What Is Cancer?
Get email updates from NCI on cancer health information, news, and other topics
Get email updates from NCI
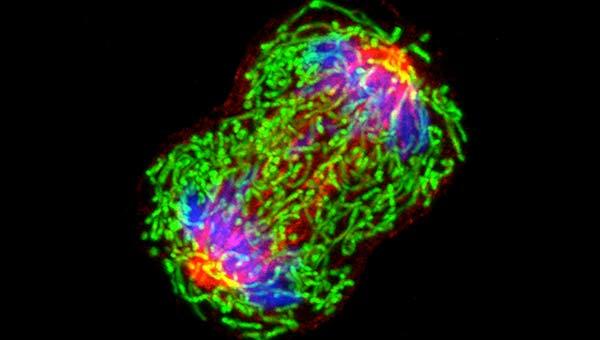
A dividing breast cancer cell.

The Definition of Cancer
Cancer is a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body.
Cancer can start almost anywhere in the human body, which is made up of trillions of cells. Normally, human cells grow and multiply (through a process called cell division) to form new cells as the body needs them. When cells grow old or become damaged, they die, and new cells take their place.
Sometimes this orderly process breaks down, and abnormal or damaged cells grow and multiply when they shouldn’t. These cells may form tumors, which are lumps of tissue. Tumors can be cancerous or not cancerous ( benign ).
Cancerous tumors spread into, or invade, nearby tissues and can travel to distant places in the body to form new tumors (a process called metastasis ). Cancerous tumors may also be called malignant tumors. Many cancers form solid tumors, but cancers of the blood, such as leukemias , generally do not.
Benign tumors do not spread into, or invade, nearby tissues. When removed, benign tumors usually don’t grow back, whereas cancerous tumors sometimes do. Benign tumors can sometimes be quite large, however. Some can cause serious symptoms or be life threatening, such as benign tumors in the brain.
Differences between Cancer Cells and Normal Cells

Get Answers >
Have questions? Connect with a Cancer Information Specialist for answers.
Cancer cells differ from normal cells in many ways. For instance, cancer cells:
- grow in the absence of signals telling them to grow. Normal cells only grow when they receive such signals.
- ignore signals that normally tell cells to stop dividing or to die (a process known as programmed cell death , or apoptosis ).
- invade into nearby areas and spread to other areas of the body. Normal cells stop growing when they encounter other cells, and most normal cells do not move around the body.
- tell blood vessels to grow toward tumors. These blood vessels supply tumors with oxygen and nutrients and remove waste products from tumors.
- hide from the immune system . The immune system normally eliminates damaged or abnormal cells.
- trick the immune system into helping cancer cells stay alive and grow. For instance, some cancer cells convince immune cells to protect the tumor instead of attacking it.
- accumulate multiple changes in their chromosomes , such as duplications and deletions of chromosome parts. Some cancer cells have double the normal number of chromosomes.
- rely on different kinds of nutrients than normal cells. In addition, some cancer cells make energy from nutrients in a different way than most normal cells. This lets cancer cells grow more quickly.
Many times, cancer cells rely so heavily on these abnormal behaviors that they can’t survive without them. Researchers have taken advantage of this fact, developing therapies that target the abnormal features of cancer cells. For example, some cancer therapies prevent blood vessels from growing toward tumors , essentially starving the tumor of needed nutrients.
How Does Cancer Develop?
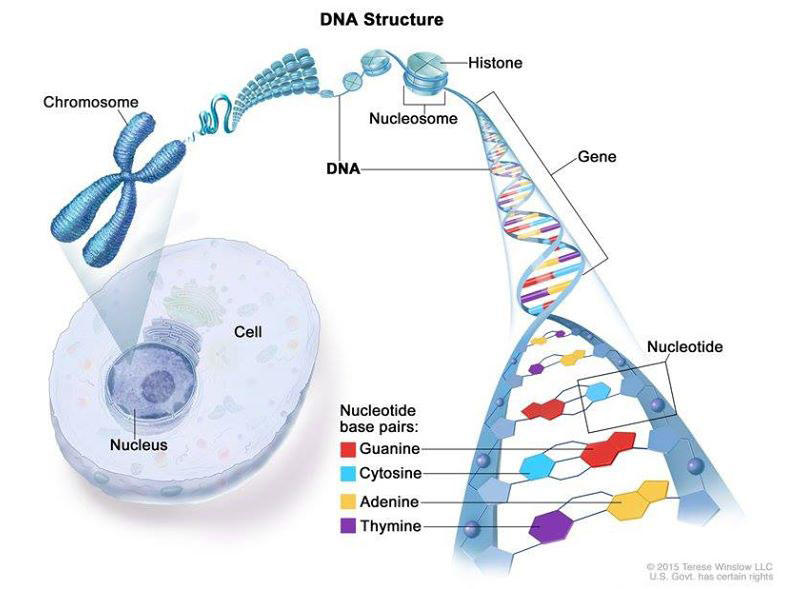
Cancer is caused by certain changes to genes, the basic physical units of inheritance. Genes are arranged in long strands of tightly packed DNA called chromosomes.
Cancer is a genetic disease—that is, it is caused by changes to genes that control the way our cells function, especially how they grow and divide.
Genetic changes that cause cancer can happen because:
- of errors that occur as cells divide.
- of damage to DNA caused by harmful substances in the environment, such as the chemicals in tobacco smoke and ultraviolet rays from the sun. (Our Cancer Causes and Prevention section has more information.)
- they were inherited from our parents.
The body normally eliminates cells with damaged DNA before they turn cancerous. But the body’s ability to do so goes down as we age. This is part of the reason why there is a higher risk of cancer later in life.
Each person’s cancer has a unique combination of genetic changes. As the cancer continues to grow, additional changes will occur. Even within the same tumor, different cells may have different genetic changes.
Fundamentals of Cancer
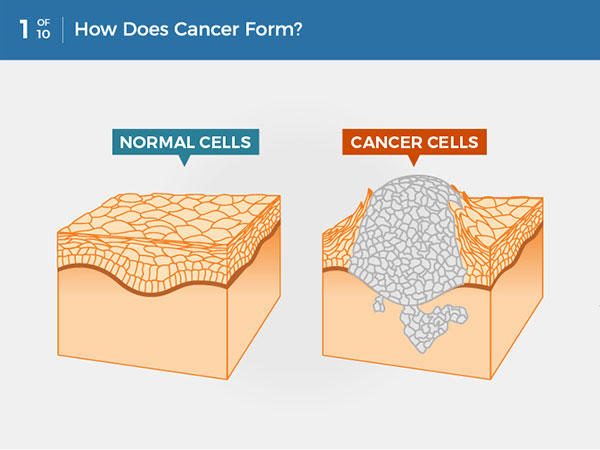
Cancer is a disease caused when cells divide uncontrollably and spread into surrounding tissues.
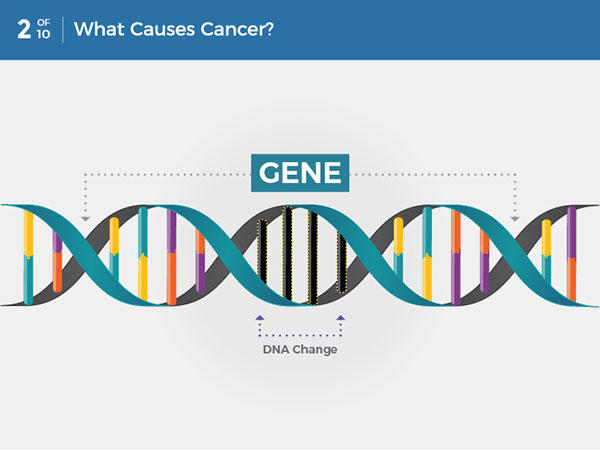
Cancer is caused by changes to DNA. Most cancer-causing DNA changes occur in sections of DNA called genes. These changes are also called genetic changes.
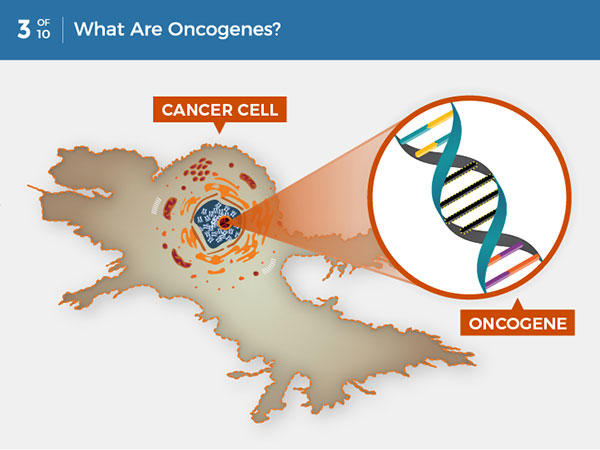
A DNA change can cause genes involved in normal cell growth to become oncogenes. Unlike normal genes, oncogenes cannot be turned off, so they cause uncontrolled cell growth.
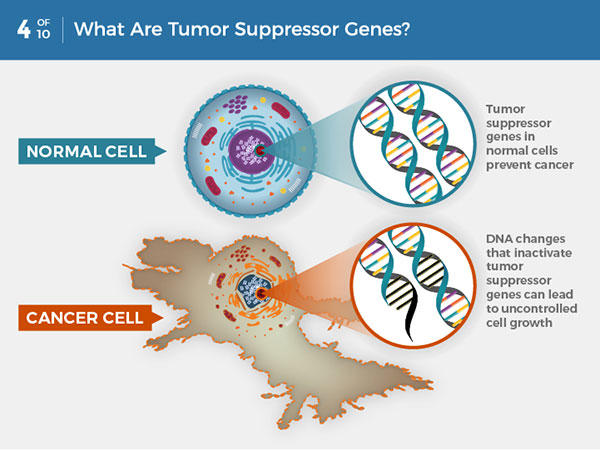
In normal cells, tumor suppressor genes prevent cancer by slowing or stopping cell growth. DNA changes that inactivate tumor suppressor genes can lead to uncontrolled cell growth and cancer.
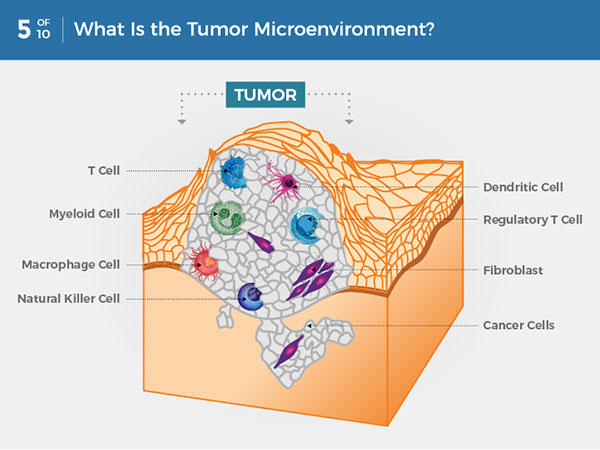
Within a tumor, cancer cells are surrounded by a variety of immune cells, fibroblasts, molecules, and blood vessels—what’s known as the tumor microenvironment. Cancer cells can change the microenvironment, which in turn can affect how cancer grows and spreads.
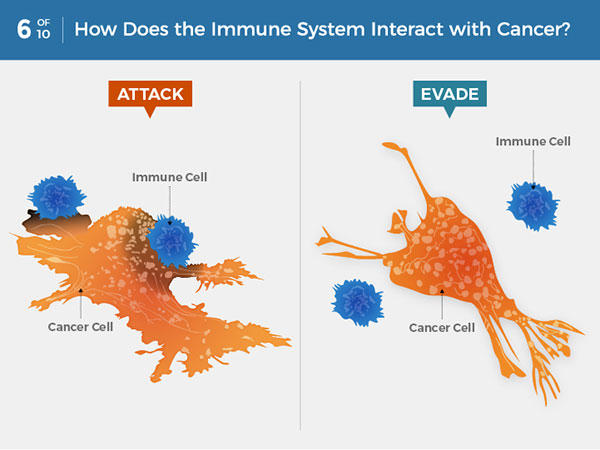
Immune system cells can detect and attack cancer cells. But some cancer cells can avoid detection or thwart an attack. Some cancer treatments can help the immune system better detect and kill cancer cells.
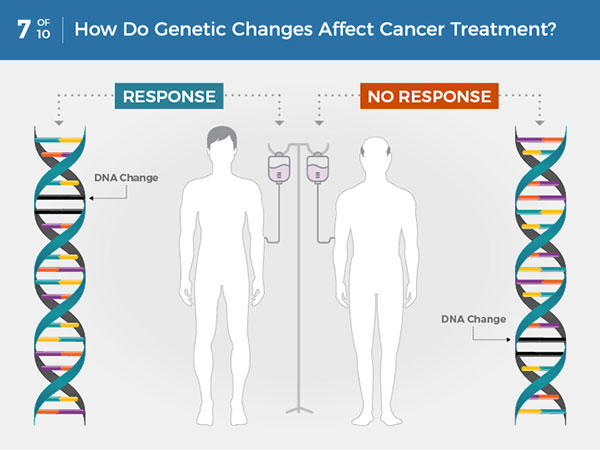
Each person’s cancer has a unique combination of genetic changes. Specific genetic changes may make a person’s cancer more or less likely to respond to certain treatments.
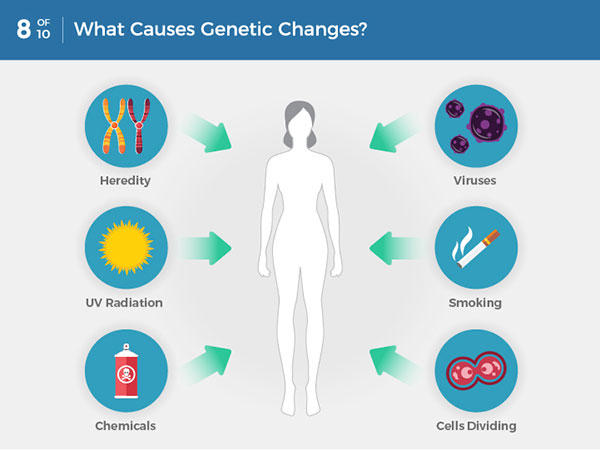
Genetic changes that cause cancer can be inherited or arise from certain environmental exposures. Genetic changes can also happen because of errors that occur as cells divide.
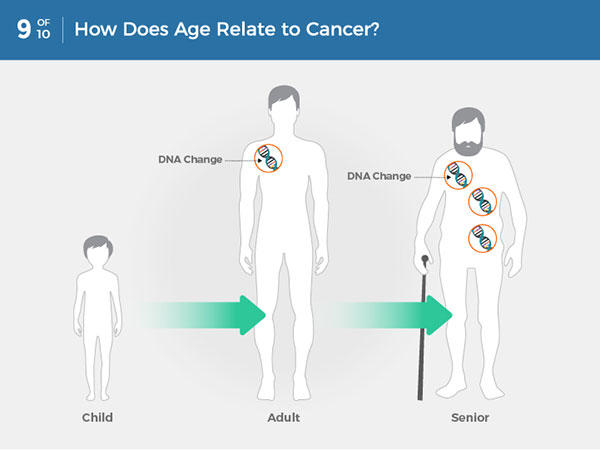
Most often, cancer-causing genetic changes accumulate slowly as a person ages, leading to a higher risk of cancer later in life.
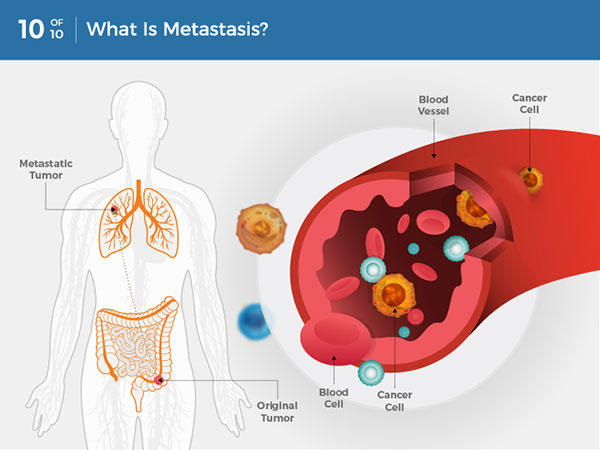
Cancer cells can break away from the original tumor and travel through the blood or lymph system to distant locations in the body, where they exit the vessels to form additional tumors. This is called metastasis.
Types of Genes that Cause Cancer
The genetic changes that contribute to cancer tend to affect three main types of genes— proto-oncogenes , tumor suppressor genes , and DNA repair genes. These changes are sometimes called “drivers” of cancer.
Proto-oncogenes are involved in normal cell growth and division. However, when these genes are altered in certain ways or are more active than normal, they may become cancer-causing genes (or oncogenes), allowing cells to grow and survive when they should not.
Tumor suppressor genes are also involved in controlling cell growth and division. Cells with certain alterations in tumor suppressor genes may divide in an uncontrolled manner.
DNA repair genes are involved in fixing damaged DNA. Cells with mutations in these genes tend to develop additional mutations in other genes and changes in their chromosomes, such as duplications and deletions of chromosome parts. Together, these mutations may cause the cells to become cancerous.
As scientists have learned more about the molecular changes that lead to cancer, they have found that certain mutations commonly occur in many types of cancer. Now there are many cancer treatments available that target gene mutations found in cancer . A few of these treatments can be used by anyone with a cancer that has the targeted mutation, no matter where the cancer started growing .
When Cancer Spreads
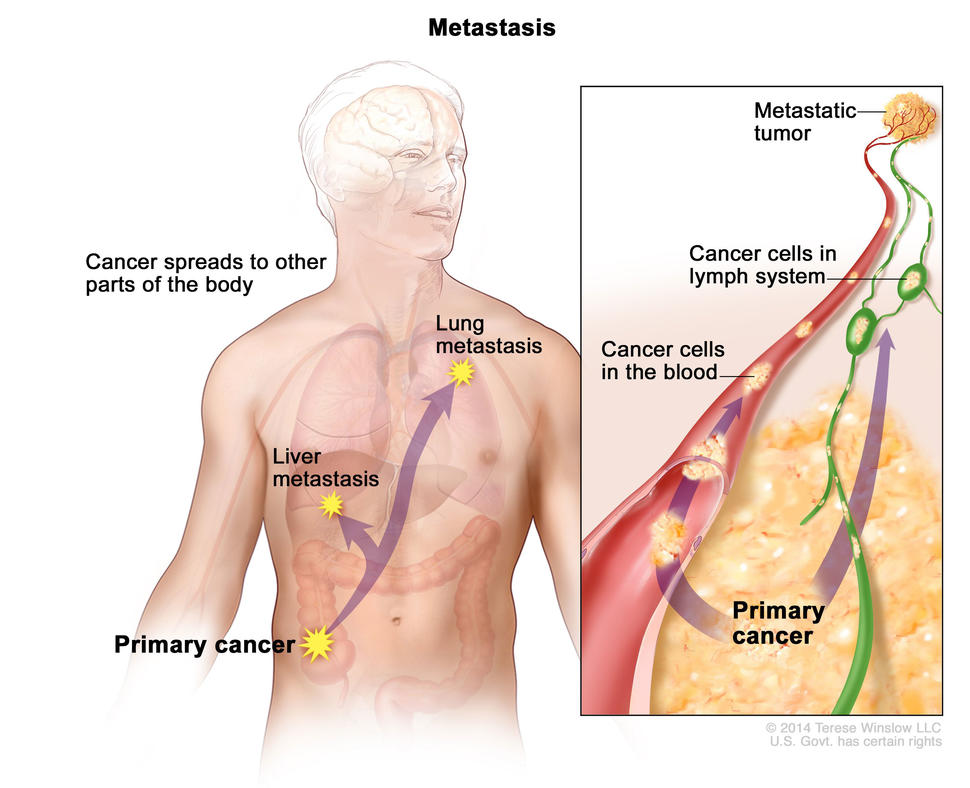
In metastasis, cancer cells break away from where they first formed and form new tumors in other parts of the body.
A cancer that has spread from the place where it first formed to another place in the body is called metastatic cancer. The process by which cancer cells spread to other parts of the body is called metastasis.
Metastatic cancer has the same name and the same type of cancer cells as the original, or primary, cancer. For example, breast cancer that forms a metastatic tumor in the lung is metastatic breast cancer, not lung cancer.
Under a microscope, metastatic cancer cells generally look the same as cells of the original cancer. Moreover, metastatic cancer cells and cells of the original cancer usually have some molecular features in common, such as the presence of specific chromosome changes.
In some cases, treatment may help prolong the lives of people with metastatic cancer. In other cases, the primary goal of treatment for metastatic cancer is to control the growth of the cancer or to relieve symptoms it is causing. Metastatic tumors can cause severe damage to how the body functions, and most people who die of cancer die of metastatic disease.
Tissue Changes that Are Not Cancer
Not every change in the body’s tissues is cancer. Some tissue changes may develop into cancer if they are not treated, however. Here are some examples of tissue changes that are not cancer but, in some cases, are monitored because they could become cancer:
- Hyperplasia occurs when cells within a tissue multiply faster than normal and extra cells build up. However, the cells and the way the tissue is organized still look normal under a microscope. Hyperplasia can be caused by several factors or conditions, including chronic irritation.
- Dysplasia is a more advanced condition than hyperplasia. In dysplasia, there is also a buildup of extra cells. But the cells look abnormal and there are changes in how the tissue is organized. In general, the more abnormal the cells and tissue look, the greater the chance that cancer will form. Some types of dysplasia may need to be monitored or treated, but others do not. An example of dysplasia is an abnormal mole (called a dysplastic nevus ) that forms on the skin. A dysplastic nevus can turn into melanoma, although most do not.
- Carcinoma in situ is an even more advanced condition. Although it is sometimes called stage 0 cancer, it is not cancer because the abnormal cells do not invade nearby tissue the way that cancer cells do. But because some carcinomas in situ may become cancer, they are usually treated.
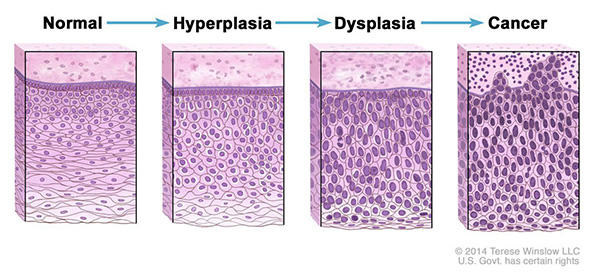
Normal cells may become cancer cells. Before cancer cells form in tissues of the body, the cells go through abnormal changes called hyperplasia and dysplasia. In hyperplasia, there is an increase in the number of cells in an organ or tissue that appear normal under a microscope. In dysplasia, the cells look abnormal under a microscope but are not cancer. Hyperplasia and dysplasia may or may not become cancer.
Types of Cancer
There are more than 100 types of cancer. Types of cancer are usually named for the organs or tissues where the cancers form. For example, lung cancer starts in the lung, and brain cancer starts in the brain. Cancers also may be described by the type of cell that formed them, such as an epithelial cell or a squamous cell .
You can search NCI’s website for information on specific types of cancer based on the cancer’s location in the body or by using our A to Z List of Cancers . We also have information on childhood cancers and cancers in adolescents and young adults .
Here are some categories of cancers that begin in specific types of cells:
Carcinomas are the most common type of cancer. They are formed by epithelial cells, which are the cells that cover the inside and outside surfaces of the body. There are many types of epithelial cells, which often have a column-like shape when viewed under a microscope.
Carcinomas that begin in different epithelial cell types have specific names:
Adenocarcinoma is a cancer that forms in epithelial cells that produce fluids or mucus. Tissues with this type of epithelial cell are sometimes called glandular tissues. Most cancers of the breast, colon, and prostate are adenocarcinomas.
Basal cell carcinoma is a cancer that begins in the lower or basal (base) layer of the epidermis, which is a person’s outer layer of skin.
Squamous cell carcinoma is a cancer that forms in squamous cells, which are epithelial cells that lie just beneath the outer surface of the skin. Squamous cells also line many other organs, including the stomach, intestines, lungs, bladder, and kidneys. Squamous cells look flat, like fish scales, when viewed under a microscope. Squamous cell carcinomas are sometimes called epidermoid carcinomas.
Transitional cell carcinoma is a cancer that forms in a type of epithelial tissue called transitional epithelium, or urothelium. This tissue, which is made up of many layers of epithelial cells that can get bigger and smaller, is found in the linings of the bladder, ureters, and part of the kidneys (renal pelvis), and a few other organs. Some cancers of the bladder, ureters, and kidneys are transitional cell carcinomas.
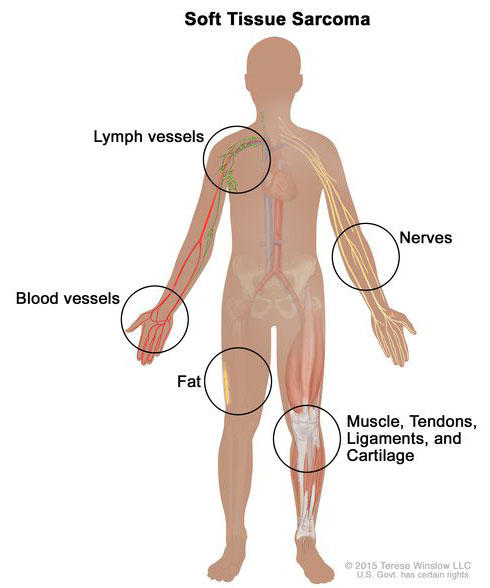
Soft tissue sarcoma forms in soft tissues of the body, including muscle, tendons, fat, blood vessels, lymph vessels, nerves, and tissue around joints.
Sarcomas are cancers that form in bone and soft tissues, including muscle, fat, blood vessels, lymph vessels , and fibrous tissue (such as tendons and ligaments).
Osteosarcoma is the most common cancer of bone. The most common types of soft tissue sarcoma are leiomyosarcoma , Kaposi sarcoma , malignant fibrous histiocytoma , liposarcoma , and dermatofibrosarcoma protuberans .
Our page on soft tissue sarcoma has more information.
Cancers that begin in the blood-forming tissue of the bone marrow are called leukemias. These cancers do not form solid tumors. Instead, large numbers of abnormal white blood cells (leukemia cells and leukemic blast cells) build up in the blood and bone marrow, crowding out normal blood cells. The low level of normal blood cells can make it harder for the body to get oxygen to its tissues, control bleeding, or fight infections.
There are four common types of leukemia, which are grouped based on how quickly the disease gets worse (acute or chronic) and on the type of blood cell the cancer starts in (lymphoblastic or myeloid). Acute forms of leukemia grow quickly and chronic forms grow more slowly.
Our page on leukemia has more information.
Lymphoma is cancer that begins in lymphocytes (T cells or B cells). These are disease-fighting white blood cells that are part of the immune system. In lymphoma, abnormal lymphocytes build up in lymph nodes and lymph vessels, as well as in other organs of the body.
There are two main types of lymphoma:
Hodgkin lymphoma – People with this disease have abnormal lymphocytes that are called Reed-Sternberg cells. These cells usually form from B cells.
Non-Hodgkin lymphoma – This is a large group of cancers that start in lymphocytes. The cancers can grow quickly or slowly and can form from B cells or T cells.
Our page on lymphoma has more information.
Multiple Myeloma
Multiple myeloma is cancer that begins in plasma cells , another type of immune cell. The abnormal plasma cells, called myeloma cells, build up in the bone marrow and form tumors in bones all through the body. Multiple myeloma is also called plasma cell myeloma and Kahler disease.
Our page on multiple myeloma and other plasma cell neoplasms has more information.
Melanoma is cancer that begins in cells that become melanocytes, which are specialized cells that make melanin (the pigment that gives skin its color). Most melanomas form on the skin, but melanomas can also form in other pigmented tissues, such as the eye.
Our pages on skin cancer and intraocular melanoma have more information.
Brain and Spinal Cord Tumors
There are different types of brain and spinal cord tumors. These tumors are named based on the type of cell in which they formed and where the tumor first formed in the central nervous system. For example, an astrocytic tumor begins in star-shaped brain cells called astrocytes , which help keep nerve cells healthy. Brain tumors can be benign (not cancer) or malignant (cancer).
Our page on brain and spinal cord tumors has more information.
Other Types of Tumors
Germ cell tumors.
Germ cell tumors are a type of tumor that begins in the cells that give rise to sperm or eggs. These tumors can occur almost anywhere in the body and can be either benign or malignant.
Our page of cancers by body location/system includes a list of germ cell tumors with links to more information.
Neuroendocrine Tumors
Neuroendocrine tumors form from cells that release hormones into the blood in response to a signal from the nervous system. These tumors, which may make higher-than-normal amounts of hormones, can cause many different symptoms. Neuroendocrine tumors may be benign or malignant.
Our definition of neuroendocrine tumors has more information.
Carcinoid Tumors
Carcinoid tumors are a type of neuroendocrine tumor. They are slow-growing tumors that are usually found in the gastrointestinal system (most often in the rectum and small intestine). Carcinoid tumors may spread to the liver or other sites in the body, and they may secrete substances such as serotonin or prostaglandins, causing carcinoid syndrome .
Our page on gastrointestinal neuroendocrine tumors has more information.
- Patient Care & Health Information
- Diseases & Conditions
Cancer refers to any one of a large number of diseases characterized by the development of abnormal cells that divide uncontrollably and have the ability to infiltrate and destroy normal body tissue. Cancer often has the ability to spread throughout your body.
Cancer is the second-leading cause of death in the world. But survival rates are improving for many types of cancer, thanks to improvements in cancer screening, treatment and prevention.
Products & Services
- A Book: Live Younger Longer
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Assortment of Pill Aids from Mayo Clinic Store
- Mayo Clinic Comprehensive Cancer Center
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Signs and symptoms caused by cancer will vary depending on what part of the body is affected.
Some general signs and symptoms associated with, but not specific to, cancer, include:
- Lump or area of thickening that can be felt under the skin
- Weight changes, including unintended loss or gain
- Skin changes, such as yellowing, darkening or redness of the skin, sores that won't heal, or changes to existing moles
- Changes in bowel or bladder habits
- Persistent cough or trouble breathing
- Difficulty swallowing
- Persistent indigestion or discomfort after eating
- Persistent, unexplained muscle or joint pain
- Persistent, unexplained fevers or night sweats
- Unexplained bleeding or bruising
When to see a doctor
Make an appointment with your doctor if you have any persistent signs or symptoms that concern you.
If you don't have any signs or symptoms, but are worried about your risk of cancer, discuss your concerns with your doctor. Ask about which cancer screening tests and procedures are appropriate for you.
Cancer is caused by changes (mutations) to the DNA within cells. The DNA inside a cell is packaged into a large number of individual genes, each of which contains a set of instructions telling the cell what functions to perform, as well as how to grow and divide. Errors in the instructions can cause the cell to stop its normal function and may allow a cell to become cancerous.
What do gene mutations do?
A gene mutation can instruct a healthy cell to:
- Allow rapid growth. A gene mutation can tell a cell to grow and divide more rapidly. This creates many new cells that all have that same mutation.
- Fail to stop uncontrolled cell growth. Normal cells know when to stop growing so that you have just the right number of each type of cell. Cancer cells lose the controls (tumor suppressor genes) that tell them when to stop growing. A mutation in a tumor suppressor gene allows cancer cells to continue growing and accumulating.
- Make mistakes when repairing DNA errors. DNA repair genes look for errors in a cell's DNA and make corrections. A mutation in a DNA repair gene may mean that other errors aren't corrected, leading cells to become cancerous.
These mutations are the most common ones found in cancer. But many other gene mutations can contribute to causing cancer.
What causes gene mutations?
Gene mutations can occur for several reasons, for instance:
- Gene mutations you're born with. You may be born with a genetic mutation that you inherited from your parents. This type of mutation accounts for a small percentage of cancers.
- Gene mutations that occur after birth. Most gene mutations occur after you're born and aren't inherited. A number of forces can cause gene mutations, such as smoking, radiation, viruses, cancer-causing chemicals (carcinogens), obesity, hormones, chronic inflammation and a lack of exercise.
Gene mutations occur frequently during normal cell growth. However, cells contain a mechanism that recognizes when a mistake occurs and repairs the mistake. Occasionally, a mistake is missed. This could cause a cell to become cancerous.
How do gene mutations interact with each other?
The gene mutations you're born with and those that you acquire throughout your life work together to cause cancer.
For instance, if you've inherited a genetic mutation that predisposes you to cancer, that doesn't mean you're certain to get cancer. Instead, you may need one or more other gene mutations to cause cancer. Your inherited gene mutation could make you more likely than other people to develop cancer when exposed to a certain cancer-causing substance.
It's not clear just how many mutations must accumulate for cancer to form. It's likely that this varies among cancer types.
More Information
Cancer care at Mayo Clinic
- Myths about cancer causes
Risk factors
While doctors have an idea of what may increase your risk of cancer, the majority of cancers occur in people who don't have any known risk factors. Factors known to increase your risk of cancer include:
Cancer can take decades to develop. That's why most people diagnosed with cancer are 65 or older. While it's more common in older adults, cancer isn't exclusively an adult disease — cancer can be diagnosed at any age.
Your habits
Certain lifestyle choices are known to increase your risk of cancer. Smoking, drinking more than one drink a day for women and up to two drinks a day for men, excessive exposure to the sun or frequent blistering sunburns, being obese, and having unsafe sex can contribute to cancer.
You can change these habits to lower your risk of cancer — though some habits are easier to change than others.
Your family history
Only a small portion of cancers are due to an inherited condition. If cancer is common in your family, it's possible that mutations are being passed from one generation to the next. You might be a candidate for genetic testing to see whether you have inherited mutations that might increase your risk of certain cancers. Keep in mind that having an inherited genetic mutation doesn't necessarily mean you'll get cancer.
Your health conditions
Some chronic health conditions, such as ulcerative colitis, can markedly increase your risk of developing certain cancers. Talk to your doctor about your risk.
Your environment
The environment around you may contain harmful chemicals that can increase your risk of cancer. Even if you don't smoke, you might inhale secondhand smoke if you go where people are smoking or if you live with someone who smokes. Chemicals in your home or workplace, such as asbestos and benzene, also are associated with an increased risk of cancer.
Complications
Cancer and its treatment can cause several complications, including:
- Pain. Pain can be caused by cancer or by cancer treatment, though not all cancer is painful. Medications and other approaches can effectively treat cancer-related pain.
- Fatigue. Fatigue in people with cancer has many causes, but it can often be managed. Fatigue associated with chemotherapy or radiation therapy treatments is common, but it's usually temporary.
- Difficulty breathing. Cancer or cancer treatment may cause a feeling of being short of breath. Treatments may bring relief.
- Nausea. Certain cancers and cancer treatments can cause nausea. Your doctor can sometimes predict if your treatment is likely to cause nausea. Medications and other treatments may help you prevent or decrease nausea.
- Diarrhea or constipation. Cancer and cancer treatment can affect your bowels and cause diarrhea or constipation.
- Weight loss. Cancer and cancer treatment may cause weight loss. Cancer steals food from normal cells and deprives them of nutrients. This is often not affected by how many calories or what kind of food is eaten; it's difficult to treat. In most cases, using artificial nutrition through tubes into the stomach or vein does not help change the weight loss.
- Chemical changes in your body. Cancer can upset the normal chemical balance in your body and increase your risk of serious complications. Signs and symptoms of chemical imbalances might include excessive thirst, frequent urination, constipation and confusion.
- Brain and nervous system problems. Cancer can press on nearby nerves and cause pain and loss of function of one part of your body. Cancer that involves the brain can cause headaches and stroke-like signs and symptoms, such as weakness on one side of your body.
- Unusual immune system reactions to cancer. In some cases the body's immune system may react to the presence of cancer by attacking healthy cells. Called paraneoplastic syndromes, these very rare reactions can lead to a variety of signs and symptoms, such as difficulty walking and seizures.
- Cancer that spreads. As cancer advances, it may spread (metastasize) to other parts of the body. Where cancer spreads depends on the type of cancer.
- Cancer that returns. Cancer survivors have a risk of cancer recurrence. Some cancers are more likely to recur than others. Ask your doctor about what you can do to reduce your risk of cancer recurrence. Your doctor may devise a follow-up care plan for you after treatment. This plan may include periodic scans and exams in the months and years after your treatment, to look for cancer recurrence.
Doctors have identified several ways to reduce your risk of cancer, such as:
- Stop smoking. If you smoke, quit. If you don't smoke, don't start. Smoking is linked to several types of cancer — not just lung cancer. Stopping now will reduce your risk of cancer in the future.
- Avoid excessive sun exposure. Harmful ultraviolet (UV) rays from the sun can increase your risk of skin cancer. Limit your sun exposure by staying in the shade, wearing protective clothing or applying sunscreen.
- Eat a healthy diet. Choose a diet rich in fruits and vegetables. Select whole grains and lean proteins. Limit your intake of processed meats.
- Exercise most days of the week. Regular exercise is linked to a lower risk of cancer. Aim for at least 30 minutes of exercise most days of the week. If you haven't been exercising regularly, start out slowly and work your way up to 30 minutes or longer.
- Maintain a healthy weight. Being overweight or obese may increase your risk of cancer. Work to achieve and maintain a healthy weight through a combination of a healthy diet and regular exercise.
- Drink alcohol in moderation, if you choose to drink. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Schedule cancer screening exams. Talk to your doctor about what types of cancer screening exams are best for you based on your risk factors.
- Ask your doctor about immunizations. Certain viruses increase your risk of cancer. Immunizations may help prevent those viruses, including hepatitis B, which increases the risk of liver cancer, and human papillomavirus (HPV), which increases the risk of cervical cancer and other cancers. Ask your doctor whether immunization against these viruses is appropriate for you.
Living with cancer?
Connect with others like you for support and answers to your questions in the Cancer support group on Mayo Clinic Connect, a patient community.
Cancer Discussions

75 Replies Fri, May 10, 2024

185 Replies Fri, May 10, 2024

48 Replies Fri, May 03, 2024
- Cancer. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed Feb. 16, 2021.
- Cancer stat facts: Cancer of any site. National Cancer Institute Surveillance, Epidemiology, and End Results Program. https://seer.cancer.gov/statfacts/html/all.html. Accessed Feb. 16, 2021.
- Symptoms of cancer. National Cancer Institute. https://www.cancer.gov/about-cancer/diagnosis-staging/symptoms. Accessed Feb. 16, 2021.
- Rock CL, et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA: A Cancer Journal for Clinicians. 2020;doi:doi.org/10.3322/caac.21591.
- Niederhuber JE, et al., eds. Genetic and epigenetic alterations in cancer. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 4, 2020.
- Ulcerative colitis. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis/all-content. Accessed Feb. 16, 2021.
- Paraneoplastic syndromes information page. National Institute of Neurological Disorder and Stroke. https://www.ninds.nih.gov/Disorders/All-Disorders/Paraneoplastic-Syndromes-Information-Page. Accessed Feb. 16, 2021.
- Deng GE, et al. Evidence-based clinical practice guidelines for integrative oncology: Complementary therapies and botanicals. Journal of the Society for Integrative Oncology. 2009;7:85.
- Taking time: Support for people with cancer. National Cancer Institute. https://www.cancer.gov/publications/patient-education/taking-time. Accessed Feb. 16, 2021.
- The American Cancer Society, eds. The principles and drivers of cancer. In: The American Cancer Society's Principles of Oncology: Prevention to Survivorship. Wiley-Blackwell; 2018.
- Hypercalcemia (high level of calcium in the blood). Merck Manual Consumer Edition. https://www.merckmanuals.com/home/hormonal-and-metabolic-disorders/electrolyte-balance/hypercalcemia-high-level-of-calcium-in-the-blood#. Accessed Feb. 16, 2021.
- What is cancer? National Cancer Institute. https://www.cancer.gov/about-cancer/understanding/what-is-cancer. Accessed Feb. 16, 2021.
- Cancer prevention overview (PDQ) — Health professional version. National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/hp-prevention-overview-pdq. Accessed Feb. 16, 2021.
- The genetics of cancer. National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/genetics. Accessed Feb. 16, 2021.
- Understanding cancer risk. Cancer.Net. https://www.cancer.net/navigating-cancer-care/prevention-and-healthy-living/understanding-cancer-risk. Accessed Feb. 16. 2021.
- Cancer screening overview (PDQ) — Health professional version. National Cancer Institute. https://www.cancer.gov/about-cancer/screening/hp-screening-overview-pdq. Accessed Feb. 16, 2021.
- How cancer is diagnosed. National Cancer Institute. https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis. Accessed Feb. 16, 2021.
- Cancer staging. National Cancer Institute. https://www.cancer.gov/about-cancer/diagnosis-staging/staging. Accessed Feb. 16, 2021.
- Making decisions about cancer treatment. Cancer.Net. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/making-decisions-about-cancer-treatment. Accessed Feb. 16, 2021.
- How cancer is treated. Cancer.Net. https://www.cancer.net/navigating-cancer-care/how-cancer-treated. Accessed Feb. 16, 2021.
- Absolute risk
- Adjuvant therapy for cancer
- Atypical cells: Are they cancer?
- Biopsy procedures
- Cancer blood tests
- Cancer diagnosis: 11 tips for coping
- Cancer pain: Relief is possible
- Cancer risk: What the numbers mean
- Cancer surgery
- Cancer survival rate
- Cancer survivors: Care for your body after treatment
- Cancer survivors: Late effects of cancer treatment
- Cancer survivors: Managing your emotions after cancer treatment
- Cancer treatment myths
- Cancer-related diarrhea
- Cancer-related fatigue
- Chemotherapy side effects: A cause of heart disease?
- Curcumin: Can it slow cancer growth?
- Eating during cancer treatment: Tips to make food tastier
- Heart cancer: Is there such a thing?
- High-dose vitamin C: Can it kill cancer cells?
- How cancer spreads
- Image-guided needle biopsy
- Infographic: Cancer Clinical Trials Offer Many Benefits
- Low blood counts
- Monoclonal antibody drugs
- Mort Crim and Cancer
- Mouth sores caused by cancer treatment: How to cope
- No appetite? How to get nutrition during cancer treatment
- PICC line placement
- Punch biopsy
- Relative risk
- Self-Image During Cancer
- Small cell, large cell cancer: What this means
- Tumor vs. cyst: What's the difference?
- What does cancer look like?
- When cancer returns: How to cope with cancer recurrence
Associated Procedures
- Biological therapy for cancer
- Bone marrow transplant
- Cancer treatment
- Chemotherapy
- Complete blood count (CBC)
- Intensity-modulated radiation therapy (IMRT)
- Needle biopsy
- Palliative care
- Radiation therapy
News from Mayo Clinic
- Mayo researchers invented a new class of AI to improve cancer research and treatments March 11, 2024, 02:55 p.m. CDT
- Can you prevent cancer with lifestyle changes? Feb. 19, 2024, 05:00 p.m. CDT
- World Cancer Day: Making a commitment to close the cancer care gap Feb. 04, 2024, 12:00 p.m. CDT
- Mayo Clinic Minute: Closing the gaps in cancer care Feb. 02, 2024, 05:30 p.m. CDT
- Highlights of Mayo Clinic research advancements in 2023 Jan. 01, 2024, 03:00 p.m. CDT
- Mayo Clinic Comprehensive Cancer Center highlights research advances in 2023 Dec. 21, 2023, 10:19 p.m. CDT
- Mayo Clinic Minute: The right way to talk with someone who has cancer Dec. 18, 2023, 05:30 p.m. CDT
- Unleashing viruses aimed at killing cancer Nov. 25, 2023, 12:00 p.m. CDT
- Telehealth's lasting impact on cancer care delivery Nov. 22, 2023, 02:05 p.m. CDT
- Mayo Clinic and Oxford Nanopore announce collaboration to advance precision medicine for cancer and genetic disorders Oct. 19, 2023, 02:07 p.m. CDT
- Mayo Clinic Q&A: How to manage dry mouth during cancer care Sept. 15, 2023, 01:30 p.m. CDT
- Mayo Clinic Q and A: Tips for cancer patients to stay safe in the summer Aug. 02, 2023, 02:00 p.m. CDT
- Mayo Clinic Minute: Is there a connection between ultraprocessed food and cancer? July 25, 2023, 03:00 p.m. CDT
- Mayo Clinic Minute: Plant-based diet is encouraged for patients with cancer July 11, 2023, 03:45 p.m. CDT
- Mayo Clinic researchers pioneer AI method to predict how cells are organized in disease microenvironments June 23, 2023, 03:00 p.m. CDT
- Mayo Clinic expert addresses cancer disparities during Black Family Cancer Awareness Week June 19, 2023, 05:33 p.m. CDT
- Mayo Clinic Minute: Preventing cancer for future generations of Black families June 19, 2023, 03:02 p.m. CDT
- Is a cancer clinical trial right for me? June 16, 2023, 01:00 p.m. CDT
- Science Saturday: Pharmacists play key role in clinical research June 03, 2023, 11:00 a.m. CDT
- Nucleus RadioPharma to open manufacturing facility in Rochester, Minnesota May 09, 2023, 03:08 p.m. CDT
- Science Saturday: Study suggests chromosomal errors may hinder some aggressive tumors April 22, 2023, 11:00 a.m. CDT
- Science Saturday: Igniting the interest of young cancer researchers April 01, 2023, 11:00 a.m. CDT
- 9 common questions about genetic testing for cancer Feb. 06, 2023, 03:00 p.m. CDT
- World Cancer Day wish from a Mayo Clinic oncologist Feb. 03, 2023, 03:00 p.m. CDT
- As cancer deaths decline, access to care remains a challenge in some communities Feb. 02, 2023, 05:30 p.m. CDT
- Science Saturday: MayoComplete next-generation sequencing -- Transforming comprehensive cancer care Jan. 07, 2023, 12:00 p.m. CDT
- Mayo Clinic Q and A: Coping with cancer and the holidays Dec. 26, 2022, 02:00 p.m. CDT
- Eclipse and Mayo Clinic create Nucleus RadioPharma to better serve cancer patients Oct. 12, 2022, 05:35 p.m. CDT
- Science Saturday: Integrative oncology -- lifestyle medicine for people with cancer Sept. 24, 2022, 11:00 a.m. CDT
- Mayo Clinic Q&A podcast: Raising awareness of childhood cancer Sept. 16, 2022, 01:00 p.m. CDT
- Mayo Clinic Q and A: Does cancer increase my risk for a blood clot? Sept. 15, 2022, 01:30 p.m. CDT
- 9 common questions about genetic testing for cancer July 27, 2022, 01:03 p.m. CDT
- Plant power: Using diet to lower cancer risk July 05, 2022, 03:00 p.m. CDT
- Science Saturday: The art and science of never giving up June 25, 2022, 11:00 a.m. CDT
- Mayo Clinic Comprehensive Cancer Center Patients, Executive Director Highlighted in American Association for Cancer Research Cancer Disparities Progress Report June 08, 2022, 10:30 p.m. CDT
- Cancer and mental health: Mayo Clinic expert dispels myths May 26, 2022, 03:30 p.m. CDT
- Immunotherapy may play role in treating nonmetastatic gastroesophageal cancer May 16, 2022, 01:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products
What to know about cancer

Cancer causes cells to divide uncontrollably. This can result in tumors, damage to the immune system, and other impairment that can be fatal.
Cancer can affect various parts of the body, such as the breasts, lungs, prostate, and skin.
In this article, we examine types of cancer, how the disease develops, and how doctors may treat it. We also explore different types of cancer and disease outlook. Finally, we answer some common questions about cancer.
Cancer resources
To discover more evidence-based information and resources for cancer, visit our dedicated hub .
What is cancer?

Cancer is a broad term. It describes the disease that results when cellular changes cause the uncontrolled growth and division of cells .
Some types of cancer cause rapid cell growth, while others cause cells to grow and divide at a slower rate.
Certain forms of cancer result in visible growths called tumors , while others, such as leukemia , do not.
Most of the body’s cells have specific functions and fixed lifespans. Cell death is part of a natural and beneficial phenomenon, which healthcare professionals call apoptosis.
A cell receives instructions to die so that the body can replace it with a newer cell that functions better. Cancerous cells lack the components that instruct them to stop dividing and to die.
As a result, they build up in the body, using oxygen and nutrients that would usually nourish other cells. Cancerous cells can form tumors, impair the immune system and cause other changes that prevent the body from functioning regularly.
Cancerous cells may appear in one area, then spread via the lymph nodes . These are clusters of immune cells located throughout the body.
There are many causes of cancer, and some are preventable.
Risk factors
Preventable risk factors for cancer include :
- heavy alcohol consumption
- excess body weight
- physical inactivity
- poor nutrition
- human papillomavirus infection
Other risk factors for cancer are not preventable. Currently, the most significant unpreventable risk factor is age. According to the American Cancer Society (ACS), doctors in the United States diagnose 88% of cancer cases in people ages 50 years or older.
Is cancer genetic?
Genetic factors can contribute to the development of cancer.
A person’s genetic code tells their cells when to divide and expire. Changes in the genes can lead to faulty instructions, and cancer can result.
Genes also influence the cells’ production of proteins, and proteins carry many of the instructions for cellular growth and division.
Some genes change proteins that would usually repair damaged cells. This can lead to a predisposition for cancer. If a parent has these genes, they may pass on the altered instructions to their offspring. A doctor may refer to this as an inherited gene mutation. These mutations may contribute to the development of up to 10% of cancer cases.
Some genetic mutations that increase the risk of developing cancer occur after birth. Healthcare professionals refer to these changes as “acquired gene mutations”. Possible causes include smoking and sun exposure. These genetic changes cause cancer more commonly than inherited gene mutations.
Other changes that can result in cancer take place in the chemical signals that determine how the cells turn specific genes on and off. Doctors may call these “epigenetic changes”.
Doctors usually prescribe treatments based on the type of cancer, its stage at diagnosis, and the person’s overall health.
Some examples of cancer treatment include :
- Chemotherapy aims to kill cancerous cells with medications that target rapidly dividing cells. The drugs can also help shrink tumors, but the side effects can be severe.
- Hormone therapy involves taking medications that change how certain hormones work or interfere with the body’s ability to produce them. When hormones play a significant role, as with prostate and breast cancers , this is a common approach.
- Immunotherapy uses medications and other treatments to boost the immune system and encourage it to fight cancerous cells.
- Radiation therapy uses high-dose radiation to kill cancerous cells. Also, a doctor may recommend using radiation to shrink a tumor before surgery or reduce tumor-related symptoms.
- Stem cell transplant can be especially beneficial for people with blood-related cancers, such as leukemia or lymphoma . It involves removing cells, such as red or white blood cells , that chemotherapy or radiation has destroyed. Lab technicians then strengthen the cells and put them back into the body.
- Surgery is often a part of a treatment plan when a person has a cancerous tumor. Also, a surgeon may remove lymph nodes to reduce or prevent the disease’s spread.
- Targeted therapies perform functions within cancerous cells to prevent them from multiplying. They can also boost the immune system. Two examples of these therapies are small-molecule drugs and monoclonal antibodies.
Doctors will often employ more than one type of treatment to maximize effectiveness.
The most common type of cancer in the U.S. is breast cancer, followed by lung and prostate cancers, according to the National Cancer Institute, which excluded nonmelanoma skin cancers from these findings.
Each year, more than 40,000 people in the country receive a diagnosis of one of the following types of cancer:
- colon and rectal
- endometrial
- non-Hodgkin’s lymphoma
Other forms are less common. According to the National Cancer Institute, there are over 100 types of cancer.
Cancer development and cell division
Doctors classify cancer by its location in the body and the tissues that it forms in.
For example, sarcomas develop in bones or soft tissues, while carcinomas form in cells that cover internal or external surfaces in the body. Basal cell carcinomas develop in the skin, while adenocarcinomas can form in the glands.
When cancerous cells spread to other parts of the body, the medical term for this is metastasis.
A person can also have more than one type of cancer at a time.
Improvements in cancer detection, increased awareness of the risks of smoking, and a drop in tobacco use have all contributed to a year-on-year decrease in the number of cancer diagnoses and deaths.
According to the ACS, the overall cancer death rate declined by 33% between 1991 and 2020.
When a person has cancer, their outlook will depend on whether the disease has spread and on its type, severity, and location.
Frequently asked questions
Below are some common questions and answers about cancer.
How do I recognize cancer before it starts to cause serious health problems?
Some cancers cause early symptoms, but others do not exhibit symptoms until they are more advanced. Many of these symptoms are often from causes unrelated to cancer.
The best way to identify cancer early is to report any unusual, persistent symptoms to a doctor so they can offer advice about any further testing that may be needed.
Can people with cancer live a long life?
Each individual’s outlook varies depending on the type of cancer they have and other factors, such as their overall health and whether the disease has spread.
However, the ACS indicates that the overall cancer death rate has declined by 33% between 1991 and 2020.
How long can someone live with cancer without knowing?
Some types of cancer do not cause symptoms in the early stages. Therefore, a person may not know they are living with the disease until it reaches more advanced stages.
For example, research indicates that carcinoid tumors may not present with any symptoms for years .
Cancer causes cells to divide uncontrollably. It also prevents them from dying at the natural point in their life cycle.
Genetic factors and lifestyle choices, such as smoking, can contribute to the development of the disease. Several elements affect the ways that DNA communicates with cells and directs their division and death.
After nonmelanoma skin cancer, breast cancer is the most common type in the U.S.
Treatments are constantly improving. Examples of current methods include chemotherapy, radiation therapy, and surgery. Some people benefit from newer options, such as stem cell transplantation and precision medicine.
The diagnosis and death rates of cancer are dropping yearly.
Last medically reviewed on January 24, 2024
- Cancer / Oncology
How we reviewed this article:
- About cancer. (n.d.). https://www.cancer.gov/about-cancer
- All about cancer. (n.d.). https://www.cancer.org/cancer.html
- Cancer facts & figures 2023. (2023). https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2023/2023-cancer-facts-and-figures.pdf
- Cingam SR, et al. (2022). Carcinoid tumors. https://www.ncbi.nlm.nih.gov/books/NBK448101/
- Common cancer types. (2018). https://www.cancer.gov/types/common-cancers
- Risk factors and cancer. (2023). https://www.cdc.gov/cancer/risk_factors.htm
Share this article
Latest news
- Depression: Virtual reality may help improve mental health
- Colorectal cancer is rising in children, teens, and young adults, study finds
- Aging white matter in the brain may affect stroke recovery, study finds
- New weight loss endoscopic procedure could help reduce 'hunger hormone'
- New oral rinse could help detect gastric cancer in early stages
Related Coverage
Radiation therapy is a treatment for cancer. A person may receive it alongside another treatment or alone. Find out why doctors recommend it, what it…
A rash can indicate mild irritation, or it could be a sign of skin cancer. It is important to find out the differences between cancerous and…
Dogs may be able to help medical professionals by detecting some types of cancer through odor signatures in a person’s breath, urine, and skin.
Udenyca is a prescription drug used to help prevent infection with chemotherapy. Learn about the serious side effects it can cause and how to manage…
A new study suggests that possible carcinogens linked to neurological issues, hormone disruption, and cancer-related death may be inside many cars.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

teacher appreciation
11 templates
memorial day
12 templates
9 templates

rain forest
23 templates
55 templates
Cancer Presentation templates
We all must do whatever is in our hands to prevent all kinds of cancer, which is the cause of millions of deaths every year. work on your health-related presentations with the help of these editable google slides and powerpoint templates..

Premium template
Unlock this template and gain unlimited access
Breast Cancer Information Brochure
Identifying the first symptoms of breast cancer can be decisive when it comes to treatment and prognosis. That’s why being well informed about them is a key factor for women all ages! With a creative and illustrative brochure like this one, you can give them the information they need so...
Rectum-related Diseases: Colon Cancer
Download the "Rectum-related Diseases: Colon Cancer" presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking...

Oncology Breakthrough
Download the Oncology Breakthrough presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news. Should there be a medical...

Skin Cancer Breakthrough
The summer has arrived, and with it, the plans in the sun: going to the beach, swimming in the pool, going on vacation… But there is a thing that we must always remember, we must wear protection! Did you know that one in five Americans will develop skin cancer by...

Breast Cancer Awareness Infographics
Did you know that 1 in 8 women will be diagnosed with breast cancer in their lifetime? It's a staggering statistic that highlights the importance of Breast Cancer Awareness Month. Thankfully, there are plenty of ways to spread awareness - and we've got just the thing. Our Google Slides &...
Endometrial Cancer Case Report
Download the "Endometrial Cancer Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...

Uterus Cancer Breakthrough
This can be one of the templates that people would love to see the most. It's been designed so that you can talk about any medical breakthroughs concerning uterus cancer. Its slides have soft shapes and a variety of pink and cream tones. There are some illustrations to contextualize your...

Pulmonary Emphysema Disease
Download the Pulmonary Emphysema Disease presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking medical...

Innovation in Chemotherapy Breakthrough
Download the "Innovation in Chemotherapy Breakthrough" presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news. Should there be...

Breast Cancer Case
Clinical cases are so convenient, the medical community is always grateful for the information provided. In this occasion, we at Slidesgo have decided to create this new presentation template, focused on breast cancer, so that you can raise awareness about this important topic and help everyone get to know what...

Breast Cancer Awareness
Raise awareness about breast cancer with this social media strategy presentation: talk about your plan and objectives to help this cause with this pink template that contains floral illustrations.

Bladder Cancer Awareness Month
Bladder cancer is a disease that affects thousands of people worldwide, usually more men than women. May is the awareness month for this type of cancer, so you can take advantage of this Slidesgo template to generate awareness about it. It has an abstract style, with waves and blue, lilac...

Ovarian Cancer Day
Download the "Ovarian Cancer Day" presentation for PowerPoint or Google Slides. Healthcare goes beyond curing patients and combating illnesses. Raising awareness about diseases, informing people about prevention methods, discussing some good practices, or even talking about a balanced diet—there are many topics related to medicine that you could be sharing...
Endometrial Cancer Detection Breakthrough
Download the "Endometrial Cancer Detection Breakthrough" presentation for PowerPoint or Google Slides. Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news. Should there...

Cancer Healthcare Center
We are all together in the fight against cancer! To give an informative slideshow about your healthcare center specialized in cancer rehabilitation, you can try this template. Let the purple tones (and the big ribbon) be a nice addition to your own contents as you explain your key numbers, statistics,...
Cancer Treatment Healthcare Center
Cancer treatment can look very different depending on the patient. Do you run a treatment clinic? What kind of professionals do you have among your staff? Do you only focus on the physical treatments, or do you also offer therapy and entertainment to improve your patient’s overall health? Speak about...

Genetic Testing for Cancer Breakthrough
A major breakthrough in the fight against cancer recently occurred in the form of a new discovery that genetic testing can be a key tool in detecting this devastating disease. While it's too early to know for sure just what impact this discovery will have, it's fair to say that...


Cervical Cancer Caused by Human Papillomavirus (HPV)
Cervical cancer is a severe health problem that affects thousands of women worldwide, and it's mostly caused by the human papillomavirus (HPV). In fact, it's the most common type of cancer caused by this nasty virus. This template can be used to provide comprehensive information about the causes, symptoms, prevention,...
- Page 1 of 9
Great presentations, faster
Slidesgo for Google Slides :
The easy way to wow
Register for free and start editing online
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Breast cancer.
Fadi M. Alkabban ; Troy Ferguson .
Affiliations
Last Update: September 26, 2022 .
- Continuing Education Activity
Breast cancer is the most common cancer diagnosed in women, accounting for more than 1 in 10 new cancer diagnoses each year. It is the second most common cause of death from cancer among women in the world. Breast cancer evolves silently, and most disease is discovered on routine screening. This activity reviews the pathophysiology, presentation and diagnosis of breast cancer and highlights the role of the interprofessional team in its management.
- Review the risk factors for breast cancer.
- Describe the histopathology of the different types of breast cancer.
- Summarize the treatment options for breast cancer.
- Outline modalities for improving care coordination among interprofessional team members to optimize outcomes for patients affected by breast cancer.
- Introduction
Breast cancer is the most common cancer diagnosed in women, accounting for more than 1 in 10 new cancer diagnoses each year. It is the second most common cause of death from cancer among women in the world. Anatomically, the breast has milk-producing glands in front of the chest wall. They lie on the pectoralis major muscle, and there are ligaments support the breast and attach it to the chest wall. Fifteen to 20 lobes circularly arranged to form the breast. The fat that covers the lobes determines the breast size and shape. Each lobe is formed by lobules containing the glands responsible for milk production in response to hormone stimulation. Breast cancer always evolves silently. Most of the patients discover their disease during their routine screening. Others may present with an accidentally discovered breast lump, change of breast shape or size, or nipple discharge. However, mastalgia is not uncommon. Physical examination, imaging, especially mammography, and tissue biopsy must be done to diagnose breast cancer. The survival rate improves with early diagnosis. The tumor tends to spread lymphatically and hematologically, leading to distant metastasis and poor prognosis. This explains and emphasizes the importance of breast cancer screening programs. [1] [2] [3]
Identifying factors associated with an increased incidence of breast cancer development is important in general health screening for women. [4] [5] Risk factors for breast cancer can be divided into 7 broad categories:
- Age: The age-adjusted incidence of breast cancer continues to increase with the advancing age of the female population.
- Gender: Most breast cancers occur in women.
- Personal history of breast cancer: A history of cancer in one breast increases the likelihood of a second primary cancer in the contralateral breast.
- Histologic risk factors: Histologic abnormalities diagnosed by breast biopsy constitute an important category of breast cancer risk factors. These abnormalities include lobular carcinoma in situ (LCIS) and proliferative changes with atypia.
- The family history of breast cancer and genetic risk factors: First-degree relatives of patients with breast cancer have a 2-fold to 3-fold excess risk for developing the disease. Five percent to 10% of all breast cancer cases are due to genetic factors, but they may account for 25% of cases in women younger than 30 years. BRCA1 and BRCA2 are the 2 most important genes responsible for increased breast cancer susceptibility.
- Reproductive risk factors: Reproductive milestones that increase a woman’s lifetime estrogen exposure are thought to increase her breast cancer risk. These include the onset of menarche before 12 years of age, first live childbirth after age 30 years, nulliparity, and menopause after age 55 years.
- Exogenous hormone use: Therapeutic or supplemental estrogen and progesterone are taken for various conditions, with the two most common scenarios being contraception in premenopausal women and hormone replacement therapy in postmenopausal women.
- Epidemiology
Invasive breast cancer affects 1 in 8 women in the United States (12.4%) during their lifetime. [6] [7] [8] In the United States, about 266,120 women will have invasive breast carcinoma in 2018, and 63,960 will have in situ breast cancer. In 2018, approximately 2550 men will have invasive breast cancer. Approximately 1 in 1000 men will have breast cancer during their lifetime. In the year 2000, the incidence of breast cancer in the United States began decreasing. This decrease may be due to the reduced use of hormone replacement therapy (HRT) by women. A connection was suggested between HRT and increased breast cancer risk. About 40,920 US women may die in 2018 from breast cancer. Larger decreases occur in women younger than 50 years old. In 2008, there were an estimated 1.38 million new cases of invasive breast cancer worldwide. The 2008 incidence of female breast cancer ranged from 19.3 cases per 100,000 in Eastern Africa to 89.9 cases per 100,000 in Western Europe. With early detection and significant advances in treatment, death rates from breast cancer have been decreasing over the past 25 years in North America and parts of Europe. In many African and Asian countries (e.g., Uganda, South Korea, and India), however, breast cancer death rates are rising. The incidence rate of breast cancer increases with age, from 1.5 cases per 100,000 in women 20 to 24 years of age to a peak of 421.3 cases per 100,000 in women 75 to 79 years of age; 95% of new cases occur in women aged 40 years or older. The median age of women at the time of breast cancer diagnosis is 61 years. According to the American Cancer Society (ACS), breast cancer rates among women from various racial and ethnic groups are as follows:
- Non-Hispanic white: 128.1 in 100,000
- African American: 124.3 in 100,000
- Hispanic/Latina: 91.0 in 100,000
- American Indian/Alaska Native: 91.9 in 100,000
- Asian American/Pacific Islander: 88.3 in 100,000
- Pathophysiology
Breast cancer develops due to DNA damage and genetic mutations that can be influenced by exposure to estrogen. Sometimes there will be an inheritance of DNA defects or pro-cancerous genes like BRCA1 and BRCA2 . Thus the family history of ovarian or breast cancer increases the risk for breast cancer development. In a normal individual, the immune system attacks cells with abnormal DNA or abnormal growth. This fails in those with breast cancer disease leading to tumor growth and spread.
- Histopathology
Breast cancer can be invasive or non-invasive according to its relation to the basement membrane. Noninvasive neoplasms of the breast are broadly divided into two major types, lobular carcinoma in situ (LCIS) and ductal carcinoma in situ (DCIS).
LCIS is regarded as a risk factor for the development of breast cancer. LCIS is recognized by its conformity to the outline of the normal lobule, with expanded and filled acini. DCIS is more morphologically heterogeneous than LCIS, and pathologists recognize four broad types of DCIS: papillary, cribriform, solid, and comedo.
DCIS is recognized as discrete spaces filled with malignant cells, usually with a recognizable basal cell layer composed of presumably normal myoepithelial cells. The papillary and cribriform types of DCIS are generally lower grade lesions and may take longer to transform into invasive cancer.
The solid and comedo types of DCIS are generally higher-grade lesions. DCIS, if not treated, usually transforms into invasive cancer. Invasive breast cancers are recognized by their lack of overall architecture, infiltration of cells haphazardly into a variable amount of stroma, or formation of sheets of continuous and monotonous cells without respect for the form and function of a glandular organ. Pathologists broadly divide invasive breast cancer into ductal and lobular histologic types.
Invasive ductal cancer tends to grow as a cohesive mass; it appears as discrete abnormalities on mammograms and is often palpable as a discrete lump in the breast smaller than lobular cancers. Invasive lobular cancer tends to permeate the breast in a single-file nature, which explains why it remains clinically occult and often escapes detection on mammography or physical examination until the disease is extensive. Invasive ductal cancer, also known as infiltrating ductal carcinoma, is the most common form of breast cancer; it accounts for 50% to 70% of invasive breast cancers.
Invasive lobular carcinoma accounts for 10% of breast cancers, and mixed ductal and lobular cancers have been increasingly recognized and described in pathology reports. When invasive ductal carcinomas take on differentiated features, they are named according to the features that they display. If the infiltrating cells form small glands lined by a single row of the bland epithelium, they are called infiltrating tubular carcinoma. The infiltrating cells may secrete copious amounts of mucin and appear to float in this material. These lesions are called mucinous or colloid tumors.
Tubular and mucinous tumors are usually low-grade (grade I) lesions; these tumors account for approximately 2% to 3% of invasive breast carcinomas. Medullary cancer is characterized by bizarre invasive cells with high-grade nuclear features, many mitoses, and lack of an in situ component. The malignancy forms sheets of cells in an almost syncytial fashion, surrounded by an infiltrate of small mononuclear lymphocytes. The borders of the tumor push into the surrounding breast rather than infiltrate or permeate the stroma. In its pure form, medullary cancer accounts for only approximately 5% of breast cancers. [9] [10] [11]
- History and Physical
Most early breast cancer patients are asymptomatic and discovered during screening mammography. With increasing size, the patient may discover cancer as a lump that is felt accidentally, mostly during combing or showering. Breast pain is an unusual symptom that happens 5% of the time. The locally advanced disease may be presented with peau d'orange, frank ulceration, or fixation to the chest wall. Inflammatory breast cancer, an advanced form of breast cancer, frequently resembles breast abscess and presents with swelling, redness, and other local signs of inflammation. Paget disease of the nipple usually presents with nipple changes that must be differentiated from nipple eczema.
Evaluation of Patients with breast cancer needs a triple assessment using clinical evaluation, imaging, and tissue biopsy. Mammography is the most commonly used modality for the diagnosis of breast cancer. Most of the asymptomatic cases are diagnosed during screening mammography. Breast cancer always presents as calcifications, dense lump, with or without architecture distortion. However, mammography is not sensitive in young women for whom breast ultrasonography can be used. Ultrasonography is useful in assessing the consistency and size of breast lumps. It has a great role in guided needle biopsy. Magnetic resonance imaging has good sensitivity for describing abnormalities in soft tissues, including the breast. It is indicated if there are occult lesions, or suspicion of multifocal or bilateral malignancy, especially ILC, and in the assessment of response to neoadjuvant chemotherapy, or when planning for breast conservation surgery and screening in the high-risk patient. Tissue biopsy is an important step in the evaluation of a breast cancer patient. There are different ways to take a tissue specimen, and these include fine-needle aspiration cytology, core biopsy (Trucut), and incisional or excisional biopsy. [12] [13] [14]
- Treatment / Management
The 2 basic principles of treatment are to reduce the chance of local recurrence and the risk of metastatic spread. Surgery with or without radiotherapy achieves local control of cancer. When there is a risk for metastatic relapse, systemic therapy is indicated in the form of hormonal therapy, chemotherapy, targeted therapy, or any combination of these. In locally advanced disease, systemic therapy is used as a palliative therapy with a small or no role for surgery. [15] [16] [17]
- Differential Diagnosis
- Breast abscess
- Fat necrosis
- Fibroadenoma
- Surgical Oncology
Surgery has a major role in the treatment of breast cancer. It is the basic way to use for local control of the disease. Radical mastectomy of Halsted, which removed the breast with axillary lymph node dissection and excision of both pectoralis muscles, is no longer recommended due to the high rate of morbidity without a survival benefit. Now, the modified radical mastectomy of Patey is more famous. It entails removing the whole breast tissue with a large part of the skin and the axillary lymph nodes. The pectoralis major and minor muscles are preserved. Breast-only removal without axillary dissection is referred to as simple mastectomy. This procedure can be performed in small tumors with negative sentinel lymph nodes. Breast-conserving surgery (BCS) is aimed at removing the tumor plus a rim of at least 1 cm of normal breast tissue (wide local excision). A quadrantectomy involves removing the entire segment of the breast that contains the tumor. The last 2 procedures are usually combined with axillary clearance through a separate incision. Axillary procedures may include sentinel lymph node biopsy, sampling, partial (II), or complete (III) axillary lymph node dissection. Lumpectomy is the removal of a benign mass without excision of the normal breast tissue.
- Radiation Oncology
Radiation therapy has a significant role in local disease control. The risk of cancer recurrence decreases by about 50% at 10 years, and the risk of breast cancer death reduces by almost 20% at 15 years when radiation therapy follows BCS. However, radiation is not necessary for women 70 years of age and older with small, lymph node-negative, hormone receptor-positive (HR+) cancers because it has not been shown to improve survival in patients who take hormonal therapy for at least 5 years. Radiation therapy is beneficial in large tumors (greater to 5 cm) or if the tumor invades skin or chest wall and if there are positive lymph nodes. It can also be used as palliative therapy in advanced cases, such as a central nervous system (CNS) or bone metastasis. It can be delivered as external beam radiation, brachytherapy, or a combination of both. [18] [19]
- Medical Oncology
Chemotherapy, hormone therapy, and targeted therapy are the systemic therapies used in breast cancer management. A 25 percent reduction in the risk of relapse over a 10 to 15-year period using a first-generation chemotherapy regimen such as cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) in a 6-month cycle. Anthracyclines (doxorubicin or epirubicin) and the newer agents such as the taxanes are modern regimens used for breast cancer. Three to 6-month period is used for adjuvant and neoadjuvant chemotherapy. Adjuvant treatment of early-stage HR+ breast cancer with tamoxifen for at least 5 years has been shown to reduce the recurrence rate by about half throughout the first 10 years and reduces breast cancer mortality by about 30% throughout the first 15 years.
More recently, studies have shown that extended use of adjuvant tamoxifen (10 years versus 5 years) further reduces the risk of breast cancer recurrence and mortality, so clinical practice guidelines now recommend consideration of adjuvant tamoxifen therapy for 10 years. The mainstay of treatment for most premenopausal women with HR+ tumors is tamoxifen. Some women may also benefit from surgical removal (oophorectomy) or chemical suppression of the ovaries, which are the main source of estrogen before menopause. Treatment guidelines recommend aromatase inhibitors (AIs) such as anastrozole should usually be included in the treatment of postmenopausal women with HR+ breast cancer. Targeted therapy is usually indicated in about 17% of breast cancers that overproduce the growth-promoting protein HER2/neu. Trastuzumab, the first approved drug, is a monoclonal antibody that directly targets the HER2 protein. It reduces the risk of recurrence and death by 52% and 33%, respectively, if combined with chemotherapy in HER2+ early breast cancer if compared to chemotherapy alone. [20] [21]
Breast cancer staging is determined clinically by physical examination and imaging studies before treatment, and breast cancer stage is determined pathologically by pathologic examination of the primary tumor and regional lymph nodes after definitive surgical treatment. Staging is performed to group patients into risk categories that define prognosis and guide treatment recommendations for patients with a similar prognosis. Breast cancer is classified with the TNM classification system, which groups patients into 4 stage groupings based on the primary tumor size (T), the regional lymph nodes status (N), and if there is any distant metastasis (M). The most widely used system is that of the American Joint Committee on Cancer:
Primary Tumor (T)
Tis: Carcinoma in-situ, Paget‘s with no tumor
T1: Less than 2 cmT1a: 0.1 to 0.5 cmT1b: 0.5 to 1.0 cmT1c: 1.0 to 2.0 cm
T2: 2 to 5 cm
T3: Larger than 5 cm
T4 T4a: Chest wall involvementT4b: Skin involvementT4c: Both 4a and 4bT4d: Inflammatory ca
Regional Lymph Nodes (N)
N1: Mobile ipsilateral axillary nodes
N2: Fixed/matted ipsilateral axillary nodes
N3 N3a – Ipsilat infraclavicular nodesN3b – Ipsilat int mammary nodesN3c – Ipsilateral supraclavicular nodes
Distant Metastases (M)
M1: Distant metastases
Stage 0 Tis
Stage I T1N0
Stage II T2N0, T3N0 T0N1, T1N1, T2N1
Stage III
*skin, rib inv., matted LNs T3 N1 T0N2, T1N2, T2N2, T3N2 Any T, N3 T4, any N Locally advanced BC
The prognosis of early breast cancer is quietly good. Stage 0 and stage I both have a 100% 5-year survival rate. The 5-year survival rate of stage II and stage III breast cancer is about 93% and 72%, respectively. When the disease spreads systemically, its prognosis worsens dramatically. Only 22% of stage IV breast cancer patients will survive their next 5 years.
- Complications
Complications can arise from the treatment, whether chemotherapy, radiation, hormonal therapy, or surgery.
Surgical complications include:
- Cosmetic issues
- Permanent scarring
- Alteration or loss of sensation in the chest area and reconstructed breasts
Chemotherapy complications include:
- Nausea/vomiting and diarrhea
- Memory loss ("chemo brain")
- Vaginal dryness
- Menopausal symptoms/fertility issues
Complications accompanying hormonal therapy include:
- Hot flashes
- Vaginal discharge dryness
- Impotence in males with breast cancer
Radiation can result in the following complications:
- Pain and skin changes
- Heart and lung issues (long-term)
- Deterrence and Patient Education
Patients usually require counseling to deal with the condition and treatment. They should be put in touch with psychological counseling, and there are also support groups available.
- Pearls and Other Issues
Breast cancer patients are advised to be followed up for life to detect early recurrence and spread. Yearly or biannual follow-up mammography is recommended for the treated and the other breast. The patient must be informed that they must visit a breast clinic if they have any suspicious manifestations. Currently, there is no role for repeated measurements of tumor markers or doing follow-up imaging other than mammography.
- Enhancing Healthcare Team Outcomes
After the treatment of breast cancer, long-term follow-up is necessary. There is a risk of local and distant relapse, and hence an interprofessional team approach is necessary. The women need regular mammograms and a pelvic exam. Also, women with risk factors for osteoporosis need a bone density exam and monitoring for tumor markers for metastatic disease. For those who are about to undergo radiation therapy, a baseline echo and cardiac evaluation are necessary. Even though many types of integrative therapies have been developed to help women with breast cancer, evidence for the majority of these treatments is weak or lacking. [22]
Over the past four decades, the survival rates of most breast cancer patients have improved. Of note is that the presence of breast cancer has gradually slowed down over the past decade, which may be due to earlier detection and improved treatments. The prognosis for patients with breast cancer is highly dependent on the status of axillary lymph nodes. The higher the number of positive lymph nodes, the worse the outcome. In general, hormone-responsive tumors tend to have a better outcome. In breast cancer survivors, adverse cardiac events are common; this is partly due to the cardiotoxic drugs to treat cancer and the presence of traditional risk factors for heart disease. The onus is on the healthcare provider to reduce the modifiable risk factors and lower the risk of adverse cardiac events. [1] [23] [Level 5)
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Breast Cancer Metastasis Sites Medical Gallery of Mikael Häggström 2014, Public Domain, via Wikimedia Commons.
Breast Mammogram. A mammographic view of the left breast demonstrates skin thickening, diffusely increased breast density, and malignant type calcifications in this patient with biopsy-proven inflammatory breast cancer. Contributed by Hassana (more...)
Breast Cancer Risk Factors 5. Kerlikowske K, Gard CC, Tice JA, et al. for the Breast Cancer Surveillance Consortium. Risk factors that increase risk of estrogen receptor-positive and -negative breast cancer. J Natl Cancer Inst. 109(5): djw276, 2016.
Interprofessional care diagram Breast cancer patients Contributed by Kathryn Malherbe (PhD candidate)
Breast Estrogen Receptor Staining Contributed by Fabiola Farci, MD
Breast Cancer Axillary Lymphadenopathy Contributed by Sunil Munakomi, MD
Breast Cancer Fine Needle Aspiration Cytology Contributed by Sunil Munakomi, MD
Clinical Signs of Breast Carcinoma Contributed by Sunil Munakomi, MD
Disclosure: Fadi Alkabban declares no relevant financial relationships with ineligible companies.
Disclosure: Troy Ferguson declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Alkabban FM, Ferguson T. Breast Cancer. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Retrospective Analysis of Women with Only Mastalgia. [J Breast Health. 2016] Retrospective Analysis of Women with Only Mastalgia. Arslan M, Küçükerdem HS, Can H, Tarcan E. J Breast Health. 2016 Oct; 12(4):151-154. Epub 2016 Oct 1.
- Preventive health care, 1999 update: 3. Follow-up after breast cancer. Canadian Task Force on Preventive Health Care. [CMAJ. 1999] Preventive health care, 1999 update: 3. Follow-up after breast cancer. Canadian Task Force on Preventive Health Care. Temple LK, Wang EE, McLeod RS. CMAJ. 1999 Oct 19; 161(8):1001-8.
- Review Common Breast Problems. [Am Fam Physician. 2019] Review Common Breast Problems. Salzman B, Collins E, Hersh L. Am Fam Physician. 2019 Apr 15; 99(8):505-514.
- Responding to the challenges of breast cancer in egypt and other arab countries. [J Egypt Natl Canc Inst. 2008] Responding to the challenges of breast cancer in egypt and other arab countries. El Saghir NS. J Egypt Natl Canc Inst. 2008 Dec; 20(4):309-12.
- Review Overview of resistance to systemic therapy in patients with breast cancer. [Adv Exp Med Biol. 2007] Review Overview of resistance to systemic therapy in patients with breast cancer. Gonzalez-Angulo AM, Morales-Vasquez F, Hortobagyi GN. Adv Exp Med Biol. 2007; 608:1-22.
Recent Activity
- Breast Cancer - StatPearls Breast Cancer - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Counseling Resource Navigation Support Groups Education Financial Assistance
Presentations and publications.
Cancer Care ’s professional oncology social workers and staff actively research, present and publish on numerous cancer-related topics that directly impact the lives of people coping with cancer.
Staff Expertise
Our staff’s publications, presentations, reports and videos are featured at national oncology and social work-related conferences, including:
- Association of Oncology Social Work (AOSW)
- American Society of Clinical Oncology (ASCO)
- American Psychosocial Oncology Society (APOS)
- Social Work Hospice and Palliative Care Network (SWHPN)
In addition to our staff's expertise, we also offer the Cancer Care Patient Access and Engagement Report , as well as the Cancer Care Patient Value Initiative .
Staff in Action
Sarah Paul, LCSW, OSW-C,
“Embracing Vicarious Resilience in Oncology Nursing: A Light in the Dark”
Cheryl Mullery, LMSW,
“Advanced Care Planning: The Gift of Empowerment for Patients With Cancer”
Sara Grisales Jaramillo, LMSW,
“Establishing a Multidisciplinary Approach to Social Determinants of Health”
Alexandra Zaleta, PhD,
“Treatment Decision Making Involvement and Informational Support Needs Among Older Adult Caregivers”
Hayley Feuchs, LMSW,
“Unveiling Disordered Eating in AYA Patients Undergoing Cancer Treatment”
Leeann Medina-Martinez, LCSW,
“How to Find Reliable and Affordable Transportation During Cancer”
Julia Manna, LMSW,
“The Transformative Power of Self-Compassion, Gratitude, and Kindness in Cancer”
Christine Calafiore, LSW,
“Steering Patients With Lung Cancer Toward Reputable Information Sources”
Samantha Fortune, LMSW,
“Psychological Concerns in the Aftermath of a Breast Cancer Diagnosis and Treatment for Young Adults”
Cassie Spector, LMSW,
“Supporting the Family Affected by a Pediatric Cancer Diagnosis: Siblings Matter, Too”
Vilmarie Rodriguez, LCSW,
“Navigating the Psychosocial Impact of Financial Toxicity and Health Equity Disparities in Oncology”
Charlotte Ference, LMSW,
“4 Ways to Help Patients With Metastatic Lung Cancer Find Meaning in Their Experiences”
Patricia Goldsmith, CEO,
“Reducing Roadblocks to Employee Health Care Through Benefit Design Implications and Unintended Consequences of Utilization Management in Cancer Treatment”
“3 Ways Employers Can Remove Barriers to Employee Health Care”
“How Benefits Brokers Can Reduce Roadblocks to Care”
“Roadblocks and Rising Costs in Cancer Treatment: What Employers Can Do”
Nikki Molfetas, LSW,
“Nurturing a Smooth Transition to Cancer Survivorship for Adolescents”
Melisa Celikoyar, LCSW,
“Wilderness Therapy Offers Benefits to Patients With Cancer”
Ellen Miller-Sonet, JD, MBA,
“Family Caregiver Roles and Challenges in Assisting Patients with Cancer Treatment Decision‐Making: Analysis of Data From a National Survey”
Allison Moskowitz Duggan, LCSW,
“How to Cope With Taking Long-Term Medication”
Shannon Coon, LMSW,
“How Do I Talk to My Teenagers About Cancer?”
Dina Smith, LMSW,
“Vicarious Trauma: Preventing, Recognizing Its Effects in Oncology Clinicians”
“As Cancer Costs Rise, Why Employee Benefits Plans Should Include Biomarker Testing”
Marissa Fors, LCSW,
“Drama Therapy Can Be a Therapeutic Tool for Helping Patients Cope With Cancer”
Laurie Feingold, LSW,
“Meeting Patients’ Spiritual Needs in Oncology Care”
Carolyn Messner, DSW, BCD, FAPOS, FAOSW, LCSW-R,
“Oncology Social Work 101: A Workshop for New Oncology Social Workers”
“What You Need To Know About Insurance Plan Restrictions In Cancer Care”
“Invisible Children: The Shifting Power Dynamics within a Sibling Relationship”
“Beyond the Diagnosis: How Cancer Treatment Could be a Catalyst for a Co-Occurring Mental Illness in the Adolescent Population”
Sarah Tennenhaus, LMSW,
“Connections and Conversation: Social Programs Addressing Social Isolation among Older Adults with Cancer”
Sarah Paul, LCSW,
“Cancer Out Loud: Not Just Another Cancer Podcast”
Sam Fortune, LMSW,
“Historical Trauma within the BIPOC Community: Implications in Psychosocial Oncology”
“How Virtual Workshops Teach Patients about Advances in Cancer Treatment during COVID & Omicron”
“Living with Cancer & Hearing Impairments: Rebuilding Meaningful Connections”
“CancerCare: An Organization with a Personal Touch”
“Preparing for the End of the U.S. Public Health Emergency (PHE): What People With Cancer Should Know”
“How Precision Medicine in Oncology Has Dramatically Changed the Way Cancer is Diagnosed and Treated”
Mary Hanley, LMSW,
“Talking With Patients About Potential Cancer Misinformation”
“Why Are Healthcare Costs So High? Blame the Middlemen”
Lucia Fanjul, LMSW,
“Immediate Interventions to Support The Newly Bereaved”
“Open Enrollment Brings New Opportunity: Insights into Today’s Complicated Health Insurance Landscape”
“How One Nonprofit Aims to Lend a Helpful Paw to Help Patients With Cancer Care for Their Pets”
“5 Ways to Reevaluate Health Benefits Design for Open Enrollment Season”
“Innovation in Cancer Therapies: Protecting Patient Access and Future Cures”
“Impact of Sexual Trauma and Need for Trauma-Informed Oncology Care”
“What HR Leaders Need to Know About Employee Health Benefits”
Leeann Medina-Martinez, LMSW,
“Addressing Disparities: Practicing Inclusion for LGBTQ+ Patients With Cancer”
Lauren Bronstein, LCSW,
“Supporting Patients Who Are Returning to Work After a Cancer Diagnosis”
Marlee Kiel, LCSW,
“How Social Media Helps AYA Patients With Cancer Find Support”
“Investing in Employee Health is Key to Retention and Recruitment”
“Books, Movies, and Journaling Aid Coping During, After Cancer Treatment”
“Covid-19 Puts Focus on Employee Health Benefits Coverage”
Marissa Fors, LCSW, OSW-C, C-ASWCM, CCM,
“Addressing the Impact of COVID-19 and Health Disparities on Cancer Screening”
“Challenges and Impacts Faced by Undocumented Cancer Patients in the Health Care System”
“Shared Decision Making Benefits Patients, Clinicians in Oncology Care”
“Peer Support Essential for Young Adults Recovering From Cancer Treatment”
Alyson Erardy, LMSW,
“How Mindfulness Can Help Caregivers Cope with Stress and Burnout”
“Contributing Factors to Delays in Diagnosis, Treatment Initiation of Cancers in Men”
“Barriers in BIPOC Populations Diagnosed With Breast Cancer”
Allison Moskowitz, LMSW,
“The Impact of Cancer on Mental Health: Recognizing Symptoms and Providing Support”
“The Role of Case Management: Improving Outcomes and Addressing Health Disparities in Cancer Care”
Claire Grainger-Valvano, LCSW, OSW-C,
“Simple Concepts to Better Serve Patients With Cancer”
William Goeren, LCSW-R, ACSW, OSW-C, SEP,
“Cancer, COVID-19, and Aging in LGBTQ+ Communities”
Danielle Saff, LMSW,
“Comprehensive Assessment Is Key for Geriatric Patients”
“COVID-19 at 1 Year: Navigating Pandemic Fatigue”
Angelique Caba, LCSW-R,
“Cultural Humility: A Way to Reduce Health Disparities in the BIPOC Community”
Karen M. Winkfield, MD, PhD; Jeanne M. Regnante, BS; Ellen Miller-Sonet, JD, MBA; Evelyn T. González, BA, MA; Karen M. Freund, MD, MPH; and Patricia M. Doykos, PhD,
“Development of an Actionable Framework to Address Cancer Care Disparities in Medically Underserved Populations in the United States: Expert Roundtable Recommendations”
Victoria Puzo, LCSW,
“Supporting Patients and Families During the Holidays: Safe Gatherings and Reducing Isolation”
“The New New Normal: Navigating Young Adult Survivorship Amid COVID-19”
Cecilia Acosta, LSW,
“How Gratitude Can Help When Coping With a Cancer Diagnosis”
“Navigating a pandemic in the nonprofit space: Lessons learned from COVID-19 responses”
Lauren Chatalian, LMSW,
“Navigating Breast Cancer Care During a Pandemic”
A.J. Cincotta-Eichenfield, LMSW,
“Understanding the Intersection of Cancer, COVID-19, and Work”
“How to Support Patients With a Young Adult or Child Caregiver During COVID-19”
“Cancer and Fibromyalgia: Addressing the Needs of Patients Despite Limited Research”
“Identifying the Needs of Men With Breast Cancer”
Sarah Kelly, LCSW,
“Navigating COVID-19: Self-Care Strategies for Oncology Professionals”
Caroline Edlund, LCSW-R,
“Coronavirus Anxiety: Helping Patients and Families Manage Fears”
“The Role of Rehabilitation Throughout Cancer Treatment”
Erin Murphy, LSW,
“Mindfulness Can Help Patients With Cancer”
Marlee Kiel, LMSW,
“The Benefits of Yoga for Cancer Patients”
“Genetic Testing and Inherited Increased Risk of Cancer”
Paige Soleimani, LMSW,
“The Importance of Caregivers During the Stem Cell Transplant Process”
Joseline Lopez, MPsy,
“Meeting Patients Where They Are: Improving Communications With Those Affected by Breast Cancer”
Patricia Goldsmith and Carole Florman,
“ICER’s concern for patients: Where’s the beef?”
“What Are the Needs of Cancer Survivors 5 Years or More After Treatment?”
“A Review of Barriers to a Successful Patient-Provider Relationship in the Hispanic Community”
“How to Apply for Medicare When You Have Cancer”
“Getting to know you: Matching cancer care to patient values”
William Goeren, LCSW-R,
“Cancer and the Transgender Community”
Richard Dickens, LCSW-R,
“Social Work Stories: Richard”
Carole Florman,
“PIPC Patient Blog: CancerCare Response to 'Mouse That Roared'”
Lauren Brailey, LMSW,
“Cancer as Trauma: How to Best Support Patients Through the Trauma of Treatment”
“Conversations on Patient Priorities and Preferences Should Take Place Before Treatment”
“How to Support Positive Body Image and High Self-Esteem in Patients With Cancer”
“Meditation Made Easy”
Sarah K. Kelly, LCSW and William Goeren, LCSW-R,
“Cancer Care - A Psychosocial Oncology Support Organization”
Ellen Miller-Sonet, MBA, JD; Jalpa A Doshi, PhD; Justin T Puckett; Henry A Glick, PhD,
“Advocating for New Patient-Centered Tools for Value-Based Treatment Choices in Oncology”
Claire Grainger, LCSW,
“The Role of Positive Psychology in Oncology Practice”
“Fertility and Family Planning: Supportive Conversations With Cancer Patients”
Patricia Goldsmith,
“Insurers Need to Focus on Patients, Not Profits”
“The Shifting Dynamics of Social Support After a Cancer Diagnosis”
“Value-Based Oncology Care Delivery Falls Short of Addressing Patients' Psychosocial Needs”
“Wounded Healers in Oncology Nursing”
“Trump pricing plans are pretentious, could impede access, and will not help much”
“Holidays Make End-of-Life Discussions Even More Challenging”
“AtlanticLIVE | Navigating Life After Cancer”
“When Clinical Trials Try Patients' Patience”
Maryrose Mongelli, LMSW,
“Effects of Parental Cancer on Children and Adolescents”
Essie Roman, LMSW,
“Finding Strength and Hope in the Midst of Breast Cancer Treatment”
“How to Make a Legacy: Tips for Young Adults with Advanced Cancer”
Andrew Chesler, LMSW,
“Anxiety, Depression in Prostate Cancer: Managing Psychosocial Effects in Male Patients”
Sonia Pacheco, LSW, LCSW,
“Hope, Gratitude and Spirituality: What They Mean to Cancer Patients”
“Re: Drug Pricing My unsolicited advice to HHS Secretary Alex Azar”
“Health-care debaters should recognize that we need innovation”
“Hope, Gratitude, and Spirituality: What They Mean to Patients with Cancer”
“The Impact of Financial Toxicity on Patients With Cancer and Families”
Ellen Miller-Sonet, JD, MBA, Jalpa A. Doshi, Justin T. Puckett and Henry Glick,
“The Need For A New Patient-Centered Decision Tool For Value-Based Treatment Choices In Oncology”
“Navigating Lung Cancer: Embracing a New Normal”
“The Caregivers' Cancer Journey”
“Patient Engagement in Cancer Care Decision-Making: Cancer Care and the Patient Values Initiative”
Marissa Fors, LMSW and Penelope Damaskos, PhD, LCSW, OSW-C,
“From Disparities to Disclosure: A Discussion on Lesbians and Breast Cancer”
“Assisting Patients With the Cost Burden of Cancer Diagnosis and Treatment: Next-Generation Sequencing Testing, Off-Label Medications, and More”
“AtlanticLIVE | A New Frontier: Biosimilars and Cancer Care”
Ellen Sonet, JD, MBA, Henry A. Glick, PhD, and Charles E. Phelps, PhD, MBA, Panelists and Jalpa A. Doshi, PhD, Moderator,
“Designing a Patient-Centered Value Framework to Guide Shared Decision Making in Oncology: Why, What, and How?”
“Challenges for Young Adult Couples Facing a Cancer Diagnosis”
“Managing Chemo Brain in Pediatric Survivors of Childhood Cancer”
Ellen Sonet, JD, MBA, Jennifer Cosenza, MA, Richard Dickens, LCSW-R, Patricia J. Goldsmith, Marcia A. Kean, MBA and Courtney Tyne, MPH,
“Decision Making at the Point of Care: Voices of Oncology Providers, A Patient Values Initiative Issue Brief”
Glenn Meuche, LCSW,
“Sitting With Silence in End-of-Life Cancer Care”
Sarah Paul, LMSW,
“Identifying the Psychosocial Needs of Young Adults with Metastatic Cancer”
Sarah Paul , LCSW,
“My Sister’s Cancer Made Me Want to Help Other Families”
“Play the Cancer Card: Dealing With Cancer During the Holiday Season”
“Patricia Goldsmith: This is the “Moonstab,” or, maybe, the “Moonshaft””
Ellen Miller-Sonet, JD, MBA, Jennifer Cosenza, MA, Richard Dickens, LCSW-R, Patricia J. Goldsmith, Marcia A. Kean, MBA, Carolyn Messner, LCSW-R and Courtney Tyne, MPH,
“Patient Values Initiative: The Many Voices of Value A Cancer Care Focus Group Assessment”
Ellen Miller-Sonet,
“Does patient activation level affect the cancer patient journey?”
Andrea Cantor, LMSW,
“Preventing Body-Trauma Triggers During Radiation Therapy for Cancer”
Maria Chi, LCSW-R,
“The Hidden Cost of Cancer: Helping Clients Cope with Financial Toxicity”
“Rare Cancers Pose a Challenge for Patients, Clinicians”
“Therapeutic Writing in Group Work for Patients With Cancer”
Marissa Fors, LMSW,
“Physical Activity Improves Outcomes for Patients with Breast Cancer and Survivors”
“Gay Men and the Stigma of a Cancer Diagnosis”
“New Patient-Focused Initiatives Presented at ASCO 2017”
Talila Marcus, LMSW,
“Hypnosis and Its Use in Cancer Treatment”
Glenn Meuche, LCSW-R,
“The Integration of Cannabis in Oncologic Care”
Ellen Miller-Sonet, MBA, JD,
“Informed decision making in cancer care: more myth than reality”
Mayra Sandoval, LMSW,
“What SUPPORT Can Do for Families Coping With Cancer During the Holidays”
Kenneth Thorpe and Patricia Goldsmith,
“Beating Cancer Shouldn’t Force Patients Into Bankruptcy”
“Dating Challenges Throughout the Cancer Journey”
“Using Cognitive-Behavioral Therapy Principles in Daily Patient Interactions”
“Improving Body Image After Cancer Treatments: Assessing the Effectiveness of an Online Mindfulness-Based Therapy (‘Me-Therapy’)”
“When Death Comes Knocking at the Door: Honoring End-of-Life Work in a Social Work Field Placement”
“The Role of Ritual in Celebration and Healing After Cancer”
Elizabeth Ezra, LCSW,
“Connecting With One’s Spiritual Identity in the Face of a Cancer Diagnosis”
“Patricia Goldsmith on Patient Access and Engagement: Results of the CancerCare Report”
“Waiting is the Worst Part of Cancer”
Claire Grainger-Valvano, LCSW,
“Coloring as a Relaxation Tool”
Stacy Lewis, LMSW,
“How Physical Changes From Breast Cancer Affect Self-Image: Considerations for Clinicians”
Michele McCourt,
“Tips and Resources for Easing the Financial Burden of Cancer Copayments”
Carolyn Messner, LCSW-R,
“Cancer and Social Work”
“Finding Meaning Amidst Meaninglessness: Addressing Existential Angst at the End of Life”
“Re-Imagining God: A Meditation on Existential Suffering at the End of Life”
“Treating Patients With Cancer and Mental Health Disorders”
Ahuva Morris, LMSW,
“Discovering Strength Through Connection: A Novel In-Person Support Group for Teens Affected by a Parent’s Cancer Diagnosis”
“Pillow Talk: How an Art Therapy Project Helps Families Talk About Cancer”
Carly O’Brien, LCSW,
“Final Wishes”
“Finding Silver Linings”
“Coping With the Loss of Fertility After Cancer”
“Unique Challenges Confront Patients With Lung Cancer”
“A Place to Grieve: Creating a Space to Reflect After a Client’s Death”
Elizabeth Ezra, LCSW and Maria Chi, LCSW-R,
“When the Other Shoe Drops: The Unique Fears and Challenges of Recurrent Disease”
“Understanding the Male Patient With Cancer”
Claire Grainger, LCSW, and Kathy Nugent, LCSW,
“The Healing Hearts Family Bereavement Camp: An Innovative Approach to Healing”
“Health Literacy and Older Adults: Strategies for Integration”
Carolyn Messner, LCSW-R and Stewart Fleishman,
“Cancer in Contemporary Society: Grounding in Oncology and Psychosocial Care”
Carolyn Messner, LCSW-R, Caroline Kornhauser and Rosalie Canosa, LCSW-R,
“The Biopsychsosocial Implications of the Site of the Cancer”
Carolyn Messner, LCSW-R, Julie Hodorowski and Caroline Kornhauser,
“The Importance of Patient Education”
Carolyn Messner, LCSW-R, Grace Christ and Lynn Behar, LICSW,
“Oncology Social Work Leadership: Inventors in a Changing World”
“An Unanticipated Awakening”
“Embracing the Oneness of All Things: A Personal Reflection on the Implications of Shamanism for Social Work Practice in End of Life and Palliative Care”
“Providing Psychosocial Care When the Patient Is a Child”
“Supporting the Cancer Patient’s Long-Distance Caregiver”
“Cancer Changed My Body: Talking About Body Image With Teens”
“A Lost Population: How to Create a Safe Harbor in the Online Community for Teens Coping with Parental Cancer”
Victoria Puzo, LMSW,
“Understanding the Triple Negative Breast Cancer Patient: Tips and Tools for Health Care Professionals”
“Oncology Social Work Field Education: An Insider’s Perspective”
Elizabeth Ezra, LCSW-R,
“Finding Hope Beyond the Pall of a Pancreatic Cancer Diagnosis; What Can We Do to Help?”
“Bridging the Gap – the CancerCare/SAGE Support Group for Older Gay Men With Cancer”
“Disclosing a Diagnosis to Children: Tell or Not Tell?”
“My Daddy Sits Upon a Star”
“Bridging Cancer Care for the Older Adult Patient”
Carolyn Messner, LCSW-R and Richard Dickens, LCSW-R,
“When A Co-Worker is Dying of Cancer: A Place for Wounded Healers”
“When a Co-Worker is Dying: Transformative Grief Educational Paradigm”
“What We So Proudly Hail: Training the Next Generation of Leaders in Oncology Social Work”
“Cancer and Palliative Care Education Programs for Night Shift Workers”
“Paradigm of Patient Education”
“Stress, Serendipity and Resilience: Keynote Address in Celebration of Social Work Month”
“The Biopsychosocial Challenges Posed by Night Shift Workers”
“Becoming One with the Cosmic Dance and Flow”
“Dying Amidst a Primordial Dawn”
Sandra Tripodi, LCSW,
“Conversations About Cancer: A Tool to Help Families Communicate”
Terms of Use and Privacy Policy
By using our website, you agree to our recently updated Privacy Policy . Here you can read more about our use of cookies which help us make continuous improvements to our website. Privacy Policy .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 16 June 2023
Antigen presentation in cancer — mechanisms and clinical implications for immunotherapy
- Kailin Yang 1 ,
- Ahmed Halima 1 &
- Timothy A. Chan ORCID: orcid.org/0000-0002-9265-0283 1 , 2 , 3 , 4
Nature Reviews Clinical Oncology volume 20 , pages 604–623 ( 2023 ) Cite this article
15k Accesses
24 Citations
28 Altmetric
Metrics details
- Immunotherapy
- Predictive markers
- Tumour immunology
Over the past decade, the emergence of effective immunotherapies has revolutionized the clinical management of many types of cancers. However, long-term durable tumour control is only achieved in a fraction of patients who receive these therapies. Understanding the mechanisms underlying clinical response and resistance to treatment is therefore essential to expanding the level of clinical benefit obtained from immunotherapies. In this Review, we describe the molecular mechanisms of antigen processing and presentation in tumours and their clinical consequences. We examine how various aspects of the antigen-presentation machinery (APM) shape tumour immunity. In particular, we discuss genomic variants in HLA alleles and other APM components, highlighting their influence on the immunopeptidomes of both malignant cells and immune cells. Understanding the APM, how it is regulated and how it changes in tumour cells is crucial for determining which patients will respond to immunotherapy and why some patients develop resistance. We focus on recently discovered molecular and genomic alterations that drive the clinical outcomes of patients receiving immune-checkpoint inhibitors. An improved understanding of how these variables mediate tumour–immune interactions is expected to guide the more precise administration of immunotherapies and reveal potentially promising directions for the development of new immunotherapeutic approaches.
The clinical success of immune-checkpoint inhibitors has improved cancer care, although long-term durable remission is only achieved in a subset of patients.
Antigen processing and presentation by tumour cells are essential for long-lasting immune surveillance.
Alterations in the genes encoding MHC components and other parts of the antigen-presentation machinery are frequently found across several cancer types and are associated with both tumour development and the effectiveness of immunotherapies.
MHC-based antigen presentation exerts strong evolutionary pressure on the immunopeptidome, which in turn shapes the mutational landscape of the tumour genome.
Germline human leukocyte antigen diversity and somatic aberrations in the antigen-presentation machinery inform the therapeutic response to immune-checkpoint inhibitors.
Development of novel therapies based on an accurate understanding of antigen presentation in the setting of tumour–immune dynamics is crucial to the development of improved therapeutic approaches.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
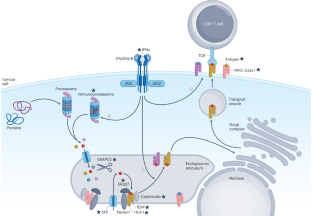
Similar content being viewed by others

Antigen presentation in cancer: insights into tumour immunogenicity and immune evasion

Towards new horizons: characterization, classification and implications of the tumour antigenic repertoire

Therapeutic cancer vaccines: advancements, challenges, and prospects
Waldman, A. D., Fritz, J. M. & Lenardo, M. J. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat. Rev. Immunol. 20 , 651–668 (2020).
Article CAS PubMed PubMed Central Google Scholar
Hodi, F. S. et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 363 , 711–723 (2010).
Larkin, J. et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med. 373 , 23–34 (2015).
Article PubMed PubMed Central Google Scholar
Schadendorf, D. et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J. Clin. Oncol. 33 , 1889–1894 (2015).
Robert, C. et al. Nivolumab in previously untreated melanoma without BRAF mutation. N. Engl. J. Med. 372 , 320–330 (2015).
Article CAS PubMed Google Scholar
Borghaei, H. et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N. Engl. J. Med. 373 , 1627–1639 (2015).
Motzer, R. J. et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 373 , 1803–1813 (2015).
Burtness, B. et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet 394 , 1915–1928 (2019).
Bellmunt, J. et al. Adjuvant atezolizumab versus observation in muscle-invasive urothelial carcinoma (IMvigor010): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 22 , 525–537 (2021).
Kelly, R. J. et al. Adjuvant nivolumab in resected esophageal or gastroesophageal junction cancer. N. Engl. J. Med. 384 , 1191–1203 (2021).
Schmid, P. et al. Atezolizumab and Nab-paclitaxel in advanced triple-negative breast cancer. N. Engl. J. Med. 379 , 2108–2121 (2018).
Ribas, A. & Wolchok, J. D. Cancer immunotherapy using checkpoint blockade. Science 359 , 1350–1355 (2018).
Antonia, S. J. et al. Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N. Engl. J. Med. 379 , 2342–2350 (2018).
Forde, P. M. et al. Neoadjuvant nivolumab plus chemotherapy in resectable lung cancer. N. Engl. J. Med. 386 , 1973–1985 (2022).
Snyder, A. et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N. Engl. J. Med. 371 , 2189–2199 (2014).
Gao, J. et al. Loss of IFN-γ pathway genes in tumor cells as a mechanism of resistance to anti-CTLA-4 therapy. Cell 167 , 397–404.e9 (2016).
Zaretsky, J. M. et al. Mutations associated with acquired resistance to PD-1 blockade in melanoma. N. Engl. J. Med. 375 , 819–829 (2016).
Zhou, X. et al. Treatment-related adverse events of PD-1 and PD-L1 inhibitor-based combination therapies in clinical trials: a systematic review and meta-analysis. Lancet Oncol. 22 , 1265–1274 (2021).
Havel, J. J., Chowell, D. & Chan, T. A. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat. Rev. Cancer 19 , 133–150 (2019).
Halima, A., Vuong, W. & Chan, T. A. Next-generation sequencing: unraveling genetic mechanisms that shape cancer immunotherapy efficacy. J. Clin. Invest. 132 , e154945 (2022).
Pietanza, M. C. et al. Phase II trial of temozolomide in patients with relapsed sensitive or refractory small cell lung cancer, with assessment of methylguanine-DNA methyltransferase as a potential biomarker. Clin. Cancer Res. 18 , 1138–1145 (2012).
Rizvi, N. A. et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 348 , 124–128 (2015).
Dudley, J. C., Lin, M. T., Le, D. T. & Eshleman, J. R. Microsatellite instability as a biomarker for PD-1 blockade. Clin. Cancer Res. 22 , 813–820 (2016).
Le, D. T. et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science 357 , 409–413 (2017).
Marcus, L., Lemery, S. J., Keegan, P. & Pazdur, R. FDA approval summary: pembrolizumab for the treatment of microsatellite instability-high solid tumors. Clin. Cancer Res. 25 , 3753–3758 (2019).
Cercek, A. et al. PD-1 blockade in mismatch repair-deficient, locally advanced rectal cancer. N. Engl. J. Med. 386 , 2363–2376 (2022).
Rosenberg, J. E. et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 387 , 1909–1920 (2016).
Gong, J., Chehrazi-Raffle, A., Reddi, S. & Salgia, R. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review of registration trials and future considerations. J. Immunother. Cancer 6 , 8 (2018).
Chan, T. A. et al. Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann. Oncol. 30 , 44–56 (2019).
Mahanty, S., Prigent, A. & Garraud, O. Immunogenicity of infectious pathogens and vaccine antigens. BMC Immunol. 16 , 31 (2015).
Pollard, A. J. & Bijker, E. M. A guide to vaccinology: from basic principles to new developments. Nat. Rev. Immunol. 21 , 83–100 (2021).
Li, F. et al. The association between CD8 + tumor-infiltrating lymphocytes and the clinical outcome of cancer immunotherapy: a systematic review and meta-analysis. EClinicalMedicine 41 , 101134 (2021).
Hellstrom, I., Hellstrom, K. E., Pierce, G. E. & Yang, J. P. Cellular and humoral immunity to different types of human neoplasms. Nature 220 , 1352–1354 (1968).
Horton, B. L. et al. Lack of CD8 + T cell effector differentiation during priming mediates checkpoint blockade resistance in non-small cell lung cancer. Sci. Immunol. 6 , eabi8800 (2021).
Lee, M. Y., Jeon, J. W., Sievers, C. & Allen, C. T. Antigen processing and presentation in cancer immunotherapy. J. Immunother. Cancer 8 , e001111 (2020).
Doherty, P. C. & Zinkernagel, R. M. A biological role for the major histocompatibility antigens. Lancet 1 , 1406–1409 (1975).
Doherty, P. C. & Zinkernagel, R. M. Enhanced immunological surveillance in mice heterozygous at the H-2 gene complex. Nature 256 , 50–52 (1975).
Parham, P. & Ohta, T. Population biology of antigen presentation by MHC class I molecules. Science 272 , 67–74 (1996).
Matsumura, M., Fremont, D. H., Peterson, P. A. & Wilson, I. A. Emerging principles for the recognition of peptide antigens by MHC class I molecules. Science 257 , 927–934 (1992).
Paul, S. et al. HLA class I alleles are associated with peptide-binding repertoires of different size, affinity, and immunogenicity. J. Immunol. 191 , 5831–5839 (2013).
Neefjes, J., Jongsma, M. L., Paul, P. & Bakke, O. Towards a systems understanding of MHC class I and MHC class II antigen presentation. Nat. Rev. Immunol. 11 , 823–836 (2011).
Colbert, J. D., Cruz, F. M. & Rock, K. L. Cross-presentation of exogenous antigens on MHC I molecules. Curr. Opin. Immunol. 64 , 1–8 (2020).
Chicz, R. M. et al. Predominant naturally processed peptides bound to HLA-DR1 are derived from MHC-related molecules and are heterogeneous in size. Nature 358 , 764–768 (1992).
Roche, P. A. & Furuta, K. The ins and outs of MHC class II-mediated antigen processing and presentation. Nat. Rev. Immunol. 15 , 203–216 (2015).
Dendrou, C. A., Petersen, J., Rossjohn, J. & Fugger, L. HLA variation and disease. Nat. Rev. Immunol. 18 , 325–339 (2018).
Arnaiz-Villena, A. et al. Evolution and molecular interactions of major histocompatibility complex (MHC)-G, -E and -F genes. Cell Mol. Life Sci. 79 , 464 (2022).
Baumeister, W., Walz, J., Zuhl, F. & Seemuller, E. The proteasome: paradigm of a self-compartmentalizing protease. Cell 92 , 367–380 (1998).
Groll, M. et al. Structure of 20S proteasome from yeast at 2.4 A resolution. Nature 386 , 463–471 (1997).
Dong, Y. et al. Cryo-EM structures and dynamics of substrate-engaged human 26S proteasome. Nature 565 , 49–55 (2019).
Cascio, P., Hilton, C., Kisselev, A. F., Rock, K. L. & Goldberg, A. L. 26S proteasomes and immunoproteasomes produce mainly N-extended versions of an antigenic peptide. EMBO J. 20 , 2357–2366 (2001).
Vigneron, N. et al. An antigenic peptide produced by peptide splicing in the proteasome. Science 304 , 587–590 (2004).
Warren, E. H. et al. An antigen produced by splicing of noncontiguous peptides in the reverse order. Science 313 , 1444–1447 (2006).
Rolfs, Z., Muller, M., Shortreed, M. R., Smith, L. M. & Bassani-Sternberg, M. Comment on “A subset of HLA-I peptides are not genomically templated: evidence for cis- and trans-spliced peptide ligands”. Sci. Immunol. 4 , eaaw1622 (2019).
Admon, A. Are there indeed spliced peptides in the immunopeptidome? Mol. Cell Proteom. 20 , 100099 (2021).
Article CAS Google Scholar
Rock, K. L. & Goldberg, A. L. Degradation of cell proteins and the generation of MHC class I-presented peptides. Annu. Rev. Immunol. 17 , 739–779 (1999).
Vigneron, N. & Van den Eynde, B. J. Proteasome subtypes and the processing of tumor antigens: increasing antigenic diversity. Curr. Opin. Immunol. 24 , 84–91 (2012).
Parcej, D. & Tampe, R. ABC proteins in antigen translocation and viral inhibition. Nat. Chem. Biol. 6 , 572–580 (2010).
Serwold, T., Gonzalez, F., Kim, J., Jacob, R. & Shastri, N. ERAAP customizes peptides for MHC class I molecules in the endoplasmic reticulum. Nature 419 , 480–483 (2002).
Pishesha, N., Harmand, T. J. & Ploegh, H. L. A guide to antigen processing and presentation. Nat. Rev. Immunol. https://doi.org/10.1038/s41577-022-00707-2 (2022).
Article PubMed Google Scholar
Garstka, M. A. et al. The first step of peptide selection in antigen presentation by MHC class I molecules. Proc. Natl Acad. Sci. USA 112 , 1505–1510 (2015).
Zarling, A. L. et al. Tapasin is a facilitator, not an editor, of class I MHC peptide binding. J. Immunol. 171 , 5287–5295 (2003).
Hermann, C. et al. TAPBPR alters MHC class I peptide presentation by functioning as a peptide exchange catalyst. eLife 4 , e09617 (2015).
Hildner, K. et al. Batf3 deficiency reveals a critical role for CD8α + dendritic cells in cytotoxic T cell immunity. Science 322 , 1097–1100 (2008).
Bonaccorsi, I. et al. Membrane transfer from tumor cells overcomes deficient phagocytic ability of plasmacytoid dendritic cells for the acquisition and presentation of tumor antigens. J. Immunol. 192 , 824–832 (2014).
Sanchez-Paulete, A. R. et al. Antigen cross-presentation and T-cell cross-priming in cancer immunology and immunotherapy. Ann. Oncol. 28 , xii44–xii55 (2017).
Blander, J. M. Regulation of the cell biology of antigen cross-presentation. Annu. Rev. Immunol. 36 , 717–753 (2018).
Canton, J. et al. The receptor DNGR-1 signals for phagosomal rupture to promote cross-presentation of dead-cell-associated antigens. Nat. Immunol. 22 , 140–153 (2021).
Shen, L., Sigal, L. J., Boes, M. & Rock, K. L. Important role of cathepsin S in generating peptides for TAP-independent MHC class I crosspresentation in vivo. Immunity 21 , 155–165 (2004).
Sanchez-Paulete, A. R. et al. Cancer immunotherapy with immunomodulatory anti-CD137 and anti-PD-1 monoclonal antibodies requires BATF3-dependent dendritic cells. Cancer Discov. 6 , 71–79 (2016).
Hanahan, D. Hallmarks of cancer: new dimensions. Cancer Discov. 12 , 31–46 (2022).
Lipsitch, M., Bergstrom, C. T. & Antia, R. Effect of human leukocyte antigen heterozygosity on infectious disease outcome: the need for allele-specific measures. BMC Med. Genet. 4 , 2 (2003).
Hraber, P., Kuiken, C. & Yusim, K. Evidence for human leukocyte antigen heterozygote advantage against hepatitis C virus infection. Hepatology 46 , 1713–1721 (2007).
Arora, J. et al. HLA heterozygote advantage against HIV-1 is driven by quantitative and qualitative differences in HLA allele-specific peptide presentation. Mol. Biol. Evol. 37 , 639–650 (2020).
Liu, Z. et al. HLA zygosity increases risk of hepatitis B virus-associated hepatocellular carcinoma. J. Infect. Dis. 224 , 1796–1805 (2021).
Gubin, M. M. et al. Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature 515 , 577–581 (2014).
Tran, E. et al. Immunogenicity of somatic mutations in human gastrointestinal cancers. Science 350 , 1387–1390 (2015).
Chowell, D. et al. Patient HLA class I genotype influences cancer response to checkpoint blockade immunotherapy. Science 359 , 582–587 (2018).
Anagnostou, V. et al. Multimodal genomic features predict outcome of immune checkpoint blockade in non-small-cell lung cancer. Nat. Cancer 1 , 99–111 (2020).
Abed, A. et al. Prognostic value of HLA-I homozygosity in patients with non-small cell lung cancer treated with single agent immunotherapy. J. Immunother. Cancer 8 , e001620 (2020).
Kobayashi, M. et al. Effect of HLA genotype on intravesical recurrence after bacillus Calmette-Guerin therapy for non-muscle-invasive bladder cancer. Cancer Immunol. Immunother. 71 , 727–736 (2022).
Chowell, D. et al. Evolutionary divergence of HLA class I genotype impacts efficacy of cancer immunotherapy. Nat. Med. 25 , 1715–1720 (2019).
Chowell, D. et al. Improved prediction of immune checkpoint blockade efficacy across multiple cancer types. Nat. Biotechnol. 40 , 499–506 (2022).
Litchfield, K. et al. Meta-analysis of tumor- and T cell-intrinsic mechanisms of sensitization to checkpoint inhibition. Cell 184 , 596–614.e14 (2021).
Cuppens, K. et al. HLA-I diversity and tumor mutational burden by comprehensive next-generation sequencing as predictive biomarkers for the treatment of non-small cell lung cancer with PD-(L)1 inhibitors. Lung Cancer 170 , 1–10 (2022).
Lu, Z. et al. Germline HLA-B evolutionary divergence influences the efficacy of immune checkpoint blockade therapy in gastrointestinal cancer. Genome Med. 13 , 175 (2021).
Lee, C. H. et al. High response rate and durability driven by HLA genetic diversity in patients with kidney cancer treated with Lenvatinib and Pembrolizumab. Mol. Cancer Res. 19 , 1510–1521 (2021).
Takahashi, S. et al. Impact of germline HLA genotypes on clinical outcomes in patients with urothelial cancer treated with pembrolizumab. Cancer Sci. https://doi.org/10.1111/cas.15488 (2022).
Roerden, M. et al. HLA evolutionary divergence as a prognostic marker for AML patients undergoing allogeneic stem cell transplantation. Cancers 12 , 1835 (2020).
Feray, C. et al. Donor HLA class 1 evolutionary divergence is a major predictor of liver allograft rejection: a retrospective cohort study. Ann. Intern. Med. 174 , 1385–1394 (2021).
Cummings, A. L. et al. Mutational landscape influences immunotherapy outcomes among patients with non-small-cell lung cancer with human leukocyte antigen supertype B44. Nat. Cancer 1 , 1167–1175 (2020).
Naranbhai, V. et al. HLA-A*03 and response to immune checkpoint blockade in cancer: an epidemiological biomarker study. Lancet Oncol. 23 , 172–184 (2022).
Pyke, R. M. et al. A machine learning algorithm with subclonal sensitivity reveals widespread pan-cancer human leukocyte antigen loss of heterozygosity. Nat. Commun. 13 , 1925 (2022).
Hazini, A., Fisher, K. & Seymour, L. Deregulation of HLA-I in cancer and its central importance for immunotherapy. J. Immunother. Cancer 9 , e002899 (2021).
Shukla, S. A. et al. Comprehensive analysis of cancer-associated somatic mutations in class I HLA genes. Nat. Biotechnol. 33 , 1152–1158 (2015).
Salter, R. D. et al. A binding site for the T-cell co-receptor CD8 on the α 3 domain of HLA-A2. Nature 345 , 41–46 (1990).
Alspach, E. et al. MHC-II neoantigens shape tumour immunity and response to immunotherapy. Nature 574 , 696–701 (2019).
Shao, X. M. et al. HLA class II immunogenic mutation burden predicts response to immune checkpoint blockade. Ann. Oncol. 33 , 728–738 (2022).
Pagliuca, S. et al. The similarity of class II HLA genotypes defines patterns of autoreactivity in idiopathic bone marrow failure disorders. Blood 138 , 2781–2798 (2021).
Daull, A. M. et al. Class I/Class II HLA evolutionary divergence ratio is an independent marker associated with disease-free and overall survival after allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia. Front. Immunol. 13 , 841470 (2022).
Steimle, V., Siegrist, C. A., Mottet, A., Lisowska-Grospierre, B. & Mach, B. Regulation of MHC class II expression by interferon-γ mediated by the transactivator gene CIITA. Science 265 , 106–109 (1994).
Rodig, S. J. et al. MHC proteins confer differential sensitivity to CTLA-4 and PD-1 blockade in untreated metastatic melanoma. Sci. Transl. Med. 10 , eaar3342 (2018).
Michelakos, T. et al. Differential role of HLA-A and HLA-B, C expression levels as prognostic markers in colon and rectal cancer. J. Immunother. Cancer 10 , e004115 (2022).
Meissner, T. B. et al. NLR family member NLRC5 is a transcriptional regulator of MHC class I genes. Proc. Natl Acad. Sci. USA 107 , 13794–13799 (2010).
Yoshihama, S. et al. NLRC5/MHC class I transactivator is a target for immune evasion in cancer. Proc. Natl Acad. Sci. USA 113 , 5999–6004 (2016).
Chew, G. L. et al. DUX4 suppresses MHC class I to promote cancer immune evasion and resistance to checkpoint blockade. Dev. Cell 50 , 658–671.e7 (2019).
Forloni, M. et al. NF-κB, and not MYCN, regulates MHC class I and endoplasmic reticulum aminopeptidases in human neuroblastoma cells. Cancer Res. 70 , 916–924 (2010).
Lorenzi, S. et al. IRF1 and NF-kB restore MHC class I-restricted tumor antigen processing and presentation to cytotoxic T cells in aggressive neuroblastoma. PLoS ONE 7 , e46928 (2012).
Yi, M. et al. The role of cancer-derived microRNAs in cancer immune escape. J. Hematol. Oncol. 13 , 25 (2020).
Mari, L. et al. microRNA 125a regulates MHC-I expression on esophageal adenocarcinoma cells, associated with suppression of antitumor immune response and poor outcomes of patients. Gastroenterology 155 , 784–798 (2018).
Colangelo, T. et al. Proteomic screening identifies calreticulin as a miR-27a direct target repressing MHC class I cell surface exposure in colorectal cancer. Cell Death Dis. 7 , e2120 (2016).
Huang, L. et al. The RNA-binding protein MEX3B mediates resistance to cancer immunotherapy by downregulating HLA-A expression. Clin. Cancer Res. 24 , 3366–3376 (2018).
Cano, F., Rapiteanu, R., Winkler, G. S. & Lehner, P. J. A non-proteolytic role for ubiquitin in deadenylation of MHC-I mRNA by the RNA-binding E3-ligase MEX-3C. Nat. Commun. 6 , 8670 (2015).
Yamamoto, K. et al. Autophagy promotes immune evasion of pancreatic cancer by degrading MHC-I. Nature 581 , 100–105 (2020).
Wang, Y. et al. Oncoprotein SND1 hijacks nascent MHC-I heavy chain to ER-associated degradation, leading to impaired CD8 + T cell response in tumor. Sci. Adv. 6 , eaba5412 (2020).
Fang, Y. et al. MAL2 drives immune evasion in breast cancer by suppressing tumor antigen presentation. J. Clin. Invest. 131 , e140837 (2021).
Jongsma, M. L. M. et al. The SPPL3-defined glycosphingolipid repertoire orchestrates HLA class I-mediated immune responses. Immunity 54 , 132–150.e9 (2021).
Rooney, M. S., Shukla, S. A., Wu, C. J., Getz, G. & Hacohen, N. Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell 160 , 48–61 (2015).
Bernal, M., Ruiz-Cabello, F., Concha, A., Paschen, A. & Garrido, F. Implication of the β2-microglobulin gene in the generation of tumor escape phenotypes. Cancer Immunol. Immunother. 61 , 1359–1371 (2012).
Gettinger, S. et al. Impaired HLA class I antigen processing and presentation as a mechanism of acquired resistance to immune checkpoint inhibitors in lung cancer. Cancer Discov. 7 , 1420–1435 (2017).
Sade-Feldman, M. et al. Resistance to checkpoint blockade therapy through inactivation of antigen presentation. Nat. Commun. 8 , 1136 (2017).
Challa-Malladi, M. et al. Combined genetic inactivation of β2-microglobulin and CD58 reveals frequent escape from immune recognition in diffuse large B cell lymphoma. Cancer Cell 20 , 728–740 (2011).
Fangazio, M. et al. Genetic mechanisms of HLA-I loss and immune escape in diffuse large B cell lymphoma. Proc. Natl Acad. Sci. USA 118 , e2104504118 (2021).
Chen, H. L. et al. A functionally defective allele of TAP1 results in loss of MHC class I antigen presentation in a human lung cancer. Nat. Genet. 13 , 210–213 (1996).
Klampfl, T. et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. N. Engl. J. Med. 369 , 2379–2390 (2013).
Arshad, N. & Cresswell, P. Tumor-associated calreticulin variants functionally compromise the peptide loading complex and impair its recruitment of MHC-I. J. Biol. Chem. 293 , 9555–9569 (2018).
Tripathi, S. C. et al. Immunoproteasome deficiency is a feature of non-small cell lung cancer with a mesenchymal phenotype and is associated with a poor outcome. Proc. Natl Acad. Sci. USA 113 , E1555–E1564 (2016).
Kalaora, S. et al. Immunoproteasome expression is associated with better prognosis and response to checkpoint therapies in melanoma. Nat. Commun. 11 , 896 (2020).
Ramsuran, V. et al. Epigenetic regulation of differential HLA-A allelic expression levels. Hum. Mol. Genet. 24 , 4268–4275 (2015).
Ye, Q. et al. Hypermethylation of HLA class I gene is associated with HLA class I down-regulation in human gastric cancer. Tissue Antigens 75 , 30–39 (2010).
Burr, M. L. et al. An evolutionarily conserved function of polycomb silences the MHC class I antigen presentation pathway and enables immune evasion in cancer. Cancer Cell 36 , 385–401.e8 (2019).
Ennishi, D. et al. Molecular and genetic characterization of MHC deficiency identifies EZH2 as therapeutic target for enhancing immune recognition. Cancer Discov. 9 , 546–563 (2019).
Guo, B., Tan, X. & Cen, H. EZH2 is a negative prognostic biomarker associated with immunosuppression in hepatocellular carcinoma. PLoS ONE 15 , e0242191 (2020).
He, P. C. & He, C. m 6 A RNA methylation: from mechanisms to therapeutic potential. EMBO J. 40 , e105977 (2021).
McFadden, M. J. et al. Post-transcriptional regulation of antiviral gene expression by N6-methyladenosine. Cell Rep. 34 , 108798 (2021).
Jin, S. et al. m 6 A RNA modification controls autophagy through upregulating ULK1 protein abundance. Cell Res. 28 , 955–957 (2018).
Wang, X. et al. m 6 A mRNA methylation controls autophagy and adipogenesis by targeting Atg5 and Atg7. Autophagy 16 , 1221–1235 (2020).
Han, D. et al. Anti-tumour immunity controlled through mRNA m 6 A methylation and YTHDF1 in dendritic cells. Nature 566 , 270–274 (2019).
Vizcaino, J. A. et al. The human immunopeptidome project: a roadmap to predict and treat immune diseases. Mol. Cell Proteom. 19 , 31–49 (2020).
Marcu, A. et al. HLA ligand atlas: a benign reference of HLA-presented peptides to improve T-cell-based cancer immunotherapy. J. Immunother. Cancer 9 , e002071 (2021).
Kubiniok, P. et al. Understanding the constitutive presentation of MHC class I immunopeptidomes in primary tissues. iScience 25 , 103768 (2022).
Phillips, E. R. & Perdue, J. F. The expression and localization of surface neoantigens in transformed and untransformed cultured cells infected with avian tumor viruses. J. Supramol. Struct. 4 , 27–44 (1976).
Lennerz, V. et al. The response of autologous T cells to a human melanoma is dominated by mutated neoantigens. Proc. Natl Acad. Sci. USA 102 , 16013–16018 (2005).
Maletzki, C., Schmidt, F., Dirks, W. G., Schmitt, M. & Linnebacher, M. Frameshift-derived neoantigens constitute immunotherapeutic targets for patients with microsatellite-instable haematological malignancies: frameshift peptides for treating MSI + blood cancers. Eur. J. Cancer 49 , 2587–2595 (2013).
McGranahan, N. et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 351 , 1463–1469 (2016).
Yang, W. et al. Immunogenic neoantigens derived from gene fusions stimulate T cell responses. Nat. Med. 25 , 767–775 (2019).
Khodadoust, M. S. et al. Antigen presentation profiling reveals recognition of lymphoma immunoglobulin neoantigens. Nature 543 , 723–727 (2017).
Haen, S. P., Loffler, M. W., Rammensee, H. G. & Brossart, P. Towards new horizons: characterization, classification and implications of the tumour antigenic repertoire. Nat. Rev. Clin. Oncol. 17 , 595–610 (2020).
Kreiter, S. et al. Mutant MHC class II epitopes drive therapeutic immune responses to cancer. Nature 520 , 692–696 (2015).
Kalaora, S. et al. Use of HLA peptidomics and whole exome sequencing to identify human immunogenic neo-antigens. Oncotarget 7 , 5110–5117 (2016).
Ott, P. A. et al. An immunogenic personal neoantigen vaccine for patients with melanoma. Nature 547 , 217–221 (2017).
Keskin, D. B. et al. Neoantigen vaccine generates intratumoral T cell responses in phase Ib glioblastoma trial. Nature 565 , 234–239 (2019).
Platten, M. et al. A vaccine targeting mutant IDH1 in newly diagnosed glioma. Nature 592 , 463–468 (2021).
Palmer, C. D. et al. Individualized, heterologous chimpanzee adenovirus and self-amplifying mRNA neoantigen vaccine for advanced metastatic solid tumors: phase 1 trial interim results. Nat. Med. 28 , 1619–1629 (2022).
Rotzschke, O. et al. Isolation and analysis of naturally processed viral peptides as recognized by cytotoxic T cells. Nature 348 , 252–254 (1990).
Hunt, D. F. et al. Characterization of peptides bound to the class I MHC molecule HLA-A2.1 by mass spectrometry. Science 255 , 1261–1263 (1992).
Bassani-Sternberg, M. et al. Direct identification of clinically relevant neoepitopes presented on native human melanoma tissue by mass spectrometry. Nat. Commun. 7 , 13404 (2016).
Schuster, H. et al. The immunopeptidomic landscape of ovarian carcinomas. Proc. Natl Acad. Sci. USA 114 , E9942–E9951 (2017).
Shao, W. et al. The SysteMHC Atlas project. Nucleic Acids Res. 46 , D1237–D1247 (2018).
Yi, X. et al. caAtlas: an immunopeptidome atlas of human cancer. iScience 24 , 103107 (2021).
Stopfer, L. E. et al. Absolute quantification of tumor antigens using embedded MHC-I isotopologue calibrants. Proc. Natl Acad. Sci. USA 118 , e2111173118 (2021).
Jaeger, A. M. et al. Deciphering the immunopeptidome in vivo reveals new tumour antigens. Nature 607 , 149–155 (2022).
Kalaora, S. et al. Identification of bacteria-derived HLA-bound peptides in melanoma. Nature 592 , 138–143 (2021).
Nielsen, M., Ternette, N. & Barra, C. The interdependence of machine learning and LC-MS approaches for an unbiased understanding of the cellular immunopeptidome. Expert. Rev. Proteom. 19 , 77–88 (2022).
Bassani-Sternberg, M. et al. Deciphering HLA-I motifs across HLA peptidomes improves neo-antigen predictions and identifies allostery regulating HLA specificity. PLoS Comput. Biol. 13 , e1005725 (2017).
Andreatta, M. et al. MS-Rescue: a computational pipeline to increase the quality and yield of immunopeptidomics experiments. Proteomics 19 , e1800357 (2019).
Alvarez, B. et al. NNAlign_MA; MHC peptidome deconvolution for accurate MHC binding motif characterization and improved T-cell epitope predictions. Mol. Cell Proteom. 18 , 2459–2477 (2019).
Jurtz, V. et al. NetMHCpan-4.0: improved peptide-MHC class I interaction predictions integrating eluted ligand and peptide binding affinity data. J. Immunol. 199 , 3360–3368 (2017).
O’Donnell, T. J., Rubinsteyn, A. & Laserson, U. MHCflurry 2.0: improved pan-allele prediction of MHC class I-presented peptides by incorporating antigen processing. Cell Syst. 11 , 418–419 (2020).
Sarkizova, S. et al. A large peptidome dataset improves HLA class I epitope prediction across most of the human population. Nat. Biotechnol. 38 , 199–209 (2020).
Chen, B. et al. Predicting HLA class II antigen presentation through integrated deep learning. Nat. Biotechnol. 37 , 1332–1343 (2019).
Erhard, F., Dolken, L., Schilling, B. & Schlosser, A. Identification of the cryptic HLA-I immunopeptidome. Cancer Immunol. Res. 8 , 1018–1026 (2020).
Ouspenskaia, T. et al. Unannotated proteins expand the MHC-I-restricted immunopeptidome in cancer. Nat. Biotechnol. 40 , 209–217 (2022).
Blass, E. & Ott, P. A. Advances in the development of personalized neoantigen-based therapeutic cancer vaccines. Nat. Rev. Clin. Oncol. 18 , 215–229 (2021).
Sahin, U. et al. Personalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancer. Nature 547 , 222–226 (2017).
Hilf, N. et al. Actively personalized vaccination trial for newly diagnosed glioblastoma. Nature 565 , 240–245 (2019).
Finn, O. J. A Believer’s overview of cancer immunosurveillance and immunotherapy. J. Immunol. 200 , 385–391 (2018).
Marty, R. et al. MHC-I genotype restricts the oncogenic mutational landscape. Cell 171 , 1272–1283.e15 (2017).
Marty Pyke, R. et al. Evolutionary pressure against MHC class II binding cancer mutations. Cell 175 , 1991 (2018).
Dersh, D., Holly, J. & Yewdell, J. W. A few good peptides: MHC class I-based cancer immunosurveillance and immunoevasion. Nat. Rev. Immunol. 21 , 116–128 (2021).
Van den Eynden, J., Jimenez-Sanchez, A., Miller, M. L. & Larsson, E. Lack of detectable neoantigen depletion signals in the untreated cancer genome. Nat. Genet. 51 , 1741–1748 (2019).
Claeys, A., Luijts, T., Marchal, K. & Van den Eynden, J. Low immunogenicity of common cancer hot spot mutations resulting in false immunogenic selection signals. PLoS Genet. 17 , e1009368 (2021).
Hoyos, D. et al. Fundamental immune-oncogenicity trade-offs define driver mutation fitness. Nature 606 , 172–179 (2022).
O’Donnell, J. S., Teng, M. W. L. & Smyth, M. J. Cancer immunoediting and resistance to T cell-based immunotherapy. Nat. Rev. Clin. Oncol. 16 , 151–167 (2019).
Balachandran, V. P. et al. Identification of unique neoantigen qualities in long-term survivors of pancreatic cancer. Nature 551 , 512–516 (2017).
Luksza, M. et al. A neoantigen fitness model predicts tumour response to checkpoint blockade immunotherapy. Nature 551 , 517–520 (2017).
Luksza, M. et al. Neoantigen quality predicts immunoediting in survivors of pancreatic cancer. Nature 606 , 389–395 (2022).
Fluckiger, A. et al. Cross-reactivity between tumor MHC class I-restricted antigens and an enterococcal bacteriophage. Science 369 , 936–942 (2020).
Zitvogel, L. & Kroemer, G. Cross-reactivity between cancer and microbial antigens. Oncoimmunology 10 , 1877416 (2021).
Au, L. et al. Determinants of anti-PD-1 response and resistance in clear cell renal cell carcinoma. Cancer Cell 39 , 1497–1518.e11 (2021).
Yarchoan, M., Hopkins, A. & Jaffee, E. M. Tumor mutational burden and response rate to PD-1 inhibition. N. Engl. J. Med. 377 , 2500–2501 (2017).
Devarakonda, S. et al. Tumor mutation burden as a biomarker in resected non-small-cell lung cancer. J. Clin. Oncol. 36 , 2995–3006 (2018).
Samstein, R. M. et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat. Genet. 51 , 202–206 (2019).
Attermann, A. S., Bjerregaard, A. M., Saini, S. K., Gronbaek, K. & Hadrup, S. R. Human endogenous retroviruses and their implication for immunotherapeutics of cancer. Ann. Oncol. 29 , 2183–2191 (2018).
Faulkner, G. J. et al. The regulated retrotransposon transcriptome of mammalian cells. Nat. Genet. 41 , 563–571 (2009).
Rycaj, K. et al. Cytotoxicity of human endogenous retrovirus K-specific T cells toward autologous ovarian cancer cells. Clin. Cancer Res. 21 , 471–483 (2015).
Jang, H. S. et al. Transposable elements drive widespread expression of oncogenes in human cancers. Nat. Genet. 51 , 611–617 (2019).
Smith, C. C. et al. Endogenous retroviral signatures predict immunotherapy response in clear cell renal cell carcinoma. J. Clin. Invest. 128 , 4804–4820 (2018).
Saini, S. K. et al. Human endogenous retroviruses form a reservoir of T cell targets in hematological cancers. Nat. Commun. 11 , 5660 (2020).
Bullman, S. et al. Analysis of Fusobacterium persistence and antibiotic response in colorectal cancer. Science 358 , 1443–1448 (2017).
Nejman, D. et al. The human tumor microbiome is composed of tumor type-specific intracellular bacteria. Science 368 , 973–980 (2020).
Jin, C. et al. Commensal microbiota promote lung cancer development via γδ T cells. Cell 176 , 998–1013.e16 (2019).
Riquelme, E. et al. Tumor microbiome diversity and composition influence pancreatic cancer outcomes. Cell 178 , 795–806.e12 (2019).
Fu, A. et al. Tumor-resident intracellular microbiota promotes metastatic colonization in breast cancer. Cell 185 , 1356–1372.e26 (2022).
Matson, V. et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science 359 , 104–108 (2018).
Routy, B. et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 359 , 91–97 (2018).
Sepich-Poore, G. D., Carter, H. & Knight, R. Intratumoral bacteria generate a new class of therapeutically relevant tumor antigens in melanoma. Cancer Cell 39 , 601–603 (2021).
Xavier, J. B. et al. The cancer microbiome: distinguishing direct and indirect effects requires a systemic view. Trends Cancer 6 , 192–204 (2020).
Yoo, S. K., Chowell, D., Valero, C., Morris, L. G. T. & Chan, T. A. Outcomes among patients with or without obesity and with cancer following treatment with immune checkpoint blockade. JAMA Netw. Open 5 , e220448 (2022).
Yoo, S. K., Chowell, D., Valero, C., Morris, L. G. T. & Chan, T. A. Pre-treatment serum albumin and mutational burden as biomarkers of response to immune checkpoint blockade. NPJ Precis. Oncol. 6 , 23 (2022).
Krishna, C., Chowell, D., Gonen, M., Elhanati, Y. & Chan, T. A. Genetic and environmental determinants of human TCR repertoire diversity. Immun. Ageing 17 , 26 (2020).
Middha, S. et al. Majority of B2M-mutant and -deficient colorectal carcinomas achieve clinical benefit from immune checkpoint inhibitor therapy and are microsatellite instability-high. JCO Precis. Oncol. 3 , PO.18.00321 (2019).
PubMed PubMed Central Google Scholar
Yeon Yeon, S. et al. Immune checkpoint blockade resistance-related B2M hotspot mutations in microsatellite-unstable colorectal carcinoma. Pathol. Res. Pract. 215 , 209–214 (2019).
Zhang, C. et al. B2M and JAK1/2-mutated MSI-H colorectal carcinomas can benefit from anti-PD-1 therapy. J. Immunother. 45 , 187–193 (2022).
Zhang, H. et al. B2M overexpression correlates with malignancy and immune signatures in human gliomas. Sci. Rep. 11 , 5045 (2021).
Li, D. et al. β2-Microglobulin maintains glioblastoma stem cells and induces M2-like polarization of tumor-associated macrophages. Cancer Res. 82 , 3321–3334 (2022).
Bern, M. D. et al. Inducible down-regulation of MHC class I results in natural killer cell tolerance. J. Exp. Med. 216 , 99–116 (2019).
McGranahan, N. et al. Allele-specific HLA loss and immune escape in lung cancer evolution. Cell 171 , 1259–1271.e11 (2017).
Gong, X. & Karchin, R. Pan-cancer HLA gene-mediated tumor immunogenicity and immune evasion. Mol. Cancer Res. 20 , 1272–1283 (2022).
Thorsson, V. et al. The immune landscape of cancer. Immunity 48 , 812–830.e14 (2018).
Shklovskaya, E. et al. Tumor MHC expression guides first-line immunotherapy selection in melanoma. Cancers 12 , 3374 (2020).
Liu, D. et al. Integrative molecular and clinical modeling of clinical outcomes to PD1 blockade in patients with metastatic melanoma. Nat. Med. 25 , 1916–1927 (2019).
Axelrod, M. L., Cook, R. S., Johnson, D. B. & Balko, J. M. Biological consequences of MHC-II expression by tumor cells in cancer. Clin. Cancer Res. 25 , 2392–2402 (2019).
Neuwelt, A. J. et al. Cancer cell-intrinsic expression of MHC II in lung cancer cell lines is actively restricted by MEK/ERK signaling and epigenetic mechanisms. J. Immunother. Cancer 8 , e000441 (2020).
Johnson, D. B. et al. Melanoma-specific MHC-II expression represents a tumour-autonomous phenotype and predicts response to anti-PD-1/PD-L1 therapy. Nat. Commun. 7 , 10582 (2016).
Roemer, M. G. M. et al. Major histocompatibility complex class II and programmed death ligand 1 expression predict outcome after programmed death 1 blockade in classic Hodgkin lymphoma. J. Clin. Oncol. 36 , 942–950 (2018).
Gonzalez-Ericsson, P. I. et al. Tumor-specific major histocompatibility-II expression predicts benefit to anti-PD-1/L1 therapy in patients with HER2-negative primary breast cancer. Clin. Cancer Res. 27 , 5299–5306 (2021).
Schirrmacher, V., Schild, H. J., Guckel, B. & von Hoegen, P. Tumour-specific CTL response requiring interactions of four different cell types and recognition of MHC class I and class II restricted tumour antigens. Immunol. Cell Biol. 71 , 311–326 (1993).
Tay, R. E., Richardson, E. K. & Toh, H. C. Revisiting the role of CD4 + T cells in cancer immunotherapy-new insights into old paradigms. Cancer Gene Ther. 28 , 5–17 (2021).
Zander, R. et al. CD4 + T cell help is required for the formation of a cytolytic CD8 + T cell subset that protects against chronic infection and cancer. Immunity 51 , 1028–1042.e4 (2019).
Rosenthal, R. et al. Neoantigen-directed immune escape in lung cancer evolution. Nature 567 , 479–485 (2019).
Thol, K., Pawlik, P. & McGranahan, N. Therapy sculpts the complex interplay between cancer and the immune system during tumour evolution. Genome Med. 14 , 137 (2022).
Homma, Y. et al. Changes in the immune cell population and cell proliferation in peripheral blood after gemcitabine-based chemotherapy for pancreatic cancer. Clin. Transl. Oncol. 16 , 330–335 (2014).
Jimenez-Sanchez, A. et al. Unraveling tumor-immune heterogeneity in advanced ovarian cancer uncovers immunogenic effect of chemotherapy. Nat. Genet. 52 , 582–593 (2020).
Szikriszt, B. et al. A comprehensive survey of the mutagenic impact of common cancer cytotoxics. Genome Biol. 17 , 99 (2016).
Wu, T. et al. Quantification of neoantigen-mediated immunoediting in cancer evolution. Cancer Res. 82 , 2226–2238 (2022).
Motzer, R. J. et al. Molecular subsets in renal cancer determine outcome to checkpoint and angiogenesis blockade. Cancer Cell 38 , 803–817.e4 (2020).
Dong, L. Q. et al. Heterogeneous immunogenomic features and distinct escape mechanisms in multifocal hepatocellular carcinoma. J. Hepatol. 72 , 896–908 (2020).
Tawbi, H. A. et al. Relatlimab and nivolumab versus nivolumab in untreated advanced melanoma. N. Engl. J. Med. 386 , 24–34 (2022).
Frampton, A. E. & Sivakumar, S. A new combination immunotherapy in advanced melanoma. N. Engl. J. Med. 386 , 91–92 (2022).
Marin-Acevedo, J. A., Kimbrough, E. O. & Lou, Y. Next generation of immune checkpoint inhibitors and beyond. J. Hematol. Oncol. 14 , 45 (2021).
Guo, E. et al. WEE1 inhibition induces anti-tumor immunity by activating ERV and the dsRNA pathway. J. Exp. Med. 219 , e20210789 (2022).
Andre, P. et al. Anti-NKG2A mAb is a checkpoint inhibitor that promotes anti-tumor immunity by unleashing both T and NK cells. Cell 175 , 1731–1743.e13 (2018).
Roschewski, M., Longo, D. L. & Wilson, W. H. CAR T-cell therapy for large B-cell lymphoma — who, when, and how? N. Engl. J. Med. 386 , 692–696 (2022).
Yarmarkovich, M. et al. Cross-HLA targeting of intracellular oncoproteins with peptide-centric CARs. Nature 599 , 477–484 (2021).
Bonaventura, P. et al. Identification of shared tumor epitopes from endogenous retroviruses inducing high-avidity cytotoxic T cells for cancer immunotherapy. Sci. Adv. 8 , eabj3671 (2022).
Rapoport, A. P. et al. NY-ESO-1-specific TCR-engineered T cells mediate sustained antigen-specific antitumor effects in myeloma. Nat. Med. 21 , 914–921 (2015).
Cameron, B. J. et al. Identification of a Titin-derived HLA-A1-presented peptide as a cross-reactive target for engineered MAGE A3-directed T cells. Sci. Transl. Med. 5 , 197ra103 (2013).
Zhao, X. et al. Tuning T cell receptor sensitivity through catch bond engineering. Science 376 , eabl5282 (2022).
Bekes, M., Langley, D. R. & Crews, C. M. PROTAC targeted protein degraders: the past is prologue. Nat. Rev. Drug Discov. 21 , 181–200 (2022).
Massafra, V. et al. Proteolysis-targeting chimeras enhance T cell bispecific antibody-driven T cell activation and effector function through increased MHC class I antigen presentation in cancer cells. J. Immunol. 207 , 493–504 (2021).
Duan, Z. & Ho, M. T-cell receptor mimic antibodies for cancer immunotherapy. Mol. Cancer Ther. 20 , 1533–1541 (2021).
Hansen, T. H., Connolly, J. M., Gould, K. G. & Fremont, D. H. Basic and translational applications of engineered MHC class I proteins. Trends Immunol. 31 , 363–369 (2010).
Chang, A. Y. et al. A therapeutic T cell receptor mimic antibody targets tumor-associated PRAME peptide/HLA-I antigens. J. Clin. Invest. 127 , 3557 (2017).
Dao, T. et al. Targeting the intracellular WT1 oncogene product with a therapeutic human antibody. Sci. Transl. Med. 5 , 176ra133 (2013).
Article Google Scholar
Carvajal, R. D. et al. Advances in the clinical management of uveal melanoma. Nat. Rev. Clin. Oncol. 20 , 99–115 (2023).
Nathan, P. et al. Overall survival benefit with tebentafusp in metastatic uveal melanoma. N. Engl. J. Med. 385 , 1196–1206 (2021).
Carvajal, R. D. et al. Phase I study of safety, tolerability, and efficacy of tebentafusp using a step-up dosing regimen and expansion in patients with metastatic uveal melanoma. J. Clin. Oncol. 40 , 1939–1948 (2022).
Liu, X. et al. Development of a TCR-like antibody and chimeric antigen receptor against NY-ESO-1/HLA-A2 for cancer immunotherapy. J. Immunother. Cancer 10 , e004035 (2022).
Hsiue, E. H. et al. Targeting a neoantigen derived from a common TP53 mutation. Science 371 , eabc8697 (2021).
Douglass, J. et al. Bispecific antibodies targeting mutant RAS neoantigens. Sci. Immunol. 6 , eabd5515 (2021).
Ma, J. et al. Bispecific antibodies: from research to clinical application. Front. Immunol. 12 , 626616 (2021).
Hegde, P. S. & Chen, D. S. Top 10 challenges in cancer immunotherapy. Immunity 52 , 17–35 (2020).
FDA. FDA Approves Pembrolizumab for Adults and children with TMB-H Solid Tumors https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-pembrolizumab-adults-and-children-tmb-h-solid-tumors (2020).
FDA. FDA Grants Accelerated Approval to Dostarlimab-gxly for dMMR Advanced Solid Tumors https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-dostarlimab-gxly-dmmr-advanced-solid-tumors (2021).
Valero, C. et al. The association between tumor mutational burden and prognosis is dependent on treatment context. Nat. Genet. 53 , 11–15 (2021).
Valero, C. et al. Response rates to anti-PD-1 immunotherapy in microsatellite-stable solid tumors with 10 or more mutations per megabase. JAMA Oncol. 7 , 739–743 (2021).
Hellmann, M. D. et al. Tumor mutational burden and efficacy of Nivolumab monotherapy and in combination with Ipilimumab in small-cell lung cancer. Cancer Cell 33 , 853–861.e4 (2018).
Wang, F. et al. Evaluation of POLE and POLD1 mutations as biomarkers for immunotherapy outcomes across multiple cancer types. JAMA Oncol. 5 , 1504–1506 (2019).
Andre, T. et al. Pembrolizumab in microsatellite-instability-high advanced colorectal cancer. N. Engl. J. Med. 383 , 2207–2218 (2020).
Le, D. T. et al. PD-1 blockade in tumors with mismatch-repair deficiency. N. Engl. J. Med. 372 , 2509–2520 (2015).
Ma, X. et al. Functional landscapes of POLE and POLD1 mutations in checkpoint blockade-dependent antitumor immunity. Nat. Genet. 54 , 996–1012 (2022).
Bauer, J. et al. The oncogenic fusion protein DNAJB1-PRKACA can be specifically targeted by peptide-based immunotherapy in fibrolamellar hepatocellular carcinoma. Nat. Commun. 13 , 6401 (2022).
Weber, D. et al. Accurate detection of tumor-specific gene fusions reveals strongly immunogenic personal neo-antigens. Nat. Biotechnol. 40 , 1276–1284 (2022).
Yoshihama, S. et al. NLRC5/CITA expression correlates with efficient response to checkpoint blockade immunotherapy. Sci. Rep. 11 , 3258 (2021).
Takahashi, A. et al. Tyrosine kinase inhibitors stimulate HLA class I expression by augmenting the IFNγ/STAT1 signaling in hepatocellular carcinoma cells. Front. Oncol. 11 , 707473 (2021).
Chang, C. H., Hammer, J., Loh, J. E., Fodor, W. L. & Flavell, R. A. The activation of major histocompatibility complex class I genes by interferon regulatory factor-1 (IRF-1). Immunogenetics 35 , 378–384 (1992).
Kriegsman, B. A. et al. Frequent loss of IRF2 in cancers leads to immune evasion through decreased MHC class I antigen presentation and increased PD-L1 expression. J. Immunol. 203 , 1999–2010 (2019).
Schaafsma, E., Fugle, C. M., Wang, X. & Cheng, C. Pan-cancer association of HLA gene expression with cancer prognosis and immunotherapy efficacy. Br. J. Cancer 125 , 422–432 (2021).
Jung, H. et al. DNA methylation loss promotes immune evasion of tumours with high mutation and copy number load. Nat. Commun. 10 , 4278 (2019).
Zhou, L., Mudianto, T., Ma, X., Riley, R. & Uppaluri, R. Targeting EZH2 enhances antigen presentation, antitumor immunity, and circumvents anti-PD-1 resistance in head and neck cancer. Clin. Cancer Res. 26 , 290–300 (2020).
Gambacorta, V. et al. Integrated multiomic profiling identifies the epigenetic regulator PRC2 as a therapeutic target to counteract leukemia immune escape and relapse. Cancer Discov. 12 , 1449–1461 (2022).
Zheng, J. et al. miR-148a-3p silences the CANX/MHC-I pathway and impairs CD8 + T cell-mediated immune attack in colorectal cancer. FASEB J. 35 , e21776 (2021).
Song, D. et al. Insights into the role of ERp57 in cancer. J. Cancer 12 , 2456–2464 (2021).
Nielsen, M. et al. Coexisting alterations of MHC class I antigen presentation and IFNγ signaling mediate acquired resistance of melanoma to post-PD-1 immunotherapy. Cancer Immunol. Res. 10 , 1254–1262 (2022).
Cromme, F. V. et al. Loss of transporter protein, encoded by the TAP-1 gene, is highly correlated with loss of HLA expression in cervical carcinomas. J. Exp. Med. 179 , 335–340 (1994).
Seliger, B. et al. Reduced membrane major histocompatibility complex class I density and stability in a subset of human renal cell carcinomas with low TAP and LMP expression. Clin. Cancer Res. 2 , 1427–1433 (1996).
CAS PubMed Google Scholar
Kaklamanis, L. et al. Loss of major histocompatibility complex-encoded transporter associated with antigen presentation (TAP) in colorectal cancer. Am. J. Pathol. 145 , 505–509 (1994).
CAS PubMed PubMed Central Google Scholar
Lopez de Castro, J. A. How ERAP1 and ERAP2 shape the peptidomes of disease-associated MHC-I proteins. Front. Immunol. 9 , 2463 (2018).
Download references
Acknowledgements
The authors are grateful for the support from NIH grants R35CA232097 (T.A.C.), R01CA205426 (T.A.C.), U54CA274513 (T.A.C.) and T32CA094186 (K.Y.), a Young Investigator Award from ASCO Conquer Cancer Foundation (K.Y.), a RSNA Research Resident Grant (K.Y.), and a Cleveland Clinic VeloSano Impact Award (K.Y.).
Author information
Authors and affiliations.
Department of Radiation Oncology, Taussig Cancer Center, Cleveland Clinic, Cleveland, OH, USA
Kailin Yang, Ahmed Halima & Timothy A. Chan
Center for Immunotherapy and Precision Immuno-Oncology, Cleveland Clinic, Cleveland, OH, USA
Timothy A. Chan
National Center for Regenerative Medicine, Cleveland, OH, USA
Case Comprehensive Cancer Center, Cleveland, OH, USA
You can also search for this author in PubMed Google Scholar
Contributions
All authors made a substantial contribution to all aspects of the preparation of this manuscript.
Corresponding author
Correspondence to Timothy A. Chan .
Ethics declarations
Competing interests.
T.A.C. is a co-founder of and holds equity in Gritstone Oncology; holds equity in An2H; acknowledges grant funding from An2H, AstraZeneca, Bristol Myers Squibb, Eisai, Illumina and Pfizer; has served as an advisor for An2H, AstraZeneca, Bristol Myers Squibb, Eisai, Illumina and MedImmune; and holds ownership of intellectual property on using tumour mutational burden to predict immunotherapy response, which has been licensed to PGDx. K.Y. and A.H. declare no competing interests.
Peer review
Peer review information.
Nature Reviews Clinical Oncology thanks J. Balko and the other, anonymous, peer reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Yang, K., Halima, A. & Chan, T.A. Antigen presentation in cancer — mechanisms and clinical implications for immunotherapy. Nat Rev Clin Oncol 20 , 604–623 (2023). https://doi.org/10.1038/s41571-023-00789-4
Download citation
Accepted : 25 May 2023
Published : 16 June 2023
Issue Date : September 2023
DOI : https://doi.org/10.1038/s41571-023-00789-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
Cancer Powerpoint Templates and Google Slides Themes
Discover a wide range of beautifully designed presentation templates tailored to raise awareness and support for cancer research and advocacy.
Explore Free Cancer Presentation Templates

Doodle Cancer Awareness Social Media Campaign Slides
Immerse your audience in an engaging, creative journey with this PowerPoint and Google Slides template specifically designed for marketing professionals. ... Read more
Retro Illustrated Breast Cancer Brochure Slides
Take your awareness campaign to the next-level with our vibrant Powerpoint and Google Slides templates. Geared towards marketers, our unique, ... Read more
Illustrated Breast Cancer Case Slides
Bring your awareness campaign to life with our pink, geometric style awareness slides template. Tailored for marketing teams, it’s a ... Read more

Illustrated Breast Cancer Healthcare Center Slides
Brighten up your message with our Pink Vibrancy Healthcare Awareness PowerPoint Template. This modern, clean design is perfect for marketing ... Read more

Cute Breast Cancer Information Brochure Slides
Grab your audience’s attention with our retro-styled, power-packed Powerpoint templates specifically designed for campaigning. Hues of pink and purple and ... Read more

Illustrated Breast Cancer Prevention Campaign Slides
The Vibrant Breast Cancer Campaign Slides template is a tastefully illustrated, pop art-inspired deck. Perfect for marketing professionals, this eye-catching ... Read more

Elegant Minimal Breast Cancer Awareness Slides
Embark on your Breast Cancer Awareness campaign with our dignified and sophisticated Powerpoint and Google Slides templates. Crafted in a ... Read more
Minimal Breast Cancer Awareness Month Slides
Revamp your marketing strategies with this highly customizable, photo-centric PowerPoint and Google Slides template. Perfectly tailored for marketers aiming to ... Read more

Illustrated Breast Cancer Treatment Breakthrough Slides
Boost the visibility of your visionary breast cancer therapy with our Powerpoint and Google Slides templates. Specifically designed for marketers, ... Read more
Bold World Breast Cancer Newsletter Slides
Make an impact with your next breast cancer awareness event with our dynamic Powerpoint and Google Slides template. Catering specifically ... Read more

Cute Illustrated Cancer Treatment Information Brochure Slides
Light up your cancer treatment campaign with our fresh, cartoon-style Powerpoint and Google Slides template. United by soft pastels, and ... Read more

Pink and Beige Breast Cancer Awareness Slides
Vibrant and soothing, these breast cancer awareness slides are easy to use as a Google Slides template, PowerPoint theme or ... Read more

Lung Cancer Awareness Slides
These lung cancer awareness slides are perfect as a Google Slides template, PowerPoint theme or Canva template. Visually striking and ... Read more
Professional designs for your presentations
SlidesCarnival templates have all the elements you need to effectively communicate your message and impress your audience.
Suitable for PowerPoint and Google Slides
Download your presentation as a PowerPoint template or use it online as a Google Slides theme. 100% free, no registration or download limits.
- Google Slides
- Editor’s Choice
- All Templates
- Frequently Asked Questions
- Google Slides Help
- PowerPoint help
- Who makes SlidesCarnival?

CANCER TYPES, CAUSES AND TREATMENT Read less
Recommended
More related content, what's hot, what's hot ( 20 ), viewers also liked, viewers also liked ( 10 ), similar to cancer ppt, similar to cancer ppt ( 20 ), more from namdeo shinde, more from namdeo shinde ( 20 ), recently uploaded, recently uploaded ( 20 ).
- 1. A PAPER PRESENTATION ON CANCER-INTRODUCTION & TREATMENT BY, Mr. NAMDEO SHINDE M. Pharm SATARA COLLEGE OF PHARMACY DEGAON, SATARA.(MH) INDIA.
- 3. What does the word cancer mean to you?
- 4. A terrifying illness.
- 8. Normal body cells grow, divide and die in an orderly fashion.
- 9. Cancer cells are different because they do not die, they just continue to grow and divide in a disorderly fashion.
- 10. Cancer can occur at any age, but 67% of cancer deaths occur in people older than 65 years
- 11. CANCER STATISTICS 30% 25% 20% 15% 10% death % 5% 0% Heart Cancer chronic Diabetes Alzheimer disease respiratory disease lower diseases
- 12. There are two types of tumours: Malignant tumors spread to other areas in the body. Benign tumors stay in one place.
- 13. Main Features
- 14. Common environmental factors leading to cancer death include: tobacco (25-30%)
- 15. Common environmental factors leading to cancer death include: diet and obesity (30-35%) tobacco (25-30%)
- 16. Common environmental factors leading to cancer death include: diet and obesity (30-35%) tobacco (25-30%) infections (15-20%)
- 17. Common environmental factors leading to cancer death include: diet and obesity (30-35%) tobacco (25-30%) Radiation infections (15-20%) Stress lack of physical activity environmental pollutants
- 18. CAUSES Benzene and other chemicals Drinking excess alcohol Environmental toxins, such as certain poisonous mushrooms and a type of poison that can grow on peanut plants (aflatoxins) Excessive sunlight exposure Genetic problems Obesity Radiation Viruses
- 20. Bladder Cancer
- 21. Bladder Cancer Lung Cancer
- 22. Bladder Cancer Lung Cancer Breast Cancer
- 23. Bladder Cancer Lung Cancer Breast Cancer Melanoma
- 24. Bladder Cancer Lung Cancer Breast Cancer Melanoma Colon and Rectal Cancer
- 25. Bladder Cancer Lung Cancer Breast Cancer Melanoma Colon and Rectal Cancer Non-Hodgkin Lymphoma
- 26. Bladder Cancer Lung Cancer Breast Cancer Melanoma Colon and Rectal Cancer Non-Hodgkin Lymphoma Endometrial Cancer
- 27. Bladder Cancer Lung Cancer Breast Cancer Melanoma Colon and Rectal Cancer Non-Hodgkin Lymphoma Endometrial Cancer Pancreatic Cancer
- 28. Bladder Cancer Lung Cancer Breast Cancer Melanoma Colon and Rectal Cancer Non-Hodgkin Lymphoma Endometrial Cancer Pancreatic Cancer Kidney (Renal Cell) Cancer
- 29. Bladder Cancer Lung Cancer Breast Cancer Melanoma Colon and Rectal Cancer Non-Hodgkin Lymphoma Endometrial Cancer Pancreatic Cancer Kidney (Renal Cell) Cancer Prostate Cancer
- 30. Bladder Cancer Lung Cancer Breast Cancer Melanoma Colon and Rectal Cancer Non-Hodgkin Lymphoma Endometrial Cancer Pancreatic Cancer Kidney (Renal Cell) Cancer Prostate Cancer Thyroid Cancer
- 31. Bladder Cancer Lung Cancer Breast Cancer Melanoma Colon and Rectal Cancer Non-Hodgkin Lymphoma Endometrial Cancer Pancreatic Cancer Kidney (Renal Cell) Cancer Prostate Cancer Thyroid Cancer
- 32. Leukemia
- 33. TESTS Biopsy of the tumor Blood tests (which look for chemicals such as tumor markers) Bone marrow biopsy (for lymphoma or leukemia) Chest x-ray Complete blood count (CBC) CT scan Liver function tests MRI scan
- 34. TREATMENT & PREVENTION
- 35. TREATMENT •Surgery •Chemotherapy •Radiation •Targeted Cancer Treatments •Small Molecule Inhibitors •Antibodies •Cell Based Immunotherapy •Gene Therapy
- 36. Chemotherapy Drugs used to kill cancer cells; disrupt some aspect of cell division. Toxic to healthy cells; hair, bone marrow, lymphocytes, and epithelial cells of intestinal lining . Side effects include hair loss, nausea, vomiting, and reduced immune responses.
- 37. Radiation therapy High-energy rays are used to kill cancer cells Stop them from growing and dividing. radiotherapy is a local treatment; it can affect cancer cells only in the treated area. side effects- Tiredness, skin reactions such as rash or redness, and loss of appetite. Temporary lowering of the WBC count.
- 38. Surgery therapy In localized cancer surgery typically attempts to remove the entire mass. Biological therapy/immunotherapy Monoclonal antibodies, interferon, interleukin- 2, and colony-stimulating factors. Side effects - Temporary flu-like symptoms such as fever and chills, muscle aches and weakness, loss of appetite and diarrhea.
- 39. Recently launched drugs- Axitinib (Inlyta) for advanced kidney cancer. Vismodegib (Erivedge) for advanced basal cell carcinoma. Carfilzomib (Kyprolis) for multiple myeloma. Ziv-aflibercept (Zaltrap) in combination with chemotherapy for metastatic colon cancer. Regorafenib (Stivarga) for metastatic colorectal cancer .
- 40. PREVENTION Eating a healthy diet. Exercising regularly. Limiting alcohol. Maintaining a healthy weight. Minimizing your exposure to radiation and toxic chemicals. Not smoking or chewing tobacco Reducing sun exposure, especially if you burn easily.
- 41. CONCLUSION Hence cancer is second leading cause of deaths following heart diseases one should care about its prevention before the occurrence of disease by varies examinations and if disease is already exists then one should go for its regular treatment. Recent treatment mainly includes radiation therapy, cell based immunotherapy, gene therapy, chemotherapy are most widely used methods used for treatment of various type of cancers.
- 42. REFERNCES www.chronicdisease.isdh.in www.cancer.gov www.chronicdisease.isdh.in.gov http://www.essense-of-life.com/moreinfo/minerals/cesium.htm http://www.micronmetals.com/55.htm http://www.stopcancer.com/toc.htm http://www.prostate90.com/sci_papers/warburg.html http://www.alternative-doctor.com/cancer/oxygen.htm http://www.advancedhealthplan.com/2cesiumchlorideforcancer2.html Cancer Facts and Figures 2012". Journalist's Resource.org http://www.medicalnewstoday.com/info/cancer-oncology http://www.news-medical.net/health/What-is-Cancer.aspx http://www.cancerresearchuk.org/ http://www.who.int/cancer/

Colorectal cancer cases more than tripled among teens over two decades, data show
C olorectal cancer incidence has steadily increased among younger people in the U.S. over the last two decades, with the youngest seeing the most dramatic jumps, according to a study scheduled for presentation at Digestive Disease Week (DDW) 2024. Between 1999 and 2020, the rate of colorectal cancers grew 500% among children ages 10 to 14, 333% among teens aged 15 to 19, and 185% among young adults ages 20 to 24, researchers said.
"Colorectal cancer is no longer considered just a disease of the elderly population," said lead researcher Islam Mohamed, MD, an internal medicine resident physician at the University of Missouri-Kansas City. "It's important that the public is aware of signs and symptoms of colorectal cancer."
Risk factors include a family history of inflammatory bowel disease or colorectal cancer. Modifiable risk factors include obesity, tobacco use, alcohol consumption and dietary habits such as low fiber intake, consumption of processed meats or sugar-sweetened beverages and a high-fat diet. Sedentary lifestyle, the presence of bacteria that tend to cause tumors, antibiotic usage, and dietary additives are potential, but not firmly established, contributors to colorectal cancer risk.
Using data from the Centers for Disease Control Wonder Database, Mohamed's team calculated trends in colorectal cancer rates for people ages 10 to 44 from 1999 to 2020.
The number of colorectal cancer cases among children and teens is not high enough to suggest widespread colonoscopy screening, but more tailored approaches should be considered, Mohamed said. In 2020, only .6 children ages 10 to14 per 100,000 population were diagnosed compared to .1 per 100,000 in 1999. Diagnoses in teens age 15 to 19 went from .3 to 1.3 per 100,000, and in young adults ages 20 to 24, cases rose from .7 to 2 per 100,000.
The most common symptoms for colorectal cancer identified in patients with early onset colorectal cancer were changes in bowel habits in terms of either constipation or diarrhea, abdominal pain, rectal bleeding and signs of iron deficiency anemia, Mohamed said.
Escalations were also found in the higher age brackets, with rates rising by 71% to 6.5 per 100,000 people in ages 30 to 34 and by 58% to 11.7 per 100,000 in ages 35 to 39 in 2020. While the 40-to-44 age group had a lower percentage increase of 37%, this group had the highest incidence rate, reaching 20 per 100,000 people in 2020.
Dr. Mohamed will present data from the study, "Evolving trends in colorectal cancer incidence among young patients under 45: A 22-year analysis of the Centers for Disease Control Wonder Database," abstract Mo1149, on Monday, May 20, at 12:30 p.m. EDT.
Provided by Digestive Disease Week

Lecia V. Sequist, MD, MPH - Screening and Early Intervention as the Keys to Success in Lung Cancer: A Practical Approach to Implementing Lung Cancer Screening for High-Risk Individuals PeerView Oncology & Hematology CME/CNE/CPE Audio Podcast
This content has been developed for healthcare professionals only. Patients who seek health information should consult with their physician or relevant patient advocacy groups. For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/AAPA/IPCE information, and to apply for credit, please visit us at PeerView.com/PJP865. CME/MOC/AAPA/IPCE credit will be available until April 16, 2025. Screening and Early Intervention as the Keys to Success in Lung Cancer: A Practical Approach to Implementing Lung Cancer Screening for High-Risk Individuals In support of improving patient care, this activity has been planned and implemented by PVI, PeerView Institute for Medical Education, and LUNGevity Foundation. PVI, PeerView Institute for Medical Education, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team. Support This activity is supported by an educational grant from Merck & Co., Inc. Disclosure information is available at the beginning of the video presentation.
- Episode Website
- More Episodes
Top Podcasts In Science
Clinical Benefit From Immunotherapy in Patients With SCLC Is Associated With Tumor Capacity for Antigen Presentation
Affiliations.
- 1 Thoracic Oncology Service, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, New York; Department of Medicine, Weill Cornell Medical College, New York, New York; Druckenmiller Center for Lung Cancer Research, Memorial Sloan Kettering Cancer Center, New York, New York. Electronic address: [email protected].
- 2 Bristol-Myers Squibb, New York, New York.
- 3 Thoracic Oncology Service, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, New York; Department of Medicine, Weill Cornell Medical College, New York, New York.
- 4 Marie-Josée and Henry R. Kravis Center for Molecular Oncology, Memorial Sloan Kettering Cancer Center, New York, New York.
- 5 Cancer Biology Program, Louis V. Gerstner Jr. Graduate School of Biomedical Sciences, Memorial Sloan Kettering Cancer Center, New York, New York.
- 6 Druckenmiller Center for Lung Cancer Research, Memorial Sloan Kettering Cancer Center, New York, New York.
- 7 Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, New York.
- 8 Perlmutter Cancer Center, New York University Langone Health, New York, New York.
- PMID: 37210008
- PMCID: PMC10524620 (available on 2024-09-01 )
- DOI: 10.1016/j.jtho.2023.05.008
Introduction: A small percentage of patients with SCLC experience durable responses to immune checkpoint blockade (ICB). Defining determinants of immune response may nominate strategies to broaden the efficacy of immunotherapy in patients with SCLC. Prior studies have been limited by small numbers or concomitant chemotherapy administration.
Methods: CheckMate 032, a multicenter, open-label, phase 1/2 trial evaluating nivolumab alone or with ipilimumab was the largest study of ICB alone in patients with SCLC. We performed comprehensive RNA sequencing of 286 pretreatment SCLC tumor samples, assessing outcome on the basis of defined SCLC subtypes (SCLC-A, -N, -P, and -Y), and expression signatures associated with durable benefit, defined as progression-free survival more than or equal to 6 months. Potential biomarkers were further explored by immunohistochemistry.
Results: None of the subtypes were associated with survival. Antigen presentation machinery signature (p = 0.000032) and presence of more than or equal to 1% infiltrating CD8+ T cells by immunohistochemistry (hazard ratio = 0.51, 95% confidence interval: 0.27-0.95) both correlated with survival in patients treated with nivolumab. Pathway enrichment analysis revealed the association between durable benefit from immunotherapy and antigen processing and presentation. Analysis of epigenetic determinants of antigen presentation identified LSD1 gene expression as a correlate of worse survival outcomes for patients treated with either nivolumab or the combination of nivolumab and ipilimumab.
Conclusions: Tumor antigen processing and presentation is a key correlate of ICB efficacy in patients with SCLC. As antigen presentation machinery is frequently epigenetically suppressed in SCLC, this study defines a targetable mechanism by which we might improve clinical benefit of ICB for patients with SCLC.
Keywords: Antigen presentation; Epigenetics; Immune checkpoint blockade; Small cell lung cancer.
Copyright © 2023 International Association for the Study of Lung Cancer. Published by Elsevier Inc. All rights reserved.
Publication types
- Clinical Trial, Phase II
- Clinical Trial, Phase I
- Multicenter Study
- Research Support, Non-U.S. Gov't
- Research Support, N.I.H., Extramural
- Antigen Presentation
- Immunotherapy
- Ipilimumab / therapeutic use
- Lung Neoplasms* / pathology
- Nivolumab / therapeutic use
- Small Cell Lung Carcinoma* / pathology
Grants and funding
- P30 CA008748/CA/NCI NIH HHS/United States
- R01 CA258784/CA/NCI NIH HHS/United States
- R35 CA263816/CA/NCI NIH HHS/United States
- U24 CA213274/CA/NCI NIH HHS/United States
- Policy Guidance
- Submitting Data
- Accessing Data
- About the Genomic Data Sharing (GDS) Policy
- Key Documents
- Preparing Genomic Data
- Extramural Grantees
- Non-NCI Funded Investigators
- Intramural Investigators
- Accessing Genomic Data
- Genomic Data Sharing Policy Contact Information
- Data Standards Services
- Cloud Resources
- Data Commons Framework
- Repositories
- ARPA-H BDF Toolbox
- Accelerating Therapeutics for Opportunities in Medicine (ATOM)
- NCI-DOE Collaboration AI/ML Resources
- NCI-DOE Publications
- U.S.-EU Artificial Intelligence Administrative Arrangement
- NCI Data Catalog
- CDISC Terminology
- FDA Terminology
- NCPDP Terminology
- Pediatric Terminology
- Metadata for Cancer Research
- Informatics Technology for Cancer Research (ITCR) Tools
- Generating and Collecting Data
- Cleaning Data
- Exploring and Analyzing Data
- Predictive Modeling
- Visualizing Data
- Sharing Data
- Cancer Data Science Course
- Training Guide Library
- Cancer Data Science Pulse Blog
- Data Science Seminar Series
- Jobs and Fellowships
- Contact CBIIT
- Organization
- CBIIT Director
- Staff Directory
- Application Support
- Genomic Data Sharing
- NCI-Department of Energy Collaborations
- Cancer Vocabulary
- Learn About Cancer Data Science
- Improve My Data Science Skills
Oncoexporter: Conversion of NCI CRDC Data to the GA4GH Phenopacket Schema
If you’re attending the EACR 2024, make sure you hear Dr. Daoud Meerzaman’s poster presentation on using Oncoexporter to convert Cancer Research Data Commons (CRDC) data into the Global Alliance for Genomics and Health (GA4GH) Phenopackets schema.
Dr. Meerzaman will illustrate the application of the Phenopacket standard to CRDC data and demonstrate a subsequent application to a simple clinical analysis.
Providing tools to convert CRDC data into the Phenopacket schema will enable further integration and analysis of a broad array of cancer data. This integration could unlock important insights into cancer development, progression, and treatment hidden in the massive reservoirs of heterogeneous cancer data sets worldwide.
The GA4GH Phenopacket schema is a common framework for capturing phenotypic and genotypic data in a way that works well with downstream machine learning applications.
The CRDC is a cloud-based infrastructure that provides public and controlled access to multiple large-scale cancer data sets . You can use NCI Cloud Resources to analyze these data sets without downloading.
Dr. Meerzaman is the Computational Genomics and Bioinformatics Branch chief at NCI’s Center for Biomedical Informatics and Information Technology. Dr. Meerzaman and his team provide bioinformatics analysis support for life sciences and clinical and translational research for intramural scientists, including NCI’s Division of Cancer Epidemiology and Genetics and Center for Cancer Research.
Enter the characters shown in the image.
SUBSCRIBE TO UPDATES
Upcoming events.
- Immuno-Oncology Translational Network (IOTN) Capstone Meeting May 14, 2024 - May 15, 2024 COnsortium of METabolomics Studies (COMETS) Analytics Workshop May 15, 2024 AI in Personalized Immunotherapies May 15, 2024 Co-Clinical Imaging Research Resource Program Annual Hybrid Meeting 2024 May 20, 2024 - May 21, 2024 Promises and Challenges: Automated Extraction of Electronic Health Record Data May 21, 2024 Machine Learning Dynamics in the Tumor Microenvironment May 22, 2024
- Presentation/Conference
- Seminar Series
Past Events
- See Past Events
- See Past Events with Videos
Help Us Help You: Take this 5-minute Survey!
We want to know what you want from this website and our weekly email. Your feedback will help us ensure we’re getting you the information you want, how you want it.
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My Portfolio
- Latest News
- Stock Market
- Premium News
- Biden Economy
- EV Deep Dive
- Stocks: Most Actives
- Stocks: Gainers
- Stocks: Losers
- Trending Tickers
- World Indices
- US Treasury Bonds
- Top Mutual Funds
- Highest Open Interest
- Highest Implied Volatility
- Stock Comparison
- Advanced Charts
- Currency Converter
- Investment Ideas
- Research Reports
- Basic Materials
- Communication Services
- Consumer Cyclical
- Consumer Defensive
- Financial Services
- Industrials
- Real Estate
- Mutual Funds
- Analyst Rating
- Technical Events
- Smart Money
- Top Holdings
- Credit cards
- Balance Transfer Cards
- Cash-back Cards
- Rewards Cards
- Travel Cards
- Personal Loans
- Student Loans
- Car Insurance
- Morning Brief
- Market Domination
- Market Domination Overtime
- Opening Bid
- Stocks in Translation
- Lead This Way
- Good Buy or Goodbye?
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo

- CA Privacy Notice
Yahoo Finance
Arvinas announces upcoming vepdegestrant poster presentations at the 2024 european society for medical oncology (esmo) breast cancer annual congress.
NEW HAVEN, Conn., May 09, 2024 (GLOBE NEWSWIRE) -- Arvinas, Inc. (Nasdaq: ARVN) today announced that two posters, including updated clinical trial data, for vepdegestrant will be presented at the 2024 European Society for Medical Oncology (ESMO) Breast Cancer Annual Congress held from May 15-17, 2024, in Berlin, Germany. Vepdegestrant is a novel investigational PROTAC ® estrogen receptor (ER) degrader that is being jointly developed by Arvinas and Pfizer for the treatment of patients with early and locally advanced or metastatic ER positive/human epidermal growth factor receptor 2 (HER2) negative (ER+/HER2-) breast cancer.
Poster session details are as follows: Date: Thursday, May 16, 2024 Time: 12:00 – 1:00 p.m. CET/ 6:00 – 7:00 a.m. ET Category: Metastatic Breast Cancer
Poster Title and Number: Vepdegestrant, a PROteolysis TArgeting Chimera (PROTAC) estrogen receptor (ER) degrader, plus palbociclib (palbo) in ER+/human epidermal growth factor receptor 2 (HER2)- advanced breast cancer: updated phase 1b cohort results, Poster 218P Presentation Type and Abstract Number: Abstract, 453
Poster Title and Number: TACTIVE-K: phase 1b/2 study of vepdegestrant, a PROteolysis TArgeting Chimera (PROTAC) estrogen receptor (ER) degrader, in combination with PF-07220060, a cyclin-dependent kinase (CDK)4 inhibitor, in ER+/human epidermal growth factor receptor 2 (HER2)- advanced breast cancer, Poster 264 Presentation Type and Abstract Number: Trial-in-Progress (TiP), 488
Abstracts are now available via the official ESMO Breast Cancer Annual Congress website here .
About Vepdegestrant Vepdegestrant is an investigational, orally bioavailable PROTAC protein degrader designed to specifically target and degrade the estrogen receptor (ER) for the treatment of patients with ER positive (ER+)/human epidermal growth factor receptor 2 (HER2) negative (ER+/HER2-) breast cancer. Vepdegestrant is being developed as a potential monotherapy and as part of combination therapy across multiple treatment settings for ER+/HER2- metastatic breast cancer.
In July 2021, Arvinas announced a global collaboration with Pfizer for the co-development and co-commercialization of vepdegestrant; Arvinas and Pfizer will share worldwide development costs, commercialization expenses, and profits.
The U.S. Food and Drug Administration (FDA) has granted vepdegestrant Fast Track designation as a monotherapy in the treatment of adults with ER+/HER2- locally advanced or metastatic breast cancer previously treated with endocrine-based therapy.
About Arvinas Arvinas is a clinical-stage biotechnology company dedicated to improving the lives of patients suffering from debilitating and life-threatening diseases through the discovery, development, and commercialization of therapies that degrade disease-causing proteins. Arvinas uses its proprietary PROTAC ® Discovery Engine platform to engineer proteolysis targeting chimeras, or PROTAC ® targeted protein degraders, that are designed to harness the body’s own natural protein disposal system to selectively and efficiently degrade and remove disease-causing proteins. In addition to its robust preclinical pipeline of PROTAC protein degraders against validated and “undruggable” targets, the company has four investigational clinical-stage programs: vepdegestrant for the treatment of patients with locally advanced or metastatic ER+/HER2- breast cancer; ARV-766 and bavdegalutamide for the treatment of men with metastatic castration-resistant prostate cancer; and ARV-102 for the treatment of patients with neurodegenerative disorders. For more information, visit www.arvinas.com .
Forward-Looking Statements This press release contains forward-looking statements within the meaning of The Private Securities Litigation Reform Act of 1995 that involve substantial risks and uncertainties, including statements regarding plans with respect to vepdegestrant as a potential monotherapy and combination across multiple treatment settings for ER+/HER2- metastatic breast cancer. All statements, other than statements of historical facts, contained in this press release, including statements regarding Arvinas’ strategy, future operations, future financial position, future revenues, projected costs, prospects, plans and objectives of management, are forward-looking statements. The words “anticipate,” “believe,” “estimate,” “expect,” “intend,” “may,” “might,” “plan,” “predict,” “project,” “target,” “potential,” “will,” “would,” “could,” “should,” “continue,” and similar expressions are intended to identify forward-looking statements, although not all forward-looking statements contain these identifying words.
Arvinas may not actually achieve the plans, intentions or expectations disclosed in these forward-looking statements, and you should not place undue reliance on such forward-looking statements. Actual results or events could differ materially from the plans, intentions and expectations disclosed in the forward-looking statements Arvinas makes as a result of various risks and uncertainties, including but not limited to: Arvinas’ and Pfizer, Inc.’s (“Pfizer”) performance of the respective obligations with respect to Arvinas’ collaboration with Pfizer; whether Arvinas and Pfizer will be able to successfully conduct and complete clinical development for vepdegestrant (ARV-471); whether Arvinas and Pfizer, as appropriate, will be able to obtain marketing approval for and commercialize vepdegestrant (ARV-471)on current timelines or at all; Arvinas’ ability to protect its intellectual property portfolio; whether Arvinas’ cash and cash equivalent resources will be sufficient to fund its foreseeable and unforeseeable operating expenses and capital expenditure requirements; and other important factors discussed in the “Risk Factors” section of Arvinas’ Annual Report on Form 10-K for the year ended December 31, 2023 and subsequent other reports on file with the U.S. Securities and Exchange Commission. The forward-looking statements contained in this press release reflect Arvinas’ current views with respect to future events, and Arvinas assumes no obligation to update any forward-looking statements, except as required by applicable law. These forward-looking statements should not be relied upon as representing Arvinas’ views as of any date subsequent to the date of this release.
Investors: Jeff Boyle +1 (347) 247-5089 [email protected]
Media: Kathleen Murphy +1 (760) 622-3771 [email protected]
Recommended Stories
Billionaire jim simons owns these 2 healthcare stocks: should you.
These stocks are both experts in their respective fields.
Moderna Tumbles After The FDA Throws A Curveball On Its Second Product
Moderna stock toppled Friday after the FDA delayed an approval decision on its RSV vaccine until the end of the month.
1 No-Brainer Growth Stock to Buy and Hold
It's hard to bet against this high-flying stock.
Q&A with Maddy Dychtwald: What the longevity revolution means for women
Women are living longer than men, but they often spend the last decade or so in "a cascade of poor health,” author Maddy Dychtwald said.
US Health Officials to Spend $100 Million on Bird Flu Surveillance
(Bloomberg) -- US health officials are putting more than $100 million toward ramping up surveillance of bird flu in cattle and people amid rising concerns that the outbreak has spread more widely than reported. Most Read from BloombergApple Nears Deal With OpenAI to Put ChatGPT on iPhoneHow One Brooklyn Neighborhood Became a Nightclub HavenTrump Pledges Across-the-Board Tax Cuts If He Returns to OfficeIce Cube’s Big3 Basketball League Sells Its First Team in $10 Million DealThe Centers for Disea
43-year-old fitness influencer ignored her GI symptoms for a year. Then she was diagnosed with stage 4 colon cancer: ‘It could happen to anyone’
"I want to create awareness that it can happen to anyone," says Maria Kang, 43.
Patients face longer trips, less access to health care after Walmart shuts clinics
For rural and lower-income patients, staying healthy will become more time-consuming after Walmart's exit from the primary care business, experts say.
Utility stocks are on fire — here are Wall Street analysts' top picks
Utility stocks are outperforming the broader markets. Here's a look at three top picks from analysts.
Should You Buy Nvidia Stock Before May 22?
Nvidia is scheduled to make a significant investor announcement that could have enormous implications for the stock price.
1 Stock (Not Nvidia) Could Be a Massive Winner From Data Center AI
This company also combines a powerful portfolio of both chips and software, not unlike what Nvidia is building.
- Get 7 Days Free
Abivax announces presentation of four abstracts for obefazimod in ulcerative colitis and preclinical colon cancer model at Digestive Disease Week 2024
PARIS, France, May 8, 2024, 8:30 a.m. CEST – Abivax SA (Euronext Paris & Nasdaq: ABVX) (“Abivax” or the “Company”), a clinical-stage biotechnology company focused on developing therapeutics that harness the body’s natural regulatory mechanisms to stabilize the immune response in patients with chronic inflammatory diseases, today announced that four scientific abstracts on its lead drug candidate, obefazimod, for the treatment of moderately to severely active ulcerative colitis (UC) and in a preclinical model on colon cancer, will be presented at Digestive Disease Week (DDW) as part of scientific exchange, taking place May 18-21, 2024, in Washington D.C., U.S.
“With four abstracts accepted for presentation at DDW 2024, we look forward to our continued exchange with the IBD community around the emerging clinical profile of obefazimod,” said Sheldon Sloan, M.D., M. Bioethics, Chief Medical Officer of Abivax. “We are excited to share new preclinical data showing obefazimod’s impact in reducing the number of tumors in the azoxymethane (AOM)/dextran sodium sulfate (DSS) mouse model of colitis-associated cancer—data in support of obefazimod’s novel mechanism of action.”
For more information, visit the Abivax booth at the DDW exhibitor hall (booth #529) or see congress details on the DDW website . Obefazimod data to be presented:
Abivax has also sponsored a Product Theater presentation titled, “ An Investigational New MOA that Can Stabilize the Inflammatory Response in Ulcerative Colitis ,” taking place on May 20, 2024, at 2:30-3:15 p.m. EDT in room “DDW Theater 1,” featuring Prof. Parambir S. Dulai, M.D., Associate Professor of Medicine in the Division of Gastroenterology and Hepatology at Northwestern University, Evanston, Illinois, U.S.
About Obefazimod Obefazimod, Abivax’s lead investigational drug candidate, is an orally administered small molecule that was demonstrated to potentially enhance the expression of a single microRNA, miR-124. Phase 2 clinical trials in patients with UC have generated positive data, resulting in the initiation of a pivotal global Phase 3 clinical trial program (ABTECT Program), with first patients enrolled in the United States in October 2022. Initiation of a Phase 2b clinical trial in Crohn’s disease is expected in Q3 2024, and exploration of potential combination therapy opportunities in UC is ongoing.
About Abivax Abivax is a clinical-stage biotechnology company focused on developing therapeutics that harness the body’s natural regulatory mechanisms to stabilize the immune response in patients with chronic inflammatory diseases. Based in France and the United States, Abivax’s lead drug candidate, obefazimod (ABX464), is in Phase 3 clinical trials for the treatment of moderately to severely active ulcerative colitis. More information on the Company is available at www.abivax.com . Follow us on LinkedIn and on X, formerly Twitter, @Abivax. Contact:
Abivax Investor Relations Patrick Malloy [email protected] +1 847 987 4878
Abivax Communications [email protected]
FORWARD-LOOKING STATEMENTS
This press release contains forward-looking statements, forecasts and estimates, including those relating to the Company’s business and financial objectives. Words such as “design,” “expect,” “forward,” “future,” “potential,” “plan,” “project” and variations of such words and similar expressions are intended to identify forward-looking statements. Although Abivax’s management believes that the expectations reflected in such forward-looking statements are reasonable, investors are cautioned that forward-looking information and statements are subject to various risks, contingencies and uncertainties, many of which are difficult to predict and generally beyond the control of Abivax, that could cause actual results and developments to differ materially from those expressed in, or implied or projected by, the forward-looking information and statements. A description of these risks, contingencies and uncertainties can be found in the documents filed by the Company with the French Autorité des Marchés Financiers pursuant to its legal obligations including its universal registration document (Document d’Enregistrement Universel) and in our Annual Report on Form 20-F filed with the U.S. Securities and Exchange Commission on April 5, 2024 under the caption “Risk Factors.” These risks, contingencies and uncertainties include, among other things, the uncertainties inherent in research and development, future clinical data and analysis, decisions by regulatory authorities, such as the FDA or the EMA, regarding whether and when to approve any drug candidate, as well as their decisions regarding labelling and other matters that could affect the availability or commercial potential of such product candidates. Special consideration should be given to the potential hurdles of clinical and pharmaceutical development including further assessment by the company and regulatory agencies and IRBs/ethics committees following the assessment of preclinical, pharmacokinetic, carcinogenicity, toxicity, CMC and clinical data. Furthermore, these forward-looking statements, forecasts and estimates are only as of the date of this press release. Readers are cautioned not to place undue reliance on these forward-looking statements. Abivax disclaims any obligation to update these forward-looking statements, forecasts or estimates to reflect any subsequent changes that the Company becomes aware of, except as required by law. Information about pharmaceutical products (including products currently in development) that is included in this press release is not intended to constitute an advertisement. This press release is for information purposes only, and the information contained herein does not constitute either an offer to sell, or the solicitation of an offer to purchase or subscribe securities of the Company in any jurisdiction. Similarly, it does not give and should not be treated as giving investment advice. It has no connection with the investment objectives, financial situation or specific needs of any recipient. It should not be regarded by recipients as a substitute for exercise of their own judgment. All opinions expressed herein are subject to change without notice. The distribution of this document may be restricted by law in certain jurisdictions. Persons into whose possession this document comes are required to inform themselves about and to observe any such restrictions.
Market Updates
5 things we learned from the q1 earnings season, after earnings, is palantir stock a buy, a sell, or fairly valued, what’s happening in the markets this week, can the fed declare victory on inflation, after earnings, is coinbase stock a buy, a sell, or fairly valued, after earnings, is albemarle stock a buy, a sell, or fairly valued, is servicenow stock a buy after earnings and its investor day, 3 stocks to buy and 3 stocks to sell after earnings, stock picks, today’s market volatility could provide tomorrow’s opportunities, 40 of the best investment picks, tech stock dividends are changing the face of dividend growth investing, roblox earnings: weakening engagement has weighed on growth, the best gaming stocks to buy, energy transfer earnings: m&a drives guidance increase in solid quarter, the best healthcare stocks to buy, going into earnings, is home depot stock a buy, a sell, or fairly valued, sponsor center.

COMMENTS
The Definition of Cancer. Cancer is a disease in which some of the body's cells grow uncontrollably and spread to other parts of the body. Cancer can start almost anywhere in the human body, which is made up of trillions of cells. Normally, human cells grow and multiply (through a process called cell division) to form new cells as the body ...
Cancer refers to any one of a large number of diseases characterized by the development of abnormal cells that divide uncontrollably and have the ability to infiltrate and destroy normal body tissue. Cancer often has the ability to spread throughout your body. Cancer is the second-leading cause of death in the world.
Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020, or nearly one in six deaths. The most common cancers are breast, lung, colon and rectum and prostate cancers. Around one-third of deaths from cancer are due to tobacco use, high body mass index, alcohol consumption, low fruit and vegetable intake, and ...
Hematologic (blood) cancers are cancers of the blood cells, including leukemia, lymphoma, and multiple myeloma. Solid tumor cancers are cancers of any of the other body organs or tissues. The most common solid tumors are breast, prostate, lung, and colorectal cancers. These cancers are alike in some ways, but can be different in the ways they ...
Understanding Cancer - Student PPT. R. Cancer. R. Lung Breast (women) Colon Bladder Prostate (men) Fat Bone Muscle Lymph nodes Bloodstream. What are some different kinds of cancer? R. How are Normal and Cancer Cell Division Different? Cancer cell division Normal cell division.
These resources include single page, front-and-back PDF fact sheets and PowerPoint presentations that offer the latest figures and trends for common cancers. Appropriate for students and health care professionals who want to learn more about these cancers. (We also have handouts for patient ...
Cancer is a broad term. It describes the disease that results when cellular changes cause the uncontrolled growth and division of cells. Some types of cancer cause rapid cell growth, while others ...
The most requested tables and figures from Cancer Facts & Figures 2022 have been assembled in an electronic format (PDF) to make it easy for you to use them. Please note that all graphic material should credit the "American Cancer Society, Cancer Facts & Figures 2022." Trends in Age-adjusted Cancer Death Rates by Site, Males, US, 1930-2019 (PDF)
Download the "Endometrial Cancer Detection Breakthrough" presentation for PowerPoint or Google Slides. Treating diseases involves a lot of prior research and clinical trials. But whenever there's a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it's great news.
About breast cancer. Cancer begins when healthy cells in the breast change and grow out of control, forming a mass or sheet of cells called a tumor. A tumor can be cancerous or noncancerous, also called benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body.
Despite specific presenting symptoms being more strongly associated with advanced stage at diagnosis than others, for most symptoms, large proportions of patients are diagnosed at stages other than stage IV. These findings provide support for early diagnosis interventions targeting common cancer symptoms, countering concerns that they might be simply expediting the detection of advanced stage ...
To elicit an effective antitumour response, antigen presentation has to be successful at two distinct events: first, cancer neoantigens have to be taken up by professional antigen-presenting cells ...
Women who have family members with breast, ovarian, tubal, or peritoneal cancer should be screened to identify a family history that may be associated with an increased risk for mutations in the breast cancer susceptibility genes BRCA1 or BRCA2. Women who have positive screening results should receive genetic counseling and then BRCA testing if ...
Breast cancer is the most common cancer diagnosed in women, accounting for more than 1 in 10 new cancer diagnoses each year. It is the second most common cause of death from cancer among women in the world. Anatomically, the breast has milk-producing glands in front of the chest wall. They lie on the pectoralis major muscle, and there are ligaments support the breast and attach it to the chest ...
Presentations and Publications. CancerCare's professional oncology social workers and staff actively research, present and publish on numerous cancer-related topics that directly impact the lives of people coping with cancer. Staff Expertise. Our staff's publications, presentations, reports and videos are featured at national oncology and ...
Several antibodies targeting PD-1 or PD-L1, including nivolumab and pembrolizumab, have since been approved for clinical use in an expanding list of tumour types, including melanoma, lung cancer ...
Download your presentation as a PowerPoint template or use it online as a Google Slides theme. 100% free, no registration or download limits. Create informative and engaging cancer presentations with these Google Slide templates. No Download Limits Free for Any Use No Signups.
Jun 2, 2009 • Download as PPT, PDF •. 199 likes • 276,796 views. Patty Melody. Health & Medicine Technology. Slideshow view. Download now. Cancer Powerpoint - Download as a PDF or view online for free.
CANCER - Download as a PDF or view online for free. 2. WHAT IS CANCER? • Cancer (medical term: malignant neoplasm) is a class of diseases in which a group of cell display uncontrolled growth through division beyond normal limits, invasion that intrudes upon and destroys adjacent tissues, and sometimes metastasis, which spreads the cells to other locations in the body via lymph or blood.
People with cancer can feel many mixed emotions, going from happiness to sadness in an instant. They feel fear and distress most of the time but also feel alone and distant from other people. These feelings are also felt by the family that are close to the person with cancer. Like sadness or fear that the person could be hurt or even die of the ...
Cancer ppt. Mar 14, 2013 • Download as PPTX, PDF •. 333 likes • 269,692 views. Namdeo Shinde. CANCER TYPES, CAUSES AND TREATMENT. Health & Medicine. Download now. Cancer ppt - Download as a PDF or view online for free.
Diagnoses in teens age 15 to 19 went from .3 to 1.3 per 100,000, and in young adults ages 20 to 24, cases rose from .7 to 2 per 100,000. The most common symptoms for colorectal cancer identified ...
Mainz Biomed N.V., a molecular genetics diagnostic company specializing in the early detection of cancer, will present an analysis from its eAArly DETECT study at Digestive Disease Week (DDW) 2024 ...
For the full presentation, downloadable Practice Aids, slides, and complete CME/MOC/AAPA/IPCE information, and to apply fo… Show PeerView Oncology & Hematology CME/CNE/CPE Audio Podcast, Ep Lecia V. Sequist, MD, MPH - Screening and Early Intervention as the Keys to Success in Lung Cancer: A Practical Approach to Implementing Lung Cancer ...
Tumor antigen processing and presentation is a key correlate of ICB efficacy in patients with SCLC. As antigen presentation machinery is frequently epigenetically suppressed in SCLC, this study defines a targetable mechanism by which we might improve clinical benefit of ICB for patients with SCLC.
PK !*pæ Z  ppt/presentation.xmlìØÝnÓ0 ð{$Þ!Ê-ê ÛIìVkÑ ! iZÇ ˜ÄÝ"œ Ùî؆xwŽ"¬= â zµ$ œü¶Ù'Ïß?6:zPÆÖ]»ŒÉY Gª-»ªnï-ñ·ÛõLÄ'u²¤îZµŒŸ" ߯޾9ï ½QVµN:è Á0]Èe|ï\¿H [Þ«FÚ³®W-dÛÎ4ÒÁ¹K*# Âð Nhš I#ë6žú›ÿéßm·u©>vå® éÇAŒÒC ö¾îíËhýÿŒ†ßâ¸$+ Ôf÷Ý*·îZgA'^Ák[]}•Ö)󥺲îÕ ...
If you're attending the EACR 2024, make sure you hear Dr. Daoud Meerzaman's poster presentation on using Oncoexporter to convert Cancer Research Data Commons (CRDC) data into the Global Alliance for Genomics and Health (GA4GH) Phenopackets schema. Register by May 27, 2024, for regular rates; from May 28 onward, you'll pay the full rate.
Presentation Type and Abstract Number: Trial-in-Progress (TiP), 488 Abstracts are now available via the official ESMO Breast Cancer Annual Congress website here . About Vepdegestrant
Abivax announces presentation of four abstracts for obefazimod in ulcerative colitis and preclinical colon cancer model at Digestive Disease Week 2024.