An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Case Rep


Case Report
Special form of osteoporosis in a 53-year-old man, simon lampart.
1 Department of Internal Medicine, Luzerner Kantonsspital, Luzern, Switzerland
Silvia Azzarello-Burri
2 Institute of Medical Genetics, University of Zurich, Schlieren-Zurich, Switzerland
Christoph Henzen
3 Division of Endocrinology and Diabetes, Luzerner Kantonsspital, Luzern, Switzerland
Stefan Fischli
Male osteoporosis often remains unrecognised. Osteoporotic fractures occur approximately 10 years later in men than in women due to higher peak bone mass. However, 30% of all hip fractures occur in men. Risk factors of osteoporotic fractures can be grouped into primary and secondary causes. We present the case of a 53-year-old man, who suffered a compression fracture of a lumbar vertebra after a generalised seizure and an atraumatic rib fracture 5 months later. We could exclude secondary causes of bone mineral loss such as primary hyperparathyroidism, glucocorticoid use and hypogonadism. However, a heterozygous missense mutation of the COL1A1 gene in exon 48 in further search of a secondary cause was found. Therapy was changed from bisphosphonate treatment to teriparatide. Considering the lack of other osteogenesis imperfecta (OI) symptoms and signs, the patient’s illness can be classified as mild. OI should be considered as differential diagnosis in unexplained cases with osteoporosis.
In contrast to female patients, osteoporosis in men often remains an unrecognised and untreated condition. Due to the higher peak bone mass in men, osteoporotic fractures (ie, hip or vertebrae) normally occur 10 years later than in women. 1 However, male osteoporosis is a relevant and common clinical problem with high morbidity and mortality. 2 Thirty per cent of all hip fractures are arising in men 3 and sustaining a hip fracture is associated with twofold to threefold increased mortality risk relative to women. 4
As in women, risk factors for bone loss and osteoporotic fractures in men can be grouped into primary (age-related, idiopathic) and secondary causes. Among secondary causes, multiple risk factors for osteoporotic fractures in men have been identified, 5 that is, hypogonadism, low body mass index (BMI), smoking, excessive alcohol drinking and the use of glucocorticoid medications. Of these, a single or a combination of multiple risk factors can lead to a reduction of bone mineral density (BMD) or even superimpose the age-related bone loss.
Therefore, a thorough identification of potential risk factors is crucial to identify persons at risk 6 and to guide further diagnostic (ie, BMD assessment by Dual Energy X-Ray Absorptiometry (DEXA)) and therapeutic (ie, bisphosphonate treatment) measures.
In this case report, we describe a patient with a rare secondary form of osteoporosis.
Case presentation
A 53-year-old man presented at our hospital with a generalised seizure for the first time, which had caused a compression fracture of the first lumbar vertebra. The medical history of the patient was uneventful, he took no medications and he denied smoking, excessive alcohol consumption and the use of glucocorticoids in the past. Although older fractures were seen on the CT scan, there was no history of previous back pain. Symptoms of hypogonadism (ie, loss of libido or decreased spontaneous/morning erections) were absent as was a reduction of his height.
Clinical examination found a patient in good clinical conditions (weight 70 kg, height 170 cm, BMI 25.1 kg/m 2 , blood pressure 152/92 mm Hg, heart rate 78/min). Further examination revealed a normal configured spine with tenderness over the lumbar spine and absence of sensorimotoric deficits in the lower extremities. There were no signs suggestive of hypercortisolism or hearing loss; sclerae were normal.
Investigations
Laboratory analysis demonstrated normal values for creatinine, transaminases, serum calcium, phosphorus, parathyroid hormone, alkaline phosphatase, total testosterone, vitamin D and thyroid stimulating hormone. Protein electrophoresis with immune fixation was normal and coeliac disease was excluded by determination of antitransglutaminase antibodies. Adult systemic mastocytosis was ruled out by a normal serum tryptase and normal examination of bone marrow aspirate (including unremarkable immunophenotyping and moleculargenetic analysis of the aspirate).
Conventional X-ray imaging and a CT scan of the whole spine found older vertebral fractures at the thoracic (Th 6, 7, 8, 9 and 11) and lumbar (L3 and 4) level with the appearance of codfish vertebrae ( figures 1 and 2 ). BMD assessed by DEXA scan demonstrated a T-score of −3.3 at the lumbar spine and a T-score of −1.5 at the femoral neck.

X-ray, lateral view showing a new fracture of L1 and older fractures of Th11, L3 and L4.

CT scan, lateral view showing multiple older fractures Th 6, 7, 8, 9 and 11, L3 and L4, and a new fracture L1.
Due to the instability of the L1 fracture, kyphoplasty with internal fixation was performed. The patient was started on a combination therapy with calcium and vitamin D and he received bisphosphonate treatment with ibandronic acid.
Outcome and follow-up
Five months later, the patient returned and was diagnosed with rib fractures, which had occurred without trauma. In a further attempt to secure a secondary cause, a molecular genetic analysis for osteogenesis imperfecta (OI) was performed. This revealed a heterozygous missense variant of the COL1A1 gene ( {"type":"entrez-nucleotide","attrs":{"text":"NM_000088","term_id":"1777425449","term_text":"NM_000088"}} NM_000088 ; c.3688G>A, p.(Glu1230Lys)). This variant has a very low minor allele frequency of 0.001% and six different in silico prediction tools indicate a deleterious effect. The affected amino acid is located in the C-terminal propeptide, and with reference to the structure, the exchange would not be expected to cause a major structural disturbance. However, the reversal of charging could lead to reduced stability of the helix. Such a mild functional effect would be in line with the mild phenotype. We therefore assume that this variant is causative, although according to the current guidelines of the American College of Medical Genetics (ACMG), it would have to be classified as variant of unknown significance.
The treatment with bisphosphonates was re-evaluated in this patient after new fractures had occurred. It was decided to change the therapy to an osteoanabolic regimen with teriparatide. This led to a clear improvement of bone density in follow-up DEXA measurements and the absence of new fractures.
Initially, the patient was only aware of postmenopausal osteoporosis in his mother. However, after the diagnosis in the patient, it became apparent that further family members showed mild signs of OI. The brother of the patient suffered an osteoporotic vertebral fracture at the age of 52. Moreover, the patients’ son was said to have had three fractures after mild traumata (hand, finger, skull) and an abnormal audiogram, and he also suffered from tinnitus. Genetic testing in the patient’s brother and son confirmed that they are also carriers of the same COL1A1 variant.
OI (‘brittle bone disease’) is a group of disorders affecting connective tissue and bone structure. OI is rare with an estimated incidence of 1 in 20 000 7 or up to 1 in 10 000 births (Orphanet report series number 2 [2018]). Most of the cases are caused by autosomal-dominant inherited mutations in genes encoding alpha-1 and alpha-2 chains of type I collagen (COL1A1 and COL1A2). 8 Rarer forms include mutations of genes that encode proteins promoting post-translational modifications of type I collagen or bone formation and osteoblast maturation ( table 1 ).
Examples of mutations outside COL1A1/COL1A2 genes in mild OI forms overlapping with early-onset osteoporosis (adapted from 19 20 )
As type I collagen is an important protein for organic bone structure, typical osseous manifestation of OI include multiple/atypical fractures often caused by minimal trauma (‘brittle bones’), bowing and deformity of long bones, short stature, scoliosis and deformity of the skull. Extra skeletal manifestations include hearing loss, blue sclerae, dentinogenesis imperfecta and hyperlaxity of ligaments. The clinical spectrum of OI is very broad, depends on the type of mutation and ranges from mild manifestations (ie, accelerated postmenopausal osteoporosis) to severe forms in children (including perinatal lethal forms). 9 10
It is well known that peak bone mass 11 and the risk for osteoporosis are strongly determined by genetic 12 and epigenetic factors 13 following a complex mechanism. In rare cases, rare genetic variants with strong functional effects, that is, a COL1A1 mutation as in this patient, can play a critical role in the development of postmenopausal 14 or male osteoporosis.
Our patient presented with advanced osteoporosis and multiple low-trauma fractures. The L1 fracture was unstable and internal fixation/kyphoplasty was mandatory. At that time, the diagnosis of OI was not made. However, it should be emphasised that caution should be kept with kyphoplasty in patients with OI due to the increased risk of fractures in the adjacent vertebral bodies after such procedures.
The patient was initially treated with ibandronate. Later, therapy was changed to teriparatide after the patient had suffered new fractures. Bisphosphonates remain the mainstay of treatment in patients with moderate and severe forms of OI. 15 However, there is a growing body of evidence that teriparatide may be helpful in patient with milder forms of OI. 16 17
A thorough search for secondary causes of osteoporosis (ie, hypogonadism, systemic mastocytosis) remained uneventful. However, due to his multiple health complaints next to the osteoporosis, including seizures, migraine and a possible histamine intolerance, the patient was referred to genetic counselling to evaluate the possibility of a genetic condition. Because of the osteoporosis and low-trauma fractures in a male patient, genetic testing for the COL1A1 and COL1A2 genes were initiated and supported the clinical suspicion of OI. Based on the clinical findings and the lack of other OI typical features (ie, deformity of long bones, absence of hearing loss and blue sclerae), the OI in this case can be classified as mild. The heterozygous missense variant in the COL1A1 gene that was found in our patient has not been described in the literature to date. However, one case with mild OI was described in the literature to harbour a variant in a similar location. 18 Based on this report and the variant characteristics detailed above, we considered it likely causal for the advanced osteoporosis in our patient. It is unknown if it is a de novo mutation or if it was inherited in an autosomal-dominant manner. However, since the brother also carries the same variant, we assume that the mother with postmenopausal osteoporosis is also a carrier. Each carrier transmits the variant with a likelihood of 50% to her or his offspring. Therefore, the opportunity of molecular genetic testing and its possible implications (ie, early risk assessment by DEXA and medical treatment) must be discussed with the relatives at risk even in mild forms of OI.
Learning points
- Male osteoporosis is often unrecognised and remains untreated. It is associated with substantial morbidity and mortality.
- As in women, the aetiology of osteoporosis in men can be grouped into primary (age-related, idiopathic) and secondary causes (ie, hypogonadism, smoking, use of glucocorticoid medications).
- Osteogenesis imperfecta (OI) remains a rare secondary cause of osteoporosis. However, it can be hypothesised that the true prevalence of this condition remains underestimated due to lack of routine genetic screening and the multiple manifestations of the disease (ie, mild clinical phenotype with lack of ‘classical’ OI features).
- OI should be considered as differential diagnosis in unexplained cases with osteoporosis after exclusion of other secondary aetiologies. The possibility of molecular testing and its implications should be discussed with the patient and his/her relatives.
Contributors: SL wrote the first draft of the article. SF reviewed the article, making substantial alterations in order to completely present the case and to fully show the scientific intent of the presentation. SA-B reviewed the section on genetical information and provided further details in this respect. CH suggested that we present the case. The patient reviewed the article several times after providing his consent.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Ms. C.S. is a 46-year-old white female, who presents to her primary care physician for further work up after being seen and treated by an orthopedic surgeon for a right distal radius fracture. Patient sustained a low impact fall from standing which led to her injury. She states generally she doesn’t have pain but rates pain in wrist seven out of ten on pain scale.
Pertinent Past Medical and Surgical History

Jones, R. (2013). Distal radius [Picture]. Retrieved from https://emrems.com/2013/10/02/distal-radius/
- Bipolar disorder, diagnosed age 23, medically treated with lithium and cognitive behavior therapy
- Hysterectomy, age 44
- Diabetes type 1, diagnosed age 2
- Depression, diagnosed age 17
Pertinent Social History
- One pack per day smoker since age 17
- Newly divorced after 25 years of marriage
- Height 5’2 weight 85 pounds
Pertinent Family History
- Father alive at age 76 with history of bipolar disorder
- Mother died of cardiac arrest after a myocardial infarction 60 days post hip replacement at age 66
- Brother alive at age 50 with history of hyperthyroidism
- Sister alive at age 52 with no pertinent medical history
The association between myasthenia gravis and risk of fracture: a systematic review and meta-analysis
- Published: 15 May 2024

Cite this article

- Chien-Ju Lin 1 ,
- Yu-Shan Lee 1 ,
- Jiann-Horng Yeh 2 , 3 ,
- Shu-Jung Liu 4 &
- Kuan-Yu Lin ORCID: orcid.org/0000-0003-0559-3514 2
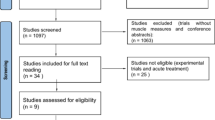
Patients with myasthenia gravis (MG), because of their muscle weakness and exposure to corticosteroids treatment, are generally considered to be at increased risk for osteoporosis or fracture. However, clinical evidence of this issue is lacking. In this review, we systematically searched databases, including Cochrane Library, PubMed, Embase, and Airiti library from inception to the end of November 2023 for cohort studies that compared participants with MG and participants without MG for incidence of osteoporosis or fracture. We used the Newcastle–Ottawa Scale for quality assessment. In total, we included 3 studies with 34,865 participants. The pooled meta-analysis using the random effect model demonstrated no significant difference in risk of fracture in the MG group (odds ratio = 1.52; 95% confidence interval = 0.74 to 3.12; I 2 = 93%; between-study variance [τ 2 ] = 0.32) compared with that for the non-MG group. Due to limited studies, we could not perform a quantitative analysis for risk of osteoporosis. In conclusion, we found no robust evidence to support the proposition that patients with MG are at higher risk for fracture than general comparators. The explanations and underlying mechanisms of this finding remain unclear, we therefore conclude that additional studies are warranted.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

The use of oral glucocorticoids and the risk of major osteoporotic fracture in patients with myasthenia gravis

Global prevalence of myasthenia gravis and the effectiveness of common drugs in its treatment: a systematic review and meta-analysis
The effect of disease-modifying anti-rheumatic drugs on skeletal muscle mass in rheumatoid arthritis patients: a systematic review with meta-analysis
Data availability.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Salari N, Fatahi B, Bartina Y, Kazeminia M, Fatahian R, Mohammadi P, Shohaimi S, Mohammadi M (2021) Global prevalence of myasthenia gravis and the effectiveness of common drugs in its treatment: a systematic review and meta-analysis. J Transl Med 19:516. https://doi.org/10.1186/s12967-021-03185-7
Article CAS PubMed PubMed Central Google Scholar
Narayanaswami P, Sanders DB, Wolfe G et al (2021) International consensus guidance for management of Myasthenia Gravis: 2020 Update. Neurology 96:114–122. https://doi.org/10.1212/wnl.0000000000011124
Article PubMed PubMed Central Google Scholar
Ruiter AM, Verschuuren J, Tannemaat MR (2020) Fatigue in patients with myasthenia gravis. A systematic review of the literature. Neuromuscul Disord 30:631–639. https://doi.org/10.1016/j.nmd.2020.06.010
Article PubMed Google Scholar
Smith EL, Gilligan C (1991) Physical activity effects on bone metabolism. Calcif Tissue Int 49(Suppl):S50-54. https://doi.org/10.1007/bf02555089
Carter MI, Hinton PS (2014) Physical activity and bone health. Mo Med 111:59–64
PubMed PubMed Central Google Scholar
Adami G, Saag KG (2019) Glucocorticoid-induced osteoporosis: 2019 concise clinical review. Osteoporos Int 30:1145–1156. https://doi.org/10.1007/s00198-019-04906-x
Article CAS PubMed Google Scholar
Lane NE (2019) Glucocorticoid-induced osteoporosis: New insights into the pathophysiology and treatments. Curr Osteoporos Rep 17:1–7. https://doi.org/10.1007/s11914-019-00498-x
Wakata N, Nemoto H, Sugimoto H, Nomoto N, Konno S, Hayashi N, Araki Y, Nakazato A (2004) Bone density in myasthenia gravis patients receiving long-term prednisolone therapy. Clin Neurol Neurosurg 106:139–141. https://doi.org/10.1016/j.clineuro.2003.12.001
Braz NFT, Rocha NP, Vieira ÉLM, Gomez RS, Barbosa IG, Malheiro OB, Kakehasi AM, Teixeira AL (2017) Negative impact of high cumulative glucocorticoid dose on bone metabolism of patients with myasthenia gravis. Neurol Sci 38:1405–1413. https://doi.org/10.1007/s10072-017-2964-z
Guan Y, Lv F, Meng Y et al (2017) Association between bone mineral density, muscle strength, and vitamin D status in patients with myasthenia gravis: a cross-sectional study. Osteoporos Int 28:2383–2390. https://doi.org/10.1007/s00198-017-4041-0
Yeh JH, Chen HJ, Chen YK, Chiu HC, Kao CH (2014) Increased risk of osteoporosis in patients with myasthenia gravis: a population-based cohort study. Neurology 83:1075–1079. https://doi.org/10.1212/wnl.0000000000000804
Kassardjian C, Widdifield J, Paterson JM, Kopp A, Nagamuthu C, Barnett C, Tu K, Breiner A (2021) Fracture risk in patients with myasthenia gravis: A population-based cohort study. J Neuromuscul Dis 8:625–632. https://doi.org/10.3233/jnd-200612
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Lo CK, Mertz D, Loeb M (2014) Newcastle-Ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14:45. https://doi.org/10.1186/1471-2288-14-45
Rstudio software. Available online: Https://www.Rstudio.Com/products/rstudio/download. Accessed 15 November 2023
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Pouwels S, de Boer A, Javaid MK, Hilton-Jones D, Verschuuren J, Cooper C, Leufkens HG, de Vries F (2013) Fracture rate in patients with myasthenia gravis: the general practice research database. Osteoporos Int 24:467–476. https://doi.org/10.1007/s00198-012-1970-5
Chiu HC, Vincent A, Newsom-Davis J, Hsieh KH, Hung T (1987) Myasthenia gravis: population differences in disease expression and acetylcholine receptor antibody titers between Chinese and Caucasians. Neurology 37:1854–1857. https://doi.org/10.1212/wnl.37.12.1854
Gregson CL, Armstrong DJ, Bowden J et al (2022) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 17:58. https://doi.org/10.1007/s11657-022-01061-5
Chowdhury SR, Chandra Das D, Sunna TC, Beyene J, Hossain A (2023) Global and regional prevalence of multimorbidity in the adult population in community settings: a systematic review and meta-analysis. EClinicalMedicine 57:101860. https://doi.org/10.1016/j.eclinm.2023.101860
Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C (2020) The epidemiology of osteoporosis. Br Med Bull 133:105–117. https://doi.org/10.1093/bmb/ldaa005
Kutsal FY, Ergin Ergani GO (2021) Vertebral compression fractures: Still an unpredictable aspect of osteoporosis. Turkish J Med Sci 51:393–399. https://doi.org/10.3906/sag-2005-315
Article Google Scholar
Alsoof D, Anderson G, McDonald CL, Basques B, Kuris E, Daniels AH (2022) Diagnosis and management of vertebral compression fracture. Am J Med 135:815–821. https://doi.org/10.1016/j.amjmed.2022.02.035
Lin CW, Chen TC, Jou JR, Woung LC (2018) Update on ocular myasthenia gravis in Taiwan. Taiwan J Ophthalmol 8:67–73. https://doi.org/10.4103/tjo.tjo_39_17
Kanis JA, Johansson H, Oden A et al (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19:893–899. https://doi.org/10.1359/jbmr.040134
Canalis E, Mazziotti G, Giustina A, Bilezikian JP (2007) Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int 18:1319–1328. https://doi.org/10.1007/s00198-007-0394-0
Sato AY, Peacock M, Bellido T (2018) Glucocorticoid excess in bone and muscle. Clin Rev Bone Miner Metab 16:33–47. https://doi.org/10.1007/s12018-018-9242-3
Safipour Z, van der Zanden R, van den Bergh J, Janssen P, Vestergaard P, de Vries F, Driessen JHM (2022) The use of oral glucocorticoids and the risk of major osteoporotic fracture in patients with myasthenia gravis. Osteoporos Int 33:649–658. https://doi.org/10.1007/s00198-021-06101-3
Konno S, Suzuki S, Masuda M, Nagane Y, Tsuda E, Murai H, Imai T, Fujioka T, Suzuki N, Utsugisawa K (2015) Association between glucocorticoid-induced osteoporosis and Myasthenia Gravis: A cross-sectional study. PLoS One 10:e0126579. https://doi.org/10.1371/journal.pone.0126579
van Staa TP, Leufkens HG, Cooper C (2002) The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 13:777–787. https://doi.org/10.1007/s001980200108
Chotiyarnwong P, McCloskey EV (2020) Pathogenesis of glucocorticoid-induced osteoporosis and options for treatment. Nat Rev Endocrinol 16:437–447. https://doi.org/10.1038/s41574-020-0341-0
En-Nosse M, Hartmann S, Trinkaus K, Alt V, Stigler B, Heiss C, Kilian O, Schnettler R, Lips KS (2009) Expression of non-neuronal cholinergic system in osteoblast-like cells and its involvement in osteogenesis. Cell Tissue Res 338:203–215. https://doi.org/10.1007/s00441-009-0871-1
Sato T, Abe T, Chida D et al (2010) Functional role of acetylcholine and the expression of cholinergic receptors and components in osteoblasts. FEBS Lett 584:817–824. https://doi.org/10.1016/j.febslet.2010.01.001
Ma Y, Elefteriou F (2020) Brain-derived acetylcholine maintains peak bone mass in adult female mice. J Bone Miner Res 35:1562–1571. https://doi.org/10.1002/jbmr.4024
Cunningham J (2005) Posttransplantation bone disease. Transplantation 79:629–634. https://doi.org/10.1097/01.tp.0000149698.79739.ef
Kuppachi S, Cheungpasitporn W, Li R et al (2022) Kidney transplantation, immunosuppression and the risk of fracture: Clinical and economic implications. Kidney Med 4:100474. https://doi.org/10.1016/j.xkme.2022.100474
Vestergaard P, Rejnmark L, Mosekilde L (2006) Methotrexate, azathioprine, cyclosporine, and risk of fracture. Calcif Tissue Int 79:69–75. https://doi.org/10.1007/s00223-006-0060-0
Dodd KC, Clay FJ, Forbes AM, Keh YS, Miller JAL, Sussman J, Lilleker JB (2023) Rituximab for myasthenia gravis. Cochrane Database Syst Rev 2023(4):CD014574. https://doi.org/10.1002/14651858.CD014574
Article PubMed Central Google Scholar
Alhaidar MK, Abumurad S, Soliven B, Rezania K (2022) Current treatment of Myasthenia Gravis. J Clin Med 11. https://doi.org/10.3390/jcm11061597
Upadhyay J, Farr OM, Mantzoros CS (2015) The role of leptin in regulating bone metabolism. Metabolism 64:105–113. https://doi.org/10.1016/j.metabol.2014.10.021
Humphrey MB, Russell L, Danila MI et al (2023) 2022 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Rheumatol (Hoboken, NJ) 75:2088–2102. https://doi.org/10.1002/art.42646
Morren JA, Li Y (2023) Myasthenia gravis: Frequently asked questions. Cleve Clin J Med 90:103–113. https://doi.org/10.3949/ccjm.90a.22017
Ebeling PR, Nguyen HH, Aleksova J, Vincent AJ, Wong P, Milat F (2022) Secondary osteoporosis. Endocr Rev 43:240–313. https://doi.org/10.1210/endrev/bnab028
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739. https://doi.org/10.1359/jbmr.2000.15.4.721
Download references
Acknowledgements
We would like to thank Enago ( www.enago.com ) for editing and proofreading this manuscript.
This research received no external funding.
Author information
Authors and affiliations.
Department of Family Medicine, Hsinchu MacKay Memorial Hospital, Hsinchu City, Taiwan
Chien-Ju Lin & Yu-Shan Lee
Department of Neurology, Shin Kong Wu Ho-Su Memorial Hospital, Taipei City, Taiwan
Jiann-Horng Yeh & Kuan-Yu Lin
School of Medicine, Fu Jen Catholic University, New Taipei City, Taiwan
Jiann-Horng Yeh
Department of Medical Library, MacKay Memorial Hospital, Tamsui Branch, New Taipei City, Taiwan
Shu-Jung Liu
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Kuan-Yu Lin .
Ethics declarations
Conflicts of interest.
Chien-Ju Lin, Yu-Shan Lee, Jiann-Horng Yeh, Shu-Jung Liu, and Kuan-Yu Lin declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 257 KB)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Lin, CJ., Lee, YS., Yeh, JH. et al. The association between myasthenia gravis and risk of fracture: a systematic review and meta-analysis. Osteoporos Int (2024). https://doi.org/10.1007/s00198-024-07097-2
Download citation
Received : 15 January 2024
Accepted : 18 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1007/s00198-024-07097-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Myasthenia gravis
- Osteoporosis
- Osteoporotic fracture
- Corticosteroid
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Osteoporosis is a disease that causes a decrease in bone mass, increasing bone fragility and fracture [ 1 ]. Osteoporosis is a common disease, and it impacts one in three post-menopausal women and one in five men worldwide. There are roughly 200 million men and women who have osteoporosis in this world. The cost and morbidity associated with ...
Understanding Osteoporosis poster Information Cards 1‐8 Normal Bone model Bag of materials for making Osteoporosis Bone model that contains: 10 white disks, 10 white star beads, 1 Osteoporosis Bone tube with lid. 4. Read The Case paragraph on page 1 aloud to the class. 5.
Abstract. Male osteoporosis often remains unrecognised. Osteoporotic fractures occur approximately 10 years later in men than in women due to higher peak bone mass. However, 30% of all hip fractures occur in men. Risk factors of osteoporotic fractures can be grouped into primary and secondary causes. We present the case of a 53-year-old man ...
Case 24-2014 — A 27-Year ... (nejmcpc1404139_disclosures.pdf) Download; ... Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO Study Group.
Osteoporosis is a disease that causes a d ecrease in bone mass, increasing bon e fragility and fracture [1]. Osteoporosis is a common disease, an d it impacts one in three post-menop ausal women ...
Osteoporosis is a chronic condition and long-term, sometimes lifelong, management is required. In individuals at high risk of fracture, the benefit versus risk profile is likely to be favourable for up to 10 years of treatment with bisphosphonates or denosumab.
Osteoporosis is a common disease that affects our elderly population. This disease usually gets undiagnosed for an extended period. Osteoporosis increases the risk of fracture in our elderly population and increases morbidity. The cost associated with osteoporosis does carry a substantial burden in our society. Here, we present a case of osteoporosis with a fracture diagnosed in clinical ...
Evidence-Based Case Studies in Osteoporosis Download book PDF ... Chapter PDF. Similar content being viewed by others. General and Specific Considerations as to why Osteoporosis-Related Care Is Often Suboptimal Article Open access 26 February 2020. Management of patients at very high risk of osteoporotic fractures through sequential treatments ...
Buy print copy. Softcover Book USD 89.99. Price excludes VAT (USA) Compact, lightweight edition. Dispatched in 3 to 5 business days. Free shipping worldwide -. This book is a cased-based, practical guide to the diagnosis and management of osteoporosis and related conditions.
A case of osteoporosis with a fracture diagnosed in clinical settings is presented and different etiology, pathophysiology, and treatment options available to treat this medical condition are discussed. Osteoporosis is a common disease that affects our elderly population. This disease usually gets undiagnosed for an extended period. Osteoporosis increases the risk of fracture in our elderly ...
Introduction. Osteoporosis, the most common bone disease in the world, leads to decreased bone strength, low bone mass, and increased risk of fractures. 1 An estimated 50% of women and 20% of men over the age of 50 will suffer an osteoporosis-related fracture, which is associated with disability, mortality, and significant financial cost to the ...
Osteoporosis is a serious disease, which results in over 200,000 fractures each year, causing severe pain and disability to individuals, at excessive cost to the National Health Service (Donaldson 2000). It is one of the few areas in which early intervention to promote and maintain bone health can make a real impact on the burden of the disease.
Patient Case Presentation. Ms. C.S. is a 46-year-old white female, who presents to her primary care physician for further work up after being seen and treated by an orthopedic surgeon for a right distal radius fracture. Patient sustained a low impact fall from standing which led to her injury.
Goyal L, Ajmera K (April 06, 2022) Osteoporosis: A Step-by-Step Case-Based Study. Cureus 14(4): e23900. DOI 10.7759/cureus.23900. FIGURE 1: Colle's distal radial fracture Discussion Pathophysiology The cause of osteoporosis [1-3] is an imbalance between bone formation and bone reabsorption. A typical
and contributing to osteoporosis[2]. Tarantal et al. proposed that persistent prenatal and postnatal tenofovir can affect bone metabolism in some animals[6]. Other studies (McComsey et al., 2011; Stellbrink et al., 2010; Haskelberg et al., 2012) suggested osteopenia and osteoporosis are more detected with TDF regimens than abacavir/lamivudine.
concepts relating osteoporosis with nutrition, exercise, and drugs mu st be addressed in detail. It is up to the group to divide the necessary research. Research will be shared with the class. Ultimately, you must consider if Jeremy's activities will have any impact on his chances of developing osteoporosis and the risks and benefits of his ...
view can reveal the humanistic impact of osteoporosis. For example, as seen below, one female participant aged 61 reported a fall and fracture, which showcased a dramatic reduction in daily activity levels and ability to manage her diabetes. CASE STUDY: OSTEOPOROSIS Person-generated health data (PGHD) provides valuable
Case Type / Diagnosis: Osteoporosis 730.2, Vertebral Fracture closed 805.8. Definition: Osteoporosis is characterized by the presence of both low bone mass and a disruption of normal bone architecture which results in loss of bone strength. According to the World Health Organization (WHO) the operational definition is a bone density measure >2 ...
the risk of fractures associated with osteoporosis. U.S. adults 50+ currently taking 13,30/0 Relative risk reduction 140/0 The risk Of fracture reduced by taking these supplements Avoidable medical events 361,507 Expected between 2022-2030 if the entire target population takes supplements at preventive intake levels 2022-2030 AVERAGE PER YEAR
Summary. This chapter discusses the case of a 68-year-old lady, Mary, who presented with osteoporosis. She attends the outpatient bone health and osteoporosis clinic in a large teaching hospital and has been referred to GP for dietetic assessment and advice. The questions raised in the chapter include queries regarding the nutrition and ...
October 25, 2004. Vol. 5 •Issue 23 • Page 32. Osteoporosis: Case Study. Case presentation and history give clues to diagnosis of osteoporosis. By Natalie Tesso Simmermacher, BSN, RN, CWOCN. T.S. is a 52-year-old white female experiencing diffuse bone pain over the past several years after menopause. She has a history of fractures to her ...
Download PDF. Osteoporosis ... the outcome of interest was not the incidence of fracture or osteoporosis; (4) studies were literature reviews, case-control studies, cross-sectional studies, or case series. ... In a Danish case-control study, which compared 124,655 patients with fractures to 373,962 age- and sex-matched control, ...
Primary biliary cholangitis was first described by Addison and Gull in 1851 in Mrs. Elizabeth, hospitalized at Guy's Hospital in London. The case report was published in the article "On a certain affection of the skin vitiligoidea—a plana, b tuberosa" in the now non-existent local medical magazine Guy's Hospital Reports [].PBC is a chronic autoimmune, non-suppurative inflammatory ...
Case studies Conversation starters Screening tools Standardized gait and balance assessment tests (with instructional videos) CDC's STEADI tools and resources can help you screen, assess, and intervene to reduce . Educational materials for providers, patients, and caregivers Information on medications linked to falls Clinical decision support for