An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Defining a Healthy Diet: Evidence for the Role of Contemporary Dietary Patterns in Health and Disease
Hellas cena.
1 Laboratory of Dietetics and Clinical Nutrition, Department of Public Health, Experimental and Forensic Medicine, University of Pavia, 27100 Pavia, Italy
2 Clinical Nutrition and Dietetics Service, Unit of Internal Medicine and Endocrinology, ICS Maugeri IRCCS, 27100 Pavia, Italy
Philip C. Calder
3 Human Development and Health, Faculty of Medicine, University of Southampton, Southampton SO16 6YD, UK
4 NIHR Southampton Biomedical Research Centre, University Hospital Southampton NHS Foundation Trust and University of Southampton, Southampton SO16 6YD, UK
The definition of what constitutes a healthy diet is continually shifting to reflect the evolving understanding of the roles that different foods, essential nutrients, and other food components play in health and disease. A large and growing body of evidence supports that intake of certain types of nutrients, specific food groups, or overarching dietary patterns positively influences health and promotes the prevention of common non-communicable diseases (NCDs). Greater consumption of health-promoting foods and limited intake of unhealthier options are intrinsic to the eating habits of certain regional diets such as the Mediterranean diet or have been constructed as part of dietary patterns designed to reduce disease risk, such as the Dietary Approaches to Stop Hypertension (DASH) or Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diets. In comparison with a more traditional Western diet, these healthier alternatives are higher in plant-based foods, including fresh fruits and vegetables, whole grains, legumes, seeds, and nuts and lower in animal-based foods, particularly fatty and processed meats. To better understand the current concept of a “healthy diet,” this review describes the features and supporting clinical and epidemiologic data for diets that have been shown to prevent disease and/or positively influence health. In total, evidence from epidemiological studies and clinical trials indicates that these types of dietary patterns reduce risks of NCDs including cardiovascular disease and cancer.
1. Introduction
Non-communicable diseases (NCDs) such as cardiovascular disease, cancer, chronic respiratory diseases, diabetes, obesity, and cognitive impairment are among the leading causes of death and disability throughout the world, affecting populations in developed as well as developing countries [ 1 ]. Although there are established genetic and environmental contributors to NCD risk, modifiable lifestyle-related factors play a large role at the individual level [ 2 , 3 , 4 ]. Dietary choices, for example, contribute to the risk for developing hypertension, hypercholesterolemia, overweight/obesity, and inflammation, which in turn increase the risk for diseases that are associated with significant morbidity and mortality, including cardiovascular disease, diabetes, and cancer [ 5 ]. Indeed, the marked rise in chronic NCDs has a causal link to global dietary patterns that are becoming increasingly Westernized [ 6 ], being characterized by high levels of fatty and processed meats, saturated fats, refined grains, salt, and sugars but lacking in fresh fruits and vegetables.
In recognition of the importance of the diet as a determinant of disease risk, the World Health Organization (WHO) Global Action Plan for the Prevention and Control of Noncommunicable Diseases includes strategies for addressing unhealthy diet patterns among its initiatives directed at reducing behavioral risk factors; the other components comprise physical inactivity, tobacco use, and harmful alcohol use [ 1 ]. Dietary changes recommended by WHO include balancing energy intake, limiting saturated and trans fats and shifting toward consumption of unsaturated fats, increasing intake of fruits and vegetables, and limiting the intake of sugar and salt. Many of these dietary targets naturally occur in regional diets such as the Mediterranean diet [ 7 ] or are included as part of evidence-based diets designed to reduce disease risk, such as the Dietary Approaches to Stop Hypertension (DASH) [ 8 ] or Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) [ 9 ] diets. To better understand the current concept of a “healthy diet”, this narrative review describes the features and supporting clinical and epidemiologic data for diets that align with the general WHO guidance and have been shown to prevent disease and/or positively influence health.
2. Components of a Healthy Diet and Their Benefits
A healthy diet is one in which macronutrients are consumed in appropriate proportions to support energetic and physiologic needs without excess intake while also providing sufficient micronutrients and hydration to meet the physiologic needs of the body [ 10 ]. Macronutrients (i.e., carbohydrates, proteins, and fats) provide the energy necessary for the cellular processes required for daily functioning [ 11 ]. Micronutrients (i.e., vitamins and minerals) are required in comparatively small amounts for normal growth, development, metabolism, and physiologic functioning [ 12 , 13 ].
Carbohydrates are the primary source of energy in the diet and are found in the greatest abundance in grains, fruits, legumes, and vegetables [ 14 ]. In terms of deriving a health benefit, whole grains are preferred over processed grains, the latter having been stripped of germ and bran during the milling process, resulting in lower amounts of fiber and micronutrients [ 15 ]. Meta-analyses of prospective cohort studies have linked increased whole-grain intake to a reduced risk of coronary heart disease, stroke, cardiovascular disease, and cancer, as well as to the decreased risk of mortality due to any cause, cardiovascular disease, cancer, respiratory disease, diabetes, and infectious disease [ 15 , 16 , 17 ]. Fresh fruits and vegetables supply energy as well as dietary fiber, which promotes the feeling of satiety and has positive effects on gastrointestinal function, cholesterol levels, and glycemic control [ 18 ]. In addition, fresh fruits and vegetables are key sources of phytochemicals (e.g., polyphenols, phytosterols, carotenoids), which are bioactive compounds believed to confer many of the health benefits associated with fruit and vegetable consumption [ 19 ]. The mechanistic effects of these various phytochemicals are unclear but include their antioxidative properties, as well as their role in regulating nuclear transcription factors, fat metabolism, and inflammatory mediators. For example, flavonoids have been shown to increase insulin secretion and reduce insulin resistance, suggesting that these phytochemicals provide some benefits in obesity and diabetes [ 20 ]. Additionally, polyphenols interact with gastrointestinal microbiota in a bi-directional manner by enhancing gut bacteria and being metabolized by these bacteria to form more bioactive compounds [ 20 ]. Fruit and vegetable intake has been shown to inversely correlate with the risk of NCDs, including hypertension [ 21 ], cardiovascular disease [ 22 , 23 ], chronic obstructive pulmonary disease [ 24 ], lung cancer [ 25 ], and metabolic syndrome [ 26 ].
Dietary proteins provide a source of energy as well as amino acids, including those that the human body requires but cannot produce on its own (i.e., essential amino acids). Dietary proteins are derived from both animal (meat, dairy, fish, and eggs) and plant (legumes, soya products, grains, nuts, and seeds) sources, with the former considered a richer source due to the array of amino acids, high digestibility, and greater bioavailability [ 27 ]. However, animal-based sources of protein contain saturated fatty acids, which have been linked to cardiovascular disease, dyslipidemia, and certain cancers. Although the mechanisms are unclear, red meat, and processed meat in particular, have been associated with an increased risk of colorectal cancer [ 28 , 29 ]. Animal-derived proteins also increase the dietary acid load, tipping the body’s acid-base balance toward acidosis [ 30 , 31 ]. The increased metabolic acid load has been linked to insulin resistance, impaired glucose homeostasis, and the development of urinary calcium stones [ 30 , 31 ].
Adequate dietary protein intake is important for maintaining lean body mass throughout the life span. In older adults, protein plays an important role in preventing age-related loss of skeletal muscle mass [ 32 ], preserving bone mass, and reducing fracture risk [ 33 ]. For older individuals not obtaining adequate protein from their diets, supplementation with amino acids can improve strength and functional status [ 34 ].
Fats (or lipids) are the primary structural components of cellular membranes and are also sources of cellular energy [ 35 ]. Dietary fats fall into 4 categories: monounsaturated fats, polyunsaturated fats, saturated fats, and trans fats. The fat content of food is generally an admixture of these different types [ 35 ]. Unsaturated fats are found in a variety of foods, including fish, many plant-derived oils, nuts, and seeds, whereas animal products (and some plant-derived oils) contribute a larger proportion of saturated fats [ 35 , 36 ]. Trans fats found in foods are predominantly the result of processing vegetable oils but are also present in small quantities in animal products (i.e., ruminant trans fats from cows, sheep, and goats) [ 35 , 36 ]. Among the types of dietary fats, unsaturated fats are associated with reduced cardiovascular and mortality risks, whereas trans fats and, to a lesser degree, saturated fats are associated with negative impacts on health, including increased mortality risk [ 36 , 37 ]. Two families of polyunsaturated fatty acids, omega-3 and omega-6, are described as essential fatty acids, because they are required for normal growth and reproduction but are not produced by the body and, therefore, must be obtained from dietary sources [ 10 ]. Omega-3 fatty acids, in particular, eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA), have been widely studied for their potential health benefits, with evidence suggesting positive effects including cardioprotection, preventing cognitive decline, reducing inflammation, sustaining muscle mass, and improving systemic insulin resistance [ 38 , 39 , 40 ]. Seafood, especially oily fish, provides EPA and DHA, and supplements are widely available for those not meeting recommended intakes with diet alone [ 41 , 42 ]. Nuts and some seeds and plant oils provide alpha-linolenic acid, the major plant omega-3 fatty acid [ 43 ].
Although required in trace amounts compared with macronutrients, micronutrients are necessary for normal growth, metabolism, physiologic functioning, and cellular integrity [ 12 , 13 ]. The shift from whole foods to processed, refined foods has reduced the micronutrient quality of the modern Western diet [ 44 ]. Vitamin and mineral inadequacies have been implicated in cellular aging and late-onset disease, as scarcity drives chronic metabolic disruption. Keeping with these observations, adequate dietary intake of, or supplementation with, micronutrients that have antioxidant properties (e.g., vitamins A, C, and E, copper, zinc, and selenium) has been suggested as a means to reduce the risk for and progression of age-related diseases [ 45 ].
Water is the principal component of the body, constituting the majority of lean body mass and total body weight [ 13 ]. Water not only provides hydration but also carries micronutrients, including trace elements and electrolytes [ 46 , 47 ]. Drinking water may supply as much as 20% of the daily recommended intake of calcium and magnesium [ 47 ]. Our understanding of water requirements and water’s effect on health and disease is limited, although the global increase in intake of high-calorie beverages has refocused attention on the importance of water for maintaining health and preventing disease [ 46 ].
3. Common Health-Promoting Dietary Patterns
Based on our understanding of nutritional requirements and their likely health impacts as described above, healthy dietary patterns can be generally described as those that are rich in health-promoting foods, including plant-based foods, fresh fruits and vegetables, antioxidants, soya, nuts, and sources of omega-3 fatty acids, and low in saturated fats and trans fats, animal-derived proteins, and added/refined sugars [ 48 ]. Patterns such as these are naturally occurring in certain regions of the world and rooted in local/regional tradition and food sources, as is the case for the traditional Mediterranean and Asian diets. Healthy dietary patterns have also been developed based on studies of nutrient intake and subsequent health measures or outcomes (e.g., the DASH [ 8 ] and MIND [ 9 ] diets) that share some common characteristics ( Figure 1 ).

A generalized healthy diet and lifestyle pyramid.
3.1. Mediterranean Diet
The Mediterranean diet is based on components of the traditional dietary patterns of Euro-Mediterranean countries and encompasses not only the types of foods consumed and their relative contributions to daily nutrient intake, but also an approach to eating that is cognizant of how foods are sourced (e.g., sustainability and eco-friendliness), cooked, and eaten, as well as lifestyle considerations such as engaging in regular physical activity, getting adequate rest, and participating in fellowship when preparing and sharing meals [ 7 ]. Within the core framework of the Mediterranean diet, variations based on geography and culture are reflected in the emphasis on the inclusion of traditional and local food products. The primary basis of daily meals in the Mediterranean diet is cereals such as whole-grain bread, pastas, couscous, and other unrefined grains that are rich in fiber and a variety of fruits and vegetables of different colors and textures that are high in micronutrients, fiber, and phytochemicals ( Table 1 ) [ 7 , 9 , 49 , 50 , 51 , 52 ]. Dairy products, preferably low-fat yogurt, cheese, or other fermented dairy products, are recommended daily in moderation as a source of calcium, which is needed for bone and heart health. Olive oil serves as the primary source of dietary lipids and is supplemented with olives, nuts, and seeds. Water (1.5–2.0 L/day or ~8 glasses) is recommended as the main source of hydration, whereas wine and other fermented alcoholic beverages are generally permitted in moderation, to be consumed with meals. Fish, white meat, and eggs are the primary sources of protein; red meat and processed meats are consumed less frequently and in smaller portions. Legumes are also a preferred source of plant-based proteins [ 7 ].
Comparison of nutritional/lifestyle components among different healthy diet options.
a Recommendations shown here are based on a 2000 calorie per day eating plan. b Contribution of total fat and quality of fat from cheese to stay within the recommended daily intake.
The health benefits of the Mediterranean diet were first described in 1975 by Ancel Keys, who observed a reduction in cardiovascular disease risk among populations whose nutritional model was consistent with practices of peoples from the Mediterranean Basin [ 53 ]. Since that time, research has revealed beneficial effects of the Mediterranean diet on a number of NCDs and related health measures, including cardiovascular and cerebrovascular disease [ 54 ], cancer [ 55 ], glycemic control [ 56 ], and cognitive function [ 57 , 58 ]. Although publication of a key intervention study (Prevención con Dieta Mediterránea; PREDIMED) conducted at multiple sites across Spain and evaluating the Mediterranean diet for the primary prevention of cardiovascular disease was retracted due to irregularities in randomization [ 59 ], a subsequent analysis adjusting for these issues reported a consistent positive effect of adhering to a Mediterranean diet supplemented with olive oil or nuts compared with a reduced-fat diet [ 59 ]. Substudies of PREDIMED have also shown that, compared with a low-fat control diet, the Mediterranean diet supplemented with olive oil or nuts is associated with a 30% reduced risk of major cardiovascular risk events [ 59 ] and reductions in systolic blood pressure (SBP) and diastolic blood pressure (DBP) of 5.8–7.3 mmHg and 3.3–3.4 mmHg, respectively [ 60 ]. In addition, cardiovascular factors such as mean internal carotid artery intima-media thickness (−0.084 mm; p < 0.05) and maximum plaque height (−0.091 mm; p < 0.05) are improved with the Mediterranean diet supplemented with nuts [ 61 ]. Greater intake of polyphenols (phytochemicals found in fruits, vegetables, tea, olive oil, and wine) correlated with a 36% reduced risk of hypertension ( p = 0.015) [ 62 ] and improvements in inflammatory biomarkers related to atherosclerosis (i.e., interleukin [IL]-6, tumor necrosis factor-alpha, soluble intercellular adhesion molecule-1, vascular cell adhesion molecule-1, and monocyte chemotactic protein-1; p < 0.05 for each), as well as in high-density lipoprotein cholesterol (HDL-C; p = 0.004) [ 62 , 63 ].
3.2. Dietary Approaches to Stop Hypertension (DASH)
The DASH diet derives its name from the Dietary Approaches to Stop Hypertension study, which evaluated the influence of dietary patterns on blood pressure [ 8 ]. Patients who consumed a diet that was rich in fruits, vegetables, and low-fat dairy and that included a reduced amount of saturated and total fat and cholesterol experienced significantly greater reductions in blood pressure than patients who consumed a control diet that was similar in composition to a typical American diet (difference in SBP/DBP, −5.5/−3.0 mmHg; p < 0.001) or a diet rich in fruits and vegetables with a reduced amount of snacks and sweets (−2.7/−1.9 mmHg; p ≤ 0.002). All 3 diets had a sodium content of 3 g per day. A subsequent study (DASH-Sodium) that explored the DASH diet or a control diet in combination with varying levels of sodium intake (high, intermediate, and low) found that the DASH diet significantly reduced SBP during the high, intermediate, and low sodium intake phases of both diets (high: −5.9 mmHg; p < 0.001; intermediate: −5.0 mmHg; p < 0.001; low: −2.2 mmHg; p < 0.05) [ 64 ]. The DASH diet also significantly reduced DBP versus the control diet during the high (−2.9 mmHg; p < 0.001) and intermediate (−2.5 mmHg; p < 0.01) sodium intake phases but not during the low intake phase (−1.0 mmHg). Although reducing sodium intake also significantly reduced blood pressure in the control diet group ( p < 0.05), the low sodium phase of the DASH diet elicited significant decreases in SBP/DBP of −8.9/−4.5 mmHg ( p < 0.001 for each) compared with high sodium intake phase of the control diet.
Subsequent controlled trials, as a whole, support the results of the DASH and DASH-Sodium studies in terms of blood pressure reduction. Moreover, these studies expanded the positive impacts of the DASH diet to include improvements in other cardiovascular risk factors or comorbidities (e.g., low-density lipoprotein cholesterol [LDL-C], total cholesterol, overweight/obesity, and insulin sensitivity) [ 65 , 66 , 67 , 68 ] and reductions in adverse outcomes such as development of cardiovascular disease, coronary heart disease, stroke, heart failure, metabolic syndrome, and diabetes (including improved pregnancy outcomes in women with gestational diabetes) [ 68 , 69 , 70 , 71 , 72 ]. Meta-analyses of studies using the DASH diet have demonstrated that LDL-C is significantly reduced by −0.1 mmol/L ( p = 0.03) [ 65 , 68 ], total cholesterol by −0.2 mmol/L ( p < 0.001) [ 65 , 68 ], body weight by −1.42 kg ( p < 0.001) [ 66 , 68 ], and fasting insulin by −0.15 μU/mL ( p < 0.001) [ 65 , 66 , 67 , 68 ]. With the DASH diet, the risk of cardiovascular disease is reduced by 20%, stroke by 19%, and heart failure by 29% ( p < 0.001 for each) [ 69 , 71 ]. The overall risk of diabetes is reduced by 18% [ 68 ], and children and adolescents with higher DASH scores (i.e., those whose diets included the highest intakes of fruits, vegetables, nuts, legumes, low-fat dairy, and whole grains) were at 64% lower risk of developing metabolic syndrome than those with the lowest DASH scores ( p = 0.023) [ 71 ]. Furthermore, rates of cesarean section decreased by 47% [ 72 ], incidence of macrosomia (birth weight > 4000 g) decreased from 39% to 4% ( p = 0.002) [ 70 ], and significantly fewer women experienced gestational diabetes that required insulin therapy on the DASH diet (23%) compared with the control diet (73%; p < 0.0001) [ 70 ].
The dietary pattern derived from the DASH study emphasizes the consumption of an array of vegetables (including colorful varieties, legumes, and starchy vegetables), fruits, fat-free or low-fat dairy products, whole grains, and various protein sources (e.g., seafood, lean meats, eggs, legumes, nuts, seeds, and soya) ( Table 1 ) [ 49 ]. Limited consumption of added sugars (< 10% of calories per day), saturated fats (< 10% of calories per day), sodium (< 2300 mg/day), and alcohol (≤ 1 drink per day for women and ≤ 2 drinks per day for men) is suggested. In addition, further reductions in blood pressure may be achievable by further reducing sodium intake, although practical challenges may limit the ability to achieve sodium intake of 1200 mg or less per day [ 49 ].
3.3. Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND)
The MIND diet combines elements of the Mediterranean and DASH diets with the goal of sustaining cognitive health throughout older age [ 9 ]. Both the Mediterranean and DASH diets have been individually linked to positive cognitive outcomes, including the prevention of cognitive decline or impairment and better cognitive performance [ 73 , 74 , 75 ]. Two high-quality cohort studies have reported associations between adherence to the MIND diet and a 53% lower risk for developing Alzheimer’s disease ( p = 0.002 for linear trend) [ 50 ] and slower declines in cognitive functioning, both overall and within specific cognitive domains (e.g., episodic, semantic, and working memory and perceptual speed and organization), such that the highest adherence rates to the MIND diet were associated with cognitive function equivalent to being 7.5 years younger [ 50 , 76 ]. Interestingly, even modest adherence to the MIND diet was associated with a 35% risk reduction for Alzheimer’s disease versus the lowest adherence group ( p = 0.002 for linear trend), whereas high adherence was needed to demonstrate 54% and 39% risk reductions with the Mediterranean and DASH diets, respectively; high adherence to the Mediterranean and DASH diet showed a statistically significant benefit [ 50 ].
The MIND diet focuses on increasing the intake of fresh fruits and vegetables and emphasizes brain-healthy foods such as green leafy vegetables, nuts, berries, beans, whole grains, fish, poultry, olive oil, and wine in moderation ( Table 1 ) [ 9 , 50 ]. Additionally, foods that are thought to be unhealthy for the brain, such as red meats, butter/margarine, cheese, pastries, sweets, and fried or fast food, are limited [ 9 ]. The specificity regarding the types of foods on the healthy and unhealthy lists differentiates MIND from the Mediterranean or DASH diets [ 50 ].
3.4. Nordic Diet
Iterations of a Nordic diet (e.g., the healthy Nordic diet, New Nordic Diet) arose from the desire to translate the Mediterranean, DASH, and other health-promoting diets into a regionally tailored dietary pattern that uses traditional, local Nordic foods and would be attractive to the public, sustainable, and eco-friendly [ 77 , 78 ]. Overarching tenets of the New Nordic Diet are to consume more (1) calories from plant sources and fewer from animal sources, (2) foods from seas and lakes, and (3) foods from the wild countryside [ 78 , 79 ]. A generalized Nordic dietary pattern would include green leafy vegetables, other vegetables, fruits, fish and seafood, potatoes, berries, whole grains (e.g., wheat, rye, oats, barley), nuts, low-fat dairy products, rapeseed, sunflower, and/or soya oils and limited intake of fresh red meat and sugar [ 78 , 80 ]. Specific dietary recommendations based on the NORDIET clinical trial are presented in Table 1 [ 51 ].
The randomized, controlled NORDIET study compared a healthy Nordic diet with a control diet (the participant’s usual Western diet) [ 77 ]. Over 6 weeks, the Nordic diet improved the lipid profile (including a 0.98 mmol/L reduction in total cholesterol [ p < 0.0001] and a 0.83 mmol/L reduction in LDL-C [ p < 0.001]), lowered SBP by 6.6 mmHg ( p = 0.008), and improved insulin sensitivity (homeostatic model assessment-insulin resistance decreased 0.11; p = 0.01) compared with the control diet. Those on the Nordic diet also experienced a 3.0 kg decrease in body weight ( p < 0.001) despite food being available ad libitum.
Results from subsequent studies conducted using Nordic diet variations are consistent with those from studies with the NORDIET study, demonstrating improvements relative to the control diet in blood lipid profile (LDL-C/HDL-C ratio, −0.15; p = 0.046) [ 81 ], inflammation (IL-1 receptor antagonist, −84 ng/L; p < 0.001) [ 81 ], blood pressure (DBP, −4.4 mmHg ( p = 0.001), and mean arterial pressure (−4.2 mmHg; p = 0.006) among patients with metabolic syndrome [ 82 ] and weight loss (−3.22 kg; p < 0.001) [ 83 ] and blood pressure reduction (SBP/DBP, −5.13/−3.24 mmHg; p < 0.05) in individuals with obesity [ 83 ]. Compared with baseline values, one study demonstrated blood pressure reductions of −6.9 mmHg (SBP) and −3.2 mmHg (DBP; p < 0.01) [ 83 , 84 ]. Additionally, a study conducted in children reported an improvement in omega-3 fatty acid status with the Nordic diet that was associated with improvements in school performance ( p < 0.05) [ 85 ]. A systematic review parsing the individual components of the Nordic diet found that evidence supported the protective effects of eating whole grains on type 2 diabetes and cardiovascular disease risk, but that there was insufficient evidence for other foods in the Nordic diet [ 86 ].
3.5. Traditional Asian Diets
Although there is substantial evidence supporting the Mediterranean and other European-based diets, traditional regional dietary patterns from other parts of the world that follow similar principles have less–well-established links to positive health outcomes. A full description of the breadth of regional diets and the associated evidence bases is beyond the scope of this publication, but we consider some Asian-based diets to be particularly relevant to this discussion.
The traditional Korean diet is composed of rice and other whole grains, fermented food, indigenous land and sea vegetables, proteins primarily from legumes and fish as opposed to red meat, medicinal herbs (e.g., garlic, green onions, ginger), and sesame and perilla oils [ 87 ]. Meals typically consist of multiple small-portion dishes are often derived from seasonal food sources and are home-cooked. Unlike the Western diet, the traditional Korean diet does not include many fried foods [ 87 ]. Epidemiologic data suggest a reduced risk of metabolic syndrome (odds ratio [OR]: 0.77; 95% CI: 0.60–0.99), obesity (OR: 0.72; 95% CI: 0.55–0.95), hypertension (OR: 0.74; 95% CI: 0.57–0.98), and hypertriglyceridemia (OR: 0.76; 95% CI: 0.59–0.99) among individuals who follow traditional Korean dietary patterns [ 88 ]. These findings are consistent with a controlled clinical trial that explored the effects of a traditional Korean diet compared with a control diet (“eat as usual”) on cardiovascular risk factors in patients with diabetes and hypertension. In that study, adherence to a traditional Korean diet favorably influenced body composition (body weight, −2.3 kg; body mass index [BMI], −0.83 kg/m 2 ; body fat, −2.2%; p < 0.01), heart rate (−7.1 bpm; p = 0.002), and glycemic control (HbA1c, −0.72%; p = 0.003) [ 89 ].
The traditional Chinese diet features rice or noodles, soups, vegetables, steamed breads or dumplings, fruits and vegetables, soy, seafood, and meat [ 90 , 91 ]. Although higher in carbohydrates and lower in fat compared with a Western diet, the traditional Chinese diet does not appear to promote weight gain in healthy, normal-weight Chinese, suggesting that carbohydrate restriction may not be a universally applicable intervention to combat obesity and cardiometabolic risk [ 92 ]. One 6-week controlled trial demonstrated that 52% of non-Chinese individuals with overweight or obesity who adhered to a traditional Chinese diet had a reduction in BMI while preserving lean body mass compared with 28% of those who followed a Western diet at the 1-year follow-up assessment [ 93 ]. In another trial, BMI decreased by 0.37 kg/m 2 and lean mass by 0.21 kg among subjects who adhered to a traditional Chinese diet for 6 weeks, whereas those who followed a Western diet had 0.26 kg/m 2 and 0.49 kg reductions in BMI and lean body mass, respectively [ 94 ]. Notably, both of these studies restricted caloric intake to 1,200 Kcal for the test and control diet groups.
Similar to the Korean diet, the traditional Japanese diet (known as Washoku) is characterized by small portions of multiple components, primarily including rice, fish (often eaten raw), soups, and pickles [ 95 ]. Fermented soybean paste (dashi) serves as the base of many of the soups that are central to the traditional Japanese diet; other ingredients include seaweed, fruits and vegetables, and mushrooms. The use of chopsticks, alternating between dishes of small portion size throughout a meal, and the base flavor of Japanese food (umami) enhance satiety and help to prevent overeating. Adherence to a traditional Japanese dietary pattern has been associated with favorable effects on blood pressure among apparently healthy Japanese adults [ 96 ]. This is consistent with data from the 2012 Japan National Health and Nutrition Survey demonstrating that adherence to a traditional Japanese diet compared with a Western diet or a meat- and fat-based dietary pattern was associated with a lower prevalence of hypertension in men [ 97 ]. However, in the same study, a traditional Japanese diet was associated with higher DBP in women, as well as higher waist circumference and BMI in men. Further study is needed to elucidate the health impacts of traditional Japanese and other Asian dietary patterns.
4. Additional Factors
While the evidence reviewed here suggests that the described dietary patterns positively influence measures of health and disease risk and outcome because they encourage the intake of foods that individually have beneficial effects and the avoidance of unhealthy options, additional factors combine to create a lifestyle that promotes health. For example, healthy diets include adequate hydration, typically in the form of water or tea/herbal infusions [ 7 , 49 , 51 , 52 ]. In addition to the dietary components, a healthy lifestyle is one that incorporates regular exercise, socialization, and adequate sleep [ 7 , 52 ], and minimizes elements that have a negative effect on health such as tobacco use, excessive alcohol consumption, physical inactivity, large amounts of screen time, and stress.
The importance of non-dietary factors is reflected in their inclusion in modern food pyramids. Built on a base of positive lifestyle factors, the lower tiers indicate daily consumption of adequate hydration and nutrient-rich, plant-based foods, with animal-derived products (meat, fish, and dairy) and sweets comprising higher tiers of the pyramid (i.e., less frequently or infrequently consumed items).
Whereas the goal may be to achieve nutrient requirements through food and water intake alone, there are situations in which food-derived nutrient intake might be inadequate due to increased need, selective eating, or food insecurity/limited access to more nutritious foods [ 98 , 99 , 100 ]. Therefore, for some individuals, dietary supplements may be required, particularly at certain life phases. For example, later in life, the recommended intake of calcium increases to sustain bone mineral density [ 101 ]; hence, supplementation with calcium may be necessary to meet recommended intake levels in older adults. Before initiating supplementation, dietary intake levels should be considered to avoid exceeding the upper tolerability limits and causing adverse events.
There are a number of other traditional regional diets that likely have similar benefits to those that we describe here. However, we made the decision to narrow our focus to those diets with evidence from randomized, controlled trials demonstrating their health benefits. For example, the African Heritage Diet focuses on traditional ingredients that may be beneficial to African American populations who experience disproportionately higher risks for chronic diseases related to their diets [ 102 ]. Future research is warranted to evaluate the impact of the African Heritage Diet and other regional dietary patterns on health.
5. Conclusions
Healthy diets, arising either by tradition or design, share many common features and generally align with the WHO Global Action Plan for the Prevention and Control of Noncommunicable Diseases. In comparison with a Western diet, these healthier alternatives are higher in plant-based foods, including fresh fruits and vegetables, whole grains, legumes, seeds, and nuts and lower in animal-based foods, particularly fatty and processed meats. Evidence from epidemiologic studies and clinical trials indicates that these types of dietary patterns reduce risks of NCDs ranging from cardiovascular disease to cancer. Further endeavors are needed to integrate these healthy dietary and lifestyle choices into daily living in communities throughout the world and to make healthy eating accessible, achievable, and sustainable.
Acknowledgments
Medical writing support was provided by Crystal Murcia, PhD, and Dennis Stancavish, MA, of Peloton Advantage, LLC, an OPEN Health company, and was funded by Pfizer Consumer Healthcare. On 1 August 2019, Pfizer Consumer Healthcare became part of GSK Consumer Healthcare.
Author Contributions
H.C. and P.C.C. contributed to the conception of the work; the acquisition, analysis, and interpretation of data; drafting; and revision of the work. Both have approved the final version for submission and agree to be personally accountable for their contributions and for ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated, resolved, and documented in the literature. All authors have read and agreed to the published version of the manuscript.
Medical writing support was funded by Pfizer Consumer Healthcare; this research received no other external funding. The APC was funded by Pfizer Consumer Healthcare. On 1 August 2019, Pfizer Consumer Healthcare became part of GSK Consumer Healthcare.
Conflicts of Interest
Hellas Cena received travel reimbursement from Pfizer Consumer Healthcare to attend a discussion meeting prior to drafting the manuscript and acts as a consultant to companies that manufacture or market dietary supplements, including Pfizer Consumer Healthcare. Philip C. Calder received travel reimbursement from Pfizer Consumer Healthcare to attend a discussion meeting prior to drafting the manuscript. Pfizer Consumer Healthcare funded this project, but the company had no role in the design, execution, interpretation, or writing of the paper.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 06 December 2017
Healthy food choices are happy food choices: Evidence from a real life sample using smartphone based assessments
- Deborah R. Wahl 1 na1 ,
- Karoline Villinger 1 na1 ,
- Laura M. König ORCID: orcid.org/0000-0003-3655-8842 1 ,
- Katrin Ziesemer 1 ,
- Harald T. Schupp 1 &
- Britta Renner 1
Scientific Reports volume 7 , Article number: 17069 ( 2017 ) Cite this article
131k Accesses
54 Citations
261 Altmetric
Metrics details
- Health sciences
- Human behaviour
Research suggests that “healthy” food choices such as eating fruits and vegetables have not only physical but also mental health benefits and might be a long-term investment in future well-being. This view contrasts with the belief that high-caloric foods taste better, make us happy, and alleviate a negative mood. To provide a more comprehensive assessment of food choice and well-being, we investigated in-the-moment eating happiness by assessing complete, real life dietary behaviour across eight days using smartphone-based ecological momentary assessment. Three main findings emerged: First, of 14 different main food categories, vegetables consumption contributed the largest share to eating happiness measured across eight days. Second, sweets on average provided comparable induced eating happiness to “healthy” food choices such as fruits or vegetables. Third, dinner elicited comparable eating happiness to snacking. These findings are discussed within the “food as health” and “food as well-being” perspectives on eating behaviour.
Similar content being viewed by others

A systematic review and multivariate meta-analysis of the physical and mental health benefits of touch interventions
Julian Packheiser, Helena Hartmann, … Frédéric Michon

Microdosing with psilocybin mushrooms: a double-blind placebo-controlled study
Federico Cavanna, Stephanie Muller, … Enzo Tagliazucchi

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers
Joseph M. Rootman, Pamela Kryskow, … Zach Walsh
Introduction
When it comes to eating, researchers, the media, and policy makers mainly focus on negative aspects of eating behaviour, like restricting certain foods, counting calories, and dieting. Likewise, health intervention efforts, including primary prevention campaigns, typically encourage consumers to trade off the expected enjoyment of hedonic and comfort foods against health benefits 1 . However, research has shown that diets and restrained eating are often counterproductive and may even enhance the risk of long-term weight gain and eating disorders 2 , 3 . A promising new perspective entails a shift from food as pure nourishment towards a more positive and well-being centred perspective of human eating behaviour 1 , 4 , 5 . In this context, Block et al . 4 have advocated a paradigm shift from “food as health” to “food as well-being” (p. 848).
Supporting this perspective of “food as well-being”, recent research suggests that “healthy” food choices, such as eating more fruits and vegetables, have not only physical but also mental health benefits 6 , 7 and might be a long-term investment in future well-being 8 . For example, in a nationally representative panel survey of over 12,000 adults from Australia, Mujcic and Oswald 8 showed that fruit and vegetable consumption predicted increases in happiness, life satisfaction, and well-being over two years. Similarly, using lagged analyses, White and colleagues 9 showed that fruit and vegetable consumption predicted improvements in positive affect on the subsequent day but not vice versa. Also, cross-sectional evidence reported by Blanchflower et al . 10 shows that eating fruits and vegetables is positively associated with well-being after adjusting for demographic variables including age, sex, or race 11 . Of note, previous research includes a wide range of time lags between actual eating occasion and well-being assessment, ranging from 24 hours 9 , 12 to 14 days 6 , to 24 months 8 . Thus, the findings support the notion that fruit and vegetable consumption has beneficial effects on different indicators of well-being, such as happiness or general life satisfaction, across a broad range of time spans.
The contention that healthy food choices such as a higher fruit and vegetable consumption is associated with greater happiness and well-being clearly contrasts with the common belief that in particular high-fat, high-sugar, or high-caloric foods taste better and make us happy while we are eating them. When it comes to eating, people usually have a spontaneous “unhealthy = tasty” association 13 and assume that chocolate is a better mood booster than an apple. According to this in-the-moment well-being perspective, consumers have to trade off the expected enjoyment of eating against the health costs of eating unhealthy foods 1 , 4 .
A wealth of research shows that the experience of negative emotions and stress leads to increased consumption in a substantial number of individuals (“emotional eating”) of unhealthy food (“comfort food”) 14 , 15 , 16 , 17 . However, this research stream focuses on emotional eating to “smooth” unpleasant experiences in response to stress or negative mood states, and the mood-boosting effect of eating is typically not assessed 18 . One of the few studies testing the effectiveness of comfort food in improving mood showed that the consumption of “unhealthy” comfort food had a mood boosting effect after a negative mood induction but not to a greater extent than non-comfort or neutral food 19 . Hence, even though people may believe that snacking on “unhealthy” foods like ice cream or chocolate provides greater pleasure and psychological benefits, the consumption of “unhealthy” foods might not actually be more psychologically beneficial than other foods.
However, both streams of research have either focused on a single food category (fruit and vegetable consumption), a single type of meal (snacking), or a single eating occasion (after negative/neutral mood induction). Accordingly, it is unknown whether the boosting effect of eating is specific to certain types of food choices and categories or whether eating has a more general boosting effect that is observable after the consumption of both “healthy” and “unhealthy” foods and across eating occasions. Accordingly, in the present study, we investigated the psychological benefits of eating that varied by food categories and meal types by assessing complete dietary behaviour across eight days in real life.
Furthermore, previous research on the impact of eating on well-being tended to rely on retrospective assessments such as food frequency questionnaires 8 , 10 and written food diaries 9 . Such retrospective self-report methods rely on the challenging task of accurately estimating average intake or remembering individual eating episodes and may lead to under-reporting food intake, particularly unhealthy food choices such as snacks 7 , 20 . To avoid memory and bias problems in the present study we used ecological momentary assessment (EMA) 21 to obtain ecologically valid and comprehensive real life data on eating behaviour and happiness as experienced in-the-moment.
In the present study, we examined the eating happiness and satisfaction experienced in-the-moment, in real time and in real life, using a smartphone based EMA approach. Specifically, healthy participants were asked to record each eating occasion, including main meals and snacks, for eight consecutive days and rate how tasty their meal/snack was, how much they enjoyed it, and how pleased they were with their meal/snack immediately after each eating episode. This intense recording of every eating episode allows assessing eating behaviour on the level of different meal types and food categories to compare experienced eating happiness across meals and categories. Following the two different research streams, we expected on a food category level that not only “unhealthy” foods like sweets would be associated with high experienced eating happiness but also “healthy” food choices such as fruits and vegetables. On a meal type level, we hypothesised that the happiness of meals differs as a function of meal type. According to previous contention, snacking in particular should be accompanied by greater happiness.
Eating episodes
Overall, during the study period, a total of 1,044 completed eating episodes were reported (see also Table 1 ). On average, participants rated their eating happiness with M = 77.59 which suggests that overall eating occasions were generally positive. However, experienced eating happiness also varied considerably between eating occasions as indicated by a range from 7.00 to 100.00 and a standard deviation of SD = 16.41.
Food categories and experienced eating happiness
All eating episodes were categorised according to their food category based on the German Nutrient Database (German: Bundeslebensmittelschlüssel), which covers the average nutritional values of approximately 10,000 foods available on the German market and is a validated standard instrument for the assessment of nutritional surveys in Germany. As shown in Table 1 , eating happiness differed significantly across all 14 food categories, F (13, 2131) = 1.78, p = 0.04. On average, experienced eating happiness varied from 71.82 ( SD = 18.65) for fish to 83.62 ( SD = 11.61) for meat substitutes. Post hoc analysis, however, did not yield significant differences in experienced eating happiness between food categories, p ≥ 0.22. Hence, on average, “unhealthy” food choices such as sweets ( M = 78.93, SD = 15.27) did not differ in experienced happiness from “healthy” food choices such as fruits ( M = 78.29, SD = 16.13) or vegetables ( M = 77.57, SD = 17.17). In addition, an intraclass correlation (ICC) of ρ = 0.22 for happiness indicated that less than a quarter of the observed variation in experienced eating happiness was due to differences between food categories, while 78% of the variation was due to differences within food categories.
However, as Figure 1 (left side) depicts, consumption frequency differed greatly across food categories. Frequently consumed food categories encompassed vegetables which were consumed at 38% of all eating occasions ( n = 400), followed by dairy products with 35% ( n = 366), and sweets with 34% ( n = 356). Conversely, rarely consumed food categories included meat substitutes, which were consumed in 2.2% of all eating occasions ( n = 23), salty extras (1.5%, n = 16), and pastries (1.3%, n = 14).
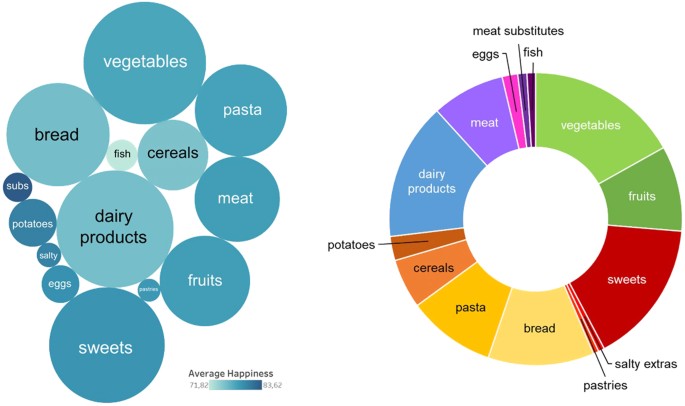
Left side: Average experienced eating happiness (colour intensity: darker colours indicate greater happiness) and consumption frequency (size of the cycle) for the 14 food categories. Right side: Absolute share of the 14 food categories in total experienced eating happiness.
Amount of experienced eating happiness by food category
To account for the frequency of consumption, we calculated and scaled the absolute experienced eating happiness according to the total sum score. As shown in Figure 1 (right side), vegetables contributed the biggest share to the total happiness followed by sweets, dairy products, and bread. Clustering food categories shows that fruits and vegetables accounted for nearly one quarter of total eating happiness score and thus, contributed to a large part of eating related happiness. Grain products such as bread, pasta, and cereals, which are main sources of carbohydrates including starch and fibre, were the second main source for eating happiness. However, “unhealthy” snacks including sweets, salty extras, and pastries represented the third biggest source of eating related happiness.
Experienced eating happiness by meal type
To further elucidate the contribution of snacks to eating happiness, analysis on the meal type level was conducted. Experienced in-the-moment eating happiness significantly varied by meal type consumed, F (4, 1039) = 11.75, p < 0.001. Frequencies of meal type consumption ranged from snacks being the most frequently logged meal type ( n = 332; see also Table 1 ) to afternoon tea being the least logged meal type ( n = 27). Figure 2 illustrates the wide dispersion within as well as between different meal types. Afternoon tea ( M = 82.41, SD = 15.26), dinner ( M = 81.47, SD = 14.73), and snacks ( M = 79.45, SD = 14.94) showed eating happiness values above the grand mean, whereas breakfast ( M = 74.28, SD = 16.35) and lunch ( M = 73.09, SD = 18.99) were below the eating happiness mean. Comparisons between meal types showed that eating happiness for snacks was significantly higher than for lunch t (533) = −4.44, p = 0.001, d = −0.38 and breakfast, t (567) = −3.78, p = 0.001, d = −0.33. However, this was also true for dinner, which induced greater eating happiness than lunch t (446) = −5.48, p < 0.001, d = −0.50 and breakfast, t (480) = −4.90, p < 0.001, d = −0.46. Finally, eating happiness for afternoon tea was greater than for lunch t (228) = −2.83, p = 0.047, d = −0.50. All other comparisons did not reach significance, t ≤ 2.49, p ≥ 0.093.
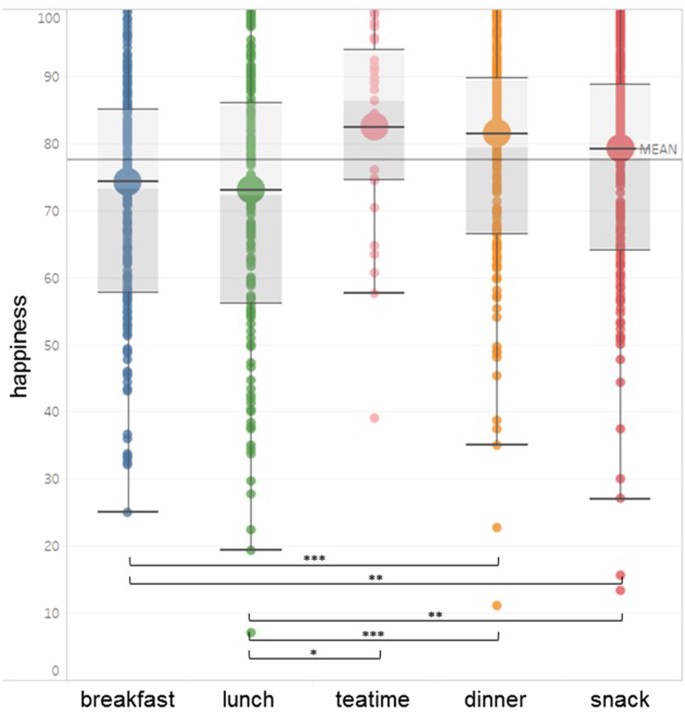
Experienced eating happiness per meal type. Small dots represent single eating events, big circles indicate average eating happiness, and the horizontal line indicates the grand mean. Boxes indicate the middle 50% (interquartile range) and median (darker/lighter shade). The whiskers above and below represent 1.5 of the interquartile range.
Control Analyses
In order to test for a potential confounding effect between experienced eating happiness, food categories, and meal type, additional control analyses within meal types were conducted. Comparing experienced eating happiness for dinner and lunch suggested that dinner did not trigger a happiness spill-over effect specific to vegetables since the foods consumed at dinner were generally associated with greater happiness than those consumed at other eating occasions (Supplementary Table S1 ). Moreover, the relative frequency of vegetables consumed at dinner (73%, n = 180 out of 245) and at lunch were comparable (69%, n = 140 out of 203), indicating that the observed happiness-vegetables link does not seem to be mainly a meal type confounding effect.
Since the present study focuses on “food effects” (Level 1) rather than “person effects” (Level 2), we analysed the data at the food item level. However, participants who were generally overall happier with their eating could have inflated the observed happiness scores for certain food categories. In order to account for person-level effects, happiness scores were person-mean centred and thereby adjusted for mean level differences in happiness. The person-mean centred happiness scores ( M cwc ) represent the difference between the individual’s average happiness score (across all single in-the-moment happiness scores per food category) and the single happiness scores of the individual within the respective food category. The centred scores indicate whether the single in-the-moment happiness score was above (indicated by positive values) or below (indicated by negative values) the individual person-mean. As Table 1 depicts, the control analyses with centred values yielded highly similar results. Vegetables were again associated on average with more happiness than other food categories (although people might differ in their general eating happiness). An additional conducted ANOVA with person-centred happiness values as dependent variables and food categories as independent variables provided also a highly similar pattern of results. Replicating the previously reported analysis, eating happiness differed significantly across all 14 food categories, F (13, 2129) = 1.94, p = 0.023, and post hoc analysis did not yield significant differences in experienced eating happiness between food categories, p ≥ 0.14. Moreover, fruits and vegetables were associated with high happiness values, and “unhealthy” food choices such as sweets did not differ in experienced happiness from “healthy” food choices such as fruits or vegetables. The only difference between the previous and control analysis was that vegetables ( M cwc = 1.16, SD = 15.14) gained slightly in importance for eating-related happiness, whereas fruits ( M cwc = −0.65, SD = 13.21), salty extras ( M cwc = −0.07, SD = 8.01), and pastries ( M cwc = −2.39, SD = 18.26) became slightly less important.
This study is the first, to our knowledge, that investigated in-the-moment experienced eating happiness in real time and real life using EMA based self-report and imagery covering the complete diversity of food intake. The present results add to and extend previous findings by suggesting that fruit and vegetable consumption has immediate beneficial psychological effects. Overall, of 14 different main food categories, vegetables consumption contributed the largest share to eating happiness measured across eight days. Thus, in addition to the investment in future well-being indicated by previous research 8 , “healthy” food choices seem to be an investment in the in-the moment well-being.
Importantly, although many cultures convey the belief that eating certain foods has a greater hedonic and mood boosting effect, the present results suggest that this might not reflect actual in-the-moment experiences accurately. Even though people often have a spontaneous “unhealthy = tasty” intuition 13 , thus indicating that a stronger happiness boosting effect of “unhealthy” food is to be expected, the induced eating happiness of sweets did not differ on average from “healthy” food choices such as fruits or vegetables. This was also true for other stereotypically “unhealthy” foods such as pastries and salty extras, which did not show the expected greater boosting effect on happiness. Moreover, analyses on the meal type level support this notion, since snacks, despite their overall positive effect, were not the most psychologically beneficial meal type, i.e., dinner had a comparable “happiness” signature to snacking. Taken together, “healthy choices” seem to be also “happy choices” and at least comparable to or even higher in their hedonic value as compared to stereotypical “unhealthy” food choices.
In general, eating happiness was high, which concurs with previous research from field studies with generally healthy participants. De Castro, Bellisle, and Dalix 22 examined weekly food diaries from 54 French subjects and found that most of the meals were rated as appealing. Also, the observed differences in average eating happiness for the 14 different food categories, albeit statistically significant, were comparable small. One could argue that this simply indicates that participants avoided selecting bad food 22 . Alternatively, this might suggest that the type of food or food categories are less decisive for experienced eating happiness than often assumed. This relates to recent findings in the field of comfort and emotional eating. Many people believe that specific types of food have greater comforting value. Also in research, the foods eaten as response to negative emotional strain, are typically characterised as being high-caloric because such foods are assumed to provide immediate psycho-physical benefits 18 . However, comparing different food types did not provide evidence for the notion that they differed in their provided comfort; rather, eating in general led to significant improvements in mood 19 . This is mirrored in the present findings. Comparing the eating happiness of “healthy” food choices such as fruits and vegetables to that of “unhealthy” food choices such as sweets shows remarkably similar patterns as, on average, they were associated with high eating happiness and their range of experiences ranged from very negative to very positive.
This raises the question of why the idea that we can eat indulgent food to compensate for life’s mishaps is so prevailing. In an innovative experimental study, Adriaanse, Prinsen, de Witt Huberts, de Ridder, and Evers 23 led participants believe that they overate. Those who characterised themselves as emotional eaters falsely attributed their over-consumption to negative emotions, demonstrating a “confabulation”-effect. This indicates that people might have restricted self-knowledge and that recalled eating episodes suffer from systematic recall biases 24 . Moreover, Boelsma, Brink, Stafleu, and Hendriks 25 examined postprandial subjective wellness and objective parameters (e.g., ghrelin, insulin, glucose) after standardised breakfast intakes and did not find direct correlations. This suggests that the impact of different food categories on wellness might not be directly related to biological effects but rather due to conditioning as food is often paired with other positive experienced situations (e.g., social interactions) or to placebo effects 18 . Moreover, experimental and field studies indicate that not only negative, but also positive, emotions trigger eating 15 , 26 . One may speculate that selective attention might contribute to the “myth” of comfort food 19 in that people attend to the consumption effect of “comfort” food in negative situation but neglect the effect in positive ones.
The present data also show that eating behaviour in the real world is a complex behaviour with many different aspects. People make more than 200 food decisions a day 27 which poses a great challenge for the measurement of eating behaviour. Studies often assess specific food categories such as fruit and vegetable consumption using Food Frequency Questionnaires, which has clear advantages in terms of cost-effectiveness. However, focusing on selective aspects of eating and food choices might provide only a selective part of the picture 15 , 17 , 22 . It is important to note that focusing solely on the “unhealthy” food choices such as sweets would have led to the conclusion that they have a high “indulgent” value. To be able to draw conclusions about which foods make people happy, the relation of different food categories needs to be considered. The more comprehensive view, considering the whole dietary behaviour across eating occasions, reveals that “healthy” food choices actually contributed the biggest share to the total experienced eating happiness. Thus, for a more comprehensive understanding of how eating behaviours are regulated, more complete and sensitive measures of the behaviour are necessary. Developments in mobile technologies hold great promise for feasible dietary assessment based on image-assisted methods 28 .
As fruits and vegetables evoked high in-the-moment happiness experiences, one could speculate that these cumulate and have spill-over effects on subsequent general well-being, including life satisfaction across time. Combing in-the-moment measures with longitudinal perspectives might be a promising avenue for future studies for understanding the pathways from eating certain food types to subjective well-being. In the literature different pathways are discussed, including physiological and biochemical aspects of specific food elements or nutrients 7 .
The present EMA based data also revealed that eating happiness varied greatly within the 14 food categories and meal types. As within food category variance represented more than two third of the total observed variance, happiness varied according to nutritional characteristics and meal type; however, a myriad of factors present in the natural environment can affect each and every meal. Thus, widening the “nourishment” perspective by including how much, when, where, how long, and with whom people eat might tell us more about experienced eating happiness. Again, mobile, in-the-moment assessment opens the possibility of assessing the behavioural signature of eating in real life. Moreover, individual factors such as eating motives, habitual eating styles, convenience, and social norms are likely to contribute to eating happiness variance 5 , 29 .
A key strength of this study is that it was the first to examine experienced eating happiness in non-clinical participants using EMA technology and imagery to assess food intake. Despite this strength, there are some limitations to this study that affect the interpretation of the results. In the present study, eating happiness was examined on a food based level. This neglects differences on the individual level and might be examined in future multilevel studies. Furthermore, as a main aim of this study was to assess real life eating behaviour, the “natural” observation level is the meal, the psychological/ecological unit of eating 30 , rather than food categories or nutrients. Therefore, we cannot exclude that specific food categories may have had a comparably higher impact on the experienced happiness of the whole meal. Sample size and therefore Type I and Type II error rates are of concern. Although the total number of observations was higher than in previous studies (see for example, Boushey et al . 28 for a review), the number of participants was small but comparable to previous studies in this field 20 , 31 , 32 , 33 . Small sample sizes can increase error rates because the number of persons is more decisive than the number of nested observations 34 . Specially, nested data can seriously increase Type I error rates, which is rather unlikely to be the case in the present study. Concerning Type II error rates, Aarts et al . 35 illustrated for lower ICCs that adding extra observations per participant also increases power, particularly in the lower observation range. Considering the ICC and the number of observations per participant, one could argue that the power in the present study is likely to be sufficient to render the observed null-differences meaningful. Finally, the predominately white and well-educated sample does limit the degree to which the results can be generalised to the wider community; these results warrant replication with a more representative sample.
Despite these limitations, we think that our study has implications for both theory and practice. The cumulative evidence of psychological benefits from healthy food choices might offer new perspectives for health promotion and public-policy programs 8 . Making people aware of the “healthy = happy” association supported by empirical evidence provides a distinct and novel perspective to the prevailing “unhealthy = tasty” folk intuition and could foster eating choices that increase both in-the-moment happiness and future well-being. Furthermore, the present research lends support to the advocated paradigm shift from “food as health” to “food as well-being” which entails a supporting and encouraging rather constraining and limiting view on eating behaviour.
The study conformed with the Declaration of Helsinki. All study protocols were approved by University of Konstanz’s Institutional Review Board and were conducted in accordance with guidelines and regulations. Upon arrival, all participants signed a written informed consent.
Participants
Thirty-eight participants (28 females: average age = 24.47, SD = 5.88, range = 18–48 years) from the University of Konstanz assessed their eating behaviour in close to real time and in their natural environment using an event-based ambulatory assessment method (EMA). No participant dropped out or had to be excluded. Thirty-three participants were students, with 52.6% studying psychology. As compensation, participants could choose between taking part in a lottery (4 × 25€) or receiving course credits (2 hours).
Participants were recruited through leaflets distributed at the university and postings on Facebook groups. Prior to participation, all participants gave written informed consent. Participants were invited to the laboratory for individual introductory sessions. During this first session, participants installed the application movisensXS (version 0.8.4203) on their own smartphones and downloaded the study survey (movisensXS Library v4065). In addition, they completed a short baseline questionnaire, including demographic variables like age, gender, education, and eating principles. Participants were instructed to log every eating occasion immediately before eating by using the smartphone to indicate the type of meal, take pictures of the food, and describe its main components using a free input field. Fluid intake was not assessed. Participants were asked to record their food intake on eight consecutive days. After finishing the study, participants were invited back to the laboratory for individual final interviews.
Immediately before eating participants were asked to indicate the type of meal with the following five options: breakfast, lunch, afternoon tea, dinner, snack. In Germany, “afternoon tea” is called “Kaffee & Kuchen” which directly translates as “coffee & cake”. It is similar to the idea of a traditional “afternoon tea” meal in UK. Specifically, in Germany, people have “Kaffee & Kuchen” in the afternoon (between 4–5 pm) and typically coffee (or tea) is served with some cake or cookies. Dinner in Germany is a main meal with mainly savoury food.
After each meal, participants were asked to rate their meal on three dimensions. They rated (1) how much they enjoyed the meal, (2) how pleased they were with their meal, and (3) how tasty their meal was. Ratings were given on a scale of one to 100. For reliability analysis, Cronbach’s Alpha was calculated to assess the internal consistency of the three items. Overall Cronbach’s alpha was calculated with α = 0.87. In addition, the average of the 38 Cronbach’s alpha scores calculated at the person level also yielded a satisfactory value with α = 0.83 ( SD = 0.24). Thirty-two of 38 participants showed a Cronbach’s alpha value above 0.70 (range = 0.42–0.97). An overall score of experienced happiness of eating was computed using the average of the three questions concerning the meals’ enjoyment, pleasure, and tastiness.
Analytical procedure
The food pictures and descriptions of their main components provided by the participants were subsequently coded by independent and trained raters. Following a standardised manual, additional components displayed in the picture were added to the description by the raters. All consumed foods were categorised into 14 different food categories (see Table 1 ) derived from the food classification system designed by the German Nutrition Society (DGE) and based on the existing food categories of the German Nutrient Database (Max Rubner Institut). Liquid intake and preparation method were not assessed. Therefore, fats and additional recipe ingredients were not included in further analyses, because they do not represent main elements of food intake. Further, salty extras were added to the categorisation.
No participant dropped out or had to be excluded due to high missing rates. Missing values were below 5% for all variables. The compliance rate at the meal level cannot be directly assessed since the numbers of meals and snacks can vary between as well as within persons (between days). As a rough compliance estimate, the numbers of meals that are expected from a “normative” perspective during the eight observation days can be used as a comparison standard (8 x breakfast, 8 × lunch, 8 × dinner = 24 meals). On average, the participants reported M = 6.3 breakfasts ( SD = 2.3), M = 5.3 lunches ( SD = 1.8), and M = 6.5 dinners ( SD = 2.0). In comparison to the “normative” expected 24 meals, these numbers indicate a good compliance (approx. 75%) with a tendency to miss six meals during the study period (approx. 25%). However, the “normative” expected 24 meals for the study period might be too high since participants might also have skipped meals (e.g. breakfast). Also, the present compliance rates are comparable to other studies. For example, Elliston et al . 36 recorded 3.3 meal/snack reports per day in an Australian adult sample and Casperson et al . 37 recorded 2.2 meal reports per day in a sample of adolescents. In the present study, on average, M = 3.4 ( SD = 1.35) meals or snacks were reported per day. These data indicate overall a satisfactory compliance rate and did not indicate selective reporting of certain food items.
To graphically visualise data, Tableau (version 10.1) was used and for further statistical analyses, IBM SPSS Statistics (version 24 for Windows).
Data availability
The dataset generated and analysed during the current study is available from the corresponding authors on reasonable request.
Cornil, Y. & Chandon, P. Pleasure as an ally of healthy eating? Contrasting visceral and epicurean eating pleasure and their association with portion size preferences and wellbeing. Appetite 104 , 52–59 (2016).
Article PubMed Google Scholar
Mann, T. et al . Medicare’s search for effective obesity treatments: Diets are not the answer. American Psychologist 62 , 220–233 (2007).
van Strien, T., Herman, C. P. & Verheijden, M. W. Dietary restraint and body mass change. A 3-year follow up study in a representative Dutch sample. Appetite 76 , 44–49 (2014).
Block, L. G. et al . From nutrients to nurturance: A conceptual introduction to food well-being. Journal of Public Policy & Marketing 30 , 5–13 (2011).
Article Google Scholar
Renner, B., Sproesser, G., Strohbach, S. & Schupp, H. T. Why we eat what we eat. The eating motivation survey (TEMS). Appetite 59 , 117–128 (2012).
Conner, T. S., Brookie, K. L., Carr, A. C., Mainvil, L. A. & Vissers, M. C. Let them eat fruit! The effect of fruit and vegetable consumption on psychological well-being in young adults: A randomized controlled trial. PloS one 12 , e0171206 (2017).
Article PubMed PubMed Central Google Scholar
Rooney, C., McKinley, M. C. & Woodside, J. V. The potential role of fruit and vegetables in aspects of psychological well-being: a review of the literature and future directions. Proceedings of the Nutrition Society 72 , 420–432 (2013).
Mujcic, R. & Oswald, A. J. Evolution of well-being and happiness after increases in consumption of fruit and vegetables. American Journal of Public Health 106 , 1504–1510 (2016).
White, B. A., Horwath, C. C. & Conner, T. S. Many apples a day keep the blues away – Daily experiences of negative and positive affect and food consumption in young adults. British Journal of Health Psychology 18 , 782–798 (2013).
Blanchflower, D. G., Oswald, A. J. & Stewart-Brown, S. Is psychological well-being linked to the consumption of fruit and vegetables? Social Indicators Research 114 , 785–801 (2013).
Grant, N., Wardle, J. & Steptoe, A. The relationship between life satisfaction and health behavior: A Cross-cultural analysis of young adults. International Journal of Behavioral Medicine 16 , 259–268 (2009).
Conner, T. S., Brookie, K. L., Richardson, A. C. & Polak, M. A. On carrots and curiosity: Eating fruit and vegetables is associated with greater flourishing in daily life. British Journal of Health Psychology 20 , 413–427 (2015).
Raghunathan, R., Naylor, R. W. & Hoyer, W. D. The unhealthy = tasty intuition and its effects on taste inferences, enjoyment, and choice of food products. Journal of Marketing 70 , 170–184 (2006).
Evers, C., Stok, F. M. & de Ridder, D. T. Feeding your feelings: Emotion regulation strategies and emotional eating. Personality and Social Psychology Bulletin 36 , 792–804 (2010).
Sproesser, G., Schupp, H. T. & Renner, B. The bright side of stress-induced eating: eating more when stressed but less when pleased. Psychological Science 25 , 58–65 (2013).
Wansink, B., Cheney, M. M. & Chan, N. Exploring comfort food preferences across age and gender. Physiology & Behavior 79 , 739–747 (2003).
Article CAS Google Scholar
Taut, D., Renner, B. & Baban, A. Reappraise the situation but express your emotions: impact of emotion regulation strategies on ad libitum food intake. Frontiers in Psychology 3 , 359 (2012).
Tomiyama, J. A., Finch, L. E. & Cummings, J. R. Did that brownie do its job? Stress, eating, and the biobehavioral effects of comfort food. Emerging Trends in the Social and Behavioral Sciences: An Interdisciplinary, Searchable, and Linkable Resource (2015).
Wagner, H. S., Ahlstrom, B., Redden, J. P., Vickers, Z. & Mann, T. The myth of comfort food. Health Psychology 33 , 1552–1557 (2014).
Schüz, B., Bower, J. & Ferguson, S. G. Stimulus control and affect in dietary behaviours. An intensive longitudinal study. Appetite 87 , 310–317 (2015).
Shiffman, S. Conceptualizing analyses of ecological momentary assessment data. Nicotine & Tobacco Research 16 , S76–S87 (2014).
de Castro, J. M., Bellisle, F. & Dalix, A.-M. Palatability and intake relationships in free-living humans: measurement and characterization in the French. Physiology & Behavior 68 , 271–277 (2000).
Adriaanse, M. A., Prinsen, S., de Witt Huberts, J. C., de Ridder, D. T. & Evers, C. ‘I ate too much so I must have been sad’: Emotions as a confabulated reason for overeating. Appetite 103 , 318–323 (2016).
Robinson, E. Relationships between expected, online and remembered enjoyment for food products. Appetite 74 , 55–60 (2014).
Boelsma, E., Brink, E. J., Stafleu, A. & Hendriks, H. F. Measures of postprandial wellness after single intake of two protein–carbohydrate meals. Appetite 54 , 456–464 (2010).
Article CAS PubMed Google Scholar
Boh, B. et al . Indulgent thinking? Ecological momentary assessment of overweight and healthy-weight participants’ cognitions and emotions. Behaviour Research and Therapy 87 , 196–206 (2016).
Wansink, B. & Sobal, J. Mindless eating: The 200 daily food decisions we overlook. Environment and Behavior 39 , 106–123 (2007).
Boushey, C., Spoden, M., Zhu, F., Delp, E. & Kerr, D. New mobile methods for dietary assessment: review of image-assisted and image-based dietary assessment methods. Proceedings of the Nutrition Society , 1–12 (2016).
Stok, F. M. et al . The DONE framework: Creation, evaluation, and updating of an interdisciplinary, dynamic framework 2.0 of determinants of nutrition and eating. PLoS ONE 12 , e0171077 (2017).
Pliner, P. & Rozin, P. In Dimensions of the meal: The science, culture, business, and art of eating (ed H Meiselman) 19–46 (Aspen Publishers, 2000).
Inauen, J., Shrout, P. E., Bolger, N., Stadler, G. & Scholz, U. Mind the gap? Anintensive longitudinal study of between-person and within-person intention-behaviorrelations. Annals of Behavioral Medicine 50 , 516–522 (2016).
Zepeda, L. & Deal, D. Think before you eat: photographic food diaries asintervention tools to change dietary decision making and attitudes. InternationalJournal of Consumer Studies 32 , 692–698 (2008).
Stein, K. F. & Corte, C. M. Ecologic momentary assessment of eating‐disordered behaviors. International Journal of Eating Disorders 34 , 349–360 (2003).
Bolger, N., Stadler, G. & Laurenceau, J. P. Power analysis for intensive longitudinal studies in Handbook of research methods for studying daily life (ed . Mehl, M. R. & Conner, T. S.) 285–301 (New York: The Guilford Press, 2012).
Aarts, E., Verhage, M., Veenvliet, J. V., Dolan, C. V. & Van Der Sluis, S. A solutionto dependency: using multilevel analysis to accommodate nested data. Natureneuroscience 17 , 491–496 (2014).
Elliston, K. G., Ferguson, S. G., Schüz, N. & Schüz, B. Situational cues andmomentary food environment predict everyday eating behavior in adults withoverweight and obesity. Health Psychology 36 , 337–345 (2017).
Casperson, S. L. et al . A mobile phone food record app to digitally capture dietary intake for adolescents in afree-living environment: usability study. JMIR mHealth and uHealth 3 , e30 (2015).
Download references
Acknowledgements
This research was supported by the Federal Ministry of Education and Research within the project SmartAct (Grant 01EL1420A, granted to B.R. & H.S.). The funding source had no involvement in the study’s design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit this article for publication. We thank Gudrun Sproesser, Helge Giese, and Angela Whale for their valuable support.
Author information
Deborah R. Wahl and Karoline Villinger contributed equally to this work.
Authors and Affiliations
Department of Psychology, University of Konstanz, Konstanz, Germany
Deborah R. Wahl, Karoline Villinger, Laura M. König, Katrin Ziesemer, Harald T. Schupp & Britta Renner
You can also search for this author in PubMed Google Scholar
Contributions
B.R. & H.S. developed the study concept. All authors participated in the generation of the study design. D.W., K.V., L.K. & K.Z. conducted the study, including participant recruitment and data collection, under the supervision of B.R. & H.S.; D.W. & K.V. conducted data analyses. D.W. & K.V. prepared the first manuscript draft, and B.R. & H.S. provided critical revisions. All authors approved the final version of the manuscript for submission.
Corresponding authors
Correspondence to Deborah R. Wahl or Britta Renner .
Ethics declarations
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary table s1, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wahl, D.R., Villinger, K., König, L.M. et al. Healthy food choices are happy food choices: Evidence from a real life sample using smartphone based assessments. Sci Rep 7 , 17069 (2017). https://doi.org/10.1038/s41598-017-17262-9
Download citation
Received : 05 June 2017
Accepted : 23 November 2017
Published : 06 December 2017
DOI : https://doi.org/10.1038/s41598-017-17262-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Financial satisfaction, food security, and shared meals are foundations of happiness among older persons in thailand.
- Sirinya Phulkerd
- Rossarin Soottipong Gray
- Sasinee Thapsuwan
BMC Geriatrics (2023)
Enrichment and Conflict Between Work and Health Behaviors: New Scales for Assessing How Work Relates to Physical Exercise and Healthy Eating
- Sabine Sonnentag
- Maria U. Kottwitz
- Jette Völker
Occupational Health Science (2023)
The value of Bayesian predictive projection for variable selection: an example of selecting lifestyle predictors of young adult well-being
- A. Bartonicek
- S. R. Wickham
- T. S. Conner
BMC Public Health (2021)
Smartphone-Based Ecological Momentary Assessment of Well-Being: A Systematic Review and Recommendations for Future Studies
- Lianne P. de Vries
- Bart M. L. Baselmans
- Meike Bartels
Journal of Happiness Studies (2021)
Exploration of nutritional, antioxidative, antibacterial and anticancer status of Russula alatoreticula: towards valorization of a traditionally preferred unique myco-food
- Somanjana Khatua
- Surashree Sen Gupta
- Krishnendu Acharya
Journal of Food Science and Technology (2021)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease
Affiliations.
- 1 Laboratory of Dietetics and Clinical Nutrition, Department of Public Health, Experimental and Forensic Medicine, University of Pavia, 27100 Pavia, Italy.
- 2 Clinical Nutrition and Dietetics Service, Unit of Internal Medicine and Endocrinology, ICS Maugeri IRCCS, 27100 Pavia, Italy.
- 3 Human Development and Health, Faculty of Medicine, University of Southampton, Southampton SO16 6YD, UK.
- 4 NIHR Southampton Biomedical Research Centre, University Hospital Southampton NHS Foundation Trust and University of Southampton, Southampton SO16 6YD, UK.
- PMID: 32012681
- PMCID: PMC7071223
- DOI: 10.3390/nu12020334
The definition of what constitutes a healthy diet is continually shifting to reflect the evolving understanding of the roles that different foods, essential nutrients, and other food components play in health and disease. A large and growing body of evidence supports that intake of certain types of nutrients, specific food groups, or overarching dietary patterns positively influences health and promotes the prevention of common non-communicable diseases (NCDs). Greater consumption of health-promoting foods and limited intake of unhealthier options are intrinsic to the eating habits of certain regional diets such as the Mediterranean diet or have been constructed as part of dietary patterns designed to reduce disease risk, such as the Dietary Approaches to Stop Hypertension (DASH) or Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diets. In comparison with a more traditional Western diet, these healthier alternatives are higher in plant-based foods, including fresh fruits and vegetables, whole grains, legumes, seeds, and nuts and lower in animal-based foods, particularly fatty and processed meats. To better understand the current concept of a "healthy diet," this review describes the features and supporting clinical and epidemiologic data for diets that have been shown to prevent disease and/or positively influence health. In total, evidence from epidemiological studies and clinical trials indicates that these types of dietary patterns reduce risks of NCDs including cardiovascular disease and cancer.
Keywords: healthy dietary patterns; macronutrients; micronutrients; non-communicable diseases; non-essential nutrients; plant-based diets.
Publication types
- Diet Surveys
- Diet, Healthy*
- Feeding Behavior*
Grants and funding
- Search Menu
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Introduction.
- < Previous

Young people and healthy eating: a systematic review of research on barriers and facilitators
- Article contents
- Figures & tables
- Supplementary Data
J Shepherd, A Harden, R Rees, G Brunton, J Garcia, S Oliver, A Oakley, Young people and healthy eating: a systematic review of research on barriers and facilitators, Health Education Research , Volume 21, Issue 2, 2006, Pages 239–257, https://doi.org/10.1093/her/cyh060
- Permissions Icon Permissions
A systematic review was conducted to examine the barriers to, and facilitators of, healthy eating among young people (11–16 years). The review focused on the wider determinants of health, examining community- and society-level interventions. Seven outcome evaluations and eight studies of young people's views were included. The effectiveness of the interventions was mixed, with improvements in knowledge and increases in healthy eating but differences according to gender. Barriers to healthy eating included poor school meal provision and ease of access to, relative cheapness of and personal taste preferences for fast food. Facilitators included support from family, wider availability of healthy foods, desire to look after one's appearance and will-power. Friends and teachers were generally not a common source of information. Some of the barriers and facilitators identified by young people had been addressed by soundly evaluated effective interventions, but significant gaps were identified where no evaluated interventions appear to have been published (e.g. better labelling of food products), or where there were no methodologically sound evaluations. Rigorous evaluation is required particularly to assess the effectiveness of increasing the availability of affordable healthy food in the public and private spaces occupied by young people.
Healthy eating contributes to an overall sense of well-being, and is a cornerstone in the prevention of a number of conditions, including heart disease, diabetes, high blood pressure, stroke, cancer, dental caries and asthma. For children and young people, healthy eating is particularly important for healthy growth and cognitive development. Eating behaviours adopted during this period are likely to be maintained into adulthood, underscoring the importance of encouraging healthy eating as early as possible [ 1 ]. Guidelines recommend consumption of at least five portions of fruit and vegetables a day, reduced intakes of saturated fat and salt and increased consumption of complex carbohydrates [ 2, 3 ]. Yet average consumption of fruit and vegetables in the UK is only about three portions a day [ 4 ]. A survey of young people aged 11–16 years found that nearly one in five did not eat breakfast before going to school [ 5 ]. Recent figures also show alarming numbers of obese and overweight children and young people [ 6 ]. Discussion about how to tackle the ‘epidemic’ of obesity is currently high on the health policy agenda [ 7 ], and effective health promotion remains a key strategy [ 8–10 ].
Evidence for the effectiveness of interventions is therefore needed to support policy and practice. The aim of this paper is to report a systematic review of the literature on young people and healthy eating. The objectives were
(i) to undertake a ‘systematic mapping’ of research on the barriers to, and facilitators of, healthy eating among young people, especially those from socially excluded groups (e.g. low-income, ethnic minority—in accordance with government health policy);
(ii) to prioritize a subset of studies to systematically review ‘in-depth’;
(iii) to ‘synthesize’ what is known from these studies about the barriers to, and facilitators of, healthy eating with young people, and how these can be addressed and
(iv) to identify gaps in existing research evidence.
General approach
This study followed standard procedures for a systematic review [ 11, 12 ]. It also sought to develop a novel approach in three key areas.
First, it adopted a conceptual framework of ‘barriers’ to and ‘facilitators’ of health. Research findings about the barriers to, and facilitators of, healthy eating among young people can help in the development of potentially effective intervention strategies. Interventions can aim to modify or remove barriers and use or build upon existing facilitators. This framework has been successfully applied in other related systematic reviews in the area of healthy eating in children [ 13 ], physical activity with children [ 14 ] and young people [ 15 ] and mental health with young people [16; S. Oliver, A. Harden, R. Rees, J. Shepherd, G. Brunton and A. Oakley, manuscript in preparation].
Second, the review was carried out in two stages: a systematic search for, and mapping of, literature on healthy eating with young people, followed by an in-depth systematic review of the quality and findings of a subset of these studies. The rationale for a two-stage review to ensure the review was as relevant as possible to users. By mapping a broad area of evidence, the key characteristics of the extant literature can be identified and discussed with review users, with the aim of prioritizing the most relevant research areas for systematic in-depth analysis [ 17, 18 ].
Third, the review utilized a ‘mixed methods’ triangulatory approach. Data from effectiveness studies (‘outcome evaluations’, primarily quantitative data) were combined with data from studies which described young people's views of factors influencing their healthy eating in negative or positive ways (‘views’ studies, primarily qualitative). We also sought data on young people's perceptions of interventions when these had been collected alongside outcomes data in outcome evaluations. However, the main source of young people's views was surveys or interview-based studies that were conducted independently of intervention evaluation (‘non-intervention’ research). The purpose was to enable us to ascertain not just whether interventions are effective, but whether they address issues important to young people, using their views as a marker of appropriateness. Few systematic reviews have attempted to synthesize evidence from both intervention and non-intervention research: most have been restricted to outcome evaluations. This study therefore represents one of the few attempts that have been made to date to integrate different study designs into systematic reviews of effectiveness [ 19–22 ].
Literature searching
A highly sensitive search strategy was developed to locate potentially relevant studies. A wide range of terms for healthy eating (e.g. nutrition, food preferences, feeding behaviour, diets and health food) were combined with health promotion terms or general or specific terms for determinants of health or ill-health (e.g. health promotion, behaviour modification, at-risk-populations, sociocultural factors and poverty) and with terms for young people (e.g. adolescent, teenager, young adult and youth). A number of electronic bibliographic databases were searched, including Medline, EMBASE, The Cochrane Library, PsycINFO, ERIC, Social Science Citation Index, CINAHL, BiblioMap and HealthPromis. The searches covered the full range of publication years available in each database up to 2001 (when the review was completed).
Full reports of potentially relevant studies identified from the literature search were obtained and classified (e.g. in terms of specific topic area, context, characteristics of young people, research design and methodological attributes).
Inclusion screening
Inclusion criteria were developed and applied to each study. The first round of screening was to identify studies to populate the map. To be included, a study had to (i) focus on healthy eating; (ii) include young people aged 11–16 years; (iii) be about the promotion of healthy eating, and/or the barriers to, or facilitators of, healthy eating; (iv) be a relevant study type: (a) an outcome evaluation or (b) a non-intervention study (e.g. cohort or case control studies, or interview studies) conducted in the UK only (to maximize relevance to UK policy and practice) and (v) be published in the English language.
The results of the map, which are reported in greater detail elsewhere [ 23 ], were used to prioritize a subset of policy relevant studies for the in-depth systematic review.
A second round of inclusion screening was performed. As before, all studies had to have healthy eating as their main focus and include young people aged 11–16 years. In addition, outcome evaluations had toFor a non-intervention study to be included it had to
(i) use a comparison or control group; report pre- and post-intervention data and, if a non-randomized trial, equivalent on sociodemographic characteristics and pre-intervention outcome variables (demonstrating their ‘potential soundness’ in advance of further quality assessment);
(ii) report an intervention that aims to make a change at the community or society level and
(iii) measure behavioural and/or physical health status outcomes.
(i) examine young people's attitudes, opinions, beliefs, feelings, understanding or experiences about healthy eating (rather than solely examine health status, behaviour or factual knowledge);
(ii) access views about one or more of the following: young people's definitions of and/or ideas about healthy eating, factors influencing their own or other young people's healthy eating and whether and how young people think healthy eating can be promoted and
(iii) privilege young people's views—presenting views directly as data that are valuable and interesting in themselves, rather than only as a route to generating variables to be tested in a predictive or causal model.
Non-intervention studies published before 1990 were excluded in order to maximize the relevance of the review findings to current policy issues.
Data extraction and quality assessment
All studies meeting inclusion criteria underwent data extraction and quality assessment, using a standardized framework [ 24 ]. Data for each study were entered independently by two researchers into a specialized computer database [ 25 ] (the full and final data extraction and quality assessment judgement for each study in the in-depth systematic review can be viewed on the Internet by visiting http://eppi.ioe.ac.uk ).
Outcome evaluations were considered methodologically ‘sound’ if they reported:Only studies meeting these criteria were used to draw conclusions about effectiveness. The results of the studies which did not meet these quality criteria were judged unclear.
(i) a control or comparison group equivalent to the intervention group on sociodemographic characteristics and pre-intervention outcome variables.
(ii) pre-intervention data for all individuals or groups recruited into the evaluation;
(iii) post-intervention data for all individuals or groups recruited into the evaluation and
(iv) on all outcomes, as described in the aims of the intervention.
Non-intervention studies were assessed according to a total of seven criteria (common to sets of criteria proposed by four research groups for qualitative research [ 26–29 ]):
(i) an explicit account of theoretical framework and/or the inclusion of a literature review which outlined a rationale for the intervention;
(ii) clearly stated aims and objectives;
(iii) a clear description of context which includes detail on factors important for interpreting the results;
(iv) a clear description of the sample;
(v) a clear description of methodology, including systematic data collection methods;
(vi) analysis of the data by more than one researcher and
(vii) the inclusion of sufficient original data to mediate between data and interpretation.
Data synthesis
Three types of analyses were performed: (i) narrative synthesis of outcome evaluations, (ii) narrative synthesis of non-intervention studies and (iii) synthesis of intervention and non-intervention studies together.
For the last of these a matrix was constructed which laid out the barriers and facilitators identified by young people alongside descriptions of the interventions included in the in-depth systematic review of outcome evaluations. The matrix was stratified by four analytical themes to characterize the levels at which the barriers and facilitators appeared to be operating: the school, family and friends, the self and practical and material resources. This methodology is described further elsewhere [ 20, 22, 30 ].
From the matrix it is possible to see:
(i) where barriers have been modified and/or facilitators built upon by soundly evaluated interventions, and ‘promising’ interventions which need further, more rigorous, evaluation (matches) and
(ii) where barriers have not been modified and facilitators not built upon by any evaluated intervention, necessitating the development and rigorous evaluation of new interventions (gaps).
Figure 1 outlines the number of studies included at various stages of the review. Of the total of 7048 reports identified, 135 reports (describing 116 studies) met the first round of screening and were included in the descriptive map. The results of the map are reported in detail in a separate publication—see Shepherd et al. [ 23 ] (the report can be downloaded free of charge via http://eppi.ioe.ac.uk ). A subset of 22 outcome evaluations and 8 studies of young people's views met the criteria for the in-depth systematic review.

The review process.
Outcome evaluations
Of the 22 outcome evaluations, most were conducted in the United States ( n = 16) [ 31–45 ], two in Finland [ 46, 47 ], and one each in the UK [ 48 ], Norway [ 49 ], Denmark [ 50 ] and Australia [ 51 ]. In addition to the main focus on promoting healthy eating, they also addressed other related issues including cardiovascular disease in general, tobacco use, accidents, obesity, alcohol and illicit drug use. Most were based in primary or secondary school settings and were delivered by teachers. Interventions varied considerably in content. While many involved some form of information provision, over half ( n = 13) involved attempts to make structural changes to young people's physical environments; half ( n = 11) trained parents in or about nutrition, seven developed health-screening resources, five provided feedback to young people on biological measures and their behavioural risk status and three aimed to provide social support systems for young people or others in the community. Social learning theory was the most common theoretical framework used to develop these interventions. Only a minority of studies included young people who could be considered socially excluded ( n = 6), primarily young people from ethnic minorities (e.g. African Americans and Hispanics).
Following detailed data extraction and critical appraisal, only seven of the 22 outcome evaluations were judged to be methodologically sound. For the remainder of this section we only report the results of these seven. Four of the seven were from the United States, with one each from the UK, Norway and Finland. The studies varied in the comprehensiveness of their reporting of the characteristics of the young people (e.g. sociodemographic/economic status). Most were White, living in middle class urban areas. All attended secondary schools. Table I details the interventions in these sound studies. Generally, they were multicomponent interventions in which classroom activities were complemented with school-wide initiatives and activities in the home. All but one of the seven sound evaluations included and an integral evaluation of the intervention processes. Some studies report results according to demographic characteristics such as age and gender.
Soundly evaluated outcome evaluations: study characteristics (n = 7)
RCT = Randomized Controlled Trial; CT = controlled trial (no randomization); PE = process evaluation.
Separate evaluations of the same intervention in two populations in New York (the Bronx and Westchester County).
The UK-based intervention was an award scheme (the ‘Wessex Healthy Schools Award’) that sought to make health-promoting changes in school ethos, organizational functioning and curriculum [ 48 ]. Changes made in schools included the introduction of health education curricula, as well as the setting of targets in key health promotion areas (including healthy eating). Knowledge levels, which were high at baseline, changed little over the course of the intervention. Intervention schools performed better in terms of healthy food choices (on audit scores). The impact on measures of healthy eating such as choosing healthy snacks varied according to age and sex. The intervention only appeared possibly to be effective for young women in Year 11 (aged 15–16 years) on these measures (statistical significance not reported).
The ‘Know Your Body’ intervention, a cardiovascular risk reduction programme, was evaluated in two separate studies in two demographically different areas of New York (the Bronx and Westchester County) [ 45 ]. Lasting for 5 years it comprised teacher-led classroom education, parental involvement activities and risk factor examination in elementary and junior high schools. In the Bronx evaluation, statistically significant increases in knowledge were reported, but favourable changes in cholesterol levels and dietary fat were not significant. In the Westchester County evaluation, we judged the effects to be unclear due to shortcomings in methods reported.
A second US-based study, the 3-year ‘Gimme 5’ programme [ 40 ], focused on increasing consumption of fruits and vegetables through a school-wide media campaign, complemented by classroom activities, parental involvement and changes to nutritional content of school meals. The intervention was effective at increasing knowledge (particularly among young women). Effects were measured in terms of changes in knowledge scores between baseline and two follow-up periods. Differences between the intervention and comparison group were significant at both follow-ups. There was a significant increase in consumption of fruit and vegetables in the intervention group, although this was not sustained.
In the third US study, the ‘Slice of Life’ intervention, peer leaders taught 10 sessions covering the benefits of fitness, healthy diets and issues concerning weight control [ 41 ]. School functioning was also addressed by student recommendations to school administrators. For young women, there were statistically significant differences between intervention and comparison groups on healthy eating scores, salt consumption scores, making healthy food choices, knowledge of healthy food, reading food labels for salt and fat content and awareness of healthy eating. However, among young men differences were only significant for salt and knowledge scores. The process evaluation suggested that having peers deliver training was acceptable to students and the peer-trainers themselves.
A Norwegian study evaluated a similar intervention to the ‘Slice of Life’ programme, employing peer educators to lead classroom activities and small group discussions on nutrition [ 49 ]. Students also analysed the availability of healthy food in their social and home environment and used a computer program to analyse the nutritional status of foods. There were significant intervention effects for reported healthy eating behaviour (but not maintained by young men) and for knowledge (not young women).
The second ‘North Karelia Youth Study’ in Finland featured classroom educational activities, a community media campaign, health-screening activities, changes to school meals and a health education initiative in the parents' workplace [ 47 ]. It was judged to be effective for healthy eating behaviour, reducing systolic blood pressure and modifying fat content of school meals, but less so for reducing cholesterol levels and diastolic blood pressure.
The evidence from the well-designed evaluations of the effectiveness of healthy eating initiatives is therefore mixed. Interventions tend to be more effective among young women than young men.
Young people's views
Table II describes the key characteristics of the eight studies of young people's views. The most consistently reported characteristics of the young people were age, gender and social class. Socioeconomic status was mixed, and in the two studies reporting ethnicity, the young people participating were predominantly White. Most studies collected data in mainstream schools and may therefore not be applicable to young people who infrequently or never attend school.
Characteristics of young people's views studies (n = 8)
All eight studies asked young people about their perceptions of, or attitudes towards, healthy eating, while none explicitly asked them what prevents them from eating healthily. Only two studies asked them what they think helps them to eat healthy foods, and only one asked for their ideas about what could or should be done to promote nutrition.
Young people tended to talk about food in terms of what they liked and disliked, rather than what was healthy/unhealthy. Healthy foods were predominantly associated with parents/adults and the home, while ‘fast food’ was associated with pleasure, friendship and social environments. Links were also made between food and appearance, with fast food perceived as having negative consequences on weight and facial appearance (and therefore a rationale for eating healthier foods). Attitudes towards healthy eating were generally positive, and the importance of a healthy diet was acknowledged. However, personal preferences for fast foods on grounds of taste tended to dominate food choice. Young people particularly valued the ability to choose what they eat.
Despite not being explicitly asked about barriers, young people discussed factors inhibiting their ability to eat healthily. These included poor availability of healthy meals at school, healthy foods sometimes being expensive and wide availability of, and personal preferences for, fast foods. Things that young people thought should be done to facilitate healthy eating included reducing the price of healthy snacks and better availability of healthy foods at school, at take-aways and in vending machines. Will-power and encouragement from the family were commonly mentioned support mechanisms for healthy eating, while teachers and peers were the least commonly cited sources of information on nutrition. Ideas for promoting healthy eating included the provision of information on nutritional content of school meals (mentioned by young women particularly) and better food labelling in general.
Table III shows the synthesis matrix which juxtaposes barriers and facilitators alongside results of outcome evaluations. There were some matches but also significant gaps between, on the one hand, what young people say are barriers to healthy eating, what helps them and what could or should be done and, on the other, soundly evaluated interventions that address these issues.
Synthesis matrix
Key to young people's views studies: Y1 , Dennison and Shepherd [ 56 ]; Y2 , Harris [ 57 ]; Y3 , McDougall [ 58 ]; Y4 , Miles and Eid [ 59 ]; Y5 , Roberts et al. [ 60 ]; Y6 , Ross [ 61 ]; Y7 , Watt and Sheiham [ 62 ]; Y8 , Watt and Sheiham [ 63 ]. Key to intervention studies: OE1 , Baranowski et al. [ 31 ]; OE2 , Bush et al. [ 32 ]; OE3 , Coates et al. [ 33 ]; OE4 , Ellison et al. [ 34 ]; OE5 , Flores [ 36 ]; OE6 , Fitzgibbon et al. [ 35 ]; OE7 , Hopper et al. [ 64 ]; OE8 , Holund [ 50 ]; OE9 , Kelder et al. [ 38 ]; OE10 , Klepp and Wilhelmsen [ 49 ]; OE11 , Moon et al. [ 48 ]; OE12 , Nader et al. [ 39 ]; OE13 , Nicklas et al. [ 40 ]; OE14 , Perry et al. [ 41 ]; OE15 , Petchers et al. [ 42 ]; OE16 , Schinke et al. [ 43 ]; OE17 , Wagner et al. [ 44 ]; OE18 , Vandongen et al. [ 51 ]; OE19 , Vartiainen et al. [ 46 ]; OE20 , Vartiainen et al. [ 47 ]; OE21 , Walter I [ 45 ]; OE22 , Walter II [ 45 ]. OE10, OE11, OE13, OE14, OE20, OE21 and OE22 denote a sound outcome evaluation. OE21 and OE22 are separate evaluations of the same intervention. Due to methodological limitations, we have judged the effects of OE22 to be unclear. Y1 and Y2 do not appear in the synthesis matrix as they did not explicitly report barriers or facilitators, and it was not possible for us to infer potential barriers or facilitators. However, these two studies did report what young people understood by healthy eating, their perceptions, and their views and opinions on the importance of eating a healthy diet. OE2, OE12, OE16 and OE17 do not appear in the synthesis matrix as they did not address any of the barriers or facilitators.
In terms of the school environment, most of the barriers identified by young people appear to have been addressed. At least two sound outcome evaluations demonstrated the effectiveness of increasing the availability of healthy foods in the school canteen [ 40, 47 ]. Furthermore, despite the low status of teachers and peers as sources of nutritional information, several soundly evaluated studies showed that they can be employed effectively to deliver nutrition interventions.
Young people associated parents and the home environment with healthy eating, and half of the sound outcome evaluations involved parents in the education of young people about nutrition. However, problems were sometimes experienced in securing parental attendance at intervention activities (e.g. seminar evenings). Why friends were not a common source of information about good nutrition is not clear. However, if peer pressure to eat unhealthy foods is a likely explanation, then it has been addressed by the peer-led interventions in three sound outcome evaluations (generally effectively) [ 41, 47, 49 ] and two outcome evaluations which did not meet the quality criteria (effectiveness unclear) [ 33, 50 ].
The fact that young people choose fast foods on grounds of taste has generally not been addressed by interventions, apart from one soundly evaluated effective intervention which included taste testings of fruit and vegetables [ 40 ]. Young people's concern over their appearance (which could be interpreted as both a barrier and a facilitator) has only been addressed in one of the sound outcome evaluations (which revealed an effective intervention) [ 41 ]. Will-power to eat healthy foods has only been examined in one outcome evaluation in the in-depth systematic review (judged to be sound and effective) (Walter I—Bronx evaluation) [ 45 ]. The need for information on nutrition was addressed by the majority of interventions in the in-depth systematic review. However, no studies were found which evaluated attempts to increase the nutritional content of school meals.
Barriers and facilitators relating to young people's practical and material resources were generally not addressed by interventions, soundly evaluated or otherwise. No studies were found which examined the effectiveness of interventions to lower the price of healthy foods. However, one soundly evaluated intervention was partially effective in increasing the availability of healthy snacks in community youth groups (Walter I—Bronx evaluation) [ 45 ]. At best, interventions have attempted to raise young people's awareness of environmental constraints on eating healthily, or encouraged them to lobby for increased availability of nutritious foods (in the case of the latter without reporting whether any changes have been effected as a result).
This review has systematically identified some of the barriers to, and facilitators of, healthy eating with young people, and illustrated to what extent they have been addressed by soundly evaluated effective interventions.
The evidence for effectiveness is mixed. Increases in knowledge of nutrition (measured in all but one study) were not consistent across studies, and changes in clinical risk factors (measured in two studies) varied, with one study detecting reductions in cholesterol and another detecting no change. Increases in reported healthy eating behaviour were observed, but mostly among young women revealing a distinct gender pattern in the findings. This was the case in four of the seven outcome evaluations (in which analysis was stratified by gender). The authors of one of the studies suggest that emphasis of the intervention on healthy weight management was more likely to appeal to young women. It was proposed that interventions directed at young men should stress the benefits of nutrition on strength, physical endurance and physical activity, particularly to appeal to those who exercise and play sports. Furthermore, age was a significant factor in determining effectiveness in one study [ 48 ]. Impact was greatest on young people in the 15- to 16-year age range (particularly for young women) in comparison with those aged 12–13 years, suggesting that dietary influences may vary with age. Tailoring the intervention to take account of age and gender is therefore crucial to ensure that interventions are as relevant and meaningful as possible.
Other systematic reviews of interventions to promote healthy eating (which included some of the studies with young people fitting the age range of this review) also show mixed results [ 52–55 ]. The findings of these reviews, while not being directly comparable in terms of conceptual framework, methods and age group, seem to offer some support for the findings of this review. The main message is that while there is some evidence to suggest effectiveness, the evidence base is limited. We have identified no comparable systematic reviews in this area.
Unlike other reviews, however, this study adopted a wider perspective through inclusion of studies of young people's views as well as effectiveness studies. A number of barriers to healthy eating were identified, including poor availability of healthy foods at school and in young people's social spaces, teachers and friends not always being a source of information/support for healthy eating, personal preferences for fast foods and healthy foods generally being expensive. Facilitating factors included information about nutritional content of foods/better labelling, parents and family members being supportive; healthy eating to improve or maintain one's personal appearance, will-power and better availability/lower pricing of healthy snacks.
Juxtaposing barriers and facilitators alongside effectiveness studies allowed us to examine the extent to which the needs of young people had been adequately addressed by evaluated interventions. To some extent they had. Most of the barriers and facilitators that related to the school and relationships with family and friends appear to have been taken into account by soundly evaluated interventions, although, as mentioned, their effectiveness varied. Many of the gaps tended to be in relation to young people as individuals (although our prioritization of interventions at the level of the community and society may have resulted in the exclusion of some of these interventions) and the wider determinants of health (‘practical and material resources’). Despite a wide search, we found few evaluations of strategies to improve nutritional labelling on foods particularly in schools or to increase the availability of affordable healthy foods particularly in settings where young people socialize. A number of initiatives are currently in place which may fill these gaps, but their effectiveness does not appear to have been reported yet. It is therefore crucial for any such schemes to be thoroughly evaluated and disseminated, at which point an updated systematic review would be timely.
This review is also constrained by the fact that its conclusions can only be supported by a relatively small proportion of the extant literature. Only seven of the 22 outcome evaluations identified were considered to be methodologically sound. As illustrated in Table III , a number of the remaining 15 interventions appear to modify barriers/build on facilitators but their results can only be judged unclear until more rigorous evaluation of these ‘promising’ interventions has been reported.
Finally, it is important to acknowledge that the majority of the outcome evaluations were conducted in the United States, and by virtue of the inclusion criteria, all the young people's views studies were UK based. The literature therefore might not be generalizable to other countries, where sociocultural values and socioeconomic circumstances may be quite different. Further evidence synthesis is needed on barriers to, and facilitators of, healthy eating and nutrition worldwide, particularly in developing countries.
The aim of this study was to survey what is known about the barriers to, and facilitators of, healthy eating among young people with a view to drawing out the implications for policy and practice. The review has mapped and quality screened the extant research in this area, and brought together the findings from evaluations of interventions aiming to promote healthy eating and studies which have elicited young people's views.
There has been much research activity in this area, yet it is disappointing that so few evaluation studies were methodologically strong enough to enable us to draw conclusions about effectiveness. There is some evidence to suggest that multicomponent school-based interventions can be effective, although effects tended to vary according to age and gender. Tailoring intervention messages accordingly is a promising approach which should therefore be evaluated. A key theme was the value young people place on choice and autonomy in relation to food. Increasing the provision and range of healthy, affordable snacks and meals in schools and social spaces will enable them to exercise their choice of healthier, tasty options.
We have identified that several barriers to, and facilitators of, healthy eating in young people have received little attention in evaluation research. Further work is needed to develop and evaluate interventions which modify or remove these barriers, and build on these facilitators. Further qualitative studies are also needed so that we can continue to listen to the views of young people. This is crucial if we are to develop and test meaningful, appropriate and effective health promotion strategies.
We would like to thank Chris Bonell and Dina Kiwan for undertaking data extraction. We would also like to acknowledge the invaluable help of Amanda Nicholas, James Thomas, Elaine Hogan, Sue Bowdler and Salma Master for support and helpful advice. The Department of Health, England, funds a specific programme of health promotion work at the EPPI-Centre. The views expressed in the report are those of the authors and not necessarily those of the Department of Health.
Google Scholar
Google Preview
- healthy diet
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Assessing the Cost of Healthy and Unhealthy Diets: A Systematic Review of Methods
- Public Health Nutrition (KE Charlton, Section Editor)
- Open access
- Published: 09 September 2022
- Volume 11 , pages 600–617, ( 2022 )
Cite this article
You have full access to this open access article

- Cherie Russell ORCID: orcid.org/0000-0003-1251-4810 1 ,
- Jillian Whelan ORCID: orcid.org/0000-0001-9434-109X 2 &
- Penelope Love ORCID: orcid.org/0000-0002-1244-3947 1 , 3
5909 Accesses
3 Citations
2 Altmetric
Explore all metrics
Purpose of Review
Poor diets are a leading risk factor for chronic disease globally. Research suggests healthy foods are often harder to access, more expensive, and of a lower quality in rural/remote or low-income/high minority areas. Food pricing studies are frequently undertaken to explore food affordability. We aimed to capture and summarise food environment costing methodologies used in both urban and rural settings.
Recent Findings
Our systematic review of high-income countries between 2006 and 2021 found 100 relevant food pricing studies. Most were conducted in the USA ( n = 47) and Australia ( n = 24), predominantly in urban areas ( n = 74) and cross-sectional in design ( n = 76). All described a data collection methodology, with just over half ( n = 57) using a named instrument. The main purpose for studies was to monitor food pricing, predominantly using the ‘food basket’, followed by the Nutrition Environment Measures Survey for Stores (NEMS-S). Comparatively, the Healthy Diets Australian Standardised Affordability and Price (ASAP) instrument supplied data on relative affordability to household incomes.
Future research would benefit from a universal instrument reflecting geographic and socio-cultural context and collecting longitudinal data to inform and evaluate initiatives targeting food affordability, availability, and accessibility.
Similar content being viewed by others

A tale of two cities: the cost, price-differential and affordability of current and healthy diets in Sydney and Canberra, Australia
Amanda J. Lee, Sarah Kane, … Meron Lewis
Healthy diets ASAP – Australian Standardised Affordability and Pricing methods protocol
Amanda J Lee, Sarah Kane, … Mathew Dick
Testing the price and affordability of healthy and current (unhealthy) diets and the potential impacts of policy change in Australia
Amanda J. Lee, Sarah Kane, … Mathew Dick
Avoid common mistakes on your manuscript.
Introduction
Poor diets, described as those low in fruits, vegetables, and whole grains, and high in red and processed meats and ultra-processed foods, are a leading risk factor for chronic disease globally [ 1 ]. In most high-income countries (HIC), poor diets disproportionally affect lower socioeconomic populations, Indigenous Peoples, and those living in rural and/or remote areas [ 2 , 3 , 4 , 5 ]. Rather than solely a consequence of individual behaviours, poor diets are critically informed by broad contextual factors, including social, commercial, environmental, and cultural influences [ 6 , 7 ]. Crucially, the consumption of a healthy diet is constrained by the range, affordability, and acceptability of foods available for sale [ 8 ]. Research suggests that healthy foods are often harder to access, more expensive, and often of a lower quality in rural, remote, or low-income/high minority areas, than in metropolitan or high-income areas [ 9 , 10 , 11 , 12 ]. Such food environments contribute to higher rates of diet-related non-communicable diseases and food insecurity [ 13 , 14 ]. In order to improve population diets, all aspects of the food environment must be addressed to ensure healthy foods are affordable, available, and of adequate nutritional quality [ 15 ].
Price is a primary factor impacting food choice, diet quality, and food security, therefore having affordable, acceptable, healthy food should be a political and social priority [ 8 , 15 , 16 ]. Some research suggests that healthy diets are associated with greater total spending [ 17 , 18 , 19 ], while other studies report that adherence to a healthy diet is less expensive than current or ‘unhealthy’ diets [ 9 , 20 , 21 ]. Regardless, the cost of a healthy diet is a proportionately large household expense (> 30% of household income) and may therefore be considered ‘unaffordable’ [ 22 ]. Additionally, public perception that healthy diets are expensive is high, which itself may be a barrier to the purchase of healthy foods [ 23 ]. Therefore, improving the affordability of healthy food could improve population diets, regardless of context [ 24 ].
To address the issue of food affordability and inform appropriate attenuating policy and intervention strategies, food pricing studies are frequently undertaken. Food pricing, however, is not a universal construct and is highly influenced by country and context. Numerous methods have been developed to measure food pricing, with data therefore not always comparable or replicable, and of limited value to inform appropriate policy [ 25 ]. Most studies that collect food pricing data conclude that food prices are rising, making healthy eating unaffordable for many populations. However, few studies to date have used this data to suggest strategies to improve affordability. Our systematic review aims to capture and summarise food environment costing methodologies used in HIC, in both urban and rural settings, between 2006 and 2021. In addressing this aim, we answer the following questions: (i) What is the stated purpose of collecting data on food prices, including whether the data is used to inform or advocate for interventions? (ii) Which instruments are being used to measure food pricing? (iii) What are the strengths and limitations of each instrument as reported by study authors?
To address the research aim, we undertook a systematic review of the literature, following the Preferred Reported Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 26 ]. We followed four steps: (i) systematic search for relevant literature; (ii) selection of studies, (iii) data extraction, and (iv) analysis and synthesis of results.
Systematic Search Strategy
After consultation with a research liaison librarian, databases used included EBSCOHOST (Academic Search Complete, CINAHL Complete, GlobalHealth, Medline Complete, and PsychINFO) and Informit. We chose these databases for their comprehensiveness and conventional use in the public health nutrition discipline. We identified search terms using a scoping review and key words used in previous food pricing reviews [ 15 , 23 , 27 , 28 ]. We searched both article abstracts and titles using the following search string: ‘food affordability’ OR ‘food cost’ OR ‘food price*’ OR ‘food promotion*’. We completed an initial search for studies published 2016–2021 in October 2021, followed by a search for studies published 2006–2015 in December 2021.
Selection of Studies
Studies were included if they were English, peer-reviewed journal articles presenting original research, monitored food prices in a high-income country/s, and were published between 2006 and 2021. The article by Glanz (2006) [ 15 ] is considered a seminal paper in food pricing research and was therefore chosen as the starting date for our search. Studies prior to this date were considered unlikely to be relevant to the research question and were thus excluded. Review articles, opinion pieces, posters, perspectives, study protocols, viewpoints, editorials, and commentaries were excluded, as well as those assessing middle- or low-income countries.
Study screening involved an initial review of all titles and removal of duplicates by A1 using online Covidence software [ 29 ], followed by abstract screening (A1), and then full text screening of remaining studies (A1). A second reviewer independently screened all articles by abstract and full text to minimise bias (A2 and A3). Disagreements were resolved through discussion between researchers; where no agreement was reached, a third party acted as an arbiter (A2 and A3). Limited hand searching was conducted given the volume of papers identified. Online Resource 1 presents a PRISMA flow chart of the study selection process.
Data Extraction
Included studies were uploaded to an Endnote (V. X9) [ 30 ] library. We systematically extracted details of each study to Microsoft Excel (V. 2112), including the author/s, year published, article title, aim, pricing instrument used (if specified), country and geographical context (e.g. urban or rural), type of data collected, number and type of locations assessed, number and type of food items captured, population (if the study used sales receipts to estimate food prices), time period of study, strengths, limitations, and conclusions.
Data Analysis and Synthesis
The coded data were used to identify major themes that were then synthesised in the results. We used an inductive thematic approach for our analysis, with the results discussed between the research team to limit researcher subjectivity [ 31 ]. We used Microsoft Excel to calculate descriptive statistics and graphical outputs.
Overview of Studies
Database searching identified 2737 studies, with 1882 studies remaining after removal of duplicates. After abstract screening, a total of 287 were identified for full-text screening, with 187 excluded, and a total of 100 studies included in this systematic review (Online Resource 1).
We observed an increasing number of studies each year, with peaks in 2013, 2014, and 2018 (Fig. 1 ).
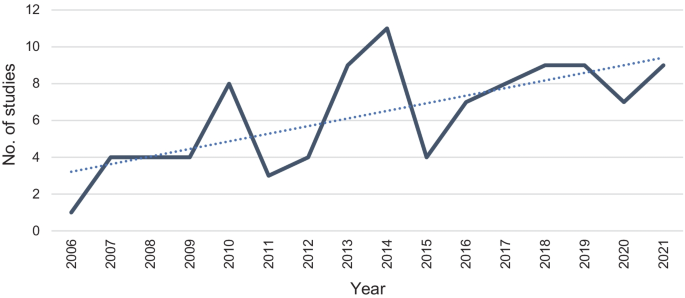
Frequency of studies published assessing food prices between 2006 and 2021
Most studies measured food prices in the USA ( n = 47), followed by Australia ( n = 25). Urban food environments were assessed more frequently ( n = 74) than rural ( n = 33). Most studies were cross-sectional ( n = 77). Most studies included instore price audits ( n = 59), followed by online price audits (supermarket websites, n = 13), or electronic point of sale data (consumer receipts, register sales, or electronic scanning of food prices in the home, n = 12), and a combination of these ( n = 17). Most studies collected food price data from more than 20 food retail outlets ( n = 34) (Table 1 ).
Details of all included studies, grouped according to data source used (instore price audits, online price audits, electronic point of sale, and combinations of these), are shown in Tables 2 , 3 , and 4 . Details include instrument used (if applicable), purpose of data collection, country, context, study type (e.g. cross-sectional, longitudinal), healthiness comparisons (between healthy and unhealthy products or diets), study author, and year. The use of a named instrument was captured to identify commonalities in usage of instruments, and not as an indication of study quality. When assessing differentials in ‘healthiness’, studies either presented a comparison of a ‘healthy diet’ with an ‘unhealthy or currently consumed diet’ or a comparison of the cost of ‘healthy’ and ‘unhealthy’ foods or product categories.
Study Purpose for Collecting Data on Food Prices
The studies included in this review had a multitude of aims (Tables 2 , 3 , and 4 ). While most studies were conducted solely to monitor food prices in a specific location/s [ 33 , 39 , 42 , 46 , 47 , 52 , 54 , 56 , 57 , 59 , 64 , 67 , 71 , 75 , 80 , 81 , 88 , 89 , 104 , 106 , 108 , 109 , 114 ], others aimed to monitor food price changes over time [ 53 , 63 , 74 , 83 , 93 , 97 , 111 , 127 ], assess food prices as a function of income, socioeconomic status, or welfare assistance [ 9 , 19 , 20 , 33 , 36 , 37 , 38 , 40 , 41 , 66 , 69 , 70 , 77 , 84 , 85 , 86 , 90 , 91 , 92 , 94 , 100 , 110 , 115 , 116 , 117 , 122 ]; assess food price in relation to geographic distance [ 19 , 77 , 91 , 92 , 94 , 98 ]; compare perceptions of food price with actual food prices [ 68 , 101 , 107 ]; and relate food price with a health outcome [ 34 , 35 , 37 , 40 , 47 , 58 , 70 , 72 , 78 , 105 , 116 , 117 , 124 , 125 ], compare the price of healthy or unhealthy foods/diets [ 9 , 20 , 34 , 43 , 50 , 51 , 55 , 60 , 61 , 62 , 63 , 64 , 65 , 76 , 85 , 86 , 93 , 94 , 95 , 96 , 99 , 102 , 110 , 111 , 112 , 120 , 121 , 123 , 124 , 126 ], assess diet costs for a specific population [ 82 , 118 ], compare food prices between brands [ 79 ], compare approaches for estimating dietary costs [ 32 ], or understand how prices impact consumption [ 44 ]. Only seven studies specifically aimed to collect data to inform policy strategies and/or community interventions to improve population health [ 10 , 11 , 49 , 80 , 87 , 103 , 113 ]. However, 26 studies did discuss their study findings on food price in relation to potential further action to improve food environments [ 9 , 19 , 20 , 33 , 36 , 37 , 40 , 43 , 47 , 49 , 50 , 54 , 55 , 59 , 63 , 64 , 81 , 85 , 86 , 87 , 88 , 103 , 104 , 105 , 110 ]. Specific suggested strategies included those targeting individuals, such as education campaigns to promote healthy and more affordable food choices [ 9 , 36 , 43 , 45 , 49 , 50 , 55 ], and those targeting environmental changes, such as taxes on ‘unhealthy’ foods [ 33 , 49 , 85 , 104 , 110 ], subsidies and exemptions for ‘healthy’ foods [ 9 , 20 , 45 , 62 , 63 , 85 , 104 , 110 ], vouchers for farmer’s markets [ 43 ], establishing more food stores [ 33 , 45 , 48 , 104 ], better public transportation for consumers to access food stores [ 59 ], generating savings at the manufacturer/wholesaler level that can be passed on to customers [ 81 ], establishing community-led food supply options [ 9 ], and increasing welfare support proportionate to food prices and geographic distances to food stores [ 37 , 40 , 50 , 73 , 85 ].
Overview of Instruments Used to Measure Food Prices
Of the 100 included studies, 57 used a named instrument to measure food prices, as described below. The remaining 43 studies did not name a pre-existing data collection instrument; instead, the authors described the data collection methodology used, for example, in store, online, or via electronic sales data.
Food Basket Instruments
The majority ( n = 30) of studies used a variation of a ‘food basket’ to estimate food prices. Food baskets capture the prices of a pre-defined list of foods, often in quantities representative of the total diet of reference families over a defined timeframe [ 9 ], and is a longstanding methodology used to investigate the availability and affordability of food. Food basket studies were mainly conducted in the USA ( n = 14) and Australia ( n = 12) [ 19 , 20 , 80 , 81 , 83 , 87 , 88 , 89 , 90 , 91 , 92 ]. Food basket studies using named instruments were conducted in the USA—using the Thrifty Food Plan Market Basket ( n = 5), the Fred Hutchinson Cancer Research Center Market Basket ( n = 3), the University of Washington’s Center for Public Health Nutrition Market Basket ( n = 3), and the USDA Market Basket ( n = 2); in Australia—using the Victorian Healthy Food Basket ( n = 4), the Food Basket informed by the INFORMAS framework ( n = 2), the Adelaide Healthy Food Basket ( n = 2), the Illawarra Healthy Food Basket ( n = 2), the Queensland Healthy Food Access Basket Survey ( n = 1), and the Northern Territory Market Basket ( n = 1); and in Canada—using the Ontario Nutritious food basket ( n = 1), the Revised Northern Food Basket ( n = 1), and an unspecified market basket ( n = 1). Food basket studies were conducted in both rural ( n = 13) [ 19 , 37 , 49 , 50 , 52 , 81 , 83 , 87 , 88 , 90 , 91 , 103 , 110 ] and urban contexts ( n = 25) [ 19 , 20 , 37 , 38 , 40 , 46 , 49 , 50 , 51 , 52 , 62 , 63 , 64 , 66 , 67 , 70 , 80 , 81 , 83 , 88 , 89 , 92 , 104 , 105 , 111 ].
All but two [ 37 , 40 ] food basket studies collected prices from physical instore locations [ 19 , 20 , 38 , 43 , 46 , 49 , 50 , 51 , 52 , 55 , 62 , 63 , 64 , 66 , 67 , 70 , 73 , 80 , 81 , 83 , 87 , 88 , 89 , 90 , 91 , 92 , 103 , 104 , 105 , 110 ], with four of these studies supplementing the data with online supermarket prices [ 62 , 63 , 64 , 81 ]. Additionally, three instruments compared the cost of a ‘healthy diet’ to either an ‘unhealthy or currently consumed diet’ [ 20 , 88 , 110 ], 13 instruments compared the cost of ‘healthy’ and ‘unhealthy’ individual foods or product categories [ 19 , 38 , 51 , 62 , 63 , 66 , 83 , 87 , 89 , 90 , 103 ], and 14 instruments did not present a comparison [ 37 , 40 , 46 , 49 , 50 , 52 , 64 , 67 , 70 , 80 , 81 , 91 , 92 , 104 , 105 ]. ‘Current’ diets were defined using national survey data [ 20 , 110 ]. Level of healthiness was defined using various benchmarks, namely the NOVA food processing classification system [ 38 ], nutrient composition and energy density [ 38 , 51 , 62 , 63 , 66 , 80 , 83 , 90 ], national Dietary Guidelines [ 19 , 43 , 70 , 87 , 88 , 89 , 90 ], and the Dietary Approaches to Stop Hypertension (DASH) dietary pattern [ 43 ]. Food affordability was benchmarked using household income [ 20 , 49 , 50 , 90 , 91 , 92 , 103 , 105 , 110 ], government subsidies [ 37 , 40 , 87 , 89 , 91 ], and minimum wage [ 38 , 66 , 70 ]; however, most studies ( n = 13) did not determine relative affordability in their analysis [ 43 , 51 , 52 , 55 , 62 , 63 , 64 , 67 , 73 , 80 , 81 , 83 , 88 ].
Healthy Diets Australian Standardised Affordability and Price (ASAP) Instrument
Following critiques of existing food baskets, the previously described INFORMAS instrument was refined to assess and compare the price and affordability of healthy and current diets in Australia, leading to the development of the Healthy Diets Australian Standardised Affordability and Price (ASAP). This instrument assesses the cost of a ‘recommended’ Australian diet (defined by the Australian Dietary Guidelines and Australian Guide to Healthy Eating) and the cost of the ‘current’ Australian diet (as reported in the 2011–12 Australian Health Survey) using the reference household of two parents and two children (boy aged 14 years; girl aged 8 years) [ 128 ]. Thus, all studies using this instrument present a comparison of the cost of a ‘healthy’ and ‘unhealthy’ diet in their analysis. Intrinsic to the instrument, the relative affordability of a healthy diet is measured against household incomes. The ASAP instrument was used by four studies to collect food price data in physical instore locations [ 9 , 85 , 86 ] or from online supermarkets [ 94 ]. Studies were conducted in both rural ( n = 2) [ 9 , 85 , 94 ] and urban ( n = 2) [ 85 , 86 , 94 ] contexts.
Nutrition Environment Measures Survey for Stores (NEMS-S) Instrument
The Nutrition Environment Measures Survey for Stores (NEMS-S) and its variants were also frequently used throughout food pricing studies ( n = 15). These included NEMS-S-Rev (Nutrition Environment Measures Survey for Stores Revised), TxNEAS (Texas Nutrition Environment Assessment), NEMS-S-NL (Nutrition Environment Measures Survey for Stores Newfoundland and Labrador), and The Bridging the Gap Food Store Observation Form. This instrument was used mostly in the USA ( n = 11) [ 11 , 33 , 36 , 44 , 47 , 48 , 54 , 57 , 68 , 71 , 107 ]. Studies were conducted in both rural ( n = 4) [ 10 , 11 , 56 , 106 ] and urban ( n = 11) [ 33 , 36 , 44 , 47 , 48 , 54 , 57 , 68 , 71 , 107 , 108 ] contexts. Compared to the food basket methodology, the NEMS-S instrument compares products in the same category that are considered ‘healthy’ or ‘unhealthy’ based on American Dietetic Association (ADA) recommended dietary guidelines, focusing on availability, price, and quality. All studies using the NEMS-S instrument collected food price data in physical instore locations. While the instrument itself does not include a calculation of relative affordability, approximately half the NEMS-S studies included this step in their methods [ 33 , 36 , 44 , 47 , 48 , 54 , 57 ], while all others did not [ 10 , 11 , 56 , 68 , 71 , 106 , 107 , 108 ].
Other Instruments
Several other named instruments were identified, used in single studies. These included the Diet and Nutrition Tool for Evaluation (DANTE) [ 101 ], the Flint Store Food Assessment Instrument [ 60 ], the Food Label Trial registry tool [ 76 ], the New Zealand Food Price Index [ 111 ], the USDA Food Store Survey Instrument [ 73 ], USDA Low-cost food plan [ 55 ] and audit forms developed by the Yale Rudd Center [ 39 ], the Hartford Advisory Commission on Food Policy [ 59 ], and the USDA Authorized Food Retailers’ Characteristics and Access Study [ 43 ]. Only three instruments compared healthy and unhealthy products [ 43 , 76 , 111 ] and none analysed the relative affordability of food.
Instrument Strengths and Limitations
The strengths and limitations of instruments commonly used across studies, as identified by study authors, are presented in Online Resource 2 . Commonly cited limitations, regardless of instrument used, included that actual purchasing behaviours were not captured (unless electronic point of sales data was utilised); culturally important and region-specific products were often not captured; tools were cross-sectional in nature, thus seasonality or changes overtime were not considered; and out-shopping, described as food purchases undertaken outside the local residential geography, including internet orders or foods purchased during travel to other communities, could not be accounted for. While some food basket studies and those using the ASAP instrument did contextualise the relative affordability of healthy foods and/or diets, this was not a part of the methodology for NEMS-S. Other limitations specific to NEMS-S included the length of the survey, and a low convergence between NEMS-S results and consumer perceptions of affordability. Specific limitations for food basket studies included results being constrained by the reference family used and the assumption that food is shared equally among household members. Additionally, most instruments did not capture geographical information regarding access to food retail outlets or availability of foods within food retail outlets.
Authors less commonly described instrument strengths. For NEMS-S, cited strengths included the ability to compare food prices between healthy and unhealthy options, that it has strong inter-rater and test-re-test reliability, and that it has been validated in multiple countries. ASAP studies, and some food basket studies, included a comparison between healthy and current (‘unhealthy’) diets (based on actual consumption) and included alcohol in the survey.
Our systematic review details the key purposes, and methodologies used, for measuring food prices in HIC between 2006 and 2021. While most studies were conducted solely to monitor food prices in specific locations, some sought to report price changes over time, and others collected data to assess comparability of food costs to healthier alternatives, average earnings, welfare payments, rurality, and socioeconomic position. Most studies measured food prices in urban areas, using instore food price audits, with an emerging use of online data collection evident. The most frequently used instruments were ‘food baskets’, used predominantly to monitor food prices; the NEMS-S instrument, used to provide data on relative cost and availability; and the ASAP instrument, use to provide data on relative affordability.
Our review differs from previous reviews of food price and affordability instruments [ 23 , 28 ] by taking a broadened focus on food pricing measures used in HIC globally and including new technology that is affording opportunities for electronic food pricing data collection. While a previous review critiqued food pricing measures for relevance specific to a rural context, our review includes both rural and urban contexts [ 28 ]. Another review [ 23 ] also describes the components of individual instruments, such as the identification of differently sized ‘food baskets’, ranging between 30 and 200 food items. Such critique was beyond the scope of our research questions.
Despite emerging options for electronic methodologies, the predominance of in person, instore data collection continues, notwithstanding the time-consuming and resource-intensive nature of this method. Studies indicate that these instore instruments can be targeted and applied within multiple contexts, such as rural [ 9 , 10 , 11 , 12 ], Indigenous [ 129 , 130 ], and low socioeconomic areas [ 85 ]. Perhaps researchers consider instore data collection as providing real-world insights at a community and population health level. Our review identified that food pricing instruments were mostly used to monitor food prices at a single point in time (cross-sectional) rather than changes at different time points (longitudinal). Instruments that enable the comparison of food prices in terms of a healthy diet (as recommended by dietary guidelines) compared with current dietary patterns (as reported through population health surveys) [ 128 ], and relative affordability for families, appear to provide data of greater practice and policy relevance with regard to community strategies, taxes, and subsidies that have potential to enhance food affordability, availability, and accessibility.
Technological innovations are an emerging alternative to in person data collection, facilitating the acquisition of online supermarket prices, a less labour-intensive method for capturing food prices [ 131 ]. To date, this method has been used within major chain-supermarkets, with a recent study reporting similar results when comparing pricing data obtained instore versus online [ 94 ]. This method therefore holds potential where an online supermarket presence exists, which was increasingly the case during the COVID-19 pandemic [ 53 ], providing rapid feedback to inform price promotions. However, for smaller and/or independent food retail outlets, frequently located in rural areas, online data collection does not appear to capture the contextual nuances of instore price promotions.
Our review found an over-representation of food pricing studies within urban areas. This is consistent with multiple studies that reflect inequities experienced within rural environments [ 132 ], and rural food environments are no exception [ 133 ]. The predominance of research within urban areas may also reflect a pragmatic researcher response to the physical proximity of stores (ease of measurement) and larger population reach (potential for greater population impact). Previous research shows significant differences in income-based variables, food environments, and the affordability of healthy food between urban and rural settings [ 134 ]. There is therefore a need for rural-specific food pricing studies, using appropriate instruments, to evaluate and inform rural-specific food environment initiatives [ 28 ].
During the period covered by this review, high level experts from the World Health Organization [ 135 ], the Lancet Commission [ 136 ], and the Food and Agricultural Organisation of the United Nations [ 137 ] have identified the potential benefits that initiatives located within food retail environments can provide in nudging dietary choices towards healthier options through instore food pricing and promotion, with the overall aim of improving population level diets [ 14 ]. Measures of food pricing, and the relative affordability of a healthy diet, are important to both inform and measure the effectiveness of such initiatives. However, few studies in our review explicitly aimed to inform initiatives or strategies, either at the community or policy level. Assessment of author-reported strengths and limitations of food pricing instruments and methodologies also identified a need for a universal instrument that reflects contextual geographic and socio-cultural information; is intended to be used repeatedly over time; and is adaptable to different country/cultural/contextual settings [ 17 , 23 ]. Future research would benefit from linking the purpose of undertaking food pricing data collection more explicitly to potential initiatives. Our review supports this call and suggests that the instrument selected should suit the context and collect longitudinal data to provide greater insights into the design and effectiveness of initiatives that make healthy food not only affordable but also available and accessible.
Strengths and Limitations
This systematic review provides a current and comprehensive overview of international food pricing studies across HIC. We acknowledge that while food prices are an important factor influencing food choice, it is only one component of the food environment; however, analysing instruments that assess food acceptability, availability, and accessibility was beyond the scope of this review. This review focused on HIC and a similar review on food pricing studies in low- and middle-income countries would be informative. This review may have missed additional relevant data as it only included English language studies and did not include grey literature or hand searching of reference lists.
Food security has come under heightened scrutiny given the food supply interruptions experienced worldwide during the COVID-19 pandemic. While studies providing a snapshot of food prices can be useful to identify areas impacted by rising food prices, much of this cross-sectional data is known. This review raises questions regarding the purpose of collecting food price data, and how this data can best be used to inform change through practice and policy strategies. We suggest that longitudinal studies using a consistent methodology, which acknowledges contextual nuances and demonstrates temporal changes in food pricing, are needed to inform and to evaluate community-based or legislative strategies to improve the relative affordability of a healthy diet.
Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, Abdollahpour I, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49.
Article Google Scholar
Australian Institute of Health and Welfare. Australia’s Health 2022: Burden of Disease. Canberra: AIHW; 2020.
Google Scholar
Sloane DC, Diamant AL, Lewis LB, Yancey AK, Flynn G, Nascimento LM, Mc Carthy WJ, Guinyard JJ, Cousineau MR. Improving the nutritional resource environment for healthy living through community-based participatory research. J Gen Intern Med. 2003;18:568–75.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–14.
Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87:1107–17.
Article CAS Google Scholar
Kickbusch I, Allen L, Franz C. The commercial determinants of health. Lancet Glob Health. 2016;4:e895–6.
Wilkinson RG, Marmot M. Social determinants of health: the solid facts, (World Health Organization). 2003.
Lee JH, Ralston RA, Truby H. Influence of food cost on diet quality and risk factors for chronic disease: a systematic review. Nutr Diet. 2011;68:248–61.
Love P, Whelan J, Bell C, Grainger F, Russell C, Lewis M, Lee A. Healthy diets in rural Victoria-cheaper than unhealthy alternatives, yet unaffordable. Int J Environ Res Public Health. 2018;15.
Whelan J, Millar L, Bell C, Russell C, Grainger F, Allender S, Love P. You can’t find healthy food in the bush: poor accessibility, availability and adequacy of food in rural Australia. Int J Environ Res Public Health. 2018;15:2316.
Pereira RF, Sidebottom AC, Boucher JL, Lindberg R, Werner R. Peer Reviewed: Assessing the Food Environment of a Rural Community: Baseline Findings From the Heart of New Ulm Project, Minnesota, 2010–2011. Prev Chronic Dis. 2014;11.
Vilaro MJ, Barnett TE. The rural food environment: a survey of food price, availability, and quality in a rural Florida community. Food Public Health. 2013;3:111–8.
Garasky S, Morton LW, Greder KA. The effects of the local food environment and social support on rural food insecurity. J Hunger Environ Nutr. 2006;1:83–103.
Swinburn B, Sacks G, Vandevijvere S, Kumanyika S, Lobstein T, Neal B, Barquera S, Friel S, Hawkes C, Kelly B. INFORMAS (I nternational N etwork for F ood and O besity/non-communicable diseases R esearch, M onitoring and A ction S upport): overview and key principles. Obes Rev. 2013;14:1–12.
Glanz K, Johnson L, Yaroch AL, Phillips M, Ayala GX, Davis EL. Measures of retail food store environments and sales: review and implications for healthy eating initiatives. J Nutr Educ Behav. 2016;48(280–288): e281.
Begemann F. Ecogeographic differentiation of bambarra groundnut (Vigna subterranea) in the collection of the International Institute of Tropical Agriculture (IITA, (Wissenschaftlicher Fachverlag). 1988.
Lee A, Mhurchu CN, Sacks G, Swinburn B, Snowdon W, Vandevijvere S, Hawkes C, L’Abbé M, Rayner M, Sanders D. Monitoring the price and affordability of foods and diets globally. Obes Rev. 2013;14:82–95.
Rao M, Afshin A, Singh G, Mozaffarian D. Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta-analysis. BMJ Open. 2013;3: e004277.
Palermo C, McCartan J, Kleve S, Sinha K, Shiell A. A longitudinal study of the cost of food in Victoria influenced by geography and nutritional quality. Aust N Z J Public Health. 2016;40:270–3.
Lee AJ, Kane S, Ramsey R, Good E, Dick M. Testing the price and affordability of healthy and current (unhealthy) diets and the potential impacts of policy change in Australia. BMC Public Health. 2016;16:1–22.
Clark P, Mendoza-Gutiérrez CF, Montiel-Ojeda D, Denova-Gutiérrez E, López-González D, Moreno-Altamirano L, Reyes A. A healthy diet is not more expensive than less healthy options: cost-analysis of different dietary patterns in Mexican children and adolescents. Nutrients. 2021;13:3871.
Burns C, Friel S. It’s time to determine the cost of a healthy diet in Australia. Aust N Z J Public Health. 2007;31:363–5.
Lewis M, Lee A. Costing ‘healthy’food baskets in Australia–a systematic review of food price and affordability monitoring tools, protocols and methods. Public Health Nutr. 2016;19:2872–86.
Moayyed H, Kelly B, Feng X, Flood V. Is living near healthier food stores associated with better food intake in regional Australia? Int J Environ Res Public Health. 2017;14:884.
Seal J. Monitoring the price and availability of healthy food–time for a national approach? Nutr Diet. 2004;61:197–200.
Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Caspi CE, Sorensen G, Subramanian S, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18:1172–87.
Love P, Whelan J, Bell C, McCracken J. Measuring rural food environments for local action in Australia: a systematic critical synthesis review. Int J Environ Res Public Health. 2019;16:2416.
Covidence systematic review software. Volume 2022. (Melbourne, Australia: Veritas Health Innovation).
The Endnote Team. Endnote. Endnote. X9 ed. Philadelphia, PA: Clarivate; 2013.
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. 2019;11:589–97.
Aaron GJ, Keim NL, Drewnowski A, Townsend MS. Estimating dietary costs of low-income women in California: a comparison of 2 approaches. Am J Clin Nutr. 2013;97:835–41.
Andreyeva T, Blumenthal DM, Schwartz MB, Long MW, Brownell KD. Availability and prices of foods across stores and neighborhoods: the case of New Haven, Connecticut. Health affairs (Project Hope). 2008;27:1381–8.
Anekwe TD, Rahkovsky I. The association between food prices and the blood glucose level of US adults with type 2 diabetes. Am J Public Health. 2014;104:678–85.
Bernstein AM, Bloom DE, Rosner BA, Franz M, Willett WC. Relation of food cost to healthfulness of diet among US women. Am J Clin Nutr. 2010;92:1197–203.
Borja K, Dieringer S. Availability of affordable healthy food in Hillsborough County, Florida. J Public Aff (14723891). 2019;19. N.PAG-N.PAG.
Bronchetti ET, Christensen G, Hoynes HW. Local food prices, SNAP purchasing power, and child health. J Health Econ. 2019;68: 102231.
Buszkiewicz J, House C, Anju A, Long M, Drewnowski A, Otten JJ. The impact of a city-level minimum wage policy on supermarket food prices by food quality metrics: a two-year follow up study. Int J Environ Res Public Health. 2019;16:102.
Caspi CE, Pelletier JE, Harnack LJ, Erickson DJ, Lenk K, Laska MN. Pricing of staple foods at supermarkets versus small food stores. Int J Environ Res Public Health. 2017;14.
Christensen G, Bronchetti ET. Local food prices and the purchasing power of SNAP benefits. Food Policy. 2020;95. N.PAG-N.PAG.
Colabianchi N, Antonakos CL, Coulton CJ, Kaestner R, Lauria M, Porter DE. The role of the built environment, food prices and neighborhood poverty in fruit and vegetable consumption: an instrumental variable analysis of the moving to opportunity experiment. Health Place. 2021;67: 102491.
Cole S, Filomena S, Morland K. Analysis of fruit and vegetable cost and quality among racially segregated neighborhoods in Brooklyn. New York J Hunger Environ Nutr. 2010;5:202–15.
Connell CL, Zoellner JM, Yadrick MK, Chekuri SC, Crook LB, Bogle ML. Energy density, nutrient adequacy, and cost per serving can provide insight into food choices in the lower Mississippi Delta. J Nutr Educ Behav. 2012;44:148–53.
DiSantis KI, Grier SA, Oakes JM, Kumanyika SK. Food prices and food shopping decisions of black women. Appetite. 2014;77:106–14.
Fan L, Canales E, Fountain B, Buys D. An assessment of the food retail environment in counties with high obesity rates in Mississippi. J Hunger Environ Nutr. 2021;16:571–93.
Franzen L, Smith C. Food system access, shopping behavior, and influences on purchasing groceries in adult Hmong living in Minnesota. Am J Health Promot. 2010;24:396–409.
Ghosh-Dastidar B, Cohen D, Hunter G, Zenk SN, Huang C, Beckman R, Dubowitz T. Distance to store, food prices, and obesity in urban food deserts. Am J Prev Med. 2014;47:587–95.
Ghosh-Dastidar M, Hunter G, Collins RL, Zenk SN, Cummins S, Beckman R, Nugroho AK, Sloan JC, Wagner LV, Dubowitz T, et al. Does opening a supermarket in a food desert change the food environment? Health Place. 2017;46:249–56.
Greenberg JA, Luick B, Alfred JM, Barber LR Jr, Bersamin A, Coleman P, Esquivel M, Fleming T, Guerrero RTL, Hollyer J, et al. The affordability of a thrifty food plan-based market basket in the United States-affiliated Pacific Region. Hawaii J Med Public Health. 2020;79:217–23.
Hardin-Fanning F, Rayens MK. Food cost disparities in rural communities. Health Promot Pract. 2015;16:383–91.
Hardin-Fanning F, Wiggins AT. Food costs are higher in counties with poor health rankings. J Cardiovasc Nurs. 2017;32:93–8.
Hilbert N, Evans-Cowley J, Reece J, Rogers C, Ake W, Hoy C. Mapping the cost of a balanced diet, as a function of travel time and food price. Journal of Agriculture, Food Systems and Community Development. 2014;5:105–27.
Hillen J. Online food prices during the COVID-19 pandemic. Agribusiness (New York). 2021;37:91–107.
Jin H, Lu Y. Evaluating consumer nutrition environment in food deserts and food swamps. Int J Environ Res Public Health. 2021;18.
Karp RJ, Wong G, Orsi M. Demonstrating nutrient cost gradients: a Brooklyn case study. Int J Vitam Nutr Res. 2014;84:244–51.
Ko LK, Enzler C, Perry CK, Rodriguez E, Mariscal N, Linde S, Duggan C. Food availability and food access in rural agricultural communities: use of mixed methods. BMC Public Health. 2018;18. N.PAG-N.PAG.
Lee Smith M, Sunil TS, Salazar CI, Rafique S, Ory MG. Disparities of food availability and affordability within convenience stores in Bexar County. Texas J Environ Public Health. 2013;2013:1–7.
Lipsky LM. Are energy-dense foods really cheaper? Reexamining the relation between food price and energy density. Am J Clin Nutr. 2009;90:1397–401.
Martin KS, Ghosh D, Page M, Wolff M, McMinimee K, Zhang M. What role do local grocery stores play in urban food environments? A case study of Hartford-Connecticut. PLoS ONE. 2014;9: e94033.
Mayfield KE, Hession SL, Weatherspoon L, Hoerr SL. A cross-sectional analysis exploring differences between food availability, food price, food quality and store size and store location in Flint Michigan. J Hunger Environ Nutr. 2020;15:643–57.
Meyerhoefer CD, Leibtag ES. A spoonful of sugar helps the medicine go down: the relationship between food prices and medical expenditures on diabetes. Am J Agr Econ. 2010;92:1271–82.
Monsivais P, Drewnowski A. The rising cost of low-energy-density foods. J Am Diet Assoc. 2007;107:2071–6.
Monsivais P, McLain J, Drewnowski A. The rising disparity in the price of healthful foods: 2004–2008. Food Policy. 2010;35:514–20.
Monsivais P, Perrigue MM, Adams SL, Drewnowski A. Measuring diet cost at the individual level: a comparison of three methods. Eur J Clin Nutr. 2013;67:1220–5.
Nansel TR, Lipsky LM, Eisenberg MH, Liu A, Mehta SN, Laffel LMB. Can families eat better without spending more? Improving diet quality does not increase diet cost in a randomized clinical trial among youth with type 1 diabetes and their parents. J Acad Nutr Diet. 2016;116:1751.
Otten JJ, Buszkiewicz J, Tang W, Anju A, Long M, Vigdor J, Drewnowski A. The impact of a city-level minimum-wage policy on supermarket food prices in Seattle-King County. Int J Environ Res Public Health. 2017;14:1039.
Richards R, Smith C. Shelter environment and placement in community affects lifestyle factors among homeless families in Minnesota. Am J Health Promot. 2006;21:36–44.
Shen Y, Clarke P, Gomez-Lopez IN, Hill AB, Romero DM, Goodspeed R, Berrocal VJ, Vydiswaran VV, Veinot TC. Using social media to assess the consumer nutrition environment: comparing Yelp reviews with a direct observation audit instrument for grocery stores. Public Health Nutr. 2019;22:257–64.
Smith C, Butterfass J, Richards R. Environment influences food access and resulting shopping and dietary behaviors among homeless Minnesotans living in food deserts. Agric Hum Values. 2010;27:141–61.
Spoden AL, Buszkiewicz JH, Drewnowski A, Long MC, Otten JJ. Seattle’s minimum wage ordinance did not affect supermarket food prices by food processing category. Public Health Nutr. 2018;21:1762–70.
Stroebele-Benschop N, Wolf K, Palmer K, Kelley CJ, Jilcott Pitts SB. Comparison of food and beverage products’ availability, variety, price and quality in German and US supermarkets. Public Health Nutr. 2020;23:3387–93.
Townsend MS, Aaron GJ, Monsivais P, Keim NL, Drewnowski A. Less-energy-dense diets of low-income women in California are associated with higher energy-adjusted diet costs. Am J Clin Nutr. 2009;89:1220–6.
Wright L, Palak G, Yoshihara K. Accessibility and affordability of healthy foods in food deserts in Florida: policy and practice implications. Florida Public Health Review. 2018;15:98–103.
Yang Y, Leung P. Price premium or price discount for locally produced food products? A temporal analysis for Hawaii. J Asian Pac Econ. 2020;25:591–610.
Zenk SN, Grigsby-Toussaint DS, Curry SJ, Berbaum M, Schneider L. Short-term temporal stability in observed retail food characteristics. J Nutr Educ Behav. 2010;42:26–32.
Abreu MD, Charlton K, Probst Y, Li N, Crino M, Wu JHY. Nutrient profiling and food prices: what is the cost of choosing healthier products? J Hum Nutr Diet. 2019;32:432–42.
Ball K, Timperio A, Crawford D. Neighbourhood socioeconomic inequalities in food access and affordability. Health Place. 2009;15:578–85.
Brimblecombe J, Ferguson M, Liberato SC, O’Dea K, Riley M. Optimisation modelling to assess cost of dietary improvement in remote aboriginal Australia. PLoS ONE. 2013;8: e83587.
Chapman K, Innes-Hughes C, Goldsbury D, Kelly B, Bauman A, Allman-Farinelli M. A comparison of the cost of generic and branded food products in Australian supermarkets. Public Health Nutr. 2013;16:894–900.
Cuttler R, Evans R, McClusky E, Purser L, Klassen KM, Palermo C. An investigation of the cost of food in the Geelong region of rural Victoria: essential data to support planning to improve access to nutritious food. Health Promot J Austr. 2019;30:124–7.
Ferguson M, O’Dea K, Chatfield M, Moodie M, Altman J, Brimblecombe J. The comparative cost of food and beverages at remote Indigenous communities, Northern Territory, Australia. Aust N Z J Public Health. 2016;40(Suppl 1):S21–6.
Ferguson M, O’Dea K, Holden S, Miles E, Brimblecombe J. Food and beverage price discounts to improve health in remote Aboriginal communities: mixed method evaluation of a natural experiment. Aust N Z J Public Health. 2017;41:32–7.
Harrison MS, Coyne T, Lee AJ, Leonard D, Lowson S, Groos A, Ashton BA. The increasing cost of the basic foods required to promote health in Queensland. Med J Aust. 2007;186:9–14.
Kettings C, Sinclair AJ, Voevodin M. A healthy diet consistent with Australian health recommendations is too expensive for welfare-dependent families. Aust N Z J Public Health. 2009;33:566–72.
Lee A, Patay D, Herron L-M, Parnell Harrison E, Lewis M. Affordability of current, and healthy, more equitable, sustainable diets by area of socioeconomic disadvantage and remoteness in Queensland: insights into food choice. Int J Equity Health. 2021;20:1–17.
Lee AJ, Kane S, Herron L-M, Matsuyama M, Lewis M. A tale of two cities: the cost, price-differential and affordability of current and healthy diets in Sydney and Canberra, Australia. Int J Behav Nutr Phys Act. 2020;17:1–13.
Palermo CE, Walker KZ, Hill P, McDonald J. The cost of healthy food in rural Victoria. Rural Remote Health. 2008;8. (1 December 2008).
Pollard CM, Landrigan TJ, Ellies PL, Kerr DA, Lester MLU, Goodchild SE. Geographic factors as determinants of food security: a Western Australian food pricing and quality study. Asia Pac J Clin Nutr. 2014;23:703–13.
Tsang A, Ndung’u MW, Coveney J, O’Dwyer L. Adelaide Healthy Food Basket: a survey on food cost, availability and affordability in five local government areas in metropolitan Adelaide, South Australia. Nutr Diet. 2007;64:241–7.
Walton K, do Rosario V, Kucherik M, Frean P, Richardson K, Turner M, Mahoney J, Charlton K, Andre do Rosario V. Identifying trends over time in food affordability: the Illawarra Healthy Food Basket survey, 2011–2019. Health Promot J Austr. 2021;1–1.
Ward PR, Coveney J, Verity F, Carter P, Schilling M. Cost and affordability of healthy food in rural South Australia. Rural Remote Health 2012;12. Article No. 1938.
Wong K, Coveney J, Ward P, Muller R, Carter P, Verity F, Tsourtos G. Availability, affordability and quality of a healthy food basket in Adelaide, South Australia. Nutr Diet. 2011;68:8–14.
Burns C, Sacks G, Gold L. Longitudinal study of Consumer Price Index (CPI) trends in core and non-core foods in Australia. Aust N Z J Public Health. 2008;32:450–3.
Zorbas C, Lee A, Peeters A, Lewis M, Landrigan T, Backholer K. Streamlined data-gathering techniques to estimate the price and affordability of healthy and unhealthy diets under different pricing scenarios. Public Health Nutr. 2021;24:1–11.
Conklin AI, Monsivais P, Khaw K, Wareham NJ, Forouhi NG. Dietary diversity, diet cost, and incidence of type 2 diabetes in the United Kingdom: a prospective cohort study. PLoS Med. 2016;13: e1002085.
Jones NRV, Tong TYN, Monsivais P. Meeting UK dietary recommendations is associated with higher estimated consumer food costs: an analysis using the National Diet and Nutrition Survey and consumer expenditure data, 2008–2012. Public Health Nutr. 2018;21:948–56.
Lan H, Lloyd T, Morgan W, Dobson PW. Are food price promotions predictable? The hazard function of supermarket discounts. J Agric Econ. 2021;1.
Mackenbach JD, Burgoine T, Lakerveld J, Forouhi NG, Griffin SJ, Wareham NJ, Monsivais P. Accessibility and affordability of supermarkets: associations with the DASH diet. Am J Prev Med. 2017;53:55–62.
Monsivais P, Scarborough P, Lloyd T, Mizdrak A, Luben R, Mulligan AA, Wareham NJ, Woodcock J. Greater accordance with the Dietary Approaches to Stop Hypertension dietary pattern is associated with lower diet-related greenhouse gas production but higher dietary costs in the United Kingdom. Am J Clin Nutr. 2015;102:138–45.
Timmins KA, Hulme C, Cade JE. The monetary value of diets consumed by British adults: an exploration into sociodemographic differences in individual-level diet costs. Public Health Nutr. 2015;18:151–9.
Timmins KA, Morris MA, Hulme C, Edwards KL, Clarke GP, Cade JE. Comparability of methods assigning monetary costs to diets: derivation from household till receipts versus cost database estimation using 4-day food diaries. Eur J Clin Nutr. 2013;67:1072–6.
Vogel C, Abbott G, Ntani G, Barker M, Cooper C, Moon G, Ball K, Baird J. Examination of how food environment and psychological factors interact in their relationship with dietary behaviours: test of a cross-sectional model. Int J Behav Nutr Phys Act. 2019;16. N.PAG-N.PAG.
Kenny T-A, Fillion M, MacLean J, Wesche SD, Chan HM. Calories are cheap, nutrients are expensive – the challenge of healthy living in Arctic communities. Food Policy. 2018;80:39–54.
Latham J, Moffat T. Determinants of variation in food cost and availability in two socioeconomically contrasting neighbourhoods of Hamilton, Ontario, Canada. Health Place. 2007;13:273–87.
Lear SA, Gasevic D, Schuurman N. Association of supermarket characteristics with the body mass index of their shoppers. Nutr J. 2013;12. (13 August 2013).
Mah CL. Taylor N. Store patterns of availability and price of food and beverage products across a rural region of Newfoundland and Labrador. Canadian journal of public health = Revue canadienne de sante publique. 2020;111:247–256.
Minaker LM, Raine KD, Wild TC, Nykiforuk CIJ, Thompson ME, Frank LD. Objective food environments and health outcomes. Am J Prev Med. 2013;45:289–96.
Minaker LM, Raine KD, Wild TC, Nykiforuk CIJ, Thompson ME, Frank LD. Construct validation of 4 food-environment assessment methods: adapting a multitrait-multimethod matrix approach for environmental measures. Am J Epidemiol. 2014;179:519–28.
Pakseresht M, Lang R, Rittmueller S, Roache C, Sheehy T, Batal M, Corriveau A, Sangita S. Food expenditure patterns in the Canadian Arctic show cause for concern for obesity and chronic disease. Int J Behav Nutr Phys Act. 2014;11. (17 April 2014).
Mackay S, Buch T, Vandevijvere S, Goodwin R, Korohina E, Funaki-Tahifote M, Lee A, Swinburn B. Cost and affordability of diets modelled on current eating patterns and on dietary guidelines, for New Zealand total population, Māori and Pacific households. Int J Environ Res Public Health. 2018;15.
Mackay S, Vandevijvere S, Lee A. Ten-year trends in the price differential between healthier and less healthy foods in New Zealand. Nutrition & dietetics: the journal of the Dietitians Association of Australia. 2019;76:271–6.
Vandevijvere S, Young N, Mackay S, Swinburn B, Gahegan M. Modelling the cost differential between healthy and current diets: the New Zealand case study. Int J Behav Nutr Phys Act. 2018;15:1–1.
Wilson N, Nghiem N, Mhurchu CN, Eyles H, Baker MG, Blakely T. Foods and dietary patterns that are healthy, low-cost, and environmentally sustainable: a case study of optimization modeling for New Zealand. PLoS ONE. 2013;8: e59648.
Alexy U, Bolzenius K, Köpper A, Clausen K, Kersting M. Diet costs and energy density in the diet of German children and adolescents. Eur J Clin Nutr. 2012;66:1362–3.
Stroebele N, Dietze P, Tinnemann P, Willich SN. Assessing the variety and pricing of selected foods in socioeconomically disparate districts of Berlin, Germany. J Public Health. 2011;19:23–8.
Albuquerque G, Moreira P, Rosário R, Araújo A, Teixeira VH, Lopes O, Moreira A, Padrão P. Adherence to the Mediterranean diet in children: Is it associated with economic cost? Porto biomedical journal. 2017;2:115–9.
Alves R, Lopes C, Rodrigues S, Perelman J. Adhering to a Mediterranean diet in a Mediterranean country: an excess cost for families? Br J Nutr. 2021;1–24.
Faria AP, Albuquerque G, Moreira P, Rosário R, Araújo A, Teixeira V, Barros R, Lopes Ó, Moreira A, Padrão P. Association between energy density and diet cost in children. Porto Biomed J. 2016;1:106–11.
Mackenbach JD, Dijkstra SC, Beulens JWJ, Seidell JC, Snijder MB, Stronks K, Monsivais P, Nicolaou M. Socioeconomic and ethnic differences in the relation between dietary costs and dietary quality: the HELIUS study. Nutr J. 2019;18. N.PAG-N.PAG.
Waterlander WE, de Haas WE, van Amstel I, Schuit AJ, Twisk JWR, Visser M, Seidell JC, Steenhuis IHM. Energy density, energy costs and income - how are they related? Public Health Nutr. 2010;13:1599–608.
Rydén P, Mattsson Sydner Y, Hagfors L. Counting the cost of healthy eating: a Swedish comparison of Mediterranean-style and ordinary diets. Int J Consum Stud. 2008;32:138–46.
Rydén PJ, Hagfors L. Diet cost, diet quality and socio-economic position: how are they related and what contributes to differences in diet costs? Public Health Nutr. 2011;14:1680–92.
Keiko S, Kentaro M, Hitomi O, Livingstone MBE, Satomi K, Hitomi S, Satoshi S. Nutritional correlates of monetary diet cost in young, middle-aged and older Japanese women. J Nutr Sci. 2017;6:1–11.
Bolarić M, Šatalić Z. The relation between food price, energy density and diet quality. Croatian Journal of Food Science and Technology. 2013;5:39–45.
Parlesak A, Tetens I, Jensen JD, Smed S, Blenkuš MG, Rayner M, Darmon N, Robertson A. Use of linear programming to develop cost-minimized nutritionally adequate health promoting food baskets. PLoS ONE. 2016;11: e0163411.
Marty L, Dubois C, Gaubard MS, Maidon A, Lesturgeon A, Gaigi H, Darmon N. Higher nutritional quality at no additional cost among low-income households: insights from food purchases of “positive deviants.” Am J Clin Nutr. 2015;102:190–8.
Ng SW, Slining MM, Popkin BM. Turning point for US diets? Recessionary effects or behavioral shifts in foods purchased and consumed. Am J Clin Nutr. 2014;99:609–16.
Lee AJ, Kane S, Lewis M, Good E, Pollard CM, Landrigan TJ, Dick M. Healthy diets ASAP–Australian standardised affordability and pricing methods protocol. Nutr J. 2018;17:1–14.
Lee A, Lewis M. Testing the price of healthy and current diets in remote Aboriginal communities to improve food security: development of the Aboriginal and Torres Strait Islander Healthy Diets ASAP (Australian Standardised Affordability and Pricing) methods. Int J Environ Res Public Health. 2018;15:2912.
Ferguson M, O’Dea K, Chatfield M, Moodie M, Altman J, Brimblecombe J. The comparative cost of food and beverages at remote Indigenous communities, Northern Territory, Australia. Aust N Z J Public Health. 2016;40:S21–6.
Zorbas C, Gilham B, Boelsen-Robinson T, Blake MR, Peeters A, Cameron AJ, Wu JH, Backholer K. The frequency and magnitude of price-promoted beverages available for sale in Australian supermarkets. Aust N Z J Public Health. 2019;43:346–51.
Bourke L, Humphreys JS, Wakerman J, Taylor J. Understanding rural and remote health: a framework for analysis in Australia. Health Place. 2012;18:496–503.
Alston LV, Bolton KA, Whelan J, Reeve E, Shee AW, Browne J, Walker T, Versace VL, Allender S, Nichols M. Retail initiatives to improve the healthiness of food environments in rural, regional and remote communities. Med J Aust. 2020;213:S5.
Cafer AM, Kaiser ML. An analysis of differences in predictors of food affordability between rural and urban counties. J Poverty. 2016;20:34–55.
Drysdale C, Sykes E, Honeysett C. WHO urges governments to promote healthy food in public facilities. 2021;2022.
Willet W. Summary report of the EAT-Lancet Commission on healthy diets from sustainable food systems. E.-L. Commission, ed. (Eat-Lancet Commission ). 2019.
Food and Organization A. The State of Food Security and Nutrition in the World 2021. (Food and Agriculture Organization Rome). 2021.
Download references
Open Access funding enabled and organized by CAUL and its Member Institutions CR is supported by an Australian Government Research Training Scholarship. This funder had no involvement in any aspect of the study. JW is funded by a Deakin University Dean’s Postdoctoral Research Fellowship. JW is also supported by the National Health and Medical Research Council (NHMRC) funded Centre of Research Excellence in Food Retail Environments for Health (RE-FRESH) (APP1152968). The opinions, analysis, and conclusions in this paper are those of the authors and should not be attributed to the NHMRC.
Author information
Authors and affiliations.
School of Exercise and Nutrition Sciences, Deakin University, Geelong, Australia
Cherie Russell & Penelope Love
School of Medicine, Institute for Health Transformation, Deakin University, Geelong, Australia
Jillian Whelan
Institute for Physical Activity and Nutrition, Deakin University, Geelong, Australia
Penelope Love
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation: Penelope Love and Jillian Whelan; Methodology: all authors; Data extraction and synthesis: Cherie Russell; Writing—original draft preparation: Cherie Russell; Writing—review and editing: all authors.
Corresponding author
Correspondence to Cherie Russell .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Public Health Nutrition
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 47 kb)
Supplementary file2 (docx 39 kb), rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Russell, C., Whelan, J. & Love, P. Assessing the Cost of Healthy and Unhealthy Diets: A Systematic Review of Methods. Curr Nutr Rep 11 , 600–617 (2022). https://doi.org/10.1007/s13668-022-00428-x
Download citation
Accepted : 11 July 2022
Published : 09 September 2022
Issue Date : December 2022
DOI : https://doi.org/10.1007/s13668-022-00428-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Food pricing
- Measurement instruments
- Food environments
Advertisement
- Find a journal
- Publish with us
- Track your research
Healthy Eating Research
- Program Staff
- National Advisory Committee
- Our Commitment to Health Equity
- Resources for Researchers
Current Funding Opportunities
Healthy Communities
- Diet Quality & Healthy Weight
Early Childhood
Food Access
Food Marketing
Food Retail
- Nutrition Policy & Programs
- Pricing & Economics
- School & After School
- List of All Research & Publications
- Ages 0-2 Feeding Recommendations
- Ages 0-5 Beverage Recommendations
- Ages 2-8 Feeding Recommendations
- Ages 5+ Beverage Recommendations
- Grantee Announcements
Supporting research on environmental and policy strategies to promote healthy eating among children to prevent childhood obesity.

Stay up to date, Sign up for email alerts
Latest News and Research

We are accepting applications for small commissioned studies and papers that address time-sensitive research questions.
focus areas
School & After School
Pricing & Economics
Nutrition Policy & Programs
Diet Quality & Healthy Weight
of afterschool sites offered fruits or vegetables during snack
Research & Publications See all
Height and weight measurement and communication with families in head start: developing a toolkit and establishing best practices.
Head start (HS) programs are required to collect children’s height and weight data. Programs also communicate these results to families. However, no standardized protocol exists to guide measurements or communicate results. The purpose of this article was to describe the development of a measurement toolkit and best practices for communication. HS programs contributed to the More
Promoting Healthier Purchases: Ultraprocessed Food Taxes and Minimally Processed Foods Subsidies for the Low Income
Fiscal policies can shift relative food prices to encourage the purchase and consumption of minimally processed foods while discouraging the purchase and consumption of unhealthy ultraprocessed foods, high in calories and nutrients of concern (sodium, sugar, and saturated fats), especially for low-income households. The 2017–2018 packaged food purchase data among U.S. households were used to More
Associations of Increased WIC Benefits for Fruits and Vegetables With Food Security and Satisfaction by Race and Ethnicity
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides nutrition support for racially and ethnically diverse populations. In 2021, the monthly cash value benefit (CVB) for the purchase of fruits and vegetables increased from $9 to $35 and was later adjusted to $24. This study investigated, by racial and ethnic groups, whether More
Centering equity in FDA regulation: Front-of-package food label effects in Latino and limited English proficiency populations
This project aims to determine the front-of-package label design that is most effective at helping Latino consumers identify and choose healthier products. The project also aims to explore whether the benefits of front-of-package design differ by English proficiency. Participants will include 4,000 US adults of parental age (18-55 years old) who identify as Latino. Participants More

IMAGES
VIDEO
COMMENTS
2. Components of a Healthy Diet and Their Benefits. A healthy diet is one in which macronutrients are consumed in appropriate proportions to support energetic and physiologic needs without excess intake while also providing sufficient micronutrients and hydration to meet the physiologic needs of the body [].Macronutrients (i.e., carbohydrates, proteins, and fats) provide the energy necessary ...
The sixth and final section identifies issues that stand out for future research on the psychology of healthy diet. ... Although reviewing these factors is beyond the scope of this paper, it is important to realise they do also affect healthy diet, and that they may interact with the determinants discussed below. In addition, we need to ...
However, research has shown that diets and restrained eating are often counterproductive and may even enhance the risk of long-term weight gain and eating disorders 2,3.
The EAT-Lancet Commission on healthy diets from sustainable food systems 32 has quantified what it believes these characteristics mean for a transformation to healthy diets by 2050; dietary practice would require a greater than 50% reduction in global consumption of red meat and highly processed foods, and a greater than 100% increase in plant ...
4 NIHR Southampton Biomedical Research Centre, University Hospital Southampton NHS Foundation Trust and University of Southampton ... DOI: 10.3390/nu12020334 Abstract The definition of what constitutes a healthy diet is continually shifting to reflect the evolving understanding of the roles that different foods, essential nutrients, and other ...
The definition of what constitutes a healthy diet is continually shifting to reflect the evolving understanding of the roles that different foods, essential nutrients, and other food components ...
A wide range of terms for healthy eating (e.g. nutrition, food preferences, feeding behaviour, diets and health food) were combined with health promotion terms or general or specific terms for determinants of health or ill-health (e.g. health promotion, behaviour modification, at-risk-populations, sociocultural factors and poverty) and with ...
The EAT-Lancet Commission1 aims to define healthy global diets that avoid environmental degradation. It adopts the planetary boundaries concept to define "a safe operating space for humanity"2,3 or more prosaically "global biophysical limits that humanity should operate within to ensure a stable and resilient Earth system".1 However, the scientific analysis is obfuscated when two ...
Healthy eating, in particular a diet rich in fruit and vegetables (FV) adds to our health; primarily because it reduces our chances of contracting a number of eating related diseases (Oyebode et al. 2014; Bazzano et al. 2002; Liu et al. 2000).Since good health adds to happiness, it is likely that healthy diets will also add to happiness, but a firm connection has not been established.
Diet has been recognized as a vital risk factor for non-communicable diseases (NCDs), climate changes, and increasing population, which has been reflected by a rapidly growing body of the literature related to healthy eating. To reveal a panorama of the topics related to healthy eating, this study aimed to characterize and visualize the knowledge structure, hotspots, and trends in this field ...
Objective: To discuss healthy diet from a psychological perspective by considering definitions of healthy diet in terms of consumer understanding; the health effects of specific dietary elements ...
Abstract. The general public's view of modern diet and human health has undergone drastic changes in recent years. There is general harmony that many chronic health problems, first noted in ...
Introduction. A transition toward healthy and environmentally sustainable food is among major global challenges. Replacing animal sources, namely red meat and milk, with plant-based sources has the potential to impact on cutting greenhouse gas emissions (Springmann et al. Citation 2018).That is a reason for the growing popularity of diets eliminating or reducing meat, milk, dairy, and eggs ...
Purpose of Review Poor diets are a leading risk factor for chronic disease globally. Research suggests healthy foods are often harder to access, more expensive, and of a lower quality in rural/remote or low-income/high minority areas. Food pricing studies are frequently undertaken to explore food affordability. We aimed to capture and summarise food environment costing methodologies used in ...
A healthy diet is associated with physical 1 and mental health. 2,3 Yet only 1% of Australians consume enough fruits and vegetables per day to meet national dietary guidelines. 4 Processed foods high in salt, saturated fat and sugars are consumed in excess, with junk food accounting for over a third of the daily energy intake in both adolescents and adults. 5 Poor diet quality constitutes a ...
The Gretchen Swanson Center for Nutrition was funded by Healthy Eating Research to conduct a study exploring how the policy changes in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) cash value benefit (CVB), or fruit and vegetable money, during the pandemic impacted the WIC program and child access to fruits and.