Loading metrics
Open Access

Qualitative Research: Understanding Patients' Needs and Experiences
- The PLoS Medicine Editors

Published: August 28, 2007
- https://doi.org/10.1371/journal.pmed.0040258
- Reader Comments
Citation: The PLoS Medicine Editors (2007) Qualitative Research: Understanding Patients' Needs and Experiences. PLoS Med 4(8): e258. https://doi.org/10.1371/journal.pmed.0040258
Copyright: © 2007 The PLoS Medicine Editors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Why do up to half of all patients with tuberculosis (TB) fail to adhere to drug treatment [ 1 ]? The answer to this question is a matter of life and death, since nonadherence contributes to disease relapse and mortality [ 2 ]. In last month's PLoS Medicine, Salla Munro and colleagues argue that qualitative studies—in which researchers listen to what patients, care givers, and health care providers have to say—can provide important insights into why nonadherence occurs [ 3 ]. Their paper is a “meta-ethnography” [ 4 ], a systematic review and synthesis of qualitative studies on adherence to TB medication. The review found a wide array of factors to explain nonadherence, such as the belief that if one's symptoms have disappeared there is no need to finish a course of treatment. We published this review because we thought it would play a role in improving the delivery of TB treatment and ultimately in reducing the enormous global burden of the disease.
PLoS Medicine has now published two such meta-ethnographies (the first looked at adherence to HIV medication [ 5 ]). We have also published a small number of individual qualitative studies. For example, in our special issue on social medicine ( http://collections.plos.org/plosmedicine/socialmedicine-2006.php ), we published a qualitative study of migrant workers in the US that found that farm working and housing conditions are organized according to ethnicity and citizenship and that this hierarchy determines health disparities [ 6 ]. We have been very selective in our editorial decisions about which qualitative studies to publish. In our decision-making process, we have been guided by two crucial questions.
The first question is whether a qualitative approach was the right way to answer the research question. Quantitative research strives to be objective: human beings, health, and illness are the objects of investigation. Such investigation has led to extraordinary biomedical advances—yet patients often fail to reap the benefits because health professionals may not understand how best to deliver them in the context of patients' multifaceted lives. The academic editor of Salla Munro and colleagues' study commented that thinking of TB drugs simply as a “biomedical intervention” without factoring in patients' needs and broader social contexts creates circumstances that increase the likelihood of poor adherence to treatment. Qualitative research is the best way to understand these needs and contexts.
Astrid Fletcher and colleagues, for example, used quantitative methods to objectively determine who (in terms of age, sex, and education level) did not use the eye-care services available in India [ 7 ]. But they adopted a qualitative approach to answer the question of why people did not use these services. David Leon and colleagues, during a quantitative study on hazardous alcohol drinking in Russia, learned that much alcohol was consumed in the form of what were described as “surrogates” [ 8 ]. Qualitative research helped to identify what these surrogates were—they included eau de Cologne and over-the-counter medications.
When researchers investigate the experiences of people receiving or failing to receive health care, identify themes in these subjective stories, and integrate these themes into the greater context of human life experience, the results are informative to care providers. The usefulness of these results lies precisely in their subjectivity: the subjects are telling us, or we are finding out through more subtle observation, what matters to them.
The results of qualitative research can also help to inform the very process of research itself. Qualitative approaches can help us to understand, for example, why some patients decline to participate in clinical trials [ 9 ], or how patients experience the trial process itself. They can even be used to refine or improve a clinical trial in “real time.” In a trial of a computerized decision support tool for patients with atrial fibrillation being considered for anticoagulation treatment, Madeleine Murtagh and colleagues used qualitative evidence in deciding to discontinue one arm of the trial (the intervention in that arm was causing confusion amongst the patients and was unlikely to produce valid data) [ 10 ]. When a quantitative study is assessing the effectiveness of a complex multifaceted intervention, qualitative methods can help to tease out why such an intervention works or fails [ 11 ]. Qualitative approaches can also help to identify which of many possible research questions should receive priority for investigation, often by asking the research participants themselves. For example, patients with asthma may value easy-to-use inhalers more highly than a new class of drug.
Once it is clear that qualitative methods constitute the right approach for a study submitted to PLoS Medicine, the second question is whether the study meets our criteria for rigor and relevance. For a study to be suitable, regardless of the methodology, it should address an important topic in clinical medicine or public health and it should have the potential to transform our understanding of the causes or treatment of disease. In assessing any study, quantitative or qualitative, we are always on the lookout for biases, poorly described methods, and limited generalizability or overinterpretation of the data. In specifically assessing qualitative studies, we additionally wish to be reassured that the researchers used some type of “quality control” in analyzing the data—for example, were the data independently analyzed by at least two researchers and did consistent themes emerge from the data each time?
One characteristic of PLoS Medicine is the very broad range of research that we have published to date. We feel that such a range is appropriate for a medical journal, since understanding the complex nature of illness and health care requires a variety of different research approaches. “What is involved is not a crossroads where we have to go left or right,” Martyn Hammersley has argued in a discussion of the false dichotomy between quantitative and qualitative research. “A better analogy is a complex maze where we are repeatedly faced with decisions, and where paths wind back on one another” [ 12 ].
- View Article
- Google Scholar
- 2. Volmink J, Garner P (2006) Directly observed therapy for treating tuberculosis. Cochrane Database Syst Rev 2, CD003343.
- 4. Noblit GW, Hare RD (1988) Meta-ethnography: Synthesizing qualitative studies. Newbury Park (CA): Sage. 88 p.
- 12. (1992) Deconstructing the qualitative–quantitative divide. In: Brannen J, editor. Mixing methods: Qualitative and quantitative research. Aldershot (United Kingdom): Avebury. pp. 39–55. editor.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 55, Issue 2
- Understanding qualitative research in health care
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
Qualitative studies are often used to research phenomena that are difficult to quantify numerically. 1,2 These may include concepts, feelings, opinions, interpretations and meanings, or why people behave in a certain way. Although qualitative research is often described in opposition to quantitative research, the approaches are complementary, and many researchers use mixed methods in their projects, combining the strengths of both approaches. 2 Many comprehensive texts exist on qualitative research methodology including those with a focus on healthcare related research. 2-4 Here we give a brief introduction to the rationale, methods and quality assessment of qualitative research.
https://doi.org/10.1136/dtb.2017.2.0457
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Key issues in qualitative research
Qualitative research allows deeper understanding of the richness and complexity of social phenomena. Qualitative methods can provide evidence on health and illness and can be used in various ways: 3
To complement quantitative methods, or when quantitative methods are impractical (e.g. when the topic is sensitive, poses measurement problems or is concerned with process and/or interaction; the research population is very small; or for intensive understanding of an innovation before widespread introduction). 3
In the exploratory stages of an applied health research programme, when they may clarify the research question and generate hypotheses. 3 Study design is often described as flexible or ‘emergent’ and researchers may have to adapt a study through a process of ‘progressive focussing’ in response to important but unanticipated findings. 3
To assess a pre-specified hypothesis, as in quantitative research. 3
To study particular experiences in depth rather than population averages or generalisations, and explore experiences from different perspectives. 3 For example, assessment of patient satisfaction is complex and varies between cultures or settings, which can make it difficult to develop quantitative measurement instruments. 5
To involve potential users in development and implementation of interventions. 6
To interpret the findings of quantitative research. 3
For example, in one study, alongside a quantitative review on the efficacy of telephone counselling for informal carers of people with dementia, qualitative methods were used to explore carers' experiences of receiving telephone counselling and counsellors' experiences of conducting telephone counselling. 7 Analysis of quantitative and qualitative results identified areas for improvement.
While the same ethical principles (autonomy, non-maleficence [doing no harm], beneficence and justice) apply equally to both quantitative and qualitative research, the application of these principles should take into account the nature of the research proposed. 3 The risks of serious physical harm arising from qualitative research are rarely as high as in quantitative medical studies. However, such research may cause psychological harm, damage to self-esteem and have an adverse impact on interpersonal relationships. Qualitative researchers should seek to minimise such risks. A ‘good’ interviewer builds rapport, encouraging trust and disclosure. In addition, the interviewer also needs to allow opportunities for the interviewee to withdraw or cease disclosure. 4
People, settings, processes, events or data are sampled in qualitative research in order to understand a particular problem, rather than to statistically represent a wider population. In contrast to quantitative methods, where many participants are sampled by randomisation, the small number of participants in qualitative research are often deliberately chosen for their ability to illuminate the research question (known as purposive sampling). 2 , 3 Such sampling may include the selection of outlier cases, cases with maximum variation or homogeneous cases.
Data collection
Methods of collecting data include observation, interviews and focus groups. 3 It is usual to write field notes, but methods can also include video or audio recordings.
Observation
Observation allows researchers to notice events and relationships in a ‘natural’ setting, which may produce insights about which the participants may not be aware. Observation (with varying levels of participation by the researcher in the events being observed) may require a prolonged time period but allows the observer to check their record against an informant's description and note discrepancies. 3
One-to-one interviews are used when the researcher wants to find out something that cannot be directly observed (e.g. how consumers evaluate health services, what understanding and attitudes underlie particular kinds of health behaviour). 3
Good questions in qualitative interviews should be open-ended, neutral, sensitive and clear to the interviewee. 8 , 9 It is usually best to start with questions that the interviewee can answer easily and then proceed to more difficult or sensitive topics. 8 Open questions allow the respondent to answer in their own words and interviews where there is a good rapport may be more likely to create a context in which respondents are prepared to discuss sensitive topics and penetrate beyond a superficial level. 2 , 3 Researchers should monitor their interviewing technique, critically appraise recordings of their interviews and ask others for their comments, noting in particular whether leading questions are being asked, whether cues are picked up or ignored, and whether interviewees are given enough time to explain what they mean. 8
Interviews can be tightly structured or more flexible: 3
A structured (standardised) interview is one in which the wording and order of all questions are exactly the same for every respondent. This aims to ensure that any differences between respondents are not attributable to differences in the questionnaire or research procedures.
A semi-structured interview covers topics on the researcher's agenda, but the phrasing and ordering of questions are tailored to the vocabulary and understanding of respondents, rather than imposing a uniform set of questions, which may be interpreted differently by respondents.
A ‘depth’ or ‘long’ interview, involves no specific set of questions. The participant's perspective on the phenomenon of interest should unfold as the participant and not the researcher views it. 3 The flexibility of such interviews may uncover new unanticipated areas or ideas.
Focus groups
Focus groups (or group interviews) are informal discussions in which participants focus collectively on a topic or issue, usually presented to them (either verbally or in written form) as a vignette to discuss. 3 , 10 Focus group participants (usually 6-8 people) may be existing clusters of people (e.g. family members, friends or work colleagues) or assembled specifically for the research. 10
The advantage of a focus group is the interaction of group participants with each other, as well as with the researcher/moderator. Such interaction is helpful to:
gain access to participants' own assumptions, meanings, vocabulary and thinking patterns;
identify concepts and practices central to the respondents, and to design subsequent questionnaires using respondents' own words or phrases, enhancing future participants' understanding of research questions;
observe how people interact to construct meanings attributed to health and illness, how opinions are formed, expressed, defended and sometimes modified in discussion and debate with others;
enable participants to have more control over the research agenda, which may generate unexpected insights into areas important to them; and
identify obstacles or objections that prevent or discourage individuals from healthy behaviours, and explore individuals' understanding of, and responses to, health-related media messages. 10
Data analysis
Whereas quantitative analysis seeks to reduce data, generating a series of statistics, qualitative analysis aims to represent data using detailed knowledge of cases. Qualitative research studies typically produce very large amounts of data, which are reduced and summarised into codes, concepts, categories, themes and theory. 3
There are many different approaches to analysis in qualitative research, including thematic analysis, framework analysis, grounded theory, interpretive phenomenological analysis, conversation analysis and discourse analysis. 2 , 3 , 11 , 12
Grounded theory derives theory from data using a constant comparative method. 2 , 3 , 11 , 12 Items in the raw data (e.g. interviews, field notes) are broken down, so that as many ideas and concepts as possible are identified and systematically coded, while at the same time comparing them with previous incidents. 2 , 3 Standardised rules are used for transcribing data to limit the risk of misinterpretation. Codes and categories can be based on the respondent's own words. 3 The data are simultaneously organised and reassembled, so that the researcher can identify relevant elements and relationships by cataloguing the substantive topics and attaching labels to concepts and themes that they see emerging from the material (rather than reflecting prior theoretical assumptions), developing core categories and ultimately explaining phenomena. 2 , 3 The analysis is iterative with the findings of preliminary analyses of data from the first phases of fieldwork informing subsequent work. 3
There should be careful documentation of all analytic decisions that lead to the creation of categories, forming an audit trail that provides evidence to support the integrity of the coding, categorisation and interpretive choices made throughout the qualitative data analysis process. 2
Researchers should also demonstrate continuous reflection on the fit between data and reality, by regarding all theoretical explanations, categories, hypotheses and questions about the data as being provisional until they are compared with the data. 3 They should give clear explanations of methods and demonstrate that they have considered alternative possible explanations for their data. 3
A study may be adapted through a process of iterative ‘progressive focussing’ in response to important unanticipated findings. 3 ‘Data saturation’ is a point at which no new themes or ideas arise from data analysis, and data collection can stop at that point.
Researchers' pre-existing assumptions are often challenged by qualitative research, as ideas are raised by respondents and new concepts and theories can develop that help to explain nuance and complexity. 13 Qualitative studies are not seeking statistical generalisability, but to provide insights with applicability to other settings and situations. It is helpful to have the qualitative researchers' description of what they have done and how it was done, so that readers can judge how transferable the findings are to other contexts. 14
Quality assessment
Qualitative methodologies are derived from many fields of social research with different philosophies and underlying assumptions. 3 There is, therefore, more than one correct way to conduct qualitative research, and there are debates and disagreements about qualitative methodology that can be confusing. 15
Quality assessment of qualitative research studies remains a contested area. 16–18 In addition, as qualitative researchers may have an impact on the data, they must show the efforts they undertook to prevent this from influencing the data. 7
Just as the quality of quantitative studies may be assessed using checklists, many checklists are available to help assess qualitative studies. 16 , 17 For example, the Critical Skills Appraisal Programme (CASP) has produced a checklist to aid evaluation of qualitative research (see Box). 19
CASP checklist 19
Screening questions:
Was there a clear statement of the aims of the research?
Is a qualitative methodology appropriate? Is it worth continuing? (Only continue if both these questions are answered ‘yes’).
Was the research design appropriate to address the aims of the research?
Was the recruitment strategy appropriate to the aims of the research?
Were the data collected in a way that addressed the research issue?
Has the relationship between researcher and participants been adequately considered?
Have ethical issues been taken into consideration?
Was the data analysis sufficiently rigorous?
Is there a clear statement of findings?
How valuable is the research?
A more detailed checklist (the COREQ) consists of 32 items in three domains: 20
The research team and reflexivity (covering items such as the researchers' sex, credentials, occupation, experience or training; the relationship with the participants; researchers' biases and assumptions).
The study design (e.g. the theoretical framework, sampling, how participants were approached, the setting, description of the sample, data collection and the audit trail)
Data analysis and reporting (e.g. the number of data coders and description of coding method, whether participant quotations were presented to illustrate the themes, whether data were consistent, and whether themes were clearly presented in the findings).
Comparison between qualitative and quantitative research
The table below summarises some key differences between qualitative and quantitative research.
- View inline
Comparison of quantitative and qualitative research 3
How can qualitative and quantitative research complement each other?
Qualitative research can complement quantitative approaches. Two examples are given below:
Survey research
Qualitative field work (e.g. using observations, interviews or focus groups) to achieve a better understanding of health problems; generation of questions and response options to capture the reality of participants' experiences; qualitative interviews to seek feedback on the perceived meanings and wording of proposed survey questions; quantitative analysis of survey responses from a large, randomly selected sample.
Intervention development and evaluation
Qualitative fieldwork to illuminate the complexity of a health problem, explore barriers and facilitators for change and explore suitable types and designs of treatment or intervention; qualitative methods to involve users in intervention design to ensure that it meets recipient needs and that it is engaging, feasible and sustainable; randomised controlled trial to assess the effectiveness of an intervention; qualitative study to explore how interventions work (and why they don't work) in the real world.
Qualitative research is a technical discipline that is important in providing valuable descriptions of complex phenomena. Qualitative studies differ from quantitative studies in that they often generate rather than test hypotheses; focus on processes, thoughts, feelings and experiences rather than outcomes; and assess small numbers of participants in depth rather than large sample sizes. Such research is designed to capture concepts that are hard to enumerate with quantitative research methods. Findings from qualitative research can enhance the design of other types of research and the implementation of health interventions. Data are often collected using observation, interviews or focus groups, usually recorded and transcribed, which allow the exploration of topics in the respondents' own words and understanding. Analysis of the information must be systematic and transparent; checklists exist to help assess the quality of qualitative studies. Qualitative methods can complement quantitative methods to add a further dimension to research, although there may be issues around the generalisability of results from one context to another. Evidence from qualitative studies can lead to a richer understanding of the complex reality of people's lives and their experience of illness and medical care.
- Understanding statistical terms: 3 . DTB 2009 ; 47 : 59 – 60 . OpenUrl Abstract / FREE Full Text
- Murphy E , et al
- Thorogood N
- Almaida RS , et al
- Bailey J , et al
- Lins S , et al
- Wilkinson S
- Glaser BG ,
- Strauss A ,
- Silverman D
- ↵ Cochrane Methods , 2011 . Supplemental handbook guidance [online]. Available: http://methods.cochrane.org/qi/supplemental-handbook-guidance [Accessed 18 January 2017] .
- ↵ Cochrane Qualitative and Implementation Methods Group , 2013 . Qualitative and implementation evidence and Cochrane reviews [online]. Available: http://methods.cochrane.org/sites/methods.cochrane.org.qi/files/public/uploads/Handbook52_QQ_Qualitative_web%20update%20Oct%202015.pdf [Accessed 18 January 2017] .
- Crabtree BF
- ↵ Critical Appraisal Skills Programme , 2013 . Qualitative research checklist [online]. Available: http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf [Accessed 18 January 2017] .
- Tong A , et al
Read the full text or download the PDF:
Advertisement

- Previous Issue
- Previous Article
- Next Article
- Box 1. What to Look for in Research Using This Method
What Is Qualitative Research?
Qualitative versus quantitative research, conducting and appraising qualitative research, conclusions, research support, competing interests, qualitative research methods in medical education.
Submitted for publication January 5, 2018. Accepted for publication November 29, 2018.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
- Search Site
Adam P. Sawatsky , John T. Ratelle , Thomas J. Beckman; Qualitative Research Methods in Medical Education. Anesthesiology 2019; 131:14–22 doi: https://doi.org/10.1097/ALN.0000000000002728
Download citation file:
- Ris (Zotero)
- Reference Manager
Qualitative research was originally developed within the social sciences. Medical education is a field that comprises multiple disciplines, including the social sciences, and utilizes qualitative research to gain a broader understanding of key phenomena within the field. Many clinician educators are unfamiliar with qualitative research. This article provides a primer for clinician educators who want to appraise or conduct qualitative research in medical education. This article discusses a definition and the philosophical underpinnings for qualitative research. Using the Standards for Reporting Qualitative Research as a guide, this article provides a step-wise approach for conducting and evaluating qualitative research in medical education. This review will enable the reader to understand when to utilize qualitative research in medical education and how to interpret reports using qualitative approaches.

Image: J. P. Rathmell and Terri Navarette.
Qualitative research provides approaches to explore and characterize the education of future anesthesiologists. For example, the practice of anesthesiology is increasingly team-based; core members of the anesthesia care team include physicians, trainees, nurse anesthetists, anesthesiologist assistants, and other healthcare team members. 1 Understanding how to work within and how to teach learners about anesthesia care teams requires the ability to conceptualize the complexity of individual psychology and social interactions that occur within teams. Qualitative research is well suited to investigate complex issues like team-based care. For example, one qualitative study observed the interactions between members of the anesthesia care team during simulated stressful situations and conducted interviews of team members; they described limited understanding of each team member’s role and perceptions about appropriate roles and responsibilities, which provided insight for interprofessional team training. 2 Another qualitative study explored the hierarchy within the anesthesia care team, highlighting residents’ reluctance to challenge the established hierarchy and outlining the strategies they use to cope with fear and intimidation. 3 Key issues in medical education and anesthesiology, particularly when exploring human experience and social interactions, may be best studied using qualitative research methodologies and methods.
Medical education is a complex field, and medical education research and practice fittingly draws from many disciplines ( e.g. , medicine, psychology, sociology, education) and synthesizes multiple perspectives to explain how people learn and how medicine should be taught. 4 , 5 The concept of a field was well described by Cristancho and Varpio 5 in their tips for early career medical educators: “A discipline is usually guided by shared paradigms, assumptions, rules and methods to present their knowledge claims— i.e. , people from the same discipline speak the same language. A field brings people from multiple disciplines together.” Qualitative research draws from the perspectives of multiple disciplines and has provided methodologies to explore the complex research questions inherent to medical education.
When appraising qualitative research in medical education, do the authors:
Clearly state the study purpose and research question?
Describe the conceptual framework that inform the study and guide analysis?
Identify their qualitative methodology and research paradigm?
Demonstrate adequate reflexivity, conveying to the reader their values, assumptions and way of thinking, being explicit about the effects these ways of thinking have on the research process?
Choose data collection methods that are congruent with the research purpose and qualitative methodology?
Select an appropriate sampling strategy, choosing participants whose perspectives or experiences are relevant to the study question?
Define their method for determining saturation, how they decided to stop data collection?
Outline their process for data processing, including the management and coding of study data?
Conduct data analysis consistent with their chosen methodology?
Consider techniques to enhance trustworthiness of their study findings?
Synthesize and interpret their data with sufficient detail and supporting quotations to explain the phenomenon of study?
Current medical training is heavily influenced by the practice of evidence-based medicine. 6 Trainees are taught the “hierarchy of evidence” for evaluating studies of clinical interventions. 7 This hierarchy prioritizes knowledge gained through systematic reviews and meta-analyses, randomized controlled trials, and observational studies, but it does not include qualitative research methodologies. This means that because of their medical training and exposure to quantitative medical literature, clinician educators may be more familiar with quantitative research and feel more comfortable engaging in studies utilizing quantitative methodologies. However, many clinician educators are not familiar with the language and application of qualitative research and feel less comfortable engaging in studies using qualitative methodologies.
Because medical education is a diverse and complex field, qualitative research is a common approach in medical education research. Clinician educators who wish to understand the medical education literature need to be familiar with qualitative research. Clinician educators involved in research may also find themselves asking questions best answered by qualitative methodologies. Our goal is to provide a broad, practical overview of qualitative research in medical education. Our objectives are to:
1) Define qualitative research.
2) Compare and contrast qualitative and quantitative research.
3) Provide a framework for conducting and appraising qualitative research in medical education.
Qualitative research in medical education has a distinct vocabulary with terminology not commonly used in other biomedical research fields. Therefore, we have provided a glossary and definitions of the common terms that are used throughout this article ( table 1 ).
Glossary of Common Terms Used in Qualitative Research

Of the many attempts to provide a comprehensive definition of qualitative research, our favorite definition comes from Denzin and Lincoln:
“Qualitative research is a situated activity that locates the observer in the world. Qualitative research consists of a set of interpretive, material practices that make the world visible. These practices…turn the world into a series of representations, including field notes, interviews, conversations, photographs, recordings, and memos to the self. At this level, qualitative research involves an interpretive, naturalistic approach to the world. This means that qualitative researchers study things in their natural settings, attempting to make sense of or interpret phenomena in terms of the meanings people bring to them.” 12
This definition reveals the following points: first, qualitative research is a “situated activity,” meaning that the research and observations are made in the real world, in this case a real life clinical or educational situation. Second, qualitative research “turns the world into a series of representations” by representing the observations, in this case of a clinical or educational situation, with qualitative data, usually taking the form of words, pictures, documents, and other symbols. Last, qualitative researchers seek to “make sense” of the meanings that research participants bring to different phenomena to allow for a greater understanding of those phenomena. Through qualitative research, observers comprehend participants’ beliefs and values and the way these beliefs and values are shaped by the context in which they are studied.
Because most clinician educators are familiar with quantitative methods, we will start by comparing qualitative and quantitative methods to gain a better understanding of qualitative research ( table 2 ). To illustrate the difference between qualitative and quantitative research in medical education, we pose the question: “What makes noon conference lectures effective for resident learning?” A qualitative approach might explore the learner perspective on learning in noon conference lectures during residency and conduct an exploratory thematic analysis to better understand what the learner thinks is effective. 13 A qualitative approach is useful to answer this question, especially if the phenomenon of interest is incompletely understood. If we wanted to compare types or attributes of conferences to assess the most effective methods of teaching in a noon conference setting, then a quantitative approach might be more appropriate, though a qualitative approach could be helpful as well. We could use qualitative data to inform the design of a survey 14 or even inform the design of a randomized control trial to compare two types of learning during noon conference. 15 Therefore, when discussing qualitative and quantitative research, the issue is not which research approach is stronger, because it is understood that each approach yields different types of knowledge when answering the research question.
Comparisons of Quantitative and Qualitative Research in Medical Education

Similarities
The first step of any research project, qualitative or quantitative, is to determine and refine the study question; this includes conducting a thorough literature review, crafting a problem statement, establishing a conceptual framework for the study, and declaring a statement of intent. 16 A common pitfall in medical education research is to start by identifying the desired methods ( e.g. , “I want to do a focus group study with medical students.”) without having a clearly refined research question, which is like putting the cart before the horse. In other words, the research question should guide the methodology and methods for both qualitative and quantitative research.
Acknowledging the conceptual framework for a study is equally important for both qualitative and quantitative research. In a systematic review of medical education research, only 55% of studies provided a conceptual framework, limiting the interpretation and meaning of the results. 17 Conceptual frameworks are often theories that represent a way of thinking about the phenomenon being studied. Conceptual frameworks guide the interpretation of data and situate the study within the larger body of literature on a specific topic. 9 Because qualitative research was developed within the social sciences, many qualitative research studies in medical education are framed by theories from social sciences. Theories from social science disciplines have the ability to “open up new ways of seeing the world and, in turn, new questions to ask, new assumptions to unearth, and new possibilities for change.” 18 Qualitative research in medical education has benefitted from these new perspectives to help understand fundamental and complex problems within medical education such as culture, power, identity, and meaning.
Differences
The fundamental difference between qualitative and quantitative methodologies centers on epistemology ( i.e. , differing views on truth and knowledge). Cleland 19 describes the differences between qualitative and quantitative philosophies of scientific inquiry: “quantitative and qualitative approaches make different assumptions about the world, about how science should be conducted and about what constitutes legitimate problems, solutions and criteria of ‘proof.’”
Quantitative research comes from objectivism , an epistemology asserting that there is an absolute truth that can be discovered; this way of thinking about knowledge leads researchers to conduct experimental study designs aimed to test hypotheses about cause and effect. 10 Qualitative research, on the other hand, comes from constructivism , an epistemology asserting that reality is constructed by our social, historical, and individual contexts, and leads researchers to utilize more naturalistic or exploratory study designs to provide explanations about phenomenon in the context that they are being studied. 10 This leads researchers to ask fundamentally different questions about a given phenomenon; quantitative research often asks questions of “What?” and “Why?” to understand causation, whereas qualitative research often asks the questions “Why?” and “How?” to understand explanations. Cook et al. 20 provide a framework for classifying the purpose of medical education research to reflect the steps in the scientific method—description (“What was done?”), justification (“Did it work?”), and clarification (“Why or how did it work?”). Qualitative research nicely fits into the categories of “description” and “clarification” by describing observations in natural settings and developing models or theories to help explain “how” and “why” educational methods work. 20
Another difference between quantitative and qualitative research is the role of the researcher in the research process. Experimental studies have explicitly stated methods for creating an “unbiased” study in which the researcher is detached ( i.e. , “blinded”) from the analysis process so that their biases do not shape the outcome of the research. 21 The term “bias” comes from the positivist paradigm underpinning quantitative research. Assessing and addressing “bias” in qualitative research is incongruous. 22 Qualitative research, based largely on a constructivist paradigm, acknowledges the role of the researcher as a “coconstructer” of knowledge and utilizes the concept of “reflexivity.” Because researchers act as coconstructors of knowledge, they must be explicit about the perspectives they bring to the research process. A reflexive researcher is one who challenges their own values, assumptions, and way of thinking and who is explicit about the effects these ways of thinking have on the research process. 23 For example, when we conducted a study on self-directed learning in residency training, we were overt regarding our roles in the residency program as core faculty, our belief in the importance of self-directed learning, and our assumptions that residents actually engaged in self-directed learning. 24 , 25 We also needed to challenge these assumptions and open ourselves to alternative questions, methods of data collection, and interpretations of the data, to ultimately ensure that we created a research team with varied perspectives. Therefore, qualitative researchers do not strive for “unbiased” research but to understand their own roles in the coconstruction of knowledge. When assessing reflexivity, it is important for the authors to define their roles, explain how those roles may affect the collection and analysis of data, and how the researchers accounted for that effect and, if needed, challenged any assumptions during the research process. Because of the role of the researcher in qualitative research, it is vital to have a member of the research team with qualitative research experience.
A Word on Mixed Methods
In mixed methods research, the researcher collects and analyzes both qualitative and quantitative data rigorously and integrates both forms of data in the results of the study. 26 Medical education research often involves complex questions that may be best addressed through both quantitative and qualitative approaches. Combining methods can complement the strengths and limitations of each method and provide data from multiple sources to create a more detailed understanding of the phenomenon of interest. Examples of uses of mixed methods that would be applicable to medical education research include: collecting qualitative and quantitative data for more complete program evaluation, collecting qualitative data to inform the research design or instrument development of a quantitative study, or collecting qualitative data to explain the meaning behind the results of a quantitative study. 26 The keys to conducting mixed methods studies are to clearly articulate your research questions, explain your rationale for use of each approach, build an appropriate research team, and carefully follow guidelines for methodologic rigor for each approach. 27
Toward Asking More “Why” Questions
We presented similarities and differences between qualitative and quantitative research to introduce the clinician educator to qualitative research but not to suggest the relative value of one these research methods over the other. Whether conducting qualitative or quantitative research in medical education, researchers should move toward asking more “why” questions to gain deeper understanding of the key phenomena and theories in medical education to move the field of medical education forward. 28 By understanding the theories and assumptions behind qualitative and quantitative research, clinicians can decide how to use these approaches to answer important questions in medical education.
There are substantial differences between qualitative and quantitative research with respect to the assessment of rigor; here we provide a framework for reading, understanding, and assessing the quality of qualitative research. O’Brien et al. 29 created a useful 21-item guide for reporting qualitative research in medical education, based upon a systematic review of reporting standards for qualitative research—the Standards for Reporting Qualitative Research. It should be noted, however, that just performing and reporting each step in these standards do not ensure research quality.
Using the Standards for Reporting Qualitative Research as a backdrop, we will highlight basic steps for clinician educators wanting to engage with qualitative research. If you use this framework to conduct qualitative research in medical education, then you should address these steps; if you are evaluating qualitative research in medical education, then you can assess whether the study investigators addressed these steps. Table 3 underscores each step and provides examples from our research in resident self-directed learning. 25
Components of Qualitative Research: Examples from a Single Research Study

Refine the study question. As with any research project, investigators should clearly define the topic of research, describe what is already known about the phenomenon that is being studied, identify gaps in the literature, and clearly state how the study will fill that gap. Considering theoretical underpinnings of qualitative research in medical education often means searching for sources outside of the biomedical literature and utilizing theories from education, sociology, psychology, or other disciplines. This is also a critical time to engage people from other disciplines to identify theories or sources of information that can help define the problem and theoretical frameworks for data collection and analysis. When evaluating the introduction of a qualitative study, the researchers should demonstrate a clear understanding of the phenomenon being studied, the previous research on the phenomenon, and conceptual frameworks that contextualize the study. Last, the problem statement and purpose of the study should be clearly stated.
Identify the qualitative methodology and research paradigm. The qualitative methodology should be chosen based on the stated purpose of the research. The qualitative methodology represents the overarching philosophy guiding the collection and analysis of data and is distinct from the research methods ( i.e. , how the data will be collected). There are a number of qualitative methodologies; we have included a list of some of the most common methodologies in table 4 . Choosing a qualitative methodology involves examining the existing literature, involving colleagues with qualitative research expertise, and considering the goals of each approach. 32 For example, explaining the processes, relationships, and theoretical understanding of a phenomenon would point the researcher to grounded theory as an appropriate approach to conducting research. Alternatively, describing the lived experiences of participants may point the researcher to a phenomenological approach. Ultimately, qualitative research should explicitly state the qualitative methodology along with the supporting rationale. Qualitative research is challenging, and you should consult or collaborate with a qualitative research expert as you shape your research question and choose an appropriate methodology. 32
Choose data collection methods. The choice of data collection methods is driven by the research question, methodology, and practical considerations. Sources of data for qualitative studies would include open-ended survey questions, interviews, focus groups, observations, and documents. Among the most important aspects of choosing the data collection method is alignment with the chosen methodology and study purpose. 33 For interviews and focus groups, there are specific methods for designing the instruments. 34 , 35 Remarkably, these instruments can change throughout the course of the study, because data analysis often informs future data collection in an iterative fashion.
Select a sampling strategy. After identifying the types of data to be collected, the next step is deciding how to sample the data sources to obtain a representative sample. Most qualitative methodologies utilize purposive sampling, which is choosing participants whose perspectives or experiences are relevant to the study question. 11 Although random sampling and convenience sampling may be simpler and less costly for the researcher than purposeful sampling, these approaches often do not provide sufficient information to answer the study question. 36 For example, in grounded theory, theoretical sampling means that the choice of subsequent participants is purposeful to aid in the building and refinement of developing theory. The criteria for selecting participants should be stated clearly. One key difference between qualitative and quantitative research is sample size: in qualitative research, sample size is usually determined during the data collection process, whereas in quantitative research, the sample size is determined a priori . Saturation is verified when the analysis of newly collected data no longer provides additional insights into the data analysis process. 10
Plan and outline a strategy for data processing. Data processing refers to how the researcher organizes, manages, and dissects the study data. Although data processing serves data analysis, it is not the analysis itself. Data processing includes practical aspects of data management, like transcribing interviews, collecting field notes, and organizing data for analysis. The next step is coding the data, which begins with organizing the raw data into chunks to allow for the identification of themes and patterns. A code is a “word or short phrase that symbolically assigns a summative, salient, essence-capturing, and/or evocative attribute for a portion of language-based or visual data.” 8 There is an artificial breakdown between data processing and analysis, because these steps may be conducted simultaneously; many consider coding as different from—yet a necessary step to facilitating—the analysis of data. 8 Qualitative software can support this process, by making it easier to organize, access, search, and code your data. However, it is noteworthy that these programs do not do the work for you, they are merely tools for supporting data processing and analysis.
Conduct the data analysis. When analyzing the data, there are several factors to consider. First, the process of data analysis begins with the initial data collection, which often informs future data collection. Researchers should be intentional when reading, reviewing, and analyzing data as it is collected, so that they can shape and enrich subsequent data collection ( e.g. , modify the interview questions). Second, data analysis is often conducted by a research team that should have the appropriate expertise and perspectives to bring to the analysis process. Therefore, when evaluating a qualitative study, you should consider the team’s composition and their reflexivity with respect to their potential biases and influences on their study subjects. Third, the overall goal is to move from the raw data to abstractions of the data that answer the research question. For example, in grounded theory, the research moves from the raw data, to the identification of themes, to categorization of themes, to identifying relationships between themes, and ultimately to the development of theoretical explanations of the phenomenon. 30 Consequently, the primary researcher or research team should be intimately involved with the data analysis, interrogating the data, writing analytic memos, and ultimately make meaning out of the data. There are differing opinions about the use of “counting” of codes or themes in qualitative research. In general, counting of themes is used during the analysis process to recognize patterns and themes; often these are not reported as numbers and percentages as in quantitative research, but may be represented by words like few , some , or many . 37
Recognize techniques to enhance trustworthiness of your study findings. Ensuring consistency between the data and the results of data analysis, along with ensuring that the data and results accurately represent the perspectives and contexts related to the data source, are crucial to ensuring trustworthiness of study findings. Methods for enhancing trustworthiness include triangulation , which is comparing findings from different methods or perspectives, and member-checking , which is presenting research findings to study participants to provide opportunities to ensure that the analysis is representative. 10
Synthesize and interpret your data. Synthesis of qualitative research is determined by the depth of the analysis and involves moving beyond description of the data to explaining the findings and situating the results within the larger body of literature on the phenomenon of interest. The reporting of data synthesis should match the research methodology. For instance, if the study is using grounded theory, does the study advance the theoretical understanding of the phenomenon being studied? It is also important to acknowledge that clarity and organization are paramount. 10 Qualitative data are rich and extensive; therefore, researchers must organize and tell a compelling story from the data. 38 This process includes the selection of representative data ( e.g. , quotations from interviews) to substantiate claims made by the research team.
Common Methodologies Used in Qualitative Research

For more information on qualitative research in medical education:
Qualitative Research and Evaluation Methods: Integrating Theory and Practice, by Michael Q. Patton (SAGE Publications, Inc., 2014)
Qualitative Inquiry and Research Design: Choosing Among Five Approaches, by John W. Cresswell (SAGE Publications, Inc. 2017)
Researching Medical Education, by Jennifer Cleland and Steven J. Durning (Wiley-Blackwell, 2015)
Qualitative Research in Medical Education, by Patricia McNally, in Oxford Textbook of Medical Education, edited by Kieren Walsh (Oxford University Press, 2013)
The Journal of Graduate Medical Education “Qualitative Rip Out Series” (Available at: http://www.jgme.org/page/ripouts )
The Standards for Reporting Qualitative Research (O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245-51.)
The Wilson Centre Qualitative Atelier (For more information: http://thewilsoncentre.ca/atelier/ )
Qualitative research is commonly used in medical education but may be unfamiliar to many clinician educators. In this article, we provided a definition of qualitative research, explored the similarities and differences between qualitative and quantitative research, and outlined a framework for conducting or appraising qualitative research in medical education. Even with advanced training, it can be difficult for clinician educators to understand and conduct qualitative research. Leaders in medical education research have proposed the following advice to clinician educators wanting to engage in qualitative medical education research: (1) clinician educators should find collaborators with knowledge of theories from other disciplines ( e.g. , sociology, cognitive psychology) and experience in qualitative research to utilize their complementary knowledge and experience to conduct research—in this way, clinician educators can identify important research questions; collaborators can inform research methodology and theoretical perspectives; and (2) clinician educators should engage with a diverse range disciplines to generate new questions and perspectives on research. 4
Support was provided solely from institutional and/or departmental sources.
The authors declare no competing interests.
Citing articles via
Most viewed, email alerts, related articles, social media, affiliations.
- ASA Practice Parameters
- Online First
- Author Resource Center
- About the Journal
- Editorial Board
- Rights & Permissions
- Online ISSN 1528-1175
- Print ISSN 0003-3022
- Anesthesiology
- ASA Monitor

- Terms & Conditions Privacy Policy
- Manage Cookie Preferences
- © Copyright 2024 American Society of Anesthesiologists
This Feature Is Available To Subscribers Only
Sign In or Create an Account

The Benefits of Research in Healthcare

- February 1, 2023
Table of Contents
The healthcare industry is always changing and evolving. With new technologies and treatments constantly being developed, it can be hard to keep up. That’s where research comes in.
Research plays a vital role in healthcare, providing the evidence that we need to decide which treatments are effective and how best to use limited resources. It can also help us understand the causes of diseases and identify potential new therapies or preventative measures. In this article, we will show you ten benefits of research in healthcare.
What Is Research in Healthcare?
Research in healthcare is an investigation of human health issues in order to gain more knowledge and understanding. It is usually funded by the government, private organizations, and pharmaceutical companies.
It aims to gain new information that may benefit patients, the community, and other researchers. Healthcare research can take different forms, such as clinical trials, which involve examining and observing people with various conditions, research on blood samples or other tissues, or tests such as scans or X-rays.
Public health research addresses larger health issues that affect society as a whole, such as the impact of giving up smoking, and social care research looks at improving the lives of people who receive care and support from social care services. Health research helps us learn why we become ill and what we can do to stay well. It is an integral part of any healthcare environment and is essential for scientific and academic innovation.
? Learn more: Why is Research Important in Healthcare?
Let’s look at some of the benefits of research in healthcare.
1. Increased knowledge and understanding of diseases and treatments
Research increases knowledge and understanding of diseases and treatments by providing doctors and scientists with a better understanding of the causes and symptoms. This allows them to identify more effective diagnosis, detection, treatment, and prevention methods.
Research leads to the development of more effective medicines and treatments and improved medical procedures, such as MRIs, CT scans, and X-rays. It also provides valuable insights into how certain cohorts of people react to treatments and medications, which can lead to more targeted and effective treatments.
2. Better care and treatment for patients
Healthcare research can improve care and treatment for patients in several ways.
Firstly, research-active hospitals are often better set up to provide more comprehensive treatment options and opportunities to be included in clinical trials, leading to better health outcomes.
Secondly, participating in research can give patients a more in-depth understanding of their condition and more time with clinical team members to identify any potential problems earlier.
Furthermore, research can allow clinicians to develop their skills and knowledge in their field while also creating a culture of learning and development. Research funded by health charities, pharmaceutical companies , and universities can provide financial support for healthcare institutions, which can help improve patient care quality.
3. Advances in medical technology
Research in healthcare has advanced medical technology in many ways. Through the development of new drugs, treatments, and cures, health research has enabled us to live longer and healthier lives. Medical research studies provide new knowledge that leads to the development of new drugs, vaccines, medical devices, and surgeries, which help to improve current treatment methods.
4. Increased safety and efficacy of drugs and treatments
Research in healthcare has increased the safety and effectiveness of drugs and medicines by providing important information about disease trends and risk factors, treatment outcomes or public health interventions, functional abilities, patterns of care, and healthcare costs and use.
Through clinical trials, researchers can control the variables that could impact the study results and provide important information about medical interventions’ efficacy and adverse effects. After approval, tracking clinical experience with the drugs is important for identifying relatively rare adverse effects and determining effectiveness in different populations or in various circumstances.
Lastly, and according to F. Barigozzi, I. Jelovac, public integration of basic research can result in lowest prices and highest efficiency .
5. Improved quality of care
Research can improve the quality of care in healthcare by providing relevant, high-quality, and safe real-world data. Quality of care can be enhanced by utilizing research to develop and implement evidence-based solutions tailored to individual patients’ needs, which can also be related to the use of AI and the digitalization of the industry.
6. Greater awareness of public health issues
Healthcare research can help increase general health awareness by providing valuable data and evidence on the efficacy of different treatment options and interventions. For example, studies such as those conducted by the Centers for Disease Control and Prevention (CDC) have provided valuable information on the safety of various drugs, treatments, and procedures, as well as the associated risks.
Research can also help to identify areas of public health that need to be addressed, such as disparities in access to care and unequal outcomes for minority populations, allowing healthcare providers to better target resources and interventions that can improve public health.
7. Greater understanding of patient perspectives
Research helps to better understand patient perspectives by providing firsthand documentation of their experiences, offering an overview of suggestions for improvement, detecting common concerns and desires associated with the quality of care, and identifying obstacles to growth and change.
Qualitative research can provide a detailed and personal account of individual experiences, allowing for a comprehensive description of the research method and participant demographics. Ethicists have long suggested greater community involvement in health research studies, including more communication about research results, to build public trust in the research community and ensure the protection process is open and accessible to all interested parties.
? Learn more : Professional ethics: An overview from health research ethics point of view by Aceme Nyika
8. Creation of new knowledge through research partnerships
Research partnerships, such as those between universities, medical schools, and funding bodies, have the potential to create new knowledge in healthcare by allowing for innovative ideas, evidence-based care, and practice to be tested and developed.
Through such collaborations, researchers can explore the causes of diseases, evaluate the effectiveness of prevention techniques, diagnose medical conditions, and create new treatments and screening programs. By harnessing the power of new genomic research and the vast amount of health-related data and stored tissue specimens, research partnerships can lead to groundbreaking discoveries that can improve the quality of life and develop safer, more effective medical care tailored to individual needs.
9. Increased funding for research
Research into causes of disease, methods of prevention, techniques for diagnosis, and new treatment approaches has led to an increase in life expectancy, reduction of infant mortality, and improved outcomes for patients with chronic diseases. This has increased funding for healthcare as more resources are put towards researching and developing new treatments and methods of care.
10. Improvements in scientific rigor and quality of research
Healthcare research can potentially improve the scientific rigor and quality of research significantly. Through increased participation in research and data sharing, health research can generate new knowledge and accelerate the pace of discovery, ultimately improving the scientific rigor and quality of research in healthcare.
Healthcare Research Benefits
Research is critical to the advancement of healthcare. By understanding the benefits of research, we can see why it is so important to invest in research initiatives and understand the industry’s digitalization . By doing so, we can improve the quality of care for all patients, advance medical technology, and create new knowledge that can be used to improve healthcare systems around the world.
Health Analytics bridges the gap between sound scientific data and market access. Phone: (410) 997-3314 Email: [email protected]
- Health Care
- Evidence Generation Planning
- Evidence Generation
- Translating to Market Access
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >

10 The role of qualitative research in arts and health
- Published: November 2015
- Cite Icon Cite
- Permissions Icon Permissions
Qualitative research designs are appropriate for researching many arts and health contexts. However, there is a wide choice of methodologies available, each with different strengths and weaknesses. In this chapter the authors draw on their extensive experience of research and evaluation to address challenges and highlight issues of best practice. An overview of common methods is provided, with discussion of key issues including sampling, data collection, and analysis and interpretation of qualitative data. This is followed by more detailed discussion of examples from health research. Approaches such as discourse analysis, narrative research, participatory, and arts-based methods are examined. The topic of ethics in qualitative research is also addressed.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Driving Innovations in Biostatistics with Denise Scholtens, PhD
“I'm continually surprised by new data types. I think that we will see the emergence of a whole new kind of technology that we probably can't even envision five years from now…When I think about where the field has come over the past 20 years, it's just phenomenal.” — Denise Scholtens, PhD
- Director, Northwestern University Data Analysis and Coordinating Center (NUDACC)
- Chief of Biostatistics in the Department of Preventive Medicine
- Professor of Preventive Medicine in the Division of Biostatistics and of Neurological Surgery
- Member of Northwestern University Clinical and Translational Sciences Institute (NUCATS)
- Member of the Robert H. Lurie Comprehensive Cancer Center
Episode Notes
Since arriving at Feinberg in 2004, Scholtens has played a central role in the dramatic expansion of biostatistics at the medical school. Now the Director of NUDACC, Scholtens brings her expertise and leadership to large-scale, multicenter studies that can lead to clinical and public health practice decision-making.
- After discovering her love of statistics as a high school math teacher, Scholtens studied bioinformatics in a PhD program before arriving at Feinberg in 2004.
- Feinberg’s commitment to biostatistics has grown substantially in recent decades. Scholtens was only one of five biostatisticians when she arrived. Now she is part of a division with almost 50 people.
- She says being a good biostatistician requires curiosity about other people’s work, knowing what questions to ask and tenacity to understand subtitles of so much data.
- At NUDACC, Scholtens and her colleagues specialize in large-scale, multicenter prospective studies and clinical trials that lead to clinical or public health practice decision-making. They operate at the executive level and oversee all aspects of the study design.
- Currently, Scholtens is involved with the launch of a large study, along with The Ohio State University, that received a $14 million grant to look at the effectiveness of aspirin in the prevention of hypertensive disorders in pregnancy.
- Scholtens first started her work in data coordinating through the Hyperglycemia Adverse Pregnancy Outcome (HAPO) study, which looked at 25,000 pregnant individuals. This led to a continued interest in fetal and maternal health.
- When it comes to supportive working environments, Scholtens celebrates the culture at Feinberg, and especially her division in biostatistics, for being collaborative as well as genuinely supportive of each other’s projects. She attributes this to strong leadership which established a culture with these guiding principles.
Additional Reading
- Read more about the ASPIRIN trial and other projects taking place at NUDACC
- Discover a study linking mothers’ obesity-related genes to babies’ birth weight, which Scholtens worked in through the HAPO study
- Browse all of Scholtens recent publications
Recorded on February 21, 2024.
Continuing Medical Education Credit
Physicians who listen to this podcast may claim continuing medical education credit after listening to an episode of this program..
Target Audience
Academic/Research, Multiple specialties
Learning Objectives
At the conclusion of this activity, participants will be able to:
- Identify the research interests and initiatives of Feinberg faculty.
- Discuss new updates in clinical and translational research.
Accreditation Statement
The Northwestern University Feinberg School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
Credit Designation Statement
The Northwestern University Feinberg School of Medicine designates this Enduring Material for a maximum of 0.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
American Board of Surgery Continuous Certification Program
Successful completion of this CME activity enables the learner to earn credit toward the CME requirement(s) of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
All the relevant financial relationships for these individuals have been mitigated.
Disclosure Statement
Denise Scholtens, PhD, has nothing to disclose. Course director, Robert Rosa, MD, has nothing to disclose. Planning committee member, Erin Spain, has nothing to disclose. FSM’s CME Leadership, Review Committee, and Staff have no relevant financial relationships with ineligible companies to disclose.
Read the Full Transcript
[00:00:00] Erin Spain, MS: This is Breakthroughs, a podcast from Northwestern University Feinberg School of Medicine. I'm Erin Spain, host of the show. Northwestern University Feinberg School of Medicine is home to a team of premier faculty and staff biostatisticians, who are the driving force of data analytic innovation and excellence here. Today, we are talking with Dr. Denise Scholtens, a leader in biostatistics at Northwestern, about the growing importance of the field, and how she leverages her skills to collaborate on several projects in Maternal and Fetal Health. She is the Director of the Northwestern University Data Analysis and Coordinating Center, NUDACC, and Chief of Biostatistics in the Department of Preventive Medicine, as well as Professor of Preventive Medicine and Neurological Surgery. Welcome to the show.
[00:01:02] Denise Scholtens, PhD: Thank you so much.
[00:01:02] Erin Spain, MS: So you have said in the past that you were drawn to this field of biostatistics because you're interested in both math and medicine, but not interested in becoming a clinician. Tell me about your path into the field and to Northwestern.
[00:01:17] Denise Scholtens, PhD: You're right. I have always been interested in both math and medicine. I knew I did not want to be involved in clinical care. Originally, fresh out of college, I was a math major and I taught high school math for a couple of years. I really enjoyed that, loved the kids, loved the teaching parts of things. Interestingly enough, my department chair at the time assigned me to teach probability and statistics to high school seniors. I had never taken a statistics course before, so I was about a week ahead of them in our classes and found that I just really enjoyed the discipline. So as much as I loved teaching, I did decide to go ahead and invest in this particular new area that I had found and I really enjoyed. So I wanted to figure out how I could engage in the field of statistics. Decided to see, you know, exactly how studying statistics could be applied to medicine. At the time, Google was brand new. So I literally typed in the two words math and medicine to see what would come up. And the discipline of biostatistics is what Google generated. And so here I am, I applied to grad school and it's been a great fit for me.
[00:02:23] Erin Spain, MS: Oh, that's fantastic. So you went on to get a PhD, and then you came to Northwestern in 2004. And so tell me a little bit about the field then and how it's changed so dramatically since.
[00:02:36] Denise Scholtens, PhD: So yes, I started here at Northwestern in 2004, just a few months after I had defended my thesis. At the time there was really an emerging field of study called bioinformatics. So I wrote my thesis in the space of genomics data analysis with what at the time was a brand new technology, microarrays. This was the first way we could measure gene transcription at a high throughput level. So I did my thesis work in that space. I studied at an institution with a lot of strengths and very classical statistics. So things that we think of in biostatistics like clinical trial design, observational study analysis, things like that. So I had really classic biostatistics training and then complimented that with sort of these emerging methods with these high dimensional data types. So I came to Northwestern here and I sort of felt like I lived in two worlds. I had sort of classic biostat clinical trials, which were certainly, you know, happening here. And, that work was thriving here at Northwestern, but I had this kind of new skillset, and I just didn't quite know how to bring the two together. That was obviously a long time ago, 20 years ago. Now we think of personalized medicine and genomic indicators for treatment and, you know, there's a whole variety of omics data variations on the theme that are closely integrated with clinical and population level health research. So there's no longer any confusion for me about how those two things come together. You know, they're two disciplines that very nicely complement each other. But yeah, I think that does speak to how the field has changed, you know, these sort of classic biostatistics methods are really nicely blended with a lot of high dimensional data types. And it's been fun to be a part of that.
[00:04:17] Erin Spain, MS: There were only a handful of folks like you at Northwestern at the time. Tell me about now and the demand for folks with your skill set.
[00:04:26] Denise Scholtens, PhD: When I came to Northwestern, I was one of a very small handful of biostatistics faculty. There were five of us. We were not even called a division of biostatistics. We were just here as the Department of Preventive Medicine. And a lot of the work we did was really very tightly integrated with the epidemiologists here in our department and we still do a lot of that for sure. There was also some work going on with the Cancer Center here at Northwestern. But yeah, a pretty small group of us, who has sort of a selected set of collaborations. You know, I contrast that now to our current division of biostatistics where we are over 20s, pushing 25, depending on exactly how you want to count. Hoping to bring a couple of new faculty on board this calendar year. We have a staff of about 25 statistical analysts. And database managers and programmers. So you know, when I came there were five faculty members and I think two master's level staff. We are now pushing, you know, pushing 50 people in our division here so it's a really thriving group.
[00:05:26] Erin Spain, MS: in your opinion, what makes a good biostatistician? Do you have to have a little bit of a tough skin to be in this field?
Denise Scholtens, PhD: I do think it's a unique person who wants to be a biostatistician. There are a variety of traits that can lead to success in this space. First of all, I think it's helpful to be wildly curious about somebody else's work. To be an excellent collaborative biostatistician, you have to be able to learn the language of another discipline. So some other clinical specialty or public health application. Another trait that makes a biostatistician successful is to be able to ask the right questions about data that will be collected or already have been collected. So understanding the subtleties there, the study design components that lead to why we have the data that we have. You know, a lot of our data, you could think of it in a simple flat file, right? Like a Microsoft Excel file with rows and columns. That certainly happens a lot, but there are a lot of incredibly innovative data types out there: wearables technology, imaging data, all kinds of high dimensional data. So I think a tenacity to understand all of the subtleties of those data and to be able to ask the right questions. And then I think for a biostatistician at a medical school like ours, being able to blend those two things, so understanding what the data are and what you have to work with and what you're heading toward, but then also facilitating the translation of those analytic findings for the audience that really wants to understand them. So for the clinicians, for the patients, for participants and the population that the findings would apply to.
Erin Spain, MS: It must feel good, though, in those situations where you are able to help uncover something to improve a study or a trial.
[00:07:07] Denise Scholtens, PhD: It really does. This is a job that's easy to get out of bed for in the morning. There's a lot of really good things that happen here. It's exciting to know that the work we do could impact clinical practice, could impact public health practice. I think in any job, you know, you can sometimes get bogged down by the amount of work or the difficulty of the work or the back and forth with team members. There's just sort of all of the day to day grind, but to be able to take a step back and remember the actual people who are affected by our own little niche in this world. It's an incredibly helpful and motivating practice that I often keep to remember exactly why I'm doing what I'm doing and who I'm doing it for.
[00:07:50] Erin Spain, MS: Well, and another important part of your work is that you are a leader. You are leading the center, NUDACC, that you mentioned, Northwestern University Data Analysis and Coordinating Center. Now, this has been open for about five years. Tell me about the center and why it's so crucial to the future of the field.
[00:08:08] Denise Scholtens, PhD: We specialize at NUDACC in large scale, multicenter prospective studies. So these are the clinical trials or the observational studies that often, most conclusively, lead to clinical or public health practice decision making. We focus specifically on multicenter work. Because it requires a lot of central coordination and we've specifically built up our NUDACC capacity to handle these multi center investigations where we have a centralized database, we have centralized and streamlined data quality assurance pipelines. We can help with central team leadership and organization for large scale networks. So we have specifically focused on those areas. There's a whole lot of project management and regulatory expertise that we have to complement our data analytics strengths as well. I think my favorite part of participating in these studies is we get involved at the very beginning. We are involved in executive level planning of these studies. We oversee all components of study design. We are intimately involved in the development of the data capture systems. And in the QA of it. We do all of this work on the front end so that we get all of the fun at the end with the statistics and can analyze data that we know are scientifically sound, are well collected, and can lead to, you know, really helpful scientific conclusions.
[00:09:33] Erin Spain, MS: Tell me about that synergy between the clinicians and the other investigators that you're working with on these projects.
[00:09:41] Denise Scholtens, PhD: It is always exciting, often entertaining. Huge range of scientific opinion and expertise and points of view, all of which are very valid and very well informed. All of the discussion that could go into designing and launching a study, it's just phenomenally interesting and trying to navigate all of that and help bring teams to consensus in terms of what is scientifically most relevant, what's going to be most impactful, what is possible given the logistical strengths. Taking all of these well informed, valid, scientific points of view and being a part of the team that helps integrate them all toward a cohesive study design and a well executed study. That's a unique part of the challenge that we face here at NUDACC, but an incredibly rewarding one. It's also such an honor and a gift to be able to work with such a uniformly gifted set of individuals. Just the clinical researchers who devote themselves to these kinds of studies are incredibly generous, incredibly thoughtful and have such care for their patients and the individuals that they serve, that to be able to sit with them and think about the next steps for a great study is a really unique privilege.
[00:10:51] Erin Spain, MS: How unique is a center like this at a medical school?
[00:10:55] Denise Scholtens, PhD: It's fairly unique to have a center like this at a medical school. Most of the premier medical research institutions do have some level of data coordinating center capacity. We're certainly working toward trying to be one of the nation's best, absolutely, and build up our capacity for doing so. I'm actually currently a part of a group of data coordinating centers where it's sort of a grassroots effort right now to organize ourselves and come up with, you know, some unified statements around the gaps that we see in our work, the challenges that we face strategizing together to improve our own work and to potentially contribute to each other's work. I think maybe the early beginnings of a new professional organization for data coordinating centers. We have a meeting coming up of about, I think it's 12 to 15 different institutions, academic research institutions, specifically medical schools that have centers like ours to try to talk through our common pain points and also celebrate our common victories.
[00:11:51] Erin Spain, MS: I want to shift gears a little bit to talk about some of your research collaborations, many of which focus on maternal and fetal health and pregnancy. You're now involved with a study with folks at the Ohio State University that received a 14 million grant looking at the effectiveness of aspirin in the prevention of hypertensive disorders in pregnancy. Tell me about this work.
[00:12:14] Denise Scholtens, PhD: Yes, this is called the aspirin study. I suppose not a very creative name, but a very appropriate one. What we'll be doing in this study is looking at two different doses of aspirin for trying to prevent maternal hypertensive disorders of pregnancy in women who are considered at high risk for these disorders. This is a huge study. Our goal is to enroll 10,742 participants. This will take place at 11 different centers across the nation. And yes, we at NUDACC will serve as the data coordinating center here, and we are partnering with the Ohio State University who will house the clinical coordinating center. So this study is designed to look at two different doses to see which is more effective at preventing hypertensive disorders of pregnancy. So that would include gestational hypertension and preeclampsia. What's really unique about this study and the reason that it is so large is that it is specifically funded to look at what's called a heterogeneity of treatment effect. What that is is a difference in the effectiveness of aspirin in preventing maternal hypertensive disorders, according to different subgroups of women. We'll specifically have sufficient statistical power to test for differences in treatment effectiveness. And we have some high priority subgroups that we'll be looking at. One is a self-identified race. There's been a noted disparity in maternal hypertensive disorders, for individuals who self identify according to different races. And so we will be powered to see if aspirin has comparable effectiveness and hopefully even better effectiveness for the groups who really need it, to bring those rates closer to equity which is, you know, certainly something we would very strongly desire to see. We'll also be able to look at subgroups of women according to obesity, according to maternal age at pregnancy, according to the start time of aspirin when aspirin use is initiated during pregnancy. So that's why the trial is so huge. For a statistician, the statisticians out there who might be listening, this is powered on a statistical interaction term, which doesn't happen very often. So it's exciting that the trial is funded in that way.
[00:14:27] Erin Spain, MS: Tell me a little bit more about this and how your specific skills are going to be utilized in this study.
[00:14:32] Denise Scholtens, PhD: Well, there are three biostatistics faculty here at Northwestern involved in this. So we're definitely dividing and conquering. Right now, we're planning this study and starting to stand it up. So we're developing our statistical analysis plans. We're developing the database. We are developing our randomization modules. So this is the piece of the study where participants are randomized to which dose of aspirin they're going to receive. Because of all of the subgroups that we're planning to study, we need to make especially sure that the assignments of which dose of aspirin are balanced within and across all of those subgroups. So we're going to be using some adaptive randomization techniques to ensure that that balance is there. So there's some fun statistical and computer programming innovation that will be applied to accomplish those things. So right now, there are usually two phases of a study that are really busy for us. That's starting to study up and that's where we are. And so yes, it is very busy for us right now. And then at the end, you know, in five years or so, once recruitment is over, then we analyze all the data,
[00:15:36] Erin Spain, MS: Are there any guidelines out there right now about the use of aspirin in pregnancy. What do you hope that this could accomplish?
Prescribing aspirin use for the prevention of hypertension during pregnancy is not uncommon at all. That is actually fairly routinely done, but that it's not outcomes based in terms of which dosage is most effective. So 81 milligrams versus 162 milligrams. That's what we will be evaluating. And my understanding is that clinicians prescribe whatever they think is better, and I'm sure those opinions are very well informed but there is very little outcome based evidence for this in this particular population that we'll be studying. So that would be the goal here, would be to hopefully very conclusively say, depending on the rates of the hypertensive disorders that we see in our study, which of the two doses of aspirin is more effective. Importantly, we will also be tracking any side effects of taking aspirin. And so that's also very much often a part of the evaluation of You know, taking a, taking a drug, right, is how safe is it? So we'll be tracking that very closely as well. Another unique part of this study is that we will be looking at factors that help explain aspirin adherence. So we are going to recommend that participants take their dose of aspirin daily. We don't necessarily expect that's always going to happen, so we are going to measure how much of their prescribed dose they are actually taking and then look at, you know, factors that contribute to that. So be they, you know, social determinants of health or a variety of other things that we'll investigate to try to understand aspirin adherence, and then also model the way in which that adherence could have affected outcomes.
Erin Spain, MS: This is not the first study that you've worked on involving maternal and fetal health. Tell me about your interest in this particular area, this particular field, and some of the other work that you've done.
[00:17:31] Denise Scholtens, PhD: So I actually first got my start in data coordinating work through the HAPO study. HAPO stands for Hyperglycemia Adverse Pregnancy Outcome. That study was started here at Northwestern before I arrived. Actually recruitment to the study occurred between 2000 and 2006. Northwestern served as the central coordinating center for that study. It was an international study of 25,000 pregnant individuals who were recruited and then outcomes were evaluated both in moms and newborns. When I was about mid career here, all the babies that were born as a part of HAPO were early teenagers. And so we conducted a follow up study on the HAPO cohort. So that's really when I got involved. It was my first introduction to being a part of a coordinating center. As I got into it, though, I saw the beauty of digging into all of these details for a huge study like this and then saw these incredible resources that were accumulated through the conduct of such a large study. So the data from the study itself is, was of course, a huge resource. But then also we have all of these different samples that sit in a biorepository, right? So like usually blood sample collection is a big part of a study like this. So all these really fun ancillary studies could spin off of the HAPO study. So we did some genomics work. We did some metabolomics work. We've integrated the two and what's called integrated omics. So, you know, my work in this space really started in the HAPO study. And I have tremendously enjoyed integrating these high dimensional data types that have come from these really rich data resources that have all, you know, resulted because of this huge multicenter longitudinal study. So I kind of accidentally fell into the space of maternal and fetal health, to be honest. But I just became phenomenally interested in it and it's been a great place.
[00:19:24] Erin Spain, MS: Would you say that this is also a population that hasn't always been studied very much in biomedical science?
[00:19:32] Denise Scholtens, PhD: I think that that is true, for sure. There are some unique vulnerabilities, right, for a pregnant individual and for the fetus, right, and in that situation. You know, the vast majority of what we do is really only pertaining to the pregnant participant but, you know, there are certainly fetal outcomes, newborn outcomes. And so, I think conducting research in this particular population is a unique opportunity and there are components of it that need to be treated with special care given sort of this unique phase of human development and this unique phase of life.
[00:20:03] Erin Spain, MS: So, as data generation just really continues to explode, and technology is advancing so fast, faster than ever, where do you see this field evolving, the field of biostatistics, where do you see it going in the next five to ten years?
[00:20:19] Denise Scholtens, PhD: That's a great question. I think all I can really tell you is that I'm continually surprised by new data types. I think that we will see an emergence of a whole new kind of technology that we probably can't even envision five years from now. And I think that the fun part about being a biostatistician is seeing what's happening and then trying to wrap your mind around the possibilities and the actual nature of the data that are collected. You know, I think back to 2004 and this whole high throughput space just felt so big. You know, we could look at gene transcription across the genome using one technology. And we could only look at one dimension of it. Right now it just seems so basic. When I think about where the field has come over the past 20 years, it's just phenomenal. I think we're seeing a similar emergence of the scale and the type of data in the imaging space and in the wearable space, with EHR data, just. You know, all these different technologies for capturing, capturing things that we just never even conceived of before. I do hope that we continue to emphasize making meaningful and translatable conclusions from these data. So actionable conclusions that can impact the way that we care for others around us. I do hope that remains a guiding principle in all that we do.
[00:21:39] Erin Spain, MS: Why is Northwestern Medicine and Northwestern Feinberg School of Medicine such a supportive environment to pursue this type of work?
[00:21:47] Denise Scholtens, PhD: That's a wonderful question and one, honestly, that faculty candidates often ask me. When we bring faculty candidates in to visit here at Northwestern, they immediately pick up on the fact that we are a collaborative group of individuals who are for each other. Who want to see each other succeed, who are happy to share the things that we know and support each other's work, and support each other's research, and help strategize around the things that we want to accomplish. There is a strong culture here, at least in my department and in my division that I've really loved that continues to persist around really genuinely collaborating and genuinely sharing lessons learned and genuinely supporting each other as we move toward common goals. We've had some really strong, generous leadership who has helped us to get there and has helped create a culture where those are the guiding principles. In my leadership role is certainly something that I strive to maintain. Really hope that's true. I'm sure I don't do it perfectly but that's absolutely something I want to see accomplished here in the division and in NUDACC for sure.
[00:22:50] Erin Spain, MS: Well, thank you so much for coming on the show and telling us about your path here to Northwestern and all of the exciting work that we can look forward to in the coming years.
[00:22:59] Denise Scholtens, PhD: Thank you so much for having me. I've really enjoyed this.
[00:23:01] Erin Spain, MS: You can listen to shows from the Northwestern Medicine Podcast Network to hear more about the latest developments in medical research, health care, and medical education. Leaders from across specialties speak to topics ranging from basic science to global health to simulation education. Learn more at feinberg. northwestern.edu/podcasts.
This paper is in the following e-collection/theme issue:
Published on 26.4.2024 in Vol 26 (2024)
Understanding Symptom Self-Monitoring Needs Among Postpartum Black Patients: Qualitative Interview Study
Authors of this article:

Original Paper
- Natalie Benda 1 , PhD ;
- Sydney Woode 2 , BSc ;
- Stephanie Niño de Rivera 1 , BS ;
- Robin B Kalish 3 , MD ;
- Laura E Riley 3 , MD ;
- Alison Hermann 4 , MD ;
- Ruth Masterson Creber 1 , MSc, PhD, RN ;
- Eric Costa Pimentel 5 , MS ;
- Jessica S Ancker 6 , MPH, PhD
1 School of Nursing, Columbia University, New York, NY, United States
2 Department of Radiology, Early Lung and Cardiac Action Program, The Mount Sinai Health System, New York, NY, United States
3 Department of Obstetrics and Gynecology, Weill Cornell Medicine, New York, NY, United States
4 Department of Psychiatry, Weill Cornell Medicine, New York, NY, United States
5 Department of Population Health Sciences, Weill Cornell Medicine, New York, NY, United States
6 Department of Biomedical Informatics, Vanderbilt University Medical Center, Nashville, TN, United States
Corresponding Author:
Natalie Benda, PhD
School of Nursing
Columbia University
560 West 168th Street
New York, NY, 10032
United States
Phone: 1 212 305 9547
Email: [email protected]
Background: Pregnancy-related death is on the rise in the United States, and there are significant disparities in outcomes for Black patients. Most solutions that address pregnancy-related death are hospital based, which rely on patients recognizing symptoms and seeking care from a health system, an area where many Black patients have reported experiencing bias. There is a need for patient-centered solutions that support and encourage postpartum people to seek care for severe symptoms.
Objective: We aimed to determine the design needs for a mobile health (mHealth) patient-reported outcomes and decision-support system to assist Black patients in assessing when to seek medical care for severe postpartum symptoms. These findings may also support different perinatal populations and minoritized groups in other clinical settings.
Methods: We conducted semistructured interviews with 36 participants—15 (42%) obstetric health professionals, 10 (28%) mental health professionals, and 11 (31%) postpartum Black patients. The interview questions included the following: current practices for symptom monitoring, barriers to and facilitators of effective monitoring, and design requirements for an mHealth system that supports monitoring for severe symptoms. Interviews were audio recorded and transcribed. We analyzed transcripts using directed content analysis and the constant comparative process. We adopted a thematic analysis approach, eliciting themes deductively using conceptual frameworks from health behavior and human information processing, while also allowing new themes to inductively arise from the data. Our team involved multiple coders to promote reliability through a consensus process.
Results: Our findings revealed considerations related to relevant symptom inputs for postpartum support, the drivers that may affect symptom processing, and the design needs for symptom self-monitoring and patient decision-support interventions. First, participants viewed both somatic and psychological symptom inputs as important to capture. Second, self-perception; previous experience; sociocultural, financial, environmental, and health systems–level factors were all perceived to impact how patients processed, made decisions about, and acted upon their symptoms. Third, participants provided recommendations for system design that involved allowing for user control and freedom. They also stressed the importance of careful wording of decision-support messages, such that messages that recommend them to seek care convey urgency but do not provoke anxiety. Alternatively, messages that recommend they may not need care should make the patient feel heard and reassured.
Conclusions: Future solutions for postpartum symptom monitoring should include both somatic and psychological symptoms, which may require combining existing measures to elicit symptoms in a nuanced manner. Solutions should allow for varied, safe interactions to suit individual needs. While mHealth or other apps may not be able to address all the social or financial needs of a person, they may at least provide information, so that patients can easily access other supportive resources.
Introduction
This study focused on designing a culturally congruent mobile health (mHealth) app to support postpartum symptom monitoring, as the current practice does not adequately support patients in identifying the warning signs of pregnancy-related death (PRD). First, we describe the public health case for symptom monitoring and decision support for PRD, specifically among US-based, Black patients, a group that faces severe disparities [ 1 , 2 ]. Next, we discuss why the current mechanisms for symptom monitoring and decision support are insufficient. We then outline the existing solutions while also emphasizing the need for new interventions, particularly why those using a combination of mHealth and patient-reported outcomes (PROs) may be appropriate. Finally, we introduce a conceptual model used to accomplish our study objectives.
PRD and Associated Health Disparities
The pregnancy-related mortality ratio has increased by >200% in the United States in the past 2 decades, and in a recent review of PRDs, experts estimated that 80% of the deaths were preventable [ 3 ]. The Centers for Disease Control and Prevention (CDC) defines PRD as “the death of a woman while pregnant or within 1 year of the end of pregnancy from any cause related to or aggravated by the pregnancy” [ 4 , 5 ]. Mental health conditions (22.7%), hemorrhage (13.7%), cardiac and coronary conditions (12.8%), infection (9.2%), thrombotic embolism (8.7%), and cardiomyopathy (8.5%) have been cited as the most common causes for PRD [ 3 ]. Although the global maternal mortality rate has declined, the global rates are still high with 287,000 people dying following childbirth in 2020. There are significant disparities in maternal mortality based on a country’s income, with almost 95% of the cases occurring in low- and middle-income countries [ 6 ]. Stark disparities in pregnancy-related outcomes in the United States, such as PRD, exist based on race. Specifically, Black or African American (henceforth, referred to as “Black”) perinatal patients experience PRD 3 times more than White perinatal patients [ 1 , 2 , 7 - 10 ].
The disparities in maternal health outcomes experienced by Black patients in the United States are based on inequitable access to care, biased treatment, and inadequate communication, driven by systemic racism and all the cascading effects it creates. Black perinatal patients are significantly more likely to be uninsured and significantly less likely to have a usual source of medical care (eg, a primary care clinician) than White patients [ 7 , 10 ]. When Black patients seek care, they face implicit biases that negatively affect care quality and health outcomes [ 1 , 7 , 10 - 12 ]. Unsurprisingly, these biases have led to reduced trust in the health care system among Black patients [ 13 - 17 ]. Black patients also receive less patient-centered communication and feel that they have poorer access to communication with their medical team [ 10 , 18 , 19 ]. Our study aimed to improve the patient centeredness of information and support for Black patients in the postpartum period through a participatory design, an approach by which representative end users are involved throughout the design process [ 20 - 23 ]. While this study focused on Black postpartum patients in the United States, we believe that our findings may provide insights for improving perinatal support for patients from minority groups globally.
Challenges to Supporting Symptom Recognition and Treatment Seeking Post Partum
Patients encounter several challenges recognizing concerning postpartum symptoms. First, the initial postpartum visit occurs 6 weeks after birth, and 86% of PRD cases occur within the first 6 weeks post partum [ 24 , 25 ]. Second, most strategies for improving postpartum outcomes focus on hospital-based solutions, which rely on people recognizing symptoms and contacting a health professional [ 7 ]. Most counseling regarding the warning signs of PRD occurs during the discharge process following delivery, when people are physically exhausted from childbirth and primarily focused on infant care [ 24 ]. As such, this is a suboptimal time for patient education about postpartum risk factors. Discharge nurses report spending <10 minutes on the warning signs of postpartum issues, and most nurses could not correctly identify the leading causes of PRD, making it unlikely that their patients could recognize the warning signs [ 26 ]. There are many measures for postpartum symptom reporting, but the most common instruments focus narrowly on specific mental health issues, many of which are not specific to postpartum mental health or postpartum health–related quality of life [ 27 ]. While these are helpful measures to use in a clinic or hospital setting, they do not provide real-time decision support regarding the full spectrum of severe symptoms that may be indicative of PRD.
Suitability of Different Solutions for Supporting Symptom Monitoring
mHealth can address the need for tailored, dynamic symptom monitoring and support. The Association of Women’s Health, Obstetric, and Neonatal Nurses and the CDC have developed 1-page summaries to help patients identify the warning signs of PRD, such as the Urgent Maternal Warning Signs (UWS) [ 28 , 29 ]. These tools represent a positive step toward improving symptom management, but these solutions do not provide real-time, tailored support. Telephone-based support staffed by health professionals has been demonstrated to decrease postpartum depression and improve maternal self-efficacy [ 30 - 33 ]. However, 24-hour hotlines can be resource intensive, and people may still experience bias when accessing these services. The goal of this study was to conduct a qualitative needs assessment for the Maternal Outcome Monitoring and Support app, an mHealth system using PROs to provide decision support for postpartum symptom monitoring.
Mobile phones offer a viable, inclusive option for intervention delivery for Black people of childbearing age. In 2020, data from the Pew Research Center indicate that 83% of Black people owned smartphones, which is comparable to smartphone ownership among White people (85%). Smartphone ownership is also higher among people aged <50 years (96%), which encompasses most postpartum patients [ 34 ]. However, Black people are twice as likely as White people to be dependent on smartphones for internet access [ 35 ]. mHealth-based apps for blood pressure and weight tracking during pregnancy have demonstrated success among diverse groups, providing evidence that mHealth may be an acceptable means for symptom reporting in the target population [ 36 - 38 ].
Symptom education and PRO-based interventions have demonstrated success in improving knowledge, self-efficacy, and outcomes. Use of PROs has improved symptom knowledge, health awareness, communication with health care professionals, and prioritization of symptoms in patients with chronic disease and cancer [ 39 - 44 ]. Multiple studies have also demonstrated that educational interventions regarding expected symptoms in the postpartum period can improve self-efficacy, resourcefulness, breastfeeding practices, and mental health [ 12 , 38 , 45 - 47 ]. However, given the issues related to trust and disparities in patient-centered communication, it is critical to understand Black patients’ perspectives about how such a system should be designed and implemented.
Conceptual Model
To study the issue of supporting symptom monitoring, we combined 2 theoretical frameworks ( Figure 1 ): the common sense model of self-regulation (health behavior) by Diefenbach and Leventhal [ 48 ] and the model of human information processing (human factors engineering) by Wickens [ 49 ]. The model by Diefenbach and Leventhal [ 48 ] depicts patients as active problem solvers with a mental model of their conditions. Patients process their symptoms, both cognitively and emotionally, and then evaluate whether action is needed [ 48 ]. The patient’s mental model of their condition, personal experiences, and sociocultural factors impact processing, evaluation, and action. In the information processing model by Wickens [ 49 ], action occurs in 2 steps—selection and execution [ 48 ]. Environmental or organizational factors also affect patients’ selection of actions and whether they can execute an action. For example, a patient may suspect that they should visit the emergency room but may not go because they do not have insurance, transportation, or childcare. Our qualitative inquiry investigated how to better support symptom processing and appropriate response selection, while also uncovering the barriers to action that may need to be mitigated.

The goal of this study was to identify the design and implementation needs of an mHealth-based symptom self-monitoring and decision-support system to support Black patients in determining when to seek care from a health professional for signs of PRD in the postpartum period. This tool will support both somatic and psychological symptoms given their complex, critical, and connected presentation. We used the described conceptual model in qualitative inquiry and pragmatic intervention design to provide contributions regarding the following: (1) relevant symptom inputs for postpartum support, (2) drivers that may affect symptom processing, and (3) how the previous 2 aspects highlight the design needs for symptom self-monitoring and patient decision support. To address our study objective, we conducted semistructured interviews with postpartum Black patients, obstetrics health professionals, and mental health professionals.
The study was conducted in 3 tertiary care hospitals and affiliated clinics within the same health system in New York City. The 3 hospitals, taken together, are involved in the delivery of >14,000 babies annually. All participants were either patients who received obstetric care in the included sites or health professionals affiliated with the sites.
Eligible patients were identified by the institutions’ research informatics team using electronic health record data. First, the patients’ providers consented to their patients being contacted, and patients’ charts were reviewed by the primary obstetrician or designate to ensure that the patient was eligible for the study and that they had a delivery experience that would allow them to participate in the interview without undue stress. Next, the patients were sent an invitation to participate via the email address listed in their record. We also posted fliers in 2 high-risk, outpatient obstetric clinics.
Obstetric and mental health professionals were eligible if they were affiliated with one of the institutions in the obstetrics or mental health department. Brief presentations were given at relevant faculty meetings, and participants were contacted individually via email or through departmental listserves.
Interested participants from all groups used a link to schedule a time to speak with a researcher.
Ethical Considerations
The study was approved by the affiliated medical schools’ institutional review board (protocol number 20-08022582). All participants provided written informed consent. Study data were coded (ie, all identifying information was removed) to protect participant privacy. Each participant was compensated US $50 for their time via a physical or electronic gift card.
Study Design and Sample
The study used semistructured interviews with 3 key stakeholder groups: recent postpartum Black patients, obstetric health professionals, and mental health professionals. Eligible patients were within 12 months post partum of a live birth, self-identified their race as Black or African American, and had at least 1 somatic or psychological high-risk feature associated with their pregnancy. High-risk features included attendance at a high-risk clinic for prenatal or postnatal care, inpatient hospitalization within 12 months post partum, a prescription of an antidepressant or benzodiazepine within 12 months of the pregnancy, or a new diagnosis of depression or anxiety within 12 months of the pregnancy. High-risk clinics treated various conditions, but the most common conditions were gestational hypertension and gestational diabetes.
We adopted an interpretivist qualitative research paradigm to study patient and health professionals’ perspectives of how symptom recognition and care seeking may be better supported [ 50 ]. Our methodological orientation involved directed content analysis, adopting an abductive reasoning approach. First, we used the previously specified conceptual model to construct questions and thematically categorize responses [ 48 ]. Then, we allowed unique subthemes to inductively emerge from the data collected [ 51 ].
Interview Guide Development
Interview guides were iteratively developed by our team of researchers with expertise in obstetrics, perinatal mental health, nursing, consumer informatics, inclusive design, and qualitative methods. The guide for each stakeholder group was reviewed and piloted before enrollment of the first participant. Interview guides were tailored for patients or health professionals but followed a similar structure, based on our conceptual model ( Figure 1 ), such that participants were first asked about barriers to and facilitators of processing symptoms cognitively and emotionally (eg, Do they notice the symptom or realize its severity?), making decisions about symptoms they are experiencing (ie, When to seek help from a health professional?), and taking action on problematic symptoms. Probing questions encouraged participants to elaborate on experiential, educational, sociocultural, organizational, environmental, or health systems–level drivers of patients’ symptom management. Then, participants were asked a series of questions related to their thoughts regarding the design of the mHealth system, including how to best report symptoms, the wording of system decision support, the desired level of involvement of the obstetrics health professionals, the means for facilitating outreach to a health professional, additional information resources, and preferences for sharing information included in the system with a trusted friend or family members. During this process, obstetrics and mental health professionals were also shown a handout that outlined the draft of the symptom management algorithm for the system being developed (CDC’s UWS) and asked if they would make any changes, additions, or deletions [ 29 ]. Full interview guides are included in Multimedia Appendix 1 .
Data Collection
All interviewees provided consent electronically before the interview. A PhD-trained qualitative research expert (NB) completing a postdoctoral study in health informatics and population health conducted all the interviews via Zoom (Zoom Video Communications) or telephone. Participants had the option to request an in-person interview, but none of them chose this option. Interviews lasted 30 to 60 minutes and were audio recorded. We explicitly described the study objectives to each participant before the interview. Following the interview, participants completed a demographics survey electronically. All electronic survey information was collected using REDCap (Research Electronic Data Capture; Vanderbilt University).
Data Preparation and Analysis
Audio recordings were converted into transcripts using an electronic software (NVivo Transcription; QSR International) and manually checked for accuracy by a study team member who did not conduct the initial interviews. We completed all data analyses using NVivo (versions 12 and 13), but we manually analyzed the data and did not use computer-aided techniques (eg, computerized emotion detection or autocoding).
Data were analyzed using thematic analysis and the constant comparative process [ 51 - 53 ]. Specifically, each analyst open coded the transcripts, by coding segments that pertained to the research questions, as opposed to coding all words and phrases. We used thematic analysis to detect the common and divergent needs for postpartum symptom monitoring. We chose this method over other approaches such as grounded theory or sentiment analysis because our needs were pragmatic to solution design, and we were not attempting to establish theory, describe phenomena, or represent collective feeling about a topic.
The first deductive analysis was conducted using an initial theoretical model derived from the common sense model by Diefenbach and Leventhal [ 48 ] and the model of human information processing by Wickens [ 49 ] ( Figure 1 ). To promote reliability, 2 coders in addition to the interviewer were involved in the analysis, and each transcript was first analyzed independently by at least 2 people (NB, SW, or SNdR), followed by meetings to resolve discrepancies based on consensus coding. The analysis team created initial codes based on the conceptual model and added new items to the codebook inductively (ie, post hoc instead of a priori, as they arose in the data). The team used NVivo to maintain a working codebook of themes, definitions, and relevant quotes derived from the data. The codebook was periodically presented to coinvestigators with expertise in obstetrics and perinatal psychiatry to improve external validity [ 51 , 52 ]. The sufficiency of sample size was assessed according to the theoretical saturation of themes encountered, specifically based on the need to add additional subthemes to the codebook [ 54 , 55 ]. After all the transcripts had been coded, at least 2 members of the coding team reviewed the data code by code to ensure that meaning remained consistent throughout the analysis and to derive key emerging themes [ 51 ].

Participant Characteristics
This study included 36 participants—15 (42%) obstetrics health professionals, 10 (28%) mental health professionals, and 11 (31%) recent postpartum Black patients. Table 1 presents the self-reported demographic information. As shown, 19% (7/36) of the health professionals and 11% (4/36) of the patients had missing data (ie, did not complete the questionnaire). Participants could also selectively choose not to answer questions. “Other” affiliations were possible for health professionals because those who had a secondary affiliation with one of the included sites but primary affiliation with another organization were eligible.
a N/A: not applicable.
b Health professionals’ self-reported role of resident psychiatrist, chief resident in psychiatry, psychologist, and patient care director was combined into the other category for analysis purposes.
Structure of Themes
Our initial theoretical model, derived from the common sense model by Diefenbach and Leventhal [ 48 ] and the model of human information processing by Wickens [ 49 ] ( Figure 1 ), described that patients experience some inputs (psychological and somatic symptoms of PRD). Then, there is a series of drivers that affect how patients cognitively and emotionally process (eg, notice and realize symptom severity), make decisions about, and act on symptoms they are experiencing. The nature of these symptoms, how they are processed, how decisions are made, and how they are acted upon then drive a conversation regarding the design needs for symptom monitoring and decision support for PRD. The emerging themes were organized into the following categories: (1) symptoms of PRD; (2) drivers of processing, decision-making, and action; and (3) design needs for a symptom-reporting and decision-support system. Quotes are labeled with study-specific identifiers: OB denotes obstetric health professional, MHP denotes mental health professional, and PT denotes patient.
Inputs: Psychological and Somatic Symptoms of PRD
Concerning and routine symptoms were reported both from a psychological and somatic perspective. Sometimes, the distinction between routine and concerning symptoms was clear. Other times, it was more challenging to differentiate routine versus concerning symptoms particularly because they were related to psychological health. Mental health professionals also noted the challenge that routine symptoms can progress to something more serious over time:
In my mind, like normal becomes abnormal, when there is any kind of functioning [loss] that like withstands two to three weeks. [MHP 04]
We really hear a lot about postpartum depression and stuff...A lot of women think...postpartum depression is you just don’t want to. You don’t have it. You go into depression where you can’t take care of your child and you don’t want to hold your child. You don’t feel connected to your child. And I learned...it can be so many different things. [PT 09]
A clear distinction was not always present between psychological and somatic symptoms:
If someone...has pain in their chest or shortness of breath, the first thing you want to think about is it sort of like clots and other kind of physiologic reasons for that. Those are also very implicated and sort of obviously [associated with] panic attacks and anxiety. So, I think though those symptoms are also relevant of physical symptoms, [they] are also relevant for mental health. [MHP 05]
Drivers of Processing, Decision-Making, and Action Based on the Symptoms Experienced
Several drivers were reported to affect symptom processing (ie, whether they noticed the symptom and its severity), patients’ capacity to decide what should be done (ie, make decisions), and whether they were able to act on concerning symptoms ( Table 2 ).
Table 2 presents exemplary quotes for emerging themes under a single driver, but many quotes were coded under multiple drivers in our analysis process. The following passage, for example, highlights how self-perception, sociocultural concerns, and the health system can overlap to present a complex set of factors that may prevent women from receiving the care they need for the symptoms they are experiencing:
A lot of times I think that does get overlooked because people feel like, well, you’re OK, you’re fine. But what research shows us is that especially for Black women, it really doesn’t matter how much money you make or your income level, like our postpartum and perinatal health outcomes are the same across the board, which is really detrimental. So, yeah, I think they get overlooked because of that. I think they get overlooked or we get overlooked in the health care system. But I also think we get overlooked by our family and friends because we’re the strong ones. So, if anybody can deal with this, it’s you. [MHP 10]
a MHP: mental health professional.
b PT: patient.
c OB: obstetric health professional.
Design Needs for a Symptom-Reporting and Decision-Support System
Obstetric health professionals, mental health professionals, and patients discussed multiple needs for improved PRD symptom reporting and decision support. The key design requirements are embedded and italicized in the following text.
Participants generally agreed that although the proposed system focuses on postpartum symptoms, it would be advantageous to introduce the system during pregnancy, particularly in the third trimester :
You have to reach women before they give birth. They might look, they might not look, they might look at it and be concerned. But then they might forget about it and not have time to call. Those first six weeks are really chaotic. [MHP 06]
I think in the third trimester would be great because often we don’t really have anything to talk about in the office. It’s very quick visits like blood pressure and you’re still pregnant and we’re just waiting. And so, I think and they start to have a lot of questions about like, well, when I get home and how’s this going to go? So, I think that time is a good time. We’re all kind of just waiting for labor to happen or full term to get there, and this kind of gives them something to feel like they can prepare for. [OB 08]
Patients were open to reminders regarding entering symptoms they were experiencing, and participants described a desire for just-in-time symptom reporting and decision support, so that they could get quick feedback as they were experiencing the symptoms:
When people get home so much in their life has changed. And it’s probably a very hectic time. So maybe I think that’s a great idea reaching out again, either a few days or a week later to make sure they’re really able to use it and engage with it to the extent that’s helpful to them. [OB 02]
I think it would be a good idea to have like a system where you can report whenever you want. [PT 03]
I think for me, I would say in the moment. But then also having something at the end of every week to just, you know, to check in with yourself. I think that would be good as well. [PT 09]
In addition to considerations about how symptoms would be recorded, participants stressed the importance of the wording of the decision-support messages that patients receive . For messages that inform the patient that their symptom did not seem to require immediate medical attention, it was important to ensure that the patient still felt heard and that they did not leave the interaction feeling stuck with nothing to do regarding a symptom that was concerning to them:
Reframe the message. You know...we apologize that you were experiencing this. We just want to reassure you that this is normal. [PT 01]
[You] don’t want to make anyone feel like their feelings aren’t valid because that’s a horrible thing, especially in health care, especially if a person is convinced that something is wrong with them and you’re telling them that it’s normal and is perfectly fine. So, in that situation, I would just, depending on what the issue is, I would also share information of what to look out for. [PT 05]
The first thing is that it’s normal, but also something that you want to be able to do for comfort. For me, I don’t have to do too much, especially if I’m having anxiety, like if I get a text back that says here are some things you can do in this very moment to handle it. And then also, here are some links or information that you can also look up. [PT 09]
In the events where a concerning symptom was reported and it was recommended that the patient should reach out to a health professional, importance of conveying a sense of urgency without scaring the patient:
You don’t want to scare people, but it’s kind of hard to get around that when something is serious, and you don’t want to dumb it down. [PT 01]
Participants wanted multiple, easy-to-do methods for connecting with their health professional team, including having the number to call pop up, scheduling a time for someone to call them, and being able to start a live web-based chat:
I like all the options, especially that form or chat you can have like, you know, those online chat where like you really chatting with someone for those who like the type. I’m the type of person I just want to make a phone call, right? So, like for me, [it] will be a call. Maybe say maybe if it’s five, five or ten minutes then that will be great. Like especially, it’s going to make me feel like, OK, there’s someone out there that will care about my health. [PT 06]
However, participants noted that they would prefer not to use a symptom-reporting and decision-support tool, but instead reach out directly via phone if they were experiencing issues.
Participants, particularly mental health professionals, described a need for improved nuance or details regarding the different psychological symptoms patients could experience that are indicative of severe mental health issues:
Thoughts of hurting yourself or someone else is a good one...I would say I would add difficulty bonding. It would add something about not being able to sleep, even if you could sleep, you know, like or your anxiety that doesn’t go away, that changes your behavior. So, it changes the way that you interact with the baby or kind of do childcare. I guess I would want to say something about. psychotic thoughts, like fear that someone else may be hurting you or...recurrent worries or anxieties that don’t go away. [MHP 02]
Patients had differing opinions regarding whether the system should be integrated with other health technologies, particularly the patient portal:
I love the patient portal. I was able to be traveling to reach out to my OB, to reach out to all, you know, the nurses and stuff like that and just experience things that I needed. [PT 09]
I feel like...it’s an integral part of my medical history. So, even if it may seem somewhat insignificant for whatever reason, I would still want to have access. [PT 09]
I didn’t find it [the patient portal] very helpful... [PT 03]
On the basis of the feedback from health professionals that it may be challenging for postpartum patients to process and recognize certain symptoms, especially those related to mental health, we explored whether patient participants would be open to sharing educational information about symptoms to expect (rather than sharing the actual symptom reports) with trusted friends or family members. Similar to other design considerations, results were mixed, but it seemed helpful to have a patient-driven option for sharing symptom-related educational information with chosen friends or family members :
I think that there’s so much going on it would help to have someone with a different perspective equipped with this information. [PT 02]
There’s a lot of shame that comes with this. I’m not sure people would actually want other people to know. I can’t speak for the majority, but I didn’t really want people to know because I don’t want the kind of energy that came with people knowing. [PT 05]
We also discovered the competing needs of balancing the patient’s desire for their health professionals to be involved in symptom reporting with the need to avoid significant increases to health professional workload :
I sort of wonder from the health care provider perspective, how involved is the provider in that in the app? Like, do they get like a PDF of all the information? Is that more work for the provider? How does the provider interpret that data? [MHP 03]
I feel like they [the health professional] should be super involved. Especially because I’m not just going off of my experience because, you know, I don’t want to feel like they’re not really like I’m experiencing. And so, it’s scaring me. So, I just want to know that, you know, you’re hands on with everything. [PT 01]
Finally, the participants desired information beyond PRD symptoms to entice them to use the system . They were supportive of including various types of information, such as breastfeeding support resources, milestones and information regarding their child, other websites and apps with trusted maternal and child health information, further support resources for how they feel mentally, and links to social services (eg, food, housing, or other assistance).
Principal Findings
In this qualitative study, we interviewed obstetric health professionals, mental health professionals, and Black postpartum patients. Our findings helped to identify the design and implementation needs of an mHealth-based, symptom self-monitoring and decision-support system designed to support Black patients in determining when to seek care from a health professional for signs of PRD in the postpartum period. We encountered important findings related to (1) inputs, including psychological and somatic symptoms; (2) drivers of processing, decision-making, and action based on the symptoms experienced; and (3) design needs for a symptom-reporting and decision-support system. We have discussed how our findings may be helpful to other postpartum populations as well as the implications of our study for patient decision-support in other clinical settings.
First, our findings related to symptom inputs revealed the challenges caused by the overlapping presentation of somatic and psychological symptoms. This provides support for our approach of including psychological and somatic issues in a single app, particularly given that mental health conditions are a leading cause of PRD. A 2021 review found 15 PRO measures for assessing postpartum recovery. The measures typically focused on mental health or health-related quality of life, but few included both psychological and somatic outcomes, and none were targeted for PRD, such as the system [ 56 ].
Moreover, related to symptom inputs, we found that current tools for pinpointing severe symptoms, such as the CDC’s UWS did not provide sufficient nuance for concerning psychological symptoms. Symptom-reporting tools for PRD will either need to consider incorporating structured assessments, such as the Edinburgh Postnatal Depression Scale (EPDS) [ 56 ], or incorporating additional symptoms. The latter approach may have advantages as the EPDS focuses on depression (while providing subscales for anxiety) and PROs evaluated for use with anxiety disorders have limitations [ 57 ]. Furthermore, the EPDS has been validated in in-person laboratory settings but not in community settings or for web-based entry [ 58 ]. We must also consider how mistrust in the health system may lead to less truthful answers. Issues expressed around stigma related to mental health indicate that the way in which these symptoms are elicited may require further assessment to promote the normalcy of the symptoms and improve candid reporting. Technology-based approaches for supporting perinatal mental health have been described as uniformly positive but having limited evidence for use [ 59 ], suggesting that further exploration is needed in this area, also considering how adding somatic issues may be perceived by patients.
Second, there were several drivers that affected symptom processing, decision-making, and action that cannot typically be solved through a symptom-reporting and decision-support system. Challenges related to self-perception and lack of experience or expectations may be addressed based on the wording for how the symptoms are elicited and by providing concise, easy-to-understand depictions of what should be expected versus what are the causes for concern. However, many of the other issues described related to sociocultural, financial, and environmental factors and the health systems’ systemic racism issues cannot be addressed directly in a simple PRO-based app and decision-support system. Directly addressing these issues will likely require more systematic, multipronged approaches. Therefore, it seems advisable to couple patient decision-support aids with other social support interventions for perinatal health [ 60 , 61 ].
Drivers of processing, decision-making, and action are still important contextual elements to be considered in the design of the system. Another study tailoring an mHealth app for Latina patients to support health during pregnancy also found it important to address issues related to financial barriers, social support, health care accessibility, and cultural differences [ 62 ]. Our best attempt to address these issues may be to promote information transparency and inclusive design. For example, there may be a “frequently asked questions” section of an app, where patients can explore things such as supportive resources for childcare while they seek medical attention or information they may show their friends or family members regarding postpartum symptoms of concern. The system may also use common human-computer interaction principles, such as information filtering [ 63 ] and organizing the suggested resources (eg, for mental health care) based on whether they accept the patient’s insurance. The built environment can also be changed through the system, but it may offer mechanisms for remote monitoring, such as telemedicine-based support or linking the system to a blood pressure cuff, when clinically appropriate [ 64 , 65 ]. As noted, the system obviously cannot address issues related to systematic racism directly [ 66 ]. Instead, we used a participatory design approach, with the hope that the nature of the information presented may be more patient centered, acceptable, and better aligned with the beliefs and values of Black patients [ 67 ]. Issues related to systematic racism have commonly been described in the US health care system, but structural inequities also exist on a global scale. Future studies should investigate how our findings regarding design needs may extend to other minoritized perinatal patient groups.
A systematic review of patient decision aids for socially disadvantaged populations across clinical settings found that such tools can improve knowledge, enhance patient-clinician communication, and reduce decisional conflict [ 68 ]. However, descriptions of patient decision aids focus on the type of tool (eg, paper vs digital), how it was delivered, when it was delivered, and by whom, as opposed to describing the content the aid provides. Therefore, it is challenging to determine how other decision-support tools have addressed information regarding environmental, financial, or health system–level factors that may affect care seeking based on the decision aid. Some tools seem to address sociocultural needs by tailoring to the target population, but the aforementioned systematic review did not find differential effects on outcomes when tools were tailored versus not tailored [ 16 ]. Future studies on patient decision aids may benefit from including non-symptom related information. Providing appropriate informational support may involve a deeper study of the systemic needs that patients may have, even if these needs may not directly be addressed by the decision aid.
Third, descriptions of the design needs for PRD symptom monitoring revealed that there is likely not a one-size-fits-all solution related to reminders, involvement of health professionals, and how the tool is incorporated with other systems (eg, the patient portal). “User control and freedom” and “flexibility of use” are two of the key items in commonly used heuristics for user interface design [ 69 ]; therefore, it is important to include options for customization and varied but safe pathways for interaction with the proposed system. For example, some participants described that they may not be likely to access the symptom-reporting system through the patient portal. Although there may be safety and convenience-related reasons for having the system as part of the patients’ medical record, if the patient chooses, the system could, on the front end, appear more like a stand-alone app than something that must be accessed through the patient portal. Patients also had varying opinions related to how they may want to reach out to a health professional if a problematic symptom was reported. These preferences may differ from instance to instance; therefore, it is helpful to ensure that patients have a choice regarding how to reach out, but system designers must also create workflows with feedback loop, so that patients who are reporting problematic symptoms are not missed (ie, if patients do not reach out themselves, they never receive attention). Patient-level customizations and options for interaction also respects patients as individuals and may promote patient-centered interactions.
Furthermore, related to design needs, participants indicated that the wording of the decision-support messages was critical. Specifically, for reports that did not include currently urgent symptoms, it was important that the message still conveyed support and validation, clarified that the patient could still reach out for help, and provided additional means for managing their symptoms, so the patient did not feel frustrated by their report [ 70 ]. Regarding messages that recommended patients to reach out to their health professional team, it was crucial to note what the symptom meant (eg, what kind of disease it could indicate), encourage the patient to reach out without increasing anxiety, and provide different avenues for easy outreach. Going forward, we plan to incorporate the aforementioned elements into the messages built into the system. We will then complete additional acceptance and comprehension testing with a larger sample of postpartum patients. These findings also indicate that care must be taken in translating such tools, and the translated materials should be reviewed with the target end user groups before implementation. This may mitigate unintended consequences or inadvertent inclusion of language that does not support the needs of minoritized groups.
Strengths and Limitations
Our study highlighted the limitations and areas that would benefit from further exploration. First, our study involved recruitment sites that were within a single health system in New York City. Second, while we achieved thematic saturation of qualitative themes (a means for determining sample sufficiency in qualitative studies) [ 54 , 55 ], our conclusions are based on a sample of 36 participants from 3 stakeholder groups. Third, given the documented disparities, we deliberately focused on the needs of Black postpartum patients, but this may not represent the needs of the postpartum patients of other races. Furthermore, our sample should not be viewed as encompassing the opinions of all Black postpartum patients. Our findings revealed the need for individual customization and varied interaction patterns on a case-by-case basis. Fourth, all interviews were conducted remotely (via Zoom or telephone), which can have effects on the interaction. On the one hand, it may be harder to connect with the interviewee, and on the other hand, people may feel more anonymous and comfortable with sharing information. Finally, although we attempted to promote external validity through the review of the coding scheme by a subject matter expert, we did not have the opportunity to perform triangulation of the findings by returning the results to participants. To address these limitations, it would be beneficial to survey a larger group of postpartum patients, powered to assess the differences based on race and ethnicity. This would allow us to come to a stronger consensus regarding design choices, assess whether there are differences in design needs or preferences, and gain feedback from patients in areas outside New York City. Future studies may also explore how other underserved groups, such as those with limited English proficiency, may benefit from tailored symptom self-monitoring and decision support.
Conclusions
In this qualitative study regarding postpartum symptom monitoring and decision support, we found that the current structured reporting measures do not include the combination of somatic and psychological symptoms that may be indicative of severe outcomes in the postpartum period. While not explicitly related to symptom reporting and decision support, patient decision aids, particularly those focusing on minoritized groups, should consider how the aids may be coupled with other structural support interventions or, at least, information about how other resources may be accessed. As stated in the commonly accepted design heuristics, we also found that user control and freedom unsurprisingly remain important for a patient decision-support aid for Black postpartum patients. Finally, decision aid–related phrases must take care to convey urgency without inducing anxiety when action may be indicated and consider respect and empathy for the patients’ symptoms when action may not be indicated to ensure that they do not feel unheard and are empowered to report new or worsening symptoms.
Acknowledgments
This study was supported by the National Institute on Minority Health and Health Disparities (K99MD015781; principal investigator: NB).
Data Availability
The data sets generated and analyzed during this study are not publicly available due to institutional review board regulations but are available from the corresponding author on reasonable request.
Authors' Contributions
NB conceptualized the study and acquired funding under the advisement of RBK, LER, AH, RMC, and JSA. NB collected the data. NB, SW, and SNdR analyzed the data with input from all other authors. ECP completed the literature review and descriptive analysis of participants’ characteristics. NB drafted the paper and received substantial inputs from all other authors.
Conflicts of Interest
LER is an Up to Date contributor and an advisory board member for the New English Journal of Medicine, and Contemporary OB/GYN. She has also been a speaker for Medscape is an an expert reviewer for Pfizer on the RSV Vaccine. AH is an Up to Date contributor, a co-founder and medical consultant for Iris Ob Health, and a consultant for Progyny.
Semistructured interview guide questions for patients and health professionals.
- Howell EA, Egorova NN, Janevic T, Brodman M, Balbierz A, Zeitlin J, et al. Race and ethnicity, medical insurance, and within-hospital severe maternal morbidity disparities. Obstet Gynecol. Feb 2020;135(2):285-293. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. May 01, 2013;70(5):490-498. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pregnancy-related deaths: data from maternal mortality review committees in 36 US States, 2017-2019. Centers for Disease Control and Prevention. URL: https://www.cdc.gov/reproductivehealth/maternal-mortality/erase-mm/data-mmrc.html [accessed 2022-11-20]
- Pregnancy mortality surveillance system. Centers for Disease Control and Prevention. 2020. URL: https://tinyurl.com/356dwufh [accessed 2024-03-23]
- Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011-2013. Obstet Gynecol. Aug 2017;130(2):366-373. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Home page. World Health Organization. URL: https://www.who.int/ [accessed 2024-03-21]
- Troiano NH, Witcher PM. Maternal mortality and morbidity in the United States: classification, causes, preventability, and critical care obstetric implications. J Perinat Neonatal Nurs. 2018;32(3):222-231. [ CrossRef ] [ Medline ]
- Creanga AA, Berg CJ, Ko JY, Farr SL, Tong VT, Bruce FC, et al. Maternal mortality and morbidity in the United States: where are we now? J Womens Health (Larchmt). Jan 2014;23(1):3-9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Campbell-Grossman C, Brage Hudson D, Keating-Lefler R, Ofe Fleck M. Community leaders' perceptions of single, low-income mothers' needs and concerns for social support. J Community Health Nurs. Dec 2005;22(4):241-257. [ CrossRef ] [ Medline ]
- New York State maternal mortality review report on pregnancy-associated deaths in 2018. New York State Department of Health. 2018. URL: https://www.health.ny.gov/community/adults/women/docs/maternal_mortality_review_2018.pdf [accessed 2024-03-23]
- Suplee PD, Kleppel L, Santa-Donato A, Bingham D. Improving postpartum education about warning signs of maternal morbidity and mortality. Nurs Womens Health. Dec 2017;20(6):552-567. [ CrossRef ] [ Medline ]
- Howell EA, Bodnar-Deren S, Balbierz A, Parides M, Bickell N. An intervention to extend breastfeeding among black and Latina mothers after delivery. Am J Obstet Gynecol. Mar 2014;210(3):239.e1-239.e5. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. Dec 2015;105(12):e60-e76. [ CrossRef ]
- Stepanikova I, Mollborn S, Cook KS, Thom DH, Kramer RM. Patients' race, ethnicity, language, and trust in a physician. J Health Soc Behav. Dec 24, 2006;47(4):390-405. [ CrossRef ] [ Medline ]
- Schwei RJ, Kadunc K, Nguyen AL, Jacobs EA. Impact of sociodemographic factors and previous interactions with the health care system on institutional trust in three racial/ethnic groups. Patient Educ Couns. Sep 2014;96(3):333-338. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Blair IV, Steiner JF, Fairclough DL, Hanratty R, Price DW, Hirsh HK, et al. Clinicians' implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Ann Fam Med. 2013;11(1):43-52. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ayanian JZ, Zaslavsky AM, Guadagnoli E, Fuchs CS, Yost KJ, Creech CM, et al. Patients' perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol. Sep 20, 2005;23(27):6576-6586. [ CrossRef ] [ Medline ]
- Reyna VF, Nelson WL, Han PK, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychol Bull. Nov 2009;135(6):943-973. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Language use in the United States: 2011. United States Census Bureau. 2011. URL: https://www.census.gov/library/publications/2013/acs/acs-22.html [accessed 2024-03-23]
- Valdez RS, Brennan PF. Exploring patients' health information communication practices with social network members as a foundation for consumer health IT design. Int J Med Inform. May 2015;84(5):363-374. [ CrossRef ] [ Medline ]
- Valdez RS, Gibbons MC, Siegel ER, Kukafka R, Brennan PF. Designing consumer health IT to enhance usability among different racial and ethnic groups within the United States. Health Technol. Jul 13, 2012;2(4):225-233. [ CrossRef ]
- Valdez RS, Holden RJ. Health care human factors/ergonomics fieldwork in home and community settings. Ergon Des. Oct 2016;24(4):4-9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Valdez RS, Holden RJ, Novak LL, Veinot TC. Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Inform Assoc. Jan 2015;22(1):2-10. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bingham D, Suplee PD, Morris MH, McBride M. Healthcare strategies for reducing pregnancy-related morbidity and mortality in the postpartum period. J Perinat Neonatal Nurs. 2018;32(3):241-249. [ CrossRef ] [ Medline ]
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. Jan 2015;125(1):5-12. [ CrossRef ] [ Medline ]
- Suplee PD, Bingham D, Kleppel L. Nurses' knowledge and teaching of possible postpartum complications. MCN Am J Matern Child Nurs. 2017;42(6):338-344. [ CrossRef ] [ Medline ]
- O'Byrne LJ, Bodunde EO, Maher GM, Khashan AS, Greene RM, Browne JP, et al. Patient-reported outcome measures evaluating postpartum maternal health and well-being: a systematic review and evaluation of measurement properties. Am J Obstet Gynecol MFM. Nov 2022;4(6):100743. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Adler A, Conte TF, Illarraza T. Improvement of Postpartum Nursing Discharge Education Through Adaptation of AWHONN’s Post-Birth Education Program. J Obstet Gynecol Neonatal Nurs. Jun 2019;48(3):S54. [ CrossRef ]
- Urgent maternal warning signs. Centers for Disease Control and Prevention. URL: https://www.cdc.gov/hearher/maternal-warning-signs/index.html [accessed 2022-12-11]
- Hannan J. APN telephone follow up to low-income first time mothers. J Clin Nurs. Jan 30, 2013;22(1-2):262-270. [ CrossRef ] [ Medline ]
- Dennis CL, Kingston D. A systematic review of telephone support for women during pregnancy and the early postpartum period. J Obstet Gynecol Neonatal Nurs. May 2008;37(3):301-314. [ CrossRef ] [ Medline ]
- Letourneau N, Secco L, Colpitts J, Aldous S, Stewart M, Dennis CL. Quasi-experimental evaluation of a telephone-based peer support intervention for maternal depression. J Adv Nurs. Jul 23, 2015;71(7):1587-1599. [ CrossRef ] [ Medline ]
- Shamshiri Milani H, Azargashb E, Beyraghi N, Defaie S, Asbaghi T. Effect of telephone-based support on postpartum depression: a randomized controlled trial. Int J Fertil Steril. 2015;9(2):247-253. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mobile fact sheet. Pew Research Center. URL: https://www.pewresearch.org/internet/fact-sheet/mobile/ [accessed 2023-02-22]
- Anderson M. Digital divide persists even as lower-income Americans make gains in tech adoption. Pew Research Center. URL: https://www.urbanismnext.org/resources/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption [accessed 2024-03-23]
- Drexler K, Cheu L, Donelan E, Kominiarek M. 415: Remote self-monitoring of perinatal weight and perinatal outcomes in low-risk women. Am J Obstet Gynecol. Jan 2020;222(1):S272-S273. [ CrossRef ]
- Marko KI, Ganju N, Krapf JM, Gaba ND, Brown JA, Benham JJ, et al. A mobile prenatal care app to reduce in-person visits: prospective controlled trial. JMIR Mhealth Uhealth. May 01, 2019;7(5):e10520. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vernon MM, Yang FM. Implementing a self-monitoring application during pregnancy and postpartum for rural and underserved women: a qualitative needs assessment study. PLoS One. Jul 19, 2022;17(7):e0270190. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Berry DL, Blumenstein BA, Halpenny B, Wolpin S, Fann JR, Austin-Seymour M, et al. Enhancing patient-provider communication with the electronic self-report assessment for cancer: a randomized trial. J Clin Oncol. Mar 10, 2011;29(8):1029-1035. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lordon RJ, Mikles SP, Kneale L, Evans HL, Munson SA, Backonja U, et al. How patient-generated health data and patient-reported outcomes affect patient-clinician relationships: a systematic review. Health Informatics J. Dec 20, 2020;26(4):2689-2706. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Todd BL, Feuerstein M, Gehrke A, Hydeman J, Beaupin L. Identifying the unmet needs of breast cancer patients post-primary treatment: the Cancer Survivor Profile (CSPro). J Cancer Surviv. Jun 29, 2015;9(2):137-160. [ CrossRef ] [ Medline ]
- Basch E, Deal AM, Dueck AC, Scher HI, Kris MG, Hudis C, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. Jul 11, 2017;318(2):197-198. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. Feb 20, 2016;34(6):557-565. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Denis F, Basch E, Septans A, Bennouna J, Urban T, Dueck AC, et al. Two-year survival comparing web-based symptom monitoring vs routine surveillance following treatment for lung cancer. JAMA. Jan 22, 2019;321(3):306-307. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Howell EA, Balbierz A, Wang J, Parides M, Zlotnick C, Leventhal H. Reducing postpartum depressive symptoms among black and Latina mothers: a randomized controlled trial. Obstet Gynecol. May 2012;119(5):942-949. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ngai FW, Chan SW, Ip WY. The effects of a childbirth psychoeducation program on learned resourcefulness, maternal role competence and perinatal depression: a quasi-experiment. Int J Nurs Stud. Oct 2009;46(10):1298-1306. [ CrossRef ] [ Medline ]
- Shorey S, Chan SW, Chong YS, He HG. A randomized controlled trial of the effectiveness of a postnatal psychoeducation programme on self-efficacy, social support and postnatal depression among primiparas. J Adv Nurs. Jun 15, 2015;71(6):1260-1273. [ CrossRef ] [ Medline ]
- Diefenbach MA, Leventhal H. The common-sense model of illness representation: theoretical and practical considerations. J Soc Distress Homeless. Jul 07, 2016;5(1):11-38. [ CrossRef ]
- Wickens CD. Multiple resources and mental workload. Hum Factors. Jun 2008;50(3):449-455. [ CrossRef ] [ Medline ]
- Gadamer HG. Philosophical Hermeneutics. Oakland, CA. University of California Press; 1976.
- Saldana J. The Coding Manual for Qualitative Researchers. Thousand Oaks, CA. Sage Publications; 2012.
- Huberman AM, Miles M, Saldana J. Qualitative Data Analysis: A Methods Sourcebook. Thousand Oaks, CA. Sage Publications; 2014.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. In: Pope C, Mays N, editors. Qualitative Research in Health Care. Hoboken, NJ. John Wiley & Sons; 2006;63-81.
- Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. Qual Rep. Sep 8, 2015;20(9):1408-1416. [ FREE Full text ] [ CrossRef ]
- Morse JM. The significance of saturation. Qual Health Res. Jul 01, 2016;5(2):147-149. [ CrossRef ]
- Sultan P, Sharawi N, Blake L, Ando K, Sultan E, Aghaeepour N, et al. Use of patient-reported outcome measures to assess outpatient postpartum recovery: a systematic review. JAMA Netw Open. May 03, 2021;4(5):e2111600. [ FREE Full text ] [ CrossRef ] [ Medline ]
- O'Carroll J, Ando K, Yun R, Panelli D, Nicklin A, Kennedy N, et al. A systematic review of patient-reported outcome measures used in maternal postpartum anxiety. Am J Obstet Gynecol MFM. Sep 2023;5(9):101076. [ CrossRef ] [ Medline ]
- Cox J. Thirty years with the Edinburgh postnatal depression scale: voices from the past and recommendations for the future. Br J Psychiatry. Mar 18, 2019;214(3):127-129. [ CrossRef ] [ Medline ]
- Novick AM, Kwitowski M, Dempsey J, Cooke DL, Dempsey AG. Technology-based approaches for supporting perinatal mental health. Curr Psychiatry Rep. Sep 23, 2022;24(9):419-429. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Guy Jr GP, Adams EK, Redd SK, Dunlop AL. Effects of Georgia's Medicaid family planning waiver on pregnancy characteristics and birth outcomes. Womens Health Issues. Dec 15, 2023. [ CrossRef ] [ Medline ]
- Zimmermann K, Haen LS, Desloge A, Handler A. The role of a local health department in advancing health equity: universal postpartum home visiting in a large urban setting. Health Equity. Oct 01, 2023;7(1):703-712. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Castillo AF, Davis AL, Krishnamurti T. Adapting a pregnancy app to address disparities in healthcare access among an emerging Latino community: qualitative study using implementation science frameworks. Research Square. Preprint posted online April 27, 2022. [ FREE Full text ] [ CrossRef ]
- Shneiderman B. The eyes have it: a task by data type taxonomy for information visualizations. In: Bederson BB, Shneiderman B, editors. The Craft of Information Visualization: Readings and Reflections. Burlington, MA. Morgan Kaufmann; 2003;364-371.
- White KM, Williamson C, Bergou N, Oetzmann C, de Angel V, Matcham F, et al. A systematic review of engagement reporting in remote measurement studies for health symptom tracking. NPJ Digit Med. Jun 29, 2022;5(1):82. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Walsh S, Golden E, Priebe S. Systematic review of patients' participation in and experiences of technology-based monitoring of mental health symptoms in the community. BMJ Open. Jun 21, 2016;6(6):e008362. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Davidson KW, Mangione CM, Barry MJ, Cabana MD, Caughey AB, Davis EM, et al. Actions to transform US preventive services task force methods to mitigate systemic racism in clinical preventive services. JAMA. Dec 21, 2021;326(23):2405-2411. [ CrossRef ] [ Medline ]
- Im EO, Chee W, Hu Y, Kim S, Choi H, Hamajima Y, et al. What to consider in a culturally tailored technology-based intervention? Comput Inform Nurs. Sep 2018;36(9):424-429. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Yen RW, Smith J, Engel J, Muscat DM, Smith SK, Mancini J, et al. A systematic review and meta-analysis of patient decision aids for socially disadvantaged populations: update from the international patient decision aid standards (IDPAS). Med Decis Making. Jun 21, 2021;41(7):870-896. [ CrossRef ]
- Nielsen J. 10 usability heuristics for user interface design. Nielsen Norman Group. 1994. URL: https://www.nngroup.com/articles/ten-usability-heuristics/ [accessed 2020-11-15]
- Ancker JS, Stabile C, Carter J, Chen LY, Stein D, Stetson PD, et al. Informing, reassuring, or alarming? Balancing patient needs in the development of a postsurgical symptom reporting system in cancer. AMIA Annu Symp Proc. 2018;2018:166-174. [ FREE Full text ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 22.03.23; peer-reviewed by C Laranjeira; comments to author 15.01.24; revised version received 20.02.24; accepted 08.03.24; published 26.04.24.
©Natalie Benda, Sydney Woode, Stephanie Niño de Rivera, Robin B Kalish, Laura E Riley, Alison Hermann, Ruth Masterson Creber, Eric Costa Pimentel, Jessica S Ancker. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 26.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
- Open access
- Published: 26 April 2024
Why are medical students so motivated to learn ultrasound skills? A qualitative study
- Anina Pless 1 na1 ,
- Roman Hari 1 na1 &
- Michael Harris 1 , 2
BMC Medical Education volume 24 , Article number: 458 ( 2024 ) Cite this article
41 Accesses
Metrics details
The introduction of ultrasound (US) courses into medical undergraduate courses is usually met with a particularly high level of student motivation. The reasons for this are unclear. The aim of this study was to investigate the factors that contribute to undergraduate medical students’ motivation to learn US skills. Understanding what motivates students to learn US will inform the efforts of faculty to foster students’ motivation to learn.
We carried out in-depth semi-structured one-to-one interviews with medical students participating in an optional US course at two Swiss universities. The interview guide consisted of 10 main questions. The content was informed by experts in the field of medical education and US, as well as by a literature review of motivation theories for learning, in particular by self-determination theory (SDT). SDT was used to guide the development of the interview guide and to reflect on the resulting themes in the discussion section. The interview guide was piloted with two medical students. The interviews lasted an average of 45 min and were audio recorded and transcribed. Thematic analysis was used to analyse the data.
Fourteen undergraduate medical students in their preclinical (year 3) and clinical studies (years 4 and 5) elaborated on a wide range of reasons for their high motivation to learn US. They were motivated for US training because of the positive nimbus of the US modality, emphasising the advantages of visualisation. Students acknowledged the potential professional benefits of learning US and described it as a fun, exciting group activity.
Conclusions
The four themes we found in our analysis can all be related to the three universal needs described in SDT. The strong focus on the visual aspect and the positive nimbus of the modality goes beyond that and reflects the visuo-centric Zeitgeist, which claims the superiority of visual information over other data. Educators should be aware that motivation to learn is affected by the Zeitgeist and ensuing preconceptions, such as the perception of the positive nimbus surrounding a topic. Other key elements that can be implemented to motivate students are just-in-time feedback, enabling group experiences and creating awareness of the clinical relevance of learning content.
Peer Review reports
The introduction of mandatory ultrasound (US) courses at our University was greeted with a standing ovation. This is not the usual reaction to the implementation of new courses and is worth exploring. We hope to understand factors that contribute to students’ motivation for learning to foster such factors when teaching.
High levels of motivation correlate with better grades throughout medical studies [ 1 , 2 ]. Kusurkar et al. examined “the effect of quality of motivation on performance” and found that motivation stemming from personal interest positively affects academic performance [ 3 ]. There is a positive correlation between motivation from personal interest and the intention to continue ones studies [ 1 ]. Motivation seems also to be correlated with learners’ well-being [ 4 ].
Several theories try to explain why students are motivated to learn. According to Self-determination theory (SDT), developed by Deci and Ryan, motivation varies not only in quantity but also in quality [ 5 ]. A central idea of the theory is that there is a distinction between autonomous motivation and controlled motivation. Autonomous motivation can be defined as engaging in an activity because one finds it interesting: doing something of one’s own free will. Controlled motivation is the norm, especially after early childhood, when social demands and roles require individuals to take responsibility for non-intrinsically interesting tasks. Students’ motivation to learn ultrasound, as perceived in our experience and as described in the literature, would mainly be classified as “autonomous” motivation in SDT, as they are engaging in an activity that they find interesting [ 6 , 7 , 8 ]. Three universal psychological needs add to the autonomous motivation: autonomy (being free to choose whatever one considers useful to do), competence (the desire to master a task and to feel effective) and relatedness (the feeling of wanting to connect with others and have a sense of belonging) [ 8 , 9 ]. Figure 1 depicts states of motivated behaviour and its relation to autonomy, competence and relatedness. At one end of the continuum is amotivation, the state of lacking an intention to act. When amotivated, people either do not act at all or they act without purpose. Amotivation results from not appreciating an activity, not feeling competent to do it, or not expecting it to achieve a desired outcome. Intrinsic motivation is placed at the other end of the continuum, emphasising that it is the essential form of self-determined activity, based solely on an internal desire to act. Extrinsically motivated behaviours cover the states between amotivation and intrinsic motivation, varying in the extent to which their regulation is autonomous [ 7 ].
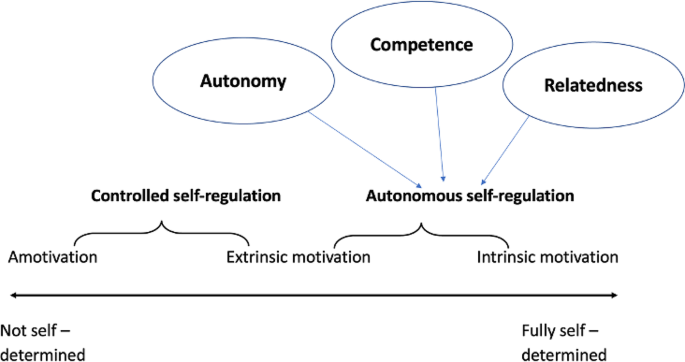
The Self-Determination Continuum, adapted from Ryan and Deci, 2000, Cook and Artino, 2016 and ten Cate et al., 2011
Our observation of students’ reception of the implementation of US teaching is in line with recent evidence [ 10 ]. Evaluations of US training programmes report positive feedback from over 95% of students, approval rates rarely seen in other fields of medical education [ 11 , 12 ]. In a USA study, 97% of students agreed that it was important for them to learn basic US skills during medical school [ 13 ]. A German questionnaire study of medical students found a similar number (98.2%) reporting a high or very high interest in curricular US in medical education, with the large majority (94.4%) of respondents agreeing or strongly agreeing that US education should be a mandatory part of their curriculum [ 14 ]. In another study, a large majority of teachers (97%) felt that the students were interested in the course [ 15 ]. Another development that underlines the attractiveness of US education for students is the introduction of extracurricular, student-led peer-tutoring initiatives [ 16 ].
The scarce evidence on why students are motivated to learn US skills, suggests that they believe that US education helps them to be prepared for clinical practice before and after graduation [ 14 , 17 ]. They also describe educational benefits beyond the mastering of US skills, for example learning physical examination skills or improving their understanding of anatomy and physiology [ 11 , 13 , 14 , 18 ]. In a recent study, Wang et al. explored why pre-clinical medical students wanted to learn US by applying Existence, Relatedness and Growth Theory, a model with three categories often used for analysing employee work performance. Students gave reasons related to all three categories, foremost existence needs (e.g. future work requirement) and growth needs (e.g. improving diagnostic skills), with relatedness needs being mentioned less often [ 19 ]. Given SDT’s three basic psychological needs of autonomy, competence and relatedness, the spectrum of reasons is likely to be broader than this.
The aim of this study was to investigate the factors that contribute to undergraduate medical students’ motivation to learn US skills, using SDT as a conceptual framework.
Study design
This was a qualitative study following a constructivist paradigm. We used semi-structured one-to-one interviews to allow the exploration of sensitive topics and motivators. We used thematic analysis to analyse the data [ 20 , 21 ]. We adhered to the Consolidated Criteria for Reporting Qualitative Research Checklist (COREQ) in the reporting of this study (for full COREQ checklist see supplementary Appendix 1) [ 22 ].
Study setting and participants
We interviewed 14 medical students from two different Swiss medical schools (University of Bern, University of Zurich) between 2019 and 2022. Both Universities had developed identical, optional medical student courses in abdominal US education that used volunteer peer-tutors. The blended learning programme was available to all Swiss medical students. The ultrasound course curriculum for the students consisted of five modules, with five hours of e-learning and 16 hours of peer-led tutoring. After completing a summative practical assessment, participants could obtain an internationally recognised course certificate in abdominal ultrasound [ 23 ]. Approximately 20% of medical students participated in these courses.
Recruitment and sampling method
We used purposive sampling. We contacted all the students that were enrolled in a voluntary, extracurricular US course ( n = 95). Potential participants were invited by an email forwarded to them by the course organisers and were also approached directly at US courses. While we had aimed to stratify participants with regards to gender, University site and age, recruitment was difficult during the COVID-19 pandemic, so we interviewed all the students willing to participate. All the students who agreed to take part had already participated in at least two tutored sessions and gave written, informed consent. After initial contact had been made, none of the participants declined to take part in the study or dropped out of it.
Ethical considerations
The study was submitted to the regional ethics committee which stated that the study does not fall under the Swiss Human Research Act (BASEC-Nr. Req-2018-00059).
All participants gave written informed consent. To ensure participant anonymity, each participant was identified only by a code after interview transcription.
Development of the interview guide
The semi-structured interview guide was informed by a literature review of motivation theories for learning, in particular by SDT, and discussions with faculty who are involved in US education, including medical educators, clinicians and US experts. Based on this information the research team discussed how to phrase questions that would be broad enough to encompass a variety of factors which can contribute to motivation according to SDT [ 7 , 9 ]. The interview guide consisted of 10 main questions which focussed on participants’ reasons to learn US and the perceived benefits (see Appendix 2). Each main question had probes to get more in-depth information. The interview guide was piloted with two students, and changes were made where necessary.
Data collection
All 14 interviews were carried out by the lead researcher AP, who had no prior relationship with the participants and was not affiliated with the US course. The interviewees were told that AP had an interest in their views of learning US skills. The risk of respondent bias, in this case the tendency to give socially desirable answers, was minimised by careful question design. The interviewer was not much older than the participants, preventing a feeling of hierarchy. Only the interviewee and AP were present during the interviews, which lasted an average of 45 min and were audio-recorded. Short field notes were made after each interview, commenting on the mood of the interview and reflecting the interviewer’s role and potential influence. The interviews were conducted at a location of the participants’ choice, most often at a public venue or at the University. Interviews were conducted in Swiss German and transcribed verbatim using High German diction. The transcriptions were done by AP as well as BB and KL, two medical students, all of whom are native Swiss German speakers. We wrote and used a transcription manual to ensure that transcripts were consistent. No repeat interviews were carried out and interview transcripts were not returned to the participants. Analysis was conducted using the High German transcripts.
Data analysis
AP, a medical doctor as well as a medical educator, did the primary analysis. She and MH, an experienced medical doctor, medical educator and qualitative researcher, independently coded three of the transcripts and compared their results to look for inconsistencies. Throughout the process, data was read and reread, using constant comparison with earlier data. Themes which derived from the data were labelled using a process of open coding to identify and later categorise phenomena in the data [ 24 ]. The interviews and analysis of the data were carried out in iterative cycles, going back and forth between the data gathering and analysis, allowing for new insights to inform changes to the interview guide [ 20 , 25 ]. Both coders regularly revised and refined the codes. No software was used.
After 14 interviews, the question of data saturation was discussed among the research team (AP, MH, RH, BB). As no new themes were arising, it was agreed that data saturation had been achieved [ 26 ].
The research team reviewed the findings individually then met to discuss the thematic structure. Each member of the team first presented their initial thoughts as to the themes. The team identified and continuously reviewed the themes until there was consensus [ 21 ]. For the sake of clarity and focus, the analysis focused on ultrasound-related factors and excluded themes related to course design in general.
We sent an overview of the key themes to four of the participants and asked for their comments. No changes needed to be made as a result of this.
14 students participated in the interviews. Table 1 shows participants’ characteristics.
We identified four US-specific themes that contribute to high levels of motivation to learn US skills. Table 2 shows the themes and subthemes.
The themes and subthemes are described in more detail below, with quotations identified by participant number.
Perception of professional benefits
All participants expressed that learning US would be an advantage professionally. This could be during their studies, or as practicing physicians. Learning US as early as possible was seen as adding to this benefit.
Benefits as a medical student
Some participants wanted to understand US images shown in lectures: Now, if we now have an US image in a lecture, I think “yes, ok, I can follow now”. (Participant(P)6)
For most participants, revising and deepening their knowledge of anatomy, as well as applying that knowledge to the patient’s body, were key benefits and motivators. Many participants felt learning US improved their spatial thinking: US gives you a different feeling of the relationships between the organs in the body. And uh, somehow you really know where the kidneys are or where the liver is. (P9)
One participant appreciated that US also put into perspective what was clinically relevant for their future career: And it was always reassuring for me that “yes, what is really relevant, I know” and if I no longer have the twenty-seventh branch of this artery in my head (…) so I was able to put in perspective the anatomical knowledge. For my future medical career. (P9)
Benefits as a physician
All participants stated that having US skills could be relevant to their future as physicians. They thought it was important to understand the indications and be able to interpret US images. Many participants were certain US would be part of their clinical life. One participant stated: Yes, it is also an examination method that is actually used in many disciplines. That means that sooner or later I will be asked to perform it on a patient. (P2) Several participants felt that they needed to be well prepared for their transition from student to resident: And that that’s my goal more or less, things that you can already acquire now, that I have them ready at hand. That at least that will work. (P2) There was also the notion that having US skills would help (…) avoid and reduce unnecessary imaging procedures and refer less patients to specialists. (P6)
The “exciting experience” component
For many participants, the motivation was connected to the feeling of experiencing something inherently fun and exciting: So, yes, it’s also a fascinating, so it’s still a “wow”. A “wow moment”. (laughs) (P3). Participants were intrinsically fascinated with the topic of US and the aspect of visualisation added to this: What I really find interesting is that my fascination still doesn’t let up (…) well, I just found it fascinating to somehow see my own organs for once (laughs). (P9)
The social aspects of learning US
Interpersonal factors played an important role, to learn and interact in small groups with other participants was described as similar to engaging in a new hobby, as well as a way of escaping everyday student life: Um, and what did I always enjoy the most? I think it was simply the interaction with the others. It’s just something that we don’t have much of in our studies. (P9)
While most participants said that the social aspect did not influence the decision to apply for the course, it was important for their positive perception of, and continuing engagement in, the course. They noted that the course gave them the opportunity to meet new people or do something with friends.
A practical skill
Many participants enjoyed doing something practical, as opposed to simply learning theory: Yes, and that’s actually kind of cool. Yeah, not exactly like a surgeon, but still a little bit hands-on. Yes. (P3)
They found learning US also enabled them to put their learning into a clinical perspective, giving them an insight into what they were working towards. One participant described how their US skills helped her become an active member of a clinical team during the practical year: I was allowed to scan a child because I said I had done this course. And afterwards I felt like one of them, not just like a trainee standing at the back, but that I had been fully interactive. (P12)
Learning US as a challenge
Participants found learning US to be a positive challenge: If you just get it or, also with the kidney, if you get it and then you recognize everything, that’s a pleasure. (P11)
Most participants performing US was not a natural gift but something they had to learn, requiring practice, diligence, and effort: Sure, there’s a mega process behind it until it’s intuitive, and it’s not the case with me at all yet, but I can imagine that, that it’s, um, doable with practice. Like the driving test, maybe. (P13)
The positive nimbus of US
Many participants said that they believed US to be an up-and-coming modality in medicine, with many advantages. We summarise these recurrent themes under the concept of the “positive nimbus” of US, referring to its positive image in public and medical discourse.
US as a modern tool
Many participants stated that US was the diagnostic tool of the future, which would become part of every physician’s basic equipment. This was often something that they had heard from others (peers, lecturers, physicians): (…) there was a doctor who said it was super important that you can do it and I should definitely take every opportunity. (P5)
Participants had a positive impression of US as a tool, ascribing many favourable attributes to it, principally that it was fast and easy. The participants found US to be versatile in terms of when and where it could be used (which body part, but also which geographical location), and for which indications to use it. They commented that they were fascinated by the breadth of what can be done with US: Yes, what I find interesting about US is that it can really be used in many different areas. (P7)
Advantages for patients
US as a tool was also described as having advantages for patients because it did not entail radiation, was non-invasive, and not painful. Another benefit for patients was that they could watch the examination “live”: You can show an image directly and that you can say to the patient “there it is and that’s how it is now. It’s good the way it is.” (P7) .
The power of visualisation
One key theme was the appeal of visualising things with US, and this contributed to the positive nimbus of US. For some participants, visualising organs was helpful because it matched their learning style: Well, personally, I’m just very much a visual person. (P8)
Most participants found it impressive to see inside the body and thereby gather a lot of information. It gave them a sense of security and the feeling that US was more objective and precise than other forms of examination: So yes, it seems to me that US is a bit more objective. (P5)
With the help of US, participants were easily able to confirm or exclude pathologies, which they found fascinating. Being able to capture an image was thought to be helpful too: some participants stated that it allowed them to show the image to others if they had any uncertainties, and to check that they had done it correctly: Something that you can see can perhaps be better discussed with other people afterwards. (P8)
Principal findings
In this qualitative interview study, medical students gave a range of reasons for their high motivation to learn US: the positive image surrounding the modality in general, with an emphasis on the advantages of visualisation; they perceived potential professional benefits; and they described it as a fun, exciting activity and a way to interact positively with other learners.
Interpretation of the results
The four themes we identified can be related to the three universal needs of autonomy, competence and relatedness described in SDT.
Mastering US skills contributed to a feeling of competence and autonomy. At the same time, feeling competent in performing US supported students in preparing for their transition from student to resident, giving them confidence in clinical situations and in interactions with patients, thus providing a professional advantage.
Learning US was described as an exciting and fun group activity. This perception aligns with the need for relatedness as described in SDT. The feeling that US was a practical alternation to their theoretical student life and a positive challenge map across to the need for competence.
The idea of learning to use a “modern”, technical tool, gave a feeling of autonomy and competence. Additionally, the fact that US is a mobile device compared to other imaging modalities was seen to offer a high degree of autonomy when deciding when and where to use it.
The visual aspect of US allows for just-in-time feedback and the immediate feeling of success when getting the right image, thus meeting the need for competence.
Whereas all four themes can be linked to the universal needs of SDT, the visual aspect of US and the positive nimbus surrounding US are more related to the “Zeitgeist”. In our study, participants’ comments suggested that they associated US with positive attributes and thought it would become increasingly important in the future. The sense that being able to visualise something was superior to other ways of examining– another subtheme we found– was central to this notion.
Comparison with existing literature
Other studies confirm that students believe learning US is an advantage in their medical studies [ 11 , 13 , 14 ]. A cross-sectional survey of graduates confirms that early US training yields physicians who are better prepared to integrate it into clinical practice [ 27 ]. While the transition from medical school to residency differs depending on the national context, it has been described as stressful and challenging in studies from different countries [ 28 , 29 ]. Early exposure to clinical environments in undergraduate years may help reduce the stress of this transition [ 29 ]. Integrating theoretical knowledge into practice in medical education has been an important issue in medical education for over a decade and remains so today. US teaching in undergraduate studies can aid professional identity formation [ 30 ]. Our results correspond with Wang et al.’s findings, that students are motivated to learn ultrasound because they believe it to be a necessity and/or advantage in their future work or current studies and because they want to learn out of interest. Wang et al. point out that relatedness played less of a role for students’ motivation, while in our study relatedness played an important role in the theme of “fun and exciting activity”. One possible explanation for this discrepancy could be that a distinction between motivation to initiate behaviour (e.g. sign up for a course) and to maintain motivation (e.g. stay motivated during the course) is seldom made. Participants in Wang et al’s study were questioned on motivation to initiate US learning, while in our study, participants had already begun or finished the US course and relatedness contributed to continuing motivation during the course but was seldom discussed as a reason for initial interest [ 19 ].
Our participants felt that visualisation enhanced the objectivity and reliability of an examination, providing a feeling of security, corresponding with Feilchenfeld et al.’s statement that “US’s visual evidence is viewed as truth, more accurate (truthful) than clinical information provided via other senses” [ 31 ]. This “Zeitgeist”, the “visuo-centric discourse” which claims the superiority of visual information over other data, may be common among medical students: a paper on body pedagogics states that “oculocentrism” (a perception of superiority of vision over other senses) is typical in Western society, especially in the medical profession [ 32 ]. The current discourse in our (medical) society that seeing is superior to, and more legitimate than, perceiving with other senses and is thus also beneficial for patient care seems to add to the “positive nimbus” of US and has an effect on students’ high motivation to learn the skill [ 26 , 28 ].
This is the first qualitative study designed to study medical students’ motivation for US education. The design of the interview guide and the interpretation of the results were guided by a consistent theoretical framework (SDT). We interviewed participants from two different medical schools. We piloted the interview guides carefully, achieved data saturation and member-checked the findings.
Limitations
Our participants were from a population taking part in a course with no curricular accreditation, making it likely that they had a high degree of motivation. The participants were students who volunteered to take part in the study, resulting in a risk of self-selection bias. We assumed that the students participating in a voluntary course and voluntarily taking part in the study would be especially highly motivated. Because our aim was to explore high levels of motivation for ultrasound, we hypothesise that the sample was in line with our research question. The factors motivating these students may not apply to other students, for example students with low motivation to learn ultrasound. Including a more varied sample might have given us other insights. Due to the COVID-19 pandemic, we could not stratify participants as intended, as US courses were put on hold for some time. Many students were busy with volunteer work at health facilities and may have been less willing to meet face-to-face. However, there was an equal number of participants from both Universities, and the gender distribution approximately reflects the gender distribution in Swiss medical studies. Also, the participants came from a homogenous group, which makes it more likely that the sample was adequate [ 33 ].
Implications for research and practice
Understanding the mechanisms of motivation in medical education helps to create a supportive learning environment and to nurture autonomous motivation. While some of our findings were specific to the modality of US, some can also be applied to other teaching areas:
Visualisation aids learning, providing immediate feedback, a sense of competence and of autonomy, adding to the motivation. For areas where visualisation is not an option, educators should consider using alternative ways to give immediate feedback, when planning educational programmes. This could mean verbally providing immediate and constructive feedback, or using a portfolio to visually track learners’ progress.
Participants found learning US fun and exciting. Not all areas of learning allow for the hands-on experience of US education, but reflecting on where practical aspects can be integrated into teaching and how to challenge students optimally– making tasks not too easy nor too difficult– could enhance students’ motivation. One example is the “gameification” of learning content, which may add to the fun factor. Educators should enable group experiences and interaction when possible. This could be supported by encouraging students to actively participate in group work, giving a structure to educational units, while also providing enough room to learn in a self-directed way as a group. Facilitators to this can be a setting of mutual trust and open dialogue, and adjusting the learning environment, for example by considering seating arrangements.
Students are motivated to learn things that will benefit them professionally, making awareness of the clinical relevance of learning content essential. Explicitly addressing concerns about transitioning from medical school to residency and providing information on how a specific skill will help for this transition could increase students’ motivation to learn. Pointing out the relevance of the subject to medical practice could help less enthusiastic students see the importance of it and result in a more autonomous– rather than controlled– choice to learn something [ 34 ].
Educators should be aware that learning happens in the context and discourse of society, and that this can affect both educators’ and learners’ perspectives and motivation. While educators cannot influence the discourse directly, it is important to understand its existence, to modify barriers and facilitate motivation. The mechanisms of such discourses and their possible impact on students’ views require more research.
Future quantitative studies could explore to which extent a more general medical student population relates to the identified themes in order to validate them. Including students with low motivation for ultrasound or students with high motivation in other areas as participants and comparing and contrasting these results with those of this study could also provide a more comprehensive view of motivational factors and be an interesting area for further research. Factors which initially sparked participants’ interest and motivation to sign up for the course may be different to those which maintained and increased their motivation during the course. Longitudinal studies would enable a deeper understanding of such nuances and other changes in motivation over time.
We found four themes that have not yet been described in the literature: US was perceived as helpful in contextualising and exemplifying other learning content and supporting the transition into professional identity and, ultimately, clinical practice; the group setting with just-in-time feedback provides a fun and positive learning experience; participants reported being motivated to learn US because it was the tool of the future, and being able to visualise something trumped other forms of examination, reflecting the visuo-centric Zeitgeist. Knowledge and understanding of these themes may be relevant to other areas of medical education.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
participant
Sobral DT. What kind of motivation drives medical students’ learning quests? Medical Education [Internet]. 2004 [cited 2019 Apr 16];38(9):950–7. https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/j.1365-2929.2004.01913.x .
Moulaert V, Verwijnen MGM, Rikers R, Scherpbier AJJA. The effects of deliberate practice in undergraduate medical education. Med Educ [Internet]. 2004 Oct [cited 2020 May 27];38(10):1044–52. https://doi.org/10.1111/j.1365-2929.2004.01954.x .
Kusurkar RA, Ten Cate TJ, Vos CMP, Westers P, Croiset G. How motivation affects academic performance: a structural equation modelling analysis. Advances in Health Sciences Education [Internet]. 2013 Mar [cited 2020 May 4];18(1):57–69. http://link.springer.com/ https://doi.org/10.1007/s10459-012-9354-3 .
Babenko O, Daniels L, Ross S, White J, Oswald A. Medical student well-being and lifelong learning: A motivational perspective. Educ Health [Internet]. 2019 [cited 2023 Jul 11];32(1):25. https://journals.lww.com/ https://doi.org/10.4103/efh.EfH_237_17 .
Ryan RM, Deci EL. Intrinsic and Extrinsic Motivations: Classic Definitions and New Directions. Contemporary Educational Psychology [Internet]. 2000 Jan [cited 2019 Jul 4];25(1):54–67. https://linkinghub.elsevier.com/retrieve/pii/S0361476X99910202 .
Kusurkar RA. Autonomous motivation in medical education. Medical Teacher [Internet]. 2019 Sep 2 [cited 2023 Jul 11];41(9):1083–4. https://www.tandfonline.com/doi/full/10.1080/0142159X.2018.1545087 .
Ryan RM, Deci EL. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. American Psychologist. 2000;11.
Cook DA, Artino AR. Motivation to learn: an overview of contemporary theories. Medical Education [Internet]. 2016 [cited 2019 Apr 10];50(10):997–1014. https://onlinelibrary.wiley.com/doi/abs/10.1111/medu.13074 .
ten Cate OTJ, Kusurkar RA, Williams GC. How self-determination theory can assist our understanding of the teaching and learning processes in medical education. AMEE Guide No. 59. Medical Teacher [Internet]. 2011 Dec [cited 2020 Sep 5];33(12):961–73. http://www.tandfonline.com/doi/full/ https://doi.org/10.3109/0142159X.2011.595435 .
Birrane J, Misran H, Creaney M, Shorten G, Nix CM. A Scoping Review of Ultrasound Teaching in Undergraduate Medical Education. MedSciEduc [Internet]. 2018 Mar [cited 2019 Jul 3];28(1):45–56. http://link.springer.com/ https://doi.org/10.1007/s40670-017-0491-4 .
Hammoudi N, Arangalage D, Boubrit L, Renaud MC, Isnard R, Collet JP et al. Ultrasound-based teaching of cardiac anatomy and physiology to undergraduate medical students. Archives of Cardiovascular Diseases [Internet]. 2013 Oct [cited 2020 May 5];106(10):487–91. https://linkinghub.elsevier.com/retrieve/pii/S1875213613001976 .
Limchareon S, Asawaworarit N, Klinwichit W, Dinchuthai P. Development of the ultrasonography learning model for undergraduate medical students: A case study of the Faculty of Medicine, Burapha University. Journal of the Chinese Medical Association [Internet]. 2016 Aug [cited 2020 May 5];79(8):445–9. https://linkinghub.elsevier.com/retrieve/pii/S1726490116300077 .
Rempell JS, Saldana F, DiSalvo D, Kumar N, Stone MB, Chan W et al. Pilot Point-of-Care Ultrasound Curriculum at Harvard Medical School: Early Experience. West J Emerg Med [Internet]. 2016 Nov [cited 2019 Jul 3];17(6):734–40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5102600/ .
Recker F, Barth G, Lo H, Haverkamp N, Nürnberg D, Kravchenko D et al. Students’ Perspectives on Curricular Ultrasound Education at German Medical Schools. Front Med [Internet]. 2021 Nov 25 [cited 2024 Mar 5];8:758255. https://www.frontiersin.org/articles/ https://doi.org/10.3389/fmed.2021.758255/full .
Dietrich CF, Hoffmann B, Abramowicz J, Badea R, Braden B, Cantisani V et al. Medical Student Ultrasound Education: A WFUMB Position Paper, Part I. Ultrasound in Medicine & Biology [Internet]. 2019 Feb [cited 2023 Jul 11];45(2):271–81. https://linkinghub.elsevier.com/retrieve/pii/S0301562918304174 .
Jahns J, Recker F, Thiessen V, Rüenauver K, Bailer B. Sono4Students– sonographische Lehre nach dem Peer-teaching Prinzip. Ultraschall in der Medizin - European Journal of Ultrasound [Internet]. 2014 Sep 24 [cited 2020 May 5];35(S 01). http://www.thieme-connect.de/DOI/DOI?10.1055/s-0034-1389403 .
Hoppmann RA, Rao VV, Bell F, Poston MB, Howe DB, Riffle S et al. The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit Ultrasound J [Internet]. 2015 Dec [cited 2020 Aug 26];7(1):18. https://theultrasoundjournal.springeropen.com/articles/ https://doi.org/10.1186/s13089-015-0035-3 .
Kefala-Karli P, Sassis L, Sassi M, Zervides C. Introduction of ultrasound-based living anatomy into the medical curriculum: a survey on medical students’ perceptions. Ultrasound J [Internet]. 2021 Dec [cited 2023 Jul 11];13(1):47. https://theultrasoundjournal.springeropen.com/articles/ https://doi.org/10.1186/s13089-021-00247-1 .
Wang TC, Chen WT, Kang YN, Lin CW, Cheng CY, Suk FM et al. Why do pre-clinical medical students learn ultrasound? Exploring learning motivation through ERG theory. BMC Med Educ [Internet]. 2021 Dec [cited 2024 Mar 5];21(1):438. https://bmcmededuc.biomedcentral.com/articles/ https://doi.org/10.1186/s12909-021-02869-4 .
Ng SL, Baker L, Cristancho S, Kennedy TJ, Lingard L. Qualitative Research in Medical Education: Methodologies and Methods. In: Swanwick T, Forrest K, O’Brien BC, editors. Understanding Medical Education [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 2018 [cited 2020 May 5]. pp. 427–41. https://doi.org/10.1002/9781119373780.ch29 .
Castleberry A, Nolen A. Thematic analysis of qualitative research data: Is it as easy as it sounds? Currents in Pharmacy Teaching and Learning [Internet]. 2018 Jun [cited 2020 May 5];10(6):807–15. https://linkinghub.elsevier.com/retrieve/pii/S1877129717300606 .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care [Internet]. 2007 Sep 16 [cited 2024 Apr 7];19(6):349–57. https://academic.oup.com/intqhc/article-lookup/doi/ https://doi.org/10.1093/intqhc/mzm042 .
Räschle N, Hari R. «Blended Learning»-Basiskurs Sonografie: Im Peer-Tutoring zu einem SGUM-akkreditierten Ultraschall-Kurs. Praxis [Internet]. 2018 Nov [cited 2024 Mar 13];107(23):1255–9. https://econtent.hogrefe.com/doi/ https://doi.org/10.1024/1661-8157/a003116 .
Charmaz K. Constructing grounded theory. 2nd edition. London; Thousand Oaks, Calif: Sage; 2014. 388 p. (Introducing qualitative methods).
Cristancho S, Goldszmidt M, Lingard L, Watling C. Qualitative research essentials for medical education. Singapore Medical Journal [Internet]. 2018 Dec [cited 2020 May 5];59(12):622–7. http://www.smj.org.sg/article/qualitative-research-essentials-medical-education .
Morse JM. The Significance of Saturation. Qualitative Health Research [Internet]. 1995 May [cited 2020 May 5];5(2):147–9. http://journals.sagepub.com/doi/10.1177/104973239500500201 .
Prats MI, Royall NA, Panchal AR, Way DP, Bahner DP. Outcomes of an Advanced Ultrasound Elective: Preparing Medical Students for Residency and Practice. Journal of Ultrasound in Medicine [Internet]. 2016 May [cited 2023 Jul 11];35(5):975–82. https://doi.org/10.7863/ultra.15.06060 .
Chang LY, Eliasz KL, Cacciatore DT, Winkel AF. The Transition From Medical Student to Resident: A Qualitative Study of New Residents’ Perspectives. Academic Medicine [Internet]. 2020 Sep [cited 2020 Sep 7];95(9):1421–7. https://journals.lww.com/ https://doi.org/10.1097/ACM.0000000000003474 .
Brennan N, Corrigan O, Allard J, Archer J, Barnes R, Bleakley A et al. The transition from medical student to junior doctor: today’s experiences of Tomorrow’s Doctors. Medical Education [Internet]. 2010 May [cited 2020 Sep 8];44(5):449–58. https://doi.org/10.1111/j.1365-2923.2009.03604.x .
Darici D, Missler M, Schober A, Masthoff M, Schnittler H, Schmitz M. Fun slipping into the doctor’s role—The relationship between sonoanatomy teaching and professional identity formation before and during the Covid-19 pandemic. Anatomical Sciences Ed [Internet]. 2022 May [cited 2023 Jul 11];15(3):447–63. https://onlinelibrary.wiley.com/doi/ https://doi.org/10.1002/ase.2178 .
Feilchenfeld Z, Kuper A, Whitehead C. Stethoscope of the 21st century: dominant discourses of ultrasound in medical education. Medical Education [Internet]. 2018 [cited 2019 Jul 3];52(12):1271–87. https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/medu.13714 .
Kelly M, Ellaway R, Scherpbier A, King N, Dornan T. Body pedagogics: embodied learning for the health professions. Med Educ [Internet]. 2019 Oct [cited 2020 Aug 11];53(10):967–77. https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/medu.13916 .
Guest G, Bunce A, Johnson L. How Many Interviews Are Enough? An Experiment with Data Saturation and Variability. Field Methods [Internet]. 2006 Feb [cited 2020 Sep 5];18(1):59–82. http://journals.sagepub.com/doi/ https://doi.org/10.1177/1525822X05279903 .
Kusurkar RA, Croiset G, Ten Cate OTJ. Twelve tips to stimulate intrinsic motivation in students through autonomy-supportive classroom teaching derived from Self-Determination Theory. Medical Teacher [Internet]. 2011 Dec [cited 2024 Mar 4];33(12):978–82. http://www.tandfonline.com/doi/full/ https://doi.org/10.3109/0142159X.2011.599896 .
Download references
Acknowledgements
We thank Benjamin Bulling for his literature review of motivation theories and for the transcription of interviews. We thank Katharina Lüscher for the interview transcription.
This research received no external funding.
Author information
Anina Pless, Roman Hari contributed equally to this work.
Authors and Affiliations
Institute of Primary Health Care (BIHAM), University of Bern, Mittelstrasse 43, 3012, Bern, Switzerland
Anina Pless, Roman Hari & Michael Harris
College of Medicine & Health, University of Exeter Medical School, Exeter, UK
Michael Harris
You can also search for this author in PubMed Google Scholar
Contributions
AP and RH contributed to the conception of the work. AP, RH and MH contributed to the design of the work. AP did the acquisition and primary analysis. AP, MH and RH interpreted the data. AP wrote the main manuscript and MH and RH substantively revised it. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Anina Pless .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
The study was submitted to the regional ethics committee (Kantonale Ehtikkommission für die Forschung, Gesundheits- und Fürsorgedirektion des Kantons Bern). A waiver was issued, stating that the study does not fall under the Swiss Human Research Act (BASEC-Nr. Req-2018-00059).
Consent for publication
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pless, A., Hari, R. & Harris, M. Why are medical students so motivated to learn ultrasound skills? A qualitative study. BMC Med Educ 24 , 458 (2024). https://doi.org/10.1186/s12909-024-05420-3
Download citation
Received : 08 February 2024
Accepted : 12 April 2024
Published : 26 April 2024
DOI : https://doi.org/10.1186/s12909-024-05420-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Medical education
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Korean J Med Educ
- v.29(2); 2017 Jun
The qualitative orientation in medical education research
Qualitative research is very important in educational research as it addresses the “how” and “why” research questions and enables deeper understanding of experiences, phenomena and context. Qualitative research allows you to ask questions that cannot be easily put into numbers to understand human experience. Getting at the everyday realities of some social phenomenon and studying important questions as they are really practiced helps extend knowledge and understanding. To do so, you need to understand the philosophical stance of qualitative research and work from this to develop the research question, study design, data collection methods and data analysis. In this article, I provide an overview of the assumptions underlying qualitative research and the role of the researcher in the qualitative process. I then go on to discuss the type of research objectives which are common in qualitative research, then introduce the main qualitative designs, data collection tools, and finally the basics of qualitative analysis. I introduce the criteria by which you can judge the quality of qualitative research. Many classic references are cited in this article, and I urge you to seek out some of these further reading to inform your qualitative research program.
Introduction
When we speak of “quantitative” or “qualitative” methodologies, we are in the final analysis speaking about an interrelated set of assumptions about the social world which are philosophical, ideological, and epistemological. They encompass more than just data collection methodologies [ 1 ].
It is easy to assume that the differences between quantitative and qualitative research are solely about how data is collected—the randomized controlled trial versus ethnographic fieldwork, the cohort study versus the semi-structured interview. However, quantitative and qualitative approaches make different assumptions about the world [ 2 ], about how science should be conducted, and about what constitutes legitimate problems, solutions and criteria of “proof” [ 3 ].
Why is it important to understand differences in assumptions, or philosophies, of research? Why not just go ahead and do a survey or carry out some interviews? First, the assumptions behind the research tools you choose provide guidance for conducting your research. They indicate whether you should be an objective observer or whether you have a contributory role in the research process. They guide whether or not you must slavishly ask each person in a study the same questions or whether your questions can evolve as the study progresses. Second, you may wish to submit your work as a dissertation or as a research paper to be considered for publication in a journal. If so, the chances are that examiners, editors, and reviewers might have knowledge of different research philosophies from yours and may be unwilling to accept the legitimacy of your approach unless you can make its assumptions clear. Third, each research paradigm has its own norms and standards, its accepted ways of doing things. You need to “do things right”. Finally, understanding the theoretical assumptions of the research approach helps you recognize what the data collection and analysis methods you are working with do well and what they do less well, and lets you design your research to take full advantage of their strengths and compensate for their weaknesses.
In this short article, I will introduce the assumptions of qualitative research and their implications for research questions, study design, methods and tools, and analysis and interpretation. Readers who wish a comparison between qualitative and quantitative approaches may find Cleland [ 4 ] useful.
Ontology and epistemology
We start with a consideration of the ontology (assumptions about the nature of reality) and epistemology (assumptions about the nature of knowledge) of qualitative research.
Qualitative research approaches are used to understand everyday human experience in all its complexity and in all its natural settings [ 5 ]. To do this, qualitative research conforms to notions that reality is socially constructed and that inquiry is unavoidably value-laden [ 6 ]. The first of these, reality is socially constructed, means reality cannot be measured directly—it exists as perceived by people and by the observer. In other words, reality is relative and multiple, perceived through socially constructed and subjective interpretations [ 7 ]. For example, what I see as an exciting event may be seen as a threat by other people. What is considered a cultural ritual in my country may be thought of as quite bizarre elsewhere. Qualitative research is concerned with how the social world is interpreted, understood, experienced, or constructed. Mann and MacLeod [ 8 ] provide a very good overview of social constructivism which is a excellent starting point for understanding this.
The idea of people seeing things in diverse ways also holds true in research process, hence inquiry being valued-laden. Different people have different views of the same thing depending on their upbringing and other experiences, their training, and professional background. Someone who has been trained as a social scientist may “see” things differently from someone who has been medically trained. A woman may see things differently to a man. A more experienced researcher will see things differently from a novice. A qualitative researcher will have very different views of the nature of “evidence” than a quantitative researcher. All these viewpoints are valid. Moreover, different researchers can study the same topic and try to find solutions to the same challenges using different study designs—and hence come up with different interpretations and different recommendations. For example, if your position is that learning is about individual, cognitive, and acquisitive processes, then you are likely to research the use of simulation training in surgery in terms of the effectiveness and efficacy of training related to mastery of technical skills [ 9 , 10 ]. However, if your stance is that learning is inherently a social activity, one which involves interactions between people or groups of people, then you will look to see how the relationships between faculty members, participants and activities during a simulation, and the wider social and cultural context, influence learning [ 11 , 12 ].
Whether researchers are explicit about it or not, ontological and epistemological assumptions will underpin how they study aspects of teaching and learning. Differences in these assumptions shape not only study design, but also what emerges as data, how this data can be analysed and even the conclusions that can be drawn and recommendations that can be made from the study. This is referred to as worldview, defined by Creswell [ 13 ] as “a general orientation about the world and the nature of research that a researcher holds.” McMillan [ 14 ] gives a very good explanation of the importance of this phenomenon in relation to medical education research. There is increasing expectation that researchers make their worldview explicit in research papers.
The research objective
Given the underlying premise that reality is socially constructed, qualitative research focuses on answering “how” and “why” questions, of understanding a phenomena or a context. For example, “Our study aimed to answer the research question: why do assessors fail to report underperformance in medical students? [ 15 ]”, “The aim of this work was to investigate how widening participation policy is translated and interpreted for implementation at the level of the individual medical school [ 4 ].”
Common verbs in qualitative research questions are identify, explore, describe, understand, and explain. If your research question includes words like test or measure or compare in your objectives, these are more appropriate for quantitative methods, as they are better suited to these types of aims. Bezuidenhout and van Schalkwyk [ 16 ] provide a good guide to developing and refining your research question. Lingard [ 17 ]’s notion of joining the conversation and the problem-gap-hook heuristic are also very useful in terms of thinking about your question and setting it out in the introduction to a paper in such a way as to interest journal editors and readers.
Do not think formulating a research question is easy. Maxwell [ 18 ] gives a good overview of some of the potential issues including being too general, making assumptions about the nature of the issue/problem and using questions which focus the study on difference rather than process. Developing relevant, focused, answerable research questions takes time and generating good questions requires that you pay attention not just to the questions themselves but to their connections with all the other components of the study (the conceptual lens/theory, the methods) [ 18 ].
Theory can be applied to qualitative studies at different times during the research process, from the selection of the research phenomenon to the write-up of the results. The application of theory at different points can be described as follows [ 19 , 20 , 21 ]: (1) Theory frames the study questions, develops the philosophical underpinnings of the study, and makes assumptions to justify or rationalize the methodological approach. (2) Qualitative investigations relate the target phenomenon to the theory. (3) Theory provides a comparative context or framework for data analysis and interpretation. (4) Theory provides triangulation of study findings.
Schwartz-Barcott et al. [ 20 ] characterized those processes as theoretical selectivity (the linking of selected concepts with existing theories), theoretical integration (the incorporation and testing of selected concepts within a particular theoretical perspective), and theory creation (the generation of relational statements and the development of a new theory). Thus, theory can be the outcome of the research project as well as the starting point [ 22 ].
However, the emerging qualitative researcher may wish a little more direction on how to use theory in practice. I direct you to two papers: Reeves et al. [ 23 ] and Bordage [ 24 ]. These authors clearly explain the utility of theory, or conceptual frameworks, in qualitative research, how theory can give researchers different “lenses” through which to look at complicated problems and social issues, focusing their attention on different aspects of the data and providing a framework within which to conduct their analysis. Bordage [ 24 ] states that “conceptual frameworks represent ways of thinking about a problem or a study, or ways of representing how complex things work the way they do. Different frameworks will emphasise different variables and outcomes.” He presents an example in his paper and illustrates how different lens highlight or emphasise different aspects of the data. Other authors suggest that two theories are potentially better than one in exploring complex social issues [ 25 ]. There is an example of this in one of my papers, where we used the theories of Bourdieu [ 26 ] and Engestrom [ 27 , 28 ] nested within an overarching framework of complexity theory [ 29 ] to help us understand learning at a surgical bootcamp. However, I suggest that for focused studies and emerging educational researchers, one theoretical framework or lens is probably sufficient.
So how to identify an appropriate theory, and when to use it? It is crucially important to read widely, to explore lots of theories, from disciplines such as (but not only) education, psychology, sociology, and economics, to see what theory is available and what may be suitable for your study. Carefully consider any theory, check its assumptions [ 30 ] are congruent with your approach, question, and context before final selection [ 31 ] before deciding which theory to use. The time you spend exploring theory will be time well spent in terms not just of interpreting a specific data set but also to broadening your knowledge. The second question, when to use it, depends on the nature of the study, but generally the use of theory in qualitative research tends to be inductive; that is, building explanations from the ground up, based on what is discovered. This typically means that theory is brought in at the analysis stage, as a lens to interpret data.
In the qualitative approach, the activities of collecting and analyzing data, developing and modifying theory, and elaborating or refocusing the research questions, are usually going on more or less simultaneously, each influencing all of the others for a useful model of qualitative research design [ 18 ]. The researcher may need to reconsider or modify any design decision during the study in response to new developments. In this way, qualitative research design is less linear than quantitative research, which is much more step-wise and fixed.
This is not the same as no structure or plan. Most qualitative projects are pre-structured at least in terms of the equivalent of a research protocol, setting out what you are doing (aims and objectives), why (why is this important), and how (theoretical underpinning, design, methods, and analysis). I have provided a brief overview of common approaches to qualitative research design below and direct you to the numerous excellent textbooks which go into this in more detail [ 32 , 33 , 34 , 35 ].
There are five basic categories of qualitative research design: ethnography, narrative, phenomenological, grounded theory, and case study [ 13 , 32 ].
2. Ethnography
In ethnography, you immerse yourself in the target participants’ environment to understand the goals, cultures, challenges, motivations, and themes that emerge. Ethnography has its roots in cultural anthropology where researchers immerse themselves within a culture, often for years. Through multiple data collection approaches—observations, interviews and documentary data, ethnographic research offers a qualitative approach with the potential to yield detailed and comprehensive accounts of different social phenomenon (actions, behavior, interactions, and beliefs). Rather than relying on interviews or surveys, you experience the environment first hand, and sometimes as a “participant observer” which gives opportunity to gather empirical insights into social practices which are normally “hidden” from the public gaze. Reeves et al. [ 36 ] give an excellent guide to ethnography in medical education which is essential reading if you are interested in using this approach.
3. Narrative
The narrative approach weaves together a sequence of events, usually from just one or two individuals to form a cohesive story. You conduct in-depth interviews, read documents, and look for themes; in other words, how does an individual story illustrate the larger life influences that created it. Often interviews are conducted over weeks, months, or even years, but the final narrative does not need to be in chronological order. Rather it can be presented as a story (or narrative) with themes, and can reconcile conflicting stories and highlight tensions and challenges which can be opportunities for innovation.
4. Phenomenology
Phenomenology is concerned with the study of experience from the perspective of the individual, “bracketing” taken-for-granted assumptions and usual ways of perceiving. Phenomenological approaches emphasise the importance of personal perspective and interpretation. As such they are powerful for understanding subjective experience, gaining insights into people’s motivations and actions, and cutting through the clutter of taken-for-granted assumptions and conventional wisdom.
Phenomenological approaches can be applied to single cases or to selected samples. A variety of methods can be used in phenomenologically-based research, including interviews, conversations, participant observation, action research, focus meetings, and analysis of personal texts. Beware though—phenomenological research generates a large quantity data for analysis.
The phenomenological approach is used in medical education research and there are some good articles which will familiarise you with this approach [ 37 , 38 ].
5. Grounded theory
Whereas a phenomenological study looks to describe the essence of an activity or event, grounded theory looks to provide an explanation or theory behind the events. Its main thrust is to generate theories regarding social phenomena: that is, to develop higher level understanding that is “grounded” in, or derived from, a systematic analysis of data [ 39 ]. Grounded theory is appropriate when the study of social interactions or experiences aims to explain a process, not to test or verify an existing theory. Rather, the theory emerges through a close and careful analysis of the data.
The key features of grounded theory are its iterative study design, theoretical (purposive) sampling, and cycles of simultaneous data collection and analysis, where analysis informs the next cycle of data collection. In keeping with this iterative design, the sample is not set at the outset but is selected purposefully as the analysis progresses; participants are chosen for their ability to confirm or challenge an emerging theory. As issues of interest are noted in the data, they are compared with other examples for similarities and differences.
Grounded theory was first proposed by Glaser and Strauss [ 40 ] in 1967 but since then there have been many interpretations of this approach, each with their own processes and norms [ 41 , 42 , 43 ].
Beware—grounded theory is often done very badly, and numerous studies are rejected by journals because they claim to use grounded theory but do not actually do so, or do so badly.
6. Case study
Researcher Yin [ 44 ] defines the case study research method as an empirical inquiry that investigates a contemporary phenomenon within its real-life context; when the boundaries between phenomenon and context are not clearly evident; and in which multiple sources of evidence are used. The case study method enables a researcher to closely examine the data within a specific context—for example, in a small geographical area or a very limited number of individuals as the subjects of study. Case studies explore and investigate contemporary real-life phenomenon through detailed contextual analysis of a limited number of events or conditions, and their relationships. A case study involves a deep understanding through multiple types of data sources. For example, we used case study methodology recently to explore the nature of the clinical learning environment in a general surgical unit, and used both documents and interviews as data sources. Case studies can be explanatory, exploratory, or describing an event [ 44 ] and case study design can be very open or more structured [ 45 ]. Case studies are a useful approach where the focus is to explain the complexities of real life situations.
While the five methods generally use similar data collection techniques (observation, interviews, and reviewing text—see below), the purpose of the study differentiates them.
Data collection methods
The qualitative methods most commonly used for research purposes can be classified in three broad categories: (1) interviews (individual or group), (2) observation methods, and (3) document review.
The qualitative research interview seeks to describe and gain understanding of certain themes in the life world of the subjects. Interviews can be organised one-to-one or group (focus groups) depending on the topic under study, the cultural context, and the aims of the project. Observational data collection in qualitative research involves the detailed observation of people and events to learn about behaviors and interactions in natural settings [ 46 ]. Such study designs are useful when the study goal is to understand cultural aspects of a setting or phenomenon [ 47 ], when the situation of interest is hidden, (tacit), or when subjects in the setting appear to have notably different views to other groups. Written materials or documents such as institutional records, personal diaries, and historical public documents may also serve as a valuable source of secondary data, providing insight into the lives and experiences of the group under study. For example, in one of my recent studies we used document analysis to uncover the thinking behind the design of a new medical school, then carried out interviews with “users” of the new building to explore how the intentions of the planners played out in reality. However, this is only one way of incorporating document analysis into a study: see Bowen [ 48 ] for an excellent introduction to the purpose and practicalities of document review within qualitative research.
See Dicicco-Bloom and Crabtree [ 49 ] for a useful summary of the content and process of the qualitative research interview, Creswell [ 50 ] for further discussion of the many different approaches in qualitative research and their common characteristics.
1. Data management
Qualitative research may use some form of quantification, but statistical forms of analysis are not central [ 51 ]. Instead, qualitative data analysis aims to uncover emerging themes, patterns, concepts, insights, and understandings [ 52 ]. The data are allowed to “speak for themselves” by the emergence of conceptual categories and descriptive themes. Trying to squeeze narratives into boxes (like “0” and “1”) would result in the loss of contextualisation and narrative layering. The researcher must immerse themselves in the data in order to be able to see meaningful patterns and themes, making notes as they go through the processes of data collection and analysis, and then using these notes to guide the analysis strategy.
Qualitative data has to be managed before it can be analysed—you can generate a lot of data from just a few interviews or observations! You may want to use a specialist qualitative database to facilitate data management and analysis. NVivo is a well-known qualitative data analysis software package (note that qualitative software packages enable you to make and store notes, and explanations of your codes, so you do not need to juggle bits of paper and electronic data files). These and similar databases are available commercially (i.e., at a cost) and are used widely by universities. The choice of database may be dictated by the resources of your institution, your personal preference, and/or what technical support is available locally. However, if you do not have access to qualitative data management software, then use paper and pencil: read and re-read transcripts, take notes on specifics and the bigger patterns, and label different themes with different coloured pen. You do all this in a software package anyway, as data management software does not describe or analyse your data for you. See Cleland et al. [ 53 ] for comprehensive guidance on how to use qualitative databases in education research.
Data analysis
While bearing in mind that qualitative data collection and analysis are iterative rather than linear (see earlier), Miles and Huberman [ 54 ] explain the process of qualitative data analysis as (1) data reduction (extracting the essence), (2) data display (organizing for meaning), and (3) drawing conclusions (explaining the findings).
Data analysis usually follows an inductive approach where the data are allowed to “speak for themselves” by the emergence of conceptual categories and descriptive themes. The researcher must be open to multiple possibilities or ways to think about a problem, engaging in “mental excursions” using multiple stimuli, “side-tracking” or “zigzagging,” changing patterns of thinking, making linkages between the “seemingly unconnected,” and “playing at it,” all with the intention of “opening the world to us in some way” [ 52 ]. The researcher must immerse themselves in the data in order to be able to see meaningful patterns and themes, making notes as they go through the processes of data collection and analysis, and then using these notes to guide the analysis strategy and the development of a coding framework.
In this way, good qualitative research has a logical chain of reasoning, multiple sources of converging evidence to support an explanation, and rules out rival hypotheses with convincing arguments and solid data. The wider literature and theory are used to derive analytical frameworks as the process of analysis develops and different interpretations of the data are likely to be considered before the final argument is built. For example, one of our own studies aimed to explore how widening access policy is translated and implemented at the level of individual medical schools [ 4 ]. Data was collected via individual interviews with key personnel. We initially conducted a primary level thematic analysis to determine themes. After the themes emerged, and following further team discussion, we explored the literature, identified and considered various theories, in some depth, before identifying the most appropriate theory or conceptual lens for a secondary, theory-driven analysis.
There are some excellent text books which discuss qualitative data analysis in detail [ 35 , 55 ].
Judging the quality of research
There are various criteria by which you can judge the quality of qualitative research. These link to efforts by the research team to consider their findings. The most common ways of doing so are triangulation, respondent validation, reflexivity, detail and process, and fair dealing [ 56 ] (but see also Varpio et al. [ 57 ] for a detailed discussion of the limitations of some of these methods).
Triangulation compares the results from either two or more different methods of data collection (for example, interviews and observation) or, more simply, two or more data sources (for example, interviews with different people). The researcher looks for patterns of convergence to develop or corroborate an overall interpretation. This is as a way of ensuring comprehensiveness. Respondent validation, or “member checking,” includes techniques in which the investigator’s account is compared with those of the research subjects to establish the level of correspondence between the two sets. Study participants’ reactions to the analyses are then incorporated into the study findings. Providing a clear account of the process of data collection and analysis is important. By the end of the study, it should be possible to provide a clear account of how early, simple coding evolved into more sophisticated coding structures and thence into clearly defined concepts and explanations for the data collected. Reflexivity is discussed earlier but in terms of analysis reflexivity means sensitivity to the ways in which the researcher and the research process have shaped the collected data, including the role of prior assumptions and experience. These two points address credibility, whether the study has been conducted well and the findings seem reasonable. It is important to pay attention to “negative cases,” data that contradict, or seem to contradict, the emerging explanation of the phenomena under study. These can be a very useful source of information in terms of refining the analysis and thinking beyond the obvious. The final technique is to ensure that the research design explicitly incorporates a wide range of different perspectives. In practice this can mean presenting data from a wide range of diverse participants. A very practical point is worth mentioning here—any reviewer will want to see quotes labelled in some way; for example, P11FFG2 would be participant 11, female, focus group 2). This helps the reader see that your data does not just represent the view of one or two people, but that there is indeed some sort of pattern or commonality to report.
Guba and Lincoln [ 58 ] provide the following criteria for judging qualitative research: credibility, transferability, dependability, and confirmability. I direct you to the original resource and to a very good explanation of these criteria in Mann and MacLeod [ 8 ].
Qualitative research is very important in educational research as it addresses the “how” and “why” research questions and enables deeper understanding of experiences, phenomena, and context. Qualitative research allows you to ask questions that cannot be easily put into numbers to understand human experience. Getting at the everyday realities of some social phenomenon and studying important questions as they are really practiced helps answer big questions. To do so, you need to understand the philosophical stance of qualitative research and work from this to develop the research question, study design, data collection methods, and data analysis.

IMAGES
VIDEO
COMMENTS
In quantitative research, importance is placed on the researcher acting as an outsider to take an objective view by keeping a certain distance from the research subject. ... In the healthcare field, qualitative research is conducted on various topics considering its characteristics and strengths. ... Han YJ. Medical litigation experience of the ...
In qualitative research, these questions explore reasons for why people do things or believe in something and tend to try to cover the drivers for behaviours, attitudes and motivations, instead of just the countable details. 2 It is important to strike a balance between a research question that is all-encompassing and one that is researchable ...
Background The interest for qualitative research methodology has expanded beyond theoretical academic research on medical education, gathering interest from all healthcare professionals. Qualitative research has potentials in exploring the social, emotional, psychological aspects of care and in broadening professionals' scientific competencies. Nonetheless, qualitative research has still not ...
In last month's PLoS Medicine, Salla Munro and colleagues argue that qualitative studies—in which researchers listen to what patients, care givers, and health care providers have to say—can provide important insights into why nonadherence occurs [ 3 ]. Their paper is a "meta-ethnography" [ 4 ], a systematic review and synthesis of ...
Qualitative studies are often used to research phenomena that are difficult to quantify numerically.1,2 These may include concepts, feelings, opinions, interpretations and meanings, or why people behave in a certain way. Although qualitative research is often described in opposition to quantitative research, the approaches are complementary, and many researchers use mixed methods in their ...
The strengths and historical dominance of quantitative research in the health care domain is well-established, but the importance of rigorous qualitative research as both a complement to, and a mechanism for, augmenting quantitative methods is increasingly being recognized and used across health-related disciplines.
The benefits of qualitative research in healthcare include: 2. Firsthand documentation of patient experiences. An overview of suggestions for improvement. The ability to detect common concerns and desires associated with the quality of care. Information about what matters most to patients.
In recent years, qualitative research methods have become increasingly prominent in medical education. The reason is simple: some of the most pressing questions in the field require qualitative approaches for meaningful answers to be found. Qualitative research examines how things unfold in real world settings.
Seven qualitative research methods are presented, defined and cited in the current literature. The qualitative research methods presented include: ethnography, grounded theory, case study, phenomenology, hermeneutics, narrative research, and action research. Data collection techniques used in all of the qualitative methods are presented and ...
Qualitative research has several applications in the medical field, and selecting the appropriate qualitative research methodology to answer a specific question is important [5]. ...
Qualitative research plays an important role in advancing practice and policy in education both inside and out of the field of medicine. 1,2 Qualitative methods allow for in- depth understanding of human be - havior and social context to provide clues as to "how" and "why" certain phenomena are occurring. 3 This can help inform understand-
Second, a processual approach may reinforce the importance of qualitative research in the field. ... Case 1 analyzed data from a course assessment based on the weekly field journals (22) of 55 medical students from two different semesters for a duration of one semester. Four weekly field journals and final reports were selected from this ...
Medical education is a complex field, and medical education research and practice fittingly draws from many disciplines (e.g., medicine, psychology, sociology, education) and synthesizes multiple perspectives to explain how people learn and how medicine should be taught. 4,5 The concept of a field was well described by Cristancho and Varpio 5 in their tips for early career medical educators ...
Qualitative research makes an important contribution to research in the medical sciences. It has a particular role in providing understanding with respect to decisions and behaviours of patients and professionals, in exploring factors affecting the implementation of new interventions, and in developing theory in fields such as illness behaviour, clinical decision making, illness prevention ...
1. Increased knowledge and understanding of diseases and treatments. Research increases knowledge and understanding of diseases and treatments by providing doctors and scientists with a better understanding of the causes and symptoms. This allows them to identify more effective diagnosis, detection, treatment, and prevention methods.
In this field, qualitative research is criticized for being subject to researcher bias and for lacking reproducibility and generalisability.10 Researchers presenting their qualitative work in health-related research are partly responsible for this view. Many qualitative researchers neglect the importance of giving an adequate description of ...
Medical Dentistry ... 1 Introduction to the field of creative arts, wellbeing, and health: achievements and current challenges Notes. Notes. 2 ... Qualitative research designs are appropriate for researching many arts and health contexts. However, there is a wide choice of methodologies available, each with different strengths and weaknesses.
Northwestern University Feinberg School of Medicine is home to a team of premier faculty and staff biostatisticians who are a driving force of data analytic innovation and excellence. In this episode, Denise Scholtens, PhD, a leader in biostatistics at Feinberg, discusses the growing importance of the field of biostatistics and how she leverages her skills to collaborate on several projects in ...
The qualities of trainees play a key role in entrustment decisions by clinical supervisors for the assignments of professional tasks and levels of supervision. A recent body of qualitative research has shown that in addition to knowledge and skills, a number of personality traits are relevant in the workplace; however, the relevance of these traits has not been investigated empirically.
Qualitative research is becoming more prominent in medicine and health care. Recently, editorials advocating a larger role for qualitative research as a way to address both "clinical" and "biopsychosocial" phenomena have appeared in, for example, the Journal of General Internal Medicine, 1 the Annals of Internal Medicine, 2 and the British Medical Journal. 3 Increasing numbers of ...
Background: Pregnancy-related death is on the rise in the United States, and there are significant disparities in outcomes for Black patients. Most solutions that address pregnancy-related death are hospital based, which rely on patients recognizing symptoms and seeking care from a health system, an area where many Black patients have reported experiencing bias.
Background The introduction of ultrasound (US) courses into medical undergraduate courses is usually met with a particularly high level of student motivation. The reasons for this are unclear. The aim of this study was to investigate the factors that contribute to undergraduate medical students' motivation to learn US skills. Understanding what motivates students to learn US will inform the ...
Abstract. Qualitative research is very important in educational research as it addresses the "how" and "why" research questions and enables deeper understanding of experiences, phenomena and context. Qualitative research allows you to ask questions that cannot be easily put into numbers to understand human experience.