Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
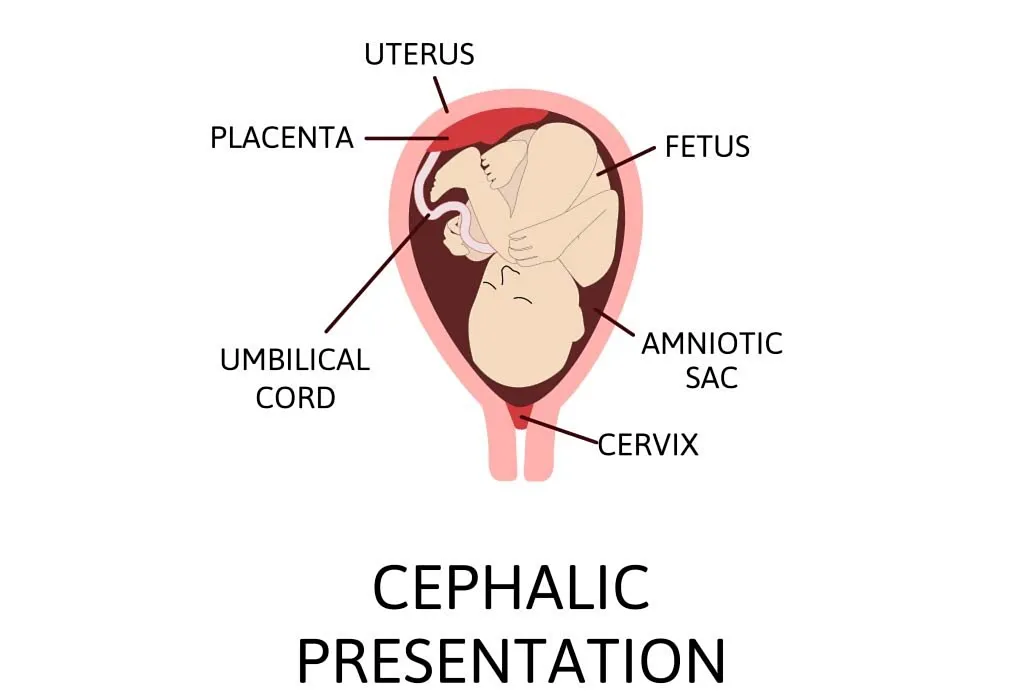
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Cephalic Position?
The ideal fetal position for labor and delivery
- Why It's Best
Risks of Other Positions
- Determining Position
- Turning a Fetus
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery.
About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy . Your healthcare provider will monitor the fetus's position during the last weeks of gestation to ensure this has happened by week 36.
If the fetus is not in the cephalic position at that point, the provider may try to turn it. If this doesn't work, some—but not all—practitioners will attempt to deliver vaginally, while others will recommend a Cesarean (C-section).
Getty Images
Why Is the Cephalic Position Best?
During labor, contractions dilate the cervix so the fetus has adequate room to come through the birth canal. The cephalic position is the easiest and safest way for the baby to pass through the birth canal.
If the fetus is in a noncephalic position, delivery becomes more challenging. Different fetal positions have a range of difficulties and varying risks.
A small percentage of babies present in noncephalic positions. This can pose risks both to the fetus and the mother, and make labor and delivery more challenging. It can also influence the way in which someone can deliver.
A fetus may actually find itself in any of these positions throughout pregnancy, as the move about the uterus. But as they grow, there will be less room to tumble around and they will settle into a final position.
It is at this point that noncephalic positions can pose significant risks.
Cephalic Posterior
A fetus may also present in an occiput or cephalic posterior position. This means they are positioned head down, but they are facing the abdomen instead of the back.
This position is also nicknamed "sunny-side up."
Presenting this way increases the chance of a painful and prolonged delivery.
There are three different types of breech fetal positioning:
- Frank breech: The legs are up with the feet near the head.
- Footling breech: One or both legs is lowered over the cervix.
- Complete breech: The fetus is bottom-first with knees bent.
A vaginal delivery is most times a safe way to deliver. But with breech positions, a vaginal delivery can be complicated.
When a baby is born in the breech position, the largest part—its head—is delivered last. This can result in them getting stuck in the birth canal (entrapped). This can cause injury or death.
The umbilical cord may also be damaged or slide down into the mouth of the womb, which can reduce or cut off the baby's oxygen supply.
Some providers are still comfortable performing a vaginal birth as long as the fetus is doing well. But breech is always a riskier delivery position compared with the cephalic position, and most cases require a C-section.
Likelihood of a Breech Baby
You are more likely to have a breech baby if you:
- Go into early labor before you're full term
- Have an abnormally shaped uterus, fibroids , or too much amniotic fluid
- Are pregnant with multiples
- Have placenta previa (when the placenta covers the cervix)
Transverse Lie
In transverse lie position, the fetus is presenting sideways across the uterus rather than vertically. They may be:
- Down, with the back facing the birth canal
- With one shoulder pointing toward the birth canal
- Up, with the hands and feet facing the birth canal
If a transverse lie is not corrected before labor, a C-section will be required. This is typically the case.
Determining Fetal Position
Your healthcare provider can determine if your baby is in cephalic presentation by performing a physical exam and ultrasound.
In the final weeks of pregnancy, your healthcare provider will feel your lower abdomen with their hands to assess the positioning of the baby. This includes where the head, back, and buttocks lie
If your healthcare provider senses that the fetus is in a breech position, they can use ultrasound to confirm their suspicion.
Turning a Fetus So They Are in Cephalic Position
External cephalic version (ECV) is a common, noninvasive procedure to turn a breech baby into cephalic position while it's still in the uterus.
This is only considered if a healthcare provider monitors presentation progress in the last trimester and notices that a fetus is maintaining a noncephalic position as your delivery date approaches.
External Cephalic Version (ECV)
ECV involves the healthcare provider applying pressure to your stomach to turn the fetus from the outside. They will attempt to rotate the head forward or backward and lift the buttocks in an upward position. Sometimes, they use ultrasound to help guide the process.
The best time to perform ECV is about 37 weeks of pregnancy. Afterward, the fetal heart rate will be monitored to make sure it’s within normal levels. You should be able to go home after having ECV done.
ECV has a 50% to 60% success rate. However, even if it does work, there is still a chance the fetus will return to the breech position before birth.
Natural Methods For Turning a Fetus
There are also natural methods that can help turn a fetus into cephalic position. There is no medical research that confirms their efficacy, however.
- Changing your position: Sometimes a fetus will move when you get into certain positions. Two specific movements that your provider may recommend include: Getting on your hands and knees and gently rocking back and forth. Another you could try is pushing your hips up in the air while laying on your back with your knees bent and feet flat on the floor (bridge pose).
- Playing stimulating sounds: Fetuses gravitate to sound. You may be successful at luring a fetus out of breech position by playing music or a recording of your voice near your lower abdomen.
- Chiropractic care: A chiropractor can try the Webster technique. This is a specific chiropractic analysis and adjustment which enables chiropractors to establish balance in the pregnant person's pelvis and reduce undue stress to the uterus and supporting ligaments.
- Acupuncture: This is a considerably safe way someone can try to turn a fetus. Some practitioners incorporate moxibustion—the burning of dried mugwort on certain areas of the body—because they believe it will enhance the chances of success.
A Word From Verywell
While most babies are born in cephalic position at delivery, this is not always the case. And while some fetuses can be turned, others may be more stubborn.
This may affect your labor and delivery wishes. Try to remember that having a healthy baby, and staying well yourself, are your ultimate priorities. That may mean diverting from your best laid plans.
Speaking to your healthcare provider about turning options and the safest route of delivery may help you adjust to this twist and feel better about how you will move ahead.
Glezerman M. Planned vaginal breech delivery: current status and the need to reconsider . Expert Rev Obstet Gynecol. 2012;7(2):159-166. doi:10.1586/eog.12.2
Cleveland Clinic. Fetal positions for birth .
MedlinePlus. Breech birth .
UT Southwestern Medical Center. Can you turn a breech baby around?
The American College of Obstetricians and Gynecologists. If your baby is breech .
Roecker CB. Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios . Journal of Chiropractic Medicine . 2013;12(2):74-78. doi:10.1016/j.jcm.2013.06.003
By Cherie Berkley, MS Berkley is a journalist with a certification in global health from Johns Hopkins University and a master's degree in journalism.
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Profile & Preferences
- My Documents
Our other sites
There's a chat in progress.
Common baby positions during pregnancy and labor

As you near the end of your third trimester, your baby will settle into position for birth. By this time in your pregnancy, your baby is likely in one of three positions.
Cephalic presentation, occiput anterior
This is the best position for labor. Your baby is head-down, their face is turned toward your back, and their chin is tucked to their chest. This allows the back of your baby’s head to easily enter your pelvis when the time is right. Most babies settle into this position by week 36 of pregnancy.
Cephalic presentation, occiput posterior position
In this case, your baby is head-down, but their face is turned toward your bellybutton instead of your back. This is also called the “sunny side up” position. If your baby is positioned this way, your labor could be longer and more difficult. Don’t be alarmed if your baby is in this position at the start of your labor. Your baby can rotate their head throughout the birthing process and may naturally turn their head to face down.
Breech position
Breech can mean any position where your baby’s head isn’t pointed down toward your pelvis. Instead, your baby’s buttocks might be positioned to enter the birth canal first. Sometimes one or both of their feet might be pointed downward.
In certain cases, babies lie crosswise inside the uterus. This position makes it more likely that the baby’s shoulder will enter the pelvis first.
If your baby is breech and they can’t be turned in the uterus, you’ll likely need a cesarean birth, or C-section. Your clinician will let you know if this is a possibility.
Turning your baby
In many cases, it’s possible to get your baby to move into the right position for birth. This is called external cephalic version. A clinician will firmly press their hands on certain parts of your belly. Babies often adjust to a head-down position when this happens.
You can also help your baby turn by changing your own position. Try getting on your hands and knees and rocking back and forth. You can also try pushing your hips upward while you lie on your back with your knees bent and your feet flat on the floor. Be sure to ask your clinician before trying to turn your baby yourself.
Stimulating music or light can sometimes encourage your baby to turn. Try placing headphones toward the bottom of your belly to see if your baby will turn toward it. Shining a light into your belly can have the same effect.
This article has been created by a national group of Kaiser Permanente ob-gyns, certified nurse-midwives, pediatricians, lactation consultants and other specialists who came together to provide you with the best pregnancy, birth, postpartum, and newborn information.
Some of the content is used and adapted with permission of The Permanente Medical Group.
- Third trimester
- Gestation period 33 weeks
DHO article page
Switching to {{aocRegion}}
Want to stay signed on?
We are unable to switch you to this area of care
We’re getting your information

ACOG Guidelines at a Glance: External Cephalic Version
Expert commentary on Practice Bulletin No. 161: External Cephalic Version
COMMITTEE ON PRACTICE BULLETINS-OBSTETRICS Practice Bulletin #161: External Cephalic Version.
American College of Obstetricians and Gynecologists. Obstet Gynecol 2016;127:e54-61. Full text of Practice Bulletin #161 is available to ACOG members at http://www.acog.org/Resources%20And%20Publications/Practice%20Bulletsin/Committee%20on%20Practice%20Bulletins%20Obstetrics/External%20Cephalic%20Version.aspx
EXTERNAL CEPHALIC VERSION In the United States, there is a widespread belief that the overall cesarean delivery rate is higher than necessary. Eff orts are being directed toward decreasing the number of these procedures, in part by encouraging physicians to make changes in their management practices. Because breech presentations are associated with a high rate of cesarean delivery, there is renewed interest in techniques such as external cephalic version (ECV) and vaginal breech delivery. The purpose of this document is to provide information about ECV by summarizing the relevant evidence presented in published studies and to make recommendations regarding its use in obstetric practice.
Used with permission. Copyright the American College of Obstetricians and Gynecologists.
ECV: A tool to prevent the first cesarean
by Stephen F Thung, MD, MSCI
Dr Thung is Associate Professor of Maternal Fetal Medicine, Clinical Chief of Obstetrics and Medical Director of Patient Flow Management, The Ohio State University, Columbus, Ohio
Preconception vaping, alcohol use not linked to spontaneous abortion risk
A pair of studies from AUA 2024 show neither drinking nor vaping by either parent is associated with significantly increased risk of a spontaneous abortion.
S1E4: Dr. Kristina Adams-Waldorf: Pandemics, pathogens and perseverance
This episode of Pap Talk by Contemporary OB/GYN features an interview with Dr. Kristina Adams-Waldorf, Professor in the Department of Obstetrics and Gynecology and Adjunct Professor in Global Health at the University of Washington (UW) School of Medicine in Seattle.

Reducing multifetal pregnancy through publicly funded IVF programs
Learn how a mandatory elective single-embryo transfer policy in publicly funded in vitro fertilization programs significantly decreases multifetal pregnancy rates, offering insights into mitigating risks in assisted reproduction.
S1E3: Dr. Emily S. Miller: Placental pathology and MVM evidence
This episode of Pap Talk by Contemporary OB/GYN features an interview with Dr. Emily S. Miller, with Northwestern Medicine in Chicago.

Higher preterm birth risk found following cesarean delivery at full dilation
Recent research highlights an association between cesarean delivery at full dilation and increased risk of subsequent preterm birth, prompting further investigation into childbirth practices and outcomes.

Unveiling the complexities of preterm birth risk from nativity, ethnicity, and race
A recent study dissected the relationships between maternal nativity, ethnicity, and race in influencing preterm birth rates, shedding light on disparities and suggesting avenues for future research.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

- Learn /
Why Is Cephalic Presentation Ideal For Childbirth?

5 Dec 2017 | 8 min Read
During labour, contractions stretch your birth canal so that your baby has adequate room to come through during birth. The cephalic presentation is the safest and easiest way for your baby to pass through the birth canal.
If your baby is in a non-cephalic position, delivery can become more challenging. Different fetal positions pose a range of difficulties and varying risks and may not be considered ideal birthing positions.
Two Kinds of Cephalic Positions
There are two kinds of cephalic positions:
- Cephalic occiput anterior , where your baby’s head is down and is facing toward your back.
- Cephalic occiput posterior , where your baby is positioned head down, but they are facing your abdomen instead of your back. This position is also nicknamed ‘sunny-side-up’ and can increase the chances of prolonged and painful delivery.
How to Know if Your Baby is In a Cephalic Position?
You can feel your baby’s position by rubbing your hand on your belly. If you feel your little one’s stomach in the upper stomach, then your baby is in a cephalic position. But if you feel their kicks in the lower stomach, then it could mean that your baby is in a breech position.
You can also determine whether your baby is in the anterior or posterior cephalic position. If your baby is in the anterior position, you may feel their movement underneath your ribs and your belly button could also pop out. If your baby is in the posterior position, then you may feel their kicks in their abdomen, and your stomach may appear rounded up instead of flat.
You can also determine your baby’s position through an ultrasound scan or a physical examination at your healthcare provider’s office.
Benefits of Cephalic Presentation in Pregnancy
Cephalic presentation is one of the most ideal birth positions, and has the following benefits:
- It is the safest way to give birth as your baby’s position is head-down and prevents the risk of any injuries.
- It can help your baby move through the delivery canal as safely and easily as possible.
- It increases the chances of smooth labour and delivery.
Are There Any Risks Involved in Cephalic Position?
Conditions like a cephalic posterior position in addition to a narrow pelvis of the mother can increase the risk of pregnancy complications during delivery. Some babies in the head-first cephalic presentation might have their heads tilted backward. This may, in some rare cases, cause preterm delivery.
What are the Risks Associated with Other Birth Positions?
A small percentage of babies may settle into a non-cephalic position before their birth. This can pose risks to both your and your baby’s health, and also influence the way in which you deliver.
In the next section, we have discussed a few positions that your baby can settle in throughout pregnancy, as they move around the uterus. But as they grow old, there will be less space for them to tumble around, and they will settle into their final position. This is when non-cephalic positions can pose a risk.
Breech Position
There are three types of breech fetal positioning:
- Frank breech : Your baby’s legs stick straight up along with their feet near their head.
- Footling breech: One or both of your baby’s legs are lowered over your cervix.
- Complete breech: Your baby is positioned bottom-first with their knees bent.
If your baby is in a breech position , vaginal delivery is considered complicated. When a baby is born in breech position, the largest part of their body, that is, their head is delivered last. This can lead to injury or even fetal distress. Moreover, the umbilical cord may also get damaged or get wrapped around your baby’s neck, cutting off their oxygen supply.
If your baby is in a breech position, your healthcare provider may recommend a c-section, or they may try ways to flip your baby’s position in a cephalic presentation.
Transverse Lie
In this position, your baby settles in sideways across the uterus rather than being in a vertical position. They may be:
- Head-down, with their back facing the birth canal
- One shoulder pointing toward the birth canal
- Up with their hands and feet facing the birth canal
If your baby settles in this position, then your healthcare provider may suggest a c-section to reduce the risk of distress in your baby and other pregnancy complications.
Turning Your Baby Into A Cephalic Position
External cephalic version (ECV) is a common, and non-invasive procedure that helps turn your baby into a cephalic position while they are in the womb. However, your healthcare provider may only consider this procedure if they consider you have a stable health condition in the last trimester, and if your baby hasn’t changed their position by the 36th week.
You can also try some natural remedies to change your baby’s position, such as:
- Lying in a bridge position: Movements like bridge position can sometimes help move your baby into a more suitable position. Lie on your back with your feet flat on the ground and your legs bent. Raise your pelvis and hips into a bridge position and hold for 5-10 minutes. Repeat several times daily.
- Chiropractic care: A chiropractor can help with the adjustment of your baby’s position and also reduce stress in them.
- Acupuncture: After your doctor’s go-ahead, you can also consider acupuncture to get your baby to settle into an ideal birthing position.
While most babies settle in a cephalic presentation by the 36th week of pregnancy, some may lie in a breech or transverse position before birth. Since the cephalic position is considered the safest, your doctor may recommend certain procedures to flip your baby’s position to make your labour and delivery smooth. You may also try the natural methods that we discussed above to get your baby into a safe birthing position and prevent risks or other pregnancy complications.
When Should A Baby Be In A Cephalic Position?
Your baby would likely naturally drop into a cephalic position between weeks 37 to 40 of your pregnancy .
Is Cephalic Position Safe?
Research shows that 95% of babies take the cephalic position a few weeks or days before their due date. It is considered to be the safest position. It ensures a smooth birthing process.
While most of the babies are in cephalic position at delivery, this is not always the case. If you have a breech baby, you can discuss the available options for delivery with your doctor.
Does cephalic presentation mean labour is near?
Head-down is the ideal position for your baby within your uterus during birth. This is known as the cephalic position. This posture allows your baby to pass through the delivery canal more easily and safely.
Can babies change from cephalic to breech?
The external cephalic version (ECV) is the most frequent procedure used for turning a breech infant.

How can I keep my baby in a cephalic position?
While your baby naturally gets into this position, you can try some exercises to ensure that they settle in cephalic presentation. Exercises such as breech tilt, forward-leaning position (spinning babies program), cat and camel pose can help.
Stitches after a normal delivery : How many stitches do you need after a vaginal delivery? Tap this post to know.
Vaginal birth after caesarean delivery : Learn all about the precautions to consider before having a vaginal delivery after a c-section procedure.
How many c-sections can you have : Tap this post to know the total number of c-sections that you can safely have.
Cover Image Credit: Freepik.com

Related Topics for you
babychakraenglish
cephalicposition
cephalicpresentation
fetaldevelopment
fetalmovement
preganancycare
Suggestions offered by doctors on BabyChakra are of advisory nature i.e., for educational and informational purposes only. Content posted on, created for, or compiled by BabyChakra is not intended or designed to replace your doctor's independent judgment about any symptom, condition, or the appropriateness or risks of a procedure or treatment for a given person.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
External cephalic version.
Meaghan M. Shanahan ; Daniel J. Martingano ; Caron J. Gray .
Affiliations
Last Update: December 13, 2023 .
- Continuing Education Activity
In carefully selected patients, an external cephalic version (ECV) may be an alternative to cesarean delivery for fetal malpresentation at term. ECV is a noninvasive procedure that manipulates fetal position through the abdominal wall of the gravida. With the global cesarean section rate reaching 34%, fetal malpresentation ranks as the third most common indication for cesarean delivery, accounting for nearly 17% of cases. Studies suggest a 60% mean success rate for ECV, emphasizing its cost-effectiveness and potential to decrease cesarean delivery rates significantly. While particularly crucial in resource-limited settings where access to medical services during labor is constrained or cesarean delivery is unavailable or unsafe, ECV presents a viable option to improve rates of vaginal delivery in singleton gestations in all settings.
This activity reviews the indications, contraindications, necessary equipment, preferred personnel, procedural technique, risks, and benefits of ECV and highlights the role of the interprofessional team in caring for patients who may benefit from this procedure.
- Select suitable candidates for an external cephalic version based on their clinical history and presentation.
- Screen patients effectively regarding the risks and benefits of an external cephalic version.
- Apply best practices when performing an external cephalic version.
- Develop and implement effective interpersonal team strategies to improve outcomes for patients undergoing external cephalic version.
- Introduction
The global cesarean section rate has increased from approximately 23% to 34% in the past decade. Fetal malpresentation is now the third-most common indication for cesarean delivery, encompassing nearly 17% of cases. Almost one-fourth of all fetuses are in a breech presentation at 28 weeks gestational age; this number decreases to between 3% and 4% at term. In current clinical practice, most pregnancies with a breech fetus are delivered by cesarean section.
Individual and institutional efforts are increasing to reduce the overall cesarean delivery rate, particularly for nulliparous patients with term, singleton, and vertex gestations. [1] [2] An alternative to cesarean delivery for fetal malpresentation at term is an external cephalic version (ECV), a procedure to correct fetal malpresentation. ECV may be indicated when the fetus is breech or in an oblique or transverse lie after 37 0/7 weeks gestation. [3] The overall success rate for ECV approaches 60%, is cost-effective, and can lead to decreased cesarean delivery rates. [4] ECV is of particular importance in resource-poor environments, where patients may have limited access to medical services during labor and delivery or where cesarean delivery is unavailable or unsafe.
- Anatomy and Physiology
ECV can be attempted when managing breech presentations or fetuses with a transverse or oblique lie. Three types of breech presentation are established concerning fetal attitude: complete, frank, and incomplete, which is sometimes referred to as footling breech. In complete breech, the fetal pelvis engages with the maternal pelvic inlet, and the fetal hips and knees are flexed. In frank breech, the fetal pelvis engages with the maternal pelvic inlet, the fetal hips are flexed, the knees are extended, and the feet are near the head. In incomplete or footling breech, one (single footling) or both (double footling) feet are extended below the level of the fetal pelvis.
A fetus with a transverse lie is positioned with their long axis, defined as the spine, at a right angle to the long axis of the gravida. The fetal head may be to the right or left side of the maternal spine. The fetus may be facing up or down. The long axis of the fetus characterizes an oblique lie at any angle to the maternal long axis that is not 90°. An oblique fetus is usually positioned with their head in the right or left lower quadrants, although this is not universal.
- Indications
ECV may be indicated in carefully selected patients. The fetus must be at or beyond 36 0/7 weeks of gestation with malpresentation, and there must be no absolute contraindications to vaginal delivery, such as placenta previa, vasa previa, or a history of classical cesarean delivery. Fetal status must be reassuring, and preprocedural nonstress testing is recommended. While ECV may be performed as early as 36 0/7 weeks gestation, many practitioners will delay ECV until 37 0/7 weeks gestation to ensure delivery of a term fetus.
ECV is more successful in multigravidas, those with a complete breech or transverse or oblique presentation, an unengaged presenting part, adequate amniotic fluid, and a posterior placenta. Nulliparous patients and those with an anterior, lateral, or cornual placenta have lower success rates. Patients with advanced cervical dilatation, obesity, oligohydramnios, or ruptured membranes also have lower success rates. Additionally, if the fetus weighs less than 2500 g, is at a low station with an engaged presenting part, is frank breech, or the spine is posterior, the success of ECV is decreased. [5]
Evidence supports the use of parenteral tocolysis, most often with the beta-2-agonist medication terbutaline, to improve the success of ECV; most studies evaluating the various aspects of ECV aspects include using a tocolytic agent. [6] [7] [8] [9] Data regarding the improved success of ECV incorporating regional anesthesia is inconsistent.
- Contraindications
Any contraindication to vaginal delivery would also be a contraindication to ECV. These contraindications include but are not limited to placenta previa, vasa previa, active genital herpes outbreak, or a history of classical cesarean delivery. A history of low transverse cesarean delivery is not an absolute contraindication to ECV. [10] The overall success rate of ECV in patients with a previous cesarean birth ranges from 50% to 84%; no cases of uterine rupture during ECV were reported in the four trials evaluating this outcome in patients with a prior cesarean delivery. [11] [12] [13] [14]
Antepartum ECV is contraindicated in multiple gestations, although it can be utilized for twin gestations that would otherwise be suitable candidates for breech extraction. [15] [16]
Patients with severe oligohydramnios, nonreassuring fetal monitoring, a hyperextended fetal head, significant fetal or uterine anomaly, fetal growth restriction, and maternal hypertension carry a low likelihood of successful ECV and a significantly increased risk of poor fetal outcomes; ECV in such situations requires careful consideration.
If a gravida who is otherwise a suitable candidate for ECV presents in early labor with fetal malpresentation, ECV may be a reasonable option if the presenting part is unengaged, the amniotic fluid index is within the normal range, and there are no contraindications to ECV or vaginal delivery. Data from the Nationwide Inpatient Sample from 1998 to 2011 noted a success rate of 65% for ECV performed in carefully selected patients during the admission for delivery. [17] ECV performed in this circumstance resulted in a significantly lower cesarean birth rate and hospital stay of greater than 7 days compared to patients with a persistent breech presentation at the time of delivery. [17]
External cephalic versions should be attempted only in settings where cesarean delivery services are readily available. Therefore, the required equipment for ECV includes all such requirements for cesarean delivery, including anesthesia services. Access to tocolytic agents, bedside ultrasonography, and external fetal heart rate monitoring equipment is also required. Following ECV, fetal status must be assessed; nonstress testing is preferred. If nonstress testing is unavailable, Doppler indices of the umbilical artery, middle cerebral artery, and ductus venosus may be performed. [18]
The personnel typically required to perform an ECV include:
- Obstetrician
- Labor and delivery nurse.
ECV may only be performed in a setting where cesarean delivery services are readily available. Personnel typically required for cesarean delivery include:
- Surgical first assistant
- Anesthesia personnel
- Surgical technician or operating room nurse
- Circulating or operating room nurse
- Pediatric personnel
- Note: for cesarean delivery, labor and delivery nurses may serve as surgical technicians, circulating, or operating room roles.
- Preparation
Before attempting ECV, informed consent must be obtained; this should include tocolysis and neuraxial analgesia if those procedures will be performed. Some clinicians will obtain consent from the patient for potential emergency cesarean delivery at this time, although this practice is not universal. Additionally, an ultrasound examination should be performed to verify fetal presentation, exclude fetal and uterine anomalies, locate the placental position, and evaluate the amniotic fluid index. Many clinicians will evaluate preprocedural fetal status with a nonstress test.
The current evidence supports the administration of terbutaline 0.25mg subcutaneously 15 to 30 minutes before the ECV but does not support using calcium channel blockers or nitroglycerin for preprocedural tocolysis. [19] While multiple studies report the increased success of ECV in patients who are administered epidural or spinal neuraxial anesthesia, overall data is insufficient to warrant a universal recommendation; neuraxial anesthesia may improve success rates for ECV in situations where tocolysis alone was unsuccessful. [20]
- Technique or Treatment
The gravida should be supine with a leftward tilt using a wedge support to relieve pressure on the great vessels. ECV is best performed using a 2-handed approach.
If the fetal presentation is breech, lift the breech out of the pelvis with one hand and apply downward pressure to the posterior fetal head to attempt a forward roll. If a forward roll is unsuccessful, a backward roll can be attempted. If the fetus is in either a transverse or oblique presentation, similar manipulation of the fetus is used to try to move the fetal head to the pelvis. [21]
Fetal well-being should be evaluated intermittently with Doppler or real-time ultrasonography during ECV. ECV should be abandoned if there is significant fetal bradycardia, patient discomfort, or if a version is not achieved easily. After a successful or unsuccessful ECV, external fetal heart rate monitoring should be performed for 30 to 60 minutes. If the gravida is Rh negative, anti-D immune globulin should be administered.
Immediate induction of labor to minimize reversion is not recommended. If the initial attempt at ECV is unsuccessful, additional attempts can be made during the same admission or at a later date.
- Complications
Complications of ECV are rare and occur in only 1% to 2% of attempts. The most common complication associated with ECV is fetal heart rate abnormalities, particularly bradycardia, occurring at a rate of 4.7% to 20%; these abnormalities usually are transient and improve upon completion or abandonment of the procedure.
More severe complications of ECV occur at a rate of less than 1% and include premature rupture of membranes, cord prolapse, vaginal bleeding, placental abruption, fetomaternal hemorrhage, emergent cesarean delivery, and stillbirth. Many of these rare complications require emergent cesarean delivery; some clinicians choose to perform ECV in the operating room, although this is neither necessary nor universal. [22]
ECV is associated with changes in Doppler indices that may reflect decreased placental perfusion. It appears these changes are short-lived and have no detrimental effects on the outcomes of uncomplicated pregnancies. A recent prospective study investigating the effects of ECV on fetal circulation in the antepartum period noted no differences in the Doppler evaluation of the middle cerebral artery or ductus venosus; all studied patients remained stable and were discharged home after the procedure. [18]
- Clinical Significance
Some data indicate that only 20% to 30% of eligible candidates are offered ECV. [23] Patients who undergo a successful ECV procedure have a lower cesarean delivery rate than patients who do not but are still at a higher risk of cesarean delivery than patients with cephalic fetuses who do not require ECV. ECV is cost-effective if the probability of a successful ECV exceeds 32%. Overall, ECV is successful in 58% of attempts, reduces the risk for CS by two-thirds, and enables 80% of these patients to deliver vaginally. [24]
- Enhancing Healthcare Team Outcomes
ECV is not a benign procedure and is most successful when performed under the care of an interprofessional team. Labor and delivery nurses play an integral role in the success of ECV as they frequently assist in the procedure, prepare the patient for ECV, and implement external fetal monitoring before, during, and after the procedure. Additionally, the support of emergent operating room staff promotes the safe delivery of a healthy fetus should complications arise during the ECV procedure. Clear and concise anticipatory interprofessional communication improves safety and outcomes for the gravida and the fetus should complications occur.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Meaghan Shanahan declares no relevant financial relationships with ineligible companies.
Disclosure: Daniel Martingano declares no relevant financial relationships with ineligible companies.
Disclosure: Caron Gray declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Shanahan MM, Martingano DJ, Gray CJ. External Cephalic Version. [Updated 2023 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Value of routine ultrasound examination at 35-37 weeks' gestation in diagnosis of non-cephalic presentation. [Ultrasound Obstet Gynecol. 2020] Value of routine ultrasound examination at 35-37 weeks' gestation in diagnosis of non-cephalic presentation. De Castro H, Ciobanu A, Formuso C, Akolekar R, Nicolaides KH. Ultrasound Obstet Gynecol. 2020 Feb; 55(2):248-256.
- External cephalic version at 38 weeks' gestation at a specialized German single center. [PLoS One. 2021] External cephalic version at 38 weeks' gestation at a specialized German single center. Zielbauer AS, Louwen F, Jennewein L. PLoS One. 2021; 16(8):e0252702. Epub 2021 Aug 30.
- External cephalic version in singleton pregnancies at term: a retrospective analysis. [Gynecol Obstet Invest. 2008] External cephalic version in singleton pregnancies at term: a retrospective analysis. Zeck W, Walcher W, Lang U. Gynecol Obstet Invest. 2008; 66(1):18-21. Epub 2008 Jan 30.
- Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - External Cephalic Version and other Interventions to turn Breech Babies to Cephalic Presentation]. [Gynecol Obstet Fertil Senol. 2...] Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - External Cephalic Version and other Interventions to turn Breech Babies to Cephalic Presentation]. Ducarme G. Gynecol Obstet Fertil Senol. 2020 Jan; 48(1):81-94. Epub 2019 Oct 31.
- Review Association between hospitals' cesarean delivery rates for breech presentation and their success rates for external cephalic version. [Eur J Obstet Gynecol Reprod Bi...] Review Association between hospitals' cesarean delivery rates for breech presentation and their success rates for external cephalic version. Athiel Y, Girault A, Le Ray C, Goffinet F. Eur J Obstet Gynecol Reprod Biol. 2022 Mar; 270:156-163. Epub 2022 Jan 13.
Recent Activity
- External Cephalic Version - StatPearls External Cephalic Version - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
What to know if your baby is breech
Find out what breech position means, how to turn a breech baby, and what having a breech baby means for your labor and delivery.

What does it mean when a baby is breech?
Signs of a breech baby, why are some babies breech, how to turn a breech baby: is it possible, will i need a c-section if my baby is breech, how to turn a breech baby naturally.
Breech is a term used to describe your baby's position in the womb. Breech position means your baby is bottom-down instead of head-down.
Babies are often active in early pregnancy, moving into different positions. But by around 8 months, there's not much room in the uterus. Most babies maximize their cramped quarters by settling in head down, in what's known as a cephalic or vertex presentation. But if you have a breech baby, it means they're poised to come out buttocks and/or feet first. At 28 weeks or less, about a quarter of babies are breech, and at 32 weeks, 7 percent are breech. By the end of pregnancy, only 3 to 4 percent of babies are in breech position. At term, a baby in breech position is unlikely to turn on their own.
There are several types of breech presentations:
- Frank breech (bottom first with feet up near the head)
- Complete breech (bottom first with legs crossed)
- Incomplete or footling breech (one or both feet are poised to come out first)
(In rare cases, a baby will be sideways in the uterus with their shoulder, back, or arm presenting first – this is called a transverse lie.)
See what these breech presentations look like .
If your baby is in breech position, you may feel them kicking in your lower belly. Or you may feel pressure under your ribcage, from their head.
By the beginning of your third trimester , your practitioner may be able to tell what position your baby is in by feeling your abdomen and locating the baby's head, back, and bottom.
If your baby's position isn't clear during an abdominal exam at 36 weeks, your caregiver may do an internal exam to try to feel what part of the baby is in your pelvis. In some cases, they may use ultrasound to confirm the baby's position.
We don't usually know why some babies are breech – in most cases it seems to be chance. While sometimes a baby with certain birth defects may not turn to a head-down position, most babies in breech position are perfectly fine. Here are some things that might increase the risk of a breech presentation:
- You're carrying multiples
- You've been pregnant before
- You've had a breech presentation before
- There's too much amniotic fluid or not enough amniotic fluid
- You have placenta previa (the placenta is covering all of part of the opening of the uterus)
- Your baby is preterm
- Your uterus is shaped abnormally or has growths, such as fibroids
- The umbilical cord is short
- You were a breech delivery, or your sibling or parent was a breech delivery
- Advanced maternal age (especially age 45 and older)
- Your baby is a low weight at delivery
- You're having a girl
There is a procedure for turning a breech baby. It's called an external cephalic version (ECV). An ob/gyn turns your baby by applying pressure to your abdomen and manually manipulating the baby into a head-down position. Some women find it very uncomfortable or even painful.
An EVC has about a 58 percent success rate, and it's more likely to work if this isn't your first baby. It's not for everyone – you can't have the procedure if you're carrying multiples or if you have too little amniotic fluid or placental abruption , for example. Your provider also won't attempt to turn your breech baby if your baby has any health problems.
The procedure is done after 36 weeks and in the hospital, where your baby can be monitored and where you'll be near a delivery room should any complications arise.
It depends, and it's something you'll want to talk with your caregiver about ahead of time. Discuss your preferences, the advantages and risks of each option ( vaginal and cesarean delivery of a breech presentation), and their experience. The biggest risk of a breech delivery is when the body delivers but the head stays entrapped within the cervix.
In the United States, most breech babies are delivered via cesarean. You may wind up having a vaginal breech delivery if your labor is so rapid that you arrive at the hospital just about to deliver. Another scenario is if you have a twin pregnancy where the first baby is in the head-first position and the second baby is not. A baby who delivers head-first will make room for the breech baby.
However, the vast majority of babies who remain breech arrive by c-section. If a c-section is planned, it will usually be scheduled at 39 weeks. To make sure your baby hasn't changed position in the meantime, you'll have an ultrasound at the hospital to confirm their position just before the surgery.
If you go into labor or your water will break s before your planned c-section, be sure to call your provider right away and head for the hospital.
In rare circumstances, if you're at low risk of complications and your caregiver is experienced delivering breech babies vaginally, you may choose to have what is called a "trial of vaginal birth." This means that you can attempt to deliver vaginally but should be prepared to have a cesarean delivery if labor isn't progressing well. You and your baby will be closely monitored during labor.
In addition to ECV, there are some alternative, natural ways to try to turn your baby. There's no proof that any of them work – or that all of them are safe. Consult your practitioner before trying them.
There's no conclusive proof that the mother's position has any effect on the baby's position, but the idea is to employ gravity to help your baby somersault into a head-down position. A few tips:
- Get into one of the following positions twice a day, starting at around 32 weeks.
- Be sure to do these moves on an empty stomach, lest your lunch comes back up.
- Make sure there's someone around to help you get up if you start feeling lightheaded.
- If you find these positions uncomfortable, stop doing them.
Position 1: Lie flat on your back and raise your pelvis so that it's 9 to 12 inches off the floor. Support your hips with a pillow and stay in this position for five to 15 minutes. Position 2: Kneel down, with your forearms on the floor in front of you, so that your bottom sticks up in the air. Stay in this position for five to 15 minutes. Sleeping position
Many women wonder if there are sleeping positions to turn a breech baby. But the positions you use to try to coax your baby head down for a short time shouldn't be used while you're sleeping. (It's not safe to sleep flat on your back in late pregnancy, for example, because the weight of your baby may compress the blood vessels that provide oxygen and nutrients to them.)
The best position for sleeping during pregnancy is on your side. Placing a pillow between your legs in this position may help open your pelvis, giving your baby room to move more easily. Support your back with plenty of pillows, too. Again, there's no proof that this works, but since it's the best sleeping position for you and your baby, you may as well give it a try.
Moxibustion
This ancient Chinese technique burns herbs to stimulate key acupressure points. To help turn a breech baby, an acupuncturist or other practitioner burns mugwort near the acupressure point of your pinky toes. According to Chinese medicine, this should stimulate your baby's activity enough that they may change position on their own. Some studies show that moxibustion in combination with acupuncture and/or positioning methods may be of some benefit. Others show moxibustion to provide no help in coaxing a baby into cephalic position. If you've discussed it with your caregiver and want to give it a try, contact your state acupuncture or Chinese medicine association and ask for the names of licensed practitioners.
One small study found that women who are regularly hypnotized into a state of deep relaxation at 37 to 40 weeks are more likely to have their baby turn than other women. If you're willing to try this technique, look for a licensed hypnotherapist with experience working with pregnant women.
Chiropractic care
There's a technique – called The Webster Breech Technique – that aims to reduce stress on the pelvis by relaxing the uterus and surrounding ligaments. The idea is that a breech baby can turn more naturally in a relaxed uterus, but research is limited as to the risks and benefits of this technique. If you're interested, talk with your provider about working with a chiropractor who's experienced with the technique.
This is a safe – and again, unproven – method based on the fact that your baby can hear sounds outside the womb. Simply play music close to the lower part of your abdomen (some women use headphones) to encourage your baby to move in the direction of the sound.
Learn more:
- C-section recovery
- Third trimester pregnancy guide and checklist
- Hospital bag checklist
Was this article helpful?
Breech, posterior, transverse lie: What position is my baby in?

Raspberry leaf tea is popular during pregnancy – but possible benefits aren't proven

Too much amniotic fluid (polyhydramnios)

C-section recovery: Timeline, aftercare tips, and expectations

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
ACOG. 2019. If your baby is breech. FAQ. The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/if-your-baby-is-breech Opens a new window [Accessed November 2021]
ACOG. 2018. Mode of term singleton breech delivery. Committee opinion number 745. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/mode-of-term-singleton-breech-delivery Opens a new window [Accessed November 2021]
Brici P et al. 2019. Turning foetal breech presentation at 32-35 weeks of gestational age by acupuncture and moxibustion. Evidence-based Complementary and Alternative Medicine https://www.hindawi.com/journals/ecam/2019/8950924/ Opens a new window [Accessed November 2021]
Ekeus C et al. 2019. Vaginal breech delivery at term and neonatal morbidity and mortality — a population-based cohort study in Sweden. Journal of Maternal Fetal Neonatal Medicine 32(2):265. https://pubmed.ncbi.nlm.nih.gov/28889774/ Opens a new window [Accessed November 2021]
Fruscalzo A et al 2014. New and old predictive factors for breech presentation: our experience in 14433 singleton pregnancies and a literature review. Journal of Maternal Fetal Neonatal Medicine 27(2): 167-72. https://pubmed.ncbi.nlm.nih.gov/23688372/ Opens a new window [Accessed November 2021]
Garcia MM et al. 2019 Effectiveness and safety of acupuncture and moxibustion in pregnant women with noncephalic presentation: An overview of systematic reviews. Evidence Based Complementary Alternative Medicine 7036914. https://pubmed.ncbi.nlm.nih.gov/31885661/ Opens a new window [Accessed November 2021]
Gray C. 2021. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed November 2021]
Meaghan M et al. 2021. External cephalic version. NCBI StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482475/ Opens a new window [Accessed November 2021]
MedlinePlus. 2020. Breech - series - Types of breech presentation. https://medlineplus.gov/ency/presentations/100193_3.htm Opens a new window [Accessed November 2020]
Noli SA et al. 2019. Preterm birth, low gestational age, low birth weight, parity, and other determinants of breech presentation: Results from a large retrospective population-based study. Biomed Research International https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6766171/ Opens a new window [Accessed November 2021]
Pistolese RA. 2002. The Webster Technique: A chiropractic technique with obstetric implications. Journal of Manipulative and Physiological Therapeutics 25(6): E1-9. https://pubmed.ncbi.nlm.nih.gov/12183701/ Opens a new window [Accessed November 2021]

Where to go next


- Vishal's account
- Prenatal Care
Fetal Cephalic Presentation During Pregnancy

What Is Cephalic Position?
Types of cephalic position, benefits of cephalic presentation, risks of cephalic position, what are some other positions and their associated risks, when does a foetus get into the cephalic position, how do you know if baby is in cephalic position, how to turn a breech baby into cephalic position, natural ways to turn a baby into cephalic position.
If your baby is moving around in the womb, it’s a good sign as it tells you that your baby is developing just fine. A baby starts moving around in the belly at around 14 weeks. And their first movements are usually called ‘ quickening’ or ‘fluttering’.
A baby can settle into many different positions throughout the pregnancy, and it’s alright. But it is only when you have reached your third and final trimester that the position of your baby in your womb will matter the most. The position that your baby takes at the end of the gestation period will most likely be how your baby will make its appearance in the world. Out of all the different positions that your baby can settle into, the cephalic position at 36 weeks is considered the best position. Read on to learn more about fetal cephalic presentation.
When it comes to cephalic presentation meaning, the following can be considered. A baby is in the cephalic position when he is in a head-down position. This is the best position for them to come out in. In case of a ‘cephalic presentation’, the chances of a smooth delivery are higher. This position is where your baby’s head has positioned itself close to the birth canal, and the feet and bottom are up. This is the best position for your baby to be in for safe and healthy delivery.
Your doctor will begin to keep an eye on the position of your baby at around 34 weeks to 36 weeks . The closer you get to your due date, the more important it is that your baby takes the cephalic position. If your baby is not in this position, your doctor will try gentle nudges to get your baby in the right position.
Though it is pretty straightforward, the cephalic position actually has two types, which are explained below:
1. Cephalic Occiput Anterior
Most babies settle in this position. Out of all the babies who settle in the cephalic position, 95% of them will settle this way. This is when a baby is in the head-down position but is facing the mother’s back. This is the preferred position as the baby is able to slide out more easily than in any other position.
2. Cephalic Occiput Posterior
In this position, the baby is in the head-down position but the baby’s face is turned towards the mother’s belly. This type of cephalic presentation is not the best position for delivery as the baby’s head could get stuck owing to its wide position. Almost 5% of the babies in cephalic presentation settle into this position. Babies who come out in this position are said to come out ‘sunny side up’.
Cephalic presentation, where the baby’s head is positioned down towards the birth canal, is the most common and optimal fetal presentation for childbirth. This positioning facilitates a smoother delivery process for both the mother and the baby. Here are several benefits associated with cephalic presentation:
1. Reduced risk of complications
Cephalic presentation decreases the likelihood of complications during labor and delivery , such as umbilical cord prolapse or shoulder dystocia, which can occur with other presentations.
2. Easier vaginal delivery
With the baby’s head positioned first, vaginal delivery is generally easier and less complicated compared to other presentations, resulting in a smoother labor process for the mother.
3. Lower risk of birth injuries
Cephalic presentation reduces the risk of birth injuries to the baby, such as head trauma or brachial plexus injuries, which may occur with other presentations, particularly breech or transverse positions.
4. Faster progression of labor
Babies in cephalic presentation often help to stimulate labor progression more effectively through their positioning, potentially shortening the duration of labor and reducing the need for medical interventions.
5. Better fetal oxygenation
Cephalic presentation typically allows for optimal positioning of the baby’s head, which facilitates adequate blood flow and oxygenation, contributing to the baby’s well-being during labor and delivery.
Factors such as the cephalic posterior position of the baby and a narrow maternal pelvis can increase the likelihood of complications during childbirth. Occasionally, infants in the cephalic presentation may exhibit a backward tilt of their heads, potentially leading to preterm delivery in rare instances.
In addition to cephalic presentation, there are several other fetal positions that can occur during pregnancy and childbirth, each with its own associated risks. These positions can impact the delivery process and may require different management strategies. Here are two common fetal positions and their associated risks:
1. Breech Presentation
- Babies in breech presentation, where the buttocks or feet are positioned to enter the birth canal first, are at higher risk of birth injuries such as hip dysplasia or brachial plexus injuries.
- Breech presentation can lead to complications during labor and delivery, including umbilical cord prolapse, entrapment of the head, or difficulty delivering the shoulders, necessitating interventions such as cesarean section.
2. Transverse Lie Presentation
- Transverse lie , where the baby is positioned sideways across the uterus, often leads to prolonged labor and increases the likelihood of cesarean section due to difficulties in the baby’s descent through the birth canal.
- The transverse position of the baby may result in compression of the umbilical cord during labor, leading to decreased oxygen supply and potential fetal distress. This situation requires careful monitoring and intervention to ensure the baby’s well-being.
When a foetus is moving into the cephalic position, it is known as ‘head engagement’. The baby stars getting into this position in the third trimester, between the 32nd and the 36th weeks, to be precise. When the head engagement begins, the foetus starts moving down into the pelvic canal. At this stage, very little of the baby is felt in the abdomen, but more is felt moving downward into the pelvic canal in preparation for birth.
You may think that in order to find out if your baby has a cephalic presentation, an ultrasound is your only option. This is not always the case. You can actually find out the position of your baby just by touching and feeling their movements.
By rubbing your hand on your belly, you might be able to feel their position. If your baby is in the cephalic position, you might feel their kicks in the upper stomach. Whereas, if the baby is in the breech position, you might feel their kicks in the lower stomach.
Even in the cephalic position, it may be possible to tell if your baby is in the anterior position or in the posterior position. When your baby is in the anterior position, they may be facing your back. You may be able to feel your baby move underneath your ribs. It is likely that your belly button will also pop out.
When your baby is in the posterior position, you will usually feel your baby start to kick you in your stomach. When your baby has its back pressed up against your back, your stomach may not look rounded out, but flat instead.
Mothers whose placentas have attached in the front, something known as anterior placenta , you may not be able to feel the movements of your baby as well as you might like to.
Breech babies can make things complicated. Both the mother and the baby will face some problems. A breech baby is positioned head-up and bottom down. In order to deliver the baby, the birth canal needs to open a lot wider than it has to in the cephalic position. Besides this, your baby can get an arm or leg entangled while coming out.
If your baby is in the breech position, there are some things that you can do to encourage the baby to get into the cephalic position. There are a few exercises that could help such as pelvic tilts , swimming , spending a bit of time upside down, and belly dancing are a few ways you can try yourself to get your baby into the head-down position .
If this is not working either, your doctor will try an ECV (External Cephalic Version) . Here, your doctor will be hands-on, applying some gentle, but firm pressure to your tummy. In order to reach a cephalic position, the baby will need to be rolled into a bottom’s up position. This technique is successful around 50% of the time. When this happens, you will be able to have a normal vaginal delivery.
Though it sounds simple enough to get the fetal presentation into cephalic, there are some risks involved with ECV. If your doctor notices your baby’s heart rate starts to become problematic, the doctor will stop the procedure right away.
Encouraging a baby to move into the cephalic position, where the head is down towards the birth canal, is often desirable for smoother labor and delivery. While medical interventions may be necessary in some cases, there are natural methods that pregnant individuals can try to help facilitate this positioning. Here are several techniques that may help turn a baby into the cephalic position:
1. Optimal Maternal Positioning
Maintaining positions such as kneeling, hands and knees, or pelvic tilts may encourage the baby to move into the cephalic position by utilizing gravity and reducing pressure on the pelvis.
2. Spinning Babies Techniques
Specific exercises and positions recommended by the Spinning Babies organization, such as Forward-Leaning Inversion or the Sidelying Release, aim to promote optimal fetal positioning and may help encourage the baby to turn cephalic.
3. Chiropractic Care or Acupuncture
Some individuals find that chiropractic adjustments or acupuncture sessions with qualified practitioners can help address pelvic misalignment or relax tight muscles, potentially creating more space for the baby to maneuver into the cephalic position.
4. Prenatal Yoga and Swimming
Engaging in gentle exercises like prenatal yoga or swimming may help promote relaxation, reduce stress on the uterine ligaments, and encourage the baby to move into the cephalic position naturally. These activities also support overall physical and mental well-being during pregnancy.
1. What factors influence whether my baby will be in cephalic presentation?
Several factors can influence your baby’s position during pregnancy, including the shape and size of your uterus, the strength of your abdominal muscles, the amount of amniotic fluid, and the position of the placenta . Additionally, your baby’s own movements and preferences play a role.
2. Is it necessary for my baby to be in cephalic presentation for a vaginal delivery?
While cephalic presentation is considered the optimal position for vaginal delivery, some babies born in non-cephalic presentations can still be safely delivered vaginally with the guidance of a skilled healthcare provider. However, certain non-cephalic presentations may increase the likelihood of needing a cesarean section.
3. What can I do to encourage my baby to stay in the cephalic presentation?
Maintaining good posture, avoiding positions that encourage the baby to settle into a breech or transverse lie, staying active with gentle exercises, and avoiding excessive reclining can all help encourage your baby to remain in the cephalic presentation. Additionally, discussing any concerns with your healthcare provider and following their recommendations can be beneficial.
This was all about fetus with cephalic presentation. Most babies get into the cephalic position on their own. This is the most ideal situation as there will be little to no complications during normal vaginal labour. There are different cephalic positions, but these should not cause a lot of issues. If your baby is in any position other than cephalic in pregnancy, you may need C-Section . Keep yourself updated on the smallest of progress during your pregnancy so that you are aware of everything that is going on. Go for regular check-ups as your doctor will be able to help you if a complication arises during acephalic presentation at 20, 28 and 30 weeks.
References/Resources:
1. Glezerman. M; Planned vaginal breech delivery: current status and the need to reconsider (Expert Review of Obstetrics & Gynecology); Taylor & Francis Online; https://www.tandfonline.com/doi/full/10.1586/eog.12.2 ; January 2014
2. Feeling your baby move during pregnancy; UT Southwestern Medical Center; https://utswmed.org/medblog/fetal-movements/
3. Fetal presentation before birth; Mayo Clinic; https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/fetal-positions/art-20546850
4. Fetal Positions; Cleveland Clinic; https://my.clevelandclinic.org/health/articles/9677-fetal-positions-for-birth
5. FAQs: If Your Baby Is Breech; American College of Obstetricians and Gynecologists; https://www.acog.org/womens-health/faqs/if-your-baby-is-breech
6. Roecker. C; Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios (Journal of Chiropractic Medicine); Science Direct; https://www.sciencedirect.com/science/article/abs/pii/S1556370713000588 ; June 2013
7. Presentation and position of baby through pregnancy and at birth; Pregnancy, Birth & Baby; https://www.pregnancybirthbaby.org.au/presentation-and-position-of-baby-through-pregnancy-and-at-birth
Belly Mapping Pregnancy Belly Growth Chart Baby in Vertex Position during Labour and Delivery
- RELATED ARTICLES
- MORE FROM AUTHOR

Cervical Cancer During Pregnancy

How to Increase Hemoglobin Levels During Pregnancy?

Using Lavender in Pregnancy: Is It Safe?

Swine Flu (H1N1) in Pregnancy

Pregnancy Abortion Pills - How Does It Work, Side Effects & Risks

Yellow Discharge During Pregnancy
Popular on parenting.

245 Rare Boy & Girl Names with Meanings

Top 22 Short Moral Stories For Kids

170 Boy & Girl Names That Mean 'Gift from God'

800+ Unique & Cute Nicknames for Boys & Girls
Latest posts.

Understanding Baby Food Labels - Easy Guide for Parents on How to Read & Use

5 Ways to Maintain Diaper Hygiene in Summer for a Happy Baby!

4 Baby Sleep-Related Questions All New Parents Have Answered by a Paediatrician!

Do Indian Babies Have Different Diaper Needs? Here's an Expert's Opinion!
Is cephalic presentation normal at 21 weeks?
You May Also Like
Planning visitors during hospital stay, you’re pregnant how these moms reacted, jump to your week of pregnancy, trending on what to expect, moms share home remedies for pregnancy morning sickness, 8 expensive products moms say are worth the money, ⚠️ you can't see this cool content because you have ad block enabled., 14 moms on what labor really feels like, what are your go-to healthy snacks, things they don't tell you about: mom edition, pregnancy brain moments let's have a laugh, help keep our community safe, to create a safe place, please, on our end, we will.

IMAGES
VIDEO
COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery. About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy.
Most babies settle into their final position somewhere between 32 to 36 weeks gestation. Head Down, Facing Down (Cephalic Presentation) This is the most common position for babies in-utero. In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest ...
Head first (called vertex or cephalic presentation) Facing backward (occiput anterior position) Spine parallel to mother's spine (longitudinal lie) Neck bent forward with chin tucked. Arms folded across the chest . If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not ...
Cephalic presentation, occiput anterior. This is the best position for labor. Your baby is head-down, their face is turned toward your back, and their chin is tucked to their chest. This allows the back of your baby's head to easily enter your pelvis when the time is right. Most babies settle into this position by week 36 of pregnancy.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation).
It has been modified from later than 36 weeks' gestation to early term-37 weeks or greater. When compared with term ECV (37+ weeks), preterm ECV (34-35 weeks) has been associated with increased short-term success with cephalic presentation, higher rates of reversion to breech in the ensuing weeks, and cesarean delivery risk reduction [RR 0. ...
Most babies settle into the cephalic presentation at 33 weeks. Your healthcare provider will carefully monitor fetal movement in the last few weeks of your gestation to ensure your baby has achieved an ideal birth position by 36 weeks of pregnancy. If your baby is not in the cephalic position by the 36th week, your healthcare provider may try a ...
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor. ... Cephalic presentation occurs in about 97% of deliveries. There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude). ...
There are other types of cephalic presentations like brow and face. These mainly describe how the fetus's neck is flexed. When does a fetus turn into a vertex presentation? Most fetuses settle into a presentation around 32 to 36 weeks of pregnancy. It's possible for a fetus to rotate into a cephalic presentation after 36 weeks.
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation, where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
The global cesarean section rate has increased from approximately 23% to 34% in the past decade. Fetal malpresentation is now the third-most common indication for cesarean delivery, encompassing nearly 17% of cases. Almost one-fourth of all fetuses are in a breech presentation at 28 weeks gestational age; this number decreases to between 3% and 4% at term. In current clinical practice, most ...
Some reports have revealed that non-cephalic ratio is relatively high until around 30 weeks of gestation (WG), and the chance of cephalic presentation increases progressively toward delivery [Citation 7]. This phenomenon is commonly called the spontaneous cephalic version (SCV).
Others show moxibustion to provide no help in coaxing a baby into cephalic position. ... Turning foetal breech presentation at 32-35 weeks of gestational age by acupuncture and moxibustion. ... 30. weeks pregnant. 31. weeks pregnant. 32. weeks pregnant. 33. weeks pregnant. 34. weeks pregnant. 35.
Introduction. Cephalic presentation is the most physiologic and frequent fetal presentation and is associated with the highest rate of successful vaginal delivery as well as with the lowest frequency of complications 1.Studies on the frequency of breech presentation by gestational age (GA) were published more than 20 years ago 2, 3, and it has been known that the prevalence of breech ...
In addition to cephalic presentation, there are several other fetal positions that can occur during pregnancy and childbirth, each with its own associated risks. ... Go for regular check-ups as your doctor will be able to help you if a complication arises during acephalic presentation at 20, 28 and 30 weeks. References/Resources: 1. Glezerman ...
29 yrs old Female asked about Cephalic presentation at 30 weeks, 5 doctors answered this and 1280 people found it useful. Get your query answered 24*7 only on | Practo Consult
Cephalic presentation just means head down and facing your back. It does not necessarily indicate that labor will be soon without other indicators like effacement, dilation, engagement. Like. m. mintyfresh21. Jan 14, 2021 at 4:41 AM. @thencomesthree,
Is cephalic presentation normal at 21 weeks? r. rubi3na. It means baby is in head down position. The doctor didn't say anything so it's probably normal. Has anyone else experienced this? Like. ... Pregnancy Week 30. Pregnancy Week 31. Pregnancy Week 32. Pregnancy Week 33. Pregnancy Week 34. Pregnancy Week 35. Pregnancy Week 36. Pregnancy Week 37.