In early 2015, NCSBN convened two panels of experts representing education, research, and practice to discuss the delegation literature and key issues, and evaluate findings from delegation research funded through NCSBN’s Center for Regulatory Excellence Grant Program. The goal was the development of national guidelines to facilitate and standardize the nursing delegation process. These National Guidelines for Nursing Delegation build on previous work by NCSBN and the American Nurses Association, and provide clarification on the responsibilities associated with delegation. Additionally, these guidelines are meant to address delegation with respect to the various levels of nursing licensure (i.e., APRN, RN, and LPN/VN, where the state NPA allows).
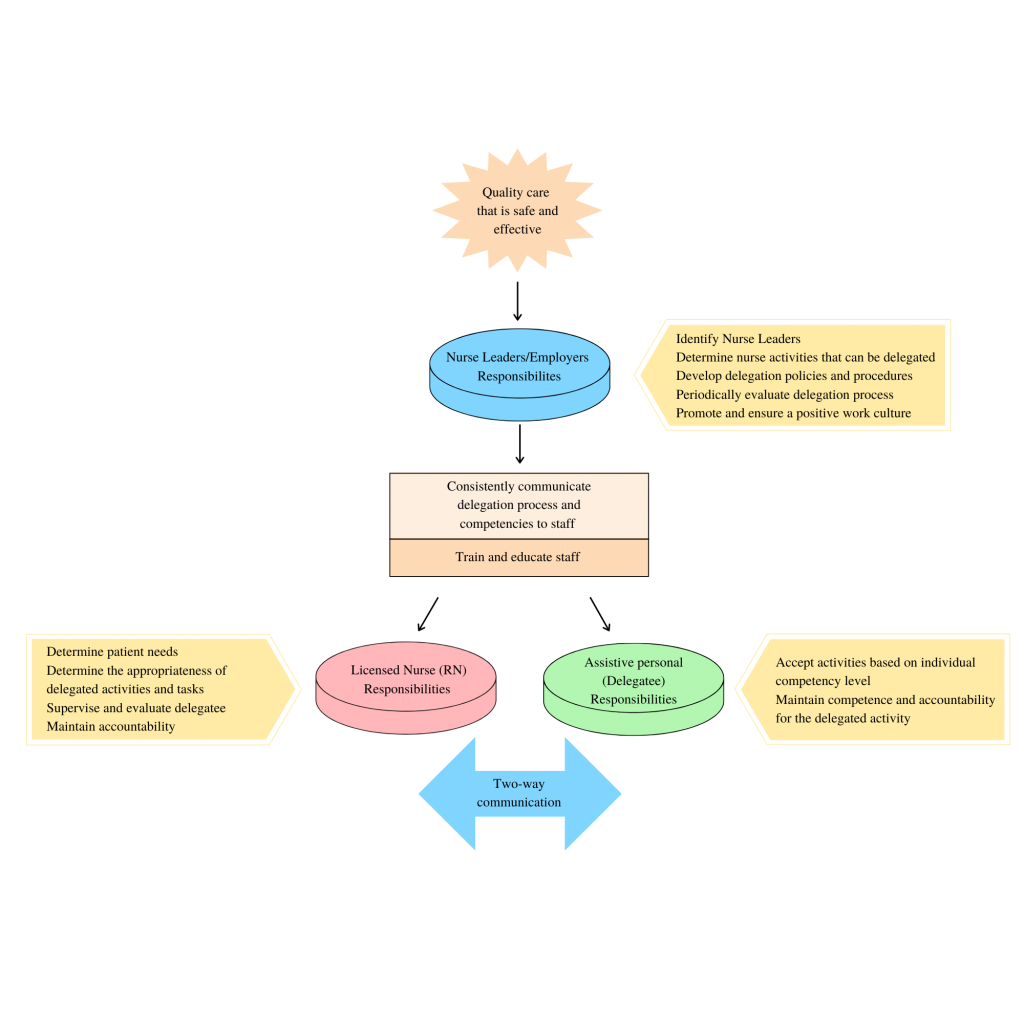
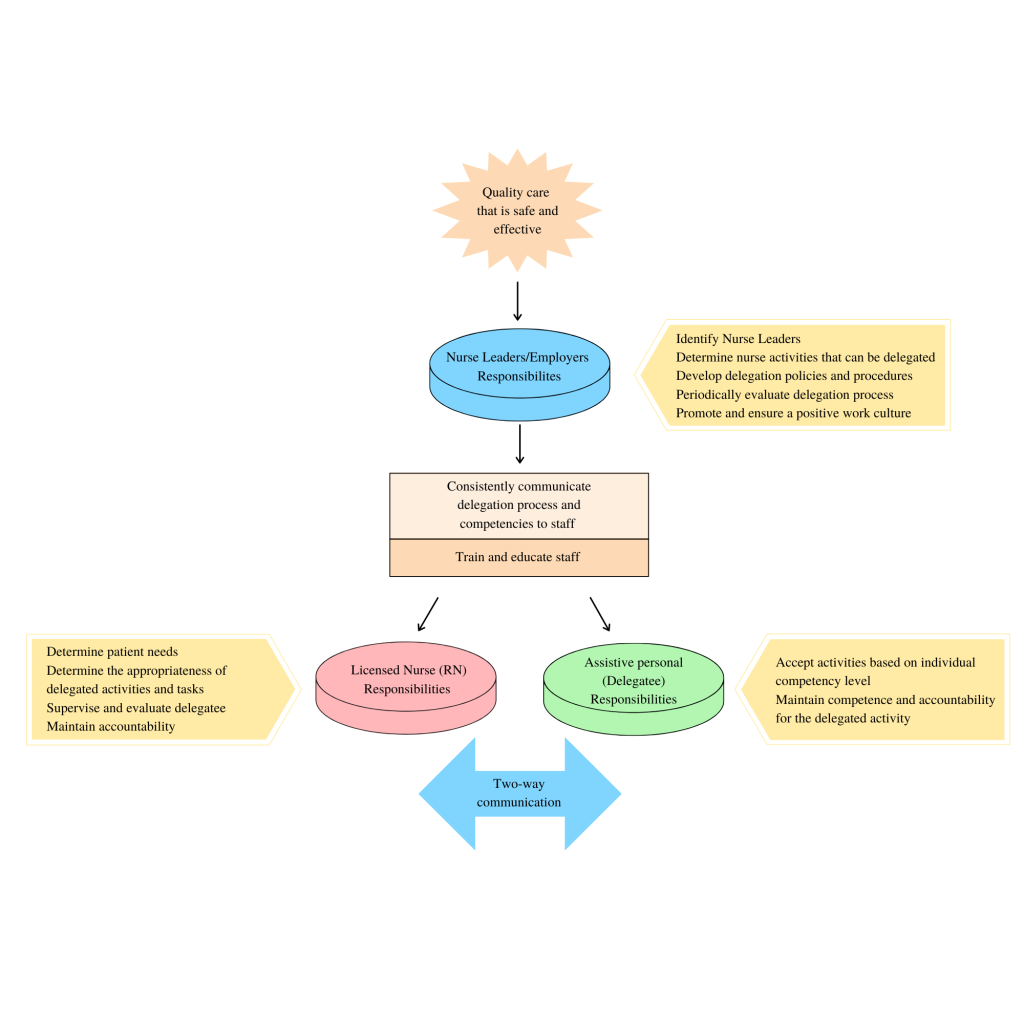
The delegation process is multifaceted. It begins with decisions made at the administrative level of the organization and extends to the staff responsible for delegating, overseeing the process, and performing the responsibilities. It involves effective communication, empowering staff to make decisions based on their judgment and support from all levels of the health care setting. The employer/nurse leader, individual licensed nurse, and delegatee all have specific responsibilities within the delegation process. (See Delegation Model below.) It is crucial to understand that states/jurisdictions have different laws and rules/regulations about delegation, and it is the responsibility of all licensed nurses to know what is permitted in their state NPA, rules/regulations, and policies.


Delegation Position Paper
NCSBN's position papers on delegation and working with others:
National Guidelines for Nursing Delegation
NCSBN and ANA Joint Position Paper on Delegation
NCSBN and the American Nurses Association (ANA) developed a joint position paper based on the guidelines developed by NCSBN in 2016 (effective 4/29/2019). This statement replaces the NCSBN and ANA 2010 Joint Statement on Delegation.
NCSBN and ANA Position Paper on the National Guidelines for Nursing Delegation
Delegating vs. assigning: What you need to know
REGISTERED NURSES (RNS) often delegate to other RNs, licensed practical nurses/vocational nurses (LPN/LVNs), and assistive personnel (AP). (In some states or jurisdictions, LPN/LVNs may be allowed to delegate, so “licensed nurses” will be used in this article.) Delegating appropriately protects patients and reduces the risk of legal liability, yet the parameters of delegation often are not fully understood.
One common area of misunderstanding is delegation vs. assignment. Knowing the differences between the two is essential to ensure you delegate appropriately. The primary difference relates to scope of practice and where the clinician learned the activities to be carried out.
According to national guidelines for nursing delegation from the National Council of State Boards of Nursing (NCSBN) and American Nurses Association (ANA), an assignment refers to the “routine care, activities, and procedures that are within the authorized scope of practice of the RN or LPN/VN or part of the routine functions of the AP.” This definition covers fundamental skills that the assignee would have learned in a basic education program. A licensed nurse is still responsible for ensuring the assignment is carried out correctly.
According to the NCSBN/ANA guideline, delegation applies when the delegatee is performing a “specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed.” As opposed to work that is part of an assignment, the work associated with delegation was not learned in a basic education program. Therefore, the delegatee must have obtained additional education and have verified competence in the delegated area for which they will be responsible. The licensed nurse maintains overall accountability for the patient, but the delegatee is responsible for the delegated activity, skill, or procedure.
Licensed nurses can’t delegate activities that involve clinical reasoning, nursing judgment, or critical decision making, and the delegated responsibility has to be within the delegator’s scope of practice under the state’s or jurisdiction’s nurse practice act (NPA).
FIVE RIGHTS OF DELEGATION
The NCSBN outlines five rights of delegation. In the case of a lawsuit, a key component would be whether you adhered to these rights:
- Right task. The task needs to fall within the delegatee’s job description or is part of organizational policies and procedures.
- Right circumstance. The patient must be stable.
- Right person. The delegatee must have the appropriate skills and knowledge to perform the task.
- Right directions and communication. Clear directions need to be given, with the delegator verifying understanding by the delegatee. Communication must be two-way, with the delegatee asking questions as needed.
- Right supervision and evaluation. The delegator needs to monitor the delegated activity, including evaluating patient outcomes.
RESPONSIBILITIES
Organizational administrators, the delegator, and the delegatee each have responsibilities when an activity, skill, or procedure is delegated.
Professionals who work at the administrative or managerial level of the organization set the cultural tone for the nursing work environment and are responsible for managing the delegation processes. Those at the administrative level within an organization define what nursing responsibilities may be delegated, to whom, and under what set(s) of circumstances. They are also responsible for developing and maintaining policies and procedures associated with delegation, periodically evaluating the efficacy and safety of delegation processes, and training and educating staff.
The delegator is responsible for determining the needs of the patient, when delegation is appropriate, and if the delegatee is competent to complete the delegated task. Delegators must follow delegation guidelines in the NPA and relevant organizational policies and procedures. Clear communication is key, and the delegator must be available as a resource to the delegatee. Delegators also need to evaluate outcomes as they maintain overall accountability for the patient. Delegators must be prepared to step in at any point if it appears the delegatee is not handling the assignment appropriately. Any problems should be reported to nursing leadership.
The delegatee is responsible for only accepting activities that fall within their competence and that they feel comfortable completing safely. Delegatees must communicate with the delegator, particularly if the patient’s condition changes, and complete the activity correctly, including fulfilling any documentation requirements. Delegatees maintain accountability for the delegated activity and need to notify the delegator immediately if they have difficulty completing the task.
ONE SPECIAL CASE
NCSBN notes that in some cases, APs are taught how to perform skills that were previously thought to be exclusively RN and LPN/LVN responsibilities, such as certified medical assistants administering injections. In these cases, it’s best to consider such tasks as being delegated and, therefore, validate competency.
KEEPING PATIENTS SAFE
Knowing the differences between assigning and delegating helps protect patients and avoid legal action should an error occur. Assignments involve routine tasks learned in basic education and that fall under designated scope of practice, while delegation involves tasks that were learned through additional education and for which competency has been determined.
Good communication and an understanding of the responsibilities of delegators and delegatees is essential to avoid misunderstanding. Remember, the licensed nurse remains accountable for the patient, but the delegatee is responsible for the delegated task.
National Council of State Boards of Nursing. National guidelines for nursing delegation. J Nurs Reg . 2016;7(1):5-12.
NCSBN, ANA . National guidelines for nursing delegation. 2019.
Disclaimer: The information offered within this article reflects general principles only and does not constitute legal advice by Nurses Service Organization (NSO) or establish appropriate or acceptable standards of professional conduct. Readers should consult with an attorney if they have specific concerns. Neither Affinity Insurance Services, Inc. nor NSO assumes any liability for how this information is applied in practice or for the accuracy of this information. Please note that Internet hyperlinks cited herein are active as of the date of publication but may be subject to change or discontinuation.
This risk management information was provided by Nurses Service Organization (NSO), the nation’s largest provider of nurses’ professional liability insurance coverage for over 550,000 nurses since 1976. The individual professional liability insurance policy administered through NSO is underwritten by American Casualty Company of Reading, Pennsylvania, a CNA company. Reproduction without permission of the publisher is prohibited. For questions, send an e-mail to [email protected] or call 1-800-247-1500. www.nso.com . Reprinted with permission from Nurses Service Organization
Content of this article has been developed in collaboration with the referenced State Nursing Association.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
More from your State Nurses Association

NNA LARC Member Spotlight
Nnf 2025 project grants – applicants needed.

Teaching Basic Genomics Concepts: Outcomes of a Team-Based Learning Activity for Nurse Practitioner Students

Nebraska Nurses Foundation – Lasting Legacy Interview Series – September 2024

Do Not Pass Over the Educators Newsletter
Nna committee updates – september 2024.

Enhancing Patient Advocacy and Care through Medicare Fluency
From the nna executive director, september 2024, from the nna president, september 2024, from the nna executive director, june 2024, from the nna president, june 2024.

Questions you should ask before volunteering
Nnf board member changes, nna region reports, june 2024.

Nebraska Nurses Foundation – Lasting Legacy Interview Series – June 2024
More from american nurse.

Stop fall prevention practices that aren’t working

Mitigating patient identification threats

Foot assessment and care
End-tidal CO 2 monitoring
Promoting health literacy

Vaccination and vaccine-hesitancy

Lyme carditis: A clinical case report

My patient is a victim of human trafficking

Medication safety and pediatric health
Tailored falls prevention plans
Chylothorax: A stepwise approach to care

3.4 Delegation
There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND). [1] These guidelines apply to all levels of nursing licensure (advanced practice registered nurses [APRN], registered nurses [RN], and licensed practical/vocational nurses [LPN/VN]) when delegating when there is no specific guidance provided by the state’s Nurse Practice Act (NPA). [2] It is important to note that states have different laws and rules/regulations regarding delegation, so it is the responsibility of all licensed nurses to know what is permitted in their jurisdiction.
The NGND defines a delegatee as an RN, LPN/VN, or UAP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN, is competent to perform the task, and verbally accepts the responsibility. [3] Delegation is allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed, but the individual has obtained additional training and validated their competence to perform the delegated responsibility. [4] However, the licensed nurse still maintains accountability for overall client care. Delegated responsibility is a nursing activity, skill, or procedure that is transferred from a licensed nurse to a delegatee. [5] Accountability is defined as being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. Therefore, if a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity themselves. [6]
Delegation is summarized in the NGND as the following [7] :
- A delegatee is allowed to perform a specific nursing activity, skill, or procedure that is outside the traditional role and basic responsibilities of the delegatee’s current job.
- The delegatee has obtained the additional education and training and validated competence to perform the care/delegated responsibility. The context and processes associated with competency validation will be different for each activity, skill, or procedure being delegated. Competency validation should be specific to the knowledge and skill needed to safely perform the delegated responsibility, as well as to the level of the practitioner (e.g., RN, LPN/VN, UAP) to whom the activity, skill, or procedure has been delegated. The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, but the delegatee bears the responsibility for completing the delegated activity, skill, or procedure.
- The licensed nurse cannot delegate nursing clinical judgment or any activity that will involve nursing clinical judgment or critical decision-making to UAP.
- Nursing responsibilities are delegated by a licensed nurse who has the authority to delegate and the delegated responsibility is within the delegator’s scope of practice.
An example of delegation is medication administration that is delegated by a licensed nurse to UAP with additional training in some agencies, according to agency policy. This task is outside the traditional role of UAP, but the delegatee has received additional training for this delegated responsibility and has completed competency validation in completing this task accurately.
An example illustrating the difference between assignment and delegation is assisting clients with eating. Feeding clients is typically part of the routine role of UAP. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or is otherwise experiencing swallowing difficulties (e.g., dysphagia), this task cannot be assigned to UAP because it is not considered routine care. Instead, the RN should perform this task themselves or delegate it to an UAP who has received additional training on feeding assistance.
The delegation process is multifaceted. See Figure 3.2 [8] for an illustration of the intersecting responsibilities of the employer/nurse leader, licensed nurse, and delegatee with two-way communication that protects the safety of the public. “Delegation begins at the administrative/nurse leader level of the organization and includes determining nursing responsibilities that can be delegated, to whom, and under what circumstances; developing delegation policies and procedures; periodically evaluating delegation processes; and promoting a positive culture/work environment. The licensed nurse is responsible for determining client needs and when to delegate, ensuring availability to the delegatee, evaluating outcomes, and maintaining accountability for delegated responsibility. Finally, the delegatee must accept activities based on their competency level, maintain competence for delegated responsibility, and maintain accountability for delegated activity.” [9]
Five Rights of Delegation
How does the RN determine what tasks can be delegated, when, and to whom? According to the National Council of State Boards of Nursing (NCSBN), RNs should use the five rights of delegation to ensure proper and appropriate delegation: right task, right circumstance, right person, right directions and communication, and right supervision and evaluation [10] :
- Right task: The activity falls within the delegatee’s job description or is included as part of the established policies and procedures of the nursing practice setting. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Right circumstance: The health condition of the client must be stable. If the client’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation. [11]
- Right person: The licensed nurse, along with the employer and the delegatee, is responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity. [12]
- Right directions and communication: Each delegation situation should be specific to the client, the nurse, and the delegatee. The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee, as part of two-way communication, should ask any clarifying questions. This communication includes any data that need to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation. The delegatee must understand the terms of the delegation and must agree to accept the delegated activity. The licensed nurse should ensure the delegatee understands they cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse. [13]
- Right supervision and evaluation: The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating client outcomes. The delegatee is responsible for communicating client information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary. The licensed nurse should ensure appropriate documentation of the activity is completed. [14]
Simply stated, the licensed nurse determines the right person is assigned the right tasks for the right clients under the right circumstances. When determining what aspects of care can be delegated, the licensed nurse uses clinical judgment while considering the client’s current clinical condition, as well as the abilities of the health care team member. The RN must also consider if the circumstances are appropriate for delegation. For example, although obtaining routine vital signs on stable clients may be appropriate to delegate to assistive personnel, obtaining vital signs on an unstable client is not appropriate to delegate.
After the decision has been made to delegate, the nurse assigning the tasks must communicate appropriately with the delegatee and provide the right directions and supervision. Communication is key to successful delegation. Clear, concise, and closed-loop communication is essential to ensure successful completion of the delegated task in a safe manner. During the final step of delegation, also referred to as supervision , the nurse verifies and evaluates that the task was performed correctly, appropriately, safely, and competently. Read more about supervision in the following section on “ Supervision .” See Table 3.4 for additional questions to consider for each “right” of delegation.
Table 3.4. Rights of Delegation [15]
| A task that can be transferred to a member of the nursing team for a specific client. | ||
| The client is stable. | ||
| The person delegating the task has the appropriate scope of practice to do so. The task is also appropriate for this delegatee’s skills and knowledge. | ||
| The task or activity is clearly defined and described. | ||
| The RN appropriately monitors the delegated activity, evaluates client outcomes, and follows up with the delegatee at the completion of the activity. |
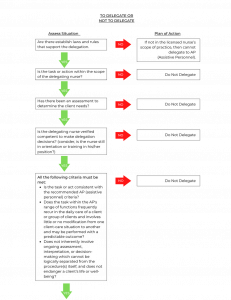
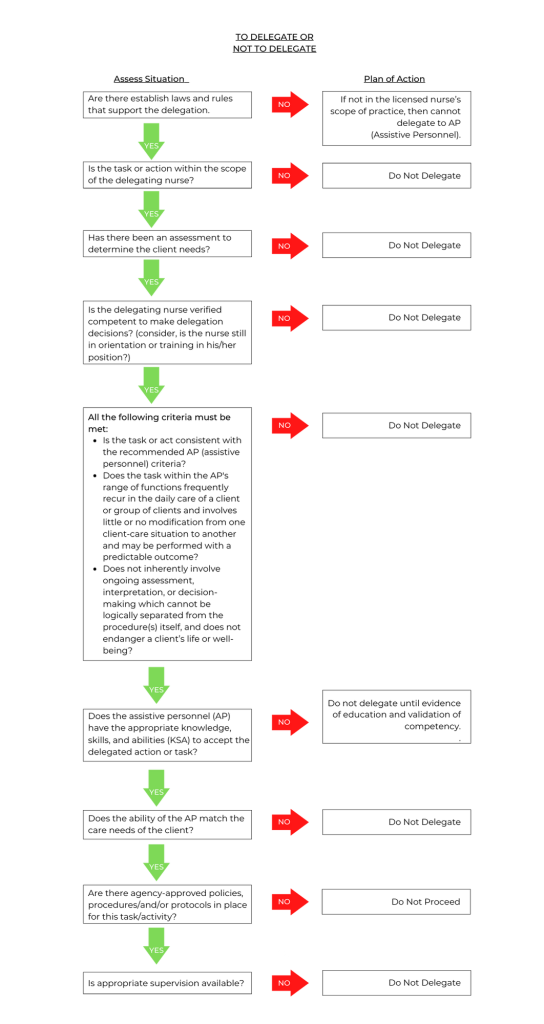
Keep in mind that any nursing intervention that requires specific nursing knowledge, clinical judgment, or use of the nursing process can only be delegated to another RN. Examples of these types of tasks include initial preoperative or admission assessments, client teaching, and creation and evaluation of a nursing care plan. See Figure 3.3 [16] for an algorithm based on the 2019 National Guidelines for Nursing Delegation that can be used when deciding if a nursing task can be delegated. [17]
Responsibilities of the Licensed Nurse
The licensed nurse has several responsibilities as part of the delegation process. According to the NGND, any decision to delegate a nursing responsibility must be based on the needs of the client or population, the stability and predictability of the client’s condition, the documented training and competence of the delegatee, and the ability of the licensed nurse to supervise the delegated responsibility and its outcome with consideration to the available staff mix and client acuity. Additionally, the licensed nurse must consider the state Nurse Practice Act regarding delegation and the employer’s policies and procedures prior to making a final decision to delegate. Licensed nurses must be aware that delegation is at the nurse’s discretion, with consideration of the particular situation. The licensed nurse maintains accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity. [18]
1. The licensed nurse must determine when and what to delegate based on the practice setting, the client’s needs and condition, the state’s/jurisdiction’s provisions for delegation, and the employer’s policies and procedures regarding delegating a specific responsibility. The licensed nurse must determine the needs of the client and whether those needs are matched by the knowledge, skills, and abilities of the delegatee and can be performed safely by the delegatee. The licensed nurse cannot delegate any activity that requires clinical reasoning, nursing judgment, or critical decision-making. The licensed nurse must ultimately make the final decision whether an activity is appropriate to delegate to the delegatee based on the “Five Rights of Delegation.”
- Rationale: The licensed nurse, who is present at the point of care, is in the best position to assess the needs of the client and what can or cannot be delegated in specific situations. [19]
2. The licensed nurse must communicate with the delegatee who will be assisting in providing client care. This should include reviewing the delegatee’s assignment and discussing delegated responsibilities, including information on the client’s condition/stability, any specific information pertaining to a certain client (e.g., no blood draws in the right arm), and any specific information about the client’s condition that should be communicated back to the licensed nurse by the delegatee.
- Rationale: Communication must be a two-way process involving both the licensed nurse delegating the activity and the delegatee being delegated the responsibility. Evidence shows that the better the communication between the nurse and the delegatee, the more optimal the outcome. The licensed nurse must provide information about the client and care requirements. This includes any specific issues related to any delegated responsibilities. These instructions should include any unique client requirements. The licensed nurse must instruct the delegatee to regularly communicate the status of the client. [20]
3. The licensed nurse must be available to the delegatee for guidance and questions, including assisting with the delegated responsibility, if necessary, or performing it themselves if the client’s condition or other circumstances warrant doing so.
- Rationale: Delegation calls for nursing judgment throughout the process. The final decision to delegate rests in the hands of the licensed nurse as they have overall accountability for the client. [21]
4. The licensed nurse must follow up with the delegatee and the client after the delegated responsibility has been completed.
- Rationale: The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. [22]
5. The licensed nurse must provide feedback information about the delegation process and any issues regarding delegatee competence level to the nurse leader. Licensed nurses in the facility need to communicate to the nurse leader responsible for delegation any issues arising related to delegation and any individual whom they identify as not being competent in a specific responsibility or unable to use good judgment and decision-making.
- Rationale: This will allow the nurse leader responsible for delegation to develop a plan to address the situation. [23]
The decision of whether or not to delegate or assign is based on the RN’s judgment concerning the condition of the client, the competence of the nursing team member, and the degree of supervision that will be required of the RN if a task is delegated. [24]
Responsibilities of the Delegatee
Everyone is responsible for the well-being of clients. While the nurse is ultimately accountable for the overall care provided to a client, the delegatee shares the responsibility for the client and is fully responsible for the delegated activity, skill, or procedure. [25] The delegatee has the following responsibilities:
1. The delegatee must accept only the delegated responsibilities that they are appropriately trained and educated to perform and feel comfortable doing given the specific circumstances in the health care setting and client’s condition. The delegatee should confirm acceptance of the responsibility to carry out the delegated activity. If the delegatee does not believe they have the appropriate competency to complete the delegated responsibility, then the delegatee should not accept the delegated responsibility. This includes informing the nursing leadership if they do not feel they have received adequate training to perform the delegated responsibility, do not perform the procedure frequently enough to do it safely, or their knowledge and skills need updating.
- Rationale: The delegatee shares the responsibility to keep clients safe, and this includes only performing activities, skills, or procedures in which they are competent and comfortable doing. [26]
2. The delegatee m ust maintain competency for the delegated responsibility.
- Rationale: Competency is an ongoing process. Even if properly taught, the delegatee may become less competent if they do not frequently perform the procedure. Given that the delegatee shares the responsibility for the client, the delegatee also has a responsibility to maintain competency. [27]
3. The delegatee must communicate with the licensed nurse in charge of the client. This includes any questions related to the delegated responsibility and follow-up on any unusual incidents that may have occurred while the delegatee was performing the delegated responsibility, any concerns about a client’s condition, and any other information important to the client’s care.
- Rationale: The delegatee is a partner in providing client care. They are interacting with the client/family and caring for the client. This information and two-way communication are important for successful delegation and optimal outcomes for the client. [28]
4. Once the delegatee verifies acceptance of the delegated responsibility, the delegatee is accountable for carrying out the delegated responsibility correctly and completing timely and accurate documentation per facility policy.
- Rationale: The delegatee cannot delegate to another individual. If the delegatee is unable to complete the responsibility or feels as though they need assistance, the delegatee should inform the licensed nurse immediately so the licensed nurse can assess the situation and provide support. Only the licensed nurse can determine if it is appropriate to delegate the activity to another individual. If at any time the licensed nurse determines they need to perform the delegated responsibility, the delegatee must relinquish responsibility upon request of the licensed nurse. [29]
Responsibilities of the Employer/Nurse Leader
The employer and nurse leaders also have responsibilities related to safe delegation of client care:
1. The employer must identify a nurse leader responsible for oversight of delegated responsibilities for the facility. If there is only one licensed nurse within the practice setting, that licensed nurse must be responsible for oversight of delegated responsibilities for the facility.
- Rationale: The nurse leader has the ability to assess the needs of the facility, understand the type of knowledge and skill needed to perform a specific nursing responsibility, and be accountable for maintaining a safe environment for clients. They are also aware of the knowledge, skill level, and limitations of the licensed nurses and UAP. Additionally, the nurse leader is positioned to develop appropriate staffing models that take into consideration the need for delegation. Therefore, the decision to delegate begins with a thorough assessment by a nurse leader designated by the institution to oversee the process. [30]
2. The designated nurse leader responsible for delegation, ideally with a committee (consisting of other nurse leaders) formed for the purposes of addressing delegation, must determine which nursing responsibilities may be delegated, to whom, and under what circumstances. The nurse leader must be aware of the state Nurse Practice Act and the laws/rules and regulations that affect the delegation process and ensure all institutional policies are in accordance with the law.
- Rationale: A systematic approach to the delegation process fosters communication and consistency of the process throughout the facility. [31]
3. Policies and procedures for delegation must be developed. The employer/nurse leader must outline specific responsibilities that can be delegated and to whom these responsibilities can be delegated. The policies and procedures should also indicate what may not be delegated. The employer must periodically review the policies and procedures for delegation to ensure they remain consistent with current nursing practice trends and that they are consistent with the state Nurse Practice Act. (Institution/employer policies can be more restrictive, but not less restrictive.)
- Rationale: Policies and procedures standardize the appropriate method of care and ensure safe practices. Having a policy and procedure specific to delegation and delegated responsibilities eliminates questions from licensed nurses and UAP about what can be delegated and how they should be performed. [32]
4. The employer/nurse leader must communicate information about delegation to the licensed nurses and UAP and educate them about what responsibilities can be delegated. This information should include the competencies of delegatees who can safely perform a specific nursing responsibility.
- Rationale: Licensed nurses must be aware of the competence level of staff and expectations for delegation (as described within the policies and procedures) to make informed decisions on whether or not delegation is appropriate for the given situahttps://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/tion. Licensed nurses maintain accountability for the client. However, the delegatee has responsibility for the delegated activity, skill, or procedure.
In summary, delegation is the transfer of the nurse’s responsibility for a task while retaining professional accountability for the client’s overall outcome. The decision to delegate is based on the nurse’s judgment, the act of delegation must be clearly defined by the nurse, and the outcomes of delegation are an extension of the nurse’s guidance and supervision. Delegation, when rooted in mutual respect and trust, is a key component to an effective health care team.
Delegation is an integral skill in the nursing profession to help manage the complexities of the dynamic and ever-changing health care environment. Delegation in nursing has been found to increase employee empowerment, decrease burnout, increase role commitment, and improve job satisfaction. [33] Cultivating delegation skills helps nurses better manage the complexities of their client care role, ensuring that their clients are safely cared for and outcomes are optimized. Delegation skills, like other nursing skills, require purposeful development and do not necessarily come easily when first transitioning into the nursing role. It is important that the new graduate nurse does not mistake delegation for pompous or arrogant behavior. Delegation requires mutual respect between the delegator and delegatee. Delegation is not seen as a sign or weakness and does not reflect one’s desire to shirk their work responsibilities. Instead, delegation reflects strong leadership and organizational skills in which the nurse leader demonstrates that they understand how to leverage their team’s strengths in order to achieve optimal care outcomes.
To help avoid any perception of arrogance in the delegation of an activity, it is important that the new graduate nurse approaches the task of delegation with humility. Clarity in the communication of the delegated responsibility is critical, and the rationale behind the delegation should be communicated to the delegatee. Within the task of delegation, the delegator should express appreciation for the delegatee and their contributions in the collaborative health care environment. Additionally, it is important to understand that no specific nurse delegated task is outside of the “nurse” role. For example, ambulating a client does not need to delegated to an unlicensed assistive personnel simply because that individual is able to perform that task. Rather, nurses must be willing to perform delegated tasks themselves when necessary. This reflects a team-oriented mindset and helps to reinforce among the care team that all roles are critical to optimizing client care. For new graduate nurses who first transition into a specific health care setting, having the opportunity to shadow individuals in various work roles helps to foster a team mindset. Asking questions of various team members regarding their work role can help a new graduate nurse demonstrate respect and value for other roles.
Examples of helpful questions may include the following:
- “What is the biggest challenge in your typical workday?”
- “What do you most enjoy about your job?”
- “How is it best to communicate with you when the unit is busy?”
- “What do you think people misunderstand most about your role?”
It is important to ensure that the team understands that care is optimized when they function as one collective unit and not in siloed roles. Each team member must feel valued and competent in their role. By understanding and practicing strategic delegation, new graduate nurses can overcome any misconceptions of arrogance and contribute positively to the healthcare team.
Review the example below to consider variation in approach to task delegation.
Scenario A: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a client. Nurse June approaches Alex in the hallway and says in an abrupt tone, “Alex, I need you to take Mr. Smith’s vital signs right now. I’m too busy to do it myself, and besides, that’s what you’re here for. Just get it done quickly.”
Analysis: June’s tone and words suggest she sees Alex’s role as less important and purely as a means to offload her tasks. June does not explain the urgency or importance of the task. June doesn’t acknowledge Alex’s effort or capability, making the request seem like a command rather than a collaborative effort.
Scenario B: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a client. Nurse June approaches Alex and says, “Hi Alex, could you please help me by taking Mr. Smith’s vital signs? I’m handling a few urgent matters right now, and it would really help to have your support. I know you’re great at this, and your thoroughness really makes a difference in our client care. Thank you so much!”
Analysis: June speaks to Alex with courtesy and acknowledges the value of his role. June clearly explains why she needs Alex’s help and the importance of the task. June acknowledges Alex’s competence and expresses gratitude, fostering feelings of value and respect.
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation . https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- “Delegation.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- NCSBN. (n.d.). Delegation. https://www.ncsbn.org/1625.htm ↵
- “Delegation Decision Tree.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- ANA. (2023, September 7). Delegation in nursing: How to build a stronger team. Retrieved from https://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/ ↵
An RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN (where the state’s Nurse Practice Act allows), is competent to perform the task, and verbally accepts the responsibility.
Allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed.
A nursing activity, skill, or procedure that is transferred from a license nurse to a delegatee.
Being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard.
Appropriate monitoring of the delegated activity, evaluation of client outcomes, and follow up with the delegatee at the completion of the activity.
Nursing Management and Professional Concepts 2e Copyright © by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
3.4 Delegation
There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND). [1] These guidelines apply to all levels of nursing licensure (advanced practice registered nurses [APRN], registered nurses [RN], and licensed practical/vocational nurses [LPN/VN]) when delegating, and there is no specific guidance provided by the state’s Nurse Practice Act (NPA). [2] It is important to note that states have different laws and rules/regulations regarding delegation, so it is the responsibility of all licensed nurses to know what is permitted in their jurisdiction.
The NGND defines a delegatee as an RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN (where the state’s Nurse Practice Act allows), is competent to perform the task, and verbally accepts the responsibility. [3] When performing a fundamental skill on the job, the delegatee is considered to be carrying out an “assignment.” Routine care, activities, and procedures are assigned based on what is included in the delegatee’s basic educational program. A licensed nurse is still responsible for ensuring an assignment is carried out completely and correctly. Delegation is defined as allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed. This definition of delegation applies to licensed nurses as well as to assistive personnel. [4]
Delegation is summarized in the NGND as the following: [5]
- A delegatee is allowed to perform a specific nursing activity, skill, or procedure that is outside the traditional role and basic responsibilities of the delegatee’s current job.
- The delegatee has obtained the additional education and training and validated competence to perform the care/delegated responsibility. The context and processes associated with competency validation will be different for each activity, skill, or procedure being delegated. Competency validation should be specific to the knowledge and skill needed to safely perform the delegated responsibility, as well as to the level of the practitioner (e.g., RN, LPN/VN, AP) to whom the activity, skill, or procedure has been delegated. The licensed nurse who delegates the “responsibility” maintains overall accountability for the client. However, the delegatee bears the responsibility for the delegated activity, skill, or procedure.
- The licensed nurse cannot delegate nursing judgment or any activity that will involve nursing judgment or critical decision-making.
- Nursing responsibilities are delegated by someone who has the authority to delegate.
- The delegated responsibility is within the delegator’s scope of practice.
- When delegating to a licensed nurse, the delegated responsibility must be within the parameters of the delegatee’s authorized scope of practice under the NPA. Regardless of how the state/jurisdiction defines delegation, as compared to assignment, appropriate delegation allows for transition of a responsibility in a safe and consistent manner. Clinical reasoning, nursing judgment, and critical decision-making cannot be delegated.
For example, in some agencies, medication administration is delegated to specially trained CNAs. This task is outside the traditional role of a CNA, but the delegatee has received additional training for this delegated responsibility. They have received competency validation in completing this task accurately, but the licensed nurse still maintains accountability for the client. Accountability is defined as being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity themselves. [6]
Another example illustrating the difference between assignment and delegation is evidenced when considering patient assistance with eating. Feeding patients is typically part of the role of assistive personnel. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or is otherwise experiencing swallowing difficulties (i.e., dysphagia), this task cannot be assigned to assistive personnel because it is not considered routine care. Instead, the RN should perform this task themselves or delegate it to a specially trained team member.
The delegation process is multifaceted. See Figure 3.2 [7] for an illustration of the intersecting responsibilities of the employer/nurse leader, licensed nurse, and delegatee with two-way communication that protects the safety of the public. “Delegation begins at the administrative/nurse leader level of the organization and includes determining nursing responsibilities that can be delegated, to whom, and under what circumstances; developing delegation policies and procedures; periodically evaluating delegation processes; and promoting a positive culture/work environment. The licensed nurse is responsible for determining client needs and when to delegate, ensuring availability to the delegatee, evaluating outcomes, and maintaining accountability for delegated responsibility. Finally, the delegatee must accept activities based on their competency level, maintain competence for delegated responsibility, and maintain accountability for delegated activity.” [8]
Five Rights of Delegation
How does the RN determine what tasks can be delegated, when, and to whom? According to the National Council of State Boards of Nursing (NCSBN), RNs should use five rights of delegation to ensure proper and appropriate delegation: right task, right circumstance, right person, right directions and communication, and right supervision and evaluation: [9]
- Right task: The activity falls within the delegatee’s job description or is included as part of the established policies and procedures of the nursing practice setting. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Right circumstance: The health condition of the client must be stable. If the client’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation. [10]
- Right person: The licensed nurse, along with the employer and the delegatee, is responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity. [11]
- Right directions and communication: Each delegation situation should be specific to the client, the nurse, and the delegatee. The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee, as part of two-way communication, should ask any clarifying questions. This communication includes any data that need to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation. The delegatee must understand the terms of the delegation and must agree to accept the delegated activity. The licensed nurse should ensure the delegatee understands they cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse. [12]
- Right supervision and evaluation: The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating client outcomes. The delegatee is responsible for communicating client information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary. The licensed nurse should ensure appropriate documentation of the activity is completed. [13]
Simply stated, the licensed nurse determines the right person is assigned the right tasks for the right clients under the right circumstances. When determining what aspects of care can be delegated, the licensed nurse uses clinical judgment while considering the client’s current clinical condition, as well as the abilities of the health care team member. The RN must also consider if the circumstances are appropriate for delegation. For example, although obtaining routine vitals signs on stable clients may be appropriate to delegate to assistive personnel, obtaining vitals signs on an unstable client is not appropriate to delegate.
After the decision has been made to delegate, the nurse assigning the tasks must communicate appropriately with the delegatee and provide the right directions and supervision. Communication is key to successful delegation. Clear, concise, and closed-loop communication is essential to ensure successful completion of the delegated task in a safe manner. During the final step of delegation, also referred to as supervision , the nurse verifies and evaluates that the task was performed correctly, appropriately, safely, and competently. Read more about supervision in the following subsection on “ Supervision .” See Table 3.4 for additional questions to consider for each “right” of delegation.
Table 3.4 Rights of Delegation [14]
| A task that can be transferred to a member of the nursing team for a specific client. | ||
| The client is stable. | ||
| The person delegating is appropriate. The task is appropriate for this delegatee’s skills and knowledge. | ||
| The task or activity is clearly defined and described. | ||
| The RN appropriately monitors the delegated activity, evaluates client outcomes, and follows up with the delegatee at the completion of the activity. |
Keep in mind that any nursing intervention that requires specific nursing knowledge, clinical judgment, or use of the nursing process can only be delegated to another RN. Examples of these types of tasks include initial preoperative or admission assessments, client teaching, and creation and evaluation of a nursing care plan. See Figure 3.3 [15] for an algorithm based on the 2019 National Guidelines for Nursing Delegation that can be used when deciding if a nursing task can be delegated. [16]
Responsibilities of the Licensed Nurse
The licensed nurse has several responsibilities as part of the delegation process. According to the NGND, any decision to delegate a nursing responsibility must be based on the needs of the client or population, the stability and predictability of the client’s condition, the documented training and competence of the delegatee, and the ability of the licensed nurse to supervise the delegated responsibility and its outcome with consideration to the available staff mix and client acuity. Additionally, the licensed nurse must consider the state Nurse Practice Act regarding delegation and the employer’s policies and procedures prior to making a final decision to delegate. Licensed nurses must be aware that delegation is at the nurse’s discretion, with consideration of the particular situation. The licensed nurse maintains accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity. [17]
1. The licensed nurse must determine when and what to delegate based on the practice setting, the client’s needs and condition, the state’s/jurisdiction’s provisions for delegation, and the employer’s policies and procedures regarding delegating a specific responsibility. The licensed nurse must determine the needs of the client and whether those needs are matched by the knowledge, skills, and abilities of the delegatee and can be performed safely by the delegatee. The licensed nurse cannot delegate any activity that requires clinical reasoning, nursing judgment, or critical decision-making. The licensed nurse must ultimately make the final decision whether an activity is appropriate to delegate to the delegatee based on the “Five Rights of Delegation.”
- Rationale: The licensed nurse, who is present at the point of care, is in the best position to assess the needs of the client and what can or cannot be delegated in specific situations. [18]
2. The licensed nurse must communicate with the delegatee who will be assisting in providing client care. This should include reviewing the delegatee’s assignment and discussing delegated responsibilities, including information on the client’s condition/stability, any specific information pertaining to a certain client (e.g., no blood draws in the right arm), and any specific information about the client’s condition that should be communicated back to the licensed nurse by the delegatee.
- Rationale: Communication must be a two-way process involving both the licensed nurse delegating the activity and the delegatee being delegated the responsibility. Evidence shows that the better the communication between the nurse and the delegatee, the more optimal the outcome. The licensed nurse must provide information about the client and care requirements. This includes any specific issues related to any delegated responsibilities. These instructions should include any unique client requirements. The licensed nurse must instruct the delegatee to regularly communicate the status of the client. [19]
3. The licensed nurse must be available to the delegatee for guidance and questions, including assisting with the delegated responsibility, if necessary, or performing it themselves if the client’s condition or other circumstances warrant doing so.
- Rationale: Delegation calls for nursing judgment throughout the process. The final decision to delegate rests in the hands of the licensed nurse as they have overall accountability for the client. [20]
4. The licensed nurse must follow up with the delegatee and the client after the delegated responsibility has been completed.
- Rationale: The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. [21]
5. The licensed nurse must provide feedback information about the delegation process and any issues regarding delegatee competence level to the nurse leader. Licensed nurses in the facility need to communicate to the nurse leader responsible for delegation any issues arising related to delegation and any individual that they identify as not being competent in a specific responsibility or unable to use good judgment and decision-making.
- Rationale: This will allow the nurse leader responsible for delegation to develop a plan to address the situation. [22]
The decision of whether or not to delegate or assign is based on the RN’s judgment concerning the condition of the client, the competence of the nursing team member, and the degree of supervision that will be required of the RN if a task is delegated. [23]
Responsibilities of the Delegatee
Everyone is responsible for the well-being of clients. While the nurse is ultimately accountable for the overall care provided to a client, the delegatee shares the responsibility for the client and is fully responsible for the delegated activity, skill, or procedure. [24] The delegatee has the following responsibilities:
1. The delegatee must accept only the delegated responsibilities that he or she is appropriately trained and educated to perform and feels comfortable doing given the specific circumstances in the health care setting and client’s condition. The delegatee should confirm acceptance of the responsibility to carry out the delegated activity. If the delegatee does not believe they have the appropriate competency to complete the delegated responsibility, then the delegatee should not accept the delegated responsibility. This includes informing the nursing leadership if they do not feel they have received adequate training to perform the delegated responsibility, is not performing the procedure frequently enough to do it safely, or their knowledge and skills need updating.
- Rationale: The delegatee shares the responsibility to keep clients safe, and this includes only performing activities, skills, or procedures in which they are competent and comfortable doing. [25]
2. The delegatee m ust maintain competency for the delegated responsibility.
- Rationale: Competency is an ongoing process. Even if properly taught, the delegatee may become less competent if they do not frequently perform the procedure. Given that the delegatee shares the responsibility for the client, the delegatee also has a responsibility to maintain competency. [26]
3. The delegatee must communicate with the licensed nurse in charge of the client. This includes any questions related to the delegated responsibility and follow-up on any unusual incidents that may have occurred while the delegatee was performing the delegated responsibility, any concerns about a client’s condition, and any other information important to the client’s care.
- Rationale: The delegatee is a partner in providing client care. They are interacting with the client/family and caring for the client. This information and two-way communication are important for successful delegation and optimal outcomes for the client. [27]
4. Once the delegatee verifies acceptance of the delegated responsibility, the delegatee is accountable for carrying out the delegated responsibility correctly and completing timely and accurate documentation per facility policy. The delegatee cannot delegate to another individual. If the delegatee is unable to complete the responsibility or feels as though they need assistance, the delegatee should inform the licensed nurse immediately so the licensed nurse can assess the situation and provide support. Only the licensed nurse can determine if it is appropriate to delegate the activity to another individual. If at any time the licensed nurse determines they need to perform the delegated responsibility, the delegatee must relinquish responsibility upon request of the licensed nurse.
- Rationale: Only a licensed nurse can delegate. In addition, because they are responsible, they need to provide direction, determine who is going to carry out the delegated responsibility, and assist or perform the responsibility themselves, if they deem that appropriate under the given circumstances. [28]
Responsibilities of the Employer/Nurse Leader
The employer and nurse leaders also have responsibilities related to safe delegation of client care:
1. The employer must identify a nurse leader responsible for oversight of delegated responsibilities for the facility. If there is only one licensed nurse within the practice setting, that licensed nurse must be responsible for oversight of delegated responsibilities for the facility.
- Rationale: The nurse leader has the ability to assess the needs of the facility, understand the type of knowledge and skill needed to perform a specific nursing responsibility, and be accountable for maintaining a safe environment for clients. They are also aware of the knowledge, skill level, and limitations of the licensed nurses and AP. Additionally, the nurse leader is positioned to develop appropriate staffing models that take into consideration the need for delegation. Therefore, the decision to delegate begins with a thorough assessment by a nurse leader designated by the institution to oversee the process. [29]
2. The designated nurse leader responsible for delegation, ideally with a committee (consisting of other nurse leaders) formed for the purposes of addressing delegation, must determine which nursing responsibilities may be delegated, to whom, and under what circumstances. The nurse leader must be aware of the state Nurse Practice Act and the laws/rules and regulations that affect the delegation process and ensure all institutional policies are in accordance with the law.
- Rationale: A systematic approach to the delegation process fosters communication and consistency of the process throughout the facility. [30]
3. Policies and procedures for delegation must be developed. The employer/nurse leader must outline specific responsibilities that can be delegated and to whom these responsibilities can be delegated. The policies and procedures should also indicate what may not be delegated. The employer must periodically review the policies and procedures for delegation to ensure they remain consistent with current nursing practice trends and that they are consistent with the state Nurse Practice Act. (Institution/employer policies can be more restrictive, but not less restrictive.)
- Rationale: Policies and procedures standardize the appropriate method of care and ensure safe practices. Having a policy and procedure specific to delegation and delegated responsibilities eliminate questions from licensed nurses and AP about what can be delegated and how they should be performed. [31]
4. The employer/nurse leader must communicate information about delegation to the licensed nurses and AP and educate them about what responsibilities can be delegated. This information should include the competencies of delegatees who can safely perform a specific nursing responsibility.
- Rationale: Licensed nurses must be aware of the competence level of staff and expectations for delegation (as described within the policies and procedures) to make informed decisions on whether or not delegation is appropriate for the given situation. Licensed nurses maintain accountability for the client. However, the delegatee has responsibility for the delegated activity, skill, or procedure.
In summary, delegation is the transfer of the nurse’s responsibility for a task while retaining professional accountability for the client’s overall outcome. The decision to delegate is based on the nurse’s judgment, the act of delegation must be clearly defined by the nurse, and the outcomes of delegation are an extension of the nurse’s guidance and supervision. Delegation, when rooted in mutual respect and trust, is a key component to an effective health care team.
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation . https://www.ncsbn.org/NGND-PosPaper_06.pdf ↵
- “Delegation.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- NCSBN. (n.d.). Delegation. https://www.ncsbn.org/1625.htm ↵
- "Delegation Decision Tree.png" by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
An RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN (where the state’s Nurse Practice Act allows), is competent to perform the task, and verbally accepts the responsibility.
Allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed.
Being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard.
Leadership and Management of Nursing Care Copyright © 2022 by Kim Belcik and Open Resources for Nursing is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
Delegating vs. assigning: What you need to know
Registered nurses (RNs) often delegate to other RNs, licensed practical nurses/vocational nurses (LPN/LVNs), and assistive personnel (AP). (In some states or jurisdictions, LPN/LVNs may be allowed to delegate, so “licensed nurses” will be used in this article.) Delegating appropriately protects patients and reduces the risk of legal liability, yet the parameters of delegation often are not fully understood.
One common area of misunderstanding is delegation vs. assignment. Knowing the differences between the two is essential to ensure you delegate appropriately. The primary difference relates to scope of practice and where the clinician learned the activities to be carried out.
According to national guidelines for nursing delegation from the National Council of State Boards of Nursing (NCSBN) and American Nurses Association (ANA), an assignment refers to the “routine care, activities, and procedures that are within the authorized scope of practice of the RN or LPN/VN or part of the routine functions of the AP.” This definition covers fundamental skills that the assignee would have learned in a basic education program. A licensed nurse is still responsible for ensuring the assignment is carried out correctly.
According to the NCSBN/ANA guideline, delegation applies when the delegatee is performing a “specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed.” As opposed to work that is part of an assignment, the work associated with delegation was not learned in a basic education program. Therefore, the delegatee must have obtained additional education and have verified competence in the delegated area for which they will be responsible. The licensed nurse maintains overall accountability for the patient, but the delegatee is responsible for the delegated activity, skill, or procedure.
Licensed nurses can’t delegate activities that involve clinical reasoning, nursing judgment, or critical decision making, and the delegated responsibility has to be within the delegator’s scope of practice under the state’s or jurisdiction’s nurse practice act (NPA).
Responsibilities
Organizational administrators, the delegator, and the delegatee each have responsibilities when an activity, skill, or procedure is delegated.
Professionals who work at the administrative or managerial level of the organization set the cultural tone for the nursing work environment and are responsible for managing the delegation processes. Those at the administrative level within an organization define what nursing responsibilities may be delegated, to whom, and under what set(s) of circumstances. They are also responsible for developing and maintaining policies and procedures associated with delegation, periodically evaluating the efficacy and safety of delegation processes, and training and educating staff.
The delegator is responsible for determining the needs of the patient, when delegation is appropriate, and if the delegatee is competent to complete the delegated task. Delegators must follow delegation guidelines in the NPA and relevant organizational policies and procedures. Clear communication is key, and the delegator must be available as a resource to the delegatee. Delegators also need to evaluate outcomes as they maintain overall accountability for the patient. Delegators must be prepared to step in at any point if it appears the delegatee is not handling the assignment appropriately. Any problems should be reported to nursing leadership.
The delegatee is responsible for only accepting activities that fall within their competence and that they feel comfortable completing safely. Delegatees must communicate with the delegator, particularly if the patient’s condition changes, and complete the activity correctly, including fulfilling any documentation requirements. Delegatees maintain accountability for the delegated activity and need to notify the delegator immediately if they have difficulty completing the task.
One special case
NCSBN notes that in some cases, APs are taught how to perform skills that were previously thought to be exclusively RN and LPN/LVN responsibilities, such as certified medical assistants administering injections. In these cases, it’s best to consider such tasks as being delegated and, therefore, validate competency.
Keeping patients safe
Knowing the differences between assigning and delegating helps protect patients and avoid legal action should an error occur. Assignments involve routine tasks learned in basic education and that fall under designated scope of practice, while delegation involves tasks that were learned through additional education and for which competency has been determined.
Good communication and an understanding of the responsibilities of delegators and delegatees is essential to avoid misunderstanding. Remember, the licensed nurse remains accountable for the patient, but the delegatee is responsible for the delegated task.
Five rights of delegation
The ncsbn outlines five rights of delegation. in the case of a lawsuit, a key component would be whether you adhered to these rights:.
- Right task . The task needs to fall within the delegatee’s job description or is part of organizational policies and procedures.
- Right circumstance . The patient must be stable.
- Right person . The delegatee must have the appropriate skills and knowledge to perform the task.
- Right directions and communication . Clear directions need to be given, with the delegator verifying understanding by the delegatee. Communication must be two-way, with the delegatee asking questions as needed.
- Right supervision and evaluation . The delegator needs to monitor the delegated activity, including evaluating patient outcomes.
Article by: Cynthia Saver, MS, RN, President of CLS Development, Inc., in Columbia, Md and Georgia Reiner, MS, CPHRM, Risk Analyst, NSO
National Council of State Boards of Nursing. National guidelines for nursing delegation. J Nurs Reg. 2016;7(1):5-12.
NCSBN, ANA. National guidelines for nursing delegation. 2019.
#Delegating #RN
Share this article:
Frequently Asked Questions
You have questions. We have answers. (It's why we're here.)
What kinds of activities might trigger a disciplinary action by a licensing board or regulatory agency?
The fact is anyone can file a complaint against you with the state board for any reason—even your own employer—and it doesn’t have to be solely connected to your professional duties. All complaints need to be taken seriously, no matter how trivial or unfounded they may appear.
How does a shared limit policy work?
The business, and all eligible employees and sub-contractors you regularly employ, will be considered when determining your practice’s premium calculation and share the same coverage limits you select for the business.
We have a shared limit policy. Are employees covered if they practice outside our office?
If your employees are moonlighting, either for pay or as a volunteer, they should carry an individual professional liability insurance policy to cover those services. Otherwise, they might not be covered for claims that arise out of these activities.
There are plenty more where those came from.
See more FAQs
More learning right here
Check out these related articles.
Nurse Case Study: Failure to monitor and inadequate documentation in home health setting
RN working in home health setting fails to monitor and properly document ulcer wounds in post-surgical Alzheimer’s patient.
Nurse Case Study: Failure to monitor high fall risk ICU patient; failure to educate family on fall prevention
This medical malpractice case study, presented by NSO and CNA, involves a registered nurse working in a critical care setting.
Joint Statement on Delegation
American nurses association (ana) and the national council of state boards of nursing (ncsbn) position statement.
Date : 2019 Adopted By : ANA and NCSBN
In 2005, both the American Nurses Association (ANA) and the National Council of State Boards of Nursing (NCSBN) adopted papers on delegation. Both papers presented the same message: delegation is an essential nursing skill. This joint statement has been updated (2019) - The National Guidelines for Nursing Delegation, reflecting an effort to standardize the nursing delegation process based on research findings and evidence in the literature and is applicable to all levels of nursing licensure (advanced practice registered nurse [APRN], registered nurse [RN], licensed practical/vocational nurse [LPN/VN]) where the nurse practice act (NPA) is silent.
The decision of whether or not to delegate or assign is based upon the RN’s judgement concerning the condition of the patient, the competence of all members of the nursing team and the degree of supervision that will be required of the RN if a task is delegated. The difference between delegation and assignment has been a source of debate for years and an attempt to distinguish between the two is captured in this document.
full position statement
Item(s) added to cart
Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password
| Property | Value |
|---|---|
| Status | |
| Version | |
| Ad File | |
| Disable Ads Flag | |
| Environment | |
| Moat Init | |
| Moat Ready | |
| Contextual Ready | |
| Contextual URL | |
| Contextual Initial Segments | |
| Contextual Used Segments | |
| AdUnit | |
| SubAdUnit | |
| Custom Targeting | |
| Ad Events | |
| Invalid Ad Sizes |
- NCSBN Member Login Submit
Access provided by

National Guidelines for Nursing Delegation
Download started
- Download PDF Download PDF
- Add to Mendeley
- evidence-based
- nursing assignment
31035-3/asset/5b80c4da-1d61-4753-b452-b588583d6440/main.assets/gr1.jpg)
Delegation Versus Assignment
Additional key definitions, literature review, guidelines for delegation, employer/nurse leader responsibilities, licensed nurse responsibilities.
- Open table in a new tab
Delegatee Responsibilities
Expert panel.
CE Posttest
Instructions, provider accreditation.
31035-3/asset/71dc2ab0-eca2-43b4-98ea-010c25cfa6bc/main.assets/fx2.jpg)
Article metrics
Related articles.
- Download Hi-res image
- Download .PPT
- Access for Developing Countries
- Articles & Issues
- Current Issue
- List of Issues
- For Authors
- Guide for Authors
- Author Services
- Permissions
- Researcher Academy
- Submit a Manuscript
- Journal Info
- About the Journal
- Contact Information
- Editorial Board
- New Content Alerts
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Health Serv Res
- PMC11075185

Delegating care as a double-edged sword for quality of nursing care: a qualitative study
Tayebeh moradi.
Trauma Nursing Research Center, Kashan University of Medical Sciences, Kashan, Iran
Mahboubeh Rezaei
Negin masoudi alavi, associated data.
No datasets were generated or analysed during the current study.
Considering the significance of care delegation in enhancing the quality of nursing care and ensuring patient safety, it is imperative to explore nurses’ experiences in this domain. As such, this study aimed to explore the experiences of Iranian nurses regarding the delegation of care.
This qualitative study was conducted between 2022 and 2023, employing the content analysis method with a conventional approach. The study utilized purposeful sampling method to select qualified participants. Data collection was carried out through in-depth and semi-structured interviews utilizing open-ended questions. The data analysis process followed the steps proposed by Graneheim and Lundman (2004) and involved the use of MAXQDA version 12 software. To ensure the trustworthiness of the data, the study employed the four rigor indices outlined by Lincoln and Guba (1985).
In the present study, a total of 15 interviews were conducted with 12 participants, the majority of whom were women. The age range of the participants fell between 25 and 40 years. Through qualitative data analysis, eight subcategories and three main categories of “insourcing of care”, “outsourcing of care” and “delegating of care to non-professionals” were identified. Additionally, the overarching theme that emerged from the analysis was “delegation of care, a double-edged sword”.
Conclusions
The results of the study revealed that the delegation of care occurred through three distinct avenues: to colleagues within the same unit, to colleagues in other units, and to non-professionals. Delegating care was found to have potential benefits, such as reducing the nursing workload and fostering teamwork. However, it was also observed that in certain instances, delegation was not only unhelpful but also led to missed nursing care. Therefore, it is crucial to adhere to standardized principles when delegating care to ensure the maintenance of high-quality nursing care.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-11054-4.
Introduction
Nurses play a crucial role in delivering healthcare services on the frontline. They serve as planners, coordinators, providers, and evaluators of care, performing a wide range of nursing tasks from the moment of admission to discharge to enhance patients’ health and facilitate their recovery [ 1 – 3 ]. Given that nurses constitute the majority of healthcare personnel worldwide, the quality of care they deliver holds significant importance [ 4 ]. Hence, any disruptions in the flow of care provided by nurses can lead to a decline in the quality of care [ 2 ].
The delegating care or delegation of authority is recognized as one of the factors that impact the quality of nursing care [ 5 ]. Various definitions of delegation of authority can be found in the related literature, but they all share a common theme: the transfer of responsibility for an activity from one person to another who accepts the responsibility to carry out the activity in an appropriate manner [ 6 ]. Nurses possess the authority to safeguard the health and well-being of each patient, allowing them to assign certain care activities to other qualified and competent individuals [ 7 ]. In the 21st century, nurses are expected to possess the ability to delegate care services while also supervising the delegated care. Delegation of care enables nurses to allocate more time to patient care, support, and education [ 8 ]. The process of delegating care involves complex decision-making, where nurses must demonstrate leadership and change management skills to establish team cohesion, support patients, and ensure the effective implementation of nursing activities [ 9 ]. In essence, delegation is viewed as a leadership skill that can significantly impact the quality of care and patient satisfaction [ 5 ]. Campbell et al. (2020) demonstrated that effective delegation of care and proper communication between nurses and nursing assistants can enhance cooperation, job satisfaction, and ultimately reduce negative outcomes for patients [ 10 ]. Delegation improves accountability, productivity, and facilitates the development of teamwork [ 11 ]. Proper and principled delegation of authority enhances nurses’ knowledge, decision-making abilities, and competence. It also improves communication skills, reduces missed care, and minimizes delays in care [ 12 , 13 ]. However, the effectiveness of teamwork and delegation between nurses and healthcare assistants varies across different unit cultures and work styles. In some settings, delegation of care may not be executed properly, leading to inefficiencies and decreased effectiveness [ 14 ]. Providing safe care is contingent upon safe delegation, and this necessitates that nurses appropriately plan, delegate, and monitor assigned tasks. Failure to delegate care activities safely and appropriately can result in adverse outcomes for patients and contribute to missed nursing care and nursing care rationing [ 15 ]. In certain instances, due to high workload, nurses may delegate complex and challenging care tasks to individuals with lower skill levels, and there may be a lack of adequate monitoring of the delegated activities. Consequently, care may be missed, duplicated, or administered improperly [ 15 ]. GransjönCraftman’s study highlighted that the high workload experienced by nurses and the challenges they face have led to the delegation of drug administration tasks to unlicensed personnel, potentially compromising the quality of care [ 16 ]. Poor delegation practices can result in nurses and nursing assistants working in parallel and separately, rather than functioning as an integrated team. It leads to ineffective communication, inappropriate work dynamics, conflicts between nurses and nursing assistants, and ultimately a decrease in the quality of care [ 14 ]. Furthermore, improper delegation of authority can result in non-compliance with care standards, inadequate documentation of provided care, and poor assessment and monitoring of patient conditions [ 17 ]. Some nurses lack understanding of the concept of delegation and do not provide proper monitoring when delegating authority. This lack of monitoring also may lead to missed nursing care and potential adverse events for patients [ 15 , 18 ].
In Iran, the delegation of care is performed by nurses, though in some cases this delegation is inappropriate. The nursing structure in Iran differs from that of other countries. The majority of nurses employed in Iranian hospitals hold a bachelor’s degree and work in hospitals and health centers under the ownership and administration of the Ministry of Health and Medical Education. Nurses in Iran face various challenges such as a shortage of nursing personnel, immediate employment after graduation without prior work experience, overtime work, undefined responsibilities, inadequate equipment, low wages, and a gap between theoretical knowledge and practical application [ 19 , 20 ]. Consequently, the delegation of care in Iran appears to be distinct from that of other countries and warrants further investigation. Rooddehghan et al. (2015) showed that Iran’s nursing care system lacks specific guidelines for delegating care. As a result, due to the nursing shortage, care is sometimes delegated to non-professionals, including the patient’s family. Additionally, due to high nursing workload, proper monitoring of these delegated tasks is not consistently carried out. Consequently, the provision of nursing care is disrupted, posing a threat to patient safety [ 8 ].
Examining the experiences of Iranian nurses regarding the delegation of care can provide valuable insights and a more realistic understanding of their perspectives on this issue. Quantitative research methods may not offer the necessary flexibility and depth required to investigate the experiential aspects of a phenomenon. Therefore, the most suitable approach to explore the experience of care delegation is through the use of qualitative research methods. These methods are particularly effective in exploring questions that involve human interpretations, mentalities, and the depth and complexity of phenomena [ 21 ]. Considering the significance of care delegation in the quality of nursing care and the limited research conducted on this topic in Iran, the purpose of this study was to explore the experiences of Iranian nurses regarding the delegation of care.
The main question of this research focused on understanding the experience of Iranian nurses in delegating care. To address this question, the appropriate research method utilized was qualitative research, with conventional content analysis approach. Qualitative content analysis is a research method commonly used to explore individuals’ understanding of everyday life phenomena and interpret the content of qualitative data. In conventional content analysis categories are directly extracted from the data [ 22 ].
Participants and sampling
The participants consisted of nurses working in various units of hospitals in Kashan city, located in the central region of Iran. The inclusion criteria for participating in the study included being a clinical nurse (a nurse who has at least a bachelor’s degree in nursing and is responsible for direct clinical care of the patients), having a minimum work experience of six months, and providing consent to participate. The exclusion criterion was the participant’s decision to leave the research during the study. The participants were selected using purposeful sampling method, taking into account the maximum variation in terms of personal and job characteristics. Sampling continued until data saturation was reached.
Data collection
After identifying eligible participants and obtaining their consent to participate in the study, information regarding personal characteristics (such as age, gender, level of education, marital status, and number of children) as well as occupational characteristics (including unit of service, work experience, and position) were collected. Data collection was conducted through in-depth and semi-structured interviews utilizing open-ended questions. The first participant was purposefully selected as a key informant among the nurses working in Kashan hospitals, and then subsequent sampling continued with maximum variation. Before the interviews, the participants were contacted by phone to arrange the details. The first researcher introduced herself and explained the purpose of the study to the participants. If the participants agreed to take part, the time and location of the interview were determined based on their preferences and convenience. With consent from the participants, the interviews were recorded using a MP3 Recorder and later transcribed verbatim. The interviews were guided by the following questions: (a) Please explain your experience of delegating care to another person; (b) What kind of care have you delegated to others, and to whom did you delegate the care? (c) What factors influenced your decision to delegate care to others? To encourage the participants and gather more in-depth information, probing questions such as “Please explain more,” “Clarify your statement further,” or “Provide an example” were asked during the interviews. The duration of the interviews ranged from 20 to 70 min. In three cases, due to fatigue of the participants during the interview, it was decided to conduct the rest of the interview in the second session.
Data analysis
The data analysis commenced after the first interview and continued alongside data collection. This iterative process allowed for a back-and-forth movement between developing concepts and gathering data, enabling subsequent data collection to acquire relevant information to address the main research question [ 22 ]. The data analysis procedure followed the steps proposed by Graneheim and Lundman (2004) [ 23 ]. The verbatim transcripts of the interviews were imported into MAXQDA software, version 12 for coding and analysis. The researchers thoroughly read the interview texts multiple times to gain a comprehensive understanding. In this research, the entire text of each interview was considered as the unit of analysis. Following that, words, sentences, or paragraphs were identified as meaning units and grouped based on their content and meaning, resulting in condensed meaning units. These condensed meaning units were abstracted, labeled, and transformed into codes. Coding was performed using the participants’ language (in vivo) or based on the researcher’s general understanding of the participants’ speech (in vitro). The codes were then compared to identify similarities and differences and then were categorized into subcategories and main categories, forming the manifest content. Through a process of careful reflection and comparison among the categories, the latent content, which was the theme of this study, was revealed. An example of how data were analyzed is provided in Table 1 .
Examples of meaning unit, condensed meaning unit, and codes
| Meaning unit | Condensed meaning unit | Codes |
|---|---|---|
| There is a problem with the demand for nurses from other units. There is no control over the work of these nurses and usually, the care by the temporary workforce isn’t done properly. | Lack of control over the work of nurses coming from other units and consequently the reduced quality of nursing care. | - Lack of control over the work of temporary nurses - Doing lower quality of care by temporary nursing staff |
| Sometimes the unit is so crowded that we’ve to delegate some work to the nurses of the next shift. If a lot of care is left to them, their workload will be increased. | An overcrowded unit forces the nurse to delegate care to the nurses of the next shift. Increased workload of the next shift nurses because of assigning a large number of cares to them. | - Mandatory delegation of care to the next shift nurses due to the overcrowded unit - High workload of the shift due to the number of cares delegated by the previous shift |
Rigor and trustworthiness
In this research, the trustworthiness of the data was assessed using four rigor indices proposed by Lincoln and Guba (1989) [ 24 ]. Prolonged engagement with the data for several months, appropriate and long-term participation and interaction with the participants, and member checking increased the credibility of the data. To increase the dependability of the data, immediate transcription of the interviews was performed, followed by seeking the opinions of two expert colleagues in the field of qualitative research (peer Checking). Moreover, the participants themselves reviewed the text of the interviews. For this purpose, several initial interviews, along with the preliminary codes derived from them, were provided to three participants involved in the interviews, allowing them to confirm or suggest corrections. The use of a sufficient and suitable sample with maximum variation in terms of demographic and occupational characteristics strengthened the confirmability of the data. Additionally, to ensure the transferability of the data, direct quotes from the participants were included, and comprehensive details related to the participants were described to provide a rich understanding of the context.
In the present study, a total of 15 interviews were conducted with 12 eligible participants. The majority of the participants were women whose ages ranged from 25 to 40 years. Additional characteristics of the participants can be found in Table 2 .
Demographic and occupational characteristics of the participants
| No. | Gender | Age (year) | Education | Marital status | No. of children | Unit | Work experience (year) | Position | Interview time (minutes) | Number of interviews |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 25 | Master’s degree | Married | No child | Internal, orthopedics, rheumatology and neurology | 2 | Nurse (rotating shift) | 25, 30 | 2 |
| 2 | Male | 36 | Bachelor’s degree | Married | 1 | ICU | 13 | Nurse (rotating shift) | 25, 30 | 2 |
| 3 | Female | 38 | Master’s degree | Married | 2 | ICU | 15 | Nurse (rotating shift) | 45 | 1 |
| 4 | Female | 40 | Bachelor’s degree | Married | 3 | Eye & ENT surgery | 17 | Nurse (rotating shift) | 20, 40 | 2 |
| 5 | Male | 25 | Master’s degree | Married | No child | CCU | 3 | Nurse (rotating shift) | 55 | 1 |
| 6 | Female | 34 | Bachelor’s degree | Married | 3 | Gastrointestinal surgery | 13 | Nurse (fixed morning shift) | 70 | 1 |
| 7 | Male | 29 | Bachelor’s degree | Married | No child | Infectious diseases | 6.5 | Nurse (fixed morning shift) | 45 | 1 |
| 8 | Female | 26 | Bachelor’s degree | Married | 1 | Pediatric and NICU | 2 | Nurse (rotating shift) | 35 | 1 |
| 9 | Female | 30 | Bachelor’s degree | Married | 1 | Pediatric | 8 | Nurse (rotating shift) | 30 | 1 |
| 10 | Female | 27 | Bachelor’s degree | Married | No child | Emergency | 4 | Nurse (rotating shift) | 35 | 1 |
| 11 | Female | 40 | Master’s degree | Single | No child | Oncology | 16 | Nurse (rotating shift) | 45 | 1 |
| 12 | Female | 35 | Master’s degree | Married | 1 | Nursing management office | 10 | Supervisor | 40 | 1 |
Qualitative data analysis resulted in the extraction of eight subcategories and three main categories as well as the theme of “delegation of care, a double-edged sword” (Table 3 ).
Results of data analysis
| Theme | Categories | Subcategories | Examples of codes |
|---|---|---|---|
| Delegation of care, a double-edged sword | Insourcing of care | Seeking assistance from colleagues in the same shift | Seeking assistance from a colleague with a lower workload Seeking assistance from a colleague with more stable patients Seeking assistance from a more experienced colleague |
| Seeking assistance from the head nurse | Seeking assistance from the head nurse for changing the dressing of orthopedic patients Seeking assistance fromthe head nurse for perform the care that the nurse is not skilled at Seeking assistance from the head nurse for changing the colostomy bag | ||
| Delegating care to colleagues on the next shift | Delegation of the patient’s dressing to the next shift Delegation of the medication to the next shift | ||
| Outsourcing of care | Patient transfer to other units | Transfer of patients with stable condition to another unit Transfer of patient with unstable condition to another unit | |
| Demand for extra nursing workforce | Requesting nursing workforce from other units Requesting nursing workforce from the nursing office Requesting for temporary nursing staff | ||
| Delegating of care to non-professionals | Delegating care to nurse assistant | Requesting the nurse assistant to do an electrocardiography Requesting the nurse assistant to perform a gavage Delegating the patient out of bed to the nurse assistant without the nurse’s supervision | |
| Delegating care to nursing students in the internship course | Delegating drug therapy to an inexperienced student Delegating the preparation of drugs to the inexperienced student Delegating unsupervised oxygen therapy to a nursing student | ||
| Delegating care to the patient’s family | Delegating of gavage to the patient’s family The patient’s change position by the patient’s family Disconnecting and reconnecting the IV drip by patient’s family |
After analyzing the data, it was found that nurses had experienced delegation of care in three ways: “insourcing of care”, “outsourcing of care” and “delegating of care to non-professionals”.
Insourcing of care
One of the categories extracted in this research was insourcing of care. Delegation of the patient’s care by the nurse to their colleagues in the same unit is called insourcing of care. In this type of delegation, the nurse delegates some of her/his patient care to other nurses in the unit for various reasons, including high workload or serious patient conditions. The insourcing of care can be accomplished through three methods: Seeking assistance from colleagues in the same shift, seeking assistance from the head nurse, or delegating care to colleagues on the next shift.
Seeking assistance from colleagues in the same shift
One form of the insourcing of care was seeking assistance from colleagues in the same shift. In the interviews, the nurses mentioned that sometimes due to the crowded unit, they asked for help from other nurses in their unit to provide care to their patients. In this regard, one of the participants said:
“When the unit is crowded, if I have a colleague whose work is less, or whose patients are more stable, or my colleague is more experienced, I get help from them, and they usually help me.” ( Participant No. 2).
Another participant said:
“Colleagues usually cooperate with me. For instance, a few days ago, the unit was extremely busy, and I had a patient with appendicitis. I asked my colleague to assist by providing the patient with clothes and completing a pre-operative form for them before going to the operating room. Also, she helped me by sending the patient’s test results. ” ( Participant No. 8).
Indeed, in delegating care to other nurses, the participants pointed out that nursing care is delegated to a colleague who has less workload, otherwise, the delegated care may be missed or overlooked. Two participants commented on this issue as follows:
“Since other colleagues may also have their own tasks to complete, we typically seek help from a colleague who less busy. This ensures that we can collectively finish all the work while allowing that colleague to assist us as well. Otherwise, our colleague may not be able to accommodate our requests or can inadvertently forget them.” ( Participant No. 4).
“Sometimes my colleagues delegate care to me, but I forget. For example, I was given an urgent care to do, or to notify sonography; I was so busy or involved in my own tasks that I forgot to do it or follow it up.” ( Participant No. 10).
Seeking assistance from the head nurse
Another subcategory of care insourcing was seeking assistance from the head nurse. Some nurses mentioned that when they face a high workload, lack of skill in caring for a specific situation, or when it is not possible to provide care due to moral or religious reasons, and other nurses are unable to help, they turn to the head nurse for assistance in performing the necessary care:
“Here, the head nurse is a man. If we’re on an all-female shift, we ask him to lend a hand with the urology patient, and he gladly pitches in. Sometimes, he assists us in changing the dressing of orthopedic patients which are big and heavy. We appreciate his help because it allows us to handle the patient’s care more efficiently.” ( Participant No. 6).
“Sometimes, nurses don’t know how to handle certain care, so they call the head nurse to come and do it, hoping to learn from them. Tasks like changing the colostomy bag, taking care of the port, removing the sheet after angiography, washing the chest bottle, and so on.” ( Participant No. 12).
Delegating care to colleagues on the next shift
In certain situations, such as overcrowding of units, patients with serious conditions and prolonged diagnostic and treatment procedures, nurses are compelled to delegate some of the patient care responsibilities for the current shift to the next shift. This practice can lead to delayed care during the next shift, or sometimes an increased workload for the nurses on the next shift. The following are the statements of some of the participants:
“For example, when a patient goes for dialysis, ultrasound, or needs a simple x-ray, it takes a while for them to return to the unit, and you won’t have enough time to fully take care of them. So, you end up leaving some of the patient’s care for the next shift .” ( Participant No. 2).
“Sometimes, the unit gets super hectic, and the patient is very ill; so that you end up having to pass on some of the tasks to the next shift. But the care gets delayed, and that puts extra pressure on the next shift .” ( Participant No. 4).
“It’s just unfortunate when a very sick patient transfers to your unit and you find out that some of his/her nursing cares weren’t done or were done incompletely, and they’re delegated to your shift. You already have your own work to handle, but now you’ve to deal with the unfinished care from the previous shift as well. It adds to your tasks and makes it hard to complete all your duties for the patient during your shift.” ( Participant No. 3).
Outsourcing of care
Another category extracted was care outsourcing. Outsourcing of care refers to transferring patient care to other units or delegating certain patient care to temporary nurses from other units. Factors such as high workload, nursing shortage, or time constraints are some reasons for nursing care outsourcing. In such cases, the nurse has to rely on temporary nurses who are transferred to the unit or transfer the patient to another unit.
Patient transfer to other units
To ensure the continuation of patient treatment and care, some nurses transferred their patients to other units. These nurses stated that when considering the transfer of a patient to another unit, they first contact the target unit. They then assess the conditions of the destination unit to ensure it meets the requirements for accepting the patient. If the unit meets the necessary conditions, the patient is subsequently transferred to that unit. Verifying the conditions of the destination unit before transferring the patient is crucial to avoid potential risks and ensure timely and appropriate care. Failing to assess the conditions of the destination unit could jeopardize the well-being of the patient and result in delays or even the absence of necessary care.
“We, in the pediatric unit, call the gynecological surgery unit. If they show us the green light, we send stable patients over five years old there. Another example is when the extra beds were all occupied and we had no choice, we sent patients with more stable conditions to the gynecological surgery unit. It helps to decrease our tasks a bit and ensures we can manage all the cares .” ( Participant No. 9).
However, another participant said:
“Sometimes a patient with “special conditions” such as a CCU patient who also needs monitoring is transferred to our unit because of an infection. Our unit is an infectious disease unit, but sometimes the large number of patients and the workload of the unit means that the nurses cannot provide the full care of them, and some care may be missed.” (Participant No.7).
Demand for extra nursing workforce
Another aspect of care outsourcing involves the demand for a nursing workforce or temporary nursing staff from other units. The nurses emphasized that they often request temporary nursing staff from the nursing management office to assist them with providing care during busy periods of the unit. Two participants expressed the following:
“Sometimes, when there’s a lot of work and the number of nurses is low, we call the nursing office and ask them to provide us with a temporary nurse .” (Participant No. 2).
“If I realize that I won’t be able to finish all the tasks before the end of my shift, I’ll ask the supervisor to provide some temporary nursing help, maybe for an hour or to fully assist us throughout the shift.” ( Participant No. 9).
Of course, the transfer of temporary staff to the unit did not always lead to all the care being done completely, and some care might be omitted or missed in this process:
“We sometimes ask for temporary staff to come into the unit as well. However, we can’t guarantee that the care will be fully carried out because the staff from other units have different routines. The type of care provided for the patients varies until they become familiar with the unit’s care practices and routines. So, it’s not always possible to complete all of care entirely .” ( Participant No. 3).
Delegating of care to non-professionals
Delegating patient care to individuals who are not qualified is referred to as delegation of care to non-professionals. In situations where nurses face an inappropriate nurse-to-patient ratio and need to provide care in any way possible, they may delegate some of their patient care responsibilities to individuals who lack the necessary qualifications. There are three types of unprincipled delegation of care to non-professionals, namely delegation to a nurse assistant, to a nursing intern, and to the patient’s family.
Delegating care to nurse assistant
Nurses mentioned that there are instances when they delegate care to non-professional nurses. Specifically, they highlighted the delegation of care to nurse assistants who may lack the necessary academic knowledge and skills required for performing certain care tasks.
“ Here, we ask the nurse assistants to perform ECG, or BS, or even in some cases do venipuncture. ” (Participant No. 8).
“ When the hospital gets busy, we usually ask the nurse assistant to do tasks like taking an ECG or performing a gavage for the patient, even though they may not be highly skilled in these areas. ” ( Participant No. 5).
Delegating care to nursing students in the internship course
Some nurses mentioned the delegation of care to nursing students in the internship course. While this practice might reduce some of the nurse’s tasks, it is important to note that nursing students are still in the learning process and may not have the ability to independently perform care without the supervision of their instructor. This type of improper delegation of care has the potential to endanger patient safety.
“Some colleagues delegate the responsibility of medication to interns. Some students, who are still learning nursing care, may not yet have the confidence to administer medication independently without supervision .” ( Participant No. 8).
Another participant stated:
“At times, nurses assign interns to care for patients, but these interns may forget to do some necessary care.” (Participant No. 11).
Delegating care to the patient’s family
Many nurses referred to the delegation of care to the patient’s family. In other words, they occasionally delegate tasks that should be performed by the nurses or other members of the healthcare team to the patient’s families. However, they acknowledged that this practice is not ideal or appropriate.
“It’s better if patients have someone accompanying them when they are hospitalized because when we’re overwhelmed with work, we often have to rely on the patient’s companion to take care of certain tasks, even though we’re aware it’s not the ideal approach .” (Participant No. 10).
“Unfortunately, there are times when nurses pass on certain care tasks to the patient’s family; Tasks such as administering tube feeding, assisting with repositioning and movement, and even providing oxygen therapy. In some cases, the nurse instructs the patient’s companion to disconnect and reconnect the IV drip, disconnect and reconnect the monitoring equipment, or administer insulin to the patient without supervision.” (Participant No. 12).
Delegation of care, a double-edged sword
The findings of this study revealed that the overarching theme extracted from the analyzed data was the “delegation of care, a double-edged sword.” Contemplating the key categories derived from the participants’ statements indicated that nurses, due to factors such as inappropriate nurse-to-patient, emergent situations, time constraints, and nursing shortage, delegate a portion of their patient care responsibilities to others. However, this care strategy can have a dual and paradoxical impact on the quality of patient care. On one hand, delegating care can reduce the workload of nurses and enable them to better attend to their other patients. On the other hand, it is associated with potential drawbacks such as delayed care, missed care, neglecting certain aspects of care, or a decrease in the overall quality of nursing care provided.
“Sometimes, because we’ve so much work to handle, we end up passing on certain care tasks to our colleagues. It helps us manage our patients’ caring tasks, but the downside is that we can’t supervise or ensure that the delegated tasks are done correctly. On the flip side, there are instances when we ask our colleague, “Did you do that?” only to find out that they completely forgot to do it .” (Participant No. 11).
This study aimed to explore the experiences of Iranian nurses regarding care delegation. It was found that in situations such as the nurses faced a high workload and insufficient staffing, they were compelled to delegate certain patient care responsibilities to others. This delegation took various forms, including delegation of care to colleagues within the same unit (insourcing), colleagues from other units (outsourcing), or non-professional individuals. In certain situations, delegating care can be beneficial as it helps to reduce the nurse’s tasks and promotes teamwork and cooperation. However, there are instances where delegation not only fails to be helpful but also diminishes the quality of care, sometimes resulting in missed or compromised care. Hence, it can be said that the delegation of care acts as a double-edged sword in terms of its impact on the quality of nursing care, with both positive and negative outcomes. Consequently, it becomes crucial to pay close attention to how care is delegated to others to minimize the negative outcomes and enhance the quality of nursing care.
In this study, nurses mentioned delegating care to colleagues within their own unit, which includes other nurses and head nurses. Ghezeljeh et al. (2020) found that increased collaboration among nurses as a result of delegating care can lead to a reduction in missed nursing care [ 25 ]. Similarly, Gibbon and Crane (2018) revealed that effective teamwork serves as a strategy to mitigate care left undone [ 26 ]. The presence of financial constraints, nursing shortage, and the high complexity of patient care have created an environment where delegation becomes necessary. Proper and standardized delegation of authority plays a crucial role in improving patient care outcomes. To ensure correct delegation of authority, three fundamental components—responsibility, authority, and accountability—must be considered. The nurse should bear the responsibility for patient care, possess the necessary authority and competence to provide care and be accountable for caring for the patient. Based on these three components and considering the five rights of delegation—namely, the right task, right circumstances, right person, right supervision, and right direction and communication—the nurse can appropriately delegate care to another individual. Among these five rights, the right of communication/direction is particularly vital in safeguarding the quality of nursing care and ensuring patient safety [ 27 ]. Hence, it is not sufficient to solely delegate care to a colleague. For a successful transfer of care, factors such as effective communication, competence, and knowledge of the receiving nurse, as well as their attitude and duties, must be taken into account [ 26 ]. In this case, Rooddehghan et al. (2015) revealed in their study that improper delegation of care can occur due to insufficient staffing and high workload, leading to a lack of proper supervision over delegated care. As a result, there is a possibility that the care assigned to another nurse may not be executed correctly [ 8 ].
In this study, nurses reported the delegating of care to the next shift. While delegating care to the next shift may decrease a nurse’s tasks, it also presents challenges such as care delays or an increased workload for the subsequent shift. Campagna et al. (2021) emphasized that nurses often delegate some care tasks to the next shift, resulting in delayed patient care, which can ultimately impact care quality [ 28 ]. Similarly, Mantovan et al. (2020) found that nurses tend to delegate care to the next shift when faced with a high workload [ 29 ]. Nurses employ strategies such as delaying care or delegating care to the next shift before omitting nursing tasks. However, any delay in the provision of nursing care diminishes its quality and have adverse consequences for the patient [ 29 – 31 ].
In the present study, the nurses identified patient transfer to other units as a significant strategy in delegating care to reduce their workload. Patient transfer within the hospital is an important aspect of patient care management, often employed to improve care provision. However, it is important to recognize that patient transfers can lead to various physiological changes that may have a negative impact on the patient’s prognosis. Therefore, patient transfers should be conducted systematically, following evidence-based guidelines. The decision to transfer a patient should be made after careful consideration of the potential benefits concerning the associated risks. It should be based on the concept of “stabilization and transfer,” starting with stabilizing the patient in the transferring center and ensuring continuity of care until the patient reaches the receiving center [ 32 , 33 ]. It is pivotal to note that transferring a patient to another unit solely to reduce the workload of the current unit may pose risks to the patient’s health.
One of the strategies mentioned by the nurses was the request for temporary nurses from other units. Studies in this area indicate that employing temporary nursing staff can help diminish the nursing workload. However, it may have adverse economic implications due to the potential increase in negative outcomes for patients. Furthermore, evidence suggests that the presence of supportive nursing staff in a unit might increase the workload for regular nurses. This is because the regular nurses must dedicate more time to supervising these individuals, and they may not be able to provide patient care to the same extent as the regular staff members of the unit [ 34 ]. Senek et al. (2020) demonstrated that the use of temporary nurses in a unit leads to an increase in unfinished nursing care [ 35 ]. Nursing managers believe that employing temporary nurses to compensate for staff shortages and high workloads in a unit does not necessarily result in an improvement in the quality of services [ 36 ].
Nurses also reported instances where they delegate care to non-professionals, such as nursing assistants or nursing students and interns. Chua et al. (2019) found that registered nurses (RNs) delegate certain routine care tasks, such as monitoring vital signs, to enrolled nurses (ENs). However, it is important to note that these nurses may not possess sufficient clinical knowledge regarding monitoring and controlling vital signs [ 37 ]. Jasemi et al. (2018) conducted a qualitative study exploring the experiences of nursing students in clinical education. The findings revealed that one of their challenges in clinical education is the delegation of nursing care to them without adequate training and supervision. The students also highlighted that the expectations of the nurses and their mentors are often unreasonable and exceed the students’ capabilities, potentially compromising patient safety [ 38 ]. In another study, nursing students expressed a desire for proper guidance and support when performing nursing care [ 39 ].
The utilization of nursing assistants or nursing students in place of registered nurses is an example of a skill mix in healthcare settings. Because of the nursing shortage and cost-cutting efforts, some hospitals have adopted a combination of professional nurses (registered nurses) and less skilled staff [ 40 ]. However, research demonstrates that the lower the ratio of registered nurses among the nursing staff responsible for direct patient care, the higher the patient mortality rates, poorer quality of care, and increased frequency of adverse outcomes [ 41 , 42 ]. Aiken et al. (2017) also showed that for every 10% decrease in the proportion of registered nurses compared to the overall nursing staff, there is an 11% increase in the likelihood of patient mortality. Beyond the risk of preventable deaths among patients, increasing the nursing skill mix can have negative results on overall care quality [ 41 ].
In the present study, it was observed that nurses delegate certain aspects of care to family members and companions of the patients. Family members play a crucial role in patient care and are considered as caregivers. They can provide valuable support in caring for patients alongside the healthcare team and nursing staff. This highlights the importance of patient- and family-centered care, where the involvement and participation of family members are emphasized. However, the role of the family in the hospital setting is primarily one of support and participation in decision-making, while the caregiver role becomes more prominent after discharge when the patient is at home [ 43 , 44 ]. Aein et al. (2009) reported that although hospital policies emphasize that nurses should not delegate nursing care tasks to the patient’s family, in certain situations, nurses may delegate some aspects of care to the patient’s family, particularly parents, to reduce their workload. However, this practice has resulted in family dissatisfaction and compromised patient safety [ 45 ]. Rooddehghan et al. (2015) also stated that some nurses delegate care responsibilities to the patient’s family or non-professional individuals. It can lead to deficiencies and errors in care, posing a potential threat to the patient’s life [ 8 ].
Strengths and limitations
This study represents the first investigation in Iran that explores nurses’ experiences with delegating care. The findings of this study can enhance the understanding of clinical nurses and nursing managers regarding delegation of care and provide better insights for potential improvements. However, it is important to acknowledge that, as a qualitative study, the generalizability of the findings may be limited to societies with similar backgrounds and cultures.
The findings of the study revealed that care delegation occurred through three methods: insourcing, outsourcing, and delegation of care to non-professionals. Nurses often resorted to delegating care to others due to reasons such as high workload, time constraints, aiming to prevent delays in care provision. This delegation of care had both positive and negative outcomes. On the one hand, it helped reduce nurses’ workload and fostered team cooperation. On the other hand, it sometimes compromises the quality of care and even leads to missed nursing care. Hence, the act of delegating care can be viewed as a double-edged sword for the quality of nursing care, with the potential for both positive and negative consequences. It is crucial to recognize that care delegation should adhere to correct and standardized principles. Incorrect delegation of care can diminish the quality of nursing care and jeopardize patient safety.
Considering the significance of correct delegation of care and its impact on enhancing nursing care, it is important for nursing managers and policymakers to develop written educational programs for nurses focusing on the proper delegation of care. This will ensure that nurses are familiar with delegation methods and principles, enabling them to effectively manage their workload and ensure comprehensive care. Furthermore, it is essential to incorporate the topic of correct delegation of care into the nursing curriculum, particularly through a nursing management course. By teaching undergraduate nursing students the appropriate methods of delegation, they will be equipped to utilize this approach correctly in their future clinical practice.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The researchers would like to express their gratitude to all the nurses who generously shared their valuable experiences. This study is a component of a nursing Ph.D. dissertation, which has received approval as a research project number 401029 from Kashan University of Medical Sciences. The researchers also appreciate the research vice-chancellor of Kashan University of Medical Sciences for providing financial support for this research.
Abbreviations
| BS | Blood Sugar |
| ECG | Electrocardiography |
| MAXQDA | MAX Qualitative Data Analysis |
Author contributions
Tayebeh Moradi, Mahboubeh Rezaei, and Negin Masoudi Alavi were responsible for the study conception/design. Tayebeh Moradi performed the data collection. Tayebeh Moradi, Mahboubeh Rezaei, and Negin Masoudi Alavi analyzed and interpreted the participants’ data. Tayebeh Moradi and Mahboubeh Rezaei were significant contributors in writing the manuscript. All the authors read and approved the final manuscript.
The article has been financially supported as a research project by the research vice-chancellor of Kashan University of Medical (Registration Number: 401029 dated 3 July 2022).
Data availability
Declarations.
After receiving approval from the ethics committee of Kashan University of Medical Sciences with the ethics code IR.KAUMS.NUHEPM.REC.1401.029, a letter of recommendation was obtained from the Research Vice-Chancellor of the university to conduct participant interviews. Before commencing the interviews, the study objectives were explained to the participants, and written informed consent was obtained from each participant to participate in the research and record the interviews in accordance with the Declaration of Helsinki. Separate written consent was obtained for each interview conducted. The participants were assured that their information would be kept confidential, and if they desired, they would be provided with the results of the research.
Not Applicable.
The authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prioritization, Delegation, and Assignment in Nursing NCLEX Practice Questions (100 Items)
In this NCLEX guide , we’ll help you review and prepare for prioritization, delegation, and assignment in your nursing exams. For this nursing test bank , improve your prioritization, delegation , and patient assignment skills by exercising with these practice questions. We will also be teaching you test-taking tips and strategies so you can tackle these questions in the NCLEX with ease. The goal of these practice quizzes and reviewers is to help student nurses establish a foundation of knowledge and skills on prioritization, delegation, and assignment.
Quiz Guidelines
Before you start, here are some examination guidelines and reminders you must read:
- Practice Exams : Engage with our Practice Exams to hone your skills in a supportive, low-pressure environment. These exams provide immediate feedback and explanations, helping you grasp core concepts, identify improvement areas, and build confidence in your knowledge and abilities.
- You’re given 2 minutes per item.
- For Challenge Exams, click on the “Start Quiz” button to start the quiz.
- Complete the quiz : Ensure that you answer the entire quiz. Only after you’ve answered every item will the score and rationales be shown.
- Learn from the rationales : After each quiz, click on the “View Questions” button to understand the explanation for each answer.
- Free access : Guess what? Our test banks are 100% FREE. Skip the hassle – no sign-ups or registrations here. A sincere promise from Nurseslabs: we have not and won’t ever request your credit card details or personal info for our practice questions. We’re dedicated to keeping this service accessible and cost-free, especially for our amazing students and nurses. So, take the leap and elevate your career hassle-free!
- Share your thoughts : We’d love your feedback, scores, and questions! Please share them in the comments below.
Prioritization, Delegation, and Assignment Practice Quiz
This section contains the practice questions to exercise your knowledge on nursing prioritization, delegation, and assignment. As with other quizzes, be sure to read and understand the question carefully. For prioritization, delegation, and assignment questions, read each choice carefully before deciding on your answer. Good luck and answer these questions at your own pace. You are here to learn.
Quizzes included in this guide are:
| Quiz No. | Quiz Title | Questions |
|---|---|---|
| 1 | 25 | |
| 2 | 25 | |
| 3 | 25 | |
| 4 | 25 |
Nursing Prioritization, Delegation and Assignment Reviewer for Nurses
This is your guide to help you answer NCLEX priority, delegation, and assignment style questions.
NCLEX Tips for Nursing Prioritization, Delegation, and Assignment questions:
Here are six tips and strategies to help you ace NCLEX questions about delegation, assignment, and prioritization.
1. Do not make decisions based on resolutions
Do not make decisions concerning the management of care issues based on resolutions you may have witnessed during your clinical experience in the hospital or clinic setting. As a student nurse , you are constantly reminded that NCLEX questions are to be solved and responded to in the context of “Ivory Tower Nursing.” That is, if you only had one patient at a time, loads of assistive personnel, countless supplies, and equipment. This is what people mean when they refer to “ textbook nursing .” But when you’re in the real world without the time and resources, you adjust. Your clinical rotation in management may have been less than ideal but remember that in NCLEX, the answers to the questions are seen in nursing textbooks or journals. Always bear in mind, “Is this textbook nursing care?”
2. Never delegate the functions of assessment, evaluation and nursing judgment.
Throughout your nursing education , you learned that assessments, nursing diagnosis , establishing expected outcomes, evaluating care and any other tasks and aspects of care including but not limited to those that entail sterile technique, critical thinking, professional judgment, and professional knowledge are the responsibilities of the registered professional nurse. You cannot give these responsibilities to nonprofessional, unlicensed assistive nursing personnel, such as nursing assistants, patient care technicians, and personal care aides.
3. Identify tasks for delegation based on the client’s needs.
Delegate activities for stable patients because some of these needs are relatively predictable and more frequently encountered. These are somewhat routinized and without the need for high levels of professional judgment and skill. But if the patient is unstable, the needs are acute and become unpredictable, ever-changing, and rarely encountered based on the patient’s changing status. These needs should not be delegated.
4. Ensure the appropriate education, skills, and experience of personnel performing delegated tasks.
Delegate activities that involve standard, consistent, and unchanged systems and procedures. The care of a patient with chest tubes and chest drainage can be delegated to either another RN or a licensed practical nurse. Therefore, the authorizing RN must ensure that the nurse is qualified, skilled, and competent to perform this intricate task, observe the patient’s response to this treatment, and ensure that the equipment is operating suitably and accurately.
The care of a stable chronically ill patient who is comparatively stable and more anticipated than a seriously ill and unstable acute patient can be assigned to the licensed practical nurse, and assistance with the activities of daily living and basic hygiene and comfort care can be assigned and delegated to an unlicensed assistive staff member like a nursing assistant or a patient care technician. Activities that frequently occur in daily patient care can be delegated. Bathing, feeding , dressing , and transferring patients are examples.
Procedures that are complex or complicated should not be delegated, especially if the patient is highly unstable.
5. Remember priorities!
Recall and understand Maslow’s Hierarchy of Needs , the ABCs (Airway, Breathing, Circulation ), and stable versus unstable. It is necessary to know and understand the priorities when deciding which patient the RN should attend to first. Remember that you can see only one patient or perform one activity when answering questions that require you to establish priorities.
Always keep in mind that improper and inappropriate assignments can lead to inadequate quality of care, unexpected care outcomes, the jeopardization of client safety, and even legal consequences. Right assignment of care to others, including nursing assistants, licensed practical nurses, and other registered nurses, is certainly one of the most significant daily decisions nurses make.
6. Additional Test Taking Tips and Strategies
- Questions using keywords such as “ best ,” “ essential ,” “ highest priority ,” “ primary ,” “ immediate ,” “ first ,” or “ initial response ” are asking for your prioritizing skills.
- Know the patient’s purpose of care, current clinical condition, and outcome of care in order to determine and plan priorities.
- Identify the priority patient based on the following: patient’s age, day of admission/ surgery , or the number of body systems involved.
- Unlicensed assistive personnel (UAP) such as nurses’ aides, certified nursing assistants, attendants, health aides are not allowed to delegate. Only a registered nurse can delegate tasks.
- In some states, Licensed Practical Nurses ( LPN ) may delegate to a UAP depending on the state nursing practice .
- Ensure the appropriate knowledge, skills, and experience of personnel performing the delegated tasks.
- Do not delegate teaching, assessment , planning , evaluating, and nursing judgment to an unlicensed nurse.
- A client with an unstable and unpredictable condition cannot be delegated to a UAP’s or LPNs.
- Delegate tasks that involve standard, simple procedures such as bathing , dressing , feeding , and transferring patients.
- Student nurses, float nurses, personal assistants, and other personnel may require levels of guidance and supervision.
Nursing Prioritization
Prioritization is deciding which needs or problems require immediate action and which ones could be delayed until later because they are not urgent. In the NCLEX, you will encounter questions that require you to use the skill of prioritizing nursing actions. These nursing prioritization questions are often presented using the multiple-choice format or via ordered-response format. For a review, in an ordered-response question format , you’ll be asked to use the computer mouse to drag and drop your nursing actions in order or priority. Based on the information presented, determine what you’ll do first, second, third, and so forth. Directions are provided with the question. To help you answer nursing prioritization questions, remember the three principles commonly used:
1. Remember ABC’s (airway, breathing, and circulation).
Patients with obvious respiratory problems or interventions to provide airway management are given priority.
2. Maslow’s Hierarchy of Needs
Use Maslow’s hierarchy of needs as a guide to prioritize by determining the order of priority by addressing the physiological needs first.
There are five different levels of Maslow’s hierarchy of needs:
- Physiological Needs. The basic physiological needs have the highest priority and must be met first. Some examples of physiological needs include oxygen, food, fluid, nutrition , shelter, sleep , clothing, and reproduction.
- Safety Needs. Safety can be divided into physical and physiological. These include health, property, employment, security of the environment, and resources.
- Social Needs. These include love, family, friendship, and intimacy.
- Esteem. These include confidence, self-esteem , respect, and achievement.
- Self-actualization. These include creativity, morality, and problem-solving.
3. Using the Nursing Process
The nursing process is a systematic approach to assess and give care to patients. Assessment should always be done first before planning or providing interventions.
Delegation in Nursing
Delegation is the transference of responsibility and authority for an activity to other health care members who are competent to do so. The “delegate” assumes responsibility for the actual performance of the task and procedure. The nurse (delegator) maintains accountability for the decision to delegate and for the appropriateness of nursing care rendered to the patient. The role of a registered nurse also includes delegating care, assigning tasks, organizing and managing care, supervising care delivered by other health care providers while effectively managing time! The NCLEX includes questions related to this unique nursing role of delegation.
5 Rights of Delegation in Nursing
The following are the five rights of delegation in nursing:
- Right Person. The licensed nurse and the employer and the delegatee are responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity.
- Right Tasks. The activity falls within the delegatees’ job description or is included as part of the nursing practice settings established written policies and procedures. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Each delegation situation should be specific to the patient, the licensed nurse, and the delegatee.
- The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee should ask any clarifying questions as part of two-way communication . This communication includes any data that needs to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation.
- The delegatee must understand the terms of the delegation and must agree to accept the delegated activity.
- The licensed nurse should ensure that the delegatee understands that she or he cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse.
- Right Circumstances. The health condition of the patient must be stable. If the patient’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation.
- The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating patient outcomes . The delegatee is responsible for communicating patient information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary.
- The licensed nurse should ensure appropriate documentation of the activity is completed.
Recommended Resources
Recommended books and resources for your NCLEX success:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Saunders Comprehensive Review for the NCLEX-RN Saunders Comprehensive Review for the NCLEX-RN Examination is often referred to as the best nursing exam review book ever. More than 5,700 practice questions are available in the text. Detailed test-taking strategies are provided for each question, with hints for analyzing and uncovering the correct answer option.

Strategies for Student Success on the Next Generation NCLEX® (NGN) Test Items Next Generation NCLEX®-style practice questions of all types are illustrated through stand-alone case studies and unfolding case studies. NCSBN Clinical Judgment Measurement Model (NCJMM) is included throughout with case scenarios that integrate the six clinical judgment cognitive skills.

Saunders Q & A Review for the NCLEX-RN® Examination This edition contains over 6,000 practice questions with each question containing a test-taking strategy and justifications for correct and incorrect answers to enhance review. Questions are organized according to the most recent NCLEX-RN test blueprint Client Needs and Integrated Processes. Questions are written at higher cognitive levels (applying, analyzing, synthesizing, evaluating, and creating) than those on the test itself.

NCLEX-RN Prep Plus by Kaplan The NCLEX-RN Prep Plus from Kaplan employs expert critical thinking techniques and targeted sample questions. This edition identifies seven types of NGN questions and explains in detail how to approach and answer each type. In addition, it provides 10 critical thinking pathways for analyzing exam questions.

Illustrated Study Guide for the NCLEX-RN® Exam The 10th edition of the Illustrated Study Guide for the NCLEX-RN Exam, 10th Edition. This study guide gives you a robust, visual, less-intimidating way to remember key facts. 2,500 review questions are now included on the Evolve companion website. 25 additional illustrations and mnemonics make the book more appealing than ever.

NCLEX RN Examination Prep Flashcards (2023 Edition) NCLEX RN Exam Review FlashCards Study Guide with Practice Test Questions [Full-Color Cards] from Test Prep Books. These flashcards are ready for use, allowing you to begin studying immediately. Each flash card is color-coded for easy subject identification.

Recommended Links
An investment in knowledge pays the best interest. Keep up the pace and continue learning with these practice quizzes:
- Nursing Test Bank: Free Practice Questions UPDATED ! Our most comprehenisve and updated nursing test bank that includes over 3,500 practice questions covering a wide range of nursing topics that are absolutely free!
- NCLEX Questions Nursing Test Bank and Review UPDATED! Over 1,000+ comprehensive NCLEX practice questions covering different nursing topics. We’ve made a significant effort to provide you with the most challenging questions along with insightful rationales for each question to reinforce learning.
11 thoughts on “Prioritization, Delegation, and Assignment in Nursing NCLEX Practice Questions (100 Items)”
Very helpful. A LPN graduate who has taken the nclex four times. It gives me a quick overview. Thanks
Love it!!! These made me think. They up there with ReMar and uWorld.
Very helpful thanks
In which order will the nurse perform the following actions as she prepares to leave the room of a client with airborne precautions after performing oral suctioning?
please your order for this question is wrong
I have learned a lot from the NursesLabs. Love it!
Nurse Pietro receives an 11-month old child with a fracture of the left femur on the pediatric unit. Which action is important for the nurse to take FIRST? First- Speak with parents as to how injury occurred??? Yes, this is going to take place but this the first thing to do? Perhaps the wording needs to change as I have been “textbook” taught, treat first, then question in cases of suspected abuse.
good questions which test your analyzing and critical thinking skils
Thank you for making this free. It is my additional resources. This has been very helpful. I really appreciate that you are helping all future nurses to be at their best .
I’m really grateful for this excercise which aids in preparing for the NCLEX. Thanks
This has help me pass my nclex !! Thanks
I am interested to join nurseslab daily question
Leave a Comment Cancel reply

IMAGES
VIDEO
COMMENTS
Delegation and assignment of nursing activities are important parts of the implementation component of practice for the licensed nurse (RN and LPN). The licensed nurse may assign and/or delegate nursing care activities to other licensed nurses and unlicensed assistive personnel (UAP) based upon their own license level,
delegation, as compared to assignment, appropriate delegation allows for transition of a responsibility in a safe and consistent manner. Clinical reasoning, nursing judgement and critical decision making cannot be delegated. The delegation process is multifaceted. It begins with the administrative level of the organization including:
Effective delegation is a skill that can take time to master, but it's essential for effective leadership and staff growth. Fortunately, ANA developed Principles for Delegation by Registered Nurses to Unlicensed Assistive Personnel (UAP). This document provides strategies for RNs to draw from when determining which tasks to delegate.
The goal was to develop national guidelines based on current research and literature to facilitate and standardize the nursing delegation process. These guidelines provide direction for employers, nurse leaders, staff nurses, and delegatees. Keywords: Delegation, evidence-based, guidelines, nursing assignment, regulation, research.
Many definitions for delegation exist in professional literature. One of the most commonly cited definitions of the word was jointly established by the American Nurses Association and the National Council of State Boards of Nursing. These groups describe delegation as the process for a nurse to direct another person to perform nursing tasks and activities. Delegation involves at least two ...
Delegation generally involves assignment of the performance of activities or tasks related to patient care to unlicensed assistive personnel while retaining accountability for the outcome. The registered nurse cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to ...
The National Council of State Boards of Nursing (NCSBN) is a not-for-profit organization whose purpose is to provide an organization through which boards of nursing act and counsel together on matters of common interest and concern affecting the public health, safety and welfare, including the development of licensing examinations in nursing.
Nursing Delegation ... A nursing activity, skill, or procedure that is transferred from a licensed ... A delegator may be an APRN, RN, or LPN/VN. • Assignment: The routine care, activities and procedures that are within the authorized scope of practice of the RN or LPN/VN or part of the routine functions of the AP.
As health care technology continues to advance, clients require increasingly complex nursing care, and as staffing becomes more challenging, health care agencies respond with an evolving variety of nursing and assistive personnel roles and responsibilities to meet these demands. As an RN, you are on the frontlines caring for ill or injured clients and their families, advocating for clients ...
According to national guidelines for nursing delegation from the National Council of State Boards of Nursing (NCSBN) and American Nurses Association (ANA), an assignment refers to the "routine care, activities, and procedures that are within the authorized scope of practice of the RN or LPN/VN or part of the routine functions of the AP.".
3.4 Delegation There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND). [1] These guidelines apply to all levels of nursing licensure (advanced ...
both defined delegation as the process for a nurse to direct another person to perform nursing tasks and activities. NCSBN describes this as the nurse transferring authority while ANA calls this a transfer of ... All decisions related to delegation and assignment are based on the fundamental principles of protection of the health, safety and ...
Delegation is allowing a delegatee to perform a specific nursing activity, skill, ... An example illustrating the difference between assignment and delegation is assisting patients with eating. Feeding patients is typically part of the routine role of AP. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or ...
3.4 Delegation There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND). [1] These guidelines apply to all levels of nursing licensure (advanced ...
A licensed nurse is still responsible for ensuring the assignment is carried out correctly. Delegation. According to the NCSBN/ANA guideline, delegation applies when the delegatee is performing a "specific nursing activity, skill, or procedure that is beyond the delegatee's traditional role and not routinely performed." As opposed to work ...
Delegation of Nursing Care ActivitiesAs a nephrology registered nurse (RN), you may be delegating to both licens. and unlicensed assistive personnel. Delegation to licensed practical nurses/licensed vocational nurses (LPNs/LVNs) is supported by the scope of practice for these nurses in the individual state's nurse practice act, which va. es ...
Date: 2019. Adopted By: ANA and NCSBN. Summary. In 2005, both the American Nurses Association (ANA) and the National Council of State Boards of Nursing (NCSBN) adopted papers on delegation. Both papers presented the same message: delegation is an essential nursing skill. This joint statement has been updated (2019) - The National Guidelines for ...
Effective delegation promotes the delivery of safe client care and permits the nurse to focus on the provision of crucial nursing activities and responsibilities. Delegation is an essential competency of nursing practice and fosters work efficiency gained by the team approach. UAP are valuable members of the team.
In early 2015, the National Council of State Boards of Nursing convened two panels of experts representing education, research, and practice. The goal was to develop national guidelines based on current research and literature to facilitate and standardize the nursing delegation process. These guidelines provide direction for employers, nurse leaders, staff nurses, and delegatees.
Delegation of care enables nurses to allocate more time to patient care, support, and education . The process of delegating care involves complex decision-making, where nurses must demonstrate leadership and change management skills to establish team cohesion, support patients, and ensure the effective implementation of nursing activities .
Directions are provided with the question. To help you answer nursing prioritization questions, remember the three principles commonly used: 1. Remember ABC's (airway, breathing, and circulation). Patients with obvious respiratory problems or interventions to provide airway management are given priority. 2.
Delegation to ensure the delegation or assignment is: a) The right task • The delegated activity must fall within the delegatee's job description and scope of practice. ... • Delegation of nursing care activities to licensed and unlicensed personnel shall comply with the following criteria:
NCBON Decision Tree for Delegation to UAP and the Position Statement on Delegation and Assignment of Nursing Activities (both available at www.ncbon.com) provide guidance for RN practice. EVALUATION is the fourth step of the nursing process and consists of determining the extent to which desired