute and long-term care, effective interventions are multimodal and include medication adjustment, environmental adjustment, alarm devices, staff safety education, calcium and vitamin D, exercise interventions, and treatment of other underlying disorders. Interventions to prevent injury in the acute and long-term care settings include limiting restraint use, lowering bedrails, using hip protectors in long-term care, calcium with vitamin D, and possibly bisphosphonates in long-term care. Across the health care continuum, effective interventions have been identified, but their use is not ubiquitous.
- Research Implications
In the community setting, identification of the best timing for screening and reassessment is needed. Identification of methods to build fall- and injury-prevention programs in the community is needed to guide policymakers. In the acute and long-term care settings, large multisite intervention studies that use multimodal interventions tailored for individual risk factors and that control for comorbidities, acuity, staffing, and other environmental factors are needed. Cost-effectiveness studies to characterize the impact of fall- and injury-prevention programs are needed in the acute and long-term care settings.
- Recommendations From Evidence-Based Practice and Research Implications
1. Recommendations for screening and assessment
- Fall and injury risk screening should be performed in all settings.
- All patients who fall should receive a comprehensive postfall assessment.
- Methods for computerized screening and followup should be explored.
Recommendations for Screening and Assessment
2. Recommendations for interventions in the community setting
- Apply multimodal interventions as identified by risk assessment.
- Participate in national reporting activities such as ANA–NDNQI.
- Examine the use of computer-based guidelines in all settings.
Recommendations for Community Setting
3. Recommendations for interventions i n the acute and long- term care settings
- Large, multi-site randomized controlled trials that evaluate tailored interventions while controlling for organizational culture, staffing, comorbidities, acuity, and other factors are needed. Injury rates should be the primary outcome of interest, since fall-rate reporting may be an imprecise measure.
- Characterize the cost effectiveness of bundles of tailored interventions.
Recommendations for Acute and Long-Term Care
Falls and related injuries are an important issue across the care continuum. National efforts in the community via Healthy People 2010, in the acute care setting via the Joint Commission’s National Patient Safety Goals, and in the long-term care setting via the Nursing Home Quality Initiative project have the potential to significantly reduce falls and related injuries. The growing number of randomized controlled trials related to fall-prevention efforts is promising. However, most of these studies have been carried out in the community and long-term care environments, with few randomized controlled trials evaluating fall- and injury-prevention measures in the acute care setting. As with other nursing-sensitive quality indicators, recent research demonstrating an association between fall rates and nurse staffing ratios needs to be more fully explored. In addition, further research needs to explore automated methods of assessing and communicating fall risk, better methods for risk identification, and the identification of prevention measures. Indeed, with coordinated efforts to apply the evidence to practice, the problem of falls might be managed more effectively.
- Search Strategy
MEDLINE, ® the Cumulative Index to Nursing and Allied Health Literature (CINAHL ® ), and Cochrane databases from inception to March 2007 were searched for medical subject heading terms, both individual terms and combinations of the following: accidental falls, patient safety, medical errors, nursing-sensitive quality indicators, and fall prevention. In addition, references from relevant articles were searched using the snowball technique, as were archives of select nursing research and gerontology journals. The Related Links function in MEDLINE was also used to maximize the search strategy. Google, Google Scholar, and citations from identified articles were also searched for additional possible references. Articles related to occupational falls, sports-related falls, alcohol-related falls, and physical abuse-related falls were excluded. Articles that reported physiologic characteristics that are suspected to preclude falls but that did not examine falls or fall-related injuries as outcomes were also excluded because the causative effect on falls and fall-related injuries is, to date, inconclusive. Further, articles that were published in a foreign language were excluded. Two hundred and twenty seven articles were reviewed. Sixty-one of these were intervention research studies related to fall and injury prevention (32 from the community setting; 33 from the acute and long-term care setting).
- Cite this Page Currie L. Fall and Injury Prevention. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 10.
- PDF version of this page (665K)
In this Page
Other titles in this collection.
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Fall and injury prevention. [Annu Rev Nurs Res. 2006] Review Fall and injury prevention. Currie LM. Annu Rev Nurs Res. 2006; 24:39-74.
- Reducing falls and resulting hip fractures among older women. [MMWR Recomm Rep. 2000] Reducing falls and resulting hip fractures among older women. Stevens JA, Olson S. MMWR Recomm Rep. 2000 Mar 31; 49(RR-2):3-12.
- A student-led demonstration project on fall prevention in a long-term care facility. [Geriatr Nurs. 2007] A student-led demonstration project on fall prevention in a long-term care facility. Bonner A, MacCulloch P, Gardner T, Chase CW. Geriatr Nurs. 2007 Sep-Oct; 28(5):312-8.
- The 6-PACK programme to decrease falls and fall-related injuries in acute hospitals: protocol for an economic evaluation alongside a cluster randomised controlled trial. [Inj Prev. 2012] The 6-PACK programme to decrease falls and fall-related injuries in acute hospitals: protocol for an economic evaluation alongside a cluster randomised controlled trial. Morello R, Barker A, Zavarsek S, Watts JJ, Haines T, Hill K, Sherrington C, Brand C, Jolley D, Stoelwinder J. Inj Prev. 2012 Apr; 18(2):e2. Epub 2012 Jan 30.
- Review Falls in the nursing home: are they preventable? [J Am Med Dir Assoc. 2004] Review Falls in the nursing home: are they preventable? Vu MQ, Weintraub N, Rubenstein LZ. J Am Med Dir Assoc. 2004 Nov-Dec; 5(6):401-6.
Recent Activity
- Fall and Injury Prevention - Patient Safety and Quality Fall and Injury Prevention - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Home / NCLEX-RN Exam / Accident/Error and Incident Prevention: NCLEX-RN
Accident/Error and Incident Prevention: NCLEX-RN
In this section of the NCLEX-RN examination, you will be expected to demonstrate your knowledge and skills of accident / error and incident prevention in order to:
- Assess clients for allergies and intervene as needed (e.g., food, latex, environmental allergies)
- Determine client/staff member knowledge of safety procedures
- Identify factors that influence accident/injury prevention (e.g., age, developmental stage, lifestyle, mental status)
- Identify deficits that may impede client safety (e.g., visual, hearing, sensory/perceptual)
- Identify and verify prescriptions for treatments that may contribute to an accident or injury (does not include medication)
- Identify and facilitate correct use of infant and child car seats
- Provide the client with appropriate method to signal staff members
- Protect the client from injury (e.g., falls, electrical hazards)
- Review necessary modifications with client to reduce stress on specific muscle or skeletal groups (e.g., frequent changing of position, routine stretching of the shoulders, neck, arms, hands, fingers)
- Implement seizure precautions for at-risk clients
- Make appropriate room assignments for cognitively impaired clients
- Ensure proper identification of client when providing care
- Verify appropriateness and/or accuracy of a treatment order
Patient, resident safety is a major concern in healthcare organizations. The Joint Commission on the Accreditation of Healthcare Organization (JCAHO) publishes patient safety goals on an annual basis to facilitate client safety.
The Hospital Patient Safety Goals for 2016 include the goals to:
- Identify patient safety risks
- Identify patients correctly
- Improve staff communication
- Use medications correctly
- Use patient safety alarms correctly
- Prevent infections
- Prevent errors and mistakes relating to surgery, other invasive procedures, and treatments
More information about the current Patient Safety Goals put forth by the Joint Commission on the Accreditation of Healthcare Organization (JCAHO) .
Assessing the Client for Allergies and Intervening as Needed
Upon first contact with the client, the nurse thoroughly assesses the client for any known allergies, in addition to many other bio-psycho-social-spiritual data. These allergies can be related to medications and other substances such as contrast media that is used for many diagnostic tests, foods, environmental factors like pet dander and air pollution and other things like an allergy to latex and products containing latex.
Nurses determine, identify and document client allergies to medications, contrast media used for diagnostic tests, foods, and environmental sources including latex.
Nurses observe for and identify any possible allergies to the medications. For example, nurses collect data relating to past medication allergic responses and they also observe patients throughout the course of care to determine if the patient is experiencing an allergic response to a new medication. For this reason, nurses must be fully informed about the signs and symptoms of an allergic response to all medications that they administer.
All allergies to medications are documented in the nursing assessment and also on the medication administration record in addition to other areas in the medical record, according to the facility's policy and procedure. Many healthcare agencies also use allergy bands and/or bar codes with embedded allergy information to enable nurses to readily identify any allergies to medications.
Similar to latex allergic responses, the degree, intensity and seriousness of allergic responses to medications can be moderate or severe.
Commonly occurring medication allergies include allergies to penicillin which can be particularly dangerous and life threatening, allergies to sulfonamides, and allergic reactions to cephalosporin medications.
Commonly occurring allergies to radiocontrast media include allergies to ionic high osmolality contrast media and nonionic low osmolality contrast media. Some of the risk factors associated with allergies to radiocontrast media include beta blocker antihypertensive medications, the elder years, female gender, and a history of renal disease and/or heart disease.
It is estimated that nearly 10% of people have a reaction to penicillin. Some of these reactions are an allergic response and others are simply a side effect. The first exposure to penicillin, referred to as the "sensitizing dose", sensitizes and prepares the body to respond to a second exposure or dose. It is then the second exposure or dose that leads to anaphylaxis, or anaphylactic shock.
The signs and symptoms of anaphylaxis and anaphylactic shock, a type of distributive shock, are the massive collapse of venules and arterioles in the body's circulatory system, decreased cardiac output, histamine release, a drop in blood pressure, pooling of venous blood, laryngeal edema, respiratory distress, a rash, a rapid bounding heart beat, and death unless it is immediately treated.
Like a penicillin allergy, allergies to latex and its effects on the body can vary among individuals in terms of its severity. For example, some clients may only be affected with an immediate local contact dermatitis, the least severe of all the allergic reactions to latex, others can be affected with a delayed contact dermatitis, and still move can respond with a life threatening allergic reaction which can be signaled with itching and flulike symptoms and progress to tachycardia, hypotension, dyspnea, chest pain tremors, and anaphylactic shock.
The signs and symptoms of immediate and delayed contact dermatitis to latex include itching and burning of the skin and skin scaling that can extend the area of contact such as the hands when latex gloves are used.
Allergies to latex can occur after long use and they can also occur with the first contact with latex.
Some of the patients at greatest risk for latex allergies are those with some immunosuppressive disorder such as HIV/AIDS, those with asthma and eczema. It is also believed that those who are allergic to some foods, like avocados, are more at risk for latex allergies than others without these food allergies.
Learn more about the role of HIV/AIDS nurses .
In summary, nurses must be knowledgeable about assessing known and possible client allergies including those to medication, other medical substances such as latex and contrast media, foods and environmental factors, the signs and symptoms of an allergic response, and interventions that must be done when the client is affected with an allergic response. Some of these interventions can include reporting, documentation and interventions to correct any allergic responses and changes that can impact on the client's healthcare status. For example, CPR and other life saving measures may be indicated when the client is affected with life threatening anaphylactic shock; and the nurse may have to administer corticosteroid medications with a doctor's order after an allergic response was communicated to the client's physician.
Determining Client and Staff Knowledge of Safety Procedures
Staff is required to have the knowledge, skills and abilities to identify safety risks, to intervene appropriately to prevent and correct safety hazards and to act accordingly when a client, family member, visitor or another staff member is actually or potentially affected by a safety hazard.
When a staff educational need related to these or other aspects of safety, the registered nurse, will plan, implement and evaluate education to meet these needs. After education is provided, the staff member will be assessed for their competency.
Some safety skills, such as using a fire extinguisher, are rarely used skills and others, such as daily surveillance of the patient care area for safety hazards and risks, are frequently used skills. Both, rarely used and frequently used safety skills, however, are associated with high risk, therefore, rarely used skills must be assessed and staff must be deemed competent on a frequent basis with observation; and frequently used safety skills can be validated for competent performance with the indirect observation of the application of these skills and the identification of any issues or discrepancies in the performance of these skills. For example, the staff member should actually demonstrate the correct use of a fire extinguisher in a planned manner and at least on an annual basis and the competency levels of staff related to frequently used safety skills can be determined and validated indirectly by observing the correct application of these skills in the area of employment.
Clients also may have safety educational needs. For example, clients at risk for incidents, accidents, and errors should be instructed about safety procedures and measures that they can use to prevent them. For example, some clients may need frequent reminders to call for help before getting out of bed to prevent a fall, and others may need the nurse to educate them for the need for grab rails and to have a carbon monoxide alarm in the home.
Identifying Factors that Influence Accident/Injury Prevention
Some of the factors that can positively impact on and influence injury and accident prevention include an age and developmental stage at which the person is able to understand safety and safe behavior; a normal, alert and awake level of consciousness, a level of cognitive ability and mental status that enables the person to have insight into safety and safe behaviors and fully aware and cognizant of their own limitations, strengths and weaknesses; and a lifestyle including exercise and an adequate diet that can enhance their health, well-being and level of safety.
In terms of age, infants, toddlers, young children and the elderly very young are at greater risk for accidents and injuries than other age groups; people with poor consumption patterns, such as illicit drug and/or alcohol abuse, are more prone to injuries and accident than those who have healthy lifestyle choices that increase their strength, stamina, agility and nutritional status.
Identifying Deficits That May Impede Client Safety (e.g., visual, hearing, sensory/perceptual)
Physical deficits like sensory losses and alterations, impaired mobility, an altered mental and emotional state, and other factors can negatively impact on the safety of the client.
Sensory and Perceptual Deficits
Physical deficits like a sensory losses and alterations can affect client safety. For example, clients with a visual impairment may trip over objects that they cannot see and they can also fail to see a sign that indicates that a floor is wet; and patients with a hearing deficit may not hear a fire or smoke alarm.
Impaired Mobility
Patients affected with permanent or temporary losses of mobility are more prone to injuries and accidents than other patients without these deficits. For example, a client with left sided paralysis as the result of a cerebrovascular accident and a client who has become weak as the result of prolonged complete bed rest are at greater risk for injuries and accident than those without these conditions.
An Altered Mental and Emotional State
High levels of stress, fatigue, the effects of some medications like sedating medications, the effects of anesthesia, and depression are risk factors associated with a greatest risk for client injuries and accidents than other clients with intact and unimpaired mental and emotional states.
A Lack of Safety Insight
A lack of good judgment and insight into safety risks place clients at risk for safety concerns.
Identifying and Verifying Prescriptions for Treatments That May Contribute to An Accident or Injury, Not Including Medications
An essential component of injury and accident protection entails the ability of the nurse to identify and verify all treatment orders and prescriptions to insure that they are not placing the client at risk for any injury or accident. When the nurse receives an order or prescription for a treatment or procedure that is questionable in terms of client appropriateness and safety, the nurse, as the nurse does with questionable medication orders, contacts the person who has prescribed the treatment or procedure and verifies the order before carrying this order out.
The treatments and procedures that are most prone to client risk, injuries and accidents and the most risky are invasive procedures including surgery and invasive diagnostic tests. It is, therefore, essential that nurses exercise extreme caution and apply their knowledge of the client's status and the risks associated with the particular treatment to the particular order to insure that undue risks are not associated with the invasive treatment or procedure that has been ordered.
Some of the procedures associated with high degrees of risk intraprocedure or treatment and after the treatment or procedure include all surgical procedures, invasive cardiac catheterizations, intubation, peripheral venous catheters, central venous catheters, chest tubes, mechanical ventilation, the administration of contrast media for diagnostic tests and other procedures and treatments, some of which will be discussed in a later section entitled The Reduction of Risk Potential .
Identifying and Facilitating the Correct Use of Infant and Child Car Seats
When properly used and fitted, infant and child death and injury secondary to motor vehicle accidents can be significantly, according to the National Highway Traffic Safety Administration (NHTSA) . It is estimated that infant and child car seats prevent death among infants by 71% and among toddlers and young children under 3 years of age by 54%.
Infant seats and car seats must be properly sized and properly installed in order for them to be effective against injures and death. For example, rears facing infant seats are always installed in the back seat facing the rear of the car when the infant or baby is less than about 2 years of age and about 20 to 30 pounds. Convertible safety seats can be both rear facing and front, or forward, facing. Regular car seat belts can be typically used when the child is at least 40 pounds and about 4 years of age.
Providing the Client with An Appropriate Method to Signal Staff Members
Many accidents and client injuries can be prevented when the client has access to a device that enables them to signal staff and when these calls to staff members are responded to in a timely manner. Nurse call bells that continue ringing for minutes without being responded to by staff can, and do, lead to unnecessary injuries and accidents that could have been prevented by a prompt staff response. Regardless of the method for alerting staff is used, calls for help and assistance must be immediately responded to.
At times the method to signal and alert nursing staff members must be modified according to the client's characteristics and needs and at other times the method to signal and alert nursing staff members must be modified according to a situation or circumstance in the environment that is not related to the client and their abilities.
Most clients are able to signal staff with a call bell and light. Others may only be able to verbally call out for help, and others may not be able to signal staff members. Clients unable to use a call bell should be placed near the nursing station or another area with high activity so the client's verbal calls for help can be heard and attended to by staff; clients unable to call for help using a call signal or verbal calls for help should not only be placed in a room near the nursing station or another area with high activity so that they can be monitored and observed on a frequent basis.
When there is a utility failure, or another environmental factor such as the malfunction of the facility's call bell system, that disrupts the use of call bells, hand held bells or buzzers should be provided to the clients so they can communicate with nursing staff despite this electrical power loss or system malfunction.
Protecting the Client from Injury
Healthcare providers and healthcare facilities are mandated to protect clients, visitors and staff from injury. Some of the commonly occurring injuries in healthcare facilities include burns, falls, electrical shock, accidental poisoning and events occurring from internal and external disasters.
Thermal injures can occur as the result of faulty warming and cooling devices and also with the improper application of heat and cold to the client, particularly when the client has a sensory and/or neurological deficit that impairs their ability to sense and feel skin damage resulting from the heat or cold application. More information about the safe and correct application of heat and cold will be discussed later in this NCLEX-RN review.
Falls a major, commonly occurring and costly accident, with or without injury, plague virtually all health care facilities. For this reason, all clients should be screened and assessed for falls risk upon admission, upon our first client contact and, also, whenever the client's condition is marked with significant physical and/or psychological or cognitive changes.
When a client is screened and assessed as a falls risk client, special interventions to prevent falls must be immediately initiated, communicated and documents.
Some of the risk factors associated with falls that are typically included in a falls risk screening and assessment are:
Incontinence
Patients who are incontinent of feces and/or urine are at greater risk for falls than clients who are not affected with these elimination problems. Incontinent patients may leave feces and/or urine of the floor which they may slip on and/or they may be in such a hurry to get to the toilet that they fail to use proper lighting and other safety measures to prevent a fall.
Confusion can lead to poor judgment and a lack of awareness of environmental factors that can lead to a fall. People who are confused may lack good judgment and they may not be aware of any hazards.
Poor vision
People who are visually impaired can trip over things they cannot see, particularly in a strange, or new, environment. Clients should be given their eyeglasses and encouraged to use them.
A delayed and slow reaction time
A delayed and slow reaction time, a normal change associated with the aging process, places clients at greater risk than others, and often younger, clients. They may not react quickly enough to avoid a hazard, such as a wet floor, that they see. This can lead to a slip and fall.
The aging population, infants and young children are the age groups that are at greatest risk for falls.
Medications
Sedating medications and other medications with some side effects, such as fatigue, muscular weakness, dizziness, and orthostatic hypotension, for example, increase a client's vulnerability to falls.
Poor muscular strength, balance, coordination, gait and range of motion (ROM)
When a client has poor balance, coordination, proper gait, and full range of motion for one reason or another, they are at greater risk for falls than other clients without these deficits. One of the most effective interventions to address these deficits is to employ the services of the physical therapist to increase the client's muscular strength, balance, coordination, gait and range of motion in order to prevent falls.
Environmental hazards
Patient rooms and client areas that have clutter, poor lighting, high glare, wet floors and/or an absence of nurse call bells are not safe. The nurse is responsible to keep the client environment safe and without any hazards.
A history of falls in the past, particularly more recent and frequent falls, place a client at future risk for falls because many of the same conditions that were present in the past, particularly the recent past, may continue to the current time. For example, paralysis secondary to a cerebrovascular accident persists over time.
Fear of falling
A client's fear of falling has been shown to be positively correlated with falls risk.
Some diseases and disorders
Some diseases and disorders, particularly those that adversely affect the client's musculoskeletal and/or neurological status, place a client at risks for falls. For example, diseases and disorders like muscular dystrophy, Parkinson's disease and a seizure disorder place a client at risk for falls.
In addition to intrinsic, patient related factors that place clients at risk for falls, there are also a number of extrinsic and environmental factors that place clients at risk for falls.
Some of these factors, all of which must be immediately corrected, include:
Inadequate patient foot wear
Poorly fitting, nonskid proof and simply dangerous shoes and slippers place clients at risk for falls. Patient footwear should be skid proof, sturdy, properly fitted and safe. Skid proof socks are highly effective in terms of fall prevention.
Broken equipment and the inappropriate use of patient equipment
Broken patient equipment such as a broken wheelchair or cane can lead to falls. All broken equipment must be reported and immediately removed from service and not used until they are repaired and deemed safe to use. All patient equipment must also be used correctly. When a staff member improperly uses a mechanical lift, for example, to move the client from the bed to the chair and the patient falls as the result of this improper use, an accident and injury has occurred as the result of this improper use of the mechanical lift.
No answers to calls for help
As previously stated, all calls from clients must be responded to promptly in order to prevent falls as well as other incidents and accidents, many of which can lead to patient injury.
In addition to assessing clients for falls risk, some of the special interventions that can prevent falls or lessen the degree of injury that a client can sustain after a fall include the following:
- The use of patient assistive devices such as walkers and canes
- Padded briefs to decrease the extent of an injury when a client does fall despite preventive measures
- The use of padded gym mats on the floor next to a bed can also decrease the extent of an injury when a client does fall despite preventive measures
- The use of low beds to decrease the extent of an injury when a client does fall despite preventive measures
- The use of bed and chair alarms to alert staff that the client is rising from the bed or the chair
- More frequent patient monitoring and observation
- The use of high toilet seats and grab bars
Electrical Safety
Like other safety hazards, health care facilities are subject to incidents and accidents associated with things and practices that are contrary to good electrical safety. For example, frayed electrical cords and using extension cords that can overwork electrical outlets and also cause client tripping and falling can occur in health care facilities unless they are eliminated from the environments within which clients receive services and staff members work.
All electrical client equipment is routinely and predictably inspected for safety, and preventive maintenance is also done and documented on these pieces of electrical equipment. When a piece of equipment is overdue for this electrical inspection and maintenance and also when it is malfunctioning and/or with a frayed wire, this piece of electrical equipment must be immediately taken out of service and sent to the appropriate department for inspection, preventive maintenance and repair. Under NO circumstances should such equipment be used even on a very temporary basis. More about the safe use of equipment will be discussed below.
Client's personal electrical equipment, such as televisions, radios, electrical razors and computers, must also be inspected and approved as safe, by a person competent to do so, before it can be used by the client in the health care environment. For this reason, patients are discouraged from bringing personal electrical equipment into the health care facility for their personal use.
Reviewing Necessary Modifications with the Client to Reduce Stress on Specific Muscle or Skeletal Groups
Some of the things that nurses can facilitate and do in order to reduce stress on specific muscle and skeletal groups include encouraging clients to perform routine stretching, range of motion exercises and also frequently changing positions into those which place the body in a safe position.
Clients who are not able to do this must be positioned and repositioned every two hours into a position that will not cause any harm such as any stressors on the muscle groups, and that prevent skin breakdown and other complications associated with immobility such as contractures.
The client positions that are used for maintaining good bodily alignment and optimal physiological functioning include the Sim's or semi prone position, the Fowler's position, the dorsal recumbent position, the prone position and the lateral position. These positions are supported and maintained with pillow, bolsters and wedges when necessary to maintain correct bodily alignment.
Routine stretching and exercising the body's full range of motion should be strongly encouraged among all clients that are able to do so and passive or assisted range of motion should be provided to the client when they are not able to perform these exercises on their own. These exercises maintain the body's ability to remain strong and mobile. Routine stretching of the shoulders, neck, arms, hands, and fingers should also be encouraged.
Implementing Seizure Precautions for At-Risk Clients
Nurses must implement seizure precautions for at-risk clients to protect them from injury. Seizures, which can be a primary diagnosis or a condition that results from another medical condition such as hypoglycemia, increased intracranial pressure and cerebrovascular accidents, result from abnormal electrical activity in the brain.
Some of the risk factors that can place a client at risk for seizures include:
- Alzheimer's disease
- The use of illicit drugs
- Some prescription drugs
- An overdose of an illicit drug
- A personal history of prior seizures
- A family history of seizures
- Cerebral tumors and infections
- Alcohol withdrawal
- Hepatic failure
- Renal failure
- Exposures to toxins
- Hypertension
- Hypoglycemia
- Extreme stress
- Some diseases such as syphilis, sickle cell anemia, Whipple's disease etc.
- Abnormal hormonal changes
The client is assessed for the presence of any seizure risk factors and when a seizure disorder is suspected the client will receive diagnostic tests such as an electroencephalogram (EEG) to assess the client's electrical activity of the brain and to determine whether or not epilepsy is the cause of the seizure activity, a MRI and CT scan to determine if there are any structural brain abnormalities like a tumor, a lumbar puncture to determine whether or not the client has an infection or cerebral bleeding, and PET imaging to determine the specific location that is causing the seizure activity.
Most seizures are short lived and they typically persist for only a few minutes; when seizures last more than 3 or 5 minutes they can be life threatening. It is also potentially life endangering when a client has several seizures in rapid succession.
When a seizure is witnessed by the nurse, the nurse must remain with the client, call for the help and assistance of others, and observe and assess the client's physical status, like their cardiac and respiratory functioning, and also implement emergency measures when they are indicated. The client should also be protected from physical injury during the seizure.
All observations and assessments of the client prior to the seizure, such as an aura, during the seizure and after the seizure are fully documented. It is also reported to the client's physician.
Clients who are at risk for seizures and a seizure disorder should be taught and educated about the need to avoid hazardous activities such as climbing to high heights with a ladder because a seizure can occur suddenly and without any warning, the warning signs of a seizure, the risk factors associated with seizures, and to wear a medical emergency tag or bracelet that alerts others to the fact that the person has a seizure disorder.
Making Appropriate Room Assignments for Cognitively Impaired Clients
In addition to more frequent monitoring, clients with a cognitive impairment should be placed in a room near a hub of activity near the nursing station, for example, to prevent injuries and accidents.
Ensuring the Proper Identification of the Client When Providing Care
Proper patient identification must be done before anything is done for or with a patient. As we previously discussed, accurate identification is necessary during all aspects of nursing care. At least two unique identifiers, other than room number, must be used.
Some examples of unique identifiers include a unique code number, the person’s first, middle and last name and/or complete date of birth including year, an encoded bar code bracelet with at least two unique identifiers imbedded into it and a photograph. Room numbers are never used as unique identifiers. Patients and residents often enter the rooms of other patients and residents, particularly when they are confused.
Patients at greatest risk for identification errors are patients who are confused, comatose, have a primary language other than English, and those patients who have an identical name or a similar name to another patient in the health care facility. For example, Mr. Smith and Mr. Smyth are at risk for identification errors when they are in the same facility.
The proper identification of patients prevents many medical errors, including wrong patient surgery, medication errors and the provision of incorrect treatments and procedures to a patient.
Health care facilities have formalized policies, procedures and mechanisms for patient identification. In addition to the use of two unique identifiers, some health care facilities also have bar coded patient identification bands, patient identification wrist bands that include any patient allergies and even wristbands to alert staff that the client is a do not resuscitate client.
Verifying the Appropriateness and/or Accuracy of a Treatment Order
An essential component of injury and accident prevention, as previously detailed with the section above entitled " Identifying and Verifying Prescriptions for Treatments That May Contribute to An Accident or Injury, Not Including Medications ", nurses must not only identify and verify all treatment orders and prescriptions to insure that they are not placing the client at risk for any injury or accident and also to verify that the order is appropriate for the client and that it is accurate and transcribed in an accurate manner.
When the nurse receives an order or prescription for a treatment or procedure that is questionable in terms of client appropriateness and safety, the nurse as the nurse manager of care, contacts the person who has prescribed the treatment or procedure, and they also clarify and verify all questionable orders.
RELATED CONTENT:
- Accident/Error and Incident Prevention (Currently here)
- Emergency Response Plans
- Ergonomic Principles
- Handling Hazardous and Infectious Materials
- Home Safety
- Reporting Incident/Event/ Irregular Occurrence/Variances
- Safe Use of Equipment
- Security Plans
- Standard Precautions/Transmission Based Precautions/Surgical Asepsis
- Use of Restraints/Safety Devices
SEE – Safety & Infection Control Practice Test Questions
- Recent Posts
Safety and Infection Control NCLEX Practice Quiz (75 Questions)
Welcome to your NCLEX practice quiz on Safety and Infection Control. According to the NCLEX-RN test plan , about 9 to 15% of questions will come from this subcategory that includes content about the “ nurse ‘s ability required to protect clients, families, and healthcare personnel from health and environmental hazards.” Good luck, and hope you will learn a lot from this quiz.
Safety and Infection Control Nursing Test Banks
For this nursing test bank , we have included 75 NCLEX practice questions related to the Safety and Infection Control subcategory divided into three sets. Patient safety and infection control are essential and vital components of quality nursing care. A nurse’s ability to think critically and use this knowledge in the delivery of nursing care is essential to the well-being of the patients.
Quiz Guidelines
Before you start, here are some examination guidelines and reminders you must read:
- Practice Exams : Engage with our Practice Exams to hone your skills in a supportive, low-pressure environment. These exams provide immediate feedback and explanations, helping you grasp core concepts, identify improvement areas, and build confidence in your knowledge and abilities.
- You’re given 2 minutes per item.
- For Challenge Exams, click on the “Start Quiz” button to start the quiz.
- Complete the quiz : Ensure that you answer the entire quiz. Only after you’ve answered every item will the score and rationales be shown.
- Learn from the rationales : After each quiz, click on the “View Questions” button to understand the explanation for each answer.
- Free access : Guess what? Our test banks are 100% FREE. Skip the hassle – no sign-ups or registrations here. A sincere promise from Nurseslabs: we have not and won’t ever request your credit card details or personal info for our practice questions. We’re dedicated to keeping this service accessible and cost-free, especially for our amazing students and nurses. So, take the leap and elevate your career hassle-free!
- Share your thoughts : We’d love your feedback, scores, and questions! Please share them in the comments below.
Quizzes included in this guide are:
Recommended Resources
Recommended books and resources for your NCLEX success:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Saunders Comprehensive Review for the NCLEX-RN Saunders Comprehensive Review for the NCLEX-RN Examination is often referred to as the best nursing exam review book ever. More than 5,700 practice questions are available in the text. Detailed test-taking strategies are provided for each question, with hints for analyzing and uncovering the correct answer option.

Strategies for Student Success on the Next Generation NCLEX® (NGN) Test Items Next Generation NCLEX®-style practice questions of all types are illustrated through stand-alone case studies and unfolding case studies. NCSBN Clinical Judgment Measurement Model (NCJMM) is included throughout with case scenarios that integrate the six clinical judgment cognitive skills.

Saunders Q & A Review for the NCLEX-RN® Examination This edition contains over 6,000 practice questions with each question containing a test-taking strategy and justifications for correct and incorrect answers to enhance review. Questions are organized according to the most recent NCLEX-RN test blueprint Client Needs and Integrated Processes. Questions are written at higher cognitive levels (applying, analyzing, synthesizing, evaluating, and creating) than those on the test itself.

NCLEX-RN Prep Plus by Kaplan The NCLEX-RN Prep Plus from Kaplan employs expert critical thinking techniques and targeted sample questions. This edition identifies seven types of NGN questions and explains in detail how to approach and answer each type. In addition, it provides 10 critical thinking pathways for analyzing exam questions.

Illustrated Study Guide for the NCLEX-RN® Exam The 10th edition of the Illustrated Study Guide for the NCLEX-RN Exam, 10th Edition. This study guide gives you a robust, visual, less-intimidating way to remember key facts. 2,500 review questions are now included on the Evolve companion website. 25 additional illustrations and mnemonics make the book more appealing than ever.

NCLEX RN Examination Prep Flashcards (2023 Edition) NCLEX RN Exam Review FlashCards Study Guide with Practice Test Questions [Full-Color Cards] from Test Prep Books. These flashcards are ready for use, allowing you to begin studying immediately. Each flash card is color-coded for easy subject identification.

Recommended Links
An investment in knowledge pays the best interest. Keep up the pace and continue learning with these practice quizzes:
- Nursing Test Bank: Free Practice Questions UPDATED ! Our most comprehenisve and updated nursing test bank that includes over 3,500 practice questions covering a wide range of nursing topics that are absolutely free!
- NCLEX Questions Nursing Test Bank and Review UPDATED! Over 1,000+ comprehensive NCLEX practice questions covering different nursing topics. We’ve made a significant effort to provide you with the most challenging questions along with insightful rationales for each question to reinforce learning.
11 thoughts on “Safety and Infection Control NCLEX Practice Quiz (75 Questions)”
In # 5 the correct answer should be letter B right?
Please review question #5 in Safety and Infection Control NCLEX Practice Exam (Set 2: 25 Questions) I chose the correct answer which was cool air dryer and it was marked wrong. But in the rationales it had it correct. Thank you
Corrected! Thank you for letting us know.
in the first set of questions #16 about doing CPR. your rational for the answer being what it is states “The nurse should use the heel of one hand at the center of the chest, then place the heel of the other hand on top of the first hand and lace fingers together and give 30 compressions that are about 1” to 1½” deep.”
this is actually incorrect. per the American Heart Association, depth of compression on children is about 2 inches. answer C is more correct than D. just think the answers should be worded better and rationale should be corrected in the depth.
Question 19 regarding the child in foster care. Foster Parents do not have permission to sign informed consent on invasive procedures and need Social Worker permission. Most often the hospital/clinic will request a signature from Social Worker. The child is in the CUSTODY of the state and the CARE of the foster parent.
Thank you very much. It is a great site, very helpful. Please kindly review the answers of the following: Safety and Infection Control NCLEX Practice Exam | Quiz #2: Question 25 The posted answers were not correspond to the Question #25. Thanks again.
Thanks Kumari, this has been fixed! :)
For Q#25 for Safety and Infection Control NCLEX Practice Exam Quiz #2, the rationale given does not match the question & its answer choices. Can you fix this, please?
Fixed. Thanks for letting us know! :)
the test was completed how i can get the certificate or anything elses to be done
Hello Piyanee, Thanks for completing the test! Just to let you know, currently, we don’t offer certificates for the quizzes on our platform. They’re mainly designed for self-assessment and practice. However, you’re welcome to try out other quizzes we have available to further strengthen your knowledge. It’s a great way to keep testing your skills and learning! If you have any other questions or need guidance on specific topics, feel free to reach out.
Leave a Comment Cancel reply

IMAGES
VIDEO
COMMENTS
One way to reduce an injury risk at school is by _______ before handling laboratory equipment. Prescription medication should be stored away from children and used ________. 1) labeled containers. 2) reading the safety notes in the laboratory manual. 3) only by the person prescribed the medication. Amelie is working with a beaker and ...
Study with Quizlet and memorize flashcards containing terms like How can a person best reduce the risk of injuries on the road? a. by always wearing a seat belt when driving b. by obeying speed limits only on highways c. by following family advice about booster seat installation d. by riding with people who only occasionally drive while intoxicated, Which may cause an individual to hesitate ...
Wear protective clothing while sleeping at home. Secure a seat belt only when riding in the front seat. Wear a cracked bicycle helmet while riding a bicycle. Put away guns in a lockbox that is secure and in a discrete location., The image shows the relationship between bike helmet use and bicycle deaths. A graph titled Bicycle Deaths and Helmet ...
Fracture. automated external defibrillator (AED) Abrasion. Non-traumatic brain injury. Contusion. Anaphylatic shock. Inflammation. Incision. Study with Quizlet and memorize flashcards containing terms like Traumatic brain injury, Concussion, Fracture and more.
Choose from 580 different sets of Safety and Injury Prevention Assignment flashcards on Quizlet. Home. Subjects Expert Solutions. Study sets, textbooks, questions. Study sets, textbooks, questions ... All results Study sets Textbooks Questions Users Classes. Study sets. 28 studiers today. Safety and Injury Prevention Assignment. 10 terms. 5 (10 ...
Study with Quizlet and memorize flashcards containing terms like Discuss the relationship between the type and severity of injury and a child's developmental stage and physical, cognitive, and psychosocial needs and skills., What are the most common causes of injuries in children: a. Birth through five months of age b. Six months through 11 months of age c. 12 through 35 months of age d. Three ...
Start studying Safety and Injury Prevention. Learn vocabulary, terms, and more with flashcards, games, and other study tools. Search. Create. Log ... Safety and Injury Prevention. STUDY. PLAY. Risk. behavior that will lead to harm or injury. Harassment. is repeated unwanted attention for any reason that may make you feel uncomfortable. C.C.C ...
Graded Assignment Unit Test Part 2: Injury Prevention and Safety (10 points) Explain the difference between intentional injuries and unintentional injuries and give examples of each. An intentional injury is when you cause physical pain or physically do something to hurt a person or animal. Example-getting shot by a terrorist would be an ...
Unit 7 focuses on injury prevention and safety promotion in schools. You will find information on children's disaster preparedness, brain injury, substance use disorder, and violence and suicide prevention. Additionally, information on sun and water safety, hearing loss, and mercury safety in schools. Lesson plans and trainings with free CEU ...
Injury prevention is an effort comprising risk assessment, hazard analysis, and inspection of the environment (e.g., home, sports facilities, or workplaces) in order to prevent or minimize the severity of physical injuries before they occur. Keeping people safe in any environment is the responsibility of safety and public health agencies; thus ...
Connect classroom design to safety and injury prevention. Discuss ways to handle unsafe behavior by understanding the function of behaviors. Describe how teachers can ensure the toys and materials they offer children do not present injury risks and are nontoxic. Explain ways adults can support safe and developmentally appropriate use of technology.
Review new technologies for their potential to be more protective, more reliable, or less costly. Action item 1: Identify control options. Action item 2: Select controls. Action item 3: Develop and update a hazard control plan. Action item 4: Select controls to protect workers during nonroutine operations and emergencies.
The Recommended Practices present a step-by-step approach to implementing a safety and health program, built around seven core elements that make up a successful program. The main goal of safety and health programs is to prevent workplace injuries, illnesses, and deaths, as well as the suffering and financial hardship these events can cause for ...
Falls and related injuries are an important issue across the care continuum. National efforts in the community via Healthy People 2010, in the acute care setting via the Joint Commission's National Patient Safety Goals, and in the long-term care setting via the Nursing Home Quality Initiative project have the potential to significantly reduce falls and related injuries. The growing number of ...
Safety and Injury Prevention quiz for 9th grade students. Find other quizzes for Physical Ed and more on Quizizz for free! Skip to Content. Enter code. Log in. Sign up Enter code. Log in. Sign up. Suggestions for you. See more. 20 Qs . Muscular System 4.5K plays 6th - 8th 13 Qs . Connective Tissues 2.6K plays 11th - 12th 15 Qs ...
View Test prep - 5.1.5 Practice_ Safety and Injury Prevention.docx from HEALTH 221 22 at Spring Valley High School. 5.1.5 Practice: Safety and Injury Prevention Health (S4116922) Points possible: ... assignment. 2021 MSC 12App Sem 1 sol (3).pdf. INARA WEEK 10 ACTIVITY .docx. Answer A The developer asks the business analyst BA to clarify key ...
Some of the factors that can positively impact on and influence injury and accident prevention include an age and developmental stage at which the person is able to understand safety and safe behavior; a normal, alert and awake level of consciousness, a level of cognitive ability and mental status that enables the person to have insight into ...
Safety and Infection Control. Adolescents (12 to 20 Years): Teaching About Safety Risks for Adolescents. fiber_manual_recordCorrect. Question Identify two (2) areas of injury prevention applicable to the adolescent client. Provide one (1) example for each area identified. Bodily harm Keep firearms in a locked cabinet or box.
Graded Assignment 6.11 Injury Prevention and Safety Prompt: Explain the difference between. AI Homework Help. Expert Help. Study Resources. ... Injury Prevention and Safety Unit Test, Part 2.docx. Foothill High School. SCIENCE 1713. Physics. pH. Injury Prevention. unhealthy risk taking behavior.
Log in to your account. Student Educator. Username
Welcome to your NCLEX practice quiz on Safety and Infection Control. According to the NCLEX-RN test plan, about 9 to 15% of questions will come from this subcategory that includes content about the "nurse's ability required to protect clients, families, and healthcare personnel from health and environmental hazards." Good luck, and hope you will learn a lot from this quiz.
Process Safety . 29. Process Safety hazards are substances or conditions which can cause injury or harm to people, processes, equipment and the environment and which are associated with the properties and behaviors of process materials. a. True . b. False 30.
The Injury and Illness Prevention Program (IIPP) is a basic, written workplace safety program. Title 8 of the California Code of Regulations (T8CCR), section 3203, requires every employer to develop and implement an effective IIPP. The main goal of an IIPP is to prevent workplace injuries and illnesses, and the financial hardship they cause ...